User login
Palliative Care: Ave atque vale
Dame Cicely Saunders, the founder of the modern hospice movement, gave me this advice early in my palliative medicine career: “Never stop thanking those who help you along.” There are many to thank and much to be thankful for since the palliative care series in ACS Surgery News commenced in September 2012. The series proposal was enthusiastically endorsed by the then Editor, Layton F. Rikkers, and promptly launched owing to the personal interest of the first series editor, Elizabeth Wood. Their strong advocacy continues with the current co-editors, Karen Deveney and Tyler Hughes and the ever-watchful eye and assistance of managing editor, Therese Borden.
The purpose of the series was to keep the concept of surgical palliative care visible to the Fellowship through the reflections of surgeons and surgeons in training, while commenting on timely issues relevant to palliative care. We were fortunate to be coupled with Peter Angelos’s astute, widely read series on ethics. Our respective areas of interest widely overlap and have come into sharper focus for the surgical community over roughly the same period of time.
It was my hope that our contributions on palliative care would emulate the qualities and quality of Dr. Angelos’s articles – commentaries that would be of interest to the entire spectrum of surgical specialties and venues of practice. While the ethics column focused on doing the right thing, we would be focused on how to do the right thing in our response to suffering. Thanks are due to ACS Surgery News for its consistent representation of the new specialty of surgical palliative care on a par with other surgical specialties. It is culturally significant that this advocacy included strong support from laypeople.
I have been gratified and am thankful for the frequent uplifting discussions and debates triggered by palliative care columns in well-thumbed copies of ACS Surgery News in our OR lounge.
I didn’t have to look far to find inspiration and direction for the advocacy of palliative care in surgical practice. My father, David D. Dunn, MD, FACS, who represented everything noble, humane, and sensible in surgery, was a community-based general surgeon practicing in an era when the “general surgeon” performed thoracic, vascular, trauma, pediatric, and plastic surgery in addition to abdominal surgery. He had extensive experience with responding to suffering in a fundamentally affirmative way. He founded the first hospice in our community to meet the needs of a proud, cantankerous, elderly man septic with a gangrenous leg who declined amputation. He also witnessed mass suffering when he commanded a field hospital tasked with the resuscitation of survivors of a liberated Nazi concentration camp. The experience could have easily destroyed him from the resulting cynicism about humanity or PTSD. But instead he claimed he learned the first step in responding to mass calamity is the resuscitation of hope. He recalled a rescued physician who was given a clean lab coat and a stethoscope even before he was given his first real meal in years. He believed the hallmarks of steadfastness and non-abandonment are the core of the surgical persona. Late in his long life that ended just before this series launched, he observed, “It’s all palliative when you get right down to it. You [meaning the next generation] have to figure out the details and do your bit.”
The future is bright to “figure out the details and do your bit” for surgeons interested in palliative care. A number of young surgeons and surgeons in training, some who have done fellowships and become ABS certified in Hospice and Palliative Medicine, have had the opportunity to be heard and their specialty field be recognized by the greater surgical community because of ACS Surgery News.
I once asked a physically and emotionally exhausted family member of an “ICU to nowhere” patient why he thought patients get “stuck” in the ICU. He answered eloquently, “People just don’t think they should die.” The prevailing biophysical and increasingly “corporate” framework for care of the seriously ill is handicapped by its inability to effectively respond to the psychological and spiritual questions raised by this comment. Inability of surgeons to reconcile personal moral imperatives with big data and corporate medicine may be contributing to burnout, one of the most frequently acknowledged problems for surgeons today. Disease management alone, even if completely evidence-based, will not break this type of gridlock nor leave patients, families, and practitioners with a lasting sense of support. We will always need a broader framework that gives us a lens through which we can see and a voice with which we can answer the serious concerns that trouble our seriously ill patients and their families. I thank ACS Surgery News for conscientiously providing us a lens and a voice over the past 7 years.
Dr. Dunn was formerly the medical director of the palliative care consultation service at the University of Pittsburgh Medical Center Hamot in Erie, Pa., and Chair of the ACS Committee on Surgical Palliative Care.
Dame Cicely Saunders, the founder of the modern hospice movement, gave me this advice early in my palliative medicine career: “Never stop thanking those who help you along.” There are many to thank and much to be thankful for since the palliative care series in ACS Surgery News commenced in September 2012. The series proposal was enthusiastically endorsed by the then Editor, Layton F. Rikkers, and promptly launched owing to the personal interest of the first series editor, Elizabeth Wood. Their strong advocacy continues with the current co-editors, Karen Deveney and Tyler Hughes and the ever-watchful eye and assistance of managing editor, Therese Borden.
The purpose of the series was to keep the concept of surgical palliative care visible to the Fellowship through the reflections of surgeons and surgeons in training, while commenting on timely issues relevant to palliative care. We were fortunate to be coupled with Peter Angelos’s astute, widely read series on ethics. Our respective areas of interest widely overlap and have come into sharper focus for the surgical community over roughly the same period of time.
It was my hope that our contributions on palliative care would emulate the qualities and quality of Dr. Angelos’s articles – commentaries that would be of interest to the entire spectrum of surgical specialties and venues of practice. While the ethics column focused on doing the right thing, we would be focused on how to do the right thing in our response to suffering. Thanks are due to ACS Surgery News for its consistent representation of the new specialty of surgical palliative care on a par with other surgical specialties. It is culturally significant that this advocacy included strong support from laypeople.
I have been gratified and am thankful for the frequent uplifting discussions and debates triggered by palliative care columns in well-thumbed copies of ACS Surgery News in our OR lounge.
I didn’t have to look far to find inspiration and direction for the advocacy of palliative care in surgical practice. My father, David D. Dunn, MD, FACS, who represented everything noble, humane, and sensible in surgery, was a community-based general surgeon practicing in an era when the “general surgeon” performed thoracic, vascular, trauma, pediatric, and plastic surgery in addition to abdominal surgery. He had extensive experience with responding to suffering in a fundamentally affirmative way. He founded the first hospice in our community to meet the needs of a proud, cantankerous, elderly man septic with a gangrenous leg who declined amputation. He also witnessed mass suffering when he commanded a field hospital tasked with the resuscitation of survivors of a liberated Nazi concentration camp. The experience could have easily destroyed him from the resulting cynicism about humanity or PTSD. But instead he claimed he learned the first step in responding to mass calamity is the resuscitation of hope. He recalled a rescued physician who was given a clean lab coat and a stethoscope even before he was given his first real meal in years. He believed the hallmarks of steadfastness and non-abandonment are the core of the surgical persona. Late in his long life that ended just before this series launched, he observed, “It’s all palliative when you get right down to it. You [meaning the next generation] have to figure out the details and do your bit.”
The future is bright to “figure out the details and do your bit” for surgeons interested in palliative care. A number of young surgeons and surgeons in training, some who have done fellowships and become ABS certified in Hospice and Palliative Medicine, have had the opportunity to be heard and their specialty field be recognized by the greater surgical community because of ACS Surgery News.
I once asked a physically and emotionally exhausted family member of an “ICU to nowhere” patient why he thought patients get “stuck” in the ICU. He answered eloquently, “People just don’t think they should die.” The prevailing biophysical and increasingly “corporate” framework for care of the seriously ill is handicapped by its inability to effectively respond to the psychological and spiritual questions raised by this comment. Inability of surgeons to reconcile personal moral imperatives with big data and corporate medicine may be contributing to burnout, one of the most frequently acknowledged problems for surgeons today. Disease management alone, even if completely evidence-based, will not break this type of gridlock nor leave patients, families, and practitioners with a lasting sense of support. We will always need a broader framework that gives us a lens through which we can see and a voice with which we can answer the serious concerns that trouble our seriously ill patients and their families. I thank ACS Surgery News for conscientiously providing us a lens and a voice over the past 7 years.
Dr. Dunn was formerly the medical director of the palliative care consultation service at the University of Pittsburgh Medical Center Hamot in Erie, Pa., and Chair of the ACS Committee on Surgical Palliative Care.
Dame Cicely Saunders, the founder of the modern hospice movement, gave me this advice early in my palliative medicine career: “Never stop thanking those who help you along.” There are many to thank and much to be thankful for since the palliative care series in ACS Surgery News commenced in September 2012. The series proposal was enthusiastically endorsed by the then Editor, Layton F. Rikkers, and promptly launched owing to the personal interest of the first series editor, Elizabeth Wood. Their strong advocacy continues with the current co-editors, Karen Deveney and Tyler Hughes and the ever-watchful eye and assistance of managing editor, Therese Borden.
The purpose of the series was to keep the concept of surgical palliative care visible to the Fellowship through the reflections of surgeons and surgeons in training, while commenting on timely issues relevant to palliative care. We were fortunate to be coupled with Peter Angelos’s astute, widely read series on ethics. Our respective areas of interest widely overlap and have come into sharper focus for the surgical community over roughly the same period of time.
It was my hope that our contributions on palliative care would emulate the qualities and quality of Dr. Angelos’s articles – commentaries that would be of interest to the entire spectrum of surgical specialties and venues of practice. While the ethics column focused on doing the right thing, we would be focused on how to do the right thing in our response to suffering. Thanks are due to ACS Surgery News for its consistent representation of the new specialty of surgical palliative care on a par with other surgical specialties. It is culturally significant that this advocacy included strong support from laypeople.
I have been gratified and am thankful for the frequent uplifting discussions and debates triggered by palliative care columns in well-thumbed copies of ACS Surgery News in our OR lounge.
I didn’t have to look far to find inspiration and direction for the advocacy of palliative care in surgical practice. My father, David D. Dunn, MD, FACS, who represented everything noble, humane, and sensible in surgery, was a community-based general surgeon practicing in an era when the “general surgeon” performed thoracic, vascular, trauma, pediatric, and plastic surgery in addition to abdominal surgery. He had extensive experience with responding to suffering in a fundamentally affirmative way. He founded the first hospice in our community to meet the needs of a proud, cantankerous, elderly man septic with a gangrenous leg who declined amputation. He also witnessed mass suffering when he commanded a field hospital tasked with the resuscitation of survivors of a liberated Nazi concentration camp. The experience could have easily destroyed him from the resulting cynicism about humanity or PTSD. But instead he claimed he learned the first step in responding to mass calamity is the resuscitation of hope. He recalled a rescued physician who was given a clean lab coat and a stethoscope even before he was given his first real meal in years. He believed the hallmarks of steadfastness and non-abandonment are the core of the surgical persona. Late in his long life that ended just before this series launched, he observed, “It’s all palliative when you get right down to it. You [meaning the next generation] have to figure out the details and do your bit.”
The future is bright to “figure out the details and do your bit” for surgeons interested in palliative care. A number of young surgeons and surgeons in training, some who have done fellowships and become ABS certified in Hospice and Palliative Medicine, have had the opportunity to be heard and their specialty field be recognized by the greater surgical community because of ACS Surgery News.
I once asked a physically and emotionally exhausted family member of an “ICU to nowhere” patient why he thought patients get “stuck” in the ICU. He answered eloquently, “People just don’t think they should die.” The prevailing biophysical and increasingly “corporate” framework for care of the seriously ill is handicapped by its inability to effectively respond to the psychological and spiritual questions raised by this comment. Inability of surgeons to reconcile personal moral imperatives with big data and corporate medicine may be contributing to burnout, one of the most frequently acknowledged problems for surgeons today. Disease management alone, even if completely evidence-based, will not break this type of gridlock nor leave patients, families, and practitioners with a lasting sense of support. We will always need a broader framework that gives us a lens through which we can see and a voice with which we can answer the serious concerns that trouble our seriously ill patients and their families. I thank ACS Surgery News for conscientiously providing us a lens and a voice over the past 7 years.
Dr. Dunn was formerly the medical director of the palliative care consultation service at the University of Pittsburgh Medical Center Hamot in Erie, Pa., and Chair of the ACS Committee on Surgical Palliative Care.
Despite interest, few liver transplant candidates discuss advance care planning with clinicians
SAN FRANCISCO – .
“Recent studies have shown that there have been low rates of these types of discussions in all areas of medicine, not just in liver transplantation per se,” Connie W. Wang, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “We were curious to see what it looked like in our practice setting.”
In an effort to evaluate current advanced care planning documentation practices in the liver transplantation setting, she and her colleagues reviewed the medical charts of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco, from January 2017 to June 2017. Next, to assess readiness to complete advanced care planning among liver transplant candidates, the researchers administered the Advanced Care Planning Engagement Survey to 41 adults who underwent an initial liver transplant evaluation from March 2018 to May 2018. The survey was scored on a Likert scale of 1-4, in which a score of 4 equaled “ready” or “confident,” and a score of 5 equaled “very ready” or “very confident.”
The mean age of the 168 transplant candidates was 53 years, 35% were female, and 52% were non-Hispanic white. Only 15 patients (9%) reported completing advanced care planning prior to their liver transplant evaluation and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record. Durable power of attorney for health care was discussed with 17 patients (10%). On logistic regression analysis, only white race was associated with completion of advanced care planning (OR 4.16; P = .03), but age, Child-Pugh score, and MELD-Na score were not.
The mean age of the 41 transplant candidates who completed the Advanced Care Planning Engagement Survey was 58 years, 39% were female, and 58% were non-Hispanic white. Nearly all respondents (93%) indicated that they were ready to appoint a durable power of attorney, 85% were ready to discuss end-of-life care, and 93% were ready to ask physicians questions about medical decisions. Similarly, 93% of patients felt confident to appoint a durable power of attorney, 88% felt confident to discuss end-of-life care, and 93% felt confident to ask physicians questions about medical decisions.
“It seems like from the patients’ perspective, they are very much open to having these conversations, but there hasn’t been [the right] environment or setting to have them,” said Dr. Wang, a third-year internal medicine resident at UCSF. “Or, there may be a barrier from the provider’s perspective. Clearly, there is a huge need that can be filled.” She noted that future research should focus on development of tools to facilitate discussions and documentation between transplant clinicians, patients, and their caregivers.
One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]: Abstract 771.
SAN FRANCISCO – .
“Recent studies have shown that there have been low rates of these types of discussions in all areas of medicine, not just in liver transplantation per se,” Connie W. Wang, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “We were curious to see what it looked like in our practice setting.”
In an effort to evaluate current advanced care planning documentation practices in the liver transplantation setting, she and her colleagues reviewed the medical charts of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco, from January 2017 to June 2017. Next, to assess readiness to complete advanced care planning among liver transplant candidates, the researchers administered the Advanced Care Planning Engagement Survey to 41 adults who underwent an initial liver transplant evaluation from March 2018 to May 2018. The survey was scored on a Likert scale of 1-4, in which a score of 4 equaled “ready” or “confident,” and a score of 5 equaled “very ready” or “very confident.”
The mean age of the 168 transplant candidates was 53 years, 35% were female, and 52% were non-Hispanic white. Only 15 patients (9%) reported completing advanced care planning prior to their liver transplant evaluation and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record. Durable power of attorney for health care was discussed with 17 patients (10%). On logistic regression analysis, only white race was associated with completion of advanced care planning (OR 4.16; P = .03), but age, Child-Pugh score, and MELD-Na score were not.
The mean age of the 41 transplant candidates who completed the Advanced Care Planning Engagement Survey was 58 years, 39% were female, and 58% were non-Hispanic white. Nearly all respondents (93%) indicated that they were ready to appoint a durable power of attorney, 85% were ready to discuss end-of-life care, and 93% were ready to ask physicians questions about medical decisions. Similarly, 93% of patients felt confident to appoint a durable power of attorney, 88% felt confident to discuss end-of-life care, and 93% felt confident to ask physicians questions about medical decisions.
“It seems like from the patients’ perspective, they are very much open to having these conversations, but there hasn’t been [the right] environment or setting to have them,” said Dr. Wang, a third-year internal medicine resident at UCSF. “Or, there may be a barrier from the provider’s perspective. Clearly, there is a huge need that can be filled.” She noted that future research should focus on development of tools to facilitate discussions and documentation between transplant clinicians, patients, and their caregivers.
One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]: Abstract 771.
SAN FRANCISCO – .
“Recent studies have shown that there have been low rates of these types of discussions in all areas of medicine, not just in liver transplantation per se,” Connie W. Wang, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “We were curious to see what it looked like in our practice setting.”
In an effort to evaluate current advanced care planning documentation practices in the liver transplantation setting, she and her colleagues reviewed the medical charts of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco, from January 2017 to June 2017. Next, to assess readiness to complete advanced care planning among liver transplant candidates, the researchers administered the Advanced Care Planning Engagement Survey to 41 adults who underwent an initial liver transplant evaluation from March 2018 to May 2018. The survey was scored on a Likert scale of 1-4, in which a score of 4 equaled “ready” or “confident,” and a score of 5 equaled “very ready” or “very confident.”
The mean age of the 168 transplant candidates was 53 years, 35% were female, and 52% were non-Hispanic white. Only 15 patients (9%) reported completing advanced care planning prior to their liver transplant evaluation and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record. Durable power of attorney for health care was discussed with 17 patients (10%). On logistic regression analysis, only white race was associated with completion of advanced care planning (OR 4.16; P = .03), but age, Child-Pugh score, and MELD-Na score were not.
The mean age of the 41 transplant candidates who completed the Advanced Care Planning Engagement Survey was 58 years, 39% were female, and 58% were non-Hispanic white. Nearly all respondents (93%) indicated that they were ready to appoint a durable power of attorney, 85% were ready to discuss end-of-life care, and 93% were ready to ask physicians questions about medical decisions. Similarly, 93% of patients felt confident to appoint a durable power of attorney, 88% felt confident to discuss end-of-life care, and 93% felt confident to ask physicians questions about medical decisions.
“It seems like from the patients’ perspective, they are very much open to having these conversations, but there hasn’t been [the right] environment or setting to have them,” said Dr. Wang, a third-year internal medicine resident at UCSF. “Or, there may be a barrier from the provider’s perspective. Clearly, there is a huge need that can be filled.” She noted that future research should focus on development of tools to facilitate discussions and documentation between transplant clinicians, patients, and their caregivers.
One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]: Abstract 771.
REPORTING FROM THE LIVER MEETING 2018
Key clinical point: There is a paucity of documentation of advance care planning or identification of a durable power of attorney in the medical record of liver transplant candidates.
Major finding: Only 9% of liver transplant candidates reported completing advanced care planning prior to their liver transplant evaluations and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record.
Study details: A retrospective review of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco.
Disclosures: One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]:Abstract 771.
Dialysis decision in elderly needs to factor in comorbidities
SAN DIEGO – The wider picture of the patient’s health and prognosis, not just chronologic age, should enter into the clinical decision to initiate dialysis, according to Bjorg Thorsteinsdottir, MD, a palliative care physician at the Mayo Clinic in Rochester, Minn.
“People perceive they have no choice [but treatment], and we perceive we have to do things to them until everything is lost, then we expect them to do a 180 [degree turn],” she said in a presentation at the meeting sponsored by the American Society of Nephrology.
“A 90-year-old fit individual, with minimal comorbidity living independently, would absolutely be a good candidate for dialysis, while a 75-year-old patient with bad peripheral vascular disease and dementia, living in a nursing home, would be unlikely to live longer on dialysis than off dialysis,” she said. “We need to weigh the risks and benefits for each individual patient against their goals and values. We need to be honest about the lack of benefit for certain subgroups of patients and the heavy treatment burdens of dialysis. Age, comorbidity, and frailty all factor into these deliberations and prognosis.”
More than 107,000 people over age 75 in the United States received dialysis in 2015, according to statistics gathered by the National Kidney Foundation. Yet the survival advantage of dialysis is more limited in elderly patients with multiple comorbidities, Dr. Thorsteinsdottir said. “It becomes important to think about the harms of treatment.”
A 2016 study from the Netherlands found no survival advantage to dialysis, compared with conservative management among kidney failure patients aged 80 and older. The survival advantage was limited with dialysis in patients aged 70 and older who also had multiple comorbidities. (Clin J Am Soc Nephrol. 2016 Apr;11(4):633-40)
In an interview, Dr. Thorsteinsdottir acknowledged that “determining who is unlikely to benefit from dialysis is complicated.” However, she said, “we know that the following comorbidities are the worst: dementia and peripheral vascular disease.”
“No one that I know of currently has an age cutoff for dialysis,” Dr. Thorsteinsdottir said in the interview, “and I do not believe the U.S. is ready for any kind of explicit limit setting by the government on dialysis treatment.”
“We must respond to legitimate concerns raised by recent studies that suggest that strong moral imperatives – to treat anyone we can treat – have created a situation where we are not pausing and asking hard questions about whether the patient in front of us is likely to benefit from dialysis,” she said in the interview. “Patients sense this and do not feel that they are given any alternatives to dialysis treatment. This needs to change.”
Dr. Thorsteinsdottir reported no relevant financial disclosures.
SAN DIEGO – The wider picture of the patient’s health and prognosis, not just chronologic age, should enter into the clinical decision to initiate dialysis, according to Bjorg Thorsteinsdottir, MD, a palliative care physician at the Mayo Clinic in Rochester, Minn.
“People perceive they have no choice [but treatment], and we perceive we have to do things to them until everything is lost, then we expect them to do a 180 [degree turn],” she said in a presentation at the meeting sponsored by the American Society of Nephrology.
“A 90-year-old fit individual, with minimal comorbidity living independently, would absolutely be a good candidate for dialysis, while a 75-year-old patient with bad peripheral vascular disease and dementia, living in a nursing home, would be unlikely to live longer on dialysis than off dialysis,” she said. “We need to weigh the risks and benefits for each individual patient against their goals and values. We need to be honest about the lack of benefit for certain subgroups of patients and the heavy treatment burdens of dialysis. Age, comorbidity, and frailty all factor into these deliberations and prognosis.”
More than 107,000 people over age 75 in the United States received dialysis in 2015, according to statistics gathered by the National Kidney Foundation. Yet the survival advantage of dialysis is more limited in elderly patients with multiple comorbidities, Dr. Thorsteinsdottir said. “It becomes important to think about the harms of treatment.”
A 2016 study from the Netherlands found no survival advantage to dialysis, compared with conservative management among kidney failure patients aged 80 and older. The survival advantage was limited with dialysis in patients aged 70 and older who also had multiple comorbidities. (Clin J Am Soc Nephrol. 2016 Apr;11(4):633-40)
In an interview, Dr. Thorsteinsdottir acknowledged that “determining who is unlikely to benefit from dialysis is complicated.” However, she said, “we know that the following comorbidities are the worst: dementia and peripheral vascular disease.”
“No one that I know of currently has an age cutoff for dialysis,” Dr. Thorsteinsdottir said in the interview, “and I do not believe the U.S. is ready for any kind of explicit limit setting by the government on dialysis treatment.”
“We must respond to legitimate concerns raised by recent studies that suggest that strong moral imperatives – to treat anyone we can treat – have created a situation where we are not pausing and asking hard questions about whether the patient in front of us is likely to benefit from dialysis,” she said in the interview. “Patients sense this and do not feel that they are given any alternatives to dialysis treatment. This needs to change.”
Dr. Thorsteinsdottir reported no relevant financial disclosures.
SAN DIEGO – The wider picture of the patient’s health and prognosis, not just chronologic age, should enter into the clinical decision to initiate dialysis, according to Bjorg Thorsteinsdottir, MD, a palliative care physician at the Mayo Clinic in Rochester, Minn.
“People perceive they have no choice [but treatment], and we perceive we have to do things to them until everything is lost, then we expect them to do a 180 [degree turn],” she said in a presentation at the meeting sponsored by the American Society of Nephrology.
“A 90-year-old fit individual, with minimal comorbidity living independently, would absolutely be a good candidate for dialysis, while a 75-year-old patient with bad peripheral vascular disease and dementia, living in a nursing home, would be unlikely to live longer on dialysis than off dialysis,” she said. “We need to weigh the risks and benefits for each individual patient against their goals and values. We need to be honest about the lack of benefit for certain subgroups of patients and the heavy treatment burdens of dialysis. Age, comorbidity, and frailty all factor into these deliberations and prognosis.”
More than 107,000 people over age 75 in the United States received dialysis in 2015, according to statistics gathered by the National Kidney Foundation. Yet the survival advantage of dialysis is more limited in elderly patients with multiple comorbidities, Dr. Thorsteinsdottir said. “It becomes important to think about the harms of treatment.”
A 2016 study from the Netherlands found no survival advantage to dialysis, compared with conservative management among kidney failure patients aged 80 and older. The survival advantage was limited with dialysis in patients aged 70 and older who also had multiple comorbidities. (Clin J Am Soc Nephrol. 2016 Apr;11(4):633-40)
In an interview, Dr. Thorsteinsdottir acknowledged that “determining who is unlikely to benefit from dialysis is complicated.” However, she said, “we know that the following comorbidities are the worst: dementia and peripheral vascular disease.”
“No one that I know of currently has an age cutoff for dialysis,” Dr. Thorsteinsdottir said in the interview, “and I do not believe the U.S. is ready for any kind of explicit limit setting by the government on dialysis treatment.”
“We must respond to legitimate concerns raised by recent studies that suggest that strong moral imperatives – to treat anyone we can treat – have created a situation where we are not pausing and asking hard questions about whether the patient in front of us is likely to benefit from dialysis,” she said in the interview. “Patients sense this and do not feel that they are given any alternatives to dialysis treatment. This needs to change.”
Dr. Thorsteinsdottir reported no relevant financial disclosures.
REPORTING FROM KIDNEY WEEK 2018
Quick Byte: Palliative care
Rapid adoption of a key program
In 2015, 75% of U.S. hospitals with more than 50 beds had palliative care programs – a sharp increase from the 25% that had palliative care in 2000.
“The rapid adoption of this high-value program, which is voluntary and runs counter to the dominant culture in U.S. hospitals, was catalyzed by tens of millions of dollars in philanthropic support for innovation, dissemination, and professionalization in the palliative care field,” according to research published in Health Affairs.
Reference
Cassel JB et al. Palliative care leadership centers are key to the diffusion of palliative care innovation. Health Aff. 2018 Feb. doi: 10.1377/hlthaff.2017.1122.
Rapid adoption of a key program
Rapid adoption of a key program
In 2015, 75% of U.S. hospitals with more than 50 beds had palliative care programs – a sharp increase from the 25% that had palliative care in 2000.
“The rapid adoption of this high-value program, which is voluntary and runs counter to the dominant culture in U.S. hospitals, was catalyzed by tens of millions of dollars in philanthropic support for innovation, dissemination, and professionalization in the palliative care field,” according to research published in Health Affairs.
Reference
Cassel JB et al. Palliative care leadership centers are key to the diffusion of palliative care innovation. Health Aff. 2018 Feb. doi: 10.1377/hlthaff.2017.1122.
In 2015, 75% of U.S. hospitals with more than 50 beds had palliative care programs – a sharp increase from the 25% that had palliative care in 2000.
“The rapid adoption of this high-value program, which is voluntary and runs counter to the dominant culture in U.S. hospitals, was catalyzed by tens of millions of dollars in philanthropic support for innovation, dissemination, and professionalization in the palliative care field,” according to research published in Health Affairs.
Reference
Cassel JB et al. Palliative care leadership centers are key to the diffusion of palliative care innovation. Health Aff. 2018 Feb. doi: 10.1377/hlthaff.2017.1122.
A physician’s response to observational studies of opioid prescribing
Several months ago, we invited readers to submit short personalized commentaries on articles that changed the way they approach a specific clinical problem and the way they take care of patients. In this issue of the Journal, addiction specialist Charles Reznikoff, MD, discusses 3 observational studies that focused on how prescribing opioids for acute pain can lead to chronic opioid use and addiction, and how these studies have influenced his practice.
Although observational studies rank lower on the level-of-evidence scale than randomized controlled trials, they can intellectually stimulate and inform us in ways that lead us to modify how we deliver clinical care.
The initial prescribing of pain medications and the management of patients with chronic pain are currently under intense scrutiny, and are the topic of much discussion in the United States. The opioid epidemic has spilled over into all aspects of daily life, far beyond the medical community. But since we physicians are the only legal and regulated source of narcotics and other pain medications, we are under the microscope—and rightly so.
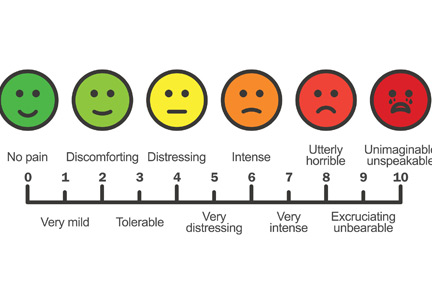
We, our patients, the pharmaceutical industry, legislators, and the law enforcement community struggle to navigate a complex maze, one with moving walls. Not long ago, physicians were told that we were not attentive enough to our patients’ suffering and needed to do better at relieving it. “Pain” became a vital sign and a recorded metric of quality care. Some excellent changes evolved from this focus, such as increased emphasis on postoperative regional and local pain control. But pain measurements continue to be recorded at every outpatient visit, an almost mindless requirement.
Recently, a patient with lupus nephritis whom I was seeing for blood pressure management reported a pain level of 8 on a scale of 10. I confess that I usually don’t even look at these metrics, but for whatever reason I saw her answer. I asked her about it. She had burned her finger while cooking and said, “I had no idea what number to pick. I picked 8. It’s no big deal.”
But the ongoing emphasis on this metric may lead some patients to expect total pain relief, a problematic expectation in those with chronic pain syndromes such as fibromyalgia. As Dr. Reznikoff points out, a large proportion of patients report they have chronic pain, and many (but clearly not all) suffer from recognized or masked chronic anxiety and depression disorders1 that may well influence how they use pain medications.
Thus, while physicians indeed are on the front lines of offering initial prescriptions for pain medications, we remain betwixt and between in the challenges of responding to the immediate needs of our patients while trying to predict the long-term effects of our prescription on the individual patient and of our prescribing patterns on society in general.
I again welcome your submissions describing how individual publications have affected your personal approach to managing patients and specific diseases. We will publish selected contributions in print and online.
- Tsang A, Von Korff M, Lee S, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain 2008; 9(10):883–891. doi:10.1016/j.jpain.2008.05.005
Several months ago, we invited readers to submit short personalized commentaries on articles that changed the way they approach a specific clinical problem and the way they take care of patients. In this issue of the Journal, addiction specialist Charles Reznikoff, MD, discusses 3 observational studies that focused on how prescribing opioids for acute pain can lead to chronic opioid use and addiction, and how these studies have influenced his practice.
Although observational studies rank lower on the level-of-evidence scale than randomized controlled trials, they can intellectually stimulate and inform us in ways that lead us to modify how we deliver clinical care.
The initial prescribing of pain medications and the management of patients with chronic pain are currently under intense scrutiny, and are the topic of much discussion in the United States. The opioid epidemic has spilled over into all aspects of daily life, far beyond the medical community. But since we physicians are the only legal and regulated source of narcotics and other pain medications, we are under the microscope—and rightly so.
We, our patients, the pharmaceutical industry, legislators, and the law enforcement community struggle to navigate a complex maze, one with moving walls. Not long ago, physicians were told that we were not attentive enough to our patients’ suffering and needed to do better at relieving it. “Pain” became a vital sign and a recorded metric of quality care. Some excellent changes evolved from this focus, such as increased emphasis on postoperative regional and local pain control. But pain measurements continue to be recorded at every outpatient visit, an almost mindless requirement.
Recently, a patient with lupus nephritis whom I was seeing for blood pressure management reported a pain level of 8 on a scale of 10. I confess that I usually don’t even look at these metrics, but for whatever reason I saw her answer. I asked her about it. She had burned her finger while cooking and said, “I had no idea what number to pick. I picked 8. It’s no big deal.”
But the ongoing emphasis on this metric may lead some patients to expect total pain relief, a problematic expectation in those with chronic pain syndromes such as fibromyalgia. As Dr. Reznikoff points out, a large proportion of patients report they have chronic pain, and many (but clearly not all) suffer from recognized or masked chronic anxiety and depression disorders1 that may well influence how they use pain medications.
Thus, while physicians indeed are on the front lines of offering initial prescriptions for pain medications, we remain betwixt and between in the challenges of responding to the immediate needs of our patients while trying to predict the long-term effects of our prescription on the individual patient and of our prescribing patterns on society in general.
I again welcome your submissions describing how individual publications have affected your personal approach to managing patients and specific diseases. We will publish selected contributions in print and online.
Several months ago, we invited readers to submit short personalized commentaries on articles that changed the way they approach a specific clinical problem and the way they take care of patients. In this issue of the Journal, addiction specialist Charles Reznikoff, MD, discusses 3 observational studies that focused on how prescribing opioids for acute pain can lead to chronic opioid use and addiction, and how these studies have influenced his practice.
Although observational studies rank lower on the level-of-evidence scale than randomized controlled trials, they can intellectually stimulate and inform us in ways that lead us to modify how we deliver clinical care.
The initial prescribing of pain medications and the management of patients with chronic pain are currently under intense scrutiny, and are the topic of much discussion in the United States. The opioid epidemic has spilled over into all aspects of daily life, far beyond the medical community. But since we physicians are the only legal and regulated source of narcotics and other pain medications, we are under the microscope—and rightly so.
We, our patients, the pharmaceutical industry, legislators, and the law enforcement community struggle to navigate a complex maze, one with moving walls. Not long ago, physicians were told that we were not attentive enough to our patients’ suffering and needed to do better at relieving it. “Pain” became a vital sign and a recorded metric of quality care. Some excellent changes evolved from this focus, such as increased emphasis on postoperative regional and local pain control. But pain measurements continue to be recorded at every outpatient visit, an almost mindless requirement.
Recently, a patient with lupus nephritis whom I was seeing for blood pressure management reported a pain level of 8 on a scale of 10. I confess that I usually don’t even look at these metrics, but for whatever reason I saw her answer. I asked her about it. She had burned her finger while cooking and said, “I had no idea what number to pick. I picked 8. It’s no big deal.”
But the ongoing emphasis on this metric may lead some patients to expect total pain relief, a problematic expectation in those with chronic pain syndromes such as fibromyalgia. As Dr. Reznikoff points out, a large proportion of patients report they have chronic pain, and many (but clearly not all) suffer from recognized or masked chronic anxiety and depression disorders1 that may well influence how they use pain medications.
Thus, while physicians indeed are on the front lines of offering initial prescriptions for pain medications, we remain betwixt and between in the challenges of responding to the immediate needs of our patients while trying to predict the long-term effects of our prescription on the individual patient and of our prescribing patterns on society in general.
I again welcome your submissions describing how individual publications have affected your personal approach to managing patients and specific diseases. We will publish selected contributions in print and online.
- Tsang A, Von Korff M, Lee S, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain 2008; 9(10):883–891. doi:10.1016/j.jpain.2008.05.005
- Tsang A, Von Korff M, Lee S, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain 2008; 9(10):883–891. doi:10.1016/j.jpain.2008.05.005
Palliative care update highlights role of nonspecialists
The new edition of providing care for critically ill patients, not just those clinicians actively specialized in palliative care.
The Clinical Practice Guidelines for Quality Palliative Care, 4th Edition, emphasizes the importance of palliative care provided by “clinicians in primary care and specialty care practices, such as oncologists,” the guideline authors stated.
The latest revision of the guideline aims to establish a foundation for “gold-standard” palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to the National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology and the Oncology Nurses Society.
One key reason for the update, according to the NCP, was to acknowledge that today’s health care system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on all clinicians who are not palliative specialists to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
This approach differs from the way palliative care is traditionally practiced, often by fellowship-trained physicians, trained nurses, and other specialists who provide that support.
The guidelines are organized into sections covering palliative care structure and processes, care for the patient nearing the end of life, and specific aspects of palliative care, including physical, psychological, and psychiatric; social; cultural, ethical, and legal; and spiritual, religious, and existential aspects.
“The expectation is that all clinicians caring for seriously ill patients will integrate palliative care competencies, such as safe and effective pain and symptom management and expert communication skills in their practice, and palliative care specialists will provide expertise for those with the most complex needs,” the guideline authors wrote.
Implications for treatment of oncology patients
These new guidelines represent a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, who is a medical oncologist, palliative care physician, and patient experience researcher at Duke University, Durham, N.C.
“Part of this report to is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” said Dr. LeBlanc.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who needs us the most, and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said in an interview.
That’s a major driver behind the emphasis in these latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, he added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists, and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
Palliative care in surgical care
These guidelines are particularly useful to surgeons in part because of their focus on what’s known as primary palliative care, said to Geoffrey P. Dunn, MD, former chair of the American College of Surgeons Committee on Surgical Palliative Care. Palliative care, the new guidelines suggest, can be implemented by nonspecialists.
Primary palliative care includes diverse skills such as breaking adverse news to patients, managing uncomplicated pain, and being able to recognize signs and symptoms of imminent demise. “These are the minimum deliverables for all people dealing with seriously ill patients,” Dr. Dunn said in an interview. “It’s palliative care that any practicing physician should be able to handle.”
Dr. Dunn concurred with Dr. LaBlanc about the workforce shortage in the palliative field. The traditional model has created a shortage of specialized clinicians to meet palliative care needs. Across the board, “staffing for palliative teams is very inconsistent,” said Dr. Dunn. “It’s a classic unfunded mandate.”
While these guidelines are a step forward in recognizing the importance of palliative care outside of the palliative care specialty, there is no reference to surgery anywhere in the text of the 141-page prepublication draft provided by the NCP, Dr. Dunn noted in the interview.
“There’s still a danger of parallel universes, where surgery is developing its own understanding of this in parallel with the more general national palliative care movement,” he said. Despite that, there is a growing connection between surgery and the broader palliative care community. That linkage is especially important given the number of seriously ill patients with high symptom burden that are seen in surgery.
“I think where surgeons are beginning to find [palliative principles] very helpful is dealing with these protracted serial discussions with families in difficult circumstances, such as how long is the life support going to be prolonged in someone with a devastating head injury, or multiple system organ failure in the elderly,” Dr. Dunn added.
The new edition of providing care for critically ill patients, not just those clinicians actively specialized in palliative care.
The Clinical Practice Guidelines for Quality Palliative Care, 4th Edition, emphasizes the importance of palliative care provided by “clinicians in primary care and specialty care practices, such as oncologists,” the guideline authors stated.
The latest revision of the guideline aims to establish a foundation for “gold-standard” palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to the National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology and the Oncology Nurses Society.
One key reason for the update, according to the NCP, was to acknowledge that today’s health care system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on all clinicians who are not palliative specialists to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
This approach differs from the way palliative care is traditionally practiced, often by fellowship-trained physicians, trained nurses, and other specialists who provide that support.
The guidelines are organized into sections covering palliative care structure and processes, care for the patient nearing the end of life, and specific aspects of palliative care, including physical, psychological, and psychiatric; social; cultural, ethical, and legal; and spiritual, religious, and existential aspects.
“The expectation is that all clinicians caring for seriously ill patients will integrate palliative care competencies, such as safe and effective pain and symptom management and expert communication skills in their practice, and palliative care specialists will provide expertise for those with the most complex needs,” the guideline authors wrote.
Implications for treatment of oncology patients
These new guidelines represent a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, who is a medical oncologist, palliative care physician, and patient experience researcher at Duke University, Durham, N.C.
“Part of this report to is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” said Dr. LeBlanc.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who needs us the most, and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said in an interview.
That’s a major driver behind the emphasis in these latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, he added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists, and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
Palliative care in surgical care
These guidelines are particularly useful to surgeons in part because of their focus on what’s known as primary palliative care, said to Geoffrey P. Dunn, MD, former chair of the American College of Surgeons Committee on Surgical Palliative Care. Palliative care, the new guidelines suggest, can be implemented by nonspecialists.
Primary palliative care includes diverse skills such as breaking adverse news to patients, managing uncomplicated pain, and being able to recognize signs and symptoms of imminent demise. “These are the minimum deliverables for all people dealing with seriously ill patients,” Dr. Dunn said in an interview. “It’s palliative care that any practicing physician should be able to handle.”
Dr. Dunn concurred with Dr. LaBlanc about the workforce shortage in the palliative field. The traditional model has created a shortage of specialized clinicians to meet palliative care needs. Across the board, “staffing for palliative teams is very inconsistent,” said Dr. Dunn. “It’s a classic unfunded mandate.”
While these guidelines are a step forward in recognizing the importance of palliative care outside of the palliative care specialty, there is no reference to surgery anywhere in the text of the 141-page prepublication draft provided by the NCP, Dr. Dunn noted in the interview.
“There’s still a danger of parallel universes, where surgery is developing its own understanding of this in parallel with the more general national palliative care movement,” he said. Despite that, there is a growing connection between surgery and the broader palliative care community. That linkage is especially important given the number of seriously ill patients with high symptom burden that are seen in surgery.
“I think where surgeons are beginning to find [palliative principles] very helpful is dealing with these protracted serial discussions with families in difficult circumstances, such as how long is the life support going to be prolonged in someone with a devastating head injury, or multiple system organ failure in the elderly,” Dr. Dunn added.
The new edition of providing care for critically ill patients, not just those clinicians actively specialized in palliative care.
The Clinical Practice Guidelines for Quality Palliative Care, 4th Edition, emphasizes the importance of palliative care provided by “clinicians in primary care and specialty care practices, such as oncologists,” the guideline authors stated.
The latest revision of the guideline aims to establish a foundation for “gold-standard” palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to the National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology and the Oncology Nurses Society.
One key reason for the update, according to the NCP, was to acknowledge that today’s health care system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on all clinicians who are not palliative specialists to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
This approach differs from the way palliative care is traditionally practiced, often by fellowship-trained physicians, trained nurses, and other specialists who provide that support.
The guidelines are organized into sections covering palliative care structure and processes, care for the patient nearing the end of life, and specific aspects of palliative care, including physical, psychological, and psychiatric; social; cultural, ethical, and legal; and spiritual, religious, and existential aspects.
“The expectation is that all clinicians caring for seriously ill patients will integrate palliative care competencies, such as safe and effective pain and symptom management and expert communication skills in their practice, and palliative care specialists will provide expertise for those with the most complex needs,” the guideline authors wrote.
Implications for treatment of oncology patients
These new guidelines represent a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, who is a medical oncologist, palliative care physician, and patient experience researcher at Duke University, Durham, N.C.
“Part of this report to is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” said Dr. LeBlanc.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who needs us the most, and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said in an interview.
That’s a major driver behind the emphasis in these latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, he added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists, and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
Palliative care in surgical care
These guidelines are particularly useful to surgeons in part because of their focus on what’s known as primary palliative care, said to Geoffrey P. Dunn, MD, former chair of the American College of Surgeons Committee on Surgical Palliative Care. Palliative care, the new guidelines suggest, can be implemented by nonspecialists.
Primary palliative care includes diverse skills such as breaking adverse news to patients, managing uncomplicated pain, and being able to recognize signs and symptoms of imminent demise. “These are the minimum deliverables for all people dealing with seriously ill patients,” Dr. Dunn said in an interview. “It’s palliative care that any practicing physician should be able to handle.”
Dr. Dunn concurred with Dr. LaBlanc about the workforce shortage in the palliative field. The traditional model has created a shortage of specialized clinicians to meet palliative care needs. Across the board, “staffing for palliative teams is very inconsistent,” said Dr. Dunn. “It’s a classic unfunded mandate.”
While these guidelines are a step forward in recognizing the importance of palliative care outside of the palliative care specialty, there is no reference to surgery anywhere in the text of the 141-page prepublication draft provided by the NCP, Dr. Dunn noted in the interview.
“There’s still a danger of parallel universes, where surgery is developing its own understanding of this in parallel with the more general national palliative care movement,” he said. Despite that, there is a growing connection between surgery and the broader palliative care community. That linkage is especially important given the number of seriously ill patients with high symptom burden that are seen in surgery.
“I think where surgeons are beginning to find [palliative principles] very helpful is dealing with these protracted serial discussions with families in difficult circumstances, such as how long is the life support going to be prolonged in someone with a devastating head injury, or multiple system organ failure in the elderly,” Dr. Dunn added.
Antipsychotic drugs failed to shorten ICU delirium
The antipsychotic medications in patients in intensive care, new research has found.
In a paper published in the New England Journal of Medicine, researchers reported the results of a randomized, double-blind, placebo-controlled trial in 566 patients with acute respiratory failure or shock and hypoactive or hyperactive delirium. Participants were randomized either to a maximum of 20 mg IV haloperidol daily, maximum 40 mg ziprasidone daily, or placebo.
At the end of the 14-day intervention period, the placebo group had a median of 8.5 days alive without delirium or coma, the haloperidol group had a median of 7.9 days, and the ziprasidone group had a median of 8.7 days. The difference between groups was not statistically significant.
There were also no significant differences between the three groups in the secondary end point of duration of delirium and coma, 30-day and 90-day survival, time to freedom from mechanical ventilation, ICU discharge, ICU readmission, or hospital discharge.
Timothy D. Girard, MD, from the department of critical care at the University of Pittsburgh, and his coauthors wrote that their findings echoed those of two previous placebo-controlled trials in smaller numbers of ICU patients.
“One possible reason that we found no evidence that the use of haloperidol or ziprasidone resulted in a fewer days with delirium or coma than placebo is that the mechanism of brain dysfunction that is considered to be targeted by antipsychotic medications – increased dopamine signaling – may not play a major role in the pathogenesis of delirium during critical illness,” they wrote.
“In the current trial, approximately 90% of the patients received one or more doses of sedatives or analgesics, and the doses of sedatives and offtrial antipsychotic medications and the durations of exposures to those agents were similar in all trial groups,” the authors added.
Most of the patients in the trial had hypotensive delirium, which made it difficult to assess the effects of antipsychotics on hypertensive delirium.
The authors also commented that the patients enrolled were a mixed group, so their findings did not rule out the possibility that certain subgroups of patients – such as nonintubated patients with hyperactive delirium, those with alcohol withdrawal, or with other delirium phenotypes – may still benefit from antipsychotics.
Patients treated with ziprasidone were more likely to experience prolongation of the corrected QT interval. Two patients in the haloperidol group developed torsades de pointes but neither had received haloperidol in the 4 days preceding the onset of the arrhythmia.
One patient in each group – including the placebo group – experienced extrapyramidal symptoms and had treatment withheld. One patient in the haloperidol group also had the trial drug withheld because of suspected neuroleptic malignant syndrome, but this was later ruled out, and one patient had haloperidol withheld because of dystonia.
The dose of haloperidol used in the study was considered high, the authors said, but they left open the possibility that even higher doses might help. However, they also noted that doses of 25 mg and above were known to have adverse effects on cognition, which is why they chose the 20-mg dosage.
The study was supported by the National Institutes of Health and the Department of Veterans Affairs Geriatric Research Education and Clinical Center. Most authors declared support from the NIH or VA during the course of the study. Four authors also reported fees and grants from private industry outside the context of the study.
SOURCE: Girard TD et al. N Engl J Med.2018 Oct 22. doi: 10.1056/NEJMoa1808217.
In a comment published with this study, Thomas P. Bleck, MD, of the department of neurologic sciences at Rush Medical College, Chicago, wrote, “A change in mental status in a patient in intensive care can be one of the most vexing problems. In the past 2 decades, the idea has arisen that antipsychotic drugs – and particularly dopamine antagonists, which ameliorate thought disorders in psychotic patients – could help patients with disordered thinking in other contexts, such as the intensive care unit. However, yet another trial has now called this idea into question.”
He noted that, in the study group, a bolus of placebo was just as effective as a bolus of active medication, which may be because of the majority of patients having hypoactive delirium, which the active drugs may not impact.
“I would still consider using dopamine agonists in patients at imminent risk of injurious behaviors but have less confidence in their benefits than I once had,” Dr. Bleck wrote.
Dr. Bleck did not report any conflicts of interest.
In a comment published with this study, Thomas P. Bleck, MD, of the department of neurologic sciences at Rush Medical College, Chicago, wrote, “A change in mental status in a patient in intensive care can be one of the most vexing problems. In the past 2 decades, the idea has arisen that antipsychotic drugs – and particularly dopamine antagonists, which ameliorate thought disorders in psychotic patients – could help patients with disordered thinking in other contexts, such as the intensive care unit. However, yet another trial has now called this idea into question.”
He noted that, in the study group, a bolus of placebo was just as effective as a bolus of active medication, which may be because of the majority of patients having hypoactive delirium, which the active drugs may not impact.
“I would still consider using dopamine agonists in patients at imminent risk of injurious behaviors but have less confidence in their benefits than I once had,” Dr. Bleck wrote.
Dr. Bleck did not report any conflicts of interest.
In a comment published with this study, Thomas P. Bleck, MD, of the department of neurologic sciences at Rush Medical College, Chicago, wrote, “A change in mental status in a patient in intensive care can be one of the most vexing problems. In the past 2 decades, the idea has arisen that antipsychotic drugs – and particularly dopamine antagonists, which ameliorate thought disorders in psychotic patients – could help patients with disordered thinking in other contexts, such as the intensive care unit. However, yet another trial has now called this idea into question.”
He noted that, in the study group, a bolus of placebo was just as effective as a bolus of active medication, which may be because of the majority of patients having hypoactive delirium, which the active drugs may not impact.
“I would still consider using dopamine agonists in patients at imminent risk of injurious behaviors but have less confidence in their benefits than I once had,” Dr. Bleck wrote.
Dr. Bleck did not report any conflicts of interest.
The antipsychotic medications in patients in intensive care, new research has found.
In a paper published in the New England Journal of Medicine, researchers reported the results of a randomized, double-blind, placebo-controlled trial in 566 patients with acute respiratory failure or shock and hypoactive or hyperactive delirium. Participants were randomized either to a maximum of 20 mg IV haloperidol daily, maximum 40 mg ziprasidone daily, or placebo.
At the end of the 14-day intervention period, the placebo group had a median of 8.5 days alive without delirium or coma, the haloperidol group had a median of 7.9 days, and the ziprasidone group had a median of 8.7 days. The difference between groups was not statistically significant.
There were also no significant differences between the three groups in the secondary end point of duration of delirium and coma, 30-day and 90-day survival, time to freedom from mechanical ventilation, ICU discharge, ICU readmission, or hospital discharge.
Timothy D. Girard, MD, from the department of critical care at the University of Pittsburgh, and his coauthors wrote that their findings echoed those of two previous placebo-controlled trials in smaller numbers of ICU patients.
“One possible reason that we found no evidence that the use of haloperidol or ziprasidone resulted in a fewer days with delirium or coma than placebo is that the mechanism of brain dysfunction that is considered to be targeted by antipsychotic medications – increased dopamine signaling – may not play a major role in the pathogenesis of delirium during critical illness,” they wrote.
“In the current trial, approximately 90% of the patients received one or more doses of sedatives or analgesics, and the doses of sedatives and offtrial antipsychotic medications and the durations of exposures to those agents were similar in all trial groups,” the authors added.
Most of the patients in the trial had hypotensive delirium, which made it difficult to assess the effects of antipsychotics on hypertensive delirium.
The authors also commented that the patients enrolled were a mixed group, so their findings did not rule out the possibility that certain subgroups of patients – such as nonintubated patients with hyperactive delirium, those with alcohol withdrawal, or with other delirium phenotypes – may still benefit from antipsychotics.
Patients treated with ziprasidone were more likely to experience prolongation of the corrected QT interval. Two patients in the haloperidol group developed torsades de pointes but neither had received haloperidol in the 4 days preceding the onset of the arrhythmia.
One patient in each group – including the placebo group – experienced extrapyramidal symptoms and had treatment withheld. One patient in the haloperidol group also had the trial drug withheld because of suspected neuroleptic malignant syndrome, but this was later ruled out, and one patient had haloperidol withheld because of dystonia.
The dose of haloperidol used in the study was considered high, the authors said, but they left open the possibility that even higher doses might help. However, they also noted that doses of 25 mg and above were known to have adverse effects on cognition, which is why they chose the 20-mg dosage.
The study was supported by the National Institutes of Health and the Department of Veterans Affairs Geriatric Research Education and Clinical Center. Most authors declared support from the NIH or VA during the course of the study. Four authors also reported fees and grants from private industry outside the context of the study.
SOURCE: Girard TD et al. N Engl J Med.2018 Oct 22. doi: 10.1056/NEJMoa1808217.
The antipsychotic medications in patients in intensive care, new research has found.
In a paper published in the New England Journal of Medicine, researchers reported the results of a randomized, double-blind, placebo-controlled trial in 566 patients with acute respiratory failure or shock and hypoactive or hyperactive delirium. Participants were randomized either to a maximum of 20 mg IV haloperidol daily, maximum 40 mg ziprasidone daily, or placebo.
At the end of the 14-day intervention period, the placebo group had a median of 8.5 days alive without delirium or coma, the haloperidol group had a median of 7.9 days, and the ziprasidone group had a median of 8.7 days. The difference between groups was not statistically significant.
There were also no significant differences between the three groups in the secondary end point of duration of delirium and coma, 30-day and 90-day survival, time to freedom from mechanical ventilation, ICU discharge, ICU readmission, or hospital discharge.
Timothy D. Girard, MD, from the department of critical care at the University of Pittsburgh, and his coauthors wrote that their findings echoed those of two previous placebo-controlled trials in smaller numbers of ICU patients.
“One possible reason that we found no evidence that the use of haloperidol or ziprasidone resulted in a fewer days with delirium or coma than placebo is that the mechanism of brain dysfunction that is considered to be targeted by antipsychotic medications – increased dopamine signaling – may not play a major role in the pathogenesis of delirium during critical illness,” they wrote.
“In the current trial, approximately 90% of the patients received one or more doses of sedatives or analgesics, and the doses of sedatives and offtrial antipsychotic medications and the durations of exposures to those agents were similar in all trial groups,” the authors added.
Most of the patients in the trial had hypotensive delirium, which made it difficult to assess the effects of antipsychotics on hypertensive delirium.
The authors also commented that the patients enrolled were a mixed group, so their findings did not rule out the possibility that certain subgroups of patients – such as nonintubated patients with hyperactive delirium, those with alcohol withdrawal, or with other delirium phenotypes – may still benefit from antipsychotics.
Patients treated with ziprasidone were more likely to experience prolongation of the corrected QT interval. Two patients in the haloperidol group developed torsades de pointes but neither had received haloperidol in the 4 days preceding the onset of the arrhythmia.
One patient in each group – including the placebo group – experienced extrapyramidal symptoms and had treatment withheld. One patient in the haloperidol group also had the trial drug withheld because of suspected neuroleptic malignant syndrome, but this was later ruled out, and one patient had haloperidol withheld because of dystonia.
The dose of haloperidol used in the study was considered high, the authors said, but they left open the possibility that even higher doses might help. However, they also noted that doses of 25 mg and above were known to have adverse effects on cognition, which is why they chose the 20-mg dosage.
The study was supported by the National Institutes of Health and the Department of Veterans Affairs Geriatric Research Education and Clinical Center. Most authors declared support from the NIH or VA during the course of the study. Four authors also reported fees and grants from private industry outside the context of the study.
SOURCE: Girard TD et al. N Engl J Med.2018 Oct 22. doi: 10.1056/NEJMoa1808217.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Antipsychotics do not reduce the duration or incidence of delirium in intensive care.
Major finding: Patients treated with antipsychotics showed similar median days without delirium or coma, compared with those treated with placebo.
Study details: A randomized, double-blind, placebo-controlled trial in 566 intensive care patients.
Disclosures: The study was supported by the National Institutes of Health and the Department of Veterans Affairs Geriatric Research Education and Clinical Center. Most authors were supported by the NIH or VA during the course of the study. Four authors also reported fees and grants from private industry outside the context of the study.
Source: Girard TD et al. N Engl J Med. 2018 Oct 22. doi: 10.1056/NEJMoa1808217.
Hospital medicine and palliative care: Wearing both hats
Dr. Barbara Egan leads SHM’s Palliative Care Work Group
Editor’s note: Each month, the Society of Hospitalist Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help improve the care of hospitalized patients.
This month, The Hospitalist spotlights Barbara Egan, MD, FACP, SFHM, chief of the hospital medicine service in the department of medicine at Memorial Sloan Kettering Cancer Center in New York. Barbara has been a member of SHM since 2005, is dual certified in hospital medicine and palliative care, and is the chair of SHM’s Palliative Care Work Group.
When did you first hear about SHM, and why did you decide to become a member?
I first learned about SHM when I was an internal medicine resident at Brigham and Women’s Hospital, Boston, in the early 2000s. BWH had an extremely strong hospitalist group; the staff I worked with served as powerful role models for me and inspired my interest in becoming a hospitalist. One of my attendings suggested that I join SHM, which I did right after I graduated from residency. I attended my first SHM Annual Conference in 2005. By then, I was working as a hospitalist at Memorial Sloan Kettering Cancer Center. SHM and the field of hospital medicine have exploded since my career first began, and I am happy to have grown alongside them. Similarly, our hospital medicine group here at MSKCC has dramatically grown, from 1 hospitalist (me) to more than 30!
How did you get involved with SHM’s Palliative Care Work Group, and what has the work group accomplished since you joined?
I was honored to be invited to join SHM’s Palliative Care Work Group in 2017 by Wendy Anderson, MD, a colleague and now a friend from University of California, San Francisco. Wendy is a visionary leader who practices and researches at the intersection of palliative care and hospital medicine. She and I met during 2015, when we were both invited to join a collaboration between SHM and the Hastings Center in Garrison, N.Y., which was aimed at improving hospitalists’ ability to provide outstanding care to hospitalized patients with life-limiting illnesses. That collaboration resulted in the Improving Communication about Serious Illness–Implementation Guide, a compilation of resources and best practices.
Wendy was chairing the SHM Palliative Care Work Group and invited me to join, which I did with great enthusiasm. This group consists of several passionate and brilliant hospitalists whose practices, in a variety of ways, involve both hospital medicine and palliative medicine. I was so honored when Wendy passed the baton to me last spring and invited me to chair the Work Group. I am lucky to have the opportunity to collaborate with this group of dynamic individuals, and we are well supported by an outstanding SHM staff member, Nick Marzano.
Are there any new projects that the work group is currently focusing on?
The primary focus of SHM’s Palliative Care Work Group is educational. That is, we aim to assess and help meet the educational needs of hospitalists, thereby helping to empower them to be outstanding providers of primary palliative care to seriously ill, hospitalized patients. To that end, we were very proud to orchestrate a palliative care mini-track for the first time at HM18. To our group’s delight, the attendance and reviews of that track were great. Thus, we were invited to further expand the palliative care offerings at HM19. We are busy planning for HM19: a full-day pre-course in palliative medicine; several podium presentations which will touch on ethical challenges, symptom management, prognostication, and other important topics; and a workshop in communication skills.
What led to your dual certification and how do your two specialties overlap?
I am board certified in internal medicine with Focused Practice in Hospital Medicine by virtue of my clinical training and my primary clinical practice as a hospitalist. As a hospitalist in a cancer center, I spend most of my time caring for patients with late- and end-stage malignancy. As such, early in my career, I had to develop a broad base of palliative medical skills, such as pain and symptom management and communication skills. I find this work extremely rewarding, albeit emotionally taxing. I have learned to redefine what clinical “success” looks like – my patients often have unfixable medical problems, but I can always strive to improve their lives in some way, even if that means helping to provide them with a painless, dignified death as opposed to curing them.
When the American Board of Medical Specialties established a board certification in Hospice and Palliative Medicine, there briefly existed a pathway to be “grandfathered” in, i.e., to qualify for board certification through an examination and clinical experience, as opposed to a fellowship. I jumped at the chance to formalize my palliative care skills and experience, and I attained board certification in 2012. This allowed me to further diversify my clinical practice here at MSKCC.
Hospital medicine is still my first love, and I spend most of my time practicing as a hospitalist on our solid tumor services. But now I also spend several weeks each year attending as a consultant on our inpatient supportive care service. In that role, I am able to collaborate with a fantastic multidisciplinary team consisting of MDs, NPs, a chaplain, a pharmacist, a social worker, and integrative medicine practitioners. I also love the opportunity to teach and mentor our palliative medicine fellows.
To me, the opportunity to marry hospital medicine and palliative medicine in my career was a natural fit. Hospitalists, particularly those caring exclusively for cancer patients like I do, need to provide excellent palliative care to our patients every day. The opportunity to further my training and to obtain board certification was a golden one, and I love being able to wear both hats here at MSKCC.
Ms. Steele is a marketing communications specialist at the Society of Hospital Medicine.
Dr. Barbara Egan leads SHM’s Palliative Care Work Group
Dr. Barbara Egan leads SHM’s Palliative Care Work Group
Editor’s note: Each month, the Society of Hospitalist Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help improve the care of hospitalized patients.
This month, The Hospitalist spotlights Barbara Egan, MD, FACP, SFHM, chief of the hospital medicine service in the department of medicine at Memorial Sloan Kettering Cancer Center in New York. Barbara has been a member of SHM since 2005, is dual certified in hospital medicine and palliative care, and is the chair of SHM’s Palliative Care Work Group.
When did you first hear about SHM, and why did you decide to become a member?
I first learned about SHM when I was an internal medicine resident at Brigham and Women’s Hospital, Boston, in the early 2000s. BWH had an extremely strong hospitalist group; the staff I worked with served as powerful role models for me and inspired my interest in becoming a hospitalist. One of my attendings suggested that I join SHM, which I did right after I graduated from residency. I attended my first SHM Annual Conference in 2005. By then, I was working as a hospitalist at Memorial Sloan Kettering Cancer Center. SHM and the field of hospital medicine have exploded since my career first began, and I am happy to have grown alongside them. Similarly, our hospital medicine group here at MSKCC has dramatically grown, from 1 hospitalist (me) to more than 30!
How did you get involved with SHM’s Palliative Care Work Group, and what has the work group accomplished since you joined?
I was honored to be invited to join SHM’s Palliative Care Work Group in 2017 by Wendy Anderson, MD, a colleague and now a friend from University of California, San Francisco. Wendy is a visionary leader who practices and researches at the intersection of palliative care and hospital medicine. She and I met during 2015, when we were both invited to join a collaboration between SHM and the Hastings Center in Garrison, N.Y., which was aimed at improving hospitalists’ ability to provide outstanding care to hospitalized patients with life-limiting illnesses. That collaboration resulted in the Improving Communication about Serious Illness–Implementation Guide, a compilation of resources and best practices.
Wendy was chairing the SHM Palliative Care Work Group and invited me to join, which I did with great enthusiasm. This group consists of several passionate and brilliant hospitalists whose practices, in a variety of ways, involve both hospital medicine and palliative medicine. I was so honored when Wendy passed the baton to me last spring and invited me to chair the Work Group. I am lucky to have the opportunity to collaborate with this group of dynamic individuals, and we are well supported by an outstanding SHM staff member, Nick Marzano.
Are there any new projects that the work group is currently focusing on?
The primary focus of SHM’s Palliative Care Work Group is educational. That is, we aim to assess and help meet the educational needs of hospitalists, thereby helping to empower them to be outstanding providers of primary palliative care to seriously ill, hospitalized patients. To that end, we were very proud to orchestrate a palliative care mini-track for the first time at HM18. To our group’s delight, the attendance and reviews of that track were great. Thus, we were invited to further expand the palliative care offerings at HM19. We are busy planning for HM19: a full-day pre-course in palliative medicine; several podium presentations which will touch on ethical challenges, symptom management, prognostication, and other important topics; and a workshop in communication skills.
What led to your dual certification and how do your two specialties overlap?
I am board certified in internal medicine with Focused Practice in Hospital Medicine by virtue of my clinical training and my primary clinical practice as a hospitalist. As a hospitalist in a cancer center, I spend most of my time caring for patients with late- and end-stage malignancy. As such, early in my career, I had to develop a broad base of palliative medical skills, such as pain and symptom management and communication skills. I find this work extremely rewarding, albeit emotionally taxing. I have learned to redefine what clinical “success” looks like – my patients often have unfixable medical problems, but I can always strive to improve their lives in some way, even if that means helping to provide them with a painless, dignified death as opposed to curing them.
When the American Board of Medical Specialties established a board certification in Hospice and Palliative Medicine, there briefly existed a pathway to be “grandfathered” in, i.e., to qualify for board certification through an examination and clinical experience, as opposed to a fellowship. I jumped at the chance to formalize my palliative care skills and experience, and I attained board certification in 2012. This allowed me to further diversify my clinical practice here at MSKCC.
Hospital medicine is still my first love, and I spend most of my time practicing as a hospitalist on our solid tumor services. But now I also spend several weeks each year attending as a consultant on our inpatient supportive care service. In that role, I am able to collaborate with a fantastic multidisciplinary team consisting of MDs, NPs, a chaplain, a pharmacist, a social worker, and integrative medicine practitioners. I also love the opportunity to teach and mentor our palliative medicine fellows.
To me, the opportunity to marry hospital medicine and palliative medicine in my career was a natural fit. Hospitalists, particularly those caring exclusively for cancer patients like I do, need to provide excellent palliative care to our patients every day. The opportunity to further my training and to obtain board certification was a golden one, and I love being able to wear both hats here at MSKCC.
Ms. Steele is a marketing communications specialist at the Society of Hospital Medicine.
Editor’s note: Each month, the Society of Hospitalist Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help improve the care of hospitalized patients.
This month, The Hospitalist spotlights Barbara Egan, MD, FACP, SFHM, chief of the hospital medicine service in the department of medicine at Memorial Sloan Kettering Cancer Center in New York. Barbara has been a member of SHM since 2005, is dual certified in hospital medicine and palliative care, and is the chair of SHM’s Palliative Care Work Group.
When did you first hear about SHM, and why did you decide to become a member?
I first learned about SHM when I was an internal medicine resident at Brigham and Women’s Hospital, Boston, in the early 2000s. BWH had an extremely strong hospitalist group; the staff I worked with served as powerful role models for me and inspired my interest in becoming a hospitalist. One of my attendings suggested that I join SHM, which I did right after I graduated from residency. I attended my first SHM Annual Conference in 2005. By then, I was working as a hospitalist at Memorial Sloan Kettering Cancer Center. SHM and the field of hospital medicine have exploded since my career first began, and I am happy to have grown alongside them. Similarly, our hospital medicine group here at MSKCC has dramatically grown, from 1 hospitalist (me) to more than 30!
How did you get involved with SHM’s Palliative Care Work Group, and what has the work group accomplished since you joined?
I was honored to be invited to join SHM’s Palliative Care Work Group in 2017 by Wendy Anderson, MD, a colleague and now a friend from University of California, San Francisco. Wendy is a visionary leader who practices and researches at the intersection of palliative care and hospital medicine. She and I met during 2015, when we were both invited to join a collaboration between SHM and the Hastings Center in Garrison, N.Y., which was aimed at improving hospitalists’ ability to provide outstanding care to hospitalized patients with life-limiting illnesses. That collaboration resulted in the Improving Communication about Serious Illness–Implementation Guide, a compilation of resources and best practices.
Wendy was chairing the SHM Palliative Care Work Group and invited me to join, which I did with great enthusiasm. This group consists of several passionate and brilliant hospitalists whose practices, in a variety of ways, involve both hospital medicine and palliative medicine. I was so honored when Wendy passed the baton to me last spring and invited me to chair the Work Group. I am lucky to have the opportunity to collaborate with this group of dynamic individuals, and we are well supported by an outstanding SHM staff member, Nick Marzano.
Are there any new projects that the work group is currently focusing on?
The primary focus of SHM’s Palliative Care Work Group is educational. That is, we aim to assess and help meet the educational needs of hospitalists, thereby helping to empower them to be outstanding providers of primary palliative care to seriously ill, hospitalized patients. To that end, we were very proud to orchestrate a palliative care mini-track for the first time at HM18. To our group’s delight, the attendance and reviews of that track were great. Thus, we were invited to further expand the palliative care offerings at HM19. We are busy planning for HM19: a full-day pre-course in palliative medicine; several podium presentations which will touch on ethical challenges, symptom management, prognostication, and other important topics; and a workshop in communication skills.
What led to your dual certification and how do your two specialties overlap?
I am board certified in internal medicine with Focused Practice in Hospital Medicine by virtue of my clinical training and my primary clinical practice as a hospitalist. As a hospitalist in a cancer center, I spend most of my time caring for patients with late- and end-stage malignancy. As such, early in my career, I had to develop a broad base of palliative medical skills, such as pain and symptom management and communication skills. I find this work extremely rewarding, albeit emotionally taxing. I have learned to redefine what clinical “success” looks like – my patients often have unfixable medical problems, but I can always strive to improve their lives in some way, even if that means helping to provide them with a painless, dignified death as opposed to curing them.
When the American Board of Medical Specialties established a board certification in Hospice and Palliative Medicine, there briefly existed a pathway to be “grandfathered” in, i.e., to qualify for board certification through an examination and clinical experience, as opposed to a fellowship. I jumped at the chance to formalize my palliative care skills and experience, and I attained board certification in 2012. This allowed me to further diversify my clinical practice here at MSKCC.
Hospital medicine is still my first love, and I spend most of my time practicing as a hospitalist on our solid tumor services. But now I also spend several weeks each year attending as a consultant on our inpatient supportive care service. In that role, I am able to collaborate with a fantastic multidisciplinary team consisting of MDs, NPs, a chaplain, a pharmacist, a social worker, and integrative medicine practitioners. I also love the opportunity to teach and mentor our palliative medicine fellows.
To me, the opportunity to marry hospital medicine and palliative medicine in my career was a natural fit. Hospitalists, particularly those caring exclusively for cancer patients like I do, need to provide excellent palliative care to our patients every day. The opportunity to further my training and to obtain board certification was a golden one, and I love being able to wear both hats here at MSKCC.
Ms. Steele is a marketing communications specialist at the Society of Hospital Medicine.
Paradigm shifts in palliative care
Better engagement with patients essential
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
Better engagement with patients essential
Better engagement with patients essential
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
Surgical palliative care – 20 years on
It was a banner year in 1998 for the moral and ethical evolution of the College. That year saw the release of its Statement of Principles of End-of-Life Care, a seminal document for the emerging framework of surgical palliative care and the first light of the work of my colleague, Peter Angelos, MD, FACS, which did much to make made ethics a less arcane element of surgical practice. These developments followed the 1997 Clinical Congress during which the College joined the then-active national debate about physician-assisted suicide.
The national debate eventually culminated with the U.S. Supreme Court’s two 1997 rulings that physician-assisted suicide is not a protected liberty interest under the Constitution. These rulings in Vacco v. Quill and Washington v. Glucksberg deferred to the states the legalization of physician-assisted suicide.
Kill the suffering, not the patient
It was ironic that the College’s attention to surgical palliative care started, literally, with a dead end. The 1997 symposium’s focus on physician-assisted suicide revealed how little there was in the surgeon’s toolbox to assist seriously ill patients and their families. At this well-attended event with a distinguished panel of surgeons and ethicists moderated by the late Thomas Krizek, MD, FACS, I heard fear of death, fear of suffering, and fear of our helplessness as practitioners in the face of our patients’ deaths. The debate was about control, not the effective response to the many species of suffering encountered in surgical practice.
Hospice care and the nascent concept of palliative care were acknowledged by both sides of the debate as beneficial but as distinctly apart from surgery. The need for improved palliative care was the one unifying idea that emerged from that day’s discussion. All sides seemed to agree that striving to mitigate suffering during the course of any serious illness would be preferable to allowing it to continue unabated until silencing it with deliberate death as a last resort. The ensuing challenge for surgeons would be the reconciliation of cure and palliation, each so much a part of surgical history, especially in the past 200 years. This would prove to be a tall order as surgeons had done such a tidy job separating these two priorities without even realizing it since the second World War. Nothing less than the soul of surgery (and medicine) would be at stake from the relentless technocratic “progress” that threatened to swallow health care and so many other aspects of our culture – a culture that perhaps has been too intoxicated by the individual “pursuit of life, liberty, and happiness” while overlooking the suffering of one’s neighbor.
Recent evidence of burnout raises the possibility that we surgeons have internalized this conflict. Because of our sacred fellowship in healing, are we now, as we were 20 years ago, in the midst of a new spiritual crisis? As the operative repertoire and our professional status become increasingly transient we will be compelled to ground our identities in something more fulfilling and enduring.
Hope in fellowship
Now, as in 1998, there is hope. Hope lies in our fellowship. The focus of palliative care as understood by surgeons has broadened considerably, encouraged by the gradual public acceptance of palliative approaches to care extending beyond hospice care and the generally favorable experiences surgeons have had with palliative care teams, some of which have been directed by surgeons. There are now dozens of surgeons currently certified in Hospice and Palliative Medicine by the American Board of Surgery who are much more skilled in palliative care than anyone practicing in 1998. The ABS’s decision (2006) to offer certification in Hospice and Palliative Medicine was, in itself, an indication of how far things had progressed since 1998.
Several challenges to contemporary surgery will benefit from the growing reservoir of palliative care expertise such as enhanced communication skill, opioid management, and burnout. The concept of shared decision making is only one example. The multidimensional understanding of suffering, a cardinal principle of palliative philosophy, could transform the current dilemma of “What do we do about opioids?” to the scientific and social research question, “What should be done with opioid receptors and countless other receptors that shape the pain experience?” And lastly, the current postgraduate educational focus on communication and burnout indicate a readiness for introspection and fellowship by surgeons, a necessary prerequisite in meeting any existential or spiritual challenge to our art.
We have come a long way in 20 years but there are still miles to go before we sleep.
Dr. Dunn was formerly the medical director of the palliative care consultation service at the University of Pittsburgh Medical Center Hamot in Erie, Pa., and Chair of the ACS Committee on Surgical Palliative Care.
It was a banner year in 1998 for the moral and ethical evolution of the College. That year saw the release of its Statement of Principles of End-of-Life Care, a seminal document for the emerging framework of surgical palliative care and the first light of the work of my colleague, Peter Angelos, MD, FACS, which did much to make made ethics a less arcane element of surgical practice. These developments followed the 1997 Clinical Congress during which the College joined the then-active national debate about physician-assisted suicide.
The national debate eventually culminated with the U.S. Supreme Court’s two 1997 rulings that physician-assisted suicide is not a protected liberty interest under the Constitution. These rulings in Vacco v. Quill and Washington v. Glucksberg deferred to the states the legalization of physician-assisted suicide.
Kill the suffering, not the patient
It was ironic that the College’s attention to surgical palliative care started, literally, with a dead end. The 1997 symposium’s focus on physician-assisted suicide revealed how little there was in the surgeon’s toolbox to assist seriously ill patients and their families. At this well-attended event with a distinguished panel of surgeons and ethicists moderated by the late Thomas Krizek, MD, FACS, I heard fear of death, fear of suffering, and fear of our helplessness as practitioners in the face of our patients’ deaths. The debate was about control, not the effective response to the many species of suffering encountered in surgical practice.
Hospice care and the nascent concept of palliative care were acknowledged by both sides of the debate as beneficial but as distinctly apart from surgery. The need for improved palliative care was the one unifying idea that emerged from that day’s discussion. All sides seemed to agree that striving to mitigate suffering during the course of any serious illness would be preferable to allowing it to continue unabated until silencing it with deliberate death as a last resort. The ensuing challenge for surgeons would be the reconciliation of cure and palliation, each so much a part of surgical history, especially in the past 200 years. This would prove to be a tall order as surgeons had done such a tidy job separating these two priorities without even realizing it since the second World War. Nothing less than the soul of surgery (and medicine) would be at stake from the relentless technocratic “progress” that threatened to swallow health care and so many other aspects of our culture – a culture that perhaps has been too intoxicated by the individual “pursuit of life, liberty, and happiness” while overlooking the suffering of one’s neighbor.
Recent evidence of burnout raises the possibility that we surgeons have internalized this conflict. Because of our sacred fellowship in healing, are we now, as we were 20 years ago, in the midst of a new spiritual crisis? As the operative repertoire and our professional status become increasingly transient we will be compelled to ground our identities in something more fulfilling and enduring.
Hope in fellowship
Now, as in 1998, there is hope. Hope lies in our fellowship. The focus of palliative care as understood by surgeons has broadened considerably, encouraged by the gradual public acceptance of palliative approaches to care extending beyond hospice care and the generally favorable experiences surgeons have had with palliative care teams, some of which have been directed by surgeons. There are now dozens of surgeons currently certified in Hospice and Palliative Medicine by the American Board of Surgery who are much more skilled in palliative care than anyone practicing in 1998. The ABS’s decision (2006) to offer certification in Hospice and Palliative Medicine was, in itself, an indication of how far things had progressed since 1998.
Several challenges to contemporary surgery will benefit from the growing reservoir of palliative care expertise such as enhanced communication skill, opioid management, and burnout. The concept of shared decision making is only one example. The multidimensional understanding of suffering, a cardinal principle of palliative philosophy, could transform the current dilemma of “What do we do about opioids?” to the scientific and social research question, “What should be done with opioid receptors and countless other receptors that shape the pain experience?” And lastly, the current postgraduate educational focus on communication and burnout indicate a readiness for introspection and fellowship by surgeons, a necessary prerequisite in meeting any existential or spiritual challenge to our art.
We have come a long way in 20 years but there are still miles to go before we sleep.
Dr. Dunn was formerly the medical director of the palliative care consultation service at the University of Pittsburgh Medical Center Hamot in Erie, Pa., and Chair of the ACS Committee on Surgical Palliative Care.
It was a banner year in 1998 for the moral and ethical evolution of the College. That year saw the release of its Statement of Principles of End-of-Life Care, a seminal document for the emerging framework of surgical palliative care and the first light of the work of my colleague, Peter Angelos, MD, FACS, which did much to make made ethics a less arcane element of surgical practice. These developments followed the 1997 Clinical Congress during which the College joined the then-active national debate about physician-assisted suicide.
The national debate eventually culminated with the U.S. Supreme Court’s two 1997 rulings that physician-assisted suicide is not a protected liberty interest under the Constitution. These rulings in Vacco v. Quill and Washington v. Glucksberg deferred to the states the legalization of physician-assisted suicide.
Kill the suffering, not the patient
It was ironic that the College’s attention to surgical palliative care started, literally, with a dead end. The 1997 symposium’s focus on physician-assisted suicide revealed how little there was in the surgeon’s toolbox to assist seriously ill patients and their families. At this well-attended event with a distinguished panel of surgeons and ethicists moderated by the late Thomas Krizek, MD, FACS, I heard fear of death, fear of suffering, and fear of our helplessness as practitioners in the face of our patients’ deaths. The debate was about control, not the effective response to the many species of suffering encountered in surgical practice.
Hospice care and the nascent concept of palliative care were acknowledged by both sides of the debate as beneficial but as distinctly apart from surgery. The need for improved palliative care was the one unifying idea that emerged from that day’s discussion. All sides seemed to agree that striving to mitigate suffering during the course of any serious illness would be preferable to allowing it to continue unabated until silencing it with deliberate death as a last resort. The ensuing challenge for surgeons would be the reconciliation of cure and palliation, each so much a part of surgical history, especially in the past 200 years. This would prove to be a tall order as surgeons had done such a tidy job separating these two priorities without even realizing it since the second World War. Nothing less than the soul of surgery (and medicine) would be at stake from the relentless technocratic “progress” that threatened to swallow health care and so many other aspects of our culture – a culture that perhaps has been too intoxicated by the individual “pursuit of life, liberty, and happiness” while overlooking the suffering of one’s neighbor.
Recent evidence of burnout raises the possibility that we surgeons have internalized this conflict. Because of our sacred fellowship in healing, are we now, as we were 20 years ago, in the midst of a new spiritual crisis? As the operative repertoire and our professional status become increasingly transient we will be compelled to ground our identities in something more fulfilling and enduring.
Hope in fellowship
Now, as in 1998, there is hope. Hope lies in our fellowship. The focus of palliative care as understood by surgeons has broadened considerably, encouraged by the gradual public acceptance of palliative approaches to care extending beyond hospice care and the generally favorable experiences surgeons have had with palliative care teams, some of which have been directed by surgeons. There are now dozens of surgeons currently certified in Hospice and Palliative Medicine by the American Board of Surgery who are much more skilled in palliative care than anyone practicing in 1998. The ABS’s decision (2006) to offer certification in Hospice and Palliative Medicine was, in itself, an indication of how far things had progressed since 1998.
Several challenges to contemporary surgery will benefit from the growing reservoir of palliative care expertise such as enhanced communication skill, opioid management, and burnout. The concept of shared decision making is only one example. The multidimensional understanding of suffering, a cardinal principle of palliative philosophy, could transform the current dilemma of “What do we do about opioids?” to the scientific and social research question, “What should be done with opioid receptors and countless other receptors that shape the pain experience?” And lastly, the current postgraduate educational focus on communication and burnout indicate a readiness for introspection and fellowship by surgeons, a necessary prerequisite in meeting any existential or spiritual challenge to our art.
We have come a long way in 20 years but there are still miles to go before we sleep.
Dr. Dunn was formerly the medical director of the palliative care consultation service at the University of Pittsburgh Medical Center Hamot in Erie, Pa., and Chair of the ACS Committee on Surgical Palliative Care.