User login
New guidelines dispel myths about COVID-19 treatment
Recommendations, as well as conspiracy theories about COVID-19, have changed at distressing rates over the past year. No disease has ever been more politicized, or more polarizing.
Experts, as well as the least educated, take a stand on what they believe is the most important way to prevent and treat this virus.
Just recently, a study was published revealing that ivermectin is not effective as a COVID-19 treatment while people continue to claim it works. It has never been more important for doctors, and especially family physicians, to have accurate and updated guidelines.
The NIH and CDC have been publishing recommendations and guidelines for the prevention and treatment of COVID-19 since the start of the pandemic. Like any new disease, these have been changing to keep up as new knowledge related to the disease becomes available.
NIH updates treatment guidelines
A recent update to the NIH COVID-19 treatment guidelines was published on March 5, 2021. While the complete guidelines are quite extensive, spanning over 200 pages, it’s most important to understand the most recent updates in them.
Since preventative medicine is an integral part of primary care, it is important to note that no medications have been advised to prevent infection with COVID-19. In fact, taking drugs for pre-exposure prophylaxis (PrEp) is not recommended even in the highest-risk patients, such as health care workers.
In the updated guidelines, tocilizumab in a single IV dose of 8 mg/kg up to a maximum of 800 mg can be given only in combination with dexamethasone (or equivalent corticosteroid) in certain hospitalized patients exhibiting rapid respiratory decompensation. These patients include recently hospitalized patients who have been admitted to the ICU within the previous 24 hours and now require mechanical ventilation or high-flow oxygen via nasal cannula. Those not in the ICU who require rapidly increasing oxygen levels and have significantly increased levels of inflammatory markers should also receive this therapy. In the new guidance, the NIH recommends treating other hospitalized patients who require oxygen with remdesivir, remdesivir + dexamethasone, or dexamethasone alone.
In outpatients, those who have mild to moderate infection and are at increased risk of developing severe disease and/or hospitalization can be treated with bamlanivimab 700 mg + etesevimab 1,400 mg. This should be started as soon as possible after a confirmed diagnosis and within 10 days of symptom onset, according to the NIH recommendations. There is no evidence to support its use in patients hospitalized because of infection. However, it can be used in patients hospitalized for other reasons who have mild to moderate infection, but should be reserved – because of limited supply – for those with the highest risk of complications.
Hydroxychloroquine and casirivimab + imdevimab
One medication that has been touted in the media as a tool to treat COVID-19 has been hydroxychloroquine. Past guidelines recommended against this medication as a treatment because it lacked efficacy and posed risks for no therapeutic benefit. The most recent guidelines also recommend against the use of hydroxychloroquine for pre- and postexposure prophylaxis.
Casirivimab + imdevimab has been another talked about therapy. However, current guidelines recommend against its use in hospitalized patients. In addition, it is advised that hospitalized patients be enrolled in a clinical trial to receive it.
Since the pandemic began, the world has seen more than 120 million infections and more than 2 million deaths. Family physicians have a vital role to play as we are often the first ones patients turn to for treatment and advice. It is imperative we stay current with the guidelines and follow the most recent updates as research data are published.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at fpnews@mdedge.com.
Recommendations, as well as conspiracy theories about COVID-19, have changed at distressing rates over the past year. No disease has ever been more politicized, or more polarizing.
Experts, as well as the least educated, take a stand on what they believe is the most important way to prevent and treat this virus.
Just recently, a study was published revealing that ivermectin is not effective as a COVID-19 treatment while people continue to claim it works. It has never been more important for doctors, and especially family physicians, to have accurate and updated guidelines.
The NIH and CDC have been publishing recommendations and guidelines for the prevention and treatment of COVID-19 since the start of the pandemic. Like any new disease, these have been changing to keep up as new knowledge related to the disease becomes available.
NIH updates treatment guidelines
A recent update to the NIH COVID-19 treatment guidelines was published on March 5, 2021. While the complete guidelines are quite extensive, spanning over 200 pages, it’s most important to understand the most recent updates in them.
Since preventative medicine is an integral part of primary care, it is important to note that no medications have been advised to prevent infection with COVID-19. In fact, taking drugs for pre-exposure prophylaxis (PrEp) is not recommended even in the highest-risk patients, such as health care workers.
In the updated guidelines, tocilizumab in a single IV dose of 8 mg/kg up to a maximum of 800 mg can be given only in combination with dexamethasone (or equivalent corticosteroid) in certain hospitalized patients exhibiting rapid respiratory decompensation. These patients include recently hospitalized patients who have been admitted to the ICU within the previous 24 hours and now require mechanical ventilation or high-flow oxygen via nasal cannula. Those not in the ICU who require rapidly increasing oxygen levels and have significantly increased levels of inflammatory markers should also receive this therapy. In the new guidance, the NIH recommends treating other hospitalized patients who require oxygen with remdesivir, remdesivir + dexamethasone, or dexamethasone alone.
In outpatients, those who have mild to moderate infection and are at increased risk of developing severe disease and/or hospitalization can be treated with bamlanivimab 700 mg + etesevimab 1,400 mg. This should be started as soon as possible after a confirmed diagnosis and within 10 days of symptom onset, according to the NIH recommendations. There is no evidence to support its use in patients hospitalized because of infection. However, it can be used in patients hospitalized for other reasons who have mild to moderate infection, but should be reserved – because of limited supply – for those with the highest risk of complications.
Hydroxychloroquine and casirivimab + imdevimab
One medication that has been touted in the media as a tool to treat COVID-19 has been hydroxychloroquine. Past guidelines recommended against this medication as a treatment because it lacked efficacy and posed risks for no therapeutic benefit. The most recent guidelines also recommend against the use of hydroxychloroquine for pre- and postexposure prophylaxis.
Casirivimab + imdevimab has been another talked about therapy. However, current guidelines recommend against its use in hospitalized patients. In addition, it is advised that hospitalized patients be enrolled in a clinical trial to receive it.
Since the pandemic began, the world has seen more than 120 million infections and more than 2 million deaths. Family physicians have a vital role to play as we are often the first ones patients turn to for treatment and advice. It is imperative we stay current with the guidelines and follow the most recent updates as research data are published.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at fpnews@mdedge.com.
Recommendations, as well as conspiracy theories about COVID-19, have changed at distressing rates over the past year. No disease has ever been more politicized, or more polarizing.
Experts, as well as the least educated, take a stand on what they believe is the most important way to prevent and treat this virus.
Just recently, a study was published revealing that ivermectin is not effective as a COVID-19 treatment while people continue to claim it works. It has never been more important for doctors, and especially family physicians, to have accurate and updated guidelines.
The NIH and CDC have been publishing recommendations and guidelines for the prevention and treatment of COVID-19 since the start of the pandemic. Like any new disease, these have been changing to keep up as new knowledge related to the disease becomes available.
NIH updates treatment guidelines
A recent update to the NIH COVID-19 treatment guidelines was published on March 5, 2021. While the complete guidelines are quite extensive, spanning over 200 pages, it’s most important to understand the most recent updates in them.
Since preventative medicine is an integral part of primary care, it is important to note that no medications have been advised to prevent infection with COVID-19. In fact, taking drugs for pre-exposure prophylaxis (PrEp) is not recommended even in the highest-risk patients, such as health care workers.
In the updated guidelines, tocilizumab in a single IV dose of 8 mg/kg up to a maximum of 800 mg can be given only in combination with dexamethasone (or equivalent corticosteroid) in certain hospitalized patients exhibiting rapid respiratory decompensation. These patients include recently hospitalized patients who have been admitted to the ICU within the previous 24 hours and now require mechanical ventilation or high-flow oxygen via nasal cannula. Those not in the ICU who require rapidly increasing oxygen levels and have significantly increased levels of inflammatory markers should also receive this therapy. In the new guidance, the NIH recommends treating other hospitalized patients who require oxygen with remdesivir, remdesivir + dexamethasone, or dexamethasone alone.
In outpatients, those who have mild to moderate infection and are at increased risk of developing severe disease and/or hospitalization can be treated with bamlanivimab 700 mg + etesevimab 1,400 mg. This should be started as soon as possible after a confirmed diagnosis and within 10 days of symptom onset, according to the NIH recommendations. There is no evidence to support its use in patients hospitalized because of infection. However, it can be used in patients hospitalized for other reasons who have mild to moderate infection, but should be reserved – because of limited supply – for those with the highest risk of complications.
Hydroxychloroquine and casirivimab + imdevimab
One medication that has been touted in the media as a tool to treat COVID-19 has been hydroxychloroquine. Past guidelines recommended against this medication as a treatment because it lacked efficacy and posed risks for no therapeutic benefit. The most recent guidelines also recommend against the use of hydroxychloroquine for pre- and postexposure prophylaxis.
Casirivimab + imdevimab has been another talked about therapy. However, current guidelines recommend against its use in hospitalized patients. In addition, it is advised that hospitalized patients be enrolled in a clinical trial to receive it.
Since the pandemic began, the world has seen more than 120 million infections and more than 2 million deaths. Family physicians have a vital role to play as we are often the first ones patients turn to for treatment and advice. It is imperative we stay current with the guidelines and follow the most recent updates as research data are published.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at fpnews@mdedge.com.
Applying lessons from Oprah to your practice
In my last column, I explained how I’m like Tom Brady. I’m not really. Brady is a Super Bowl–winning quarterback worth over $200 million. No, I’m like Oprah. Well, trying anyway.
Brady and Oprah, in addition to being gazillionaires, have in common that they’re arguably the GOATs (Greatest Of All Time) in their fields. Watching Oprah interview Meghan Markle and Prince Harry was like watching Tom Brady on the jumbotron – she made it look easy. Her ability to create conversation and coax information from guests is hall-of-fame good. But although they are both admirable, trying to be like Brady is useful only for next Thanksgiving when you’re trying to beat your cousins from Massachusetts in touch football. .
1. Prepare ahead. It’s clear that Oprah has binders of notes about her guests and thoroughly reviewed them before she invites them to sit down. We should do the same. Open the chart and read as much as you can before you open the door. Have important information in your head so you don’t have to break from your interview to refer to it.
2. Sprinkle pleasantry. She’d never start an interview with: So why are you here? Nor should we. Even one nonscripted question or comment can help build a little rapport before getting to the work.
3. Be brief. Oprah gets her question out fast, then gets out of the way. And as a bonus, this is the easiest place to shave a few minutes from your appointments from your own end. Think for a second before you speak and try to find the shortest route to your question. Try to keep your questions to just a sentence or two.
4. Stay on it. Once you’ve discovered something relevant, stay with it, resisting the urge to finish the review of symptoms. This is not just to make a diagnosis, but as importantly, trying to diagnose “the real reason” for the visit. Then, when the question is done, own the transition. Oprah uses: “Let’s move on.” This is a bit abrupt for us, but it can be helpful if used sparingly and gently. I might soften this a little by adding “I want to be sure we have enough time to get through everything for you.”
5. Wait. A few seconds seems an eternity on the air (and in clinic), but sometimes the silent pause is just what’s needed to help the patient expand and share.
6. Be nonjudgmental. Most of us believe we’re pretty good at this, yet, it’s sometimes a blind spot. It’s easy to blame the obese patient for his stasis dermatitis or the hidradenitis patient who hasn’t stop smoking for her cysts. It also helps to be nontransactional. If you make patients feel that you’re asking questions only to extract information, you’ll never reach Oprah level.
7. Be in the moment. It is difficult, but when possible, avoid typing notes while you’re still interviewing. We’re not just there to get the facts, we’re also trying to get the story and that sometimes takes really listening.
I’m no more like Oprah than Brady, of course. But it is more fun to close my eyes and imagine myself being her when I see my next patient. That is, until Thanksgiving. Watch out, Bedards from Attleboro.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
In my last column, I explained how I’m like Tom Brady. I’m not really. Brady is a Super Bowl–winning quarterback worth over $200 million. No, I’m like Oprah. Well, trying anyway.
Brady and Oprah, in addition to being gazillionaires, have in common that they’re arguably the GOATs (Greatest Of All Time) in their fields. Watching Oprah interview Meghan Markle and Prince Harry was like watching Tom Brady on the jumbotron – she made it look easy. Her ability to create conversation and coax information from guests is hall-of-fame good. But although they are both admirable, trying to be like Brady is useful only for next Thanksgiving when you’re trying to beat your cousins from Massachusetts in touch football. .
1. Prepare ahead. It’s clear that Oprah has binders of notes about her guests and thoroughly reviewed them before she invites them to sit down. We should do the same. Open the chart and read as much as you can before you open the door. Have important information in your head so you don’t have to break from your interview to refer to it.
2. Sprinkle pleasantry. She’d never start an interview with: So why are you here? Nor should we. Even one nonscripted question or comment can help build a little rapport before getting to the work.
3. Be brief. Oprah gets her question out fast, then gets out of the way. And as a bonus, this is the easiest place to shave a few minutes from your appointments from your own end. Think for a second before you speak and try to find the shortest route to your question. Try to keep your questions to just a sentence or two.
4. Stay on it. Once you’ve discovered something relevant, stay with it, resisting the urge to finish the review of symptoms. This is not just to make a diagnosis, but as importantly, trying to diagnose “the real reason” for the visit. Then, when the question is done, own the transition. Oprah uses: “Let’s move on.” This is a bit abrupt for us, but it can be helpful if used sparingly and gently. I might soften this a little by adding “I want to be sure we have enough time to get through everything for you.”
5. Wait. A few seconds seems an eternity on the air (and in clinic), but sometimes the silent pause is just what’s needed to help the patient expand and share.
6. Be nonjudgmental. Most of us believe we’re pretty good at this, yet, it’s sometimes a blind spot. It’s easy to blame the obese patient for his stasis dermatitis or the hidradenitis patient who hasn’t stop smoking for her cysts. It also helps to be nontransactional. If you make patients feel that you’re asking questions only to extract information, you’ll never reach Oprah level.
7. Be in the moment. It is difficult, but when possible, avoid typing notes while you’re still interviewing. We’re not just there to get the facts, we’re also trying to get the story and that sometimes takes really listening.
I’m no more like Oprah than Brady, of course. But it is more fun to close my eyes and imagine myself being her when I see my next patient. That is, until Thanksgiving. Watch out, Bedards from Attleboro.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
In my last column, I explained how I’m like Tom Brady. I’m not really. Brady is a Super Bowl–winning quarterback worth over $200 million. No, I’m like Oprah. Well, trying anyway.
Brady and Oprah, in addition to being gazillionaires, have in common that they’re arguably the GOATs (Greatest Of All Time) in their fields. Watching Oprah interview Meghan Markle and Prince Harry was like watching Tom Brady on the jumbotron – she made it look easy. Her ability to create conversation and coax information from guests is hall-of-fame good. But although they are both admirable, trying to be like Brady is useful only for next Thanksgiving when you’re trying to beat your cousins from Massachusetts in touch football. .
1. Prepare ahead. It’s clear that Oprah has binders of notes about her guests and thoroughly reviewed them before she invites them to sit down. We should do the same. Open the chart and read as much as you can before you open the door. Have important information in your head so you don’t have to break from your interview to refer to it.
2. Sprinkle pleasantry. She’d never start an interview with: So why are you here? Nor should we. Even one nonscripted question or comment can help build a little rapport before getting to the work.
3. Be brief. Oprah gets her question out fast, then gets out of the way. And as a bonus, this is the easiest place to shave a few minutes from your appointments from your own end. Think for a second before you speak and try to find the shortest route to your question. Try to keep your questions to just a sentence or two.
4. Stay on it. Once you’ve discovered something relevant, stay with it, resisting the urge to finish the review of symptoms. This is not just to make a diagnosis, but as importantly, trying to diagnose “the real reason” for the visit. Then, when the question is done, own the transition. Oprah uses: “Let’s move on.” This is a bit abrupt for us, but it can be helpful if used sparingly and gently. I might soften this a little by adding “I want to be sure we have enough time to get through everything for you.”
5. Wait. A few seconds seems an eternity on the air (and in clinic), but sometimes the silent pause is just what’s needed to help the patient expand and share.
6. Be nonjudgmental. Most of us believe we’re pretty good at this, yet, it’s sometimes a blind spot. It’s easy to blame the obese patient for his stasis dermatitis or the hidradenitis patient who hasn’t stop smoking for her cysts. It also helps to be nontransactional. If you make patients feel that you’re asking questions only to extract information, you’ll never reach Oprah level.
7. Be in the moment. It is difficult, but when possible, avoid typing notes while you’re still interviewing. We’re not just there to get the facts, we’re also trying to get the story and that sometimes takes really listening.
I’m no more like Oprah than Brady, of course. But it is more fun to close my eyes and imagine myself being her when I see my next patient. That is, until Thanksgiving. Watch out, Bedards from Attleboro.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
School refusal and COVID-19: The pediatrician's role
Hooray for back to school! But not for everyone. ... what to do with those who have trouble transitioning back?
As we have now passed a year since COVID-19–related shutdowns were implemented throughout the United States; and with returns to in-person schooling continuing to vary based on location, many of us either in our personal lives, or through conversations with patients and families, are experiencing a yearning for the “good old days” of fully in-person schooling. As the place where children and adolescents spend a good portion of their waking hours, school is integral to not just children’s academic development, but to emotional and social development as well. One interesting phenomenon I’ve seen working with many children and families is that the strong desire to go back to school is not universal. Some of my patients are perfectly happy to be doing “remote schooling”, as it reduces the stress that they were experiencing in this setting before the pandemic.1 These families find themselves wondering – how will I get my child to return to school? As we (hopefully) turn the corner toward a return to normalcy, I believe many of us may find ourselves counseling families on whether a return to in-person schooling is in their child’s best interest. Even when a family decides it is best for their child to return, we might encounter scenarios in which children and adolescents outright refuse to go to school, or engage in avoidant behavior, which is broadly known as “school refusal.” Discussion of a treatment approach to this often challenging clinical scenario is warranted.
The first step in addressing the issue is defining it. School refusal is not a “diagnosis” in psychiatric lexicon, rather it describes a behavior which may be a symptom or manifestation of any number of underlying factors. One helpful definition proposed is (a) missing 25% of total school time for at least 2 weeks or (b) experiencing difficulty attending school such that there is significant interference in the child’s or family’s daily routine for at least 2 weeks, or (c) missing at least 10 days of school over a period of 15 weeks.2 The common thread of this, and any other definition, is sustained absenteeism or avoidance with significant impact to education, family life, or both. It is estimated that the prevalence of this phenomenon is between 1% and 2% of school-aged children.
Next to consider is what might be prompting or underlying the behavior. A comprehensive evaluation approach should include consideration of environmental factors such as bullying and learning difficulties, as well as presence of an anxiety or depressive disorder. Awareness of whether the child/adolescent has a 504 plan or individualized education program (IEP) is vital, as these can be marshaled for additional support. Family factors, including parental illness (medical and/or psychiatric), should also be considered. As school avoidance behaviors often include somatic symptoms of anxiety such as palpitations, shortness of breath, and abdominal pain; a rule out of medical etiology is recommended, as well as a caution to consider both medical and behavioral factors simultaneously, as focus on either separately can lead to missing the other.
Separation anxiety and social anxiety disorders are two specific conditions that may manifest in school refusal and should be evaluated for specifically. Separation anxiety is characterized by developmentally inappropriate, excessive worry or distress associated with separation from a primary caregiver or major attachment figure. Social anxiety is characterized by excessive fear or worry about being negatively evaluated by others in social situations.3 One publicly available tool that can be helpful for screening for a variety of anxiety disorders in children and adolescents is the SCARED.4 The PHQ-9 Adolescent5 is one such screening instrument for depression, which can be a driving factor or co-occur in children with school refusal.
When it comes to treatment, the best evidence out there is for a cognitive-behavioral therapy (CBT)–based approach motivated toward a return to the school setting as soon as possible.6,7 This will involve looking at how thoughts, behaviors, and feelings are interacting with each other in the clinical scenario and how these might be challenged or changed in a positive manner. Coping and problem-solving skills are often incorporated. This approach may also involve gradual exposure to the anxiety-producing situation in a hierarchical fashion starting with less anxiety-provoking scenarios and moving toward increasingly challenging ones. CBT for school refusal is likely most effective when including both school and family involvement to ensure consistency across settings. Making sure that there are not inadvertent reinforcing factors motivating staying home (for instance unrestricted access to electronic devices) is an important step to consider. If anxiety or depression is moderately to severely impairing – which is frequently the case when school refusal comes to clinical attention, consider use of medication as part of the treatment strategy. Selective serotonin reuptake inhibitors as a class are the most commonly used medications and deserve strong consideration.
To summarize, school refusal can occur for a variety of reasons. Early identification and comprehensive treatment taking into account child and family preference and using a multimodal approach to encourage and support a quick return to the school environment is considered best practice.
Dr. Hoffnung is a pediatric psychiatrist at the University of Vermont Children’s Hospital and an assistant professor of psychiatry at the Robert Larner, M.D. College of Medicine at the University of Vermont, both in Burlington. He has no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. See, for example: www.npr.org/2021/03/08/971457441/as-many-parents-fret-over-remote-learning-some-find-their-kids-are-thriving.
2. Kearney CA. Educ Psychol Rev. 2008;20:257-82.
3. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, Va.: American Psychiatric Association, 2013.
4. Available at: www.pediatricbipolar.pitt.edu/resources/instruments.
5. Available at: www.aacap.org/App_Themes/AACAP/docs/member_resources/toolbox_for_clinical_practice_and_outcomes/symptoms/GLAD-PC_PHQ-9.pdf.
6. Elliott JG and Place M. J Child Psychol Psychiatry. 2019;60(1):4-15.
7. Prabhuswamy M. J Paed Child Health. 2018;54(10):1117-20.
Hooray for back to school! But not for everyone. ... what to do with those who have trouble transitioning back?
As we have now passed a year since COVID-19–related shutdowns were implemented throughout the United States; and with returns to in-person schooling continuing to vary based on location, many of us either in our personal lives, or through conversations with patients and families, are experiencing a yearning for the “good old days” of fully in-person schooling. As the place where children and adolescents spend a good portion of their waking hours, school is integral to not just children’s academic development, but to emotional and social development as well. One interesting phenomenon I’ve seen working with many children and families is that the strong desire to go back to school is not universal. Some of my patients are perfectly happy to be doing “remote schooling”, as it reduces the stress that they were experiencing in this setting before the pandemic.1 These families find themselves wondering – how will I get my child to return to school? As we (hopefully) turn the corner toward a return to normalcy, I believe many of us may find ourselves counseling families on whether a return to in-person schooling is in their child’s best interest. Even when a family decides it is best for their child to return, we might encounter scenarios in which children and adolescents outright refuse to go to school, or engage in avoidant behavior, which is broadly known as “school refusal.” Discussion of a treatment approach to this often challenging clinical scenario is warranted.
The first step in addressing the issue is defining it. School refusal is not a “diagnosis” in psychiatric lexicon, rather it describes a behavior which may be a symptom or manifestation of any number of underlying factors. One helpful definition proposed is (a) missing 25% of total school time for at least 2 weeks or (b) experiencing difficulty attending school such that there is significant interference in the child’s or family’s daily routine for at least 2 weeks, or (c) missing at least 10 days of school over a period of 15 weeks.2 The common thread of this, and any other definition, is sustained absenteeism or avoidance with significant impact to education, family life, or both. It is estimated that the prevalence of this phenomenon is between 1% and 2% of school-aged children.
Next to consider is what might be prompting or underlying the behavior. A comprehensive evaluation approach should include consideration of environmental factors such as bullying and learning difficulties, as well as presence of an anxiety or depressive disorder. Awareness of whether the child/adolescent has a 504 plan or individualized education program (IEP) is vital, as these can be marshaled for additional support. Family factors, including parental illness (medical and/or psychiatric), should also be considered. As school avoidance behaviors often include somatic symptoms of anxiety such as palpitations, shortness of breath, and abdominal pain; a rule out of medical etiology is recommended, as well as a caution to consider both medical and behavioral factors simultaneously, as focus on either separately can lead to missing the other.
Separation anxiety and social anxiety disorders are two specific conditions that may manifest in school refusal and should be evaluated for specifically. Separation anxiety is characterized by developmentally inappropriate, excessive worry or distress associated with separation from a primary caregiver or major attachment figure. Social anxiety is characterized by excessive fear or worry about being negatively evaluated by others in social situations.3 One publicly available tool that can be helpful for screening for a variety of anxiety disorders in children and adolescents is the SCARED.4 The PHQ-9 Adolescent5 is one such screening instrument for depression, which can be a driving factor or co-occur in children with school refusal.
When it comes to treatment, the best evidence out there is for a cognitive-behavioral therapy (CBT)–based approach motivated toward a return to the school setting as soon as possible.6,7 This will involve looking at how thoughts, behaviors, and feelings are interacting with each other in the clinical scenario and how these might be challenged or changed in a positive manner. Coping and problem-solving skills are often incorporated. This approach may also involve gradual exposure to the anxiety-producing situation in a hierarchical fashion starting with less anxiety-provoking scenarios and moving toward increasingly challenging ones. CBT for school refusal is likely most effective when including both school and family involvement to ensure consistency across settings. Making sure that there are not inadvertent reinforcing factors motivating staying home (for instance unrestricted access to electronic devices) is an important step to consider. If anxiety or depression is moderately to severely impairing – which is frequently the case when school refusal comes to clinical attention, consider use of medication as part of the treatment strategy. Selective serotonin reuptake inhibitors as a class are the most commonly used medications and deserve strong consideration.
To summarize, school refusal can occur for a variety of reasons. Early identification and comprehensive treatment taking into account child and family preference and using a multimodal approach to encourage and support a quick return to the school environment is considered best practice.
Dr. Hoffnung is a pediatric psychiatrist at the University of Vermont Children’s Hospital and an assistant professor of psychiatry at the Robert Larner, M.D. College of Medicine at the University of Vermont, both in Burlington. He has no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. See, for example: www.npr.org/2021/03/08/971457441/as-many-parents-fret-over-remote-learning-some-find-their-kids-are-thriving.
2. Kearney CA. Educ Psychol Rev. 2008;20:257-82.
3. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, Va.: American Psychiatric Association, 2013.
4. Available at: www.pediatricbipolar.pitt.edu/resources/instruments.
5. Available at: www.aacap.org/App_Themes/AACAP/docs/member_resources/toolbox_for_clinical_practice_and_outcomes/symptoms/GLAD-PC_PHQ-9.pdf.
6. Elliott JG and Place M. J Child Psychol Psychiatry. 2019;60(1):4-15.
7. Prabhuswamy M. J Paed Child Health. 2018;54(10):1117-20.
Hooray for back to school! But not for everyone. ... what to do with those who have trouble transitioning back?
As we have now passed a year since COVID-19–related shutdowns were implemented throughout the United States; and with returns to in-person schooling continuing to vary based on location, many of us either in our personal lives, or through conversations with patients and families, are experiencing a yearning for the “good old days” of fully in-person schooling. As the place where children and adolescents spend a good portion of their waking hours, school is integral to not just children’s academic development, but to emotional and social development as well. One interesting phenomenon I’ve seen working with many children and families is that the strong desire to go back to school is not universal. Some of my patients are perfectly happy to be doing “remote schooling”, as it reduces the stress that they were experiencing in this setting before the pandemic.1 These families find themselves wondering – how will I get my child to return to school? As we (hopefully) turn the corner toward a return to normalcy, I believe many of us may find ourselves counseling families on whether a return to in-person schooling is in their child’s best interest. Even when a family decides it is best for their child to return, we might encounter scenarios in which children and adolescents outright refuse to go to school, or engage in avoidant behavior, which is broadly known as “school refusal.” Discussion of a treatment approach to this often challenging clinical scenario is warranted.
The first step in addressing the issue is defining it. School refusal is not a “diagnosis” in psychiatric lexicon, rather it describes a behavior which may be a symptom or manifestation of any number of underlying factors. One helpful definition proposed is (a) missing 25% of total school time for at least 2 weeks or (b) experiencing difficulty attending school such that there is significant interference in the child’s or family’s daily routine for at least 2 weeks, or (c) missing at least 10 days of school over a period of 15 weeks.2 The common thread of this, and any other definition, is sustained absenteeism or avoidance with significant impact to education, family life, or both. It is estimated that the prevalence of this phenomenon is between 1% and 2% of school-aged children.
Next to consider is what might be prompting or underlying the behavior. A comprehensive evaluation approach should include consideration of environmental factors such as bullying and learning difficulties, as well as presence of an anxiety or depressive disorder. Awareness of whether the child/adolescent has a 504 plan or individualized education program (IEP) is vital, as these can be marshaled for additional support. Family factors, including parental illness (medical and/or psychiatric), should also be considered. As school avoidance behaviors often include somatic symptoms of anxiety such as palpitations, shortness of breath, and abdominal pain; a rule out of medical etiology is recommended, as well as a caution to consider both medical and behavioral factors simultaneously, as focus on either separately can lead to missing the other.
Separation anxiety and social anxiety disorders are two specific conditions that may manifest in school refusal and should be evaluated for specifically. Separation anxiety is characterized by developmentally inappropriate, excessive worry or distress associated with separation from a primary caregiver or major attachment figure. Social anxiety is characterized by excessive fear or worry about being negatively evaluated by others in social situations.3 One publicly available tool that can be helpful for screening for a variety of anxiety disorders in children and adolescents is the SCARED.4 The PHQ-9 Adolescent5 is one such screening instrument for depression, which can be a driving factor or co-occur in children with school refusal.
When it comes to treatment, the best evidence out there is for a cognitive-behavioral therapy (CBT)–based approach motivated toward a return to the school setting as soon as possible.6,7 This will involve looking at how thoughts, behaviors, and feelings are interacting with each other in the clinical scenario and how these might be challenged or changed in a positive manner. Coping and problem-solving skills are often incorporated. This approach may also involve gradual exposure to the anxiety-producing situation in a hierarchical fashion starting with less anxiety-provoking scenarios and moving toward increasingly challenging ones. CBT for school refusal is likely most effective when including both school and family involvement to ensure consistency across settings. Making sure that there are not inadvertent reinforcing factors motivating staying home (for instance unrestricted access to electronic devices) is an important step to consider. If anxiety or depression is moderately to severely impairing – which is frequently the case when school refusal comes to clinical attention, consider use of medication as part of the treatment strategy. Selective serotonin reuptake inhibitors as a class are the most commonly used medications and deserve strong consideration.
To summarize, school refusal can occur for a variety of reasons. Early identification and comprehensive treatment taking into account child and family preference and using a multimodal approach to encourage and support a quick return to the school environment is considered best practice.
Dr. Hoffnung is a pediatric psychiatrist at the University of Vermont Children’s Hospital and an assistant professor of psychiatry at the Robert Larner, M.D. College of Medicine at the University of Vermont, both in Burlington. He has no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. See, for example: www.npr.org/2021/03/08/971457441/as-many-parents-fret-over-remote-learning-some-find-their-kids-are-thriving.
2. Kearney CA. Educ Psychol Rev. 2008;20:257-82.
3. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, Va.: American Psychiatric Association, 2013.
4. Available at: www.pediatricbipolar.pitt.edu/resources/instruments.
5. Available at: www.aacap.org/App_Themes/AACAP/docs/member_resources/toolbox_for_clinical_practice_and_outcomes/symptoms/GLAD-PC_PHQ-9.pdf.
6. Elliott JG and Place M. J Child Psychol Psychiatry. 2019;60(1):4-15.
7. Prabhuswamy M. J Paed Child Health. 2018;54(10):1117-20.
Office etiquette: Answering patient phone calls
In my office, one of the many consequences of the COVID-19 pandemic has been a dramatic increase in telephone traffic. I’m sure there are multiple reasons for this, but a major one is calls from patients who remain reluctant to visit our office in person.
Our veteran front-office staff members were adept at handling phone traffic at any level, but most of them retired because of the pandemic. The young folks who replaced them have struggled at times. You would think that millennials, who spend so much time on phones, would have little to learn in that department – until you remember that Twitter, Twitch, and TikTok do not demand polished interpersonal skills.
To address this issue, I have a memo in my office, which I have written, that establishes clear rules for proper professional telephone etiquette. If you want to adapt it for your own office, feel free to do so:
1. You only have one chance to make a first impression. The way we answer it determines, to a significant extent, how the community thinks of us, as people and as health care providers.
2. Answer all incoming calls before the third ring.
3. Answer warmly, enthusiastically, and professionally. Since the caller cannot see you, your voice is the only impression of our office a first-time caller will get.
4. Identify yourself and our office immediately. “Good morning, Doctor Eastern’s office. This is _____. How may I help you?” No one should ever have to ask what office they have reached, or to whom they are speaking.
5. Speak softly. This is to ensure confidentiality (more on that next), and because most people find loud telephone voices unpleasant.
6. Maintaining patient confidentiality is a top priority. It makes patients feel secure about being treated in our office, and it is also the law. Keep in mind that patients and others in the office may be able to overhear your phone conversations. Keep your voice down; never use the phone’s hands-free “speaker” function.
Be cautious about all information that is given over the phone. Don’t disclose any personal information unless you are absolutely certain you are talking to the correct patient. If the caller is not the patient, never discuss personal information without the patient’s permission.
7. Adopt a positive vocabulary – one that focuses on helping people. For example, rather than saying, “I don’t know,” say, “Let me find out for you,” or “I’ll find out who can help you with that.”
8. Offer to take a message if the caller has a question or issue you cannot address. Assure the patient that the appropriate staffer will call back later that day. That way, office workflow is not interrupted, and the patient still receives a prompt (and correct) answer.
9. All messages left overnight with the answering service must be returned as early as possible the very next business day. This is a top priority each morning. Few things annoy callers trying to reach their doctors more than unreturned calls. If the office will be closed for a holiday, or a response will be delayed for any other reason, make sure the service knows, and passes it on to patients.
10. Everyone in the office must answer calls when necessary. If you notice that a phone is ringing and the receptionists are swamped, please answer it; an incoming call must never go unanswered.
11. If the phone rings while you are dealing with a patient in person, the patient in front of you is your first priority. Put the caller on hold, but always ask permission before doing so, and wait for an answer. Never leave a caller on hold for more than a minute or two unless absolutely unavoidable.
12. NEVER answer, “Doctor’s office, please hold.” To a patient, that is even worse than not answering at all. No matter how often your hold message tells callers how important they are, they know they are being ignored. Such encounters never end well: Those who wait will be grumpy and rude when you get back to them; those who hang up will be even more grumpy and rude when they call back. Worst of all are those who don’t call back and seek care elsewhere – often leaving a nasty comment on social media besides.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
In my office, one of the many consequences of the COVID-19 pandemic has been a dramatic increase in telephone traffic. I’m sure there are multiple reasons for this, but a major one is calls from patients who remain reluctant to visit our office in person.
Our veteran front-office staff members were adept at handling phone traffic at any level, but most of them retired because of the pandemic. The young folks who replaced them have struggled at times. You would think that millennials, who spend so much time on phones, would have little to learn in that department – until you remember that Twitter, Twitch, and TikTok do not demand polished interpersonal skills.
To address this issue, I have a memo in my office, which I have written, that establishes clear rules for proper professional telephone etiquette. If you want to adapt it for your own office, feel free to do so:
1. You only have one chance to make a first impression. The way we answer it determines, to a significant extent, how the community thinks of us, as people and as health care providers.
2. Answer all incoming calls before the third ring.
3. Answer warmly, enthusiastically, and professionally. Since the caller cannot see you, your voice is the only impression of our office a first-time caller will get.
4. Identify yourself and our office immediately. “Good morning, Doctor Eastern’s office. This is _____. How may I help you?” No one should ever have to ask what office they have reached, or to whom they are speaking.
5. Speak softly. This is to ensure confidentiality (more on that next), and because most people find loud telephone voices unpleasant.
6. Maintaining patient confidentiality is a top priority. It makes patients feel secure about being treated in our office, and it is also the law. Keep in mind that patients and others in the office may be able to overhear your phone conversations. Keep your voice down; never use the phone’s hands-free “speaker” function.
Be cautious about all information that is given over the phone. Don’t disclose any personal information unless you are absolutely certain you are talking to the correct patient. If the caller is not the patient, never discuss personal information without the patient’s permission.
7. Adopt a positive vocabulary – one that focuses on helping people. For example, rather than saying, “I don’t know,” say, “Let me find out for you,” or “I’ll find out who can help you with that.”
8. Offer to take a message if the caller has a question or issue you cannot address. Assure the patient that the appropriate staffer will call back later that day. That way, office workflow is not interrupted, and the patient still receives a prompt (and correct) answer.
9. All messages left overnight with the answering service must be returned as early as possible the very next business day. This is a top priority each morning. Few things annoy callers trying to reach their doctors more than unreturned calls. If the office will be closed for a holiday, or a response will be delayed for any other reason, make sure the service knows, and passes it on to patients.
10. Everyone in the office must answer calls when necessary. If you notice that a phone is ringing and the receptionists are swamped, please answer it; an incoming call must never go unanswered.
11. If the phone rings while you are dealing with a patient in person, the patient in front of you is your first priority. Put the caller on hold, but always ask permission before doing so, and wait for an answer. Never leave a caller on hold for more than a minute or two unless absolutely unavoidable.
12. NEVER answer, “Doctor’s office, please hold.” To a patient, that is even worse than not answering at all. No matter how often your hold message tells callers how important they are, they know they are being ignored. Such encounters never end well: Those who wait will be grumpy and rude when you get back to them; those who hang up will be even more grumpy and rude when they call back. Worst of all are those who don’t call back and seek care elsewhere – often leaving a nasty comment on social media besides.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
In my office, one of the many consequences of the COVID-19 pandemic has been a dramatic increase in telephone traffic. I’m sure there are multiple reasons for this, but a major one is calls from patients who remain reluctant to visit our office in person.
Our veteran front-office staff members were adept at handling phone traffic at any level, but most of them retired because of the pandemic. The young folks who replaced them have struggled at times. You would think that millennials, who spend so much time on phones, would have little to learn in that department – until you remember that Twitter, Twitch, and TikTok do not demand polished interpersonal skills.
To address this issue, I have a memo in my office, which I have written, that establishes clear rules for proper professional telephone etiquette. If you want to adapt it for your own office, feel free to do so:
1. You only have one chance to make a first impression. The way we answer it determines, to a significant extent, how the community thinks of us, as people and as health care providers.
2. Answer all incoming calls before the third ring.
3. Answer warmly, enthusiastically, and professionally. Since the caller cannot see you, your voice is the only impression of our office a first-time caller will get.
4. Identify yourself and our office immediately. “Good morning, Doctor Eastern’s office. This is _____. How may I help you?” No one should ever have to ask what office they have reached, or to whom they are speaking.
5. Speak softly. This is to ensure confidentiality (more on that next), and because most people find loud telephone voices unpleasant.
6. Maintaining patient confidentiality is a top priority. It makes patients feel secure about being treated in our office, and it is also the law. Keep in mind that patients and others in the office may be able to overhear your phone conversations. Keep your voice down; never use the phone’s hands-free “speaker” function.
Be cautious about all information that is given over the phone. Don’t disclose any personal information unless you are absolutely certain you are talking to the correct patient. If the caller is not the patient, never discuss personal information without the patient’s permission.
7. Adopt a positive vocabulary – one that focuses on helping people. For example, rather than saying, “I don’t know,” say, “Let me find out for you,” or “I’ll find out who can help you with that.”
8. Offer to take a message if the caller has a question or issue you cannot address. Assure the patient that the appropriate staffer will call back later that day. That way, office workflow is not interrupted, and the patient still receives a prompt (and correct) answer.
9. All messages left overnight with the answering service must be returned as early as possible the very next business day. This is a top priority each morning. Few things annoy callers trying to reach their doctors more than unreturned calls. If the office will be closed for a holiday, or a response will be delayed for any other reason, make sure the service knows, and passes it on to patients.
10. Everyone in the office must answer calls when necessary. If you notice that a phone is ringing and the receptionists are swamped, please answer it; an incoming call must never go unanswered.
11. If the phone rings while you are dealing with a patient in person, the patient in front of you is your first priority. Put the caller on hold, but always ask permission before doing so, and wait for an answer. Never leave a caller on hold for more than a minute or two unless absolutely unavoidable.
12. NEVER answer, “Doctor’s office, please hold.” To a patient, that is even worse than not answering at all. No matter how often your hold message tells callers how important they are, they know they are being ignored. Such encounters never end well: Those who wait will be grumpy and rude when you get back to them; those who hang up will be even more grumpy and rude when they call back. Worst of all are those who don’t call back and seek care elsewhere – often leaving a nasty comment on social media besides.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Virtual is the new real
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
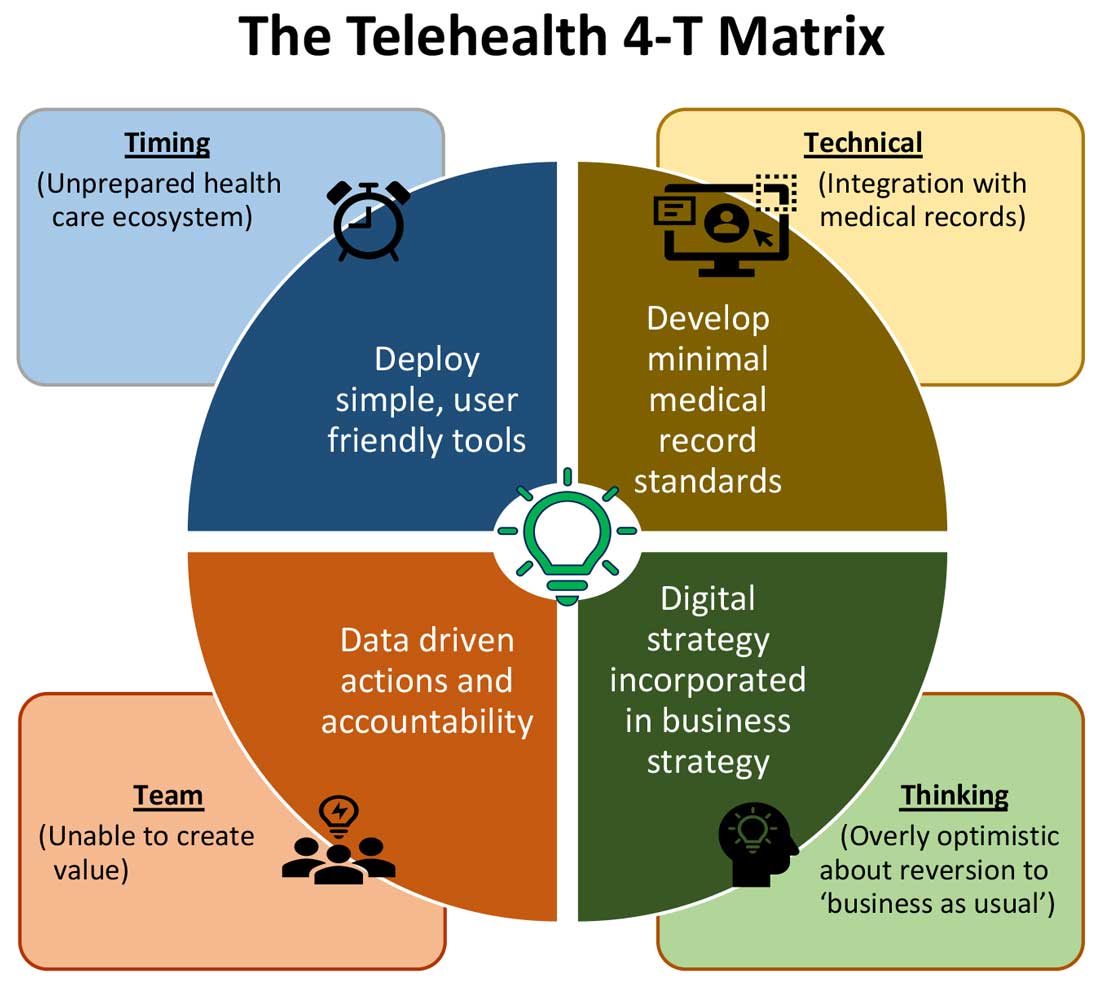
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
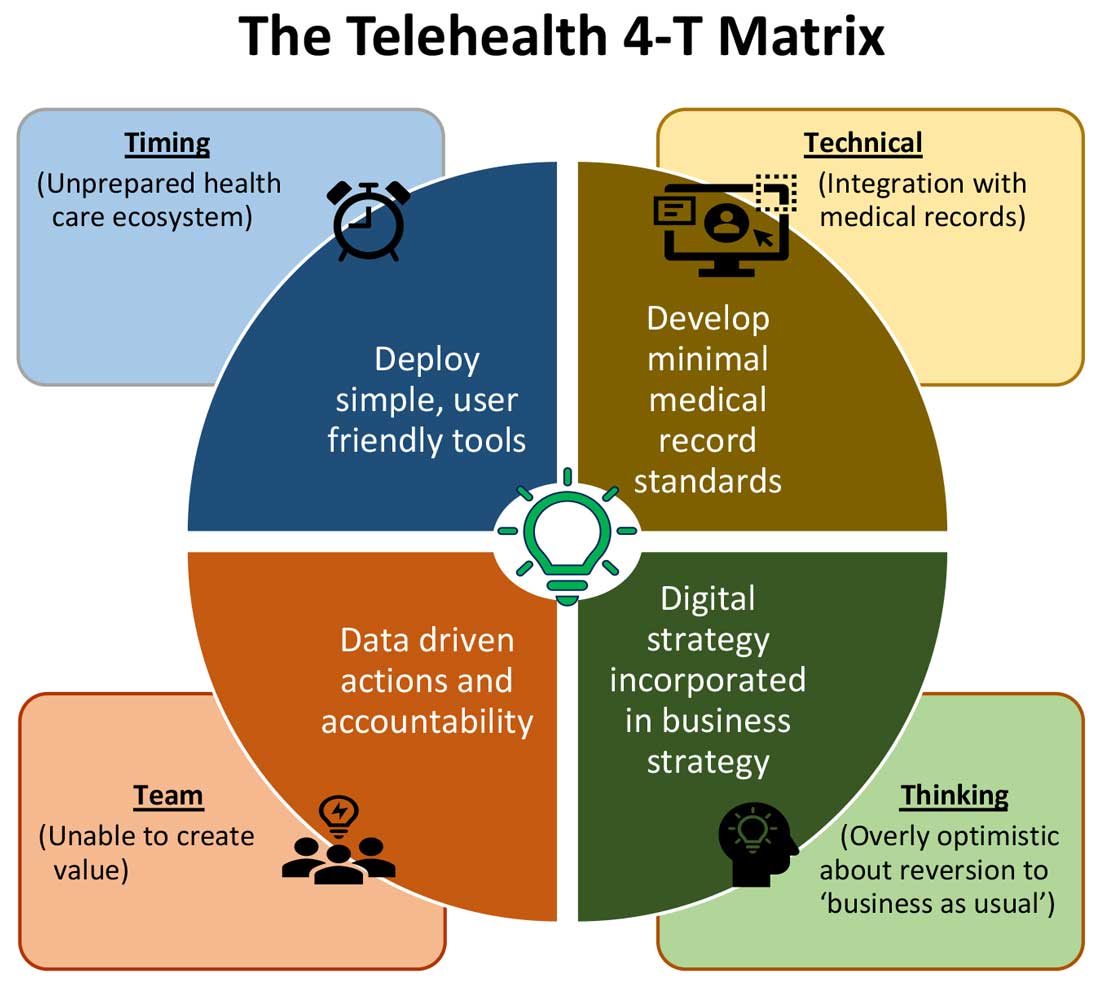
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
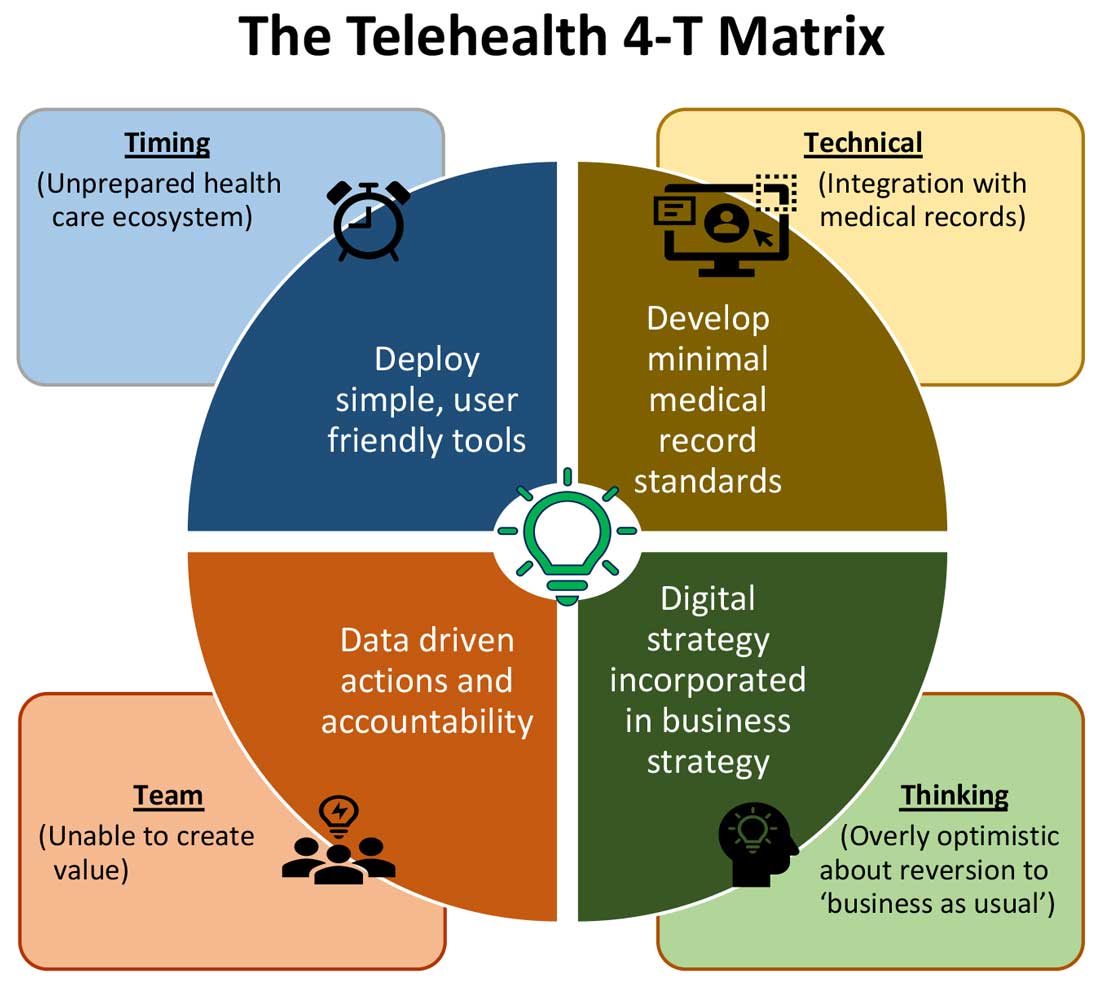
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
The siesta solution
Are you a napper? Unless you’re retired that may sound like a ridiculous question. When could you possibly fit in the time to doze off for even 20 minutes? I suspect there may be one or two of you who, although you are still working, have found a way to schedule a nap into your schedules. The rest of us must wait until we no longer have clinical responsibilities.
In my experience, you regular nappers seem to be the lucky few who have discovered the art of nodding off after lunch and waking up refreshed and ready to take on a full afternoon of patients. We in the unlucky majority may have tried taking a nap but run the risk of its flowing into a deep slumber the length of which we can’t control. Or, more likely, we find that we wake feeling groggy and disoriented and, even worse, the daytime nod off has messed up our nighttime schedule.
Well, it turns out the ability to take daytime naps and reap their cardiometabolic benefits is not just luck but has a significant genetic component. Investigators at Massachusetts General Hospital in Boston have recently published a study in which they report finding more than a score of gene regions that determine a person’s propensity to take daytime naps.. The researchers have also unearthed preliminary evidence supporting a link between daytime napping and cardiometabolic health. My mother began napping when my sister and I were infants and never gave it up. Unfortunately, I seem to have ended up on the wrong side of the genomic shuffle.
Although this new research is interesting, I don’t think the investigators have enough information to answer one of the questions that every pediatrician fields multiple times each week. “When should my toddler grow out of his afternoon nap?” Although it looks like we may be getting closer to a gene-based answer, I have always couched my reply in terms of behavior modification and the fostering of habit-forming associations.
As a child begins to transition from multiple short naps interspersed with feedings to a pattern of two distinct naps, I suggest to parents that they begin to think of the afternoon nap as a siesta. In other words, the nap is something that always comes immediately after lunch with no intervening shenanigans. No playtime, no Teletubbies videos, no quick trips to the grocery store, nothing, nada, zip.
At least for me, lunch has always been soporific. And I suspect we will learn eventually that association cuts across the entire genetic landscape to one degree or another. It makes sense to take advantage of that association and remove all other distractions. For some parents, that means creating the illusion that they too are taking a siesta: No TV, no phone calls. Imagine that the whole household has suddenly moved to Spain for the next hour or two. If you’ve ever been a tourist in rural Spain and tried to do anything, buy anything, or visit a museum between 2 and 4 p.m. you’ve got the idea.
When the child is young he or she will probably fall asleep as long as his parents have been reasonably successful at maintaining sleep hygiene practices. As the child is gaining more stamina and gives up the morning nap, the siesta will remain as a quiet time because that’s the way it’s always been in the household. The child may sleep or play quietly, or be read a sleep-inducing story because no other options will be available until some predetermined time. An hour is usually reasonable. If sleep hasn’t overtaken them, an earlier bedtime will probably be in order. The child will outgrow the napping part of the siesta when his or her sleep need is gone. But, the siesta/quiet time can remain as an option until all-day school intervenes. This scheme works if you can get parents to appropriately prioritize their child’s sleep needs. That’s not always an easy sell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Are you a napper? Unless you’re retired that may sound like a ridiculous question. When could you possibly fit in the time to doze off for even 20 minutes? I suspect there may be one or two of you who, although you are still working, have found a way to schedule a nap into your schedules. The rest of us must wait until we no longer have clinical responsibilities.
In my experience, you regular nappers seem to be the lucky few who have discovered the art of nodding off after lunch and waking up refreshed and ready to take on a full afternoon of patients. We in the unlucky majority may have tried taking a nap but run the risk of its flowing into a deep slumber the length of which we can’t control. Or, more likely, we find that we wake feeling groggy and disoriented and, even worse, the daytime nod off has messed up our nighttime schedule.
Well, it turns out the ability to take daytime naps and reap their cardiometabolic benefits is not just luck but has a significant genetic component. Investigators at Massachusetts General Hospital in Boston have recently published a study in which they report finding more than a score of gene regions that determine a person’s propensity to take daytime naps.. The researchers have also unearthed preliminary evidence supporting a link between daytime napping and cardiometabolic health. My mother began napping when my sister and I were infants and never gave it up. Unfortunately, I seem to have ended up on the wrong side of the genomic shuffle.
Although this new research is interesting, I don’t think the investigators have enough information to answer one of the questions that every pediatrician fields multiple times each week. “When should my toddler grow out of his afternoon nap?” Although it looks like we may be getting closer to a gene-based answer, I have always couched my reply in terms of behavior modification and the fostering of habit-forming associations.
As a child begins to transition from multiple short naps interspersed with feedings to a pattern of two distinct naps, I suggest to parents that they begin to think of the afternoon nap as a siesta. In other words, the nap is something that always comes immediately after lunch with no intervening shenanigans. No playtime, no Teletubbies videos, no quick trips to the grocery store, nothing, nada, zip.
At least for me, lunch has always been soporific. And I suspect we will learn eventually that association cuts across the entire genetic landscape to one degree or another. It makes sense to take advantage of that association and remove all other distractions. For some parents, that means creating the illusion that they too are taking a siesta: No TV, no phone calls. Imagine that the whole household has suddenly moved to Spain for the next hour or two. If you’ve ever been a tourist in rural Spain and tried to do anything, buy anything, or visit a museum between 2 and 4 p.m. you’ve got the idea.
When the child is young he or she will probably fall asleep as long as his parents have been reasonably successful at maintaining sleep hygiene practices. As the child is gaining more stamina and gives up the morning nap, the siesta will remain as a quiet time because that’s the way it’s always been in the household. The child may sleep or play quietly, or be read a sleep-inducing story because no other options will be available until some predetermined time. An hour is usually reasonable. If sleep hasn’t overtaken them, an earlier bedtime will probably be in order. The child will outgrow the napping part of the siesta when his or her sleep need is gone. But, the siesta/quiet time can remain as an option until all-day school intervenes. This scheme works if you can get parents to appropriately prioritize their child’s sleep needs. That’s not always an easy sell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Are you a napper? Unless you’re retired that may sound like a ridiculous question. When could you possibly fit in the time to doze off for even 20 minutes? I suspect there may be one or two of you who, although you are still working, have found a way to schedule a nap into your schedules. The rest of us must wait until we no longer have clinical responsibilities.
In my experience, you regular nappers seem to be the lucky few who have discovered the art of nodding off after lunch and waking up refreshed and ready to take on a full afternoon of patients. We in the unlucky majority may have tried taking a nap but run the risk of its flowing into a deep slumber the length of which we can’t control. Or, more likely, we find that we wake feeling groggy and disoriented and, even worse, the daytime nod off has messed up our nighttime schedule.
Well, it turns out the ability to take daytime naps and reap their cardiometabolic benefits is not just luck but has a significant genetic component. Investigators at Massachusetts General Hospital in Boston have recently published a study in which they report finding more than a score of gene regions that determine a person’s propensity to take daytime naps.. The researchers have also unearthed preliminary evidence supporting a link between daytime napping and cardiometabolic health. My mother began napping when my sister and I were infants and never gave it up. Unfortunately, I seem to have ended up on the wrong side of the genomic shuffle.
Although this new research is interesting, I don’t think the investigators have enough information to answer one of the questions that every pediatrician fields multiple times each week. “When should my toddler grow out of his afternoon nap?” Although it looks like we may be getting closer to a gene-based answer, I have always couched my reply in terms of behavior modification and the fostering of habit-forming associations.
As a child begins to transition from multiple short naps interspersed with feedings to a pattern of two distinct naps, I suggest to parents that they begin to think of the afternoon nap as a siesta. In other words, the nap is something that always comes immediately after lunch with no intervening shenanigans. No playtime, no Teletubbies videos, no quick trips to the grocery store, nothing, nada, zip.
At least for me, lunch has always been soporific. And I suspect we will learn eventually that association cuts across the entire genetic landscape to one degree or another. It makes sense to take advantage of that association and remove all other distractions. For some parents, that means creating the illusion that they too are taking a siesta: No TV, no phone calls. Imagine that the whole household has suddenly moved to Spain for the next hour or two. If you’ve ever been a tourist in rural Spain and tried to do anything, buy anything, or visit a museum between 2 and 4 p.m. you’ve got the idea.
When the child is young he or she will probably fall asleep as long as his parents have been reasonably successful at maintaining sleep hygiene practices. As the child is gaining more stamina and gives up the morning nap, the siesta will remain as a quiet time because that’s the way it’s always been in the household. The child may sleep or play quietly, or be read a sleep-inducing story because no other options will be available until some predetermined time. An hour is usually reasonable. If sleep hasn’t overtaken them, an earlier bedtime will probably be in order. The child will outgrow the napping part of the siesta when his or her sleep need is gone. But, the siesta/quiet time can remain as an option until all-day school intervenes. This scheme works if you can get parents to appropriately prioritize their child’s sleep needs. That’s not always an easy sell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Point-Counterpoint: The future of rheumatology is sub-subspecialization
Sub-subspecialization would be counterproductive: Orrin M. Troum, MD
The much-discussed looming rheumatology workforce shortage is actually here already. And it’s going to worsen rapidly. Add to that the striking geographic maldistribution of rheumatologists across the United States, and it makes little sense for some rheumatologists to declare they’re only going to see patients with psoriatic arthritis, or gout, or lupus. Such sub-subspecialization will only worsen the workforce problem, Orrin M. Troum, MD, asserted at the 2021 Rheumatology Winter Clinical Symposium.
Besides, surveys indicate that most rheumatologists like what they do now, despite their status as the lowest-paid subspecialists within internal medicine. They enjoy a sense of satisfaction stemming from their ability to help patients with chronic debilitating diseases turn their lives around as a result of revolutionary treatment advances in the last 2 decades, said Dr. Troum, a rheumatologist at the University of Southern California, Los Angeles, and in private practice in Santa Monica.
The 2015 American College of Rheumatology Workforce Study concluded that the demand for adult rheumatology services already outstripped the supply by 12.9% in 2015. And as current rheumatologists retire in tandem with a growing aged general population saddled with an accompanying burgeoning prevalence of rheumatic and musculoskeletal diseases, demand is expected to exceed supply by a whopping 102% in 2030.
The Workforce Study also highlighted the geographic maldistribution problem, with 21% of all adult rheumatologists now practicing in the Northeast and only 3.9% in the Southwest. Rheumatologists are also few and far between across large swaths of the South Central, North Central, and Northwest United States.
Today rheumatologists spend about half their working hours seeing patients with rheumatic diseases, one-quarter of their time in administrative tasks, 20% seeing patients with nonrheumatic diseases such as osteoarthritis, and the rest in teaching or research. It could be argued that, if rheumatologists declined to see patients with osteoarthritis, a nonrheumatic disease, it would put a sizeable dent in the workforce shortage, but it’s clear that nonrheumatologists can’t reliably differentiate inflammatory from noninflammatory arthritis. And there’s another problem with the idea of rheumatologists barring the office door to patients with nonrheumatic diseases: imagine a young clinical rheumatologist going out into practice and trying to tell referring internists, family physicians, and orthopedists that he or she doesn’t want to see patients with osteoarthritis, noninflammatory back pain, or fibromyalgia.
“How busy do you think you’re going to be, ever, if you tell the referring docs that you’re not going to see patients they think they need help with? And who’s going to make the correct diagnosis if we don’t at least see these patients initially?” Dr. Troum asked.
The case for sub-subspecialization: Martin J. Bergman, MD
Think about how many patients you’re treating for vasculitis, systemic lupus erythematosus, Behçet’s disease, or systemic sclerosis. Do you think you’re doing the best job that’s possible when you’re seeing just a handful of these patients, or would outcomes be better if they were seen at centers where the focus is specifically on these somewhat rare diseases? asked Martin J. Bergman, MD, a rheumatologist at Drexel University, Philadelphia, and in private practice in Ridley Park, Pa.
We can take a lesson from other specialties. It’s well-documented that higher surgical volume brings better care and better outcomes for cardiovascular and cancer surgery. Specialized high-level trauma centers achieve 20%-30% better outcomes. And outcomes are also improved when joint replacement surgery is done at specialty centers. Why would we expect rheumatology to be any different?
Actually, there is already evidence from within our own field to support this concept. A longitudinal study of 150 consecutive SLE patients – half treated at the general rheumatology clinic at Rush University, Chicago, and the other half at the medical center’s specialized lupus clinic – showed demonstrably better quality-of-care outcomes for the patients seen in the dedicated lupus clinic. They were roughly twice as likely to undergo antiphospholipid antibody testing and were also significantly more likely to have bone mineral density testing, pneumococcal vaccination, and sunscreen counseling.
Look, I get it. This is not going to be possible everywhere. In underserved geographic areas, it may not be feasible. But I would think that, even in places where you can’t have sub-subspecialty clinics, maybe it’s time for rheumatologists to start thinking in terms of sub-specializing their own practice and getting out of areas where we can make little or no impact beyond what other physicians can accomplish. Most of us provide very little value for patients with fibromyalgia and chronic fatigue syndrome. We have only so much time, and rather than taking care of anybody who has an ache or a pain we should focus on where we can make the most impact, and that’s inflammatory disease.
The speakers reported having no financial conflicts regarding their presentations.
Sub-subspecialization would be counterproductive: Orrin M. Troum, MD
The much-discussed looming rheumatology workforce shortage is actually here already. And it’s going to worsen rapidly. Add to that the striking geographic maldistribution of rheumatologists across the United States, and it makes little sense for some rheumatologists to declare they’re only going to see patients with psoriatic arthritis, or gout, or lupus. Such sub-subspecialization will only worsen the workforce problem, Orrin M. Troum, MD, asserted at the 2021 Rheumatology Winter Clinical Symposium.
Besides, surveys indicate that most rheumatologists like what they do now, despite their status as the lowest-paid subspecialists within internal medicine. They enjoy a sense of satisfaction stemming from their ability to help patients with chronic debilitating diseases turn their lives around as a result of revolutionary treatment advances in the last 2 decades, said Dr. Troum, a rheumatologist at the University of Southern California, Los Angeles, and in private practice in Santa Monica.
The 2015 American College of Rheumatology Workforce Study concluded that the demand for adult rheumatology services already outstripped the supply by 12.9% in 2015. And as current rheumatologists retire in tandem with a growing aged general population saddled with an accompanying burgeoning prevalence of rheumatic and musculoskeletal diseases, demand is expected to exceed supply by a whopping 102% in 2030.
The Workforce Study also highlighted the geographic maldistribution problem, with 21% of all adult rheumatologists now practicing in the Northeast and only 3.9% in the Southwest. Rheumatologists are also few and far between across large swaths of the South Central, North Central, and Northwest United States.
Today rheumatologists spend about half their working hours seeing patients with rheumatic diseases, one-quarter of their time in administrative tasks, 20% seeing patients with nonrheumatic diseases such as osteoarthritis, and the rest in teaching or research. It could be argued that, if rheumatologists declined to see patients with osteoarthritis, a nonrheumatic disease, it would put a sizeable dent in the workforce shortage, but it’s clear that nonrheumatologists can’t reliably differentiate inflammatory from noninflammatory arthritis. And there’s another problem with the idea of rheumatologists barring the office door to patients with nonrheumatic diseases: imagine a young clinical rheumatologist going out into practice and trying to tell referring internists, family physicians, and orthopedists that he or she doesn’t want to see patients with osteoarthritis, noninflammatory back pain, or fibromyalgia.
“How busy do you think you’re going to be, ever, if you tell the referring docs that you’re not going to see patients they think they need help with? And who’s going to make the correct diagnosis if we don’t at least see these patients initially?” Dr. Troum asked.
The case for sub-subspecialization: Martin J. Bergman, MD
Think about how many patients you’re treating for vasculitis, systemic lupus erythematosus, Behçet’s disease, or systemic sclerosis. Do you think you’re doing the best job that’s possible when you’re seeing just a handful of these patients, or would outcomes be better if they were seen at centers where the focus is specifically on these somewhat rare diseases? asked Martin J. Bergman, MD, a rheumatologist at Drexel University, Philadelphia, and in private practice in Ridley Park, Pa.
We can take a lesson from other specialties. It’s well-documented that higher surgical volume brings better care and better outcomes for cardiovascular and cancer surgery. Specialized high-level trauma centers achieve 20%-30% better outcomes. And outcomes are also improved when joint replacement surgery is done at specialty centers. Why would we expect rheumatology to be any different?
Actually, there is already evidence from within our own field to support this concept. A longitudinal study of 150 consecutive SLE patients – half treated at the general rheumatology clinic at Rush University, Chicago, and the other half at the medical center’s specialized lupus clinic – showed demonstrably better quality-of-care outcomes for the patients seen in the dedicated lupus clinic. They were roughly twice as likely to undergo antiphospholipid antibody testing and were also significantly more likely to have bone mineral density testing, pneumococcal vaccination, and sunscreen counseling.
Look, I get it. This is not going to be possible everywhere. In underserved geographic areas, it may not be feasible. But I would think that, even in places where you can’t have sub-subspecialty clinics, maybe it’s time for rheumatologists to start thinking in terms of sub-specializing their own practice and getting out of areas where we can make little or no impact beyond what other physicians can accomplish. Most of us provide very little value for patients with fibromyalgia and chronic fatigue syndrome. We have only so much time, and rather than taking care of anybody who has an ache or a pain we should focus on where we can make the most impact, and that’s inflammatory disease.
The speakers reported having no financial conflicts regarding their presentations.
Sub-subspecialization would be counterproductive: Orrin M. Troum, MD
The much-discussed looming rheumatology workforce shortage is actually here already. And it’s going to worsen rapidly. Add to that the striking geographic maldistribution of rheumatologists across the United States, and it makes little sense for some rheumatologists to declare they’re only going to see patients with psoriatic arthritis, or gout, or lupus. Such sub-subspecialization will only worsen the workforce problem, Orrin M. Troum, MD, asserted at the 2021 Rheumatology Winter Clinical Symposium.
Besides, surveys indicate that most rheumatologists like what they do now, despite their status as the lowest-paid subspecialists within internal medicine. They enjoy a sense of satisfaction stemming from their ability to help patients with chronic debilitating diseases turn their lives around as a result of revolutionary treatment advances in the last 2 decades, said Dr. Troum, a rheumatologist at the University of Southern California, Los Angeles, and in private practice in Santa Monica.
The 2015 American College of Rheumatology Workforce Study concluded that the demand for adult rheumatology services already outstripped the supply by 12.9% in 2015. And as current rheumatologists retire in tandem with a growing aged general population saddled with an accompanying burgeoning prevalence of rheumatic and musculoskeletal diseases, demand is expected to exceed supply by a whopping 102% in 2030.
The Workforce Study also highlighted the geographic maldistribution problem, with 21% of all adult rheumatologists now practicing in the Northeast and only 3.9% in the Southwest. Rheumatologists are also few and far between across large swaths of the South Central, North Central, and Northwest United States.
Today rheumatologists spend about half their working hours seeing patients with rheumatic diseases, one-quarter of their time in administrative tasks, 20% seeing patients with nonrheumatic diseases such as osteoarthritis, and the rest in teaching or research. It could be argued that, if rheumatologists declined to see patients with osteoarthritis, a nonrheumatic disease, it would put a sizeable dent in the workforce shortage, but it’s clear that nonrheumatologists can’t reliably differentiate inflammatory from noninflammatory arthritis. And there’s another problem with the idea of rheumatologists barring the office door to patients with nonrheumatic diseases: imagine a young clinical rheumatologist going out into practice and trying to tell referring internists, family physicians, and orthopedists that he or she doesn’t want to see patients with osteoarthritis, noninflammatory back pain, or fibromyalgia.
“How busy do you think you’re going to be, ever, if you tell the referring docs that you’re not going to see patients they think they need help with? And who’s going to make the correct diagnosis if we don’t at least see these patients initially?” Dr. Troum asked.
The case for sub-subspecialization: Martin J. Bergman, MD
Think about how many patients you’re treating for vasculitis, systemic lupus erythematosus, Behçet’s disease, or systemic sclerosis. Do you think you’re doing the best job that’s possible when you’re seeing just a handful of these patients, or would outcomes be better if they were seen at centers where the focus is specifically on these somewhat rare diseases? asked Martin J. Bergman, MD, a rheumatologist at Drexel University, Philadelphia, and in private practice in Ridley Park, Pa.
We can take a lesson from other specialties. It’s well-documented that higher surgical volume brings better care and better outcomes for cardiovascular and cancer surgery. Specialized high-level trauma centers achieve 20%-30% better outcomes. And outcomes are also improved when joint replacement surgery is done at specialty centers. Why would we expect rheumatology to be any different?
Actually, there is already evidence from within our own field to support this concept. A longitudinal study of 150 consecutive SLE patients – half treated at the general rheumatology clinic at Rush University, Chicago, and the other half at the medical center’s specialized lupus clinic – showed demonstrably better quality-of-care outcomes for the patients seen in the dedicated lupus clinic. They were roughly twice as likely to undergo antiphospholipid antibody testing and were also significantly more likely to have bone mineral density testing, pneumococcal vaccination, and sunscreen counseling.
Look, I get it. This is not going to be possible everywhere. In underserved geographic areas, it may not be feasible. But I would think that, even in places where you can’t have sub-subspecialty clinics, maybe it’s time for rheumatologists to start thinking in terms of sub-specializing their own practice and getting out of areas where we can make little or no impact beyond what other physicians can accomplish. Most of us provide very little value for patients with fibromyalgia and chronic fatigue syndrome. We have only so much time, and rather than taking care of anybody who has an ache or a pain we should focus on where we can make the most impact, and that’s inflammatory disease.
The speakers reported having no financial conflicts regarding their presentations.
FROM RWCS 2021
Helping parents deal with children’s transition to in-person school
This spring may bring an unusual transition for families: a return to in-person school after nearly a year in a virtual classroom. This will undoubtedly come as a welcome relief to many parents worried about their children’s education and development and struggling with running school from home. But it is important for parents to remember that transitions, even happy ones, are difficult. You can help parents to anticipate what may be challenging about this transition for their children so that they are all prepared and can diminish struggles and support their children’s mastery.
Be curious about their children’s thoughts and feelings
Parents should adopt a truly curious and open-minded approach with their children. Remind parents that, while they are experts on their own children, they should not assume they know what their children are thinking or feeling about the return to school. Some children, especially ones struggling with learning problems or difficulty with peers, will have grown very comfortable being at home with parents or siblings. Some children, especially pre- and early teens, may have changed substantially in the year and might feel uncertain about returning to a prior team or group of friends. Some children may feel concerned about leaving a pet at home alone. Some children may be going to a new school and be anxious about facing such a big transition without the usual planning and supports. Those on a college track may be worried they are “behind” academically or in college preparation.
Parents can show up when and where their children are most likely to talk, perhaps bath time or bedtime for younger children or in the car together with their adolescents. They can ask: “Have you been thinking about what it might be like to go back to school? Have your friends been chatting about it?” They might be curious together about what might have changed in a year. What might be really great about being back in a classroom? What might they miss about home school? And what might be new? Are you worried about the work, any of your friends, or not being home? If children can begin to anticipate both the good and the difficult, they will be better equipped to face and manage the challenges and appreciate the delights.
Children in elementary school are built to master new situations but are also prone to anxiety about new expectations and demands. Parents can be calmly curious about what their thoughts, feelings, and questions are and look for answers together. Often all they need is to see parents being calm in the face of uncertainty, bearing the strong feelings that may come, and preserving curiosity and compassion. Adolescents may be grieving the things they have missed, or they may have concerns about relationships and practical matters such as the implications for applying to college. Parents can offer compassion and validation and help them to devise their own strategies to face the practical challenges they are concerned about.
Be mindful of their children’s vulnerabilities
While most children will find the transition back to school easier than they may anticipate, there will be some for whom the transition will be very challenging. Children who have been bullied at school may have found themselves able to concentrate and learn free of the fear and stress of a classmate’s taunts or stares. Children with learning disabilities or ADHD have probably struggled with online school, but they have also likely established strategies and supports during the year that have enabled them to get enough individualized help to get their work done. These children are vulnerable to falling behind and getting discouraged when these supports are lost, and possibly not replaced with new ones in the chaos of transition. Parents should reassure their children that they will work with the school to make sure that they can succeed in the classroom as they did at home.
Children with an inhibited or shy temperament might have found that it was easier to focus and listen in the comfortable setting of home than in a busy, stimulating classroom. Children who suffer from anxiety disorders that may make separating from parents or managing the performance and social demands of school extra difficult will find the return to school especially challenging. Some younger children may have experienced the emergence of an anxiety disorder during the past year, and the return to school may mark the challenge that brings heretofore quiet symptoms into full relief.
These children have all enjoyed being able to avoid the discomfort of certain anxiety-provoking situations, and they may be particularly stressed by anticipating a return to school. Younger children may begin to have stomach aches and other physical complaints as the return to school gets close, older children may seem more withdrawn or irritable or begin discussing ways to continue school from home. Parents should help their children try to identify and describe their worries. For anxious children, having a chance to practice may be very helpful. Visiting their school, especially if it is a new school, or having a planned hangout with a friend (with appropriate precautions) is the kind of exposure that can lessen anticipatory anxiety. If this is not enough, parents should not hesitate to bring in other caring, supportive adults, such as school counselors or therapists that may be essential to helping their children face and manage what may be intense anxiety.
Consider routines to support their transition
Just as parents begin to return their children to an earlier bedtime toward the end of summer, it will be helpful to consider how changing certain routines will support their children now. If children will need to get up earlier to be ready for a bus or a team practice, they should start moving bedtime and wake-up time earlier gradually. Uniforms or backpacks that have not been seen for a year should be dug out. Children who are planning a return to a sport may benefit from gradually increasing their exercise or starting training now. This will have the added benefit of improving sleep and energy and fortifying children for the challenges of change. Parents might consider reaching out to other parents in the same class as their children and having a virtual conversation to share their thoughts.
If their family has developed some new “COVID routines” that they have come to enjoy, they should find a way to preserve them. Perhaps they are having dinner together more often or have established a family game night or Netflix night. Help parents consider how to avoid falling back into overscheduling their children and themselves. If they created a time to Zoom with distant or vulnerable loved ones, they might decide to continue this. School may determine some of their routines, but they should also prioritize their family connections and well-being in deciding how to schedule their days.
Find opportunity for mastery and meaning
As parents are listening, validating, and planning with their children, they might use this time to reflect on valuable lessons. They might point out the value of patience: Adjusting to change takes time and happens in fits and starts. It has been 12 months since many of the pandemic changes started and it will take more than a few days to adjust as schools reopen. They might point out how proud they are of what their children have been able to learn, build, or do during this year, what they admire about them. It may be a time to consider what their family may have lost and gained during the past year, what they are eager to leave behind, and what they might like to keep. And it is also a chance for parents to observe that change is an inevitable part of life (especially when growing up). It is always challenging, and often brings loss and sadness. But if we pay attention, there are also the green shoots of what is new and possible.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
This spring may bring an unusual transition for families: a return to in-person school after nearly a year in a virtual classroom. This will undoubtedly come as a welcome relief to many parents worried about their children’s education and development and struggling with running school from home. But it is important for parents to remember that transitions, even happy ones, are difficult. You can help parents to anticipate what may be challenging about this transition for their children so that they are all prepared and can diminish struggles and support their children’s mastery.
Be curious about their children’s thoughts and feelings
Parents should adopt a truly curious and open-minded approach with their children. Remind parents that, while they are experts on their own children, they should not assume they know what their children are thinking or feeling about the return to school. Some children, especially ones struggling with learning problems or difficulty with peers, will have grown very comfortable being at home with parents or siblings. Some children, especially pre- and early teens, may have changed substantially in the year and might feel uncertain about returning to a prior team or group of friends. Some children may feel concerned about leaving a pet at home alone. Some children may be going to a new school and be anxious about facing such a big transition without the usual planning and supports. Those on a college track may be worried they are “behind” academically or in college preparation.
Parents can show up when and where their children are most likely to talk, perhaps bath time or bedtime for younger children or in the car together with their adolescents. They can ask: “Have you been thinking about what it might be like to go back to school? Have your friends been chatting about it?” They might be curious together about what might have changed in a year. What might be really great about being back in a classroom? What might they miss about home school? And what might be new? Are you worried about the work, any of your friends, or not being home? If children can begin to anticipate both the good and the difficult, they will be better equipped to face and manage the challenges and appreciate the delights.
Children in elementary school are built to master new situations but are also prone to anxiety about new expectations and demands. Parents can be calmly curious about what their thoughts, feelings, and questions are and look for answers together. Often all they need is to see parents being calm in the face of uncertainty, bearing the strong feelings that may come, and preserving curiosity and compassion. Adolescents may be grieving the things they have missed, or they may have concerns about relationships and practical matters such as the implications for applying to college. Parents can offer compassion and validation and help them to devise their own strategies to face the practical challenges they are concerned about.
Be mindful of their children’s vulnerabilities
While most children will find the transition back to school easier than they may anticipate, there will be some for whom the transition will be very challenging. Children who have been bullied at school may have found themselves able to concentrate and learn free of the fear and stress of a classmate’s taunts or stares. Children with learning disabilities or ADHD have probably struggled with online school, but they have also likely established strategies and supports during the year that have enabled them to get enough individualized help to get their work done. These children are vulnerable to falling behind and getting discouraged when these supports are lost, and possibly not replaced with new ones in the chaos of transition. Parents should reassure their children that they will work with the school to make sure that they can succeed in the classroom as they did at home.
Children with an inhibited or shy temperament might have found that it was easier to focus and listen in the comfortable setting of home than in a busy, stimulating classroom. Children who suffer from anxiety disorders that may make separating from parents or managing the performance and social demands of school extra difficult will find the return to school especially challenging. Some younger children may have experienced the emergence of an anxiety disorder during the past year, and the return to school may mark the challenge that brings heretofore quiet symptoms into full relief.
These children have all enjoyed being able to avoid the discomfort of certain anxiety-provoking situations, and they may be particularly stressed by anticipating a return to school. Younger children may begin to have stomach aches and other physical complaints as the return to school gets close, older children may seem more withdrawn or irritable or begin discussing ways to continue school from home. Parents should help their children try to identify and describe their worries. For anxious children, having a chance to practice may be very helpful. Visiting their school, especially if it is a new school, or having a planned hangout with a friend (with appropriate precautions) is the kind of exposure that can lessen anticipatory anxiety. If this is not enough, parents should not hesitate to bring in other caring, supportive adults, such as school counselors or therapists that may be essential to helping their children face and manage what may be intense anxiety.
Consider routines to support their transition
Just as parents begin to return their children to an earlier bedtime toward the end of summer, it will be helpful to consider how changing certain routines will support their children now. If children will need to get up earlier to be ready for a bus or a team practice, they should start moving bedtime and wake-up time earlier gradually. Uniforms or backpacks that have not been seen for a year should be dug out. Children who are planning a return to a sport may benefit from gradually increasing their exercise or starting training now. This will have the added benefit of improving sleep and energy and fortifying children for the challenges of change. Parents might consider reaching out to other parents in the same class as their children and having a virtual conversation to share their thoughts.
If their family has developed some new “COVID routines” that they have come to enjoy, they should find a way to preserve them. Perhaps they are having dinner together more often or have established a family game night or Netflix night. Help parents consider how to avoid falling back into overscheduling their children and themselves. If they created a time to Zoom with distant or vulnerable loved ones, they might decide to continue this. School may determine some of their routines, but they should also prioritize their family connections and well-being in deciding how to schedule their days.
Find opportunity for mastery and meaning
As parents are listening, validating, and planning with their children, they might use this time to reflect on valuable lessons. They might point out the value of patience: Adjusting to change takes time and happens in fits and starts. It has been 12 months since many of the pandemic changes started and it will take more than a few days to adjust as schools reopen. They might point out how proud they are of what their children have been able to learn, build, or do during this year, what they admire about them. It may be a time to consider what their family may have lost and gained during the past year, what they are eager to leave behind, and what they might like to keep. And it is also a chance for parents to observe that change is an inevitable part of life (especially when growing up). It is always challenging, and often brings loss and sadness. But if we pay attention, there are also the green shoots of what is new and possible.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
This spring may bring an unusual transition for families: a return to in-person school after nearly a year in a virtual classroom. This will undoubtedly come as a welcome relief to many parents worried about their children’s education and development and struggling with running school from home. But it is important for parents to remember that transitions, even happy ones, are difficult. You can help parents to anticipate what may be challenging about this transition for their children so that they are all prepared and can diminish struggles and support their children’s mastery.
Be curious about their children’s thoughts and feelings
Parents should adopt a truly curious and open-minded approach with their children. Remind parents that, while they are experts on their own children, they should not assume they know what their children are thinking or feeling about the return to school. Some children, especially ones struggling with learning problems or difficulty with peers, will have grown very comfortable being at home with parents or siblings. Some children, especially pre- and early teens, may have changed substantially in the year and might feel uncertain about returning to a prior team or group of friends. Some children may feel concerned about leaving a pet at home alone. Some children may be going to a new school and be anxious about facing such a big transition without the usual planning and supports. Those on a college track may be worried they are “behind” academically or in college preparation.
Parents can show up when and where their children are most likely to talk, perhaps bath time or bedtime for younger children or in the car together with their adolescents. They can ask: “Have you been thinking about what it might be like to go back to school? Have your friends been chatting about it?” They might be curious together about what might have changed in a year. What might be really great about being back in a classroom? What might they miss about home school? And what might be new? Are you worried about the work, any of your friends, or not being home? If children can begin to anticipate both the good and the difficult, they will be better equipped to face and manage the challenges and appreciate the delights.
Children in elementary school are built to master new situations but are also prone to anxiety about new expectations and demands. Parents can be calmly curious about what their thoughts, feelings, and questions are and look for answers together. Often all they need is to see parents being calm in the face of uncertainty, bearing the strong feelings that may come, and preserving curiosity and compassion. Adolescents may be grieving the things they have missed, or they may have concerns about relationships and practical matters such as the implications for applying to college. Parents can offer compassion and validation and help them to devise their own strategies to face the practical challenges they are concerned about.
Be mindful of their children’s vulnerabilities
While most children will find the transition back to school easier than they may anticipate, there will be some for whom the transition will be very challenging. Children who have been bullied at school may have found themselves able to concentrate and learn free of the fear and stress of a classmate’s taunts or stares. Children with learning disabilities or ADHD have probably struggled with online school, but they have also likely established strategies and supports during the year that have enabled them to get enough individualized help to get their work done. These children are vulnerable to falling behind and getting discouraged when these supports are lost, and possibly not replaced with new ones in the chaos of transition. Parents should reassure their children that they will work with the school to make sure that they can succeed in the classroom as they did at home.
Children with an inhibited or shy temperament might have found that it was easier to focus and listen in the comfortable setting of home than in a busy, stimulating classroom. Children who suffer from anxiety disorders that may make separating from parents or managing the performance and social demands of school extra difficult will find the return to school especially challenging. Some younger children may have experienced the emergence of an anxiety disorder during the past year, and the return to school may mark the challenge that brings heretofore quiet symptoms into full relief.
These children have all enjoyed being able to avoid the discomfort of certain anxiety-provoking situations, and they may be particularly stressed by anticipating a return to school. Younger children may begin to have stomach aches and other physical complaints as the return to school gets close, older children may seem more withdrawn or irritable or begin discussing ways to continue school from home. Parents should help their children try to identify and describe their worries. For anxious children, having a chance to practice may be very helpful. Visiting their school, especially if it is a new school, or having a planned hangout with a friend (with appropriate precautions) is the kind of exposure that can lessen anticipatory anxiety. If this is not enough, parents should not hesitate to bring in other caring, supportive adults, such as school counselors or therapists that may be essential to helping their children face and manage what may be intense anxiety.
Consider routines to support their transition
Just as parents begin to return their children to an earlier bedtime toward the end of summer, it will be helpful to consider how changing certain routines will support their children now. If children will need to get up earlier to be ready for a bus or a team practice, they should start moving bedtime and wake-up time earlier gradually. Uniforms or backpacks that have not been seen for a year should be dug out. Children who are planning a return to a sport may benefit from gradually increasing their exercise or starting training now. This will have the added benefit of improving sleep and energy and fortifying children for the challenges of change. Parents might consider reaching out to other parents in the same class as their children and having a virtual conversation to share their thoughts.
If their family has developed some new “COVID routines” that they have come to enjoy, they should find a way to preserve them. Perhaps they are having dinner together more often or have established a family game night or Netflix night. Help parents consider how to avoid falling back into overscheduling their children and themselves. If they created a time to Zoom with distant or vulnerable loved ones, they might decide to continue this. School may determine some of their routines, but they should also prioritize their family connections and well-being in deciding how to schedule their days.
Find opportunity for mastery and meaning
As parents are listening, validating, and planning with their children, they might use this time to reflect on valuable lessons. They might point out the value of patience: Adjusting to change takes time and happens in fits and starts. It has been 12 months since many of the pandemic changes started and it will take more than a few days to adjust as schools reopen. They might point out how proud they are of what their children have been able to learn, build, or do during this year, what they admire about them. It may be a time to consider what their family may have lost and gained during the past year, what they are eager to leave behind, and what they might like to keep. And it is also a chance for parents to observe that change is an inevitable part of life (especially when growing up). It is always challenging, and often brings loss and sadness. But if we pay attention, there are also the green shoots of what is new and possible.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
mCODE: Improving data sharing to enhance cancer care
An initiative designed to improve sharing of patient data may provide “tremendous benefits” in cancer care and research, according to authors of a review article.
The goals of the initiative, called Minimal Common Oncology Data Elements (mCODE), were to identify the data elements in electronic health records that are “essential” for making treatment decisions and create “a standardized computable data format” that would improve the exchange of data across EHRs, according to the mCODE website.
Travis J. Osterman, DO, of Vanderbilt University Medical Center in Nashville, Tenn., and colleagues described the mCODE initiative in a review published in JCO Clinical Cancer Informatics.
At present, commercially available EHRs are poorly designed to support modern oncology workflow, requiring laborious data entry and lacking a common library of oncology-specific discrete data elements. As an example, most EHRs poorly support the needs of precision oncology and clinical genetics, since next-generation sequencing and genetic test results are almost universally reported in PDF files.
In addition, basic, operational oncology data (e.g., cancer staging, adverse event documentation, response to treatment, etc.) are captured in EHRs primarily as an unstructured narrative.
Computable, analytical data are found for only the small percentage of patients in clinical trials. Even then, some degree of manual data abstraction is regularly required.
Interoperability of EHRs between practices and health care institutions is often so poor that the transfer of basic cancer-related information as analyzable data is difficult or even impossible.
Making progress: The 21st Century Cures Act
The American Society of Clinical Oncology has a more than 15-year history of developing oncology data standards. Unfortunately, progress in implementing these standards has been glacially slow. Impediments have included:
- A lack of conformance with clinical workflows.
- Failure to test standards on specific-use cases during pilot testing.
- A focus on data exchange, rather than the practical impediments to data entry.
- Poor engagement with EHR vendors in distributing clinical information modules with an oncology-specific focus
- Instability of data interoperability technologies.
The 21st Century Cures Act, which became law in December 2016, mandated improvement in the interoperability of health information through the development of data standards and application programming interfaces.
In early 2020, final rules for implementation required technology vendors to employ application programming interfaces using a single interoperability resource. In addition, payers were required to use the United States Core Data for Interoperability Standard for data exchange. These requirements were intended to provide patients with access to their own health care data “without special effort.”
As a fortunate byproduct, since EHR vendors are required to implement application program interfaces using the Health Level Seven International (HL7) Fast Healthcare Interoperability Resource (FHIR) Specification, the final rules could enable systems like mCODE to be more easily integrated with existing EHRs.
Lessons from CancerLinQ
ASCO created the health technology platform CancerLinQ in 2014, envisioning that it could become an oncology-focused learning health system – a system in which internal data and experience are systematically integrated with external evidence, allowing knowledge to be put into practice.
CancerLinQ extracts data from EHRs and other sources via direct software connections. CancerLinQ then aggregates, harmonizes, and normalizes the data in a cloud-based environment.
The data are available to participating practices for quality improvement in patient care and secondary research. In 2020, records of cancer patients in the CancerLinQ database surpassed 2 million.
CancerLinQ has been successful. However, because of the nature of the EHR ecosystem and the scope and variability of data capture by clinicians, supporting a true learning health system has proven to be a formidable task. Postprocessing manual review using trained human curators is laborious and unsustainable.
The CancerLinQ experience illustrated that basic cancer-pertinent data should be standardized in the EHR and collected prospectively.
The mCODE model
The mCODE initiative seeks to facilitate progress in care quality, clinical research, and health care policy by developing and maintaining a standard, computable, interoperable data format.
Guiding principles that were adopted early in mCODE’s development included:
- A collaborative, noncommercial, use case–driven developmental model.
- Iterative processes.
- User-driven development, refinement, and maintenance.
- Low ongoing maintenance requirements.
A foundational moment in mCODE’s development involved achieving consensus among stakeholders that the project would fail if EHR vendors required additional data entry by users.
After pilot work, a real-world endpoints project, working-group deliberation, public comment, and refinement, the final data standard included six primary domains: patient, disease, laboratory data/vital signs, genomics, treatment, and outcome.
Each domain is further divided into several concepts with specific associated data elements. The data elements are modeled into value sets that specify the possible values for the data element.
To test mCODE, eight organizations representing oncology EHR vendors, standards developers, and research organizations participated in a cancer interoperability track. The comments helped refine mCODE version 1.0, which was released in March 2020 and is accessible via the mCODE website.
Additions will likely be reviewed by a technical review group after external piloting of new use cases.
Innovation, not regulation
Every interaction between a patient and care provider yields information that could lead to improved safety and better outcomes. To be successful, the information must be collected in a computable format so it can be aggregated with data from other patients, analyzed without manual curation, and shared through interoperable systems. Those data should also be secure enough to protect the privacy of individual patients.
mCODE is a consensus data standard for oncology that provides an infrastructure to share patient data between oncology practices and health care systems while promising little to no additional data entry on the part of clinicians. Adoption by sites will be critical, however.
Publishing the standard through the HL7 FHIR technology demonstrated to EHR vendors and regulatory agencies the stability of HL7, an essential requirement for its incorporation into software.
EHR vendors and others are engaged in the CodeX HL7 FHIR Accelerator to design projects to expand and/or modify mCODE. Their creativity and innovativeness via the external advisory mCODE council and/or CodeX will be encouraged to help mCODE reach its full potential.
As part of CodeX, the Community of Practice, an open forum for end users, was established to provide regular updates about mCODE-related initiatives and use cases to solicit in-progress input, according to Robert S. Miller, MD, medical director of CancerLinQ and an author of the mCODE review.
For mCODE to be embraced by all stakeholders, there should be no additional regulations. By engaging stakeholders in an enterprise that supports innovation and collaboration – without additional regulation – mCODE could maximize the potential of EHRs that, until now, have assisted us only marginally in accomplishing those goals.
mCODE is a joint venture of ASCO/CancerLinQ, the Alliance for Clinical Trials in Oncology Foundation, the MITRE Corporation, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Dr. Osterman disclosed a grant from the National Cancer Institute and relationships with Infostratix, eHealth, AstraZeneca, Outcomes Insights, Biodesix, MD Outlook, GenomOncology, Cota Healthcare, GE Healthcare, and Microsoft. Dr. Miller and the third review author disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
An initiative designed to improve sharing of patient data may provide “tremendous benefits” in cancer care and research, according to authors of a review article.
The goals of the initiative, called Minimal Common Oncology Data Elements (mCODE), were to identify the data elements in electronic health records that are “essential” for making treatment decisions and create “a standardized computable data format” that would improve the exchange of data across EHRs, according to the mCODE website.
Travis J. Osterman, DO, of Vanderbilt University Medical Center in Nashville, Tenn., and colleagues described the mCODE initiative in a review published in JCO Clinical Cancer Informatics.
At present, commercially available EHRs are poorly designed to support modern oncology workflow, requiring laborious data entry and lacking a common library of oncology-specific discrete data elements. As an example, most EHRs poorly support the needs of precision oncology and clinical genetics, since next-generation sequencing and genetic test results are almost universally reported in PDF files.
In addition, basic, operational oncology data (e.g., cancer staging, adverse event documentation, response to treatment, etc.) are captured in EHRs primarily as an unstructured narrative.
Computable, analytical data are found for only the small percentage of patients in clinical trials. Even then, some degree of manual data abstraction is regularly required.
Interoperability of EHRs between practices and health care institutions is often so poor that the transfer of basic cancer-related information as analyzable data is difficult or even impossible.
Making progress: The 21st Century Cures Act
The American Society of Clinical Oncology has a more than 15-year history of developing oncology data standards. Unfortunately, progress in implementing these standards has been glacially slow. Impediments have included:
- A lack of conformance with clinical workflows.
- Failure to test standards on specific-use cases during pilot testing.
- A focus on data exchange, rather than the practical impediments to data entry.
- Poor engagement with EHR vendors in distributing clinical information modules with an oncology-specific focus
- Instability of data interoperability technologies.
The 21st Century Cures Act, which became law in December 2016, mandated improvement in the interoperability of health information through the development of data standards and application programming interfaces.
In early 2020, final rules for implementation required technology vendors to employ application programming interfaces using a single interoperability resource. In addition, payers were required to use the United States Core Data for Interoperability Standard for data exchange. These requirements were intended to provide patients with access to their own health care data “without special effort.”
As a fortunate byproduct, since EHR vendors are required to implement application program interfaces using the Health Level Seven International (HL7) Fast Healthcare Interoperability Resource (FHIR) Specification, the final rules could enable systems like mCODE to be more easily integrated with existing EHRs.
Lessons from CancerLinQ
ASCO created the health technology platform CancerLinQ in 2014, envisioning that it could become an oncology-focused learning health system – a system in which internal data and experience are systematically integrated with external evidence, allowing knowledge to be put into practice.
CancerLinQ extracts data from EHRs and other sources via direct software connections. CancerLinQ then aggregates, harmonizes, and normalizes the data in a cloud-based environment.
The data are available to participating practices for quality improvement in patient care and secondary research. In 2020, records of cancer patients in the CancerLinQ database surpassed 2 million.
CancerLinQ has been successful. However, because of the nature of the EHR ecosystem and the scope and variability of data capture by clinicians, supporting a true learning health system has proven to be a formidable task. Postprocessing manual review using trained human curators is laborious and unsustainable.
The CancerLinQ experience illustrated that basic cancer-pertinent data should be standardized in the EHR and collected prospectively.
The mCODE model
The mCODE initiative seeks to facilitate progress in care quality, clinical research, and health care policy by developing and maintaining a standard, computable, interoperable data format.
Guiding principles that were adopted early in mCODE’s development included:
- A collaborative, noncommercial, use case–driven developmental model.
- Iterative processes.
- User-driven development, refinement, and maintenance.
- Low ongoing maintenance requirements.
A foundational moment in mCODE’s development involved achieving consensus among stakeholders that the project would fail if EHR vendors required additional data entry by users.
After pilot work, a real-world endpoints project, working-group deliberation, public comment, and refinement, the final data standard included six primary domains: patient, disease, laboratory data/vital signs, genomics, treatment, and outcome.
Each domain is further divided into several concepts with specific associated data elements. The data elements are modeled into value sets that specify the possible values for the data element.
To test mCODE, eight organizations representing oncology EHR vendors, standards developers, and research organizations participated in a cancer interoperability track. The comments helped refine mCODE version 1.0, which was released in March 2020 and is accessible via the mCODE website.
Additions will likely be reviewed by a technical review group after external piloting of new use cases.
Innovation, not regulation
Every interaction between a patient and care provider yields information that could lead to improved safety and better outcomes. To be successful, the information must be collected in a computable format so it can be aggregated with data from other patients, analyzed without manual curation, and shared through interoperable systems. Those data should also be secure enough to protect the privacy of individual patients.
mCODE is a consensus data standard for oncology that provides an infrastructure to share patient data between oncology practices and health care systems while promising little to no additional data entry on the part of clinicians. Adoption by sites will be critical, however.
Publishing the standard through the HL7 FHIR technology demonstrated to EHR vendors and regulatory agencies the stability of HL7, an essential requirement for its incorporation into software.
EHR vendors and others are engaged in the CodeX HL7 FHIR Accelerator to design projects to expand and/or modify mCODE. Their creativity and innovativeness via the external advisory mCODE council and/or CodeX will be encouraged to help mCODE reach its full potential.
As part of CodeX, the Community of Practice, an open forum for end users, was established to provide regular updates about mCODE-related initiatives and use cases to solicit in-progress input, according to Robert S. Miller, MD, medical director of CancerLinQ and an author of the mCODE review.
For mCODE to be embraced by all stakeholders, there should be no additional regulations. By engaging stakeholders in an enterprise that supports innovation and collaboration – without additional regulation – mCODE could maximize the potential of EHRs that, until now, have assisted us only marginally in accomplishing those goals.
mCODE is a joint venture of ASCO/CancerLinQ, the Alliance for Clinical Trials in Oncology Foundation, the MITRE Corporation, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Dr. Osterman disclosed a grant from the National Cancer Institute and relationships with Infostratix, eHealth, AstraZeneca, Outcomes Insights, Biodesix, MD Outlook, GenomOncology, Cota Healthcare, GE Healthcare, and Microsoft. Dr. Miller and the third review author disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
An initiative designed to improve sharing of patient data may provide “tremendous benefits” in cancer care and research, according to authors of a review article.
The goals of the initiative, called Minimal Common Oncology Data Elements (mCODE), were to identify the data elements in electronic health records that are “essential” for making treatment decisions and create “a standardized computable data format” that would improve the exchange of data across EHRs, according to the mCODE website.
Travis J. Osterman, DO, of Vanderbilt University Medical Center in Nashville, Tenn., and colleagues described the mCODE initiative in a review published in JCO Clinical Cancer Informatics.
At present, commercially available EHRs are poorly designed to support modern oncology workflow, requiring laborious data entry and lacking a common library of oncology-specific discrete data elements. As an example, most EHRs poorly support the needs of precision oncology and clinical genetics, since next-generation sequencing and genetic test results are almost universally reported in PDF files.
In addition, basic, operational oncology data (e.g., cancer staging, adverse event documentation, response to treatment, etc.) are captured in EHRs primarily as an unstructured narrative.
Computable, analytical data are found for only the small percentage of patients in clinical trials. Even then, some degree of manual data abstraction is regularly required.
Interoperability of EHRs between practices and health care institutions is often so poor that the transfer of basic cancer-related information as analyzable data is difficult or even impossible.
Making progress: The 21st Century Cures Act
The American Society of Clinical Oncology has a more than 15-year history of developing oncology data standards. Unfortunately, progress in implementing these standards has been glacially slow. Impediments have included:
- A lack of conformance with clinical workflows.
- Failure to test standards on specific-use cases during pilot testing.
- A focus on data exchange, rather than the practical impediments to data entry.
- Poor engagement with EHR vendors in distributing clinical information modules with an oncology-specific focus
- Instability of data interoperability technologies.
The 21st Century Cures Act, which became law in December 2016, mandated improvement in the interoperability of health information through the development of data standards and application programming interfaces.
In early 2020, final rules for implementation required technology vendors to employ application programming interfaces using a single interoperability resource. In addition, payers were required to use the United States Core Data for Interoperability Standard for data exchange. These requirements were intended to provide patients with access to their own health care data “without special effort.”
As a fortunate byproduct, since EHR vendors are required to implement application program interfaces using the Health Level Seven International (HL7) Fast Healthcare Interoperability Resource (FHIR) Specification, the final rules could enable systems like mCODE to be more easily integrated with existing EHRs.
Lessons from CancerLinQ
ASCO created the health technology platform CancerLinQ in 2014, envisioning that it could become an oncology-focused learning health system – a system in which internal data and experience are systematically integrated with external evidence, allowing knowledge to be put into practice.
CancerLinQ extracts data from EHRs and other sources via direct software connections. CancerLinQ then aggregates, harmonizes, and normalizes the data in a cloud-based environment.
The data are available to participating practices for quality improvement in patient care and secondary research. In 2020, records of cancer patients in the CancerLinQ database surpassed 2 million.
CancerLinQ has been successful. However, because of the nature of the EHR ecosystem and the scope and variability of data capture by clinicians, supporting a true learning health system has proven to be a formidable task. Postprocessing manual review using trained human curators is laborious and unsustainable.
The CancerLinQ experience illustrated that basic cancer-pertinent data should be standardized in the EHR and collected prospectively.
The mCODE model
The mCODE initiative seeks to facilitate progress in care quality, clinical research, and health care policy by developing and maintaining a standard, computable, interoperable data format.
Guiding principles that were adopted early in mCODE’s development included:
- A collaborative, noncommercial, use case–driven developmental model.
- Iterative processes.
- User-driven development, refinement, and maintenance.
- Low ongoing maintenance requirements.
A foundational moment in mCODE’s development involved achieving consensus among stakeholders that the project would fail if EHR vendors required additional data entry by users.
After pilot work, a real-world endpoints project, working-group deliberation, public comment, and refinement, the final data standard included six primary domains: patient, disease, laboratory data/vital signs, genomics, treatment, and outcome.
Each domain is further divided into several concepts with specific associated data elements. The data elements are modeled into value sets that specify the possible values for the data element.
To test mCODE, eight organizations representing oncology EHR vendors, standards developers, and research organizations participated in a cancer interoperability track. The comments helped refine mCODE version 1.0, which was released in March 2020 and is accessible via the mCODE website.
Additions will likely be reviewed by a technical review group after external piloting of new use cases.
Innovation, not regulation
Every interaction between a patient and care provider yields information that could lead to improved safety and better outcomes. To be successful, the information must be collected in a computable format so it can be aggregated with data from other patients, analyzed without manual curation, and shared through interoperable systems. Those data should also be secure enough to protect the privacy of individual patients.
mCODE is a consensus data standard for oncology that provides an infrastructure to share patient data between oncology practices and health care systems while promising little to no additional data entry on the part of clinicians. Adoption by sites will be critical, however.
Publishing the standard through the HL7 FHIR technology demonstrated to EHR vendors and regulatory agencies the stability of HL7, an essential requirement for its incorporation into software.
EHR vendors and others are engaged in the CodeX HL7 FHIR Accelerator to design projects to expand and/or modify mCODE. Their creativity and innovativeness via the external advisory mCODE council and/or CodeX will be encouraged to help mCODE reach its full potential.
As part of CodeX, the Community of Practice, an open forum for end users, was established to provide regular updates about mCODE-related initiatives and use cases to solicit in-progress input, according to Robert S. Miller, MD, medical director of CancerLinQ and an author of the mCODE review.
For mCODE to be embraced by all stakeholders, there should be no additional regulations. By engaging stakeholders in an enterprise that supports innovation and collaboration – without additional regulation – mCODE could maximize the potential of EHRs that, until now, have assisted us only marginally in accomplishing those goals.
mCODE is a joint venture of ASCO/CancerLinQ, the Alliance for Clinical Trials in Oncology Foundation, the MITRE Corporation, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Dr. Osterman disclosed a grant from the National Cancer Institute and relationships with Infostratix, eHealth, AstraZeneca, Outcomes Insights, Biodesix, MD Outlook, GenomOncology, Cota Healthcare, GE Healthcare, and Microsoft. Dr. Miller and the third review author disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM JCO CLINICAL CANCER INFORMATICS
The vanguard of HIV care: Don’t forget this screening
In response, clinical care is continually adapting to the dramatically altered natural history of disease.
Today, the cutting edge of clinical care overlaps with primary care. The clinical vanguard addresses the medical vulnerabilities of patients with HIV, seeking to eliminate preventable morbidity and premature death. Among this clinical vanguard is the screening for and prevention of anal cancer. With the increased longevity of people living with HIV and the nearly universal exposure to human papillomavirus (HPV), there is now potential for progression to mucosal cellular dysplasia and eventual malignancy.
We know that prevention is possible because of the example of cervical cancer, the etiology of which is exposure to oncogenic serotypes of HPV (16 and 18 are most common). Screenings for cervical cancer (regular clinical examinations and Pap smears) and treatments to eliminate high-grade dysplasia have decreased the incidence rate by over 50% since the 1970s. Vaccination against HPV has been available since 2006 and offers the prospect of preventing HPV-associated malignancies, including head and neck cancer, in future decades.
However, rates of anal cancer are increasing. The CDC estimates that about 4,700 new cases of HPV-associated anal cancers are diagnosed in women and about 2,300 are diagnosed in men each year in the United States. Anal cancer rates in individuals with HIV have increased in the era of effective antiretrovirals and greater longevity. The highest rates, at 95 per 100,000, are in HIV-positive men who have sex with men. Very similar rates were noted in a more recent study that found increased risk with advancing age and in those with an AIDS diagnosis.
All patients with HIV should be screened
The New York State AIDS Institute Clinical Guidelines Program recommends screening for anal dysplasia in all patients with HIV. A proactive approach similar to cervical cancer screening is appropriate and includes measures easily implemented by all clinicians.
- History: Assess for rectal symptoms, anal pain, discharge, and lumps.
- Physical exam: Assess for presence of perianal lesions; perform a thorough digital rectal exam.
- Anal Pap test for anal cytology: Insert a Dacron swab moistened with tap water about 3 inches into the anal canal, applying pressure to lateral anal walls and rotating the swab. Then remove and place the swab into liquid cytology solution, shake vigorously for a full 30 seconds, and assess for any dysplasia (high-grade squamous intraepithelial lesion, low-grade intraepithelial lesion, atypical squamous cells of undetermined significance), which would warrant further evaluation by high-resolution anoscopy (HRA).
High-resolution anoscopy
HRA for anal dysplasia corresponds to colposcopy for cervical dysplasia. The ability to treat and eliminate high-risk precursor lesions interrupts the progression to malignancy. The efficacy of this strategy is being evaluated in a National Institutes of Health prospective trial called the Anchor Study. The epidemiology of HPV; the clinical horror of witnessing the painful, preventable deaths of young patients with well-controlled HIV caused by anal cancer; and the example of controlling cervical cancer have motivated my practice to assure comprehensive care for our patients.
Unfortunately, establishing HRA in one’s practice is challenging. Barriers to practice include the expense of required equipment and the absence of consensus on specific products. In addition, hands-on precepting to ease newcomers to competence is not generally available. Considerable skill is required for complete visualization of the anal transformative zone in the folds of the anal canal, and recognizing high-risk lesions requires study and accumulated experience. The International Anal Neoplasia Society is a useful resource that also offers a training course. We are invited to train ourselves, and to rely on the eventual feedback of biopsy results and the forbearance of our early patients.
The expanding scope of our medical practices must shift to meet the evolving needs of the growing population of virologically suppressed patients who are living longer. HIV care involves curing life-threatening opportunistic infections, encouraging antiretroviral adherence, and providing comprehensive care – which now includes preventing anal cancer.
A version of this article first appeared on Medscape.com.
In response, clinical care is continually adapting to the dramatically altered natural history of disease.
Today, the cutting edge of clinical care overlaps with primary care. The clinical vanguard addresses the medical vulnerabilities of patients with HIV, seeking to eliminate preventable morbidity and premature death. Among this clinical vanguard is the screening for and prevention of anal cancer. With the increased longevity of people living with HIV and the nearly universal exposure to human papillomavirus (HPV), there is now potential for progression to mucosal cellular dysplasia and eventual malignancy.
We know that prevention is possible because of the example of cervical cancer, the etiology of which is exposure to oncogenic serotypes of HPV (16 and 18 are most common). Screenings for cervical cancer (regular clinical examinations and Pap smears) and treatments to eliminate high-grade dysplasia have decreased the incidence rate by over 50% since the 1970s. Vaccination against HPV has been available since 2006 and offers the prospect of preventing HPV-associated malignancies, including head and neck cancer, in future decades.
However, rates of anal cancer are increasing. The CDC estimates that about 4,700 new cases of HPV-associated anal cancers are diagnosed in women and about 2,300 are diagnosed in men each year in the United States. Anal cancer rates in individuals with HIV have increased in the era of effective antiretrovirals and greater longevity. The highest rates, at 95 per 100,000, are in HIV-positive men who have sex with men. Very similar rates were noted in a more recent study that found increased risk with advancing age and in those with an AIDS diagnosis.
All patients with HIV should be screened
The New York State AIDS Institute Clinical Guidelines Program recommends screening for anal dysplasia in all patients with HIV. A proactive approach similar to cervical cancer screening is appropriate and includes measures easily implemented by all clinicians.
- History: Assess for rectal symptoms, anal pain, discharge, and lumps.
- Physical exam: Assess for presence of perianal lesions; perform a thorough digital rectal exam.
- Anal Pap test for anal cytology: Insert a Dacron swab moistened with tap water about 3 inches into the anal canal, applying pressure to lateral anal walls and rotating the swab. Then remove and place the swab into liquid cytology solution, shake vigorously for a full 30 seconds, and assess for any dysplasia (high-grade squamous intraepithelial lesion, low-grade intraepithelial lesion, atypical squamous cells of undetermined significance), which would warrant further evaluation by high-resolution anoscopy (HRA).
High-resolution anoscopy
HRA for anal dysplasia corresponds to colposcopy for cervical dysplasia. The ability to treat and eliminate high-risk precursor lesions interrupts the progression to malignancy. The efficacy of this strategy is being evaluated in a National Institutes of Health prospective trial called the Anchor Study. The epidemiology of HPV; the clinical horror of witnessing the painful, preventable deaths of young patients with well-controlled HIV caused by anal cancer; and the example of controlling cervical cancer have motivated my practice to assure comprehensive care for our patients.
Unfortunately, establishing HRA in one’s practice is challenging. Barriers to practice include the expense of required equipment and the absence of consensus on specific products. In addition, hands-on precepting to ease newcomers to competence is not generally available. Considerable skill is required for complete visualization of the anal transformative zone in the folds of the anal canal, and recognizing high-risk lesions requires study and accumulated experience. The International Anal Neoplasia Society is a useful resource that also offers a training course. We are invited to train ourselves, and to rely on the eventual feedback of biopsy results and the forbearance of our early patients.
The expanding scope of our medical practices must shift to meet the evolving needs of the growing population of virologically suppressed patients who are living longer. HIV care involves curing life-threatening opportunistic infections, encouraging antiretroviral adherence, and providing comprehensive care – which now includes preventing anal cancer.
A version of this article first appeared on Medscape.com.
In response, clinical care is continually adapting to the dramatically altered natural history of disease.
Today, the cutting edge of clinical care overlaps with primary care. The clinical vanguard addresses the medical vulnerabilities of patients with HIV, seeking to eliminate preventable morbidity and premature death. Among this clinical vanguard is the screening for and prevention of anal cancer. With the increased longevity of people living with HIV and the nearly universal exposure to human papillomavirus (HPV), there is now potential for progression to mucosal cellular dysplasia and eventual malignancy.
We know that prevention is possible because of the example of cervical cancer, the etiology of which is exposure to oncogenic serotypes of HPV (16 and 18 are most common). Screenings for cervical cancer (regular clinical examinations and Pap smears) and treatments to eliminate high-grade dysplasia have decreased the incidence rate by over 50% since the 1970s. Vaccination against HPV has been available since 2006 and offers the prospect of preventing HPV-associated malignancies, including head and neck cancer, in future decades.
However, rates of anal cancer are increasing. The CDC estimates that about 4,700 new cases of HPV-associated anal cancers are diagnosed in women and about 2,300 are diagnosed in men each year in the United States. Anal cancer rates in individuals with HIV have increased in the era of effective antiretrovirals and greater longevity. The highest rates, at 95 per 100,000, are in HIV-positive men who have sex with men. Very similar rates were noted in a more recent study that found increased risk with advancing age and in those with an AIDS diagnosis.
All patients with HIV should be screened
The New York State AIDS Institute Clinical Guidelines Program recommends screening for anal dysplasia in all patients with HIV. A proactive approach similar to cervical cancer screening is appropriate and includes measures easily implemented by all clinicians.
- History: Assess for rectal symptoms, anal pain, discharge, and lumps.
- Physical exam: Assess for presence of perianal lesions; perform a thorough digital rectal exam.
- Anal Pap test for anal cytology: Insert a Dacron swab moistened with tap water about 3 inches into the anal canal, applying pressure to lateral anal walls and rotating the swab. Then remove and place the swab into liquid cytology solution, shake vigorously for a full 30 seconds, and assess for any dysplasia (high-grade squamous intraepithelial lesion, low-grade intraepithelial lesion, atypical squamous cells of undetermined significance), which would warrant further evaluation by high-resolution anoscopy (HRA).
High-resolution anoscopy
HRA for anal dysplasia corresponds to colposcopy for cervical dysplasia. The ability to treat and eliminate high-risk precursor lesions interrupts the progression to malignancy. The efficacy of this strategy is being evaluated in a National Institutes of Health prospective trial called the Anchor Study. The epidemiology of HPV; the clinical horror of witnessing the painful, preventable deaths of young patients with well-controlled HIV caused by anal cancer; and the example of controlling cervical cancer have motivated my practice to assure comprehensive care for our patients.
Unfortunately, establishing HRA in one’s practice is challenging. Barriers to practice include the expense of required equipment and the absence of consensus on specific products. In addition, hands-on precepting to ease newcomers to competence is not generally available. Considerable skill is required for complete visualization of the anal transformative zone in the folds of the anal canal, and recognizing high-risk lesions requires study and accumulated experience. The International Anal Neoplasia Society is a useful resource that also offers a training course. We are invited to train ourselves, and to rely on the eventual feedback of biopsy results and the forbearance of our early patients.
The expanding scope of our medical practices must shift to meet the evolving needs of the growing population of virologically suppressed patients who are living longer. HIV care involves curing life-threatening opportunistic infections, encouraging antiretroviral adherence, and providing comprehensive care – which now includes preventing anal cancer.
A version of this article first appeared on Medscape.com.