User login
Pediatricians at odds over gender-affirming care for trans kids
Some members of the American Academy of Pediatrics say its association leadership is blocking discussion about a resolution asking for a “rigorous systematic review” of gender-affirming care guidelines.
At issue is 2018 guidance that states children can undergo hormonal therapy after they are deemed appropriate candidates following a thorough mental health evaluation.
Critics say minors under age 18 may be getting “fast-tracked” to hormonal treatment too quickly or inappropriately and can end up regretting the decision and facing medical conditions like sterility.
Five AAP members, which has a total membership of around 67,000 pediatricians in the United States and Canada, this year penned Resolution 27, calling for a possible update of the guidelines following consultation with stakeholders that include mental health and medical clinicians, parents, and patients “with diverse views and experiences.”
Those members and others in written comments on a members-only website accuse the AAP of deliberately silencing debate on the issue and changing resolution rules. Any AAP member can submit a resolution for consideration by the group’s leadership at its annual policy meeting.
This year, the AAP sent an email to members stating it would not allow comments on resolutions that had not been “sponsored” by one of the group’s 66 chapters or 88 internal committees, councils, or sections.
That’s why comments were not allowed on Resolution 27, said Mark Del Monte, the AAP’s CEO. A second attempt to get sponsorship during the annual leadership forum, held earlier this month in Chicago, also failed, he noted. Mr. Del Monte told this news organization that changes to the resolution process are made every year and that no rule changes were directly associated with Resolution 27.
But one of the resolution’s authors said there was sponsorship when members first drafted the suggestion. Julia Mason, MD, a board member for the Society for Evidence-based Gender Medicine and a pediatrician in private practice in Gresham, Ore., says an AAP chapter president agreed to second Resolution 27 but backed off after attending a different AAP meeting. Dr. Mason did not name the member.
On Aug. 10, AAP President Moira Szilagyi, MD, PhD, wrote in a blog on the AAP website – after the AAP leadership meeting in Chicago – that the lack of sponsorship “meant no one was willing to support their proposal.”
The AAP Leadership Council’s 154 voting entities approved 48 resolutions at the meeting, all of which will be referred to the AAP Board of Directors for potential, but not definite, action as the Board only takes resolutions under advisement, Mr. Del Monte notes.
In an email allowing members to comment on a resolution (number 28) regarding education support for caring for transgender patients, 23 chose to support Resolution 27 instead.
“I am wholeheartedly in support of Resolution 27, which interestingly has been removed from the list of resolutions for member comment,” one comment read. “I can no longer trust the AAP to provide medical evidence-based education with regard to care for transgender individuals.”
“We don’t need a formal resolution to look at the evidence around the care of transgender young people. Evaluating the evidence behind our recommendations, which the unsponsored resolution called for, is a routine part of the Academy’s policy-writing process,” wrote Dr. Szilagyi in her blog.
Mr. Del Monte says that “the 2018 policy is under review now.”
So far, “the evidence that we have seen reinforces our policy that gender-affirming care is the correct approach,” Mr. Del Monte stresses. “It is supported by every mainstream medical society in the world and is the standard of care,” he maintains.
Among those societies is the World Professional Association for Transgender Health, which in the draft of its latest Standards of Care (SOC8) – the first new guidance on the issue for 10 years – reportedly lowers the age for “top surgery” to 15 years.
The final SOC8 will most likely be published to coincide with WPATH’s annual meeting in September in Montreal.
Opponents plan to protest outside the AAP’s annual meeting, in Anaheim in October, Dr. Mason says.
“I’m concerned that kids with a transient gender identity are being funneled into medicalization that does not serve them,” Dr. Mason says. “I am worried that the trans identity is valued over the possibility of desistance,” she adds, admitting that her goal is to have fewer children transition gender.
Last summer, AAP found itself in hot water on the same topic when it barred SEGM from having a booth at the AAP annual meeting in 2021, as reported by this news organization.
A version of this article first appeared on Medscape.com.
Some members of the American Academy of Pediatrics say its association leadership is blocking discussion about a resolution asking for a “rigorous systematic review” of gender-affirming care guidelines.
At issue is 2018 guidance that states children can undergo hormonal therapy after they are deemed appropriate candidates following a thorough mental health evaluation.
Critics say minors under age 18 may be getting “fast-tracked” to hormonal treatment too quickly or inappropriately and can end up regretting the decision and facing medical conditions like sterility.
Five AAP members, which has a total membership of around 67,000 pediatricians in the United States and Canada, this year penned Resolution 27, calling for a possible update of the guidelines following consultation with stakeholders that include mental health and medical clinicians, parents, and patients “with diverse views and experiences.”
Those members and others in written comments on a members-only website accuse the AAP of deliberately silencing debate on the issue and changing resolution rules. Any AAP member can submit a resolution for consideration by the group’s leadership at its annual policy meeting.
This year, the AAP sent an email to members stating it would not allow comments on resolutions that had not been “sponsored” by one of the group’s 66 chapters or 88 internal committees, councils, or sections.
That’s why comments were not allowed on Resolution 27, said Mark Del Monte, the AAP’s CEO. A second attempt to get sponsorship during the annual leadership forum, held earlier this month in Chicago, also failed, he noted. Mr. Del Monte told this news organization that changes to the resolution process are made every year and that no rule changes were directly associated with Resolution 27.
But one of the resolution’s authors said there was sponsorship when members first drafted the suggestion. Julia Mason, MD, a board member for the Society for Evidence-based Gender Medicine and a pediatrician in private practice in Gresham, Ore., says an AAP chapter president agreed to second Resolution 27 but backed off after attending a different AAP meeting. Dr. Mason did not name the member.
On Aug. 10, AAP President Moira Szilagyi, MD, PhD, wrote in a blog on the AAP website – after the AAP leadership meeting in Chicago – that the lack of sponsorship “meant no one was willing to support their proposal.”
The AAP Leadership Council’s 154 voting entities approved 48 resolutions at the meeting, all of which will be referred to the AAP Board of Directors for potential, but not definite, action as the Board only takes resolutions under advisement, Mr. Del Monte notes.
In an email allowing members to comment on a resolution (number 28) regarding education support for caring for transgender patients, 23 chose to support Resolution 27 instead.
“I am wholeheartedly in support of Resolution 27, which interestingly has been removed from the list of resolutions for member comment,” one comment read. “I can no longer trust the AAP to provide medical evidence-based education with regard to care for transgender individuals.”
“We don’t need a formal resolution to look at the evidence around the care of transgender young people. Evaluating the evidence behind our recommendations, which the unsponsored resolution called for, is a routine part of the Academy’s policy-writing process,” wrote Dr. Szilagyi in her blog.
Mr. Del Monte says that “the 2018 policy is under review now.”
So far, “the evidence that we have seen reinforces our policy that gender-affirming care is the correct approach,” Mr. Del Monte stresses. “It is supported by every mainstream medical society in the world and is the standard of care,” he maintains.
Among those societies is the World Professional Association for Transgender Health, which in the draft of its latest Standards of Care (SOC8) – the first new guidance on the issue for 10 years – reportedly lowers the age for “top surgery” to 15 years.
The final SOC8 will most likely be published to coincide with WPATH’s annual meeting in September in Montreal.
Opponents plan to protest outside the AAP’s annual meeting, in Anaheim in October, Dr. Mason says.
“I’m concerned that kids with a transient gender identity are being funneled into medicalization that does not serve them,” Dr. Mason says. “I am worried that the trans identity is valued over the possibility of desistance,” she adds, admitting that her goal is to have fewer children transition gender.
Last summer, AAP found itself in hot water on the same topic when it barred SEGM from having a booth at the AAP annual meeting in 2021, as reported by this news organization.
A version of this article first appeared on Medscape.com.
Some members of the American Academy of Pediatrics say its association leadership is blocking discussion about a resolution asking for a “rigorous systematic review” of gender-affirming care guidelines.
At issue is 2018 guidance that states children can undergo hormonal therapy after they are deemed appropriate candidates following a thorough mental health evaluation.
Critics say minors under age 18 may be getting “fast-tracked” to hormonal treatment too quickly or inappropriately and can end up regretting the decision and facing medical conditions like sterility.
Five AAP members, which has a total membership of around 67,000 pediatricians in the United States and Canada, this year penned Resolution 27, calling for a possible update of the guidelines following consultation with stakeholders that include mental health and medical clinicians, parents, and patients “with diverse views and experiences.”
Those members and others in written comments on a members-only website accuse the AAP of deliberately silencing debate on the issue and changing resolution rules. Any AAP member can submit a resolution for consideration by the group’s leadership at its annual policy meeting.
This year, the AAP sent an email to members stating it would not allow comments on resolutions that had not been “sponsored” by one of the group’s 66 chapters or 88 internal committees, councils, or sections.
That’s why comments were not allowed on Resolution 27, said Mark Del Monte, the AAP’s CEO. A second attempt to get sponsorship during the annual leadership forum, held earlier this month in Chicago, also failed, he noted. Mr. Del Monte told this news organization that changes to the resolution process are made every year and that no rule changes were directly associated with Resolution 27.
But one of the resolution’s authors said there was sponsorship when members first drafted the suggestion. Julia Mason, MD, a board member for the Society for Evidence-based Gender Medicine and a pediatrician in private practice in Gresham, Ore., says an AAP chapter president agreed to second Resolution 27 but backed off after attending a different AAP meeting. Dr. Mason did not name the member.
On Aug. 10, AAP President Moira Szilagyi, MD, PhD, wrote in a blog on the AAP website – after the AAP leadership meeting in Chicago – that the lack of sponsorship “meant no one was willing to support their proposal.”
The AAP Leadership Council’s 154 voting entities approved 48 resolutions at the meeting, all of which will be referred to the AAP Board of Directors for potential, but not definite, action as the Board only takes resolutions under advisement, Mr. Del Monte notes.
In an email allowing members to comment on a resolution (number 28) regarding education support for caring for transgender patients, 23 chose to support Resolution 27 instead.
“I am wholeheartedly in support of Resolution 27, which interestingly has been removed from the list of resolutions for member comment,” one comment read. “I can no longer trust the AAP to provide medical evidence-based education with regard to care for transgender individuals.”
“We don’t need a formal resolution to look at the evidence around the care of transgender young people. Evaluating the evidence behind our recommendations, which the unsponsored resolution called for, is a routine part of the Academy’s policy-writing process,” wrote Dr. Szilagyi in her blog.
Mr. Del Monte says that “the 2018 policy is under review now.”
So far, “the evidence that we have seen reinforces our policy that gender-affirming care is the correct approach,” Mr. Del Monte stresses. “It is supported by every mainstream medical society in the world and is the standard of care,” he maintains.
Among those societies is the World Professional Association for Transgender Health, which in the draft of its latest Standards of Care (SOC8) – the first new guidance on the issue for 10 years – reportedly lowers the age for “top surgery” to 15 years.
The final SOC8 will most likely be published to coincide with WPATH’s annual meeting in September in Montreal.
Opponents plan to protest outside the AAP’s annual meeting, in Anaheim in October, Dr. Mason says.
“I’m concerned that kids with a transient gender identity are being funneled into medicalization that does not serve them,” Dr. Mason says. “I am worried that the trans identity is valued over the possibility of desistance,” she adds, admitting that her goal is to have fewer children transition gender.
Last summer, AAP found itself in hot water on the same topic when it barred SEGM from having a booth at the AAP annual meeting in 2021, as reported by this news organization.
A version of this article first appeared on Medscape.com.
Children and COVID: ED visits and new admissions change course
New child cases of COVID-19 made at least a temporary transition from slow increase to decrease, and emergency department visits and new admissions seem to be following a downward trend.
, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. For some historical perspective, the latest weekly count falls below last year’s Delta surge figure of 121,000 (Aug. 6-12) but above the summer 2020 total of 26,000 (Aug. 7-13).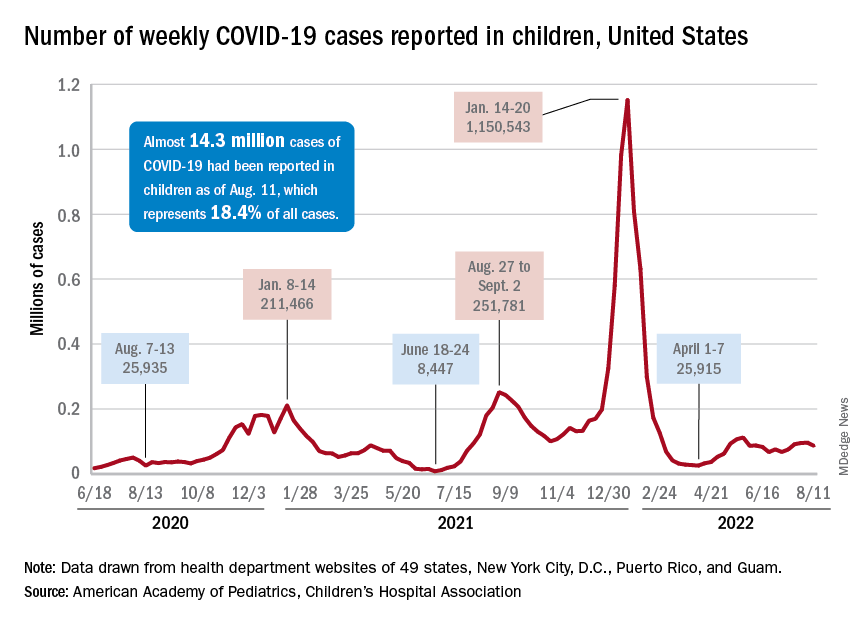
Measures of serious illness finally head downward
The prolonged rise in ED visits and new admissions over the last 5 months, which continued even through late spring when cases were declining, seems to have peaked, CDC data suggest.
That upward trend, driven largely by continued increases among younger children, peaked in late July, when 6.7% of all ED visits for children aged 0-11 years involved diagnosed COVID-19. The corresponding peaks for older children occurred around the same time but were only about half as high: 3.4% for 12- to 15-year-olds and 3.6% for those aged 16-17, the CDC reported.
The data for new admissions present a similar scenario: an increase starting in mid-April that continued unabated into late July despite the decline in new cases. By the time admissions among children aged 0-17 years peaked at 0.46 per 100,000 population in late July, they had reached the same level seen during the Delta surge. By Aug. 7, the rate of new hospitalizations was down to 0.42 per 100,000, the CDC said on its COVID Data Tracker.
The vaccine is ready for all students, but …
As children all over the country start or get ready to start a new school year, the only large-scale student vaccine mandate belongs to the District of Columbia. California has a mandate pending, but it will not go into effect until after July 1, 2023. There are, however, 20 states that have banned vaccine mandates for students, according to the National Academy for State Health Policy.
Nonmandated vaccination of the youngest children against COVID-19 continues to be slow. In the approximately 7 weeks (June 19 to Aug. 9) since the vaccine was approved for use in children younger than 5 years, just 4.4% of that age group has received at least one dose and 0.7% are fully vaccinated. Among those aged 5-11 years, who have been vaccine-eligible since early November of last year, 37.6% have received at least one dose and 30.2% are fully vaccinated, the CDC said.
New child cases of COVID-19 made at least a temporary transition from slow increase to decrease, and emergency department visits and new admissions seem to be following a downward trend.
, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. For some historical perspective, the latest weekly count falls below last year’s Delta surge figure of 121,000 (Aug. 6-12) but above the summer 2020 total of 26,000 (Aug. 7-13).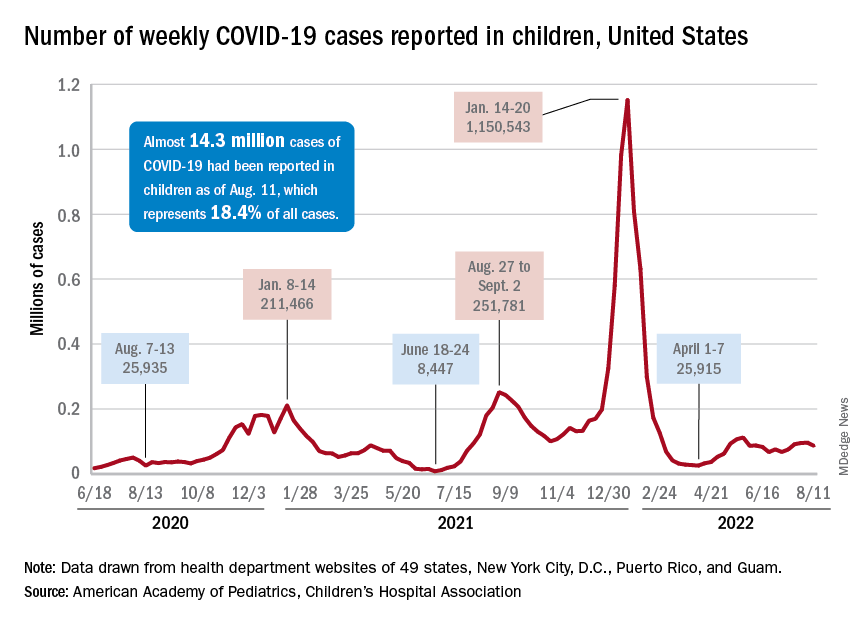
Measures of serious illness finally head downward
The prolonged rise in ED visits and new admissions over the last 5 months, which continued even through late spring when cases were declining, seems to have peaked, CDC data suggest.
That upward trend, driven largely by continued increases among younger children, peaked in late July, when 6.7% of all ED visits for children aged 0-11 years involved diagnosed COVID-19. The corresponding peaks for older children occurred around the same time but were only about half as high: 3.4% for 12- to 15-year-olds and 3.6% for those aged 16-17, the CDC reported.
The data for new admissions present a similar scenario: an increase starting in mid-April that continued unabated into late July despite the decline in new cases. By the time admissions among children aged 0-17 years peaked at 0.46 per 100,000 population in late July, they had reached the same level seen during the Delta surge. By Aug. 7, the rate of new hospitalizations was down to 0.42 per 100,000, the CDC said on its COVID Data Tracker.
The vaccine is ready for all students, but …
As children all over the country start or get ready to start a new school year, the only large-scale student vaccine mandate belongs to the District of Columbia. California has a mandate pending, but it will not go into effect until after July 1, 2023. There are, however, 20 states that have banned vaccine mandates for students, according to the National Academy for State Health Policy.
Nonmandated vaccination of the youngest children against COVID-19 continues to be slow. In the approximately 7 weeks (June 19 to Aug. 9) since the vaccine was approved for use in children younger than 5 years, just 4.4% of that age group has received at least one dose and 0.7% are fully vaccinated. Among those aged 5-11 years, who have been vaccine-eligible since early November of last year, 37.6% have received at least one dose and 30.2% are fully vaccinated, the CDC said.
New child cases of COVID-19 made at least a temporary transition from slow increase to decrease, and emergency department visits and new admissions seem to be following a downward trend.
, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. For some historical perspective, the latest weekly count falls below last year’s Delta surge figure of 121,000 (Aug. 6-12) but above the summer 2020 total of 26,000 (Aug. 7-13).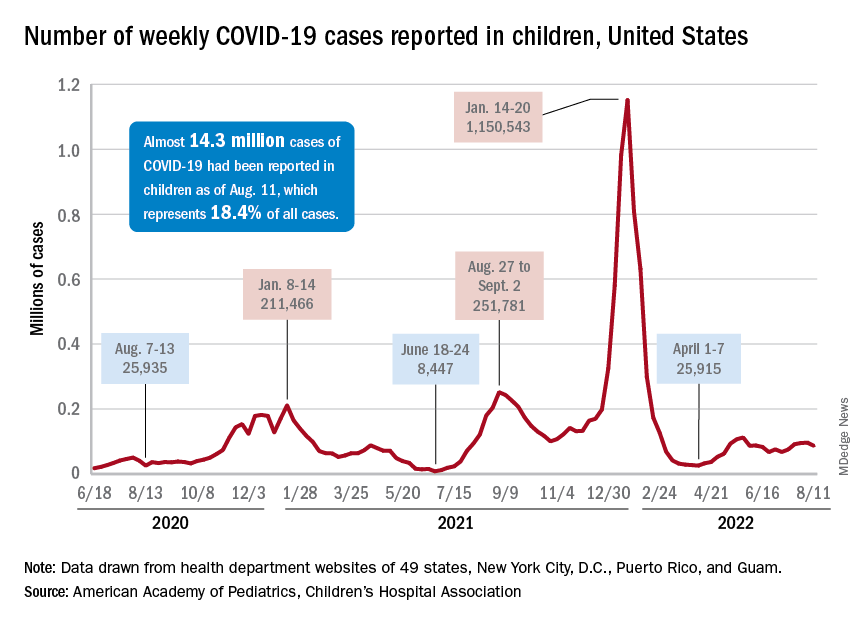
Measures of serious illness finally head downward
The prolonged rise in ED visits and new admissions over the last 5 months, which continued even through late spring when cases were declining, seems to have peaked, CDC data suggest.
That upward trend, driven largely by continued increases among younger children, peaked in late July, when 6.7% of all ED visits for children aged 0-11 years involved diagnosed COVID-19. The corresponding peaks for older children occurred around the same time but were only about half as high: 3.4% for 12- to 15-year-olds and 3.6% for those aged 16-17, the CDC reported.
The data for new admissions present a similar scenario: an increase starting in mid-April that continued unabated into late July despite the decline in new cases. By the time admissions among children aged 0-17 years peaked at 0.46 per 100,000 population in late July, they had reached the same level seen during the Delta surge. By Aug. 7, the rate of new hospitalizations was down to 0.42 per 100,000, the CDC said on its COVID Data Tracker.
The vaccine is ready for all students, but …
As children all over the country start or get ready to start a new school year, the only large-scale student vaccine mandate belongs to the District of Columbia. California has a mandate pending, but it will not go into effect until after July 1, 2023. There are, however, 20 states that have banned vaccine mandates for students, according to the National Academy for State Health Policy.
Nonmandated vaccination of the youngest children against COVID-19 continues to be slow. In the approximately 7 weeks (June 19 to Aug. 9) since the vaccine was approved for use in children younger than 5 years, just 4.4% of that age group has received at least one dose and 0.7% are fully vaccinated. Among those aged 5-11 years, who have been vaccine-eligible since early November of last year, 37.6% have received at least one dose and 30.2% are fully vaccinated, the CDC said.
Prematurity, family environment linked to lower rate of school readiness
Among children born prematurely, rates of school readiness were lower, compared with rates for children born full term, new data indicate.
In a Canadian cohort study that included more than 60,000 children, 35% of children born prematurely had scores on the Early Development Instrument (EDI) that indicated they were vulnerable to developmental problems, compared with 28% of children born full term.
“Our take-home message is that being born prematurely, even if all was well, is a risk factor for not being ready for school, and these families should be identified early, screened for any difficulties, and offered early intervention,” senior author Chelsea A. Ruth, MD, assistant professor of pediatrics and child health at the University of Manitoba, Winnipeg, told this news organization.
The findings were published online in JAMA Pediatrics.
Gestational age gradient
The investigators examined two cohorts of children who were in kindergarten at the time of data collection. One of them, the population-based cohort, included children born between 2000 and 2011 whose school readiness was assessed using the EDI data. Preterm birth was defined as a gestational age (GA) of less than 37 weeks. The other, the sibling cohort, was a subset of the population cohort and included children born prematurely and their closest-in-age siblings who were born full term.
The main outcome was vulnerability in the EDI, which was defined as having a score below the 10th percentile of the Canadian population norms for one or more of the five EDI domains. These domains are physical health and well-being, social competence, emotional maturity, language and cognitive development, and communication skills and general knowledge.
A total of 63,277 children were included in the analyses, of whom 4,352 were born prematurely (mean GA, 34 weeks; 53% boys) and 58,925 were born full term (mean GA, 39 weeks; 51% boys).
After data adjustment, 35% of children born prematurely were vulnerable in the EDI, compared with 28% of those born full term (adjusted odds ratio, 1.32).
The investigators found a clear GA gradient. Children born at earlier GAs (< 28 weeks or 28-33 weeks) were at higher risk of being vulnerable than those born at later GAs (34-36 weeks) in any EDI domain (48% vs. 40%) and in each of the five EDI domains. Earlier GA was associated with greater risk for vulnerability in physical health and well-being (34% vs. 22%) and in the Multiple Challenge Index (25% vs. 17%). It also was associated with greater risk for need for additional support in kindergarten (22% vs. 5%).
Furthermore, 12% of children born at less than 28 weeks’ gestation were vulnerable in two EDI domains, and 8% were vulnerable in three domains. The corresponding proportions were 9% and 7%, respectively, for those born between 28 and 33 weeks and 7% and 5% for those born between 34 and 36 weeks.
“The study confirmed what we see in practice, that being born even a little bit early increases the chance for not being ready for school, and the earlier a child is born, the more likely they are to have troubles,” said Dr. Ruth.
Cause or manifestation?
In the population cohort, prematurity (< 34 weeks’ GA: AOR, 1.72; 34-36 weeks’ GA: AOR, 1.23), male sex (AOR, 2.24), small for GA (AOR, 1.31), and various maternal medical and sociodemographic factors were associated with EDI vulnerability.
In the sibling subset, EDI outcomes were similar for children born prematurely and their siblings born full term, except for the communication skills and general knowledge domain (AOR, 1.39) and the Multiple Challenge Index (AOR, 1.43). Male sex (AOR, 2.19) was associated with EDI vulnerability in this cohort as well, as was maternal age at delivery (AOR, 1.53).
“Whether prematurity is a cause or a manifestation of an altered family ecosystem is difficult to ascertain,” Lauren Neel, MD, a neonatologist at Emory University, Atlanta, and colleagues write in an accompanying editorial. “However, research on this topic is much needed, along with novel interventions to change academic trajectories and care models that implement these findings in practice. As we begin to understand the factors in and interventions for promoting resilience in preterm-born children, we may need to change our research question to this: Could we optimize resilience and long-term academic trajectories to include the family as well?”
Six crucial years
Commenting on the study, Veronica Bordes Edgar, PhD, associate professor of psychiatry and pediatrics at the University of Texas Southwestern Medical Center’s Peter O’Donnell Jr. Brain Institute, Dallas, said, “None of the findings surprised me, but I was very pleased that they looked at such a broad sample.”
Pediatricians should monitor and screen children for early academic readiness, since these factors are associated with later academic outcomes, Dr. Edgar added. “Early intervention does not stop at age 3, but rather the first 6 years are so crucial to lay the foundation for future success. The pediatrician can play a role in preparing children and families by promoting early reading, such as through Reach Out and Read, encouraging language-rich play, and providing guidance on early childhood education and developmental needs.
“Further examination of long-term outcomes for these children to capture the longitudinal trend would help to document what is often observed clinically, in that children who start off with difficulties do not always catch up once they are in the academic environment,” Dr. Edgar concluded.
The study was supported by Research Manitoba and the Children’s Research Institute of Manitoba. Dr. Ruth, Dr. Neel, and Dr. Edgar have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among children born prematurely, rates of school readiness were lower, compared with rates for children born full term, new data indicate.
In a Canadian cohort study that included more than 60,000 children, 35% of children born prematurely had scores on the Early Development Instrument (EDI) that indicated they were vulnerable to developmental problems, compared with 28% of children born full term.
“Our take-home message is that being born prematurely, even if all was well, is a risk factor for not being ready for school, and these families should be identified early, screened for any difficulties, and offered early intervention,” senior author Chelsea A. Ruth, MD, assistant professor of pediatrics and child health at the University of Manitoba, Winnipeg, told this news organization.
The findings were published online in JAMA Pediatrics.
Gestational age gradient
The investigators examined two cohorts of children who were in kindergarten at the time of data collection. One of them, the population-based cohort, included children born between 2000 and 2011 whose school readiness was assessed using the EDI data. Preterm birth was defined as a gestational age (GA) of less than 37 weeks. The other, the sibling cohort, was a subset of the population cohort and included children born prematurely and their closest-in-age siblings who were born full term.
The main outcome was vulnerability in the EDI, which was defined as having a score below the 10th percentile of the Canadian population norms for one or more of the five EDI domains. These domains are physical health and well-being, social competence, emotional maturity, language and cognitive development, and communication skills and general knowledge.
A total of 63,277 children were included in the analyses, of whom 4,352 were born prematurely (mean GA, 34 weeks; 53% boys) and 58,925 were born full term (mean GA, 39 weeks; 51% boys).
After data adjustment, 35% of children born prematurely were vulnerable in the EDI, compared with 28% of those born full term (adjusted odds ratio, 1.32).
The investigators found a clear GA gradient. Children born at earlier GAs (< 28 weeks or 28-33 weeks) were at higher risk of being vulnerable than those born at later GAs (34-36 weeks) in any EDI domain (48% vs. 40%) and in each of the five EDI domains. Earlier GA was associated with greater risk for vulnerability in physical health and well-being (34% vs. 22%) and in the Multiple Challenge Index (25% vs. 17%). It also was associated with greater risk for need for additional support in kindergarten (22% vs. 5%).
Furthermore, 12% of children born at less than 28 weeks’ gestation were vulnerable in two EDI domains, and 8% were vulnerable in three domains. The corresponding proportions were 9% and 7%, respectively, for those born between 28 and 33 weeks and 7% and 5% for those born between 34 and 36 weeks.
“The study confirmed what we see in practice, that being born even a little bit early increases the chance for not being ready for school, and the earlier a child is born, the more likely they are to have troubles,” said Dr. Ruth.
Cause or manifestation?
In the population cohort, prematurity (< 34 weeks’ GA: AOR, 1.72; 34-36 weeks’ GA: AOR, 1.23), male sex (AOR, 2.24), small for GA (AOR, 1.31), and various maternal medical and sociodemographic factors were associated with EDI vulnerability.
In the sibling subset, EDI outcomes were similar for children born prematurely and their siblings born full term, except for the communication skills and general knowledge domain (AOR, 1.39) and the Multiple Challenge Index (AOR, 1.43). Male sex (AOR, 2.19) was associated with EDI vulnerability in this cohort as well, as was maternal age at delivery (AOR, 1.53).
“Whether prematurity is a cause or a manifestation of an altered family ecosystem is difficult to ascertain,” Lauren Neel, MD, a neonatologist at Emory University, Atlanta, and colleagues write in an accompanying editorial. “However, research on this topic is much needed, along with novel interventions to change academic trajectories and care models that implement these findings in practice. As we begin to understand the factors in and interventions for promoting resilience in preterm-born children, we may need to change our research question to this: Could we optimize resilience and long-term academic trajectories to include the family as well?”
Six crucial years
Commenting on the study, Veronica Bordes Edgar, PhD, associate professor of psychiatry and pediatrics at the University of Texas Southwestern Medical Center’s Peter O’Donnell Jr. Brain Institute, Dallas, said, “None of the findings surprised me, but I was very pleased that they looked at such a broad sample.”
Pediatricians should monitor and screen children for early academic readiness, since these factors are associated with later academic outcomes, Dr. Edgar added. “Early intervention does not stop at age 3, but rather the first 6 years are so crucial to lay the foundation for future success. The pediatrician can play a role in preparing children and families by promoting early reading, such as through Reach Out and Read, encouraging language-rich play, and providing guidance on early childhood education and developmental needs.
“Further examination of long-term outcomes for these children to capture the longitudinal trend would help to document what is often observed clinically, in that children who start off with difficulties do not always catch up once they are in the academic environment,” Dr. Edgar concluded.
The study was supported by Research Manitoba and the Children’s Research Institute of Manitoba. Dr. Ruth, Dr. Neel, and Dr. Edgar have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among children born prematurely, rates of school readiness were lower, compared with rates for children born full term, new data indicate.
In a Canadian cohort study that included more than 60,000 children, 35% of children born prematurely had scores on the Early Development Instrument (EDI) that indicated they were vulnerable to developmental problems, compared with 28% of children born full term.
“Our take-home message is that being born prematurely, even if all was well, is a risk factor for not being ready for school, and these families should be identified early, screened for any difficulties, and offered early intervention,” senior author Chelsea A. Ruth, MD, assistant professor of pediatrics and child health at the University of Manitoba, Winnipeg, told this news organization.
The findings were published online in JAMA Pediatrics.
Gestational age gradient
The investigators examined two cohorts of children who were in kindergarten at the time of data collection. One of them, the population-based cohort, included children born between 2000 and 2011 whose school readiness was assessed using the EDI data. Preterm birth was defined as a gestational age (GA) of less than 37 weeks. The other, the sibling cohort, was a subset of the population cohort and included children born prematurely and their closest-in-age siblings who were born full term.
The main outcome was vulnerability in the EDI, which was defined as having a score below the 10th percentile of the Canadian population norms for one or more of the five EDI domains. These domains are physical health and well-being, social competence, emotional maturity, language and cognitive development, and communication skills and general knowledge.
A total of 63,277 children were included in the analyses, of whom 4,352 were born prematurely (mean GA, 34 weeks; 53% boys) and 58,925 were born full term (mean GA, 39 weeks; 51% boys).
After data adjustment, 35% of children born prematurely were vulnerable in the EDI, compared with 28% of those born full term (adjusted odds ratio, 1.32).
The investigators found a clear GA gradient. Children born at earlier GAs (< 28 weeks or 28-33 weeks) were at higher risk of being vulnerable than those born at later GAs (34-36 weeks) in any EDI domain (48% vs. 40%) and in each of the five EDI domains. Earlier GA was associated with greater risk for vulnerability in physical health and well-being (34% vs. 22%) and in the Multiple Challenge Index (25% vs. 17%). It also was associated with greater risk for need for additional support in kindergarten (22% vs. 5%).
Furthermore, 12% of children born at less than 28 weeks’ gestation were vulnerable in two EDI domains, and 8% were vulnerable in three domains. The corresponding proportions were 9% and 7%, respectively, for those born between 28 and 33 weeks and 7% and 5% for those born between 34 and 36 weeks.
“The study confirmed what we see in practice, that being born even a little bit early increases the chance for not being ready for school, and the earlier a child is born, the more likely they are to have troubles,” said Dr. Ruth.
Cause or manifestation?
In the population cohort, prematurity (< 34 weeks’ GA: AOR, 1.72; 34-36 weeks’ GA: AOR, 1.23), male sex (AOR, 2.24), small for GA (AOR, 1.31), and various maternal medical and sociodemographic factors were associated with EDI vulnerability.
In the sibling subset, EDI outcomes were similar for children born prematurely and their siblings born full term, except for the communication skills and general knowledge domain (AOR, 1.39) and the Multiple Challenge Index (AOR, 1.43). Male sex (AOR, 2.19) was associated with EDI vulnerability in this cohort as well, as was maternal age at delivery (AOR, 1.53).
“Whether prematurity is a cause or a manifestation of an altered family ecosystem is difficult to ascertain,” Lauren Neel, MD, a neonatologist at Emory University, Atlanta, and colleagues write in an accompanying editorial. “However, research on this topic is much needed, along with novel interventions to change academic trajectories and care models that implement these findings in practice. As we begin to understand the factors in and interventions for promoting resilience in preterm-born children, we may need to change our research question to this: Could we optimize resilience and long-term academic trajectories to include the family as well?”
Six crucial years
Commenting on the study, Veronica Bordes Edgar, PhD, associate professor of psychiatry and pediatrics at the University of Texas Southwestern Medical Center’s Peter O’Donnell Jr. Brain Institute, Dallas, said, “None of the findings surprised me, but I was very pleased that they looked at such a broad sample.”
Pediatricians should monitor and screen children for early academic readiness, since these factors are associated with later academic outcomes, Dr. Edgar added. “Early intervention does not stop at age 3, but rather the first 6 years are so crucial to lay the foundation for future success. The pediatrician can play a role in preparing children and families by promoting early reading, such as through Reach Out and Read, encouraging language-rich play, and providing guidance on early childhood education and developmental needs.
“Further examination of long-term outcomes for these children to capture the longitudinal trend would help to document what is often observed clinically, in that children who start off with difficulties do not always catch up once they are in the academic environment,” Dr. Edgar concluded.
The study was supported by Research Manitoba and the Children’s Research Institute of Manitoba. Dr. Ruth, Dr. Neel, and Dr. Edgar have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PEDIATRICS
What’s in a mother’s song?
How do a baby’s body and brain respond when their mother sings a lullaby?
Shannon de l’Etoile, PhD, is hoping to find out. Dr. de l’Etoile, professor of music therapy at the University of Miami, began watching interactions between typically functioning mothers and infants, mothers with postpartum depression and their babies, and mothers and infants with Down Syndrome.
The infants she studied became highly attentive to their mothers’ singing and showed “a contented state of arousal,” she said. Mothers, meanwhile, became more engaged with their babies.
To examine the issue more scientifically, Dr. de l’Etoile has launched a study of infant-directed singing, a method connecting babies and mothers through song. With the help of a nearly $20,000 grant from the Grammy Museum – a Los Angeles nonprofit that hosts and funds exhibits and other music programs – Dr. de l’Etoile plans to recruit 20 women whose children attend programming at the Linda Ray Intervention Center at the University of Miami. The early intervention program targets children under age 2 who have disabilities or slower development, or who may have been exposed to drugs in utero. The study will last 1 year, with plans for an extension.
“By helping the mothers to become more sensitive, we are simultaneously helping infants learn how to regulate, so that by the time they’re in preschool, they can manage their behavior and have a successful, positive experience,” Dr. de l’Etoile said. She hopes her project will help women gain the confidence they need for families emotionally.
Mothers who practice infant-directed singing communicate with their babies through a variety of songs, from happy, playful versions of the ABCs, to more somber, drawn-out lullabies. In turn, their babies learn the emotional cues that go along with songs, potentially going from crying to playing, or watching their mother attentively.
Later in life, children raised with infant-directed singing might sing to themselves when they are stressed or need to go to sleep, Dr. de l’Etoile said.
A caregiving method like singing may be less intuitive for women facing basic survival challenges, like maintaining safe housing or putting food on the table, Dr. d’Etoile said.
Interest in studying infant-directed singing has grown in the past few years, although according to Sandra Trehub, PhD, an expert in infant-directed singing, studies of the phenomenon began in the early 1990s. In her own work, Dr. Trehub found that infants appear to be more engaged with parents who sing directly to them than those who sing around but not at them.
Dr. Trehub said singing can be an additional resource for a mother to overcome socioeconomic hardships and bond with their child.
“Songs sung to an infant repeatedly become almost like a special signal between mother and child, a way for them to bond with each other,” she said.
Isabel Santana Chica, MS, executive director of the Linda Ray Intervention Center, expressed enthusiasm for the project.
“Music is a great way to support language, social, and emotional development,” Ms. Chica said. “My hope is that through infant-directed singing, mothers will have one additional tool to connect to their infants and enhance development.”
A version of this article first appeared on Medscape.com.
How do a baby’s body and brain respond when their mother sings a lullaby?
Shannon de l’Etoile, PhD, is hoping to find out. Dr. de l’Etoile, professor of music therapy at the University of Miami, began watching interactions between typically functioning mothers and infants, mothers with postpartum depression and their babies, and mothers and infants with Down Syndrome.
The infants she studied became highly attentive to their mothers’ singing and showed “a contented state of arousal,” she said. Mothers, meanwhile, became more engaged with their babies.
To examine the issue more scientifically, Dr. de l’Etoile has launched a study of infant-directed singing, a method connecting babies and mothers through song. With the help of a nearly $20,000 grant from the Grammy Museum – a Los Angeles nonprofit that hosts and funds exhibits and other music programs – Dr. de l’Etoile plans to recruit 20 women whose children attend programming at the Linda Ray Intervention Center at the University of Miami. The early intervention program targets children under age 2 who have disabilities or slower development, or who may have been exposed to drugs in utero. The study will last 1 year, with plans for an extension.
“By helping the mothers to become more sensitive, we are simultaneously helping infants learn how to regulate, so that by the time they’re in preschool, they can manage their behavior and have a successful, positive experience,” Dr. de l’Etoile said. She hopes her project will help women gain the confidence they need for families emotionally.
Mothers who practice infant-directed singing communicate with their babies through a variety of songs, from happy, playful versions of the ABCs, to more somber, drawn-out lullabies. In turn, their babies learn the emotional cues that go along with songs, potentially going from crying to playing, or watching their mother attentively.
Later in life, children raised with infant-directed singing might sing to themselves when they are stressed or need to go to sleep, Dr. de l’Etoile said.
A caregiving method like singing may be less intuitive for women facing basic survival challenges, like maintaining safe housing or putting food on the table, Dr. d’Etoile said.
Interest in studying infant-directed singing has grown in the past few years, although according to Sandra Trehub, PhD, an expert in infant-directed singing, studies of the phenomenon began in the early 1990s. In her own work, Dr. Trehub found that infants appear to be more engaged with parents who sing directly to them than those who sing around but not at them.
Dr. Trehub said singing can be an additional resource for a mother to overcome socioeconomic hardships and bond with their child.
“Songs sung to an infant repeatedly become almost like a special signal between mother and child, a way for them to bond with each other,” she said.
Isabel Santana Chica, MS, executive director of the Linda Ray Intervention Center, expressed enthusiasm for the project.
“Music is a great way to support language, social, and emotional development,” Ms. Chica said. “My hope is that through infant-directed singing, mothers will have one additional tool to connect to their infants and enhance development.”
A version of this article first appeared on Medscape.com.
How do a baby’s body and brain respond when their mother sings a lullaby?
Shannon de l’Etoile, PhD, is hoping to find out. Dr. de l’Etoile, professor of music therapy at the University of Miami, began watching interactions between typically functioning mothers and infants, mothers with postpartum depression and their babies, and mothers and infants with Down Syndrome.
The infants she studied became highly attentive to their mothers’ singing and showed “a contented state of arousal,” she said. Mothers, meanwhile, became more engaged with their babies.
To examine the issue more scientifically, Dr. de l’Etoile has launched a study of infant-directed singing, a method connecting babies and mothers through song. With the help of a nearly $20,000 grant from the Grammy Museum – a Los Angeles nonprofit that hosts and funds exhibits and other music programs – Dr. de l’Etoile plans to recruit 20 women whose children attend programming at the Linda Ray Intervention Center at the University of Miami. The early intervention program targets children under age 2 who have disabilities or slower development, or who may have been exposed to drugs in utero. The study will last 1 year, with plans for an extension.
“By helping the mothers to become more sensitive, we are simultaneously helping infants learn how to regulate, so that by the time they’re in preschool, they can manage their behavior and have a successful, positive experience,” Dr. de l’Etoile said. She hopes her project will help women gain the confidence they need for families emotionally.
Mothers who practice infant-directed singing communicate with their babies through a variety of songs, from happy, playful versions of the ABCs, to more somber, drawn-out lullabies. In turn, their babies learn the emotional cues that go along with songs, potentially going from crying to playing, or watching their mother attentively.
Later in life, children raised with infant-directed singing might sing to themselves when they are stressed or need to go to sleep, Dr. de l’Etoile said.
A caregiving method like singing may be less intuitive for women facing basic survival challenges, like maintaining safe housing or putting food on the table, Dr. d’Etoile said.
Interest in studying infant-directed singing has grown in the past few years, although according to Sandra Trehub, PhD, an expert in infant-directed singing, studies of the phenomenon began in the early 1990s. In her own work, Dr. Trehub found that infants appear to be more engaged with parents who sing directly to them than those who sing around but not at them.
Dr. Trehub said singing can be an additional resource for a mother to overcome socioeconomic hardships and bond with their child.
“Songs sung to an infant repeatedly become almost like a special signal between mother and child, a way for them to bond with each other,” she said.
Isabel Santana Chica, MS, executive director of the Linda Ray Intervention Center, expressed enthusiasm for the project.
“Music is a great way to support language, social, and emotional development,” Ms. Chica said. “My hope is that through infant-directed singing, mothers will have one additional tool to connect to their infants and enhance development.”
A version of this article first appeared on Medscape.com.
Managing maternal and infant mental health
An overwhelmed mother presents to your office with her 2-month-old son for his check-up. She seems distant and dysphoric, often shrugging her shoulders with an empty stare when asked about her son’s development. Her baby cries loudly in her arms and you can see that she is uncomfortable soothing him as she frantically rocks him back and forth. He appears to have gained little weight since the last appointment occurring 6 days post partum and his mother describes him as “difficult and fussy all the time.” The father was unable to attend the appointment due to work obligations and often leaves the baby alone with the mother for 10 hours per day. As you examine her son, you counsel the mother on how to care for her baby while also caring for herself. The mother immediately begins to sob into her hands and states: “I can’t do this anymore. I am not meant to be a mother.”
Major depressive disorder with peripartum onset – also known as postpartum depression – is a major public health concern that affects approximately 20% of women in industrial societies like the United States. It is among the most prevalent psychiatric disorders in the world and remains largely underdiagnosed because of lack of access to care, symptom underreporting secondary to stigma, and lack of education regarding illness.1 Adequate treatment of perinatal depression is of paramount importance, as this condition can have significant negative consequences for both mother and child.
Infants raised by depressed mothers show early disruptions in social and emotional development, including diminished security of attachment with their mothers and reduced ability to self-regulate.2 Later in development, the offspring of depressed mothers are at greater risk for psychopathology – most notably anxiety and depression as well as impaired social behavior. 3,4 Rates of depression in school-aged and adolescent children of depressed mothers have been reported to be between 20% and 41%.4 Not only are rates of depression higher, but depression in children of depressed parents, relative to depression in same-age children of nondepressed parents, has an earlier age of onset, longer duration, and is associated with greater functional impairment and risk of relapse.5
In addition, evidence shows that infants of depressed mothers show more negative affect and more self-directed regulatory behaviors, while toddlers show more dysregulated aggression and heightened mood lability.6 Given that these infants also already have an increased genetic risk for depression and anxiety, it is essential that mothers are identified and treated early to prevent these early disruptions to the parent-child relationship.
Pediatricians sit at the intersection of motherhood and infant development. This offers a unique opportunity to influence the trajectory of the child through bolstering supports for the mother. Understandably, time is limited during these brief touchpoints occurring over the first postpartum year, although a heartfelt “How are you?” can make all the difference. In asking this simple question in a disarming way, you may prevent multiple adverse childhood experiences for your tiniest patients.
Further, evidence has shown that toxic stress experienced during sensitive periods of brain development in infants and young children can negatively affect brain architecture. Brain pathways that are rarely used are pruned away, whereas pathways that are readily accessed grow stronger. If children are exposed to toxic stress, whether it be from abuse, mental illness of a caregiver such as severe maternal depression, witnessed domestic violence, or worse, they may begin to experience the world as dangerous and uncertain. This can strengthen connections in parts of the brain associated with fear, arousal, and emotional regulation at the cost of other parts of the brain associated with learning and safety.
Particularly focusing on infancy through preschool, children depend on sensitive, responsive caregivers to learn how to understand emotions and begin to self-soothe. Pediatricians have access to this critical period and can help lead the way toward secure attachment between mother and child. Through taking this dyadic, integrated approach, not only can downstream problems in the child be attenuated or even prevented (that is, disrupted social-emotional development and depression/anxiety), but a mother’s identity can form around her strengths in parenting rather than negative cognitive distortions. Here are some ways to quickly assess a mother for major depressive disorder with peripartum onset so that treatment can be secured, allowing children to develop and learn in a safe, supportive, loving environment:
- Add a standardized instrument to the check-in process during baby’s first year of life. The Edinburgh Postnatal Depression Scale (EPDS) is the most commonly used screening tool, consisting of 10 questions with a score of 10 or greater suggestive of maternal depression. Recently, it was found that the EPDS may be further abbreviated to a three-question version with a sensitivity of 95% and a negative predictive value of 98%.
- Dedicate 5 minutes during each appointment to ask the mother, in earnest, how she is doing and to create space to hear her concerns. This high-yield discussion can be the catalyst the mother needs to identify that something is not right.
- Obtain collateral information from the mother’s partner, if available, in a way that feels collaborative and supportive. You may ask the partner during the appointment if they have any concerns about how both parents are coping with their new parenting roles.
- If the mother has multiple risk factors for major depressive disorder with peripartum onset – past history of depression, family history of perinatal depression, lack of social supports, or past history of major depressive disorder with peripartum onset with an earlier child (elevating their risk to about 50%) – you may dedicate a bit more time to assess the patient and/or provide mental health resources directly upon wrapping up the appointment.
- Finally, you may add an educational blurb about major depressive disorder with peripartum onset in all after-visit summaries for new parents and infants with a list of mental health resources that includes reproductive psychiatrists, therapists, and a link to robust resources like Postpartum Support International.
By taking the extra step to leverage the relationship between mother and infant at this highly vulnerable time, you have the ability to positively affect the trajectory of a family. And, at the end of the day, this dyadic approach to patient care is the secret ingredient to improved outcomes all around.
References
1. Muzik M and Hamilton SE. Matern Child Health J. 2016;20(11):2268-79.
2. Granat A et al. Emotion. 2017;17(1):11-27.
3. Conroy S et al. J Am Acad Child Adolesc Psychiatry. 2012;51(1):51-61.
4. Goodman SH. Annu Rev Clin Psychol. 2007;3:107-35.
5. Keller MB et al. Arch Gen Psychiatry. 1986;43(10):930-7.
6. Tronick EZ and Gianino AF. New Dir Child Dev. 1986;34:5-11.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
An overwhelmed mother presents to your office with her 2-month-old son for his check-up. She seems distant and dysphoric, often shrugging her shoulders with an empty stare when asked about her son’s development. Her baby cries loudly in her arms and you can see that she is uncomfortable soothing him as she frantically rocks him back and forth. He appears to have gained little weight since the last appointment occurring 6 days post partum and his mother describes him as “difficult and fussy all the time.” The father was unable to attend the appointment due to work obligations and often leaves the baby alone with the mother for 10 hours per day. As you examine her son, you counsel the mother on how to care for her baby while also caring for herself. The mother immediately begins to sob into her hands and states: “I can’t do this anymore. I am not meant to be a mother.”
Major depressive disorder with peripartum onset – also known as postpartum depression – is a major public health concern that affects approximately 20% of women in industrial societies like the United States. It is among the most prevalent psychiatric disorders in the world and remains largely underdiagnosed because of lack of access to care, symptom underreporting secondary to stigma, and lack of education regarding illness.1 Adequate treatment of perinatal depression is of paramount importance, as this condition can have significant negative consequences for both mother and child.
Infants raised by depressed mothers show early disruptions in social and emotional development, including diminished security of attachment with their mothers and reduced ability to self-regulate.2 Later in development, the offspring of depressed mothers are at greater risk for psychopathology – most notably anxiety and depression as well as impaired social behavior. 3,4 Rates of depression in school-aged and adolescent children of depressed mothers have been reported to be between 20% and 41%.4 Not only are rates of depression higher, but depression in children of depressed parents, relative to depression in same-age children of nondepressed parents, has an earlier age of onset, longer duration, and is associated with greater functional impairment and risk of relapse.5
In addition, evidence shows that infants of depressed mothers show more negative affect and more self-directed regulatory behaviors, while toddlers show more dysregulated aggression and heightened mood lability.6 Given that these infants also already have an increased genetic risk for depression and anxiety, it is essential that mothers are identified and treated early to prevent these early disruptions to the parent-child relationship.
Pediatricians sit at the intersection of motherhood and infant development. This offers a unique opportunity to influence the trajectory of the child through bolstering supports for the mother. Understandably, time is limited during these brief touchpoints occurring over the first postpartum year, although a heartfelt “How are you?” can make all the difference. In asking this simple question in a disarming way, you may prevent multiple adverse childhood experiences for your tiniest patients.
Further, evidence has shown that toxic stress experienced during sensitive periods of brain development in infants and young children can negatively affect brain architecture. Brain pathways that are rarely used are pruned away, whereas pathways that are readily accessed grow stronger. If children are exposed to toxic stress, whether it be from abuse, mental illness of a caregiver such as severe maternal depression, witnessed domestic violence, or worse, they may begin to experience the world as dangerous and uncertain. This can strengthen connections in parts of the brain associated with fear, arousal, and emotional regulation at the cost of other parts of the brain associated with learning and safety.
Particularly focusing on infancy through preschool, children depend on sensitive, responsive caregivers to learn how to understand emotions and begin to self-soothe. Pediatricians have access to this critical period and can help lead the way toward secure attachment between mother and child. Through taking this dyadic, integrated approach, not only can downstream problems in the child be attenuated or even prevented (that is, disrupted social-emotional development and depression/anxiety), but a mother’s identity can form around her strengths in parenting rather than negative cognitive distortions. Here are some ways to quickly assess a mother for major depressive disorder with peripartum onset so that treatment can be secured, allowing children to develop and learn in a safe, supportive, loving environment:
- Add a standardized instrument to the check-in process during baby’s first year of life. The Edinburgh Postnatal Depression Scale (EPDS) is the most commonly used screening tool, consisting of 10 questions with a score of 10 or greater suggestive of maternal depression. Recently, it was found that the EPDS may be further abbreviated to a three-question version with a sensitivity of 95% and a negative predictive value of 98%.
- Dedicate 5 minutes during each appointment to ask the mother, in earnest, how she is doing and to create space to hear her concerns. This high-yield discussion can be the catalyst the mother needs to identify that something is not right.
- Obtain collateral information from the mother’s partner, if available, in a way that feels collaborative and supportive. You may ask the partner during the appointment if they have any concerns about how both parents are coping with their new parenting roles.
- If the mother has multiple risk factors for major depressive disorder with peripartum onset – past history of depression, family history of perinatal depression, lack of social supports, or past history of major depressive disorder with peripartum onset with an earlier child (elevating their risk to about 50%) – you may dedicate a bit more time to assess the patient and/or provide mental health resources directly upon wrapping up the appointment.
- Finally, you may add an educational blurb about major depressive disorder with peripartum onset in all after-visit summaries for new parents and infants with a list of mental health resources that includes reproductive psychiatrists, therapists, and a link to robust resources like Postpartum Support International.
By taking the extra step to leverage the relationship between mother and infant at this highly vulnerable time, you have the ability to positively affect the trajectory of a family. And, at the end of the day, this dyadic approach to patient care is the secret ingredient to improved outcomes all around.
References
1. Muzik M and Hamilton SE. Matern Child Health J. 2016;20(11):2268-79.
2. Granat A et al. Emotion. 2017;17(1):11-27.
3. Conroy S et al. J Am Acad Child Adolesc Psychiatry. 2012;51(1):51-61.
4. Goodman SH. Annu Rev Clin Psychol. 2007;3:107-35.
5. Keller MB et al. Arch Gen Psychiatry. 1986;43(10):930-7.
6. Tronick EZ and Gianino AF. New Dir Child Dev. 1986;34:5-11.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
An overwhelmed mother presents to your office with her 2-month-old son for his check-up. She seems distant and dysphoric, often shrugging her shoulders with an empty stare when asked about her son’s development. Her baby cries loudly in her arms and you can see that she is uncomfortable soothing him as she frantically rocks him back and forth. He appears to have gained little weight since the last appointment occurring 6 days post partum and his mother describes him as “difficult and fussy all the time.” The father was unable to attend the appointment due to work obligations and often leaves the baby alone with the mother for 10 hours per day. As you examine her son, you counsel the mother on how to care for her baby while also caring for herself. The mother immediately begins to sob into her hands and states: “I can’t do this anymore. I am not meant to be a mother.”
Major depressive disorder with peripartum onset – also known as postpartum depression – is a major public health concern that affects approximately 20% of women in industrial societies like the United States. It is among the most prevalent psychiatric disorders in the world and remains largely underdiagnosed because of lack of access to care, symptom underreporting secondary to stigma, and lack of education regarding illness.1 Adequate treatment of perinatal depression is of paramount importance, as this condition can have significant negative consequences for both mother and child.
Infants raised by depressed mothers show early disruptions in social and emotional development, including diminished security of attachment with their mothers and reduced ability to self-regulate.2 Later in development, the offspring of depressed mothers are at greater risk for psychopathology – most notably anxiety and depression as well as impaired social behavior. 3,4 Rates of depression in school-aged and adolescent children of depressed mothers have been reported to be between 20% and 41%.4 Not only are rates of depression higher, but depression in children of depressed parents, relative to depression in same-age children of nondepressed parents, has an earlier age of onset, longer duration, and is associated with greater functional impairment and risk of relapse.5
In addition, evidence shows that infants of depressed mothers show more negative affect and more self-directed regulatory behaviors, while toddlers show more dysregulated aggression and heightened mood lability.6 Given that these infants also already have an increased genetic risk for depression and anxiety, it is essential that mothers are identified and treated early to prevent these early disruptions to the parent-child relationship.
Pediatricians sit at the intersection of motherhood and infant development. This offers a unique opportunity to influence the trajectory of the child through bolstering supports for the mother. Understandably, time is limited during these brief touchpoints occurring over the first postpartum year, although a heartfelt “How are you?” can make all the difference. In asking this simple question in a disarming way, you may prevent multiple adverse childhood experiences for your tiniest patients.
Further, evidence has shown that toxic stress experienced during sensitive periods of brain development in infants and young children can negatively affect brain architecture. Brain pathways that are rarely used are pruned away, whereas pathways that are readily accessed grow stronger. If children are exposed to toxic stress, whether it be from abuse, mental illness of a caregiver such as severe maternal depression, witnessed domestic violence, or worse, they may begin to experience the world as dangerous and uncertain. This can strengthen connections in parts of the brain associated with fear, arousal, and emotional regulation at the cost of other parts of the brain associated with learning and safety.
Particularly focusing on infancy through preschool, children depend on sensitive, responsive caregivers to learn how to understand emotions and begin to self-soothe. Pediatricians have access to this critical period and can help lead the way toward secure attachment between mother and child. Through taking this dyadic, integrated approach, not only can downstream problems in the child be attenuated or even prevented (that is, disrupted social-emotional development and depression/anxiety), but a mother’s identity can form around her strengths in parenting rather than negative cognitive distortions. Here are some ways to quickly assess a mother for major depressive disorder with peripartum onset so that treatment can be secured, allowing children to develop and learn in a safe, supportive, loving environment:
- Add a standardized instrument to the check-in process during baby’s first year of life. The Edinburgh Postnatal Depression Scale (EPDS) is the most commonly used screening tool, consisting of 10 questions with a score of 10 or greater suggestive of maternal depression. Recently, it was found that the EPDS may be further abbreviated to a three-question version with a sensitivity of 95% and a negative predictive value of 98%.
- Dedicate 5 minutes during each appointment to ask the mother, in earnest, how she is doing and to create space to hear her concerns. This high-yield discussion can be the catalyst the mother needs to identify that something is not right.
- Obtain collateral information from the mother’s partner, if available, in a way that feels collaborative and supportive. You may ask the partner during the appointment if they have any concerns about how both parents are coping with their new parenting roles.
- If the mother has multiple risk factors for major depressive disorder with peripartum onset – past history of depression, family history of perinatal depression, lack of social supports, or past history of major depressive disorder with peripartum onset with an earlier child (elevating their risk to about 50%) – you may dedicate a bit more time to assess the patient and/or provide mental health resources directly upon wrapping up the appointment.
- Finally, you may add an educational blurb about major depressive disorder with peripartum onset in all after-visit summaries for new parents and infants with a list of mental health resources that includes reproductive psychiatrists, therapists, and a link to robust resources like Postpartum Support International.
By taking the extra step to leverage the relationship between mother and infant at this highly vulnerable time, you have the ability to positively affect the trajectory of a family. And, at the end of the day, this dyadic approach to patient care is the secret ingredient to improved outcomes all around.
References
1. Muzik M and Hamilton SE. Matern Child Health J. 2016;20(11):2268-79.
2. Granat A et al. Emotion. 2017;17(1):11-27.
3. Conroy S et al. J Am Acad Child Adolesc Psychiatry. 2012;51(1):51-61.
4. Goodman SH. Annu Rev Clin Psychol. 2007;3:107-35.
5. Keller MB et al. Arch Gen Psychiatry. 1986;43(10):930-7.
6. Tronick EZ and Gianino AF. New Dir Child Dev. 1986;34:5-11.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
A 9-year-old girl was evaluated for a week-long history of rash on the feet
A complete body examination failed to reveal any other lesions suggestive of a fungal infection. A blood count and urinalysis were within normal limits. She had no lymphadenopathy or hepatosplenomegaly. She was diagnosed with cutaneous larva migrans (CLM) given the clinical appearance of the lesions and the recent travel history.
CLM is a zoonotic infection caused by several hookworms such as Ancylostoma braziliense, Ancylostoma caninum, and Uncinaria stenocephala, as well as human hookworms such as Ancylostoma duodenale and Necator americanus. The hookworms can be present in contaminated soils and sandy beaches on the coastal regions of South America, the Caribbean, the Southeastern United States, Southeast Asia, and Africa.1-5
It is a common disease in the tourist population visiting tropical countries because of exposure to the hookworms in the soil without use of proper foot protection.
The clinical features are of an erythematous linear serpiginous plaque that is pruritic and can progress from millimeters to centimeters in size within a few days to weeks. Vesicles and multiple tracks can also be seen. The most common locations are the feet, buttocks, and thighs.
The larvae in the soil come from eggs excreted in the feces of infected cats and dogs. The infection is caused by direct contact of the larvae with the stratum corneum of the skin creating a burrow and an inflammatory response that will cause erythema, edema, track formation, and pruritus.
Diagnosis is made clinically. Rarely, a skin biopsy is warranted. The differential diagnosis includes tinea pedis, granuloma annulare, larva currens, contact dermatitis, and herpes zoster.
Tinea pedis is a fungal infection of the skin of the feet, commonly localized on the web spaces. The risk factors are a hot and humid environment, prolonged wear of occlusive footwear, excess sweating, and prolonged exposure to water.6 Diagnosis is confirmed by microscopic evaluation of skin scrapings with potassium hydroxide or a fungal culture. The infection is treated with topical antifungal creams and, in severe cases, systemic antifungals. Granuloma annulare is a benign chronic skin condition that presents with annular-shaped lesions. Its etiology is unknown. The lesions may be asymptomatic or mildly pruritic. Localized granuloma annulare typically presents as reddish-brown papules or plaques on the fingers, hands, elbows, dorsal feet, or ankles. The feature distinguishing granuloma annulare from other annular lesions is its absence of scale.
Allergic contact dermatitis is caused by skin exposure to an allergen and a secondary inflammatory response to this material on the skin causing inflammation, vesiculation, and pruritus. Lesions are treated with topical corticosteroids and avoidance of the allergen.
Herpes zoster is caused by a viral infection of the latent varicella-zoster virus. Its reactivation causes the presence of vesicles with an erythematous base that have a dermatomal distribution. The lesions are usually tender. Treatment is recommended to be started within 72 hours of the eruption with antivirals such as acyclovir or valacyclovir.
Cutaneous larva currens is caused by the cutaneous infection with Strongyloides stercoralis. In comparison with CLM, the lesions progress faster, at up to a centimeter within hours.
CLM is usually self-limited. If the patient has multiple lesions or more severe disease, oral albendazole or ivermectin can be prescribed. Other treatments, though not preferred, include freezing and topical thiabendazole solutions.
As our patient had several lesions, oral ivermectin was chosen as treatment and the lesions cleared within a week. Also, she was recommended to always wear shoes when walking on the beach.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Dr. Valderrama is a pediatric dermatologist at Fundación Cardioinfantil, Bogota, Colombia.
References
1. Feldmeier H and Schuster A. Eur J Clin Microbiol Infect Dis. 2012 Jun;31(6):915-8.
2. Jacobson CC and Abel EA. J Am Acad Dermatol. 2007 Jun;56(6):1026-43.
3. Kincaid L et al. Travel Med Infect Dis. 2015 Sep-Oct;13(5):382-7.
4. Gill N et al. Adv Skin Wound Care. 2020 Jul;33(7):356-9.
5. Rodenas-Herranz T et al. Dermatol Ther. 2020 May;33(3):e13316.
6. Pramod K et al. In: StatPearls [Internet]. Treasure Island (Fla): StatPearls Publishing; 2022 Jan.
A complete body examination failed to reveal any other lesions suggestive of a fungal infection. A blood count and urinalysis were within normal limits. She had no lymphadenopathy or hepatosplenomegaly. She was diagnosed with cutaneous larva migrans (CLM) given the clinical appearance of the lesions and the recent travel history.
CLM is a zoonotic infection caused by several hookworms such as Ancylostoma braziliense, Ancylostoma caninum, and Uncinaria stenocephala, as well as human hookworms such as Ancylostoma duodenale and Necator americanus. The hookworms can be present in contaminated soils and sandy beaches on the coastal regions of South America, the Caribbean, the Southeastern United States, Southeast Asia, and Africa.1-5
It is a common disease in the tourist population visiting tropical countries because of exposure to the hookworms in the soil without use of proper foot protection.
The clinical features are of an erythematous linear serpiginous plaque that is pruritic and can progress from millimeters to centimeters in size within a few days to weeks. Vesicles and multiple tracks can also be seen. The most common locations are the feet, buttocks, and thighs.
The larvae in the soil come from eggs excreted in the feces of infected cats and dogs. The infection is caused by direct contact of the larvae with the stratum corneum of the skin creating a burrow and an inflammatory response that will cause erythema, edema, track formation, and pruritus.
Diagnosis is made clinically. Rarely, a skin biopsy is warranted. The differential diagnosis includes tinea pedis, granuloma annulare, larva currens, contact dermatitis, and herpes zoster.
Tinea pedis is a fungal infection of the skin of the feet, commonly localized on the web spaces. The risk factors are a hot and humid environment, prolonged wear of occlusive footwear, excess sweating, and prolonged exposure to water.6 Diagnosis is confirmed by microscopic evaluation of skin scrapings with potassium hydroxide or a fungal culture. The infection is treated with topical antifungal creams and, in severe cases, systemic antifungals. Granuloma annulare is a benign chronic skin condition that presents with annular-shaped lesions. Its etiology is unknown. The lesions may be asymptomatic or mildly pruritic. Localized granuloma annulare typically presents as reddish-brown papules or plaques on the fingers, hands, elbows, dorsal feet, or ankles. The feature distinguishing granuloma annulare from other annular lesions is its absence of scale.
Allergic contact dermatitis is caused by skin exposure to an allergen and a secondary inflammatory response to this material on the skin causing inflammation, vesiculation, and pruritus. Lesions are treated with topical corticosteroids and avoidance of the allergen.
Herpes zoster is caused by a viral infection of the latent varicella-zoster virus. Its reactivation causes the presence of vesicles with an erythematous base that have a dermatomal distribution. The lesions are usually tender. Treatment is recommended to be started within 72 hours of the eruption with antivirals such as acyclovir or valacyclovir.
Cutaneous larva currens is caused by the cutaneous infection with Strongyloides stercoralis. In comparison with CLM, the lesions progress faster, at up to a centimeter within hours.
CLM is usually self-limited. If the patient has multiple lesions or more severe disease, oral albendazole or ivermectin can be prescribed. Other treatments, though not preferred, include freezing and topical thiabendazole solutions.
As our patient had several lesions, oral ivermectin was chosen as treatment and the lesions cleared within a week. Also, she was recommended to always wear shoes when walking on the beach.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Dr. Valderrama is a pediatric dermatologist at Fundación Cardioinfantil, Bogota, Colombia.
References
1. Feldmeier H and Schuster A. Eur J Clin Microbiol Infect Dis. 2012 Jun;31(6):915-8.
2. Jacobson CC and Abel EA. J Am Acad Dermatol. 2007 Jun;56(6):1026-43.
3. Kincaid L et al. Travel Med Infect Dis. 2015 Sep-Oct;13(5):382-7.
4. Gill N et al. Adv Skin Wound Care. 2020 Jul;33(7):356-9.
5. Rodenas-Herranz T et al. Dermatol Ther. 2020 May;33(3):e13316.
6. Pramod K et al. In: StatPearls [Internet]. Treasure Island (Fla): StatPearls Publishing; 2022 Jan.
A complete body examination failed to reveal any other lesions suggestive of a fungal infection. A blood count and urinalysis were within normal limits. She had no lymphadenopathy or hepatosplenomegaly. She was diagnosed with cutaneous larva migrans (CLM) given the clinical appearance of the lesions and the recent travel history.
CLM is a zoonotic infection caused by several hookworms such as Ancylostoma braziliense, Ancylostoma caninum, and Uncinaria stenocephala, as well as human hookworms such as Ancylostoma duodenale and Necator americanus. The hookworms can be present in contaminated soils and sandy beaches on the coastal regions of South America, the Caribbean, the Southeastern United States, Southeast Asia, and Africa.1-5
It is a common disease in the tourist population visiting tropical countries because of exposure to the hookworms in the soil without use of proper foot protection.
The clinical features are of an erythematous linear serpiginous plaque that is pruritic and can progress from millimeters to centimeters in size within a few days to weeks. Vesicles and multiple tracks can also be seen. The most common locations are the feet, buttocks, and thighs.
The larvae in the soil come from eggs excreted in the feces of infected cats and dogs. The infection is caused by direct contact of the larvae with the stratum corneum of the skin creating a burrow and an inflammatory response that will cause erythema, edema, track formation, and pruritus.
Diagnosis is made clinically. Rarely, a skin biopsy is warranted. The differential diagnosis includes tinea pedis, granuloma annulare, larva currens, contact dermatitis, and herpes zoster.
Tinea pedis is a fungal infection of the skin of the feet, commonly localized on the web spaces. The risk factors are a hot and humid environment, prolonged wear of occlusive footwear, excess sweating, and prolonged exposure to water.6 Diagnosis is confirmed by microscopic evaluation of skin scrapings with potassium hydroxide or a fungal culture. The infection is treated with topical antifungal creams and, in severe cases, systemic antifungals. Granuloma annulare is a benign chronic skin condition that presents with annular-shaped lesions. Its etiology is unknown. The lesions may be asymptomatic or mildly pruritic. Localized granuloma annulare typically presents as reddish-brown papules or plaques on the fingers, hands, elbows, dorsal feet, or ankles. The feature distinguishing granuloma annulare from other annular lesions is its absence of scale.
Allergic contact dermatitis is caused by skin exposure to an allergen and a secondary inflammatory response to this material on the skin causing inflammation, vesiculation, and pruritus. Lesions are treated with topical corticosteroids and avoidance of the allergen.
Herpes zoster is caused by a viral infection of the latent varicella-zoster virus. Its reactivation causes the presence of vesicles with an erythematous base that have a dermatomal distribution. The lesions are usually tender. Treatment is recommended to be started within 72 hours of the eruption with antivirals such as acyclovir or valacyclovir.
Cutaneous larva currens is caused by the cutaneous infection with Strongyloides stercoralis. In comparison with CLM, the lesions progress faster, at up to a centimeter within hours.
CLM is usually self-limited. If the patient has multiple lesions or more severe disease, oral albendazole or ivermectin can be prescribed. Other treatments, though not preferred, include freezing and topical thiabendazole solutions.
As our patient had several lesions, oral ivermectin was chosen as treatment and the lesions cleared within a week. Also, she was recommended to always wear shoes when walking on the beach.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Dr. Valderrama is a pediatric dermatologist at Fundación Cardioinfantil, Bogota, Colombia.
References
1. Feldmeier H and Schuster A. Eur J Clin Microbiol Infect Dis. 2012 Jun;31(6):915-8.
2. Jacobson CC and Abel EA. J Am Acad Dermatol. 2007 Jun;56(6):1026-43.
3. Kincaid L et al. Travel Med Infect Dis. 2015 Sep-Oct;13(5):382-7.
4. Gill N et al. Adv Skin Wound Care. 2020 Jul;33(7):356-9.
5. Rodenas-Herranz T et al. Dermatol Ther. 2020 May;33(3):e13316.
6. Pramod K et al. In: StatPearls [Internet]. Treasure Island (Fla): StatPearls Publishing; 2022 Jan.
Her mother reported recent travel to a beachside city in Colombia. A review of systems was negative. She was not taking any other medications or vitamin supplements. There were no pets at home and no other affected family members. Physical exam was notable for an erythematous curvilinear plaque on the feet and a small vesicle.
Risk factors in children linked to stroke as soon as 30s, 40s
In a case-control study, atherosclerotic risk factors were uncommon in childhood and did not appear to be associated with the pathogenesis of arterial ischemic stroke in children or in early young adulthood.
But by the fourth and fifth decades of life, these risk factors were strongly associated with a significant risk for stroke, heightening that risk almost tenfold.
“While strokes in childhood and very early adulthood are not likely caused by atherosclerotic risk factors, it does look like these risk factors increase throughout early and young adulthood and become significant risk factors for stroke in the 30s and 40s,” lead author Sharon N. Poisson, MD, MAS, associate professor of neurology at the University of Colorado at Denver, Aurora, said in an interview.
The findings were published online in JAMA Neurology.
In this study, the researchers focused on arterial ischemic stroke, not hemorrhagic stroke. “We know that high blood pressure, diabetes, smoking, obesity, all of these are risk factors for ischemic stroke, but what we didn’t know is at what age do those atherosclerotic risk factors actually start to cause stroke,” Dr. Poisson said.
To find out more, she and her team did a case control study of data in the Kaiser Permanente Northern California system, which had been accumulating relevant data over a period of 14 years, from Jan. 1, 2000, through Dec. 31, 2014.
The analysis included 141 children and 455 young adults with arterial ischemic stroke and 1,382 age-matched controls.
The children were divided into two age categories: ages 29 days to 9 years and ages 10-19 years.
In the younger group, there were 69 cases of arterial ischemic stroke. In the older age group, there were 72 cases.
Young adults were divided into three age categories: 20-29 years (n = 71 cases), 30-39 years (144 cases), and 40-49 years (240 cases).
Among pediatric controls, 168 children aged 29 days to 9 years (46.5%) and 196 children aged 10-19 years (53.8%) developed arterial ischemic stroke.
There were 121 cases of ischemic stroke among young adult controls aged 20-29 years, 298 cases among controls aged 30-39 years, and 599 cases in those aged 40-49 years.
Both childhood cases and controls had a low prevalence of documented diagnoses of atherosclerotic risk factors (ARFs). The odds ratio of having any ARFs on arterial ischemic stroke was 1.87 for ages 0-9 years, and 1.00 for ages 10-19.
However, cases rose with age.
The OR was 2.3 for age range 20-29 years, 3.57 for age range 30-39 years, and 4.91 for age range 40-49 years.
The analysis also showed that the OR associated with multiple ARFs was 5.29 for age range 0-9 years, 2.75 for age range 10-19 years, 7.33 for age range 20-29 years, 9.86 for age range 30-39 years, and 9.35 for age range 40-49 years.
Multiple risk factors were rare in children but became more prevalent with each decade of young adult life.
The presumed cause of arterial ischemic stroke was atherosclerosis. Evidence of atherosclerosis was present in 1.4% of those aged 10-19 years, 8.5% of those aged 20-29 years, 21.5% of those aged 30-39 years, and 42.5% of those aged 40-49 years.
“This study tells us that, while stroke in adolescence and very early adulthood may not be caused by atherosclerotic risk factors, starting to accumulate those risk factors early in life clearly increases the risk of stroke in the 30s and 40s. I hope we can get this message across, because the sooner we can treat the risk factors, the better the outcome,” Dr. Poisson said.
Prevention starts in childhood
Prevention of cardiovascular disease begins in childhood, which is a paradigm shift from the way cardiovascular disease was thought of a couple of decades ago, noted pediatric cardiologist Guilherme Baptista de Faia, MD, from the Ann & Robert H. Lurie Children’s Hospital in Chicago.
“Our guidelines for risk factor reduction in children aim to address how or when do we screen for these risk factors, how or when do we intervene, and do these interventions impact cardiovascular outcomes later in life? This article is part of the mounting research that aims to understand the relationship between childhood cardiovascular risk factors and early cardiovascular disease,” Dr. Baptista de Faia said.
“There has been an interesting progression in our understanding of the impact of CV risk factors early in life. Large cohorts such as Bogalusa Heart Study, Risk in Young Finns Study, Muscatine Study, the Childhood Determinants of Adult Health, CARDIA, and the International Childhood Cardiovascular Cohorts (i3C) have been instrumental in evaluating this question,” he said.
The knowledge that atherosclerotic risk factors in children can lead to acceleration of atherosclerosis in later life opens the door to preventive medicine, said Dr. Baptista de Faia, who was not part of the study.
“This is where preventive medicine comes in. If we can identify the children at increased risk, can we intervene to improve outcomes later in life?” he said. Familial hypercholesterolemia is “a great example of this. We can screen children early in life, there is an effective treatment, and we know from populations studies that early treatment significantly decreases the risk for cardiovascular disease later in life.”
Dr. Poisson reported that she received grants from the National Institutes of Health during the conduct of this study, which was supported by the NIH.
A version of this article first appeared on Medscape.com.
In a case-control study, atherosclerotic risk factors were uncommon in childhood and did not appear to be associated with the pathogenesis of arterial ischemic stroke in children or in early young adulthood.
But by the fourth and fifth decades of life, these risk factors were strongly associated with a significant risk for stroke, heightening that risk almost tenfold.
“While strokes in childhood and very early adulthood are not likely caused by atherosclerotic risk factors, it does look like these risk factors increase throughout early and young adulthood and become significant risk factors for stroke in the 30s and 40s,” lead author Sharon N. Poisson, MD, MAS, associate professor of neurology at the University of Colorado at Denver, Aurora, said in an interview.
The findings were published online in JAMA Neurology.
In this study, the researchers focused on arterial ischemic stroke, not hemorrhagic stroke. “We know that high blood pressure, diabetes, smoking, obesity, all of these are risk factors for ischemic stroke, but what we didn’t know is at what age do those atherosclerotic risk factors actually start to cause stroke,” Dr. Poisson said.
To find out more, she and her team did a case control study of data in the Kaiser Permanente Northern California system, which had been accumulating relevant data over a period of 14 years, from Jan. 1, 2000, through Dec. 31, 2014.
The analysis included 141 children and 455 young adults with arterial ischemic stroke and 1,382 age-matched controls.
The children were divided into two age categories: ages 29 days to 9 years and ages 10-19 years.
In the younger group, there were 69 cases of arterial ischemic stroke. In the older age group, there were 72 cases.
Young adults were divided into three age categories: 20-29 years (n = 71 cases), 30-39 years (144 cases), and 40-49 years (240 cases).
Among pediatric controls, 168 children aged 29 days to 9 years (46.5%) and 196 children aged 10-19 years (53.8%) developed arterial ischemic stroke.
There were 121 cases of ischemic stroke among young adult controls aged 20-29 years, 298 cases among controls aged 30-39 years, and 599 cases in those aged 40-49 years.
Both childhood cases and controls had a low prevalence of documented diagnoses of atherosclerotic risk factors (ARFs). The odds ratio of having any ARFs on arterial ischemic stroke was 1.87 for ages 0-9 years, and 1.00 for ages 10-19.
However, cases rose with age.
The OR was 2.3 for age range 20-29 years, 3.57 for age range 30-39 years, and 4.91 for age range 40-49 years.
The analysis also showed that the OR associated with multiple ARFs was 5.29 for age range 0-9 years, 2.75 for age range 10-19 years, 7.33 for age range 20-29 years, 9.86 for age range 30-39 years, and 9.35 for age range 40-49 years.
Multiple risk factors were rare in children but became more prevalent with each decade of young adult life.
The presumed cause of arterial ischemic stroke was atherosclerosis. Evidence of atherosclerosis was present in 1.4% of those aged 10-19 years, 8.5% of those aged 20-29 years, 21.5% of those aged 30-39 years, and 42.5% of those aged 40-49 years.
“This study tells us that, while stroke in adolescence and very early adulthood may not be caused by atherosclerotic risk factors, starting to accumulate those risk factors early in life clearly increases the risk of stroke in the 30s and 40s. I hope we can get this message across, because the sooner we can treat the risk factors, the better the outcome,” Dr. Poisson said.
Prevention starts in childhood
Prevention of cardiovascular disease begins in childhood, which is a paradigm shift from the way cardiovascular disease was thought of a couple of decades ago, noted pediatric cardiologist Guilherme Baptista de Faia, MD, from the Ann & Robert H. Lurie Children’s Hospital in Chicago.
“Our guidelines for risk factor reduction in children aim to address how or when do we screen for these risk factors, how or when do we intervene, and do these interventions impact cardiovascular outcomes later in life? This article is part of the mounting research that aims to understand the relationship between childhood cardiovascular risk factors and early cardiovascular disease,” Dr. Baptista de Faia said.
“There has been an interesting progression in our understanding of the impact of CV risk factors early in life. Large cohorts such as Bogalusa Heart Study, Risk in Young Finns Study, Muscatine Study, the Childhood Determinants of Adult Health, CARDIA, and the International Childhood Cardiovascular Cohorts (i3C) have been instrumental in evaluating this question,” he said.
The knowledge that atherosclerotic risk factors in children can lead to acceleration of atherosclerosis in later life opens the door to preventive medicine, said Dr. Baptista de Faia, who was not part of the study.
“This is where preventive medicine comes in. If we can identify the children at increased risk, can we intervene to improve outcomes later in life?” he said. Familial hypercholesterolemia is “a great example of this. We can screen children early in life, there is an effective treatment, and we know from populations studies that early treatment significantly decreases the risk for cardiovascular disease later in life.”
Dr. Poisson reported that she received grants from the National Institutes of Health during the conduct of this study, which was supported by the NIH.
A version of this article first appeared on Medscape.com.
In a case-control study, atherosclerotic risk factors were uncommon in childhood and did not appear to be associated with the pathogenesis of arterial ischemic stroke in children or in early young adulthood.
But by the fourth and fifth decades of life, these risk factors were strongly associated with a significant risk for stroke, heightening that risk almost tenfold.
“While strokes in childhood and very early adulthood are not likely caused by atherosclerotic risk factors, it does look like these risk factors increase throughout early and young adulthood and become significant risk factors for stroke in the 30s and 40s,” lead author Sharon N. Poisson, MD, MAS, associate professor of neurology at the University of Colorado at Denver, Aurora, said in an interview.
The findings were published online in JAMA Neurology.
In this study, the researchers focused on arterial ischemic stroke, not hemorrhagic stroke. “We know that high blood pressure, diabetes, smoking, obesity, all of these are risk factors for ischemic stroke, but what we didn’t know is at what age do those atherosclerotic risk factors actually start to cause stroke,” Dr. Poisson said.
To find out more, she and her team did a case control study of data in the Kaiser Permanente Northern California system, which had been accumulating relevant data over a period of 14 years, from Jan. 1, 2000, through Dec. 31, 2014.
The analysis included 141 children and 455 young adults with arterial ischemic stroke and 1,382 age-matched controls.
The children were divided into two age categories: ages 29 days to 9 years and ages 10-19 years.
In the younger group, there were 69 cases of arterial ischemic stroke. In the older age group, there were 72 cases.
Young adults were divided into three age categories: 20-29 years (n = 71 cases), 30-39 years (144 cases), and 40-49 years (240 cases).
Among pediatric controls, 168 children aged 29 days to 9 years (46.5%) and 196 children aged 10-19 years (53.8%) developed arterial ischemic stroke.
There were 121 cases of ischemic stroke among young adult controls aged 20-29 years, 298 cases among controls aged 30-39 years, and 599 cases in those aged 40-49 years.
Both childhood cases and controls had a low prevalence of documented diagnoses of atherosclerotic risk factors (ARFs). The odds ratio of having any ARFs on arterial ischemic stroke was 1.87 for ages 0-9 years, and 1.00 for ages 10-19.
However, cases rose with age.
The OR was 2.3 for age range 20-29 years, 3.57 for age range 30-39 years, and 4.91 for age range 40-49 years.
The analysis also showed that the OR associated with multiple ARFs was 5.29 for age range 0-9 years, 2.75 for age range 10-19 years, 7.33 for age range 20-29 years, 9.86 for age range 30-39 years, and 9.35 for age range 40-49 years.
Multiple risk factors were rare in children but became more prevalent with each decade of young adult life.
The presumed cause of arterial ischemic stroke was atherosclerosis. Evidence of atherosclerosis was present in 1.4% of those aged 10-19 years, 8.5% of those aged 20-29 years, 21.5% of those aged 30-39 years, and 42.5% of those aged 40-49 years.
“This study tells us that, while stroke in adolescence and very early adulthood may not be caused by atherosclerotic risk factors, starting to accumulate those risk factors early in life clearly increases the risk of stroke in the 30s and 40s. I hope we can get this message across, because the sooner we can treat the risk factors, the better the outcome,” Dr. Poisson said.
Prevention starts in childhood
Prevention of cardiovascular disease begins in childhood, which is a paradigm shift from the way cardiovascular disease was thought of a couple of decades ago, noted pediatric cardiologist Guilherme Baptista de Faia, MD, from the Ann & Robert H. Lurie Children’s Hospital in Chicago.
“Our guidelines for risk factor reduction in children aim to address how or when do we screen for these risk factors, how or when do we intervene, and do these interventions impact cardiovascular outcomes later in life? This article is part of the mounting research that aims to understand the relationship between childhood cardiovascular risk factors and early cardiovascular disease,” Dr. Baptista de Faia said.
“There has been an interesting progression in our understanding of the impact of CV risk factors early in life. Large cohorts such as Bogalusa Heart Study, Risk in Young Finns Study, Muscatine Study, the Childhood Determinants of Adult Health, CARDIA, and the International Childhood Cardiovascular Cohorts (i3C) have been instrumental in evaluating this question,” he said.
The knowledge that atherosclerotic risk factors in children can lead to acceleration of atherosclerosis in later life opens the door to preventive medicine, said Dr. Baptista de Faia, who was not part of the study.
“This is where preventive medicine comes in. If we can identify the children at increased risk, can we intervene to improve outcomes later in life?” he said. Familial hypercholesterolemia is “a great example of this. We can screen children early in life, there is an effective treatment, and we know from populations studies that early treatment significantly decreases the risk for cardiovascular disease later in life.”
Dr. Poisson reported that she received grants from the National Institutes of Health during the conduct of this study, which was supported by the NIH.
A version of this article first appeared on Medscape.com.
FROM JAMA NEUROLOGY
Acute otitis media pneumococcal disease burden in children due to serotypes not included in vaccines
My group in Rochester, N.Y., examined the current pneumococcal serotypes causing AOM in children. From our data, we can determine the PCV13 vaccine types that escape prevention and cause AOM and understand what effect to expect from the new pneumococcal conjugate vaccines (PCVs) that will be coming soon. There are limited data from middle ear fluid (MEF) cultures on which to base such analyses. Tympanocentesis is the preferred method for securing MEF for culture and our group is unique in providing such data to the Centers for Disease Control and publishing our results on a periodic basis to inform clinicians.
Pneumococci are the second most common cause of acute otitis media (AOM) since the introduction of pneumococcal conjugate vaccines (PCVs) more than 2 decades ago.1,2 Pneumococcal AOM causes more severe acute disease and more often causes suppurative complications than Haemophilus influenzae, which is the most common cause of AOM. Prevention of pneumococcal AOM will be a highly relevant contributor to cost-effectiveness analyses for the anticipated introduction of PCV15 (Merck) and PCV20 (Pfizer). Both PCV15 and PCV20 have been licensed for adult use; PCV15 licensure for infants and children occurred in June 2022 for invasive pneumococcal disease and is anticipated in the near future for PCV20. They are improvements over PCV13 because they add serotypes that cause invasive pneumococcal diseases, although less so for prevention of AOM, on the basis of our data.
Nasopharyngeal colonization is a necessary pathogenic step in progression to pneumococcal disease. However, not all strains of pneumococci expressing different capsular serotypes are equally virulent and likely to cause disease. In PCV-vaccinated populations, vaccine pressure and antibiotic resistance drive PCV serotype replacement with nonvaccine serotypes (NVTs), gradually reducing the net effectiveness of the vaccines. Therefore, knowledge of prevalent NVTs colonizing the nasopharynx identifies future pneumococcal serotypes most likely to emerge as pathogenic.
We published an effectiveness study of PCV13.3 A relative reduction of 86% in AOM caused by strains expressing PCV13 serotypes was observed in the first few years after PCV13 introduction. The greatest reduction in MEF samples was in serotype 19A, with a relative reduction of 91%. However, over time the vaccine type efficacy of PCV13 against MEF-positive pneumococcal AOM has eroded. There was no clear efficacy against serotype 3, and we still observed cases of serotype 19A and 19F. PCV13 vaccine failures have been even more frequent in Europe (nearly 30% of pneumococcal AOM in Europe is caused by vaccine serotypes) than our data indicate, where about 10% of AOM is caused by PCV13 serotypes.
In our most recent publication covering 2015-2019, we described results from 589 children, aged 6-36 months, from whom we collected 2,042 nasopharyngeal samples.2,4 During AOM, 495 MEF samples from 319 AOM-infected children were collected (during bilateral infections, tympanocentesis was performed in both ears). Whether bacteria were isolated was based per AOM case, not per tap. The average age of children with AOM was 15 months (range 6-31 months). The three most prevalent nasopharyngeal pneumococcal serotypes were 35B, 23B, and 15B/C. Serotype 35B was the most common at AOM visits in both the nasopharynx and MEF samples followed by serotype 15B/C. Nonsusceptibility among pneumococci to penicillin, azithromycin, and multiple other antibiotics was high. Increasing resistance to ceftriaxone was also observed.
Based on our results, if PCV15 (PCV13 + 22F and 33F) effectiveness is identical to PCV13 for the included serotypes and 100% efficacy for the added serotypes is presumed, PCV15 will reduce pneumococcal AOMs by 8%, pneumococcal nasopharyngeal colonization events at onset of AOM by 6%, and pneumococcal nasopharyngeal colonization events during health by 3%. As for the projected reductions brought about by PCV20 (PCV15 + 8, 10A, 11A, 12F, and 15B), presuming serotype 15B is efficacious against serotype 15C and 100% efficacy for the added serotypes, PCV20 will reduce pneumococcal AOMs by 22%, pneumococcal nasopharyngeal colonization events at onset of AOM by 20%, and pneumococcal nasopharyngeal colonization events during health by 3% (Figure).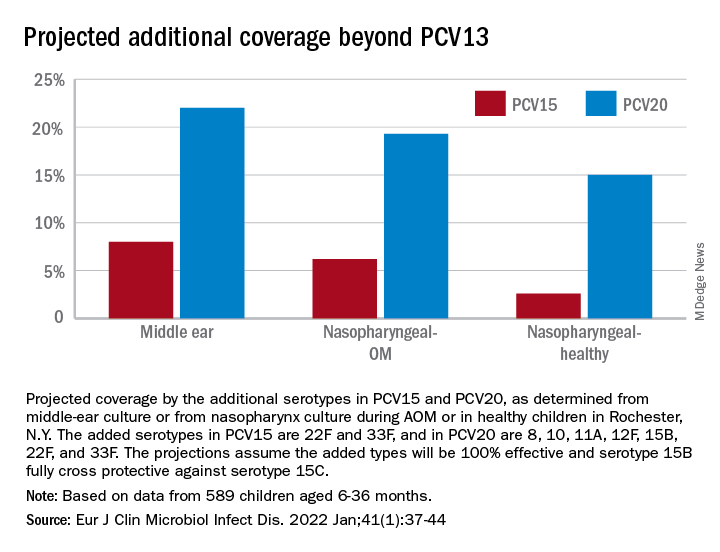
The CDC estimated that, in 2004, pneumococcal disease in the United States caused 4 million illness episodes, 22,000 deaths, 445,000 hospitalizations, 774,000 emergency department visits, 5 million outpatient visits, and 4.1 million outpatient antibiotic prescriptions. Direct medical costs totaled $3.5 billion. Pneumonia (866,000 cases) accounted for 22% of all cases and 72% of pneumococcal costs. AOM and sinusitis (1.5 million cases each) composed 75% of cases and 16% of direct medical costs.5 However, if indirect costs are taken into account, such as work loss by parents of young children, the cost of pneumococcal disease caused by AOM alone may exceed $6 billion annually6 and become dominant in the cost-effectiveness analysis in high-income countries.
Despite widespread use of PCV13, Pneumococcus has shown its resilience under vaccine pressure such that the organism remains a very common AOM pathogen. All-cause AOM has declined modestly and pneumococcal AOM caused by the specific serotypes in PCVs has declined dramatically since the introduction of PCVs. However, the burden of pneumococcal AOM disease is still considerable.
The notion that strains expressing serotypes that were not included in PCV7 were less virulent was proven wrong within a few years after introduction of PCV7, with the emergence of strains expressing serotype 19A, and others. The same cycle occurred after introduction of PCV13. It appears to take about 4 years after introduction of a PCV before peak effectiveness is achieved – which then begins to erode with emergence of NVTs. First, the NVTs are observed to colonize the nasopharynx as commensals and then from among those strains new disease-causing strains emerge.
At the most recent meeting of the International Society of Pneumococci and Pneumococcal Diseases in Toronto in June, many presentations focused on the fact that PCVs elicit highly effective protective serotype-specific antibodies to the capsular polysaccharides of included types. However, 100 serotypes are known. The limitations of PCVs are becoming increasingly apparent. They are costly and consume a large portion of the Vaccines for Children budget. Children in the developing world remain largely unvaccinated because of the high cost. NVTs that have emerged to cause disease vary by country, vary by adult vs. pediatric populations, and are dynamically changing year to year. Forthcoming PCVs of 15 and 20 serotypes will be even more costly than PCV13, will not include many newly emerged serotypes, and will probably likewise encounter “serotype replacement” because of high immune evasion by pneumococci.
When Merck and Pfizer made their decisions on serotype composition for PCV15 and PCV20, respectively, they were based on available data at the time regarding predominant serotypes causing invasive pneumococcal disease in countries that had the best data and would be the market for their products. However, from the time of the decision to licensure of vaccine is many years, and during that time the pneumococcal serotypes have changed, more so for AOM, and I predict more change will occur in the future.
In the past 3 years, Dr. Pichichero has received honoraria from Merck to attend 1-day consulting meetings and his institution has received investigator-initiated research grants to study aspects of PCV15. In the past 3 years, he was reimbursed for expenses to attend the ISPPD meeting in Toronto to present a poster on potential efficacy of PCV20 to prevent complicated AOM.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital.
References
1. Kaur R et al. Pediatrics. 2017;140(3).
2. Kaur R et al. Eur J Clin Microbiol Infect Dis. 2021;41:37-44..
3. Pichichero M et al. Lancet Child Adolesc Health. 2018;2(8):561-8.
4. Zhou F et al. Pediatrics. 2008;121(2):253-60.
5. Huang SS et al. Vaccine. 2011;29(18):3398-412.
6. Casey JR and Pichichero ME. Clin Pediatr (Phila). 2014;53(9):865-73. .
My group in Rochester, N.Y., examined the current pneumococcal serotypes causing AOM in children. From our data, we can determine the PCV13 vaccine types that escape prevention and cause AOM and understand what effect to expect from the new pneumococcal conjugate vaccines (PCVs) that will be coming soon. There are limited data from middle ear fluid (MEF) cultures on which to base such analyses. Tympanocentesis is the preferred method for securing MEF for culture and our group is unique in providing such data to the Centers for Disease Control and publishing our results on a periodic basis to inform clinicians.
Pneumococci are the second most common cause of acute otitis media (AOM) since the introduction of pneumococcal conjugate vaccines (PCVs) more than 2 decades ago.1,2 Pneumococcal AOM causes more severe acute disease and more often causes suppurative complications than Haemophilus influenzae, which is the most common cause of AOM. Prevention of pneumococcal AOM will be a highly relevant contributor to cost-effectiveness analyses for the anticipated introduction of PCV15 (Merck) and PCV20 (Pfizer). Both PCV15 and PCV20 have been licensed for adult use; PCV15 licensure for infants and children occurred in June 2022 for invasive pneumococcal disease and is anticipated in the near future for PCV20. They are improvements over PCV13 because they add serotypes that cause invasive pneumococcal diseases, although less so for prevention of AOM, on the basis of our data.
Nasopharyngeal colonization is a necessary pathogenic step in progression to pneumococcal disease. However, not all strains of pneumococci expressing different capsular serotypes are equally virulent and likely to cause disease. In PCV-vaccinated populations, vaccine pressure and antibiotic resistance drive PCV serotype replacement with nonvaccine serotypes (NVTs), gradually reducing the net effectiveness of the vaccines. Therefore, knowledge of prevalent NVTs colonizing the nasopharynx identifies future pneumococcal serotypes most likely to emerge as pathogenic.
We published an effectiveness study of PCV13.3 A relative reduction of 86% in AOM caused by strains expressing PCV13 serotypes was observed in the first few years after PCV13 introduction. The greatest reduction in MEF samples was in serotype 19A, with a relative reduction of 91%. However, over time the vaccine type efficacy of PCV13 against MEF-positive pneumococcal AOM has eroded. There was no clear efficacy against serotype 3, and we still observed cases of serotype 19A and 19F. PCV13 vaccine failures have been even more frequent in Europe (nearly 30% of pneumococcal AOM in Europe is caused by vaccine serotypes) than our data indicate, where about 10% of AOM is caused by PCV13 serotypes.
In our most recent publication covering 2015-2019, we described results from 589 children, aged 6-36 months, from whom we collected 2,042 nasopharyngeal samples.2,4 During AOM, 495 MEF samples from 319 AOM-infected children were collected (during bilateral infections, tympanocentesis was performed in both ears). Whether bacteria were isolated was based per AOM case, not per tap. The average age of children with AOM was 15 months (range 6-31 months). The three most prevalent nasopharyngeal pneumococcal serotypes were 35B, 23B, and 15B/C. Serotype 35B was the most common at AOM visits in both the nasopharynx and MEF samples followed by serotype 15B/C. Nonsusceptibility among pneumococci to penicillin, azithromycin, and multiple other antibiotics was high. Increasing resistance to ceftriaxone was also observed.
Based on our results, if PCV15 (PCV13 + 22F and 33F) effectiveness is identical to PCV13 for the included serotypes and 100% efficacy for the added serotypes is presumed, PCV15 will reduce pneumococcal AOMs by 8%, pneumococcal nasopharyngeal colonization events at onset of AOM by 6%, and pneumococcal nasopharyngeal colonization events during health by 3%. As for the projected reductions brought about by PCV20 (PCV15 + 8, 10A, 11A, 12F, and 15B), presuming serotype 15B is efficacious against serotype 15C and 100% efficacy for the added serotypes, PCV20 will reduce pneumococcal AOMs by 22%, pneumococcal nasopharyngeal colonization events at onset of AOM by 20%, and pneumococcal nasopharyngeal colonization events during health by 3% (Figure).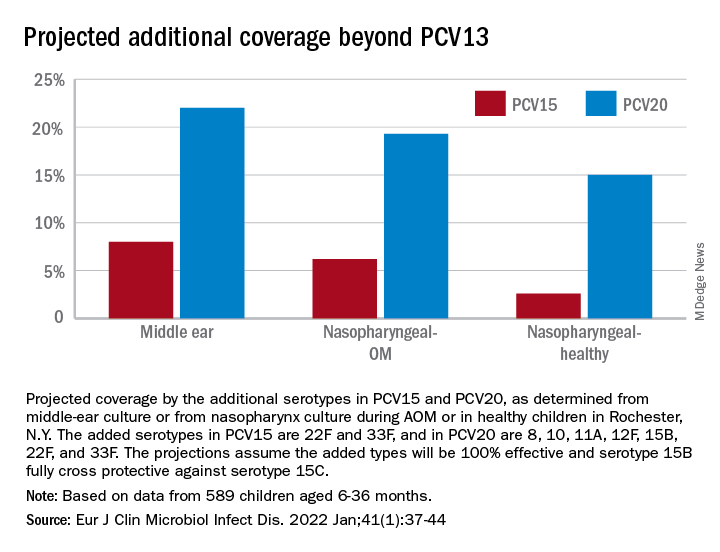
The CDC estimated that, in 2004, pneumococcal disease in the United States caused 4 million illness episodes, 22,000 deaths, 445,000 hospitalizations, 774,000 emergency department visits, 5 million outpatient visits, and 4.1 million outpatient antibiotic prescriptions. Direct medical costs totaled $3.5 billion. Pneumonia (866,000 cases) accounted for 22% of all cases and 72% of pneumococcal costs. AOM and sinusitis (1.5 million cases each) composed 75% of cases and 16% of direct medical costs.5 However, if indirect costs are taken into account, such as work loss by parents of young children, the cost of pneumococcal disease caused by AOM alone may exceed $6 billion annually6 and become dominant in the cost-effectiveness analysis in high-income countries.
Despite widespread use of PCV13, Pneumococcus has shown its resilience under vaccine pressure such that the organism remains a very common AOM pathogen. All-cause AOM has declined modestly and pneumococcal AOM caused by the specific serotypes in PCVs has declined dramatically since the introduction of PCVs. However, the burden of pneumococcal AOM disease is still considerable.
The notion that strains expressing serotypes that were not included in PCV7 were less virulent was proven wrong within a few years after introduction of PCV7, with the emergence of strains expressing serotype 19A, and others. The same cycle occurred after introduction of PCV13. It appears to take about 4 years after introduction of a PCV before peak effectiveness is achieved – which then begins to erode with emergence of NVTs. First, the NVTs are observed to colonize the nasopharynx as commensals and then from among those strains new disease-causing strains emerge.
At the most recent meeting of the International Society of Pneumococci and Pneumococcal Diseases in Toronto in June, many presentations focused on the fact that PCVs elicit highly effective protective serotype-specific antibodies to the capsular polysaccharides of included types. However, 100 serotypes are known. The limitations of PCVs are becoming increasingly apparent. They are costly and consume a large portion of the Vaccines for Children budget. Children in the developing world remain largely unvaccinated because of the high cost. NVTs that have emerged to cause disease vary by country, vary by adult vs. pediatric populations, and are dynamically changing year to year. Forthcoming PCVs of 15 and 20 serotypes will be even more costly than PCV13, will not include many newly emerged serotypes, and will probably likewise encounter “serotype replacement” because of high immune evasion by pneumococci.
When Merck and Pfizer made their decisions on serotype composition for PCV15 and PCV20, respectively, they were based on available data at the time regarding predominant serotypes causing invasive pneumococcal disease in countries that had the best data and would be the market for their products. However, from the time of the decision to licensure of vaccine is many years, and during that time the pneumococcal serotypes have changed, more so for AOM, and I predict more change will occur in the future.
In the past 3 years, Dr. Pichichero has received honoraria from Merck to attend 1-day consulting meetings and his institution has received investigator-initiated research grants to study aspects of PCV15. In the past 3 years, he was reimbursed for expenses to attend the ISPPD meeting in Toronto to present a poster on potential efficacy of PCV20 to prevent complicated AOM.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital.
References
1. Kaur R et al. Pediatrics. 2017;140(3).
2. Kaur R et al. Eur J Clin Microbiol Infect Dis. 2021;41:37-44..
3. Pichichero M et al. Lancet Child Adolesc Health. 2018;2(8):561-8.
4. Zhou F et al. Pediatrics. 2008;121(2):253-60.
5. Huang SS et al. Vaccine. 2011;29(18):3398-412.
6. Casey JR and Pichichero ME. Clin Pediatr (Phila). 2014;53(9):865-73. .
My group in Rochester, N.Y., examined the current pneumococcal serotypes causing AOM in children. From our data, we can determine the PCV13 vaccine types that escape prevention and cause AOM and understand what effect to expect from the new pneumococcal conjugate vaccines (PCVs) that will be coming soon. There are limited data from middle ear fluid (MEF) cultures on which to base such analyses. Tympanocentesis is the preferred method for securing MEF for culture and our group is unique in providing such data to the Centers for Disease Control and publishing our results on a periodic basis to inform clinicians.
Pneumococci are the second most common cause of acute otitis media (AOM) since the introduction of pneumococcal conjugate vaccines (PCVs) more than 2 decades ago.1,2 Pneumococcal AOM causes more severe acute disease and more often causes suppurative complications than Haemophilus influenzae, which is the most common cause of AOM. Prevention of pneumococcal AOM will be a highly relevant contributor to cost-effectiveness analyses for the anticipated introduction of PCV15 (Merck) and PCV20 (Pfizer). Both PCV15 and PCV20 have been licensed for adult use; PCV15 licensure for infants and children occurred in June 2022 for invasive pneumococcal disease and is anticipated in the near future for PCV20. They are improvements over PCV13 because they add serotypes that cause invasive pneumococcal diseases, although less so for prevention of AOM, on the basis of our data.
Nasopharyngeal colonization is a necessary pathogenic step in progression to pneumococcal disease. However, not all strains of pneumococci expressing different capsular serotypes are equally virulent and likely to cause disease. In PCV-vaccinated populations, vaccine pressure and antibiotic resistance drive PCV serotype replacement with nonvaccine serotypes (NVTs), gradually reducing the net effectiveness of the vaccines. Therefore, knowledge of prevalent NVTs colonizing the nasopharynx identifies future pneumococcal serotypes most likely to emerge as pathogenic.
We published an effectiveness study of PCV13.3 A relative reduction of 86% in AOM caused by strains expressing PCV13 serotypes was observed in the first few years after PCV13 introduction. The greatest reduction in MEF samples was in serotype 19A, with a relative reduction of 91%. However, over time the vaccine type efficacy of PCV13 against MEF-positive pneumococcal AOM has eroded. There was no clear efficacy against serotype 3, and we still observed cases of serotype 19A and 19F. PCV13 vaccine failures have been even more frequent in Europe (nearly 30% of pneumococcal AOM in Europe is caused by vaccine serotypes) than our data indicate, where about 10% of AOM is caused by PCV13 serotypes.
In our most recent publication covering 2015-2019, we described results from 589 children, aged 6-36 months, from whom we collected 2,042 nasopharyngeal samples.2,4 During AOM, 495 MEF samples from 319 AOM-infected children were collected (during bilateral infections, tympanocentesis was performed in both ears). Whether bacteria were isolated was based per AOM case, not per tap. The average age of children with AOM was 15 months (range 6-31 months). The three most prevalent nasopharyngeal pneumococcal serotypes were 35B, 23B, and 15B/C. Serotype 35B was the most common at AOM visits in both the nasopharynx and MEF samples followed by serotype 15B/C. Nonsusceptibility among pneumococci to penicillin, azithromycin, and multiple other antibiotics was high. Increasing resistance to ceftriaxone was also observed.
Based on our results, if PCV15 (PCV13 + 22F and 33F) effectiveness is identical to PCV13 for the included serotypes and 100% efficacy for the added serotypes is presumed, PCV15 will reduce pneumococcal AOMs by 8%, pneumococcal nasopharyngeal colonization events at onset of AOM by 6%, and pneumococcal nasopharyngeal colonization events during health by 3%. As for the projected reductions brought about by PCV20 (PCV15 + 8, 10A, 11A, 12F, and 15B), presuming serotype 15B is efficacious against serotype 15C and 100% efficacy for the added serotypes, PCV20 will reduce pneumococcal AOMs by 22%, pneumococcal nasopharyngeal colonization events at onset of AOM by 20%, and pneumococcal nasopharyngeal colonization events during health by 3% (Figure).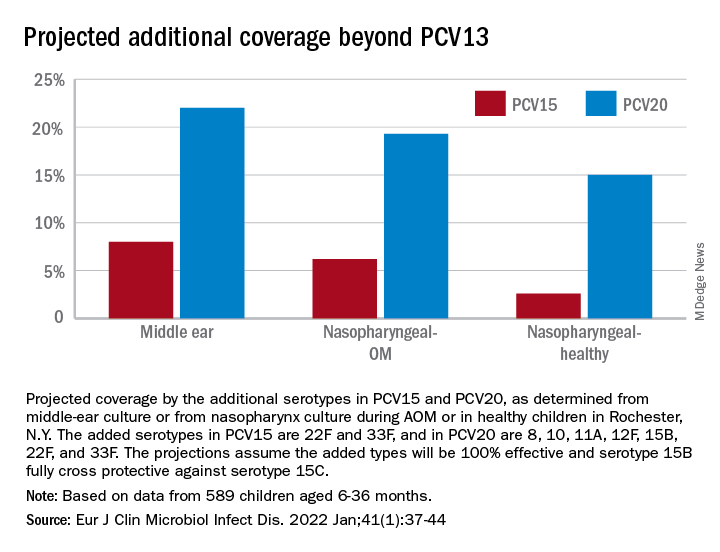
The CDC estimated that, in 2004, pneumococcal disease in the United States caused 4 million illness episodes, 22,000 deaths, 445,000 hospitalizations, 774,000 emergency department visits, 5 million outpatient visits, and 4.1 million outpatient antibiotic prescriptions. Direct medical costs totaled $3.5 billion. Pneumonia (866,000 cases) accounted for 22% of all cases and 72% of pneumococcal costs. AOM and sinusitis (1.5 million cases each) composed 75% of cases and 16% of direct medical costs.5 However, if indirect costs are taken into account, such as work loss by parents of young children, the cost of pneumococcal disease caused by AOM alone may exceed $6 billion annually6 and become dominant in the cost-effectiveness analysis in high-income countries.
Despite widespread use of PCV13, Pneumococcus has shown its resilience under vaccine pressure such that the organism remains a very common AOM pathogen. All-cause AOM has declined modestly and pneumococcal AOM caused by the specific serotypes in PCVs has declined dramatically since the introduction of PCVs. However, the burden of pneumococcal AOM disease is still considerable.
The notion that strains expressing serotypes that were not included in PCV7 were less virulent was proven wrong within a few years after introduction of PCV7, with the emergence of strains expressing serotype 19A, and others. The same cycle occurred after introduction of PCV13. It appears to take about 4 years after introduction of a PCV before peak effectiveness is achieved – which then begins to erode with emergence of NVTs. First, the NVTs are observed to colonize the nasopharynx as commensals and then from among those strains new disease-causing strains emerge.
At the most recent meeting of the International Society of Pneumococci and Pneumococcal Diseases in Toronto in June, many presentations focused on the fact that PCVs elicit highly effective protective serotype-specific antibodies to the capsular polysaccharides of included types. However, 100 serotypes are known. The limitations of PCVs are becoming increasingly apparent. They are costly and consume a large portion of the Vaccines for Children budget. Children in the developing world remain largely unvaccinated because of the high cost. NVTs that have emerged to cause disease vary by country, vary by adult vs. pediatric populations, and are dynamically changing year to year. Forthcoming PCVs of 15 and 20 serotypes will be even more costly than PCV13, will not include many newly emerged serotypes, and will probably likewise encounter “serotype replacement” because of high immune evasion by pneumococci.
When Merck and Pfizer made their decisions on serotype composition for PCV15 and PCV20, respectively, they were based on available data at the time regarding predominant serotypes causing invasive pneumococcal disease in countries that had the best data and would be the market for their products. However, from the time of the decision to licensure of vaccine is many years, and during that time the pneumococcal serotypes have changed, more so for AOM, and I predict more change will occur in the future.
In the past 3 years, Dr. Pichichero has received honoraria from Merck to attend 1-day consulting meetings and his institution has received investigator-initiated research grants to study aspects of PCV15. In the past 3 years, he was reimbursed for expenses to attend the ISPPD meeting in Toronto to present a poster on potential efficacy of PCV20 to prevent complicated AOM.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital.
References
1. Kaur R et al. Pediatrics. 2017;140(3).
2. Kaur R et al. Eur J Clin Microbiol Infect Dis. 2021;41:37-44..
3. Pichichero M et al. Lancet Child Adolesc Health. 2018;2(8):561-8.
4. Zhou F et al. Pediatrics. 2008;121(2):253-60.
5. Huang SS et al. Vaccine. 2011;29(18):3398-412.
6. Casey JR and Pichichero ME. Clin Pediatr (Phila). 2014;53(9):865-73. .
Active shooter drills may be harming children, but doctors offer help
The drills can range from staging lockdowns and sheltering in place to quasi dramas with mock shooters roaming the halls. Although the goals of these training exercises are important, equally important are the potential negative effects of drills on students’ mental health, according to doctors with expertise in pediatrics and mental health.
“Dramatic simulation of an active shooter event at school would be expected to provoke the same stress response as the real thing,” said Peter L. Loper Jr., MD, a pediatrician and psychiatrist, in an interview. “While ensuring their physical safety is very important, we must be intentional about making sure that we are not doing so at the expense of their psychosocial or emotional safety.”
“Children may not be able to differentiate a dramatic drill from a real event,” emphasized Dr. Loper, of the neuropsychiatry and behavioral science departments at the University of South Carolina, Columbia. “The parts of the brain responsible for our flight-fight-or-freeze response would interpret both simulated and real events identically and produce the same neurohormonal stress-response.”
Indeed, a study published in the journal Humanities & Social Sciences Communications suggested children experienced mental health problems related to participating in active shooter drills. In the large study, a team of statisticians from the Georgia Institute of Technology found that students reported a 42% increase in stress and anxiety and a 38.7% increase in depression during the 90 days following active shooter drills, compared with the 90 days before the drills.
The authors of this study, including Mai ElSherief, PhD, drew these conclusions after analyzing 54 million social media posts before and after drills in 114 schools across 33 states. The researchers analyzed the language of the social media posts by teachers, parents, and students and found increased use of the words hope, love, home, school, kids, community, support, and help after the drills. The researchers considered posting with these terms in the aftermath of the drills to be indicative of having high anxiety.
They included examples of how high stress, anxiety, and depression manifested in specific posts from parents in their report. The following is an example of a poster expressing high anxiety and stress: “are we really gonna normalize school shooter drills?! holy sh* there has to be a real way to avoid these tragedies. sh*t like this cannot be normalized. teachers injured after being shot with plastic pellets ‘execution style’ in active shooter drill.”
The authors also shared this post to serve as an example of a person who seems depressed: “and now we are revisiting the trauma on our kids, forcing them to act out school drills monthly. i don’t get why gen x parents buy into this concept wholeheartedly. things need to change.”
The published material did not include posts from students, but the researchers’ analysis of the content of posts overall showed increased concerns for health and increased concerns about death during the period after drills, compared with before drills.
The authors also conducted focus groups in communities in which drills occurred, and many teachers and parents reported anecdotal evidence of children who were nervous long after the drills were over, with some showing extreme reactions such as panic over a standard fire alarm at school. Overall, the results show that school shooter drills can negatively affect school communities over prolonged periods of time, they concluded.
According to a statement from the American Academy of Pediatrics, “there is a need to be cautious about the potential psychological risks and other unintended consequences of directly involving children in live exercises and drills.”
“These risks and consequences are especially a concern when children are deceived and led to believe there is an actual attack and not a drill,” wrote David Schonfeld, MD, the lead author of the statement on Participation of Children and Adolescents in Live Crisis Drills and Exercises, and colleagues.
Managing the fallout
Physicians can help students experiencing mental health problems from these drills, according to doctors interviewed for this piece.
It’s important for providers to know that stress will show up differently in children than in adults, said Chelsea Younghans, MD, a psychiatrist and military officer in Bethesda, Md., in an interview.
“They may see children with headaches, stomach aches, or nonspecific complaints. They may also see children who have not had difficulty with sleep present with nightmares or bed wetting,” she added.
For teens and preteens, validated tools such as the Child PTSD Symptom Scale (CPSS-5) and Child and Adolescent Trauma Screen (CATS) to assess PTSD in youth, may help serve as a starting point for a conversation between providers and their older child population, she noted.
Children who exhibit avoidance or withdrawal behaviors including consistent school refusal, an increase in reassurance-seeking behaviors, or somatic symptoms like vague abdominal pain or headaches that prevent school attendance after participating in a drill, may need more robust mental health services, Dr. Loper noted.
Dr. Schonfeld, who is also director of the National Center for School Crisis and Bereavement at Children’s Hospital Los Angeles, called for health care providers to be available to help children process traumatic reactions to these exercises.
Agreeing with Dr. Schonfeld, Dr. Younghans said: “It is vital to debrief with students and staff after drills, making sure that students have a safe space and ample time to speak with trusted staff. As children will undoubtedly have questions and concerns, creating open lines of communication will help alleviate any traumatic effect these drills may have.”
Communicating with various stakeholders
Experts also gave recommendations for how clinicians communicate with leaders in their area’s school districts and other members of their communities about these training exercises.
“For primary care providers, it is important to establish meaningful relationships within your community and patient population as much as possible,” Dr. Younghans said. “Having a good relationship with the local schools and being part of the conversation can help increase school and community awareness on the impact these drills can have on students and staff,” she added.
For those pediatricians or other health care providers who serve as consultants to schools, Dr. Schonfeld advised they ask about policies related to exercises and drills, such as what are the limits to what children might be exposed to in a drill, and what requirements there might be at the local and state level in terms of frequency and what the drills will and will not involve.
He also noted that clinicians should encourage school leaders to consider the fact that kids may have personal histories of trauma that are completely unknown to the school when they design these exercises.
School staff and health care providers should explain the nature and reasons for drills, invite family members to express concerns, and make accommodations if necessary for some children to participate in drills in a more limited way, noted Dr. Schonfeld, who is also clinical professor of pediatrics at the University of Southern California, Los Angeles.
“I think health care providers should work with legislators, so that if they require a drill, it must be done in a way that is physically and emotionally safe,” he added.
Executing better drills for students’ mental health
Experts also advised on ways to execute these drills that will be least damaging to students.
The AAP statement on Participation of Children and Adolescents in Live Crisis Drills and Exercises, for example, advocates eliminating high-intensity drills, prohibiting deception in drills, and providing accommodations based on children’s vulnerabilities.
Dr. Schonfeld also emphasized, in an interview, that training for an attack need not be extremely realistic to be effective.
“When you are preparing for a crisis, the drills and exercises are for children to practice and develop mastery over something they don’t know how to do fully yet,” said Dr. Schonfeld.
Citing a suggestion from a 2020 report conducted by Everytown for Gun Safety on keeping schools safe from gun violence, Dr. Younghans said, “Schools should be in clear communication with communities and families regarding when drills will be happening,” and advised ensuring that the explanation of drills is developmentally appropriate to the age of the children participating.
The report also recommends conducting drills that do not simulate an actual incident, combining drills with trauma-informed approaches to address students’ well-being during and for a sustained period after the drills, and tracking data on the efficacy and effects of drills.
Dr. Loper suggested ways that clinicians and parents can help navigate the tricky territory of school safety drills.
In his view, they should not be random or unexpected, and anticipatory guidance should be given regarding any visual or auditory stimuli, such as flashing lights or sirens, alarms, or announcements.
“A preventive approach should be utilized to ensure that any child who is experiencing extreme drill-distress be excused from any future disaster drills to prevent retraumatization,” Dr. Loper said.
Physicians interviewed for this piece also provided tips on how to talk about these events with children in a way that is beneficial to their mental health.
“What we want to do is [have a] calm discussion [with kids] about what we are doing and why we are doing it” and guide them through the movements, Dr. Schonfeld said.
When teaching children how to respond to an emergency, some elements of uncertainty need to be discussed. Children need to anticipate “what you might do if you are not in the classroom if something occurs, such as being in the bathroom, or out at recess,” he continued.
Dr. Younghans recommended that parents and staff schedule time to prepare children for the drill and practice in advance, and that behavioral health providers, counselors, and/or primary care providers should be involved in the planning and execution of the drill.
The Georgia Tech study was supported through a grant from Everytown for Gun Safety.
The study authors and experts interviewed for this piece had no financial conflicts to disclose.
The drills can range from staging lockdowns and sheltering in place to quasi dramas with mock shooters roaming the halls. Although the goals of these training exercises are important, equally important are the potential negative effects of drills on students’ mental health, according to doctors with expertise in pediatrics and mental health.
“Dramatic simulation of an active shooter event at school would be expected to provoke the same stress response as the real thing,” said Peter L. Loper Jr., MD, a pediatrician and psychiatrist, in an interview. “While ensuring their physical safety is very important, we must be intentional about making sure that we are not doing so at the expense of their psychosocial or emotional safety.”
“Children may not be able to differentiate a dramatic drill from a real event,” emphasized Dr. Loper, of the neuropsychiatry and behavioral science departments at the University of South Carolina, Columbia. “The parts of the brain responsible for our flight-fight-or-freeze response would interpret both simulated and real events identically and produce the same neurohormonal stress-response.”
Indeed, a study published in the journal Humanities & Social Sciences Communications suggested children experienced mental health problems related to participating in active shooter drills. In the large study, a team of statisticians from the Georgia Institute of Technology found that students reported a 42% increase in stress and anxiety and a 38.7% increase in depression during the 90 days following active shooter drills, compared with the 90 days before the drills.
The authors of this study, including Mai ElSherief, PhD, drew these conclusions after analyzing 54 million social media posts before and after drills in 114 schools across 33 states. The researchers analyzed the language of the social media posts by teachers, parents, and students and found increased use of the words hope, love, home, school, kids, community, support, and help after the drills. The researchers considered posting with these terms in the aftermath of the drills to be indicative of having high anxiety.
They included examples of how high stress, anxiety, and depression manifested in specific posts from parents in their report. The following is an example of a poster expressing high anxiety and stress: “are we really gonna normalize school shooter drills?! holy sh* there has to be a real way to avoid these tragedies. sh*t like this cannot be normalized. teachers injured after being shot with plastic pellets ‘execution style’ in active shooter drill.”
The authors also shared this post to serve as an example of a person who seems depressed: “and now we are revisiting the trauma on our kids, forcing them to act out school drills monthly. i don’t get why gen x parents buy into this concept wholeheartedly. things need to change.”
The published material did not include posts from students, but the researchers’ analysis of the content of posts overall showed increased concerns for health and increased concerns about death during the period after drills, compared with before drills.
The authors also conducted focus groups in communities in which drills occurred, and many teachers and parents reported anecdotal evidence of children who were nervous long after the drills were over, with some showing extreme reactions such as panic over a standard fire alarm at school. Overall, the results show that school shooter drills can negatively affect school communities over prolonged periods of time, they concluded.
According to a statement from the American Academy of Pediatrics, “there is a need to be cautious about the potential psychological risks and other unintended consequences of directly involving children in live exercises and drills.”
“These risks and consequences are especially a concern when children are deceived and led to believe there is an actual attack and not a drill,” wrote David Schonfeld, MD, the lead author of the statement on Participation of Children and Adolescents in Live Crisis Drills and Exercises, and colleagues.
Managing the fallout
Physicians can help students experiencing mental health problems from these drills, according to doctors interviewed for this piece.
It’s important for providers to know that stress will show up differently in children than in adults, said Chelsea Younghans, MD, a psychiatrist and military officer in Bethesda, Md., in an interview.
“They may see children with headaches, stomach aches, or nonspecific complaints. They may also see children who have not had difficulty with sleep present with nightmares or bed wetting,” she added.
For teens and preteens, validated tools such as the Child PTSD Symptom Scale (CPSS-5) and Child and Adolescent Trauma Screen (CATS) to assess PTSD in youth, may help serve as a starting point for a conversation between providers and their older child population, she noted.
Children who exhibit avoidance or withdrawal behaviors including consistent school refusal, an increase in reassurance-seeking behaviors, or somatic symptoms like vague abdominal pain or headaches that prevent school attendance after participating in a drill, may need more robust mental health services, Dr. Loper noted.
Dr. Schonfeld, who is also director of the National Center for School Crisis and Bereavement at Children’s Hospital Los Angeles, called for health care providers to be available to help children process traumatic reactions to these exercises.
Agreeing with Dr. Schonfeld, Dr. Younghans said: “It is vital to debrief with students and staff after drills, making sure that students have a safe space and ample time to speak with trusted staff. As children will undoubtedly have questions and concerns, creating open lines of communication will help alleviate any traumatic effect these drills may have.”
Communicating with various stakeholders
Experts also gave recommendations for how clinicians communicate with leaders in their area’s school districts and other members of their communities about these training exercises.
“For primary care providers, it is important to establish meaningful relationships within your community and patient population as much as possible,” Dr. Younghans said. “Having a good relationship with the local schools and being part of the conversation can help increase school and community awareness on the impact these drills can have on students and staff,” she added.
For those pediatricians or other health care providers who serve as consultants to schools, Dr. Schonfeld advised they ask about policies related to exercises and drills, such as what are the limits to what children might be exposed to in a drill, and what requirements there might be at the local and state level in terms of frequency and what the drills will and will not involve.
He also noted that clinicians should encourage school leaders to consider the fact that kids may have personal histories of trauma that are completely unknown to the school when they design these exercises.
School staff and health care providers should explain the nature and reasons for drills, invite family members to express concerns, and make accommodations if necessary for some children to participate in drills in a more limited way, noted Dr. Schonfeld, who is also clinical professor of pediatrics at the University of Southern California, Los Angeles.
“I think health care providers should work with legislators, so that if they require a drill, it must be done in a way that is physically and emotionally safe,” he added.
Executing better drills for students’ mental health
Experts also advised on ways to execute these drills that will be least damaging to students.
The AAP statement on Participation of Children and Adolescents in Live Crisis Drills and Exercises, for example, advocates eliminating high-intensity drills, prohibiting deception in drills, and providing accommodations based on children’s vulnerabilities.
Dr. Schonfeld also emphasized, in an interview, that training for an attack need not be extremely realistic to be effective.
“When you are preparing for a crisis, the drills and exercises are for children to practice and develop mastery over something they don’t know how to do fully yet,” said Dr. Schonfeld.
Citing a suggestion from a 2020 report conducted by Everytown for Gun Safety on keeping schools safe from gun violence, Dr. Younghans said, “Schools should be in clear communication with communities and families regarding when drills will be happening,” and advised ensuring that the explanation of drills is developmentally appropriate to the age of the children participating.
The report also recommends conducting drills that do not simulate an actual incident, combining drills with trauma-informed approaches to address students’ well-being during and for a sustained period after the drills, and tracking data on the efficacy and effects of drills.
Dr. Loper suggested ways that clinicians and parents can help navigate the tricky territory of school safety drills.
In his view, they should not be random or unexpected, and anticipatory guidance should be given regarding any visual or auditory stimuli, such as flashing lights or sirens, alarms, or announcements.
“A preventive approach should be utilized to ensure that any child who is experiencing extreme drill-distress be excused from any future disaster drills to prevent retraumatization,” Dr. Loper said.
Physicians interviewed for this piece also provided tips on how to talk about these events with children in a way that is beneficial to their mental health.
“What we want to do is [have a] calm discussion [with kids] about what we are doing and why we are doing it” and guide them through the movements, Dr. Schonfeld said.
When teaching children how to respond to an emergency, some elements of uncertainty need to be discussed. Children need to anticipate “what you might do if you are not in the classroom if something occurs, such as being in the bathroom, or out at recess,” he continued.
Dr. Younghans recommended that parents and staff schedule time to prepare children for the drill and practice in advance, and that behavioral health providers, counselors, and/or primary care providers should be involved in the planning and execution of the drill.
The Georgia Tech study was supported through a grant from Everytown for Gun Safety.
The study authors and experts interviewed for this piece had no financial conflicts to disclose.
The drills can range from staging lockdowns and sheltering in place to quasi dramas with mock shooters roaming the halls. Although the goals of these training exercises are important, equally important are the potential negative effects of drills on students’ mental health, according to doctors with expertise in pediatrics and mental health.
“Dramatic simulation of an active shooter event at school would be expected to provoke the same stress response as the real thing,” said Peter L. Loper Jr., MD, a pediatrician and psychiatrist, in an interview. “While ensuring their physical safety is very important, we must be intentional about making sure that we are not doing so at the expense of their psychosocial or emotional safety.”
“Children may not be able to differentiate a dramatic drill from a real event,” emphasized Dr. Loper, of the neuropsychiatry and behavioral science departments at the University of South Carolina, Columbia. “The parts of the brain responsible for our flight-fight-or-freeze response would interpret both simulated and real events identically and produce the same neurohormonal stress-response.”
Indeed, a study published in the journal Humanities & Social Sciences Communications suggested children experienced mental health problems related to participating in active shooter drills. In the large study, a team of statisticians from the Georgia Institute of Technology found that students reported a 42% increase in stress and anxiety and a 38.7% increase in depression during the 90 days following active shooter drills, compared with the 90 days before the drills.
The authors of this study, including Mai ElSherief, PhD, drew these conclusions after analyzing 54 million social media posts before and after drills in 114 schools across 33 states. The researchers analyzed the language of the social media posts by teachers, parents, and students and found increased use of the words hope, love, home, school, kids, community, support, and help after the drills. The researchers considered posting with these terms in the aftermath of the drills to be indicative of having high anxiety.
They included examples of how high stress, anxiety, and depression manifested in specific posts from parents in their report. The following is an example of a poster expressing high anxiety and stress: “are we really gonna normalize school shooter drills?! holy sh* there has to be a real way to avoid these tragedies. sh*t like this cannot be normalized. teachers injured after being shot with plastic pellets ‘execution style’ in active shooter drill.”
The authors also shared this post to serve as an example of a person who seems depressed: “and now we are revisiting the trauma on our kids, forcing them to act out school drills monthly. i don’t get why gen x parents buy into this concept wholeheartedly. things need to change.”
The published material did not include posts from students, but the researchers’ analysis of the content of posts overall showed increased concerns for health and increased concerns about death during the period after drills, compared with before drills.
The authors also conducted focus groups in communities in which drills occurred, and many teachers and parents reported anecdotal evidence of children who were nervous long after the drills were over, with some showing extreme reactions such as panic over a standard fire alarm at school. Overall, the results show that school shooter drills can negatively affect school communities over prolonged periods of time, they concluded.
According to a statement from the American Academy of Pediatrics, “there is a need to be cautious about the potential psychological risks and other unintended consequences of directly involving children in live exercises and drills.”
“These risks and consequences are especially a concern when children are deceived and led to believe there is an actual attack and not a drill,” wrote David Schonfeld, MD, the lead author of the statement on Participation of Children and Adolescents in Live Crisis Drills and Exercises, and colleagues.
Managing the fallout
Physicians can help students experiencing mental health problems from these drills, according to doctors interviewed for this piece.
It’s important for providers to know that stress will show up differently in children than in adults, said Chelsea Younghans, MD, a psychiatrist and military officer in Bethesda, Md., in an interview.
“They may see children with headaches, stomach aches, or nonspecific complaints. They may also see children who have not had difficulty with sleep present with nightmares or bed wetting,” she added.
For teens and preteens, validated tools such as the Child PTSD Symptom Scale (CPSS-5) and Child and Adolescent Trauma Screen (CATS) to assess PTSD in youth, may help serve as a starting point for a conversation between providers and their older child population, she noted.
Children who exhibit avoidance or withdrawal behaviors including consistent school refusal, an increase in reassurance-seeking behaviors, or somatic symptoms like vague abdominal pain or headaches that prevent school attendance after participating in a drill, may need more robust mental health services, Dr. Loper noted.
Dr. Schonfeld, who is also director of the National Center for School Crisis and Bereavement at Children’s Hospital Los Angeles, called for health care providers to be available to help children process traumatic reactions to these exercises.
Agreeing with Dr. Schonfeld, Dr. Younghans said: “It is vital to debrief with students and staff after drills, making sure that students have a safe space and ample time to speak with trusted staff. As children will undoubtedly have questions and concerns, creating open lines of communication will help alleviate any traumatic effect these drills may have.”
Communicating with various stakeholders
Experts also gave recommendations for how clinicians communicate with leaders in their area’s school districts and other members of their communities about these training exercises.
“For primary care providers, it is important to establish meaningful relationships within your community and patient population as much as possible,” Dr. Younghans said. “Having a good relationship with the local schools and being part of the conversation can help increase school and community awareness on the impact these drills can have on students and staff,” she added.
For those pediatricians or other health care providers who serve as consultants to schools, Dr. Schonfeld advised they ask about policies related to exercises and drills, such as what are the limits to what children might be exposed to in a drill, and what requirements there might be at the local and state level in terms of frequency and what the drills will and will not involve.
He also noted that clinicians should encourage school leaders to consider the fact that kids may have personal histories of trauma that are completely unknown to the school when they design these exercises.
School staff and health care providers should explain the nature and reasons for drills, invite family members to express concerns, and make accommodations if necessary for some children to participate in drills in a more limited way, noted Dr. Schonfeld, who is also clinical professor of pediatrics at the University of Southern California, Los Angeles.
“I think health care providers should work with legislators, so that if they require a drill, it must be done in a way that is physically and emotionally safe,” he added.
Executing better drills for students’ mental health
Experts also advised on ways to execute these drills that will be least damaging to students.
The AAP statement on Participation of Children and Adolescents in Live Crisis Drills and Exercises, for example, advocates eliminating high-intensity drills, prohibiting deception in drills, and providing accommodations based on children’s vulnerabilities.
Dr. Schonfeld also emphasized, in an interview, that training for an attack need not be extremely realistic to be effective.
“When you are preparing for a crisis, the drills and exercises are for children to practice and develop mastery over something they don’t know how to do fully yet,” said Dr. Schonfeld.
Citing a suggestion from a 2020 report conducted by Everytown for Gun Safety on keeping schools safe from gun violence, Dr. Younghans said, “Schools should be in clear communication with communities and families regarding when drills will be happening,” and advised ensuring that the explanation of drills is developmentally appropriate to the age of the children participating.
The report also recommends conducting drills that do not simulate an actual incident, combining drills with trauma-informed approaches to address students’ well-being during and for a sustained period after the drills, and tracking data on the efficacy and effects of drills.
Dr. Loper suggested ways that clinicians and parents can help navigate the tricky territory of school safety drills.
In his view, they should not be random or unexpected, and anticipatory guidance should be given regarding any visual or auditory stimuli, such as flashing lights or sirens, alarms, or announcements.
“A preventive approach should be utilized to ensure that any child who is experiencing extreme drill-distress be excused from any future disaster drills to prevent retraumatization,” Dr. Loper said.
Physicians interviewed for this piece also provided tips on how to talk about these events with children in a way that is beneficial to their mental health.
“What we want to do is [have a] calm discussion [with kids] about what we are doing and why we are doing it” and guide them through the movements, Dr. Schonfeld said.
When teaching children how to respond to an emergency, some elements of uncertainty need to be discussed. Children need to anticipate “what you might do if you are not in the classroom if something occurs, such as being in the bathroom, or out at recess,” he continued.
Dr. Younghans recommended that parents and staff schedule time to prepare children for the drill and practice in advance, and that behavioral health providers, counselors, and/or primary care providers should be involved in the planning and execution of the drill.
The Georgia Tech study was supported through a grant from Everytown for Gun Safety.
The study authors and experts interviewed for this piece had no financial conflicts to disclose.
Biosimilar-to-biosimilar switches deemed safe and effective, systematic review reveals
Switching from one biosimilar medication to another is safe and effective, a new systematic review indicates, even though this clinical practice is not governed by current health authority regulations or guidance.
“No reduction in effectiveness or increase in adverse events was detected in biosimilar-to-biosimilar switching studies conducted to date,” the review’s authors noted in their study, published online in BioDrugs.
“The possibility of multiple switches between biosimilars of the same reference biologic is already a reality, and these types of switches are expected to become more common in the future. ... Although it is not covered by current health authority regulations or guidance,” added the authors, led by Hillel P. Cohen, PhD, executive director of scientific affairs at Sandoz, a division of Novartis.
The researchers searched electronic databases through December 2021 and found 23 observational studies that met their search criteria, of which 13 were published in peer-reviewed journals; the remainder appeared in abstract form. The studies totaled 3,657 patients. The researchers did not identify any randomized clinical trials.
“The studies were heterogeneous in size, design, and endpoints, providing data on safety, effectiveness, immunogenicity, pharmacokinetics, patient retention, patient and physician perceptions, and drug-use patterns,” the authors wrote.
The authors found that the majority of studies evaluated switches between biosimilars of infliximab, but they also identified switches between biosimilars of adalimumab, etanercept, and rituximab.
“Some health care providers are hesitant to switch patients from one biosimilar to another biosimilar because of a perceived lack of clinical data on such switches,” Dr. Cohen said in an interview.
The review’s findings – that there were no clinically relevant differences when switching patients from one biosimilar to another – are consistent with the science, Dr. Cohen said. “Physicians should have confidence that the data demonstrate that safety and effectiveness are not impacted if patients switch from one biosimilar to another biosimilar of the same reference biologic,” he said.
Currently, the published data include biosimilars to only four reference biologics. “However, I anticipate additional biosimilar-to-biosimilar switching data will become available in the future,” Dr. Cohen said. “In fact, several new studies have been published in recent months, after the cut-off date for inclusion in our systematic review.”
Switching common in rheumatology, dermatology, and gastroenterology
Biosimilar-to-biosimilar switching was observed most commonly in rheumatology practice, but also was seen in the specialties of dermatology and gastroenterology.
Jeffrey Weinberg, MD, clinical professor of dermatology, Icahn School of Medicine at Mount Sinai, New York City, said in an interview that the study is among the best to date showing that switching biosimilars does not compromise efficacy or safety.
“I would hypothesize that the interchangeability would apply to psoriasis patients,” Dr. Weinberg said. However, “over the next few years, we will have an increasing number of biosimilars for an increasing number of different molecules. We will need to be vigilant to observe if similar behavior is observed with the biosimilars yet to come.”
Keith Choate, MD, PhD, professor of dermatology, pathology, and genetics, and associate dean for physician-scientist development at Yale University, New Haven, Conn., said that biosimilars have comparable efficacy to the branded medication they replace. “If response is lost to an individual agent, we would not typically then switch to a biosimilar, but would favor another class of therapy or a distinct therapeutic which targets the same pathway.”
When physicians prescribe a biosimilar for rheumatoid arthritis or psoriatic arthritis, in 9 out 10 people, “it’s going to work as well, and it’s not going to cause any more side effects,” said Stanford Shoor, MD, clinical professor of medicine and rheumatology, Stanford (Calif.) University.
The systematic review, even within its limitations, reinforces confidence in the antitumor necrosis factor biosimilars, said Jean-Frederic Colombel, MD, codirector of the Feinstein Inflammatory Bowel Disease Clinical Center at Mount Sinai, New York, and professor of medicine, division of gastroenterology, Icahn School of Medicine at Mount Sinai.
“Still, studies with longer follow-up are needed,” Dr. Colombel said, adding that the remaining questions relate to the efficacy and safety of switching multiple times, which will likely occur in the near future. There will be a “need to provide information to the patient regarding what originator or biosimilar(s) he has been exposed to during the course of his disease.”
Switching will increasingly become the norm, said Miguel Regueiro, MD, chair of the Digestive Disease & Surgery Institute, Cleveland Clinic. In his clinical practice, he has the most experience with Crohn’s disease and ulcerative colitis, and biosimilar-to-biosimilar infliximab switches. “Unless there are data that emerge, I have no concerns with this.”
He added that it’s an “interesting study that affirms my findings in clinical practice – that one can switch from a biosimilar to biosimilar (of the same reference product).”
The review’s results also make sense from an economic standpoint, said Rajat Bhatt, MD, owner of Prime Rheumatology in Richmond, Tex., and an adjunct faculty member at Caribbean Medical University, Willemstad, Curaçao. “Switching to biosimilars will result in cost savings for the health care system.” Patients on certain insurances also will save by switching to a biosimilar with a lower copay.
However, the review is limited by a relatively small number of studies that have provided primary data on this topic, and most of these were switching from infliximab to a biosimilar for inflammatory bowel disease, said Alfred Kim, MD, PhD, an adult rheumatologist at Barnes-Jewish Hospital, St. Louis, and assistant professor of medicine at Washington University in St. Louis.
As with any meta-analysis evaluating a small number of studies, “broad applicability to all conditions and reference/biosimilar pair can only be assumed. Also, many of the studies used for this meta-analysis are observational, which can introduce a variety of biases that can be difficult to adjust for,” Dr. Kim said. “Nevertheless, these analyses are an important first step in validating the [Food and Drug Administration’s] approach to evaluating biosimilars, as the clinical outcomes are consistent between different biosimilars.”
This systematic review is not enough to prove that all patients will do fine when switching from one biosimilar to another, said Florence Aslinia, MD, a gastroenterologist at the University of Kansas Health System in Kansas City. It’s possible that some patients may not do as well, she said, noting that, in one study of patients with inflammatory bowel disease, 10% of patients on a biosimilar infliximab needed to switch back to the originator infliximab (Remicade, Janssen) because of side effects attributed to the biosimilar. The same thing may or may not happen with biosimilar-to-biosimilar switching, and it requires further study.
The authors did not receive any funding for writing this review. Dr. Cohen is an employee of Sandoz, a division of Novartis. He may own stock in Novartis. Two coauthors are also employees of Sandoz. The other three coauthors reported having financial relationships with numerous pharmaceutical companies, including Sandoz and/or Novartis. Dr. Colombel reported financial relationships with many pharmaceutical companies, including Novartis and other manufacturers of biosimilars. Dr. Regueiro reports financial relationships with numerous pharmaceutical companies, including some manufacturers of biosimilars. Dr. Weinberg reported financial relationships with Celgene, AbbVie, Eli Lilly, and Novartis. Kim reports financial relationships with GlaxoSmithKline, Pfizer, and AstraZeneca. Dr. Aslinia, Dr. Shoor, Dr. Choate, and Dr. Bhatt reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Switching from one biosimilar medication to another is safe and effective, a new systematic review indicates, even though this clinical practice is not governed by current health authority regulations or guidance.
“No reduction in effectiveness or increase in adverse events was detected in biosimilar-to-biosimilar switching studies conducted to date,” the review’s authors noted in their study, published online in BioDrugs.
“The possibility of multiple switches between biosimilars of the same reference biologic is already a reality, and these types of switches are expected to become more common in the future. ... Although it is not covered by current health authority regulations or guidance,” added the authors, led by Hillel P. Cohen, PhD, executive director of scientific affairs at Sandoz, a division of Novartis.
The researchers searched electronic databases through December 2021 and found 23 observational studies that met their search criteria, of which 13 were published in peer-reviewed journals; the remainder appeared in abstract form. The studies totaled 3,657 patients. The researchers did not identify any randomized clinical trials.
“The studies were heterogeneous in size, design, and endpoints, providing data on safety, effectiveness, immunogenicity, pharmacokinetics, patient retention, patient and physician perceptions, and drug-use patterns,” the authors wrote.
The authors found that the majority of studies evaluated switches between biosimilars of infliximab, but they also identified switches between biosimilars of adalimumab, etanercept, and rituximab.
“Some health care providers are hesitant to switch patients from one biosimilar to another biosimilar because of a perceived lack of clinical data on such switches,” Dr. Cohen said in an interview.
The review’s findings – that there were no clinically relevant differences when switching patients from one biosimilar to another – are consistent with the science, Dr. Cohen said. “Physicians should have confidence that the data demonstrate that safety and effectiveness are not impacted if patients switch from one biosimilar to another biosimilar of the same reference biologic,” he said.
Currently, the published data include biosimilars to only four reference biologics. “However, I anticipate additional biosimilar-to-biosimilar switching data will become available in the future,” Dr. Cohen said. “In fact, several new studies have been published in recent months, after the cut-off date for inclusion in our systematic review.”
Switching common in rheumatology, dermatology, and gastroenterology
Biosimilar-to-biosimilar switching was observed most commonly in rheumatology practice, but also was seen in the specialties of dermatology and gastroenterology.
Jeffrey Weinberg, MD, clinical professor of dermatology, Icahn School of Medicine at Mount Sinai, New York City, said in an interview that the study is among the best to date showing that switching biosimilars does not compromise efficacy or safety.
“I would hypothesize that the interchangeability would apply to psoriasis patients,” Dr. Weinberg said. However, “over the next few years, we will have an increasing number of biosimilars for an increasing number of different molecules. We will need to be vigilant to observe if similar behavior is observed with the biosimilars yet to come.”
Keith Choate, MD, PhD, professor of dermatology, pathology, and genetics, and associate dean for physician-scientist development at Yale University, New Haven, Conn., said that biosimilars have comparable efficacy to the branded medication they replace. “If response is lost to an individual agent, we would not typically then switch to a biosimilar, but would favor another class of therapy or a distinct therapeutic which targets the same pathway.”
When physicians prescribe a biosimilar for rheumatoid arthritis or psoriatic arthritis, in 9 out 10 people, “it’s going to work as well, and it’s not going to cause any more side effects,” said Stanford Shoor, MD, clinical professor of medicine and rheumatology, Stanford (Calif.) University.
The systematic review, even within its limitations, reinforces confidence in the antitumor necrosis factor biosimilars, said Jean-Frederic Colombel, MD, codirector of the Feinstein Inflammatory Bowel Disease Clinical Center at Mount Sinai, New York, and professor of medicine, division of gastroenterology, Icahn School of Medicine at Mount Sinai.
“Still, studies with longer follow-up are needed,” Dr. Colombel said, adding that the remaining questions relate to the efficacy and safety of switching multiple times, which will likely occur in the near future. There will be a “need to provide information to the patient regarding what originator or biosimilar(s) he has been exposed to during the course of his disease.”
Switching will increasingly become the norm, said Miguel Regueiro, MD, chair of the Digestive Disease & Surgery Institute, Cleveland Clinic. In his clinical practice, he has the most experience with Crohn’s disease and ulcerative colitis, and biosimilar-to-biosimilar infliximab switches. “Unless there are data that emerge, I have no concerns with this.”
He added that it’s an “interesting study that affirms my findings in clinical practice – that one can switch from a biosimilar to biosimilar (of the same reference product).”
The review’s results also make sense from an economic standpoint, said Rajat Bhatt, MD, owner of Prime Rheumatology in Richmond, Tex., and an adjunct faculty member at Caribbean Medical University, Willemstad, Curaçao. “Switching to biosimilars will result in cost savings for the health care system.” Patients on certain insurances also will save by switching to a biosimilar with a lower copay.
However, the review is limited by a relatively small number of studies that have provided primary data on this topic, and most of these were switching from infliximab to a biosimilar for inflammatory bowel disease, said Alfred Kim, MD, PhD, an adult rheumatologist at Barnes-Jewish Hospital, St. Louis, and assistant professor of medicine at Washington University in St. Louis.
As with any meta-analysis evaluating a small number of studies, “broad applicability to all conditions and reference/biosimilar pair can only be assumed. Also, many of the studies used for this meta-analysis are observational, which can introduce a variety of biases that can be difficult to adjust for,” Dr. Kim said. “Nevertheless, these analyses are an important first step in validating the [Food and Drug Administration’s] approach to evaluating biosimilars, as the clinical outcomes are consistent between different biosimilars.”
This systematic review is not enough to prove that all patients will do fine when switching from one biosimilar to another, said Florence Aslinia, MD, a gastroenterologist at the University of Kansas Health System in Kansas City. It’s possible that some patients may not do as well, she said, noting that, in one study of patients with inflammatory bowel disease, 10% of patients on a biosimilar infliximab needed to switch back to the originator infliximab (Remicade, Janssen) because of side effects attributed to the biosimilar. The same thing may or may not happen with biosimilar-to-biosimilar switching, and it requires further study.
The authors did not receive any funding for writing this review. Dr. Cohen is an employee of Sandoz, a division of Novartis. He may own stock in Novartis. Two coauthors are also employees of Sandoz. The other three coauthors reported having financial relationships with numerous pharmaceutical companies, including Sandoz and/or Novartis. Dr. Colombel reported financial relationships with many pharmaceutical companies, including Novartis and other manufacturers of biosimilars. Dr. Regueiro reports financial relationships with numerous pharmaceutical companies, including some manufacturers of biosimilars. Dr. Weinberg reported financial relationships with Celgene, AbbVie, Eli Lilly, and Novartis. Kim reports financial relationships with GlaxoSmithKline, Pfizer, and AstraZeneca. Dr. Aslinia, Dr. Shoor, Dr. Choate, and Dr. Bhatt reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Switching from one biosimilar medication to another is safe and effective, a new systematic review indicates, even though this clinical practice is not governed by current health authority regulations or guidance.
“No reduction in effectiveness or increase in adverse events was detected in biosimilar-to-biosimilar switching studies conducted to date,” the review’s authors noted in their study, published online in BioDrugs.
“The possibility of multiple switches between biosimilars of the same reference biologic is already a reality, and these types of switches are expected to become more common in the future. ... Although it is not covered by current health authority regulations or guidance,” added the authors, led by Hillel P. Cohen, PhD, executive director of scientific affairs at Sandoz, a division of Novartis.
The researchers searched electronic databases through December 2021 and found 23 observational studies that met their search criteria, of which 13 were published in peer-reviewed journals; the remainder appeared in abstract form. The studies totaled 3,657 patients. The researchers did not identify any randomized clinical trials.
“The studies were heterogeneous in size, design, and endpoints, providing data on safety, effectiveness, immunogenicity, pharmacokinetics, patient retention, patient and physician perceptions, and drug-use patterns,” the authors wrote.
The authors found that the majority of studies evaluated switches between biosimilars of infliximab, but they also identified switches between biosimilars of adalimumab, etanercept, and rituximab.
“Some health care providers are hesitant to switch patients from one biosimilar to another biosimilar because of a perceived lack of clinical data on such switches,” Dr. Cohen said in an interview.
The review’s findings – that there were no clinically relevant differences when switching patients from one biosimilar to another – are consistent with the science, Dr. Cohen said. “Physicians should have confidence that the data demonstrate that safety and effectiveness are not impacted if patients switch from one biosimilar to another biosimilar of the same reference biologic,” he said.
Currently, the published data include biosimilars to only four reference biologics. “However, I anticipate additional biosimilar-to-biosimilar switching data will become available in the future,” Dr. Cohen said. “In fact, several new studies have been published in recent months, after the cut-off date for inclusion in our systematic review.”
Switching common in rheumatology, dermatology, and gastroenterology
Biosimilar-to-biosimilar switching was observed most commonly in rheumatology practice, but also was seen in the specialties of dermatology and gastroenterology.
Jeffrey Weinberg, MD, clinical professor of dermatology, Icahn School of Medicine at Mount Sinai, New York City, said in an interview that the study is among the best to date showing that switching biosimilars does not compromise efficacy or safety.
“I would hypothesize that the interchangeability would apply to psoriasis patients,” Dr. Weinberg said. However, “over the next few years, we will have an increasing number of biosimilars for an increasing number of different molecules. We will need to be vigilant to observe if similar behavior is observed with the biosimilars yet to come.”
Keith Choate, MD, PhD, professor of dermatology, pathology, and genetics, and associate dean for physician-scientist development at Yale University, New Haven, Conn., said that biosimilars have comparable efficacy to the branded medication they replace. “If response is lost to an individual agent, we would not typically then switch to a biosimilar, but would favor another class of therapy or a distinct therapeutic which targets the same pathway.”
When physicians prescribe a biosimilar for rheumatoid arthritis or psoriatic arthritis, in 9 out 10 people, “it’s going to work as well, and it’s not going to cause any more side effects,” said Stanford Shoor, MD, clinical professor of medicine and rheumatology, Stanford (Calif.) University.
The systematic review, even within its limitations, reinforces confidence in the antitumor necrosis factor biosimilars, said Jean-Frederic Colombel, MD, codirector of the Feinstein Inflammatory Bowel Disease Clinical Center at Mount Sinai, New York, and professor of medicine, division of gastroenterology, Icahn School of Medicine at Mount Sinai.
“Still, studies with longer follow-up are needed,” Dr. Colombel said, adding that the remaining questions relate to the efficacy and safety of switching multiple times, which will likely occur in the near future. There will be a “need to provide information to the patient regarding what originator or biosimilar(s) he has been exposed to during the course of his disease.”
Switching will increasingly become the norm, said Miguel Regueiro, MD, chair of the Digestive Disease & Surgery Institute, Cleveland Clinic. In his clinical practice, he has the most experience with Crohn’s disease and ulcerative colitis, and biosimilar-to-biosimilar infliximab switches. “Unless there are data that emerge, I have no concerns with this.”
He added that it’s an “interesting study that affirms my findings in clinical practice – that one can switch from a biosimilar to biosimilar (of the same reference product).”
The review’s results also make sense from an economic standpoint, said Rajat Bhatt, MD, owner of Prime Rheumatology in Richmond, Tex., and an adjunct faculty member at Caribbean Medical University, Willemstad, Curaçao. “Switching to biosimilars will result in cost savings for the health care system.” Patients on certain insurances also will save by switching to a biosimilar with a lower copay.
However, the review is limited by a relatively small number of studies that have provided primary data on this topic, and most of these were switching from infliximab to a biosimilar for inflammatory bowel disease, said Alfred Kim, MD, PhD, an adult rheumatologist at Barnes-Jewish Hospital, St. Louis, and assistant professor of medicine at Washington University in St. Louis.
As with any meta-analysis evaluating a small number of studies, “broad applicability to all conditions and reference/biosimilar pair can only be assumed. Also, many of the studies used for this meta-analysis are observational, which can introduce a variety of biases that can be difficult to adjust for,” Dr. Kim said. “Nevertheless, these analyses are an important first step in validating the [Food and Drug Administration’s] approach to evaluating biosimilars, as the clinical outcomes are consistent between different biosimilars.”
This systematic review is not enough to prove that all patients will do fine when switching from one biosimilar to another, said Florence Aslinia, MD, a gastroenterologist at the University of Kansas Health System in Kansas City. It’s possible that some patients may not do as well, she said, noting that, in one study of patients with inflammatory bowel disease, 10% of patients on a biosimilar infliximab needed to switch back to the originator infliximab (Remicade, Janssen) because of side effects attributed to the biosimilar. The same thing may or may not happen with biosimilar-to-biosimilar switching, and it requires further study.
The authors did not receive any funding for writing this review. Dr. Cohen is an employee of Sandoz, a division of Novartis. He may own stock in Novartis. Two coauthors are also employees of Sandoz. The other three coauthors reported having financial relationships with numerous pharmaceutical companies, including Sandoz and/or Novartis. Dr. Colombel reported financial relationships with many pharmaceutical companies, including Novartis and other manufacturers of biosimilars. Dr. Regueiro reports financial relationships with numerous pharmaceutical companies, including some manufacturers of biosimilars. Dr. Weinberg reported financial relationships with Celgene, AbbVie, Eli Lilly, and Novartis. Kim reports financial relationships with GlaxoSmithKline, Pfizer, and AstraZeneca. Dr. Aslinia, Dr. Shoor, Dr. Choate, and Dr. Bhatt reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM BIODRUGS







