User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Roots of physician burnout: It’s the work load
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
FROM THE JOINT COMMISSION JOURNAL ON QUALITY AND PATIENT SAFETY
CDC chief lays out attack plan for COVID variants
earlier this week.
As part of JAMA’s Q&A series with JAMA editor in chief Howard Bauchner, MD, Dr. Walensky referenced the blueprint she coathored with Anthony Fauci, MD, the nation’s top infectious disease expert, and Henry T. Walke, MD, MPH, of the CDC, which was published on Feb. 17 in JAMA.
In the viewpoint article, they explain that the Department of Health & Human Services has established the SARS-CoV-2 Interagency Group to improve coordination among the CDC, the National Institutes of Health, the Food and Drug Administration, the Biomedical Advanced Research and Development Authority, the Department of Agriculture, and the Department of Defense.
Dr. Walensky said the first objective is to reinforce vigilance regarding public health mitigation strategies to decrease the amount of virus that’s circulating.
As part of that strategy, she said, the CDC strongly urges against nonessential travel.
In addition, public health leaders are working on a surveillance system to better understand the SARS-CoV-2 variants. That will take ramping up genome sequencing of the SARS-CoV-2 virus and ensuring that sampling is geographically representative.
She said the CDC is partnering with state health labs to obtain about 750 samples every week and is teaming up with commercial labs and academic centers to obtain an interim target of 6,000 samples per week.
She acknowledged the United States “is not where we need to be” with sequencing but has come a long way since January. At that time, they were sequencing 250 samples every week; they are currently sequencing thousands each week.
Data analysis is another concern: “We need to be able to understand at the basic science level what the information means,” Dr. Walensky said.
Researchers aren’t sure how the variants might affect use of convalescent plasma or monoclonal antibody treatments. It is expected that 5% of persons who are vaccinated against COVID-19 will nevertheless contract the disease. Sequencing will help answer whether such persons who have been vaccinated and who subsequently contract the virus are among those 5% or whether have been infected by a variant that evades the vaccine.
Accelerating vaccine administration globally and in the United States is essential, Dr. Walensky said.
As of Feb. 17, 56 million doses had been administered in the United States.
Top three threats
She updated the numbers on the three biggest variant threats.
Regarding B.1.1.7, which originated in the United Kingdom, she said: “So far, we’ve had over 1,200 cases in 41 states.” She noted that the variant is likely to be about 50% more transmissible and 30% to 50% more virulent.
“So far, it looks like that strain doesn’t have any real decrease in susceptibility to our vaccines,” she said.
The strain from South Africa (B.1.351) has been found in 19 cases in the United States.
The P.1. variant, which originated in Brazil, has been identified in two cases in two states.
Outlook for March and April
Dr. Bauchner asked Dr. Walensky what she envisions for March and April. He noted that public optimism is high in light of the continued reductions in COVID-19 case numbers, hospitalizations, and deaths, as well as the fact that warmer weather is coming and that more vaccinations are on the horizon.
“While I really am hopeful for what could happen in March and April,” Dr. Walensky said, “I really do know that this could go bad so fast. We saw it in November. We saw it in December.”
CDC models have projected that, by March, the more transmissible B.1.1.7 strain is likely to be the dominant strain, she reiterated.
“I worry that it will be spring, and we will all have had enough,” Dr. Walensky said. She noted that some states are already relaxing mask mandates.
“Around that time, life will look and feel a little better, and the motivation for those who might be vaccine hesitant may be diminished,” she said.
Dr. Bauchner also asked her to weigh in on whether a third vaccine, from Johnson & Johnson (J&J), may soon gain FDA emergency-use authorization – and whether its lower expected efficacy rate may result in a tiered system of vaccinations, with higher-risk populations receiving the more efficacious vaccines.
Dr. Walensky said more data are needed before that question can be answered.
“It may very well be that the data point us to the best populations in which to use this vaccine,” she said.
In phase 3 data, the J&J vaccine was shown to be 72% effective in the United States for moderate to severe disease.
Dr. Walensky said it’s important to remember that the projected efficacy for that vaccine is higher than that for the flu shot as well as many other vaccines currently in use for other diseases.
She said it also has several advantages. The vaccine has less-stringent storage requirements, requires just one dose, and protects against hospitalization and death, although it’s less efficacious in protecting against contracting the disease.
“I think many people would opt to get that one if they could get it sooner,” she said.
A version of this article first appeared on Medscape.com.
earlier this week.
As part of JAMA’s Q&A series with JAMA editor in chief Howard Bauchner, MD, Dr. Walensky referenced the blueprint she coathored with Anthony Fauci, MD, the nation’s top infectious disease expert, and Henry T. Walke, MD, MPH, of the CDC, which was published on Feb. 17 in JAMA.
In the viewpoint article, they explain that the Department of Health & Human Services has established the SARS-CoV-2 Interagency Group to improve coordination among the CDC, the National Institutes of Health, the Food and Drug Administration, the Biomedical Advanced Research and Development Authority, the Department of Agriculture, and the Department of Defense.
Dr. Walensky said the first objective is to reinforce vigilance regarding public health mitigation strategies to decrease the amount of virus that’s circulating.
As part of that strategy, she said, the CDC strongly urges against nonessential travel.
In addition, public health leaders are working on a surveillance system to better understand the SARS-CoV-2 variants. That will take ramping up genome sequencing of the SARS-CoV-2 virus and ensuring that sampling is geographically representative.
She said the CDC is partnering with state health labs to obtain about 750 samples every week and is teaming up with commercial labs and academic centers to obtain an interim target of 6,000 samples per week.
She acknowledged the United States “is not where we need to be” with sequencing but has come a long way since January. At that time, they were sequencing 250 samples every week; they are currently sequencing thousands each week.
Data analysis is another concern: “We need to be able to understand at the basic science level what the information means,” Dr. Walensky said.
Researchers aren’t sure how the variants might affect use of convalescent plasma or monoclonal antibody treatments. It is expected that 5% of persons who are vaccinated against COVID-19 will nevertheless contract the disease. Sequencing will help answer whether such persons who have been vaccinated and who subsequently contract the virus are among those 5% or whether have been infected by a variant that evades the vaccine.
Accelerating vaccine administration globally and in the United States is essential, Dr. Walensky said.
As of Feb. 17, 56 million doses had been administered in the United States.
Top three threats
She updated the numbers on the three biggest variant threats.
Regarding B.1.1.7, which originated in the United Kingdom, she said: “So far, we’ve had over 1,200 cases in 41 states.” She noted that the variant is likely to be about 50% more transmissible and 30% to 50% more virulent.
“So far, it looks like that strain doesn’t have any real decrease in susceptibility to our vaccines,” she said.
The strain from South Africa (B.1.351) has been found in 19 cases in the United States.
The P.1. variant, which originated in Brazil, has been identified in two cases in two states.
Outlook for March and April
Dr. Bauchner asked Dr. Walensky what she envisions for March and April. He noted that public optimism is high in light of the continued reductions in COVID-19 case numbers, hospitalizations, and deaths, as well as the fact that warmer weather is coming and that more vaccinations are on the horizon.
“While I really am hopeful for what could happen in March and April,” Dr. Walensky said, “I really do know that this could go bad so fast. We saw it in November. We saw it in December.”
CDC models have projected that, by March, the more transmissible B.1.1.7 strain is likely to be the dominant strain, she reiterated.
“I worry that it will be spring, and we will all have had enough,” Dr. Walensky said. She noted that some states are already relaxing mask mandates.
“Around that time, life will look and feel a little better, and the motivation for those who might be vaccine hesitant may be diminished,” she said.
Dr. Bauchner also asked her to weigh in on whether a third vaccine, from Johnson & Johnson (J&J), may soon gain FDA emergency-use authorization – and whether its lower expected efficacy rate may result in a tiered system of vaccinations, with higher-risk populations receiving the more efficacious vaccines.
Dr. Walensky said more data are needed before that question can be answered.
“It may very well be that the data point us to the best populations in which to use this vaccine,” she said.
In phase 3 data, the J&J vaccine was shown to be 72% effective in the United States for moderate to severe disease.
Dr. Walensky said it’s important to remember that the projected efficacy for that vaccine is higher than that for the flu shot as well as many other vaccines currently in use for other diseases.
She said it also has several advantages. The vaccine has less-stringent storage requirements, requires just one dose, and protects against hospitalization and death, although it’s less efficacious in protecting against contracting the disease.
“I think many people would opt to get that one if they could get it sooner,” she said.
A version of this article first appeared on Medscape.com.
earlier this week.
As part of JAMA’s Q&A series with JAMA editor in chief Howard Bauchner, MD, Dr. Walensky referenced the blueprint she coathored with Anthony Fauci, MD, the nation’s top infectious disease expert, and Henry T. Walke, MD, MPH, of the CDC, which was published on Feb. 17 in JAMA.
In the viewpoint article, they explain that the Department of Health & Human Services has established the SARS-CoV-2 Interagency Group to improve coordination among the CDC, the National Institutes of Health, the Food and Drug Administration, the Biomedical Advanced Research and Development Authority, the Department of Agriculture, and the Department of Defense.
Dr. Walensky said the first objective is to reinforce vigilance regarding public health mitigation strategies to decrease the amount of virus that’s circulating.
As part of that strategy, she said, the CDC strongly urges against nonessential travel.
In addition, public health leaders are working on a surveillance system to better understand the SARS-CoV-2 variants. That will take ramping up genome sequencing of the SARS-CoV-2 virus and ensuring that sampling is geographically representative.
She said the CDC is partnering with state health labs to obtain about 750 samples every week and is teaming up with commercial labs and academic centers to obtain an interim target of 6,000 samples per week.
She acknowledged the United States “is not where we need to be” with sequencing but has come a long way since January. At that time, they were sequencing 250 samples every week; they are currently sequencing thousands each week.
Data analysis is another concern: “We need to be able to understand at the basic science level what the information means,” Dr. Walensky said.
Researchers aren’t sure how the variants might affect use of convalescent plasma or monoclonal antibody treatments. It is expected that 5% of persons who are vaccinated against COVID-19 will nevertheless contract the disease. Sequencing will help answer whether such persons who have been vaccinated and who subsequently contract the virus are among those 5% or whether have been infected by a variant that evades the vaccine.
Accelerating vaccine administration globally and in the United States is essential, Dr. Walensky said.
As of Feb. 17, 56 million doses had been administered in the United States.
Top three threats
She updated the numbers on the three biggest variant threats.
Regarding B.1.1.7, which originated in the United Kingdom, she said: “So far, we’ve had over 1,200 cases in 41 states.” She noted that the variant is likely to be about 50% more transmissible and 30% to 50% more virulent.
“So far, it looks like that strain doesn’t have any real decrease in susceptibility to our vaccines,” she said.
The strain from South Africa (B.1.351) has been found in 19 cases in the United States.
The P.1. variant, which originated in Brazil, has been identified in two cases in two states.
Outlook for March and April
Dr. Bauchner asked Dr. Walensky what she envisions for March and April. He noted that public optimism is high in light of the continued reductions in COVID-19 case numbers, hospitalizations, and deaths, as well as the fact that warmer weather is coming and that more vaccinations are on the horizon.
“While I really am hopeful for what could happen in March and April,” Dr. Walensky said, “I really do know that this could go bad so fast. We saw it in November. We saw it in December.”
CDC models have projected that, by March, the more transmissible B.1.1.7 strain is likely to be the dominant strain, she reiterated.
“I worry that it will be spring, and we will all have had enough,” Dr. Walensky said. She noted that some states are already relaxing mask mandates.
“Around that time, life will look and feel a little better, and the motivation for those who might be vaccine hesitant may be diminished,” she said.
Dr. Bauchner also asked her to weigh in on whether a third vaccine, from Johnson & Johnson (J&J), may soon gain FDA emergency-use authorization – and whether its lower expected efficacy rate may result in a tiered system of vaccinations, with higher-risk populations receiving the more efficacious vaccines.
Dr. Walensky said more data are needed before that question can be answered.
“It may very well be that the data point us to the best populations in which to use this vaccine,” she said.
In phase 3 data, the J&J vaccine was shown to be 72% effective in the United States for moderate to severe disease.
Dr. Walensky said it’s important to remember that the projected efficacy for that vaccine is higher than that for the flu shot as well as many other vaccines currently in use for other diseases.
She said it also has several advantages. The vaccine has less-stringent storage requirements, requires just one dose, and protects against hospitalization and death, although it’s less efficacious in protecting against contracting the disease.
“I think many people would opt to get that one if they could get it sooner,” she said.
A version of this article first appeared on Medscape.com.
Alien cells may explain COVID-19 brain fog
, a new report suggests.
The authors report five separate post-mortem cases from patients who died with COVID-19 in which large cells resembling megakaryocytes were identified in cortical capillaries. Immunohistochemistry subsequently confirmed their megakaryocyte identity.
They point out that the finding is of interest as – to their knowledge – megakaryocytes have not been found in the brain before.
The observations are described in a research letter published online Feb. 12 in JAMA Neurology.
Bone marrow cells in the brain
Lead author David Nauen, MD, PhD, a neuropathologist from Johns Hopkins University, Baltimore, reported that he identified these cells in the first analysis of post-mortem brain tissue from a patient who had COVID-19.
“Some other viruses cause changes in the brain such as encephalopathy, and as neurologic symptoms are often reported in COVID-19, I was curious to see if similar effects were seen in brain post-mortem samples from patients who had died with the infection,” Dr. Nauen said.
On his first analysis of the brain tissue of a patient who had COVID-19, Dr. Nauen saw no evidence of viral encephalitis, but he observed some “unusually large” cells in the brain capillaries.
“I was taken aback; I couldn’t figure out what they were. Then I realized these cells were megakaryocytes from the bone marrow. I have never seen these cells in the brain before. I asked several colleagues and none of them had either. After extensive literature searches, I could find no evidence of megakaryocytes being in the brain,” Dr. Nauen noted.
Megakaryocytes, he explained, are “very large cells, and the brain capillaries are very small – just large enough to let red blood cells and lymphocytes pass through. To see these very large cells in such vessels is extremely unusual. It looks like they are causing occlusions.”
By occluding flow through individual capillaries, these large cells could cause ischemic alteration in a distinct pattern, potentially resulting in an atypical form of neurologic impairment, the authors suggest.
“This might alter the hemodynamics and put pressure on other vessels, possibly contributing to the increased risk of stroke that has been reported in COVID-19,” Dr. Nauen said. None of the samples he examined came from patients with COVID-19 who had had a stroke, he reported.
Other than the presence of megakaryocytes in the capillaries, the brain looked normal, he said. He has now examined samples from 15 brains of patients who had COVID-19 and megakaryocytes have been found in the brain capillaries in five cases.
New neurologic complication
Classic encephalitis found with other viruses has not been reported in brain post-mortem examinations from patients who had COVID-19, Dr. Nauen noted. “The cognitive issues such as grogginess associated with COVID-19 would indicate problems with the cortex but that hasn’t been documented. This occlusion of a multitude of tiny vessels by megalokaryocytes may offer some explanation of the cognitive issues. This is a new kind of vascular insult seen on pathology, and suggests a new kind of neurologic complication,” he added.
The big question is what these megakaryocytes are doing in the brain.
“Megakaryocytes are bone marrow cells. They are not immune cells. Their job is to produce platelets to help the blood clot. They are not normally found outside the bone marrow, but they have been reported in other organs in COVID-19 patients.
“But the big puzzle associated with finding them in the brain is how they get through the very fine network of blood vessels in the lungs. The geometry just doesn’t work. We don’t know which part of the COVID inflammatory response makes this happen,” said Dr. Nauen.
The authors suggest one possibility is that altered endothelial or other signaling is recruiting megakaryocytes into the circulation and somehow permitting them to pass through the lungs.
“We need to try and understand if there is anything distinctive about these megakaryocytes – which proteins are they expressing that may explain why they are behaving in such an unusual way,” said Dr. Nauen.
Noting that many patients with severe COVID-19 have problems with clotting, and megakaryocytes are part of the clotting system, he speculated that some sort of aberrant message is being sent to these cells.
“It is notable that we found megakaryocytes in cortical capillaries in 33% of cases examined. Because the standard brain autopsy sections taken sampled at random [are] only a minute portion of the cortical volume, finding these cells suggests the total burden could be considerable,” the authors wrote.
Dr. Nauen added that to his knowledge, this is the first report of such observations, and the next step is to look for similar findings in larger sample sizes.
A version of this article first appeared on Medscape.com.
, a new report suggests.
The authors report five separate post-mortem cases from patients who died with COVID-19 in which large cells resembling megakaryocytes were identified in cortical capillaries. Immunohistochemistry subsequently confirmed their megakaryocyte identity.
They point out that the finding is of interest as – to their knowledge – megakaryocytes have not been found in the brain before.
The observations are described in a research letter published online Feb. 12 in JAMA Neurology.
Bone marrow cells in the brain
Lead author David Nauen, MD, PhD, a neuropathologist from Johns Hopkins University, Baltimore, reported that he identified these cells in the first analysis of post-mortem brain tissue from a patient who had COVID-19.
“Some other viruses cause changes in the brain such as encephalopathy, and as neurologic symptoms are often reported in COVID-19, I was curious to see if similar effects were seen in brain post-mortem samples from patients who had died with the infection,” Dr. Nauen said.
On his first analysis of the brain tissue of a patient who had COVID-19, Dr. Nauen saw no evidence of viral encephalitis, but he observed some “unusually large” cells in the brain capillaries.
“I was taken aback; I couldn’t figure out what they were. Then I realized these cells were megakaryocytes from the bone marrow. I have never seen these cells in the brain before. I asked several colleagues and none of them had either. After extensive literature searches, I could find no evidence of megakaryocytes being in the brain,” Dr. Nauen noted.
Megakaryocytes, he explained, are “very large cells, and the brain capillaries are very small – just large enough to let red blood cells and lymphocytes pass through. To see these very large cells in such vessels is extremely unusual. It looks like they are causing occlusions.”
By occluding flow through individual capillaries, these large cells could cause ischemic alteration in a distinct pattern, potentially resulting in an atypical form of neurologic impairment, the authors suggest.
“This might alter the hemodynamics and put pressure on other vessels, possibly contributing to the increased risk of stroke that has been reported in COVID-19,” Dr. Nauen said. None of the samples he examined came from patients with COVID-19 who had had a stroke, he reported.
Other than the presence of megakaryocytes in the capillaries, the brain looked normal, he said. He has now examined samples from 15 brains of patients who had COVID-19 and megakaryocytes have been found in the brain capillaries in five cases.
New neurologic complication
Classic encephalitis found with other viruses has not been reported in brain post-mortem examinations from patients who had COVID-19, Dr. Nauen noted. “The cognitive issues such as grogginess associated with COVID-19 would indicate problems with the cortex but that hasn’t been documented. This occlusion of a multitude of tiny vessels by megalokaryocytes may offer some explanation of the cognitive issues. This is a new kind of vascular insult seen on pathology, and suggests a new kind of neurologic complication,” he added.
The big question is what these megakaryocytes are doing in the brain.
“Megakaryocytes are bone marrow cells. They are not immune cells. Their job is to produce platelets to help the blood clot. They are not normally found outside the bone marrow, but they have been reported in other organs in COVID-19 patients.
“But the big puzzle associated with finding them in the brain is how they get through the very fine network of blood vessels in the lungs. The geometry just doesn’t work. We don’t know which part of the COVID inflammatory response makes this happen,” said Dr. Nauen.
The authors suggest one possibility is that altered endothelial or other signaling is recruiting megakaryocytes into the circulation and somehow permitting them to pass through the lungs.
“We need to try and understand if there is anything distinctive about these megakaryocytes – which proteins are they expressing that may explain why they are behaving in such an unusual way,” said Dr. Nauen.
Noting that many patients with severe COVID-19 have problems with clotting, and megakaryocytes are part of the clotting system, he speculated that some sort of aberrant message is being sent to these cells.
“It is notable that we found megakaryocytes in cortical capillaries in 33% of cases examined. Because the standard brain autopsy sections taken sampled at random [are] only a minute portion of the cortical volume, finding these cells suggests the total burden could be considerable,” the authors wrote.
Dr. Nauen added that to his knowledge, this is the first report of such observations, and the next step is to look for similar findings in larger sample sizes.
A version of this article first appeared on Medscape.com.
, a new report suggests.
The authors report five separate post-mortem cases from patients who died with COVID-19 in which large cells resembling megakaryocytes were identified in cortical capillaries. Immunohistochemistry subsequently confirmed their megakaryocyte identity.
They point out that the finding is of interest as – to their knowledge – megakaryocytes have not been found in the brain before.
The observations are described in a research letter published online Feb. 12 in JAMA Neurology.
Bone marrow cells in the brain
Lead author David Nauen, MD, PhD, a neuropathologist from Johns Hopkins University, Baltimore, reported that he identified these cells in the first analysis of post-mortem brain tissue from a patient who had COVID-19.
“Some other viruses cause changes in the brain such as encephalopathy, and as neurologic symptoms are often reported in COVID-19, I was curious to see if similar effects were seen in brain post-mortem samples from patients who had died with the infection,” Dr. Nauen said.
On his first analysis of the brain tissue of a patient who had COVID-19, Dr. Nauen saw no evidence of viral encephalitis, but he observed some “unusually large” cells in the brain capillaries.
“I was taken aback; I couldn’t figure out what they were. Then I realized these cells were megakaryocytes from the bone marrow. I have never seen these cells in the brain before. I asked several colleagues and none of them had either. After extensive literature searches, I could find no evidence of megakaryocytes being in the brain,” Dr. Nauen noted.
Megakaryocytes, he explained, are “very large cells, and the brain capillaries are very small – just large enough to let red blood cells and lymphocytes pass through. To see these very large cells in such vessels is extremely unusual. It looks like they are causing occlusions.”
By occluding flow through individual capillaries, these large cells could cause ischemic alteration in a distinct pattern, potentially resulting in an atypical form of neurologic impairment, the authors suggest.
“This might alter the hemodynamics and put pressure on other vessels, possibly contributing to the increased risk of stroke that has been reported in COVID-19,” Dr. Nauen said. None of the samples he examined came from patients with COVID-19 who had had a stroke, he reported.
Other than the presence of megakaryocytes in the capillaries, the brain looked normal, he said. He has now examined samples from 15 brains of patients who had COVID-19 and megakaryocytes have been found in the brain capillaries in five cases.
New neurologic complication
Classic encephalitis found with other viruses has not been reported in brain post-mortem examinations from patients who had COVID-19, Dr. Nauen noted. “The cognitive issues such as grogginess associated with COVID-19 would indicate problems with the cortex but that hasn’t been documented. This occlusion of a multitude of tiny vessels by megalokaryocytes may offer some explanation of the cognitive issues. This is a new kind of vascular insult seen on pathology, and suggests a new kind of neurologic complication,” he added.
The big question is what these megakaryocytes are doing in the brain.
“Megakaryocytes are bone marrow cells. They are not immune cells. Their job is to produce platelets to help the blood clot. They are not normally found outside the bone marrow, but they have been reported in other organs in COVID-19 patients.
“But the big puzzle associated with finding them in the brain is how they get through the very fine network of blood vessels in the lungs. The geometry just doesn’t work. We don’t know which part of the COVID inflammatory response makes this happen,” said Dr. Nauen.
The authors suggest one possibility is that altered endothelial or other signaling is recruiting megakaryocytes into the circulation and somehow permitting them to pass through the lungs.
“We need to try and understand if there is anything distinctive about these megakaryocytes – which proteins are they expressing that may explain why they are behaving in such an unusual way,” said Dr. Nauen.
Noting that many patients with severe COVID-19 have problems with clotting, and megakaryocytes are part of the clotting system, he speculated that some sort of aberrant message is being sent to these cells.
“It is notable that we found megakaryocytes in cortical capillaries in 33% of cases examined. Because the standard brain autopsy sections taken sampled at random [are] only a minute portion of the cortical volume, finding these cells suggests the total burden could be considerable,” the authors wrote.
Dr. Nauen added that to his knowledge, this is the first report of such observations, and the next step is to look for similar findings in larger sample sizes.
A version of this article first appeared on Medscape.com.
FROM JAMA NEUROLOGY
Victorious endurance: To pass the breaking point and not break
I’ve been thinking a lot about endurance recently.
COVID-19 is surging in the United States. Health care workers exhausted from the first and second waves are quickly reaching the verge of collapse. I’m seeing more and more heartbreaking articles about the bone-deep fatigue, fear, and frustration health care workers are facing, and I weep. As horrible as it is to be fighting this terrifying, little-understood, invisible virus, health care workers are also fighting an equally distressing war against misinformation, recklessness, apathy, and outright denial.
As if that wasn’t enough, we are also dealing with racial and social unrest not seen in decades. The most significant cultural divisions and political animosity perhaps since the Civil War. A contested election. The fraying of our democratic institutions and our standing in the global community. The weakest economy since the Great Depression. Record unemployment. Many individuals and families facing or already experiencing eviction and food insecurity. Record-setting fires, hurricanes, and other natural disasters that are only projected to intensify due to climate change.
That’s a lot to endure. And we don’t have much choice other than to live through it. Some of us will break under the strain; others will disengage by giving up clinical work or even leaving health care altogether. Some of us will pack it in and retire, walk away from relationships with family members or longtime friends, or even emigrate to another country (New Zealand, anyone?). Some of us will passively hunker down, letting the challenges of this time overwhelm us and just hoping we can hang on long enough to emerge, albeit beaten and scarred, on the other side.
But some of us will experience victorious endurance – the kind that doesn’t just accept suffering but finds a way to triumph over it. I came across the concept of victorious endurance in the Bible, but its origin is earlier, from classical Greece. It comes from the ancient Greek word hupomone, which literally means “abiding under” – as in disciplining oneself to bear up under a trial when one would more naturally rebel, or just give up. The ancient Greeks were big on virtues like self-control, long-suffering, and perseverance in the face of seemingly insurmountable difficulties; Odysseus was a poster child for hupomone. I believe the concept of victorious endurance can be applicable for people across many belief systems, philosophies, and ways of life.
The late William Barclay, former professor of divinity and biblical criticism at the University of Glasgow, Scotland, said of hupomone:
It is untranslatable. It does not describe the frame of mind which can sit down with folded hands and bowed head and let a torrent of troubles sweep over it in passive resignation. It describes the ability to bear things in such a triumphant way that it transfigures them. Chrysostom has a great panegyric on this hupomone. He calls it “the root of all goods, the mother of piety, the fruit that never withers, a fortress that is never taken, a harbour that knows no storms” and “the queen of virtues, the foundation of right actions, peace in war, calm in tempest, security in plots.” It is the courageous and triumphant ability to pass the breaking-point and not to break and always to greet the unseen with a cheer. It is the alchemy which transmutes tribulation into strength and glory.
Barclay further noted that “Cicero defines patientia, its Latin equivalent, as: ‘The voluntary and daily suffering of hard and difficult things, for the sake of honour and usefulness.”
In the midst of the most challenging public health emergency of our lifetimes, I am seeing hospitalists – and nurses, respiratory therapists, and countless other health care workers – doing exactly this, every day. I’m so incredibly proud of you all, and thankful beyond words.
I doubt that victorious endurance comes naturally to any of us; it’s something we work at, pursue and nurture. What’s the secret to cultivating victorious endurance in the midst of unimaginable stress? I’m pretty sure there’s no specific formula. I don’t mean to sound like a Pollyanna or to make light of the tumult and turmoil of these times, but here are a few things that, based on my own experiences, may help cultivate this valuable virtue.
Be part of a support network. In the midst of great stress, and especially during this time of social distancing, it’s especially tempting to just hunker down, close in on ourselves, and shut others out – sometimes even our closest friends and loved ones. Maintaining relationships is just too exhausting. But you need people who can come alongside you and offer words of encouragement when you are at your lowest. And there’s nothing that will bring out the best in you like being there to encourage and support someone else. We all need to both receive and to give emotional support at a time like this.
Take the long view. When we’re in the middle of a serious crisis, it seems like the problems we’re facing will last forever. There’s no light at the end of the tunnel, no port in the storm. But even this pandemic won’t last forever. If we can keep in mind the fact that things will eventually get better and that the current situation isn’t permanent, it can help us maintain our perspective and have more patience with the current dysfunction.
Focus on who you want to be in this moment. This is the hardest time most of us have ever lived through, both professionally and personally. But let me throw you a challenge. When you look back on this time from the perspective of five years from now, or maybe ten, how will you want to remember yourself? Who will you want to have been during this time? Looking back, what will make you proud of how you handled this challenge? Be that person.
Look for things to be thankful for. In the midst of the chaos that is our lives and our work right now, I believe we can still occasionally see moments of grace if we keep our eyes open for them. If we aren’t looking for them, we may miss them entirely. And those small moments of love, touches of compassion, displays of selflessness, and even flashes of victorious endurance in yourself or others are gifts to be treasured and held on to – to give thanks for.
Embrace a cause greater than yourself. May I suggest that one thing that might help our efforts to cultivate the virtue of victorious endurance during difficult times might be to embrace a cause that is bigger than yourself; that is, one that lures you to focus beyond your immediate circumstances? What are you passionate about, outside of your life’s normal routine?
If you don’t have a passion, consider what you might become passionate about, with a little effort. For some of us, like me, this will be our faith in God. For others it may be advocating for an end to racism or for broader social justice issues. Maybe it’s working to overcome our cultural and political divisions or to strengthen the institutions of our democracy. Perhaps it’s getting involved with efforts to mitigate climate change. Maybe it’s reaching out to the homeless or hungry in your own community or mentoring a child who is being left behind by the demands of remote learning.
Or perhaps what you embrace is even closer to home: maybe it’s working to eliminate health disparities in your institution or health system, or figuring out how to use technology and resources differently to improve how care is being delivered during or after this pandemic. Maybe it’s as simple as re-committing yourself to personally care for every patient you see today with the very best you have to offer, and with patience, compassion, and grace.
Find something that sets your heart on fire. Something that makes you want to take this difficult time and “transmute tribulation into strength and glory.” Something that, when you look back on these days, will make you thankful that you didn’t just hunker down and subsist through them. Instead, you accomplished great things; you learned; you contributed; and you grew stronger and better.
That’s victorious endurance.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey. This essay was published initially on The Hospital Leader, the official blog of SHM.
I’ve been thinking a lot about endurance recently.
COVID-19 is surging in the United States. Health care workers exhausted from the first and second waves are quickly reaching the verge of collapse. I’m seeing more and more heartbreaking articles about the bone-deep fatigue, fear, and frustration health care workers are facing, and I weep. As horrible as it is to be fighting this terrifying, little-understood, invisible virus, health care workers are also fighting an equally distressing war against misinformation, recklessness, apathy, and outright denial.
As if that wasn’t enough, we are also dealing with racial and social unrest not seen in decades. The most significant cultural divisions and political animosity perhaps since the Civil War. A contested election. The fraying of our democratic institutions and our standing in the global community. The weakest economy since the Great Depression. Record unemployment. Many individuals and families facing or already experiencing eviction and food insecurity. Record-setting fires, hurricanes, and other natural disasters that are only projected to intensify due to climate change.
That’s a lot to endure. And we don’t have much choice other than to live through it. Some of us will break under the strain; others will disengage by giving up clinical work or even leaving health care altogether. Some of us will pack it in and retire, walk away from relationships with family members or longtime friends, or even emigrate to another country (New Zealand, anyone?). Some of us will passively hunker down, letting the challenges of this time overwhelm us and just hoping we can hang on long enough to emerge, albeit beaten and scarred, on the other side.
But some of us will experience victorious endurance – the kind that doesn’t just accept suffering but finds a way to triumph over it. I came across the concept of victorious endurance in the Bible, but its origin is earlier, from classical Greece. It comes from the ancient Greek word hupomone, which literally means “abiding under” – as in disciplining oneself to bear up under a trial when one would more naturally rebel, or just give up. The ancient Greeks were big on virtues like self-control, long-suffering, and perseverance in the face of seemingly insurmountable difficulties; Odysseus was a poster child for hupomone. I believe the concept of victorious endurance can be applicable for people across many belief systems, philosophies, and ways of life.
The late William Barclay, former professor of divinity and biblical criticism at the University of Glasgow, Scotland, said of hupomone:
It is untranslatable. It does not describe the frame of mind which can sit down with folded hands and bowed head and let a torrent of troubles sweep over it in passive resignation. It describes the ability to bear things in such a triumphant way that it transfigures them. Chrysostom has a great panegyric on this hupomone. He calls it “the root of all goods, the mother of piety, the fruit that never withers, a fortress that is never taken, a harbour that knows no storms” and “the queen of virtues, the foundation of right actions, peace in war, calm in tempest, security in plots.” It is the courageous and triumphant ability to pass the breaking-point and not to break and always to greet the unseen with a cheer. It is the alchemy which transmutes tribulation into strength and glory.
Barclay further noted that “Cicero defines patientia, its Latin equivalent, as: ‘The voluntary and daily suffering of hard and difficult things, for the sake of honour and usefulness.”
In the midst of the most challenging public health emergency of our lifetimes, I am seeing hospitalists – and nurses, respiratory therapists, and countless other health care workers – doing exactly this, every day. I’m so incredibly proud of you all, and thankful beyond words.
I doubt that victorious endurance comes naturally to any of us; it’s something we work at, pursue and nurture. What’s the secret to cultivating victorious endurance in the midst of unimaginable stress? I’m pretty sure there’s no specific formula. I don’t mean to sound like a Pollyanna or to make light of the tumult and turmoil of these times, but here are a few things that, based on my own experiences, may help cultivate this valuable virtue.
Be part of a support network. In the midst of great stress, and especially during this time of social distancing, it’s especially tempting to just hunker down, close in on ourselves, and shut others out – sometimes even our closest friends and loved ones. Maintaining relationships is just too exhausting. But you need people who can come alongside you and offer words of encouragement when you are at your lowest. And there’s nothing that will bring out the best in you like being there to encourage and support someone else. We all need to both receive and to give emotional support at a time like this.
Take the long view. When we’re in the middle of a serious crisis, it seems like the problems we’re facing will last forever. There’s no light at the end of the tunnel, no port in the storm. But even this pandemic won’t last forever. If we can keep in mind the fact that things will eventually get better and that the current situation isn’t permanent, it can help us maintain our perspective and have more patience with the current dysfunction.
Focus on who you want to be in this moment. This is the hardest time most of us have ever lived through, both professionally and personally. But let me throw you a challenge. When you look back on this time from the perspective of five years from now, or maybe ten, how will you want to remember yourself? Who will you want to have been during this time? Looking back, what will make you proud of how you handled this challenge? Be that person.
Look for things to be thankful for. In the midst of the chaos that is our lives and our work right now, I believe we can still occasionally see moments of grace if we keep our eyes open for them. If we aren’t looking for them, we may miss them entirely. And those small moments of love, touches of compassion, displays of selflessness, and even flashes of victorious endurance in yourself or others are gifts to be treasured and held on to – to give thanks for.
Embrace a cause greater than yourself. May I suggest that one thing that might help our efforts to cultivate the virtue of victorious endurance during difficult times might be to embrace a cause that is bigger than yourself; that is, one that lures you to focus beyond your immediate circumstances? What are you passionate about, outside of your life’s normal routine?
If you don’t have a passion, consider what you might become passionate about, with a little effort. For some of us, like me, this will be our faith in God. For others it may be advocating for an end to racism or for broader social justice issues. Maybe it’s working to overcome our cultural and political divisions or to strengthen the institutions of our democracy. Perhaps it’s getting involved with efforts to mitigate climate change. Maybe it’s reaching out to the homeless or hungry in your own community or mentoring a child who is being left behind by the demands of remote learning.
Or perhaps what you embrace is even closer to home: maybe it’s working to eliminate health disparities in your institution or health system, or figuring out how to use technology and resources differently to improve how care is being delivered during or after this pandemic. Maybe it’s as simple as re-committing yourself to personally care for every patient you see today with the very best you have to offer, and with patience, compassion, and grace.
Find something that sets your heart on fire. Something that makes you want to take this difficult time and “transmute tribulation into strength and glory.” Something that, when you look back on these days, will make you thankful that you didn’t just hunker down and subsist through them. Instead, you accomplished great things; you learned; you contributed; and you grew stronger and better.
That’s victorious endurance.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey. This essay was published initially on The Hospital Leader, the official blog of SHM.
I’ve been thinking a lot about endurance recently.
COVID-19 is surging in the United States. Health care workers exhausted from the first and second waves are quickly reaching the verge of collapse. I’m seeing more and more heartbreaking articles about the bone-deep fatigue, fear, and frustration health care workers are facing, and I weep. As horrible as it is to be fighting this terrifying, little-understood, invisible virus, health care workers are also fighting an equally distressing war against misinformation, recklessness, apathy, and outright denial.
As if that wasn’t enough, we are also dealing with racial and social unrest not seen in decades. The most significant cultural divisions and political animosity perhaps since the Civil War. A contested election. The fraying of our democratic institutions and our standing in the global community. The weakest economy since the Great Depression. Record unemployment. Many individuals and families facing or already experiencing eviction and food insecurity. Record-setting fires, hurricanes, and other natural disasters that are only projected to intensify due to climate change.
That’s a lot to endure. And we don’t have much choice other than to live through it. Some of us will break under the strain; others will disengage by giving up clinical work or even leaving health care altogether. Some of us will pack it in and retire, walk away from relationships with family members or longtime friends, or even emigrate to another country (New Zealand, anyone?). Some of us will passively hunker down, letting the challenges of this time overwhelm us and just hoping we can hang on long enough to emerge, albeit beaten and scarred, on the other side.
But some of us will experience victorious endurance – the kind that doesn’t just accept suffering but finds a way to triumph over it. I came across the concept of victorious endurance in the Bible, but its origin is earlier, from classical Greece. It comes from the ancient Greek word hupomone, which literally means “abiding under” – as in disciplining oneself to bear up under a trial when one would more naturally rebel, or just give up. The ancient Greeks were big on virtues like self-control, long-suffering, and perseverance in the face of seemingly insurmountable difficulties; Odysseus was a poster child for hupomone. I believe the concept of victorious endurance can be applicable for people across many belief systems, philosophies, and ways of life.
The late William Barclay, former professor of divinity and biblical criticism at the University of Glasgow, Scotland, said of hupomone:
It is untranslatable. It does not describe the frame of mind which can sit down with folded hands and bowed head and let a torrent of troubles sweep over it in passive resignation. It describes the ability to bear things in such a triumphant way that it transfigures them. Chrysostom has a great panegyric on this hupomone. He calls it “the root of all goods, the mother of piety, the fruit that never withers, a fortress that is never taken, a harbour that knows no storms” and “the queen of virtues, the foundation of right actions, peace in war, calm in tempest, security in plots.” It is the courageous and triumphant ability to pass the breaking-point and not to break and always to greet the unseen with a cheer. It is the alchemy which transmutes tribulation into strength and glory.
Barclay further noted that “Cicero defines patientia, its Latin equivalent, as: ‘The voluntary and daily suffering of hard and difficult things, for the sake of honour and usefulness.”
In the midst of the most challenging public health emergency of our lifetimes, I am seeing hospitalists – and nurses, respiratory therapists, and countless other health care workers – doing exactly this, every day. I’m so incredibly proud of you all, and thankful beyond words.
I doubt that victorious endurance comes naturally to any of us; it’s something we work at, pursue and nurture. What’s the secret to cultivating victorious endurance in the midst of unimaginable stress? I’m pretty sure there’s no specific formula. I don’t mean to sound like a Pollyanna or to make light of the tumult and turmoil of these times, but here are a few things that, based on my own experiences, may help cultivate this valuable virtue.
Be part of a support network. In the midst of great stress, and especially during this time of social distancing, it’s especially tempting to just hunker down, close in on ourselves, and shut others out – sometimes even our closest friends and loved ones. Maintaining relationships is just too exhausting. But you need people who can come alongside you and offer words of encouragement when you are at your lowest. And there’s nothing that will bring out the best in you like being there to encourage and support someone else. We all need to both receive and to give emotional support at a time like this.
Take the long view. When we’re in the middle of a serious crisis, it seems like the problems we’re facing will last forever. There’s no light at the end of the tunnel, no port in the storm. But even this pandemic won’t last forever. If we can keep in mind the fact that things will eventually get better and that the current situation isn’t permanent, it can help us maintain our perspective and have more patience with the current dysfunction.
Focus on who you want to be in this moment. This is the hardest time most of us have ever lived through, both professionally and personally. But let me throw you a challenge. When you look back on this time from the perspective of five years from now, or maybe ten, how will you want to remember yourself? Who will you want to have been during this time? Looking back, what will make you proud of how you handled this challenge? Be that person.
Look for things to be thankful for. In the midst of the chaos that is our lives and our work right now, I believe we can still occasionally see moments of grace if we keep our eyes open for them. If we aren’t looking for them, we may miss them entirely. And those small moments of love, touches of compassion, displays of selflessness, and even flashes of victorious endurance in yourself or others are gifts to be treasured and held on to – to give thanks for.
Embrace a cause greater than yourself. May I suggest that one thing that might help our efforts to cultivate the virtue of victorious endurance during difficult times might be to embrace a cause that is bigger than yourself; that is, one that lures you to focus beyond your immediate circumstances? What are you passionate about, outside of your life’s normal routine?
If you don’t have a passion, consider what you might become passionate about, with a little effort. For some of us, like me, this will be our faith in God. For others it may be advocating for an end to racism or for broader social justice issues. Maybe it’s working to overcome our cultural and political divisions or to strengthen the institutions of our democracy. Perhaps it’s getting involved with efforts to mitigate climate change. Maybe it’s reaching out to the homeless or hungry in your own community or mentoring a child who is being left behind by the demands of remote learning.
Or perhaps what you embrace is even closer to home: maybe it’s working to eliminate health disparities in your institution or health system, or figuring out how to use technology and resources differently to improve how care is being delivered during or after this pandemic. Maybe it’s as simple as re-committing yourself to personally care for every patient you see today with the very best you have to offer, and with patience, compassion, and grace.
Find something that sets your heart on fire. Something that makes you want to take this difficult time and “transmute tribulation into strength and glory.” Something that, when you look back on these days, will make you thankful that you didn’t just hunker down and subsist through them. Instead, you accomplished great things; you learned; you contributed; and you grew stronger and better.
That’s victorious endurance.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey. This essay was published initially on The Hospital Leader, the official blog of SHM.
When the X-Waiver gets X’ed: Implications for hospitalists
There are two pandemics permeating the United States: COVID-19 and addiction. To date, more than 468,000 people have died from COVID-19 in the U.S. In the 12-month period ending in May 2020, over 80,000 died from a drug related cause – the highest number ever recorded in a year. Many of these deaths involved opioids.
COVID-19 has worsened outcomes for people with addiction. There is less access to treatment, increased isolation, and worsening psychosocial and economic stressors. These factors may drive new, increased, or more risky substance use and return to use for people in recovery. As hospitalists, we have been responders in both COVID-19 and our country’s worsening overdose and addiction crisis.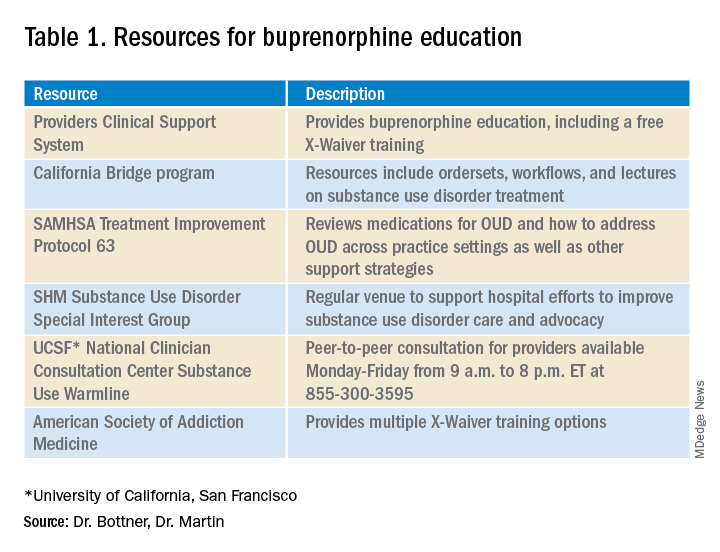
In December 2020’s Journal of Hospital Medicine article “Converging Crises: Caring for hospitalized adults with substance use disorder in the time of COVID-19”, Dr. Honora Englander and her coauthors called on hospitalists to actively engage patients with substance use disorders during hospitalization. The article highlights the colliding crises of addiction and COVID-19 and provides eight practical approaches for hospitalists to address substance use disorders during the pandemic, including initiating buprenorphine for opioid withdrawal and prescribing it for opioid use disorder (OUD) treatment.
Buprenorphine effectively treats opioid withdrawal, reduces OUD-related mortality, and decreases hospital readmissions related to OUD. To prescribe buprenorphine for OUD in the outpatient setting or on hospital discharge, providers need an X-Waiver. The X-Waiver is a result of the Drug Addiction Treatment Act 2000 (DATA 2000), which was enacted in 2000. It permits physicians to prescribe buprenorphine for OUD treatment after an 8-hour training. In 2016, the Comprehensive Addiction and Recovery Act extended buprenorphine prescribing to physician assistants (PAs) and advanced-practice nurses (APNs). However, PAs and APNs are required to complete a 24-hour training to receive the waiver.
On Jan. 14, 2021, the U.S. Department of Health and Human Services under the Trump administration announced it was removing the X-Waiver training previously required for physicians to prescribe this life-saving medication. However, on Jan. 20, 2021, the Biden administration froze the training requirement removal pending a 60-day review. The excitement about the waiver’s eradication further dampened on Jan. 25, when the plan was halted due to procedural factors coupled with the concern that HHS may not have the authority to void requirements mandated by Congress.
Many of us continue to be hopeful that the X-Waiver will soon be gone. The Substance Abuse and Mental Health Services Administration has committed to working with federal agencies to increase access to buprenorphine. The Biden administration also committed to addressing our country’s addiction crisis, including a plan to “make effective prevention, treatment, and recovery services available to all, including through a $125 billion federal investment.”
Despite the pause on HHS’s recent attempt to “X the X-Waiver,” we now have renewed attention and interest in this critical issue and an opportunity for greater and longer-lasting legislative impact. SHM supports that Congress repeal the legislative requirement for buprenorphine training dictated by DATA 2000 so that it cannot be rolled back by future administrations. To further increase access to buprenorphine treatment, the training requirement should be removed for all providers who care for individuals with OUD.
The X-Waiver has been a barrier to hospitalist adoption of this critical, life-saving medication. HHS’s stance to nix the waiver, though fleeting, should be interpreted as an urgent call to the medical community, including us as hospitalists, to learn about buprenorphine with the many resources available (see table 1). As hospital medicine providers, we can order buprenorphine for patients with OUD during hospitalization. It is discharge prescriptions that have been limited to providers with an X-Waiver.
What can we do now to prepare for the eventual X-Waiver training removal? We can start by educating ourselves with the resources listed in table 1. Those of us who are already buprenorphine champions could lead trainings in our home institutions. In a future without the waiver there will be more flexibility to develop hospitalist-focused buprenorphine trainings, as the previous ones were geared for outpatient providers. Hospitalist organizations could support hospitalist-specific buprenorphine trainings and extend the models to include additional medications for addiction.
There is a large body of evidence regarding buprenorphine’s safety and efficacy in OUD treatment. With a worsening overdose crisis, there have been increasing opioid-related hospitalizations. When new medications for diabetes, hypertension, or DVT treatment become available, as hospitalists we incorporate them into our toolbox. As buprenorphine becomes more accessible, we can be leaders in further adopting it (and other substance use disorder medications while we are at it) as our standard of care for people with OUD.
Dr. Bottner is a physician assistant in the Division of Hospital Medicine at Dell Medical School at The University of Texas at Austin and director of the hospital’s Buprenorphine Team. Dr. Martin is a board-certified addiction medicine physician and hospitalist at University of California, San Francisco, and director of the Addiction Care Team at San Francisco General Hospital. Dr. Bottner and Dr. Martin colead the SHM Substance Use Disorder Special Interest Group.
There are two pandemics permeating the United States: COVID-19 and addiction. To date, more than 468,000 people have died from COVID-19 in the U.S. In the 12-month period ending in May 2020, over 80,000 died from a drug related cause – the highest number ever recorded in a year. Many of these deaths involved opioids.
COVID-19 has worsened outcomes for people with addiction. There is less access to treatment, increased isolation, and worsening psychosocial and economic stressors. These factors may drive new, increased, or more risky substance use and return to use for people in recovery. As hospitalists, we have been responders in both COVID-19 and our country’s worsening overdose and addiction crisis.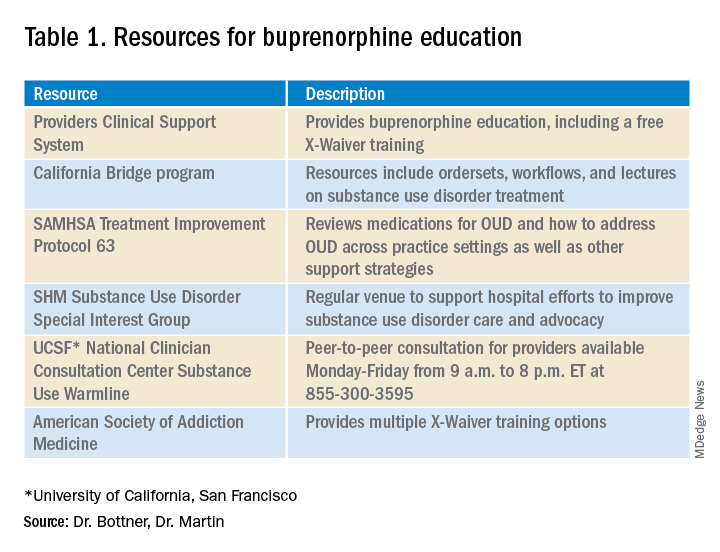
In December 2020’s Journal of Hospital Medicine article “Converging Crises: Caring for hospitalized adults with substance use disorder in the time of COVID-19”, Dr. Honora Englander and her coauthors called on hospitalists to actively engage patients with substance use disorders during hospitalization. The article highlights the colliding crises of addiction and COVID-19 and provides eight practical approaches for hospitalists to address substance use disorders during the pandemic, including initiating buprenorphine for opioid withdrawal and prescribing it for opioid use disorder (OUD) treatment.
Buprenorphine effectively treats opioid withdrawal, reduces OUD-related mortality, and decreases hospital readmissions related to OUD. To prescribe buprenorphine for OUD in the outpatient setting or on hospital discharge, providers need an X-Waiver. The X-Waiver is a result of the Drug Addiction Treatment Act 2000 (DATA 2000), which was enacted in 2000. It permits physicians to prescribe buprenorphine for OUD treatment after an 8-hour training. In 2016, the Comprehensive Addiction and Recovery Act extended buprenorphine prescribing to physician assistants (PAs) and advanced-practice nurses (APNs). However, PAs and APNs are required to complete a 24-hour training to receive the waiver.
On Jan. 14, 2021, the U.S. Department of Health and Human Services under the Trump administration announced it was removing the X-Waiver training previously required for physicians to prescribe this life-saving medication. However, on Jan. 20, 2021, the Biden administration froze the training requirement removal pending a 60-day review. The excitement about the waiver’s eradication further dampened on Jan. 25, when the plan was halted due to procedural factors coupled with the concern that HHS may not have the authority to void requirements mandated by Congress.
Many of us continue to be hopeful that the X-Waiver will soon be gone. The Substance Abuse and Mental Health Services Administration has committed to working with federal agencies to increase access to buprenorphine. The Biden administration also committed to addressing our country’s addiction crisis, including a plan to “make effective prevention, treatment, and recovery services available to all, including through a $125 billion federal investment.”
Despite the pause on HHS’s recent attempt to “X the X-Waiver,” we now have renewed attention and interest in this critical issue and an opportunity for greater and longer-lasting legislative impact. SHM supports that Congress repeal the legislative requirement for buprenorphine training dictated by DATA 2000 so that it cannot be rolled back by future administrations. To further increase access to buprenorphine treatment, the training requirement should be removed for all providers who care for individuals with OUD.
The X-Waiver has been a barrier to hospitalist adoption of this critical, life-saving medication. HHS’s stance to nix the waiver, though fleeting, should be interpreted as an urgent call to the medical community, including us as hospitalists, to learn about buprenorphine with the many resources available (see table 1). As hospital medicine providers, we can order buprenorphine for patients with OUD during hospitalization. It is discharge prescriptions that have been limited to providers with an X-Waiver.
What can we do now to prepare for the eventual X-Waiver training removal? We can start by educating ourselves with the resources listed in table 1. Those of us who are already buprenorphine champions could lead trainings in our home institutions. In a future without the waiver there will be more flexibility to develop hospitalist-focused buprenorphine trainings, as the previous ones were geared for outpatient providers. Hospitalist organizations could support hospitalist-specific buprenorphine trainings and extend the models to include additional medications for addiction.
There is a large body of evidence regarding buprenorphine’s safety and efficacy in OUD treatment. With a worsening overdose crisis, there have been increasing opioid-related hospitalizations. When new medications for diabetes, hypertension, or DVT treatment become available, as hospitalists we incorporate them into our toolbox. As buprenorphine becomes more accessible, we can be leaders in further adopting it (and other substance use disorder medications while we are at it) as our standard of care for people with OUD.
Dr. Bottner is a physician assistant in the Division of Hospital Medicine at Dell Medical School at The University of Texas at Austin and director of the hospital’s Buprenorphine Team. Dr. Martin is a board-certified addiction medicine physician and hospitalist at University of California, San Francisco, and director of the Addiction Care Team at San Francisco General Hospital. Dr. Bottner and Dr. Martin colead the SHM Substance Use Disorder Special Interest Group.
There are two pandemics permeating the United States: COVID-19 and addiction. To date, more than 468,000 people have died from COVID-19 in the U.S. In the 12-month period ending in May 2020, over 80,000 died from a drug related cause – the highest number ever recorded in a year. Many of these deaths involved opioids.
COVID-19 has worsened outcomes for people with addiction. There is less access to treatment, increased isolation, and worsening psychosocial and economic stressors. These factors may drive new, increased, or more risky substance use and return to use for people in recovery. As hospitalists, we have been responders in both COVID-19 and our country’s worsening overdose and addiction crisis.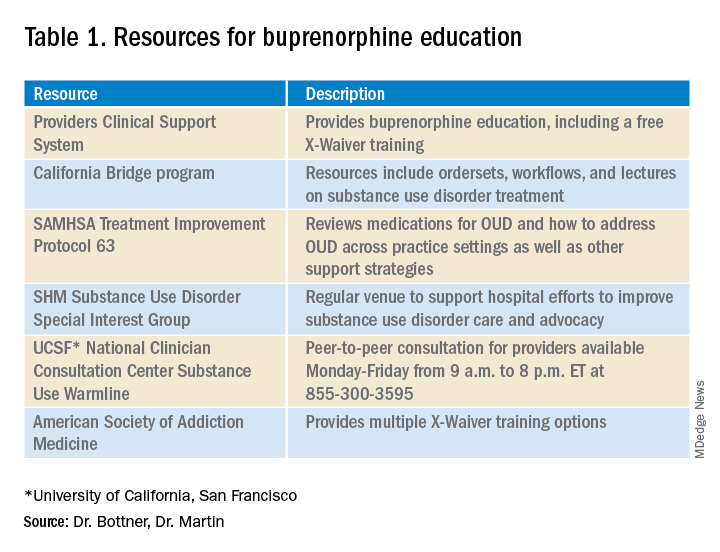
In December 2020’s Journal of Hospital Medicine article “Converging Crises: Caring for hospitalized adults with substance use disorder in the time of COVID-19”, Dr. Honora Englander and her coauthors called on hospitalists to actively engage patients with substance use disorders during hospitalization. The article highlights the colliding crises of addiction and COVID-19 and provides eight practical approaches for hospitalists to address substance use disorders during the pandemic, including initiating buprenorphine for opioid withdrawal and prescribing it for opioid use disorder (OUD) treatment.
Buprenorphine effectively treats opioid withdrawal, reduces OUD-related mortality, and decreases hospital readmissions related to OUD. To prescribe buprenorphine for OUD in the outpatient setting or on hospital discharge, providers need an X-Waiver. The X-Waiver is a result of the Drug Addiction Treatment Act 2000 (DATA 2000), which was enacted in 2000. It permits physicians to prescribe buprenorphine for OUD treatment after an 8-hour training. In 2016, the Comprehensive Addiction and Recovery Act extended buprenorphine prescribing to physician assistants (PAs) and advanced-practice nurses (APNs). However, PAs and APNs are required to complete a 24-hour training to receive the waiver.
On Jan. 14, 2021, the U.S. Department of Health and Human Services under the Trump administration announced it was removing the X-Waiver training previously required for physicians to prescribe this life-saving medication. However, on Jan. 20, 2021, the Biden administration froze the training requirement removal pending a 60-day review. The excitement about the waiver’s eradication further dampened on Jan. 25, when the plan was halted due to procedural factors coupled with the concern that HHS may not have the authority to void requirements mandated by Congress.
Many of us continue to be hopeful that the X-Waiver will soon be gone. The Substance Abuse and Mental Health Services Administration has committed to working with federal agencies to increase access to buprenorphine. The Biden administration also committed to addressing our country’s addiction crisis, including a plan to “make effective prevention, treatment, and recovery services available to all, including through a $125 billion federal investment.”
Despite the pause on HHS’s recent attempt to “X the X-Waiver,” we now have renewed attention and interest in this critical issue and an opportunity for greater and longer-lasting legislative impact. SHM supports that Congress repeal the legislative requirement for buprenorphine training dictated by DATA 2000 so that it cannot be rolled back by future administrations. To further increase access to buprenorphine treatment, the training requirement should be removed for all providers who care for individuals with OUD.
The X-Waiver has been a barrier to hospitalist adoption of this critical, life-saving medication. HHS’s stance to nix the waiver, though fleeting, should be interpreted as an urgent call to the medical community, including us as hospitalists, to learn about buprenorphine with the many resources available (see table 1). As hospital medicine providers, we can order buprenorphine for patients with OUD during hospitalization. It is discharge prescriptions that have been limited to providers with an X-Waiver.
What can we do now to prepare for the eventual X-Waiver training removal? We can start by educating ourselves with the resources listed in table 1. Those of us who are already buprenorphine champions could lead trainings in our home institutions. In a future without the waiver there will be more flexibility to develop hospitalist-focused buprenorphine trainings, as the previous ones were geared for outpatient providers. Hospitalist organizations could support hospitalist-specific buprenorphine trainings and extend the models to include additional medications for addiction.
There is a large body of evidence regarding buprenorphine’s safety and efficacy in OUD treatment. With a worsening overdose crisis, there have been increasing opioid-related hospitalizations. When new medications for diabetes, hypertension, or DVT treatment become available, as hospitalists we incorporate them into our toolbox. As buprenorphine becomes more accessible, we can be leaders in further adopting it (and other substance use disorder medications while we are at it) as our standard of care for people with OUD.
Dr. Bottner is a physician assistant in the Division of Hospital Medicine at Dell Medical School at The University of Texas at Austin and director of the hospital’s Buprenorphine Team. Dr. Martin is a board-certified addiction medicine physician and hospitalist at University of California, San Francisco, and director of the Addiction Care Team at San Francisco General Hospital. Dr. Bottner and Dr. Martin colead the SHM Substance Use Disorder Special Interest Group.
New child COVID-19 cases decline as total passes 3 million
New COVID-19 cases in children continue to drop each week, but the total number of cases has now surpassed 3 million since the start of the pandemic, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.

It was still enough, though, to bring the total to 3.03 million children infected with SARS-CoV-19 in the United States, the AAP and the CHA said in their weekly report.
The nation also hit a couple of other ignominious milestones. The cumulative rate of COVID-19 infection now stands at 4,030 per 100,000, so 4% of all children have been infected. Also, children represented 16.9% of all new cases for the week, which equals the highest proportion seen throughout the pandemic, based on data from health departments in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
There have been 241 COVID-19–related deaths in children so far, with 14 reported during the week of Feb. 5-11. Kansas just recorded its first pediatric death, which leaves 10 states that have had no fatalities. Texas, with 39 deaths, has had more than any other state, among the 43 that are reporting mortality by age, the AAP/CHA report showed.
New COVID-19 cases in children continue to drop each week, but the total number of cases has now surpassed 3 million since the start of the pandemic, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.

It was still enough, though, to bring the total to 3.03 million children infected with SARS-CoV-19 in the United States, the AAP and the CHA said in their weekly report.
The nation also hit a couple of other ignominious milestones. The cumulative rate of COVID-19 infection now stands at 4,030 per 100,000, so 4% of all children have been infected. Also, children represented 16.9% of all new cases for the week, which equals the highest proportion seen throughout the pandemic, based on data from health departments in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
There have been 241 COVID-19–related deaths in children so far, with 14 reported during the week of Feb. 5-11. Kansas just recorded its first pediatric death, which leaves 10 states that have had no fatalities. Texas, with 39 deaths, has had more than any other state, among the 43 that are reporting mortality by age, the AAP/CHA report showed.
New COVID-19 cases in children continue to drop each week, but the total number of cases has now surpassed 3 million since the start of the pandemic, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.

It was still enough, though, to bring the total to 3.03 million children infected with SARS-CoV-19 in the United States, the AAP and the CHA said in their weekly report.
The nation also hit a couple of other ignominious milestones. The cumulative rate of COVID-19 infection now stands at 4,030 per 100,000, so 4% of all children have been infected. Also, children represented 16.9% of all new cases for the week, which equals the highest proportion seen throughout the pandemic, based on data from health departments in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
There have been 241 COVID-19–related deaths in children so far, with 14 reported during the week of Feb. 5-11. Kansas just recorded its first pediatric death, which leaves 10 states that have had no fatalities. Texas, with 39 deaths, has had more than any other state, among the 43 that are reporting mortality by age, the AAP/CHA report showed.
FDA expands sacubitril/valsartan indication to embrace some HFpEF
The Food and Drug Administration has approved a groundbreaking expanded indication for sacubitril/valsartan (Entresto), making it the first drug in the United States indicated for chronic heart failure not specifically characterized by ejection fraction.
The new labeling, as provided by Novartis, grants physicians a good deal of discretion in prescribing sacubitril/valsartan for patients with HF beyond those with HF and reduced ejection fraction (HFrEF), for which the drug was approved in 2015 primarily on the basis of the PARADIGM-HF trial.
The indication now reads, “to reduce the risk of cardiovascular death and hospitalization for heart failure in adult patients with chronic heart failure. Benefits are most clearly evident in patients with left ventricular ejection fraction (LVEF) below normal.”
Of note, the labeling cautions that “LVEF is a variable measure, so use clinical judgment in deciding whom to treat.”
The expanded indication essentially extends the sacubitril/valsartan option to many patients with HF and preserved LVEF (HFpEF), who in practice are most likely to have an LVEF in the range adjacent to “reduced,” long defined as “preserved” but lately categorized as “mid-range.”
But the FDA did not get so specific. In granting the expanded indication, which Novartis announced Feb. 16 in a press release, the agency accommodated the Dec. 15 majority recommendation of its Cardiovascular and Renal Drugs Advisory Committee that the PARAGON-HF trial “provided sufficient evidence to support” an indication beyond HFrEF.
The nature of the PARAGON-HF trial, along with detailed discussion among committee members after their vote tally, made it clear that the 12-to-1 majority favored an indication that would include clinically appropriate patients with “below normal” LVEF.
PARAGON-HF had assigned more than 4,800 patients whose LVEF was 45% or higher and were in NYHA class 2-4 to receive sacubitril/valsartan or valsartan only. Those taking the combo drug showed a 13% drop in risk for HF hospitalization or cardiovascular deaths over an average of 3 years, which narrowly missed significance (P = .059).
But a subgroup analysis garnered attention for its hint of benefit for patients with “mid-range” LVEF, in this case, below the median of 57%. The finding was supported by a later PARAGON-HF and PARADIGM-HF meta-analysis that pointed to a significant benefit for patients with HFpEF at its lowest LVEF levels, especially in women.
The expanded approval “is a significant advancement, providing a treatment to many patients who were not eligible for treatment before, because their ejection fraction was above the region we normally considered reduced,” Scott Solomon, MD, of Brigham and Women’s Hospital, Boston, said in the Novartis press release. “We can now offer a treatment to a wider range of patients who have an LVEF below normal,” added Dr. Solomon, PARAGON-HF executive committee cochair.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a groundbreaking expanded indication for sacubitril/valsartan (Entresto), making it the first drug in the United States indicated for chronic heart failure not specifically characterized by ejection fraction.
The new labeling, as provided by Novartis, grants physicians a good deal of discretion in prescribing sacubitril/valsartan for patients with HF beyond those with HF and reduced ejection fraction (HFrEF), for which the drug was approved in 2015 primarily on the basis of the PARADIGM-HF trial.
The indication now reads, “to reduce the risk of cardiovascular death and hospitalization for heart failure in adult patients with chronic heart failure. Benefits are most clearly evident in patients with left ventricular ejection fraction (LVEF) below normal.”
Of note, the labeling cautions that “LVEF is a variable measure, so use clinical judgment in deciding whom to treat.”
The expanded indication essentially extends the sacubitril/valsartan option to many patients with HF and preserved LVEF (HFpEF), who in practice are most likely to have an LVEF in the range adjacent to “reduced,” long defined as “preserved” but lately categorized as “mid-range.”
But the FDA did not get so specific. In granting the expanded indication, which Novartis announced Feb. 16 in a press release, the agency accommodated the Dec. 15 majority recommendation of its Cardiovascular and Renal Drugs Advisory Committee that the PARAGON-HF trial “provided sufficient evidence to support” an indication beyond HFrEF.
The nature of the PARAGON-HF trial, along with detailed discussion among committee members after their vote tally, made it clear that the 12-to-1 majority favored an indication that would include clinically appropriate patients with “below normal” LVEF.
PARAGON-HF had assigned more than 4,800 patients whose LVEF was 45% or higher and were in NYHA class 2-4 to receive sacubitril/valsartan or valsartan only. Those taking the combo drug showed a 13% drop in risk for HF hospitalization or cardiovascular deaths over an average of 3 years, which narrowly missed significance (P = .059).
But a subgroup analysis garnered attention for its hint of benefit for patients with “mid-range” LVEF, in this case, below the median of 57%. The finding was supported by a later PARAGON-HF and PARADIGM-HF meta-analysis that pointed to a significant benefit for patients with HFpEF at its lowest LVEF levels, especially in women.
The expanded approval “is a significant advancement, providing a treatment to many patients who were not eligible for treatment before, because their ejection fraction was above the region we normally considered reduced,” Scott Solomon, MD, of Brigham and Women’s Hospital, Boston, said in the Novartis press release. “We can now offer a treatment to a wider range of patients who have an LVEF below normal,” added Dr. Solomon, PARAGON-HF executive committee cochair.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a groundbreaking expanded indication for sacubitril/valsartan (Entresto), making it the first drug in the United States indicated for chronic heart failure not specifically characterized by ejection fraction.
The new labeling, as provided by Novartis, grants physicians a good deal of discretion in prescribing sacubitril/valsartan for patients with HF beyond those with HF and reduced ejection fraction (HFrEF), for which the drug was approved in 2015 primarily on the basis of the PARADIGM-HF trial.
The indication now reads, “to reduce the risk of cardiovascular death and hospitalization for heart failure in adult patients with chronic heart failure. Benefits are most clearly evident in patients with left ventricular ejection fraction (LVEF) below normal.”
Of note, the labeling cautions that “LVEF is a variable measure, so use clinical judgment in deciding whom to treat.”
The expanded indication essentially extends the sacubitril/valsartan option to many patients with HF and preserved LVEF (HFpEF), who in practice are most likely to have an LVEF in the range adjacent to “reduced,” long defined as “preserved” but lately categorized as “mid-range.”
But the FDA did not get so specific. In granting the expanded indication, which Novartis announced Feb. 16 in a press release, the agency accommodated the Dec. 15 majority recommendation of its Cardiovascular and Renal Drugs Advisory Committee that the PARAGON-HF trial “provided sufficient evidence to support” an indication beyond HFrEF.
The nature of the PARAGON-HF trial, along with detailed discussion among committee members after their vote tally, made it clear that the 12-to-1 majority favored an indication that would include clinically appropriate patients with “below normal” LVEF.
PARAGON-HF had assigned more than 4,800 patients whose LVEF was 45% or higher and were in NYHA class 2-4 to receive sacubitril/valsartan or valsartan only. Those taking the combo drug showed a 13% drop in risk for HF hospitalization or cardiovascular deaths over an average of 3 years, which narrowly missed significance (P = .059).
But a subgroup analysis garnered attention for its hint of benefit for patients with “mid-range” LVEF, in this case, below the median of 57%. The finding was supported by a later PARAGON-HF and PARADIGM-HF meta-analysis that pointed to a significant benefit for patients with HFpEF at its lowest LVEF levels, especially in women.
The expanded approval “is a significant advancement, providing a treatment to many patients who were not eligible for treatment before, because their ejection fraction was above the region we normally considered reduced,” Scott Solomon, MD, of Brigham and Women’s Hospital, Boston, said in the Novartis press release. “We can now offer a treatment to a wider range of patients who have an LVEF below normal,” added Dr. Solomon, PARAGON-HF executive committee cochair.
A version of this article first appeared on Medscape.com.
One-third of health care workers leery of getting COVID-19 vaccine, survey shows
Moreover, 54% of direct care providers indicated that they would take the vaccine if offered, compared with 60% of noncare providers.
The findings come from what is believed to be the largest survey of health care provider attitudes toward COVID-19 vaccination, published online Jan. 25 in Clinical Infectious Diseases.
“We have shown that self-reported willingness to receive vaccination against COVID-19 differs by age, gender, race and hospital role, with physicians and research scientists showing the highest acceptance,” Jana Shaw, MD, MPH, State University of New York, Syracuse, N.Y, the study’s corresponding author, told this news organization. “Building trust in authorities and confidence in vaccines is a complex and time-consuming process that requires commitment and resources. We have to make those investments as hesitancy can severely undermine vaccination coverage. Because health care providers are members of our communities, it is possible that their views are shared by the public at large. Our findings can assist public health professionals as a starting point of discussion and engagement with communities to ensure that we vaccinate at least 80% of the public to end the pandemic.”
For the study, Dr. Shaw and her colleagues emailed an anonymous survey to 9,565 employees of State University of New York Upstate Medical University, Syracuse, an academic medical center that cares for an estimated 1.8 million people. The survey, which contained questions intended to evaluate attitudes, belief, and willingness to get vaccinated, took place between Nov. 23 and Dec. 5, about a week before the U.S. Food and Drug Administration granted the first emergency use authorization for the Pfizer-BioNTech BNT162b2 mRNA vaccine.
Survey recipients included physicians, nurse practitioners, physician assistants, nurses, pharmacists, medical and nursing students, allied health professionals, and nonclinical ancillary staff.
Of the 9,565 surveys sent, 5,287 responses were collected and used in the final analysis, for a response rate of 55%. The mean age of respondents was 43, 73% were female, 85% were White, 6% were Asian, 5% were Black/African American, and the rest were Native American, Native Hawaiian/Pacific Islander, or from other races. More than half of respondents (59%) reported that they provided direct patient care, and 32% said they provided care for patients with COVID-19.
Of all survey respondents, 58% expressed their intent to receive a COVID-19 vaccine, but this varied by their role in the health care system. For example, in response to the statement, “If a vaccine were offered free of charge, I would take it,” 80% of scientists and physicians agreed that they would, while colleagues in other roles were unsure whether they would take the vaccine, including 34% of registered nurses, 32% of allied health professionals, and 32% of master’s-level clinicians. These differences across roles were significant (P less than .001).
The researchers also found that direct patient care or care for COVID-19 patients was associated with lower vaccination intent. For example, 54% of direct care providers and 62% of non-care providers indicated they would take the vaccine if offered, compared with 52% of those who had provided care for COVID-19 patients vs. 61% of those who had not (P less than .001).
“This was a really surprising finding,” said Dr. Shaw, who is a pediatric infectious diseases physician at SUNY Upstate. “In general, one would expect that perceived severity of disease would lead to a greater desire to get vaccinated. Because our question did not address severity of disease, it is possible that we oversampled respondents who took care of patients with mild disease (i.e., in an outpatient setting). This could have led to an underestimation of disease severity and resulted in lower vaccination intent.”
A focus on rebuilding trust
Survey respondents who agreed or strongly agreed that they would accept a vaccine were older (a mean age of 44 years), compared with those who were not sure or who disagreed (a mean age of 42 vs. 38 years, respectively; P less than .001). In addition, fewer females agreed or strongly agreed that they would accept a vaccine (54% vs. 73% of males), whereas those who self-identified as Black/African American were least likely to want to get vaccinated, compared with those from other ethnic groups (31%, compared with 74% of Asians, 58% of Whites, and 39% of American Indians or Alaska Natives).
“We are deeply aware of the poor decisions scientists made in the past, which led to a prevailing skepticism and ‘feeling like guinea pigs’ among people of color, especially Black adults,” Dr. Shaw said. “Black adults are less likely, compared [with] White adults, to have confidence that scientists act in the public interest. Rebuilding trust will take time and has to start with addressing health care disparities. In addition, we need to acknowledge contributions of Black researchers to science. For example, until recently very few knew that the Moderna vaccine was developed [with the help of] Dr. Kizzmekia Corbett, who is Black.”
The top five main areas of unease that all respondents expressed about a COVID-19 vaccine were concern about adverse events/side effects (47%), efficacy (15%), rushed release (11%), safety (11%), and the research and authorization process (3%).
“I think it is important that fellow clinicians recognize that, in order to boost vaccine confidence we will need careful, individually tailored communication strategies,” Dr. Shaw said. “A consideration should be given to those [strategies] that utilize interpersonal channels that deliver leadership by example and leverage influencers in the institution to encourage wider adoption of vaccination.”
Aaron M. Milstone, MD, MHS, asked to comment on the research, recommended that health care workers advocate for the vaccine and encourage their patients, friends, and loved ones to get vaccinated. “Soon, COVID-19 will have taken more than half a million lives in the U.S.,” said Dr. Milstone, a pediatric epidemiologist at Johns Hopkins University, Baltimore. “Although vaccines can have side effects like fever and muscle aches, and very, very rare more serious side effects, the risks of dying from COVID are much greater than the risk of a serious vaccine reaction. The study’s authors shed light on the ongoing need for leaders of all communities to support the COVID vaccines, not just the scientific community, but religious leaders, political leaders, and community leaders.”
Addressing vaccine hesitancy
Informed by their own survey, Dr. Shaw and her colleagues have developed a plan to address vaccine hesitancy to ensure high vaccine uptake at SUNY Upstate. Those strategies include, but aren’t limited to, institution-wide forums for all employees on COVID-19 vaccine safety, risks, and benefits followed by Q&A sessions, grand rounds for providers summarizing clinical trial data on mRNA vaccines, development of an Ask COVID email line for staff to ask vaccine-related questions, and a detailed vaccine-specific FAQ document.
In addition, SUNY Upstate experts have engaged in numerous media interviews to provide education and updates on the benefits of vaccination to public and staff, stationary vaccine locations, and mobile COVID-19 vaccine carts. “To date, the COVID-19 vaccination process has been well received, and we anticipate strong vaccine uptake,” she said.
Dr. Shaw acknowledged certain limitations of the survey, including its cross-sectional design and the fact that it was conducted in a single health care system in the northeastern United States. “Thus, generalizability to other regions of the U.S. and other countries may be limited,” Dr. Shaw said. “The study was also conducted before EUA [emergency use authorization] was granted to either the Moderna or Pfizer-BioNTech vaccines. It is therefore likely that vaccine acceptance will change over time as more people get vaccinated.”
The authors have disclosed no relevant financial relationships. Dr. Milstone disclosed that he has received a research grant from Merck, but it is not related to vaccines.
A version of this article first appeared on Medscape.com.
Moreover, 54% of direct care providers indicated that they would take the vaccine if offered, compared with 60% of noncare providers.
The findings come from what is believed to be the largest survey of health care provider attitudes toward COVID-19 vaccination, published online Jan. 25 in Clinical Infectious Diseases.
“We have shown that self-reported willingness to receive vaccination against COVID-19 differs by age, gender, race and hospital role, with physicians and research scientists showing the highest acceptance,” Jana Shaw, MD, MPH, State University of New York, Syracuse, N.Y, the study’s corresponding author, told this news organization. “Building trust in authorities and confidence in vaccines is a complex and time-consuming process that requires commitment and resources. We have to make those investments as hesitancy can severely undermine vaccination coverage. Because health care providers are members of our communities, it is possible that their views are shared by the public at large. Our findings can assist public health professionals as a starting point of discussion and engagement with communities to ensure that we vaccinate at least 80% of the public to end the pandemic.”
For the study, Dr. Shaw and her colleagues emailed an anonymous survey to 9,565 employees of State University of New York Upstate Medical University, Syracuse, an academic medical center that cares for an estimated 1.8 million people. The survey, which contained questions intended to evaluate attitudes, belief, and willingness to get vaccinated, took place between Nov. 23 and Dec. 5, about a week before the U.S. Food and Drug Administration granted the first emergency use authorization for the Pfizer-BioNTech BNT162b2 mRNA vaccine.
Survey recipients included physicians, nurse practitioners, physician assistants, nurses, pharmacists, medical and nursing students, allied health professionals, and nonclinical ancillary staff.
Of the 9,565 surveys sent, 5,287 responses were collected and used in the final analysis, for a response rate of 55%. The mean age of respondents was 43, 73% were female, 85% were White, 6% were Asian, 5% were Black/African American, and the rest were Native American, Native Hawaiian/Pacific Islander, or from other races. More than half of respondents (59%) reported that they provided direct patient care, and 32% said they provided care for patients with COVID-19.
Of all survey respondents, 58% expressed their intent to receive a COVID-19 vaccine, but this varied by their role in the health care system. For example, in response to the statement, “If a vaccine were offered free of charge, I would take it,” 80% of scientists and physicians agreed that they would, while colleagues in other roles were unsure whether they would take the vaccine, including 34% of registered nurses, 32% of allied health professionals, and 32% of master’s-level clinicians. These differences across roles were significant (P less than .001).
The researchers also found that direct patient care or care for COVID-19 patients was associated with lower vaccination intent. For example, 54% of direct care providers and 62% of non-care providers indicated they would take the vaccine if offered, compared with 52% of those who had provided care for COVID-19 patients vs. 61% of those who had not (P less than .001).
“This was a really surprising finding,” said Dr. Shaw, who is a pediatric infectious diseases physician at SUNY Upstate. “In general, one would expect that perceived severity of disease would lead to a greater desire to get vaccinated. Because our question did not address severity of disease, it is possible that we oversampled respondents who took care of patients with mild disease (i.e., in an outpatient setting). This could have led to an underestimation of disease severity and resulted in lower vaccination intent.”
A focus on rebuilding trust
Survey respondents who agreed or strongly agreed that they would accept a vaccine were older (a mean age of 44 years), compared with those who were not sure or who disagreed (a mean age of 42 vs. 38 years, respectively; P less than .001). In addition, fewer females agreed or strongly agreed that they would accept a vaccine (54% vs. 73% of males), whereas those who self-identified as Black/African American were least likely to want to get vaccinated, compared with those from other ethnic groups (31%, compared with 74% of Asians, 58% of Whites, and 39% of American Indians or Alaska Natives).
“We are deeply aware of the poor decisions scientists made in the past, which led to a prevailing skepticism and ‘feeling like guinea pigs’ among people of color, especially Black adults,” Dr. Shaw said. “Black adults are less likely, compared [with] White adults, to have confidence that scientists act in the public interest. Rebuilding trust will take time and has to start with addressing health care disparities. In addition, we need to acknowledge contributions of Black researchers to science. For example, until recently very few knew that the Moderna vaccine was developed [with the help of] Dr. Kizzmekia Corbett, who is Black.”
The top five main areas of unease that all respondents expressed about a COVID-19 vaccine were concern about adverse events/side effects (47%), efficacy (15%), rushed release (11%), safety (11%), and the research and authorization process (3%).
“I think it is important that fellow clinicians recognize that, in order to boost vaccine confidence we will need careful, individually tailored communication strategies,” Dr. Shaw said. “A consideration should be given to those [strategies] that utilize interpersonal channels that deliver leadership by example and leverage influencers in the institution to encourage wider adoption of vaccination.”
Aaron M. Milstone, MD, MHS, asked to comment on the research, recommended that health care workers advocate for the vaccine and encourage their patients, friends, and loved ones to get vaccinated. “Soon, COVID-19 will have taken more than half a million lives in the U.S.,” said Dr. Milstone, a pediatric epidemiologist at Johns Hopkins University, Baltimore. “Although vaccines can have side effects like fever and muscle aches, and very, very rare more serious side effects, the risks of dying from COVID are much greater than the risk of a serious vaccine reaction. The study’s authors shed light on the ongoing need for leaders of all communities to support the COVID vaccines, not just the scientific community, but religious leaders, political leaders, and community leaders.”
Addressing vaccine hesitancy
Informed by their own survey, Dr. Shaw and her colleagues have developed a plan to address vaccine hesitancy to ensure high vaccine uptake at SUNY Upstate. Those strategies include, but aren’t limited to, institution-wide forums for all employees on COVID-19 vaccine safety, risks, and benefits followed by Q&A sessions, grand rounds for providers summarizing clinical trial data on mRNA vaccines, development of an Ask COVID email line for staff to ask vaccine-related questions, and a detailed vaccine-specific FAQ document.
In addition, SUNY Upstate experts have engaged in numerous media interviews to provide education and updates on the benefits of vaccination to public and staff, stationary vaccine locations, and mobile COVID-19 vaccine carts. “To date, the COVID-19 vaccination process has been well received, and we anticipate strong vaccine uptake,” she said.
Dr. Shaw acknowledged certain limitations of the survey, including its cross-sectional design and the fact that it was conducted in a single health care system in the northeastern United States. “Thus, generalizability to other regions of the U.S. and other countries may be limited,” Dr. Shaw said. “The study was also conducted before EUA [emergency use authorization] was granted to either the Moderna or Pfizer-BioNTech vaccines. It is therefore likely that vaccine acceptance will change over time as more people get vaccinated.”
The authors have disclosed no relevant financial relationships. Dr. Milstone disclosed that he has received a research grant from Merck, but it is not related to vaccines.
A version of this article first appeared on Medscape.com.
Moreover, 54% of direct care providers indicated that they would take the vaccine if offered, compared with 60% of noncare providers.
The findings come from what is believed to be the largest survey of health care provider attitudes toward COVID-19 vaccination, published online Jan. 25 in Clinical Infectious Diseases.
“We have shown that self-reported willingness to receive vaccination against COVID-19 differs by age, gender, race and hospital role, with physicians and research scientists showing the highest acceptance,” Jana Shaw, MD, MPH, State University of New York, Syracuse, N.Y, the study’s corresponding author, told this news organization. “Building trust in authorities and confidence in vaccines is a complex and time-consuming process that requires commitment and resources. We have to make those investments as hesitancy can severely undermine vaccination coverage. Because health care providers are members of our communities, it is possible that their views are shared by the public at large. Our findings can assist public health professionals as a starting point of discussion and engagement with communities to ensure that we vaccinate at least 80% of the public to end the pandemic.”
For the study, Dr. Shaw and her colleagues emailed an anonymous survey to 9,565 employees of State University of New York Upstate Medical University, Syracuse, an academic medical center that cares for an estimated 1.8 million people. The survey, which contained questions intended to evaluate attitudes, belief, and willingness to get vaccinated, took place between Nov. 23 and Dec. 5, about a week before the U.S. Food and Drug Administration granted the first emergency use authorization for the Pfizer-BioNTech BNT162b2 mRNA vaccine.
Survey recipients included physicians, nurse practitioners, physician assistants, nurses, pharmacists, medical and nursing students, allied health professionals, and nonclinical ancillary staff.
Of the 9,565 surveys sent, 5,287 responses were collected and used in the final analysis, for a response rate of 55%. The mean age of respondents was 43, 73% were female, 85% were White, 6% were Asian, 5% were Black/African American, and the rest were Native American, Native Hawaiian/Pacific Islander, or from other races. More than half of respondents (59%) reported that they provided direct patient care, and 32% said they provided care for patients with COVID-19.
Of all survey respondents, 58% expressed their intent to receive a COVID-19 vaccine, but this varied by their role in the health care system. For example, in response to the statement, “If a vaccine were offered free of charge, I would take it,” 80% of scientists and physicians agreed that they would, while colleagues in other roles were unsure whether they would take the vaccine, including 34% of registered nurses, 32% of allied health professionals, and 32% of master’s-level clinicians. These differences across roles were significant (P less than .001).
The researchers also found that direct patient care or care for COVID-19 patients was associated with lower vaccination intent. For example, 54% of direct care providers and 62% of non-care providers indicated they would take the vaccine if offered, compared with 52% of those who had provided care for COVID-19 patients vs. 61% of those who had not (P less than .001).
“This was a really surprising finding,” said Dr. Shaw, who is a pediatric infectious diseases physician at SUNY Upstate. “In general, one would expect that perceived severity of disease would lead to a greater desire to get vaccinated. Because our question did not address severity of disease, it is possible that we oversampled respondents who took care of patients with mild disease (i.e., in an outpatient setting). This could have led to an underestimation of disease severity and resulted in lower vaccination intent.”
A focus on rebuilding trust
Survey respondents who agreed or strongly agreed that they would accept a vaccine were older (a mean age of 44 years), compared with those who were not sure or who disagreed (a mean age of 42 vs. 38 years, respectively; P less than .001). In addition, fewer females agreed or strongly agreed that they would accept a vaccine (54% vs. 73% of males), whereas those who self-identified as Black/African American were least likely to want to get vaccinated, compared with those from other ethnic groups (31%, compared with 74% of Asians, 58% of Whites, and 39% of American Indians or Alaska Natives).
“We are deeply aware of the poor decisions scientists made in the past, which led to a prevailing skepticism and ‘feeling like guinea pigs’ among people of color, especially Black adults,” Dr. Shaw said. “Black adults are less likely, compared [with] White adults, to have confidence that scientists act in the public interest. Rebuilding trust will take time and has to start with addressing health care disparities. In addition, we need to acknowledge contributions of Black researchers to science. For example, until recently very few knew that the Moderna vaccine was developed [with the help of] Dr. Kizzmekia Corbett, who is Black.”
The top five main areas of unease that all respondents expressed about a COVID-19 vaccine were concern about adverse events/side effects (47%), efficacy (15%), rushed release (11%), safety (11%), and the research and authorization process (3%).
“I think it is important that fellow clinicians recognize that, in order to boost vaccine confidence we will need careful, individually tailored communication strategies,” Dr. Shaw said. “A consideration should be given to those [strategies] that utilize interpersonal channels that deliver leadership by example and leverage influencers in the institution to encourage wider adoption of vaccination.”
Aaron M. Milstone, MD, MHS, asked to comment on the research, recommended that health care workers advocate for the vaccine and encourage their patients, friends, and loved ones to get vaccinated. “Soon, COVID-19 will have taken more than half a million lives in the U.S.,” said Dr. Milstone, a pediatric epidemiologist at Johns Hopkins University, Baltimore. “Although vaccines can have side effects like fever and muscle aches, and very, very rare more serious side effects, the risks of dying from COVID are much greater than the risk of a serious vaccine reaction. The study’s authors shed light on the ongoing need for leaders of all communities to support the COVID vaccines, not just the scientific community, but religious leaders, political leaders, and community leaders.”
Addressing vaccine hesitancy
Informed by their own survey, Dr. Shaw and her colleagues have developed a plan to address vaccine hesitancy to ensure high vaccine uptake at SUNY Upstate. Those strategies include, but aren’t limited to, institution-wide forums for all employees on COVID-19 vaccine safety, risks, and benefits followed by Q&A sessions, grand rounds for providers summarizing clinical trial data on mRNA vaccines, development of an Ask COVID email line for staff to ask vaccine-related questions, and a detailed vaccine-specific FAQ document.
In addition, SUNY Upstate experts have engaged in numerous media interviews to provide education and updates on the benefits of vaccination to public and staff, stationary vaccine locations, and mobile COVID-19 vaccine carts. “To date, the COVID-19 vaccination process has been well received, and we anticipate strong vaccine uptake,” she said.
Dr. Shaw acknowledged certain limitations of the survey, including its cross-sectional design and the fact that it was conducted in a single health care system in the northeastern United States. “Thus, generalizability to other regions of the U.S. and other countries may be limited,” Dr. Shaw said. “The study was also conducted before EUA [emergency use authorization] was granted to either the Moderna or Pfizer-BioNTech vaccines. It is therefore likely that vaccine acceptance will change over time as more people get vaccinated.”
The authors have disclosed no relevant financial relationships. Dr. Milstone disclosed that he has received a research grant from Merck, but it is not related to vaccines.
A version of this article first appeared on Medscape.com.
More Americans hospitalized, readmitted for heart failure
Overall primary HF hospitalization rates per 1,000 adults declined from 4.4 in 2010 to 4.1 in 2013, and then increased from 4.2 in 2014 to 4.9 in 2017.
Rates of unique patient visits for HF were also on the way down – falling from 3.4 in 2010 to 3.2 in 2013 and 2014 – before climbing to 3.8 in 2017.
Similar trends were observed for rates of postdischarge HF readmissions (from 1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (from 0.8 in 2010 to 0.7 in 2014 to 0.9 in 2017).
“We should be emphasizing the things we know work to reduce heart failure hospitalization, which is, No. 1, prevention,” senior author Boback Ziaeian, MD, PhD, said in an interview.
Comorbidities that can lead to heart failure crept up over the study period, such that by 2017, hypertension was present in 91.4% of patients, diabetes in 48.9%, and lipid disorders in 53.1%, up from 76.5%, 44.9%, and 40.4%, respectively, in 2010. Half of all patients had coronary artery disease at both time points. Renal disease shot up from 45.9% to 60.6% by 2017.
“If we did a better job of controlling our known risk factors, we would really cut down on the incidence of heart failure being developed and then, among those estimated 6.6 million heart failure patients, we need to get them on our cornerstone therapies,” said Dr. Ziaeian, of the Veterans Affairts Greater Los Angeles Healthcare System and the University of California, Los Angeles.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors, which have shown clear efficacy and safety in trials like DAPA-HF and EMPEROR-Reduced, provide a “huge opportunity” to add on to standard therapies, he noted. Competition for VA contracts has brought the price down to about $50 a month for veterans, compared with a cash price of about $500-$600 a month.
Yet in routine practice, only 8% of veterans with HF at his center are on an SGLT2 inhibitor, compared with 80% on ACE inhibitors or beta blockers, observed Dr. Ziaeian. “This medication has been indicated for the last year and a half and we’re only at 8% in a system where we have pretty easy access to medications.”
As reported online Feb. 10 in JAMA Cardiology, notable sex differences were found in hospitalization, with higher rates per 1,000 persons among men.
In contrast, a 2020 report on HF trends in the VA system showed a 2% decrease in unadjusted 30-day readmissions from 2007 to 2017 and a decline in the adjusted 30-day readmission risk.
The present study did not risk-adjust readmission risk and included a population that was 51% male, compared with about 98% male in the VA, the investigators noted.
“The increasing hospitalization rate in our study may represent an actual increase in HF hospitalizations or shifts in administrative coding practices, increased use of HF biomarkers, or lower thresholds for diagnosis of HF with preserved ejection fraction,” they wrote.
The analysis was based on data from the Nationwide Readmission Database, which included 35,197,725 hospitalizations with a primary or secondary diagnosis of HF and 8,273,270 primary HF hospitalizations from January 2010 to December 2017.
A single primary HF admission occurred in 5,092,626 unique patients and 1,269,109 had two or more HF hospitalizations. The mean age was 72.1 years.
The administrative database did not include clinical data, so it wasn’t possible to differentiate between HF with preserved or reduced ejection fraction, the authors noted. Patient race and ethnicity data also were not available.
“Future studies are needed to verify our findings to better develop and improve individualized strategies for HF prevention, management, and surveillance for men and women,” the investigators concluded.
One coauthor reporting receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, CHF Solutions, Edwards Lifesciences, Janssen Pharmaceuticals, Medtronic, Merck, and Novartis. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
Overall primary HF hospitalization rates per 1,000 adults declined from 4.4 in 2010 to 4.1 in 2013, and then increased from 4.2 in 2014 to 4.9 in 2017.
Rates of unique patient visits for HF were also on the way down – falling from 3.4 in 2010 to 3.2 in 2013 and 2014 – before climbing to 3.8 in 2017.
Similar trends were observed for rates of postdischarge HF readmissions (from 1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (from 0.8 in 2010 to 0.7 in 2014 to 0.9 in 2017).
“We should be emphasizing the things we know work to reduce heart failure hospitalization, which is, No. 1, prevention,” senior author Boback Ziaeian, MD, PhD, said in an interview.
Comorbidities that can lead to heart failure crept up over the study period, such that by 2017, hypertension was present in 91.4% of patients, diabetes in 48.9%, and lipid disorders in 53.1%, up from 76.5%, 44.9%, and 40.4%, respectively, in 2010. Half of all patients had coronary artery disease at both time points. Renal disease shot up from 45.9% to 60.6% by 2017.
“If we did a better job of controlling our known risk factors, we would really cut down on the incidence of heart failure being developed and then, among those estimated 6.6 million heart failure patients, we need to get them on our cornerstone therapies,” said Dr. Ziaeian, of the Veterans Affairts Greater Los Angeles Healthcare System and the University of California, Los Angeles.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors, which have shown clear efficacy and safety in trials like DAPA-HF and EMPEROR-Reduced, provide a “huge opportunity” to add on to standard therapies, he noted. Competition for VA contracts has brought the price down to about $50 a month for veterans, compared with a cash price of about $500-$600 a month.
Yet in routine practice, only 8% of veterans with HF at his center are on an SGLT2 inhibitor, compared with 80% on ACE inhibitors or beta blockers, observed Dr. Ziaeian. “This medication has been indicated for the last year and a half and we’re only at 8% in a system where we have pretty easy access to medications.”
As reported online Feb. 10 in JAMA Cardiology, notable sex differences were found in hospitalization, with higher rates per 1,000 persons among men.
In contrast, a 2020 report on HF trends in the VA system showed a 2% decrease in unadjusted 30-day readmissions from 2007 to 2017 and a decline in the adjusted 30-day readmission risk.
The present study did not risk-adjust readmission risk and included a population that was 51% male, compared with about 98% male in the VA, the investigators noted.
“The increasing hospitalization rate in our study may represent an actual increase in HF hospitalizations or shifts in administrative coding practices, increased use of HF biomarkers, or lower thresholds for diagnosis of HF with preserved ejection fraction,” they wrote.
The analysis was based on data from the Nationwide Readmission Database, which included 35,197,725 hospitalizations with a primary or secondary diagnosis of HF and 8,273,270 primary HF hospitalizations from January 2010 to December 2017.
A single primary HF admission occurred in 5,092,626 unique patients and 1,269,109 had two or more HF hospitalizations. The mean age was 72.1 years.
The administrative database did not include clinical data, so it wasn’t possible to differentiate between HF with preserved or reduced ejection fraction, the authors noted. Patient race and ethnicity data also were not available.
“Future studies are needed to verify our findings to better develop and improve individualized strategies for HF prevention, management, and surveillance for men and women,” the investigators concluded.
One coauthor reporting receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, CHF Solutions, Edwards Lifesciences, Janssen Pharmaceuticals, Medtronic, Merck, and Novartis. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
Overall primary HF hospitalization rates per 1,000 adults declined from 4.4 in 2010 to 4.1 in 2013, and then increased from 4.2 in 2014 to 4.9 in 2017.
Rates of unique patient visits for HF were also on the way down – falling from 3.4 in 2010 to 3.2 in 2013 and 2014 – before climbing to 3.8 in 2017.
Similar trends were observed for rates of postdischarge HF readmissions (from 1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (from 0.8 in 2010 to 0.7 in 2014 to 0.9 in 2017).
“We should be emphasizing the things we know work to reduce heart failure hospitalization, which is, No. 1, prevention,” senior author Boback Ziaeian, MD, PhD, said in an interview.
Comorbidities that can lead to heart failure crept up over the study period, such that by 2017, hypertension was present in 91.4% of patients, diabetes in 48.9%, and lipid disorders in 53.1%, up from 76.5%, 44.9%, and 40.4%, respectively, in 2010. Half of all patients had coronary artery disease at both time points. Renal disease shot up from 45.9% to 60.6% by 2017.
“If we did a better job of controlling our known risk factors, we would really cut down on the incidence of heart failure being developed and then, among those estimated 6.6 million heart failure patients, we need to get them on our cornerstone therapies,” said Dr. Ziaeian, of the Veterans Affairts Greater Los Angeles Healthcare System and the University of California, Los Angeles.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors, which have shown clear efficacy and safety in trials like DAPA-HF and EMPEROR-Reduced, provide a “huge opportunity” to add on to standard therapies, he noted. Competition for VA contracts has brought the price down to about $50 a month for veterans, compared with a cash price of about $500-$600 a month.
Yet in routine practice, only 8% of veterans with HF at his center are on an SGLT2 inhibitor, compared with 80% on ACE inhibitors or beta blockers, observed Dr. Ziaeian. “This medication has been indicated for the last year and a half and we’re only at 8% in a system where we have pretty easy access to medications.”
As reported online Feb. 10 in JAMA Cardiology, notable sex differences were found in hospitalization, with higher rates per 1,000 persons among men.
In contrast, a 2020 report on HF trends in the VA system showed a 2% decrease in unadjusted 30-day readmissions from 2007 to 2017 and a decline in the adjusted 30-day readmission risk.
The present study did not risk-adjust readmission risk and included a population that was 51% male, compared with about 98% male in the VA, the investigators noted.
“The increasing hospitalization rate in our study may represent an actual increase in HF hospitalizations or shifts in administrative coding practices, increased use of HF biomarkers, or lower thresholds for diagnosis of HF with preserved ejection fraction,” they wrote.
The analysis was based on data from the Nationwide Readmission Database, which included 35,197,725 hospitalizations with a primary or secondary diagnosis of HF and 8,273,270 primary HF hospitalizations from January 2010 to December 2017.
A single primary HF admission occurred in 5,092,626 unique patients and 1,269,109 had two or more HF hospitalizations. The mean age was 72.1 years.
The administrative database did not include clinical data, so it wasn’t possible to differentiate between HF with preserved or reduced ejection fraction, the authors noted. Patient race and ethnicity data also were not available.
“Future studies are needed to verify our findings to better develop and improve individualized strategies for HF prevention, management, and surveillance for men and women,” the investigators concluded.
One coauthor reporting receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, CHF Solutions, Edwards Lifesciences, Janssen Pharmaceuticals, Medtronic, Merck, and Novartis. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
Back in session
Before the pandemic, the biggest parent-related challenge for Charlie Wray, DO, MS, a hospitalist and assistant clinical professor of medicine at the University of California, San Francisco, was “figuring out what I was going to pack in my kids’ lunches. Like most people, we were very much in our groove – we knew when my wife was going to leave work, and which day I’d pick up the kids,” Dr. Wray said. “I reflect back on that and think how easy it was.”
The old life – the one that seems so comparatively effortless – has been gone for close to a year now. And with the reopening of schools in the fall of 2020, hospitalists with school-age kids felt – and are still feeling – the strain in a variety of ways.
‘Podding up’
“The largest struggles that we have had involve dealing with the daily logistics of doing at-home learning,” said Dr. Wray, father to a 6-year-old and a 3-year-old. Dr. Wray and his wife are both physicians and have been juggling full work schedules with virtual school for their older child, who is not old enough to be autonomous. “For parents who have younger children who require one-on-one attention for the vast majority of their learning, that certainly takes more of a toll on your time, energy, and resources.”
Uncertainty has created anxiety about the future. “We have no idea what’s going to be happening next month. How do we plan for that? How do we allocate our time for that? That has been a real struggle for us, especially for a two-physician household where we are both considered front line and are both needing to be at the hospital or the clinic on a fairly regular basis,” he said.
Then there is the never-ending stress. Dr. Wray observed that physicians are used to operating under stress, especially at work. “What I think is gnawing at me, and probably a lot of other physicians out there, is you go home and that stress is still there. It’s really hard to escape it. And you wake up in the morning and it’s there, whereas in the past, you could have a nice day. There’s little separation between work and domestic life right now.”
Having to work later into the evening has eaten into time for himself and time with his wife too. “That’s another side effect of the pandemic – it not only takes your time during the day, it takes the time you used to have at night to relax.”
To manage these challenges, Dr. Wray said he and his wife regularly double check their schedules. The family has also created a pod – “I think ‘podded up’ is a verb now,” he laughed – with another family and hired a recent college graduate to help the kids with their virtual learning. “Is it as good as being at school and amongst friends and having an actual teacher there? Of course not. But I think it’s the best that we can do.”
Dr. Wray said his employers have been flexible and understanding regarding scheduling conflicts that parents can have. “It’s really difficult for us, so oftentimes I struggle to see how other people are pulling this off. We recognize how fortunate we are, so that’s something I never want to overlook.”
Dividing and conquering
The biggest prepandemic issue for Sridevi Alla, MD, a hospitalist at Baptist Memorial Health in Jackson, Miss., and mother to four children – a 10-year-old, 6-year-old, 2-year-old, and a 9-month-old – was finding a babysitter on the weekend to take her kids out somewhere to burn off energy.
That’s a noticeable departure from the current demand to be not just a parent, but a teacher and a counselor too, thanks to virtual school, noted Dr. Alla. “You are their everything now,” she said. “They don’t have friends. They don’t have any other atmosphere or learning environment to let out their energy, their emotions. You have become their world.”
The beginning of the pandemic was particularly stressful for Dr. Alla, who is in the United States on an H-1B visa. “It was totally worrisome because you’re putting yourself at risk with patients who have the coronavirus, despite not knowing what your future itself is going to be like or what your family’s future is going to be like if anything happens to you,” she said. “We are fortunate we have our jobs. A lot of my immigrant friends lost theirs in the middle of this and they’re still trying to find jobs.”
Dr. Alla’s first challenge was whether to send her older two children to school or keep them at home to do virtual learning. The lack of information from the schools at first did not help that process, but she and her husband ended up choosing virtual school, a decision they still occasionally question.
Next, they had to find child care, and not just someone who could look after the younger two kids – they needed someone with the ability to also help the older ones with their homework.
Though initially the family had help, their first nanny had to quit because her roommate contracted COVID. “After that, we didn’t have help and my husband decided to work from home,” said Dr. Alla. “As of now, we’re still looking for child care. And the main issues are the late hours and the hospitalist week-on, week-off schedule.”
“It’s extremely hard,” she reflected. “At home, there’s no line. A 2-year-old doesn’t understand office time or personal time.” Still, Dr. Alla and her husband are maintaining by dividing up responsibilities and making sure they are always planning ahead.
Maintaining a routine
The greatest challenge for Heather Nye, MD, PhD, a hospitalist and professor of clinical medicine at UCSF, has been “maintaining normalcy for the kids.” She mourns the loss of a normal childhood for her kids, however temporary. “Living with abandon, feeling like you’re invincible, going out there and breaking your arm, meeting people, not fearing the world – those are not things we can instill in them right now,” she said.
The mother of an eighth grader and a second grader, Dr. Nye said their school district did not communicate well about how school would proceed. The district ended up offering only virtual school, with no plans for even hybrid learning in the future, leaving parents scrambling to plan.
Dr. Nye lucked out when her youngest child was accepted for a slot at a day camp offered through a partnership between the YMCA and UCSF. However, her eighth grader did not do well with distance learning in the spring, so having that virtual school as the only option has been difficult.
“Neither of the kids are doing really well in school,” she said. Her older one is overwhelmed by all the disparate online platforms and her youngest is having a hard time adjusting to differences like using a virtual pen. “The learning itself without question has suffered. You wonder about evaluation and this whole cohort of children in what will probably be more or less a lost year.”
Routines are the backbone of the family’s survival. “I think one of the most important things for kids in any stage of development is having a routine and being comfortable with that routine because that creates a sense of wellbeing in this time of uncertainty,” Dr. Nye said.
Neither Dr. Nye nor her husband, a geriatrician, have cut back on their work, so they are balancing a full plate of activities with parenting. Though their family is managing, “there are streaks of days where we’re like: ‘Are we failing our children?’ I’m sure every parent out there is asking themselves: ‘Am I doing enough?’” But she said, “We’re very, very lucky. We got that [camp] slot, we have the money to pay for it, and we both have flexible jobs.”
Rallying resources
Avital O’Glasser, MD, a hospitalist and associate professor of medicine at Oregon Health and Science University, Portland, fervently wished she could clone herself when the pandemic first started. Not only were her kids suddenly thrown into online classes, but she was pulled in to create a new service line for the COVID response at her clinic.
“The number of times that I said I think I need a time turner from Harry Potter. ... I felt that nothing was getting done even close to adequately because we were cutting corners left and right,” she said.
Thankfully, things have simmered down and Dr. O’Glasser is now working from home 5 or 6 days a week while her husband, a lawyer, goes to his job. “I think stress is lower now, but that’s in large part because, by the end of June, I really had to just stop and acknowledge how stressed I was and do a dramatic realignment of what I was doing for myself in terms of mental health support and bandwidth,” she said. Part of that involved realizing that the family needed a homeschool nanny for their 10-year-old and 7-year-old. “It’s been a lifesaver,” said Dr. O’Glasser.
Though life is on more of an even keel now, stress pops up in unexpected ways. “My youngest has pretty intense separation anxiety from me. Even with getting attention all day from our homeschool nanny, the day after I’m out of the house at the hospital, he really clings to me,” Dr. O’Glasser said. There’s sibling rivalry too, in an attempt to get parental attention.
Setting boundaries between work and home was her biggest challenge prepandemic, and that has not changed. “You’re trying to find that happy balance between professional development and family,” Dr. O’Glasser said. “Where do I cut corners? Do I try to multitask but spread myself thin? How do I say no to things? When am I going to find time to do laundry? When am I disconnecting? I think that now it’s facets of the same conundrum, but just manifested in different ways.”
She emphasized that parents should go easy on themselves right now. “A lot of parenting rules went out the window. My kids have had more screen time…and the amount of junk food they eat right now? Celebrate the wins.” Dr. O’Glasser chuckled about how her definition of a “win” has changed. “The bar now is something that I may never have considered a win before. Just seize those small moments. If my 7-year-old needs to do reading at my feet while I’m finishing notes from the day before, that’s okay,” she said.
How hospitalist groups can help
All four hospitalists had ideas about how hospitalist groups can help parents with school-age kids during the pandemic.
Providing child care at health care systems gives employees additional support, said Dr. Alla. Some of her friends have been unable to find child care because they are physicians who care for COVID patients and people do not want the extra risk. “I think any institution should think about this option because it’s very beneficial for an employee, especially for the long hours.”
Dr. Wray said he saw a program that matches up a hospitalist who has kids with one who does not in a type of buddy system, and they check in with each other. Then, if the parent has something come up, the other hospitalist can fill in and the parent can “pay it back” at another time. “This doesn’t put all the impetus on the schedule or on a single individual but spreads the risk out a little more and gives parents a bit of a parachute to make them feel like the system is supporting them,” he said.
“I would encourage groups to reach appropriate accommodations that are equitable and that don’t create discord because they’re perceived as unfair,” said Dr. O’Glasser. For instance, giving child care stipends, but limiting them to care at a licensed facility when some people might need to pay for a homeschool tutor. “Some of the policies that I saw seem to leave out the elementary school lot. You can’t just lump all kids together.”
Dr. Nye thought group leaders should take unseen pressures into account when evaluating employee performance. “I think we’re going to need to shift our yardstick because we can’t do everything now,” she said. “I’m talking about the extra things that people do that they’re evaluated on at the end of the year like volunteering for more shifts, sitting on committees, the things that likely aren’t in their job description. We’re going to have times when people are filling every last minute for their families. Face it with kindness and understanding and know that, in future years, things are going to go back to normal.”
Before the pandemic, the biggest parent-related challenge for Charlie Wray, DO, MS, a hospitalist and assistant clinical professor of medicine at the University of California, San Francisco, was “figuring out what I was going to pack in my kids’ lunches. Like most people, we were very much in our groove – we knew when my wife was going to leave work, and which day I’d pick up the kids,” Dr. Wray said. “I reflect back on that and think how easy it was.”
The old life – the one that seems so comparatively effortless – has been gone for close to a year now. And with the reopening of schools in the fall of 2020, hospitalists with school-age kids felt – and are still feeling – the strain in a variety of ways.
‘Podding up’
“The largest struggles that we have had involve dealing with the daily logistics of doing at-home learning,” said Dr. Wray, father to a 6-year-old and a 3-year-old. Dr. Wray and his wife are both physicians and have been juggling full work schedules with virtual school for their older child, who is not old enough to be autonomous. “For parents who have younger children who require one-on-one attention for the vast majority of their learning, that certainly takes more of a toll on your time, energy, and resources.”
Uncertainty has created anxiety about the future. “We have no idea what’s going to be happening next month. How do we plan for that? How do we allocate our time for that? That has been a real struggle for us, especially for a two-physician household where we are both considered front line and are both needing to be at the hospital or the clinic on a fairly regular basis,” he said.
Then there is the never-ending stress. Dr. Wray observed that physicians are used to operating under stress, especially at work. “What I think is gnawing at me, and probably a lot of other physicians out there, is you go home and that stress is still there. It’s really hard to escape it. And you wake up in the morning and it’s there, whereas in the past, you could have a nice day. There’s little separation between work and domestic life right now.”
Having to work later into the evening has eaten into time for himself and time with his wife too. “That’s another side effect of the pandemic – it not only takes your time during the day, it takes the time you used to have at night to relax.”
To manage these challenges, Dr. Wray said he and his wife regularly double check their schedules. The family has also created a pod – “I think ‘podded up’ is a verb now,” he laughed – with another family and hired a recent college graduate to help the kids with their virtual learning. “Is it as good as being at school and amongst friends and having an actual teacher there? Of course not. But I think it’s the best that we can do.”
Dr. Wray said his employers have been flexible and understanding regarding scheduling conflicts that parents can have. “It’s really difficult for us, so oftentimes I struggle to see how other people are pulling this off. We recognize how fortunate we are, so that’s something I never want to overlook.”
Dividing and conquering
The biggest prepandemic issue for Sridevi Alla, MD, a hospitalist at Baptist Memorial Health in Jackson, Miss., and mother to four children – a 10-year-old, 6-year-old, 2-year-old, and a 9-month-old – was finding a babysitter on the weekend to take her kids out somewhere to burn off energy.
That’s a noticeable departure from the current demand to be not just a parent, but a teacher and a counselor too, thanks to virtual school, noted Dr. Alla. “You are their everything now,” she said. “They don’t have friends. They don’t have any other atmosphere or learning environment to let out their energy, their emotions. You have become their world.”
The beginning of the pandemic was particularly stressful for Dr. Alla, who is in the United States on an H-1B visa. “It was totally worrisome because you’re putting yourself at risk with patients who have the coronavirus, despite not knowing what your future itself is going to be like or what your family’s future is going to be like if anything happens to you,” she said. “We are fortunate we have our jobs. A lot of my immigrant friends lost theirs in the middle of this and they’re still trying to find jobs.”
Dr. Alla’s first challenge was whether to send her older two children to school or keep them at home to do virtual learning. The lack of information from the schools at first did not help that process, but she and her husband ended up choosing virtual school, a decision they still occasionally question.
Next, they had to find child care, and not just someone who could look after the younger two kids – they needed someone with the ability to also help the older ones with their homework.
Though initially the family had help, their first nanny had to quit because her roommate contracted COVID. “After that, we didn’t have help and my husband decided to work from home,” said Dr. Alla. “As of now, we’re still looking for child care. And the main issues are the late hours and the hospitalist week-on, week-off schedule.”
“It’s extremely hard,” she reflected. “At home, there’s no line. A 2-year-old doesn’t understand office time or personal time.” Still, Dr. Alla and her husband are maintaining by dividing up responsibilities and making sure they are always planning ahead.
Maintaining a routine
The greatest challenge for Heather Nye, MD, PhD, a hospitalist and professor of clinical medicine at UCSF, has been “maintaining normalcy for the kids.” She mourns the loss of a normal childhood for her kids, however temporary. “Living with abandon, feeling like you’re invincible, going out there and breaking your arm, meeting people, not fearing the world – those are not things we can instill in them right now,” she said.
The mother of an eighth grader and a second grader, Dr. Nye said their school district did not communicate well about how school would proceed. The district ended up offering only virtual school, with no plans for even hybrid learning in the future, leaving parents scrambling to plan.
Dr. Nye lucked out when her youngest child was accepted for a slot at a day camp offered through a partnership between the YMCA and UCSF. However, her eighth grader did not do well with distance learning in the spring, so having that virtual school as the only option has been difficult.
“Neither of the kids are doing really well in school,” she said. Her older one is overwhelmed by all the disparate online platforms and her youngest is having a hard time adjusting to differences like using a virtual pen. “The learning itself without question has suffered. You wonder about evaluation and this whole cohort of children in what will probably be more or less a lost year.”
Routines are the backbone of the family’s survival. “I think one of the most important things for kids in any stage of development is having a routine and being comfortable with that routine because that creates a sense of wellbeing in this time of uncertainty,” Dr. Nye said.
Neither Dr. Nye nor her husband, a geriatrician, have cut back on their work, so they are balancing a full plate of activities with parenting. Though their family is managing, “there are streaks of days where we’re like: ‘Are we failing our children?’ I’m sure every parent out there is asking themselves: ‘Am I doing enough?’” But she said, “We’re very, very lucky. We got that [camp] slot, we have the money to pay for it, and we both have flexible jobs.”
Rallying resources
Avital O’Glasser, MD, a hospitalist and associate professor of medicine at Oregon Health and Science University, Portland, fervently wished she could clone herself when the pandemic first started. Not only were her kids suddenly thrown into online classes, but she was pulled in to create a new service line for the COVID response at her clinic.
“The number of times that I said I think I need a time turner from Harry Potter. ... I felt that nothing was getting done even close to adequately because we were cutting corners left and right,” she said.
Thankfully, things have simmered down and Dr. O’Glasser is now working from home 5 or 6 days a week while her husband, a lawyer, goes to his job. “I think stress is lower now, but that’s in large part because, by the end of June, I really had to just stop and acknowledge how stressed I was and do a dramatic realignment of what I was doing for myself in terms of mental health support and bandwidth,” she said. Part of that involved realizing that the family needed a homeschool nanny for their 10-year-old and 7-year-old. “It’s been a lifesaver,” said Dr. O’Glasser.
Though life is on more of an even keel now, stress pops up in unexpected ways. “My youngest has pretty intense separation anxiety from me. Even with getting attention all day from our homeschool nanny, the day after I’m out of the house at the hospital, he really clings to me,” Dr. O’Glasser said. There’s sibling rivalry too, in an attempt to get parental attention.
Setting boundaries between work and home was her biggest challenge prepandemic, and that has not changed. “You’re trying to find that happy balance between professional development and family,” Dr. O’Glasser said. “Where do I cut corners? Do I try to multitask but spread myself thin? How do I say no to things? When am I going to find time to do laundry? When am I disconnecting? I think that now it’s facets of the same conundrum, but just manifested in different ways.”
She emphasized that parents should go easy on themselves right now. “A lot of parenting rules went out the window. My kids have had more screen time…and the amount of junk food they eat right now? Celebrate the wins.” Dr. O’Glasser chuckled about how her definition of a “win” has changed. “The bar now is something that I may never have considered a win before. Just seize those small moments. If my 7-year-old needs to do reading at my feet while I’m finishing notes from the day before, that’s okay,” she said.
How hospitalist groups can help
All four hospitalists had ideas about how hospitalist groups can help parents with school-age kids during the pandemic.
Providing child care at health care systems gives employees additional support, said Dr. Alla. Some of her friends have been unable to find child care because they are physicians who care for COVID patients and people do not want the extra risk. “I think any institution should think about this option because it’s very beneficial for an employee, especially for the long hours.”
Dr. Wray said he saw a program that matches up a hospitalist who has kids with one who does not in a type of buddy system, and they check in with each other. Then, if the parent has something come up, the other hospitalist can fill in and the parent can “pay it back” at another time. “This doesn’t put all the impetus on the schedule or on a single individual but spreads the risk out a little more and gives parents a bit of a parachute to make them feel like the system is supporting them,” he said.
“I would encourage groups to reach appropriate accommodations that are equitable and that don’t create discord because they’re perceived as unfair,” said Dr. O’Glasser. For instance, giving child care stipends, but limiting them to care at a licensed facility when some people might need to pay for a homeschool tutor. “Some of the policies that I saw seem to leave out the elementary school lot. You can’t just lump all kids together.”
Dr. Nye thought group leaders should take unseen pressures into account when evaluating employee performance. “I think we’re going to need to shift our yardstick because we can’t do everything now,” she said. “I’m talking about the extra things that people do that they’re evaluated on at the end of the year like volunteering for more shifts, sitting on committees, the things that likely aren’t in their job description. We’re going to have times when people are filling every last minute for their families. Face it with kindness and understanding and know that, in future years, things are going to go back to normal.”
Before the pandemic, the biggest parent-related challenge for Charlie Wray, DO, MS, a hospitalist and assistant clinical professor of medicine at the University of California, San Francisco, was “figuring out what I was going to pack in my kids’ lunches. Like most people, we were very much in our groove – we knew when my wife was going to leave work, and which day I’d pick up the kids,” Dr. Wray said. “I reflect back on that and think how easy it was.”
The old life – the one that seems so comparatively effortless – has been gone for close to a year now. And with the reopening of schools in the fall of 2020, hospitalists with school-age kids felt – and are still feeling – the strain in a variety of ways.
‘Podding up’
“The largest struggles that we have had involve dealing with the daily logistics of doing at-home learning,” said Dr. Wray, father to a 6-year-old and a 3-year-old. Dr. Wray and his wife are both physicians and have been juggling full work schedules with virtual school for their older child, who is not old enough to be autonomous. “For parents who have younger children who require one-on-one attention for the vast majority of their learning, that certainly takes more of a toll on your time, energy, and resources.”
Uncertainty has created anxiety about the future. “We have no idea what’s going to be happening next month. How do we plan for that? How do we allocate our time for that? That has been a real struggle for us, especially for a two-physician household where we are both considered front line and are both needing to be at the hospital or the clinic on a fairly regular basis,” he said.
Then there is the never-ending stress. Dr. Wray observed that physicians are used to operating under stress, especially at work. “What I think is gnawing at me, and probably a lot of other physicians out there, is you go home and that stress is still there. It’s really hard to escape it. And you wake up in the morning and it’s there, whereas in the past, you could have a nice day. There’s little separation between work and domestic life right now.”
Having to work later into the evening has eaten into time for himself and time with his wife too. “That’s another side effect of the pandemic – it not only takes your time during the day, it takes the time you used to have at night to relax.”
To manage these challenges, Dr. Wray said he and his wife regularly double check their schedules. The family has also created a pod – “I think ‘podded up’ is a verb now,” he laughed – with another family and hired a recent college graduate to help the kids with their virtual learning. “Is it as good as being at school and amongst friends and having an actual teacher there? Of course not. But I think it’s the best that we can do.”
Dr. Wray said his employers have been flexible and understanding regarding scheduling conflicts that parents can have. “It’s really difficult for us, so oftentimes I struggle to see how other people are pulling this off. We recognize how fortunate we are, so that’s something I never want to overlook.”
Dividing and conquering
The biggest prepandemic issue for Sridevi Alla, MD, a hospitalist at Baptist Memorial Health in Jackson, Miss., and mother to four children – a 10-year-old, 6-year-old, 2-year-old, and a 9-month-old – was finding a babysitter on the weekend to take her kids out somewhere to burn off energy.
That’s a noticeable departure from the current demand to be not just a parent, but a teacher and a counselor too, thanks to virtual school, noted Dr. Alla. “You are their everything now,” she said. “They don’t have friends. They don’t have any other atmosphere or learning environment to let out their energy, their emotions. You have become their world.”
The beginning of the pandemic was particularly stressful for Dr. Alla, who is in the United States on an H-1B visa. “It was totally worrisome because you’re putting yourself at risk with patients who have the coronavirus, despite not knowing what your future itself is going to be like or what your family’s future is going to be like if anything happens to you,” she said. “We are fortunate we have our jobs. A lot of my immigrant friends lost theirs in the middle of this and they’re still trying to find jobs.”
Dr. Alla’s first challenge was whether to send her older two children to school or keep them at home to do virtual learning. The lack of information from the schools at first did not help that process, but she and her husband ended up choosing virtual school, a decision they still occasionally question.
Next, they had to find child care, and not just someone who could look after the younger two kids – they needed someone with the ability to also help the older ones with their homework.
Though initially the family had help, their first nanny had to quit because her roommate contracted COVID. “After that, we didn’t have help and my husband decided to work from home,” said Dr. Alla. “As of now, we’re still looking for child care. And the main issues are the late hours and the hospitalist week-on, week-off schedule.”
“It’s extremely hard,” she reflected. “At home, there’s no line. A 2-year-old doesn’t understand office time or personal time.” Still, Dr. Alla and her husband are maintaining by dividing up responsibilities and making sure they are always planning ahead.
Maintaining a routine
The greatest challenge for Heather Nye, MD, PhD, a hospitalist and professor of clinical medicine at UCSF, has been “maintaining normalcy for the kids.” She mourns the loss of a normal childhood for her kids, however temporary. “Living with abandon, feeling like you’re invincible, going out there and breaking your arm, meeting people, not fearing the world – those are not things we can instill in them right now,” she said.
The mother of an eighth grader and a second grader, Dr. Nye said their school district did not communicate well about how school would proceed. The district ended up offering only virtual school, with no plans for even hybrid learning in the future, leaving parents scrambling to plan.
Dr. Nye lucked out when her youngest child was accepted for a slot at a day camp offered through a partnership between the YMCA and UCSF. However, her eighth grader did not do well with distance learning in the spring, so having that virtual school as the only option has been difficult.
“Neither of the kids are doing really well in school,” she said. Her older one is overwhelmed by all the disparate online platforms and her youngest is having a hard time adjusting to differences like using a virtual pen. “The learning itself without question has suffered. You wonder about evaluation and this whole cohort of children in what will probably be more or less a lost year.”
Routines are the backbone of the family’s survival. “I think one of the most important things for kids in any stage of development is having a routine and being comfortable with that routine because that creates a sense of wellbeing in this time of uncertainty,” Dr. Nye said.
Neither Dr. Nye nor her husband, a geriatrician, have cut back on their work, so they are balancing a full plate of activities with parenting. Though their family is managing, “there are streaks of days where we’re like: ‘Are we failing our children?’ I’m sure every parent out there is asking themselves: ‘Am I doing enough?’” But she said, “We’re very, very lucky. We got that [camp] slot, we have the money to pay for it, and we both have flexible jobs.”
Rallying resources
Avital O’Glasser, MD, a hospitalist and associate professor of medicine at Oregon Health and Science University, Portland, fervently wished she could clone herself when the pandemic first started. Not only were her kids suddenly thrown into online classes, but she was pulled in to create a new service line for the COVID response at her clinic.
“The number of times that I said I think I need a time turner from Harry Potter. ... I felt that nothing was getting done even close to adequately because we were cutting corners left and right,” she said.
Thankfully, things have simmered down and Dr. O’Glasser is now working from home 5 or 6 days a week while her husband, a lawyer, goes to his job. “I think stress is lower now, but that’s in large part because, by the end of June, I really had to just stop and acknowledge how stressed I was and do a dramatic realignment of what I was doing for myself in terms of mental health support and bandwidth,” she said. Part of that involved realizing that the family needed a homeschool nanny for their 10-year-old and 7-year-old. “It’s been a lifesaver,” said Dr. O’Glasser.
Though life is on more of an even keel now, stress pops up in unexpected ways. “My youngest has pretty intense separation anxiety from me. Even with getting attention all day from our homeschool nanny, the day after I’m out of the house at the hospital, he really clings to me,” Dr. O’Glasser said. There’s sibling rivalry too, in an attempt to get parental attention.
Setting boundaries between work and home was her biggest challenge prepandemic, and that has not changed. “You’re trying to find that happy balance between professional development and family,” Dr. O’Glasser said. “Where do I cut corners? Do I try to multitask but spread myself thin? How do I say no to things? When am I going to find time to do laundry? When am I disconnecting? I think that now it’s facets of the same conundrum, but just manifested in different ways.”
She emphasized that parents should go easy on themselves right now. “A lot of parenting rules went out the window. My kids have had more screen time…and the amount of junk food they eat right now? Celebrate the wins.” Dr. O’Glasser chuckled about how her definition of a “win” has changed. “The bar now is something that I may never have considered a win before. Just seize those small moments. If my 7-year-old needs to do reading at my feet while I’m finishing notes from the day before, that’s okay,” she said.
How hospitalist groups can help
All four hospitalists had ideas about how hospitalist groups can help parents with school-age kids during the pandemic.
Providing child care at health care systems gives employees additional support, said Dr. Alla. Some of her friends have been unable to find child care because they are physicians who care for COVID patients and people do not want the extra risk. “I think any institution should think about this option because it’s very beneficial for an employee, especially for the long hours.”
Dr. Wray said he saw a program that matches up a hospitalist who has kids with one who does not in a type of buddy system, and they check in with each other. Then, if the parent has something come up, the other hospitalist can fill in and the parent can “pay it back” at another time. “This doesn’t put all the impetus on the schedule or on a single individual but spreads the risk out a little more and gives parents a bit of a parachute to make them feel like the system is supporting them,” he said.
“I would encourage groups to reach appropriate accommodations that are equitable and that don’t create discord because they’re perceived as unfair,” said Dr. O’Glasser. For instance, giving child care stipends, but limiting them to care at a licensed facility when some people might need to pay for a homeschool tutor. “Some of the policies that I saw seem to leave out the elementary school lot. You can’t just lump all kids together.”
Dr. Nye thought group leaders should take unseen pressures into account when evaluating employee performance. “I think we’re going to need to shift our yardstick because we can’t do everything now,” she said. “I’m talking about the extra things that people do that they’re evaluated on at the end of the year like volunteering for more shifts, sitting on committees, the things that likely aren’t in their job description. We’re going to have times when people are filling every last minute for their families. Face it with kindness and understanding and know that, in future years, things are going to go back to normal.”













