User login
LGBTQ students would get new protections under Biden plan
On the 50th anniversary of Title IX’s inception, the Biden administration has proposed changes to the law that would protect transgender students and assault survivors on college and university campuses.
With these changes, the protections provided by Title IX – a civil rights law that prohibits sex-based discrimination in schools that receive federal funding – would now be extended to students who identify as trans. The update would ensure that government-funded schools make proper accommodations for a trans student population, such as allowing students to use bathrooms and other facilities that align with their gender identity, and enforcing the use of students’ correct pronouns.
The revisions also seek to undo amendments made to the law by Betsy DeVos, who was secretary of education during the Trump presidency, which strengthened due process protections for students accused of sexual assault and narrowed the definition of sexual harassment. These rules “weakened protections for survivors of sexual assault and diminished the promise of an education free from discrimination,” the Biden administration said.
“Our proposed changes will allow us to continue that progress and ensure all our nation’s students – no matter where they live, who they are, or whom they love – can learn, grow, and thrive in school,” Education Secretary Miguel Cardona, PhD, said in a news release. “We welcome public comment on these critical regulations so we can further the Biden-Harris Administration’s mission of creating educational environments free from sex discrimination and sexual violence.”
The revisions will go through a long period of public comment before they are set into law. Still, the proposed changes mark a way forward for trans students who are not explicitly protected under Title IX, and they offer solace to assault survivors who may have felt discouraged to come forward and report under Ms. DeVos’s rules.
“The proposed regulations reflect the [Education] Department’s commitment to give full effect to Title IX, ensuring that no person experiences sex discrimination in education, and that school procedures for addressing complaints of sex discrimination, including sexual violence and other forms of sex-based harassment, are clear, effective, and fair to all involved,” said Catherine Lhamon, JD, assistant secretary for the Education Department’s Office Of Civil Rights.
More specific rules about transgender students’ participation in school sports are still to come.
A version of this article first appeared on WebMD.com.
On the 50th anniversary of Title IX’s inception, the Biden administration has proposed changes to the law that would protect transgender students and assault survivors on college and university campuses.
With these changes, the protections provided by Title IX – a civil rights law that prohibits sex-based discrimination in schools that receive federal funding – would now be extended to students who identify as trans. The update would ensure that government-funded schools make proper accommodations for a trans student population, such as allowing students to use bathrooms and other facilities that align with their gender identity, and enforcing the use of students’ correct pronouns.
The revisions also seek to undo amendments made to the law by Betsy DeVos, who was secretary of education during the Trump presidency, which strengthened due process protections for students accused of sexual assault and narrowed the definition of sexual harassment. These rules “weakened protections for survivors of sexual assault and diminished the promise of an education free from discrimination,” the Biden administration said.
“Our proposed changes will allow us to continue that progress and ensure all our nation’s students – no matter where they live, who they are, or whom they love – can learn, grow, and thrive in school,” Education Secretary Miguel Cardona, PhD, said in a news release. “We welcome public comment on these critical regulations so we can further the Biden-Harris Administration’s mission of creating educational environments free from sex discrimination and sexual violence.”
The revisions will go through a long period of public comment before they are set into law. Still, the proposed changes mark a way forward for trans students who are not explicitly protected under Title IX, and they offer solace to assault survivors who may have felt discouraged to come forward and report under Ms. DeVos’s rules.
“The proposed regulations reflect the [Education] Department’s commitment to give full effect to Title IX, ensuring that no person experiences sex discrimination in education, and that school procedures for addressing complaints of sex discrimination, including sexual violence and other forms of sex-based harassment, are clear, effective, and fair to all involved,” said Catherine Lhamon, JD, assistant secretary for the Education Department’s Office Of Civil Rights.
More specific rules about transgender students’ participation in school sports are still to come.
A version of this article first appeared on WebMD.com.
On the 50th anniversary of Title IX’s inception, the Biden administration has proposed changes to the law that would protect transgender students and assault survivors on college and university campuses.
With these changes, the protections provided by Title IX – a civil rights law that prohibits sex-based discrimination in schools that receive federal funding – would now be extended to students who identify as trans. The update would ensure that government-funded schools make proper accommodations for a trans student population, such as allowing students to use bathrooms and other facilities that align with their gender identity, and enforcing the use of students’ correct pronouns.
The revisions also seek to undo amendments made to the law by Betsy DeVos, who was secretary of education during the Trump presidency, which strengthened due process protections for students accused of sexual assault and narrowed the definition of sexual harassment. These rules “weakened protections for survivors of sexual assault and diminished the promise of an education free from discrimination,” the Biden administration said.
“Our proposed changes will allow us to continue that progress and ensure all our nation’s students – no matter where they live, who they are, or whom they love – can learn, grow, and thrive in school,” Education Secretary Miguel Cardona, PhD, said in a news release. “We welcome public comment on these critical regulations so we can further the Biden-Harris Administration’s mission of creating educational environments free from sex discrimination and sexual violence.”
The revisions will go through a long period of public comment before they are set into law. Still, the proposed changes mark a way forward for trans students who are not explicitly protected under Title IX, and they offer solace to assault survivors who may have felt discouraged to come forward and report under Ms. DeVos’s rules.
“The proposed regulations reflect the [Education] Department’s commitment to give full effect to Title IX, ensuring that no person experiences sex discrimination in education, and that school procedures for addressing complaints of sex discrimination, including sexual violence and other forms of sex-based harassment, are clear, effective, and fair to all involved,” said Catherine Lhamon, JD, assistant secretary for the Education Department’s Office Of Civil Rights.
More specific rules about transgender students’ participation in school sports are still to come.
A version of this article first appeared on WebMD.com.
Roe v. Wade: Medical groups react to Supreme Court decision
The country’s top medical organizations condemned the overturning of Roe v. Wade, saying the removal of federal protections for women to access abortion services marks a “dark day.”
“It is unfathomable. It is unfair. It is wrong,” said the President of the American College of Obstetricians and Gynecologists (ACOG) Iffath Abbasi Hoskins, MD.
“Today is a very dark day in health care. It is a dark day, indeed, for the tens of millions of patients who have suddenly and unfairly lost access to safe legal and evidence-based abortion care,” Dr. Hoskins said at a press conference June 24 sponsored by ACOG.
“It is dark for the thousands of clinicians who now, instead of focusing on providing health care to their patients, have to live with the threats of legal, civil, and even professional penalties,” Dr. Hoskins added.
ACOG has 62,000 members and is the leading group of doctors that provides obstetric and gynecologic care.
Dilemma for some doctors?
“I’d like to take a moment to talk about the future of the medical profession,” said ACOG Chief Executive Officer Maureen G. Phipps, MD, MPH. “[The] decision is, as Dr. Hoskins clearly said, a tragic one for our patients in states across the country, but the harm does not end there.”
Dr. Phipps described overturning Roe v. Wade as “the boldest act of legislative interference that we have seen in this country. It will allow state legislators to tell physicians what care they can and cannot provide to their patients.”
“It will leave physicians looking over our shoulders, wondering if a patient is in enough of a crisis to permit an exception to a law,” Dr. Phipps added. “This is an affront to all that drew my colleagues and me into medicine.”
Although the impact on doctor training remains to be seen, she said 44% of ob.gyn. residents are trained in states now empowered to ban abortions.
The effect of the Supreme Court decision on miscarriage management is another unknown.
“It’s going to be very difficult for us, the clinicians, to manage miscarriage,” Dr. Hoskins said. “Many miscarriages could be what we call ‘incomplete’ in the beginning,” where there is still a heartbeat and the patient is cramping and/or bleeding.
In that instance, Dr. Hoskins said, clinicians may be thinking that they have to wait.
“They may be needing to get additional opinions, whether it’s a legal opinion ... or another medical opinion.”
“It’s going to have a devastating effect on every aspect of a woman’s health care, including if she is spontaneously miscarrying,” Dr. Hoskins predicted.
Physician protect thyself?
To what extent doctors can shield themselves from potential prosecution “is a hard question to answer,” Molly Meegan, JD, ACOG’s chief legal officer and general counsel, said.
Ms. Meegan recommended members speak to the risk managers at their individual institutions for guidance.
“It is a real patchwork [of laws] out there, she said. “And that patchwork itself is a danger to people as they seek essential reproductive health care.”
Also, she added, “If a doctor can’t tell what the law is at the time they’re trying to provide the care, it has a terribly chilling effect on medical care.”
Another potential threat to doctors in states that still allow abortion services is action from a neighboring state.
“We are going to be advocating very strongly that states do not have extra-territorial jurisdiction to reach beyond the edges of their state.”
The worry is if a doctor in New Mexico, where abortion is legal, performs an abortion for a person from Texas, where it will soon be illegal, is then prosecuted by Texas, for example.
Medication abortion
Asked about any potential effects on medication abortions, ACOG’s Jen Villavicencio, MD, said it remains to be seen.
“Certainly many of the laws that we have seen, including trigger ban laws, encompass medication abortion,” she said. Several states have these so-called trigger laws, which put into effect laws passed to ban abortion in case Roe was overturned.
This means, she said, that any abortion option, whether it’s procedural or medication, could be and will be banned in some of these states.
Ms. Meegan added that ACOG will continue to support access to medication abortion and that it should be decided by the U.S. Food and Drug Administration and not individual states.
Maternal mortality may rise
“Maternal mortality in and of itself is a very difficult topic,” Dr. Hoskins said, but [the] decision amplifies the implications. “I think of the patients who will have to manage severe complications and mental health challenges while they are carrying a pregnancy that they are forced to carry.”
“I also think of the patients who need to end their pregnancies in order to save their own lives,” Dr. Hoskins added.
Dr. Hoskins said the United States already has a high maternal mortality rate. This new law, she added, could force women into higher-risk situations if they experience high blood pressure, preeclampsia, or bleeding after the birth of the baby.
Growing inequality possible?
“The grievous inequities that exist in this country will grow and expand unchecked without safe access to legal abortion,” Dr. Phipps said.
She noted that women, based on location, will continue “to have protected access to safe evidence-based abortion. Others will have the means and resources and opportunities to secure the care.”
But the same may not be true for women in underserved or disadvantaged communities, Dr. Phipps added.
American Medical Association
ACOG was not the only group to react. “The American Medical Association is deeply disturbed by the U.S. Supreme Court’s decision to overturn nearly a half century of precedent protecting patients’ right to critical reproductive health care,” President Jack Resneck Jr., MD, said in a statement.
The decision represents “an egregious allowance of government intrusion into the medical examination room, a direct attack on the practice of medicine and the patient-physician relationship, and a brazen violation of patients’ rights to evidence-based reproductive health services.”
American Academy of Family Physicians
“The American Academy of Family Physicians is disappointed and disheartened by the Supreme Court’s decision to strike down longstanding protections afforded by Roe v. Wade and Planned Parenthood v. Casey,” President Sterling N. Ransone Jr., MD, said in a statement.
The organization has 127,600 physician and medical student members.
“This decision negatively impacts our practices and our patients by undermining the patient-physician relationship and potentially criminalizing evidence-based medical care,” added Dr. Ransone.
American College of Physicians
“A patient’s decision about whether to continue a pregnancy should be a private decision made in consultation with a physician or other health care professional, without interference from the government,” President Ryan D. Mire, MD, said in a statement. “We strongly oppose medically unnecessary government restrictions on any health care services,” added Dr. Mire on behalf of the group’s 161,000 members.
American Academy of Pediatrics
“This decision carries grave consequences for our adolescent patients, who already face many more barriers than adults in accessing comprehensive reproductive health care services and abortion care,” President Moira Szilagyi, MD, PhD, said in a statement.
“In the wake of this ruling, the American Academy of Pediatrics will continue to support our chapters as states consider policies affecting access to abortion care, and pediatricians will continue to support our patients,” Dr. Szilagyi added.
American Public Health Association
The court’s decision “is a catastrophic judicial failure that will reverberate differently in each state and portends to jeopardize the health and lives of all Americans,” Executive Director Georges C. Benjamin, MD, said in a statement.
American Urogynecologic Society
“The American Urogynecologic Society opposes any ruling that restricts a person’s access to health care and criminalizes the practice of medicine,” the group said in a statement. “This ruling ultimately poses a serious threat to the patient-provider relationship and subsequent decisionmaking necessary to ensure optimal outcomes for patients. As practitioners, we should be free to provide what is in the best interest of our patients.”
A version of this article first appeared on Medscape.com.
The country’s top medical organizations condemned the overturning of Roe v. Wade, saying the removal of federal protections for women to access abortion services marks a “dark day.”
“It is unfathomable. It is unfair. It is wrong,” said the President of the American College of Obstetricians and Gynecologists (ACOG) Iffath Abbasi Hoskins, MD.
“Today is a very dark day in health care. It is a dark day, indeed, for the tens of millions of patients who have suddenly and unfairly lost access to safe legal and evidence-based abortion care,” Dr. Hoskins said at a press conference June 24 sponsored by ACOG.
“It is dark for the thousands of clinicians who now, instead of focusing on providing health care to their patients, have to live with the threats of legal, civil, and even professional penalties,” Dr. Hoskins added.
ACOG has 62,000 members and is the leading group of doctors that provides obstetric and gynecologic care.
Dilemma for some doctors?
“I’d like to take a moment to talk about the future of the medical profession,” said ACOG Chief Executive Officer Maureen G. Phipps, MD, MPH. “[The] decision is, as Dr. Hoskins clearly said, a tragic one for our patients in states across the country, but the harm does not end there.”
Dr. Phipps described overturning Roe v. Wade as “the boldest act of legislative interference that we have seen in this country. It will allow state legislators to tell physicians what care they can and cannot provide to their patients.”
“It will leave physicians looking over our shoulders, wondering if a patient is in enough of a crisis to permit an exception to a law,” Dr. Phipps added. “This is an affront to all that drew my colleagues and me into medicine.”
Although the impact on doctor training remains to be seen, she said 44% of ob.gyn. residents are trained in states now empowered to ban abortions.
The effect of the Supreme Court decision on miscarriage management is another unknown.
“It’s going to be very difficult for us, the clinicians, to manage miscarriage,” Dr. Hoskins said. “Many miscarriages could be what we call ‘incomplete’ in the beginning,” where there is still a heartbeat and the patient is cramping and/or bleeding.
In that instance, Dr. Hoskins said, clinicians may be thinking that they have to wait.
“They may be needing to get additional opinions, whether it’s a legal opinion ... or another medical opinion.”
“It’s going to have a devastating effect on every aspect of a woman’s health care, including if she is spontaneously miscarrying,” Dr. Hoskins predicted.
Physician protect thyself?
To what extent doctors can shield themselves from potential prosecution “is a hard question to answer,” Molly Meegan, JD, ACOG’s chief legal officer and general counsel, said.
Ms. Meegan recommended members speak to the risk managers at their individual institutions for guidance.
“It is a real patchwork [of laws] out there, she said. “And that patchwork itself is a danger to people as they seek essential reproductive health care.”
Also, she added, “If a doctor can’t tell what the law is at the time they’re trying to provide the care, it has a terribly chilling effect on medical care.”
Another potential threat to doctors in states that still allow abortion services is action from a neighboring state.
“We are going to be advocating very strongly that states do not have extra-territorial jurisdiction to reach beyond the edges of their state.”
The worry is if a doctor in New Mexico, where abortion is legal, performs an abortion for a person from Texas, where it will soon be illegal, is then prosecuted by Texas, for example.
Medication abortion
Asked about any potential effects on medication abortions, ACOG’s Jen Villavicencio, MD, said it remains to be seen.
“Certainly many of the laws that we have seen, including trigger ban laws, encompass medication abortion,” she said. Several states have these so-called trigger laws, which put into effect laws passed to ban abortion in case Roe was overturned.
This means, she said, that any abortion option, whether it’s procedural or medication, could be and will be banned in some of these states.
Ms. Meegan added that ACOG will continue to support access to medication abortion and that it should be decided by the U.S. Food and Drug Administration and not individual states.
Maternal mortality may rise
“Maternal mortality in and of itself is a very difficult topic,” Dr. Hoskins said, but [the] decision amplifies the implications. “I think of the patients who will have to manage severe complications and mental health challenges while they are carrying a pregnancy that they are forced to carry.”
“I also think of the patients who need to end their pregnancies in order to save their own lives,” Dr. Hoskins added.
Dr. Hoskins said the United States already has a high maternal mortality rate. This new law, she added, could force women into higher-risk situations if they experience high blood pressure, preeclampsia, or bleeding after the birth of the baby.
Growing inequality possible?
“The grievous inequities that exist in this country will grow and expand unchecked without safe access to legal abortion,” Dr. Phipps said.
She noted that women, based on location, will continue “to have protected access to safe evidence-based abortion. Others will have the means and resources and opportunities to secure the care.”
But the same may not be true for women in underserved or disadvantaged communities, Dr. Phipps added.
American Medical Association
ACOG was not the only group to react. “The American Medical Association is deeply disturbed by the U.S. Supreme Court’s decision to overturn nearly a half century of precedent protecting patients’ right to critical reproductive health care,” President Jack Resneck Jr., MD, said in a statement.
The decision represents “an egregious allowance of government intrusion into the medical examination room, a direct attack on the practice of medicine and the patient-physician relationship, and a brazen violation of patients’ rights to evidence-based reproductive health services.”
American Academy of Family Physicians
“The American Academy of Family Physicians is disappointed and disheartened by the Supreme Court’s decision to strike down longstanding protections afforded by Roe v. Wade and Planned Parenthood v. Casey,” President Sterling N. Ransone Jr., MD, said in a statement.
The organization has 127,600 physician and medical student members.
“This decision negatively impacts our practices and our patients by undermining the patient-physician relationship and potentially criminalizing evidence-based medical care,” added Dr. Ransone.
American College of Physicians
“A patient’s decision about whether to continue a pregnancy should be a private decision made in consultation with a physician or other health care professional, without interference from the government,” President Ryan D. Mire, MD, said in a statement. “We strongly oppose medically unnecessary government restrictions on any health care services,” added Dr. Mire on behalf of the group’s 161,000 members.
American Academy of Pediatrics
“This decision carries grave consequences for our adolescent patients, who already face many more barriers than adults in accessing comprehensive reproductive health care services and abortion care,” President Moira Szilagyi, MD, PhD, said in a statement.
“In the wake of this ruling, the American Academy of Pediatrics will continue to support our chapters as states consider policies affecting access to abortion care, and pediatricians will continue to support our patients,” Dr. Szilagyi added.
American Public Health Association
The court’s decision “is a catastrophic judicial failure that will reverberate differently in each state and portends to jeopardize the health and lives of all Americans,” Executive Director Georges C. Benjamin, MD, said in a statement.
American Urogynecologic Society
“The American Urogynecologic Society opposes any ruling that restricts a person’s access to health care and criminalizes the practice of medicine,” the group said in a statement. “This ruling ultimately poses a serious threat to the patient-provider relationship and subsequent decisionmaking necessary to ensure optimal outcomes for patients. As practitioners, we should be free to provide what is in the best interest of our patients.”
A version of this article first appeared on Medscape.com.
The country’s top medical organizations condemned the overturning of Roe v. Wade, saying the removal of federal protections for women to access abortion services marks a “dark day.”
“It is unfathomable. It is unfair. It is wrong,” said the President of the American College of Obstetricians and Gynecologists (ACOG) Iffath Abbasi Hoskins, MD.
“Today is a very dark day in health care. It is a dark day, indeed, for the tens of millions of patients who have suddenly and unfairly lost access to safe legal and evidence-based abortion care,” Dr. Hoskins said at a press conference June 24 sponsored by ACOG.
“It is dark for the thousands of clinicians who now, instead of focusing on providing health care to their patients, have to live with the threats of legal, civil, and even professional penalties,” Dr. Hoskins added.
ACOG has 62,000 members and is the leading group of doctors that provides obstetric and gynecologic care.
Dilemma for some doctors?
“I’d like to take a moment to talk about the future of the medical profession,” said ACOG Chief Executive Officer Maureen G. Phipps, MD, MPH. “[The] decision is, as Dr. Hoskins clearly said, a tragic one for our patients in states across the country, but the harm does not end there.”
Dr. Phipps described overturning Roe v. Wade as “the boldest act of legislative interference that we have seen in this country. It will allow state legislators to tell physicians what care they can and cannot provide to their patients.”
“It will leave physicians looking over our shoulders, wondering if a patient is in enough of a crisis to permit an exception to a law,” Dr. Phipps added. “This is an affront to all that drew my colleagues and me into medicine.”
Although the impact on doctor training remains to be seen, she said 44% of ob.gyn. residents are trained in states now empowered to ban abortions.
The effect of the Supreme Court decision on miscarriage management is another unknown.
“It’s going to be very difficult for us, the clinicians, to manage miscarriage,” Dr. Hoskins said. “Many miscarriages could be what we call ‘incomplete’ in the beginning,” where there is still a heartbeat and the patient is cramping and/or bleeding.
In that instance, Dr. Hoskins said, clinicians may be thinking that they have to wait.
“They may be needing to get additional opinions, whether it’s a legal opinion ... or another medical opinion.”
“It’s going to have a devastating effect on every aspect of a woman’s health care, including if she is spontaneously miscarrying,” Dr. Hoskins predicted.
Physician protect thyself?
To what extent doctors can shield themselves from potential prosecution “is a hard question to answer,” Molly Meegan, JD, ACOG’s chief legal officer and general counsel, said.
Ms. Meegan recommended members speak to the risk managers at their individual institutions for guidance.
“It is a real patchwork [of laws] out there, she said. “And that patchwork itself is a danger to people as they seek essential reproductive health care.”
Also, she added, “If a doctor can’t tell what the law is at the time they’re trying to provide the care, it has a terribly chilling effect on medical care.”
Another potential threat to doctors in states that still allow abortion services is action from a neighboring state.
“We are going to be advocating very strongly that states do not have extra-territorial jurisdiction to reach beyond the edges of their state.”
The worry is if a doctor in New Mexico, where abortion is legal, performs an abortion for a person from Texas, where it will soon be illegal, is then prosecuted by Texas, for example.
Medication abortion
Asked about any potential effects on medication abortions, ACOG’s Jen Villavicencio, MD, said it remains to be seen.
“Certainly many of the laws that we have seen, including trigger ban laws, encompass medication abortion,” she said. Several states have these so-called trigger laws, which put into effect laws passed to ban abortion in case Roe was overturned.
This means, she said, that any abortion option, whether it’s procedural or medication, could be and will be banned in some of these states.
Ms. Meegan added that ACOG will continue to support access to medication abortion and that it should be decided by the U.S. Food and Drug Administration and not individual states.
Maternal mortality may rise
“Maternal mortality in and of itself is a very difficult topic,” Dr. Hoskins said, but [the] decision amplifies the implications. “I think of the patients who will have to manage severe complications and mental health challenges while they are carrying a pregnancy that they are forced to carry.”
“I also think of the patients who need to end their pregnancies in order to save their own lives,” Dr. Hoskins added.
Dr. Hoskins said the United States already has a high maternal mortality rate. This new law, she added, could force women into higher-risk situations if they experience high blood pressure, preeclampsia, or bleeding after the birth of the baby.
Growing inequality possible?
“The grievous inequities that exist in this country will grow and expand unchecked without safe access to legal abortion,” Dr. Phipps said.
She noted that women, based on location, will continue “to have protected access to safe evidence-based abortion. Others will have the means and resources and opportunities to secure the care.”
But the same may not be true for women in underserved or disadvantaged communities, Dr. Phipps added.
American Medical Association
ACOG was not the only group to react. “The American Medical Association is deeply disturbed by the U.S. Supreme Court’s decision to overturn nearly a half century of precedent protecting patients’ right to critical reproductive health care,” President Jack Resneck Jr., MD, said in a statement.
The decision represents “an egregious allowance of government intrusion into the medical examination room, a direct attack on the practice of medicine and the patient-physician relationship, and a brazen violation of patients’ rights to evidence-based reproductive health services.”
American Academy of Family Physicians
“The American Academy of Family Physicians is disappointed and disheartened by the Supreme Court’s decision to strike down longstanding protections afforded by Roe v. Wade and Planned Parenthood v. Casey,” President Sterling N. Ransone Jr., MD, said in a statement.
The organization has 127,600 physician and medical student members.
“This decision negatively impacts our practices and our patients by undermining the patient-physician relationship and potentially criminalizing evidence-based medical care,” added Dr. Ransone.
American College of Physicians
“A patient’s decision about whether to continue a pregnancy should be a private decision made in consultation with a physician or other health care professional, without interference from the government,” President Ryan D. Mire, MD, said in a statement. “We strongly oppose medically unnecessary government restrictions on any health care services,” added Dr. Mire on behalf of the group’s 161,000 members.
American Academy of Pediatrics
“This decision carries grave consequences for our adolescent patients, who already face many more barriers than adults in accessing comprehensive reproductive health care services and abortion care,” President Moira Szilagyi, MD, PhD, said in a statement.
“In the wake of this ruling, the American Academy of Pediatrics will continue to support our chapters as states consider policies affecting access to abortion care, and pediatricians will continue to support our patients,” Dr. Szilagyi added.
American Public Health Association
The court’s decision “is a catastrophic judicial failure that will reverberate differently in each state and portends to jeopardize the health and lives of all Americans,” Executive Director Georges C. Benjamin, MD, said in a statement.
American Urogynecologic Society
“The American Urogynecologic Society opposes any ruling that restricts a person’s access to health care and criminalizes the practice of medicine,” the group said in a statement. “This ruling ultimately poses a serious threat to the patient-provider relationship and subsequent decisionmaking necessary to ensure optimal outcomes for patients. As practitioners, we should be free to provide what is in the best interest of our patients.”
A version of this article first appeared on Medscape.com.
‘Can I survive without payments from insurers?’
It took Michael Golden, MD, 5 years to decide to switch to a concierge practice, in which patients pay a monthly or annual fee for more personalized care. Dr. Golden, an internist in Beverly, Mass., changed course in 2021, during the COVID-19 pandemic.
“I’m not sure why I hesitated for so long,” said Dr. Golden.
But taking the plunge is a big step that they sometimes put off for years.
“The main factors for waiting are fear, uncertainty, and doubt,” said Leigh “Jack” Forbush, DO, a family physician who runs a DPC practice in Hampden, Maine, and mentors doctors contemplating the switch.
According to Dr. Forbush, the critical questions doctors ask themselves are, “Will I be able to find enough paying patients?” and – in the case of DPC practices, which cancel insurance – “Can I live without the money I get from insurers?”
Terry Bauer, CEO of Specialdocs Consultants in Highland Park, Ill., which helps doctors move to a concierge practice, said many of his clients put off the decision for as long as 15 years.
“Clients became progressively worn out – or even burnt out – by the demands of fee-for-service medicine,” said Dr. Bauer. “For women, the tipping point can be when their kids ask, ‘Mom, do you like your job better than me?’ For men, it may be more about feeling tired and unsatisfied with their work.”
But once these doctors make the switch, it’s with all their heart. “A client recently told me that if he couldn’t open a concierge practice, he might have to quit medicine,” Dr. Bauer said. “And he’s only 51.”
Few doctors regret switching
A 2020 survey of DPC physicians for the Society of Actuaries found that 99% reported having better or much better overall personal and professional satisfaction.
Retainer-based physicians report feeling much more relaxed after they start a concierge practice. On many workdays, Dr. Golden takes a walk on a trail in the woods behind his office. “That’s something I couldn’t do before,” he said. “And I go to my kids’ soccer games. I’m able to be present in their lives now.”
Since retainer-based doctors have markedly fewer patients, they can form personal relationships with each one. When Dr. Golden switched, he “went from having a couple of thousand patients to a few hundred,” he said.
“I know each patient now,” said Dorothy Cohen Serna, MD, an internist in Cypress, Tex., who moved to concierge in 2017. “I don’t need to look at their chart to know who they are.”
Dr. Serna said patients’ close relationship with her helped them get through the worst months of the pandemic. “They were scared, depressed, and concerned, and they needed a lot of individual attention,” she said.
Because they see fewer patients, concierge doctors can lengthen appointment times to about 30 minutes – or longer, if necessary. They no longer have a problem answering patients’ “doorknob questions” – wholly new concerns brought up at the end of the visit.
“The appointment might be for a sprained ankle, and then the patient might mention they haven’t been sleeping well,” Dr. Golden said. “I have time to talk about that without worrying that my schedule is getting backed up.”
Why patients sign up
Retainer-based practices are still an exotic concept in many areas, but patients are beginning to understand the value, said Shalini Kaneriya, MD, an internist in Herndon, Va,, who switched her practice to concierge in 2018.
Several hundred patients followed her into her new practice because “people realized their care would be better if they had a concierge doctor,” she said. Two years ago, partly because of growing demand, she recruited another physician as an associate.
“People want a relationship with their doctor,” Dr. Serna added. “It’s hard to provide that in a regular practice.”
Todd Granger, MD, an internist who opened a DPC practice in Chapel Hill, N.C., in 2016, said new patients often mention feeling rushed through appointments with their previous doctors. Also, “it’s hard to get to see a doctor around here.”
Scott Bernstein, MD, an internist who runs a DPC practice in Scottsdale, Ariz., said he can arrange to have patients see specialists much faster than if they try to make appointments on their own. “I personally call specialists and then prep my patients on how to deal with the appointment,” he said.
Retainer-based practices tend to have a greater number of older and chronically ill patients, but they also attract patients who need less care. “The healthier patients find value in our proactive approach to prevention and wellness,” Dr. Serna said.
Some concierge physicians charge higher fees to patients who need more care, but many decide this is too complicated and charge everyone the same fee. Dr. Granger said he initially had a variable fee schedule, but when some lower-paying patients began to need more visits, he had to consider charging them extra. “Now I basically have just one fee,” he said.
Not a good fit for many physicians
Dr. Bauer said a lot of physicians are interested in retainer-based practice, but many of them might not make the income they had hoped for. Specialdocs interviews physicians who inquire about the model and ultimately doesn’t contract with 80% of them, Dr. Bauer said.
To be able to sign up and retain enough patients, the doctor’s attitude is important. “You have to be driven by the desire to go deep with patients -- to work hard with them and deal with their issues,” said Erika Bliss, MD, who runs a DPC practice in Seattle.
Dr. Bernstein said retainer-based physicians have to be interested in lifestyle issues, such as diet, exercise, and sleep. “I spend a lot of time dealing with issues like how to incorporate physical activity into daily routines,” he said. “Some doctors wouldn’t enjoy doing that.”
Also, concierge physicians have to be available all the time. “Patients have my cell phone number,” Dr. Granger said. “They could call in the middle of the night, but they usually don’t.”
To ensure that they get some time off, many concierge physicians have partners. Dr. Bernstein and another DPC doctor maintain separate practices but cover for each other. Each takes every other weekend off plus 6 weeks every year.
Can you attract enough patients?
A key challenge is finding enough patients to sustain a concierge practice. Planning the switch involves setting a target number of patients needed for the doctor to make a decent income after paying practice expenses. For example, a doctor charging $300 a month to 250 patients would gross $900,000 per year, and then pay practice expenses from that.
Attracting the target number of patients can take months or even years. After almost 6 years, Dr. Granger said, he has around 240 patients ― well below his target number of 440.
Partly because the practice model is not well known in North Carolina, Dr. Granger set his fee very low, at $60 a month, then raised it to $75. That means his practice has been grossing just $216,000 a year. But he is not about to give up. He plans to raise his fee in July and hopes that word of mouth will add more patients.
If physicians cannot earn enough in their concierge practice, Dr. Bauer said, they may moonlight at a local hospital or work for a telemedicine company. He hasn’t heard of physicians closing their concierge practice and returning to their previous practice model. “They didn’t like what they were doing before,” he said.
Opening up to lower-income patients
Dr. Granger’s $75 monthly fee is an example of how retainer-based medicine has transformed itself from a gold-plated service for rich people to a service that middle-class and even lower-income people can afford. DPC practices like Dr. Granger’s have dramatically lowered expenses by cutting out the need to bill insurance companies. Some DPC practices further reduce expenses by not having any staff and by renting out office space.
Dr. Forbush’s Pine Tree State patients are mostly blue-collar workers – electricians, plumbers, people who work in small businesses. He charges them $150 a month, which most patients who don’t have health insurance can afford. He said three-quarters of his patients lack health insurance, although some have back-up finances, such as health savings accounts.
Since his patients have to pay out of pocket for tests and specialists, Dr. Forbush keeps referrals in check by handling many problems himself. “Since I have more time to spend with the patient, I can often work out issues that other doctors might ask specialists to deal with,” he said.
He has learned some dermatologic procedures. “There are plenty of things I can handle on my own,” he said.
Dr. Granger adds that by examining patients during longer appointments, expensive diagnostic exams are not always necessary.
The challenges for this model
Many experts warn that retainer-based practices won’t work for doctors who want to leave employment or for doctors fresh out of residency. Not having your own patients to bring into the new practice is a big minus, because this is the best way to start the new practice.
Still, there are other ways to find patients. Dr. Bauer said physicians can advertise online, make themselves known by giving speeches in the community, or contract with small employers to treat their workers.
Dr. Bauer said some of his clients were employed physicians, and he thinks they will become a bigger factor now that fewer doctors remain in private practice. The chief barrier for employed physicians is the restrictive covenant that prevents them from setting up a practice nearby. But Dr. Bauer said some employers are willing to waive restrictive covenants for retainer-based doctors.
New physicians are also adopting the concierge model. Dr. Forbush said physicians straight out of residency have set up DPC practices in Maine. They signed up patients for their new practices even before they graduated, he said.
Retainer-based medicine is still mainly limited to primary care physicians, but according to Dr. Bauer, it can also work for specialists who have long-term relationships with patients, such as cardiologists, ob.gyns., rheumatologists, neurologists, and endocrinologists.
No going back
Most doctors who make the switch to retainer-based practice understand that there’s likely no going back. When Dr. Bernstein switched, he announced the change to patients and canceled insurance contracts. “It was make or break,” he said. “I had no parachute.”
A version of this article first appeared on Medscape.com.
It took Michael Golden, MD, 5 years to decide to switch to a concierge practice, in which patients pay a monthly or annual fee for more personalized care. Dr. Golden, an internist in Beverly, Mass., changed course in 2021, during the COVID-19 pandemic.
“I’m not sure why I hesitated for so long,” said Dr. Golden.
But taking the plunge is a big step that they sometimes put off for years.
“The main factors for waiting are fear, uncertainty, and doubt,” said Leigh “Jack” Forbush, DO, a family physician who runs a DPC practice in Hampden, Maine, and mentors doctors contemplating the switch.
According to Dr. Forbush, the critical questions doctors ask themselves are, “Will I be able to find enough paying patients?” and – in the case of DPC practices, which cancel insurance – “Can I live without the money I get from insurers?”
Terry Bauer, CEO of Specialdocs Consultants in Highland Park, Ill., which helps doctors move to a concierge practice, said many of his clients put off the decision for as long as 15 years.
“Clients became progressively worn out – or even burnt out – by the demands of fee-for-service medicine,” said Dr. Bauer. “For women, the tipping point can be when their kids ask, ‘Mom, do you like your job better than me?’ For men, it may be more about feeling tired and unsatisfied with their work.”
But once these doctors make the switch, it’s with all their heart. “A client recently told me that if he couldn’t open a concierge practice, he might have to quit medicine,” Dr. Bauer said. “And he’s only 51.”
Few doctors regret switching
A 2020 survey of DPC physicians for the Society of Actuaries found that 99% reported having better or much better overall personal and professional satisfaction.
Retainer-based physicians report feeling much more relaxed after they start a concierge practice. On many workdays, Dr. Golden takes a walk on a trail in the woods behind his office. “That’s something I couldn’t do before,” he said. “And I go to my kids’ soccer games. I’m able to be present in their lives now.”
Since retainer-based doctors have markedly fewer patients, they can form personal relationships with each one. When Dr. Golden switched, he “went from having a couple of thousand patients to a few hundred,” he said.
“I know each patient now,” said Dorothy Cohen Serna, MD, an internist in Cypress, Tex., who moved to concierge in 2017. “I don’t need to look at their chart to know who they are.”
Dr. Serna said patients’ close relationship with her helped them get through the worst months of the pandemic. “They were scared, depressed, and concerned, and they needed a lot of individual attention,” she said.
Because they see fewer patients, concierge doctors can lengthen appointment times to about 30 minutes – or longer, if necessary. They no longer have a problem answering patients’ “doorknob questions” – wholly new concerns brought up at the end of the visit.
“The appointment might be for a sprained ankle, and then the patient might mention they haven’t been sleeping well,” Dr. Golden said. “I have time to talk about that without worrying that my schedule is getting backed up.”
Why patients sign up
Retainer-based practices are still an exotic concept in many areas, but patients are beginning to understand the value, said Shalini Kaneriya, MD, an internist in Herndon, Va,, who switched her practice to concierge in 2018.
Several hundred patients followed her into her new practice because “people realized their care would be better if they had a concierge doctor,” she said. Two years ago, partly because of growing demand, she recruited another physician as an associate.
“People want a relationship with their doctor,” Dr. Serna added. “It’s hard to provide that in a regular practice.”
Todd Granger, MD, an internist who opened a DPC practice in Chapel Hill, N.C., in 2016, said new patients often mention feeling rushed through appointments with their previous doctors. Also, “it’s hard to get to see a doctor around here.”
Scott Bernstein, MD, an internist who runs a DPC practice in Scottsdale, Ariz., said he can arrange to have patients see specialists much faster than if they try to make appointments on their own. “I personally call specialists and then prep my patients on how to deal with the appointment,” he said.
Retainer-based practices tend to have a greater number of older and chronically ill patients, but they also attract patients who need less care. “The healthier patients find value in our proactive approach to prevention and wellness,” Dr. Serna said.
Some concierge physicians charge higher fees to patients who need more care, but many decide this is too complicated and charge everyone the same fee. Dr. Granger said he initially had a variable fee schedule, but when some lower-paying patients began to need more visits, he had to consider charging them extra. “Now I basically have just one fee,” he said.
Not a good fit for many physicians
Dr. Bauer said a lot of physicians are interested in retainer-based practice, but many of them might not make the income they had hoped for. Specialdocs interviews physicians who inquire about the model and ultimately doesn’t contract with 80% of them, Dr. Bauer said.
To be able to sign up and retain enough patients, the doctor’s attitude is important. “You have to be driven by the desire to go deep with patients -- to work hard with them and deal with their issues,” said Erika Bliss, MD, who runs a DPC practice in Seattle.
Dr. Bernstein said retainer-based physicians have to be interested in lifestyle issues, such as diet, exercise, and sleep. “I spend a lot of time dealing with issues like how to incorporate physical activity into daily routines,” he said. “Some doctors wouldn’t enjoy doing that.”
Also, concierge physicians have to be available all the time. “Patients have my cell phone number,” Dr. Granger said. “They could call in the middle of the night, but they usually don’t.”
To ensure that they get some time off, many concierge physicians have partners. Dr. Bernstein and another DPC doctor maintain separate practices but cover for each other. Each takes every other weekend off plus 6 weeks every year.
Can you attract enough patients?
A key challenge is finding enough patients to sustain a concierge practice. Planning the switch involves setting a target number of patients needed for the doctor to make a decent income after paying practice expenses. For example, a doctor charging $300 a month to 250 patients would gross $900,000 per year, and then pay practice expenses from that.
Attracting the target number of patients can take months or even years. After almost 6 years, Dr. Granger said, he has around 240 patients ― well below his target number of 440.
Partly because the practice model is not well known in North Carolina, Dr. Granger set his fee very low, at $60 a month, then raised it to $75. That means his practice has been grossing just $216,000 a year. But he is not about to give up. He plans to raise his fee in July and hopes that word of mouth will add more patients.
If physicians cannot earn enough in their concierge practice, Dr. Bauer said, they may moonlight at a local hospital or work for a telemedicine company. He hasn’t heard of physicians closing their concierge practice and returning to their previous practice model. “They didn’t like what they were doing before,” he said.
Opening up to lower-income patients
Dr. Granger’s $75 monthly fee is an example of how retainer-based medicine has transformed itself from a gold-plated service for rich people to a service that middle-class and even lower-income people can afford. DPC practices like Dr. Granger’s have dramatically lowered expenses by cutting out the need to bill insurance companies. Some DPC practices further reduce expenses by not having any staff and by renting out office space.
Dr. Forbush’s Pine Tree State patients are mostly blue-collar workers – electricians, plumbers, people who work in small businesses. He charges them $150 a month, which most patients who don’t have health insurance can afford. He said three-quarters of his patients lack health insurance, although some have back-up finances, such as health savings accounts.
Since his patients have to pay out of pocket for tests and specialists, Dr. Forbush keeps referrals in check by handling many problems himself. “Since I have more time to spend with the patient, I can often work out issues that other doctors might ask specialists to deal with,” he said.
He has learned some dermatologic procedures. “There are plenty of things I can handle on my own,” he said.
Dr. Granger adds that by examining patients during longer appointments, expensive diagnostic exams are not always necessary.
The challenges for this model
Many experts warn that retainer-based practices won’t work for doctors who want to leave employment or for doctors fresh out of residency. Not having your own patients to bring into the new practice is a big minus, because this is the best way to start the new practice.
Still, there are other ways to find patients. Dr. Bauer said physicians can advertise online, make themselves known by giving speeches in the community, or contract with small employers to treat their workers.
Dr. Bauer said some of his clients were employed physicians, and he thinks they will become a bigger factor now that fewer doctors remain in private practice. The chief barrier for employed physicians is the restrictive covenant that prevents them from setting up a practice nearby. But Dr. Bauer said some employers are willing to waive restrictive covenants for retainer-based doctors.
New physicians are also adopting the concierge model. Dr. Forbush said physicians straight out of residency have set up DPC practices in Maine. They signed up patients for their new practices even before they graduated, he said.
Retainer-based medicine is still mainly limited to primary care physicians, but according to Dr. Bauer, it can also work for specialists who have long-term relationships with patients, such as cardiologists, ob.gyns., rheumatologists, neurologists, and endocrinologists.
No going back
Most doctors who make the switch to retainer-based practice understand that there’s likely no going back. When Dr. Bernstein switched, he announced the change to patients and canceled insurance contracts. “It was make or break,” he said. “I had no parachute.”
A version of this article first appeared on Medscape.com.
It took Michael Golden, MD, 5 years to decide to switch to a concierge practice, in which patients pay a monthly or annual fee for more personalized care. Dr. Golden, an internist in Beverly, Mass., changed course in 2021, during the COVID-19 pandemic.
“I’m not sure why I hesitated for so long,” said Dr. Golden.
But taking the plunge is a big step that they sometimes put off for years.
“The main factors for waiting are fear, uncertainty, and doubt,” said Leigh “Jack” Forbush, DO, a family physician who runs a DPC practice in Hampden, Maine, and mentors doctors contemplating the switch.
According to Dr. Forbush, the critical questions doctors ask themselves are, “Will I be able to find enough paying patients?” and – in the case of DPC practices, which cancel insurance – “Can I live without the money I get from insurers?”
Terry Bauer, CEO of Specialdocs Consultants in Highland Park, Ill., which helps doctors move to a concierge practice, said many of his clients put off the decision for as long as 15 years.
“Clients became progressively worn out – or even burnt out – by the demands of fee-for-service medicine,” said Dr. Bauer. “For women, the tipping point can be when their kids ask, ‘Mom, do you like your job better than me?’ For men, it may be more about feeling tired and unsatisfied with their work.”
But once these doctors make the switch, it’s with all their heart. “A client recently told me that if he couldn’t open a concierge practice, he might have to quit medicine,” Dr. Bauer said. “And he’s only 51.”
Few doctors regret switching
A 2020 survey of DPC physicians for the Society of Actuaries found that 99% reported having better or much better overall personal and professional satisfaction.
Retainer-based physicians report feeling much more relaxed after they start a concierge practice. On many workdays, Dr. Golden takes a walk on a trail in the woods behind his office. “That’s something I couldn’t do before,” he said. “And I go to my kids’ soccer games. I’m able to be present in their lives now.”
Since retainer-based doctors have markedly fewer patients, they can form personal relationships with each one. When Dr. Golden switched, he “went from having a couple of thousand patients to a few hundred,” he said.
“I know each patient now,” said Dorothy Cohen Serna, MD, an internist in Cypress, Tex., who moved to concierge in 2017. “I don’t need to look at their chart to know who they are.”
Dr. Serna said patients’ close relationship with her helped them get through the worst months of the pandemic. “They were scared, depressed, and concerned, and they needed a lot of individual attention,” she said.
Because they see fewer patients, concierge doctors can lengthen appointment times to about 30 minutes – or longer, if necessary. They no longer have a problem answering patients’ “doorknob questions” – wholly new concerns brought up at the end of the visit.
“The appointment might be for a sprained ankle, and then the patient might mention they haven’t been sleeping well,” Dr. Golden said. “I have time to talk about that without worrying that my schedule is getting backed up.”
Why patients sign up
Retainer-based practices are still an exotic concept in many areas, but patients are beginning to understand the value, said Shalini Kaneriya, MD, an internist in Herndon, Va,, who switched her practice to concierge in 2018.
Several hundred patients followed her into her new practice because “people realized their care would be better if they had a concierge doctor,” she said. Two years ago, partly because of growing demand, she recruited another physician as an associate.
“People want a relationship with their doctor,” Dr. Serna added. “It’s hard to provide that in a regular practice.”
Todd Granger, MD, an internist who opened a DPC practice in Chapel Hill, N.C., in 2016, said new patients often mention feeling rushed through appointments with their previous doctors. Also, “it’s hard to get to see a doctor around here.”
Scott Bernstein, MD, an internist who runs a DPC practice in Scottsdale, Ariz., said he can arrange to have patients see specialists much faster than if they try to make appointments on their own. “I personally call specialists and then prep my patients on how to deal with the appointment,” he said.
Retainer-based practices tend to have a greater number of older and chronically ill patients, but they also attract patients who need less care. “The healthier patients find value in our proactive approach to prevention and wellness,” Dr. Serna said.
Some concierge physicians charge higher fees to patients who need more care, but many decide this is too complicated and charge everyone the same fee. Dr. Granger said he initially had a variable fee schedule, but when some lower-paying patients began to need more visits, he had to consider charging them extra. “Now I basically have just one fee,” he said.
Not a good fit for many physicians
Dr. Bauer said a lot of physicians are interested in retainer-based practice, but many of them might not make the income they had hoped for. Specialdocs interviews physicians who inquire about the model and ultimately doesn’t contract with 80% of them, Dr. Bauer said.
To be able to sign up and retain enough patients, the doctor’s attitude is important. “You have to be driven by the desire to go deep with patients -- to work hard with them and deal with their issues,” said Erika Bliss, MD, who runs a DPC practice in Seattle.
Dr. Bernstein said retainer-based physicians have to be interested in lifestyle issues, such as diet, exercise, and sleep. “I spend a lot of time dealing with issues like how to incorporate physical activity into daily routines,” he said. “Some doctors wouldn’t enjoy doing that.”
Also, concierge physicians have to be available all the time. “Patients have my cell phone number,” Dr. Granger said. “They could call in the middle of the night, but they usually don’t.”
To ensure that they get some time off, many concierge physicians have partners. Dr. Bernstein and another DPC doctor maintain separate practices but cover for each other. Each takes every other weekend off plus 6 weeks every year.
Can you attract enough patients?
A key challenge is finding enough patients to sustain a concierge practice. Planning the switch involves setting a target number of patients needed for the doctor to make a decent income after paying practice expenses. For example, a doctor charging $300 a month to 250 patients would gross $900,000 per year, and then pay practice expenses from that.
Attracting the target number of patients can take months or even years. After almost 6 years, Dr. Granger said, he has around 240 patients ― well below his target number of 440.
Partly because the practice model is not well known in North Carolina, Dr. Granger set his fee very low, at $60 a month, then raised it to $75. That means his practice has been grossing just $216,000 a year. But he is not about to give up. He plans to raise his fee in July and hopes that word of mouth will add more patients.
If physicians cannot earn enough in their concierge practice, Dr. Bauer said, they may moonlight at a local hospital or work for a telemedicine company. He hasn’t heard of physicians closing their concierge practice and returning to their previous practice model. “They didn’t like what they were doing before,” he said.
Opening up to lower-income patients
Dr. Granger’s $75 monthly fee is an example of how retainer-based medicine has transformed itself from a gold-plated service for rich people to a service that middle-class and even lower-income people can afford. DPC practices like Dr. Granger’s have dramatically lowered expenses by cutting out the need to bill insurance companies. Some DPC practices further reduce expenses by not having any staff and by renting out office space.
Dr. Forbush’s Pine Tree State patients are mostly blue-collar workers – electricians, plumbers, people who work in small businesses. He charges them $150 a month, which most patients who don’t have health insurance can afford. He said three-quarters of his patients lack health insurance, although some have back-up finances, such as health savings accounts.
Since his patients have to pay out of pocket for tests and specialists, Dr. Forbush keeps referrals in check by handling many problems himself. “Since I have more time to spend with the patient, I can often work out issues that other doctors might ask specialists to deal with,” he said.
He has learned some dermatologic procedures. “There are plenty of things I can handle on my own,” he said.
Dr. Granger adds that by examining patients during longer appointments, expensive diagnostic exams are not always necessary.
The challenges for this model
Many experts warn that retainer-based practices won’t work for doctors who want to leave employment or for doctors fresh out of residency. Not having your own patients to bring into the new practice is a big minus, because this is the best way to start the new practice.
Still, there are other ways to find patients. Dr. Bauer said physicians can advertise online, make themselves known by giving speeches in the community, or contract with small employers to treat their workers.
Dr. Bauer said some of his clients were employed physicians, and he thinks they will become a bigger factor now that fewer doctors remain in private practice. The chief barrier for employed physicians is the restrictive covenant that prevents them from setting up a practice nearby. But Dr. Bauer said some employers are willing to waive restrictive covenants for retainer-based doctors.
New physicians are also adopting the concierge model. Dr. Forbush said physicians straight out of residency have set up DPC practices in Maine. They signed up patients for their new practices even before they graduated, he said.
Retainer-based medicine is still mainly limited to primary care physicians, but according to Dr. Bauer, it can also work for specialists who have long-term relationships with patients, such as cardiologists, ob.gyns., rheumatologists, neurologists, and endocrinologists.
No going back
Most doctors who make the switch to retainer-based practice understand that there’s likely no going back. When Dr. Bernstein switched, he announced the change to patients and canceled insurance contracts. “It was make or break,” he said. “I had no parachute.”
A version of this article first appeared on Medscape.com.
$3 billion in cancer drug waste: Can it be salvaged?
Three billion dollars: It’s enough to finance the annual out-of-pocket costs for 1 in 7 patients with cancer. It would cover almost half of the National Cancer Institute’s annual budget. And it could fund President Biden’s entire Cancer Moonshot program, with more than a billion to spare.
It’s also how much the United States spends on unused cancer drugs each year, some experts estimate.
Drug companies typically sell infused drugs in one or two single-dose vial sizes, but patients don’t come in such neat packages. A patient may need 300 mg of a drug that is only sold as 200 mg vials, which means half of a vial will go to waste.
Although most oncology drugs don’t incur substantial waste, even small volumes can translate to millions of dollars a year.
But can this money be saved or reallocated, if only we delivered drugs more efficiently?
Some experts don’t believe that’s possible.
“Attempts to recoup money for discarded drugs wouldn’t happen in a vacuum,” said Robin Yabroff, PhD, MBA, an epidemiologist and scientific vice president of Health Services Research at the American Cancer Society, who was part of a committee commissioned to evaluate the costs associated with discarded drugs.
The potential catch of any widespread effort to seek repayment or reduce the amount of discarded drugs, Dr. Yabroff and colleagues note, is that manufacturers would “simply increase the price of the vial.”
In other words, attempting to fix one problem may lead to another — essentially a whack-a-mole of cancer costs, which are projected to balloon to $246 billion by 2030.
What this means is without sweeping policies to rein in cancer care costs, oncologists can only do so much. And every little bit counts.
“We are left chipping away at this monster of cancer care costs,” said Adam Binder, MD, a medical oncologist at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Millions spent on “reasonable amount” of waste
Michal Sarfaty, MD, was excited when enfortumab vedotin came on the market to treat advanced urothelial cancer in late 2019.
The cost of the drug, however, tempered her enthusiasm.
Enfortumab vedotin is a “great drug,” said Dr. Sarfaty, an oncologist at the Sheba Medical Center, Ramat Gan, Israel. But it can cost upwards of $500,000 a year for an average-weight man.
Given the expense, Dr. Sarfaty wanted to understand how much of the drug gets thrown away. During a fellowship at Memorial Sloan Kettering (MSK) Cancer Center in New York, Dr. Sarfaty explored the amount of unused enfortumab vedotin among the 64 patients who received the drug in 2020. She, along with a team at MSK, calculated the price tag of that waste and extrapolated those estimates for patients across the country.
Although waste occurred in almost half of administered doses (367 of 793), only a small volume got discarded — 2.9% per dose, on average.
Multiplying unused milligrams by the cost per milligram, Dr. Sarfaty and colleagues estimated that, for each patient, $3,127 of the drug got discarded. When calculated over the year, the cost came to just over $200,000 at MSK, and nearly $15 million when projected across the approved patient population in the United States.
“Ultimately, we did not see a lot of waste with this specific drug,” Dr. Sarfaty said. “Under 2.9% is considered a reasonable amount, below the 3% threshold Peter Bach, MD, and colleagues recommend. But even with this small amount of waste, the cost per patient and to the system remains notable.”
The problem with recouping drug waste
Estimates from the Centers for Medicare & Medicaid Services (CMS), which tracks costs associated with discarded weight-based drugs covered under Medicare Part B, support the notion that small quantities of discarded drugs can still translate to big bucks.
Since 2017, CMS has required healthcare providers to report the volume of drugs discarded from a single-dose vial using a code, known as the JW modifier. The JW modifier means that providers can be reimbursed for the entire vial amount, not just the quantity the patient used.
In 2019, claims data from Medicare Part B showed that 1.85% of discarded rituximab came to $33.3 million. For infliximab, the 1.55% of discarded liquid translated to $15 million, and just 0.36% of discarded pembrolizumab reached $10 million.
However, experts question whether the JW modifier accurately reflects the quantity of drugs discarded.
According to the 2021 report from the National Academies of Sciences, Engineering, and Medicine (NASEM), most physicians don’t use the JW modifier. Among Medicare claims, 16.2% included the JW modifier in 2017 and 16.9% did in 2018.
The rate was significantly lower for private insurance. Of more than 4 million private insurance claims on 77 drugs made in 2017 and 2018, only 3.6% included the JW modifier; 15 of these drugs had no JW claims.
“Although we found that most physicians don’t use the JW modifier, even those who do, don’t use it consistently, even for the same patient,” said Dr. Yabroff, a co-author on the report.
Going a step further, Dr. Yabroff and colleagues argue that even if everyone used the JW modifier as intended, manufacturers would probably increase the price of drugs to compensate for any loss, potentially eliminating savings for payers.
That’s because, in the United States, manufacturers typically base drug prices on a patient and payers’ “willingness to pay for better health,” not on the volume of liquid used. Take a patient who pays $2,000 to receive the dose they need. If that dose is 600 mg but requires using two vials of 400 mg, then “to the patient, the 600-mg dose is worth $2,000, and the remainder has no value whatsoever,” the NASEM authors argue.
The authors parallel this scenario to purchasing a designer coat or dress. If that item requires alterations that remove a section of material, “the customer does not typically get a rebate because all the fabric was not needed,” the NASEM team writes.
But there’s a flaw in this rationale, argues Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel. A person’s willingness to pay for better health assumes that the price of a drug is based on proper market forces, where a drug’s cost and its effectiveness are in harmony.
“The problem is we’re operating in a broken market where the prices of oncology drugs have no real bearing on their efficacy,” said Dr. Goldstein.
And, as Dr. Bach noted in a 2021 Health Affairs piece, willingness to pay also requires that consumers know what they’re paying and allows them to walk away from an excessively high price.
But neither is a reality.
For one, Dr. Bach explains, companies may lowball the monthly price of a drug. In 2020, GlaxoSmithKline (GSK) announced that its new drug Blenrep would carry a list price of $8,277 per vial, or about $23,900 per month for an average 79 kg (175 lb) patient. That price accounts for two vials of the drug. But, according to Dr. Bach, “what GSK left out is that 44% of U.S. adults weigh more than 80 kg, and above that weight, three vials are needed per dose.” That would raise the average monthly cost to $30,479.
Perhaps more importantly, consumers can’t easily walk away.
“Medicare can’t negotiate prices and is forced to pay what a drug company says,” Dr. Goldstein said. “This is very different to when I buy a coat. If the price is too high, I can walk away.”
Fixed dosing: A solution or a new problem?
Efforts to reduce the financial impact of discarded cancer drugs can blow back on physicians, patients, and payers in other unanticipated ways. Take fixed dosing. Although chemotherapy dosing remains weight-based, many targeted therapies — such as nivolumab and pembrolizumab — recently transitioned to a fixed dosing regimen.
Administering a fixed, instead of weight-based, dose eliminates waste but can create new problems.
“Patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” said Dr. Goldstein. In a 2017 analysis, Dr. Goldstein and colleagues compared dosing strategies in patients with metastatic non–small cell lung cancer who received pembrolizumab. The team found that the total annual cost of weight-based dosing was $2.6 billion, whereas the cost of the fixed dosing strategy was $3.44 billion — 24% more. In other words, personalized weight-based dosing would save more than $825 million dollars in the United States each year.
A 2020 analysis based in France found a similar cost increase of 26% for fixed dosing of pembrolizumab as well as nivolumab.
“I’ve argued we should go back to weight-based dosing,” Dr. Goldstein said. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
Does dose rounding work?
Rose DiMarco, PharmD, BCPS, BCOP, keeps a tight watch on patients being treated at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Dr. DiMarco educates patients about their treatment plan, reviews their lab results, and monitors them for side effects and drug interactions.
She also thinks a lot about costs.
“We spend about $100,000 a day on oncology drugs, and we want to make sure we’re not being wasteful,” Dr. DiMarco said in an interview.
One major initiative to curb waste and reduce costs at Jefferson has centered on dose rounding, which calculates whether a specific dose can be altered slightly to conserve vials and prevent waste. According to the Hematology/Oncology Pharmacy Association, a patient can receive up to 10% more or less of a weight-based dose without impacting treatment efficacy.
If, for instance, a patient requires 380 mg, but two vials come to 400 mg, rounding up that dose by approximately 5% means eliminating 20 mg that would go unused. But if that patient requires 420 mg, rounding down about 5% means substantial savings from not opening a new vial.
At Jefferson, Dr. DiMarco and her pharmacy colleagues map out dose ranges for all patients. Anyone who falls inside the 10% may be eligible for dose rounding. Anyone who doesn’t will receive the usual dose.
Although it is a challenge to implement, dose rounding has become standard of care at many cancer centers across the United States and is linked to substantial savings.
A 2018 analysis projected annual savings of $865,000 associated with rounding down eight monoclonal antibodies for patients with metastatic disease at a community cancer center. A more recent analysis from the Mayo Clinic found that dose rounding saved a total of 9,814 drug vials — 4485 of which were cancer drugs and 5329 of which were biologics — and resulted in $7.3 million in savings over 6 months in 2019 — $1.56 million from oncology agents and $5.7 from biologics.
And in a small 2019 analysis, researchers at Jefferson showed dose rounding of one monoclonal antibody saved approximately $30,000 in just 3 months, Dr. DiMarco noted.
“Not only does this process reduce costs and waste, but it also standardizes the preparation of hazardous medications, which can help prevent medication errors,” Dr. DiMarco said.
Nibbling around the edges
Despite estimates that scale into the billions of dollars, “drug wastage is just a small part of overall cancer costs,” Dr. Sarfaty said.
Fumiko Chino, MD, a radiation oncologist at MSK, agrees. “When we talk about affordability and cost, we can nibble around the edges of what’s really important,” Dr. Chino said. “Discarded drugs may cost a lot when you consider them in aggregate, but they are not as important as negotiated drug prices, which could substantially reduce overall costs.”
And until drug prices are addressed on a broader policy level, the cost of cancer care likely won’t improve in a meaningful way.
“But for the patient sitting in front of me, my focus will always be to provide the best care possible,” Dr. Binder said.
A version of this article first appeared on Medscape.com.
Three billion dollars: It’s enough to finance the annual out-of-pocket costs for 1 in 7 patients with cancer. It would cover almost half of the National Cancer Institute’s annual budget. And it could fund President Biden’s entire Cancer Moonshot program, with more than a billion to spare.
It’s also how much the United States spends on unused cancer drugs each year, some experts estimate.
Drug companies typically sell infused drugs in one or two single-dose vial sizes, but patients don’t come in such neat packages. A patient may need 300 mg of a drug that is only sold as 200 mg vials, which means half of a vial will go to waste.
Although most oncology drugs don’t incur substantial waste, even small volumes can translate to millions of dollars a year.
But can this money be saved or reallocated, if only we delivered drugs more efficiently?
Some experts don’t believe that’s possible.
“Attempts to recoup money for discarded drugs wouldn’t happen in a vacuum,” said Robin Yabroff, PhD, MBA, an epidemiologist and scientific vice president of Health Services Research at the American Cancer Society, who was part of a committee commissioned to evaluate the costs associated with discarded drugs.
The potential catch of any widespread effort to seek repayment or reduce the amount of discarded drugs, Dr. Yabroff and colleagues note, is that manufacturers would “simply increase the price of the vial.”
In other words, attempting to fix one problem may lead to another — essentially a whack-a-mole of cancer costs, which are projected to balloon to $246 billion by 2030.
What this means is without sweeping policies to rein in cancer care costs, oncologists can only do so much. And every little bit counts.
“We are left chipping away at this monster of cancer care costs,” said Adam Binder, MD, a medical oncologist at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Millions spent on “reasonable amount” of waste
Michal Sarfaty, MD, was excited when enfortumab vedotin came on the market to treat advanced urothelial cancer in late 2019.
The cost of the drug, however, tempered her enthusiasm.
Enfortumab vedotin is a “great drug,” said Dr. Sarfaty, an oncologist at the Sheba Medical Center, Ramat Gan, Israel. But it can cost upwards of $500,000 a year for an average-weight man.
Given the expense, Dr. Sarfaty wanted to understand how much of the drug gets thrown away. During a fellowship at Memorial Sloan Kettering (MSK) Cancer Center in New York, Dr. Sarfaty explored the amount of unused enfortumab vedotin among the 64 patients who received the drug in 2020. She, along with a team at MSK, calculated the price tag of that waste and extrapolated those estimates for patients across the country.
Although waste occurred in almost half of administered doses (367 of 793), only a small volume got discarded — 2.9% per dose, on average.
Multiplying unused milligrams by the cost per milligram, Dr. Sarfaty and colleagues estimated that, for each patient, $3,127 of the drug got discarded. When calculated over the year, the cost came to just over $200,000 at MSK, and nearly $15 million when projected across the approved patient population in the United States.
“Ultimately, we did not see a lot of waste with this specific drug,” Dr. Sarfaty said. “Under 2.9% is considered a reasonable amount, below the 3% threshold Peter Bach, MD, and colleagues recommend. But even with this small amount of waste, the cost per patient and to the system remains notable.”
The problem with recouping drug waste
Estimates from the Centers for Medicare & Medicaid Services (CMS), which tracks costs associated with discarded weight-based drugs covered under Medicare Part B, support the notion that small quantities of discarded drugs can still translate to big bucks.
Since 2017, CMS has required healthcare providers to report the volume of drugs discarded from a single-dose vial using a code, known as the JW modifier. The JW modifier means that providers can be reimbursed for the entire vial amount, not just the quantity the patient used.
In 2019, claims data from Medicare Part B showed that 1.85% of discarded rituximab came to $33.3 million. For infliximab, the 1.55% of discarded liquid translated to $15 million, and just 0.36% of discarded pembrolizumab reached $10 million.
However, experts question whether the JW modifier accurately reflects the quantity of drugs discarded.
According to the 2021 report from the National Academies of Sciences, Engineering, and Medicine (NASEM), most physicians don’t use the JW modifier. Among Medicare claims, 16.2% included the JW modifier in 2017 and 16.9% did in 2018.
The rate was significantly lower for private insurance. Of more than 4 million private insurance claims on 77 drugs made in 2017 and 2018, only 3.6% included the JW modifier; 15 of these drugs had no JW claims.
“Although we found that most physicians don’t use the JW modifier, even those who do, don’t use it consistently, even for the same patient,” said Dr. Yabroff, a co-author on the report.
Going a step further, Dr. Yabroff and colleagues argue that even if everyone used the JW modifier as intended, manufacturers would probably increase the price of drugs to compensate for any loss, potentially eliminating savings for payers.
That’s because, in the United States, manufacturers typically base drug prices on a patient and payers’ “willingness to pay for better health,” not on the volume of liquid used. Take a patient who pays $2,000 to receive the dose they need. If that dose is 600 mg but requires using two vials of 400 mg, then “to the patient, the 600-mg dose is worth $2,000, and the remainder has no value whatsoever,” the NASEM authors argue.
The authors parallel this scenario to purchasing a designer coat or dress. If that item requires alterations that remove a section of material, “the customer does not typically get a rebate because all the fabric was not needed,” the NASEM team writes.
But there’s a flaw in this rationale, argues Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel. A person’s willingness to pay for better health assumes that the price of a drug is based on proper market forces, where a drug’s cost and its effectiveness are in harmony.
“The problem is we’re operating in a broken market where the prices of oncology drugs have no real bearing on their efficacy,” said Dr. Goldstein.
And, as Dr. Bach noted in a 2021 Health Affairs piece, willingness to pay also requires that consumers know what they’re paying and allows them to walk away from an excessively high price.
But neither is a reality.
For one, Dr. Bach explains, companies may lowball the monthly price of a drug. In 2020, GlaxoSmithKline (GSK) announced that its new drug Blenrep would carry a list price of $8,277 per vial, or about $23,900 per month for an average 79 kg (175 lb) patient. That price accounts for two vials of the drug. But, according to Dr. Bach, “what GSK left out is that 44% of U.S. adults weigh more than 80 kg, and above that weight, three vials are needed per dose.” That would raise the average monthly cost to $30,479.
Perhaps more importantly, consumers can’t easily walk away.
“Medicare can’t negotiate prices and is forced to pay what a drug company says,” Dr. Goldstein said. “This is very different to when I buy a coat. If the price is too high, I can walk away.”
Fixed dosing: A solution or a new problem?
Efforts to reduce the financial impact of discarded cancer drugs can blow back on physicians, patients, and payers in other unanticipated ways. Take fixed dosing. Although chemotherapy dosing remains weight-based, many targeted therapies — such as nivolumab and pembrolizumab — recently transitioned to a fixed dosing regimen.
Administering a fixed, instead of weight-based, dose eliminates waste but can create new problems.
“Patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” said Dr. Goldstein. In a 2017 analysis, Dr. Goldstein and colleagues compared dosing strategies in patients with metastatic non–small cell lung cancer who received pembrolizumab. The team found that the total annual cost of weight-based dosing was $2.6 billion, whereas the cost of the fixed dosing strategy was $3.44 billion — 24% more. In other words, personalized weight-based dosing would save more than $825 million dollars in the United States each year.
A 2020 analysis based in France found a similar cost increase of 26% for fixed dosing of pembrolizumab as well as nivolumab.
“I’ve argued we should go back to weight-based dosing,” Dr. Goldstein said. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
Does dose rounding work?
Rose DiMarco, PharmD, BCPS, BCOP, keeps a tight watch on patients being treated at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Dr. DiMarco educates patients about their treatment plan, reviews their lab results, and monitors them for side effects and drug interactions.
She also thinks a lot about costs.
“We spend about $100,000 a day on oncology drugs, and we want to make sure we’re not being wasteful,” Dr. DiMarco said in an interview.
One major initiative to curb waste and reduce costs at Jefferson has centered on dose rounding, which calculates whether a specific dose can be altered slightly to conserve vials and prevent waste. According to the Hematology/Oncology Pharmacy Association, a patient can receive up to 10% more or less of a weight-based dose without impacting treatment efficacy.
If, for instance, a patient requires 380 mg, but two vials come to 400 mg, rounding up that dose by approximately 5% means eliminating 20 mg that would go unused. But if that patient requires 420 mg, rounding down about 5% means substantial savings from not opening a new vial.
At Jefferson, Dr. DiMarco and her pharmacy colleagues map out dose ranges for all patients. Anyone who falls inside the 10% may be eligible for dose rounding. Anyone who doesn’t will receive the usual dose.
Although it is a challenge to implement, dose rounding has become standard of care at many cancer centers across the United States and is linked to substantial savings.
A 2018 analysis projected annual savings of $865,000 associated with rounding down eight monoclonal antibodies for patients with metastatic disease at a community cancer center. A more recent analysis from the Mayo Clinic found that dose rounding saved a total of 9,814 drug vials — 4485 of which were cancer drugs and 5329 of which were biologics — and resulted in $7.3 million in savings over 6 months in 2019 — $1.56 million from oncology agents and $5.7 from biologics.
And in a small 2019 analysis, researchers at Jefferson showed dose rounding of one monoclonal antibody saved approximately $30,000 in just 3 months, Dr. DiMarco noted.
“Not only does this process reduce costs and waste, but it also standardizes the preparation of hazardous medications, which can help prevent medication errors,” Dr. DiMarco said.
Nibbling around the edges
Despite estimates that scale into the billions of dollars, “drug wastage is just a small part of overall cancer costs,” Dr. Sarfaty said.
Fumiko Chino, MD, a radiation oncologist at MSK, agrees. “When we talk about affordability and cost, we can nibble around the edges of what’s really important,” Dr. Chino said. “Discarded drugs may cost a lot when you consider them in aggregate, but they are not as important as negotiated drug prices, which could substantially reduce overall costs.”
And until drug prices are addressed on a broader policy level, the cost of cancer care likely won’t improve in a meaningful way.
“But for the patient sitting in front of me, my focus will always be to provide the best care possible,” Dr. Binder said.
A version of this article first appeared on Medscape.com.
Three billion dollars: It’s enough to finance the annual out-of-pocket costs for 1 in 7 patients with cancer. It would cover almost half of the National Cancer Institute’s annual budget. And it could fund President Biden’s entire Cancer Moonshot program, with more than a billion to spare.
It’s also how much the United States spends on unused cancer drugs each year, some experts estimate.
Drug companies typically sell infused drugs in one or two single-dose vial sizes, but patients don’t come in such neat packages. A patient may need 300 mg of a drug that is only sold as 200 mg vials, which means half of a vial will go to waste.
Although most oncology drugs don’t incur substantial waste, even small volumes can translate to millions of dollars a year.
But can this money be saved or reallocated, if only we delivered drugs more efficiently?
Some experts don’t believe that’s possible.
“Attempts to recoup money for discarded drugs wouldn’t happen in a vacuum,” said Robin Yabroff, PhD, MBA, an epidemiologist and scientific vice president of Health Services Research at the American Cancer Society, who was part of a committee commissioned to evaluate the costs associated with discarded drugs.
The potential catch of any widespread effort to seek repayment or reduce the amount of discarded drugs, Dr. Yabroff and colleagues note, is that manufacturers would “simply increase the price of the vial.”
In other words, attempting to fix one problem may lead to another — essentially a whack-a-mole of cancer costs, which are projected to balloon to $246 billion by 2030.
What this means is without sweeping policies to rein in cancer care costs, oncologists can only do so much. And every little bit counts.
“We are left chipping away at this monster of cancer care costs,” said Adam Binder, MD, a medical oncologist at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Millions spent on “reasonable amount” of waste
Michal Sarfaty, MD, was excited when enfortumab vedotin came on the market to treat advanced urothelial cancer in late 2019.
The cost of the drug, however, tempered her enthusiasm.
Enfortumab vedotin is a “great drug,” said Dr. Sarfaty, an oncologist at the Sheba Medical Center, Ramat Gan, Israel. But it can cost upwards of $500,000 a year for an average-weight man.
Given the expense, Dr. Sarfaty wanted to understand how much of the drug gets thrown away. During a fellowship at Memorial Sloan Kettering (MSK) Cancer Center in New York, Dr. Sarfaty explored the amount of unused enfortumab vedotin among the 64 patients who received the drug in 2020. She, along with a team at MSK, calculated the price tag of that waste and extrapolated those estimates for patients across the country.
Although waste occurred in almost half of administered doses (367 of 793), only a small volume got discarded — 2.9% per dose, on average.
Multiplying unused milligrams by the cost per milligram, Dr. Sarfaty and colleagues estimated that, for each patient, $3,127 of the drug got discarded. When calculated over the year, the cost came to just over $200,000 at MSK, and nearly $15 million when projected across the approved patient population in the United States.
“Ultimately, we did not see a lot of waste with this specific drug,” Dr. Sarfaty said. “Under 2.9% is considered a reasonable amount, below the 3% threshold Peter Bach, MD, and colleagues recommend. But even with this small amount of waste, the cost per patient and to the system remains notable.”
The problem with recouping drug waste
Estimates from the Centers for Medicare & Medicaid Services (CMS), which tracks costs associated with discarded weight-based drugs covered under Medicare Part B, support the notion that small quantities of discarded drugs can still translate to big bucks.
Since 2017, CMS has required healthcare providers to report the volume of drugs discarded from a single-dose vial using a code, known as the JW modifier. The JW modifier means that providers can be reimbursed for the entire vial amount, not just the quantity the patient used.
In 2019, claims data from Medicare Part B showed that 1.85% of discarded rituximab came to $33.3 million. For infliximab, the 1.55% of discarded liquid translated to $15 million, and just 0.36% of discarded pembrolizumab reached $10 million.
However, experts question whether the JW modifier accurately reflects the quantity of drugs discarded.
According to the 2021 report from the National Academies of Sciences, Engineering, and Medicine (NASEM), most physicians don’t use the JW modifier. Among Medicare claims, 16.2% included the JW modifier in 2017 and 16.9% did in 2018.
The rate was significantly lower for private insurance. Of more than 4 million private insurance claims on 77 drugs made in 2017 and 2018, only 3.6% included the JW modifier; 15 of these drugs had no JW claims.
“Although we found that most physicians don’t use the JW modifier, even those who do, don’t use it consistently, even for the same patient,” said Dr. Yabroff, a co-author on the report.
Going a step further, Dr. Yabroff and colleagues argue that even if everyone used the JW modifier as intended, manufacturers would probably increase the price of drugs to compensate for any loss, potentially eliminating savings for payers.
That’s because, in the United States, manufacturers typically base drug prices on a patient and payers’ “willingness to pay for better health,” not on the volume of liquid used. Take a patient who pays $2,000 to receive the dose they need. If that dose is 600 mg but requires using two vials of 400 mg, then “to the patient, the 600-mg dose is worth $2,000, and the remainder has no value whatsoever,” the NASEM authors argue.
The authors parallel this scenario to purchasing a designer coat or dress. If that item requires alterations that remove a section of material, “the customer does not typically get a rebate because all the fabric was not needed,” the NASEM team writes.
But there’s a flaw in this rationale, argues Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel. A person’s willingness to pay for better health assumes that the price of a drug is based on proper market forces, where a drug’s cost and its effectiveness are in harmony.
“The problem is we’re operating in a broken market where the prices of oncology drugs have no real bearing on their efficacy,” said Dr. Goldstein.
And, as Dr. Bach noted in a 2021 Health Affairs piece, willingness to pay also requires that consumers know what they’re paying and allows them to walk away from an excessively high price.
But neither is a reality.
For one, Dr. Bach explains, companies may lowball the monthly price of a drug. In 2020, GlaxoSmithKline (GSK) announced that its new drug Blenrep would carry a list price of $8,277 per vial, or about $23,900 per month for an average 79 kg (175 lb) patient. That price accounts for two vials of the drug. But, according to Dr. Bach, “what GSK left out is that 44% of U.S. adults weigh more than 80 kg, and above that weight, three vials are needed per dose.” That would raise the average monthly cost to $30,479.
Perhaps more importantly, consumers can’t easily walk away.
“Medicare can’t negotiate prices and is forced to pay what a drug company says,” Dr. Goldstein said. “This is very different to when I buy a coat. If the price is too high, I can walk away.”
Fixed dosing: A solution or a new problem?
Efforts to reduce the financial impact of discarded cancer drugs can blow back on physicians, patients, and payers in other unanticipated ways. Take fixed dosing. Although chemotherapy dosing remains weight-based, many targeted therapies — such as nivolumab and pembrolizumab — recently transitioned to a fixed dosing regimen.
Administering a fixed, instead of weight-based, dose eliminates waste but can create new problems.
“Patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” said Dr. Goldstein. In a 2017 analysis, Dr. Goldstein and colleagues compared dosing strategies in patients with metastatic non–small cell lung cancer who received pembrolizumab. The team found that the total annual cost of weight-based dosing was $2.6 billion, whereas the cost of the fixed dosing strategy was $3.44 billion — 24% more. In other words, personalized weight-based dosing would save more than $825 million dollars in the United States each year.
A 2020 analysis based in France found a similar cost increase of 26% for fixed dosing of pembrolizumab as well as nivolumab.
“I’ve argued we should go back to weight-based dosing,” Dr. Goldstein said. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
Does dose rounding work?
Rose DiMarco, PharmD, BCPS, BCOP, keeps a tight watch on patients being treated at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Dr. DiMarco educates patients about their treatment plan, reviews their lab results, and monitors them for side effects and drug interactions.
She also thinks a lot about costs.
“We spend about $100,000 a day on oncology drugs, and we want to make sure we’re not being wasteful,” Dr. DiMarco said in an interview.
One major initiative to curb waste and reduce costs at Jefferson has centered on dose rounding, which calculates whether a specific dose can be altered slightly to conserve vials and prevent waste. According to the Hematology/Oncology Pharmacy Association, a patient can receive up to 10% more or less of a weight-based dose without impacting treatment efficacy.
If, for instance, a patient requires 380 mg, but two vials come to 400 mg, rounding up that dose by approximately 5% means eliminating 20 mg that would go unused. But if that patient requires 420 mg, rounding down about 5% means substantial savings from not opening a new vial.
At Jefferson, Dr. DiMarco and her pharmacy colleagues map out dose ranges for all patients. Anyone who falls inside the 10% may be eligible for dose rounding. Anyone who doesn’t will receive the usual dose.
Although it is a challenge to implement, dose rounding has become standard of care at many cancer centers across the United States and is linked to substantial savings.
A 2018 analysis projected annual savings of $865,000 associated with rounding down eight monoclonal antibodies for patients with metastatic disease at a community cancer center. A more recent analysis from the Mayo Clinic found that dose rounding saved a total of 9,814 drug vials — 4485 of which were cancer drugs and 5329 of which were biologics — and resulted in $7.3 million in savings over 6 months in 2019 — $1.56 million from oncology agents and $5.7 from biologics.
And in a small 2019 analysis, researchers at Jefferson showed dose rounding of one monoclonal antibody saved approximately $30,000 in just 3 months, Dr. DiMarco noted.
“Not only does this process reduce costs and waste, but it also standardizes the preparation of hazardous medications, which can help prevent medication errors,” Dr. DiMarco said.
Nibbling around the edges
Despite estimates that scale into the billions of dollars, “drug wastage is just a small part of overall cancer costs,” Dr. Sarfaty said.
Fumiko Chino, MD, a radiation oncologist at MSK, agrees. “When we talk about affordability and cost, we can nibble around the edges of what’s really important,” Dr. Chino said. “Discarded drugs may cost a lot when you consider them in aggregate, but they are not as important as negotiated drug prices, which could substantially reduce overall costs.”
And until drug prices are addressed on a broader policy level, the cost of cancer care likely won’t improve in a meaningful way.
“But for the patient sitting in front of me, my focus will always be to provide the best care possible,” Dr. Binder said.
A version of this article first appeared on Medscape.com.
Advance directives for psychiatric care reduce compulsory admissions
, new research shows.
Results of a randomized trial showed the peer worker PAD group had a 42% reduction in compulsory admission over the following 12 months. This study group also had lower symptom scores, greater rates of recovery, and increased empowerment, compared with patients assigned to usual care.
In addition to proving that PADs are effective in reducing compulsory admission, the results show that facilitation by peer workers is relevant, study investigator Aurélie Tinland, MD, PhD, Faculté de Médecine Timone, Aix-Marseille University, Marseille, France, told delegates attending the virtual European Psychiatric Association (EPA) 2022 Congress. The study was simultaneously published online in JAMA Psychiatry.
However, Dr. Tinland noted that more research that includes “harder to reach” populations is needed. In addition, greater use of PADs is also key to reducing compulsory admissions.
‘Most coercive’ country
The researchers note that respect for patient autonomy is a strong pillar of health care, such that “involuntary treatment should be unusual.” However, they point out that “compulsory psychiatric admissions are far too common in countries of all income levels.”
In France, said Dr. Tinland, 24% of psychiatric hospitalizations are compulsory. The country is ranked the sixth “most coercive” country in the world, and there are concerns about human rights in French psychiatric facilities.
She added that advance care statements are the most efficient tool for reducing coercion, with one study suggesting they could cut rates by 25%, compared with usual care.
However, she noted there is an “asymmetry” between medical professionals and patients and a risk of “undue influence” when clinicians facilitate the completion of care statements.
To examine the impact on clinical outcomes of peer-worker facilitated PADs, the researchers studied adults with a diagnosis of schizophrenia, bipolar I disorder, or schizoaffective disorder who were admitted to a psychiatric hospital within the previous 12 months. Peer workers are individuals who have lived experience with mental illness and help inform and guide current patients about care options in the event of a mental health crisis.
Study participants were randomly assigned 1:1 to an intervention group or a usual care control group. The intervention group received a PAD document and were assigned a peer worker while the usual care group received comprehensive information about the PAD concept at study entry and were free to complete it, but they were not connected with a peer worker.
The PAD document included information about future treatment and support preferences, early signs of relapse, and coping strategies. Participants could meet the peer worker in a place of their choice and be supported in drafting the document and in sharing it with health care professionals.
In all, 394 individuals completed the study. The majority (61%) of participants were male and 66% had completed post-secondary education. Schizophrenia was diagnosed in 45%, bipolar I disorder in 36%, and schizoaffective disorder in 19%.
Participants in the intervention group were significantly younger than those in the control group, with a mean of 37.4 years versus 41 years (P = .003) and were less likely to have one or more somatic comorbidities, at 61.2% versus 69.2%.
A PAD was completed by 54.6% of individuals in the intervention group versus 7.1% of controls (P < .001). The PAD was written with peer worker support by 41.3% of those in the intervention and by 2% of controls. Of those who completed a PAD, 75.7% met care facilitators, and 27.1% used it during a crisis over the following 12 months.
Results showed that the rate of compulsory admissions was significantly lower in the peer worker PAD group, at 27% versus 39.9% in control participants, at an odds ratio of 0.58 (P = .007).
Participants in the intervention group had lower symptoms on the modified Colorado Symptom Score than usual care patients with an effect size of -0.20 (P = .03) and higher scores on the Empowerment Scale (effect size 0.30, P = .003).
Scores on the Recovery Assessment Scale were also significantly higher in the peer worker PAD group versus controls with an effect size of 0.44 (P < .001). There were no significant differences, however, in overall admission rates, the quality of the therapeutic alliance, or quality of life.
Putting patients in the driver’s seat
Commenting on the findings, Robert Dabney Jr., MA, MDiv, peer apprentice program manager at the Depression and Bipolar Support Alliance, Chicago, said the study “tells us there are many benefits to completing a psychiatric advance directive, but perhaps the most powerful one is putting the person receiving mental health care in the driver’s seat of their own recovery.”
However, he noted that “many people living with mental health conditions don’t know the option exists to decide on their treatment plan in advance of a crisis.”
“This is where peer support specialists can come in. Having a peer who has been through similar experiences and can guide you through the process is as comforting as it is empowering. I have witnessed and experienced firsthand the power of peer support,” he said.
“It’s my personal hope and the goal of the Depression and Bipolar Support Alliance to empower more people to either become peer support specialists or seek out peer support services, because we know it improves and even saves lives,” Mr. Dabney added.
Virginia A. Brown, PhD, department of psychiatry & behavioral sciences, University of Texas at Austin Dell Medical School, noted there are huge differences between the health care systems in France and the United States.
She explained that two of the greatest barriers to PADs in the United States is that until 2016, filling one out was not billable and that “practitioners don’t know anything about advanced care plans.”
Dr. Brown said her own work shows that individuals who support patients during a crisis believe it would be “really helpful if we had some kind of document that we could share with the health care system that says: ‘Hey, look, I’m the designated person to speak for this patient, they’ve identified me through a document.’ So, people were actually describing a need for this document but didn’t know that it existed.”
Another problem is that in the United States, hospitals operate in a “closed system” and cannot talk to an unrelated hospital or to the police department “to get information to those first responders during an emergency about who to talk to about their wishes and preferences.”
“There are a lot of hurdles that we’ve got to get over to make a more robust system that protects the autonomy of people who live with serious mental illness,” Dr. Brown said, as “losing capacity during a crisis is time-limited, and it requires us to respond to it as a medical emergency.”
The study was supported by an institutional grant from the French 2017 National Program of Health Services Research. The Clinical Research Direction of Assistance Publique Hôpitaux de Marseille sponsored the trial. Dr. Tinland declares grants from the French Ministry of Health Directorate General of Health Care Services during the conduct of the study.
A version of this article first appeared on Medscape.com.
, new research shows.
Results of a randomized trial showed the peer worker PAD group had a 42% reduction in compulsory admission over the following 12 months. This study group also had lower symptom scores, greater rates of recovery, and increased empowerment, compared with patients assigned to usual care.
In addition to proving that PADs are effective in reducing compulsory admission, the results show that facilitation by peer workers is relevant, study investigator Aurélie Tinland, MD, PhD, Faculté de Médecine Timone, Aix-Marseille University, Marseille, France, told delegates attending the virtual European Psychiatric Association (EPA) 2022 Congress. The study was simultaneously published online in JAMA Psychiatry.
However, Dr. Tinland noted that more research that includes “harder to reach” populations is needed. In addition, greater use of PADs is also key to reducing compulsory admissions.
‘Most coercive’ country
The researchers note that respect for patient autonomy is a strong pillar of health care, such that “involuntary treatment should be unusual.” However, they point out that “compulsory psychiatric admissions are far too common in countries of all income levels.”
In France, said Dr. Tinland, 24% of psychiatric hospitalizations are compulsory. The country is ranked the sixth “most coercive” country in the world, and there are concerns about human rights in French psychiatric facilities.
She added that advance care statements are the most efficient tool for reducing coercion, with one study suggesting they could cut rates by 25%, compared with usual care.
However, she noted there is an “asymmetry” between medical professionals and patients and a risk of “undue influence” when clinicians facilitate the completion of care statements.
To examine the impact on clinical outcomes of peer-worker facilitated PADs, the researchers studied adults with a diagnosis of schizophrenia, bipolar I disorder, or schizoaffective disorder who were admitted to a psychiatric hospital within the previous 12 months. Peer workers are individuals who have lived experience with mental illness and help inform and guide current patients about care options in the event of a mental health crisis.
Study participants were randomly assigned 1:1 to an intervention group or a usual care control group. The intervention group received a PAD document and were assigned a peer worker while the usual care group received comprehensive information about the PAD concept at study entry and were free to complete it, but they were not connected with a peer worker.
The PAD document included information about future treatment and support preferences, early signs of relapse, and coping strategies. Participants could meet the peer worker in a place of their choice and be supported in drafting the document and in sharing it with health care professionals.
In all, 394 individuals completed the study. The majority (61%) of participants were male and 66% had completed post-secondary education. Schizophrenia was diagnosed in 45%, bipolar I disorder in 36%, and schizoaffective disorder in 19%.
Participants in the intervention group were significantly younger than those in the control group, with a mean of 37.4 years versus 41 years (P = .003) and were less likely to have one or more somatic comorbidities, at 61.2% versus 69.2%.
A PAD was completed by 54.6% of individuals in the intervention group versus 7.1% of controls (P < .001). The PAD was written with peer worker support by 41.3% of those in the intervention and by 2% of controls. Of those who completed a PAD, 75.7% met care facilitators, and 27.1% used it during a crisis over the following 12 months.
Results showed that the rate of compulsory admissions was significantly lower in the peer worker PAD group, at 27% versus 39.9% in control participants, at an odds ratio of 0.58 (P = .007).
Participants in the intervention group had lower symptoms on the modified Colorado Symptom Score than usual care patients with an effect size of -0.20 (P = .03) and higher scores on the Empowerment Scale (effect size 0.30, P = .003).
Scores on the Recovery Assessment Scale were also significantly higher in the peer worker PAD group versus controls with an effect size of 0.44 (P < .001). There were no significant differences, however, in overall admission rates, the quality of the therapeutic alliance, or quality of life.
Putting patients in the driver’s seat
Commenting on the findings, Robert Dabney Jr., MA, MDiv, peer apprentice program manager at the Depression and Bipolar Support Alliance, Chicago, said the study “tells us there are many benefits to completing a psychiatric advance directive, but perhaps the most powerful one is putting the person receiving mental health care in the driver’s seat of their own recovery.”
However, he noted that “many people living with mental health conditions don’t know the option exists to decide on their treatment plan in advance of a crisis.”
“This is where peer support specialists can come in. Having a peer who has been through similar experiences and can guide you through the process is as comforting as it is empowering. I have witnessed and experienced firsthand the power of peer support,” he said.
“It’s my personal hope and the goal of the Depression and Bipolar Support Alliance to empower more people to either become peer support specialists or seek out peer support services, because we know it improves and even saves lives,” Mr. Dabney added.
Virginia A. Brown, PhD, department of psychiatry & behavioral sciences, University of Texas at Austin Dell Medical School, noted there are huge differences between the health care systems in France and the United States.
She explained that two of the greatest barriers to PADs in the United States is that until 2016, filling one out was not billable and that “practitioners don’t know anything about advanced care plans.”
Dr. Brown said her own work shows that individuals who support patients during a crisis believe it would be “really helpful if we had some kind of document that we could share with the health care system that says: ‘Hey, look, I’m the designated person to speak for this patient, they’ve identified me through a document.’ So, people were actually describing a need for this document but didn’t know that it existed.”
Another problem is that in the United States, hospitals operate in a “closed system” and cannot talk to an unrelated hospital or to the police department “to get information to those first responders during an emergency about who to talk to about their wishes and preferences.”
“There are a lot of hurdles that we’ve got to get over to make a more robust system that protects the autonomy of people who live with serious mental illness,” Dr. Brown said, as “losing capacity during a crisis is time-limited, and it requires us to respond to it as a medical emergency.”
The study was supported by an institutional grant from the French 2017 National Program of Health Services Research. The Clinical Research Direction of Assistance Publique Hôpitaux de Marseille sponsored the trial. Dr. Tinland declares grants from the French Ministry of Health Directorate General of Health Care Services during the conduct of the study.
A version of this article first appeared on Medscape.com.
, new research shows.
Results of a randomized trial showed the peer worker PAD group had a 42% reduction in compulsory admission over the following 12 months. This study group also had lower symptom scores, greater rates of recovery, and increased empowerment, compared with patients assigned to usual care.
In addition to proving that PADs are effective in reducing compulsory admission, the results show that facilitation by peer workers is relevant, study investigator Aurélie Tinland, MD, PhD, Faculté de Médecine Timone, Aix-Marseille University, Marseille, France, told delegates attending the virtual European Psychiatric Association (EPA) 2022 Congress. The study was simultaneously published online in JAMA Psychiatry.
However, Dr. Tinland noted that more research that includes “harder to reach” populations is needed. In addition, greater use of PADs is also key to reducing compulsory admissions.
‘Most coercive’ country
The researchers note that respect for patient autonomy is a strong pillar of health care, such that “involuntary treatment should be unusual.” However, they point out that “compulsory psychiatric admissions are far too common in countries of all income levels.”
In France, said Dr. Tinland, 24% of psychiatric hospitalizations are compulsory. The country is ranked the sixth “most coercive” country in the world, and there are concerns about human rights in French psychiatric facilities.
She added that advance care statements are the most efficient tool for reducing coercion, with one study suggesting they could cut rates by 25%, compared with usual care.
However, she noted there is an “asymmetry” between medical professionals and patients and a risk of “undue influence” when clinicians facilitate the completion of care statements.
To examine the impact on clinical outcomes of peer-worker facilitated PADs, the researchers studied adults with a diagnosis of schizophrenia, bipolar I disorder, or schizoaffective disorder who were admitted to a psychiatric hospital within the previous 12 months. Peer workers are individuals who have lived experience with mental illness and help inform and guide current patients about care options in the event of a mental health crisis.
Study participants were randomly assigned 1:1 to an intervention group or a usual care control group. The intervention group received a PAD document and were assigned a peer worker while the usual care group received comprehensive information about the PAD concept at study entry and were free to complete it, but they were not connected with a peer worker.
The PAD document included information about future treatment and support preferences, early signs of relapse, and coping strategies. Participants could meet the peer worker in a place of their choice and be supported in drafting the document and in sharing it with health care professionals.
In all, 394 individuals completed the study. The majority (61%) of participants were male and 66% had completed post-secondary education. Schizophrenia was diagnosed in 45%, bipolar I disorder in 36%, and schizoaffective disorder in 19%.
Participants in the intervention group were significantly younger than those in the control group, with a mean of 37.4 years versus 41 years (P = .003) and were less likely to have one or more somatic comorbidities, at 61.2% versus 69.2%.
A PAD was completed by 54.6% of individuals in the intervention group versus 7.1% of controls (P < .001). The PAD was written with peer worker support by 41.3% of those in the intervention and by 2% of controls. Of those who completed a PAD, 75.7% met care facilitators, and 27.1% used it during a crisis over the following 12 months.
Results showed that the rate of compulsory admissions was significantly lower in the peer worker PAD group, at 27% versus 39.9% in control participants, at an odds ratio of 0.58 (P = .007).
Participants in the intervention group had lower symptoms on the modified Colorado Symptom Score than usual care patients with an effect size of -0.20 (P = .03) and higher scores on the Empowerment Scale (effect size 0.30, P = .003).
Scores on the Recovery Assessment Scale were also significantly higher in the peer worker PAD group versus controls with an effect size of 0.44 (P < .001). There were no significant differences, however, in overall admission rates, the quality of the therapeutic alliance, or quality of life.
Putting patients in the driver’s seat
Commenting on the findings, Robert Dabney Jr., MA, MDiv, peer apprentice program manager at the Depression and Bipolar Support Alliance, Chicago, said the study “tells us there are many benefits to completing a psychiatric advance directive, but perhaps the most powerful one is putting the person receiving mental health care in the driver’s seat of their own recovery.”
However, he noted that “many people living with mental health conditions don’t know the option exists to decide on their treatment plan in advance of a crisis.”
“This is where peer support specialists can come in. Having a peer who has been through similar experiences and can guide you through the process is as comforting as it is empowering. I have witnessed and experienced firsthand the power of peer support,” he said.
“It’s my personal hope and the goal of the Depression and Bipolar Support Alliance to empower more people to either become peer support specialists or seek out peer support services, because we know it improves and even saves lives,” Mr. Dabney added.
Virginia A. Brown, PhD, department of psychiatry & behavioral sciences, University of Texas at Austin Dell Medical School, noted there are huge differences between the health care systems in France and the United States.
She explained that two of the greatest barriers to PADs in the United States is that until 2016, filling one out was not billable and that “practitioners don’t know anything about advanced care plans.”
Dr. Brown said her own work shows that individuals who support patients during a crisis believe it would be “really helpful if we had some kind of document that we could share with the health care system that says: ‘Hey, look, I’m the designated person to speak for this patient, they’ve identified me through a document.’ So, people were actually describing a need for this document but didn’t know that it existed.”
Another problem is that in the United States, hospitals operate in a “closed system” and cannot talk to an unrelated hospital or to the police department “to get information to those first responders during an emergency about who to talk to about their wishes and preferences.”
“There are a lot of hurdles that we’ve got to get over to make a more robust system that protects the autonomy of people who live with serious mental illness,” Dr. Brown said, as “losing capacity during a crisis is time-limited, and it requires us to respond to it as a medical emergency.”
The study was supported by an institutional grant from the French 2017 National Program of Health Services Research. The Clinical Research Direction of Assistance Publique Hôpitaux de Marseille sponsored the trial. Dr. Tinland declares grants from the French Ministry of Health Directorate General of Health Care Services during the conduct of the study.
A version of this article first appeared on Medscape.com.
FROM EPA 2022
Fridays at the oasis
Growing up, my dad would often go to his law office on weekends to get work done.
As a kid I didn’t really understand this. Dad had an office at home, and could close the door if he needed to. Usually he did this, but sometimes he left to go to his REAL office.
And now ... I sometimes do the same thing.
I don’t see patients on Fridays these days. In the postpandemic world my schedule still hasn’t returned to normal (maybe it never will and this is the new normal), and with research and case reviews and other stuff it seemed logical to just work from home and do them that day. My staff works from home, so if I’m not seeing patients, why can’t I?
After a few Fridays of this, I began going to my empty office, too, and understood where my dad was coming from.
My little solo office, as non-fancy as it is (the carpeting and interior are all from 1993), is quiet. From my back office I can’t hear the corridor hustle and bustle of people going to their appointments or arguing on a cell phone. Just the hum of the air conditioner and the occasional few seconds of a car alarm outside. If I put on iTunes no one complains about my musical tastes.
There isn’t much to do there BUT work, which is the idea. The building’s wifi is too slow to stream or watch Youtube. I’m not tempted to work on a puzzle with my daughter, take a book off a shelf, play with my dogs, or go down the hall for a nap. All the little things we do to procrastinate aren’t there, like convincing myself that I need to clean the pool or balance the checkbook ASAP.
I don’t have the distractions of my dogs barking at passing cars, or kids going up and down the hall, or the phone ringing with people asking who I’m voting for.
My little office is a private oasis, of sorts. Quiet and undisturbed.
Not quite Superman’s Fortress of Solitude, but close enough for me.
And, with all due respect to the Man of Steel, the Fortress of Solitude doesn’t have a Keurig.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Growing up, my dad would often go to his law office on weekends to get work done.
As a kid I didn’t really understand this. Dad had an office at home, and could close the door if he needed to. Usually he did this, but sometimes he left to go to his REAL office.
And now ... I sometimes do the same thing.
I don’t see patients on Fridays these days. In the postpandemic world my schedule still hasn’t returned to normal (maybe it never will and this is the new normal), and with research and case reviews and other stuff it seemed logical to just work from home and do them that day. My staff works from home, so if I’m not seeing patients, why can’t I?
After a few Fridays of this, I began going to my empty office, too, and understood where my dad was coming from.
My little solo office, as non-fancy as it is (the carpeting and interior are all from 1993), is quiet. From my back office I can’t hear the corridor hustle and bustle of people going to their appointments or arguing on a cell phone. Just the hum of the air conditioner and the occasional few seconds of a car alarm outside. If I put on iTunes no one complains about my musical tastes.
There isn’t much to do there BUT work, which is the idea. The building’s wifi is too slow to stream or watch Youtube. I’m not tempted to work on a puzzle with my daughter, take a book off a shelf, play with my dogs, or go down the hall for a nap. All the little things we do to procrastinate aren’t there, like convincing myself that I need to clean the pool or balance the checkbook ASAP.
I don’t have the distractions of my dogs barking at passing cars, or kids going up and down the hall, or the phone ringing with people asking who I’m voting for.
My little office is a private oasis, of sorts. Quiet and undisturbed.
Not quite Superman’s Fortress of Solitude, but close enough for me.
And, with all due respect to the Man of Steel, the Fortress of Solitude doesn’t have a Keurig.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Growing up, my dad would often go to his law office on weekends to get work done.
As a kid I didn’t really understand this. Dad had an office at home, and could close the door if he needed to. Usually he did this, but sometimes he left to go to his REAL office.
And now ... I sometimes do the same thing.
I don’t see patients on Fridays these days. In the postpandemic world my schedule still hasn’t returned to normal (maybe it never will and this is the new normal), and with research and case reviews and other stuff it seemed logical to just work from home and do them that day. My staff works from home, so if I’m not seeing patients, why can’t I?
After a few Fridays of this, I began going to my empty office, too, and understood where my dad was coming from.
My little solo office, as non-fancy as it is (the carpeting and interior are all from 1993), is quiet. From my back office I can’t hear the corridor hustle and bustle of people going to their appointments or arguing on a cell phone. Just the hum of the air conditioner and the occasional few seconds of a car alarm outside. If I put on iTunes no one complains about my musical tastes.
There isn’t much to do there BUT work, which is the idea. The building’s wifi is too slow to stream or watch Youtube. I’m not tempted to work on a puzzle with my daughter, take a book off a shelf, play with my dogs, or go down the hall for a nap. All the little things we do to procrastinate aren’t there, like convincing myself that I need to clean the pool or balance the checkbook ASAP.
I don’t have the distractions of my dogs barking at passing cars, or kids going up and down the hall, or the phone ringing with people asking who I’m voting for.
My little office is a private oasis, of sorts. Quiet and undisturbed.
Not quite Superman’s Fortress of Solitude, but close enough for me.
And, with all due respect to the Man of Steel, the Fortress of Solitude doesn’t have a Keurig.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“How long, how long to sing this song?”
“My soul is in deep anguish. How long, Lord, how long?” – Psalm 6
. A once-common word in the 1800s, it fell steeply in popularity in the 20th century. Lately, I see it everywhere. It’s a beautiful word, capturing not only sorrow, but also weariness. It is also audacious, facing injustice and acknowledging that it ought not be this way, and communal, bearing witness to the shared hardship of being human. The Hebrew scriptures captured the experience of lament in the form of psalms, from the Greek, psalmoi or “words to accompany the music.” A few thousand years later, the words still resonate, especially in times of grief. “I am weary with my groaning; all the night make I my bed to swim; I water my couch with my tears.”
“Hair loss” is not the chief complaint you want to see when running behind in clinic – it’s never a 15-minute visit. A woman in her late 30s with wavy, light-brown hair that grew to her waistline was seated on the exam chair. When I sat across from her, I couldn’t see her scalp. No erythema or scale. No frontal band of hair loss. Just a bit thin everywhere. Perhaps another post-COVID telogen? This might be easy. I blew right by her mother, who was sitting in the corner of the room. Her black and white horizontal striped shirt seemed to match her gray and white hair. She looked worried.
Having perused my patient’s labs and done an exam, I announced that the diagnosis was telogen effluvium. “There are many possible causes, stress is a common one. Have you been under a lot of stress lately?” (The answer is always yes, thus providing a good foothold to climb out of a hair-loss visit). “Yes. My 1-year-old daughter died last year. She had choked on a cashew from a granola bar given by her sister.” I gasped and turned from her green eyes to her mom’s. Without saying a word, mom pleaded with me to help. “I don’t know what to say,” I said, “I’m so sorry.” Neither replied.
On the commute home that day I listened to a live recording of the U2 song, “40.” I had recently read about it in a touching essay about lament by Enuma Okoro of the Financial Times. I thought about my patient’s suffering and the brutal injustice of fate. It feels like it’s everywhere lately. Reporting from the events in Ukraine, Buffalo, Uvalde, Tulsa has put agonized faces like hers in the public square for us all to gape at and quietly mourn.
Even from a secular lens, it can be seen that a beauty of psalms is how they move from despair to hope. Prayers will be answered. Things will get better. Turn up the volume and feel the urgency and pathos Bono injects into your soul as he sings the refrain; “How long, how long? How long to sing this song?” In the live version we the audience take over for him. The words accompanying the music swell over the crowd. How much longer? How much more suffering? My patient’s hair will grow back. It will take years. All we can do is lament with her.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“My soul is in deep anguish. How long, Lord, how long?” – Psalm 6
. A once-common word in the 1800s, it fell steeply in popularity in the 20th century. Lately, I see it everywhere. It’s a beautiful word, capturing not only sorrow, but also weariness. It is also audacious, facing injustice and acknowledging that it ought not be this way, and communal, bearing witness to the shared hardship of being human. The Hebrew scriptures captured the experience of lament in the form of psalms, from the Greek, psalmoi or “words to accompany the music.” A few thousand years later, the words still resonate, especially in times of grief. “I am weary with my groaning; all the night make I my bed to swim; I water my couch with my tears.”
“Hair loss” is not the chief complaint you want to see when running behind in clinic – it’s never a 15-minute visit. A woman in her late 30s with wavy, light-brown hair that grew to her waistline was seated on the exam chair. When I sat across from her, I couldn’t see her scalp. No erythema or scale. No frontal band of hair loss. Just a bit thin everywhere. Perhaps another post-COVID telogen? This might be easy. I blew right by her mother, who was sitting in the corner of the room. Her black and white horizontal striped shirt seemed to match her gray and white hair. She looked worried.
Having perused my patient’s labs and done an exam, I announced that the diagnosis was telogen effluvium. “There are many possible causes, stress is a common one. Have you been under a lot of stress lately?” (The answer is always yes, thus providing a good foothold to climb out of a hair-loss visit). “Yes. My 1-year-old daughter died last year. She had choked on a cashew from a granola bar given by her sister.” I gasped and turned from her green eyes to her mom’s. Without saying a word, mom pleaded with me to help. “I don’t know what to say,” I said, “I’m so sorry.” Neither replied.
On the commute home that day I listened to a live recording of the U2 song, “40.” I had recently read about it in a touching essay about lament by Enuma Okoro of the Financial Times. I thought about my patient’s suffering and the brutal injustice of fate. It feels like it’s everywhere lately. Reporting from the events in Ukraine, Buffalo, Uvalde, Tulsa has put agonized faces like hers in the public square for us all to gape at and quietly mourn.
Even from a secular lens, it can be seen that a beauty of psalms is how they move from despair to hope. Prayers will be answered. Things will get better. Turn up the volume and feel the urgency and pathos Bono injects into your soul as he sings the refrain; “How long, how long? How long to sing this song?” In the live version we the audience take over for him. The words accompanying the music swell over the crowd. How much longer? How much more suffering? My patient’s hair will grow back. It will take years. All we can do is lament with her.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“My soul is in deep anguish. How long, Lord, how long?” – Psalm 6
. A once-common word in the 1800s, it fell steeply in popularity in the 20th century. Lately, I see it everywhere. It’s a beautiful word, capturing not only sorrow, but also weariness. It is also audacious, facing injustice and acknowledging that it ought not be this way, and communal, bearing witness to the shared hardship of being human. The Hebrew scriptures captured the experience of lament in the form of psalms, from the Greek, psalmoi or “words to accompany the music.” A few thousand years later, the words still resonate, especially in times of grief. “I am weary with my groaning; all the night make I my bed to swim; I water my couch with my tears.”
“Hair loss” is not the chief complaint you want to see when running behind in clinic – it’s never a 15-minute visit. A woman in her late 30s with wavy, light-brown hair that grew to her waistline was seated on the exam chair. When I sat across from her, I couldn’t see her scalp. No erythema or scale. No frontal band of hair loss. Just a bit thin everywhere. Perhaps another post-COVID telogen? This might be easy. I blew right by her mother, who was sitting in the corner of the room. Her black and white horizontal striped shirt seemed to match her gray and white hair. She looked worried.
Having perused my patient’s labs and done an exam, I announced that the diagnosis was telogen effluvium. “There are many possible causes, stress is a common one. Have you been under a lot of stress lately?” (The answer is always yes, thus providing a good foothold to climb out of a hair-loss visit). “Yes. My 1-year-old daughter died last year. She had choked on a cashew from a granola bar given by her sister.” I gasped and turned from her green eyes to her mom’s. Without saying a word, mom pleaded with me to help. “I don’t know what to say,” I said, “I’m so sorry.” Neither replied.
On the commute home that day I listened to a live recording of the U2 song, “40.” I had recently read about it in a touching essay about lament by Enuma Okoro of the Financial Times. I thought about my patient’s suffering and the brutal injustice of fate. It feels like it’s everywhere lately. Reporting from the events in Ukraine, Buffalo, Uvalde, Tulsa has put agonized faces like hers in the public square for us all to gape at and quietly mourn.
Even from a secular lens, it can be seen that a beauty of psalms is how they move from despair to hope. Prayers will be answered. Things will get better. Turn up the volume and feel the urgency and pathos Bono injects into your soul as he sings the refrain; “How long, how long? How long to sing this song?” In the live version we the audience take over for him. The words accompanying the music swell over the crowd. How much longer? How much more suffering? My patient’s hair will grow back. It will take years. All we can do is lament with her.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Heart failure: Medicare cost sharing may put quadruple therapy out of reach
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.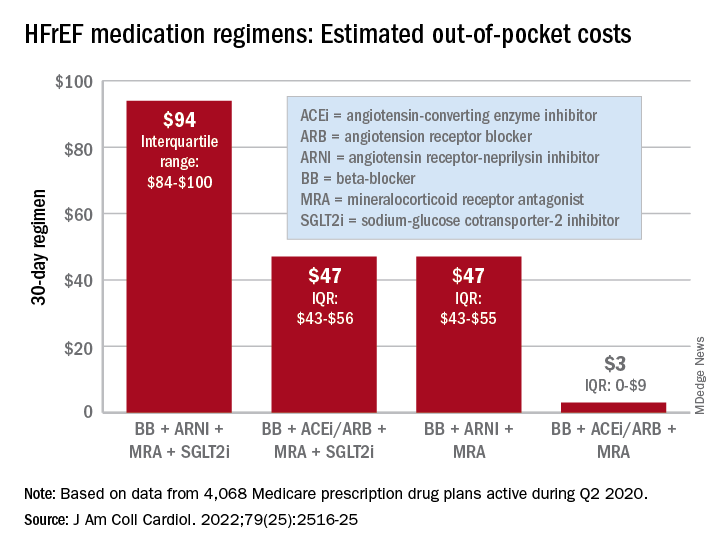
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.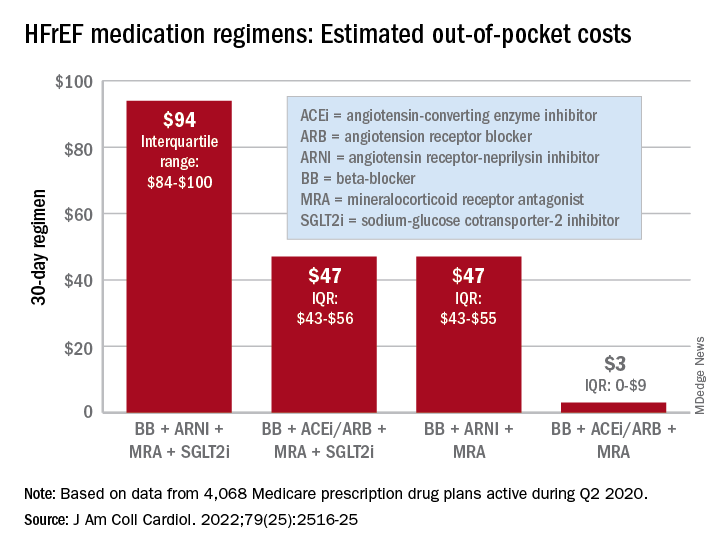
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.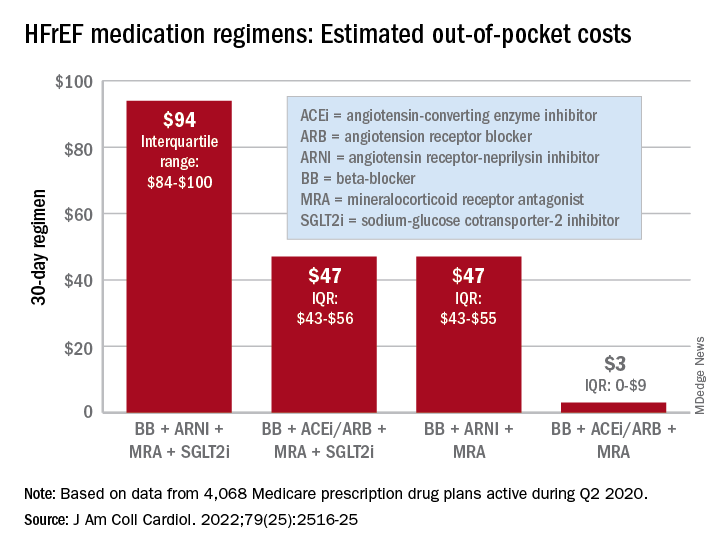
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
FROM THE JOURNAL Of the AMERICAN COLLEGE OF CARDIOLOGY
More Black mothers deliver by cesarean, not always by choice
When 29-year-old Sakeenah Fowler was pregnant with her first child, doctors kept a close watch. Ms. Fowler has lupus, high blood pressure, a history of blood clotting, and kidney problems that all could have endangered her or the health of her unborn baby.
She saw maternal-fetal specialists who could keep watch of her high-risk pregnancy, and she collected urine samples every 24 hours to make sure her kidneys were functioning properly from her home in Roebuck, S.C.
But the pregnancy ultimately proved uneventful; even her kidneys remained stable. So Ms. Fowler said she was shocked when her doctors ordered an emergency cesarean delivery after she had gone into active labor.
“I was already dilated all the way to 6 cm,” but the baby’s heart rate had decreased by a small amount, she says. “They thought it was best to just go ahead with a C-section.”
Ms. Fowler, who is Black, said she believes the surgical intervention was unnecessary and that she wasn’t given a chance to discuss her options for a vaginal childbirth.
“They already had it in their minds that I wasn’t going to make it through the pregnancy without any issues; then when I did, it was like they wanted to find something that made me have to have a C-section,” Ms. Fowler said. “It was close to the holidays; everybody was ready to go home. It was just like I was pushed to do what they wanted me to do.”
Ms. Fowler’s sense of a lack of choice is important beyond the measure of patient experience. While cesarean deliveries can be a lifeline for mother and baby, they can put up massive roadblocks to maternal and infant health when not necessary.
“The risk of hemorrhage, infection – on average, all of these go up when you have surgery instead of a vaginal delivery,” says Kimberly B. Glazer, PhD, a perinatal epidemiologist at the Icahn School of Medicine at Mount Sinai, New York.
“Birth is one of the most salient experiences you can have. People want to feel like their values and preferences – whatever they may be – were honored and respected. Even if the delivery goes a different way than you wanted, feeling like your values were taken into account is very important.”
More than 1 million women undergo cesarean deliveries in the United States every year, composing over 31% of all births in 2020, according to the Centers for Disease Control and Prevention.
The World Health Organization, meanwhile, recommends a rate of cesarean delivery of no more than 15% per region. Whether or not all the U.S. procedures were medically warranted is unclear, however.
Black women have higher odds of undergoing a cesarean: 36% undergo surgical deliveries annually, compared with about 30% of White women. Black women are also about three times more likely to die of pregnancy-related causes than White women.
Risk becomes reality
Ms. Fowler eventually developed an infection in her cesarean surgical wound, but her doctors initially insisted her alternating chills and fever were merely postpartum hormonal swings, she says.
“I thought something had to be wrong, but they just kept saying nothing was wrong,” she says.
By the time her doctors caught the infection, Ms. Fowler was readmitted to the hospital for several days of IV antibiotic therapy. The infection “almost got into my bloodstream and could have killed me,” she says.
While cesarean deliveries are associated with decreases in maternal, neonatal, and infant mortality, the benefits are only seen up to a certain threshold. The WHO, for instance, has reported that over the 15% threshold, that lower mortality benefit disappears.
“When medically necessary, cesarean delivery can improve outcomes for mother and baby. But the fact that cesarean section rates have increased in recent years without a corresponding improvement in health outcomes indicates overreliance on the procedure,” Dr. Glazer says.
Clinical discretion leads to biased judgment calls
Rates of cesarean deliveries are even higher among low-risk pregnancies in women of color than in White women. Between 2016 and 2019, the overall rate of cesarean deliveries for low-risk births was 23%, according to a recent analysis. But the rate was almost 18% higher among Black women than among White women (27% vs. 22%).
“When you see data about these subjective indications varying by race and ethnicity, I think that’s pointing us toward some answers,” Dr. Glazer says. “Once you adjust for all these measures, prepregnancy characteristics, and risk factors, the research identifies variation in quality and outcomes that is rooted in structural and systemic racism in health care, implicit bias from clinicians.”
Researchers investigating cesarean deliveries have found that Black women are more likely to undergo the surgery for reasons that are highly subjective, such as fetal distress.
“There is a huge range of how concerning a fetal heart rate can be, and some health providers might perform a C-section for only minor changes in the fetal heart rate, while others might wait until it is much worse,” said Rebecca Hamm, MD, an assistant professor of obstetrics and gynecology at the Perelman School of Medicine at the University of Pennsylvania.
At least some of the differences in care can be explained by where women deliver their babies, studies have shown. Women of color disproportionately deliver at hospitals with poorer quality outcomes for moms and babies.
Dealing with the aftermath
There can be costs that reverberate throughout the life of a mother, child, and their family as the result of surgical delivery.
“Cesarean sections cost a lot more,” says Jamila Taylor, PhD, director of health care reform and a senior fellow with The Century Foundation, a progressive policy think tank in Washington, D.C. The cost of a cesarean delivery averages about $17,000, compared with about $12,200 for a vaginal birth; for uninsured patients, surgical deliveries cost about $9,000 more than vaginal deliveries.
Dr. Taylor, who has studied the historical mistreatment of Black women in obstetrics, noted that this cost includes not just the bill for surgery but also a prolonged recovery time that is often spent in a hospital bed.
Beyond the detrimental effect that a large hospital bill for delivery and aftercare can have on families, other costs can crop up later. Infants delivered by cesarean surgery are more likely to develop an infection, breathing problems, and to spend time in the neonatal intensive care unit than babies born vaginally. Although studies suggest these outcomes may result from a medically necessary health concern that spurred the cesarean surgery, they often stem from the delivery itself.
Babies born surgically also miss out on the benefits of passing through the birth canal, such as supporting a newborn’s immune system and preparing their lungs to breathe oxygen after birth.
Most of the efforts to reduce inequities in maternal care are happening at the clinical level, aimed at both patients and providers, Dr. Taylor says.
“As advocates, we’re talking about how we can help Black women be advocates for themselves in the health care system – if the physician suggests a C-section, getting a second opinion, or walking through what a [surgical delivery] will mean and what their recovery will look like,” she says.
Women are also increasingly choosing non-hospital settings to deliver when possible, Dr. Taylor says. Including doulas or midwife practitioners in the maternal care team can reduce unnecessary cesarean deliveries among Black women, according to Camille Clare, MD, chair of the New York chapter of the American College of Obstetricians and Gynecologists.
Also, last year, race was removed from the vaginal birth after C-section (VBAC) calculator, which is used to gauge the safety of vaginal delivery in women with a history of surgical birth. The original calculator included race-based correction factors for Black women and Hispanic women. It predicted a lower likelihood of successful vaginal deliveries for women who already had a C-section and who identify as Black or Hispanic than for White women with otherwise identical characteristics, such as age, weight, and a history of cesarean delivery.
“Those are things that over time should reduce the high rates of cesarean section for Black women in particular,” Dr. Clare says.
In addition to embracing the updated calculator and including nurse-midwives and doulas in their obstetrics services, Penn Medicine, Philadelphia received a federal grant to study the impact of creating a standard plan for deliveries. This includes standardizing the induction of labor and any effect that might have on reducing C-section rates.
“This idea that biases lead to difference in decisionmaking, and that by standardizing practices we could address these differences – people were somewhat resistant at first,” Dr. Hamm says. “They didn’t believe there were differences in their practices.”
People struggle to recognize those differences, she says, and “it takes active participation in reducing disparities to make that happen.”
At the community level, Synergistic Sisters in Science (SIS), a group of maternal health experts and health equity advocates, is working on a project called PM3, to reduce maternal mortality through mobile technology.
The smartphone app will provide information for new moms to empower them to start conversations with health care providers. It also connects users to social support and resources. SIS is especially hoping to engage Black women living in rural areas.
“There is so much mistrust due to things like unnecessary C-sections and the fact that Black women feel they aren’t heard,” said Natalie Hernandez, PhD, executive director of the Center for Maternal Health Equity at Morehouse School of Medicine, Atlanta. “Here is a tool that gives a woman information that’s culturally centered, looks like her, and was informed by her voice.”
A version of this article first appeared on WebMD.com.
When 29-year-old Sakeenah Fowler was pregnant with her first child, doctors kept a close watch. Ms. Fowler has lupus, high blood pressure, a history of blood clotting, and kidney problems that all could have endangered her or the health of her unborn baby.
She saw maternal-fetal specialists who could keep watch of her high-risk pregnancy, and she collected urine samples every 24 hours to make sure her kidneys were functioning properly from her home in Roebuck, S.C.
But the pregnancy ultimately proved uneventful; even her kidneys remained stable. So Ms. Fowler said she was shocked when her doctors ordered an emergency cesarean delivery after she had gone into active labor.
“I was already dilated all the way to 6 cm,” but the baby’s heart rate had decreased by a small amount, she says. “They thought it was best to just go ahead with a C-section.”
Ms. Fowler, who is Black, said she believes the surgical intervention was unnecessary and that she wasn’t given a chance to discuss her options for a vaginal childbirth.
“They already had it in their minds that I wasn’t going to make it through the pregnancy without any issues; then when I did, it was like they wanted to find something that made me have to have a C-section,” Ms. Fowler said. “It was close to the holidays; everybody was ready to go home. It was just like I was pushed to do what they wanted me to do.”
Ms. Fowler’s sense of a lack of choice is important beyond the measure of patient experience. While cesarean deliveries can be a lifeline for mother and baby, they can put up massive roadblocks to maternal and infant health when not necessary.
“The risk of hemorrhage, infection – on average, all of these go up when you have surgery instead of a vaginal delivery,” says Kimberly B. Glazer, PhD, a perinatal epidemiologist at the Icahn School of Medicine at Mount Sinai, New York.
“Birth is one of the most salient experiences you can have. People want to feel like their values and preferences – whatever they may be – were honored and respected. Even if the delivery goes a different way than you wanted, feeling like your values were taken into account is very important.”
More than 1 million women undergo cesarean deliveries in the United States every year, composing over 31% of all births in 2020, according to the Centers for Disease Control and Prevention.
The World Health Organization, meanwhile, recommends a rate of cesarean delivery of no more than 15% per region. Whether or not all the U.S. procedures were medically warranted is unclear, however.
Black women have higher odds of undergoing a cesarean: 36% undergo surgical deliveries annually, compared with about 30% of White women. Black women are also about three times more likely to die of pregnancy-related causes than White women.
Risk becomes reality
Ms. Fowler eventually developed an infection in her cesarean surgical wound, but her doctors initially insisted her alternating chills and fever were merely postpartum hormonal swings, she says.
“I thought something had to be wrong, but they just kept saying nothing was wrong,” she says.
By the time her doctors caught the infection, Ms. Fowler was readmitted to the hospital for several days of IV antibiotic therapy. The infection “almost got into my bloodstream and could have killed me,” she says.
While cesarean deliveries are associated with decreases in maternal, neonatal, and infant mortality, the benefits are only seen up to a certain threshold. The WHO, for instance, has reported that over the 15% threshold, that lower mortality benefit disappears.
“When medically necessary, cesarean delivery can improve outcomes for mother and baby. But the fact that cesarean section rates have increased in recent years without a corresponding improvement in health outcomes indicates overreliance on the procedure,” Dr. Glazer says.
Clinical discretion leads to biased judgment calls
Rates of cesarean deliveries are even higher among low-risk pregnancies in women of color than in White women. Between 2016 and 2019, the overall rate of cesarean deliveries for low-risk births was 23%, according to a recent analysis. But the rate was almost 18% higher among Black women than among White women (27% vs. 22%).
“When you see data about these subjective indications varying by race and ethnicity, I think that’s pointing us toward some answers,” Dr. Glazer says. “Once you adjust for all these measures, prepregnancy characteristics, and risk factors, the research identifies variation in quality and outcomes that is rooted in structural and systemic racism in health care, implicit bias from clinicians.”
Researchers investigating cesarean deliveries have found that Black women are more likely to undergo the surgery for reasons that are highly subjective, such as fetal distress.
“There is a huge range of how concerning a fetal heart rate can be, and some health providers might perform a C-section for only minor changes in the fetal heart rate, while others might wait until it is much worse,” said Rebecca Hamm, MD, an assistant professor of obstetrics and gynecology at the Perelman School of Medicine at the University of Pennsylvania.
At least some of the differences in care can be explained by where women deliver their babies, studies have shown. Women of color disproportionately deliver at hospitals with poorer quality outcomes for moms and babies.
Dealing with the aftermath
There can be costs that reverberate throughout the life of a mother, child, and their family as the result of surgical delivery.
“Cesarean sections cost a lot more,” says Jamila Taylor, PhD, director of health care reform and a senior fellow with The Century Foundation, a progressive policy think tank in Washington, D.C. The cost of a cesarean delivery averages about $17,000, compared with about $12,200 for a vaginal birth; for uninsured patients, surgical deliveries cost about $9,000 more than vaginal deliveries.
Dr. Taylor, who has studied the historical mistreatment of Black women in obstetrics, noted that this cost includes not just the bill for surgery but also a prolonged recovery time that is often spent in a hospital bed.
Beyond the detrimental effect that a large hospital bill for delivery and aftercare can have on families, other costs can crop up later. Infants delivered by cesarean surgery are more likely to develop an infection, breathing problems, and to spend time in the neonatal intensive care unit than babies born vaginally. Although studies suggest these outcomes may result from a medically necessary health concern that spurred the cesarean surgery, they often stem from the delivery itself.
Babies born surgically also miss out on the benefits of passing through the birth canal, such as supporting a newborn’s immune system and preparing their lungs to breathe oxygen after birth.
Most of the efforts to reduce inequities in maternal care are happening at the clinical level, aimed at both patients and providers, Dr. Taylor says.
“As advocates, we’re talking about how we can help Black women be advocates for themselves in the health care system – if the physician suggests a C-section, getting a second opinion, or walking through what a [surgical delivery] will mean and what their recovery will look like,” she says.
Women are also increasingly choosing non-hospital settings to deliver when possible, Dr. Taylor says. Including doulas or midwife practitioners in the maternal care team can reduce unnecessary cesarean deliveries among Black women, according to Camille Clare, MD, chair of the New York chapter of the American College of Obstetricians and Gynecologists.
Also, last year, race was removed from the vaginal birth after C-section (VBAC) calculator, which is used to gauge the safety of vaginal delivery in women with a history of surgical birth. The original calculator included race-based correction factors for Black women and Hispanic women. It predicted a lower likelihood of successful vaginal deliveries for women who already had a C-section and who identify as Black or Hispanic than for White women with otherwise identical characteristics, such as age, weight, and a history of cesarean delivery.
“Those are things that over time should reduce the high rates of cesarean section for Black women in particular,” Dr. Clare says.
In addition to embracing the updated calculator and including nurse-midwives and doulas in their obstetrics services, Penn Medicine, Philadelphia received a federal grant to study the impact of creating a standard plan for deliveries. This includes standardizing the induction of labor and any effect that might have on reducing C-section rates.
“This idea that biases lead to difference in decisionmaking, and that by standardizing practices we could address these differences – people were somewhat resistant at first,” Dr. Hamm says. “They didn’t believe there were differences in their practices.”
People struggle to recognize those differences, she says, and “it takes active participation in reducing disparities to make that happen.”
At the community level, Synergistic Sisters in Science (SIS), a group of maternal health experts and health equity advocates, is working on a project called PM3, to reduce maternal mortality through mobile technology.
The smartphone app will provide information for new moms to empower them to start conversations with health care providers. It also connects users to social support and resources. SIS is especially hoping to engage Black women living in rural areas.
“There is so much mistrust due to things like unnecessary C-sections and the fact that Black women feel they aren’t heard,” said Natalie Hernandez, PhD, executive director of the Center for Maternal Health Equity at Morehouse School of Medicine, Atlanta. “Here is a tool that gives a woman information that’s culturally centered, looks like her, and was informed by her voice.”
A version of this article first appeared on WebMD.com.
When 29-year-old Sakeenah Fowler was pregnant with her first child, doctors kept a close watch. Ms. Fowler has lupus, high blood pressure, a history of blood clotting, and kidney problems that all could have endangered her or the health of her unborn baby.
She saw maternal-fetal specialists who could keep watch of her high-risk pregnancy, and she collected urine samples every 24 hours to make sure her kidneys were functioning properly from her home in Roebuck, S.C.
But the pregnancy ultimately proved uneventful; even her kidneys remained stable. So Ms. Fowler said she was shocked when her doctors ordered an emergency cesarean delivery after she had gone into active labor.
“I was already dilated all the way to 6 cm,” but the baby’s heart rate had decreased by a small amount, she says. “They thought it was best to just go ahead with a C-section.”
Ms. Fowler, who is Black, said she believes the surgical intervention was unnecessary and that she wasn’t given a chance to discuss her options for a vaginal childbirth.
“They already had it in their minds that I wasn’t going to make it through the pregnancy without any issues; then when I did, it was like they wanted to find something that made me have to have a C-section,” Ms. Fowler said. “It was close to the holidays; everybody was ready to go home. It was just like I was pushed to do what they wanted me to do.”
Ms. Fowler’s sense of a lack of choice is important beyond the measure of patient experience. While cesarean deliveries can be a lifeline for mother and baby, they can put up massive roadblocks to maternal and infant health when not necessary.
“The risk of hemorrhage, infection – on average, all of these go up when you have surgery instead of a vaginal delivery,” says Kimberly B. Glazer, PhD, a perinatal epidemiologist at the Icahn School of Medicine at Mount Sinai, New York.
“Birth is one of the most salient experiences you can have. People want to feel like their values and preferences – whatever they may be – were honored and respected. Even if the delivery goes a different way than you wanted, feeling like your values were taken into account is very important.”
More than 1 million women undergo cesarean deliveries in the United States every year, composing over 31% of all births in 2020, according to the Centers for Disease Control and Prevention.
The World Health Organization, meanwhile, recommends a rate of cesarean delivery of no more than 15% per region. Whether or not all the U.S. procedures were medically warranted is unclear, however.
Black women have higher odds of undergoing a cesarean: 36% undergo surgical deliveries annually, compared with about 30% of White women. Black women are also about three times more likely to die of pregnancy-related causes than White women.
Risk becomes reality
Ms. Fowler eventually developed an infection in her cesarean surgical wound, but her doctors initially insisted her alternating chills and fever were merely postpartum hormonal swings, she says.
“I thought something had to be wrong, but they just kept saying nothing was wrong,” she says.
By the time her doctors caught the infection, Ms. Fowler was readmitted to the hospital for several days of IV antibiotic therapy. The infection “almost got into my bloodstream and could have killed me,” she says.
While cesarean deliveries are associated with decreases in maternal, neonatal, and infant mortality, the benefits are only seen up to a certain threshold. The WHO, for instance, has reported that over the 15% threshold, that lower mortality benefit disappears.
“When medically necessary, cesarean delivery can improve outcomes for mother and baby. But the fact that cesarean section rates have increased in recent years without a corresponding improvement in health outcomes indicates overreliance on the procedure,” Dr. Glazer says.
Clinical discretion leads to biased judgment calls
Rates of cesarean deliveries are even higher among low-risk pregnancies in women of color than in White women. Between 2016 and 2019, the overall rate of cesarean deliveries for low-risk births was 23%, according to a recent analysis. But the rate was almost 18% higher among Black women than among White women (27% vs. 22%).
“When you see data about these subjective indications varying by race and ethnicity, I think that’s pointing us toward some answers,” Dr. Glazer says. “Once you adjust for all these measures, prepregnancy characteristics, and risk factors, the research identifies variation in quality and outcomes that is rooted in structural and systemic racism in health care, implicit bias from clinicians.”
Researchers investigating cesarean deliveries have found that Black women are more likely to undergo the surgery for reasons that are highly subjective, such as fetal distress.
“There is a huge range of how concerning a fetal heart rate can be, and some health providers might perform a C-section for only minor changes in the fetal heart rate, while others might wait until it is much worse,” said Rebecca Hamm, MD, an assistant professor of obstetrics and gynecology at the Perelman School of Medicine at the University of Pennsylvania.
At least some of the differences in care can be explained by where women deliver their babies, studies have shown. Women of color disproportionately deliver at hospitals with poorer quality outcomes for moms and babies.
Dealing with the aftermath
There can be costs that reverberate throughout the life of a mother, child, and their family as the result of surgical delivery.
“Cesarean sections cost a lot more,” says Jamila Taylor, PhD, director of health care reform and a senior fellow with The Century Foundation, a progressive policy think tank in Washington, D.C. The cost of a cesarean delivery averages about $17,000, compared with about $12,200 for a vaginal birth; for uninsured patients, surgical deliveries cost about $9,000 more than vaginal deliveries.
Dr. Taylor, who has studied the historical mistreatment of Black women in obstetrics, noted that this cost includes not just the bill for surgery but also a prolonged recovery time that is often spent in a hospital bed.
Beyond the detrimental effect that a large hospital bill for delivery and aftercare can have on families, other costs can crop up later. Infants delivered by cesarean surgery are more likely to develop an infection, breathing problems, and to spend time in the neonatal intensive care unit than babies born vaginally. Although studies suggest these outcomes may result from a medically necessary health concern that spurred the cesarean surgery, they often stem from the delivery itself.
Babies born surgically also miss out on the benefits of passing through the birth canal, such as supporting a newborn’s immune system and preparing their lungs to breathe oxygen after birth.
Most of the efforts to reduce inequities in maternal care are happening at the clinical level, aimed at both patients and providers, Dr. Taylor says.
“As advocates, we’re talking about how we can help Black women be advocates for themselves in the health care system – if the physician suggests a C-section, getting a second opinion, or walking through what a [surgical delivery] will mean and what their recovery will look like,” she says.
Women are also increasingly choosing non-hospital settings to deliver when possible, Dr. Taylor says. Including doulas or midwife practitioners in the maternal care team can reduce unnecessary cesarean deliveries among Black women, according to Camille Clare, MD, chair of the New York chapter of the American College of Obstetricians and Gynecologists.
Also, last year, race was removed from the vaginal birth after C-section (VBAC) calculator, which is used to gauge the safety of vaginal delivery in women with a history of surgical birth. The original calculator included race-based correction factors for Black women and Hispanic women. It predicted a lower likelihood of successful vaginal deliveries for women who already had a C-section and who identify as Black or Hispanic than for White women with otherwise identical characteristics, such as age, weight, and a history of cesarean delivery.
“Those are things that over time should reduce the high rates of cesarean section for Black women in particular,” Dr. Clare says.
In addition to embracing the updated calculator and including nurse-midwives and doulas in their obstetrics services, Penn Medicine, Philadelphia received a federal grant to study the impact of creating a standard plan for deliveries. This includes standardizing the induction of labor and any effect that might have on reducing C-section rates.
“This idea that biases lead to difference in decisionmaking, and that by standardizing practices we could address these differences – people were somewhat resistant at first,” Dr. Hamm says. “They didn’t believe there were differences in their practices.”
People struggle to recognize those differences, she says, and “it takes active participation in reducing disparities to make that happen.”
At the community level, Synergistic Sisters in Science (SIS), a group of maternal health experts and health equity advocates, is working on a project called PM3, to reduce maternal mortality through mobile technology.
The smartphone app will provide information for new moms to empower them to start conversations with health care providers. It also connects users to social support and resources. SIS is especially hoping to engage Black women living in rural areas.
“There is so much mistrust due to things like unnecessary C-sections and the fact that Black women feel they aren’t heard,” said Natalie Hernandez, PhD, executive director of the Center for Maternal Health Equity at Morehouse School of Medicine, Atlanta. “Here is a tool that gives a woman information that’s culturally centered, looks like her, and was informed by her voice.”
A version of this article first appeared on WebMD.com.
AMA: Insurance should cover treatment for infertility caused by gender-affirming care
CHICAGO – Health insurance should cover treatment for infertility caused by gender-affirming medical interventions, the American Medical Association said June 13 at its House of Delegates meeting.
Speaking on behalf of the Medical Student Section, Justin Magrath, of Louisiana, said, “We as a section feel that these interventions should be considered as additional causes of iatrogenic infertility and be covered by insurance.”
Iatrogenic infertility is infertility caused by surgery, radiotherapy, chemotherapy, or other medically necessary treatment. The AMA voted June 13 to support including the phrase, “impaired fertility as a consequence of gender-affirming hormone therapy and gender-affirming surgery,” in that definition.
The AMA also supports access to fertility preservation services for people who undergo those treatments.
“I’ve had many friends who went through transitions and gender-affirming care and had no idea that these options were available and others who did know they were available but they were so expensive that they couldn’t access them,” said emergency medicine resident Sophia Spadafore, MD, delegate for the Resident and Fellow Section. “So while people might be able to access gender-affirming care, sometimes they have to make the decision between future fertility and having children and accessing this kind of lifesaving care that we support.”
The AMA already had policies that support insurance coverage of treatments for gender dysphoria and the right to seek fertility preservation services for people who undergo gender-affirming hormone therapy or surgery, but until this week, it had not addressed insurance coverage for preserving fertility in those cases.
“The transgender population already faces many barriers to care, such as provider discrimination, legal concerns, financial burden, and emotional cost,” Mr. Magrath said during a reference committee hearing on June 11. “We as a section ask our organization to continue to serve as an ally, providing equitable care for diverse populations and expanding coverage for medically necessary treatments.”
“I am a gender surgeon, so this is pretty important to me,” said Sean Figy, MD, of Nebraska, a delegate for the American Society for Reconstructive Microsurgery.
The original resolution included the words “medically necessary” when referring to gender-affirming treatments, and Dr. Figy expressed hesitancy about those words. An amendment removed them.
“I’ve seen that phrase weaponized against gender-nonconforming patients,” he said.
Ophthalmologist Charles Hickey, MD, of the Ohio delegation, spoke in favor of referral or of waiting to adopt the resolution.
“I think the different amendments being discussed here are evidence that this needs a more thorough and careful treatment than we can do at this point right now,” he said.
A version of this article first appeared on Medscape.com.
CHICAGO – Health insurance should cover treatment for infertility caused by gender-affirming medical interventions, the American Medical Association said June 13 at its House of Delegates meeting.
Speaking on behalf of the Medical Student Section, Justin Magrath, of Louisiana, said, “We as a section feel that these interventions should be considered as additional causes of iatrogenic infertility and be covered by insurance.”
Iatrogenic infertility is infertility caused by surgery, radiotherapy, chemotherapy, or other medically necessary treatment. The AMA voted June 13 to support including the phrase, “impaired fertility as a consequence of gender-affirming hormone therapy and gender-affirming surgery,” in that definition.
The AMA also supports access to fertility preservation services for people who undergo those treatments.
“I’ve had many friends who went through transitions and gender-affirming care and had no idea that these options were available and others who did know they were available but they were so expensive that they couldn’t access them,” said emergency medicine resident Sophia Spadafore, MD, delegate for the Resident and Fellow Section. “So while people might be able to access gender-affirming care, sometimes they have to make the decision between future fertility and having children and accessing this kind of lifesaving care that we support.”
The AMA already had policies that support insurance coverage of treatments for gender dysphoria and the right to seek fertility preservation services for people who undergo gender-affirming hormone therapy or surgery, but until this week, it had not addressed insurance coverage for preserving fertility in those cases.
“The transgender population already faces many barriers to care, such as provider discrimination, legal concerns, financial burden, and emotional cost,” Mr. Magrath said during a reference committee hearing on June 11. “We as a section ask our organization to continue to serve as an ally, providing equitable care for diverse populations and expanding coverage for medically necessary treatments.”
“I am a gender surgeon, so this is pretty important to me,” said Sean Figy, MD, of Nebraska, a delegate for the American Society for Reconstructive Microsurgery.
The original resolution included the words “medically necessary” when referring to gender-affirming treatments, and Dr. Figy expressed hesitancy about those words. An amendment removed them.
“I’ve seen that phrase weaponized against gender-nonconforming patients,” he said.
Ophthalmologist Charles Hickey, MD, of the Ohio delegation, spoke in favor of referral or of waiting to adopt the resolution.
“I think the different amendments being discussed here are evidence that this needs a more thorough and careful treatment than we can do at this point right now,” he said.
A version of this article first appeared on Medscape.com.
CHICAGO – Health insurance should cover treatment for infertility caused by gender-affirming medical interventions, the American Medical Association said June 13 at its House of Delegates meeting.
Speaking on behalf of the Medical Student Section, Justin Magrath, of Louisiana, said, “We as a section feel that these interventions should be considered as additional causes of iatrogenic infertility and be covered by insurance.”
Iatrogenic infertility is infertility caused by surgery, radiotherapy, chemotherapy, or other medically necessary treatment. The AMA voted June 13 to support including the phrase, “impaired fertility as a consequence of gender-affirming hormone therapy and gender-affirming surgery,” in that definition.
The AMA also supports access to fertility preservation services for people who undergo those treatments.
“I’ve had many friends who went through transitions and gender-affirming care and had no idea that these options were available and others who did know they were available but they were so expensive that they couldn’t access them,” said emergency medicine resident Sophia Spadafore, MD, delegate for the Resident and Fellow Section. “So while people might be able to access gender-affirming care, sometimes they have to make the decision between future fertility and having children and accessing this kind of lifesaving care that we support.”
The AMA already had policies that support insurance coverage of treatments for gender dysphoria and the right to seek fertility preservation services for people who undergo gender-affirming hormone therapy or surgery, but until this week, it had not addressed insurance coverage for preserving fertility in those cases.
“The transgender population already faces many barriers to care, such as provider discrimination, legal concerns, financial burden, and emotional cost,” Mr. Magrath said during a reference committee hearing on June 11. “We as a section ask our organization to continue to serve as an ally, providing equitable care for diverse populations and expanding coverage for medically necessary treatments.”
“I am a gender surgeon, so this is pretty important to me,” said Sean Figy, MD, of Nebraska, a delegate for the American Society for Reconstructive Microsurgery.
The original resolution included the words “medically necessary” when referring to gender-affirming treatments, and Dr. Figy expressed hesitancy about those words. An amendment removed them.
“I’ve seen that phrase weaponized against gender-nonconforming patients,” he said.
Ophthalmologist Charles Hickey, MD, of the Ohio delegation, spoke in favor of referral or of waiting to adopt the resolution.
“I think the different amendments being discussed here are evidence that this needs a more thorough and careful treatment than we can do at this point right now,” he said.
A version of this article first appeared on Medscape.com.



