User login
Caps on malpractice damages
Question: Which of the following statements regarding statutory caps on malpractice damages is best?
A. All states have such a statutory provision.
B. The provision limits the recovery of both economic and noneconomic losses.
C. It’s constitutional.
D. It’s not constitutional.
E. Whether it’s constitutional depends on the jurisdiction.
Answer: E. In 1975, California enacted its historic Medical Injury Compensation Reform Act (MICRA),1 the state legislature declaring that there was “a major health care crisis in the State of California attributable to skyrocketing malpractice premium costs and resulting in a potential breakdown of the health delivery system.”
The rationale was to provide some predictability, because noneconomic damages are difficult to quantify, and jury sympathy may result in unrealistically high payments. It was believed that damages for pain and suffering, for example, often contributed to runaway jury verdicts, prompting one indignant observer to write: “In making arguments for pain and suffering awards, both sides attempt to win the jurors’ sympathies with highly emotional evidence. A blind plaintiff will receive careful instruction to come to court with his [guide] dog, and to dab at his eyes with a handkerchief.”2
One of the main provisions of MICRA is to limit noneconomic recovery for injuries arising out of medical negligence. It caps noneconomic damages – for example, pain and suffering, disfigurement, emotional distress, loss of consortium, and other nonpecuniary losses – at $250,000. The law does not restrict recovery of economic damages such as wage loss, medical expenses, and future lost income.
California is the pioneer state to institute this tort reform measure, and about a dozen other states have followed suit, such as Proposition 12 in Texas, which limits noneconomic damages to $750,000 – $250,000 from the defendant doctor and $500,000 from the hospital.
Many tort reformists hail MICRA as the prototype success story, crediting it for bringing California’s malpractice insurance premiums from one of the highest levels in the nation to one of its lowest. A 2004 study reported that states with caps have a loss ratio (losses plus costs over premiums) that is 12% lower than in those without damage caps.3 Lower premiums in turn are linked to greater physician entry into the locality, especially for high-risk specialists.
In addition, caps may have a salutary effect on the wasteful practice of defensive medicine. A 2007 report by the American Medical Association confirms and extends an earlier study that reached such conclusions.
However, recent medical malpractice rates are generally no longer rising or even falling – both in states that had enacted tort reform and in states that had not. This may mean that other interventions such as medical error recognition and reduction are also effective.
Unsurprisingly, caps on damages have been challenged on constitutional grounds, as a violation of the equal rights amendment and the patient’s right to a jury trial. Two recent cases with divergent results – one on California, and the other in Florida – illustrate the state of flux over this controversy.
In Chan v. Curran, the plaintiff sought to relitigate the constitutionality of the California damage cap, but the appellate court ruled for the doctor defendant.4 The case alleged a wrongful death when the patient died from hemorrhage related to warfarin (Coumadin) use during open heart surgery.
The plaintiff argued that MICRA’s rationale was irrelevant, because there was no longer a malpractice insurance crisis in California – thus, restrictions placed on the quantum of damages are not rationally related to any legitimate state interest.
Furthermore, by limiting the amount of noneconomic damages to $250,000, MICRA violated equal protection and discouraged or inhibited attorneys from taking up malpractice cases on a contingency fee basis. Finally, the plaintiff argued that under the statute, a litigant is deprived of the right to a jury trial.
The court rejected all of these arguments, and reaffirmed the constitutionality of MICRA in line with earlier decisions that began with California’s Supreme Court decision in the Fein v. Permanente Medical Group case.5
On the other hand, the recent case of Estate of Michelle Evette McCall v. U.S. found the Florida Supreme Court ruling for the plaintiff.6 There, the court deemed unconstitutional Florida’s statute limiting wrongful death damages in medical malpractice to $1 million.
The case involved a young mother who died of massive hemorrhage following a cesarean section. In a 5-2 decision, the court held that the statute was arbitrary, reasoning that “the statutory cap on wrongful death noneconomic damages fails because it imposes unfair and illogical burdens on injured parties.”
Unlike California, the Florida court found that the cap bears no rational relationship to any perceived malpractice insurance crisis. And, while saving a modest amount for many, the statute imposed devastating costs on those who are most grievously injured, as well as on cases affecting multiple claimants.
The court commented that “the finding by the Legislature and the Task Force that Florida was in the midst of a bona fide medical malpractice crisis, threatening the access of Floridians to health care, is dubious and questionable at the very best.” The court also noted that four malpractice carriers actually increased their net income by more than 4,300% between 2003 and 2010.
In 2010, the Illinois Supreme Court also held in Lebron v. Gottlieb Memorial Hospital that the state’s $500,000 cap for noneconomic damages was unconstitutional, being in violation of the separation of powers doctrine.7 Only judges are empowered to reduce excessive verdicts, termed a remittitur. Thus, a statutory damage cap amounted to a “legislative remittitur” that invaded the power of the judiciary and violated the constitutional requirement of separation of powers.
The battle over caps continues unabated, with the trend appearing to favor the plaintiff bar. Florida’s ruling was the eighth state supreme court decision that held damage caps unconstitutional, joining Alabama, Georgia, Illinois, Missouri, New Hampshire, Oregon, and Washington. Five other states – Arizona, Arkansas, Kentucky, Pennsylvania, and Wyoming – already have state constitutional prohibitions on damage caps.
References
1. Medical Injury Compensation Reform Act of 1975, Cal. Civ. Proc. Code § 3333.2 (West 1982).
2. O’Connell, J. Offers That Can’t Be Refused: Foreclosure of Personal Injury Claims by Defendants’ Prompt Tender of Claimants’ Net Economic Losses. 77 N.W.U.L. Rev. 589, 591 (1982).
3. Thorpe, K. The Medical Malpractice Crisis: Recent Trends and the Impact of State Tort Reforms, Health Affairs 2004, Jan 21 [doi:10.1377/hlthaff.w4.20].
4. Chan v. Curran, 237 Cal. App. 4th 601 (Cal.Ct.App. 2015).
5. Fein v. Permanente Medical Group, 695 P.2d 665 (Cal. 1985).
6. Estate of Michelle Evette McCall v. U.S., 2014 Fla. LEXIS 933 (Fla. Mar. 13, 2014).
7. Lebron v. Gottlieb Memorial Hospital, 930 N.E.2d 895 (Ill. 2010).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at siang@hawaii.edu.
Question: Which of the following statements regarding statutory caps on malpractice damages is best?
A. All states have such a statutory provision.
B. The provision limits the recovery of both economic and noneconomic losses.
C. It’s constitutional.
D. It’s not constitutional.
E. Whether it’s constitutional depends on the jurisdiction.
Answer: E. In 1975, California enacted its historic Medical Injury Compensation Reform Act (MICRA),1 the state legislature declaring that there was “a major health care crisis in the State of California attributable to skyrocketing malpractice premium costs and resulting in a potential breakdown of the health delivery system.”
The rationale was to provide some predictability, because noneconomic damages are difficult to quantify, and jury sympathy may result in unrealistically high payments. It was believed that damages for pain and suffering, for example, often contributed to runaway jury verdicts, prompting one indignant observer to write: “In making arguments for pain and suffering awards, both sides attempt to win the jurors’ sympathies with highly emotional evidence. A blind plaintiff will receive careful instruction to come to court with his [guide] dog, and to dab at his eyes with a handkerchief.”2
One of the main provisions of MICRA is to limit noneconomic recovery for injuries arising out of medical negligence. It caps noneconomic damages – for example, pain and suffering, disfigurement, emotional distress, loss of consortium, and other nonpecuniary losses – at $250,000. The law does not restrict recovery of economic damages such as wage loss, medical expenses, and future lost income.
California is the pioneer state to institute this tort reform measure, and about a dozen other states have followed suit, such as Proposition 12 in Texas, which limits noneconomic damages to $750,000 – $250,000 from the defendant doctor and $500,000 from the hospital.
Many tort reformists hail MICRA as the prototype success story, crediting it for bringing California’s malpractice insurance premiums from one of the highest levels in the nation to one of its lowest. A 2004 study reported that states with caps have a loss ratio (losses plus costs over premiums) that is 12% lower than in those without damage caps.3 Lower premiums in turn are linked to greater physician entry into the locality, especially for high-risk specialists.
In addition, caps may have a salutary effect on the wasteful practice of defensive medicine. A 2007 report by the American Medical Association confirms and extends an earlier study that reached such conclusions.
However, recent medical malpractice rates are generally no longer rising or even falling – both in states that had enacted tort reform and in states that had not. This may mean that other interventions such as medical error recognition and reduction are also effective.
Unsurprisingly, caps on damages have been challenged on constitutional grounds, as a violation of the equal rights amendment and the patient’s right to a jury trial. Two recent cases with divergent results – one on California, and the other in Florida – illustrate the state of flux over this controversy.
In Chan v. Curran, the plaintiff sought to relitigate the constitutionality of the California damage cap, but the appellate court ruled for the doctor defendant.4 The case alleged a wrongful death when the patient died from hemorrhage related to warfarin (Coumadin) use during open heart surgery.
The plaintiff argued that MICRA’s rationale was irrelevant, because there was no longer a malpractice insurance crisis in California – thus, restrictions placed on the quantum of damages are not rationally related to any legitimate state interest.
Furthermore, by limiting the amount of noneconomic damages to $250,000, MICRA violated equal protection and discouraged or inhibited attorneys from taking up malpractice cases on a contingency fee basis. Finally, the plaintiff argued that under the statute, a litigant is deprived of the right to a jury trial.
The court rejected all of these arguments, and reaffirmed the constitutionality of MICRA in line with earlier decisions that began with California’s Supreme Court decision in the Fein v. Permanente Medical Group case.5
On the other hand, the recent case of Estate of Michelle Evette McCall v. U.S. found the Florida Supreme Court ruling for the plaintiff.6 There, the court deemed unconstitutional Florida’s statute limiting wrongful death damages in medical malpractice to $1 million.
The case involved a young mother who died of massive hemorrhage following a cesarean section. In a 5-2 decision, the court held that the statute was arbitrary, reasoning that “the statutory cap on wrongful death noneconomic damages fails because it imposes unfair and illogical burdens on injured parties.”
Unlike California, the Florida court found that the cap bears no rational relationship to any perceived malpractice insurance crisis. And, while saving a modest amount for many, the statute imposed devastating costs on those who are most grievously injured, as well as on cases affecting multiple claimants.
The court commented that “the finding by the Legislature and the Task Force that Florida was in the midst of a bona fide medical malpractice crisis, threatening the access of Floridians to health care, is dubious and questionable at the very best.” The court also noted that four malpractice carriers actually increased their net income by more than 4,300% between 2003 and 2010.
In 2010, the Illinois Supreme Court also held in Lebron v. Gottlieb Memorial Hospital that the state’s $500,000 cap for noneconomic damages was unconstitutional, being in violation of the separation of powers doctrine.7 Only judges are empowered to reduce excessive verdicts, termed a remittitur. Thus, a statutory damage cap amounted to a “legislative remittitur” that invaded the power of the judiciary and violated the constitutional requirement of separation of powers.
The battle over caps continues unabated, with the trend appearing to favor the plaintiff bar. Florida’s ruling was the eighth state supreme court decision that held damage caps unconstitutional, joining Alabama, Georgia, Illinois, Missouri, New Hampshire, Oregon, and Washington. Five other states – Arizona, Arkansas, Kentucky, Pennsylvania, and Wyoming – already have state constitutional prohibitions on damage caps.
References
1. Medical Injury Compensation Reform Act of 1975, Cal. Civ. Proc. Code § 3333.2 (West 1982).
2. O’Connell, J. Offers That Can’t Be Refused: Foreclosure of Personal Injury Claims by Defendants’ Prompt Tender of Claimants’ Net Economic Losses. 77 N.W.U.L. Rev. 589, 591 (1982).
3. Thorpe, K. The Medical Malpractice Crisis: Recent Trends and the Impact of State Tort Reforms, Health Affairs 2004, Jan 21 [doi:10.1377/hlthaff.w4.20].
4. Chan v. Curran, 237 Cal. App. 4th 601 (Cal.Ct.App. 2015).
5. Fein v. Permanente Medical Group, 695 P.2d 665 (Cal. 1985).
6. Estate of Michelle Evette McCall v. U.S., 2014 Fla. LEXIS 933 (Fla. Mar. 13, 2014).
7. Lebron v. Gottlieb Memorial Hospital, 930 N.E.2d 895 (Ill. 2010).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at siang@hawaii.edu.
Question: Which of the following statements regarding statutory caps on malpractice damages is best?
A. All states have such a statutory provision.
B. The provision limits the recovery of both economic and noneconomic losses.
C. It’s constitutional.
D. It’s not constitutional.
E. Whether it’s constitutional depends on the jurisdiction.
Answer: E. In 1975, California enacted its historic Medical Injury Compensation Reform Act (MICRA),1 the state legislature declaring that there was “a major health care crisis in the State of California attributable to skyrocketing malpractice premium costs and resulting in a potential breakdown of the health delivery system.”
The rationale was to provide some predictability, because noneconomic damages are difficult to quantify, and jury sympathy may result in unrealistically high payments. It was believed that damages for pain and suffering, for example, often contributed to runaway jury verdicts, prompting one indignant observer to write: “In making arguments for pain and suffering awards, both sides attempt to win the jurors’ sympathies with highly emotional evidence. A blind plaintiff will receive careful instruction to come to court with his [guide] dog, and to dab at his eyes with a handkerchief.”2
One of the main provisions of MICRA is to limit noneconomic recovery for injuries arising out of medical negligence. It caps noneconomic damages – for example, pain and suffering, disfigurement, emotional distress, loss of consortium, and other nonpecuniary losses – at $250,000. The law does not restrict recovery of economic damages such as wage loss, medical expenses, and future lost income.
California is the pioneer state to institute this tort reform measure, and about a dozen other states have followed suit, such as Proposition 12 in Texas, which limits noneconomic damages to $750,000 – $250,000 from the defendant doctor and $500,000 from the hospital.
Many tort reformists hail MICRA as the prototype success story, crediting it for bringing California’s malpractice insurance premiums from one of the highest levels in the nation to one of its lowest. A 2004 study reported that states with caps have a loss ratio (losses plus costs over premiums) that is 12% lower than in those without damage caps.3 Lower premiums in turn are linked to greater physician entry into the locality, especially for high-risk specialists.
In addition, caps may have a salutary effect on the wasteful practice of defensive medicine. A 2007 report by the American Medical Association confirms and extends an earlier study that reached such conclusions.
However, recent medical malpractice rates are generally no longer rising or even falling – both in states that had enacted tort reform and in states that had not. This may mean that other interventions such as medical error recognition and reduction are also effective.
Unsurprisingly, caps on damages have been challenged on constitutional grounds, as a violation of the equal rights amendment and the patient’s right to a jury trial. Two recent cases with divergent results – one on California, and the other in Florida – illustrate the state of flux over this controversy.
In Chan v. Curran, the plaintiff sought to relitigate the constitutionality of the California damage cap, but the appellate court ruled for the doctor defendant.4 The case alleged a wrongful death when the patient died from hemorrhage related to warfarin (Coumadin) use during open heart surgery.
The plaintiff argued that MICRA’s rationale was irrelevant, because there was no longer a malpractice insurance crisis in California – thus, restrictions placed on the quantum of damages are not rationally related to any legitimate state interest.
Furthermore, by limiting the amount of noneconomic damages to $250,000, MICRA violated equal protection and discouraged or inhibited attorneys from taking up malpractice cases on a contingency fee basis. Finally, the plaintiff argued that under the statute, a litigant is deprived of the right to a jury trial.
The court rejected all of these arguments, and reaffirmed the constitutionality of MICRA in line with earlier decisions that began with California’s Supreme Court decision in the Fein v. Permanente Medical Group case.5
On the other hand, the recent case of Estate of Michelle Evette McCall v. U.S. found the Florida Supreme Court ruling for the plaintiff.6 There, the court deemed unconstitutional Florida’s statute limiting wrongful death damages in medical malpractice to $1 million.
The case involved a young mother who died of massive hemorrhage following a cesarean section. In a 5-2 decision, the court held that the statute was arbitrary, reasoning that “the statutory cap on wrongful death noneconomic damages fails because it imposes unfair and illogical burdens on injured parties.”
Unlike California, the Florida court found that the cap bears no rational relationship to any perceived malpractice insurance crisis. And, while saving a modest amount for many, the statute imposed devastating costs on those who are most grievously injured, as well as on cases affecting multiple claimants.
The court commented that “the finding by the Legislature and the Task Force that Florida was in the midst of a bona fide medical malpractice crisis, threatening the access of Floridians to health care, is dubious and questionable at the very best.” The court also noted that four malpractice carriers actually increased their net income by more than 4,300% between 2003 and 2010.
In 2010, the Illinois Supreme Court also held in Lebron v. Gottlieb Memorial Hospital that the state’s $500,000 cap for noneconomic damages was unconstitutional, being in violation of the separation of powers doctrine.7 Only judges are empowered to reduce excessive verdicts, termed a remittitur. Thus, a statutory damage cap amounted to a “legislative remittitur” that invaded the power of the judiciary and violated the constitutional requirement of separation of powers.
The battle over caps continues unabated, with the trend appearing to favor the plaintiff bar. Florida’s ruling was the eighth state supreme court decision that held damage caps unconstitutional, joining Alabama, Georgia, Illinois, Missouri, New Hampshire, Oregon, and Washington. Five other states – Arizona, Arkansas, Kentucky, Pennsylvania, and Wyoming – already have state constitutional prohibitions on damage caps.
References
1. Medical Injury Compensation Reform Act of 1975, Cal. Civ. Proc. Code § 3333.2 (West 1982).
2. O’Connell, J. Offers That Can’t Be Refused: Foreclosure of Personal Injury Claims by Defendants’ Prompt Tender of Claimants’ Net Economic Losses. 77 N.W.U.L. Rev. 589, 591 (1982).
3. Thorpe, K. The Medical Malpractice Crisis: Recent Trends and the Impact of State Tort Reforms, Health Affairs 2004, Jan 21 [doi:10.1377/hlthaff.w4.20].
4. Chan v. Curran, 237 Cal. App. 4th 601 (Cal.Ct.App. 2015).
5. Fein v. Permanente Medical Group, 695 P.2d 665 (Cal. 1985).
6. Estate of Michelle Evette McCall v. U.S., 2014 Fla. LEXIS 933 (Fla. Mar. 13, 2014).
7. Lebron v. Gottlieb Memorial Hospital, 930 N.E.2d 895 (Ill. 2010).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at siang@hawaii.edu.
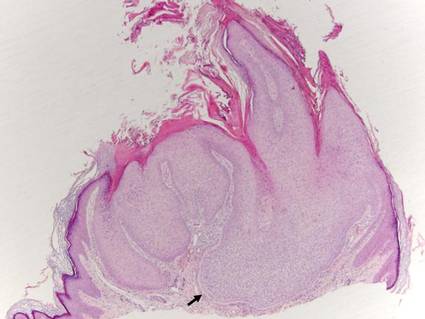
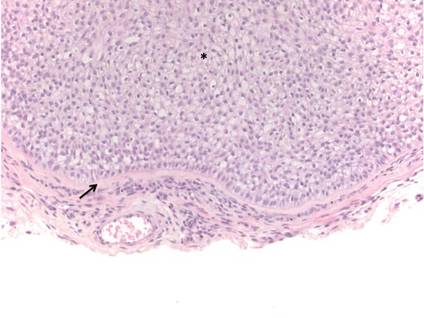
What Is Your Diagnosis? Verrucous Carcinoma
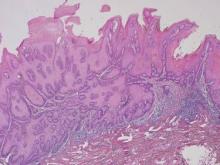
An 81-year-old woman presented for evaluation of a nodule on the right labia majora that had been present for 1 year. She had a history of intertriginous psoriasis, and several biopsies were performed at an outside facility over the last 5 years that revealed psoriasis but were otherwise noncontributory. Physical examination revealed erythema and scaling on the buttocks with maceration in the intertriginous area (top) and the perineum associated with a verrucous nodule (bottom).
The Diagnosis: Verrucous Carcinoma
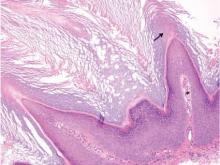
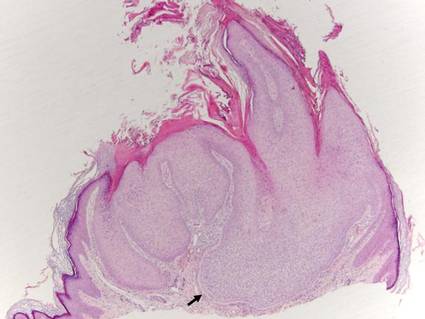
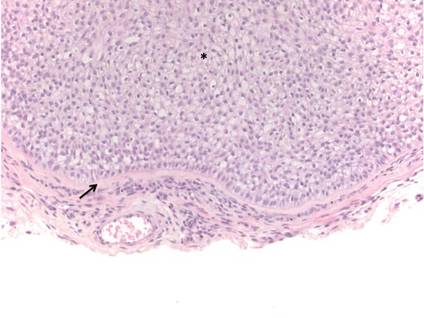
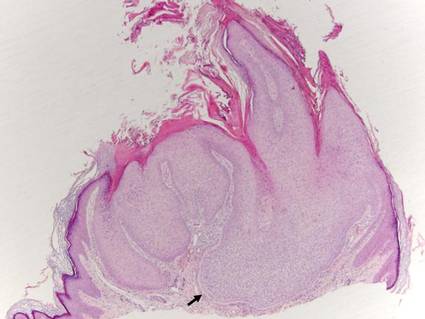
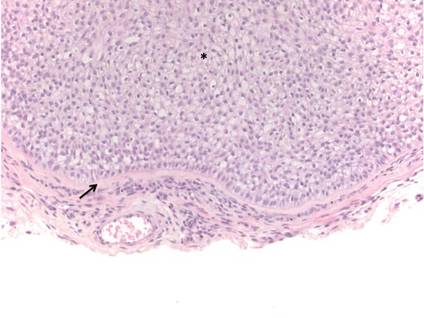
Biopsies of early lesions often may be difficult to interpret without clinicopathological correlation. Our patient’s tumor was associated with intertriginous psoriasis, which was the only abnormality previously noted on superficial biopsies performed at an outside facility. The patient was scheduled for an excisional biopsy due to the large tumor size and clinical suspicion that the prior biopsies were inadequate and failed to demonstrate the primary underlying pathology. Excisional biopsy of the verrucous tumor revealed epithelium composed of keratinocytes with glassy cytoplasm. Papillomatosis was noted along with an endophytic component of well-differentiated epithelial cells extending into the dermis in a bulbous pattern consistent with the verrucous carcinoma variant of squamous cell carcinoma (SCC)(Figure). Verrucous carcinoma often requires correlation with both the clinical and histopathologic findings for definitive diagnosis, as keratinocytes often appear to be well differentiated.1
Verrucous carcinoma may begin as an innocuous papule that slowly grows into a large fungating tumor. Verrucous carcinomas typically are slow growing, exophytic, and low grade. The etiology of verrucous carcinoma is not clear, and the role of human papillomavirus (HPV) infection is controversial.2 Best classified as a well-differentiated SCC, verrucous carcinoma rarely metastasizes but may invade adjacent tissues.
Differential diagnoses include a giant inflamed seborrheic keratosis, condyloma acuminatum, rupioid psoriasis, and inflammatory linear verrucous epidermal nevus (ILVEN). Although large and inflamed seborrheic keratoses may have squamous eddies that mimic SCC, seborrheic keratoses do not invade the dermis and typically have a well-circumscribed stuck-on appearance. Abnormal mitotic figures are not identified. Condylomas are genital warts caused by HPV infection that often are clustered, well circumscribed, and exophytic. Large lesions can be difficult to distinguish from verrucous carcinomas, and biopsy generally reveals koilocytes identified by perinuclear clearing and raisinlike nuclei. Immunohistochemical staining and in situ hybridization studies can be of value in diagnosis and in identifying those lesions that are at high risk for malignant transformation. High-risk condylomas are associated with HPV-16, HPV-18, HPV-31, HPV-33, HPV-35, and HPV-39, as well as other types, whereas low-risk condylomas are associated with HPV-6, HPV-11, HPV-42, and others.2 Differentiating squamous cell hyperplasia from squamous cell carcinoma in situ also can be aided by immunohistochemistry. Squamous cell hyperplasia is usually negative for INK4 p16Ink4A and p53 and exhibits variable Ki-67 staining. Differentiated squamous cell carcinoma in situ exhibits a profile that is p16Ink4A negative, Ki-67 positive, and exhibits variable p53 staining.3 Basaloid and warty intraepithelial neoplasia is consistently p16Ink4A positive, Ki-67 positive, and variably positive for p53.3 Therefore, p16 staining of high-grade areas is a useful biomarker that can help establish diagnosis of associated squamous cell carcinoma.4 The role of papillomaviruses in the development of nonmelanoma skin cancer is an area of active study, and research suggests that papillomaviruses may have a much greater role than previously suspected.5
At times, psoriasis may be markedly hyperkeratotic, clinically mimicking a verrucous neoplasm. This hyperkeratotic type of psoriasis is known as rupioid psoriasis. However, these psoriatic lesions are exophytic, are associated with spongiform pustules, and lack the atypia and endophytic pattern typically seen with verrucous carcinoma. An ILVEN also lacks atypia and an endophytic pattern and usually presents in childhood as a persistent linear plaque, rather than the verrucous plaque noted in our patient. Squamous cell carcinoma has been reported to arise in the setting of verrucoid ILVEN but is exceptionally uncommon.6
Successful treatment of verrucous carcinoma is best achieved by complete excision. Oral retinoids and immunomodulators such as imiquimod also may be of value.7 Our patient’s tumor qualifies as T2N0M0 because it was greater than 2 cm in size.8 A Breslow thickness of 2 mm or greater and Clark level IV are high-risk features associated with a worse prognosis, but clinical evaluation of our patient’s lymph nodes was unremarkable and no distant metastases were identified. Our patient continues to do well with no evidence of recurrence.
1. Bambao C, Nofech-Mozes S, Shier M. Giant condyloma versus verrucous carcinoma: a case report. J Low Genit Tract Dis. 2010;14:230-233.
2. Asiaf A, Ahmad ST, Mohannad SO, et al. Review of the current knowledge on the epidemiology, pathogenesis, and prevention of human papillomavirus infection. Eur J Cancer Prev. 2014;23:206-224.
3. Chaux A, Pfannl R, Rodríguez IM, et al. Distinctive immunohistochemical profile of penile intraepithelial lesions: a study of 74 cases. Am J Surg Pathol. 2011;35:553-562.
4. Darragh TM, Colgan TJ, Cox JT, et al. The lower anogenital squamous terminology standardization project for HPV-associated lesions: background and consensus recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Arch Pathol Lab Med. 2012;136:1266-1297.
5. Aldabagh B, Angeles J, Cardones AR, et al. Cutaneous squamous cell carcinoma and human papillomavirus: is there an association? Dermatol Surg. 2013;39:1-23.
6. Turk BG, Ertam I, Urkmez A, et al. Development of squamous cell carcinoma on an inflammatory linear verrucous epidermal nevus in the genital area. Cutis. 2012;89:273-275.
7. Erkek E, Basar H, Bozdogan O, et al. Giant condyloma acuminata of Buschke-Löwenstein: successful treatment with a combination of surgical excision, oral acitretin and topical imiquimod. Clin Exp Dermatol. 2009;34:366-368.
8. Cutaneous squamous cell carcinoma and other cutaneous carcinomas. In: Edge SB, Byrd DR, Compton CC, et al, eds. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer; 2010:301-314.
An 81-year-old woman presented for evaluation of a nodule on the right labia majora that had been present for 1 year. She had a history of intertriginous psoriasis, and several biopsies were performed at an outside facility over the last 5 years that revealed psoriasis but were otherwise noncontributory. Physical examination revealed erythema and scaling on the buttocks with maceration in the intertriginous area (top) and the perineum associated with a verrucous nodule (bottom).
The Diagnosis: Verrucous Carcinoma
Biopsies of early lesions often may be difficult to interpret without clinicopathological correlation. Our patient’s tumor was associated with intertriginous psoriasis, which was the only abnormality previously noted on superficial biopsies performed at an outside facility. The patient was scheduled for an excisional biopsy due to the large tumor size and clinical suspicion that the prior biopsies were inadequate and failed to demonstrate the primary underlying pathology. Excisional biopsy of the verrucous tumor revealed epithelium composed of keratinocytes with glassy cytoplasm. Papillomatosis was noted along with an endophytic component of well-differentiated epithelial cells extending into the dermis in a bulbous pattern consistent with the verrucous carcinoma variant of squamous cell carcinoma (SCC)(Figure). Verrucous carcinoma often requires correlation with both the clinical and histopathologic findings for definitive diagnosis, as keratinocytes often appear to be well differentiated.1
Verrucous carcinoma may begin as an innocuous papule that slowly grows into a large fungating tumor. Verrucous carcinomas typically are slow growing, exophytic, and low grade. The etiology of verrucous carcinoma is not clear, and the role of human papillomavirus (HPV) infection is controversial.2 Best classified as a well-differentiated SCC, verrucous carcinoma rarely metastasizes but may invade adjacent tissues.
Differential diagnoses include a giant inflamed seborrheic keratosis, condyloma acuminatum, rupioid psoriasis, and inflammatory linear verrucous epidermal nevus (ILVEN). Although large and inflamed seborrheic keratoses may have squamous eddies that mimic SCC, seborrheic keratoses do not invade the dermis and typically have a well-circumscribed stuck-on appearance. Abnormal mitotic figures are not identified. Condylomas are genital warts caused by HPV infection that often are clustered, well circumscribed, and exophytic. Large lesions can be difficult to distinguish from verrucous carcinomas, and biopsy generally reveals koilocytes identified by perinuclear clearing and raisinlike nuclei. Immunohistochemical staining and in situ hybridization studies can be of value in diagnosis and in identifying those lesions that are at high risk for malignant transformation. High-risk condylomas are associated with HPV-16, HPV-18, HPV-31, HPV-33, HPV-35, and HPV-39, as well as other types, whereas low-risk condylomas are associated with HPV-6, HPV-11, HPV-42, and others.2 Differentiating squamous cell hyperplasia from squamous cell carcinoma in situ also can be aided by immunohistochemistry. Squamous cell hyperplasia is usually negative for INK4 p16Ink4A and p53 and exhibits variable Ki-67 staining. Differentiated squamous cell carcinoma in situ exhibits a profile that is p16Ink4A negative, Ki-67 positive, and exhibits variable p53 staining.3 Basaloid and warty intraepithelial neoplasia is consistently p16Ink4A positive, Ki-67 positive, and variably positive for p53.3 Therefore, p16 staining of high-grade areas is a useful biomarker that can help establish diagnosis of associated squamous cell carcinoma.4 The role of papillomaviruses in the development of nonmelanoma skin cancer is an area of active study, and research suggests that papillomaviruses may have a much greater role than previously suspected.5
At times, psoriasis may be markedly hyperkeratotic, clinically mimicking a verrucous neoplasm. This hyperkeratotic type of psoriasis is known as rupioid psoriasis. However, these psoriatic lesions are exophytic, are associated with spongiform pustules, and lack the atypia and endophytic pattern typically seen with verrucous carcinoma. An ILVEN also lacks atypia and an endophytic pattern and usually presents in childhood as a persistent linear plaque, rather than the verrucous plaque noted in our patient. Squamous cell carcinoma has been reported to arise in the setting of verrucoid ILVEN but is exceptionally uncommon.6
Successful treatment of verrucous carcinoma is best achieved by complete excision. Oral retinoids and immunomodulators such as imiquimod also may be of value.7 Our patient’s tumor qualifies as T2N0M0 because it was greater than 2 cm in size.8 A Breslow thickness of 2 mm or greater and Clark level IV are high-risk features associated with a worse prognosis, but clinical evaluation of our patient’s lymph nodes was unremarkable and no distant metastases were identified. Our patient continues to do well with no evidence of recurrence.
An 81-year-old woman presented for evaluation of a nodule on the right labia majora that had been present for 1 year. She had a history of intertriginous psoriasis, and several biopsies were performed at an outside facility over the last 5 years that revealed psoriasis but were otherwise noncontributory. Physical examination revealed erythema and scaling on the buttocks with maceration in the intertriginous area (top) and the perineum associated with a verrucous nodule (bottom).
The Diagnosis: Verrucous Carcinoma
Biopsies of early lesions often may be difficult to interpret without clinicopathological correlation. Our patient’s tumor was associated with intertriginous psoriasis, which was the only abnormality previously noted on superficial biopsies performed at an outside facility. The patient was scheduled for an excisional biopsy due to the large tumor size and clinical suspicion that the prior biopsies were inadequate and failed to demonstrate the primary underlying pathology. Excisional biopsy of the verrucous tumor revealed epithelium composed of keratinocytes with glassy cytoplasm. Papillomatosis was noted along with an endophytic component of well-differentiated epithelial cells extending into the dermis in a bulbous pattern consistent with the verrucous carcinoma variant of squamous cell carcinoma (SCC)(Figure). Verrucous carcinoma often requires correlation with both the clinical and histopathologic findings for definitive diagnosis, as keratinocytes often appear to be well differentiated.1
Verrucous carcinoma may begin as an innocuous papule that slowly grows into a large fungating tumor. Verrucous carcinomas typically are slow growing, exophytic, and low grade. The etiology of verrucous carcinoma is not clear, and the role of human papillomavirus (HPV) infection is controversial.2 Best classified as a well-differentiated SCC, verrucous carcinoma rarely metastasizes but may invade adjacent tissues.
Differential diagnoses include a giant inflamed seborrheic keratosis, condyloma acuminatum, rupioid psoriasis, and inflammatory linear verrucous epidermal nevus (ILVEN). Although large and inflamed seborrheic keratoses may have squamous eddies that mimic SCC, seborrheic keratoses do not invade the dermis and typically have a well-circumscribed stuck-on appearance. Abnormal mitotic figures are not identified. Condylomas are genital warts caused by HPV infection that often are clustered, well circumscribed, and exophytic. Large lesions can be difficult to distinguish from verrucous carcinomas, and biopsy generally reveals koilocytes identified by perinuclear clearing and raisinlike nuclei. Immunohistochemical staining and in situ hybridization studies can be of value in diagnosis and in identifying those lesions that are at high risk for malignant transformation. High-risk condylomas are associated with HPV-16, HPV-18, HPV-31, HPV-33, HPV-35, and HPV-39, as well as other types, whereas low-risk condylomas are associated with HPV-6, HPV-11, HPV-42, and others.2 Differentiating squamous cell hyperplasia from squamous cell carcinoma in situ also can be aided by immunohistochemistry. Squamous cell hyperplasia is usually negative for INK4 p16Ink4A and p53 and exhibits variable Ki-67 staining. Differentiated squamous cell carcinoma in situ exhibits a profile that is p16Ink4A negative, Ki-67 positive, and exhibits variable p53 staining.3 Basaloid and warty intraepithelial neoplasia is consistently p16Ink4A positive, Ki-67 positive, and variably positive for p53.3 Therefore, p16 staining of high-grade areas is a useful biomarker that can help establish diagnosis of associated squamous cell carcinoma.4 The role of papillomaviruses in the development of nonmelanoma skin cancer is an area of active study, and research suggests that papillomaviruses may have a much greater role than previously suspected.5
At times, psoriasis may be markedly hyperkeratotic, clinically mimicking a verrucous neoplasm. This hyperkeratotic type of psoriasis is known as rupioid psoriasis. However, these psoriatic lesions are exophytic, are associated with spongiform pustules, and lack the atypia and endophytic pattern typically seen with verrucous carcinoma. An ILVEN also lacks atypia and an endophytic pattern and usually presents in childhood as a persistent linear plaque, rather than the verrucous plaque noted in our patient. Squamous cell carcinoma has been reported to arise in the setting of verrucoid ILVEN but is exceptionally uncommon.6
Successful treatment of verrucous carcinoma is best achieved by complete excision. Oral retinoids and immunomodulators such as imiquimod also may be of value.7 Our patient’s tumor qualifies as T2N0M0 because it was greater than 2 cm in size.8 A Breslow thickness of 2 mm or greater and Clark level IV are high-risk features associated with a worse prognosis, but clinical evaluation of our patient’s lymph nodes was unremarkable and no distant metastases were identified. Our patient continues to do well with no evidence of recurrence.
1. Bambao C, Nofech-Mozes S, Shier M. Giant condyloma versus verrucous carcinoma: a case report. J Low Genit Tract Dis. 2010;14:230-233.
2. Asiaf A, Ahmad ST, Mohannad SO, et al. Review of the current knowledge on the epidemiology, pathogenesis, and prevention of human papillomavirus infection. Eur J Cancer Prev. 2014;23:206-224.
3. Chaux A, Pfannl R, Rodríguez IM, et al. Distinctive immunohistochemical profile of penile intraepithelial lesions: a study of 74 cases. Am J Surg Pathol. 2011;35:553-562.
4. Darragh TM, Colgan TJ, Cox JT, et al. The lower anogenital squamous terminology standardization project for HPV-associated lesions: background and consensus recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Arch Pathol Lab Med. 2012;136:1266-1297.
5. Aldabagh B, Angeles J, Cardones AR, et al. Cutaneous squamous cell carcinoma and human papillomavirus: is there an association? Dermatol Surg. 2013;39:1-23.
6. Turk BG, Ertam I, Urkmez A, et al. Development of squamous cell carcinoma on an inflammatory linear verrucous epidermal nevus in the genital area. Cutis. 2012;89:273-275.
7. Erkek E, Basar H, Bozdogan O, et al. Giant condyloma acuminata of Buschke-Löwenstein: successful treatment with a combination of surgical excision, oral acitretin and topical imiquimod. Clin Exp Dermatol. 2009;34:366-368.
8. Cutaneous squamous cell carcinoma and other cutaneous carcinomas. In: Edge SB, Byrd DR, Compton CC, et al, eds. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer; 2010:301-314.
1. Bambao C, Nofech-Mozes S, Shier M. Giant condyloma versus verrucous carcinoma: a case report. J Low Genit Tract Dis. 2010;14:230-233.
2. Asiaf A, Ahmad ST, Mohannad SO, et al. Review of the current knowledge on the epidemiology, pathogenesis, and prevention of human papillomavirus infection. Eur J Cancer Prev. 2014;23:206-224.
3. Chaux A, Pfannl R, Rodríguez IM, et al. Distinctive immunohistochemical profile of penile intraepithelial lesions: a study of 74 cases. Am J Surg Pathol. 2011;35:553-562.
4. Darragh TM, Colgan TJ, Cox JT, et al. The lower anogenital squamous terminology standardization project for HPV-associated lesions: background and consensus recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Arch Pathol Lab Med. 2012;136:1266-1297.
5. Aldabagh B, Angeles J, Cardones AR, et al. Cutaneous squamous cell carcinoma and human papillomavirus: is there an association? Dermatol Surg. 2013;39:1-23.
6. Turk BG, Ertam I, Urkmez A, et al. Development of squamous cell carcinoma on an inflammatory linear verrucous epidermal nevus in the genital area. Cutis. 2012;89:273-275.
7. Erkek E, Basar H, Bozdogan O, et al. Giant condyloma acuminata of Buschke-Löwenstein: successful treatment with a combination of surgical excision, oral acitretin and topical imiquimod. Clin Exp Dermatol. 2009;34:366-368.
8. Cutaneous squamous cell carcinoma and other cutaneous carcinomas. In: Edge SB, Byrd DR, Compton CC, et al, eds. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer; 2010:301-314.
ACIP releases 2015-2016 flu vaccine recommendations
Influenza vaccination is recommended for all patients aged 6 months and older, as long as they don’t have a contraindication, according to a report Aug. 7 in Morbidity and Mortality Weekly Report.
Trivalent influenza vaccines for the 2015-2016 season will contain hemagglutinin (HA) derived from an H1N1-like virus, an H3N2-like virus, and a B/Phuket/3073/2013-like (Yamagata lineage) virus. Quadrivalent vaccines will contain those components, as well as a B/Brisbane/60/2008-like (Victoria lineage) virus, the same virus recommended for quadrivalent formulations in the 2013-14 and 2014-15 seasons, ACIP said in a statement.
New FDA-approved vaccines include Afluria, the Fluzone Intradermal Quadrivalent vaccine (both approved in 2014 for adults aged 18-64 years), and an expanded age indication for Flublok, which is now indicated for adults aged 18 years and older.
The live attenuated influenza vaccine (LAIV) should not be used in certain populations, including those aged less than 2 years or greater than 49 years; children aged 2-17 years taking aspirin; pateints with severe allergic reactions to the vaccine; pregnant women; and those with egg allergies, among others. Either the LAIV or the inactivated influenza vaccine (IIV) is appropriate for administration in healthy children aged 2-8 years, ACIP said.
For a detailed explanation of the recommendations, see MMWR.
Influenza vaccination is recommended for all patients aged 6 months and older, as long as they don’t have a contraindication, according to a report Aug. 7 in Morbidity and Mortality Weekly Report.
Trivalent influenza vaccines for the 2015-2016 season will contain hemagglutinin (HA) derived from an H1N1-like virus, an H3N2-like virus, and a B/Phuket/3073/2013-like (Yamagata lineage) virus. Quadrivalent vaccines will contain those components, as well as a B/Brisbane/60/2008-like (Victoria lineage) virus, the same virus recommended for quadrivalent formulations in the 2013-14 and 2014-15 seasons, ACIP said in a statement.
New FDA-approved vaccines include Afluria, the Fluzone Intradermal Quadrivalent vaccine (both approved in 2014 for adults aged 18-64 years), and an expanded age indication for Flublok, which is now indicated for adults aged 18 years and older.
The live attenuated influenza vaccine (LAIV) should not be used in certain populations, including those aged less than 2 years or greater than 49 years; children aged 2-17 years taking aspirin; pateints with severe allergic reactions to the vaccine; pregnant women; and those with egg allergies, among others. Either the LAIV or the inactivated influenza vaccine (IIV) is appropriate for administration in healthy children aged 2-8 years, ACIP said.
For a detailed explanation of the recommendations, see MMWR.
Influenza vaccination is recommended for all patients aged 6 months and older, as long as they don’t have a contraindication, according to a report Aug. 7 in Morbidity and Mortality Weekly Report.
Trivalent influenza vaccines for the 2015-2016 season will contain hemagglutinin (HA) derived from an H1N1-like virus, an H3N2-like virus, and a B/Phuket/3073/2013-like (Yamagata lineage) virus. Quadrivalent vaccines will contain those components, as well as a B/Brisbane/60/2008-like (Victoria lineage) virus, the same virus recommended for quadrivalent formulations in the 2013-14 and 2014-15 seasons, ACIP said in a statement.
New FDA-approved vaccines include Afluria, the Fluzone Intradermal Quadrivalent vaccine (both approved in 2014 for adults aged 18-64 years), and an expanded age indication for Flublok, which is now indicated for adults aged 18 years and older.
The live attenuated influenza vaccine (LAIV) should not be used in certain populations, including those aged less than 2 years or greater than 49 years; children aged 2-17 years taking aspirin; pateints with severe allergic reactions to the vaccine; pregnant women; and those with egg allergies, among others. Either the LAIV or the inactivated influenza vaccine (IIV) is appropriate for administration in healthy children aged 2-8 years, ACIP said.
For a detailed explanation of the recommendations, see MMWR.
Modifiable risk factors foretell colonic anastomotic leak
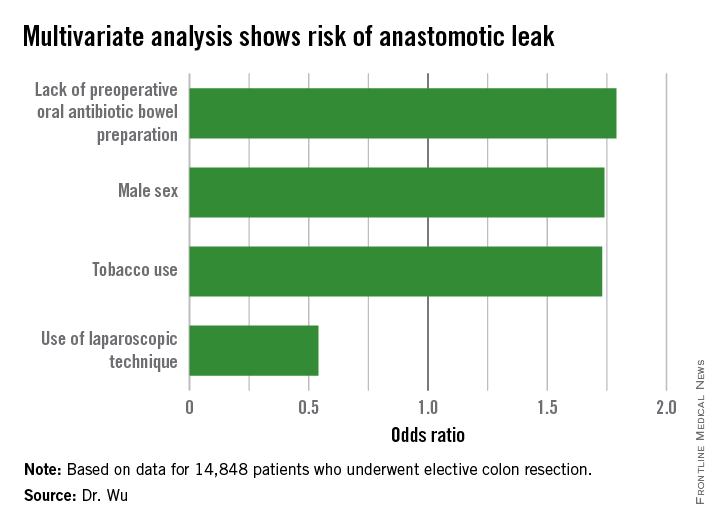
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
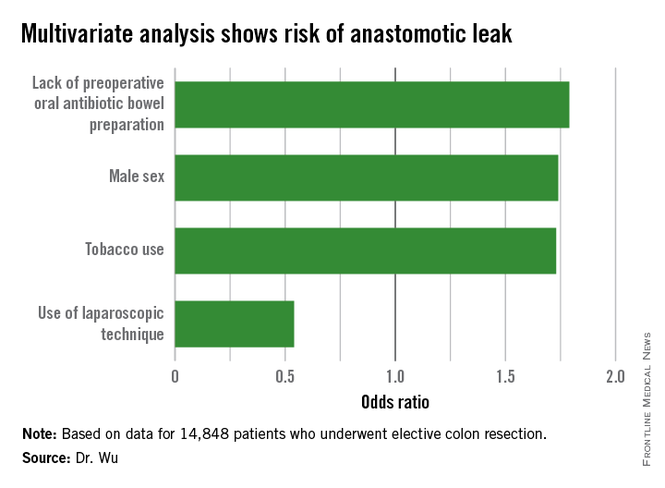
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
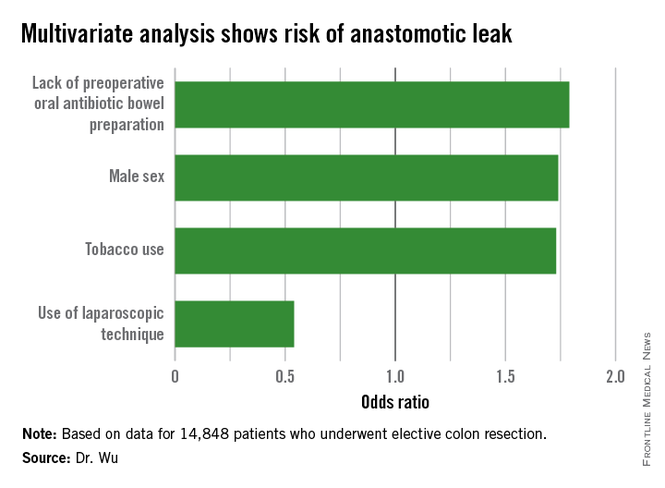
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
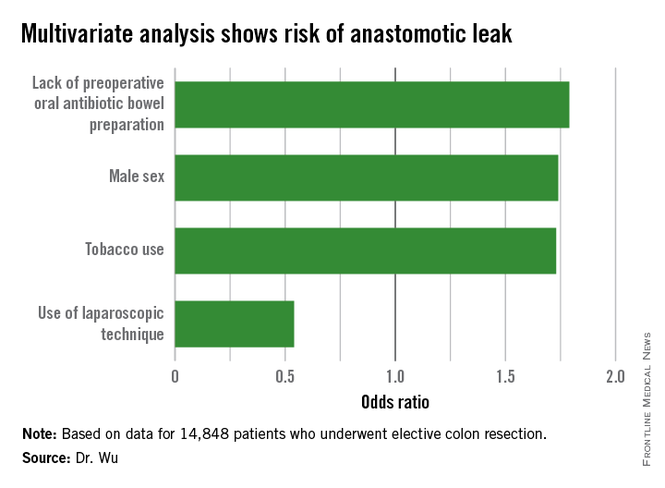
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Altering specific patient and operative factors can modify the risk of anastomotic leakage after colectomy.
Major finding: Male sex (OR, 1.74), tobacco use (OR, 1.73), and lack of an oral antibiotic bowel preparation (OR, 1.79) predicted anastomotic leak.
Data source: A retrospective study of 14,848 elective colectomies.
Disclosures: The authors reported having no relevant financial disclosures.
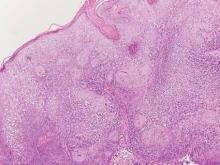
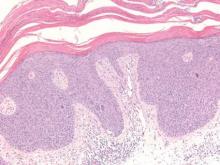
Trichilemmoma
Trichilemmomas are benign follicular neoplasms that exhibit differentiation toward the outer root sheath of the pilosebaceous follicular epithelium.1 Trichilemmomas clinically present as individual or multiple, slowly growing, verrucous papules appearing most commonly on the face or neck. The lesions may coalesce to form small plaques. Although trichilemmomas typically are isolated, patients with multiple trichilemmomas require a cancer screening workup due to their association with Cowden disease, which results from a mutation in the phosphatase and tensin homolog tumor suppressor gene, PTEN.2 An easy way to remember the association between trichilemmomas and Cowden disease is to alter the spelling to “trichile-moo-moo,” using the “moo moo” sound of an animal cow as a clue linking the tumor to Cowden disease.
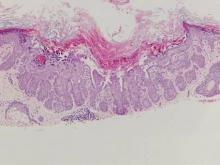
Histologically, trichilemmomas exhibit a lobular epidermal downgrowth into the dermis (Figure 1). The surface of the lesion may be hyperkeratotic and somewhat papillomatous. Cells toward the center of the lobule are pale staining, periodic acid–Schiff positive, and diastase labile due to high levels of intracellular glycogen (Figure 2). Cells toward the periphery of the lobule usually appear basophilic with a palisading arrangement of the peripheral cells. The entire lobule is enclosed within an eosinophilic basement membrane that stains positively with periodic acid–Schiff (Figure 2).1 Consistent with the tumor’s differentiation toward the outer root sheath of the hair follicle, trichilemmomas have been reported to express CD34 focally or diffusely.3
 |  |
Similar to trichilemmoma, inverted follicular keratosis (IFK) commonly presents as a solitary asymptomatic papule on the face. Inverted follicular keratosis is a somewhat controversial entity, with some authorities arguing IFK is a variant of verruca vulgaris or seborrheic keratosis. Histologically, IFKs can be differentiated by the presence of squamous eddies (concentric layers of squamous cells in a whorled pattern), which are diagnostic, and central longitudinal crypts that contain keratin and are lined by squamous epithelium.4 Basaloid cells can be seen at the periphery of the tumors; however, IFKs lack an eosinophilic basement membrane surrounding the tumor (Figure 3).
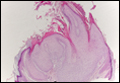
Squamous cell carcinoma in situ classically appears as an erythematous hyperkeratotic papule or plaque on sun-exposed sites that can become crusted or ulcerated. Microscopically, squamous cell carcinoma in situ displays full-thickness disorderly maturation of keratinocytes. The keratinocytes exhibit nuclear pleomorphism. Atypical mitotic figures and dyskeratotic keratinocytes also can be seen throughout the full thickness of the epidermis (Figure 4).5
Verruca vulgaris (Figure 5) histologically demonstrates hyperkeratosis with tiers of parakeratosis, digitated epidermal hyperplasia, and dilated tortuous capillaries within the dermal papillae. At the edges of the lesion there often is inward turning of elongated rete ridges,6,7 which can be thought of as the rete reaching out for a hug of sorts to spread the human papillomavirus infection. Although the surface of a trichilemmoma can bear resemblance to a verruca vulgaris, the remainder of the histologic features can be used to help differentiate these tumors. Additionally, there has been no evidence suggestive of a viral etiology for trichilemmomas.8
Warty dyskeratoma features an umbilicated papule, usually on the face, head, or neck, that is associated with a follicular unit. The papule shows a cup-shaped, keratin-filled invagination; suprabasilar clefting; and acantholytic dyskeratotic cells, which are features that are not seen in trichilemmomas (Figure 6).9
Acknowledgment—The authors would like to thank Brandon Litzner, MD, St Louis, Missouri, for proofreading the manuscript.
1. Brownstein MH, Shapiro L. Trichilemmoma: analysis of 40 new cases. Arch Dermatol. 1973;107:866-869.
2. Al-Zaid T, Ditelberg J, Prieto V, et al. Trichilemmomas show loss of PTEN in Cowden syndrome but only rarely in sporadic tumors. J Cutan Pathol. 2012;39:493-499.
3. Tardío JC. CD34-reactive tumors of the skin. an updated review of an ever-growing list of lesions. J Cutan Pathol. 2009;36:89-102.
4. Mehregan A. Inverted follicular keratosis is a distinct follicular tumor. Am J Dermatopathol. 1983;5:467-470.
5. Cockerell CJ. Histopathology of incipient intraepidermal squamous cell carcinoma (“actinic keratosis”). J Am Acad Dermatol. 2000;42(1, pt 2):11-17.
6. Jabłonska S, Majewski S, Obalek S, et al. Cutaneous warts. Clin Dermatol. 1997;15:309-319.
7. Hardin J, Gardner J, Colome M, et al. Verrucous cyst with melanocytic and sebaceous differentiation. Arch Path Lab Med. 2013;137:576-579.
8. Johnson BL, Kramer EM, Lavker RM. The keratotic tumors of Cowden’s disease: an electron microscopy study. J Cutan Pathol. 1987;14:291-298.
9. Kaddu S, Dong H, Mayer G, et al. Warty dyskeratoma—“follicular dyskeratoma”: analysis of clinicopathologic features of a distinctive follicular adnexal neoplasm. J Am Acad Dermatol. 2002;47:423-428.
Trichilemmomas are benign follicular neoplasms that exhibit differentiation toward the outer root sheath of the pilosebaceous follicular epithelium.1 Trichilemmomas clinically present as individual or multiple, slowly growing, verrucous papules appearing most commonly on the face or neck. The lesions may coalesce to form small plaques. Although trichilemmomas typically are isolated, patients with multiple trichilemmomas require a cancer screening workup due to their association with Cowden disease, which results from a mutation in the phosphatase and tensin homolog tumor suppressor gene, PTEN.2 An easy way to remember the association between trichilemmomas and Cowden disease is to alter the spelling to “trichile-moo-moo,” using the “moo moo” sound of an animal cow as a clue linking the tumor to Cowden disease.
Histologically, trichilemmomas exhibit a lobular epidermal downgrowth into the dermis (Figure 1). The surface of the lesion may be hyperkeratotic and somewhat papillomatous. Cells toward the center of the lobule are pale staining, periodic acid–Schiff positive, and diastase labile due to high levels of intracellular glycogen (Figure 2). Cells toward the periphery of the lobule usually appear basophilic with a palisading arrangement of the peripheral cells. The entire lobule is enclosed within an eosinophilic basement membrane that stains positively with periodic acid–Schiff (Figure 2).1 Consistent with the tumor’s differentiation toward the outer root sheath of the hair follicle, trichilemmomas have been reported to express CD34 focally or diffusely.3
 |  |
Similar to trichilemmoma, inverted follicular keratosis (IFK) commonly presents as a solitary asymptomatic papule on the face. Inverted follicular keratosis is a somewhat controversial entity, with some authorities arguing IFK is a variant of verruca vulgaris or seborrheic keratosis. Histologically, IFKs can be differentiated by the presence of squamous eddies (concentric layers of squamous cells in a whorled pattern), which are diagnostic, and central longitudinal crypts that contain keratin and are lined by squamous epithelium.4 Basaloid cells can be seen at the periphery of the tumors; however, IFKs lack an eosinophilic basement membrane surrounding the tumor (Figure 3).
Squamous cell carcinoma in situ classically appears as an erythematous hyperkeratotic papule or plaque on sun-exposed sites that can become crusted or ulcerated. Microscopically, squamous cell carcinoma in situ displays full-thickness disorderly maturation of keratinocytes. The keratinocytes exhibit nuclear pleomorphism. Atypical mitotic figures and dyskeratotic keratinocytes also can be seen throughout the full thickness of the epidermis (Figure 4).5
Verruca vulgaris (Figure 5) histologically demonstrates hyperkeratosis with tiers of parakeratosis, digitated epidermal hyperplasia, and dilated tortuous capillaries within the dermal papillae. At the edges of the lesion there often is inward turning of elongated rete ridges,6,7 which can be thought of as the rete reaching out for a hug of sorts to spread the human papillomavirus infection. Although the surface of a trichilemmoma can bear resemblance to a verruca vulgaris, the remainder of the histologic features can be used to help differentiate these tumors. Additionally, there has been no evidence suggestive of a viral etiology for trichilemmomas.8
Warty dyskeratoma features an umbilicated papule, usually on the face, head, or neck, that is associated with a follicular unit. The papule shows a cup-shaped, keratin-filled invagination; suprabasilar clefting; and acantholytic dyskeratotic cells, which are features that are not seen in trichilemmomas (Figure 6).9
Acknowledgment—The authors would like to thank Brandon Litzner, MD, St Louis, Missouri, for proofreading the manuscript.
Trichilemmomas are benign follicular neoplasms that exhibit differentiation toward the outer root sheath of the pilosebaceous follicular epithelium.1 Trichilemmomas clinically present as individual or multiple, slowly growing, verrucous papules appearing most commonly on the face or neck. The lesions may coalesce to form small plaques. Although trichilemmomas typically are isolated, patients with multiple trichilemmomas require a cancer screening workup due to their association with Cowden disease, which results from a mutation in the phosphatase and tensin homolog tumor suppressor gene, PTEN.2 An easy way to remember the association between trichilemmomas and Cowden disease is to alter the spelling to “trichile-moo-moo,” using the “moo moo” sound of an animal cow as a clue linking the tumor to Cowden disease.
Histologically, trichilemmomas exhibit a lobular epidermal downgrowth into the dermis (Figure 1). The surface of the lesion may be hyperkeratotic and somewhat papillomatous. Cells toward the center of the lobule are pale staining, periodic acid–Schiff positive, and diastase labile due to high levels of intracellular glycogen (Figure 2). Cells toward the periphery of the lobule usually appear basophilic with a palisading arrangement of the peripheral cells. The entire lobule is enclosed within an eosinophilic basement membrane that stains positively with periodic acid–Schiff (Figure 2).1 Consistent with the tumor’s differentiation toward the outer root sheath of the hair follicle, trichilemmomas have been reported to express CD34 focally or diffusely.3
 |  |
Similar to trichilemmoma, inverted follicular keratosis (IFK) commonly presents as a solitary asymptomatic papule on the face. Inverted follicular keratosis is a somewhat controversial entity, with some authorities arguing IFK is a variant of verruca vulgaris or seborrheic keratosis. Histologically, IFKs can be differentiated by the presence of squamous eddies (concentric layers of squamous cells in a whorled pattern), which are diagnostic, and central longitudinal crypts that contain keratin and are lined by squamous epithelium.4 Basaloid cells can be seen at the periphery of the tumors; however, IFKs lack an eosinophilic basement membrane surrounding the tumor (Figure 3).
Squamous cell carcinoma in situ classically appears as an erythematous hyperkeratotic papule or plaque on sun-exposed sites that can become crusted or ulcerated. Microscopically, squamous cell carcinoma in situ displays full-thickness disorderly maturation of keratinocytes. The keratinocytes exhibit nuclear pleomorphism. Atypical mitotic figures and dyskeratotic keratinocytes also can be seen throughout the full thickness of the epidermis (Figure 4).5
Verruca vulgaris (Figure 5) histologically demonstrates hyperkeratosis with tiers of parakeratosis, digitated epidermal hyperplasia, and dilated tortuous capillaries within the dermal papillae. At the edges of the lesion there often is inward turning of elongated rete ridges,6,7 which can be thought of as the rete reaching out for a hug of sorts to spread the human papillomavirus infection. Although the surface of a trichilemmoma can bear resemblance to a verruca vulgaris, the remainder of the histologic features can be used to help differentiate these tumors. Additionally, there has been no evidence suggestive of a viral etiology for trichilemmomas.8
Warty dyskeratoma features an umbilicated papule, usually on the face, head, or neck, that is associated with a follicular unit. The papule shows a cup-shaped, keratin-filled invagination; suprabasilar clefting; and acantholytic dyskeratotic cells, which are features that are not seen in trichilemmomas (Figure 6).9
Acknowledgment—The authors would like to thank Brandon Litzner, MD, St Louis, Missouri, for proofreading the manuscript.
1. Brownstein MH, Shapiro L. Trichilemmoma: analysis of 40 new cases. Arch Dermatol. 1973;107:866-869.
2. Al-Zaid T, Ditelberg J, Prieto V, et al. Trichilemmomas show loss of PTEN in Cowden syndrome but only rarely in sporadic tumors. J Cutan Pathol. 2012;39:493-499.
3. Tardío JC. CD34-reactive tumors of the skin. an updated review of an ever-growing list of lesions. J Cutan Pathol. 2009;36:89-102.
4. Mehregan A. Inverted follicular keratosis is a distinct follicular tumor. Am J Dermatopathol. 1983;5:467-470.
5. Cockerell CJ. Histopathology of incipient intraepidermal squamous cell carcinoma (“actinic keratosis”). J Am Acad Dermatol. 2000;42(1, pt 2):11-17.
6. Jabłonska S, Majewski S, Obalek S, et al. Cutaneous warts. Clin Dermatol. 1997;15:309-319.
7. Hardin J, Gardner J, Colome M, et al. Verrucous cyst with melanocytic and sebaceous differentiation. Arch Path Lab Med. 2013;137:576-579.
8. Johnson BL, Kramer EM, Lavker RM. The keratotic tumors of Cowden’s disease: an electron microscopy study. J Cutan Pathol. 1987;14:291-298.
9. Kaddu S, Dong H, Mayer G, et al. Warty dyskeratoma—“follicular dyskeratoma”: analysis of clinicopathologic features of a distinctive follicular adnexal neoplasm. J Am Acad Dermatol. 2002;47:423-428.
1. Brownstein MH, Shapiro L. Trichilemmoma: analysis of 40 new cases. Arch Dermatol. 1973;107:866-869.
2. Al-Zaid T, Ditelberg J, Prieto V, et al. Trichilemmomas show loss of PTEN in Cowden syndrome but only rarely in sporadic tumors. J Cutan Pathol. 2012;39:493-499.
3. Tardío JC. CD34-reactive tumors of the skin. an updated review of an ever-growing list of lesions. J Cutan Pathol. 2009;36:89-102.
4. Mehregan A. Inverted follicular keratosis is a distinct follicular tumor. Am J Dermatopathol. 1983;5:467-470.
5. Cockerell CJ. Histopathology of incipient intraepidermal squamous cell carcinoma (“actinic keratosis”). J Am Acad Dermatol. 2000;42(1, pt 2):11-17.
6. Jabłonska S, Majewski S, Obalek S, et al. Cutaneous warts. Clin Dermatol. 1997;15:309-319.
7. Hardin J, Gardner J, Colome M, et al. Verrucous cyst with melanocytic and sebaceous differentiation. Arch Path Lab Med. 2013;137:576-579.
8. Johnson BL, Kramer EM, Lavker RM. The keratotic tumors of Cowden’s disease: an electron microscopy study. J Cutan Pathol. 1987;14:291-298.
9. Kaddu S, Dong H, Mayer G, et al. Warty dyskeratoma—“follicular dyskeratoma”: analysis of clinicopathologic features of a distinctive follicular adnexal neoplasm. J Am Acad Dermatol. 2002;47:423-428.
Catching up on brain stimulation with Dr. Irving Reti
Psychiatry is a field where the treatment of our disorders remains perplexing: We’re still trying to figure out if the best way to treat psychiatric conditions is through psychotherapy, with medications, or for more resistant conditions, by stimulating activity in the brain in several different ways.
The field of brain stimulation includes electroconvulsive therapy, as well as transcranial magnetic stimulation (TMS), direct transcranial current stimulation (tDCS), and deep brain stimulation (DBS), all of which are examples of treatments that are still just coming into their own.
In search of an update on brain stimulation, I met with Dr. Irving Reti, director of the Johns Hopkins Hospital Brain Stimulation Program and editor of “Brain Stimulation: Methodologies and Interventions” (Hoboken, N.J.: Wiley-Blackwell, 2015). We met at a Starbucks in Baltimore, and I’ll tell you that a one-on-one conversation with an expert is a wonderful way to learn about state-of-the-art treatments, the only downside being that Starbucks does not offer CME credit.
Dr. Reti, who went to medical school at the University of Sydney and speaks with a charming Australian accent, trained in psychiatry at Johns Hopkins, and then did a neuroscience fellowship.
“I’d just finished residency training, and I was giving ECT to rats. We were looking at the expression of immediate-early genes. At the same time, I started doing consults in the mood disorders clinic.”
In 2006, Dr. Reti took over as director of ECT at Hopkins, and that same year, Dr. Jimmy Potash got funding to study TMS. Dr. Potash has since moved to the University of Iowa, and Dr. Reti took over TMS administration at Hopkins. Dr. Reti was flattered to be approached by Wiley to edit “Brain Stimulation,” and he talked about how he was pleased with the final edition of the book.
“I ended up getting the top people to write the chapters, people like Sarah Lisanby, Michael Nitsche, John Rothwell, and Mark George. These are the leaders in the field of brain stimulation.”
I asked Dr. Reti to walk me through what was happening in each brain stimulation area.
“In ECT,” he said, “we know a lot more now about how both the settings and the anesthesia regimen affect the outcomes. We didn’t know this when I trained in the ’90s.” Dr. Reti estimated that he’s administered ECT to close to 2,000 patients.
TMS is done less often at Hopkins; he estimated that 10-20 patients receive the treatment, and each patient comes 30-40 times, with each session lasting 40 minutes.
“It’s better than medicine but not as effective as ECT. We’re seeing an efficacy rate around 50%-60%,” and he noted that some patients have trouble tolerating the procedure as the magnetic stimulation can be uncomfortable. “The TMS coil stimulates the scalp nerves and muscles immediately under the coil, which causes discomfort.” He noted that some patients need to premedicate with over-the-counter pain medicines.
“We’re also finding that low-frequency stimulation on the right can be helpful for anxiety,” Dr. Reti said.
He talked about treating patients with psychotherapy along with TMS. The brain changes are thought to increase the brain’s plasticity and perhaps make psychotherapy more effective.
“It’s being studied in drug treatment. You can show someone with an addiction stimuli to trigger cravings, and doing this with TMS may block the response,” he said.
He talked for a while about direct transcranial brain stimulation, which I was not very familiar with. Because it is being used to improve focus-playing video games, the equipment is not being marketed as a psychiatric treatment and doesn’t fall under the domain of the Food and Drug Administration.
“Kids are using it to improve their concentration and performance with video games; all you need is a 9-volt battery and some electrodes that are attached to the scalp. The kits cost about $250, but you can burn your scalp,” he said.
Dr. Reti referred me to an article in the New Yorker on tDCS, “Electrified: Adventures in transcranial direct-current stimulation” by Elif Batuman. He noted that there are studies in progress to look at therapeutic uses for tDCS, including one at Johns Hopkins where neuropsychologist David Schretlen is looking at improving cognition in schizophrenia. Dr. Reti is interested in seeing if tDCS might be helpful in decreasing self-injurious behaviors in autistic children, as ECT has been effective in severe cases. He noted that while ECT and TMS stimulate neurons in the brain to fire, tDCS changes the stimulation threshold without directly causing the neurons to discharge.
Finally, we talked a little about deep brain stimulation. Thin electrodes directly target nodes in brain circuits that can modulate the activity of those circuits. He noted that deep brain stimulation was being used at Johns Hopkins to treat Parkinson’s disease, and other centers have looked at its use for severe obsessive-compulsive disorder and treatment-resistant depression.
“We know that the response habituates; now they are trying on-demand DBS,” Dr. Reti noted.
So, although I got no continuing medical education credits, I did get to try a new Starbucks drink while having a very stimulating discussion on the latest convulsive and nonconvulsive psychiatric brain research.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Psychiatry is a field where the treatment of our disorders remains perplexing: We’re still trying to figure out if the best way to treat psychiatric conditions is through psychotherapy, with medications, or for more resistant conditions, by stimulating activity in the brain in several different ways.
The field of brain stimulation includes electroconvulsive therapy, as well as transcranial magnetic stimulation (TMS), direct transcranial current stimulation (tDCS), and deep brain stimulation (DBS), all of which are examples of treatments that are still just coming into their own.
In search of an update on brain stimulation, I met with Dr. Irving Reti, director of the Johns Hopkins Hospital Brain Stimulation Program and editor of “Brain Stimulation: Methodologies and Interventions” (Hoboken, N.J.: Wiley-Blackwell, 2015). We met at a Starbucks in Baltimore, and I’ll tell you that a one-on-one conversation with an expert is a wonderful way to learn about state-of-the-art treatments, the only downside being that Starbucks does not offer CME credit.
Dr. Reti, who went to medical school at the University of Sydney and speaks with a charming Australian accent, trained in psychiatry at Johns Hopkins, and then did a neuroscience fellowship.
“I’d just finished residency training, and I was giving ECT to rats. We were looking at the expression of immediate-early genes. At the same time, I started doing consults in the mood disorders clinic.”
In 2006, Dr. Reti took over as director of ECT at Hopkins, and that same year, Dr. Jimmy Potash got funding to study TMS. Dr. Potash has since moved to the University of Iowa, and Dr. Reti took over TMS administration at Hopkins. Dr. Reti was flattered to be approached by Wiley to edit “Brain Stimulation,” and he talked about how he was pleased with the final edition of the book.
“I ended up getting the top people to write the chapters, people like Sarah Lisanby, Michael Nitsche, John Rothwell, and Mark George. These are the leaders in the field of brain stimulation.”
I asked Dr. Reti to walk me through what was happening in each brain stimulation area.
“In ECT,” he said, “we know a lot more now about how both the settings and the anesthesia regimen affect the outcomes. We didn’t know this when I trained in the ’90s.” Dr. Reti estimated that he’s administered ECT to close to 2,000 patients.
TMS is done less often at Hopkins; he estimated that 10-20 patients receive the treatment, and each patient comes 30-40 times, with each session lasting 40 minutes.
“It’s better than medicine but not as effective as ECT. We’re seeing an efficacy rate around 50%-60%,” and he noted that some patients have trouble tolerating the procedure as the magnetic stimulation can be uncomfortable. “The TMS coil stimulates the scalp nerves and muscles immediately under the coil, which causes discomfort.” He noted that some patients need to premedicate with over-the-counter pain medicines.
“We’re also finding that low-frequency stimulation on the right can be helpful for anxiety,” Dr. Reti said.
He talked about treating patients with psychotherapy along with TMS. The brain changes are thought to increase the brain’s plasticity and perhaps make psychotherapy more effective.
“It’s being studied in drug treatment. You can show someone with an addiction stimuli to trigger cravings, and doing this with TMS may block the response,” he said.
He talked for a while about direct transcranial brain stimulation, which I was not very familiar with. Because it is being used to improve focus-playing video games, the equipment is not being marketed as a psychiatric treatment and doesn’t fall under the domain of the Food and Drug Administration.
“Kids are using it to improve their concentration and performance with video games; all you need is a 9-volt battery and some electrodes that are attached to the scalp. The kits cost about $250, but you can burn your scalp,” he said.
Dr. Reti referred me to an article in the New Yorker on tDCS, “Electrified: Adventures in transcranial direct-current stimulation” by Elif Batuman. He noted that there are studies in progress to look at therapeutic uses for tDCS, including one at Johns Hopkins where neuropsychologist David Schretlen is looking at improving cognition in schizophrenia. Dr. Reti is interested in seeing if tDCS might be helpful in decreasing self-injurious behaviors in autistic children, as ECT has been effective in severe cases. He noted that while ECT and TMS stimulate neurons in the brain to fire, tDCS changes the stimulation threshold without directly causing the neurons to discharge.
Finally, we talked a little about deep brain stimulation. Thin electrodes directly target nodes in brain circuits that can modulate the activity of those circuits. He noted that deep brain stimulation was being used at Johns Hopkins to treat Parkinson’s disease, and other centers have looked at its use for severe obsessive-compulsive disorder and treatment-resistant depression.
“We know that the response habituates; now they are trying on-demand DBS,” Dr. Reti noted.
So, although I got no continuing medical education credits, I did get to try a new Starbucks drink while having a very stimulating discussion on the latest convulsive and nonconvulsive psychiatric brain research.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Psychiatry is a field where the treatment of our disorders remains perplexing: We’re still trying to figure out if the best way to treat psychiatric conditions is through psychotherapy, with medications, or for more resistant conditions, by stimulating activity in the brain in several different ways.
The field of brain stimulation includes electroconvulsive therapy, as well as transcranial magnetic stimulation (TMS), direct transcranial current stimulation (tDCS), and deep brain stimulation (DBS), all of which are examples of treatments that are still just coming into their own.
In search of an update on brain stimulation, I met with Dr. Irving Reti, director of the Johns Hopkins Hospital Brain Stimulation Program and editor of “Brain Stimulation: Methodologies and Interventions” (Hoboken, N.J.: Wiley-Blackwell, 2015). We met at a Starbucks in Baltimore, and I’ll tell you that a one-on-one conversation with an expert is a wonderful way to learn about state-of-the-art treatments, the only downside being that Starbucks does not offer CME credit.
Dr. Reti, who went to medical school at the University of Sydney and speaks with a charming Australian accent, trained in psychiatry at Johns Hopkins, and then did a neuroscience fellowship.
“I’d just finished residency training, and I was giving ECT to rats. We were looking at the expression of immediate-early genes. At the same time, I started doing consults in the mood disorders clinic.”
In 2006, Dr. Reti took over as director of ECT at Hopkins, and that same year, Dr. Jimmy Potash got funding to study TMS. Dr. Potash has since moved to the University of Iowa, and Dr. Reti took over TMS administration at Hopkins. Dr. Reti was flattered to be approached by Wiley to edit “Brain Stimulation,” and he talked about how he was pleased with the final edition of the book.
“I ended up getting the top people to write the chapters, people like Sarah Lisanby, Michael Nitsche, John Rothwell, and Mark George. These are the leaders in the field of brain stimulation.”
I asked Dr. Reti to walk me through what was happening in each brain stimulation area.
“In ECT,” he said, “we know a lot more now about how both the settings and the anesthesia regimen affect the outcomes. We didn’t know this when I trained in the ’90s.” Dr. Reti estimated that he’s administered ECT to close to 2,000 patients.
TMS is done less often at Hopkins; he estimated that 10-20 patients receive the treatment, and each patient comes 30-40 times, with each session lasting 40 minutes.
“It’s better than medicine but not as effective as ECT. We’re seeing an efficacy rate around 50%-60%,” and he noted that some patients have trouble tolerating the procedure as the magnetic stimulation can be uncomfortable. “The TMS coil stimulates the scalp nerves and muscles immediately under the coil, which causes discomfort.” He noted that some patients need to premedicate with over-the-counter pain medicines.
“We’re also finding that low-frequency stimulation on the right can be helpful for anxiety,” Dr. Reti said.
He talked about treating patients with psychotherapy along with TMS. The brain changes are thought to increase the brain’s plasticity and perhaps make psychotherapy more effective.
“It’s being studied in drug treatment. You can show someone with an addiction stimuli to trigger cravings, and doing this with TMS may block the response,” he said.
He talked for a while about direct transcranial brain stimulation, which I was not very familiar with. Because it is being used to improve focus-playing video games, the equipment is not being marketed as a psychiatric treatment and doesn’t fall under the domain of the Food and Drug Administration.
“Kids are using it to improve their concentration and performance with video games; all you need is a 9-volt battery and some electrodes that are attached to the scalp. The kits cost about $250, but you can burn your scalp,” he said.
Dr. Reti referred me to an article in the New Yorker on tDCS, “Electrified: Adventures in transcranial direct-current stimulation” by Elif Batuman. He noted that there are studies in progress to look at therapeutic uses for tDCS, including one at Johns Hopkins where neuropsychologist David Schretlen is looking at improving cognition in schizophrenia. Dr. Reti is interested in seeing if tDCS might be helpful in decreasing self-injurious behaviors in autistic children, as ECT has been effective in severe cases. He noted that while ECT and TMS stimulate neurons in the brain to fire, tDCS changes the stimulation threshold without directly causing the neurons to discharge.
Finally, we talked a little about deep brain stimulation. Thin electrodes directly target nodes in brain circuits that can modulate the activity of those circuits. He noted that deep brain stimulation was being used at Johns Hopkins to treat Parkinson’s disease, and other centers have looked at its use for severe obsessive-compulsive disorder and treatment-resistant depression.
“We know that the response habituates; now they are trying on-demand DBS,” Dr. Reti noted.
So, although I got no continuing medical education credits, I did get to try a new Starbucks drink while having a very stimulating discussion on the latest convulsive and nonconvulsive psychiatric brain research.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Top 10 treatments for vitiligo
PARK CITY, UTAH – At the annual meeting of the Pacific Dermatologic Association, Dr. Sancy A. Leachman offered a top 10 list of new agents and technologies for the treatment of vitiligo.
No. 10: Ultraviolet A1 (UVA1) phototherapy
Dr. Harvey Lui at the University of British Columbia in Vancouver is leading a phase II trial to evaluate the potential for UVA1 to induce repigmentation within vitiligo patches and to assess the side effect profile of the treatment. “I think it might work,” said Dr. Leachman, professor and chair of dermatology at Oregon Health & Science University (OHSU), Portland.
No. 9: Ginkgo biloba
The use of ginko biloba 40-60 mg 2-3 times per day, 10 minutes before a meal, was mentioned in a Cochrane Review of vitiligo treatments published on Feb. 24, 2015. “I think I’m going to give this a try in people who have failed other treatments and see if I can get some response,” Dr. Leachman said.
No. 8: Red light
Dr. Lui is leading a randomized phase II trial of low-intensity and high-intensity red light versus no treatment for vitiligo patches. Treatments will be given twice weekly for 10 weeks, with follow-up assessments at 4, 8, and 12 weeks post treatment.
No. 7: Micrografting
A novel suction blister device known as the CelluTome epidermal harvesting system uses heat and slight vacuum pressure to harvest healthy epidermal skin tissue without damaging the donor site. Dr. Leachman characterized the technology as “semiautomating the process of suction graft transplantation.”
No. 6: The ReCell device
Manufactured by Avita Medical, this investigational autologous cell harvesting device is used after CO2 abrasion and enables clinicians to create regenerative epithelial suspension with a small sample of the patient’s skin. A phase IV trial in the Netherlands is underway to assess the efficacy and safety of autologous epidermal cell suspension grafting with the ReCell device after CO2 laser abrasion, compared with CO2 laser abrasion alone and no treatment, in patients with piebaldism and stable vitiligo.
No. 5: Topical Photocil
In a pilot study sponsored by Applied Biology, researchers are enrolling patients with vitiligo to assess the safety and efficacy of Photocil. The primary outcome measure is the Vitiligo Area Severity Index (VASI). “When this cream is activated by sunlight, it degrades into narrow-band and UVB light, so you can put a topical cream on that will administer narrow-band UVB only in that spot,” said Dr. Leachman, who is also director of OHSU’s Knight Melanoma Research Program. “That’s amazing to me.”
No. 4: Afamelanotide
This is an analogue of a melanocyte-stimulating hormone. A randomized study conducted at two academic medical centers found that the combination of afamelanotide implant and narrow-band UVB phototherapy resulted in statistically superior and faster repigmentation, compared with narrow-band UVB monotherapy (JAMA Dermatol. 2015 Jan;151(1):42-50).
No. 3: Abatacept (Orencia)
This is a soluble fusion protein consisting of human cytotoxic T-lymphocyte–associated antigen 4 (CTLA4), which prevents T-cell activation. A phase I trial is underway at Brigham and Women’s Hospital in Boston to determine if weekly self-injections of the agent lead to clinical improvements of vitiligo lesions. The primary outcome measure is change in repigmentation with abatacept therapy based on the VASI score.
No. 2. Simvastatin
The notion of its use is based on STAT1 inhibition reducing interferon-gamma–dependent activation of CD8-positive T cells, according to Dr. Leachman. The concept has been successful in a mouse model, and a study in humans was recently completed by Dr. John Harris at the University of Massachusetts, Worcester. “What we have is the ability to apply an existing drug (Simvastatin) to the process and see if it works,” she said. “Wouldn’t it be cool if we could give a statin and improve vitiligo?”
No 1: Tofacitinib
This is a Janus kinase inhibitor commonly used for rheumatoid arthritis. According to Dr. Leachman, Janus kinase inhibition prevents STAT activation, “which prevents [interferon]-gamma production, which reduces activation of CD8-positive T cells via CXCL10 binding to CXCR3,” she said. A case report demonstrating its efficacy in a 53-year-old patient was recently published in JAMA Dermatology by Dr. Brett A. King and Dr. Brittany Craiglow, dermatologists at Yale School of Medicine, New Haven, Conn. “I’m hopeful that this [agent] will be made into a topical cream because these drugs do have substantial side effects,” Dr. Leachman said.
Dr. Leachman disclosed that she is a member of the medical and scientific advisory board for Myriad Genetics Laboratory. She has also participated in an advisory board meeting for Castle Biosciences and has participated in the DecisionDx registry.
PARK CITY, UTAH – At the annual meeting of the Pacific Dermatologic Association, Dr. Sancy A. Leachman offered a top 10 list of new agents and technologies for the treatment of vitiligo.
No. 10: Ultraviolet A1 (UVA1) phototherapy
Dr. Harvey Lui at the University of British Columbia in Vancouver is leading a phase II trial to evaluate the potential for UVA1 to induce repigmentation within vitiligo patches and to assess the side effect profile of the treatment. “I think it might work,” said Dr. Leachman, professor and chair of dermatology at Oregon Health & Science University (OHSU), Portland.
No. 9: Ginkgo biloba
The use of ginko biloba 40-60 mg 2-3 times per day, 10 minutes before a meal, was mentioned in a Cochrane Review of vitiligo treatments published on Feb. 24, 2015. “I think I’m going to give this a try in people who have failed other treatments and see if I can get some response,” Dr. Leachman said.
No. 8: Red light
Dr. Lui is leading a randomized phase II trial of low-intensity and high-intensity red light versus no treatment for vitiligo patches. Treatments will be given twice weekly for 10 weeks, with follow-up assessments at 4, 8, and 12 weeks post treatment.
No. 7: Micrografting
A novel suction blister device known as the CelluTome epidermal harvesting system uses heat and slight vacuum pressure to harvest healthy epidermal skin tissue without damaging the donor site. Dr. Leachman characterized the technology as “semiautomating the process of suction graft transplantation.”
No. 6: The ReCell device
Manufactured by Avita Medical, this investigational autologous cell harvesting device is used after CO2 abrasion and enables clinicians to create regenerative epithelial suspension with a small sample of the patient’s skin. A phase IV trial in the Netherlands is underway to assess the efficacy and safety of autologous epidermal cell suspension grafting with the ReCell device after CO2 laser abrasion, compared with CO2 laser abrasion alone and no treatment, in patients with piebaldism and stable vitiligo.
No. 5: Topical Photocil
In a pilot study sponsored by Applied Biology, researchers are enrolling patients with vitiligo to assess the safety and efficacy of Photocil. The primary outcome measure is the Vitiligo Area Severity Index (VASI). “When this cream is activated by sunlight, it degrades into narrow-band and UVB light, so you can put a topical cream on that will administer narrow-band UVB only in that spot,” said Dr. Leachman, who is also director of OHSU’s Knight Melanoma Research Program. “That’s amazing to me.”
No. 4: Afamelanotide
This is an analogue of a melanocyte-stimulating hormone. A randomized study conducted at two academic medical centers found that the combination of afamelanotide implant and narrow-band UVB phototherapy resulted in statistically superior and faster repigmentation, compared with narrow-band UVB monotherapy (JAMA Dermatol. 2015 Jan;151(1):42-50).
No. 3: Abatacept (Orencia)
This is a soluble fusion protein consisting of human cytotoxic T-lymphocyte–associated antigen 4 (CTLA4), which prevents T-cell activation. A phase I trial is underway at Brigham and Women’s Hospital in Boston to determine if weekly self-injections of the agent lead to clinical improvements of vitiligo lesions. The primary outcome measure is change in repigmentation with abatacept therapy based on the VASI score.
No. 2. Simvastatin
The notion of its use is based on STAT1 inhibition reducing interferon-gamma–dependent activation of CD8-positive T cells, according to Dr. Leachman. The concept has been successful in a mouse model, and a study in humans was recently completed by Dr. John Harris at the University of Massachusetts, Worcester. “What we have is the ability to apply an existing drug (Simvastatin) to the process and see if it works,” she said. “Wouldn’t it be cool if we could give a statin and improve vitiligo?”
No 1: Tofacitinib
This is a Janus kinase inhibitor commonly used for rheumatoid arthritis. According to Dr. Leachman, Janus kinase inhibition prevents STAT activation, “which prevents [interferon]-gamma production, which reduces activation of CD8-positive T cells via CXCL10 binding to CXCR3,” she said. A case report demonstrating its efficacy in a 53-year-old patient was recently published in JAMA Dermatology by Dr. Brett A. King and Dr. Brittany Craiglow, dermatologists at Yale School of Medicine, New Haven, Conn. “I’m hopeful that this [agent] will be made into a topical cream because these drugs do have substantial side effects,” Dr. Leachman said.
Dr. Leachman disclosed that she is a member of the medical and scientific advisory board for Myriad Genetics Laboratory. She has also participated in an advisory board meeting for Castle Biosciences and has participated in the DecisionDx registry.
PARK CITY, UTAH – At the annual meeting of the Pacific Dermatologic Association, Dr. Sancy A. Leachman offered a top 10 list of new agents and technologies for the treatment of vitiligo.
No. 10: Ultraviolet A1 (UVA1) phototherapy
Dr. Harvey Lui at the University of British Columbia in Vancouver is leading a phase II trial to evaluate the potential for UVA1 to induce repigmentation within vitiligo patches and to assess the side effect profile of the treatment. “I think it might work,” said Dr. Leachman, professor and chair of dermatology at Oregon Health & Science University (OHSU), Portland.
No. 9: Ginkgo biloba
The use of ginko biloba 40-60 mg 2-3 times per day, 10 minutes before a meal, was mentioned in a Cochrane Review of vitiligo treatments published on Feb. 24, 2015. “I think I’m going to give this a try in people who have failed other treatments and see if I can get some response,” Dr. Leachman said.
No. 8: Red light
Dr. Lui is leading a randomized phase II trial of low-intensity and high-intensity red light versus no treatment for vitiligo patches. Treatments will be given twice weekly for 10 weeks, with follow-up assessments at 4, 8, and 12 weeks post treatment.
No. 7: Micrografting
A novel suction blister device known as the CelluTome epidermal harvesting system uses heat and slight vacuum pressure to harvest healthy epidermal skin tissue without damaging the donor site. Dr. Leachman characterized the technology as “semiautomating the process of suction graft transplantation.”
No. 6: The ReCell device
Manufactured by Avita Medical, this investigational autologous cell harvesting device is used after CO2 abrasion and enables clinicians to create regenerative epithelial suspension with a small sample of the patient’s skin. A phase IV trial in the Netherlands is underway to assess the efficacy and safety of autologous epidermal cell suspension grafting with the ReCell device after CO2 laser abrasion, compared with CO2 laser abrasion alone and no treatment, in patients with piebaldism and stable vitiligo.
No. 5: Topical Photocil
In a pilot study sponsored by Applied Biology, researchers are enrolling patients with vitiligo to assess the safety and efficacy of Photocil. The primary outcome measure is the Vitiligo Area Severity Index (VASI). “When this cream is activated by sunlight, it degrades into narrow-band and UVB light, so you can put a topical cream on that will administer narrow-band UVB only in that spot,” said Dr. Leachman, who is also director of OHSU’s Knight Melanoma Research Program. “That’s amazing to me.”
No. 4: Afamelanotide
This is an analogue of a melanocyte-stimulating hormone. A randomized study conducted at two academic medical centers found that the combination of afamelanotide implant and narrow-band UVB phototherapy resulted in statistically superior and faster repigmentation, compared with narrow-band UVB monotherapy (JAMA Dermatol. 2015 Jan;151(1):42-50).
No. 3: Abatacept (Orencia)
This is a soluble fusion protein consisting of human cytotoxic T-lymphocyte–associated antigen 4 (CTLA4), which prevents T-cell activation. A phase I trial is underway at Brigham and Women’s Hospital in Boston to determine if weekly self-injections of the agent lead to clinical improvements of vitiligo lesions. The primary outcome measure is change in repigmentation with abatacept therapy based on the VASI score.
No. 2. Simvastatin
The notion of its use is based on STAT1 inhibition reducing interferon-gamma–dependent activation of CD8-positive T cells, according to Dr. Leachman. The concept has been successful in a mouse model, and a study in humans was recently completed by Dr. John Harris at the University of Massachusetts, Worcester. “What we have is the ability to apply an existing drug (Simvastatin) to the process and see if it works,” she said. “Wouldn’t it be cool if we could give a statin and improve vitiligo?”
No 1: Tofacitinib
This is a Janus kinase inhibitor commonly used for rheumatoid arthritis. According to Dr. Leachman, Janus kinase inhibition prevents STAT activation, “which prevents [interferon]-gamma production, which reduces activation of CD8-positive T cells via CXCL10 binding to CXCR3,” she said. A case report demonstrating its efficacy in a 53-year-old patient was recently published in JAMA Dermatology by Dr. Brett A. King and Dr. Brittany Craiglow, dermatologists at Yale School of Medicine, New Haven, Conn. “I’m hopeful that this [agent] will be made into a topical cream because these drugs do have substantial side effects,” Dr. Leachman said.
Dr. Leachman disclosed that she is a member of the medical and scientific advisory board for Myriad Genetics Laboratory. She has also participated in an advisory board meeting for Castle Biosciences and has participated in the DecisionDx registry.
EXPERT ANALYSIS AT PDA 2015
LISTEN NOW: Tales from the Research, Innovations, and Clinical Vignette (RIV) Poster Competition
Hospitalists who presented RIV posters at HM15 talk about their projects. Dr. Brian Poustinchian worked on a bedside rounding study at Midwestern University in Illinois, and Dr. Jennifer Pascoe worked on a poster about patients leaving the hospital against medical advice, focusing on a case of her own at the University of Rochester.
Hospitalists who presented RIV posters at HM15 talk about their projects. Dr. Brian Poustinchian worked on a bedside rounding study at Midwestern University in Illinois, and Dr. Jennifer Pascoe worked on a poster about patients leaving the hospital against medical advice, focusing on a case of her own at the University of Rochester.
Hospitalists who presented RIV posters at HM15 talk about their projects. Dr. Brian Poustinchian worked on a bedside rounding study at Midwestern University in Illinois, and Dr. Jennifer Pascoe worked on a poster about patients leaving the hospital against medical advice, focusing on a case of her own at the University of Rochester.
Similar Early Outcomes in nvAF Regardless of Anticoagulant Type
NEW YORK - In the early months of anticoagulant treatment, patients with nonvalvular atrial fibrillation (nvAF) have similar rates of bleeding and arterial clots with dabigatran, rivaroxaban and vitamin K antagonists (VKA) like warfarin, researchers from France report.
Large randomized trials have shown the newer non-VKA oral anticoagulants (NOAC) to have superior safety and efficacy relative to warfarin, but subsequent observational studies have yielded conflicting results.
Dr. Géric Maura from National Health Insurance (CNAMTS) in Paris and colleagues used the French National Health Insurance information system to assess the bleeding and arterial thrombotic risks of dabigatran and rivaroxaban, each compared with VKA, during the first few months of therapy in 32,807 newly treated patients with nvAF.
There was no significant difference in bleeding between VKA- and dabigatran- or rivaroxaban-treated patients on propensity-matched analysis, regardless of whether patients were treated with low or high doses of each NOAC, the researchers report in Circulation, online July 21.
The composite outcome comprising hospitalization for bleeding and death occurred with similar frequency in the different treatment groups.
Among the secondary endpoints, there were no significant differences between treatments in arterial thromboembolic events or in the composite outcome comprising stroke, systemic embolism and death.
"Although our overall results are reassuring in relation to initiation of NOAC in nvAF patients in France with no marked excess thromboembolic or bleeding risk, they also suggest that particular caution is required when initiating NOAC," the researchers conclude. "But on the basis of this study comparing NOAC to VKA, NOAC cannot be considered to be safer than VKA during the early phase of treatment. On the contrary, the clinical implications of our results are that physicians must be just as cautious when initiating NOAC as when initiating VKA, particularly in view of the absence of an antidote and objective monitoring of the extent of anticoagulation."
"Similar analyses should be extended to other NOAC such as apixaban and observational studies should now focus on NOAC head-to-head comparison in a non-inferiority design," they suggest.
The study had no commercial funding and the authors reported no conflicts of interest.
Dr. Maura did not respond to a request for comment.
NEW YORK - In the early months of anticoagulant treatment, patients with nonvalvular atrial fibrillation (nvAF) have similar rates of bleeding and arterial clots with dabigatran, rivaroxaban and vitamin K antagonists (VKA) like warfarin, researchers from France report.
Large randomized trials have shown the newer non-VKA oral anticoagulants (NOAC) to have superior safety and efficacy relative to warfarin, but subsequent observational studies have yielded conflicting results.
Dr. Géric Maura from National Health Insurance (CNAMTS) in Paris and colleagues used the French National Health Insurance information system to assess the bleeding and arterial thrombotic risks of dabigatran and rivaroxaban, each compared with VKA, during the first few months of therapy in 32,807 newly treated patients with nvAF.
There was no significant difference in bleeding between VKA- and dabigatran- or rivaroxaban-treated patients on propensity-matched analysis, regardless of whether patients were treated with low or high doses of each NOAC, the researchers report in Circulation, online July 21.
The composite outcome comprising hospitalization for bleeding and death occurred with similar frequency in the different treatment groups.
Among the secondary endpoints, there were no significant differences between treatments in arterial thromboembolic events or in the composite outcome comprising stroke, systemic embolism and death.
"Although our overall results are reassuring in relation to initiation of NOAC in nvAF patients in France with no marked excess thromboembolic or bleeding risk, they also suggest that particular caution is required when initiating NOAC," the researchers conclude. "But on the basis of this study comparing NOAC to VKA, NOAC cannot be considered to be safer than VKA during the early phase of treatment. On the contrary, the clinical implications of our results are that physicians must be just as cautious when initiating NOAC as when initiating VKA, particularly in view of the absence of an antidote and objective monitoring of the extent of anticoagulation."
"Similar analyses should be extended to other NOAC such as apixaban and observational studies should now focus on NOAC head-to-head comparison in a non-inferiority design," they suggest.
The study had no commercial funding and the authors reported no conflicts of interest.
Dr. Maura did not respond to a request for comment.
NEW YORK - In the early months of anticoagulant treatment, patients with nonvalvular atrial fibrillation (nvAF) have similar rates of bleeding and arterial clots with dabigatran, rivaroxaban and vitamin K antagonists (VKA) like warfarin, researchers from France report.
Large randomized trials have shown the newer non-VKA oral anticoagulants (NOAC) to have superior safety and efficacy relative to warfarin, but subsequent observational studies have yielded conflicting results.
Dr. Géric Maura from National Health Insurance (CNAMTS) in Paris and colleagues used the French National Health Insurance information system to assess the bleeding and arterial thrombotic risks of dabigatran and rivaroxaban, each compared with VKA, during the first few months of therapy in 32,807 newly treated patients with nvAF.
There was no significant difference in bleeding between VKA- and dabigatran- or rivaroxaban-treated patients on propensity-matched analysis, regardless of whether patients were treated with low or high doses of each NOAC, the researchers report in Circulation, online July 21.
The composite outcome comprising hospitalization for bleeding and death occurred with similar frequency in the different treatment groups.
Among the secondary endpoints, there were no significant differences between treatments in arterial thromboembolic events or in the composite outcome comprising stroke, systemic embolism and death.
"Although our overall results are reassuring in relation to initiation of NOAC in nvAF patients in France with no marked excess thromboembolic or bleeding risk, they also suggest that particular caution is required when initiating NOAC," the researchers conclude. "But on the basis of this study comparing NOAC to VKA, NOAC cannot be considered to be safer than VKA during the early phase of treatment. On the contrary, the clinical implications of our results are that physicians must be just as cautious when initiating NOAC as when initiating VKA, particularly in view of the absence of an antidote and objective monitoring of the extent of anticoagulation."
"Similar analyses should be extended to other NOAC such as apixaban and observational studies should now focus on NOAC head-to-head comparison in a non-inferiority design," they suggest.
The study had no commercial funding and the authors reported no conflicts of interest.
Dr. Maura did not respond to a request for comment.
New prognostic model for follicular lymphoma

Photo courtesy of NIH
A newly developed prognostic model can identify follicular lymphoma (FL) patients at the highest risk for treatment failure, according to researchers.
To create this model, called m7-FLIPI, the team combined the Follicular Lymphoma International Prognostic Index (FLIPI), Eastern Cooperative Oncology Group (ECOG) performance status, and the mutation status of 7 genes—EZH2, ARID1A, MEF2B, EP300, FOXO1, CREBBP, and CARD11.
The researchers said this is the first prognostic model for FL that accounts for both clinical factors and genetic mutations.
They described the creation and testing of the model in The Lancet Oncology.
“We set out to determine, at the time of diagnosis, which patients’ disease will have sustained responses after treatment and whether new genetic data could help inform which patients are at risk for developing progressive lymphoma so clinicians would be able to offer these high-risk patients more effective therapies,” said Randy Gascoyne, MD, of the British Columbia Cancer Agency in Vancouver, Canada.
He and his colleagues created the m7-FLIPI by conducting a retrospective analysis of genetic mutations and clinical risk factors in 2 cohorts of patients with symptomatic, advanced stage, or bulky FL grade 1, 2, or 3A.
The patients had a biopsy specimen collected 12 months or less before they began first-line treatment with an immunochemotherapy regimen containing rituximab.
Training cohort
The training cohort consisted of 151 FL patients who received R-CHOP. The median follow-up for these patients was 7.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found 28% of patients (43/151) were defined as high-risk, with a 5-year failure-free survival (FFS) rate of 38.29%.
And 72% of patients (108/151) were defined as low-risk, with a 5-year FFS of 77.21%. The hazard ratio was 4.14 (P<0.0001).
The positive predictive value for 5-year FFS was 64%, and the negative predictive value was 78%. The m7-FLIPI outperformed a prognostic model of only gene mutations and the FLIPI-2.
Validation cohort
The validation cohort consisted of 107 patients who received R-CVP. The median follow-up for these patients was 6.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found that 22% of patients (24/107) were defined as high-risk, with a 5-year FFS of 25%.
And 78% of patients (83/107) were defined as low-risk, with a 5-year FFS of 68.24%. The hazard ratio was 3.58 (P<0.0001).
The positive predictive value for 5-year FFS was 72%, and the negative predictive value was 68%. The m7-FLIPI outperformed the FLIPI alone and the FLIPI combined with ECOG performance status.
Overall survival
Although the m7-FLIPI was designed specifically for FFS, the researchers also tested its prognostic utility for overall survival (OS).
In the training cohort, high-risk disease according to the m7-FLIPI was associated with a 5-year OS of 65.25%, compared to 89.98% for low-risk disease (P=0.00031).
In the validation cohort, 5-year OS was 41.67% for patients with high-risk disease and 84.01% for patients with low-risk disease (P<0.0001). In both cohorts, the m7-FLIPI outperformed the FLIPI alone.
Based on these results, the researchers believe the m7-FLIPI could be utilized in a clinical setting to test all new FL patients at diagnosis and identify patients who harbor the most aggressive disease.
“The m7-FLIPI could be extremely significant for the medical community,” Dr Gascoyne said, “changing the story for high-risk patients who are currently destined to not respond well to standard treatment.” ![]()

Photo courtesy of NIH
A newly developed prognostic model can identify follicular lymphoma (FL) patients at the highest risk for treatment failure, according to researchers.
To create this model, called m7-FLIPI, the team combined the Follicular Lymphoma International Prognostic Index (FLIPI), Eastern Cooperative Oncology Group (ECOG) performance status, and the mutation status of 7 genes—EZH2, ARID1A, MEF2B, EP300, FOXO1, CREBBP, and CARD11.
The researchers said this is the first prognostic model for FL that accounts for both clinical factors and genetic mutations.
They described the creation and testing of the model in The Lancet Oncology.
“We set out to determine, at the time of diagnosis, which patients’ disease will have sustained responses after treatment and whether new genetic data could help inform which patients are at risk for developing progressive lymphoma so clinicians would be able to offer these high-risk patients more effective therapies,” said Randy Gascoyne, MD, of the British Columbia Cancer Agency in Vancouver, Canada.
He and his colleagues created the m7-FLIPI by conducting a retrospective analysis of genetic mutations and clinical risk factors in 2 cohorts of patients with symptomatic, advanced stage, or bulky FL grade 1, 2, or 3A.
The patients had a biopsy specimen collected 12 months or less before they began first-line treatment with an immunochemotherapy regimen containing rituximab.
Training cohort
The training cohort consisted of 151 FL patients who received R-CHOP. The median follow-up for these patients was 7.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found 28% of patients (43/151) were defined as high-risk, with a 5-year failure-free survival (FFS) rate of 38.29%.
And 72% of patients (108/151) were defined as low-risk, with a 5-year FFS of 77.21%. The hazard ratio was 4.14 (P<0.0001).
The positive predictive value for 5-year FFS was 64%, and the negative predictive value was 78%. The m7-FLIPI outperformed a prognostic model of only gene mutations and the FLIPI-2.
Validation cohort
The validation cohort consisted of 107 patients who received R-CVP. The median follow-up for these patients was 6.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found that 22% of patients (24/107) were defined as high-risk, with a 5-year FFS of 25%.
And 78% of patients (83/107) were defined as low-risk, with a 5-year FFS of 68.24%. The hazard ratio was 3.58 (P<0.0001).
The positive predictive value for 5-year FFS was 72%, and the negative predictive value was 68%. The m7-FLIPI outperformed the FLIPI alone and the FLIPI combined with ECOG performance status.
Overall survival
Although the m7-FLIPI was designed specifically for FFS, the researchers also tested its prognostic utility for overall survival (OS).
In the training cohort, high-risk disease according to the m7-FLIPI was associated with a 5-year OS of 65.25%, compared to 89.98% for low-risk disease (P=0.00031).
In the validation cohort, 5-year OS was 41.67% for patients with high-risk disease and 84.01% for patients with low-risk disease (P<0.0001). In both cohorts, the m7-FLIPI outperformed the FLIPI alone.
Based on these results, the researchers believe the m7-FLIPI could be utilized in a clinical setting to test all new FL patients at diagnosis and identify patients who harbor the most aggressive disease.
“The m7-FLIPI could be extremely significant for the medical community,” Dr Gascoyne said, “changing the story for high-risk patients who are currently destined to not respond well to standard treatment.” ![]()

Photo courtesy of NIH
A newly developed prognostic model can identify follicular lymphoma (FL) patients at the highest risk for treatment failure, according to researchers.
To create this model, called m7-FLIPI, the team combined the Follicular Lymphoma International Prognostic Index (FLIPI), Eastern Cooperative Oncology Group (ECOG) performance status, and the mutation status of 7 genes—EZH2, ARID1A, MEF2B, EP300, FOXO1, CREBBP, and CARD11.
The researchers said this is the first prognostic model for FL that accounts for both clinical factors and genetic mutations.
They described the creation and testing of the model in The Lancet Oncology.
“We set out to determine, at the time of diagnosis, which patients’ disease will have sustained responses after treatment and whether new genetic data could help inform which patients are at risk for developing progressive lymphoma so clinicians would be able to offer these high-risk patients more effective therapies,” said Randy Gascoyne, MD, of the British Columbia Cancer Agency in Vancouver, Canada.
He and his colleagues created the m7-FLIPI by conducting a retrospective analysis of genetic mutations and clinical risk factors in 2 cohorts of patients with symptomatic, advanced stage, or bulky FL grade 1, 2, or 3A.
The patients had a biopsy specimen collected 12 months or less before they began first-line treatment with an immunochemotherapy regimen containing rituximab.
Training cohort
The training cohort consisted of 151 FL patients who received R-CHOP. The median follow-up for these patients was 7.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found 28% of patients (43/151) were defined as high-risk, with a 5-year failure-free survival (FFS) rate of 38.29%.
And 72% of patients (108/151) were defined as low-risk, with a 5-year FFS of 77.21%. The hazard ratio was 4.14 (P<0.0001).
The positive predictive value for 5-year FFS was 64%, and the negative predictive value was 78%. The m7-FLIPI outperformed a prognostic model of only gene mutations and the FLIPI-2.
Validation cohort
The validation cohort consisted of 107 patients who received R-CVP. The median follow-up for these patients was 6.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found that 22% of patients (24/107) were defined as high-risk, with a 5-year FFS of 25%.
And 78% of patients (83/107) were defined as low-risk, with a 5-year FFS of 68.24%. The hazard ratio was 3.58 (P<0.0001).
The positive predictive value for 5-year FFS was 72%, and the negative predictive value was 68%. The m7-FLIPI outperformed the FLIPI alone and the FLIPI combined with ECOG performance status.
Overall survival
Although the m7-FLIPI was designed specifically for FFS, the researchers also tested its prognostic utility for overall survival (OS).
In the training cohort, high-risk disease according to the m7-FLIPI was associated with a 5-year OS of 65.25%, compared to 89.98% for low-risk disease (P=0.00031).
In the validation cohort, 5-year OS was 41.67% for patients with high-risk disease and 84.01% for patients with low-risk disease (P<0.0001). In both cohorts, the m7-FLIPI outperformed the FLIPI alone.
Based on these results, the researchers believe the m7-FLIPI could be utilized in a clinical setting to test all new FL patients at diagnosis and identify patients who harbor the most aggressive disease.
“The m7-FLIPI could be extremely significant for the medical community,” Dr Gascoyne said, “changing the story for high-risk patients who are currently destined to not respond well to standard treatment.” ![]()