User login
Preterm C-sections, induced deliveries dropped during COVID-19 pandemic
Premature births from cesarean (C-section) and induced deliveries dropped abruptly by 6.5% from the projected number in the first month of the COVID-19 pandemic and stayed at the lower rate consistently throughout the year, researchers have found.
Results of the study, led by Daniel Dench, PhD, assistant professor at the Georgia Institute of Technology School of Economics in Atlanta, were published online in Pediatrics.
The authors say their findings help answer the question of whether numbers of preterm (less than 37 weeks gestation) C-sections and induced deliveries would change if women didn’t see their physicians during pregnancy as often, especially in person, and raise the question of whether some birth interventions by physicians may not be necessary. The pandemic gave researchers a natural, ethical way to study the question.
The researchers found that in March 2020 – the start of business closures and stay-at-home orders around the country – preterm births from C-sections or induced deliveries immediately fell from the forecast number for the month by 0.4 percentage points. For the rest of 2020, the number remained on average 0.35 percentage points below the numbers predicted.
That means 350 fewer preterm C-sections and induced deliveries per 100,000 live births, or 10,000 fewer overall, the authors said.
Dr. Dench told this publication the numbers for those births had been steady from January 2010 to February 2020, but the pattern “diverges from this trend very clearly beginning exactly in March 2020 and does not return to trend by December 2020.”
Meanwhile, during the study period, the number of full-term cesarean and induced deliveries stayed steady and started to increase slightly in 2020. Researchers also adjusted for seasonality as, for example, preterm births are higher on average in February than in March.
So far, Dr. Dench said in a press release, it’s not clear whether the lower numbers mean physicians didn’t deliver babies that ended up surviving in the womb anyway or if they missed some that would die in the womb without intervention.
To better understand those implications, Dr. Dench says he is turning to fetal death records for March-December 2020 and he said he expects to have those results analyzed by the end of the year.
If there was no change in fetal deaths at the same time as the drop in preterm births, Dr. Dench said, that could point to physician interventions that may not have been necessary.
Mya R. Zapata, MD, an obstetrician-gynecologist with UCLA Health, who was not involved with the study, told this publication that checking the fetal deaths is a good start and an objective outcome in answering the question, but she points out there are other outcomes that will take a deeper analysis, such as whether there are differences later in developmental outcomes after fewer physician visits.
“It’s always a good question for health care,” she said, “are we doing more than we need to?”
Dr. Zapata is the obstetrics service chief for UCLA’s labor and delivery unit and was an integral part of decision-making as to what services were essential and for which patients. She said the fewer visits and fewer ultrasounds the researchers describe fit with what ob.gyns. at UCLA experienced as the pandemic hit.
“We really tried to hone in on people who were at highest risk for an adverse outcome,” she said. “I still have the question of whether there were things we missed in low-risk people. It will take time to get the entire answer. But it does make us reflect that perhaps less intervention could be better for patients and easier. It’s our job in medicine to keep asking the question of what is essential and safe and not just continue with current practice because that’s what we’ve always done.”
The amount of data gave the researchers an unusual view. They studied 38,891,271 singleton births in the United States from 2010 to 2020 with data from the National Center for Health Statistics.
“If you look at 1,000 births in a single hospital, or even at 30,000 births across a hospital system, you wouldn’t be able to see the drop as clearly,” Dr. Dench said. “The drop we detected is a huge change, but you might miss it in a small sample.”
The researchers acknowledge a limitation of the study is that half of all preterm C-sections and induced deliveries happen because of a ruptured membrane, a spontaneous cause. Those instances can’t be distinguished from the ones caused by doctors’ interventions in this study.
“Still, these findings are significant because the causes for preterm births are not always known,” the authors wrote in the press release.
The study authors and Dr. Zapata reported no relevant financial relationships.
Premature births from cesarean (C-section) and induced deliveries dropped abruptly by 6.5% from the projected number in the first month of the COVID-19 pandemic and stayed at the lower rate consistently throughout the year, researchers have found.
Results of the study, led by Daniel Dench, PhD, assistant professor at the Georgia Institute of Technology School of Economics in Atlanta, were published online in Pediatrics.
The authors say their findings help answer the question of whether numbers of preterm (less than 37 weeks gestation) C-sections and induced deliveries would change if women didn’t see their physicians during pregnancy as often, especially in person, and raise the question of whether some birth interventions by physicians may not be necessary. The pandemic gave researchers a natural, ethical way to study the question.
The researchers found that in March 2020 – the start of business closures and stay-at-home orders around the country – preterm births from C-sections or induced deliveries immediately fell from the forecast number for the month by 0.4 percentage points. For the rest of 2020, the number remained on average 0.35 percentage points below the numbers predicted.
That means 350 fewer preterm C-sections and induced deliveries per 100,000 live births, or 10,000 fewer overall, the authors said.
Dr. Dench told this publication the numbers for those births had been steady from January 2010 to February 2020, but the pattern “diverges from this trend very clearly beginning exactly in March 2020 and does not return to trend by December 2020.”
Meanwhile, during the study period, the number of full-term cesarean and induced deliveries stayed steady and started to increase slightly in 2020. Researchers also adjusted for seasonality as, for example, preterm births are higher on average in February than in March.
So far, Dr. Dench said in a press release, it’s not clear whether the lower numbers mean physicians didn’t deliver babies that ended up surviving in the womb anyway or if they missed some that would die in the womb without intervention.
To better understand those implications, Dr. Dench says he is turning to fetal death records for March-December 2020 and he said he expects to have those results analyzed by the end of the year.
If there was no change in fetal deaths at the same time as the drop in preterm births, Dr. Dench said, that could point to physician interventions that may not have been necessary.
Mya R. Zapata, MD, an obstetrician-gynecologist with UCLA Health, who was not involved with the study, told this publication that checking the fetal deaths is a good start and an objective outcome in answering the question, but she points out there are other outcomes that will take a deeper analysis, such as whether there are differences later in developmental outcomes after fewer physician visits.
“It’s always a good question for health care,” she said, “are we doing more than we need to?”
Dr. Zapata is the obstetrics service chief for UCLA’s labor and delivery unit and was an integral part of decision-making as to what services were essential and for which patients. She said the fewer visits and fewer ultrasounds the researchers describe fit with what ob.gyns. at UCLA experienced as the pandemic hit.
“We really tried to hone in on people who were at highest risk for an adverse outcome,” she said. “I still have the question of whether there were things we missed in low-risk people. It will take time to get the entire answer. But it does make us reflect that perhaps less intervention could be better for patients and easier. It’s our job in medicine to keep asking the question of what is essential and safe and not just continue with current practice because that’s what we’ve always done.”
The amount of data gave the researchers an unusual view. They studied 38,891,271 singleton births in the United States from 2010 to 2020 with data from the National Center for Health Statistics.
“If you look at 1,000 births in a single hospital, or even at 30,000 births across a hospital system, you wouldn’t be able to see the drop as clearly,” Dr. Dench said. “The drop we detected is a huge change, but you might miss it in a small sample.”
The researchers acknowledge a limitation of the study is that half of all preterm C-sections and induced deliveries happen because of a ruptured membrane, a spontaneous cause. Those instances can’t be distinguished from the ones caused by doctors’ interventions in this study.
“Still, these findings are significant because the causes for preterm births are not always known,” the authors wrote in the press release.
The study authors and Dr. Zapata reported no relevant financial relationships.
Premature births from cesarean (C-section) and induced deliveries dropped abruptly by 6.5% from the projected number in the first month of the COVID-19 pandemic and stayed at the lower rate consistently throughout the year, researchers have found.
Results of the study, led by Daniel Dench, PhD, assistant professor at the Georgia Institute of Technology School of Economics in Atlanta, were published online in Pediatrics.
The authors say their findings help answer the question of whether numbers of preterm (less than 37 weeks gestation) C-sections and induced deliveries would change if women didn’t see their physicians during pregnancy as often, especially in person, and raise the question of whether some birth interventions by physicians may not be necessary. The pandemic gave researchers a natural, ethical way to study the question.
The researchers found that in March 2020 – the start of business closures and stay-at-home orders around the country – preterm births from C-sections or induced deliveries immediately fell from the forecast number for the month by 0.4 percentage points. For the rest of 2020, the number remained on average 0.35 percentage points below the numbers predicted.
That means 350 fewer preterm C-sections and induced deliveries per 100,000 live births, or 10,000 fewer overall, the authors said.
Dr. Dench told this publication the numbers for those births had been steady from January 2010 to February 2020, but the pattern “diverges from this trend very clearly beginning exactly in March 2020 and does not return to trend by December 2020.”
Meanwhile, during the study period, the number of full-term cesarean and induced deliveries stayed steady and started to increase slightly in 2020. Researchers also adjusted for seasonality as, for example, preterm births are higher on average in February than in March.
So far, Dr. Dench said in a press release, it’s not clear whether the lower numbers mean physicians didn’t deliver babies that ended up surviving in the womb anyway or if they missed some that would die in the womb without intervention.
To better understand those implications, Dr. Dench says he is turning to fetal death records for March-December 2020 and he said he expects to have those results analyzed by the end of the year.
If there was no change in fetal deaths at the same time as the drop in preterm births, Dr. Dench said, that could point to physician interventions that may not have been necessary.
Mya R. Zapata, MD, an obstetrician-gynecologist with UCLA Health, who was not involved with the study, told this publication that checking the fetal deaths is a good start and an objective outcome in answering the question, but she points out there are other outcomes that will take a deeper analysis, such as whether there are differences later in developmental outcomes after fewer physician visits.
“It’s always a good question for health care,” she said, “are we doing more than we need to?”
Dr. Zapata is the obstetrics service chief for UCLA’s labor and delivery unit and was an integral part of decision-making as to what services were essential and for which patients. She said the fewer visits and fewer ultrasounds the researchers describe fit with what ob.gyns. at UCLA experienced as the pandemic hit.
“We really tried to hone in on people who were at highest risk for an adverse outcome,” she said. “I still have the question of whether there were things we missed in low-risk people. It will take time to get the entire answer. But it does make us reflect that perhaps less intervention could be better for patients and easier. It’s our job in medicine to keep asking the question of what is essential and safe and not just continue with current practice because that’s what we’ve always done.”
The amount of data gave the researchers an unusual view. They studied 38,891,271 singleton births in the United States from 2010 to 2020 with data from the National Center for Health Statistics.
“If you look at 1,000 births in a single hospital, or even at 30,000 births across a hospital system, you wouldn’t be able to see the drop as clearly,” Dr. Dench said. “The drop we detected is a huge change, but you might miss it in a small sample.”
The researchers acknowledge a limitation of the study is that half of all preterm C-sections and induced deliveries happen because of a ruptured membrane, a spontaneous cause. Those instances can’t be distinguished from the ones caused by doctors’ interventions in this study.
“Still, these findings are significant because the causes for preterm births are not always known,” the authors wrote in the press release.
The study authors and Dr. Zapata reported no relevant financial relationships.
FROM PEDIATRICS
Hospital factors drive many discharges against medical advice
The analysis found that in about 1 in 5 cases, shortcomings in the quality of care and other factors beyond patients’ control explain why they leave the hospital before completing recommended treatment.
Clinicians may be quick to blame patients for so-called discharges against medical advice (AMA), which comprise up to 2% of hospital admissions and are associated with an increased risk of mortality and readmission. But “we as providers are very much involved in the reasons why these patients left,” Kushinga Bvute, MD, MPH, a second-year internal medicine resident at Florida Atlantic University, Boca Raton, who led the new study, told this news organization. Dr. Bvute and her colleagues presented their findings April 6 at the Society of General Internal Medicine (SGIM) 2022 Annual Meeting, Orlando, Florida.
Dr. Bvute and her colleagues reviewed the records of 548 AMA discharges – out of a total of 354,767 discharges – from Boca Raton Regional Hospital from January 2020 to January 2021. In 44% of cases, patients cited their own reasons for leaving. But in nearly 20% of AMA discharges, the researchers identified factors linked to treatment.
Hospital-related reasons patients cited for leaving AMA were general wait times (3.5%), provider wait times (2.6%), provider care (2.9%), the hospital environment (2.7%), wanting a private room (2%), and seeking medical care elsewhere (6.2%).
Patient-related factors were refusing treatment (27%), feeling better (3.5%), addiction problems (2.9%), financial complications (2.9%), and dependent care (2.4%). Ten (1.8%) eloped, according to the researchers.
Nearly 60% of patients who were discharged AMA were men, with a mean age of 56 years (standard deviation, 19.13). The average stay was 1.64 days.
In roughly one-third of cases, there was no documented reason for the departure – underscoring the need for better reporting, according to the researchers.
To address AMA discharges, hospitals “need to focus on factors they influence, such as high-quality patient care, the hospital environment, and provider-patient relationships,” the researchers report.
New procedures needed
The hospital is working on procedures to ensure that reasons for AMA discharges are documented. The administration also is implementing preventive steps, such as communicating with patients about the risks of leaving and providing discharge plans to reduce the likelihood that a patient will return, Dr. Bvute told this news organization.
Dr. Bvute said the findings should encourage individual clinicians to “remove any stereotypes that sometimes come attached to having those three letters on your charts.”
Data were collected during the COVID-19 pandemic, but Dr. Bvute does not believe that fear of coronavirus exposure drove many patients to leave the hospital prematurely.
The study is notable for approaching AMA discharges from a quality improvement perspective, David Alfandre, MD, MPH, a health care ethicist at the VA National Center for Ethics in Health Care, Washington, D.C., said in an interview.
Dr. Alfandre, who was not involved in the study, said it reflects growing recognition that hospitals can take steps to reduce adverse outcomes associated with AMA discharges. “It’s starting to shift the conversation to saying, this isn’t just the patient’s problem, but this is the health care provider’s problem,” he said.
Dr. Alfandre co-authored a 2021 analysis showing that hospital characteristics account for 7.3% of variation in the probability of a patient being discharged AMA. However, research is needed to identify effective interventions besides the established use of buprenorphine and naloxone for patients with opioid use disorder. “I think everybody recognizes the quality of communication is poor, but that doesn’t really help us operationalize that to know what to do,” he said.
Emily Holmes, MD, MPH, medical director of the Changing Health Outcomes Through Integrated Care Excellence Program at IU Health, Indianapolis, cautioned that data may be biased because defining AMA discharge can be subjective.
Reasons are not consistently documented and can be difficult to capture because they are often multifactorial, Dr. Holmes said. “For example, long wait times are more problematic when a patient is worried about finances and care for a child,” she said.
But Dr. Holmes, who was not involved in the study, said it does encourage clinicians “to think about what we can do systematically to reduce AMA discharges.”
Dr. Bvute, Dr. Alfandre, and Dr. Holmes reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The analysis found that in about 1 in 5 cases, shortcomings in the quality of care and other factors beyond patients’ control explain why they leave the hospital before completing recommended treatment.
Clinicians may be quick to blame patients for so-called discharges against medical advice (AMA), which comprise up to 2% of hospital admissions and are associated with an increased risk of mortality and readmission. But “we as providers are very much involved in the reasons why these patients left,” Kushinga Bvute, MD, MPH, a second-year internal medicine resident at Florida Atlantic University, Boca Raton, who led the new study, told this news organization. Dr. Bvute and her colleagues presented their findings April 6 at the Society of General Internal Medicine (SGIM) 2022 Annual Meeting, Orlando, Florida.
Dr. Bvute and her colleagues reviewed the records of 548 AMA discharges – out of a total of 354,767 discharges – from Boca Raton Regional Hospital from January 2020 to January 2021. In 44% of cases, patients cited their own reasons for leaving. But in nearly 20% of AMA discharges, the researchers identified factors linked to treatment.
Hospital-related reasons patients cited for leaving AMA were general wait times (3.5%), provider wait times (2.6%), provider care (2.9%), the hospital environment (2.7%), wanting a private room (2%), and seeking medical care elsewhere (6.2%).
Patient-related factors were refusing treatment (27%), feeling better (3.5%), addiction problems (2.9%), financial complications (2.9%), and dependent care (2.4%). Ten (1.8%) eloped, according to the researchers.
Nearly 60% of patients who were discharged AMA were men, with a mean age of 56 years (standard deviation, 19.13). The average stay was 1.64 days.
In roughly one-third of cases, there was no documented reason for the departure – underscoring the need for better reporting, according to the researchers.
To address AMA discharges, hospitals “need to focus on factors they influence, such as high-quality patient care, the hospital environment, and provider-patient relationships,” the researchers report.
New procedures needed
The hospital is working on procedures to ensure that reasons for AMA discharges are documented. The administration also is implementing preventive steps, such as communicating with patients about the risks of leaving and providing discharge plans to reduce the likelihood that a patient will return, Dr. Bvute told this news organization.
Dr. Bvute said the findings should encourage individual clinicians to “remove any stereotypes that sometimes come attached to having those three letters on your charts.”
Data were collected during the COVID-19 pandemic, but Dr. Bvute does not believe that fear of coronavirus exposure drove many patients to leave the hospital prematurely.
The study is notable for approaching AMA discharges from a quality improvement perspective, David Alfandre, MD, MPH, a health care ethicist at the VA National Center for Ethics in Health Care, Washington, D.C., said in an interview.
Dr. Alfandre, who was not involved in the study, said it reflects growing recognition that hospitals can take steps to reduce adverse outcomes associated with AMA discharges. “It’s starting to shift the conversation to saying, this isn’t just the patient’s problem, but this is the health care provider’s problem,” he said.
Dr. Alfandre co-authored a 2021 analysis showing that hospital characteristics account for 7.3% of variation in the probability of a patient being discharged AMA. However, research is needed to identify effective interventions besides the established use of buprenorphine and naloxone for patients with opioid use disorder. “I think everybody recognizes the quality of communication is poor, but that doesn’t really help us operationalize that to know what to do,” he said.
Emily Holmes, MD, MPH, medical director of the Changing Health Outcomes Through Integrated Care Excellence Program at IU Health, Indianapolis, cautioned that data may be biased because defining AMA discharge can be subjective.
Reasons are not consistently documented and can be difficult to capture because they are often multifactorial, Dr. Holmes said. “For example, long wait times are more problematic when a patient is worried about finances and care for a child,” she said.
But Dr. Holmes, who was not involved in the study, said it does encourage clinicians “to think about what we can do systematically to reduce AMA discharges.”
Dr. Bvute, Dr. Alfandre, and Dr. Holmes reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The analysis found that in about 1 in 5 cases, shortcomings in the quality of care and other factors beyond patients’ control explain why they leave the hospital before completing recommended treatment.
Clinicians may be quick to blame patients for so-called discharges against medical advice (AMA), which comprise up to 2% of hospital admissions and are associated with an increased risk of mortality and readmission. But “we as providers are very much involved in the reasons why these patients left,” Kushinga Bvute, MD, MPH, a second-year internal medicine resident at Florida Atlantic University, Boca Raton, who led the new study, told this news organization. Dr. Bvute and her colleagues presented their findings April 6 at the Society of General Internal Medicine (SGIM) 2022 Annual Meeting, Orlando, Florida.
Dr. Bvute and her colleagues reviewed the records of 548 AMA discharges – out of a total of 354,767 discharges – from Boca Raton Regional Hospital from January 2020 to January 2021. In 44% of cases, patients cited their own reasons for leaving. But in nearly 20% of AMA discharges, the researchers identified factors linked to treatment.
Hospital-related reasons patients cited for leaving AMA were general wait times (3.5%), provider wait times (2.6%), provider care (2.9%), the hospital environment (2.7%), wanting a private room (2%), and seeking medical care elsewhere (6.2%).
Patient-related factors were refusing treatment (27%), feeling better (3.5%), addiction problems (2.9%), financial complications (2.9%), and dependent care (2.4%). Ten (1.8%) eloped, according to the researchers.
Nearly 60% of patients who were discharged AMA were men, with a mean age of 56 years (standard deviation, 19.13). The average stay was 1.64 days.
In roughly one-third of cases, there was no documented reason for the departure – underscoring the need for better reporting, according to the researchers.
To address AMA discharges, hospitals “need to focus on factors they influence, such as high-quality patient care, the hospital environment, and provider-patient relationships,” the researchers report.
New procedures needed
The hospital is working on procedures to ensure that reasons for AMA discharges are documented. The administration also is implementing preventive steps, such as communicating with patients about the risks of leaving and providing discharge plans to reduce the likelihood that a patient will return, Dr. Bvute told this news organization.
Dr. Bvute said the findings should encourage individual clinicians to “remove any stereotypes that sometimes come attached to having those three letters on your charts.”
Data were collected during the COVID-19 pandemic, but Dr. Bvute does not believe that fear of coronavirus exposure drove many patients to leave the hospital prematurely.
The study is notable for approaching AMA discharges from a quality improvement perspective, David Alfandre, MD, MPH, a health care ethicist at the VA National Center for Ethics in Health Care, Washington, D.C., said in an interview.
Dr. Alfandre, who was not involved in the study, said it reflects growing recognition that hospitals can take steps to reduce adverse outcomes associated with AMA discharges. “It’s starting to shift the conversation to saying, this isn’t just the patient’s problem, but this is the health care provider’s problem,” he said.
Dr. Alfandre co-authored a 2021 analysis showing that hospital characteristics account for 7.3% of variation in the probability of a patient being discharged AMA. However, research is needed to identify effective interventions besides the established use of buprenorphine and naloxone for patients with opioid use disorder. “I think everybody recognizes the quality of communication is poor, but that doesn’t really help us operationalize that to know what to do,” he said.
Emily Holmes, MD, MPH, medical director of the Changing Health Outcomes Through Integrated Care Excellence Program at IU Health, Indianapolis, cautioned that data may be biased because defining AMA discharge can be subjective.
Reasons are not consistently documented and can be difficult to capture because they are often multifactorial, Dr. Holmes said. “For example, long wait times are more problematic when a patient is worried about finances and care for a child,” she said.
But Dr. Holmes, who was not involved in the study, said it does encourage clinicians “to think about what we can do systematically to reduce AMA discharges.”
Dr. Bvute, Dr. Alfandre, and Dr. Holmes reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SGIM 2022
‘Outbid on three houses!’ Doc frustrated by crazy market
After more than a decade of moving because of medical school, residencies, and international fellowships, Abhi Kole, MD, PhD, is ready to put down roots. But he’s learning that buying a house in today’s housing market is easier said than done.
In the past 6 months, Dr. Kole, an internist at Grady Hospital in Atlanta, put in offers on three houses. None resulted in a purchase. Dr. Kole says he’s learned how to be more competitive with each subsequent offer, starting out with a bid significantly above the asking price and waiving his right to an appraisal or financing contingencies.
The experience has been surprising and disappointing.
“I knew the market was bad when I started looking and that home prices had gone up,” Dr. Kole says. “What I didn’t realize was that it would still be so hard for me. I have a good job, no debt, and great credit.”
Another frustration for Dr. Kole: He’s been approved for a physician’s loan (a type of mortgage that requires a lower down payment and does not count student loans in debt-to-income calculations) from a national bank, but sellers seem to prefer buyers who work with local lenders. Dr. Kole has been willing to waive the appraisal and mortgage contingency on the right home, but he draws the line at waiving the inspection, a trend that some other buyers in his area are going along with.
“With each house, I learn more about how this works and what amount of risk I can safely assume,” Dr. Kobe says. “There are certain things I definitely wouldn’t give up.”
“Potential homebuyers are really facing a triple threat right now,” says Clare Losey, an assistant research economist with the Texas Real Estate Research Center. “There’s high home appreciation, high mortgage rates, and low inventory of homes for sale.”
It’s still possible to find — and buy — your dream home, even in today’s market with all its challenges. Here are some important steps that can help you.
1. Do not low ball.
There may be some cases in which you can save money by making an offer significantly below the asking price on a property. However, with most housing areas across the country experiencing a seller’s market, you run the risk of offending the buyer or being dismissed as not having a serious offer.
In today’s market, a better strategy is to go in with close to your best and final offer from the start, realtors say. It can help to waive the appraisal or financing contingency as well, although it’s important to understand the risk associated with doing so. Last month, the average home sold for 103% of the list price, according to data compiled from Statista.
2. Get credit ready.
The better your credit, the easier time you’ll have getting a mortgage — and the lower the rate you’ll pay for the loan. The average first-time homebuyer has a credit score of 746, according to a recent paper by Fannie Mae. If you know you’re going to buy a home in the next few months, you can improve your credit by making sure to pay all your bills on time and by avoiding taking on any new debt.
This is also a good opportunity to check your credit report (get all three reports for free from AnnualCreditReport.com) to see whether there are any mistakes or other problems that you’ll need to clear up before applying for a loan. Also, take a look at your credit-utilization ratio (the amount of credit you use compared to the amount available to you). Experts recommend keeping this number below 30%.
3. Prepare to move quickly.
Among homes that closed in March, the average number of days on the market (the amount of time between listing and closing) was just 38 days, according to Realtor.com. In busy markets, homes are moving even faster, realtors say, with sellers commonly accepting offers within days of listing their house for sale.
“It’s crazy,” says Sarah Scattini, president of the Reno/Sparks Association of Realtors. “The market is moving extremely fast here. If you list your home, your sale is pending within 5 days.”
In addition to moving quickly to make your initial offer, do the same if a buyer counters with a negotiation. A speedy response will show the buyer that you’re very interested — and to beat out any other bidders who may have also received a counteroffer.
4. Shop around for mortgages.
Especially for first-time homebuyers, the process will go much more smoothly if you’ve got a team of professionals to help you. Look for a realtor and a mortgage lender who have experience working with first-time homebuyers and with physicians, if possible.
Since mortgage rates can vary wildly, you’ll want to shop around a bit before settling on a lender. Get quotes from a local lender, an online lender, and, potentially, a credit union or a mortgage broker to get a sense of the types of mortgages and rates available to you.
“With multiple offers on every single listing, you really want to align yourself with a great realtor who can negotiate for you on your behalf and navigate you through this very tricky market,” says Ms. Scattini.
For both your realtor and your lender, you’ll want to know up front how they get paid and how they calculate their fees. Typically, the real estate agents for buyers and sellers split a 6% commission on home sales, meaning that your realtor will likely take home 3% of the purchase price.
5. Get preapproved.
Once you’ve settled on a lender, getting preapproved for a mortgage can make your offer more appealing to potential buyers. Preapproval is an in-depth process in which lenders pull your credit and look at other financial factors, such as your income and assets, to tell you ahead of time how much you could borrow under their standards and how much that might cost you.
These days, a large number of buyers are coming in with a cash offer, which in former times was considered very appealing to sellers. However, preapproval helps equalize buyers, and as one seller noted, “I don’t care if it’s cash or mortgage, as long as I get the money.”
If, like most homebuyers, you need a mortgage to finance the purchase, having preapproval can provide some assurance to sellers that your offer won’t fall through because you can’t qualify for the mortgage you expected. Once you’ve received preapproval, don’t open any new credit accounts. If your credit score goes down, the amount you can borrow could decline as well.
6. Firm up your budget.
While the preapproval process will tell you how much a lender thinks you can afford, it typically makes sense to come up with your own budget as well. That’s because banks and other mortgage lenders may approve you for much more than you want or are able to pay for a home.
You’ll want to factor in future costs of homeowners as well as any other (current or future) expenses for which the lender may not have accounted. For example, if you’re planning to have children soon, you may want to lower your budget to factor in the cost of childcare.
Knowing your budget ahead of time, and looking only at houses that fall within it, will prevent you from falling in love with a house that you really can’t afford.
7. Stick with it.
Buying a house in today’s market is no easy task. The first part of the process requires simply looking at multiple houses to get a sense of how far your budget will go and whether there are homes that meet your requirements.
If you’re sure that purchasing a home is the best financial move for you, don’t give up. Instead, consider whether you can make adjustments that could widen your pool of potential homes. That may mean changing your budget, moving a little further out geographically, or opting for a house that needs a little more work than you expected.
That said, while the pace of price increases will likely moderate, it’s unlikely prices will go down significantly in the future.
“We might see home price appreciation subside to levels close to 10% to 15% [from 20% last year] or even just 5% to 10%,” Ms. Losey says. “When you do the math, home prices just can’t continue to go up 20% year over year.”
Dr. Kobe is planning to keep looking for his home for at least the next several months.
“Prices are still going up, but we are hearing that the inventory will increase over the summer,” he says. “I’m still out looking for the right house, and I’m ready to make an offer.”
A version of this article first appeared on Medscape.com.
After more than a decade of moving because of medical school, residencies, and international fellowships, Abhi Kole, MD, PhD, is ready to put down roots. But he’s learning that buying a house in today’s housing market is easier said than done.
In the past 6 months, Dr. Kole, an internist at Grady Hospital in Atlanta, put in offers on three houses. None resulted in a purchase. Dr. Kole says he’s learned how to be more competitive with each subsequent offer, starting out with a bid significantly above the asking price and waiving his right to an appraisal or financing contingencies.
The experience has been surprising and disappointing.
“I knew the market was bad when I started looking and that home prices had gone up,” Dr. Kole says. “What I didn’t realize was that it would still be so hard for me. I have a good job, no debt, and great credit.”
Another frustration for Dr. Kole: He’s been approved for a physician’s loan (a type of mortgage that requires a lower down payment and does not count student loans in debt-to-income calculations) from a national bank, but sellers seem to prefer buyers who work with local lenders. Dr. Kole has been willing to waive the appraisal and mortgage contingency on the right home, but he draws the line at waiving the inspection, a trend that some other buyers in his area are going along with.
“With each house, I learn more about how this works and what amount of risk I can safely assume,” Dr. Kobe says. “There are certain things I definitely wouldn’t give up.”
“Potential homebuyers are really facing a triple threat right now,” says Clare Losey, an assistant research economist with the Texas Real Estate Research Center. “There’s high home appreciation, high mortgage rates, and low inventory of homes for sale.”
It’s still possible to find — and buy — your dream home, even in today’s market with all its challenges. Here are some important steps that can help you.
1. Do not low ball.
There may be some cases in which you can save money by making an offer significantly below the asking price on a property. However, with most housing areas across the country experiencing a seller’s market, you run the risk of offending the buyer or being dismissed as not having a serious offer.
In today’s market, a better strategy is to go in with close to your best and final offer from the start, realtors say. It can help to waive the appraisal or financing contingency as well, although it’s important to understand the risk associated with doing so. Last month, the average home sold for 103% of the list price, according to data compiled from Statista.
2. Get credit ready.
The better your credit, the easier time you’ll have getting a mortgage — and the lower the rate you’ll pay for the loan. The average first-time homebuyer has a credit score of 746, according to a recent paper by Fannie Mae. If you know you’re going to buy a home in the next few months, you can improve your credit by making sure to pay all your bills on time and by avoiding taking on any new debt.
This is also a good opportunity to check your credit report (get all three reports for free from AnnualCreditReport.com) to see whether there are any mistakes or other problems that you’ll need to clear up before applying for a loan. Also, take a look at your credit-utilization ratio (the amount of credit you use compared to the amount available to you). Experts recommend keeping this number below 30%.
3. Prepare to move quickly.
Among homes that closed in March, the average number of days on the market (the amount of time between listing and closing) was just 38 days, according to Realtor.com. In busy markets, homes are moving even faster, realtors say, with sellers commonly accepting offers within days of listing their house for sale.
“It’s crazy,” says Sarah Scattini, president of the Reno/Sparks Association of Realtors. “The market is moving extremely fast here. If you list your home, your sale is pending within 5 days.”
In addition to moving quickly to make your initial offer, do the same if a buyer counters with a negotiation. A speedy response will show the buyer that you’re very interested — and to beat out any other bidders who may have also received a counteroffer.
4. Shop around for mortgages.
Especially for first-time homebuyers, the process will go much more smoothly if you’ve got a team of professionals to help you. Look for a realtor and a mortgage lender who have experience working with first-time homebuyers and with physicians, if possible.
Since mortgage rates can vary wildly, you’ll want to shop around a bit before settling on a lender. Get quotes from a local lender, an online lender, and, potentially, a credit union or a mortgage broker to get a sense of the types of mortgages and rates available to you.
“With multiple offers on every single listing, you really want to align yourself with a great realtor who can negotiate for you on your behalf and navigate you through this very tricky market,” says Ms. Scattini.
For both your realtor and your lender, you’ll want to know up front how they get paid and how they calculate their fees. Typically, the real estate agents for buyers and sellers split a 6% commission on home sales, meaning that your realtor will likely take home 3% of the purchase price.
5. Get preapproved.
Once you’ve settled on a lender, getting preapproved for a mortgage can make your offer more appealing to potential buyers. Preapproval is an in-depth process in which lenders pull your credit and look at other financial factors, such as your income and assets, to tell you ahead of time how much you could borrow under their standards and how much that might cost you.
These days, a large number of buyers are coming in with a cash offer, which in former times was considered very appealing to sellers. However, preapproval helps equalize buyers, and as one seller noted, “I don’t care if it’s cash or mortgage, as long as I get the money.”
If, like most homebuyers, you need a mortgage to finance the purchase, having preapproval can provide some assurance to sellers that your offer won’t fall through because you can’t qualify for the mortgage you expected. Once you’ve received preapproval, don’t open any new credit accounts. If your credit score goes down, the amount you can borrow could decline as well.
6. Firm up your budget.
While the preapproval process will tell you how much a lender thinks you can afford, it typically makes sense to come up with your own budget as well. That’s because banks and other mortgage lenders may approve you for much more than you want or are able to pay for a home.
You’ll want to factor in future costs of homeowners as well as any other (current or future) expenses for which the lender may not have accounted. For example, if you’re planning to have children soon, you may want to lower your budget to factor in the cost of childcare.
Knowing your budget ahead of time, and looking only at houses that fall within it, will prevent you from falling in love with a house that you really can’t afford.
7. Stick with it.
Buying a house in today’s market is no easy task. The first part of the process requires simply looking at multiple houses to get a sense of how far your budget will go and whether there are homes that meet your requirements.
If you’re sure that purchasing a home is the best financial move for you, don’t give up. Instead, consider whether you can make adjustments that could widen your pool of potential homes. That may mean changing your budget, moving a little further out geographically, or opting for a house that needs a little more work than you expected.
That said, while the pace of price increases will likely moderate, it’s unlikely prices will go down significantly in the future.
“We might see home price appreciation subside to levels close to 10% to 15% [from 20% last year] or even just 5% to 10%,” Ms. Losey says. “When you do the math, home prices just can’t continue to go up 20% year over year.”
Dr. Kobe is planning to keep looking for his home for at least the next several months.
“Prices are still going up, but we are hearing that the inventory will increase over the summer,” he says. “I’m still out looking for the right house, and I’m ready to make an offer.”
A version of this article first appeared on Medscape.com.
After more than a decade of moving because of medical school, residencies, and international fellowships, Abhi Kole, MD, PhD, is ready to put down roots. But he’s learning that buying a house in today’s housing market is easier said than done.
In the past 6 months, Dr. Kole, an internist at Grady Hospital in Atlanta, put in offers on three houses. None resulted in a purchase. Dr. Kole says he’s learned how to be more competitive with each subsequent offer, starting out with a bid significantly above the asking price and waiving his right to an appraisal or financing contingencies.
The experience has been surprising and disappointing.
“I knew the market was bad when I started looking and that home prices had gone up,” Dr. Kole says. “What I didn’t realize was that it would still be so hard for me. I have a good job, no debt, and great credit.”
Another frustration for Dr. Kole: He’s been approved for a physician’s loan (a type of mortgage that requires a lower down payment and does not count student loans in debt-to-income calculations) from a national bank, but sellers seem to prefer buyers who work with local lenders. Dr. Kole has been willing to waive the appraisal and mortgage contingency on the right home, but he draws the line at waiving the inspection, a trend that some other buyers in his area are going along with.
“With each house, I learn more about how this works and what amount of risk I can safely assume,” Dr. Kobe says. “There are certain things I definitely wouldn’t give up.”
“Potential homebuyers are really facing a triple threat right now,” says Clare Losey, an assistant research economist with the Texas Real Estate Research Center. “There’s high home appreciation, high mortgage rates, and low inventory of homes for sale.”
It’s still possible to find — and buy — your dream home, even in today’s market with all its challenges. Here are some important steps that can help you.
1. Do not low ball.
There may be some cases in which you can save money by making an offer significantly below the asking price on a property. However, with most housing areas across the country experiencing a seller’s market, you run the risk of offending the buyer or being dismissed as not having a serious offer.
In today’s market, a better strategy is to go in with close to your best and final offer from the start, realtors say. It can help to waive the appraisal or financing contingency as well, although it’s important to understand the risk associated with doing so. Last month, the average home sold for 103% of the list price, according to data compiled from Statista.
2. Get credit ready.
The better your credit, the easier time you’ll have getting a mortgage — and the lower the rate you’ll pay for the loan. The average first-time homebuyer has a credit score of 746, according to a recent paper by Fannie Mae. If you know you’re going to buy a home in the next few months, you can improve your credit by making sure to pay all your bills on time and by avoiding taking on any new debt.
This is also a good opportunity to check your credit report (get all three reports for free from AnnualCreditReport.com) to see whether there are any mistakes or other problems that you’ll need to clear up before applying for a loan. Also, take a look at your credit-utilization ratio (the amount of credit you use compared to the amount available to you). Experts recommend keeping this number below 30%.
3. Prepare to move quickly.
Among homes that closed in March, the average number of days on the market (the amount of time between listing and closing) was just 38 days, according to Realtor.com. In busy markets, homes are moving even faster, realtors say, with sellers commonly accepting offers within days of listing their house for sale.
“It’s crazy,” says Sarah Scattini, president of the Reno/Sparks Association of Realtors. “The market is moving extremely fast here. If you list your home, your sale is pending within 5 days.”
In addition to moving quickly to make your initial offer, do the same if a buyer counters with a negotiation. A speedy response will show the buyer that you’re very interested — and to beat out any other bidders who may have also received a counteroffer.
4. Shop around for mortgages.
Especially for first-time homebuyers, the process will go much more smoothly if you’ve got a team of professionals to help you. Look for a realtor and a mortgage lender who have experience working with first-time homebuyers and with physicians, if possible.
Since mortgage rates can vary wildly, you’ll want to shop around a bit before settling on a lender. Get quotes from a local lender, an online lender, and, potentially, a credit union or a mortgage broker to get a sense of the types of mortgages and rates available to you.
“With multiple offers on every single listing, you really want to align yourself with a great realtor who can negotiate for you on your behalf and navigate you through this very tricky market,” says Ms. Scattini.
For both your realtor and your lender, you’ll want to know up front how they get paid and how they calculate their fees. Typically, the real estate agents for buyers and sellers split a 6% commission on home sales, meaning that your realtor will likely take home 3% of the purchase price.
5. Get preapproved.
Once you’ve settled on a lender, getting preapproved for a mortgage can make your offer more appealing to potential buyers. Preapproval is an in-depth process in which lenders pull your credit and look at other financial factors, such as your income and assets, to tell you ahead of time how much you could borrow under their standards and how much that might cost you.
These days, a large number of buyers are coming in with a cash offer, which in former times was considered very appealing to sellers. However, preapproval helps equalize buyers, and as one seller noted, “I don’t care if it’s cash or mortgage, as long as I get the money.”
If, like most homebuyers, you need a mortgage to finance the purchase, having preapproval can provide some assurance to sellers that your offer won’t fall through because you can’t qualify for the mortgage you expected. Once you’ve received preapproval, don’t open any new credit accounts. If your credit score goes down, the amount you can borrow could decline as well.
6. Firm up your budget.
While the preapproval process will tell you how much a lender thinks you can afford, it typically makes sense to come up with your own budget as well. That’s because banks and other mortgage lenders may approve you for much more than you want or are able to pay for a home.
You’ll want to factor in future costs of homeowners as well as any other (current or future) expenses for which the lender may not have accounted. For example, if you’re planning to have children soon, you may want to lower your budget to factor in the cost of childcare.
Knowing your budget ahead of time, and looking only at houses that fall within it, will prevent you from falling in love with a house that you really can’t afford.
7. Stick with it.
Buying a house in today’s market is no easy task. The first part of the process requires simply looking at multiple houses to get a sense of how far your budget will go and whether there are homes that meet your requirements.
If you’re sure that purchasing a home is the best financial move for you, don’t give up. Instead, consider whether you can make adjustments that could widen your pool of potential homes. That may mean changing your budget, moving a little further out geographically, or opting for a house that needs a little more work than you expected.
That said, while the pace of price increases will likely moderate, it’s unlikely prices will go down significantly in the future.
“We might see home price appreciation subside to levels close to 10% to 15% [from 20% last year] or even just 5% to 10%,” Ms. Losey says. “When you do the math, home prices just can’t continue to go up 20% year over year.”
Dr. Kobe is planning to keep looking for his home for at least the next several months.
“Prices are still going up, but we are hearing that the inventory will increase over the summer,” he says. “I’m still out looking for the right house, and I’m ready to make an offer.”
A version of this article first appeared on Medscape.com.
Tebipenem pivoxil hydrobromide offers oral option for complex UTIs
“No new oral antibiotic alternative has emerged to treat these conditions in more than 25 years,” corresponding author Angela K. Talley, MD, said in an interview. The new research was published in the New England Journal of Medicine.
Patients with complicated urinary tract infection (cUTI), including acute pyelonephritis (AP), are often hospitalized and treated with intravenous therapy because of the lack of oral options, especially in cases of antibiotic-resistant pathogens, explained Dr. Talley, of Spero Therapeutics.
In their new phase 3, double-blind randomized trial, the researchers evaluated the safety and effectiveness of oral TBP-PI-HBr, compared with intravenous ertapenem in hospitalized patients with cUTIs or AP. Oral tebipenem is an investigational carbapenem with demonstrated activity against uropathogenic Enterobacterales, and it has shown effectiveness in animal models, the researchers noted in their paper.
Methods and results
The researchers randomized 1,372 adult patients. The microbiologic intent-to-treat population included 449 patients who received TBP-PI-HBr (600 mg every 8 hours) and 419 who received ertapenem (1 g every 24 hours) for 7-10 days or up to 14 days for patients with bacteremia.
The primary endpoint was a composite of clinical cure and favorable microbiologic response, assessed at a test-of-cure visit on day 19. Clinical cure was defined as “complete resolution or clinically significant alleviation of baseline signs and symptoms of complicated urinary tract infection or acute pyelonephritis and no new symptoms, such that no further antimicrobial therapy was warranted,” the researchers wrote. Microbiologic response was defined as a reduction to less than 103 CFU per milliliter in uropathogen levels from baseline at day 19.
Overall, the clinical response occurred in 58.8% of patients who received TBP-PI-HBr and 61.6% of those who received ertapenem at the test-of-cure visit.
Clinical cure rates were similar in the TBP-PI-HBr and ertapenem groups (93.1% vs. 93.6%) at the test-of-cure visit.
Both treatment groups showed similar responses to Enterobacterales pathogens at the test-of-cure visit (62.7% for TBP-PI-HBr and 65.2% for ertapenem).
Among patients with bacteremia at baseline, overall response rates were 72.3% and 66.0% for TBP-PI-HBr and ertapenem, respectively, at the test-of-cure visit, and 93.6% and 96.2%, respectively, at the end-of-treatment visit on or around day 25.
The overall incidence of adverse events was approximately 26% in both treatment groups. Most adverse events were mild or moderate in severity and did not limit treatment, the researchers wrote.
The mean age of the patients was 58.1 years; 46.1% were aged 65 and older, and 11.5% had bacteremia at baseline.
The study findings were limited by several factors, including the mandated 7- to 10-day course of antibiotics, which may not reflect the standard of care in other settings in the United States. The study’s trial sites were located in the United States, South Africa, and Europe. The study population was primarily White and from Central and Eastern Europe. Other limitations included the randomization of patients before confirming the baseline pathogen, although this was done to limit potential confounding from previous antibiotics, the researchers noted.
Safety and efficacy support application for approval
“To our knowledge, this is the first head-to-head evaluation of an IV vs. an oral drug for the treatment of cUTI and acute pyelonephritis,” Dr. Talley said in an interview.
“The findings demonstrate that almost all patients in the study achieved complete resolution of the signs and symptoms of their infection,” she said.
TBP-PI-HBr has not been approved by the Food and Drug Administration, but a new drug application that included data from the current study was submitted to the FDA and is currently under review, Dr. Talley noted.
As for additional research, the current study was conducted in hospitalized patients, and the use of TBP-PI-HBr in the outpatient setting has not yet been evaluated, she said.
Approval and use of oral carbapenem will change practice
The current study is very important because it provides a viable and effective alternative form of antibiotic delivery for the patients with complicated UTI, Noel N. Deep, MD, emphasized in an interview.
“Currently these patients have to be treated with IV carbapenem antibiotics either in a hospital or through a home health nurse,” Dr. Deep, a general internist in group practice in Antigo, Wisc., explained.
Current IV strategies also carry the inherent risk associated with the insertion of an IV catheter that is left in place for several days or replaced periodically. “The oral antibiotic eliminates these risks and higher health care costs and provides a safer and equally efficacious option,” Dr. Deep said.
In the current study, “I was definitely surprised at the effectiveness of the oral carbapenem,” Dr. Deep said. “I am absolutely delighted with this new treatment option that physicians can now add to their armamentarium [assuming FDA approval] as we provide care to our patients,” he said.
If approved, TBP-PI-HBr will definitely change the treatment spectrum for the multidrug-resistant bacterial UTIs, said Dr. Deep. “Carbapenems have continued to be effective and low antibiotic resistance to carbapenems has been recorded.”
As for additional research, “I would like to see studies done in other ethnicities and different countries to ascertain the effectiveness of this antibiotic in those populations and against other bacterial strains with potentially different resistance mechanisms,” Dr. Deep said.
The study was supported by Spero Therapeutics and the Department of Health and Human Services. Lead author Paul B. Eckburg, MD, of Stanford (Calif.) University, and Dr. Talley are employees of Spero Therapeutics. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News.
“No new oral antibiotic alternative has emerged to treat these conditions in more than 25 years,” corresponding author Angela K. Talley, MD, said in an interview. The new research was published in the New England Journal of Medicine.
Patients with complicated urinary tract infection (cUTI), including acute pyelonephritis (AP), are often hospitalized and treated with intravenous therapy because of the lack of oral options, especially in cases of antibiotic-resistant pathogens, explained Dr. Talley, of Spero Therapeutics.
In their new phase 3, double-blind randomized trial, the researchers evaluated the safety and effectiveness of oral TBP-PI-HBr, compared with intravenous ertapenem in hospitalized patients with cUTIs or AP. Oral tebipenem is an investigational carbapenem with demonstrated activity against uropathogenic Enterobacterales, and it has shown effectiveness in animal models, the researchers noted in their paper.
Methods and results
The researchers randomized 1,372 adult patients. The microbiologic intent-to-treat population included 449 patients who received TBP-PI-HBr (600 mg every 8 hours) and 419 who received ertapenem (1 g every 24 hours) for 7-10 days or up to 14 days for patients with bacteremia.
The primary endpoint was a composite of clinical cure and favorable microbiologic response, assessed at a test-of-cure visit on day 19. Clinical cure was defined as “complete resolution or clinically significant alleviation of baseline signs and symptoms of complicated urinary tract infection or acute pyelonephritis and no new symptoms, such that no further antimicrobial therapy was warranted,” the researchers wrote. Microbiologic response was defined as a reduction to less than 103 CFU per milliliter in uropathogen levels from baseline at day 19.
Overall, the clinical response occurred in 58.8% of patients who received TBP-PI-HBr and 61.6% of those who received ertapenem at the test-of-cure visit.
Clinical cure rates were similar in the TBP-PI-HBr and ertapenem groups (93.1% vs. 93.6%) at the test-of-cure visit.
Both treatment groups showed similar responses to Enterobacterales pathogens at the test-of-cure visit (62.7% for TBP-PI-HBr and 65.2% for ertapenem).
Among patients with bacteremia at baseline, overall response rates were 72.3% and 66.0% for TBP-PI-HBr and ertapenem, respectively, at the test-of-cure visit, and 93.6% and 96.2%, respectively, at the end-of-treatment visit on or around day 25.
The overall incidence of adverse events was approximately 26% in both treatment groups. Most adverse events were mild or moderate in severity and did not limit treatment, the researchers wrote.
The mean age of the patients was 58.1 years; 46.1% were aged 65 and older, and 11.5% had bacteremia at baseline.
The study findings were limited by several factors, including the mandated 7- to 10-day course of antibiotics, which may not reflect the standard of care in other settings in the United States. The study’s trial sites were located in the United States, South Africa, and Europe. The study population was primarily White and from Central and Eastern Europe. Other limitations included the randomization of patients before confirming the baseline pathogen, although this was done to limit potential confounding from previous antibiotics, the researchers noted.
Safety and efficacy support application for approval
“To our knowledge, this is the first head-to-head evaluation of an IV vs. an oral drug for the treatment of cUTI and acute pyelonephritis,” Dr. Talley said in an interview.
“The findings demonstrate that almost all patients in the study achieved complete resolution of the signs and symptoms of their infection,” she said.
TBP-PI-HBr has not been approved by the Food and Drug Administration, but a new drug application that included data from the current study was submitted to the FDA and is currently under review, Dr. Talley noted.
As for additional research, the current study was conducted in hospitalized patients, and the use of TBP-PI-HBr in the outpatient setting has not yet been evaluated, she said.
Approval and use of oral carbapenem will change practice
The current study is very important because it provides a viable and effective alternative form of antibiotic delivery for the patients with complicated UTI, Noel N. Deep, MD, emphasized in an interview.
“Currently these patients have to be treated with IV carbapenem antibiotics either in a hospital or through a home health nurse,” Dr. Deep, a general internist in group practice in Antigo, Wisc., explained.
Current IV strategies also carry the inherent risk associated with the insertion of an IV catheter that is left in place for several days or replaced periodically. “The oral antibiotic eliminates these risks and higher health care costs and provides a safer and equally efficacious option,” Dr. Deep said.
In the current study, “I was definitely surprised at the effectiveness of the oral carbapenem,” Dr. Deep said. “I am absolutely delighted with this new treatment option that physicians can now add to their armamentarium [assuming FDA approval] as we provide care to our patients,” he said.
If approved, TBP-PI-HBr will definitely change the treatment spectrum for the multidrug-resistant bacterial UTIs, said Dr. Deep. “Carbapenems have continued to be effective and low antibiotic resistance to carbapenems has been recorded.”
As for additional research, “I would like to see studies done in other ethnicities and different countries to ascertain the effectiveness of this antibiotic in those populations and against other bacterial strains with potentially different resistance mechanisms,” Dr. Deep said.
The study was supported by Spero Therapeutics and the Department of Health and Human Services. Lead author Paul B. Eckburg, MD, of Stanford (Calif.) University, and Dr. Talley are employees of Spero Therapeutics. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News.
“No new oral antibiotic alternative has emerged to treat these conditions in more than 25 years,” corresponding author Angela K. Talley, MD, said in an interview. The new research was published in the New England Journal of Medicine.
Patients with complicated urinary tract infection (cUTI), including acute pyelonephritis (AP), are often hospitalized and treated with intravenous therapy because of the lack of oral options, especially in cases of antibiotic-resistant pathogens, explained Dr. Talley, of Spero Therapeutics.
In their new phase 3, double-blind randomized trial, the researchers evaluated the safety and effectiveness of oral TBP-PI-HBr, compared with intravenous ertapenem in hospitalized patients with cUTIs or AP. Oral tebipenem is an investigational carbapenem with demonstrated activity against uropathogenic Enterobacterales, and it has shown effectiveness in animal models, the researchers noted in their paper.
Methods and results
The researchers randomized 1,372 adult patients. The microbiologic intent-to-treat population included 449 patients who received TBP-PI-HBr (600 mg every 8 hours) and 419 who received ertapenem (1 g every 24 hours) for 7-10 days or up to 14 days for patients with bacteremia.
The primary endpoint was a composite of clinical cure and favorable microbiologic response, assessed at a test-of-cure visit on day 19. Clinical cure was defined as “complete resolution or clinically significant alleviation of baseline signs and symptoms of complicated urinary tract infection or acute pyelonephritis and no new symptoms, such that no further antimicrobial therapy was warranted,” the researchers wrote. Microbiologic response was defined as a reduction to less than 103 CFU per milliliter in uropathogen levels from baseline at day 19.
Overall, the clinical response occurred in 58.8% of patients who received TBP-PI-HBr and 61.6% of those who received ertapenem at the test-of-cure visit.
Clinical cure rates were similar in the TBP-PI-HBr and ertapenem groups (93.1% vs. 93.6%) at the test-of-cure visit.
Both treatment groups showed similar responses to Enterobacterales pathogens at the test-of-cure visit (62.7% for TBP-PI-HBr and 65.2% for ertapenem).
Among patients with bacteremia at baseline, overall response rates were 72.3% and 66.0% for TBP-PI-HBr and ertapenem, respectively, at the test-of-cure visit, and 93.6% and 96.2%, respectively, at the end-of-treatment visit on or around day 25.
The overall incidence of adverse events was approximately 26% in both treatment groups. Most adverse events were mild or moderate in severity and did not limit treatment, the researchers wrote.
The mean age of the patients was 58.1 years; 46.1% were aged 65 and older, and 11.5% had bacteremia at baseline.
The study findings were limited by several factors, including the mandated 7- to 10-day course of antibiotics, which may not reflect the standard of care in other settings in the United States. The study’s trial sites were located in the United States, South Africa, and Europe. The study population was primarily White and from Central and Eastern Europe. Other limitations included the randomization of patients before confirming the baseline pathogen, although this was done to limit potential confounding from previous antibiotics, the researchers noted.
Safety and efficacy support application for approval
“To our knowledge, this is the first head-to-head evaluation of an IV vs. an oral drug for the treatment of cUTI and acute pyelonephritis,” Dr. Talley said in an interview.
“The findings demonstrate that almost all patients in the study achieved complete resolution of the signs and symptoms of their infection,” she said.
TBP-PI-HBr has not been approved by the Food and Drug Administration, but a new drug application that included data from the current study was submitted to the FDA and is currently under review, Dr. Talley noted.
As for additional research, the current study was conducted in hospitalized patients, and the use of TBP-PI-HBr in the outpatient setting has not yet been evaluated, she said.
Approval and use of oral carbapenem will change practice
The current study is very important because it provides a viable and effective alternative form of antibiotic delivery for the patients with complicated UTI, Noel N. Deep, MD, emphasized in an interview.
“Currently these patients have to be treated with IV carbapenem antibiotics either in a hospital or through a home health nurse,” Dr. Deep, a general internist in group practice in Antigo, Wisc., explained.
Current IV strategies also carry the inherent risk associated with the insertion of an IV catheter that is left in place for several days or replaced periodically. “The oral antibiotic eliminates these risks and higher health care costs and provides a safer and equally efficacious option,” Dr. Deep said.
In the current study, “I was definitely surprised at the effectiveness of the oral carbapenem,” Dr. Deep said. “I am absolutely delighted with this new treatment option that physicians can now add to their armamentarium [assuming FDA approval] as we provide care to our patients,” he said.
If approved, TBP-PI-HBr will definitely change the treatment spectrum for the multidrug-resistant bacterial UTIs, said Dr. Deep. “Carbapenems have continued to be effective and low antibiotic resistance to carbapenems has been recorded.”
As for additional research, “I would like to see studies done in other ethnicities and different countries to ascertain the effectiveness of this antibiotic in those populations and against other bacterial strains with potentially different resistance mechanisms,” Dr. Deep said.
The study was supported by Spero Therapeutics and the Department of Health and Human Services. Lead author Paul B. Eckburg, MD, of Stanford (Calif.) University, and Dr. Talley are employees of Spero Therapeutics. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Abnormal growth of the amygdala in infants tied to autism
A new study suggests that overgrowth of the amygdala in infants during the first 6-12 months of life is tied to a later diagnosis of autism spectrum disorder (ASD).
“The faster the amygdala grew in infancy, the more social difficulties the child showed when diagnosed with autism a year later,” first author Mark Shen, PhD, assistant professor of psychiatry and neuroscience, University of North Carolina, Chapel Hill, told this news organization.
The study was published online in the American Journal of Psychiatry.
Unique to autism
The amygdala plays a key role in processing memory, emotional responses, and decisionmaking.
It’s long been known that the amygdala is abnormally large in school-aged children with ASD, but until now, it was not known precisely when aberrant amygdala growth happens, what the clinical consequences may be, and whether amygdala overgrowth is unique to autism.
To investigate, Dr. Shen and colleagues evaluated 1,099 longitudinal MRI scans obtained during natural sleep at 6, 12, and 24 months of age in 408 infants in the Infant Brain Imaging Study (IBIS) Network.
The cohort included 58 infants at high likelihood of developing ASD who were later diagnosed with the disorder, 212 infants at high likelihood of ASD who did not develop ASD, 109 typically-developing control infants, and 29 infants with fragile X syndrome.
At 6 months, infants who developed ASD had typically sized amygdala volumes but showed significantly faster amygdala growth between 6 and 24 months, such that by 12 months the ASD group had significantly larger amygdala volume (Cohen’s d = 0.56), compared with all other groups.
Amygdala growth rate between 6 and 12 months was significantly associated with greater social deficits at 24 months when the children were diagnosed with ASD.
“We found that the amygdala grows too rapidly between 6 and 12 months of age, during a presymptomatic period in autism, prior to when the diagnostic symptoms of autism (social difficulties and repetitive behaviors) are evident and lead to the later diagnosis of autism,” Dr. Shen said in an interview.
This brain growth pattern appears to be unique to autism, as babies with the genetic disorder fragile X syndrome – another neurodevelopmental condition – showed a markedly different brain growth pattern: no differences in amygdala growth but enlargement of a different brain structure, the caudate, which was linked to increased repetitive behaviors, the investigators found.
Earlier intervention
Prior research has shown that children who are later diagnosed with ASD often display problems in infancy with how they attend to visual stimuli in their surroundings.
These early problems with processing visual and sensory information may put increased stress on the amygdala, potentially leading to amygdala hyperactivity, deficits in pruning dendritic connections, and overgrowth, Dr. Shen and colleagues hypothesize.
Amygdala overgrowth has also been linked to chronic stress in studies of other psychiatric conditions, such as depression and anxiety, and may provide a clue to understanding this observation in infants who later develop autism.
“This research suggests that an optimal time to begin supports for children who are at the highest likelihood of developing autism may be during the first year of life: to improve early precursors to social development, such as sensory processing, in babies even before social difficulties arise,” Dr. Shen said.
Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University, St. Louis, said, “What makes this study important is the finding of abnormally increased amygdala growth rate in autism using a longitudinal design that focuses on earlier development.”
“While we are typically used to understanding brain structure as abnormally decreasing over time in certain disorders like Alzheimer’s disease, this study challenges us to understand that too much brain volume growth can also be abnormal in specific conditions,” Dr. Raji added.
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, and National Institute of Mental Health, along with Autism Speaks and the Simons Foundation. Dr. Shen and Dr. Raji have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study suggests that overgrowth of the amygdala in infants during the first 6-12 months of life is tied to a later diagnosis of autism spectrum disorder (ASD).
“The faster the amygdala grew in infancy, the more social difficulties the child showed when diagnosed with autism a year later,” first author Mark Shen, PhD, assistant professor of psychiatry and neuroscience, University of North Carolina, Chapel Hill, told this news organization.
The study was published online in the American Journal of Psychiatry.
Unique to autism
The amygdala plays a key role in processing memory, emotional responses, and decisionmaking.
It’s long been known that the amygdala is abnormally large in school-aged children with ASD, but until now, it was not known precisely when aberrant amygdala growth happens, what the clinical consequences may be, and whether amygdala overgrowth is unique to autism.
To investigate, Dr. Shen and colleagues evaluated 1,099 longitudinal MRI scans obtained during natural sleep at 6, 12, and 24 months of age in 408 infants in the Infant Brain Imaging Study (IBIS) Network.
The cohort included 58 infants at high likelihood of developing ASD who were later diagnosed with the disorder, 212 infants at high likelihood of ASD who did not develop ASD, 109 typically-developing control infants, and 29 infants with fragile X syndrome.
At 6 months, infants who developed ASD had typically sized amygdala volumes but showed significantly faster amygdala growth between 6 and 24 months, such that by 12 months the ASD group had significantly larger amygdala volume (Cohen’s d = 0.56), compared with all other groups.
Amygdala growth rate between 6 and 12 months was significantly associated with greater social deficits at 24 months when the children were diagnosed with ASD.
“We found that the amygdala grows too rapidly between 6 and 12 months of age, during a presymptomatic period in autism, prior to when the diagnostic symptoms of autism (social difficulties and repetitive behaviors) are evident and lead to the later diagnosis of autism,” Dr. Shen said in an interview.
This brain growth pattern appears to be unique to autism, as babies with the genetic disorder fragile X syndrome – another neurodevelopmental condition – showed a markedly different brain growth pattern: no differences in amygdala growth but enlargement of a different brain structure, the caudate, which was linked to increased repetitive behaviors, the investigators found.
Earlier intervention
Prior research has shown that children who are later diagnosed with ASD often display problems in infancy with how they attend to visual stimuli in their surroundings.
These early problems with processing visual and sensory information may put increased stress on the amygdala, potentially leading to amygdala hyperactivity, deficits in pruning dendritic connections, and overgrowth, Dr. Shen and colleagues hypothesize.
Amygdala overgrowth has also been linked to chronic stress in studies of other psychiatric conditions, such as depression and anxiety, and may provide a clue to understanding this observation in infants who later develop autism.
“This research suggests that an optimal time to begin supports for children who are at the highest likelihood of developing autism may be during the first year of life: to improve early precursors to social development, such as sensory processing, in babies even before social difficulties arise,” Dr. Shen said.
Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University, St. Louis, said, “What makes this study important is the finding of abnormally increased amygdala growth rate in autism using a longitudinal design that focuses on earlier development.”
“While we are typically used to understanding brain structure as abnormally decreasing over time in certain disorders like Alzheimer’s disease, this study challenges us to understand that too much brain volume growth can also be abnormal in specific conditions,” Dr. Raji added.
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, and National Institute of Mental Health, along with Autism Speaks and the Simons Foundation. Dr. Shen and Dr. Raji have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study suggests that overgrowth of the amygdala in infants during the first 6-12 months of life is tied to a later diagnosis of autism spectrum disorder (ASD).
“The faster the amygdala grew in infancy, the more social difficulties the child showed when diagnosed with autism a year later,” first author Mark Shen, PhD, assistant professor of psychiatry and neuroscience, University of North Carolina, Chapel Hill, told this news organization.
The study was published online in the American Journal of Psychiatry.
Unique to autism
The amygdala plays a key role in processing memory, emotional responses, and decisionmaking.
It’s long been known that the amygdala is abnormally large in school-aged children with ASD, but until now, it was not known precisely when aberrant amygdala growth happens, what the clinical consequences may be, and whether amygdala overgrowth is unique to autism.
To investigate, Dr. Shen and colleagues evaluated 1,099 longitudinal MRI scans obtained during natural sleep at 6, 12, and 24 months of age in 408 infants in the Infant Brain Imaging Study (IBIS) Network.
The cohort included 58 infants at high likelihood of developing ASD who were later diagnosed with the disorder, 212 infants at high likelihood of ASD who did not develop ASD, 109 typically-developing control infants, and 29 infants with fragile X syndrome.
At 6 months, infants who developed ASD had typically sized amygdala volumes but showed significantly faster amygdala growth between 6 and 24 months, such that by 12 months the ASD group had significantly larger amygdala volume (Cohen’s d = 0.56), compared with all other groups.
Amygdala growth rate between 6 and 12 months was significantly associated with greater social deficits at 24 months when the children were diagnosed with ASD.
“We found that the amygdala grows too rapidly between 6 and 12 months of age, during a presymptomatic period in autism, prior to when the diagnostic symptoms of autism (social difficulties and repetitive behaviors) are evident and lead to the later diagnosis of autism,” Dr. Shen said in an interview.
This brain growth pattern appears to be unique to autism, as babies with the genetic disorder fragile X syndrome – another neurodevelopmental condition – showed a markedly different brain growth pattern: no differences in amygdala growth but enlargement of a different brain structure, the caudate, which was linked to increased repetitive behaviors, the investigators found.
Earlier intervention
Prior research has shown that children who are later diagnosed with ASD often display problems in infancy with how they attend to visual stimuli in their surroundings.
These early problems with processing visual and sensory information may put increased stress on the amygdala, potentially leading to amygdala hyperactivity, deficits in pruning dendritic connections, and overgrowth, Dr. Shen and colleagues hypothesize.
Amygdala overgrowth has also been linked to chronic stress in studies of other psychiatric conditions, such as depression and anxiety, and may provide a clue to understanding this observation in infants who later develop autism.
“This research suggests that an optimal time to begin supports for children who are at the highest likelihood of developing autism may be during the first year of life: to improve early precursors to social development, such as sensory processing, in babies even before social difficulties arise,” Dr. Shen said.
Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University, St. Louis, said, “What makes this study important is the finding of abnormally increased amygdala growth rate in autism using a longitudinal design that focuses on earlier development.”
“While we are typically used to understanding brain structure as abnormally decreasing over time in certain disorders like Alzheimer’s disease, this study challenges us to understand that too much brain volume growth can also be abnormal in specific conditions,” Dr. Raji added.
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, and National Institute of Mental Health, along with Autism Speaks and the Simons Foundation. Dr. Shen and Dr. Raji have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Bellies up to the bar, the weight gain is on us
I’d do anything for weight loss (but I won’t do that)
Weight loss isn’t a multibillion-dollar industry for nothing. How many people step onto the scale in the morning and sigh, wishing they could lose that last 10 pounds?
Alcohol also isn’t a multibillion-dollar industry for nothing. If there’s one thing more universal than wishing you could lose weight, it’s drinking to forget your woes about being unable to lose weight.
Naturally, and unfortunately for those of us who rather enjoy a good beer, one of the best ways to lose weight is to stop drinking. Alcohol is almost the definition of empty calories. So, which wins out: The unstoppable force of wanting to lose weight, or the immovable object of alcohol? According to a survey from DrugAbuse.com, it’s alcohol, and it’s not even close.
Even in a state with as health conscious a reputation as California, not only are people not willing to give up alcohol to lose weight, they’re willing to gain a noticeable amount of weight in order to continue drinking. It’s 14 pounds for Californians, which is in the middle of the road for America, which overall averaged 13 pounds to keep drinking. Hawaiians, South Dakotans, Utahns, and Vermonters were at the bottom, willing to add only 8 pounds to keep booze in their diet. At the other end of the scale, willing to add 28 whole pounds to keep the beer flowing, is humble little Rhode Island, followed by Wyoming at 23 pounds, Maryland at 22, and Tennessee at 21.
Obviously, that’s a lot of weight to gain, but to drive home the exact quantity of just how much weight, KRON-TV noted that adding the U.S. average of 13 pounds to your body is the equivalent of strapping 224 slices of bacon to yourself, which, to us, is just the poorest choice of comparison. If there’s one thing we’re less willing to give up than alcohol, it’s probably bacon. Or if you’re feeling especially ambitious, you could go for bacon-scented beer from the Waffle House. Now that’s a drink.
This looks like a job for the ‘magnetic slime robot’
What’s that? While you were in the process of gaining 14 pounds so you could keep drinking alcohol you swallowed something that you shouldn’t have? Did you swallow a lot of aggression?
You swallowed a what? An ear bud? But how did you manage that? No, never mind, we don’t really want to hear about your personal life. Lucky for you, though, today’s LOTME phrase that pays is “magnetic turd” and it’s just the thing for the busy executive/child with a foreign object stuck in their … whatever.
Yes, we said magnetic turd. Or, if you prefer, a “magnetic slime robot.” The black-brown–colored blob/robot/turd in question is an investigational substance that can be controlled magnetically to move through very narrow spaces and encircle small objects that have been accidentally swallowed, its cocreator, Li Zhang of the Chinese University of Hong Kong, told the Guardian.
It’s made by combining the polymer polyvinyl alcohol with borax and particles of neodymium magnet. And since those neodymium particles are not particularly friendly to humans, Dr. Zhang and the research team coated the slime with silica to seal in the toxicity. The slime has the consistency of custard and exhibits “visco-elastic properties,” Dr. Zhang said, meaning that “sometimes it behaves like a solid, sometimes it behaves like a liquid.”
We could go on, telling you about the substance’s self-healing ability and electrical conductivity and how it does look very, very turd-like. Instead, we offer this link to the team’s really freaky video.
We’re going to be seeing that in our nightmares.
Fish: More than meets the fry?
When you think of fish, intelligence isn’t usually the first thing to pop into your head. Their short memory spans, which can be as little as 3 seconds, probably don’t help their cause.
Recently, though, it has become apparent that fish can be trained to do simple math problems like adding and subtracting. Research conducted in Germany has shown that cichlids – tropical fish often found in home aquariums – and stingrays can observe small quantities and know how many things are there without actually counting, kind of like how a human can look at a bowl of apples and know about how many are in it.
Fish, once thought to be not very smart, may be on the same level of intelligence as birds, suggested Vera Schluessel, PhD, of the University of Bonn’s Institute of Zoology, and associates.
“Successful fish showed abilities far above chance level, specifically in the stingrays. Again, this raises the question of what abilities fish may be capable of if being asked the ‘right’ question,” the researchers said in Scientific Reports.
They tried to teach the cichlids and stingrays how to add and subtract by recognizing colors: Blue meant to add one and yellow meant to subtract one. Gates were set up and when the fish chose a correct answer, they were rewarded with food. Although it took many sessions for the fish to completely catch on, they did figure it out eventually.
If fish are smarter than we thought, maybe we can stop paying for math tutors for our kids and just have the family goldfish do it.
For earthworms, not all plastics are created equal
Everything living on the earth has to deal with pollution in some way, including earthworms. Not only have they have adapted to eating plastics found in soil, they have preferences.
The earthworm is a little creature with a big job. The materials and minerals they munch on as they go through the earth get recycled through their tiny bodies to create more fertile soil for things to grow – making them the hidden heroes of every garden. But what about soil that’s full of microscopic plastic pieces? Well, turns out earthworms will eat that too, investigators from Nankai University in Tianjin, China, reported in Environmental Science & Technology.
The researchers looked at how these eating machines were digesting the plastic and found that they actually have preferences. Soils with bio-based polylactic acid (PLA) or petroleum-derived polyethylene terephthalate (PET) particles were a hit. Another test showed that the worms broke the PLA particles down into smaller fragments than the PET ones. So at least the “healthier” option agreed with them more. More work is needed, however, to determine if the worms are being harmed by all the waste they’re digesting.
So what does this mean for the evolution or even survival of this unsung hero of the planet? Scientists still need to dig into that question. No pun intended.
I’d do anything for weight loss (but I won’t do that)
Weight loss isn’t a multibillion-dollar industry for nothing. How many people step onto the scale in the morning and sigh, wishing they could lose that last 10 pounds?
Alcohol also isn’t a multibillion-dollar industry for nothing. If there’s one thing more universal than wishing you could lose weight, it’s drinking to forget your woes about being unable to lose weight.
Naturally, and unfortunately for those of us who rather enjoy a good beer, one of the best ways to lose weight is to stop drinking. Alcohol is almost the definition of empty calories. So, which wins out: The unstoppable force of wanting to lose weight, or the immovable object of alcohol? According to a survey from DrugAbuse.com, it’s alcohol, and it’s not even close.
Even in a state with as health conscious a reputation as California, not only are people not willing to give up alcohol to lose weight, they’re willing to gain a noticeable amount of weight in order to continue drinking. It’s 14 pounds for Californians, which is in the middle of the road for America, which overall averaged 13 pounds to keep drinking. Hawaiians, South Dakotans, Utahns, and Vermonters were at the bottom, willing to add only 8 pounds to keep booze in their diet. At the other end of the scale, willing to add 28 whole pounds to keep the beer flowing, is humble little Rhode Island, followed by Wyoming at 23 pounds, Maryland at 22, and Tennessee at 21.
Obviously, that’s a lot of weight to gain, but to drive home the exact quantity of just how much weight, KRON-TV noted that adding the U.S. average of 13 pounds to your body is the equivalent of strapping 224 slices of bacon to yourself, which, to us, is just the poorest choice of comparison. If there’s one thing we’re less willing to give up than alcohol, it’s probably bacon. Or if you’re feeling especially ambitious, you could go for bacon-scented beer from the Waffle House. Now that’s a drink.
This looks like a job for the ‘magnetic slime robot’
What’s that? While you were in the process of gaining 14 pounds so you could keep drinking alcohol you swallowed something that you shouldn’t have? Did you swallow a lot of aggression?
You swallowed a what? An ear bud? But how did you manage that? No, never mind, we don’t really want to hear about your personal life. Lucky for you, though, today’s LOTME phrase that pays is “magnetic turd” and it’s just the thing for the busy executive/child with a foreign object stuck in their … whatever.
Yes, we said magnetic turd. Or, if you prefer, a “magnetic slime robot.” The black-brown–colored blob/robot/turd in question is an investigational substance that can be controlled magnetically to move through very narrow spaces and encircle small objects that have been accidentally swallowed, its cocreator, Li Zhang of the Chinese University of Hong Kong, told the Guardian.
It’s made by combining the polymer polyvinyl alcohol with borax and particles of neodymium magnet. And since those neodymium particles are not particularly friendly to humans, Dr. Zhang and the research team coated the slime with silica to seal in the toxicity. The slime has the consistency of custard and exhibits “visco-elastic properties,” Dr. Zhang said, meaning that “sometimes it behaves like a solid, sometimes it behaves like a liquid.”
We could go on, telling you about the substance’s self-healing ability and electrical conductivity and how it does look very, very turd-like. Instead, we offer this link to the team’s really freaky video.
We’re going to be seeing that in our nightmares.
Fish: More than meets the fry?
When you think of fish, intelligence isn’t usually the first thing to pop into your head. Their short memory spans, which can be as little as 3 seconds, probably don’t help their cause.
Recently, though, it has become apparent that fish can be trained to do simple math problems like adding and subtracting. Research conducted in Germany has shown that cichlids – tropical fish often found in home aquariums – and stingrays can observe small quantities and know how many things are there without actually counting, kind of like how a human can look at a bowl of apples and know about how many are in it.
Fish, once thought to be not very smart, may be on the same level of intelligence as birds, suggested Vera Schluessel, PhD, of the University of Bonn’s Institute of Zoology, and associates.
“Successful fish showed abilities far above chance level, specifically in the stingrays. Again, this raises the question of what abilities fish may be capable of if being asked the ‘right’ question,” the researchers said in Scientific Reports.
They tried to teach the cichlids and stingrays how to add and subtract by recognizing colors: Blue meant to add one and yellow meant to subtract one. Gates were set up and when the fish chose a correct answer, they were rewarded with food. Although it took many sessions for the fish to completely catch on, they did figure it out eventually.
If fish are smarter than we thought, maybe we can stop paying for math tutors for our kids and just have the family goldfish do it.
For earthworms, not all plastics are created equal
Everything living on the earth has to deal with pollution in some way, including earthworms. Not only have they have adapted to eating plastics found in soil, they have preferences.
The earthworm is a little creature with a big job. The materials and minerals they munch on as they go through the earth get recycled through their tiny bodies to create more fertile soil for things to grow – making them the hidden heroes of every garden. But what about soil that’s full of microscopic plastic pieces? Well, turns out earthworms will eat that too, investigators from Nankai University in Tianjin, China, reported in Environmental Science & Technology.
The researchers looked at how these eating machines were digesting the plastic and found that they actually have preferences. Soils with bio-based polylactic acid (PLA) or petroleum-derived polyethylene terephthalate (PET) particles were a hit. Another test showed that the worms broke the PLA particles down into smaller fragments than the PET ones. So at least the “healthier” option agreed with them more. More work is needed, however, to determine if the worms are being harmed by all the waste they’re digesting.
So what does this mean for the evolution or even survival of this unsung hero of the planet? Scientists still need to dig into that question. No pun intended.
I’d do anything for weight loss (but I won’t do that)
Weight loss isn’t a multibillion-dollar industry for nothing. How many people step onto the scale in the morning and sigh, wishing they could lose that last 10 pounds?
Alcohol also isn’t a multibillion-dollar industry for nothing. If there’s one thing more universal than wishing you could lose weight, it’s drinking to forget your woes about being unable to lose weight.
Naturally, and unfortunately for those of us who rather enjoy a good beer, one of the best ways to lose weight is to stop drinking. Alcohol is almost the definition of empty calories. So, which wins out: The unstoppable force of wanting to lose weight, or the immovable object of alcohol? According to a survey from DrugAbuse.com, it’s alcohol, and it’s not even close.
Even in a state with as health conscious a reputation as California, not only are people not willing to give up alcohol to lose weight, they’re willing to gain a noticeable amount of weight in order to continue drinking. It’s 14 pounds for Californians, which is in the middle of the road for America, which overall averaged 13 pounds to keep drinking. Hawaiians, South Dakotans, Utahns, and Vermonters were at the bottom, willing to add only 8 pounds to keep booze in their diet. At the other end of the scale, willing to add 28 whole pounds to keep the beer flowing, is humble little Rhode Island, followed by Wyoming at 23 pounds, Maryland at 22, and Tennessee at 21.
Obviously, that’s a lot of weight to gain, but to drive home the exact quantity of just how much weight, KRON-TV noted that adding the U.S. average of 13 pounds to your body is the equivalent of strapping 224 slices of bacon to yourself, which, to us, is just the poorest choice of comparison. If there’s one thing we’re less willing to give up than alcohol, it’s probably bacon. Or if you’re feeling especially ambitious, you could go for bacon-scented beer from the Waffle House. Now that’s a drink.
This looks like a job for the ‘magnetic slime robot’
What’s that? While you were in the process of gaining 14 pounds so you could keep drinking alcohol you swallowed something that you shouldn’t have? Did you swallow a lot of aggression?
You swallowed a what? An ear bud? But how did you manage that? No, never mind, we don’t really want to hear about your personal life. Lucky for you, though, today’s LOTME phrase that pays is “magnetic turd” and it’s just the thing for the busy executive/child with a foreign object stuck in their … whatever.
Yes, we said magnetic turd. Or, if you prefer, a “magnetic slime robot.” The black-brown–colored blob/robot/turd in question is an investigational substance that can be controlled magnetically to move through very narrow spaces and encircle small objects that have been accidentally swallowed, its cocreator, Li Zhang of the Chinese University of Hong Kong, told the Guardian.
It’s made by combining the polymer polyvinyl alcohol with borax and particles of neodymium magnet. And since those neodymium particles are not particularly friendly to humans, Dr. Zhang and the research team coated the slime with silica to seal in the toxicity. The slime has the consistency of custard and exhibits “visco-elastic properties,” Dr. Zhang said, meaning that “sometimes it behaves like a solid, sometimes it behaves like a liquid.”
We could go on, telling you about the substance’s self-healing ability and electrical conductivity and how it does look very, very turd-like. Instead, we offer this link to the team’s really freaky video.
We’re going to be seeing that in our nightmares.
Fish: More than meets the fry?
When you think of fish, intelligence isn’t usually the first thing to pop into your head. Their short memory spans, which can be as little as 3 seconds, probably don’t help their cause.
Recently, though, it has become apparent that fish can be trained to do simple math problems like adding and subtracting. Research conducted in Germany has shown that cichlids – tropical fish often found in home aquariums – and stingrays can observe small quantities and know how many things are there without actually counting, kind of like how a human can look at a bowl of apples and know about how many are in it.
Fish, once thought to be not very smart, may be on the same level of intelligence as birds, suggested Vera Schluessel, PhD, of the University of Bonn’s Institute of Zoology, and associates.
“Successful fish showed abilities far above chance level, specifically in the stingrays. Again, this raises the question of what abilities fish may be capable of if being asked the ‘right’ question,” the researchers said in Scientific Reports.
They tried to teach the cichlids and stingrays how to add and subtract by recognizing colors: Blue meant to add one and yellow meant to subtract one. Gates were set up and when the fish chose a correct answer, they were rewarded with food. Although it took many sessions for the fish to completely catch on, they did figure it out eventually.
If fish are smarter than we thought, maybe we can stop paying for math tutors for our kids and just have the family goldfish do it.
For earthworms, not all plastics are created equal
Everything living on the earth has to deal with pollution in some way, including earthworms. Not only have they have adapted to eating plastics found in soil, they have preferences.
The earthworm is a little creature with a big job. The materials and minerals they munch on as they go through the earth get recycled through their tiny bodies to create more fertile soil for things to grow – making them the hidden heroes of every garden. But what about soil that’s full of microscopic plastic pieces? Well, turns out earthworms will eat that too, investigators from Nankai University in Tianjin, China, reported in Environmental Science & Technology.
The researchers looked at how these eating machines were digesting the plastic and found that they actually have preferences. Soils with bio-based polylactic acid (PLA) or petroleum-derived polyethylene terephthalate (PET) particles were a hit. Another test showed that the worms broke the PLA particles down into smaller fragments than the PET ones. So at least the “healthier” option agreed with them more. More work is needed, however, to determine if the worms are being harmed by all the waste they’re digesting.
So what does this mean for the evolution or even survival of this unsung hero of the planet? Scientists still need to dig into that question. No pun intended.
Could AI tool identify type 1 diabetes earlier in childhood?
An artificial intelligence (AI)–based predictive tool may be able to identify type 1 diabetes in children earlier, before they are diagnosed as a result of potentially fatal diabetic ketoacidosis (DKA), suggests a new U.K. study.
The tool was developed by Julia Townson, PhD, senior trial manager in children and young people at Cardiff University, U.K., and colleagues.
Her team had previously shown that children who develop type 1 diabetes have a different pattern of contact with primary care in the 6 months leading up to their diagnosis.
Symptoms of type 1 diabetes include going to the toilet more and being thirsty, tired, and thin, but GPs can still miss these signs.
So they tested different combinations of factors from GP records – such as urinary tract infections or bedwetting, being prescribed antibiotics or family history of type 1 diabetes – in approximately 1 million children in Wales, more than 2,000 of whom had been diagnosed with type 1 diabetes, to train the predictive tool.
In a separate study of around 1.5 million children in England, they found that the algorithm could identify type 1 diabetes in 75% of affected children 11 days earlier than without the tool, if it was set up as an alert at every one in 10 general practice consultations.
Dr. Townson presented her research at the recent Diabetes UK Professional Conference 2022.
One-quarter of kids diagnosed with type 1 diabetes are in DKA
During her presentation, Dr. Townson explained that, in the U.K., approximately 25% of children with type 1 diabetes are diagnosed while they are in DKA, a figure that has remained unchanged for 25 years.
“We know that delayed- and misdiagnosis are the most common reasons for a child presenting in DKA at diagnosis,” she said. “And of course, the reason why it’s so important to prevent presentation in DKA is because of the considerable morbidity and potentially mortality associated with it.”
Indeed, with a simple internet search, Dr. Townson was able to identify four children who lost their lives to DKA in the past 8 years in the U.K.
“It’s encouraging to see that this research could save many families a potentially traumatic trip to the hospital by helping family doctors diagnose type 1 diabetes more rapidly,” Conor McKeever, research communications manager at the type 1 diabetes charity JDRF, told this news organization.
“This approach could go hand-in-hand with population screening, which has the potential to identify people at high risk of developing type 1 diabetes before they experience any symptoms,” he added. The hope is that “far fewer families experience DKA at the start of their type 1 diabetes journey.”
“Finding a way to catch the condition and treat it early could help to avoid emergency hospital treatment and save lives,” agreed Lucy Chambers, PhD, head of research communications at Diabetes UK, which funded the research.
How to integrate tool into GP systems
“We are now looking to see how this tool might work with primary care computer systems,” Dr. Townson said. She said in an interview that they are exploring “how it could be ‘bolted’ on to the GP’s software system.”
“It works on many different levels, but one level is frequency of consultations in relation to the frequency of previous consultations, so it needs to be able to ‘look’ through the electronic health records, at the time of the consultation, to come up with a predictive score.”
Dr. Townson said it is not clear how “easy it will be to integrate it into current systems, and I do not know of any other machine learning applications which have been used like this in primary care.”
“But we are hopeful, and we have started to contact companies who are involved in providing these systems.”
The research was funded by Diabetes UK, and the Clinical Trials Unit was funded by Health and Care Research Wales. No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
An artificial intelligence (AI)–based predictive tool may be able to identify type 1 diabetes in children earlier, before they are diagnosed as a result of potentially fatal diabetic ketoacidosis (DKA), suggests a new U.K. study.
The tool was developed by Julia Townson, PhD, senior trial manager in children and young people at Cardiff University, U.K., and colleagues.
Her team had previously shown that children who develop type 1 diabetes have a different pattern of contact with primary care in the 6 months leading up to their diagnosis.
Symptoms of type 1 diabetes include going to the toilet more and being thirsty, tired, and thin, but GPs can still miss these signs.
So they tested different combinations of factors from GP records – such as urinary tract infections or bedwetting, being prescribed antibiotics or family history of type 1 diabetes – in approximately 1 million children in Wales, more than 2,000 of whom had been diagnosed with type 1 diabetes, to train the predictive tool.
In a separate study of around 1.5 million children in England, they found that the algorithm could identify type 1 diabetes in 75% of affected children 11 days earlier than without the tool, if it was set up as an alert at every one in 10 general practice consultations.
Dr. Townson presented her research at the recent Diabetes UK Professional Conference 2022.
One-quarter of kids diagnosed with type 1 diabetes are in DKA
During her presentation, Dr. Townson explained that, in the U.K., approximately 25% of children with type 1 diabetes are diagnosed while they are in DKA, a figure that has remained unchanged for 25 years.
“We know that delayed- and misdiagnosis are the most common reasons for a child presenting in DKA at diagnosis,” she said. “And of course, the reason why it’s so important to prevent presentation in DKA is because of the considerable morbidity and potentially mortality associated with it.”
Indeed, with a simple internet search, Dr. Townson was able to identify four children who lost their lives to DKA in the past 8 years in the U.K.
“It’s encouraging to see that this research could save many families a potentially traumatic trip to the hospital by helping family doctors diagnose type 1 diabetes more rapidly,” Conor McKeever, research communications manager at the type 1 diabetes charity JDRF, told this news organization.
“This approach could go hand-in-hand with population screening, which has the potential to identify people at high risk of developing type 1 diabetes before they experience any symptoms,” he added. The hope is that “far fewer families experience DKA at the start of their type 1 diabetes journey.”
“Finding a way to catch the condition and treat it early could help to avoid emergency hospital treatment and save lives,” agreed Lucy Chambers, PhD, head of research communications at Diabetes UK, which funded the research.
How to integrate tool into GP systems
“We are now looking to see how this tool might work with primary care computer systems,” Dr. Townson said. She said in an interview that they are exploring “how it could be ‘bolted’ on to the GP’s software system.”
“It works on many different levels, but one level is frequency of consultations in relation to the frequency of previous consultations, so it needs to be able to ‘look’ through the electronic health records, at the time of the consultation, to come up with a predictive score.”
Dr. Townson said it is not clear how “easy it will be to integrate it into current systems, and I do not know of any other machine learning applications which have been used like this in primary care.”
“But we are hopeful, and we have started to contact companies who are involved in providing these systems.”
The research was funded by Diabetes UK, and the Clinical Trials Unit was funded by Health and Care Research Wales. No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
An artificial intelligence (AI)–based predictive tool may be able to identify type 1 diabetes in children earlier, before they are diagnosed as a result of potentially fatal diabetic ketoacidosis (DKA), suggests a new U.K. study.
The tool was developed by Julia Townson, PhD, senior trial manager in children and young people at Cardiff University, U.K., and colleagues.
Her team had previously shown that children who develop type 1 diabetes have a different pattern of contact with primary care in the 6 months leading up to their diagnosis.
Symptoms of type 1 diabetes include going to the toilet more and being thirsty, tired, and thin, but GPs can still miss these signs.
So they tested different combinations of factors from GP records – such as urinary tract infections or bedwetting, being prescribed antibiotics or family history of type 1 diabetes – in approximately 1 million children in Wales, more than 2,000 of whom had been diagnosed with type 1 diabetes, to train the predictive tool.
In a separate study of around 1.5 million children in England, they found that the algorithm could identify type 1 diabetes in 75% of affected children 11 days earlier than without the tool, if it was set up as an alert at every one in 10 general practice consultations.
Dr. Townson presented her research at the recent Diabetes UK Professional Conference 2022.
One-quarter of kids diagnosed with type 1 diabetes are in DKA
During her presentation, Dr. Townson explained that, in the U.K., approximately 25% of children with type 1 diabetes are diagnosed while they are in DKA, a figure that has remained unchanged for 25 years.
“We know that delayed- and misdiagnosis are the most common reasons for a child presenting in DKA at diagnosis,” she said. “And of course, the reason why it’s so important to prevent presentation in DKA is because of the considerable morbidity and potentially mortality associated with it.”
Indeed, with a simple internet search, Dr. Townson was able to identify four children who lost their lives to DKA in the past 8 years in the U.K.
“It’s encouraging to see that this research could save many families a potentially traumatic trip to the hospital by helping family doctors diagnose type 1 diabetes more rapidly,” Conor McKeever, research communications manager at the type 1 diabetes charity JDRF, told this news organization.
“This approach could go hand-in-hand with population screening, which has the potential to identify people at high risk of developing type 1 diabetes before they experience any symptoms,” he added. The hope is that “far fewer families experience DKA at the start of their type 1 diabetes journey.”
“Finding a way to catch the condition and treat it early could help to avoid emergency hospital treatment and save lives,” agreed Lucy Chambers, PhD, head of research communications at Diabetes UK, which funded the research.
How to integrate tool into GP systems
“We are now looking to see how this tool might work with primary care computer systems,” Dr. Townson said. She said in an interview that they are exploring “how it could be ‘bolted’ on to the GP’s software system.”
“It works on many different levels, but one level is frequency of consultations in relation to the frequency of previous consultations, so it needs to be able to ‘look’ through the electronic health records, at the time of the consultation, to come up with a predictive score.”
Dr. Townson said it is not clear how “easy it will be to integrate it into current systems, and I do not know of any other machine learning applications which have been used like this in primary care.”
“But we are hopeful, and we have started to contact companies who are involved in providing these systems.”
The research was funded by Diabetes UK, and the Clinical Trials Unit was funded by Health and Care Research Wales. No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
Nanoparticle shows promise for ALS
SEATTLE – , which was the change in the summated motor unit index (MUNIX) from baseline to week 36.
The drug, CNM-Au8, is being developed by Clene, and would represent a novel mechanism of action. “This is a brand-new approach. We used it complementary with riluzole and it was well tolerated, so I see this as an add-on therapy. I think if we can show some more positivity and longer-term results, it’s going to be a game changer for ALS,” Matthew Kiernan, MBBS, PhD, said in an interview. Dr. Kiernan presented the results at the 2022 annual meeting of the American Academy of Neurology.
Riluzole (Rilutek), which received Food and Drug Administration approval in 1995, inhibits glutamate release to counter excitotoxicity, which is believed to play a role in ALS, Huntington’s disease, ischemia, and other acute and chronic neurodegenerative diseases. The other FDA-approved agent for ALS is the neuroprotective agent and free-radical scavenger edaravone (Radicava), approved in 2017.
CNM-Au8 is made up of catalytically active gold nanocrystals that cross the blood-brain barrier, but lacks the toxicity associated with other synthetic gold compounds, according to the company. The formulation is also being investigated for the treatment of Parkinson’s disease and multiple sclerosis. Basic research has shown that it stabilizes mitochondria and reduces accumulation of the TDP-43 protein, which is linked to spread of ALS through the brain, Dr. Kiernan said during his presentation.
The treatment is well tolerated. “Normally in an ALS trial, we see about a 25% dropout rate. There were no dropouts on the active compound in the clinical trial. There are less deaths, so improved survival,” said Dr. Kiernan, the Bushell chair of neurology at the University of Sydney and codirector of the Brain and Mind Center in Sydney.
Good safety signal
The fact that the trial missed its primary endpoint isn’t too concerning, according to Nicholas Johnson, MD, who comoderated the session where the study was presented. “ALS clinical trials are incredibly difficult to conduct, especially a phase 2 learning-phase clinical trial. At this phase, I’m much more buoyed by the fact that they have a good safety signal, and that they’re willing to move forward to that phase 3 clinical trial,” Dr. Johnson said in an interview. He is vice chair of research at Virginia Commonwealth University, Richmond.
A phase 3 clinical trial is in development in the United States and Europe. The drug also is included as part of the HEALEY ALS Platform Trial, which is testing multiple ALS therapies simultaneously. “The results from that should be available by the second half of this year and it will also inform us as to what the approach should be,” said Dr. Kiernan.
Dr. Johnson also was enthusiastic. “I’m excited to see the results in terms of the primary endpoints for that next phase 3 clinical trial,” he said.
Ongoing research
In September 2021, Clene announced a second expanded access program for people with ALS.
The study included a 36-week double-blind treatment period followed by long-term, open-label follow-up. Twenty-three patients received 30 mg CNM-Au8, and 22 received placebo. In the first 36 weeks, the treatment group was more likely to have no disease progression, defined as death, tracheostomy, noninvasive ventilation, or a gastronomy tube (P = .0125). The researchers compared the probability of experiencing a less than 6-point decline in the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale. At 12 weeks, it was about 85% in both groups. At 24 weeks, it was about 60% to 50% in favor of the CNM-Au8 group, and at 36 weeks it was about 50% to 20% (P = .0350).
At 36 weeks, quality of life as measured by the ALS Specific Quality of Life–Short Form was better in the treatment group at 36 weeks (mean change, 0.9; P = .0177).
Survival was better in the treatment group at 96 weeks than the mortality derived from a European Network for the Cure of ALS prediction model (hazard ratio [HR], 0.2974; P = .0068). This benefit also was experienced by patients who received drug throughout the study (HR, 0.36; 95% confidence interval [CI], 0.12-1.1) and those who started out on placebo and converted to active drug during the open-label period (HR, 0.24; 95% CI, 0.064-0.88).
The study was funded by Clene and FightMND. Dr. Kiernan and Dr. Johnson have no relevant financial disclosures.
SEATTLE – , which was the change in the summated motor unit index (MUNIX) from baseline to week 36.
The drug, CNM-Au8, is being developed by Clene, and would represent a novel mechanism of action. “This is a brand-new approach. We used it complementary with riluzole and it was well tolerated, so I see this as an add-on therapy. I think if we can show some more positivity and longer-term results, it’s going to be a game changer for ALS,” Matthew Kiernan, MBBS, PhD, said in an interview. Dr. Kiernan presented the results at the 2022 annual meeting of the American Academy of Neurology.
Riluzole (Rilutek), which received Food and Drug Administration approval in 1995, inhibits glutamate release to counter excitotoxicity, which is believed to play a role in ALS, Huntington’s disease, ischemia, and other acute and chronic neurodegenerative diseases. The other FDA-approved agent for ALS is the neuroprotective agent and free-radical scavenger edaravone (Radicava), approved in 2017.
CNM-Au8 is made up of catalytically active gold nanocrystals that cross the blood-brain barrier, but lacks the toxicity associated with other synthetic gold compounds, according to the company. The formulation is also being investigated for the treatment of Parkinson’s disease and multiple sclerosis. Basic research has shown that it stabilizes mitochondria and reduces accumulation of the TDP-43 protein, which is linked to spread of ALS through the brain, Dr. Kiernan said during his presentation.
The treatment is well tolerated. “Normally in an ALS trial, we see about a 25% dropout rate. There were no dropouts on the active compound in the clinical trial. There are less deaths, so improved survival,” said Dr. Kiernan, the Bushell chair of neurology at the University of Sydney and codirector of the Brain and Mind Center in Sydney.
Good safety signal
The fact that the trial missed its primary endpoint isn’t too concerning, according to Nicholas Johnson, MD, who comoderated the session where the study was presented. “ALS clinical trials are incredibly difficult to conduct, especially a phase 2 learning-phase clinical trial. At this phase, I’m much more buoyed by the fact that they have a good safety signal, and that they’re willing to move forward to that phase 3 clinical trial,” Dr. Johnson said in an interview. He is vice chair of research at Virginia Commonwealth University, Richmond.
A phase 3 clinical trial is in development in the United States and Europe. The drug also is included as part of the HEALEY ALS Platform Trial, which is testing multiple ALS therapies simultaneously. “The results from that should be available by the second half of this year and it will also inform us as to what the approach should be,” said Dr. Kiernan.
Dr. Johnson also was enthusiastic. “I’m excited to see the results in terms of the primary endpoints for that next phase 3 clinical trial,” he said.
Ongoing research
In September 2021, Clene announced a second expanded access program for people with ALS.
The study included a 36-week double-blind treatment period followed by long-term, open-label follow-up. Twenty-three patients received 30 mg CNM-Au8, and 22 received placebo. In the first 36 weeks, the treatment group was more likely to have no disease progression, defined as death, tracheostomy, noninvasive ventilation, or a gastronomy tube (P = .0125). The researchers compared the probability of experiencing a less than 6-point decline in the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale. At 12 weeks, it was about 85% in both groups. At 24 weeks, it was about 60% to 50% in favor of the CNM-Au8 group, and at 36 weeks it was about 50% to 20% (P = .0350).
At 36 weeks, quality of life as measured by the ALS Specific Quality of Life–Short Form was better in the treatment group at 36 weeks (mean change, 0.9; P = .0177).
Survival was better in the treatment group at 96 weeks than the mortality derived from a European Network for the Cure of ALS prediction model (hazard ratio [HR], 0.2974; P = .0068). This benefit also was experienced by patients who received drug throughout the study (HR, 0.36; 95% confidence interval [CI], 0.12-1.1) and those who started out on placebo and converted to active drug during the open-label period (HR, 0.24; 95% CI, 0.064-0.88).
The study was funded by Clene and FightMND. Dr. Kiernan and Dr. Johnson have no relevant financial disclosures.
SEATTLE – , which was the change in the summated motor unit index (MUNIX) from baseline to week 36.
The drug, CNM-Au8, is being developed by Clene, and would represent a novel mechanism of action. “This is a brand-new approach. We used it complementary with riluzole and it was well tolerated, so I see this as an add-on therapy. I think if we can show some more positivity and longer-term results, it’s going to be a game changer for ALS,” Matthew Kiernan, MBBS, PhD, said in an interview. Dr. Kiernan presented the results at the 2022 annual meeting of the American Academy of Neurology.
Riluzole (Rilutek), which received Food and Drug Administration approval in 1995, inhibits glutamate release to counter excitotoxicity, which is believed to play a role in ALS, Huntington’s disease, ischemia, and other acute and chronic neurodegenerative diseases. The other FDA-approved agent for ALS is the neuroprotective agent and free-radical scavenger edaravone (Radicava), approved in 2017.
CNM-Au8 is made up of catalytically active gold nanocrystals that cross the blood-brain barrier, but lacks the toxicity associated with other synthetic gold compounds, according to the company. The formulation is also being investigated for the treatment of Parkinson’s disease and multiple sclerosis. Basic research has shown that it stabilizes mitochondria and reduces accumulation of the TDP-43 protein, which is linked to spread of ALS through the brain, Dr. Kiernan said during his presentation.
The treatment is well tolerated. “Normally in an ALS trial, we see about a 25% dropout rate. There were no dropouts on the active compound in the clinical trial. There are less deaths, so improved survival,” said Dr. Kiernan, the Bushell chair of neurology at the University of Sydney and codirector of the Brain and Mind Center in Sydney.
Good safety signal
The fact that the trial missed its primary endpoint isn’t too concerning, according to Nicholas Johnson, MD, who comoderated the session where the study was presented. “ALS clinical trials are incredibly difficult to conduct, especially a phase 2 learning-phase clinical trial. At this phase, I’m much more buoyed by the fact that they have a good safety signal, and that they’re willing to move forward to that phase 3 clinical trial,” Dr. Johnson said in an interview. He is vice chair of research at Virginia Commonwealth University, Richmond.
A phase 3 clinical trial is in development in the United States and Europe. The drug also is included as part of the HEALEY ALS Platform Trial, which is testing multiple ALS therapies simultaneously. “The results from that should be available by the second half of this year and it will also inform us as to what the approach should be,” said Dr. Kiernan.
Dr. Johnson also was enthusiastic. “I’m excited to see the results in terms of the primary endpoints for that next phase 3 clinical trial,” he said.
Ongoing research
In September 2021, Clene announced a second expanded access program for people with ALS.
The study included a 36-week double-blind treatment period followed by long-term, open-label follow-up. Twenty-three patients received 30 mg CNM-Au8, and 22 received placebo. In the first 36 weeks, the treatment group was more likely to have no disease progression, defined as death, tracheostomy, noninvasive ventilation, or a gastronomy tube (P = .0125). The researchers compared the probability of experiencing a less than 6-point decline in the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale. At 12 weeks, it was about 85% in both groups. At 24 weeks, it was about 60% to 50% in favor of the CNM-Au8 group, and at 36 weeks it was about 50% to 20% (P = .0350).
At 36 weeks, quality of life as measured by the ALS Specific Quality of Life–Short Form was better in the treatment group at 36 weeks (mean change, 0.9; P = .0177).
Survival was better in the treatment group at 96 weeks than the mortality derived from a European Network for the Cure of ALS prediction model (hazard ratio [HR], 0.2974; P = .0068). This benefit also was experienced by patients who received drug throughout the study (HR, 0.36; 95% confidence interval [CI], 0.12-1.1) and those who started out on placebo and converted to active drug during the open-label period (HR, 0.24; 95% CI, 0.064-0.88).
The study was funded by Clene and FightMND. Dr. Kiernan and Dr. Johnson have no relevant financial disclosures.
AT AAN 2022
Extraction of infected implanted cardiac devices rare, despite guidelines
The rates of infection involving cardiac implanted electronic devices (CIEDs), like pacemakers and cardioverter defibrillators (ICDs), are substantial, but only a minority of patients in the United States receive the guideline-directed recommendation of device removal, according to data from a Medicare population.
The study was conducted on the hypothesis that adherence to guidelines were low, “but we were surprised by how low the extraction rates turned out to be,” Sean D. Pokorney, MD, an electrophysiologist at the Duke Clinical Research Institute, Durham, N.C., reported at the annual scientific sessions of the American College of Cardiology.
The major U.S. and European guidelines are uniform in recommending complete extraction for a CIED infection. The American Heart Association and the Heart Rhythm Society and two out of the three other guidelines cited by Dr. Pokorney not only recommend extraction but specify prompt extraction.
Neither complete extraction nor prompt extraction are typical.
Of the 11,619 CIED infection cases identified in the Medicare database, 18.2% underwent extraction within 30 days of diagnosis. Only 13% were extracted within 6 days.
Lack of extraction may cause avoidable mortality
The result is likely to be avoidable mortality. Among those with extraction within 30 days, 80% were still alive 1 year later. Survival at 1 year fell to 67.6% in those without an extraction within this time frame.
This translated to a 22% lower rate of death at 1 year (hazard ratio, 0.78; P = .008) in those who underwent extraction within 30 days.
For those in whom the device was extracted within 7 days, the associated HR for death at 1 year was more than 40% lower (HR, 0.59; P < .001), reported Dr. Pokorney, who characterized these reductions as occurring in “a dose-response fashion.”
The very high risk of relapse despite antibiotics is the reason that “there is a class 1 indication for complete hardware removal,” Dr. Pokorney. He cited five studies that addressed this question. With partial device removal or medical therapy alone, relapse was consistently 50% or greater. In one study, it was 67%. In another it was 100%.
With complete removal, the rate of infection relapse was 1% or lower in four. In the fifth, the rate was 4.2%.
Infections can occur early or late after implantation, but cases accumulate over time. In the Medicare data sample, infection rates climbed from 0.3% at 1 year to 0.6% at 2 years and then to 1.1% at 3 years, Dr. Pokorney reported.
Other studies have also shown a steady increase in the proportion of implanted devices associated with infection over time. In a cohort study conducted in Olmstead County, Minnesota, the cumulative probability of a CIED infection reached 6.2% after 15 years and 11.7% after 25 years. While about half of these were infections localized to the device pocket, the others were potentially life-threatening systemic infections, according to Dr. Pokorney, who cited this study.
In his analysis of the Medicare data, all fee-for-service patients receiving a first CIED implant over a period of 14 years were included. The 14-year period ended just before the COVID-19 epidemic.
The more than 11,000 CIED infections were identified in 1,065,549 total CIED patients. Most (72%) had received a pacemaker. Of the others , more than half received an ICD and the others received a cardiac resynchronization device. The median age was 78 years.
Female and Black patients even less likely to undergo extraction
About half (49.1%) of the overall study population was female, but females represented only about 40% of those who developed an infection. Blacks represented just under 8% of the population but nearly 16% of the CIED infections. Both females and Blacks were significantly less likely than the overall study population to undergo extraction for their infection (P < .001 for both).
Perhaps predictably, patients with comorbidities were more likely to develop CIED infections. For example, 87% of those with infection, versus only 64.9% of the overall population, were in heart failure at the time of implantation. Diabetes (68.3% vs. 49.3%), ischemic heart disease (91.9% vs. 79.4%), renal disease (70.5% vs. 37.9%), and chronic obstructive pulmonary disease (70.6% vs. 55.0%) were also more common at baseline in those who went on to a CIED infection than in the overall population.
Based on the evidence that there is a large unmet need to improve adherence to the guidelines, Dr. Pokorney called for care pathways and other quality initiatives to address the problem.
The reasons that so many patients are not undergoing prompt device extraction at the time of infection is unclear, but Dr. Pokorney offered some hypotheses.
“There appears to be a false belief in the efficacy of antibiotics for treating CIED infections,” Dr. Pokorney said.
Comorbidities shouldn’t delay extraction
It is also possible that clinicians are concerned about performing extractions in patients with multiple comorbidities. If clinicians are delaying extractions for this reason, Dr. Pokorney suggested this behavior is misdirected given the fact that delays appear to increase mortality risk.
Several experts, including Rachel Lambert, MD, an electrophysiologist and professor of medicine at Yale University, New Haven, Conn., agreed that these data deserve a response.
“I was not surprised by the mortality data, but I was surprised at this low extraction rate,” said Dr. Lambert, who concurs with the guidelines. She indicated this study provides teeth to prompt action.
“It is great to have these data about the increased mortality risk to back up the guidelines,” she said.
More information is needed to understand exactly why CIED infection is not now leading to guideline-directed care. Dr. Pokorney said: “Where do we go from here is a key question.”
While several different types of initiatives might be needed, Dr. Pokorney called for regionalization of care to address the fact that not every center that places CIEDs has the capability to perform extractions.
“Extraction is not available at every center, and it probably should not be available at every center, so mechanisms are need to get patients with infection to the specialized centers that provide care,” he said.
Dr. Pokorney has financial relationships with Boston Scientific, Bristol-Myers Squibb, Gilead, Janssen, Medtronic, Pfizer, and Philips. Dr. Lambert reported financial relationships with Abbott, Amgen, and Medtronic.
The rates of infection involving cardiac implanted electronic devices (CIEDs), like pacemakers and cardioverter defibrillators (ICDs), are substantial, but only a minority of patients in the United States receive the guideline-directed recommendation of device removal, according to data from a Medicare population.
The study was conducted on the hypothesis that adherence to guidelines were low, “but we were surprised by how low the extraction rates turned out to be,” Sean D. Pokorney, MD, an electrophysiologist at the Duke Clinical Research Institute, Durham, N.C., reported at the annual scientific sessions of the American College of Cardiology.
The major U.S. and European guidelines are uniform in recommending complete extraction for a CIED infection. The American Heart Association and the Heart Rhythm Society and two out of the three other guidelines cited by Dr. Pokorney not only recommend extraction but specify prompt extraction.
Neither complete extraction nor prompt extraction are typical.
Of the 11,619 CIED infection cases identified in the Medicare database, 18.2% underwent extraction within 30 days of diagnosis. Only 13% were extracted within 6 days.
Lack of extraction may cause avoidable mortality
The result is likely to be avoidable mortality. Among those with extraction within 30 days, 80% were still alive 1 year later. Survival at 1 year fell to 67.6% in those without an extraction within this time frame.
This translated to a 22% lower rate of death at 1 year (hazard ratio, 0.78; P = .008) in those who underwent extraction within 30 days.
For those in whom the device was extracted within 7 days, the associated HR for death at 1 year was more than 40% lower (HR, 0.59; P < .001), reported Dr. Pokorney, who characterized these reductions as occurring in “a dose-response fashion.”
The very high risk of relapse despite antibiotics is the reason that “there is a class 1 indication for complete hardware removal,” Dr. Pokorney. He cited five studies that addressed this question. With partial device removal or medical therapy alone, relapse was consistently 50% or greater. In one study, it was 67%. In another it was 100%.
With complete removal, the rate of infection relapse was 1% or lower in four. In the fifth, the rate was 4.2%.
Infections can occur early or late after implantation, but cases accumulate over time. In the Medicare data sample, infection rates climbed from 0.3% at 1 year to 0.6% at 2 years and then to 1.1% at 3 years, Dr. Pokorney reported.
Other studies have also shown a steady increase in the proportion of implanted devices associated with infection over time. In a cohort study conducted in Olmstead County, Minnesota, the cumulative probability of a CIED infection reached 6.2% after 15 years and 11.7% after 25 years. While about half of these were infections localized to the device pocket, the others were potentially life-threatening systemic infections, according to Dr. Pokorney, who cited this study.
In his analysis of the Medicare data, all fee-for-service patients receiving a first CIED implant over a period of 14 years were included. The 14-year period ended just before the COVID-19 epidemic.
The more than 11,000 CIED infections were identified in 1,065,549 total CIED patients. Most (72%) had received a pacemaker. Of the others , more than half received an ICD and the others received a cardiac resynchronization device. The median age was 78 years.
Female and Black patients even less likely to undergo extraction
About half (49.1%) of the overall study population was female, but females represented only about 40% of those who developed an infection. Blacks represented just under 8% of the population but nearly 16% of the CIED infections. Both females and Blacks were significantly less likely than the overall study population to undergo extraction for their infection (P < .001 for both).
Perhaps predictably, patients with comorbidities were more likely to develop CIED infections. For example, 87% of those with infection, versus only 64.9% of the overall population, were in heart failure at the time of implantation. Diabetes (68.3% vs. 49.3%), ischemic heart disease (91.9% vs. 79.4%), renal disease (70.5% vs. 37.9%), and chronic obstructive pulmonary disease (70.6% vs. 55.0%) were also more common at baseline in those who went on to a CIED infection than in the overall population.
Based on the evidence that there is a large unmet need to improve adherence to the guidelines, Dr. Pokorney called for care pathways and other quality initiatives to address the problem.
The reasons that so many patients are not undergoing prompt device extraction at the time of infection is unclear, but Dr. Pokorney offered some hypotheses.
“There appears to be a false belief in the efficacy of antibiotics for treating CIED infections,” Dr. Pokorney said.
Comorbidities shouldn’t delay extraction
It is also possible that clinicians are concerned about performing extractions in patients with multiple comorbidities. If clinicians are delaying extractions for this reason, Dr. Pokorney suggested this behavior is misdirected given the fact that delays appear to increase mortality risk.
Several experts, including Rachel Lambert, MD, an electrophysiologist and professor of medicine at Yale University, New Haven, Conn., agreed that these data deserve a response.
“I was not surprised by the mortality data, but I was surprised at this low extraction rate,” said Dr. Lambert, who concurs with the guidelines. She indicated this study provides teeth to prompt action.
“It is great to have these data about the increased mortality risk to back up the guidelines,” she said.
More information is needed to understand exactly why CIED infection is not now leading to guideline-directed care. Dr. Pokorney said: “Where do we go from here is a key question.”
While several different types of initiatives might be needed, Dr. Pokorney called for regionalization of care to address the fact that not every center that places CIEDs has the capability to perform extractions.
“Extraction is not available at every center, and it probably should not be available at every center, so mechanisms are need to get patients with infection to the specialized centers that provide care,” he said.
Dr. Pokorney has financial relationships with Boston Scientific, Bristol-Myers Squibb, Gilead, Janssen, Medtronic, Pfizer, and Philips. Dr. Lambert reported financial relationships with Abbott, Amgen, and Medtronic.
The rates of infection involving cardiac implanted electronic devices (CIEDs), like pacemakers and cardioverter defibrillators (ICDs), are substantial, but only a minority of patients in the United States receive the guideline-directed recommendation of device removal, according to data from a Medicare population.
The study was conducted on the hypothesis that adherence to guidelines were low, “but we were surprised by how low the extraction rates turned out to be,” Sean D. Pokorney, MD, an electrophysiologist at the Duke Clinical Research Institute, Durham, N.C., reported at the annual scientific sessions of the American College of Cardiology.
The major U.S. and European guidelines are uniform in recommending complete extraction for a CIED infection. The American Heart Association and the Heart Rhythm Society and two out of the three other guidelines cited by Dr. Pokorney not only recommend extraction but specify prompt extraction.
Neither complete extraction nor prompt extraction are typical.
Of the 11,619 CIED infection cases identified in the Medicare database, 18.2% underwent extraction within 30 days of diagnosis. Only 13% were extracted within 6 days.
Lack of extraction may cause avoidable mortality
The result is likely to be avoidable mortality. Among those with extraction within 30 days, 80% were still alive 1 year later. Survival at 1 year fell to 67.6% in those without an extraction within this time frame.
This translated to a 22% lower rate of death at 1 year (hazard ratio, 0.78; P = .008) in those who underwent extraction within 30 days.
For those in whom the device was extracted within 7 days, the associated HR for death at 1 year was more than 40% lower (HR, 0.59; P < .001), reported Dr. Pokorney, who characterized these reductions as occurring in “a dose-response fashion.”
The very high risk of relapse despite antibiotics is the reason that “there is a class 1 indication for complete hardware removal,” Dr. Pokorney. He cited five studies that addressed this question. With partial device removal or medical therapy alone, relapse was consistently 50% or greater. In one study, it was 67%. In another it was 100%.
With complete removal, the rate of infection relapse was 1% or lower in four. In the fifth, the rate was 4.2%.
Infections can occur early or late after implantation, but cases accumulate over time. In the Medicare data sample, infection rates climbed from 0.3% at 1 year to 0.6% at 2 years and then to 1.1% at 3 years, Dr. Pokorney reported.
Other studies have also shown a steady increase in the proportion of implanted devices associated with infection over time. In a cohort study conducted in Olmstead County, Minnesota, the cumulative probability of a CIED infection reached 6.2% after 15 years and 11.7% after 25 years. While about half of these were infections localized to the device pocket, the others were potentially life-threatening systemic infections, according to Dr. Pokorney, who cited this study.
In his analysis of the Medicare data, all fee-for-service patients receiving a first CIED implant over a period of 14 years were included. The 14-year period ended just before the COVID-19 epidemic.
The more than 11,000 CIED infections were identified in 1,065,549 total CIED patients. Most (72%) had received a pacemaker. Of the others , more than half received an ICD and the others received a cardiac resynchronization device. The median age was 78 years.
Female and Black patients even less likely to undergo extraction
About half (49.1%) of the overall study population was female, but females represented only about 40% of those who developed an infection. Blacks represented just under 8% of the population but nearly 16% of the CIED infections. Both females and Blacks were significantly less likely than the overall study population to undergo extraction for their infection (P < .001 for both).
Perhaps predictably, patients with comorbidities were more likely to develop CIED infections. For example, 87% of those with infection, versus only 64.9% of the overall population, were in heart failure at the time of implantation. Diabetes (68.3% vs. 49.3%), ischemic heart disease (91.9% vs. 79.4%), renal disease (70.5% vs. 37.9%), and chronic obstructive pulmonary disease (70.6% vs. 55.0%) were also more common at baseline in those who went on to a CIED infection than in the overall population.
Based on the evidence that there is a large unmet need to improve adherence to the guidelines, Dr. Pokorney called for care pathways and other quality initiatives to address the problem.
The reasons that so many patients are not undergoing prompt device extraction at the time of infection is unclear, but Dr. Pokorney offered some hypotheses.
“There appears to be a false belief in the efficacy of antibiotics for treating CIED infections,” Dr. Pokorney said.
Comorbidities shouldn’t delay extraction
It is also possible that clinicians are concerned about performing extractions in patients with multiple comorbidities. If clinicians are delaying extractions for this reason, Dr. Pokorney suggested this behavior is misdirected given the fact that delays appear to increase mortality risk.
Several experts, including Rachel Lambert, MD, an electrophysiologist and professor of medicine at Yale University, New Haven, Conn., agreed that these data deserve a response.
“I was not surprised by the mortality data, but I was surprised at this low extraction rate,” said Dr. Lambert, who concurs with the guidelines. She indicated this study provides teeth to prompt action.
“It is great to have these data about the increased mortality risk to back up the guidelines,” she said.
More information is needed to understand exactly why CIED infection is not now leading to guideline-directed care. Dr. Pokorney said: “Where do we go from here is a key question.”
While several different types of initiatives might be needed, Dr. Pokorney called for regionalization of care to address the fact that not every center that places CIEDs has the capability to perform extractions.
“Extraction is not available at every center, and it probably should not be available at every center, so mechanisms are need to get patients with infection to the specialized centers that provide care,” he said.
Dr. Pokorney has financial relationships with Boston Scientific, Bristol-Myers Squibb, Gilead, Janssen, Medtronic, Pfizer, and Philips. Dr. Lambert reported financial relationships with Abbott, Amgen, and Medtronic.
FROM ACC 2022
Physical fitness tied to lower risk of Alzheimer’s disease
, new findings suggest. “One exciting finding of this study is that as people’s fitness improved, their risk of Alzheimer’s disease decreased – it was not an all-or-nothing proposition,” study investigator Edward Zamrini, MD, of the Washington DC VA Medical Center, said in a news release.
The findings suggest that people can work toward making incremental changes and improvements in their physical fitness, which may help decrease their risk of dementia, Dr. Zamrini added.
The findings were presented at the 2022 annual meeting of the American Academy of Neurology.
Effective prevention strategy
Using the Veterans Health Administration database, Dr. Zamrini and colleagues identified 649,605 veterans (mean age, 61 years) free of Alzheimer’s disease and related disorders (ADRD) when they completed standardized exercise treadmill tests between 2000 and 2017.
They divided participants into five age-specific fitness groups, from least fit to most fit, based on peak metabolic equivalents (METs) achieved during the treadmill test: lowest-fit (METs, ±3.8), low-fit (METs, ±5.8), moderate-fit (METs, ±7.5), fit (METs, ±9.2), and highest-fit (METs, ±11.7).
In unadjusted analysis, veterans with the lowest cardiorespiratory fitness developed ADRD at a rate of 9.5 cases per 1,000 person-years, compared with a rate of 6.4 cases per 1,000 person-years for the most fit group (P < .001).
After adjusting for factors that could affect risk of ADRD, compared with the lowest-fit group, the highest-fit and fit groups were 33% and 26% less likely to develop ADRD, respectively, while the moderate-fit and low-fit groups were 20% and 13% less likely to develop the disease, respectively.
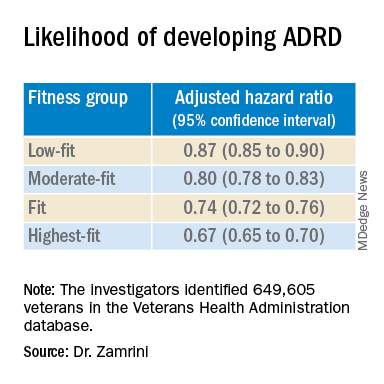
The findings suggest that the association between cardiorespiratory fitness and ADRD risk is “inverse, independent, and graded,” the researchers said in their conference abstract.
“The idea that you can reduce your risk for Alzheimer’s disease by simply increasing your activity is very promising, especially since there are no adequate treatments to prevent or stop the progression of the disease,” Dr. Zamrini added in the news release.
“We hope to develop a simple scale that can be individualized so people can see the benefits that even incremental improvements in fitness can deliver,” he said.
The next vital sign?
Commenting on the study, Shaheen E. Lakhan, MD, PhD, a neurologist in Boston, noted that “for decades and with increasing body of support from studies like this, we have known that preventing dementia is based on healthy behaviors for the brain including a proper diet (NASH and/or Mediterranean), exercise regimen (aerobic/cardio more than anaerobic/weight-lifting), sleep hygiene, and social and intellectual engagements.”
“Frankly, what’s good for the body is good for the brain,” said Dr. Lakhan.
“It should be noted that the measure studied here is cardiorespiratory fitness, which has been associated with heart disease and resulting death, death from any cause, and now brain health,” Dr. Lakhan said.
“This powerful predictor may in fact be the next vital sign, after your heart rate and blood pressure, from which your primary care provider can make a personalized treatment plan,” he added.
“Accelerating this process, the ability to measure cardiorespiratory fitness traditionally from huge stationary machines down to wearables like a watch or ring, or even your iPhone or Android, is just on the horizon,” Dr. Lakhan said.
“Instead of tracking just your weight, shape, and BMI, personal fitness may be tailored to optimizing this indicator and further empowering individuals to take charge of their health,” he said.
The study was supported by the National Institute on Aging, the National Institutes of Health, the U.S. Department of Veterans Affairs, the Washington DC VA Medical Center, and George Washington University. Dr. Zamrini and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new findings suggest. “One exciting finding of this study is that as people’s fitness improved, their risk of Alzheimer’s disease decreased – it was not an all-or-nothing proposition,” study investigator Edward Zamrini, MD, of the Washington DC VA Medical Center, said in a news release.
The findings suggest that people can work toward making incremental changes and improvements in their physical fitness, which may help decrease their risk of dementia, Dr. Zamrini added.
The findings were presented at the 2022 annual meeting of the American Academy of Neurology.
Effective prevention strategy
Using the Veterans Health Administration database, Dr. Zamrini and colleagues identified 649,605 veterans (mean age, 61 years) free of Alzheimer’s disease and related disorders (ADRD) when they completed standardized exercise treadmill tests between 2000 and 2017.
They divided participants into five age-specific fitness groups, from least fit to most fit, based on peak metabolic equivalents (METs) achieved during the treadmill test: lowest-fit (METs, ±3.8), low-fit (METs, ±5.8), moderate-fit (METs, ±7.5), fit (METs, ±9.2), and highest-fit (METs, ±11.7).
In unadjusted analysis, veterans with the lowest cardiorespiratory fitness developed ADRD at a rate of 9.5 cases per 1,000 person-years, compared with a rate of 6.4 cases per 1,000 person-years for the most fit group (P < .001).
After adjusting for factors that could affect risk of ADRD, compared with the lowest-fit group, the highest-fit and fit groups were 33% and 26% less likely to develop ADRD, respectively, while the moderate-fit and low-fit groups were 20% and 13% less likely to develop the disease, respectively.
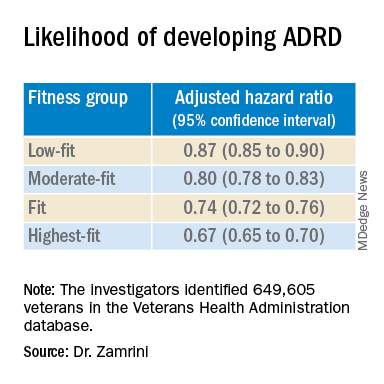
The findings suggest that the association between cardiorespiratory fitness and ADRD risk is “inverse, independent, and graded,” the researchers said in their conference abstract.
“The idea that you can reduce your risk for Alzheimer’s disease by simply increasing your activity is very promising, especially since there are no adequate treatments to prevent or stop the progression of the disease,” Dr. Zamrini added in the news release.
“We hope to develop a simple scale that can be individualized so people can see the benefits that even incremental improvements in fitness can deliver,” he said.
The next vital sign?
Commenting on the study, Shaheen E. Lakhan, MD, PhD, a neurologist in Boston, noted that “for decades and with increasing body of support from studies like this, we have known that preventing dementia is based on healthy behaviors for the brain including a proper diet (NASH and/or Mediterranean), exercise regimen (aerobic/cardio more than anaerobic/weight-lifting), sleep hygiene, and social and intellectual engagements.”
“Frankly, what’s good for the body is good for the brain,” said Dr. Lakhan.
“It should be noted that the measure studied here is cardiorespiratory fitness, which has been associated with heart disease and resulting death, death from any cause, and now brain health,” Dr. Lakhan said.
“This powerful predictor may in fact be the next vital sign, after your heart rate and blood pressure, from which your primary care provider can make a personalized treatment plan,” he added.
“Accelerating this process, the ability to measure cardiorespiratory fitness traditionally from huge stationary machines down to wearables like a watch or ring, or even your iPhone or Android, is just on the horizon,” Dr. Lakhan said.
“Instead of tracking just your weight, shape, and BMI, personal fitness may be tailored to optimizing this indicator and further empowering individuals to take charge of their health,” he said.
The study was supported by the National Institute on Aging, the National Institutes of Health, the U.S. Department of Veterans Affairs, the Washington DC VA Medical Center, and George Washington University. Dr. Zamrini and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new findings suggest. “One exciting finding of this study is that as people’s fitness improved, their risk of Alzheimer’s disease decreased – it was not an all-or-nothing proposition,” study investigator Edward Zamrini, MD, of the Washington DC VA Medical Center, said in a news release.
The findings suggest that people can work toward making incremental changes and improvements in their physical fitness, which may help decrease their risk of dementia, Dr. Zamrini added.
The findings were presented at the 2022 annual meeting of the American Academy of Neurology.
Effective prevention strategy
Using the Veterans Health Administration database, Dr. Zamrini and colleagues identified 649,605 veterans (mean age, 61 years) free of Alzheimer’s disease and related disorders (ADRD) when they completed standardized exercise treadmill tests between 2000 and 2017.
They divided participants into five age-specific fitness groups, from least fit to most fit, based on peak metabolic equivalents (METs) achieved during the treadmill test: lowest-fit (METs, ±3.8), low-fit (METs, ±5.8), moderate-fit (METs, ±7.5), fit (METs, ±9.2), and highest-fit (METs, ±11.7).
In unadjusted analysis, veterans with the lowest cardiorespiratory fitness developed ADRD at a rate of 9.5 cases per 1,000 person-years, compared with a rate of 6.4 cases per 1,000 person-years for the most fit group (P < .001).
After adjusting for factors that could affect risk of ADRD, compared with the lowest-fit group, the highest-fit and fit groups were 33% and 26% less likely to develop ADRD, respectively, while the moderate-fit and low-fit groups were 20% and 13% less likely to develop the disease, respectively.
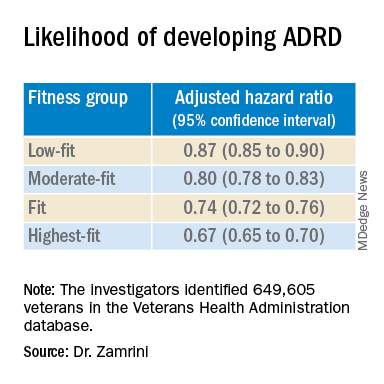
The findings suggest that the association between cardiorespiratory fitness and ADRD risk is “inverse, independent, and graded,” the researchers said in their conference abstract.
“The idea that you can reduce your risk for Alzheimer’s disease by simply increasing your activity is very promising, especially since there are no adequate treatments to prevent or stop the progression of the disease,” Dr. Zamrini added in the news release.
“We hope to develop a simple scale that can be individualized so people can see the benefits that even incremental improvements in fitness can deliver,” he said.
The next vital sign?
Commenting on the study, Shaheen E. Lakhan, MD, PhD, a neurologist in Boston, noted that “for decades and with increasing body of support from studies like this, we have known that preventing dementia is based on healthy behaviors for the brain including a proper diet (NASH and/or Mediterranean), exercise regimen (aerobic/cardio more than anaerobic/weight-lifting), sleep hygiene, and social and intellectual engagements.”
“Frankly, what’s good for the body is good for the brain,” said Dr. Lakhan.
“It should be noted that the measure studied here is cardiorespiratory fitness, which has been associated with heart disease and resulting death, death from any cause, and now brain health,” Dr. Lakhan said.
“This powerful predictor may in fact be the next vital sign, after your heart rate and blood pressure, from which your primary care provider can make a personalized treatment plan,” he added.
“Accelerating this process, the ability to measure cardiorespiratory fitness traditionally from huge stationary machines down to wearables like a watch or ring, or even your iPhone or Android, is just on the horizon,” Dr. Lakhan said.
“Instead of tracking just your weight, shape, and BMI, personal fitness may be tailored to optimizing this indicator and further empowering individuals to take charge of their health,” he said.
The study was supported by the National Institute on Aging, the National Institutes of Health, the U.S. Department of Veterans Affairs, the Washington DC VA Medical Center, and George Washington University. Dr. Zamrini and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAN 2022











