User login
Walking App Works Only if Users Think It Does
TOPLINE:
Apps designed to increase physical activity may be useful in increasing daily step counts for users who believe the intervention beneficial, but not for those who do not. The app’s effectiveness is notably influenced by how users perceive its utility.
METHODOLOGY:
- Researchers conducted a randomized controlled trial from February 2021 to May 2022 to evaluate the effectiveness of SNapp, an adaptive app designed to promote walking through tailored coaching content.
- Overall, 176 adults (76% women; mean age, 56 years) were randomly assigned to use the app plus tailored coaching content (SNapp group; n = 87) or only the step counter app (control group; n = 89).
- SNapp’s coaching content provided personalized feedback on step counts and recommendations for increasing walking, while also considering individual preferences for behavior change techniques.
- The primary outcome was the daily step count recorded by the app, which was updated on an hourly basis in a database over an intervention period of 12 months.
- Perceptions of ease of use and usefulness were assessed to determine their effect on the effectiveness of the app.
TAKEAWAY:
- Intervention group participants used the app nearly 30% of days, while those using the app alone showed almost identical use.
- The SNapp intervention did not significantly affect the step counts on average over time (B, −202.30; 95% CI, −889.7 to 485.1).
- Perceived usefulness significantly moderated the intervention effect of SNapp (B, 344.38; 90% CI, 40.4-648.3), but perceived ease of use did not (B, 38.60; 90% CI, −276.5 to 353.7).
- Among participants with a high perceived usefulness, the SNapp group had a higher median step count than the control group (median difference, 1260 steps; 90% CI, −3243.7 to 1298.2); however, this difference was not statistically significant.
IN PRACTICE:
“This study shows that perceived usefulness is also an important factor influencing behavioral effects. Hence, it is essential for apps to be perceived as useful to effectively improve users’ activity levels,” the authors wrote.
SOURCE:
The study was led by Anne L. Vos, PhD, of the Amsterdam School of Communication Research at the University of Amsterdam, in the Netherlands. It was published online on September 16, 2024, in the American Journal of Preventive Medicine.
LIMITATIONS:
The study’s recruitment strategy primarily attracted highly educated individuals, limiting generalizability. The app’s accuracy in measuring steps could be improved, as it sometimes underestimated step counts. Researchers also were unable to check if participants read messages from coaches.
DISCLOSURES:
The study was supported by grants from the Dutch Heart Foundation and the Netherlands Organisation for Health Research and Development. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Apps designed to increase physical activity may be useful in increasing daily step counts for users who believe the intervention beneficial, but not for those who do not. The app’s effectiveness is notably influenced by how users perceive its utility.
METHODOLOGY:
- Researchers conducted a randomized controlled trial from February 2021 to May 2022 to evaluate the effectiveness of SNapp, an adaptive app designed to promote walking through tailored coaching content.
- Overall, 176 adults (76% women; mean age, 56 years) were randomly assigned to use the app plus tailored coaching content (SNapp group; n = 87) or only the step counter app (control group; n = 89).
- SNapp’s coaching content provided personalized feedback on step counts and recommendations for increasing walking, while also considering individual preferences for behavior change techniques.
- The primary outcome was the daily step count recorded by the app, which was updated on an hourly basis in a database over an intervention period of 12 months.
- Perceptions of ease of use and usefulness were assessed to determine their effect on the effectiveness of the app.
TAKEAWAY:
- Intervention group participants used the app nearly 30% of days, while those using the app alone showed almost identical use.
- The SNapp intervention did not significantly affect the step counts on average over time (B, −202.30; 95% CI, −889.7 to 485.1).
- Perceived usefulness significantly moderated the intervention effect of SNapp (B, 344.38; 90% CI, 40.4-648.3), but perceived ease of use did not (B, 38.60; 90% CI, −276.5 to 353.7).
- Among participants with a high perceived usefulness, the SNapp group had a higher median step count than the control group (median difference, 1260 steps; 90% CI, −3243.7 to 1298.2); however, this difference was not statistically significant.
IN PRACTICE:
“This study shows that perceived usefulness is also an important factor influencing behavioral effects. Hence, it is essential for apps to be perceived as useful to effectively improve users’ activity levels,” the authors wrote.
SOURCE:
The study was led by Anne L. Vos, PhD, of the Amsterdam School of Communication Research at the University of Amsterdam, in the Netherlands. It was published online on September 16, 2024, in the American Journal of Preventive Medicine.
LIMITATIONS:
The study’s recruitment strategy primarily attracted highly educated individuals, limiting generalizability. The app’s accuracy in measuring steps could be improved, as it sometimes underestimated step counts. Researchers also were unable to check if participants read messages from coaches.
DISCLOSURES:
The study was supported by grants from the Dutch Heart Foundation and the Netherlands Organisation for Health Research and Development. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Apps designed to increase physical activity may be useful in increasing daily step counts for users who believe the intervention beneficial, but not for those who do not. The app’s effectiveness is notably influenced by how users perceive its utility.
METHODOLOGY:
- Researchers conducted a randomized controlled trial from February 2021 to May 2022 to evaluate the effectiveness of SNapp, an adaptive app designed to promote walking through tailored coaching content.
- Overall, 176 adults (76% women; mean age, 56 years) were randomly assigned to use the app plus tailored coaching content (SNapp group; n = 87) or only the step counter app (control group; n = 89).
- SNapp’s coaching content provided personalized feedback on step counts and recommendations for increasing walking, while also considering individual preferences for behavior change techniques.
- The primary outcome was the daily step count recorded by the app, which was updated on an hourly basis in a database over an intervention period of 12 months.
- Perceptions of ease of use and usefulness were assessed to determine their effect on the effectiveness of the app.
TAKEAWAY:
- Intervention group participants used the app nearly 30% of days, while those using the app alone showed almost identical use.
- The SNapp intervention did not significantly affect the step counts on average over time (B, −202.30; 95% CI, −889.7 to 485.1).
- Perceived usefulness significantly moderated the intervention effect of SNapp (B, 344.38; 90% CI, 40.4-648.3), but perceived ease of use did not (B, 38.60; 90% CI, −276.5 to 353.7).
- Among participants with a high perceived usefulness, the SNapp group had a higher median step count than the control group (median difference, 1260 steps; 90% CI, −3243.7 to 1298.2); however, this difference was not statistically significant.
IN PRACTICE:
“This study shows that perceived usefulness is also an important factor influencing behavioral effects. Hence, it is essential for apps to be perceived as useful to effectively improve users’ activity levels,” the authors wrote.
SOURCE:
The study was led by Anne L. Vos, PhD, of the Amsterdam School of Communication Research at the University of Amsterdam, in the Netherlands. It was published online on September 16, 2024, in the American Journal of Preventive Medicine.
LIMITATIONS:
The study’s recruitment strategy primarily attracted highly educated individuals, limiting generalizability. The app’s accuracy in measuring steps could be improved, as it sometimes underestimated step counts. Researchers also were unable to check if participants read messages from coaches.
DISCLOSURES:
The study was supported by grants from the Dutch Heart Foundation and the Netherlands Organisation for Health Research and Development. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Environmental, Metabolic Factors Driving Global Rise in Stroke
Air pollution, high temperatures, and metabolic risk factors are driving global increases in stroke, contributing to 12 million cases and more than 7 million deaths from stroke each year, new data from the Global Burden of Disease (GBD) study showed.
Between 1990 and 2021, the number of people who experienced a stroke increased to 11.9 million (up by 70% since 1990), while the number of stroke survivors rose to 93.8 million (up by 86%), and stroke-related deaths rose to 7.3 million (up by 44%), making stroke the third leading cause of death worldwide after ischemic heart disease and COVID-19, investigators found.
Stroke is highly preventable, the investigators noted, with 84% of the stroke burden in 2021 attributable to 23 modifiable risk factors, including air pollution, excess body weight, high blood pressure, smoking, and physical inactivity.
This means there are “tremendous opportunities to alter the trajectory of stroke risk for the next generation,” Catherine O. Johnson, MPH, PhD, co-author and lead research scientist at the Institute for Health Metrics and Evaluation (IHME), University of Washington, Seattle, said in a news release.
The study was published online in The Lancet Neurology.
Top Risk Factor for Subarachnoid Hemorrhage
Since 1990, the contribution of high temperatures to poor health and early death due to stroke has risen 72%, a trend likely to increase in the future — underscoring the impact of environmental factors on the growing stroke burden, the authors said.
“Given that ambient air pollution is reciprocally linked with ambient temperature and climate change, the importance of urgent climate actions and measures to reduce air pollution cannot be overestimated,” Dr. Johnson said.
Mitchell S.V. Elkind, MD, MS, chief clinical science officer for the American Heart Association, who wasn’t involved in the study, told this news organization that environmental factors such as air pollution, particulate matter from wildfires and other sources, and excessive heat are now recognized as major contributors to the risk for stroke. “This should not be surprising as we have long recognized the risks of stroke associated with toxins in cigarette smoke, which likely share mechanisms for vascular damage with pollutants,” Dr. Elkind said.
The data also reveal for the first time that ambient particulate matter air pollution is a top risk factor for subarachnoid hemorrhage, contributing to 14% of the death and disability caused by this serious stroke subtype, on a par with smoking.
Dr. Elkind noted that smoking is “a major risk factor for subarachnoid hemorrhage. It makes sense that particulate air pollution would therefore similarly be a risk factor for subarachnoid hemorrhage, which similarly damages blood vessels. Prior studies were likely too small or did not assess the role of air pollution in subarachnoid hemorrhage.”
The analysis also showed substantial increases between 1990 and 2021 in the global stroke burden linked to high body mass index (up by 88%), high blood sugar (up 32%), a diet high in sugar-sweetened drinks (up 23%), low physical activity (up 11%), high systolic blood pressure (up 7%), and a diet low in omega-6 polyunsaturated fatty acids (up 5%).
“And with increasing exposure to risk factors such as high blood sugar and diet high in sugar-sweetened drinks, there is a critical need for interventions focused on obesity and metabolic syndromes,” Dr. Johnson said.
“Identifying sustainable ways to work with communities to take action to prevent and control modifiable risk factors for stroke is essential to address this growing crisis,” she added.
Prevention Strategies Fall Short
The data also showed that stroke-related disability-adjusted life-years rose from around 121.4 million years of healthy life lost in 1990 to 160.5 million years in 2021, making stroke the fourth leading cause of health loss worldwide after COVID-19, ischemic heart disease, and neonatal disorders.
“The global growth of the number of people who develop stroke and died from or remain disabled by stroke is growing fast, strongly suggesting that currently used stroke prevention strategies are not sufficiently effective,” lead author Valery L. Feigin, MD, PhD, from Auckland University of Technology, Auckland, New Zealand, and affiliate professor at IHME, said in the release.
“New, proven effective population-wide and motivational individual prevention strategies that could be applied to all people at risk of having a stroke, regardless of the level of risk, as recommended in the recent Lancet Neurology Commission on Stroke should be implemented across the globe urgently,” said Dr. Feigin.
Dr. Elkind said the AHA supports research on the effects of air quality on risk for vascular injury and stroke and has “long advocated for policies to mitigate the adverse health impacts of air pollutants, including reduction of vehicle emissions and renewable portfolio standards, taking into account racial, ethnic, and economic disparities.”
“AHA, and the healthcare sector more broadly, must take a leadership role in recommending policies to improve environmental air quality and in working with the private sector and industry to improve air quality,” Dr. Elkind said.
In an accompanying commentary, Ming Liu, MD, and Simiao Wu, MD, PhD, West China Hospital, Sichuan University, Chengdu, China, wrote that “pragmatic solutions to the enormous and increasing stroke burden include surveillance, prevention, acute care, and rehabilitation.”
“Surveillance strategies include establishing a national-level framework for regular monitoring of stroke burden, risk factors, and healthcare services via community-based surveys and health records,” they noted.
“Artificial intelligence and mobile technologies might not only facilitate the dissemination of evidence-based health services but also increase the number of data sources and encourage participation of multidisciplinary collaborators, potentially improving the validity and accuracy of future GBD estimates,” they added.
This study was funded by the Bill & Melinda Gates Foundation. Author disclosures are listed with the original article.
A version of this article first appeared on Medscape.com.
Air pollution, high temperatures, and metabolic risk factors are driving global increases in stroke, contributing to 12 million cases and more than 7 million deaths from stroke each year, new data from the Global Burden of Disease (GBD) study showed.
Between 1990 and 2021, the number of people who experienced a stroke increased to 11.9 million (up by 70% since 1990), while the number of stroke survivors rose to 93.8 million (up by 86%), and stroke-related deaths rose to 7.3 million (up by 44%), making stroke the third leading cause of death worldwide after ischemic heart disease and COVID-19, investigators found.
Stroke is highly preventable, the investigators noted, with 84% of the stroke burden in 2021 attributable to 23 modifiable risk factors, including air pollution, excess body weight, high blood pressure, smoking, and physical inactivity.
This means there are “tremendous opportunities to alter the trajectory of stroke risk for the next generation,” Catherine O. Johnson, MPH, PhD, co-author and lead research scientist at the Institute for Health Metrics and Evaluation (IHME), University of Washington, Seattle, said in a news release.
The study was published online in The Lancet Neurology.
Top Risk Factor for Subarachnoid Hemorrhage
Since 1990, the contribution of high temperatures to poor health and early death due to stroke has risen 72%, a trend likely to increase in the future — underscoring the impact of environmental factors on the growing stroke burden, the authors said.
“Given that ambient air pollution is reciprocally linked with ambient temperature and climate change, the importance of urgent climate actions and measures to reduce air pollution cannot be overestimated,” Dr. Johnson said.
Mitchell S.V. Elkind, MD, MS, chief clinical science officer for the American Heart Association, who wasn’t involved in the study, told this news organization that environmental factors such as air pollution, particulate matter from wildfires and other sources, and excessive heat are now recognized as major contributors to the risk for stroke. “This should not be surprising as we have long recognized the risks of stroke associated with toxins in cigarette smoke, which likely share mechanisms for vascular damage with pollutants,” Dr. Elkind said.
The data also reveal for the first time that ambient particulate matter air pollution is a top risk factor for subarachnoid hemorrhage, contributing to 14% of the death and disability caused by this serious stroke subtype, on a par with smoking.
Dr. Elkind noted that smoking is “a major risk factor for subarachnoid hemorrhage. It makes sense that particulate air pollution would therefore similarly be a risk factor for subarachnoid hemorrhage, which similarly damages blood vessels. Prior studies were likely too small or did not assess the role of air pollution in subarachnoid hemorrhage.”
The analysis also showed substantial increases between 1990 and 2021 in the global stroke burden linked to high body mass index (up by 88%), high blood sugar (up 32%), a diet high in sugar-sweetened drinks (up 23%), low physical activity (up 11%), high systolic blood pressure (up 7%), and a diet low in omega-6 polyunsaturated fatty acids (up 5%).
“And with increasing exposure to risk factors such as high blood sugar and diet high in sugar-sweetened drinks, there is a critical need for interventions focused on obesity and metabolic syndromes,” Dr. Johnson said.
“Identifying sustainable ways to work with communities to take action to prevent and control modifiable risk factors for stroke is essential to address this growing crisis,” she added.
Prevention Strategies Fall Short
The data also showed that stroke-related disability-adjusted life-years rose from around 121.4 million years of healthy life lost in 1990 to 160.5 million years in 2021, making stroke the fourth leading cause of health loss worldwide after COVID-19, ischemic heart disease, and neonatal disorders.
“The global growth of the number of people who develop stroke and died from or remain disabled by stroke is growing fast, strongly suggesting that currently used stroke prevention strategies are not sufficiently effective,” lead author Valery L. Feigin, MD, PhD, from Auckland University of Technology, Auckland, New Zealand, and affiliate professor at IHME, said in the release.
“New, proven effective population-wide and motivational individual prevention strategies that could be applied to all people at risk of having a stroke, regardless of the level of risk, as recommended in the recent Lancet Neurology Commission on Stroke should be implemented across the globe urgently,” said Dr. Feigin.
Dr. Elkind said the AHA supports research on the effects of air quality on risk for vascular injury and stroke and has “long advocated for policies to mitigate the adverse health impacts of air pollutants, including reduction of vehicle emissions and renewable portfolio standards, taking into account racial, ethnic, and economic disparities.”
“AHA, and the healthcare sector more broadly, must take a leadership role in recommending policies to improve environmental air quality and in working with the private sector and industry to improve air quality,” Dr. Elkind said.
In an accompanying commentary, Ming Liu, MD, and Simiao Wu, MD, PhD, West China Hospital, Sichuan University, Chengdu, China, wrote that “pragmatic solutions to the enormous and increasing stroke burden include surveillance, prevention, acute care, and rehabilitation.”
“Surveillance strategies include establishing a national-level framework for regular monitoring of stroke burden, risk factors, and healthcare services via community-based surveys and health records,” they noted.
“Artificial intelligence and mobile technologies might not only facilitate the dissemination of evidence-based health services but also increase the number of data sources and encourage participation of multidisciplinary collaborators, potentially improving the validity and accuracy of future GBD estimates,” they added.
This study was funded by the Bill & Melinda Gates Foundation. Author disclosures are listed with the original article.
A version of this article first appeared on Medscape.com.
Air pollution, high temperatures, and metabolic risk factors are driving global increases in stroke, contributing to 12 million cases and more than 7 million deaths from stroke each year, new data from the Global Burden of Disease (GBD) study showed.
Between 1990 and 2021, the number of people who experienced a stroke increased to 11.9 million (up by 70% since 1990), while the number of stroke survivors rose to 93.8 million (up by 86%), and stroke-related deaths rose to 7.3 million (up by 44%), making stroke the third leading cause of death worldwide after ischemic heart disease and COVID-19, investigators found.
Stroke is highly preventable, the investigators noted, with 84% of the stroke burden in 2021 attributable to 23 modifiable risk factors, including air pollution, excess body weight, high blood pressure, smoking, and physical inactivity.
This means there are “tremendous opportunities to alter the trajectory of stroke risk for the next generation,” Catherine O. Johnson, MPH, PhD, co-author and lead research scientist at the Institute for Health Metrics and Evaluation (IHME), University of Washington, Seattle, said in a news release.
The study was published online in The Lancet Neurology.
Top Risk Factor for Subarachnoid Hemorrhage
Since 1990, the contribution of high temperatures to poor health and early death due to stroke has risen 72%, a trend likely to increase in the future — underscoring the impact of environmental factors on the growing stroke burden, the authors said.
“Given that ambient air pollution is reciprocally linked with ambient temperature and climate change, the importance of urgent climate actions and measures to reduce air pollution cannot be overestimated,” Dr. Johnson said.
Mitchell S.V. Elkind, MD, MS, chief clinical science officer for the American Heart Association, who wasn’t involved in the study, told this news organization that environmental factors such as air pollution, particulate matter from wildfires and other sources, and excessive heat are now recognized as major contributors to the risk for stroke. “This should not be surprising as we have long recognized the risks of stroke associated with toxins in cigarette smoke, which likely share mechanisms for vascular damage with pollutants,” Dr. Elkind said.
The data also reveal for the first time that ambient particulate matter air pollution is a top risk factor for subarachnoid hemorrhage, contributing to 14% of the death and disability caused by this serious stroke subtype, on a par with smoking.
Dr. Elkind noted that smoking is “a major risk factor for subarachnoid hemorrhage. It makes sense that particulate air pollution would therefore similarly be a risk factor for subarachnoid hemorrhage, which similarly damages blood vessels. Prior studies were likely too small or did not assess the role of air pollution in subarachnoid hemorrhage.”
The analysis also showed substantial increases between 1990 and 2021 in the global stroke burden linked to high body mass index (up by 88%), high blood sugar (up 32%), a diet high in sugar-sweetened drinks (up 23%), low physical activity (up 11%), high systolic blood pressure (up 7%), and a diet low in omega-6 polyunsaturated fatty acids (up 5%).
“And with increasing exposure to risk factors such as high blood sugar and diet high in sugar-sweetened drinks, there is a critical need for interventions focused on obesity and metabolic syndromes,” Dr. Johnson said.
“Identifying sustainable ways to work with communities to take action to prevent and control modifiable risk factors for stroke is essential to address this growing crisis,” she added.
Prevention Strategies Fall Short
The data also showed that stroke-related disability-adjusted life-years rose from around 121.4 million years of healthy life lost in 1990 to 160.5 million years in 2021, making stroke the fourth leading cause of health loss worldwide after COVID-19, ischemic heart disease, and neonatal disorders.
“The global growth of the number of people who develop stroke and died from or remain disabled by stroke is growing fast, strongly suggesting that currently used stroke prevention strategies are not sufficiently effective,” lead author Valery L. Feigin, MD, PhD, from Auckland University of Technology, Auckland, New Zealand, and affiliate professor at IHME, said in the release.
“New, proven effective population-wide and motivational individual prevention strategies that could be applied to all people at risk of having a stroke, regardless of the level of risk, as recommended in the recent Lancet Neurology Commission on Stroke should be implemented across the globe urgently,” said Dr. Feigin.
Dr. Elkind said the AHA supports research on the effects of air quality on risk for vascular injury and stroke and has “long advocated for policies to mitigate the adverse health impacts of air pollutants, including reduction of vehicle emissions and renewable portfolio standards, taking into account racial, ethnic, and economic disparities.”
“AHA, and the healthcare sector more broadly, must take a leadership role in recommending policies to improve environmental air quality and in working with the private sector and industry to improve air quality,” Dr. Elkind said.
In an accompanying commentary, Ming Liu, MD, and Simiao Wu, MD, PhD, West China Hospital, Sichuan University, Chengdu, China, wrote that “pragmatic solutions to the enormous and increasing stroke burden include surveillance, prevention, acute care, and rehabilitation.”
“Surveillance strategies include establishing a national-level framework for regular monitoring of stroke burden, risk factors, and healthcare services via community-based surveys and health records,” they noted.
“Artificial intelligence and mobile technologies might not only facilitate the dissemination of evidence-based health services but also increase the number of data sources and encourage participation of multidisciplinary collaborators, potentially improving the validity and accuracy of future GBD estimates,” they added.
This study was funded by the Bill & Melinda Gates Foundation. Author disclosures are listed with the original article.
A version of this article first appeared on Medscape.com.
Controlling Six Risk Factors Can Combat CKD in Obesity
TOPLINE:
Optimal management of blood pressure, A1c levels, low-density lipoprotein cholesterol (LDL-C), albuminuria, smoking, and physical activity may reduce the excess risk for chronic kidney disease (CKD) typically linked to obesity. The protective effect is more pronounced in men, in those with lower healthy food scores, and in users of diabetes medication.
METHODOLOGY:
- Obesity is a significant risk factor for CKD, but it is unknown if managing multiple other obesity-related CKD risk factors can mitigate the excess CKD risk.
- Researchers assessed CKD risk factor control in 97,538 participants with obesity from the UK Biobank and compared them with an equal number of age- and sex-matched control participants with normal body weight and no CKD at baseline.
- Participants with obesity were assessed for six modifiable risk factors: Blood pressure, A1c levels, LDL-C, albuminuria, smoking, and physical activity.
- Overall, 2487, 12,720, 32,388, 36,988, and 15,381 participants with obesity had at most two, three, four, five, and six risk factors under combined control, respectively, with the two or fewer group serving as the reference.
- The primary outcome was incident CKD and the degree of combined risk factor control in persons. The CKD risk and risk factor control in participants with obesity were also compared with CKD incidence in matched normal weight participants.
TAKEAWAY:
- During a median follow-up period of 10.8 years, 3954 cases of incident CKD were reported in participants with obesity and 1498 cases in matched persons of normal body mass index (BMI).
- In a stepwise pattern, optimal control of each additional risk factor was associated with 11% (adjusted hazard ratio [aHR], 0.89; 95% CI, 0.86-0.91) reduction in the incidence of CKD events, down to a 49% reduction in CKD incidence (aHR, 0.51; 95% CI, 0.43-0.61) for combined control of all six risk factors in participants with obesity.
- The protective effect of combined control of risk factors was more pronounced in men vs women, in those with lower vs higher healthy diet scores, and in users vs nonusers of diabetes medication.
- A similar stepwise pattern emerged between the number of risk factors controlled and CKD risk in participants with obesity compared with matched individuals of normal BMI, with the excess CKD risk eliminated in participants with obesity with six risk factors under control.
IN PRACTICE:
“Comprehensive control of risk factors might effectively neutralize the excessive CKD risk associated with obesity, emphasizing the potential of a joint management approach in the prevention of CKD in this population,” the authors wrote.
SOURCE:
The study was led by Rui Tang, MS, Department of Epidemiology, School of Public Health and Tropical Medicine, Tulane University, New Orleans, Louisiana. It was published online in Diabetes, Obesity and Metabolism.
LIMITATIONS:
The evaluated risk factors for CKD were arbitrarily selected, which may not represent the ideal group. The study did not consider the time-varying effect of joint risk factor control owing to the lack of some variables such as A1c. The generalizability of the findings was limited because over 90% of the UK Biobank cohort is composed of White people and individuals with healthier behaviors compared with the overall UK population.
DISCLOSURES:
The study was supported by grants from the US National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Optimal management of blood pressure, A1c levels, low-density lipoprotein cholesterol (LDL-C), albuminuria, smoking, and physical activity may reduce the excess risk for chronic kidney disease (CKD) typically linked to obesity. The protective effect is more pronounced in men, in those with lower healthy food scores, and in users of diabetes medication.
METHODOLOGY:
- Obesity is a significant risk factor for CKD, but it is unknown if managing multiple other obesity-related CKD risk factors can mitigate the excess CKD risk.
- Researchers assessed CKD risk factor control in 97,538 participants with obesity from the UK Biobank and compared them with an equal number of age- and sex-matched control participants with normal body weight and no CKD at baseline.
- Participants with obesity were assessed for six modifiable risk factors: Blood pressure, A1c levels, LDL-C, albuminuria, smoking, and physical activity.
- Overall, 2487, 12,720, 32,388, 36,988, and 15,381 participants with obesity had at most two, three, four, five, and six risk factors under combined control, respectively, with the two or fewer group serving as the reference.
- The primary outcome was incident CKD and the degree of combined risk factor control in persons. The CKD risk and risk factor control in participants with obesity were also compared with CKD incidence in matched normal weight participants.
TAKEAWAY:
- During a median follow-up period of 10.8 years, 3954 cases of incident CKD were reported in participants with obesity and 1498 cases in matched persons of normal body mass index (BMI).
- In a stepwise pattern, optimal control of each additional risk factor was associated with 11% (adjusted hazard ratio [aHR], 0.89; 95% CI, 0.86-0.91) reduction in the incidence of CKD events, down to a 49% reduction in CKD incidence (aHR, 0.51; 95% CI, 0.43-0.61) for combined control of all six risk factors in participants with obesity.
- The protective effect of combined control of risk factors was more pronounced in men vs women, in those with lower vs higher healthy diet scores, and in users vs nonusers of diabetes medication.
- A similar stepwise pattern emerged between the number of risk factors controlled and CKD risk in participants with obesity compared with matched individuals of normal BMI, with the excess CKD risk eliminated in participants with obesity with six risk factors under control.
IN PRACTICE:
“Comprehensive control of risk factors might effectively neutralize the excessive CKD risk associated with obesity, emphasizing the potential of a joint management approach in the prevention of CKD in this population,” the authors wrote.
SOURCE:
The study was led by Rui Tang, MS, Department of Epidemiology, School of Public Health and Tropical Medicine, Tulane University, New Orleans, Louisiana. It was published online in Diabetes, Obesity and Metabolism.
LIMITATIONS:
The evaluated risk factors for CKD were arbitrarily selected, which may not represent the ideal group. The study did not consider the time-varying effect of joint risk factor control owing to the lack of some variables such as A1c. The generalizability of the findings was limited because over 90% of the UK Biobank cohort is composed of White people and individuals with healthier behaviors compared with the overall UK population.
DISCLOSURES:
The study was supported by grants from the US National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Optimal management of blood pressure, A1c levels, low-density lipoprotein cholesterol (LDL-C), albuminuria, smoking, and physical activity may reduce the excess risk for chronic kidney disease (CKD) typically linked to obesity. The protective effect is more pronounced in men, in those with lower healthy food scores, and in users of diabetes medication.
METHODOLOGY:
- Obesity is a significant risk factor for CKD, but it is unknown if managing multiple other obesity-related CKD risk factors can mitigate the excess CKD risk.
- Researchers assessed CKD risk factor control in 97,538 participants with obesity from the UK Biobank and compared them with an equal number of age- and sex-matched control participants with normal body weight and no CKD at baseline.
- Participants with obesity were assessed for six modifiable risk factors: Blood pressure, A1c levels, LDL-C, albuminuria, smoking, and physical activity.
- Overall, 2487, 12,720, 32,388, 36,988, and 15,381 participants with obesity had at most two, three, four, five, and six risk factors under combined control, respectively, with the two or fewer group serving as the reference.
- The primary outcome was incident CKD and the degree of combined risk factor control in persons. The CKD risk and risk factor control in participants with obesity were also compared with CKD incidence in matched normal weight participants.
TAKEAWAY:
- During a median follow-up period of 10.8 years, 3954 cases of incident CKD were reported in participants with obesity and 1498 cases in matched persons of normal body mass index (BMI).
- In a stepwise pattern, optimal control of each additional risk factor was associated with 11% (adjusted hazard ratio [aHR], 0.89; 95% CI, 0.86-0.91) reduction in the incidence of CKD events, down to a 49% reduction in CKD incidence (aHR, 0.51; 95% CI, 0.43-0.61) for combined control of all six risk factors in participants with obesity.
- The protective effect of combined control of risk factors was more pronounced in men vs women, in those with lower vs higher healthy diet scores, and in users vs nonusers of diabetes medication.
- A similar stepwise pattern emerged between the number of risk factors controlled and CKD risk in participants with obesity compared with matched individuals of normal BMI, with the excess CKD risk eliminated in participants with obesity with six risk factors under control.
IN PRACTICE:
“Comprehensive control of risk factors might effectively neutralize the excessive CKD risk associated with obesity, emphasizing the potential of a joint management approach in the prevention of CKD in this population,” the authors wrote.
SOURCE:
The study was led by Rui Tang, MS, Department of Epidemiology, School of Public Health and Tropical Medicine, Tulane University, New Orleans, Louisiana. It was published online in Diabetes, Obesity and Metabolism.
LIMITATIONS:
The evaluated risk factors for CKD were arbitrarily selected, which may not represent the ideal group. The study did not consider the time-varying effect of joint risk factor control owing to the lack of some variables such as A1c. The generalizability of the findings was limited because over 90% of the UK Biobank cohort is composed of White people and individuals with healthier behaviors compared with the overall UK population.
DISCLOSURES:
The study was supported by grants from the US National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Rheumatology Clinic Interventions for Smoking, Blood Pressure ‘Make a Big Difference’
Two relatively simple interventions — addressing high blood pressure (BP) and smoking cessation — could make a huge difference for patients with rheumatic disease. Patients with autoimmune disease are up to three times more likely to develop cardiovascular disease (CVD) than the general population. In addition to compounding CVD, smoking is tied to the development of certain autoimmune conditions, as well as worse outcomes. Christie Bartels, MD, chief of the Division of Rheumatology at the University of Wisconsin School of Medicine and Public Health, Madison, has focused her research on improving cardiac health in inflammatory diseases. This news organization spoke with Bartels about two short interventions she developed that tackle hypertension and smoking cessation during regular visits, each taking less than 3 minutes.
How Do These Programs Address Cardiac Disease Prevention?
The BP and Quit Connect programs help clinics systematically address the two most modifiable risk factors for CVD: high BP and smoking. There’s also evidence that addressing these two risk factors improves outcomes in rheumatic diseases. Hypertension predicts an increase in lupus damage. Particularly in lupus nephritis, hypertension will increase the risk for CVD and kidney failure. People who use tobacco have worse outcomes in diseases like rheumatoid arthritis, psoriatic arthritis, and lupus, as well as more CVD, and antirheumatic drugs may not work as well.
In 90 seconds to 3 minutes, staff can do protocol-based care, which we’ve done across 20,000-plus visits. We showed we can improve population level rates of high BP and BP control, as well as increase smoking quitting rates across different patient settings.
What Is the Quit Connect Program?
The Quit Connect program is a 10- to 90-second point of care intervention. During rooming, staff (medical assistants and nurses) ask patients: “A) Do you smoke? and B) Have you thought about cutting back or quitting in the next 30 days?”
It turns out, when you ask the question that way, between a third and a half of people say that they’ve thought about cutting back or quitting. Then, we can get patients connected directly to Quitline, a free public service across all 50 states that smokers can use to get cessation support.
If patients are ready, we ask if we can arrange for them to receive a call from a Quitline coach about setting a quit date or receiving free nicotine replacement therapy. The beautiful thing is when that all happens, A) it’s free to the patient, and B) the results from the Quitline can be recorded right back to the electronic health record.
In our most recent publication in Arthritis Care & Research, we documented bringing Quit Connect to Grady Hospital in downtown Atlanta. It’s a safety net hospital, where 80% patients are Black and 70%-80% patients are on public insurance or uninsured. Using this protocol, we improved Quitline referrals 20-fold.
What Is the BP Connect Program?
At least half of the encounters in United States happen in specialty clinics. Unfortunately, when patients get their BP measured in a specialty clinic that’s not a cardiology or a vascular clinic, often, even if the pressure is high, the clinic doesn’t give patients feedback on that. The problem is because we haven’t said anything, that gives people the false reassurance that their BP is okay.
We’ve developed a 3-minute protocol to ask, advise, and connect. The idea is that if we measure a high BP, then we remeasure and confirm that it’s high. Then, we advise why it matters in rheumatic disease: Patients with rheumatic diseases are already at an increased risk for heart disease, and controlling BP can make a big difference. Then, we connect patients with high BP back to primary care.
Specifically, a SmartSet — an electronic medical record feature — prompts different actions based on confirmed high BP readings:
- If systolic BP ≥ 140-159, the SmartSet directs scheduling a visit to a nurse or primary care provider.
- If systolic BP ≥ 160-179, the next primary care visit anticipates the need to see a prescriber.
- If systolic BP ≥ 180, then the medical assistant or nurse at the visit is instructed to notify the provider who can arrange a provider-to-provider handoff for safety to exclude a hypertensive emergency.
That order goes to the scheduler to call primary care to coordinate follow-up. BP Connect doubled the likelihood of a guideline-recommended follow-up in primary care within 30 days. All patients benefited, and disparities decreased. BP Connect has had 1100 downloads, and both BP and Quit Connect programs are endorsed by the Centers for Disease Control and Prevention and Million Hearts.
How Do These Programs Affect Clinical Practice?
We developed these interventions with a health system engineer, and we time stamped everything. Part of the sustainability of this model is that it fits within a regular workflow. As a practicing rheumatologist, I understand that time is a precious commodity.
The interventions are in partnership with frontline staff. We’ve received feedback that they feel pride participating in these initiatives. They can say, because of me, 30 patients followed up last month for high BP, or 10 patients took a referral to the Quitline last year. We celebrate these accomplishments with the staff.
What Are the Next Steps for These Programs?
Public-facing toolkits for both BP and Quit Connect programs are available online. We have implemented [these programs] in a rural setting, in an urban setting, in Milwaukee and in Atlanta, and we are looking in the future to do a larger, multistate implementation study. If folks are interested, we’d love to partner with them to look at disseminating this further.
A version of this article appeared on Medscape.com.
Two relatively simple interventions — addressing high blood pressure (BP) and smoking cessation — could make a huge difference for patients with rheumatic disease. Patients with autoimmune disease are up to three times more likely to develop cardiovascular disease (CVD) than the general population. In addition to compounding CVD, smoking is tied to the development of certain autoimmune conditions, as well as worse outcomes. Christie Bartels, MD, chief of the Division of Rheumatology at the University of Wisconsin School of Medicine and Public Health, Madison, has focused her research on improving cardiac health in inflammatory diseases. This news organization spoke with Bartels about two short interventions she developed that tackle hypertension and smoking cessation during regular visits, each taking less than 3 minutes.
How Do These Programs Address Cardiac Disease Prevention?
The BP and Quit Connect programs help clinics systematically address the two most modifiable risk factors for CVD: high BP and smoking. There’s also evidence that addressing these two risk factors improves outcomes in rheumatic diseases. Hypertension predicts an increase in lupus damage. Particularly in lupus nephritis, hypertension will increase the risk for CVD and kidney failure. People who use tobacco have worse outcomes in diseases like rheumatoid arthritis, psoriatic arthritis, and lupus, as well as more CVD, and antirheumatic drugs may not work as well.
In 90 seconds to 3 minutes, staff can do protocol-based care, which we’ve done across 20,000-plus visits. We showed we can improve population level rates of high BP and BP control, as well as increase smoking quitting rates across different patient settings.
What Is the Quit Connect Program?
The Quit Connect program is a 10- to 90-second point of care intervention. During rooming, staff (medical assistants and nurses) ask patients: “A) Do you smoke? and B) Have you thought about cutting back or quitting in the next 30 days?”
It turns out, when you ask the question that way, between a third and a half of people say that they’ve thought about cutting back or quitting. Then, we can get patients connected directly to Quitline, a free public service across all 50 states that smokers can use to get cessation support.
If patients are ready, we ask if we can arrange for them to receive a call from a Quitline coach about setting a quit date or receiving free nicotine replacement therapy. The beautiful thing is when that all happens, A) it’s free to the patient, and B) the results from the Quitline can be recorded right back to the electronic health record.
In our most recent publication in Arthritis Care & Research, we documented bringing Quit Connect to Grady Hospital in downtown Atlanta. It’s a safety net hospital, where 80% patients are Black and 70%-80% patients are on public insurance or uninsured. Using this protocol, we improved Quitline referrals 20-fold.
What Is the BP Connect Program?
At least half of the encounters in United States happen in specialty clinics. Unfortunately, when patients get their BP measured in a specialty clinic that’s not a cardiology or a vascular clinic, often, even if the pressure is high, the clinic doesn’t give patients feedback on that. The problem is because we haven’t said anything, that gives people the false reassurance that their BP is okay.
We’ve developed a 3-minute protocol to ask, advise, and connect. The idea is that if we measure a high BP, then we remeasure and confirm that it’s high. Then, we advise why it matters in rheumatic disease: Patients with rheumatic diseases are already at an increased risk for heart disease, and controlling BP can make a big difference. Then, we connect patients with high BP back to primary care.
Specifically, a SmartSet — an electronic medical record feature — prompts different actions based on confirmed high BP readings:
- If systolic BP ≥ 140-159, the SmartSet directs scheduling a visit to a nurse or primary care provider.
- If systolic BP ≥ 160-179, the next primary care visit anticipates the need to see a prescriber.
- If systolic BP ≥ 180, then the medical assistant or nurse at the visit is instructed to notify the provider who can arrange a provider-to-provider handoff for safety to exclude a hypertensive emergency.
That order goes to the scheduler to call primary care to coordinate follow-up. BP Connect doubled the likelihood of a guideline-recommended follow-up in primary care within 30 days. All patients benefited, and disparities decreased. BP Connect has had 1100 downloads, and both BP and Quit Connect programs are endorsed by the Centers for Disease Control and Prevention and Million Hearts.
How Do These Programs Affect Clinical Practice?
We developed these interventions with a health system engineer, and we time stamped everything. Part of the sustainability of this model is that it fits within a regular workflow. As a practicing rheumatologist, I understand that time is a precious commodity.
The interventions are in partnership with frontline staff. We’ve received feedback that they feel pride participating in these initiatives. They can say, because of me, 30 patients followed up last month for high BP, or 10 patients took a referral to the Quitline last year. We celebrate these accomplishments with the staff.
What Are the Next Steps for These Programs?
Public-facing toolkits for both BP and Quit Connect programs are available online. We have implemented [these programs] in a rural setting, in an urban setting, in Milwaukee and in Atlanta, and we are looking in the future to do a larger, multistate implementation study. If folks are interested, we’d love to partner with them to look at disseminating this further.
A version of this article appeared on Medscape.com.
Two relatively simple interventions — addressing high blood pressure (BP) and smoking cessation — could make a huge difference for patients with rheumatic disease. Patients with autoimmune disease are up to three times more likely to develop cardiovascular disease (CVD) than the general population. In addition to compounding CVD, smoking is tied to the development of certain autoimmune conditions, as well as worse outcomes. Christie Bartels, MD, chief of the Division of Rheumatology at the University of Wisconsin School of Medicine and Public Health, Madison, has focused her research on improving cardiac health in inflammatory diseases. This news organization spoke with Bartels about two short interventions she developed that tackle hypertension and smoking cessation during regular visits, each taking less than 3 minutes.
How Do These Programs Address Cardiac Disease Prevention?
The BP and Quit Connect programs help clinics systematically address the two most modifiable risk factors for CVD: high BP and smoking. There’s also evidence that addressing these two risk factors improves outcomes in rheumatic diseases. Hypertension predicts an increase in lupus damage. Particularly in lupus nephritis, hypertension will increase the risk for CVD and kidney failure. People who use tobacco have worse outcomes in diseases like rheumatoid arthritis, psoriatic arthritis, and lupus, as well as more CVD, and antirheumatic drugs may not work as well.
In 90 seconds to 3 minutes, staff can do protocol-based care, which we’ve done across 20,000-plus visits. We showed we can improve population level rates of high BP and BP control, as well as increase smoking quitting rates across different patient settings.
What Is the Quit Connect Program?
The Quit Connect program is a 10- to 90-second point of care intervention. During rooming, staff (medical assistants and nurses) ask patients: “A) Do you smoke? and B) Have you thought about cutting back or quitting in the next 30 days?”
It turns out, when you ask the question that way, between a third and a half of people say that they’ve thought about cutting back or quitting. Then, we can get patients connected directly to Quitline, a free public service across all 50 states that smokers can use to get cessation support.
If patients are ready, we ask if we can arrange for them to receive a call from a Quitline coach about setting a quit date or receiving free nicotine replacement therapy. The beautiful thing is when that all happens, A) it’s free to the patient, and B) the results from the Quitline can be recorded right back to the electronic health record.
In our most recent publication in Arthritis Care & Research, we documented bringing Quit Connect to Grady Hospital in downtown Atlanta. It’s a safety net hospital, where 80% patients are Black and 70%-80% patients are on public insurance or uninsured. Using this protocol, we improved Quitline referrals 20-fold.
What Is the BP Connect Program?
At least half of the encounters in United States happen in specialty clinics. Unfortunately, when patients get their BP measured in a specialty clinic that’s not a cardiology or a vascular clinic, often, even if the pressure is high, the clinic doesn’t give patients feedback on that. The problem is because we haven’t said anything, that gives people the false reassurance that their BP is okay.
We’ve developed a 3-minute protocol to ask, advise, and connect. The idea is that if we measure a high BP, then we remeasure and confirm that it’s high. Then, we advise why it matters in rheumatic disease: Patients with rheumatic diseases are already at an increased risk for heart disease, and controlling BP can make a big difference. Then, we connect patients with high BP back to primary care.
Specifically, a SmartSet — an electronic medical record feature — prompts different actions based on confirmed high BP readings:
- If systolic BP ≥ 140-159, the SmartSet directs scheduling a visit to a nurse or primary care provider.
- If systolic BP ≥ 160-179, the next primary care visit anticipates the need to see a prescriber.
- If systolic BP ≥ 180, then the medical assistant or nurse at the visit is instructed to notify the provider who can arrange a provider-to-provider handoff for safety to exclude a hypertensive emergency.
That order goes to the scheduler to call primary care to coordinate follow-up. BP Connect doubled the likelihood of a guideline-recommended follow-up in primary care within 30 days. All patients benefited, and disparities decreased. BP Connect has had 1100 downloads, and both BP and Quit Connect programs are endorsed by the Centers for Disease Control and Prevention and Million Hearts.
How Do These Programs Affect Clinical Practice?
We developed these interventions with a health system engineer, and we time stamped everything. Part of the sustainability of this model is that it fits within a regular workflow. As a practicing rheumatologist, I understand that time is a precious commodity.
The interventions are in partnership with frontline staff. We’ve received feedback that they feel pride participating in these initiatives. They can say, because of me, 30 patients followed up last month for high BP, or 10 patients took a referral to the Quitline last year. We celebrate these accomplishments with the staff.
What Are the Next Steps for These Programs?
Public-facing toolkits for both BP and Quit Connect programs are available online. We have implemented [these programs] in a rural setting, in an urban setting, in Milwaukee and in Atlanta, and we are looking in the future to do a larger, multistate implementation study. If folks are interested, we’d love to partner with them to look at disseminating this further.
A version of this article appeared on Medscape.com.
Coffee’s ‘Sweet Spot’: Daily Consumption and Cardiometabolic Risk
Each and every day, 1 billion people on this planet ingest a particular psychoactive substance. This chemical has fairly profound physiologic effects. It increases levels of nitric oxide in the blood, leads to vasodilation, and, of course, makes you feel more awake. The substance comes in many forms but almost always in a liquid medium. Do you have it yet? That’s right. The substance is caffeine, quite possibly the healthiest recreational drug that has ever been discovered.
This might be my New England upbringing speaking, but when it comes to lifestyle and health, one of the rules I’ve internalized is that things that are pleasurable are generally bad for you. I know, I know — some of you love to exercise. Some of you love doing crosswords. But you know what I mean. I’m talking French fries, smoked meats, drugs, smoking, alcohol, binge-watching Firefly. You’d be suspicious if a study came out suggesting that eating ice cream in bed reduces your risk for heart attack, and so would I. So I’m always on the lookout for those unicorns of lifestyle factors, those rare things that you want to do and are also good for you.
So far, the data are strong for three things: sleeping, (safe) sexual activity, and coffee. You’ll have to stay tuned for articles about the first two. Today, we’re brewing up some deeper insights about the power of java.
I was inspired to write this article because of a paper, “Habitual Coffee, Tea, and Caffeine Consumption, Circulating Metabolites, and the Risk of Cardiometabolic Multimorbidity,” appearing September 17 in The Journal of Clinical Endocrinology and Metabolism (JCEM).
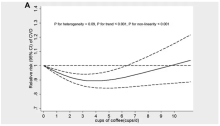
This is not the first study to suggest that coffee intake may be beneficial. A 2013 meta-analysis summarized the results of 36 studies with more than a million participants and found a U-shaped relationship between coffee intake and cardiovascular risk. The sweet spot was at three to five cups a day; people drinking that much coffee had about a 15% reduced risk for cardiovascular disease compared with nondrinkers.
But here’s the thing. Coffee contains caffeine, but it is much more than that. It is a heady brew of various chemicals and compounds, phenols, and chlorogenic acids. And, of course, you can get caffeine from stuff that isn’t coffee — natural things like tea — and decidedly unnatural things like energy drinks. How do you figure out where the benefit really lies?
The JCEM study leveraged the impressive UK Biobank dataset to figure this out. The Biobank recruited more than half a million people from the UK between 2006 and 2010 and collected a wealth of data from each of them: surveys, blood samples, biometrics, medical imaging — the works. And then they followed what would happen to those people medically over time. It’s a pretty amazing resource.
But for the purposes of this study, what you need to know is that just under 200,000 of those participants met the key criteria for this study: being free from cardiovascular disease at baseline; having completed a detailed survey about their coffee, tea, and other caffeinated beverage intake; and having adequate follow-up. A subset of that number, just under 100,000, had metabolomic data — which is where this study really gets interesting.
We’ll dive into the metabolome in a moment, but first let’s just talk about the main finding, the relationship between coffee, tea, or caffeine and cardiovascular disease. But to do that, we need to acknowledge that people who drink a lot of coffee are different from people who don’t, and it might be those differences, not the coffee itself, that are beneficial.
What were those differences? People who drank more coffee tended to be a bit older, were less likely to be female, and were slightly more likely to engage in physical activity. They ate less processed meat but also fewer vegetables. Some of those factors, like being female, are generally protective against cardiovascular disease; but some, like age, are definitely not. The authors adjusted for these and multiple other factors, including alcohol intake, BMI, kidney function, and many others to try to disentangle the effect of being the type of person who drinks a lot of coffee from the drinking a lot of coffee itself.
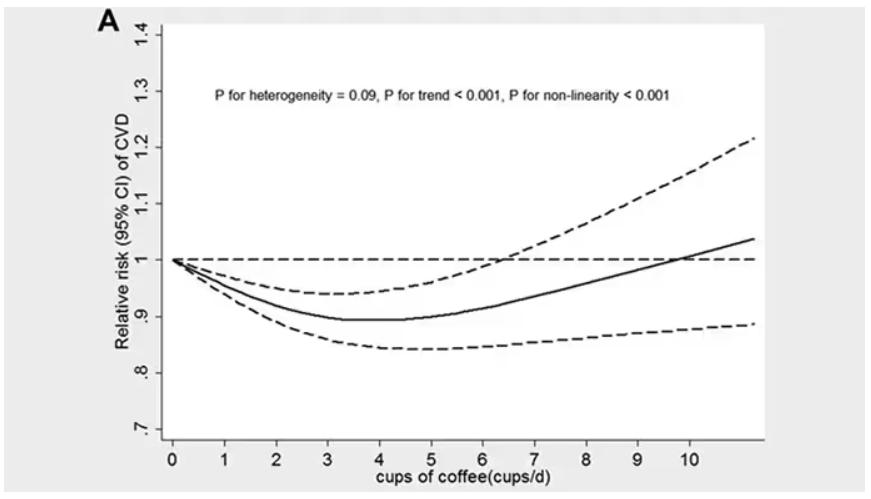
These are the results of the fully adjusted model. Compared with nonconsumers, you can see that people in the higher range of coffee, tea, or just caffeine intake have almost a 40% reduction in cardiovascular disease in follow-up.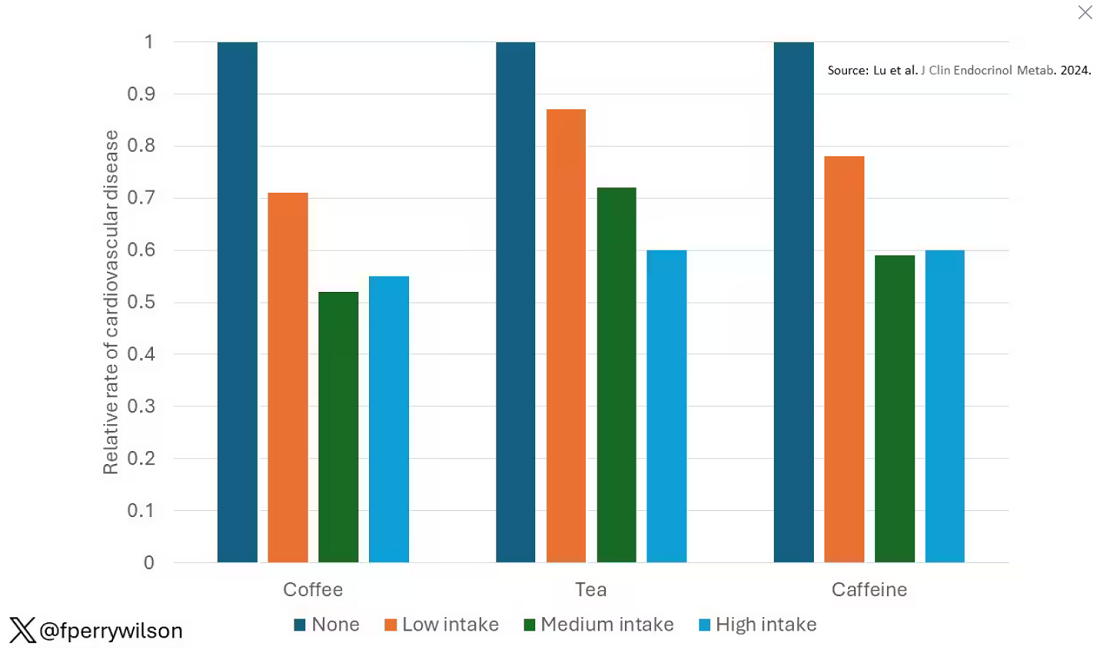
Looking at the benefit across the spectrum of intake, you again see that U-shaped curve, suggesting that a sweet spot for daily consumption can be found around 3 cups of coffee or tea (or 250 mg of caffeine). A standard energy drink contains about 120 mg of caffeine. 
But if this is true, it would be good to know why. To figure that out, the authors turned to the metabolome. The idea here is that your body is constantly breaking stuff down, taking all these proteins and chemicals and compounds that we ingest and turning them into metabolites. Using advanced measurement techniques, researchers can measure hundreds or even thousands of metabolites from a single blood sample. They provide information, obviously, about the food you eat and the drinks you drink, but what is really intriguing is that some metabolites are associated with better health and some with worse
In this study, researchers measured 168 individual metabolites. Eighty of them, nearly half, were significantly altered in people who drank more coffee.
This figure summarizes the findings, and yes, this is way too complicated. 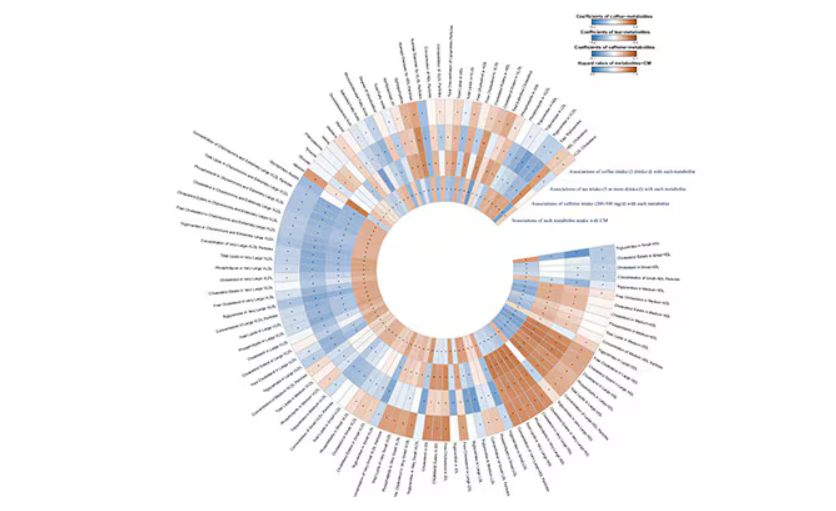
But here’s how to interpret it. The inner ring shows you how certain metabolites are associated with cardiovascular disease. The outer rings show you how those metabolites are associated with coffee, tea, or caffeine. The interesting part is that the sections of the ring (outer rings and inner rings) are very different colors.
Like here.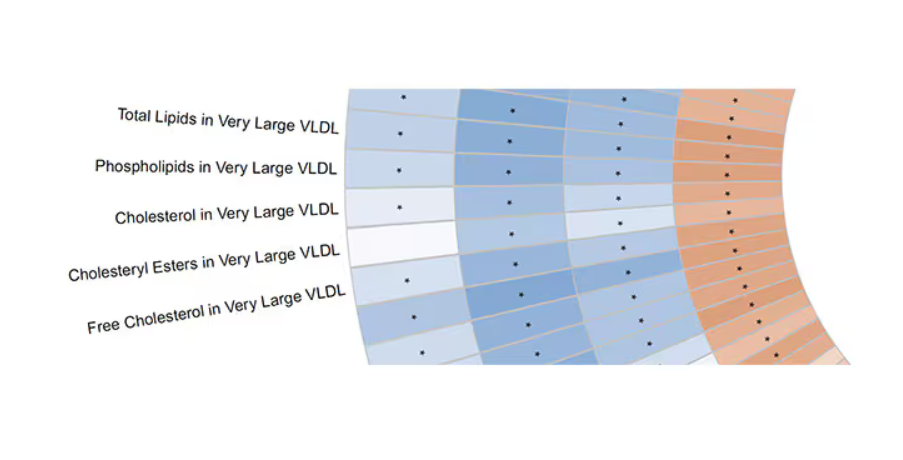
What you see here is a fairly profound effect that coffee, tea, or caffeine intake has on metabolites of VLDL — bad cholesterol. The beverages lower it, and, of course, higher levels lead to cardiovascular disease. This means that this is a potential causal pathway from coffee intake to heart protection.
And that’s not the only one.
You see a similar relationship for saturated fatty acids. Higher levels lead to cardiovascular disease, and coffee intake lowers levels. The reverse works too: Lower levels of histidine (an amino acid) increase cardiovascular risk, and coffee seems to raise those levels.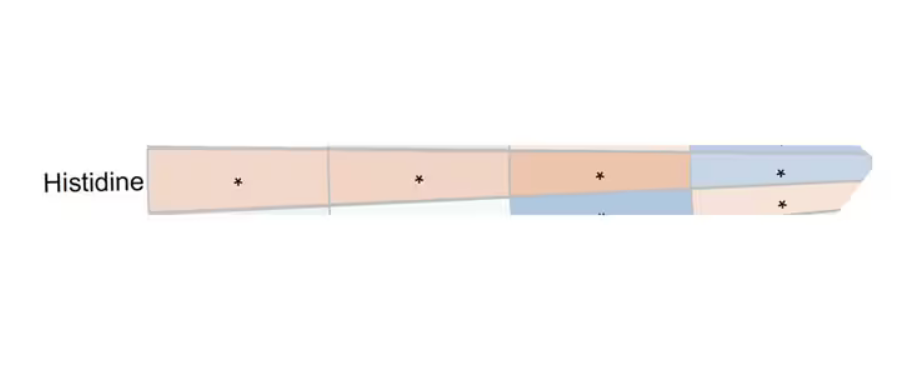
Is this all too good to be true? It’s hard to say. The data on coffee’s benefits have been remarkably consistent. Still, I wouldn’t be a good doctor if I didn’t mention that clearly there is a difference between a cup of black coffee and a venti caramel Frappuccino.
Nevertheless, coffee remains firmly in my holy trinity of enjoyable things that are, for whatever reason, still good for you. So, when you’re having that second, or third, or maybe fourth cup of the day, you can take that to heart.
Dr. Wilson, associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Each and every day, 1 billion people on this planet ingest a particular psychoactive substance. This chemical has fairly profound physiologic effects. It increases levels of nitric oxide in the blood, leads to vasodilation, and, of course, makes you feel more awake. The substance comes in many forms but almost always in a liquid medium. Do you have it yet? That’s right. The substance is caffeine, quite possibly the healthiest recreational drug that has ever been discovered.
This might be my New England upbringing speaking, but when it comes to lifestyle and health, one of the rules I’ve internalized is that things that are pleasurable are generally bad for you. I know, I know — some of you love to exercise. Some of you love doing crosswords. But you know what I mean. I’m talking French fries, smoked meats, drugs, smoking, alcohol, binge-watching Firefly. You’d be suspicious if a study came out suggesting that eating ice cream in bed reduces your risk for heart attack, and so would I. So I’m always on the lookout for those unicorns of lifestyle factors, those rare things that you want to do and are also good for you.
So far, the data are strong for three things: sleeping, (safe) sexual activity, and coffee. You’ll have to stay tuned for articles about the first two. Today, we’re brewing up some deeper insights about the power of java.
I was inspired to write this article because of a paper, “Habitual Coffee, Tea, and Caffeine Consumption, Circulating Metabolites, and the Risk of Cardiometabolic Multimorbidity,” appearing September 17 in The Journal of Clinical Endocrinology and Metabolism (JCEM).
This is not the first study to suggest that coffee intake may be beneficial. A 2013 meta-analysis summarized the results of 36 studies with more than a million participants and found a U-shaped relationship between coffee intake and cardiovascular risk. The sweet spot was at three to five cups a day; people drinking that much coffee had about a 15% reduced risk for cardiovascular disease compared with nondrinkers.
But here’s the thing. Coffee contains caffeine, but it is much more than that. It is a heady brew of various chemicals and compounds, phenols, and chlorogenic acids. And, of course, you can get caffeine from stuff that isn’t coffee — natural things like tea — and decidedly unnatural things like energy drinks. How do you figure out where the benefit really lies?
The JCEM study leveraged the impressive UK Biobank dataset to figure this out. The Biobank recruited more than half a million people from the UK between 2006 and 2010 and collected a wealth of data from each of them: surveys, blood samples, biometrics, medical imaging — the works. And then they followed what would happen to those people medically over time. It’s a pretty amazing resource.
But for the purposes of this study, what you need to know is that just under 200,000 of those participants met the key criteria for this study: being free from cardiovascular disease at baseline; having completed a detailed survey about their coffee, tea, and other caffeinated beverage intake; and having adequate follow-up. A subset of that number, just under 100,000, had metabolomic data — which is where this study really gets interesting.
We’ll dive into the metabolome in a moment, but first let’s just talk about the main finding, the relationship between coffee, tea, or caffeine and cardiovascular disease. But to do that, we need to acknowledge that people who drink a lot of coffee are different from people who don’t, and it might be those differences, not the coffee itself, that are beneficial.
What were those differences? People who drank more coffee tended to be a bit older, were less likely to be female, and were slightly more likely to engage in physical activity. They ate less processed meat but also fewer vegetables. Some of those factors, like being female, are generally protective against cardiovascular disease; but some, like age, are definitely not. The authors adjusted for these and multiple other factors, including alcohol intake, BMI, kidney function, and many others to try to disentangle the effect of being the type of person who drinks a lot of coffee from the drinking a lot of coffee itself.
These are the results of the fully adjusted model. Compared with nonconsumers, you can see that people in the higher range of coffee, tea, or just caffeine intake have almost a 40% reduction in cardiovascular disease in follow-up.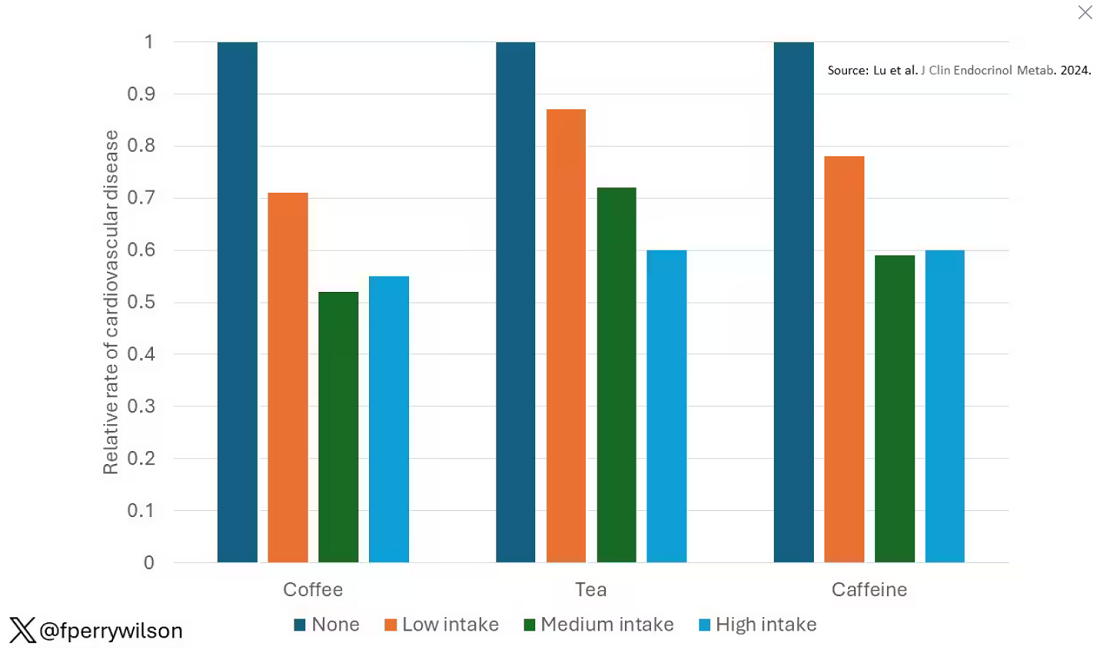
Looking at the benefit across the spectrum of intake, you again see that U-shaped curve, suggesting that a sweet spot for daily consumption can be found around 3 cups of coffee or tea (or 250 mg of caffeine). A standard energy drink contains about 120 mg of caffeine. 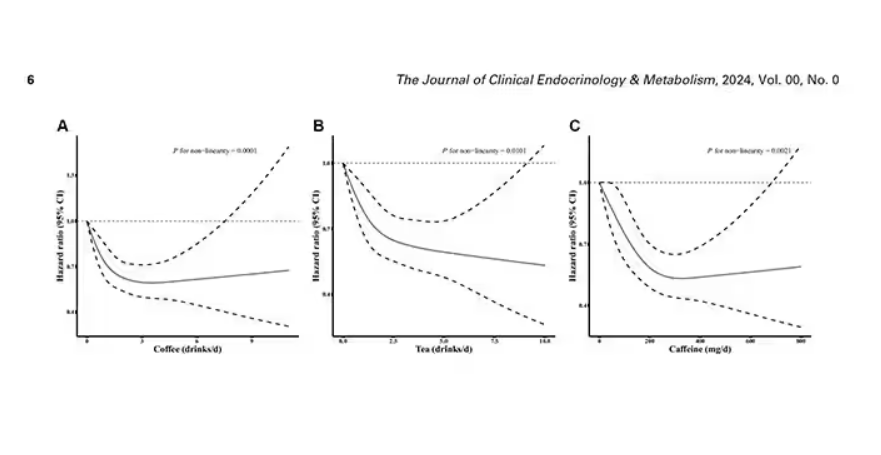
But if this is true, it would be good to know why. To figure that out, the authors turned to the metabolome. The idea here is that your body is constantly breaking stuff down, taking all these proteins and chemicals and compounds that we ingest and turning them into metabolites. Using advanced measurement techniques, researchers can measure hundreds or even thousands of metabolites from a single blood sample. They provide information, obviously, about the food you eat and the drinks you drink, but what is really intriguing is that some metabolites are associated with better health and some with worse
In this study, researchers measured 168 individual metabolites. Eighty of them, nearly half, were significantly altered in people who drank more coffee.
This figure summarizes the findings, and yes, this is way too complicated. 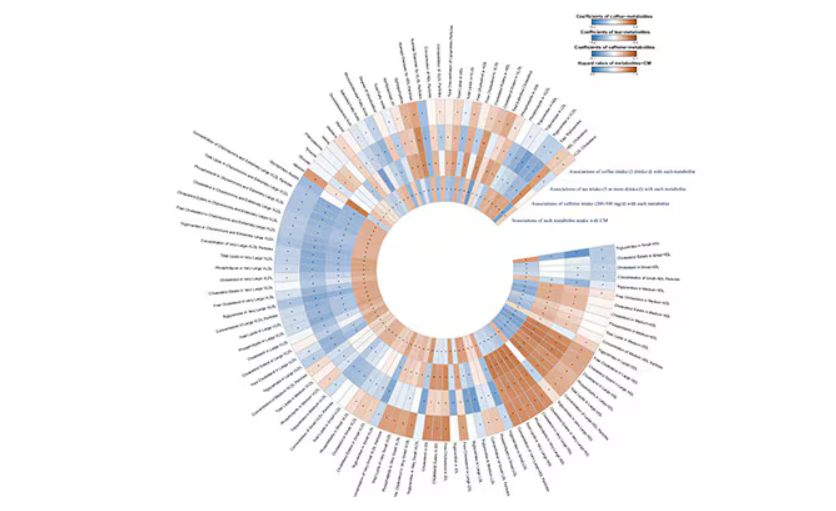
But here’s how to interpret it. The inner ring shows you how certain metabolites are associated with cardiovascular disease. The outer rings show you how those metabolites are associated with coffee, tea, or caffeine. The interesting part is that the sections of the ring (outer rings and inner rings) are very different colors.
Like here.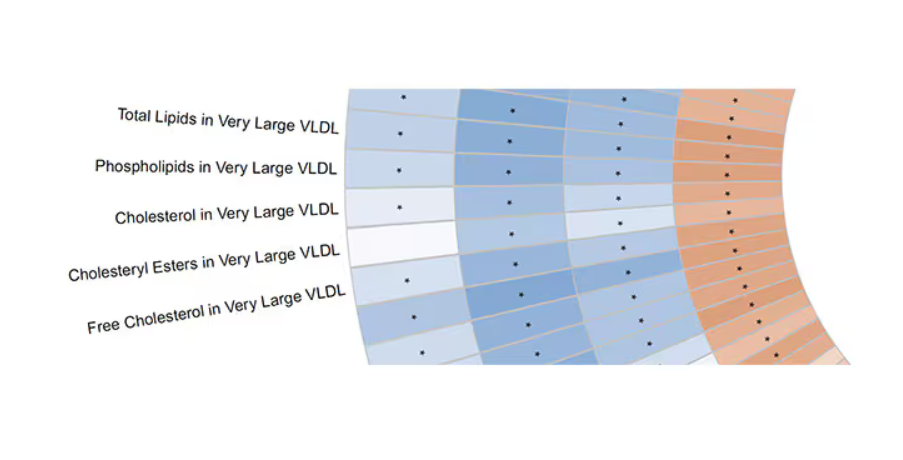
What you see here is a fairly profound effect that coffee, tea, or caffeine intake has on metabolites of VLDL — bad cholesterol. The beverages lower it, and, of course, higher levels lead to cardiovascular disease. This means that this is a potential causal pathway from coffee intake to heart protection.
And that’s not the only one.
You see a similar relationship for saturated fatty acids. Higher levels lead to cardiovascular disease, and coffee intake lowers levels. The reverse works too: Lower levels of histidine (an amino acid) increase cardiovascular risk, and coffee seems to raise those levels.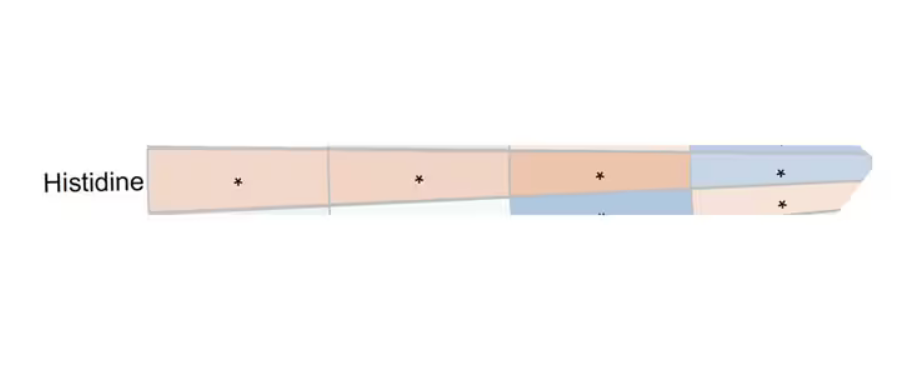
Is this all too good to be true? It’s hard to say. The data on coffee’s benefits have been remarkably consistent. Still, I wouldn’t be a good doctor if I didn’t mention that clearly there is a difference between a cup of black coffee and a venti caramel Frappuccino.
Nevertheless, coffee remains firmly in my holy trinity of enjoyable things that are, for whatever reason, still good for you. So, when you’re having that second, or third, or maybe fourth cup of the day, you can take that to heart.
Dr. Wilson, associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Each and every day, 1 billion people on this planet ingest a particular psychoactive substance. This chemical has fairly profound physiologic effects. It increases levels of nitric oxide in the blood, leads to vasodilation, and, of course, makes you feel more awake. The substance comes in many forms but almost always in a liquid medium. Do you have it yet? That’s right. The substance is caffeine, quite possibly the healthiest recreational drug that has ever been discovered.
This might be my New England upbringing speaking, but when it comes to lifestyle and health, one of the rules I’ve internalized is that things that are pleasurable are generally bad for you. I know, I know — some of you love to exercise. Some of you love doing crosswords. But you know what I mean. I’m talking French fries, smoked meats, drugs, smoking, alcohol, binge-watching Firefly. You’d be suspicious if a study came out suggesting that eating ice cream in bed reduces your risk for heart attack, and so would I. So I’m always on the lookout for those unicorns of lifestyle factors, those rare things that you want to do and are also good for you.
So far, the data are strong for three things: sleeping, (safe) sexual activity, and coffee. You’ll have to stay tuned for articles about the first two. Today, we’re brewing up some deeper insights about the power of java.
I was inspired to write this article because of a paper, “Habitual Coffee, Tea, and Caffeine Consumption, Circulating Metabolites, and the Risk of Cardiometabolic Multimorbidity,” appearing September 17 in The Journal of Clinical Endocrinology and Metabolism (JCEM).
This is not the first study to suggest that coffee intake may be beneficial. A 2013 meta-analysis summarized the results of 36 studies with more than a million participants and found a U-shaped relationship between coffee intake and cardiovascular risk. The sweet spot was at three to five cups a day; people drinking that much coffee had about a 15% reduced risk for cardiovascular disease compared with nondrinkers.
But here’s the thing. Coffee contains caffeine, but it is much more than that. It is a heady brew of various chemicals and compounds, phenols, and chlorogenic acids. And, of course, you can get caffeine from stuff that isn’t coffee — natural things like tea — and decidedly unnatural things like energy drinks. How do you figure out where the benefit really lies?
The JCEM study leveraged the impressive UK Biobank dataset to figure this out. The Biobank recruited more than half a million people from the UK between 2006 and 2010 and collected a wealth of data from each of them: surveys, blood samples, biometrics, medical imaging — the works. And then they followed what would happen to those people medically over time. It’s a pretty amazing resource.
But for the purposes of this study, what you need to know is that just under 200,000 of those participants met the key criteria for this study: being free from cardiovascular disease at baseline; having completed a detailed survey about their coffee, tea, and other caffeinated beverage intake; and having adequate follow-up. A subset of that number, just under 100,000, had metabolomic data — which is where this study really gets interesting.
We’ll dive into the metabolome in a moment, but first let’s just talk about the main finding, the relationship between coffee, tea, or caffeine and cardiovascular disease. But to do that, we need to acknowledge that people who drink a lot of coffee are different from people who don’t, and it might be those differences, not the coffee itself, that are beneficial.
What were those differences? People who drank more coffee tended to be a bit older, were less likely to be female, and were slightly more likely to engage in physical activity. They ate less processed meat but also fewer vegetables. Some of those factors, like being female, are generally protective against cardiovascular disease; but some, like age, are definitely not. The authors adjusted for these and multiple other factors, including alcohol intake, BMI, kidney function, and many others to try to disentangle the effect of being the type of person who drinks a lot of coffee from the drinking a lot of coffee itself.
These are the results of the fully adjusted model. Compared with nonconsumers, you can see that people in the higher range of coffee, tea, or just caffeine intake have almost a 40% reduction in cardiovascular disease in follow-up.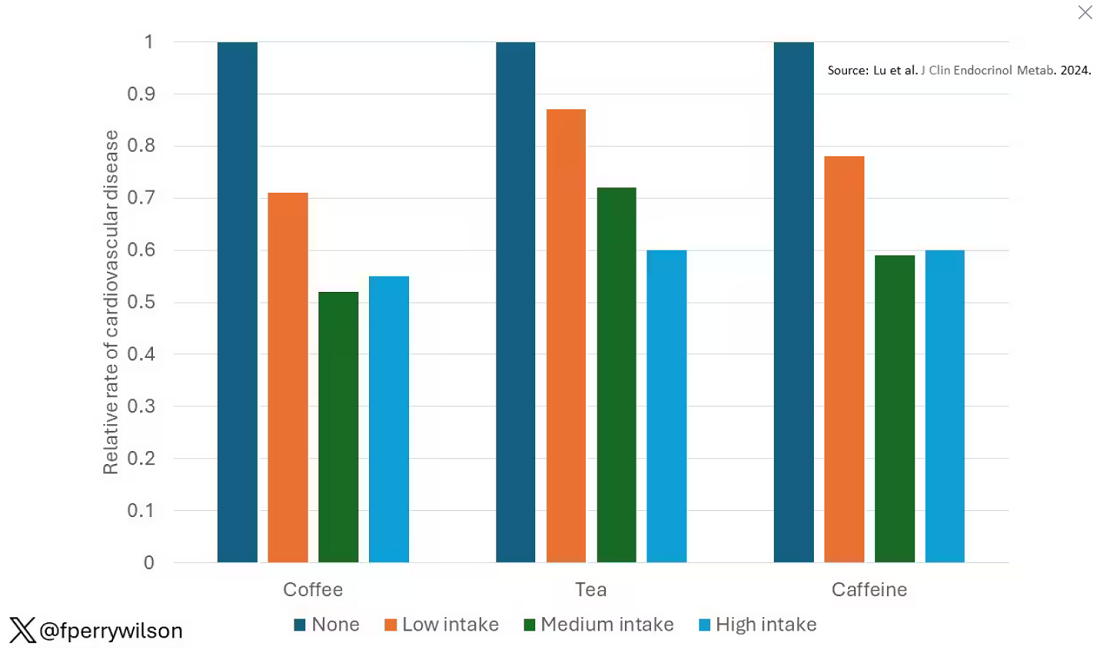
Looking at the benefit across the spectrum of intake, you again see that U-shaped curve, suggesting that a sweet spot for daily consumption can be found around 3 cups of coffee or tea (or 250 mg of caffeine). A standard energy drink contains about 120 mg of caffeine. 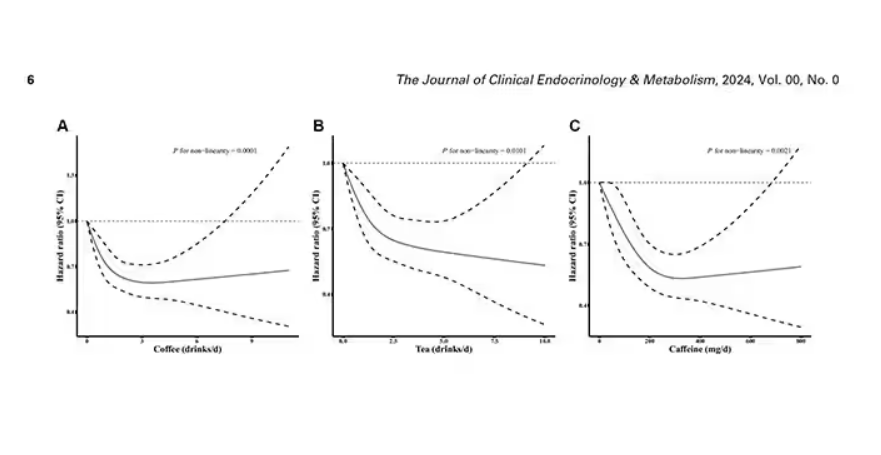
But if this is true, it would be good to know why. To figure that out, the authors turned to the metabolome. The idea here is that your body is constantly breaking stuff down, taking all these proteins and chemicals and compounds that we ingest and turning them into metabolites. Using advanced measurement techniques, researchers can measure hundreds or even thousands of metabolites from a single blood sample. They provide information, obviously, about the food you eat and the drinks you drink, but what is really intriguing is that some metabolites are associated with better health and some with worse
In this study, researchers measured 168 individual metabolites. Eighty of them, nearly half, were significantly altered in people who drank more coffee.
This figure summarizes the findings, and yes, this is way too complicated. 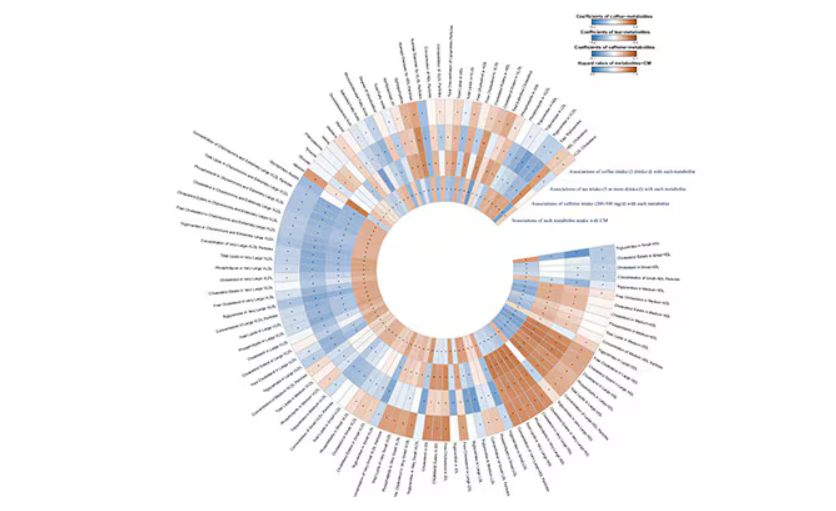
But here’s how to interpret it. The inner ring shows you how certain metabolites are associated with cardiovascular disease. The outer rings show you how those metabolites are associated with coffee, tea, or caffeine. The interesting part is that the sections of the ring (outer rings and inner rings) are very different colors.
Like here.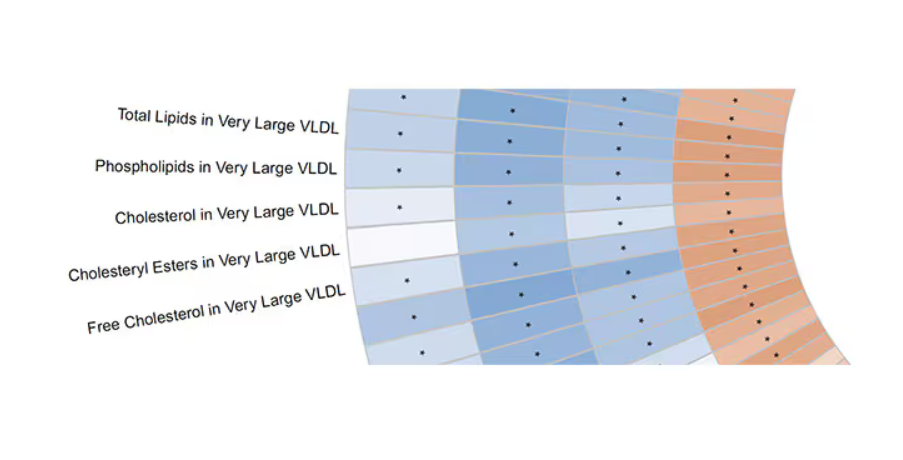
What you see here is a fairly profound effect that coffee, tea, or caffeine intake has on metabolites of VLDL — bad cholesterol. The beverages lower it, and, of course, higher levels lead to cardiovascular disease. This means that this is a potential causal pathway from coffee intake to heart protection.
And that’s not the only one.
You see a similar relationship for saturated fatty acids. Higher levels lead to cardiovascular disease, and coffee intake lowers levels. The reverse works too: Lower levels of histidine (an amino acid) increase cardiovascular risk, and coffee seems to raise those levels.
Is this all too good to be true? It’s hard to say. The data on coffee’s benefits have been remarkably consistent. Still, I wouldn’t be a good doctor if I didn’t mention that clearly there is a difference between a cup of black coffee and a venti caramel Frappuccino.
Nevertheless, coffee remains firmly in my holy trinity of enjoyable things that are, for whatever reason, still good for you. So, when you’re having that second, or third, or maybe fourth cup of the day, you can take that to heart.
Dr. Wilson, associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Can AI Improve Cardiomyopathy Detection in Pregnant Women?
TOPLINE:
Artificial intelligence (AI)–guided screening using digital stethoscopes doubled the detection of left ventricular systolic dysfunction (LVSD) in pregnant and postpartum women in Nigeria. Cardiomyopathy during pregnancy and post partum is challenging to diagnose because of symptom overlap with normal pregnancy changes. AI-guided screening showed a significant improvement in diagnosis rates, compared with usual care.
METHODOLOGY:
- Researchers conducted an open-label, randomized clinical trial involving 1232 pregnant and postpartum women in Nigeria.
- Participants were randomized to either AI-guided screening using digital stethoscopes and 12-lead ECGs or usual care.
- The primary outcome was the identification of LVSD confirmed by echocardiography.
- Secondary outcomes were AI model performance across subgroups and the effectiveness of AI in identifying various levels of LVSD.
TAKEAWAY:
- AI-guided screening using digital stethoscopes detected LVSD in 4.1% of participants, compared with 2.0% of controls (P = .032).
- The 12-lead AI-ECG model detected LVSD in 3.4% of participants in the intervention arm, compared with 2.0% of those in the control arm (P = .125).
- No serious adverse events related to study participation were reported.
- The study highlighted the potential of AI-guided screening to improve the diagnosis of pregnancy-related cardiomyopathy.
IN PRACTICE:
“Delays in the diagnosis of cardiomyopathy during the peripartum period is associated with poorer outcomes as such, it is imperative that we are able to identify cardiac dysfunction early so that appropriate care can be initiated to reduce associated adverse maternal and infant outcomes,” wrote the authors of the study.
SOURCE:
This study was led by Demilade A. Adedinsewo, MBchB, Mayo Clinic in Jacksonville, Florida. It was published online in Nature Medicine.
LIMITATIONS:
The study’s pragmatic design and enrollment at teaching hospitals with echocardiography capabilities limited generalizability. Two thirds of participants were in the third trimester or postpartum at study entry, which limited follow-up visits. The study did not require completion of all seven visits, which led to potential attrition bias. The selected cutoff for LVSD (left ventricular ejection fraction < 50%) did not match the original model specifications, which potentially affected results.
DISCLOSURES:
Dr. Adedinsewo disclosed receiving grants from the Mayo Clinic BIRCWH program funded by the National Institutes of Health. Two coauthors reported holding patents for AI algorithms licensed to Anumana, AliveCor, and Eko Health. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Artificial intelligence (AI)–guided screening using digital stethoscopes doubled the detection of left ventricular systolic dysfunction (LVSD) in pregnant and postpartum women in Nigeria. Cardiomyopathy during pregnancy and post partum is challenging to diagnose because of symptom overlap with normal pregnancy changes. AI-guided screening showed a significant improvement in diagnosis rates, compared with usual care.
METHODOLOGY:
- Researchers conducted an open-label, randomized clinical trial involving 1232 pregnant and postpartum women in Nigeria.
- Participants were randomized to either AI-guided screening using digital stethoscopes and 12-lead ECGs or usual care.
- The primary outcome was the identification of LVSD confirmed by echocardiography.
- Secondary outcomes were AI model performance across subgroups and the effectiveness of AI in identifying various levels of LVSD.
TAKEAWAY:
- AI-guided screening using digital stethoscopes detected LVSD in 4.1% of participants, compared with 2.0% of controls (P = .032).
- The 12-lead AI-ECG model detected LVSD in 3.4% of participants in the intervention arm, compared with 2.0% of those in the control arm (P = .125).
- No serious adverse events related to study participation were reported.
- The study highlighted the potential of AI-guided screening to improve the diagnosis of pregnancy-related cardiomyopathy.
IN PRACTICE:
“Delays in the diagnosis of cardiomyopathy during the peripartum period is associated with poorer outcomes as such, it is imperative that we are able to identify cardiac dysfunction early so that appropriate care can be initiated to reduce associated adverse maternal and infant outcomes,” wrote the authors of the study.
SOURCE:
This study was led by Demilade A. Adedinsewo, MBchB, Mayo Clinic in Jacksonville, Florida. It was published online in Nature Medicine.
LIMITATIONS:
The study’s pragmatic design and enrollment at teaching hospitals with echocardiography capabilities limited generalizability. Two thirds of participants were in the third trimester or postpartum at study entry, which limited follow-up visits. The study did not require completion of all seven visits, which led to potential attrition bias. The selected cutoff for LVSD (left ventricular ejection fraction < 50%) did not match the original model specifications, which potentially affected results.
DISCLOSURES:
Dr. Adedinsewo disclosed receiving grants from the Mayo Clinic BIRCWH program funded by the National Institutes of Health. Two coauthors reported holding patents for AI algorithms licensed to Anumana, AliveCor, and Eko Health. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Artificial intelligence (AI)–guided screening using digital stethoscopes doubled the detection of left ventricular systolic dysfunction (LVSD) in pregnant and postpartum women in Nigeria. Cardiomyopathy during pregnancy and post partum is challenging to diagnose because of symptom overlap with normal pregnancy changes. AI-guided screening showed a significant improvement in diagnosis rates, compared with usual care.
METHODOLOGY:
- Researchers conducted an open-label, randomized clinical trial involving 1232 pregnant and postpartum women in Nigeria.
- Participants were randomized to either AI-guided screening using digital stethoscopes and 12-lead ECGs or usual care.
- The primary outcome was the identification of LVSD confirmed by echocardiography.
- Secondary outcomes were AI model performance across subgroups and the effectiveness of AI in identifying various levels of LVSD.
TAKEAWAY:
- AI-guided screening using digital stethoscopes detected LVSD in 4.1% of participants, compared with 2.0% of controls (P = .032).
- The 12-lead AI-ECG model detected LVSD in 3.4% of participants in the intervention arm, compared with 2.0% of those in the control arm (P = .125).
- No serious adverse events related to study participation were reported.
- The study highlighted the potential of AI-guided screening to improve the diagnosis of pregnancy-related cardiomyopathy.
IN PRACTICE:
“Delays in the diagnosis of cardiomyopathy during the peripartum period is associated with poorer outcomes as such, it is imperative that we are able to identify cardiac dysfunction early so that appropriate care can be initiated to reduce associated adverse maternal and infant outcomes,” wrote the authors of the study.
SOURCE:
This study was led by Demilade A. Adedinsewo, MBchB, Mayo Clinic in Jacksonville, Florida. It was published online in Nature Medicine.
LIMITATIONS:
The study’s pragmatic design and enrollment at teaching hospitals with echocardiography capabilities limited generalizability. Two thirds of participants were in the third trimester or postpartum at study entry, which limited follow-up visits. The study did not require completion of all seven visits, which led to potential attrition bias. The selected cutoff for LVSD (left ventricular ejection fraction < 50%) did not match the original model specifications, which potentially affected results.
DISCLOSURES:
Dr. Adedinsewo disclosed receiving grants from the Mayo Clinic BIRCWH program funded by the National Institutes of Health. Two coauthors reported holding patents for AI algorithms licensed to Anumana, AliveCor, and Eko Health. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Beyond Weight Loss, Limited Bariatric Surgery Benefits in Older Adults
TOPLINE:
For older adults with obesity, bariatric surgery does not appear to significantly reduce the risk for obesity-related cancer and cardiovascular disease (CVD), as it does in younger adults.
METHODOLOGY:
- Bariatric surgery has been shown to decrease the risk for obesity-related cancer and CVD but is typically reserved for patients aged < 60 years. Whether the same holds for patients who undergo surgery at older ages is unclear.
- Researchers analyzed nationwide data from three countries (Denmark, Finland, and Sweden) to compare patients with no history of cancer or CVD and age ≥ 60 years who underwent bariatric surgery against matched controls who received nonoperative treatment for obesity.
- The main outcome was obesity-related cancer, defined as a composite outcome of breast, endometrial, esophageal, colorectal, and kidney cancer. The secondary outcome was CVD, defined as a composite of myocardial infarction, ischemic stroke, and cerebral hemorrhage.
- Analyses were adjusted for diabetes, hypertension, peripheral vascular disease, chronic obstructive pulmonary disease, kidney disease, and frailty.
TAKEAWAY:
- Of the 15,300 patients (66.4% women) included, 2550 underwent bariatric surgery (including gastric bypass in 1930) and 12,750 matched controls received nonoperative treatment for obesity.
- During a median 5.8 years of follow-up, 658 (4.3%) people developed obesity-related cancer and 1436 (9.4%) developed CVD.
- Bariatric surgery in adults aged ≥ 60 years was not associated with a reduced risk for obesity-related cancer (hazard ratio [HR], 0.81) or CVD (HR, 0.86) compared with matched nonoperative controls.
- Bariatric surgery appeared to be associated with a decreased risk for obesity-related cancer in women (HR, 0.76).
- There was a decreased risk for both obesity-related cancer (HR, 0.74) and CVD (HR, 0.82) in patients who underwent gastric bypass.
IN PRACTICE:
“The findings from this study suggest a limited role of bariatric surgery in older patients for the prevention of obesity-related cancer or cardiovascular disease,” the authors wrote, noting that this “may be explained by the poorer weight loss and resolution of comorbidities observed in patients who underwent surgery at an older age.”
SOURCE:
The study, with first author Peter Gerber, MD, PhD, Department of Surgery, Capio St Göran’s Hospital, Stockholm, Sweden, was published online in JAMA Network Open.
LIMITATIONS:
Data on smoking status and body mass index were not available. The observational design limited the ability to draw causal inferences. The null association between bariatric surgery and outcomes may be due to limited power.
DISCLOSURES:
The study was funded by the Swedish Society of Medicine. The authors reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
For older adults with obesity, bariatric surgery does not appear to significantly reduce the risk for obesity-related cancer and cardiovascular disease (CVD), as it does in younger adults.
METHODOLOGY:
- Bariatric surgery has been shown to decrease the risk for obesity-related cancer and CVD but is typically reserved for patients aged < 60 years. Whether the same holds for patients who undergo surgery at older ages is unclear.
- Researchers analyzed nationwide data from three countries (Denmark, Finland, and Sweden) to compare patients with no history of cancer or CVD and age ≥ 60 years who underwent bariatric surgery against matched controls who received nonoperative treatment for obesity.
- The main outcome was obesity-related cancer, defined as a composite outcome of breast, endometrial, esophageal, colorectal, and kidney cancer. The secondary outcome was CVD, defined as a composite of myocardial infarction, ischemic stroke, and cerebral hemorrhage.
- Analyses were adjusted for diabetes, hypertension, peripheral vascular disease, chronic obstructive pulmonary disease, kidney disease, and frailty.
TAKEAWAY:
- Of the 15,300 patients (66.4% women) included, 2550 underwent bariatric surgery (including gastric bypass in 1930) and 12,750 matched controls received nonoperative treatment for obesity.
- During a median 5.8 years of follow-up, 658 (4.3%) people developed obesity-related cancer and 1436 (9.4%) developed CVD.
- Bariatric surgery in adults aged ≥ 60 years was not associated with a reduced risk for obesity-related cancer (hazard ratio [HR], 0.81) or CVD (HR, 0.86) compared with matched nonoperative controls.
- Bariatric surgery appeared to be associated with a decreased risk for obesity-related cancer in women (HR, 0.76).
- There was a decreased risk for both obesity-related cancer (HR, 0.74) and CVD (HR, 0.82) in patients who underwent gastric bypass.
IN PRACTICE:
“The findings from this study suggest a limited role of bariatric surgery in older patients for the prevention of obesity-related cancer or cardiovascular disease,” the authors wrote, noting that this “may be explained by the poorer weight loss and resolution of comorbidities observed in patients who underwent surgery at an older age.”
SOURCE:
The study, with first author Peter Gerber, MD, PhD, Department of Surgery, Capio St Göran’s Hospital, Stockholm, Sweden, was published online in JAMA Network Open.
LIMITATIONS:
Data on smoking status and body mass index were not available. The observational design limited the ability to draw causal inferences. The null association between bariatric surgery and outcomes may be due to limited power.
DISCLOSURES:
The study was funded by the Swedish Society of Medicine. The authors reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
For older adults with obesity, bariatric surgery does not appear to significantly reduce the risk for obesity-related cancer and cardiovascular disease (CVD), as it does in younger adults.
METHODOLOGY:
- Bariatric surgery has been shown to decrease the risk for obesity-related cancer and CVD but is typically reserved for patients aged < 60 years. Whether the same holds for patients who undergo surgery at older ages is unclear.
- Researchers analyzed nationwide data from three countries (Denmark, Finland, and Sweden) to compare patients with no history of cancer or CVD and age ≥ 60 years who underwent bariatric surgery against matched controls who received nonoperative treatment for obesity.
- The main outcome was obesity-related cancer, defined as a composite outcome of breast, endometrial, esophageal, colorectal, and kidney cancer. The secondary outcome was CVD, defined as a composite of myocardial infarction, ischemic stroke, and cerebral hemorrhage.
- Analyses were adjusted for diabetes, hypertension, peripheral vascular disease, chronic obstructive pulmonary disease, kidney disease, and frailty.
TAKEAWAY:
- Of the 15,300 patients (66.4% women) included, 2550 underwent bariatric surgery (including gastric bypass in 1930) and 12,750 matched controls received nonoperative treatment for obesity.
- During a median 5.8 years of follow-up, 658 (4.3%) people developed obesity-related cancer and 1436 (9.4%) developed CVD.
- Bariatric surgery in adults aged ≥ 60 years was not associated with a reduced risk for obesity-related cancer (hazard ratio [HR], 0.81) or CVD (HR, 0.86) compared with matched nonoperative controls.
- Bariatric surgery appeared to be associated with a decreased risk for obesity-related cancer in women (HR, 0.76).
- There was a decreased risk for both obesity-related cancer (HR, 0.74) and CVD (HR, 0.82) in patients who underwent gastric bypass.
IN PRACTICE:
“The findings from this study suggest a limited role of bariatric surgery in older patients for the prevention of obesity-related cancer or cardiovascular disease,” the authors wrote, noting that this “may be explained by the poorer weight loss and resolution of comorbidities observed in patients who underwent surgery at an older age.”
SOURCE:
The study, with first author Peter Gerber, MD, PhD, Department of Surgery, Capio St Göran’s Hospital, Stockholm, Sweden, was published online in JAMA Network Open.
LIMITATIONS:
Data on smoking status and body mass index were not available. The observational design limited the ability to draw causal inferences. The null association between bariatric surgery and outcomes may be due to limited power.
DISCLOSURES:
The study was funded by the Swedish Society of Medicine. The authors reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Old, Frail Patients: Study More, Intervene Less?
Lessons From SENIOR-RITA
The ability to save cardiac muscle during an acute coronary syndrome with percutaneous coronary intervention (PCI) made cardiology one of the most popular fields in medicine.
But acute coronary syndromes come in different categories. While rapid PCI clearly benefits patients with ST-segment elevation myocardial infarction (STEMI), the best use of angiography and PCI for patients with non–ST-segment elevation myocardial infarction (NSTEMI) is more complex.
There have been many trials and meta-analyses, and generally, outcomes are similar with either approach. Perhaps if one looks with enough optimism, there is a benefit for the more aggressive approach in higher-risk patients.
Despite the similar outcomes with the two strategies, most patients are treated with the early invasive approach. Early and invasive fit the spirit of modern cardiology.
Yet, older patients with acute coronary syndromes present a different challenge. NSTEMI trials, like most trials, enrolled mostly younger adults.
Whether evidence obtained in young people applies to older patients is one of the most common and important questions in all of medical practice. Older patients may be at higher risk for a primary outcome, but they also have greater risks for harm from therapy as well as more competing causes of morbidity and mortality.
Only a handful of smaller trials have enrolled older patients with NSTEMI. These trials have produced little evidence that an early invasive approach should be preferred.
The SENIOR-RITA Trial
At ESC, Vijay Kunadian, MD, from Newcastle, England, presented results of SENIOR-RITA, a large trial comparing an invasive vs conservative strategy in NSTEMI patients 75 years of age or older.
In the conservative arm, coronary angiography was allowed if the patient deteriorated and the procedure was clinically indicated in the judgment of the treating physicians.
Slightly more than 1500 patients with NSTEMI were randomly assigned to either strategy in 48 centers in the United Kingdom. Their mean age was 82 years, nearly half were women, and about a third were frail.
Over 4 years of follow-up, the primary outcome of cardiovascular (CV) death or MI occurred at a similar rate in both arms: 25.6% vs 26.3% for invasive vs conservative, respectively (HR, 0.94; 95% CI, 0.77-1.14; P =.53).
Rates of CV death were also not significantly different (15.8% vs 14.2%; HR, 1.11; 95% CI, 0.86-1.44).
The rate of nonfatal MI was slightly lower in the invasive arm (11.7% vs 15.0%; HR, 0.75; 95% CI, 0.57-0.99).
Some other notable findings: Fewer than half of patients in the invasive arm underwent revascularization. Coronary angiography was done in about a quarter of patients in the conservative arm, and revascularization in only 14%.
Comments
Because medicine has improved and patients live longer, cardiologists increasingly see older adults with frailty. It’s important to study these patients.
The authors tell us that 1 in 5 patients screened were enrolled, and those not enrolled were similar in age and were treated nearly equally with either strategy. Not all trials offer this information; it’s important because knowing that patients in a trial are representative helps us translate evidence to our actual patients.
Another positive was the investigators’ smart choice of cardiovascular death and MI as their primary outcome. Strategy trials are usually open label. If they had included an outcome that requires a decision from a clinician, such as unplanned revascularization, then bias becomes a possibility when patients and clinicians are aware of the treatment assignment. (I wrote about poor endpoint choice in the ABYSS trial.)
The most notable finding in SENIOR-RITA was that approximately 76% of patients in the conservative arm did not have a coronary angiogram and 86% were not revascularized.
Yet, the rate of CV death and MI were similar during 4 years of follow-up. This observation is nearly identical to the findings in chronic stable disease, seen in the ISCHEMIA trial. (See Figure 6a in the paper’s supplement.)
I take two messages from this consistent observation: One is that medical therapy is quite good at treating coronary artery disease not associated with acute vessel closure in STEMI.
The other is that using coronary angiography and revascularization as a bailout, in only a fraction of cases, achieves the same result, so the conservative strategy should be preferred.
I am not sure that the SENIOR-RITA researchers see it this way. They write in their discussion that “clinicians are often reluctant to offer an invasive strategy to frail older adults.” They then remind readers that modern PCI techniques (radial approach) have low rates of adverse events.
Perhaps I misread their message, but that paragraph seemed like it was reinforcing our tendency to offer invasive approaches to patients with NSTEMI.
I feel differently. When a trial reports similar outcomes with two strategies, I think we should favor the one with less intervention. I feel even more strongly about this philosophy in older patients with frailty.
Are we not in the business of helping people with the least amount of intervention?
The greatest challenge for the cardiologist of today is not a lack of treatment options, but whether we should use all options in older, frailer adults.
Good on the SENIOR-RITA investigators, for they have shown that we can avoid intervention in the vast majority of older adults presenting with NSTEMI.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Kentucky, and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Lessons From SENIOR-RITA
Lessons From SENIOR-RITA
The ability to save cardiac muscle during an acute coronary syndrome with percutaneous coronary intervention (PCI) made cardiology one of the most popular fields in medicine.
But acute coronary syndromes come in different categories. While rapid PCI clearly benefits patients with ST-segment elevation myocardial infarction (STEMI), the best use of angiography and PCI for patients with non–ST-segment elevation myocardial infarction (NSTEMI) is more complex.
There have been many trials and meta-analyses, and generally, outcomes are similar with either approach. Perhaps if one looks with enough optimism, there is a benefit for the more aggressive approach in higher-risk patients.
Despite the similar outcomes with the two strategies, most patients are treated with the early invasive approach. Early and invasive fit the spirit of modern cardiology.
Yet, older patients with acute coronary syndromes present a different challenge. NSTEMI trials, like most trials, enrolled mostly younger adults.
Whether evidence obtained in young people applies to older patients is one of the most common and important questions in all of medical practice. Older patients may be at higher risk for a primary outcome, but they also have greater risks for harm from therapy as well as more competing causes of morbidity and mortality.
Only a handful of smaller trials have enrolled older patients with NSTEMI. These trials have produced little evidence that an early invasive approach should be preferred.
The SENIOR-RITA Trial
At ESC, Vijay Kunadian, MD, from Newcastle, England, presented results of SENIOR-RITA, a large trial comparing an invasive vs conservative strategy in NSTEMI patients 75 years of age or older.
In the conservative arm, coronary angiography was allowed if the patient deteriorated and the procedure was clinically indicated in the judgment of the treating physicians.
Slightly more than 1500 patients with NSTEMI were randomly assigned to either strategy in 48 centers in the United Kingdom. Their mean age was 82 years, nearly half were women, and about a third were frail.
Over 4 years of follow-up, the primary outcome of cardiovascular (CV) death or MI occurred at a similar rate in both arms: 25.6% vs 26.3% for invasive vs conservative, respectively (HR, 0.94; 95% CI, 0.77-1.14; P =.53).
Rates of CV death were also not significantly different (15.8% vs 14.2%; HR, 1.11; 95% CI, 0.86-1.44).
The rate of nonfatal MI was slightly lower in the invasive arm (11.7% vs 15.0%; HR, 0.75; 95% CI, 0.57-0.99).
Some other notable findings: Fewer than half of patients in the invasive arm underwent revascularization. Coronary angiography was done in about a quarter of patients in the conservative arm, and revascularization in only 14%.
Comments
Because medicine has improved and patients live longer, cardiologists increasingly see older adults with frailty. It’s important to study these patients.
The authors tell us that 1 in 5 patients screened were enrolled, and those not enrolled were similar in age and were treated nearly equally with either strategy. Not all trials offer this information; it’s important because knowing that patients in a trial are representative helps us translate evidence to our actual patients.
Another positive was the investigators’ smart choice of cardiovascular death and MI as their primary outcome. Strategy trials are usually open label. If they had included an outcome that requires a decision from a clinician, such as unplanned revascularization, then bias becomes a possibility when patients and clinicians are aware of the treatment assignment. (I wrote about poor endpoint choice in the ABYSS trial.)
The most notable finding in SENIOR-RITA was that approximately 76% of patients in the conservative arm did not have a coronary angiogram and 86% were not revascularized.
Yet, the rate of CV death and MI were similar during 4 years of follow-up. This observation is nearly identical to the findings in chronic stable disease, seen in the ISCHEMIA trial. (See Figure 6a in the paper’s supplement.)
I take two messages from this consistent observation: One is that medical therapy is quite good at treating coronary artery disease not associated with acute vessel closure in STEMI.
The other is that using coronary angiography and revascularization as a bailout, in only a fraction of cases, achieves the same result, so the conservative strategy should be preferred.
I am not sure that the SENIOR-RITA researchers see it this way. They write in their discussion that “clinicians are often reluctant to offer an invasive strategy to frail older adults.” They then remind readers that modern PCI techniques (radial approach) have low rates of adverse events.
Perhaps I misread their message, but that paragraph seemed like it was reinforcing our tendency to offer invasive approaches to patients with NSTEMI.
I feel differently. When a trial reports similar outcomes with two strategies, I think we should favor the one with less intervention. I feel even more strongly about this philosophy in older patients with frailty.
Are we not in the business of helping people with the least amount of intervention?
The greatest challenge for the cardiologist of today is not a lack of treatment options, but whether we should use all options in older, frailer adults.
Good on the SENIOR-RITA investigators, for they have shown that we can avoid intervention in the vast majority of older adults presenting with NSTEMI.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Kentucky, and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The ability to save cardiac muscle during an acute coronary syndrome with percutaneous coronary intervention (PCI) made cardiology one of the most popular fields in medicine.
But acute coronary syndromes come in different categories. While rapid PCI clearly benefits patients with ST-segment elevation myocardial infarction (STEMI), the best use of angiography and PCI for patients with non–ST-segment elevation myocardial infarction (NSTEMI) is more complex.
There have been many trials and meta-analyses, and generally, outcomes are similar with either approach. Perhaps if one looks with enough optimism, there is a benefit for the more aggressive approach in higher-risk patients.
Despite the similar outcomes with the two strategies, most patients are treated with the early invasive approach. Early and invasive fit the spirit of modern cardiology.
Yet, older patients with acute coronary syndromes present a different challenge. NSTEMI trials, like most trials, enrolled mostly younger adults.
Whether evidence obtained in young people applies to older patients is one of the most common and important questions in all of medical practice. Older patients may be at higher risk for a primary outcome, but they also have greater risks for harm from therapy as well as more competing causes of morbidity and mortality.
Only a handful of smaller trials have enrolled older patients with NSTEMI. These trials have produced little evidence that an early invasive approach should be preferred.
The SENIOR-RITA Trial
At ESC, Vijay Kunadian, MD, from Newcastle, England, presented results of SENIOR-RITA, a large trial comparing an invasive vs conservative strategy in NSTEMI patients 75 years of age or older.
In the conservative arm, coronary angiography was allowed if the patient deteriorated and the procedure was clinically indicated in the judgment of the treating physicians.
Slightly more than 1500 patients with NSTEMI were randomly assigned to either strategy in 48 centers in the United Kingdom. Their mean age was 82 years, nearly half were women, and about a third were frail.
Over 4 years of follow-up, the primary outcome of cardiovascular (CV) death or MI occurred at a similar rate in both arms: 25.6% vs 26.3% for invasive vs conservative, respectively (HR, 0.94; 95% CI, 0.77-1.14; P =.53).
Rates of CV death were also not significantly different (15.8% vs 14.2%; HR, 1.11; 95% CI, 0.86-1.44).
The rate of nonfatal MI was slightly lower in the invasive arm (11.7% vs 15.0%; HR, 0.75; 95% CI, 0.57-0.99).
Some other notable findings: Fewer than half of patients in the invasive arm underwent revascularization. Coronary angiography was done in about a quarter of patients in the conservative arm, and revascularization in only 14%.
Comments
Because medicine has improved and patients live longer, cardiologists increasingly see older adults with frailty. It’s important to study these patients.
The authors tell us that 1 in 5 patients screened were enrolled, and those not enrolled were similar in age and were treated nearly equally with either strategy. Not all trials offer this information; it’s important because knowing that patients in a trial are representative helps us translate evidence to our actual patients.
Another positive was the investigators’ smart choice of cardiovascular death and MI as their primary outcome. Strategy trials are usually open label. If they had included an outcome that requires a decision from a clinician, such as unplanned revascularization, then bias becomes a possibility when patients and clinicians are aware of the treatment assignment. (I wrote about poor endpoint choice in the ABYSS trial.)
The most notable finding in SENIOR-RITA was that approximately 76% of patients in the conservative arm did not have a coronary angiogram and 86% were not revascularized.
Yet, the rate of CV death and MI were similar during 4 years of follow-up. This observation is nearly identical to the findings in chronic stable disease, seen in the ISCHEMIA trial. (See Figure 6a in the paper’s supplement.)
I take two messages from this consistent observation: One is that medical therapy is quite good at treating coronary artery disease not associated with acute vessel closure in STEMI.
The other is that using coronary angiography and revascularization as a bailout, in only a fraction of cases, achieves the same result, so the conservative strategy should be preferred.
I am not sure that the SENIOR-RITA researchers see it this way. They write in their discussion that “clinicians are often reluctant to offer an invasive strategy to frail older adults.” They then remind readers that modern PCI techniques (radial approach) have low rates of adverse events.
Perhaps I misread their message, but that paragraph seemed like it was reinforcing our tendency to offer invasive approaches to patients with NSTEMI.
I feel differently. When a trial reports similar outcomes with two strategies, I think we should favor the one with less intervention. I feel even more strongly about this philosophy in older patients with frailty.
Are we not in the business of helping people with the least amount of intervention?
The greatest challenge for the cardiologist of today is not a lack of treatment options, but whether we should use all options in older, frailer adults.
Good on the SENIOR-RITA investigators, for they have shown that we can avoid intervention in the vast majority of older adults presenting with NSTEMI.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Kentucky, and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Variation in Cardiovascular Risk Assessment Status in Patients Receiving Oral Anti-Cancer Therapies: A Focus on Equity throughout VISN (Veteran Integrated Service Network) 12
Background
Oral anti-cancer therapies have quickly moved to the forefront of cancer treatment for several oncologic disease states. While these treatments have led to improvements in prognosis and ease of administration, many of these agents carry the risk of serious short- and long-term toxicities affecting the cardiovascular system. This prompted the Journal of the American Heart Association (JAHA) to release special guidance focused on cardiovascular monitoring strategies for anti-cancer agents. The primary objective of this retrospective review was to evaluate compliance with cardiovascular monitoring based on JAHA cardio-oncologic guidelines. The secondary objective was to assess disparities in cardiovascular monitoring based on markers of equity such as race/ ethnicity, rurality, socioeconomic status and gender.
Methods
Patients who initiated pazopanib, cabozantinib, lenvatinib, axitinib, regorafenib, nilotinib, ibrutinib, sorafenib, sunitinib, ponatinib or everolimus between January 1, 2019 and December 31, 2022 at a VHA VISN 12 site with oncology services were followed forward until treatment discontinuation or 12 months of therapy had been completed. Data was acquired utilizing the VA Informatics and Computing Infrastructure (VINCI) and the Corporate Data Warehouse (CDW). The following cardiovascular monitoring markers were recorded at baseline and months 3, 6, 9 and 12 after initiation anti-cancer therapy: blood pressure, blood glucose, cholesterol, ECG and echocardiogram. Descriptive statistics were used to examine all continuous variables, while frequencies were used to examine categorical variables. Univariate statistics were performed on all items respectively.
Results
A total of 219 patients were identified initiating pre-specified oral anti-cancer therapies during the study time period. Of these, a total of n=145 met study inclusion criteria. 97% were male (n=141), 80% (n=116) had a racial background of white, 36% (n=52) live in rural or highly rural locations and 23% (n=34) lived in a high poverty area. Based on the primary endpoint, the mean compliance with recommended cardiovascular monitoring was 44.95% [IQR 12]. There was no statistically significant difference in cardiovascular monitoring based on equity.
Conclusions
Overall uptake of cardiovascular monitoring markers recommended by JAHA guidance is low. We plan to evaluate methods to increase these measures, utilizing clinical pharmacy provider support throughout VISN 12.
Background
Oral anti-cancer therapies have quickly moved to the forefront of cancer treatment for several oncologic disease states. While these treatments have led to improvements in prognosis and ease of administration, many of these agents carry the risk of serious short- and long-term toxicities affecting the cardiovascular system. This prompted the Journal of the American Heart Association (JAHA) to release special guidance focused on cardiovascular monitoring strategies for anti-cancer agents. The primary objective of this retrospective review was to evaluate compliance with cardiovascular monitoring based on JAHA cardio-oncologic guidelines. The secondary objective was to assess disparities in cardiovascular monitoring based on markers of equity such as race/ ethnicity, rurality, socioeconomic status and gender.
Methods
Patients who initiated pazopanib, cabozantinib, lenvatinib, axitinib, regorafenib, nilotinib, ibrutinib, sorafenib, sunitinib, ponatinib or everolimus between January 1, 2019 and December 31, 2022 at a VHA VISN 12 site with oncology services were followed forward until treatment discontinuation or 12 months of therapy had been completed. Data was acquired utilizing the VA Informatics and Computing Infrastructure (VINCI) and the Corporate Data Warehouse (CDW). The following cardiovascular monitoring markers were recorded at baseline and months 3, 6, 9 and 12 after initiation anti-cancer therapy: blood pressure, blood glucose, cholesterol, ECG and echocardiogram. Descriptive statistics were used to examine all continuous variables, while frequencies were used to examine categorical variables. Univariate statistics were performed on all items respectively.
Results
A total of 219 patients were identified initiating pre-specified oral anti-cancer therapies during the study time period. Of these, a total of n=145 met study inclusion criteria. 97% were male (n=141), 80% (n=116) had a racial background of white, 36% (n=52) live in rural or highly rural locations and 23% (n=34) lived in a high poverty area. Based on the primary endpoint, the mean compliance with recommended cardiovascular monitoring was 44.95% [IQR 12]. There was no statistically significant difference in cardiovascular monitoring based on equity.
Conclusions
Overall uptake of cardiovascular monitoring markers recommended by JAHA guidance is low. We plan to evaluate methods to increase these measures, utilizing clinical pharmacy provider support throughout VISN 12.
Background
Oral anti-cancer therapies have quickly moved to the forefront of cancer treatment for several oncologic disease states. While these treatments have led to improvements in prognosis and ease of administration, many of these agents carry the risk of serious short- and long-term toxicities affecting the cardiovascular system. This prompted the Journal of the American Heart Association (JAHA) to release special guidance focused on cardiovascular monitoring strategies for anti-cancer agents. The primary objective of this retrospective review was to evaluate compliance with cardiovascular monitoring based on JAHA cardio-oncologic guidelines. The secondary objective was to assess disparities in cardiovascular monitoring based on markers of equity such as race/ ethnicity, rurality, socioeconomic status and gender.
Methods
Patients who initiated pazopanib, cabozantinib, lenvatinib, axitinib, regorafenib, nilotinib, ibrutinib, sorafenib, sunitinib, ponatinib or everolimus between January 1, 2019 and December 31, 2022 at a VHA VISN 12 site with oncology services were followed forward until treatment discontinuation or 12 months of therapy had been completed. Data was acquired utilizing the VA Informatics and Computing Infrastructure (VINCI) and the Corporate Data Warehouse (CDW). The following cardiovascular monitoring markers were recorded at baseline and months 3, 6, 9 and 12 after initiation anti-cancer therapy: blood pressure, blood glucose, cholesterol, ECG and echocardiogram. Descriptive statistics were used to examine all continuous variables, while frequencies were used to examine categorical variables. Univariate statistics were performed on all items respectively.
Results
A total of 219 patients were identified initiating pre-specified oral anti-cancer therapies during the study time period. Of these, a total of n=145 met study inclusion criteria. 97% were male (n=141), 80% (n=116) had a racial background of white, 36% (n=52) live in rural or highly rural locations and 23% (n=34) lived in a high poverty area. Based on the primary endpoint, the mean compliance with recommended cardiovascular monitoring was 44.95% [IQR 12]. There was no statistically significant difference in cardiovascular monitoring based on equity.
Conclusions
Overall uptake of cardiovascular monitoring markers recommended by JAHA guidance is low. We plan to evaluate methods to increase these measures, utilizing clinical pharmacy provider support throughout VISN 12.
Eating the Right Fats May Help Patients Live Longer
These are the results of a study published in JAMA Internal Medicine that followed more than 600,000 participants over 2 decades.
Bin Zhao, PhD, of the National Clinical Research Center for Metabolic Diseases at the Key Laboratory of Diabetes Immunology in Changsha, China, and colleagues concluded from these data that consuming plant-based fats instead of animal fats could be beneficial for health and improve survival.
It may not be so simple, however. “We are one step ahead of the publication: We no longer just distinguish between animal and plant fats but mainly consider the composition,” said Stefan Lorkowski, PhD, chair of biochemistry and physiology of nutrition at the Institute of Nutritional Sciences at the University of Jena in Germany, in response to inquiries from this news organization.
What’s in a Fat?
Although Dr. Zhao and colleagues studied the effect of different plant and animal fat sources (eg, grains, nuts, legumes, plant oils, red and white meat, dairy, eggs, and fish), they did not consider the composition of the fatty acids that they contained. “It matters which dairy products, which plant oils, and which fish are consumed,” said Dr. Lorkowski.
The data analyzed in the Chinese study come from a prospective cohort study (NIH-AARP Diet and Health Study) conducted in the United States from 1995 to 2019. At the beginning, the 407,531 study participants (average age, 61 years) filled out dietary questionnaires once. They were then followed for up to 24 years for total and cardiovascular mortality.
During this period, 185,111 study participants died, including 58,526 from cardiovascular diseases. Participants who consumed the most plant-based fats, according to the dietary questionnaires filled out in 1995, had a lower risk for death than those who consumed the least plant-based fats. Their overall mortality risk was 9% lower, and their cardiovascular mortality risk was 14% lower. This finding was especially noticeable when it came to plant fats from grains or plant oils.
Animal Fat and Mortality
In contrast, a higher intake of animal fat was associated with both a higher overall mortality risk (16%) and a higher cardiovascular mortality risk (14%). This was especially true for fat from dairy products and eggs.
A trend towards a reduced overall and cardiovascular mortality risk was observed for fat from fish. “The fact that only a trend towards fish consumption was observed may be due to the study having many more meat eaters than fish eaters,” said Dr. Lorkowski.
Another imbalance limits the significance of the study, he added. The two groups, those who primarily consumed plant fats and those who primarily consumed animal fats, were already distinct at the beginning of the study. Those who consumed more plant fats were more likely to have diabetes, a higher body mass index (BMI), higher energy intake, and higher alcohol consumption but consumed more fiber, fruits, and vegetables and were more physically active. “They may have been trying to live healthier because they were sicker,” said Dr. Lorkowski.
Potential Confounding
Dr. Zhao and his team adjusted the results for various potential confounding factors, including age, gender, BMI, ethnicity, smoking, physical activity, education, marital status, diabetes, health status, vitamin intake, protein, carbohydrates, fiber, trans fats, cholesterol intake, and alcohol consumption. However, according to Dr. Lorkowski, “statistical adjustment is always incomplete, and confounding cannot be completely ruled out.”
Nevertheless, these results provide relevant insights for dietary recommendations that could help improve health and related outcomes, according to the authors. “Replacement of 5% energy from animal fat with 5% energy from plant fat, particularly fat from grains or vegetable oils, was associated with a lower risk for mortality: 4%-24% reduction in overall mortality and 5%-30% reduction in cardiovascular disease mortality.”
Fat Composition Matters
Animal fat, however, should not simply be replaced with plant fat, said Dr. Lorkowski. “Cold-water fish, which provides important long-chain omega-3 fatty acids, is also considered animal fat. And palm and coconut fat, while plant-based, contain unhealthy long-chain saturated fats. And the type of plant oils also makes a difference, whether one uses corn germ or sunflower oil rich in omega-6 fatty acids or flaxseed or rapeseed oil rich in omega-3 fatty acids.
“A diet rich in unsaturated fats, with sufficient and balanced intake of omega-3 and omega-6 fatty acids, that is also abundant in fiber-rich carbohydrate sources and plant-based protein, is always better than too much fat from animal sources.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
These are the results of a study published in JAMA Internal Medicine that followed more than 600,000 participants over 2 decades.
Bin Zhao, PhD, of the National Clinical Research Center for Metabolic Diseases at the Key Laboratory of Diabetes Immunology in Changsha, China, and colleagues concluded from these data that consuming plant-based fats instead of animal fats could be beneficial for health and improve survival.
It may not be so simple, however. “We are one step ahead of the publication: We no longer just distinguish between animal and plant fats but mainly consider the composition,” said Stefan Lorkowski, PhD, chair of biochemistry and physiology of nutrition at the Institute of Nutritional Sciences at the University of Jena in Germany, in response to inquiries from this news organization.
What’s in a Fat?
Although Dr. Zhao and colleagues studied the effect of different plant and animal fat sources (eg, grains, nuts, legumes, plant oils, red and white meat, dairy, eggs, and fish), they did not consider the composition of the fatty acids that they contained. “It matters which dairy products, which plant oils, and which fish are consumed,” said Dr. Lorkowski.
The data analyzed in the Chinese study come from a prospective cohort study (NIH-AARP Diet and Health Study) conducted in the United States from 1995 to 2019. At the beginning, the 407,531 study participants (average age, 61 years) filled out dietary questionnaires once. They were then followed for up to 24 years for total and cardiovascular mortality.
During this period, 185,111 study participants died, including 58,526 from cardiovascular diseases. Participants who consumed the most plant-based fats, according to the dietary questionnaires filled out in 1995, had a lower risk for death than those who consumed the least plant-based fats. Their overall mortality risk was 9% lower, and their cardiovascular mortality risk was 14% lower. This finding was especially noticeable when it came to plant fats from grains or plant oils.
Animal Fat and Mortality
In contrast, a higher intake of animal fat was associated with both a higher overall mortality risk (16%) and a higher cardiovascular mortality risk (14%). This was especially true for fat from dairy products and eggs.
A trend towards a reduced overall and cardiovascular mortality risk was observed for fat from fish. “The fact that only a trend towards fish consumption was observed may be due to the study having many more meat eaters than fish eaters,” said Dr. Lorkowski.
Another imbalance limits the significance of the study, he added. The two groups, those who primarily consumed plant fats and those who primarily consumed animal fats, were already distinct at the beginning of the study. Those who consumed more plant fats were more likely to have diabetes, a higher body mass index (BMI), higher energy intake, and higher alcohol consumption but consumed more fiber, fruits, and vegetables and were more physically active. “They may have been trying to live healthier because they were sicker,” said Dr. Lorkowski.
Potential Confounding
Dr. Zhao and his team adjusted the results for various potential confounding factors, including age, gender, BMI, ethnicity, smoking, physical activity, education, marital status, diabetes, health status, vitamin intake, protein, carbohydrates, fiber, trans fats, cholesterol intake, and alcohol consumption. However, according to Dr. Lorkowski, “statistical adjustment is always incomplete, and confounding cannot be completely ruled out.”
Nevertheless, these results provide relevant insights for dietary recommendations that could help improve health and related outcomes, according to the authors. “Replacement of 5% energy from animal fat with 5% energy from plant fat, particularly fat from grains or vegetable oils, was associated with a lower risk for mortality: 4%-24% reduction in overall mortality and 5%-30% reduction in cardiovascular disease mortality.”
Fat Composition Matters
Animal fat, however, should not simply be replaced with plant fat, said Dr. Lorkowski. “Cold-water fish, which provides important long-chain omega-3 fatty acids, is also considered animal fat. And palm and coconut fat, while plant-based, contain unhealthy long-chain saturated fats. And the type of plant oils also makes a difference, whether one uses corn germ or sunflower oil rich in omega-6 fatty acids or flaxseed or rapeseed oil rich in omega-3 fatty acids.
“A diet rich in unsaturated fats, with sufficient and balanced intake of omega-3 and omega-6 fatty acids, that is also abundant in fiber-rich carbohydrate sources and plant-based protein, is always better than too much fat from animal sources.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
These are the results of a study published in JAMA Internal Medicine that followed more than 600,000 participants over 2 decades.
Bin Zhao, PhD, of the National Clinical Research Center for Metabolic Diseases at the Key Laboratory of Diabetes Immunology in Changsha, China, and colleagues concluded from these data that consuming plant-based fats instead of animal fats could be beneficial for health and improve survival.
It may not be so simple, however. “We are one step ahead of the publication: We no longer just distinguish between animal and plant fats but mainly consider the composition,” said Stefan Lorkowski, PhD, chair of biochemistry and physiology of nutrition at the Institute of Nutritional Sciences at the University of Jena in Germany, in response to inquiries from this news organization.
What’s in a Fat?
Although Dr. Zhao and colleagues studied the effect of different plant and animal fat sources (eg, grains, nuts, legumes, plant oils, red and white meat, dairy, eggs, and fish), they did not consider the composition of the fatty acids that they contained. “It matters which dairy products, which plant oils, and which fish are consumed,” said Dr. Lorkowski.
The data analyzed in the Chinese study come from a prospective cohort study (NIH-AARP Diet and Health Study) conducted in the United States from 1995 to 2019. At the beginning, the 407,531 study participants (average age, 61 years) filled out dietary questionnaires once. They were then followed for up to 24 years for total and cardiovascular mortality.
During this period, 185,111 study participants died, including 58,526 from cardiovascular diseases. Participants who consumed the most plant-based fats, according to the dietary questionnaires filled out in 1995, had a lower risk for death than those who consumed the least plant-based fats. Their overall mortality risk was 9% lower, and their cardiovascular mortality risk was 14% lower. This finding was especially noticeable when it came to plant fats from grains or plant oils.
Animal Fat and Mortality
In contrast, a higher intake of animal fat was associated with both a higher overall mortality risk (16%) and a higher cardiovascular mortality risk (14%). This was especially true for fat from dairy products and eggs.
A trend towards a reduced overall and cardiovascular mortality risk was observed for fat from fish. “The fact that only a trend towards fish consumption was observed may be due to the study having many more meat eaters than fish eaters,” said Dr. Lorkowski.
Another imbalance limits the significance of the study, he added. The two groups, those who primarily consumed plant fats and those who primarily consumed animal fats, were already distinct at the beginning of the study. Those who consumed more plant fats were more likely to have diabetes, a higher body mass index (BMI), higher energy intake, and higher alcohol consumption but consumed more fiber, fruits, and vegetables and were more physically active. “They may have been trying to live healthier because they were sicker,” said Dr. Lorkowski.
Potential Confounding
Dr. Zhao and his team adjusted the results for various potential confounding factors, including age, gender, BMI, ethnicity, smoking, physical activity, education, marital status, diabetes, health status, vitamin intake, protein, carbohydrates, fiber, trans fats, cholesterol intake, and alcohol consumption. However, according to Dr. Lorkowski, “statistical adjustment is always incomplete, and confounding cannot be completely ruled out.”
Nevertheless, these results provide relevant insights for dietary recommendations that could help improve health and related outcomes, according to the authors. “Replacement of 5% energy from animal fat with 5% energy from plant fat, particularly fat from grains or vegetable oils, was associated with a lower risk for mortality: 4%-24% reduction in overall mortality and 5%-30% reduction in cardiovascular disease mortality.”
Fat Composition Matters
Animal fat, however, should not simply be replaced with plant fat, said Dr. Lorkowski. “Cold-water fish, which provides important long-chain omega-3 fatty acids, is also considered animal fat. And palm and coconut fat, while plant-based, contain unhealthy long-chain saturated fats. And the type of plant oils also makes a difference, whether one uses corn germ or sunflower oil rich in omega-6 fatty acids or flaxseed or rapeseed oil rich in omega-3 fatty acids.
“A diet rich in unsaturated fats, with sufficient and balanced intake of omega-3 and omega-6 fatty acids, that is also abundant in fiber-rich carbohydrate sources and plant-based protein, is always better than too much fat from animal sources.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
FROM JAMA INTERNAL MEDICINE