User login
Pandemic restrictions ignite innovative pivot for psychiatry
As medical school faculty members – and our students – know well, the COVID-19 pandemic forced us to become creative and shift much of our curricula online. Many hospitals chose to limit medical student rotations because of safety concerns. Students fell victim to canceled psychiatry rotations and electives during the pandemic’s early days. Privacy issues, combined with stigma tied to mental illness, made this shift to virtual instruction particularly challenging. But as a field, we persevered! And, as we learned during our shift toward telemedicine, many of the changes we made in medical education are probably here to stay.
Our team at the New York Institute of Technology College of Osteopathic Medicine (NYITCOM) was able to implement a novel curriculum that allowed our students to learn psychiatry and maintain high-quality medical school education.
We developed an online course for third-year students’ rotation in psychiatry, with several modules that focused on a variety of psychiatric topics and disorders, including the basic classifications and categories of depression, anxiety, personality disorders, and psychotic disorders. There were also video encounters available showing actual patient encounters. On completion of the online module, a faculty session was held to discuss topics of concern/confusion to the students, areas of interest, and a variety of related topics, such as professionalism in psychiatry, essentials of the mental status exam, management of diverse populations, and COVID repercussions in psychiatry.
For fourth-year students, we developed a telemedicine psychiatry elective, which allowed the students to observe psychiatric evaluations, psychiatric medication review visits, and even follow-up psychotherapy sessions, with the school’s clinical psychologists. The new method was minimally invasive, and it was accepted by patients and welcomed by the students.
During a time when hospitals were limiting onsite student rotations and discouraging patient contact, medical students still needed to experience patient interactions. As the director of the school’s Center for Behavioral Health, I designed an additional program that allowed students to participate in observing patients who presented with psychiatric complaints and symptoms. It had to be confidential in nature, accessible, and safe.
I recalled my own training in a hospital setting, where students and residents were allowed to observe a patient being evaluated by an attending, through a one-way mirror. It was a method that was acceptable at the time in a hospital, but unfortunately, not in a private office setting. As such, students and residents experienced such an interaction in acute inpatient and/or outpatient clinics of a hospital. The experience was invaluable.
The concept was simple, yet very efficient. The clinicians in the Center for Behavioral Health were seeing all patients with psychiatric needs via a HIPAA-compliant telemedicine platform. Access was granted for students – with the patient’s consent – and they “entered the session” without being seen or heard. This presented little to no distraction to the patient, and the student was able to observe a range of clinical sessions.
The course also provided online supplemental modules, including essential psychiatric topics, psychopharmacology, and a psychotherapeutic module that discussed a myriad of therapeutic interventions. In addition, the student was supervised weekly by the course director, the psychopharmacologist, and the clinical psychologist. The course director provided daily wrap-up reviews as well.
Originally, this new approach was envisioned as a temporary solution for use during the pandemic. But it has become clear that this approach would be beneficial post pandemic as well. Most of the students who participated in the course were actually interested in pursuing psychiatry as their future specialty. It allowed them to observe a population of patients firsthand that they might encounter in private practice, as opposed to only hospital settings.
Being present in a session with a patient with psychiatric symptoms and diagnoses has always been a challenge. Many patients refuse to have another medical professional in the room because of the intimate details being discussed and their associated stigma. The patients’ inability to see or hear the student during the sessions allows them to ignore the students’ presence – or at least not be intimidated by it. This, therefore, allows the students access and affords them a unique and memorable educational experience.
The pandemic curtailed and altered medical students’ traditional exposure to patients, but we found innovative ways to redefine it. As difficult as COVID-19 has been for the health care community, we have been able to use the restrictions forced by the pandemic to identify innovative ways to improve the education of our medical students.
In addition to serving as director of the Center for Behavioral Health at NYITCOM in Old Westbury, N.Y., Dr. Jarkon is assistant professor in the department of family medicine. She has no disclosures.
As medical school faculty members – and our students – know well, the COVID-19 pandemic forced us to become creative and shift much of our curricula online. Many hospitals chose to limit medical student rotations because of safety concerns. Students fell victim to canceled psychiatry rotations and electives during the pandemic’s early days. Privacy issues, combined with stigma tied to mental illness, made this shift to virtual instruction particularly challenging. But as a field, we persevered! And, as we learned during our shift toward telemedicine, many of the changes we made in medical education are probably here to stay.
Our team at the New York Institute of Technology College of Osteopathic Medicine (NYITCOM) was able to implement a novel curriculum that allowed our students to learn psychiatry and maintain high-quality medical school education.
We developed an online course for third-year students’ rotation in psychiatry, with several modules that focused on a variety of psychiatric topics and disorders, including the basic classifications and categories of depression, anxiety, personality disorders, and psychotic disorders. There were also video encounters available showing actual patient encounters. On completion of the online module, a faculty session was held to discuss topics of concern/confusion to the students, areas of interest, and a variety of related topics, such as professionalism in psychiatry, essentials of the mental status exam, management of diverse populations, and COVID repercussions in psychiatry.
For fourth-year students, we developed a telemedicine psychiatry elective, which allowed the students to observe psychiatric evaluations, psychiatric medication review visits, and even follow-up psychotherapy sessions, with the school’s clinical psychologists. The new method was minimally invasive, and it was accepted by patients and welcomed by the students.
During a time when hospitals were limiting onsite student rotations and discouraging patient contact, medical students still needed to experience patient interactions. As the director of the school’s Center for Behavioral Health, I designed an additional program that allowed students to participate in observing patients who presented with psychiatric complaints and symptoms. It had to be confidential in nature, accessible, and safe.
I recalled my own training in a hospital setting, where students and residents were allowed to observe a patient being evaluated by an attending, through a one-way mirror. It was a method that was acceptable at the time in a hospital, but unfortunately, not in a private office setting. As such, students and residents experienced such an interaction in acute inpatient and/or outpatient clinics of a hospital. The experience was invaluable.
The concept was simple, yet very efficient. The clinicians in the Center for Behavioral Health were seeing all patients with psychiatric needs via a HIPAA-compliant telemedicine platform. Access was granted for students – with the patient’s consent – and they “entered the session” without being seen or heard. This presented little to no distraction to the patient, and the student was able to observe a range of clinical sessions.
The course also provided online supplemental modules, including essential psychiatric topics, psychopharmacology, and a psychotherapeutic module that discussed a myriad of therapeutic interventions. In addition, the student was supervised weekly by the course director, the psychopharmacologist, and the clinical psychologist. The course director provided daily wrap-up reviews as well.
Originally, this new approach was envisioned as a temporary solution for use during the pandemic. But it has become clear that this approach would be beneficial post pandemic as well. Most of the students who participated in the course were actually interested in pursuing psychiatry as their future specialty. It allowed them to observe a population of patients firsthand that they might encounter in private practice, as opposed to only hospital settings.
Being present in a session with a patient with psychiatric symptoms and diagnoses has always been a challenge. Many patients refuse to have another medical professional in the room because of the intimate details being discussed and their associated stigma. The patients’ inability to see or hear the student during the sessions allows them to ignore the students’ presence – or at least not be intimidated by it. This, therefore, allows the students access and affords them a unique and memorable educational experience.
The pandemic curtailed and altered medical students’ traditional exposure to patients, but we found innovative ways to redefine it. As difficult as COVID-19 has been for the health care community, we have been able to use the restrictions forced by the pandemic to identify innovative ways to improve the education of our medical students.
In addition to serving as director of the Center for Behavioral Health at NYITCOM in Old Westbury, N.Y., Dr. Jarkon is assistant professor in the department of family medicine. She has no disclosures.
As medical school faculty members – and our students – know well, the COVID-19 pandemic forced us to become creative and shift much of our curricula online. Many hospitals chose to limit medical student rotations because of safety concerns. Students fell victim to canceled psychiatry rotations and electives during the pandemic’s early days. Privacy issues, combined with stigma tied to mental illness, made this shift to virtual instruction particularly challenging. But as a field, we persevered! And, as we learned during our shift toward telemedicine, many of the changes we made in medical education are probably here to stay.
Our team at the New York Institute of Technology College of Osteopathic Medicine (NYITCOM) was able to implement a novel curriculum that allowed our students to learn psychiatry and maintain high-quality medical school education.
We developed an online course for third-year students’ rotation in psychiatry, with several modules that focused on a variety of psychiatric topics and disorders, including the basic classifications and categories of depression, anxiety, personality disorders, and psychotic disorders. There were also video encounters available showing actual patient encounters. On completion of the online module, a faculty session was held to discuss topics of concern/confusion to the students, areas of interest, and a variety of related topics, such as professionalism in psychiatry, essentials of the mental status exam, management of diverse populations, and COVID repercussions in psychiatry.
For fourth-year students, we developed a telemedicine psychiatry elective, which allowed the students to observe psychiatric evaluations, psychiatric medication review visits, and even follow-up psychotherapy sessions, with the school’s clinical psychologists. The new method was minimally invasive, and it was accepted by patients and welcomed by the students.
During a time when hospitals were limiting onsite student rotations and discouraging patient contact, medical students still needed to experience patient interactions. As the director of the school’s Center for Behavioral Health, I designed an additional program that allowed students to participate in observing patients who presented with psychiatric complaints and symptoms. It had to be confidential in nature, accessible, and safe.
I recalled my own training in a hospital setting, where students and residents were allowed to observe a patient being evaluated by an attending, through a one-way mirror. It was a method that was acceptable at the time in a hospital, but unfortunately, not in a private office setting. As such, students and residents experienced such an interaction in acute inpatient and/or outpatient clinics of a hospital. The experience was invaluable.
The concept was simple, yet very efficient. The clinicians in the Center for Behavioral Health were seeing all patients with psychiatric needs via a HIPAA-compliant telemedicine platform. Access was granted for students – with the patient’s consent – and they “entered the session” without being seen or heard. This presented little to no distraction to the patient, and the student was able to observe a range of clinical sessions.
The course also provided online supplemental modules, including essential psychiatric topics, psychopharmacology, and a psychotherapeutic module that discussed a myriad of therapeutic interventions. In addition, the student was supervised weekly by the course director, the psychopharmacologist, and the clinical psychologist. The course director provided daily wrap-up reviews as well.
Originally, this new approach was envisioned as a temporary solution for use during the pandemic. But it has become clear that this approach would be beneficial post pandemic as well. Most of the students who participated in the course were actually interested in pursuing psychiatry as their future specialty. It allowed them to observe a population of patients firsthand that they might encounter in private practice, as opposed to only hospital settings.
Being present in a session with a patient with psychiatric symptoms and diagnoses has always been a challenge. Many patients refuse to have another medical professional in the room because of the intimate details being discussed and their associated stigma. The patients’ inability to see or hear the student during the sessions allows them to ignore the students’ presence – or at least not be intimidated by it. This, therefore, allows the students access and affords them a unique and memorable educational experience.
The pandemic curtailed and altered medical students’ traditional exposure to patients, but we found innovative ways to redefine it. As difficult as COVID-19 has been for the health care community, we have been able to use the restrictions forced by the pandemic to identify innovative ways to improve the education of our medical students.
In addition to serving as director of the Center for Behavioral Health at NYITCOM in Old Westbury, N.Y., Dr. Jarkon is assistant professor in the department of family medicine. She has no disclosures.
Should I get a COVID-19 booster shot?
When I was in Florida a few weeks ago, I met a friend outside who approached me wearing an N-95 mask. He said he was wearing it because the Delta variant was running wild in Florida, and several of his younger unvaccinated employees had contracted it, and he encouraged me to get a COVID booster shot. In the late summer, although the federal government recommended booster shots for anyone 8 months after their original vaccination series, national confusion still reigns, with an Food and Drug Administration advisory panel more recently recommending against a Pfizer booster for all adults, but supporting a booster for those ages 65 and older or at a high risk for severe COVID-19.
At the end of December, I was excited when the local hospital whose staff I am on made the Moderna vaccine available. I had to wait several hours but it was worth it, and I did not care about the low-grade fever and malaise I experienced after the second dose. Astoundingly, I still have patients who have not been vaccinated, although many of them are elderly, frail, or immunocompromised. I think people who publicly argue against vaccination need to visit their local intensive care unit.
While less so than some other physicians, – and you must lean in to see anything. We take all reasonable precautions, wearing masks, wiping down exam rooms and door handles, keeping the waiting room as empty as possible, using HEPA filters, and keeping exhaust fans going in the rooms continuously. My staff have all been vaccinated (I’m lucky there).
Still, if you are seeing 30 or 40 patients a day of all age groups and working in small unventilated rooms, you could be exposed to the Delta variant. While breakthrough infections among fully vaccinated immunocompetent individuals may be rare, if you do develop a breakthrough case, even if mild or asymptomatic, CDC recommendations include quarantining for at least 10 days. Obviously, this can be disastrous to your practice as a COVID infection works through your office.
This brings us to back to booster shots. Personally, I think all health care workers should be eager to get a booster shot. I also think individuals who have wide public exposure, particularly indoors, such as teachers and retail sales workers, should be eager to get one too. Here are some of the pros, as well as some cons for boosters.
Arguments for booster shots
- Booster shots should elevate your antibody levels and make you more resistant to breakthrough infections, but this is still theoretical. Antibody levels decline over time – more rapidly in those over 56 years of age.
- Vaccine doses go to waste every month in the United States, although specific numbers are lacking.
- Vaccinated individuals almost never get hospitalized and die from COVID, presumably even fewer do so after receiving a booster.
- You could unwittingly become a vector. Many of the breakthrough infections are mild and without symptoms. If you do test positive, it could be devastating to your patients, and your medical practice.
Arguments against booster shots
- These vaccine doses should be going to other countries that have low vaccination levels where many of the nasty variants are developing.
- You may have side effects from the vaccine, though thrombosis has only been seen with the Astra-Zeneca and Johnson and Johnson vaccines. Myocarditis is usually seen in younger patients and is almost always self limited.
- Breakthrough infections are rare.
This COVID pandemic is moving and changing so fast, it is bewildering. But with a little luck, COVID could eventually become an annual nuisance like the flu, and the COVID vaccine will become an annual shot based on the newest mutations. For now, my opinion is, get your booster shot.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
When I was in Florida a few weeks ago, I met a friend outside who approached me wearing an N-95 mask. He said he was wearing it because the Delta variant was running wild in Florida, and several of his younger unvaccinated employees had contracted it, and he encouraged me to get a COVID booster shot. In the late summer, although the federal government recommended booster shots for anyone 8 months after their original vaccination series, national confusion still reigns, with an Food and Drug Administration advisory panel more recently recommending against a Pfizer booster for all adults, but supporting a booster for those ages 65 and older or at a high risk for severe COVID-19.
At the end of December, I was excited when the local hospital whose staff I am on made the Moderna vaccine available. I had to wait several hours but it was worth it, and I did not care about the low-grade fever and malaise I experienced after the second dose. Astoundingly, I still have patients who have not been vaccinated, although many of them are elderly, frail, or immunocompromised. I think people who publicly argue against vaccination need to visit their local intensive care unit.
While less so than some other physicians, – and you must lean in to see anything. We take all reasonable precautions, wearing masks, wiping down exam rooms and door handles, keeping the waiting room as empty as possible, using HEPA filters, and keeping exhaust fans going in the rooms continuously. My staff have all been vaccinated (I’m lucky there).
Still, if you are seeing 30 or 40 patients a day of all age groups and working in small unventilated rooms, you could be exposed to the Delta variant. While breakthrough infections among fully vaccinated immunocompetent individuals may be rare, if you do develop a breakthrough case, even if mild or asymptomatic, CDC recommendations include quarantining for at least 10 days. Obviously, this can be disastrous to your practice as a COVID infection works through your office.
This brings us to back to booster shots. Personally, I think all health care workers should be eager to get a booster shot. I also think individuals who have wide public exposure, particularly indoors, such as teachers and retail sales workers, should be eager to get one too. Here are some of the pros, as well as some cons for boosters.
Arguments for booster shots
- Booster shots should elevate your antibody levels and make you more resistant to breakthrough infections, but this is still theoretical. Antibody levels decline over time – more rapidly in those over 56 years of age.
- Vaccine doses go to waste every month in the United States, although specific numbers are lacking.
- Vaccinated individuals almost never get hospitalized and die from COVID, presumably even fewer do so after receiving a booster.
- You could unwittingly become a vector. Many of the breakthrough infections are mild and without symptoms. If you do test positive, it could be devastating to your patients, and your medical practice.
Arguments against booster shots
- These vaccine doses should be going to other countries that have low vaccination levels where many of the nasty variants are developing.
- You may have side effects from the vaccine, though thrombosis has only been seen with the Astra-Zeneca and Johnson and Johnson vaccines. Myocarditis is usually seen in younger patients and is almost always self limited.
- Breakthrough infections are rare.
This COVID pandemic is moving and changing so fast, it is bewildering. But with a little luck, COVID could eventually become an annual nuisance like the flu, and the COVID vaccine will become an annual shot based on the newest mutations. For now, my opinion is, get your booster shot.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
When I was in Florida a few weeks ago, I met a friend outside who approached me wearing an N-95 mask. He said he was wearing it because the Delta variant was running wild in Florida, and several of his younger unvaccinated employees had contracted it, and he encouraged me to get a COVID booster shot. In the late summer, although the federal government recommended booster shots for anyone 8 months after their original vaccination series, national confusion still reigns, with an Food and Drug Administration advisory panel more recently recommending against a Pfizer booster for all adults, but supporting a booster for those ages 65 and older or at a high risk for severe COVID-19.
At the end of December, I was excited when the local hospital whose staff I am on made the Moderna vaccine available. I had to wait several hours but it was worth it, and I did not care about the low-grade fever and malaise I experienced after the second dose. Astoundingly, I still have patients who have not been vaccinated, although many of them are elderly, frail, or immunocompromised. I think people who publicly argue against vaccination need to visit their local intensive care unit.
While less so than some other physicians, – and you must lean in to see anything. We take all reasonable precautions, wearing masks, wiping down exam rooms and door handles, keeping the waiting room as empty as possible, using HEPA filters, and keeping exhaust fans going in the rooms continuously. My staff have all been vaccinated (I’m lucky there).
Still, if you are seeing 30 or 40 patients a day of all age groups and working in small unventilated rooms, you could be exposed to the Delta variant. While breakthrough infections among fully vaccinated immunocompetent individuals may be rare, if you do develop a breakthrough case, even if mild or asymptomatic, CDC recommendations include quarantining for at least 10 days. Obviously, this can be disastrous to your practice as a COVID infection works through your office.
This brings us to back to booster shots. Personally, I think all health care workers should be eager to get a booster shot. I also think individuals who have wide public exposure, particularly indoors, such as teachers and retail sales workers, should be eager to get one too. Here are some of the pros, as well as some cons for boosters.
Arguments for booster shots
- Booster shots should elevate your antibody levels and make you more resistant to breakthrough infections, but this is still theoretical. Antibody levels decline over time – more rapidly in those over 56 years of age.
- Vaccine doses go to waste every month in the United States, although specific numbers are lacking.
- Vaccinated individuals almost never get hospitalized and die from COVID, presumably even fewer do so after receiving a booster.
- You could unwittingly become a vector. Many of the breakthrough infections are mild and without symptoms. If you do test positive, it could be devastating to your patients, and your medical practice.
Arguments against booster shots
- These vaccine doses should be going to other countries that have low vaccination levels where many of the nasty variants are developing.
- You may have side effects from the vaccine, though thrombosis has only been seen with the Astra-Zeneca and Johnson and Johnson vaccines. Myocarditis is usually seen in younger patients and is almost always self limited.
- Breakthrough infections are rare.
This COVID pandemic is moving and changing so fast, it is bewildering. But with a little luck, COVID could eventually become an annual nuisance like the flu, and the COVID vaccine will become an annual shot based on the newest mutations. For now, my opinion is, get your booster shot.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
Noise in medicine
A 26-year-old woman who reports a history of acyclovir-resistant herpes complains of a recurring, stinging rash around her mouth. Topical tacrolimus made it worse, she said. On exam, she has somewhat grouped pustules on her cutaneous lip. I mentioned her to colleagues, saying: “I’ve a patient with acyclovir-resistant herpes who isn’t improving on high-dose Valtrex.” They proffered a few alternative diagnoses and treatment recommendations. I tried several to no avail.
(it is after all only one condition). Nobel Prize–winning economist Daniel Kahneman, PhD, with two other authors, has written a brilliant book about this cognitive unreliability called “Noise: A Flaw in Human Judgment” (New York: Hachette Book Group, 2021).
Both bias and noise create trouble for us. Although biases get more attention, noise is both more prevalent and insidious. In a 2016 article, Dr. Kahneman and coauthors use a bathroom scale as an analogy to explain the difference. “We would say that the scale is biased if its readings are generally either too high or too low. A scale that consistently underestimates true weight by exactly 4 pounds is seriously biased but free of noise. A scale that gives two different readings when you step on it twice is noisy.” In the case presented, “measurements” by me and my colleagues were returning different “readings.” There is one true diagnosis and best treatment, yet because of noise, we waste time and resources by not getting it right the first time.
There is also evidence of bias in this case. For example, there’s probably some confirmation bias: The patient said she has a history of antiviral-resistant herpes; therefore, her rash might appear to be herpes. Also there might be salience bias: it’s easy to see how prominent pustules might be herpes simplex virus. Noise is an issue in many misdiagnoses, but trickier to see. In most instances, we don’t have the opportunity to get multiple assessments of the same case. When examined though, interrater reliability in medicine is often found to be shockingly low, an indication of how much noise there is in our clinical judgments. This leads to waste, frustration – and can even be dangerous when we’re trying to diagnose cancers such as melanoma, lung, or breast cancer.
Dr. Kahneman and colleagues have excellent recommendations on how to reduce noise, such as tips for good decision hygiene (e.g., using differential diagnoses) and using algorithms (e.g., calculating Apgar or LACE scores). I also liked their strategy of aggregating expert opinions. Fascinatingly, averaging multiple independent assessments is mathematically guaranteed to reduce noise. (God, I love economists). This is true of measurements and opinions: If you use 100 judgments for a case, you reduce noise by 90% (the noise is divided by the square root of the number of judgments averaged). So 20 colleagues’ opinions would reduce noise by almost 80%. However, those 20 opinions must be independent to avoid spurious agreement. (Again, math for the win.)
I showed photos of my patient to a few other dermatologists. They independently returned the same result: perioral dermatitis. This was the correct diagnosis and reminded me why grand rounds and tumor boards are such a great help. Multiple, independent assessments are more likely to get it right than just one opinion because we are canceling out the noise. But remember, grand rounds has to be old-school style – no looking at your coresident answers before giving yours!
Our patient cleared after restarting her topical tacrolimus and a bit of doxycycline. Credit the wisdom of the crowd. Reassuringly though, Dr. Kahneman also shows that expertise does matter in minimizing error. So that fellowship you did was still a great idea.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. He reports having no conflicts of interest. Write to him at dermnews@mdedge.com.
A 26-year-old woman who reports a history of acyclovir-resistant herpes complains of a recurring, stinging rash around her mouth. Topical tacrolimus made it worse, she said. On exam, she has somewhat grouped pustules on her cutaneous lip. I mentioned her to colleagues, saying: “I’ve a patient with acyclovir-resistant herpes who isn’t improving on high-dose Valtrex.” They proffered a few alternative diagnoses and treatment recommendations. I tried several to no avail.
(it is after all only one condition). Nobel Prize–winning economist Daniel Kahneman, PhD, with two other authors, has written a brilliant book about this cognitive unreliability called “Noise: A Flaw in Human Judgment” (New York: Hachette Book Group, 2021).
Both bias and noise create trouble for us. Although biases get more attention, noise is both more prevalent and insidious. In a 2016 article, Dr. Kahneman and coauthors use a bathroom scale as an analogy to explain the difference. “We would say that the scale is biased if its readings are generally either too high or too low. A scale that consistently underestimates true weight by exactly 4 pounds is seriously biased but free of noise. A scale that gives two different readings when you step on it twice is noisy.” In the case presented, “measurements” by me and my colleagues were returning different “readings.” There is one true diagnosis and best treatment, yet because of noise, we waste time and resources by not getting it right the first time.
There is also evidence of bias in this case. For example, there’s probably some confirmation bias: The patient said she has a history of antiviral-resistant herpes; therefore, her rash might appear to be herpes. Also there might be salience bias: it’s easy to see how prominent pustules might be herpes simplex virus. Noise is an issue in many misdiagnoses, but trickier to see. In most instances, we don’t have the opportunity to get multiple assessments of the same case. When examined though, interrater reliability in medicine is often found to be shockingly low, an indication of how much noise there is in our clinical judgments. This leads to waste, frustration – and can even be dangerous when we’re trying to diagnose cancers such as melanoma, lung, or breast cancer.
Dr. Kahneman and colleagues have excellent recommendations on how to reduce noise, such as tips for good decision hygiene (e.g., using differential diagnoses) and using algorithms (e.g., calculating Apgar or LACE scores). I also liked their strategy of aggregating expert opinions. Fascinatingly, averaging multiple independent assessments is mathematically guaranteed to reduce noise. (God, I love economists). This is true of measurements and opinions: If you use 100 judgments for a case, you reduce noise by 90% (the noise is divided by the square root of the number of judgments averaged). So 20 colleagues’ opinions would reduce noise by almost 80%. However, those 20 opinions must be independent to avoid spurious agreement. (Again, math for the win.)
I showed photos of my patient to a few other dermatologists. They independently returned the same result: perioral dermatitis. This was the correct diagnosis and reminded me why grand rounds and tumor boards are such a great help. Multiple, independent assessments are more likely to get it right than just one opinion because we are canceling out the noise. But remember, grand rounds has to be old-school style – no looking at your coresident answers before giving yours!
Our patient cleared after restarting her topical tacrolimus and a bit of doxycycline. Credit the wisdom of the crowd. Reassuringly though, Dr. Kahneman also shows that expertise does matter in minimizing error. So that fellowship you did was still a great idea.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. He reports having no conflicts of interest. Write to him at dermnews@mdedge.com.
A 26-year-old woman who reports a history of acyclovir-resistant herpes complains of a recurring, stinging rash around her mouth. Topical tacrolimus made it worse, she said. On exam, she has somewhat grouped pustules on her cutaneous lip. I mentioned her to colleagues, saying: “I’ve a patient with acyclovir-resistant herpes who isn’t improving on high-dose Valtrex.” They proffered a few alternative diagnoses and treatment recommendations. I tried several to no avail.
(it is after all only one condition). Nobel Prize–winning economist Daniel Kahneman, PhD, with two other authors, has written a brilliant book about this cognitive unreliability called “Noise: A Flaw in Human Judgment” (New York: Hachette Book Group, 2021).
Both bias and noise create trouble for us. Although biases get more attention, noise is both more prevalent and insidious. In a 2016 article, Dr. Kahneman and coauthors use a bathroom scale as an analogy to explain the difference. “We would say that the scale is biased if its readings are generally either too high or too low. A scale that consistently underestimates true weight by exactly 4 pounds is seriously biased but free of noise. A scale that gives two different readings when you step on it twice is noisy.” In the case presented, “measurements” by me and my colleagues were returning different “readings.” There is one true diagnosis and best treatment, yet because of noise, we waste time and resources by not getting it right the first time.
There is also evidence of bias in this case. For example, there’s probably some confirmation bias: The patient said she has a history of antiviral-resistant herpes; therefore, her rash might appear to be herpes. Also there might be salience bias: it’s easy to see how prominent pustules might be herpes simplex virus. Noise is an issue in many misdiagnoses, but trickier to see. In most instances, we don’t have the opportunity to get multiple assessments of the same case. When examined though, interrater reliability in medicine is often found to be shockingly low, an indication of how much noise there is in our clinical judgments. This leads to waste, frustration – and can even be dangerous when we’re trying to diagnose cancers such as melanoma, lung, or breast cancer.
Dr. Kahneman and colleagues have excellent recommendations on how to reduce noise, such as tips for good decision hygiene (e.g., using differential diagnoses) and using algorithms (e.g., calculating Apgar or LACE scores). I also liked their strategy of aggregating expert opinions. Fascinatingly, averaging multiple independent assessments is mathematically guaranteed to reduce noise. (God, I love economists). This is true of measurements and opinions: If you use 100 judgments for a case, you reduce noise by 90% (the noise is divided by the square root of the number of judgments averaged). So 20 colleagues’ opinions would reduce noise by almost 80%. However, those 20 opinions must be independent to avoid spurious agreement. (Again, math for the win.)
I showed photos of my patient to a few other dermatologists. They independently returned the same result: perioral dermatitis. This was the correct diagnosis and reminded me why grand rounds and tumor boards are such a great help. Multiple, independent assessments are more likely to get it right than just one opinion because we are canceling out the noise. But remember, grand rounds has to be old-school style – no looking at your coresident answers before giving yours!
Our patient cleared after restarting her topical tacrolimus and a bit of doxycycline. Credit the wisdom of the crowd. Reassuringly though, Dr. Kahneman also shows that expertise does matter in minimizing error. So that fellowship you did was still a great idea.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. He reports having no conflicts of interest. Write to him at dermnews@mdedge.com.
Adolescent immunizations and protecting our children from COVID-19
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)

It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)

It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)

It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Expert advice
I once answered online skin questions. The most popular one was, “Is my penis supposed to look like that?”
Then the site was bought by an entrepreneur with a corporate sensibility. He opened two forums: for 15 bucks, you could access the Medical Forum and ask a doctor. For 10, you could join the Community Forum and ask anybody with an opinion. One guess about which forum was more popular.
Years later, a colleague referred a fellow who had run a poison ivy website for a decade and wanted to interview a doctor. He had never spoken with one before, “because it never occurred to me.” His site featured the usual folklore: that blister fluid spreads the poison, that you can catch it from your dog. His website had many pictures. Some were in focus, and a few actually showed poison ivy.
I checked a year later and found that he had never uploaded our interview to his website. When I emailed to ask how come, he said he’d been busy, and did I want him to? I told him I was OK.
What made me think of these old episodes was a phone chat I had the other day with an IT guy about my laptop.
After I told him my problem, he said, “Since you’re a doctor, could I ask you a medical question?”
“Sure.”
“Is the COVID vaccine safe?” he asked.
“I had two shots myself,” I said, “and I’m planning a third. Does that tell you what I think about how safe it is?”
He didn’t answer, and we got back to the laptop.
Five minutes later he said, “I just wonder whether we should mess with vaccines. Maybe we should let nature take its course.”
“How about polio and diphtheria?” I said. “Should we let nature take its course with them?”
He thought for a moment and said, “If you don’t get vaccinated, can you spread the virus to other people?”
“Yes, you can,” I said. “It’s not just that you can get sick, but you can make other people sick, and possibly die if they’re old or vulnerable.”
Again, no response. We finished up with the laptop.
“Thanks for your medical advice,” he said. “I get conflicting information from so many sources.”
Yes, he does. He and everybody else always have. When the issues are poison ivy and genital blotchiness, the stakes are not high enough for anyone to talk about. To a large extent, people have always made their minds up about things based on what their friends think and tell them.
If your friends all wear masks, they will stare at you if you don’t. If your friends don’t wear masks, they will stare at you if you do. Or more than that. Very few people like to be stared at. Or worse.
or another: social media disinformation, distrust of the establishment, personal freedom. When the stakes are low, no reasons are needed. Who cares why someone blames Fido for his poison ivy?
Addressing the reasons people give for their positions, or the reasons others assign to them, may sometimes help people reconsider. For all those other times, the old adage applies: You cannot reason someone out of what he never reasoned himself into.
When it comes to contact dermatitis or penile blotches, you can try to straighten people out, but it doesn’t matter much if you fail. When the people you are trying to convince are spreading disease, filling up ICUs, or dying, it matters a great deal, which does not necessarily increase your odds of succeeding.
There have always been “Medical Forums” – where you ask a professional with official credentials – and “Community Forums” – where you ask Jerry next door or Hortense on Instagram. There always will be. Most of the time this is a curiosity of little general interest. Though not always.
Of course I believe in expert advice. I spent my whole career dispensing it.
Still, modesty is proper. Knowledge may be evolving and tentative, and sensible advice often ignored.
As Hippocrates said a long time ago: Life is short, and art long, opportunity fleeting, experimentation perilous, and judgment difficult.
They all still are.
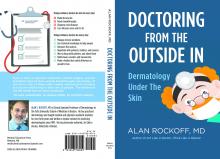
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now retired, after more than 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His latest book, “Doctoring from the Outside In,” was recently published. This is his last column for Dermatology News. Write to him at dermnews@mdedge.com.
I once answered online skin questions. The most popular one was, “Is my penis supposed to look like that?”
Then the site was bought by an entrepreneur with a corporate sensibility. He opened two forums: for 15 bucks, you could access the Medical Forum and ask a doctor. For 10, you could join the Community Forum and ask anybody with an opinion. One guess about which forum was more popular.
Years later, a colleague referred a fellow who had run a poison ivy website for a decade and wanted to interview a doctor. He had never spoken with one before, “because it never occurred to me.” His site featured the usual folklore: that blister fluid spreads the poison, that you can catch it from your dog. His website had many pictures. Some were in focus, and a few actually showed poison ivy.
I checked a year later and found that he had never uploaded our interview to his website. When I emailed to ask how come, he said he’d been busy, and did I want him to? I told him I was OK.
What made me think of these old episodes was a phone chat I had the other day with an IT guy about my laptop.
After I told him my problem, he said, “Since you’re a doctor, could I ask you a medical question?”
“Sure.”
“Is the COVID vaccine safe?” he asked.
“I had two shots myself,” I said, “and I’m planning a third. Does that tell you what I think about how safe it is?”
He didn’t answer, and we got back to the laptop.
Five minutes later he said, “I just wonder whether we should mess with vaccines. Maybe we should let nature take its course.”
“How about polio and diphtheria?” I said. “Should we let nature take its course with them?”
He thought for a moment and said, “If you don’t get vaccinated, can you spread the virus to other people?”
“Yes, you can,” I said. “It’s not just that you can get sick, but you can make other people sick, and possibly die if they’re old or vulnerable.”
Again, no response. We finished up with the laptop.
“Thanks for your medical advice,” he said. “I get conflicting information from so many sources.”
Yes, he does. He and everybody else always have. When the issues are poison ivy and genital blotchiness, the stakes are not high enough for anyone to talk about. To a large extent, people have always made their minds up about things based on what their friends think and tell them.
If your friends all wear masks, they will stare at you if you don’t. If your friends don’t wear masks, they will stare at you if you do. Or more than that. Very few people like to be stared at. Or worse.
or another: social media disinformation, distrust of the establishment, personal freedom. When the stakes are low, no reasons are needed. Who cares why someone blames Fido for his poison ivy?
Addressing the reasons people give for their positions, or the reasons others assign to them, may sometimes help people reconsider. For all those other times, the old adage applies: You cannot reason someone out of what he never reasoned himself into.
When it comes to contact dermatitis or penile blotches, you can try to straighten people out, but it doesn’t matter much if you fail. When the people you are trying to convince are spreading disease, filling up ICUs, or dying, it matters a great deal, which does not necessarily increase your odds of succeeding.
There have always been “Medical Forums” – where you ask a professional with official credentials – and “Community Forums” – where you ask Jerry next door or Hortense on Instagram. There always will be. Most of the time this is a curiosity of little general interest. Though not always.
Of course I believe in expert advice. I spent my whole career dispensing it.
Still, modesty is proper. Knowledge may be evolving and tentative, and sensible advice often ignored.
As Hippocrates said a long time ago: Life is short, and art long, opportunity fleeting, experimentation perilous, and judgment difficult.
They all still are.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now retired, after more than 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His latest book, “Doctoring from the Outside In,” was recently published. This is his last column for Dermatology News. Write to him at dermnews@mdedge.com.
I once answered online skin questions. The most popular one was, “Is my penis supposed to look like that?”
Then the site was bought by an entrepreneur with a corporate sensibility. He opened two forums: for 15 bucks, you could access the Medical Forum and ask a doctor. For 10, you could join the Community Forum and ask anybody with an opinion. One guess about which forum was more popular.
Years later, a colleague referred a fellow who had run a poison ivy website for a decade and wanted to interview a doctor. He had never spoken with one before, “because it never occurred to me.” His site featured the usual folklore: that blister fluid spreads the poison, that you can catch it from your dog. His website had many pictures. Some were in focus, and a few actually showed poison ivy.
I checked a year later and found that he had never uploaded our interview to his website. When I emailed to ask how come, he said he’d been busy, and did I want him to? I told him I was OK.
What made me think of these old episodes was a phone chat I had the other day with an IT guy about my laptop.
After I told him my problem, he said, “Since you’re a doctor, could I ask you a medical question?”
“Sure.”
“Is the COVID vaccine safe?” he asked.
“I had two shots myself,” I said, “and I’m planning a third. Does that tell you what I think about how safe it is?”
He didn’t answer, and we got back to the laptop.
Five minutes later he said, “I just wonder whether we should mess with vaccines. Maybe we should let nature take its course.”
“How about polio and diphtheria?” I said. “Should we let nature take its course with them?”
He thought for a moment and said, “If you don’t get vaccinated, can you spread the virus to other people?”
“Yes, you can,” I said. “It’s not just that you can get sick, but you can make other people sick, and possibly die if they’re old or vulnerable.”
Again, no response. We finished up with the laptop.
“Thanks for your medical advice,” he said. “I get conflicting information from so many sources.”
Yes, he does. He and everybody else always have. When the issues are poison ivy and genital blotchiness, the stakes are not high enough for anyone to talk about. To a large extent, people have always made their minds up about things based on what their friends think and tell them.
If your friends all wear masks, they will stare at you if you don’t. If your friends don’t wear masks, they will stare at you if you do. Or more than that. Very few people like to be stared at. Or worse.
or another: social media disinformation, distrust of the establishment, personal freedom. When the stakes are low, no reasons are needed. Who cares why someone blames Fido for his poison ivy?
Addressing the reasons people give for their positions, or the reasons others assign to them, may sometimes help people reconsider. For all those other times, the old adage applies: You cannot reason someone out of what he never reasoned himself into.
When it comes to contact dermatitis or penile blotches, you can try to straighten people out, but it doesn’t matter much if you fail. When the people you are trying to convince are spreading disease, filling up ICUs, or dying, it matters a great deal, which does not necessarily increase your odds of succeeding.
There have always been “Medical Forums” – where you ask a professional with official credentials – and “Community Forums” – where you ask Jerry next door or Hortense on Instagram. There always will be. Most of the time this is a curiosity of little general interest. Though not always.
Of course I believe in expert advice. I spent my whole career dispensing it.
Still, modesty is proper. Knowledge may be evolving and tentative, and sensible advice often ignored.
As Hippocrates said a long time ago: Life is short, and art long, opportunity fleeting, experimentation perilous, and judgment difficult.
They all still are.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now retired, after more than 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His latest book, “Doctoring from the Outside In,” was recently published. This is his last column for Dermatology News. Write to him at dermnews@mdedge.com.
Acid series: Lactic acid
One of the most commonly used organic acids used on the skin, lactic acid, has been used for over 3 decades. Originally derived from milk or plant-derived sugars, this gentle exfoliating acid can be used in peels, serums, masks, and toners, and has the additional benefit of hydrating the skin. Lactic acid is formulated in concentrations from 2% to 50%; however, because of its large molecular size, it doesn’t penetrate the deeper layers of the dermis to the same extent as the other alpha-hydroxy acids (AHAs), such as glycolic acid. Thus, it is one of the gentler exfoliants and one that can be used in sensitive skin or darker skin types.
Despite its mild peeling effects, lactic acid is best used to treat xerotic skin because of its function as a humectant, drawing moisture into the stratum corneum. Similar to the other AHAs, lactic acid has also been shown to decrease melanogenesis and is a gentle treatment for skin hyperpigmentation, particularly in skin of color. Side effects include peeling, stinging, erythema, photosensitivity, and hyperpigmentation when improperly used.
Very little clinical research has been reported in the last 20 years as to the uses and benefits of lactic acid in skincare. In my clinical experience, daily use of lactic acid is more effective and has more long-term benefits for hydration and rejuvenation of the skin than the other AHAs. Concentrations of 10%-15% used daily on the skin as a mild exfoliant and humectant have shown to improve texture, decrease pigmentation and improve fine lines – without thinning of the skin seen with the deeper dermal penetrating acids.
Confusion in the market has also risen as many over-the-counter brands have included ammonium lactate in their portfolio of moisturizers. Ammonium lactate is a combination of ammonium hydroxide and lactic acid, or the salt of lactic acid. A comparative study evaluating the difference between 5% lactic acid and 12% ammonium lactate for the treatment of xerosis showed that ammonium lactate was significantly more effective at reducing xerosis. It is widely used in the treatment of keratosis pilaris, calluses, xerosis, and ichthyosis.
Widespread use of lactic acid has not gotten as much glory as that of glycolic acid. However, in clinical practice, its functions are more widespread. It is a much safer acid to use, and its added benefit of increasing hydration of the skin is crucial in its long-term use for both photoaging and the prevention of wrinkles. With any acid, the exfoliating properties must be treated with adequate hydration and barrier repair.
The intrinsic moisturizing effect of lactic acid makes it a much more well-rounded acid and that can be used for longer periods of time in a broader spectrum of patients.
Dr. Lily Talakoub and Dr. Naissan O. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at dermnews@mdedge.com. They had no relevant disclosures.
One of the most commonly used organic acids used on the skin, lactic acid, has been used for over 3 decades. Originally derived from milk or plant-derived sugars, this gentle exfoliating acid can be used in peels, serums, masks, and toners, and has the additional benefit of hydrating the skin. Lactic acid is formulated in concentrations from 2% to 50%; however, because of its large molecular size, it doesn’t penetrate the deeper layers of the dermis to the same extent as the other alpha-hydroxy acids (AHAs), such as glycolic acid. Thus, it is one of the gentler exfoliants and one that can be used in sensitive skin or darker skin types.
Despite its mild peeling effects, lactic acid is best used to treat xerotic skin because of its function as a humectant, drawing moisture into the stratum corneum. Similar to the other AHAs, lactic acid has also been shown to decrease melanogenesis and is a gentle treatment for skin hyperpigmentation, particularly in skin of color. Side effects include peeling, stinging, erythema, photosensitivity, and hyperpigmentation when improperly used.
Very little clinical research has been reported in the last 20 years as to the uses and benefits of lactic acid in skincare. In my clinical experience, daily use of lactic acid is more effective and has more long-term benefits for hydration and rejuvenation of the skin than the other AHAs. Concentrations of 10%-15% used daily on the skin as a mild exfoliant and humectant have shown to improve texture, decrease pigmentation and improve fine lines – without thinning of the skin seen with the deeper dermal penetrating acids.
Confusion in the market has also risen as many over-the-counter brands have included ammonium lactate in their portfolio of moisturizers. Ammonium lactate is a combination of ammonium hydroxide and lactic acid, or the salt of lactic acid. A comparative study evaluating the difference between 5% lactic acid and 12% ammonium lactate for the treatment of xerosis showed that ammonium lactate was significantly more effective at reducing xerosis. It is widely used in the treatment of keratosis pilaris, calluses, xerosis, and ichthyosis.
Widespread use of lactic acid has not gotten as much glory as that of glycolic acid. However, in clinical practice, its functions are more widespread. It is a much safer acid to use, and its added benefit of increasing hydration of the skin is crucial in its long-term use for both photoaging and the prevention of wrinkles. With any acid, the exfoliating properties must be treated with adequate hydration and barrier repair.
The intrinsic moisturizing effect of lactic acid makes it a much more well-rounded acid and that can be used for longer periods of time in a broader spectrum of patients.
Dr. Lily Talakoub and Dr. Naissan O. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at dermnews@mdedge.com. They had no relevant disclosures.
One of the most commonly used organic acids used on the skin, lactic acid, has been used for over 3 decades. Originally derived from milk or plant-derived sugars, this gentle exfoliating acid can be used in peels, serums, masks, and toners, and has the additional benefit of hydrating the skin. Lactic acid is formulated in concentrations from 2% to 50%; however, because of its large molecular size, it doesn’t penetrate the deeper layers of the dermis to the same extent as the other alpha-hydroxy acids (AHAs), such as glycolic acid. Thus, it is one of the gentler exfoliants and one that can be used in sensitive skin or darker skin types.
Despite its mild peeling effects, lactic acid is best used to treat xerotic skin because of its function as a humectant, drawing moisture into the stratum corneum. Similar to the other AHAs, lactic acid has also been shown to decrease melanogenesis and is a gentle treatment for skin hyperpigmentation, particularly in skin of color. Side effects include peeling, stinging, erythema, photosensitivity, and hyperpigmentation when improperly used.
Very little clinical research has been reported in the last 20 years as to the uses and benefits of lactic acid in skincare. In my clinical experience, daily use of lactic acid is more effective and has more long-term benefits for hydration and rejuvenation of the skin than the other AHAs. Concentrations of 10%-15% used daily on the skin as a mild exfoliant and humectant have shown to improve texture, decrease pigmentation and improve fine lines – without thinning of the skin seen with the deeper dermal penetrating acids.
Confusion in the market has also risen as many over-the-counter brands have included ammonium lactate in their portfolio of moisturizers. Ammonium lactate is a combination of ammonium hydroxide and lactic acid, or the salt of lactic acid. A comparative study evaluating the difference between 5% lactic acid and 12% ammonium lactate for the treatment of xerosis showed that ammonium lactate was significantly more effective at reducing xerosis. It is widely used in the treatment of keratosis pilaris, calluses, xerosis, and ichthyosis.
Widespread use of lactic acid has not gotten as much glory as that of glycolic acid. However, in clinical practice, its functions are more widespread. It is a much safer acid to use, and its added benefit of increasing hydration of the skin is crucial in its long-term use for both photoaging and the prevention of wrinkles. With any acid, the exfoliating properties must be treated with adequate hydration and barrier repair.
The intrinsic moisturizing effect of lactic acid makes it a much more well-rounded acid and that can be used for longer periods of time in a broader spectrum of patients.
Dr. Lily Talakoub and Dr. Naissan O. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at dermnews@mdedge.com. They had no relevant disclosures.
Vetiver: More than a pleasant aroma?
An important ingredient in the contemporary perfume and cosmetics industries, vetiver, is the only grass cultivated throughout the world to retain its essential oil, which contains sesquiterpene alcohols and hydrocarbons.1-3 Field and glasshouse studies have revealed that vetiver grass can tolerate extreme variations in climate well, including protracted drought, floods, submergence, temperature, and soils high in acidity, alkalinity, and various heavy metals. Its heartiness may explain its continuing or even increasing use in fragrances and other products pertinent to skin health as humanity strives to adapt to climate change.4 In a 2017 review of various commercial essential oils as antimicrobial therapy for cutaneous disorders, Orchard and van Vuuren identified vetiver as warranting particular attention for its capacity to confer broad benefits to the skin in addressing acne, cuts, eczema, oiliness, sores, wounds, and aging skin.5 The focus of this column will be the dermatologic potential of vetiver.
Chemical constituents
Vetiver is thought to be one of the most complex of the essential oils owing to the hundreds of sesquiterpene derivatives with large structural diversity that contribute to its composition. 3
In a 2012 analysis of the components of South Indian vetiver oils, Mallavarapu et al. found an abundance of sesquiterpenes and oxygenated sesquiterpenes with cedrane, bisabolane, eudesmane, eremophilane, and zizaane skeletons. The primary constituents identified in the four oils evaluated included eudesma-4,6-diene (delta-selinene) + beta-vetispirene (3.9%-6.1%), beta-vetivenene (0.9%-9.4%), 13-nor-trans-eudesma-4(15),7-dien-11-one + amorph-4-en-10-ol (5.0%-6.4%), trans-eudesma-4(15),7-dien-12-ol (vetiselinenol) + (E)-opposita-4(15),7(11)-dien-12-ol (3.7%-5.9%), eremophila-1 (10),11-dien-2alpha-ol (nootkatol) + ziza-6(13)-en-12-ol (khusimol) (16.1%-19.2%), and eremophila-1(10),7(11)-dien-2alpha-ol (isonootkatol) + (E)-eremophila-1(10),7(11)-12-ol (isovalencenol) (5.6%-6.9%).6
Antimicrobial activity
In 2012, Saikia et al. assessed the antimycobacterial activity of Vetiveria zizanioides against Mycobacterium tuberculosis H(37)Rv and H(37)Ra strains. Their results showed that ethanolic extracts and hexane fractions displayed robust antimycobacterial properties, buttressing the traditional medical uses of the plant, as well as consideration of this agent as a modern antituberculosis agent.7
Two years later, Dos Santos et al. showed that Vetiveria zizanioides roots grown in Brazil exhibited notable antimicrobial effects against various pathogenic organisms.8In 2017, Burger et al. showed that vetiver essential oil primarily contributes its scent to cosmetic formulations but also displayed antimicrobial activity against Gram-positive bacterial strains, as well as one strain of Candida glabrata. They suggest that vetiver should be considered for its antimicrobial capacity as an added bonus to cosmetic formulations.2
In a 2018 study to ascertain the antimicrobial activity of 247 essential oil combinations against five reference strains of wound pathogens, Orchard et al. found that 26 combinations exhibited extensive antimicrobial activity. Sandalwood and vetiver were found to contribute most to antimicrobial function when used in combination. The investigators concluded that such combinations warrant consideration for wound therapy.9
Antiacne activity
In 2018, Orchard et al. conducted another study of the efficacy of commercial essential oil combinations against the two pathogens responsible for acne, Propionibacterium acnes and Staphlyococcus epidermidis. They investigated 408 combinations, of which 167 exhibited notable antimicrobial activity. They observed that the combination with the lowest minimum inhibitory concentration value against P. acnes and S. epidermidis was vetiver and cinnamon bark.10 This usage points to the potential of vetiver use as an antiacne ingredient.
Safety
The Scientific Committee on Consumer Safety (SCCS) offered a final opinion on the safety of the fragrance ingredient acetylated vetiver oil in 2019, declaring its use with 1% alpha-tocopherol in cosmetic leave-on and rinse-off products safe at proposed concentration levels. They noted that acetylated vetiver oil has been used for several years without provoking contact allergies.11
Conclusion
Much more research is necessary to determine just what kind of a role this perfumery powerhouse can play in dermatology.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at dermnews@mdedge.com.
References
1. Del Giudice L et al. Environ Microbiol. 2008 Oct;10(10):2824-41.
2. Burger P et al. Medicines (Basel). 2017 Jun 16;4(2):41.
3. Belhassen E et al. Chem Biodivers. 2014 Nov;11(11):1821–42.
4. Danh LT et al. Int J Phytoremediation. 2009 Oct-Dec;11(8):664–91.
5. Orchard A and van Vuuren S. Evid Based Complement Alternat Med. 2017;2017:4517971.
6. Mallavarapu GR et al. Nat Prod Commun. 2012 Feb;7(2):223–5.
7. Saikia D et al. Complement Ther Med. 2012 Dec;20(6):434–6.
8. Dos Santos DS et al. Acta Pharm. 2014 Dec;64(4):495-501.
9. Orchard A et al. Chem Biodivers. 2018 Dec;15(12):e1800405.
10. Orchard A et al. Int J Cosmet Sci. 2018 Mar 24. [Epub ahead of print].
11. SCCS members & External experts. Regul Toxicol Pharmacol. 2019 Oct;107:104389.
An important ingredient in the contemporary perfume and cosmetics industries, vetiver, is the only grass cultivated throughout the world to retain its essential oil, which contains sesquiterpene alcohols and hydrocarbons.1-3 Field and glasshouse studies have revealed that vetiver grass can tolerate extreme variations in climate well, including protracted drought, floods, submergence, temperature, and soils high in acidity, alkalinity, and various heavy metals. Its heartiness may explain its continuing or even increasing use in fragrances and other products pertinent to skin health as humanity strives to adapt to climate change.4 In a 2017 review of various commercial essential oils as antimicrobial therapy for cutaneous disorders, Orchard and van Vuuren identified vetiver as warranting particular attention for its capacity to confer broad benefits to the skin in addressing acne, cuts, eczema, oiliness, sores, wounds, and aging skin.5 The focus of this column will be the dermatologic potential of vetiver.
Chemical constituents
Vetiver is thought to be one of the most complex of the essential oils owing to the hundreds of sesquiterpene derivatives with large structural diversity that contribute to its composition. 3
In a 2012 analysis of the components of South Indian vetiver oils, Mallavarapu et al. found an abundance of sesquiterpenes and oxygenated sesquiterpenes with cedrane, bisabolane, eudesmane, eremophilane, and zizaane skeletons. The primary constituents identified in the four oils evaluated included eudesma-4,6-diene (delta-selinene) + beta-vetispirene (3.9%-6.1%), beta-vetivenene (0.9%-9.4%), 13-nor-trans-eudesma-4(15),7-dien-11-one + amorph-4-en-10-ol (5.0%-6.4%), trans-eudesma-4(15),7-dien-12-ol (vetiselinenol) + (E)-opposita-4(15),7(11)-dien-12-ol (3.7%-5.9%), eremophila-1 (10),11-dien-2alpha-ol (nootkatol) + ziza-6(13)-en-12-ol (khusimol) (16.1%-19.2%), and eremophila-1(10),7(11)-dien-2alpha-ol (isonootkatol) + (E)-eremophila-1(10),7(11)-12-ol (isovalencenol) (5.6%-6.9%).6
Antimicrobial activity
In 2012, Saikia et al. assessed the antimycobacterial activity of Vetiveria zizanioides against Mycobacterium tuberculosis H(37)Rv and H(37)Ra strains. Their results showed that ethanolic extracts and hexane fractions displayed robust antimycobacterial properties, buttressing the traditional medical uses of the plant, as well as consideration of this agent as a modern antituberculosis agent.7
Two years later, Dos Santos et al. showed that Vetiveria zizanioides roots grown in Brazil exhibited notable antimicrobial effects against various pathogenic organisms.8In 2017, Burger et al. showed that vetiver essential oil primarily contributes its scent to cosmetic formulations but also displayed antimicrobial activity against Gram-positive bacterial strains, as well as one strain of Candida glabrata. They suggest that vetiver should be considered for its antimicrobial capacity as an added bonus to cosmetic formulations.2
In a 2018 study to ascertain the antimicrobial activity of 247 essential oil combinations against five reference strains of wound pathogens, Orchard et al. found that 26 combinations exhibited extensive antimicrobial activity. Sandalwood and vetiver were found to contribute most to antimicrobial function when used in combination. The investigators concluded that such combinations warrant consideration for wound therapy.9
Antiacne activity
In 2018, Orchard et al. conducted another study of the efficacy of commercial essential oil combinations against the two pathogens responsible for acne, Propionibacterium acnes and Staphlyococcus epidermidis. They investigated 408 combinations, of which 167 exhibited notable antimicrobial activity. They observed that the combination with the lowest minimum inhibitory concentration value against P. acnes and S. epidermidis was vetiver and cinnamon bark.10 This usage points to the potential of vetiver use as an antiacne ingredient.
Safety
The Scientific Committee on Consumer Safety (SCCS) offered a final opinion on the safety of the fragrance ingredient acetylated vetiver oil in 2019, declaring its use with 1% alpha-tocopherol in cosmetic leave-on and rinse-off products safe at proposed concentration levels. They noted that acetylated vetiver oil has been used for several years without provoking contact allergies.11
Conclusion
Much more research is necessary to determine just what kind of a role this perfumery powerhouse can play in dermatology.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at dermnews@mdedge.com.
References
1. Del Giudice L et al. Environ Microbiol. 2008 Oct;10(10):2824-41.
2. Burger P et al. Medicines (Basel). 2017 Jun 16;4(2):41.
3. Belhassen E et al. Chem Biodivers. 2014 Nov;11(11):1821–42.
4. Danh LT et al. Int J Phytoremediation. 2009 Oct-Dec;11(8):664–91.
5. Orchard A and van Vuuren S. Evid Based Complement Alternat Med. 2017;2017:4517971.
6. Mallavarapu GR et al. Nat Prod Commun. 2012 Feb;7(2):223–5.
7. Saikia D et al. Complement Ther Med. 2012 Dec;20(6):434–6.
8. Dos Santos DS et al. Acta Pharm. 2014 Dec;64(4):495-501.
9. Orchard A et al. Chem Biodivers. 2018 Dec;15(12):e1800405.
10. Orchard A et al. Int J Cosmet Sci. 2018 Mar 24. [Epub ahead of print].
11. SCCS members & External experts. Regul Toxicol Pharmacol. 2019 Oct;107:104389.
An important ingredient in the contemporary perfume and cosmetics industries, vetiver, is the only grass cultivated throughout the world to retain its essential oil, which contains sesquiterpene alcohols and hydrocarbons.1-3 Field and glasshouse studies have revealed that vetiver grass can tolerate extreme variations in climate well, including protracted drought, floods, submergence, temperature, and soils high in acidity, alkalinity, and various heavy metals. Its heartiness may explain its continuing or even increasing use in fragrances and other products pertinent to skin health as humanity strives to adapt to climate change.4 In a 2017 review of various commercial essential oils as antimicrobial therapy for cutaneous disorders, Orchard and van Vuuren identified vetiver as warranting particular attention for its capacity to confer broad benefits to the skin in addressing acne, cuts, eczema, oiliness, sores, wounds, and aging skin.5 The focus of this column will be the dermatologic potential of vetiver.
Chemical constituents
Vetiver is thought to be one of the most complex of the essential oils owing to the hundreds of sesquiterpene derivatives with large structural diversity that contribute to its composition. 3
In a 2012 analysis of the components of South Indian vetiver oils, Mallavarapu et al. found an abundance of sesquiterpenes and oxygenated sesquiterpenes with cedrane, bisabolane, eudesmane, eremophilane, and zizaane skeletons. The primary constituents identified in the four oils evaluated included eudesma-4,6-diene (delta-selinene) + beta-vetispirene (3.9%-6.1%), beta-vetivenene (0.9%-9.4%), 13-nor-trans-eudesma-4(15),7-dien-11-one + amorph-4-en-10-ol (5.0%-6.4%), trans-eudesma-4(15),7-dien-12-ol (vetiselinenol) + (E)-opposita-4(15),7(11)-dien-12-ol (3.7%-5.9%), eremophila-1 (10),11-dien-2alpha-ol (nootkatol) + ziza-6(13)-en-12-ol (khusimol) (16.1%-19.2%), and eremophila-1(10),7(11)-dien-2alpha-ol (isonootkatol) + (E)-eremophila-1(10),7(11)-12-ol (isovalencenol) (5.6%-6.9%).6
Antimicrobial activity
In 2012, Saikia et al. assessed the antimycobacterial activity of Vetiveria zizanioides against Mycobacterium tuberculosis H(37)Rv and H(37)Ra strains. Their results showed that ethanolic extracts and hexane fractions displayed robust antimycobacterial properties, buttressing the traditional medical uses of the plant, as well as consideration of this agent as a modern antituberculosis agent.7
Two years later, Dos Santos et al. showed that Vetiveria zizanioides roots grown in Brazil exhibited notable antimicrobial effects against various pathogenic organisms.8In 2017, Burger et al. showed that vetiver essential oil primarily contributes its scent to cosmetic formulations but also displayed antimicrobial activity against Gram-positive bacterial strains, as well as one strain of Candida glabrata. They suggest that vetiver should be considered for its antimicrobial capacity as an added bonus to cosmetic formulations.2
In a 2018 study to ascertain the antimicrobial activity of 247 essential oil combinations against five reference strains of wound pathogens, Orchard et al. found that 26 combinations exhibited extensive antimicrobial activity. Sandalwood and vetiver were found to contribute most to antimicrobial function when used in combination. The investigators concluded that such combinations warrant consideration for wound therapy.9
Antiacne activity
In 2018, Orchard et al. conducted another study of the efficacy of commercial essential oil combinations against the two pathogens responsible for acne, Propionibacterium acnes and Staphlyococcus epidermidis. They investigated 408 combinations, of which 167 exhibited notable antimicrobial activity. They observed that the combination with the lowest minimum inhibitory concentration value against P. acnes and S. epidermidis was vetiver and cinnamon bark.10 This usage points to the potential of vetiver use as an antiacne ingredient.
Safety
The Scientific Committee on Consumer Safety (SCCS) offered a final opinion on the safety of the fragrance ingredient acetylated vetiver oil in 2019, declaring its use with 1% alpha-tocopherol in cosmetic leave-on and rinse-off products safe at proposed concentration levels. They noted that acetylated vetiver oil has been used for several years without provoking contact allergies.11
Conclusion
Much more research is necessary to determine just what kind of a role this perfumery powerhouse can play in dermatology.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at dermnews@mdedge.com.
References
1. Del Giudice L et al. Environ Microbiol. 2008 Oct;10(10):2824-41.
2. Burger P et al. Medicines (Basel). 2017 Jun 16;4(2):41.
3. Belhassen E et al. Chem Biodivers. 2014 Nov;11(11):1821–42.
4. Danh LT et al. Int J Phytoremediation. 2009 Oct-Dec;11(8):664–91.
5. Orchard A and van Vuuren S. Evid Based Complement Alternat Med. 2017;2017:4517971.
6. Mallavarapu GR et al. Nat Prod Commun. 2012 Feb;7(2):223–5.
7. Saikia D et al. Complement Ther Med. 2012 Dec;20(6):434–6.
8. Dos Santos DS et al. Acta Pharm. 2014 Dec;64(4):495-501.
9. Orchard A et al. Chem Biodivers. 2018 Dec;15(12):e1800405.
10. Orchard A et al. Int J Cosmet Sci. 2018 Mar 24. [Epub ahead of print].
11. SCCS members & External experts. Regul Toxicol Pharmacol. 2019 Oct;107:104389.
Pandemic goal deficiency disorder
In August I shared with you my observations on two opposing op-ed pieces from two major newspapers, one was in favor of masking mandates for public schools, the other against. (Masking in school: A battle of the op-eds. MDedge Pediatrics. Letters from Maine, 2021 Aug 12). Neither group of authors could offer us evidence from controlled studies to support their views. However, both agreed that returning children to school deserves a high priority. But neither the authors nor I treaded into the uncharted waters of exactly how masking fits into our national goals for managing the pandemic because ... no one in this country has articulated what these goals should be. A third op-ed appearing 3 weeks later suggests why we are floundering in this goal-deficient limbo.
Writing in the New York Times, two epidemiologists in Boston ask the simple question: “What are we actually trying to achieve in the United States?” when it comes to the pandemic. (Allen AG and Jenkins H. The Hard Covid-19 Questions We’re Not Asking. 2021 Aug 30). Is our goal zero infections? Is it hammering on the virus until we can treat it like the seasonal flu? We do seem to agree that not having kids in school has been a disaster economically, educationally, and psychologically. But, where does the goal of getting them back in school fit into a larger and as yet undefined national goal? Without that target we have little idea of what compromises and risks we should be willing to accept.
How much serious pediatric disease is acceptable? It appears that the number of fatal complications in the pediatric population is very small in comparison with other demographic groups. Although few in number, there have been and there will continue to be pediatric deaths because of COVID. Is our goal zero pediatric deaths? If it is then this dictates a level of response that ripples back upstream to every child in every classroom and could threaten our overarching goal of returning children to school. Because none of us likes the thought of a child dying, some of us may be hesitant to even consider a strategy that doesn’t include zero pediatric deaths as a goal.
Are we looking to have zero serious pediatric infections? Achieving this goal is unlikely. Even if we develop a pediatric vaccine in the near future it probably won’t be in the arms of enough children by the end of this school year to make a significant dent in the number of serious pediatric infections. Waiting until an optimal number of children are immunized doesn’t feel like it will achieve a primary goal of getting kids back in school if we continue to focus on driving the level of serious pediatric infections to zero. We have already endured a year in which many communities made decisions that seemed to have prioritized an unstated goal of no school exposure–related educator deaths. Again, a goal based on little if any evidence.
The problem we face in this country is that our response to the pandemic has been nonuniform. Here in Brunswick, Maine, 99% of the eligible adults have been vaccinated. Even with the recent surge, we may be ready for a strategy that avoids wholesale quarantining. A targeted and robust antibody testing system might work for us and make an unproven and unpopular masking mandate unnecessary. Britain seems to be moving in a similar direction to meet its goal of keeping children in school.
However, there are large population groups in regions of this country that have stumbled at taking the initial steps to get the pandemic under control. Articulating a national goal that covers both communities where the response to the pandemic has been less thoughtful and robust along with states that have been more successful is going to be difficult. But it must be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
In August I shared with you my observations on two opposing op-ed pieces from two major newspapers, one was in favor of masking mandates for public schools, the other against. (Masking in school: A battle of the op-eds. MDedge Pediatrics. Letters from Maine, 2021 Aug 12). Neither group of authors could offer us evidence from controlled studies to support their views. However, both agreed that returning children to school deserves a high priority. But neither the authors nor I treaded into the uncharted waters of exactly how masking fits into our national goals for managing the pandemic because ... no one in this country has articulated what these goals should be. A third op-ed appearing 3 weeks later suggests why we are floundering in this goal-deficient limbo.
Writing in the New York Times, two epidemiologists in Boston ask the simple question: “What are we actually trying to achieve in the United States?” when it comes to the pandemic. (Allen AG and Jenkins H. The Hard Covid-19 Questions We’re Not Asking. 2021 Aug 30). Is our goal zero infections? Is it hammering on the virus until we can treat it like the seasonal flu? We do seem to agree that not having kids in school has been a disaster economically, educationally, and psychologically. But, where does the goal of getting them back in school fit into a larger and as yet undefined national goal? Without that target we have little idea of what compromises and risks we should be willing to accept.
How much serious pediatric disease is acceptable? It appears that the number of fatal complications in the pediatric population is very small in comparison with other demographic groups. Although few in number, there have been and there will continue to be pediatric deaths because of COVID. Is our goal zero pediatric deaths? If it is then this dictates a level of response that ripples back upstream to every child in every classroom and could threaten our overarching goal of returning children to school. Because none of us likes the thought of a child dying, some of us may be hesitant to even consider a strategy that doesn’t include zero pediatric deaths as a goal.
Are we looking to have zero serious pediatric infections? Achieving this goal is unlikely. Even if we develop a pediatric vaccine in the near future it probably won’t be in the arms of enough children by the end of this school year to make a significant dent in the number of serious pediatric infections. Waiting until an optimal number of children are immunized doesn’t feel like it will achieve a primary goal of getting kids back in school if we continue to focus on driving the level of serious pediatric infections to zero. We have already endured a year in which many communities made decisions that seemed to have prioritized an unstated goal of no school exposure–related educator deaths. Again, a goal based on little if any evidence.
The problem we face in this country is that our response to the pandemic has been nonuniform. Here in Brunswick, Maine, 99% of the eligible adults have been vaccinated. Even with the recent surge, we may be ready for a strategy that avoids wholesale quarantining. A targeted and robust antibody testing system might work for us and make an unproven and unpopular masking mandate unnecessary. Britain seems to be moving in a similar direction to meet its goal of keeping children in school.
However, there are large population groups in regions of this country that have stumbled at taking the initial steps to get the pandemic under control. Articulating a national goal that covers both communities where the response to the pandemic has been less thoughtful and robust along with states that have been more successful is going to be difficult. But it must be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
In August I shared with you my observations on two opposing op-ed pieces from two major newspapers, one was in favor of masking mandates for public schools, the other against. (Masking in school: A battle of the op-eds. MDedge Pediatrics. Letters from Maine, 2021 Aug 12). Neither group of authors could offer us evidence from controlled studies to support their views. However, both agreed that returning children to school deserves a high priority. But neither the authors nor I treaded into the uncharted waters of exactly how masking fits into our national goals for managing the pandemic because ... no one in this country has articulated what these goals should be. A third op-ed appearing 3 weeks later suggests why we are floundering in this goal-deficient limbo.
Writing in the New York Times, two epidemiologists in Boston ask the simple question: “What are we actually trying to achieve in the United States?” when it comes to the pandemic. (Allen AG and Jenkins H. The Hard Covid-19 Questions We’re Not Asking. 2021 Aug 30). Is our goal zero infections? Is it hammering on the virus until we can treat it like the seasonal flu? We do seem to agree that not having kids in school has been a disaster economically, educationally, and psychologically. But, where does the goal of getting them back in school fit into a larger and as yet undefined national goal? Without that target we have little idea of what compromises and risks we should be willing to accept.
How much serious pediatric disease is acceptable? It appears that the number of fatal complications in the pediatric population is very small in comparison with other demographic groups. Although few in number, there have been and there will continue to be pediatric deaths because of COVID. Is our goal zero pediatric deaths? If it is then this dictates a level of response that ripples back upstream to every child in every classroom and could threaten our overarching goal of returning children to school. Because none of us likes the thought of a child dying, some of us may be hesitant to even consider a strategy that doesn’t include zero pediatric deaths as a goal.
Are we looking to have zero serious pediatric infections? Achieving this goal is unlikely. Even if we develop a pediatric vaccine in the near future it probably won’t be in the arms of enough children by the end of this school year to make a significant dent in the number of serious pediatric infections. Waiting until an optimal number of children are immunized doesn’t feel like it will achieve a primary goal of getting kids back in school if we continue to focus on driving the level of serious pediatric infections to zero. We have already endured a year in which many communities made decisions that seemed to have prioritized an unstated goal of no school exposure–related educator deaths. Again, a goal based on little if any evidence.
The problem we face in this country is that our response to the pandemic has been nonuniform. Here in Brunswick, Maine, 99% of the eligible adults have been vaccinated. Even with the recent surge, we may be ready for a strategy that avoids wholesale quarantining. A targeted and robust antibody testing system might work for us and make an unproven and unpopular masking mandate unnecessary. Britain seems to be moving in a similar direction to meet its goal of keeping children in school.
However, there are large population groups in regions of this country that have stumbled at taking the initial steps to get the pandemic under control. Articulating a national goal that covers both communities where the response to the pandemic has been less thoughtful and robust along with states that have been more successful is going to be difficult. But it must be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Finding employees during a pandemic
.
My own office is prime example: I have had job listings for both front- and back-office positions posted on all the major job boards and other employment portals for months, with a disappointing response. Of the few who do respond, many, incredibly, do not show up for their interviews!
It turns out that this is a widespread problem, and not just in medicine. A recent survey by the National Federation of Independent Business found that 42% of business owners, in all walks of life, had job openings that could not be filled, a record high. Over 90% of those hiring reported few or no qualified applicants and an increase in interview no-shows.
Clearly, this is a huge obstacle to growth – and even to conducting normal operations – for my practice and many others.
Reasons for the situation vary, but a big one has been the unfortunate fact that many open job positions actually pay less than the expanded unemployment benefits that many people have received under the March 2020 CARES Act. By one estimate, almost 70% of unemployed workers have been collecting more on unemployment than they earned while working. The CARES benefits expired in early September, but many potential workers continue to receive payments through a newer FEMA program, and some states have their own ongoing benefit programs.
Other reasons have been offered: Some candidates are unvaccinated (an immediate deal-breaker in my office), and some working parents continue to face a lack of childcare or in-person schooling for their children. Some applicants – regardless of vaccination status – have said they are hesitant to work in a medical office setting and risk getting COVID-19, despite all the precautions we have in place. Others have said they are waiting until the job market improves.
There are no easy solutions to this complicated problem, but here are a few suggestions culled from my research and conversations with HR professionals and others.
One obvious option is to offer higher wages, and perhaps even signing bonuses. “Whenever anyone says they can’t find the workers they need,” a consultant told me, “they are really saying they can’t find them at the wages they want to pay.” There are limits to the wages and benefits a private office with a very finite salary budget can offer, of course – but a few higher-paid employees may be preferable to no new workers at all.
For job candidates who fear COVID-19 exposure, assure them that their health and safety is a priority by spelling out the procedures your office is following (social distancing, reduced patient capacity, interaction barriers, face masks, avoidance of handshakes, enhanced cleaning procedures, symptom questionnaires, temperature checks, etc.) to minimize the risk of exposure.
You also may need to rework your interview process. In the Zoom era, most preliminary interviews can be conducted remotely. For on-site interviews, explain how you’re maintaining a safe interview environment by applying the same office safety policies to interactions with interviewees.
If a promising candidate doesn’t show up for an interview, the applicant could be making a token effort to obtain a job in order to perpetuate unemployment payments, but don’t jump to that conclusion. There may be extenuating circumstances, such as an emergency, illness, or traffic issues. Also, consider the possibility that it was your fault. If you waited too long to schedule the interview, another office could have lured them away. Or you may not have adequately explained your COVID-19 exposure safeguards. At the very least, a drawn-out process or a lack of transparency can make applicants apprehensive about accepting a job with you, particularly if other employers are pursuing them.
To counter the shortsighted appeal of collecting unemployment benefits, it may help to highlight the long-term growth opportunities available at your office. Consider outlining typical career tracks, or providing specific examples of how people have advanced their careers at your facility. I frequently cite the example of my current office manager, who began as an assistant receptionist almost 30 years ago.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
.
My own office is prime example: I have had job listings for both front- and back-office positions posted on all the major job boards and other employment portals for months, with a disappointing response. Of the few who do respond, many, incredibly, do not show up for their interviews!
It turns out that this is a widespread problem, and not just in medicine. A recent survey by the National Federation of Independent Business found that 42% of business owners, in all walks of life, had job openings that could not be filled, a record high. Over 90% of those hiring reported few or no qualified applicants and an increase in interview no-shows.
Clearly, this is a huge obstacle to growth – and even to conducting normal operations – for my practice and many others.
Reasons for the situation vary, but a big one has been the unfortunate fact that many open job positions actually pay less than the expanded unemployment benefits that many people have received under the March 2020 CARES Act. By one estimate, almost 70% of unemployed workers have been collecting more on unemployment than they earned while working. The CARES benefits expired in early September, but many potential workers continue to receive payments through a newer FEMA program, and some states have their own ongoing benefit programs.
Other reasons have been offered: Some candidates are unvaccinated (an immediate deal-breaker in my office), and some working parents continue to face a lack of childcare or in-person schooling for their children. Some applicants – regardless of vaccination status – have said they are hesitant to work in a medical office setting and risk getting COVID-19, despite all the precautions we have in place. Others have said they are waiting until the job market improves.
There are no easy solutions to this complicated problem, but here are a few suggestions culled from my research and conversations with HR professionals and others.
One obvious option is to offer higher wages, and perhaps even signing bonuses. “Whenever anyone says they can’t find the workers they need,” a consultant told me, “they are really saying they can’t find them at the wages they want to pay.” There are limits to the wages and benefits a private office with a very finite salary budget can offer, of course – but a few higher-paid employees may be preferable to no new workers at all.
For job candidates who fear COVID-19 exposure, assure them that their health and safety is a priority by spelling out the procedures your office is following (social distancing, reduced patient capacity, interaction barriers, face masks, avoidance of handshakes, enhanced cleaning procedures, symptom questionnaires, temperature checks, etc.) to minimize the risk of exposure.
You also may need to rework your interview process. In the Zoom era, most preliminary interviews can be conducted remotely. For on-site interviews, explain how you’re maintaining a safe interview environment by applying the same office safety policies to interactions with interviewees.
If a promising candidate doesn’t show up for an interview, the applicant could be making a token effort to obtain a job in order to perpetuate unemployment payments, but don’t jump to that conclusion. There may be extenuating circumstances, such as an emergency, illness, or traffic issues. Also, consider the possibility that it was your fault. If you waited too long to schedule the interview, another office could have lured them away. Or you may not have adequately explained your COVID-19 exposure safeguards. At the very least, a drawn-out process or a lack of transparency can make applicants apprehensive about accepting a job with you, particularly if other employers are pursuing them.
To counter the shortsighted appeal of collecting unemployment benefits, it may help to highlight the long-term growth opportunities available at your office. Consider outlining typical career tracks, or providing specific examples of how people have advanced their careers at your facility. I frequently cite the example of my current office manager, who began as an assistant receptionist almost 30 years ago.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
.
My own office is prime example: I have had job listings for both front- and back-office positions posted on all the major job boards and other employment portals for months, with a disappointing response. Of the few who do respond, many, incredibly, do not show up for their interviews!
It turns out that this is a widespread problem, and not just in medicine. A recent survey by the National Federation of Independent Business found that 42% of business owners, in all walks of life, had job openings that could not be filled, a record high. Over 90% of those hiring reported few or no qualified applicants and an increase in interview no-shows.
Clearly, this is a huge obstacle to growth – and even to conducting normal operations – for my practice and many others.
Reasons for the situation vary, but a big one has been the unfortunate fact that many open job positions actually pay less than the expanded unemployment benefits that many people have received under the March 2020 CARES Act. By one estimate, almost 70% of unemployed workers have been collecting more on unemployment than they earned while working. The CARES benefits expired in early September, but many potential workers continue to receive payments through a newer FEMA program, and some states have their own ongoing benefit programs.
Other reasons have been offered: Some candidates are unvaccinated (an immediate deal-breaker in my office), and some working parents continue to face a lack of childcare or in-person schooling for their children. Some applicants – regardless of vaccination status – have said they are hesitant to work in a medical office setting and risk getting COVID-19, despite all the precautions we have in place. Others have said they are waiting until the job market improves.
There are no easy solutions to this complicated problem, but here are a few suggestions culled from my research and conversations with HR professionals and others.
One obvious option is to offer higher wages, and perhaps even signing bonuses. “Whenever anyone says they can’t find the workers they need,” a consultant told me, “they are really saying they can’t find them at the wages they want to pay.” There are limits to the wages and benefits a private office with a very finite salary budget can offer, of course – but a few higher-paid employees may be preferable to no new workers at all.
For job candidates who fear COVID-19 exposure, assure them that their health and safety is a priority by spelling out the procedures your office is following (social distancing, reduced patient capacity, interaction barriers, face masks, avoidance of handshakes, enhanced cleaning procedures, symptom questionnaires, temperature checks, etc.) to minimize the risk of exposure.
You also may need to rework your interview process. In the Zoom era, most preliminary interviews can be conducted remotely. For on-site interviews, explain how you’re maintaining a safe interview environment by applying the same office safety policies to interactions with interviewees.
If a promising candidate doesn’t show up for an interview, the applicant could be making a token effort to obtain a job in order to perpetuate unemployment payments, but don’t jump to that conclusion. There may be extenuating circumstances, such as an emergency, illness, or traffic issues. Also, consider the possibility that it was your fault. If you waited too long to schedule the interview, another office could have lured them away. Or you may not have adequately explained your COVID-19 exposure safeguards. At the very least, a drawn-out process or a lack of transparency can make applicants apprehensive about accepting a job with you, particularly if other employers are pursuing them.
To counter the shortsighted appeal of collecting unemployment benefits, it may help to highlight the long-term growth opportunities available at your office. Consider outlining typical career tracks, or providing specific examples of how people have advanced their careers at your facility. I frequently cite the example of my current office manager, who began as an assistant receptionist almost 30 years ago.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Online mental health treatment: Is this the answer we’ve been waiting for?
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.