User login
COVID-19 shifts telehealth to the center of cardiology
during the COVID-19 pandemic.
During a recent telehealth webinar, Ami Bhatt, MD, director of the adult congenital heart disease program, Massachusetts General Hospital, Boston, said they’ve gone from seeing 400 patients a day in their clinic to fewer than 40 and are trying to push that number even lower and use virtual care as much as possible.
“The reason is we are having to send home physicians who are exposed and it’s cutting into our workforce very quickly. So the more people you could have at home doing work virtually is important because you’re going to need to call them in [during] the next couple of weeks,” she said. “And our PPE [personal protective equipment] is running low. So if we can afford to not have someone come in the office and not wear a mask because they had a cough, that’s a mask that can be used by someone performing CPR in an ICU.”
The hospital also adopted a train-the-trainer method to bring its existing telehealth program to cardiology, said Dr. Bhatt, who coauthored the American College of Cardiology’s recent guidance on establishing telehealth in the cardiology clinic.
“We find that sending people tip sheets and PowerPoints in addition to everything that is happening ... is too much,” Dr. Bhatt observed. “So actually holding your friend’s hand and walking them through it once you’ve learned how to do it has been really great in terms of adoption. Otherwise, everyone would fall back on phone, which is OK for now, but we need to establish a long-term plan.”
During the same March 20 webinar, David Konur, CEO of the Cardiovascular Institute of the South, Houma, La., said they began doing telecardiology more than 5 years ago and now do about 30,000 “patient touches” a month with 24/7 access.
“This is certainly an unprecedented time,” he said. “COVID-19 is shining a very bright light on the barriers that exist in health care, as well as the friction that exists to accessing care for all of our patients.”
New mandates
A new Food and Drug Administration policy, temporarily relaxing prior guidance on certain connected remote monitoring devices such as ECGs and cardiac monitors, is part of a shifting landscape to reduce barriers to telehealth during the ongoing pandemic. The increased flexibility may increase access to important patient physiological data, while eliminating unnecessary patient contact and easing the burden on healthcare facilities and providers, the agency said in the new guidance, issued March 20.
As such, the FDA “does not intend to object to limited modifications to the indications, claims, functionality, or hardware or software of FDA-cleared noninvasive remote monitoring devices that are used to support patient monitoring.”
Modifications could include the addition of monitoring statements for patients with COVID-19 or coexisting conditions such as hypertension and heart failure; a change to the indications or claims related to home use of devices previously cleared for use only in health care settings; and changes to hardware or software to increase remote monitoring capability. The approved devices listed in the guidance are clinical electronic thermometers, ECGs, cardiac monitors, ECG software for over-the-counter use, pulse oximetry, noninvasive blood pressure monitors, respiratory rate/breathing frequency monitors, and electronic stethoscopes.
The FDA policy comes just days after the Centers for Medicare & Medicaid Services expanded telehealth coverage to Medicare beneficiaries and the Office for Civil Rights at the U.S. Department of Health & Human Services said it would not penalize health care providers for using such non–HIPAA compliant third-party apps as Skype or Google Hangouts video. The HHS also signaled that physicians would be allowed to practice across state lines during the COVID-19 crisis.
“All these mandates have come in a time of desperation where we’re doing the best that we can to provide for patients and keep them safe,” Eugenia Gianos, MD, system director of cardiovascular prevention at Northwell Health and director of the Women’s Cardiovascular Center, Lenox Hill Hospital, New York, said in an interview. “Realistically, the whole digital realm has a lot of promise for our patients.” She noted that telehealth programs are still being developed for the department, but that office visits have been purposely scaled back by more than 75% to protect patients as well as health care providers. “In times of need, the most promising technologies we have, have to come to the forefront,” Dr. Gianos said. “So using the data from the home – whether they have a blood pressure cuff or something that tracks their heart rate or their weight – when we don’t otherwise have data, is of great value.”
Andrew M. Freeman, MD, director of clinical cardiology and operations at National Jewish Hospital in Denver, said “in the current situation, telehealth is the most viable option because it keeps patients safe and physicians safe. So it wouldn’t surprise me if every institution in the country, if not worldwide, is very rapidly pursuing this kind of approach.”
Exactly how many programs or cardiologists were already using telehealth is impossible to say, although the ACC is planning to survey its members on their practices during the COVID-19 pandemic, he noted.
The situation is so fluid that ACC is already revising its March 13 telehealth guidance to reflect the recent policy changes. Another document is being prepared to provide physicians with a template for the telehealth space, said Dr. Freeman, who coauthored the telehealth guidance and also serves on the ACC’s Innovation Leadership Council.
The new FDA policy allowing greater flexibility on remote monitoring devices is somewhat “vaguely worded,” Dr. Freeman noted, but highlights the ability of existing technology to provide essential patient data from home. “I think as we add adjuncts to the things we’re used to in the normal face-to-face visit, it’s going to make the face-to-face visit less required,” he said.
Questions remain, however, on implementing telehealth for new patients and whether payers will follow HHS’s decision not to conduct audits to ensure a prior relationship existed. The potential for telehealth to reach across state lines also is being viewed cautiously until tested legally, Dr. Freeman observed.
“If there’s one blessing in this awful disease that we have received, is that it may really give the power to clinicians, hospital systems, and payers to make telehealth a true viable, sustainable solution for good care that’s readily available to folks,” he said.
Fast-tracked research
On March 24, the American Heart Association announced it is committing $2.5 million for fast-tracked research grants for projects than can turn around results within 9-12 months and focus on how this novel coronavirus affects heart and brain health.
Additional funding also will be made available to the AHA’s new Center for Health Technology & Innovation’s Strategically Focused Research Networks to develop rapid technology solutions to aid in dealing with the pandemic.
The rapid response grant is an “unprecedented but logical move for the organization in these extraordinary times,” AHA President Bob Harrington, MD, chair of medicine at Stanford (Calif.) University, said in a statement. “We are committed to quickly bringing together and supporting some of the brightest minds in research science and clinical care who are shovel ready with the laboratories, tools, and data resources to immediately begin work on addressing this emergent issue.”
Dr. Freeman and Dr. Bhatt have disclosed no relevant financial relationships. Dr. Harrington is on the editorial board for Medscape Cardiology.
A version of this article originally appeared on Medscape.com
during the COVID-19 pandemic.
During a recent telehealth webinar, Ami Bhatt, MD, director of the adult congenital heart disease program, Massachusetts General Hospital, Boston, said they’ve gone from seeing 400 patients a day in their clinic to fewer than 40 and are trying to push that number even lower and use virtual care as much as possible.
“The reason is we are having to send home physicians who are exposed and it’s cutting into our workforce very quickly. So the more people you could have at home doing work virtually is important because you’re going to need to call them in [during] the next couple of weeks,” she said. “And our PPE [personal protective equipment] is running low. So if we can afford to not have someone come in the office and not wear a mask because they had a cough, that’s a mask that can be used by someone performing CPR in an ICU.”
The hospital also adopted a train-the-trainer method to bring its existing telehealth program to cardiology, said Dr. Bhatt, who coauthored the American College of Cardiology’s recent guidance on establishing telehealth in the cardiology clinic.
“We find that sending people tip sheets and PowerPoints in addition to everything that is happening ... is too much,” Dr. Bhatt observed. “So actually holding your friend’s hand and walking them through it once you’ve learned how to do it has been really great in terms of adoption. Otherwise, everyone would fall back on phone, which is OK for now, but we need to establish a long-term plan.”
During the same March 20 webinar, David Konur, CEO of the Cardiovascular Institute of the South, Houma, La., said they began doing telecardiology more than 5 years ago and now do about 30,000 “patient touches” a month with 24/7 access.
“This is certainly an unprecedented time,” he said. “COVID-19 is shining a very bright light on the barriers that exist in health care, as well as the friction that exists to accessing care for all of our patients.”
New mandates
A new Food and Drug Administration policy, temporarily relaxing prior guidance on certain connected remote monitoring devices such as ECGs and cardiac monitors, is part of a shifting landscape to reduce barriers to telehealth during the ongoing pandemic. The increased flexibility may increase access to important patient physiological data, while eliminating unnecessary patient contact and easing the burden on healthcare facilities and providers, the agency said in the new guidance, issued March 20.
As such, the FDA “does not intend to object to limited modifications to the indications, claims, functionality, or hardware or software of FDA-cleared noninvasive remote monitoring devices that are used to support patient monitoring.”
Modifications could include the addition of monitoring statements for patients with COVID-19 or coexisting conditions such as hypertension and heart failure; a change to the indications or claims related to home use of devices previously cleared for use only in health care settings; and changes to hardware or software to increase remote monitoring capability. The approved devices listed in the guidance are clinical electronic thermometers, ECGs, cardiac monitors, ECG software for over-the-counter use, pulse oximetry, noninvasive blood pressure monitors, respiratory rate/breathing frequency monitors, and electronic stethoscopes.
The FDA policy comes just days after the Centers for Medicare & Medicaid Services expanded telehealth coverage to Medicare beneficiaries and the Office for Civil Rights at the U.S. Department of Health & Human Services said it would not penalize health care providers for using such non–HIPAA compliant third-party apps as Skype or Google Hangouts video. The HHS also signaled that physicians would be allowed to practice across state lines during the COVID-19 crisis.
“All these mandates have come in a time of desperation where we’re doing the best that we can to provide for patients and keep them safe,” Eugenia Gianos, MD, system director of cardiovascular prevention at Northwell Health and director of the Women’s Cardiovascular Center, Lenox Hill Hospital, New York, said in an interview. “Realistically, the whole digital realm has a lot of promise for our patients.” She noted that telehealth programs are still being developed for the department, but that office visits have been purposely scaled back by more than 75% to protect patients as well as health care providers. “In times of need, the most promising technologies we have, have to come to the forefront,” Dr. Gianos said. “So using the data from the home – whether they have a blood pressure cuff or something that tracks their heart rate or their weight – when we don’t otherwise have data, is of great value.”
Andrew M. Freeman, MD, director of clinical cardiology and operations at National Jewish Hospital in Denver, said “in the current situation, telehealth is the most viable option because it keeps patients safe and physicians safe. So it wouldn’t surprise me if every institution in the country, if not worldwide, is very rapidly pursuing this kind of approach.”
Exactly how many programs or cardiologists were already using telehealth is impossible to say, although the ACC is planning to survey its members on their practices during the COVID-19 pandemic, he noted.
The situation is so fluid that ACC is already revising its March 13 telehealth guidance to reflect the recent policy changes. Another document is being prepared to provide physicians with a template for the telehealth space, said Dr. Freeman, who coauthored the telehealth guidance and also serves on the ACC’s Innovation Leadership Council.
The new FDA policy allowing greater flexibility on remote monitoring devices is somewhat “vaguely worded,” Dr. Freeman noted, but highlights the ability of existing technology to provide essential patient data from home. “I think as we add adjuncts to the things we’re used to in the normal face-to-face visit, it’s going to make the face-to-face visit less required,” he said.
Questions remain, however, on implementing telehealth for new patients and whether payers will follow HHS’s decision not to conduct audits to ensure a prior relationship existed. The potential for telehealth to reach across state lines also is being viewed cautiously until tested legally, Dr. Freeman observed.
“If there’s one blessing in this awful disease that we have received, is that it may really give the power to clinicians, hospital systems, and payers to make telehealth a true viable, sustainable solution for good care that’s readily available to folks,” he said.
Fast-tracked research
On March 24, the American Heart Association announced it is committing $2.5 million for fast-tracked research grants for projects than can turn around results within 9-12 months and focus on how this novel coronavirus affects heart and brain health.
Additional funding also will be made available to the AHA’s new Center for Health Technology & Innovation’s Strategically Focused Research Networks to develop rapid technology solutions to aid in dealing with the pandemic.
The rapid response grant is an “unprecedented but logical move for the organization in these extraordinary times,” AHA President Bob Harrington, MD, chair of medicine at Stanford (Calif.) University, said in a statement. “We are committed to quickly bringing together and supporting some of the brightest minds in research science and clinical care who are shovel ready with the laboratories, tools, and data resources to immediately begin work on addressing this emergent issue.”
Dr. Freeman and Dr. Bhatt have disclosed no relevant financial relationships. Dr. Harrington is on the editorial board for Medscape Cardiology.
A version of this article originally appeared on Medscape.com
during the COVID-19 pandemic.
During a recent telehealth webinar, Ami Bhatt, MD, director of the adult congenital heart disease program, Massachusetts General Hospital, Boston, said they’ve gone from seeing 400 patients a day in their clinic to fewer than 40 and are trying to push that number even lower and use virtual care as much as possible.
“The reason is we are having to send home physicians who are exposed and it’s cutting into our workforce very quickly. So the more people you could have at home doing work virtually is important because you’re going to need to call them in [during] the next couple of weeks,” she said. “And our PPE [personal protective equipment] is running low. So if we can afford to not have someone come in the office and not wear a mask because they had a cough, that’s a mask that can be used by someone performing CPR in an ICU.”
The hospital also adopted a train-the-trainer method to bring its existing telehealth program to cardiology, said Dr. Bhatt, who coauthored the American College of Cardiology’s recent guidance on establishing telehealth in the cardiology clinic.
“We find that sending people tip sheets and PowerPoints in addition to everything that is happening ... is too much,” Dr. Bhatt observed. “So actually holding your friend’s hand and walking them through it once you’ve learned how to do it has been really great in terms of adoption. Otherwise, everyone would fall back on phone, which is OK for now, but we need to establish a long-term plan.”
During the same March 20 webinar, David Konur, CEO of the Cardiovascular Institute of the South, Houma, La., said they began doing telecardiology more than 5 years ago and now do about 30,000 “patient touches” a month with 24/7 access.
“This is certainly an unprecedented time,” he said. “COVID-19 is shining a very bright light on the barriers that exist in health care, as well as the friction that exists to accessing care for all of our patients.”
New mandates
A new Food and Drug Administration policy, temporarily relaxing prior guidance on certain connected remote monitoring devices such as ECGs and cardiac monitors, is part of a shifting landscape to reduce barriers to telehealth during the ongoing pandemic. The increased flexibility may increase access to important patient physiological data, while eliminating unnecessary patient contact and easing the burden on healthcare facilities and providers, the agency said in the new guidance, issued March 20.
As such, the FDA “does not intend to object to limited modifications to the indications, claims, functionality, or hardware or software of FDA-cleared noninvasive remote monitoring devices that are used to support patient monitoring.”
Modifications could include the addition of monitoring statements for patients with COVID-19 or coexisting conditions such as hypertension and heart failure; a change to the indications or claims related to home use of devices previously cleared for use only in health care settings; and changes to hardware or software to increase remote monitoring capability. The approved devices listed in the guidance are clinical electronic thermometers, ECGs, cardiac monitors, ECG software for over-the-counter use, pulse oximetry, noninvasive blood pressure monitors, respiratory rate/breathing frequency monitors, and electronic stethoscopes.
The FDA policy comes just days after the Centers for Medicare & Medicaid Services expanded telehealth coverage to Medicare beneficiaries and the Office for Civil Rights at the U.S. Department of Health & Human Services said it would not penalize health care providers for using such non–HIPAA compliant third-party apps as Skype or Google Hangouts video. The HHS also signaled that physicians would be allowed to practice across state lines during the COVID-19 crisis.
“All these mandates have come in a time of desperation where we’re doing the best that we can to provide for patients and keep them safe,” Eugenia Gianos, MD, system director of cardiovascular prevention at Northwell Health and director of the Women’s Cardiovascular Center, Lenox Hill Hospital, New York, said in an interview. “Realistically, the whole digital realm has a lot of promise for our patients.” She noted that telehealth programs are still being developed for the department, but that office visits have been purposely scaled back by more than 75% to protect patients as well as health care providers. “In times of need, the most promising technologies we have, have to come to the forefront,” Dr. Gianos said. “So using the data from the home – whether they have a blood pressure cuff or something that tracks their heart rate or their weight – when we don’t otherwise have data, is of great value.”
Andrew M. Freeman, MD, director of clinical cardiology and operations at National Jewish Hospital in Denver, said “in the current situation, telehealth is the most viable option because it keeps patients safe and physicians safe. So it wouldn’t surprise me if every institution in the country, if not worldwide, is very rapidly pursuing this kind of approach.”
Exactly how many programs or cardiologists were already using telehealth is impossible to say, although the ACC is planning to survey its members on their practices during the COVID-19 pandemic, he noted.
The situation is so fluid that ACC is already revising its March 13 telehealth guidance to reflect the recent policy changes. Another document is being prepared to provide physicians with a template for the telehealth space, said Dr. Freeman, who coauthored the telehealth guidance and also serves on the ACC’s Innovation Leadership Council.
The new FDA policy allowing greater flexibility on remote monitoring devices is somewhat “vaguely worded,” Dr. Freeman noted, but highlights the ability of existing technology to provide essential patient data from home. “I think as we add adjuncts to the things we’re used to in the normal face-to-face visit, it’s going to make the face-to-face visit less required,” he said.
Questions remain, however, on implementing telehealth for new patients and whether payers will follow HHS’s decision not to conduct audits to ensure a prior relationship existed. The potential for telehealth to reach across state lines also is being viewed cautiously until tested legally, Dr. Freeman observed.
“If there’s one blessing in this awful disease that we have received, is that it may really give the power to clinicians, hospital systems, and payers to make telehealth a true viable, sustainable solution for good care that’s readily available to folks,” he said.
Fast-tracked research
On March 24, the American Heart Association announced it is committing $2.5 million for fast-tracked research grants for projects than can turn around results within 9-12 months and focus on how this novel coronavirus affects heart and brain health.
Additional funding also will be made available to the AHA’s new Center for Health Technology & Innovation’s Strategically Focused Research Networks to develop rapid technology solutions to aid in dealing with the pandemic.
The rapid response grant is an “unprecedented but logical move for the organization in these extraordinary times,” AHA President Bob Harrington, MD, chair of medicine at Stanford (Calif.) University, said in a statement. “We are committed to quickly bringing together and supporting some of the brightest minds in research science and clinical care who are shovel ready with the laboratories, tools, and data resources to immediately begin work on addressing this emergent issue.”
Dr. Freeman and Dr. Bhatt have disclosed no relevant financial relationships. Dr. Harrington is on the editorial board for Medscape Cardiology.
A version of this article originally appeared on Medscape.com
FDA to allow alternative respiratory devices to treat COVID-19
“Whenever possible, health care facilities should use FDA-cleared conventional/standard full-featured ventilators when necessary to support patients with respiratory failure, or a device subject to an Emergency Use Authorization (EUA), if any,” FDA stated in a guidance document issued March 22.
“However, to help ensure the availability of the greatest possible number of devices for this purpose, ... FDA does not intend to object to limited modifications to indications, claims, functionality, or to the hardware, software, or materials of FDA-cleared devices used to support patients with respiratory failure or respiratory insufficiency, without prior submission of a premarket notification” for the duration of the declared national emergency related to the COVID-19 pandemic.
FDA Commissioner Stephen Hahn, MD, said in a statement that the agency is doing everything it can to support patients, health care professionals, and others during this pandemic.
“One of the most impactful steps we can take is to help with access and availability to life-saving medical treatments,” he said. “Our policy issued today demonstrates our ability to react and adapt quickly during this pandemic and help very ill patients access the lifesaving ventilator support they need. To do that, we are providing maximum regulatory flexibility to facilitate an increase in ventilator inventory, while still providing crucial FDA oversight. We believe this action will immediately increase ventilator availability.”
The document identified examples of where modifications would not create undue risk, including the use of powered emergency ventilators and anesthesia gas machines for patients needing mechanical ventilation; the use of ventilators outside of their cleared environment; the use of devices used to treat patients with sleep apnea, such as CPAPs and BiPAPs, to treat respiratory insufficiency when appropriate design mitigations are in place to minimize aerosolization; and the use of oxygen concentrators for primary supply when medically necessary and clinically appropriate.
The agency also is allowing for changes to the hardware, software, and materials to FDA-cleared ventilators and anesthesia gas machines, such as modifications to motors, batteries, or other electrical components; material changes to components in the gas pathways or with other patient tissue contact; the introduction of filtration to minimize aerosolization; and other hardware and software modifications.
FDA is also allowing for products to be used past their indicated shelf life.
“Whenever possible, health care facilities should use FDA-cleared conventional/standard full-featured ventilators when necessary to support patients with respiratory failure, or a device subject to an Emergency Use Authorization (EUA), if any,” FDA stated in a guidance document issued March 22.
“However, to help ensure the availability of the greatest possible number of devices for this purpose, ... FDA does not intend to object to limited modifications to indications, claims, functionality, or to the hardware, software, or materials of FDA-cleared devices used to support patients with respiratory failure or respiratory insufficiency, without prior submission of a premarket notification” for the duration of the declared national emergency related to the COVID-19 pandemic.
FDA Commissioner Stephen Hahn, MD, said in a statement that the agency is doing everything it can to support patients, health care professionals, and others during this pandemic.
“One of the most impactful steps we can take is to help with access and availability to life-saving medical treatments,” he said. “Our policy issued today demonstrates our ability to react and adapt quickly during this pandemic and help very ill patients access the lifesaving ventilator support they need. To do that, we are providing maximum regulatory flexibility to facilitate an increase in ventilator inventory, while still providing crucial FDA oversight. We believe this action will immediately increase ventilator availability.”
The document identified examples of where modifications would not create undue risk, including the use of powered emergency ventilators and anesthesia gas machines for patients needing mechanical ventilation; the use of ventilators outside of their cleared environment; the use of devices used to treat patients with sleep apnea, such as CPAPs and BiPAPs, to treat respiratory insufficiency when appropriate design mitigations are in place to minimize aerosolization; and the use of oxygen concentrators for primary supply when medically necessary and clinically appropriate.
The agency also is allowing for changes to the hardware, software, and materials to FDA-cleared ventilators and anesthesia gas machines, such as modifications to motors, batteries, or other electrical components; material changes to components in the gas pathways or with other patient tissue contact; the introduction of filtration to minimize aerosolization; and other hardware and software modifications.
FDA is also allowing for products to be used past their indicated shelf life.
“Whenever possible, health care facilities should use FDA-cleared conventional/standard full-featured ventilators when necessary to support patients with respiratory failure, or a device subject to an Emergency Use Authorization (EUA), if any,” FDA stated in a guidance document issued March 22.
“However, to help ensure the availability of the greatest possible number of devices for this purpose, ... FDA does not intend to object to limited modifications to indications, claims, functionality, or to the hardware, software, or materials of FDA-cleared devices used to support patients with respiratory failure or respiratory insufficiency, without prior submission of a premarket notification” for the duration of the declared national emergency related to the COVID-19 pandemic.
FDA Commissioner Stephen Hahn, MD, said in a statement that the agency is doing everything it can to support patients, health care professionals, and others during this pandemic.
“One of the most impactful steps we can take is to help with access and availability to life-saving medical treatments,” he said. “Our policy issued today demonstrates our ability to react and adapt quickly during this pandemic and help very ill patients access the lifesaving ventilator support they need. To do that, we are providing maximum regulatory flexibility to facilitate an increase in ventilator inventory, while still providing crucial FDA oversight. We believe this action will immediately increase ventilator availability.”
The document identified examples of where modifications would not create undue risk, including the use of powered emergency ventilators and anesthesia gas machines for patients needing mechanical ventilation; the use of ventilators outside of their cleared environment; the use of devices used to treat patients with sleep apnea, such as CPAPs and BiPAPs, to treat respiratory insufficiency when appropriate design mitigations are in place to minimize aerosolization; and the use of oxygen concentrators for primary supply when medically necessary and clinically appropriate.
The agency also is allowing for changes to the hardware, software, and materials to FDA-cleared ventilators and anesthesia gas machines, such as modifications to motors, batteries, or other electrical components; material changes to components in the gas pathways or with other patient tissue contact; the introduction of filtration to minimize aerosolization; and other hardware and software modifications.
FDA is also allowing for products to be used past their indicated shelf life.
Survey explores the role of social media in choosing a dermatologist
Fewer than one-quarter of consumers rely heavily on social media for choosing a dermatologist, results from an online survey suggest.
In a video presentation during a virtual meeting held by the George Washington University department of dermatology, Kamaria Nelson, MD, said that, as of 2019, 79% of Americans have a social media account, with the majority using platforms such as Facebook, Instagram, Twitter, and YouTube. “There’s also a high predominance of social media use in the dermatology field, with many dermatologists assuming that it will improve their personal brands,” said Dr. Nelson, a research fellow in the department of dermatology at George Washington University, Washington. “Some even hire social media managers to monitor online reviews and mitigate any damage. So, although social media is commonly used, it’s unknown if it impacts patient knowledge, access to health care, or provider choice.”
To evaluate how social media influences patients when choosing a dermatologist, she and her colleagues used Survey Monkey to create a 10-item questionnaire that they distributed to 1,481 individuals in the general U.S. population in May 2019. Individuals qualified for the study if they used social media and if they had ever been to a dermatologist. Dr. Nelson reported that 726 individuals (58%) qualified for the survey and 715 completed it, for a response rate of 98%. The researchers used Chi-square tests to compare frequency and importance of social media by visit type, age, gender, and educational level.
When the respondents were stratified by visit type, 43% who saw a dermatologist for cosmetic reasons were more likely to view social media as “extremely important” or “very important,” compared with 15% of patients who saw a dermatologist for medical reasons (P less than .0001).
When stratified by age, about 12% of respondents between the ages of 18 and 44 years considered social media as extremely important when choosing a dermatologist, compared with only 9% of those aged 45-60 years and about 2% of those older than age 60 (P less than .0001).
When stratified by educational level, 30% of respondents with a high school degree or less were more likely to view social media as extremely important or very important when choosing a dermatologist, while 62% of those with more than a high school degree were more likely to view social media as “not at all important” or only “slightly important” (P = .0006).
One of the survey questions was, “When choosing a dermatologist to see, how important is his or her social media site?” Only 9% of respondents said extremely important, 13% said very important, 21% said “moderately important,” 24% said slightly important, and 33% said not at all important. “This left about 22% of respondents who viewed the social media site as extremely important or very important when choosing a dermatologist,” Dr. Nelson said.
Factors deemed important on a dermatologist’s social media profile were patient reviews (68%), years of experience (61%), and the amount of medical information written by the dermatologist (59%).
“There seems to be a low reliance on social media when selecting a dermatologist,” Dr. Nelson concluded. “We also found that cosmetic patients, patients with lower levels of education, and younger patients were more likely to value social media. Therefore, social media may only be useful for targeting specific patient populations. When doing so, medical information written by a provider is most often desired.”
The virtual meeting included presentations that had been slated for the annual meeting of the American Academy of Dermatology, which was canceled because of the COVID-19 pandemic. Dr. Nelson reported having no disclosures.
Fewer than one-quarter of consumers rely heavily on social media for choosing a dermatologist, results from an online survey suggest.
In a video presentation during a virtual meeting held by the George Washington University department of dermatology, Kamaria Nelson, MD, said that, as of 2019, 79% of Americans have a social media account, with the majority using platforms such as Facebook, Instagram, Twitter, and YouTube. “There’s also a high predominance of social media use in the dermatology field, with many dermatologists assuming that it will improve their personal brands,” said Dr. Nelson, a research fellow in the department of dermatology at George Washington University, Washington. “Some even hire social media managers to monitor online reviews and mitigate any damage. So, although social media is commonly used, it’s unknown if it impacts patient knowledge, access to health care, or provider choice.”
To evaluate how social media influences patients when choosing a dermatologist, she and her colleagues used Survey Monkey to create a 10-item questionnaire that they distributed to 1,481 individuals in the general U.S. population in May 2019. Individuals qualified for the study if they used social media and if they had ever been to a dermatologist. Dr. Nelson reported that 726 individuals (58%) qualified for the survey and 715 completed it, for a response rate of 98%. The researchers used Chi-square tests to compare frequency and importance of social media by visit type, age, gender, and educational level.
When the respondents were stratified by visit type, 43% who saw a dermatologist for cosmetic reasons were more likely to view social media as “extremely important” or “very important,” compared with 15% of patients who saw a dermatologist for medical reasons (P less than .0001).
When stratified by age, about 12% of respondents between the ages of 18 and 44 years considered social media as extremely important when choosing a dermatologist, compared with only 9% of those aged 45-60 years and about 2% of those older than age 60 (P less than .0001).
When stratified by educational level, 30% of respondents with a high school degree or less were more likely to view social media as extremely important or very important when choosing a dermatologist, while 62% of those with more than a high school degree were more likely to view social media as “not at all important” or only “slightly important” (P = .0006).
One of the survey questions was, “When choosing a dermatologist to see, how important is his or her social media site?” Only 9% of respondents said extremely important, 13% said very important, 21% said “moderately important,” 24% said slightly important, and 33% said not at all important. “This left about 22% of respondents who viewed the social media site as extremely important or very important when choosing a dermatologist,” Dr. Nelson said.
Factors deemed important on a dermatologist’s social media profile were patient reviews (68%), years of experience (61%), and the amount of medical information written by the dermatologist (59%).
“There seems to be a low reliance on social media when selecting a dermatologist,” Dr. Nelson concluded. “We also found that cosmetic patients, patients with lower levels of education, and younger patients were more likely to value social media. Therefore, social media may only be useful for targeting specific patient populations. When doing so, medical information written by a provider is most often desired.”
The virtual meeting included presentations that had been slated for the annual meeting of the American Academy of Dermatology, which was canceled because of the COVID-19 pandemic. Dr. Nelson reported having no disclosures.
Fewer than one-quarter of consumers rely heavily on social media for choosing a dermatologist, results from an online survey suggest.
In a video presentation during a virtual meeting held by the George Washington University department of dermatology, Kamaria Nelson, MD, said that, as of 2019, 79% of Americans have a social media account, with the majority using platforms such as Facebook, Instagram, Twitter, and YouTube. “There’s also a high predominance of social media use in the dermatology field, with many dermatologists assuming that it will improve their personal brands,” said Dr. Nelson, a research fellow in the department of dermatology at George Washington University, Washington. “Some even hire social media managers to monitor online reviews and mitigate any damage. So, although social media is commonly used, it’s unknown if it impacts patient knowledge, access to health care, or provider choice.”
To evaluate how social media influences patients when choosing a dermatologist, she and her colleagues used Survey Monkey to create a 10-item questionnaire that they distributed to 1,481 individuals in the general U.S. population in May 2019. Individuals qualified for the study if they used social media and if they had ever been to a dermatologist. Dr. Nelson reported that 726 individuals (58%) qualified for the survey and 715 completed it, for a response rate of 98%. The researchers used Chi-square tests to compare frequency and importance of social media by visit type, age, gender, and educational level.
When the respondents were stratified by visit type, 43% who saw a dermatologist for cosmetic reasons were more likely to view social media as “extremely important” or “very important,” compared with 15% of patients who saw a dermatologist for medical reasons (P less than .0001).
When stratified by age, about 12% of respondents between the ages of 18 and 44 years considered social media as extremely important when choosing a dermatologist, compared with only 9% of those aged 45-60 years and about 2% of those older than age 60 (P less than .0001).
When stratified by educational level, 30% of respondents with a high school degree or less were more likely to view social media as extremely important or very important when choosing a dermatologist, while 62% of those with more than a high school degree were more likely to view social media as “not at all important” or only “slightly important” (P = .0006).
One of the survey questions was, “When choosing a dermatologist to see, how important is his or her social media site?” Only 9% of respondents said extremely important, 13% said very important, 21% said “moderately important,” 24% said slightly important, and 33% said not at all important. “This left about 22% of respondents who viewed the social media site as extremely important or very important when choosing a dermatologist,” Dr. Nelson said.
Factors deemed important on a dermatologist’s social media profile were patient reviews (68%), years of experience (61%), and the amount of medical information written by the dermatologist (59%).
“There seems to be a low reliance on social media when selecting a dermatologist,” Dr. Nelson concluded. “We also found that cosmetic patients, patients with lower levels of education, and younger patients were more likely to value social media. Therefore, social media may only be useful for targeting specific patient populations. When doing so, medical information written by a provider is most often desired.”
The virtual meeting included presentations that had been slated for the annual meeting of the American Academy of Dermatology, which was canceled because of the COVID-19 pandemic. Dr. Nelson reported having no disclosures.
7 tips for running your practice in the coronavirus crisis
At one large practice in Bergen County, New Jersey, the waiting room is empty — but its patients are still receiving care. As of mid-March, the practice is still operating, thanks to the group’s willingness to adapt its work flow, sometimes radically, to mitigate the threat of the COVID-19 pandemic.
For example, patients now call the receptionist from their vehicles when they arrive, and wait there until receiving a call back telling them the clinician is ready. The practice has also started using telemedicine for the first time, to the extent it can be adopted in a hurry, and some clinicians are working from home on tasks such as medication refills.
Still, the rapidly increasing numbers of COVID-19 cases in the United States raises the possibility that some physician offices will decide or be forced to close temporarily, as occurred in London last month.
Many practices across the country are having to adjust the way they operate, amid daily changes in the pandemic. What should you do to adapt to this new way of operating your practice?
1. Create a task force to manage change
The readiness of medical practices to address the myriad challenges posed by this crisis has so far been a mixed bag, said Owen Dahl, MBA, a Texas-based medical practice management consultant. “Leadership is going to have to assess what’s happening in the community, what’s happening with staff members who may or may not have the disease and may or may not have to self-quarantine,” Dahl said.
The physicians, the administrator, CEO, or managing partner should be involved in decision making as the global crisis unfolds, added Laurie Morgan, MBA, a California-based practice management consultant. And depending on the size of the practice, it may be useful to delegate specific components of this work to various department managers or other individuals in the group.
The team should assess:
- Recommendations and/or mandates from local, state, and federal governments
- Guidance from specialty and state medical societies
- How to triage patients over the phone, virtual visits, or referral to an alternate site of care
- Where to send patients for testing
- The practice’s inventory of personal protective equipment (PPE)
- Review of and possible revision of current infection control policies
- Possible collaborations within the community
- Reimbursement policies for suspected COVID-19 triage, testing, and follow-up treatment — in office or virtually
- Whether some employees’ work (eg, billing, coding) can be done remotely
- Options for paying personnel in the case of a temporary shutdown
- What’s covered and excluded by the group’s business interruption insurance
2. Consider postponing nonessential appointments
What’s more, it’s crucial for practices to form a strategy that does not involve bringing patients into the office, said Javeed Siddiqui, MD, MPH, an infectious disease physician, epidemiologist, and chief medical officer of TeleMed2U. “One thing we really have to recognize in this pandemic is that we don’t want people going and sitting in our waiting room. We don’t want people coming, and not only exposing other patients, but also further exposing staff. Forward triaging is going to be essential in this type of pandemic.”
Reliant Medical Group, with multiple locations in Massachusetts, for example, announced to patients recently that it will postpone appointments for some routine and elective procedures, as determined by the group’s physicians and clinical staff.
“Taking this step will help limit the number of people passing through our facilities, which will help slow the spread of illness [as recommended by the CDC],” noted an email blast to patients.
3. Overcommunicate to patients
With a situation as dynamic and unprecedented as this, constant and clear communication with patients is crucial. “In general, in my experience, practices don’t realize how much communication is necessary,” said Morgan. “In order to be effective and get the word out, you have to be overcommunicating.”
Today’s practices have multiple ways to communicate to keep people informed, including email, text messaging, social media, patient portals, and even local television and radio.
One email or text message to the patient population can help direct them to the appropriate streams of information. Helping direct patients to updated information is critical.
In contrast, having the front desk field multitudes of calls from concerned patients ties up precious resources, according Siddiqui. “Right now, practices are absolutely inundated, patients are waiting on hold, and that creates a great deal of frustration,” he said.
“We really need to take a page from every other industry in the United States, and that is using secure SMS, email communication, and telehealth,” Siddiqui said. “Healthcare generally tends to be a laggard in this because so many people think, ‘Well, you can’t do that in healthcare,’ as opposed to thinking, ‘How can we do that in healthcare?’”
4. Take advantage of telemedicine
Fortunately, technology to interact with patients remotely is almost ubiquitous. Even for practices with little experience in this arena, various vendors exist that can get secure, HIPAA-compliant technologies up and running quickly.
Various payers have issued guidance regarding reimbursement for telemedicine specific to COVID-19, and on March 6, Congress passed a law regarding Medicare coverage and payment for virtual services during a government-declared state of emergency. Some of the rules about HIPAA compliance in telemedicine have been eased for this emergency.
But even with well-established telemedicine modalities in place, it’s crunch time for applying it to COVID-19. “You need to find a way to have telemedicine available and use it, because depending on how this goes, that’s going to be clearly the safest, best way to care for a huge number of people,” said Darryl Elmouchi, MD, MBA, chief medical officer of Spectrum Health System and president of Spectrum Health Medical Group in Michigan.
“What we recognize now, both with our past experience with telehealth for many years and specifically with this coronavirus testing we’ve done, is that it’s incredibly useful both for the clinicians and the patients,” Elmouchi said.
One possibility to consider is the tactic used by Spectrum, a large integrated healthcare system. The company mobilized its existing telemedicine program to offer free virtual screenings for anyone in Michigan showing possible symptoms of COVID-19. “We wanted to keep people out of our clinics, emergency rooms, and urgent care centers if they didn’t need to be there, and help allay fears,” he said.
Elmouchi said his company faced the problems that other physicians would also have to deal with. “It was a ton of work with a dedicated team that was focused on this. The hardest part was probably trying to determine how we can staff it,” he said.
With their dedicated virtual team still seeing regularly scheduled virtual patients, the system had to reassign its traditional teams, such as urgent care and primary care clinicians, to the virtual screening effort. “Then we had to figure out how we could operationalize it. It was a lot of work,” Elmouchi said.
Telemedicine capabilities are not limited to screening patients, but can also be used to stay in touch with patients who may be quarantined and provide follow-up care, he noted.
5. Identify COVID-19 testing sites
Access to tests remains a problem in the US, but is improving by the week. For practices that can attain the tests themselves, it will still require some creativity to administer them with as little risk as possible. In South Korea, for example, and increasingly in the United States, healthcare organizations are instructing patients waiting to be tested to stay in their cars and have a practitioner wearing the proper PPE go out to patients to test them there.
Alternatively, some practices may opt to have PPE-wearing staff members bring PPE to patients in their cars and then escort them to a designated testing area in the building —through the back door if noninfected patients are still being seen.
“Once in the office, you still need to isolate virus patients in any way you can,” Dahl said. “In fact, you want a negative-pressure environment if possible, with the air being sucked out rather than circulating,” he said, adding that a large restroom with a ventilation system could be repurposed as a makeshift exam room.
Community testing sites are another possibility, given proper coordination with other healthcare organizations and community officials. Siddiqui has been working with several communities in which individual clinics and hospitals are unable to handle testing on their own, and have instead collaborated to create community testing sites in tents on local athletic fields.
“One of our communities is looking at using the local college parking lot to do drive-through testing there,” he said. “We really need to embrace collaboration much more than we’ve ever done.”
Collaboration also requires sharing supplies and PPE, noted Dahl. “Don’t hoard them because of the shortage. Look at your inventory and make sure you can help out whomever you may be sending patients to.” And if your office is falling short, Dahl advises checking with offices in your community that may be closing — such as dentists or plastic surgeons — for supplies you can purchase or simply have.
The US Food and Drug Administration has issued some guidance to healthcare providers about shortages of surgical masks and gowns, including advice about reusable cloth alternatives to gowns.
In addition, some hospitals have asked clinicians to keep their masks and provided guidance on how to conserve supplies.
6. Preparing to potentially shut down
A temporary closure may be inevitable for some practices. “Maybe the physician owners will not feel like they have a choice,” said Morgan. “They might feel like they want to stay open for as long as they can; but if it’s not safe for patients or not safe for employees, maybe they’ll feel it’s better if they check out for a bit.”
Should practices make the decision to close or reduce hours, multimodal communication with patients and the public is paramount. Patients will want to know whom to call if they are feeling ill for any reason, where to seek care, and when the practice expects to reopen. Again, proactive outreach will be more efficient and comforting to patients.
Handling financial ramifications of closure is a top priority as well, and will require a full understanding of what is and isn’t covered by the practice’s business interruption insurance. Practices that don’t have a line of credit should reach out to banks and the Small Business Administration immediately, according to Dahl. Practices that have lines of credit already may want to ask for an increase, added Morgan.
Protecting employees’ income is challenging as well. For employees who are furloughed, consider allowing them to use their sick and vacation time during the shutdown — and possibly let staff ‘borrow’ not-yet accrued paid time off.
“However, there’s a risk with certain jobs in a medical practice that tend to have extremely high turnover, so physicians and administrators may be reluctant to pay people too much because they don’t know for sure those employees will come back to those jobs,” Morgan said. “On the other hand, if you have had a stable team for a very long time and feel confident that those employees are going to stay, then you may make a different decision.”
7. Seize work-from-home opportunities
Even if the practice isn’t seeing patients, there may be opportunities for some employees, such as billers and schedulers, to continue to work from home,” Morgan noted. Particularly if a practice is behind on its billing, a closure or slowdown is an ideal time to catch up. This measure will keep at least some people working — perhaps including some individuals who can be cross-trained to do other tasks — and maintain some cashflow when the practice needs it most.
Other remote-friendly jobs that often fall by the wayside when practices are busy include marketing tasks such as setting up or updating Google business pages, Healthgrades profiles, and so on, noted Morgan.
“Another thing that can be even more important, and is often overlooked, is making sure health plan directories have correct information about your practice,” she added. “These are pesky, often tedious tasks that may require repeated contact with health plans to fix things — perfect things to do when the office is not busy or closed.”
For administrators and billers, if the practice is able to keep paying these employees while partially or fully closed, it can also be an excellent time to do the sort of analysis that takes a lot of focused attention and is hard to do when busy. Some examples: a detailed comparison of payer performance, analysis of referral patterns, or a review of coding accuracy, Morgan suggested.
Although practices have varying levels of comfort in letting employees work from home, it’s not much different from working with external billing or scheduling services that have grown more popular in recent years, Morgan said.
As with many technologies, HIPAA is a leading concern, though it needn’t be, according to Morgan. “If you are on a cloud-based electronic medical record and practice management system, there’s a good chance that it’s very straightforward to set someone up to work from elsewhere and have that data be secure,” she said.
Finally, as the crisis begins to abate, practices must keep working in teams to evaluate and structure an orderly return to business as usual, gleaning best practices from colleagues whenever possible.
“I would tell practices this is not a time when anyone is competing with anyone,” said Elmouchi. “The more collaboration between practices and health systems that have larger resources, the better.”
This article was originally published on Medscape.com.
At one large practice in Bergen County, New Jersey, the waiting room is empty — but its patients are still receiving care. As of mid-March, the practice is still operating, thanks to the group’s willingness to adapt its work flow, sometimes radically, to mitigate the threat of the COVID-19 pandemic.
For example, patients now call the receptionist from their vehicles when they arrive, and wait there until receiving a call back telling them the clinician is ready. The practice has also started using telemedicine for the first time, to the extent it can be adopted in a hurry, and some clinicians are working from home on tasks such as medication refills.
Still, the rapidly increasing numbers of COVID-19 cases in the United States raises the possibility that some physician offices will decide or be forced to close temporarily, as occurred in London last month.
Many practices across the country are having to adjust the way they operate, amid daily changes in the pandemic. What should you do to adapt to this new way of operating your practice?
1. Create a task force to manage change
The readiness of medical practices to address the myriad challenges posed by this crisis has so far been a mixed bag, said Owen Dahl, MBA, a Texas-based medical practice management consultant. “Leadership is going to have to assess what’s happening in the community, what’s happening with staff members who may or may not have the disease and may or may not have to self-quarantine,” Dahl said.
The physicians, the administrator, CEO, or managing partner should be involved in decision making as the global crisis unfolds, added Laurie Morgan, MBA, a California-based practice management consultant. And depending on the size of the practice, it may be useful to delegate specific components of this work to various department managers or other individuals in the group.
The team should assess:
- Recommendations and/or mandates from local, state, and federal governments
- Guidance from specialty and state medical societies
- How to triage patients over the phone, virtual visits, or referral to an alternate site of care
- Where to send patients for testing
- The practice’s inventory of personal protective equipment (PPE)
- Review of and possible revision of current infection control policies
- Possible collaborations within the community
- Reimbursement policies for suspected COVID-19 triage, testing, and follow-up treatment — in office or virtually
- Whether some employees’ work (eg, billing, coding) can be done remotely
- Options for paying personnel in the case of a temporary shutdown
- What’s covered and excluded by the group’s business interruption insurance
2. Consider postponing nonessential appointments
What’s more, it’s crucial for practices to form a strategy that does not involve bringing patients into the office, said Javeed Siddiqui, MD, MPH, an infectious disease physician, epidemiologist, and chief medical officer of TeleMed2U. “One thing we really have to recognize in this pandemic is that we don’t want people going and sitting in our waiting room. We don’t want people coming, and not only exposing other patients, but also further exposing staff. Forward triaging is going to be essential in this type of pandemic.”
Reliant Medical Group, with multiple locations in Massachusetts, for example, announced to patients recently that it will postpone appointments for some routine and elective procedures, as determined by the group’s physicians and clinical staff.
“Taking this step will help limit the number of people passing through our facilities, which will help slow the spread of illness [as recommended by the CDC],” noted an email blast to patients.
3. Overcommunicate to patients
With a situation as dynamic and unprecedented as this, constant and clear communication with patients is crucial. “In general, in my experience, practices don’t realize how much communication is necessary,” said Morgan. “In order to be effective and get the word out, you have to be overcommunicating.”
Today’s practices have multiple ways to communicate to keep people informed, including email, text messaging, social media, patient portals, and even local television and radio.
One email or text message to the patient population can help direct them to the appropriate streams of information. Helping direct patients to updated information is critical.
In contrast, having the front desk field multitudes of calls from concerned patients ties up precious resources, according Siddiqui. “Right now, practices are absolutely inundated, patients are waiting on hold, and that creates a great deal of frustration,” he said.
“We really need to take a page from every other industry in the United States, and that is using secure SMS, email communication, and telehealth,” Siddiqui said. “Healthcare generally tends to be a laggard in this because so many people think, ‘Well, you can’t do that in healthcare,’ as opposed to thinking, ‘How can we do that in healthcare?’”
4. Take advantage of telemedicine
Fortunately, technology to interact with patients remotely is almost ubiquitous. Even for practices with little experience in this arena, various vendors exist that can get secure, HIPAA-compliant technologies up and running quickly.
Various payers have issued guidance regarding reimbursement for telemedicine specific to COVID-19, and on March 6, Congress passed a law regarding Medicare coverage and payment for virtual services during a government-declared state of emergency. Some of the rules about HIPAA compliance in telemedicine have been eased for this emergency.
But even with well-established telemedicine modalities in place, it’s crunch time for applying it to COVID-19. “You need to find a way to have telemedicine available and use it, because depending on how this goes, that’s going to be clearly the safest, best way to care for a huge number of people,” said Darryl Elmouchi, MD, MBA, chief medical officer of Spectrum Health System and president of Spectrum Health Medical Group in Michigan.
“What we recognize now, both with our past experience with telehealth for many years and specifically with this coronavirus testing we’ve done, is that it’s incredibly useful both for the clinicians and the patients,” Elmouchi said.
One possibility to consider is the tactic used by Spectrum, a large integrated healthcare system. The company mobilized its existing telemedicine program to offer free virtual screenings for anyone in Michigan showing possible symptoms of COVID-19. “We wanted to keep people out of our clinics, emergency rooms, and urgent care centers if they didn’t need to be there, and help allay fears,” he said.
Elmouchi said his company faced the problems that other physicians would also have to deal with. “It was a ton of work with a dedicated team that was focused on this. The hardest part was probably trying to determine how we can staff it,” he said.
With their dedicated virtual team still seeing regularly scheduled virtual patients, the system had to reassign its traditional teams, such as urgent care and primary care clinicians, to the virtual screening effort. “Then we had to figure out how we could operationalize it. It was a lot of work,” Elmouchi said.
Telemedicine capabilities are not limited to screening patients, but can also be used to stay in touch with patients who may be quarantined and provide follow-up care, he noted.
5. Identify COVID-19 testing sites
Access to tests remains a problem in the US, but is improving by the week. For practices that can attain the tests themselves, it will still require some creativity to administer them with as little risk as possible. In South Korea, for example, and increasingly in the United States, healthcare organizations are instructing patients waiting to be tested to stay in their cars and have a practitioner wearing the proper PPE go out to patients to test them there.
Alternatively, some practices may opt to have PPE-wearing staff members bring PPE to patients in their cars and then escort them to a designated testing area in the building —through the back door if noninfected patients are still being seen.
“Once in the office, you still need to isolate virus patients in any way you can,” Dahl said. “In fact, you want a negative-pressure environment if possible, with the air being sucked out rather than circulating,” he said, adding that a large restroom with a ventilation system could be repurposed as a makeshift exam room.
Community testing sites are another possibility, given proper coordination with other healthcare organizations and community officials. Siddiqui has been working with several communities in which individual clinics and hospitals are unable to handle testing on their own, and have instead collaborated to create community testing sites in tents on local athletic fields.
“One of our communities is looking at using the local college parking lot to do drive-through testing there,” he said. “We really need to embrace collaboration much more than we’ve ever done.”
Collaboration also requires sharing supplies and PPE, noted Dahl. “Don’t hoard them because of the shortage. Look at your inventory and make sure you can help out whomever you may be sending patients to.” And if your office is falling short, Dahl advises checking with offices in your community that may be closing — such as dentists or plastic surgeons — for supplies you can purchase or simply have.
The US Food and Drug Administration has issued some guidance to healthcare providers about shortages of surgical masks and gowns, including advice about reusable cloth alternatives to gowns.
In addition, some hospitals have asked clinicians to keep their masks and provided guidance on how to conserve supplies.
6. Preparing to potentially shut down
A temporary closure may be inevitable for some practices. “Maybe the physician owners will not feel like they have a choice,” said Morgan. “They might feel like they want to stay open for as long as they can; but if it’s not safe for patients or not safe for employees, maybe they’ll feel it’s better if they check out for a bit.”
Should practices make the decision to close or reduce hours, multimodal communication with patients and the public is paramount. Patients will want to know whom to call if they are feeling ill for any reason, where to seek care, and when the practice expects to reopen. Again, proactive outreach will be more efficient and comforting to patients.
Handling financial ramifications of closure is a top priority as well, and will require a full understanding of what is and isn’t covered by the practice’s business interruption insurance. Practices that don’t have a line of credit should reach out to banks and the Small Business Administration immediately, according to Dahl. Practices that have lines of credit already may want to ask for an increase, added Morgan.
Protecting employees’ income is challenging as well. For employees who are furloughed, consider allowing them to use their sick and vacation time during the shutdown — and possibly let staff ‘borrow’ not-yet accrued paid time off.
“However, there’s a risk with certain jobs in a medical practice that tend to have extremely high turnover, so physicians and administrators may be reluctant to pay people too much because they don’t know for sure those employees will come back to those jobs,” Morgan said. “On the other hand, if you have had a stable team for a very long time and feel confident that those employees are going to stay, then you may make a different decision.”
7. Seize work-from-home opportunities
Even if the practice isn’t seeing patients, there may be opportunities for some employees, such as billers and schedulers, to continue to work from home,” Morgan noted. Particularly if a practice is behind on its billing, a closure or slowdown is an ideal time to catch up. This measure will keep at least some people working — perhaps including some individuals who can be cross-trained to do other tasks — and maintain some cashflow when the practice needs it most.
Other remote-friendly jobs that often fall by the wayside when practices are busy include marketing tasks such as setting up or updating Google business pages, Healthgrades profiles, and so on, noted Morgan.
“Another thing that can be even more important, and is often overlooked, is making sure health plan directories have correct information about your practice,” she added. “These are pesky, often tedious tasks that may require repeated contact with health plans to fix things — perfect things to do when the office is not busy or closed.”
For administrators and billers, if the practice is able to keep paying these employees while partially or fully closed, it can also be an excellent time to do the sort of analysis that takes a lot of focused attention and is hard to do when busy. Some examples: a detailed comparison of payer performance, analysis of referral patterns, or a review of coding accuracy, Morgan suggested.
Although practices have varying levels of comfort in letting employees work from home, it’s not much different from working with external billing or scheduling services that have grown more popular in recent years, Morgan said.
As with many technologies, HIPAA is a leading concern, though it needn’t be, according to Morgan. “If you are on a cloud-based electronic medical record and practice management system, there’s a good chance that it’s very straightforward to set someone up to work from elsewhere and have that data be secure,” she said.
Finally, as the crisis begins to abate, practices must keep working in teams to evaluate and structure an orderly return to business as usual, gleaning best practices from colleagues whenever possible.
“I would tell practices this is not a time when anyone is competing with anyone,” said Elmouchi. “The more collaboration between practices and health systems that have larger resources, the better.”
This article was originally published on Medscape.com.
At one large practice in Bergen County, New Jersey, the waiting room is empty — but its patients are still receiving care. As of mid-March, the practice is still operating, thanks to the group’s willingness to adapt its work flow, sometimes radically, to mitigate the threat of the COVID-19 pandemic.
For example, patients now call the receptionist from their vehicles when they arrive, and wait there until receiving a call back telling them the clinician is ready. The practice has also started using telemedicine for the first time, to the extent it can be adopted in a hurry, and some clinicians are working from home on tasks such as medication refills.
Still, the rapidly increasing numbers of COVID-19 cases in the United States raises the possibility that some physician offices will decide or be forced to close temporarily, as occurred in London last month.
Many practices across the country are having to adjust the way they operate, amid daily changes in the pandemic. What should you do to adapt to this new way of operating your practice?
1. Create a task force to manage change
The readiness of medical practices to address the myriad challenges posed by this crisis has so far been a mixed bag, said Owen Dahl, MBA, a Texas-based medical practice management consultant. “Leadership is going to have to assess what’s happening in the community, what’s happening with staff members who may or may not have the disease and may or may not have to self-quarantine,” Dahl said.
The physicians, the administrator, CEO, or managing partner should be involved in decision making as the global crisis unfolds, added Laurie Morgan, MBA, a California-based practice management consultant. And depending on the size of the practice, it may be useful to delegate specific components of this work to various department managers or other individuals in the group.
The team should assess:
- Recommendations and/or mandates from local, state, and federal governments
- Guidance from specialty and state medical societies
- How to triage patients over the phone, virtual visits, or referral to an alternate site of care
- Where to send patients for testing
- The practice’s inventory of personal protective equipment (PPE)
- Review of and possible revision of current infection control policies
- Possible collaborations within the community
- Reimbursement policies for suspected COVID-19 triage, testing, and follow-up treatment — in office or virtually
- Whether some employees’ work (eg, billing, coding) can be done remotely
- Options for paying personnel in the case of a temporary shutdown
- What’s covered and excluded by the group’s business interruption insurance
2. Consider postponing nonessential appointments
What’s more, it’s crucial for practices to form a strategy that does not involve bringing patients into the office, said Javeed Siddiqui, MD, MPH, an infectious disease physician, epidemiologist, and chief medical officer of TeleMed2U. “One thing we really have to recognize in this pandemic is that we don’t want people going and sitting in our waiting room. We don’t want people coming, and not only exposing other patients, but also further exposing staff. Forward triaging is going to be essential in this type of pandemic.”
Reliant Medical Group, with multiple locations in Massachusetts, for example, announced to patients recently that it will postpone appointments for some routine and elective procedures, as determined by the group’s physicians and clinical staff.
“Taking this step will help limit the number of people passing through our facilities, which will help slow the spread of illness [as recommended by the CDC],” noted an email blast to patients.
3. Overcommunicate to patients
With a situation as dynamic and unprecedented as this, constant and clear communication with patients is crucial. “In general, in my experience, practices don’t realize how much communication is necessary,” said Morgan. “In order to be effective and get the word out, you have to be overcommunicating.”
Today’s practices have multiple ways to communicate to keep people informed, including email, text messaging, social media, patient portals, and even local television and radio.
One email or text message to the patient population can help direct them to the appropriate streams of information. Helping direct patients to updated information is critical.
In contrast, having the front desk field multitudes of calls from concerned patients ties up precious resources, according Siddiqui. “Right now, practices are absolutely inundated, patients are waiting on hold, and that creates a great deal of frustration,” he said.
“We really need to take a page from every other industry in the United States, and that is using secure SMS, email communication, and telehealth,” Siddiqui said. “Healthcare generally tends to be a laggard in this because so many people think, ‘Well, you can’t do that in healthcare,’ as opposed to thinking, ‘How can we do that in healthcare?’”
4. Take advantage of telemedicine
Fortunately, technology to interact with patients remotely is almost ubiquitous. Even for practices with little experience in this arena, various vendors exist that can get secure, HIPAA-compliant technologies up and running quickly.
Various payers have issued guidance regarding reimbursement for telemedicine specific to COVID-19, and on March 6, Congress passed a law regarding Medicare coverage and payment for virtual services during a government-declared state of emergency. Some of the rules about HIPAA compliance in telemedicine have been eased for this emergency.
But even with well-established telemedicine modalities in place, it’s crunch time for applying it to COVID-19. “You need to find a way to have telemedicine available and use it, because depending on how this goes, that’s going to be clearly the safest, best way to care for a huge number of people,” said Darryl Elmouchi, MD, MBA, chief medical officer of Spectrum Health System and president of Spectrum Health Medical Group in Michigan.
“What we recognize now, both with our past experience with telehealth for many years and specifically with this coronavirus testing we’ve done, is that it’s incredibly useful both for the clinicians and the patients,” Elmouchi said.
One possibility to consider is the tactic used by Spectrum, a large integrated healthcare system. The company mobilized its existing telemedicine program to offer free virtual screenings for anyone in Michigan showing possible symptoms of COVID-19. “We wanted to keep people out of our clinics, emergency rooms, and urgent care centers if they didn’t need to be there, and help allay fears,” he said.
Elmouchi said his company faced the problems that other physicians would also have to deal with. “It was a ton of work with a dedicated team that was focused on this. The hardest part was probably trying to determine how we can staff it,” he said.
With their dedicated virtual team still seeing regularly scheduled virtual patients, the system had to reassign its traditional teams, such as urgent care and primary care clinicians, to the virtual screening effort. “Then we had to figure out how we could operationalize it. It was a lot of work,” Elmouchi said.
Telemedicine capabilities are not limited to screening patients, but can also be used to stay in touch with patients who may be quarantined and provide follow-up care, he noted.
5. Identify COVID-19 testing sites
Access to tests remains a problem in the US, but is improving by the week. For practices that can attain the tests themselves, it will still require some creativity to administer them with as little risk as possible. In South Korea, for example, and increasingly in the United States, healthcare organizations are instructing patients waiting to be tested to stay in their cars and have a practitioner wearing the proper PPE go out to patients to test them there.
Alternatively, some practices may opt to have PPE-wearing staff members bring PPE to patients in their cars and then escort them to a designated testing area in the building —through the back door if noninfected patients are still being seen.
“Once in the office, you still need to isolate virus patients in any way you can,” Dahl said. “In fact, you want a negative-pressure environment if possible, with the air being sucked out rather than circulating,” he said, adding that a large restroom with a ventilation system could be repurposed as a makeshift exam room.
Community testing sites are another possibility, given proper coordination with other healthcare organizations and community officials. Siddiqui has been working with several communities in which individual clinics and hospitals are unable to handle testing on their own, and have instead collaborated to create community testing sites in tents on local athletic fields.
“One of our communities is looking at using the local college parking lot to do drive-through testing there,” he said. “We really need to embrace collaboration much more than we’ve ever done.”
Collaboration also requires sharing supplies and PPE, noted Dahl. “Don’t hoard them because of the shortage. Look at your inventory and make sure you can help out whomever you may be sending patients to.” And if your office is falling short, Dahl advises checking with offices in your community that may be closing — such as dentists or plastic surgeons — for supplies you can purchase or simply have.
The US Food and Drug Administration has issued some guidance to healthcare providers about shortages of surgical masks and gowns, including advice about reusable cloth alternatives to gowns.
In addition, some hospitals have asked clinicians to keep their masks and provided guidance on how to conserve supplies.
6. Preparing to potentially shut down
A temporary closure may be inevitable for some practices. “Maybe the physician owners will not feel like they have a choice,” said Morgan. “They might feel like they want to stay open for as long as they can; but if it’s not safe for patients or not safe for employees, maybe they’ll feel it’s better if they check out for a bit.”
Should practices make the decision to close or reduce hours, multimodal communication with patients and the public is paramount. Patients will want to know whom to call if they are feeling ill for any reason, where to seek care, and when the practice expects to reopen. Again, proactive outreach will be more efficient and comforting to patients.
Handling financial ramifications of closure is a top priority as well, and will require a full understanding of what is and isn’t covered by the practice’s business interruption insurance. Practices that don’t have a line of credit should reach out to banks and the Small Business Administration immediately, according to Dahl. Practices that have lines of credit already may want to ask for an increase, added Morgan.
Protecting employees’ income is challenging as well. For employees who are furloughed, consider allowing them to use their sick and vacation time during the shutdown — and possibly let staff ‘borrow’ not-yet accrued paid time off.
“However, there’s a risk with certain jobs in a medical practice that tend to have extremely high turnover, so physicians and administrators may be reluctant to pay people too much because they don’t know for sure those employees will come back to those jobs,” Morgan said. “On the other hand, if you have had a stable team for a very long time and feel confident that those employees are going to stay, then you may make a different decision.”
7. Seize work-from-home opportunities
Even if the practice isn’t seeing patients, there may be opportunities for some employees, such as billers and schedulers, to continue to work from home,” Morgan noted. Particularly if a practice is behind on its billing, a closure or slowdown is an ideal time to catch up. This measure will keep at least some people working — perhaps including some individuals who can be cross-trained to do other tasks — and maintain some cashflow when the practice needs it most.
Other remote-friendly jobs that often fall by the wayside when practices are busy include marketing tasks such as setting up or updating Google business pages, Healthgrades profiles, and so on, noted Morgan.
“Another thing that can be even more important, and is often overlooked, is making sure health plan directories have correct information about your practice,” she added. “These are pesky, often tedious tasks that may require repeated contact with health plans to fix things — perfect things to do when the office is not busy or closed.”
For administrators and billers, if the practice is able to keep paying these employees while partially or fully closed, it can also be an excellent time to do the sort of analysis that takes a lot of focused attention and is hard to do when busy. Some examples: a detailed comparison of payer performance, analysis of referral patterns, or a review of coding accuracy, Morgan suggested.
Although practices have varying levels of comfort in letting employees work from home, it’s not much different from working with external billing or scheduling services that have grown more popular in recent years, Morgan said.
As with many technologies, HIPAA is a leading concern, though it needn’t be, according to Morgan. “If you are on a cloud-based electronic medical record and practice management system, there’s a good chance that it’s very straightforward to set someone up to work from elsewhere and have that data be secure,” she said.
Finally, as the crisis begins to abate, practices must keep working in teams to evaluate and structure an orderly return to business as usual, gleaning best practices from colleagues whenever possible.
“I would tell practices this is not a time when anyone is competing with anyone,” said Elmouchi. “The more collaboration between practices and health systems that have larger resources, the better.”
This article was originally published on Medscape.com.
Give me an occupation, Miss Dashwood
“I’ve been watching YouTube videos on how to set a ventilator,” said one of our dermatologists. The absurdity, levity, and gravity of that statement captures in a single sentence where we are today.
None of us alive have experience with such a crisis. It is as if our planet passed through a wormhole and we’ve been transported to the late medieval period: We doctors fighting the Black Death donned in beaked masks filled with juniper berries, mint, and clove to protect us from the miasma. Now, though, we spray store-bought lavender disinfectant on surgical masks.
“A crisis shows you a person’s soul,” said New York Governor Andrew Cuomo, adding: “It shows you what they’re made of, the weaknesses explode and the strengths ... emboldened.” Most of us have traveled through life with no experience of peril. Such mortal danger explodes and emboldens us, dividing us in two, the fearful or the phlegmatic.
When President Trump proclaimed that plaquenil was a promising treatment for the virus, prescriptions for the drug soared so quickly that four of eight manufacturers reported being in shortage by the end of the day. Many of those prescriptions were written by physicians for themselves and their families. Private Facebook physician groups shared insider tips for how to get around constraints and find the drug – as hoardable as toilet paper. As a department chief and fellow human being, I understand why some of us might behave this way. We didn’t sign up to be dermatologists or nephrologists or surgeons or pulmonologists agreeing that, to do so, we might die. We are all afraid.
The track of this epic storm became clear last week and now, terrifyingly, it appears it will be a direct hit. I braced for an onslaught of anxiety from our doctors and staff. But as the forecast became more grim, the courage began to well up and creativity climbed. Doctors went to local stores and bought all the masks and shields on their own. Rolls of toilet paper and diapers began magically appearing in our mom-doctors’ offices, delivered by angels in scrubs. I’ve practically had to install a velvet rope at my door to organize the queue of people wanting to talk to me about their ideas to help – keep 6 feet apart please! Stories like this abound. Even at the EvergreenHealth hospital in Washington they’ve not had shortages of staff. Rather than calling out sick, they called in: “If you need me, I’m available.”
Doctors are afraid and frustrated. Some of the things we will do in the coming weeks will first do no good, perhaps even harm. But I believe it’s because we’ve yet to embolden our strengths. It’s our job as leaders, attendings, administrators to inform and enable them.
When Marianne fell deathly ill in “Sense and Sensibility,” Colonel Branden wrung his hands and paced the floor. “Give me an occupation, Miss Dashwood, or I shall run mad.” Doctors are running, mad. And, just in case, some dermatologists are relearning how to intubate, waiting for that occupation to be given.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He has no relevant conflicts of interest related to this column. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“I’ve been watching YouTube videos on how to set a ventilator,” said one of our dermatologists. The absurdity, levity, and gravity of that statement captures in a single sentence where we are today.
None of us alive have experience with such a crisis. It is as if our planet passed through a wormhole and we’ve been transported to the late medieval period: We doctors fighting the Black Death donned in beaked masks filled with juniper berries, mint, and clove to protect us from the miasma. Now, though, we spray store-bought lavender disinfectant on surgical masks.
“A crisis shows you a person’s soul,” said New York Governor Andrew Cuomo, adding: “It shows you what they’re made of, the weaknesses explode and the strengths ... emboldened.” Most of us have traveled through life with no experience of peril. Such mortal danger explodes and emboldens us, dividing us in two, the fearful or the phlegmatic.
When President Trump proclaimed that plaquenil was a promising treatment for the virus, prescriptions for the drug soared so quickly that four of eight manufacturers reported being in shortage by the end of the day. Many of those prescriptions were written by physicians for themselves and their families. Private Facebook physician groups shared insider tips for how to get around constraints and find the drug – as hoardable as toilet paper. As a department chief and fellow human being, I understand why some of us might behave this way. We didn’t sign up to be dermatologists or nephrologists or surgeons or pulmonologists agreeing that, to do so, we might die. We are all afraid.
The track of this epic storm became clear last week and now, terrifyingly, it appears it will be a direct hit. I braced for an onslaught of anxiety from our doctors and staff. But as the forecast became more grim, the courage began to well up and creativity climbed. Doctors went to local stores and bought all the masks and shields on their own. Rolls of toilet paper and diapers began magically appearing in our mom-doctors’ offices, delivered by angels in scrubs. I’ve practically had to install a velvet rope at my door to organize the queue of people wanting to talk to me about their ideas to help – keep 6 feet apart please! Stories like this abound. Even at the EvergreenHealth hospital in Washington they’ve not had shortages of staff. Rather than calling out sick, they called in: “If you need me, I’m available.”
Doctors are afraid and frustrated. Some of the things we will do in the coming weeks will first do no good, perhaps even harm. But I believe it’s because we’ve yet to embolden our strengths. It’s our job as leaders, attendings, administrators to inform and enable them.
When Marianne fell deathly ill in “Sense and Sensibility,” Colonel Branden wrung his hands and paced the floor. “Give me an occupation, Miss Dashwood, or I shall run mad.” Doctors are running, mad. And, just in case, some dermatologists are relearning how to intubate, waiting for that occupation to be given.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He has no relevant conflicts of interest related to this column. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“I’ve been watching YouTube videos on how to set a ventilator,” said one of our dermatologists. The absurdity, levity, and gravity of that statement captures in a single sentence where we are today.
None of us alive have experience with such a crisis. It is as if our planet passed through a wormhole and we’ve been transported to the late medieval period: We doctors fighting the Black Death donned in beaked masks filled with juniper berries, mint, and clove to protect us from the miasma. Now, though, we spray store-bought lavender disinfectant on surgical masks.
“A crisis shows you a person’s soul,” said New York Governor Andrew Cuomo, adding: “It shows you what they’re made of, the weaknesses explode and the strengths ... emboldened.” Most of us have traveled through life with no experience of peril. Such mortal danger explodes and emboldens us, dividing us in two, the fearful or the phlegmatic.
When President Trump proclaimed that plaquenil was a promising treatment for the virus, prescriptions for the drug soared so quickly that four of eight manufacturers reported being in shortage by the end of the day. Many of those prescriptions were written by physicians for themselves and their families. Private Facebook physician groups shared insider tips for how to get around constraints and find the drug – as hoardable as toilet paper. As a department chief and fellow human being, I understand why some of us might behave this way. We didn’t sign up to be dermatologists or nephrologists or surgeons or pulmonologists agreeing that, to do so, we might die. We are all afraid.
The track of this epic storm became clear last week and now, terrifyingly, it appears it will be a direct hit. I braced for an onslaught of anxiety from our doctors and staff. But as the forecast became more grim, the courage began to well up and creativity climbed. Doctors went to local stores and bought all the masks and shields on their own. Rolls of toilet paper and diapers began magically appearing in our mom-doctors’ offices, delivered by angels in scrubs. I’ve practically had to install a velvet rope at my door to organize the queue of people wanting to talk to me about their ideas to help – keep 6 feet apart please! Stories like this abound. Even at the EvergreenHealth hospital in Washington they’ve not had shortages of staff. Rather than calling out sick, they called in: “If you need me, I’m available.”
Doctors are afraid and frustrated. Some of the things we will do in the coming weeks will first do no good, perhaps even harm. But I believe it’s because we’ve yet to embolden our strengths. It’s our job as leaders, attendings, administrators to inform and enable them.
When Marianne fell deathly ill in “Sense and Sensibility,” Colonel Branden wrung his hands and paced the floor. “Give me an occupation, Miss Dashwood, or I shall run mad.” Doctors are running, mad. And, just in case, some dermatologists are relearning how to intubate, waiting for that occupation to be given.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He has no relevant conflicts of interest related to this column. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Preventable diseases could gain a foothold because of COVID-19
There is a highly infectious virus spreading around the world and it is targeting the most vulnerable among us. It is among the most contagious of human diseases, spreading through the air unseen. No, it isn’t the novel coronavirus, COVID-19. It’s measles.
Remember measles? Outbreaks in recent years have brought the disease, which once was declared eliminated in the United States, back into the news and public awareness, but measles never has really gone away. Every year there are millions of cases worldwide – in 2018 alone there were nearly 10 million estimated cases and 142,300 deaths, according to the World Health Organization. The good news is that measles vaccination is highly effective, at about 97% after the recommended two doses. According to the Centers for Disease Control and Prevention, “because of vaccination, more than 21 million lives have been saved and measles deaths have been reduced by 80% since 2000.” This is a tremendous public health success and a cause for celebration. But our work is not done. The recent increases in vaccine hesitancy and refusal in many countries has contributed to the resurgence of measles worldwide.
Influenza still is in full swing with the CDC reporting high activity in 1 states for the week ending April 4th. Seasonal influenza, according to currently available data, has a lower fatality rate than COVID-19, but that doesn’t mean it is harmless. Thus far in the 2019-2020 flu season, there have been at least 24,000 deaths because of influenza in the United States alone, 166 of which were among pediatric patients.*
Like many pediatricians, I have seen firsthand the impact of vaccine-preventable illnesses like influenza, pertussis, and varicella. I have personally cared for an infant with pertussis who had to be intubated and on a ventilator for nearly a week. I have told the family of a child with cancer that they would have to be admitted to the hospital yet again for intravenous antiviral medication because that little rash turned out to be varicella. I have performed CPR on a previously healthy teenager with the flu whose heart was failing despite maximum ventilator support. All these illnesses might have been prevented had these patients or those around them been appropriately vaccinated.
Right now, the United States and governments around the world are taking unprecedented public health measures to prevent the spread of COVID-19, directing the public to stay home, avoid unnecessary contact with other people, practice good hand-washing and infection-control techniques. In order to promote social distancing, many primary care clinics are canceling nonurgent appointments or converting them to virtual visits, including some visits for routine vaccinations for older children, teens, and adults. This is a responsible choice to keep potentially asymptomatic people from spreading COVID-19, but once restrictions begin to lift, we all will need to act to help our patients catch up on these missing vaccinations.
This pandemic has made it more apparent than ever that we all rely upon each other to stay healthy. While this pandemic has disrupted nearly every aspect of daily life, we can’t let it disrupt one of the great successes in health care today: the prevention of serious illnesses. As soon as it is safe to do so, we must help and encourage patients to catch up on missing vaccinations. It’s rare that preventative public health measures and vaccine developments are in the nightly news, so we should use this increased public awareness to ensure patients are well educated and protected from every disease. As part of this, we must continue our efforts to share accurate information on the safety and efficacy of routine vaccination. And when there is a vaccine for COVID-19? Let’s make sure everyone gets that too.
Dr. Leighton is a pediatrician in the ED at Children’s National Hospital and currently is completing her MPH in health policy at George Washington University, both in Washington. She had no relevant financial disclosures.*
* This article was updated 4/10/2020.
There is a highly infectious virus spreading around the world and it is targeting the most vulnerable among us. It is among the most contagious of human diseases, spreading through the air unseen. No, it isn’t the novel coronavirus, COVID-19. It’s measles.
Remember measles? Outbreaks in recent years have brought the disease, which once was declared eliminated in the United States, back into the news and public awareness, but measles never has really gone away. Every year there are millions of cases worldwide – in 2018 alone there were nearly 10 million estimated cases and 142,300 deaths, according to the World Health Organization. The good news is that measles vaccination is highly effective, at about 97% after the recommended two doses. According to the Centers for Disease Control and Prevention, “because of vaccination, more than 21 million lives have been saved and measles deaths have been reduced by 80% since 2000.” This is a tremendous public health success and a cause for celebration. But our work is not done. The recent increases in vaccine hesitancy and refusal in many countries has contributed to the resurgence of measles worldwide.
Influenza still is in full swing with the CDC reporting high activity in 1 states for the week ending April 4th. Seasonal influenza, according to currently available data, has a lower fatality rate than COVID-19, but that doesn’t mean it is harmless. Thus far in the 2019-2020 flu season, there have been at least 24,000 deaths because of influenza in the United States alone, 166 of which were among pediatric patients.*
Like many pediatricians, I have seen firsthand the impact of vaccine-preventable illnesses like influenza, pertussis, and varicella. I have personally cared for an infant with pertussis who had to be intubated and on a ventilator for nearly a week. I have told the family of a child with cancer that they would have to be admitted to the hospital yet again for intravenous antiviral medication because that little rash turned out to be varicella. I have performed CPR on a previously healthy teenager with the flu whose heart was failing despite maximum ventilator support. All these illnesses might have been prevented had these patients or those around them been appropriately vaccinated.
Right now, the United States and governments around the world are taking unprecedented public health measures to prevent the spread of COVID-19, directing the public to stay home, avoid unnecessary contact with other people, practice good hand-washing and infection-control techniques. In order to promote social distancing, many primary care clinics are canceling nonurgent appointments or converting them to virtual visits, including some visits for routine vaccinations for older children, teens, and adults. This is a responsible choice to keep potentially asymptomatic people from spreading COVID-19, but once restrictions begin to lift, we all will need to act to help our patients catch up on these missing vaccinations.
This pandemic has made it more apparent than ever that we all rely upon each other to stay healthy. While this pandemic has disrupted nearly every aspect of daily life, we can’t let it disrupt one of the great successes in health care today: the prevention of serious illnesses. As soon as it is safe to do so, we must help and encourage patients to catch up on missing vaccinations. It’s rare that preventative public health measures and vaccine developments are in the nightly news, so we should use this increased public awareness to ensure patients are well educated and protected from every disease. As part of this, we must continue our efforts to share accurate information on the safety and efficacy of routine vaccination. And when there is a vaccine for COVID-19? Let’s make sure everyone gets that too.
Dr. Leighton is a pediatrician in the ED at Children’s National Hospital and currently is completing her MPH in health policy at George Washington University, both in Washington. She had no relevant financial disclosures.*
* This article was updated 4/10/2020.
There is a highly infectious virus spreading around the world and it is targeting the most vulnerable among us. It is among the most contagious of human diseases, spreading through the air unseen. No, it isn’t the novel coronavirus, COVID-19. It’s measles.
Remember measles? Outbreaks in recent years have brought the disease, which once was declared eliminated in the United States, back into the news and public awareness, but measles never has really gone away. Every year there are millions of cases worldwide – in 2018 alone there were nearly 10 million estimated cases and 142,300 deaths, according to the World Health Organization. The good news is that measles vaccination is highly effective, at about 97% after the recommended two doses. According to the Centers for Disease Control and Prevention, “because of vaccination, more than 21 million lives have been saved and measles deaths have been reduced by 80% since 2000.” This is a tremendous public health success and a cause for celebration. But our work is not done. The recent increases in vaccine hesitancy and refusal in many countries has contributed to the resurgence of measles worldwide.
Influenza still is in full swing with the CDC reporting high activity in 1 states for the week ending April 4th. Seasonal influenza, according to currently available data, has a lower fatality rate than COVID-19, but that doesn’t mean it is harmless. Thus far in the 2019-2020 flu season, there have been at least 24,000 deaths because of influenza in the United States alone, 166 of which were among pediatric patients.*
Like many pediatricians, I have seen firsthand the impact of vaccine-preventable illnesses like influenza, pertussis, and varicella. I have personally cared for an infant with pertussis who had to be intubated and on a ventilator for nearly a week. I have told the family of a child with cancer that they would have to be admitted to the hospital yet again for intravenous antiviral medication because that little rash turned out to be varicella. I have performed CPR on a previously healthy teenager with the flu whose heart was failing despite maximum ventilator support. All these illnesses might have been prevented had these patients or those around them been appropriately vaccinated.
Right now, the United States and governments around the world are taking unprecedented public health measures to prevent the spread of COVID-19, directing the public to stay home, avoid unnecessary contact with other people, practice good hand-washing and infection-control techniques. In order to promote social distancing, many primary care clinics are canceling nonurgent appointments or converting them to virtual visits, including some visits for routine vaccinations for older children, teens, and adults. This is a responsible choice to keep potentially asymptomatic people from spreading COVID-19, but once restrictions begin to lift, we all will need to act to help our patients catch up on these missing vaccinations.
This pandemic has made it more apparent than ever that we all rely upon each other to stay healthy. While this pandemic has disrupted nearly every aspect of daily life, we can’t let it disrupt one of the great successes in health care today: the prevention of serious illnesses. As soon as it is safe to do so, we must help and encourage patients to catch up on missing vaccinations. It’s rare that preventative public health measures and vaccine developments are in the nightly news, so we should use this increased public awareness to ensure patients are well educated and protected from every disease. As part of this, we must continue our efforts to share accurate information on the safety and efficacy of routine vaccination. And when there is a vaccine for COVID-19? Let’s make sure everyone gets that too.
Dr. Leighton is a pediatrician in the ED at Children’s National Hospital and currently is completing her MPH in health policy at George Washington University, both in Washington. She had no relevant financial disclosures.*
* This article was updated 4/10/2020.
Milestone Match Day sees record highs; soar in DO applicants
Unifying allopathic (MD) and osteopathic (DO) applicants for the first time in a single matching program, 2020’s Match Day results underscored the continuing growth of DOs in the field, boosting numbers in primary care medicine and the Match as a whole.
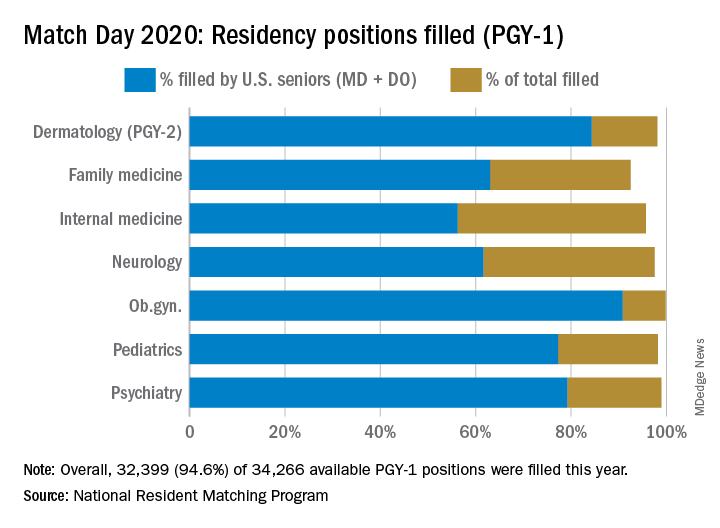
The 2020 Main Residency Match bested 2019’s record as the largest in the history of the National Resident Matching Program (NRMP), with 40,084 applicants submitting program choices for 37,256 positions. This compares with 38,376 applicants vying for 35,185 positions last year.
It’s the seventh consecutive year in which overall match numbers are up, according to the NRMP. Although the number of applicants increased, so did the number of positions, resulting in a slight drop in the percent of positions filled during 2019-2020.
Available first-year (PGY-1) positions rose to 34,266, an increase of 2,072 (6.4%) over 2019. “This was, in part, due to the last migration of osteopathic program positions into the Main Residency Match,” Donna L. Lamb, DHSc, NRMP president and CEO, said in an interview. An agreement the Accreditation Council for Graduate Medical Education, American Osteopathic Association and American Association of Colleges of Osteopathic Medicine reached in 2014 recognized ACGME as the primary accrediting body for graduate medical education programs by 2020.
This led to the first single match for U.S. MD and DO senior students and graduates and the inclusion of DO senior students as sponsored applicants in 2020, Dr. Lamb noted.
Gains, trends in 2020 match
Growth in U.S. DO senior participation also pushed this year’s Match to record highs. There were 6,581 U.S. DO medical school seniors who submitted rank order lists, 1,103 more than in 2019. Among those seniors, 90.7% matched to PGY-1 positions, driving the match rate for U.S. DO seniors up 2.6 percentage points from 2019.
Since 2016, the number of U.S. DO seniors seeking positions has risen by 3,599 or 120%. “Of course, the number of U.S. MD seniors who submitted program choices was also record-high: 19,326, an increase of 401 over 2019. The 93.7% match rate to first-year positions for this group has remained very consistent for many years,” Dr. Lamb said.
Among individual specialties, the NRMP reported extremely high fill rates for dermatology, medicine-emergency medicine, neurological surgery, physical medicine and rehabilitation (categorical), integrated plastic surgery, and thoracic surgery. Other competitive specialties included medicine-pediatrics, orthopedic surgery, otolaryngology, and vascular surgery.
Participation of international medical school students and graduates (IMGs) went up in 2020, breaking a 3-year cycle of decline. More than 61% matched to first-year positions, 2.5 percentage points higher than 2019 – and the highest match rate since 1990. “IMGs generally are having the most success matching to primary care specialties, including internal medicine, family medicine, and pediatrics,” Dr. Lamb said.
Primary care benefits from DO growth
DO candidates also helped drive up the numbers in primary care.
Internal medicine offered 8,697 categorical positions, 581 more than in 2019, reflecting a fill rate of 95.7%. More than 40% of these slots were filled by U.S. MD seniors, a category that’s seen decreases over the last 5 years, due in part to administrative and financial burdens associated with primary care internal medicine.
“In addition, the steady growth of internal medicine has increased the overall number of training positions available, and with the growth of other specialties in parallel, it has also likely had some effect on decreasing the percentage of U.S. graduates entering the field,” Phil Masters, MD, vice president of membership and global engagement at the American College of Physicians, said in an interview.
However, fill rates for U.S. DO seniors reached 16% in 2020, a notable rise from 6.9% in 2016. “As the number of osteopathic trainees increases, we are happy that more are choosing internal medicine as a career path,” Dr. Masters said, adding that the slightly different training and practice orientation of osteopathic physicians “complements that of their allopathic colleagues, and add richness to the many different practice settings that internal medicine encompasses.”
A record number of DO seniors also matched in family medicine (1,392), accounting for nearly 30% of all applicants. The single match led to an important net increase in filled family medicine residency positions, Clif Knight, MD, senior vice president for education at the American Academy of Family Physicians, said in an interview.
Overall, family medicine filled 92.5% of its 4,662 positions, 555 more than in 2019. The results show that family medicine and primary care are on solid footing, Dr. Knight said. “We are excited that the number of filled family medicine residency positions increased from last year. This is important as we work to meet the significant primary care workforce shortage,” he added.
In other specialties:
- Pediatrics filled more than 98% of its 2,864 categorical positions, 17 more than in 2019. U.S. MD seniors filled 1,731 (60.4%) of those slots. “We’re very excited about our newly matched pediatricians,” Sara “Sally” H. Goza, MD, president of the American Academy of Pediatrics, said in an interview. “The coronavirus outbreak has shown us how valuable the pediatric workforce is and how much we’re needed.’’
- Dermatology offered 478 positions, achieving a fill rate of 98.1%. “Looking at our own program’s Match results, I feel very satisfied that we are accomplishing our specific aim to serve rural populations and to create a diverse workforce in dermatology,” Erik Stratman, MD, an expert on dermatologic education in U.S. medical schools/residency programs, and a member of the American Academy of Dermatology, said in an interview. “It’s nice to see the fruits of the specialty’s expanding efforts to get the right people in the specialty who reflect those populations we serve.”
- Obstetrics-gynecology offered 1,433 first-year positions – 48 more than in 2019 – achieving a fill rate of 99.8%, with U.S. MD seniors filling more than 75% of those slots.
- Neurology filled more than 97.5% of 682 offered positions in 2020. However, U.S. MD seniors represented just under half of those filled positions (46.5%).
- Psychiatry offered 1,858 positions in 2020, achieving an overall fill rate of 98.9%, 61.2% for U.S. MD seniors.
- Emergency Medicine filled 99.5% of the 2,665 positions offered this year. In this profession, the U.S. MD fill rate was 64.3%. These new interns are sorely needed at a time when EM physicians are on the front lines of a pandemic, Hannah R. Hughes, MD, president of the Emergency Medicine Residents’ Association, said in an interview.
Unifying allopathic (MD) and osteopathic (DO) applicants for the first time in a single matching program, 2020’s Match Day results underscored the continuing growth of DOs in the field, boosting numbers in primary care medicine and the Match as a whole.
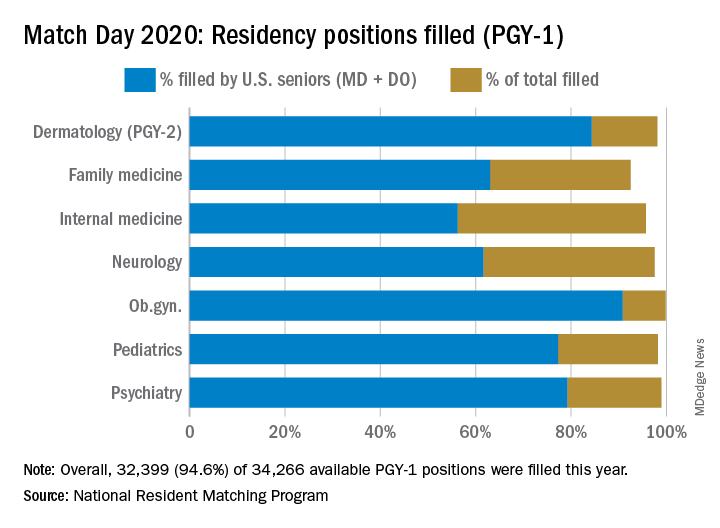
The 2020 Main Residency Match bested 2019’s record as the largest in the history of the National Resident Matching Program (NRMP), with 40,084 applicants submitting program choices for 37,256 positions. This compares with 38,376 applicants vying for 35,185 positions last year.
It’s the seventh consecutive year in which overall match numbers are up, according to the NRMP. Although the number of applicants increased, so did the number of positions, resulting in a slight drop in the percent of positions filled during 2019-2020.
Available first-year (PGY-1) positions rose to 34,266, an increase of 2,072 (6.4%) over 2019. “This was, in part, due to the last migration of osteopathic program positions into the Main Residency Match,” Donna L. Lamb, DHSc, NRMP president and CEO, said in an interview. An agreement the Accreditation Council for Graduate Medical Education, American Osteopathic Association and American Association of Colleges of Osteopathic Medicine reached in 2014 recognized ACGME as the primary accrediting body for graduate medical education programs by 2020.
This led to the first single match for U.S. MD and DO senior students and graduates and the inclusion of DO senior students as sponsored applicants in 2020, Dr. Lamb noted.
Gains, trends in 2020 match
Growth in U.S. DO senior participation also pushed this year’s Match to record highs. There were 6,581 U.S. DO medical school seniors who submitted rank order lists, 1,103 more than in 2019. Among those seniors, 90.7% matched to PGY-1 positions, driving the match rate for U.S. DO seniors up 2.6 percentage points from 2019.
Since 2016, the number of U.S. DO seniors seeking positions has risen by 3,599 or 120%. “Of course, the number of U.S. MD seniors who submitted program choices was also record-high: 19,326, an increase of 401 over 2019. The 93.7% match rate to first-year positions for this group has remained very consistent for many years,” Dr. Lamb said.
Among individual specialties, the NRMP reported extremely high fill rates for dermatology, medicine-emergency medicine, neurological surgery, physical medicine and rehabilitation (categorical), integrated plastic surgery, and thoracic surgery. Other competitive specialties included medicine-pediatrics, orthopedic surgery, otolaryngology, and vascular surgery.
Participation of international medical school students and graduates (IMGs) went up in 2020, breaking a 3-year cycle of decline. More than 61% matched to first-year positions, 2.5 percentage points higher than 2019 – and the highest match rate since 1990. “IMGs generally are having the most success matching to primary care specialties, including internal medicine, family medicine, and pediatrics,” Dr. Lamb said.
Primary care benefits from DO growth
DO candidates also helped drive up the numbers in primary care.
Internal medicine offered 8,697 categorical positions, 581 more than in 2019, reflecting a fill rate of 95.7%. More than 40% of these slots were filled by U.S. MD seniors, a category that’s seen decreases over the last 5 years, due in part to administrative and financial burdens associated with primary care internal medicine.
“In addition, the steady growth of internal medicine has increased the overall number of training positions available, and with the growth of other specialties in parallel, it has also likely had some effect on decreasing the percentage of U.S. graduates entering the field,” Phil Masters, MD, vice president of membership and global engagement at the American College of Physicians, said in an interview.
However, fill rates for U.S. DO seniors reached 16% in 2020, a notable rise from 6.9% in 2016. “As the number of osteopathic trainees increases, we are happy that more are choosing internal medicine as a career path,” Dr. Masters said, adding that the slightly different training and practice orientation of osteopathic physicians “complements that of their allopathic colleagues, and add richness to the many different practice settings that internal medicine encompasses.”
A record number of DO seniors also matched in family medicine (1,392), accounting for nearly 30% of all applicants. The single match led to an important net increase in filled family medicine residency positions, Clif Knight, MD, senior vice president for education at the American Academy of Family Physicians, said in an interview.
Overall, family medicine filled 92.5% of its 4,662 positions, 555 more than in 2019. The results show that family medicine and primary care are on solid footing, Dr. Knight said. “We are excited that the number of filled family medicine residency positions increased from last year. This is important as we work to meet the significant primary care workforce shortage,” he added.
In other specialties:
- Pediatrics filled more than 98% of its 2,864 categorical positions, 17 more than in 2019. U.S. MD seniors filled 1,731 (60.4%) of those slots. “We’re very excited about our newly matched pediatricians,” Sara “Sally” H. Goza, MD, president of the American Academy of Pediatrics, said in an interview. “The coronavirus outbreak has shown us how valuable the pediatric workforce is and how much we’re needed.’’
- Dermatology offered 478 positions, achieving a fill rate of 98.1%. “Looking at our own program’s Match results, I feel very satisfied that we are accomplishing our specific aim to serve rural populations and to create a diverse workforce in dermatology,” Erik Stratman, MD, an expert on dermatologic education in U.S. medical schools/residency programs, and a member of the American Academy of Dermatology, said in an interview. “It’s nice to see the fruits of the specialty’s expanding efforts to get the right people in the specialty who reflect those populations we serve.”
- Obstetrics-gynecology offered 1,433 first-year positions – 48 more than in 2019 – achieving a fill rate of 99.8%, with U.S. MD seniors filling more than 75% of those slots.
- Neurology filled more than 97.5% of 682 offered positions in 2020. However, U.S. MD seniors represented just under half of those filled positions (46.5%).
- Psychiatry offered 1,858 positions in 2020, achieving an overall fill rate of 98.9%, 61.2% for U.S. MD seniors.
- Emergency Medicine filled 99.5% of the 2,665 positions offered this year. In this profession, the U.S. MD fill rate was 64.3%. These new interns are sorely needed at a time when EM physicians are on the front lines of a pandemic, Hannah R. Hughes, MD, president of the Emergency Medicine Residents’ Association, said in an interview.
Unifying allopathic (MD) and osteopathic (DO) applicants for the first time in a single matching program, 2020’s Match Day results underscored the continuing growth of DOs in the field, boosting numbers in primary care medicine and the Match as a whole.
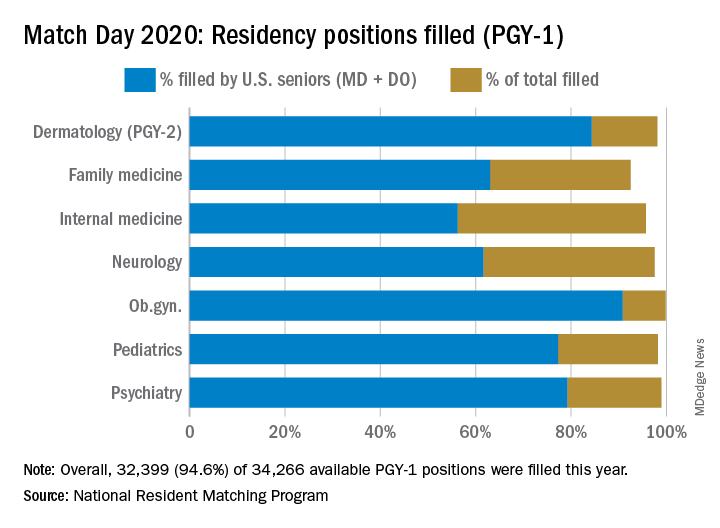
The 2020 Main Residency Match bested 2019’s record as the largest in the history of the National Resident Matching Program (NRMP), with 40,084 applicants submitting program choices for 37,256 positions. This compares with 38,376 applicants vying for 35,185 positions last year.
It’s the seventh consecutive year in which overall match numbers are up, according to the NRMP. Although the number of applicants increased, so did the number of positions, resulting in a slight drop in the percent of positions filled during 2019-2020.
Available first-year (PGY-1) positions rose to 34,266, an increase of 2,072 (6.4%) over 2019. “This was, in part, due to the last migration of osteopathic program positions into the Main Residency Match,” Donna L. Lamb, DHSc, NRMP president and CEO, said in an interview. An agreement the Accreditation Council for Graduate Medical Education, American Osteopathic Association and American Association of Colleges of Osteopathic Medicine reached in 2014 recognized ACGME as the primary accrediting body for graduate medical education programs by 2020.
This led to the first single match for U.S. MD and DO senior students and graduates and the inclusion of DO senior students as sponsored applicants in 2020, Dr. Lamb noted.
Gains, trends in 2020 match
Growth in U.S. DO senior participation also pushed this year’s Match to record highs. There were 6,581 U.S. DO medical school seniors who submitted rank order lists, 1,103 more than in 2019. Among those seniors, 90.7% matched to PGY-1 positions, driving the match rate for U.S. DO seniors up 2.6 percentage points from 2019.
Since 2016, the number of U.S. DO seniors seeking positions has risen by 3,599 or 120%. “Of course, the number of U.S. MD seniors who submitted program choices was also record-high: 19,326, an increase of 401 over 2019. The 93.7% match rate to first-year positions for this group has remained very consistent for many years,” Dr. Lamb said.
Among individual specialties, the NRMP reported extremely high fill rates for dermatology, medicine-emergency medicine, neurological surgery, physical medicine and rehabilitation (categorical), integrated plastic surgery, and thoracic surgery. Other competitive specialties included medicine-pediatrics, orthopedic surgery, otolaryngology, and vascular surgery.
Participation of international medical school students and graduates (IMGs) went up in 2020, breaking a 3-year cycle of decline. More than 61% matched to first-year positions, 2.5 percentage points higher than 2019 – and the highest match rate since 1990. “IMGs generally are having the most success matching to primary care specialties, including internal medicine, family medicine, and pediatrics,” Dr. Lamb said.
Primary care benefits from DO growth
DO candidates also helped drive up the numbers in primary care.
Internal medicine offered 8,697 categorical positions, 581 more than in 2019, reflecting a fill rate of 95.7%. More than 40% of these slots were filled by U.S. MD seniors, a category that’s seen decreases over the last 5 years, due in part to administrative and financial burdens associated with primary care internal medicine.
“In addition, the steady growth of internal medicine has increased the overall number of training positions available, and with the growth of other specialties in parallel, it has also likely had some effect on decreasing the percentage of U.S. graduates entering the field,” Phil Masters, MD, vice president of membership and global engagement at the American College of Physicians, said in an interview.
However, fill rates for U.S. DO seniors reached 16% in 2020, a notable rise from 6.9% in 2016. “As the number of osteopathic trainees increases, we are happy that more are choosing internal medicine as a career path,” Dr. Masters said, adding that the slightly different training and practice orientation of osteopathic physicians “complements that of their allopathic colleagues, and add richness to the many different practice settings that internal medicine encompasses.”
A record number of DO seniors also matched in family medicine (1,392), accounting for nearly 30% of all applicants. The single match led to an important net increase in filled family medicine residency positions, Clif Knight, MD, senior vice president for education at the American Academy of Family Physicians, said in an interview.
Overall, family medicine filled 92.5% of its 4,662 positions, 555 more than in 2019. The results show that family medicine and primary care are on solid footing, Dr. Knight said. “We are excited that the number of filled family medicine residency positions increased from last year. This is important as we work to meet the significant primary care workforce shortage,” he added.
In other specialties:
- Pediatrics filled more than 98% of its 2,864 categorical positions, 17 more than in 2019. U.S. MD seniors filled 1,731 (60.4%) of those slots. “We’re very excited about our newly matched pediatricians,” Sara “Sally” H. Goza, MD, president of the American Academy of Pediatrics, said in an interview. “The coronavirus outbreak has shown us how valuable the pediatric workforce is and how much we’re needed.’’
- Dermatology offered 478 positions, achieving a fill rate of 98.1%. “Looking at our own program’s Match results, I feel very satisfied that we are accomplishing our specific aim to serve rural populations and to create a diverse workforce in dermatology,” Erik Stratman, MD, an expert on dermatologic education in U.S. medical schools/residency programs, and a member of the American Academy of Dermatology, said in an interview. “It’s nice to see the fruits of the specialty’s expanding efforts to get the right people in the specialty who reflect those populations we serve.”
- Obstetrics-gynecology offered 1,433 first-year positions – 48 more than in 2019 – achieving a fill rate of 99.8%, with U.S. MD seniors filling more than 75% of those slots.
- Neurology filled more than 97.5% of 682 offered positions in 2020. However, U.S. MD seniors represented just under half of those filled positions (46.5%).
- Psychiatry offered 1,858 positions in 2020, achieving an overall fill rate of 98.9%, 61.2% for U.S. MD seniors.
- Emergency Medicine filled 99.5% of the 2,665 positions offered this year. In this profession, the U.S. MD fill rate was 64.3%. These new interns are sorely needed at a time when EM physicians are on the front lines of a pandemic, Hannah R. Hughes, MD, president of the Emergency Medicine Residents’ Association, said in an interview.
Emergency Rule: Docs can bill for telehealth and COVID-19 tests. Here’s how
Many medical practices have long wanted to use telehealth to perform office visits and other evaluation and management (E/M) services. The technology readily exists and many electronic health records are set up to do telehealth visits. The problem has been getting paid for those visits. Medicare limited telehealth services to patients in underserved areas, and commercial insurances wouldn’t pay. But amid the COVID-19 crisis, things have changed.
On March 17, Congress passed a law allowing Medicare to waive some telehealth restrictions during a government state of emergency only, which we are in now. Specifically, the patient no longer needs to be in a medically underserved area and no longer needs to go to an originating site, such as a hospital. The patient can be located anywhere in the country and be in their own home.
Further, the Centers for Medicare & Medicaid is waiving the requirement that the practitioner use a HIPAA-compliant platform for the telehealth service. The service must still be provided using a real-time audiovisual platform, but that could be via FaceTime or Skype, both of which are readily available via a patient’s smartphone or home computer. Audio alone – that is, phone calls between physician and patient – is still insufficient.
Billing for telemedicine
There are two lists of services that you can bill for telehealth. One of the lists is in Medicare’s telehealth fact sheet and includes both CPT and HCPCS codes. The second is in your CPT book, Appendix P, and lists only CPT codes.
Practices may bill all of the Medicare-covered telehealth services using these new rules. This includes new and established patient visits 99201–99215. It includes inpatient and skilled nursing services, for which CMS uses HCPCS codes in place of CPT codes.
Some notable additional services that you may bill via telehealth are: smoking cessation, transitional care management, advanced care planning, psychiatric diagnostic interviews and psychotherapy, and initial and subsequent Medicare wellness visits. The Welcome to Medicare visit is not on the list.
Report these services to Medicare with the correct CPT code and use place of service 02 (telehealth) on the claim. There is a CPT modifier for telehealth (Modifier -95 Synchronous Telemedicine Service Rendered Via a Real-Time Interactive Audio and Video Telecommunications System) but Medicare does not require it.
If you perform an office visit and also do smoking cessation, document those just as you would if you saw the patient in person. Document the history; observational exam, if relevant; and the assessment and plan. Note the additional time spent in smoking cessation counseling. If it was a level three established patient, code 99213-25 and 99406 (smoking and tobacco use cessation counseling visit, intermediate, 3-10 minutes).
The Office of Inspector General is allowing practices to reduce or waive copays and patient due amounts. However, a practice is not required to waive the copay or patient due amount for a telehealth service.
Medicare Advantage plans are required to cover all services that original Medicare covers. State Medicaid plans and Medicaid managed care organizations can set their own rules.
What about commercial payers?
While CMS has issued its Medicare guidelines, commercial insurance companies can also set their own rules about covering telehealth services. Many of them have rushed to update their policies to allow office visits to be billed via telehealth.
Unfortunately, each payer can set its own rules about whether to cover telehealth and if the place of service 02 and/or modifier -95 is needed. UnitedHealthcare is covering telehealth visits for all of its Medicare Advantage, Medicaid, and commercial accounts.
Humana also is covering telemedicine for urgent care needs. Some private insurers are continuing to offer virtual visits with their contracted telehealth provider, not with the patient’s own physician. It is likely that this will change in the days ahead, but it means practices must check their payer policies and pay attention to the emails they receive from the payers. If patient foot traffic is slow, this may be a good time to call each payer to not only find out their telehealth rules, but to also learn what else is being suspended during the COVID-19 pandemic.
This would also be a good job for an employee to do from home versus coming into the practice.
None of the payers are limiting the diagnosis code for telemedicine services. The patient does not need to have a cough or fever to have telemedicine covered. Any diagnosis or condition is eligible to be billed via telehealth.
The waived restrictions by Medicare are in place only as long as the government state of emergency. Commercial payers are also describing these as temporary. However, it may be hard to put the genie back in the bottle. Medical practices and patients may find that these visits are just what the doctor ordered.
COVID-19 testing
Although testing is still not widely available, the American Medical Association has developed a CPT code for the test:
- 87635: Infectious agent detection by nucleic acid (DNA or RNA); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]), amplified probe technique
CMS has also developed codes for testing for this new coronavirus. One (U0001) is specifically for tests done in the CDC lab. The second (U0002) was for other labs, but it seems likely that the CPT code will replace it.
In February, the U.S. Food and Drug Administration issued a new policy for certain labs to develop their own validated COVID-19 diagnostics. This second HCPCS code could be used for such tests when submitting claims to Medicare or other insurers.
The hope by CMS is that having these specific codes will encourage further testing and improve tracking of the virus.
This article first appeared on Medscape.com.
Many medical practices have long wanted to use telehealth to perform office visits and other evaluation and management (E/M) services. The technology readily exists and many electronic health records are set up to do telehealth visits. The problem has been getting paid for those visits. Medicare limited telehealth services to patients in underserved areas, and commercial insurances wouldn’t pay. But amid the COVID-19 crisis, things have changed.
On March 17, Congress passed a law allowing Medicare to waive some telehealth restrictions during a government state of emergency only, which we are in now. Specifically, the patient no longer needs to be in a medically underserved area and no longer needs to go to an originating site, such as a hospital. The patient can be located anywhere in the country and be in their own home.
Further, the Centers for Medicare & Medicaid is waiving the requirement that the practitioner use a HIPAA-compliant platform for the telehealth service. The service must still be provided using a real-time audiovisual platform, but that could be via FaceTime or Skype, both of which are readily available via a patient’s smartphone or home computer. Audio alone – that is, phone calls between physician and patient – is still insufficient.
Billing for telemedicine
There are two lists of services that you can bill for telehealth. One of the lists is in Medicare’s telehealth fact sheet and includes both CPT and HCPCS codes. The second is in your CPT book, Appendix P, and lists only CPT codes.
Practices may bill all of the Medicare-covered telehealth services using these new rules. This includes new and established patient visits 99201–99215. It includes inpatient and skilled nursing services, for which CMS uses HCPCS codes in place of CPT codes.
Some notable additional services that you may bill via telehealth are: smoking cessation, transitional care management, advanced care planning, psychiatric diagnostic interviews and psychotherapy, and initial and subsequent Medicare wellness visits. The Welcome to Medicare visit is not on the list.
Report these services to Medicare with the correct CPT code and use place of service 02 (telehealth) on the claim. There is a CPT modifier for telehealth (Modifier -95 Synchronous Telemedicine Service Rendered Via a Real-Time Interactive Audio and Video Telecommunications System) but Medicare does not require it.
If you perform an office visit and also do smoking cessation, document those just as you would if you saw the patient in person. Document the history; observational exam, if relevant; and the assessment and plan. Note the additional time spent in smoking cessation counseling. If it was a level three established patient, code 99213-25 and 99406 (smoking and tobacco use cessation counseling visit, intermediate, 3-10 minutes).
The Office of Inspector General is allowing practices to reduce or waive copays and patient due amounts. However, a practice is not required to waive the copay or patient due amount for a telehealth service.
Medicare Advantage plans are required to cover all services that original Medicare covers. State Medicaid plans and Medicaid managed care organizations can set their own rules.
What about commercial payers?
While CMS has issued its Medicare guidelines, commercial insurance companies can also set their own rules about covering telehealth services. Many of them have rushed to update their policies to allow office visits to be billed via telehealth.
Unfortunately, each payer can set its own rules about whether to cover telehealth and if the place of service 02 and/or modifier -95 is needed. UnitedHealthcare is covering telehealth visits for all of its Medicare Advantage, Medicaid, and commercial accounts.
Humana also is covering telemedicine for urgent care needs. Some private insurers are continuing to offer virtual visits with their contracted telehealth provider, not with the patient’s own physician. It is likely that this will change in the days ahead, but it means practices must check their payer policies and pay attention to the emails they receive from the payers. If patient foot traffic is slow, this may be a good time to call each payer to not only find out their telehealth rules, but to also learn what else is being suspended during the COVID-19 pandemic.
This would also be a good job for an employee to do from home versus coming into the practice.
None of the payers are limiting the diagnosis code for telemedicine services. The patient does not need to have a cough or fever to have telemedicine covered. Any diagnosis or condition is eligible to be billed via telehealth.
The waived restrictions by Medicare are in place only as long as the government state of emergency. Commercial payers are also describing these as temporary. However, it may be hard to put the genie back in the bottle. Medical practices and patients may find that these visits are just what the doctor ordered.
COVID-19 testing
Although testing is still not widely available, the American Medical Association has developed a CPT code for the test:
- 87635: Infectious agent detection by nucleic acid (DNA or RNA); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]), amplified probe technique
CMS has also developed codes for testing for this new coronavirus. One (U0001) is specifically for tests done in the CDC lab. The second (U0002) was for other labs, but it seems likely that the CPT code will replace it.
In February, the U.S. Food and Drug Administration issued a new policy for certain labs to develop their own validated COVID-19 diagnostics. This second HCPCS code could be used for such tests when submitting claims to Medicare or other insurers.
The hope by CMS is that having these specific codes will encourage further testing and improve tracking of the virus.
This article first appeared on Medscape.com.
Many medical practices have long wanted to use telehealth to perform office visits and other evaluation and management (E/M) services. The technology readily exists and many electronic health records are set up to do telehealth visits. The problem has been getting paid for those visits. Medicare limited telehealth services to patients in underserved areas, and commercial insurances wouldn’t pay. But amid the COVID-19 crisis, things have changed.
On March 17, Congress passed a law allowing Medicare to waive some telehealth restrictions during a government state of emergency only, which we are in now. Specifically, the patient no longer needs to be in a medically underserved area and no longer needs to go to an originating site, such as a hospital. The patient can be located anywhere in the country and be in their own home.
Further, the Centers for Medicare & Medicaid is waiving the requirement that the practitioner use a HIPAA-compliant platform for the telehealth service. The service must still be provided using a real-time audiovisual platform, but that could be via FaceTime or Skype, both of which are readily available via a patient’s smartphone or home computer. Audio alone – that is, phone calls between physician and patient – is still insufficient.
Billing for telemedicine
There are two lists of services that you can bill for telehealth. One of the lists is in Medicare’s telehealth fact sheet and includes both CPT and HCPCS codes. The second is in your CPT book, Appendix P, and lists only CPT codes.
Practices may bill all of the Medicare-covered telehealth services using these new rules. This includes new and established patient visits 99201–99215. It includes inpatient and skilled nursing services, for which CMS uses HCPCS codes in place of CPT codes.
Some notable additional services that you may bill via telehealth are: smoking cessation, transitional care management, advanced care planning, psychiatric diagnostic interviews and psychotherapy, and initial and subsequent Medicare wellness visits. The Welcome to Medicare visit is not on the list.
Report these services to Medicare with the correct CPT code and use place of service 02 (telehealth) on the claim. There is a CPT modifier for telehealth (Modifier -95 Synchronous Telemedicine Service Rendered Via a Real-Time Interactive Audio and Video Telecommunications System) but Medicare does not require it.
If you perform an office visit and also do smoking cessation, document those just as you would if you saw the patient in person. Document the history; observational exam, if relevant; and the assessment and plan. Note the additional time spent in smoking cessation counseling. If it was a level three established patient, code 99213-25 and 99406 (smoking and tobacco use cessation counseling visit, intermediate, 3-10 minutes).
The Office of Inspector General is allowing practices to reduce or waive copays and patient due amounts. However, a practice is not required to waive the copay or patient due amount for a telehealth service.
Medicare Advantage plans are required to cover all services that original Medicare covers. State Medicaid plans and Medicaid managed care organizations can set their own rules.
What about commercial payers?
While CMS has issued its Medicare guidelines, commercial insurance companies can also set their own rules about covering telehealth services. Many of them have rushed to update their policies to allow office visits to be billed via telehealth.
Unfortunately, each payer can set its own rules about whether to cover telehealth and if the place of service 02 and/or modifier -95 is needed. UnitedHealthcare is covering telehealth visits for all of its Medicare Advantage, Medicaid, and commercial accounts.
Humana also is covering telemedicine for urgent care needs. Some private insurers are continuing to offer virtual visits with their contracted telehealth provider, not with the patient’s own physician. It is likely that this will change in the days ahead, but it means practices must check their payer policies and pay attention to the emails they receive from the payers. If patient foot traffic is slow, this may be a good time to call each payer to not only find out their telehealth rules, but to also learn what else is being suspended during the COVID-19 pandemic.
This would also be a good job for an employee to do from home versus coming into the practice.
None of the payers are limiting the diagnosis code for telemedicine services. The patient does not need to have a cough or fever to have telemedicine covered. Any diagnosis or condition is eligible to be billed via telehealth.
The waived restrictions by Medicare are in place only as long as the government state of emergency. Commercial payers are also describing these as temporary. However, it may be hard to put the genie back in the bottle. Medical practices and patients may find that these visits are just what the doctor ordered.
COVID-19 testing
Although testing is still not widely available, the American Medical Association has developed a CPT code for the test:
- 87635: Infectious agent detection by nucleic acid (DNA or RNA); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]), amplified probe technique
CMS has also developed codes for testing for this new coronavirus. One (U0001) is specifically for tests done in the CDC lab. The second (U0002) was for other labs, but it seems likely that the CPT code will replace it.
In February, the U.S. Food and Drug Administration issued a new policy for certain labs to develop their own validated COVID-19 diagnostics. This second HCPCS code could be used for such tests when submitting claims to Medicare or other insurers.
The hope by CMS is that having these specific codes will encourage further testing and improve tracking of the virus.
This article first appeared on Medscape.com.
Coronavirus resources from AAD target safe office practices, new telemedicine guidance
The American Academy of Dermatology (
The guidance pages are publicly viewable. Additionally, AAD has made a collection of COVID-19 articles from the Journal of the American Academy of Dermatology freely available for the next 6 months.
George Hruza, MD, AAD president, detailed regulatory updates and other federal actions as well as guidance regarding telemedicine and clinical practice in a message to AAD members.
“While many questions still need answers, I have appointed an Ad Hoc Task Force to assess dermatology’s needs, share knowledge, and provide ongoing guidance and information throughout the crisis,” Dr. Hruza wrote.
“The situation is changing rapidly, and we are committed to keeping you updated with reliable and practical information to help you adapt to the circumstances,” he noted, referring dermatologists to the AAD’s information hub for the coronavirus outbreak. “We are keeping this page updated frequently, and it will serve as your primary source for what we know now,” he noted.
The Centers for Medicare & Medicaid Services has recently relaxed key regulations regarding technology to provide telemedicine so that physicians and patients can use existing platforms such as FaceTime and Skype for virtual visits. The usual fines for HIPAA noncompliance have been waived. Additionally, telemedicine visits can now be reimbursed at the same rate as in-person visits.
Private payers are beginning to follow suit, said Dr. Hruza, noting that the AAD Association is working to harmonize private coverage with public reimbursement. The AAD also is tracking which payers are coming in line with federal policies on its teledermatology page.
These changes in regulation around telemedicine apply to patient encounters for any purpose, not just coronavirus-related encounters, noted Dr. Hruza. “The good news is that the government has taken action to make it much easier for us to provide virtual consults to patients. Dermatology has always been a leader in telemedicine, and it will be an important way to offer care to patients who can’t or don’t need to come into the office or clinic,” he added.
Importantly, said Dr. Hruza, CMS is allowing practices to have discretion over whether copays are collected, or collected in full, so that these payments don’t present a barrier to patient care in the current crisis environment.
For dermatologists who are new to telemedicine, AAD has created an online resource that includes information about various telemedicine platforms, updated guidance regarding regulations, and best practices for accurate coding and documentation of telemedicine visits.
The Academy has also been developing dermatology-specific guidance, including how to address the concerns of patients who are receiving biologic therapies and how to conserve personal protective equipment while still protecting physicians, staff, and patients from COVID-19 infection.
For patients on biologic therapy who show no sign of coronavirus infection, the decision to continue or stop biologics should be made on a case-by-case basis. Factors to be considered include patient age, comorbidities, and the severity of the original indication for biologic use.
Initiation of biologics should only be done after a similar risk-benefit analysis, with a recommendation to consider deferring initiation for patients 60 and older and those with comorbidities that may portend a worse course in the event of coronavirus infection. Biologics should be discontinued for patients who test positive for COVID-19.
Dr. Hruza outlined some of the federal measures taken that may affect the business side of dermatology practices. These include a $20 million transfer to the Small Business Administration to offset administrative expenses associated with increased loan volumes related to the coronavirus outbreak. Eligible expenses for loans may include new devices and environmental adjustments to accommodate telehealth services.
Additionally, it is anticipated that as employers are required to provide paid sick and family leave, a payroll tax credit will be issued to employers. Some self-employed individuals will also be able to claim a tax credit for sick and family leave.
A recent news release from the AAD encourages the public to use high-emollient moisturizers after handwashing. The release also provides other tips, such as using petrolatum at bedtime for hands that are particularly dry and focusing on the fingertips when moisturizing, as these areas are prone to cracking. The release also reaffirms that the most effective way to clean hands is soap and water, and that moisturizing after handwashing does not negate the antiviral effects of cleansing, contrary to some social media reports.
koakes@mdedge.com
The American Academy of Dermatology (
The guidance pages are publicly viewable. Additionally, AAD has made a collection of COVID-19 articles from the Journal of the American Academy of Dermatology freely available for the next 6 months.
George Hruza, MD, AAD president, detailed regulatory updates and other federal actions as well as guidance regarding telemedicine and clinical practice in a message to AAD members.
“While many questions still need answers, I have appointed an Ad Hoc Task Force to assess dermatology’s needs, share knowledge, and provide ongoing guidance and information throughout the crisis,” Dr. Hruza wrote.
“The situation is changing rapidly, and we are committed to keeping you updated with reliable and practical information to help you adapt to the circumstances,” he noted, referring dermatologists to the AAD’s information hub for the coronavirus outbreak. “We are keeping this page updated frequently, and it will serve as your primary source for what we know now,” he noted.
The Centers for Medicare & Medicaid Services has recently relaxed key regulations regarding technology to provide telemedicine so that physicians and patients can use existing platforms such as FaceTime and Skype for virtual visits. The usual fines for HIPAA noncompliance have been waived. Additionally, telemedicine visits can now be reimbursed at the same rate as in-person visits.
Private payers are beginning to follow suit, said Dr. Hruza, noting that the AAD Association is working to harmonize private coverage with public reimbursement. The AAD also is tracking which payers are coming in line with federal policies on its teledermatology page.
These changes in regulation around telemedicine apply to patient encounters for any purpose, not just coronavirus-related encounters, noted Dr. Hruza. “The good news is that the government has taken action to make it much easier for us to provide virtual consults to patients. Dermatology has always been a leader in telemedicine, and it will be an important way to offer care to patients who can’t or don’t need to come into the office or clinic,” he added.
Importantly, said Dr. Hruza, CMS is allowing practices to have discretion over whether copays are collected, or collected in full, so that these payments don’t present a barrier to patient care in the current crisis environment.
For dermatologists who are new to telemedicine, AAD has created an online resource that includes information about various telemedicine platforms, updated guidance regarding regulations, and best practices for accurate coding and documentation of telemedicine visits.
The Academy has also been developing dermatology-specific guidance, including how to address the concerns of patients who are receiving biologic therapies and how to conserve personal protective equipment while still protecting physicians, staff, and patients from COVID-19 infection.
For patients on biologic therapy who show no sign of coronavirus infection, the decision to continue or stop biologics should be made on a case-by-case basis. Factors to be considered include patient age, comorbidities, and the severity of the original indication for biologic use.
Initiation of biologics should only be done after a similar risk-benefit analysis, with a recommendation to consider deferring initiation for patients 60 and older and those with comorbidities that may portend a worse course in the event of coronavirus infection. Biologics should be discontinued for patients who test positive for COVID-19.
Dr. Hruza outlined some of the federal measures taken that may affect the business side of dermatology practices. These include a $20 million transfer to the Small Business Administration to offset administrative expenses associated with increased loan volumes related to the coronavirus outbreak. Eligible expenses for loans may include new devices and environmental adjustments to accommodate telehealth services.
Additionally, it is anticipated that as employers are required to provide paid sick and family leave, a payroll tax credit will be issued to employers. Some self-employed individuals will also be able to claim a tax credit for sick and family leave.
A recent news release from the AAD encourages the public to use high-emollient moisturizers after handwashing. The release also provides other tips, such as using petrolatum at bedtime for hands that are particularly dry and focusing on the fingertips when moisturizing, as these areas are prone to cracking. The release also reaffirms that the most effective way to clean hands is soap and water, and that moisturizing after handwashing does not negate the antiviral effects of cleansing, contrary to some social media reports.
koakes@mdedge.com
The American Academy of Dermatology (
The guidance pages are publicly viewable. Additionally, AAD has made a collection of COVID-19 articles from the Journal of the American Academy of Dermatology freely available for the next 6 months.
George Hruza, MD, AAD president, detailed regulatory updates and other federal actions as well as guidance regarding telemedicine and clinical practice in a message to AAD members.
“While many questions still need answers, I have appointed an Ad Hoc Task Force to assess dermatology’s needs, share knowledge, and provide ongoing guidance and information throughout the crisis,” Dr. Hruza wrote.
“The situation is changing rapidly, and we are committed to keeping you updated with reliable and practical information to help you adapt to the circumstances,” he noted, referring dermatologists to the AAD’s information hub for the coronavirus outbreak. “We are keeping this page updated frequently, and it will serve as your primary source for what we know now,” he noted.
The Centers for Medicare & Medicaid Services has recently relaxed key regulations regarding technology to provide telemedicine so that physicians and patients can use existing platforms such as FaceTime and Skype for virtual visits. The usual fines for HIPAA noncompliance have been waived. Additionally, telemedicine visits can now be reimbursed at the same rate as in-person visits.
Private payers are beginning to follow suit, said Dr. Hruza, noting that the AAD Association is working to harmonize private coverage with public reimbursement. The AAD also is tracking which payers are coming in line with federal policies on its teledermatology page.
These changes in regulation around telemedicine apply to patient encounters for any purpose, not just coronavirus-related encounters, noted Dr. Hruza. “The good news is that the government has taken action to make it much easier for us to provide virtual consults to patients. Dermatology has always been a leader in telemedicine, and it will be an important way to offer care to patients who can’t or don’t need to come into the office or clinic,” he added.
Importantly, said Dr. Hruza, CMS is allowing practices to have discretion over whether copays are collected, or collected in full, so that these payments don’t present a barrier to patient care in the current crisis environment.
For dermatologists who are new to telemedicine, AAD has created an online resource that includes information about various telemedicine platforms, updated guidance regarding regulations, and best practices for accurate coding and documentation of telemedicine visits.
The Academy has also been developing dermatology-specific guidance, including how to address the concerns of patients who are receiving biologic therapies and how to conserve personal protective equipment while still protecting physicians, staff, and patients from COVID-19 infection.
For patients on biologic therapy who show no sign of coronavirus infection, the decision to continue or stop biologics should be made on a case-by-case basis. Factors to be considered include patient age, comorbidities, and the severity of the original indication for biologic use.
Initiation of biologics should only be done after a similar risk-benefit analysis, with a recommendation to consider deferring initiation for patients 60 and older and those with comorbidities that may portend a worse course in the event of coronavirus infection. Biologics should be discontinued for patients who test positive for COVID-19.
Dr. Hruza outlined some of the federal measures taken that may affect the business side of dermatology practices. These include a $20 million transfer to the Small Business Administration to offset administrative expenses associated with increased loan volumes related to the coronavirus outbreak. Eligible expenses for loans may include new devices and environmental adjustments to accommodate telehealth services.
Additionally, it is anticipated that as employers are required to provide paid sick and family leave, a payroll tax credit will be issued to employers. Some self-employed individuals will also be able to claim a tax credit for sick and family leave.
A recent news release from the AAD encourages the public to use high-emollient moisturizers after handwashing. The release also provides other tips, such as using petrolatum at bedtime for hands that are particularly dry and focusing on the fingertips when moisturizing, as these areas are prone to cracking. The release also reaffirms that the most effective way to clean hands is soap and water, and that moisturizing after handwashing does not negate the antiviral effects of cleansing, contrary to some social media reports.
koakes@mdedge.com
The apricot tree
My apricot tree has bloomed. It is a foolish tree planted by a foolish man since it blossoms, with beautiful pink then white flowers, at least 3 weeks too early in Northern Kentucky. Nonetheless, I am hopeful that it will produce fruit, maybe this year.
The apricot tree takes me back to my early childhood in Oklahoma City. We had a small apricot tree in the backyard of our rental house, and my dad would talk about how there was nothing finer than a sun ripened apricot. Those were happy times. My dad was a milkman and was home every day by late afternoon, though he was still taking classes at night to try to finish his degree. My mother was at home and my older brother in first grade down the street. My little sister was small and tried to keep up.
My time was unstructured, and I reveled in the backyard. In retrospect, the backyard was an open display of broken and hoped for dreams. There was a junked car my best friend Alvin and I would sit in, there was a huge tree stump we sat on and played around, we had an old slow dog named Pooch, gifted to us when my mom’s sister moved to Alaska. We ran around with no shirts or shoes, played and pretended, and carefully watched the apricot tree.
I remember one time when the apricots finally ripened. My father climbed up and got me one, and it was so sweet I did not notice that the juice ran down my face and my bare chest. It was the sweetest and most wonderful thing I have ever tasted. All the better for having to wait for it.
. I have had four major meetings canceled and though my livelihood and life are at risk, I feel oddly free and happy. I am no longer under those pressures to research, write, and present, and am spending at lot of time at home with my wife and daughter. I think I will clean out the garage (who knows what I will find?) and work in the backyard – and keep a close watch on the apricot tree.
As many of you have, I have awkwardly embraced telemedicine in the past. It is interesting now, how HIPAA regulations and state licensing requirements have finally been tossed aside, making it possible to practice telemedicine. I suspect things will stay that way if it is demonstrated they are unnecessary.
In my office, we are depopulating the waiting room and autoclaving face masks. I am cleaning out the stockroom and donating extra gloves, gowns, and masks to the local hospital. We may shut down altogether. There is little more I can do unless called to man a ventilator. I hope it doesn’t come to that, but I will serve if called.
I suggest you embrace your current unstructured time and use it to let your mind roam. It is a reprieve from today’s hyperconnected, hurly burly world. I also suggest you check COVID-19 news updates only once a day and turn off television news altogether. Other than following the recommendations and guidance of public health authorities, there is nothing you can do to speed up the resolution of this pandemic.
No matter how awful, this will pass. It is a warm spring and it is possible the apricot tree will not be bitten by frost, and we may have fruit this year. We should know in about 2 months. I am going to keep a close watch on it.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
My apricot tree has bloomed. It is a foolish tree planted by a foolish man since it blossoms, with beautiful pink then white flowers, at least 3 weeks too early in Northern Kentucky. Nonetheless, I am hopeful that it will produce fruit, maybe this year.
The apricot tree takes me back to my early childhood in Oklahoma City. We had a small apricot tree in the backyard of our rental house, and my dad would talk about how there was nothing finer than a sun ripened apricot. Those were happy times. My dad was a milkman and was home every day by late afternoon, though he was still taking classes at night to try to finish his degree. My mother was at home and my older brother in first grade down the street. My little sister was small and tried to keep up.
My time was unstructured, and I reveled in the backyard. In retrospect, the backyard was an open display of broken and hoped for dreams. There was a junked car my best friend Alvin and I would sit in, there was a huge tree stump we sat on and played around, we had an old slow dog named Pooch, gifted to us when my mom’s sister moved to Alaska. We ran around with no shirts or shoes, played and pretended, and carefully watched the apricot tree.
I remember one time when the apricots finally ripened. My father climbed up and got me one, and it was so sweet I did not notice that the juice ran down my face and my bare chest. It was the sweetest and most wonderful thing I have ever tasted. All the better for having to wait for it.
. I have had four major meetings canceled and though my livelihood and life are at risk, I feel oddly free and happy. I am no longer under those pressures to research, write, and present, and am spending at lot of time at home with my wife and daughter. I think I will clean out the garage (who knows what I will find?) and work in the backyard – and keep a close watch on the apricot tree.
As many of you have, I have awkwardly embraced telemedicine in the past. It is interesting now, how HIPAA regulations and state licensing requirements have finally been tossed aside, making it possible to practice telemedicine. I suspect things will stay that way if it is demonstrated they are unnecessary.
In my office, we are depopulating the waiting room and autoclaving face masks. I am cleaning out the stockroom and donating extra gloves, gowns, and masks to the local hospital. We may shut down altogether. There is little more I can do unless called to man a ventilator. I hope it doesn’t come to that, but I will serve if called.
I suggest you embrace your current unstructured time and use it to let your mind roam. It is a reprieve from today’s hyperconnected, hurly burly world. I also suggest you check COVID-19 news updates only once a day and turn off television news altogether. Other than following the recommendations and guidance of public health authorities, there is nothing you can do to speed up the resolution of this pandemic.
No matter how awful, this will pass. It is a warm spring and it is possible the apricot tree will not be bitten by frost, and we may have fruit this year. We should know in about 2 months. I am going to keep a close watch on it.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
My apricot tree has bloomed. It is a foolish tree planted by a foolish man since it blossoms, with beautiful pink then white flowers, at least 3 weeks too early in Northern Kentucky. Nonetheless, I am hopeful that it will produce fruit, maybe this year.
The apricot tree takes me back to my early childhood in Oklahoma City. We had a small apricot tree in the backyard of our rental house, and my dad would talk about how there was nothing finer than a sun ripened apricot. Those were happy times. My dad was a milkman and was home every day by late afternoon, though he was still taking classes at night to try to finish his degree. My mother was at home and my older brother in first grade down the street. My little sister was small and tried to keep up.
My time was unstructured, and I reveled in the backyard. In retrospect, the backyard was an open display of broken and hoped for dreams. There was a junked car my best friend Alvin and I would sit in, there was a huge tree stump we sat on and played around, we had an old slow dog named Pooch, gifted to us when my mom’s sister moved to Alaska. We ran around with no shirts or shoes, played and pretended, and carefully watched the apricot tree.
I remember one time when the apricots finally ripened. My father climbed up and got me one, and it was so sweet I did not notice that the juice ran down my face and my bare chest. It was the sweetest and most wonderful thing I have ever tasted. All the better for having to wait for it.
. I have had four major meetings canceled and though my livelihood and life are at risk, I feel oddly free and happy. I am no longer under those pressures to research, write, and present, and am spending at lot of time at home with my wife and daughter. I think I will clean out the garage (who knows what I will find?) and work in the backyard – and keep a close watch on the apricot tree.
As many of you have, I have awkwardly embraced telemedicine in the past. It is interesting now, how HIPAA regulations and state licensing requirements have finally been tossed aside, making it possible to practice telemedicine. I suspect things will stay that way if it is demonstrated they are unnecessary.
In my office, we are depopulating the waiting room and autoclaving face masks. I am cleaning out the stockroom and donating extra gloves, gowns, and masks to the local hospital. We may shut down altogether. There is little more I can do unless called to man a ventilator. I hope it doesn’t come to that, but I will serve if called.
I suggest you embrace your current unstructured time and use it to let your mind roam. It is a reprieve from today’s hyperconnected, hurly burly world. I also suggest you check COVID-19 news updates only once a day and turn off television news altogether. Other than following the recommendations and guidance of public health authorities, there is nothing you can do to speed up the resolution of this pandemic.
No matter how awful, this will pass. It is a warm spring and it is possible the apricot tree will not be bitten by frost, and we may have fruit this year. We should know in about 2 months. I am going to keep a close watch on it.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.











