User login
Black patients most likely to be restrained in EDs, Latino patients least likely
SAN FRANCISCO – .
In contrast, Hispanic/Latino patients were less likely to be restrained than both Black and White patients, researchers reported in a poster presented at the annual meeting of the American Psychiatric Association. The study authors also found that clinicians rarely turned to restraints, using them in just 2,712 of 882,390 ED visits (0.3%) over a 7-year period.
The study doesn’t examine why the disparities exist. But lead author Erika Chang-Sing, a medical student at Yale University, New Haven, Conn., said in an interview that it’s clear that racial bias is the cause of the differences in restraint rates among White, Black, and Hispanics/Latino patients. “We think that there are multiple contributing factors to the higher rates of restraint for Black patients brought to the hospital by police, and all of them are rooted in systemic racism,” she said, adding that “the lower odds of restraint in the Hispanic or Latino group are also rooted in systemic racism and inequity.”
According to Ms. Chang-Sing, researchers launched the study to gain insight into the use of the restraints in the Southeast and to see what’s happening in light of the recent publicizing of killings of Black people by police. Being taken to the hospital by police “might contribute both to the individual patient’s behavior and the health care provider’s assessment of risk in determining whether or not to apply restraints,” she said.
Other research has linked ethnicity to higher rates of restraint use. For example, a 2021 study of 32,054 cases of patients under mandatory psychiatric hold in 11 Massachusetts emergency rooms found that Black (adjusted odds ratio, 1.22) and Hispanic (aOR, 1.45) patients were more likely to be restrained than White patients.
For the new study, researchers retrospectively tracked 885,102 emergency room visits at three North Carolina emergency departments from 2015 to 2022, including 9,130 who were brought in by police and 2,712 who were physically restrained because of the perceived risk of violence. “Providers use restraints, or straps, to secure the patient’s wrists and ankles to the bed,” Ms. Chang-Sing said.
Among all patients, 52.5% were Black, but 66% of those who were restrained were Black. The numbers for White patients were 35.7% and 23.9%, respectively, and 5.7% and 3.2% for Hispanics/Latino patients. Black patients were less likely than White patients to get a psychiatric primary emergency department diagnosis (aOR, 0.67), but those in that category were more likely than their White counterparts to be restrained (aOR, 1.36).
The higher risk of restraint use in Black patients overall disappeared when researchers adjusted their statistics to account for the effects of sex, age, and type of insurance (aOR, 0.86). Ms. Chang-Sing said the study team is reanalyzing the data since they think insurance may not be a confounder.
Why might Hispanic/Latino ethnicity be protective against restraint use? “This may be due to language barriers, fear of law enforcement, and avoidance of the hospital in the first place,” Ms. Chang-Sing said.
Emergency physician Wendy Macias-Konstantopoulos, MD, MPH, MBA, of Harvard Medical School and Massachusetts General Hospital, both in Boston, coauthored the 2021 study on police restraints. In an interview, she said the new findings add to previous research by providing data about the role played by the police who bring patients to the ED. She added that there is no evidence that certain populations simply need more restraints.
What can be done to reduce disparities in restraint use? Mental health teams can make a difference by responding to mental health emergencies, Ms. Chang-Sing said. “These providers can be instrumental in communicating to patients that the intention is to care for them, not to punish them.”
Another strategy is to increase the number of clinics and crisis response centers, she said. Hospital-based crisis response teams can also be helpful, she said. “Because these teams are focused only on behavioral emergencies, they can be more thoughtful in avoiding the use of restraints.”
No study funding was reported. The study authors and Dr. Macias-Konstantopoulos have no disclosures.
SAN FRANCISCO – .
In contrast, Hispanic/Latino patients were less likely to be restrained than both Black and White patients, researchers reported in a poster presented at the annual meeting of the American Psychiatric Association. The study authors also found that clinicians rarely turned to restraints, using them in just 2,712 of 882,390 ED visits (0.3%) over a 7-year period.
The study doesn’t examine why the disparities exist. But lead author Erika Chang-Sing, a medical student at Yale University, New Haven, Conn., said in an interview that it’s clear that racial bias is the cause of the differences in restraint rates among White, Black, and Hispanics/Latino patients. “We think that there are multiple contributing factors to the higher rates of restraint for Black patients brought to the hospital by police, and all of them are rooted in systemic racism,” she said, adding that “the lower odds of restraint in the Hispanic or Latino group are also rooted in systemic racism and inequity.”
According to Ms. Chang-Sing, researchers launched the study to gain insight into the use of the restraints in the Southeast and to see what’s happening in light of the recent publicizing of killings of Black people by police. Being taken to the hospital by police “might contribute both to the individual patient’s behavior and the health care provider’s assessment of risk in determining whether or not to apply restraints,” she said.
Other research has linked ethnicity to higher rates of restraint use. For example, a 2021 study of 32,054 cases of patients under mandatory psychiatric hold in 11 Massachusetts emergency rooms found that Black (adjusted odds ratio, 1.22) and Hispanic (aOR, 1.45) patients were more likely to be restrained than White patients.
For the new study, researchers retrospectively tracked 885,102 emergency room visits at three North Carolina emergency departments from 2015 to 2022, including 9,130 who were brought in by police and 2,712 who were physically restrained because of the perceived risk of violence. “Providers use restraints, or straps, to secure the patient’s wrists and ankles to the bed,” Ms. Chang-Sing said.
Among all patients, 52.5% were Black, but 66% of those who were restrained were Black. The numbers for White patients were 35.7% and 23.9%, respectively, and 5.7% and 3.2% for Hispanics/Latino patients. Black patients were less likely than White patients to get a psychiatric primary emergency department diagnosis (aOR, 0.67), but those in that category were more likely than their White counterparts to be restrained (aOR, 1.36).
The higher risk of restraint use in Black patients overall disappeared when researchers adjusted their statistics to account for the effects of sex, age, and type of insurance (aOR, 0.86). Ms. Chang-Sing said the study team is reanalyzing the data since they think insurance may not be a confounder.
Why might Hispanic/Latino ethnicity be protective against restraint use? “This may be due to language barriers, fear of law enforcement, and avoidance of the hospital in the first place,” Ms. Chang-Sing said.
Emergency physician Wendy Macias-Konstantopoulos, MD, MPH, MBA, of Harvard Medical School and Massachusetts General Hospital, both in Boston, coauthored the 2021 study on police restraints. In an interview, she said the new findings add to previous research by providing data about the role played by the police who bring patients to the ED. She added that there is no evidence that certain populations simply need more restraints.
What can be done to reduce disparities in restraint use? Mental health teams can make a difference by responding to mental health emergencies, Ms. Chang-Sing said. “These providers can be instrumental in communicating to patients that the intention is to care for them, not to punish them.”
Another strategy is to increase the number of clinics and crisis response centers, she said. Hospital-based crisis response teams can also be helpful, she said. “Because these teams are focused only on behavioral emergencies, they can be more thoughtful in avoiding the use of restraints.”
No study funding was reported. The study authors and Dr. Macias-Konstantopoulos have no disclosures.
SAN FRANCISCO – .
In contrast, Hispanic/Latino patients were less likely to be restrained than both Black and White patients, researchers reported in a poster presented at the annual meeting of the American Psychiatric Association. The study authors also found that clinicians rarely turned to restraints, using them in just 2,712 of 882,390 ED visits (0.3%) over a 7-year period.
The study doesn’t examine why the disparities exist. But lead author Erika Chang-Sing, a medical student at Yale University, New Haven, Conn., said in an interview that it’s clear that racial bias is the cause of the differences in restraint rates among White, Black, and Hispanics/Latino patients. “We think that there are multiple contributing factors to the higher rates of restraint for Black patients brought to the hospital by police, and all of them are rooted in systemic racism,” she said, adding that “the lower odds of restraint in the Hispanic or Latino group are also rooted in systemic racism and inequity.”
According to Ms. Chang-Sing, researchers launched the study to gain insight into the use of the restraints in the Southeast and to see what’s happening in light of the recent publicizing of killings of Black people by police. Being taken to the hospital by police “might contribute both to the individual patient’s behavior and the health care provider’s assessment of risk in determining whether or not to apply restraints,” she said.
Other research has linked ethnicity to higher rates of restraint use. For example, a 2021 study of 32,054 cases of patients under mandatory psychiatric hold in 11 Massachusetts emergency rooms found that Black (adjusted odds ratio, 1.22) and Hispanic (aOR, 1.45) patients were more likely to be restrained than White patients.
For the new study, researchers retrospectively tracked 885,102 emergency room visits at three North Carolina emergency departments from 2015 to 2022, including 9,130 who were brought in by police and 2,712 who were physically restrained because of the perceived risk of violence. “Providers use restraints, or straps, to secure the patient’s wrists and ankles to the bed,” Ms. Chang-Sing said.
Among all patients, 52.5% were Black, but 66% of those who were restrained were Black. The numbers for White patients were 35.7% and 23.9%, respectively, and 5.7% and 3.2% for Hispanics/Latino patients. Black patients were less likely than White patients to get a psychiatric primary emergency department diagnosis (aOR, 0.67), but those in that category were more likely than their White counterparts to be restrained (aOR, 1.36).
The higher risk of restraint use in Black patients overall disappeared when researchers adjusted their statistics to account for the effects of sex, age, and type of insurance (aOR, 0.86). Ms. Chang-Sing said the study team is reanalyzing the data since they think insurance may not be a confounder.
Why might Hispanic/Latino ethnicity be protective against restraint use? “This may be due to language barriers, fear of law enforcement, and avoidance of the hospital in the first place,” Ms. Chang-Sing said.
Emergency physician Wendy Macias-Konstantopoulos, MD, MPH, MBA, of Harvard Medical School and Massachusetts General Hospital, both in Boston, coauthored the 2021 study on police restraints. In an interview, she said the new findings add to previous research by providing data about the role played by the police who bring patients to the ED. She added that there is no evidence that certain populations simply need more restraints.
What can be done to reduce disparities in restraint use? Mental health teams can make a difference by responding to mental health emergencies, Ms. Chang-Sing said. “These providers can be instrumental in communicating to patients that the intention is to care for them, not to punish them.”
Another strategy is to increase the number of clinics and crisis response centers, she said. Hospital-based crisis response teams can also be helpful, she said. “Because these teams are focused only on behavioral emergencies, they can be more thoughtful in avoiding the use of restraints.”
No study funding was reported. The study authors and Dr. Macias-Konstantopoulos have no disclosures.
AT APA 2023
Differences in 30-Day Readmission Rates in Older Adults With Dementia
Study 1 Overview (Park et al)
Objective: To compare rates of adverse events and 30-day readmission among patients with dementia who undergo percutaneous coronary intervention (PCI) with those without dementia.
Design: This cohort study used a national database of hospital readmissions developed by the Agency for Healthcare Research and Quality.
Setting and participants: Data from State Inpatient Databases were used to derive this national readmissions database representing 80% of hospitals from 28 states that contribute data. The study included all individuals aged 18 years and older who were identified to have had a PCI procedure in the years 2017 and 2018. International Classification of Diseases, Tenth Revision (ICD-10) codes were used to identify PCI procedures, including drug-eluting stent placement, bare-metal stent placement, and balloon angioplasty, performed in patients who presented with myocardial infarction and unstable angina and those with stable ischemic heart disease. Patients were stratified into those with or without dementia, also defined using ICD-10 codes. A total of 755,406 index hospitalizations were included; 2.3% of the patients had dementia.
Main outcome measures: The primary study outcome was 30-day all-cause readmission, with the cause classified as cardiovascular or noncardiovascular. Secondary outcome measures examined were delirium, in-hospital mortality, cardiac arrest, blood transfusion, acute kidney injury, fall in hospital, length of hospital stay, and other adverse outcomes. Location at discharge was also examined. Other covariates included in the analysis were age, sex, comorbidities, hospital characteristics, primary payer, and median income. For analysis, a propensity score matching algorithm was applied to match patients with and without dementia. Kaplan-Meier curves were used to examine 30-day readmission rates, and a Cox proportional hazards model was used to calculate hazard ratios (HR) for those with and without dementia. For secondary outcomes, logistic regression models were used to calculate odds ratios (OR) of outcomes between those with and without dementia.
Main results: The average age of those with dementia was 78.8 years vs 64.9 years in those without dementia. Women made up 42.8% of those with dementia and 31.3% of those without dementia. Those with dementia also had higher rates of comorbidities, such as heart failure, renal failure, and depression. After propensity score matching, 17,309 and 17,187 patients with and without dementia, respectively, were included. Covariates were balanced between the 2 groups after matching. For the primary outcome, patients with dementia were more likely to be readmitted at 30 days (HR, 1.11; 95% CI, 1.05-1.18; P < .01) when compared to those without dementia. For other adverse outcomes, delirium was significantly more likely to occur for those with dementia (OR, 4.37; 95% CI, 3.69-5.16; P < .01). Patients with dementia were also more likely to die in hospital (OR, 1.15; 95% CI, 1.01-1.30; P = .03), have cardiac arrest (OR, 1.19; 95% CI, 1.01-1.39; P = .04), receive a blood transfusion (OR, 1.17; 95% CI, 1.00-1.36; P = .05), experience acute kidney injury (OR, 1.30; 95% CI, 1.21-1.39; P < .01), and fall in hospital (OR, 2.51; 95% CI, 2.06-3.07; P < .01). Hospital length of stay was higher for those with dementia, with a mean difference of 1.43 days. For discharge location, patients with dementia were more likely to be sent to a skilled nursing facility (30.1% vs 12.2%) and less likely to be discharged home.
Conclusion: Patients with dementia are more likely to experience adverse events, including delirium, mortality, kidney injury, and falls after PCI, and are more likely to be readmitted to the hospital in 30 days compared to those without dementia.
Study 2 Overview (Gilmore-Bykovskyi et al)
Objective: To examine the association between race and 30-day readmissions in Black and non-Hispanic White Medicare beneficiaries with dementia.
Design: This was a retrospective cohort study that used 100% Medicare fee-for service claims data from all hospitalizations between January 1, 2014, and November 30, 2014, for all enrollees with a dementia diagnosis. The claims data were linked to the patient, hospital stay, and hospital factors. Patients with dementia were identified using a validated algorithm that requires an inpatient, skilled nursing facility, home health, or Part B institutional or noninstitutional claim with a qualifying diagnostic code during a 3-year period. Persons enrolled in a health maintenance organization plan were excluded.
Main outcome measures: The primary outcome examined in this study was 30-day all-cause readmission. Self-reported race and ethnic identity was a baseline covariate. Persons who self-reported Black or non-Hispanic White race were included in the study; other categories of race and ethnicity were excluded because of prior evidence suggesting low accuracy of these categories in Medicare claims data. Other covariates included neighborhood disadvantage, measured using the Area Deprivation Index (ADI), and rurality; hospital-level and hospital stay–level characteristics such as for-profit status and number of annual discharges; and individual demographic characteristics and comorbidities. The ADI is constructed using variables of poverty, education, housing, and employment and is represented as a percentile ranking of level of disadvantage. Unadjusted and adjusted analyses of 30-day hospital readmission were conducted. Models using various levels of adjustment were constructed to examine the contributions of the identified covariates to the estimated association between 30-day readmission and race.
Main results: A total of 1,523,142 index hospital stays among 945,481 beneficiaries were included; 215,815 episodes were among Black beneficiaries and 1,307,327 episodes were among non-Hispanic White beneficiaries. Mean age was 81.5 years, and approximately 61% of beneficiaries were female. Black beneficiaries were younger but had higher rates of dual Medicare/Medicaid eligibility and disability; they were also more likely to reside in disadvantaged neighborhoods. Black beneficiaries had a 30-day readmission rate of 24.1% compared with 18.5% in non-Hispanic White beneficiaries (unadjusted OR, 1.37; 95% CI, 1.35-1.39). The differences in outcomes persisted after adjusting for geographic factors, social factors, hospital characteristics, hospital stay factors, demographics, and comorbidities, suggesting that unmeasured underlying racial disparities not included in this model accounted for the differences. The effects of certain variables, such as neighborhood, differed by race; for example, the protective effect of living in a less disadvantaged neighborhood was observed among White beneficiaries but not Black beneficiaries.
Conclusion: Racial and geographic disparities in 30-day readmission rates were observed among Medicare beneficiaries with dementia. Protective effects associated with neighborhood advantage may confer different levels of benefit for people of different race.
Commentary
Adults living with dementia are at higher risk of adverse outcomes across settings. In the first study, by Park et al, among adults who underwent a cardiac procedure (PCI), those with dementia were more likely to experience adverse events compared to those without dementia. These outcomes include increased rates of 30-day readmissions, delirium, cardiac arrest, and falls. These findings are consistent with other studies that found a similar association among patients who underwent other cardiac procedures, such as transcatheter aortic valve replacement.1 Because dementia is a strong predisposing factor for delirium, it is not surprising that delirium is observed across patients who underwent different procedures or hospitalization episodes.2 Because of the potential hazards for inpatients with dementia, hospitals have developed risk-reduction programs, such as those that promote recognition of dementia, and management strategies that reduce the risk of delirium.3 Delirium prevention may also impact other adverse outcomes, such as falls, discharge to institutional care, and readmissions.
Racial disparities in care outcomes have been documented across settings, including hospital4 and hospice care settings.5 In study 2, by Gilmore-Bykovskyi et al, the findings of higher rates of hospital readmission among Black patients when compared to non-Hispanic White patients were not surprising. The central finding of this study is that even when accounting for various levels of factors, including hospital-level, hospital stay–level, individual (demographics, comorbidities), and neighborhood characteristics (disadvantage), the observed disparity diminished but persisted, suggesting that while these various levels of factors contributed to the observed disparity, other unmeasured factors also contributed. Another key finding is that the effect of the various factors examined in this study may affect different subgroups in different ways, suggesting underlying factors, and thus potential solutions to reduce disparities in care outcomes, could differ among subgroups.
Applications for Clinical Practice and System Implementation
These 2 studies add to the literature on factors that can affect 30-day hospital readmission rates in patients with dementia. These data could allow for more robust discussions of what to anticipate when adults with dementia undergo specific procedures, and also further build the case that improvements in care, such as delirium prevention programs, could offer benefits. The observation about racial and ethnic disparities in care outcomes among patients with dementia highlights the continued need to better understand the drivers of these disparities so that hospital systems and policy makers can consider and test possible solutions. Future studies should further disentangle the relationships among the various levels of factors and observed disparities in outcomes, especially for this vulnerable population of adults living with dementia.
Practice Points
- Clinicians should be aware of the additional risks for poor outcomes that dementia confers.
- Awareness of this increased risk will inform discussions of risks and benefits for older adults considered for procedures.
–William W. Hung, MD, MPH
1. Park DY, Sana MK, Shoura S, et al. Readmission and in-hospital outcomes after transcatheter aortic valve replacement in patients with dementia. Cardiovasc Revasc Med. 2023;46:70-77. doi:10.1016/j.carrev.2022.08.016
2. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51(5):591-598. doi:10.1034/j.1600-0579.2003.00201.x
3. Weldingh NM, Mellingsæter MR, Hegna BW, et al. Impact of a dementia-friendly program on detection and management of patients with cognitive impairment and delirium in acute-care hospital units: a controlled clinical trial design. BMC Geriatr. 2022;22(1):266. doi:10.1186/s12877-022-02949-0
4. Hermosura AH, Noonan CJ, Fyfe-Johnson AL, et al. Hospital disparities between native Hawaiian and other pacific islanders and non-Hispanic whites with Alzheimer’s disease and related dementias. J Aging Health. 2020;32(10):1579-1590. doi:10.1177/0898264320945177
5. Zhang Y, Shao H, Zhang M, Li J. Healthcare utilization and mortality after hospice live discharge among Medicare patients with and without Alzheimer’s disease and related dementias. J Gen Intern Med. 2023 Jan 17. doi:10.1007/s11606-023-08031-8
Study 1 Overview (Park et al)
Objective: To compare rates of adverse events and 30-day readmission among patients with dementia who undergo percutaneous coronary intervention (PCI) with those without dementia.
Design: This cohort study used a national database of hospital readmissions developed by the Agency for Healthcare Research and Quality.
Setting and participants: Data from State Inpatient Databases were used to derive this national readmissions database representing 80% of hospitals from 28 states that contribute data. The study included all individuals aged 18 years and older who were identified to have had a PCI procedure in the years 2017 and 2018. International Classification of Diseases, Tenth Revision (ICD-10) codes were used to identify PCI procedures, including drug-eluting stent placement, bare-metal stent placement, and balloon angioplasty, performed in patients who presented with myocardial infarction and unstable angina and those with stable ischemic heart disease. Patients were stratified into those with or without dementia, also defined using ICD-10 codes. A total of 755,406 index hospitalizations were included; 2.3% of the patients had dementia.
Main outcome measures: The primary study outcome was 30-day all-cause readmission, with the cause classified as cardiovascular or noncardiovascular. Secondary outcome measures examined were delirium, in-hospital mortality, cardiac arrest, blood transfusion, acute kidney injury, fall in hospital, length of hospital stay, and other adverse outcomes. Location at discharge was also examined. Other covariates included in the analysis were age, sex, comorbidities, hospital characteristics, primary payer, and median income. For analysis, a propensity score matching algorithm was applied to match patients with and without dementia. Kaplan-Meier curves were used to examine 30-day readmission rates, and a Cox proportional hazards model was used to calculate hazard ratios (HR) for those with and without dementia. For secondary outcomes, logistic regression models were used to calculate odds ratios (OR) of outcomes between those with and without dementia.
Main results: The average age of those with dementia was 78.8 years vs 64.9 years in those without dementia. Women made up 42.8% of those with dementia and 31.3% of those without dementia. Those with dementia also had higher rates of comorbidities, such as heart failure, renal failure, and depression. After propensity score matching, 17,309 and 17,187 patients with and without dementia, respectively, were included. Covariates were balanced between the 2 groups after matching. For the primary outcome, patients with dementia were more likely to be readmitted at 30 days (HR, 1.11; 95% CI, 1.05-1.18; P < .01) when compared to those without dementia. For other adverse outcomes, delirium was significantly more likely to occur for those with dementia (OR, 4.37; 95% CI, 3.69-5.16; P < .01). Patients with dementia were also more likely to die in hospital (OR, 1.15; 95% CI, 1.01-1.30; P = .03), have cardiac arrest (OR, 1.19; 95% CI, 1.01-1.39; P = .04), receive a blood transfusion (OR, 1.17; 95% CI, 1.00-1.36; P = .05), experience acute kidney injury (OR, 1.30; 95% CI, 1.21-1.39; P < .01), and fall in hospital (OR, 2.51; 95% CI, 2.06-3.07; P < .01). Hospital length of stay was higher for those with dementia, with a mean difference of 1.43 days. For discharge location, patients with dementia were more likely to be sent to a skilled nursing facility (30.1% vs 12.2%) and less likely to be discharged home.
Conclusion: Patients with dementia are more likely to experience adverse events, including delirium, mortality, kidney injury, and falls after PCI, and are more likely to be readmitted to the hospital in 30 days compared to those without dementia.
Study 2 Overview (Gilmore-Bykovskyi et al)
Objective: To examine the association between race and 30-day readmissions in Black and non-Hispanic White Medicare beneficiaries with dementia.
Design: This was a retrospective cohort study that used 100% Medicare fee-for service claims data from all hospitalizations between January 1, 2014, and November 30, 2014, for all enrollees with a dementia diagnosis. The claims data were linked to the patient, hospital stay, and hospital factors. Patients with dementia were identified using a validated algorithm that requires an inpatient, skilled nursing facility, home health, or Part B institutional or noninstitutional claim with a qualifying diagnostic code during a 3-year period. Persons enrolled in a health maintenance organization plan were excluded.
Main outcome measures: The primary outcome examined in this study was 30-day all-cause readmission. Self-reported race and ethnic identity was a baseline covariate. Persons who self-reported Black or non-Hispanic White race were included in the study; other categories of race and ethnicity were excluded because of prior evidence suggesting low accuracy of these categories in Medicare claims data. Other covariates included neighborhood disadvantage, measured using the Area Deprivation Index (ADI), and rurality; hospital-level and hospital stay–level characteristics such as for-profit status and number of annual discharges; and individual demographic characteristics and comorbidities. The ADI is constructed using variables of poverty, education, housing, and employment and is represented as a percentile ranking of level of disadvantage. Unadjusted and adjusted analyses of 30-day hospital readmission were conducted. Models using various levels of adjustment were constructed to examine the contributions of the identified covariates to the estimated association between 30-day readmission and race.
Main results: A total of 1,523,142 index hospital stays among 945,481 beneficiaries were included; 215,815 episodes were among Black beneficiaries and 1,307,327 episodes were among non-Hispanic White beneficiaries. Mean age was 81.5 years, and approximately 61% of beneficiaries were female. Black beneficiaries were younger but had higher rates of dual Medicare/Medicaid eligibility and disability; they were also more likely to reside in disadvantaged neighborhoods. Black beneficiaries had a 30-day readmission rate of 24.1% compared with 18.5% in non-Hispanic White beneficiaries (unadjusted OR, 1.37; 95% CI, 1.35-1.39). The differences in outcomes persisted after adjusting for geographic factors, social factors, hospital characteristics, hospital stay factors, demographics, and comorbidities, suggesting that unmeasured underlying racial disparities not included in this model accounted for the differences. The effects of certain variables, such as neighborhood, differed by race; for example, the protective effect of living in a less disadvantaged neighborhood was observed among White beneficiaries but not Black beneficiaries.
Conclusion: Racial and geographic disparities in 30-day readmission rates were observed among Medicare beneficiaries with dementia. Protective effects associated with neighborhood advantage may confer different levels of benefit for people of different race.
Commentary
Adults living with dementia are at higher risk of adverse outcomes across settings. In the first study, by Park et al, among adults who underwent a cardiac procedure (PCI), those with dementia were more likely to experience adverse events compared to those without dementia. These outcomes include increased rates of 30-day readmissions, delirium, cardiac arrest, and falls. These findings are consistent with other studies that found a similar association among patients who underwent other cardiac procedures, such as transcatheter aortic valve replacement.1 Because dementia is a strong predisposing factor for delirium, it is not surprising that delirium is observed across patients who underwent different procedures or hospitalization episodes.2 Because of the potential hazards for inpatients with dementia, hospitals have developed risk-reduction programs, such as those that promote recognition of dementia, and management strategies that reduce the risk of delirium.3 Delirium prevention may also impact other adverse outcomes, such as falls, discharge to institutional care, and readmissions.
Racial disparities in care outcomes have been documented across settings, including hospital4 and hospice care settings.5 In study 2, by Gilmore-Bykovskyi et al, the findings of higher rates of hospital readmission among Black patients when compared to non-Hispanic White patients were not surprising. The central finding of this study is that even when accounting for various levels of factors, including hospital-level, hospital stay–level, individual (demographics, comorbidities), and neighborhood characteristics (disadvantage), the observed disparity diminished but persisted, suggesting that while these various levels of factors contributed to the observed disparity, other unmeasured factors also contributed. Another key finding is that the effect of the various factors examined in this study may affect different subgroups in different ways, suggesting underlying factors, and thus potential solutions to reduce disparities in care outcomes, could differ among subgroups.
Applications for Clinical Practice and System Implementation
These 2 studies add to the literature on factors that can affect 30-day hospital readmission rates in patients with dementia. These data could allow for more robust discussions of what to anticipate when adults with dementia undergo specific procedures, and also further build the case that improvements in care, such as delirium prevention programs, could offer benefits. The observation about racial and ethnic disparities in care outcomes among patients with dementia highlights the continued need to better understand the drivers of these disparities so that hospital systems and policy makers can consider and test possible solutions. Future studies should further disentangle the relationships among the various levels of factors and observed disparities in outcomes, especially for this vulnerable population of adults living with dementia.
Practice Points
- Clinicians should be aware of the additional risks for poor outcomes that dementia confers.
- Awareness of this increased risk will inform discussions of risks and benefits for older adults considered for procedures.
–William W. Hung, MD, MPH
Study 1 Overview (Park et al)
Objective: To compare rates of adverse events and 30-day readmission among patients with dementia who undergo percutaneous coronary intervention (PCI) with those without dementia.
Design: This cohort study used a national database of hospital readmissions developed by the Agency for Healthcare Research and Quality.
Setting and participants: Data from State Inpatient Databases were used to derive this national readmissions database representing 80% of hospitals from 28 states that contribute data. The study included all individuals aged 18 years and older who were identified to have had a PCI procedure in the years 2017 and 2018. International Classification of Diseases, Tenth Revision (ICD-10) codes were used to identify PCI procedures, including drug-eluting stent placement, bare-metal stent placement, and balloon angioplasty, performed in patients who presented with myocardial infarction and unstable angina and those with stable ischemic heart disease. Patients were stratified into those with or without dementia, also defined using ICD-10 codes. A total of 755,406 index hospitalizations were included; 2.3% of the patients had dementia.
Main outcome measures: The primary study outcome was 30-day all-cause readmission, with the cause classified as cardiovascular or noncardiovascular. Secondary outcome measures examined were delirium, in-hospital mortality, cardiac arrest, blood transfusion, acute kidney injury, fall in hospital, length of hospital stay, and other adverse outcomes. Location at discharge was also examined. Other covariates included in the analysis were age, sex, comorbidities, hospital characteristics, primary payer, and median income. For analysis, a propensity score matching algorithm was applied to match patients with and without dementia. Kaplan-Meier curves were used to examine 30-day readmission rates, and a Cox proportional hazards model was used to calculate hazard ratios (HR) for those with and without dementia. For secondary outcomes, logistic regression models were used to calculate odds ratios (OR) of outcomes between those with and without dementia.
Main results: The average age of those with dementia was 78.8 years vs 64.9 years in those without dementia. Women made up 42.8% of those with dementia and 31.3% of those without dementia. Those with dementia also had higher rates of comorbidities, such as heart failure, renal failure, and depression. After propensity score matching, 17,309 and 17,187 patients with and without dementia, respectively, were included. Covariates were balanced between the 2 groups after matching. For the primary outcome, patients with dementia were more likely to be readmitted at 30 days (HR, 1.11; 95% CI, 1.05-1.18; P < .01) when compared to those without dementia. For other adverse outcomes, delirium was significantly more likely to occur for those with dementia (OR, 4.37; 95% CI, 3.69-5.16; P < .01). Patients with dementia were also more likely to die in hospital (OR, 1.15; 95% CI, 1.01-1.30; P = .03), have cardiac arrest (OR, 1.19; 95% CI, 1.01-1.39; P = .04), receive a blood transfusion (OR, 1.17; 95% CI, 1.00-1.36; P = .05), experience acute kidney injury (OR, 1.30; 95% CI, 1.21-1.39; P < .01), and fall in hospital (OR, 2.51; 95% CI, 2.06-3.07; P < .01). Hospital length of stay was higher for those with dementia, with a mean difference of 1.43 days. For discharge location, patients with dementia were more likely to be sent to a skilled nursing facility (30.1% vs 12.2%) and less likely to be discharged home.
Conclusion: Patients with dementia are more likely to experience adverse events, including delirium, mortality, kidney injury, and falls after PCI, and are more likely to be readmitted to the hospital in 30 days compared to those without dementia.
Study 2 Overview (Gilmore-Bykovskyi et al)
Objective: To examine the association between race and 30-day readmissions in Black and non-Hispanic White Medicare beneficiaries with dementia.
Design: This was a retrospective cohort study that used 100% Medicare fee-for service claims data from all hospitalizations between January 1, 2014, and November 30, 2014, for all enrollees with a dementia diagnosis. The claims data were linked to the patient, hospital stay, and hospital factors. Patients with dementia were identified using a validated algorithm that requires an inpatient, skilled nursing facility, home health, or Part B institutional or noninstitutional claim with a qualifying diagnostic code during a 3-year period. Persons enrolled in a health maintenance organization plan were excluded.
Main outcome measures: The primary outcome examined in this study was 30-day all-cause readmission. Self-reported race and ethnic identity was a baseline covariate. Persons who self-reported Black or non-Hispanic White race were included in the study; other categories of race and ethnicity were excluded because of prior evidence suggesting low accuracy of these categories in Medicare claims data. Other covariates included neighborhood disadvantage, measured using the Area Deprivation Index (ADI), and rurality; hospital-level and hospital stay–level characteristics such as for-profit status and number of annual discharges; and individual demographic characteristics and comorbidities. The ADI is constructed using variables of poverty, education, housing, and employment and is represented as a percentile ranking of level of disadvantage. Unadjusted and adjusted analyses of 30-day hospital readmission were conducted. Models using various levels of adjustment were constructed to examine the contributions of the identified covariates to the estimated association between 30-day readmission and race.
Main results: A total of 1,523,142 index hospital stays among 945,481 beneficiaries were included; 215,815 episodes were among Black beneficiaries and 1,307,327 episodes were among non-Hispanic White beneficiaries. Mean age was 81.5 years, and approximately 61% of beneficiaries were female. Black beneficiaries were younger but had higher rates of dual Medicare/Medicaid eligibility and disability; they were also more likely to reside in disadvantaged neighborhoods. Black beneficiaries had a 30-day readmission rate of 24.1% compared with 18.5% in non-Hispanic White beneficiaries (unadjusted OR, 1.37; 95% CI, 1.35-1.39). The differences in outcomes persisted after adjusting for geographic factors, social factors, hospital characteristics, hospital stay factors, demographics, and comorbidities, suggesting that unmeasured underlying racial disparities not included in this model accounted for the differences. The effects of certain variables, such as neighborhood, differed by race; for example, the protective effect of living in a less disadvantaged neighborhood was observed among White beneficiaries but not Black beneficiaries.
Conclusion: Racial and geographic disparities in 30-day readmission rates were observed among Medicare beneficiaries with dementia. Protective effects associated with neighborhood advantage may confer different levels of benefit for people of different race.
Commentary
Adults living with dementia are at higher risk of adverse outcomes across settings. In the first study, by Park et al, among adults who underwent a cardiac procedure (PCI), those with dementia were more likely to experience adverse events compared to those without dementia. These outcomes include increased rates of 30-day readmissions, delirium, cardiac arrest, and falls. These findings are consistent with other studies that found a similar association among patients who underwent other cardiac procedures, such as transcatheter aortic valve replacement.1 Because dementia is a strong predisposing factor for delirium, it is not surprising that delirium is observed across patients who underwent different procedures or hospitalization episodes.2 Because of the potential hazards for inpatients with dementia, hospitals have developed risk-reduction programs, such as those that promote recognition of dementia, and management strategies that reduce the risk of delirium.3 Delirium prevention may also impact other adverse outcomes, such as falls, discharge to institutional care, and readmissions.
Racial disparities in care outcomes have been documented across settings, including hospital4 and hospice care settings.5 In study 2, by Gilmore-Bykovskyi et al, the findings of higher rates of hospital readmission among Black patients when compared to non-Hispanic White patients were not surprising. The central finding of this study is that even when accounting for various levels of factors, including hospital-level, hospital stay–level, individual (demographics, comorbidities), and neighborhood characteristics (disadvantage), the observed disparity diminished but persisted, suggesting that while these various levels of factors contributed to the observed disparity, other unmeasured factors also contributed. Another key finding is that the effect of the various factors examined in this study may affect different subgroups in different ways, suggesting underlying factors, and thus potential solutions to reduce disparities in care outcomes, could differ among subgroups.
Applications for Clinical Practice and System Implementation
These 2 studies add to the literature on factors that can affect 30-day hospital readmission rates in patients with dementia. These data could allow for more robust discussions of what to anticipate when adults with dementia undergo specific procedures, and also further build the case that improvements in care, such as delirium prevention programs, could offer benefits. The observation about racial and ethnic disparities in care outcomes among patients with dementia highlights the continued need to better understand the drivers of these disparities so that hospital systems and policy makers can consider and test possible solutions. Future studies should further disentangle the relationships among the various levels of factors and observed disparities in outcomes, especially for this vulnerable population of adults living with dementia.
Practice Points
- Clinicians should be aware of the additional risks for poor outcomes that dementia confers.
- Awareness of this increased risk will inform discussions of risks and benefits for older adults considered for procedures.
–William W. Hung, MD, MPH
1. Park DY, Sana MK, Shoura S, et al. Readmission and in-hospital outcomes after transcatheter aortic valve replacement in patients with dementia. Cardiovasc Revasc Med. 2023;46:70-77. doi:10.1016/j.carrev.2022.08.016
2. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51(5):591-598. doi:10.1034/j.1600-0579.2003.00201.x
3. Weldingh NM, Mellingsæter MR, Hegna BW, et al. Impact of a dementia-friendly program on detection and management of patients with cognitive impairment and delirium in acute-care hospital units: a controlled clinical trial design. BMC Geriatr. 2022;22(1):266. doi:10.1186/s12877-022-02949-0
4. Hermosura AH, Noonan CJ, Fyfe-Johnson AL, et al. Hospital disparities between native Hawaiian and other pacific islanders and non-Hispanic whites with Alzheimer’s disease and related dementias. J Aging Health. 2020;32(10):1579-1590. doi:10.1177/0898264320945177
5. Zhang Y, Shao H, Zhang M, Li J. Healthcare utilization and mortality after hospice live discharge among Medicare patients with and without Alzheimer’s disease and related dementias. J Gen Intern Med. 2023 Jan 17. doi:10.1007/s11606-023-08031-8
1. Park DY, Sana MK, Shoura S, et al. Readmission and in-hospital outcomes after transcatheter aortic valve replacement in patients with dementia. Cardiovasc Revasc Med. 2023;46:70-77. doi:10.1016/j.carrev.2022.08.016
2. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51(5):591-598. doi:10.1034/j.1600-0579.2003.00201.x
3. Weldingh NM, Mellingsæter MR, Hegna BW, et al. Impact of a dementia-friendly program on detection and management of patients with cognitive impairment and delirium in acute-care hospital units: a controlled clinical trial design. BMC Geriatr. 2022;22(1):266. doi:10.1186/s12877-022-02949-0
4. Hermosura AH, Noonan CJ, Fyfe-Johnson AL, et al. Hospital disparities between native Hawaiian and other pacific islanders and non-Hispanic whites with Alzheimer’s disease and related dementias. J Aging Health. 2020;32(10):1579-1590. doi:10.1177/0898264320945177
5. Zhang Y, Shao H, Zhang M, Li J. Healthcare utilization and mortality after hospice live discharge among Medicare patients with and without Alzheimer’s disease and related dementias. J Gen Intern Med. 2023 Jan 17. doi:10.1007/s11606-023-08031-8
Persistent Wounds Refractory to Broad-Spectrum Antibiotics
The Diagnosis: PASH (Pyoderma Gangrenosum, Acne, Hidradenitis Suppurativa) Syndrome
Obtaining our patient’s history of hidradenitis suppurativa (HS), a hallmark sterile neutrophilic dermatosis, was key to making the correct diagnosis of PASH (pyoderma gangrenosum, acne, HS) syndrome. In our patient, the history of HS increased the consideration of pyoderma gangrenosum (PG) due to the persistent breast and leg wounds. Additionally, it was important to consider a diagnosis of PG in lesions that were not responding to broad-spectrum antimicrobial treatment. In our patient, the concurrent presentation of draining abscesses in the axillae (Figure, A) and inflammatory nodulocystic facial acne (Figure, B) were additional diagnostic clues that suggested the triad of PASH syndrome.

Although SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome also can present with cutaneous features of acne and HS, the lack of bone and joint involvement in our patient made this diagnosis less likely. Calciphylaxis can present as ulcerations on the lower extremities, but it usually presents with a livedolike pattern with overlying black eschar and is unlikely in the absence of underlying metabolic or renal disease. PAPA (pyogenic arthritis, PG, acne) syndrome is characterized by recurrent joint involvement and lacks features of HS. Lastly, our patient was immunocompetent with no risk factors for mycobacterial infection.
PASH syndrome is a rare inherited syndrome, but its constituent inflammatory conditions are ubiquitous. They share a common underlying mechanism consisting of overactivation of the innate immune systems driven by increased production of the inflammatory cytokines IL-1, IL-17, and tumor necrosis factor α, resulting in sterile neutrophilic dermatoses.1 The diagnosis is based on the clinical presentation, as laboratory investigations are nondiagnostic. Biopsies and cultures can be performed to rule out infectious etiologies. Additionally, PASH syndrome is considered part of a larger spectrum of syndromes including PAPA and PAPASH (pyogenic arthritis, acne, PG, HS) syndromes. The absence of pyogenic arthritis distinguishes PASH syndrome from PAPA and PAPASH syndromes.2 Clinically, PASH syndrome and the related sterile neutrophilic dermatoses share the characteristic of pronounced cutaneous involvement that substantially alters the patient’s quality of life. Cigarette smoking is an exacerbating factor and has a well-established association with HS.3 Therefore, smoking cessation should be encouraged in these patients to avoid exacerbation of the disease process.
Maintaining adequate immunosuppression is key to managing the underlying disease processes. Classic immunosuppressive agents such as systemic glucocorticoids and methotrexate may fail to satisfactorily control the disease.4 Treatment options currently are somewhat limited and are aimed at targeting the inflammatory cytokines that propagate the disease. The most consistent responses have been observed with anti–tumor necrosis factor α antagonists such as adalimumab, infliximab, and etanercept.5 Additionally, there is varied response to anakinra, suggesting the importance of selectively targeting IL-1β.6 Unfortunately, misdiagnosis for an infectious etiology is common, and antibiotics and debridement are of limited use for the underlying pathophysiology of PASH syndrome. Importantly, biopsy and debridement often are discouraged due to the risk of pathergy.7
Our case demonstrates the importance of maintaining a high clinical suspicion for immune-mediated lesions that are refractory to antimicrobial agents. Additionally, prior history of multiple neutrophilic dermatoses should prompt consideration for the PASH/PAPA/PAPASH disease spectrum. Early and accurate identification of neutrophilic dermatoses such as PG and HS are crucial to initiating proper cytokine-targeting treatment and achieving disease remission.
- Cugno M, Borghi A, Marzano AV. PAPA, PASH and PAPASH syndromes: pathophysiology, presentation and treatment. Am J Clin Dermatol. 2017;18:555-562.
- Genovese G, Moltrasio C, Garcovich S, et al. PAPA spectrum disorders. G Ital Dermatol Venereol. 2020;155:542-550.
- König A, Lehmann C, Rompel R, et al. Cigarette smoking as a triggering factor of hidradenitis suppurativa. Dermatology. 1999;198:261-264.
- Ahn C, Negus D, Huang W. Pyoderma gangrenosum: a review of pathogenesis and treatment. Expert Rev Clin Immunol. 2018;14:225-233.
- Saint-Georges V, Peternel S, Kaštelan M, et al. Tumor necrosis factor antagonists in the treatment of pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH) syndrome. Acta Dermatovenerol Croat. 2018;26:173-178.
- Braun-Falco M, Kovnerystyy O, Lohse P, et al. Pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH)—a new autoinflammatory syndrome distinct from PAPA syndrome. J Am Acad Dermatol. 2012;66:409-415.
- Patel DK, Locke M, Jarrett P. Pyoderma gangrenosum with pathergy: a potentially significant complication following breast reconstruction. J Plast Reconstr Aesthet Surg. 2017;70:884-892.
The Diagnosis: PASH (Pyoderma Gangrenosum, Acne, Hidradenitis Suppurativa) Syndrome
Obtaining our patient’s history of hidradenitis suppurativa (HS), a hallmark sterile neutrophilic dermatosis, was key to making the correct diagnosis of PASH (pyoderma gangrenosum, acne, HS) syndrome. In our patient, the history of HS increased the consideration of pyoderma gangrenosum (PG) due to the persistent breast and leg wounds. Additionally, it was important to consider a diagnosis of PG in lesions that were not responding to broad-spectrum antimicrobial treatment. In our patient, the concurrent presentation of draining abscesses in the axillae (Figure, A) and inflammatory nodulocystic facial acne (Figure, B) were additional diagnostic clues that suggested the triad of PASH syndrome.

Although SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome also can present with cutaneous features of acne and HS, the lack of bone and joint involvement in our patient made this diagnosis less likely. Calciphylaxis can present as ulcerations on the lower extremities, but it usually presents with a livedolike pattern with overlying black eschar and is unlikely in the absence of underlying metabolic or renal disease. PAPA (pyogenic arthritis, PG, acne) syndrome is characterized by recurrent joint involvement and lacks features of HS. Lastly, our patient was immunocompetent with no risk factors for mycobacterial infection.
PASH syndrome is a rare inherited syndrome, but its constituent inflammatory conditions are ubiquitous. They share a common underlying mechanism consisting of overactivation of the innate immune systems driven by increased production of the inflammatory cytokines IL-1, IL-17, and tumor necrosis factor α, resulting in sterile neutrophilic dermatoses.1 The diagnosis is based on the clinical presentation, as laboratory investigations are nondiagnostic. Biopsies and cultures can be performed to rule out infectious etiologies. Additionally, PASH syndrome is considered part of a larger spectrum of syndromes including PAPA and PAPASH (pyogenic arthritis, acne, PG, HS) syndromes. The absence of pyogenic arthritis distinguishes PASH syndrome from PAPA and PAPASH syndromes.2 Clinically, PASH syndrome and the related sterile neutrophilic dermatoses share the characteristic of pronounced cutaneous involvement that substantially alters the patient’s quality of life. Cigarette smoking is an exacerbating factor and has a well-established association with HS.3 Therefore, smoking cessation should be encouraged in these patients to avoid exacerbation of the disease process.
Maintaining adequate immunosuppression is key to managing the underlying disease processes. Classic immunosuppressive agents such as systemic glucocorticoids and methotrexate may fail to satisfactorily control the disease.4 Treatment options currently are somewhat limited and are aimed at targeting the inflammatory cytokines that propagate the disease. The most consistent responses have been observed with anti–tumor necrosis factor α antagonists such as adalimumab, infliximab, and etanercept.5 Additionally, there is varied response to anakinra, suggesting the importance of selectively targeting IL-1β.6 Unfortunately, misdiagnosis for an infectious etiology is common, and antibiotics and debridement are of limited use for the underlying pathophysiology of PASH syndrome. Importantly, biopsy and debridement often are discouraged due to the risk of pathergy.7
Our case demonstrates the importance of maintaining a high clinical suspicion for immune-mediated lesions that are refractory to antimicrobial agents. Additionally, prior history of multiple neutrophilic dermatoses should prompt consideration for the PASH/PAPA/PAPASH disease spectrum. Early and accurate identification of neutrophilic dermatoses such as PG and HS are crucial to initiating proper cytokine-targeting treatment and achieving disease remission.
The Diagnosis: PASH (Pyoderma Gangrenosum, Acne, Hidradenitis Suppurativa) Syndrome
Obtaining our patient’s history of hidradenitis suppurativa (HS), a hallmark sterile neutrophilic dermatosis, was key to making the correct diagnosis of PASH (pyoderma gangrenosum, acne, HS) syndrome. In our patient, the history of HS increased the consideration of pyoderma gangrenosum (PG) due to the persistent breast and leg wounds. Additionally, it was important to consider a diagnosis of PG in lesions that were not responding to broad-spectrum antimicrobial treatment. In our patient, the concurrent presentation of draining abscesses in the axillae (Figure, A) and inflammatory nodulocystic facial acne (Figure, B) were additional diagnostic clues that suggested the triad of PASH syndrome.

Although SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome also can present with cutaneous features of acne and HS, the lack of bone and joint involvement in our patient made this diagnosis less likely. Calciphylaxis can present as ulcerations on the lower extremities, but it usually presents with a livedolike pattern with overlying black eschar and is unlikely in the absence of underlying metabolic or renal disease. PAPA (pyogenic arthritis, PG, acne) syndrome is characterized by recurrent joint involvement and lacks features of HS. Lastly, our patient was immunocompetent with no risk factors for mycobacterial infection.
PASH syndrome is a rare inherited syndrome, but its constituent inflammatory conditions are ubiquitous. They share a common underlying mechanism consisting of overactivation of the innate immune systems driven by increased production of the inflammatory cytokines IL-1, IL-17, and tumor necrosis factor α, resulting in sterile neutrophilic dermatoses.1 The diagnosis is based on the clinical presentation, as laboratory investigations are nondiagnostic. Biopsies and cultures can be performed to rule out infectious etiologies. Additionally, PASH syndrome is considered part of a larger spectrum of syndromes including PAPA and PAPASH (pyogenic arthritis, acne, PG, HS) syndromes. The absence of pyogenic arthritis distinguishes PASH syndrome from PAPA and PAPASH syndromes.2 Clinically, PASH syndrome and the related sterile neutrophilic dermatoses share the characteristic of pronounced cutaneous involvement that substantially alters the patient’s quality of life. Cigarette smoking is an exacerbating factor and has a well-established association with HS.3 Therefore, smoking cessation should be encouraged in these patients to avoid exacerbation of the disease process.
Maintaining adequate immunosuppression is key to managing the underlying disease processes. Classic immunosuppressive agents such as systemic glucocorticoids and methotrexate may fail to satisfactorily control the disease.4 Treatment options currently are somewhat limited and are aimed at targeting the inflammatory cytokines that propagate the disease. The most consistent responses have been observed with anti–tumor necrosis factor α antagonists such as adalimumab, infliximab, and etanercept.5 Additionally, there is varied response to anakinra, suggesting the importance of selectively targeting IL-1β.6 Unfortunately, misdiagnosis for an infectious etiology is common, and antibiotics and debridement are of limited use for the underlying pathophysiology of PASH syndrome. Importantly, biopsy and debridement often are discouraged due to the risk of pathergy.7
Our case demonstrates the importance of maintaining a high clinical suspicion for immune-mediated lesions that are refractory to antimicrobial agents. Additionally, prior history of multiple neutrophilic dermatoses should prompt consideration for the PASH/PAPA/PAPASH disease spectrum. Early and accurate identification of neutrophilic dermatoses such as PG and HS are crucial to initiating proper cytokine-targeting treatment and achieving disease remission.
- Cugno M, Borghi A, Marzano AV. PAPA, PASH and PAPASH syndromes: pathophysiology, presentation and treatment. Am J Clin Dermatol. 2017;18:555-562.
- Genovese G, Moltrasio C, Garcovich S, et al. PAPA spectrum disorders. G Ital Dermatol Venereol. 2020;155:542-550.
- König A, Lehmann C, Rompel R, et al. Cigarette smoking as a triggering factor of hidradenitis suppurativa. Dermatology. 1999;198:261-264.
- Ahn C, Negus D, Huang W. Pyoderma gangrenosum: a review of pathogenesis and treatment. Expert Rev Clin Immunol. 2018;14:225-233.
- Saint-Georges V, Peternel S, Kaštelan M, et al. Tumor necrosis factor antagonists in the treatment of pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH) syndrome. Acta Dermatovenerol Croat. 2018;26:173-178.
- Braun-Falco M, Kovnerystyy O, Lohse P, et al. Pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH)—a new autoinflammatory syndrome distinct from PAPA syndrome. J Am Acad Dermatol. 2012;66:409-415.
- Patel DK, Locke M, Jarrett P. Pyoderma gangrenosum with pathergy: a potentially significant complication following breast reconstruction. J Plast Reconstr Aesthet Surg. 2017;70:884-892.
- Cugno M, Borghi A, Marzano AV. PAPA, PASH and PAPASH syndromes: pathophysiology, presentation and treatment. Am J Clin Dermatol. 2017;18:555-562.
- Genovese G, Moltrasio C, Garcovich S, et al. PAPA spectrum disorders. G Ital Dermatol Venereol. 2020;155:542-550.
- König A, Lehmann C, Rompel R, et al. Cigarette smoking as a triggering factor of hidradenitis suppurativa. Dermatology. 1999;198:261-264.
- Ahn C, Negus D, Huang W. Pyoderma gangrenosum: a review of pathogenesis and treatment. Expert Rev Clin Immunol. 2018;14:225-233.
- Saint-Georges V, Peternel S, Kaštelan M, et al. Tumor necrosis factor antagonists in the treatment of pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH) syndrome. Acta Dermatovenerol Croat. 2018;26:173-178.
- Braun-Falco M, Kovnerystyy O, Lohse P, et al. Pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH)—a new autoinflammatory syndrome distinct from PAPA syndrome. J Am Acad Dermatol. 2012;66:409-415.
- Patel DK, Locke M, Jarrett P. Pyoderma gangrenosum with pathergy: a potentially significant complication following breast reconstruction. J Plast Reconstr Aesthet Surg. 2017;70:884-892.
A 28-year-old Black woman presented to the hospital for evaluation of worsening leg wounds as well as a similar eroding plaque on the left breast of 1 month’s duration. Broad-spectrum antibiotics prescribed during a prior emergency department visit resulted in no improvement. Her medical history was notable for hidradenitis suppurativa that previously was well controlled on adalimumab prior to discontinuation 1 year prior. A review of systems was negative for fever, chills, shortness of breath, chest pain, night sweats, and arthralgia. The patient had discontinued the antibiotics and was not taking any other medications at the time of presentation. She reported a history of smoking cigarettes (5 pack years). Physical examination revealed hyperkeratotic eroded plaques with violaceous borders circumferentially around the left breast (top) and legs with notable undermining (bottom). Inflammatory nodulocystic acne of the face as well as sinus tract formation with purulent drainage in the axillae also were present. Laboratory workup revealed an elevated erythrocyte sedimentation rate (116 mm/h [reference range, <20 mm/h]). Computed tomography of the leg wound was negative for soft-tissue infection. Aerobic and anaerobic tissue cultures demonstrated no growth.

Number of cancer survivors with functional limitations doubled in 20 years
Vishal Patel, BS, a student at the Dell Medical School at The University of Texas at Austin, and colleagues identified 51,258 cancer survivors from the National Health Interview Survey, representing a weighted population of approximately 178.8 million from 1999 to 2018.
Most survivors were women (60.2%) and were at least 65 years old (55.4%). In 1999, 3.6 million weighted survivors reported functional limitation. In 2018, the number increased to 8.2 million, a 2.25-fold increase.
The number of survivors who reported no limitations also increased, but not by as much. That group grew 1.34-fold during the study period.
For context, “the 70% prevalence of functional limitation among survivors in 2018 is nearly twice that of the general population,” the authors wrote.
Patients surveyed on function
Functional limitation was defined as “self-reported difficulty performing any of 12 routine physical or social activities without assistance.” Examples of the activities included difficulty sitting for more than 2 hours, difficulty participating in social activities or difficulty pushing or pulling an object the size of a living room chair.
Over the 2 decades analyzed, the adjusted prevalence of functional limitation was highest among survivors of pancreatic cancer (80.3%) and lung cancer (76.5%). Prevalence was lowest for survivors of melanoma (62.2%), breast (61.8%) and prostate (59.5%) cancers.
Not just a result of living longer
Mr. Patel told this publication that one assumption people might make when they read these results is that people are just living longer with cancer and losing functional ability accordingly.
“But, in fact, we found that the youngest [– those less than 65 years–] actually contributed to this trend more than the oldest people, which means it’s not just [happening], because people are getting older,” he said.
Hispanic and Black individuals had disproportionately higher increases in functional limitation; percentage point increases over the 2 decades were 19.5 for Black people, 25.1 for Hispanic people and 12.5 for White people. There may be a couple of reasons for that, Mr. Patel noted.
Those who are Black or Hispanic tend to have less access to cancer survivorship care for reasons including insurance status and historic health care inequities, he noted.
“The other potential reason is that they have had less access to cancer care historically. And if, 20 years ago Black and Hispanic individuals didn’t have access to some chemotherapies, and now they do, maybe it’s the increased access to care that’s causing these functional limitations. Because chemotherapy can sometimes be very toxic. It may be sort of a catch-up toxicity,” he said.
Quality of life beyond survivorship
Mr. Patel said the results seem to call for building on improved survival rates by tracking and improving function.
“It’s good to celebrate that there are more survivors. But now that we can keep people alive longer, maybe we can shift gears to improving their quality of life,” he said.
The more-than-doubling of functional limitations over 2 decades “is a very sobering trend,” he noted, while pointing out that the functional limitations applied to 8 million people in the United States – people whose needs are not being met.
There’s no sign of the trend stopping, he continued. “We saw no downward trend, only an upward trend.”
Increasingly, including functionality as an endpoint in cancer trials, in addition to improvements in mortality, is one place to start, he added.
“Our findings suggest an urgent need for care teams to understand and address function, for researchers to evaluate function as a core outcome in trials, and for health systems and policy makers to reimagine survivorship care, recognizing the burden of cancer and its treatment on physical, psychosocial, and cognitive function,” the authors wrote in their paper. Limitations of the study include the potential for recall bias, lack of cancer staging or treatment information, and the subjective perception of function.
A coauthor reported personal fees from Astellas, AstraZeneca, AAA, Blue Earth, Janssen, Lantheus, Myovant, Myriad Genetics, Novartis, Telix, and Sanofi, as well as grants from Pfizer and Bayer during the conduct of the study. No other disclosures were reported.
Vishal Patel, BS, a student at the Dell Medical School at The University of Texas at Austin, and colleagues identified 51,258 cancer survivors from the National Health Interview Survey, representing a weighted population of approximately 178.8 million from 1999 to 2018.
Most survivors were women (60.2%) and were at least 65 years old (55.4%). In 1999, 3.6 million weighted survivors reported functional limitation. In 2018, the number increased to 8.2 million, a 2.25-fold increase.
The number of survivors who reported no limitations also increased, but not by as much. That group grew 1.34-fold during the study period.
For context, “the 70% prevalence of functional limitation among survivors in 2018 is nearly twice that of the general population,” the authors wrote.
Patients surveyed on function
Functional limitation was defined as “self-reported difficulty performing any of 12 routine physical or social activities without assistance.” Examples of the activities included difficulty sitting for more than 2 hours, difficulty participating in social activities or difficulty pushing or pulling an object the size of a living room chair.
Over the 2 decades analyzed, the adjusted prevalence of functional limitation was highest among survivors of pancreatic cancer (80.3%) and lung cancer (76.5%). Prevalence was lowest for survivors of melanoma (62.2%), breast (61.8%) and prostate (59.5%) cancers.
Not just a result of living longer
Mr. Patel told this publication that one assumption people might make when they read these results is that people are just living longer with cancer and losing functional ability accordingly.
“But, in fact, we found that the youngest [– those less than 65 years–] actually contributed to this trend more than the oldest people, which means it’s not just [happening], because people are getting older,” he said.
Hispanic and Black individuals had disproportionately higher increases in functional limitation; percentage point increases over the 2 decades were 19.5 for Black people, 25.1 for Hispanic people and 12.5 for White people. There may be a couple of reasons for that, Mr. Patel noted.
Those who are Black or Hispanic tend to have less access to cancer survivorship care for reasons including insurance status and historic health care inequities, he noted.
“The other potential reason is that they have had less access to cancer care historically. And if, 20 years ago Black and Hispanic individuals didn’t have access to some chemotherapies, and now they do, maybe it’s the increased access to care that’s causing these functional limitations. Because chemotherapy can sometimes be very toxic. It may be sort of a catch-up toxicity,” he said.
Quality of life beyond survivorship
Mr. Patel said the results seem to call for building on improved survival rates by tracking and improving function.
“It’s good to celebrate that there are more survivors. But now that we can keep people alive longer, maybe we can shift gears to improving their quality of life,” he said.
The more-than-doubling of functional limitations over 2 decades “is a very sobering trend,” he noted, while pointing out that the functional limitations applied to 8 million people in the United States – people whose needs are not being met.
There’s no sign of the trend stopping, he continued. “We saw no downward trend, only an upward trend.”
Increasingly, including functionality as an endpoint in cancer trials, in addition to improvements in mortality, is one place to start, he added.
“Our findings suggest an urgent need for care teams to understand and address function, for researchers to evaluate function as a core outcome in trials, and for health systems and policy makers to reimagine survivorship care, recognizing the burden of cancer and its treatment on physical, psychosocial, and cognitive function,” the authors wrote in their paper. Limitations of the study include the potential for recall bias, lack of cancer staging or treatment information, and the subjective perception of function.
A coauthor reported personal fees from Astellas, AstraZeneca, AAA, Blue Earth, Janssen, Lantheus, Myovant, Myriad Genetics, Novartis, Telix, and Sanofi, as well as grants from Pfizer and Bayer during the conduct of the study. No other disclosures were reported.
Vishal Patel, BS, a student at the Dell Medical School at The University of Texas at Austin, and colleagues identified 51,258 cancer survivors from the National Health Interview Survey, representing a weighted population of approximately 178.8 million from 1999 to 2018.
Most survivors were women (60.2%) and were at least 65 years old (55.4%). In 1999, 3.6 million weighted survivors reported functional limitation. In 2018, the number increased to 8.2 million, a 2.25-fold increase.
The number of survivors who reported no limitations also increased, but not by as much. That group grew 1.34-fold during the study period.
For context, “the 70% prevalence of functional limitation among survivors in 2018 is nearly twice that of the general population,” the authors wrote.
Patients surveyed on function
Functional limitation was defined as “self-reported difficulty performing any of 12 routine physical or social activities without assistance.” Examples of the activities included difficulty sitting for more than 2 hours, difficulty participating in social activities or difficulty pushing or pulling an object the size of a living room chair.
Over the 2 decades analyzed, the adjusted prevalence of functional limitation was highest among survivors of pancreatic cancer (80.3%) and lung cancer (76.5%). Prevalence was lowest for survivors of melanoma (62.2%), breast (61.8%) and prostate (59.5%) cancers.
Not just a result of living longer
Mr. Patel told this publication that one assumption people might make when they read these results is that people are just living longer with cancer and losing functional ability accordingly.
“But, in fact, we found that the youngest [– those less than 65 years–] actually contributed to this trend more than the oldest people, which means it’s not just [happening], because people are getting older,” he said.
Hispanic and Black individuals had disproportionately higher increases in functional limitation; percentage point increases over the 2 decades were 19.5 for Black people, 25.1 for Hispanic people and 12.5 for White people. There may be a couple of reasons for that, Mr. Patel noted.
Those who are Black or Hispanic tend to have less access to cancer survivorship care for reasons including insurance status and historic health care inequities, he noted.
“The other potential reason is that they have had less access to cancer care historically. And if, 20 years ago Black and Hispanic individuals didn’t have access to some chemotherapies, and now they do, maybe it’s the increased access to care that’s causing these functional limitations. Because chemotherapy can sometimes be very toxic. It may be sort of a catch-up toxicity,” he said.
Quality of life beyond survivorship
Mr. Patel said the results seem to call for building on improved survival rates by tracking and improving function.
“It’s good to celebrate that there are more survivors. But now that we can keep people alive longer, maybe we can shift gears to improving their quality of life,” he said.
The more-than-doubling of functional limitations over 2 decades “is a very sobering trend,” he noted, while pointing out that the functional limitations applied to 8 million people in the United States – people whose needs are not being met.
There’s no sign of the trend stopping, he continued. “We saw no downward trend, only an upward trend.”
Increasingly, including functionality as an endpoint in cancer trials, in addition to improvements in mortality, is one place to start, he added.
“Our findings suggest an urgent need for care teams to understand and address function, for researchers to evaluate function as a core outcome in trials, and for health systems and policy makers to reimagine survivorship care, recognizing the burden of cancer and its treatment on physical, psychosocial, and cognitive function,” the authors wrote in their paper. Limitations of the study include the potential for recall bias, lack of cancer staging or treatment information, and the subjective perception of function.
A coauthor reported personal fees from Astellas, AstraZeneca, AAA, Blue Earth, Janssen, Lantheus, Myovant, Myriad Genetics, Novartis, Telix, and Sanofi, as well as grants from Pfizer and Bayer during the conduct of the study. No other disclosures were reported.
FROM JAMA ONCOLOGY
Diversity – We’re not one size fits all
The United States has often been described as a “melting pot,” defined as diverse cultures and ethnicities coming together to form the rich fabric of our nation. These days, it seems that our fabric is a bit frayed.
DEIB (diversity, equity, inclusion, and belonging) is dawning as a significant conversation. Each and every one of us is unique by age, gender, culture/ethnicity, religion, socioeconomic status, geographical location, race, and sexual identity – to name just a few aspects of our identity. Keeping these differences in mind, it is evident that none of us fits a “one size fits all” mold.
Some of these differences, such as cross-cultural cuisine and holidays, are enjoyed and celebrated as wonderful opportunities to learn from others, embrace our distinctions, and have them beneficially contribute to our lives. Other differences, however, are not understood or embraced and are, in fact, belittled and stigmatized. Sexual identity falls into this category. It behooves us as a country to become more aware and educated about this category in our identities, in order to understand it, quell our unfounded fear, learn to support one another, and improve our collective mental health.
Recent reports have shown that exposing students and teachers to sexual identity diversity education has sparked some backlash from parents and communities alike. Those opposed are citing concerns over introducing children to LGBTQ+ information, either embedded in the school curriculum or made available in school library reading materials. “Children should remain innocent” seems to be the message. Perhaps parents prefer to discuss this topic privately, at home. Either way, teaching about diversity does not damage one’s innocence or deprive parents of private conversations. In fact, it educates children by improving their awareness, tolerance, and acceptance of others’ differences, and can serve as a catalyst to further parental conversation.
There are kids everywhere who are starting to develop and understand their identities. Wouldn’t it be wonderful for them to know that whichever way they identify is okay, that they are not ‘weird’ or ‘different,’ but that in fact we are all different? Wouldn’t it be great for them to be able to explore and discuss their identities and journeys openly, and not have to hide for fear of retribution or bullying?
It is important for these children to know that they are not alone, that they have options, and that they don’t need to contemplate suicide because they believe that their identity makes them not worthy of being in this world.
Starting the conversation early on in life can empower our youth by planting the seed that people are not “one size fits all,” which is the element responsible for our being unique and human. Diversity can be woven into the rich fabric that defines our nation, rather than be a factor that unravels it.
April was National Diversity Awareness Month and we took time to celebrate our country’s cultural melting pot. By embracing our differences, we can show our children and ourselves how to better navigate diversity, which can help us all fit in.
Dr. Jarkon is a psychiatrist and director of the Center for Behavioral Health at the New York Institute of Technology College of Osteopathic Medicine in Old Westbury, N.Y.
The United States has often been described as a “melting pot,” defined as diverse cultures and ethnicities coming together to form the rich fabric of our nation. These days, it seems that our fabric is a bit frayed.
DEIB (diversity, equity, inclusion, and belonging) is dawning as a significant conversation. Each and every one of us is unique by age, gender, culture/ethnicity, religion, socioeconomic status, geographical location, race, and sexual identity – to name just a few aspects of our identity. Keeping these differences in mind, it is evident that none of us fits a “one size fits all” mold.
Some of these differences, such as cross-cultural cuisine and holidays, are enjoyed and celebrated as wonderful opportunities to learn from others, embrace our distinctions, and have them beneficially contribute to our lives. Other differences, however, are not understood or embraced and are, in fact, belittled and stigmatized. Sexual identity falls into this category. It behooves us as a country to become more aware and educated about this category in our identities, in order to understand it, quell our unfounded fear, learn to support one another, and improve our collective mental health.
Recent reports have shown that exposing students and teachers to sexual identity diversity education has sparked some backlash from parents and communities alike. Those opposed are citing concerns over introducing children to LGBTQ+ information, either embedded in the school curriculum or made available in school library reading materials. “Children should remain innocent” seems to be the message. Perhaps parents prefer to discuss this topic privately, at home. Either way, teaching about diversity does not damage one’s innocence or deprive parents of private conversations. In fact, it educates children by improving their awareness, tolerance, and acceptance of others’ differences, and can serve as a catalyst to further parental conversation.
There are kids everywhere who are starting to develop and understand their identities. Wouldn’t it be wonderful for them to know that whichever way they identify is okay, that they are not ‘weird’ or ‘different,’ but that in fact we are all different? Wouldn’t it be great for them to be able to explore and discuss their identities and journeys openly, and not have to hide for fear of retribution or bullying?
It is important for these children to know that they are not alone, that they have options, and that they don’t need to contemplate suicide because they believe that their identity makes them not worthy of being in this world.
Starting the conversation early on in life can empower our youth by planting the seed that people are not “one size fits all,” which is the element responsible for our being unique and human. Diversity can be woven into the rich fabric that defines our nation, rather than be a factor that unravels it.
April was National Diversity Awareness Month and we took time to celebrate our country’s cultural melting pot. By embracing our differences, we can show our children and ourselves how to better navigate diversity, which can help us all fit in.
Dr. Jarkon is a psychiatrist and director of the Center for Behavioral Health at the New York Institute of Technology College of Osteopathic Medicine in Old Westbury, N.Y.
The United States has often been described as a “melting pot,” defined as diverse cultures and ethnicities coming together to form the rich fabric of our nation. These days, it seems that our fabric is a bit frayed.
DEIB (diversity, equity, inclusion, and belonging) is dawning as a significant conversation. Each and every one of us is unique by age, gender, culture/ethnicity, religion, socioeconomic status, geographical location, race, and sexual identity – to name just a few aspects of our identity. Keeping these differences in mind, it is evident that none of us fits a “one size fits all” mold.
Some of these differences, such as cross-cultural cuisine and holidays, are enjoyed and celebrated as wonderful opportunities to learn from others, embrace our distinctions, and have them beneficially contribute to our lives. Other differences, however, are not understood or embraced and are, in fact, belittled and stigmatized. Sexual identity falls into this category. It behooves us as a country to become more aware and educated about this category in our identities, in order to understand it, quell our unfounded fear, learn to support one another, and improve our collective mental health.
Recent reports have shown that exposing students and teachers to sexual identity diversity education has sparked some backlash from parents and communities alike. Those opposed are citing concerns over introducing children to LGBTQ+ information, either embedded in the school curriculum or made available in school library reading materials. “Children should remain innocent” seems to be the message. Perhaps parents prefer to discuss this topic privately, at home. Either way, teaching about diversity does not damage one’s innocence or deprive parents of private conversations. In fact, it educates children by improving their awareness, tolerance, and acceptance of others’ differences, and can serve as a catalyst to further parental conversation.
There are kids everywhere who are starting to develop and understand their identities. Wouldn’t it be wonderful for them to know that whichever way they identify is okay, that they are not ‘weird’ or ‘different,’ but that in fact we are all different? Wouldn’t it be great for them to be able to explore and discuss their identities and journeys openly, and not have to hide for fear of retribution or bullying?
It is important for these children to know that they are not alone, that they have options, and that they don’t need to contemplate suicide because they believe that their identity makes them not worthy of being in this world.
Starting the conversation early on in life can empower our youth by planting the seed that people are not “one size fits all,” which is the element responsible for our being unique and human. Diversity can be woven into the rich fabric that defines our nation, rather than be a factor that unravels it.
April was National Diversity Awareness Month and we took time to celebrate our country’s cultural melting pot. By embracing our differences, we can show our children and ourselves how to better navigate diversity, which can help us all fit in.
Dr. Jarkon is a psychiatrist and director of the Center for Behavioral Health at the New York Institute of Technology College of Osteopathic Medicine in Old Westbury, N.Y.
CLL: Black patients die sooner than Whites
The findings, published in the American Journal of Hematology, hint that the racial disparity has shrunk over time, especially within the first few years of the targeted-therapy era. Still, “Black patients had a shorter median overall survival of 7 years compared to 9 years for White patients,” study coauthor Deborah Stephens, DO, of the University of Utah Huntsman Cancer Institute, said in an interview. “Clearly, more research is needed to tease out the biologic or economic barriers to achieving prolonged survival.”
As the researchers noted, CLL is far more common among White patients (5.1 cases per 100,000) than other races (Black patients: 3.2 cases per 100,000; Hispanic patients: 2.1 cases per 100,000; Asian American patients: 1.1 per 100,000). In total, non-White patients make up just 11%-13% of CLL cases in the United States.
According to Dr. Stephens, “little is known or published” about Black patients with CLL, “and it is still a mystery why fewer patients that are Black develop CLL and why this group would have shorter survival.”
Dr. Stephens and colleagues launched the new study – the largest of its kind to date – to understand disparities between White and Black patients over most of the past 20 years. The researchers especially wanted to analyze trends during the last decade, when targeted therapies revolutionized treatment of the disease.
The study authors analyzed data in the National Cancer Database for 97,804 patients diagnosed from 2004 to 2018 (90.7% White, 7.6% Black, 0.6% Asian, 1.1% other). Of patients who reported ethnicity (n = 93,555), 2.6% were Hispanic.
Black patients were more likely to have begun CLL therapy at diagnosis (35.9%) than were White patients (23.6%), a sign that Black patients had more advanced disease. Black patients also had shorter overall survival (7.0 years, 95% confidence interval [CI], 6.7–7.3 years) vs. White patients (9.1 years, 95% CI, 9.0–9.3 years, P < .001).
“This finding could be due to underlying biologic differences in the pathology of CLL, when comparing patients across racial groups,” Dr. Stephens said. “Additionally, there could be differences in access to care. Notably, there are fewer racial minorities enrolled in clinical trials, and perhaps we are not individualizing therapy for unique biologic factors seen in CLL affecting racial minorities.”
Other factors also could be at play. Black patients were more likely than were White patients to have one or more comorbidities (27.9% vs. 21.3%, P < .001), lack insurance (6.6% vs. 2.1%, P < .001) and live in lower-income neighborhoods (47.7% vs. 13.1%, P < .001).
What explains the gap in outcomes? In an interview, study lead author Victoria Vardell, MD, of the University of Utah, Salt Lake City, noted that researchers often attribute worse medical outcomes in Black patients to economic and social disparities.
“However, when we adjusted for a number of surrogate markers of health care access, including income, comorbidities, and location, among others, this disparity remained. That indicates that this may be a more complex problem in CLL in particular. Certainly, we cannot adjust for all the socioeconomic strain placed on Black Americans, including those with CLL, but there may be molecular features related to ancestry or environmental exposures that also play a role,” Dr. Vardell said.
She added that “the high cost and difficulty obtaining many novel therapies, particularly in the clinical trial setting, places significantly higher burdens on already disadvantaged populations.”
There is some good news in the new report. “Promisingly, our data suggest that the survival disparity between White and Black patients with CLL may be improving, particularly within the last 5 years, though longer follow-up is needed to confirm significance,” the researchers reported.
Alessandra Ferrajoli, MD, of M.D. Anderson Cancer Center, Houston, who has studied racial disparities in CLL, praised the study in an interview. As she noted, it examines an impressively large population.
The explanations for the disparities are still elusive, she said, although it seems clear there are multiple factors at play. “We don’t know if the disease has the same characteristics in African-Americans as in Whites,” Dr. Ferrajoli said. However, she noted, there’s “no indication that the response to treatment is different according to race.”
Moving forward, she said, the study findings “reinforce the fact that we need to pay attention to this population and be quite attentive to their characteristics.”
No study funding was reported. The authors and Dr. Ferrajoli have no disclosures.
The findings, published in the American Journal of Hematology, hint that the racial disparity has shrunk over time, especially within the first few years of the targeted-therapy era. Still, “Black patients had a shorter median overall survival of 7 years compared to 9 years for White patients,” study coauthor Deborah Stephens, DO, of the University of Utah Huntsman Cancer Institute, said in an interview. “Clearly, more research is needed to tease out the biologic or economic barriers to achieving prolonged survival.”
As the researchers noted, CLL is far more common among White patients (5.1 cases per 100,000) than other races (Black patients: 3.2 cases per 100,000; Hispanic patients: 2.1 cases per 100,000; Asian American patients: 1.1 per 100,000). In total, non-White patients make up just 11%-13% of CLL cases in the United States.
According to Dr. Stephens, “little is known or published” about Black patients with CLL, “and it is still a mystery why fewer patients that are Black develop CLL and why this group would have shorter survival.”
Dr. Stephens and colleagues launched the new study – the largest of its kind to date – to understand disparities between White and Black patients over most of the past 20 years. The researchers especially wanted to analyze trends during the last decade, when targeted therapies revolutionized treatment of the disease.
The study authors analyzed data in the National Cancer Database for 97,804 patients diagnosed from 2004 to 2018 (90.7% White, 7.6% Black, 0.6% Asian, 1.1% other). Of patients who reported ethnicity (n = 93,555), 2.6% were Hispanic.
Black patients were more likely to have begun CLL therapy at diagnosis (35.9%) than were White patients (23.6%), a sign that Black patients had more advanced disease. Black patients also had shorter overall survival (7.0 years, 95% confidence interval [CI], 6.7–7.3 years) vs. White patients (9.1 years, 95% CI, 9.0–9.3 years, P < .001).
“This finding could be due to underlying biologic differences in the pathology of CLL, when comparing patients across racial groups,” Dr. Stephens said. “Additionally, there could be differences in access to care. Notably, there are fewer racial minorities enrolled in clinical trials, and perhaps we are not individualizing therapy for unique biologic factors seen in CLL affecting racial minorities.”
Other factors also could be at play. Black patients were more likely than were White patients to have one or more comorbidities (27.9% vs. 21.3%, P < .001), lack insurance (6.6% vs. 2.1%, P < .001) and live in lower-income neighborhoods (47.7% vs. 13.1%, P < .001).
What explains the gap in outcomes? In an interview, study lead author Victoria Vardell, MD, of the University of Utah, Salt Lake City, noted that researchers often attribute worse medical outcomes in Black patients to economic and social disparities.
“However, when we adjusted for a number of surrogate markers of health care access, including income, comorbidities, and location, among others, this disparity remained. That indicates that this may be a more complex problem in CLL in particular. Certainly, we cannot adjust for all the socioeconomic strain placed on Black Americans, including those with CLL, but there may be molecular features related to ancestry or environmental exposures that also play a role,” Dr. Vardell said.
She added that “the high cost and difficulty obtaining many novel therapies, particularly in the clinical trial setting, places significantly higher burdens on already disadvantaged populations.”
There is some good news in the new report. “Promisingly, our data suggest that the survival disparity between White and Black patients with CLL may be improving, particularly within the last 5 years, though longer follow-up is needed to confirm significance,” the researchers reported.
Alessandra Ferrajoli, MD, of M.D. Anderson Cancer Center, Houston, who has studied racial disparities in CLL, praised the study in an interview. As she noted, it examines an impressively large population.
The explanations for the disparities are still elusive, she said, although it seems clear there are multiple factors at play. “We don’t know if the disease has the same characteristics in African-Americans as in Whites,” Dr. Ferrajoli said. However, she noted, there’s “no indication that the response to treatment is different according to race.”
Moving forward, she said, the study findings “reinforce the fact that we need to pay attention to this population and be quite attentive to their characteristics.”
No study funding was reported. The authors and Dr. Ferrajoli have no disclosures.
The findings, published in the American Journal of Hematology, hint that the racial disparity has shrunk over time, especially within the first few years of the targeted-therapy era. Still, “Black patients had a shorter median overall survival of 7 years compared to 9 years for White patients,” study coauthor Deborah Stephens, DO, of the University of Utah Huntsman Cancer Institute, said in an interview. “Clearly, more research is needed to tease out the biologic or economic barriers to achieving prolonged survival.”
As the researchers noted, CLL is far more common among White patients (5.1 cases per 100,000) than other races (Black patients: 3.2 cases per 100,000; Hispanic patients: 2.1 cases per 100,000; Asian American patients: 1.1 per 100,000). In total, non-White patients make up just 11%-13% of CLL cases in the United States.
According to Dr. Stephens, “little is known or published” about Black patients with CLL, “and it is still a mystery why fewer patients that are Black develop CLL and why this group would have shorter survival.”
Dr. Stephens and colleagues launched the new study – the largest of its kind to date – to understand disparities between White and Black patients over most of the past 20 years. The researchers especially wanted to analyze trends during the last decade, when targeted therapies revolutionized treatment of the disease.
The study authors analyzed data in the National Cancer Database for 97,804 patients diagnosed from 2004 to 2018 (90.7% White, 7.6% Black, 0.6% Asian, 1.1% other). Of patients who reported ethnicity (n = 93,555), 2.6% were Hispanic.
Black patients were more likely to have begun CLL therapy at diagnosis (35.9%) than were White patients (23.6%), a sign that Black patients had more advanced disease. Black patients also had shorter overall survival (7.0 years, 95% confidence interval [CI], 6.7–7.3 years) vs. White patients (9.1 years, 95% CI, 9.0–9.3 years, P < .001).
“This finding could be due to underlying biologic differences in the pathology of CLL, when comparing patients across racial groups,” Dr. Stephens said. “Additionally, there could be differences in access to care. Notably, there are fewer racial minorities enrolled in clinical trials, and perhaps we are not individualizing therapy for unique biologic factors seen in CLL affecting racial minorities.”
Other factors also could be at play. Black patients were more likely than were White patients to have one or more comorbidities (27.9% vs. 21.3%, P < .001), lack insurance (6.6% vs. 2.1%, P < .001) and live in lower-income neighborhoods (47.7% vs. 13.1%, P < .001).
What explains the gap in outcomes? In an interview, study lead author Victoria Vardell, MD, of the University of Utah, Salt Lake City, noted that researchers often attribute worse medical outcomes in Black patients to economic and social disparities.
“However, when we adjusted for a number of surrogate markers of health care access, including income, comorbidities, and location, among others, this disparity remained. That indicates that this may be a more complex problem in CLL in particular. Certainly, we cannot adjust for all the socioeconomic strain placed on Black Americans, including those with CLL, but there may be molecular features related to ancestry or environmental exposures that also play a role,” Dr. Vardell said.
She added that “the high cost and difficulty obtaining many novel therapies, particularly in the clinical trial setting, places significantly higher burdens on already disadvantaged populations.”
There is some good news in the new report. “Promisingly, our data suggest that the survival disparity between White and Black patients with CLL may be improving, particularly within the last 5 years, though longer follow-up is needed to confirm significance,” the researchers reported.
Alessandra Ferrajoli, MD, of M.D. Anderson Cancer Center, Houston, who has studied racial disparities in CLL, praised the study in an interview. As she noted, it examines an impressively large population.
The explanations for the disparities are still elusive, she said, although it seems clear there are multiple factors at play. “We don’t know if the disease has the same characteristics in African-Americans as in Whites,” Dr. Ferrajoli said. However, she noted, there’s “no indication that the response to treatment is different according to race.”
Moving forward, she said, the study findings “reinforce the fact that we need to pay attention to this population and be quite attentive to their characteristics.”
No study funding was reported. The authors and Dr. Ferrajoli have no disclosures.
FROM AMERICAN JOURNAL OF HEMATOLOGY
Disparities in Melanoma Demographics, Tumor Stage, and Metastases in Hispanic and Latino Patients: A Retrospective Study
To the Editor:
Melanoma is an aggressive form of skin cancer with a high rate of metastasis and poor prognosis.1 Historically, Hispanic and/or Latino patients have presented with more advanced-stage melanomas and have lower survival rates compared with non-Hispanic and/or non-Latino White patients.2 In this study, we evaluated recent data from the last decade to investigate if disparities in melanoma tumor stage at diagnosis and risk for metastases continue to exist in the Hispanic and/or Latino population.
We conducted a retrospective review of melanoma patients at 2 major medical centers in Los Angeles, California—Keck Medicine of USC and Los Angeles County-USC Medical Center—from January 2010 to January 2020. The data collected from electronic medical records included age at melanoma diagnosis, sex, race and ethnicity, insurance type, Breslow depth of lesion, presence of ulceration, and presence of lymph node or distant metastases. Melanoma tumor stage was determined using the American Joint Committee on Cancer classification. Patients who self-reported their ethnicity as not Hispanic and/or Latino were designated to this group regardless of their reported race. Those patients who reported their ethnicity as not Hispanic and/or Latino and reported their race as White were designated as non-Hispanic and/or non-Latino White. This study was approved by the institutional review board of the University of Southern California (Los Angeles). Data analysis was performed using the Pearson χ2 test, Fisher exact test, and Wilcoxon rank sum test. Statistical significance was determined at P<.05.
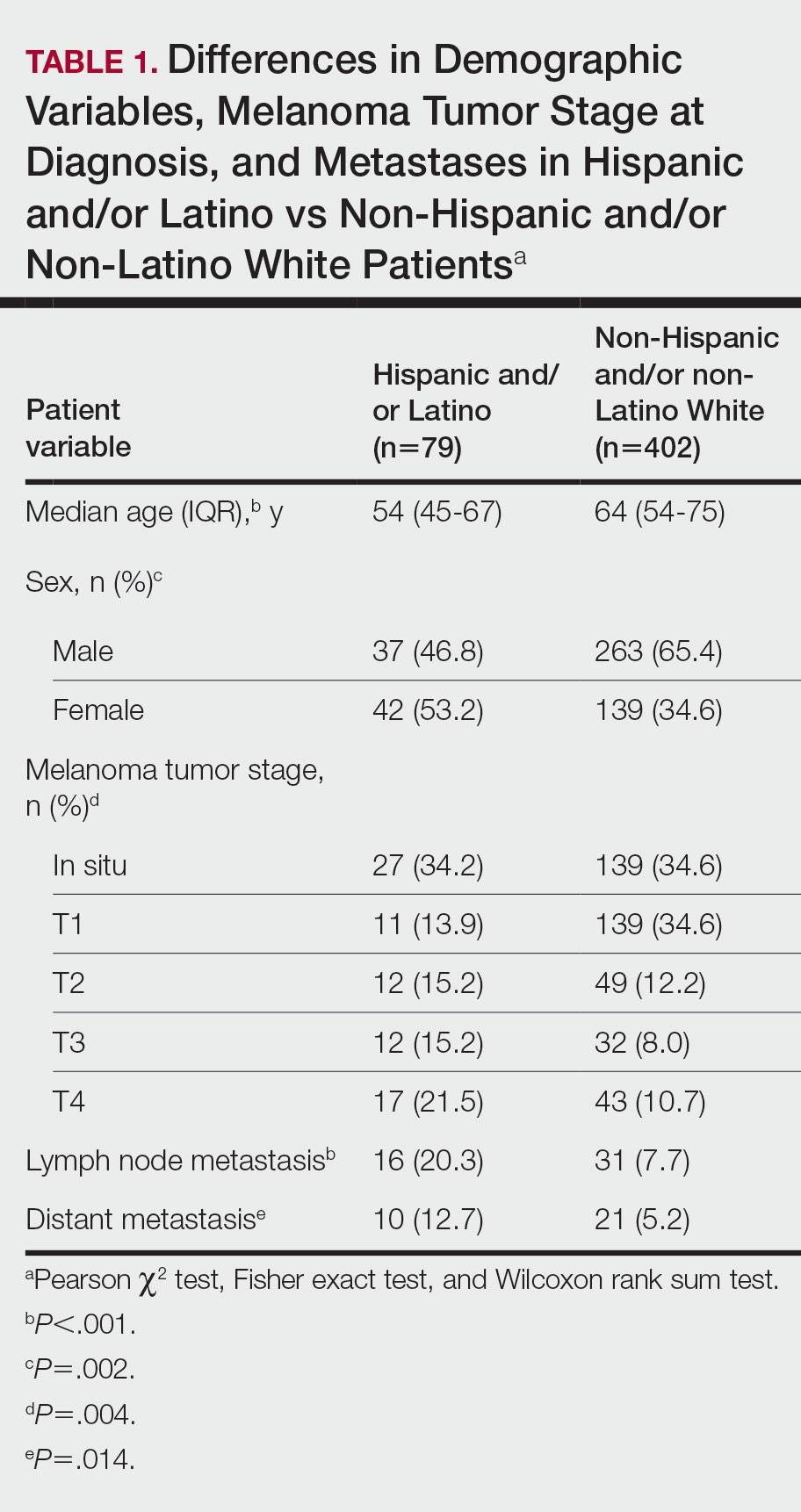
The final cohort of patients included 79 Hispanic and/or Latino patients and 402 non-Hispanic and/or non-Latino White patients. The median age for the Hispanic and/or Latino group was 54 years and 64 years for the non-Hispanic and/or non-Latino White group (P<.001). There was a greater percentage of females in the Hispanic and/or Latino group compared with the non-Hispanic and/or non-Latino White group (53.2% vs 34.6%)(P=.002). Hispanic and/or Latino patients presented with more advanced tumor stage melanomas (T3: 15.2%; T4: 21.5%) compared with non-Hispanic and/or non-Latino White patients (T3: 8.0%; T4: 10.7%)(P=.004). Furthermore, Hispanic and/or Latino patients had higher rates of lymph node metastases compared with non-Hispanic and/or non-Latino White patients (20.3% vs 7.7% [P<.001]) and higher rates of distant metastases (12.7% vs 5.2% [P=.014])(Table 1). The majority of Hispanic and/or Latino patients had Medicaid (39.2%), while most non-Hispanic and/or non-Latino White patients had a preferred provider organization insurance plan (37.3%) or Medicare (34.3%)(P<.001)(Table 2).
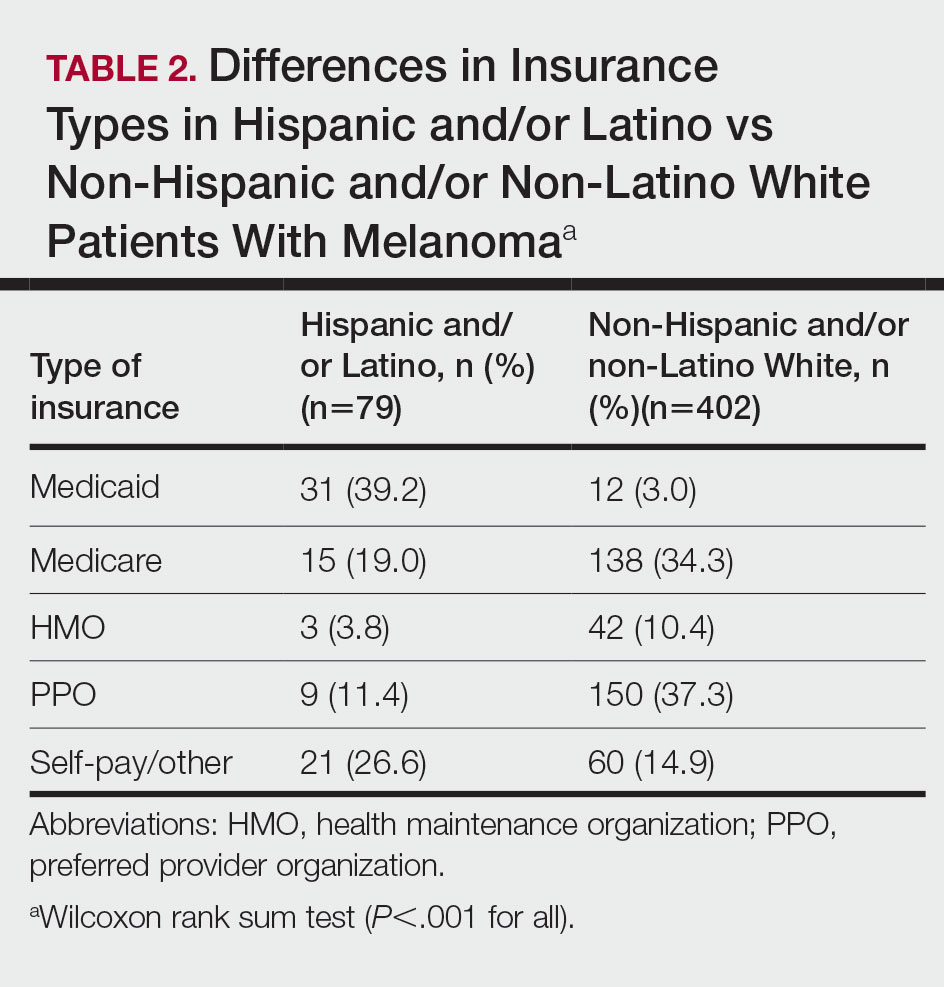
This retrospective study analyzing nearly 10 years of recent melanoma data found that disparities in melanoma diagnosis and treatment continue to exist among Hispanic and/or Latino patients. Compared to non-Hispanic and/or non-Latino White patients, Hispanic and/or Latino patients were diagnosed with melanoma at a younger age and the proportion of females with melanoma was higher. Cormier et al2 also reported that Hispanic patients were younger at melanoma diagnosis, and females represented a larger majority of patients in the Hispanic population compared with the White population. Hispanic and/or Latino patients in our study had more advanced melanoma tumor stage at diagnosis and a higher risk of lymph node and distant metastases, similar to findings reported by Koblinksi et al.3
Our retrospective cohort study demonstrated that the demographics of Hispanic and/or Latino patients with melanoma differ from non-Hispanic and/or non-Latino White patients, specifically with a greater proportion of younger and female patients in the Hispanic and/or Latino population. We also found that Hispanic and/or Latino patients continue to experience worse melanoma outcomes compared with non-Hispanic and/or non-Latino White patients. Further studies are needed to investigate the etiologies behind these health care disparities and potential interventions to address them. In addition, there needs to be increased awareness of the risk for melanoma in Hispanic and/or Latino patients among both health care providers and patients.
Limitations of this study included a smaller sample size of patients from one geographic region. The retrospective design of this study also increased the risk for selection bias, as some of the patients may have had incomplete records or were lost to follow-up. Therefore, the study cohort may not be representative of the general population. Additionally, patients’ skin types could not be determined using standardized tools such as the Fitzpatrick scale, thus we could not assess how patient skin type may have affected melanoma outcomes.
- Aggarwal P, Knabel P, Fleischer AB. United States burden of melanoma and non-melanoma skin cancer from 1990 to 2019. J Am Acad Dermatol. 2021;85:388-395. doi:10.1016/j.jaad.2021.03.109
- Cormier JN, Xing Y, Ding M, et al. Ethnic differences among patients with cutaneous melanoma. Arch Intern Med. 2006;166:1907. doi:10.1001/archinte.166.17.1907
- Koblinski JE, Maykowski P, Zeitouni NC. Disparities in melanoma stage at diagnosis in Arizona: a 10-year Arizona Cancer Registry study. J Am Acad Dermatol. 2021;84:1776-1779. doi:10.1016/j.jaad.2021.02.045
To the Editor:
Melanoma is an aggressive form of skin cancer with a high rate of metastasis and poor prognosis.1 Historically, Hispanic and/or Latino patients have presented with more advanced-stage melanomas and have lower survival rates compared with non-Hispanic and/or non-Latino White patients.2 In this study, we evaluated recent data from the last decade to investigate if disparities in melanoma tumor stage at diagnosis and risk for metastases continue to exist in the Hispanic and/or Latino population.
We conducted a retrospective review of melanoma patients at 2 major medical centers in Los Angeles, California—Keck Medicine of USC and Los Angeles County-USC Medical Center—from January 2010 to January 2020. The data collected from electronic medical records included age at melanoma diagnosis, sex, race and ethnicity, insurance type, Breslow depth of lesion, presence of ulceration, and presence of lymph node or distant metastases. Melanoma tumor stage was determined using the American Joint Committee on Cancer classification. Patients who self-reported their ethnicity as not Hispanic and/or Latino were designated to this group regardless of their reported race. Those patients who reported their ethnicity as not Hispanic and/or Latino and reported their race as White were designated as non-Hispanic and/or non-Latino White. This study was approved by the institutional review board of the University of Southern California (Los Angeles). Data analysis was performed using the Pearson χ2 test, Fisher exact test, and Wilcoxon rank sum test. Statistical significance was determined at P<.05.
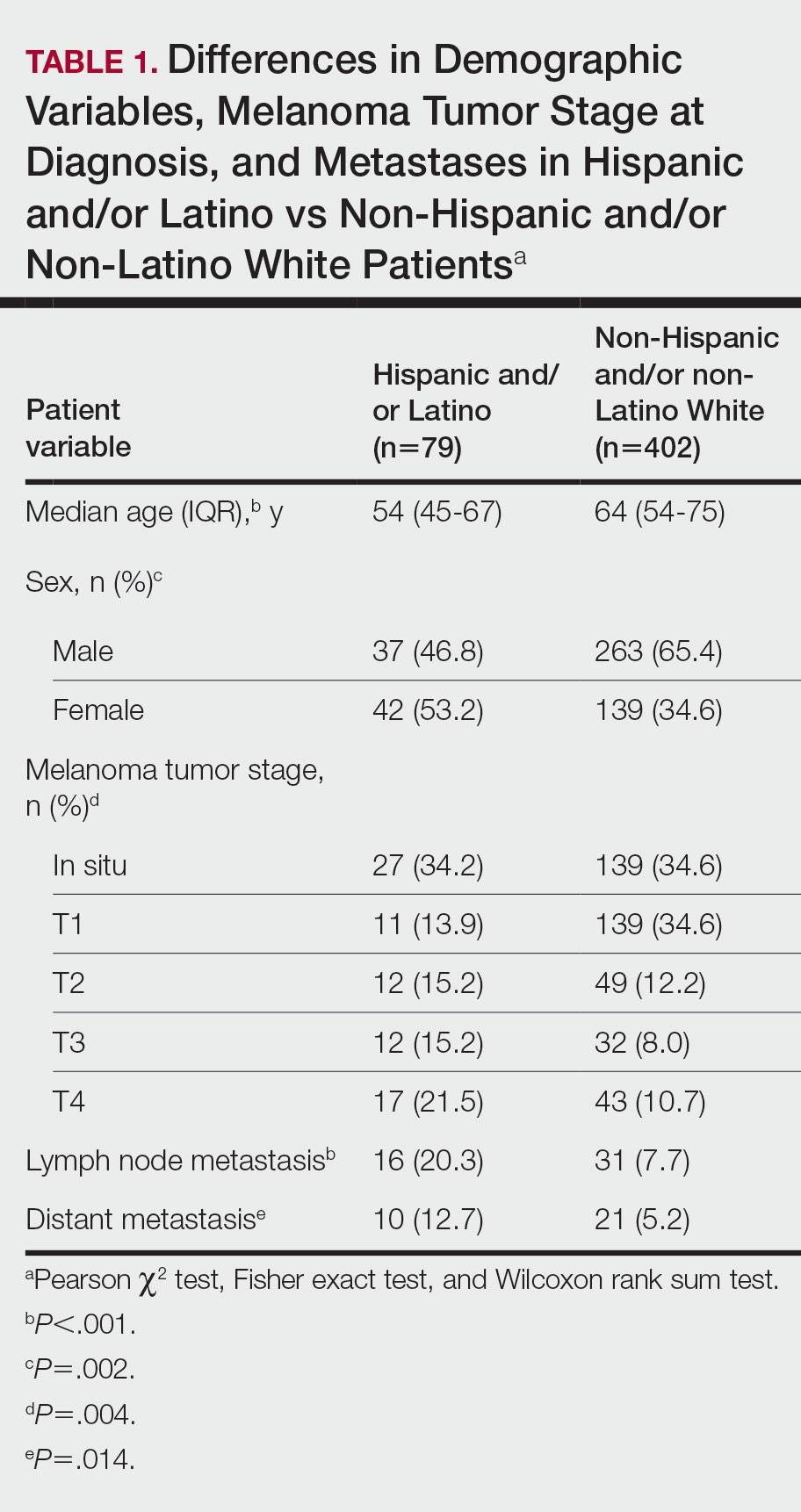
The final cohort of patients included 79 Hispanic and/or Latino patients and 402 non-Hispanic and/or non-Latino White patients. The median age for the Hispanic and/or Latino group was 54 years and 64 years for the non-Hispanic and/or non-Latino White group (P<.001). There was a greater percentage of females in the Hispanic and/or Latino group compared with the non-Hispanic and/or non-Latino White group (53.2% vs 34.6%)(P=.002). Hispanic and/or Latino patients presented with more advanced tumor stage melanomas (T3: 15.2%; T4: 21.5%) compared with non-Hispanic and/or non-Latino White patients (T3: 8.0%; T4: 10.7%)(P=.004). Furthermore, Hispanic and/or Latino patients had higher rates of lymph node metastases compared with non-Hispanic and/or non-Latino White patients (20.3% vs 7.7% [P<.001]) and higher rates of distant metastases (12.7% vs 5.2% [P=.014])(Table 1). The majority of Hispanic and/or Latino patients had Medicaid (39.2%), while most non-Hispanic and/or non-Latino White patients had a preferred provider organization insurance plan (37.3%) or Medicare (34.3%)(P<.001)(Table 2).
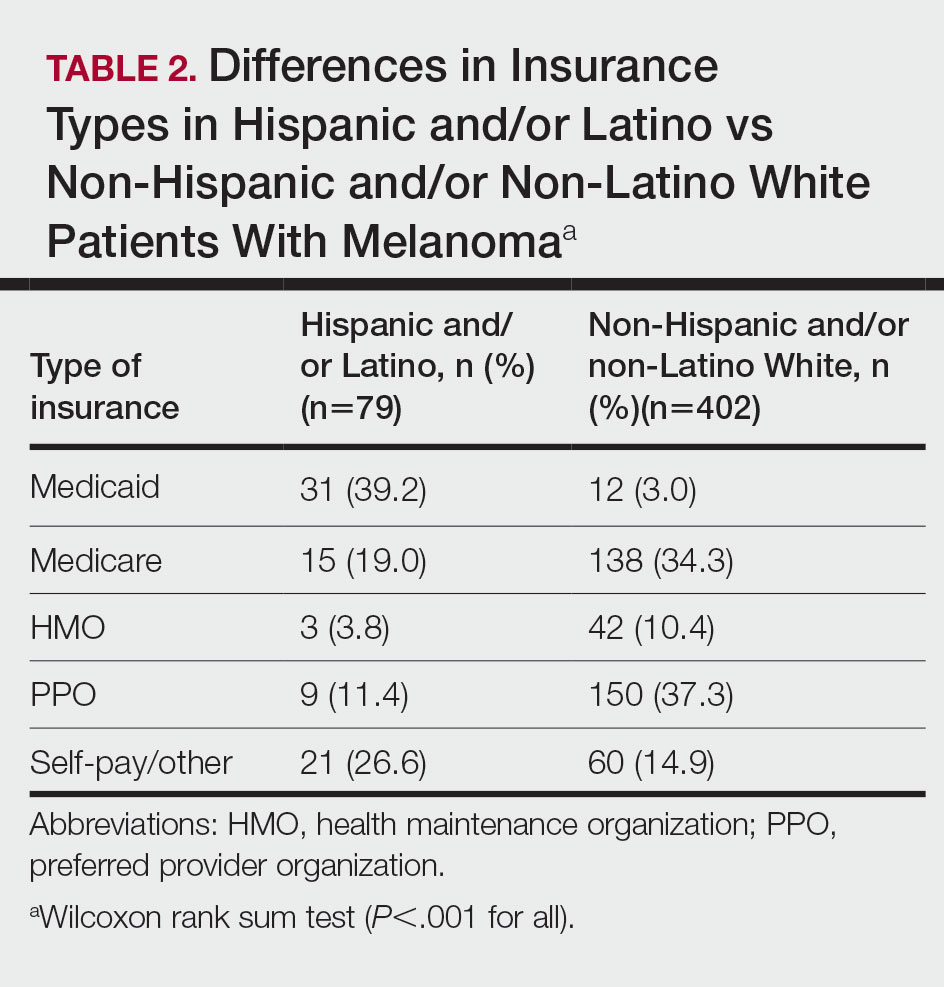
This retrospective study analyzing nearly 10 years of recent melanoma data found that disparities in melanoma diagnosis and treatment continue to exist among Hispanic and/or Latino patients. Compared to non-Hispanic and/or non-Latino White patients, Hispanic and/or Latino patients were diagnosed with melanoma at a younger age and the proportion of females with melanoma was higher. Cormier et al2 also reported that Hispanic patients were younger at melanoma diagnosis, and females represented a larger majority of patients in the Hispanic population compared with the White population. Hispanic and/or Latino patients in our study had more advanced melanoma tumor stage at diagnosis and a higher risk of lymph node and distant metastases, similar to findings reported by Koblinksi et al.3
Our retrospective cohort study demonstrated that the demographics of Hispanic and/or Latino patients with melanoma differ from non-Hispanic and/or non-Latino White patients, specifically with a greater proportion of younger and female patients in the Hispanic and/or Latino population. We also found that Hispanic and/or Latino patients continue to experience worse melanoma outcomes compared with non-Hispanic and/or non-Latino White patients. Further studies are needed to investigate the etiologies behind these health care disparities and potential interventions to address them. In addition, there needs to be increased awareness of the risk for melanoma in Hispanic and/or Latino patients among both health care providers and patients.
Limitations of this study included a smaller sample size of patients from one geographic region. The retrospective design of this study also increased the risk for selection bias, as some of the patients may have had incomplete records or were lost to follow-up. Therefore, the study cohort may not be representative of the general population. Additionally, patients’ skin types could not be determined using standardized tools such as the Fitzpatrick scale, thus we could not assess how patient skin type may have affected melanoma outcomes.
To the Editor:
Melanoma is an aggressive form of skin cancer with a high rate of metastasis and poor prognosis.1 Historically, Hispanic and/or Latino patients have presented with more advanced-stage melanomas and have lower survival rates compared with non-Hispanic and/or non-Latino White patients.2 In this study, we evaluated recent data from the last decade to investigate if disparities in melanoma tumor stage at diagnosis and risk for metastases continue to exist in the Hispanic and/or Latino population.
We conducted a retrospective review of melanoma patients at 2 major medical centers in Los Angeles, California—Keck Medicine of USC and Los Angeles County-USC Medical Center—from January 2010 to January 2020. The data collected from electronic medical records included age at melanoma diagnosis, sex, race and ethnicity, insurance type, Breslow depth of lesion, presence of ulceration, and presence of lymph node or distant metastases. Melanoma tumor stage was determined using the American Joint Committee on Cancer classification. Patients who self-reported their ethnicity as not Hispanic and/or Latino were designated to this group regardless of their reported race. Those patients who reported their ethnicity as not Hispanic and/or Latino and reported their race as White were designated as non-Hispanic and/or non-Latino White. This study was approved by the institutional review board of the University of Southern California (Los Angeles). Data analysis was performed using the Pearson χ2 test, Fisher exact test, and Wilcoxon rank sum test. Statistical significance was determined at P<.05.
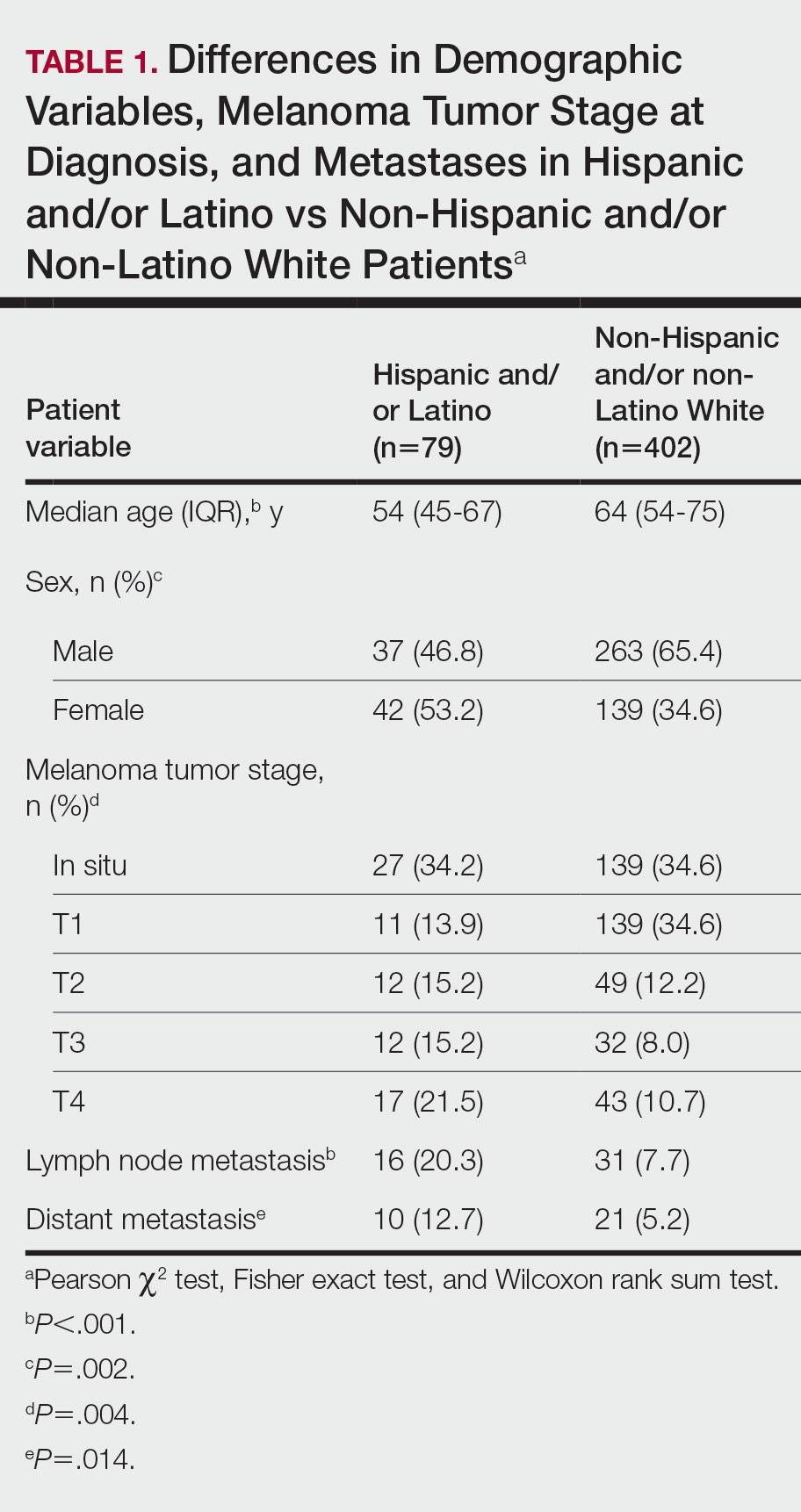
The final cohort of patients included 79 Hispanic and/or Latino patients and 402 non-Hispanic and/or non-Latino White patients. The median age for the Hispanic and/or Latino group was 54 years and 64 years for the non-Hispanic and/or non-Latino White group (P<.001). There was a greater percentage of females in the Hispanic and/or Latino group compared with the non-Hispanic and/or non-Latino White group (53.2% vs 34.6%)(P=.002). Hispanic and/or Latino patients presented with more advanced tumor stage melanomas (T3: 15.2%; T4: 21.5%) compared with non-Hispanic and/or non-Latino White patients (T3: 8.0%; T4: 10.7%)(P=.004). Furthermore, Hispanic and/or Latino patients had higher rates of lymph node metastases compared with non-Hispanic and/or non-Latino White patients (20.3% vs 7.7% [P<.001]) and higher rates of distant metastases (12.7% vs 5.2% [P=.014])(Table 1). The majority of Hispanic and/or Latino patients had Medicaid (39.2%), while most non-Hispanic and/or non-Latino White patients had a preferred provider organization insurance plan (37.3%) or Medicare (34.3%)(P<.001)(Table 2).
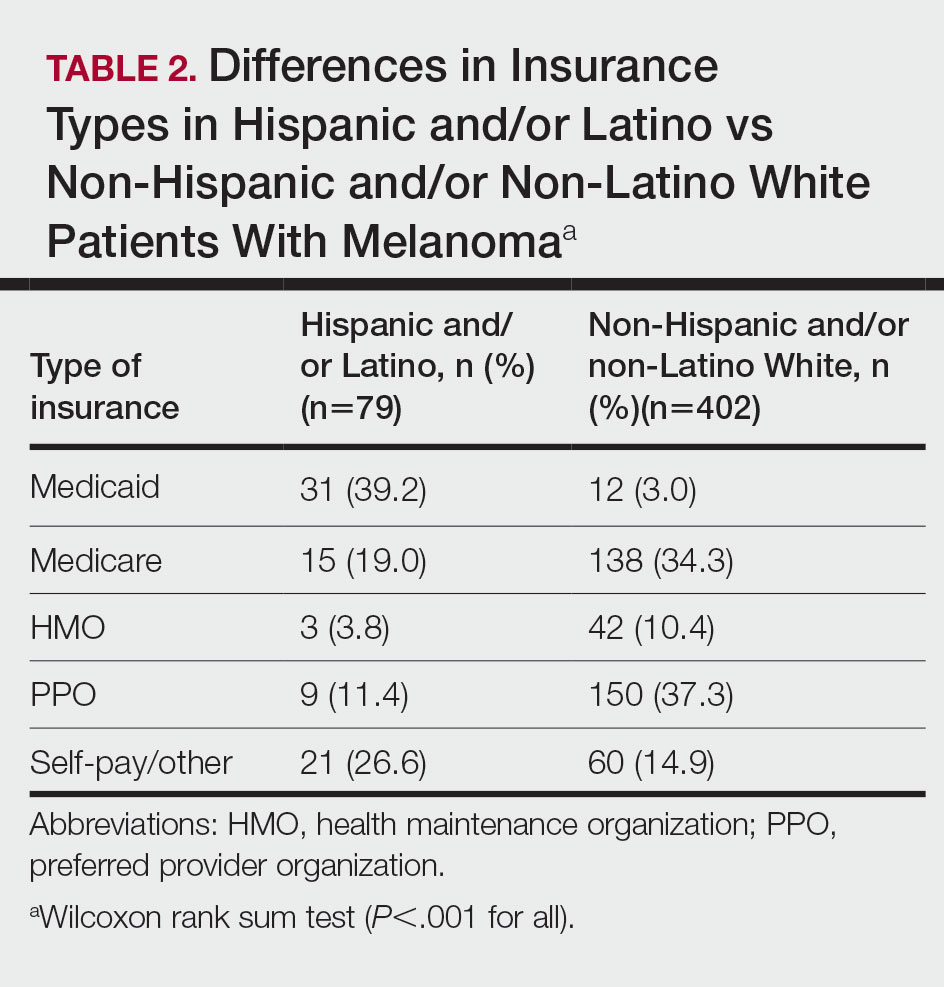
This retrospective study analyzing nearly 10 years of recent melanoma data found that disparities in melanoma diagnosis and treatment continue to exist among Hispanic and/or Latino patients. Compared to non-Hispanic and/or non-Latino White patients, Hispanic and/or Latino patients were diagnosed with melanoma at a younger age and the proportion of females with melanoma was higher. Cormier et al2 also reported that Hispanic patients were younger at melanoma diagnosis, and females represented a larger majority of patients in the Hispanic population compared with the White population. Hispanic and/or Latino patients in our study had more advanced melanoma tumor stage at diagnosis and a higher risk of lymph node and distant metastases, similar to findings reported by Koblinksi et al.3
Our retrospective cohort study demonstrated that the demographics of Hispanic and/or Latino patients with melanoma differ from non-Hispanic and/or non-Latino White patients, specifically with a greater proportion of younger and female patients in the Hispanic and/or Latino population. We also found that Hispanic and/or Latino patients continue to experience worse melanoma outcomes compared with non-Hispanic and/or non-Latino White patients. Further studies are needed to investigate the etiologies behind these health care disparities and potential interventions to address them. In addition, there needs to be increased awareness of the risk for melanoma in Hispanic and/or Latino patients among both health care providers and patients.
Limitations of this study included a smaller sample size of patients from one geographic region. The retrospective design of this study also increased the risk for selection bias, as some of the patients may have had incomplete records or were lost to follow-up. Therefore, the study cohort may not be representative of the general population. Additionally, patients’ skin types could not be determined using standardized tools such as the Fitzpatrick scale, thus we could not assess how patient skin type may have affected melanoma outcomes.
- Aggarwal P, Knabel P, Fleischer AB. United States burden of melanoma and non-melanoma skin cancer from 1990 to 2019. J Am Acad Dermatol. 2021;85:388-395. doi:10.1016/j.jaad.2021.03.109
- Cormier JN, Xing Y, Ding M, et al. Ethnic differences among patients with cutaneous melanoma. Arch Intern Med. 2006;166:1907. doi:10.1001/archinte.166.17.1907
- Koblinski JE, Maykowski P, Zeitouni NC. Disparities in melanoma stage at diagnosis in Arizona: a 10-year Arizona Cancer Registry study. J Am Acad Dermatol. 2021;84:1776-1779. doi:10.1016/j.jaad.2021.02.045
- Aggarwal P, Knabel P, Fleischer AB. United States burden of melanoma and non-melanoma skin cancer from 1990 to 2019. J Am Acad Dermatol. 2021;85:388-395. doi:10.1016/j.jaad.2021.03.109
- Cormier JN, Xing Y, Ding M, et al. Ethnic differences among patients with cutaneous melanoma. Arch Intern Med. 2006;166:1907. doi:10.1001/archinte.166.17.1907
- Koblinski JE, Maykowski P, Zeitouni NC. Disparities in melanoma stage at diagnosis in Arizona: a 10-year Arizona Cancer Registry study. J Am Acad Dermatol. 2021;84:1776-1779. doi:10.1016/j.jaad.2021.02.045
Practice Points
- Hispanic and/or Latino patients often present with more advanced-stage melanomas and have decreased survival rates compared with non-Hispanic and/or non-Latino White patients.
- More education and awareness on the risk for melanoma as well as sun-protective behaviors in the Hispanic and/or Latino population is needed among both health care providers and patients to prevent diagnosis of melanoma in later stages and improve outcomes.
De-pathologizing gender identity: Psychiatry’s role
Treating patients who are transgender or gender diverse (TGGD) requires an understanding of the social and psychological factors that have a unique impact on this population. As clinicians, it is our responsibility to understand the social, cultural, and political issues our patients face, both historically and currently. In this article, we provide information about the nature of gender and gender identity as separate from biological sex and informed by a person’s perception of self as male, female, nonbinary, or other variation.
Psychiatrists must be aware of how individuals who are TGGD have been perceived, classified, and treated by the medical profession, as this history is often a source of mistrust and a barrier to treatment for patients who need psychiatric care. This includes awareness of the “gatekeeping” role that persists in medical institutions today: applying strict eligibility criteria to determine the “fitness” of individuals who are transgender to pursue medical transition, as compared to the informed-consent model that is widely applied to other medical interventions. Our review of minority stress theory, as applicable to this patient population, provides a context and framework for empathic approaches to care for patients who are TGGD. Recognizing barriers to care and ways in which we can create a supportive environment for treatment will allow for tailored approaches that better fit the unique needs of this patient population.
The gender binary
In Western societies, gender has often been viewed as “binary,” oppositional, and directly correlated with physical sex or presumed anatomy.1 The theory of gender essentialism insists that sex and gender are indistinguishable from one another and provide 2 “natural” and distinct categories: women and men. The “gender/sex” binary refers to the belief that individuals born with 2 X chromosomes will inherently develop into and fulfill the social roles of women, and those born with an X and a Y chromosome will develop into and fulfill the social roles of men.1 In this context, “sex” refers to biological characteristics of individuals, including combinations of sex chromosomes, anatomy, and the development of sex characteristics during puberty. The term “gender” refers to the social, cultural, and behavioral aspects of being a man, woman, both, or neither, and “gender identity” refers to one’s internal, individual sense of self and experience of gender (Figure 12). Many Western cultures are now facing destabilization of the gender/sex binary in social, political, and interpersonal contexts.1 This is perhaps most clearly seen in the battle for self-determination and protection by laws affecting individuals who are transgender as well as the determination of other groups to maintain traditional sex and gender roles, often through political action. Historically, individuals who are TGGD have been present in a variety of cultures. For example, most Native American cultures have revered other-gendered individuals, more recently referred to as “two-spirited.” Similarly, the Bugis people of South Sulawesi, Indonesia, recognize 5 genders that exist on a nonbinary spectrum.3
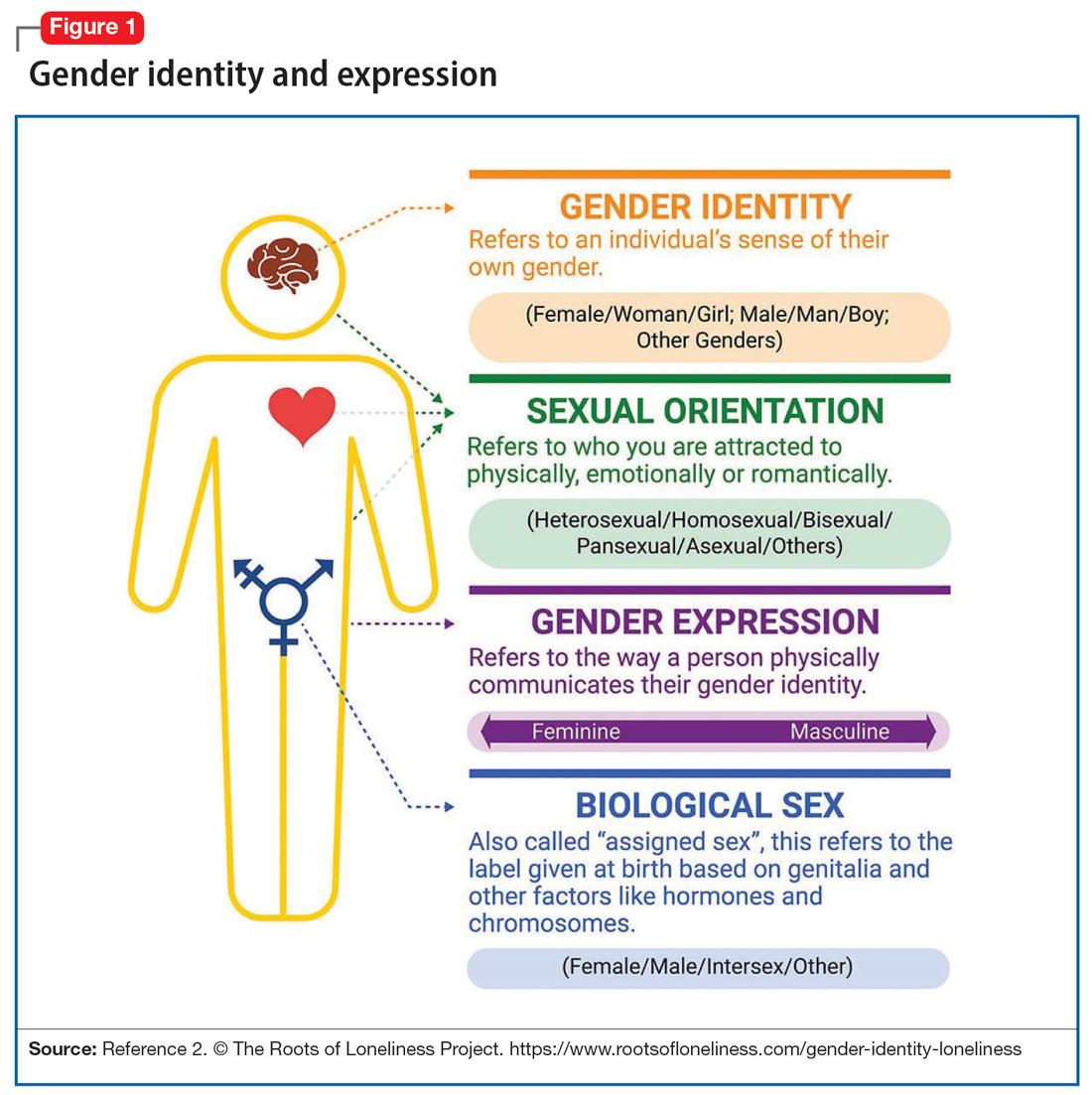
Despite its prevalence in Western society, scientific evidence for the gender/sex binary is lacking. The gender similarities hypothesis states that males and females are similar in most, but not all, psychological variables and is supported by multiple meta-analyses examining psychological gender differences.4 In a 2005 review of 46 meta-analyses of gender-differences, studied through behavior analysis, effect sizes for gender differences were trivial or small in almost 75% of examined variables.5 Analyzing for internal consistency among studies showing large gender/sex differences, Joel et al6 found that, on measures of personality traits, attitudes, interests, and behaviors were rarely homogenous in the brains of males or females. In fact, <1% of study participants showed only masculine or feminine traits, whereas 55% showed a combination, or mosaic, of these traits.6 These findings were supported by further research in behavioral neuroendocrinology that demonstrated a lack of hormonal evidence for 2 distinct sexes. Both estrogen (the “female” hormone) and testosterone (the “male” hormone) are produced by both biological males and females. Further, levels of estradiol do not significantly differ between males and females, and, in fact, in nonpregnant females, estradiol levels are more similar to those of males than to those of pregnant females.1 In the last decade, imaging studies of the human brain have shown that brain structure and connectivity in individuals who are transgender are more similar to those of their experienced gender than of their natal sex.7 In social analyses of intersex individuals (individuals born with ambiguous physical sex characteristics), surgical assignment into the binary gender system did not improve—and often worsened—feelings of isolation and shame.1
The National Institutes of Health defines gender as “socially constructed and enacted roles and behaviors which occur in a historical and cultural context and vary across societies and time.”8 The World Health Organization (WHO) provides a similar definition, and the evidence to support this exists in social-role theory, social-identity theory, and the stereotype-content model. However, despite evidence disputing a gender/sex binary, this method of classifying individuals into a dyad persists in many areas of modern culture, from gender-specific physical spaces (bathrooms, classrooms, store brands), language (pronouns), and laws. This desire for categorization helps fulfill social and psychological needs of groups and individuals by providing group identities and giving structure to the complexity of modern-day life. Identity and group membership provide a sense of belonging, source of self-esteem, and avoidance of ambiguity. Binary gender stereotypes provide expectations that allow anticipation and prediction of our social environments.9 However, the harm of perpetuating the false gender/sex binary is well documented and includes social and economic penalties, extreme violence, and even death. The field of medicine has not been immune from practices that implicitly endorse the gender/sex connection, as seen in the erroneous use of gender in biomedical writings at the highest levels and evidenced in research examining “gender” differences in disease incidence.
Gender diversity as a pathology
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM) has been a source of pathologizing gender diversity since the 1960s, with the introduction of “transsexualism” in DSM-II10 and “gender identity disorder of childhood” in DSM-III.11 These diagnoses were listed under the headings of “sexual deviations” and “psychosexual disorders” in the respective DSM editions. This illustrates how gender diversity was viewed as a mental illness/defect. As the DSM developed through various revisions, so have these diagnoses. DSM-IV used the diagnosis “gender identity disorder.”12 Psychiatry has evolved away from this line of thinking by focusing on the distress from biological sex characteristics that are “incongruent” with an individual’s gender identity, leading to the development of the gender dysphoria diagnosis.13 While this has been a positive step in psychiatry’s efforts to de-pathologize individuals who are gender-diverse, it raises the question: should such diagnoses be included in the DSM at all?
The gender dysphoria diagnosis continues to be needed by many individuals who are TGGD in order to access gender-affirming health care services. Mental health professionals are placed in a gatekeeping role by the expectation that they provide letters of “support” to indicate an individual is of sound mind and consistent gender identity to have services covered by insurance providers. In this way, the insurance industry and the field of medicine continue to believe that individuals who are TGGD need psychiatric permission and/or counsel regarding their gender identity. This can place psychiatry in a role of controlling access to necessary care while also creating a possible distrust in our ability to provide care to patients who are gender-diverse. This is particularly problematic given the high rates of depression, anxiety, trauma, and substance use within these communities.14 In the WHO’s ICD-11, gender dysphoria was changed to gender incongruence and is contained in the category of “Conditions related to sexual health.”15 This indicates continued evolution of how medicine views individuals who are TGGD, and offers hope that psychiatry and the DSM will follow suit.
Continue to: Minority stress theory
Minority stress theory
Ilan Meyer’s minority stress theory explores how cultural and social factors impact mental health functioning (Figure 216). Minority stress theory, which was originally developed for what at the time was described as the lesbian, gay, and bisexual communities, purports that the higher prevalence of mental health disorders among such individuals is likely due to social stigma, discrimination, and stressors associated with minority status. More recently, minority stress theory has been expanded to provide framework for individuals who are TGGD. Hendricks et al17 explain how distal, proximal, and resilience factors contribute to mental health outcomes among these individuals. Distal factors, such as gender-related discrimination, harassment, violence, and rejection, explain how systemic, cultural, and environmental events lead to overt stress. Proximal factors consist of an individual’s expectation and anticipation of negative and stressful events and the internalization of negative attitudes and prejudice (ie, internalized transphobia). Resilience factors consist of community connectedness and within-group identification and can help mediate the negative effects of distal and proximal factors.
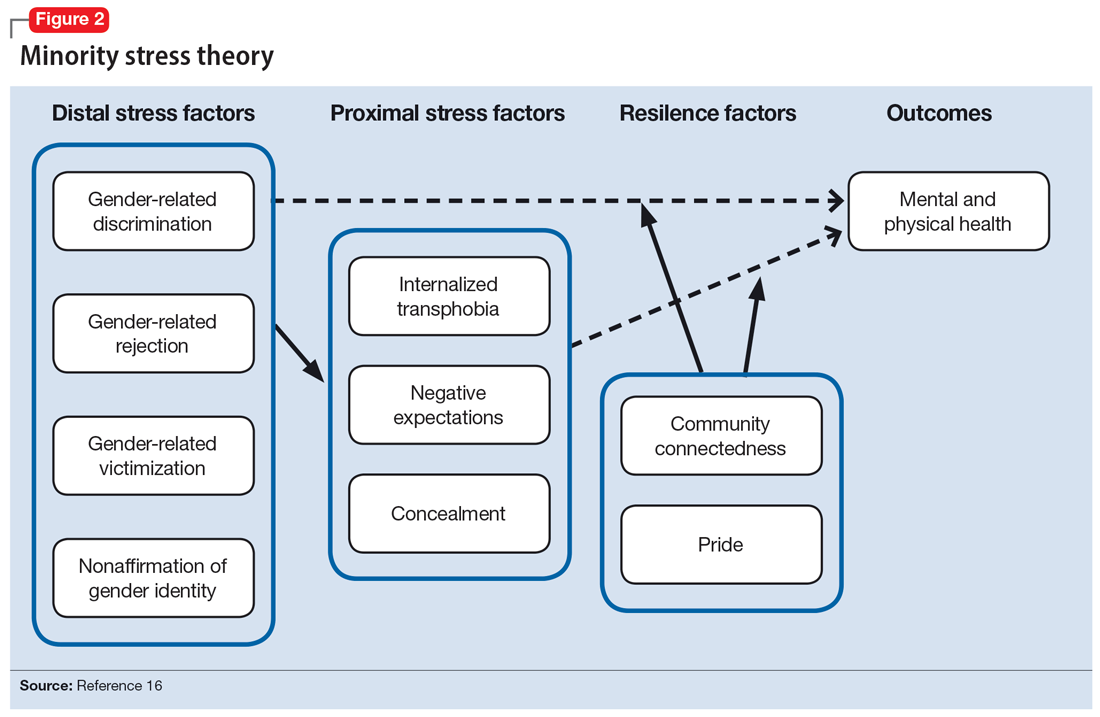
As clinicians, understanding our patients’ experiences and expectations can help us better engage with them and create an environment of safety and healing. Minority stress theory framework suggests that patients may start treatment with distrust or suspicion in light of previous negative experiences. They may also be likely to expect clinicians to be judgmental or to lack understanding of them. The 2015 US Transgender Survey found that 33% of individuals who are TGGD who sought medical treatment in the past year had at least 1 negative experience related to their gender identity (Table 118). Twenty-four percent reported having to educate their clinician about people who are TGGD, while 15% reported the health care professional asked invasive or unnecessary questions about their gender status that were unrelated to their visit. While psychiatry is often distinct from the larger medical field, it is important to understand the negative encounters individuals who are TGGD have likely experienced in medicine, and how those events may skew their feelings about psychiatric treatment. This is especially salient given the higher prevalence of various psychiatric disorders among individuals who are TGGD.18
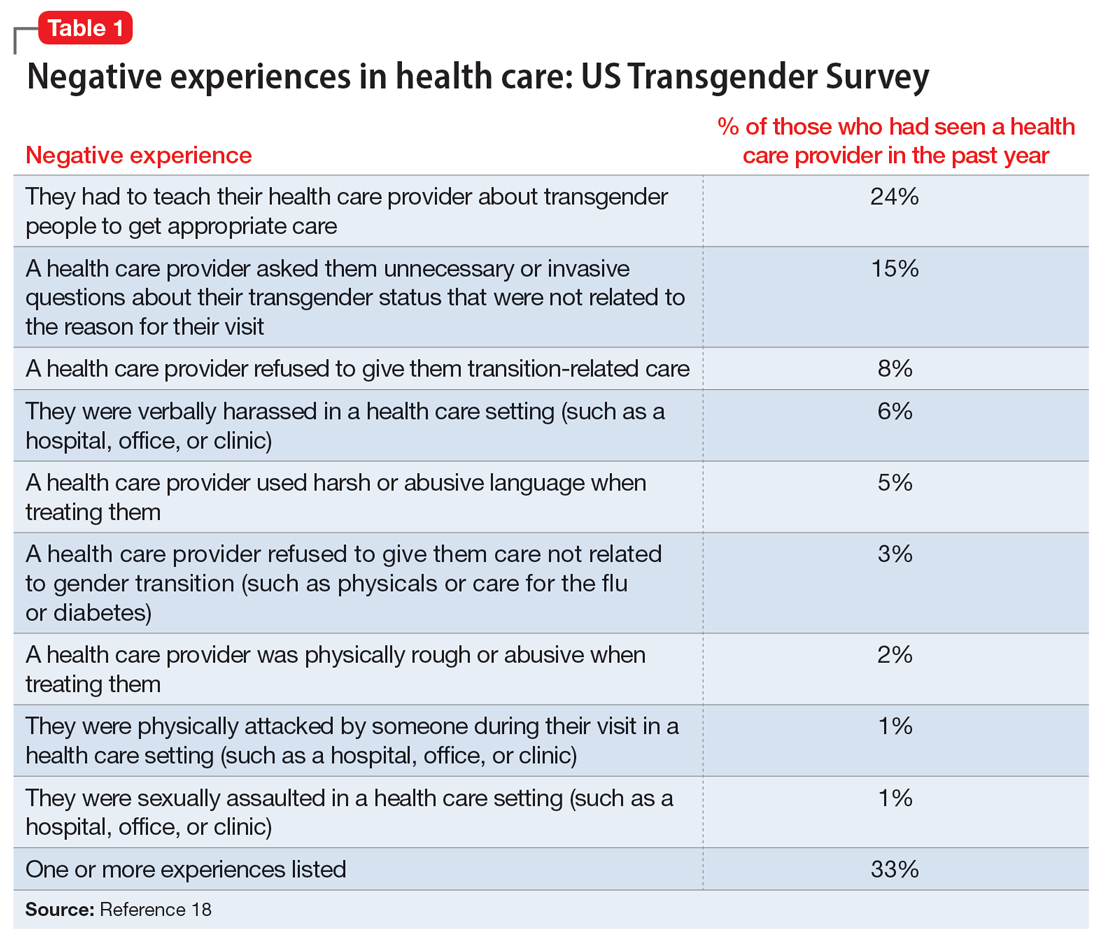
According to the US Transgender Survey, 39% of participants were currently experiencing serious psychological distress, which is nearly 8 times the rate in the US population (5%).18 When extrapolated, this data indicates that we in psychiatry are likely to work with individuals who identify as TGGD, regardless of our expertise. Additionally, research indicates that having access to gender-affirming care—such as hormone replacement therapy, gender-affirming surgery, voice therapy, and other treatments—greatly improves mental health issues such as anxiety, depression, and suicidality among individuals who are TGGD.19,20 It is in this way we in psychiatry must do more than just care for our patients by becoming advocates for them to receive the care they need and deserve. While at times we may want to stay out of politics and other public discourse, it is becoming increasingly necessary as health care is entrenched in politics.
Clinical applicability
Because individuals who are TGGD experience higher rates of depression, anxiety, substance use, and other psychiatric disorders,14 it is increasingly likely that many clinicians will be presented with opportunities to treat such individuals. Despite high rates of psychiatric disorders, individuals who are TGGD often avoid treatment due to concerns about being pathologized, stereotyped, and/or encountering professionals who lack the knowledge to treat them as they are.21 Several studies recommend clinicians better equip themselves to appropriately provide services to individuals who are TGGD.21 Some advise seeking education to understand the unique needs of these patients and to help stay current with appropriate terminology and language (Table 222). This also implies not relying on patients to educate clinicians in understanding their specific needs and experiences.
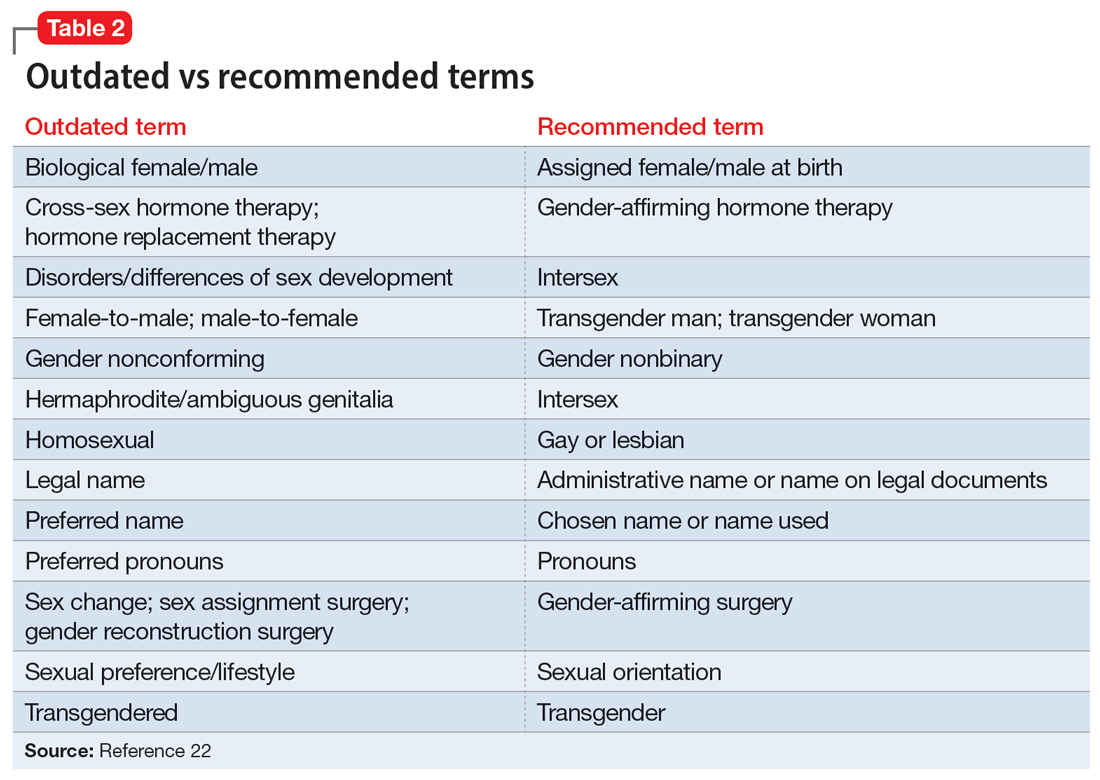
Making assumptions about a patient’s identity is one of the most commonly reported issues by individuals who are TGGD. Therefore, it is critical to avoid making assumptions about patients based on binary stereotypes.23,24 We can circumvent these mistakes by asking every patient for their name and pronouns, and introducing ourselves with our pronouns. This illustrates an openness and understanding of the importance of identity and language, and makes it common practice from the outset. Integrating the use of gender-neutral language into paperwork, intake forms, charting, and conversation will also help avoid the pitfalls of misgendering and making false assumptions. This will also allow for support staff, medical assistants, and others to use correct language with patients. Having a patient’s used name and pronouns visible for everyone who works with the patient is necessary to effectively meet the patient’s needs. Additionally, understanding that the range of experiences and needs for individuals who are TGGD is heterogeneous can help reduce assumptions and ensure we are asking for needed information. It is also important to ask for only relevant information needed to provide treatment.
Continue to: Resources are widely available...
Resources are widely available to aid in the care of individuals who are TGGD. In 2022, the World Professional Association for Transgender Health released new guidelines—Standards of Care 8—for working with individuals who are TGGD.25 While these standards include a section dedicated to mental health, they also provide guidelines on education, assessments, specific demographic groups, hormone therapy, primary care, and sexual health. Additionally, while we may not want the role of gatekeeping for individuals to receive gender-affirming care, we work within a health care and insurance system that continues to require psychiatric assessment for such surgeries. In this role, we must do our part to educate ourselves in how to best provide these assessments and letters of support to help patients receive appropriate and life-saving care.
Finally, in order to provide a more comfortable and affirming space for individuals who are TGGD, develop ways to self-assess and monitor the policies, procedures, and language used within your practice, clinic, or institution. Monitoring the language used in charting to ensure consistency with the individual’s gender identity is important for our own understanding of the patient, and for patients to feel seen. This is especially true given patients’ access to medical records under the Cures Act. Moreover, it is essential to be cognizant of how you present clients to others in consultation or care coordination to ensure the patient is identified correctly and consistently by clinicians and staff.
Bottom Line
Understanding the social, cultural, and medical discrimination faced by patients who are transgender or gender diverse can make us better suited to engage and treat these individuals in an affirming and supportive way.
Related Resources
- World Professional Association of Transgender Health (WPATH) Standards of Care—8th edition. https://www.tandfonline.com/doi/pdf/10.1080/26895269.2022.2100644
- The Fenway Institute: National LGBTQIA+ Health Education Center. https://fenwayhealth.org/the-fenway-institute/education/the-national-lgbtia-health-education-center/
1. Morgenroth T, Ryan MK. The effects of gender trouble: an integrative theoretical framework of the perpetuation and disruption of the gender/sex binary. Perspect Psychol Sci. 2021;16(6):1113-1142. doi:10.1177/1745691620902442
2. The Roots of Loneliness Project. Accessed April 8, 2023. https://www.rootsofloneliness.com/gender-identity-loneliness
3. Davies SG. Challenging Gender Norms: Five Genders Among Bugis in Indonesia. Thomson Wadsworth; 2007.
4. Hyde JS. The gender similarities hypothesis. Am Psychol. 2005;60(6):581-592. doi:10.1037/0003-066X.60.6.581
5. Joel D. Beyond the binary: rethinking sex and the brain. Neurosci Biobehav Rev. 2021;122:165-175. doi:10.1016/j.neubiorev.2020.22.018
6. Joel D, Berman Z, Tavor I, et al. Sex beyond the genitalia: the human brain mosaic. Proc Natl Acad Sci U S A. 2015;112(50):15468-15473. doi:10.1073/pnas.1509654112
7. Palmer BF, Clegg DJ. A universally accepted definition of gender will positively impact societal understanding, acceptance, and appropriateness of health care. Mayo Clin Proc. 2020;95(10):2235-2243. doi:10.1016/j.mayocp.2020.01.031
8. Office of Research on Women’s Health. Sex & Gender. National Institutes of Health. Accessed April 6, 2023. https://orwh.od.nih.gov/sex-gender
9. Morgenroth T, Sendén MG, Lindqvist A, et al. Defending the sex/gender binary: the role of gender identification and need for closure. Soc Psychol Pers Sci. 2021;12(5):731-740.
10. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 2nd ed. American Psychiatric Association; 1968.
11. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. American Psychiatric Association; 1980.
12. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; 1994.
13. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Publishing; 2013.
14. Wanta JW, Niforatos JD, Durbak E, et al. Mental health diagnoses among transgender patients in the clinical setting: an all-payer electronic health record study. Transgend Health. 2019;4(1):313-315.
15. World Health Organization. International Statistical Classification of Diseases. 11th ed. World Health Organization; 2019.
16. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674-697. doi:10.1037/0033-2909.129.5.674
17. Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the Minority Stress Model. Profess Psychol: Res Pract. 2012;43(5):460-467. doi:10.1037/a0029597
18. James SE, Herman J, Keisling M, et al. The Report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality; 2016. Accessed April 6, 2023. https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf
19. Almazan AN, Keuroghlian AS. Association between gender-affirming surgeries and mental health outcomes. JAMA Surg. 2021;156(7):611-618. doi:10.1001/jamasurg.2021.0952
20. Tordoff DM, Wanta JW, Collin A, et al. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Netw Open. 2022;5(2):e220978. doi:10.1001/jamanetworkopen.2022.0978
21. Snow A, Cerel J, Loeffler DN, et al. Barriers to mental health care for transgender and gender-nonconforming adults: a systematic literature review. Health Soc Work. 2019;44(3):149-155. doi:10.1093/hsw/hlz016
22. National LGBTQIA+ Health Education Center. Accessed April 8, 2023. https://www.lgbtqiahealtheducation.org
23. Baldwin A, Dodge B, Schick VR, et al. Transgender and genderqueer individuals’ experiences with health care providers: what’s working, what’s not, and where do we go from here? J Health Care Poor Underserved. 2018;29(4):1300-1318. doi:10.1353/hpu.2018.0097
24. Kcomt L, Gorey KM, Barrett BJ, et al. Healthcare avoidance due to anticipated discrimination among transgender people: a call to create trans-affirmative environments. SSM-Popul Health. 2020;11:100608. doi:10.1016/j.ssmph.2020.100608
25. Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgender Health. 2022;23(Suppl 1):S1-S259.
Treating patients who are transgender or gender diverse (TGGD) requires an understanding of the social and psychological factors that have a unique impact on this population. As clinicians, it is our responsibility to understand the social, cultural, and political issues our patients face, both historically and currently. In this article, we provide information about the nature of gender and gender identity as separate from biological sex and informed by a person’s perception of self as male, female, nonbinary, or other variation.
Psychiatrists must be aware of how individuals who are TGGD have been perceived, classified, and treated by the medical profession, as this history is often a source of mistrust and a barrier to treatment for patients who need psychiatric care. This includes awareness of the “gatekeeping” role that persists in medical institutions today: applying strict eligibility criteria to determine the “fitness” of individuals who are transgender to pursue medical transition, as compared to the informed-consent model that is widely applied to other medical interventions. Our review of minority stress theory, as applicable to this patient population, provides a context and framework for empathic approaches to care for patients who are TGGD. Recognizing barriers to care and ways in which we can create a supportive environment for treatment will allow for tailored approaches that better fit the unique needs of this patient population.
The gender binary
In Western societies, gender has often been viewed as “binary,” oppositional, and directly correlated with physical sex or presumed anatomy.1 The theory of gender essentialism insists that sex and gender are indistinguishable from one another and provide 2 “natural” and distinct categories: women and men. The “gender/sex” binary refers to the belief that individuals born with 2 X chromosomes will inherently develop into and fulfill the social roles of women, and those born with an X and a Y chromosome will develop into and fulfill the social roles of men.1 In this context, “sex” refers to biological characteristics of individuals, including combinations of sex chromosomes, anatomy, and the development of sex characteristics during puberty. The term “gender” refers to the social, cultural, and behavioral aspects of being a man, woman, both, or neither, and “gender identity” refers to one’s internal, individual sense of self and experience of gender (Figure 12). Many Western cultures are now facing destabilization of the gender/sex binary in social, political, and interpersonal contexts.1 This is perhaps most clearly seen in the battle for self-determination and protection by laws affecting individuals who are transgender as well as the determination of other groups to maintain traditional sex and gender roles, often through political action. Historically, individuals who are TGGD have been present in a variety of cultures. For example, most Native American cultures have revered other-gendered individuals, more recently referred to as “two-spirited.” Similarly, the Bugis people of South Sulawesi, Indonesia, recognize 5 genders that exist on a nonbinary spectrum.3
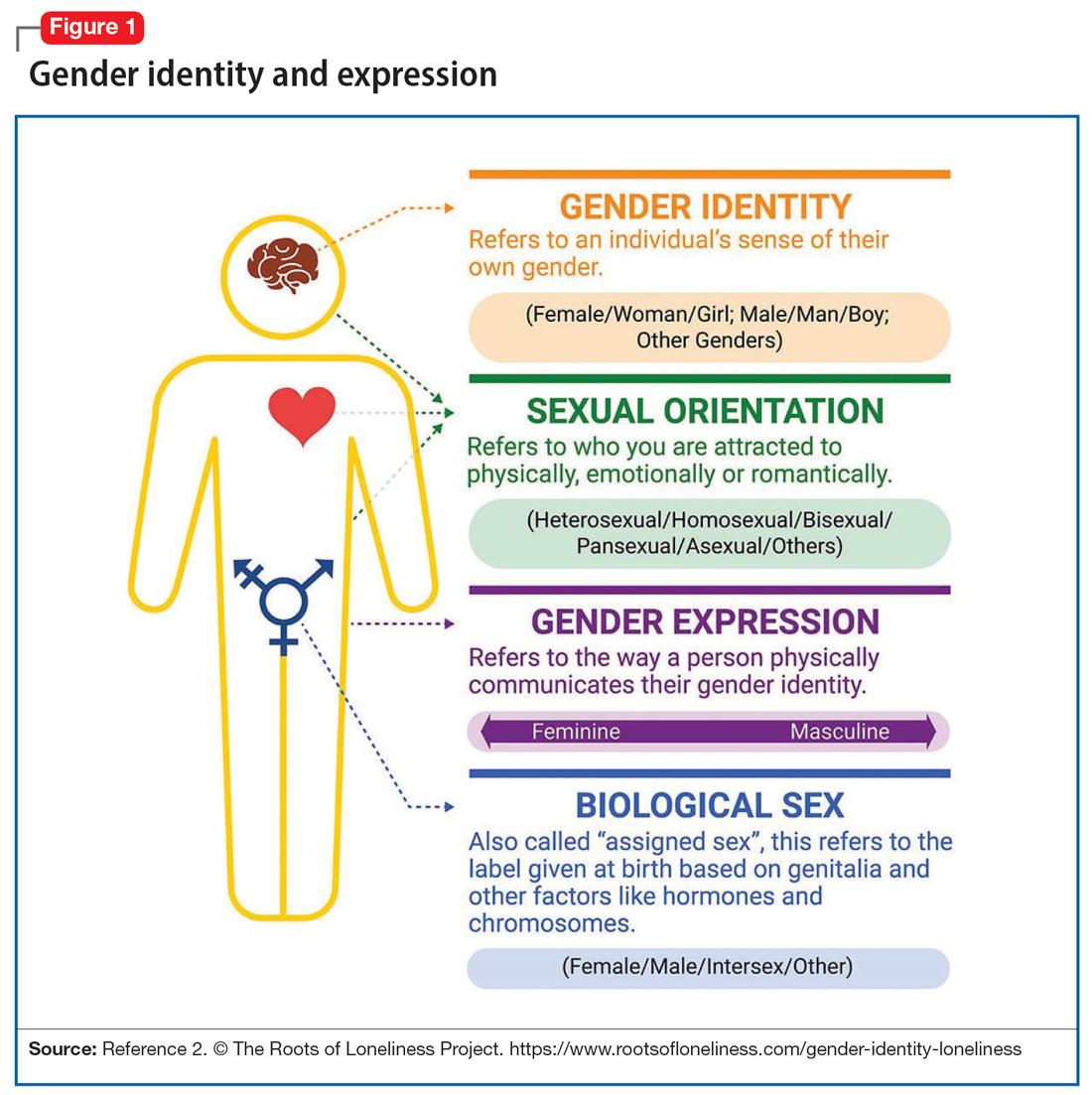
Despite its prevalence in Western society, scientific evidence for the gender/sex binary is lacking. The gender similarities hypothesis states that males and females are similar in most, but not all, psychological variables and is supported by multiple meta-analyses examining psychological gender differences.4 In a 2005 review of 46 meta-analyses of gender-differences, studied through behavior analysis, effect sizes for gender differences were trivial or small in almost 75% of examined variables.5 Analyzing for internal consistency among studies showing large gender/sex differences, Joel et al6 found that, on measures of personality traits, attitudes, interests, and behaviors were rarely homogenous in the brains of males or females. In fact, <1% of study participants showed only masculine or feminine traits, whereas 55% showed a combination, or mosaic, of these traits.6 These findings were supported by further research in behavioral neuroendocrinology that demonstrated a lack of hormonal evidence for 2 distinct sexes. Both estrogen (the “female” hormone) and testosterone (the “male” hormone) are produced by both biological males and females. Further, levels of estradiol do not significantly differ between males and females, and, in fact, in nonpregnant females, estradiol levels are more similar to those of males than to those of pregnant females.1 In the last decade, imaging studies of the human brain have shown that brain structure and connectivity in individuals who are transgender are more similar to those of their experienced gender than of their natal sex.7 In social analyses of intersex individuals (individuals born with ambiguous physical sex characteristics), surgical assignment into the binary gender system did not improve—and often worsened—feelings of isolation and shame.1
The National Institutes of Health defines gender as “socially constructed and enacted roles and behaviors which occur in a historical and cultural context and vary across societies and time.”8 The World Health Organization (WHO) provides a similar definition, and the evidence to support this exists in social-role theory, social-identity theory, and the stereotype-content model. However, despite evidence disputing a gender/sex binary, this method of classifying individuals into a dyad persists in many areas of modern culture, from gender-specific physical spaces (bathrooms, classrooms, store brands), language (pronouns), and laws. This desire for categorization helps fulfill social and psychological needs of groups and individuals by providing group identities and giving structure to the complexity of modern-day life. Identity and group membership provide a sense of belonging, source of self-esteem, and avoidance of ambiguity. Binary gender stereotypes provide expectations that allow anticipation and prediction of our social environments.9 However, the harm of perpetuating the false gender/sex binary is well documented and includes social and economic penalties, extreme violence, and even death. The field of medicine has not been immune from practices that implicitly endorse the gender/sex connection, as seen in the erroneous use of gender in biomedical writings at the highest levels and evidenced in research examining “gender” differences in disease incidence.
Gender diversity as a pathology
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM) has been a source of pathologizing gender diversity since the 1960s, with the introduction of “transsexualism” in DSM-II10 and “gender identity disorder of childhood” in DSM-III.11 These diagnoses were listed under the headings of “sexual deviations” and “psychosexual disorders” in the respective DSM editions. This illustrates how gender diversity was viewed as a mental illness/defect. As the DSM developed through various revisions, so have these diagnoses. DSM-IV used the diagnosis “gender identity disorder.”12 Psychiatry has evolved away from this line of thinking by focusing on the distress from biological sex characteristics that are “incongruent” with an individual’s gender identity, leading to the development of the gender dysphoria diagnosis.13 While this has been a positive step in psychiatry’s efforts to de-pathologize individuals who are gender-diverse, it raises the question: should such diagnoses be included in the DSM at all?
The gender dysphoria diagnosis continues to be needed by many individuals who are TGGD in order to access gender-affirming health care services. Mental health professionals are placed in a gatekeeping role by the expectation that they provide letters of “support” to indicate an individual is of sound mind and consistent gender identity to have services covered by insurance providers. In this way, the insurance industry and the field of medicine continue to believe that individuals who are TGGD need psychiatric permission and/or counsel regarding their gender identity. This can place psychiatry in a role of controlling access to necessary care while also creating a possible distrust in our ability to provide care to patients who are gender-diverse. This is particularly problematic given the high rates of depression, anxiety, trauma, and substance use within these communities.14 In the WHO’s ICD-11, gender dysphoria was changed to gender incongruence and is contained in the category of “Conditions related to sexual health.”15 This indicates continued evolution of how medicine views individuals who are TGGD, and offers hope that psychiatry and the DSM will follow suit.
Continue to: Minority stress theory
Minority stress theory
Ilan Meyer’s minority stress theory explores how cultural and social factors impact mental health functioning (Figure 216). Minority stress theory, which was originally developed for what at the time was described as the lesbian, gay, and bisexual communities, purports that the higher prevalence of mental health disorders among such individuals is likely due to social stigma, discrimination, and stressors associated with minority status. More recently, minority stress theory has been expanded to provide framework for individuals who are TGGD. Hendricks et al17 explain how distal, proximal, and resilience factors contribute to mental health outcomes among these individuals. Distal factors, such as gender-related discrimination, harassment, violence, and rejection, explain how systemic, cultural, and environmental events lead to overt stress. Proximal factors consist of an individual’s expectation and anticipation of negative and stressful events and the internalization of negative attitudes and prejudice (ie, internalized transphobia). Resilience factors consist of community connectedness and within-group identification and can help mediate the negative effects of distal and proximal factors.
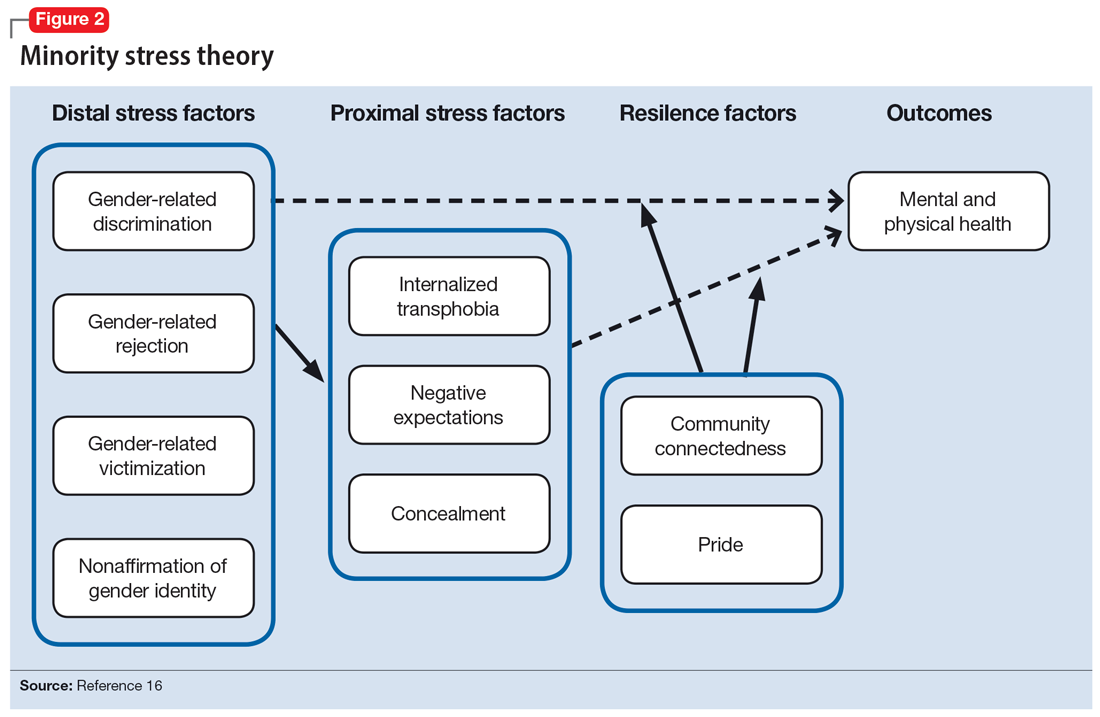
As clinicians, understanding our patients’ experiences and expectations can help us better engage with them and create an environment of safety and healing. Minority stress theory framework suggests that patients may start treatment with distrust or suspicion in light of previous negative experiences. They may also be likely to expect clinicians to be judgmental or to lack understanding of them. The 2015 US Transgender Survey found that 33% of individuals who are TGGD who sought medical treatment in the past year had at least 1 negative experience related to their gender identity (Table 118). Twenty-four percent reported having to educate their clinician about people who are TGGD, while 15% reported the health care professional asked invasive or unnecessary questions about their gender status that were unrelated to their visit. While psychiatry is often distinct from the larger medical field, it is important to understand the negative encounters individuals who are TGGD have likely experienced in medicine, and how those events may skew their feelings about psychiatric treatment. This is especially salient given the higher prevalence of various psychiatric disorders among individuals who are TGGD.18
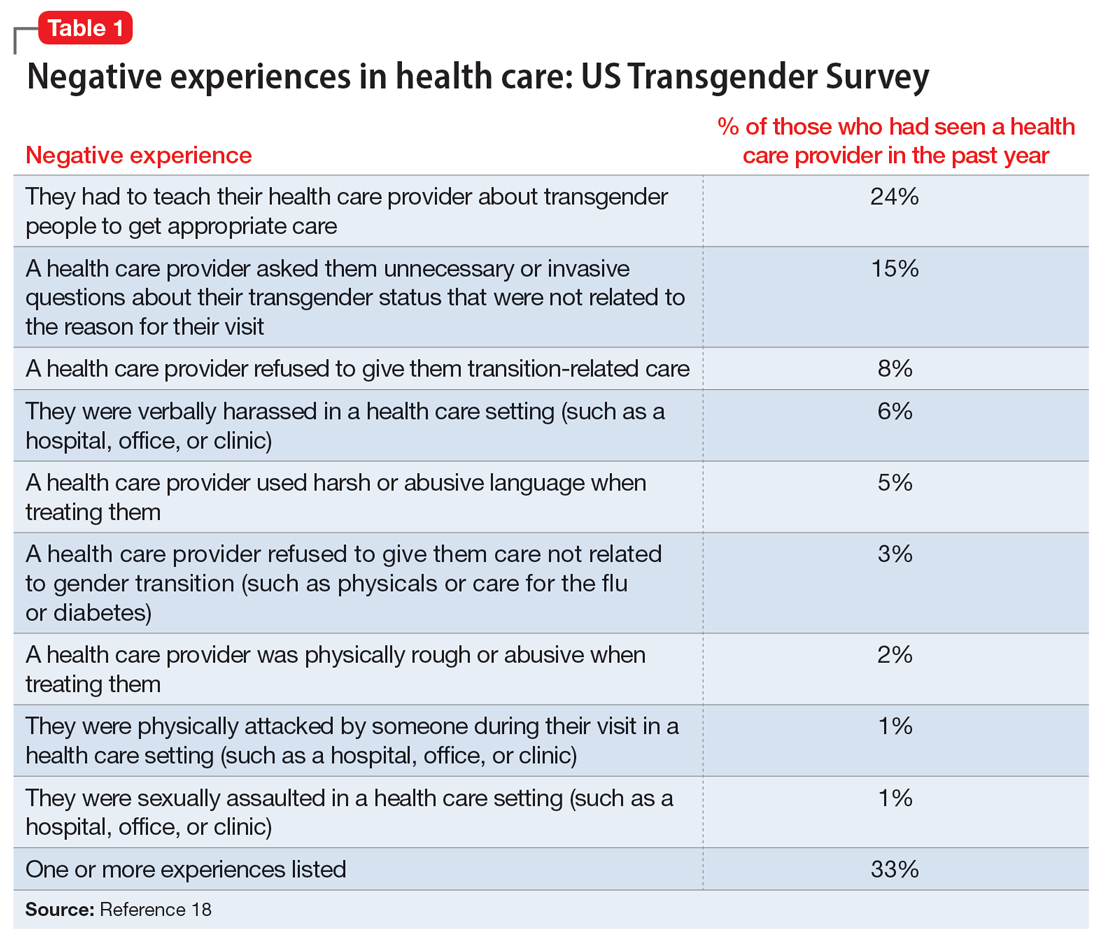
According to the US Transgender Survey, 39% of participants were currently experiencing serious psychological distress, which is nearly 8 times the rate in the US population (5%).18 When extrapolated, this data indicates that we in psychiatry are likely to work with individuals who identify as TGGD, regardless of our expertise. Additionally, research indicates that having access to gender-affirming care—such as hormone replacement therapy, gender-affirming surgery, voice therapy, and other treatments—greatly improves mental health issues such as anxiety, depression, and suicidality among individuals who are TGGD.19,20 It is in this way we in psychiatry must do more than just care for our patients by becoming advocates for them to receive the care they need and deserve. While at times we may want to stay out of politics and other public discourse, it is becoming increasingly necessary as health care is entrenched in politics.
Clinical applicability
Because individuals who are TGGD experience higher rates of depression, anxiety, substance use, and other psychiatric disorders,14 it is increasingly likely that many clinicians will be presented with opportunities to treat such individuals. Despite high rates of psychiatric disorders, individuals who are TGGD often avoid treatment due to concerns about being pathologized, stereotyped, and/or encountering professionals who lack the knowledge to treat them as they are.21 Several studies recommend clinicians better equip themselves to appropriately provide services to individuals who are TGGD.21 Some advise seeking education to understand the unique needs of these patients and to help stay current with appropriate terminology and language (Table 222). This also implies not relying on patients to educate clinicians in understanding their specific needs and experiences.
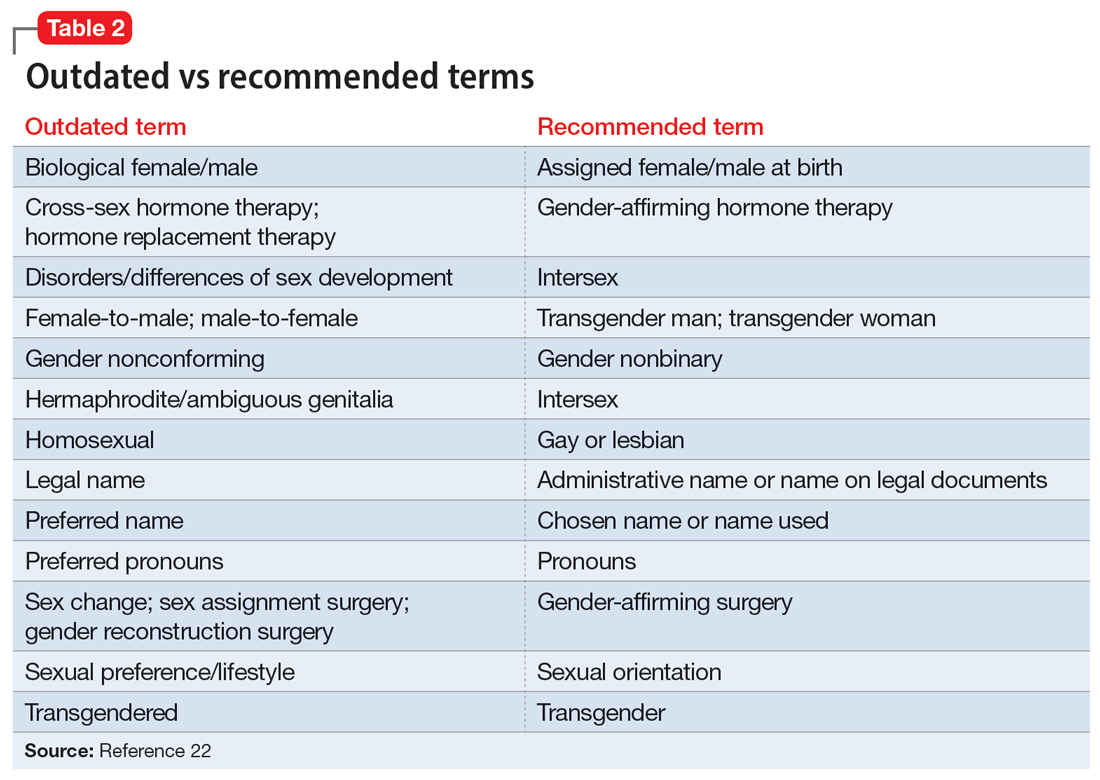
Making assumptions about a patient’s identity is one of the most commonly reported issues by individuals who are TGGD. Therefore, it is critical to avoid making assumptions about patients based on binary stereotypes.23,24 We can circumvent these mistakes by asking every patient for their name and pronouns, and introducing ourselves with our pronouns. This illustrates an openness and understanding of the importance of identity and language, and makes it common practice from the outset. Integrating the use of gender-neutral language into paperwork, intake forms, charting, and conversation will also help avoid the pitfalls of misgendering and making false assumptions. This will also allow for support staff, medical assistants, and others to use correct language with patients. Having a patient’s used name and pronouns visible for everyone who works with the patient is necessary to effectively meet the patient’s needs. Additionally, understanding that the range of experiences and needs for individuals who are TGGD is heterogeneous can help reduce assumptions and ensure we are asking for needed information. It is also important to ask for only relevant information needed to provide treatment.
Continue to: Resources are widely available...
Resources are widely available to aid in the care of individuals who are TGGD. In 2022, the World Professional Association for Transgender Health released new guidelines—Standards of Care 8—for working with individuals who are TGGD.25 While these standards include a section dedicated to mental health, they also provide guidelines on education, assessments, specific demographic groups, hormone therapy, primary care, and sexual health. Additionally, while we may not want the role of gatekeeping for individuals to receive gender-affirming care, we work within a health care and insurance system that continues to require psychiatric assessment for such surgeries. In this role, we must do our part to educate ourselves in how to best provide these assessments and letters of support to help patients receive appropriate and life-saving care.
Finally, in order to provide a more comfortable and affirming space for individuals who are TGGD, develop ways to self-assess and monitor the policies, procedures, and language used within your practice, clinic, or institution. Monitoring the language used in charting to ensure consistency with the individual’s gender identity is important for our own understanding of the patient, and for patients to feel seen. This is especially true given patients’ access to medical records under the Cures Act. Moreover, it is essential to be cognizant of how you present clients to others in consultation or care coordination to ensure the patient is identified correctly and consistently by clinicians and staff.
Bottom Line
Understanding the social, cultural, and medical discrimination faced by patients who are transgender or gender diverse can make us better suited to engage and treat these individuals in an affirming and supportive way.
Related Resources
- World Professional Association of Transgender Health (WPATH) Standards of Care—8th edition. https://www.tandfonline.com/doi/pdf/10.1080/26895269.2022.2100644
- The Fenway Institute: National LGBTQIA+ Health Education Center. https://fenwayhealth.org/the-fenway-institute/education/the-national-lgbtia-health-education-center/
Treating patients who are transgender or gender diverse (TGGD) requires an understanding of the social and psychological factors that have a unique impact on this population. As clinicians, it is our responsibility to understand the social, cultural, and political issues our patients face, both historically and currently. In this article, we provide information about the nature of gender and gender identity as separate from biological sex and informed by a person’s perception of self as male, female, nonbinary, or other variation.
Psychiatrists must be aware of how individuals who are TGGD have been perceived, classified, and treated by the medical profession, as this history is often a source of mistrust and a barrier to treatment for patients who need psychiatric care. This includes awareness of the “gatekeeping” role that persists in medical institutions today: applying strict eligibility criteria to determine the “fitness” of individuals who are transgender to pursue medical transition, as compared to the informed-consent model that is widely applied to other medical interventions. Our review of minority stress theory, as applicable to this patient population, provides a context and framework for empathic approaches to care for patients who are TGGD. Recognizing barriers to care and ways in which we can create a supportive environment for treatment will allow for tailored approaches that better fit the unique needs of this patient population.
The gender binary
In Western societies, gender has often been viewed as “binary,” oppositional, and directly correlated with physical sex or presumed anatomy.1 The theory of gender essentialism insists that sex and gender are indistinguishable from one another and provide 2 “natural” and distinct categories: women and men. The “gender/sex” binary refers to the belief that individuals born with 2 X chromosomes will inherently develop into and fulfill the social roles of women, and those born with an X and a Y chromosome will develop into and fulfill the social roles of men.1 In this context, “sex” refers to biological characteristics of individuals, including combinations of sex chromosomes, anatomy, and the development of sex characteristics during puberty. The term “gender” refers to the social, cultural, and behavioral aspects of being a man, woman, both, or neither, and “gender identity” refers to one’s internal, individual sense of self and experience of gender (Figure 12). Many Western cultures are now facing destabilization of the gender/sex binary in social, political, and interpersonal contexts.1 This is perhaps most clearly seen in the battle for self-determination and protection by laws affecting individuals who are transgender as well as the determination of other groups to maintain traditional sex and gender roles, often through political action. Historically, individuals who are TGGD have been present in a variety of cultures. For example, most Native American cultures have revered other-gendered individuals, more recently referred to as “two-spirited.” Similarly, the Bugis people of South Sulawesi, Indonesia, recognize 5 genders that exist on a nonbinary spectrum.3
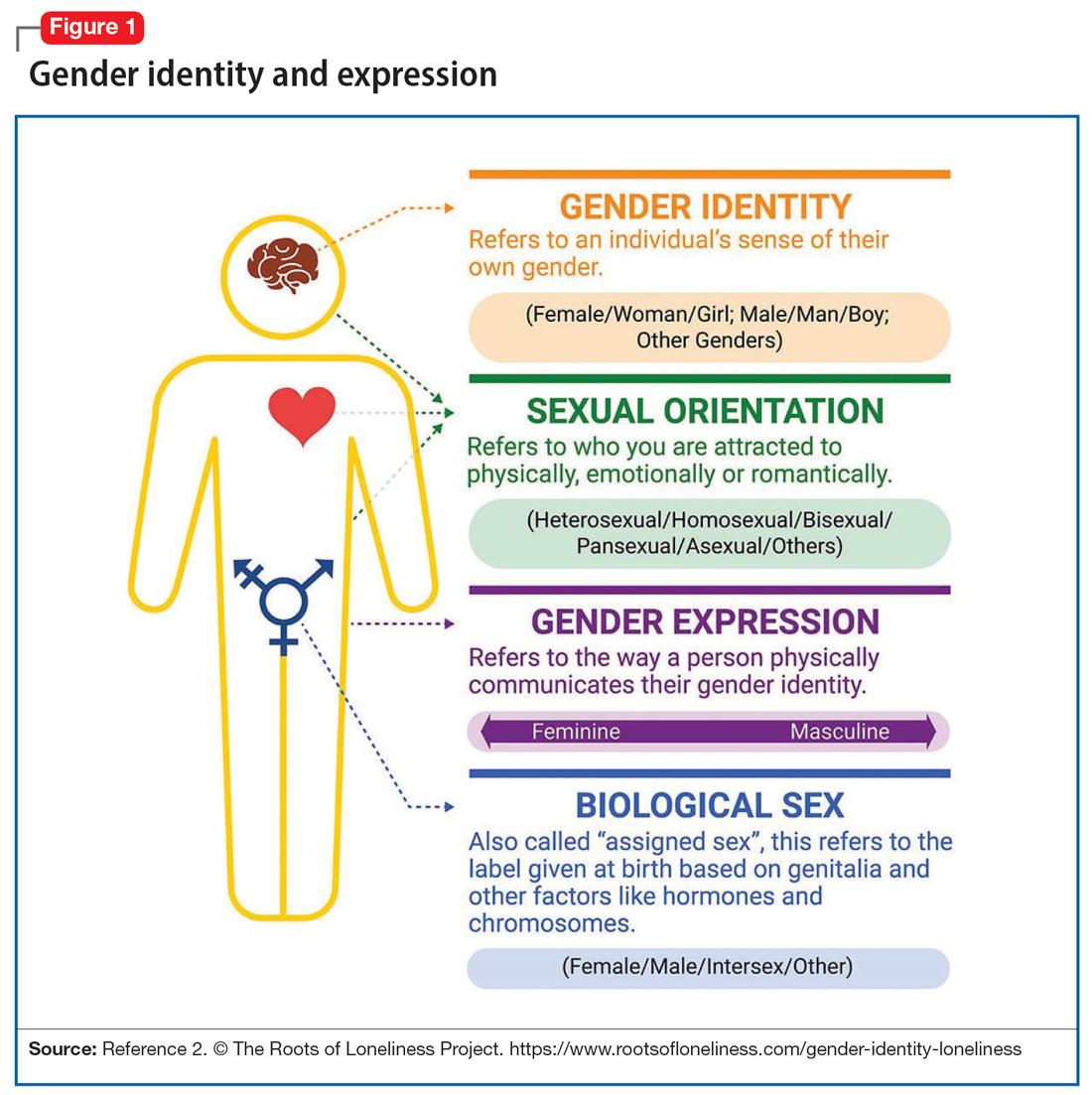
Despite its prevalence in Western society, scientific evidence for the gender/sex binary is lacking. The gender similarities hypothesis states that males and females are similar in most, but not all, psychological variables and is supported by multiple meta-analyses examining psychological gender differences.4 In a 2005 review of 46 meta-analyses of gender-differences, studied through behavior analysis, effect sizes for gender differences were trivial or small in almost 75% of examined variables.5 Analyzing for internal consistency among studies showing large gender/sex differences, Joel et al6 found that, on measures of personality traits, attitudes, interests, and behaviors were rarely homogenous in the brains of males or females. In fact, <1% of study participants showed only masculine or feminine traits, whereas 55% showed a combination, or mosaic, of these traits.6 These findings were supported by further research in behavioral neuroendocrinology that demonstrated a lack of hormonal evidence for 2 distinct sexes. Both estrogen (the “female” hormone) and testosterone (the “male” hormone) are produced by both biological males and females. Further, levels of estradiol do not significantly differ between males and females, and, in fact, in nonpregnant females, estradiol levels are more similar to those of males than to those of pregnant females.1 In the last decade, imaging studies of the human brain have shown that brain structure and connectivity in individuals who are transgender are more similar to those of their experienced gender than of their natal sex.7 In social analyses of intersex individuals (individuals born with ambiguous physical sex characteristics), surgical assignment into the binary gender system did not improve—and often worsened—feelings of isolation and shame.1
The National Institutes of Health defines gender as “socially constructed and enacted roles and behaviors which occur in a historical and cultural context and vary across societies and time.”8 The World Health Organization (WHO) provides a similar definition, and the evidence to support this exists in social-role theory, social-identity theory, and the stereotype-content model. However, despite evidence disputing a gender/sex binary, this method of classifying individuals into a dyad persists in many areas of modern culture, from gender-specific physical spaces (bathrooms, classrooms, store brands), language (pronouns), and laws. This desire for categorization helps fulfill social and psychological needs of groups and individuals by providing group identities and giving structure to the complexity of modern-day life. Identity and group membership provide a sense of belonging, source of self-esteem, and avoidance of ambiguity. Binary gender stereotypes provide expectations that allow anticipation and prediction of our social environments.9 However, the harm of perpetuating the false gender/sex binary is well documented and includes social and economic penalties, extreme violence, and even death. The field of medicine has not been immune from practices that implicitly endorse the gender/sex connection, as seen in the erroneous use of gender in biomedical writings at the highest levels and evidenced in research examining “gender” differences in disease incidence.
Gender diversity as a pathology
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM) has been a source of pathologizing gender diversity since the 1960s, with the introduction of “transsexualism” in DSM-II10 and “gender identity disorder of childhood” in DSM-III.11 These diagnoses were listed under the headings of “sexual deviations” and “psychosexual disorders” in the respective DSM editions. This illustrates how gender diversity was viewed as a mental illness/defect. As the DSM developed through various revisions, so have these diagnoses. DSM-IV used the diagnosis “gender identity disorder.”12 Psychiatry has evolved away from this line of thinking by focusing on the distress from biological sex characteristics that are “incongruent” with an individual’s gender identity, leading to the development of the gender dysphoria diagnosis.13 While this has been a positive step in psychiatry’s efforts to de-pathologize individuals who are gender-diverse, it raises the question: should such diagnoses be included in the DSM at all?
The gender dysphoria diagnosis continues to be needed by many individuals who are TGGD in order to access gender-affirming health care services. Mental health professionals are placed in a gatekeeping role by the expectation that they provide letters of “support” to indicate an individual is of sound mind and consistent gender identity to have services covered by insurance providers. In this way, the insurance industry and the field of medicine continue to believe that individuals who are TGGD need psychiatric permission and/or counsel regarding their gender identity. This can place psychiatry in a role of controlling access to necessary care while also creating a possible distrust in our ability to provide care to patients who are gender-diverse. This is particularly problematic given the high rates of depression, anxiety, trauma, and substance use within these communities.14 In the WHO’s ICD-11, gender dysphoria was changed to gender incongruence and is contained in the category of “Conditions related to sexual health.”15 This indicates continued evolution of how medicine views individuals who are TGGD, and offers hope that psychiatry and the DSM will follow suit.
Continue to: Minority stress theory
Minority stress theory
Ilan Meyer’s minority stress theory explores how cultural and social factors impact mental health functioning (Figure 216). Minority stress theory, which was originally developed for what at the time was described as the lesbian, gay, and bisexual communities, purports that the higher prevalence of mental health disorders among such individuals is likely due to social stigma, discrimination, and stressors associated with minority status. More recently, minority stress theory has been expanded to provide framework for individuals who are TGGD. Hendricks et al17 explain how distal, proximal, and resilience factors contribute to mental health outcomes among these individuals. Distal factors, such as gender-related discrimination, harassment, violence, and rejection, explain how systemic, cultural, and environmental events lead to overt stress. Proximal factors consist of an individual’s expectation and anticipation of negative and stressful events and the internalization of negative attitudes and prejudice (ie, internalized transphobia). Resilience factors consist of community connectedness and within-group identification and can help mediate the negative effects of distal and proximal factors.
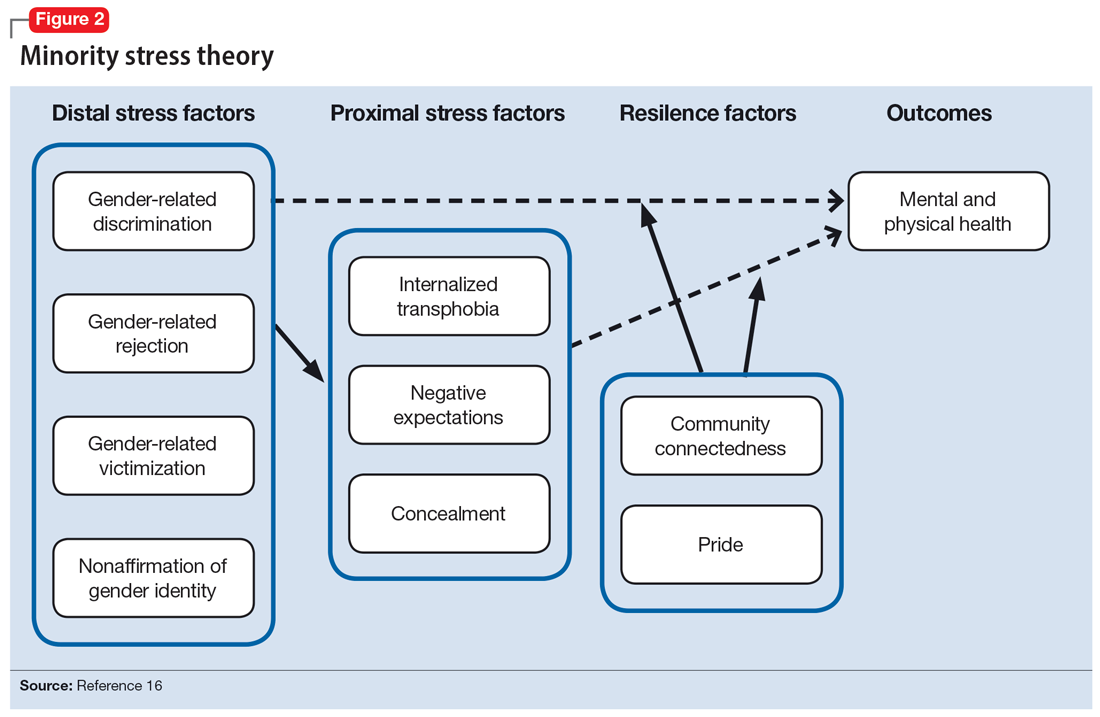
As clinicians, understanding our patients’ experiences and expectations can help us better engage with them and create an environment of safety and healing. Minority stress theory framework suggests that patients may start treatment with distrust or suspicion in light of previous negative experiences. They may also be likely to expect clinicians to be judgmental or to lack understanding of them. The 2015 US Transgender Survey found that 33% of individuals who are TGGD who sought medical treatment in the past year had at least 1 negative experience related to their gender identity (Table 118). Twenty-four percent reported having to educate their clinician about people who are TGGD, while 15% reported the health care professional asked invasive or unnecessary questions about their gender status that were unrelated to their visit. While psychiatry is often distinct from the larger medical field, it is important to understand the negative encounters individuals who are TGGD have likely experienced in medicine, and how those events may skew their feelings about psychiatric treatment. This is especially salient given the higher prevalence of various psychiatric disorders among individuals who are TGGD.18
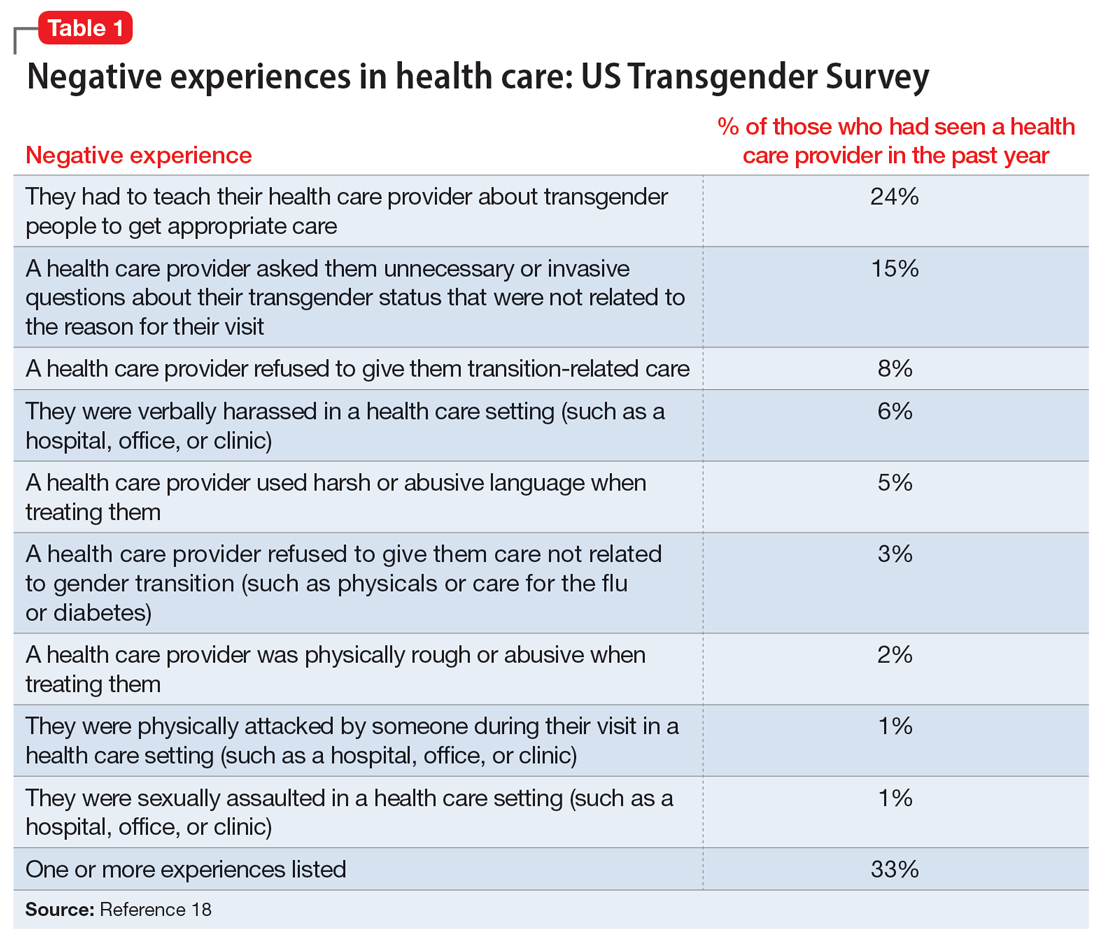
According to the US Transgender Survey, 39% of participants were currently experiencing serious psychological distress, which is nearly 8 times the rate in the US population (5%).18 When extrapolated, this data indicates that we in psychiatry are likely to work with individuals who identify as TGGD, regardless of our expertise. Additionally, research indicates that having access to gender-affirming care—such as hormone replacement therapy, gender-affirming surgery, voice therapy, and other treatments—greatly improves mental health issues such as anxiety, depression, and suicidality among individuals who are TGGD.19,20 It is in this way we in psychiatry must do more than just care for our patients by becoming advocates for them to receive the care they need and deserve. While at times we may want to stay out of politics and other public discourse, it is becoming increasingly necessary as health care is entrenched in politics.
Clinical applicability
Because individuals who are TGGD experience higher rates of depression, anxiety, substance use, and other psychiatric disorders,14 it is increasingly likely that many clinicians will be presented with opportunities to treat such individuals. Despite high rates of psychiatric disorders, individuals who are TGGD often avoid treatment due to concerns about being pathologized, stereotyped, and/or encountering professionals who lack the knowledge to treat them as they are.21 Several studies recommend clinicians better equip themselves to appropriately provide services to individuals who are TGGD.21 Some advise seeking education to understand the unique needs of these patients and to help stay current with appropriate terminology and language (Table 222). This also implies not relying on patients to educate clinicians in understanding their specific needs and experiences.
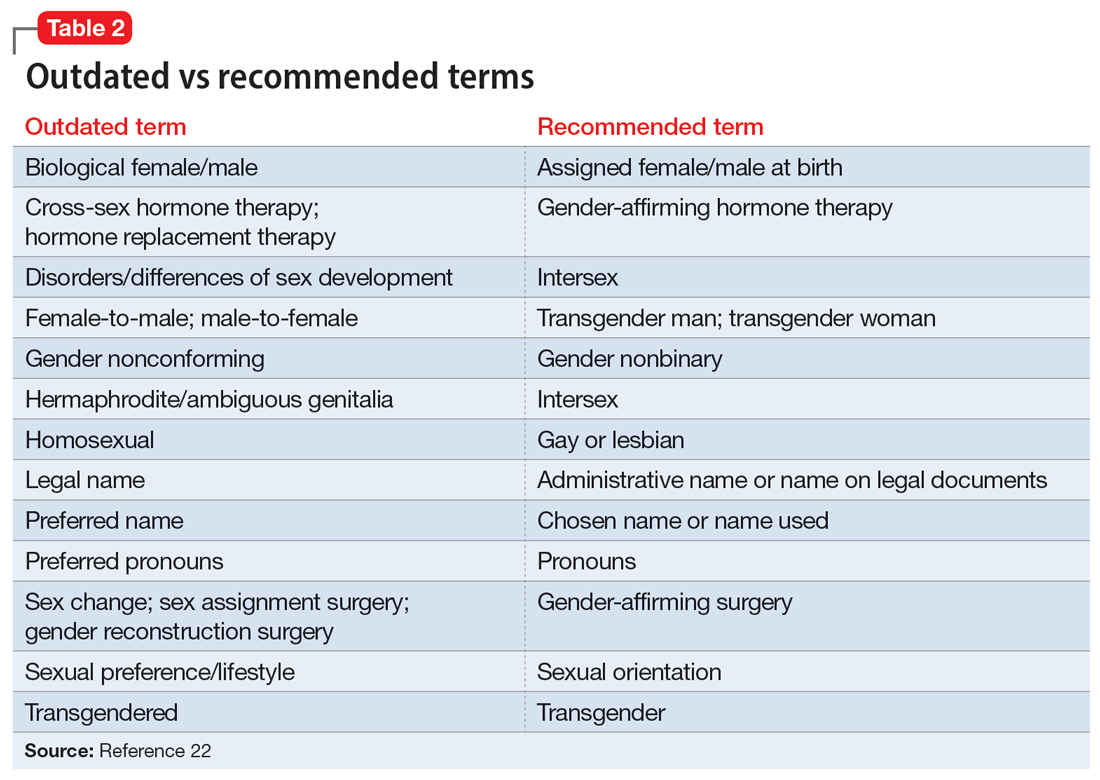
Making assumptions about a patient’s identity is one of the most commonly reported issues by individuals who are TGGD. Therefore, it is critical to avoid making assumptions about patients based on binary stereotypes.23,24 We can circumvent these mistakes by asking every patient for their name and pronouns, and introducing ourselves with our pronouns. This illustrates an openness and understanding of the importance of identity and language, and makes it common practice from the outset. Integrating the use of gender-neutral language into paperwork, intake forms, charting, and conversation will also help avoid the pitfalls of misgendering and making false assumptions. This will also allow for support staff, medical assistants, and others to use correct language with patients. Having a patient’s used name and pronouns visible for everyone who works with the patient is necessary to effectively meet the patient’s needs. Additionally, understanding that the range of experiences and needs for individuals who are TGGD is heterogeneous can help reduce assumptions and ensure we are asking for needed information. It is also important to ask for only relevant information needed to provide treatment.
Continue to: Resources are widely available...
Resources are widely available to aid in the care of individuals who are TGGD. In 2022, the World Professional Association for Transgender Health released new guidelines—Standards of Care 8—for working with individuals who are TGGD.25 While these standards include a section dedicated to mental health, they also provide guidelines on education, assessments, specific demographic groups, hormone therapy, primary care, and sexual health. Additionally, while we may not want the role of gatekeeping for individuals to receive gender-affirming care, we work within a health care and insurance system that continues to require psychiatric assessment for such surgeries. In this role, we must do our part to educate ourselves in how to best provide these assessments and letters of support to help patients receive appropriate and life-saving care.
Finally, in order to provide a more comfortable and affirming space for individuals who are TGGD, develop ways to self-assess and monitor the policies, procedures, and language used within your practice, clinic, or institution. Monitoring the language used in charting to ensure consistency with the individual’s gender identity is important for our own understanding of the patient, and for patients to feel seen. This is especially true given patients’ access to medical records under the Cures Act. Moreover, it is essential to be cognizant of how you present clients to others in consultation or care coordination to ensure the patient is identified correctly and consistently by clinicians and staff.
Bottom Line
Understanding the social, cultural, and medical discrimination faced by patients who are transgender or gender diverse can make us better suited to engage and treat these individuals in an affirming and supportive way.
Related Resources
- World Professional Association of Transgender Health (WPATH) Standards of Care—8th edition. https://www.tandfonline.com/doi/pdf/10.1080/26895269.2022.2100644
- The Fenway Institute: National LGBTQIA+ Health Education Center. https://fenwayhealth.org/the-fenway-institute/education/the-national-lgbtia-health-education-center/
1. Morgenroth T, Ryan MK. The effects of gender trouble: an integrative theoretical framework of the perpetuation and disruption of the gender/sex binary. Perspect Psychol Sci. 2021;16(6):1113-1142. doi:10.1177/1745691620902442
2. The Roots of Loneliness Project. Accessed April 8, 2023. https://www.rootsofloneliness.com/gender-identity-loneliness
3. Davies SG. Challenging Gender Norms: Five Genders Among Bugis in Indonesia. Thomson Wadsworth; 2007.
4. Hyde JS. The gender similarities hypothesis. Am Psychol. 2005;60(6):581-592. doi:10.1037/0003-066X.60.6.581
5. Joel D. Beyond the binary: rethinking sex and the brain. Neurosci Biobehav Rev. 2021;122:165-175. doi:10.1016/j.neubiorev.2020.22.018
6. Joel D, Berman Z, Tavor I, et al. Sex beyond the genitalia: the human brain mosaic. Proc Natl Acad Sci U S A. 2015;112(50):15468-15473. doi:10.1073/pnas.1509654112
7. Palmer BF, Clegg DJ. A universally accepted definition of gender will positively impact societal understanding, acceptance, and appropriateness of health care. Mayo Clin Proc. 2020;95(10):2235-2243. doi:10.1016/j.mayocp.2020.01.031
8. Office of Research on Women’s Health. Sex & Gender. National Institutes of Health. Accessed April 6, 2023. https://orwh.od.nih.gov/sex-gender
9. Morgenroth T, Sendén MG, Lindqvist A, et al. Defending the sex/gender binary: the role of gender identification and need for closure. Soc Psychol Pers Sci. 2021;12(5):731-740.
10. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 2nd ed. American Psychiatric Association; 1968.
11. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. American Psychiatric Association; 1980.
12. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; 1994.
13. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Publishing; 2013.
14. Wanta JW, Niforatos JD, Durbak E, et al. Mental health diagnoses among transgender patients in the clinical setting: an all-payer electronic health record study. Transgend Health. 2019;4(1):313-315.
15. World Health Organization. International Statistical Classification of Diseases. 11th ed. World Health Organization; 2019.
16. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674-697. doi:10.1037/0033-2909.129.5.674
17. Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the Minority Stress Model. Profess Psychol: Res Pract. 2012;43(5):460-467. doi:10.1037/a0029597
18. James SE, Herman J, Keisling M, et al. The Report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality; 2016. Accessed April 6, 2023. https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf
19. Almazan AN, Keuroghlian AS. Association between gender-affirming surgeries and mental health outcomes. JAMA Surg. 2021;156(7):611-618. doi:10.1001/jamasurg.2021.0952
20. Tordoff DM, Wanta JW, Collin A, et al. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Netw Open. 2022;5(2):e220978. doi:10.1001/jamanetworkopen.2022.0978
21. Snow A, Cerel J, Loeffler DN, et al. Barriers to mental health care for transgender and gender-nonconforming adults: a systematic literature review. Health Soc Work. 2019;44(3):149-155. doi:10.1093/hsw/hlz016
22. National LGBTQIA+ Health Education Center. Accessed April 8, 2023. https://www.lgbtqiahealtheducation.org
23. Baldwin A, Dodge B, Schick VR, et al. Transgender and genderqueer individuals’ experiences with health care providers: what’s working, what’s not, and where do we go from here? J Health Care Poor Underserved. 2018;29(4):1300-1318. doi:10.1353/hpu.2018.0097
24. Kcomt L, Gorey KM, Barrett BJ, et al. Healthcare avoidance due to anticipated discrimination among transgender people: a call to create trans-affirmative environments. SSM-Popul Health. 2020;11:100608. doi:10.1016/j.ssmph.2020.100608
25. Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgender Health. 2022;23(Suppl 1):S1-S259.
1. Morgenroth T, Ryan MK. The effects of gender trouble: an integrative theoretical framework of the perpetuation and disruption of the gender/sex binary. Perspect Psychol Sci. 2021;16(6):1113-1142. doi:10.1177/1745691620902442
2. The Roots of Loneliness Project. Accessed April 8, 2023. https://www.rootsofloneliness.com/gender-identity-loneliness
3. Davies SG. Challenging Gender Norms: Five Genders Among Bugis in Indonesia. Thomson Wadsworth; 2007.
4. Hyde JS. The gender similarities hypothesis. Am Psychol. 2005;60(6):581-592. doi:10.1037/0003-066X.60.6.581
5. Joel D. Beyond the binary: rethinking sex and the brain. Neurosci Biobehav Rev. 2021;122:165-175. doi:10.1016/j.neubiorev.2020.22.018
6. Joel D, Berman Z, Tavor I, et al. Sex beyond the genitalia: the human brain mosaic. Proc Natl Acad Sci U S A. 2015;112(50):15468-15473. doi:10.1073/pnas.1509654112
7. Palmer BF, Clegg DJ. A universally accepted definition of gender will positively impact societal understanding, acceptance, and appropriateness of health care. Mayo Clin Proc. 2020;95(10):2235-2243. doi:10.1016/j.mayocp.2020.01.031
8. Office of Research on Women’s Health. Sex & Gender. National Institutes of Health. Accessed April 6, 2023. https://orwh.od.nih.gov/sex-gender
9. Morgenroth T, Sendén MG, Lindqvist A, et al. Defending the sex/gender binary: the role of gender identification and need for closure. Soc Psychol Pers Sci. 2021;12(5):731-740.
10. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 2nd ed. American Psychiatric Association; 1968.
11. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. American Psychiatric Association; 1980.
12. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; 1994.
13. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Publishing; 2013.
14. Wanta JW, Niforatos JD, Durbak E, et al. Mental health diagnoses among transgender patients in the clinical setting: an all-payer electronic health record study. Transgend Health. 2019;4(1):313-315.
15. World Health Organization. International Statistical Classification of Diseases. 11th ed. World Health Organization; 2019.
16. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674-697. doi:10.1037/0033-2909.129.5.674
17. Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the Minority Stress Model. Profess Psychol: Res Pract. 2012;43(5):460-467. doi:10.1037/a0029597
18. James SE, Herman J, Keisling M, et al. The Report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality; 2016. Accessed April 6, 2023. https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf
19. Almazan AN, Keuroghlian AS. Association between gender-affirming surgeries and mental health outcomes. JAMA Surg. 2021;156(7):611-618. doi:10.1001/jamasurg.2021.0952
20. Tordoff DM, Wanta JW, Collin A, et al. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Netw Open. 2022;5(2):e220978. doi:10.1001/jamanetworkopen.2022.0978
21. Snow A, Cerel J, Loeffler DN, et al. Barriers to mental health care for transgender and gender-nonconforming adults: a systematic literature review. Health Soc Work. 2019;44(3):149-155. doi:10.1093/hsw/hlz016
22. National LGBTQIA+ Health Education Center. Accessed April 8, 2023. https://www.lgbtqiahealtheducation.org
23. Baldwin A, Dodge B, Schick VR, et al. Transgender and genderqueer individuals’ experiences with health care providers: what’s working, what’s not, and where do we go from here? J Health Care Poor Underserved. 2018;29(4):1300-1318. doi:10.1353/hpu.2018.0097
24. Kcomt L, Gorey KM, Barrett BJ, et al. Healthcare avoidance due to anticipated discrimination among transgender people: a call to create trans-affirmative environments. SSM-Popul Health. 2020;11:100608. doi:10.1016/j.ssmph.2020.100608
25. Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgender Health. 2022;23(Suppl 1):S1-S259.
Guidelines for assessing cancer risk may need updating
The authors of the clinical trial suggest that these guidelines may need to be revised.
Individuals with hereditary breast and ovarian cancer (HBOC) have an 80% lifetime risk of breast cancer and are at greater risk of ovarian cancer, pancreatic cancer, prostate cancer, and melanoma. Those with Lynch syndrome (LS) have an 80% lifetime risk of colorectal cancer, a 60% lifetime risk of endometrial cancer, and heightened risk of upper gastrointestinal, urinary tract, skin, and other tumors, said study coauthor N. Jewel Samadder, MD in a statement.
The National Cancer Control Network has guidelines for determining family risk for colorectal cancer and breast, ovarian, and pancreatic cancer to identify individuals who should be screened for LS and HBOC, but these rely on personal and family health histories.
“These criteria were created at a time when genetic testing was cost prohibitive and thus aimed to identify those at the greatest chance of being a mutation carrier in the absence of population-wide whole-exome sequencing. However, [LS and HBOC] are poorly identified in current practice, and many patients are not aware of their cancer risk,” said Dr. Samadder, professor of medicine and coleader of the precision oncology program at the Mayo Clinic Comprehensive Cancer Center, Phoenix, in the statement.
Whole-exome sequencing covers only protein-coding regions of the genome, which is less than 2% of the total genome but includes more than 85% of known disease-related genetic variants, according to Emily Gay, who presented the trial results (Abstract 5768) on April 18 at the annual meeting of the American Association for Cancer Research.
“In recent years, the cost of whole-exome sequencing has been rapidly decreasing, allowing us to complete this test on saliva samples from thousands, if not tens of thousands of patients covering large populations and large health systems,” said Ms. Gay, a genetic counseling graduate student at the University of Arizona, during her presentation.
She described results from the TAPESTRY clinical trial, with 44,306 participants from Mayo Clinic centers in Arizona, Florida, and Minnesota, who were identified as definitely or likely to be harboring pathogenic mutations and consented to whole-exome sequencing from saliva samples. They used electronic health records to determine whether patients would satisfy the testing criteria from NCCN guidelines.
The researchers identified 1.24% of participants to be carriers of HBOC or LS. Of the HBOC carriers, 62.8% were female, and of the LS carriers, 62.6% were female. The percentages of HBOC and LS carriers who were White were 88.6 and 94.5, respectively. The median age of both groups was 57 years. Of HBOC carriers, 47.3% had personal histories of cancers; for LS carries, the percentage was 44.2.
Of HBOC carriers, 49.1% had been previously unaware of their genetic condition, while an even higher percentage of patients with LS – 59.3% – fell into that category. Thirty-two percent of those with HBOC and 56.2% of those with LS would not have qualified for screening using the relevant NCCN guidelines.
“Most strikingly,” 63.8% of individuals with mutations in the MSH6 gene and 83.7% of those mutations in the PMS2 gene would not have met NCCN criteria, Ms. Gay said.
Having a cancer type not known to be related to a genetic syndrome was a reason for 58.6% of individuals failing to meet NCCN guidelines, while 60.5% did not meet the guidelines because of an insufficient number of relatives known to have a history of cancer, and 63.3% did not because they had no personal history of cancer. Among individuals with a pathogenic mutation who met NCCN criteria, 34% were not aware of their condition.
“This suggests that the NCCN guidelines are underutilized in clinical practice, potentially due to the busy schedule of clinicians or because the complexity of using these criteria,” said Ms. Gay.
The numbers were even more striking among minorities: “There is additional data analysis and research needed in this area, but based on our preliminary findings, we saw that nearly 50% of the individuals who are [part of an underrepresented minority group] did not meet criteria, compared with 32% of the white cohort,” said Ms. Gay.
Asked what new NCCN guidelines should be, Ms. Gay replied: “I think maybe limiting the number of relatives that you have to have with a certain type of cancer, especially as we see families get smaller and smaller, especially in the United States – that family data isn’t necessarily available or as useful. And then also, I think, incorporating in the size of a family into the calculation, so more of maybe a point-based system like we see with other genetic conditions rather than a ‘yes you meet or no, you don’t.’ More of a range to say ‘you fall on the low-risk, medium-risk, or high-risk stage,’” said Ms. Gay.
During the Q&A period, session cochair Andrew Godwin, PhD, who is a professor of molecular oncology and pathology at University of Kansas Medical Center, Kansas City, said he wondered if whole-exome sequencing was capable of picking up cancer risk mutations that standard targeted tests don’t look for.
Dr. Samadder, who was in the audience, answered the question, saying that targeted tests are actually better at picking up some types of mutations like intronic mutations, single-nucleotide polymorphisms, and deletions.
“There are some limitations to whole-exome sequencing. Our estimate here of 1.2% [of participants carrying HBOC or LS mutations] is probably an underestimate. There are additional variants that exome sequencing probably doesn’t pick up easily or as well. That’s why we qualify that exome sequencing is a screening test, not a diagnostic,” he continued.
Ms. Gay and Dr. Samadder have no relevant financial disclosures. Dr. Godwin has financial relationships with Clara Biotech, VITRAC Therapeutics, and Sinochips Diagnostics.
The authors of the clinical trial suggest that these guidelines may need to be revised.
Individuals with hereditary breast and ovarian cancer (HBOC) have an 80% lifetime risk of breast cancer and are at greater risk of ovarian cancer, pancreatic cancer, prostate cancer, and melanoma. Those with Lynch syndrome (LS) have an 80% lifetime risk of colorectal cancer, a 60% lifetime risk of endometrial cancer, and heightened risk of upper gastrointestinal, urinary tract, skin, and other tumors, said study coauthor N. Jewel Samadder, MD in a statement.
The National Cancer Control Network has guidelines for determining family risk for colorectal cancer and breast, ovarian, and pancreatic cancer to identify individuals who should be screened for LS and HBOC, but these rely on personal and family health histories.
“These criteria were created at a time when genetic testing was cost prohibitive and thus aimed to identify those at the greatest chance of being a mutation carrier in the absence of population-wide whole-exome sequencing. However, [LS and HBOC] are poorly identified in current practice, and many patients are not aware of their cancer risk,” said Dr. Samadder, professor of medicine and coleader of the precision oncology program at the Mayo Clinic Comprehensive Cancer Center, Phoenix, in the statement.
Whole-exome sequencing covers only protein-coding regions of the genome, which is less than 2% of the total genome but includes more than 85% of known disease-related genetic variants, according to Emily Gay, who presented the trial results (Abstract 5768) on April 18 at the annual meeting of the American Association for Cancer Research.
“In recent years, the cost of whole-exome sequencing has been rapidly decreasing, allowing us to complete this test on saliva samples from thousands, if not tens of thousands of patients covering large populations and large health systems,” said Ms. Gay, a genetic counseling graduate student at the University of Arizona, during her presentation.
She described results from the TAPESTRY clinical trial, with 44,306 participants from Mayo Clinic centers in Arizona, Florida, and Minnesota, who were identified as definitely or likely to be harboring pathogenic mutations and consented to whole-exome sequencing from saliva samples. They used electronic health records to determine whether patients would satisfy the testing criteria from NCCN guidelines.
The researchers identified 1.24% of participants to be carriers of HBOC or LS. Of the HBOC carriers, 62.8% were female, and of the LS carriers, 62.6% were female. The percentages of HBOC and LS carriers who were White were 88.6 and 94.5, respectively. The median age of both groups was 57 years. Of HBOC carriers, 47.3% had personal histories of cancers; for LS carries, the percentage was 44.2.
Of HBOC carriers, 49.1% had been previously unaware of their genetic condition, while an even higher percentage of patients with LS – 59.3% – fell into that category. Thirty-two percent of those with HBOC and 56.2% of those with LS would not have qualified for screening using the relevant NCCN guidelines.
“Most strikingly,” 63.8% of individuals with mutations in the MSH6 gene and 83.7% of those mutations in the PMS2 gene would not have met NCCN criteria, Ms. Gay said.
Having a cancer type not known to be related to a genetic syndrome was a reason for 58.6% of individuals failing to meet NCCN guidelines, while 60.5% did not meet the guidelines because of an insufficient number of relatives known to have a history of cancer, and 63.3% did not because they had no personal history of cancer. Among individuals with a pathogenic mutation who met NCCN criteria, 34% were not aware of their condition.
“This suggests that the NCCN guidelines are underutilized in clinical practice, potentially due to the busy schedule of clinicians or because the complexity of using these criteria,” said Ms. Gay.
The numbers were even more striking among minorities: “There is additional data analysis and research needed in this area, but based on our preliminary findings, we saw that nearly 50% of the individuals who are [part of an underrepresented minority group] did not meet criteria, compared with 32% of the white cohort,” said Ms. Gay.
Asked what new NCCN guidelines should be, Ms. Gay replied: “I think maybe limiting the number of relatives that you have to have with a certain type of cancer, especially as we see families get smaller and smaller, especially in the United States – that family data isn’t necessarily available or as useful. And then also, I think, incorporating in the size of a family into the calculation, so more of maybe a point-based system like we see with other genetic conditions rather than a ‘yes you meet or no, you don’t.’ More of a range to say ‘you fall on the low-risk, medium-risk, or high-risk stage,’” said Ms. Gay.
During the Q&A period, session cochair Andrew Godwin, PhD, who is a professor of molecular oncology and pathology at University of Kansas Medical Center, Kansas City, said he wondered if whole-exome sequencing was capable of picking up cancer risk mutations that standard targeted tests don’t look for.
Dr. Samadder, who was in the audience, answered the question, saying that targeted tests are actually better at picking up some types of mutations like intronic mutations, single-nucleotide polymorphisms, and deletions.
“There are some limitations to whole-exome sequencing. Our estimate here of 1.2% [of participants carrying HBOC or LS mutations] is probably an underestimate. There are additional variants that exome sequencing probably doesn’t pick up easily or as well. That’s why we qualify that exome sequencing is a screening test, not a diagnostic,” he continued.
Ms. Gay and Dr. Samadder have no relevant financial disclosures. Dr. Godwin has financial relationships with Clara Biotech, VITRAC Therapeutics, and Sinochips Diagnostics.
The authors of the clinical trial suggest that these guidelines may need to be revised.
Individuals with hereditary breast and ovarian cancer (HBOC) have an 80% lifetime risk of breast cancer and are at greater risk of ovarian cancer, pancreatic cancer, prostate cancer, and melanoma. Those with Lynch syndrome (LS) have an 80% lifetime risk of colorectal cancer, a 60% lifetime risk of endometrial cancer, and heightened risk of upper gastrointestinal, urinary tract, skin, and other tumors, said study coauthor N. Jewel Samadder, MD in a statement.
The National Cancer Control Network has guidelines for determining family risk for colorectal cancer and breast, ovarian, and pancreatic cancer to identify individuals who should be screened for LS and HBOC, but these rely on personal and family health histories.
“These criteria were created at a time when genetic testing was cost prohibitive and thus aimed to identify those at the greatest chance of being a mutation carrier in the absence of population-wide whole-exome sequencing. However, [LS and HBOC] are poorly identified in current practice, and many patients are not aware of their cancer risk,” said Dr. Samadder, professor of medicine and coleader of the precision oncology program at the Mayo Clinic Comprehensive Cancer Center, Phoenix, in the statement.
Whole-exome sequencing covers only protein-coding regions of the genome, which is less than 2% of the total genome but includes more than 85% of known disease-related genetic variants, according to Emily Gay, who presented the trial results (Abstract 5768) on April 18 at the annual meeting of the American Association for Cancer Research.
“In recent years, the cost of whole-exome sequencing has been rapidly decreasing, allowing us to complete this test on saliva samples from thousands, if not tens of thousands of patients covering large populations and large health systems,” said Ms. Gay, a genetic counseling graduate student at the University of Arizona, during her presentation.
She described results from the TAPESTRY clinical trial, with 44,306 participants from Mayo Clinic centers in Arizona, Florida, and Minnesota, who were identified as definitely or likely to be harboring pathogenic mutations and consented to whole-exome sequencing from saliva samples. They used electronic health records to determine whether patients would satisfy the testing criteria from NCCN guidelines.
The researchers identified 1.24% of participants to be carriers of HBOC or LS. Of the HBOC carriers, 62.8% were female, and of the LS carriers, 62.6% were female. The percentages of HBOC and LS carriers who were White were 88.6 and 94.5, respectively. The median age of both groups was 57 years. Of HBOC carriers, 47.3% had personal histories of cancers; for LS carries, the percentage was 44.2.
Of HBOC carriers, 49.1% had been previously unaware of their genetic condition, while an even higher percentage of patients with LS – 59.3% – fell into that category. Thirty-two percent of those with HBOC and 56.2% of those with LS would not have qualified for screening using the relevant NCCN guidelines.
“Most strikingly,” 63.8% of individuals with mutations in the MSH6 gene and 83.7% of those mutations in the PMS2 gene would not have met NCCN criteria, Ms. Gay said.
Having a cancer type not known to be related to a genetic syndrome was a reason for 58.6% of individuals failing to meet NCCN guidelines, while 60.5% did not meet the guidelines because of an insufficient number of relatives known to have a history of cancer, and 63.3% did not because they had no personal history of cancer. Among individuals with a pathogenic mutation who met NCCN criteria, 34% were not aware of their condition.
“This suggests that the NCCN guidelines are underutilized in clinical practice, potentially due to the busy schedule of clinicians or because the complexity of using these criteria,” said Ms. Gay.
The numbers were even more striking among minorities: “There is additional data analysis and research needed in this area, but based on our preliminary findings, we saw that nearly 50% of the individuals who are [part of an underrepresented minority group] did not meet criteria, compared with 32% of the white cohort,” said Ms. Gay.
Asked what new NCCN guidelines should be, Ms. Gay replied: “I think maybe limiting the number of relatives that you have to have with a certain type of cancer, especially as we see families get smaller and smaller, especially in the United States – that family data isn’t necessarily available or as useful. And then also, I think, incorporating in the size of a family into the calculation, so more of maybe a point-based system like we see with other genetic conditions rather than a ‘yes you meet or no, you don’t.’ More of a range to say ‘you fall on the low-risk, medium-risk, or high-risk stage,’” said Ms. Gay.
During the Q&A period, session cochair Andrew Godwin, PhD, who is a professor of molecular oncology and pathology at University of Kansas Medical Center, Kansas City, said he wondered if whole-exome sequencing was capable of picking up cancer risk mutations that standard targeted tests don’t look for.
Dr. Samadder, who was in the audience, answered the question, saying that targeted tests are actually better at picking up some types of mutations like intronic mutations, single-nucleotide polymorphisms, and deletions.
“There are some limitations to whole-exome sequencing. Our estimate here of 1.2% [of participants carrying HBOC or LS mutations] is probably an underestimate. There are additional variants that exome sequencing probably doesn’t pick up easily or as well. That’s why we qualify that exome sequencing is a screening test, not a diagnostic,” he continued.
Ms. Gay and Dr. Samadder have no relevant financial disclosures. Dr. Godwin has financial relationships with Clara Biotech, VITRAC Therapeutics, and Sinochips Diagnostics.
FROM AACR 2023
Poor representation of patients with darker skin phototypes in laser and light device studies
, according to a systematic review of the literature, the authors reported.
“While there broadly appears to be skin of color representation [in such studies], a more granular understanding of the data shows a large discrepancy in representation between ‘lighter’ and ‘darker’ skin of color patients,” Priya Manjaly and associates wrote in the Journal of Cosmetic Dermatology.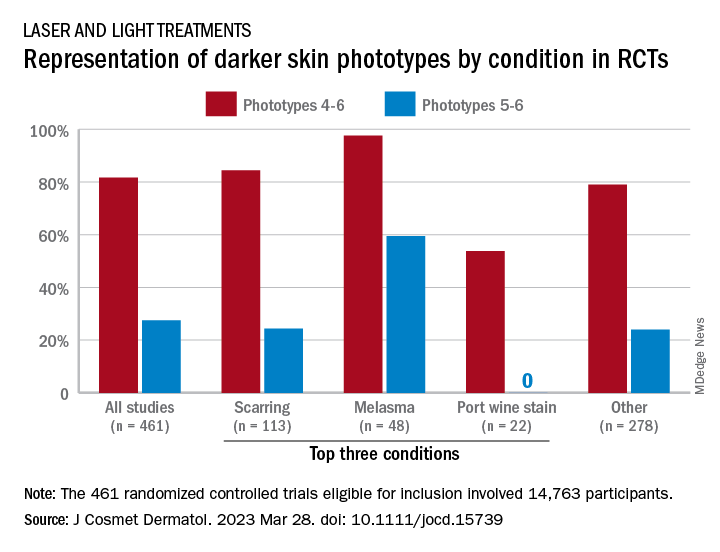
Among the 461 randomized controlled trials (RCTs) eligible for inclusion, most (81.7%) included participants with skin phototypes 4-6, which is considered skin of color. When only phototypes 5 and 6 were included, however, representation in studies involving laser and light devices was only 27.5%, said Ms. Manjaly, a research fellow in the department of dermatology at Boston University, and associates.
“This trend of excluding darker skin phototypes persisted when the results were stratified by condition, laser of study, study location, journal type, and funding source,” the investigators noted.
RCTs of laser/light devices for scarring, the most common dermatologic condition represented, included phototypes 5 and 6 in 24.4% of studies, compared with 84.4% for phototypes 4-6. The gap was smaller for melasma, but not for port wine stains. Among the devices examined, RCTs of diode lasers and intense pulsed light had the smallest gaps between inclusion of the two groups of phototypes, while pulsed-dye laser studies had the largest, they reported.
Stratification by journal showed the largest gap in studies published by Lasers in Medical Science and the smallest gap coming from Lasers in Surgery and Medicine. Funding was not specified for the majority of the eligible device RCTs, but those funded by industry had the smallest discrepancy between types 5-6 and types 4-6 and those supported by foundations/nonprofits the largest, Ms. Manjaly and associates said.
“With projections estimating that more than 50% of the U.S. population is set to identify as Hispanic or nonwhite by 2045 ... the lack of information has important consequences for clinical practice, as clinicians are unable to counsel patients on the efficacy and possible complications of various devices in patient with skin of color,” they wrote.
The investigators did not declare any conflicts of interest or funding sources.
, according to a systematic review of the literature, the authors reported.
“While there broadly appears to be skin of color representation [in such studies], a more granular understanding of the data shows a large discrepancy in representation between ‘lighter’ and ‘darker’ skin of color patients,” Priya Manjaly and associates wrote in the Journal of Cosmetic Dermatology.
Among the 461 randomized controlled trials (RCTs) eligible for inclusion, most (81.7%) included participants with skin phototypes 4-6, which is considered skin of color. When only phototypes 5 and 6 were included, however, representation in studies involving laser and light devices was only 27.5%, said Ms. Manjaly, a research fellow in the department of dermatology at Boston University, and associates.
“This trend of excluding darker skin phototypes persisted when the results were stratified by condition, laser of study, study location, journal type, and funding source,” the investigators noted.
RCTs of laser/light devices for scarring, the most common dermatologic condition represented, included phototypes 5 and 6 in 24.4% of studies, compared with 84.4% for phototypes 4-6. The gap was smaller for melasma, but not for port wine stains. Among the devices examined, RCTs of diode lasers and intense pulsed light had the smallest gaps between inclusion of the two groups of phototypes, while pulsed-dye laser studies had the largest, they reported.
Stratification by journal showed the largest gap in studies published by Lasers in Medical Science and the smallest gap coming from Lasers in Surgery and Medicine. Funding was not specified for the majority of the eligible device RCTs, but those funded by industry had the smallest discrepancy between types 5-6 and types 4-6 and those supported by foundations/nonprofits the largest, Ms. Manjaly and associates said.
“With projections estimating that more than 50% of the U.S. population is set to identify as Hispanic or nonwhite by 2045 ... the lack of information has important consequences for clinical practice, as clinicians are unable to counsel patients on the efficacy and possible complications of various devices in patient with skin of color,” they wrote.
The investigators did not declare any conflicts of interest or funding sources.
, according to a systematic review of the literature, the authors reported.
“While there broadly appears to be skin of color representation [in such studies], a more granular understanding of the data shows a large discrepancy in representation between ‘lighter’ and ‘darker’ skin of color patients,” Priya Manjaly and associates wrote in the Journal of Cosmetic Dermatology.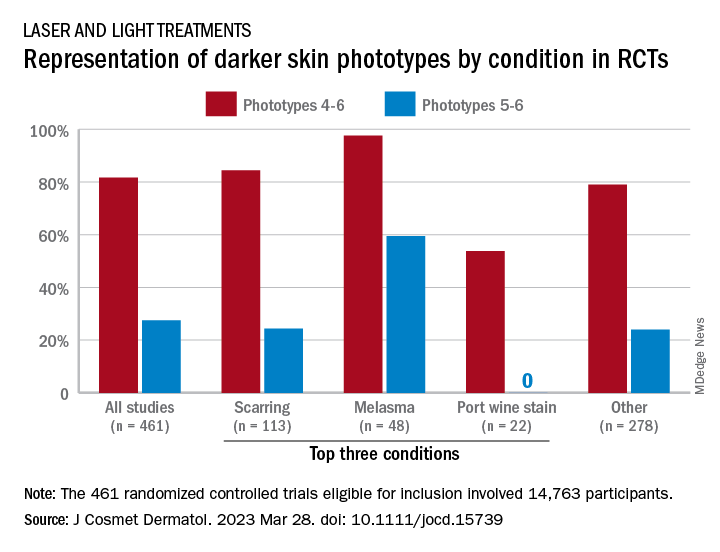
Among the 461 randomized controlled trials (RCTs) eligible for inclusion, most (81.7%) included participants with skin phototypes 4-6, which is considered skin of color. When only phototypes 5 and 6 were included, however, representation in studies involving laser and light devices was only 27.5%, said Ms. Manjaly, a research fellow in the department of dermatology at Boston University, and associates.
“This trend of excluding darker skin phototypes persisted when the results were stratified by condition, laser of study, study location, journal type, and funding source,” the investigators noted.
RCTs of laser/light devices for scarring, the most common dermatologic condition represented, included phototypes 5 and 6 in 24.4% of studies, compared with 84.4% for phototypes 4-6. The gap was smaller for melasma, but not for port wine stains. Among the devices examined, RCTs of diode lasers and intense pulsed light had the smallest gaps between inclusion of the two groups of phototypes, while pulsed-dye laser studies had the largest, they reported.
Stratification by journal showed the largest gap in studies published by Lasers in Medical Science and the smallest gap coming from Lasers in Surgery and Medicine. Funding was not specified for the majority of the eligible device RCTs, but those funded by industry had the smallest discrepancy between types 5-6 and types 4-6 and those supported by foundations/nonprofits the largest, Ms. Manjaly and associates said.
“With projections estimating that more than 50% of the U.S. population is set to identify as Hispanic or nonwhite by 2045 ... the lack of information has important consequences for clinical practice, as clinicians are unable to counsel patients on the efficacy and possible complications of various devices in patient with skin of color,” they wrote.
The investigators did not declare any conflicts of interest or funding sources.
FROM THE JOURNAL OF COSMETIC DERMATOLOGY



