User login
For MD-IQ use only
Lack of food for thought: Starve a bacterium, feed an infection
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
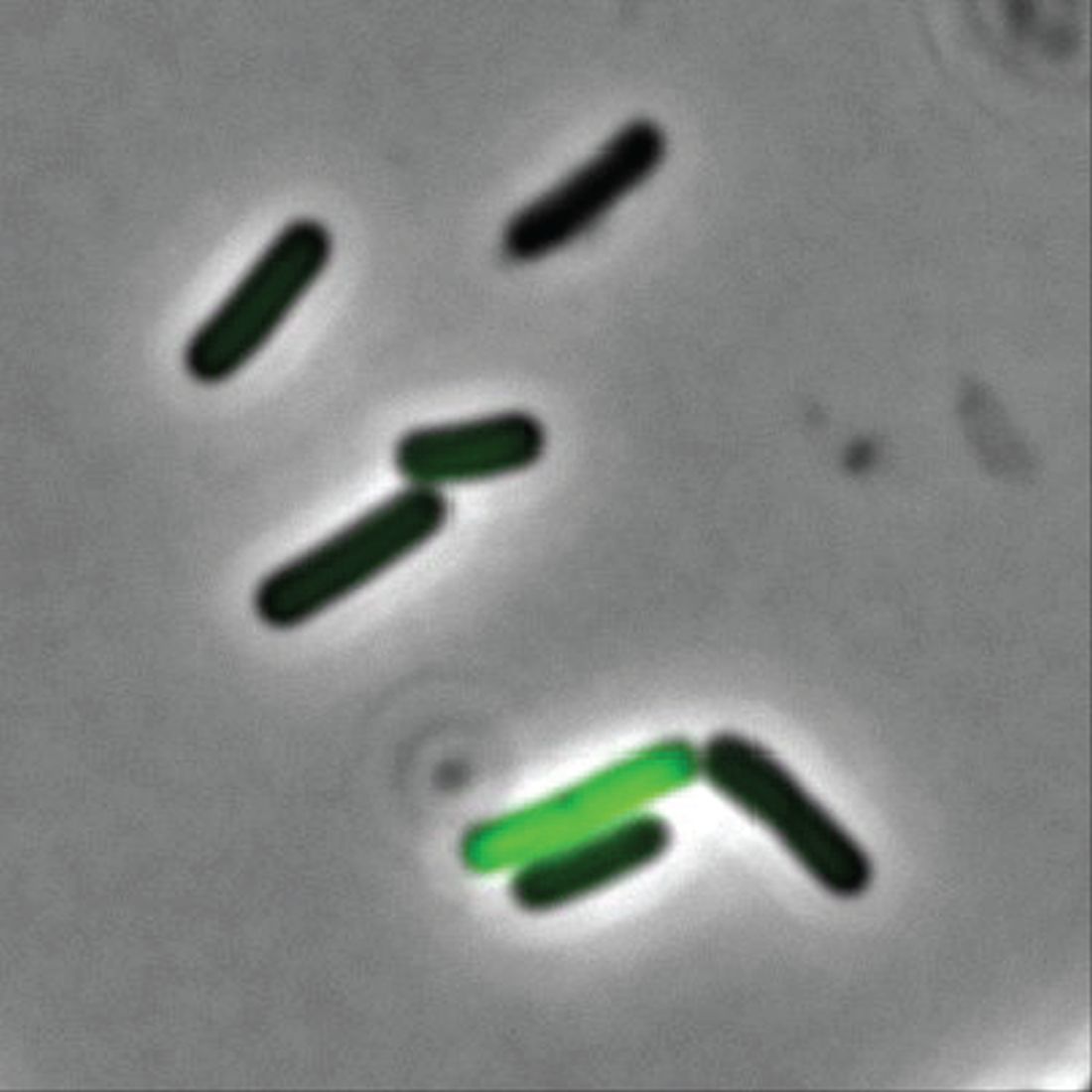
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
The sacrifice of orthodoxy: Maintaining collegiality in psychiatry
Psychiatrists practice in a wide array of ways. We approach our work and our patients with beliefs and preconceptions that develop over time. Our training has significant influence, though our own personalities and biases also affect our understanding.
Psychiatrists have philosophical lenses through which they see patients. We can reflect and see some standard archetypes. We are familiar with the reductionistic pharmacologist, the somatic treatment specialist, the psychodynamic ‘guru,’ and the medicolegally paralyzed practitioner. It is without judgment that we lay these out, for our very point is that we have these constituent parts within our own clinical identities. The intensity with which we subscribe to these clinical sensibilities could contribute to a biased orthodoxy.
Orthodoxy can be defined as an accepted theory that stems from an authoritative entity. This is a well-known phenomenon that continues to be visible. For example, one can quickly peruse psychodynamic literature to find one school of thought criticizing another. It is not without some confrontation and even interpersonal rifts that the lineage of psychoanalytic theory has evolved. This has always been of interest to us. A core facet of psychoanalysis is empathy, truly knowing the inner state of a different person. And yet, the very bastions of this clinical sensibility frequently resort to veiled attacks on those in their field who have opposing views. It then begs the question: If even enlightened institutions fail at a nonjudgmental approach toward their colleagues, what hope is there for the rest of us clinicians, mired in the thick of day-to-day clinical practice?
It is our contention that the odds are against us. Even the aforementioned critique of psychoanalytic orthodoxy is just another example of how we humans organize our experience. Even as we write an article in argument against unbridled critique, we find it difficult to do so without engaging in it. For to criticize another is to help shore up our own personal identities. This is especially the case when clinicians deal with issues that we feel strongly about. The human psyche has a need to organize its experience, as “our experience of ourselves is fundamental to how we operate in the world. Our subjective experience is the phenomenology of all that one might be aware of.”1
In this vein, we would like to cite attribution theory. This is a view of human behavior within social psychology. The Austrian psychologist Fritz Heider, PhD, investigated “the domain of social interactions, wondering how people perceive each other in interaction and especially how they make sense of each other’s behavior.”2 Attribution theory suggests that as humans organize our social interactions, we may make two basic assumptions. One is that our own behavior is highly affected by an environment that is beyond our control. The second is that when judging the behavior of others, we are more likely to attribute it to internal traits that they have. A classic example is automobile traffic. When we see someone driving erratically, we are more likely to blame them for being an inherently bad driver. However, if attention is called to our own driving, we are more likely to cite external factors such as rush hour, a bad driver around us, or a faulty vehicle.
We would like to reference one last model of human behavior. It has become customary within the field of neuroscience to view the brain as a predictive organ: “Theories of prediction in perception, action, and learning suggest that the brain serves to reduce the discrepancies between expectation and actual experience, i.e., by reducing the prediction error.”3 Perception itself has recently been described as a controlled hallucination, where the brain makes predictions of what it thinks it is about to see based on past experiences. Visual stimulus ultimately takes time to enter our eyes and be processed in the brain – “predictions would need to preactivate neural representations that would typically be driven by sensory input, before the actual arrival of that input.”4 It thus seems to be an inherent method of the brain to anticipate visual and even social events to help human beings sustain themselves.
Having spoken of a psychoanalytic conceptualization of self-organization, the theory of attribution, and research into social neuroscience, we turn our attention back to the central question that this article would like to address.
When we find ourselves busy in rote clinical practice, we believe the likelihood of intercollegiate mentalization is low; our ability to relate to our peers becomes strained. We ultimately do not practice in a vacuum. Psychiatrists, even those in a solo private practice, are ultimately part of a community of providers who, more or less, follow some emergent ‘standard of care.’ This can be a vague concept; but one that takes on a concrete form in the minds of certain clinicians and certainly in the setting of a medicolegal court. Yet, the psychiatrists that we know all have very stereotyped ways of practice. And at the heart of it, we all think that we are right.
We can use polypharmacy as an example. Imagine that you have a new patient intake, who tells you that they are transferring care from another psychiatrist. They inform you of their medication regimen. This patient presents on eight or more psychotropics. Many of us may have a visceral reaction at this point and, following the aforementioned attribution theory, we may ask ourselves what ‘quack’ of a doctor would do this. Yet some among us would think that a very competent psychopharmacologist was daring enough to use the full armamentarium of psychopharmacology to help this patient, who must be treatment refractory.
When speaking with such a patient, we would be quick to reflect on our own parsimonious use of medications. We would tell ourselves that we are responsible providers and would be quick to recommend discontinuation of medications. This would help us feel better about ourselves, and would of course assuage the ever-present medicolegal ‘big brother’ in our minds. It is through this very process that we affirm our self-identities. For if this patient’s previous physician was a bad psychiatrist, then we are a good psychiatrist. It is through this process that our clinical selves find confirmation.
We do not mean to reduce the complexities of human behavior to quick stereotypes. However, it is our belief that when confronted with clinical or philosophical disputes with our colleagues, the basic rules of human behavior will attempt to dissolve and override efforts at mentalization, collegiality, or interpersonal sensitivity. For to accept a clinical practice view that is different from ours would be akin to giving up the essence of our clinical identities. It could be compared to the fragmentation process of a vulnerable psyche when confronted with a reality that is at odds with preconceived notions and experiences.
While we may be able to appreciate the nuances and sensibilities of another provider, we believe it would be particularly difficult for most of us to actually attempt to practice in a fashion that is not congruent with our own organizers of experience. Whether or not our practice style is ‘perfect,’ it has worked for us. Social neuroscience and our understanding of the organization of the self would predict that we would hold onto our way of practice with all the mind’s defenses. Externalization, denial, and projection could all be called into action in this battle against existential fragmentation.
Do we seek to portray a clinical world where there is no hope for genuine modeling of clinical sensibilities to other psychiatrists? That is not our intention. Yet it seems that many of the theoretical frameworks that we subscribe to argue against this possibility. We would be hypocritical if we did not here state that our own theoretical frameworks are yet other examples of “organizers of experience.” Attribution theory, intersubjectivity, and social neuroscience are simply our ways of organizing the chaos of perceptions, ideas, and intricacies of human behavior.
If we accept that psychiatrists, like all human beings, are trapped in a subjective experience, then we can be more playful and flexible when interacting with our colleagues. We do not have to be as defensive of our practices and accusatory of others. If we practice daily according to some orthodoxy, then we color our experiences of the patient and of our colleagues’ ways of practice. We automatically start off on the wrong foot. And yet, to give up this orthodoxy would, by definition, be disorganizing and fragmenting to us. For as Nietzsche said, “truth is an illusion without which a certain species could not survive.”5
Dr. Khalafian practices full time as a general outpatient psychiatrist. He trained at the University of California, San Diego, for his psychiatric residency and currently works as a telepsychiatrist, serving an outpatient clinic population in northern California. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Badre and Dr. Khalafian have no conflicts of interest.
References
1. Buirski P and Haglund P. Making sense together: The intersubjective approach to psychotherapy. Northvale, NJ: Jason Aronson; 2001.
2. Malle BF. Attribution theories: How people make sense of behavior. In Chadee D (ed.), Theories in social psychology. pp. 72-95. Wiley-Blackwell; 2011.
3. Brown EC and Brune M. The role of prediction in social neuroscience. Front Hum Neurosci. 2012 May 24;6:147. doi: 10.3389/fnhum.2012.00147.
4. Blom T et al. Predictions drive neural representations of visual events ahead of incoming sensory information. Proc Natl Acad Sci USA. 2020 Mar 31;117(13):7510-7515. doi: 10.1073/pnas.1917777117.
5. Yalom I. The Gift of Therapy. Harper Perennial; 2002.
Psychiatrists practice in a wide array of ways. We approach our work and our patients with beliefs and preconceptions that develop over time. Our training has significant influence, though our own personalities and biases also affect our understanding.
Psychiatrists have philosophical lenses through which they see patients. We can reflect and see some standard archetypes. We are familiar with the reductionistic pharmacologist, the somatic treatment specialist, the psychodynamic ‘guru,’ and the medicolegally paralyzed practitioner. It is without judgment that we lay these out, for our very point is that we have these constituent parts within our own clinical identities. The intensity with which we subscribe to these clinical sensibilities could contribute to a biased orthodoxy.
Orthodoxy can be defined as an accepted theory that stems from an authoritative entity. This is a well-known phenomenon that continues to be visible. For example, one can quickly peruse psychodynamic literature to find one school of thought criticizing another. It is not without some confrontation and even interpersonal rifts that the lineage of psychoanalytic theory has evolved. This has always been of interest to us. A core facet of psychoanalysis is empathy, truly knowing the inner state of a different person. And yet, the very bastions of this clinical sensibility frequently resort to veiled attacks on those in their field who have opposing views. It then begs the question: If even enlightened institutions fail at a nonjudgmental approach toward their colleagues, what hope is there for the rest of us clinicians, mired in the thick of day-to-day clinical practice?
It is our contention that the odds are against us. Even the aforementioned critique of psychoanalytic orthodoxy is just another example of how we humans organize our experience. Even as we write an article in argument against unbridled critique, we find it difficult to do so without engaging in it. For to criticize another is to help shore up our own personal identities. This is especially the case when clinicians deal with issues that we feel strongly about. The human psyche has a need to organize its experience, as “our experience of ourselves is fundamental to how we operate in the world. Our subjective experience is the phenomenology of all that one might be aware of.”1
In this vein, we would like to cite attribution theory. This is a view of human behavior within social psychology. The Austrian psychologist Fritz Heider, PhD, investigated “the domain of social interactions, wondering how people perceive each other in interaction and especially how they make sense of each other’s behavior.”2 Attribution theory suggests that as humans organize our social interactions, we may make two basic assumptions. One is that our own behavior is highly affected by an environment that is beyond our control. The second is that when judging the behavior of others, we are more likely to attribute it to internal traits that they have. A classic example is automobile traffic. When we see someone driving erratically, we are more likely to blame them for being an inherently bad driver. However, if attention is called to our own driving, we are more likely to cite external factors such as rush hour, a bad driver around us, or a faulty vehicle.
We would like to reference one last model of human behavior. It has become customary within the field of neuroscience to view the brain as a predictive organ: “Theories of prediction in perception, action, and learning suggest that the brain serves to reduce the discrepancies between expectation and actual experience, i.e., by reducing the prediction error.”3 Perception itself has recently been described as a controlled hallucination, where the brain makes predictions of what it thinks it is about to see based on past experiences. Visual stimulus ultimately takes time to enter our eyes and be processed in the brain – “predictions would need to preactivate neural representations that would typically be driven by sensory input, before the actual arrival of that input.”4 It thus seems to be an inherent method of the brain to anticipate visual and even social events to help human beings sustain themselves.
Having spoken of a psychoanalytic conceptualization of self-organization, the theory of attribution, and research into social neuroscience, we turn our attention back to the central question that this article would like to address.
When we find ourselves busy in rote clinical practice, we believe the likelihood of intercollegiate mentalization is low; our ability to relate to our peers becomes strained. We ultimately do not practice in a vacuum. Psychiatrists, even those in a solo private practice, are ultimately part of a community of providers who, more or less, follow some emergent ‘standard of care.’ This can be a vague concept; but one that takes on a concrete form in the minds of certain clinicians and certainly in the setting of a medicolegal court. Yet, the psychiatrists that we know all have very stereotyped ways of practice. And at the heart of it, we all think that we are right.
We can use polypharmacy as an example. Imagine that you have a new patient intake, who tells you that they are transferring care from another psychiatrist. They inform you of their medication regimen. This patient presents on eight or more psychotropics. Many of us may have a visceral reaction at this point and, following the aforementioned attribution theory, we may ask ourselves what ‘quack’ of a doctor would do this. Yet some among us would think that a very competent psychopharmacologist was daring enough to use the full armamentarium of psychopharmacology to help this patient, who must be treatment refractory.
When speaking with such a patient, we would be quick to reflect on our own parsimonious use of medications. We would tell ourselves that we are responsible providers and would be quick to recommend discontinuation of medications. This would help us feel better about ourselves, and would of course assuage the ever-present medicolegal ‘big brother’ in our minds. It is through this very process that we affirm our self-identities. For if this patient’s previous physician was a bad psychiatrist, then we are a good psychiatrist. It is through this process that our clinical selves find confirmation.
We do not mean to reduce the complexities of human behavior to quick stereotypes. However, it is our belief that when confronted with clinical or philosophical disputes with our colleagues, the basic rules of human behavior will attempt to dissolve and override efforts at mentalization, collegiality, or interpersonal sensitivity. For to accept a clinical practice view that is different from ours would be akin to giving up the essence of our clinical identities. It could be compared to the fragmentation process of a vulnerable psyche when confronted with a reality that is at odds with preconceived notions and experiences.
While we may be able to appreciate the nuances and sensibilities of another provider, we believe it would be particularly difficult for most of us to actually attempt to practice in a fashion that is not congruent with our own organizers of experience. Whether or not our practice style is ‘perfect,’ it has worked for us. Social neuroscience and our understanding of the organization of the self would predict that we would hold onto our way of practice with all the mind’s defenses. Externalization, denial, and projection could all be called into action in this battle against existential fragmentation.
Do we seek to portray a clinical world where there is no hope for genuine modeling of clinical sensibilities to other psychiatrists? That is not our intention. Yet it seems that many of the theoretical frameworks that we subscribe to argue against this possibility. We would be hypocritical if we did not here state that our own theoretical frameworks are yet other examples of “organizers of experience.” Attribution theory, intersubjectivity, and social neuroscience are simply our ways of organizing the chaos of perceptions, ideas, and intricacies of human behavior.
If we accept that psychiatrists, like all human beings, are trapped in a subjective experience, then we can be more playful and flexible when interacting with our colleagues. We do not have to be as defensive of our practices and accusatory of others. If we practice daily according to some orthodoxy, then we color our experiences of the patient and of our colleagues’ ways of practice. We automatically start off on the wrong foot. And yet, to give up this orthodoxy would, by definition, be disorganizing and fragmenting to us. For as Nietzsche said, “truth is an illusion without which a certain species could not survive.”5
Dr. Khalafian practices full time as a general outpatient psychiatrist. He trained at the University of California, San Diego, for his psychiatric residency and currently works as a telepsychiatrist, serving an outpatient clinic population in northern California. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Badre and Dr. Khalafian have no conflicts of interest.
References
1. Buirski P and Haglund P. Making sense together: The intersubjective approach to psychotherapy. Northvale, NJ: Jason Aronson; 2001.
2. Malle BF. Attribution theories: How people make sense of behavior. In Chadee D (ed.), Theories in social psychology. pp. 72-95. Wiley-Blackwell; 2011.
3. Brown EC and Brune M. The role of prediction in social neuroscience. Front Hum Neurosci. 2012 May 24;6:147. doi: 10.3389/fnhum.2012.00147.
4. Blom T et al. Predictions drive neural representations of visual events ahead of incoming sensory information. Proc Natl Acad Sci USA. 2020 Mar 31;117(13):7510-7515. doi: 10.1073/pnas.1917777117.
5. Yalom I. The Gift of Therapy. Harper Perennial; 2002.
Psychiatrists practice in a wide array of ways. We approach our work and our patients with beliefs and preconceptions that develop over time. Our training has significant influence, though our own personalities and biases also affect our understanding.
Psychiatrists have philosophical lenses through which they see patients. We can reflect and see some standard archetypes. We are familiar with the reductionistic pharmacologist, the somatic treatment specialist, the psychodynamic ‘guru,’ and the medicolegally paralyzed practitioner. It is without judgment that we lay these out, for our very point is that we have these constituent parts within our own clinical identities. The intensity with which we subscribe to these clinical sensibilities could contribute to a biased orthodoxy.
Orthodoxy can be defined as an accepted theory that stems from an authoritative entity. This is a well-known phenomenon that continues to be visible. For example, one can quickly peruse psychodynamic literature to find one school of thought criticizing another. It is not without some confrontation and even interpersonal rifts that the lineage of psychoanalytic theory has evolved. This has always been of interest to us. A core facet of psychoanalysis is empathy, truly knowing the inner state of a different person. And yet, the very bastions of this clinical sensibility frequently resort to veiled attacks on those in their field who have opposing views. It then begs the question: If even enlightened institutions fail at a nonjudgmental approach toward their colleagues, what hope is there for the rest of us clinicians, mired in the thick of day-to-day clinical practice?
It is our contention that the odds are against us. Even the aforementioned critique of psychoanalytic orthodoxy is just another example of how we humans organize our experience. Even as we write an article in argument against unbridled critique, we find it difficult to do so without engaging in it. For to criticize another is to help shore up our own personal identities. This is especially the case when clinicians deal with issues that we feel strongly about. The human psyche has a need to organize its experience, as “our experience of ourselves is fundamental to how we operate in the world. Our subjective experience is the phenomenology of all that one might be aware of.”1
In this vein, we would like to cite attribution theory. This is a view of human behavior within social psychology. The Austrian psychologist Fritz Heider, PhD, investigated “the domain of social interactions, wondering how people perceive each other in interaction and especially how they make sense of each other’s behavior.”2 Attribution theory suggests that as humans organize our social interactions, we may make two basic assumptions. One is that our own behavior is highly affected by an environment that is beyond our control. The second is that when judging the behavior of others, we are more likely to attribute it to internal traits that they have. A classic example is automobile traffic. When we see someone driving erratically, we are more likely to blame them for being an inherently bad driver. However, if attention is called to our own driving, we are more likely to cite external factors such as rush hour, a bad driver around us, or a faulty vehicle.
We would like to reference one last model of human behavior. It has become customary within the field of neuroscience to view the brain as a predictive organ: “Theories of prediction in perception, action, and learning suggest that the brain serves to reduce the discrepancies between expectation and actual experience, i.e., by reducing the prediction error.”3 Perception itself has recently been described as a controlled hallucination, where the brain makes predictions of what it thinks it is about to see based on past experiences. Visual stimulus ultimately takes time to enter our eyes and be processed in the brain – “predictions would need to preactivate neural representations that would typically be driven by sensory input, before the actual arrival of that input.”4 It thus seems to be an inherent method of the brain to anticipate visual and even social events to help human beings sustain themselves.
Having spoken of a psychoanalytic conceptualization of self-organization, the theory of attribution, and research into social neuroscience, we turn our attention back to the central question that this article would like to address.
When we find ourselves busy in rote clinical practice, we believe the likelihood of intercollegiate mentalization is low; our ability to relate to our peers becomes strained. We ultimately do not practice in a vacuum. Psychiatrists, even those in a solo private practice, are ultimately part of a community of providers who, more or less, follow some emergent ‘standard of care.’ This can be a vague concept; but one that takes on a concrete form in the minds of certain clinicians and certainly in the setting of a medicolegal court. Yet, the psychiatrists that we know all have very stereotyped ways of practice. And at the heart of it, we all think that we are right.
We can use polypharmacy as an example. Imagine that you have a new patient intake, who tells you that they are transferring care from another psychiatrist. They inform you of their medication regimen. This patient presents on eight or more psychotropics. Many of us may have a visceral reaction at this point and, following the aforementioned attribution theory, we may ask ourselves what ‘quack’ of a doctor would do this. Yet some among us would think that a very competent psychopharmacologist was daring enough to use the full armamentarium of psychopharmacology to help this patient, who must be treatment refractory.
When speaking with such a patient, we would be quick to reflect on our own parsimonious use of medications. We would tell ourselves that we are responsible providers and would be quick to recommend discontinuation of medications. This would help us feel better about ourselves, and would of course assuage the ever-present medicolegal ‘big brother’ in our minds. It is through this very process that we affirm our self-identities. For if this patient’s previous physician was a bad psychiatrist, then we are a good psychiatrist. It is through this process that our clinical selves find confirmation.
We do not mean to reduce the complexities of human behavior to quick stereotypes. However, it is our belief that when confronted with clinical or philosophical disputes with our colleagues, the basic rules of human behavior will attempt to dissolve and override efforts at mentalization, collegiality, or interpersonal sensitivity. For to accept a clinical practice view that is different from ours would be akin to giving up the essence of our clinical identities. It could be compared to the fragmentation process of a vulnerable psyche when confronted with a reality that is at odds with preconceived notions and experiences.
While we may be able to appreciate the nuances and sensibilities of another provider, we believe it would be particularly difficult for most of us to actually attempt to practice in a fashion that is not congruent with our own organizers of experience. Whether or not our practice style is ‘perfect,’ it has worked for us. Social neuroscience and our understanding of the organization of the self would predict that we would hold onto our way of practice with all the mind’s defenses. Externalization, denial, and projection could all be called into action in this battle against existential fragmentation.
Do we seek to portray a clinical world where there is no hope for genuine modeling of clinical sensibilities to other psychiatrists? That is not our intention. Yet it seems that many of the theoretical frameworks that we subscribe to argue against this possibility. We would be hypocritical if we did not here state that our own theoretical frameworks are yet other examples of “organizers of experience.” Attribution theory, intersubjectivity, and social neuroscience are simply our ways of organizing the chaos of perceptions, ideas, and intricacies of human behavior.
If we accept that psychiatrists, like all human beings, are trapped in a subjective experience, then we can be more playful and flexible when interacting with our colleagues. We do not have to be as defensive of our practices and accusatory of others. If we practice daily according to some orthodoxy, then we color our experiences of the patient and of our colleagues’ ways of practice. We automatically start off on the wrong foot. And yet, to give up this orthodoxy would, by definition, be disorganizing and fragmenting to us. For as Nietzsche said, “truth is an illusion without which a certain species could not survive.”5
Dr. Khalafian practices full time as a general outpatient psychiatrist. He trained at the University of California, San Diego, for his psychiatric residency and currently works as a telepsychiatrist, serving an outpatient clinic population in northern California. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Badre and Dr. Khalafian have no conflicts of interest.
References
1. Buirski P and Haglund P. Making sense together: The intersubjective approach to psychotherapy. Northvale, NJ: Jason Aronson; 2001.
2. Malle BF. Attribution theories: How people make sense of behavior. In Chadee D (ed.), Theories in social psychology. pp. 72-95. Wiley-Blackwell; 2011.
3. Brown EC and Brune M. The role of prediction in social neuroscience. Front Hum Neurosci. 2012 May 24;6:147. doi: 10.3389/fnhum.2012.00147.
4. Blom T et al. Predictions drive neural representations of visual events ahead of incoming sensory information. Proc Natl Acad Sci USA. 2020 Mar 31;117(13):7510-7515. doi: 10.1073/pnas.1917777117.
5. Yalom I. The Gift of Therapy. Harper Perennial; 2002.
Deadly bacteria in recalled eye drops can spread person-to-person
according to a new report.
Scientists are concerned that the once-rare treatment-resistant bacteria found in the eyedrops can spread person-to-person, posing a risk of becoming a recurrent problem in the United States, The New York Times reported.
In January, EzriCare and Delsam Pharma artificial tears and ointment products were recalled after being linked to the bacterium P. aeruginosa. The bacteria have caused at least 68 infections, including three deaths and at least eight cases of blindness. The eyedrops were imported to the United States from India, and many of the cases occurred after the bacteria spread person-to-person at a long-term care facility in Connecticut, according to the Times, which cited FDA and Centers for Disease Control and Prevention lead investigator Maroya Walters, PhD.
Dr. Walters said the cases that caused death or blindness were traced to the EzriCare artificial tears product.
“It’s very hard to get rid of,” University of North Carolina at Chapel Hill infectious disease specialist David van Duin, MD, PhD, told the Times, noting that the bacteria cling to sink drains, water faucets, and other moist places.
The FDA said it had halted the import of the recalled products and has since visited the plant in India where they were made, which is owned by Global Pharma Healthcare. In a citation to the company dated March 2, the FDA listed nearly a dozen problems, such as dirty equipment and the absence of safety procedures and tests.
A version of this article originally appeared on WebMD.com.
according to a new report.
Scientists are concerned that the once-rare treatment-resistant bacteria found in the eyedrops can spread person-to-person, posing a risk of becoming a recurrent problem in the United States, The New York Times reported.
In January, EzriCare and Delsam Pharma artificial tears and ointment products were recalled after being linked to the bacterium P. aeruginosa. The bacteria have caused at least 68 infections, including three deaths and at least eight cases of blindness. The eyedrops were imported to the United States from India, and many of the cases occurred after the bacteria spread person-to-person at a long-term care facility in Connecticut, according to the Times, which cited FDA and Centers for Disease Control and Prevention lead investigator Maroya Walters, PhD.
Dr. Walters said the cases that caused death or blindness were traced to the EzriCare artificial tears product.
“It’s very hard to get rid of,” University of North Carolina at Chapel Hill infectious disease specialist David van Duin, MD, PhD, told the Times, noting that the bacteria cling to sink drains, water faucets, and other moist places.
The FDA said it had halted the import of the recalled products and has since visited the plant in India where they were made, which is owned by Global Pharma Healthcare. In a citation to the company dated March 2, the FDA listed nearly a dozen problems, such as dirty equipment and the absence of safety procedures and tests.
A version of this article originally appeared on WebMD.com.
according to a new report.
Scientists are concerned that the once-rare treatment-resistant bacteria found in the eyedrops can spread person-to-person, posing a risk of becoming a recurrent problem in the United States, The New York Times reported.
In January, EzriCare and Delsam Pharma artificial tears and ointment products were recalled after being linked to the bacterium P. aeruginosa. The bacteria have caused at least 68 infections, including three deaths and at least eight cases of blindness. The eyedrops were imported to the United States from India, and many of the cases occurred after the bacteria spread person-to-person at a long-term care facility in Connecticut, according to the Times, which cited FDA and Centers for Disease Control and Prevention lead investigator Maroya Walters, PhD.
Dr. Walters said the cases that caused death or blindness were traced to the EzriCare artificial tears product.
“It’s very hard to get rid of,” University of North Carolina at Chapel Hill infectious disease specialist David van Duin, MD, PhD, told the Times, noting that the bacteria cling to sink drains, water faucets, and other moist places.
The FDA said it had halted the import of the recalled products and has since visited the plant in India where they were made, which is owned by Global Pharma Healthcare. In a citation to the company dated March 2, the FDA listed nearly a dozen problems, such as dirty equipment and the absence of safety procedures and tests.
A version of this article originally appeared on WebMD.com.
The end of the telemedicine era?
I started taking care of Jim, a 68-year-old man with metastatic renal cell carcinoma back in the fall of 2018. Jim lived far from our clinic in the rural western Sierra Mountains and had a hard time getting to Santa Monica, but needed ongoing pain and symptom management, as well as follow-up visits with oncology and discussions with our teams about preparing for the end of life.
Luckily for Jim, the Centers for Medicare & Medicaid Services had relaxed the rules around telehealth because of the public health emergency, and we were easily able to provide telemedicine visits throughout the pandemic ensuring that Jim retained access to the care team that had managed his cancer for several years at that point. This would not have been possible without the use of telemedicine – at least not without great effort and expense by Jim to make frequent trips to our Santa Monica clinic.
So, you can imagine my apprehension when I received an email the other day from our billing department, informing billing providers like myself that “telehealth visits are still covered through the end of the year.” While this initially seemed like reassuring news, it immediately begged the question – what happens at the end of the year? What will care look like for patients like Jim who live at a significant distance from their providers?
The end of the COVID-19 public health emergency on May 11 has prompted states to reevaluate the future of telehealth for Medicaid and Medicare recipients. Most states plan to make some telehealth services permanent, particularly in rural areas. While other telehealth services have been extended through Dec. 31, 2024, under the Consolidated Appropriations Act of 2023.
But still, We can now see very ill patients in their own homes without imposing an undue burden on them to come in for yet another office visit. Prior to the public health emergency, our embedded palliative care program would see patients only when they were in the oncology clinic so as to not burden them with having to travel to yet another clinic. This made our palliative providers less efficient since patients were being seen by multiple providers in the same space, which led to some time spent waiting around. It also frequently tied up our clinic exam rooms for long periods of time, delaying care for patients sitting in the waiting room.
Telehealth changed that virtually overnight. With the widespread availability of smartphones and tablets, patients could stay at home and speak more comfortably in their own surroundings – especially about the difficult topics we tend to dig into in palliative care – such as fears, suffering, grief, loss, legacy, regret, trauma, gratitude, dying – without the impersonal, aseptic environment of a clinic. We could visit with their family/caregivers, kids, and their pets. We could tour their living space and see how they were managing from a functional standpoint. We could get to know aspects of our patients’ lives that we’d never have seen in the clinic that could help us understand their goals and values better and help care for them more fully.
The benefit to the institution was also measurable. We could see our patients faster – the time from referral to consult dropped dramatically because patients could be scheduled for next-day virtual visits instead of having to wait for them to come back to an oncology visit. We could do quick symptom-focused visits that prior to telehealth would have been conducted by phone without the ability to perform at the very least an observational physical exam of the patient, which is important when prescribing medications to medically frail populations.
If telemedicine goes, how will it affect outpatient palliative care?
If that goes away, I do not know what will happen to outpatient palliative care. I can tell you we will be much less efficient in terms of when we see patients. There will probably be a higher clinic burden to patients, as well as higher financial toxicity to patients (Parking in the structure attached to my office building is $22 per day). And, what about the uncaptured costs associated with transportation for those whose illness prevents them from driving themselves? This can range from Uber costs to the time cost for a patient’s family member to take off work and arrange for childcare in order to drive the patient to a clinic for a visit.
In February, I received emails from the Drug Enforcement Agency suggesting that they, too, may roll back providers’ ability to prescribe controlled substances to patients who are mainly receiving telehealth services. While I understand and fully support the need to curb inappropriate overprescribing of controlled medications, I am concerned about the unintended consequences to cancer patients who live at a remote distance from their oncologists and palliative care providers. I remain hopeful that DEA will consider a carveout exception for those patients who have cancer, are receiving palliative care services, or are deemed to be at the end of life, much like the chronic opioid guidelines developed by the Centers for Disease Control and Prevention have done.
Telemedicine in essential care
Back to Jim. Using telehealth and electronic prescribing, our oncology and palliative care programs were able to keep Jim comfortable and at home through the end of his life. He did not have to travel 3 hours each way to get care. He did not have to spend money on parking and gas, and his daughter did not have to take days off work and arrange for a babysitter in order to drive him to our clinic. We partnered with a local pharmacy that was willing to special order medications for Jim when his pain became worse and he required a long-acting opioid. We partnered with a local home health company that kept a close eye on Jim and let us know when he seemed to be declining further, prompting discussions about transitioning to hospice.
I’m proud of the fact that our group helped Jim stay in comfortable surroundings and out of the clinic and hospital over the last 6 months of his life, but that would never have happened without the safe and thoughtful use of telehealth by our team.
Ironically, because of a public health emergency, we were able to provide efficient and high-quality palliative care at the right time, to the right person, in the right place, satisfying CMS goals to provide better care for patients and whole populations at lower costs.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
I started taking care of Jim, a 68-year-old man with metastatic renal cell carcinoma back in the fall of 2018. Jim lived far from our clinic in the rural western Sierra Mountains and had a hard time getting to Santa Monica, but needed ongoing pain and symptom management, as well as follow-up visits with oncology and discussions with our teams about preparing for the end of life.
Luckily for Jim, the Centers for Medicare & Medicaid Services had relaxed the rules around telehealth because of the public health emergency, and we were easily able to provide telemedicine visits throughout the pandemic ensuring that Jim retained access to the care team that had managed his cancer for several years at that point. This would not have been possible without the use of telemedicine – at least not without great effort and expense by Jim to make frequent trips to our Santa Monica clinic.
So, you can imagine my apprehension when I received an email the other day from our billing department, informing billing providers like myself that “telehealth visits are still covered through the end of the year.” While this initially seemed like reassuring news, it immediately begged the question – what happens at the end of the year? What will care look like for patients like Jim who live at a significant distance from their providers?
The end of the COVID-19 public health emergency on May 11 has prompted states to reevaluate the future of telehealth for Medicaid and Medicare recipients. Most states plan to make some telehealth services permanent, particularly in rural areas. While other telehealth services have been extended through Dec. 31, 2024, under the Consolidated Appropriations Act of 2023.
But still, We can now see very ill patients in their own homes without imposing an undue burden on them to come in for yet another office visit. Prior to the public health emergency, our embedded palliative care program would see patients only when they were in the oncology clinic so as to not burden them with having to travel to yet another clinic. This made our palliative providers less efficient since patients were being seen by multiple providers in the same space, which led to some time spent waiting around. It also frequently tied up our clinic exam rooms for long periods of time, delaying care for patients sitting in the waiting room.
Telehealth changed that virtually overnight. With the widespread availability of smartphones and tablets, patients could stay at home and speak more comfortably in their own surroundings – especially about the difficult topics we tend to dig into in palliative care – such as fears, suffering, grief, loss, legacy, regret, trauma, gratitude, dying – without the impersonal, aseptic environment of a clinic. We could visit with their family/caregivers, kids, and their pets. We could tour their living space and see how they were managing from a functional standpoint. We could get to know aspects of our patients’ lives that we’d never have seen in the clinic that could help us understand their goals and values better and help care for them more fully.
The benefit to the institution was also measurable. We could see our patients faster – the time from referral to consult dropped dramatically because patients could be scheduled for next-day virtual visits instead of having to wait for them to come back to an oncology visit. We could do quick symptom-focused visits that prior to telehealth would have been conducted by phone without the ability to perform at the very least an observational physical exam of the patient, which is important when prescribing medications to medically frail populations.
If telemedicine goes, how will it affect outpatient palliative care?
If that goes away, I do not know what will happen to outpatient palliative care. I can tell you we will be much less efficient in terms of when we see patients. There will probably be a higher clinic burden to patients, as well as higher financial toxicity to patients (Parking in the structure attached to my office building is $22 per day). And, what about the uncaptured costs associated with transportation for those whose illness prevents them from driving themselves? This can range from Uber costs to the time cost for a patient’s family member to take off work and arrange for childcare in order to drive the patient to a clinic for a visit.
In February, I received emails from the Drug Enforcement Agency suggesting that they, too, may roll back providers’ ability to prescribe controlled substances to patients who are mainly receiving telehealth services. While I understand and fully support the need to curb inappropriate overprescribing of controlled medications, I am concerned about the unintended consequences to cancer patients who live at a remote distance from their oncologists and palliative care providers. I remain hopeful that DEA will consider a carveout exception for those patients who have cancer, are receiving palliative care services, or are deemed to be at the end of life, much like the chronic opioid guidelines developed by the Centers for Disease Control and Prevention have done.
Telemedicine in essential care
Back to Jim. Using telehealth and electronic prescribing, our oncology and palliative care programs were able to keep Jim comfortable and at home through the end of his life. He did not have to travel 3 hours each way to get care. He did not have to spend money on parking and gas, and his daughter did not have to take days off work and arrange for a babysitter in order to drive him to our clinic. We partnered with a local pharmacy that was willing to special order medications for Jim when his pain became worse and he required a long-acting opioid. We partnered with a local home health company that kept a close eye on Jim and let us know when he seemed to be declining further, prompting discussions about transitioning to hospice.
I’m proud of the fact that our group helped Jim stay in comfortable surroundings and out of the clinic and hospital over the last 6 months of his life, but that would never have happened without the safe and thoughtful use of telehealth by our team.
Ironically, because of a public health emergency, we were able to provide efficient and high-quality palliative care at the right time, to the right person, in the right place, satisfying CMS goals to provide better care for patients and whole populations at lower costs.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
I started taking care of Jim, a 68-year-old man with metastatic renal cell carcinoma back in the fall of 2018. Jim lived far from our clinic in the rural western Sierra Mountains and had a hard time getting to Santa Monica, but needed ongoing pain and symptom management, as well as follow-up visits with oncology and discussions with our teams about preparing for the end of life.
Luckily for Jim, the Centers for Medicare & Medicaid Services had relaxed the rules around telehealth because of the public health emergency, and we were easily able to provide telemedicine visits throughout the pandemic ensuring that Jim retained access to the care team that had managed his cancer for several years at that point. This would not have been possible without the use of telemedicine – at least not without great effort and expense by Jim to make frequent trips to our Santa Monica clinic.
So, you can imagine my apprehension when I received an email the other day from our billing department, informing billing providers like myself that “telehealth visits are still covered through the end of the year.” While this initially seemed like reassuring news, it immediately begged the question – what happens at the end of the year? What will care look like for patients like Jim who live at a significant distance from their providers?
The end of the COVID-19 public health emergency on May 11 has prompted states to reevaluate the future of telehealth for Medicaid and Medicare recipients. Most states plan to make some telehealth services permanent, particularly in rural areas. While other telehealth services have been extended through Dec. 31, 2024, under the Consolidated Appropriations Act of 2023.
But still, We can now see very ill patients in their own homes without imposing an undue burden on them to come in for yet another office visit. Prior to the public health emergency, our embedded palliative care program would see patients only when they were in the oncology clinic so as to not burden them with having to travel to yet another clinic. This made our palliative providers less efficient since patients were being seen by multiple providers in the same space, which led to some time spent waiting around. It also frequently tied up our clinic exam rooms for long periods of time, delaying care for patients sitting in the waiting room.
Telehealth changed that virtually overnight. With the widespread availability of smartphones and tablets, patients could stay at home and speak more comfortably in their own surroundings – especially about the difficult topics we tend to dig into in palliative care – such as fears, suffering, grief, loss, legacy, regret, trauma, gratitude, dying – without the impersonal, aseptic environment of a clinic. We could visit with their family/caregivers, kids, and their pets. We could tour their living space and see how they were managing from a functional standpoint. We could get to know aspects of our patients’ lives that we’d never have seen in the clinic that could help us understand their goals and values better and help care for them more fully.
The benefit to the institution was also measurable. We could see our patients faster – the time from referral to consult dropped dramatically because patients could be scheduled for next-day virtual visits instead of having to wait for them to come back to an oncology visit. We could do quick symptom-focused visits that prior to telehealth would have been conducted by phone without the ability to perform at the very least an observational physical exam of the patient, which is important when prescribing medications to medically frail populations.
If telemedicine goes, how will it affect outpatient palliative care?
If that goes away, I do not know what will happen to outpatient palliative care. I can tell you we will be much less efficient in terms of when we see patients. There will probably be a higher clinic burden to patients, as well as higher financial toxicity to patients (Parking in the structure attached to my office building is $22 per day). And, what about the uncaptured costs associated with transportation for those whose illness prevents them from driving themselves? This can range from Uber costs to the time cost for a patient’s family member to take off work and arrange for childcare in order to drive the patient to a clinic for a visit.
In February, I received emails from the Drug Enforcement Agency suggesting that they, too, may roll back providers’ ability to prescribe controlled substances to patients who are mainly receiving telehealth services. While I understand and fully support the need to curb inappropriate overprescribing of controlled medications, I am concerned about the unintended consequences to cancer patients who live at a remote distance from their oncologists and palliative care providers. I remain hopeful that DEA will consider a carveout exception for those patients who have cancer, are receiving palliative care services, or are deemed to be at the end of life, much like the chronic opioid guidelines developed by the Centers for Disease Control and Prevention have done.
Telemedicine in essential care
Back to Jim. Using telehealth and electronic prescribing, our oncology and palliative care programs were able to keep Jim comfortable and at home through the end of his life. He did not have to travel 3 hours each way to get care. He did not have to spend money on parking and gas, and his daughter did not have to take days off work and arrange for a babysitter in order to drive him to our clinic. We partnered with a local pharmacy that was willing to special order medications for Jim when his pain became worse and he required a long-acting opioid. We partnered with a local home health company that kept a close eye on Jim and let us know when he seemed to be declining further, prompting discussions about transitioning to hospice.
I’m proud of the fact that our group helped Jim stay in comfortable surroundings and out of the clinic and hospital over the last 6 months of his life, but that would never have happened without the safe and thoughtful use of telehealth by our team.
Ironically, because of a public health emergency, we were able to provide efficient and high-quality palliative care at the right time, to the right person, in the right place, satisfying CMS goals to provide better care for patients and whole populations at lower costs.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
Heart rate, cardiac phase influence perception of time
People’s perception of time is subjective and based not only on their emotional state but also on heartbeat and heart rate (HR), two new studies suggest.
Researchers studied young adults with an electrocardiogram (ECG), measuring electrical activity at millisecond resolution while participants listened to tones that varied in duration. Participants were asked to report whether certain tones were longer or shorter, in relation to others.
The researchers found that the momentary perception of time was not continuous but rather expanded or contracted with each heartbeat. When the heartbeat preceding a tone was shorter, participants regarded the tone as longer in duration; but when the preceding heartbeat was longer, the participants experienced the tone as shorter.
“Our findings suggest that there is a unique role that cardiac dynamics play in the momentary experience of time,” lead author Saeedah Sadeghi, MSc, a doctoral candidate in the department of psychology at Cornell University, Ithaca, N.Y., said in an interview.
The study was published online in Psychophysiology.
In a second study, published in the journal Current Biology, a separate team of researchers asked participants to judge whether a brief event – the presentation of a tone or an image – was shorter or longer than a reference duration. ECG was used to track systole and diastole when participants were presented with these events.
The researchers found that the durations were underestimated during systole and overestimated during diastole, suggesting that time seemed to “speed up” or “slow down,” based on cardiac contraction and relaxation. When participants rated the events as more arousing, their perceived durations contracted, even during diastole.
“In our new paper, we show that our heart shapes the perceived duration of events, so time passes quicker when the heart contracts but slower when the heart relaxes,” lead author Irena Arslanova, PhD, postdoctoral researcher in cognitive neuroscience, Royal Holloway University of London, told this news organization.
Temporal ‘wrinkles’
“Subjective time is malleable,” observed Ms. Sadeghi and colleagues in their report. “Rather than being a uniform dimension, perceived duration has ‘wrinkles,’ with certain intervals appearing to dilate or contract relative to objective time” – a phenomenon sometimes referred to as “distortion.”
“We have known that people aren’t always consistent in how they perceive time, and objective duration doesn’t always explain subjective perception of time,” Ms. Sadeghi said.
Although the potential role of the heart in the experience of time has been hypothesized, research into the heart-time connection has been limited, with previous studies focusing primarily on estimating the average cardiac measures on longer time scales over seconds to minutes.
The current study sought to investigate “the beat-by-beat fluctuations of the heart period on the experience of brief moments in time” because, compared with longer time scales, subsecond temporal perception “has different underlying mechanisms” and a subsecond stimulus can be a “small fraction of a heartbeat.”
To home in on this small fraction, the researchers studied 45 participants (aged 18-21), who listened to 210 tones ranging in duration from 80 ms (short) to 188 ms (long). The tones were linearly spaced at 18-ms increments (80, 98, 116, 134, 152, 170, 188).
Participants were asked to categorize each tone as “short” or “long.” All tones were randomly assigned to be synchronized either with the systolic or diastolic phase of the cardiac cycle (50% each). The tones were triggered by participants’ heartbeats.
In addition, participants engaged in a heartbeat-counting activity, in which they were asked not to touch their pulse but to count their heartbeats by tuning in to their bodily sensations at intervals of 25, 35, and 45 seconds.
‘Classical’ response
“Participants exhibited an increased heart period after tone onset, which returned to baseline following an average canonical bell shape,” the authors reported.
The researchers performed regression analyses to determine how, on average, the heart rate before the tone was related to perceived duration or how the amount of change after the tone was related to perceived duration.
They found that when the heart rate was higher before the tone, participants tended to be more accurate in their time perception. When the heartbeat preceding a tone was shorter, participants experienced the tone as longer; conversely, when the heartbeat was longer, they experienced the duration of the identical sound as shorter.
When participants focused their attention on the sounds, their heart rate was affected such that their orienting responses actually changed their heart rate and, in turn, their temporal perception.
“The orienting response is classical,” Ms. Sadeghi said. “When you attend to something unpredictable or novel, the act of orienting attention decreases the HR.”
She explained that the heartbeats are “noise to the brain.” When people need to perceive external events, “a decrease in HR facilitates the intake of things from outside and facilitates sensory intake.”
A lower HR “makes it easier for the person to take in the tone and perceive it, so it feels as though they perceive more of the tone and the duration seems longer – similarly, when the HR decreases.”
It is unknown whether this is a causal relationship, she cautioned, “but it seems as though the decrease in HR somehow makes it easier to ‘get’ more of the tone, which then appears to have longer duration.”
Bidirectional relationship
“We know that experienced time can be distorted,” said Dr. Arslanova. “Time flies by when we’re busy or having fun but drags on when we’re bored or waiting for something, yet we still don’t know how the brain gives rise to such elastic experience of time.”
The brain controls the heart in response to the information the heart provides about the state of the body, she noted, “but we have begun to see more research showing that the heart–brain relationship is bidirectional.”
This means that the heart plays a role in shaping “how we process information and experience emotions.” In this analysis, Dr. Arslanova and colleagues “wanted to study whether the heart also shapes the experience of time.”
To do so, they conducted two experiments.
In the first, participants (n = 28) were presented with brief events during systole or during diastole. The events took the form of an emotionally neutral visual shape or auditory tone, shown for durations of 200 to 400 ms.
Participants were asked whether these events were of longer or shorter duration, compared with a reference duration.
The researchers found significant main effect of cardiac phase systole (F(1,27) = 8.1, P =.01), with stimuli presented at diastole regarded, on average, as 7 ms longer than those presented at systole.
They also found a significant main effect of modality (F(1,27) = 5.7, P = .02), with tones judged, on average, as 13 ms longer than visual stimuli.
“This means that time ‘sped up’ during the heart’s contraction and ‘slowed down’ during the heart’s relaxation,” Dr. Arslanova said.
The effect of cardiac phase on duration perception was independent of changes in HR, the authors noted.
In the second experiment, participants performed a similar task, but this time, it involved the images of faces containing emotional expressions. The researchers again observed a similar pattern of time appearing to speed up during systole and slow down during diastole, with stimuli present at diastole regarded as being an average 9 ms longer than those presented at systole.
These opposing effects of systole and diastole on time perception were present only for low and average arousal ratings (b = 14.4 [SE 3.2], P < .001 and b = 9.2 [2.3], P <.001, respectively). However, this effect disappeared when arousal ratings increased (b = 4.1 [3.2] P =.21).
“Interestingly, when participants rated the events as more arousing, their perceived durations contracted, even during the heart’s relaxation,” Dr. Arslanova observed. “This means that in a nonaroused state, the two cardiac phases pull the experienced duration in opposite directions – time contracts, then expands.”
The findings “also predict that increasing HR would speed up passing time, making events seem shorter, because there will be a stronger influence from the heart’s contractions,” she said.
She described the relationship between time perception and emotion as complex, noting that the findings are important because they show “that the way we experience time cannot be examined in isolation from our body,” she said.
Converging evidence
Martin Wiener, PhD, assistant professor, George Mason University, Fairfax, Va., said both papers “provide converging evidence on the role of the heart in our perception of time.”
Together, “the results share that our sense of time – that is, our incoming sensory perception of the present ‘moment’ – is adjusted or ‘gated’ by both our HR and cardiac phase,” said Dr. Wiener, executive director of the Timing Research Forum.
The studies “provide a link between the body and the brain, in terms of our perception, and that we cannot study one without the context of the other,” said Dr. Wiener, who was not involved with the current study.
“All of this opens up a new avenue of research, and so it is very exciting to see,” Dr. Wiener stated.
No source of funding was listed for the study by Ms. Sadeghi and coauthors. They declared no relevant financial relationships.
Dr. Arslanova and coauthors declared no competing interests. Senior author Manos Tsakiris, PhD, receives funding from the European Research Council Consolidator Grant. Dr. Wiener declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People’s perception of time is subjective and based not only on their emotional state but also on heartbeat and heart rate (HR), two new studies suggest.
Researchers studied young adults with an electrocardiogram (ECG), measuring electrical activity at millisecond resolution while participants listened to tones that varied in duration. Participants were asked to report whether certain tones were longer or shorter, in relation to others.
The researchers found that the momentary perception of time was not continuous but rather expanded or contracted with each heartbeat. When the heartbeat preceding a tone was shorter, participants regarded the tone as longer in duration; but when the preceding heartbeat was longer, the participants experienced the tone as shorter.
“Our findings suggest that there is a unique role that cardiac dynamics play in the momentary experience of time,” lead author Saeedah Sadeghi, MSc, a doctoral candidate in the department of psychology at Cornell University, Ithaca, N.Y., said in an interview.
The study was published online in Psychophysiology.
In a second study, published in the journal Current Biology, a separate team of researchers asked participants to judge whether a brief event – the presentation of a tone or an image – was shorter or longer than a reference duration. ECG was used to track systole and diastole when participants were presented with these events.
The researchers found that the durations were underestimated during systole and overestimated during diastole, suggesting that time seemed to “speed up” or “slow down,” based on cardiac contraction and relaxation. When participants rated the events as more arousing, their perceived durations contracted, even during diastole.
“In our new paper, we show that our heart shapes the perceived duration of events, so time passes quicker when the heart contracts but slower when the heart relaxes,” lead author Irena Arslanova, PhD, postdoctoral researcher in cognitive neuroscience, Royal Holloway University of London, told this news organization.
Temporal ‘wrinkles’
“Subjective time is malleable,” observed Ms. Sadeghi and colleagues in their report. “Rather than being a uniform dimension, perceived duration has ‘wrinkles,’ with certain intervals appearing to dilate or contract relative to objective time” – a phenomenon sometimes referred to as “distortion.”
“We have known that people aren’t always consistent in how they perceive time, and objective duration doesn’t always explain subjective perception of time,” Ms. Sadeghi said.
Although the potential role of the heart in the experience of time has been hypothesized, research into the heart-time connection has been limited, with previous studies focusing primarily on estimating the average cardiac measures on longer time scales over seconds to minutes.
The current study sought to investigate “the beat-by-beat fluctuations of the heart period on the experience of brief moments in time” because, compared with longer time scales, subsecond temporal perception “has different underlying mechanisms” and a subsecond stimulus can be a “small fraction of a heartbeat.”
To home in on this small fraction, the researchers studied 45 participants (aged 18-21), who listened to 210 tones ranging in duration from 80 ms (short) to 188 ms (long). The tones were linearly spaced at 18-ms increments (80, 98, 116, 134, 152, 170, 188).
Participants were asked to categorize each tone as “short” or “long.” All tones were randomly assigned to be synchronized either with the systolic or diastolic phase of the cardiac cycle (50% each). The tones were triggered by participants’ heartbeats.
In addition, participants engaged in a heartbeat-counting activity, in which they were asked not to touch their pulse but to count their heartbeats by tuning in to their bodily sensations at intervals of 25, 35, and 45 seconds.
‘Classical’ response
“Participants exhibited an increased heart period after tone onset, which returned to baseline following an average canonical bell shape,” the authors reported.
The researchers performed regression analyses to determine how, on average, the heart rate before the tone was related to perceived duration or how the amount of change after the tone was related to perceived duration.
They found that when the heart rate was higher before the tone, participants tended to be more accurate in their time perception. When the heartbeat preceding a tone was shorter, participants experienced the tone as longer; conversely, when the heartbeat was longer, they experienced the duration of the identical sound as shorter.
When participants focused their attention on the sounds, their heart rate was affected such that their orienting responses actually changed their heart rate and, in turn, their temporal perception.
“The orienting response is classical,” Ms. Sadeghi said. “When you attend to something unpredictable or novel, the act of orienting attention decreases the HR.”
She explained that the heartbeats are “noise to the brain.” When people need to perceive external events, “a decrease in HR facilitates the intake of things from outside and facilitates sensory intake.”
A lower HR “makes it easier for the person to take in the tone and perceive it, so it feels as though they perceive more of the tone and the duration seems longer – similarly, when the HR decreases.”
It is unknown whether this is a causal relationship, she cautioned, “but it seems as though the decrease in HR somehow makes it easier to ‘get’ more of the tone, which then appears to have longer duration.”
Bidirectional relationship
“We know that experienced time can be distorted,” said Dr. Arslanova. “Time flies by when we’re busy or having fun but drags on when we’re bored or waiting for something, yet we still don’t know how the brain gives rise to such elastic experience of time.”
The brain controls the heart in response to the information the heart provides about the state of the body, she noted, “but we have begun to see more research showing that the heart–brain relationship is bidirectional.”
This means that the heart plays a role in shaping “how we process information and experience emotions.” In this analysis, Dr. Arslanova and colleagues “wanted to study whether the heart also shapes the experience of time.”
To do so, they conducted two experiments.
In the first, participants (n = 28) were presented with brief events during systole or during diastole. The events took the form of an emotionally neutral visual shape or auditory tone, shown for durations of 200 to 400 ms.
Participants were asked whether these events were of longer or shorter duration, compared with a reference duration.
The researchers found significant main effect of cardiac phase systole (F(1,27) = 8.1, P =.01), with stimuli presented at diastole regarded, on average, as 7 ms longer than those presented at systole.
They also found a significant main effect of modality (F(1,27) = 5.7, P = .02), with tones judged, on average, as 13 ms longer than visual stimuli.
“This means that time ‘sped up’ during the heart’s contraction and ‘slowed down’ during the heart’s relaxation,” Dr. Arslanova said.
The effect of cardiac phase on duration perception was independent of changes in HR, the authors noted.
In the second experiment, participants performed a similar task, but this time, it involved the images of faces containing emotional expressions. The researchers again observed a similar pattern of time appearing to speed up during systole and slow down during diastole, with stimuli present at diastole regarded as being an average 9 ms longer than those presented at systole.
These opposing effects of systole and diastole on time perception were present only for low and average arousal ratings (b = 14.4 [SE 3.2], P < .001 and b = 9.2 [2.3], P <.001, respectively). However, this effect disappeared when arousal ratings increased (b = 4.1 [3.2] P =.21).
“Interestingly, when participants rated the events as more arousing, their perceived durations contracted, even during the heart’s relaxation,” Dr. Arslanova observed. “This means that in a nonaroused state, the two cardiac phases pull the experienced duration in opposite directions – time contracts, then expands.”
The findings “also predict that increasing HR would speed up passing time, making events seem shorter, because there will be a stronger influence from the heart’s contractions,” she said.
She described the relationship between time perception and emotion as complex, noting that the findings are important because they show “that the way we experience time cannot be examined in isolation from our body,” she said.
Converging evidence
Martin Wiener, PhD, assistant professor, George Mason University, Fairfax, Va., said both papers “provide converging evidence on the role of the heart in our perception of time.”
Together, “the results share that our sense of time – that is, our incoming sensory perception of the present ‘moment’ – is adjusted or ‘gated’ by both our HR and cardiac phase,” said Dr. Wiener, executive director of the Timing Research Forum.
The studies “provide a link between the body and the brain, in terms of our perception, and that we cannot study one without the context of the other,” said Dr. Wiener, who was not involved with the current study.
“All of this opens up a new avenue of research, and so it is very exciting to see,” Dr. Wiener stated.
No source of funding was listed for the study by Ms. Sadeghi and coauthors. They declared no relevant financial relationships.
Dr. Arslanova and coauthors declared no competing interests. Senior author Manos Tsakiris, PhD, receives funding from the European Research Council Consolidator Grant. Dr. Wiener declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People’s perception of time is subjective and based not only on their emotional state but also on heartbeat and heart rate (HR), two new studies suggest.
Researchers studied young adults with an electrocardiogram (ECG), measuring electrical activity at millisecond resolution while participants listened to tones that varied in duration. Participants were asked to report whether certain tones were longer or shorter, in relation to others.
The researchers found that the momentary perception of time was not continuous but rather expanded or contracted with each heartbeat. When the heartbeat preceding a tone was shorter, participants regarded the tone as longer in duration; but when the preceding heartbeat was longer, the participants experienced the tone as shorter.
“Our findings suggest that there is a unique role that cardiac dynamics play in the momentary experience of time,” lead author Saeedah Sadeghi, MSc, a doctoral candidate in the department of psychology at Cornell University, Ithaca, N.Y., said in an interview.
The study was published online in Psychophysiology.
In a second study, published in the journal Current Biology, a separate team of researchers asked participants to judge whether a brief event – the presentation of a tone or an image – was shorter or longer than a reference duration. ECG was used to track systole and diastole when participants were presented with these events.
The researchers found that the durations were underestimated during systole and overestimated during diastole, suggesting that time seemed to “speed up” or “slow down,” based on cardiac contraction and relaxation. When participants rated the events as more arousing, their perceived durations contracted, even during diastole.
“In our new paper, we show that our heart shapes the perceived duration of events, so time passes quicker when the heart contracts but slower when the heart relaxes,” lead author Irena Arslanova, PhD, postdoctoral researcher in cognitive neuroscience, Royal Holloway University of London, told this news organization.
Temporal ‘wrinkles’
“Subjective time is malleable,” observed Ms. Sadeghi and colleagues in their report. “Rather than being a uniform dimension, perceived duration has ‘wrinkles,’ with certain intervals appearing to dilate or contract relative to objective time” – a phenomenon sometimes referred to as “distortion.”
“We have known that people aren’t always consistent in how they perceive time, and objective duration doesn’t always explain subjective perception of time,” Ms. Sadeghi said.
Although the potential role of the heart in the experience of time has been hypothesized, research into the heart-time connection has been limited, with previous studies focusing primarily on estimating the average cardiac measures on longer time scales over seconds to minutes.
The current study sought to investigate “the beat-by-beat fluctuations of the heart period on the experience of brief moments in time” because, compared with longer time scales, subsecond temporal perception “has different underlying mechanisms” and a subsecond stimulus can be a “small fraction of a heartbeat.”
To home in on this small fraction, the researchers studied 45 participants (aged 18-21), who listened to 210 tones ranging in duration from 80 ms (short) to 188 ms (long). The tones were linearly spaced at 18-ms increments (80, 98, 116, 134, 152, 170, 188).
Participants were asked to categorize each tone as “short” or “long.” All tones were randomly assigned to be synchronized either with the systolic or diastolic phase of the cardiac cycle (50% each). The tones were triggered by participants’ heartbeats.
In addition, participants engaged in a heartbeat-counting activity, in which they were asked not to touch their pulse but to count their heartbeats by tuning in to their bodily sensations at intervals of 25, 35, and 45 seconds.
‘Classical’ response
“Participants exhibited an increased heart period after tone onset, which returned to baseline following an average canonical bell shape,” the authors reported.
The researchers performed regression analyses to determine how, on average, the heart rate before the tone was related to perceived duration or how the amount of change after the tone was related to perceived duration.
They found that when the heart rate was higher before the tone, participants tended to be more accurate in their time perception. When the heartbeat preceding a tone was shorter, participants experienced the tone as longer; conversely, when the heartbeat was longer, they experienced the duration of the identical sound as shorter.
When participants focused their attention on the sounds, their heart rate was affected such that their orienting responses actually changed their heart rate and, in turn, their temporal perception.
“The orienting response is classical,” Ms. Sadeghi said. “When you attend to something unpredictable or novel, the act of orienting attention decreases the HR.”
She explained that the heartbeats are “noise to the brain.” When people need to perceive external events, “a decrease in HR facilitates the intake of things from outside and facilitates sensory intake.”
A lower HR “makes it easier for the person to take in the tone and perceive it, so it feels as though they perceive more of the tone and the duration seems longer – similarly, when the HR decreases.”
It is unknown whether this is a causal relationship, she cautioned, “but it seems as though the decrease in HR somehow makes it easier to ‘get’ more of the tone, which then appears to have longer duration.”
Bidirectional relationship
“We know that experienced time can be distorted,” said Dr. Arslanova. “Time flies by when we’re busy or having fun but drags on when we’re bored or waiting for something, yet we still don’t know how the brain gives rise to such elastic experience of time.”
The brain controls the heart in response to the information the heart provides about the state of the body, she noted, “but we have begun to see more research showing that the heart–brain relationship is bidirectional.”
This means that the heart plays a role in shaping “how we process information and experience emotions.” In this analysis, Dr. Arslanova and colleagues “wanted to study whether the heart also shapes the experience of time.”
To do so, they conducted two experiments.
In the first, participants (n = 28) were presented with brief events during systole or during diastole. The events took the form of an emotionally neutral visual shape or auditory tone, shown for durations of 200 to 400 ms.
Participants were asked whether these events were of longer or shorter duration, compared with a reference duration.
The researchers found significant main effect of cardiac phase systole (F(1,27) = 8.1, P =.01), with stimuli presented at diastole regarded, on average, as 7 ms longer than those presented at systole.
They also found a significant main effect of modality (F(1,27) = 5.7, P = .02), with tones judged, on average, as 13 ms longer than visual stimuli.
“This means that time ‘sped up’ during the heart’s contraction and ‘slowed down’ during the heart’s relaxation,” Dr. Arslanova said.
The effect of cardiac phase on duration perception was independent of changes in HR, the authors noted.
In the second experiment, participants performed a similar task, but this time, it involved the images of faces containing emotional expressions. The researchers again observed a similar pattern of time appearing to speed up during systole and slow down during diastole, with stimuli present at diastole regarded as being an average 9 ms longer than those presented at systole.
These opposing effects of systole and diastole on time perception were present only for low and average arousal ratings (b = 14.4 [SE 3.2], P < .001 and b = 9.2 [2.3], P <.001, respectively). However, this effect disappeared when arousal ratings increased (b = 4.1 [3.2] P =.21).
“Interestingly, when participants rated the events as more arousing, their perceived durations contracted, even during the heart’s relaxation,” Dr. Arslanova observed. “This means that in a nonaroused state, the two cardiac phases pull the experienced duration in opposite directions – time contracts, then expands.”
The findings “also predict that increasing HR would speed up passing time, making events seem shorter, because there will be a stronger influence from the heart’s contractions,” she said.
She described the relationship between time perception and emotion as complex, noting that the findings are important because they show “that the way we experience time cannot be examined in isolation from our body,” she said.
Converging evidence
Martin Wiener, PhD, assistant professor, George Mason University, Fairfax, Va., said both papers “provide converging evidence on the role of the heart in our perception of time.”
Together, “the results share that our sense of time – that is, our incoming sensory perception of the present ‘moment’ – is adjusted or ‘gated’ by both our HR and cardiac phase,” said Dr. Wiener, executive director of the Timing Research Forum.
The studies “provide a link between the body and the brain, in terms of our perception, and that we cannot study one without the context of the other,” said Dr. Wiener, who was not involved with the current study.
“All of this opens up a new avenue of research, and so it is very exciting to see,” Dr. Wiener stated.
No source of funding was listed for the study by Ms. Sadeghi and coauthors. They declared no relevant financial relationships.
Dr. Arslanova and coauthors declared no competing interests. Senior author Manos Tsakiris, PhD, receives funding from the European Research Council Consolidator Grant. Dr. Wiener declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PSYCHOPHYSIOLOGY
Kickback Scheme Nets Prison Time for Philadelphia VAMC Service Chief
A former manager at the Philadelphia Veterans Affairs Medical Center (VAMC) has been sentenced to 6 months in federal prison for his part in a bribery scheme.
Ralph Johnson was convicted of accepting $30,000 in kickbacks and bribes for steering contracts to Earron and Carlicha Starks, who ran Ekno Medical Supply and Collondale Medical Supply from 2009 to 2019. Johnson served as chief of environmental services at the medical center. He admitted to receiving cash in binders and packages mailed to his home between 2018 and 2019.
The Starkses pleaded guilty first to paying kickbacks on $7 million worth of contracts to Florida VA facilities, then participated in a sting that implicated Johnson.
The VA Office of Inspector General began investigating Johnson in 2018 after the Starkses, who were indicted for bribing staff at US Department of Veterans Affairs (VA) hospitals in Miami and West Palm Beach, Florida, said they also paid officials in VA facilities on the East Coast.
According to the Philadelphia Inquirer, the judge credited Johnson’s past military service and his “extensive cooperation” with federal authorities investigating fraud within the VA. Johnson apologized to his former employers: “Throughout these 2 and a half years [since the arrest] there’s not a day I don’t think about the wrongness that I did.”
In addition to the prison sentence, Johnson has been ordered to pay back, at $50 a month, the $440,000-plus he cost the Philadelphia VAMC in fraudulent and bloated contracts.
Johnson is at least the third Philadelphia VAMC employee indicted or sentenced for fraud since 2020.
A former manager at the Philadelphia Veterans Affairs Medical Center (VAMC) has been sentenced to 6 months in federal prison for his part in a bribery scheme.
Ralph Johnson was convicted of accepting $30,000 in kickbacks and bribes for steering contracts to Earron and Carlicha Starks, who ran Ekno Medical Supply and Collondale Medical Supply from 2009 to 2019. Johnson served as chief of environmental services at the medical center. He admitted to receiving cash in binders and packages mailed to his home between 2018 and 2019.
The Starkses pleaded guilty first to paying kickbacks on $7 million worth of contracts to Florida VA facilities, then participated in a sting that implicated Johnson.
The VA Office of Inspector General began investigating Johnson in 2018 after the Starkses, who were indicted for bribing staff at US Department of Veterans Affairs (VA) hospitals in Miami and West Palm Beach, Florida, said they also paid officials in VA facilities on the East Coast.
According to the Philadelphia Inquirer, the judge credited Johnson’s past military service and his “extensive cooperation” with federal authorities investigating fraud within the VA. Johnson apologized to his former employers: “Throughout these 2 and a half years [since the arrest] there’s not a day I don’t think about the wrongness that I did.”
In addition to the prison sentence, Johnson has been ordered to pay back, at $50 a month, the $440,000-plus he cost the Philadelphia VAMC in fraudulent and bloated contracts.
Johnson is at least the third Philadelphia VAMC employee indicted or sentenced for fraud since 2020.
A former manager at the Philadelphia Veterans Affairs Medical Center (VAMC) has been sentenced to 6 months in federal prison for his part in a bribery scheme.
Ralph Johnson was convicted of accepting $30,000 in kickbacks and bribes for steering contracts to Earron and Carlicha Starks, who ran Ekno Medical Supply and Collondale Medical Supply from 2009 to 2019. Johnson served as chief of environmental services at the medical center. He admitted to receiving cash in binders and packages mailed to his home between 2018 and 2019.
The Starkses pleaded guilty first to paying kickbacks on $7 million worth of contracts to Florida VA facilities, then participated in a sting that implicated Johnson.
The VA Office of Inspector General began investigating Johnson in 2018 after the Starkses, who were indicted for bribing staff at US Department of Veterans Affairs (VA) hospitals in Miami and West Palm Beach, Florida, said they also paid officials in VA facilities on the East Coast.
According to the Philadelphia Inquirer, the judge credited Johnson’s past military service and his “extensive cooperation” with federal authorities investigating fraud within the VA. Johnson apologized to his former employers: “Throughout these 2 and a half years [since the arrest] there’s not a day I don’t think about the wrongness that I did.”
In addition to the prison sentence, Johnson has been ordered to pay back, at $50 a month, the $440,000-plus he cost the Philadelphia VAMC in fraudulent and bloated contracts.
Johnson is at least the third Philadelphia VAMC employee indicted or sentenced for fraud since 2020.
Song stuck in your head? What earworms reveal about health
If Miley Cyrus has planted “Flowers” in your head, rest assured you’re not alone.
An earworm – a bit of music you can’t shake from your brain – happens to almost everyone.
The culprit is typically a song you’ve heard repeatedly with a strong rhythm and melody (like Miley’s No. 1 hit this year).
It pops into your head and stays there, unbidden and often unwanted. As you fish for something new on Spotify, there’s always a chance that a catchy hook holds an earworm.
“A catchy tune or melody is the part of a song most likely to get stuck in a person’s head, often a bit from the chorus,” said Elizabeth H. Margulis, PhD, a professor at Princeton (N.J.) University and director of its music cognition lab. The phenomenon, which has been studied since 1885 (way before earbuds), goes by such names as stuck song syndrome, sticky music, musical imagery repetition, intrusive musical imagery, or the semi-official term, involuntary musical imagery, or INMI.
Research confirms how common it is. A 2020 study of American college students found that 97% had experienced an earworm in the past month, similar to findings from a larger Finnish survey done more than 10 years ago.
One in five people had experienced an earworm more than once a day, the study found. The typical length was 10-30 minutes, though 8.5% said theirs lasted more than 3 hours. Levels of “distress and interference” that earworms caused was mostly “mild to moderate.”
Some 86% said they tried to stop it – most frequently by distraction, like talking to a friend or listening to another song.
If music is important to you, your earworms are more likely to last longer and be harder to control, earlier research found. And women are thought to be more likely to have them.
“Very musical people may have more earworms because it’s easy for them to conjure up a certain tune,” says David Silbersweig, MD, chairman of the department of psychiatry and codirector of the Institute for the Neurosciences at Brigham and Women’s Hospital in Boston.
Moreover, people who lack “psychological flexibility” may find earworms more bothersome. The more they try to avoid or control intrusive thoughts (or songs), the more persistent those thoughts become.
“This is consistent with OCD (obsessive-compulsive disorder) research on the paradoxical effect of thought suppression,” the authors of the 2020 study wrote. In fact, people who report very annoying or stressful earworms are more likely to have obsessive-compulsive symptoms.
That makes them worth a closer look.
Digging for the source of earworms
Scientists trace earworms to the auditory cortex in the temporal lobe of the brain, which controls how you perceive music, as well as deep temporal lobe areas that are responsible for retrieving memories. Your amygdala and ventral striatum, parts of your brain that involve emotion, also tie into the making of an earworm.
MRI experiments found that “INMI is a common internal experience recruiting brain networks involved in perception, emotions, memory and spontaneous thoughts,” a 2015 paper in Consciousness and Cognition reported.
These brain networks work in tandem if you connect a song to an emotional memory – that’s when you’re more likely to experience it as an earworm. The “loop” of music you’ll hear in your head is usually a 20-second snippet.
Think of it as a “cognitive itch,” as researchers from the Netherlands put it. An earworm can be triggered by associating a song with a specific situation or emotion. Trying to suppress it just reminds you it’s there, “scratching” the itch and making it worse. “The more one tries to suppress the songs, the more their impetus increases, a mental process known as ironic process theory,” they wrote.
“It’s also worth pointing out that earworms don’t always occur right after a song ends,” said Michael K. Scullin, PhD, an associate professor of psychology and neuroscience at Baylor University in Waco, Tex. “Sometimes they only occur many hours later, and sometimes the earworm isn’t the song you were most recently listening to.”
These processes aren’t fully understood, he said, “but they likely represent memory consolidation mechanisms; that is, the brain trying to reactivate and stabilize musical memories.” Kind of like switching “radio stations” in your head.
When to worry
Earworms are most often harmless. “They’re part of a healthy brain,” said Dr. Silbersweig. But in rare cases, they indicate certain medical conditions. People with OCD, for example, have been shown to have earworms during times of stress. If this is the case, cognitive-behavioral therapy as well as some antidepressants may help.
Take an earworm seriously if it’s linked to other symptoms, said Elaine Jones, MD, a neurologist in Hilton Head, S.C., and a fellow of the American Academy of Neurology. Those symptoms could include “loss of consciousness or confusion, visual loss or changes, speech arrest, tremors of arms or legs,” she said.
“Most worrisome would be a seizure, but other causes could include a migraine aura. In a younger person, less than 20 years old, this kind of earworm could indicate a psychiatric condition like schizophrenia.” Drug toxicity or brain damage can also present with earworms.
Her bottom line: “If an earworm is persistent for more than 24 hours, or if it is associated with the other symptoms mentioned above, it would be important to reach out to your primary care doctor to ensure that nothing more serious is going on,” said Dr. Jones. With no other symptoms, “it is more likely to be just an earworm.”
Japanese research also indicates that an earworm that lasts for several hours in a day can be linked to depression. If a person has symptoms such as low mood, insomnia, and loss of appetite, along with earworms that last several hours a day, treatment may help.
There’s another category called “musical hallucinations” – where the person thinks they are actually hearing music, which could be a symptom of depression, although scientists don’t know for sure. The drug vortioxetine, which may help boost serotonin in the brain, has shown some promise in reducing earworms.
Some research has shown that diseases that damage the auditory pathway in the brain have a link to musical hallucinations.
How to stop a simple earworm
Here are six easy ways to make it stop:
- Mix up your playlist. “Listening to songs repeatedly does increase the likelihood that they’ll get stuck,” said Dr. Margulis.
- Take breaks from your tunes throughout the day. “Longer listening durations are more likely to lead to earworms,” Dr. Scullin said.
- Use your feet. than the beat of your earworm. This will interrupt your memory of the tempo and can help chase away the earworm.
- Stick with that song. “Listen to a song all the way through,” said Dr. Silbersweig. If you only listen to snippets of a song, the can take hold. That’s the brain’s tendency to remember things that are interrupted more easily than completed things.
- Distract yourself. Lose yourself in a book, a movie, your work, or a hobby that requires concentration. “Redirecting attention to an absorbing task can be an effective way to dislodge an earworm,” said Dr. Margulis.
- Chew gum. shows that the action of doing so interferes with repetitive memories and stops your mind from “scanning” a song. Then enjoy the sound of silence!
A version of this article first appeared on WebMD.com.
If Miley Cyrus has planted “Flowers” in your head, rest assured you’re not alone.
An earworm – a bit of music you can’t shake from your brain – happens to almost everyone.
The culprit is typically a song you’ve heard repeatedly with a strong rhythm and melody (like Miley’s No. 1 hit this year).
It pops into your head and stays there, unbidden and often unwanted. As you fish for something new on Spotify, there’s always a chance that a catchy hook holds an earworm.
“A catchy tune or melody is the part of a song most likely to get stuck in a person’s head, often a bit from the chorus,” said Elizabeth H. Margulis, PhD, a professor at Princeton (N.J.) University and director of its music cognition lab. The phenomenon, which has been studied since 1885 (way before earbuds), goes by such names as stuck song syndrome, sticky music, musical imagery repetition, intrusive musical imagery, or the semi-official term, involuntary musical imagery, or INMI.
Research confirms how common it is. A 2020 study of American college students found that 97% had experienced an earworm in the past month, similar to findings from a larger Finnish survey done more than 10 years ago.
One in five people had experienced an earworm more than once a day, the study found. The typical length was 10-30 minutes, though 8.5% said theirs lasted more than 3 hours. Levels of “distress and interference” that earworms caused was mostly “mild to moderate.”
Some 86% said they tried to stop it – most frequently by distraction, like talking to a friend or listening to another song.
If music is important to you, your earworms are more likely to last longer and be harder to control, earlier research found. And women are thought to be more likely to have them.
“Very musical people may have more earworms because it’s easy for them to conjure up a certain tune,” says David Silbersweig, MD, chairman of the department of psychiatry and codirector of the Institute for the Neurosciences at Brigham and Women’s Hospital in Boston.
Moreover, people who lack “psychological flexibility” may find earworms more bothersome. The more they try to avoid or control intrusive thoughts (or songs), the more persistent those thoughts become.
“This is consistent with OCD (obsessive-compulsive disorder) research on the paradoxical effect of thought suppression,” the authors of the 2020 study wrote. In fact, people who report very annoying or stressful earworms are more likely to have obsessive-compulsive symptoms.
That makes them worth a closer look.
Digging for the source of earworms
Scientists trace earworms to the auditory cortex in the temporal lobe of the brain, which controls how you perceive music, as well as deep temporal lobe areas that are responsible for retrieving memories. Your amygdala and ventral striatum, parts of your brain that involve emotion, also tie into the making of an earworm.
MRI experiments found that “INMI is a common internal experience recruiting brain networks involved in perception, emotions, memory and spontaneous thoughts,” a 2015 paper in Consciousness and Cognition reported.
These brain networks work in tandem if you connect a song to an emotional memory – that’s when you’re more likely to experience it as an earworm. The “loop” of music you’ll hear in your head is usually a 20-second snippet.
Think of it as a “cognitive itch,” as researchers from the Netherlands put it. An earworm can be triggered by associating a song with a specific situation or emotion. Trying to suppress it just reminds you it’s there, “scratching” the itch and making it worse. “The more one tries to suppress the songs, the more their impetus increases, a mental process known as ironic process theory,” they wrote.
“It’s also worth pointing out that earworms don’t always occur right after a song ends,” said Michael K. Scullin, PhD, an associate professor of psychology and neuroscience at Baylor University in Waco, Tex. “Sometimes they only occur many hours later, and sometimes the earworm isn’t the song you were most recently listening to.”
These processes aren’t fully understood, he said, “but they likely represent memory consolidation mechanisms; that is, the brain trying to reactivate and stabilize musical memories.” Kind of like switching “radio stations” in your head.
When to worry
Earworms are most often harmless. “They’re part of a healthy brain,” said Dr. Silbersweig. But in rare cases, they indicate certain medical conditions. People with OCD, for example, have been shown to have earworms during times of stress. If this is the case, cognitive-behavioral therapy as well as some antidepressants may help.
Take an earworm seriously if it’s linked to other symptoms, said Elaine Jones, MD, a neurologist in Hilton Head, S.C., and a fellow of the American Academy of Neurology. Those symptoms could include “loss of consciousness or confusion, visual loss or changes, speech arrest, tremors of arms or legs,” she said.
“Most worrisome would be a seizure, but other causes could include a migraine aura. In a younger person, less than 20 years old, this kind of earworm could indicate a psychiatric condition like schizophrenia.” Drug toxicity or brain damage can also present with earworms.
Her bottom line: “If an earworm is persistent for more than 24 hours, or if it is associated with the other symptoms mentioned above, it would be important to reach out to your primary care doctor to ensure that nothing more serious is going on,” said Dr. Jones. With no other symptoms, “it is more likely to be just an earworm.”
Japanese research also indicates that an earworm that lasts for several hours in a day can be linked to depression. If a person has symptoms such as low mood, insomnia, and loss of appetite, along with earworms that last several hours a day, treatment may help.
There’s another category called “musical hallucinations” – where the person thinks they are actually hearing music, which could be a symptom of depression, although scientists don’t know for sure. The drug vortioxetine, which may help boost serotonin in the brain, has shown some promise in reducing earworms.
Some research has shown that diseases that damage the auditory pathway in the brain have a link to musical hallucinations.
How to stop a simple earworm
Here are six easy ways to make it stop:
- Mix up your playlist. “Listening to songs repeatedly does increase the likelihood that they’ll get stuck,” said Dr. Margulis.
- Take breaks from your tunes throughout the day. “Longer listening durations are more likely to lead to earworms,” Dr. Scullin said.
- Use your feet. than the beat of your earworm. This will interrupt your memory of the tempo and can help chase away the earworm.
- Stick with that song. “Listen to a song all the way through,” said Dr. Silbersweig. If you only listen to snippets of a song, the can take hold. That’s the brain’s tendency to remember things that are interrupted more easily than completed things.
- Distract yourself. Lose yourself in a book, a movie, your work, or a hobby that requires concentration. “Redirecting attention to an absorbing task can be an effective way to dislodge an earworm,” said Dr. Margulis.
- Chew gum. shows that the action of doing so interferes with repetitive memories and stops your mind from “scanning” a song. Then enjoy the sound of silence!
A version of this article first appeared on WebMD.com.
If Miley Cyrus has planted “Flowers” in your head, rest assured you’re not alone.
An earworm – a bit of music you can’t shake from your brain – happens to almost everyone.
The culprit is typically a song you’ve heard repeatedly with a strong rhythm and melody (like Miley’s No. 1 hit this year).
It pops into your head and stays there, unbidden and often unwanted. As you fish for something new on Spotify, there’s always a chance that a catchy hook holds an earworm.
“A catchy tune or melody is the part of a song most likely to get stuck in a person’s head, often a bit from the chorus,” said Elizabeth H. Margulis, PhD, a professor at Princeton (N.J.) University and director of its music cognition lab. The phenomenon, which has been studied since 1885 (way before earbuds), goes by such names as stuck song syndrome, sticky music, musical imagery repetition, intrusive musical imagery, or the semi-official term, involuntary musical imagery, or INMI.
Research confirms how common it is. A 2020 study of American college students found that 97% had experienced an earworm in the past month, similar to findings from a larger Finnish survey done more than 10 years ago.
One in five people had experienced an earworm more than once a day, the study found. The typical length was 10-30 minutes, though 8.5% said theirs lasted more than 3 hours. Levels of “distress and interference” that earworms caused was mostly “mild to moderate.”
Some 86% said they tried to stop it – most frequently by distraction, like talking to a friend or listening to another song.
If music is important to you, your earworms are more likely to last longer and be harder to control, earlier research found. And women are thought to be more likely to have them.
“Very musical people may have more earworms because it’s easy for them to conjure up a certain tune,” says David Silbersweig, MD, chairman of the department of psychiatry and codirector of the Institute for the Neurosciences at Brigham and Women’s Hospital in Boston.
Moreover, people who lack “psychological flexibility” may find earworms more bothersome. The more they try to avoid or control intrusive thoughts (or songs), the more persistent those thoughts become.
“This is consistent with OCD (obsessive-compulsive disorder) research on the paradoxical effect of thought suppression,” the authors of the 2020 study wrote. In fact, people who report very annoying or stressful earworms are more likely to have obsessive-compulsive symptoms.
That makes them worth a closer look.
Digging for the source of earworms
Scientists trace earworms to the auditory cortex in the temporal lobe of the brain, which controls how you perceive music, as well as deep temporal lobe areas that are responsible for retrieving memories. Your amygdala and ventral striatum, parts of your brain that involve emotion, also tie into the making of an earworm.
MRI experiments found that “INMI is a common internal experience recruiting brain networks involved in perception, emotions, memory and spontaneous thoughts,” a 2015 paper in Consciousness and Cognition reported.
These brain networks work in tandem if you connect a song to an emotional memory – that’s when you’re more likely to experience it as an earworm. The “loop” of music you’ll hear in your head is usually a 20-second snippet.
Think of it as a “cognitive itch,” as researchers from the Netherlands put it. An earworm can be triggered by associating a song with a specific situation or emotion. Trying to suppress it just reminds you it’s there, “scratching” the itch and making it worse. “The more one tries to suppress the songs, the more their impetus increases, a mental process known as ironic process theory,” they wrote.
“It’s also worth pointing out that earworms don’t always occur right after a song ends,” said Michael K. Scullin, PhD, an associate professor of psychology and neuroscience at Baylor University in Waco, Tex. “Sometimes they only occur many hours later, and sometimes the earworm isn’t the song you were most recently listening to.”
These processes aren’t fully understood, he said, “but they likely represent memory consolidation mechanisms; that is, the brain trying to reactivate and stabilize musical memories.” Kind of like switching “radio stations” in your head.
When to worry
Earworms are most often harmless. “They’re part of a healthy brain,” said Dr. Silbersweig. But in rare cases, they indicate certain medical conditions. People with OCD, for example, have been shown to have earworms during times of stress. If this is the case, cognitive-behavioral therapy as well as some antidepressants may help.
Take an earworm seriously if it’s linked to other symptoms, said Elaine Jones, MD, a neurologist in Hilton Head, S.C., and a fellow of the American Academy of Neurology. Those symptoms could include “loss of consciousness or confusion, visual loss or changes, speech arrest, tremors of arms or legs,” she said.
“Most worrisome would be a seizure, but other causes could include a migraine aura. In a younger person, less than 20 years old, this kind of earworm could indicate a psychiatric condition like schizophrenia.” Drug toxicity or brain damage can also present with earworms.
Her bottom line: “If an earworm is persistent for more than 24 hours, or if it is associated with the other symptoms mentioned above, it would be important to reach out to your primary care doctor to ensure that nothing more serious is going on,” said Dr. Jones. With no other symptoms, “it is more likely to be just an earworm.”
Japanese research also indicates that an earworm that lasts for several hours in a day can be linked to depression. If a person has symptoms such as low mood, insomnia, and loss of appetite, along with earworms that last several hours a day, treatment may help.
There’s another category called “musical hallucinations” – where the person thinks they are actually hearing music, which could be a symptom of depression, although scientists don’t know for sure. The drug vortioxetine, which may help boost serotonin in the brain, has shown some promise in reducing earworms.
Some research has shown that diseases that damage the auditory pathway in the brain have a link to musical hallucinations.
How to stop a simple earworm
Here are six easy ways to make it stop:
- Mix up your playlist. “Listening to songs repeatedly does increase the likelihood that they’ll get stuck,” said Dr. Margulis.
- Take breaks from your tunes throughout the day. “Longer listening durations are more likely to lead to earworms,” Dr. Scullin said.
- Use your feet. than the beat of your earworm. This will interrupt your memory of the tempo and can help chase away the earworm.
- Stick with that song. “Listen to a song all the way through,” said Dr. Silbersweig. If you only listen to snippets of a song, the can take hold. That’s the brain’s tendency to remember things that are interrupted more easily than completed things.
- Distract yourself. Lose yourself in a book, a movie, your work, or a hobby that requires concentration. “Redirecting attention to an absorbing task can be an effective way to dislodge an earworm,” said Dr. Margulis.
- Chew gum. shows that the action of doing so interferes with repetitive memories and stops your mind from “scanning” a song. Then enjoy the sound of silence!
A version of this article first appeared on WebMD.com.
Implicit bias in medicine and beyond
Recently, I reported to the Washtenaw County Circuit Courthouse in Ann Arbor, Mich., to fulfill my civic responsibility of jury duty. After check-in, a pool of 250 potential jurors were shown a video about implicit bias and shuttled off to different courtrooms for the jury selection process (voir dire, or “to speak the truth” in French). While not personally called up to the juror box on this day, I did have the opportunity to observe the attorneys and judge as they questioned potential jurors to uncover any indication that they might not be fair or impartial in judging the facts of this criminal case. After over 3 hours of questioning and several peremptory challenges, a jury was empaneled, and the rest of us were dismissed for the day.
In the legal system, implicit bias can adversely affect legal outcomes by impacting the beliefs and attitudes of multiple stakeholders, including attorneys and judges, litigants, witnesses, and of course jurors, threatening one of our society’s most fundamental principles of equal justice under the law. In the health care arena, implicit bias has been shown to impact patient-clinician communication and contribute to racial and ethnic disparities in patient outcomes. As a medical community, acknowledging and accepting the existence of implicit bias, its manifestations, and its impact is a critical first step to ensuring that every patient that walks into our exam rooms receives equitable care, and we can begin to move the needle in addressing persistent health disparities in patients with gastrointestinal diseases and beyond. While this is regrettably a politically charged topic in our current environment, I urge you to join me in reflecting on whether and how unconscious attitudes or stereotypes may unintentionally color the way in which you interact with patients in the clinic and serve to create or perpetuate inequities in treatment. (I also urge you to show up for jury duty!)
Turning to our April issue, we highlight two recent studies from AGA’s flagship journals, one showing an unexpected rise in pancreatic cancer incidence among women under the age of 55, and another evaluating survival outcomes by fibrosis stage in biopsy-proven nonalcoholic fatty liver disease. In this month’s Member Spotlight column, we introduce you to gastroenterologist Daniel Leffler, MD, who shares his experiences transitioning from a traditional academic career to a job in industry to further scientific advancements in celiac disease treatment. We hope you enjoy these articles and all the content included in our April issue!
Megan A. Adams, MD, JD, MSc
Recently, I reported to the Washtenaw County Circuit Courthouse in Ann Arbor, Mich., to fulfill my civic responsibility of jury duty. After check-in, a pool of 250 potential jurors were shown a video about implicit bias and shuttled off to different courtrooms for the jury selection process (voir dire, or “to speak the truth” in French). While not personally called up to the juror box on this day, I did have the opportunity to observe the attorneys and judge as they questioned potential jurors to uncover any indication that they might not be fair or impartial in judging the facts of this criminal case. After over 3 hours of questioning and several peremptory challenges, a jury was empaneled, and the rest of us were dismissed for the day.
In the legal system, implicit bias can adversely affect legal outcomes by impacting the beliefs and attitudes of multiple stakeholders, including attorneys and judges, litigants, witnesses, and of course jurors, threatening one of our society’s most fundamental principles of equal justice under the law. In the health care arena, implicit bias has been shown to impact patient-clinician communication and contribute to racial and ethnic disparities in patient outcomes. As a medical community, acknowledging and accepting the existence of implicit bias, its manifestations, and its impact is a critical first step to ensuring that every patient that walks into our exam rooms receives equitable care, and we can begin to move the needle in addressing persistent health disparities in patients with gastrointestinal diseases and beyond. While this is regrettably a politically charged topic in our current environment, I urge you to join me in reflecting on whether and how unconscious attitudes or stereotypes may unintentionally color the way in which you interact with patients in the clinic and serve to create or perpetuate inequities in treatment. (I also urge you to show up for jury duty!)
Turning to our April issue, we highlight two recent studies from AGA’s flagship journals, one showing an unexpected rise in pancreatic cancer incidence among women under the age of 55, and another evaluating survival outcomes by fibrosis stage in biopsy-proven nonalcoholic fatty liver disease. In this month’s Member Spotlight column, we introduce you to gastroenterologist Daniel Leffler, MD, who shares his experiences transitioning from a traditional academic career to a job in industry to further scientific advancements in celiac disease treatment. We hope you enjoy these articles and all the content included in our April issue!
Megan A. Adams, MD, JD, MSc
Recently, I reported to the Washtenaw County Circuit Courthouse in Ann Arbor, Mich., to fulfill my civic responsibility of jury duty. After check-in, a pool of 250 potential jurors were shown a video about implicit bias and shuttled off to different courtrooms for the jury selection process (voir dire, or “to speak the truth” in French). While not personally called up to the juror box on this day, I did have the opportunity to observe the attorneys and judge as they questioned potential jurors to uncover any indication that they might not be fair or impartial in judging the facts of this criminal case. After over 3 hours of questioning and several peremptory challenges, a jury was empaneled, and the rest of us were dismissed for the day.
In the legal system, implicit bias can adversely affect legal outcomes by impacting the beliefs and attitudes of multiple stakeholders, including attorneys and judges, litigants, witnesses, and of course jurors, threatening one of our society’s most fundamental principles of equal justice under the law. In the health care arena, implicit bias has been shown to impact patient-clinician communication and contribute to racial and ethnic disparities in patient outcomes. As a medical community, acknowledging and accepting the existence of implicit bias, its manifestations, and its impact is a critical first step to ensuring that every patient that walks into our exam rooms receives equitable care, and we can begin to move the needle in addressing persistent health disparities in patients with gastrointestinal diseases and beyond. While this is regrettably a politically charged topic in our current environment, I urge you to join me in reflecting on whether and how unconscious attitudes or stereotypes may unintentionally color the way in which you interact with patients in the clinic and serve to create or perpetuate inequities in treatment. (I also urge you to show up for jury duty!)
Turning to our April issue, we highlight two recent studies from AGA’s flagship journals, one showing an unexpected rise in pancreatic cancer incidence among women under the age of 55, and another evaluating survival outcomes by fibrosis stage in biopsy-proven nonalcoholic fatty liver disease. In this month’s Member Spotlight column, we introduce you to gastroenterologist Daniel Leffler, MD, who shares his experiences transitioning from a traditional academic career to a job in industry to further scientific advancements in celiac disease treatment. We hope you enjoy these articles and all the content included in our April issue!
Megan A. Adams, MD, JD, MSc
GI lends itself to multiple career paths, says Boston physician
Daniel Leffler, MD, MS, AGAF, has some advice for young physicians starting out in their careers: Don’t be afraid of change.
“Just because you’re a doctor doesn’t mean you have to spend the rest of your career doing patient care. We don’t teach that in medical school as well as we should,” said Dr. Leffler. “If you’re interested in a skill set and move in a different direction, that’s totally okay. Many people have major career shifts, whether it’s early, mid- or late career.”
Dr. Leffler followed his own advice in 2016 when he left his longtime job as an associate professor at Harvard Medical School and accepted a position with Takeda Pharmaceuticals. As its medical director, he had a specific goal: To find more therapeutic options for patients with celiac disease.
“Gastroenterology is a fantastic field of medicine, and it somehow continues to get more and more exciting,” said Dr. Leffler, who continues to see patients at Beth Israel Deaconess Medical Center in Boston. “There are just so many careers you can have within gastroenterology, whether you are a full-time endoscopist, in a teaching career, or doing lab work.”
He discussed the events that led to this career change in an interview with GI & Hepatology News.
Q: Why did you choose GI?
Dr. Leffler: I think for a lot of people GI is just an incredibly diverse field where you can see all types of patients and you have an unusually wide armamentarium of diagnostic and therapeutic options. Our ability to see inside in the GI tract relatively easily and obtain tissue and do functional studies is unique. It makes it a very dynamic field.
Q: What gives you the most joy in your day-to-day practice?
Dr. Leffler: I think it’s taking a fresh look at somebody whose symptoms have been incorrectly diagnosed or diagnosed preliminarily as one thing and opening different options and working with the patient to hopefully find a more targeted therapy based on a more definitive diagnosis.
Q: Describe your biggest practice-related challenge and what you are doing to address it.
Dr. Leffler: There are two challenges. For celiac disease, all I have is a gluten-free diet. It would be nice to have other options, the same way we do with almost every other GI disease, whether it’s acid-related disorders or chronic constipation or inflammatory bowel disease. We have a range of therapies we can pick and choose from, tailoring those to the individual. We are not there yet, unfortunately, in celiac disease, so that’s a huge challenge.
Another challenge is awareness of celiac disease. It’s not what it should be. We see a lot of patients who either were misdiagnosed or went many years without getting a proper diagnosis or got diagnosed and did not have proper education or follow up.
Q: How has your job changed since you first began your career? Perhaps we could discuss your switch from Harvard/Beth Israel Deaconess to Takeda Pharmaceuticals.
Dr. Leffler: I became convinced some years ago that the next big thing for celiac disease was an effective therapy beyond the gluten-free diet. Takeda had acquired rights to two of the therapies that I was most interested in, even though they were very early. There was a new glutenase, TAK-062, and a new immune-tolerizing molecule that became TAK-101. Takeda had moved its research center to Boston, and they were looking for someone to work on their celiac program. Moving from an academic position, which I loved, was a really difficult decision.
I didn’t leave without a conversation with the division chief at the time, Tom Lamont, MD. I basically said, “If this doesn’t work out, will you take me back?” I wasn’t sure how much I’d like working in industry. The other thing, on both sides, was that I was allowed to keep a clinic. I still see patients on Fridays and really, to me, I have the best of both worlds.
Q: What teacher or mentor had the greatest impact on you?
Dr. Leffler: I really think of Ciaran Kelly, MD at Beth Israel Deaconess, Detlef Schuppan, MD, who also was at Beth Israel Deaconess, but is now at the University of Mainz in Germany. And Peter Green, MD at Columbia University. These three are the physicians I’ve interacted with the most and learned the most from.
Q: What habits have you established that have benefited your career most?
Dr. Leffler: I do try to focus on being a good collaborator. Playing that long game of working for the good of the project and not necessarily what is next for you, has served me very well over the years.
Lightening round
Superpower?
Optimism
Favorite movie to quote?
The Big Lebowski
What is your favorite form of exercise?
Elliptical
Name one thing on your bucket list.
Ethiopia travel
How many cups of coffee do you drink per day?
Two-ish
Dr. Leffler is on LinkedIn.
Daniel Leffler, MD, MS, AGAF, has some advice for young physicians starting out in their careers: Don’t be afraid of change.
“Just because you’re a doctor doesn’t mean you have to spend the rest of your career doing patient care. We don’t teach that in medical school as well as we should,” said Dr. Leffler. “If you’re interested in a skill set and move in a different direction, that’s totally okay. Many people have major career shifts, whether it’s early, mid- or late career.”
Dr. Leffler followed his own advice in 2016 when he left his longtime job as an associate professor at Harvard Medical School and accepted a position with Takeda Pharmaceuticals. As its medical director, he had a specific goal: To find more therapeutic options for patients with celiac disease.
“Gastroenterology is a fantastic field of medicine, and it somehow continues to get more and more exciting,” said Dr. Leffler, who continues to see patients at Beth Israel Deaconess Medical Center in Boston. “There are just so many careers you can have within gastroenterology, whether you are a full-time endoscopist, in a teaching career, or doing lab work.”
He discussed the events that led to this career change in an interview with GI & Hepatology News.
Q: Why did you choose GI?
Dr. Leffler: I think for a lot of people GI is just an incredibly diverse field where you can see all types of patients and you have an unusually wide armamentarium of diagnostic and therapeutic options. Our ability to see inside in the GI tract relatively easily and obtain tissue and do functional studies is unique. It makes it a very dynamic field.
Q: What gives you the most joy in your day-to-day practice?
Dr. Leffler: I think it’s taking a fresh look at somebody whose symptoms have been incorrectly diagnosed or diagnosed preliminarily as one thing and opening different options and working with the patient to hopefully find a more targeted therapy based on a more definitive diagnosis.
Q: Describe your biggest practice-related challenge and what you are doing to address it.
Dr. Leffler: There are two challenges. For celiac disease, all I have is a gluten-free diet. It would be nice to have other options, the same way we do with almost every other GI disease, whether it’s acid-related disorders or chronic constipation or inflammatory bowel disease. We have a range of therapies we can pick and choose from, tailoring those to the individual. We are not there yet, unfortunately, in celiac disease, so that’s a huge challenge.
Another challenge is awareness of celiac disease. It’s not what it should be. We see a lot of patients who either were misdiagnosed or went many years without getting a proper diagnosis or got diagnosed and did not have proper education or follow up.
Q: How has your job changed since you first began your career? Perhaps we could discuss your switch from Harvard/Beth Israel Deaconess to Takeda Pharmaceuticals.
Dr. Leffler: I became convinced some years ago that the next big thing for celiac disease was an effective therapy beyond the gluten-free diet. Takeda had acquired rights to two of the therapies that I was most interested in, even though they were very early. There was a new glutenase, TAK-062, and a new immune-tolerizing molecule that became TAK-101. Takeda had moved its research center to Boston, and they were looking for someone to work on their celiac program. Moving from an academic position, which I loved, was a really difficult decision.
I didn’t leave without a conversation with the division chief at the time, Tom Lamont, MD. I basically said, “If this doesn’t work out, will you take me back?” I wasn’t sure how much I’d like working in industry. The other thing, on both sides, was that I was allowed to keep a clinic. I still see patients on Fridays and really, to me, I have the best of both worlds.
Q: What teacher or mentor had the greatest impact on you?
Dr. Leffler: I really think of Ciaran Kelly, MD at Beth Israel Deaconess, Detlef Schuppan, MD, who also was at Beth Israel Deaconess, but is now at the University of Mainz in Germany. And Peter Green, MD at Columbia University. These three are the physicians I’ve interacted with the most and learned the most from.
Q: What habits have you established that have benefited your career most?
Dr. Leffler: I do try to focus on being a good collaborator. Playing that long game of working for the good of the project and not necessarily what is next for you, has served me very well over the years.
Lightening round
Superpower?
Optimism
Favorite movie to quote?
The Big Lebowski
What is your favorite form of exercise?
Elliptical
Name one thing on your bucket list.
Ethiopia travel
How many cups of coffee do you drink per day?
Two-ish
Dr. Leffler is on LinkedIn.
Daniel Leffler, MD, MS, AGAF, has some advice for young physicians starting out in their careers: Don’t be afraid of change.
“Just because you’re a doctor doesn’t mean you have to spend the rest of your career doing patient care. We don’t teach that in medical school as well as we should,” said Dr. Leffler. “If you’re interested in a skill set and move in a different direction, that’s totally okay. Many people have major career shifts, whether it’s early, mid- or late career.”
Dr. Leffler followed his own advice in 2016 when he left his longtime job as an associate professor at Harvard Medical School and accepted a position with Takeda Pharmaceuticals. As its medical director, he had a specific goal: To find more therapeutic options for patients with celiac disease.
“Gastroenterology is a fantastic field of medicine, and it somehow continues to get more and more exciting,” said Dr. Leffler, who continues to see patients at Beth Israel Deaconess Medical Center in Boston. “There are just so many careers you can have within gastroenterology, whether you are a full-time endoscopist, in a teaching career, or doing lab work.”
He discussed the events that led to this career change in an interview with GI & Hepatology News.
Q: Why did you choose GI?
Dr. Leffler: I think for a lot of people GI is just an incredibly diverse field where you can see all types of patients and you have an unusually wide armamentarium of diagnostic and therapeutic options. Our ability to see inside in the GI tract relatively easily and obtain tissue and do functional studies is unique. It makes it a very dynamic field.
Q: What gives you the most joy in your day-to-day practice?
Dr. Leffler: I think it’s taking a fresh look at somebody whose symptoms have been incorrectly diagnosed or diagnosed preliminarily as one thing and opening different options and working with the patient to hopefully find a more targeted therapy based on a more definitive diagnosis.
Q: Describe your biggest practice-related challenge and what you are doing to address it.
Dr. Leffler: There are two challenges. For celiac disease, all I have is a gluten-free diet. It would be nice to have other options, the same way we do with almost every other GI disease, whether it’s acid-related disorders or chronic constipation or inflammatory bowel disease. We have a range of therapies we can pick and choose from, tailoring those to the individual. We are not there yet, unfortunately, in celiac disease, so that’s a huge challenge.
Another challenge is awareness of celiac disease. It’s not what it should be. We see a lot of patients who either were misdiagnosed or went many years without getting a proper diagnosis or got diagnosed and did not have proper education or follow up.
Q: How has your job changed since you first began your career? Perhaps we could discuss your switch from Harvard/Beth Israel Deaconess to Takeda Pharmaceuticals.
Dr. Leffler: I became convinced some years ago that the next big thing for celiac disease was an effective therapy beyond the gluten-free diet. Takeda had acquired rights to two of the therapies that I was most interested in, even though they were very early. There was a new glutenase, TAK-062, and a new immune-tolerizing molecule that became TAK-101. Takeda had moved its research center to Boston, and they were looking for someone to work on their celiac program. Moving from an academic position, which I loved, was a really difficult decision.
I didn’t leave without a conversation with the division chief at the time, Tom Lamont, MD. I basically said, “If this doesn’t work out, will you take me back?” I wasn’t sure how much I’d like working in industry. The other thing, on both sides, was that I was allowed to keep a clinic. I still see patients on Fridays and really, to me, I have the best of both worlds.
Q: What teacher or mentor had the greatest impact on you?
Dr. Leffler: I really think of Ciaran Kelly, MD at Beth Israel Deaconess, Detlef Schuppan, MD, who also was at Beth Israel Deaconess, but is now at the University of Mainz in Germany. And Peter Green, MD at Columbia University. These three are the physicians I’ve interacted with the most and learned the most from.
Q: What habits have you established that have benefited your career most?
Dr. Leffler: I do try to focus on being a good collaborator. Playing that long game of working for the good of the project and not necessarily what is next for you, has served me very well over the years.
Lightening round
Superpower?
Optimism
Favorite movie to quote?
The Big Lebowski
What is your favorite form of exercise?
Elliptical
Name one thing on your bucket list.
Ethiopia travel
How many cups of coffee do you drink per day?
Two-ish
Dr. Leffler is on LinkedIn.
Frustration over iPLEDGE evident at FDA meeting
During 2 days of after the chaotic rollout of the new REMS platform at the end of 2021.
On March 29, at the end of the FDA’s joint meeting of two advisory committees that addressed ways to improve the iPLEDGE program, most panelists voted to change the 19-day lockout period for patients who can become pregnant, and the requirement that every month, providers must document counseling of those who cannot get pregnant and are taking the drug for acne.
However, there was no consensus on whether there should be a lockout at all or for how long, and what an appropriate interval for counseling those who cannot get pregnant would be, if not monthly. Those voting on the questions repeatedly cited a lack of data to make well-informed decisions.
The meeting of the two panels, the FDA’s Drug Safety and Risk Management Advisory Committee and the Dermatologic and Ophthalmic Drugs Advisory Committee, was held March 28-29, to discuss proposed changes to iPLEDGE requirements, to minimize the program’s burden on patients, prescribers, and pharmacies – while maintaining safe use of the highly teratogenic drug.
Lockout based on outdated reasoning
John S. Barbieri, MD, a dermatologist and epidemiologist, and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital in Boston, speaking as deputy chair of the American Academy of Dermatology Association (AADA) iPLEDGE work group, described the burden of getting the drug to patients. He was not on the panel, but spoke during the open public hearing.
“Compared to other acne medications, the time it takes to successfully go from prescribed (isotretinoin) to when the patient actually has it in their hands is 5- to 10-fold higher,” he said.
Among the barriers is the 19-day lockout period for people who can get pregnant and miss the 7-day window for picking up their prescriptions. They must then wait 19 days to get a pregnancy test to clear them for receiving the medication.
Gregory Wedin, PharmD, pharmacovigilance and risk management director of Upsher-Smith Laboratories, who spoke on behalf of the Isotretinoin Products Manufacturer Group (IPMG), which manages iPLEDGE, said, “The rationale for the 19-day wait is to ensure the next confirmatory pregnancy test is completed after the most fertile period of the menstrual cycle is passed.”
Many don’t have a monthly cycle
But Dr. Barbieri said that reasoning is outdated.
“The current program’s focus on the menstrual cycle is really an antiquated approach,” he said. “Many patients do not have a monthly cycle due to medical conditions like polycystic ovarian syndrome, or due to [certain kinds of] contraception.”
He added, “By removing this 19-day lockout and, really, the archaic timing around the menstrual cycle in general in this program, we can simplify the program, improve it, and better align it with the real-world biology of our patients.” He added that patients are often missing the 7-day window for picking up their prescriptions through no fault of their own. Speakers at the hearing also mentioned insurance hassles and ordering delays.
Communication with IPMG
Ilona Frieden, MD, professor of dermatology and pediatrics at the University of California, San Francisco, and outgoing chair of the AADA iPLEDGE work group, cited difficulty in working with IPMG on modifications as another barrier. She also spoke during the open public hearing.
“Despite many, many attempts to work with the IPMG, we are not aware of any organizational structure or key leaders to communicate with. Instead we have been given repeatedly a generic email address for trying to establish a working relationship and we believe this may explain the inaction of the IPMG since our proposals 4 years ago in 2019.”
Among those proposals, she said, were allowing telemedicine visits as part of the iPLEDGE REMS program and reducing counseling attestation to every 6 months instead of monthly for those who cannot become pregnant.
She pointed to the chaotic rollout of modifications to the iPLEDGE program on a new website at the end of 2021.
In 2021, she said, “despite 6 months of notification, no prescriber input was solicited before revamping the website. This lack of transparency and accountability has been a major hurdle in improving iPLEDGE.”
Dr. Barbieri called the rollout “a debacle” that could have been mitigated with communication with IPMG. “We warned about every issue that happened and talked about ways to mitigate it and were largely ignored,” he said.
“By including dermatologists and key stakeholders in these discussions, as we move forward with changes to improve this program, we can make sure that it’s patient-centered.”
IPMG did not address the specific complaints about the working relationship with the AADA workgroup at the meeting.
Monthly attestation for counseling patients who cannot get pregnant
Dr. Barbieri said the monthly requirement to counsel patients who cannot get pregnant and document that counseling unfairly burdens clinicians and patients. “We’re essentially asking patients to come in monthly just to tell them not to share their drugs [or] donate blood,” he said.
Ken Katz, MD, MSc, a dermatologist at Kaiser Permanente in San Francisco, was among the panel members voting not to continue the 19-day lockout.
“I think this places an unduly high burden physically and psychologically on our patients. It seems arbitrary,” he said. “Likely we will miss some pregnancies; we are missing some already. But the burden is not matched by the benefit.”
IPMG representative Dr. Wedin, said, “while we cannot support eliminating or extending the confirmation interval to a year, the [iPLEDGE] sponsors are agreeable [to] a 120-day confirmation interval.”
He said that while an extension to 120 days would reduce burden on prescribers, it comes with the risk in reducing oversight by a certified iPLEDGE prescriber and potentially increasing the risk for drug sharing.
“A patient may be more likely to share their drug with another person the further along with therapy they get as their condition improves,” Dr. Wedin said.
Home pregnancy testing
The advisory groups were also tasked with discussing whether home pregnancy tests, allowed during the COVID-19 public health emergency, should continue to be allowed. Most committee members and those in the public hearing who spoke on the issue agreed that home tests should continue in an effort to increase access and decrease burden.
During the pandemic, iPLEDGE rules have been relaxed from having a pregnancy test done only at a Clinical Laboratory Improvement Amendments–certified laboratory.
Lindsey Crist, PharmD, a risk management analyst at the FDA, who presented the FDA review committee’s analysis, said that the FDA’s review committee recommends ending the allowance of home tests, citing insufficient data on use and the discovery of instances of falsification of pregnancy tests.
“One study at an academic medical center reviewed the medical records of 89 patients who used home pregnancy tests while taking isotretinoin during the public health emergency. It found that 15.7% submitted falsified pregnancy test results,” Dr. Crist said.
Dr. Crist added, however, that the review committee recommends allowing the tests to be done in a provider’s office as an alternative.
Workaround to avoid falsification
Advisory committee member Brian P. Green, DO, associate professor of dermatology at Penn State University, Hershey, Pa., spoke in support of home pregnancy tests.
“What we have people do for telemedicine is take the stick, write their name, write the date on it, and send a picture of that the same day as their visit,” he said. “That way we have the pregnancy test the same day. Allowing this to continue to happen at home is important. Bringing people in is burdensome and costly.”
Emmy Graber, MD, a dermatologist who practices in Boston, and a director of the American Acne and Rosacea Society (AARS), relayed an example of the burden for a patient using isotretinoin who lives 1.5 hours away from the dermatology office. She is able to meet the requirements of iPLEDGE only through telehealth.
“Home pregnancy tests are highly sensitive, equal to the ones done in CLIA-certified labs, and highly accurate when interpreted by a dermatology provider,” said Dr. Graber, who spoke on behalf of the AARS during the open public hearing.
“Notably, CLIA [Clinical Laboratory Improvement Amendments] certification is not required by other REMS programs” for teratogenic drugs, she added.
Dr. Graber said it’s important to note that in the time the pandemic exceptions have been made for isotretinoin patients, “there has been no reported spike in pregnancy in the past three years.
“We do have some data to show that it is not imposing additional harms,” she said.
Suggestions for improvement
At the end of the hearing, advisory committee members were asked to propose improvements to the iPLEDGE REMS program.
Dr. Green advocated for the addition of an iPLEDGE mobile app.
“Most people go to their phones rather than their computers, particularly teenagers and younger people,” he noted.
Advisory committee member Megha M. Tollefson, MD, professor of dermatology and pediatric and adolescent medicine at Mayo Clinic in Rochester, Minn., echoed the need for an iPLEDGE app.
The young patients getting isotretinoin “don’t respond to email, they don’t necessarily go onto web pages. If we’re going to be as effective as possible, it’s going to have to be through an app-based system.”
Dr. Tollefson said she would like to see patient counseling standardized through the app. “I think there’s a lot of variability in what counseling is given when it’s left to the individual prescriber or practice,” she said.
Exceptions for long-acting contraceptives?
Advisory committee member Abbey B. Berenson, MD, PhD, professor of obstetrics and gynecology at University of Texas Medical Branch in Galveston, said that patients taking long-acting reversible contraceptives (LARCs) may need to be considered differently when deciding the intervals for attestation or whether to have a lockout period.
“LARC methods’ rate of failure is extremely low,” she said. “While it is true, as it has been pointed out, that all methods can fail, when they’re over 99% effective, I think that we can treat those methods differently than we treat methods such as birth control pills or abstinence that fail far more often. That is one way we could minimize burden on the providers and the patients.”
She also suggested using members of the health care team other than physicians to complete counseling, such as a nurse or pharmacist.
Prescriptions for emergency contraception
Advisory committee member Sascha Dublin, MD, PhD, senior scientific investigator for Kaiser Permanente Washington Health Research Institute in Seattle, said most patients taking the drug who can get pregnant should get a prescription for emergency contraception at the time of the first isotretinoin prescription.
“They don’t have to buy it, but to make it available at the very beginning sets the expectation that it would be good to have in your medicine cabinet, particularly if the [contraception] choice is abstinence or birth control pills.”
Dr. Dublin also called for better transparency surrounding the role of IPMG.
She said IPMG should be expected to collect data in a way that allows examination of health disparities, including by race and ethnicity and insurance status. Dr. Dublin added that she was concerned about the poor communication between dermatological societies and IPMG.
“The FDA should really require that IPMG hold periodic, regularly scheduled stakeholder forums,” she said. “There has to be a mechanism in place for IPMG to listen to those concerns in real time and respond.”
The advisory committees’ recommendations to the FDA are nonbinding, but the FDA generally follows the recommendations of advisory panels.
During 2 days of after the chaotic rollout of the new REMS platform at the end of 2021.
On March 29, at the end of the FDA’s joint meeting of two advisory committees that addressed ways to improve the iPLEDGE program, most panelists voted to change the 19-day lockout period for patients who can become pregnant, and the requirement that every month, providers must document counseling of those who cannot get pregnant and are taking the drug for acne.
However, there was no consensus on whether there should be a lockout at all or for how long, and what an appropriate interval for counseling those who cannot get pregnant would be, if not monthly. Those voting on the questions repeatedly cited a lack of data to make well-informed decisions.
The meeting of the two panels, the FDA’s Drug Safety and Risk Management Advisory Committee and the Dermatologic and Ophthalmic Drugs Advisory Committee, was held March 28-29, to discuss proposed changes to iPLEDGE requirements, to minimize the program’s burden on patients, prescribers, and pharmacies – while maintaining safe use of the highly teratogenic drug.
Lockout based on outdated reasoning
John S. Barbieri, MD, a dermatologist and epidemiologist, and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital in Boston, speaking as deputy chair of the American Academy of Dermatology Association (AADA) iPLEDGE work group, described the burden of getting the drug to patients. He was not on the panel, but spoke during the open public hearing.
“Compared to other acne medications, the time it takes to successfully go from prescribed (isotretinoin) to when the patient actually has it in their hands is 5- to 10-fold higher,” he said.
Among the barriers is the 19-day lockout period for people who can get pregnant and miss the 7-day window for picking up their prescriptions. They must then wait 19 days to get a pregnancy test to clear them for receiving the medication.
Gregory Wedin, PharmD, pharmacovigilance and risk management director of Upsher-Smith Laboratories, who spoke on behalf of the Isotretinoin Products Manufacturer Group (IPMG), which manages iPLEDGE, said, “The rationale for the 19-day wait is to ensure the next confirmatory pregnancy test is completed after the most fertile period of the menstrual cycle is passed.”
Many don’t have a monthly cycle
But Dr. Barbieri said that reasoning is outdated.
“The current program’s focus on the menstrual cycle is really an antiquated approach,” he said. “Many patients do not have a monthly cycle due to medical conditions like polycystic ovarian syndrome, or due to [certain kinds of] contraception.”
He added, “By removing this 19-day lockout and, really, the archaic timing around the menstrual cycle in general in this program, we can simplify the program, improve it, and better align it with the real-world biology of our patients.” He added that patients are often missing the 7-day window for picking up their prescriptions through no fault of their own. Speakers at the hearing also mentioned insurance hassles and ordering delays.
Communication with IPMG
Ilona Frieden, MD, professor of dermatology and pediatrics at the University of California, San Francisco, and outgoing chair of the AADA iPLEDGE work group, cited difficulty in working with IPMG on modifications as another barrier. She also spoke during the open public hearing.
“Despite many, many attempts to work with the IPMG, we are not aware of any organizational structure or key leaders to communicate with. Instead we have been given repeatedly a generic email address for trying to establish a working relationship and we believe this may explain the inaction of the IPMG since our proposals 4 years ago in 2019.”
Among those proposals, she said, were allowing telemedicine visits as part of the iPLEDGE REMS program and reducing counseling attestation to every 6 months instead of monthly for those who cannot become pregnant.
She pointed to the chaotic rollout of modifications to the iPLEDGE program on a new website at the end of 2021.
In 2021, she said, “despite 6 months of notification, no prescriber input was solicited before revamping the website. This lack of transparency and accountability has been a major hurdle in improving iPLEDGE.”
Dr. Barbieri called the rollout “a debacle” that could have been mitigated with communication with IPMG. “We warned about every issue that happened and talked about ways to mitigate it and were largely ignored,” he said.
“By including dermatologists and key stakeholders in these discussions, as we move forward with changes to improve this program, we can make sure that it’s patient-centered.”
IPMG did not address the specific complaints about the working relationship with the AADA workgroup at the meeting.
Monthly attestation for counseling patients who cannot get pregnant
Dr. Barbieri said the monthly requirement to counsel patients who cannot get pregnant and document that counseling unfairly burdens clinicians and patients. “We’re essentially asking patients to come in monthly just to tell them not to share their drugs [or] donate blood,” he said.
Ken Katz, MD, MSc, a dermatologist at Kaiser Permanente in San Francisco, was among the panel members voting not to continue the 19-day lockout.
“I think this places an unduly high burden physically and psychologically on our patients. It seems arbitrary,” he said. “Likely we will miss some pregnancies; we are missing some already. But the burden is not matched by the benefit.”
IPMG representative Dr. Wedin, said, “while we cannot support eliminating or extending the confirmation interval to a year, the [iPLEDGE] sponsors are agreeable [to] a 120-day confirmation interval.”
He said that while an extension to 120 days would reduce burden on prescribers, it comes with the risk in reducing oversight by a certified iPLEDGE prescriber and potentially increasing the risk for drug sharing.
“A patient may be more likely to share their drug with another person the further along with therapy they get as their condition improves,” Dr. Wedin said.
Home pregnancy testing
The advisory groups were also tasked with discussing whether home pregnancy tests, allowed during the COVID-19 public health emergency, should continue to be allowed. Most committee members and those in the public hearing who spoke on the issue agreed that home tests should continue in an effort to increase access and decrease burden.
During the pandemic, iPLEDGE rules have been relaxed from having a pregnancy test done only at a Clinical Laboratory Improvement Amendments–certified laboratory.
Lindsey Crist, PharmD, a risk management analyst at the FDA, who presented the FDA review committee’s analysis, said that the FDA’s review committee recommends ending the allowance of home tests, citing insufficient data on use and the discovery of instances of falsification of pregnancy tests.
“One study at an academic medical center reviewed the medical records of 89 patients who used home pregnancy tests while taking isotretinoin during the public health emergency. It found that 15.7% submitted falsified pregnancy test results,” Dr. Crist said.
Dr. Crist added, however, that the review committee recommends allowing the tests to be done in a provider’s office as an alternative.
Workaround to avoid falsification
Advisory committee member Brian P. Green, DO, associate professor of dermatology at Penn State University, Hershey, Pa., spoke in support of home pregnancy tests.
“What we have people do for telemedicine is take the stick, write their name, write the date on it, and send a picture of that the same day as their visit,” he said. “That way we have the pregnancy test the same day. Allowing this to continue to happen at home is important. Bringing people in is burdensome and costly.”
Emmy Graber, MD, a dermatologist who practices in Boston, and a director of the American Acne and Rosacea Society (AARS), relayed an example of the burden for a patient using isotretinoin who lives 1.5 hours away from the dermatology office. She is able to meet the requirements of iPLEDGE only through telehealth.
“Home pregnancy tests are highly sensitive, equal to the ones done in CLIA-certified labs, and highly accurate when interpreted by a dermatology provider,” said Dr. Graber, who spoke on behalf of the AARS during the open public hearing.
“Notably, CLIA [Clinical Laboratory Improvement Amendments] certification is not required by other REMS programs” for teratogenic drugs, she added.
Dr. Graber said it’s important to note that in the time the pandemic exceptions have been made for isotretinoin patients, “there has been no reported spike in pregnancy in the past three years.
“We do have some data to show that it is not imposing additional harms,” she said.
Suggestions for improvement
At the end of the hearing, advisory committee members were asked to propose improvements to the iPLEDGE REMS program.
Dr. Green advocated for the addition of an iPLEDGE mobile app.
“Most people go to their phones rather than their computers, particularly teenagers and younger people,” he noted.
Advisory committee member Megha M. Tollefson, MD, professor of dermatology and pediatric and adolescent medicine at Mayo Clinic in Rochester, Minn., echoed the need for an iPLEDGE app.
The young patients getting isotretinoin “don’t respond to email, they don’t necessarily go onto web pages. If we’re going to be as effective as possible, it’s going to have to be through an app-based system.”
Dr. Tollefson said she would like to see patient counseling standardized through the app. “I think there’s a lot of variability in what counseling is given when it’s left to the individual prescriber or practice,” she said.
Exceptions for long-acting contraceptives?
Advisory committee member Abbey B. Berenson, MD, PhD, professor of obstetrics and gynecology at University of Texas Medical Branch in Galveston, said that patients taking long-acting reversible contraceptives (LARCs) may need to be considered differently when deciding the intervals for attestation or whether to have a lockout period.
“LARC methods’ rate of failure is extremely low,” she said. “While it is true, as it has been pointed out, that all methods can fail, when they’re over 99% effective, I think that we can treat those methods differently than we treat methods such as birth control pills or abstinence that fail far more often. That is one way we could minimize burden on the providers and the patients.”
She also suggested using members of the health care team other than physicians to complete counseling, such as a nurse or pharmacist.
Prescriptions for emergency contraception
Advisory committee member Sascha Dublin, MD, PhD, senior scientific investigator for Kaiser Permanente Washington Health Research Institute in Seattle, said most patients taking the drug who can get pregnant should get a prescription for emergency contraception at the time of the first isotretinoin prescription.
“They don’t have to buy it, but to make it available at the very beginning sets the expectation that it would be good to have in your medicine cabinet, particularly if the [contraception] choice is abstinence or birth control pills.”
Dr. Dublin also called for better transparency surrounding the role of IPMG.
She said IPMG should be expected to collect data in a way that allows examination of health disparities, including by race and ethnicity and insurance status. Dr. Dublin added that she was concerned about the poor communication between dermatological societies and IPMG.
“The FDA should really require that IPMG hold periodic, regularly scheduled stakeholder forums,” she said. “There has to be a mechanism in place for IPMG to listen to those concerns in real time and respond.”
The advisory committees’ recommendations to the FDA are nonbinding, but the FDA generally follows the recommendations of advisory panels.
During 2 days of after the chaotic rollout of the new REMS platform at the end of 2021.
On March 29, at the end of the FDA’s joint meeting of two advisory committees that addressed ways to improve the iPLEDGE program, most panelists voted to change the 19-day lockout period for patients who can become pregnant, and the requirement that every month, providers must document counseling of those who cannot get pregnant and are taking the drug for acne.
However, there was no consensus on whether there should be a lockout at all or for how long, and what an appropriate interval for counseling those who cannot get pregnant would be, if not monthly. Those voting on the questions repeatedly cited a lack of data to make well-informed decisions.
The meeting of the two panels, the FDA’s Drug Safety and Risk Management Advisory Committee and the Dermatologic and Ophthalmic Drugs Advisory Committee, was held March 28-29, to discuss proposed changes to iPLEDGE requirements, to minimize the program’s burden on patients, prescribers, and pharmacies – while maintaining safe use of the highly teratogenic drug.
Lockout based on outdated reasoning
John S. Barbieri, MD, a dermatologist and epidemiologist, and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital in Boston, speaking as deputy chair of the American Academy of Dermatology Association (AADA) iPLEDGE work group, described the burden of getting the drug to patients. He was not on the panel, but spoke during the open public hearing.
“Compared to other acne medications, the time it takes to successfully go from prescribed (isotretinoin) to when the patient actually has it in their hands is 5- to 10-fold higher,” he said.
Among the barriers is the 19-day lockout period for people who can get pregnant and miss the 7-day window for picking up their prescriptions. They must then wait 19 days to get a pregnancy test to clear them for receiving the medication.
Gregory Wedin, PharmD, pharmacovigilance and risk management director of Upsher-Smith Laboratories, who spoke on behalf of the Isotretinoin Products Manufacturer Group (IPMG), which manages iPLEDGE, said, “The rationale for the 19-day wait is to ensure the next confirmatory pregnancy test is completed after the most fertile period of the menstrual cycle is passed.”
Many don’t have a monthly cycle
But Dr. Barbieri said that reasoning is outdated.
“The current program’s focus on the menstrual cycle is really an antiquated approach,” he said. “Many patients do not have a monthly cycle due to medical conditions like polycystic ovarian syndrome, or due to [certain kinds of] contraception.”
He added, “By removing this 19-day lockout and, really, the archaic timing around the menstrual cycle in general in this program, we can simplify the program, improve it, and better align it with the real-world biology of our patients.” He added that patients are often missing the 7-day window for picking up their prescriptions through no fault of their own. Speakers at the hearing also mentioned insurance hassles and ordering delays.
Communication with IPMG
Ilona Frieden, MD, professor of dermatology and pediatrics at the University of California, San Francisco, and outgoing chair of the AADA iPLEDGE work group, cited difficulty in working with IPMG on modifications as another barrier. She also spoke during the open public hearing.
“Despite many, many attempts to work with the IPMG, we are not aware of any organizational structure or key leaders to communicate with. Instead we have been given repeatedly a generic email address for trying to establish a working relationship and we believe this may explain the inaction of the IPMG since our proposals 4 years ago in 2019.”
Among those proposals, she said, were allowing telemedicine visits as part of the iPLEDGE REMS program and reducing counseling attestation to every 6 months instead of monthly for those who cannot become pregnant.
She pointed to the chaotic rollout of modifications to the iPLEDGE program on a new website at the end of 2021.
In 2021, she said, “despite 6 months of notification, no prescriber input was solicited before revamping the website. This lack of transparency and accountability has been a major hurdle in improving iPLEDGE.”
Dr. Barbieri called the rollout “a debacle” that could have been mitigated with communication with IPMG. “We warned about every issue that happened and talked about ways to mitigate it and were largely ignored,” he said.
“By including dermatologists and key stakeholders in these discussions, as we move forward with changes to improve this program, we can make sure that it’s patient-centered.”
IPMG did not address the specific complaints about the working relationship with the AADA workgroup at the meeting.
Monthly attestation for counseling patients who cannot get pregnant
Dr. Barbieri said the monthly requirement to counsel patients who cannot get pregnant and document that counseling unfairly burdens clinicians and patients. “We’re essentially asking patients to come in monthly just to tell them not to share their drugs [or] donate blood,” he said.
Ken Katz, MD, MSc, a dermatologist at Kaiser Permanente in San Francisco, was among the panel members voting not to continue the 19-day lockout.
“I think this places an unduly high burden physically and psychologically on our patients. It seems arbitrary,” he said. “Likely we will miss some pregnancies; we are missing some already. But the burden is not matched by the benefit.”
IPMG representative Dr. Wedin, said, “while we cannot support eliminating or extending the confirmation interval to a year, the [iPLEDGE] sponsors are agreeable [to] a 120-day confirmation interval.”
He said that while an extension to 120 days would reduce burden on prescribers, it comes with the risk in reducing oversight by a certified iPLEDGE prescriber and potentially increasing the risk for drug sharing.
“A patient may be more likely to share their drug with another person the further along with therapy they get as their condition improves,” Dr. Wedin said.
Home pregnancy testing
The advisory groups were also tasked with discussing whether home pregnancy tests, allowed during the COVID-19 public health emergency, should continue to be allowed. Most committee members and those in the public hearing who spoke on the issue agreed that home tests should continue in an effort to increase access and decrease burden.
During the pandemic, iPLEDGE rules have been relaxed from having a pregnancy test done only at a Clinical Laboratory Improvement Amendments–certified laboratory.
Lindsey Crist, PharmD, a risk management analyst at the FDA, who presented the FDA review committee’s analysis, said that the FDA’s review committee recommends ending the allowance of home tests, citing insufficient data on use and the discovery of instances of falsification of pregnancy tests.
“One study at an academic medical center reviewed the medical records of 89 patients who used home pregnancy tests while taking isotretinoin during the public health emergency. It found that 15.7% submitted falsified pregnancy test results,” Dr. Crist said.
Dr. Crist added, however, that the review committee recommends allowing the tests to be done in a provider’s office as an alternative.
Workaround to avoid falsification
Advisory committee member Brian P. Green, DO, associate professor of dermatology at Penn State University, Hershey, Pa., spoke in support of home pregnancy tests.
“What we have people do for telemedicine is take the stick, write their name, write the date on it, and send a picture of that the same day as their visit,” he said. “That way we have the pregnancy test the same day. Allowing this to continue to happen at home is important. Bringing people in is burdensome and costly.”
Emmy Graber, MD, a dermatologist who practices in Boston, and a director of the American Acne and Rosacea Society (AARS), relayed an example of the burden for a patient using isotretinoin who lives 1.5 hours away from the dermatology office. She is able to meet the requirements of iPLEDGE only through telehealth.
“Home pregnancy tests are highly sensitive, equal to the ones done in CLIA-certified labs, and highly accurate when interpreted by a dermatology provider,” said Dr. Graber, who spoke on behalf of the AARS during the open public hearing.
“Notably, CLIA [Clinical Laboratory Improvement Amendments] certification is not required by other REMS programs” for teratogenic drugs, she added.
Dr. Graber said it’s important to note that in the time the pandemic exceptions have been made for isotretinoin patients, “there has been no reported spike in pregnancy in the past three years.
“We do have some data to show that it is not imposing additional harms,” she said.
Suggestions for improvement
At the end of the hearing, advisory committee members were asked to propose improvements to the iPLEDGE REMS program.
Dr. Green advocated for the addition of an iPLEDGE mobile app.
“Most people go to their phones rather than their computers, particularly teenagers and younger people,” he noted.
Advisory committee member Megha M. Tollefson, MD, professor of dermatology and pediatric and adolescent medicine at Mayo Clinic in Rochester, Minn., echoed the need for an iPLEDGE app.
The young patients getting isotretinoin “don’t respond to email, they don’t necessarily go onto web pages. If we’re going to be as effective as possible, it’s going to have to be through an app-based system.”
Dr. Tollefson said she would like to see patient counseling standardized through the app. “I think there’s a lot of variability in what counseling is given when it’s left to the individual prescriber or practice,” she said.
Exceptions for long-acting contraceptives?
Advisory committee member Abbey B. Berenson, MD, PhD, professor of obstetrics and gynecology at University of Texas Medical Branch in Galveston, said that patients taking long-acting reversible contraceptives (LARCs) may need to be considered differently when deciding the intervals for attestation or whether to have a lockout period.
“LARC methods’ rate of failure is extremely low,” she said. “While it is true, as it has been pointed out, that all methods can fail, when they’re over 99% effective, I think that we can treat those methods differently than we treat methods such as birth control pills or abstinence that fail far more often. That is one way we could minimize burden on the providers and the patients.”
She also suggested using members of the health care team other than physicians to complete counseling, such as a nurse or pharmacist.
Prescriptions for emergency contraception
Advisory committee member Sascha Dublin, MD, PhD, senior scientific investigator for Kaiser Permanente Washington Health Research Institute in Seattle, said most patients taking the drug who can get pregnant should get a prescription for emergency contraception at the time of the first isotretinoin prescription.
“They don’t have to buy it, but to make it available at the very beginning sets the expectation that it would be good to have in your medicine cabinet, particularly if the [contraception] choice is abstinence or birth control pills.”
Dr. Dublin also called for better transparency surrounding the role of IPMG.
She said IPMG should be expected to collect data in a way that allows examination of health disparities, including by race and ethnicity and insurance status. Dr. Dublin added that she was concerned about the poor communication between dermatological societies and IPMG.
“The FDA should really require that IPMG hold periodic, regularly scheduled stakeholder forums,” she said. “There has to be a mechanism in place for IPMG to listen to those concerns in real time and respond.”
The advisory committees’ recommendations to the FDA are nonbinding, but the FDA generally follows the recommendations of advisory panels.