User login
Don’t skip contraception talk for women with complex health conditions
.
In an installment of the American College of Physicians’ In the Clinic series, Rachel Cannon, MD, Kelly Treder, MD, and Elisabeth J. Woodhams, MD, all of Boston Medical Center, presented an article on the complex topic of contraception for patients with chronic illness.
“Many patients with chronic illness or complex medical issues interact with a primary care provider on a frequent basis, which provides a great access point for contraceptive counseling with a provider they trust and know,” said Dr. Cannon and Dr. Treder in a joint interview. “We wanted to create a ‘go to’ resource for primary care physicians to review contraceptive options and counseling best practices for all of their patients. Contraceptive care is part of overall health care and should be included in the primary care encounter.”
The authors discussed the types of contraception, as well as risks and benefits, and offered guidance for choosing a contraceptive method for medically complex patients.
“In recent years, there has been a shift in contraceptive counseling toward shared decision-making, a counseling strategy that honors the patient as the expert in their body and their life experiences and emphasizes their autonomy and values,” the authors said. “For providers, this translates to understanding that contraceptive efficacy is not the only important characteristic to patients, and that many other important factors contribute to an individual’s decision to use a particular method or not use birth control at all,” they said.
Start the conversation
Start by assessing a patient’s interest in and readiness for pregnancy, if applicable, the authors said. One example of a screen, the PATH questionnaire (Parent/Pregnancy Attitudes, Timing, and How important), is designed for patients in any demographic, and includes questions about the timing and desire for pregnancy and feelings about birth control, as well as options for patients to express uncertainty or ambivalence about pregnancy and contraception.
Some patients may derive benefits from hormonal contraceptives beyond pregnancy prevention, the authors wrote. Combined hormonal contraceptives (CHCs) may improve menorrhagia, and data suggest that CHC use also may reduce risk for some cancer types, including endometrial and ovarian cancers, they said.
Overall, contraceptive counseling should include discussions of safety, efficacy, and the patient’s lived experience.
Clinical considerations and contraindications
Medically complex patients who desire contraception may consider hormonal or nonhormonal methods based on their preferences and medical conditions, but clinicians need to consider comorbidities and contraindications, the authors wrote.
When a woman of childbearing age with any complex medical issue starts a new medication or receives a new diagnosis, contraception and pregnancy planning should be part of the discussion, the authors said. Safe and successful pregnancies are possible for women with complex medical issues when underlying health concerns are identified and addressed in advance, they added. Alternatively, for patients seeking to avoid pregnancy permanently, options for sterilization can be part of an informed discussion.
The Centers for Disease Control and Prevention’s Medical Eligibility Criteria for Contraceptive Use offers clinicians detailed information about the risks of both contraceptives and pregnancy for patients with various medical conditions, according to the authors.
The CDC document lists medical conditions associated with an increased risk for adverse health events if the individual becomes pregnant. These conditions include breast cancer, complicated valvular heart disease, cystic fibrosis, diabetes, endometrial or ovarian cancer, epilepsy, hypertension, bariatric surgery within 2 years of the pregnancy, HIV, ischemic heart disease, severe cirrhosis, stroke, lupus, solid organ transplant within 2 years of the pregnancy, and tuberculosis. Women with these and other conditions associated with increased risk of adverse events if pregnancy occurs should be advised of the high failure rate of barrier and behavior-based contraceptive methods, and informed about options for long-acting contraceptives, according to the CDC.
Risks, benefits, and balance
“It is important to remember that the alternative to contraception for many patients is pregnancy – for many patients with complex medical conditions, pregnancy is far more dangerous than any contraceptive method,” Dr. Cannon and Dr. Treder said in an interview. “This is important to consider when thinking about relative contraindications to a certain method or when thinking about ‘less effective’ contraception methods. The most effective method is a method the patient will actually continue to use,” they said.
The recent approval of the over-the-counter minipill is “a huge win for reproductive health care,” said Dr. Cannon and Dr. Treder. The minipill has very few contraindications, and it is the most effective over-the-counter contraceptive now available, they said.
“An over-the-counter contraceptive pill can increase access to contraception without having to see a physician in the clinic, freeing patients from many of the challenges of navigating the health care system,” the authors added.
As for additional research, the establishment of a long-term safety record may help support other OTC contraceptive methods in the future, the authors said.
Contraceptive counseling is everyone’s specialty
In an accompanying editorial, Amy A. Sarma, MD, a cardiologist at Massachusetts General Hospital, Boston, shared an example of the importance of contraceptive discussions with medically complex patients outside of an ob.gyn. setting. A young woman with a family history of myocardial infarction had neglected her own primary care until an MI of her own sent her to the hospital. While hospitalized, the patient was diagnosed with diabetes, hypertension, and hyperlipidemia.
“Her cardiology care team made every effort to optimize her cardiac care, but no one considered that she was also a woman of childbearing potential despite the teratogenic potential of several of her prescribed medications,” Dr. Sarma wrote. When the patient visited Dr. Sarma to discuss prevention of future MIs, Dr. Sarma took the opportunity to discuss the cardiovascular risks of pregnancy and the risks for this patient not only because of her recent MI, but also because of her chronic health conditions.
As it happened, the woman did not want a high-risk pregnancy and was interested in contraceptive methods. Dr. Sarma pointed out that, had the woman been engaged in routine primary care, these issues would have arisen in that setting, but like many younger women with cardiovascular disease, she did not make her own primary care a priority, and had missed out on other opportunities to discuss contraception. “Her MI opened a window of opportunity to help prevent an unintended and high-risk pregnancy,” Dr. Sarma noted.
Dr. Sarma’s patient anecdote illustrated the point of the In the Clinic review: that any clinician can discuss pregnancy and contraception with patients of childbearing age who have medical comorbidities that could affect a pregnancy. “All clinicians who care for patients of reproductive potential should become comfortable discussing pregnancy intent, preconception risk assessment, and contraceptive counseling,” Dr. Sarma said.
The research for this article was funded by the American College of Physicians. The review authors had no financial conflicts to disclose. Dr. Sarma had no financial conflicts to disclose.
.
In an installment of the American College of Physicians’ In the Clinic series, Rachel Cannon, MD, Kelly Treder, MD, and Elisabeth J. Woodhams, MD, all of Boston Medical Center, presented an article on the complex topic of contraception for patients with chronic illness.
“Many patients with chronic illness or complex medical issues interact with a primary care provider on a frequent basis, which provides a great access point for contraceptive counseling with a provider they trust and know,” said Dr. Cannon and Dr. Treder in a joint interview. “We wanted to create a ‘go to’ resource for primary care physicians to review contraceptive options and counseling best practices for all of their patients. Contraceptive care is part of overall health care and should be included in the primary care encounter.”
The authors discussed the types of contraception, as well as risks and benefits, and offered guidance for choosing a contraceptive method for medically complex patients.
“In recent years, there has been a shift in contraceptive counseling toward shared decision-making, a counseling strategy that honors the patient as the expert in their body and their life experiences and emphasizes their autonomy and values,” the authors said. “For providers, this translates to understanding that contraceptive efficacy is not the only important characteristic to patients, and that many other important factors contribute to an individual’s decision to use a particular method or not use birth control at all,” they said.
Start the conversation
Start by assessing a patient’s interest in and readiness for pregnancy, if applicable, the authors said. One example of a screen, the PATH questionnaire (Parent/Pregnancy Attitudes, Timing, and How important), is designed for patients in any demographic, and includes questions about the timing and desire for pregnancy and feelings about birth control, as well as options for patients to express uncertainty or ambivalence about pregnancy and contraception.
Some patients may derive benefits from hormonal contraceptives beyond pregnancy prevention, the authors wrote. Combined hormonal contraceptives (CHCs) may improve menorrhagia, and data suggest that CHC use also may reduce risk for some cancer types, including endometrial and ovarian cancers, they said.
Overall, contraceptive counseling should include discussions of safety, efficacy, and the patient’s lived experience.
Clinical considerations and contraindications
Medically complex patients who desire contraception may consider hormonal or nonhormonal methods based on their preferences and medical conditions, but clinicians need to consider comorbidities and contraindications, the authors wrote.
When a woman of childbearing age with any complex medical issue starts a new medication or receives a new diagnosis, contraception and pregnancy planning should be part of the discussion, the authors said. Safe and successful pregnancies are possible for women with complex medical issues when underlying health concerns are identified and addressed in advance, they added. Alternatively, for patients seeking to avoid pregnancy permanently, options for sterilization can be part of an informed discussion.
The Centers for Disease Control and Prevention’s Medical Eligibility Criteria for Contraceptive Use offers clinicians detailed information about the risks of both contraceptives and pregnancy for patients with various medical conditions, according to the authors.
The CDC document lists medical conditions associated with an increased risk for adverse health events if the individual becomes pregnant. These conditions include breast cancer, complicated valvular heart disease, cystic fibrosis, diabetes, endometrial or ovarian cancer, epilepsy, hypertension, bariatric surgery within 2 years of the pregnancy, HIV, ischemic heart disease, severe cirrhosis, stroke, lupus, solid organ transplant within 2 years of the pregnancy, and tuberculosis. Women with these and other conditions associated with increased risk of adverse events if pregnancy occurs should be advised of the high failure rate of barrier and behavior-based contraceptive methods, and informed about options for long-acting contraceptives, according to the CDC.
Risks, benefits, and balance
“It is important to remember that the alternative to contraception for many patients is pregnancy – for many patients with complex medical conditions, pregnancy is far more dangerous than any contraceptive method,” Dr. Cannon and Dr. Treder said in an interview. “This is important to consider when thinking about relative contraindications to a certain method or when thinking about ‘less effective’ contraception methods. The most effective method is a method the patient will actually continue to use,” they said.
The recent approval of the over-the-counter minipill is “a huge win for reproductive health care,” said Dr. Cannon and Dr. Treder. The minipill has very few contraindications, and it is the most effective over-the-counter contraceptive now available, they said.
“An over-the-counter contraceptive pill can increase access to contraception without having to see a physician in the clinic, freeing patients from many of the challenges of navigating the health care system,” the authors added.
As for additional research, the establishment of a long-term safety record may help support other OTC contraceptive methods in the future, the authors said.
Contraceptive counseling is everyone’s specialty
In an accompanying editorial, Amy A. Sarma, MD, a cardiologist at Massachusetts General Hospital, Boston, shared an example of the importance of contraceptive discussions with medically complex patients outside of an ob.gyn. setting. A young woman with a family history of myocardial infarction had neglected her own primary care until an MI of her own sent her to the hospital. While hospitalized, the patient was diagnosed with diabetes, hypertension, and hyperlipidemia.
“Her cardiology care team made every effort to optimize her cardiac care, but no one considered that she was also a woman of childbearing potential despite the teratogenic potential of several of her prescribed medications,” Dr. Sarma wrote. When the patient visited Dr. Sarma to discuss prevention of future MIs, Dr. Sarma took the opportunity to discuss the cardiovascular risks of pregnancy and the risks for this patient not only because of her recent MI, but also because of her chronic health conditions.
As it happened, the woman did not want a high-risk pregnancy and was interested in contraceptive methods. Dr. Sarma pointed out that, had the woman been engaged in routine primary care, these issues would have arisen in that setting, but like many younger women with cardiovascular disease, she did not make her own primary care a priority, and had missed out on other opportunities to discuss contraception. “Her MI opened a window of opportunity to help prevent an unintended and high-risk pregnancy,” Dr. Sarma noted.
Dr. Sarma’s patient anecdote illustrated the point of the In the Clinic review: that any clinician can discuss pregnancy and contraception with patients of childbearing age who have medical comorbidities that could affect a pregnancy. “All clinicians who care for patients of reproductive potential should become comfortable discussing pregnancy intent, preconception risk assessment, and contraceptive counseling,” Dr. Sarma said.
The research for this article was funded by the American College of Physicians. The review authors had no financial conflicts to disclose. Dr. Sarma had no financial conflicts to disclose.
.
In an installment of the American College of Physicians’ In the Clinic series, Rachel Cannon, MD, Kelly Treder, MD, and Elisabeth J. Woodhams, MD, all of Boston Medical Center, presented an article on the complex topic of contraception for patients with chronic illness.
“Many patients with chronic illness or complex medical issues interact with a primary care provider on a frequent basis, which provides a great access point for contraceptive counseling with a provider they trust and know,” said Dr. Cannon and Dr. Treder in a joint interview. “We wanted to create a ‘go to’ resource for primary care physicians to review contraceptive options and counseling best practices for all of their patients. Contraceptive care is part of overall health care and should be included in the primary care encounter.”
The authors discussed the types of contraception, as well as risks and benefits, and offered guidance for choosing a contraceptive method for medically complex patients.
“In recent years, there has been a shift in contraceptive counseling toward shared decision-making, a counseling strategy that honors the patient as the expert in their body and their life experiences and emphasizes their autonomy and values,” the authors said. “For providers, this translates to understanding that contraceptive efficacy is not the only important characteristic to patients, and that many other important factors contribute to an individual’s decision to use a particular method or not use birth control at all,” they said.
Start the conversation
Start by assessing a patient’s interest in and readiness for pregnancy, if applicable, the authors said. One example of a screen, the PATH questionnaire (Parent/Pregnancy Attitudes, Timing, and How important), is designed for patients in any demographic, and includes questions about the timing and desire for pregnancy and feelings about birth control, as well as options for patients to express uncertainty or ambivalence about pregnancy and contraception.
Some patients may derive benefits from hormonal contraceptives beyond pregnancy prevention, the authors wrote. Combined hormonal contraceptives (CHCs) may improve menorrhagia, and data suggest that CHC use also may reduce risk for some cancer types, including endometrial and ovarian cancers, they said.
Overall, contraceptive counseling should include discussions of safety, efficacy, and the patient’s lived experience.
Clinical considerations and contraindications
Medically complex patients who desire contraception may consider hormonal or nonhormonal methods based on their preferences and medical conditions, but clinicians need to consider comorbidities and contraindications, the authors wrote.
When a woman of childbearing age with any complex medical issue starts a new medication or receives a new diagnosis, contraception and pregnancy planning should be part of the discussion, the authors said. Safe and successful pregnancies are possible for women with complex medical issues when underlying health concerns are identified and addressed in advance, they added. Alternatively, for patients seeking to avoid pregnancy permanently, options for sterilization can be part of an informed discussion.
The Centers for Disease Control and Prevention’s Medical Eligibility Criteria for Contraceptive Use offers clinicians detailed information about the risks of both contraceptives and pregnancy for patients with various medical conditions, according to the authors.
The CDC document lists medical conditions associated with an increased risk for adverse health events if the individual becomes pregnant. These conditions include breast cancer, complicated valvular heart disease, cystic fibrosis, diabetes, endometrial or ovarian cancer, epilepsy, hypertension, bariatric surgery within 2 years of the pregnancy, HIV, ischemic heart disease, severe cirrhosis, stroke, lupus, solid organ transplant within 2 years of the pregnancy, and tuberculosis. Women with these and other conditions associated with increased risk of adverse events if pregnancy occurs should be advised of the high failure rate of barrier and behavior-based contraceptive methods, and informed about options for long-acting contraceptives, according to the CDC.
Risks, benefits, and balance
“It is important to remember that the alternative to contraception for many patients is pregnancy – for many patients with complex medical conditions, pregnancy is far more dangerous than any contraceptive method,” Dr. Cannon and Dr. Treder said in an interview. “This is important to consider when thinking about relative contraindications to a certain method or when thinking about ‘less effective’ contraception methods. The most effective method is a method the patient will actually continue to use,” they said.
The recent approval of the over-the-counter minipill is “a huge win for reproductive health care,” said Dr. Cannon and Dr. Treder. The minipill has very few contraindications, and it is the most effective over-the-counter contraceptive now available, they said.
“An over-the-counter contraceptive pill can increase access to contraception without having to see a physician in the clinic, freeing patients from many of the challenges of navigating the health care system,” the authors added.
As for additional research, the establishment of a long-term safety record may help support other OTC contraceptive methods in the future, the authors said.
Contraceptive counseling is everyone’s specialty
In an accompanying editorial, Amy A. Sarma, MD, a cardiologist at Massachusetts General Hospital, Boston, shared an example of the importance of contraceptive discussions with medically complex patients outside of an ob.gyn. setting. A young woman with a family history of myocardial infarction had neglected her own primary care until an MI of her own sent her to the hospital. While hospitalized, the patient was diagnosed with diabetes, hypertension, and hyperlipidemia.
“Her cardiology care team made every effort to optimize her cardiac care, but no one considered that she was also a woman of childbearing potential despite the teratogenic potential of several of her prescribed medications,” Dr. Sarma wrote. When the patient visited Dr. Sarma to discuss prevention of future MIs, Dr. Sarma took the opportunity to discuss the cardiovascular risks of pregnancy and the risks for this patient not only because of her recent MI, but also because of her chronic health conditions.
As it happened, the woman did not want a high-risk pregnancy and was interested in contraceptive methods. Dr. Sarma pointed out that, had the woman been engaged in routine primary care, these issues would have arisen in that setting, but like many younger women with cardiovascular disease, she did not make her own primary care a priority, and had missed out on other opportunities to discuss contraception. “Her MI opened a window of opportunity to help prevent an unintended and high-risk pregnancy,” Dr. Sarma noted.
Dr. Sarma’s patient anecdote illustrated the point of the In the Clinic review: that any clinician can discuss pregnancy and contraception with patients of childbearing age who have medical comorbidities that could affect a pregnancy. “All clinicians who care for patients of reproductive potential should become comfortable discussing pregnancy intent, preconception risk assessment, and contraceptive counseling,” Dr. Sarma said.
The research for this article was funded by the American College of Physicians. The review authors had no financial conflicts to disclose. Dr. Sarma had no financial conflicts to disclose.
FROM THE ANNALS OF INTERNAL MEDICINE
Addressing disparities in goals-of-care conversations
Critical Care Network
Nonrespiratory Critical Care Section
Goals-of-care discussions are essential to management of the intensive care unit (ICU) patient. Racial inequities in end-of-life decision making have been documented for many years, with literature demonstrating that marginalized populations are less likely to have EHR-documented goals-of-care discussions and more likely to have concerns regarding clinician communication.
A recently published randomized control trial in JAMA highlights an intervention that offers promise in addressing disparities in goals-of-care conversations. Curtis, et al. studied whether priming physicians with a communication guide advising on discussion prompts and language for goals-of-care could improve the rate of documented goals-of-care discussions among hospitalized older adults with serious illness. The study found that for patients in the intervention arm, there was a significant increase in proportion of goals-of-care discussions within 30 days. Notably, the difference in documented goals-of-care discussions between arms was greater in the subgroup of patients from underserved groups (Curtis JR, et al. JAMA. 2023;329[23]:2028-37).
Nevertheless, while interventions may help increase the rate of goals-of-care discussions, it is also important to address the content of discussions themselves. You and colleagues recently published a mixed-methods study assessing the impact of race on shared decision-making behaviors during family/caregiver meetings. The authors found that while ICU physicians approached shared decision making with White and Black families similarly, Black families felt their physicians provided less validation of the family role in decision making than White families did (You H, et al. Ann Am Thorac Soc. 2023 May;20[5]:759-62). These findings highlight the importance of ongoing work that focuses not only on quantity but also on quality of communication regarding goals-of-care for patients from diverse backgrounds.
Divya Shankar MD
Section Fellow-in-Training
Muhammad Hayat-Syed MD
Section Vice Chair
Critical Care Network
Nonrespiratory Critical Care Section
Goals-of-care discussions are essential to management of the intensive care unit (ICU) patient. Racial inequities in end-of-life decision making have been documented for many years, with literature demonstrating that marginalized populations are less likely to have EHR-documented goals-of-care discussions and more likely to have concerns regarding clinician communication.
A recently published randomized control trial in JAMA highlights an intervention that offers promise in addressing disparities in goals-of-care conversations. Curtis, et al. studied whether priming physicians with a communication guide advising on discussion prompts and language for goals-of-care could improve the rate of documented goals-of-care discussions among hospitalized older adults with serious illness. The study found that for patients in the intervention arm, there was a significant increase in proportion of goals-of-care discussions within 30 days. Notably, the difference in documented goals-of-care discussions between arms was greater in the subgroup of patients from underserved groups (Curtis JR, et al. JAMA. 2023;329[23]:2028-37).
Nevertheless, while interventions may help increase the rate of goals-of-care discussions, it is also important to address the content of discussions themselves. You and colleagues recently published a mixed-methods study assessing the impact of race on shared decision-making behaviors during family/caregiver meetings. The authors found that while ICU physicians approached shared decision making with White and Black families similarly, Black families felt their physicians provided less validation of the family role in decision making than White families did (You H, et al. Ann Am Thorac Soc. 2023 May;20[5]:759-62). These findings highlight the importance of ongoing work that focuses not only on quantity but also on quality of communication regarding goals-of-care for patients from diverse backgrounds.
Divya Shankar MD
Section Fellow-in-Training
Muhammad Hayat-Syed MD
Section Vice Chair
Critical Care Network
Nonrespiratory Critical Care Section
Goals-of-care discussions are essential to management of the intensive care unit (ICU) patient. Racial inequities in end-of-life decision making have been documented for many years, with literature demonstrating that marginalized populations are less likely to have EHR-documented goals-of-care discussions and more likely to have concerns regarding clinician communication.
A recently published randomized control trial in JAMA highlights an intervention that offers promise in addressing disparities in goals-of-care conversations. Curtis, et al. studied whether priming physicians with a communication guide advising on discussion prompts and language for goals-of-care could improve the rate of documented goals-of-care discussions among hospitalized older adults with serious illness. The study found that for patients in the intervention arm, there was a significant increase in proportion of goals-of-care discussions within 30 days. Notably, the difference in documented goals-of-care discussions between arms was greater in the subgroup of patients from underserved groups (Curtis JR, et al. JAMA. 2023;329[23]:2028-37).
Nevertheless, while interventions may help increase the rate of goals-of-care discussions, it is also important to address the content of discussions themselves. You and colleagues recently published a mixed-methods study assessing the impact of race on shared decision-making behaviors during family/caregiver meetings. The authors found that while ICU physicians approached shared decision making with White and Black families similarly, Black families felt their physicians provided less validation of the family role in decision making than White families did (You H, et al. Ann Am Thorac Soc. 2023 May;20[5]:759-62). These findings highlight the importance of ongoing work that focuses not only on quantity but also on quality of communication regarding goals-of-care for patients from diverse backgrounds.
Divya Shankar MD
Section Fellow-in-Training
Muhammad Hayat-Syed MD
Section Vice Chair
Social needs case management cuts acute care usage
Hospitalizations fell by 11% in patients assigned to integrated social needs case management, a randomized controlled study conducted in California found.
The reduction in acute care use was likely because of the 3% increase in primary care visits with this approach, according to lead study author Mark D. Fleming, PhD, MS, assistant professor of health and social behavior at the University of California, Berkeley. The study was published in Annals of Internal Medicine.
The findings provide evidence for the theory that social needs case management can decrease acute care use by facilitating access to primary care, Dr. Fleming said in an interview. “While an increasing number of studies have measured the effects of social needs case management on hospital use, the findings have been inconsistent, with some studies showing a decrease in hospital use and others showing no change.” There was no strong evidence of an effect on acute care.
A 2018 study, however, found that liaising with community care workers substantially reduced hospital days in disadvantaged patients.
Case management, a complex approach linking medical and social needs, can overcome barriers to care by facilitating access to transportation and helping patients navigate the health care system, the authors noted. It can also streamline patient access to insurance coverage and social benefits.
The study
The current data came from a secondary analysis of a randomized encouragement study in Costa County, Calif., during 2017 and 2018. That study allocated adult California Medicaid beneficiaries of diverse race and ethnicity, relatively high social needs, and high risk for acute care use to two arms: social needs case management (n = 21,422) or administrative observation (22,389 weighted). Chronic health issues ranged from arthritis, diabetes, and back conditions to heart or lung disease, and psychological disorders. About 50% in both groups were younger than age 40 and 60% were women.
Case managers assessed patient needs, created a patient-centered care plan, and facilitated community resource referrals, primary care visits, and applications for public benefits.
The professionally diverse managers included public health nurses, social workers, substance misuse counselors, and mental health clinicians, as well as homeless service specialists and community health workers. Case management was offered as in-person or remote telephonic services for 1 year.
While rates of primary care visits were significantly higher in the case management group – incidence rate 1.03 (95% confidence interval [CI],1.00-1.07) – no intergroup differences emerged in visits for specialty care, behavioral health, psychiatric emergency visits, or jail intakes.
Although the analysis could not measure a direct effect of primary care use on hospitalizations, the results suggested it would take 6.6 primary care visits to avert one hospitalization. As a limitation, the outcomes were studied for only 1 year, but further effects of case management on health and service use could take longer to appear.
Commenting on the analysis but not involved in it, Laura Gottlieb, MD, MPH, professor in the department of family and community medicine at the University of California, San Francisco, said a few studies have suggested several pathways through which case management might influence health and health care utilization – and not solely through access to social services.
“The current findings underscore that one of those pathways is likely via connection to health care services,” she said.
As to the cost effectiveness of social needs case management given the necessary increase in personnel costs, she added, that it is a matter of society’s priorities. “If we want to achieve equity, we need to invest dollars differently. That is not a hospital-level issue. It is a society-level issue. Hospitals need to be able to stay afloat, so health care policies need to enable them to make different decisions,” she added. Broadly implementing such an approach will obviously take investment, Dr. Gottlieb continued.
“California Medicaid is trying to enable this shift in investments, but it is hard to move existing structures.” She added that more data are needed on the interaction between social services, patient experiences of care, and self-efficacy to understand a wider array of mechanisms through which case management might affect outcomes.
This analysis was supported by the Agency for Healthcare Research and Quality and Contra Costa Health Services. The authors disclosed no relevant conflicts of interest.
Hospitalizations fell by 11% in patients assigned to integrated social needs case management, a randomized controlled study conducted in California found.
The reduction in acute care use was likely because of the 3% increase in primary care visits with this approach, according to lead study author Mark D. Fleming, PhD, MS, assistant professor of health and social behavior at the University of California, Berkeley. The study was published in Annals of Internal Medicine.
The findings provide evidence for the theory that social needs case management can decrease acute care use by facilitating access to primary care, Dr. Fleming said in an interview. “While an increasing number of studies have measured the effects of social needs case management on hospital use, the findings have been inconsistent, with some studies showing a decrease in hospital use and others showing no change.” There was no strong evidence of an effect on acute care.
A 2018 study, however, found that liaising with community care workers substantially reduced hospital days in disadvantaged patients.
Case management, a complex approach linking medical and social needs, can overcome barriers to care by facilitating access to transportation and helping patients navigate the health care system, the authors noted. It can also streamline patient access to insurance coverage and social benefits.
The study
The current data came from a secondary analysis of a randomized encouragement study in Costa County, Calif., during 2017 and 2018. That study allocated adult California Medicaid beneficiaries of diverse race and ethnicity, relatively high social needs, and high risk for acute care use to two arms: social needs case management (n = 21,422) or administrative observation (22,389 weighted). Chronic health issues ranged from arthritis, diabetes, and back conditions to heart or lung disease, and psychological disorders. About 50% in both groups were younger than age 40 and 60% were women.
Case managers assessed patient needs, created a patient-centered care plan, and facilitated community resource referrals, primary care visits, and applications for public benefits.
The professionally diverse managers included public health nurses, social workers, substance misuse counselors, and mental health clinicians, as well as homeless service specialists and community health workers. Case management was offered as in-person or remote telephonic services for 1 year.
While rates of primary care visits were significantly higher in the case management group – incidence rate 1.03 (95% confidence interval [CI],1.00-1.07) – no intergroup differences emerged in visits for specialty care, behavioral health, psychiatric emergency visits, or jail intakes.
Although the analysis could not measure a direct effect of primary care use on hospitalizations, the results suggested it would take 6.6 primary care visits to avert one hospitalization. As a limitation, the outcomes were studied for only 1 year, but further effects of case management on health and service use could take longer to appear.
Commenting on the analysis but not involved in it, Laura Gottlieb, MD, MPH, professor in the department of family and community medicine at the University of California, San Francisco, said a few studies have suggested several pathways through which case management might influence health and health care utilization – and not solely through access to social services.
“The current findings underscore that one of those pathways is likely via connection to health care services,” she said.
As to the cost effectiveness of social needs case management given the necessary increase in personnel costs, she added, that it is a matter of society’s priorities. “If we want to achieve equity, we need to invest dollars differently. That is not a hospital-level issue. It is a society-level issue. Hospitals need to be able to stay afloat, so health care policies need to enable them to make different decisions,” she added. Broadly implementing such an approach will obviously take investment, Dr. Gottlieb continued.
“California Medicaid is trying to enable this shift in investments, but it is hard to move existing structures.” She added that more data are needed on the interaction between social services, patient experiences of care, and self-efficacy to understand a wider array of mechanisms through which case management might affect outcomes.
This analysis was supported by the Agency for Healthcare Research and Quality and Contra Costa Health Services. The authors disclosed no relevant conflicts of interest.
Hospitalizations fell by 11% in patients assigned to integrated social needs case management, a randomized controlled study conducted in California found.
The reduction in acute care use was likely because of the 3% increase in primary care visits with this approach, according to lead study author Mark D. Fleming, PhD, MS, assistant professor of health and social behavior at the University of California, Berkeley. The study was published in Annals of Internal Medicine.
The findings provide evidence for the theory that social needs case management can decrease acute care use by facilitating access to primary care, Dr. Fleming said in an interview. “While an increasing number of studies have measured the effects of social needs case management on hospital use, the findings have been inconsistent, with some studies showing a decrease in hospital use and others showing no change.” There was no strong evidence of an effect on acute care.
A 2018 study, however, found that liaising with community care workers substantially reduced hospital days in disadvantaged patients.
Case management, a complex approach linking medical and social needs, can overcome barriers to care by facilitating access to transportation and helping patients navigate the health care system, the authors noted. It can also streamline patient access to insurance coverage and social benefits.
The study
The current data came from a secondary analysis of a randomized encouragement study in Costa County, Calif., during 2017 and 2018. That study allocated adult California Medicaid beneficiaries of diverse race and ethnicity, relatively high social needs, and high risk for acute care use to two arms: social needs case management (n = 21,422) or administrative observation (22,389 weighted). Chronic health issues ranged from arthritis, diabetes, and back conditions to heart or lung disease, and psychological disorders. About 50% in both groups were younger than age 40 and 60% were women.
Case managers assessed patient needs, created a patient-centered care plan, and facilitated community resource referrals, primary care visits, and applications for public benefits.
The professionally diverse managers included public health nurses, social workers, substance misuse counselors, and mental health clinicians, as well as homeless service specialists and community health workers. Case management was offered as in-person or remote telephonic services for 1 year.
While rates of primary care visits were significantly higher in the case management group – incidence rate 1.03 (95% confidence interval [CI],1.00-1.07) – no intergroup differences emerged in visits for specialty care, behavioral health, psychiatric emergency visits, or jail intakes.
Although the analysis could not measure a direct effect of primary care use on hospitalizations, the results suggested it would take 6.6 primary care visits to avert one hospitalization. As a limitation, the outcomes were studied for only 1 year, but further effects of case management on health and service use could take longer to appear.
Commenting on the analysis but not involved in it, Laura Gottlieb, MD, MPH, professor in the department of family and community medicine at the University of California, San Francisco, said a few studies have suggested several pathways through which case management might influence health and health care utilization – and not solely through access to social services.
“The current findings underscore that one of those pathways is likely via connection to health care services,” she said.
As to the cost effectiveness of social needs case management given the necessary increase in personnel costs, she added, that it is a matter of society’s priorities. “If we want to achieve equity, we need to invest dollars differently. That is not a hospital-level issue. It is a society-level issue. Hospitals need to be able to stay afloat, so health care policies need to enable them to make different decisions,” she added. Broadly implementing such an approach will obviously take investment, Dr. Gottlieb continued.
“California Medicaid is trying to enable this shift in investments, but it is hard to move existing structures.” She added that more data are needed on the interaction between social services, patient experiences of care, and self-efficacy to understand a wider array of mechanisms through which case management might affect outcomes.
This analysis was supported by the Agency for Healthcare Research and Quality and Contra Costa Health Services. The authors disclosed no relevant conflicts of interest.
FROM ANNALS of INTERNAL MEDICINE
Squamous Cell Carcinoma
THE COMPARISON
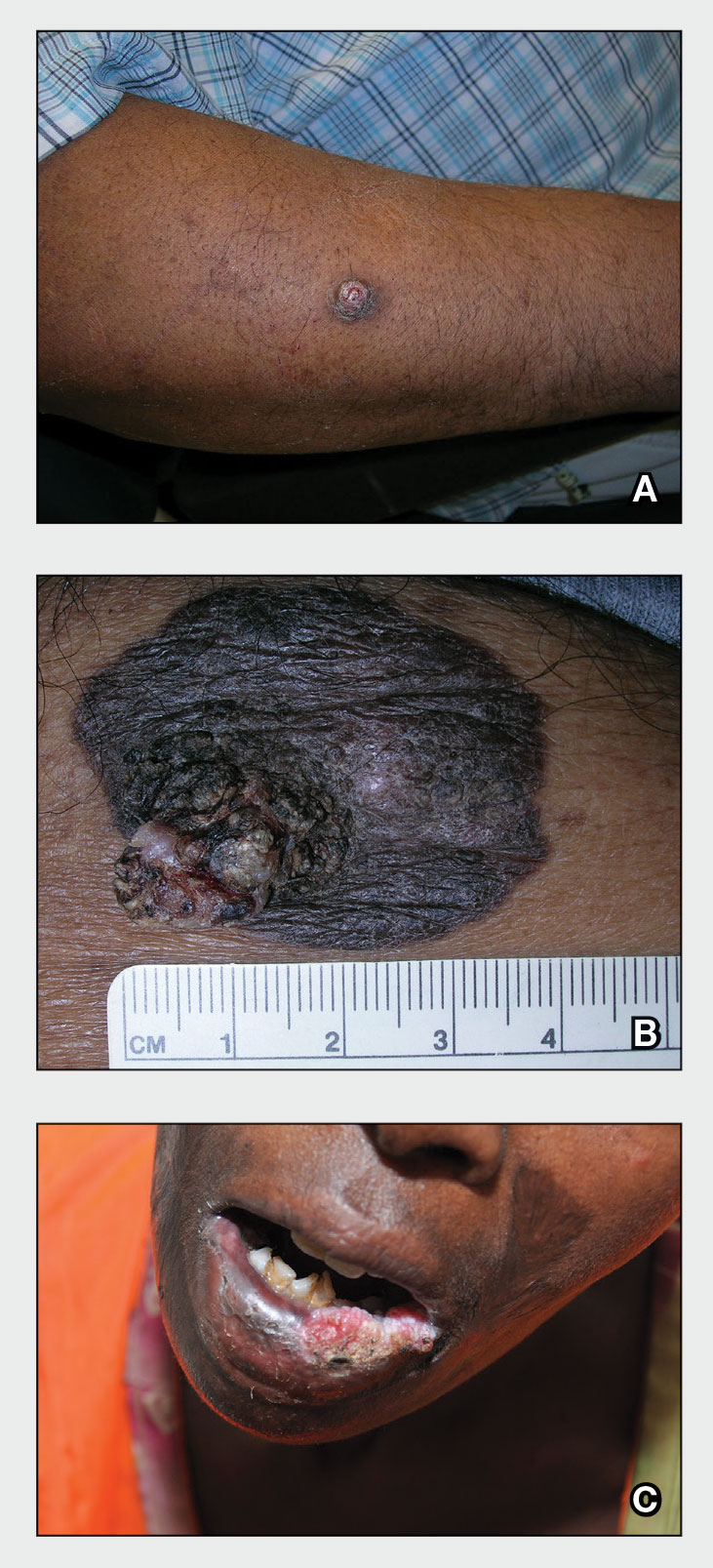
A A 51-year-old Hispanic man with a squamous cell carcinoma (SCC) of the keratoacanthoma type on the arm.
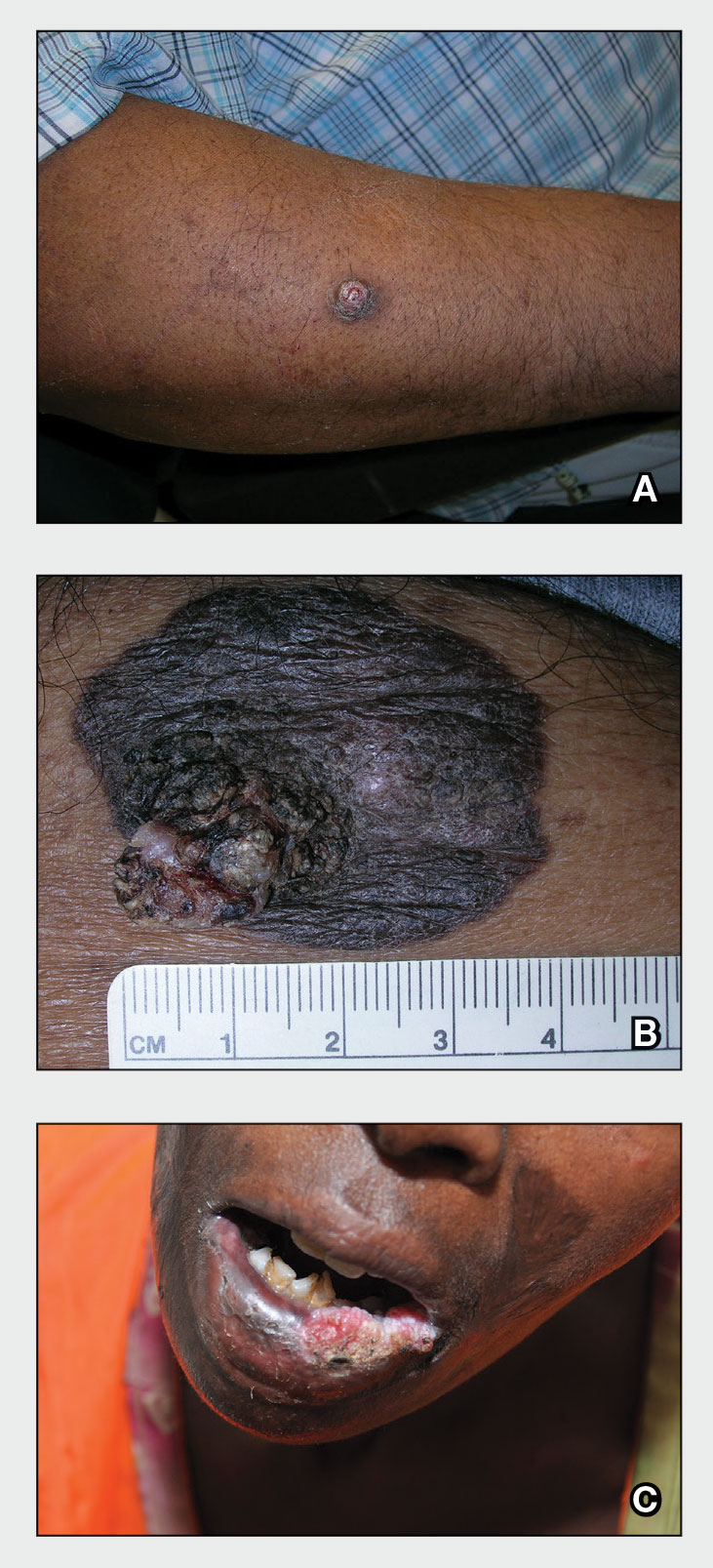
B A 75-year-old Black man with an SCC of the keratoacanthoma type on the abdomen.
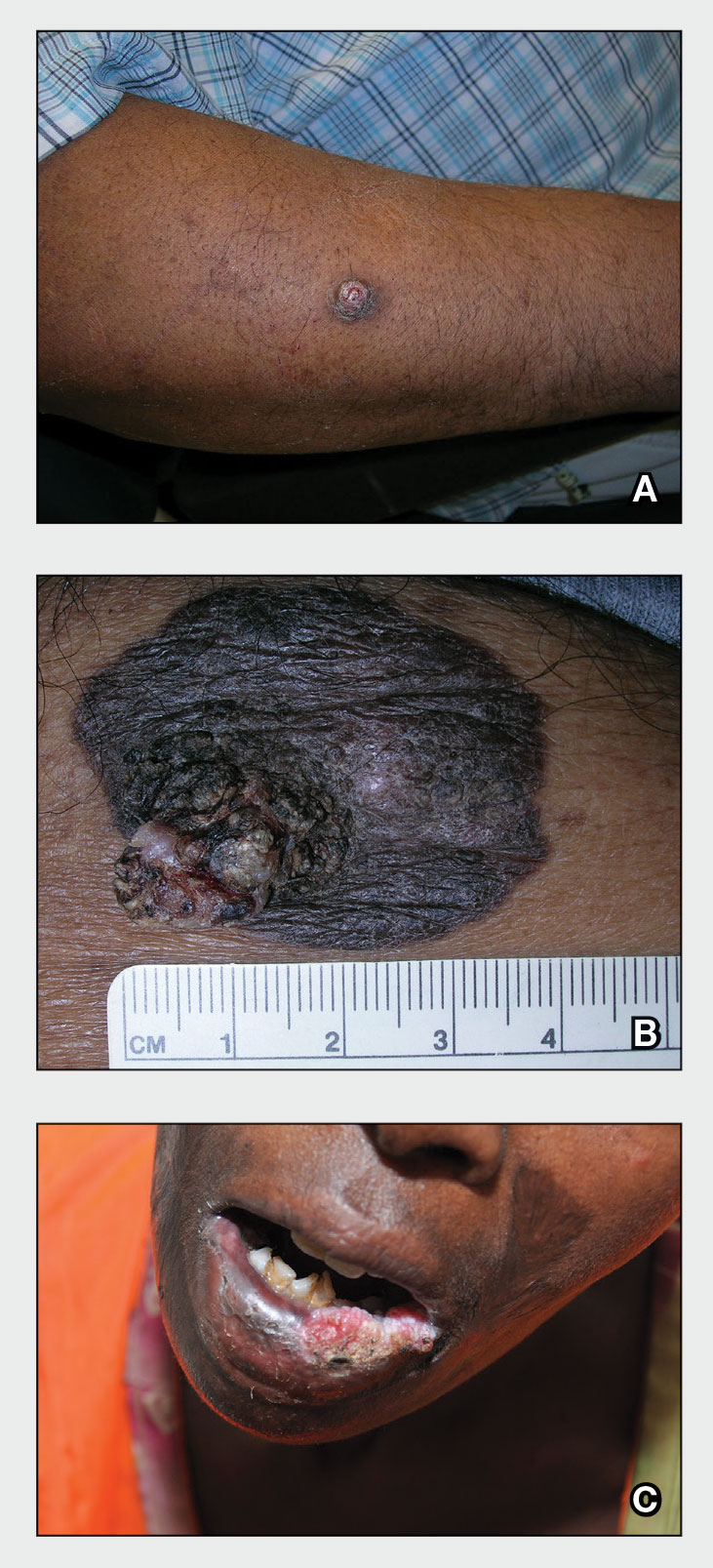
C An African woman with an SCC on the lower lip decades after a large facial burn, which is known as a Marjolin ulcer.
Cutaneous squamous cell carcinoma (SCC) develops from a malignant tumor of the keratinocytes, eccrine glands, or pilosebaceous units that invades the dermis. Risk factors include lighter skin tone, higher cumulative sun exposure, human papillomavirus (HPV) infection, hidradenitis suppurativa (HS), lichen sclerosus, family history of skin cancer,1 and immunosuppression.2 It typically affects sun-exposed areas of the body such as the face, scalp, neck, and extensor surfaces of the arms (Figure, A).3,4 However, in those with darker skin tones, the most common anatomic sites are those that are not exposed to the sun (Figure, B). Squamous cell carcinoma is diagnosed via skin biopsy. Treatment options include surgical excision, destructive methods such as electrodesiccation and curettage, and Mohs micrographic surgery. Cutaneous SCC has a cure rate of more than 95% and a mortality rate of 1.5% to 2% in the United States.3
Epidemiology
Squamous cell carcinoma is the most common skin cancer occurring in Black individuals, manifesting primarily in the fifth decade of life.5-7 It is the second most common skin cancer in White, Hispanic, and Asian individuals and is more common in males.8 In a study of organ transplant recipients (N=413), Pritchett et al9 reported that HPV infection was a major risk factor in Hispanic patients because 66.7% of those with SCC had a history of HPV. However, HPV is a risk factor for SCC in all ethnic groups.10
Key clinical features in people with darker skin tones
Anatomic location
- The lower legs and anogenital areas are the most common sites for SCC in patients with skin of color.4,11
- In Black women, SCC occurs more often on sun-exposed areas such as the arms and legs compared to Black men.7,12-14
- The genitalia, perianal area, ocular mucosa, and oral mucosa are the least likely areas to be routinely examined, even in skin cancer clinics that see high-risk patients, despite the SCC risk in the anogenital area.15,16
- Squamous cell carcinoma of the lips and scalp is more likely to occur in Black women vs Black men.4,7,17 Clinical appearance
- In those with darker skin tones, SCCs may appear hyperpigmented4 or hyperkeratotic with a lack of erythema and an inconsistent appearance.6,7,18
- A nonhealing ulceration of the skin should prompt a biopsy to rule out SCC.3,19
Worth noting
In patients with darker skin tones, the risk for SCC increases in areas with chronic inflammation and scarring of the skin.4,6,7,11,18,20-22 In Black patients, 20% to 40% of cases of SCC occur in the setting of chronic inflammation and scarring.6,7,18 Chronic inflammatory conditions include ulcers, lupus vulgaris, discoid lupus erythematosus, and HPV. In patients with discoid lupus erythematosus, there is an additive effect of sun exposure on the scars, which may play a role in the pathogenesis and metastasis risk for skin cancer in Black patients.4 Other scarring conditions include thermal or chemical burn scars, areas of physical trauma, and prior sites of radiation treatment.14,23 Squamous cell carcinoma arising in a burn scar is called a Marjolin ulcer or malignant degeneration of a scar (Figure, C). It is reported more often in lower-income, underresourced countries, which may suggest the need for early detection in populations with skin of color.24
Squamous cell carcinoma is more aggressive in sites that are not exposed to sun compared to sun-exposed areas.17,25
The risk for SCC is increased in immunocompromised patients,2 especially those with HPV.10
The prevalence of SCC in those with HS is approximately 4.6%. The chronic inflammation and irritation from HS in association with other risk factors such as tobacco use may contribute to the malignant transformation to SCC.26
Health disparity highlight
- The risk for metastasis from SCC is 20% to 40% in Black patients vs 1% to 4% in White patients.4,6,27
- Penile SCC was associated with a lower overall survival rate in patients of African descent.20,21
- The increased morbidity and mortality from SCC in patients with skin of color may be attributed to delays in diagnosis and treatment as well as an incomplete understanding of tumor genetics.4,6,18
Acknowledgment—The authors thank Elyse Gadra (Philadelphia, Pennsylvania) for assistance in the preparation of this manuscript.
- Asgari MM, Warton EM, Whittemore AS. Family history of skin cancer is associated with increased risk of cutaneous squamous cell carcinoma. Dermatol Surg. 2015;41:481-486. doi:10.1097/DSS.0000000000000292
- Harwood CA, Surentheran T, McGregor JM, et al. Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol. 2000;61:289-297. doi:10.1002/1096-9071(200007)61:3<289::aid-jmv2>3.0.co;2-z
- Kallini JR, Nouran H, Khachemoune A. Squamous cell carcinoma of the skin: epidemiology, classification, management, and novel trends. Int J Dermatol. 2015;54:130-140. https://doi.org/10.1111/ijd.12553.
- Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public [published online January 28, 2014]. J Am Acad Dermatol. 2014;70:748-762. doi:10.1016/j.jaad.2013.11.038
- Bradford PT. Skin cancer in skin of color. Dermatol Nurse. 2009;21:170-177.
- Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760.
- Davis DS, Robinson C, Callender VD. Skin cancer in women of color: epidemiology, pathogenesis and clinical manifestations. Int J Womens Dermatol. 2021;7:127-134. https://doi.org/10.1016/j.ijwd.2021.01.017
- Baum B, Duarte AM. Skin cancer epidemic in American Hispanic and Latino patients. In: Silverberg N, Duran-McKinster C, Tay Y-K, eds. Pediatric Skin of Color. Springer; 2015:453-460.
- Pritchett EN, Doyle A, Shaver CM, et al. Nonmelanoma skin cancer in nonwhite organ transplant recipients. JAMA Dermatol. 2016;152: 1348-1353. doi:10.1001/jamadermatol.2016.3328
- Karagas MR, Nelson HH, Sehr P, et al. Human papillomavirus infection and incidence of squamous cell and basal cell carcinomas of the skin. J Natl Cancer Inst. 2006;98:389-395. doi:10.1093/jnci/djj092
- Gohara M. Skin cancer: an African perspective. Br J Dermatol. 2015;173: 17-21. https://doi.org/10.1111/bjd.13380
- Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8-18. doi:10.1016/s1011-1344(01)00198-1
- Halder RM, Bang KM. Skin cancer in African Americans in the United States. Dermatol Clin. 1988;6:397-407.
- Mora RG, Perniciaro C. Cancer of the skin in blacks. I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543. doi:10.1016/s0190-9622(81)70113-0
- Bajaj S, Wolner ZJ, Dusza SW, et al. Total body skin examination practices: a survey study amongst dermatologists at high-risk skin cancer clinics. Dermatol Pract Concept. 2019;9:132-138. doi:10.5826/dpc.0902a09
- Rieder EA, Mu EW, Wang J, et al. Dermatologist practices during total body skin examinations: a survey study. J Drugs Dermatol. 2018;17:516-520.
- Halder RM, Ara CJ. Skin cancer and photoaging in ethnic skin. Dermatol Clin. 2003;21:725-732, x. doi: 10.1016/s0733-8635(03)00085-8
- Higgins S, Nazemi A, Chow M, et al. Review of nonmelanoma skin cancer in African Americans, Hispanics, and Asians. Dermatol Surg. 2018;44:903-910.
- Sng J, Koh D, Siong WC, et al. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009;61:426-432.
- Shao K, Feng H. Racial and ethnic healthcare disparities in skin cancer in the United States: a review of existing inequities, contributing factors, and potential solutions. J Clin Aesthet Dermatol. 2022;15:16-22.
- Shao K, Hooper J, Feng H. Racial and ethnic health disparities in dermatology in the United States. part 2: disease-specific epidemiology, characteristics, management, and outcomes. J Am Acad Dermatol. 2022;87:733-744. https://doi.org/10.1016/j.jaad.2021.12.062
- Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137-151. https://doi.org/10.1007/s40257-021-00662-z
- Copcu E, Aktas A, Sis¸man N, et al. Thirty-one cases of Marjolin’s ulcer. Clin Exp Dermatol. 2003;28:138-141. doi:10.1046/j.1365-2230.2003.01210.x
- Abdi MA, Yan M, Hanna TP. Systematic review of modern case series of squamous cell cancer arising in a chronic ulcer (Marjolin’s ulcer) of the skin. JCO Glob Oncol. 2020;6:809-818. doi:10.1200/GO.20.00094
- Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi:10.1016/j.det.2019.05.009
- Chapman S, Delgadillo D, Barber C, et al. Cutanteous squamous cell complicating hidradenitis suppurativa: a review of the prevalence, pathogenesis, and treatment of this dreaded complication. Acta Dermatovenerol Al Pannocica Adriat. 2018;27:25-28.
- Kailas A, Botwin AL, Pritchett EN, et al. Assessing the effectiveness of knowledge-based interventions in increasing skin cancer awareness, knowledge, and protective behaviors in skin of color populations. Cutis. 2017;100:235-240.
THE COMPARISON
A A 51-year-old Hispanic man with a squamous cell carcinoma (SCC) of the keratoacanthoma type on the arm.
B A 75-year-old Black man with an SCC of the keratoacanthoma type on the abdomen.
C An African woman with an SCC on the lower lip decades after a large facial burn, which is known as a Marjolin ulcer.
Cutaneous squamous cell carcinoma (SCC) develops from a malignant tumor of the keratinocytes, eccrine glands, or pilosebaceous units that invades the dermis. Risk factors include lighter skin tone, higher cumulative sun exposure, human papillomavirus (HPV) infection, hidradenitis suppurativa (HS), lichen sclerosus, family history of skin cancer,1 and immunosuppression.2 It typically affects sun-exposed areas of the body such as the face, scalp, neck, and extensor surfaces of the arms (Figure, A).3,4 However, in those with darker skin tones, the most common anatomic sites are those that are not exposed to the sun (Figure, B). Squamous cell carcinoma is diagnosed via skin biopsy. Treatment options include surgical excision, destructive methods such as electrodesiccation and curettage, and Mohs micrographic surgery. Cutaneous SCC has a cure rate of more than 95% and a mortality rate of 1.5% to 2% in the United States.3
Epidemiology
Squamous cell carcinoma is the most common skin cancer occurring in Black individuals, manifesting primarily in the fifth decade of life.5-7 It is the second most common skin cancer in White, Hispanic, and Asian individuals and is more common in males.8 In a study of organ transplant recipients (N=413), Pritchett et al9 reported that HPV infection was a major risk factor in Hispanic patients because 66.7% of those with SCC had a history of HPV. However, HPV is a risk factor for SCC in all ethnic groups.10
Key clinical features in people with darker skin tones
Anatomic location
- The lower legs and anogenital areas are the most common sites for SCC in patients with skin of color.4,11
- In Black women, SCC occurs more often on sun-exposed areas such as the arms and legs compared to Black men.7,12-14
- The genitalia, perianal area, ocular mucosa, and oral mucosa are the least likely areas to be routinely examined, even in skin cancer clinics that see high-risk patients, despite the SCC risk in the anogenital area.15,16
- Squamous cell carcinoma of the lips and scalp is more likely to occur in Black women vs Black men.4,7,17 Clinical appearance
- In those with darker skin tones, SCCs may appear hyperpigmented4 or hyperkeratotic with a lack of erythema and an inconsistent appearance.6,7,18
- A nonhealing ulceration of the skin should prompt a biopsy to rule out SCC.3,19
Worth noting
In patients with darker skin tones, the risk for SCC increases in areas with chronic inflammation and scarring of the skin.4,6,7,11,18,20-22 In Black patients, 20% to 40% of cases of SCC occur in the setting of chronic inflammation and scarring.6,7,18 Chronic inflammatory conditions include ulcers, lupus vulgaris, discoid lupus erythematosus, and HPV. In patients with discoid lupus erythematosus, there is an additive effect of sun exposure on the scars, which may play a role in the pathogenesis and metastasis risk for skin cancer in Black patients.4 Other scarring conditions include thermal or chemical burn scars, areas of physical trauma, and prior sites of radiation treatment.14,23 Squamous cell carcinoma arising in a burn scar is called a Marjolin ulcer or malignant degeneration of a scar (Figure, C). It is reported more often in lower-income, underresourced countries, which may suggest the need for early detection in populations with skin of color.24
Squamous cell carcinoma is more aggressive in sites that are not exposed to sun compared to sun-exposed areas.17,25
The risk for SCC is increased in immunocompromised patients,2 especially those with HPV.10
The prevalence of SCC in those with HS is approximately 4.6%. The chronic inflammation and irritation from HS in association with other risk factors such as tobacco use may contribute to the malignant transformation to SCC.26
Health disparity highlight
- The risk for metastasis from SCC is 20% to 40% in Black patients vs 1% to 4% in White patients.4,6,27
- Penile SCC was associated with a lower overall survival rate in patients of African descent.20,21
- The increased morbidity and mortality from SCC in patients with skin of color may be attributed to delays in diagnosis and treatment as well as an incomplete understanding of tumor genetics.4,6,18
Acknowledgment—The authors thank Elyse Gadra (Philadelphia, Pennsylvania) for assistance in the preparation of this manuscript.
THE COMPARISON
A A 51-year-old Hispanic man with a squamous cell carcinoma (SCC) of the keratoacanthoma type on the arm.
B A 75-year-old Black man with an SCC of the keratoacanthoma type on the abdomen.
C An African woman with an SCC on the lower lip decades after a large facial burn, which is known as a Marjolin ulcer.
Cutaneous squamous cell carcinoma (SCC) develops from a malignant tumor of the keratinocytes, eccrine glands, or pilosebaceous units that invades the dermis. Risk factors include lighter skin tone, higher cumulative sun exposure, human papillomavirus (HPV) infection, hidradenitis suppurativa (HS), lichen sclerosus, family history of skin cancer,1 and immunosuppression.2 It typically affects sun-exposed areas of the body such as the face, scalp, neck, and extensor surfaces of the arms (Figure, A).3,4 However, in those with darker skin tones, the most common anatomic sites are those that are not exposed to the sun (Figure, B). Squamous cell carcinoma is diagnosed via skin biopsy. Treatment options include surgical excision, destructive methods such as electrodesiccation and curettage, and Mohs micrographic surgery. Cutaneous SCC has a cure rate of more than 95% and a mortality rate of 1.5% to 2% in the United States.3
Epidemiology
Squamous cell carcinoma is the most common skin cancer occurring in Black individuals, manifesting primarily in the fifth decade of life.5-7 It is the second most common skin cancer in White, Hispanic, and Asian individuals and is more common in males.8 In a study of organ transplant recipients (N=413), Pritchett et al9 reported that HPV infection was a major risk factor in Hispanic patients because 66.7% of those with SCC had a history of HPV. However, HPV is a risk factor for SCC in all ethnic groups.10
Key clinical features in people with darker skin tones
Anatomic location
- The lower legs and anogenital areas are the most common sites for SCC in patients with skin of color.4,11
- In Black women, SCC occurs more often on sun-exposed areas such as the arms and legs compared to Black men.7,12-14
- The genitalia, perianal area, ocular mucosa, and oral mucosa are the least likely areas to be routinely examined, even in skin cancer clinics that see high-risk patients, despite the SCC risk in the anogenital area.15,16
- Squamous cell carcinoma of the lips and scalp is more likely to occur in Black women vs Black men.4,7,17 Clinical appearance
- In those with darker skin tones, SCCs may appear hyperpigmented4 or hyperkeratotic with a lack of erythema and an inconsistent appearance.6,7,18
- A nonhealing ulceration of the skin should prompt a biopsy to rule out SCC.3,19
Worth noting
In patients with darker skin tones, the risk for SCC increases in areas with chronic inflammation and scarring of the skin.4,6,7,11,18,20-22 In Black patients, 20% to 40% of cases of SCC occur in the setting of chronic inflammation and scarring.6,7,18 Chronic inflammatory conditions include ulcers, lupus vulgaris, discoid lupus erythematosus, and HPV. In patients with discoid lupus erythematosus, there is an additive effect of sun exposure on the scars, which may play a role in the pathogenesis and metastasis risk for skin cancer in Black patients.4 Other scarring conditions include thermal or chemical burn scars, areas of physical trauma, and prior sites of radiation treatment.14,23 Squamous cell carcinoma arising in a burn scar is called a Marjolin ulcer or malignant degeneration of a scar (Figure, C). It is reported more often in lower-income, underresourced countries, which may suggest the need for early detection in populations with skin of color.24
Squamous cell carcinoma is more aggressive in sites that are not exposed to sun compared to sun-exposed areas.17,25
The risk for SCC is increased in immunocompromised patients,2 especially those with HPV.10
The prevalence of SCC in those with HS is approximately 4.6%. The chronic inflammation and irritation from HS in association with other risk factors such as tobacco use may contribute to the malignant transformation to SCC.26
Health disparity highlight
- The risk for metastasis from SCC is 20% to 40% in Black patients vs 1% to 4% in White patients.4,6,27
- Penile SCC was associated with a lower overall survival rate in patients of African descent.20,21
- The increased morbidity and mortality from SCC in patients with skin of color may be attributed to delays in diagnosis and treatment as well as an incomplete understanding of tumor genetics.4,6,18
Acknowledgment—The authors thank Elyse Gadra (Philadelphia, Pennsylvania) for assistance in the preparation of this manuscript.
- Asgari MM, Warton EM, Whittemore AS. Family history of skin cancer is associated with increased risk of cutaneous squamous cell carcinoma. Dermatol Surg. 2015;41:481-486. doi:10.1097/DSS.0000000000000292
- Harwood CA, Surentheran T, McGregor JM, et al. Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol. 2000;61:289-297. doi:10.1002/1096-9071(200007)61:3<289::aid-jmv2>3.0.co;2-z
- Kallini JR, Nouran H, Khachemoune A. Squamous cell carcinoma of the skin: epidemiology, classification, management, and novel trends. Int J Dermatol. 2015;54:130-140. https://doi.org/10.1111/ijd.12553.
- Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public [published online January 28, 2014]. J Am Acad Dermatol. 2014;70:748-762. doi:10.1016/j.jaad.2013.11.038
- Bradford PT. Skin cancer in skin of color. Dermatol Nurse. 2009;21:170-177.
- Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760.
- Davis DS, Robinson C, Callender VD. Skin cancer in women of color: epidemiology, pathogenesis and clinical manifestations. Int J Womens Dermatol. 2021;7:127-134. https://doi.org/10.1016/j.ijwd.2021.01.017
- Baum B, Duarte AM. Skin cancer epidemic in American Hispanic and Latino patients. In: Silverberg N, Duran-McKinster C, Tay Y-K, eds. Pediatric Skin of Color. Springer; 2015:453-460.
- Pritchett EN, Doyle A, Shaver CM, et al. Nonmelanoma skin cancer in nonwhite organ transplant recipients. JAMA Dermatol. 2016;152: 1348-1353. doi:10.1001/jamadermatol.2016.3328
- Karagas MR, Nelson HH, Sehr P, et al. Human papillomavirus infection and incidence of squamous cell and basal cell carcinomas of the skin. J Natl Cancer Inst. 2006;98:389-395. doi:10.1093/jnci/djj092
- Gohara M. Skin cancer: an African perspective. Br J Dermatol. 2015;173: 17-21. https://doi.org/10.1111/bjd.13380
- Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8-18. doi:10.1016/s1011-1344(01)00198-1
- Halder RM, Bang KM. Skin cancer in African Americans in the United States. Dermatol Clin. 1988;6:397-407.
- Mora RG, Perniciaro C. Cancer of the skin in blacks. I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543. doi:10.1016/s0190-9622(81)70113-0
- Bajaj S, Wolner ZJ, Dusza SW, et al. Total body skin examination practices: a survey study amongst dermatologists at high-risk skin cancer clinics. Dermatol Pract Concept. 2019;9:132-138. doi:10.5826/dpc.0902a09
- Rieder EA, Mu EW, Wang J, et al. Dermatologist practices during total body skin examinations: a survey study. J Drugs Dermatol. 2018;17:516-520.
- Halder RM, Ara CJ. Skin cancer and photoaging in ethnic skin. Dermatol Clin. 2003;21:725-732, x. doi: 10.1016/s0733-8635(03)00085-8
- Higgins S, Nazemi A, Chow M, et al. Review of nonmelanoma skin cancer in African Americans, Hispanics, and Asians. Dermatol Surg. 2018;44:903-910.
- Sng J, Koh D, Siong WC, et al. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009;61:426-432.
- Shao K, Feng H. Racial and ethnic healthcare disparities in skin cancer in the United States: a review of existing inequities, contributing factors, and potential solutions. J Clin Aesthet Dermatol. 2022;15:16-22.
- Shao K, Hooper J, Feng H. Racial and ethnic health disparities in dermatology in the United States. part 2: disease-specific epidemiology, characteristics, management, and outcomes. J Am Acad Dermatol. 2022;87:733-744. https://doi.org/10.1016/j.jaad.2021.12.062
- Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137-151. https://doi.org/10.1007/s40257-021-00662-z
- Copcu E, Aktas A, Sis¸man N, et al. Thirty-one cases of Marjolin’s ulcer. Clin Exp Dermatol. 2003;28:138-141. doi:10.1046/j.1365-2230.2003.01210.x
- Abdi MA, Yan M, Hanna TP. Systematic review of modern case series of squamous cell cancer arising in a chronic ulcer (Marjolin’s ulcer) of the skin. JCO Glob Oncol. 2020;6:809-818. doi:10.1200/GO.20.00094
- Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi:10.1016/j.det.2019.05.009
- Chapman S, Delgadillo D, Barber C, et al. Cutanteous squamous cell complicating hidradenitis suppurativa: a review of the prevalence, pathogenesis, and treatment of this dreaded complication. Acta Dermatovenerol Al Pannocica Adriat. 2018;27:25-28.
- Kailas A, Botwin AL, Pritchett EN, et al. Assessing the effectiveness of knowledge-based interventions in increasing skin cancer awareness, knowledge, and protective behaviors in skin of color populations. Cutis. 2017;100:235-240.
- Asgari MM, Warton EM, Whittemore AS. Family history of skin cancer is associated with increased risk of cutaneous squamous cell carcinoma. Dermatol Surg. 2015;41:481-486. doi:10.1097/DSS.0000000000000292
- Harwood CA, Surentheran T, McGregor JM, et al. Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol. 2000;61:289-297. doi:10.1002/1096-9071(200007)61:3<289::aid-jmv2>3.0.co;2-z
- Kallini JR, Nouran H, Khachemoune A. Squamous cell carcinoma of the skin: epidemiology, classification, management, and novel trends. Int J Dermatol. 2015;54:130-140. https://doi.org/10.1111/ijd.12553.
- Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public [published online January 28, 2014]. J Am Acad Dermatol. 2014;70:748-762. doi:10.1016/j.jaad.2013.11.038
- Bradford PT. Skin cancer in skin of color. Dermatol Nurse. 2009;21:170-177.
- Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760.
- Davis DS, Robinson C, Callender VD. Skin cancer in women of color: epidemiology, pathogenesis and clinical manifestations. Int J Womens Dermatol. 2021;7:127-134. https://doi.org/10.1016/j.ijwd.2021.01.017
- Baum B, Duarte AM. Skin cancer epidemic in American Hispanic and Latino patients. In: Silverberg N, Duran-McKinster C, Tay Y-K, eds. Pediatric Skin of Color. Springer; 2015:453-460.
- Pritchett EN, Doyle A, Shaver CM, et al. Nonmelanoma skin cancer in nonwhite organ transplant recipients. JAMA Dermatol. 2016;152: 1348-1353. doi:10.1001/jamadermatol.2016.3328
- Karagas MR, Nelson HH, Sehr P, et al. Human papillomavirus infection and incidence of squamous cell and basal cell carcinomas of the skin. J Natl Cancer Inst. 2006;98:389-395. doi:10.1093/jnci/djj092
- Gohara M. Skin cancer: an African perspective. Br J Dermatol. 2015;173: 17-21. https://doi.org/10.1111/bjd.13380
- Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8-18. doi:10.1016/s1011-1344(01)00198-1
- Halder RM, Bang KM. Skin cancer in African Americans in the United States. Dermatol Clin. 1988;6:397-407.
- Mora RG, Perniciaro C. Cancer of the skin in blacks. I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543. doi:10.1016/s0190-9622(81)70113-0
- Bajaj S, Wolner ZJ, Dusza SW, et al. Total body skin examination practices: a survey study amongst dermatologists at high-risk skin cancer clinics. Dermatol Pract Concept. 2019;9:132-138. doi:10.5826/dpc.0902a09
- Rieder EA, Mu EW, Wang J, et al. Dermatologist practices during total body skin examinations: a survey study. J Drugs Dermatol. 2018;17:516-520.
- Halder RM, Ara CJ. Skin cancer and photoaging in ethnic skin. Dermatol Clin. 2003;21:725-732, x. doi: 10.1016/s0733-8635(03)00085-8
- Higgins S, Nazemi A, Chow M, et al. Review of nonmelanoma skin cancer in African Americans, Hispanics, and Asians. Dermatol Surg. 2018;44:903-910.
- Sng J, Koh D, Siong WC, et al. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009;61:426-432.
- Shao K, Feng H. Racial and ethnic healthcare disparities in skin cancer in the United States: a review of existing inequities, contributing factors, and potential solutions. J Clin Aesthet Dermatol. 2022;15:16-22.
- Shao K, Hooper J, Feng H. Racial and ethnic health disparities in dermatology in the United States. part 2: disease-specific epidemiology, characteristics, management, and outcomes. J Am Acad Dermatol. 2022;87:733-744. https://doi.org/10.1016/j.jaad.2021.12.062
- Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137-151. https://doi.org/10.1007/s40257-021-00662-z
- Copcu E, Aktas A, Sis¸man N, et al. Thirty-one cases of Marjolin’s ulcer. Clin Exp Dermatol. 2003;28:138-141. doi:10.1046/j.1365-2230.2003.01210.x
- Abdi MA, Yan M, Hanna TP. Systematic review of modern case series of squamous cell cancer arising in a chronic ulcer (Marjolin’s ulcer) of the skin. JCO Glob Oncol. 2020;6:809-818. doi:10.1200/GO.20.00094
- Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi:10.1016/j.det.2019.05.009
- Chapman S, Delgadillo D, Barber C, et al. Cutanteous squamous cell complicating hidradenitis suppurativa: a review of the prevalence, pathogenesis, and treatment of this dreaded complication. Acta Dermatovenerol Al Pannocica Adriat. 2018;27:25-28.
- Kailas A, Botwin AL, Pritchett EN, et al. Assessing the effectiveness of knowledge-based interventions in increasing skin cancer awareness, knowledge, and protective behaviors in skin of color populations. Cutis. 2017;100:235-240.
Black women weigh emerging risks of ‘creamy crack’ hair straighteners
Deanna Denham Hughes was stunned when she was diagnosed with ovarian cancer in 2022. She was only 32. She had no family history of cancer, and tests found no genetic link. Ms. Hughes wondered why she, an otherwise healthy Black mother of two, would develop a malignancy known as a “silent killer.”
After emergency surgery to remove the mass, along with her ovaries, uterus, fallopian tubes, and appendix, Ms. Hughes said, she saw an Instagram post in which a woman with uterine cancer linked her condition to chemical hair straighteners.
“I almost fell over,” she said from her home in Smyrna, Ga.
When Ms. Hughes was about 4, her mother began applying a chemical straightener, or relaxer, to her hair every 6-8 weeks. “It burned, and it smelled awful,” Ms. Hughes recalled. “But it was just part of our routine to ‘deal with my hair.’ ”
The routine continued until she went to college and met other Black women who wore their hair naturally. Soon, Ms. Hughes quit relaxers.
Social and economic pressures have long compelled Black girls and women to straighten their hair to conform to Eurocentric beauty standards. But chemical straighteners are stinky and costly and sometimes cause painful scalp burns. Mounting evidence now shows they could be a health hazard.
Relaxers can contain carcinogens, such as formaldehyde-releasing agents, phthalates, and other endocrine-disrupting compounds, according to National Institutes of Health studies. The compounds can mimic the body’s hormones and have been linked to breast, uterine, and ovarian cancers, studies show.
African American women’s often frequent and lifelong application of chemical relaxers to their hair and scalp might explain why hormone-related cancers kill disproportionately more Black than White women, say researchers and cancer doctors.
“What’s in these products is harmful,” said Tamarra James-Todd, PhD, an epidemiology professor at Harvard T.H. Chan School of Public Health, Boston, who has studied straightening products for the past 20 years.
She believes manufacturers, policymakers, and physicians should warn consumers that relaxers might cause cancer and other health problems.
But regulators have been slow to act, physicians have been reluctant to take up the cause, and racism continues to dictate fashion standards that make it tough for women to quit relaxers, products so addictive they’re known as “creamy crack.”
Michelle Obama straightened her hair when Barack Obama served as president because she believed Americans were “not ready” to see her in braids, the former first lady said after leaving the White House. The U.S. military still prohibited popular Black hairstyles such as dreadlocks and twists while the nation’s first Black president was in office.
California in 2019 became the first of nearly two dozen states to ban race-based hair discrimination. Last year, the U.S. House of Representatives passed similar legislation, known as the CROWN Act, for Creating a Respectful and Open World for Natural Hair. But the bill failed in the Senate.
The need for legislation underscores the challenges Black girls and women face at school and in the workplace.
“You have to pick your struggles,” said Atlanta-based surgical oncologist Ryland J. Gore, MD. She informs her breast cancer patients about the increased cancer risk from relaxers. Despite her knowledge, however, Dr. Gore continues to use chemical straighteners on her own hair, as she has since she was about 7 years old.
“Your hair tells a story,” she said.
In conversations with patients, Dr. Gore sometimes talks about how African American women once wove messages into their braids about the route to take on the Underground Railroad as they sought freedom from slavery.
“It’s just a deep discussion,” one that touches on culture, history, and research into current hairstyling practices, she said. “The data is out there. So patients should be warned, and then they can make a decision.”
The first hint of a connection between hair products and health issues surfaced in the 1990s. Doctors began seeing signs of sexual maturation in Black babies and young girls who developed breasts and pubic hair after using shampoo containing estrogen or placental extract. When the girls stopped using the shampoo, the hair and breast development receded, according to a study published in the journal Clinical Pediatrics in 1998.
Since then, Dr. James-Todd and other researchers have linked chemicals in hair products to a variety of health issues more prevalent among Black women – from early puberty to preterm birth, obesity, and diabetes.
In recent years, researchers have focused on a possible connection between ingredients in chemical relaxers and hormone-related cancers, like the one Ms. Hughes developed, which tend to be more aggressive and deadly in Black women.
A 2017 study found White women who used chemical relaxers were nearly twice as likely to develop breast cancer as those who did not use them. Because the vast majority of the Black study participants used relaxers, researchers could not effectively test the association in Black women, said lead author Adana Llanos, PhD, associate professor of epidemiology at Columbia University’s Mailman School of Public Health, New York.
Researchers did test it in 2020.
The so-called Sister Study, a landmark National Institute of Environmental Health Sciences investigation into the causes of breast cancer and related diseases, followed 50,000 U.S. women whose sisters had been diagnosed with breast cancer and who were cancer-free when they enrolled. Regardless of race, women who reported using relaxers in the prior year were 18% more likely to be diagnosed with breast cancer. Those who used relaxers at least every 5-8 weeks had a 31% higher breast cancer risk.
Nearly 75% of the Black sisters used relaxers in the prior year, compared with 3% of the non-Hispanic White sisters. Three-quarters of Black women self-reported using the straighteners as adolescents, and frequent use of chemical straighteners during adolescence raised the risk of premenopausal breast cancer, a 2021 NIH-funded study in the International Journal of Cancer found.
Another 2021 analysis of the Sister Study data showed sisters who self-reported that they frequently used relaxers or pressing products doubled their ovarian cancer risk. In 2022, another study found frequent use more than doubled uterine cancer risk.
After researchers discovered the link with uterine cancer, some called for policy changes and other measures to reduce exposure to chemical relaxers.
“It is time to intervene,” Dr. Llanos and her colleagues wrote in a Journal of the National Cancer Institute editorial accompanying the uterine cancer analysis. While acknowledging the need for more research, they issued a “call for action.”
No one can say that using permanent hair straighteners will give you cancer, Dr. Llanos said in an interview. “That’s not how cancer works,” she said, noting that some smokers never develop lung cancer, despite tobacco use being a known risk factor.
The body of research linking hair straighteners and cancer is more limited, said Dr. Llanos, who quit using chemical relaxers 15 years ago. But, she asked rhetorically, “Do we need to do the research for 50 more years to know that chemical relaxers are harmful?”
Charlotte R. Gamble, MD, a gynecological oncologist whose Washington, D.C., practice includes Black women with uterine and ovarian cancer, said she and her colleagues see the uterine cancer study findings as worthy of further exploration – but not yet worthy of discussion with patients.
“The jury’s out for me personally,” she said. “There’s so much more data that’s needed.”
Meanwhile, Dr. James-Todd and other researchers believe they have built a solid body of evidence.
“There are enough things we do know to begin taking action, developing interventions, providing useful information to clinicians and patients and the general public,” said Traci N. Bethea, PhD, assistant professor in the Office of Minority Health and Health Disparities Research at Georgetown University.
Responsibility for regulating personal-care products, including chemical hair straighteners and hair dyes – which also have been linked to hormone-related cancers – lies with the Food and Drug Administration. But the FDA does not subject personal-care products to the same approval process it uses for food and drugs. The FDA restricts only 11 categories of chemicals used in cosmetics, while concerns about health effects have prompted the European Union to restrict the use of at least 2,400 substances.
In March, Reps. Ayanna Pressley (D-Mass.) and Shontel Brown (D-Ohio) asked the FDA to investigate the potential health threat posed by chemical relaxers. An FDA representative said the agency would look into it.
Natural hairstyles are enjoying a resurgence among Black girls and women, but many continue to rely on the creamy crack, said Dede Teteh, DrPH, assistant professor of public health at Chapman University, Irvine, Calif.
She had her first straightening perm at 8 and has struggled to withdraw from relaxers as an adult, said Dr. Teteh, who now wears locs. Not long ago, she considered chemically straightening her hair for an academic job interview because she didn’t want her hair to “be a hindrance” when she appeared before White professors.
Dr. Teteh led “The Cost of Beauty,” a hair-health research project published in 2017. She and her team interviewed 91 Black women in Southern California. Some became “combative” at the idea of quitting relaxers and claimed “everything can cause cancer.”
Their reactions speak to the challenges Black women face in America, Dr. Teteh said.
“It’s not that people do not want to hear the information related to their health,” she said. “But they want people to share the information in a way that it’s really empathetic to the plight of being Black here in the United States.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – the independent source for health policy research, polling, and journalism.
Deanna Denham Hughes was stunned when she was diagnosed with ovarian cancer in 2022. She was only 32. She had no family history of cancer, and tests found no genetic link. Ms. Hughes wondered why she, an otherwise healthy Black mother of two, would develop a malignancy known as a “silent killer.”
After emergency surgery to remove the mass, along with her ovaries, uterus, fallopian tubes, and appendix, Ms. Hughes said, she saw an Instagram post in which a woman with uterine cancer linked her condition to chemical hair straighteners.
“I almost fell over,” she said from her home in Smyrna, Ga.
When Ms. Hughes was about 4, her mother began applying a chemical straightener, or relaxer, to her hair every 6-8 weeks. “It burned, and it smelled awful,” Ms. Hughes recalled. “But it was just part of our routine to ‘deal with my hair.’ ”
The routine continued until she went to college and met other Black women who wore their hair naturally. Soon, Ms. Hughes quit relaxers.
Social and economic pressures have long compelled Black girls and women to straighten their hair to conform to Eurocentric beauty standards. But chemical straighteners are stinky and costly and sometimes cause painful scalp burns. Mounting evidence now shows they could be a health hazard.
Relaxers can contain carcinogens, such as formaldehyde-releasing agents, phthalates, and other endocrine-disrupting compounds, according to National Institutes of Health studies. The compounds can mimic the body’s hormones and have been linked to breast, uterine, and ovarian cancers, studies show.
African American women’s often frequent and lifelong application of chemical relaxers to their hair and scalp might explain why hormone-related cancers kill disproportionately more Black than White women, say researchers and cancer doctors.
“What’s in these products is harmful,” said Tamarra James-Todd, PhD, an epidemiology professor at Harvard T.H. Chan School of Public Health, Boston, who has studied straightening products for the past 20 years.
She believes manufacturers, policymakers, and physicians should warn consumers that relaxers might cause cancer and other health problems.
But regulators have been slow to act, physicians have been reluctant to take up the cause, and racism continues to dictate fashion standards that make it tough for women to quit relaxers, products so addictive they’re known as “creamy crack.”
Michelle Obama straightened her hair when Barack Obama served as president because she believed Americans were “not ready” to see her in braids, the former first lady said after leaving the White House. The U.S. military still prohibited popular Black hairstyles such as dreadlocks and twists while the nation’s first Black president was in office.
California in 2019 became the first of nearly two dozen states to ban race-based hair discrimination. Last year, the U.S. House of Representatives passed similar legislation, known as the CROWN Act, for Creating a Respectful and Open World for Natural Hair. But the bill failed in the Senate.
The need for legislation underscores the challenges Black girls and women face at school and in the workplace.
“You have to pick your struggles,” said Atlanta-based surgical oncologist Ryland J. Gore, MD. She informs her breast cancer patients about the increased cancer risk from relaxers. Despite her knowledge, however, Dr. Gore continues to use chemical straighteners on her own hair, as she has since she was about 7 years old.
“Your hair tells a story,” she said.
In conversations with patients, Dr. Gore sometimes talks about how African American women once wove messages into their braids about the route to take on the Underground Railroad as they sought freedom from slavery.
“It’s just a deep discussion,” one that touches on culture, history, and research into current hairstyling practices, she said. “The data is out there. So patients should be warned, and then they can make a decision.”
The first hint of a connection between hair products and health issues surfaced in the 1990s. Doctors began seeing signs of sexual maturation in Black babies and young girls who developed breasts and pubic hair after using shampoo containing estrogen or placental extract. When the girls stopped using the shampoo, the hair and breast development receded, according to a study published in the journal Clinical Pediatrics in 1998.
Since then, Dr. James-Todd and other researchers have linked chemicals in hair products to a variety of health issues more prevalent among Black women – from early puberty to preterm birth, obesity, and diabetes.
In recent years, researchers have focused on a possible connection between ingredients in chemical relaxers and hormone-related cancers, like the one Ms. Hughes developed, which tend to be more aggressive and deadly in Black women.
A 2017 study found White women who used chemical relaxers were nearly twice as likely to develop breast cancer as those who did not use them. Because the vast majority of the Black study participants used relaxers, researchers could not effectively test the association in Black women, said lead author Adana Llanos, PhD, associate professor of epidemiology at Columbia University’s Mailman School of Public Health, New York.
Researchers did test it in 2020.
The so-called Sister Study, a landmark National Institute of Environmental Health Sciences investigation into the causes of breast cancer and related diseases, followed 50,000 U.S. women whose sisters had been diagnosed with breast cancer and who were cancer-free when they enrolled. Regardless of race, women who reported using relaxers in the prior year were 18% more likely to be diagnosed with breast cancer. Those who used relaxers at least every 5-8 weeks had a 31% higher breast cancer risk.
Nearly 75% of the Black sisters used relaxers in the prior year, compared with 3% of the non-Hispanic White sisters. Three-quarters of Black women self-reported using the straighteners as adolescents, and frequent use of chemical straighteners during adolescence raised the risk of premenopausal breast cancer, a 2021 NIH-funded study in the International Journal of Cancer found.
Another 2021 analysis of the Sister Study data showed sisters who self-reported that they frequently used relaxers or pressing products doubled their ovarian cancer risk. In 2022, another study found frequent use more than doubled uterine cancer risk.
After researchers discovered the link with uterine cancer, some called for policy changes and other measures to reduce exposure to chemical relaxers.
“It is time to intervene,” Dr. Llanos and her colleagues wrote in a Journal of the National Cancer Institute editorial accompanying the uterine cancer analysis. While acknowledging the need for more research, they issued a “call for action.”
No one can say that using permanent hair straighteners will give you cancer, Dr. Llanos said in an interview. “That’s not how cancer works,” she said, noting that some smokers never develop lung cancer, despite tobacco use being a known risk factor.
The body of research linking hair straighteners and cancer is more limited, said Dr. Llanos, who quit using chemical relaxers 15 years ago. But, she asked rhetorically, “Do we need to do the research for 50 more years to know that chemical relaxers are harmful?”
Charlotte R. Gamble, MD, a gynecological oncologist whose Washington, D.C., practice includes Black women with uterine and ovarian cancer, said she and her colleagues see the uterine cancer study findings as worthy of further exploration – but not yet worthy of discussion with patients.
“The jury’s out for me personally,” she said. “There’s so much more data that’s needed.”
Meanwhile, Dr. James-Todd and other researchers believe they have built a solid body of evidence.
“There are enough things we do know to begin taking action, developing interventions, providing useful information to clinicians and patients and the general public,” said Traci N. Bethea, PhD, assistant professor in the Office of Minority Health and Health Disparities Research at Georgetown University.
Responsibility for regulating personal-care products, including chemical hair straighteners and hair dyes – which also have been linked to hormone-related cancers – lies with the Food and Drug Administration. But the FDA does not subject personal-care products to the same approval process it uses for food and drugs. The FDA restricts only 11 categories of chemicals used in cosmetics, while concerns about health effects have prompted the European Union to restrict the use of at least 2,400 substances.
In March, Reps. Ayanna Pressley (D-Mass.) and Shontel Brown (D-Ohio) asked the FDA to investigate the potential health threat posed by chemical relaxers. An FDA representative said the agency would look into it.
Natural hairstyles are enjoying a resurgence among Black girls and women, but many continue to rely on the creamy crack, said Dede Teteh, DrPH, assistant professor of public health at Chapman University, Irvine, Calif.
She had her first straightening perm at 8 and has struggled to withdraw from relaxers as an adult, said Dr. Teteh, who now wears locs. Not long ago, she considered chemically straightening her hair for an academic job interview because she didn’t want her hair to “be a hindrance” when she appeared before White professors.
Dr. Teteh led “The Cost of Beauty,” a hair-health research project published in 2017. She and her team interviewed 91 Black women in Southern California. Some became “combative” at the idea of quitting relaxers and claimed “everything can cause cancer.”
Their reactions speak to the challenges Black women face in America, Dr. Teteh said.
“It’s not that people do not want to hear the information related to their health,” she said. “But they want people to share the information in a way that it’s really empathetic to the plight of being Black here in the United States.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – the independent source for health policy research, polling, and journalism.
Deanna Denham Hughes was stunned when she was diagnosed with ovarian cancer in 2022. She was only 32. She had no family history of cancer, and tests found no genetic link. Ms. Hughes wondered why she, an otherwise healthy Black mother of two, would develop a malignancy known as a “silent killer.”
After emergency surgery to remove the mass, along with her ovaries, uterus, fallopian tubes, and appendix, Ms. Hughes said, she saw an Instagram post in which a woman with uterine cancer linked her condition to chemical hair straighteners.
“I almost fell over,” she said from her home in Smyrna, Ga.
When Ms. Hughes was about 4, her mother began applying a chemical straightener, or relaxer, to her hair every 6-8 weeks. “It burned, and it smelled awful,” Ms. Hughes recalled. “But it was just part of our routine to ‘deal with my hair.’ ”
The routine continued until she went to college and met other Black women who wore their hair naturally. Soon, Ms. Hughes quit relaxers.
Social and economic pressures have long compelled Black girls and women to straighten their hair to conform to Eurocentric beauty standards. But chemical straighteners are stinky and costly and sometimes cause painful scalp burns. Mounting evidence now shows they could be a health hazard.
Relaxers can contain carcinogens, such as formaldehyde-releasing agents, phthalates, and other endocrine-disrupting compounds, according to National Institutes of Health studies. The compounds can mimic the body’s hormones and have been linked to breast, uterine, and ovarian cancers, studies show.
African American women’s often frequent and lifelong application of chemical relaxers to their hair and scalp might explain why hormone-related cancers kill disproportionately more Black than White women, say researchers and cancer doctors.
“What’s in these products is harmful,” said Tamarra James-Todd, PhD, an epidemiology professor at Harvard T.H. Chan School of Public Health, Boston, who has studied straightening products for the past 20 years.
She believes manufacturers, policymakers, and physicians should warn consumers that relaxers might cause cancer and other health problems.
But regulators have been slow to act, physicians have been reluctant to take up the cause, and racism continues to dictate fashion standards that make it tough for women to quit relaxers, products so addictive they’re known as “creamy crack.”
Michelle Obama straightened her hair when Barack Obama served as president because she believed Americans were “not ready” to see her in braids, the former first lady said after leaving the White House. The U.S. military still prohibited popular Black hairstyles such as dreadlocks and twists while the nation’s first Black president was in office.
California in 2019 became the first of nearly two dozen states to ban race-based hair discrimination. Last year, the U.S. House of Representatives passed similar legislation, known as the CROWN Act, for Creating a Respectful and Open World for Natural Hair. But the bill failed in the Senate.
The need for legislation underscores the challenges Black girls and women face at school and in the workplace.
“You have to pick your struggles,” said Atlanta-based surgical oncologist Ryland J. Gore, MD. She informs her breast cancer patients about the increased cancer risk from relaxers. Despite her knowledge, however, Dr. Gore continues to use chemical straighteners on her own hair, as she has since she was about 7 years old.
“Your hair tells a story,” she said.
In conversations with patients, Dr. Gore sometimes talks about how African American women once wove messages into their braids about the route to take on the Underground Railroad as they sought freedom from slavery.
“It’s just a deep discussion,” one that touches on culture, history, and research into current hairstyling practices, she said. “The data is out there. So patients should be warned, and then they can make a decision.”
The first hint of a connection between hair products and health issues surfaced in the 1990s. Doctors began seeing signs of sexual maturation in Black babies and young girls who developed breasts and pubic hair after using shampoo containing estrogen or placental extract. When the girls stopped using the shampoo, the hair and breast development receded, according to a study published in the journal Clinical Pediatrics in 1998.
Since then, Dr. James-Todd and other researchers have linked chemicals in hair products to a variety of health issues more prevalent among Black women – from early puberty to preterm birth, obesity, and diabetes.
In recent years, researchers have focused on a possible connection between ingredients in chemical relaxers and hormone-related cancers, like the one Ms. Hughes developed, which tend to be more aggressive and deadly in Black women.
A 2017 study found White women who used chemical relaxers were nearly twice as likely to develop breast cancer as those who did not use them. Because the vast majority of the Black study participants used relaxers, researchers could not effectively test the association in Black women, said lead author Adana Llanos, PhD, associate professor of epidemiology at Columbia University’s Mailman School of Public Health, New York.
Researchers did test it in 2020.
The so-called Sister Study, a landmark National Institute of Environmental Health Sciences investigation into the causes of breast cancer and related diseases, followed 50,000 U.S. women whose sisters had been diagnosed with breast cancer and who were cancer-free when they enrolled. Regardless of race, women who reported using relaxers in the prior year were 18% more likely to be diagnosed with breast cancer. Those who used relaxers at least every 5-8 weeks had a 31% higher breast cancer risk.
Nearly 75% of the Black sisters used relaxers in the prior year, compared with 3% of the non-Hispanic White sisters. Three-quarters of Black women self-reported using the straighteners as adolescents, and frequent use of chemical straighteners during adolescence raised the risk of premenopausal breast cancer, a 2021 NIH-funded study in the International Journal of Cancer found.
Another 2021 analysis of the Sister Study data showed sisters who self-reported that they frequently used relaxers or pressing products doubled their ovarian cancer risk. In 2022, another study found frequent use more than doubled uterine cancer risk.
After researchers discovered the link with uterine cancer, some called for policy changes and other measures to reduce exposure to chemical relaxers.
“It is time to intervene,” Dr. Llanos and her colleagues wrote in a Journal of the National Cancer Institute editorial accompanying the uterine cancer analysis. While acknowledging the need for more research, they issued a “call for action.”
No one can say that using permanent hair straighteners will give you cancer, Dr. Llanos said in an interview. “That’s not how cancer works,” she said, noting that some smokers never develop lung cancer, despite tobacco use being a known risk factor.
The body of research linking hair straighteners and cancer is more limited, said Dr. Llanos, who quit using chemical relaxers 15 years ago. But, she asked rhetorically, “Do we need to do the research for 50 more years to know that chemical relaxers are harmful?”
Charlotte R. Gamble, MD, a gynecological oncologist whose Washington, D.C., practice includes Black women with uterine and ovarian cancer, said she and her colleagues see the uterine cancer study findings as worthy of further exploration – but not yet worthy of discussion with patients.
“The jury’s out for me personally,” she said. “There’s so much more data that’s needed.”
Meanwhile, Dr. James-Todd and other researchers believe they have built a solid body of evidence.
“There are enough things we do know to begin taking action, developing interventions, providing useful information to clinicians and patients and the general public,” said Traci N. Bethea, PhD, assistant professor in the Office of Minority Health and Health Disparities Research at Georgetown University.
Responsibility for regulating personal-care products, including chemical hair straighteners and hair dyes – which also have been linked to hormone-related cancers – lies with the Food and Drug Administration. But the FDA does not subject personal-care products to the same approval process it uses for food and drugs. The FDA restricts only 11 categories of chemicals used in cosmetics, while concerns about health effects have prompted the European Union to restrict the use of at least 2,400 substances.
In March, Reps. Ayanna Pressley (D-Mass.) and Shontel Brown (D-Ohio) asked the FDA to investigate the potential health threat posed by chemical relaxers. An FDA representative said the agency would look into it.
Natural hairstyles are enjoying a resurgence among Black girls and women, but many continue to rely on the creamy crack, said Dede Teteh, DrPH, assistant professor of public health at Chapman University, Irvine, Calif.
She had her first straightening perm at 8 and has struggled to withdraw from relaxers as an adult, said Dr. Teteh, who now wears locs. Not long ago, she considered chemically straightening her hair for an academic job interview because she didn’t want her hair to “be a hindrance” when she appeared before White professors.
Dr. Teteh led “The Cost of Beauty,” a hair-health research project published in 2017. She and her team interviewed 91 Black women in Southern California. Some became “combative” at the idea of quitting relaxers and claimed “everything can cause cancer.”
Their reactions speak to the challenges Black women face in America, Dr. Teteh said.
“It’s not that people do not want to hear the information related to their health,” she said. “But they want people to share the information in a way that it’s really empathetic to the plight of being Black here in the United States.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – the independent source for health policy research, polling, and journalism.
New tech promises better blood oxygen readings on dark skin
A recent study adds weight to earlier findings that their device works.
“It is a new, first-in-class technology,” said Sanjay Gokhale, MD, the bioengineer who is leading this research at the University of Texas at Arlington. “The team conducted extensive preclinical work and carried out phase 1 studies in human volunteers, demonstrating sensitivity and accuracy.”
It’s one of several projects underway to update pulse oximetry, a technology based on research in lighter-skinned people that has not changed much in 50 years.
The pulse oximeter, or “pulse ox,” measures the saturation of oxygen in your hemoglobin (a protein in red blood cells). But it tends to overestimate the oxygen saturation in patients with darker skin by about 2%-3%. That may not sound like a lot, but it’s enough to delay major treatment for respiratory issues like COVID-19.
“Falsely elevated readings from commercial oximeters have delayed treatment of Black COVID-19 patients for hours in some cases,” said Divya Chander, MD, PhD, an anesthesiologist in Oakland, Calif., and chair of neuroscience at The Singularity Group. (Dr. Chander was not involved in the UT Arlington research.)
Early research happening separately at Brown University and Tufts University aims to redesign the pulse oximeter to get accurate readings in patients of all skin tones. University of California, San Diego, researchers are looking into a method that measures blood oxygen using sound in combination with light. Other solutions try to correct for skin tone with algorithms.
The device from UT Arlington uses an algorithm too, but its main innovation is that it replaces red light with green light.
Red light, green light
Traditional oximetry devices, which typically clip on to the patient’s fingertip, use LEDs to beam light through the skin at two wavelengths: one in the red part of the spectrum, the other in the infrared. The light transmits from one side of the clip to the other, passing through arterial blood as it pulses.
The device calculates a patient’s oxygenation based on how much light of each wavelength is absorbed by hemoglobin in the blood. Oxygenated hemoglobin absorbs the light differently than deoxygenated hemoglobin, so oxygenation can be represented as a percentage; 100% means all hemoglobin is completely oxygenated. But the melanin in skin can interfere with the absorption of light and affect the results.
The green light strategy measures not absorption but reflectance – how much of the light bounces back. As with traditional oximetry, the green-light method uses two wavelengths. Each is a different shade of green, and the two forms of hemoglobin reflect them differently.
Using an algorithm developed by the researchers, the device can capture readings in patients of all skin tones, the researchers say. And because it works on the wrist rather than a finger, the device also eliminates issues with cold fingers and dark nail polish – both known to reduce accuracy in traditional oximetry.
In the latest experiments, the researchers tested the technology on synthetic skin samples with varying amounts of melanin, Dr. Gokhale said. The device picked up changes in blood oxygen saturation even in samples with high melanin levels.
In a study published last year, the technology was tested in 16 people against an invasive handheld blood analyzer and a noninvasive commercial pulse oximeter, and found to be comparable to the invasive method.
A drawback
The green light approach could be “game changing,” Dr. Chander said. But there is a drawback.
Since green light doesn’t penetrate as deeply, this approach measures blood oxygen saturation in capillary beds (small blood vessels very close to the skin surface). By contrast, traditional oximetry measures oxygen saturation in an artery as it pulses – thus the name pulse oximetry.
Valuable information can be obtained from an arterial pulse.
Changes in arterial pulse, known as the waveforms, “can tell us about a patient’s hydration status [for instance],” Dr. Chander said. “In a mechanically ventilated patient, this variation with a patient’s respiratory cycle can give us feedback about how responsive the patient will be to fluid resuscitation if their blood pressure is too low.”
Given such considerations, the green light method may be useful as an adjunct, not a full replacement, to a standard pulse ox, Dr. Chander noted.
A version of this article appeared on WebMD.com.
A recent study adds weight to earlier findings that their device works.
“It is a new, first-in-class technology,” said Sanjay Gokhale, MD, the bioengineer who is leading this research at the University of Texas at Arlington. “The team conducted extensive preclinical work and carried out phase 1 studies in human volunteers, demonstrating sensitivity and accuracy.”
It’s one of several projects underway to update pulse oximetry, a technology based on research in lighter-skinned people that has not changed much in 50 years.
The pulse oximeter, or “pulse ox,” measures the saturation of oxygen in your hemoglobin (a protein in red blood cells). But it tends to overestimate the oxygen saturation in patients with darker skin by about 2%-3%. That may not sound like a lot, but it’s enough to delay major treatment for respiratory issues like COVID-19.
“Falsely elevated readings from commercial oximeters have delayed treatment of Black COVID-19 patients for hours in some cases,” said Divya Chander, MD, PhD, an anesthesiologist in Oakland, Calif., and chair of neuroscience at The Singularity Group. (Dr. Chander was not involved in the UT Arlington research.)
Early research happening separately at Brown University and Tufts University aims to redesign the pulse oximeter to get accurate readings in patients of all skin tones. University of California, San Diego, researchers are looking into a method that measures blood oxygen using sound in combination with light. Other solutions try to correct for skin tone with algorithms.
The device from UT Arlington uses an algorithm too, but its main innovation is that it replaces red light with green light.
Red light, green light
Traditional oximetry devices, which typically clip on to the patient’s fingertip, use LEDs to beam light through the skin at two wavelengths: one in the red part of the spectrum, the other in the infrared. The light transmits from one side of the clip to the other, passing through arterial blood as it pulses.
The device calculates a patient’s oxygenation based on how much light of each wavelength is absorbed by hemoglobin in the blood. Oxygenated hemoglobin absorbs the light differently than deoxygenated hemoglobin, so oxygenation can be represented as a percentage; 100% means all hemoglobin is completely oxygenated. But the melanin in skin can interfere with the absorption of light and affect the results.
The green light strategy measures not absorption but reflectance – how much of the light bounces back. As with traditional oximetry, the green-light method uses two wavelengths. Each is a different shade of green, and the two forms of hemoglobin reflect them differently.
Using an algorithm developed by the researchers, the device can capture readings in patients of all skin tones, the researchers say. And because it works on the wrist rather than a finger, the device also eliminates issues with cold fingers and dark nail polish – both known to reduce accuracy in traditional oximetry.
In the latest experiments, the researchers tested the technology on synthetic skin samples with varying amounts of melanin, Dr. Gokhale said. The device picked up changes in blood oxygen saturation even in samples with high melanin levels.
In a study published last year, the technology was tested in 16 people against an invasive handheld blood analyzer and a noninvasive commercial pulse oximeter, and found to be comparable to the invasive method.
A drawback
The green light approach could be “game changing,” Dr. Chander said. But there is a drawback.
Since green light doesn’t penetrate as deeply, this approach measures blood oxygen saturation in capillary beds (small blood vessels very close to the skin surface). By contrast, traditional oximetry measures oxygen saturation in an artery as it pulses – thus the name pulse oximetry.
Valuable information can be obtained from an arterial pulse.
Changes in arterial pulse, known as the waveforms, “can tell us about a patient’s hydration status [for instance],” Dr. Chander said. “In a mechanically ventilated patient, this variation with a patient’s respiratory cycle can give us feedback about how responsive the patient will be to fluid resuscitation if their blood pressure is too low.”
Given such considerations, the green light method may be useful as an adjunct, not a full replacement, to a standard pulse ox, Dr. Chander noted.
A version of this article appeared on WebMD.com.
A recent study adds weight to earlier findings that their device works.
“It is a new, first-in-class technology,” said Sanjay Gokhale, MD, the bioengineer who is leading this research at the University of Texas at Arlington. “The team conducted extensive preclinical work and carried out phase 1 studies in human volunteers, demonstrating sensitivity and accuracy.”
It’s one of several projects underway to update pulse oximetry, a technology based on research in lighter-skinned people that has not changed much in 50 years.
The pulse oximeter, or “pulse ox,” measures the saturation of oxygen in your hemoglobin (a protein in red blood cells). But it tends to overestimate the oxygen saturation in patients with darker skin by about 2%-3%. That may not sound like a lot, but it’s enough to delay major treatment for respiratory issues like COVID-19.
“Falsely elevated readings from commercial oximeters have delayed treatment of Black COVID-19 patients for hours in some cases,” said Divya Chander, MD, PhD, an anesthesiologist in Oakland, Calif., and chair of neuroscience at The Singularity Group. (Dr. Chander was not involved in the UT Arlington research.)
Early research happening separately at Brown University and Tufts University aims to redesign the pulse oximeter to get accurate readings in patients of all skin tones. University of California, San Diego, researchers are looking into a method that measures blood oxygen using sound in combination with light. Other solutions try to correct for skin tone with algorithms.
The device from UT Arlington uses an algorithm too, but its main innovation is that it replaces red light with green light.
Red light, green light
Traditional oximetry devices, which typically clip on to the patient’s fingertip, use LEDs to beam light through the skin at two wavelengths: one in the red part of the spectrum, the other in the infrared. The light transmits from one side of the clip to the other, passing through arterial blood as it pulses.
The device calculates a patient’s oxygenation based on how much light of each wavelength is absorbed by hemoglobin in the blood. Oxygenated hemoglobin absorbs the light differently than deoxygenated hemoglobin, so oxygenation can be represented as a percentage; 100% means all hemoglobin is completely oxygenated. But the melanin in skin can interfere with the absorption of light and affect the results.
The green light strategy measures not absorption but reflectance – how much of the light bounces back. As with traditional oximetry, the green-light method uses two wavelengths. Each is a different shade of green, and the two forms of hemoglobin reflect them differently.
Using an algorithm developed by the researchers, the device can capture readings in patients of all skin tones, the researchers say. And because it works on the wrist rather than a finger, the device also eliminates issues with cold fingers and dark nail polish – both known to reduce accuracy in traditional oximetry.
In the latest experiments, the researchers tested the technology on synthetic skin samples with varying amounts of melanin, Dr. Gokhale said. The device picked up changes in blood oxygen saturation even in samples with high melanin levels.
In a study published last year, the technology was tested in 16 people against an invasive handheld blood analyzer and a noninvasive commercial pulse oximeter, and found to be comparable to the invasive method.
A drawback
The green light approach could be “game changing,” Dr. Chander said. But there is a drawback.
Since green light doesn’t penetrate as deeply, this approach measures blood oxygen saturation in capillary beds (small blood vessels very close to the skin surface). By contrast, traditional oximetry measures oxygen saturation in an artery as it pulses – thus the name pulse oximetry.
Valuable information can be obtained from an arterial pulse.
Changes in arterial pulse, known as the waveforms, “can tell us about a patient’s hydration status [for instance],” Dr. Chander said. “In a mechanically ventilated patient, this variation with a patient’s respiratory cycle can give us feedback about how responsive the patient will be to fluid resuscitation if their blood pressure is too low.”
Given such considerations, the green light method may be useful as an adjunct, not a full replacement, to a standard pulse ox, Dr. Chander noted.
A version of this article appeared on WebMD.com.
Squamous cell carcinoma
THE COMPARISON
A A 51-year-old Hispanic man with a squamous cell carcinoma (SCC) of the keratoacanthoma type on the arm.
B A 75-year-old Black man with an SCC of the keratoacanthoma type on the abdomen.
C An African woman with an SCC on the lower lip decades after a large facial burn, which is known as a Marjolin ulcer.
Cutaneous squamous cell carcinoma (SCC) develops from a malignant tumor of the keratinocytes, eccrine glands, or pilosebaceous units that invades the dermis. Risk factors include lighter skin tone, higher cumulative sun exposure, human papillomavirus (HPV) infection, hidradenitis suppurativa (HS), lichen sclerosus, family history of skin cancer,1 and immunosuppression.2 It typically affects sun-exposed areas of the body such as the face, scalp, neck, and extensor surfaces of the arms (FIGURE A).3,4 However, in those with darker skin tones, the most common anatomic sites are those that are not exposed to the sun (FIGURE B). SCC is diagnosed via skin biopsy. Treatment options include surgical excision, destructive methods such as electrodesiccation and curettage, and Mohs micrographic surgery. Cutaneous SCC has a cure rate of more than 95% and a mortality rate of 1.5% to 2% in the United States.3
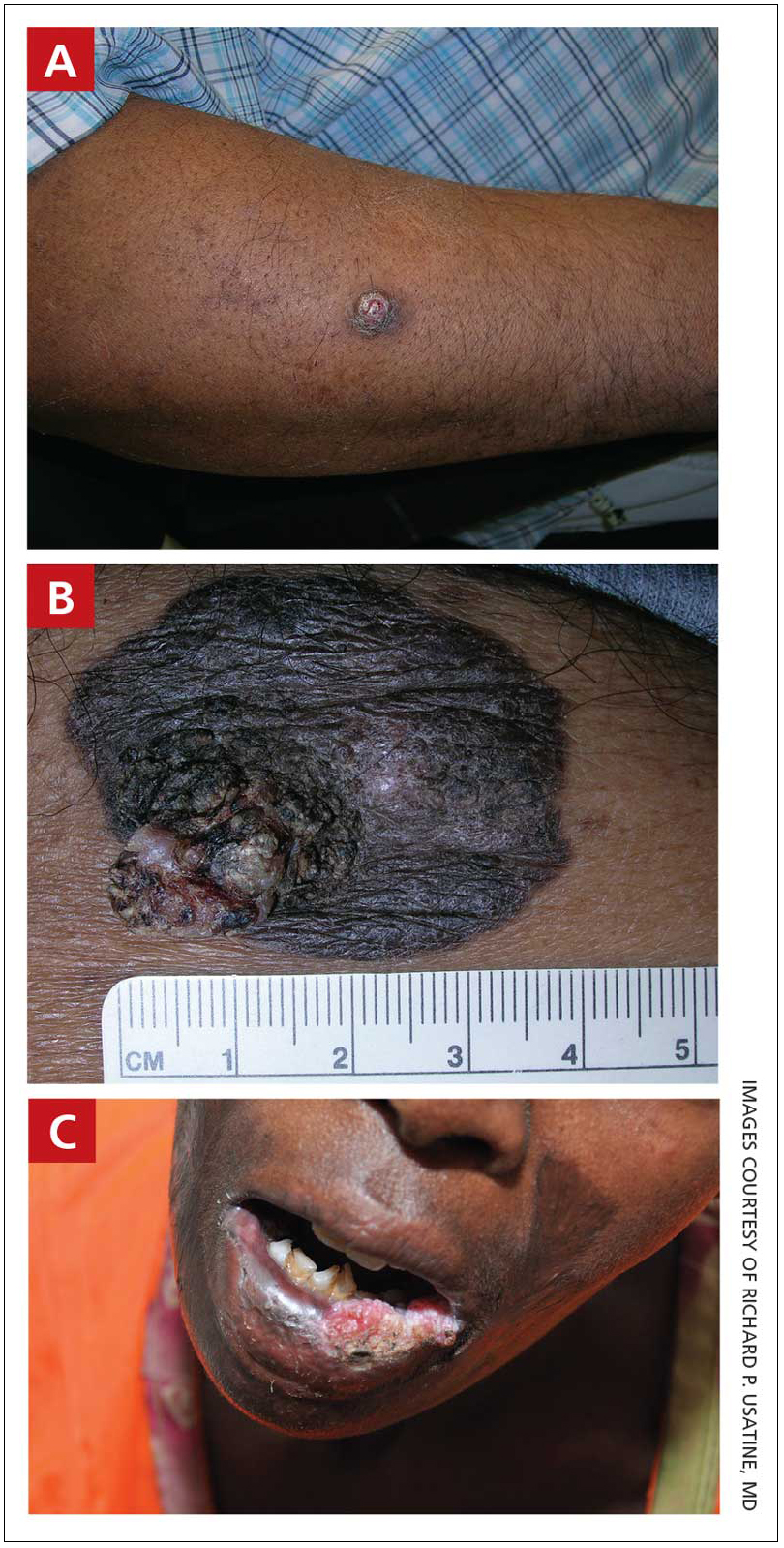
Epidemiology
SCC is the most common skin cancer occurring in Black individuals, manifesting primarily in the fifth decade of life.5-7 It is the second most common skin cancer in White, Hispanic, and Asian individuals and is more common in males.8 In a study of organ transplant recipients (N = 413), Pritchett et al9 reported that HPV infection was a major risk factor in Hispanic patients because 66.7% of those with SCC had a history of HPV. However, HPV is a risk factor for SCC in all ethnic groups.10
Key clinical features in people with darker skin tones
Anatomic location
- The lower legs and anogenital areas are the most common sites for SCC in patients with skin of color.4,11
- In Black women, SCC occurs more often on sun-exposed areas such as the arms and legs compared to Black men.7,12-14
- The genitalia, perianal area, ocular mucosa, and oral mucosa are the least likely areas to be routinely examined, even in skin cancer clinics that see highrisk patients, despite the SCC risk in the anogenital area.15,16
- Squamous cell carcinoma of the lips and scalp is more likely to occur in Black women vs Black men.4,7,17
Clinical appearance
- In those with darker skin tones, SCCs may appear hyperpigmented4 or hyperkeratotic with a lack of erythema and an inconsistent appearance.6,7,18
- A nonhealing ulceration of the skin should prompt a biopsy to rule out SCC.3,19
Worth noting
In patients with darker skin tones, the risk for SCC increases in areas with chronic inflammation and scarring of the skin.4,6,7,11,18,20-22 In Black patients, 20% to 40% of cases of SCC occur in the setting of chronic inflammation and scarring.6,7,18 Chronic inflammatory conditions include ulcers, lupus vulgaris, discoid lupus erythematosus, and HPV. In patients with discoid lupus erythematosus, there is an additive effect of sun exposure on the scars, which may play a role in the pathogenesis and metastasis risk for skin cancer in Black patients.4 Other scarring conditions include thermal or chemical burn scars, areas of physical trauma, and prior sites of radiation treatment.14,23 SCC arising in a burn scar is called a Marjolin ulcer or malignant degeneration of a scar (FIGURE C). It is reported more often in lower-income, underresourced countries, which may suggest the need for early detection in populations with skin of color.24
SCC is more aggressive in sites that are not exposed to sun compared to sun-exposed areas.17,25
Continue to: The risk for SCC...
The risk for SCC is increased in immunocompromised patients,2 especially those with HPV.10
The prevalence of SCC in those with HS is approximately 4.6%. The chronic inflammation and irritation from HS in association with other risk factors such as tobacco use may contribute to the malignant transformation to SCC.26
Health disparity highlight
- The risk for metastasis from SCC is 20% to 40% in Black patients vs 1% to 4% in White patients.4,6,27
- Penile SCC was associated with a lower overall survival rate in patients of African descent.20,21
- The increased morbidity and mortality from SCC in patients with skin of color may be attributed to delays in diagnosis and treatment as well as an incomplete understanding of tumor genetics.4,6,18
ACKNOWLEDGMENT
The authors thank Elyse Gadra (Philadelphia, Pennsylvania) for assistance in the preparation of this manuscript.
1. Asgari MM, Warton EM, Whittemore AS. Family history of skin cancer is associated with increased risk of cutaneous squamous cell carcinoma. Dermatol Surg. 2015;41:481-486. doi: 10.1097/ DSS.0000000000000292
2. Harwood CA, Surentheran T, McGregor JM, et al. Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol. 2000;61:289-297. doi: 10.1002/1096-9071(200007)61:3<289::aidjmv2> 3.0.co;2-z
3. Kallini JR, Nouran H, Khachemoune A. Squamous cell carcinoma of the skin: epidemiology, classification, management, and novel trends. Int J Dermatol. 2015;54:130-140. doi: 10.1111/ijd.12553.
4. Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public J Am Acad Dermatol. 2014;70:748-762. doi: 10.1016/j.jaad.2013.11.038
5. Bradford PT. Skin cancer in skin of color. Dermatol Nurse. 2009;21:170-177.
6. Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760.
7. Davis DS, Robinson C, Callender VD. Skin cancer in women of color: epidemiology, pathogenesis and clinical manifestations. Int J Womens Dermatol. 2021;7:127-134. doi: 10.1016/ j.ijwd.2021.01.017
8. Baum B, Duarte AM. Skin cancer epidemic in American Hispanic and Latino patients. In: Silverberg N, Duran-McKinster C, Tay Y-K, eds. Pediatric Skin of Color. Springer; 2015:453-460.
9. Pritchett EN, Doyle A, Shaver CM, et al. Nonmelanoma skin cancer in nonwhite organ transplant recipients. JAMA Dermatol. 2016;152: 1348-1353. doi: 10.1001/jamadermatol.2016.3328
10. Karagas MR, Nelson HH, Sehr P, et al. Human papillomavirus infection and incidence of squamous cell and basal cell carcinomas of the skin. J Natl Cancer Inst. 2006;98:389-395. doi: 10.1093/jnci/ djj092
11. Gohara M. Skin cancer: an African perspective. Br J Dermatol. 2015;173:17-21. doi: 10.1111/bjd.13380
12. Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8-18. doi: 10.1016/ s1011-1344(01)00198-1
13. Halder RM, Bang KM. Skin cancer in African Americans in the United States. Dermatol Clin. 1988;6:397-407.
14. Mora RG, Perniciaro C. Cancer of the skin in blacks. I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543. doi: 10.1016/s0190-9622 (81)70113-0
15. Bajaj S, Wolner ZJ, Dusza SW, et al. Total body skin examination practices: a survey study amongst dermatologists at high-risk skin cancer clinics. Dermatol Pract Concept. 2019;9:132-138. doi: 10.5826/dpc.0902a09
16. Rieder EA, Mu EW, Wang J, et al. Dermatologist practices during total body skin examinations: a survey study. J Drugs Dermatol. 2018;17:516-520.
17. Halder RM, Ara CJ. Skin cancer and photoaging in ethnic skin. Dermatol Clin. 2003;21:725-732, x. doi: 10.1016/s0733-8635 (03)00085-8
18. Higgins S, Nazemi A, Chow M, et al. Review of nonmelanoma skin cancer in African Americans, Hispanics, and Asians. Dermatol Surg. 2018;44:903-910.
19. Sng J, Koh D, Siong WC, et al. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009; 61:426-432.
20. Shao K, Feng H. Racial and ethnic healthcare disparities in skin cancer in the United States: a review of existing inequities, contributing factors, and potential solutions. J Clin Aesthet Dermatol. 2022;15:16-22.
21. Shao K, Hooper J, Feng H. Racial and ethnic health disparities in dermatology in the United States. Part 2: disease-specific epidemiology, characteristics, management, and outcomes. J Am Acad Dermatol. 2022;87:733-744. doi: 10.1016/j.jaad.2021. 12.062
22. Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137- 151. doi: 10.1007/s40257-021-00662-z
23. Copcu E, Aktas A, Sis¸man N, et al. Thirty-one cases of Marjolin’s ulcer. Clin Exp Dermatol. 2003;28:138-141. doi: 10.1046/j.1365- 2230.2003.01210.x
24. Abdi MA, Yan M, Hanna TP. Systematic review of modern case series of squamous cell cancer arising in a chronic ulcer (Marjolin’s ulcer) of the skin. JCO Glob Oncol. 2020;6:809-818. doi: 10.1200/ GO.20.00094
25. Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi: 10.1016/j.det.2019.05.009
26. Chapman S, Delgadillo D, Barber C, et al. Cutanteous squamous cell complicating hidradenitis suppurativa: a review of the prevalence, pathogenesis, and treatment of this dreaded complication. Acta Dermatovenerol Al Pannocica Adriat. 2018;27:25-28.
27. Kailas A, Botwin AL, Pritchett EN, et al. Assessing the effectiveness of knowledge-based interventions in increasing skin cancer awareness, knowledge, and protective behaviors in skin of color populations. Cutis. 2017;100:235-240.
THE COMPARISON
A A 51-year-old Hispanic man with a squamous cell carcinoma (SCC) of the keratoacanthoma type on the arm.
B A 75-year-old Black man with an SCC of the keratoacanthoma type on the abdomen.
C An African woman with an SCC on the lower lip decades after a large facial burn, which is known as a Marjolin ulcer.
Cutaneous squamous cell carcinoma (SCC) develops from a malignant tumor of the keratinocytes, eccrine glands, or pilosebaceous units that invades the dermis. Risk factors include lighter skin tone, higher cumulative sun exposure, human papillomavirus (HPV) infection, hidradenitis suppurativa (HS), lichen sclerosus, family history of skin cancer,1 and immunosuppression.2 It typically affects sun-exposed areas of the body such as the face, scalp, neck, and extensor surfaces of the arms (FIGURE A).3,4 However, in those with darker skin tones, the most common anatomic sites are those that are not exposed to the sun (FIGURE B). SCC is diagnosed via skin biopsy. Treatment options include surgical excision, destructive methods such as electrodesiccation and curettage, and Mohs micrographic surgery. Cutaneous SCC has a cure rate of more than 95% and a mortality rate of 1.5% to 2% in the United States.3
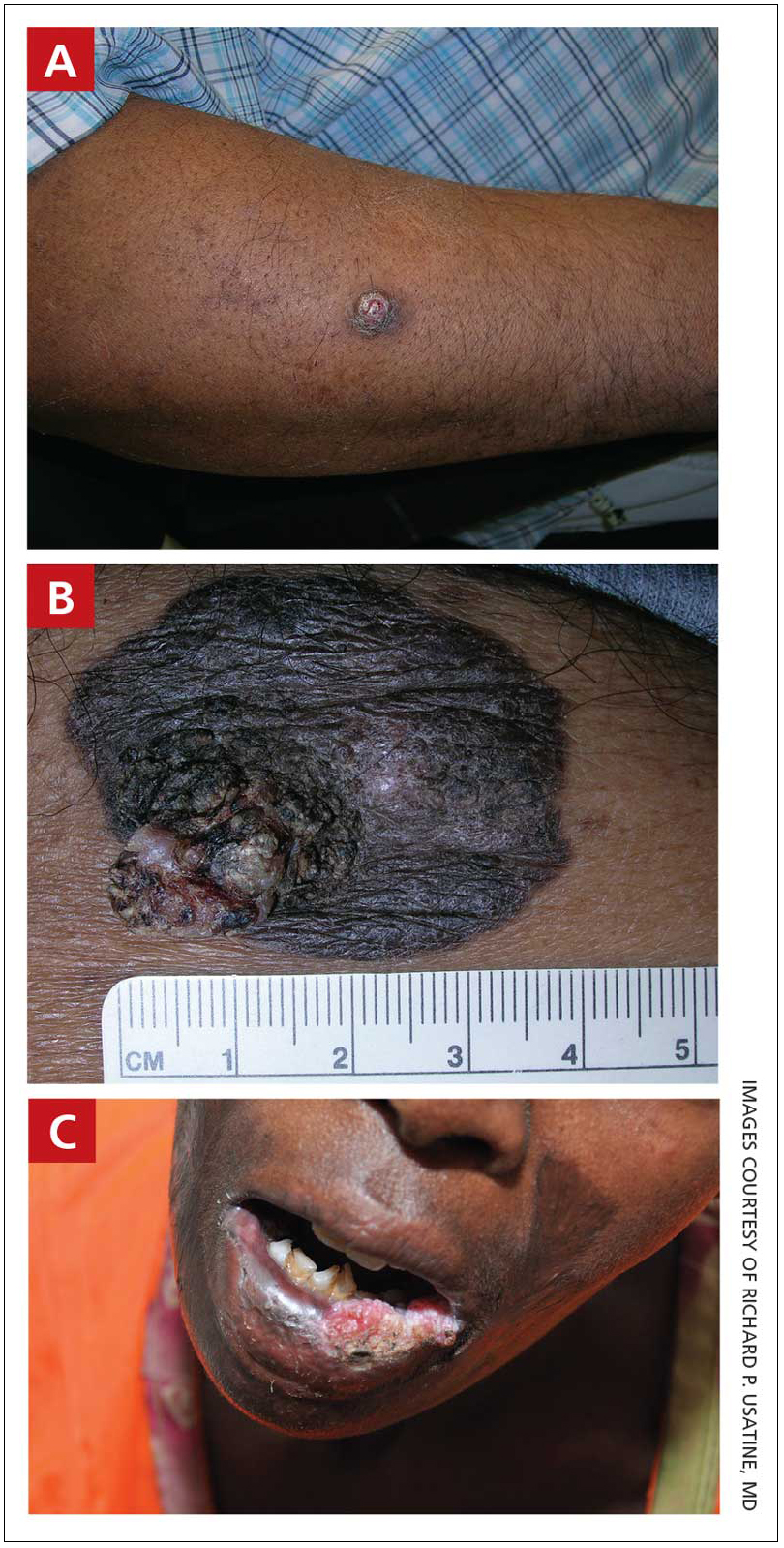
Epidemiology
SCC is the most common skin cancer occurring in Black individuals, manifesting primarily in the fifth decade of life.5-7 It is the second most common skin cancer in White, Hispanic, and Asian individuals and is more common in males.8 In a study of organ transplant recipients (N = 413), Pritchett et al9 reported that HPV infection was a major risk factor in Hispanic patients because 66.7% of those with SCC had a history of HPV. However, HPV is a risk factor for SCC in all ethnic groups.10
Key clinical features in people with darker skin tones
Anatomic location
- The lower legs and anogenital areas are the most common sites for SCC in patients with skin of color.4,11
- In Black women, SCC occurs more often on sun-exposed areas such as the arms and legs compared to Black men.7,12-14
- The genitalia, perianal area, ocular mucosa, and oral mucosa are the least likely areas to be routinely examined, even in skin cancer clinics that see highrisk patients, despite the SCC risk in the anogenital area.15,16
- Squamous cell carcinoma of the lips and scalp is more likely to occur in Black women vs Black men.4,7,17
Clinical appearance
- In those with darker skin tones, SCCs may appear hyperpigmented4 or hyperkeratotic with a lack of erythema and an inconsistent appearance.6,7,18
- A nonhealing ulceration of the skin should prompt a biopsy to rule out SCC.3,19
Worth noting
In patients with darker skin tones, the risk for SCC increases in areas with chronic inflammation and scarring of the skin.4,6,7,11,18,20-22 In Black patients, 20% to 40% of cases of SCC occur in the setting of chronic inflammation and scarring.6,7,18 Chronic inflammatory conditions include ulcers, lupus vulgaris, discoid lupus erythematosus, and HPV. In patients with discoid lupus erythematosus, there is an additive effect of sun exposure on the scars, which may play a role in the pathogenesis and metastasis risk for skin cancer in Black patients.4 Other scarring conditions include thermal or chemical burn scars, areas of physical trauma, and prior sites of radiation treatment.14,23 SCC arising in a burn scar is called a Marjolin ulcer or malignant degeneration of a scar (FIGURE C). It is reported more often in lower-income, underresourced countries, which may suggest the need for early detection in populations with skin of color.24
SCC is more aggressive in sites that are not exposed to sun compared to sun-exposed areas.17,25
Continue to: The risk for SCC...
The risk for SCC is increased in immunocompromised patients,2 especially those with HPV.10
The prevalence of SCC in those with HS is approximately 4.6%. The chronic inflammation and irritation from HS in association with other risk factors such as tobacco use may contribute to the malignant transformation to SCC.26
Health disparity highlight
- The risk for metastasis from SCC is 20% to 40% in Black patients vs 1% to 4% in White patients.4,6,27
- Penile SCC was associated with a lower overall survival rate in patients of African descent.20,21
- The increased morbidity and mortality from SCC in patients with skin of color may be attributed to delays in diagnosis and treatment as well as an incomplete understanding of tumor genetics.4,6,18
ACKNOWLEDGMENT
The authors thank Elyse Gadra (Philadelphia, Pennsylvania) for assistance in the preparation of this manuscript.
THE COMPARISON
A A 51-year-old Hispanic man with a squamous cell carcinoma (SCC) of the keratoacanthoma type on the arm.
B A 75-year-old Black man with an SCC of the keratoacanthoma type on the abdomen.
C An African woman with an SCC on the lower lip decades after a large facial burn, which is known as a Marjolin ulcer.
Cutaneous squamous cell carcinoma (SCC) develops from a malignant tumor of the keratinocytes, eccrine glands, or pilosebaceous units that invades the dermis. Risk factors include lighter skin tone, higher cumulative sun exposure, human papillomavirus (HPV) infection, hidradenitis suppurativa (HS), lichen sclerosus, family history of skin cancer,1 and immunosuppression.2 It typically affects sun-exposed areas of the body such as the face, scalp, neck, and extensor surfaces of the arms (FIGURE A).3,4 However, in those with darker skin tones, the most common anatomic sites are those that are not exposed to the sun (FIGURE B). SCC is diagnosed via skin biopsy. Treatment options include surgical excision, destructive methods such as electrodesiccation and curettage, and Mohs micrographic surgery. Cutaneous SCC has a cure rate of more than 95% and a mortality rate of 1.5% to 2% in the United States.3
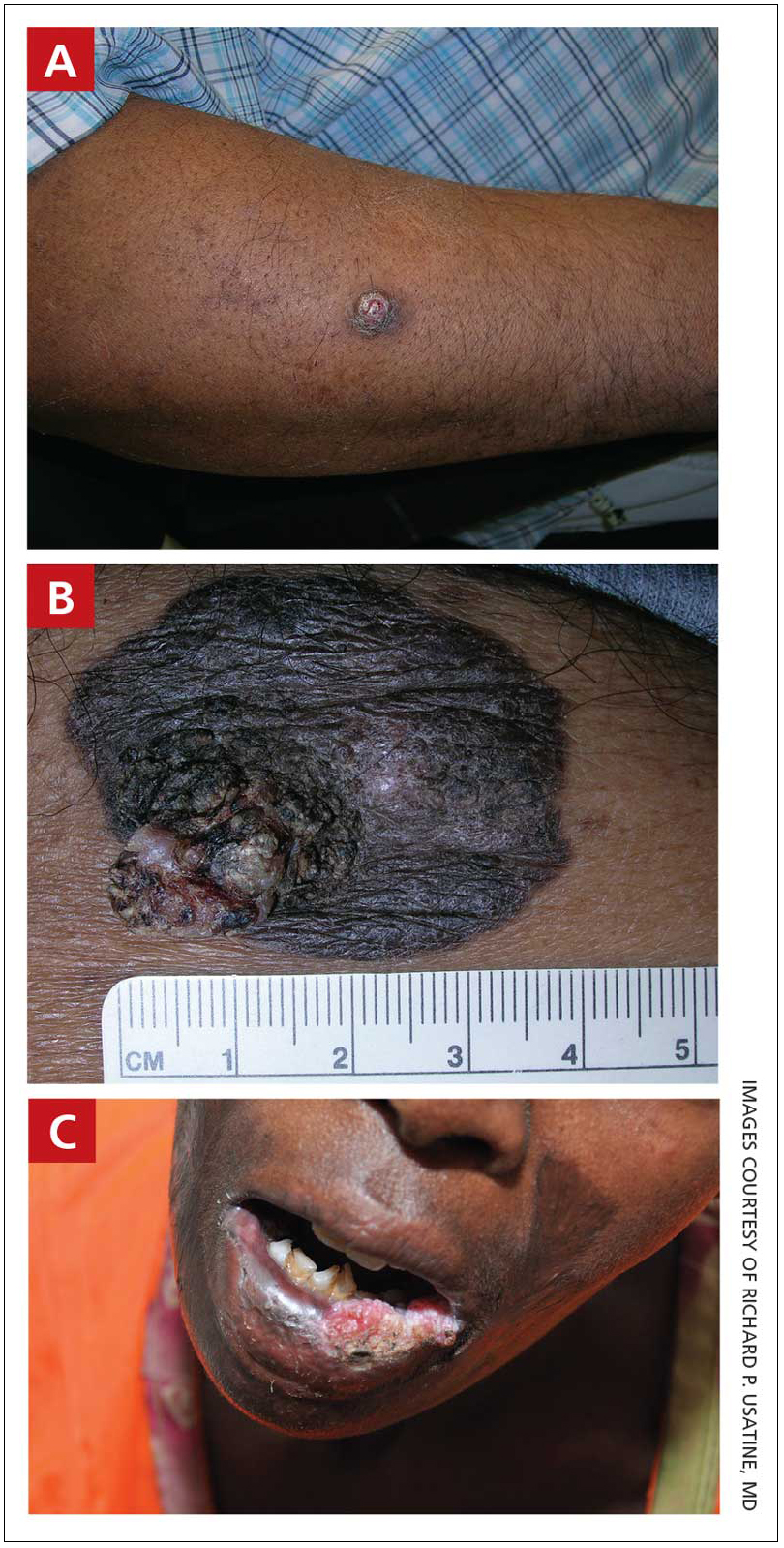
Epidemiology
SCC is the most common skin cancer occurring in Black individuals, manifesting primarily in the fifth decade of life.5-7 It is the second most common skin cancer in White, Hispanic, and Asian individuals and is more common in males.8 In a study of organ transplant recipients (N = 413), Pritchett et al9 reported that HPV infection was a major risk factor in Hispanic patients because 66.7% of those with SCC had a history of HPV. However, HPV is a risk factor for SCC in all ethnic groups.10
Key clinical features in people with darker skin tones
Anatomic location
- The lower legs and anogenital areas are the most common sites for SCC in patients with skin of color.4,11
- In Black women, SCC occurs more often on sun-exposed areas such as the arms and legs compared to Black men.7,12-14
- The genitalia, perianal area, ocular mucosa, and oral mucosa are the least likely areas to be routinely examined, even in skin cancer clinics that see highrisk patients, despite the SCC risk in the anogenital area.15,16
- Squamous cell carcinoma of the lips and scalp is more likely to occur in Black women vs Black men.4,7,17
Clinical appearance
- In those with darker skin tones, SCCs may appear hyperpigmented4 or hyperkeratotic with a lack of erythema and an inconsistent appearance.6,7,18
- A nonhealing ulceration of the skin should prompt a biopsy to rule out SCC.3,19
Worth noting
In patients with darker skin tones, the risk for SCC increases in areas with chronic inflammation and scarring of the skin.4,6,7,11,18,20-22 In Black patients, 20% to 40% of cases of SCC occur in the setting of chronic inflammation and scarring.6,7,18 Chronic inflammatory conditions include ulcers, lupus vulgaris, discoid lupus erythematosus, and HPV. In patients with discoid lupus erythematosus, there is an additive effect of sun exposure on the scars, which may play a role in the pathogenesis and metastasis risk for skin cancer in Black patients.4 Other scarring conditions include thermal or chemical burn scars, areas of physical trauma, and prior sites of radiation treatment.14,23 SCC arising in a burn scar is called a Marjolin ulcer or malignant degeneration of a scar (FIGURE C). It is reported more often in lower-income, underresourced countries, which may suggest the need for early detection in populations with skin of color.24
SCC is more aggressive in sites that are not exposed to sun compared to sun-exposed areas.17,25
Continue to: The risk for SCC...
The risk for SCC is increased in immunocompromised patients,2 especially those with HPV.10
The prevalence of SCC in those with HS is approximately 4.6%. The chronic inflammation and irritation from HS in association with other risk factors such as tobacco use may contribute to the malignant transformation to SCC.26
Health disparity highlight
- The risk for metastasis from SCC is 20% to 40% in Black patients vs 1% to 4% in White patients.4,6,27
- Penile SCC was associated with a lower overall survival rate in patients of African descent.20,21
- The increased morbidity and mortality from SCC in patients with skin of color may be attributed to delays in diagnosis and treatment as well as an incomplete understanding of tumor genetics.4,6,18
ACKNOWLEDGMENT
The authors thank Elyse Gadra (Philadelphia, Pennsylvania) for assistance in the preparation of this manuscript.
1. Asgari MM, Warton EM, Whittemore AS. Family history of skin cancer is associated with increased risk of cutaneous squamous cell carcinoma. Dermatol Surg. 2015;41:481-486. doi: 10.1097/ DSS.0000000000000292
2. Harwood CA, Surentheran T, McGregor JM, et al. Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol. 2000;61:289-297. doi: 10.1002/1096-9071(200007)61:3<289::aidjmv2> 3.0.co;2-z
3. Kallini JR, Nouran H, Khachemoune A. Squamous cell carcinoma of the skin: epidemiology, classification, management, and novel trends. Int J Dermatol. 2015;54:130-140. doi: 10.1111/ijd.12553.
4. Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public J Am Acad Dermatol. 2014;70:748-762. doi: 10.1016/j.jaad.2013.11.038
5. Bradford PT. Skin cancer in skin of color. Dermatol Nurse. 2009;21:170-177.
6. Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760.
7. Davis DS, Robinson C, Callender VD. Skin cancer in women of color: epidemiology, pathogenesis and clinical manifestations. Int J Womens Dermatol. 2021;7:127-134. doi: 10.1016/ j.ijwd.2021.01.017
8. Baum B, Duarte AM. Skin cancer epidemic in American Hispanic and Latino patients. In: Silverberg N, Duran-McKinster C, Tay Y-K, eds. Pediatric Skin of Color. Springer; 2015:453-460.
9. Pritchett EN, Doyle A, Shaver CM, et al. Nonmelanoma skin cancer in nonwhite organ transplant recipients. JAMA Dermatol. 2016;152: 1348-1353. doi: 10.1001/jamadermatol.2016.3328
10. Karagas MR, Nelson HH, Sehr P, et al. Human papillomavirus infection and incidence of squamous cell and basal cell carcinomas of the skin. J Natl Cancer Inst. 2006;98:389-395. doi: 10.1093/jnci/ djj092
11. Gohara M. Skin cancer: an African perspective. Br J Dermatol. 2015;173:17-21. doi: 10.1111/bjd.13380
12. Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8-18. doi: 10.1016/ s1011-1344(01)00198-1
13. Halder RM, Bang KM. Skin cancer in African Americans in the United States. Dermatol Clin. 1988;6:397-407.
14. Mora RG, Perniciaro C. Cancer of the skin in blacks. I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543. doi: 10.1016/s0190-9622 (81)70113-0
15. Bajaj S, Wolner ZJ, Dusza SW, et al. Total body skin examination practices: a survey study amongst dermatologists at high-risk skin cancer clinics. Dermatol Pract Concept. 2019;9:132-138. doi: 10.5826/dpc.0902a09
16. Rieder EA, Mu EW, Wang J, et al. Dermatologist practices during total body skin examinations: a survey study. J Drugs Dermatol. 2018;17:516-520.
17. Halder RM, Ara CJ. Skin cancer and photoaging in ethnic skin. Dermatol Clin. 2003;21:725-732, x. doi: 10.1016/s0733-8635 (03)00085-8
18. Higgins S, Nazemi A, Chow M, et al. Review of nonmelanoma skin cancer in African Americans, Hispanics, and Asians. Dermatol Surg. 2018;44:903-910.
19. Sng J, Koh D, Siong WC, et al. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009; 61:426-432.
20. Shao K, Feng H. Racial and ethnic healthcare disparities in skin cancer in the United States: a review of existing inequities, contributing factors, and potential solutions. J Clin Aesthet Dermatol. 2022;15:16-22.
21. Shao K, Hooper J, Feng H. Racial and ethnic health disparities in dermatology in the United States. Part 2: disease-specific epidemiology, characteristics, management, and outcomes. J Am Acad Dermatol. 2022;87:733-744. doi: 10.1016/j.jaad.2021. 12.062
22. Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137- 151. doi: 10.1007/s40257-021-00662-z
23. Copcu E, Aktas A, Sis¸man N, et al. Thirty-one cases of Marjolin’s ulcer. Clin Exp Dermatol. 2003;28:138-141. doi: 10.1046/j.1365- 2230.2003.01210.x
24. Abdi MA, Yan M, Hanna TP. Systematic review of modern case series of squamous cell cancer arising in a chronic ulcer (Marjolin’s ulcer) of the skin. JCO Glob Oncol. 2020;6:809-818. doi: 10.1200/ GO.20.00094
25. Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi: 10.1016/j.det.2019.05.009
26. Chapman S, Delgadillo D, Barber C, et al. Cutanteous squamous cell complicating hidradenitis suppurativa: a review of the prevalence, pathogenesis, and treatment of this dreaded complication. Acta Dermatovenerol Al Pannocica Adriat. 2018;27:25-28.
27. Kailas A, Botwin AL, Pritchett EN, et al. Assessing the effectiveness of knowledge-based interventions in increasing skin cancer awareness, knowledge, and protective behaviors in skin of color populations. Cutis. 2017;100:235-240.
1. Asgari MM, Warton EM, Whittemore AS. Family history of skin cancer is associated with increased risk of cutaneous squamous cell carcinoma. Dermatol Surg. 2015;41:481-486. doi: 10.1097/ DSS.0000000000000292
2. Harwood CA, Surentheran T, McGregor JM, et al. Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol. 2000;61:289-297. doi: 10.1002/1096-9071(200007)61:3<289::aidjmv2> 3.0.co;2-z
3. Kallini JR, Nouran H, Khachemoune A. Squamous cell carcinoma of the skin: epidemiology, classification, management, and novel trends. Int J Dermatol. 2015;54:130-140. doi: 10.1111/ijd.12553.
4. Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public J Am Acad Dermatol. 2014;70:748-762. doi: 10.1016/j.jaad.2013.11.038
5. Bradford PT. Skin cancer in skin of color. Dermatol Nurse. 2009;21:170-177.
6. Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760.
7. Davis DS, Robinson C, Callender VD. Skin cancer in women of color: epidemiology, pathogenesis and clinical manifestations. Int J Womens Dermatol. 2021;7:127-134. doi: 10.1016/ j.ijwd.2021.01.017
8. Baum B, Duarte AM. Skin cancer epidemic in American Hispanic and Latino patients. In: Silverberg N, Duran-McKinster C, Tay Y-K, eds. Pediatric Skin of Color. Springer; 2015:453-460.
9. Pritchett EN, Doyle A, Shaver CM, et al. Nonmelanoma skin cancer in nonwhite organ transplant recipients. JAMA Dermatol. 2016;152: 1348-1353. doi: 10.1001/jamadermatol.2016.3328
10. Karagas MR, Nelson HH, Sehr P, et al. Human papillomavirus infection and incidence of squamous cell and basal cell carcinomas of the skin. J Natl Cancer Inst. 2006;98:389-395. doi: 10.1093/jnci/ djj092
11. Gohara M. Skin cancer: an African perspective. Br J Dermatol. 2015;173:17-21. doi: 10.1111/bjd.13380
12. Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8-18. doi: 10.1016/ s1011-1344(01)00198-1
13. Halder RM, Bang KM. Skin cancer in African Americans in the United States. Dermatol Clin. 1988;6:397-407.
14. Mora RG, Perniciaro C. Cancer of the skin in blacks. I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543. doi: 10.1016/s0190-9622 (81)70113-0
15. Bajaj S, Wolner ZJ, Dusza SW, et al. Total body skin examination practices: a survey study amongst dermatologists at high-risk skin cancer clinics. Dermatol Pract Concept. 2019;9:132-138. doi: 10.5826/dpc.0902a09
16. Rieder EA, Mu EW, Wang J, et al. Dermatologist practices during total body skin examinations: a survey study. J Drugs Dermatol. 2018;17:516-520.
17. Halder RM, Ara CJ. Skin cancer and photoaging in ethnic skin. Dermatol Clin. 2003;21:725-732, x. doi: 10.1016/s0733-8635 (03)00085-8
18. Higgins S, Nazemi A, Chow M, et al. Review of nonmelanoma skin cancer in African Americans, Hispanics, and Asians. Dermatol Surg. 2018;44:903-910.
19. Sng J, Koh D, Siong WC, et al. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009; 61:426-432.
20. Shao K, Feng H. Racial and ethnic healthcare disparities in skin cancer in the United States: a review of existing inequities, contributing factors, and potential solutions. J Clin Aesthet Dermatol. 2022;15:16-22.
21. Shao K, Hooper J, Feng H. Racial and ethnic health disparities in dermatology in the United States. Part 2: disease-specific epidemiology, characteristics, management, and outcomes. J Am Acad Dermatol. 2022;87:733-744. doi: 10.1016/j.jaad.2021. 12.062
22. Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137- 151. doi: 10.1007/s40257-021-00662-z
23. Copcu E, Aktas A, Sis¸man N, et al. Thirty-one cases of Marjolin’s ulcer. Clin Exp Dermatol. 2003;28:138-141. doi: 10.1046/j.1365- 2230.2003.01210.x
24. Abdi MA, Yan M, Hanna TP. Systematic review of modern case series of squamous cell cancer arising in a chronic ulcer (Marjolin’s ulcer) of the skin. JCO Glob Oncol. 2020;6:809-818. doi: 10.1200/ GO.20.00094
25. Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi: 10.1016/j.det.2019.05.009
26. Chapman S, Delgadillo D, Barber C, et al. Cutanteous squamous cell complicating hidradenitis suppurativa: a review of the prevalence, pathogenesis, and treatment of this dreaded complication. Acta Dermatovenerol Al Pannocica Adriat. 2018;27:25-28.
27. Kailas A, Botwin AL, Pritchett EN, et al. Assessing the effectiveness of knowledge-based interventions in increasing skin cancer awareness, knowledge, and protective behaviors in skin of color populations. Cutis. 2017;100:235-240.
Indian Health Service dermatologist: ‘I saw a real need to be of service’
After completing his dermatology residency at Johns Hopkins Hospital in 2010, Christopher Bengson, MD, MHS, then a Lieutenant Commander in the U.S. Public Health Service, accepted an offer to become a full-time dermatologist at Phoenix Indian Medical Center (PIMC) in Arizona, fulfilling a long desire to provide care for underserved individuals. Thirteen years later, .
As one of the largest hospitals in the IHS system, PIMC provides direct health care services to a population of more than 156,000, including tribal members from The Fort McDowell Yavapai Nation, the Salt River Pima-Maricopa Indian Community, and the San Lucy District of the Tohono O’odham Nation, the Tonto Apache Tribe, the Yavapai-Apache Indian Tribe, and the Yavapai-Prescott Indian Tribe. Dr. Bengson also cares for tribal members who travel to PIMC from as far away as Washington State and Hawaii to receive dermatologic care.
“There is a disproportionate number of Native American patients that come in with severe psoriasis, hidradenitis suppurativa, and dissecting cellulitis of the scalp compared to the general U.S. population, and I’ve been surprised by how many have nonmelanoma skin cancers and autoimmune connective tissue diseases like lupus, as the prevailing sentiment among his patients is that Native people do not get skin cancer,” he said in an interview. “Those who travel great distances are those who come see me for the surgical removal of skin cancers.”
Interesting cases he’s seen in his nearly 13 years on the job include Epstein-Barr virus-induced NK/T-cell lymphoma, anaplastic large cell lymphoma, subcutaneous panniculitis-like T-cell lymphoma, and necrobiotic xanthogranuloma, “tumors that have generally gone to tertiary care facilities for treatment, but we’ve been able to manage here.”
In 2017, Dr. Bengson was appointed as the IHS’s first chief clinical consultant for dermatology, a post that provides him the opportunity to interface with Native people and IHS-affiliated clinicians nationwide regarding skin-related questions and concerns. As the only full-time dermatologist employed by the IHS, he also views his role as providing an opportunity to change the perception that some Native Americans may still hold about federally delivered health care, “where there may be a cultural distrust of government health care in indigenous communities, driven by generational historical traumas that have come out of boarding schools, population relocation to desolate and isolated areas of the country, and contracts that were simply not honored,” he explained.
“While none of these issues are new, what has been great for me is that I’m going on 13 years of being at the same facility, and I’ve treated family members, their kids, and even their grandkids. In some ways the primary barrier of continuity of care – at least at PIMC – has been eliminated by me just being here for a long period of time.”
In Dr. Bengson’s opinion, efforts to improve access to attract more Native Americans to dermatology are laudable, including the American Academy of Dermatology’s Pathways Program, which aims to increase the number of dermatology residents from Black, Latino, and indigenous communities from approximately 100 residents to 250 residents by 2027, or by over 150%, through community-based engagement strategies that begin in high school.
“To have an objective benchmark is encouraging,” he said. However, he encourages dermatology residency program directors to rethink how they recruit Native Americans, many of whom hail from rural areas. “If you’re recruiting primarily from urban settings, you’re very unlikely to include Native Americans as a larger group of minorities,” he said. “When you look at the number of department chairs who are Native American, it’s on the order of 0.1%, [so] it’s no surprise that dermatologists coming out of a residency program don’t want to go to reservations to provide dermatologic care. We pay a lot of lip service to mentorship programs and things like that, but you need a mentor who follows you through the process – and it’s a long process.”
He believes that residency program directors should reconsider the metrics used to select dermatology residents and should consider the degree of adversity that a Native American applicant may have had to overcome to make it to the residency selection committees.
Despite obstacles to attracting young Native Americans to a career in medicine, Dr. Bengson sees encouraging signs ahead. Some of his Native American patients and family members of patients have enrolled in medical school and have asked to rotate with him at PIMC at the premedical and medical student level. “Some have moved on, not necessarily to dermatology, but to other specialties and careers in health care,” he said. “When you have such high rates of obesity, diabetes, hypertension, coronary artery disease, and stroke in Native American communities, nodulocystic acne and other skin conditions that are not threats to life and limb become less of a priority. We need to get more people in the pipeline to deliver medical services even if it may not be in dermatology, as the need for dedicated health care professionals is so great across all disciplines.”
After completing his dermatology residency at Johns Hopkins Hospital in 2010, Christopher Bengson, MD, MHS, then a Lieutenant Commander in the U.S. Public Health Service, accepted an offer to become a full-time dermatologist at Phoenix Indian Medical Center (PIMC) in Arizona, fulfilling a long desire to provide care for underserved individuals. Thirteen years later, .
As one of the largest hospitals in the IHS system, PIMC provides direct health care services to a population of more than 156,000, including tribal members from The Fort McDowell Yavapai Nation, the Salt River Pima-Maricopa Indian Community, and the San Lucy District of the Tohono O’odham Nation, the Tonto Apache Tribe, the Yavapai-Apache Indian Tribe, and the Yavapai-Prescott Indian Tribe. Dr. Bengson also cares for tribal members who travel to PIMC from as far away as Washington State and Hawaii to receive dermatologic care.
“There is a disproportionate number of Native American patients that come in with severe psoriasis, hidradenitis suppurativa, and dissecting cellulitis of the scalp compared to the general U.S. population, and I’ve been surprised by how many have nonmelanoma skin cancers and autoimmune connective tissue diseases like lupus, as the prevailing sentiment among his patients is that Native people do not get skin cancer,” he said in an interview. “Those who travel great distances are those who come see me for the surgical removal of skin cancers.”
Interesting cases he’s seen in his nearly 13 years on the job include Epstein-Barr virus-induced NK/T-cell lymphoma, anaplastic large cell lymphoma, subcutaneous panniculitis-like T-cell lymphoma, and necrobiotic xanthogranuloma, “tumors that have generally gone to tertiary care facilities for treatment, but we’ve been able to manage here.”
In 2017, Dr. Bengson was appointed as the IHS’s first chief clinical consultant for dermatology, a post that provides him the opportunity to interface with Native people and IHS-affiliated clinicians nationwide regarding skin-related questions and concerns. As the only full-time dermatologist employed by the IHS, he also views his role as providing an opportunity to change the perception that some Native Americans may still hold about federally delivered health care, “where there may be a cultural distrust of government health care in indigenous communities, driven by generational historical traumas that have come out of boarding schools, population relocation to desolate and isolated areas of the country, and contracts that were simply not honored,” he explained.
“While none of these issues are new, what has been great for me is that I’m going on 13 years of being at the same facility, and I’ve treated family members, their kids, and even their grandkids. In some ways the primary barrier of continuity of care – at least at PIMC – has been eliminated by me just being here for a long period of time.”
In Dr. Bengson’s opinion, efforts to improve access to attract more Native Americans to dermatology are laudable, including the American Academy of Dermatology’s Pathways Program, which aims to increase the number of dermatology residents from Black, Latino, and indigenous communities from approximately 100 residents to 250 residents by 2027, or by over 150%, through community-based engagement strategies that begin in high school.
“To have an objective benchmark is encouraging,” he said. However, he encourages dermatology residency program directors to rethink how they recruit Native Americans, many of whom hail from rural areas. “If you’re recruiting primarily from urban settings, you’re very unlikely to include Native Americans as a larger group of minorities,” he said. “When you look at the number of department chairs who are Native American, it’s on the order of 0.1%, [so] it’s no surprise that dermatologists coming out of a residency program don’t want to go to reservations to provide dermatologic care. We pay a lot of lip service to mentorship programs and things like that, but you need a mentor who follows you through the process – and it’s a long process.”
He believes that residency program directors should reconsider the metrics used to select dermatology residents and should consider the degree of adversity that a Native American applicant may have had to overcome to make it to the residency selection committees.
Despite obstacles to attracting young Native Americans to a career in medicine, Dr. Bengson sees encouraging signs ahead. Some of his Native American patients and family members of patients have enrolled in medical school and have asked to rotate with him at PIMC at the premedical and medical student level. “Some have moved on, not necessarily to dermatology, but to other specialties and careers in health care,” he said. “When you have such high rates of obesity, diabetes, hypertension, coronary artery disease, and stroke in Native American communities, nodulocystic acne and other skin conditions that are not threats to life and limb become less of a priority. We need to get more people in the pipeline to deliver medical services even if it may not be in dermatology, as the need for dedicated health care professionals is so great across all disciplines.”
After completing his dermatology residency at Johns Hopkins Hospital in 2010, Christopher Bengson, MD, MHS, then a Lieutenant Commander in the U.S. Public Health Service, accepted an offer to become a full-time dermatologist at Phoenix Indian Medical Center (PIMC) in Arizona, fulfilling a long desire to provide care for underserved individuals. Thirteen years later, .
As one of the largest hospitals in the IHS system, PIMC provides direct health care services to a population of more than 156,000, including tribal members from The Fort McDowell Yavapai Nation, the Salt River Pima-Maricopa Indian Community, and the San Lucy District of the Tohono O’odham Nation, the Tonto Apache Tribe, the Yavapai-Apache Indian Tribe, and the Yavapai-Prescott Indian Tribe. Dr. Bengson also cares for tribal members who travel to PIMC from as far away as Washington State and Hawaii to receive dermatologic care.
“There is a disproportionate number of Native American patients that come in with severe psoriasis, hidradenitis suppurativa, and dissecting cellulitis of the scalp compared to the general U.S. population, and I’ve been surprised by how many have nonmelanoma skin cancers and autoimmune connective tissue diseases like lupus, as the prevailing sentiment among his patients is that Native people do not get skin cancer,” he said in an interview. “Those who travel great distances are those who come see me for the surgical removal of skin cancers.”
Interesting cases he’s seen in his nearly 13 years on the job include Epstein-Barr virus-induced NK/T-cell lymphoma, anaplastic large cell lymphoma, subcutaneous panniculitis-like T-cell lymphoma, and necrobiotic xanthogranuloma, “tumors that have generally gone to tertiary care facilities for treatment, but we’ve been able to manage here.”
In 2017, Dr. Bengson was appointed as the IHS’s first chief clinical consultant for dermatology, a post that provides him the opportunity to interface with Native people and IHS-affiliated clinicians nationwide regarding skin-related questions and concerns. As the only full-time dermatologist employed by the IHS, he also views his role as providing an opportunity to change the perception that some Native Americans may still hold about federally delivered health care, “where there may be a cultural distrust of government health care in indigenous communities, driven by generational historical traumas that have come out of boarding schools, population relocation to desolate and isolated areas of the country, and contracts that were simply not honored,” he explained.
“While none of these issues are new, what has been great for me is that I’m going on 13 years of being at the same facility, and I’ve treated family members, their kids, and even their grandkids. In some ways the primary barrier of continuity of care – at least at PIMC – has been eliminated by me just being here for a long period of time.”
In Dr. Bengson’s opinion, efforts to improve access to attract more Native Americans to dermatology are laudable, including the American Academy of Dermatology’s Pathways Program, which aims to increase the number of dermatology residents from Black, Latino, and indigenous communities from approximately 100 residents to 250 residents by 2027, or by over 150%, through community-based engagement strategies that begin in high school.
“To have an objective benchmark is encouraging,” he said. However, he encourages dermatology residency program directors to rethink how they recruit Native Americans, many of whom hail from rural areas. “If you’re recruiting primarily from urban settings, you’re very unlikely to include Native Americans as a larger group of minorities,” he said. “When you look at the number of department chairs who are Native American, it’s on the order of 0.1%, [so] it’s no surprise that dermatologists coming out of a residency program don’t want to go to reservations to provide dermatologic care. We pay a lot of lip service to mentorship programs and things like that, but you need a mentor who follows you through the process – and it’s a long process.”
He believes that residency program directors should reconsider the metrics used to select dermatology residents and should consider the degree of adversity that a Native American applicant may have had to overcome to make it to the residency selection committees.
Despite obstacles to attracting young Native Americans to a career in medicine, Dr. Bengson sees encouraging signs ahead. Some of his Native American patients and family members of patients have enrolled in medical school and have asked to rotate with him at PIMC at the premedical and medical student level. “Some have moved on, not necessarily to dermatology, but to other specialties and careers in health care,” he said. “When you have such high rates of obesity, diabetes, hypertension, coronary artery disease, and stroke in Native American communities, nodulocystic acne and other skin conditions that are not threats to life and limb become less of a priority. We need to get more people in the pipeline to deliver medical services even if it may not be in dermatology, as the need for dedicated health care professionals is so great across all disciplines.”
Top 50 Authors in Dermatology by Publication Rate (2017-2022)
To the Editor:
Citation number and Hirsch index (h-index) have long been employed as metrics of productivity for academic scholarship. The h-index is defined as the highest number of publications (the maximum h value) of an author who has published at least h papers, each cited by other authors at least h times.1 In a bibliometric analysis of the most frequently cited authors in dermatology from 1974 to 2019 (N=378,276), females comprised 12% of first and 11% of senior authors of the most cited publications, and 6 of the most cited authors in dermatology were women.2 In another study analyzing the most prolific dermatologic authors based on h-index, 0% from 1980 to 1989 and 19% from 2010 to 2019 were female (N=393,488).3 Because citation number and h-index favor longer-practicing dermatologists, we examined dermatology author productivity and gender trends by recent publication rates.
The Scopus database was searched for dermatology publications by using the field category “dermatology”from January 1, 2017, to October 7, 2022. Nondermatologists and authors with the same initials were excluded. Authors were ranked by number of publications, including original articles, case reports, letters, and reviews. Sex, degree, and years of experience were determined via a Google search of the author’s name. The h-index; number of citations; and percentages of first, middle, and last authorship were recorded.
Of the top 50 published dermatologists, 30% were female (n=15) and 56% (n=28) held both MD and PhD degrees (Table). The mean years of experience was 26.27 years (range, 6–44 years), with a mean of 29.23 years in females and 25.87 years in males. The mean h-index was 27.96 (range, 8–88), with 24.87 for females and 29.29 for males. The mean number of citations was 4032.64 (range, 235–36,908), with 2891.13 for females and 4521.86 for males. Thirty-one authors were most frequently middle authors, 18 were senior authors, and 1 was a first author. On average (SD), authors were senior or first author in 47.97% (20.08%) of their publications (range, 6.32%–94.93%).
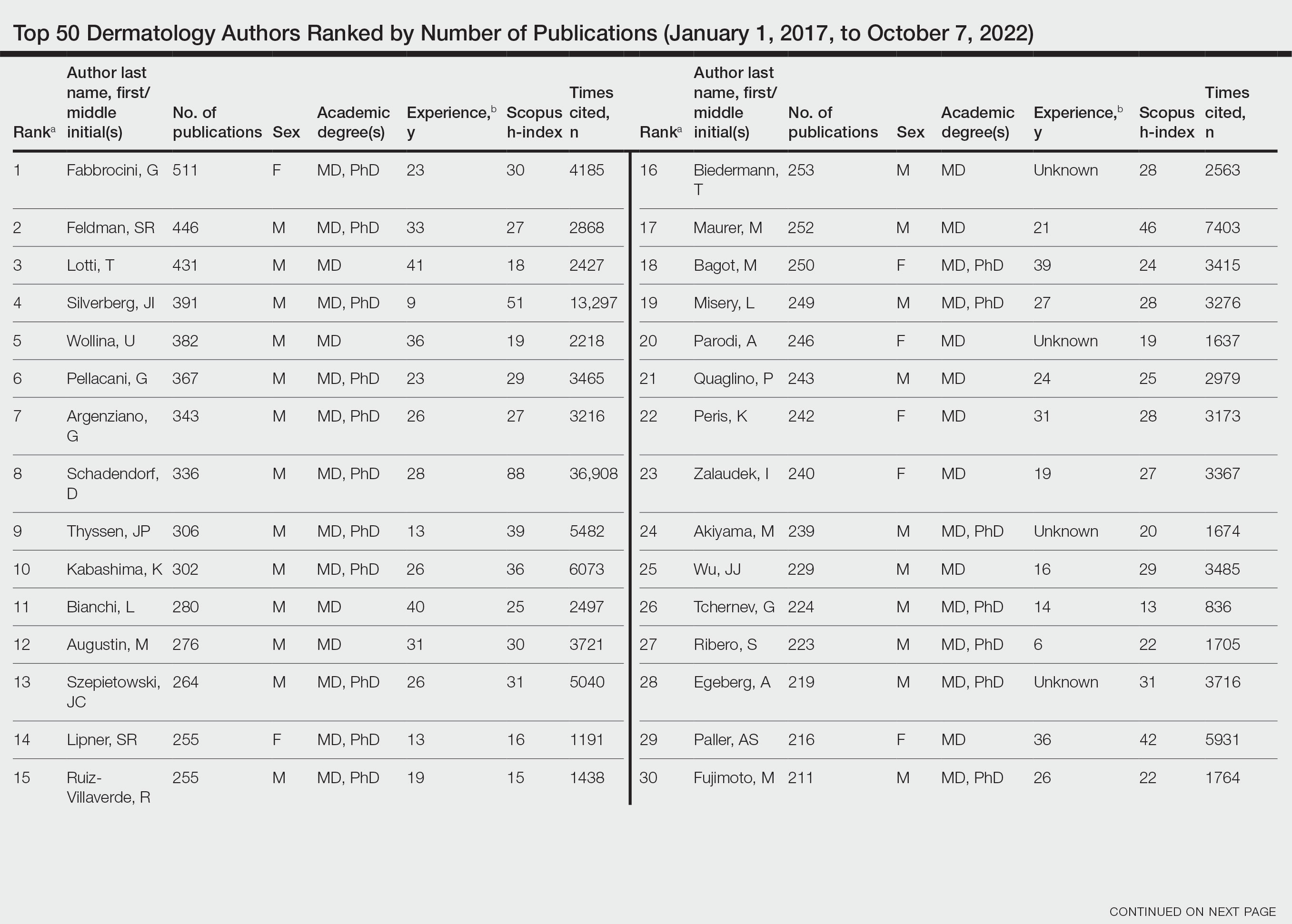
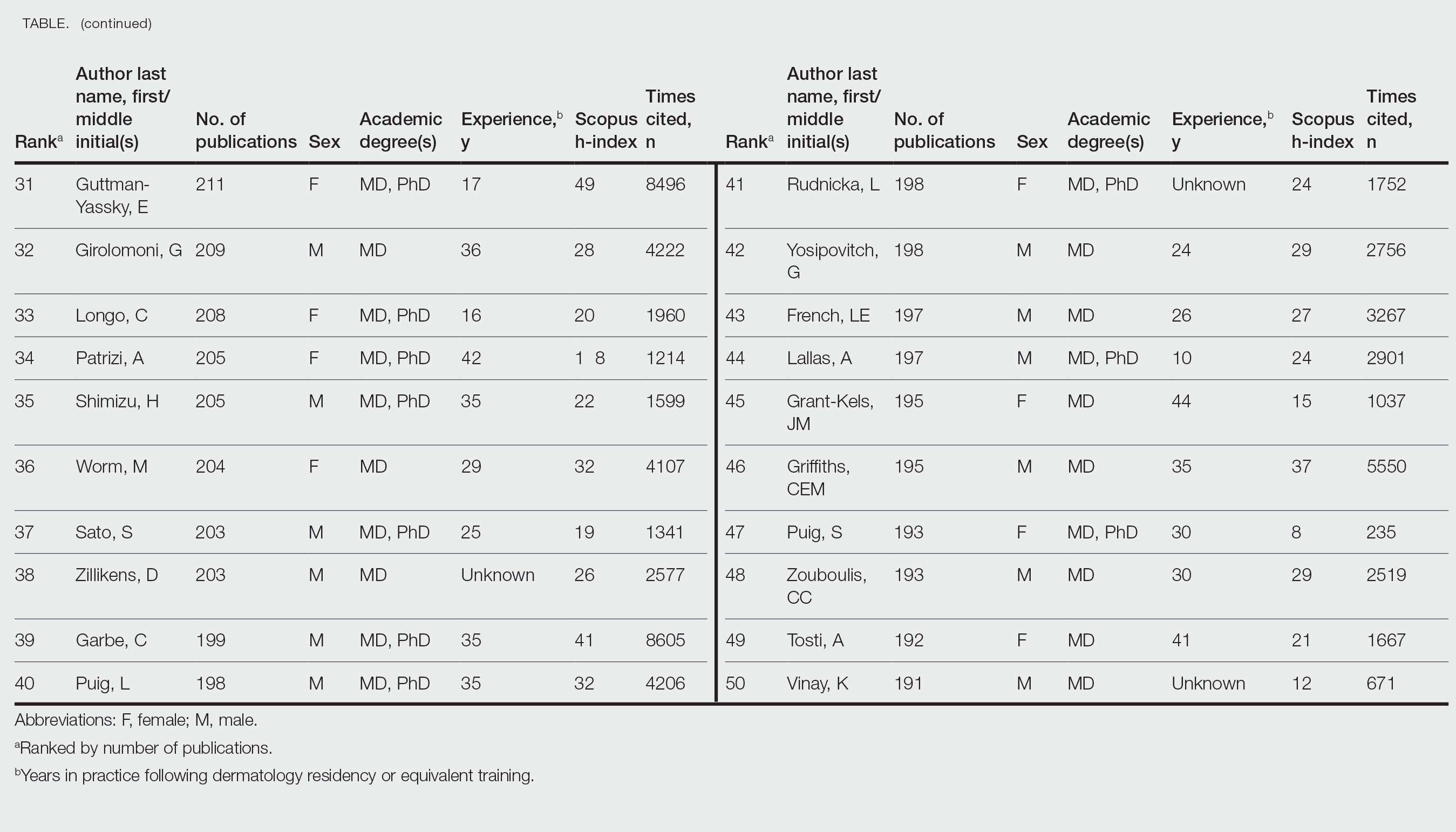
Our study shows that females were more highly represented as top dermatology authors (30%) as measured by publication numbers from 2017 to 2022 than in studies measuring citation rate from 1974 to 2019 (12%)2 or h-index from 2010 to 2019 (19%).3 Similarly, in a study of dermatology authorship from 2009 to 2019, on average, females represented 51.06% first and 38.18% last authors.4
The proportion of females in the dermatology workforce has increased, with 3964 of 10,385 (38.2%) active dermatologists in 20075 being female vs 6372 of 12,505 (51.0%) in 2019.6 The lower proportion of practicing female dermatologists in earlier years likely accounts for the lower percentage of females in dermatology citations and h-index top lists during that time, given that citation and h-index metrics are biased to dermatologists with longer careers.
Although our data are encouraging, females still accounted for less than one-third of the top 50 authors by publication numbers. Gender inequalities persist, with only one-third of a total of 1292 National Institutes of Health dermatology grants and one-fourth of Research Project Grant Program (R01) grants being awarded to females in the years 2009 to 2014.7 Therefore, formal and informal mentorship, protected time for research, resources for childcare, and opportunities for funding will be critical in supporting female dermatologists to both publish highly impactful research and obtain research grants.
Limitations of our study include the omission of authors with identical initials and the inability to account for name changes. Furthermore, Scopus does not include all articles published by each author. Finally, publication number reflects quantity but may not reflect quality.
By quantitating dermatology author publication numbers, we found better representation of female authors compared with studies measuring citation number and h-index. With higher proportions of female dermatology trainees and efforts to increase mentorship and research support for female dermatologists, we expect improved equality in top lists of dermatology citations and h-index values.
- Dysart J. Measuring research impact and quality: h-index. Accessed July 11, 2023. https://libraryguides.missouri.edu/impact/hindex
- Maymone MBC, Laughter M, Vashi NA, et al. The most cited articles and authors in dermatology: a bibliometric analysis of 1974-2019. J Am Acad Dermatol. 2020;83:201-205. doi:10.1016/j.jaad.2019.06.1308
- Szeto MD, Presley CL, Maymone MBC, et al. Top authors in dermatology by h-index: a bibliometric analysis of 1980-2020. J Am Acad Dermatol. 2021;85:1573-1579. doi:10.1016/j.jaad.2020.10.087
- Laughter MR, Yemc MG, Presley CL, et al. Gender representation in the authorship of dermatology publications. J Am Acad Dermatol. 2022;86:698-700. doi:10.1016/j.jaad.2021.03.019
- Association of American Medical Colleges. 2008 physician specialty data report. Accessed July 11, 2023. https://www.aamc.org/media/33491/download
- Association of American Medical Colleges. 2019 physician specialty data report. Accessed July 11, 2023. https://www.aamc.org/data-reports/workforce/data/active-physicians-sex-and-specialty-2019
- Cheng MY, Sukhov A, Sultani H, et al. Trends in National Institutes of Health funding of principal investigators in dermatology research by academic degree and sex. JAMA Dermatol. 2016;152:883-888. doi:10.1001/jamadermatol.2016.0271
To the Editor:
Citation number and Hirsch index (h-index) have long been employed as metrics of productivity for academic scholarship. The h-index is defined as the highest number of publications (the maximum h value) of an author who has published at least h papers, each cited by other authors at least h times.1 In a bibliometric analysis of the most frequently cited authors in dermatology from 1974 to 2019 (N=378,276), females comprised 12% of first and 11% of senior authors of the most cited publications, and 6 of the most cited authors in dermatology were women.2 In another study analyzing the most prolific dermatologic authors based on h-index, 0% from 1980 to 1989 and 19% from 2010 to 2019 were female (N=393,488).3 Because citation number and h-index favor longer-practicing dermatologists, we examined dermatology author productivity and gender trends by recent publication rates.
The Scopus database was searched for dermatology publications by using the field category “dermatology”from January 1, 2017, to October 7, 2022. Nondermatologists and authors with the same initials were excluded. Authors were ranked by number of publications, including original articles, case reports, letters, and reviews. Sex, degree, and years of experience were determined via a Google search of the author’s name. The h-index; number of citations; and percentages of first, middle, and last authorship were recorded.
Of the top 50 published dermatologists, 30% were female (n=15) and 56% (n=28) held both MD and PhD degrees (Table). The mean years of experience was 26.27 years (range, 6–44 years), with a mean of 29.23 years in females and 25.87 years in males. The mean h-index was 27.96 (range, 8–88), with 24.87 for females and 29.29 for males. The mean number of citations was 4032.64 (range, 235–36,908), with 2891.13 for females and 4521.86 for males. Thirty-one authors were most frequently middle authors, 18 were senior authors, and 1 was a first author. On average (SD), authors were senior or first author in 47.97% (20.08%) of their publications (range, 6.32%–94.93%).
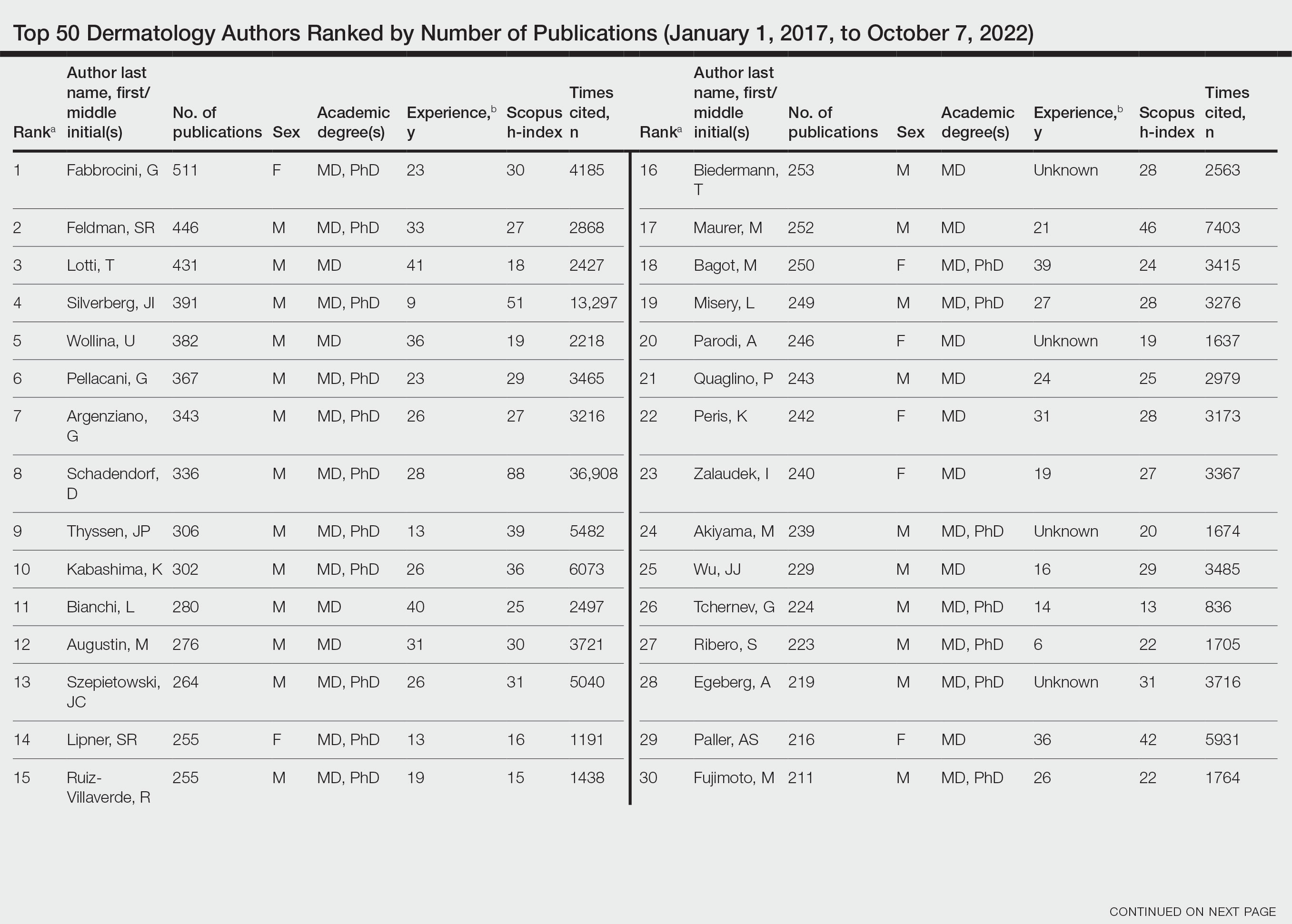
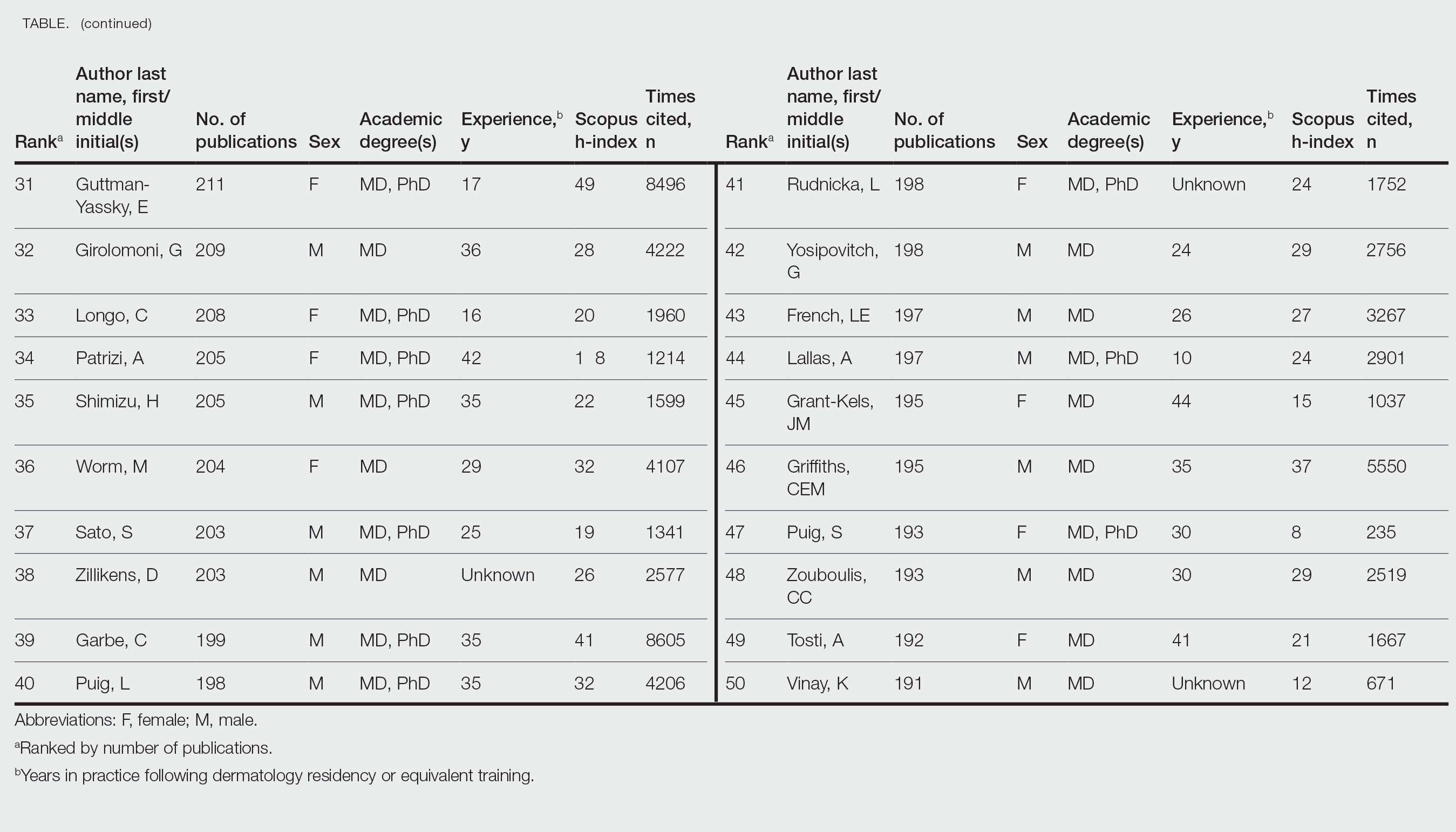
Our study shows that females were more highly represented as top dermatology authors (30%) as measured by publication numbers from 2017 to 2022 than in studies measuring citation rate from 1974 to 2019 (12%)2 or h-index from 2010 to 2019 (19%).3 Similarly, in a study of dermatology authorship from 2009 to 2019, on average, females represented 51.06% first and 38.18% last authors.4
The proportion of females in the dermatology workforce has increased, with 3964 of 10,385 (38.2%) active dermatologists in 20075 being female vs 6372 of 12,505 (51.0%) in 2019.6 The lower proportion of practicing female dermatologists in earlier years likely accounts for the lower percentage of females in dermatology citations and h-index top lists during that time, given that citation and h-index metrics are biased to dermatologists with longer careers.
Although our data are encouraging, females still accounted for less than one-third of the top 50 authors by publication numbers. Gender inequalities persist, with only one-third of a total of 1292 National Institutes of Health dermatology grants and one-fourth of Research Project Grant Program (R01) grants being awarded to females in the years 2009 to 2014.7 Therefore, formal and informal mentorship, protected time for research, resources for childcare, and opportunities for funding will be critical in supporting female dermatologists to both publish highly impactful research and obtain research grants.
Limitations of our study include the omission of authors with identical initials and the inability to account for name changes. Furthermore, Scopus does not include all articles published by each author. Finally, publication number reflects quantity but may not reflect quality.
By quantitating dermatology author publication numbers, we found better representation of female authors compared with studies measuring citation number and h-index. With higher proportions of female dermatology trainees and efforts to increase mentorship and research support for female dermatologists, we expect improved equality in top lists of dermatology citations and h-index values.
To the Editor:
Citation number and Hirsch index (h-index) have long been employed as metrics of productivity for academic scholarship. The h-index is defined as the highest number of publications (the maximum h value) of an author who has published at least h papers, each cited by other authors at least h times.1 In a bibliometric analysis of the most frequently cited authors in dermatology from 1974 to 2019 (N=378,276), females comprised 12% of first and 11% of senior authors of the most cited publications, and 6 of the most cited authors in dermatology were women.2 In another study analyzing the most prolific dermatologic authors based on h-index, 0% from 1980 to 1989 and 19% from 2010 to 2019 were female (N=393,488).3 Because citation number and h-index favor longer-practicing dermatologists, we examined dermatology author productivity and gender trends by recent publication rates.
The Scopus database was searched for dermatology publications by using the field category “dermatology”from January 1, 2017, to October 7, 2022. Nondermatologists and authors with the same initials were excluded. Authors were ranked by number of publications, including original articles, case reports, letters, and reviews. Sex, degree, and years of experience were determined via a Google search of the author’s name. The h-index; number of citations; and percentages of first, middle, and last authorship were recorded.
Of the top 50 published dermatologists, 30% were female (n=15) and 56% (n=28) held both MD and PhD degrees (Table). The mean years of experience was 26.27 years (range, 6–44 years), with a mean of 29.23 years in females and 25.87 years in males. The mean h-index was 27.96 (range, 8–88), with 24.87 for females and 29.29 for males. The mean number of citations was 4032.64 (range, 235–36,908), with 2891.13 for females and 4521.86 for males. Thirty-one authors were most frequently middle authors, 18 were senior authors, and 1 was a first author. On average (SD), authors were senior or first author in 47.97% (20.08%) of their publications (range, 6.32%–94.93%).
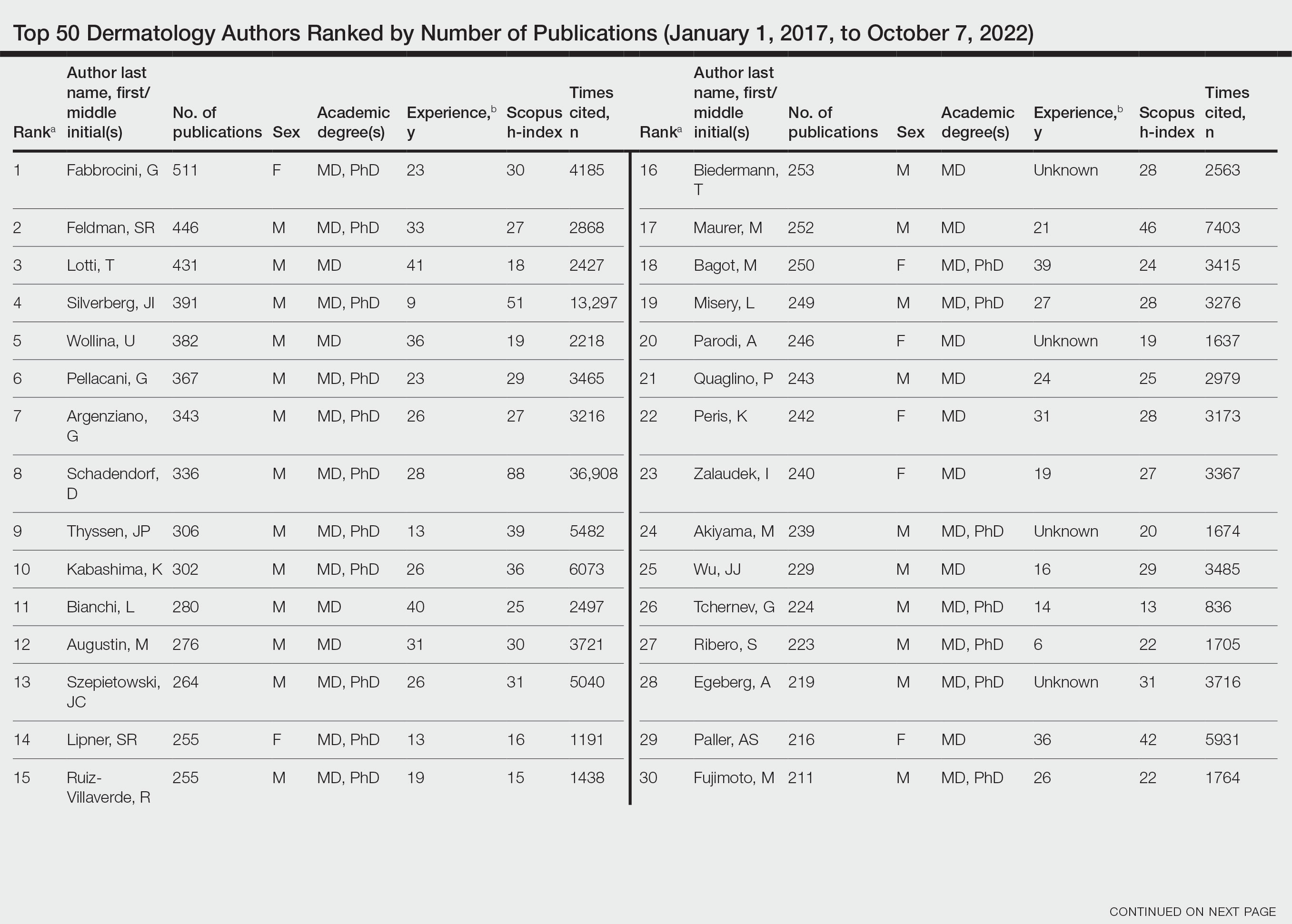
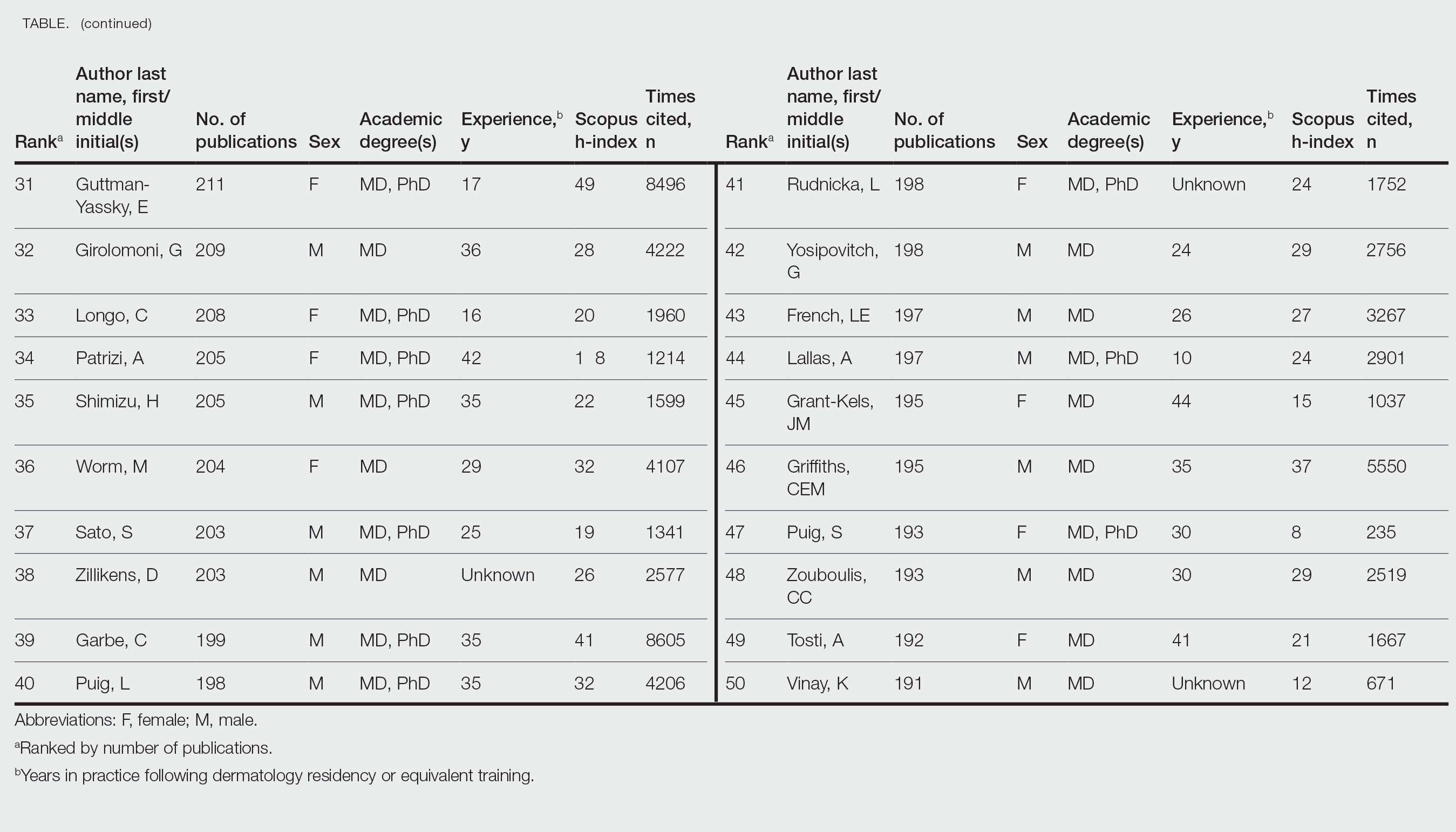
Our study shows that females were more highly represented as top dermatology authors (30%) as measured by publication numbers from 2017 to 2022 than in studies measuring citation rate from 1974 to 2019 (12%)2 or h-index from 2010 to 2019 (19%).3 Similarly, in a study of dermatology authorship from 2009 to 2019, on average, females represented 51.06% first and 38.18% last authors.4
The proportion of females in the dermatology workforce has increased, with 3964 of 10,385 (38.2%) active dermatologists in 20075 being female vs 6372 of 12,505 (51.0%) in 2019.6 The lower proportion of practicing female dermatologists in earlier years likely accounts for the lower percentage of females in dermatology citations and h-index top lists during that time, given that citation and h-index metrics are biased to dermatologists with longer careers.
Although our data are encouraging, females still accounted for less than one-third of the top 50 authors by publication numbers. Gender inequalities persist, with only one-third of a total of 1292 National Institutes of Health dermatology grants and one-fourth of Research Project Grant Program (R01) grants being awarded to females in the years 2009 to 2014.7 Therefore, formal and informal mentorship, protected time for research, resources for childcare, and opportunities for funding will be critical in supporting female dermatologists to both publish highly impactful research and obtain research grants.
Limitations of our study include the omission of authors with identical initials and the inability to account for name changes. Furthermore, Scopus does not include all articles published by each author. Finally, publication number reflects quantity but may not reflect quality.
By quantitating dermatology author publication numbers, we found better representation of female authors compared with studies measuring citation number and h-index. With higher proportions of female dermatology trainees and efforts to increase mentorship and research support for female dermatologists, we expect improved equality in top lists of dermatology citations and h-index values.
- Dysart J. Measuring research impact and quality: h-index. Accessed July 11, 2023. https://libraryguides.missouri.edu/impact/hindex
- Maymone MBC, Laughter M, Vashi NA, et al. The most cited articles and authors in dermatology: a bibliometric analysis of 1974-2019. J Am Acad Dermatol. 2020;83:201-205. doi:10.1016/j.jaad.2019.06.1308
- Szeto MD, Presley CL, Maymone MBC, et al. Top authors in dermatology by h-index: a bibliometric analysis of 1980-2020. J Am Acad Dermatol. 2021;85:1573-1579. doi:10.1016/j.jaad.2020.10.087
- Laughter MR, Yemc MG, Presley CL, et al. Gender representation in the authorship of dermatology publications. J Am Acad Dermatol. 2022;86:698-700. doi:10.1016/j.jaad.2021.03.019
- Association of American Medical Colleges. 2008 physician specialty data report. Accessed July 11, 2023. https://www.aamc.org/media/33491/download
- Association of American Medical Colleges. 2019 physician specialty data report. Accessed July 11, 2023. https://www.aamc.org/data-reports/workforce/data/active-physicians-sex-and-specialty-2019
- Cheng MY, Sukhov A, Sultani H, et al. Trends in National Institutes of Health funding of principal investigators in dermatology research by academic degree and sex. JAMA Dermatol. 2016;152:883-888. doi:10.1001/jamadermatol.2016.0271
- Dysart J. Measuring research impact and quality: h-index. Accessed July 11, 2023. https://libraryguides.missouri.edu/impact/hindex
- Maymone MBC, Laughter M, Vashi NA, et al. The most cited articles and authors in dermatology: a bibliometric analysis of 1974-2019. J Am Acad Dermatol. 2020;83:201-205. doi:10.1016/j.jaad.2019.06.1308
- Szeto MD, Presley CL, Maymone MBC, et al. Top authors in dermatology by h-index: a bibliometric analysis of 1980-2020. J Am Acad Dermatol. 2021;85:1573-1579. doi:10.1016/j.jaad.2020.10.087
- Laughter MR, Yemc MG, Presley CL, et al. Gender representation in the authorship of dermatology publications. J Am Acad Dermatol. 2022;86:698-700. doi:10.1016/j.jaad.2021.03.019
- Association of American Medical Colleges. 2008 physician specialty data report. Accessed July 11, 2023. https://www.aamc.org/media/33491/download
- Association of American Medical Colleges. 2019 physician specialty data report. Accessed July 11, 2023. https://www.aamc.org/data-reports/workforce/data/active-physicians-sex-and-specialty-2019
- Cheng MY, Sukhov A, Sultani H, et al. Trends in National Institutes of Health funding of principal investigators in dermatology research by academic degree and sex. JAMA Dermatol. 2016;152:883-888. doi:10.1001/jamadermatol.2016.0271
Practice Points
- Academic scholarship often is measured by number of citations and h-index. Using these measures, female dermatologists are infrequently represented on top author lists.
- Using the Scopus database to search for the 50 most published dermatology authors from January 1, 2017, to October 7, 2022, 30% were female.
- Higher proportions of female dermatology trainees as well as efforts to increase mentorship and research support for female dermatologists may improve equality in top lists of dermatology citations and h-index values.
Dermatologic care in Indian Country marked by unique challenges, opportunities
As a proud member of the Oglala Lakota Nation from the Pine Ridge Indian Reservation in southwestern South Dakota, Drew Hicks grew up with limited access to basic health care, let alone the luxury of scheduling an appointment with a dermatologist or another medical specialist.
The area – once home to the Lakota war leader Crazy Horse – encompasses nearly 47,000 residents scattered over about 2.2 million acres, larger than the size of Rhode Island, with land marked by rolling mixed grass prairie, sandhills, and badlands. Some of the Oglala Lakota people live in substandard housing and lack regular access to food, running water, and refrigeration, not to mention cell phone and Internet service. “It’s sparse,” said Mr. Hicks, the son of Tribal ranchers who now is a 3rd-year medical student at the Mayo Clinic College of Medicine and Science in Rochester, Minn., and has an early interest in pursuing dermatology. “There is a lot of territory and not a lot of health care serving the population.” From the Hicks home, the nearest place to receive health care is a family medicine practice in Martin, S.D. – about a 15-minute drive on gravel roads in the best of conditions, but in poor weather, it can be difficult, he said. “So, there are environmental challenges besides the limited number of health care providers.”
Clinicians in the practice “did have to be the point of care for everything from dermatologic issues to emergency medicine to delivering a baby, because the next-closest medical facility of any magnitude is 2 hours away,” he said.
Challenges of health literacy and limited access to comprehensive health care at Pine Ridge and other American Indian (AI) and Alaska Native (AN) reservations have long-term consequences. “My own mom struggled to control her blood pressure for years and now has chronic kidney disease,” Mr. Hicks said. “It’s not an uncommon story. Diabetes on the reservation is a big issue.” Then there’s his father, who survived two bouts with melanoma that was diagnosed at an advanced stage. “I think about how that has impacted him, and wonder, had we had a dermatologist who serviced our area, would we have caught things sooner?” he said. “I feel there is so much room for impactful health care deliveries to communities like Pine Ridge.” At the same time, he emphasized, “this isn’t poverty porn. We’re a resilient people. Any effort to engage with AIs or ANs should be from a perspective of a learner, having cultural humility, and seeking out community leaders to help lead you.”
According to the 2020 Census, there are 574 federally recognized sovereign tribal nations in the United States and federal- and state-recognized American Indian reservations in 35 states. AI/AN people make up about 2.9% of the total U.S. population, or 9.7 million, and their life expectancy is an average of 4.4 years less, compared with the general population (a mean of 73.7 vs. 78.1 years, respectively). Because of limited access to dermatologic care in these areas, the risk for developing significant skin conditions and diseases that may go undetected for long stretches of time is increased.
“That can mean advanced skin cancers like basal cell carcinomas that have become larger than what you would see in a typical metropolitan population,” said Lucinda Kohn, MD, assistant professor of dermatology in the Centers for American Indian and Alaska Native Health at the University of Colorado at Denver, Aurora, who spent part of her dermatology residency rotating at the Chinle (Ariz.) Service Unit, an Indian Health Service facility, in 2017 and now provides teledermatology and regular in-person dermatology care at that clinic. “The climate there is dry, so you can see bad eczema and dry skin. There’s also a lot of acne and hidradenitis suppurativa. I think the acne and HS is due to the hyperglycemic index diet from the food deserts. Skin disease reflects the climate, the food desert, and the lack of close specialty care.”
Acne scarring common
Some published evidence suggests that acne is more prevalent and severe in AI/AN individuals. In a survey of 158 AI/AN individuals with a mean age of 32 years, 79.1% reported a history of acne, 55.1% reported acne scarring, and 31% reported having active lesions. “Looking back on my experience in high school, I definitely see that in myself and in my peers,” Mr. Hicks said. And, while there are limited published studies about the incidence of melanoma in this population, an analysis from 2006 found that the incidence was 3.1 per 100,000 between 2001 and 2005, which was an increase from 1.6 per 100,000 reported between 1992 and 2000.
There’s a lot to unpack for dermatologists caring for the AI/AN population besides the raw health disparities: a long history of distrust between AI/AN people and the federal government, structural racism, geographic isolation, health literacy challenges, and high rates of poverty and unemployment. And while individuals from federally recognized tribes have a legal right to receive health care provided by the Indian Health Service, a component of the Department of Health & Human Services, the U.S. Government Accountability Office found that in 2017 per capita spending available to the IHS was $4,078, compared with $8,109 for Medicaid, $10,692 for the Veterans Health Administration, and $13,185 for Medicare.
“Everyone deserves healthy skin and good health,” said Dr. Kohn, whose husband is AI and works in AI law. “Knowing that there are pockets of people who lack that access to care really bothers me. I think the American Indians are frequently overlooked. They’re just not even counted for in certain surveys,” she added, noting that categories are usually defined as Black, Hispanic, Asian, or White.
According to Dr. Kohn, who coauthored a chapter titled “Dermatology on American Indian and Alaska Native Reservations,” for the 2021 book “Dermatology in Rural Settings”, 70% of AIs live in urban areas, “so it’s not just people who live on reservations, though the disparity is greatest there.” To help deliver dermatologic care in the rural areas “where you’re on tribal lands, you must partner with the tribes,” she added. “You must get their permission, operate under their laws and regulations and their rules, learn the local customs, learn about the culture, learn the people, and learn their resources before you practice. That’s the only ethical way to practice.” This also means appreciating the fact that some AI/AN individuals may not understand what a dermatologist could do for them. “One of the bigger hurdles to overcome,” she said, is educating the population that dermatologists can cure skin diseases and that there are good medications for treating the diseases.
Shortcomings of teledermatology
Some dermatologists perform teledermatology visits for tribes, often from an office located in a different time zone. “And, they don’t have a sense of what resources are available for the people they’re serving,” Dr. Kohn said. “For example, if they diagnose a potential skin cancer on the face and say, ‘you need a biopsy,’ but the closest dermatologist is 4 hours away, is that really serving the patient? Or, if you tell a patient, ‘I want you to go out and buy Vanicream for your skin,’ but Vanicream costs $17 and the patient can’t even afford to buy food, are you really doing them a service?”
In a survey-based study of 238 AI individuals that is scheduled to be published in late 2023, Dr. Kohn and colleagues asked respondents at two regional powwows in Denver if they would be open to teledermatology – either in their home or in a primary care clinic. Most respondents (70%) lived in urban areas, the rest in rural settings. Nearly half of respondents (42%) “did not want to do teledermatology, even though they couldn’t access in-person dermatology,” Dr. Kohn said. “So, for people who think teledermatology is the answer [to improving access], the respondents to our survey weren’t interested in pursuing that as a solution. I was surprised by that.” When the researchers broke down the responses by age, teenage respondents were even less interested in teledermatology than adults were. “I think there’s something about having someone see you in person, knowing who you are,” she said.
Partnerships with tribes
To foster more sustainable change in the delivery of skin care beyond remote teledermatology and periodic visits from volunteers, some dermatology residencies have established partnerships with tribes, including Massachusetts General Hospital’s teaching partnership with the Rosebud Sioux tribe in Rosebud, S.D., and the University of Utah dermatology department’s resident continuity clinic with Navajo Nation in Montezuma Creek, Utah. In 2016, officials from the Utah Navajo Health System reached out to the University of Utah’s dermatology department to inquire about the potential for creating a teledermatology clinic to serve patients who receive primary care at the Montezuma Creek Community Health Center, located in Southeastern Utah on the northern tip of the Navajo Nation.
Stephanie Klein, MD, associate professor of dermatology at the university, spearheaded the clinic’s launch but soon encountered obstacles that ranged from not being able to visualize the patient’s skin clearly on her computer screen to difficulty making a personal connection with patients despite help from Navajo translators. “It was hard to build a relationship,” she said. A few years later, she drove down to meet with officials of the health system and posed the question: “What is the ideal thing you would want from dermatology?”
Continuity, they told her. “They said that a lot of the services they receive in the form of outreach are rotational, where someone might come in for a day, or a week, or five people may rotate throughout the year,” which did not serve them well, said Dr. Klein, who subsequently collaborated with Utah Navajo Health System clinicians to establish a resident continuity clinic, which launched in January 2021.
The arrangement also serves as a continuity clinic for Dr. Klein as an attending physician. Each month, she and one dermatology resident drive 6.5 hours from Salt Lake City to Montezuma Creek, where they spend 1 or 2 full days seeing about 25 patients referred by the primary care clinicians who work there. About one-quarter of the time they fly, thanks to financial support from a private donor. The flight takes about an hour, then it’s an hour-long drive to the actual clinic. “It’s a commitment,” Dr. Klein said. “A resident can come with me if they commit to the clinic for at least 1 year. This enables us to have continuity of care; it allows us to build relationships with the patients and with the care team there.” As for the prior teledermatology visits she had with residents, “I still do those, but now I do them in between the in-person visits, so I’m not meeting people over telehealth; I’m just following up with them.”

Situated in the high desert among rock formations, the estimated population of Montezuma Creek is just over 320 people. “It’s a beautiful place with otherworldly buttes and mesas, and the Blue Mountains rising up in the distance,” said Lowell Nicholson, MD, a dermatology resident at the University of Utah who is in his second year of a 2-year commitment to the clinic. “But the landscape can be harsh, and it is underserved from an infrastructure perspective,” with large areas with no cell phone service and limited access to running water and refrigeration. “People in general travel quite far to get their medical care and most of the roads are dirt or gravel, so after a big snowstorm or if it’s been raining, they can become impassable.”
Dermatologic conditions they often encounter include vitiligo, photodermatoses, hidradenitis suppurativa, eczema, psoriasis, and severe acne, often with lots of acne-associated scarring. “In general, we tend to see dramatic or advanced presentations of general dermatology diagnoses,” Dr. Nicholson said. “We see a lot of really extensive psoriasis, which can be socially stigmatizing.”
He recalled one middle-aged man who isolated himself from others because his psoriasis became unbearable. The man refused to leave his house, visit family members, or attend tribal meetups. “He tried to see his regular doctor about it and was given topicals, but his disease was just too extensive,” said Dr. Nicholson, who suggested trying a biologic but learned that the man did not have regular access to refrigeration. “That wasn’t going to work, but we started him on an oral medication, apremilast, which has completely cleared his skin,” he said. “He’s doing great. The last time we saw him he was re-engaged with his family, and he told us he was going on dates. We really improved his quality of life.”
Dr. Klein recalled seeing a 6-year-old girl at the clinic with atopic dermatitis so severe that it caused her to miss several days of school. “When she was in school, she was so distracted by the itching – it was so overwhelming,” she said. She was struggling with topical medicines that weren’t effective, but Dr. Klein got her on dupilumab, and during a follow-up visit the girl told her, “This is the first time in my life I can think about things” other than itching.
According to Dr. Nicholson, some patients seen at the Montezuma Creek clinic are on Medicare or carry standard insurance. “Others have a mix, and others are getting all their medications through the Montezuma Creek clinic or through the IHS clinics,” he said. “I have been surprised at the formulary and our ability to get relatively expensive medications for our patients, like biologics and TNF inhibitors. But it takes some creativity to know what is going to work for your patients’ living situation.”
Training more AI/AN dermatologists key
While efforts to increase the culturally respectful and sustainable dermatologic care for AI/AN individuals continue through programs like the continuity clinic at Montezuma Creek, sources interviewed for this story emphasized the importance of training more AI/AN dermatologists. “Of the people who graduate from high school, AIs have the lowest rate of going on to college,” said Dr. Kohn, who serves as a mentor to Mr. Hicks. “Let’s say they get all the way to medical school; it’s about good mentorship and support in what they’re pursuing. We are seeing more AIs in medical school now, something that I personally notice, and I notice it from what Chinle Service Unit tells me. They have received many requests from Native medical students and premed students who want to rotate at Chinle. Native trainees want the experience of being there.”
According to the Association of American Medical Colleges, the number of AI/AN applicants to medical schools increased from 72 in 2020-2021 to 105 in 2021-2022 but dipped slightly to 94 in 2022-2023. Inspired by a passion to serve Pine Ridge or a community like it, Mr. Hicks decided to apply for medical school. While he doesn’t want to “close any doors” on which medical specialty he ultimately chooses to practice, the current front-runner is dermatology, he said, largely because of the influence of Dr. Kohn and two Mayo dermatologists who have become mentors: Molly Lohman, MD, and Hafsa M. Cantwell, MD. “I didn’t see anyone from my background who was a doctor, so having those role models is so important for Native kids to think, ‘I can do this, too,’ and to pursue it,” he said.
As a proud member of the Oglala Lakota Nation from the Pine Ridge Indian Reservation in southwestern South Dakota, Drew Hicks grew up with limited access to basic health care, let alone the luxury of scheduling an appointment with a dermatologist or another medical specialist.
The area – once home to the Lakota war leader Crazy Horse – encompasses nearly 47,000 residents scattered over about 2.2 million acres, larger than the size of Rhode Island, with land marked by rolling mixed grass prairie, sandhills, and badlands. Some of the Oglala Lakota people live in substandard housing and lack regular access to food, running water, and refrigeration, not to mention cell phone and Internet service. “It’s sparse,” said Mr. Hicks, the son of Tribal ranchers who now is a 3rd-year medical student at the Mayo Clinic College of Medicine and Science in Rochester, Minn., and has an early interest in pursuing dermatology. “There is a lot of territory and not a lot of health care serving the population.” From the Hicks home, the nearest place to receive health care is a family medicine practice in Martin, S.D. – about a 15-minute drive on gravel roads in the best of conditions, but in poor weather, it can be difficult, he said. “So, there are environmental challenges besides the limited number of health care providers.”
Clinicians in the practice “did have to be the point of care for everything from dermatologic issues to emergency medicine to delivering a baby, because the next-closest medical facility of any magnitude is 2 hours away,” he said.
Challenges of health literacy and limited access to comprehensive health care at Pine Ridge and other American Indian (AI) and Alaska Native (AN) reservations have long-term consequences. “My own mom struggled to control her blood pressure for years and now has chronic kidney disease,” Mr. Hicks said. “It’s not an uncommon story. Diabetes on the reservation is a big issue.” Then there’s his father, who survived two bouts with melanoma that was diagnosed at an advanced stage. “I think about how that has impacted him, and wonder, had we had a dermatologist who serviced our area, would we have caught things sooner?” he said. “I feel there is so much room for impactful health care deliveries to communities like Pine Ridge.” At the same time, he emphasized, “this isn’t poverty porn. We’re a resilient people. Any effort to engage with AIs or ANs should be from a perspective of a learner, having cultural humility, and seeking out community leaders to help lead you.”
According to the 2020 Census, there are 574 federally recognized sovereign tribal nations in the United States and federal- and state-recognized American Indian reservations in 35 states. AI/AN people make up about 2.9% of the total U.S. population, or 9.7 million, and their life expectancy is an average of 4.4 years less, compared with the general population (a mean of 73.7 vs. 78.1 years, respectively). Because of limited access to dermatologic care in these areas, the risk for developing significant skin conditions and diseases that may go undetected for long stretches of time is increased.
“That can mean advanced skin cancers like basal cell carcinomas that have become larger than what you would see in a typical metropolitan population,” said Lucinda Kohn, MD, assistant professor of dermatology in the Centers for American Indian and Alaska Native Health at the University of Colorado at Denver, Aurora, who spent part of her dermatology residency rotating at the Chinle (Ariz.) Service Unit, an Indian Health Service facility, in 2017 and now provides teledermatology and regular in-person dermatology care at that clinic. “The climate there is dry, so you can see bad eczema and dry skin. There’s also a lot of acne and hidradenitis suppurativa. I think the acne and HS is due to the hyperglycemic index diet from the food deserts. Skin disease reflects the climate, the food desert, and the lack of close specialty care.”
Acne scarring common
Some published evidence suggests that acne is more prevalent and severe in AI/AN individuals. In a survey of 158 AI/AN individuals with a mean age of 32 years, 79.1% reported a history of acne, 55.1% reported acne scarring, and 31% reported having active lesions. “Looking back on my experience in high school, I definitely see that in myself and in my peers,” Mr. Hicks said. And, while there are limited published studies about the incidence of melanoma in this population, an analysis from 2006 found that the incidence was 3.1 per 100,000 between 2001 and 2005, which was an increase from 1.6 per 100,000 reported between 1992 and 2000.
There’s a lot to unpack for dermatologists caring for the AI/AN population besides the raw health disparities: a long history of distrust between AI/AN people and the federal government, structural racism, geographic isolation, health literacy challenges, and high rates of poverty and unemployment. And while individuals from federally recognized tribes have a legal right to receive health care provided by the Indian Health Service, a component of the Department of Health & Human Services, the U.S. Government Accountability Office found that in 2017 per capita spending available to the IHS was $4,078, compared with $8,109 for Medicaid, $10,692 for the Veterans Health Administration, and $13,185 for Medicare.
“Everyone deserves healthy skin and good health,” said Dr. Kohn, whose husband is AI and works in AI law. “Knowing that there are pockets of people who lack that access to care really bothers me. I think the American Indians are frequently overlooked. They’re just not even counted for in certain surveys,” she added, noting that categories are usually defined as Black, Hispanic, Asian, or White.
According to Dr. Kohn, who coauthored a chapter titled “Dermatology on American Indian and Alaska Native Reservations,” for the 2021 book “Dermatology in Rural Settings”, 70% of AIs live in urban areas, “so it’s not just people who live on reservations, though the disparity is greatest there.” To help deliver dermatologic care in the rural areas “where you’re on tribal lands, you must partner with the tribes,” she added. “You must get their permission, operate under their laws and regulations and their rules, learn the local customs, learn about the culture, learn the people, and learn their resources before you practice. That’s the only ethical way to practice.” This also means appreciating the fact that some AI/AN individuals may not understand what a dermatologist could do for them. “One of the bigger hurdles to overcome,” she said, is educating the population that dermatologists can cure skin diseases and that there are good medications for treating the diseases.
Shortcomings of teledermatology
Some dermatologists perform teledermatology visits for tribes, often from an office located in a different time zone. “And, they don’t have a sense of what resources are available for the people they’re serving,” Dr. Kohn said. “For example, if they diagnose a potential skin cancer on the face and say, ‘you need a biopsy,’ but the closest dermatologist is 4 hours away, is that really serving the patient? Or, if you tell a patient, ‘I want you to go out and buy Vanicream for your skin,’ but Vanicream costs $17 and the patient can’t even afford to buy food, are you really doing them a service?”
In a survey-based study of 238 AI individuals that is scheduled to be published in late 2023, Dr. Kohn and colleagues asked respondents at two regional powwows in Denver if they would be open to teledermatology – either in their home or in a primary care clinic. Most respondents (70%) lived in urban areas, the rest in rural settings. Nearly half of respondents (42%) “did not want to do teledermatology, even though they couldn’t access in-person dermatology,” Dr. Kohn said. “So, for people who think teledermatology is the answer [to improving access], the respondents to our survey weren’t interested in pursuing that as a solution. I was surprised by that.” When the researchers broke down the responses by age, teenage respondents were even less interested in teledermatology than adults were. “I think there’s something about having someone see you in person, knowing who you are,” she said.
Partnerships with tribes
To foster more sustainable change in the delivery of skin care beyond remote teledermatology and periodic visits from volunteers, some dermatology residencies have established partnerships with tribes, including Massachusetts General Hospital’s teaching partnership with the Rosebud Sioux tribe in Rosebud, S.D., and the University of Utah dermatology department’s resident continuity clinic with Navajo Nation in Montezuma Creek, Utah. In 2016, officials from the Utah Navajo Health System reached out to the University of Utah’s dermatology department to inquire about the potential for creating a teledermatology clinic to serve patients who receive primary care at the Montezuma Creek Community Health Center, located in Southeastern Utah on the northern tip of the Navajo Nation.
Stephanie Klein, MD, associate professor of dermatology at the university, spearheaded the clinic’s launch but soon encountered obstacles that ranged from not being able to visualize the patient’s skin clearly on her computer screen to difficulty making a personal connection with patients despite help from Navajo translators. “It was hard to build a relationship,” she said. A few years later, she drove down to meet with officials of the health system and posed the question: “What is the ideal thing you would want from dermatology?”
Continuity, they told her. “They said that a lot of the services they receive in the form of outreach are rotational, where someone might come in for a day, or a week, or five people may rotate throughout the year,” which did not serve them well, said Dr. Klein, who subsequently collaborated with Utah Navajo Health System clinicians to establish a resident continuity clinic, which launched in January 2021.
The arrangement also serves as a continuity clinic for Dr. Klein as an attending physician. Each month, she and one dermatology resident drive 6.5 hours from Salt Lake City to Montezuma Creek, where they spend 1 or 2 full days seeing about 25 patients referred by the primary care clinicians who work there. About one-quarter of the time they fly, thanks to financial support from a private donor. The flight takes about an hour, then it’s an hour-long drive to the actual clinic. “It’s a commitment,” Dr. Klein said. “A resident can come with me if they commit to the clinic for at least 1 year. This enables us to have continuity of care; it allows us to build relationships with the patients and with the care team there.” As for the prior teledermatology visits she had with residents, “I still do those, but now I do them in between the in-person visits, so I’m not meeting people over telehealth; I’m just following up with them.”

Situated in the high desert among rock formations, the estimated population of Montezuma Creek is just over 320 people. “It’s a beautiful place with otherworldly buttes and mesas, and the Blue Mountains rising up in the distance,” said Lowell Nicholson, MD, a dermatology resident at the University of Utah who is in his second year of a 2-year commitment to the clinic. “But the landscape can be harsh, and it is underserved from an infrastructure perspective,” with large areas with no cell phone service and limited access to running water and refrigeration. “People in general travel quite far to get their medical care and most of the roads are dirt or gravel, so after a big snowstorm or if it’s been raining, they can become impassable.”
Dermatologic conditions they often encounter include vitiligo, photodermatoses, hidradenitis suppurativa, eczema, psoriasis, and severe acne, often with lots of acne-associated scarring. “In general, we tend to see dramatic or advanced presentations of general dermatology diagnoses,” Dr. Nicholson said. “We see a lot of really extensive psoriasis, which can be socially stigmatizing.”
He recalled one middle-aged man who isolated himself from others because his psoriasis became unbearable. The man refused to leave his house, visit family members, or attend tribal meetups. “He tried to see his regular doctor about it and was given topicals, but his disease was just too extensive,” said Dr. Nicholson, who suggested trying a biologic but learned that the man did not have regular access to refrigeration. “That wasn’t going to work, but we started him on an oral medication, apremilast, which has completely cleared his skin,” he said. “He’s doing great. The last time we saw him he was re-engaged with his family, and he told us he was going on dates. We really improved his quality of life.”
Dr. Klein recalled seeing a 6-year-old girl at the clinic with atopic dermatitis so severe that it caused her to miss several days of school. “When she was in school, she was so distracted by the itching – it was so overwhelming,” she said. She was struggling with topical medicines that weren’t effective, but Dr. Klein got her on dupilumab, and during a follow-up visit the girl told her, “This is the first time in my life I can think about things” other than itching.
According to Dr. Nicholson, some patients seen at the Montezuma Creek clinic are on Medicare or carry standard insurance. “Others have a mix, and others are getting all their medications through the Montezuma Creek clinic or through the IHS clinics,” he said. “I have been surprised at the formulary and our ability to get relatively expensive medications for our patients, like biologics and TNF inhibitors. But it takes some creativity to know what is going to work for your patients’ living situation.”
Training more AI/AN dermatologists key
While efforts to increase the culturally respectful and sustainable dermatologic care for AI/AN individuals continue through programs like the continuity clinic at Montezuma Creek, sources interviewed for this story emphasized the importance of training more AI/AN dermatologists. “Of the people who graduate from high school, AIs have the lowest rate of going on to college,” said Dr. Kohn, who serves as a mentor to Mr. Hicks. “Let’s say they get all the way to medical school; it’s about good mentorship and support in what they’re pursuing. We are seeing more AIs in medical school now, something that I personally notice, and I notice it from what Chinle Service Unit tells me. They have received many requests from Native medical students and premed students who want to rotate at Chinle. Native trainees want the experience of being there.”
According to the Association of American Medical Colleges, the number of AI/AN applicants to medical schools increased from 72 in 2020-2021 to 105 in 2021-2022 but dipped slightly to 94 in 2022-2023. Inspired by a passion to serve Pine Ridge or a community like it, Mr. Hicks decided to apply for medical school. While he doesn’t want to “close any doors” on which medical specialty he ultimately chooses to practice, the current front-runner is dermatology, he said, largely because of the influence of Dr. Kohn and two Mayo dermatologists who have become mentors: Molly Lohman, MD, and Hafsa M. Cantwell, MD. “I didn’t see anyone from my background who was a doctor, so having those role models is so important for Native kids to think, ‘I can do this, too,’ and to pursue it,” he said.
As a proud member of the Oglala Lakota Nation from the Pine Ridge Indian Reservation in southwestern South Dakota, Drew Hicks grew up with limited access to basic health care, let alone the luxury of scheduling an appointment with a dermatologist or another medical specialist.
The area – once home to the Lakota war leader Crazy Horse – encompasses nearly 47,000 residents scattered over about 2.2 million acres, larger than the size of Rhode Island, with land marked by rolling mixed grass prairie, sandhills, and badlands. Some of the Oglala Lakota people live in substandard housing and lack regular access to food, running water, and refrigeration, not to mention cell phone and Internet service. “It’s sparse,” said Mr. Hicks, the son of Tribal ranchers who now is a 3rd-year medical student at the Mayo Clinic College of Medicine and Science in Rochester, Minn., and has an early interest in pursuing dermatology. “There is a lot of territory and not a lot of health care serving the population.” From the Hicks home, the nearest place to receive health care is a family medicine practice in Martin, S.D. – about a 15-minute drive on gravel roads in the best of conditions, but in poor weather, it can be difficult, he said. “So, there are environmental challenges besides the limited number of health care providers.”
Clinicians in the practice “did have to be the point of care for everything from dermatologic issues to emergency medicine to delivering a baby, because the next-closest medical facility of any magnitude is 2 hours away,” he said.
Challenges of health literacy and limited access to comprehensive health care at Pine Ridge and other American Indian (AI) and Alaska Native (AN) reservations have long-term consequences. “My own mom struggled to control her blood pressure for years and now has chronic kidney disease,” Mr. Hicks said. “It’s not an uncommon story. Diabetes on the reservation is a big issue.” Then there’s his father, who survived two bouts with melanoma that was diagnosed at an advanced stage. “I think about how that has impacted him, and wonder, had we had a dermatologist who serviced our area, would we have caught things sooner?” he said. “I feel there is so much room for impactful health care deliveries to communities like Pine Ridge.” At the same time, he emphasized, “this isn’t poverty porn. We’re a resilient people. Any effort to engage with AIs or ANs should be from a perspective of a learner, having cultural humility, and seeking out community leaders to help lead you.”
According to the 2020 Census, there are 574 federally recognized sovereign tribal nations in the United States and federal- and state-recognized American Indian reservations in 35 states. AI/AN people make up about 2.9% of the total U.S. population, or 9.7 million, and their life expectancy is an average of 4.4 years less, compared with the general population (a mean of 73.7 vs. 78.1 years, respectively). Because of limited access to dermatologic care in these areas, the risk for developing significant skin conditions and diseases that may go undetected for long stretches of time is increased.
“That can mean advanced skin cancers like basal cell carcinomas that have become larger than what you would see in a typical metropolitan population,” said Lucinda Kohn, MD, assistant professor of dermatology in the Centers for American Indian and Alaska Native Health at the University of Colorado at Denver, Aurora, who spent part of her dermatology residency rotating at the Chinle (Ariz.) Service Unit, an Indian Health Service facility, in 2017 and now provides teledermatology and regular in-person dermatology care at that clinic. “The climate there is dry, so you can see bad eczema and dry skin. There’s also a lot of acne and hidradenitis suppurativa. I think the acne and HS is due to the hyperglycemic index diet from the food deserts. Skin disease reflects the climate, the food desert, and the lack of close specialty care.”
Acne scarring common
Some published evidence suggests that acne is more prevalent and severe in AI/AN individuals. In a survey of 158 AI/AN individuals with a mean age of 32 years, 79.1% reported a history of acne, 55.1% reported acne scarring, and 31% reported having active lesions. “Looking back on my experience in high school, I definitely see that in myself and in my peers,” Mr. Hicks said. And, while there are limited published studies about the incidence of melanoma in this population, an analysis from 2006 found that the incidence was 3.1 per 100,000 between 2001 and 2005, which was an increase from 1.6 per 100,000 reported between 1992 and 2000.
There’s a lot to unpack for dermatologists caring for the AI/AN population besides the raw health disparities: a long history of distrust between AI/AN people and the federal government, structural racism, geographic isolation, health literacy challenges, and high rates of poverty and unemployment. And while individuals from federally recognized tribes have a legal right to receive health care provided by the Indian Health Service, a component of the Department of Health & Human Services, the U.S. Government Accountability Office found that in 2017 per capita spending available to the IHS was $4,078, compared with $8,109 for Medicaid, $10,692 for the Veterans Health Administration, and $13,185 for Medicare.
“Everyone deserves healthy skin and good health,” said Dr. Kohn, whose husband is AI and works in AI law. “Knowing that there are pockets of people who lack that access to care really bothers me. I think the American Indians are frequently overlooked. They’re just not even counted for in certain surveys,” she added, noting that categories are usually defined as Black, Hispanic, Asian, or White.
According to Dr. Kohn, who coauthored a chapter titled “Dermatology on American Indian and Alaska Native Reservations,” for the 2021 book “Dermatology in Rural Settings”, 70% of AIs live in urban areas, “so it’s not just people who live on reservations, though the disparity is greatest there.” To help deliver dermatologic care in the rural areas “where you’re on tribal lands, you must partner with the tribes,” she added. “You must get their permission, operate under their laws and regulations and their rules, learn the local customs, learn about the culture, learn the people, and learn their resources before you practice. That’s the only ethical way to practice.” This also means appreciating the fact that some AI/AN individuals may not understand what a dermatologist could do for them. “One of the bigger hurdles to overcome,” she said, is educating the population that dermatologists can cure skin diseases and that there are good medications for treating the diseases.
Shortcomings of teledermatology
Some dermatologists perform teledermatology visits for tribes, often from an office located in a different time zone. “And, they don’t have a sense of what resources are available for the people they’re serving,” Dr. Kohn said. “For example, if they diagnose a potential skin cancer on the face and say, ‘you need a biopsy,’ but the closest dermatologist is 4 hours away, is that really serving the patient? Or, if you tell a patient, ‘I want you to go out and buy Vanicream for your skin,’ but Vanicream costs $17 and the patient can’t even afford to buy food, are you really doing them a service?”
In a survey-based study of 238 AI individuals that is scheduled to be published in late 2023, Dr. Kohn and colleagues asked respondents at two regional powwows in Denver if they would be open to teledermatology – either in their home or in a primary care clinic. Most respondents (70%) lived in urban areas, the rest in rural settings. Nearly half of respondents (42%) “did not want to do teledermatology, even though they couldn’t access in-person dermatology,” Dr. Kohn said. “So, for people who think teledermatology is the answer [to improving access], the respondents to our survey weren’t interested in pursuing that as a solution. I was surprised by that.” When the researchers broke down the responses by age, teenage respondents were even less interested in teledermatology than adults were. “I think there’s something about having someone see you in person, knowing who you are,” she said.
Partnerships with tribes
To foster more sustainable change in the delivery of skin care beyond remote teledermatology and periodic visits from volunteers, some dermatology residencies have established partnerships with tribes, including Massachusetts General Hospital’s teaching partnership with the Rosebud Sioux tribe in Rosebud, S.D., and the University of Utah dermatology department’s resident continuity clinic with Navajo Nation in Montezuma Creek, Utah. In 2016, officials from the Utah Navajo Health System reached out to the University of Utah’s dermatology department to inquire about the potential for creating a teledermatology clinic to serve patients who receive primary care at the Montezuma Creek Community Health Center, located in Southeastern Utah on the northern tip of the Navajo Nation.
Stephanie Klein, MD, associate professor of dermatology at the university, spearheaded the clinic’s launch but soon encountered obstacles that ranged from not being able to visualize the patient’s skin clearly on her computer screen to difficulty making a personal connection with patients despite help from Navajo translators. “It was hard to build a relationship,” she said. A few years later, she drove down to meet with officials of the health system and posed the question: “What is the ideal thing you would want from dermatology?”
Continuity, they told her. “They said that a lot of the services they receive in the form of outreach are rotational, where someone might come in for a day, or a week, or five people may rotate throughout the year,” which did not serve them well, said Dr. Klein, who subsequently collaborated with Utah Navajo Health System clinicians to establish a resident continuity clinic, which launched in January 2021.
The arrangement also serves as a continuity clinic for Dr. Klein as an attending physician. Each month, she and one dermatology resident drive 6.5 hours from Salt Lake City to Montezuma Creek, where they spend 1 or 2 full days seeing about 25 patients referred by the primary care clinicians who work there. About one-quarter of the time they fly, thanks to financial support from a private donor. The flight takes about an hour, then it’s an hour-long drive to the actual clinic. “It’s a commitment,” Dr. Klein said. “A resident can come with me if they commit to the clinic for at least 1 year. This enables us to have continuity of care; it allows us to build relationships with the patients and with the care team there.” As for the prior teledermatology visits she had with residents, “I still do those, but now I do them in between the in-person visits, so I’m not meeting people over telehealth; I’m just following up with them.”

Situated in the high desert among rock formations, the estimated population of Montezuma Creek is just over 320 people. “It’s a beautiful place with otherworldly buttes and mesas, and the Blue Mountains rising up in the distance,” said Lowell Nicholson, MD, a dermatology resident at the University of Utah who is in his second year of a 2-year commitment to the clinic. “But the landscape can be harsh, and it is underserved from an infrastructure perspective,” with large areas with no cell phone service and limited access to running water and refrigeration. “People in general travel quite far to get their medical care and most of the roads are dirt or gravel, so after a big snowstorm or if it’s been raining, they can become impassable.”
Dermatologic conditions they often encounter include vitiligo, photodermatoses, hidradenitis suppurativa, eczema, psoriasis, and severe acne, often with lots of acne-associated scarring. “In general, we tend to see dramatic or advanced presentations of general dermatology diagnoses,” Dr. Nicholson said. “We see a lot of really extensive psoriasis, which can be socially stigmatizing.”
He recalled one middle-aged man who isolated himself from others because his psoriasis became unbearable. The man refused to leave his house, visit family members, or attend tribal meetups. “He tried to see his regular doctor about it and was given topicals, but his disease was just too extensive,” said Dr. Nicholson, who suggested trying a biologic but learned that the man did not have regular access to refrigeration. “That wasn’t going to work, but we started him on an oral medication, apremilast, which has completely cleared his skin,” he said. “He’s doing great. The last time we saw him he was re-engaged with his family, and he told us he was going on dates. We really improved his quality of life.”
Dr. Klein recalled seeing a 6-year-old girl at the clinic with atopic dermatitis so severe that it caused her to miss several days of school. “When she was in school, she was so distracted by the itching – it was so overwhelming,” she said. She was struggling with topical medicines that weren’t effective, but Dr. Klein got her on dupilumab, and during a follow-up visit the girl told her, “This is the first time in my life I can think about things” other than itching.
According to Dr. Nicholson, some patients seen at the Montezuma Creek clinic are on Medicare or carry standard insurance. “Others have a mix, and others are getting all their medications through the Montezuma Creek clinic or through the IHS clinics,” he said. “I have been surprised at the formulary and our ability to get relatively expensive medications for our patients, like biologics and TNF inhibitors. But it takes some creativity to know what is going to work for your patients’ living situation.”
Training more AI/AN dermatologists key
While efforts to increase the culturally respectful and sustainable dermatologic care for AI/AN individuals continue through programs like the continuity clinic at Montezuma Creek, sources interviewed for this story emphasized the importance of training more AI/AN dermatologists. “Of the people who graduate from high school, AIs have the lowest rate of going on to college,” said Dr. Kohn, who serves as a mentor to Mr. Hicks. “Let’s say they get all the way to medical school; it’s about good mentorship and support in what they’re pursuing. We are seeing more AIs in medical school now, something that I personally notice, and I notice it from what Chinle Service Unit tells me. They have received many requests from Native medical students and premed students who want to rotate at Chinle. Native trainees want the experience of being there.”
According to the Association of American Medical Colleges, the number of AI/AN applicants to medical schools increased from 72 in 2020-2021 to 105 in 2021-2022 but dipped slightly to 94 in 2022-2023. Inspired by a passion to serve Pine Ridge or a community like it, Mr. Hicks decided to apply for medical school. While he doesn’t want to “close any doors” on which medical specialty he ultimately chooses to practice, the current front-runner is dermatology, he said, largely because of the influence of Dr. Kohn and two Mayo dermatologists who have become mentors: Molly Lohman, MD, and Hafsa M. Cantwell, MD. “I didn’t see anyone from my background who was a doctor, so having those role models is so important for Native kids to think, ‘I can do this, too,’ and to pursue it,” he said.







