User login
Rivaroxaban monitoring kit launched in Europe

Instrumentation Laboratory, a company that develops in vitro diagnostic instruments, has announced the commercialization of the HemosIL Rivaroxaban Testing Solution in Europe.
This testing kit consists of the HemosIL Liquid Anti-Xa Assay, Rivaroxaban Calibrators, and Rivaroxaban Controls, which can be used with ACL TOP Hemostasis Testing Systems to monitor patients taking the oral anticoagulant rivaroxaban (Xarelto).
The assay, calibrators, and controls are now CE IVD Marked under the European IVD Directive 98/79/EC.
This allows Instrumentation Laboratory to distribute the HemosIL Rivaroxaban Testing Solution in the European Union and other international territories.
Although monitoring is generally not required for patients on rivaroxaban, there are cases in which measuring rivaroxaban may be necessary.
This includes patients who present with bleeding, require reversal of anticoagulation, experience deteriorating renal function, or must undergo surgery or an invasive procedure and have taken rivaroxaban within 24 hours or longer if creatinine clearance is < 50 mL min-1.
Liquid Anti-Xa Assay
The HemosIL Liquid Anti-Xa kit is a one-stage chromogenic assay based on a synthetic chromogenic substrate and factor Xa inactivation. Rivaroxaban levels in patient plasma are measured automatically on an ACL TOP Hemostasis Testing System when this assay is calibrated with the HemosIL Rivaroxaban Calibrators.
The Anti-Xa Assay kit consists of:
- Factor Xa reagent: 5 x 2.5 mL vial of a liquid preparation containing purified bovine factor Xa (approximately 5.5 nkat/mL), Tris-Buffer, EDTA, dextran sulfate, sodium chloride, and bovine serum albumin.
- Chromogenic substrate: 5 x 3 mL vial of liquid chromogenic substrate S-2732 (approximately 1.2 mg/mL) and bulking agent.
Rivaroxaban Calibrators
The HemosIL Rivaroxaban Calibrators are intended for the calibration of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized calibrators prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban are used by the instrument to automatically prepare a calibration curve.
The Rivaroxaban Calibrator kit consists of:
- Rivaroxaban Calibrator 1: 5 x 1 mL vials of a lyophilized human plasma containing buffers and stabilizers.
- Rivaroxaban Calibrator 2: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, buffers, and stabilizers.
Rivaroxaban Controls
HemosIL Rivaroxaban Controls are intended for the quality control of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized controls are prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban. Use of both controls is recommended for a complete quality control program.
The Rivaroxaban Controls kit consists of:
- Rivaroxaban Low Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.
- Rivaroxaban High Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.


Instrumentation Laboratory, a company that develops in vitro diagnostic instruments, has announced the commercialization of the HemosIL Rivaroxaban Testing Solution in Europe.
This testing kit consists of the HemosIL Liquid Anti-Xa Assay, Rivaroxaban Calibrators, and Rivaroxaban Controls, which can be used with ACL TOP Hemostasis Testing Systems to monitor patients taking the oral anticoagulant rivaroxaban (Xarelto).
The assay, calibrators, and controls are now CE IVD Marked under the European IVD Directive 98/79/EC.
This allows Instrumentation Laboratory to distribute the HemosIL Rivaroxaban Testing Solution in the European Union and other international territories.
Although monitoring is generally not required for patients on rivaroxaban, there are cases in which measuring rivaroxaban may be necessary.
This includes patients who present with bleeding, require reversal of anticoagulation, experience deteriorating renal function, or must undergo surgery or an invasive procedure and have taken rivaroxaban within 24 hours or longer if creatinine clearance is < 50 mL min-1.
Liquid Anti-Xa Assay
The HemosIL Liquid Anti-Xa kit is a one-stage chromogenic assay based on a synthetic chromogenic substrate and factor Xa inactivation. Rivaroxaban levels in patient plasma are measured automatically on an ACL TOP Hemostasis Testing System when this assay is calibrated with the HemosIL Rivaroxaban Calibrators.
The Anti-Xa Assay kit consists of:
- Factor Xa reagent: 5 x 2.5 mL vial of a liquid preparation containing purified bovine factor Xa (approximately 5.5 nkat/mL), Tris-Buffer, EDTA, dextran sulfate, sodium chloride, and bovine serum albumin.
- Chromogenic substrate: 5 x 3 mL vial of liquid chromogenic substrate S-2732 (approximately 1.2 mg/mL) and bulking agent.
Rivaroxaban Calibrators
The HemosIL Rivaroxaban Calibrators are intended for the calibration of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized calibrators prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban are used by the instrument to automatically prepare a calibration curve.
The Rivaroxaban Calibrator kit consists of:
- Rivaroxaban Calibrator 1: 5 x 1 mL vials of a lyophilized human plasma containing buffers and stabilizers.
- Rivaroxaban Calibrator 2: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, buffers, and stabilizers.
Rivaroxaban Controls
HemosIL Rivaroxaban Controls are intended for the quality control of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized controls are prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban. Use of both controls is recommended for a complete quality control program.
The Rivaroxaban Controls kit consists of:
- Rivaroxaban Low Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.
- Rivaroxaban High Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.


Instrumentation Laboratory, a company that develops in vitro diagnostic instruments, has announced the commercialization of the HemosIL Rivaroxaban Testing Solution in Europe.
This testing kit consists of the HemosIL Liquid Anti-Xa Assay, Rivaroxaban Calibrators, and Rivaroxaban Controls, which can be used with ACL TOP Hemostasis Testing Systems to monitor patients taking the oral anticoagulant rivaroxaban (Xarelto).
The assay, calibrators, and controls are now CE IVD Marked under the European IVD Directive 98/79/EC.
This allows Instrumentation Laboratory to distribute the HemosIL Rivaroxaban Testing Solution in the European Union and other international territories.
Although monitoring is generally not required for patients on rivaroxaban, there are cases in which measuring rivaroxaban may be necessary.
This includes patients who present with bleeding, require reversal of anticoagulation, experience deteriorating renal function, or must undergo surgery or an invasive procedure and have taken rivaroxaban within 24 hours or longer if creatinine clearance is < 50 mL min-1.
Liquid Anti-Xa Assay
The HemosIL Liquid Anti-Xa kit is a one-stage chromogenic assay based on a synthetic chromogenic substrate and factor Xa inactivation. Rivaroxaban levels in patient plasma are measured automatically on an ACL TOP Hemostasis Testing System when this assay is calibrated with the HemosIL Rivaroxaban Calibrators.
The Anti-Xa Assay kit consists of:
- Factor Xa reagent: 5 x 2.5 mL vial of a liquid preparation containing purified bovine factor Xa (approximately 5.5 nkat/mL), Tris-Buffer, EDTA, dextran sulfate, sodium chloride, and bovine serum albumin.
- Chromogenic substrate: 5 x 3 mL vial of liquid chromogenic substrate S-2732 (approximately 1.2 mg/mL) and bulking agent.
Rivaroxaban Calibrators
The HemosIL Rivaroxaban Calibrators are intended for the calibration of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized calibrators prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban are used by the instrument to automatically prepare a calibration curve.
The Rivaroxaban Calibrator kit consists of:
- Rivaroxaban Calibrator 1: 5 x 1 mL vials of a lyophilized human plasma containing buffers and stabilizers.
- Rivaroxaban Calibrator 2: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, buffers, and stabilizers.
Rivaroxaban Controls
HemosIL Rivaroxaban Controls are intended for the quality control of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized controls are prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban. Use of both controls is recommended for a complete quality control program.
The Rivaroxaban Controls kit consists of:
- Rivaroxaban Low Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.
- Rivaroxaban High Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.

Platform simplifies data analysis, team says

Photo by Rhoda Baer
Researchers say they have developed a user-friendly platform for analyzing transcriptomic and epigenomic sequencing data.
This platform, BioWardrobe, was designed to help biomedical researchers analyze data that might answer questions about diseases and basic biology.
“Although biologists can perform experiments and obtain the data, they often lack the programming expertise required to perform computational data analysis,” said Artem Barski, PhD, of the University of Cincinnati in Ohio.
“BioWardrobe aims to empower researchers by bridging this gap between data and knowledge.”
Dr Barski and Andrey Kartashov, also of the University of Cincinnati, described BioWardrobe in Genome Biology.
The pair said the recent proliferation of sequencing-based methods for analysis of gene expression, chromatin structure, and protein-DNA interactions has widened our horizons, but the volume of data obtained from sequencing requires computational data analysis.
Unfortunately, the bioinformatics and programming expertise required for this analysis may be absent in biomedical laboratories. And this can result in data inaccessibility or delays in applying modern sequencing-based technologies to pressing questions in basic and health-related research.
Dr Barski and Kartashov believe BioWardrobe can solve those problems by providing a “biologist-friendly” web interface.
BioWardrobe users can download data from institutional facilities or public databases, map reads, and visualize results on a genome browser. The platform also allows for differential gene expression and binding analysis, and it can create average tag-density profiles and heatmaps.
Dr Barski and Kartashov plan to continue improving BioWardrobe and continue using the platform in their own research on epigenetic regulation in the immune system, as well as in collaborative projects with other investigators. ![]()

Photo by Rhoda Baer
Researchers say they have developed a user-friendly platform for analyzing transcriptomic and epigenomic sequencing data.
This platform, BioWardrobe, was designed to help biomedical researchers analyze data that might answer questions about diseases and basic biology.
“Although biologists can perform experiments and obtain the data, they often lack the programming expertise required to perform computational data analysis,” said Artem Barski, PhD, of the University of Cincinnati in Ohio.
“BioWardrobe aims to empower researchers by bridging this gap between data and knowledge.”
Dr Barski and Andrey Kartashov, also of the University of Cincinnati, described BioWardrobe in Genome Biology.
The pair said the recent proliferation of sequencing-based methods for analysis of gene expression, chromatin structure, and protein-DNA interactions has widened our horizons, but the volume of data obtained from sequencing requires computational data analysis.
Unfortunately, the bioinformatics and programming expertise required for this analysis may be absent in biomedical laboratories. And this can result in data inaccessibility or delays in applying modern sequencing-based technologies to pressing questions in basic and health-related research.
Dr Barski and Kartashov believe BioWardrobe can solve those problems by providing a “biologist-friendly” web interface.
BioWardrobe users can download data from institutional facilities or public databases, map reads, and visualize results on a genome browser. The platform also allows for differential gene expression and binding analysis, and it can create average tag-density profiles and heatmaps.
Dr Barski and Kartashov plan to continue improving BioWardrobe and continue using the platform in their own research on epigenetic regulation in the immune system, as well as in collaborative projects with other investigators. ![]()

Photo by Rhoda Baer
Researchers say they have developed a user-friendly platform for analyzing transcriptomic and epigenomic sequencing data.
This platform, BioWardrobe, was designed to help biomedical researchers analyze data that might answer questions about diseases and basic biology.
“Although biologists can perform experiments and obtain the data, they often lack the programming expertise required to perform computational data analysis,” said Artem Barski, PhD, of the University of Cincinnati in Ohio.
“BioWardrobe aims to empower researchers by bridging this gap between data and knowledge.”
Dr Barski and Andrey Kartashov, also of the University of Cincinnati, described BioWardrobe in Genome Biology.
The pair said the recent proliferation of sequencing-based methods for analysis of gene expression, chromatin structure, and protein-DNA interactions has widened our horizons, but the volume of data obtained from sequencing requires computational data analysis.
Unfortunately, the bioinformatics and programming expertise required for this analysis may be absent in biomedical laboratories. And this can result in data inaccessibility or delays in applying modern sequencing-based technologies to pressing questions in basic and health-related research.
Dr Barski and Kartashov believe BioWardrobe can solve those problems by providing a “biologist-friendly” web interface.
BioWardrobe users can download data from institutional facilities or public databases, map reads, and visualize results on a genome browser. The platform also allows for differential gene expression and binding analysis, and it can create average tag-density profiles and heatmaps.
Dr Barski and Kartashov plan to continue improving BioWardrobe and continue using the platform in their own research on epigenetic regulation in the immune system, as well as in collaborative projects with other investigators. ![]()
Family-centered care in the NICU
Hospitals are slow to change, especially when changes – such as the inclusion of families in patient care – are not big money makers. Even so, in a competitive marketplace, hospitals are beginning to realize that patient and family satisfaction develops loyal customers.
When patients and families have a good experience, they are likely to return to the hospital and recommend the hospital to others. From a business perspective, it makes sense to develop family-oriented care in hospital specialty units such as the neonatal intensive care unit.
Involving families in the NICU also reduces the neonate’s length of stay (Nurs Adm Q. 2009 Jan-Mar;33[1]32-7).
COPE is a manualized intervention program comprising DVDs and a workbook.
The DVDs provide parents with educational information about the appearance and behavioral characteristics of their premature infants and about how they can participate in their infants’ care, meet their needs, enhance the quality of interaction with their infants, and facilitate their development.
The workbook skills-building activities assist parents in implementing the educational information (for example, learning how to read their infants’ awake states and stress cues, keeping track of important developmental milestones, determining what behaviors are helpful when their infants are stressed).
Parents listen to the COPE educational information on DVDs as they read it in their workbooks. The first intervention in COPE is delivered to the parents 2-4 days after the infant is admitted to the NICU. The second COPE intervention is delivered 2-4 days after the first intervention, and the third intervention is delivered to parents 1-4 days prior to the infant’s discharge from the NICU. Parents receive the fourth COPE intervention 1 week after the infant is discharged from the hospital. Each of the four DVDs has corresponding skills-building activities that parents complete after they listen to the educational information on the DVDs.
The problem
In NICUs, families are not the primary focus of care. To nursing staff, parents are an unknown factor. Parents may silence alarms or open cribs to touch the baby, not realizing that by doing so, they are dysregulating the neonate’s delicate environment. They see nurses moving things around, and so feel they should be able to do it, too. Parents come in many varieties. Some parents sit quietly and appear overwhelmed. Some parents behave erratically. Some parents may smell of alcohol or marijuana, putting everyone in the NICU on alert. Assessing and intervening with parents is helpful to nurses, reduces tension between nurse and parent, and ensures that the daily caring for the neonate is smooth and optimal. Nurses are eager to help with parents.
Nursing perspective
From the nurses’ perspective, the parents are not the patient! Nurses have not been trained to assess and manage distressed parents. Nurses can provide basic education about the baby’s medical condition but do not have time to explain the details that overanxious parents might demand. The nurses recognize that some parents are under severe stress and do not want to leave the bedside, even to care for their own needs. The nurses recognize that some parents have their own health conditions but are unsure how to approach this issue. Nurses welcome education about how to intervene and how to refer parents to appropriate resources.
Parental perspective
Parents are distressed and uncertain about the fate of their newborns. There is an immediate need to gain as much information as possible about the baby’s medical condition and to understand what the nurses are “doing to our baby.” There may be concern that the nurse seems more bonded to the baby than the parents. There may be a lack of understanding of when the babies can be handled and what and when they can be fed. There is significant emotional distress about “not being able to take the baby home.” Parents may want to assign blame or may feel overwhelmed with guilt. For families with poor coping skills, fear and anger may predominate and can be directed at the nurses – an immediate and ever available target. Generally, parents want to be included as much as possible in the care of their children.
Postpartum disorders in the NICU
It is expected that having a baby in the NICU is stressful. However, a meta-analysis of 38 studies of stress in parents of preterm infants, compared with term infants, found that parents of preterm children experience only slightly more stress than do parents of term children. There is decreasing parental stress from the 1980s onward, probably because of the increased quality of care for preterm infants. These studies included 3,025 parents of preterm and low-birth-weight infants (PLoS One 2013;8[2]:e54992).
Over the long term, the psychological functioning of NICU parents is no different from that of control parents. A prospective randomized controlled study defined psychological distress as meeting one or more of the following criteria: any psychiatric diagnosis on the Mini-International Neuropsychiatric Interview at 2 years; Edinburgh Postnatal Depression Scale score more than 12.5 at 2 years; Hospital Anxiety and Depression Scale score more than 11.0 at 2 years, receiving treatment with antidepressants/psychotherapy/counseling over the previous 15 months (Psychosomatics 2014;55[6]:613-20).
In the short term, NICU parents are at risk for postpartum depression (PPD) with the resultant difficulty in establishing good attachment with their babies. The prevalence of PPD in mothers of term newborns is 10%-15%, compared with 28%-70% among NICU mothers (Int J Womens Health. 2014;2014[6]:975-87).
Fathers are known as the forgotten parents and experience a high prevalence of depressive symptoms. Fathers of term newborns experience depression at rates of 2%-10%, but rates of up to 60% have been reported in NICU fathers (Adv Neonatal Care. 2010 Aug;10[4]:200-3).
Prevention of psychiatric illness in family members
The NICU environment is often dimly lighted, and improving lighting prevents depression in NICU mothers. A 3-week bright-light therapy intervention improved the sleep and health outcomes of NICU mothers, who experienced less morning fatigue and depressive symptoms, and improved quality of life, compared with the control group (Biol Res Nurs. 2013 Oct;15[4] 398-406). An architect on our team is designing “quiet spaces” for parents and creating more ambient light and daylighting in our NICU.
For parents who do not want to leave the NICU, mobile computer terminals can bring education to the bedside. For parents who can leave the bedside, family educational interventions are well received (Adv Neonatal Care. 2013 Apr;13[2]:115-26).
In current practice, in our labor and delivery suite and in many NICUs, mothers are screened for postpartum depression via the Edinburgh Postnatal Depression Scale (EPDS) (Br J Psychiatry 1987 Jun;150[6]:782-6). If mothers score over 13, they are referred for further assessment. Treatment often consists of referral for individual intervention for the mother (usually sertraline and disclosures/instructions about breastfeeding, as well as supportive psychotherapy).
What does family-centered care look like?
A family perspective supports the screening of both parents, using the EPDS. This can occur on admission of the baby to the NICU and at 2-week intervals thereafter and again at discharge (J Perinatol 2013 Oct;33[10]748-53). Ideally, family functioning also can be assessed, and if needed, intervention can be offered to the whole family system.
Family screening occurs in other pediatric medical settings. High-risk families can be identified with the Psychosocial Assessment Tool (PAT) (Acta Oncol. 2015 May;54[5]:574-80).
The PAT is a brief parent self-report composed of items that assess risk associated with the child, family, and broader systems. It is currently used at 50 sites in 28 states in the United States. The PAT has been translated into Spanish, Columbian Spanish, Dutch, Brazilian Portuguese, Hebrew, Greek, Polish, Italian, Japanese, Chinese, and Korean, and is used internationally. English adaptations for Canada, the United Kingdom, Australia, New Zealand, and Singapore also are available. It has been modified for use in NICUs.
The screening enables health care providers to refer families to the appropriate service: support groups (low risk), psychoeducation (medium risk), or intensive outpatient services (high risk). This stratification allows for the appropriate use of services.
Likewise, family interventions can be thought about in tiers, similar to the risk stratification of the PAT. Tier 1 is a universal educational intervention for all parents, tier 2 parents have higher needs, and tier 3 parents need immediate intervention. The following descriptions show how this might work in practice.
Family intervention: Tier 1
•All families can be given educational material about the mental health needs of parents with a newborn in the NICU. Ideally, this material can be provided through handouts, references for further reading, and through websites accessed in the NICU. For parents who are willing to leave the NICU, they can attend support groups.
•All parents can be screened at initial contact in the NICU and then on discharge from the NICU. If the neonate stays an extended time, the parents can be screened at 2-week intervals. A high score on the EPDS screen indicates an immediate need to refer a parent. A family assessment tool, such as the PAT, can identify high-risk families for immediate referral.
•NICU nursing staff can actively address coparenting struggles. Our NICU nurses provide formal letters between nurses and parents to establish the parameters of the care of the baby, and provide direction for coparenting.
Family intervention: Tier 2
Parents identified on the PAT as having higher needs can be enrolled in psychoeducational groups, led by staff members who have behavioral health training and experience.
Family intervention: Tier 3
These parents are identified on the PAT as high risk and need significant health care services. The NICU social worker can actively work on consultation with addiction medicine, mental health, or social services.
In summary, a family approach in the NICU improves nurse-parent interactions. A focus on coparenting sets the stage for cooperation, trust, and better family outcomes. Some basic training in systems concepts and family dynamics can provide NICU staff with basic clinical skills to provide psychoeducation. Adequate screening can triage high-risk parents appropriately. For NICUs that want to implement a psychoeducational program, Melnyk’s COPE program is an evidenced-based program that is well worth implementation.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She thanks other members of the NICU team at the University of Colorado Hospital: Christy Math, Katherine Perica, and John J. White.
Hospitals are slow to change, especially when changes – such as the inclusion of families in patient care – are not big money makers. Even so, in a competitive marketplace, hospitals are beginning to realize that patient and family satisfaction develops loyal customers.
When patients and families have a good experience, they are likely to return to the hospital and recommend the hospital to others. From a business perspective, it makes sense to develop family-oriented care in hospital specialty units such as the neonatal intensive care unit.
Involving families in the NICU also reduces the neonate’s length of stay (Nurs Adm Q. 2009 Jan-Mar;33[1]32-7).
COPE is a manualized intervention program comprising DVDs and a workbook.
The DVDs provide parents with educational information about the appearance and behavioral characteristics of their premature infants and about how they can participate in their infants’ care, meet their needs, enhance the quality of interaction with their infants, and facilitate their development.
The workbook skills-building activities assist parents in implementing the educational information (for example, learning how to read their infants’ awake states and stress cues, keeping track of important developmental milestones, determining what behaviors are helpful when their infants are stressed).
Parents listen to the COPE educational information on DVDs as they read it in their workbooks. The first intervention in COPE is delivered to the parents 2-4 days after the infant is admitted to the NICU. The second COPE intervention is delivered 2-4 days after the first intervention, and the third intervention is delivered to parents 1-4 days prior to the infant’s discharge from the NICU. Parents receive the fourth COPE intervention 1 week after the infant is discharged from the hospital. Each of the four DVDs has corresponding skills-building activities that parents complete after they listen to the educational information on the DVDs.
The problem
In NICUs, families are not the primary focus of care. To nursing staff, parents are an unknown factor. Parents may silence alarms or open cribs to touch the baby, not realizing that by doing so, they are dysregulating the neonate’s delicate environment. They see nurses moving things around, and so feel they should be able to do it, too. Parents come in many varieties. Some parents sit quietly and appear overwhelmed. Some parents behave erratically. Some parents may smell of alcohol or marijuana, putting everyone in the NICU on alert. Assessing and intervening with parents is helpful to nurses, reduces tension between nurse and parent, and ensures that the daily caring for the neonate is smooth and optimal. Nurses are eager to help with parents.
Nursing perspective
From the nurses’ perspective, the parents are not the patient! Nurses have not been trained to assess and manage distressed parents. Nurses can provide basic education about the baby’s medical condition but do not have time to explain the details that overanxious parents might demand. The nurses recognize that some parents are under severe stress and do not want to leave the bedside, even to care for their own needs. The nurses recognize that some parents have their own health conditions but are unsure how to approach this issue. Nurses welcome education about how to intervene and how to refer parents to appropriate resources.
Parental perspective
Parents are distressed and uncertain about the fate of their newborns. There is an immediate need to gain as much information as possible about the baby’s medical condition and to understand what the nurses are “doing to our baby.” There may be concern that the nurse seems more bonded to the baby than the parents. There may be a lack of understanding of when the babies can be handled and what and when they can be fed. There is significant emotional distress about “not being able to take the baby home.” Parents may want to assign blame or may feel overwhelmed with guilt. For families with poor coping skills, fear and anger may predominate and can be directed at the nurses – an immediate and ever available target. Generally, parents want to be included as much as possible in the care of their children.
Postpartum disorders in the NICU
It is expected that having a baby in the NICU is stressful. However, a meta-analysis of 38 studies of stress in parents of preterm infants, compared with term infants, found that parents of preterm children experience only slightly more stress than do parents of term children. There is decreasing parental stress from the 1980s onward, probably because of the increased quality of care for preterm infants. These studies included 3,025 parents of preterm and low-birth-weight infants (PLoS One 2013;8[2]:e54992).
Over the long term, the psychological functioning of NICU parents is no different from that of control parents. A prospective randomized controlled study defined psychological distress as meeting one or more of the following criteria: any psychiatric diagnosis on the Mini-International Neuropsychiatric Interview at 2 years; Edinburgh Postnatal Depression Scale score more than 12.5 at 2 years; Hospital Anxiety and Depression Scale score more than 11.0 at 2 years, receiving treatment with antidepressants/psychotherapy/counseling over the previous 15 months (Psychosomatics 2014;55[6]:613-20).
In the short term, NICU parents are at risk for postpartum depression (PPD) with the resultant difficulty in establishing good attachment with their babies. The prevalence of PPD in mothers of term newborns is 10%-15%, compared with 28%-70% among NICU mothers (Int J Womens Health. 2014;2014[6]:975-87).
Fathers are known as the forgotten parents and experience a high prevalence of depressive symptoms. Fathers of term newborns experience depression at rates of 2%-10%, but rates of up to 60% have been reported in NICU fathers (Adv Neonatal Care. 2010 Aug;10[4]:200-3).
Prevention of psychiatric illness in family members
The NICU environment is often dimly lighted, and improving lighting prevents depression in NICU mothers. A 3-week bright-light therapy intervention improved the sleep and health outcomes of NICU mothers, who experienced less morning fatigue and depressive symptoms, and improved quality of life, compared with the control group (Biol Res Nurs. 2013 Oct;15[4] 398-406). An architect on our team is designing “quiet spaces” for parents and creating more ambient light and daylighting in our NICU.
For parents who do not want to leave the NICU, mobile computer terminals can bring education to the bedside. For parents who can leave the bedside, family educational interventions are well received (Adv Neonatal Care. 2013 Apr;13[2]:115-26).
In current practice, in our labor and delivery suite and in many NICUs, mothers are screened for postpartum depression via the Edinburgh Postnatal Depression Scale (EPDS) (Br J Psychiatry 1987 Jun;150[6]:782-6). If mothers score over 13, they are referred for further assessment. Treatment often consists of referral for individual intervention for the mother (usually sertraline and disclosures/instructions about breastfeeding, as well as supportive psychotherapy).
What does family-centered care look like?
A family perspective supports the screening of both parents, using the EPDS. This can occur on admission of the baby to the NICU and at 2-week intervals thereafter and again at discharge (J Perinatol 2013 Oct;33[10]748-53). Ideally, family functioning also can be assessed, and if needed, intervention can be offered to the whole family system.
Family screening occurs in other pediatric medical settings. High-risk families can be identified with the Psychosocial Assessment Tool (PAT) (Acta Oncol. 2015 May;54[5]:574-80).
The PAT is a brief parent self-report composed of items that assess risk associated with the child, family, and broader systems. It is currently used at 50 sites in 28 states in the United States. The PAT has been translated into Spanish, Columbian Spanish, Dutch, Brazilian Portuguese, Hebrew, Greek, Polish, Italian, Japanese, Chinese, and Korean, and is used internationally. English adaptations for Canada, the United Kingdom, Australia, New Zealand, and Singapore also are available. It has been modified for use in NICUs.
The screening enables health care providers to refer families to the appropriate service: support groups (low risk), psychoeducation (medium risk), or intensive outpatient services (high risk). This stratification allows for the appropriate use of services.
Likewise, family interventions can be thought about in tiers, similar to the risk stratification of the PAT. Tier 1 is a universal educational intervention for all parents, tier 2 parents have higher needs, and tier 3 parents need immediate intervention. The following descriptions show how this might work in practice.
Family intervention: Tier 1
•All families can be given educational material about the mental health needs of parents with a newborn in the NICU. Ideally, this material can be provided through handouts, references for further reading, and through websites accessed in the NICU. For parents who are willing to leave the NICU, they can attend support groups.
•All parents can be screened at initial contact in the NICU and then on discharge from the NICU. If the neonate stays an extended time, the parents can be screened at 2-week intervals. A high score on the EPDS screen indicates an immediate need to refer a parent. A family assessment tool, such as the PAT, can identify high-risk families for immediate referral.
•NICU nursing staff can actively address coparenting struggles. Our NICU nurses provide formal letters between nurses and parents to establish the parameters of the care of the baby, and provide direction for coparenting.
Family intervention: Tier 2
Parents identified on the PAT as having higher needs can be enrolled in psychoeducational groups, led by staff members who have behavioral health training and experience.
Family intervention: Tier 3
These parents are identified on the PAT as high risk and need significant health care services. The NICU social worker can actively work on consultation with addiction medicine, mental health, or social services.
In summary, a family approach in the NICU improves nurse-parent interactions. A focus on coparenting sets the stage for cooperation, trust, and better family outcomes. Some basic training in systems concepts and family dynamics can provide NICU staff with basic clinical skills to provide psychoeducation. Adequate screening can triage high-risk parents appropriately. For NICUs that want to implement a psychoeducational program, Melnyk’s COPE program is an evidenced-based program that is well worth implementation.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She thanks other members of the NICU team at the University of Colorado Hospital: Christy Math, Katherine Perica, and John J. White.
Hospitals are slow to change, especially when changes – such as the inclusion of families in patient care – are not big money makers. Even so, in a competitive marketplace, hospitals are beginning to realize that patient and family satisfaction develops loyal customers.
When patients and families have a good experience, they are likely to return to the hospital and recommend the hospital to others. From a business perspective, it makes sense to develop family-oriented care in hospital specialty units such as the neonatal intensive care unit.
Involving families in the NICU also reduces the neonate’s length of stay (Nurs Adm Q. 2009 Jan-Mar;33[1]32-7).
COPE is a manualized intervention program comprising DVDs and a workbook.
The DVDs provide parents with educational information about the appearance and behavioral characteristics of their premature infants and about how they can participate in their infants’ care, meet their needs, enhance the quality of interaction with their infants, and facilitate their development.
The workbook skills-building activities assist parents in implementing the educational information (for example, learning how to read their infants’ awake states and stress cues, keeping track of important developmental milestones, determining what behaviors are helpful when their infants are stressed).
Parents listen to the COPE educational information on DVDs as they read it in their workbooks. The first intervention in COPE is delivered to the parents 2-4 days after the infant is admitted to the NICU. The second COPE intervention is delivered 2-4 days after the first intervention, and the third intervention is delivered to parents 1-4 days prior to the infant’s discharge from the NICU. Parents receive the fourth COPE intervention 1 week after the infant is discharged from the hospital. Each of the four DVDs has corresponding skills-building activities that parents complete after they listen to the educational information on the DVDs.
The problem
In NICUs, families are not the primary focus of care. To nursing staff, parents are an unknown factor. Parents may silence alarms or open cribs to touch the baby, not realizing that by doing so, they are dysregulating the neonate’s delicate environment. They see nurses moving things around, and so feel they should be able to do it, too. Parents come in many varieties. Some parents sit quietly and appear overwhelmed. Some parents behave erratically. Some parents may smell of alcohol or marijuana, putting everyone in the NICU on alert. Assessing and intervening with parents is helpful to nurses, reduces tension between nurse and parent, and ensures that the daily caring for the neonate is smooth and optimal. Nurses are eager to help with parents.
Nursing perspective
From the nurses’ perspective, the parents are not the patient! Nurses have not been trained to assess and manage distressed parents. Nurses can provide basic education about the baby’s medical condition but do not have time to explain the details that overanxious parents might demand. The nurses recognize that some parents are under severe stress and do not want to leave the bedside, even to care for their own needs. The nurses recognize that some parents have their own health conditions but are unsure how to approach this issue. Nurses welcome education about how to intervene and how to refer parents to appropriate resources.
Parental perspective
Parents are distressed and uncertain about the fate of their newborns. There is an immediate need to gain as much information as possible about the baby’s medical condition and to understand what the nurses are “doing to our baby.” There may be concern that the nurse seems more bonded to the baby than the parents. There may be a lack of understanding of when the babies can be handled and what and when they can be fed. There is significant emotional distress about “not being able to take the baby home.” Parents may want to assign blame or may feel overwhelmed with guilt. For families with poor coping skills, fear and anger may predominate and can be directed at the nurses – an immediate and ever available target. Generally, parents want to be included as much as possible in the care of their children.
Postpartum disorders in the NICU
It is expected that having a baby in the NICU is stressful. However, a meta-analysis of 38 studies of stress in parents of preterm infants, compared with term infants, found that parents of preterm children experience only slightly more stress than do parents of term children. There is decreasing parental stress from the 1980s onward, probably because of the increased quality of care for preterm infants. These studies included 3,025 parents of preterm and low-birth-weight infants (PLoS One 2013;8[2]:e54992).
Over the long term, the psychological functioning of NICU parents is no different from that of control parents. A prospective randomized controlled study defined psychological distress as meeting one or more of the following criteria: any psychiatric diagnosis on the Mini-International Neuropsychiatric Interview at 2 years; Edinburgh Postnatal Depression Scale score more than 12.5 at 2 years; Hospital Anxiety and Depression Scale score more than 11.0 at 2 years, receiving treatment with antidepressants/psychotherapy/counseling over the previous 15 months (Psychosomatics 2014;55[6]:613-20).
In the short term, NICU parents are at risk for postpartum depression (PPD) with the resultant difficulty in establishing good attachment with their babies. The prevalence of PPD in mothers of term newborns is 10%-15%, compared with 28%-70% among NICU mothers (Int J Womens Health. 2014;2014[6]:975-87).
Fathers are known as the forgotten parents and experience a high prevalence of depressive symptoms. Fathers of term newborns experience depression at rates of 2%-10%, but rates of up to 60% have been reported in NICU fathers (Adv Neonatal Care. 2010 Aug;10[4]:200-3).
Prevention of psychiatric illness in family members
The NICU environment is often dimly lighted, and improving lighting prevents depression in NICU mothers. A 3-week bright-light therapy intervention improved the sleep and health outcomes of NICU mothers, who experienced less morning fatigue and depressive symptoms, and improved quality of life, compared with the control group (Biol Res Nurs. 2013 Oct;15[4] 398-406). An architect on our team is designing “quiet spaces” for parents and creating more ambient light and daylighting in our NICU.
For parents who do not want to leave the NICU, mobile computer terminals can bring education to the bedside. For parents who can leave the bedside, family educational interventions are well received (Adv Neonatal Care. 2013 Apr;13[2]:115-26).
In current practice, in our labor and delivery suite and in many NICUs, mothers are screened for postpartum depression via the Edinburgh Postnatal Depression Scale (EPDS) (Br J Psychiatry 1987 Jun;150[6]:782-6). If mothers score over 13, they are referred for further assessment. Treatment often consists of referral for individual intervention for the mother (usually sertraline and disclosures/instructions about breastfeeding, as well as supportive psychotherapy).
What does family-centered care look like?
A family perspective supports the screening of both parents, using the EPDS. This can occur on admission of the baby to the NICU and at 2-week intervals thereafter and again at discharge (J Perinatol 2013 Oct;33[10]748-53). Ideally, family functioning also can be assessed, and if needed, intervention can be offered to the whole family system.
Family screening occurs in other pediatric medical settings. High-risk families can be identified with the Psychosocial Assessment Tool (PAT) (Acta Oncol. 2015 May;54[5]:574-80).
The PAT is a brief parent self-report composed of items that assess risk associated with the child, family, and broader systems. It is currently used at 50 sites in 28 states in the United States. The PAT has been translated into Spanish, Columbian Spanish, Dutch, Brazilian Portuguese, Hebrew, Greek, Polish, Italian, Japanese, Chinese, and Korean, and is used internationally. English adaptations for Canada, the United Kingdom, Australia, New Zealand, and Singapore also are available. It has been modified for use in NICUs.
The screening enables health care providers to refer families to the appropriate service: support groups (low risk), psychoeducation (medium risk), or intensive outpatient services (high risk). This stratification allows for the appropriate use of services.
Likewise, family interventions can be thought about in tiers, similar to the risk stratification of the PAT. Tier 1 is a universal educational intervention for all parents, tier 2 parents have higher needs, and tier 3 parents need immediate intervention. The following descriptions show how this might work in practice.
Family intervention: Tier 1
•All families can be given educational material about the mental health needs of parents with a newborn in the NICU. Ideally, this material can be provided through handouts, references for further reading, and through websites accessed in the NICU. For parents who are willing to leave the NICU, they can attend support groups.
•All parents can be screened at initial contact in the NICU and then on discharge from the NICU. If the neonate stays an extended time, the parents can be screened at 2-week intervals. A high score on the EPDS screen indicates an immediate need to refer a parent. A family assessment tool, such as the PAT, can identify high-risk families for immediate referral.
•NICU nursing staff can actively address coparenting struggles. Our NICU nurses provide formal letters between nurses and parents to establish the parameters of the care of the baby, and provide direction for coparenting.
Family intervention: Tier 2
Parents identified on the PAT as having higher needs can be enrolled in psychoeducational groups, led by staff members who have behavioral health training and experience.
Family intervention: Tier 3
These parents are identified on the PAT as high risk and need significant health care services. The NICU social worker can actively work on consultation with addiction medicine, mental health, or social services.
In summary, a family approach in the NICU improves nurse-parent interactions. A focus on coparenting sets the stage for cooperation, trust, and better family outcomes. Some basic training in systems concepts and family dynamics can provide NICU staff with basic clinical skills to provide psychoeducation. Adequate screening can triage high-risk parents appropriately. For NICUs that want to implement a psychoeducational program, Melnyk’s COPE program is an evidenced-based program that is well worth implementation.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She thanks other members of the NICU team at the University of Colorado Hospital: Christy Math, Katherine Perica, and John J. White.
OpenNotes: Transparency in health care
Transparency, until recently, was rarely associated with health care. Not anymore. For better and sometimes worse, there is a revolutionary movement toward transparency in all facets of health care: transparency of costs, outcomes, quality, service, and reputation. Full transparency has now come to medical records in the form of OpenNotes. This is a patient-centered initiative that allows patients full access to their charts, including all their doctors’ notes.
Patients have always had the right to see their records. Ordinarily though, they would be required to go to the medical records office, fill out paperwork, and request copies of their charts. They’d have to supply a reason and usually pay a fee. OpenNotes changes that. Open patient charts are free and easy to access, usually digitally. OpenNotes programs are still rare, and before we go any further, it’s important to examine what we’ve learned about them.
In 2010, Beth Israel Deaconess Medical Center in Boston, Geisinger Health System in Pennsylvania, and Harborview Medical Center in Seattle invited 105 primary care physicians to open their notes to nearly 14,000 patients. The results were overwhelmingly (and to me, surprisingly) positive: More than 85% of patients accessed their notes at least once. Nearly 100% of patients wanted the program to continue. Patients reported a better understanding of their medical issues, better medication adherence, increased adoption of healthy habits, and less anxiety about their health. I would have expected more confusion and anxiety among the patients.
What about the physicians? According to the initiative, whereas 1 in 3 patients thought they should have unfettered access to their physicians’ notes, only 1 in 10 physicians did. That’s understandable. The physicians in the pilot shared many of the same concerns you and I have, namely that OpenNotes would lead to an increased workload to explain esoteric notes to patients and to allay anxieties.
Yet, this extra workload didn’t occur. Only 3% of physicians reported spending more time answering patients’ questions. One-fifth did report that they changed the language they used when writing notes, primarily to avoid offending patients. Every physician in the initiative said he or she would continue using OpenNotes. Surprised? So was I.
Even the usually conservative SERMO physician audience responded in an unexpected manner. According to a poll conducted this June, SERMO asked 2,300 physicians if patients should have access to their medical records (including MD notes). Forty-nine percent said “only on a case-by-case basis,” 34% said “yes, always,” and 17% said “no, never.”
So, are OpenNotes a success? Let’s take a closer look at some of the challenges: First, we physicians use language that will confuse patients at best and lead them to incorrect conclusions at worst. “Acne necrotica?” Sounds like a case of medieval pimples, but actually it’s pretty harmless. Or consider, “Differential diagnosis includes neuroendocrine tumor.” It doesn’t mean you have it, but some patients will believe they do. Will we have to dumb down our charts then to appease them? Won’t this degrade note quality, one of the primary objectives we are trying to avoid? It’s unclear.
The purpose of a patient note is to inform other providers and to remind ourselves of the critical information needed to care for a patient. It must be pithy and honest. It often reflects our inchoate thoughts as much as our diagnoses. It must also include the sundry requirements we know and love that are needed only to bill for the visit. These are not characteristics that make for a good patient read.
Indeed, the benefits of transparency are not limitless. In some instances, more transparency is worse. Imagine if all your emails and texts were transparent to everyone. Or if everything you’ve ever said about your mother-in-law were viewable by her. That would clearly be a case of bad transparency. Not sharing everything doesn’t mean we are dishonest or duplicitous. It means we are civil. It doesn’t mean we don’t care; it means we do care. We care about our friends and family. We care about our patients and the best way to make them well.
Unless we make it clear to patients that the notes they are viewing are not written for them, I’m worried simply opening charts could damage the doctor-patient relationship as much as it fosters it. Interestingly, there are companies trying to build a technical solution for this conundrum. Others are advocating for standardization of pathology and lab reports that are patient friendly. I’ll research these topics and let you know what I find out in a future column.
Perhaps I shouldn’t have been surprised by the positive results from the OpenNotes initiative. After all, for the last several years, I have given patients their actual pathology report for every biopsy I’ve done (which numbers in the many thousands). I have had fewer than five follow-up questions from patients that I can remember. Pretty much all were legitimate, as I recall, including a wrong site error in a report.
Today, more than 5 million patients have access to their providers’ notes on OpenNotes. That number will grow. Our biggest risk is to not be involved. “Just say no” didn’t work for Nancy Reagan; it won’t do our cause any good either.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
Transparency, until recently, was rarely associated with health care. Not anymore. For better and sometimes worse, there is a revolutionary movement toward transparency in all facets of health care: transparency of costs, outcomes, quality, service, and reputation. Full transparency has now come to medical records in the form of OpenNotes. This is a patient-centered initiative that allows patients full access to their charts, including all their doctors’ notes.
Patients have always had the right to see their records. Ordinarily though, they would be required to go to the medical records office, fill out paperwork, and request copies of their charts. They’d have to supply a reason and usually pay a fee. OpenNotes changes that. Open patient charts are free and easy to access, usually digitally. OpenNotes programs are still rare, and before we go any further, it’s important to examine what we’ve learned about them.
In 2010, Beth Israel Deaconess Medical Center in Boston, Geisinger Health System in Pennsylvania, and Harborview Medical Center in Seattle invited 105 primary care physicians to open their notes to nearly 14,000 patients. The results were overwhelmingly (and to me, surprisingly) positive: More than 85% of patients accessed their notes at least once. Nearly 100% of patients wanted the program to continue. Patients reported a better understanding of their medical issues, better medication adherence, increased adoption of healthy habits, and less anxiety about their health. I would have expected more confusion and anxiety among the patients.
What about the physicians? According to the initiative, whereas 1 in 3 patients thought they should have unfettered access to their physicians’ notes, only 1 in 10 physicians did. That’s understandable. The physicians in the pilot shared many of the same concerns you and I have, namely that OpenNotes would lead to an increased workload to explain esoteric notes to patients and to allay anxieties.
Yet, this extra workload didn’t occur. Only 3% of physicians reported spending more time answering patients’ questions. One-fifth did report that they changed the language they used when writing notes, primarily to avoid offending patients. Every physician in the initiative said he or she would continue using OpenNotes. Surprised? So was I.
Even the usually conservative SERMO physician audience responded in an unexpected manner. According to a poll conducted this June, SERMO asked 2,300 physicians if patients should have access to their medical records (including MD notes). Forty-nine percent said “only on a case-by-case basis,” 34% said “yes, always,” and 17% said “no, never.”
So, are OpenNotes a success? Let’s take a closer look at some of the challenges: First, we physicians use language that will confuse patients at best and lead them to incorrect conclusions at worst. “Acne necrotica?” Sounds like a case of medieval pimples, but actually it’s pretty harmless. Or consider, “Differential diagnosis includes neuroendocrine tumor.” It doesn’t mean you have it, but some patients will believe they do. Will we have to dumb down our charts then to appease them? Won’t this degrade note quality, one of the primary objectives we are trying to avoid? It’s unclear.
The purpose of a patient note is to inform other providers and to remind ourselves of the critical information needed to care for a patient. It must be pithy and honest. It often reflects our inchoate thoughts as much as our diagnoses. It must also include the sundry requirements we know and love that are needed only to bill for the visit. These are not characteristics that make for a good patient read.
Indeed, the benefits of transparency are not limitless. In some instances, more transparency is worse. Imagine if all your emails and texts were transparent to everyone. Or if everything you’ve ever said about your mother-in-law were viewable by her. That would clearly be a case of bad transparency. Not sharing everything doesn’t mean we are dishonest or duplicitous. It means we are civil. It doesn’t mean we don’t care; it means we do care. We care about our friends and family. We care about our patients and the best way to make them well.
Unless we make it clear to patients that the notes they are viewing are not written for them, I’m worried simply opening charts could damage the doctor-patient relationship as much as it fosters it. Interestingly, there are companies trying to build a technical solution for this conundrum. Others are advocating for standardization of pathology and lab reports that are patient friendly. I’ll research these topics and let you know what I find out in a future column.
Perhaps I shouldn’t have been surprised by the positive results from the OpenNotes initiative. After all, for the last several years, I have given patients their actual pathology report for every biopsy I’ve done (which numbers in the many thousands). I have had fewer than five follow-up questions from patients that I can remember. Pretty much all were legitimate, as I recall, including a wrong site error in a report.
Today, more than 5 million patients have access to their providers’ notes on OpenNotes. That number will grow. Our biggest risk is to not be involved. “Just say no” didn’t work for Nancy Reagan; it won’t do our cause any good either.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
Transparency, until recently, was rarely associated with health care. Not anymore. For better and sometimes worse, there is a revolutionary movement toward transparency in all facets of health care: transparency of costs, outcomes, quality, service, and reputation. Full transparency has now come to medical records in the form of OpenNotes. This is a patient-centered initiative that allows patients full access to their charts, including all their doctors’ notes.
Patients have always had the right to see their records. Ordinarily though, they would be required to go to the medical records office, fill out paperwork, and request copies of their charts. They’d have to supply a reason and usually pay a fee. OpenNotes changes that. Open patient charts are free and easy to access, usually digitally. OpenNotes programs are still rare, and before we go any further, it’s important to examine what we’ve learned about them.
In 2010, Beth Israel Deaconess Medical Center in Boston, Geisinger Health System in Pennsylvania, and Harborview Medical Center in Seattle invited 105 primary care physicians to open their notes to nearly 14,000 patients. The results were overwhelmingly (and to me, surprisingly) positive: More than 85% of patients accessed their notes at least once. Nearly 100% of patients wanted the program to continue. Patients reported a better understanding of their medical issues, better medication adherence, increased adoption of healthy habits, and less anxiety about their health. I would have expected more confusion and anxiety among the patients.
What about the physicians? According to the initiative, whereas 1 in 3 patients thought they should have unfettered access to their physicians’ notes, only 1 in 10 physicians did. That’s understandable. The physicians in the pilot shared many of the same concerns you and I have, namely that OpenNotes would lead to an increased workload to explain esoteric notes to patients and to allay anxieties.
Yet, this extra workload didn’t occur. Only 3% of physicians reported spending more time answering patients’ questions. One-fifth did report that they changed the language they used when writing notes, primarily to avoid offending patients. Every physician in the initiative said he or she would continue using OpenNotes. Surprised? So was I.
Even the usually conservative SERMO physician audience responded in an unexpected manner. According to a poll conducted this June, SERMO asked 2,300 physicians if patients should have access to their medical records (including MD notes). Forty-nine percent said “only on a case-by-case basis,” 34% said “yes, always,” and 17% said “no, never.”
So, are OpenNotes a success? Let’s take a closer look at some of the challenges: First, we physicians use language that will confuse patients at best and lead them to incorrect conclusions at worst. “Acne necrotica?” Sounds like a case of medieval pimples, but actually it’s pretty harmless. Or consider, “Differential diagnosis includes neuroendocrine tumor.” It doesn’t mean you have it, but some patients will believe they do. Will we have to dumb down our charts then to appease them? Won’t this degrade note quality, one of the primary objectives we are trying to avoid? It’s unclear.
The purpose of a patient note is to inform other providers and to remind ourselves of the critical information needed to care for a patient. It must be pithy and honest. It often reflects our inchoate thoughts as much as our diagnoses. It must also include the sundry requirements we know and love that are needed only to bill for the visit. These are not characteristics that make for a good patient read.
Indeed, the benefits of transparency are not limitless. In some instances, more transparency is worse. Imagine if all your emails and texts were transparent to everyone. Or if everything you’ve ever said about your mother-in-law were viewable by her. That would clearly be a case of bad transparency. Not sharing everything doesn’t mean we are dishonest or duplicitous. It means we are civil. It doesn’t mean we don’t care; it means we do care. We care about our friends and family. We care about our patients and the best way to make them well.
Unless we make it clear to patients that the notes they are viewing are not written for them, I’m worried simply opening charts could damage the doctor-patient relationship as much as it fosters it. Interestingly, there are companies trying to build a technical solution for this conundrum. Others are advocating for standardization of pathology and lab reports that are patient friendly. I’ll research these topics and let you know what I find out in a future column.
Perhaps I shouldn’t have been surprised by the positive results from the OpenNotes initiative. After all, for the last several years, I have given patients their actual pathology report for every biopsy I’ve done (which numbers in the many thousands). I have had fewer than five follow-up questions from patients that I can remember. Pretty much all were legitimate, as I recall, including a wrong site error in a report.
Today, more than 5 million patients have access to their providers’ notes on OpenNotes. That number will grow. Our biggest risk is to not be involved. “Just say no” didn’t work for Nancy Reagan; it won’t do our cause any good either.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
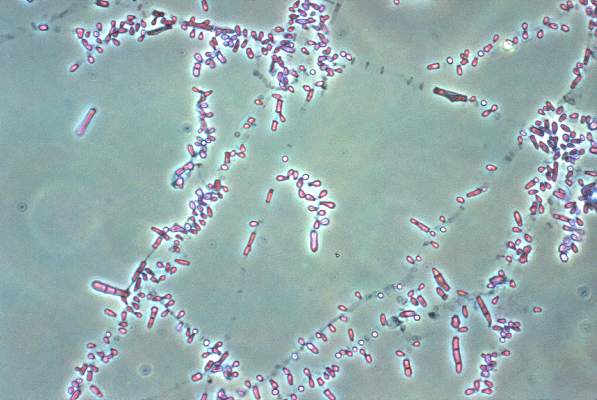
Fungal foot infections risk secondary infection in diabetic patients
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM WCD 2015
One dollar and forty-two cents
No good deed goes unpunished.
We froze Myrna’s keratosis off her forehead. Gratis, of course.
This was followed by repeated calls from Myrna: the spot was red, it was painful, it wasn’t healing right.
So we mailed her an envelope filled with cream to help heal the skin. Although we used our regular postage meter, somehow Myrna got the package with $1.42 postage due.
Not going to work.
Myrna called to complain. Then she drove over and walked into the office, but we weren’t there. Then she called again and left a message. “I’m coming in this afternoon,” she said. “I expect to pick up my $1.42.”
Really.
Later that morning, Stephanie came by for a skin check. Because Stephanie is catering manager at a downtown ultra-upscale hotel, I knew she would both appreciate the tale of $1.42 and be able to top it. Everyone in her field can fill several books of client encounters no one could make up.
When I asked her to share some stories, Stephanie did not disappoint.
“Sure,” she said. “People plan lavish weddings, no expense spared. But when they send gift baskets, we have to charge $3.50 each to pay the livery people who deliver them. That they object to.
“But what’s even worse,” she went on, “is when it comes to feeding the band. We discount the meals for musicians 60%-70% below the per-plate rate for guests.
“That’s not low enough for some people, though. We explain to them that the band members do have to eat. ‘Yes,’ say some of the brides, ‘but do we have to give them a whole meal? Can’t we just give them a sandwich or something?’ This is from people who are spending six figures on food alone.”
“Sounds like Marie Antoinette,” I said. “What do you tell them?”
“We say, OK, we’ll see if we can discount the band meals even more,” Stephanie said.
Not an hour later, Ken came in. Ken manages an art-house movie theater in a close-in, affluent suburb. As I knew he would, Ken had stories, too.
“People are always angling for some kind of special privilege,” he said. ‘I’ve been a patron for years,” they say. ‘Can’t you do something for me?’
“What do they want?” I ask. “Free tickets?”
“Yes, or preferential seating,” said Ken, “but we tell them that if we do that for them, we’d have to do it for everybody.
“Or else it’s a cold, winter night and the theater is a little chilly. Some of the patrons want us to give them free popcorn.” Ken sighed.
Anybody in the service business is going to meet up with behavior like this. We probably should be grateful that most patients have enough respect for our profession to dissuade them from:
• Demanding to be seen for free or have us waive the copay since “the treatment didn’t work.”
• Refusing to hand over the copay for a follow-up, because, “It was just a quick check, didn’t take any time.”
• Insist on having us treat the wart or skin tag again at no charge, because “you missed a spot.”
And so on. At least even our demanding patients don’t ask for popcorn.
Myrna did show up that afternoon, by the way. I don’t know how much she spent on gas to come in. Our office manager Fatima took care of things. She gave Myrna her Buck-42:
Three quarters.
Two dimes.
Five nickels.
And 22 pennies.
Fatima is really good at keeping a straight face.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
No good deed goes unpunished.
We froze Myrna’s keratosis off her forehead. Gratis, of course.
This was followed by repeated calls from Myrna: the spot was red, it was painful, it wasn’t healing right.
So we mailed her an envelope filled with cream to help heal the skin. Although we used our regular postage meter, somehow Myrna got the package with $1.42 postage due.
Not going to work.
Myrna called to complain. Then she drove over and walked into the office, but we weren’t there. Then she called again and left a message. “I’m coming in this afternoon,” she said. “I expect to pick up my $1.42.”
Really.
Later that morning, Stephanie came by for a skin check. Because Stephanie is catering manager at a downtown ultra-upscale hotel, I knew she would both appreciate the tale of $1.42 and be able to top it. Everyone in her field can fill several books of client encounters no one could make up.
When I asked her to share some stories, Stephanie did not disappoint.
“Sure,” she said. “People plan lavish weddings, no expense spared. But when they send gift baskets, we have to charge $3.50 each to pay the livery people who deliver them. That they object to.
“But what’s even worse,” she went on, “is when it comes to feeding the band. We discount the meals for musicians 60%-70% below the per-plate rate for guests.
“That’s not low enough for some people, though. We explain to them that the band members do have to eat. ‘Yes,’ say some of the brides, ‘but do we have to give them a whole meal? Can’t we just give them a sandwich or something?’ This is from people who are spending six figures on food alone.”
“Sounds like Marie Antoinette,” I said. “What do you tell them?”
“We say, OK, we’ll see if we can discount the band meals even more,” Stephanie said.
Not an hour later, Ken came in. Ken manages an art-house movie theater in a close-in, affluent suburb. As I knew he would, Ken had stories, too.
“People are always angling for some kind of special privilege,” he said. ‘I’ve been a patron for years,” they say. ‘Can’t you do something for me?’
“What do they want?” I ask. “Free tickets?”
“Yes, or preferential seating,” said Ken, “but we tell them that if we do that for them, we’d have to do it for everybody.
“Or else it’s a cold, winter night and the theater is a little chilly. Some of the patrons want us to give them free popcorn.” Ken sighed.
Anybody in the service business is going to meet up with behavior like this. We probably should be grateful that most patients have enough respect for our profession to dissuade them from:
• Demanding to be seen for free or have us waive the copay since “the treatment didn’t work.”
• Refusing to hand over the copay for a follow-up, because, “It was just a quick check, didn’t take any time.”
• Insist on having us treat the wart or skin tag again at no charge, because “you missed a spot.”
And so on. At least even our demanding patients don’t ask for popcorn.
Myrna did show up that afternoon, by the way. I don’t know how much she spent on gas to come in. Our office manager Fatima took care of things. She gave Myrna her Buck-42:
Three quarters.
Two dimes.
Five nickels.
And 22 pennies.
Fatima is really good at keeping a straight face.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
No good deed goes unpunished.
We froze Myrna’s keratosis off her forehead. Gratis, of course.
This was followed by repeated calls from Myrna: the spot was red, it was painful, it wasn’t healing right.
So we mailed her an envelope filled with cream to help heal the skin. Although we used our regular postage meter, somehow Myrna got the package with $1.42 postage due.
Not going to work.
Myrna called to complain. Then she drove over and walked into the office, but we weren’t there. Then she called again and left a message. “I’m coming in this afternoon,” she said. “I expect to pick up my $1.42.”
Really.
Later that morning, Stephanie came by for a skin check. Because Stephanie is catering manager at a downtown ultra-upscale hotel, I knew she would both appreciate the tale of $1.42 and be able to top it. Everyone in her field can fill several books of client encounters no one could make up.
When I asked her to share some stories, Stephanie did not disappoint.
“Sure,” she said. “People plan lavish weddings, no expense spared. But when they send gift baskets, we have to charge $3.50 each to pay the livery people who deliver them. That they object to.
“But what’s even worse,” she went on, “is when it comes to feeding the band. We discount the meals for musicians 60%-70% below the per-plate rate for guests.
“That’s not low enough for some people, though. We explain to them that the band members do have to eat. ‘Yes,’ say some of the brides, ‘but do we have to give them a whole meal? Can’t we just give them a sandwich or something?’ This is from people who are spending six figures on food alone.”
“Sounds like Marie Antoinette,” I said. “What do you tell them?”
“We say, OK, we’ll see if we can discount the band meals even more,” Stephanie said.
Not an hour later, Ken came in. Ken manages an art-house movie theater in a close-in, affluent suburb. As I knew he would, Ken had stories, too.
“People are always angling for some kind of special privilege,” he said. ‘I’ve been a patron for years,” they say. ‘Can’t you do something for me?’
“What do they want?” I ask. “Free tickets?”
“Yes, or preferential seating,” said Ken, “but we tell them that if we do that for them, we’d have to do it for everybody.
“Or else it’s a cold, winter night and the theater is a little chilly. Some of the patrons want us to give them free popcorn.” Ken sighed.
Anybody in the service business is going to meet up with behavior like this. We probably should be grateful that most patients have enough respect for our profession to dissuade them from:
• Demanding to be seen for free or have us waive the copay since “the treatment didn’t work.”
• Refusing to hand over the copay for a follow-up, because, “It was just a quick check, didn’t take any time.”
• Insist on having us treat the wart or skin tag again at no charge, because “you missed a spot.”
And so on. At least even our demanding patients don’t ask for popcorn.
Myrna did show up that afternoon, by the way. I don’t know how much she spent on gas to come in. Our office manager Fatima took care of things. She gave Myrna her Buck-42:
Three quarters.
Two dimes.
Five nickels.
And 22 pennies.
Fatima is really good at keeping a straight face.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
China's Healthcare Reform Drive Stuck in First Gear
SHANGHAI (Reuters) - Li Tiantian, a Chinese doctor turned tech entrepreneur, is a leading light of the country's much-trumpeted healthcare reform drive. His medical networking platform DXY.com links two million doctors across China and has attracted funding from tech giants like Tencent.
DXY is exactly what Beijing has said it's looking to support after it pinpointed remote healthcare, Internet and technology as drivers to solve its healthcare woes in a 5-year roadmap in March.
The reality is rather different: DXY is curbing plans to work with public hospitals to help connect doctors and patients online because of a lack of support by Beijing and obstacles working with China's huge, fragmented public healthcare sector.
"We've heard a lot of good stories from the top - Internet +, driving force, policy changing - but see nothing happen at the bottom," Li told Reuters. "It's not about market, capital or even tech - these things are already developed very well ... rather it's the regulations, laws and systems of support."
Li's position reflects wider obstacles to healthcare reforms in technology, online drug sales, hospital privatization and doctors' pay, drivers that are a major lure for investors and firms betting billions of dollars on China opening up a market set to be worth around $1.3 trillion by 2020.
"(Investors) always ask: is there actually a macro tailwind, and is the government and regulatory environment - which is very important in China - supportive of this?" said Alexander Ng, associate principal at McKinsey & Co.
"If there's a lot of negative voices it might make investors back off or calculate a much higher risk premium."
China has ramped up its healthcare reform rhetoric, touting greater access for foreign investors to healthcare services, a bigger role for technology and pushing drug sales from mostly state-run hospitals towards the retail market.
This has helped draw in close to $30 billion worth of healthcare merger and acquisition investment so far this year, a fivefold leap from the same period in 2014, according to Reuters data. Healthcare M&A already leapt last year.
But, despite the government's longer-term ambitions, industry insiders say reforms are being held up because of technical issues such as crumbling and fragmented IT systems to in-fighting between regulators and push-back from the state-run firms who dominate the sector - and don't want change.
"With so many vested interests - dealers, hospitals, insurance departments and others - reform is not very fast," said Frank Zhao, chief financial officer at China Jo Jo Drugstores Inc.
Privately, some health policy advisers admit reforms are falling behind, while the public line is that reform has "hit up against the Yangtze River," a reference to the obstacle famously overcome by Mao Zedong's Communist forces in 1949.
The healthcare ministry did not respond to faxed queries seeking comment for this article.
Zhao points to the expected approval for online prescription drug sales, which he and other industry insiders say has been delayed this year due to regulatory concerns and opposition from state-run hospitals and distributors.
These hold-ups are a frustration for pharmacy chains like Jo Jo as it looks to increase its business online, but also for tech giants like Alibaba Group Holding Ltd, which wants to get into the online prescription drug space.
One big draw for investors has been China's privatization drive of healthcare services - touted as key to revamping an unpopular healthcare system, blighted by crowded hospitals, corruption and simmering tension between patients and staff.
But, despite the fast growth of private investment in hospitals, the public sector still dominates around 90% of all patient visits, according to a Deutsche Bank 2015 healthcare report. Investors cite issues with insurance schemes, access to Chinese doctors and a still tightly-controlled market.
"With things still not market-led, organizations like ours are facing huge challenges and difficulties," Hu Lan, President and Director of hospital investment firm AMCARE Corporation, said at a conference in Shanghai in June.
Healthcare spending as a slice of China's GDP also remains small at around 6% in 2013 compared to 17% in the United States, World Health Organization (WHO) data show.
Reforms to reduce hospitals' reliance on drug sales also faces a revolt from doctors who argue this will take away a key revenue stream at a time when medical staff are overworked, underpaid and often violently abused by angry patients.
"Every few days you hear about a doctor being beaten or even killed. This situation is a huge mental burden for doctors," said Wu Xiaobo a doctor at the Wangjing Hospital in Beijing in a recent viral video campaign for doctors' rights.
As for DXY's Li, his firm now plans to change tack and set up an offline clinic in the eastern city of Hangzhou this year to pilot potential healthcare reforms - outside the state sector.
"We were hoping we could leverage changing policy and do something on mobile and digital," Li said. "We found it's just too slow, so the only way to do it is out on our own."
SHANGHAI (Reuters) - Li Tiantian, a Chinese doctor turned tech entrepreneur, is a leading light of the country's much-trumpeted healthcare reform drive. His medical networking platform DXY.com links two million doctors across China and has attracted funding from tech giants like Tencent.
DXY is exactly what Beijing has said it's looking to support after it pinpointed remote healthcare, Internet and technology as drivers to solve its healthcare woes in a 5-year roadmap in March.
The reality is rather different: DXY is curbing plans to work with public hospitals to help connect doctors and patients online because of a lack of support by Beijing and obstacles working with China's huge, fragmented public healthcare sector.
"We've heard a lot of good stories from the top - Internet +, driving force, policy changing - but see nothing happen at the bottom," Li told Reuters. "It's not about market, capital or even tech - these things are already developed very well ... rather it's the regulations, laws and systems of support."
Li's position reflects wider obstacles to healthcare reforms in technology, online drug sales, hospital privatization and doctors' pay, drivers that are a major lure for investors and firms betting billions of dollars on China opening up a market set to be worth around $1.3 trillion by 2020.
"(Investors) always ask: is there actually a macro tailwind, and is the government and regulatory environment - which is very important in China - supportive of this?" said Alexander Ng, associate principal at McKinsey & Co.
"If there's a lot of negative voices it might make investors back off or calculate a much higher risk premium."
China has ramped up its healthcare reform rhetoric, touting greater access for foreign investors to healthcare services, a bigger role for technology and pushing drug sales from mostly state-run hospitals towards the retail market.
This has helped draw in close to $30 billion worth of healthcare merger and acquisition investment so far this year, a fivefold leap from the same period in 2014, according to Reuters data. Healthcare M&A already leapt last year.
But, despite the government's longer-term ambitions, industry insiders say reforms are being held up because of technical issues such as crumbling and fragmented IT systems to in-fighting between regulators and push-back from the state-run firms who dominate the sector - and don't want change.
"With so many vested interests - dealers, hospitals, insurance departments and others - reform is not very fast," said Frank Zhao, chief financial officer at China Jo Jo Drugstores Inc.
Privately, some health policy advisers admit reforms are falling behind, while the public line is that reform has "hit up against the Yangtze River," a reference to the obstacle famously overcome by Mao Zedong's Communist forces in 1949.
The healthcare ministry did not respond to faxed queries seeking comment for this article.
Zhao points to the expected approval for online prescription drug sales, which he and other industry insiders say has been delayed this year due to regulatory concerns and opposition from state-run hospitals and distributors.
These hold-ups are a frustration for pharmacy chains like Jo Jo as it looks to increase its business online, but also for tech giants like Alibaba Group Holding Ltd, which wants to get into the online prescription drug space.
One big draw for investors has been China's privatization drive of healthcare services - touted as key to revamping an unpopular healthcare system, blighted by crowded hospitals, corruption and simmering tension between patients and staff.
But, despite the fast growth of private investment in hospitals, the public sector still dominates around 90% of all patient visits, according to a Deutsche Bank 2015 healthcare report. Investors cite issues with insurance schemes, access to Chinese doctors and a still tightly-controlled market.
"With things still not market-led, organizations like ours are facing huge challenges and difficulties," Hu Lan, President and Director of hospital investment firm AMCARE Corporation, said at a conference in Shanghai in June.
Healthcare spending as a slice of China's GDP also remains small at around 6% in 2013 compared to 17% in the United States, World Health Organization (WHO) data show.
Reforms to reduce hospitals' reliance on drug sales also faces a revolt from doctors who argue this will take away a key revenue stream at a time when medical staff are overworked, underpaid and often violently abused by angry patients.
"Every few days you hear about a doctor being beaten or even killed. This situation is a huge mental burden for doctors," said Wu Xiaobo a doctor at the Wangjing Hospital in Beijing in a recent viral video campaign for doctors' rights.
As for DXY's Li, his firm now plans to change tack and set up an offline clinic in the eastern city of Hangzhou this year to pilot potential healthcare reforms - outside the state sector.
"We were hoping we could leverage changing policy and do something on mobile and digital," Li said. "We found it's just too slow, so the only way to do it is out on our own."
SHANGHAI (Reuters) - Li Tiantian, a Chinese doctor turned tech entrepreneur, is a leading light of the country's much-trumpeted healthcare reform drive. His medical networking platform DXY.com links two million doctors across China and has attracted funding from tech giants like Tencent.
DXY is exactly what Beijing has said it's looking to support after it pinpointed remote healthcare, Internet and technology as drivers to solve its healthcare woes in a 5-year roadmap in March.
The reality is rather different: DXY is curbing plans to work with public hospitals to help connect doctors and patients online because of a lack of support by Beijing and obstacles working with China's huge, fragmented public healthcare sector.
"We've heard a lot of good stories from the top - Internet +, driving force, policy changing - but see nothing happen at the bottom," Li told Reuters. "It's not about market, capital or even tech - these things are already developed very well ... rather it's the regulations, laws and systems of support."
Li's position reflects wider obstacles to healthcare reforms in technology, online drug sales, hospital privatization and doctors' pay, drivers that are a major lure for investors and firms betting billions of dollars on China opening up a market set to be worth around $1.3 trillion by 2020.
"(Investors) always ask: is there actually a macro tailwind, and is the government and regulatory environment - which is very important in China - supportive of this?" said Alexander Ng, associate principal at McKinsey & Co.
"If there's a lot of negative voices it might make investors back off or calculate a much higher risk premium."
China has ramped up its healthcare reform rhetoric, touting greater access for foreign investors to healthcare services, a bigger role for technology and pushing drug sales from mostly state-run hospitals towards the retail market.
This has helped draw in close to $30 billion worth of healthcare merger and acquisition investment so far this year, a fivefold leap from the same period in 2014, according to Reuters data. Healthcare M&A already leapt last year.
But, despite the government's longer-term ambitions, industry insiders say reforms are being held up because of technical issues such as crumbling and fragmented IT systems to in-fighting between regulators and push-back from the state-run firms who dominate the sector - and don't want change.
"With so many vested interests - dealers, hospitals, insurance departments and others - reform is not very fast," said Frank Zhao, chief financial officer at China Jo Jo Drugstores Inc.
Privately, some health policy advisers admit reforms are falling behind, while the public line is that reform has "hit up against the Yangtze River," a reference to the obstacle famously overcome by Mao Zedong's Communist forces in 1949.
The healthcare ministry did not respond to faxed queries seeking comment for this article.
Zhao points to the expected approval for online prescription drug sales, which he and other industry insiders say has been delayed this year due to regulatory concerns and opposition from state-run hospitals and distributors.
These hold-ups are a frustration for pharmacy chains like Jo Jo as it looks to increase its business online, but also for tech giants like Alibaba Group Holding Ltd, which wants to get into the online prescription drug space.
One big draw for investors has been China's privatization drive of healthcare services - touted as key to revamping an unpopular healthcare system, blighted by crowded hospitals, corruption and simmering tension between patients and staff.
But, despite the fast growth of private investment in hospitals, the public sector still dominates around 90% of all patient visits, according to a Deutsche Bank 2015 healthcare report. Investors cite issues with insurance schemes, access to Chinese doctors and a still tightly-controlled market.
"With things still not market-led, organizations like ours are facing huge challenges and difficulties," Hu Lan, President and Director of hospital investment firm AMCARE Corporation, said at a conference in Shanghai in June.
Healthcare spending as a slice of China's GDP also remains small at around 6% in 2013 compared to 17% in the United States, World Health Organization (WHO) data show.
Reforms to reduce hospitals' reliance on drug sales also faces a revolt from doctors who argue this will take away a key revenue stream at a time when medical staff are overworked, underpaid and often violently abused by angry patients.
"Every few days you hear about a doctor being beaten or even killed. This situation is a huge mental burden for doctors," said Wu Xiaobo a doctor at the Wangjing Hospital in Beijing in a recent viral video campaign for doctors' rights.
As for DXY's Li, his firm now plans to change tack and set up an offline clinic in the eastern city of Hangzhou this year to pilot potential healthcare reforms - outside the state sector.
"We were hoping we could leverage changing policy and do something on mobile and digital," Li said. "We found it's just too slow, so the only way to do it is out on our own."
Health care transition practices continue to evolve
It’s been nearly 13 years since the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians released its Consensus Policy Statement on Health Care Transitions for Young Adults With Special Needs and 4 years since the AAP, AAFP, ACP Clinical Report: Supporting Health Care Transition (HCT) from Adolescence to Adulthood in the Medical Home was published, but formal adoption of suggested approaches has remained minimal.
A recent survey of 158 members of the Childhood Arthritis and Rheumatology Research Alliance in North America found that fewer than 10% of respondents were familiar with the consensus statement and the HCT clinical report, only 8% have a formal written transition policy, while 42% use an informal approach (J. Rheumatol. 2014;41:768-79). Respondents ranked fragmented adult health care and lack of time to provide sufficient services as the two major barriers to transition.
“Until recently, there hasn’t been a lot of focus on transition in fellowship training, and I don’t know how well the consensus policy statement and HCT clinical report are publicized in residency or fellowship training,” one of the study authors, Dr. Tova Ronis, said in an interview. “There’s definitely a role for more education about the policy statement and HCT clinical report.” As a result of inconsistent transition practices, some patients fall through the cracks in the transition from pediatric to adult rheumatology care. Transition can be difficult and even patients who receive transition care can have challenges, said Dr. Ronis of the pediatric rheumatology division at Children’s National Health System, Washington. She spoke of one young patient with severe systemic disease who was referred to ongoing adult care with an expert in the field. The patient “went to the adult office but didn’t like it there; she didn’t feel like she was being listened to and didn’t feel like the new doctor knew her well. She would come back to us, go back and forth, so her care became very fragmented. We communicated with the adult doctor but there wasn’t one person making the plan [of care].” In addition, other clinicians who had been providing subspecialty care and had not transitioned her to adult practice “were still at the children’s hospital, so when she experienced health problems or pain, she would come to the pediatric emergency department,” Dr. Ronis recalled. “She hadn’t identified the new institution as her medical home, so her care became very fragmented during that transition process. She actually missed some therapy because she didn’t like the new office, so wasn’t seen anywhere for a while.”
Dr. Paul T. Jensen said that most clinicians “have a gut feeling” that the current health care transition landscape has limitations, despite the availability of such tools as the Got Transition website, the Transition Readiness Assessment Questionnaire (TRAQ), as well as studies of novel approaches such as having a social worker serve as a transition coordinator(Pediatr. Rheumatol. 2015;13:17 [doi:10.1186/s12969-015-0013-0]) or having clinicians from adult practices see patients at a pediatric institution (Pediatr. Pulmonol. 2013;48:658-65). “I think that most, if not all, pediatric providers, including pediatric rheumatologists, worry about their patients as they get older, especially those who have a decreased maturity level,” said Dr. Jensen, who is a fellow in both adult and pediatric rheumatology at the Ohio State University Wexner Medical Center and Nationwide Children’s Hospital, Columbus. “But I think there’s a large lack of knowledge about what resources are available.”
Choosing transition practices that work for you
Dr. Patience White, a pediatric and adult rheumatologist who in 2011 coauthored the HCT Clinical Report, is familiar with such sentiment. She says that the topic of transition has “come to the forefront because the pediatric rheumatology field has grown. On top of that, many of our patients have grown up and moved on to other aspects of adulthood, so now pediatric providers will need to prepare to ‘let them go to adult health care.’ The perfect storm is happening.” Dr. White codirects the Got Transition Center for Health Care Transition Improvement, a federally funded program located at the National Alliance to Advance Adolescent Health. One of the center’s goals is to expand the use of the Six Core Elements of Health Care Transition that were developed to help make the 2011 Health Care Transitions Clinical Report actionable. These include practice quality improvement strategies such as establishing a transition policy, tracking progress, offering transition readiness assessments, creating a transition plan, transferring to an adult provider, and assessing the youth’s and family’s experience with the transition. The original Six Core Elements of Health Care Transition were tested in learning collaboratives across the United States and have been updated with input from the learning collaboratives and national transition experts into three separate packages of tools and evaluation approaches for transitioning youth to adult health care providers, transitioning to an adult approach to health care without changing providers, and integrating young adults into adult health care. For example, recommendations when transitioning youth to adult health care providers include developing a transition policy/statement “with input from youth and families that describes the practice’s approach to transition, including privacy and consent information,” as well as conducting regular transition readiness assessments, beginning at age 14 years, “to identify and discuss with youth and parent/caregiver their needs and goals in self-care.” Other tools available from the Got Transition website include a set of frequently asked transition questions developed by and for youth/young adults, as well as many transition resources.
While she acknowledged it may not be feasible for pediatric and adult rheumatologists to implement all Six Core Elements in their practice, Dr. White suggests providers might try implementing at least one or two and, for pediatric rheumatologists, start the discussion of the transition process when their patients reach the age of 13 years as recommended by the HCT clinical report. “Everybody says it’s hard, and I agree, changing practice processes to improve health care is hard work,” she said. “We know preparation for the youth and family needs to happen. We know transfer and communication has to occur, and that the accepting adult provider has to be informed and comfortable to make the transition process a success. It is about choosing one or two Six Core Element tools that can work for you, your practice, and your patients to help them through the transition process. If you’re an adult provider, you might choose to offer a welcome letter to my practice and a self-care assessment for the new young adult patients joining the practice so the adult health care provider can understand how proficient the young adults are with respect to their self-care skills and knowledge of the adult health care system.”
Disease-specific toolkits coming in 2016
Dr. White is also a consultant to the Pediatric to Adult Health Care Transitions Workgroup, an effort of the ACP Council of Subspecialty Societies to address gaps in care that exist with the transition of pediatric patients into adult health care. According to an ACP document describing the effort, the goal of workgroup is to identify “common tools/templates for a ‘general’ transition process, and subspecialty societies will utilize the templates to develop customized toolkits for specific diseases/conditions. The toolkits will then be collected and broadly disseminated,” with release targeted for May 2016 at the ACP national meeting. Dr. Stacy P. Ardoin, who is leading the rheumatology subspecialty group on behalf of the American College of Rheumatology, said the fact that this effort was initiated by the ACP “is great, because historically most of the interest in transition has bubbled up from the pediatric side. I think that adult providers are realizing more and more that patients who come to them with complex childhood onset conditions are challenging to manage, and that we really need to partner together to make things the best for our patients.”
Dr. Ardoin, a rheumatologist in the department of internal medicine at the Ohio State University Wexner Medical Center and in the department of pediatrics at Nationwide Children’s Hospital, characterized the final product as “not so much a definite protocol that everybody has to follow, but more just providing recommendations to the practitioner saying, ‘these are the things that we recommend and here are some tools to accomplish it.’ There’s such a lack of standardization for anything with transition despite the fact that we have consensus statements that have been put out in the past. Perhaps part of the problem is that they were too vague or not considered individually for each specialty. Hopefully, having each specialty take this on and look at their unique needs in the transition process will make people more willing to participate.”
Preparing patients to become health care self-advocates
Not all physicians are convinced that more recommendations will help clinicians navigate the intricacies of health care transition, however. “If children come to you as a physician at a young age (most of the kids with arthritis) or very ill (most of the children with systemic lupus erythematosus), good care over time represents a significant bonding experience,” said Dr. Thomas J. A. Lehman, chief of the division of pediatric rheumatology at the Hospital for Special Surgery in New York. “The children come to see you as a significant other in their life. If they then are suddenly ‘cast out’ because they reach a certain age it doesn’t go down any better than it would if a significant relative ‘cast them out.’ The doctors like to think they are transitioning the patients. The patients who have bonded feel they are being rejected. I don’t have an answer to this problem. However, none of the past HCT policy statements adequately recognize this aspect.”
For her part, Dr. White, who is also professor of medicine and pediatrics at George Washington University, Washington, said that in some published studies pediatric providers acknowledged that they are reluctant to transition patients to adult health care providers “and can overprotect their young patients as some parents do. This approach can result in the young adult being a poor self-advocate in the adult health care environment and not receiving developmentally appropriate health care. If a pediatric patient and family have not been informed of when they can no longer come to the pediatric rheumatology practice and have not discussed a transition to adult health care plan, they often assume they can stay with their pediatric rheumatologist forever.”
In addition, Dr. White continued, “some pediatric rheumatologists might say, ‘adult providers don’t know how to care for pediatric rheumatology [patients].’ Well, that may due to the adult providers not having received training in specific pediatric onset conditions. Communication between the pediatric and adult providers is key to a good transition experience for everyone. Trying to quickly build a new relationship with a new young adult patient to keep them engaged in their care and who has been used to the same pediatric provider for years is challenging, and the young adult and the adult provider need the pediatric provider’s support and availability to be a consultant to support the adult provider in the areas where they have little disease-specific experience.”
Dr. Jensen makes it a point to talk to his patients about health care transition in early adolescence, helps them set goals, and encourages them to “take more ownership in late adolescence for his or her own health: making their own appointments for follow-up visits, giving time to the patient in the room alone, and asking patients to maybe monitor medication adherence but not to lay the medications out for the patient in the morning,” he said. “When patients are given that opportunity, they may mature.”
Dr. Ronis, who is implementing a health care transition program at Children’s National Health System, thinks about health care transition as “a time where there’s risk for potentially worsening disease and negative outcomes due to perceived fragmentation of care. The more prepared we are and the more we prepare our patients to do this successfully, the better outcomes our patients will have.”
The Got Transition Center for Health Care Transition Improvement is funded by the Health Resources and Services Administration. The physicians interviewed for this story reported having no financial disclosures.
It’s been nearly 13 years since the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians released its Consensus Policy Statement on Health Care Transitions for Young Adults With Special Needs and 4 years since the AAP, AAFP, ACP Clinical Report: Supporting Health Care Transition (HCT) from Adolescence to Adulthood in the Medical Home was published, but formal adoption of suggested approaches has remained minimal.
A recent survey of 158 members of the Childhood Arthritis and Rheumatology Research Alliance in North America found that fewer than 10% of respondents were familiar with the consensus statement and the HCT clinical report, only 8% have a formal written transition policy, while 42% use an informal approach (J. Rheumatol. 2014;41:768-79). Respondents ranked fragmented adult health care and lack of time to provide sufficient services as the two major barriers to transition.
“Until recently, there hasn’t been a lot of focus on transition in fellowship training, and I don’t know how well the consensus policy statement and HCT clinical report are publicized in residency or fellowship training,” one of the study authors, Dr. Tova Ronis, said in an interview. “There’s definitely a role for more education about the policy statement and HCT clinical report.” As a result of inconsistent transition practices, some patients fall through the cracks in the transition from pediatric to adult rheumatology care. Transition can be difficult and even patients who receive transition care can have challenges, said Dr. Ronis of the pediatric rheumatology division at Children’s National Health System, Washington. She spoke of one young patient with severe systemic disease who was referred to ongoing adult care with an expert in the field. The patient “went to the adult office but didn’t like it there; she didn’t feel like she was being listened to and didn’t feel like the new doctor knew her well. She would come back to us, go back and forth, so her care became very fragmented. We communicated with the adult doctor but there wasn’t one person making the plan [of care].” In addition, other clinicians who had been providing subspecialty care and had not transitioned her to adult practice “were still at the children’s hospital, so when she experienced health problems or pain, she would come to the pediatric emergency department,” Dr. Ronis recalled. “She hadn’t identified the new institution as her medical home, so her care became very fragmented during that transition process. She actually missed some therapy because she didn’t like the new office, so wasn’t seen anywhere for a while.”
Dr. Paul T. Jensen said that most clinicians “have a gut feeling” that the current health care transition landscape has limitations, despite the availability of such tools as the Got Transition website, the Transition Readiness Assessment Questionnaire (TRAQ), as well as studies of novel approaches such as having a social worker serve as a transition coordinator(Pediatr. Rheumatol. 2015;13:17 [doi:10.1186/s12969-015-0013-0]) or having clinicians from adult practices see patients at a pediatric institution (Pediatr. Pulmonol. 2013;48:658-65). “I think that most, if not all, pediatric providers, including pediatric rheumatologists, worry about their patients as they get older, especially those who have a decreased maturity level,” said Dr. Jensen, who is a fellow in both adult and pediatric rheumatology at the Ohio State University Wexner Medical Center and Nationwide Children’s Hospital, Columbus. “But I think there’s a large lack of knowledge about what resources are available.”
Choosing transition practices that work for you
Dr. Patience White, a pediatric and adult rheumatologist who in 2011 coauthored the HCT Clinical Report, is familiar with such sentiment. She says that the topic of transition has “come to the forefront because the pediatric rheumatology field has grown. On top of that, many of our patients have grown up and moved on to other aspects of adulthood, so now pediatric providers will need to prepare to ‘let them go to adult health care.’ The perfect storm is happening.” Dr. White codirects the Got Transition Center for Health Care Transition Improvement, a federally funded program located at the National Alliance to Advance Adolescent Health. One of the center’s goals is to expand the use of the Six Core Elements of Health Care Transition that were developed to help make the 2011 Health Care Transitions Clinical Report actionable. These include practice quality improvement strategies such as establishing a transition policy, tracking progress, offering transition readiness assessments, creating a transition plan, transferring to an adult provider, and assessing the youth’s and family’s experience with the transition. The original Six Core Elements of Health Care Transition were tested in learning collaboratives across the United States and have been updated with input from the learning collaboratives and national transition experts into three separate packages of tools and evaluation approaches for transitioning youth to adult health care providers, transitioning to an adult approach to health care without changing providers, and integrating young adults into adult health care. For example, recommendations when transitioning youth to adult health care providers include developing a transition policy/statement “with input from youth and families that describes the practice’s approach to transition, including privacy and consent information,” as well as conducting regular transition readiness assessments, beginning at age 14 years, “to identify and discuss with youth and parent/caregiver their needs and goals in self-care.” Other tools available from the Got Transition website include a set of frequently asked transition questions developed by and for youth/young adults, as well as many transition resources.
While she acknowledged it may not be feasible for pediatric and adult rheumatologists to implement all Six Core Elements in their practice, Dr. White suggests providers might try implementing at least one or two and, for pediatric rheumatologists, start the discussion of the transition process when their patients reach the age of 13 years as recommended by the HCT clinical report. “Everybody says it’s hard, and I agree, changing practice processes to improve health care is hard work,” she said. “We know preparation for the youth and family needs to happen. We know transfer and communication has to occur, and that the accepting adult provider has to be informed and comfortable to make the transition process a success. It is about choosing one or two Six Core Element tools that can work for you, your practice, and your patients to help them through the transition process. If you’re an adult provider, you might choose to offer a welcome letter to my practice and a self-care assessment for the new young adult patients joining the practice so the adult health care provider can understand how proficient the young adults are with respect to their self-care skills and knowledge of the adult health care system.”
Disease-specific toolkits coming in 2016
Dr. White is also a consultant to the Pediatric to Adult Health Care Transitions Workgroup, an effort of the ACP Council of Subspecialty Societies to address gaps in care that exist with the transition of pediatric patients into adult health care. According to an ACP document describing the effort, the goal of workgroup is to identify “common tools/templates for a ‘general’ transition process, and subspecialty societies will utilize the templates to develop customized toolkits for specific diseases/conditions. The toolkits will then be collected and broadly disseminated,” with release targeted for May 2016 at the ACP national meeting. Dr. Stacy P. Ardoin, who is leading the rheumatology subspecialty group on behalf of the American College of Rheumatology, said the fact that this effort was initiated by the ACP “is great, because historically most of the interest in transition has bubbled up from the pediatric side. I think that adult providers are realizing more and more that patients who come to them with complex childhood onset conditions are challenging to manage, and that we really need to partner together to make things the best for our patients.”
Dr. Ardoin, a rheumatologist in the department of internal medicine at the Ohio State University Wexner Medical Center and in the department of pediatrics at Nationwide Children’s Hospital, characterized the final product as “not so much a definite protocol that everybody has to follow, but more just providing recommendations to the practitioner saying, ‘these are the things that we recommend and here are some tools to accomplish it.’ There’s such a lack of standardization for anything with transition despite the fact that we have consensus statements that have been put out in the past. Perhaps part of the problem is that they were too vague or not considered individually for each specialty. Hopefully, having each specialty take this on and look at their unique needs in the transition process will make people more willing to participate.”
Preparing patients to become health care self-advocates
Not all physicians are convinced that more recommendations will help clinicians navigate the intricacies of health care transition, however. “If children come to you as a physician at a young age (most of the kids with arthritis) or very ill (most of the children with systemic lupus erythematosus), good care over time represents a significant bonding experience,” said Dr. Thomas J. A. Lehman, chief of the division of pediatric rheumatology at the Hospital for Special Surgery in New York. “The children come to see you as a significant other in their life. If they then are suddenly ‘cast out’ because they reach a certain age it doesn’t go down any better than it would if a significant relative ‘cast them out.’ The doctors like to think they are transitioning the patients. The patients who have bonded feel they are being rejected. I don’t have an answer to this problem. However, none of the past HCT policy statements adequately recognize this aspect.”
For her part, Dr. White, who is also professor of medicine and pediatrics at George Washington University, Washington, said that in some published studies pediatric providers acknowledged that they are reluctant to transition patients to adult health care providers “and can overprotect their young patients as some parents do. This approach can result in the young adult being a poor self-advocate in the adult health care environment and not receiving developmentally appropriate health care. If a pediatric patient and family have not been informed of when they can no longer come to the pediatric rheumatology practice and have not discussed a transition to adult health care plan, they often assume they can stay with their pediatric rheumatologist forever.”
In addition, Dr. White continued, “some pediatric rheumatologists might say, ‘adult providers don’t know how to care for pediatric rheumatology [patients].’ Well, that may due to the adult providers not having received training in specific pediatric onset conditions. Communication between the pediatric and adult providers is key to a good transition experience for everyone. Trying to quickly build a new relationship with a new young adult patient to keep them engaged in their care and who has been used to the same pediatric provider for years is challenging, and the young adult and the adult provider need the pediatric provider’s support and availability to be a consultant to support the adult provider in the areas where they have little disease-specific experience.”
Dr. Jensen makes it a point to talk to his patients about health care transition in early adolescence, helps them set goals, and encourages them to “take more ownership in late adolescence for his or her own health: making their own appointments for follow-up visits, giving time to the patient in the room alone, and asking patients to maybe monitor medication adherence but not to lay the medications out for the patient in the morning,” he said. “When patients are given that opportunity, they may mature.”
Dr. Ronis, who is implementing a health care transition program at Children’s National Health System, thinks about health care transition as “a time where there’s risk for potentially worsening disease and negative outcomes due to perceived fragmentation of care. The more prepared we are and the more we prepare our patients to do this successfully, the better outcomes our patients will have.”
The Got Transition Center for Health Care Transition Improvement is funded by the Health Resources and Services Administration. The physicians interviewed for this story reported having no financial disclosures.
It’s been nearly 13 years since the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians released its Consensus Policy Statement on Health Care Transitions for Young Adults With Special Needs and 4 years since the AAP, AAFP, ACP Clinical Report: Supporting Health Care Transition (HCT) from Adolescence to Adulthood in the Medical Home was published, but formal adoption of suggested approaches has remained minimal.
A recent survey of 158 members of the Childhood Arthritis and Rheumatology Research Alliance in North America found that fewer than 10% of respondents were familiar with the consensus statement and the HCT clinical report, only 8% have a formal written transition policy, while 42% use an informal approach (J. Rheumatol. 2014;41:768-79). Respondents ranked fragmented adult health care and lack of time to provide sufficient services as the two major barriers to transition.
“Until recently, there hasn’t been a lot of focus on transition in fellowship training, and I don’t know how well the consensus policy statement and HCT clinical report are publicized in residency or fellowship training,” one of the study authors, Dr. Tova Ronis, said in an interview. “There’s definitely a role for more education about the policy statement and HCT clinical report.” As a result of inconsistent transition practices, some patients fall through the cracks in the transition from pediatric to adult rheumatology care. Transition can be difficult and even patients who receive transition care can have challenges, said Dr. Ronis of the pediatric rheumatology division at Children’s National Health System, Washington. She spoke of one young patient with severe systemic disease who was referred to ongoing adult care with an expert in the field. The patient “went to the adult office but didn’t like it there; she didn’t feel like she was being listened to and didn’t feel like the new doctor knew her well. She would come back to us, go back and forth, so her care became very fragmented. We communicated with the adult doctor but there wasn’t one person making the plan [of care].” In addition, other clinicians who had been providing subspecialty care and had not transitioned her to adult practice “were still at the children’s hospital, so when she experienced health problems or pain, she would come to the pediatric emergency department,” Dr. Ronis recalled. “She hadn’t identified the new institution as her medical home, so her care became very fragmented during that transition process. She actually missed some therapy because she didn’t like the new office, so wasn’t seen anywhere for a while.”
Dr. Paul T. Jensen said that most clinicians “have a gut feeling” that the current health care transition landscape has limitations, despite the availability of such tools as the Got Transition website, the Transition Readiness Assessment Questionnaire (TRAQ), as well as studies of novel approaches such as having a social worker serve as a transition coordinator(Pediatr. Rheumatol. 2015;13:17 [doi:10.1186/s12969-015-0013-0]) or having clinicians from adult practices see patients at a pediatric institution (Pediatr. Pulmonol. 2013;48:658-65). “I think that most, if not all, pediatric providers, including pediatric rheumatologists, worry about their patients as they get older, especially those who have a decreased maturity level,” said Dr. Jensen, who is a fellow in both adult and pediatric rheumatology at the Ohio State University Wexner Medical Center and Nationwide Children’s Hospital, Columbus. “But I think there’s a large lack of knowledge about what resources are available.”
Choosing transition practices that work for you
Dr. Patience White, a pediatric and adult rheumatologist who in 2011 coauthored the HCT Clinical Report, is familiar with such sentiment. She says that the topic of transition has “come to the forefront because the pediatric rheumatology field has grown. On top of that, many of our patients have grown up and moved on to other aspects of adulthood, so now pediatric providers will need to prepare to ‘let them go to adult health care.’ The perfect storm is happening.” Dr. White codirects the Got Transition Center for Health Care Transition Improvement, a federally funded program located at the National Alliance to Advance Adolescent Health. One of the center’s goals is to expand the use of the Six Core Elements of Health Care Transition that were developed to help make the 2011 Health Care Transitions Clinical Report actionable. These include practice quality improvement strategies such as establishing a transition policy, tracking progress, offering transition readiness assessments, creating a transition plan, transferring to an adult provider, and assessing the youth’s and family’s experience with the transition. The original Six Core Elements of Health Care Transition were tested in learning collaboratives across the United States and have been updated with input from the learning collaboratives and national transition experts into three separate packages of tools and evaluation approaches for transitioning youth to adult health care providers, transitioning to an adult approach to health care without changing providers, and integrating young adults into adult health care. For example, recommendations when transitioning youth to adult health care providers include developing a transition policy/statement “with input from youth and families that describes the practice’s approach to transition, including privacy and consent information,” as well as conducting regular transition readiness assessments, beginning at age 14 years, “to identify and discuss with youth and parent/caregiver their needs and goals in self-care.” Other tools available from the Got Transition website include a set of frequently asked transition questions developed by and for youth/young adults, as well as many transition resources.
While she acknowledged it may not be feasible for pediatric and adult rheumatologists to implement all Six Core Elements in their practice, Dr. White suggests providers might try implementing at least one or two and, for pediatric rheumatologists, start the discussion of the transition process when their patients reach the age of 13 years as recommended by the HCT clinical report. “Everybody says it’s hard, and I agree, changing practice processes to improve health care is hard work,” she said. “We know preparation for the youth and family needs to happen. We know transfer and communication has to occur, and that the accepting adult provider has to be informed and comfortable to make the transition process a success. It is about choosing one or two Six Core Element tools that can work for you, your practice, and your patients to help them through the transition process. If you’re an adult provider, you might choose to offer a welcome letter to my practice and a self-care assessment for the new young adult patients joining the practice so the adult health care provider can understand how proficient the young adults are with respect to their self-care skills and knowledge of the adult health care system.”
Disease-specific toolkits coming in 2016
Dr. White is also a consultant to the Pediatric to Adult Health Care Transitions Workgroup, an effort of the ACP Council of Subspecialty Societies to address gaps in care that exist with the transition of pediatric patients into adult health care. According to an ACP document describing the effort, the goal of workgroup is to identify “common tools/templates for a ‘general’ transition process, and subspecialty societies will utilize the templates to develop customized toolkits for specific diseases/conditions. The toolkits will then be collected and broadly disseminated,” with release targeted for May 2016 at the ACP national meeting. Dr. Stacy P. Ardoin, who is leading the rheumatology subspecialty group on behalf of the American College of Rheumatology, said the fact that this effort was initiated by the ACP “is great, because historically most of the interest in transition has bubbled up from the pediatric side. I think that adult providers are realizing more and more that patients who come to them with complex childhood onset conditions are challenging to manage, and that we really need to partner together to make things the best for our patients.”
Dr. Ardoin, a rheumatologist in the department of internal medicine at the Ohio State University Wexner Medical Center and in the department of pediatrics at Nationwide Children’s Hospital, characterized the final product as “not so much a definite protocol that everybody has to follow, but more just providing recommendations to the practitioner saying, ‘these are the things that we recommend and here are some tools to accomplish it.’ There’s such a lack of standardization for anything with transition despite the fact that we have consensus statements that have been put out in the past. Perhaps part of the problem is that they were too vague or not considered individually for each specialty. Hopefully, having each specialty take this on and look at their unique needs in the transition process will make people more willing to participate.”
Preparing patients to become health care self-advocates
Not all physicians are convinced that more recommendations will help clinicians navigate the intricacies of health care transition, however. “If children come to you as a physician at a young age (most of the kids with arthritis) or very ill (most of the children with systemic lupus erythematosus), good care over time represents a significant bonding experience,” said Dr. Thomas J. A. Lehman, chief of the division of pediatric rheumatology at the Hospital for Special Surgery in New York. “The children come to see you as a significant other in their life. If they then are suddenly ‘cast out’ because they reach a certain age it doesn’t go down any better than it would if a significant relative ‘cast them out.’ The doctors like to think they are transitioning the patients. The patients who have bonded feel they are being rejected. I don’t have an answer to this problem. However, none of the past HCT policy statements adequately recognize this aspect.”
For her part, Dr. White, who is also professor of medicine and pediatrics at George Washington University, Washington, said that in some published studies pediatric providers acknowledged that they are reluctant to transition patients to adult health care providers “and can overprotect their young patients as some parents do. This approach can result in the young adult being a poor self-advocate in the adult health care environment and not receiving developmentally appropriate health care. If a pediatric patient and family have not been informed of when they can no longer come to the pediatric rheumatology practice and have not discussed a transition to adult health care plan, they often assume they can stay with their pediatric rheumatologist forever.”
In addition, Dr. White continued, “some pediatric rheumatologists might say, ‘adult providers don’t know how to care for pediatric rheumatology [patients].’ Well, that may due to the adult providers not having received training in specific pediatric onset conditions. Communication between the pediatric and adult providers is key to a good transition experience for everyone. Trying to quickly build a new relationship with a new young adult patient to keep them engaged in their care and who has been used to the same pediatric provider for years is challenging, and the young adult and the adult provider need the pediatric provider’s support and availability to be a consultant to support the adult provider in the areas where they have little disease-specific experience.”
Dr. Jensen makes it a point to talk to his patients about health care transition in early adolescence, helps them set goals, and encourages them to “take more ownership in late adolescence for his or her own health: making their own appointments for follow-up visits, giving time to the patient in the room alone, and asking patients to maybe monitor medication adherence but not to lay the medications out for the patient in the morning,” he said. “When patients are given that opportunity, they may mature.”
Dr. Ronis, who is implementing a health care transition program at Children’s National Health System, thinks about health care transition as “a time where there’s risk for potentially worsening disease and negative outcomes due to perceived fragmentation of care. The more prepared we are and the more we prepare our patients to do this successfully, the better outcomes our patients will have.”
The Got Transition Center for Health Care Transition Improvement is funded by the Health Resources and Services Administration. The physicians interviewed for this story reported having no financial disclosures.
How CLL evades the immune system

Photo courtesy of
Monash University
A study published in Leukemia has revealed a mechanism by which chronic lymphocytic leukemia (CLL) evades the immune system.
“It turns out that cancer cells are very good at sabotaging the immune system, using various tricks that confuse immune cells and ‘smoke screens’ preventing immune cells from recognizing the cancer,” said study author Fabienne Mackay, PhD, of Monash University in Melbourne, Victoria, Australia.
She and her colleagues believe they have determined exactly how CLL confuses the immune system and devised a way to stop it without destroying the patient’s immune system.
The team noted that B cells rely on the protein BAFF to survive. And each B cell has 3 different kinds of receptors that detect the presence of BAFF in the blood—TACI, BAFF-R, and BCMA.
The researchers discovered that, in CLL patients, the TACI receptors of cancerous B cells over-produce interleukin-10 (IL-10), which tricks the immune system into thinking nothing is wrong, allowing CLL to thrive undetected.
“We found that, when the receptor called TACI was blocked, it prevented the secretion of IL-10 without eliminating normal B cells,” Dr Mackay said. “Without IL-10, the tumor can no longer keep the immune system at bay, which means the patient’s immune system can be ‘kick-started’ again to fight infections and cancers.”
“This is very exciting because it means that B cells stay alive and well to do their job in the immune system fighting other infections. It also means the over-production of IL-10 is stopped, and the CLL cells are now exposed to immune cells specialized in fighting cancers.”
Dr Mackay said her team’s discovery may be relevant for cancers other than CLL and could change the way they are treated.
“The best weapon we have for fighting cancer is the immune system itself,” Dr Mackay noted. “It can sense the presence of an infection but also the emergence of a cancer.” ![]()

Photo courtesy of
Monash University
A study published in Leukemia has revealed a mechanism by which chronic lymphocytic leukemia (CLL) evades the immune system.
“It turns out that cancer cells are very good at sabotaging the immune system, using various tricks that confuse immune cells and ‘smoke screens’ preventing immune cells from recognizing the cancer,” said study author Fabienne Mackay, PhD, of Monash University in Melbourne, Victoria, Australia.
She and her colleagues believe they have determined exactly how CLL confuses the immune system and devised a way to stop it without destroying the patient’s immune system.
The team noted that B cells rely on the protein BAFF to survive. And each B cell has 3 different kinds of receptors that detect the presence of BAFF in the blood—TACI, BAFF-R, and BCMA.
The researchers discovered that, in CLL patients, the TACI receptors of cancerous B cells over-produce interleukin-10 (IL-10), which tricks the immune system into thinking nothing is wrong, allowing CLL to thrive undetected.
“We found that, when the receptor called TACI was blocked, it prevented the secretion of IL-10 without eliminating normal B cells,” Dr Mackay said. “Without IL-10, the tumor can no longer keep the immune system at bay, which means the patient’s immune system can be ‘kick-started’ again to fight infections and cancers.”
“This is very exciting because it means that B cells stay alive and well to do their job in the immune system fighting other infections. It also means the over-production of IL-10 is stopped, and the CLL cells are now exposed to immune cells specialized in fighting cancers.”
Dr Mackay said her team’s discovery may be relevant for cancers other than CLL and could change the way they are treated.
“The best weapon we have for fighting cancer is the immune system itself,” Dr Mackay noted. “It can sense the presence of an infection but also the emergence of a cancer.” ![]()

Photo courtesy of
Monash University
A study published in Leukemia has revealed a mechanism by which chronic lymphocytic leukemia (CLL) evades the immune system.
“It turns out that cancer cells are very good at sabotaging the immune system, using various tricks that confuse immune cells and ‘smoke screens’ preventing immune cells from recognizing the cancer,” said study author Fabienne Mackay, PhD, of Monash University in Melbourne, Victoria, Australia.
She and her colleagues believe they have determined exactly how CLL confuses the immune system and devised a way to stop it without destroying the patient’s immune system.
The team noted that B cells rely on the protein BAFF to survive. And each B cell has 3 different kinds of receptors that detect the presence of BAFF in the blood—TACI, BAFF-R, and BCMA.
The researchers discovered that, in CLL patients, the TACI receptors of cancerous B cells over-produce interleukin-10 (IL-10), which tricks the immune system into thinking nothing is wrong, allowing CLL to thrive undetected.
“We found that, when the receptor called TACI was blocked, it prevented the secretion of IL-10 without eliminating normal B cells,” Dr Mackay said. “Without IL-10, the tumor can no longer keep the immune system at bay, which means the patient’s immune system can be ‘kick-started’ again to fight infections and cancers.”
“This is very exciting because it means that B cells stay alive and well to do their job in the immune system fighting other infections. It also means the over-production of IL-10 is stopped, and the CLL cells are now exposed to immune cells specialized in fighting cancers.”
Dr Mackay said her team’s discovery may be relevant for cancers other than CLL and could change the way they are treated.
“The best weapon we have for fighting cancer is the immune system itself,” Dr Mackay noted. “It can sense the presence of an infection but also the emergence of a cancer.” ![]()
FDA extends storage of platelets in plasma

Photo by Charles Haymond
The US Food and Drug Administration (FDA) has cleared a labeling change for the Terumo BCT Trima Accel Automated Blood Collection System.
The change means platelets in plasma that are collected via this system can now be stored for 7 days instead of 5, but the blood products must be tested for bacterial contamination.
The label change also allows for use of a wireless feature designed to enhance the mobility and flexibility of the system.
The Trima Accel system includes the Trima Accel device, a tubing set, and Trima Accel software. The system uses a centrifuge to separate whole blood into platelets, plasma, and red blood cells. It then collects the components based on customer-configured priorities and the donor’s physiology and blood count.
Platelet storage
The FDA is now allowing platelets in 100% plasma that are collected via the Trima Accel system to be stored for up to 7 days post-collection. But platelets in isoplate solution can only be stored for up to 5 days.
For platelet storage up to 7 days, the FDA requires that every product be tested with a bacterial detection device cleared by the FDA and labeled as a “safety measure.”
Wireless feature
The newly cleared wireless feature connects the Trima Accel system to software applications such as the Cadence Data Collection System or the Vista Information System through the blood center’s or hospital’s existing wireless network.
This enables access to electronic donor information and reporting capabilities, with the goals of streamlining collections, simplifying data management, and allowing operators to focus on donor care, even when a wired connection is unavailable.
The wireless feature enables blood centers to either purchase a compatible wireless appliance from Terumo BCT or choose an appliance of their own for attachment to the Trima Accel system using a mounting bracket on the back of the system. ![]()

Photo by Charles Haymond
The US Food and Drug Administration (FDA) has cleared a labeling change for the Terumo BCT Trima Accel Automated Blood Collection System.
The change means platelets in plasma that are collected via this system can now be stored for 7 days instead of 5, but the blood products must be tested for bacterial contamination.
The label change also allows for use of a wireless feature designed to enhance the mobility and flexibility of the system.
The Trima Accel system includes the Trima Accel device, a tubing set, and Trima Accel software. The system uses a centrifuge to separate whole blood into platelets, plasma, and red blood cells. It then collects the components based on customer-configured priorities and the donor’s physiology and blood count.
Platelet storage
The FDA is now allowing platelets in 100% plasma that are collected via the Trima Accel system to be stored for up to 7 days post-collection. But platelets in isoplate solution can only be stored for up to 5 days.
For platelet storage up to 7 days, the FDA requires that every product be tested with a bacterial detection device cleared by the FDA and labeled as a “safety measure.”
Wireless feature
The newly cleared wireless feature connects the Trima Accel system to software applications such as the Cadence Data Collection System or the Vista Information System through the blood center’s or hospital’s existing wireless network.
This enables access to electronic donor information and reporting capabilities, with the goals of streamlining collections, simplifying data management, and allowing operators to focus on donor care, even when a wired connection is unavailable.
The wireless feature enables blood centers to either purchase a compatible wireless appliance from Terumo BCT or choose an appliance of their own for attachment to the Trima Accel system using a mounting bracket on the back of the system. ![]()

Photo by Charles Haymond
The US Food and Drug Administration (FDA) has cleared a labeling change for the Terumo BCT Trima Accel Automated Blood Collection System.
The change means platelets in plasma that are collected via this system can now be stored for 7 days instead of 5, but the blood products must be tested for bacterial contamination.
The label change also allows for use of a wireless feature designed to enhance the mobility and flexibility of the system.
The Trima Accel system includes the Trima Accel device, a tubing set, and Trima Accel software. The system uses a centrifuge to separate whole blood into platelets, plasma, and red blood cells. It then collects the components based on customer-configured priorities and the donor’s physiology and blood count.
Platelet storage
The FDA is now allowing platelets in 100% plasma that are collected via the Trima Accel system to be stored for up to 7 days post-collection. But platelets in isoplate solution can only be stored for up to 5 days.
For platelet storage up to 7 days, the FDA requires that every product be tested with a bacterial detection device cleared by the FDA and labeled as a “safety measure.”
Wireless feature
The newly cleared wireless feature connects the Trima Accel system to software applications such as the Cadence Data Collection System or the Vista Information System through the blood center’s or hospital’s existing wireless network.
This enables access to electronic donor information and reporting capabilities, with the goals of streamlining collections, simplifying data management, and allowing operators to focus on donor care, even when a wired connection is unavailable.
The wireless feature enables blood centers to either purchase a compatible wireless appliance from Terumo BCT or choose an appliance of their own for attachment to the Trima Accel system using a mounting bracket on the back of the system. ![]()