User login
Children and COVID: Nearly 200,000 new cases reported in 1 week
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
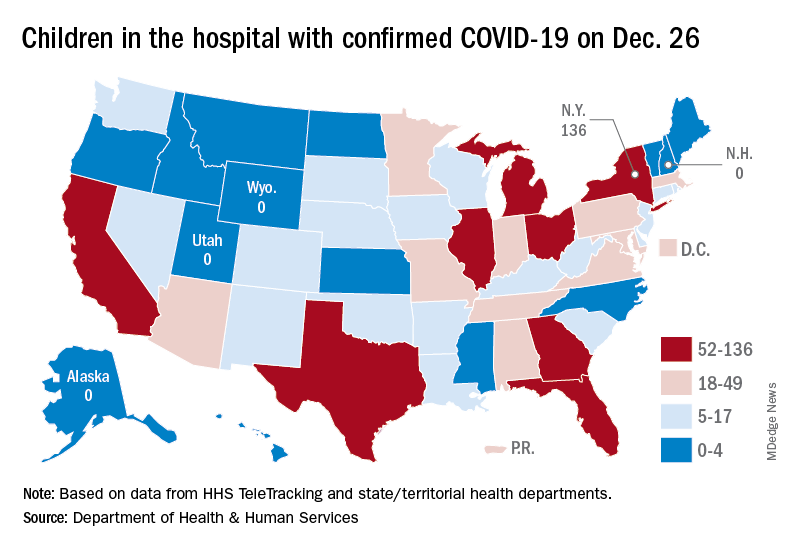
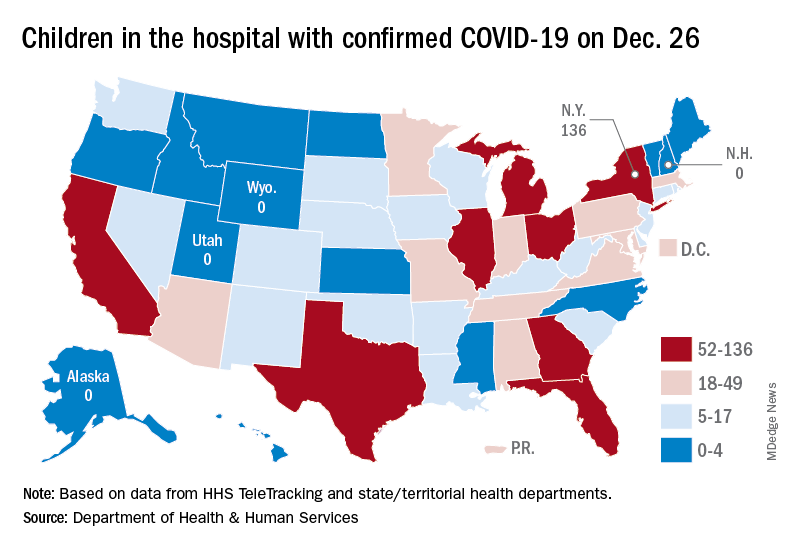
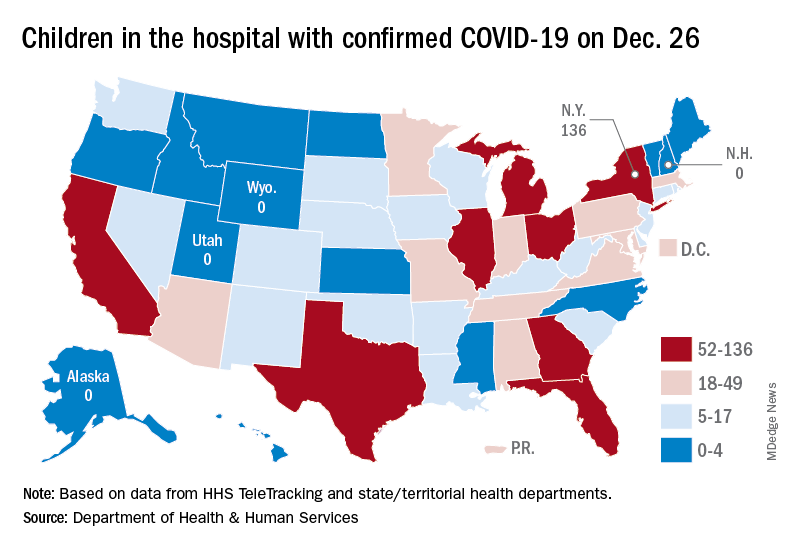
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
COVID-19 vaccinations in people with HIV reflect general rates despite higher mortality risk, study says
Around the world, people with HIV show variations in COVID-19 vaccination rates similar to those seen in the general population, raising concerns because of their increased risk for morbidity and mortality from COVID-19 infection.
“To our knowledge, this analysis presents the first and largest investigation of vaccination rates among people with HIV,” reported the authors in research published in the Journal of Infectious Diseases.
The findings reflect data on nearly 7,000 people with HIV participating in the REPRIEVE clinical trial. As of July, COVID-19 vaccination rates ranged from a high of 71% in higher income regions to just 18% in sub-Saharan Africa and bottomed out at 0% in Haiti.
“This disparity in COVID-19 vaccination rates among people with HIV across income regions may increase morbidity from COVID-19 in the most vulnerable HIV populations,” the authors noted.
In general, people with HIV have been shown in recent research to have as much as 29% higher odds of morality from COVID-19 than the general population, and a 20% higher odds of hospitalization, hence their need for vaccination is especially pressing.
To understand the vaccination rates, the authors looked at data from the ongoing REPRIEVE trial, designed to investigate primary cardiovascular prevention worldwide among people with HIV. The trial includes data on COVID-19 vaccination status, providing a unique opportunity to capture those rates.
The study specifically included 6,952 people with HIV aged 40-75 years and on stable antiretroviral therapy (ART), without known cardiovascular disease, and a low to moderate atherosclerotic cardiovascular disease (ASCVD) risk.
The diverse participants with HIV were from 12 countries, including 66% who were people of color, as well as 32% women. Countries represented include Brazil (n = 1,042), Botswana (n = 273), Canada (n = 123), Haiti (n = 136), India (n = 469), Peru (n = 142), South Africa (n = 527), Spain (n = 198), Thailand (n = 582), Uganda (n = 175), United States (n = 3,162), and Zimbabwe (n = 123).
With vaccination defined as having received at least one vaccine shot, the overall cumulative COVID-19 vaccination rate in the study was 55% through July 2021.
By region, the highest cumulative rates were in the high-income countries of the United States and Canada (71%), followed by Latin America and the Caribbean (59%) – all consistent with the general population in these areas
Lower cumulative vaccination rates were observed in South Asia (49%), Southeast/East Asia (41%), and sub-Saharan Africa (18%), also reflecting the regional vaccination rates.
The United States had the highest country-specific COVID-19 vaccination rate of 72%, followed by Peru (69%) and Brazil (63%). Countries with the lowest vaccination rates were South Africa (18%), Uganda (3%), and Haiti (0%).
Of note, South Africa and Botswana have the largest share of deaths from HIV/AIDS, and both had very low COVID-19 vaccination rates in general, compared with high-income countries.
Overall, factors linked to the likelihood of being vaccinated included residing in the high-income U.S./Canada Global Burden of Disease superregion, as well as being White, male, older, having a higher body mass index (BMI), a higher ASCVD risk score, and longer duration of ART.
Participants’ decisions regarding COVID-19 vaccination in the study were made individually and were not based on any study-related recommendations or requirements, the authors noted.
Vaccination rates were higher among men than women in most regions, with the exception of sub-Saharan Africa. Vaccination rates were higher among Whites than Blacks in the U.S./Canada high-income region, with a high proportion of participants from the United States.
“It was surprising to us – and unfortunate – that in the high-income superregion vaccination rates were higher among individuals who identified as White than those who identified as Black and among men,” senior author Steven K. Grinspoon, MD, said in an interview.
“Given data for higher morbidity from COVID-19 among people of color with HIV, this disparity is likely to have significant public health implications,” said Dr. Grinspoon, a professor of medicine at Harvard Medical School and chief of the metabolism unit at Massachusetts General Hospital, both in Boston.
Newer data from the REPRIEVE study through October has shown continued steady increases in the cumulative vaccination rates in all regions, Dr. Grinspoon noted, with the largest increases in the Southeast/East Asia, South Asia, and sub-Saharan Africa, whereas a leveling off of rates was observed in the high-income regions.
Overall, “it is encouraging that rates among people with HIV are similar to and, in many regions, higher than the general population,” Dr. Grinspoon said.
However, with the data showing a higher risk for COVID-19 death in people with HIV, “it is critical that people with HIV, representing a vulnerable and immunocompromised population, be vaccinated for COVID-19,” Dr. Grinspoon said.
Commenting on the study, Monica Gandhi, MD, MPH, director of the Gladstone Center for AIDS Research at the University of California, San Francisco, agreed that “it is encouraging that these rates are as high as the general population, showing that there is not excess hesitancy among those living with HIV.”
Unlike other immunocompromised groups, people with HIV were not necessarily prioritized for vaccination, since antiretroviral therapy can reconstitute the immune system, “so I am not surprised the [vaccination] rates aren’t higher,” Dr. Gandhi, who was not involved with the study, said in an interview.
Nevertheless, “it is important that those with risk factors for more severe disease, such as higher BMI and higher cardiovascular disease, are prioritized for COVID-19 vaccination, [as] these are important groups in which to increase rates,” she said.
“The take-home message is that we have to increase our rates of vaccination in this critically important population,” Dr. Gandhi emphasized. “Global vaccine equity is paramount given that the burden of HIV infections remains in sub-Saharan Africa.”
The study received support from the National Institutes of Health and funding from Kowa Pharmaceuticals and Gilead Sciences. The authors and Dr. Gandhi disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Around the world, people with HIV show variations in COVID-19 vaccination rates similar to those seen in the general population, raising concerns because of their increased risk for morbidity and mortality from COVID-19 infection.
“To our knowledge, this analysis presents the first and largest investigation of vaccination rates among people with HIV,” reported the authors in research published in the Journal of Infectious Diseases.
The findings reflect data on nearly 7,000 people with HIV participating in the REPRIEVE clinical trial. As of July, COVID-19 vaccination rates ranged from a high of 71% in higher income regions to just 18% in sub-Saharan Africa and bottomed out at 0% in Haiti.
“This disparity in COVID-19 vaccination rates among people with HIV across income regions may increase morbidity from COVID-19 in the most vulnerable HIV populations,” the authors noted.
In general, people with HIV have been shown in recent research to have as much as 29% higher odds of morality from COVID-19 than the general population, and a 20% higher odds of hospitalization, hence their need for vaccination is especially pressing.
To understand the vaccination rates, the authors looked at data from the ongoing REPRIEVE trial, designed to investigate primary cardiovascular prevention worldwide among people with HIV. The trial includes data on COVID-19 vaccination status, providing a unique opportunity to capture those rates.
The study specifically included 6,952 people with HIV aged 40-75 years and on stable antiretroviral therapy (ART), without known cardiovascular disease, and a low to moderate atherosclerotic cardiovascular disease (ASCVD) risk.
The diverse participants with HIV were from 12 countries, including 66% who were people of color, as well as 32% women. Countries represented include Brazil (n = 1,042), Botswana (n = 273), Canada (n = 123), Haiti (n = 136), India (n = 469), Peru (n = 142), South Africa (n = 527), Spain (n = 198), Thailand (n = 582), Uganda (n = 175), United States (n = 3,162), and Zimbabwe (n = 123).
With vaccination defined as having received at least one vaccine shot, the overall cumulative COVID-19 vaccination rate in the study was 55% through July 2021.
By region, the highest cumulative rates were in the high-income countries of the United States and Canada (71%), followed by Latin America and the Caribbean (59%) – all consistent with the general population in these areas
Lower cumulative vaccination rates were observed in South Asia (49%), Southeast/East Asia (41%), and sub-Saharan Africa (18%), also reflecting the regional vaccination rates.
The United States had the highest country-specific COVID-19 vaccination rate of 72%, followed by Peru (69%) and Brazil (63%). Countries with the lowest vaccination rates were South Africa (18%), Uganda (3%), and Haiti (0%).
Of note, South Africa and Botswana have the largest share of deaths from HIV/AIDS, and both had very low COVID-19 vaccination rates in general, compared with high-income countries.
Overall, factors linked to the likelihood of being vaccinated included residing in the high-income U.S./Canada Global Burden of Disease superregion, as well as being White, male, older, having a higher body mass index (BMI), a higher ASCVD risk score, and longer duration of ART.
Participants’ decisions regarding COVID-19 vaccination in the study were made individually and were not based on any study-related recommendations or requirements, the authors noted.
Vaccination rates were higher among men than women in most regions, with the exception of sub-Saharan Africa. Vaccination rates were higher among Whites than Blacks in the U.S./Canada high-income region, with a high proportion of participants from the United States.
“It was surprising to us – and unfortunate – that in the high-income superregion vaccination rates were higher among individuals who identified as White than those who identified as Black and among men,” senior author Steven K. Grinspoon, MD, said in an interview.
“Given data for higher morbidity from COVID-19 among people of color with HIV, this disparity is likely to have significant public health implications,” said Dr. Grinspoon, a professor of medicine at Harvard Medical School and chief of the metabolism unit at Massachusetts General Hospital, both in Boston.
Newer data from the REPRIEVE study through October has shown continued steady increases in the cumulative vaccination rates in all regions, Dr. Grinspoon noted, with the largest increases in the Southeast/East Asia, South Asia, and sub-Saharan Africa, whereas a leveling off of rates was observed in the high-income regions.
Overall, “it is encouraging that rates among people with HIV are similar to and, in many regions, higher than the general population,” Dr. Grinspoon said.
However, with the data showing a higher risk for COVID-19 death in people with HIV, “it is critical that people with HIV, representing a vulnerable and immunocompromised population, be vaccinated for COVID-19,” Dr. Grinspoon said.
Commenting on the study, Monica Gandhi, MD, MPH, director of the Gladstone Center for AIDS Research at the University of California, San Francisco, agreed that “it is encouraging that these rates are as high as the general population, showing that there is not excess hesitancy among those living with HIV.”
Unlike other immunocompromised groups, people with HIV were not necessarily prioritized for vaccination, since antiretroviral therapy can reconstitute the immune system, “so I am not surprised the [vaccination] rates aren’t higher,” Dr. Gandhi, who was not involved with the study, said in an interview.
Nevertheless, “it is important that those with risk factors for more severe disease, such as higher BMI and higher cardiovascular disease, are prioritized for COVID-19 vaccination, [as] these are important groups in which to increase rates,” she said.
“The take-home message is that we have to increase our rates of vaccination in this critically important population,” Dr. Gandhi emphasized. “Global vaccine equity is paramount given that the burden of HIV infections remains in sub-Saharan Africa.”
The study received support from the National Institutes of Health and funding from Kowa Pharmaceuticals and Gilead Sciences. The authors and Dr. Gandhi disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Around the world, people with HIV show variations in COVID-19 vaccination rates similar to those seen in the general population, raising concerns because of their increased risk for morbidity and mortality from COVID-19 infection.
“To our knowledge, this analysis presents the first and largest investigation of vaccination rates among people with HIV,” reported the authors in research published in the Journal of Infectious Diseases.
The findings reflect data on nearly 7,000 people with HIV participating in the REPRIEVE clinical trial. As of July, COVID-19 vaccination rates ranged from a high of 71% in higher income regions to just 18% in sub-Saharan Africa and bottomed out at 0% in Haiti.
“This disparity in COVID-19 vaccination rates among people with HIV across income regions may increase morbidity from COVID-19 in the most vulnerable HIV populations,” the authors noted.
In general, people with HIV have been shown in recent research to have as much as 29% higher odds of morality from COVID-19 than the general population, and a 20% higher odds of hospitalization, hence their need for vaccination is especially pressing.
To understand the vaccination rates, the authors looked at data from the ongoing REPRIEVE trial, designed to investigate primary cardiovascular prevention worldwide among people with HIV. The trial includes data on COVID-19 vaccination status, providing a unique opportunity to capture those rates.
The study specifically included 6,952 people with HIV aged 40-75 years and on stable antiretroviral therapy (ART), without known cardiovascular disease, and a low to moderate atherosclerotic cardiovascular disease (ASCVD) risk.
The diverse participants with HIV were from 12 countries, including 66% who were people of color, as well as 32% women. Countries represented include Brazil (n = 1,042), Botswana (n = 273), Canada (n = 123), Haiti (n = 136), India (n = 469), Peru (n = 142), South Africa (n = 527), Spain (n = 198), Thailand (n = 582), Uganda (n = 175), United States (n = 3,162), and Zimbabwe (n = 123).
With vaccination defined as having received at least one vaccine shot, the overall cumulative COVID-19 vaccination rate in the study was 55% through July 2021.
By region, the highest cumulative rates were in the high-income countries of the United States and Canada (71%), followed by Latin America and the Caribbean (59%) – all consistent with the general population in these areas
Lower cumulative vaccination rates were observed in South Asia (49%), Southeast/East Asia (41%), and sub-Saharan Africa (18%), also reflecting the regional vaccination rates.
The United States had the highest country-specific COVID-19 vaccination rate of 72%, followed by Peru (69%) and Brazil (63%). Countries with the lowest vaccination rates were South Africa (18%), Uganda (3%), and Haiti (0%).
Of note, South Africa and Botswana have the largest share of deaths from HIV/AIDS, and both had very low COVID-19 vaccination rates in general, compared with high-income countries.
Overall, factors linked to the likelihood of being vaccinated included residing in the high-income U.S./Canada Global Burden of Disease superregion, as well as being White, male, older, having a higher body mass index (BMI), a higher ASCVD risk score, and longer duration of ART.
Participants’ decisions regarding COVID-19 vaccination in the study were made individually and were not based on any study-related recommendations or requirements, the authors noted.
Vaccination rates were higher among men than women in most regions, with the exception of sub-Saharan Africa. Vaccination rates were higher among Whites than Blacks in the U.S./Canada high-income region, with a high proportion of participants from the United States.
“It was surprising to us – and unfortunate – that in the high-income superregion vaccination rates were higher among individuals who identified as White than those who identified as Black and among men,” senior author Steven K. Grinspoon, MD, said in an interview.
“Given data for higher morbidity from COVID-19 among people of color with HIV, this disparity is likely to have significant public health implications,” said Dr. Grinspoon, a professor of medicine at Harvard Medical School and chief of the metabolism unit at Massachusetts General Hospital, both in Boston.
Newer data from the REPRIEVE study through October has shown continued steady increases in the cumulative vaccination rates in all regions, Dr. Grinspoon noted, with the largest increases in the Southeast/East Asia, South Asia, and sub-Saharan Africa, whereas a leveling off of rates was observed in the high-income regions.
Overall, “it is encouraging that rates among people with HIV are similar to and, in many regions, higher than the general population,” Dr. Grinspoon said.
However, with the data showing a higher risk for COVID-19 death in people with HIV, “it is critical that people with HIV, representing a vulnerable and immunocompromised population, be vaccinated for COVID-19,” Dr. Grinspoon said.
Commenting on the study, Monica Gandhi, MD, MPH, director of the Gladstone Center for AIDS Research at the University of California, San Francisco, agreed that “it is encouraging that these rates are as high as the general population, showing that there is not excess hesitancy among those living with HIV.”
Unlike other immunocompromised groups, people with HIV were not necessarily prioritized for vaccination, since antiretroviral therapy can reconstitute the immune system, “so I am not surprised the [vaccination] rates aren’t higher,” Dr. Gandhi, who was not involved with the study, said in an interview.
Nevertheless, “it is important that those with risk factors for more severe disease, such as higher BMI and higher cardiovascular disease, are prioritized for COVID-19 vaccination, [as] these are important groups in which to increase rates,” she said.
“The take-home message is that we have to increase our rates of vaccination in this critically important population,” Dr. Gandhi emphasized. “Global vaccine equity is paramount given that the burden of HIV infections remains in sub-Saharan Africa.”
The study received support from the National Institutes of Health and funding from Kowa Pharmaceuticals and Gilead Sciences. The authors and Dr. Gandhi disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF INFECTIOUS DISEASES
Spesolimab speeds lesion clearance in generalized pustular psoriasis
GPP is a life-threatening skin condition involving the widespread eruption of sterile pustules, with a clinical course that “can be relapsing with recurrent flares or persistent with intermittent flares,” Hervé Bachelez, MD, of the Université de Paris and coauthors wrote. GPP patients are often hospitalized, and mortality ranges from 2% to 16% from causes that include sepsis and cardiorespiratory failure.
“The role of the interleukin-36 pathway in GPP is supported by the finding of loss-of-function mutations in the interleukin-36 receptor antagonist gene (IL36RN) and associated genes (CARD14, AP1S3, SERPINA3, and MPO) and by the overexpression of interleukin-36 cytokines in GPP skin lesions,” therefore, IL-36 is a potential treatment target to manage flares, they explained.
In the multicenter, double-blind trial, published in the New England Journal of Medicine, the researchers randomized 35 adults with GPP flares to a single 900-mg intravenous dose of spesolimab and 18 to placebo. Patients in both groups could receive an open-label dose of spesolimab after day 8; all patients were followed for 12 weeks.
The primary study endpoint was the Generalized Pustular Psoriasis Physician Global Assessment (GPPGA) pustulation subscore of 0 at 1 week after treatment. The GPPGA ranges from 0 (no visible pustules) to 4 (severe pustules). At baseline, 46% spesolimab patients and 39% placebo patients had a GPPGA pustulation subscore of 3, and 37% and 33%, respectively, had a pustulation subscore of 4.
After 1 week, 54% of the spesolimab patients had no visible pustules, compared with 6% of placebo patients; the difference was statistically significant (P < .001). The main secondary endpoint was a score of 0 or 1 (clear or almost clear skin) on the GPPGA total score after 1 week. Significantly more spesolimab patients had GPPGA total scores of 0 or 1, compared with placebo patients (43% vs. 11%, respectively; P = .02).
Overall, 6 of 35 spesolimab patients (17%) and 6% of those in the placebo groups developed infections during the first week, and 24 of 51 patients (47%) who had received spesolimab at any point during the study developed infections by week 12. Infections included urinary tract infections (three cases), influenza (three), otitis externa (two), folliculitis (two), upper respiratory tract infection (two), and pustule (two).
In the first week, 6% of spesolimab patients and none of the placebo patients reported serious adverse events; at week 12, 12% of patients who had received at least one spesolimab dose reported a serious adverse event. In addition, antidrug antibodies were identified in 23 (46%) of the 50 patients who received at least one dose of spesolimab.
“Symptoms that were observed in two patients who received spesolimab were reported as a drug reaction with eosinophilia and systemic symptoms (DRESS),” the authors noted. One patient had a RegiSCAR (European Registry of Severe Cutaneous Adverse Reactions) score and the other had a score of 3; a score below 2 indicates no DRESS, and a score of 2 or 3 indicates “possible DRESS,” they added.
“Because 15 of the 18 patients who were assigned to the placebo group received open-label spesolimab, the effect of spesolimab as compared with that of placebo could not be determined after week 1,” the researchers noted.
The study findings were limited by several factors including the short randomization period and small study population, the researchers noted. However, the effect sizes for both the primary and secondary endpoints were large, which strengthened the results.
The results support data from previous studies suggesting a role for IL-36 in the pathogenesis of GPP, and support the need for longer and larger studies of the safety and effectiveness of spesolimab for GPP patients, they concluded.
No FDA-approved therapy
“GPP is a very rare but devastating life-threatening disease that presents with the sudden onset of pustules throughout the skin,” Joel Gelfand, MD, professor of dermatology and director of the psoriasis and phototherapy center at the University of Pennsylvania, Philadelphia, said in an interview. “Without rapid treatment, GPP can result in death. Currently there are no [Food and Drug Administration]–approved treatments for this orphan disease.”
Dr. Gelfand said he was surprised by the degree of efficacy and the speed of the patient response to spesolimab, compared with placebo, which he described as “truly remarkable.” Based on the current study results, “spesolimab offers a tremendous step forward for our patients,” he added.
Looking ahead, Dr. Gelfand noted that “longer-term studies with a comparator, such as a biologic that targets IL-17, would be helpful to more fully understand the safety, efficacy, and role that spesolimab will have in real-world patients.”
On Dec. 15, Boehringer Ingelheim announced that the FDA had granted priority review for spesolimab for treating GPP flares.
The study was supported by Boehringer Ingelheim. Lead author Dr. Bachelez had no financial conflicts to disclose. Several authors are employees of Boehringer Ingelheim. Dr. Gelfand is a consultant for the study sponsor Boehringer Ingelheim and has received research grants from Boehringer Ingelheim to his institution to support an investigator-initiated study. He also disclosed serving as a consultant and receiving research grants from other manufacturers of psoriasis products.
GPP is a life-threatening skin condition involving the widespread eruption of sterile pustules, with a clinical course that “can be relapsing with recurrent flares or persistent with intermittent flares,” Hervé Bachelez, MD, of the Université de Paris and coauthors wrote. GPP patients are often hospitalized, and mortality ranges from 2% to 16% from causes that include sepsis and cardiorespiratory failure.
“The role of the interleukin-36 pathway in GPP is supported by the finding of loss-of-function mutations in the interleukin-36 receptor antagonist gene (IL36RN) and associated genes (CARD14, AP1S3, SERPINA3, and MPO) and by the overexpression of interleukin-36 cytokines in GPP skin lesions,” therefore, IL-36 is a potential treatment target to manage flares, they explained.
In the multicenter, double-blind trial, published in the New England Journal of Medicine, the researchers randomized 35 adults with GPP flares to a single 900-mg intravenous dose of spesolimab and 18 to placebo. Patients in both groups could receive an open-label dose of spesolimab after day 8; all patients were followed for 12 weeks.
The primary study endpoint was the Generalized Pustular Psoriasis Physician Global Assessment (GPPGA) pustulation subscore of 0 at 1 week after treatment. The GPPGA ranges from 0 (no visible pustules) to 4 (severe pustules). At baseline, 46% spesolimab patients and 39% placebo patients had a GPPGA pustulation subscore of 3, and 37% and 33%, respectively, had a pustulation subscore of 4.
After 1 week, 54% of the spesolimab patients had no visible pustules, compared with 6% of placebo patients; the difference was statistically significant (P < .001). The main secondary endpoint was a score of 0 or 1 (clear or almost clear skin) on the GPPGA total score after 1 week. Significantly more spesolimab patients had GPPGA total scores of 0 or 1, compared with placebo patients (43% vs. 11%, respectively; P = .02).
Overall, 6 of 35 spesolimab patients (17%) and 6% of those in the placebo groups developed infections during the first week, and 24 of 51 patients (47%) who had received spesolimab at any point during the study developed infections by week 12. Infections included urinary tract infections (three cases), influenza (three), otitis externa (two), folliculitis (two), upper respiratory tract infection (two), and pustule (two).
In the first week, 6% of spesolimab patients and none of the placebo patients reported serious adverse events; at week 12, 12% of patients who had received at least one spesolimab dose reported a serious adverse event. In addition, antidrug antibodies were identified in 23 (46%) of the 50 patients who received at least one dose of spesolimab.
“Symptoms that were observed in two patients who received spesolimab were reported as a drug reaction with eosinophilia and systemic symptoms (DRESS),” the authors noted. One patient had a RegiSCAR (European Registry of Severe Cutaneous Adverse Reactions) score and the other had a score of 3; a score below 2 indicates no DRESS, and a score of 2 or 3 indicates “possible DRESS,” they added.
“Because 15 of the 18 patients who were assigned to the placebo group received open-label spesolimab, the effect of spesolimab as compared with that of placebo could not be determined after week 1,” the researchers noted.
The study findings were limited by several factors including the short randomization period and small study population, the researchers noted. However, the effect sizes for both the primary and secondary endpoints were large, which strengthened the results.
The results support data from previous studies suggesting a role for IL-36 in the pathogenesis of GPP, and support the need for longer and larger studies of the safety and effectiveness of spesolimab for GPP patients, they concluded.
No FDA-approved therapy
“GPP is a very rare but devastating life-threatening disease that presents with the sudden onset of pustules throughout the skin,” Joel Gelfand, MD, professor of dermatology and director of the psoriasis and phototherapy center at the University of Pennsylvania, Philadelphia, said in an interview. “Without rapid treatment, GPP can result in death. Currently there are no [Food and Drug Administration]–approved treatments for this orphan disease.”
Dr. Gelfand said he was surprised by the degree of efficacy and the speed of the patient response to spesolimab, compared with placebo, which he described as “truly remarkable.” Based on the current study results, “spesolimab offers a tremendous step forward for our patients,” he added.
Looking ahead, Dr. Gelfand noted that “longer-term studies with a comparator, such as a biologic that targets IL-17, would be helpful to more fully understand the safety, efficacy, and role that spesolimab will have in real-world patients.”
On Dec. 15, Boehringer Ingelheim announced that the FDA had granted priority review for spesolimab for treating GPP flares.
The study was supported by Boehringer Ingelheim. Lead author Dr. Bachelez had no financial conflicts to disclose. Several authors are employees of Boehringer Ingelheim. Dr. Gelfand is a consultant for the study sponsor Boehringer Ingelheim and has received research grants from Boehringer Ingelheim to his institution to support an investigator-initiated study. He also disclosed serving as a consultant and receiving research grants from other manufacturers of psoriasis products.
GPP is a life-threatening skin condition involving the widespread eruption of sterile pustules, with a clinical course that “can be relapsing with recurrent flares or persistent with intermittent flares,” Hervé Bachelez, MD, of the Université de Paris and coauthors wrote. GPP patients are often hospitalized, and mortality ranges from 2% to 16% from causes that include sepsis and cardiorespiratory failure.
“The role of the interleukin-36 pathway in GPP is supported by the finding of loss-of-function mutations in the interleukin-36 receptor antagonist gene (IL36RN) and associated genes (CARD14, AP1S3, SERPINA3, and MPO) and by the overexpression of interleukin-36 cytokines in GPP skin lesions,” therefore, IL-36 is a potential treatment target to manage flares, they explained.
In the multicenter, double-blind trial, published in the New England Journal of Medicine, the researchers randomized 35 adults with GPP flares to a single 900-mg intravenous dose of spesolimab and 18 to placebo. Patients in both groups could receive an open-label dose of spesolimab after day 8; all patients were followed for 12 weeks.
The primary study endpoint was the Generalized Pustular Psoriasis Physician Global Assessment (GPPGA) pustulation subscore of 0 at 1 week after treatment. The GPPGA ranges from 0 (no visible pustules) to 4 (severe pustules). At baseline, 46% spesolimab patients and 39% placebo patients had a GPPGA pustulation subscore of 3, and 37% and 33%, respectively, had a pustulation subscore of 4.
After 1 week, 54% of the spesolimab patients had no visible pustules, compared with 6% of placebo patients; the difference was statistically significant (P < .001). The main secondary endpoint was a score of 0 or 1 (clear or almost clear skin) on the GPPGA total score after 1 week. Significantly more spesolimab patients had GPPGA total scores of 0 or 1, compared with placebo patients (43% vs. 11%, respectively; P = .02).
Overall, 6 of 35 spesolimab patients (17%) and 6% of those in the placebo groups developed infections during the first week, and 24 of 51 patients (47%) who had received spesolimab at any point during the study developed infections by week 12. Infections included urinary tract infections (three cases), influenza (three), otitis externa (two), folliculitis (two), upper respiratory tract infection (two), and pustule (two).
In the first week, 6% of spesolimab patients and none of the placebo patients reported serious adverse events; at week 12, 12% of patients who had received at least one spesolimab dose reported a serious adverse event. In addition, antidrug antibodies were identified in 23 (46%) of the 50 patients who received at least one dose of spesolimab.
“Symptoms that were observed in two patients who received spesolimab were reported as a drug reaction with eosinophilia and systemic symptoms (DRESS),” the authors noted. One patient had a RegiSCAR (European Registry of Severe Cutaneous Adverse Reactions) score and the other had a score of 3; a score below 2 indicates no DRESS, and a score of 2 or 3 indicates “possible DRESS,” they added.
“Because 15 of the 18 patients who were assigned to the placebo group received open-label spesolimab, the effect of spesolimab as compared with that of placebo could not be determined after week 1,” the researchers noted.
The study findings were limited by several factors including the short randomization period and small study population, the researchers noted. However, the effect sizes for both the primary and secondary endpoints were large, which strengthened the results.
The results support data from previous studies suggesting a role for IL-36 in the pathogenesis of GPP, and support the need for longer and larger studies of the safety and effectiveness of spesolimab for GPP patients, they concluded.
No FDA-approved therapy
“GPP is a very rare but devastating life-threatening disease that presents with the sudden onset of pustules throughout the skin,” Joel Gelfand, MD, professor of dermatology and director of the psoriasis and phototherapy center at the University of Pennsylvania, Philadelphia, said in an interview. “Without rapid treatment, GPP can result in death. Currently there are no [Food and Drug Administration]–approved treatments for this orphan disease.”
Dr. Gelfand said he was surprised by the degree of efficacy and the speed of the patient response to spesolimab, compared with placebo, which he described as “truly remarkable.” Based on the current study results, “spesolimab offers a tremendous step forward for our patients,” he added.
Looking ahead, Dr. Gelfand noted that “longer-term studies with a comparator, such as a biologic that targets IL-17, would be helpful to more fully understand the safety, efficacy, and role that spesolimab will have in real-world patients.”
On Dec. 15, Boehringer Ingelheim announced that the FDA had granted priority review for spesolimab for treating GPP flares.
The study was supported by Boehringer Ingelheim. Lead author Dr. Bachelez had no financial conflicts to disclose. Several authors are employees of Boehringer Ingelheim. Dr. Gelfand is a consultant for the study sponsor Boehringer Ingelheim and has received research grants from Boehringer Ingelheim to his institution to support an investigator-initiated study. He also disclosed serving as a consultant and receiving research grants from other manufacturers of psoriasis products.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
FDA OKs emergency use of Merck pill for COVID-19
Similar to FDA authorization of another antiviral pill regimen – ritonavir plus nirmatrelvir, or Paxlovid – granted to Pfizer on Wednesday, molnupiravir (brand name Lagevrio) should be taken early in the course of COVID-19 illness.
Pfizer’s drug is authorized for anyone aged 12 and up. But Merck’s is only for adults aged 18 and older.
Merck filed an application for emergency use authorization with the FDA in October. The company included results of its phase 3 study showing the treatment could lead to a 50% reduction in COVID-19 hospitalizations. Data later showed this efficacy at closer to a 30% reduction. In November, an FDA advisory panel narrowly recommended the agency grant authorization by a 13-10 vote.
Animal studies found the drug may harm a fetus, so it is not recommended for pregnant people, the FDA says. It may be prescribed to a pregnant person only after their doctor determines the benefits outweigh the risks and the patient is told of those risks.
Women who may get pregnant should use a reliable method of birth control if being treated with molnupiravir and for 4 days after the final dose.
Two weapons against COVID
Two antiviral pills could be better than one, at least in terms of making more COVID-19 treatments available in early 2022. It is yet to be seen if the drugmakers will be able to keep up with demand, which could substantially increase with an expected surge in Omicron variant cases.
Ritonavir and molnupiravir join remdesivir (brand name Veklury) as available antivirals to treat COVID-19. Remdesivir is fully approved by the FDA but is given only through an IV to people in the hospital.
Officials point out that COVID-19 treatments in tablet form are more convenient for patients in the United States and across the globe, particularly where IV infusion services may be limited.
In March 2021, experts accurately predicted that the molnupiravir pill would be available by year’s end.
Interestingly, in September, Merck announced the findings of laboratory studies suggesting that molnupiravir would work against variants of SARS-CoV-2 because the agent does not target the virus’s spike protein.
Perhaps in part because of early promising results, the U.S. government announced in November intentions to purchase $1 billion worth of molnupiravir. That new order came on top of $1.2 billion worth of the pills the U.S. ordered in June.
A version of this article first appeared on WebMD.com.
Similar to FDA authorization of another antiviral pill regimen – ritonavir plus nirmatrelvir, or Paxlovid – granted to Pfizer on Wednesday, molnupiravir (brand name Lagevrio) should be taken early in the course of COVID-19 illness.
Pfizer’s drug is authorized for anyone aged 12 and up. But Merck’s is only for adults aged 18 and older.
Merck filed an application for emergency use authorization with the FDA in October. The company included results of its phase 3 study showing the treatment could lead to a 50% reduction in COVID-19 hospitalizations. Data later showed this efficacy at closer to a 30% reduction. In November, an FDA advisory panel narrowly recommended the agency grant authorization by a 13-10 vote.
Animal studies found the drug may harm a fetus, so it is not recommended for pregnant people, the FDA says. It may be prescribed to a pregnant person only after their doctor determines the benefits outweigh the risks and the patient is told of those risks.
Women who may get pregnant should use a reliable method of birth control if being treated with molnupiravir and for 4 days after the final dose.
Two weapons against COVID
Two antiviral pills could be better than one, at least in terms of making more COVID-19 treatments available in early 2022. It is yet to be seen if the drugmakers will be able to keep up with demand, which could substantially increase with an expected surge in Omicron variant cases.
Ritonavir and molnupiravir join remdesivir (brand name Veklury) as available antivirals to treat COVID-19. Remdesivir is fully approved by the FDA but is given only through an IV to people in the hospital.
Officials point out that COVID-19 treatments in tablet form are more convenient for patients in the United States and across the globe, particularly where IV infusion services may be limited.
In March 2021, experts accurately predicted that the molnupiravir pill would be available by year’s end.
Interestingly, in September, Merck announced the findings of laboratory studies suggesting that molnupiravir would work against variants of SARS-CoV-2 because the agent does not target the virus’s spike protein.
Perhaps in part because of early promising results, the U.S. government announced in November intentions to purchase $1 billion worth of molnupiravir. That new order came on top of $1.2 billion worth of the pills the U.S. ordered in June.
A version of this article first appeared on WebMD.com.
Similar to FDA authorization of another antiviral pill regimen – ritonavir plus nirmatrelvir, or Paxlovid – granted to Pfizer on Wednesday, molnupiravir (brand name Lagevrio) should be taken early in the course of COVID-19 illness.
Pfizer’s drug is authorized for anyone aged 12 and up. But Merck’s is only for adults aged 18 and older.
Merck filed an application for emergency use authorization with the FDA in October. The company included results of its phase 3 study showing the treatment could lead to a 50% reduction in COVID-19 hospitalizations. Data later showed this efficacy at closer to a 30% reduction. In November, an FDA advisory panel narrowly recommended the agency grant authorization by a 13-10 vote.
Animal studies found the drug may harm a fetus, so it is not recommended for pregnant people, the FDA says. It may be prescribed to a pregnant person only after their doctor determines the benefits outweigh the risks and the patient is told of those risks.
Women who may get pregnant should use a reliable method of birth control if being treated with molnupiravir and for 4 days after the final dose.
Two weapons against COVID
Two antiviral pills could be better than one, at least in terms of making more COVID-19 treatments available in early 2022. It is yet to be seen if the drugmakers will be able to keep up with demand, which could substantially increase with an expected surge in Omicron variant cases.
Ritonavir and molnupiravir join remdesivir (brand name Veklury) as available antivirals to treat COVID-19. Remdesivir is fully approved by the FDA but is given only through an IV to people in the hospital.
Officials point out that COVID-19 treatments in tablet form are more convenient for patients in the United States and across the globe, particularly where IV infusion services may be limited.
In March 2021, experts accurately predicted that the molnupiravir pill would be available by year’s end.
Interestingly, in September, Merck announced the findings of laboratory studies suggesting that molnupiravir would work against variants of SARS-CoV-2 because the agent does not target the virus’s spike protein.
Perhaps in part because of early promising results, the U.S. government announced in November intentions to purchase $1 billion worth of molnupiravir. That new order came on top of $1.2 billion worth of the pills the U.S. ordered in June.
A version of this article first appeared on WebMD.com.
Bamlanivimab’s effects in COVID-19 depend on antibodies
In the randomized controlled trial, in both the group who received bamlanivimab and the group who received placebo, higher antigen and viral RNA levels were associated with a lower proportion of patients achieving recovery.
Other studies have shown that the use of monoclonal antibodies reduces hospitalization risk in outpatients with early COVID-19, and appears to promote viral load decline in the nasopharynx, wrote Jens D. Lundgren, MD, of the University of Copenhagen and colleagues in their article published in the Annals of Internal Medicine. What had been missing prior to this new research was final results from hospitalized patients, the authors said.
In the new study, the researchers randomized 314 adults hospitalized with COVID-19 but without end-organ failure to receive 7,000 mg bamlanivimab (163 patients) or a placebo (151 patients). All patients received study-supplied remdesivir unless contraindicated. The researchers compared the efficacy of bamlanivimab versus placebo, but considered remdesivir the standard of care in this study.
At baseline, 50% of patients overall had antispike endogenous neutralizing antibodies (nAbs), and 50% had SARS-CoV-2 nucleocapsid plasma antigen levels of at least 1,000 ng/L.
The median time to sustained recovery, 19 days, was not significantly different between the bamlanivimab and placebo groups (subhazard ratio, 0.99).
“As hypothesized, among those who were negative for nAb, the difference between bamlanivimab and placebo was more evident if levels of plasma antigen or nasal-swab viral RNA were above the median entry levels,” with subhazard ratios of 1.48 and 1.89, respectively, the researchers explained.
However, the hazard ratio for death for bamlanivimab vs. placebo was 0.45 for patients negative for nAb vs. 3.53 for those positive for nAb. These differences with respect to nAb status were similar across all 90 elements of a composite safety outcome, the researchers said.
Potential benefits remain unclear
The use of neutralizing monoclonal antibodies has been extensively documented as an effective treatment for COVID-19 among ambulatory patients, corresponding author Dr. Lundgren said in an interview.
“Conversely, among admitted patients with COVID-19 pneumonia, the benefit has been questionable,” he said.
The researchers examined a hypothesis that the null finding in hospitalized patients may stem from differences in underlying mechanisms, “either from uncontrolled viral replication – which would be predicted to occur in particular among those not yet been able to mount an endogenous immune response – or from hyperinflammation among those that have mounted such a response,” Dr. Lundgren said.
The study findings supported the stated hypothesis, said Dr. Lundgren. “However, it was surprising that not only was the neutralizing antibody without any benefit among those that had mounted an endogenous immune response, but it actually may have been harmful,” he said.
Bamlanivimab was effective against the viral strain that circulated at the time of enrollment in the study, but subsequent viral strains have appeared to be unaffected by the neutralizing activity of the antibody, said Dr. Lundgren.
From a practical standpoint, “the findings would suggest that use of neutralizing monoclonal antibodies for patients admitted to a hospital with COVID pneumonia should be restricted to those that have not yet mounted an endogenous immune response, as determined by lack of detectable neutralizing antibodies at the time of admission,” Dr. Lundgren said.
Looking ahead, studies are currently underway to examine how the findings translate to vaccinated patients, he added. Other questions to be addressed include whether the benefits and harms apply to some or all neutralizing antibody products, he said.
In addition, “our research consortium is currently doing field testing of several point-of-care test candidates to examine their reliability and functionality,” for how quickly they might identify an endogenous neutralizing antibody response in an admitted COVID pneumonia patient,” Dr. Lundgren noted.
Findings show bamlanivimab’s limits
“Based on the findings of the current study, no clear subgroup of patients could be identified who would benefit from bamlanivimab when hospitalized with COVID-19,” said Suman Pal, MD, of the University of New Mexico, Albuquerque, in an interview.
“The study findings also show possible harm of using bamlanivimab in hospitalized COVID-19 patients who were seropositive for neutralizing antibodies prior to receiving therapy,” Dr. Pal emphasized. “Moreover, the study did not include participants with COVID-19 from variant strains, such as delta and omicron, which currently account for a large number of cases.” “Therefore, the results of this study do not support the use of bamlanivimab in the clinical setting until further evidence is available to guide the selection of patients who may benefit from therapy,” he explained.
“The possible benefit of bamlanivimab does not outweigh the risks in patients hospitalized with COVID-19,” he concluded.
Dr. Pal emphasized the need for larger prospective studies to establish whether bamlanivimab may have benefits in a subgroup of patients, but “well-validated point-of-care tests to identify such patients need to be readily available before this therapy can be considered by clinicians at the bedside,” he concluded.
Diligent screening required before use
Monoclonal antibody treatment has been administered to individuals with diagnosis of COVID-19 infection as outpatients as well as for hospitalized inpatients, said Noel Deep, MD, an internist in Antigo, Wisc., in an interview. “This study is important because it helps physicians and health care institutions to evaluate whether continued use of the monoclonal antibodies would be beneficial and, if so, in what patient populations,” he said.
The findings present interesting implications for the care of COVID-19 patients, said Dr. Deep. “This study indicates that bamlanivimab does not provide the benefit that was initially envisioned when the monoclonal antibody infusions were initially initiated in the treatment of COVID-19 infections. “Serological screening of the patients would help to identify that subgroup of individuals who could benefit from this monoclonal antibody rather than administering it to every COVID-19–positive individual,” he explained.
However, “it is important to note that the emergency use authorization (EUA) for single-agent bamlanivimab has been revoked,” Dr. Deep said.
“The potential benefits of bamlanivimab can be realized only if adequate attention is paid to identifying the appropriate candidates based on serological screening, and administering bamlanivimab to those who are already producing endogenous antibodies could lead to increased risk to those individuals,” he said. Dr. Deep added that he would favor administration of bamlanivimab “in those appropriately screened and eligible candidates, and it is my opinion that the benefits outweigh the risks in those individuals.”
Although the EUA for single-agent bamlanivimab has been revoked, “alternative monoclonal antibody therapies remain available under EUA, including REGEN-COV (casirivimab and imdevimab, administered together), and bamlanivimab and etesevimab administered together, for the same uses as previously authorized for bamlanivimab alone,” Dr. Deep said. “The FDA believes that these alternative monoclonal antibody therapies remain appropriate to treat patients with COVID-19, and I would like to see some data about the benefits and risks of these agents,” he noted.
Limitations, funding, and disclosures
The main limitation of the study was the small size and the fact that it was a subgroup analysis of a trial that ended early because of futility, the researchers wrote. However, the Therapeutics for Inpatients With COVID-19 (TICO) platform will proceed with clinical evaluation of additional COVID-19 treatments, they said.
The study was supported primarily by the U.S. government Operation Warp Speed and the National Institute of Allergy and Infectious Diseases. Other funding sources included the Division of Clinical Research and Leidos Biomedical Research for the INSIGHT (International Network for Strategic Initiatives in Global HIV Trials) Network, as well as an agreement between the National Heart, Lung, and Blood Institute and the Research Triangle Institute for the PETAL (Prevention & Early Treatment of Acute Lung Injury) Network and CTSN (Cardiothoracic Surgical Trials Network). Other support came from the U.S. Department of Veterans Affairs and the governments of Denmark (National Research Foundation), Australia (National Health and Medical Research Council), and the United Kingdom (Medical Research Council).
The medications used in the study were donated by Gilead Sciences and Eli Lilly.
The researchers had no financial conflicts do disclose. Dr. Deep and Dr. Pal had no relevant financial conflicts to disclose.
In the randomized controlled trial, in both the group who received bamlanivimab and the group who received placebo, higher antigen and viral RNA levels were associated with a lower proportion of patients achieving recovery.
Other studies have shown that the use of monoclonal antibodies reduces hospitalization risk in outpatients with early COVID-19, and appears to promote viral load decline in the nasopharynx, wrote Jens D. Lundgren, MD, of the University of Copenhagen and colleagues in their article published in the Annals of Internal Medicine. What had been missing prior to this new research was final results from hospitalized patients, the authors said.
In the new study, the researchers randomized 314 adults hospitalized with COVID-19 but without end-organ failure to receive 7,000 mg bamlanivimab (163 patients) or a placebo (151 patients). All patients received study-supplied remdesivir unless contraindicated. The researchers compared the efficacy of bamlanivimab versus placebo, but considered remdesivir the standard of care in this study.
At baseline, 50% of patients overall had antispike endogenous neutralizing antibodies (nAbs), and 50% had SARS-CoV-2 nucleocapsid plasma antigen levels of at least 1,000 ng/L.
The median time to sustained recovery, 19 days, was not significantly different between the bamlanivimab and placebo groups (subhazard ratio, 0.99).
“As hypothesized, among those who were negative for nAb, the difference between bamlanivimab and placebo was more evident if levels of plasma antigen or nasal-swab viral RNA were above the median entry levels,” with subhazard ratios of 1.48 and 1.89, respectively, the researchers explained.
However, the hazard ratio for death for bamlanivimab vs. placebo was 0.45 for patients negative for nAb vs. 3.53 for those positive for nAb. These differences with respect to nAb status were similar across all 90 elements of a composite safety outcome, the researchers said.
Potential benefits remain unclear
The use of neutralizing monoclonal antibodies has been extensively documented as an effective treatment for COVID-19 among ambulatory patients, corresponding author Dr. Lundgren said in an interview.
“Conversely, among admitted patients with COVID-19 pneumonia, the benefit has been questionable,” he said.
The researchers examined a hypothesis that the null finding in hospitalized patients may stem from differences in underlying mechanisms, “either from uncontrolled viral replication – which would be predicted to occur in particular among those not yet been able to mount an endogenous immune response – or from hyperinflammation among those that have mounted such a response,” Dr. Lundgren said.
The study findings supported the stated hypothesis, said Dr. Lundgren. “However, it was surprising that not only was the neutralizing antibody without any benefit among those that had mounted an endogenous immune response, but it actually may have been harmful,” he said.
Bamlanivimab was effective against the viral strain that circulated at the time of enrollment in the study, but subsequent viral strains have appeared to be unaffected by the neutralizing activity of the antibody, said Dr. Lundgren.
From a practical standpoint, “the findings would suggest that use of neutralizing monoclonal antibodies for patients admitted to a hospital with COVID pneumonia should be restricted to those that have not yet mounted an endogenous immune response, as determined by lack of detectable neutralizing antibodies at the time of admission,” Dr. Lundgren said.
Looking ahead, studies are currently underway to examine how the findings translate to vaccinated patients, he added. Other questions to be addressed include whether the benefits and harms apply to some or all neutralizing antibody products, he said.
In addition, “our research consortium is currently doing field testing of several point-of-care test candidates to examine their reliability and functionality,” for how quickly they might identify an endogenous neutralizing antibody response in an admitted COVID pneumonia patient,” Dr. Lundgren noted.
Findings show bamlanivimab’s limits
“Based on the findings of the current study, no clear subgroup of patients could be identified who would benefit from bamlanivimab when hospitalized with COVID-19,” said Suman Pal, MD, of the University of New Mexico, Albuquerque, in an interview.
“The study findings also show possible harm of using bamlanivimab in hospitalized COVID-19 patients who were seropositive for neutralizing antibodies prior to receiving therapy,” Dr. Pal emphasized. “Moreover, the study did not include participants with COVID-19 from variant strains, such as delta and omicron, which currently account for a large number of cases.” “Therefore, the results of this study do not support the use of bamlanivimab in the clinical setting until further evidence is available to guide the selection of patients who may benefit from therapy,” he explained.
“The possible benefit of bamlanivimab does not outweigh the risks in patients hospitalized with COVID-19,” he concluded.
Dr. Pal emphasized the need for larger prospective studies to establish whether bamlanivimab may have benefits in a subgroup of patients, but “well-validated point-of-care tests to identify such patients need to be readily available before this therapy can be considered by clinicians at the bedside,” he concluded.
Diligent screening required before use
Monoclonal antibody treatment has been administered to individuals with diagnosis of COVID-19 infection as outpatients as well as for hospitalized inpatients, said Noel Deep, MD, an internist in Antigo, Wisc., in an interview. “This study is important because it helps physicians and health care institutions to evaluate whether continued use of the monoclonal antibodies would be beneficial and, if so, in what patient populations,” he said.
The findings present interesting implications for the care of COVID-19 patients, said Dr. Deep. “This study indicates that bamlanivimab does not provide the benefit that was initially envisioned when the monoclonal antibody infusions were initially initiated in the treatment of COVID-19 infections. “Serological screening of the patients would help to identify that subgroup of individuals who could benefit from this monoclonal antibody rather than administering it to every COVID-19–positive individual,” he explained.
However, “it is important to note that the emergency use authorization (EUA) for single-agent bamlanivimab has been revoked,” Dr. Deep said.
“The potential benefits of bamlanivimab can be realized only if adequate attention is paid to identifying the appropriate candidates based on serological screening, and administering bamlanivimab to those who are already producing endogenous antibodies could lead to increased risk to those individuals,” he said. Dr. Deep added that he would favor administration of bamlanivimab “in those appropriately screened and eligible candidates, and it is my opinion that the benefits outweigh the risks in those individuals.”
Although the EUA for single-agent bamlanivimab has been revoked, “alternative monoclonal antibody therapies remain available under EUA, including REGEN-COV (casirivimab and imdevimab, administered together), and bamlanivimab and etesevimab administered together, for the same uses as previously authorized for bamlanivimab alone,” Dr. Deep said. “The FDA believes that these alternative monoclonal antibody therapies remain appropriate to treat patients with COVID-19, and I would like to see some data about the benefits and risks of these agents,” he noted.
Limitations, funding, and disclosures
The main limitation of the study was the small size and the fact that it was a subgroup analysis of a trial that ended early because of futility, the researchers wrote. However, the Therapeutics for Inpatients With COVID-19 (TICO) platform will proceed with clinical evaluation of additional COVID-19 treatments, they said.
The study was supported primarily by the U.S. government Operation Warp Speed and the National Institute of Allergy and Infectious Diseases. Other funding sources included the Division of Clinical Research and Leidos Biomedical Research for the INSIGHT (International Network for Strategic Initiatives in Global HIV Trials) Network, as well as an agreement between the National Heart, Lung, and Blood Institute and the Research Triangle Institute for the PETAL (Prevention & Early Treatment of Acute Lung Injury) Network and CTSN (Cardiothoracic Surgical Trials Network). Other support came from the U.S. Department of Veterans Affairs and the governments of Denmark (National Research Foundation), Australia (National Health and Medical Research Council), and the United Kingdom (Medical Research Council).
The medications used in the study were donated by Gilead Sciences and Eli Lilly.
The researchers had no financial conflicts do disclose. Dr. Deep and Dr. Pal had no relevant financial conflicts to disclose.
In the randomized controlled trial, in both the group who received bamlanivimab and the group who received placebo, higher antigen and viral RNA levels were associated with a lower proportion of patients achieving recovery.
Other studies have shown that the use of monoclonal antibodies reduces hospitalization risk in outpatients with early COVID-19, and appears to promote viral load decline in the nasopharynx, wrote Jens D. Lundgren, MD, of the University of Copenhagen and colleagues in their article published in the Annals of Internal Medicine. What had been missing prior to this new research was final results from hospitalized patients, the authors said.
In the new study, the researchers randomized 314 adults hospitalized with COVID-19 but without end-organ failure to receive 7,000 mg bamlanivimab (163 patients) or a placebo (151 patients). All patients received study-supplied remdesivir unless contraindicated. The researchers compared the efficacy of bamlanivimab versus placebo, but considered remdesivir the standard of care in this study.
At baseline, 50% of patients overall had antispike endogenous neutralizing antibodies (nAbs), and 50% had SARS-CoV-2 nucleocapsid plasma antigen levels of at least 1,000 ng/L.
The median time to sustained recovery, 19 days, was not significantly different between the bamlanivimab and placebo groups (subhazard ratio, 0.99).
“As hypothesized, among those who were negative for nAb, the difference between bamlanivimab and placebo was more evident if levels of plasma antigen or nasal-swab viral RNA were above the median entry levels,” with subhazard ratios of 1.48 and 1.89, respectively, the researchers explained.
However, the hazard ratio for death for bamlanivimab vs. placebo was 0.45 for patients negative for nAb vs. 3.53 for those positive for nAb. These differences with respect to nAb status were similar across all 90 elements of a composite safety outcome, the researchers said.
Potential benefits remain unclear
The use of neutralizing monoclonal antibodies has been extensively documented as an effective treatment for COVID-19 among ambulatory patients, corresponding author Dr. Lundgren said in an interview.
“Conversely, among admitted patients with COVID-19 pneumonia, the benefit has been questionable,” he said.
The researchers examined a hypothesis that the null finding in hospitalized patients may stem from differences in underlying mechanisms, “either from uncontrolled viral replication – which would be predicted to occur in particular among those not yet been able to mount an endogenous immune response – or from hyperinflammation among those that have mounted such a response,” Dr. Lundgren said.
The study findings supported the stated hypothesis, said Dr. Lundgren. “However, it was surprising that not only was the neutralizing antibody without any benefit among those that had mounted an endogenous immune response, but it actually may have been harmful,” he said.
Bamlanivimab was effective against the viral strain that circulated at the time of enrollment in the study, but subsequent viral strains have appeared to be unaffected by the neutralizing activity of the antibody, said Dr. Lundgren.
From a practical standpoint, “the findings would suggest that use of neutralizing monoclonal antibodies for patients admitted to a hospital with COVID pneumonia should be restricted to those that have not yet mounted an endogenous immune response, as determined by lack of detectable neutralizing antibodies at the time of admission,” Dr. Lundgren said.
Looking ahead, studies are currently underway to examine how the findings translate to vaccinated patients, he added. Other questions to be addressed include whether the benefits and harms apply to some or all neutralizing antibody products, he said.
In addition, “our research consortium is currently doing field testing of several point-of-care test candidates to examine their reliability and functionality,” for how quickly they might identify an endogenous neutralizing antibody response in an admitted COVID pneumonia patient,” Dr. Lundgren noted.
Findings show bamlanivimab’s limits
“Based on the findings of the current study, no clear subgroup of patients could be identified who would benefit from bamlanivimab when hospitalized with COVID-19,” said Suman Pal, MD, of the University of New Mexico, Albuquerque, in an interview.
“The study findings also show possible harm of using bamlanivimab in hospitalized COVID-19 patients who were seropositive for neutralizing antibodies prior to receiving therapy,” Dr. Pal emphasized. “Moreover, the study did not include participants with COVID-19 from variant strains, such as delta and omicron, which currently account for a large number of cases.” “Therefore, the results of this study do not support the use of bamlanivimab in the clinical setting until further evidence is available to guide the selection of patients who may benefit from therapy,” he explained.
“The possible benefit of bamlanivimab does not outweigh the risks in patients hospitalized with COVID-19,” he concluded.
Dr. Pal emphasized the need for larger prospective studies to establish whether bamlanivimab may have benefits in a subgroup of patients, but “well-validated point-of-care tests to identify such patients need to be readily available before this therapy can be considered by clinicians at the bedside,” he concluded.
Diligent screening required before use
Monoclonal antibody treatment has been administered to individuals with diagnosis of COVID-19 infection as outpatients as well as for hospitalized inpatients, said Noel Deep, MD, an internist in Antigo, Wisc., in an interview. “This study is important because it helps physicians and health care institutions to evaluate whether continued use of the monoclonal antibodies would be beneficial and, if so, in what patient populations,” he said.
The findings present interesting implications for the care of COVID-19 patients, said Dr. Deep. “This study indicates that bamlanivimab does not provide the benefit that was initially envisioned when the monoclonal antibody infusions were initially initiated in the treatment of COVID-19 infections. “Serological screening of the patients would help to identify that subgroup of individuals who could benefit from this monoclonal antibody rather than administering it to every COVID-19–positive individual,” he explained.
However, “it is important to note that the emergency use authorization (EUA) for single-agent bamlanivimab has been revoked,” Dr. Deep said.
“The potential benefits of bamlanivimab can be realized only if adequate attention is paid to identifying the appropriate candidates based on serological screening, and administering bamlanivimab to those who are already producing endogenous antibodies could lead to increased risk to those individuals,” he said. Dr. Deep added that he would favor administration of bamlanivimab “in those appropriately screened and eligible candidates, and it is my opinion that the benefits outweigh the risks in those individuals.”
Although the EUA for single-agent bamlanivimab has been revoked, “alternative monoclonal antibody therapies remain available under EUA, including REGEN-COV (casirivimab and imdevimab, administered together), and bamlanivimab and etesevimab administered together, for the same uses as previously authorized for bamlanivimab alone,” Dr. Deep said. “The FDA believes that these alternative monoclonal antibody therapies remain appropriate to treat patients with COVID-19, and I would like to see some data about the benefits and risks of these agents,” he noted.
Limitations, funding, and disclosures
The main limitation of the study was the small size and the fact that it was a subgroup analysis of a trial that ended early because of futility, the researchers wrote. However, the Therapeutics for Inpatients With COVID-19 (TICO) platform will proceed with clinical evaluation of additional COVID-19 treatments, they said.
The study was supported primarily by the U.S. government Operation Warp Speed and the National Institute of Allergy and Infectious Diseases. Other funding sources included the Division of Clinical Research and Leidos Biomedical Research for the INSIGHT (International Network for Strategic Initiatives in Global HIV Trials) Network, as well as an agreement between the National Heart, Lung, and Blood Institute and the Research Triangle Institute for the PETAL (Prevention & Early Treatment of Acute Lung Injury) Network and CTSN (Cardiothoracic Surgical Trials Network). Other support came from the U.S. Department of Veterans Affairs and the governments of Denmark (National Research Foundation), Australia (National Health and Medical Research Council), and the United Kingdom (Medical Research Council).
The medications used in the study were donated by Gilead Sciences and Eli Lilly.
The researchers had no financial conflicts do disclose. Dr. Deep and Dr. Pal had no relevant financial conflicts to disclose.
FROM ANNALS OF INTERNAL MEDICINE
Children and COVID: New cases up slightly, vaccinations continue to slow
New COVID-19 vaccinations in children were down by almost 24% in the last week as new cases rose by just 3.5%, based on new data.
That fairly low number suggests the latest case count from the American Academy of Pediatrics and the Children’s Hospital Association has not caught up yet to the reality of the Omicron variant, which has sent new cases climbing among all ages and now represents the majority of COVID-19 infections nationwide, the Centers for Disease Control and Prevention said.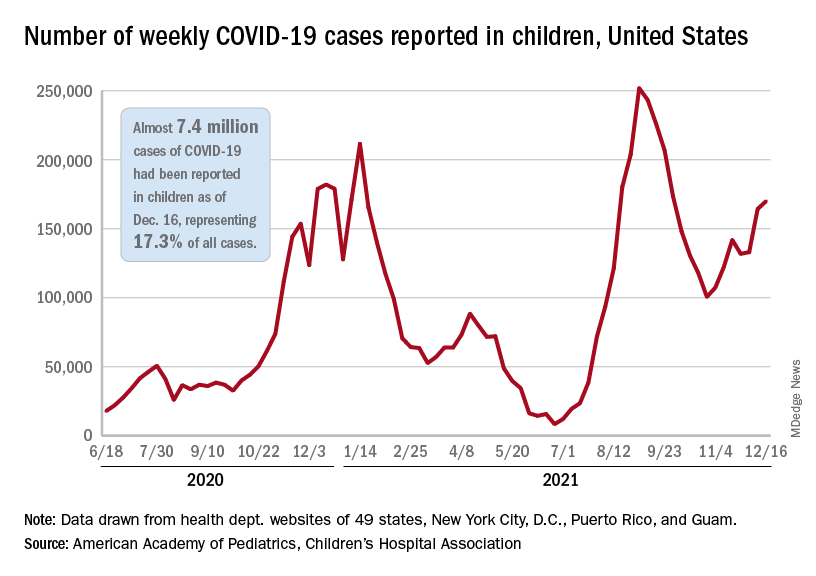
Meanwhile, in the midst of the latest surge, the United States just passed yet another sobering COVID milestone: 1,000 deaths in children aged 17 and under. The total as of Dec. 20 was 1,015, according to the CDC, with the largest share, almost 32%, occurring in children less than 5 years of age.
Regionally, the majority of that increase came in the Northeast, with a small rise in the South and decreases in the Midwest and West, the AAP and CHA said in their weekly COVID report.
At the state level, the largest percent increases in cases over the past 2 weeks were seen in Maine and New Hampshire, as well as Vermont, which has the nation’s highest vaccination rates for children aged 5-11 (51%) and 12-17 (84%), the AAP said in its vaccination trends report.
Nationally, new COVID vaccinations in children continue to trend downward. The number of children aged 5-17 years who had received at least one dose increased by about 498,000 for the week of Dec. 13-19, down from 654,000 (–23.9%) the previous week. Children aged 5-11 years still represented the largest share (22.7%) of all vaccine initiators in the last 2 weeks, but that proportion was 42.8% just before Thanksgiving, according to data from the CDC.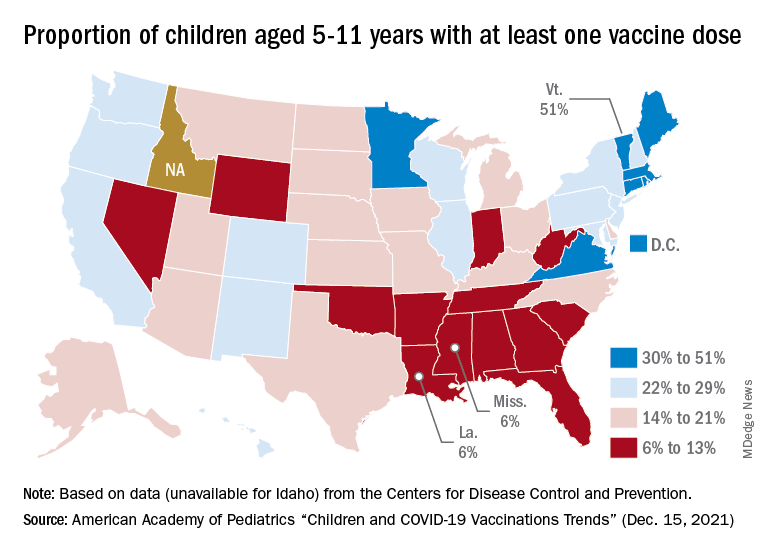
On a more positive note, children aged 5-11 made up 51% of all Americans who completed the vaccine regimen during the 2 weeks ending Dec. 20. The cumulative completion count is 3.6 million in that age group, along with almost 13.4 million children aged 12-17, and the CDC data show that 6.1 million children aged 5-11 and 15.9 million children aged 12-17 have received at least one dose.
On a less positive note, however, that means almost half (47%) of 12- to 17-year-olds still are not fully vaccinated and that over a third (37%) have received no vaccine at all, according to the COVID Data Tracker.
New COVID-19 vaccinations in children were down by almost 24% in the last week as new cases rose by just 3.5%, based on new data.
That fairly low number suggests the latest case count from the American Academy of Pediatrics and the Children’s Hospital Association has not caught up yet to the reality of the Omicron variant, which has sent new cases climbing among all ages and now represents the majority of COVID-19 infections nationwide, the Centers for Disease Control and Prevention said.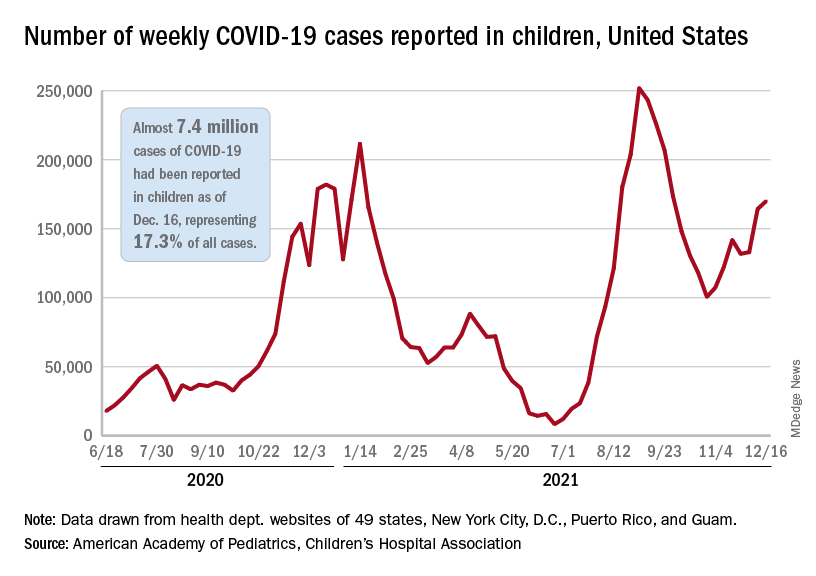
Meanwhile, in the midst of the latest surge, the United States just passed yet another sobering COVID milestone: 1,000 deaths in children aged 17 and under. The total as of Dec. 20 was 1,015, according to the CDC, with the largest share, almost 32%, occurring in children less than 5 years of age.
Regionally, the majority of that increase came in the Northeast, with a small rise in the South and decreases in the Midwest and West, the AAP and CHA said in their weekly COVID report.
At the state level, the largest percent increases in cases over the past 2 weeks were seen in Maine and New Hampshire, as well as Vermont, which has the nation’s highest vaccination rates for children aged 5-11 (51%) and 12-17 (84%), the AAP said in its vaccination trends report.
Nationally, new COVID vaccinations in children continue to trend downward. The number of children aged 5-17 years who had received at least one dose increased by about 498,000 for the week of Dec. 13-19, down from 654,000 (–23.9%) the previous week. Children aged 5-11 years still represented the largest share (22.7%) of all vaccine initiators in the last 2 weeks, but that proportion was 42.8% just before Thanksgiving, according to data from the CDC.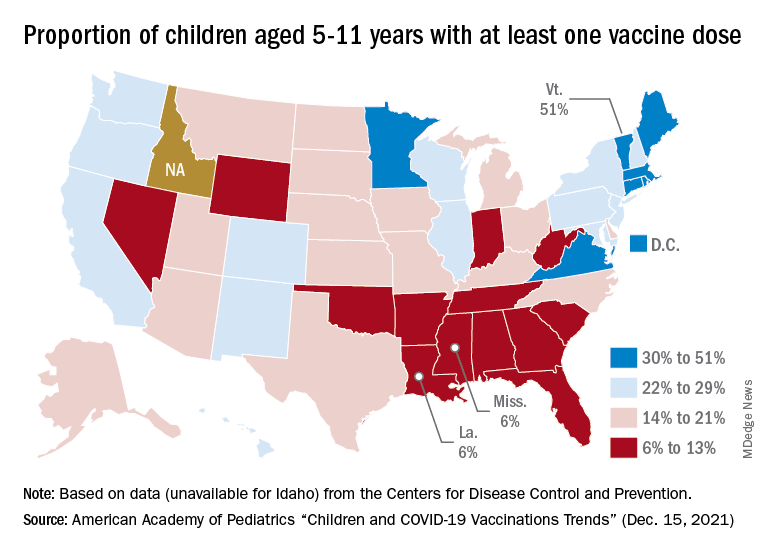
On a more positive note, children aged 5-11 made up 51% of all Americans who completed the vaccine regimen during the 2 weeks ending Dec. 20. The cumulative completion count is 3.6 million in that age group, along with almost 13.4 million children aged 12-17, and the CDC data show that 6.1 million children aged 5-11 and 15.9 million children aged 12-17 have received at least one dose.
On a less positive note, however, that means almost half (47%) of 12- to 17-year-olds still are not fully vaccinated and that over a third (37%) have received no vaccine at all, according to the COVID Data Tracker.
New COVID-19 vaccinations in children were down by almost 24% in the last week as new cases rose by just 3.5%, based on new data.
That fairly low number suggests the latest case count from the American Academy of Pediatrics and the Children’s Hospital Association has not caught up yet to the reality of the Omicron variant, which has sent new cases climbing among all ages and now represents the majority of COVID-19 infections nationwide, the Centers for Disease Control and Prevention said.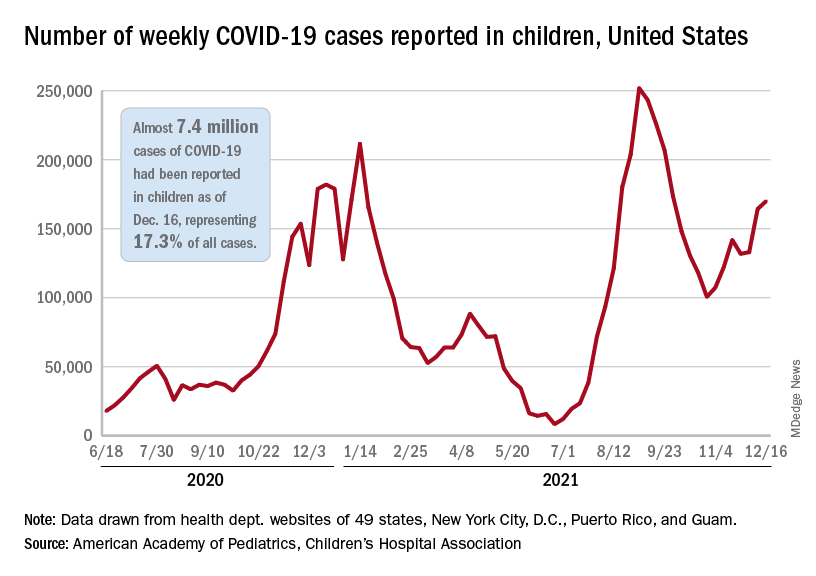
Meanwhile, in the midst of the latest surge, the United States just passed yet another sobering COVID milestone: 1,000 deaths in children aged 17 and under. The total as of Dec. 20 was 1,015, according to the CDC, with the largest share, almost 32%, occurring in children less than 5 years of age.
Regionally, the majority of that increase came in the Northeast, with a small rise in the South and decreases in the Midwest and West, the AAP and CHA said in their weekly COVID report.
At the state level, the largest percent increases in cases over the past 2 weeks were seen in Maine and New Hampshire, as well as Vermont, which has the nation’s highest vaccination rates for children aged 5-11 (51%) and 12-17 (84%), the AAP said in its vaccination trends report.
Nationally, new COVID vaccinations in children continue to trend downward. The number of children aged 5-17 years who had received at least one dose increased by about 498,000 for the week of Dec. 13-19, down from 654,000 (–23.9%) the previous week. Children aged 5-11 years still represented the largest share (22.7%) of all vaccine initiators in the last 2 weeks, but that proportion was 42.8% just before Thanksgiving, according to data from the CDC.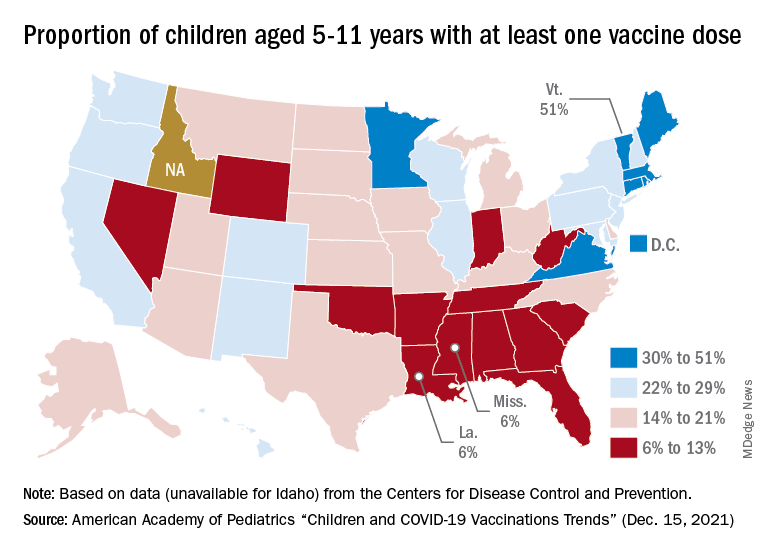
On a more positive note, children aged 5-11 made up 51% of all Americans who completed the vaccine regimen during the 2 weeks ending Dec. 20. The cumulative completion count is 3.6 million in that age group, along with almost 13.4 million children aged 12-17, and the CDC data show that 6.1 million children aged 5-11 and 15.9 million children aged 12-17 have received at least one dose.
On a less positive note, however, that means almost half (47%) of 12- to 17-year-olds still are not fully vaccinated and that over a third (37%) have received no vaccine at all, according to the COVID Data Tracker.
RSV resurgence likely in wake of COVID-19
The impact of respiratory syncytial virus (RSV)will likely be greater in 2021 and 2022 in the United States than in previous years as a result of the ongoing COVID-19 pandemic, based on data from a simulation-modeling study involving approximately 19 million individuals.
Although RSV usually follows consistent patterns of timing and duration, the disease all but disappeared starting in March 2020 after the introduction of measures to mitigate the spread of COVID-19, Zhe Zheng, MBBS, of Yale University, New Haven, Conn., and colleagues wrote.
However, lifting of mitigation measures has resulted in emergence of RSV in various parts of the world in early 2021, and trends may be similar in the United States, but data are needed to plan for prophylaxis and hospital use, they noted.
In a study published in JAMA Network Open, the researchers developed a simulation model for epidemics of RSV based on historical data. They acquired inpatient records from New York during 2005-2014 and from California during 2003-2011. The primary clinical outcome was the estimated monthly hospitalizations for RSV.
The simulated study population was 19.45 million individuals. After evaluating several scenarios including continued low transmission associated with social distancing and other mitigation measures, the researchers focused on the likely scenario that introduction of RSV from other regions would likely spark RSV epidemics in the United States.
They determined that spring and summer 2021 would show an increase in hospitalizations for RSV. Overall, higher rates of virus introduction from other regions were associated with more intense spring and summer RSV epidemics, with the trade-off of smaller winter epidemics. In the model, the expected RSV epidemic in spring and summer 2021 in New York was small, with a peak incidence of 419 hospitalizations per 100,000 people in April; by contrast, for states with less seasonal variability, such as Florida, the model predicted a larger summer epidemic.
In the model, the mean age of hospitalization for children younger than 5 years for January 2022 was expected to be 1.17 years, compared with 0.84 years in January 2019, the researchers noted.
Across all age groups, the greatest relative increase in the incidence of RSV infection was predicted for children aged 1-4 years (ranging from 82% to 86%), as were lower respiratory infections (87%-101%) and hospitalization (99%-119%), compared with prepandemic levels.
Hospitalizations for children aged 1 year were predicted to double compared with prepandemic seasons; 707 per 100,000 children per year for 2021 and 2022 versus 355 per 100,000 children per year in a typical prepandemic season. However, the largest incidence of lower respiratory infections (30,075 per 100,000) was predicted for infants aged 3-5 months, and the largest incidence of hospitalizations (3,116 per 100,000) was predicted for infants younger than 3 months.
“Without virus importation, the risk of RSV infections across all age groups in the winter of 2021 and 2022 would be greater, as more susceptible individuals were spared from infections in the absence of summer epidemics,” the researchers noted.
The older mean hospitalization age seen in the model was similar to the reported median patient age in Australia both before the pandemic and during the reemergent RSV epidemic.
“This makes intuitive sense, since many children born in 2020 were spared from RSV infection due to the low virus activity; these children will be older when they get infected for the first time during the reemergent epidemics,” the researchers wrote. “Consequently, stakeholders should consider modifying prophylaxis guidelines to include high-risk infants less than 2 years of age for the 2021-2022 season.”
The study findings were limited by several factors including the lack of data on level of virus introduction or on the impact of lack of boosting on infants with only transplacentally acquired RSV antibodies, the researchers noted. Other limitations include the use of historical data and the lack of data on values outside those included in the model, as well as the inability to control for other factors that could influence RSV, such as vaccines or long-lasting antibodies.
However, the results suggest that the rate of imported infections is associated with RSV hospitalizations, and the model effectively captured the RSV epidemics in the United States in spring and summer 2021.
Models can guide clinical preparations
“Health care simulation modeling is a growing field, with very exciting implications,” Lenore Jarvis, MD, of George Washington University, Washington, said in an interview. The field has the potential ability to influence health care in a data-driven way, including, but not limited to, staffing and other hospital operations, as well as patient care decision-making. “In short, accurate modeling and predictions can help us to make informed health care decisions that can lead to increased quality of care, potential cost savings, and even to help save lives,” she said.
Although the details of transmission modeling were not mentioned in the study, the authors evaluated the performances of several models and scenarios. “Scenario 4, for example, was focused on in particular because it best captured the observed dynamics [for RSV] that emerged during the spring and summer of 2021,” Dr. Jarvis said.
“Pediatricians can speak to these trends firsthand. A decrease in expected RSV infections and hospitalizations in 2020, followed by an unprecedented and early increase in RSV infections and severity in 2021, and the factors that the authors account for make sense, such as reintroduction of RSV from other regions and low immunity in the population,” she said. “It also makes sense that, in these transmission modeling scenarios, the expected mean age of hospitalization because of RSV increased with a temporary (hopefully) increase in RSV hospitalizations in the 2021 season, and potentially the 2022 RSV season.”
As for additional research, Dr. Jarvis said she would like to see follow-up data on the RSV transmission modeling. “For example, with scenario 4, does this scenario continue to perform well in other time periods, such as the winter? If the modeling continues to be accurate during other periods of evaluation and reevaluation, this modeling could be very useful in helping pediatric clinics and hospitals to prepare for RSV care and hospital capacity management.”
The study was supported by grants to various researchers from the National Institute of Allergy and Infectious Diseases/National Institutes of Health, the National Center for Advancing Translational Science at the National Institutes of Health, and NIH Roadmap for Medical Research. Lead author Ms. Zheng had no financial conflicts to disclose. Her study coauthors disclosed relationships with companies including AbbVie, Merck, Pfizer, GlaxoSmithKline, MedImmune, and Janssen. Dr. Jarvis had no financial conflicts to disclose and serves on the Pediatric News editorial advisory board.
The impact of respiratory syncytial virus (RSV)will likely be greater in 2021 and 2022 in the United States than in previous years as a result of the ongoing COVID-19 pandemic, based on data from a simulation-modeling study involving approximately 19 million individuals.
Although RSV usually follows consistent patterns of timing and duration, the disease all but disappeared starting in March 2020 after the introduction of measures to mitigate the spread of COVID-19, Zhe Zheng, MBBS, of Yale University, New Haven, Conn., and colleagues wrote.
However, lifting of mitigation measures has resulted in emergence of RSV in various parts of the world in early 2021, and trends may be similar in the United States, but data are needed to plan for prophylaxis and hospital use, they noted.
In a study published in JAMA Network Open, the researchers developed a simulation model for epidemics of RSV based on historical data. They acquired inpatient records from New York during 2005-2014 and from California during 2003-2011. The primary clinical outcome was the estimated monthly hospitalizations for RSV.
The simulated study population was 19.45 million individuals. After evaluating several scenarios including continued low transmission associated with social distancing and other mitigation measures, the researchers focused on the likely scenario that introduction of RSV from other regions would likely spark RSV epidemics in the United States.
They determined that spring and summer 2021 would show an increase in hospitalizations for RSV. Overall, higher rates of virus introduction from other regions were associated with more intense spring and summer RSV epidemics, with the trade-off of smaller winter epidemics. In the model, the expected RSV epidemic in spring and summer 2021 in New York was small, with a peak incidence of 419 hospitalizations per 100,000 people in April; by contrast, for states with less seasonal variability, such as Florida, the model predicted a larger summer epidemic.
In the model, the mean age of hospitalization for children younger than 5 years for January 2022 was expected to be 1.17 years, compared with 0.84 years in January 2019, the researchers noted.
Across all age groups, the greatest relative increase in the incidence of RSV infection was predicted for children aged 1-4 years (ranging from 82% to 86%), as were lower respiratory infections (87%-101%) and hospitalization (99%-119%), compared with prepandemic levels.
Hospitalizations for children aged 1 year were predicted to double compared with prepandemic seasons; 707 per 100,000 children per year for 2021 and 2022 versus 355 per 100,000 children per year in a typical prepandemic season. However, the largest incidence of lower respiratory infections (30,075 per 100,000) was predicted for infants aged 3-5 months, and the largest incidence of hospitalizations (3,116 per 100,000) was predicted for infants younger than 3 months.
“Without virus importation, the risk of RSV infections across all age groups in the winter of 2021 and 2022 would be greater, as more susceptible individuals were spared from infections in the absence of summer epidemics,” the researchers noted.
The older mean hospitalization age seen in the model was similar to the reported median patient age in Australia both before the pandemic and during the reemergent RSV epidemic.
“This makes intuitive sense, since many children born in 2020 were spared from RSV infection due to the low virus activity; these children will be older when they get infected for the first time during the reemergent epidemics,” the researchers wrote. “Consequently, stakeholders should consider modifying prophylaxis guidelines to include high-risk infants less than 2 years of age for the 2021-2022 season.”
The study findings were limited by several factors including the lack of data on level of virus introduction or on the impact of lack of boosting on infants with only transplacentally acquired RSV antibodies, the researchers noted. Other limitations include the use of historical data and the lack of data on values outside those included in the model, as well as the inability to control for other factors that could influence RSV, such as vaccines or long-lasting antibodies.
However, the results suggest that the rate of imported infections is associated with RSV hospitalizations, and the model effectively captured the RSV epidemics in the United States in spring and summer 2021.
Models can guide clinical preparations
“Health care simulation modeling is a growing field, with very exciting implications,” Lenore Jarvis, MD, of George Washington University, Washington, said in an interview. The field has the potential ability to influence health care in a data-driven way, including, but not limited to, staffing and other hospital operations, as well as patient care decision-making. “In short, accurate modeling and predictions can help us to make informed health care decisions that can lead to increased quality of care, potential cost savings, and even to help save lives,” she said.
Although the details of transmission modeling were not mentioned in the study, the authors evaluated the performances of several models and scenarios. “Scenario 4, for example, was focused on in particular because it best captured the observed dynamics [for RSV] that emerged during the spring and summer of 2021,” Dr. Jarvis said.
“Pediatricians can speak to these trends firsthand. A decrease in expected RSV infections and hospitalizations in 2020, followed by an unprecedented and early increase in RSV infections and severity in 2021, and the factors that the authors account for make sense, such as reintroduction of RSV from other regions and low immunity in the population,” she said. “It also makes sense that, in these transmission modeling scenarios, the expected mean age of hospitalization because of RSV increased with a temporary (hopefully) increase in RSV hospitalizations in the 2021 season, and potentially the 2022 RSV season.”
As for additional research, Dr. Jarvis said she would like to see follow-up data on the RSV transmission modeling. “For example, with scenario 4, does this scenario continue to perform well in other time periods, such as the winter? If the modeling continues to be accurate during other periods of evaluation and reevaluation, this modeling could be very useful in helping pediatric clinics and hospitals to prepare for RSV care and hospital capacity management.”
The study was supported by grants to various researchers from the National Institute of Allergy and Infectious Diseases/National Institutes of Health, the National Center for Advancing Translational Science at the National Institutes of Health, and NIH Roadmap for Medical Research. Lead author Ms. Zheng had no financial conflicts to disclose. Her study coauthors disclosed relationships with companies including AbbVie, Merck, Pfizer, GlaxoSmithKline, MedImmune, and Janssen. Dr. Jarvis had no financial conflicts to disclose and serves on the Pediatric News editorial advisory board.
The impact of respiratory syncytial virus (RSV)will likely be greater in 2021 and 2022 in the United States than in previous years as a result of the ongoing COVID-19 pandemic, based on data from a simulation-modeling study involving approximately 19 million individuals.
Although RSV usually follows consistent patterns of timing and duration, the disease all but disappeared starting in March 2020 after the introduction of measures to mitigate the spread of COVID-19, Zhe Zheng, MBBS, of Yale University, New Haven, Conn., and colleagues wrote.
However, lifting of mitigation measures has resulted in emergence of RSV in various parts of the world in early 2021, and trends may be similar in the United States, but data are needed to plan for prophylaxis and hospital use, they noted.
In a study published in JAMA Network Open, the researchers developed a simulation model for epidemics of RSV based on historical data. They acquired inpatient records from New York during 2005-2014 and from California during 2003-2011. The primary clinical outcome was the estimated monthly hospitalizations for RSV.
The simulated study population was 19.45 million individuals. After evaluating several scenarios including continued low transmission associated with social distancing and other mitigation measures, the researchers focused on the likely scenario that introduction of RSV from other regions would likely spark RSV epidemics in the United States.
They determined that spring and summer 2021 would show an increase in hospitalizations for RSV. Overall, higher rates of virus introduction from other regions were associated with more intense spring and summer RSV epidemics, with the trade-off of smaller winter epidemics. In the model, the expected RSV epidemic in spring and summer 2021 in New York was small, with a peak incidence of 419 hospitalizations per 100,000 people in April; by contrast, for states with less seasonal variability, such as Florida, the model predicted a larger summer epidemic.
In the model, the mean age of hospitalization for children younger than 5 years for January 2022 was expected to be 1.17 years, compared with 0.84 years in January 2019, the researchers noted.
Across all age groups, the greatest relative increase in the incidence of RSV infection was predicted for children aged 1-4 years (ranging from 82% to 86%), as were lower respiratory infections (87%-101%) and hospitalization (99%-119%), compared with prepandemic levels.
Hospitalizations for children aged 1 year were predicted to double compared with prepandemic seasons; 707 per 100,000 children per year for 2021 and 2022 versus 355 per 100,000 children per year in a typical prepandemic season. However, the largest incidence of lower respiratory infections (30,075 per 100,000) was predicted for infants aged 3-5 months, and the largest incidence of hospitalizations (3,116 per 100,000) was predicted for infants younger than 3 months.
“Without virus importation, the risk of RSV infections across all age groups in the winter of 2021 and 2022 would be greater, as more susceptible individuals were spared from infections in the absence of summer epidemics,” the researchers noted.
The older mean hospitalization age seen in the model was similar to the reported median patient age in Australia both before the pandemic and during the reemergent RSV epidemic.
“This makes intuitive sense, since many children born in 2020 were spared from RSV infection due to the low virus activity; these children will be older when they get infected for the first time during the reemergent epidemics,” the researchers wrote. “Consequently, stakeholders should consider modifying prophylaxis guidelines to include high-risk infants less than 2 years of age for the 2021-2022 season.”
The study findings were limited by several factors including the lack of data on level of virus introduction or on the impact of lack of boosting on infants with only transplacentally acquired RSV antibodies, the researchers noted. Other limitations include the use of historical data and the lack of data on values outside those included in the model, as well as the inability to control for other factors that could influence RSV, such as vaccines or long-lasting antibodies.
However, the results suggest that the rate of imported infections is associated with RSV hospitalizations, and the model effectively captured the RSV epidemics in the United States in spring and summer 2021.
Models can guide clinical preparations
“Health care simulation modeling is a growing field, with very exciting implications,” Lenore Jarvis, MD, of George Washington University, Washington, said in an interview. The field has the potential ability to influence health care in a data-driven way, including, but not limited to, staffing and other hospital operations, as well as patient care decision-making. “In short, accurate modeling and predictions can help us to make informed health care decisions that can lead to increased quality of care, potential cost savings, and even to help save lives,” she said.
Although the details of transmission modeling were not mentioned in the study, the authors evaluated the performances of several models and scenarios. “Scenario 4, for example, was focused on in particular because it best captured the observed dynamics [for RSV] that emerged during the spring and summer of 2021,” Dr. Jarvis said.
“Pediatricians can speak to these trends firsthand. A decrease in expected RSV infections and hospitalizations in 2020, followed by an unprecedented and early increase in RSV infections and severity in 2021, and the factors that the authors account for make sense, such as reintroduction of RSV from other regions and low immunity in the population,” she said. “It also makes sense that, in these transmission modeling scenarios, the expected mean age of hospitalization because of RSV increased with a temporary (hopefully) increase in RSV hospitalizations in the 2021 season, and potentially the 2022 RSV season.”
As for additional research, Dr. Jarvis said she would like to see follow-up data on the RSV transmission modeling. “For example, with scenario 4, does this scenario continue to perform well in other time periods, such as the winter? If the modeling continues to be accurate during other periods of evaluation and reevaluation, this modeling could be very useful in helping pediatric clinics and hospitals to prepare for RSV care and hospital capacity management.”
The study was supported by grants to various researchers from the National Institute of Allergy and Infectious Diseases/National Institutes of Health, the National Center for Advancing Translational Science at the National Institutes of Health, and NIH Roadmap for Medical Research. Lead author Ms. Zheng had no financial conflicts to disclose. Her study coauthors disclosed relationships with companies including AbbVie, Merck, Pfizer, GlaxoSmithKline, MedImmune, and Janssen. Dr. Jarvis had no financial conflicts to disclose and serves on the Pediatric News editorial advisory board.
FROM JAMA NETWORK OPEN
FDA approves cabotegravir LA; New HIV PrEP option fills an important gap
SILVER SPRING, MD – .
The priority review approval was based on phase 2b-3 clinical trial data submitted to the agency this past August, after the study was stopped early due to encouraging efficacy results of the first pre-planned interim end-point analysis.
“Although TDF-FTC PrEP could be almost astoundingly effective in preventing HIV acquisition across populations and risk exposures, the adherence to the daily protocols was really challenging and difficult to attain initially and to maintain for some of our most vulnerable populations,” Raphael Landovitz, MD, MDC, lead study investigator and co-director of The Center for HIV Identification, Prevention, and Treatment Services at UCLA, Los Angeles, told this news organization.
Dr. Landovitz noted that population level benefits observed with PrEP were limited to people who were highly engaged in health care and well resourced, but the same benefits were not observed in the most vulnerable, highest-risk populations.
“The idea was, is there anything that we can do to improve ... choices for different options, some of which – like long-acting agents – would remove the obligation to adhere to daily prescribing or a post-coital and be more discreet,” he said.
Data demonstrated superiority versus TDF-FTC
Details of the prospective, phase 2b-3 randomized, double-blind, double-dummy, active-controlled trial among 4,566 cisgender MSM (men who have sex with men) and transgender women highlighted the superiority of CAB 600 mg intramuscularly versus placebo or active TDF-FTC (300 mg/200 mg), with CAB-LA reducing HIV infection risk by 66%. These results were published August 11 in the New England Journal of Medicine and previously reported by this news organization.
Investigators identified HIV infections in 57 participants (including 52 who acquired HIV infections after enrollment). The hazard ratio for incident HIV infection versus TDG-FTC was 0.34, P < .001. Notably, effects were consistent across prespecified subgroups and populations.
Additionally, integrase strand-transfer inhibitor (INSTI) resistance mutations were detected in 1 of 4 of baseline HIV infection cases among CAB participants, while 2 of 39 incident infections in TDF-FTC participants occurred despite drug concentrations indicating good PrEP adherence.
Adverse events, breakthrough infections, and other important considerations
Because the trial was halted early, long-term safety data were lacking, thereby prompting investigators to launch an ongoing, open-label extension. In the initial trial, injection site reactions were reported in 81.4% (1,724) of CAB participants, most beginning a median of 1 day (IQR 0-2 days) post-injection, mild to moderate in severity (60.8% pain, 23.7% tenderness), and lasting a median of 3 days (IQR 2-6 days). In comparison, injection site reactions were reported in 31.3% of TDF-FTC participants (who, incidentally, received at least one placebo injection).
Severe adverse events (grade 3 or higher) were similar between CAB and TDF-FTC groups, They consisted mostly of an increase in creatine kinase level (14.2% with CAB vs. 13.5% with TDF-FTC) and a decrease in creatinine clearance (7.0% with CAB vs. 8.3% with TDF-FTC).
Although weight gain was higher among CAB participants (1.23 kg/year vs. 0.37 kg/year, TDF-FTC participants), most of the differences were observed during the first 40 weeks and were driven by weight loss in the TDF-FDC group. Weight changes were similar (~1 kg/year) thereafter.
Importantly, study participants assigned CAB underwent an oral-tablet, 5-week lead-in phase, which might have contributed to eventual treatment failure.
In a companion piece published Nov. 1 in the Journal of Infectious Diseases, investigators noted that adherence to the oral lead-in was poor in roughly one-third of participants with incident, breakthrough infections. They wrote that the barriers to adherence with daily oral PrEP regimens coupled with the favorable CAB-LA safety profile suggested that “the oral phase before CAB-LA initiation might not be necessary or desirable.”
The question remains as to whether or not strategies entailing viral load or other RNA screening tests at follow-up clinic visits might be warranted.
“It’s one of the biggest sort of ‘what’s next’ questions that’s come out of this study,” Dr. Landovitz said. “We’re now testing the strategy of using viral load or RNA screening at every visit to see if, in fact, we can catch these breakthrough infections earlier and potentially avoid resistance,” he added.
Until more data are available, Dr. Landovitz said that “the guidance for the clinician would be that until you have resistance testing back on someone who breaks through cabotegravir PrEP to use a protease inhibitor-based treatment regimen, at least initially.”
Institutional changes to ensure delivery of injections, tracking, and follow-up to ensure optimal use of long-acting PrEP agents are likely to challenge already overburdened health care systems and may require additional strategies for implementation (for example, pharmacy or at-home administration). Despite these factors, CAB-LA approval is welcome news to clinicians and patients alike.
“We’re constantly searching for new drugs to expand our repertoire of what we can provide patients,” Lina Rosengren-Hovee, MD, MPH, assistant professor of medicine and infectious disease specialist at UNC Health, Chapel Hill, N.C., said in an interview. Dr. Rosengren-Hovee was not involved in the study.
“For folks under 30, the sexual and gender minority, Black, and Latino, they are the ones with the highest need for PrEP, that are in a position that places them at higher risk for HIV. Being able to offer an injectable option is ... a game changer,” she said.
Dr. Rosengren-Hovee reports no relevant financial relationships. Dr. Landovitz has consulting relationships with Gilead, Janssen, Roche, and Cepheus.
A version of this article first appeared on Medscape.com.
SILVER SPRING, MD – .
The priority review approval was based on phase 2b-3 clinical trial data submitted to the agency this past August, after the study was stopped early due to encouraging efficacy results of the first pre-planned interim end-point analysis.
“Although TDF-FTC PrEP could be almost astoundingly effective in preventing HIV acquisition across populations and risk exposures, the adherence to the daily protocols was really challenging and difficult to attain initially and to maintain for some of our most vulnerable populations,” Raphael Landovitz, MD, MDC, lead study investigator and co-director of The Center for HIV Identification, Prevention, and Treatment Services at UCLA, Los Angeles, told this news organization.
Dr. Landovitz noted that population level benefits observed with PrEP were limited to people who were highly engaged in health care and well resourced, but the same benefits were not observed in the most vulnerable, highest-risk populations.
“The idea was, is there anything that we can do to improve ... choices for different options, some of which – like long-acting agents – would remove the obligation to adhere to daily prescribing or a post-coital and be more discreet,” he said.
Data demonstrated superiority versus TDF-FTC
Details of the prospective, phase 2b-3 randomized, double-blind, double-dummy, active-controlled trial among 4,566 cisgender MSM (men who have sex with men) and transgender women highlighted the superiority of CAB 600 mg intramuscularly versus placebo or active TDF-FTC (300 mg/200 mg), with CAB-LA reducing HIV infection risk by 66%. These results were published August 11 in the New England Journal of Medicine and previously reported by this news organization.
Investigators identified HIV infections in 57 participants (including 52 who acquired HIV infections after enrollment). The hazard ratio for incident HIV infection versus TDG-FTC was 0.34, P < .001. Notably, effects were consistent across prespecified subgroups and populations.
Additionally, integrase strand-transfer inhibitor (INSTI) resistance mutations were detected in 1 of 4 of baseline HIV infection cases among CAB participants, while 2 of 39 incident infections in TDF-FTC participants occurred despite drug concentrations indicating good PrEP adherence.
Adverse events, breakthrough infections, and other important considerations
Because the trial was halted early, long-term safety data were lacking, thereby prompting investigators to launch an ongoing, open-label extension. In the initial trial, injection site reactions were reported in 81.4% (1,724) of CAB participants, most beginning a median of 1 day (IQR 0-2 days) post-injection, mild to moderate in severity (60.8% pain, 23.7% tenderness), and lasting a median of 3 days (IQR 2-6 days). In comparison, injection site reactions were reported in 31.3% of TDF-FTC participants (who, incidentally, received at least one placebo injection).
Severe adverse events (grade 3 or higher) were similar between CAB and TDF-FTC groups, They consisted mostly of an increase in creatine kinase level (14.2% with CAB vs. 13.5% with TDF-FTC) and a decrease in creatinine clearance (7.0% with CAB vs. 8.3% with TDF-FTC).
Although weight gain was higher among CAB participants (1.23 kg/year vs. 0.37 kg/year, TDF-FTC participants), most of the differences were observed during the first 40 weeks and were driven by weight loss in the TDF-FDC group. Weight changes were similar (~1 kg/year) thereafter.
Importantly, study participants assigned CAB underwent an oral-tablet, 5-week lead-in phase, which might have contributed to eventual treatment failure.
In a companion piece published Nov. 1 in the Journal of Infectious Diseases, investigators noted that adherence to the oral lead-in was poor in roughly one-third of participants with incident, breakthrough infections. They wrote that the barriers to adherence with daily oral PrEP regimens coupled with the favorable CAB-LA safety profile suggested that “the oral phase before CAB-LA initiation might not be necessary or desirable.”
The question remains as to whether or not strategies entailing viral load or other RNA screening tests at follow-up clinic visits might be warranted.
“It’s one of the biggest sort of ‘what’s next’ questions that’s come out of this study,” Dr. Landovitz said. “We’re now testing the strategy of using viral load or RNA screening at every visit to see if, in fact, we can catch these breakthrough infections earlier and potentially avoid resistance,” he added.
Until more data are available, Dr. Landovitz said that “the guidance for the clinician would be that until you have resistance testing back on someone who breaks through cabotegravir PrEP to use a protease inhibitor-based treatment regimen, at least initially.”
Institutional changes to ensure delivery of injections, tracking, and follow-up to ensure optimal use of long-acting PrEP agents are likely to challenge already overburdened health care systems and may require additional strategies for implementation (for example, pharmacy or at-home administration). Despite these factors, CAB-LA approval is welcome news to clinicians and patients alike.
“We’re constantly searching for new drugs to expand our repertoire of what we can provide patients,” Lina Rosengren-Hovee, MD, MPH, assistant professor of medicine and infectious disease specialist at UNC Health, Chapel Hill, N.C., said in an interview. Dr. Rosengren-Hovee was not involved in the study.
“For folks under 30, the sexual and gender minority, Black, and Latino, they are the ones with the highest need for PrEP, that are in a position that places them at higher risk for HIV. Being able to offer an injectable option is ... a game changer,” she said.
Dr. Rosengren-Hovee reports no relevant financial relationships. Dr. Landovitz has consulting relationships with Gilead, Janssen, Roche, and Cepheus.
A version of this article first appeared on Medscape.com.
SILVER SPRING, MD – .
The priority review approval was based on phase 2b-3 clinical trial data submitted to the agency this past August, after the study was stopped early due to encouraging efficacy results of the first pre-planned interim end-point analysis.
“Although TDF-FTC PrEP could be almost astoundingly effective in preventing HIV acquisition across populations and risk exposures, the adherence to the daily protocols was really challenging and difficult to attain initially and to maintain for some of our most vulnerable populations,” Raphael Landovitz, MD, MDC, lead study investigator and co-director of The Center for HIV Identification, Prevention, and Treatment Services at UCLA, Los Angeles, told this news organization.
Dr. Landovitz noted that population level benefits observed with PrEP were limited to people who were highly engaged in health care and well resourced, but the same benefits were not observed in the most vulnerable, highest-risk populations.
“The idea was, is there anything that we can do to improve ... choices for different options, some of which – like long-acting agents – would remove the obligation to adhere to daily prescribing or a post-coital and be more discreet,” he said.
Data demonstrated superiority versus TDF-FTC
Details of the prospective, phase 2b-3 randomized, double-blind, double-dummy, active-controlled trial among 4,566 cisgender MSM (men who have sex with men) and transgender women highlighted the superiority of CAB 600 mg intramuscularly versus placebo or active TDF-FTC (300 mg/200 mg), with CAB-LA reducing HIV infection risk by 66%. These results were published August 11 in the New England Journal of Medicine and previously reported by this news organization.
Investigators identified HIV infections in 57 participants (including 52 who acquired HIV infections after enrollment). The hazard ratio for incident HIV infection versus TDG-FTC was 0.34, P < .001. Notably, effects were consistent across prespecified subgroups and populations.
Additionally, integrase strand-transfer inhibitor (INSTI) resistance mutations were detected in 1 of 4 of baseline HIV infection cases among CAB participants, while 2 of 39 incident infections in TDF-FTC participants occurred despite drug concentrations indicating good PrEP adherence.
Adverse events, breakthrough infections, and other important considerations
Because the trial was halted early, long-term safety data were lacking, thereby prompting investigators to launch an ongoing, open-label extension. In the initial trial, injection site reactions were reported in 81.4% (1,724) of CAB participants, most beginning a median of 1 day (IQR 0-2 days) post-injection, mild to moderate in severity (60.8% pain, 23.7% tenderness), and lasting a median of 3 days (IQR 2-6 days). In comparison, injection site reactions were reported in 31.3% of TDF-FTC participants (who, incidentally, received at least one placebo injection).
Severe adverse events (grade 3 or higher) were similar between CAB and TDF-FTC groups, They consisted mostly of an increase in creatine kinase level (14.2% with CAB vs. 13.5% with TDF-FTC) and a decrease in creatinine clearance (7.0% with CAB vs. 8.3% with TDF-FTC).
Although weight gain was higher among CAB participants (1.23 kg/year vs. 0.37 kg/year, TDF-FTC participants), most of the differences were observed during the first 40 weeks and were driven by weight loss in the TDF-FDC group. Weight changes were similar (~1 kg/year) thereafter.
Importantly, study participants assigned CAB underwent an oral-tablet, 5-week lead-in phase, which might have contributed to eventual treatment failure.
In a companion piece published Nov. 1 in the Journal of Infectious Diseases, investigators noted that adherence to the oral lead-in was poor in roughly one-third of participants with incident, breakthrough infections. They wrote that the barriers to adherence with daily oral PrEP regimens coupled with the favorable CAB-LA safety profile suggested that “the oral phase before CAB-LA initiation might not be necessary or desirable.”
The question remains as to whether or not strategies entailing viral load or other RNA screening tests at follow-up clinic visits might be warranted.
“It’s one of the biggest sort of ‘what’s next’ questions that’s come out of this study,” Dr. Landovitz said. “We’re now testing the strategy of using viral load or RNA screening at every visit to see if, in fact, we can catch these breakthrough infections earlier and potentially avoid resistance,” he added.
Until more data are available, Dr. Landovitz said that “the guidance for the clinician would be that until you have resistance testing back on someone who breaks through cabotegravir PrEP to use a protease inhibitor-based treatment regimen, at least initially.”
Institutional changes to ensure delivery of injections, tracking, and follow-up to ensure optimal use of long-acting PrEP agents are likely to challenge already overburdened health care systems and may require additional strategies for implementation (for example, pharmacy or at-home administration). Despite these factors, CAB-LA approval is welcome news to clinicians and patients alike.
“We’re constantly searching for new drugs to expand our repertoire of what we can provide patients,” Lina Rosengren-Hovee, MD, MPH, assistant professor of medicine and infectious disease specialist at UNC Health, Chapel Hill, N.C., said in an interview. Dr. Rosengren-Hovee was not involved in the study.
“For folks under 30, the sexual and gender minority, Black, and Latino, they are the ones with the highest need for PrEP, that are in a position that places them at higher risk for HIV. Being able to offer an injectable option is ... a game changer,” she said.
Dr. Rosengren-Hovee reports no relevant financial relationships. Dr. Landovitz has consulting relationships with Gilead, Janssen, Roche, and Cepheus.
A version of this article first appeared on Medscape.com.
Axilla swelling after COVID booster puts focus on mammogram timing
This inflammation is caused by the enlargement of lymph nodes and can show up as an abnormal finding on mammograms and other types of chest scans, causing concern and even the need for additional imaging and follow up, wrote Constance D. Lehman, MD, PhD, and colleagues in an article published in Journal of the American College of Radiology.
Lymph node swelling is a normal immune system reaction to vaccination, and “COVID-19 vaccinations in the arm are a well-documented cause of inflammatory unilateral axillary adenopathy,” noted Dr. Lehman, in an interview. The side effect will occur on the side of the body where the patient received a vaccine, and it is not always noticeable to the woman experiencing it, she said.
“We’re finding that the patients’ bodies are responding to the booster in many ways that are similar to the initial COVID vaccines, with lymph node swelling, muscle aches and pains, headaches, and so on,” said Dr. Lehman, who is chief of breast imaging at the Massachusetts General Hospital, Boston. There have been no real differences in reactions between the Moderna and Pfizer vaccines, she added.
Because axillary lymph node swelling can obscure mammogram results, staff of at least a few imaging centers, including Penn State Breast Center in Hershey, Pa., and Providence Women’s Imaging Center in Torrance, Calif., told this news organization that they are asking women to delay mammogram imaging either 6 weeks or 4-6 weeks after getting a COVID-19 booster.
Experts’ suggestions on mammograms, boosters timing
Other experts, including Jessica Leung, MD, acknowledged that vaccine-related reactive adenopathy is seen after the booster dose and provided recommendations for the timing of getting mammograms and the booster with this in mind.
“I would recommend getting the screening mammogram first, which can be followed immediately by vaccination, even on the same day,” said Jessica Leung, MD, a professor of diagnostic radiology at the University of Texas MD Anderson Cancer Center in Houston, Tex.
“If this is not possible from the scheduling perspective, then the patient should consult her health care provider regarding whether it is okay to wait a bit after receiving the vaccine before getting her screening mammogram.”
The answer to that question will likely depend on the time interval since the prior mammogram and the patient’s personal risk factors for developing breast cancer. Dr. Leung noted. “This is all predicated on the assumption that the patient is asymptomatic. If she has any symptoms, for example a palpable breast lump, then she should seek medical attention regardless of timing of vaccination.”
The same holds true for boosters, she said.
She emphasized that careful consideration should be given before delaying the mammogram. “The medical community has a great deal more knowledge at this time than in the early days of COVID-19 vaccination, so we are often able to identify reactive adenopathy related to vaccination. If patients were to delay the mammogram, any reactive adenopathy may persist, on average, for 4-6 weeks.”
Debra Patt, MD, PhD, MBA, executive vice president at Texas Oncology, professor at the University of Texas at Austin, provided a specific example of when a patient should not delay the diagnostic imaging, which is “in the event that there is an abnormal mass in the breast that requires evaluation.”
Providers are now prepared to address these issues, she added.
Dr. Lehman’s nuanced recommendations
“It’s easy to get both a mammogram and booster, and just a matter of timing them – so that the reaction doesn’t interfere with the mammography results,” Dr. Lehman said.
But she emphasized that women should not be choosing between their mammograms or a booster. “We are now saying the same thing that we did with the initial vaccine,” said Dr. Lehman. “We don’t want patients delaying their mammograms, and we don’t want them delaying their boosters – both are critical to staying healthy.”
In her center, a model was developed to navigate vaccine-associated adenopathy. While this approach was developed for the primary vaccine series, the same applies for the booster, which is essentially a third dose of the same vaccine, explained Dr. Lehman.
When patients present for mammography, ultrasound, or MRI, the technologist will document their COVID-19 vaccination status (first or second dose or booster), the date it was given, and the location. Adding vaccination documentation to intake forms helps to support appropriate management of patients who undergo imaging after COVID-19 vaccination. Six weeks is used as the cutoff point for defining “recent” vaccination.
For patients who are getting a screening mammography or MRI, and who have no symptoms beyond unilateral axillary adenopathy on the same side of the body where they received the COVID-19 vaccination (given in the arm) within a 6-week period, the following is included in the screening mammography or screening MRI report: “In the specific setting of a patient with documented recent (within the past 6 weeks) COVID-19 vaccination in the ipsilateral arm, axillary adenopathy is a benign imaging finding. No further imaging is indicated at this time. If there is clinical concern that persists more than 6 weeks after the patient received the final vaccine dose, axillary ultrasound is recommended.”
The experts interviewed reported no conflicts of interest.
This inflammation is caused by the enlargement of lymph nodes and can show up as an abnormal finding on mammograms and other types of chest scans, causing concern and even the need for additional imaging and follow up, wrote Constance D. Lehman, MD, PhD, and colleagues in an article published in Journal of the American College of Radiology.
Lymph node swelling is a normal immune system reaction to vaccination, and “COVID-19 vaccinations in the arm are a well-documented cause of inflammatory unilateral axillary adenopathy,” noted Dr. Lehman, in an interview. The side effect will occur on the side of the body where the patient received a vaccine, and it is not always noticeable to the woman experiencing it, she said.
“We’re finding that the patients’ bodies are responding to the booster in many ways that are similar to the initial COVID vaccines, with lymph node swelling, muscle aches and pains, headaches, and so on,” said Dr. Lehman, who is chief of breast imaging at the Massachusetts General Hospital, Boston. There have been no real differences in reactions between the Moderna and Pfizer vaccines, she added.
Because axillary lymph node swelling can obscure mammogram results, staff of at least a few imaging centers, including Penn State Breast Center in Hershey, Pa., and Providence Women’s Imaging Center in Torrance, Calif., told this news organization that they are asking women to delay mammogram imaging either 6 weeks or 4-6 weeks after getting a COVID-19 booster.
Experts’ suggestions on mammograms, boosters timing
Other experts, including Jessica Leung, MD, acknowledged that vaccine-related reactive adenopathy is seen after the booster dose and provided recommendations for the timing of getting mammograms and the booster with this in mind.
“I would recommend getting the screening mammogram first, which can be followed immediately by vaccination, even on the same day,” said Jessica Leung, MD, a professor of diagnostic radiology at the University of Texas MD Anderson Cancer Center in Houston, Tex.
“If this is not possible from the scheduling perspective, then the patient should consult her health care provider regarding whether it is okay to wait a bit after receiving the vaccine before getting her screening mammogram.”
The answer to that question will likely depend on the time interval since the prior mammogram and the patient’s personal risk factors for developing breast cancer. Dr. Leung noted. “This is all predicated on the assumption that the patient is asymptomatic. If she has any symptoms, for example a palpable breast lump, then she should seek medical attention regardless of timing of vaccination.”
The same holds true for boosters, she said.
She emphasized that careful consideration should be given before delaying the mammogram. “The medical community has a great deal more knowledge at this time than in the early days of COVID-19 vaccination, so we are often able to identify reactive adenopathy related to vaccination. If patients were to delay the mammogram, any reactive adenopathy may persist, on average, for 4-6 weeks.”
Debra Patt, MD, PhD, MBA, executive vice president at Texas Oncology, professor at the University of Texas at Austin, provided a specific example of when a patient should not delay the diagnostic imaging, which is “in the event that there is an abnormal mass in the breast that requires evaluation.”
Providers are now prepared to address these issues, she added.
Dr. Lehman’s nuanced recommendations
“It’s easy to get both a mammogram and booster, and just a matter of timing them – so that the reaction doesn’t interfere with the mammography results,” Dr. Lehman said.
But she emphasized that women should not be choosing between their mammograms or a booster. “We are now saying the same thing that we did with the initial vaccine,” said Dr. Lehman. “We don’t want patients delaying their mammograms, and we don’t want them delaying their boosters – both are critical to staying healthy.”
In her center, a model was developed to navigate vaccine-associated adenopathy. While this approach was developed for the primary vaccine series, the same applies for the booster, which is essentially a third dose of the same vaccine, explained Dr. Lehman.
When patients present for mammography, ultrasound, or MRI, the technologist will document their COVID-19 vaccination status (first or second dose or booster), the date it was given, and the location. Adding vaccination documentation to intake forms helps to support appropriate management of patients who undergo imaging after COVID-19 vaccination. Six weeks is used as the cutoff point for defining “recent” vaccination.
For patients who are getting a screening mammography or MRI, and who have no symptoms beyond unilateral axillary adenopathy on the same side of the body where they received the COVID-19 vaccination (given in the arm) within a 6-week period, the following is included in the screening mammography or screening MRI report: “In the specific setting of a patient with documented recent (within the past 6 weeks) COVID-19 vaccination in the ipsilateral arm, axillary adenopathy is a benign imaging finding. No further imaging is indicated at this time. If there is clinical concern that persists more than 6 weeks after the patient received the final vaccine dose, axillary ultrasound is recommended.”
The experts interviewed reported no conflicts of interest.
This inflammation is caused by the enlargement of lymph nodes and can show up as an abnormal finding on mammograms and other types of chest scans, causing concern and even the need for additional imaging and follow up, wrote Constance D. Lehman, MD, PhD, and colleagues in an article published in Journal of the American College of Radiology.
Lymph node swelling is a normal immune system reaction to vaccination, and “COVID-19 vaccinations in the arm are a well-documented cause of inflammatory unilateral axillary adenopathy,” noted Dr. Lehman, in an interview. The side effect will occur on the side of the body where the patient received a vaccine, and it is not always noticeable to the woman experiencing it, she said.
“We’re finding that the patients’ bodies are responding to the booster in many ways that are similar to the initial COVID vaccines, with lymph node swelling, muscle aches and pains, headaches, and so on,” said Dr. Lehman, who is chief of breast imaging at the Massachusetts General Hospital, Boston. There have been no real differences in reactions between the Moderna and Pfizer vaccines, she added.
Because axillary lymph node swelling can obscure mammogram results, staff of at least a few imaging centers, including Penn State Breast Center in Hershey, Pa., and Providence Women’s Imaging Center in Torrance, Calif., told this news organization that they are asking women to delay mammogram imaging either 6 weeks or 4-6 weeks after getting a COVID-19 booster.
Experts’ suggestions on mammograms, boosters timing
Other experts, including Jessica Leung, MD, acknowledged that vaccine-related reactive adenopathy is seen after the booster dose and provided recommendations for the timing of getting mammograms and the booster with this in mind.
“I would recommend getting the screening mammogram first, which can be followed immediately by vaccination, even on the same day,” said Jessica Leung, MD, a professor of diagnostic radiology at the University of Texas MD Anderson Cancer Center in Houston, Tex.
“If this is not possible from the scheduling perspective, then the patient should consult her health care provider regarding whether it is okay to wait a bit after receiving the vaccine before getting her screening mammogram.”
The answer to that question will likely depend on the time interval since the prior mammogram and the patient’s personal risk factors for developing breast cancer. Dr. Leung noted. “This is all predicated on the assumption that the patient is asymptomatic. If she has any symptoms, for example a palpable breast lump, then she should seek medical attention regardless of timing of vaccination.”
The same holds true for boosters, she said.
She emphasized that careful consideration should be given before delaying the mammogram. “The medical community has a great deal more knowledge at this time than in the early days of COVID-19 vaccination, so we are often able to identify reactive adenopathy related to vaccination. If patients were to delay the mammogram, any reactive adenopathy may persist, on average, for 4-6 weeks.”
Debra Patt, MD, PhD, MBA, executive vice president at Texas Oncology, professor at the University of Texas at Austin, provided a specific example of when a patient should not delay the diagnostic imaging, which is “in the event that there is an abnormal mass in the breast that requires evaluation.”
Providers are now prepared to address these issues, she added.
Dr. Lehman’s nuanced recommendations
“It’s easy to get both a mammogram and booster, and just a matter of timing them – so that the reaction doesn’t interfere with the mammography results,” Dr. Lehman said.
But she emphasized that women should not be choosing between their mammograms or a booster. “We are now saying the same thing that we did with the initial vaccine,” said Dr. Lehman. “We don’t want patients delaying their mammograms, and we don’t want them delaying their boosters – both are critical to staying healthy.”
In her center, a model was developed to navigate vaccine-associated adenopathy. While this approach was developed for the primary vaccine series, the same applies for the booster, which is essentially a third dose of the same vaccine, explained Dr. Lehman.
When patients present for mammography, ultrasound, or MRI, the technologist will document their COVID-19 vaccination status (first or second dose or booster), the date it was given, and the location. Adding vaccination documentation to intake forms helps to support appropriate management of patients who undergo imaging after COVID-19 vaccination. Six weeks is used as the cutoff point for defining “recent” vaccination.
For patients who are getting a screening mammography or MRI, and who have no symptoms beyond unilateral axillary adenopathy on the same side of the body where they received the COVID-19 vaccination (given in the arm) within a 6-week period, the following is included in the screening mammography or screening MRI report: “In the specific setting of a patient with documented recent (within the past 6 weeks) COVID-19 vaccination in the ipsilateral arm, axillary adenopathy is a benign imaging finding. No further imaging is indicated at this time. If there is clinical concern that persists more than 6 weeks after the patient received the final vaccine dose, axillary ultrasound is recommended.”
The experts interviewed reported no conflicts of interest.
AAP updates guidance on HIV testing and prophylaxis in youth
Pediatricians should take a more proactive role in protecting children and adolescents from HIV infections, according to updated guidance from the American Academy of Pediatrics. The comprehensive new recommendations stress winning the trust and confidence of pediatric patients and reaffirm support for testing and treating adolescents without parental consent where state laws allow.
While the number of HIV-infected people in the United States remains high, most sexually active youth do not believe they are at risk and have never been tested, noted authors Katherine K. Hsu, MD, MPH, of the Massachusetts Department of Public Health and Boston University Medical Center, and Natella Yurievna Rakhmanina, MD, PhD, of Children’s National Hospital and George Washington University, both in Washington.
That is a knowledge gap that pediatricians are well situated to fill. “Pediatricians can play a key role in preventing and controlling HIV infection by promoting risk-reduction counseling and offering routine HIV testing and prophylaxis to adolescent and young adult (youth) patients,” they wrote on Dec. 20, 2021, in their study published in Pediatrics.
Key components of youth encounters, they stressed, is creating safe environments for obtaining an accurate sexual and reproductive health assessment and providing nonstigmatizing risk counseling.
According to Dr. Rakhmanina, major barriers to addressing preventive HIV counseling have included pediatricians’ lack of time, cultural differences, adolescents’ inaccurate responses, discomfort discussing sexual issues, and adolescents’ fear of parent or caregiver notification. Other concerns have been lack of adequate payment and insufficient training in how to talk to adolescents about sexual and reproductive issues.
According to the Centers for Disease Control and Prevention, at year end in 2018 an estimated 1,173,900 people age 13 or older were living with HIV infection in the United States, of whom 47,800 (4%) were adolescents and young adults 13-24 years of age.
These estimates include diagnosed and undiagnosed individuals. Between 2014 and 2018, new diagnoses of HIV infection accounted for 21% (7,817 of 37,515) of all new HIV diagnoses in the United States.
The new AAP clinical report updates policy statements from 2001 and again 2011 that encouraged HIV testing of all sexually active youth.
It reflects changes in epidemiology, advances in diagnostic testing with improved immunoassays, and updated recommendations for HIV testing and postexposure prophylaxis (PEP), as well as new guidance for pre-exposure prophylaxis (PrEP).
A 2017 study found that the 2011 HIV testing guidelines was associated with only a slight increase in HIV screening and a shift toward testing younger people and away from testing on the basis of risk.
Against this backdrop of persistent HIV infection and to-date modest uptake of earlier guidance, the 2021 statement made 14 main recommendations to pediatricians. Among these:
- Foster open discussion of gender and sexual orientation and behavior, as well as reproductive health issues.
- Recognize the clinical presentation of the acute retroviral syndrome, which can present as syndromes resembling infectious mononucleosis and influenza.
- Consider including virologic testing in the diagnostic workup of sexually active youth.
- Consider routine HIV screening for all youth 15 years or older at least once and rescreening high-risk youth. Those at higher risk should be rescreened at least annually, and potentially as frequently as every 3-6 months.
- Youth at substantial risk should be routinely offered PrEP, while PEP with antiretroviral drugs is indicated after unsafe exposures such as unsafe sexual activity, unsafe needle use, or sexual violence. Survivors of sexual violence should have baseline HIV testing and sexually transmitted infection (STI) screening and treatment. They should also be offered mental health and other supportive counseling.
- Test youth who request HIV screening at any time even in the absence of reported risk factors. Although parent or guardian involvement is preferable, in most legal settings the adolescent’s consent should suffice for testing and treatment.
- For youth with a positive HIV test, facilitate and confirm prompt linkage to age-appropriate HIV specialty care.
Will the current report’s recommendations be met with greater uptake than previous iterations? Yes, according to Maria E. Trent, MD, MPH, chief of the division of adolescent/young adult medicine at Johns Hopkins University, Baltimore, but a fundamental first step will be the establishment of honesty and confidentiality. “Pediatricians are essential stakeholders in HIV prevention and intervention efforts in the United States. Recent data, however, suggest that pediatricians often struggle to create the essential alone time with adolescents and young adults to conduct critical sexual health conversations that allow for adequate STI/HIV risk screening,” said Dr. Trent, who was not involved in the report. “Consistently creating that space will be the first task for ensuring adherence to these recommendations.”
Strategies to optimize risk screening for clinical decision support, such as confidential online previsit questionnaires that link to the electronic medical record, may facilitate discussions during the visit while maintaining clinician efficiency, she added.
Furthermore, while one-time general HIV screening during adolescence will be an easy goal, “integrating annual testing, biomedical intervention for PrEP/PEP, and ongoing follow-up and testing for those on biomedical intervention may present practical but not insurmountable challenges,” Dr. Trent said.
When pediatricians recognize that care is suboptimal in practice, ensuring that pediatricians have established linkages to adolescent-friendly services for free or low-cost HIV testing, PrEP/PEP, and HIV management will prevent gaps in care, Dr. Trent continued. “The most exciting development in health care is that telemedicine can now be used to work with young people, giving the practicing pediatrician more opportunities and flexibility to deliver and triage care.”
Will any of the guidelines such as an adolescent’s right to independent consent be considered unacceptable by parents? “While this part of the recommendations is not new, the thought that their adolescent can initiate and receive confidential care for HIV prevention or intervention without their knowledge or consent may initially be challenging to process,” Dr. Trent said. “Ultimately, what I’ve observed in practice is that parents are relieved and often proud of their young person for taking the initiative to engage in self-care to maintain their health and relieved to be involved as a critical support person.”
She added that pediatricians need to make their practice policies clear and have information available for parents on state laws related to confidential care. “They also need to carefully use the electronic health record to avoid errors in disclosures to proxies without patient consent.”
Dr. Rakhmanina agreed there will likely be greater adherence to this round of recommendations. “The culture of addressing sexual and reproductive health issues among adolescents in the U.S. is changing among pediatric providers, and we start seeing more champions of PrEP and HIV testing in our communities,” she said.
This study received no external funding. The authors had no financial relationships or potential conflicts of interest to disclose. Dr. Trent disclosed no competing interests relevant to her comments.
Pediatricians should take a more proactive role in protecting children and adolescents from HIV infections, according to updated guidance from the American Academy of Pediatrics. The comprehensive new recommendations stress winning the trust and confidence of pediatric patients and reaffirm support for testing and treating adolescents without parental consent where state laws allow.
While the number of HIV-infected people in the United States remains high, most sexually active youth do not believe they are at risk and have never been tested, noted authors Katherine K. Hsu, MD, MPH, of the Massachusetts Department of Public Health and Boston University Medical Center, and Natella Yurievna Rakhmanina, MD, PhD, of Children’s National Hospital and George Washington University, both in Washington.
That is a knowledge gap that pediatricians are well situated to fill. “Pediatricians can play a key role in preventing and controlling HIV infection by promoting risk-reduction counseling and offering routine HIV testing and prophylaxis to adolescent and young adult (youth) patients,” they wrote on Dec. 20, 2021, in their study published in Pediatrics.
Key components of youth encounters, they stressed, is creating safe environments for obtaining an accurate sexual and reproductive health assessment and providing nonstigmatizing risk counseling.
According to Dr. Rakhmanina, major barriers to addressing preventive HIV counseling have included pediatricians’ lack of time, cultural differences, adolescents’ inaccurate responses, discomfort discussing sexual issues, and adolescents’ fear of parent or caregiver notification. Other concerns have been lack of adequate payment and insufficient training in how to talk to adolescents about sexual and reproductive issues.
According to the Centers for Disease Control and Prevention, at year end in 2018 an estimated 1,173,900 people age 13 or older were living with HIV infection in the United States, of whom 47,800 (4%) were adolescents and young adults 13-24 years of age.
These estimates include diagnosed and undiagnosed individuals. Between 2014 and 2018, new diagnoses of HIV infection accounted for 21% (7,817 of 37,515) of all new HIV diagnoses in the United States.
The new AAP clinical report updates policy statements from 2001 and again 2011 that encouraged HIV testing of all sexually active youth.
It reflects changes in epidemiology, advances in diagnostic testing with improved immunoassays, and updated recommendations for HIV testing and postexposure prophylaxis (PEP), as well as new guidance for pre-exposure prophylaxis (PrEP).
A 2017 study found that the 2011 HIV testing guidelines was associated with only a slight increase in HIV screening and a shift toward testing younger people and away from testing on the basis of risk.
Against this backdrop of persistent HIV infection and to-date modest uptake of earlier guidance, the 2021 statement made 14 main recommendations to pediatricians. Among these:
- Foster open discussion of gender and sexual orientation and behavior, as well as reproductive health issues.
- Recognize the clinical presentation of the acute retroviral syndrome, which can present as syndromes resembling infectious mononucleosis and influenza.
- Consider including virologic testing in the diagnostic workup of sexually active youth.
- Consider routine HIV screening for all youth 15 years or older at least once and rescreening high-risk youth. Those at higher risk should be rescreened at least annually, and potentially as frequently as every 3-6 months.
- Youth at substantial risk should be routinely offered PrEP, while PEP with antiretroviral drugs is indicated after unsafe exposures such as unsafe sexual activity, unsafe needle use, or sexual violence. Survivors of sexual violence should have baseline HIV testing and sexually transmitted infection (STI) screening and treatment. They should also be offered mental health and other supportive counseling.
- Test youth who request HIV screening at any time even in the absence of reported risk factors. Although parent or guardian involvement is preferable, in most legal settings the adolescent’s consent should suffice for testing and treatment.
- For youth with a positive HIV test, facilitate and confirm prompt linkage to age-appropriate HIV specialty care.
Will the current report’s recommendations be met with greater uptake than previous iterations? Yes, according to Maria E. Trent, MD, MPH, chief of the division of adolescent/young adult medicine at Johns Hopkins University, Baltimore, but a fundamental first step will be the establishment of honesty and confidentiality. “Pediatricians are essential stakeholders in HIV prevention and intervention efforts in the United States. Recent data, however, suggest that pediatricians often struggle to create the essential alone time with adolescents and young adults to conduct critical sexual health conversations that allow for adequate STI/HIV risk screening,” said Dr. Trent, who was not involved in the report. “Consistently creating that space will be the first task for ensuring adherence to these recommendations.”
Strategies to optimize risk screening for clinical decision support, such as confidential online previsit questionnaires that link to the electronic medical record, may facilitate discussions during the visit while maintaining clinician efficiency, she added.
Furthermore, while one-time general HIV screening during adolescence will be an easy goal, “integrating annual testing, biomedical intervention for PrEP/PEP, and ongoing follow-up and testing for those on biomedical intervention may present practical but not insurmountable challenges,” Dr. Trent said.
When pediatricians recognize that care is suboptimal in practice, ensuring that pediatricians have established linkages to adolescent-friendly services for free or low-cost HIV testing, PrEP/PEP, and HIV management will prevent gaps in care, Dr. Trent continued. “The most exciting development in health care is that telemedicine can now be used to work with young people, giving the practicing pediatrician more opportunities and flexibility to deliver and triage care.”
Will any of the guidelines such as an adolescent’s right to independent consent be considered unacceptable by parents? “While this part of the recommendations is not new, the thought that their adolescent can initiate and receive confidential care for HIV prevention or intervention without their knowledge or consent may initially be challenging to process,” Dr. Trent said. “Ultimately, what I’ve observed in practice is that parents are relieved and often proud of their young person for taking the initiative to engage in self-care to maintain their health and relieved to be involved as a critical support person.”
She added that pediatricians need to make their practice policies clear and have information available for parents on state laws related to confidential care. “They also need to carefully use the electronic health record to avoid errors in disclosures to proxies without patient consent.”
Dr. Rakhmanina agreed there will likely be greater adherence to this round of recommendations. “The culture of addressing sexual and reproductive health issues among adolescents in the U.S. is changing among pediatric providers, and we start seeing more champions of PrEP and HIV testing in our communities,” she said.
This study received no external funding. The authors had no financial relationships or potential conflicts of interest to disclose. Dr. Trent disclosed no competing interests relevant to her comments.
Pediatricians should take a more proactive role in protecting children and adolescents from HIV infections, according to updated guidance from the American Academy of Pediatrics. The comprehensive new recommendations stress winning the trust and confidence of pediatric patients and reaffirm support for testing and treating adolescents without parental consent where state laws allow.
While the number of HIV-infected people in the United States remains high, most sexually active youth do not believe they are at risk and have never been tested, noted authors Katherine K. Hsu, MD, MPH, of the Massachusetts Department of Public Health and Boston University Medical Center, and Natella Yurievna Rakhmanina, MD, PhD, of Children’s National Hospital and George Washington University, both in Washington.
That is a knowledge gap that pediatricians are well situated to fill. “Pediatricians can play a key role in preventing and controlling HIV infection by promoting risk-reduction counseling and offering routine HIV testing and prophylaxis to adolescent and young adult (youth) patients,” they wrote on Dec. 20, 2021, in their study published in Pediatrics.
Key components of youth encounters, they stressed, is creating safe environments for obtaining an accurate sexual and reproductive health assessment and providing nonstigmatizing risk counseling.
According to Dr. Rakhmanina, major barriers to addressing preventive HIV counseling have included pediatricians’ lack of time, cultural differences, adolescents’ inaccurate responses, discomfort discussing sexual issues, and adolescents’ fear of parent or caregiver notification. Other concerns have been lack of adequate payment and insufficient training in how to talk to adolescents about sexual and reproductive issues.
According to the Centers for Disease Control and Prevention, at year end in 2018 an estimated 1,173,900 people age 13 or older were living with HIV infection in the United States, of whom 47,800 (4%) were adolescents and young adults 13-24 years of age.
These estimates include diagnosed and undiagnosed individuals. Between 2014 and 2018, new diagnoses of HIV infection accounted for 21% (7,817 of 37,515) of all new HIV diagnoses in the United States.
The new AAP clinical report updates policy statements from 2001 and again 2011 that encouraged HIV testing of all sexually active youth.
It reflects changes in epidemiology, advances in diagnostic testing with improved immunoassays, and updated recommendations for HIV testing and postexposure prophylaxis (PEP), as well as new guidance for pre-exposure prophylaxis (PrEP).
A 2017 study found that the 2011 HIV testing guidelines was associated with only a slight increase in HIV screening and a shift toward testing younger people and away from testing on the basis of risk.
Against this backdrop of persistent HIV infection and to-date modest uptake of earlier guidance, the 2021 statement made 14 main recommendations to pediatricians. Among these:
- Foster open discussion of gender and sexual orientation and behavior, as well as reproductive health issues.
- Recognize the clinical presentation of the acute retroviral syndrome, which can present as syndromes resembling infectious mononucleosis and influenza.
- Consider including virologic testing in the diagnostic workup of sexually active youth.
- Consider routine HIV screening for all youth 15 years or older at least once and rescreening high-risk youth. Those at higher risk should be rescreened at least annually, and potentially as frequently as every 3-6 months.
- Youth at substantial risk should be routinely offered PrEP, while PEP with antiretroviral drugs is indicated after unsafe exposures such as unsafe sexual activity, unsafe needle use, or sexual violence. Survivors of sexual violence should have baseline HIV testing and sexually transmitted infection (STI) screening and treatment. They should also be offered mental health and other supportive counseling.
- Test youth who request HIV screening at any time even in the absence of reported risk factors. Although parent or guardian involvement is preferable, in most legal settings the adolescent’s consent should suffice for testing and treatment.
- For youth with a positive HIV test, facilitate and confirm prompt linkage to age-appropriate HIV specialty care.
Will the current report’s recommendations be met with greater uptake than previous iterations? Yes, according to Maria E. Trent, MD, MPH, chief of the division of adolescent/young adult medicine at Johns Hopkins University, Baltimore, but a fundamental first step will be the establishment of honesty and confidentiality. “Pediatricians are essential stakeholders in HIV prevention and intervention efforts in the United States. Recent data, however, suggest that pediatricians often struggle to create the essential alone time with adolescents and young adults to conduct critical sexual health conversations that allow for adequate STI/HIV risk screening,” said Dr. Trent, who was not involved in the report. “Consistently creating that space will be the first task for ensuring adherence to these recommendations.”
Strategies to optimize risk screening for clinical decision support, such as confidential online previsit questionnaires that link to the electronic medical record, may facilitate discussions during the visit while maintaining clinician efficiency, she added.
Furthermore, while one-time general HIV screening during adolescence will be an easy goal, “integrating annual testing, biomedical intervention for PrEP/PEP, and ongoing follow-up and testing for those on biomedical intervention may present practical but not insurmountable challenges,” Dr. Trent said.
When pediatricians recognize that care is suboptimal in practice, ensuring that pediatricians have established linkages to adolescent-friendly services for free or low-cost HIV testing, PrEP/PEP, and HIV management will prevent gaps in care, Dr. Trent continued. “The most exciting development in health care is that telemedicine can now be used to work with young people, giving the practicing pediatrician more opportunities and flexibility to deliver and triage care.”
Will any of the guidelines such as an adolescent’s right to independent consent be considered unacceptable by parents? “While this part of the recommendations is not new, the thought that their adolescent can initiate and receive confidential care for HIV prevention or intervention without their knowledge or consent may initially be challenging to process,” Dr. Trent said. “Ultimately, what I’ve observed in practice is that parents are relieved and often proud of their young person for taking the initiative to engage in self-care to maintain their health and relieved to be involved as a critical support person.”
She added that pediatricians need to make their practice policies clear and have information available for parents on state laws related to confidential care. “They also need to carefully use the electronic health record to avoid errors in disclosures to proxies without patient consent.”
Dr. Rakhmanina agreed there will likely be greater adherence to this round of recommendations. “The culture of addressing sexual and reproductive health issues among adolescents in the U.S. is changing among pediatric providers, and we start seeing more champions of PrEP and HIV testing in our communities,” she said.
This study received no external funding. The authors had no financial relationships or potential conflicts of interest to disclose. Dr. Trent disclosed no competing interests relevant to her comments.
FROM PEDIATRICS