User login
‘Unprecedented’ responses to neoadjuvant treatment in dMMR colon cancer
PARIS – was given before surgery to patients with DNA mismatch repair deficient (dMMR) colon cancer, say researchers reporting new results from the NICHE-2 trial.
The trial involved 112 patients with dMMR colon cancer who were given one cycle of low-dose ipilimumab and two cycles of nivolumab followed by surgery.
The results show that 95% of patients had a major pathologic response (MPR), and 67% had a pathologic complete response (pCR) to immunotherapy.
To date, none of these patients have had disease recurrence after a median follow-up of 13.1 months.
Study presenter Myriam Chalabi, MD, an oncologist at the Netherlands Cancer Institute, Amsterdam, described the findings as “unprecedented,” especially as many of the patients had stage 3 and high-risk disease, and the expected disease recurrence rate with standard-of-care adjuvant chemotherapy in these patients would usually have been around 15%.
“Importantly, this treatment was very well-tolerated,” she added.
Dr. Chalabi presented the new results during a presidential session at the European Society for Medical Oncology Congress 2022, held in Paris.
Neoadjuvant immunotherapy “has the potential to become standard of care” in these patients, she said, adding that the “future has never been brighter” for dMMR colon cancer.
Around 10%-15% of colon cancers are dMMR, and around 33% of these are associated with Lynch syndrome, she noted.
She also urged pharmaceutical companies to seek approval for immunotherapy in this patient population, to warm applause from the audience.
Commenting on the results, Andrés Cervantes, MD, PhD, professor of medicine at the University of Valencia, Spain, said in an ESMO press release that the “innovative” study “questions the need for surgery and postoperative chemotherapy in all patients in whom the primary tumor has disappeared.”
He observed that adjuvant chemotherapy has remained standard of care, “despite the fact that chemotherapy is not so active, and a complete disappearance of the tumor in the surgical specimen is not observed.”
Overall, Dr. Cervantes said that dMMR status is a “strong predictor of the positive effect observed with this short-course immunotherapy,” adding that “determining dMMR can be easily done by immunohistochemistry in the conventional pathology lab, without the need for complex molecular testing.”
The “minimal toxicity” seen in the study “may also facilitate the implementation of this strategy, potentially sparing patients from surgery.”
Details of the new results
For the NICHE-2 study, patients with stage cT3 dMMR colon cancer and/or nodal involvement but without metastases and no signs of obstruction received one dose of ipilimumab 1 mg/kg and two doses of nivolumab 3 mg/kg before undergoing surgery within 6 weeks of enrollment.
The 112 participants were a median age of 60 years, and just over half were women. High-risk stage 3 disease was present in 74% of patients, which included 64% of patients with clinical T4a or T4b tumors and 62% with radiologic N2 stage cancer.
Median time from the first immunotherapy dose to surgery was 5.4 weeks.
Immune-related adverse events were seen in 61% of patients, but just 4% of patients experienced grade 3-4 immune-related adverse events, and 2% consequently had a delay in surgery, meaning the study met its primary safety endpoint.
In the end, all patients underwent surgery, with 100% having R0 resections.
A pathologic response was seen in 99% of patients, with 95% having an MPR, defined as less than or equal to 10% residual viable tumor, and 4% a partial response, defined as 10% to less than or equal to 50% residual viable tumor. A pCR, which included both the tumor bed and lymph nodes, was seen in 67% of participants.
There was a borderline significant difference in pCR patients between the 66 patients with sporadic tumors and the 32 with Lynch syndrome, at 58% versus 78% (P = .056).
At the meeting, discussant James Larkin, MD, PhD, consultant medical oncologist, The Royal Marsden, London, who was not involved with the study, agreed that the results were “striking,” with “brief treatment ... [showing] a major effect.”
However, he emphasized that it will be “important” to see the prespecified 3-year disease-free survival data, and he questioned whether the single low dose of ipilimumab was, in fact, necessary.
Dr. Larkin also emphasized that organ-sparing strategies in colon cancer are less “clear cut” than they are in rectal cancer and would require ongoing follow-up with colonoscopies and, potentially, biopsies. He also said it is “critical” to get patients’ views on the desirability of organ sparing.
The study was funded by Bristol Myers Squibb. Dr. Chalabi has reported no financial interests. Disclosures for the other authors are listed with the abstract. Dr. Larkin has declared relationships with Eisai, Novartis, Merck, Pfizer, BMS, iOnctura, Debiopharm, Incyte, MSD, Pierre Fabre, Ibsen, Roche, EUSA Pharma, AstraZeneca, GSK, Calithera, Ultimovacs, Seagen, and Nektar Therapeutics.
A version of this article first appeared on Medscape.com.
PARIS – was given before surgery to patients with DNA mismatch repair deficient (dMMR) colon cancer, say researchers reporting new results from the NICHE-2 trial.
The trial involved 112 patients with dMMR colon cancer who were given one cycle of low-dose ipilimumab and two cycles of nivolumab followed by surgery.
The results show that 95% of patients had a major pathologic response (MPR), and 67% had a pathologic complete response (pCR) to immunotherapy.
To date, none of these patients have had disease recurrence after a median follow-up of 13.1 months.
Study presenter Myriam Chalabi, MD, an oncologist at the Netherlands Cancer Institute, Amsterdam, described the findings as “unprecedented,” especially as many of the patients had stage 3 and high-risk disease, and the expected disease recurrence rate with standard-of-care adjuvant chemotherapy in these patients would usually have been around 15%.
“Importantly, this treatment was very well-tolerated,” she added.
Dr. Chalabi presented the new results during a presidential session at the European Society for Medical Oncology Congress 2022, held in Paris.
Neoadjuvant immunotherapy “has the potential to become standard of care” in these patients, she said, adding that the “future has never been brighter” for dMMR colon cancer.
Around 10%-15% of colon cancers are dMMR, and around 33% of these are associated with Lynch syndrome, she noted.
She also urged pharmaceutical companies to seek approval for immunotherapy in this patient population, to warm applause from the audience.
Commenting on the results, Andrés Cervantes, MD, PhD, professor of medicine at the University of Valencia, Spain, said in an ESMO press release that the “innovative” study “questions the need for surgery and postoperative chemotherapy in all patients in whom the primary tumor has disappeared.”
He observed that adjuvant chemotherapy has remained standard of care, “despite the fact that chemotherapy is not so active, and a complete disappearance of the tumor in the surgical specimen is not observed.”
Overall, Dr. Cervantes said that dMMR status is a “strong predictor of the positive effect observed with this short-course immunotherapy,” adding that “determining dMMR can be easily done by immunohistochemistry in the conventional pathology lab, without the need for complex molecular testing.”
The “minimal toxicity” seen in the study “may also facilitate the implementation of this strategy, potentially sparing patients from surgery.”
Details of the new results
For the NICHE-2 study, patients with stage cT3 dMMR colon cancer and/or nodal involvement but without metastases and no signs of obstruction received one dose of ipilimumab 1 mg/kg and two doses of nivolumab 3 mg/kg before undergoing surgery within 6 weeks of enrollment.
The 112 participants were a median age of 60 years, and just over half were women. High-risk stage 3 disease was present in 74% of patients, which included 64% of patients with clinical T4a or T4b tumors and 62% with radiologic N2 stage cancer.
Median time from the first immunotherapy dose to surgery was 5.4 weeks.
Immune-related adverse events were seen in 61% of patients, but just 4% of patients experienced grade 3-4 immune-related adverse events, and 2% consequently had a delay in surgery, meaning the study met its primary safety endpoint.
In the end, all patients underwent surgery, with 100% having R0 resections.
A pathologic response was seen in 99% of patients, with 95% having an MPR, defined as less than or equal to 10% residual viable tumor, and 4% a partial response, defined as 10% to less than or equal to 50% residual viable tumor. A pCR, which included both the tumor bed and lymph nodes, was seen in 67% of participants.
There was a borderline significant difference in pCR patients between the 66 patients with sporadic tumors and the 32 with Lynch syndrome, at 58% versus 78% (P = .056).
At the meeting, discussant James Larkin, MD, PhD, consultant medical oncologist, The Royal Marsden, London, who was not involved with the study, agreed that the results were “striking,” with “brief treatment ... [showing] a major effect.”
However, he emphasized that it will be “important” to see the prespecified 3-year disease-free survival data, and he questioned whether the single low dose of ipilimumab was, in fact, necessary.
Dr. Larkin also emphasized that organ-sparing strategies in colon cancer are less “clear cut” than they are in rectal cancer and would require ongoing follow-up with colonoscopies and, potentially, biopsies. He also said it is “critical” to get patients’ views on the desirability of organ sparing.
The study was funded by Bristol Myers Squibb. Dr. Chalabi has reported no financial interests. Disclosures for the other authors are listed with the abstract. Dr. Larkin has declared relationships with Eisai, Novartis, Merck, Pfizer, BMS, iOnctura, Debiopharm, Incyte, MSD, Pierre Fabre, Ibsen, Roche, EUSA Pharma, AstraZeneca, GSK, Calithera, Ultimovacs, Seagen, and Nektar Therapeutics.
A version of this article first appeared on Medscape.com.
PARIS – was given before surgery to patients with DNA mismatch repair deficient (dMMR) colon cancer, say researchers reporting new results from the NICHE-2 trial.
The trial involved 112 patients with dMMR colon cancer who were given one cycle of low-dose ipilimumab and two cycles of nivolumab followed by surgery.
The results show that 95% of patients had a major pathologic response (MPR), and 67% had a pathologic complete response (pCR) to immunotherapy.
To date, none of these patients have had disease recurrence after a median follow-up of 13.1 months.
Study presenter Myriam Chalabi, MD, an oncologist at the Netherlands Cancer Institute, Amsterdam, described the findings as “unprecedented,” especially as many of the patients had stage 3 and high-risk disease, and the expected disease recurrence rate with standard-of-care adjuvant chemotherapy in these patients would usually have been around 15%.
“Importantly, this treatment was very well-tolerated,” she added.
Dr. Chalabi presented the new results during a presidential session at the European Society for Medical Oncology Congress 2022, held in Paris.
Neoadjuvant immunotherapy “has the potential to become standard of care” in these patients, she said, adding that the “future has never been brighter” for dMMR colon cancer.
Around 10%-15% of colon cancers are dMMR, and around 33% of these are associated with Lynch syndrome, she noted.
She also urged pharmaceutical companies to seek approval for immunotherapy in this patient population, to warm applause from the audience.
Commenting on the results, Andrés Cervantes, MD, PhD, professor of medicine at the University of Valencia, Spain, said in an ESMO press release that the “innovative” study “questions the need for surgery and postoperative chemotherapy in all patients in whom the primary tumor has disappeared.”
He observed that adjuvant chemotherapy has remained standard of care, “despite the fact that chemotherapy is not so active, and a complete disappearance of the tumor in the surgical specimen is not observed.”
Overall, Dr. Cervantes said that dMMR status is a “strong predictor of the positive effect observed with this short-course immunotherapy,” adding that “determining dMMR can be easily done by immunohistochemistry in the conventional pathology lab, without the need for complex molecular testing.”
The “minimal toxicity” seen in the study “may also facilitate the implementation of this strategy, potentially sparing patients from surgery.”
Details of the new results
For the NICHE-2 study, patients with stage cT3 dMMR colon cancer and/or nodal involvement but without metastases and no signs of obstruction received one dose of ipilimumab 1 mg/kg and two doses of nivolumab 3 mg/kg before undergoing surgery within 6 weeks of enrollment.
The 112 participants were a median age of 60 years, and just over half were women. High-risk stage 3 disease was present in 74% of patients, which included 64% of patients with clinical T4a or T4b tumors and 62% with radiologic N2 stage cancer.
Median time from the first immunotherapy dose to surgery was 5.4 weeks.
Immune-related adverse events were seen in 61% of patients, but just 4% of patients experienced grade 3-4 immune-related adverse events, and 2% consequently had a delay in surgery, meaning the study met its primary safety endpoint.
In the end, all patients underwent surgery, with 100% having R0 resections.
A pathologic response was seen in 99% of patients, with 95% having an MPR, defined as less than or equal to 10% residual viable tumor, and 4% a partial response, defined as 10% to less than or equal to 50% residual viable tumor. A pCR, which included both the tumor bed and lymph nodes, was seen in 67% of participants.
There was a borderline significant difference in pCR patients between the 66 patients with sporadic tumors and the 32 with Lynch syndrome, at 58% versus 78% (P = .056).
At the meeting, discussant James Larkin, MD, PhD, consultant medical oncologist, The Royal Marsden, London, who was not involved with the study, agreed that the results were “striking,” with “brief treatment ... [showing] a major effect.”
However, he emphasized that it will be “important” to see the prespecified 3-year disease-free survival data, and he questioned whether the single low dose of ipilimumab was, in fact, necessary.
Dr. Larkin also emphasized that organ-sparing strategies in colon cancer are less “clear cut” than they are in rectal cancer and would require ongoing follow-up with colonoscopies and, potentially, biopsies. He also said it is “critical” to get patients’ views on the desirability of organ sparing.
The study was funded by Bristol Myers Squibb. Dr. Chalabi has reported no financial interests. Disclosures for the other authors are listed with the abstract. Dr. Larkin has declared relationships with Eisai, Novartis, Merck, Pfizer, BMS, iOnctura, Debiopharm, Incyte, MSD, Pierre Fabre, Ibsen, Roche, EUSA Pharma, AstraZeneca, GSK, Calithera, Ultimovacs, Seagen, and Nektar Therapeutics.
A version of this article first appeared on Medscape.com.
TBI is an unrecognized risk factor for cardiovascular disease
(CVD). More severe TBI is associated with higher risk of CVD, new research shows.
Given the relatively young age of post-9/11–era veterans with TBI, there may be an increased burden of heart disease in the future as these veterans age and develop traditional risk factors for CVD, the investigators, led by Ian J. Stewart, MD, with Uniformed Services University, Bethesda, Md., wrote.
The study was published online in JAMA Neurology.
Novel data
Since Sept. 11, 2001, 4.5 million people have served in the U.S. military, with their time in service defined by the long-running wars in Iraq and Afghanistan. Estimates suggest that up to 20% of post-9/11 veterans sustained a TBI.
While some evidence suggests that TBI increases the risk of CVD, prior reports have focused mainly on cerebrovascular outcomes. Until now, the potential association of TBI with CVD has not been comprehensively examined in post-9/11–era veterans.
The retrospective cohort study included 1,559,928 predominantly male post-9/11 veterans, including 301,169 (19.3%) with a history of TBI and 1,258,759 (81%) with no TBI history.
In fully adjusted models, compared with veterans with no TBI history, a history of mild, moderate/severe, or penetrating TBI was associated with increased risk of developing the composite CVD endpoint (coronary artery disease, stroke, peripheral artery disease, and CVD death).
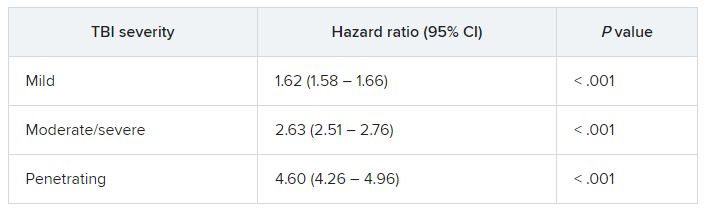
TBIs of all severities were associated with the individual components of the composite outcome, except penetrating TBI and CVD death.
“The association of TBI with subsequent CVD was not attenuated in multivariable models, suggesting that TBI may be accounting for risk that is independent from the other variables,” Dr. Stewart and colleagues wrote.
They noted that the risk was highest shortly after injury, but TBI remained significantly associated with CVD for years after the initial insult.
Why TBI may raise the risk of subsequent CVD remains unclear.
It’s possible that patients with TBI develop more traditional risk factors for CVD through time than do patients without TBI. A study in mice found that TBI led to increased rates of atherosclerosis, the researchers said.
An additional mechanism may be disruption of autonomic regulation, which has been known to occur after TBI.
Another potential pathway is through mental health diagnoses, such as posttraumatic stress disorder; a large body of work has identified associations between PTSD and CVD, including among post-9/11 veterans.
Further work is needed to determine how this risk can be modified to improve outcomes for post-9/11–era veterans, the researchers write.
Unrecognized CVD risk factor?
Reached for comment, Shaheen E. Lakhan, MD, PhD, a neurologist and researcher from Boston who wasn’t involved in the study, said the effects of TBI on heart health are “very underreported, and most clinicians would not make the link.”
“When the brain suffers a traumatic injury, it activates a cascade of neuro-inflammation that goes haywire in an attempt to protect further brain damage. Oftentimes, these inflammatory by-products leak into the body, especially in trauma, when the barriers are broken between brain and body, and can cause systemic body inflammation, which is well associated with heart disease,” Dr. Lakhan said.
In addition, Dr. Lakhan said, “TBI itself localized to just the brain can negatively affect good health habits, leading to worsening heart health, too.”
“Research like this brings light where not much exists and underscores the importance of protecting our brains from physical trauma,” he said.
The study was supported by the assistant secretary of defense for health affairs, endorsed by the Department of Defense through the Psychological Health/Traumatic Brain Injury Research Program Long-Term Impact of Military-Relevant Brain Injury Consortium, and by the U.S. Department of Veterans Affairs. Dr. Stewart and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(CVD). More severe TBI is associated with higher risk of CVD, new research shows.
Given the relatively young age of post-9/11–era veterans with TBI, there may be an increased burden of heart disease in the future as these veterans age and develop traditional risk factors for CVD, the investigators, led by Ian J. Stewart, MD, with Uniformed Services University, Bethesda, Md., wrote.
The study was published online in JAMA Neurology.
Novel data
Since Sept. 11, 2001, 4.5 million people have served in the U.S. military, with their time in service defined by the long-running wars in Iraq and Afghanistan. Estimates suggest that up to 20% of post-9/11 veterans sustained a TBI.
While some evidence suggests that TBI increases the risk of CVD, prior reports have focused mainly on cerebrovascular outcomes. Until now, the potential association of TBI with CVD has not been comprehensively examined in post-9/11–era veterans.
The retrospective cohort study included 1,559,928 predominantly male post-9/11 veterans, including 301,169 (19.3%) with a history of TBI and 1,258,759 (81%) with no TBI history.
In fully adjusted models, compared with veterans with no TBI history, a history of mild, moderate/severe, or penetrating TBI was associated with increased risk of developing the composite CVD endpoint (coronary artery disease, stroke, peripheral artery disease, and CVD death).
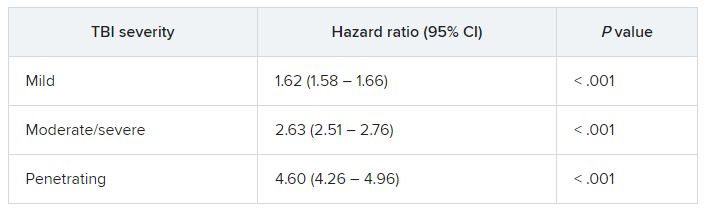
TBIs of all severities were associated with the individual components of the composite outcome, except penetrating TBI and CVD death.
“The association of TBI with subsequent CVD was not attenuated in multivariable models, suggesting that TBI may be accounting for risk that is independent from the other variables,” Dr. Stewart and colleagues wrote.
They noted that the risk was highest shortly after injury, but TBI remained significantly associated with CVD for years after the initial insult.
Why TBI may raise the risk of subsequent CVD remains unclear.
It’s possible that patients with TBI develop more traditional risk factors for CVD through time than do patients without TBI. A study in mice found that TBI led to increased rates of atherosclerosis, the researchers said.
An additional mechanism may be disruption of autonomic regulation, which has been known to occur after TBI.
Another potential pathway is through mental health diagnoses, such as posttraumatic stress disorder; a large body of work has identified associations between PTSD and CVD, including among post-9/11 veterans.
Further work is needed to determine how this risk can be modified to improve outcomes for post-9/11–era veterans, the researchers write.
Unrecognized CVD risk factor?
Reached for comment, Shaheen E. Lakhan, MD, PhD, a neurologist and researcher from Boston who wasn’t involved in the study, said the effects of TBI on heart health are “very underreported, and most clinicians would not make the link.”
“When the brain suffers a traumatic injury, it activates a cascade of neuro-inflammation that goes haywire in an attempt to protect further brain damage. Oftentimes, these inflammatory by-products leak into the body, especially in trauma, when the barriers are broken between brain and body, and can cause systemic body inflammation, which is well associated with heart disease,” Dr. Lakhan said.
In addition, Dr. Lakhan said, “TBI itself localized to just the brain can negatively affect good health habits, leading to worsening heart health, too.”
“Research like this brings light where not much exists and underscores the importance of protecting our brains from physical trauma,” he said.
The study was supported by the assistant secretary of defense for health affairs, endorsed by the Department of Defense through the Psychological Health/Traumatic Brain Injury Research Program Long-Term Impact of Military-Relevant Brain Injury Consortium, and by the U.S. Department of Veterans Affairs. Dr. Stewart and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(CVD). More severe TBI is associated with higher risk of CVD, new research shows.
Given the relatively young age of post-9/11–era veterans with TBI, there may be an increased burden of heart disease in the future as these veterans age and develop traditional risk factors for CVD, the investigators, led by Ian J. Stewart, MD, with Uniformed Services University, Bethesda, Md., wrote.
The study was published online in JAMA Neurology.
Novel data
Since Sept. 11, 2001, 4.5 million people have served in the U.S. military, with their time in service defined by the long-running wars in Iraq and Afghanistan. Estimates suggest that up to 20% of post-9/11 veterans sustained a TBI.
While some evidence suggests that TBI increases the risk of CVD, prior reports have focused mainly on cerebrovascular outcomes. Until now, the potential association of TBI with CVD has not been comprehensively examined in post-9/11–era veterans.
The retrospective cohort study included 1,559,928 predominantly male post-9/11 veterans, including 301,169 (19.3%) with a history of TBI and 1,258,759 (81%) with no TBI history.
In fully adjusted models, compared with veterans with no TBI history, a history of mild, moderate/severe, or penetrating TBI was associated with increased risk of developing the composite CVD endpoint (coronary artery disease, stroke, peripheral artery disease, and CVD death).
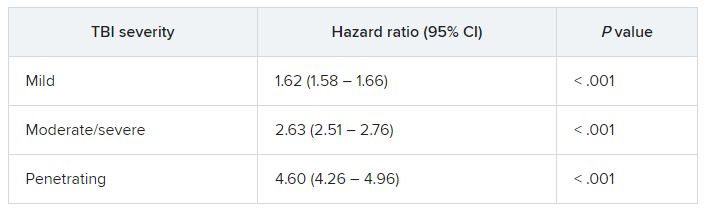
TBIs of all severities were associated with the individual components of the composite outcome, except penetrating TBI and CVD death.
“The association of TBI with subsequent CVD was not attenuated in multivariable models, suggesting that TBI may be accounting for risk that is independent from the other variables,” Dr. Stewart and colleagues wrote.
They noted that the risk was highest shortly after injury, but TBI remained significantly associated with CVD for years after the initial insult.
Why TBI may raise the risk of subsequent CVD remains unclear.
It’s possible that patients with TBI develop more traditional risk factors for CVD through time than do patients without TBI. A study in mice found that TBI led to increased rates of atherosclerosis, the researchers said.
An additional mechanism may be disruption of autonomic regulation, which has been known to occur after TBI.
Another potential pathway is through mental health diagnoses, such as posttraumatic stress disorder; a large body of work has identified associations between PTSD and CVD, including among post-9/11 veterans.
Further work is needed to determine how this risk can be modified to improve outcomes for post-9/11–era veterans, the researchers write.
Unrecognized CVD risk factor?
Reached for comment, Shaheen E. Lakhan, MD, PhD, a neurologist and researcher from Boston who wasn’t involved in the study, said the effects of TBI on heart health are “very underreported, and most clinicians would not make the link.”
“When the brain suffers a traumatic injury, it activates a cascade of neuro-inflammation that goes haywire in an attempt to protect further brain damage. Oftentimes, these inflammatory by-products leak into the body, especially in trauma, when the barriers are broken between brain and body, and can cause systemic body inflammation, which is well associated with heart disease,” Dr. Lakhan said.
In addition, Dr. Lakhan said, “TBI itself localized to just the brain can negatively affect good health habits, leading to worsening heart health, too.”
“Research like this brings light where not much exists and underscores the importance of protecting our brains from physical trauma,” he said.
The study was supported by the assistant secretary of defense for health affairs, endorsed by the Department of Defense through the Psychological Health/Traumatic Brain Injury Research Program Long-Term Impact of Military-Relevant Brain Injury Consortium, and by the U.S. Department of Veterans Affairs. Dr. Stewart and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pembro/chemo combo fails to improve event-free survival in head and neck cancer
PARIS – compared with CRT plus placebo as first-line therapy for patients with locally advanced head and neck squamous cell cancers (HNSCC), reported investigators of the KEYNOTE-412 trial.
Among 804 patients with newly diagnosed, pathologically proven, unresected locally advanced head and neck squamous cell carcinomas who were followed for a median of 47.7 months, the event-free survival (EFS) rate with the pembrolizumab/CRT combination followed by maintenance pembrolizumab was 63.2%, compared with 56.2% for CRT plus placebo. This translated into a nonsignificant hazard ratio of 0.83, said Jean-Pascal Machiels, MD, PhD, at the annual meeting of the European Society for Medical Oncology.
Despite the trial failing to meet its primary endpoint, Dr. Machiels expressed optimism about the results.
“Pembrolizumab with chemoradiation was associated with a favorable trend toward improved event-free survival versus placebo plus chemoradiation in patients with locally advanced head and neck cancer,” he said.
He noted that the 2-year EFS rate was 63% with pembrolizumab, compared with 56% with placebo.
The data also support the hypothesis that programmed death–ligand 1 (PD-L1) expression as measured by a combined positive score (CPS) could be a predictive biomarker for identifying those patients most likely to respond to the immune checkpoint inhibitor, he added.
KEYNOTE-412 details
The rationale for combining the checkpoint inhibitors pembrolizumab with chemoradiotherapy comes from the KEYNOTE-048 trial results of which showed a survival improvement for the use of pembrolizumab plus a platinum-containing regimen as a first-line therapy for recurrent or metastatic HNSCC, as well as pembrolizumab monotherapy for patients with PD-L1 CPS of 1 or greater.
In the current study, Dr. Machiels and colleagues studied whether adding pembrolizumab to CRT could benefit patients with treatment-naive unresected, locally advanced HNSCC.
Eligible patients included those with stage T3 or T4, N0-N3 or any N2a-3 (T1-T4) cancers of the larynx, hypopharynx, or oral cavity, and either p16-negative oropharynx cancers or T4 or N3 p16-positive oropharynx cancer. Patients were required to be eligible for high-dose cisplatin-based CRT.
A total of 804 patients were randomized, 402 in each arm, to receive either pembrolizumab 200 mg intravenously every 3 weeks for 3 cycles plus CRT followed by maintenance pembrolizumab for 14 cycles, or to placebo plus CRT followed by placebo maintenance.
As noted before, there was no significant difference between the study arms for the primary endpoint of EFS. The 24-month EFS rate was 63.2% for the pembrolizumab group, compared with 56.2% for controls. The respective 6-month EFS rates were 57.4% versus 52.1%.
In a post hoc analysis, both EFS and overall survival were numerically with pembrolizumab among patients with PD-L1 CPS of 20 or greater. The respective 2- and 3-year EFS rates were 71.2% versus 62.6%, and 66.7% versus 57.2%.
The 24-months overall survival rates were 83.3% with pembrolizumab and 79.9% with placebo, and 36-month rates were 79.1% and 73%, respectively.
Neither EFS rates nor OS rates among patients in this subgroup differed significantly; however, there were no new safety signals with the combination, Dr. Machiels said. The incidence of grade 3 or greater adverse events was 92.2% in the pembrolizumab arm versus 88.4% in the placebo arm. Four patients in the pembrolizumab arm and six in the control arm died from treatment-related causes.
Benefit still to be proven
In a media briefing held prior to his presentation, Dr. Machiels was asked how he could justify his conclusions about a benefit for adding pembrolizumab given that there was no difference between the treatment groups for the primary endpoint.
He said that when the investigators designed the trial 7 years ago, the CPS score for PD-L1 expression had not yet been developed, and that if it had been they might have designed the trial to explore the effect of the pembrolizumab chemoradiation combination according to CPS subgroups.
He also pointed to the numerically superior 2-year EFS and overall rates.
In the presidential symposium, James Larkin, MD, PhD, an invited discussant from the Royal Marsden Hospital, London, said that chemotherapy and anti–PD-1 therapies are known to offer benefit in advanced cancers despite the trial’s failure.
“There is a signal, particularly as we’ve seen in the high PD-L1 group,” he said, noting that the signal was consistent with that seen in the JAVELIN 100 study, which was also a negative trial. He cautioned against relying too heavily on the comparison, however, as JAVELIN 100 was conducted with avelumab, a PD-L1 inhibitor, whereas pembrolizumab is a PD-1 inhibitor.
“Could there be an issue here with treatment schedule? An example and a comparison might be the PACIFIC study in non–small cell lung cancer, which is a positive trial, where actually the checkpoint inhibit with durvalumab was given immediately after the chemoradiotherapy, leading to benefit, rather than being concurrent,” he said.
Dr. Larkin also questioned whether, as codiscussant Sherene Loi, MD, PhD, from the Peter MacCallum Cancer Center, Melbourne, suggested radiotherapy to lymph nodes might alter the immune response to checkpoint inhibitors.
“Clearly radiotherapy is the central component of treatment in this setting, so it would be quite difficult to scale too much on that, but the question is: ‘Could it be modified?’ For example, just to irradiate the primary tumor and involved lymph nodes and potentially spare noninvolved lymph nodes,” he said.
The KEYNOTE-412 study was funded by Merck Sharp & Dohme. Dr. Machiels reported uncompensated consulting to the company. Dr. Larkin reported consulting for and receiving honoraria from Merck and others. Dr. Loi reported uncompensated advisory board activity for Merck and others.
PARIS – compared with CRT plus placebo as first-line therapy for patients with locally advanced head and neck squamous cell cancers (HNSCC), reported investigators of the KEYNOTE-412 trial.
Among 804 patients with newly diagnosed, pathologically proven, unresected locally advanced head and neck squamous cell carcinomas who were followed for a median of 47.7 months, the event-free survival (EFS) rate with the pembrolizumab/CRT combination followed by maintenance pembrolizumab was 63.2%, compared with 56.2% for CRT plus placebo. This translated into a nonsignificant hazard ratio of 0.83, said Jean-Pascal Machiels, MD, PhD, at the annual meeting of the European Society for Medical Oncology.
Despite the trial failing to meet its primary endpoint, Dr. Machiels expressed optimism about the results.
“Pembrolizumab with chemoradiation was associated with a favorable trend toward improved event-free survival versus placebo plus chemoradiation in patients with locally advanced head and neck cancer,” he said.
He noted that the 2-year EFS rate was 63% with pembrolizumab, compared with 56% with placebo.
The data also support the hypothesis that programmed death–ligand 1 (PD-L1) expression as measured by a combined positive score (CPS) could be a predictive biomarker for identifying those patients most likely to respond to the immune checkpoint inhibitor, he added.
KEYNOTE-412 details
The rationale for combining the checkpoint inhibitors pembrolizumab with chemoradiotherapy comes from the KEYNOTE-048 trial results of which showed a survival improvement for the use of pembrolizumab plus a platinum-containing regimen as a first-line therapy for recurrent or metastatic HNSCC, as well as pembrolizumab monotherapy for patients with PD-L1 CPS of 1 or greater.
In the current study, Dr. Machiels and colleagues studied whether adding pembrolizumab to CRT could benefit patients with treatment-naive unresected, locally advanced HNSCC.
Eligible patients included those with stage T3 or T4, N0-N3 or any N2a-3 (T1-T4) cancers of the larynx, hypopharynx, or oral cavity, and either p16-negative oropharynx cancers or T4 or N3 p16-positive oropharynx cancer. Patients were required to be eligible for high-dose cisplatin-based CRT.
A total of 804 patients were randomized, 402 in each arm, to receive either pembrolizumab 200 mg intravenously every 3 weeks for 3 cycles plus CRT followed by maintenance pembrolizumab for 14 cycles, or to placebo plus CRT followed by placebo maintenance.
As noted before, there was no significant difference between the study arms for the primary endpoint of EFS. The 24-month EFS rate was 63.2% for the pembrolizumab group, compared with 56.2% for controls. The respective 6-month EFS rates were 57.4% versus 52.1%.
In a post hoc analysis, both EFS and overall survival were numerically with pembrolizumab among patients with PD-L1 CPS of 20 or greater. The respective 2- and 3-year EFS rates were 71.2% versus 62.6%, and 66.7% versus 57.2%.
The 24-months overall survival rates were 83.3% with pembrolizumab and 79.9% with placebo, and 36-month rates were 79.1% and 73%, respectively.
Neither EFS rates nor OS rates among patients in this subgroup differed significantly; however, there were no new safety signals with the combination, Dr. Machiels said. The incidence of grade 3 or greater adverse events was 92.2% in the pembrolizumab arm versus 88.4% in the placebo arm. Four patients in the pembrolizumab arm and six in the control arm died from treatment-related causes.
Benefit still to be proven
In a media briefing held prior to his presentation, Dr. Machiels was asked how he could justify his conclusions about a benefit for adding pembrolizumab given that there was no difference between the treatment groups for the primary endpoint.
He said that when the investigators designed the trial 7 years ago, the CPS score for PD-L1 expression had not yet been developed, and that if it had been they might have designed the trial to explore the effect of the pembrolizumab chemoradiation combination according to CPS subgroups.
He also pointed to the numerically superior 2-year EFS and overall rates.
In the presidential symposium, James Larkin, MD, PhD, an invited discussant from the Royal Marsden Hospital, London, said that chemotherapy and anti–PD-1 therapies are known to offer benefit in advanced cancers despite the trial’s failure.
“There is a signal, particularly as we’ve seen in the high PD-L1 group,” he said, noting that the signal was consistent with that seen in the JAVELIN 100 study, which was also a negative trial. He cautioned against relying too heavily on the comparison, however, as JAVELIN 100 was conducted with avelumab, a PD-L1 inhibitor, whereas pembrolizumab is a PD-1 inhibitor.
“Could there be an issue here with treatment schedule? An example and a comparison might be the PACIFIC study in non–small cell lung cancer, which is a positive trial, where actually the checkpoint inhibit with durvalumab was given immediately after the chemoradiotherapy, leading to benefit, rather than being concurrent,” he said.
Dr. Larkin also questioned whether, as codiscussant Sherene Loi, MD, PhD, from the Peter MacCallum Cancer Center, Melbourne, suggested radiotherapy to lymph nodes might alter the immune response to checkpoint inhibitors.
“Clearly radiotherapy is the central component of treatment in this setting, so it would be quite difficult to scale too much on that, but the question is: ‘Could it be modified?’ For example, just to irradiate the primary tumor and involved lymph nodes and potentially spare noninvolved lymph nodes,” he said.
The KEYNOTE-412 study was funded by Merck Sharp & Dohme. Dr. Machiels reported uncompensated consulting to the company. Dr. Larkin reported consulting for and receiving honoraria from Merck and others. Dr. Loi reported uncompensated advisory board activity for Merck and others.
PARIS – compared with CRT plus placebo as first-line therapy for patients with locally advanced head and neck squamous cell cancers (HNSCC), reported investigators of the KEYNOTE-412 trial.
Among 804 patients with newly diagnosed, pathologically proven, unresected locally advanced head and neck squamous cell carcinomas who were followed for a median of 47.7 months, the event-free survival (EFS) rate with the pembrolizumab/CRT combination followed by maintenance pembrolizumab was 63.2%, compared with 56.2% for CRT plus placebo. This translated into a nonsignificant hazard ratio of 0.83, said Jean-Pascal Machiels, MD, PhD, at the annual meeting of the European Society for Medical Oncology.
Despite the trial failing to meet its primary endpoint, Dr. Machiels expressed optimism about the results.
“Pembrolizumab with chemoradiation was associated with a favorable trend toward improved event-free survival versus placebo plus chemoradiation in patients with locally advanced head and neck cancer,” he said.
He noted that the 2-year EFS rate was 63% with pembrolizumab, compared with 56% with placebo.
The data also support the hypothesis that programmed death–ligand 1 (PD-L1) expression as measured by a combined positive score (CPS) could be a predictive biomarker for identifying those patients most likely to respond to the immune checkpoint inhibitor, he added.
KEYNOTE-412 details
The rationale for combining the checkpoint inhibitors pembrolizumab with chemoradiotherapy comes from the KEYNOTE-048 trial results of which showed a survival improvement for the use of pembrolizumab plus a platinum-containing regimen as a first-line therapy for recurrent or metastatic HNSCC, as well as pembrolizumab monotherapy for patients with PD-L1 CPS of 1 or greater.
In the current study, Dr. Machiels and colleagues studied whether adding pembrolizumab to CRT could benefit patients with treatment-naive unresected, locally advanced HNSCC.
Eligible patients included those with stage T3 or T4, N0-N3 or any N2a-3 (T1-T4) cancers of the larynx, hypopharynx, or oral cavity, and either p16-negative oropharynx cancers or T4 or N3 p16-positive oropharynx cancer. Patients were required to be eligible for high-dose cisplatin-based CRT.
A total of 804 patients were randomized, 402 in each arm, to receive either pembrolizumab 200 mg intravenously every 3 weeks for 3 cycles plus CRT followed by maintenance pembrolizumab for 14 cycles, or to placebo plus CRT followed by placebo maintenance.
As noted before, there was no significant difference between the study arms for the primary endpoint of EFS. The 24-month EFS rate was 63.2% for the pembrolizumab group, compared with 56.2% for controls. The respective 6-month EFS rates were 57.4% versus 52.1%.
In a post hoc analysis, both EFS and overall survival were numerically with pembrolizumab among patients with PD-L1 CPS of 20 or greater. The respective 2- and 3-year EFS rates were 71.2% versus 62.6%, and 66.7% versus 57.2%.
The 24-months overall survival rates were 83.3% with pembrolizumab and 79.9% with placebo, and 36-month rates were 79.1% and 73%, respectively.
Neither EFS rates nor OS rates among patients in this subgroup differed significantly; however, there were no new safety signals with the combination, Dr. Machiels said. The incidence of grade 3 or greater adverse events was 92.2% in the pembrolizumab arm versus 88.4% in the placebo arm. Four patients in the pembrolizumab arm and six in the control arm died from treatment-related causes.
Benefit still to be proven
In a media briefing held prior to his presentation, Dr. Machiels was asked how he could justify his conclusions about a benefit for adding pembrolizumab given that there was no difference between the treatment groups for the primary endpoint.
He said that when the investigators designed the trial 7 years ago, the CPS score for PD-L1 expression had not yet been developed, and that if it had been they might have designed the trial to explore the effect of the pembrolizumab chemoradiation combination according to CPS subgroups.
He also pointed to the numerically superior 2-year EFS and overall rates.
In the presidential symposium, James Larkin, MD, PhD, an invited discussant from the Royal Marsden Hospital, London, said that chemotherapy and anti–PD-1 therapies are known to offer benefit in advanced cancers despite the trial’s failure.
“There is a signal, particularly as we’ve seen in the high PD-L1 group,” he said, noting that the signal was consistent with that seen in the JAVELIN 100 study, which was also a negative trial. He cautioned against relying too heavily on the comparison, however, as JAVELIN 100 was conducted with avelumab, a PD-L1 inhibitor, whereas pembrolizumab is a PD-1 inhibitor.
“Could there be an issue here with treatment schedule? An example and a comparison might be the PACIFIC study in non–small cell lung cancer, which is a positive trial, where actually the checkpoint inhibit with durvalumab was given immediately after the chemoradiotherapy, leading to benefit, rather than being concurrent,” he said.
Dr. Larkin also questioned whether, as codiscussant Sherene Loi, MD, PhD, from the Peter MacCallum Cancer Center, Melbourne, suggested radiotherapy to lymph nodes might alter the immune response to checkpoint inhibitors.
“Clearly radiotherapy is the central component of treatment in this setting, so it would be quite difficult to scale too much on that, but the question is: ‘Could it be modified?’ For example, just to irradiate the primary tumor and involved lymph nodes and potentially spare noninvolved lymph nodes,” he said.
The KEYNOTE-412 study was funded by Merck Sharp & Dohme. Dr. Machiels reported uncompensated consulting to the company. Dr. Larkin reported consulting for and receiving honoraria from Merck and others. Dr. Loi reported uncompensated advisory board activity for Merck and others.
AT ESMO CONGRESS 2022
In NSCLC, not all EGFR mutations are the same
In non–small cell lung cancer (NSCLC), . However, there is a range of different EGFR mutations, and different mutation combinations can lead to different tumor characteristics that might in turn affect response to therapy.
A new real-world analysis of 159 NSCLC patients found that a combination of a mutation of the TP53 tumor suppressor gene and the EGFR Ex20 mutation is associated with worse disease outcomes, compared to patients with the EGFR Ex20 mutation alone. But the news wasn’t all bad. The same group of patients also responded better to ICB (immune checkpoint blockade) therapy than did the broader population of EGFR Ex20 patients.
The EGFR Ex20 mutation occurs in about 4% of NSCLC cases, while TP53 is quite common: The new study found a frequency of 43.9%. “We first have to mention that the findings regarding TP53 do not reach statistical significance; however, the trend is very strong, and results might be hampered due to small sample sizes. We think it is [appropriate] to exhaust more treatment options for these patients, especially targeted approaches with newer drugs that specifically target exon 20 insertions, as these drugs were not applied in our cohort,” Anna Kron, Dr. rer. medic., said in an email exchange. Dr. Kron presented the results at a poster session in Paris at the ESMO Congress. She is a researcher at University Hospital of Cologne, Germany.
The ImmunoTarget study, published in 2019, examined over 500 NSCLC patients with a range of driver mutations including EGFR and found that they responded poorly to ICIs in comparison to KRAS mutations.
But Dr. Kron’s group was not convinced. “Ex20 mutations differ clinically from other tyrosine kinase mutations in EGFR. We set out this study to rechallenge the paradigm of impaired benefit from ICI in EGFR-mutated patients, as we consider these mutations not interchangeable with other EGFR mutations,” Dr. Kron said.
“We would postulate that in EGFR Exon 20 mutations, ICI and specific inhibitors should be part of the therapeutic course. In patients with co-occurring TP53 mutations, treatment escalation could be considered,” Dr. Kron said.
The study included 159 patients with advanced NSCLC with the EGFR exon 20 insertion, who were treated between 2014 and 2020 at German hospitals. Among the patients, 37.7% were female; mean age at diagnosis was 65.87 years; 50.3% had a smoking history and 38.4% did not (data were unavailable for the rest); and 9.4% of tumors were stage I, 4.4% stage II, 8.2% stage IIIA, 3.8% stage IIIB, and 74.2% stage IV.
Over a follow-up of 4.1 years, there was a trend toward longer survival among patients with TP53 wild type (OS, 20 versus 12 months; P = .092). Sixty-six patients who received ICI therapy had better OS compared with those who did not (22 versus 10 months; P = .018). Among patients with co-occurring TP53 mutations, receipt of ICI therapy was associated with longer OS (16 versus 8 months; P = .048). There was a trend toward patients with TP53 wild type treated with ICI faring better than those who didn’t receive ICI (27.0 months versus 11.0 months; P = .109).
The researchers are continuing to study patients with EGFR Ex20 to better understand the role of TP53 and ICI therapy in these patients.
The study received no funding. Dr. Kron has no relevant financial disclosures.
In non–small cell lung cancer (NSCLC), . However, there is a range of different EGFR mutations, and different mutation combinations can lead to different tumor characteristics that might in turn affect response to therapy.
A new real-world analysis of 159 NSCLC patients found that a combination of a mutation of the TP53 tumor suppressor gene and the EGFR Ex20 mutation is associated with worse disease outcomes, compared to patients with the EGFR Ex20 mutation alone. But the news wasn’t all bad. The same group of patients also responded better to ICB (immune checkpoint blockade) therapy than did the broader population of EGFR Ex20 patients.
The EGFR Ex20 mutation occurs in about 4% of NSCLC cases, while TP53 is quite common: The new study found a frequency of 43.9%. “We first have to mention that the findings regarding TP53 do not reach statistical significance; however, the trend is very strong, and results might be hampered due to small sample sizes. We think it is [appropriate] to exhaust more treatment options for these patients, especially targeted approaches with newer drugs that specifically target exon 20 insertions, as these drugs were not applied in our cohort,” Anna Kron, Dr. rer. medic., said in an email exchange. Dr. Kron presented the results at a poster session in Paris at the ESMO Congress. She is a researcher at University Hospital of Cologne, Germany.
The ImmunoTarget study, published in 2019, examined over 500 NSCLC patients with a range of driver mutations including EGFR and found that they responded poorly to ICIs in comparison to KRAS mutations.
But Dr. Kron’s group was not convinced. “Ex20 mutations differ clinically from other tyrosine kinase mutations in EGFR. We set out this study to rechallenge the paradigm of impaired benefit from ICI in EGFR-mutated patients, as we consider these mutations not interchangeable with other EGFR mutations,” Dr. Kron said.
“We would postulate that in EGFR Exon 20 mutations, ICI and specific inhibitors should be part of the therapeutic course. In patients with co-occurring TP53 mutations, treatment escalation could be considered,” Dr. Kron said.
The study included 159 patients with advanced NSCLC with the EGFR exon 20 insertion, who were treated between 2014 and 2020 at German hospitals. Among the patients, 37.7% were female; mean age at diagnosis was 65.87 years; 50.3% had a smoking history and 38.4% did not (data were unavailable for the rest); and 9.4% of tumors were stage I, 4.4% stage II, 8.2% stage IIIA, 3.8% stage IIIB, and 74.2% stage IV.
Over a follow-up of 4.1 years, there was a trend toward longer survival among patients with TP53 wild type (OS, 20 versus 12 months; P = .092). Sixty-six patients who received ICI therapy had better OS compared with those who did not (22 versus 10 months; P = .018). Among patients with co-occurring TP53 mutations, receipt of ICI therapy was associated with longer OS (16 versus 8 months; P = .048). There was a trend toward patients with TP53 wild type treated with ICI faring better than those who didn’t receive ICI (27.0 months versus 11.0 months; P = .109).
The researchers are continuing to study patients with EGFR Ex20 to better understand the role of TP53 and ICI therapy in these patients.
The study received no funding. Dr. Kron has no relevant financial disclosures.
In non–small cell lung cancer (NSCLC), . However, there is a range of different EGFR mutations, and different mutation combinations can lead to different tumor characteristics that might in turn affect response to therapy.
A new real-world analysis of 159 NSCLC patients found that a combination of a mutation of the TP53 tumor suppressor gene and the EGFR Ex20 mutation is associated with worse disease outcomes, compared to patients with the EGFR Ex20 mutation alone. But the news wasn’t all bad. The same group of patients also responded better to ICB (immune checkpoint blockade) therapy than did the broader population of EGFR Ex20 patients.
The EGFR Ex20 mutation occurs in about 4% of NSCLC cases, while TP53 is quite common: The new study found a frequency of 43.9%. “We first have to mention that the findings regarding TP53 do not reach statistical significance; however, the trend is very strong, and results might be hampered due to small sample sizes. We think it is [appropriate] to exhaust more treatment options for these patients, especially targeted approaches with newer drugs that specifically target exon 20 insertions, as these drugs were not applied in our cohort,” Anna Kron, Dr. rer. medic., said in an email exchange. Dr. Kron presented the results at a poster session in Paris at the ESMO Congress. She is a researcher at University Hospital of Cologne, Germany.
The ImmunoTarget study, published in 2019, examined over 500 NSCLC patients with a range of driver mutations including EGFR and found that they responded poorly to ICIs in comparison to KRAS mutations.
But Dr. Kron’s group was not convinced. “Ex20 mutations differ clinically from other tyrosine kinase mutations in EGFR. We set out this study to rechallenge the paradigm of impaired benefit from ICI in EGFR-mutated patients, as we consider these mutations not interchangeable with other EGFR mutations,” Dr. Kron said.
“We would postulate that in EGFR Exon 20 mutations, ICI and specific inhibitors should be part of the therapeutic course. In patients with co-occurring TP53 mutations, treatment escalation could be considered,” Dr. Kron said.
The study included 159 patients with advanced NSCLC with the EGFR exon 20 insertion, who were treated between 2014 and 2020 at German hospitals. Among the patients, 37.7% were female; mean age at diagnosis was 65.87 years; 50.3% had a smoking history and 38.4% did not (data were unavailable for the rest); and 9.4% of tumors were stage I, 4.4% stage II, 8.2% stage IIIA, 3.8% stage IIIB, and 74.2% stage IV.
Over a follow-up of 4.1 years, there was a trend toward longer survival among patients with TP53 wild type (OS, 20 versus 12 months; P = .092). Sixty-six patients who received ICI therapy had better OS compared with those who did not (22 versus 10 months; P = .018). Among patients with co-occurring TP53 mutations, receipt of ICI therapy was associated with longer OS (16 versus 8 months; P = .048). There was a trend toward patients with TP53 wild type treated with ICI faring better than those who didn’t receive ICI (27.0 months versus 11.0 months; P = .109).
The researchers are continuing to study patients with EGFR Ex20 to better understand the role of TP53 and ICI therapy in these patients.
The study received no funding. Dr. Kron has no relevant financial disclosures.
FROM ESMO CONGRESS 2022
Spondyloarthritis disease activity measurement with ASDAS not influenced by gender
GHENT, BELGIUM – The Ankylosing Spondylitis Disease Activity Score (ASDAS) should be the preferred tool for disease activity assessment in patients with axial spondyloarthritis (axSpA) because it is not influenced by gender, according to new data on gender and patient outcomes as assessed by commonly used scoring methods and indices across the spectrum of SpA disease subtypes.
In contrast, researchers led by Diego Benavent, MD, a rheumatologist at La Paz University Hospital, Madrid, found that gender influenced the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) in all three disease subtypes: axSpA, peripheral SpA (pSpA), and psoriatic arthritis (PsA).
In addition, data show that women with axSpA, pSpA, or PsA reported higher disease activity, functional limitation, and poorer overall health.
Dr. Benavent presented the results at the 13th International Congress on Spondyloarthritides. The study was also published online Sept. 12 in RMD Open.
“The ASDAS is more likely to be the activity score used because we are reassured that it performs well in both men and women. However, there is a need for more appropriate validated indices that are not affected by gender in peripheral spondyloarthropathies and psoriatic arthritis,” Dr. Benavent said.
So far, most data concerning gender differences have been described in patients with axSpA, and with various measurement instruments available to assess disease activity, function, and overall health. Dr. Benavent and his colleagues wanted to investigate the influence of gender on disease outcomes across not only axSpA but pSpA and PsA, too, to see if there were differences in the relationship between gender and these other disease subtypes.
In previous studies, ASDAS has shown better psychometric properties than the BASDAI for disease activity in axSpA. “But there is little validation in pSpA and PsA, and the influence of gender in the outcomes assessed by these instruments is unknown.
“Compared with men, women with an axSpA diagnosis tend to have more frequent peripheral and extramusculoskeletal manifestations, such as enthesitis and inflammatory bowel disease,” Dr. Benavent said in an interview. “However, males with axSpA present more radiographic damage and objective signs of inflammation.”
Martin Rudwaleit, MD, head of the department of internal medicine and rheumatology at Klinikum Bielefeld (Germany), who attended the talk, reflected on the findings.
“Decades ago, ankylosing spondylitis was largely considered a male disease as found in 80%-90% of cases. Later, with MRI, we started to diagnose patients earlier and learned that more females have the disease and that females have less structural damage in the spine than men. As such, male gender is a predictor for worse radiographic progression,” Dr. Rudwaleit said.
“The question is whether the female patients who are considered to have axSpA really have axSpA, or do they have other origins of their back pain?” he continued.
“Also, this study shows us that females report a wider spectrum of symptoms than males. For example, headache, general discomfort, and overall, a broader spectrum of symptoms than men. This might have contributed to the fact that, previously, diagnoses of axSpA might have been made later in females than males.”
Large study across SpA phenotypes and disease-scoring methods
A total of 4,185 patients from 24 countries participated, with 65% having axSpA, 10% pSpA, and 25% PsA. Females totaled 38.8% of patients across all three types of spondyloarthritis. The researchers drew the data from the Assessment of SpondyloArthritis International Society (ASAS)-perSpA study.
The researchers looked for associations between gender and disease activity as measured by ASDAS and BASDAI, C-reactive protein (CRP), physical function with the Bath Ankylosing Spondylitis Functional Index (BASFI), overall health with the ASAS Health Index (ASAS HI), and European Quality of Life Five Dimensions (EQ-5D) outcomes.
In axSpA, there was a split of 68% men vs. 32% women. The researchers observed certain factors that were more common among men: smoking (49% vs. 32%), HLA-B27 positivity (83% vs. 70%), and elevated CRP (75% vs. 66%). Women more often had enthesitis (45% vs. 39%) and fibromyalgia (17% vs. 3%).
In pSpA, the gender split was approximately equal at 47% men and 53% women. But compared with women, men had more inflammatory back pain (62% vs. 50%), HLA-B27 positivity (70% vs. 54%), and elevated CRP (75% vs. 66%). Women more frequently had inflammatory bowel disease (IBD, 8% vs. 3%) and fibromyalgia (18% vs. 3%).
An approximately equal gender split was also found with PsA (48.5% men vs. 51.5% women). Men more frequently reported ever drinking alcohol than did women (63% vs. 26%), whereas women had a greater family history of both spondyloarthritis (41% vs. 32%) and psoriasis (41% vs. 31%). Women also more often reported enthesitis (49% vs. 42%) and fibromyalgia (19% vs. 3%) than men.
“These data strongly suggest that female patients showed significantly more fibromyalgia across all disease subtypes, and the magnitude of the difference with men is notable,” Dr. Benavent said.”Fibromyalgia is associated with pain and worse patient-reported outcomes, which may bias outcomes with disease activity scores.”
When the researchers analyzed outcomes by the different scores and indices for each disease subtype, they found that females had worse scores for most indices (ASDAS, BASDAI, patient’s global assessment (PtGA), BASFI, ASAS HI, and EQ-5D). “However, for CRP, men presented worse scores across axSpA and pSpA, and no differences were found with women in PsA,” Dr. Benavent added.
Although there are differences between the genders according to the scores, these differences may be confounded and this will affect the score outcome: for example, confounding by fibromyalgia in women, he explained.
To avoid the confounding effect, multivariable regression models were used, including the dependent variable as the explored outcome: for example, with BASDAI or ASDAS serving as the dependent variable and gender as the main independent variable, along with adjustments for potential confounders. When the influence of gender on BASDAI was considered, Dr. Benavent and colleagues found that being female increased all scores across the spectrum: axSpA (0.39 units; 95% confidence interval, 0.2-0.58), pSpA (1.22 units; 95% CI, 0.77-1.69), and PsA (0.88 units; 95% CI, 0.59-1.19). When the influence of gender on ASDAS was considered, the researchers found that being female had no effect on axSpA (0.02 units; 95% CI, –0.07 to 0.11), but did for pSpA (0.36 units; 95% CI, 0.15-0.58) and PsA (0.25 units; 95% CI, 0.12-0.38).
“ASDAS is better than BASDAI because it is similar in males and females, but this only holds true in axSpA, not in pSpA or PsA,” Dr. Benavent concluded.
Dr. Benavent declared serving on speakers bureaus for Janssen, Galapagos, and AbbVie, and receiving grant or research support from Novartis outside the submitted work. Dr. Rudwaleit declared financial relationships with AbbVie, UCB, and Lilly.
GHENT, BELGIUM – The Ankylosing Spondylitis Disease Activity Score (ASDAS) should be the preferred tool for disease activity assessment in patients with axial spondyloarthritis (axSpA) because it is not influenced by gender, according to new data on gender and patient outcomes as assessed by commonly used scoring methods and indices across the spectrum of SpA disease subtypes.
In contrast, researchers led by Diego Benavent, MD, a rheumatologist at La Paz University Hospital, Madrid, found that gender influenced the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) in all three disease subtypes: axSpA, peripheral SpA (pSpA), and psoriatic arthritis (PsA).
In addition, data show that women with axSpA, pSpA, or PsA reported higher disease activity, functional limitation, and poorer overall health.
Dr. Benavent presented the results at the 13th International Congress on Spondyloarthritides. The study was also published online Sept. 12 in RMD Open.
“The ASDAS is more likely to be the activity score used because we are reassured that it performs well in both men and women. However, there is a need for more appropriate validated indices that are not affected by gender in peripheral spondyloarthropathies and psoriatic arthritis,” Dr. Benavent said.
So far, most data concerning gender differences have been described in patients with axSpA, and with various measurement instruments available to assess disease activity, function, and overall health. Dr. Benavent and his colleagues wanted to investigate the influence of gender on disease outcomes across not only axSpA but pSpA and PsA, too, to see if there were differences in the relationship between gender and these other disease subtypes.
In previous studies, ASDAS has shown better psychometric properties than the BASDAI for disease activity in axSpA. “But there is little validation in pSpA and PsA, and the influence of gender in the outcomes assessed by these instruments is unknown.
“Compared with men, women with an axSpA diagnosis tend to have more frequent peripheral and extramusculoskeletal manifestations, such as enthesitis and inflammatory bowel disease,” Dr. Benavent said in an interview. “However, males with axSpA present more radiographic damage and objective signs of inflammation.”
Martin Rudwaleit, MD, head of the department of internal medicine and rheumatology at Klinikum Bielefeld (Germany), who attended the talk, reflected on the findings.
“Decades ago, ankylosing spondylitis was largely considered a male disease as found in 80%-90% of cases. Later, with MRI, we started to diagnose patients earlier and learned that more females have the disease and that females have less structural damage in the spine than men. As such, male gender is a predictor for worse radiographic progression,” Dr. Rudwaleit said.
“The question is whether the female patients who are considered to have axSpA really have axSpA, or do they have other origins of their back pain?” he continued.
“Also, this study shows us that females report a wider spectrum of symptoms than males. For example, headache, general discomfort, and overall, a broader spectrum of symptoms than men. This might have contributed to the fact that, previously, diagnoses of axSpA might have been made later in females than males.”
Large study across SpA phenotypes and disease-scoring methods
A total of 4,185 patients from 24 countries participated, with 65% having axSpA, 10% pSpA, and 25% PsA. Females totaled 38.8% of patients across all three types of spondyloarthritis. The researchers drew the data from the Assessment of SpondyloArthritis International Society (ASAS)-perSpA study.
The researchers looked for associations between gender and disease activity as measured by ASDAS and BASDAI, C-reactive protein (CRP), physical function with the Bath Ankylosing Spondylitis Functional Index (BASFI), overall health with the ASAS Health Index (ASAS HI), and European Quality of Life Five Dimensions (EQ-5D) outcomes.
In axSpA, there was a split of 68% men vs. 32% women. The researchers observed certain factors that were more common among men: smoking (49% vs. 32%), HLA-B27 positivity (83% vs. 70%), and elevated CRP (75% vs. 66%). Women more often had enthesitis (45% vs. 39%) and fibromyalgia (17% vs. 3%).
In pSpA, the gender split was approximately equal at 47% men and 53% women. But compared with women, men had more inflammatory back pain (62% vs. 50%), HLA-B27 positivity (70% vs. 54%), and elevated CRP (75% vs. 66%). Women more frequently had inflammatory bowel disease (IBD, 8% vs. 3%) and fibromyalgia (18% vs. 3%).
An approximately equal gender split was also found with PsA (48.5% men vs. 51.5% women). Men more frequently reported ever drinking alcohol than did women (63% vs. 26%), whereas women had a greater family history of both spondyloarthritis (41% vs. 32%) and psoriasis (41% vs. 31%). Women also more often reported enthesitis (49% vs. 42%) and fibromyalgia (19% vs. 3%) than men.
“These data strongly suggest that female patients showed significantly more fibromyalgia across all disease subtypes, and the magnitude of the difference with men is notable,” Dr. Benavent said.”Fibromyalgia is associated with pain and worse patient-reported outcomes, which may bias outcomes with disease activity scores.”
When the researchers analyzed outcomes by the different scores and indices for each disease subtype, they found that females had worse scores for most indices (ASDAS, BASDAI, patient’s global assessment (PtGA), BASFI, ASAS HI, and EQ-5D). “However, for CRP, men presented worse scores across axSpA and pSpA, and no differences were found with women in PsA,” Dr. Benavent added.
Although there are differences between the genders according to the scores, these differences may be confounded and this will affect the score outcome: for example, confounding by fibromyalgia in women, he explained.
To avoid the confounding effect, multivariable regression models were used, including the dependent variable as the explored outcome: for example, with BASDAI or ASDAS serving as the dependent variable and gender as the main independent variable, along with adjustments for potential confounders. When the influence of gender on BASDAI was considered, Dr. Benavent and colleagues found that being female increased all scores across the spectrum: axSpA (0.39 units; 95% confidence interval, 0.2-0.58), pSpA (1.22 units; 95% CI, 0.77-1.69), and PsA (0.88 units; 95% CI, 0.59-1.19). When the influence of gender on ASDAS was considered, the researchers found that being female had no effect on axSpA (0.02 units; 95% CI, –0.07 to 0.11), but did for pSpA (0.36 units; 95% CI, 0.15-0.58) and PsA (0.25 units; 95% CI, 0.12-0.38).
“ASDAS is better than BASDAI because it is similar in males and females, but this only holds true in axSpA, not in pSpA or PsA,” Dr. Benavent concluded.
Dr. Benavent declared serving on speakers bureaus for Janssen, Galapagos, and AbbVie, and receiving grant or research support from Novartis outside the submitted work. Dr. Rudwaleit declared financial relationships with AbbVie, UCB, and Lilly.
GHENT, BELGIUM – The Ankylosing Spondylitis Disease Activity Score (ASDAS) should be the preferred tool for disease activity assessment in patients with axial spondyloarthritis (axSpA) because it is not influenced by gender, according to new data on gender and patient outcomes as assessed by commonly used scoring methods and indices across the spectrum of SpA disease subtypes.
In contrast, researchers led by Diego Benavent, MD, a rheumatologist at La Paz University Hospital, Madrid, found that gender influenced the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) in all three disease subtypes: axSpA, peripheral SpA (pSpA), and psoriatic arthritis (PsA).
In addition, data show that women with axSpA, pSpA, or PsA reported higher disease activity, functional limitation, and poorer overall health.
Dr. Benavent presented the results at the 13th International Congress on Spondyloarthritides. The study was also published online Sept. 12 in RMD Open.
“The ASDAS is more likely to be the activity score used because we are reassured that it performs well in both men and women. However, there is a need for more appropriate validated indices that are not affected by gender in peripheral spondyloarthropathies and psoriatic arthritis,” Dr. Benavent said.
So far, most data concerning gender differences have been described in patients with axSpA, and with various measurement instruments available to assess disease activity, function, and overall health. Dr. Benavent and his colleagues wanted to investigate the influence of gender on disease outcomes across not only axSpA but pSpA and PsA, too, to see if there were differences in the relationship between gender and these other disease subtypes.
In previous studies, ASDAS has shown better psychometric properties than the BASDAI for disease activity in axSpA. “But there is little validation in pSpA and PsA, and the influence of gender in the outcomes assessed by these instruments is unknown.
“Compared with men, women with an axSpA diagnosis tend to have more frequent peripheral and extramusculoskeletal manifestations, such as enthesitis and inflammatory bowel disease,” Dr. Benavent said in an interview. “However, males with axSpA present more radiographic damage and objective signs of inflammation.”
Martin Rudwaleit, MD, head of the department of internal medicine and rheumatology at Klinikum Bielefeld (Germany), who attended the talk, reflected on the findings.
“Decades ago, ankylosing spondylitis was largely considered a male disease as found in 80%-90% of cases. Later, with MRI, we started to diagnose patients earlier and learned that more females have the disease and that females have less structural damage in the spine than men. As such, male gender is a predictor for worse radiographic progression,” Dr. Rudwaleit said.
“The question is whether the female patients who are considered to have axSpA really have axSpA, or do they have other origins of their back pain?” he continued.
“Also, this study shows us that females report a wider spectrum of symptoms than males. For example, headache, general discomfort, and overall, a broader spectrum of symptoms than men. This might have contributed to the fact that, previously, diagnoses of axSpA might have been made later in females than males.”
Large study across SpA phenotypes and disease-scoring methods
A total of 4,185 patients from 24 countries participated, with 65% having axSpA, 10% pSpA, and 25% PsA. Females totaled 38.8% of patients across all three types of spondyloarthritis. The researchers drew the data from the Assessment of SpondyloArthritis International Society (ASAS)-perSpA study.
The researchers looked for associations between gender and disease activity as measured by ASDAS and BASDAI, C-reactive protein (CRP), physical function with the Bath Ankylosing Spondylitis Functional Index (BASFI), overall health with the ASAS Health Index (ASAS HI), and European Quality of Life Five Dimensions (EQ-5D) outcomes.
In axSpA, there was a split of 68% men vs. 32% women. The researchers observed certain factors that were more common among men: smoking (49% vs. 32%), HLA-B27 positivity (83% vs. 70%), and elevated CRP (75% vs. 66%). Women more often had enthesitis (45% vs. 39%) and fibromyalgia (17% vs. 3%).
In pSpA, the gender split was approximately equal at 47% men and 53% women. But compared with women, men had more inflammatory back pain (62% vs. 50%), HLA-B27 positivity (70% vs. 54%), and elevated CRP (75% vs. 66%). Women more frequently had inflammatory bowel disease (IBD, 8% vs. 3%) and fibromyalgia (18% vs. 3%).
An approximately equal gender split was also found with PsA (48.5% men vs. 51.5% women). Men more frequently reported ever drinking alcohol than did women (63% vs. 26%), whereas women had a greater family history of both spondyloarthritis (41% vs. 32%) and psoriasis (41% vs. 31%). Women also more often reported enthesitis (49% vs. 42%) and fibromyalgia (19% vs. 3%) than men.
“These data strongly suggest that female patients showed significantly more fibromyalgia across all disease subtypes, and the magnitude of the difference with men is notable,” Dr. Benavent said.”Fibromyalgia is associated with pain and worse patient-reported outcomes, which may bias outcomes with disease activity scores.”
When the researchers analyzed outcomes by the different scores and indices for each disease subtype, they found that females had worse scores for most indices (ASDAS, BASDAI, patient’s global assessment (PtGA), BASFI, ASAS HI, and EQ-5D). “However, for CRP, men presented worse scores across axSpA and pSpA, and no differences were found with women in PsA,” Dr. Benavent added.
Although there are differences between the genders according to the scores, these differences may be confounded and this will affect the score outcome: for example, confounding by fibromyalgia in women, he explained.
To avoid the confounding effect, multivariable regression models were used, including the dependent variable as the explored outcome: for example, with BASDAI or ASDAS serving as the dependent variable and gender as the main independent variable, along with adjustments for potential confounders. When the influence of gender on BASDAI was considered, Dr. Benavent and colleagues found that being female increased all scores across the spectrum: axSpA (0.39 units; 95% confidence interval, 0.2-0.58), pSpA (1.22 units; 95% CI, 0.77-1.69), and PsA (0.88 units; 95% CI, 0.59-1.19). When the influence of gender on ASDAS was considered, the researchers found that being female had no effect on axSpA (0.02 units; 95% CI, –0.07 to 0.11), but did for pSpA (0.36 units; 95% CI, 0.15-0.58) and PsA (0.25 units; 95% CI, 0.12-0.38).
“ASDAS is better than BASDAI because it is similar in males and females, but this only holds true in axSpA, not in pSpA or PsA,” Dr. Benavent concluded.
Dr. Benavent declared serving on speakers bureaus for Janssen, Galapagos, and AbbVie, and receiving grant or research support from Novartis outside the submitted work. Dr. Rudwaleit declared financial relationships with AbbVie, UCB, and Lilly.
AT THE 2022 SPA CONGRESS
In early NSCLC, comorbidities linked to survival
Cardiometabolic and respiratory comorbidities are associated with worse survival in patients with non–small cell lung cancer (NSCLC), and new research suggests a potential mechanism.
Prior studies had shown mixed results when it came to these comorbidities and survival, according to study coauthor author Geoffrey Liu, MD, who is an epidemiology researcher at the University of Toronto Princess Margaret Cancer Centre. The new work represents data from multiple continents, from various ethnicities and cultures.
“We found that comorbidities had much greater impact on earlier than later stages of lung cancer, consistent with this previous study,” said Dr. Liu in an email. The study was presented by Miguel Garcia-Pardo, who is a researcher at University of Toronto Princess Margaret Cancer Centre, during a poster session at the annual meeting of the European Society for Medical Oncology.
“Deaths from [cardiometabolic] comorbidities were mainly from non–lung cancer competing causes, whereas the deaths from respiratory comorbidities were primarily driven by lung cancer specific survival, i.e., deaths from lung cancer itself. We conclude that Dr. Liu said.
Dr. Liu noted that controlling cardiometabolic risk factors like diabetes and hypertension is typically de-emphasized after diagnosis with early-stage lung cancer. The rationale is often that the lung cancer is a more acute concern than longer-term cardiometabolic risks. “The data from our analyses suggest a rethinking of this strategy. We need to pay more attention to controlling cardiovascular risk factors in early-stage lung cancer,” Dr. Liu said.
The findings also suggest that respiratory comorbidities should be managed more aggressively. That would allow more patients to undergo treatments like surgery and stereotactic radiation.
The Clinical Outcome Studies of the International Lung Cancer Consortium drew from two dozen studies conducted across five continents. It examined clinical, epidemiologic, genetic, and genomic factors and their potential influence on NSCLC outcomes. Cardiometabolic comorbidities included coronary artery disease, diabetes, vascular related diseases, and other heart diseases. Respiratory comorbidities included chronic obstructive pulmonary disease and asthma.
The analysis included 16,354 patients. Among patients with stage I NSCLC, there was an association between reduced overall survival (OS) and cardiometabolic comorbidity (adjusted hazard ratio, 1.17; P = .01) and respiratory comorbidity (aHR, 1.36; P < .001). For stage II/III patients, there was no significant association between OS and cardiometabolic comorbidities, but respiratory comorbidity was associated with worse OS (aHR, 1.15; P < .001). In stage 4, worse OS was associated with both cardiometabolic health comorbidity (aHR, 1.11; P = .03), but not respiratory comorbidity.
Among patients with stage IV NSCLC, there were no associations between overall survival or lung cancer–specific survival (LCSS) and respiratory or cardiometabolic risk factors. However, an examination of cause of death found a different pattern in patients with stage IB-IIIA disease: LCSS was worse among patients with respiratory comorbidities (aHR, 1.21; 95% CI, 1.09-1.34). Among those with cardiovascular comorbidities, the risk of non-NSCLC mortality was higher (aHR, 1.36; 95% CI, 1.15-1.63). The presence of respiratory comorbidity was associated with a reduced probability of undergoing surgical resection for both stage I (adjusted odds ratio, 0.45; 95% CI, 0.35-0.59) and stage II/III patients (aOR, 0.66; 95% CI, 0.53-0.80).
There was an association between non-NSCLC mortality and cardiometabolic comorbidities in stage IA (aHR, 1.37; 95% CI, 1.06-1.77) and in stages IB-IIIA (aHR, 1.32; 95% CI, 1.03-1.71) NSCLC. There were also associations between NSCLC mortality and respiratory comorbidity among stage IA (aHR, 1.51; 95% CI, 1.17-1.95) and stages IB-IIIA (aHR, 1.20; 95% CI, 1.06-1.36) NSCLC. There were no associations between respiratory comorbidity and non-NSCLC mortality.
Respiratory comorbidity was associated with a lower chance of undergoing surgical resection in stage IA (aHR, 0.54; 95% CI, 0.35-0.83) and stage IB-IIIA (aHR, 0.57; 95% CI, 0.46-0.70) cancers. Cardiometabolic comorbidity was associated with a lower rate of surgical resection only in stage 1B-3A patients (aHR, 0.73; 95% CI, 0.56-0.96). Among those who underwent resection, stage IA patients were less likely to die of lung cancer (aHR, 0.38; 95% CI, 0.28-0.52) but more likely to die of other causes (aHR, 1.73; 95% CI, 1.07-1.78). Stage IB-IIIA patients who underwent resection were less likely to die of lung cancer (aHR, 0.37; 95%, 0.32-0.42), but there was no significant association with non–lung cancer mortality.
The study was funded by the Lusi Wong Family Fund and the Alan Brown Chair. Dr. Liu has no relevant financial disclosures.
Cardiometabolic and respiratory comorbidities are associated with worse survival in patients with non–small cell lung cancer (NSCLC), and new research suggests a potential mechanism.
Prior studies had shown mixed results when it came to these comorbidities and survival, according to study coauthor author Geoffrey Liu, MD, who is an epidemiology researcher at the University of Toronto Princess Margaret Cancer Centre. The new work represents data from multiple continents, from various ethnicities and cultures.
“We found that comorbidities had much greater impact on earlier than later stages of lung cancer, consistent with this previous study,” said Dr. Liu in an email. The study was presented by Miguel Garcia-Pardo, who is a researcher at University of Toronto Princess Margaret Cancer Centre, during a poster session at the annual meeting of the European Society for Medical Oncology.
“Deaths from [cardiometabolic] comorbidities were mainly from non–lung cancer competing causes, whereas the deaths from respiratory comorbidities were primarily driven by lung cancer specific survival, i.e., deaths from lung cancer itself. We conclude that Dr. Liu said.
Dr. Liu noted that controlling cardiometabolic risk factors like diabetes and hypertension is typically de-emphasized after diagnosis with early-stage lung cancer. The rationale is often that the lung cancer is a more acute concern than longer-term cardiometabolic risks. “The data from our analyses suggest a rethinking of this strategy. We need to pay more attention to controlling cardiovascular risk factors in early-stage lung cancer,” Dr. Liu said.
The findings also suggest that respiratory comorbidities should be managed more aggressively. That would allow more patients to undergo treatments like surgery and stereotactic radiation.
The Clinical Outcome Studies of the International Lung Cancer Consortium drew from two dozen studies conducted across five continents. It examined clinical, epidemiologic, genetic, and genomic factors and their potential influence on NSCLC outcomes. Cardiometabolic comorbidities included coronary artery disease, diabetes, vascular related diseases, and other heart diseases. Respiratory comorbidities included chronic obstructive pulmonary disease and asthma.
The analysis included 16,354 patients. Among patients with stage I NSCLC, there was an association between reduced overall survival (OS) and cardiometabolic comorbidity (adjusted hazard ratio, 1.17; P = .01) and respiratory comorbidity (aHR, 1.36; P < .001). For stage II/III patients, there was no significant association between OS and cardiometabolic comorbidities, but respiratory comorbidity was associated with worse OS (aHR, 1.15; P < .001). In stage 4, worse OS was associated with both cardiometabolic health comorbidity (aHR, 1.11; P = .03), but not respiratory comorbidity.
Among patients with stage IV NSCLC, there were no associations between overall survival or lung cancer–specific survival (LCSS) and respiratory or cardiometabolic risk factors. However, an examination of cause of death found a different pattern in patients with stage IB-IIIA disease: LCSS was worse among patients with respiratory comorbidities (aHR, 1.21; 95% CI, 1.09-1.34). Among those with cardiovascular comorbidities, the risk of non-NSCLC mortality was higher (aHR, 1.36; 95% CI, 1.15-1.63). The presence of respiratory comorbidity was associated with a reduced probability of undergoing surgical resection for both stage I (adjusted odds ratio, 0.45; 95% CI, 0.35-0.59) and stage II/III patients (aOR, 0.66; 95% CI, 0.53-0.80).
There was an association between non-NSCLC mortality and cardiometabolic comorbidities in stage IA (aHR, 1.37; 95% CI, 1.06-1.77) and in stages IB-IIIA (aHR, 1.32; 95% CI, 1.03-1.71) NSCLC. There were also associations between NSCLC mortality and respiratory comorbidity among stage IA (aHR, 1.51; 95% CI, 1.17-1.95) and stages IB-IIIA (aHR, 1.20; 95% CI, 1.06-1.36) NSCLC. There were no associations between respiratory comorbidity and non-NSCLC mortality.
Respiratory comorbidity was associated with a lower chance of undergoing surgical resection in stage IA (aHR, 0.54; 95% CI, 0.35-0.83) and stage IB-IIIA (aHR, 0.57; 95% CI, 0.46-0.70) cancers. Cardiometabolic comorbidity was associated with a lower rate of surgical resection only in stage 1B-3A patients (aHR, 0.73; 95% CI, 0.56-0.96). Among those who underwent resection, stage IA patients were less likely to die of lung cancer (aHR, 0.38; 95% CI, 0.28-0.52) but more likely to die of other causes (aHR, 1.73; 95% CI, 1.07-1.78). Stage IB-IIIA patients who underwent resection were less likely to die of lung cancer (aHR, 0.37; 95%, 0.32-0.42), but there was no significant association with non–lung cancer mortality.
The study was funded by the Lusi Wong Family Fund and the Alan Brown Chair. Dr. Liu has no relevant financial disclosures.
Cardiometabolic and respiratory comorbidities are associated with worse survival in patients with non–small cell lung cancer (NSCLC), and new research suggests a potential mechanism.
Prior studies had shown mixed results when it came to these comorbidities and survival, according to study coauthor author Geoffrey Liu, MD, who is an epidemiology researcher at the University of Toronto Princess Margaret Cancer Centre. The new work represents data from multiple continents, from various ethnicities and cultures.
“We found that comorbidities had much greater impact on earlier than later stages of lung cancer, consistent with this previous study,” said Dr. Liu in an email. The study was presented by Miguel Garcia-Pardo, who is a researcher at University of Toronto Princess Margaret Cancer Centre, during a poster session at the annual meeting of the European Society for Medical Oncology.
“Deaths from [cardiometabolic] comorbidities were mainly from non–lung cancer competing causes, whereas the deaths from respiratory comorbidities were primarily driven by lung cancer specific survival, i.e., deaths from lung cancer itself. We conclude that Dr. Liu said.
Dr. Liu noted that controlling cardiometabolic risk factors like diabetes and hypertension is typically de-emphasized after diagnosis with early-stage lung cancer. The rationale is often that the lung cancer is a more acute concern than longer-term cardiometabolic risks. “The data from our analyses suggest a rethinking of this strategy. We need to pay more attention to controlling cardiovascular risk factors in early-stage lung cancer,” Dr. Liu said.
The findings also suggest that respiratory comorbidities should be managed more aggressively. That would allow more patients to undergo treatments like surgery and stereotactic radiation.
The Clinical Outcome Studies of the International Lung Cancer Consortium drew from two dozen studies conducted across five continents. It examined clinical, epidemiologic, genetic, and genomic factors and their potential influence on NSCLC outcomes. Cardiometabolic comorbidities included coronary artery disease, diabetes, vascular related diseases, and other heart diseases. Respiratory comorbidities included chronic obstructive pulmonary disease and asthma.
The analysis included 16,354 patients. Among patients with stage I NSCLC, there was an association between reduced overall survival (OS) and cardiometabolic comorbidity (adjusted hazard ratio, 1.17; P = .01) and respiratory comorbidity (aHR, 1.36; P < .001). For stage II/III patients, there was no significant association between OS and cardiometabolic comorbidities, but respiratory comorbidity was associated with worse OS (aHR, 1.15; P < .001). In stage 4, worse OS was associated with both cardiometabolic health comorbidity (aHR, 1.11; P = .03), but not respiratory comorbidity.
Among patients with stage IV NSCLC, there were no associations between overall survival or lung cancer–specific survival (LCSS) and respiratory or cardiometabolic risk factors. However, an examination of cause of death found a different pattern in patients with stage IB-IIIA disease: LCSS was worse among patients with respiratory comorbidities (aHR, 1.21; 95% CI, 1.09-1.34). Among those with cardiovascular comorbidities, the risk of non-NSCLC mortality was higher (aHR, 1.36; 95% CI, 1.15-1.63). The presence of respiratory comorbidity was associated with a reduced probability of undergoing surgical resection for both stage I (adjusted odds ratio, 0.45; 95% CI, 0.35-0.59) and stage II/III patients (aOR, 0.66; 95% CI, 0.53-0.80).
There was an association between non-NSCLC mortality and cardiometabolic comorbidities in stage IA (aHR, 1.37; 95% CI, 1.06-1.77) and in stages IB-IIIA (aHR, 1.32; 95% CI, 1.03-1.71) NSCLC. There were also associations between NSCLC mortality and respiratory comorbidity among stage IA (aHR, 1.51; 95% CI, 1.17-1.95) and stages IB-IIIA (aHR, 1.20; 95% CI, 1.06-1.36) NSCLC. There were no associations between respiratory comorbidity and non-NSCLC mortality.
Respiratory comorbidity was associated with a lower chance of undergoing surgical resection in stage IA (aHR, 0.54; 95% CI, 0.35-0.83) and stage IB-IIIA (aHR, 0.57; 95% CI, 0.46-0.70) cancers. Cardiometabolic comorbidity was associated with a lower rate of surgical resection only in stage 1B-3A patients (aHR, 0.73; 95% CI, 0.56-0.96). Among those who underwent resection, stage IA patients were less likely to die of lung cancer (aHR, 0.38; 95% CI, 0.28-0.52) but more likely to die of other causes (aHR, 1.73; 95% CI, 1.07-1.78). Stage IB-IIIA patients who underwent resection were less likely to die of lung cancer (aHR, 0.37; 95%, 0.32-0.42), but there was no significant association with non–lung cancer mortality.
The study was funded by the Lusi Wong Family Fund and the Alan Brown Chair. Dr. Liu has no relevant financial disclosures.
FROM ESMO CONGRESS 2022
Your poop may hold the secret to long life
Lots of things can disrupt your gut health over the years. A high-sugar diet, stress, antibiotics – all are linked to bad changes in the gut microbiome, the microbes that live in your intestinal tract. And this can raise the risk of diseases.
It could be possible, scientists say, by having people take a sample of their own stool when they are young to be put back into their colons when they are older.
While the science to back this up isn’t quite there yet, some researchers are saying we shouldn’t wait. They are calling on existing stool banks to let people start banking their stool now, so it’s there for them to use if the science becomes available.
But how would that work?
First, you’d go to a stool bank and provide a fresh sample of your poop, which would be screened for diseases, washed, processed, and deposited into a long-term storage facility.
Then, down the road, if you get a condition such as inflammatory bowel disease, heart disease, or type 2 diabetes – or if you have a procedure that wipes out your microbiome, like a course of antibiotics or chemotherapy – doctors could use your preserved stool to “re-colonize” your gut, restoring it to its earlier, healthier state, said Scott Weiss, MD, professor of medicine at Harvard Medical School, Boston, and a coauthor of a recent paper on the topic. They would do that using fecal microbiota transplantation, or FMT.
Timing is everything. You’d want a sample from when you’re healthy – say, between the ages of 18 and 35, or before a chronic condition is likely, said Dr. Weiss. But if you’re still healthy into your late 30s, 40s, or even 50s, providing a sample then could still benefit you later in life.
If we could pull off a banking system like this, it could have the potential to treat autoimmune disease, inflammatory bowel disease, diabetes, obesity, and heart disease – or even reverse the effects of aging. How can we make this happen?
Stool banks of today
While stool banks do exist today, the samples inside are destined not for the original donors but rather for sick patients hoping to treat an illness. Using FMT, doctors transfer the fecal material to the patient’s colon, restoring helpful gut microbiota.
Some research shows FMT may help treat inflammatory bowel diseases, such as Crohn’s or ulcerative colitis. Animal studies suggest it could help treat obesity, lengthen lifespan, and reverse some effects of aging, such as age-related decline in brain function. Other clinical trials are looking into its potential as a cancer treatment, said Dr. Weiss.
But outside the lab, FMT is mainly used for one purpose: to treat Clostridioides difficile infection. It works even better than antibiotics, research shows.
But first you need to find a healthy donor, and that’s harder than you might think.
Finding healthy stool samples
Banking our bodily substances is nothing new. Blood banks, for example, are common throughout the United States, and cord blood banking – preserving blood from a baby’s umbilical cord to aid possible future medical needs of the child – is becoming more popular. Sperm donors are highly sought after, and doctors regularly transplant kidneys and bone marrow to patients in need.
So why are we so particular about poop?
Part of the reason may be because feces (like blood, for that matter) can harbor disease – which is why it’s so important to find healthy stool donors. Problem is, this can be surprisingly hard to do.
To donate fecal matter, people must go through a rigorous screening process, said Majdi Osman, MD, chief medical officer for OpenBiome, a nonprofit microbiome research organization.
Until recently, OpenBiome operated a stool donation program, though it has since shifted its focus to research. Potential donors were screened for diseases and mental health conditions, pathogens, and antibiotic resistance. The pass rate was less than 3%.
“We take a very cautious approach because the association between diseases and the microbiome is still being understood,” Dr. Osman said.
FMT also carries risks – though so far, they seem mild. Side effects include mild diarrhea, nausea, belly pain, and fatigue. (The reason? Even the healthiest donor stool may not mix perfectly with your own.)
That’s where the idea of using your own stool comes in, said Yang-Yu Liu, PhD, a Harvard researcher who studies the microbiome and the lead author of the paper mentioned above. It’s not just more appealing but may also be a better “match” for your body.
Should you bank your stool?
While the researchers say we have reason to be optimistic about the future, it’s important to remember that many challenges remain. FMT is early in development, and there’s a lot about the microbiome we still don’t know.
There’s no guarantee, for example, that restoring a person’s microbiome to its formerly disease-free state will keep diseases at bay forever, said Dr. Weiss. If your genes raise your odds of having Crohn’s, for instance, it’s possible the disease could come back.
We also don’t know how long stool samples can be preserved, said Dr. Liu. Stool banks currently store fecal matter for 1 or 2 years, not decades. To protect the proteins and DNA structures for that long, samples would likely need to be stashed at the liquid nitrogen storage temperature of –196° C. (Currently, samples are stored at about –80° C.) Even then, testing would be needed to confirm if the fragile microorganisms in the stool can survive.
This raises another question: Who’s going to regulate all this?
The FDA regulates the use of FMT as a drug for the treatment of C. diff, but as Dr. Liu pointed out, many gastroenterologists consider the gut microbiota an organ. In that case, human fecal matter could be regulated the same way blood, bone, or even egg cells are.
Cord blood banking may be a helpful model, Dr. Liu said.
“We don’t have to start from scratch.”
Then there’s the question of cost. Cord blood banks could be a point of reference for that too, the researchers say. They charge about $1,500 to $2,820 for the first collection and processing, plus a yearly storage fee of $185 to $370.
Despite the unknowns, one thing is for sure: The interest in fecal banking is real – and growing. At least one microbiome firm, Cordlife Group Limited, based in Singapore, announced that it has started to allow people to bank their stool for future use.
“More people should talk about it and think about it,” said Dr. Liu.
A version of this article first appeared on WebMD.com.
Lots of things can disrupt your gut health over the years. A high-sugar diet, stress, antibiotics – all are linked to bad changes in the gut microbiome, the microbes that live in your intestinal tract. And this can raise the risk of diseases.
It could be possible, scientists say, by having people take a sample of their own stool when they are young to be put back into their colons when they are older.
While the science to back this up isn’t quite there yet, some researchers are saying we shouldn’t wait. They are calling on existing stool banks to let people start banking their stool now, so it’s there for them to use if the science becomes available.
But how would that work?
First, you’d go to a stool bank and provide a fresh sample of your poop, which would be screened for diseases, washed, processed, and deposited into a long-term storage facility.
Then, down the road, if you get a condition such as inflammatory bowel disease, heart disease, or type 2 diabetes – or if you have a procedure that wipes out your microbiome, like a course of antibiotics or chemotherapy – doctors could use your preserved stool to “re-colonize” your gut, restoring it to its earlier, healthier state, said Scott Weiss, MD, professor of medicine at Harvard Medical School, Boston, and a coauthor of a recent paper on the topic. They would do that using fecal microbiota transplantation, or FMT.
Timing is everything. You’d want a sample from when you’re healthy – say, between the ages of 18 and 35, or before a chronic condition is likely, said Dr. Weiss. But if you’re still healthy into your late 30s, 40s, or even 50s, providing a sample then could still benefit you later in life.
If we could pull off a banking system like this, it could have the potential to treat autoimmune disease, inflammatory bowel disease, diabetes, obesity, and heart disease – or even reverse the effects of aging. How can we make this happen?
Stool banks of today
While stool banks do exist today, the samples inside are destined not for the original donors but rather for sick patients hoping to treat an illness. Using FMT, doctors transfer the fecal material to the patient’s colon, restoring helpful gut microbiota.
Some research shows FMT may help treat inflammatory bowel diseases, such as Crohn’s or ulcerative colitis. Animal studies suggest it could help treat obesity, lengthen lifespan, and reverse some effects of aging, such as age-related decline in brain function. Other clinical trials are looking into its potential as a cancer treatment, said Dr. Weiss.
But outside the lab, FMT is mainly used for one purpose: to treat Clostridioides difficile infection. It works even better than antibiotics, research shows.
But first you need to find a healthy donor, and that’s harder than you might think.
Finding healthy stool samples
Banking our bodily substances is nothing new. Blood banks, for example, are common throughout the United States, and cord blood banking – preserving blood from a baby’s umbilical cord to aid possible future medical needs of the child – is becoming more popular. Sperm donors are highly sought after, and doctors regularly transplant kidneys and bone marrow to patients in need.
So why are we so particular about poop?
Part of the reason may be because feces (like blood, for that matter) can harbor disease – which is why it’s so important to find healthy stool donors. Problem is, this can be surprisingly hard to do.
To donate fecal matter, people must go through a rigorous screening process, said Majdi Osman, MD, chief medical officer for OpenBiome, a nonprofit microbiome research organization.
Until recently, OpenBiome operated a stool donation program, though it has since shifted its focus to research. Potential donors were screened for diseases and mental health conditions, pathogens, and antibiotic resistance. The pass rate was less than 3%.
“We take a very cautious approach because the association between diseases and the microbiome is still being understood,” Dr. Osman said.
FMT also carries risks – though so far, they seem mild. Side effects include mild diarrhea, nausea, belly pain, and fatigue. (The reason? Even the healthiest donor stool may not mix perfectly with your own.)
That’s where the idea of using your own stool comes in, said Yang-Yu Liu, PhD, a Harvard researcher who studies the microbiome and the lead author of the paper mentioned above. It’s not just more appealing but may also be a better “match” for your body.
Should you bank your stool?
While the researchers say we have reason to be optimistic about the future, it’s important to remember that many challenges remain. FMT is early in development, and there’s a lot about the microbiome we still don’t know.
There’s no guarantee, for example, that restoring a person’s microbiome to its formerly disease-free state will keep diseases at bay forever, said Dr. Weiss. If your genes raise your odds of having Crohn’s, for instance, it’s possible the disease could come back.
We also don’t know how long stool samples can be preserved, said Dr. Liu. Stool banks currently store fecal matter for 1 or 2 years, not decades. To protect the proteins and DNA structures for that long, samples would likely need to be stashed at the liquid nitrogen storage temperature of –196° C. (Currently, samples are stored at about –80° C.) Even then, testing would be needed to confirm if the fragile microorganisms in the stool can survive.
This raises another question: Who’s going to regulate all this?
The FDA regulates the use of FMT as a drug for the treatment of C. diff, but as Dr. Liu pointed out, many gastroenterologists consider the gut microbiota an organ. In that case, human fecal matter could be regulated the same way blood, bone, or even egg cells are.
Cord blood banking may be a helpful model, Dr. Liu said.
“We don’t have to start from scratch.”
Then there’s the question of cost. Cord blood banks could be a point of reference for that too, the researchers say. They charge about $1,500 to $2,820 for the first collection and processing, plus a yearly storage fee of $185 to $370.
Despite the unknowns, one thing is for sure: The interest in fecal banking is real – and growing. At least one microbiome firm, Cordlife Group Limited, based in Singapore, announced that it has started to allow people to bank their stool for future use.
“More people should talk about it and think about it,” said Dr. Liu.
A version of this article first appeared on WebMD.com.
Lots of things can disrupt your gut health over the years. A high-sugar diet, stress, antibiotics – all are linked to bad changes in the gut microbiome, the microbes that live in your intestinal tract. And this can raise the risk of diseases.
It could be possible, scientists say, by having people take a sample of their own stool when they are young to be put back into their colons when they are older.
While the science to back this up isn’t quite there yet, some researchers are saying we shouldn’t wait. They are calling on existing stool banks to let people start banking their stool now, so it’s there for them to use if the science becomes available.
But how would that work?
First, you’d go to a stool bank and provide a fresh sample of your poop, which would be screened for diseases, washed, processed, and deposited into a long-term storage facility.
Then, down the road, if you get a condition such as inflammatory bowel disease, heart disease, or type 2 diabetes – or if you have a procedure that wipes out your microbiome, like a course of antibiotics or chemotherapy – doctors could use your preserved stool to “re-colonize” your gut, restoring it to its earlier, healthier state, said Scott Weiss, MD, professor of medicine at Harvard Medical School, Boston, and a coauthor of a recent paper on the topic. They would do that using fecal microbiota transplantation, or FMT.
Timing is everything. You’d want a sample from when you’re healthy – say, between the ages of 18 and 35, or before a chronic condition is likely, said Dr. Weiss. But if you’re still healthy into your late 30s, 40s, or even 50s, providing a sample then could still benefit you later in life.
If we could pull off a banking system like this, it could have the potential to treat autoimmune disease, inflammatory bowel disease, diabetes, obesity, and heart disease – or even reverse the effects of aging. How can we make this happen?
Stool banks of today
While stool banks do exist today, the samples inside are destined not for the original donors but rather for sick patients hoping to treat an illness. Using FMT, doctors transfer the fecal material to the patient’s colon, restoring helpful gut microbiota.
Some research shows FMT may help treat inflammatory bowel diseases, such as Crohn’s or ulcerative colitis. Animal studies suggest it could help treat obesity, lengthen lifespan, and reverse some effects of aging, such as age-related decline in brain function. Other clinical trials are looking into its potential as a cancer treatment, said Dr. Weiss.
But outside the lab, FMT is mainly used for one purpose: to treat Clostridioides difficile infection. It works even better than antibiotics, research shows.
But first you need to find a healthy donor, and that’s harder than you might think.
Finding healthy stool samples
Banking our bodily substances is nothing new. Blood banks, for example, are common throughout the United States, and cord blood banking – preserving blood from a baby’s umbilical cord to aid possible future medical needs of the child – is becoming more popular. Sperm donors are highly sought after, and doctors regularly transplant kidneys and bone marrow to patients in need.
So why are we so particular about poop?
Part of the reason may be because feces (like blood, for that matter) can harbor disease – which is why it’s so important to find healthy stool donors. Problem is, this can be surprisingly hard to do.
To donate fecal matter, people must go through a rigorous screening process, said Majdi Osman, MD, chief medical officer for OpenBiome, a nonprofit microbiome research organization.
Until recently, OpenBiome operated a stool donation program, though it has since shifted its focus to research. Potential donors were screened for diseases and mental health conditions, pathogens, and antibiotic resistance. The pass rate was less than 3%.
“We take a very cautious approach because the association between diseases and the microbiome is still being understood,” Dr. Osman said.
FMT also carries risks – though so far, they seem mild. Side effects include mild diarrhea, nausea, belly pain, and fatigue. (The reason? Even the healthiest donor stool may not mix perfectly with your own.)
That’s where the idea of using your own stool comes in, said Yang-Yu Liu, PhD, a Harvard researcher who studies the microbiome and the lead author of the paper mentioned above. It’s not just more appealing but may also be a better “match” for your body.
Should you bank your stool?
While the researchers say we have reason to be optimistic about the future, it’s important to remember that many challenges remain. FMT is early in development, and there’s a lot about the microbiome we still don’t know.
There’s no guarantee, for example, that restoring a person’s microbiome to its formerly disease-free state will keep diseases at bay forever, said Dr. Weiss. If your genes raise your odds of having Crohn’s, for instance, it’s possible the disease could come back.
We also don’t know how long stool samples can be preserved, said Dr. Liu. Stool banks currently store fecal matter for 1 or 2 years, not decades. To protect the proteins and DNA structures for that long, samples would likely need to be stashed at the liquid nitrogen storage temperature of –196° C. (Currently, samples are stored at about –80° C.) Even then, testing would be needed to confirm if the fragile microorganisms in the stool can survive.
This raises another question: Who’s going to regulate all this?
The FDA regulates the use of FMT as a drug for the treatment of C. diff, but as Dr. Liu pointed out, many gastroenterologists consider the gut microbiota an organ. In that case, human fecal matter could be regulated the same way blood, bone, or even egg cells are.
Cord blood banking may be a helpful model, Dr. Liu said.
“We don’t have to start from scratch.”
Then there’s the question of cost. Cord blood banks could be a point of reference for that too, the researchers say. They charge about $1,500 to $2,820 for the first collection and processing, plus a yearly storage fee of $185 to $370.
Despite the unknowns, one thing is for sure: The interest in fecal banking is real – and growing. At least one microbiome firm, Cordlife Group Limited, based in Singapore, announced that it has started to allow people to bank their stool for future use.
“More people should talk about it and think about it,” said Dr. Liu.
A version of this article first appeared on WebMD.com.
AMA joins in lawsuit accusing Cigna of underpaying physicians
, the nation’s largest third-party network.
The American Medical Association, the Medical Society of New Jersey, and the Washington State Medical Association on Sept. 12 entered into a legal battle between the giant insurers and patients.
At issue are claims involving the firm MultiPlan as an intermediary. Cigna had not responded to this news organization at press time following multiple requests for comment.
According to the legal complaint AMA and the two state medical societies joined, MultiPlan has contracts with more than 1.2 million clinicians. Under these agreements, medical professionals agree to accept a set percentage of billed charges as payment in full, while not holding patients responsible for the difference between the original billed charges and the discounted rate.
But the complaint alleges that MultiPlan failed to stick with that bargain. In a statement, AMA President Jack Resneck Jr, MD, said the physician groups joined the legal action “to shed light on Cigna’s misconduct and create remedies so that patients and physicians can look forward to getting what they are promised.”
Dr. Resneck said Cigna’s approach “is riddled with conflicts of interest and manipulations that routinely shortchanged payments to MultiPlan Network physicians and interfered with the patient-physician relationship by ignoring the MultiPlan contracts and making incorrect statements to patients about their liability for the unpaid portion of the billed charges.”
According to the complaint, Cigna used a company called Zelis to “unilaterally re-price’’ claims at an amount far lower than that called for by the MultiPlan Contract. The three cases cited in the lawsuit stem from a 2017 spine surgery in Washington and 2018 orthopedic and 2020 breast reconstruction surgeries in New Jersey. The decisions to ignore the previous agreements and cut the reimbursement led the physicians involved to eventually bill patients for some of the money in dispute, according to the complaint.
“The providers were left in a very untenable situation,” D. Brian Hufford, an attorney involved in the case, told this news organization. “Their only choice was to go after the insurance company and sue them or they have to go after the patient. That interferes with the patient-doctor relationship.”
Mr. Hufford, who’s a partner at law firm Zuckerman Spaeder, said that these kinds of cases fall beyond the protections provided by the No Surprises Act. Plaintiffs in these cases were enrolled in what are called self-insured plans provided by employers, through which they were supposed to be allowed to seek out-of-network care.
Highly concerning are the messages that insurers send to patients through explanation of benefits (EOB) statements, Mr. Hufford said. Thus in this case against Cigna, physicians and patients have the “same interest in trying to make sure the insurance companies are paying the appropriate amounts for these services,” he said.
Cigna “is telling the patients that the provider has accepted something, and that the patient does not have to worry about paying for that, when in fact that’s not true,” Mr. Hufford said. “That goes beyond merely not complying with the plan documents, but also engaging in conduct that we believe was inappropriate.”
A version of this article first appeared on Medscape.com.
, the nation’s largest third-party network.
The American Medical Association, the Medical Society of New Jersey, and the Washington State Medical Association on Sept. 12 entered into a legal battle between the giant insurers and patients.
At issue are claims involving the firm MultiPlan as an intermediary. Cigna had not responded to this news organization at press time following multiple requests for comment.
According to the legal complaint AMA and the two state medical societies joined, MultiPlan has contracts with more than 1.2 million clinicians. Under these agreements, medical professionals agree to accept a set percentage of billed charges as payment in full, while not holding patients responsible for the difference between the original billed charges and the discounted rate.
But the complaint alleges that MultiPlan failed to stick with that bargain. In a statement, AMA President Jack Resneck Jr, MD, said the physician groups joined the legal action “to shed light on Cigna’s misconduct and create remedies so that patients and physicians can look forward to getting what they are promised.”
Dr. Resneck said Cigna’s approach “is riddled with conflicts of interest and manipulations that routinely shortchanged payments to MultiPlan Network physicians and interfered with the patient-physician relationship by ignoring the MultiPlan contracts and making incorrect statements to patients about their liability for the unpaid portion of the billed charges.”
According to the complaint, Cigna used a company called Zelis to “unilaterally re-price’’ claims at an amount far lower than that called for by the MultiPlan Contract. The three cases cited in the lawsuit stem from a 2017 spine surgery in Washington and 2018 orthopedic and 2020 breast reconstruction surgeries in New Jersey. The decisions to ignore the previous agreements and cut the reimbursement led the physicians involved to eventually bill patients for some of the money in dispute, according to the complaint.
“The providers were left in a very untenable situation,” D. Brian Hufford, an attorney involved in the case, told this news organization. “Their only choice was to go after the insurance company and sue them or they have to go after the patient. That interferes with the patient-doctor relationship.”
Mr. Hufford, who’s a partner at law firm Zuckerman Spaeder, said that these kinds of cases fall beyond the protections provided by the No Surprises Act. Plaintiffs in these cases were enrolled in what are called self-insured plans provided by employers, through which they were supposed to be allowed to seek out-of-network care.
Highly concerning are the messages that insurers send to patients through explanation of benefits (EOB) statements, Mr. Hufford said. Thus in this case against Cigna, physicians and patients have the “same interest in trying to make sure the insurance companies are paying the appropriate amounts for these services,” he said.
Cigna “is telling the patients that the provider has accepted something, and that the patient does not have to worry about paying for that, when in fact that’s not true,” Mr. Hufford said. “That goes beyond merely not complying with the plan documents, but also engaging in conduct that we believe was inappropriate.”
A version of this article first appeared on Medscape.com.
, the nation’s largest third-party network.
The American Medical Association, the Medical Society of New Jersey, and the Washington State Medical Association on Sept. 12 entered into a legal battle between the giant insurers and patients.
At issue are claims involving the firm MultiPlan as an intermediary. Cigna had not responded to this news organization at press time following multiple requests for comment.
According to the legal complaint AMA and the two state medical societies joined, MultiPlan has contracts with more than 1.2 million clinicians. Under these agreements, medical professionals agree to accept a set percentage of billed charges as payment in full, while not holding patients responsible for the difference between the original billed charges and the discounted rate.
But the complaint alleges that MultiPlan failed to stick with that bargain. In a statement, AMA President Jack Resneck Jr, MD, said the physician groups joined the legal action “to shed light on Cigna’s misconduct and create remedies so that patients and physicians can look forward to getting what they are promised.”
Dr. Resneck said Cigna’s approach “is riddled with conflicts of interest and manipulations that routinely shortchanged payments to MultiPlan Network physicians and interfered with the patient-physician relationship by ignoring the MultiPlan contracts and making incorrect statements to patients about their liability for the unpaid portion of the billed charges.”
According to the complaint, Cigna used a company called Zelis to “unilaterally re-price’’ claims at an amount far lower than that called for by the MultiPlan Contract. The three cases cited in the lawsuit stem from a 2017 spine surgery in Washington and 2018 orthopedic and 2020 breast reconstruction surgeries in New Jersey. The decisions to ignore the previous agreements and cut the reimbursement led the physicians involved to eventually bill patients for some of the money in dispute, according to the complaint.
“The providers were left in a very untenable situation,” D. Brian Hufford, an attorney involved in the case, told this news organization. “Their only choice was to go after the insurance company and sue them or they have to go after the patient. That interferes with the patient-doctor relationship.”
Mr. Hufford, who’s a partner at law firm Zuckerman Spaeder, said that these kinds of cases fall beyond the protections provided by the No Surprises Act. Plaintiffs in these cases were enrolled in what are called self-insured plans provided by employers, through which they were supposed to be allowed to seek out-of-network care.
Highly concerning are the messages that insurers send to patients through explanation of benefits (EOB) statements, Mr. Hufford said. Thus in this case against Cigna, physicians and patients have the “same interest in trying to make sure the insurance companies are paying the appropriate amounts for these services,” he said.
Cigna “is telling the patients that the provider has accepted something, and that the patient does not have to worry about paying for that, when in fact that’s not true,” Mr. Hufford said. “That goes beyond merely not complying with the plan documents, but also engaging in conduct that we believe was inappropriate.”
A version of this article first appeared on Medscape.com.
‘Smoking gun–level’ evidence found linking air pollution with lung cancer
PARIS – Air pollution has been recognized as a risk factor for lung cancer for about 2 decades, and already present in normal lung cells to cause cancer.
Think of it as “smoking gun–level” evidence that may explain why many nonsmokers still develop non–small cell lung cancer, said Charles Swanton, PhD, from the Francis Crick Institute and Cancer Research UK Chief Clinician, London.
“What this work shows is that air pollution is directly causing lung cancer but through a slightly unexpected pathway,” he said at a briefing prior to his presentation of the data in a presidential symposium held earlier this month in Paris at the European Society for Medical Oncology Congress 2022.
Importantly, he and his team also propose a mechanism for blocking the effects of air pollution with monoclonal antibodies directed against the inflammatory cytokine interleukein-1 beta.
Carcinogenesis explored
Lung cancer in never-smokers has a low mutational burden, with about 5- to 10-fold fewer mutations in a nonsmoker, compared with an ever smoker or current smoker, Dr. Swanton noted.
“The other thing to say about never-smokers is that they don’t have a clear environmental carcinogenic signature. So how do you square the circle? You’ve got the problem that you know that air pollution is associated with lung cancer – we don’t know if it causes it – but we also see that we’ve got no DNA mutations due to an environmental carcinogen,” he said during his symposium presentation.
The traditional model proposed to explain how carcinogens cause cancer holds that exposure to a carcinogen causes DNA mutations that lead to clonal expansion and tumor growth.
“But there are some major problems with this model,” Dr. Swanton said.
For example, normal skin contains a “patchwork of mutant clones,” but skin cancer is still uncommon, he said, and in studies in mice, 17 of 20 environmental carcinogens did not induce DNA mutations. He also noted that a common melanoma driver mutation, BRAF V600E, is not induced by exposure to a ultraviolet light.
“Any explanation for never-smoking lung cancer would have to fulfill three criteria: one, you have to explain why geographic variation exists; two, you have to prove causation; and three, you have to explain how cancers can be initiated without directly causing DNA mutations,” he said.
Normal lung tissues in nonsmoking adults can harbor pre-existing mutations, with the number of mutations increasing likely as a consequence of aging. In fact, more than 50% of normal lung biopsy tissues have been shown to harbor driver KRAS and/or EGFR mutations, Dr. Swanton said.
“In our research, these mutations alone only weakly potentiated cancer in laboratory models. However, when lung cells with these mutations were exposed to air pollutants, we saw more cancers and these occurred more quickly than when lung cells with these mutations were not exposed to pollutants, suggesting that air pollution promotes the initiation of lung cancer in cells harboring driver gene mutations. The next step is to discover why some lung cells with mutations become cancerous when exposed to pollutants while others don’t,” he said.
Geographical exposures
Looking at data on 447,932 participants in the UK Biobank, the investigators found that increasing exposure to ambient air particles smaller than 2.5 mcm (PM2.5) was significantly associated with seven cancer types, including lung cancer. They also saw an association between PM2.5 exposure levels and EGFR-mutated lung cancer incidence in the United Kingdom, South Korea, and Taiwan.
And crucially, as Dr. Swanton and associates showed in mouse models, exposure of lung cells bearing somatic EGFR and KRAS mutations to PM2.5 causes recruitment of macrophages that in turn secrete IL-1B, resulting in a transdifferentiation of EGFR-mutated cells into a cancer stem cell state, and tumor formation.
Importantly, pollution-induced tumor formation can be blocked by antibodies directed against IL-1B, Dr. Swanton said.
He pointed to a 2017 study in The Lancet suggesting that anti-inflammatory therapy with the anti–IL-1 antibody canakinumab (Ilaris) could reduce incident lung cancer and lung cancer deaths.
‘Elegant first demonstration’
“This is a very meaningful demonstration, from epidemiological data to preclinical models of the role of PM2.5 air pollutants in the promotion of lung cancer, and it provides us with very important insights into the mechanism through which nonsmokers can get lung cancer,” commented Suzette Delaloge, MD, from the cancer interception program at Institut Goustave Roussy in Villejuif, France, the invited discussant.
“But beyond that, it also has a great impact on our vision of carcinogenesis, with this very elegant first demonstration of the alternative nonmutagenic, carcinogenetic promotion hypothesis for fine particulate matter,” she said.
Questions still to be answered include whether PM2.5 pollutants could also be mutagenic, is the oncogenic pathway ubiquitous in tissue, which components of PM2.5 might drive the effect, how long of an exposure is required to promote lung cancer, and why and how persons without cancer develop specific driver mutations such as EGFR, she said.
“This research is intriguing and exciting as it means that we can ask whether, in the future, it will be possible to use lung scans to look for precancerous lesions in the lungs and try to reverse them with medicines such as interleukin-1B inhibitors,” said Tony Mok, MD, a lung cancer specialist at the Chinese University of Hong Kong, who was not involved in the study.
“We don’t yet know whether it will be possible to use highly sensitive EGFR profiling on blood or other samples to find nonsmokers who are predisposed to lung cancer and may benefit from lung scanning, so discussions are still very speculative,” he said in a statement.
The study was supported by Cancer Research UK, the Lung Cancer Research Foundations, Rosetrees Trust, the Mark Foundation for Cancer Research and the Ruth Strauss Foundation. Dr. Swanton disclosed grants/research support, honoraria, and stock ownership with multiple entities. Dr. Delaloge disclosed institutional financing and research funding from multiple companies. Dr. Mok disclosed stock ownership and honoraria with multiple companies.
PARIS – Air pollution has been recognized as a risk factor for lung cancer for about 2 decades, and already present in normal lung cells to cause cancer.
Think of it as “smoking gun–level” evidence that may explain why many nonsmokers still develop non–small cell lung cancer, said Charles Swanton, PhD, from the Francis Crick Institute and Cancer Research UK Chief Clinician, London.
“What this work shows is that air pollution is directly causing lung cancer but through a slightly unexpected pathway,” he said at a briefing prior to his presentation of the data in a presidential symposium held earlier this month in Paris at the European Society for Medical Oncology Congress 2022.
Importantly, he and his team also propose a mechanism for blocking the effects of air pollution with monoclonal antibodies directed against the inflammatory cytokine interleukein-1 beta.
Carcinogenesis explored
Lung cancer in never-smokers has a low mutational burden, with about 5- to 10-fold fewer mutations in a nonsmoker, compared with an ever smoker or current smoker, Dr. Swanton noted.
“The other thing to say about never-smokers is that they don’t have a clear environmental carcinogenic signature. So how do you square the circle? You’ve got the problem that you know that air pollution is associated with lung cancer – we don’t know if it causes it – but we also see that we’ve got no DNA mutations due to an environmental carcinogen,” he said during his symposium presentation.
The traditional model proposed to explain how carcinogens cause cancer holds that exposure to a carcinogen causes DNA mutations that lead to clonal expansion and tumor growth.
“But there are some major problems with this model,” Dr. Swanton said.
For example, normal skin contains a “patchwork of mutant clones,” but skin cancer is still uncommon, he said, and in studies in mice, 17 of 20 environmental carcinogens did not induce DNA mutations. He also noted that a common melanoma driver mutation, BRAF V600E, is not induced by exposure to a ultraviolet light.
“Any explanation for never-smoking lung cancer would have to fulfill three criteria: one, you have to explain why geographic variation exists; two, you have to prove causation; and three, you have to explain how cancers can be initiated without directly causing DNA mutations,” he said.
Normal lung tissues in nonsmoking adults can harbor pre-existing mutations, with the number of mutations increasing likely as a consequence of aging. In fact, more than 50% of normal lung biopsy tissues have been shown to harbor driver KRAS and/or EGFR mutations, Dr. Swanton said.
“In our research, these mutations alone only weakly potentiated cancer in laboratory models. However, when lung cells with these mutations were exposed to air pollutants, we saw more cancers and these occurred more quickly than when lung cells with these mutations were not exposed to pollutants, suggesting that air pollution promotes the initiation of lung cancer in cells harboring driver gene mutations. The next step is to discover why some lung cells with mutations become cancerous when exposed to pollutants while others don’t,” he said.
Geographical exposures
Looking at data on 447,932 participants in the UK Biobank, the investigators found that increasing exposure to ambient air particles smaller than 2.5 mcm (PM2.5) was significantly associated with seven cancer types, including lung cancer. They also saw an association between PM2.5 exposure levels and EGFR-mutated lung cancer incidence in the United Kingdom, South Korea, and Taiwan.
And crucially, as Dr. Swanton and associates showed in mouse models, exposure of lung cells bearing somatic EGFR and KRAS mutations to PM2.5 causes recruitment of macrophages that in turn secrete IL-1B, resulting in a transdifferentiation of EGFR-mutated cells into a cancer stem cell state, and tumor formation.
Importantly, pollution-induced tumor formation can be blocked by antibodies directed against IL-1B, Dr. Swanton said.
He pointed to a 2017 study in The Lancet suggesting that anti-inflammatory therapy with the anti–IL-1 antibody canakinumab (Ilaris) could reduce incident lung cancer and lung cancer deaths.
‘Elegant first demonstration’
“This is a very meaningful demonstration, from epidemiological data to preclinical models of the role of PM2.5 air pollutants in the promotion of lung cancer, and it provides us with very important insights into the mechanism through which nonsmokers can get lung cancer,” commented Suzette Delaloge, MD, from the cancer interception program at Institut Goustave Roussy in Villejuif, France, the invited discussant.
“But beyond that, it also has a great impact on our vision of carcinogenesis, with this very elegant first demonstration of the alternative nonmutagenic, carcinogenetic promotion hypothesis for fine particulate matter,” she said.
Questions still to be answered include whether PM2.5 pollutants could also be mutagenic, is the oncogenic pathway ubiquitous in tissue, which components of PM2.5 might drive the effect, how long of an exposure is required to promote lung cancer, and why and how persons without cancer develop specific driver mutations such as EGFR, she said.
“This research is intriguing and exciting as it means that we can ask whether, in the future, it will be possible to use lung scans to look for precancerous lesions in the lungs and try to reverse them with medicines such as interleukin-1B inhibitors,” said Tony Mok, MD, a lung cancer specialist at the Chinese University of Hong Kong, who was not involved in the study.
“We don’t yet know whether it will be possible to use highly sensitive EGFR profiling on blood or other samples to find nonsmokers who are predisposed to lung cancer and may benefit from lung scanning, so discussions are still very speculative,” he said in a statement.
The study was supported by Cancer Research UK, the Lung Cancer Research Foundations, Rosetrees Trust, the Mark Foundation for Cancer Research and the Ruth Strauss Foundation. Dr. Swanton disclosed grants/research support, honoraria, and stock ownership with multiple entities. Dr. Delaloge disclosed institutional financing and research funding from multiple companies. Dr. Mok disclosed stock ownership and honoraria with multiple companies.
PARIS – Air pollution has been recognized as a risk factor for lung cancer for about 2 decades, and already present in normal lung cells to cause cancer.
Think of it as “smoking gun–level” evidence that may explain why many nonsmokers still develop non–small cell lung cancer, said Charles Swanton, PhD, from the Francis Crick Institute and Cancer Research UK Chief Clinician, London.
“What this work shows is that air pollution is directly causing lung cancer but through a slightly unexpected pathway,” he said at a briefing prior to his presentation of the data in a presidential symposium held earlier this month in Paris at the European Society for Medical Oncology Congress 2022.
Importantly, he and his team also propose a mechanism for blocking the effects of air pollution with monoclonal antibodies directed against the inflammatory cytokine interleukein-1 beta.
Carcinogenesis explored
Lung cancer in never-smokers has a low mutational burden, with about 5- to 10-fold fewer mutations in a nonsmoker, compared with an ever smoker or current smoker, Dr. Swanton noted.
“The other thing to say about never-smokers is that they don’t have a clear environmental carcinogenic signature. So how do you square the circle? You’ve got the problem that you know that air pollution is associated with lung cancer – we don’t know if it causes it – but we also see that we’ve got no DNA mutations due to an environmental carcinogen,” he said during his symposium presentation.
The traditional model proposed to explain how carcinogens cause cancer holds that exposure to a carcinogen causes DNA mutations that lead to clonal expansion and tumor growth.
“But there are some major problems with this model,” Dr. Swanton said.
For example, normal skin contains a “patchwork of mutant clones,” but skin cancer is still uncommon, he said, and in studies in mice, 17 of 20 environmental carcinogens did not induce DNA mutations. He also noted that a common melanoma driver mutation, BRAF V600E, is not induced by exposure to a ultraviolet light.
“Any explanation for never-smoking lung cancer would have to fulfill three criteria: one, you have to explain why geographic variation exists; two, you have to prove causation; and three, you have to explain how cancers can be initiated without directly causing DNA mutations,” he said.
Normal lung tissues in nonsmoking adults can harbor pre-existing mutations, with the number of mutations increasing likely as a consequence of aging. In fact, more than 50% of normal lung biopsy tissues have been shown to harbor driver KRAS and/or EGFR mutations, Dr. Swanton said.
“In our research, these mutations alone only weakly potentiated cancer in laboratory models. However, when lung cells with these mutations were exposed to air pollutants, we saw more cancers and these occurred more quickly than when lung cells with these mutations were not exposed to pollutants, suggesting that air pollution promotes the initiation of lung cancer in cells harboring driver gene mutations. The next step is to discover why some lung cells with mutations become cancerous when exposed to pollutants while others don’t,” he said.
Geographical exposures
Looking at data on 447,932 participants in the UK Biobank, the investigators found that increasing exposure to ambient air particles smaller than 2.5 mcm (PM2.5) was significantly associated with seven cancer types, including lung cancer. They also saw an association between PM2.5 exposure levels and EGFR-mutated lung cancer incidence in the United Kingdom, South Korea, and Taiwan.
And crucially, as Dr. Swanton and associates showed in mouse models, exposure of lung cells bearing somatic EGFR and KRAS mutations to PM2.5 causes recruitment of macrophages that in turn secrete IL-1B, resulting in a transdifferentiation of EGFR-mutated cells into a cancer stem cell state, and tumor formation.
Importantly, pollution-induced tumor formation can be blocked by antibodies directed against IL-1B, Dr. Swanton said.
He pointed to a 2017 study in The Lancet suggesting that anti-inflammatory therapy with the anti–IL-1 antibody canakinumab (Ilaris) could reduce incident lung cancer and lung cancer deaths.
‘Elegant first demonstration’
“This is a very meaningful demonstration, from epidemiological data to preclinical models of the role of PM2.5 air pollutants in the promotion of lung cancer, and it provides us with very important insights into the mechanism through which nonsmokers can get lung cancer,” commented Suzette Delaloge, MD, from the cancer interception program at Institut Goustave Roussy in Villejuif, France, the invited discussant.
“But beyond that, it also has a great impact on our vision of carcinogenesis, with this very elegant first demonstration of the alternative nonmutagenic, carcinogenetic promotion hypothesis for fine particulate matter,” she said.
Questions still to be answered include whether PM2.5 pollutants could also be mutagenic, is the oncogenic pathway ubiquitous in tissue, which components of PM2.5 might drive the effect, how long of an exposure is required to promote lung cancer, and why and how persons without cancer develop specific driver mutations such as EGFR, she said.
“This research is intriguing and exciting as it means that we can ask whether, in the future, it will be possible to use lung scans to look for precancerous lesions in the lungs and try to reverse them with medicines such as interleukin-1B inhibitors,” said Tony Mok, MD, a lung cancer specialist at the Chinese University of Hong Kong, who was not involved in the study.
“We don’t yet know whether it will be possible to use highly sensitive EGFR profiling on blood or other samples to find nonsmokers who are predisposed to lung cancer and may benefit from lung scanning, so discussions are still very speculative,” he said in a statement.
The study was supported by Cancer Research UK, the Lung Cancer Research Foundations, Rosetrees Trust, the Mark Foundation for Cancer Research and the Ruth Strauss Foundation. Dr. Swanton disclosed grants/research support, honoraria, and stock ownership with multiple entities. Dr. Delaloge disclosed institutional financing and research funding from multiple companies. Dr. Mok disclosed stock ownership and honoraria with multiple companies.
AT ESMO CONGRESS 2022
Optimizing Narrowband UVB Phototherapy: Is It More Challenging for Your Older Patients?
Even with recent pharmacologic treatment advances, narrowband UVB (NB-UVB) phototherapy remains a versatile, safe, and efficacious adjunctive or exclusive treatment for multiple dermatologic conditions, including psoriasis and atopic dermatitis.
In a prior study, Matthews et al13 reported that 96% (50/52) of patients older than 65 years achieved medium to high levels of clearance with NB-UVB phototherapy. Nonetheless, 2 other findings in this study related to the number of treatments required to achieve clearance (ie, clearance rates) and erythema rates prompted further investigation. The first finding was higher-than-expected clearance rates. Older adults had a clearance rate with a mean of 33 treatments compared to prior studies featuring mean clearance rates of 20 to 28 treatments.7,8,14-16 This finding resembled a study in the United Kingdom17 with a median clearance rate in older adults of 30 treatments. In contrast, the median clearance rate from a study in Turkey18 was 42 treatments in older adults. We hypothesized that more photosensitizing medications used in older vs younger adults prompted more dose adjustments with NB-UVB phototherapy to avoid burning (ie, erythema) at baseline and throughout the treatment course. These dose adjustments may have increased the overall clearance rates. If true, we predicted that younger adults treated with the same protocol would have cleared more quickly, either because of age-related differences or because they likely had fewer comorbidities and therefore fewer medications.
The second finding from Matthews et al13 that warranted further investigation was a higher erythema rate compared to the older adult study from the United Kingdom.17 We hypothesized that potentially greater use of photosensitizing medications in the United States could explain the higher erythema rates. Although medication-induced photosensitivity is less likely with NB-UVB phototherapy than with UVA, certain medications can cause UVB photosensitivity, including thiazides, quinidine, calcium channel antagonists, phenothiazines, and nonsteroidal anti-inflammatory drugs.8,19,20 Therefore, photosensitizing medication use either at baseline or during a course of NB-UVB phototherapy could increase the risk for erythema. Age-related skin changes also have been considered as a
This retrospective study aimed to determine if NB-UVB phototherapy is equally effective in both older and younger adults treated with the same protocol; to examine the association between the use of photosensitizing medications and clearance rates in both older and younger adults; and to examine the association between the use of photosensitizing medications and erythema rates in older vs younger adults.
Methods
Study Design and Patients—This retrospective cohort study used billing records to identify patients who received NB-UVB phototherapy at 3 different clinical sites within a large US health care system in Washington (Group Health Cooperative, now Kaiser Permanente Washington), serving more than 600,000 patients between January 1, 2012, and December 31, 2016. The institutional review board of Kaiser Permanente Washington Health Research Institute approved this study (IRB 1498087-4). Younger adults were classified as those 64 years or younger and older adults as those 65 years and older at the start of their phototherapy regimen. A power analysis determined that the optimal sample size for this study was 250 patients.
Individuals were excluded if they had fewer than 6 phototherapy treatments; a diagnosis of vitiligo, photosensitivity dermatitis, morphea, or pityriasis rubra pilaris; and/or treatment of the hands or feet only.
Phototherapy Protocol—Using a 48-lamp NB-UVB unit, trained phototherapy nurses provided all treatments following standardized treatment protocols13 based on previously published phototherapy guidelines.24 Nurses determined each patient’s disease clearance level using a 3-point clearance scale (high, medium, low).13 Each patient’s starting dose was determined based on the estimated MED for their skin phototype.
Statistical Analysis—Data were analyzed using Stata statistical software (StataCorp LLC). Univariate analyses were used to examine the data and identify outliers, bad values, and missing data, as well as to calculate descriptive statistics. Pearson χ2 and Fisher exact statistics were used to calculate differences in categorical variables. Linear multivariate regression models and logistic multivariate models were used to examine statistical relationships between variables. Statistical significance was defined as P≤.05.
Results
Patient Characteristics—Medical records were reviewed for 172 patients who received phototherapy between 2012 and 2016. Patients ranged in age from 23 to 91 years, with 102 patients 64 years and younger and 70 patients 65 years and older. Tables 1 and 2 outline the patient characteristics and conditions treated.

Phototherapy Effectiveness—

Photosensitizing Medications, Clearance Levels, and Clearance Rates—

Frequency of Treatments and Clearance Rates—Older adults more consistently completed the recommended frequency of treatments—3 times weekly—compared to younger adults (74.3% vs 58.5%). However, all patients who completed 3 treatments per week required a similar number of treatments to clear (older adults, mean [SD]: 35.7 [21.6]; younger adults, mean [SD]: 34.7 [19.0]; P=.85). Among patients completing 2 or fewer treatments per week, older adults required a mean (SD) of only 31 (9.0) treatments to clear vs 41.5 (21.3) treatments to clear for younger adults, but the difference was not statistically significant (P=.08). However, even those with suboptimal frequency ultimately achieved similar clearance levels.


Photosensitizing Medications and Erythema Rates—

Overall, phototherapy nurses adjusted the starting dose according to the phototype-based protocol an average of 69% of the time for patients on medications with photosensitivity listed as a potential side effect. However, the frequency depended significantly on the clinic (clinic A, 24%; clinic B, 92%; clinic C, 87%)(P≤.001). Nurses across all clinics consistently decreased the treatment dose when patients reported starting new photosensitizing medications. Patients with adjusted starting doses had slightly but not significantly higher clearance rates compared to those without (mean, 37.8 vs 35.5; t(104)=0.58; P=.56).

Comment
Impact of Photosensitizing Medications on Clearance—Photosensitizing medications and treatment frequency were 2 factors that might explain the slower clearance rates in younger adults. In this study, both groups of patients used similar numbers of photosensitizing medications, but more older adults were taking 3 or more medications (Table 3). We found no statistically significant relationship between taking photosensitizing medications and either the clearance rates or the level of clearance achieved in either age group.
Impact of Treatment Frequency—Weekly treatment frequency also was examined. One prior study demonstrated that treatments 3 times weekly led to a faster clearance time and higher clearance levels compared with twice-weekly treatment.7 When patients completed treatments twice weekly, it took an average of 1.5 times more days to clear, which impacted cost and clinical resource availability. The patients ranged in age from 17 to 80 years, but outcomes in older patients were not described separately.7 Interestingly, our study seemed to find a difference between age groups when the impact of treatment frequency was examined. Older adults completed nearly 4 fewer mean treatments to clear when treating less often, with more than 80% achieving high levels of clearance, whereas the younger adults required almost 7 more treatments to clear when they came in less frequently, with approximately 80% achieving a high level of clearance. As a result, our study found that in both age groups, slowing the treatment frequency extended the treatment time to clearance—more for the younger adults than the older adults—but did not significantly change the percentage of individuals reaching full clearance in either group.
Erythema Rates—There was no association between photosensitizing medications and erythema rates except when patients were taking at least 3 medications. Most medications that listed photosensitivity as a possible side effect did not specify their relevant range of UV radiation; therefore, all such medications were examined during this analysis. Prior research has shown UVB range photosensitizing medications include thiazides, quinidine, calcium channel antagonists, phenothiazines, and nonsteroidal anti-inflammatory drugs.19 A sensitivity analysis that focused only on these medications found no association between them and any particular grade of erythema. However, patients taking 3 or more of any medications listing photosensitivity as a side effect had an increased risk for grade 2 erythema.
Erythema rates in this study were consistent with a 2013 systematic review that reported 57% of patients with asymptomatic grade 1 erythema.25 In the 2 other comparative older adult studies, erythema rates varied widely: 35% in a study from Turkey18compared to only1.89% in a study from the United Kingdom.17
The starting dose for NB-UVB may drive erythema rates. The current study’s protocols were based on an estimated MED that is subjectively determined by the dermatology provider’s assessment of the patient’s skin sensitivity via examination and questions to the patient about their response to environmental sun exposure (ie, burning and tanning)26 and is frequently used to determine the starting dose and subsequent dose escalation. Certain medications have been found to increase photosensitivity and erythema,20 which can change an individual’s MED. If photosensitizing medications are started prior to or during a course of NB-UVB without a pretreatment MED, they might increase the risk for erythema. This study did not identify specific erythema-inducing medications but did find that taking 3 or more photosensitizing medications was associated with increased episodes of grade 2 erythema. Similarly, Harrop et al8 found that patients who were taking photosensitizing medications were more likely to have grade 2 or higher erythema, despite baseline MED testing, which is an established safety mechanism to reduce the risk and severity of erythema.14,20,27 The authors of a recent study of older adults in Taiwan specifically recommended MED testing due to the unpredictable influence of polypharmacy on MED calculations in this population.28 Therefore, this study’s use of an estimated MED in older adults may have influenced the starting dose as well as the incidence and severity of erythemic events. Age-related skin changes likely are ruled out as a consideration for mild erythema by the similarity of grade 1 erythema rates in both older and younger adults. Other studies have identified differences between the age groups, where older patients experienced more intense erythema in the late phase of UVB treatments.22,23 This phenomenon could increase the risk for a grade 2 erythema, which may correspond with this study’s findings.
Other potential causes of erythema were ruled out during our study, including erythema related to missed treatments and shielding mishaps. Other factors, however, may impact the level of sensitivity each patient has to phototherapy, including genetics, epigenetics, and cumulative sun damage. With NB-UVB, near-erythemogenic doses are optimal to achieve effective treatments but require a delicate balance to achieve, which may be more problematic for older adults, especially those taking several medications.
Study Limitations—Our study design made it difficult to draw conclusions about rarer dermatologic conditions. Some patients received treatments over years that were not included in the study period. Finally, power calculations suggested that our actual sample size was too small, with approximately one-third of the required sample missing.
Practical Implications—The goals of phototherapy are to achieve a high level of disease clearance with the fewest number of treatments possible and minimal side effects.
The extra staff training and patient monitoring required for MED testing likely is to add value and preserve resources if faster clearance rates could be achieved and may warrant further investigation. Phototherapy centers require standardized treatment protocols, diligent well-trained staff, and program monitoring to ensure consistent care to all patients. This study highlighted the ongoing opportunity for health care organizations to conduct evidence-based practice inquiries to continually optimize care for their patients.
- Fernández-Guarino M, Aboin-Gonzalez S, Barchino L, et al. Treatment of moderate and severe adult chronic atopic dermatitis with narrow-band UVB and the combination of narrow-band UVB/UVA phototherapy. Dermatol Ther. 2016;29:19-23.
- Foerster J, Boswell K, West J, et al. Narrowband UVB treatment is highly effective and causes a strong reduction in the use of steroid and other creams in psoriasis patients in clinical practice. PLoS One. 2017;12:e0181813.
- Gambichler T, Breuckmann F, Boms S, et al. Narrowband UVB phototherapy in skin conditions beyond psoriasis. J Am Acad Dermatol. 2005;52:660-670.
- Ryu HH, Choe YS, Jo S, et al. Remission period in psoriasis after multiple cycles of narrowband ultraviolet B phototherapy. J Dermatol. 2014;41:622-627.
- Schneider LA, Hinrichs R, Scharffetter-Kochanek K. Phototherapy and photochemotherapy. Clin Dermatol. 2008;26:464-476.
- Tintle S, Shemer A, Suárez-Fariñas M, et al. Reversal of atopic dermatitis with narrow-band UVB phototherapy and biomarkers for therapeutic response. J Allergy Clin Immunol. 2011;128:583-593.e581-584.
- Cameron H, Dawe RS, Yule S, et al. A randomized, observer-blinded trial of twice vs. three times weekly narrowband ultraviolet B phototherapy for chronic plaque psoriasis. Br J Dermatol. 2002;147:973-978.
- Harrop G, Dawe RS, Ibbotson S. Are photosensitizing medications associated with increased risk of important erythemal reactions during ultraviolet B phototherapy? Br J Dermatol. 2018;179:1184-1185.
- Torres AE, Lyons AB, Hamzavi IH, et al. Role of phototherapy in the era of biologics. J Am Acad Dermatol. 2021;84:479-485.
- Bukvic´ć Mokos Z, Jovic´ A, Cˇeovic´ R, et al. Therapeutic challenges in the mature patient. Clin Dermatol. 2018;36:128-139.
- Di Lernia V, Goldust M. An overview of the efficacy and safety of systemic treatments for psoriasis in the elderly. Expert Opin Biol Ther. 2018;18:897-903.
- Oliveira C, Torres T. More than skin deep: the systemic nature of atopic dermatitis. Eur J Dermatol. 2019;29:250-258.
- Matthews S, Pike K, Chien A. Phototherapy: safe and effective for challenging skin conditions in older adults. Cutis. 2021;108:E15-E21.
- Rodríguez-Granados MT, Estany-Gestal A, Pousa-Martínez M, et al. Is it useful to calculate minimal erythema dose before narrowband UV-B phototherapy? Actas Dermosifiliogr. 2017;108:852-858.
- Parlak N, Kundakci N, Parlak A, et al. Narrowband ultraviolet B phototherapy starting and incremental dose in patients with psoriasis: comparison of percentage dose and fixed dose protocols. Photodermatol Photoimmunol Photomed. 2015;31:90-97.
- Kleinpenning MM, Smits T, Boezeman J, et al. Narrowband ultraviolet B therapy in psoriasis: randomized double-blind comparison of high-dose and low-dose irradiation regimens. Br J Dermatol. 2009;161:1351-1356.
- Powell JB, Gach JE. Phototherapy in the elderly. Clin Exp Dermatol. 2015;40:605-610.
- Bulur I, Erdogan HK, Aksu AE, et al. The efficacy and safety of phototherapy in geriatric patients: a retrospective study. An Bras Dermatol. 2018;93:33-38.
- Dawe RS, Ibbotson SH. Drug-induced photosensitivity. Dermatol Clin. 2014;32:363-368, ix.
- Cameron H, Dawe RS. Photosensitizing drugs may lower the narrow-band ultraviolet B (TL-01) minimal erythema dose. Br J Dermatol. 2000;142:389-390.
- Elmets CA, Lim HW, Stoff B, et al. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis with phototherapy. J Am Acad Dermatol. 2019;81:775-804.
- Gloor M, Scherotzke A. Age dependence of ultraviolet light-induced erythema following narrow-band UVB exposure. Photodermatol Photoimmunol Photomed. 2002;18:121-126.
- Cox NH, Diffey BL, Farr PM. The relationship between chronological age and the erythemal response to ultraviolet B radiation. Br J Dermatol. 1992;126:315-319.
- Morrison W. Phototherapy and Photochemotherapy for Skin Disease. 2nd ed. Informa Healthcare; 2005.
- Almutawa F, Alnomair N, Wang Y, et al. Systematic review of UV-based therapy for psoriasis. Am J Clin Dermatol. 2013;14:87-109.
- Trakatelli M, Bylaite-Bucinskiene M, Correia O, et al. Clinical assessment of skin phototypes: watch your words! Eur J Dermatol. 2017;27:615-619.
- Kwon IH, Kwon HH, Na SJ, et al. Could colorimetric method replace the individual minimal erythemal dose (MED) measurements in determining the initial dose of narrow-band UVB treatment for psoriasis patients with skin phototype III-V? J Eur Acad Dermatol Venereol. 2013;27:494-498.
- Chen WA, Chang CM. The minimal erythema dose of narrowband ultraviolet B in elderly Taiwanese [published online September 1, 2021]. Photodermatol Photoimmunol Photomed. doi:10.1111/phpp.12730
Even with recent pharmacologic treatment advances, narrowband UVB (NB-UVB) phototherapy remains a versatile, safe, and efficacious adjunctive or exclusive treatment for multiple dermatologic conditions, including psoriasis and atopic dermatitis.
In a prior study, Matthews et al13 reported that 96% (50/52) of patients older than 65 years achieved medium to high levels of clearance with NB-UVB phototherapy. Nonetheless, 2 other findings in this study related to the number of treatments required to achieve clearance (ie, clearance rates) and erythema rates prompted further investigation. The first finding was higher-than-expected clearance rates. Older adults had a clearance rate with a mean of 33 treatments compared to prior studies featuring mean clearance rates of 20 to 28 treatments.7,8,14-16 This finding resembled a study in the United Kingdom17 with a median clearance rate in older adults of 30 treatments. In contrast, the median clearance rate from a study in Turkey18 was 42 treatments in older adults. We hypothesized that more photosensitizing medications used in older vs younger adults prompted more dose adjustments with NB-UVB phototherapy to avoid burning (ie, erythema) at baseline and throughout the treatment course. These dose adjustments may have increased the overall clearance rates. If true, we predicted that younger adults treated with the same protocol would have cleared more quickly, either because of age-related differences or because they likely had fewer comorbidities and therefore fewer medications.
The second finding from Matthews et al13 that warranted further investigation was a higher erythema rate compared to the older adult study from the United Kingdom.17 We hypothesized that potentially greater use of photosensitizing medications in the United States could explain the higher erythema rates. Although medication-induced photosensitivity is less likely with NB-UVB phototherapy than with UVA, certain medications can cause UVB photosensitivity, including thiazides, quinidine, calcium channel antagonists, phenothiazines, and nonsteroidal anti-inflammatory drugs.8,19,20 Therefore, photosensitizing medication use either at baseline or during a course of NB-UVB phototherapy could increase the risk for erythema. Age-related skin changes also have been considered as a
This retrospective study aimed to determine if NB-UVB phototherapy is equally effective in both older and younger adults treated with the same protocol; to examine the association between the use of photosensitizing medications and clearance rates in both older and younger adults; and to examine the association between the use of photosensitizing medications and erythema rates in older vs younger adults.
Methods
Study Design and Patients—This retrospective cohort study used billing records to identify patients who received NB-UVB phototherapy at 3 different clinical sites within a large US health care system in Washington (Group Health Cooperative, now Kaiser Permanente Washington), serving more than 600,000 patients between January 1, 2012, and December 31, 2016. The institutional review board of Kaiser Permanente Washington Health Research Institute approved this study (IRB 1498087-4). Younger adults were classified as those 64 years or younger and older adults as those 65 years and older at the start of their phototherapy regimen. A power analysis determined that the optimal sample size for this study was 250 patients.
Individuals were excluded if they had fewer than 6 phototherapy treatments; a diagnosis of vitiligo, photosensitivity dermatitis, morphea, or pityriasis rubra pilaris; and/or treatment of the hands or feet only.
Phototherapy Protocol—Using a 48-lamp NB-UVB unit, trained phototherapy nurses provided all treatments following standardized treatment protocols13 based on previously published phototherapy guidelines.24 Nurses determined each patient’s disease clearance level using a 3-point clearance scale (high, medium, low).13 Each patient’s starting dose was determined based on the estimated MED for their skin phototype.
Statistical Analysis—Data were analyzed using Stata statistical software (StataCorp LLC). Univariate analyses were used to examine the data and identify outliers, bad values, and missing data, as well as to calculate descriptive statistics. Pearson χ2 and Fisher exact statistics were used to calculate differences in categorical variables. Linear multivariate regression models and logistic multivariate models were used to examine statistical relationships between variables. Statistical significance was defined as P≤.05.
Results
Patient Characteristics—Medical records were reviewed for 172 patients who received phototherapy between 2012 and 2016. Patients ranged in age from 23 to 91 years, with 102 patients 64 years and younger and 70 patients 65 years and older. Tables 1 and 2 outline the patient characteristics and conditions treated.

Phototherapy Effectiveness—

Photosensitizing Medications, Clearance Levels, and Clearance Rates—

Frequency of Treatments and Clearance Rates—Older adults more consistently completed the recommended frequency of treatments—3 times weekly—compared to younger adults (74.3% vs 58.5%). However, all patients who completed 3 treatments per week required a similar number of treatments to clear (older adults, mean [SD]: 35.7 [21.6]; younger adults, mean [SD]: 34.7 [19.0]; P=.85). Among patients completing 2 or fewer treatments per week, older adults required a mean (SD) of only 31 (9.0) treatments to clear vs 41.5 (21.3) treatments to clear for younger adults, but the difference was not statistically significant (P=.08). However, even those with suboptimal frequency ultimately achieved similar clearance levels.


Photosensitizing Medications and Erythema Rates—

Overall, phototherapy nurses adjusted the starting dose according to the phototype-based protocol an average of 69% of the time for patients on medications with photosensitivity listed as a potential side effect. However, the frequency depended significantly on the clinic (clinic A, 24%; clinic B, 92%; clinic C, 87%)(P≤.001). Nurses across all clinics consistently decreased the treatment dose when patients reported starting new photosensitizing medications. Patients with adjusted starting doses had slightly but not significantly higher clearance rates compared to those without (mean, 37.8 vs 35.5; t(104)=0.58; P=.56).

Comment
Impact of Photosensitizing Medications on Clearance—Photosensitizing medications and treatment frequency were 2 factors that might explain the slower clearance rates in younger adults. In this study, both groups of patients used similar numbers of photosensitizing medications, but more older adults were taking 3 or more medications (Table 3). We found no statistically significant relationship between taking photosensitizing medications and either the clearance rates or the level of clearance achieved in either age group.
Impact of Treatment Frequency—Weekly treatment frequency also was examined. One prior study demonstrated that treatments 3 times weekly led to a faster clearance time and higher clearance levels compared with twice-weekly treatment.7 When patients completed treatments twice weekly, it took an average of 1.5 times more days to clear, which impacted cost and clinical resource availability. The patients ranged in age from 17 to 80 years, but outcomes in older patients were not described separately.7 Interestingly, our study seemed to find a difference between age groups when the impact of treatment frequency was examined. Older adults completed nearly 4 fewer mean treatments to clear when treating less often, with more than 80% achieving high levels of clearance, whereas the younger adults required almost 7 more treatments to clear when they came in less frequently, with approximately 80% achieving a high level of clearance. As a result, our study found that in both age groups, slowing the treatment frequency extended the treatment time to clearance—more for the younger adults than the older adults—but did not significantly change the percentage of individuals reaching full clearance in either group.
Erythema Rates—There was no association between photosensitizing medications and erythema rates except when patients were taking at least 3 medications. Most medications that listed photosensitivity as a possible side effect did not specify their relevant range of UV radiation; therefore, all such medications were examined during this analysis. Prior research has shown UVB range photosensitizing medications include thiazides, quinidine, calcium channel antagonists, phenothiazines, and nonsteroidal anti-inflammatory drugs.19 A sensitivity analysis that focused only on these medications found no association between them and any particular grade of erythema. However, patients taking 3 or more of any medications listing photosensitivity as a side effect had an increased risk for grade 2 erythema.
Erythema rates in this study were consistent with a 2013 systematic review that reported 57% of patients with asymptomatic grade 1 erythema.25 In the 2 other comparative older adult studies, erythema rates varied widely: 35% in a study from Turkey18compared to only1.89% in a study from the United Kingdom.17
The starting dose for NB-UVB may drive erythema rates. The current study’s protocols were based on an estimated MED that is subjectively determined by the dermatology provider’s assessment of the patient’s skin sensitivity via examination and questions to the patient about their response to environmental sun exposure (ie, burning and tanning)26 and is frequently used to determine the starting dose and subsequent dose escalation. Certain medications have been found to increase photosensitivity and erythema,20 which can change an individual’s MED. If photosensitizing medications are started prior to or during a course of NB-UVB without a pretreatment MED, they might increase the risk for erythema. This study did not identify specific erythema-inducing medications but did find that taking 3 or more photosensitizing medications was associated with increased episodes of grade 2 erythema. Similarly, Harrop et al8 found that patients who were taking photosensitizing medications were more likely to have grade 2 or higher erythema, despite baseline MED testing, which is an established safety mechanism to reduce the risk and severity of erythema.14,20,27 The authors of a recent study of older adults in Taiwan specifically recommended MED testing due to the unpredictable influence of polypharmacy on MED calculations in this population.28 Therefore, this study’s use of an estimated MED in older adults may have influenced the starting dose as well as the incidence and severity of erythemic events. Age-related skin changes likely are ruled out as a consideration for mild erythema by the similarity of grade 1 erythema rates in both older and younger adults. Other studies have identified differences between the age groups, where older patients experienced more intense erythema in the late phase of UVB treatments.22,23 This phenomenon could increase the risk for a grade 2 erythema, which may correspond with this study’s findings.
Other potential causes of erythema were ruled out during our study, including erythema related to missed treatments and shielding mishaps. Other factors, however, may impact the level of sensitivity each patient has to phototherapy, including genetics, epigenetics, and cumulative sun damage. With NB-UVB, near-erythemogenic doses are optimal to achieve effective treatments but require a delicate balance to achieve, which may be more problematic for older adults, especially those taking several medications.
Study Limitations—Our study design made it difficult to draw conclusions about rarer dermatologic conditions. Some patients received treatments over years that were not included in the study period. Finally, power calculations suggested that our actual sample size was too small, with approximately one-third of the required sample missing.
Practical Implications—The goals of phototherapy are to achieve a high level of disease clearance with the fewest number of treatments possible and minimal side effects.
The extra staff training and patient monitoring required for MED testing likely is to add value and preserve resources if faster clearance rates could be achieved and may warrant further investigation. Phototherapy centers require standardized treatment protocols, diligent well-trained staff, and program monitoring to ensure consistent care to all patients. This study highlighted the ongoing opportunity for health care organizations to conduct evidence-based practice inquiries to continually optimize care for their patients.
Even with recent pharmacologic treatment advances, narrowband UVB (NB-UVB) phototherapy remains a versatile, safe, and efficacious adjunctive or exclusive treatment for multiple dermatologic conditions, including psoriasis and atopic dermatitis.
In a prior study, Matthews et al13 reported that 96% (50/52) of patients older than 65 years achieved medium to high levels of clearance with NB-UVB phototherapy. Nonetheless, 2 other findings in this study related to the number of treatments required to achieve clearance (ie, clearance rates) and erythema rates prompted further investigation. The first finding was higher-than-expected clearance rates. Older adults had a clearance rate with a mean of 33 treatments compared to prior studies featuring mean clearance rates of 20 to 28 treatments.7,8,14-16 This finding resembled a study in the United Kingdom17 with a median clearance rate in older adults of 30 treatments. In contrast, the median clearance rate from a study in Turkey18 was 42 treatments in older adults. We hypothesized that more photosensitizing medications used in older vs younger adults prompted more dose adjustments with NB-UVB phototherapy to avoid burning (ie, erythema) at baseline and throughout the treatment course. These dose adjustments may have increased the overall clearance rates. If true, we predicted that younger adults treated with the same protocol would have cleared more quickly, either because of age-related differences or because they likely had fewer comorbidities and therefore fewer medications.
The second finding from Matthews et al13 that warranted further investigation was a higher erythema rate compared to the older adult study from the United Kingdom.17 We hypothesized that potentially greater use of photosensitizing medications in the United States could explain the higher erythema rates. Although medication-induced photosensitivity is less likely with NB-UVB phototherapy than with UVA, certain medications can cause UVB photosensitivity, including thiazides, quinidine, calcium channel antagonists, phenothiazines, and nonsteroidal anti-inflammatory drugs.8,19,20 Therefore, photosensitizing medication use either at baseline or during a course of NB-UVB phototherapy could increase the risk for erythema. Age-related skin changes also have been considered as a
This retrospective study aimed to determine if NB-UVB phototherapy is equally effective in both older and younger adults treated with the same protocol; to examine the association between the use of photosensitizing medications and clearance rates in both older and younger adults; and to examine the association between the use of photosensitizing medications and erythema rates in older vs younger adults.
Methods
Study Design and Patients—This retrospective cohort study used billing records to identify patients who received NB-UVB phototherapy at 3 different clinical sites within a large US health care system in Washington (Group Health Cooperative, now Kaiser Permanente Washington), serving more than 600,000 patients between January 1, 2012, and December 31, 2016. The institutional review board of Kaiser Permanente Washington Health Research Institute approved this study (IRB 1498087-4). Younger adults were classified as those 64 years or younger and older adults as those 65 years and older at the start of their phototherapy regimen. A power analysis determined that the optimal sample size for this study was 250 patients.
Individuals were excluded if they had fewer than 6 phototherapy treatments; a diagnosis of vitiligo, photosensitivity dermatitis, morphea, or pityriasis rubra pilaris; and/or treatment of the hands or feet only.
Phototherapy Protocol—Using a 48-lamp NB-UVB unit, trained phototherapy nurses provided all treatments following standardized treatment protocols13 based on previously published phototherapy guidelines.24 Nurses determined each patient’s disease clearance level using a 3-point clearance scale (high, medium, low).13 Each patient’s starting dose was determined based on the estimated MED for their skin phototype.
Statistical Analysis—Data were analyzed using Stata statistical software (StataCorp LLC). Univariate analyses were used to examine the data and identify outliers, bad values, and missing data, as well as to calculate descriptive statistics. Pearson χ2 and Fisher exact statistics were used to calculate differences in categorical variables. Linear multivariate regression models and logistic multivariate models were used to examine statistical relationships between variables. Statistical significance was defined as P≤.05.
Results
Patient Characteristics—Medical records were reviewed for 172 patients who received phototherapy between 2012 and 2016. Patients ranged in age from 23 to 91 years, with 102 patients 64 years and younger and 70 patients 65 years and older. Tables 1 and 2 outline the patient characteristics and conditions treated.

Phototherapy Effectiveness—

Photosensitizing Medications, Clearance Levels, and Clearance Rates—

Frequency of Treatments and Clearance Rates—Older adults more consistently completed the recommended frequency of treatments—3 times weekly—compared to younger adults (74.3% vs 58.5%). However, all patients who completed 3 treatments per week required a similar number of treatments to clear (older adults, mean [SD]: 35.7 [21.6]; younger adults, mean [SD]: 34.7 [19.0]; P=.85). Among patients completing 2 or fewer treatments per week, older adults required a mean (SD) of only 31 (9.0) treatments to clear vs 41.5 (21.3) treatments to clear for younger adults, but the difference was not statistically significant (P=.08). However, even those with suboptimal frequency ultimately achieved similar clearance levels.


Photosensitizing Medications and Erythema Rates—

Overall, phototherapy nurses adjusted the starting dose according to the phototype-based protocol an average of 69% of the time for patients on medications with photosensitivity listed as a potential side effect. However, the frequency depended significantly on the clinic (clinic A, 24%; clinic B, 92%; clinic C, 87%)(P≤.001). Nurses across all clinics consistently decreased the treatment dose when patients reported starting new photosensitizing medications. Patients with adjusted starting doses had slightly but not significantly higher clearance rates compared to those without (mean, 37.8 vs 35.5; t(104)=0.58; P=.56).

Comment
Impact of Photosensitizing Medications on Clearance—Photosensitizing medications and treatment frequency were 2 factors that might explain the slower clearance rates in younger adults. In this study, both groups of patients used similar numbers of photosensitizing medications, but more older adults were taking 3 or more medications (Table 3). We found no statistically significant relationship between taking photosensitizing medications and either the clearance rates or the level of clearance achieved in either age group.
Impact of Treatment Frequency—Weekly treatment frequency also was examined. One prior study demonstrated that treatments 3 times weekly led to a faster clearance time and higher clearance levels compared with twice-weekly treatment.7 When patients completed treatments twice weekly, it took an average of 1.5 times more days to clear, which impacted cost and clinical resource availability. The patients ranged in age from 17 to 80 years, but outcomes in older patients were not described separately.7 Interestingly, our study seemed to find a difference between age groups when the impact of treatment frequency was examined. Older adults completed nearly 4 fewer mean treatments to clear when treating less often, with more than 80% achieving high levels of clearance, whereas the younger adults required almost 7 more treatments to clear when they came in less frequently, with approximately 80% achieving a high level of clearance. As a result, our study found that in both age groups, slowing the treatment frequency extended the treatment time to clearance—more for the younger adults than the older adults—but did not significantly change the percentage of individuals reaching full clearance in either group.
Erythema Rates—There was no association between photosensitizing medications and erythema rates except when patients were taking at least 3 medications. Most medications that listed photosensitivity as a possible side effect did not specify their relevant range of UV radiation; therefore, all such medications were examined during this analysis. Prior research has shown UVB range photosensitizing medications include thiazides, quinidine, calcium channel antagonists, phenothiazines, and nonsteroidal anti-inflammatory drugs.19 A sensitivity analysis that focused only on these medications found no association between them and any particular grade of erythema. However, patients taking 3 or more of any medications listing photosensitivity as a side effect had an increased risk for grade 2 erythema.
Erythema rates in this study were consistent with a 2013 systematic review that reported 57% of patients with asymptomatic grade 1 erythema.25 In the 2 other comparative older adult studies, erythema rates varied widely: 35% in a study from Turkey18compared to only1.89% in a study from the United Kingdom.17
The starting dose for NB-UVB may drive erythema rates. The current study’s protocols were based on an estimated MED that is subjectively determined by the dermatology provider’s assessment of the patient’s skin sensitivity via examination and questions to the patient about their response to environmental sun exposure (ie, burning and tanning)26 and is frequently used to determine the starting dose and subsequent dose escalation. Certain medications have been found to increase photosensitivity and erythema,20 which can change an individual’s MED. If photosensitizing medications are started prior to or during a course of NB-UVB without a pretreatment MED, they might increase the risk for erythema. This study did not identify specific erythema-inducing medications but did find that taking 3 or more photosensitizing medications was associated with increased episodes of grade 2 erythema. Similarly, Harrop et al8 found that patients who were taking photosensitizing medications were more likely to have grade 2 or higher erythema, despite baseline MED testing, which is an established safety mechanism to reduce the risk and severity of erythema.14,20,27 The authors of a recent study of older adults in Taiwan specifically recommended MED testing due to the unpredictable influence of polypharmacy on MED calculations in this population.28 Therefore, this study’s use of an estimated MED in older adults may have influenced the starting dose as well as the incidence and severity of erythemic events. Age-related skin changes likely are ruled out as a consideration for mild erythema by the similarity of grade 1 erythema rates in both older and younger adults. Other studies have identified differences between the age groups, where older patients experienced more intense erythema in the late phase of UVB treatments.22,23 This phenomenon could increase the risk for a grade 2 erythema, which may correspond with this study’s findings.
Other potential causes of erythema were ruled out during our study, including erythema related to missed treatments and shielding mishaps. Other factors, however, may impact the level of sensitivity each patient has to phototherapy, including genetics, epigenetics, and cumulative sun damage. With NB-UVB, near-erythemogenic doses are optimal to achieve effective treatments but require a delicate balance to achieve, which may be more problematic for older adults, especially those taking several medications.
Study Limitations—Our study design made it difficult to draw conclusions about rarer dermatologic conditions. Some patients received treatments over years that were not included in the study period. Finally, power calculations suggested that our actual sample size was too small, with approximately one-third of the required sample missing.
Practical Implications—The goals of phototherapy are to achieve a high level of disease clearance with the fewest number of treatments possible and minimal side effects.
The extra staff training and patient monitoring required for MED testing likely is to add value and preserve resources if faster clearance rates could be achieved and may warrant further investigation. Phototherapy centers require standardized treatment protocols, diligent well-trained staff, and program monitoring to ensure consistent care to all patients. This study highlighted the ongoing opportunity for health care organizations to conduct evidence-based practice inquiries to continually optimize care for their patients.
- Fernández-Guarino M, Aboin-Gonzalez S, Barchino L, et al. Treatment of moderate and severe adult chronic atopic dermatitis with narrow-band UVB and the combination of narrow-band UVB/UVA phototherapy. Dermatol Ther. 2016;29:19-23.
- Foerster J, Boswell K, West J, et al. Narrowband UVB treatment is highly effective and causes a strong reduction in the use of steroid and other creams in psoriasis patients in clinical practice. PLoS One. 2017;12:e0181813.
- Gambichler T, Breuckmann F, Boms S, et al. Narrowband UVB phototherapy in skin conditions beyond psoriasis. J Am Acad Dermatol. 2005;52:660-670.
- Ryu HH, Choe YS, Jo S, et al. Remission period in psoriasis after multiple cycles of narrowband ultraviolet B phototherapy. J Dermatol. 2014;41:622-627.
- Schneider LA, Hinrichs R, Scharffetter-Kochanek K. Phototherapy and photochemotherapy. Clin Dermatol. 2008;26:464-476.
- Tintle S, Shemer A, Suárez-Fariñas M, et al. Reversal of atopic dermatitis with narrow-band UVB phototherapy and biomarkers for therapeutic response. J Allergy Clin Immunol. 2011;128:583-593.e581-584.
- Cameron H, Dawe RS, Yule S, et al. A randomized, observer-blinded trial of twice vs. three times weekly narrowband ultraviolet B phototherapy for chronic plaque psoriasis. Br J Dermatol. 2002;147:973-978.
- Harrop G, Dawe RS, Ibbotson S. Are photosensitizing medications associated with increased risk of important erythemal reactions during ultraviolet B phototherapy? Br J Dermatol. 2018;179:1184-1185.
- Torres AE, Lyons AB, Hamzavi IH, et al. Role of phototherapy in the era of biologics. J Am Acad Dermatol. 2021;84:479-485.
- Bukvic´ć Mokos Z, Jovic´ A, Cˇeovic´ R, et al. Therapeutic challenges in the mature patient. Clin Dermatol. 2018;36:128-139.
- Di Lernia V, Goldust M. An overview of the efficacy and safety of systemic treatments for psoriasis in the elderly. Expert Opin Biol Ther. 2018;18:897-903.
- Oliveira C, Torres T. More than skin deep: the systemic nature of atopic dermatitis. Eur J Dermatol. 2019;29:250-258.
- Matthews S, Pike K, Chien A. Phototherapy: safe and effective for challenging skin conditions in older adults. Cutis. 2021;108:E15-E21.
- Rodríguez-Granados MT, Estany-Gestal A, Pousa-Martínez M, et al. Is it useful to calculate minimal erythema dose before narrowband UV-B phototherapy? Actas Dermosifiliogr. 2017;108:852-858.
- Parlak N, Kundakci N, Parlak A, et al. Narrowband ultraviolet B phototherapy starting and incremental dose in patients with psoriasis: comparison of percentage dose and fixed dose protocols. Photodermatol Photoimmunol Photomed. 2015;31:90-97.
- Kleinpenning MM, Smits T, Boezeman J, et al. Narrowband ultraviolet B therapy in psoriasis: randomized double-blind comparison of high-dose and low-dose irradiation regimens. Br J Dermatol. 2009;161:1351-1356.
- Powell JB, Gach JE. Phototherapy in the elderly. Clin Exp Dermatol. 2015;40:605-610.
- Bulur I, Erdogan HK, Aksu AE, et al. The efficacy and safety of phototherapy in geriatric patients: a retrospective study. An Bras Dermatol. 2018;93:33-38.
- Dawe RS, Ibbotson SH. Drug-induced photosensitivity. Dermatol Clin. 2014;32:363-368, ix.
- Cameron H, Dawe RS. Photosensitizing drugs may lower the narrow-band ultraviolet B (TL-01) minimal erythema dose. Br J Dermatol. 2000;142:389-390.
- Elmets CA, Lim HW, Stoff B, et al. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis with phototherapy. J Am Acad Dermatol. 2019;81:775-804.
- Gloor M, Scherotzke A. Age dependence of ultraviolet light-induced erythema following narrow-band UVB exposure. Photodermatol Photoimmunol Photomed. 2002;18:121-126.
- Cox NH, Diffey BL, Farr PM. The relationship between chronological age and the erythemal response to ultraviolet B radiation. Br J Dermatol. 1992;126:315-319.
- Morrison W. Phototherapy and Photochemotherapy for Skin Disease. 2nd ed. Informa Healthcare; 2005.
- Almutawa F, Alnomair N, Wang Y, et al. Systematic review of UV-based therapy for psoriasis. Am J Clin Dermatol. 2013;14:87-109.
- Trakatelli M, Bylaite-Bucinskiene M, Correia O, et al. Clinical assessment of skin phototypes: watch your words! Eur J Dermatol. 2017;27:615-619.
- Kwon IH, Kwon HH, Na SJ, et al. Could colorimetric method replace the individual minimal erythemal dose (MED) measurements in determining the initial dose of narrow-band UVB treatment for psoriasis patients with skin phototype III-V? J Eur Acad Dermatol Venereol. 2013;27:494-498.
- Chen WA, Chang CM. The minimal erythema dose of narrowband ultraviolet B in elderly Taiwanese [published online September 1, 2021]. Photodermatol Photoimmunol Photomed. doi:10.1111/phpp.12730
- Fernández-Guarino M, Aboin-Gonzalez S, Barchino L, et al. Treatment of moderate and severe adult chronic atopic dermatitis with narrow-band UVB and the combination of narrow-band UVB/UVA phototherapy. Dermatol Ther. 2016;29:19-23.
- Foerster J, Boswell K, West J, et al. Narrowband UVB treatment is highly effective and causes a strong reduction in the use of steroid and other creams in psoriasis patients in clinical practice. PLoS One. 2017;12:e0181813.
- Gambichler T, Breuckmann F, Boms S, et al. Narrowband UVB phototherapy in skin conditions beyond psoriasis. J Am Acad Dermatol. 2005;52:660-670.
- Ryu HH, Choe YS, Jo S, et al. Remission period in psoriasis after multiple cycles of narrowband ultraviolet B phototherapy. J Dermatol. 2014;41:622-627.
- Schneider LA, Hinrichs R, Scharffetter-Kochanek K. Phototherapy and photochemotherapy. Clin Dermatol. 2008;26:464-476.
- Tintle S, Shemer A, Suárez-Fariñas M, et al. Reversal of atopic dermatitis with narrow-band UVB phototherapy and biomarkers for therapeutic response. J Allergy Clin Immunol. 2011;128:583-593.e581-584.
- Cameron H, Dawe RS, Yule S, et al. A randomized, observer-blinded trial of twice vs. three times weekly narrowband ultraviolet B phototherapy for chronic plaque psoriasis. Br J Dermatol. 2002;147:973-978.
- Harrop G, Dawe RS, Ibbotson S. Are photosensitizing medications associated with increased risk of important erythemal reactions during ultraviolet B phototherapy? Br J Dermatol. 2018;179:1184-1185.
- Torres AE, Lyons AB, Hamzavi IH, et al. Role of phototherapy in the era of biologics. J Am Acad Dermatol. 2021;84:479-485.
- Bukvic´ć Mokos Z, Jovic´ A, Cˇeovic´ R, et al. Therapeutic challenges in the mature patient. Clin Dermatol. 2018;36:128-139.
- Di Lernia V, Goldust M. An overview of the efficacy and safety of systemic treatments for psoriasis in the elderly. Expert Opin Biol Ther. 2018;18:897-903.
- Oliveira C, Torres T. More than skin deep: the systemic nature of atopic dermatitis. Eur J Dermatol. 2019;29:250-258.
- Matthews S, Pike K, Chien A. Phototherapy: safe and effective for challenging skin conditions in older adults. Cutis. 2021;108:E15-E21.
- Rodríguez-Granados MT, Estany-Gestal A, Pousa-Martínez M, et al. Is it useful to calculate minimal erythema dose before narrowband UV-B phototherapy? Actas Dermosifiliogr. 2017;108:852-858.
- Parlak N, Kundakci N, Parlak A, et al. Narrowband ultraviolet B phototherapy starting and incremental dose in patients with psoriasis: comparison of percentage dose and fixed dose protocols. Photodermatol Photoimmunol Photomed. 2015;31:90-97.
- Kleinpenning MM, Smits T, Boezeman J, et al. Narrowband ultraviolet B therapy in psoriasis: randomized double-blind comparison of high-dose and low-dose irradiation regimens. Br J Dermatol. 2009;161:1351-1356.
- Powell JB, Gach JE. Phototherapy in the elderly. Clin Exp Dermatol. 2015;40:605-610.
- Bulur I, Erdogan HK, Aksu AE, et al. The efficacy and safety of phototherapy in geriatric patients: a retrospective study. An Bras Dermatol. 2018;93:33-38.
- Dawe RS, Ibbotson SH. Drug-induced photosensitivity. Dermatol Clin. 2014;32:363-368, ix.
- Cameron H, Dawe RS. Photosensitizing drugs may lower the narrow-band ultraviolet B (TL-01) minimal erythema dose. Br J Dermatol. 2000;142:389-390.
- Elmets CA, Lim HW, Stoff B, et al. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis with phototherapy. J Am Acad Dermatol. 2019;81:775-804.
- Gloor M, Scherotzke A. Age dependence of ultraviolet light-induced erythema following narrow-band UVB exposure. Photodermatol Photoimmunol Photomed. 2002;18:121-126.
- Cox NH, Diffey BL, Farr PM. The relationship between chronological age and the erythemal response to ultraviolet B radiation. Br J Dermatol. 1992;126:315-319.
- Morrison W. Phototherapy and Photochemotherapy for Skin Disease. 2nd ed. Informa Healthcare; 2005.
- Almutawa F, Alnomair N, Wang Y, et al. Systematic review of UV-based therapy for psoriasis. Am J Clin Dermatol. 2013;14:87-109.
- Trakatelli M, Bylaite-Bucinskiene M, Correia O, et al. Clinical assessment of skin phototypes: watch your words! Eur J Dermatol. 2017;27:615-619.
- Kwon IH, Kwon HH, Na SJ, et al. Could colorimetric method replace the individual minimal erythemal dose (MED) measurements in determining the initial dose of narrow-band UVB treatment for psoriasis patients with skin phototype III-V? J Eur Acad Dermatol Venereol. 2013;27:494-498.
- Chen WA, Chang CM. The minimal erythema dose of narrowband ultraviolet B in elderly Taiwanese [published online September 1, 2021]. Photodermatol Photoimmunol Photomed. doi:10.1111/phpp.12730
Practice Points
- Narrowband UVB (NB-UVB) phototherapy remains a safe and efficacious nonpharmacologic treatment for dermatologic conditions in older and younger adults.
- Compared to younger adults, older adults using the same protocols need similar or even fewer treatments to achieve high levels of clearance.
- Individuals taking 3 or more photosensitizing medications, regardless of age, may be at higher risk for substantial erythema with NB-UVB phototherapy.
- Phototherapy program monitoring is important to ensure quality care and investigate opportunities for care optimization.