User login
Detransition, baby: Examining factors leading to ‘detransitioning’ and regret in the transgender community
Over the holiday season I had the pleasure of finally reading the national bestseller, Detransition, Baby. On the surface, the story depicts the complex relationships between Reese, a transgender woman who strongly desires a family, her ex-wife, Ames – a transgender woman who detransitioned to live as a cisgender man – and Ames’ cisgender female partner, who is unexpectedly pregnant with his child. The story delves much deeper than the relationships between these characters, as it exceptionally articulates many of the emotional intricacies of the transgender experience and addresses one of the most taboo topics in the transgender community – detransitioning and regret.
The terms “transition” and “detransition” have fallen out of favor in the vernacular of the transgender population as they incorrectly imply that gender identity is contingent upon gender-affirmation processes.1,2 More importantly, the terms “detransition” and regret are not synonymous. Conflating these terms has undermined the intrinsic nature of gender identity, which has resulted in political and legal consequences seeking to limit or outright ban care for transgender patients.
As a gender-affirming surgeon, one of the most common questions I get asked is the rate of regret patients have after their surgeries. While I have no issue answering the question when it is presented, I do not hesitate to point out some of the problematic subtext inherent in such inquiries. Within the line of questioning, many often comment, “It’s so permanent,” “I can’t believe people can do this to their bodies,” or “How sure are patients before undergoing these surgeries?” While these comments and queries can be downright offensive, they seem to stem from the difficulty people have comprehending gender dysphoria and the painstaking steps people take to affirm their identity. The implication of these comments also reveals a more deep-seated issue – general distrust of individual bodily autonomy, personal identity, and choice.
For the obstetrician-gynecologist, understanding the concept of autonomous, patient-centered decision-making should be second nature, as we face a similar line of interrogation when discussing abortion, contraception, and pregnancy. No other field faces this level of scrutiny when it comes to defending a patient’s bodily autonomy. For example, given the history of reproductive injustice with tubal ligation procedures, the American College of Obstetricians and Gynecologists has issued clear guidelines regarding counseling of women while acknowledging the tenuous history of these procedures with minority subgroups. According to their committee opinion, ethical counseling for such a permanent procedure involves understanding the content of information presented to the patient, how that information is conveyed, and self-reflection on the part of the provider.3 The approach to counseling and understanding gender-affirming care is no different.
I want to be clear that regret after gender-affirming surgery is rare, occurring in 0%-3.8% of patients.4-6 In a separate study, 91% of patients expressed significant improvement in quality of life after surgery.7 However, what is disheartening about patients who experience surgical regret is that it originates from continued difficulty from the transition process itself and ongoing discrimination – even though the patient’s physical characteristics match their gender identity.4-6 Similarly, in another survey which examined 17,151 participants who had pursued gender affirmation (broadly defined), approximately 2,242 (13.1%) reported a history of detransition.2 Among these adults, the vast majority (82.5%), cited external factors such as school harassment, sexual violence, family pressure, and social stigma as reasons for detransitioning.2 Other associated factors included male sex assigned at birth, nonbinary gender identity, bisexual orientation, and having an unsupportive family.2
When Ames is explaining his “detransition” to his cisfemale partner, he states: “I got sick of living as trans …[sic]… I am trans, but I don’t need to do trans.”8 While there is still more research needed to further understand detransitioning and surgical regret, these few studies demonstrate a heart-breaking reality – in many aspects of our society it is still extremely difficult to live as a transgender person.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. She did not report any disclosures.
References
1. National LGBTQIA+ Health Education Center, A program of the Fenway Institute: LGBTQIA+ glossary of terms for health care teams. 2020. Available at www.lgbtqiahealtheducation.org/wp-content/uploads/2020/10/Glossary-2020.08.30.pdf. Accessed Dec. 30, 2021.
2. Turban JL et al. LGBT Health 2021;8(4):273-80.
3. Sterilization of women: Ethical issues and considerations. Committee Opinion No. 695. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;129:e109-16.
4. Ruppin U, Pfafflin F. Arch Sex Behav. 2015;44:1321-9.
5. Lawrence AA. Arch Sex Behav. 2003;32:299-315.
6. Landen M et al. Acta Psychiatr Scand. 1998;97:284-9.
7. Papdopulos NA et al. J Sex Med. 2017;14(5):721-30.
8. Peters T. Detransition, Baby. New York: Penguin Random House, 2021.
Over the holiday season I had the pleasure of finally reading the national bestseller, Detransition, Baby. On the surface, the story depicts the complex relationships between Reese, a transgender woman who strongly desires a family, her ex-wife, Ames – a transgender woman who detransitioned to live as a cisgender man – and Ames’ cisgender female partner, who is unexpectedly pregnant with his child. The story delves much deeper than the relationships between these characters, as it exceptionally articulates many of the emotional intricacies of the transgender experience and addresses one of the most taboo topics in the transgender community – detransitioning and regret.
The terms “transition” and “detransition” have fallen out of favor in the vernacular of the transgender population as they incorrectly imply that gender identity is contingent upon gender-affirmation processes.1,2 More importantly, the terms “detransition” and regret are not synonymous. Conflating these terms has undermined the intrinsic nature of gender identity, which has resulted in political and legal consequences seeking to limit or outright ban care for transgender patients.
As a gender-affirming surgeon, one of the most common questions I get asked is the rate of regret patients have after their surgeries. While I have no issue answering the question when it is presented, I do not hesitate to point out some of the problematic subtext inherent in such inquiries. Within the line of questioning, many often comment, “It’s so permanent,” “I can’t believe people can do this to their bodies,” or “How sure are patients before undergoing these surgeries?” While these comments and queries can be downright offensive, they seem to stem from the difficulty people have comprehending gender dysphoria and the painstaking steps people take to affirm their identity. The implication of these comments also reveals a more deep-seated issue – general distrust of individual bodily autonomy, personal identity, and choice.
For the obstetrician-gynecologist, understanding the concept of autonomous, patient-centered decision-making should be second nature, as we face a similar line of interrogation when discussing abortion, contraception, and pregnancy. No other field faces this level of scrutiny when it comes to defending a patient’s bodily autonomy. For example, given the history of reproductive injustice with tubal ligation procedures, the American College of Obstetricians and Gynecologists has issued clear guidelines regarding counseling of women while acknowledging the tenuous history of these procedures with minority subgroups. According to their committee opinion, ethical counseling for such a permanent procedure involves understanding the content of information presented to the patient, how that information is conveyed, and self-reflection on the part of the provider.3 The approach to counseling and understanding gender-affirming care is no different.
I want to be clear that regret after gender-affirming surgery is rare, occurring in 0%-3.8% of patients.4-6 In a separate study, 91% of patients expressed significant improvement in quality of life after surgery.7 However, what is disheartening about patients who experience surgical regret is that it originates from continued difficulty from the transition process itself and ongoing discrimination – even though the patient’s physical characteristics match their gender identity.4-6 Similarly, in another survey which examined 17,151 participants who had pursued gender affirmation (broadly defined), approximately 2,242 (13.1%) reported a history of detransition.2 Among these adults, the vast majority (82.5%), cited external factors such as school harassment, sexual violence, family pressure, and social stigma as reasons for detransitioning.2 Other associated factors included male sex assigned at birth, nonbinary gender identity, bisexual orientation, and having an unsupportive family.2
When Ames is explaining his “detransition” to his cisfemale partner, he states: “I got sick of living as trans …[sic]… I am trans, but I don’t need to do trans.”8 While there is still more research needed to further understand detransitioning and surgical regret, these few studies demonstrate a heart-breaking reality – in many aspects of our society it is still extremely difficult to live as a transgender person.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. She did not report any disclosures.
References
1. National LGBTQIA+ Health Education Center, A program of the Fenway Institute: LGBTQIA+ glossary of terms for health care teams. 2020. Available at www.lgbtqiahealtheducation.org/wp-content/uploads/2020/10/Glossary-2020.08.30.pdf. Accessed Dec. 30, 2021.
2. Turban JL et al. LGBT Health 2021;8(4):273-80.
3. Sterilization of women: Ethical issues and considerations. Committee Opinion No. 695. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;129:e109-16.
4. Ruppin U, Pfafflin F. Arch Sex Behav. 2015;44:1321-9.
5. Lawrence AA. Arch Sex Behav. 2003;32:299-315.
6. Landen M et al. Acta Psychiatr Scand. 1998;97:284-9.
7. Papdopulos NA et al. J Sex Med. 2017;14(5):721-30.
8. Peters T. Detransition, Baby. New York: Penguin Random House, 2021.
Over the holiday season I had the pleasure of finally reading the national bestseller, Detransition, Baby. On the surface, the story depicts the complex relationships between Reese, a transgender woman who strongly desires a family, her ex-wife, Ames – a transgender woman who detransitioned to live as a cisgender man – and Ames’ cisgender female partner, who is unexpectedly pregnant with his child. The story delves much deeper than the relationships between these characters, as it exceptionally articulates many of the emotional intricacies of the transgender experience and addresses one of the most taboo topics in the transgender community – detransitioning and regret.
The terms “transition” and “detransition” have fallen out of favor in the vernacular of the transgender population as they incorrectly imply that gender identity is contingent upon gender-affirmation processes.1,2 More importantly, the terms “detransition” and regret are not synonymous. Conflating these terms has undermined the intrinsic nature of gender identity, which has resulted in political and legal consequences seeking to limit or outright ban care for transgender patients.
As a gender-affirming surgeon, one of the most common questions I get asked is the rate of regret patients have after their surgeries. While I have no issue answering the question when it is presented, I do not hesitate to point out some of the problematic subtext inherent in such inquiries. Within the line of questioning, many often comment, “It’s so permanent,” “I can’t believe people can do this to their bodies,” or “How sure are patients before undergoing these surgeries?” While these comments and queries can be downright offensive, they seem to stem from the difficulty people have comprehending gender dysphoria and the painstaking steps people take to affirm their identity. The implication of these comments also reveals a more deep-seated issue – general distrust of individual bodily autonomy, personal identity, and choice.
For the obstetrician-gynecologist, understanding the concept of autonomous, patient-centered decision-making should be second nature, as we face a similar line of interrogation when discussing abortion, contraception, and pregnancy. No other field faces this level of scrutiny when it comes to defending a patient’s bodily autonomy. For example, given the history of reproductive injustice with tubal ligation procedures, the American College of Obstetricians and Gynecologists has issued clear guidelines regarding counseling of women while acknowledging the tenuous history of these procedures with minority subgroups. According to their committee opinion, ethical counseling for such a permanent procedure involves understanding the content of information presented to the patient, how that information is conveyed, and self-reflection on the part of the provider.3 The approach to counseling and understanding gender-affirming care is no different.
I want to be clear that regret after gender-affirming surgery is rare, occurring in 0%-3.8% of patients.4-6 In a separate study, 91% of patients expressed significant improvement in quality of life after surgery.7 However, what is disheartening about patients who experience surgical regret is that it originates from continued difficulty from the transition process itself and ongoing discrimination – even though the patient’s physical characteristics match their gender identity.4-6 Similarly, in another survey which examined 17,151 participants who had pursued gender affirmation (broadly defined), approximately 2,242 (13.1%) reported a history of detransition.2 Among these adults, the vast majority (82.5%), cited external factors such as school harassment, sexual violence, family pressure, and social stigma as reasons for detransitioning.2 Other associated factors included male sex assigned at birth, nonbinary gender identity, bisexual orientation, and having an unsupportive family.2
When Ames is explaining his “detransition” to his cisfemale partner, he states: “I got sick of living as trans …[sic]… I am trans, but I don’t need to do trans.”8 While there is still more research needed to further understand detransitioning and surgical regret, these few studies demonstrate a heart-breaking reality – in many aspects of our society it is still extremely difficult to live as a transgender person.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. She did not report any disclosures.
References
1. National LGBTQIA+ Health Education Center, A program of the Fenway Institute: LGBTQIA+ glossary of terms for health care teams. 2020. Available at www.lgbtqiahealtheducation.org/wp-content/uploads/2020/10/Glossary-2020.08.30.pdf. Accessed Dec. 30, 2021.
2. Turban JL et al. LGBT Health 2021;8(4):273-80.
3. Sterilization of women: Ethical issues and considerations. Committee Opinion No. 695. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;129:e109-16.
4. Ruppin U, Pfafflin F. Arch Sex Behav. 2015;44:1321-9.
5. Lawrence AA. Arch Sex Behav. 2003;32:299-315.
6. Landen M et al. Acta Psychiatr Scand. 1998;97:284-9.
7. Papdopulos NA et al. J Sex Med. 2017;14(5):721-30.
8. Peters T. Detransition, Baby. New York: Penguin Random House, 2021.
Could stopping ‘thousand cuts’ by insurers and PBMs help rheumatology’s workforce shortage?
I am hearing more and more often from colleagues about the number of rheumatologists taking early retirement because of the frustration of having doctor-patient shared decision-making taken out of their hands and given to the insurance companies and their pharmacy benefit managers (PBMs). Often the right medication for the patient is not available on the formulary, causing unnecessary administrative barriers to providing care. When you put that together with the decreased reimbursement and the many obstacles to the “buy-and-bill” model, many rheumatologists have just had enough and called it quits earlier than they thought they would. This is a significant contributor to the growing workforce problem in rheumatology.
Many of the issues affecting the availability of medications happen throughout the development and distribution of a drug treatment – regulatory approval and obstacles to commercial launch, such as patent thickets, “pay for delay,” and other anticompetitive tactics by the manufacturers. And once a medication is launched on to the marketplace, rheumatologists are at the mercy of the health plans and PBMs as to whether, when, and even where a medication can be used. Here is where much of the frustration begins, amplified by the knowledge that profit for the PBM is the driving force behind formulary construction.
To support rheumatologists in addressing these challenges, the Coalition of State Rheumatology Organizations started a “Reporting Insurance/Payer Issues” page. Here, rheumatologists can describe issues or complaints they have with payers regarding patient care. The responses we’ve received so far always have a sense of urgency and frustration in the description of whatever obstacle to care is being thrown up by an insurance company or PBM.
One of the recent issues that has arisen via the CSRO’s reporting form involves a new policy for an insurance plan that removes the availability of the intravenous formulation of a medication if it has a subcutaneous (sub Q) formulation. It is a commercial version of the Medicare self-administered drug list, but worse. At least Medicare takes the time to look at the actual usage of a formulation before moving it from Part B to Part D. This new policy flatly states that no patients will have access to the IV formulation until the sub Q formulation has been tried. This includes switching all stable IV patients over to the sub Q formulation. Because the IV formulation is weight based, switching patients from IV to sub Q can reduce their dosage by more than 50%. It appears that loss of disease control is a small price to pay for increased PBM profits (called “savings” by the PBM). Notably, IV medications through physician “buy and bill” offer no revenue to the insurance company, while sub Q medications increase profits through rebates, fees, and other price concessions.
The CSRO outlined these concerns in its Jan. 18, 2022, response to the insurance company’s reply to the coalition’s original letter, urging them to value patients over profits. In this response, the CSRO addressed nonmedical switching, site of care cost, outcome documentation, and grandfathering stable patients, and finished with a discussion on ERISA (Employee Retirement Income Security Act of 1974) protections.
While our Reporting Insurance/Payer Issues form cannot handle reimbursement issues, there needs to be a word about money and profit when it comes to physicians. Physicians whose specialties have few to no procedures, including rheumatologists, rely on office visits and ancillary services such as infusion suites for income. That income sustains their practice and maintains all their attendant expenses. Many of the recent policies put forth by health plans not only intrude on the doctor-patient relationship in treatment decisions, but also reduce reimbursements and place obstacles to “buy and bill,” shifting revenue from the physician to the insurance company.
All these insurance/payer issues boil down to a version of “death by a thousand cuts.” These cuts harm patients and impede rheumatologists’ ability to sustain their practices. They are a type of moral injury (among the many we see in health care providers) that are causing rheumatologists to retire early. Clearly, these issues ultimately affect the workforce. We need advocacy on many levels if we have any hope of dulling the knives that are delivering these “cuts.”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is President of the CSRO, past chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.
I am hearing more and more often from colleagues about the number of rheumatologists taking early retirement because of the frustration of having doctor-patient shared decision-making taken out of their hands and given to the insurance companies and their pharmacy benefit managers (PBMs). Often the right medication for the patient is not available on the formulary, causing unnecessary administrative barriers to providing care. When you put that together with the decreased reimbursement and the many obstacles to the “buy-and-bill” model, many rheumatologists have just had enough and called it quits earlier than they thought they would. This is a significant contributor to the growing workforce problem in rheumatology.
Many of the issues affecting the availability of medications happen throughout the development and distribution of a drug treatment – regulatory approval and obstacles to commercial launch, such as patent thickets, “pay for delay,” and other anticompetitive tactics by the manufacturers. And once a medication is launched on to the marketplace, rheumatologists are at the mercy of the health plans and PBMs as to whether, when, and even where a medication can be used. Here is where much of the frustration begins, amplified by the knowledge that profit for the PBM is the driving force behind formulary construction.
To support rheumatologists in addressing these challenges, the Coalition of State Rheumatology Organizations started a “Reporting Insurance/Payer Issues” page. Here, rheumatologists can describe issues or complaints they have with payers regarding patient care. The responses we’ve received so far always have a sense of urgency and frustration in the description of whatever obstacle to care is being thrown up by an insurance company or PBM.
One of the recent issues that has arisen via the CSRO’s reporting form involves a new policy for an insurance plan that removes the availability of the intravenous formulation of a medication if it has a subcutaneous (sub Q) formulation. It is a commercial version of the Medicare self-administered drug list, but worse. At least Medicare takes the time to look at the actual usage of a formulation before moving it from Part B to Part D. This new policy flatly states that no patients will have access to the IV formulation until the sub Q formulation has been tried. This includes switching all stable IV patients over to the sub Q formulation. Because the IV formulation is weight based, switching patients from IV to sub Q can reduce their dosage by more than 50%. It appears that loss of disease control is a small price to pay for increased PBM profits (called “savings” by the PBM). Notably, IV medications through physician “buy and bill” offer no revenue to the insurance company, while sub Q medications increase profits through rebates, fees, and other price concessions.
The CSRO outlined these concerns in its Jan. 18, 2022, response to the insurance company’s reply to the coalition’s original letter, urging them to value patients over profits. In this response, the CSRO addressed nonmedical switching, site of care cost, outcome documentation, and grandfathering stable patients, and finished with a discussion on ERISA (Employee Retirement Income Security Act of 1974) protections.
While our Reporting Insurance/Payer Issues form cannot handle reimbursement issues, there needs to be a word about money and profit when it comes to physicians. Physicians whose specialties have few to no procedures, including rheumatologists, rely on office visits and ancillary services such as infusion suites for income. That income sustains their practice and maintains all their attendant expenses. Many of the recent policies put forth by health plans not only intrude on the doctor-patient relationship in treatment decisions, but also reduce reimbursements and place obstacles to “buy and bill,” shifting revenue from the physician to the insurance company.
All these insurance/payer issues boil down to a version of “death by a thousand cuts.” These cuts harm patients and impede rheumatologists’ ability to sustain their practices. They are a type of moral injury (among the many we see in health care providers) that are causing rheumatologists to retire early. Clearly, these issues ultimately affect the workforce. We need advocacy on many levels if we have any hope of dulling the knives that are delivering these “cuts.”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is President of the CSRO, past chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.
I am hearing more and more often from colleagues about the number of rheumatologists taking early retirement because of the frustration of having doctor-patient shared decision-making taken out of their hands and given to the insurance companies and their pharmacy benefit managers (PBMs). Often the right medication for the patient is not available on the formulary, causing unnecessary administrative barriers to providing care. When you put that together with the decreased reimbursement and the many obstacles to the “buy-and-bill” model, many rheumatologists have just had enough and called it quits earlier than they thought they would. This is a significant contributor to the growing workforce problem in rheumatology.
Many of the issues affecting the availability of medications happen throughout the development and distribution of a drug treatment – regulatory approval and obstacles to commercial launch, such as patent thickets, “pay for delay,” and other anticompetitive tactics by the manufacturers. And once a medication is launched on to the marketplace, rheumatologists are at the mercy of the health plans and PBMs as to whether, when, and even where a medication can be used. Here is where much of the frustration begins, amplified by the knowledge that profit for the PBM is the driving force behind formulary construction.
To support rheumatologists in addressing these challenges, the Coalition of State Rheumatology Organizations started a “Reporting Insurance/Payer Issues” page. Here, rheumatologists can describe issues or complaints they have with payers regarding patient care. The responses we’ve received so far always have a sense of urgency and frustration in the description of whatever obstacle to care is being thrown up by an insurance company or PBM.
One of the recent issues that has arisen via the CSRO’s reporting form involves a new policy for an insurance plan that removes the availability of the intravenous formulation of a medication if it has a subcutaneous (sub Q) formulation. It is a commercial version of the Medicare self-administered drug list, but worse. At least Medicare takes the time to look at the actual usage of a formulation before moving it from Part B to Part D. This new policy flatly states that no patients will have access to the IV formulation until the sub Q formulation has been tried. This includes switching all stable IV patients over to the sub Q formulation. Because the IV formulation is weight based, switching patients from IV to sub Q can reduce their dosage by more than 50%. It appears that loss of disease control is a small price to pay for increased PBM profits (called “savings” by the PBM). Notably, IV medications through physician “buy and bill” offer no revenue to the insurance company, while sub Q medications increase profits through rebates, fees, and other price concessions.
The CSRO outlined these concerns in its Jan. 18, 2022, response to the insurance company’s reply to the coalition’s original letter, urging them to value patients over profits. In this response, the CSRO addressed nonmedical switching, site of care cost, outcome documentation, and grandfathering stable patients, and finished with a discussion on ERISA (Employee Retirement Income Security Act of 1974) protections.
While our Reporting Insurance/Payer Issues form cannot handle reimbursement issues, there needs to be a word about money and profit when it comes to physicians. Physicians whose specialties have few to no procedures, including rheumatologists, rely on office visits and ancillary services such as infusion suites for income. That income sustains their practice and maintains all their attendant expenses. Many of the recent policies put forth by health plans not only intrude on the doctor-patient relationship in treatment decisions, but also reduce reimbursements and place obstacles to “buy and bill,” shifting revenue from the physician to the insurance company.
All these insurance/payer issues boil down to a version of “death by a thousand cuts.” These cuts harm patients and impede rheumatologists’ ability to sustain their practices. They are a type of moral injury (among the many we see in health care providers) that are causing rheumatologists to retire early. Clearly, these issues ultimately affect the workforce. We need advocacy on many levels if we have any hope of dulling the knives that are delivering these “cuts.”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is President of the CSRO, past chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.
When the patient wants to speak to a manager
A patient swore at me the other day. Not as in “she used a curse word.” As in she spewed fury, spitting out a vulgar, adverbial word before “... terrible doctor” while jabbing her finger toward me. In my 15 years of practice, I’d never had that happen before. Equally surprising, I was not surprised by her outburst. The level of incivility from patients is at an all-time high.
Her anger was misdirected. She wanted me to write a letter to her employer excusing her from getting a vaccine. It was neither indicated nor ethical for me to do so. I did my best to redirect her, but without success. As our chief of service, I often help with service concerns and am happy to see patients who want another opinion or want to speak with the department head (aka, “the manager”). Usually I can help. Lately, it’s become harder.
Not only are such rude incidents more frequent, but they are also more dramatic and inappropriate. For example, I cannot imagine writing a complaint against a doctor stating that she must be a foreign medical grad (as it happens, she’s Ivy League-trained) or demanding money back when a biopsy result turned out to be benign, or threatening to report a doctor to the medical board because he failed to schedule a follow-up appointment (that doctor had been retired for months). Patients have hung up on our staff mid-sentence and slammed a clinic door when they left in a huff. Why are so many previously sensible people throwing childlike tantrums?
It’s the same phenomenon happening to our fellow service agents across all industries. The Federal Aviation Administration’s graph of unruly passenger incidents is a flat line from 1995 to 2019, then it goes straight vertical. A recent survey showed that Americans’ sense of civility is low and worse, that people’s expectations that civility will improve is going down. It’s palpable. Last month, I witnessed a man and woman screaming at each other over Christmas lights in a busy store. An army of aproned walkie-talkie staff surrounded them and escorted them out – their coordination and efficiency clearly indicated they’d done this before. Customers everywhere are mad, frustrated, disenfranchised. Lately, a lot of things just are not working out for them. Supplies are out. Kids are sent home from school. No elective surgery appointments are available. The insta-gratification they’ve grown accustomed to from Amazon and DoorDash is colliding with the reality that not everything works that way.
The word “patient’’ you’ll recall comes from the Latin “patior,” meaning to suffer or bear. With virus variants raging, inflation growing, and call center wait times approaching infinity, many of our patients, it seems, cannot bear any more. I’m confident this situation will improve and our patients will be more reasonable in their expectations, but I am afraid that, in the end, we’ll have lost some decorum and dignity that we may never find again in medicine.
For my potty-mouthed patient, I made an excuse to leave the room to get my dermatoscope and walked out. It gave her time to calm down. I returned in a few minutes to do a skin exam. As I was wrapping up, I advised her that she cannot raise her voice or use offensive language and that she should know that I and everyone in our office cares about her and wants to help. She did apologize for her behavior, but then had to add that, if I really cared, I’d write the letter for her.
I guess the customer is not always right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
A patient swore at me the other day. Not as in “she used a curse word.” As in she spewed fury, spitting out a vulgar, adverbial word before “... terrible doctor” while jabbing her finger toward me. In my 15 years of practice, I’d never had that happen before. Equally surprising, I was not surprised by her outburst. The level of incivility from patients is at an all-time high.
Her anger was misdirected. She wanted me to write a letter to her employer excusing her from getting a vaccine. It was neither indicated nor ethical for me to do so. I did my best to redirect her, but without success. As our chief of service, I often help with service concerns and am happy to see patients who want another opinion or want to speak with the department head (aka, “the manager”). Usually I can help. Lately, it’s become harder.
Not only are such rude incidents more frequent, but they are also more dramatic and inappropriate. For example, I cannot imagine writing a complaint against a doctor stating that she must be a foreign medical grad (as it happens, she’s Ivy League-trained) or demanding money back when a biopsy result turned out to be benign, or threatening to report a doctor to the medical board because he failed to schedule a follow-up appointment (that doctor had been retired for months). Patients have hung up on our staff mid-sentence and slammed a clinic door when they left in a huff. Why are so many previously sensible people throwing childlike tantrums?
It’s the same phenomenon happening to our fellow service agents across all industries. The Federal Aviation Administration’s graph of unruly passenger incidents is a flat line from 1995 to 2019, then it goes straight vertical. A recent survey showed that Americans’ sense of civility is low and worse, that people’s expectations that civility will improve is going down. It’s palpable. Last month, I witnessed a man and woman screaming at each other over Christmas lights in a busy store. An army of aproned walkie-talkie staff surrounded them and escorted them out – their coordination and efficiency clearly indicated they’d done this before. Customers everywhere are mad, frustrated, disenfranchised. Lately, a lot of things just are not working out for them. Supplies are out. Kids are sent home from school. No elective surgery appointments are available. The insta-gratification they’ve grown accustomed to from Amazon and DoorDash is colliding with the reality that not everything works that way.
The word “patient’’ you’ll recall comes from the Latin “patior,” meaning to suffer or bear. With virus variants raging, inflation growing, and call center wait times approaching infinity, many of our patients, it seems, cannot bear any more. I’m confident this situation will improve and our patients will be more reasonable in their expectations, but I am afraid that, in the end, we’ll have lost some decorum and dignity that we may never find again in medicine.
For my potty-mouthed patient, I made an excuse to leave the room to get my dermatoscope and walked out. It gave her time to calm down. I returned in a few minutes to do a skin exam. As I was wrapping up, I advised her that she cannot raise her voice or use offensive language and that she should know that I and everyone in our office cares about her and wants to help. She did apologize for her behavior, but then had to add that, if I really cared, I’d write the letter for her.
I guess the customer is not always right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
A patient swore at me the other day. Not as in “she used a curse word.” As in she spewed fury, spitting out a vulgar, adverbial word before “... terrible doctor” while jabbing her finger toward me. In my 15 years of practice, I’d never had that happen before. Equally surprising, I was not surprised by her outburst. The level of incivility from patients is at an all-time high.
Her anger was misdirected. She wanted me to write a letter to her employer excusing her from getting a vaccine. It was neither indicated nor ethical for me to do so. I did my best to redirect her, but without success. As our chief of service, I often help with service concerns and am happy to see patients who want another opinion or want to speak with the department head (aka, “the manager”). Usually I can help. Lately, it’s become harder.
Not only are such rude incidents more frequent, but they are also more dramatic and inappropriate. For example, I cannot imagine writing a complaint against a doctor stating that she must be a foreign medical grad (as it happens, she’s Ivy League-trained) or demanding money back when a biopsy result turned out to be benign, or threatening to report a doctor to the medical board because he failed to schedule a follow-up appointment (that doctor had been retired for months). Patients have hung up on our staff mid-sentence and slammed a clinic door when they left in a huff. Why are so many previously sensible people throwing childlike tantrums?
It’s the same phenomenon happening to our fellow service agents across all industries. The Federal Aviation Administration’s graph of unruly passenger incidents is a flat line from 1995 to 2019, then it goes straight vertical. A recent survey showed that Americans’ sense of civility is low and worse, that people’s expectations that civility will improve is going down. It’s palpable. Last month, I witnessed a man and woman screaming at each other over Christmas lights in a busy store. An army of aproned walkie-talkie staff surrounded them and escorted them out – their coordination and efficiency clearly indicated they’d done this before. Customers everywhere are mad, frustrated, disenfranchised. Lately, a lot of things just are not working out for them. Supplies are out. Kids are sent home from school. No elective surgery appointments are available. The insta-gratification they’ve grown accustomed to from Amazon and DoorDash is colliding with the reality that not everything works that way.
The word “patient’’ you’ll recall comes from the Latin “patior,” meaning to suffer or bear. With virus variants raging, inflation growing, and call center wait times approaching infinity, many of our patients, it seems, cannot bear any more. I’m confident this situation will improve and our patients will be more reasonable in their expectations, but I am afraid that, in the end, we’ll have lost some decorum and dignity that we may never find again in medicine.
For my potty-mouthed patient, I made an excuse to leave the room to get my dermatoscope and walked out. It gave her time to calm down. I returned in a few minutes to do a skin exam. As I was wrapping up, I advised her that she cannot raise her voice or use offensive language and that she should know that I and everyone in our office cares about her and wants to help. She did apologize for her behavior, but then had to add that, if I really cared, I’d write the letter for her.
I guess the customer is not always right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Should you dismiss that patient?
After a recent column about the dilemma of dealing with patients who refuse to be vaccinated against COVID-19, several readers raised the
Contrary to what seems to be the popular opinion, there are no statutory laws that I am aware of that directly apply to patient dismissal, beyond the obvious ones prohibiting discrimination that I’ve discussed many times. The more realistic concern is leaving yourself vulnerable to civil litigation – usually charges of abandonment.
Criteria will vary by region, jurisdiction, and practice. Since there are no hard and fast rules, your reasons for dismissal should be determined in advance, written out, and included in your practice manual. Once you have laid down your rules, follow them. Exceptions should be rare and made only under extraordinary circumstances.
Most patients are dismissed because of interpersonal conflicts between physician or staff members. Usually, that involves noncompliance with a reasonable treatment plan (including vaccinations), but there are other valid reasons. These include threats of violence, inappropriate sexual advances, providing false or misleading medical history, demands for inappropriate treatments or medications, and repeated failure to keep appointments or pay bills. And most ethics experts agree that you can dismiss someone who insists on treatment outside your area of expertise, or at a location other than your private office.
Even when circumstances warrant, dismissal should be a last resort. As with most interpersonal conflicts, your best option is usually reconciliation. Sit down with the patient, explain your concerns, and discuss what must be done if your doctor-patient relationship is to continue. Often, such patients are not aware (or willing to admit) that they are violating your office policies. Honest communication will often save such relationships. But be sure to make it clear that failure to address the problems you have outlined will result in dismissal from your practice. Document this conversation in detail in the patient’s chart, and follow up with a written communication reconfirming what you discussed.
If, despite your best (documented) efforts, the problems continue and dismissal becomes necessary, following a few generally accepted guidelines will help keep the process smooth and consequence free.
First, try to avoid dismissing a patient in the middle of a course of treatment. If that is unavoidable, you might want to contact your malpractice carrier and review the case with them prior to doing so.
Inform the patient, preferably by certified mail, of your decision. Spell out your reasons, with a reminder that these problems were discussed, and that a warning was issued and not heeded. If the patient belongs to a third-party health plan, be certain that you are acting within the stipulations of your contract with that plan, and inform the payer in writing of your action.
Once again, you must clearly document in the patient’s chart exactly how he or she violated your office policies. This will minimize grounds for charges of discrimination of any sort. Be especially diligent about this step if the patient has any known physical or mental disability.
Give the patient a reasonable amount of time (30 days is common) to find another physician, and mention that you will address any emergent problems within the scope of your specialty within that 30-day period. To minimize any potential allegations of abandonment, include a list of competent physicians in your area (without any guarantees) who might be willing to assume the patient’s care. Alternatively, you can list the phone number or website of a local medical society that they can contact to find a replacement. Offer to transfer medical records to the new physician upon receipt of written permission.
File a copy or scan of the letter, the certified delivery receipt, and the returned signature card in the patient’s chart. While the law states that a first-class letter, properly addressed and stamped, is presumed to have been delivered, you don’t want any question as to whether the patient received written notice of dismissal.
Forcibly ending a physician-patient relationship is a significant event that should not be undertaken lightly. Again, dismissal should be a rare occurrence, a last resort.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
After a recent column about the dilemma of dealing with patients who refuse to be vaccinated against COVID-19, several readers raised the
Contrary to what seems to be the popular opinion, there are no statutory laws that I am aware of that directly apply to patient dismissal, beyond the obvious ones prohibiting discrimination that I’ve discussed many times. The more realistic concern is leaving yourself vulnerable to civil litigation – usually charges of abandonment.
Criteria will vary by region, jurisdiction, and practice. Since there are no hard and fast rules, your reasons for dismissal should be determined in advance, written out, and included in your practice manual. Once you have laid down your rules, follow them. Exceptions should be rare and made only under extraordinary circumstances.
Most patients are dismissed because of interpersonal conflicts between physician or staff members. Usually, that involves noncompliance with a reasonable treatment plan (including vaccinations), but there are other valid reasons. These include threats of violence, inappropriate sexual advances, providing false or misleading medical history, demands for inappropriate treatments or medications, and repeated failure to keep appointments or pay bills. And most ethics experts agree that you can dismiss someone who insists on treatment outside your area of expertise, or at a location other than your private office.
Even when circumstances warrant, dismissal should be a last resort. As with most interpersonal conflicts, your best option is usually reconciliation. Sit down with the patient, explain your concerns, and discuss what must be done if your doctor-patient relationship is to continue. Often, such patients are not aware (or willing to admit) that they are violating your office policies. Honest communication will often save such relationships. But be sure to make it clear that failure to address the problems you have outlined will result in dismissal from your practice. Document this conversation in detail in the patient’s chart, and follow up with a written communication reconfirming what you discussed.
If, despite your best (documented) efforts, the problems continue and dismissal becomes necessary, following a few generally accepted guidelines will help keep the process smooth and consequence free.
First, try to avoid dismissing a patient in the middle of a course of treatment. If that is unavoidable, you might want to contact your malpractice carrier and review the case with them prior to doing so.
Inform the patient, preferably by certified mail, of your decision. Spell out your reasons, with a reminder that these problems were discussed, and that a warning was issued and not heeded. If the patient belongs to a third-party health plan, be certain that you are acting within the stipulations of your contract with that plan, and inform the payer in writing of your action.
Once again, you must clearly document in the patient’s chart exactly how he or she violated your office policies. This will minimize grounds for charges of discrimination of any sort. Be especially diligent about this step if the patient has any known physical or mental disability.
Give the patient a reasonable amount of time (30 days is common) to find another physician, and mention that you will address any emergent problems within the scope of your specialty within that 30-day period. To minimize any potential allegations of abandonment, include a list of competent physicians in your area (without any guarantees) who might be willing to assume the patient’s care. Alternatively, you can list the phone number or website of a local medical society that they can contact to find a replacement. Offer to transfer medical records to the new physician upon receipt of written permission.
File a copy or scan of the letter, the certified delivery receipt, and the returned signature card in the patient’s chart. While the law states that a first-class letter, properly addressed and stamped, is presumed to have been delivered, you don’t want any question as to whether the patient received written notice of dismissal.
Forcibly ending a physician-patient relationship is a significant event that should not be undertaken lightly. Again, dismissal should be a rare occurrence, a last resort.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
After a recent column about the dilemma of dealing with patients who refuse to be vaccinated against COVID-19, several readers raised the
Contrary to what seems to be the popular opinion, there are no statutory laws that I am aware of that directly apply to patient dismissal, beyond the obvious ones prohibiting discrimination that I’ve discussed many times. The more realistic concern is leaving yourself vulnerable to civil litigation – usually charges of abandonment.
Criteria will vary by region, jurisdiction, and practice. Since there are no hard and fast rules, your reasons for dismissal should be determined in advance, written out, and included in your practice manual. Once you have laid down your rules, follow them. Exceptions should be rare and made only under extraordinary circumstances.
Most patients are dismissed because of interpersonal conflicts between physician or staff members. Usually, that involves noncompliance with a reasonable treatment plan (including vaccinations), but there are other valid reasons. These include threats of violence, inappropriate sexual advances, providing false or misleading medical history, demands for inappropriate treatments or medications, and repeated failure to keep appointments or pay bills. And most ethics experts agree that you can dismiss someone who insists on treatment outside your area of expertise, or at a location other than your private office.
Even when circumstances warrant, dismissal should be a last resort. As with most interpersonal conflicts, your best option is usually reconciliation. Sit down with the patient, explain your concerns, and discuss what must be done if your doctor-patient relationship is to continue. Often, such patients are not aware (or willing to admit) that they are violating your office policies. Honest communication will often save such relationships. But be sure to make it clear that failure to address the problems you have outlined will result in dismissal from your practice. Document this conversation in detail in the patient’s chart, and follow up with a written communication reconfirming what you discussed.
If, despite your best (documented) efforts, the problems continue and dismissal becomes necessary, following a few generally accepted guidelines will help keep the process smooth and consequence free.
First, try to avoid dismissing a patient in the middle of a course of treatment. If that is unavoidable, you might want to contact your malpractice carrier and review the case with them prior to doing so.
Inform the patient, preferably by certified mail, of your decision. Spell out your reasons, with a reminder that these problems were discussed, and that a warning was issued and not heeded. If the patient belongs to a third-party health plan, be certain that you are acting within the stipulations of your contract with that plan, and inform the payer in writing of your action.
Once again, you must clearly document in the patient’s chart exactly how he or she violated your office policies. This will minimize grounds for charges of discrimination of any sort. Be especially diligent about this step if the patient has any known physical or mental disability.
Give the patient a reasonable amount of time (30 days is common) to find another physician, and mention that you will address any emergent problems within the scope of your specialty within that 30-day period. To minimize any potential allegations of abandonment, include a list of competent physicians in your area (without any guarantees) who might be willing to assume the patient’s care. Alternatively, you can list the phone number or website of a local medical society that they can contact to find a replacement. Offer to transfer medical records to the new physician upon receipt of written permission.
File a copy or scan of the letter, the certified delivery receipt, and the returned signature card in the patient’s chart. While the law states that a first-class letter, properly addressed and stamped, is presumed to have been delivered, you don’t want any question as to whether the patient received written notice of dismissal.
Forcibly ending a physician-patient relationship is a significant event that should not be undertaken lightly. Again, dismissal should be a rare occurrence, a last resort.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
The limits of education
For more than a decade, studies on the dubious value of education in the face of vaccine refusal and hesitancy have been accumulating. But, too often, the research has been ignored by folks who believe that they can teach the “misinformed” into dropping their resistance. Among some circles education ranks right up there with apple pie and motherhood as one of the pillars of Americana. Those wedded to the education mantra may acknowledge that teaching and preaching hasn’t worked well in the past. But, they may claim it’s because we haven’t done enough of it or hit the right buttons. The notion that if we can just share the facts with the uninformed everything will be fine is a myth that obviously is going to die slowly.
In a recent op-ed piece in the New York Times two physicians at Harvard Medical School reported on their study of about three-quarters of a million children who were eligible to receive HPV vaccines (2021 Dec 21. “Facts alone aren’t going to win over the unvaccinated. This might,” Anupam B. Jena and Christopher M. Worsham). The researchers found that children whose mothers had been diagnosed with cervical cancer were no more likely to be immunized than those children whose mothers had not had the disease. Who could be better informed about risks and hazards of contracting HPV than women with cervical cancer? If the facts won’t motivate, where does that leave us?
Those of you born before 1960 may remember or at least have heard about a television show called “Truth or Consequences.” It was a silly farce of a game show which has no bearing on our nation’s crisis of widespread vaccine refusal. However, buried in its title is the answer. If the truth isn’t convincing the resistors, then the obvious choice is consequences.
I hope that you have discovered that same strategy when counseling parents of misbehaving children. Talk is cheap and often ineffective. Explaining the error of his ways to a child who probably already knows what he is doing wrong is a waste of everyone’s time and unpleasant for those within earshot. At some point, sooner better than later, it’s time to say there is going to be a consequence for this misbehavior – going home from the playground, spending a few minutes in time-out, removing a privilege, etc. If consequences are chosen well and instituted with a minimum of idle threats, they work.
And, we are beginning to see it work in the face of pandemic shot refusal. Here in Maine the governor mandated that all health care workers be vaccinated. There was plenty of gnashing of teeth and threats of mass job walk offs. And, there were a few hospital workers who quit, but in the end it worked.
The trick is choosing consequences that have some teeth and make sense. Clearly, some folks who have read about the consequences of not getting vaccinated and may have even lost family members to the disease don’t see those losses as significant consequences for whatever reason. The threat of losing a job is likely to get their attention.
Threats must be carried out even though they may be disruptive in the short term. The good thing about well-crafted mandates is that they can be a win-win for everyone. The vaccine resisters don’t need to admit they were wrong. “Those shots are B.S., but the governor made me do it.” The problem is finding leaders who understand that education has its limits and who have the courage to create and administer the consequences.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
For more than a decade, studies on the dubious value of education in the face of vaccine refusal and hesitancy have been accumulating. But, too often, the research has been ignored by folks who believe that they can teach the “misinformed” into dropping their resistance. Among some circles education ranks right up there with apple pie and motherhood as one of the pillars of Americana. Those wedded to the education mantra may acknowledge that teaching and preaching hasn’t worked well in the past. But, they may claim it’s because we haven’t done enough of it or hit the right buttons. The notion that if we can just share the facts with the uninformed everything will be fine is a myth that obviously is going to die slowly.
In a recent op-ed piece in the New York Times two physicians at Harvard Medical School reported on their study of about three-quarters of a million children who were eligible to receive HPV vaccines (2021 Dec 21. “Facts alone aren’t going to win over the unvaccinated. This might,” Anupam B. Jena and Christopher M. Worsham). The researchers found that children whose mothers had been diagnosed with cervical cancer were no more likely to be immunized than those children whose mothers had not had the disease. Who could be better informed about risks and hazards of contracting HPV than women with cervical cancer? If the facts won’t motivate, where does that leave us?
Those of you born before 1960 may remember or at least have heard about a television show called “Truth or Consequences.” It was a silly farce of a game show which has no bearing on our nation’s crisis of widespread vaccine refusal. However, buried in its title is the answer. If the truth isn’t convincing the resistors, then the obvious choice is consequences.
I hope that you have discovered that same strategy when counseling parents of misbehaving children. Talk is cheap and often ineffective. Explaining the error of his ways to a child who probably already knows what he is doing wrong is a waste of everyone’s time and unpleasant for those within earshot. At some point, sooner better than later, it’s time to say there is going to be a consequence for this misbehavior – going home from the playground, spending a few minutes in time-out, removing a privilege, etc. If consequences are chosen well and instituted with a minimum of idle threats, they work.
And, we are beginning to see it work in the face of pandemic shot refusal. Here in Maine the governor mandated that all health care workers be vaccinated. There was plenty of gnashing of teeth and threats of mass job walk offs. And, there were a few hospital workers who quit, but in the end it worked.
The trick is choosing consequences that have some teeth and make sense. Clearly, some folks who have read about the consequences of not getting vaccinated and may have even lost family members to the disease don’t see those losses as significant consequences for whatever reason. The threat of losing a job is likely to get their attention.
Threats must be carried out even though they may be disruptive in the short term. The good thing about well-crafted mandates is that they can be a win-win for everyone. The vaccine resisters don’t need to admit they were wrong. “Those shots are B.S., but the governor made me do it.” The problem is finding leaders who understand that education has its limits and who have the courage to create and administer the consequences.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
For more than a decade, studies on the dubious value of education in the face of vaccine refusal and hesitancy have been accumulating. But, too often, the research has been ignored by folks who believe that they can teach the “misinformed” into dropping their resistance. Among some circles education ranks right up there with apple pie and motherhood as one of the pillars of Americana. Those wedded to the education mantra may acknowledge that teaching and preaching hasn’t worked well in the past. But, they may claim it’s because we haven’t done enough of it or hit the right buttons. The notion that if we can just share the facts with the uninformed everything will be fine is a myth that obviously is going to die slowly.
In a recent op-ed piece in the New York Times two physicians at Harvard Medical School reported on their study of about three-quarters of a million children who were eligible to receive HPV vaccines (2021 Dec 21. “Facts alone aren’t going to win over the unvaccinated. This might,” Anupam B. Jena and Christopher M. Worsham). The researchers found that children whose mothers had been diagnosed with cervical cancer were no more likely to be immunized than those children whose mothers had not had the disease. Who could be better informed about risks and hazards of contracting HPV than women with cervical cancer? If the facts won’t motivate, where does that leave us?
Those of you born before 1960 may remember or at least have heard about a television show called “Truth or Consequences.” It was a silly farce of a game show which has no bearing on our nation’s crisis of widespread vaccine refusal. However, buried in its title is the answer. If the truth isn’t convincing the resistors, then the obvious choice is consequences.
I hope that you have discovered that same strategy when counseling parents of misbehaving children. Talk is cheap and often ineffective. Explaining the error of his ways to a child who probably already knows what he is doing wrong is a waste of everyone’s time and unpleasant for those within earshot. At some point, sooner better than later, it’s time to say there is going to be a consequence for this misbehavior – going home from the playground, spending a few minutes in time-out, removing a privilege, etc. If consequences are chosen well and instituted with a minimum of idle threats, they work.
And, we are beginning to see it work in the face of pandemic shot refusal. Here in Maine the governor mandated that all health care workers be vaccinated. There was plenty of gnashing of teeth and threats of mass job walk offs. And, there were a few hospital workers who quit, but in the end it worked.
The trick is choosing consequences that have some teeth and make sense. Clearly, some folks who have read about the consequences of not getting vaccinated and may have even lost family members to the disease don’t see those losses as significant consequences for whatever reason. The threat of losing a job is likely to get their attention.
Threats must be carried out even though they may be disruptive in the short term. The good thing about well-crafted mandates is that they can be a win-win for everyone. The vaccine resisters don’t need to admit they were wrong. “Those shots are B.S., but the governor made me do it.” The problem is finding leaders who understand that education has its limits and who have the courage to create and administer the consequences.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
What is the diagnosis?
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition that is becoming more recognized in children. It has a variable presentation, most commonly presenting as painful, recurrent cysts, abscesses, nodules, and/or pustules in classic locations with associated scarring and sinus tract formation.
The majority of patients present with bilateral lesions found most commonly in the axillae and inguinal folds.1 There are myriad other potential sites of involvement including the inframammary folds, inner thighs, buttocks, and groin.1 Diagnosis is made based on history and physical exam. There is a standard severity classification scheme called the Hurley score, which stratifies disease severity based on the presence of sinus tracts and extent of disease.1 HS is associated with comorbid conditions such as obesity, overweight, acne, and inflammatory bowel and joint disease.2 This painful, persistent condition is well documented to have a negative impact on quality of life in adult patients, and similar impairment has been found in pediatric patients.3,4
HS may be increasing in pediatric and adolescent patients, with recent studies showing onset coinciding most commonly with the onset of puberty.1,2 There is often a period of several years between symptom onset and diagnosis.1 A recent editorial highlighted the disparities that exist in HS, with disease more common in Black children and limited information about disease prevalence in Hispanic children.5
What’s the treatment plan?
HS is a difficult disease to treat, with few patients achieving remission and a significant proportion of patients with treatment-refractory disease.1 There are limited studies of HS treatment in pediatric patients. Topical and systemic antibiotic therapy are mainstays of HS treatment, with tetracyclines and a combination of clindamycin plus rifampin commonly used in adults and children alike. Topical therapies including topical antibiotics and antibacterial solutions are frequently used as adjunctive therapy.6 Adalimumab, a tumor necrosis factor receptor blocker, has been Food and Drug Administration approved for HS for ages 12 and up and is currently the only FDA-approved medication for HS in pediatric patients. Our patient was started on 100 mg doxycycline twice daily, with short-dose topical corticosteroids for symptom management of the most inflamed lesions.
What’s on the differential?
Acne conglobata
Acne conglobata is an uncommon, severe variant of acne vulgaris which arise in patients with a history of acne vulgaris and presents with comedones, cysts, abscesses, and scarring with possible drainage of pus. Lesions can present diffusely on the face, back, and body, including in the axillae, groin, and buttocks, and as such can be confused with HS.7
However, in contrast with HS, patients with acne conglobata will also develop disease in non–apocrine gland–bearing skin. This patient’s lack of preceding acne and restriction of lesions to the axillae, inguinal folds, and buttocks makes acne conglobata less likely.
Epidermal inclusion cyst
Epidermal inclusion cyst (EIC) is a common cutaneous cyst, presenting as a well-circumscribed nodule(s) with a central punctum. If not excised, lesions can sometimes become infected and painful.8 In contrast with HS, EIC presents only uncommonly as multiple lesions arising in different areas, and spontaneous drainage is uncommon. Our patient’s development of multiple draining lesions makes this diagnosis unlikely.
Furunculosis
Furunculosis is a common bacterial infection of the skin, presenting with inflammatory nodules or pustules centered around the hair follicle. Lesions may commonly present at sites of skin trauma and are found most frequently on the extremities.9 Though furunculosis lesions may drain pus and can coalesce to form larger “carbuncles,” our patient’s presence of significant scarring and lack of extremity involvement makes HS more likely.
Recurrent MRSA abscesses
Methicillin-resistant Staphylococcus aureus skin and soft-tissue infections are not uncommon in the pediatric population, with presentation of infection ranging from cellulitis to fluid-containing abscesses.10 Recurrent abscesses may be seen in MRSA infection, however in this patient the presence of draining, scarring lesions in multiple locations typical for HS over time is more consistent with a diagnosis of HS.
Dr. Eichenfield is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego, and Rady Children’s Hospital, San Diego. Ms. Appiah is a pediatric dermatology research associate in the division of pediatric and adolescent dermatology at the University of California, San Diego, and Rady Children’s Hospital. Dr. Eichenfield and Ms. Appiah have no relevant financial disclosures.
References
1. Liy-Wong C et al. JAMA Dermatol. 2021;157(4):385-91.
2. Choi E et al. J Am Acad Dermatol. 2022;86(1):140-7.
3. Machado MO et al. JAMA Dermatol. 2019;155(8):939-45.
4. McAndrew R et al. J Am Acad Dermatol. 2021;84(3):829-30.
5. Kirby JS and Zaenglein AL. JAMA Dermatol. 2021;157(4):379-80.
6. Alikhan A et al. J Am Acad Dermatol. 2019;81(1):91-101.
7. Greydanus DE et al. Dis Mon. 2021;67(4):101103.
8. Weir CB, St. Hilaire NJ. Epidermal Inclusion Cyst, in “StatPearls.” Treasure Island, Fla: StatPearls Publishing, 2021.
9. Atanaskova N and Tomecki KJ. Dermatol Clin. 2010;28(3):479-87.
10. Papastefan ST et al. J Surg Res. 2019;242:70-7.
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition that is becoming more recognized in children. It has a variable presentation, most commonly presenting as painful, recurrent cysts, abscesses, nodules, and/or pustules in classic locations with associated scarring and sinus tract formation.
The majority of patients present with bilateral lesions found most commonly in the axillae and inguinal folds.1 There are myriad other potential sites of involvement including the inframammary folds, inner thighs, buttocks, and groin.1 Diagnosis is made based on history and physical exam. There is a standard severity classification scheme called the Hurley score, which stratifies disease severity based on the presence of sinus tracts and extent of disease.1 HS is associated with comorbid conditions such as obesity, overweight, acne, and inflammatory bowel and joint disease.2 This painful, persistent condition is well documented to have a negative impact on quality of life in adult patients, and similar impairment has been found in pediatric patients.3,4
HS may be increasing in pediatric and adolescent patients, with recent studies showing onset coinciding most commonly with the onset of puberty.1,2 There is often a period of several years between symptom onset and diagnosis.1 A recent editorial highlighted the disparities that exist in HS, with disease more common in Black children and limited information about disease prevalence in Hispanic children.5
What’s the treatment plan?
HS is a difficult disease to treat, with few patients achieving remission and a significant proportion of patients with treatment-refractory disease.1 There are limited studies of HS treatment in pediatric patients. Topical and systemic antibiotic therapy are mainstays of HS treatment, with tetracyclines and a combination of clindamycin plus rifampin commonly used in adults and children alike. Topical therapies including topical antibiotics and antibacterial solutions are frequently used as adjunctive therapy.6 Adalimumab, a tumor necrosis factor receptor blocker, has been Food and Drug Administration approved for HS for ages 12 and up and is currently the only FDA-approved medication for HS in pediatric patients. Our patient was started on 100 mg doxycycline twice daily, with short-dose topical corticosteroids for symptom management of the most inflamed lesions.
What’s on the differential?
Acne conglobata
Acne conglobata is an uncommon, severe variant of acne vulgaris which arise in patients with a history of acne vulgaris and presents with comedones, cysts, abscesses, and scarring with possible drainage of pus. Lesions can present diffusely on the face, back, and body, including in the axillae, groin, and buttocks, and as such can be confused with HS.7
However, in contrast with HS, patients with acne conglobata will also develop disease in non–apocrine gland–bearing skin. This patient’s lack of preceding acne and restriction of lesions to the axillae, inguinal folds, and buttocks makes acne conglobata less likely.
Epidermal inclusion cyst
Epidermal inclusion cyst (EIC) is a common cutaneous cyst, presenting as a well-circumscribed nodule(s) with a central punctum. If not excised, lesions can sometimes become infected and painful.8 In contrast with HS, EIC presents only uncommonly as multiple lesions arising in different areas, and spontaneous drainage is uncommon. Our patient’s development of multiple draining lesions makes this diagnosis unlikely.
Furunculosis
Furunculosis is a common bacterial infection of the skin, presenting with inflammatory nodules or pustules centered around the hair follicle. Lesions may commonly present at sites of skin trauma and are found most frequently on the extremities.9 Though furunculosis lesions may drain pus and can coalesce to form larger “carbuncles,” our patient’s presence of significant scarring and lack of extremity involvement makes HS more likely.
Recurrent MRSA abscesses
Methicillin-resistant Staphylococcus aureus skin and soft-tissue infections are not uncommon in the pediatric population, with presentation of infection ranging from cellulitis to fluid-containing abscesses.10 Recurrent abscesses may be seen in MRSA infection, however in this patient the presence of draining, scarring lesions in multiple locations typical for HS over time is more consistent with a diagnosis of HS.
Dr. Eichenfield is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego, and Rady Children’s Hospital, San Diego. Ms. Appiah is a pediatric dermatology research associate in the division of pediatric and adolescent dermatology at the University of California, San Diego, and Rady Children’s Hospital. Dr. Eichenfield and Ms. Appiah have no relevant financial disclosures.
References
1. Liy-Wong C et al. JAMA Dermatol. 2021;157(4):385-91.
2. Choi E et al. J Am Acad Dermatol. 2022;86(1):140-7.
3. Machado MO et al. JAMA Dermatol. 2019;155(8):939-45.
4. McAndrew R et al. J Am Acad Dermatol. 2021;84(3):829-30.
5. Kirby JS and Zaenglein AL. JAMA Dermatol. 2021;157(4):379-80.
6. Alikhan A et al. J Am Acad Dermatol. 2019;81(1):91-101.
7. Greydanus DE et al. Dis Mon. 2021;67(4):101103.
8. Weir CB, St. Hilaire NJ. Epidermal Inclusion Cyst, in “StatPearls.” Treasure Island, Fla: StatPearls Publishing, 2021.
9. Atanaskova N and Tomecki KJ. Dermatol Clin. 2010;28(3):479-87.
10. Papastefan ST et al. J Surg Res. 2019;242:70-7.
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition that is becoming more recognized in children. It has a variable presentation, most commonly presenting as painful, recurrent cysts, abscesses, nodules, and/or pustules in classic locations with associated scarring and sinus tract formation.
The majority of patients present with bilateral lesions found most commonly in the axillae and inguinal folds.1 There are myriad other potential sites of involvement including the inframammary folds, inner thighs, buttocks, and groin.1 Diagnosis is made based on history and physical exam. There is a standard severity classification scheme called the Hurley score, which stratifies disease severity based on the presence of sinus tracts and extent of disease.1 HS is associated with comorbid conditions such as obesity, overweight, acne, and inflammatory bowel and joint disease.2 This painful, persistent condition is well documented to have a negative impact on quality of life in adult patients, and similar impairment has been found in pediatric patients.3,4
HS may be increasing in pediatric and adolescent patients, with recent studies showing onset coinciding most commonly with the onset of puberty.1,2 There is often a period of several years between symptom onset and diagnosis.1 A recent editorial highlighted the disparities that exist in HS, with disease more common in Black children and limited information about disease prevalence in Hispanic children.5
What’s the treatment plan?
HS is a difficult disease to treat, with few patients achieving remission and a significant proportion of patients with treatment-refractory disease.1 There are limited studies of HS treatment in pediatric patients. Topical and systemic antibiotic therapy are mainstays of HS treatment, with tetracyclines and a combination of clindamycin plus rifampin commonly used in adults and children alike. Topical therapies including topical antibiotics and antibacterial solutions are frequently used as adjunctive therapy.6 Adalimumab, a tumor necrosis factor receptor blocker, has been Food and Drug Administration approved for HS for ages 12 and up and is currently the only FDA-approved medication for HS in pediatric patients. Our patient was started on 100 mg doxycycline twice daily, with short-dose topical corticosteroids for symptom management of the most inflamed lesions.
What’s on the differential?
Acne conglobata
Acne conglobata is an uncommon, severe variant of acne vulgaris which arise in patients with a history of acne vulgaris and presents with comedones, cysts, abscesses, and scarring with possible drainage of pus. Lesions can present diffusely on the face, back, and body, including in the axillae, groin, and buttocks, and as such can be confused with HS.7
However, in contrast with HS, patients with acne conglobata will also develop disease in non–apocrine gland–bearing skin. This patient’s lack of preceding acne and restriction of lesions to the axillae, inguinal folds, and buttocks makes acne conglobata less likely.
Epidermal inclusion cyst
Epidermal inclusion cyst (EIC) is a common cutaneous cyst, presenting as a well-circumscribed nodule(s) with a central punctum. If not excised, lesions can sometimes become infected and painful.8 In contrast with HS, EIC presents only uncommonly as multiple lesions arising in different areas, and spontaneous drainage is uncommon. Our patient’s development of multiple draining lesions makes this diagnosis unlikely.
Furunculosis
Furunculosis is a common bacterial infection of the skin, presenting with inflammatory nodules or pustules centered around the hair follicle. Lesions may commonly present at sites of skin trauma and are found most frequently on the extremities.9 Though furunculosis lesions may drain pus and can coalesce to form larger “carbuncles,” our patient’s presence of significant scarring and lack of extremity involvement makes HS more likely.
Recurrent MRSA abscesses
Methicillin-resistant Staphylococcus aureus skin and soft-tissue infections are not uncommon in the pediatric population, with presentation of infection ranging from cellulitis to fluid-containing abscesses.10 Recurrent abscesses may be seen in MRSA infection, however in this patient the presence of draining, scarring lesions in multiple locations typical for HS over time is more consistent with a diagnosis of HS.
Dr. Eichenfield is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego, and Rady Children’s Hospital, San Diego. Ms. Appiah is a pediatric dermatology research associate in the division of pediatric and adolescent dermatology at the University of California, San Diego, and Rady Children’s Hospital. Dr. Eichenfield and Ms. Appiah have no relevant financial disclosures.
References
1. Liy-Wong C et al. JAMA Dermatol. 2021;157(4):385-91.
2. Choi E et al. J Am Acad Dermatol. 2022;86(1):140-7.
3. Machado MO et al. JAMA Dermatol. 2019;155(8):939-45.
4. McAndrew R et al. J Am Acad Dermatol. 2021;84(3):829-30.
5. Kirby JS and Zaenglein AL. JAMA Dermatol. 2021;157(4):379-80.
6. Alikhan A et al. J Am Acad Dermatol. 2019;81(1):91-101.
7. Greydanus DE et al. Dis Mon. 2021;67(4):101103.
8. Weir CB, St. Hilaire NJ. Epidermal Inclusion Cyst, in “StatPearls.” Treasure Island, Fla: StatPearls Publishing, 2021.
9. Atanaskova N and Tomecki KJ. Dermatol Clin. 2010;28(3):479-87.
10. Papastefan ST et al. J Surg Res. 2019;242:70-7.
Physician as trusted counselor
Pediatricians play many roles as they fulfill their duties and responsibilities. Among these is the role of trusted counselor.
A pediatrician is a risk manager. Not the risk manager at a brokerage firm assessing financial risks. Not the hospital lawyer providing legal advice to minimize lawsuits against the hospital. The pediatrician, as risk manager, is a fiduciary, confidant, partner, and guide for parents seeking to protect and maximize the health of their children.
The practice of pediatrics deals with many low-probability, high-impact threats. This begins before birth. The obstetrician has already ordered a litany of prenatal screens, blood tests, and ultrasounds. Many of these have a positive predictive value of less than 20%. That means the alarming positive results are wrong more than 80% of the time. Tests done purportedly to reassure the parents are likely to falsely terrify them. This devilish process continues immediately after birth. The newborns are subjected to a wide variety of screening tests that they must pass before being stamped USDA Prime baby. Early in my career, a thorough newborn physical exam was the key means of identifying problems. Modern medicine employs a wide variety of blood tests, a hearing screen, a pulse ox check, and a transcutaneous bilirubin test before discharge. It is a gauntlet that few escape unscathed. Even the totally normal infant is going to flunk a handful of these screens. Then the nursery doctor is ready to erect additional hoops to jump through. Too big or too small? You need glucose checks. Breech presentation? A hip ultrasound. Too long in labor? Blood tests. Too pale or too ruddy? Blood tests. Not acting quite right? Temperature too high? Temperature too low? Too irritable? Too lethargic? Baby, you’ve hit the jackpot for extra blood tests, an app to estimate the risk of early-onset sepsis, and maybe a trip to the NICU.
Many of these protocols have poor positive predictive value results that are not easy to explain to lay people. The ideas are not easily taught to medical students. Those results can be even harder to communicate to new parents with health care careers. A little knowledge goes a long ways toward long, sleepless nights of worrying even though the baby is just fine. Even cute. Snuggly. A good baby! Parents, hug your baby! Feed the baby! Let the professional do most of the worrying.
What does a professional worrier offer? First, a comprehension of the science. The professional understands sensitivity and specificity, false-positive rates, prevalence, and positive predictive value. Second, particular knowledge of the various tests involved, including the confirmatory tests and the risk-benefit of treatment. Third, experienced clinical judgment that knows that lotteries are bad investments even though two people are splitting a $600 million lottery win this week. Most people don’t emotionally cope with small risks. Fourth, the ability to do values clarification. There is not a one-size-fits-all bedside approach in pediatrics. Parents have differing expectations, differing levels of risk aversion, and different methods for handling anxiety. First-time parents may be very risk intolerant with their baby. Some people deal with fear by seeking more information. Others are looking for evidence that the expert physician is committed to compassionately providing whatever is best for their child.
How has medicine evolved recently? I will highlight four items. First, as described earlier, there has been a large increase in the number of these screens that will be failed. Typical office practice continues the methodology with well child exams and developmental screening. Second, many screens have been introduced that have very low positive predictive value. This leads to many anxious parents who will benefit from pediatricians with the bedside manner to guide the parents and their precious baby through this maze of scientific interventions. The science is difficult enough to master during training. It takes more time to learn the art of counseling parents, listening to their concerns, and earning their trust. That art is practiced in face-to-face encounters with the parents. The classic approach to residency training limits the opportunity to observe and mentor the knowledge, skills, and empathy of a good bedside manner.
A third evolution, more recent, has been the widespread pollution of scientific knowledge with misinformation and disinformation through social media. I addressed that issue in my columns in January and March 2019.
Fourth, most recently, I believe the pandemic has emphasized to the public that nothing in life is totally risk free. Extreme efforts to reduce risk produce unwanted consequences. There is a window of opportunity here to work with parents and patients to build relationships that help people to assess risks and make more rational and beneficial choices. For example, when is the risk of meningitis in a febrile young infant low enough to manage at home? The risk will never be zero. But admission to the hospital “just in case” is not risk free either. People are acutely aware of that right now.
Health care professionals can position themselves as the trusted source of health information specific to a particular person’s situation. Health care professionals can be competent, committed, and compassionate listeners to what really worries people. In this way, we manage risk. This role also involves addressing the mental health crisis causing so much suicide and addiction. Severe problems should be referred to specialists, but I anticipate in the near future that most pediatricians will require more skills dealing with risk and anxiety rather than microbes.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Pediatricians play many roles as they fulfill their duties and responsibilities. Among these is the role of trusted counselor.
A pediatrician is a risk manager. Not the risk manager at a brokerage firm assessing financial risks. Not the hospital lawyer providing legal advice to minimize lawsuits against the hospital. The pediatrician, as risk manager, is a fiduciary, confidant, partner, and guide for parents seeking to protect and maximize the health of their children.
The practice of pediatrics deals with many low-probability, high-impact threats. This begins before birth. The obstetrician has already ordered a litany of prenatal screens, blood tests, and ultrasounds. Many of these have a positive predictive value of less than 20%. That means the alarming positive results are wrong more than 80% of the time. Tests done purportedly to reassure the parents are likely to falsely terrify them. This devilish process continues immediately after birth. The newborns are subjected to a wide variety of screening tests that they must pass before being stamped USDA Prime baby. Early in my career, a thorough newborn physical exam was the key means of identifying problems. Modern medicine employs a wide variety of blood tests, a hearing screen, a pulse ox check, and a transcutaneous bilirubin test before discharge. It is a gauntlet that few escape unscathed. Even the totally normal infant is going to flunk a handful of these screens. Then the nursery doctor is ready to erect additional hoops to jump through. Too big or too small? You need glucose checks. Breech presentation? A hip ultrasound. Too long in labor? Blood tests. Too pale or too ruddy? Blood tests. Not acting quite right? Temperature too high? Temperature too low? Too irritable? Too lethargic? Baby, you’ve hit the jackpot for extra blood tests, an app to estimate the risk of early-onset sepsis, and maybe a trip to the NICU.
Many of these protocols have poor positive predictive value results that are not easy to explain to lay people. The ideas are not easily taught to medical students. Those results can be even harder to communicate to new parents with health care careers. A little knowledge goes a long ways toward long, sleepless nights of worrying even though the baby is just fine. Even cute. Snuggly. A good baby! Parents, hug your baby! Feed the baby! Let the professional do most of the worrying.
What does a professional worrier offer? First, a comprehension of the science. The professional understands sensitivity and specificity, false-positive rates, prevalence, and positive predictive value. Second, particular knowledge of the various tests involved, including the confirmatory tests and the risk-benefit of treatment. Third, experienced clinical judgment that knows that lotteries are bad investments even though two people are splitting a $600 million lottery win this week. Most people don’t emotionally cope with small risks. Fourth, the ability to do values clarification. There is not a one-size-fits-all bedside approach in pediatrics. Parents have differing expectations, differing levels of risk aversion, and different methods for handling anxiety. First-time parents may be very risk intolerant with their baby. Some people deal with fear by seeking more information. Others are looking for evidence that the expert physician is committed to compassionately providing whatever is best for their child.
How has medicine evolved recently? I will highlight four items. First, as described earlier, there has been a large increase in the number of these screens that will be failed. Typical office practice continues the methodology with well child exams and developmental screening. Second, many screens have been introduced that have very low positive predictive value. This leads to many anxious parents who will benefit from pediatricians with the bedside manner to guide the parents and their precious baby through this maze of scientific interventions. The science is difficult enough to master during training. It takes more time to learn the art of counseling parents, listening to their concerns, and earning their trust. That art is practiced in face-to-face encounters with the parents. The classic approach to residency training limits the opportunity to observe and mentor the knowledge, skills, and empathy of a good bedside manner.
A third evolution, more recent, has been the widespread pollution of scientific knowledge with misinformation and disinformation through social media. I addressed that issue in my columns in January and March 2019.
Fourth, most recently, I believe the pandemic has emphasized to the public that nothing in life is totally risk free. Extreme efforts to reduce risk produce unwanted consequences. There is a window of opportunity here to work with parents and patients to build relationships that help people to assess risks and make more rational and beneficial choices. For example, when is the risk of meningitis in a febrile young infant low enough to manage at home? The risk will never be zero. But admission to the hospital “just in case” is not risk free either. People are acutely aware of that right now.
Health care professionals can position themselves as the trusted source of health information specific to a particular person’s situation. Health care professionals can be competent, committed, and compassionate listeners to what really worries people. In this way, we manage risk. This role also involves addressing the mental health crisis causing so much suicide and addiction. Severe problems should be referred to specialists, but I anticipate in the near future that most pediatricians will require more skills dealing with risk and anxiety rather than microbes.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Pediatricians play many roles as they fulfill their duties and responsibilities. Among these is the role of trusted counselor.
A pediatrician is a risk manager. Not the risk manager at a brokerage firm assessing financial risks. Not the hospital lawyer providing legal advice to minimize lawsuits against the hospital. The pediatrician, as risk manager, is a fiduciary, confidant, partner, and guide for parents seeking to protect and maximize the health of their children.
The practice of pediatrics deals with many low-probability, high-impact threats. This begins before birth. The obstetrician has already ordered a litany of prenatal screens, blood tests, and ultrasounds. Many of these have a positive predictive value of less than 20%. That means the alarming positive results are wrong more than 80% of the time. Tests done purportedly to reassure the parents are likely to falsely terrify them. This devilish process continues immediately after birth. The newborns are subjected to a wide variety of screening tests that they must pass before being stamped USDA Prime baby. Early in my career, a thorough newborn physical exam was the key means of identifying problems. Modern medicine employs a wide variety of blood tests, a hearing screen, a pulse ox check, and a transcutaneous bilirubin test before discharge. It is a gauntlet that few escape unscathed. Even the totally normal infant is going to flunk a handful of these screens. Then the nursery doctor is ready to erect additional hoops to jump through. Too big or too small? You need glucose checks. Breech presentation? A hip ultrasound. Too long in labor? Blood tests. Too pale or too ruddy? Blood tests. Not acting quite right? Temperature too high? Temperature too low? Too irritable? Too lethargic? Baby, you’ve hit the jackpot for extra blood tests, an app to estimate the risk of early-onset sepsis, and maybe a trip to the NICU.
Many of these protocols have poor positive predictive value results that are not easy to explain to lay people. The ideas are not easily taught to medical students. Those results can be even harder to communicate to new parents with health care careers. A little knowledge goes a long ways toward long, sleepless nights of worrying even though the baby is just fine. Even cute. Snuggly. A good baby! Parents, hug your baby! Feed the baby! Let the professional do most of the worrying.
What does a professional worrier offer? First, a comprehension of the science. The professional understands sensitivity and specificity, false-positive rates, prevalence, and positive predictive value. Second, particular knowledge of the various tests involved, including the confirmatory tests and the risk-benefit of treatment. Third, experienced clinical judgment that knows that lotteries are bad investments even though two people are splitting a $600 million lottery win this week. Most people don’t emotionally cope with small risks. Fourth, the ability to do values clarification. There is not a one-size-fits-all bedside approach in pediatrics. Parents have differing expectations, differing levels of risk aversion, and different methods for handling anxiety. First-time parents may be very risk intolerant with their baby. Some people deal with fear by seeking more information. Others are looking for evidence that the expert physician is committed to compassionately providing whatever is best for their child.
How has medicine evolved recently? I will highlight four items. First, as described earlier, there has been a large increase in the number of these screens that will be failed. Typical office practice continues the methodology with well child exams and developmental screening. Second, many screens have been introduced that have very low positive predictive value. This leads to many anxious parents who will benefit from pediatricians with the bedside manner to guide the parents and their precious baby through this maze of scientific interventions. The science is difficult enough to master during training. It takes more time to learn the art of counseling parents, listening to their concerns, and earning their trust. That art is practiced in face-to-face encounters with the parents. The classic approach to residency training limits the opportunity to observe and mentor the knowledge, skills, and empathy of a good bedside manner.
A third evolution, more recent, has been the widespread pollution of scientific knowledge with misinformation and disinformation through social media. I addressed that issue in my columns in January and March 2019.
Fourth, most recently, I believe the pandemic has emphasized to the public that nothing in life is totally risk free. Extreme efforts to reduce risk produce unwanted consequences. There is a window of opportunity here to work with parents and patients to build relationships that help people to assess risks and make more rational and beneficial choices. For example, when is the risk of meningitis in a febrile young infant low enough to manage at home? The risk will never be zero. But admission to the hospital “just in case” is not risk free either. People are acutely aware of that right now.
Health care professionals can position themselves as the trusted source of health information specific to a particular person’s situation. Health care professionals can be competent, committed, and compassionate listeners to what really worries people. In this way, we manage risk. This role also involves addressing the mental health crisis causing so much suicide and addiction. Severe problems should be referred to specialists, but I anticipate in the near future that most pediatricians will require more skills dealing with risk and anxiety rather than microbes.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Pediatric depression and parents
In October of 2021, the American Academy of Child and Adolescent Psychiatry, the American Academy of Pediatrics, and the Children’s Hospital Association jointly declared a National State of Emergency in Children’s Mental Health and called on policy makers to address a host of challenges that have impeded access to effective mental health care for youth.
In November, we wrote about how pediatricians may increase their use of screening for adolescent depression and initiate treatment when appropriate.
Now we complement that piece with guidance you may offer the parents of your depressed adolescent patients. Adolescent depression is a common pediatric disorder, especially in the COVID-19 era when so many relationships and activities have been limited or cut off. With treatment, most adolescents recover. Accepting that it may be taking longer to find a therapist, you can make treatment recommendations, support the teenager and parents, address safety concerns and, if the depression is of moderate or more serious severity, start medications. Parents are your natural partners as they are concerned about their children’s health and safety and eager for guidance on how to best support their recovery.
Adolescence is a time in which parents transition to more of a consulting than a controlling posture with their children, but illness calls for a shift toward setting rules and routines that will support health and healing. Prepare both the teenager (in a 1:1 discussion) and parents for this temporary shift, and for some teenagers, expect resistance. Depression will make the teenager more unhappy and irritable. It also causes withdrawal, by sapping energy and making one feel unwelcome at activities, believing his or her presence will be a burden to others. Treatment includes something called “behavioral activation,” or continuous nudging, to keep the patient involved in social, intellectual, and physical activities. Parents (and siblings) are the keys to this behavioral activation, whether nudging to participate in a board game or a walk. Reassure parents they should not take it personally when their teen resists, and not be discouraged if they fail sometimes. Their focus is on calmly, warmly, and repeatedly prompting their children with nudges toward these routines and activities. They should be ready to remind them why they are “nagging,” framing these efforts explicitly as supporting recovery from depression. If possible, applying these rules to everyone at home will help. They need to avoid being drawn into conflict, focusing instead on staying connected to their teens. Their task is to keep planning and cajoling, giving their children multiple opportunities to participate, pushing back against depression’s gravitational pull for total withdrawal.
Sleep
One of the most important thing parents can do for their depressed adolescents is to support their healthy restful sleep. During adolescence, the timing of sleep naturally shifts later, and the need for restful sleep increases. Working against the demands of homework, extracurricular activities, and social connections, sleep often suffers during adolescence. Further sleep disruptions, including difficulty falling asleep and frequent awakening during sleep or in the early morning, are typical of depression. Restful sleep is instrumental to recovery, and parents need to help their depressed teens set good sleep habits. This includes setting a time for bed that is realistic and consistent and turning off screens 30 minutes before lights out. A soothing, consistent bedtime routine, including a hot shower and reading in bed, is a powerful cue for sleep. Getting daily exercise and avoiding a heavy meal and caffeine in the hours before bed supports both falling and staying asleep. Having light reading near bed (magazines or comics) instead of screens can provide a way to pass 30 minutes if they wake up during the night (ideally reading out of bed), one that will not make it harder for them to go back to sleep. Finally, teens should not be allowed to spend all day in bed or nap in the afternoon. This may be the hardest task for parents, as adolescents naturally treat their beds like their center of operations and depression lowers their energy and initiative. If parents set these rules and routines for all members of the family, it can improve the chances that their depressed adolescents may begin to return to healthy sleep.
Exercise
Vigorous exercise (for 20 minutes three times weekly) is as effective as SSRIs in treating mild to moderate depression. Even in severe depression, exercise may accelerate recovery and certainly contributes to returning to restful sleep and a feeling of improved energy. Inviting their depressed teens to join them on a trip to the gym may seem like a fool’s errand to parents, but they should prioritize getting their children moving. Don’t offer choices or ask what activity they would like to do. Most invitations will be met with “no, thanks” (or probably something less polite). Instead, initiate simple activities and then cajole the children with “let’s go!” They should use loving persistence to get them out the door. Parents are the experts on their children and will know if there is an activity that they are more likely to enjoy. Make any activities group ones, easy to start and not too long. They could initiate family walks or bike rides in their neighborhood. If it helps, they can blame you, “these are doctor’s orders!” This approach of warm persistence should be applied across the board, helping their depressed teens participate in mealtimes and other activities. Prepare parents that this can feel unnatural, if they have been letting their healthy teenagers have more space and independence and less time in family activities.
Social connections
Behavioral activation includes keeping a depressed teen engaged in social activities. Friendships are a potent motivator in the lives of healthy adolescents. If depressed teens can stay connected to close friends, it is a powerful force for recovery. Find out if their friends know about their depression, whom do they trust to tell about it? Help them find comfortable language to speak about their depression with trusted friends. Parents can use their behavioral activation strategies to prompt their teenagers to participate in social activities. If texting, video chatting, or social media platforms are how they stay connected with close friends, support their use of these platforms. But be mindful that social media promotes social comparison over connection, and depression sets them up to feel less than others even without assistance. Parents should support real time with their friends in small groups, for short periods during the time of day when they have the most energy.
Safety
Suicide is the second leading cause of death for adolescents in the United States, and the rate of attempted and completed suicide in adolescents has been steadily climbing over the past decade according to the CDC. The rate is higher in older adolescents, though thankfully relatively uncommon (about 1 in 10,000 a year), and, although we know risk factors, no one has been able to predict reliably the risk for an individual teenager at a point in time. In a clinically referred sample, 85% of depressed adolescents will have suicidal ideation and 32% will make a suicide attempt. The risk is higher in those adolescents with more than one psychiatric diagnosis and with a history of impulsive behaviors, substance abuse, prior suicide attempts, and a family history of suicide. It is important that parents hear that asking about suicidal thoughts will not cause them. On the contrary, preserving open communication and a warm relationship is very protective. Adolescent suicide attempts are likely to be impulsive, so helping the family to consider ways to “put up obstacles” that would slow down any possible attempt is an effective way to improve safety. Ask your patients about suicidal thoughts, plans, and what keeps them safe. Find out if they worry about sharing these thoughts with their parents and why. Ask if there are ways their parents can check on them that “aren’t too annoying.” Determine if there are guns in the home, and if so, are they safely stored (locked, separate from ammunition)? More than 50% of completed adolescent suicides involve firearms, so this question is critical. What about access to medications that could be dangerous in overdose in your home or a relative’s home they may visit? Discussing these facts with your patients and their parents together will make it easier for them to continue the conversation outside of your office and can make an enormous difference in their recovery.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
Reference
Kovacs M et al. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):8-20.
In October of 2021, the American Academy of Child and Adolescent Psychiatry, the American Academy of Pediatrics, and the Children’s Hospital Association jointly declared a National State of Emergency in Children’s Mental Health and called on policy makers to address a host of challenges that have impeded access to effective mental health care for youth.
In November, we wrote about how pediatricians may increase their use of screening for adolescent depression and initiate treatment when appropriate.
Now we complement that piece with guidance you may offer the parents of your depressed adolescent patients. Adolescent depression is a common pediatric disorder, especially in the COVID-19 era when so many relationships and activities have been limited or cut off. With treatment, most adolescents recover. Accepting that it may be taking longer to find a therapist, you can make treatment recommendations, support the teenager and parents, address safety concerns and, if the depression is of moderate or more serious severity, start medications. Parents are your natural partners as they are concerned about their children’s health and safety and eager for guidance on how to best support their recovery.
Adolescence is a time in which parents transition to more of a consulting than a controlling posture with their children, but illness calls for a shift toward setting rules and routines that will support health and healing. Prepare both the teenager (in a 1:1 discussion) and parents for this temporary shift, and for some teenagers, expect resistance. Depression will make the teenager more unhappy and irritable. It also causes withdrawal, by sapping energy and making one feel unwelcome at activities, believing his or her presence will be a burden to others. Treatment includes something called “behavioral activation,” or continuous nudging, to keep the patient involved in social, intellectual, and physical activities. Parents (and siblings) are the keys to this behavioral activation, whether nudging to participate in a board game or a walk. Reassure parents they should not take it personally when their teen resists, and not be discouraged if they fail sometimes. Their focus is on calmly, warmly, and repeatedly prompting their children with nudges toward these routines and activities. They should be ready to remind them why they are “nagging,” framing these efforts explicitly as supporting recovery from depression. If possible, applying these rules to everyone at home will help. They need to avoid being drawn into conflict, focusing instead on staying connected to their teens. Their task is to keep planning and cajoling, giving their children multiple opportunities to participate, pushing back against depression’s gravitational pull for total withdrawal.
Sleep
One of the most important thing parents can do for their depressed adolescents is to support their healthy restful sleep. During adolescence, the timing of sleep naturally shifts later, and the need for restful sleep increases. Working against the demands of homework, extracurricular activities, and social connections, sleep often suffers during adolescence. Further sleep disruptions, including difficulty falling asleep and frequent awakening during sleep or in the early morning, are typical of depression. Restful sleep is instrumental to recovery, and parents need to help their depressed teens set good sleep habits. This includes setting a time for bed that is realistic and consistent and turning off screens 30 minutes before lights out. A soothing, consistent bedtime routine, including a hot shower and reading in bed, is a powerful cue for sleep. Getting daily exercise and avoiding a heavy meal and caffeine in the hours before bed supports both falling and staying asleep. Having light reading near bed (magazines or comics) instead of screens can provide a way to pass 30 minutes if they wake up during the night (ideally reading out of bed), one that will not make it harder for them to go back to sleep. Finally, teens should not be allowed to spend all day in bed or nap in the afternoon. This may be the hardest task for parents, as adolescents naturally treat their beds like their center of operations and depression lowers their energy and initiative. If parents set these rules and routines for all members of the family, it can improve the chances that their depressed adolescents may begin to return to healthy sleep.
Exercise
Vigorous exercise (for 20 minutes three times weekly) is as effective as SSRIs in treating mild to moderate depression. Even in severe depression, exercise may accelerate recovery and certainly contributes to returning to restful sleep and a feeling of improved energy. Inviting their depressed teens to join them on a trip to the gym may seem like a fool’s errand to parents, but they should prioritize getting their children moving. Don’t offer choices or ask what activity they would like to do. Most invitations will be met with “no, thanks” (or probably something less polite). Instead, initiate simple activities and then cajole the children with “let’s go!” They should use loving persistence to get them out the door. Parents are the experts on their children and will know if there is an activity that they are more likely to enjoy. Make any activities group ones, easy to start and not too long. They could initiate family walks or bike rides in their neighborhood. If it helps, they can blame you, “these are doctor’s orders!” This approach of warm persistence should be applied across the board, helping their depressed teens participate in mealtimes and other activities. Prepare parents that this can feel unnatural, if they have been letting their healthy teenagers have more space and independence and less time in family activities.
Social connections
Behavioral activation includes keeping a depressed teen engaged in social activities. Friendships are a potent motivator in the lives of healthy adolescents. If depressed teens can stay connected to close friends, it is a powerful force for recovery. Find out if their friends know about their depression, whom do they trust to tell about it? Help them find comfortable language to speak about their depression with trusted friends. Parents can use their behavioral activation strategies to prompt their teenagers to participate in social activities. If texting, video chatting, or social media platforms are how they stay connected with close friends, support their use of these platforms. But be mindful that social media promotes social comparison over connection, and depression sets them up to feel less than others even without assistance. Parents should support real time with their friends in small groups, for short periods during the time of day when they have the most energy.
Safety
Suicide is the second leading cause of death for adolescents in the United States, and the rate of attempted and completed suicide in adolescents has been steadily climbing over the past decade according to the CDC. The rate is higher in older adolescents, though thankfully relatively uncommon (about 1 in 10,000 a year), and, although we know risk factors, no one has been able to predict reliably the risk for an individual teenager at a point in time. In a clinically referred sample, 85% of depressed adolescents will have suicidal ideation and 32% will make a suicide attempt. The risk is higher in those adolescents with more than one psychiatric diagnosis and with a history of impulsive behaviors, substance abuse, prior suicide attempts, and a family history of suicide. It is important that parents hear that asking about suicidal thoughts will not cause them. On the contrary, preserving open communication and a warm relationship is very protective. Adolescent suicide attempts are likely to be impulsive, so helping the family to consider ways to “put up obstacles” that would slow down any possible attempt is an effective way to improve safety. Ask your patients about suicidal thoughts, plans, and what keeps them safe. Find out if they worry about sharing these thoughts with their parents and why. Ask if there are ways their parents can check on them that “aren’t too annoying.” Determine if there are guns in the home, and if so, are they safely stored (locked, separate from ammunition)? More than 50% of completed adolescent suicides involve firearms, so this question is critical. What about access to medications that could be dangerous in overdose in your home or a relative’s home they may visit? Discussing these facts with your patients and their parents together will make it easier for them to continue the conversation outside of your office and can make an enormous difference in their recovery.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
Reference
Kovacs M et al. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):8-20.
In October of 2021, the American Academy of Child and Adolescent Psychiatry, the American Academy of Pediatrics, and the Children’s Hospital Association jointly declared a National State of Emergency in Children’s Mental Health and called on policy makers to address a host of challenges that have impeded access to effective mental health care for youth.
In November, we wrote about how pediatricians may increase their use of screening for adolescent depression and initiate treatment when appropriate.
Now we complement that piece with guidance you may offer the parents of your depressed adolescent patients. Adolescent depression is a common pediatric disorder, especially in the COVID-19 era when so many relationships and activities have been limited or cut off. With treatment, most adolescents recover. Accepting that it may be taking longer to find a therapist, you can make treatment recommendations, support the teenager and parents, address safety concerns and, if the depression is of moderate or more serious severity, start medications. Parents are your natural partners as they are concerned about their children’s health and safety and eager for guidance on how to best support their recovery.
Adolescence is a time in which parents transition to more of a consulting than a controlling posture with their children, but illness calls for a shift toward setting rules and routines that will support health and healing. Prepare both the teenager (in a 1:1 discussion) and parents for this temporary shift, and for some teenagers, expect resistance. Depression will make the teenager more unhappy and irritable. It also causes withdrawal, by sapping energy and making one feel unwelcome at activities, believing his or her presence will be a burden to others. Treatment includes something called “behavioral activation,” or continuous nudging, to keep the patient involved in social, intellectual, and physical activities. Parents (and siblings) are the keys to this behavioral activation, whether nudging to participate in a board game or a walk. Reassure parents they should not take it personally when their teen resists, and not be discouraged if they fail sometimes. Their focus is on calmly, warmly, and repeatedly prompting their children with nudges toward these routines and activities. They should be ready to remind them why they are “nagging,” framing these efforts explicitly as supporting recovery from depression. If possible, applying these rules to everyone at home will help. They need to avoid being drawn into conflict, focusing instead on staying connected to their teens. Their task is to keep planning and cajoling, giving their children multiple opportunities to participate, pushing back against depression’s gravitational pull for total withdrawal.
Sleep
One of the most important thing parents can do for their depressed adolescents is to support their healthy restful sleep. During adolescence, the timing of sleep naturally shifts later, and the need for restful sleep increases. Working against the demands of homework, extracurricular activities, and social connections, sleep often suffers during adolescence. Further sleep disruptions, including difficulty falling asleep and frequent awakening during sleep or in the early morning, are typical of depression. Restful sleep is instrumental to recovery, and parents need to help their depressed teens set good sleep habits. This includes setting a time for bed that is realistic and consistent and turning off screens 30 minutes before lights out. A soothing, consistent bedtime routine, including a hot shower and reading in bed, is a powerful cue for sleep. Getting daily exercise and avoiding a heavy meal and caffeine in the hours before bed supports both falling and staying asleep. Having light reading near bed (magazines or comics) instead of screens can provide a way to pass 30 minutes if they wake up during the night (ideally reading out of bed), one that will not make it harder for them to go back to sleep. Finally, teens should not be allowed to spend all day in bed or nap in the afternoon. This may be the hardest task for parents, as adolescents naturally treat their beds like their center of operations and depression lowers their energy and initiative. If parents set these rules and routines for all members of the family, it can improve the chances that their depressed adolescents may begin to return to healthy sleep.
Exercise
Vigorous exercise (for 20 minutes three times weekly) is as effective as SSRIs in treating mild to moderate depression. Even in severe depression, exercise may accelerate recovery and certainly contributes to returning to restful sleep and a feeling of improved energy. Inviting their depressed teens to join them on a trip to the gym may seem like a fool’s errand to parents, but they should prioritize getting their children moving. Don’t offer choices or ask what activity they would like to do. Most invitations will be met with “no, thanks” (or probably something less polite). Instead, initiate simple activities and then cajole the children with “let’s go!” They should use loving persistence to get them out the door. Parents are the experts on their children and will know if there is an activity that they are more likely to enjoy. Make any activities group ones, easy to start and not too long. They could initiate family walks or bike rides in their neighborhood. If it helps, they can blame you, “these are doctor’s orders!” This approach of warm persistence should be applied across the board, helping their depressed teens participate in mealtimes and other activities. Prepare parents that this can feel unnatural, if they have been letting their healthy teenagers have more space and independence and less time in family activities.
Social connections
Behavioral activation includes keeping a depressed teen engaged in social activities. Friendships are a potent motivator in the lives of healthy adolescents. If depressed teens can stay connected to close friends, it is a powerful force for recovery. Find out if their friends know about their depression, whom do they trust to tell about it? Help them find comfortable language to speak about their depression with trusted friends. Parents can use their behavioral activation strategies to prompt their teenagers to participate in social activities. If texting, video chatting, or social media platforms are how they stay connected with close friends, support their use of these platforms. But be mindful that social media promotes social comparison over connection, and depression sets them up to feel less than others even without assistance. Parents should support real time with their friends in small groups, for short periods during the time of day when they have the most energy.
Safety
Suicide is the second leading cause of death for adolescents in the United States, and the rate of attempted and completed suicide in adolescents has been steadily climbing over the past decade according to the CDC. The rate is higher in older adolescents, though thankfully relatively uncommon (about 1 in 10,000 a year), and, although we know risk factors, no one has been able to predict reliably the risk for an individual teenager at a point in time. In a clinically referred sample, 85% of depressed adolescents will have suicidal ideation and 32% will make a suicide attempt. The risk is higher in those adolescents with more than one psychiatric diagnosis and with a history of impulsive behaviors, substance abuse, prior suicide attempts, and a family history of suicide. It is important that parents hear that asking about suicidal thoughts will not cause them. On the contrary, preserving open communication and a warm relationship is very protective. Adolescent suicide attempts are likely to be impulsive, so helping the family to consider ways to “put up obstacles” that would slow down any possible attempt is an effective way to improve safety. Ask your patients about suicidal thoughts, plans, and what keeps them safe. Find out if they worry about sharing these thoughts with their parents and why. Ask if there are ways their parents can check on them that “aren’t too annoying.” Determine if there are guns in the home, and if so, are they safely stored (locked, separate from ammunition)? More than 50% of completed adolescent suicides involve firearms, so this question is critical. What about access to medications that could be dangerous in overdose in your home or a relative’s home they may visit? Discussing these facts with your patients and their parents together will make it easier for them to continue the conversation outside of your office and can make an enormous difference in their recovery.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
Reference
Kovacs M et al. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):8-20.
The etiology of acute otitis media in young children in recent years
Since the COVID-19 pandemic began, pediatricians have been seeing fewer cases of all respiratory illnesses, including acute otitis media (AOM). However, as I prepare this column, an uptick has commenced and likely will continue in an upward trajectory as we emerge from the pandemic into an endemic coronavirus era. Our group in Rochester, N.Y., has continued prospective studies of AOM throughout the pandemic. We found that nasopharyngeal colonization by Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae, and Moraxella catarrhalis remained prevalent in our study cohort of children aged 6-36 months. However, with all the precautions of masking, social distancing, hand washing, and quick exclusion from day care when illness occurred, the frequency of detecting these common otopathogens decreased, as one might expect.1
Leading up to the pandemic, we had an abundance of data to characterize AOM etiology and found that the cause of AOM continues to change following the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar 13). Our most recent report on otopathogen distribution and antibiotic susceptibility covered the years 2015-2019.2 A total of 589 children were enrolled prospectively and we collected 495 middle ear fluid samples (MEF) from 319 AOM cases using tympanocentesis. The frequency of isolates was H. influenzae (34%), pneumococcus (24%), and M. catarrhalis (15%). Beta-lactamase–positive H. influenzae strains were identified among 49% of the isolates, rendering them resistant to amoxicillin. PCV13 serotypes were infrequently isolated. However, we did isolate vaccine types (VTs) in some children from MEF, notably serotypes 19F, 19A, and 3. Non-PCV13 pneumococcus serotypes 35B, 23B, and 15B/C emerged as the most common serotypes. Amoxicillin resistance was identified among 25% of pneumococcal strains. Out of 16 antibiotics tested, 9 (56%) showed a significant increase in nonsusceptibility among pneumococcal isolates. 100% of M. catarrhalis isolates were beta-lactamase producers and therefore resistant to amoxicillin.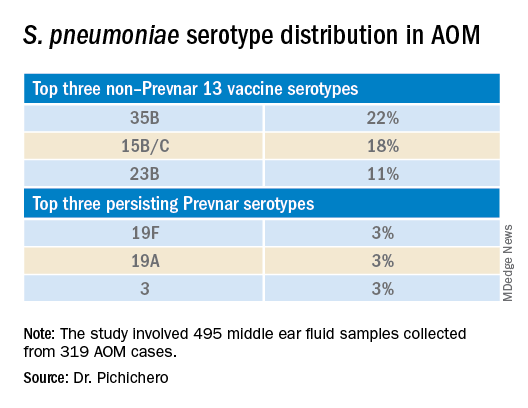
PCV13 has resulted in a decline in both invasive and noninvasive pneumococcal infections caused by strains expressing the 13 capsular serotypes included in the vaccine. However, the emergence of replacement serotypes occurred after introduction of PCV73,4 and continues to occur during the PCV13 era, as shown from the results presented here. Non-PCV13 serotypes accounted for more than 90% of MEF isolates during 2015-2019, with 35B, 21 and 23B being the most commonly isolated. Other emergent serotypes of potential importance were nonvaccine serotypes 15A, 15B, 15C, 23A and 11A. This is highly relevant because forthcoming higher-valency PCVs – PCV15 (manufactured by Merck) and PCV20 (manufactured by Pfizer) will not include many of the dominant capsular serotypes of pneumococcus strains causing AOM. Consequently, the impact of higher-valency PCVs on AOM will not be as great as was observed with the introduction of PCV7 or PCV13.
Of special interest, 22% of pneumococcus isolates from MEF were serotype 35B, making it the most prevalent. Recently we reported a significant rise in antibiotic nonsusceptibility in Spn isolates, contributed mainly by serotype 35B5 and we have been studying how 35B strains transitioned from commensal to otopathogen in children.6 Because serotype 35B strains are increasingly prevalent and often antibiotic resistant, absence of this serotype from PCV15 and PCV20 is cause for concern.
The frequency of isolation of H. influenzae and M. catarrhalis has remained stable across the PCV13 era as the No. 1 and No. 3 pathogens. Similarly, the production of beta-lactamase among strains causing AOM has remained stable at close to 50% and 100%, respectively. Use of amoxicillin, either high dose or standard dose, would not be expected to kill these bacteria.
Our study design has limitations. The population is derived from a predominantly middle-class, suburban population of children in upstate New York and may not be representative of other types of populations in the United States. The children are 6-36 months old, the age when most AOM occurs. MEF samples that were culture negative for bacteria were not further tested by polymerase chain reaction methods.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Kaur R et al. Front Pediatr. 2021;9:722483.
2. Kaur R et al. Euro J Clin Microbiol Infect Dis. 2021;41:37-44
3. Pelton SI et al. Pediatr Infect Disease J. 2004;23:1015-22.
4. Farrell DJ et al. Pediatr Infect Disease J. 2007;26:123-8..
5. Kaur R et al. Clin Infect Dis 2021;72(5):797-805.
6. Fuji N et al. Front Cell Infect Microbiol. 2021;11:744742.
Since the COVID-19 pandemic began, pediatricians have been seeing fewer cases of all respiratory illnesses, including acute otitis media (AOM). However, as I prepare this column, an uptick has commenced and likely will continue in an upward trajectory as we emerge from the pandemic into an endemic coronavirus era. Our group in Rochester, N.Y., has continued prospective studies of AOM throughout the pandemic. We found that nasopharyngeal colonization by Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae, and Moraxella catarrhalis remained prevalent in our study cohort of children aged 6-36 months. However, with all the precautions of masking, social distancing, hand washing, and quick exclusion from day care when illness occurred, the frequency of detecting these common otopathogens decreased, as one might expect.1
Leading up to the pandemic, we had an abundance of data to characterize AOM etiology and found that the cause of AOM continues to change following the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar 13). Our most recent report on otopathogen distribution and antibiotic susceptibility covered the years 2015-2019.2 A total of 589 children were enrolled prospectively and we collected 495 middle ear fluid samples (MEF) from 319 AOM cases using tympanocentesis. The frequency of isolates was H. influenzae (34%), pneumococcus (24%), and M. catarrhalis (15%). Beta-lactamase–positive H. influenzae strains were identified among 49% of the isolates, rendering them resistant to amoxicillin. PCV13 serotypes were infrequently isolated. However, we did isolate vaccine types (VTs) in some children from MEF, notably serotypes 19F, 19A, and 3. Non-PCV13 pneumococcus serotypes 35B, 23B, and 15B/C emerged as the most common serotypes. Amoxicillin resistance was identified among 25% of pneumococcal strains. Out of 16 antibiotics tested, 9 (56%) showed a significant increase in nonsusceptibility among pneumococcal isolates. 100% of M. catarrhalis isolates were beta-lactamase producers and therefore resistant to amoxicillin.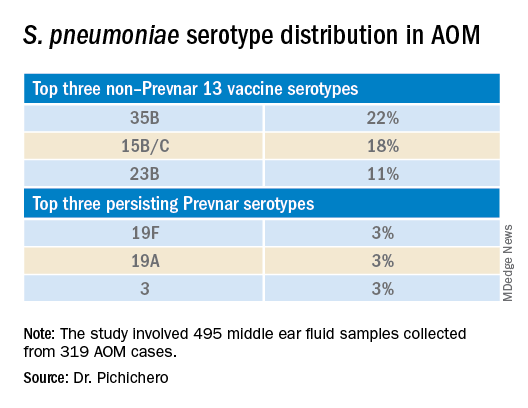
PCV13 has resulted in a decline in both invasive and noninvasive pneumococcal infections caused by strains expressing the 13 capsular serotypes included in the vaccine. However, the emergence of replacement serotypes occurred after introduction of PCV73,4 and continues to occur during the PCV13 era, as shown from the results presented here. Non-PCV13 serotypes accounted for more than 90% of MEF isolates during 2015-2019, with 35B, 21 and 23B being the most commonly isolated. Other emergent serotypes of potential importance were nonvaccine serotypes 15A, 15B, 15C, 23A and 11A. This is highly relevant because forthcoming higher-valency PCVs – PCV15 (manufactured by Merck) and PCV20 (manufactured by Pfizer) will not include many of the dominant capsular serotypes of pneumococcus strains causing AOM. Consequently, the impact of higher-valency PCVs on AOM will not be as great as was observed with the introduction of PCV7 or PCV13.
Of special interest, 22% of pneumococcus isolates from MEF were serotype 35B, making it the most prevalent. Recently we reported a significant rise in antibiotic nonsusceptibility in Spn isolates, contributed mainly by serotype 35B5 and we have been studying how 35B strains transitioned from commensal to otopathogen in children.6 Because serotype 35B strains are increasingly prevalent and often antibiotic resistant, absence of this serotype from PCV15 and PCV20 is cause for concern.
The frequency of isolation of H. influenzae and M. catarrhalis has remained stable across the PCV13 era as the No. 1 and No. 3 pathogens. Similarly, the production of beta-lactamase among strains causing AOM has remained stable at close to 50% and 100%, respectively. Use of amoxicillin, either high dose or standard dose, would not be expected to kill these bacteria.
Our study design has limitations. The population is derived from a predominantly middle-class, suburban population of children in upstate New York and may not be representative of other types of populations in the United States. The children are 6-36 months old, the age when most AOM occurs. MEF samples that were culture negative for bacteria were not further tested by polymerase chain reaction methods.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Kaur R et al. Front Pediatr. 2021;9:722483.
2. Kaur R et al. Euro J Clin Microbiol Infect Dis. 2021;41:37-44
3. Pelton SI et al. Pediatr Infect Disease J. 2004;23:1015-22.
4. Farrell DJ et al. Pediatr Infect Disease J. 2007;26:123-8..
5. Kaur R et al. Clin Infect Dis 2021;72(5):797-805.
6. Fuji N et al. Front Cell Infect Microbiol. 2021;11:744742.
Since the COVID-19 pandemic began, pediatricians have been seeing fewer cases of all respiratory illnesses, including acute otitis media (AOM). However, as I prepare this column, an uptick has commenced and likely will continue in an upward trajectory as we emerge from the pandemic into an endemic coronavirus era. Our group in Rochester, N.Y., has continued prospective studies of AOM throughout the pandemic. We found that nasopharyngeal colonization by Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae, and Moraxella catarrhalis remained prevalent in our study cohort of children aged 6-36 months. However, with all the precautions of masking, social distancing, hand washing, and quick exclusion from day care when illness occurred, the frequency of detecting these common otopathogens decreased, as one might expect.1
Leading up to the pandemic, we had an abundance of data to characterize AOM etiology and found that the cause of AOM continues to change following the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar 13). Our most recent report on otopathogen distribution and antibiotic susceptibility covered the years 2015-2019.2 A total of 589 children were enrolled prospectively and we collected 495 middle ear fluid samples (MEF) from 319 AOM cases using tympanocentesis. The frequency of isolates was H. influenzae (34%), pneumococcus (24%), and M. catarrhalis (15%). Beta-lactamase–positive H. influenzae strains were identified among 49% of the isolates, rendering them resistant to amoxicillin. PCV13 serotypes were infrequently isolated. However, we did isolate vaccine types (VTs) in some children from MEF, notably serotypes 19F, 19A, and 3. Non-PCV13 pneumococcus serotypes 35B, 23B, and 15B/C emerged as the most common serotypes. Amoxicillin resistance was identified among 25% of pneumococcal strains. Out of 16 antibiotics tested, 9 (56%) showed a significant increase in nonsusceptibility among pneumococcal isolates. 100% of M. catarrhalis isolates were beta-lactamase producers and therefore resistant to amoxicillin.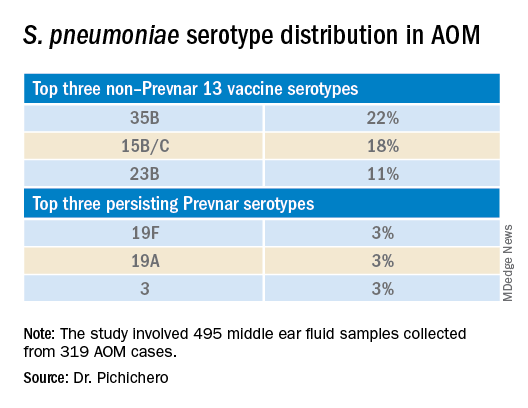
PCV13 has resulted in a decline in both invasive and noninvasive pneumococcal infections caused by strains expressing the 13 capsular serotypes included in the vaccine. However, the emergence of replacement serotypes occurred after introduction of PCV73,4 and continues to occur during the PCV13 era, as shown from the results presented here. Non-PCV13 serotypes accounted for more than 90% of MEF isolates during 2015-2019, with 35B, 21 and 23B being the most commonly isolated. Other emergent serotypes of potential importance were nonvaccine serotypes 15A, 15B, 15C, 23A and 11A. This is highly relevant because forthcoming higher-valency PCVs – PCV15 (manufactured by Merck) and PCV20 (manufactured by Pfizer) will not include many of the dominant capsular serotypes of pneumococcus strains causing AOM. Consequently, the impact of higher-valency PCVs on AOM will not be as great as was observed with the introduction of PCV7 or PCV13.
Of special interest, 22% of pneumococcus isolates from MEF were serotype 35B, making it the most prevalent. Recently we reported a significant rise in antibiotic nonsusceptibility in Spn isolates, contributed mainly by serotype 35B5 and we have been studying how 35B strains transitioned from commensal to otopathogen in children.6 Because serotype 35B strains are increasingly prevalent and often antibiotic resistant, absence of this serotype from PCV15 and PCV20 is cause for concern.
The frequency of isolation of H. influenzae and M. catarrhalis has remained stable across the PCV13 era as the No. 1 and No. 3 pathogens. Similarly, the production of beta-lactamase among strains causing AOM has remained stable at close to 50% and 100%, respectively. Use of amoxicillin, either high dose or standard dose, would not be expected to kill these bacteria.
Our study design has limitations. The population is derived from a predominantly middle-class, suburban population of children in upstate New York and may not be representative of other types of populations in the United States. The children are 6-36 months old, the age when most AOM occurs. MEF samples that were culture negative for bacteria were not further tested by polymerase chain reaction methods.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Kaur R et al. Front Pediatr. 2021;9:722483.
2. Kaur R et al. Euro J Clin Microbiol Infect Dis. 2021;41:37-44
3. Pelton SI et al. Pediatr Infect Disease J. 2004;23:1015-22.
4. Farrell DJ et al. Pediatr Infect Disease J. 2007;26:123-8..
5. Kaur R et al. Clin Infect Dis 2021;72(5):797-805.
6. Fuji N et al. Front Cell Infect Microbiol. 2021;11:744742.
Should psychiatry categorize ‘substance-induced paraphilia?’
‘substance-induced paraphilia?’
The dopamine receptors of the brain get their fair share amid the didactics we receive in residency. From discussions of antipsychotics and schizophrenia to stimulants and ADHD, dopamine plays a key role. Depending on the program and interest of faculty, methamphetamine may get its own lecture or be mixed in with other stimulants of abuse. During that discussion, a comment might be made in passing on the impact of methamphetamine on sexual desire and activity.
Experiences in the emergency department caring for patients who are intoxicated from methamphetamine then effectively make up for any gaps in trainees’ knowledge base. From patients engaging in self-pleasing pursuits in the emergency room to unfiltered reports of sexual exploits and desires, the impact of methamphetamine on sexual behavior quickly becomes apparent. Those experiences are later reinforced when residents are exposed to more long-term rehabilitation programs and have more in-depth conversations with patients about the sex-culture surrounding methamphetamine.
It is common to hear that, under the influence of methamphetamine, any available body will become an acceptable sexual partner – at times resulting in significant regrets, dangerous sexual activity, and complicated questions surrounding consent. Some early studies have found up to 72% increase in risky sexual behavior in methamphetamine users.1 This is particularly problematic as society has recently taken on the difficult and important work to re-examine the role and nature of consent in sexual activities. This falls within the larger #MeToo movement and has led to advocating for harsher sentencing of sexual offenders.
Yet simultaneously, society has also reconsidered its approach to apportioning blame on drug users.2 This shift to a more compassionate stance has resulted in a desire to treat and care for a disorder, rather than punish and condemn a poor choice. As forensic psychiatrists, we have noted this significant change. Where substance use disorders were once considered a risk factor for recidivism, they are now considered a disability that not only warrants treatment but can also diminish the share of blame one may be responsible for.
The convergence of those two societal movements often plays out in the courtroom, and in our experience when faced with those two opposing viewpoints, triers of fact (judges and juries) often favor punishing sexual offense over empathizing with an addictive disorder. While certainly not implying methamphetamine use condones sexual offense, we do posit the particular relationship between methamphetamine use and sexual activity should be explained to those entrusted with deciding guilt.
Examples of such problems are extremely common. A routine case involves IK,3 a 48-year-old male without significant history of legal problems, arrested for indecent exposure. His history of mental illness is closely intertwined with a history of substance use, leading to many psychiatric hospitalizations for methamphetamine-induced psychosis. After many hospitalizations he was placed in an assertive community treatment (ACT) team.
One day, IK is approached by an industrious drug dealer who frequents multiple board-and-cares in search for customers interested in relapsing. IK uses methamphetamine and within hours finds himself having walked miles away, naked, in the middle of an RV park. He subsequently describes the experience of unrelenting sexual desire, accompanied by ideas of reference involving billboards encouraging him to demonstrate his sexual prowess, as well as auditory hallucinations of women cheering him on. This leads to him pleasing himself publicly and his subsequent arrest.
Interviewing IK, 3 months later, he is embarrassed and apologetic. He is cognizant of the inappropriate nature of the incident and the foolishness of his actions. However, when asked whether he considers himself a sexual offender, he protests that he would never act in such a manner if not under the influence of methamphetamine. He points to his lack of significant sexual urges when sober, his lack of prior sexual offense, his lack of sexually violent offense, and his lack of unusual sexual interests.
It is unclear to us how society will or should adjudicate on such a case. It is not under the purview of forensic psychiatry to become a trier of fact. However, psychiatry should have a better working framework of how to discuss and conceptualize such situations, especially considering the dire consequences for those involved.
While any criminal conviction already has the potential to destroy a person’s life, sexual crimes bring particularly serious consequences. Entry into the national sex offender registry, in addition to carrying an unshakable stigma, comes with additional degrees of lost freedom. These individuals are prohibited from living or working in areas that have children in proximity, subjecting them to the outskirts of society and greatly restricting any chance of economic escape from poverty. Parks, libraries, and shopping malls can become off limits. Privacy for these individuals is nonexistent; from websites they visit to where they travel physically can be monitored. Even where they live and a detailed physical description are often easily accessible by members of their community.
When should it be permissible to consider sex offender status for someone on the grounds of a mental illness? A patient with obsessive-compulsive disorder might have sadistic obsessions and compulsions to commit violent sexual acts, which, along with being repugnant to society, are entirely ego-dystonic to the suffering patient. Psychosis is often characterized as involving a loss of insight and impaired reality testing. If society accepts insanity as grounds to mitigate sentencing, then why not permit it for grounds to wave the designation of sex offender to those with certain disorders, including substance use disorder? Wherever we come down on this issue,
Should IK have to register as a sex offender? Regardless of the circumstances, he did publicly masturbate. Society has determined that public sexual displays are a crime worth carrying the pariah status of sex offender – why should an exception be made for methamphetamine use? On the other hand, it is difficult to claim that IK’s behavior was entirely of his own free will. Most triers of fact will have never experienced that amount of dopamine reward. They can’t attest to the remaining free will after experiencing more pleasurable salience and positive reinforcement than ever naturally possible.
How we deal with the behavioral consequences, and other sequelae, of methamphetamine use is a growing problem. Access to and use of methamphetamine is no longer reserved for soldiers patrolling the jungles of Vietnam. Once thought to be a scourge of the West Coast, methamphetamine is now widely available throughout the United States.4 The use of methamphetamine is likely to continue to expand as society keeps pursuing the decriminalizing of drug use. Psychiatrists practicing in areas heavily affected by methamphetamine see firsthand the burden it places on community resources in the form of increased psychosis, emergency room utilization, medical resource strain, and encounters with police.5
The presence of mental illness is tied to a small but statistically significant risk of violence. However, substance use is a well-established risk factor for violence.6 What is often missed is that many sexual offenders have not committed a violent offense. However, like IK, they have been charged with indecent exposure or other nonviolent sexual offenses, such as prostitution and solicitation. Those nonviolent offenses are driven by poor judgment and impulsivity, the trademarks of substance use. The answer cannot be to incarcerate, and eventually add to the sex offender registry, the growing number of these individuals.
Yet, as psychiatrists, we seem at a loss for how to treat these patients. The prescription of allowing them to spend a night in the ED with a complementary sandwich garnished with olanzapine often feels like enabling. Substance use treatment programs are too limited, and the wait list is rarely shorter than the time it takes our patient to purchase their next hit.
There are no effective pharmacologic treatments for methamphetamine use disorder.7 The recommendations of cognitive-behavioral therapy, family and group therapy, contingency management, and a 12-step program may be sufficient for the most motivated and well-supported patients but are inadequate for the vast majority.8 As much as we want to laud the merits of community psychiatry and the ACT [assertive community treatment] model of care, it is hard to carry that banner while confronted with the reality these patients face on a day-to-day basis during any shift in the emergency room. Eventually the countless encounters with homeless, helplessly meth-addicted patients ending in discharge back to the streets begins to tarnish the bright rhetoric surrounding community care, which starts to sound more and more like abandonment of patients to suffer in futility.9
It is not up to forensic psychiatrists, or even psychiatry as a whole, to fix the myriad of inadequacies surrounding how society handles those suffering from methamphetamine addiction. However, it is essential for psychiatry to study and educate society on the interaction of methamphetamine use and sexual behavior. There has been some exploration into other risk factors for paraphilic behavior while under the influence of substances, but there is a dearth of information on this topic. Establishing a nomenclature called “substance-induced paraphilia” might be a way to bring clarity to such instances in both a forensic and general psychiatric setting.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research. Dr. Compton has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Psychol Addict Behav. 2016;30(2)147-57.
2. Monitor Psychol. 2019;50(6).
3. IK’s case has been modified in certain ways to maintain confidentiality.
4. J Psychoactive Drugs. 2000;(2):137-41.
5. Acad Emerg Med. 2020 Nov;27(11):1116-25.
6. Swanson JW. Mental disorder, substance abuse, and community violence: An epidemiological approach, in: Monahan J and Steadman HJ, eds. “Violence and Mental Disorder: Developments in Risk Assessment” (Chicago: University of Chicago Press, 1994, pp. 101-36).
7. Addiction. 2004 Jun;99(6)708-17.
8. Am Fam Physician. 2007 Oct 15;76(8):1169-74.
9. Perspect Biol Med. 2021;64(1)70-81.
The dopamine receptors of the brain get their fair share amid the didactics we receive in residency. From discussions of antipsychotics and schizophrenia to stimulants and ADHD, dopamine plays a key role. Depending on the program and interest of faculty, methamphetamine may get its own lecture or be mixed in with other stimulants of abuse. During that discussion, a comment might be made in passing on the impact of methamphetamine on sexual desire and activity.
Experiences in the emergency department caring for patients who are intoxicated from methamphetamine then effectively make up for any gaps in trainees’ knowledge base. From patients engaging in self-pleasing pursuits in the emergency room to unfiltered reports of sexual exploits and desires, the impact of methamphetamine on sexual behavior quickly becomes apparent. Those experiences are later reinforced when residents are exposed to more long-term rehabilitation programs and have more in-depth conversations with patients about the sex-culture surrounding methamphetamine.
It is common to hear that, under the influence of methamphetamine, any available body will become an acceptable sexual partner – at times resulting in significant regrets, dangerous sexual activity, and complicated questions surrounding consent. Some early studies have found up to 72% increase in risky sexual behavior in methamphetamine users.1 This is particularly problematic as society has recently taken on the difficult and important work to re-examine the role and nature of consent in sexual activities. This falls within the larger #MeToo movement and has led to advocating for harsher sentencing of sexual offenders.
Yet simultaneously, society has also reconsidered its approach to apportioning blame on drug users.2 This shift to a more compassionate stance has resulted in a desire to treat and care for a disorder, rather than punish and condemn a poor choice. As forensic psychiatrists, we have noted this significant change. Where substance use disorders were once considered a risk factor for recidivism, they are now considered a disability that not only warrants treatment but can also diminish the share of blame one may be responsible for.
The convergence of those two societal movements often plays out in the courtroom, and in our experience when faced with those two opposing viewpoints, triers of fact (judges and juries) often favor punishing sexual offense over empathizing with an addictive disorder. While certainly not implying methamphetamine use condones sexual offense, we do posit the particular relationship between methamphetamine use and sexual activity should be explained to those entrusted with deciding guilt.
Examples of such problems are extremely common. A routine case involves IK,3 a 48-year-old male without significant history of legal problems, arrested for indecent exposure. His history of mental illness is closely intertwined with a history of substance use, leading to many psychiatric hospitalizations for methamphetamine-induced psychosis. After many hospitalizations he was placed in an assertive community treatment (ACT) team.
One day, IK is approached by an industrious drug dealer who frequents multiple board-and-cares in search for customers interested in relapsing. IK uses methamphetamine and within hours finds himself having walked miles away, naked, in the middle of an RV park. He subsequently describes the experience of unrelenting sexual desire, accompanied by ideas of reference involving billboards encouraging him to demonstrate his sexual prowess, as well as auditory hallucinations of women cheering him on. This leads to him pleasing himself publicly and his subsequent arrest.
Interviewing IK, 3 months later, he is embarrassed and apologetic. He is cognizant of the inappropriate nature of the incident and the foolishness of his actions. However, when asked whether he considers himself a sexual offender, he protests that he would never act in such a manner if not under the influence of methamphetamine. He points to his lack of significant sexual urges when sober, his lack of prior sexual offense, his lack of sexually violent offense, and his lack of unusual sexual interests.
It is unclear to us how society will or should adjudicate on such a case. It is not under the purview of forensic psychiatry to become a trier of fact. However, psychiatry should have a better working framework of how to discuss and conceptualize such situations, especially considering the dire consequences for those involved.
While any criminal conviction already has the potential to destroy a person’s life, sexual crimes bring particularly serious consequences. Entry into the national sex offender registry, in addition to carrying an unshakable stigma, comes with additional degrees of lost freedom. These individuals are prohibited from living or working in areas that have children in proximity, subjecting them to the outskirts of society and greatly restricting any chance of economic escape from poverty. Parks, libraries, and shopping malls can become off limits. Privacy for these individuals is nonexistent; from websites they visit to where they travel physically can be monitored. Even where they live and a detailed physical description are often easily accessible by members of their community.
When should it be permissible to consider sex offender status for someone on the grounds of a mental illness? A patient with obsessive-compulsive disorder might have sadistic obsessions and compulsions to commit violent sexual acts, which, along with being repugnant to society, are entirely ego-dystonic to the suffering patient. Psychosis is often characterized as involving a loss of insight and impaired reality testing. If society accepts insanity as grounds to mitigate sentencing, then why not permit it for grounds to wave the designation of sex offender to those with certain disorders, including substance use disorder? Wherever we come down on this issue,
Should IK have to register as a sex offender? Regardless of the circumstances, he did publicly masturbate. Society has determined that public sexual displays are a crime worth carrying the pariah status of sex offender – why should an exception be made for methamphetamine use? On the other hand, it is difficult to claim that IK’s behavior was entirely of his own free will. Most triers of fact will have never experienced that amount of dopamine reward. They can’t attest to the remaining free will after experiencing more pleasurable salience and positive reinforcement than ever naturally possible.
How we deal with the behavioral consequences, and other sequelae, of methamphetamine use is a growing problem. Access to and use of methamphetamine is no longer reserved for soldiers patrolling the jungles of Vietnam. Once thought to be a scourge of the West Coast, methamphetamine is now widely available throughout the United States.4 The use of methamphetamine is likely to continue to expand as society keeps pursuing the decriminalizing of drug use. Psychiatrists practicing in areas heavily affected by methamphetamine see firsthand the burden it places on community resources in the form of increased psychosis, emergency room utilization, medical resource strain, and encounters with police.5
The presence of mental illness is tied to a small but statistically significant risk of violence. However, substance use is a well-established risk factor for violence.6 What is often missed is that many sexual offenders have not committed a violent offense. However, like IK, they have been charged with indecent exposure or other nonviolent sexual offenses, such as prostitution and solicitation. Those nonviolent offenses are driven by poor judgment and impulsivity, the trademarks of substance use. The answer cannot be to incarcerate, and eventually add to the sex offender registry, the growing number of these individuals.
Yet, as psychiatrists, we seem at a loss for how to treat these patients. The prescription of allowing them to spend a night in the ED with a complementary sandwich garnished with olanzapine often feels like enabling. Substance use treatment programs are too limited, and the wait list is rarely shorter than the time it takes our patient to purchase their next hit.
There are no effective pharmacologic treatments for methamphetamine use disorder.7 The recommendations of cognitive-behavioral therapy, family and group therapy, contingency management, and a 12-step program may be sufficient for the most motivated and well-supported patients but are inadequate for the vast majority.8 As much as we want to laud the merits of community psychiatry and the ACT [assertive community treatment] model of care, it is hard to carry that banner while confronted with the reality these patients face on a day-to-day basis during any shift in the emergency room. Eventually the countless encounters with homeless, helplessly meth-addicted patients ending in discharge back to the streets begins to tarnish the bright rhetoric surrounding community care, which starts to sound more and more like abandonment of patients to suffer in futility.9
It is not up to forensic psychiatrists, or even psychiatry as a whole, to fix the myriad of inadequacies surrounding how society handles those suffering from methamphetamine addiction. However, it is essential for psychiatry to study and educate society on the interaction of methamphetamine use and sexual behavior. There has been some exploration into other risk factors for paraphilic behavior while under the influence of substances, but there is a dearth of information on this topic. Establishing a nomenclature called “substance-induced paraphilia” might be a way to bring clarity to such instances in both a forensic and general psychiatric setting.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research. Dr. Compton has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Psychol Addict Behav. 2016;30(2)147-57.
2. Monitor Psychol. 2019;50(6).
3. IK’s case has been modified in certain ways to maintain confidentiality.
4. J Psychoactive Drugs. 2000;(2):137-41.
5. Acad Emerg Med. 2020 Nov;27(11):1116-25.
6. Swanson JW. Mental disorder, substance abuse, and community violence: An epidemiological approach, in: Monahan J and Steadman HJ, eds. “Violence and Mental Disorder: Developments in Risk Assessment” (Chicago: University of Chicago Press, 1994, pp. 101-36).
7. Addiction. 2004 Jun;99(6)708-17.
8. Am Fam Physician. 2007 Oct 15;76(8):1169-74.
9. Perspect Biol Med. 2021;64(1)70-81.
The dopamine receptors of the brain get their fair share amid the didactics we receive in residency. From discussions of antipsychotics and schizophrenia to stimulants and ADHD, dopamine plays a key role. Depending on the program and interest of faculty, methamphetamine may get its own lecture or be mixed in with other stimulants of abuse. During that discussion, a comment might be made in passing on the impact of methamphetamine on sexual desire and activity.
Experiences in the emergency department caring for patients who are intoxicated from methamphetamine then effectively make up for any gaps in trainees’ knowledge base. From patients engaging in self-pleasing pursuits in the emergency room to unfiltered reports of sexual exploits and desires, the impact of methamphetamine on sexual behavior quickly becomes apparent. Those experiences are later reinforced when residents are exposed to more long-term rehabilitation programs and have more in-depth conversations with patients about the sex-culture surrounding methamphetamine.
It is common to hear that, under the influence of methamphetamine, any available body will become an acceptable sexual partner – at times resulting in significant regrets, dangerous sexual activity, and complicated questions surrounding consent. Some early studies have found up to 72% increase in risky sexual behavior in methamphetamine users.1 This is particularly problematic as society has recently taken on the difficult and important work to re-examine the role and nature of consent in sexual activities. This falls within the larger #MeToo movement and has led to advocating for harsher sentencing of sexual offenders.
Yet simultaneously, society has also reconsidered its approach to apportioning blame on drug users.2 This shift to a more compassionate stance has resulted in a desire to treat and care for a disorder, rather than punish and condemn a poor choice. As forensic psychiatrists, we have noted this significant change. Where substance use disorders were once considered a risk factor for recidivism, they are now considered a disability that not only warrants treatment but can also diminish the share of blame one may be responsible for.
The convergence of those two societal movements often plays out in the courtroom, and in our experience when faced with those two opposing viewpoints, triers of fact (judges and juries) often favor punishing sexual offense over empathizing with an addictive disorder. While certainly not implying methamphetamine use condones sexual offense, we do posit the particular relationship between methamphetamine use and sexual activity should be explained to those entrusted with deciding guilt.
Examples of such problems are extremely common. A routine case involves IK,3 a 48-year-old male without significant history of legal problems, arrested for indecent exposure. His history of mental illness is closely intertwined with a history of substance use, leading to many psychiatric hospitalizations for methamphetamine-induced psychosis. After many hospitalizations he was placed in an assertive community treatment (ACT) team.
One day, IK is approached by an industrious drug dealer who frequents multiple board-and-cares in search for customers interested in relapsing. IK uses methamphetamine and within hours finds himself having walked miles away, naked, in the middle of an RV park. He subsequently describes the experience of unrelenting sexual desire, accompanied by ideas of reference involving billboards encouraging him to demonstrate his sexual prowess, as well as auditory hallucinations of women cheering him on. This leads to him pleasing himself publicly and his subsequent arrest.
Interviewing IK, 3 months later, he is embarrassed and apologetic. He is cognizant of the inappropriate nature of the incident and the foolishness of his actions. However, when asked whether he considers himself a sexual offender, he protests that he would never act in such a manner if not under the influence of methamphetamine. He points to his lack of significant sexual urges when sober, his lack of prior sexual offense, his lack of sexually violent offense, and his lack of unusual sexual interests.
It is unclear to us how society will or should adjudicate on such a case. It is not under the purview of forensic psychiatry to become a trier of fact. However, psychiatry should have a better working framework of how to discuss and conceptualize such situations, especially considering the dire consequences for those involved.
While any criminal conviction already has the potential to destroy a person’s life, sexual crimes bring particularly serious consequences. Entry into the national sex offender registry, in addition to carrying an unshakable stigma, comes with additional degrees of lost freedom. These individuals are prohibited from living or working in areas that have children in proximity, subjecting them to the outskirts of society and greatly restricting any chance of economic escape from poverty. Parks, libraries, and shopping malls can become off limits. Privacy for these individuals is nonexistent; from websites they visit to where they travel physically can be monitored. Even where they live and a detailed physical description are often easily accessible by members of their community.
When should it be permissible to consider sex offender status for someone on the grounds of a mental illness? A patient with obsessive-compulsive disorder might have sadistic obsessions and compulsions to commit violent sexual acts, which, along with being repugnant to society, are entirely ego-dystonic to the suffering patient. Psychosis is often characterized as involving a loss of insight and impaired reality testing. If society accepts insanity as grounds to mitigate sentencing, then why not permit it for grounds to wave the designation of sex offender to those with certain disorders, including substance use disorder? Wherever we come down on this issue,
Should IK have to register as a sex offender? Regardless of the circumstances, he did publicly masturbate. Society has determined that public sexual displays are a crime worth carrying the pariah status of sex offender – why should an exception be made for methamphetamine use? On the other hand, it is difficult to claim that IK’s behavior was entirely of his own free will. Most triers of fact will have never experienced that amount of dopamine reward. They can’t attest to the remaining free will after experiencing more pleasurable salience and positive reinforcement than ever naturally possible.
How we deal with the behavioral consequences, and other sequelae, of methamphetamine use is a growing problem. Access to and use of methamphetamine is no longer reserved for soldiers patrolling the jungles of Vietnam. Once thought to be a scourge of the West Coast, methamphetamine is now widely available throughout the United States.4 The use of methamphetamine is likely to continue to expand as society keeps pursuing the decriminalizing of drug use. Psychiatrists practicing in areas heavily affected by methamphetamine see firsthand the burden it places on community resources in the form of increased psychosis, emergency room utilization, medical resource strain, and encounters with police.5
The presence of mental illness is tied to a small but statistically significant risk of violence. However, substance use is a well-established risk factor for violence.6 What is often missed is that many sexual offenders have not committed a violent offense. However, like IK, they have been charged with indecent exposure or other nonviolent sexual offenses, such as prostitution and solicitation. Those nonviolent offenses are driven by poor judgment and impulsivity, the trademarks of substance use. The answer cannot be to incarcerate, and eventually add to the sex offender registry, the growing number of these individuals.
Yet, as psychiatrists, we seem at a loss for how to treat these patients. The prescription of allowing them to spend a night in the ED with a complementary sandwich garnished with olanzapine often feels like enabling. Substance use treatment programs are too limited, and the wait list is rarely shorter than the time it takes our patient to purchase their next hit.
There are no effective pharmacologic treatments for methamphetamine use disorder.7 The recommendations of cognitive-behavioral therapy, family and group therapy, contingency management, and a 12-step program may be sufficient for the most motivated and well-supported patients but are inadequate for the vast majority.8 As much as we want to laud the merits of community psychiatry and the ACT [assertive community treatment] model of care, it is hard to carry that banner while confronted with the reality these patients face on a day-to-day basis during any shift in the emergency room. Eventually the countless encounters with homeless, helplessly meth-addicted patients ending in discharge back to the streets begins to tarnish the bright rhetoric surrounding community care, which starts to sound more and more like abandonment of patients to suffer in futility.9
It is not up to forensic psychiatrists, or even psychiatry as a whole, to fix the myriad of inadequacies surrounding how society handles those suffering from methamphetamine addiction. However, it is essential for psychiatry to study and educate society on the interaction of methamphetamine use and sexual behavior. There has been some exploration into other risk factors for paraphilic behavior while under the influence of substances, but there is a dearth of information on this topic. Establishing a nomenclature called “substance-induced paraphilia” might be a way to bring clarity to such instances in both a forensic and general psychiatric setting.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research. Dr. Compton has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Psychol Addict Behav. 2016;30(2)147-57.
2. Monitor Psychol. 2019;50(6).
3. IK’s case has been modified in certain ways to maintain confidentiality.
4. J Psychoactive Drugs. 2000;(2):137-41.
5. Acad Emerg Med. 2020 Nov;27(11):1116-25.
6. Swanson JW. Mental disorder, substance abuse, and community violence: An epidemiological approach, in: Monahan J and Steadman HJ, eds. “Violence and Mental Disorder: Developments in Risk Assessment” (Chicago: University of Chicago Press, 1994, pp. 101-36).
7. Addiction. 2004 Jun;99(6)708-17.
8. Am Fam Physician. 2007 Oct 15;76(8):1169-74.
9. Perspect Biol Med. 2021;64(1)70-81.
‘substance-induced paraphilia?’
‘substance-induced paraphilia?’






















