User login
EMA recommends PreHevbri hepatitis B vaccine for approval
The European Medicines Agency’s (EMA’s) human medicines committee has recommended approval of a hepatitis B vaccine for adults.
The agency’s Committee for Medicinal Products for Human Use (CHMP) granted a positive opinion for PreHevbri on Feb. 24 for active immunization against hepatitis B virus (HBV) infection. PreHevbri (PreHevBrio in the United States and Sci-B-Vac in Israel) received approval from the Food and Drug Administration on Nov. 30, 2021. The vaccine is produced by VBI Vaccines (Delaware) Inc., based in Cambridge, Mass.
The World Health Organization estimates that more than 290 million people globally are infected with HBV. HBV is the leading cause of liver disease, and an estimated 900,000 people die every year from complications from chronic HBV infection, according to a VBI Vaccine press release. A 2019 report from the European Centre for Disease Prevention and Control found that adults in the European Union aged 35-44 had the highest rates of acute infections with HBV, and people aged 25-34 had the highest rate of chronic HBV infections. Vaccination programs are key interventions in preventing transmission of the virus, the report noted.
PreHevbri is a hepatitis B vaccine composed of three surface antigens of the hepatitis B virus. The vaccine is administered via injection in three doses on a 0-, 1-, and 6-month schedule and is indicated for use in adults aged 18 years and older.
The CHMP recommendation was based on data from a safety and immunogenicity study, which included 1,607 participants aged 18 and older, and a lot-to-lot study, which included 2,838 adults aged 18-45, according the VBI vaccine press release.
The recommendation will now be reviewed by the European Commission. If approved, PreHevbri will be the only three-antigen HBV vaccine for adults approved in the European Union.
A version of this article first appeared on Medscape.com.
The European Medicines Agency’s (EMA’s) human medicines committee has recommended approval of a hepatitis B vaccine for adults.
The agency’s Committee for Medicinal Products for Human Use (CHMP) granted a positive opinion for PreHevbri on Feb. 24 for active immunization against hepatitis B virus (HBV) infection. PreHevbri (PreHevBrio in the United States and Sci-B-Vac in Israel) received approval from the Food and Drug Administration on Nov. 30, 2021. The vaccine is produced by VBI Vaccines (Delaware) Inc., based in Cambridge, Mass.
The World Health Organization estimates that more than 290 million people globally are infected with HBV. HBV is the leading cause of liver disease, and an estimated 900,000 people die every year from complications from chronic HBV infection, according to a VBI Vaccine press release. A 2019 report from the European Centre for Disease Prevention and Control found that adults in the European Union aged 35-44 had the highest rates of acute infections with HBV, and people aged 25-34 had the highest rate of chronic HBV infections. Vaccination programs are key interventions in preventing transmission of the virus, the report noted.
PreHevbri is a hepatitis B vaccine composed of three surface antigens of the hepatitis B virus. The vaccine is administered via injection in three doses on a 0-, 1-, and 6-month schedule and is indicated for use in adults aged 18 years and older.
The CHMP recommendation was based on data from a safety and immunogenicity study, which included 1,607 participants aged 18 and older, and a lot-to-lot study, which included 2,838 adults aged 18-45, according the VBI vaccine press release.
The recommendation will now be reviewed by the European Commission. If approved, PreHevbri will be the only three-antigen HBV vaccine for adults approved in the European Union.
A version of this article first appeared on Medscape.com.
The European Medicines Agency’s (EMA’s) human medicines committee has recommended approval of a hepatitis B vaccine for adults.
The agency’s Committee for Medicinal Products for Human Use (CHMP) granted a positive opinion for PreHevbri on Feb. 24 for active immunization against hepatitis B virus (HBV) infection. PreHevbri (PreHevBrio in the United States and Sci-B-Vac in Israel) received approval from the Food and Drug Administration on Nov. 30, 2021. The vaccine is produced by VBI Vaccines (Delaware) Inc., based in Cambridge, Mass.
The World Health Organization estimates that more than 290 million people globally are infected with HBV. HBV is the leading cause of liver disease, and an estimated 900,000 people die every year from complications from chronic HBV infection, according to a VBI Vaccine press release. A 2019 report from the European Centre for Disease Prevention and Control found that adults in the European Union aged 35-44 had the highest rates of acute infections with HBV, and people aged 25-34 had the highest rate of chronic HBV infections. Vaccination programs are key interventions in preventing transmission of the virus, the report noted.
PreHevbri is a hepatitis B vaccine composed of three surface antigens of the hepatitis B virus. The vaccine is administered via injection in three doses on a 0-, 1-, and 6-month schedule and is indicated for use in adults aged 18 years and older.
The CHMP recommendation was based on data from a safety and immunogenicity study, which included 1,607 participants aged 18 and older, and a lot-to-lot study, which included 2,838 adults aged 18-45, according the VBI vaccine press release.
The recommendation will now be reviewed by the European Commission. If approved, PreHevbri will be the only three-antigen HBV vaccine for adults approved in the European Union.
A version of this article first appeared on Medscape.com.
Evidence mounts for paramagnetic rim lesions in diagnosing MS
WEST PALM BEACH, FLA. – , new research suggests.
Results from two studies add to the mounting evidence underscoring the importance of the imaging features, researchers noted. “Our data suggest that the presence and number of iron rim lesions hold a prognostic value for long-term disability in MS, especially the presence of four or more rim lesions,” said Amjad I. AlTokhis, School of Medicine, University of Nottingham, United Kingdom, and Division of Clinical Neuroscience, Nottingham University Hospitals NHS Trust, who was the lead author of both studies.
Importantly, the effect of the rim lesions on disability was greater than that of established prognostic biomarkers of T2 white matter lesion count and volume, she noted.
“This could support the use of iron rim lesions as an imaging biomarker for disease severity and worse prognosis,” said Dr. AlTokhis. “These findings also support that iron rim lesions might be clinically useful not only diagnostically but also for disease progression and predicting future disability in MS,” she added.
The findings were presented at the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) Forum 2022.
Sign of aggressive disease?
Dozens of studies have linked rim lesions, which are also known as iron rim lesions because of their composition of iron-laden macrophages/microglia, to more severe disease course in MS, as well as to having potential as an important imaging biomarker for diagnosis. However, studies have often been limited to smaller longitudinal cohorts.
In the first study, Dr. AlTokhis and colleagues enrolled 91 patients with MS (56 women) between 2008 and 2013 for whom 7 Tesla (7T) MRI was available with SWI-filtered phase sequencing.
At baseline, among 42 patients with clinically isolated syndrome, 50% had one or more of the rim lesions. The corresponding rates were 38% among 34 patients with relapsing-remitting MS, 38% among 18 patients with primary-progressive MS, and as high as 71% among 17 patients with secondary-progressive MS (P < .05 vs. primary progressive MS and clinically isolated syndrome).
At a median follow-up of 9 years, 18 of the patients with clinically isolated syndrome and relapsing-remitting MS progressed to secondary progressive MS; and among them, 56% had at least one rim lesion.
Of 24 who did not progress to secondary progressive MS, only 33% had at least one rim lesion.
The median baseline level of disease severity in the entire cohort, as measured by Age-Related Multiple Sclerosis Score (ARMSS), was 5.4. However, the median score among patients with rim lesions was higher, compared with those without the lesions (ARMSS, 6.7 vs. 5.0).
After the median 9-year follow-up, disease severity remained higher among those with versus those without the lesions (ARMSS, 7.3 vs. 6.3).
Patients with rim lesions had more white matter lesions overall; and a further analysis surprisingly showed that the number of rim lesions was indeed associated with long-term disability (P = .005).
“Detecting four or more iron rim lesions could be a sign of more aggressive disease and disability – thus, possibly useful in earlier treatment and a potential target for therapies,” Dr. AlTokhis said.
“Also, for clinical practicality, [the number of] iron rim lesions had the most direct effect on disability compared to white matter lesion count and volume, supporting its role as an independent prognostic imaging biomarker,” she added.
Dr. AlTokhis noted that “detecting and counting rim lesions is much easier than assessing all white matter lesions, adding to the clinical utility of this sign.”
Diagnostic value
The second study, presented at the meeting by coinvestigator Brian Renner, MD, Department of Neurology at Cedars Sinai, Los Angeles, reported on the significance of the rim lesions in MS diagnosis. It included 95 patients who had presented for new evaluation on suspicion of MS at 10 centers in the North American Imaging in MS Cooperative (NAIMS).
Of these participants, 44 (46%) were positively diagnosed according to McDonald 2017 criteria (MC2017) for MS, while 37 (39%) were given an alternative diagnosis to MS. Fourteen were considered at risk for MS with diagnoses of clinically isolating syndrome or radiologically isolating syndrome.
Overall, among the 44 with an MS diagnosis, 34 had one or more rim lesions; among the 51 who did not meet an MS diagnosis, only six had one or more of the rim lesions. One or more rim lesions were further observed in three patients with radiologically isolating syndrome and one patient with clinically isolating syndrome.
Among those with one or more of the rim lesions, a diagnosis of MS with MC2017 MS criteria was identified with a high sensitivity of 80%, high specificity of 88%, accuracy of 84%, and an AUC of 81%.
“We’ve shown that paramagnetic rim lesions are highly specific for MS, and the sensitivity of rim lesions for MS is higher than previously reported, despite similar techniques in rating, processing, and evaluation – which was likely related to the nature of the cohort,” Dr. Renner said.
Promising data
During the NAIMS symposium, Christopher C. Hemond, MD, assistant professor or neurology at the University of Massachusetts Medical School, Worcester, noted to meeting attendees that the rim lesions were seen across the entire course of the MS disease spectrum, spanning from radiologically isolating syndrome to secondary progressive MS.
“We know paramagnetic rim lesions are visible at all disease stages. They are uniquely larger and more destructive than their rimless peers and are associated with stronger disease severity,” said Dr. Hemond, who was not involved with the research.
“There is promising data at this point suggesting that [the rim lesions] may represent a biomarker predictive of future disability accumulation,” he added.
Dr. Hemond noted that, unlike in Dr. Renner’s study, the bulk of previous studies have indicated that rim lesions “are associated with a high specificity but only modest sensitivity, in the mid-50% range, for the diagnosis of MS in comparison to some conditions that mimic MS.”
Commenting on the findings, Dr. Hemond noted the results from Dr. Renner’s ongoing study “are critical in building confidence in the translational use of this biomarker to assist in ruling in a diagnosis of MS,” while Dr. AlTokis’ study “adds to and is consistent with the growing literature of pathological associations of paramagnetic rim lesions in MS.”
Dr. Hemond added that the NAIMS cooperative plans to publish guidance in the area in the coming months.
“Although paramagnetic rim lesions have strong pathological associations in MS, it remains unclear if the presence of these lesions should change MS clinical management at the present time,” he said.
During the NAIMS session, Francesca Bagnato, MD, PhD, Vanderbilt University Medical Center, Nashville, Tenn., noted the growing importance of the role of rim lesions in clinical research. “It is clear that these paramagnetic rim lesions are going to be the new biomarker for the next generation of clinical trials,” she said.
Dr. Renner’s study received funding from the Race to Erase MS Foundation. Dr. AlTokhis, Dr. Renner, and Dr. Hemond have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
WEST PALM BEACH, FLA. – , new research suggests.
Results from two studies add to the mounting evidence underscoring the importance of the imaging features, researchers noted. “Our data suggest that the presence and number of iron rim lesions hold a prognostic value for long-term disability in MS, especially the presence of four or more rim lesions,” said Amjad I. AlTokhis, School of Medicine, University of Nottingham, United Kingdom, and Division of Clinical Neuroscience, Nottingham University Hospitals NHS Trust, who was the lead author of both studies.
Importantly, the effect of the rim lesions on disability was greater than that of established prognostic biomarkers of T2 white matter lesion count and volume, she noted.
“This could support the use of iron rim lesions as an imaging biomarker for disease severity and worse prognosis,” said Dr. AlTokhis. “These findings also support that iron rim lesions might be clinically useful not only diagnostically but also for disease progression and predicting future disability in MS,” she added.
The findings were presented at the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) Forum 2022.
Sign of aggressive disease?
Dozens of studies have linked rim lesions, which are also known as iron rim lesions because of their composition of iron-laden macrophages/microglia, to more severe disease course in MS, as well as to having potential as an important imaging biomarker for diagnosis. However, studies have often been limited to smaller longitudinal cohorts.
In the first study, Dr. AlTokhis and colleagues enrolled 91 patients with MS (56 women) between 2008 and 2013 for whom 7 Tesla (7T) MRI was available with SWI-filtered phase sequencing.
At baseline, among 42 patients with clinically isolated syndrome, 50% had one or more of the rim lesions. The corresponding rates were 38% among 34 patients with relapsing-remitting MS, 38% among 18 patients with primary-progressive MS, and as high as 71% among 17 patients with secondary-progressive MS (P < .05 vs. primary progressive MS and clinically isolated syndrome).
At a median follow-up of 9 years, 18 of the patients with clinically isolated syndrome and relapsing-remitting MS progressed to secondary progressive MS; and among them, 56% had at least one rim lesion.
Of 24 who did not progress to secondary progressive MS, only 33% had at least one rim lesion.
The median baseline level of disease severity in the entire cohort, as measured by Age-Related Multiple Sclerosis Score (ARMSS), was 5.4. However, the median score among patients with rim lesions was higher, compared with those without the lesions (ARMSS, 6.7 vs. 5.0).
After the median 9-year follow-up, disease severity remained higher among those with versus those without the lesions (ARMSS, 7.3 vs. 6.3).
Patients with rim lesions had more white matter lesions overall; and a further analysis surprisingly showed that the number of rim lesions was indeed associated with long-term disability (P = .005).
“Detecting four or more iron rim lesions could be a sign of more aggressive disease and disability – thus, possibly useful in earlier treatment and a potential target for therapies,” Dr. AlTokhis said.
“Also, for clinical practicality, [the number of] iron rim lesions had the most direct effect on disability compared to white matter lesion count and volume, supporting its role as an independent prognostic imaging biomarker,” she added.
Dr. AlTokhis noted that “detecting and counting rim lesions is much easier than assessing all white matter lesions, adding to the clinical utility of this sign.”
Diagnostic value
The second study, presented at the meeting by coinvestigator Brian Renner, MD, Department of Neurology at Cedars Sinai, Los Angeles, reported on the significance of the rim lesions in MS diagnosis. It included 95 patients who had presented for new evaluation on suspicion of MS at 10 centers in the North American Imaging in MS Cooperative (NAIMS).
Of these participants, 44 (46%) were positively diagnosed according to McDonald 2017 criteria (MC2017) for MS, while 37 (39%) were given an alternative diagnosis to MS. Fourteen were considered at risk for MS with diagnoses of clinically isolating syndrome or radiologically isolating syndrome.
Overall, among the 44 with an MS diagnosis, 34 had one or more rim lesions; among the 51 who did not meet an MS diagnosis, only six had one or more of the rim lesions. One or more rim lesions were further observed in three patients with radiologically isolating syndrome and one patient with clinically isolating syndrome.
Among those with one or more of the rim lesions, a diagnosis of MS with MC2017 MS criteria was identified with a high sensitivity of 80%, high specificity of 88%, accuracy of 84%, and an AUC of 81%.
“We’ve shown that paramagnetic rim lesions are highly specific for MS, and the sensitivity of rim lesions for MS is higher than previously reported, despite similar techniques in rating, processing, and evaluation – which was likely related to the nature of the cohort,” Dr. Renner said.
Promising data
During the NAIMS symposium, Christopher C. Hemond, MD, assistant professor or neurology at the University of Massachusetts Medical School, Worcester, noted to meeting attendees that the rim lesions were seen across the entire course of the MS disease spectrum, spanning from radiologically isolating syndrome to secondary progressive MS.
“We know paramagnetic rim lesions are visible at all disease stages. They are uniquely larger and more destructive than their rimless peers and are associated with stronger disease severity,” said Dr. Hemond, who was not involved with the research.
“There is promising data at this point suggesting that [the rim lesions] may represent a biomarker predictive of future disability accumulation,” he added.
Dr. Hemond noted that, unlike in Dr. Renner’s study, the bulk of previous studies have indicated that rim lesions “are associated with a high specificity but only modest sensitivity, in the mid-50% range, for the diagnosis of MS in comparison to some conditions that mimic MS.”
Commenting on the findings, Dr. Hemond noted the results from Dr. Renner’s ongoing study “are critical in building confidence in the translational use of this biomarker to assist in ruling in a diagnosis of MS,” while Dr. AlTokis’ study “adds to and is consistent with the growing literature of pathological associations of paramagnetic rim lesions in MS.”
Dr. Hemond added that the NAIMS cooperative plans to publish guidance in the area in the coming months.
“Although paramagnetic rim lesions have strong pathological associations in MS, it remains unclear if the presence of these lesions should change MS clinical management at the present time,” he said.
During the NAIMS session, Francesca Bagnato, MD, PhD, Vanderbilt University Medical Center, Nashville, Tenn., noted the growing importance of the role of rim lesions in clinical research. “It is clear that these paramagnetic rim lesions are going to be the new biomarker for the next generation of clinical trials,” she said.
Dr. Renner’s study received funding from the Race to Erase MS Foundation. Dr. AlTokhis, Dr. Renner, and Dr. Hemond have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
WEST PALM BEACH, FLA. – , new research suggests.
Results from two studies add to the mounting evidence underscoring the importance of the imaging features, researchers noted. “Our data suggest that the presence and number of iron rim lesions hold a prognostic value for long-term disability in MS, especially the presence of four or more rim lesions,” said Amjad I. AlTokhis, School of Medicine, University of Nottingham, United Kingdom, and Division of Clinical Neuroscience, Nottingham University Hospitals NHS Trust, who was the lead author of both studies.
Importantly, the effect of the rim lesions on disability was greater than that of established prognostic biomarkers of T2 white matter lesion count and volume, she noted.
“This could support the use of iron rim lesions as an imaging biomarker for disease severity and worse prognosis,” said Dr. AlTokhis. “These findings also support that iron rim lesions might be clinically useful not only diagnostically but also for disease progression and predicting future disability in MS,” she added.
The findings were presented at the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) Forum 2022.
Sign of aggressive disease?
Dozens of studies have linked rim lesions, which are also known as iron rim lesions because of their composition of iron-laden macrophages/microglia, to more severe disease course in MS, as well as to having potential as an important imaging biomarker for diagnosis. However, studies have often been limited to smaller longitudinal cohorts.
In the first study, Dr. AlTokhis and colleagues enrolled 91 patients with MS (56 women) between 2008 and 2013 for whom 7 Tesla (7T) MRI was available with SWI-filtered phase sequencing.
At baseline, among 42 patients with clinically isolated syndrome, 50% had one or more of the rim lesions. The corresponding rates were 38% among 34 patients with relapsing-remitting MS, 38% among 18 patients with primary-progressive MS, and as high as 71% among 17 patients with secondary-progressive MS (P < .05 vs. primary progressive MS and clinically isolated syndrome).
At a median follow-up of 9 years, 18 of the patients with clinically isolated syndrome and relapsing-remitting MS progressed to secondary progressive MS; and among them, 56% had at least one rim lesion.
Of 24 who did not progress to secondary progressive MS, only 33% had at least one rim lesion.
The median baseline level of disease severity in the entire cohort, as measured by Age-Related Multiple Sclerosis Score (ARMSS), was 5.4. However, the median score among patients with rim lesions was higher, compared with those without the lesions (ARMSS, 6.7 vs. 5.0).
After the median 9-year follow-up, disease severity remained higher among those with versus those without the lesions (ARMSS, 7.3 vs. 6.3).
Patients with rim lesions had more white matter lesions overall; and a further analysis surprisingly showed that the number of rim lesions was indeed associated with long-term disability (P = .005).
“Detecting four or more iron rim lesions could be a sign of more aggressive disease and disability – thus, possibly useful in earlier treatment and a potential target for therapies,” Dr. AlTokhis said.
“Also, for clinical practicality, [the number of] iron rim lesions had the most direct effect on disability compared to white matter lesion count and volume, supporting its role as an independent prognostic imaging biomarker,” she added.
Dr. AlTokhis noted that “detecting and counting rim lesions is much easier than assessing all white matter lesions, adding to the clinical utility of this sign.”
Diagnostic value
The second study, presented at the meeting by coinvestigator Brian Renner, MD, Department of Neurology at Cedars Sinai, Los Angeles, reported on the significance of the rim lesions in MS diagnosis. It included 95 patients who had presented for new evaluation on suspicion of MS at 10 centers in the North American Imaging in MS Cooperative (NAIMS).
Of these participants, 44 (46%) were positively diagnosed according to McDonald 2017 criteria (MC2017) for MS, while 37 (39%) were given an alternative diagnosis to MS. Fourteen were considered at risk for MS with diagnoses of clinically isolating syndrome or radiologically isolating syndrome.
Overall, among the 44 with an MS diagnosis, 34 had one or more rim lesions; among the 51 who did not meet an MS diagnosis, only six had one or more of the rim lesions. One or more rim lesions were further observed in three patients with radiologically isolating syndrome and one patient with clinically isolating syndrome.
Among those with one or more of the rim lesions, a diagnosis of MS with MC2017 MS criteria was identified with a high sensitivity of 80%, high specificity of 88%, accuracy of 84%, and an AUC of 81%.
“We’ve shown that paramagnetic rim lesions are highly specific for MS, and the sensitivity of rim lesions for MS is higher than previously reported, despite similar techniques in rating, processing, and evaluation – which was likely related to the nature of the cohort,” Dr. Renner said.
Promising data
During the NAIMS symposium, Christopher C. Hemond, MD, assistant professor or neurology at the University of Massachusetts Medical School, Worcester, noted to meeting attendees that the rim lesions were seen across the entire course of the MS disease spectrum, spanning from radiologically isolating syndrome to secondary progressive MS.
“We know paramagnetic rim lesions are visible at all disease stages. They are uniquely larger and more destructive than their rimless peers and are associated with stronger disease severity,” said Dr. Hemond, who was not involved with the research.
“There is promising data at this point suggesting that [the rim lesions] may represent a biomarker predictive of future disability accumulation,” he added.
Dr. Hemond noted that, unlike in Dr. Renner’s study, the bulk of previous studies have indicated that rim lesions “are associated with a high specificity but only modest sensitivity, in the mid-50% range, for the diagnosis of MS in comparison to some conditions that mimic MS.”
Commenting on the findings, Dr. Hemond noted the results from Dr. Renner’s ongoing study “are critical in building confidence in the translational use of this biomarker to assist in ruling in a diagnosis of MS,” while Dr. AlTokis’ study “adds to and is consistent with the growing literature of pathological associations of paramagnetic rim lesions in MS.”
Dr. Hemond added that the NAIMS cooperative plans to publish guidance in the area in the coming months.
“Although paramagnetic rim lesions have strong pathological associations in MS, it remains unclear if the presence of these lesions should change MS clinical management at the present time,” he said.
During the NAIMS session, Francesca Bagnato, MD, PhD, Vanderbilt University Medical Center, Nashville, Tenn., noted the growing importance of the role of rim lesions in clinical research. “It is clear that these paramagnetic rim lesions are going to be the new biomarker for the next generation of clinical trials,” she said.
Dr. Renner’s study received funding from the Race to Erase MS Foundation. Dr. AlTokhis, Dr. Renner, and Dr. Hemond have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
REPORTING FROM ACTRIMS FORUM 2022
Spinal cord atrophy predicts ‘silent progression’ in MS
WEST PALM BEACH, FLA. – , new research shows. Study results suggest that this is a potentially important biomarker for disease progression that may otherwise go unrecognized by clinicians and patients, investigators noted.
“We found that cervical cord atrophy at the C1 level, as obtained from routine brain MRI, is the strongest indicator of silent progression and secondary progressive MS conversion,” said lead author Antje Bischof, MD, department of neurology and Institute of Translational Neurology, University Hospital, Munster, Germany.
“Silent progression and secondary progressive MS conversion are each predominantly related to spinal cord atrophy,” she added.
Dr. Bischof presented the findings at the annual meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS).
Relatively new concept
Secondary progressive MS (SPMS) generally occurs when relapsing-remitting MS (RRMS) progresses, with relapses ceasing and a more steady accumulation of disability occurring.
However, a relapse-free “silent progression” of MS, described in previous research as occurring in as many as one-third or more of patients with relapsing MS, emerges at a much earlier stage prior to secondary progression. This potentially involves widespread neurodegeneration in early disease stages.
“Because the concept of silent progression is relatively new and directly challenges the long-accepted two-stage hypothesis, many clinicians have yet to actively identify silent progression in clinical practice,” said coinvestigator Bruce A. C. Cree, MD, PhD, professor of clinical neurology at the University of California, San Francisco).
To investigate the underlying structural or pathophysiologic changes that are linked to silent progression, the researchers focused on spinal cord measures, which are known to strongly correlate with disability.
They evaluated 360 patients with RRMS and 47 with SPMS and compared outcomes with 80 participants who acted as the study controls. The groups were matched for age, sex, disease duration, and treatments over a 12-year observation period using data from the UCSF MS Center.
To examine spinal cord changes in areas that could affect MS, the investigators used a novel orientation of MRI brain scans to capture the upper cervical cord area.
Among the patients with RRMS, 54 converted to SPMS over 12 years; 159 had silent progression during the period. Silent progression was defined as the onset of irreversible worsening of scores on the Expanded Disability Status Scale (EDSS). Silent progression was confirmed over 12 months and occurred independently of relapses.
‘Strongest predictor’
The analysis showed spinal cord atrophy at the C1 vertebral level to be the strongest predictor of silent progression, with each 1% increase in spinal cord atrophy associated with a 69% shorter time to silent clinical progression (P < .0001).
Those who converted from RRMS to SPMS showed spinal atrophy rates of –2.19% per year, versus –0.88% per year among those who did not convert (P < .001).
“C1A atrophy rates in patients with silent progression were faster even when combining RRMS and SPMS patients,” Dr. Bischof said.
Of note, the patients who silently progressed showed a lower EDSS score at baseline, she added.
Next to spinal atrophy, ventricular enlargement was the second strongest MRI metric associated with silent progression over the 12 years. Each 1% increase in lateral ventricle size was associated with a 16% reduced time to silent clinical progression (P = .007).
“These findings extend the prognostic value of spinal cord atrophy not only for the conversion to SPMS but also silent progression,” Dr. Bischof said. “Furthermore, we show that the enlargement of the lateral ventricles is the second strongest indicator of impending silent progression and the strongest of all brain measures,” she said.
Standard of care?
While the unique MRI techniques used in the study may not be easily obtained in standard practice, Dr. Cree noted that efforts are underway to facilitate the process. “Development of a fully automated software package to obtain those measurements for both clinical trials and in some [clinical settings] is underway,” he said.
Dr. Cree noted that once those technologies are available, the assessment of spinal cord atrophy could become standard in MS care. “I predict that when upper cervical cord measurements can be readily measured, assessment for decrease in the upper cervical cord area will be an essential component of routine care of relapsing MS patients,” he said.
“Because decreases in upper cervical cord areas herald disability worsening, there may well be a window of opportunity to use highly effective treatments to arrest or even reverse this process before irreversible disability accumulates,” Dr. Cree added.
Treatment implications
Commenting on the findings, ACTRIMS program cochair Anne Cross, MD, professor of neurology and the Manny and Rosalyn Rosenthal–Dr John Trotter MS Chair in Neuroimmunology, Washington University, St. Louis, noted that the study is important for two key reasons.
“We lack a good prognostic marker of future progression, but this could have very important implications for the choice of treatment of patients, particularly if the findings are applicable not only at the group level, as in the study, but also at the level of the individual patient,” said Dr. Cross, who was not involved with the research.
Secondly, the results suggest benefits in the selection of patients for clinical trials of agents that might stop progression. “Choosing patients who would deliver the most impact in studies of potential new treatments for progressive MS” is important, Dr. Cross said.
“We don’t want to dilute our trial patient populations with patients who might not be destined to progress in the ensuing years,” she added.
Also commenting on the findings, Benjamin Segal, MD, director of the University of Michigan’s Multiple Sclerosis Center and the Holtom-Garrett Program in Neuroimmunology, Ann Arbor, agreed that the study offers valuable insights. “These findings are striking in that they underscore the fact that even patients with relapsing-remitting MS undergo functional decline in between overt clinical exacerbations, although the decline is more subtle than that experienced by people with progressive forms of MS,” Dr. Segal said.
He noted that the strong correlation between silent progression and spinal cord atrophy, more so than with brain measures, “is not so surprising, since clinical decline was measured using the EDSS scale – which emphasizes ambulation over other functions,” such as cognition.
“It would be interesting to correlate silent progression with serum neurofilament light chain levels, at baseline as well as change over time,” Dr. Segal added.
Dr. Bischof and Dr. Segal have reported no relevant financial relationships. Dr. Cree has received personal compensation for consulting from Biogen, EMD Serono, and Novartis.
A version of this article first appeared on Medscape.com.
WEST PALM BEACH, FLA. – , new research shows. Study results suggest that this is a potentially important biomarker for disease progression that may otherwise go unrecognized by clinicians and patients, investigators noted.
“We found that cervical cord atrophy at the C1 level, as obtained from routine brain MRI, is the strongest indicator of silent progression and secondary progressive MS conversion,” said lead author Antje Bischof, MD, department of neurology and Institute of Translational Neurology, University Hospital, Munster, Germany.
“Silent progression and secondary progressive MS conversion are each predominantly related to spinal cord atrophy,” she added.
Dr. Bischof presented the findings at the annual meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS).
Relatively new concept
Secondary progressive MS (SPMS) generally occurs when relapsing-remitting MS (RRMS) progresses, with relapses ceasing and a more steady accumulation of disability occurring.
However, a relapse-free “silent progression” of MS, described in previous research as occurring in as many as one-third or more of patients with relapsing MS, emerges at a much earlier stage prior to secondary progression. This potentially involves widespread neurodegeneration in early disease stages.
“Because the concept of silent progression is relatively new and directly challenges the long-accepted two-stage hypothesis, many clinicians have yet to actively identify silent progression in clinical practice,” said coinvestigator Bruce A. C. Cree, MD, PhD, professor of clinical neurology at the University of California, San Francisco).
To investigate the underlying structural or pathophysiologic changes that are linked to silent progression, the researchers focused on spinal cord measures, which are known to strongly correlate with disability.
They evaluated 360 patients with RRMS and 47 with SPMS and compared outcomes with 80 participants who acted as the study controls. The groups were matched for age, sex, disease duration, and treatments over a 12-year observation period using data from the UCSF MS Center.
To examine spinal cord changes in areas that could affect MS, the investigators used a novel orientation of MRI brain scans to capture the upper cervical cord area.
Among the patients with RRMS, 54 converted to SPMS over 12 years; 159 had silent progression during the period. Silent progression was defined as the onset of irreversible worsening of scores on the Expanded Disability Status Scale (EDSS). Silent progression was confirmed over 12 months and occurred independently of relapses.
‘Strongest predictor’
The analysis showed spinal cord atrophy at the C1 vertebral level to be the strongest predictor of silent progression, with each 1% increase in spinal cord atrophy associated with a 69% shorter time to silent clinical progression (P < .0001).
Those who converted from RRMS to SPMS showed spinal atrophy rates of –2.19% per year, versus –0.88% per year among those who did not convert (P < .001).
“C1A atrophy rates in patients with silent progression were faster even when combining RRMS and SPMS patients,” Dr. Bischof said.
Of note, the patients who silently progressed showed a lower EDSS score at baseline, she added.
Next to spinal atrophy, ventricular enlargement was the second strongest MRI metric associated with silent progression over the 12 years. Each 1% increase in lateral ventricle size was associated with a 16% reduced time to silent clinical progression (P = .007).
“These findings extend the prognostic value of spinal cord atrophy not only for the conversion to SPMS but also silent progression,” Dr. Bischof said. “Furthermore, we show that the enlargement of the lateral ventricles is the second strongest indicator of impending silent progression and the strongest of all brain measures,” she said.
Standard of care?
While the unique MRI techniques used in the study may not be easily obtained in standard practice, Dr. Cree noted that efforts are underway to facilitate the process. “Development of a fully automated software package to obtain those measurements for both clinical trials and in some [clinical settings] is underway,” he said.
Dr. Cree noted that once those technologies are available, the assessment of spinal cord atrophy could become standard in MS care. “I predict that when upper cervical cord measurements can be readily measured, assessment for decrease in the upper cervical cord area will be an essential component of routine care of relapsing MS patients,” he said.
“Because decreases in upper cervical cord areas herald disability worsening, there may well be a window of opportunity to use highly effective treatments to arrest or even reverse this process before irreversible disability accumulates,” Dr. Cree added.
Treatment implications
Commenting on the findings, ACTRIMS program cochair Anne Cross, MD, professor of neurology and the Manny and Rosalyn Rosenthal–Dr John Trotter MS Chair in Neuroimmunology, Washington University, St. Louis, noted that the study is important for two key reasons.
“We lack a good prognostic marker of future progression, but this could have very important implications for the choice of treatment of patients, particularly if the findings are applicable not only at the group level, as in the study, but also at the level of the individual patient,” said Dr. Cross, who was not involved with the research.
Secondly, the results suggest benefits in the selection of patients for clinical trials of agents that might stop progression. “Choosing patients who would deliver the most impact in studies of potential new treatments for progressive MS” is important, Dr. Cross said.
“We don’t want to dilute our trial patient populations with patients who might not be destined to progress in the ensuing years,” she added.
Also commenting on the findings, Benjamin Segal, MD, director of the University of Michigan’s Multiple Sclerosis Center and the Holtom-Garrett Program in Neuroimmunology, Ann Arbor, agreed that the study offers valuable insights. “These findings are striking in that they underscore the fact that even patients with relapsing-remitting MS undergo functional decline in between overt clinical exacerbations, although the decline is more subtle than that experienced by people with progressive forms of MS,” Dr. Segal said.
He noted that the strong correlation between silent progression and spinal cord atrophy, more so than with brain measures, “is not so surprising, since clinical decline was measured using the EDSS scale – which emphasizes ambulation over other functions,” such as cognition.
“It would be interesting to correlate silent progression with serum neurofilament light chain levels, at baseline as well as change over time,” Dr. Segal added.
Dr. Bischof and Dr. Segal have reported no relevant financial relationships. Dr. Cree has received personal compensation for consulting from Biogen, EMD Serono, and Novartis.
A version of this article first appeared on Medscape.com.
WEST PALM BEACH, FLA. – , new research shows. Study results suggest that this is a potentially important biomarker for disease progression that may otherwise go unrecognized by clinicians and patients, investigators noted.
“We found that cervical cord atrophy at the C1 level, as obtained from routine brain MRI, is the strongest indicator of silent progression and secondary progressive MS conversion,” said lead author Antje Bischof, MD, department of neurology and Institute of Translational Neurology, University Hospital, Munster, Germany.
“Silent progression and secondary progressive MS conversion are each predominantly related to spinal cord atrophy,” she added.
Dr. Bischof presented the findings at the annual meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS).
Relatively new concept
Secondary progressive MS (SPMS) generally occurs when relapsing-remitting MS (RRMS) progresses, with relapses ceasing and a more steady accumulation of disability occurring.
However, a relapse-free “silent progression” of MS, described in previous research as occurring in as many as one-third or more of patients with relapsing MS, emerges at a much earlier stage prior to secondary progression. This potentially involves widespread neurodegeneration in early disease stages.
“Because the concept of silent progression is relatively new and directly challenges the long-accepted two-stage hypothesis, many clinicians have yet to actively identify silent progression in clinical practice,” said coinvestigator Bruce A. C. Cree, MD, PhD, professor of clinical neurology at the University of California, San Francisco).
To investigate the underlying structural or pathophysiologic changes that are linked to silent progression, the researchers focused on spinal cord measures, which are known to strongly correlate with disability.
They evaluated 360 patients with RRMS and 47 with SPMS and compared outcomes with 80 participants who acted as the study controls. The groups were matched for age, sex, disease duration, and treatments over a 12-year observation period using data from the UCSF MS Center.
To examine spinal cord changes in areas that could affect MS, the investigators used a novel orientation of MRI brain scans to capture the upper cervical cord area.
Among the patients with RRMS, 54 converted to SPMS over 12 years; 159 had silent progression during the period. Silent progression was defined as the onset of irreversible worsening of scores on the Expanded Disability Status Scale (EDSS). Silent progression was confirmed over 12 months and occurred independently of relapses.
‘Strongest predictor’
The analysis showed spinal cord atrophy at the C1 vertebral level to be the strongest predictor of silent progression, with each 1% increase in spinal cord atrophy associated with a 69% shorter time to silent clinical progression (P < .0001).
Those who converted from RRMS to SPMS showed spinal atrophy rates of –2.19% per year, versus –0.88% per year among those who did not convert (P < .001).
“C1A atrophy rates in patients with silent progression were faster even when combining RRMS and SPMS patients,” Dr. Bischof said.
Of note, the patients who silently progressed showed a lower EDSS score at baseline, she added.
Next to spinal atrophy, ventricular enlargement was the second strongest MRI metric associated with silent progression over the 12 years. Each 1% increase in lateral ventricle size was associated with a 16% reduced time to silent clinical progression (P = .007).
“These findings extend the prognostic value of spinal cord atrophy not only for the conversion to SPMS but also silent progression,” Dr. Bischof said. “Furthermore, we show that the enlargement of the lateral ventricles is the second strongest indicator of impending silent progression and the strongest of all brain measures,” she said.
Standard of care?
While the unique MRI techniques used in the study may not be easily obtained in standard practice, Dr. Cree noted that efforts are underway to facilitate the process. “Development of a fully automated software package to obtain those measurements for both clinical trials and in some [clinical settings] is underway,” he said.
Dr. Cree noted that once those technologies are available, the assessment of spinal cord atrophy could become standard in MS care. “I predict that when upper cervical cord measurements can be readily measured, assessment for decrease in the upper cervical cord area will be an essential component of routine care of relapsing MS patients,” he said.
“Because decreases in upper cervical cord areas herald disability worsening, there may well be a window of opportunity to use highly effective treatments to arrest or even reverse this process before irreversible disability accumulates,” Dr. Cree added.
Treatment implications
Commenting on the findings, ACTRIMS program cochair Anne Cross, MD, professor of neurology and the Manny and Rosalyn Rosenthal–Dr John Trotter MS Chair in Neuroimmunology, Washington University, St. Louis, noted that the study is important for two key reasons.
“We lack a good prognostic marker of future progression, but this could have very important implications for the choice of treatment of patients, particularly if the findings are applicable not only at the group level, as in the study, but also at the level of the individual patient,” said Dr. Cross, who was not involved with the research.
Secondly, the results suggest benefits in the selection of patients for clinical trials of agents that might stop progression. “Choosing patients who would deliver the most impact in studies of potential new treatments for progressive MS” is important, Dr. Cross said.
“We don’t want to dilute our trial patient populations with patients who might not be destined to progress in the ensuing years,” she added.
Also commenting on the findings, Benjamin Segal, MD, director of the University of Michigan’s Multiple Sclerosis Center and the Holtom-Garrett Program in Neuroimmunology, Ann Arbor, agreed that the study offers valuable insights. “These findings are striking in that they underscore the fact that even patients with relapsing-remitting MS undergo functional decline in between overt clinical exacerbations, although the decline is more subtle than that experienced by people with progressive forms of MS,” Dr. Segal said.
He noted that the strong correlation between silent progression and spinal cord atrophy, more so than with brain measures, “is not so surprising, since clinical decline was measured using the EDSS scale – which emphasizes ambulation over other functions,” such as cognition.
“It would be interesting to correlate silent progression with serum neurofilament light chain levels, at baseline as well as change over time,” Dr. Segal added.
Dr. Bischof and Dr. Segal have reported no relevant financial relationships. Dr. Cree has received personal compensation for consulting from Biogen, EMD Serono, and Novartis.
A version of this article first appeared on Medscape.com.
REPORTING FROM ACTRIMS FORUM 2022
Some physicians still lack access to COVID-19 vaccines
It would be overused and trite to say that the pandemic has drastically altered all of our lives and will cause lasting impact on how we function in society and medicine for years to come. While it seems that the current trend of the latest Omicron variant is on the downslope, the path to get to this point has been fraught with challenges that have struck at the very core of our society. As a primary care physician on the front lines seeing COVID patients, I have had to deal with not only the disease but the politics around it. I practice in Florida, and I still cannot give COVID vaccines in my office.
I am a firm believer in the ability for physicians to be able to give all the necessary adult vaccines and provide them for their patients. The COVID vaccine exacerbated a majorly flawed system that further increased the health care disparities in the country. The current vaccine system for the majority of adult vaccines involves the physician’s being able to directly purchase supplies from the vaccine manufacturer, administer them to the patients, and be reimbursed.
Third parties can purchase vaccines at lower rates than those for physicians
The Affordable Care Act mandates that all vaccines approved by the Advisory Committee on Immunization Practices (ACIP) at the Centers for Disease Control and Prevention must be covered. This allows for better access to care as physicians will be able to purchase, store, and deliver vaccines to their patients. The fallacy in this system is that third parties get involved and rebates or incentives are given to these groups to purchase vaccines at a rate lower than those for physicians.
In addition, many organizations can get access to vaccines before physicians and at a lower cost. That system was flawed to begin with and created a deterrent for access to care and physician involvement in the vaccination process. This was worsened by different states being given the ability to decide how vaccines would be distributed for COVID.
Many pharmacies were able to give out COVID vaccines while many physician offices still have not received access to any of the vaccines. One of the major safety issues with this is that no physicians were involved in the administration of the vaccine, and it is unclear what training was given to the individuals injecting that vaccine. Finally, different places were interpreting the recommendations from ACIP on their own and not necessarily following the appropriate guidelines. All of these factors have further widened the health care disparity gap and made it difficult to provide the COVID vaccines in doctors’ offices.
Recommended next steps, solutions to problem
The question is what to do about this. The most important thing is to get the vaccines in arms so they can save lives. In addition, doctors need to be able to get the vaccines in their offices.
Many patients trust their physicians to advise them on what to do regarding health care. The majority of patients want to know if they should get the vaccine and ask for counseling. Physicians answering patients’ questions about vaccines is an important step in overcoming vaccine hesitancy.
Also, doctors need to be informed and supportive of the vaccine process.
The next step is the governmental aspect with those in power making sure that vaccines are accessible to all. Even if the vaccine cannot be given in the office, doctors should still be recommending that patients receive them. Plus, doctors should take every opportunity to ask about what vaccines their patients have received and encourage their patients to get vaccinated.
The COVID-19 vaccines are safe and effective and have been monitored for safety more than any other vaccine. There are multiple systems in place to look for any signals that could indicate an issue was caused by a COVID-19 vaccine. These vaccines can be administered with other vaccines, and there is a great opportunity for physicians to encourage patients to receive these life-saving vaccines.
While it may seem that the COVID-19 case counts are on the downslope, the importance of continuing to vaccinate is predicated on the very real concern that the disease is still circulating and the unvaccinated are still at risk for severe infection.
Dr. Goldman is immediate past governor of the Florida chapter of the American College of Physicians, a regent for the American College of Physicians, vice-president of the Florida Medical Association, and president of the Florida Medical Association Political Action Committee. You can reach Dr. Goldman at imnews@mdedge.com.
It would be overused and trite to say that the pandemic has drastically altered all of our lives and will cause lasting impact on how we function in society and medicine for years to come. While it seems that the current trend of the latest Omicron variant is on the downslope, the path to get to this point has been fraught with challenges that have struck at the very core of our society. As a primary care physician on the front lines seeing COVID patients, I have had to deal with not only the disease but the politics around it. I practice in Florida, and I still cannot give COVID vaccines in my office.
I am a firm believer in the ability for physicians to be able to give all the necessary adult vaccines and provide them for their patients. The COVID vaccine exacerbated a majorly flawed system that further increased the health care disparities in the country. The current vaccine system for the majority of adult vaccines involves the physician’s being able to directly purchase supplies from the vaccine manufacturer, administer them to the patients, and be reimbursed.
Third parties can purchase vaccines at lower rates than those for physicians
The Affordable Care Act mandates that all vaccines approved by the Advisory Committee on Immunization Practices (ACIP) at the Centers for Disease Control and Prevention must be covered. This allows for better access to care as physicians will be able to purchase, store, and deliver vaccines to their patients. The fallacy in this system is that third parties get involved and rebates or incentives are given to these groups to purchase vaccines at a rate lower than those for physicians.
In addition, many organizations can get access to vaccines before physicians and at a lower cost. That system was flawed to begin with and created a deterrent for access to care and physician involvement in the vaccination process. This was worsened by different states being given the ability to decide how vaccines would be distributed for COVID.
Many pharmacies were able to give out COVID vaccines while many physician offices still have not received access to any of the vaccines. One of the major safety issues with this is that no physicians were involved in the administration of the vaccine, and it is unclear what training was given to the individuals injecting that vaccine. Finally, different places were interpreting the recommendations from ACIP on their own and not necessarily following the appropriate guidelines. All of these factors have further widened the health care disparity gap and made it difficult to provide the COVID vaccines in doctors’ offices.
Recommended next steps, solutions to problem
The question is what to do about this. The most important thing is to get the vaccines in arms so they can save lives. In addition, doctors need to be able to get the vaccines in their offices.
Many patients trust their physicians to advise them on what to do regarding health care. The majority of patients want to know if they should get the vaccine and ask for counseling. Physicians answering patients’ questions about vaccines is an important step in overcoming vaccine hesitancy.
Also, doctors need to be informed and supportive of the vaccine process.
The next step is the governmental aspect with those in power making sure that vaccines are accessible to all. Even if the vaccine cannot be given in the office, doctors should still be recommending that patients receive them. Plus, doctors should take every opportunity to ask about what vaccines their patients have received and encourage their patients to get vaccinated.
The COVID-19 vaccines are safe and effective and have been monitored for safety more than any other vaccine. There are multiple systems in place to look for any signals that could indicate an issue was caused by a COVID-19 vaccine. These vaccines can be administered with other vaccines, and there is a great opportunity for physicians to encourage patients to receive these life-saving vaccines.
While it may seem that the COVID-19 case counts are on the downslope, the importance of continuing to vaccinate is predicated on the very real concern that the disease is still circulating and the unvaccinated are still at risk for severe infection.
Dr. Goldman is immediate past governor of the Florida chapter of the American College of Physicians, a regent for the American College of Physicians, vice-president of the Florida Medical Association, and president of the Florida Medical Association Political Action Committee. You can reach Dr. Goldman at imnews@mdedge.com.
It would be overused and trite to say that the pandemic has drastically altered all of our lives and will cause lasting impact on how we function in society and medicine for years to come. While it seems that the current trend of the latest Omicron variant is on the downslope, the path to get to this point has been fraught with challenges that have struck at the very core of our society. As a primary care physician on the front lines seeing COVID patients, I have had to deal with not only the disease but the politics around it. I practice in Florida, and I still cannot give COVID vaccines in my office.
I am a firm believer in the ability for physicians to be able to give all the necessary adult vaccines and provide them for their patients. The COVID vaccine exacerbated a majorly flawed system that further increased the health care disparities in the country. The current vaccine system for the majority of adult vaccines involves the physician’s being able to directly purchase supplies from the vaccine manufacturer, administer them to the patients, and be reimbursed.
Third parties can purchase vaccines at lower rates than those for physicians
The Affordable Care Act mandates that all vaccines approved by the Advisory Committee on Immunization Practices (ACIP) at the Centers for Disease Control and Prevention must be covered. This allows for better access to care as physicians will be able to purchase, store, and deliver vaccines to their patients. The fallacy in this system is that third parties get involved and rebates or incentives are given to these groups to purchase vaccines at a rate lower than those for physicians.
In addition, many organizations can get access to vaccines before physicians and at a lower cost. That system was flawed to begin with and created a deterrent for access to care and physician involvement in the vaccination process. This was worsened by different states being given the ability to decide how vaccines would be distributed for COVID.
Many pharmacies were able to give out COVID vaccines while many physician offices still have not received access to any of the vaccines. One of the major safety issues with this is that no physicians were involved in the administration of the vaccine, and it is unclear what training was given to the individuals injecting that vaccine. Finally, different places were interpreting the recommendations from ACIP on their own and not necessarily following the appropriate guidelines. All of these factors have further widened the health care disparity gap and made it difficult to provide the COVID vaccines in doctors’ offices.
Recommended next steps, solutions to problem
The question is what to do about this. The most important thing is to get the vaccines in arms so they can save lives. In addition, doctors need to be able to get the vaccines in their offices.
Many patients trust their physicians to advise them on what to do regarding health care. The majority of patients want to know if they should get the vaccine and ask for counseling. Physicians answering patients’ questions about vaccines is an important step in overcoming vaccine hesitancy.
Also, doctors need to be informed and supportive of the vaccine process.
The next step is the governmental aspect with those in power making sure that vaccines are accessible to all. Even if the vaccine cannot be given in the office, doctors should still be recommending that patients receive them. Plus, doctors should take every opportunity to ask about what vaccines their patients have received and encourage their patients to get vaccinated.
The COVID-19 vaccines are safe and effective and have been monitored for safety more than any other vaccine. There are multiple systems in place to look for any signals that could indicate an issue was caused by a COVID-19 vaccine. These vaccines can be administered with other vaccines, and there is a great opportunity for physicians to encourage patients to receive these life-saving vaccines.
While it may seem that the COVID-19 case counts are on the downslope, the importance of continuing to vaccinate is predicated on the very real concern that the disease is still circulating and the unvaccinated are still at risk for severe infection.
Dr. Goldman is immediate past governor of the Florida chapter of the American College of Physicians, a regent for the American College of Physicians, vice-president of the Florida Medical Association, and president of the Florida Medical Association Political Action Committee. You can reach Dr. Goldman at imnews@mdedge.com.
Should all women be routinely screened for lung cancer?
especially those with a history of breast cancer, according to a new study published in BJS Open.
The 2021 screening guidelines include adults aged between 50 and 80 years who have a 20–pack-year smoking history and currently smoke or have quit within the past 15 years, but the guidelines do not include nonsmokers or patients with a history of previous malignancies, such as breast cancer.
Led by Daniela Molena, MD, a thoracic surgeon and director of esophageal surgery at Memorial Sloan Kettering Cancer Center, New York, researchers conducted an analysis of 2,192 women with first-time lung cancer who underwent lung resections at Memorial Sloan Kettering between January 2000 and December 2017. The study’s objective was to determine stage at diagnosis, survival, and eligibility for lung cancer screening among patients with lung cancer who had a previous breast cancer diagnosis and those who did not have a history of breast cancer.
Only 331 (15.1%) patients were previously diagnosed with breast cancer, which was not statistically significant. “Overall, there were no statistically significant differences in genomic or oncogenic pathway alterations between the two groups, which suggests that lung cancer in patients who previously had breast cancer may not be affected at the genomic level by the previous breast cancer,” the authors wrote.
However, at 58.4%, more than half of patients in the study (1,281 patients) were prior smokers and only 33.3% met the USPSTF criteria for lung cancer screening, which the authors said was concerning.
“The most important finding of the study was that a high percentage of women with lung cancer, regardless of breast cancer history, did not meet the current USPSTF criteria for lung cancer screening. This is very important given the observation that nearly half of the women included in the study did not have a history of smoking. As such, the role of imaging for other causes, such as cancer surveillance, becomes especially important for early cancer diagnosis,” Dr. Molena and colleagues wrote. “To reduce late-stage cancer diagnoses, further assessment of guidelines for lung cancer screening for all women may be needed.”
Instead, for almost half of women in the study group with a history of breast cancer, the lung cancer was detected on a routine follow-up imaging scan.
USPSTF guidelines for lung cancer screening do not include previous malignancy as a high-risk feature requiring evaluation, which may explain why so few women in this study were screened for lung cancer, even though lung cancer is more common in breast cancer survivors than the general population. Approximately 10% of women who have had breast cancer will develop a second malignancy within 10 years and in most cases, it will be lung cancer. Plus, according to the National Cancer Institute, breast, lung, and colorectal cancers are the three most common cancers in women and account for approximately 50% of all new cancer diagnoses in women in 2020.
A 2018 analysis published in Frontiers in Oncology found that, of more than 6,000 women with secondary primary lung cancer after having had breast cancer, 42% had distant-stage disease at the time of diagnosis which, Dr. Molena and colleagues said, suggests an ongoing need to update screening recommendations.
“Given that lung cancer has a 5-year overall survival rate of less than 20% (highlighting the benefits of early-stage diagnosis), a better understanding of lung cancer in women with a history of breast cancer could have important implications for screening and surveillance,” the authors wrote.
Estrogen is known to play a role in the development of lung cancer by activating the epidermal growth factor receptor (EGFR). Previous research has shown an increased risk of lung cancer in patients with estrogen receptor–negative, progesterone receptor–negative, HER2-negative, or triple-negative breast cancer.
“Antiestrogen treatment has been demonstrated to decrease the incidence of lung cancer and has been associated with improved long-term survival in patients with lung cancer after breast cancer. Future studies should seek to identify high-risk populations on the basis of hormone receptor status and antiestrogen therapy use,” the authors wrote.
The authors noted a number of limitations to the study, including the single hospital as the sole source of data, plus, the analysis did not account for the length of time since patients quit smoking and a lung cancer diagnosis. Nor did it consider other risk factors, such as radiation, chemotherapy, or antiestrogen therapies.
The authors did not disclose any study-related conflicts of interests.
This article was updated 3/2/22.
especially those with a history of breast cancer, according to a new study published in BJS Open.
The 2021 screening guidelines include adults aged between 50 and 80 years who have a 20–pack-year smoking history and currently smoke or have quit within the past 15 years, but the guidelines do not include nonsmokers or patients with a history of previous malignancies, such as breast cancer.
Led by Daniela Molena, MD, a thoracic surgeon and director of esophageal surgery at Memorial Sloan Kettering Cancer Center, New York, researchers conducted an analysis of 2,192 women with first-time lung cancer who underwent lung resections at Memorial Sloan Kettering between January 2000 and December 2017. The study’s objective was to determine stage at diagnosis, survival, and eligibility for lung cancer screening among patients with lung cancer who had a previous breast cancer diagnosis and those who did not have a history of breast cancer.
Only 331 (15.1%) patients were previously diagnosed with breast cancer, which was not statistically significant. “Overall, there were no statistically significant differences in genomic or oncogenic pathway alterations between the two groups, which suggests that lung cancer in patients who previously had breast cancer may not be affected at the genomic level by the previous breast cancer,” the authors wrote.
However, at 58.4%, more than half of patients in the study (1,281 patients) were prior smokers and only 33.3% met the USPSTF criteria for lung cancer screening, which the authors said was concerning.
“The most important finding of the study was that a high percentage of women with lung cancer, regardless of breast cancer history, did not meet the current USPSTF criteria for lung cancer screening. This is very important given the observation that nearly half of the women included in the study did not have a history of smoking. As such, the role of imaging for other causes, such as cancer surveillance, becomes especially important for early cancer diagnosis,” Dr. Molena and colleagues wrote. “To reduce late-stage cancer diagnoses, further assessment of guidelines for lung cancer screening for all women may be needed.”
Instead, for almost half of women in the study group with a history of breast cancer, the lung cancer was detected on a routine follow-up imaging scan.
USPSTF guidelines for lung cancer screening do not include previous malignancy as a high-risk feature requiring evaluation, which may explain why so few women in this study were screened for lung cancer, even though lung cancer is more common in breast cancer survivors than the general population. Approximately 10% of women who have had breast cancer will develop a second malignancy within 10 years and in most cases, it will be lung cancer. Plus, according to the National Cancer Institute, breast, lung, and colorectal cancers are the three most common cancers in women and account for approximately 50% of all new cancer diagnoses in women in 2020.
A 2018 analysis published in Frontiers in Oncology found that, of more than 6,000 women with secondary primary lung cancer after having had breast cancer, 42% had distant-stage disease at the time of diagnosis which, Dr. Molena and colleagues said, suggests an ongoing need to update screening recommendations.
“Given that lung cancer has a 5-year overall survival rate of less than 20% (highlighting the benefits of early-stage diagnosis), a better understanding of lung cancer in women with a history of breast cancer could have important implications for screening and surveillance,” the authors wrote.
Estrogen is known to play a role in the development of lung cancer by activating the epidermal growth factor receptor (EGFR). Previous research has shown an increased risk of lung cancer in patients with estrogen receptor–negative, progesterone receptor–negative, HER2-negative, or triple-negative breast cancer.
“Antiestrogen treatment has been demonstrated to decrease the incidence of lung cancer and has been associated with improved long-term survival in patients with lung cancer after breast cancer. Future studies should seek to identify high-risk populations on the basis of hormone receptor status and antiestrogen therapy use,” the authors wrote.
The authors noted a number of limitations to the study, including the single hospital as the sole source of data, plus, the analysis did not account for the length of time since patients quit smoking and a lung cancer diagnosis. Nor did it consider other risk factors, such as radiation, chemotherapy, or antiestrogen therapies.
The authors did not disclose any study-related conflicts of interests.
This article was updated 3/2/22.
especially those with a history of breast cancer, according to a new study published in BJS Open.
The 2021 screening guidelines include adults aged between 50 and 80 years who have a 20–pack-year smoking history and currently smoke or have quit within the past 15 years, but the guidelines do not include nonsmokers or patients with a history of previous malignancies, such as breast cancer.
Led by Daniela Molena, MD, a thoracic surgeon and director of esophageal surgery at Memorial Sloan Kettering Cancer Center, New York, researchers conducted an analysis of 2,192 women with first-time lung cancer who underwent lung resections at Memorial Sloan Kettering between January 2000 and December 2017. The study’s objective was to determine stage at diagnosis, survival, and eligibility for lung cancer screening among patients with lung cancer who had a previous breast cancer diagnosis and those who did not have a history of breast cancer.
Only 331 (15.1%) patients were previously diagnosed with breast cancer, which was not statistically significant. “Overall, there were no statistically significant differences in genomic or oncogenic pathway alterations between the two groups, which suggests that lung cancer in patients who previously had breast cancer may not be affected at the genomic level by the previous breast cancer,” the authors wrote.
However, at 58.4%, more than half of patients in the study (1,281 patients) were prior smokers and only 33.3% met the USPSTF criteria for lung cancer screening, which the authors said was concerning.
“The most important finding of the study was that a high percentage of women with lung cancer, regardless of breast cancer history, did not meet the current USPSTF criteria for lung cancer screening. This is very important given the observation that nearly half of the women included in the study did not have a history of smoking. As such, the role of imaging for other causes, such as cancer surveillance, becomes especially important for early cancer diagnosis,” Dr. Molena and colleagues wrote. “To reduce late-stage cancer diagnoses, further assessment of guidelines for lung cancer screening for all women may be needed.”
Instead, for almost half of women in the study group with a history of breast cancer, the lung cancer was detected on a routine follow-up imaging scan.
USPSTF guidelines for lung cancer screening do not include previous malignancy as a high-risk feature requiring evaluation, which may explain why so few women in this study were screened for lung cancer, even though lung cancer is more common in breast cancer survivors than the general population. Approximately 10% of women who have had breast cancer will develop a second malignancy within 10 years and in most cases, it will be lung cancer. Plus, according to the National Cancer Institute, breast, lung, and colorectal cancers are the three most common cancers in women and account for approximately 50% of all new cancer diagnoses in women in 2020.
A 2018 analysis published in Frontiers in Oncology found that, of more than 6,000 women with secondary primary lung cancer after having had breast cancer, 42% had distant-stage disease at the time of diagnosis which, Dr. Molena and colleagues said, suggests an ongoing need to update screening recommendations.
“Given that lung cancer has a 5-year overall survival rate of less than 20% (highlighting the benefits of early-stage diagnosis), a better understanding of lung cancer in women with a history of breast cancer could have important implications for screening and surveillance,” the authors wrote.
Estrogen is known to play a role in the development of lung cancer by activating the epidermal growth factor receptor (EGFR). Previous research has shown an increased risk of lung cancer in patients with estrogen receptor–negative, progesterone receptor–negative, HER2-negative, or triple-negative breast cancer.
“Antiestrogen treatment has been demonstrated to decrease the incidence of lung cancer and has been associated with improved long-term survival in patients with lung cancer after breast cancer. Future studies should seek to identify high-risk populations on the basis of hormone receptor status and antiestrogen therapy use,” the authors wrote.
The authors noted a number of limitations to the study, including the single hospital as the sole source of data, plus, the analysis did not account for the length of time since patients quit smoking and a lung cancer diagnosis. Nor did it consider other risk factors, such as radiation, chemotherapy, or antiestrogen therapies.
The authors did not disclose any study-related conflicts of interests.
This article was updated 3/2/22.
FROM BJS OPEN
IBD-VTE score serves as reminder to assess postdischarge risk
The chances of developing a blood clot after hospital admission for inflammatory bowel disease (IBD) may persist for several months after being discharged, but a new simple score might help clinicians identify patients who are at greatest risk.
The score – which takes eight, easily captured factors into consideration – had a reasonable ability to distinguish between people who did and did not develop venous thromboembolism (VTE), with an area under the curve of 0.71 (95% confidence interval, 0.69-0.72).
“There is clearly an excess of risk for VTE in patients admitted for IBD in the 90 days following their hospital discharge,” said Philip Harvey, MD, a consultant gastroenterologist with the Royal Wolverhampton (England) NHS Trust at the 17th congress of the European Crohn’s and Colitis Organisation.
“Advancing age, male gender, emergency admission, longer admissions, and ulcerative colitis are particularly important risk factors,” he noted.
“We have proposed a risk-scoring system that will be generalizable to patients under the age of 60 using readily identifiable clinical data so that clinicians can identify patients who are at the greatest risk,” Dr. Harvey added when presenting the work.
“This research provides much needed evidence to guide posthospitalization anticoagulation in patients hospitalized for IBD flares,” Bharati Kochar, MD, MS, independently commented.
“Surgeons are already discharging select patients on anticoagulation for DVT [deep vein thrombosis] prophylaxis [but] we need to consider this more systematically after medical IBD admissions,” suggested Dr. Kochar, who is a gastroenterologist and IBD specialist at Massachusetts General Hospital in Boston.
“This research should spur prospective investigation into type of anticoagulation upon discharge, dose, duration and whether the intervention makes a difference in postdischarge clotting events in patients hospitalized for a flare of IBD,” she added.
VTE risk in IBD patients
The risk and prevention of VTE and arterial thrombosis in IBD patients was the focus of a recent international consensus project in which 14 international IBD experts and three thrombosis experts from 12 countries came together to develop evidence-based guidance. Nineteen statements and 10 core recommendations were made, notably that “patients with IBD should be screened for VTE risk factors” and that “thromboprophylaxis should be given to patients with IBD during hospitalization of any cause and maintained during the inpatient period.”
Although met with a high level of agreement among the expert panel, these recommendations were supported by a low (grade C/D) level of evidence.
The expert panel observed in their conclusions that “development of specific risk-assessment tools for thrombotic complications in patients with IBD are needed, as they might influence management in some clinical scenarios (such as thromboprophylaxis during ambulatory flares).”
Large hospitalized IBD population considered
Dr. Harvey and fellow investigators’ IBD-VTE risk score was created using data from almost 102,000 patients (49,385 of whom were men) with just greater than 201,000 hospital admissions between 2006 and 2019. These data were taken from the Hospital Episode Statistics (HES), a “data warehouse” that collects details of all emergency, routine, and outpatient hospital attendances at NHS hospitals in England.
“The HES database is advantageous due to its size because VTE events are relatively uncommon in this group, and therefore it’s important to capture as many patients as possible,” Dr. Harvey explained.
All admissions, from emergencies without surgery to those involving surgery, and those for more routine cases of elective surgery were considered, with the most common (79.3%) admission type being nonsurgical emergencies.
A multilevel logistic regression model was used to identify patient and admission factors that might influence the risk for VTE.
With regard to the number of VTE events seen, Dr. Harvey noted: “There was an enormous excess of events and risk in that 0-90 day period, compared to 180-270 days later. This was true across all admission types.”
Indeed, VTE rates per 100,000 people in the 0-90 day postoperative period were 36.9 for emergency surgical admissions, and 15.6 for both nonsurgical emergencies and elective surgeries. Rates in the later period were a respective 0.84, 1.59, and 1.70.
Key risk factors for VTE were male gender, older age, emergency admission with or without surgery, longer hospital stays, and having ulcerative colitis which were included in the scoring system together with number of prior IBD hospital admissions in the past 3 months, ethnicity, and number of comorbidities.
Ideal thromboprophylaxis duration under investigation
“A higher risk of DVT is known in these patients and all should be considered for postoperative VTE prevention,” said Robert Neil Goldstone, MD, who is assistant professor of surgery at Massachusetts General Hospital.
“Many scores can be used, including the Caprini score, which also adds a point for patient history of IBD,” he observed.
The flip-side of VTE is of course the risk for postsurgical bleeding. While this is something clinicians need to be cognizant of there is “not generally increased risk” with some of the more commonly used anticoagulants, Dr. Goldstone noted. In his practice, “high-risk” IBD patients who have undergone bowel surgery will commonly be discharged on a low-molecular-weight heparin treatment for at least 3-4 weeks.
“The bigger question that remains is whether prolonged postoperative thromboprophylaxis is required,” Dr. Goldstone said. This is something that needs examining in a large randomized controlled trial.
Dr. Harvey and coinvestigators had no conflicts of interest to disclose. Dr. Kochar is on the Board of Editors for GI & Hepatology News but had no other conflicts of interest. Dr. Goldstone was also not involved in the study and had nothing to disclose.
The chances of developing a blood clot after hospital admission for inflammatory bowel disease (IBD) may persist for several months after being discharged, but a new simple score might help clinicians identify patients who are at greatest risk.
The score – which takes eight, easily captured factors into consideration – had a reasonable ability to distinguish between people who did and did not develop venous thromboembolism (VTE), with an area under the curve of 0.71 (95% confidence interval, 0.69-0.72).
“There is clearly an excess of risk for VTE in patients admitted for IBD in the 90 days following their hospital discharge,” said Philip Harvey, MD, a consultant gastroenterologist with the Royal Wolverhampton (England) NHS Trust at the 17th congress of the European Crohn’s and Colitis Organisation.
“Advancing age, male gender, emergency admission, longer admissions, and ulcerative colitis are particularly important risk factors,” he noted.
“We have proposed a risk-scoring system that will be generalizable to patients under the age of 60 using readily identifiable clinical data so that clinicians can identify patients who are at the greatest risk,” Dr. Harvey added when presenting the work.
“This research provides much needed evidence to guide posthospitalization anticoagulation in patients hospitalized for IBD flares,” Bharati Kochar, MD, MS, independently commented.
“Surgeons are already discharging select patients on anticoagulation for DVT [deep vein thrombosis] prophylaxis [but] we need to consider this more systematically after medical IBD admissions,” suggested Dr. Kochar, who is a gastroenterologist and IBD specialist at Massachusetts General Hospital in Boston.
“This research should spur prospective investigation into type of anticoagulation upon discharge, dose, duration and whether the intervention makes a difference in postdischarge clotting events in patients hospitalized for a flare of IBD,” she added.
VTE risk in IBD patients
The risk and prevention of VTE and arterial thrombosis in IBD patients was the focus of a recent international consensus project in which 14 international IBD experts and three thrombosis experts from 12 countries came together to develop evidence-based guidance. Nineteen statements and 10 core recommendations were made, notably that “patients with IBD should be screened for VTE risk factors” and that “thromboprophylaxis should be given to patients with IBD during hospitalization of any cause and maintained during the inpatient period.”
Although met with a high level of agreement among the expert panel, these recommendations were supported by a low (grade C/D) level of evidence.
The expert panel observed in their conclusions that “development of specific risk-assessment tools for thrombotic complications in patients with IBD are needed, as they might influence management in some clinical scenarios (such as thromboprophylaxis during ambulatory flares).”
Large hospitalized IBD population considered
Dr. Harvey and fellow investigators’ IBD-VTE risk score was created using data from almost 102,000 patients (49,385 of whom were men) with just greater than 201,000 hospital admissions between 2006 and 2019. These data were taken from the Hospital Episode Statistics (HES), a “data warehouse” that collects details of all emergency, routine, and outpatient hospital attendances at NHS hospitals in England.
“The HES database is advantageous due to its size because VTE events are relatively uncommon in this group, and therefore it’s important to capture as many patients as possible,” Dr. Harvey explained.
All admissions, from emergencies without surgery to those involving surgery, and those for more routine cases of elective surgery were considered, with the most common (79.3%) admission type being nonsurgical emergencies.
A multilevel logistic regression model was used to identify patient and admission factors that might influence the risk for VTE.
With regard to the number of VTE events seen, Dr. Harvey noted: “There was an enormous excess of events and risk in that 0-90 day period, compared to 180-270 days later. This was true across all admission types.”
Indeed, VTE rates per 100,000 people in the 0-90 day postoperative period were 36.9 for emergency surgical admissions, and 15.6 for both nonsurgical emergencies and elective surgeries. Rates in the later period were a respective 0.84, 1.59, and 1.70.
Key risk factors for VTE were male gender, older age, emergency admission with or without surgery, longer hospital stays, and having ulcerative colitis which were included in the scoring system together with number of prior IBD hospital admissions in the past 3 months, ethnicity, and number of comorbidities.
Ideal thromboprophylaxis duration under investigation
“A higher risk of DVT is known in these patients and all should be considered for postoperative VTE prevention,” said Robert Neil Goldstone, MD, who is assistant professor of surgery at Massachusetts General Hospital.
“Many scores can be used, including the Caprini score, which also adds a point for patient history of IBD,” he observed.
The flip-side of VTE is of course the risk for postsurgical bleeding. While this is something clinicians need to be cognizant of there is “not generally increased risk” with some of the more commonly used anticoagulants, Dr. Goldstone noted. In his practice, “high-risk” IBD patients who have undergone bowel surgery will commonly be discharged on a low-molecular-weight heparin treatment for at least 3-4 weeks.
“The bigger question that remains is whether prolonged postoperative thromboprophylaxis is required,” Dr. Goldstone said. This is something that needs examining in a large randomized controlled trial.
Dr. Harvey and coinvestigators had no conflicts of interest to disclose. Dr. Kochar is on the Board of Editors for GI & Hepatology News but had no other conflicts of interest. Dr. Goldstone was also not involved in the study and had nothing to disclose.
The chances of developing a blood clot after hospital admission for inflammatory bowel disease (IBD) may persist for several months after being discharged, but a new simple score might help clinicians identify patients who are at greatest risk.
The score – which takes eight, easily captured factors into consideration – had a reasonable ability to distinguish between people who did and did not develop venous thromboembolism (VTE), with an area under the curve of 0.71 (95% confidence interval, 0.69-0.72).
“There is clearly an excess of risk for VTE in patients admitted for IBD in the 90 days following their hospital discharge,” said Philip Harvey, MD, a consultant gastroenterologist with the Royal Wolverhampton (England) NHS Trust at the 17th congress of the European Crohn’s and Colitis Organisation.
“Advancing age, male gender, emergency admission, longer admissions, and ulcerative colitis are particularly important risk factors,” he noted.
“We have proposed a risk-scoring system that will be generalizable to patients under the age of 60 using readily identifiable clinical data so that clinicians can identify patients who are at the greatest risk,” Dr. Harvey added when presenting the work.
“This research provides much needed evidence to guide posthospitalization anticoagulation in patients hospitalized for IBD flares,” Bharati Kochar, MD, MS, independently commented.
“Surgeons are already discharging select patients on anticoagulation for DVT [deep vein thrombosis] prophylaxis [but] we need to consider this more systematically after medical IBD admissions,” suggested Dr. Kochar, who is a gastroenterologist and IBD specialist at Massachusetts General Hospital in Boston.
“This research should spur prospective investigation into type of anticoagulation upon discharge, dose, duration and whether the intervention makes a difference in postdischarge clotting events in patients hospitalized for a flare of IBD,” she added.
VTE risk in IBD patients
The risk and prevention of VTE and arterial thrombosis in IBD patients was the focus of a recent international consensus project in which 14 international IBD experts and three thrombosis experts from 12 countries came together to develop evidence-based guidance. Nineteen statements and 10 core recommendations were made, notably that “patients with IBD should be screened for VTE risk factors” and that “thromboprophylaxis should be given to patients with IBD during hospitalization of any cause and maintained during the inpatient period.”
Although met with a high level of agreement among the expert panel, these recommendations were supported by a low (grade C/D) level of evidence.
The expert panel observed in their conclusions that “development of specific risk-assessment tools for thrombotic complications in patients with IBD are needed, as they might influence management in some clinical scenarios (such as thromboprophylaxis during ambulatory flares).”
Large hospitalized IBD population considered
Dr. Harvey and fellow investigators’ IBD-VTE risk score was created using data from almost 102,000 patients (49,385 of whom were men) with just greater than 201,000 hospital admissions between 2006 and 2019. These data were taken from the Hospital Episode Statistics (HES), a “data warehouse” that collects details of all emergency, routine, and outpatient hospital attendances at NHS hospitals in England.
“The HES database is advantageous due to its size because VTE events are relatively uncommon in this group, and therefore it’s important to capture as many patients as possible,” Dr. Harvey explained.
All admissions, from emergencies without surgery to those involving surgery, and those for more routine cases of elective surgery were considered, with the most common (79.3%) admission type being nonsurgical emergencies.
A multilevel logistic regression model was used to identify patient and admission factors that might influence the risk for VTE.
With regard to the number of VTE events seen, Dr. Harvey noted: “There was an enormous excess of events and risk in that 0-90 day period, compared to 180-270 days later. This was true across all admission types.”
Indeed, VTE rates per 100,000 people in the 0-90 day postoperative period were 36.9 for emergency surgical admissions, and 15.6 for both nonsurgical emergencies and elective surgeries. Rates in the later period were a respective 0.84, 1.59, and 1.70.
Key risk factors for VTE were male gender, older age, emergency admission with or without surgery, longer hospital stays, and having ulcerative colitis which were included in the scoring system together with number of prior IBD hospital admissions in the past 3 months, ethnicity, and number of comorbidities.
Ideal thromboprophylaxis duration under investigation
“A higher risk of DVT is known in these patients and all should be considered for postoperative VTE prevention,” said Robert Neil Goldstone, MD, who is assistant professor of surgery at Massachusetts General Hospital.
“Many scores can be used, including the Caprini score, which also adds a point for patient history of IBD,” he observed.
The flip-side of VTE is of course the risk for postsurgical bleeding. While this is something clinicians need to be cognizant of there is “not generally increased risk” with some of the more commonly used anticoagulants, Dr. Goldstone noted. In his practice, “high-risk” IBD patients who have undergone bowel surgery will commonly be discharged on a low-molecular-weight heparin treatment for at least 3-4 weeks.
“The bigger question that remains is whether prolonged postoperative thromboprophylaxis is required,” Dr. Goldstone said. This is something that needs examining in a large randomized controlled trial.
Dr. Harvey and coinvestigators had no conflicts of interest to disclose. Dr. Kochar is on the Board of Editors for GI & Hepatology News but had no other conflicts of interest. Dr. Goldstone was also not involved in the study and had nothing to disclose.
FROM ECCO 2022
Needle-free epinephrine products could be available in 2023
Longstanding anxiety around use of epinephrine autoinjectors has prompted research into alternative delivery routes for this life-saving medication. Several companies presented posters on their needle-free epinephrine products at the American Academy of Allergy, Asthma & Immunology (AAAAI) Annual Meeting.
Intranasal formulations are under development at ARS Pharmaceuticals (San Diego) and Bryn Pharma (Raleigh, N.C.). And Aquestive Therapeutics (Warren, N.J.) is working on a sublingual film that delivers epinephrine prodrug when applied under the tongue.
Epinephrine is essential for stopping life-threatening allergic reactions, yet patients often don’t carry their autoinjectors and many hesitate to use them. “It’s needle phobia,” said ARS Pharmaceuticals CEO Richard Lowenthal in an interview with this news organization. “They’re afraid to use it. They don’t like to inject their children, so they hesitate.”
Both nasal sprays reached maximal plasma concentration in 20-30 minutes. ARS Pharmaceuticals compared its intranasal product (Neffy 1 mg) against manual intramuscular injection (0.3 mg) and two autoinjectors (EpiPen 0.3 mg and Symjepi 0.3 mg) by analyzing data from multiple randomized crossover Phase 1 studies examining pharmacokinetics and pharmacodynamics in 175 healthy adults. In this integrated analysis, EpiPen was fastest (20 minutes) at reaching maximal concentration (Tmax), followed by Symjepi and Neffy (both 30 minutes) and epinephrine 0.3 mg IM (45 minutes). In a human factors analysis, ARS Pharmaceuticals reported that untrained participants were able to administer the Neffy spray to themselves or another participant safely and effectively during a simulated emergency scenario.
Bryn Pharma compared pharmacokinetics of its nasal spray product (BRYN-NDS1C 6.6 mg) when self-administered or administered by trained professionals and found comparable profiles for each. Tmax values were also similar: 21.63 minutes (trained professional) and 19.82 minutes (self-administered).
Aquestive Therapeutics is developing a postage stamp-sized product (AQST-109) that delivers epinephrine and begins dissolving when placed under the tongue. No water or swallowing is required for administration, and its packaging is thinner and smaller than a credit card, according to CEO Keith Kendall.
Its analysis showed that the epinephrine reaches maximum plasma concentration in about 15 minutes, with a Tmax range narrower than that of the EpiPen. “The results showed dosing with AQST-109 resulted in PK concentration and Tmax values comparable to published data from autoinjectors,” said John Oppenheimer, MD, of Rutgers University School of Medicine, in a prerecorded poster summary.
Aquestive aims to move forward to the manufacture of registration batches and a pivotal pharmacokinetic study in the second half of 2022. Mr. Lowenthal said ARS Pharmaceuticals is hoping for approval and launch of its nasal spray by summer 2023.
“Having a non-needle delivery device would help many people overcome that fear and hopefully increase use in anaphylaxis,” said David Stukus, MD, an allergist-immunologist and professor of clinical pediatrics at Nationwide Children’s Hospital, Columbus, who was not involved with any of the studies on EpiPen alternatives. And “it’s not just food allergy – anaphylaxis can occur from venom stings, medications, or idiopathic causes.”
Mr. Lowenthal is the CEO of ARS Pharmaceuticals. Mr. Kendall is CEO of Aquestive Therapeutics. Dr. Oppenheimer is a consultant for Aquestive, GSK, Amgen, Sanofi, and Aimmune and sits on Aquestive’s advisory board. Dr. Stukus is a consultant for Novartis.
A version of this article first appeared on Medscape.com.
Longstanding anxiety around use of epinephrine autoinjectors has prompted research into alternative delivery routes for this life-saving medication. Several companies presented posters on their needle-free epinephrine products at the American Academy of Allergy, Asthma & Immunology (AAAAI) Annual Meeting.
Intranasal formulations are under development at ARS Pharmaceuticals (San Diego) and Bryn Pharma (Raleigh, N.C.). And Aquestive Therapeutics (Warren, N.J.) is working on a sublingual film that delivers epinephrine prodrug when applied under the tongue.
Epinephrine is essential for stopping life-threatening allergic reactions, yet patients often don’t carry their autoinjectors and many hesitate to use them. “It’s needle phobia,” said ARS Pharmaceuticals CEO Richard Lowenthal in an interview with this news organization. “They’re afraid to use it. They don’t like to inject their children, so they hesitate.”
Both nasal sprays reached maximal plasma concentration in 20-30 minutes. ARS Pharmaceuticals compared its intranasal product (Neffy 1 mg) against manual intramuscular injection (0.3 mg) and two autoinjectors (EpiPen 0.3 mg and Symjepi 0.3 mg) by analyzing data from multiple randomized crossover Phase 1 studies examining pharmacokinetics and pharmacodynamics in 175 healthy adults. In this integrated analysis, EpiPen was fastest (20 minutes) at reaching maximal concentration (Tmax), followed by Symjepi and Neffy (both 30 minutes) and epinephrine 0.3 mg IM (45 minutes). In a human factors analysis, ARS Pharmaceuticals reported that untrained participants were able to administer the Neffy spray to themselves or another participant safely and effectively during a simulated emergency scenario.
Bryn Pharma compared pharmacokinetics of its nasal spray product (BRYN-NDS1C 6.6 mg) when self-administered or administered by trained professionals and found comparable profiles for each. Tmax values were also similar: 21.63 minutes (trained professional) and 19.82 minutes (self-administered).
Aquestive Therapeutics is developing a postage stamp-sized product (AQST-109) that delivers epinephrine and begins dissolving when placed under the tongue. No water or swallowing is required for administration, and its packaging is thinner and smaller than a credit card, according to CEO Keith Kendall.
Its analysis showed that the epinephrine reaches maximum plasma concentration in about 15 minutes, with a Tmax range narrower than that of the EpiPen. “The results showed dosing with AQST-109 resulted in PK concentration and Tmax values comparable to published data from autoinjectors,” said John Oppenheimer, MD, of Rutgers University School of Medicine, in a prerecorded poster summary.
Aquestive aims to move forward to the manufacture of registration batches and a pivotal pharmacokinetic study in the second half of 2022. Mr. Lowenthal said ARS Pharmaceuticals is hoping for approval and launch of its nasal spray by summer 2023.
“Having a non-needle delivery device would help many people overcome that fear and hopefully increase use in anaphylaxis,” said David Stukus, MD, an allergist-immunologist and professor of clinical pediatrics at Nationwide Children’s Hospital, Columbus, who was not involved with any of the studies on EpiPen alternatives. And “it’s not just food allergy – anaphylaxis can occur from venom stings, medications, or idiopathic causes.”
Mr. Lowenthal is the CEO of ARS Pharmaceuticals. Mr. Kendall is CEO of Aquestive Therapeutics. Dr. Oppenheimer is a consultant for Aquestive, GSK, Amgen, Sanofi, and Aimmune and sits on Aquestive’s advisory board. Dr. Stukus is a consultant for Novartis.
A version of this article first appeared on Medscape.com.
Longstanding anxiety around use of epinephrine autoinjectors has prompted research into alternative delivery routes for this life-saving medication. Several companies presented posters on their needle-free epinephrine products at the American Academy of Allergy, Asthma & Immunology (AAAAI) Annual Meeting.
Intranasal formulations are under development at ARS Pharmaceuticals (San Diego) and Bryn Pharma (Raleigh, N.C.). And Aquestive Therapeutics (Warren, N.J.) is working on a sublingual film that delivers epinephrine prodrug when applied under the tongue.
Epinephrine is essential for stopping life-threatening allergic reactions, yet patients often don’t carry their autoinjectors and many hesitate to use them. “It’s needle phobia,” said ARS Pharmaceuticals CEO Richard Lowenthal in an interview with this news organization. “They’re afraid to use it. They don’t like to inject their children, so they hesitate.”
Both nasal sprays reached maximal plasma concentration in 20-30 minutes. ARS Pharmaceuticals compared its intranasal product (Neffy 1 mg) against manual intramuscular injection (0.3 mg) and two autoinjectors (EpiPen 0.3 mg and Symjepi 0.3 mg) by analyzing data from multiple randomized crossover Phase 1 studies examining pharmacokinetics and pharmacodynamics in 175 healthy adults. In this integrated analysis, EpiPen was fastest (20 minutes) at reaching maximal concentration (Tmax), followed by Symjepi and Neffy (both 30 minutes) and epinephrine 0.3 mg IM (45 minutes). In a human factors analysis, ARS Pharmaceuticals reported that untrained participants were able to administer the Neffy spray to themselves or another participant safely and effectively during a simulated emergency scenario.
Bryn Pharma compared pharmacokinetics of its nasal spray product (BRYN-NDS1C 6.6 mg) when self-administered or administered by trained professionals and found comparable profiles for each. Tmax values were also similar: 21.63 minutes (trained professional) and 19.82 minutes (self-administered).
Aquestive Therapeutics is developing a postage stamp-sized product (AQST-109) that delivers epinephrine and begins dissolving when placed under the tongue. No water or swallowing is required for administration, and its packaging is thinner and smaller than a credit card, according to CEO Keith Kendall.
Its analysis showed that the epinephrine reaches maximum plasma concentration in about 15 minutes, with a Tmax range narrower than that of the EpiPen. “The results showed dosing with AQST-109 resulted in PK concentration and Tmax values comparable to published data from autoinjectors,” said John Oppenheimer, MD, of Rutgers University School of Medicine, in a prerecorded poster summary.
Aquestive aims to move forward to the manufacture of registration batches and a pivotal pharmacokinetic study in the second half of 2022. Mr. Lowenthal said ARS Pharmaceuticals is hoping for approval and launch of its nasal spray by summer 2023.
“Having a non-needle delivery device would help many people overcome that fear and hopefully increase use in anaphylaxis,” said David Stukus, MD, an allergist-immunologist and professor of clinical pediatrics at Nationwide Children’s Hospital, Columbus, who was not involved with any of the studies on EpiPen alternatives. And “it’s not just food allergy – anaphylaxis can occur from venom stings, medications, or idiopathic causes.”
Mr. Lowenthal is the CEO of ARS Pharmaceuticals. Mr. Kendall is CEO of Aquestive Therapeutics. Dr. Oppenheimer is a consultant for Aquestive, GSK, Amgen, Sanofi, and Aimmune and sits on Aquestive’s advisory board. Dr. Stukus is a consultant for Novartis.
A version of this article first appeared on Medscape.com.
FROM AAAAI
GI involvement may signal risk for MIS-C after COVID
While evaluating an adolescent who had endured a several-day history of vomiting and diarrhea, I mentioned the likelihood of a viral causation, including SARS-CoV-2 infection. His well-informed mother responded, “He has no respiratory symptoms. Does COVID cause GI disease?”
Indeed, not only is the gastrointestinal tract a potential portal of entry of the virus but it may well be the site of mediation of both local and remote injury and thus a harbinger of more severe clinical phenotypes.
As we learn more about the clinical spectrum of COVID, it is becoming increasingly clear that certain features of GI tract involvement may allow us to establish a timeline of the clinical course and perhaps predict the outcome.
The GI tract’s involvement isn’t surprising
The ways in which the GI tract serves as a target organ of SARS-CoV-2 have been postulated in the literature. In part, this is related to the presence of abundant receptors for SARS-CoV-2 cell binding and internalization. The virus uses angiotensin-converting enzyme 2 receptors to enter various cells. These receptors are highly expressed on not only lung cells but also enterocytes. Binding of SARS-CoV-2 to ACE2 receptors allows GI involvement, leading to microscopic mucosal inflammation, increased permeability, and altered intestinal absorption.
The clinical GI manifestations of this include anorexia, nausea, vomiting, diarrhea, and abdominal pain, which may be the earliest, or sole, symptoms of COVID-19, often noted before the onset of fever or respiratory symptoms. In fact, John Ong, MBBS, and colleagues, in a discussion about patients with primary GI SARS-CoV-2 infection and symptoms, use the term “GI-COVID.”
Clinical course of GI manifestations
After SARS-CoV-2 exposure, adults most commonly present with respiratory symptoms, with GI symptoms reported in 10%-15% of cases. However, the overall incidence of GI involvement during SARS-CoV-2 infection varies according to age, with children more likely than adults to manifest intestinal symptoms.
There are also differences in incidence reported when comparing hospitalized with nonhospitalized individuals. In early reports from the onset of the COVID-19 pandemic, 11%-43% of hospitalized adult patients manifested GI symptoms. Of note, the presence of GI symptoms was associated with more severe disease and thus predictive of outcomes in those admitted to hospitals.
In a multicenter study that assessed pediatric inpatients with COVID-19, GI manifestations were present in 57% of patients and were the first manifestation in 14%. Adjusted by confounding factors, those with GI symptoms had a higher risk for pediatric intensive care unit admission. Patients admitted to the PICU also had higher serum C-reactive protein and aspartate aminotransferase values.
Emerging data on MIS-C
In previously healthy children and adolescents, the severe, life-threatening complication of multisystem inflammatory syndrome in children (MIS-C) may present 2-6 weeks after acute infection with SARS-CoV-2. MIS-C appears to be an immune activation syndrome and is presumed to be the delayed immunologic sequelae of mild/asymptomatic SARS-CoV-2 infection. This response manifests as hyperinflammation in conjunction with a peak in antibody production a few weeks later.
One report of 186 children with MIS-C in the United States noted that the involved organ system included the GI tract in 92%, followed by cardiovascular in 80%, hematologic in 76%, mucocutaneous in 74%, and respiratory in 70%. Affected children were hospitalized for a median of 7 days, with 80% requiring intensive care, 20% receiving mechanical ventilation, and 48% receiving vasoactive support; 2% died. In a similar study of patients hospitalized in New York, 88% had GI symptoms (abdominal pain, vomiting, and/or diarrhea). A retrospective chart review of patients with MIS-C found that the majority had GI symptoms with any portion of the GI tract potentially involved, but ileal and colonic inflammation predominated.
Elizabeth Whittaker, MD, and colleagues described the clinical characteristics of children in eight hospitals in England who met criteria for MIS-C that were temporally associated with SARS-CoV-2. At presentation, all of the patients manifested fever and nonspecific GI symptoms, including vomiting (45%), abdominal pain (53%), and diarrhea (52%). During hospitalization, 50% developed shock with evidence of myocardial dysfunction.
Ermias D. Belay, MD, and colleagues described the clinical characteristics of a large cohort of patients with MIS-C that were reported to the U.S. Centers for Disease Control and Prevention. Of 1,733 patients identified, GI symptoms were reported in 53%-67%. Over half developed hypotension or shock and were admitted for intensive care. Younger children more frequently presented with abdominal pain in contrast with adolescents, who more frequently manifest respiratory symptoms.
In a multicenter retrospective study of Italian children with COVID-19 that was conducted from the onset of the pandemic to early 2021, GI symptoms were noted in 38%. These manifestations were mild and self-limiting, comparable to other viral intestinal infections. However, a subset of children (9.5%) had severe GI manifestations of MIS-C, defined as a medical and/or radiologic diagnosis of acute abdomen, appendicitis, intussusception, pancreatitis, abdominal fluid collection, or diffuse adenomesenteritis requiring surgical consultation. Overall, 42% of this group underwent surgery. The authors noted that the clinical presentation of abdominal pain, lymphopenia, and increased C-reactive protein and ferritin levels were associated with a 9- to 30-fold increased probability of these severe sequelae. In addition, the severity of the GI manifestations was correlated with age (5-10 years: overall response, 8.33; >10 years: OR, 6.37). Again, the presence of GI symptoms was a harbinger of hospitalization and PICU admission.
Given that GI symptoms are a common presentation of MIS-C, its diagnosis may be delayed as clinicians first consider other GI/viral infections, inflammatory bowel disease, or Kawasaki disease. Prompt identification of GI involvement and awareness of the potential outcomes may guide the management and improve the outcome.
These studies provide a clear picture of the differential presenting features of COVID-19 and MIS-C. Although there may be other environmental/genetic factors that govern the incidence, impact, and manifestations, COVID’s status as an ongoing pandemic gives these observations worldwide relevance. This is evident in a recent report documenting pronounced GI symptoms in African children with COVID-19.
It should be noted, however, that the published data cited here reflect the impact of the initial variants of SARS-CoV-2. The GI binding, effects, and aftermath of infection with the Delta and Omicron variants is not yet known.
Cause and effect, or simply coincidental?
Some insight into MIS-C pathogenesis was provided by Lael M. Yonker, MD, and colleagues in their analysis of biospecimens from 100 children: 19 with MIS-C, 26 with acute COVID-19, and 55 controls. They demonstrated that in children with MIS-C the prolonged presence of SARS-CoV-2 in the GI tract led to the release of zonulin, a biomarker of intestinal permeability, with subsequent trafficking of SARS-CoV-2 antigens into the bloodstream, leading to hyperinflammation. They were then able to decrease plasma SARS-CoV-2 spike antigen levels and inflammatory markers, with resulting clinical improvement after administration of larazotide, a zonulin antagonist.
These observations regarding the potential mechanism and triggers of MIS-C may offer biomarkers for early detection and/or strategies for prevention and treatment of MIS-C.
Bottom line
The GI tract is the target of an immune-mediated inflammatory response that is triggered by SARS-CoV-2, with MIS-C being the major manifestation of the resultant high degree of inflammation. These observations will allow an increased awareness of nonrespiratory symptoms of SARS-CoV-2 infection by clinicians working in emergency departments and primary care settings.
Clues that may enhance the ability of pediatric clinicians to recognize the potential for severe GI involvement include the occurrence of abdominal pain, leukopenia, and elevated inflammatory markers. Their presence should raise suspicion of MIS-C and lead to early evaluation.
Of note, COVID-19 mRNA vaccination is associated with a lower incidence of MIS-C in adolescents. This underscores the importance of COVID vaccination for all eligible children. Yet, we clearly have our work cut out for us. Of 107 children with MIS-C who were hospitalized in France, 31% were adolescents eligible for vaccination; however, none had been fully vaccinated. At the end of 2021, CDC data noted that less than 1% of vaccine-eligible children (12-17 years) were fully vaccinated.
The Pfizer-BioNTech vaccine is now authorized for receipt by children aged 5-11 years, the age group that is at highest risk for MIS-C. However, despite the approval of vaccines for these younger children, there is limited access in some parts of the United States at a time of rising incidence.
We look forward to broad availability of pediatric vaccination strategies. In addition, with the intense focus on safe and effective therapeutics for SARS-CoV-2 infection, we hope to soon have strategies to prevent and/or treat the life-threatening manifestations and long-term consequences of MIS-C. For example, the recently reported central role of the gut microbiota in immunity against SARS-CoV-2 infection offer the possibility that “microbiota modulation” may both reduce GI injury and enhance vaccine efficacy.
Dr. Balistreri has disclosed no relevant financial relationships.
William F. Balistreri, MD, is the Dorothy M.M. Kersten Professor of Pediatrics; director emeritus, Pediatric Liver Care Center; medical director emeritus, liver transplantation; and professor, University of Cincinnati College of Medicine, department of pediatrics, Cincinnati Children’s Hospital Medical Center. He has served as director of the division of gastroenterology, hepatology, and nutrition at Cincinnati Children’s for 25 years and frequently covers gastroenterology, liver, and nutrition-related topics for this news organization. Dr Balistreri is currently editor-in-chief of the Journal of Pediatrics, having previously served as editor-in-chief of several journals and textbooks. He also became the first pediatrician to act as president of the American Association for the Study of Liver Diseases. In his spare time, he coaches youth lacrosse.
A version of this article first appeared on Medscape.com.
While evaluating an adolescent who had endured a several-day history of vomiting and diarrhea, I mentioned the likelihood of a viral causation, including SARS-CoV-2 infection. His well-informed mother responded, “He has no respiratory symptoms. Does COVID cause GI disease?”
Indeed, not only is the gastrointestinal tract a potential portal of entry of the virus but it may well be the site of mediation of both local and remote injury and thus a harbinger of more severe clinical phenotypes.
As we learn more about the clinical spectrum of COVID, it is becoming increasingly clear that certain features of GI tract involvement may allow us to establish a timeline of the clinical course and perhaps predict the outcome.
The GI tract’s involvement isn’t surprising
The ways in which the GI tract serves as a target organ of SARS-CoV-2 have been postulated in the literature. In part, this is related to the presence of abundant receptors for SARS-CoV-2 cell binding and internalization. The virus uses angiotensin-converting enzyme 2 receptors to enter various cells. These receptors are highly expressed on not only lung cells but also enterocytes. Binding of SARS-CoV-2 to ACE2 receptors allows GI involvement, leading to microscopic mucosal inflammation, increased permeability, and altered intestinal absorption.
The clinical GI manifestations of this include anorexia, nausea, vomiting, diarrhea, and abdominal pain, which may be the earliest, or sole, symptoms of COVID-19, often noted before the onset of fever or respiratory symptoms. In fact, John Ong, MBBS, and colleagues, in a discussion about patients with primary GI SARS-CoV-2 infection and symptoms, use the term “GI-COVID.”
Clinical course of GI manifestations
After SARS-CoV-2 exposure, adults most commonly present with respiratory symptoms, with GI symptoms reported in 10%-15% of cases. However, the overall incidence of GI involvement during SARS-CoV-2 infection varies according to age, with children more likely than adults to manifest intestinal symptoms.
There are also differences in incidence reported when comparing hospitalized with nonhospitalized individuals. In early reports from the onset of the COVID-19 pandemic, 11%-43% of hospitalized adult patients manifested GI symptoms. Of note, the presence of GI symptoms was associated with more severe disease and thus predictive of outcomes in those admitted to hospitals.
In a multicenter study that assessed pediatric inpatients with COVID-19, GI manifestations were present in 57% of patients and were the first manifestation in 14%. Adjusted by confounding factors, those with GI symptoms had a higher risk for pediatric intensive care unit admission. Patients admitted to the PICU also had higher serum C-reactive protein and aspartate aminotransferase values.
Emerging data on MIS-C
In previously healthy children and adolescents, the severe, life-threatening complication of multisystem inflammatory syndrome in children (MIS-C) may present 2-6 weeks after acute infection with SARS-CoV-2. MIS-C appears to be an immune activation syndrome and is presumed to be the delayed immunologic sequelae of mild/asymptomatic SARS-CoV-2 infection. This response manifests as hyperinflammation in conjunction with a peak in antibody production a few weeks later.
One report of 186 children with MIS-C in the United States noted that the involved organ system included the GI tract in 92%, followed by cardiovascular in 80%, hematologic in 76%, mucocutaneous in 74%, and respiratory in 70%. Affected children were hospitalized for a median of 7 days, with 80% requiring intensive care, 20% receiving mechanical ventilation, and 48% receiving vasoactive support; 2% died. In a similar study of patients hospitalized in New York, 88% had GI symptoms (abdominal pain, vomiting, and/or diarrhea). A retrospective chart review of patients with MIS-C found that the majority had GI symptoms with any portion of the GI tract potentially involved, but ileal and colonic inflammation predominated.
Elizabeth Whittaker, MD, and colleagues described the clinical characteristics of children in eight hospitals in England who met criteria for MIS-C that were temporally associated with SARS-CoV-2. At presentation, all of the patients manifested fever and nonspecific GI symptoms, including vomiting (45%), abdominal pain (53%), and diarrhea (52%). During hospitalization, 50% developed shock with evidence of myocardial dysfunction.
Ermias D. Belay, MD, and colleagues described the clinical characteristics of a large cohort of patients with MIS-C that were reported to the U.S. Centers for Disease Control and Prevention. Of 1,733 patients identified, GI symptoms were reported in 53%-67%. Over half developed hypotension or shock and were admitted for intensive care. Younger children more frequently presented with abdominal pain in contrast with adolescents, who more frequently manifest respiratory symptoms.
In a multicenter retrospective study of Italian children with COVID-19 that was conducted from the onset of the pandemic to early 2021, GI symptoms were noted in 38%. These manifestations were mild and self-limiting, comparable to other viral intestinal infections. However, a subset of children (9.5%) had severe GI manifestations of MIS-C, defined as a medical and/or radiologic diagnosis of acute abdomen, appendicitis, intussusception, pancreatitis, abdominal fluid collection, or diffuse adenomesenteritis requiring surgical consultation. Overall, 42% of this group underwent surgery. The authors noted that the clinical presentation of abdominal pain, lymphopenia, and increased C-reactive protein and ferritin levels were associated with a 9- to 30-fold increased probability of these severe sequelae. In addition, the severity of the GI manifestations was correlated with age (5-10 years: overall response, 8.33; >10 years: OR, 6.37). Again, the presence of GI symptoms was a harbinger of hospitalization and PICU admission.
Given that GI symptoms are a common presentation of MIS-C, its diagnosis may be delayed as clinicians first consider other GI/viral infections, inflammatory bowel disease, or Kawasaki disease. Prompt identification of GI involvement and awareness of the potential outcomes may guide the management and improve the outcome.
These studies provide a clear picture of the differential presenting features of COVID-19 and MIS-C. Although there may be other environmental/genetic factors that govern the incidence, impact, and manifestations, COVID’s status as an ongoing pandemic gives these observations worldwide relevance. This is evident in a recent report documenting pronounced GI symptoms in African children with COVID-19.
It should be noted, however, that the published data cited here reflect the impact of the initial variants of SARS-CoV-2. The GI binding, effects, and aftermath of infection with the Delta and Omicron variants is not yet known.
Cause and effect, or simply coincidental?
Some insight into MIS-C pathogenesis was provided by Lael M. Yonker, MD, and colleagues in their analysis of biospecimens from 100 children: 19 with MIS-C, 26 with acute COVID-19, and 55 controls. They demonstrated that in children with MIS-C the prolonged presence of SARS-CoV-2 in the GI tract led to the release of zonulin, a biomarker of intestinal permeability, with subsequent trafficking of SARS-CoV-2 antigens into the bloodstream, leading to hyperinflammation. They were then able to decrease plasma SARS-CoV-2 spike antigen levels and inflammatory markers, with resulting clinical improvement after administration of larazotide, a zonulin antagonist.
These observations regarding the potential mechanism and triggers of MIS-C may offer biomarkers for early detection and/or strategies for prevention and treatment of MIS-C.
Bottom line
The GI tract is the target of an immune-mediated inflammatory response that is triggered by SARS-CoV-2, with MIS-C being the major manifestation of the resultant high degree of inflammation. These observations will allow an increased awareness of nonrespiratory symptoms of SARS-CoV-2 infection by clinicians working in emergency departments and primary care settings.
Clues that may enhance the ability of pediatric clinicians to recognize the potential for severe GI involvement include the occurrence of abdominal pain, leukopenia, and elevated inflammatory markers. Their presence should raise suspicion of MIS-C and lead to early evaluation.
Of note, COVID-19 mRNA vaccination is associated with a lower incidence of MIS-C in adolescents. This underscores the importance of COVID vaccination for all eligible children. Yet, we clearly have our work cut out for us. Of 107 children with MIS-C who were hospitalized in France, 31% were adolescents eligible for vaccination; however, none had been fully vaccinated. At the end of 2021, CDC data noted that less than 1% of vaccine-eligible children (12-17 years) were fully vaccinated.
The Pfizer-BioNTech vaccine is now authorized for receipt by children aged 5-11 years, the age group that is at highest risk for MIS-C. However, despite the approval of vaccines for these younger children, there is limited access in some parts of the United States at a time of rising incidence.
We look forward to broad availability of pediatric vaccination strategies. In addition, with the intense focus on safe and effective therapeutics for SARS-CoV-2 infection, we hope to soon have strategies to prevent and/or treat the life-threatening manifestations and long-term consequences of MIS-C. For example, the recently reported central role of the gut microbiota in immunity against SARS-CoV-2 infection offer the possibility that “microbiota modulation” may both reduce GI injury and enhance vaccine efficacy.
Dr. Balistreri has disclosed no relevant financial relationships.
William F. Balistreri, MD, is the Dorothy M.M. Kersten Professor of Pediatrics; director emeritus, Pediatric Liver Care Center; medical director emeritus, liver transplantation; and professor, University of Cincinnati College of Medicine, department of pediatrics, Cincinnati Children’s Hospital Medical Center. He has served as director of the division of gastroenterology, hepatology, and nutrition at Cincinnati Children’s for 25 years and frequently covers gastroenterology, liver, and nutrition-related topics for this news organization. Dr Balistreri is currently editor-in-chief of the Journal of Pediatrics, having previously served as editor-in-chief of several journals and textbooks. He also became the first pediatrician to act as president of the American Association for the Study of Liver Diseases. In his spare time, he coaches youth lacrosse.
A version of this article first appeared on Medscape.com.
While evaluating an adolescent who had endured a several-day history of vomiting and diarrhea, I mentioned the likelihood of a viral causation, including SARS-CoV-2 infection. His well-informed mother responded, “He has no respiratory symptoms. Does COVID cause GI disease?”
Indeed, not only is the gastrointestinal tract a potential portal of entry of the virus but it may well be the site of mediation of both local and remote injury and thus a harbinger of more severe clinical phenotypes.
As we learn more about the clinical spectrum of COVID, it is becoming increasingly clear that certain features of GI tract involvement may allow us to establish a timeline of the clinical course and perhaps predict the outcome.
The GI tract’s involvement isn’t surprising
The ways in which the GI tract serves as a target organ of SARS-CoV-2 have been postulated in the literature. In part, this is related to the presence of abundant receptors for SARS-CoV-2 cell binding and internalization. The virus uses angiotensin-converting enzyme 2 receptors to enter various cells. These receptors are highly expressed on not only lung cells but also enterocytes. Binding of SARS-CoV-2 to ACE2 receptors allows GI involvement, leading to microscopic mucosal inflammation, increased permeability, and altered intestinal absorption.
The clinical GI manifestations of this include anorexia, nausea, vomiting, diarrhea, and abdominal pain, which may be the earliest, or sole, symptoms of COVID-19, often noted before the onset of fever or respiratory symptoms. In fact, John Ong, MBBS, and colleagues, in a discussion about patients with primary GI SARS-CoV-2 infection and symptoms, use the term “GI-COVID.”
Clinical course of GI manifestations
After SARS-CoV-2 exposure, adults most commonly present with respiratory symptoms, with GI symptoms reported in 10%-15% of cases. However, the overall incidence of GI involvement during SARS-CoV-2 infection varies according to age, with children more likely than adults to manifest intestinal symptoms.
There are also differences in incidence reported when comparing hospitalized with nonhospitalized individuals. In early reports from the onset of the COVID-19 pandemic, 11%-43% of hospitalized adult patients manifested GI symptoms. Of note, the presence of GI symptoms was associated with more severe disease and thus predictive of outcomes in those admitted to hospitals.
In a multicenter study that assessed pediatric inpatients with COVID-19, GI manifestations were present in 57% of patients and were the first manifestation in 14%. Adjusted by confounding factors, those with GI symptoms had a higher risk for pediatric intensive care unit admission. Patients admitted to the PICU also had higher serum C-reactive protein and aspartate aminotransferase values.
Emerging data on MIS-C
In previously healthy children and adolescents, the severe, life-threatening complication of multisystem inflammatory syndrome in children (MIS-C) may present 2-6 weeks after acute infection with SARS-CoV-2. MIS-C appears to be an immune activation syndrome and is presumed to be the delayed immunologic sequelae of mild/asymptomatic SARS-CoV-2 infection. This response manifests as hyperinflammation in conjunction with a peak in antibody production a few weeks later.
One report of 186 children with MIS-C in the United States noted that the involved organ system included the GI tract in 92%, followed by cardiovascular in 80%, hematologic in 76%, mucocutaneous in 74%, and respiratory in 70%. Affected children were hospitalized for a median of 7 days, with 80% requiring intensive care, 20% receiving mechanical ventilation, and 48% receiving vasoactive support; 2% died. In a similar study of patients hospitalized in New York, 88% had GI symptoms (abdominal pain, vomiting, and/or diarrhea). A retrospective chart review of patients with MIS-C found that the majority had GI symptoms with any portion of the GI tract potentially involved, but ileal and colonic inflammation predominated.
Elizabeth Whittaker, MD, and colleagues described the clinical characteristics of children in eight hospitals in England who met criteria for MIS-C that were temporally associated with SARS-CoV-2. At presentation, all of the patients manifested fever and nonspecific GI symptoms, including vomiting (45%), abdominal pain (53%), and diarrhea (52%). During hospitalization, 50% developed shock with evidence of myocardial dysfunction.
Ermias D. Belay, MD, and colleagues described the clinical characteristics of a large cohort of patients with MIS-C that were reported to the U.S. Centers for Disease Control and Prevention. Of 1,733 patients identified, GI symptoms were reported in 53%-67%. Over half developed hypotension or shock and were admitted for intensive care. Younger children more frequently presented with abdominal pain in contrast with adolescents, who more frequently manifest respiratory symptoms.
In a multicenter retrospective study of Italian children with COVID-19 that was conducted from the onset of the pandemic to early 2021, GI symptoms were noted in 38%. These manifestations were mild and self-limiting, comparable to other viral intestinal infections. However, a subset of children (9.5%) had severe GI manifestations of MIS-C, defined as a medical and/or radiologic diagnosis of acute abdomen, appendicitis, intussusception, pancreatitis, abdominal fluid collection, or diffuse adenomesenteritis requiring surgical consultation. Overall, 42% of this group underwent surgery. The authors noted that the clinical presentation of abdominal pain, lymphopenia, and increased C-reactive protein and ferritin levels were associated with a 9- to 30-fold increased probability of these severe sequelae. In addition, the severity of the GI manifestations was correlated with age (5-10 years: overall response, 8.33; >10 years: OR, 6.37). Again, the presence of GI symptoms was a harbinger of hospitalization and PICU admission.
Given that GI symptoms are a common presentation of MIS-C, its diagnosis may be delayed as clinicians first consider other GI/viral infections, inflammatory bowel disease, or Kawasaki disease. Prompt identification of GI involvement and awareness of the potential outcomes may guide the management and improve the outcome.
These studies provide a clear picture of the differential presenting features of COVID-19 and MIS-C. Although there may be other environmental/genetic factors that govern the incidence, impact, and manifestations, COVID’s status as an ongoing pandemic gives these observations worldwide relevance. This is evident in a recent report documenting pronounced GI symptoms in African children with COVID-19.
It should be noted, however, that the published data cited here reflect the impact of the initial variants of SARS-CoV-2. The GI binding, effects, and aftermath of infection with the Delta and Omicron variants is not yet known.
Cause and effect, or simply coincidental?
Some insight into MIS-C pathogenesis was provided by Lael M. Yonker, MD, and colleagues in their analysis of biospecimens from 100 children: 19 with MIS-C, 26 with acute COVID-19, and 55 controls. They demonstrated that in children with MIS-C the prolonged presence of SARS-CoV-2 in the GI tract led to the release of zonulin, a biomarker of intestinal permeability, with subsequent trafficking of SARS-CoV-2 antigens into the bloodstream, leading to hyperinflammation. They were then able to decrease plasma SARS-CoV-2 spike antigen levels and inflammatory markers, with resulting clinical improvement after administration of larazotide, a zonulin antagonist.
These observations regarding the potential mechanism and triggers of MIS-C may offer biomarkers for early detection and/or strategies for prevention and treatment of MIS-C.
Bottom line
The GI tract is the target of an immune-mediated inflammatory response that is triggered by SARS-CoV-2, with MIS-C being the major manifestation of the resultant high degree of inflammation. These observations will allow an increased awareness of nonrespiratory symptoms of SARS-CoV-2 infection by clinicians working in emergency departments and primary care settings.
Clues that may enhance the ability of pediatric clinicians to recognize the potential for severe GI involvement include the occurrence of abdominal pain, leukopenia, and elevated inflammatory markers. Their presence should raise suspicion of MIS-C and lead to early evaluation.
Of note, COVID-19 mRNA vaccination is associated with a lower incidence of MIS-C in adolescents. This underscores the importance of COVID vaccination for all eligible children. Yet, we clearly have our work cut out for us. Of 107 children with MIS-C who were hospitalized in France, 31% were adolescents eligible for vaccination; however, none had been fully vaccinated. At the end of 2021, CDC data noted that less than 1% of vaccine-eligible children (12-17 years) were fully vaccinated.
The Pfizer-BioNTech vaccine is now authorized for receipt by children aged 5-11 years, the age group that is at highest risk for MIS-C. However, despite the approval of vaccines for these younger children, there is limited access in some parts of the United States at a time of rising incidence.
We look forward to broad availability of pediatric vaccination strategies. In addition, with the intense focus on safe and effective therapeutics for SARS-CoV-2 infection, we hope to soon have strategies to prevent and/or treat the life-threatening manifestations and long-term consequences of MIS-C. For example, the recently reported central role of the gut microbiota in immunity against SARS-CoV-2 infection offer the possibility that “microbiota modulation” may both reduce GI injury and enhance vaccine efficacy.
Dr. Balistreri has disclosed no relevant financial relationships.
William F. Balistreri, MD, is the Dorothy M.M. Kersten Professor of Pediatrics; director emeritus, Pediatric Liver Care Center; medical director emeritus, liver transplantation; and professor, University of Cincinnati College of Medicine, department of pediatrics, Cincinnati Children’s Hospital Medical Center. He has served as director of the division of gastroenterology, hepatology, and nutrition at Cincinnati Children’s for 25 years and frequently covers gastroenterology, liver, and nutrition-related topics for this news organization. Dr Balistreri is currently editor-in-chief of the Journal of Pediatrics, having previously served as editor-in-chief of several journals and textbooks. He also became the first pediatrician to act as president of the American Association for the Study of Liver Diseases. In his spare time, he coaches youth lacrosse.
A version of this article first appeared on Medscape.com.
Children and COVID: New cases down to pre-Omicron level
New cases of COVID-19 in U.S. children dropped for the fifth consecutive week, but the rate of decline slowed considerably, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The national count of new cases has now fallen for five straight weeks since peaking Jan. 14-20, and this week’s figure is the lowest since the pre-Omicron days of mid-November, based on data collected by the AAP and CHA from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.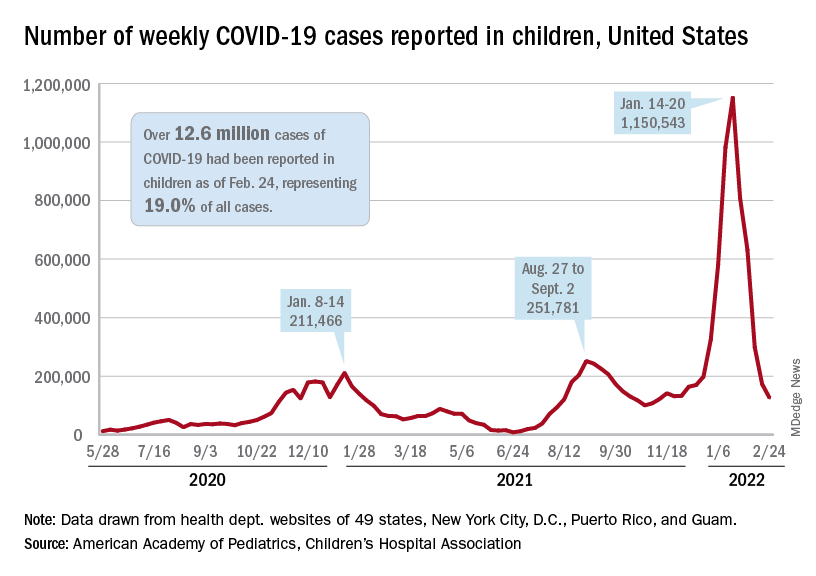
Over 12.6 million pediatric cases have been reported by those jurisdictions since the start of the pandemic, representing 19.0% of all cases in the United States, the AAP and CHA said in their weekly COVID report.
The highest cumulative rate among the states, 27.5%, can be found in Vermont, followed by New Hampshire (26.7%) and Alaska (26.6%). Alabama’s 12.1% is lower than any other jurisdiction, but the state stopped reporting during the summer of 2021, just as the Delta surge was beginning. The next two lowest states, Florida (12.8%) and Utah (13.9%), both define children as those aged 0-14 years, so the state with the lowest rate and no qualifiers is Idaho at 14.3%, the AAP/CHA data show.
The downward trend in new cases is reflected in other national measures. The daily rate of new hospital admissions for children aged 0-17 years was 0.32 per 100,000 population on Feb. 26, which is a drop of 75% since admissions peaked at 1.25 per 100,000 on Jan. 15, according to the Centers for Disease Control and Prevention.
The most recent 7-day average (Feb. 20-26) for child admissions with confirmed COVID-19 was 237 per day, compared with 914 per day during the peak week of Jan. 10-16. Emergency department visits with diagnosed COVID, measured as a percentage of all ED visits by age group, are down even more. The 7-day average was 1.2% on Feb. 25 for children aged 0-11 years, compared with a peak of 13.9% in mid-January, the CDC said on its COVID Data Tracker. The current rates for older children are even lower.
The decline of the Omicron surge over the last few weeks is allowing states to end mask mandates in schools around the country. The governors of California, Oregon, and Washington just announced that their states will be lifting their mask requirements on March 11, and New York State will end its mandate on March 2, while New York City is scheduled to go mask-free as of March 7, according to District Administration.
Those types of government moves, however, do not seem to be entirely supported by the public. In a survey conducted Feb. 9-21 by the Kaiser Family Foundation, 43% of the 1,502 respondents said that all students and staff should be required to wear masks in schools, while 40% said that there should be no mask requirements at all.
New cases of COVID-19 in U.S. children dropped for the fifth consecutive week, but the rate of decline slowed considerably, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The national count of new cases has now fallen for five straight weeks since peaking Jan. 14-20, and this week’s figure is the lowest since the pre-Omicron days of mid-November, based on data collected by the AAP and CHA from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.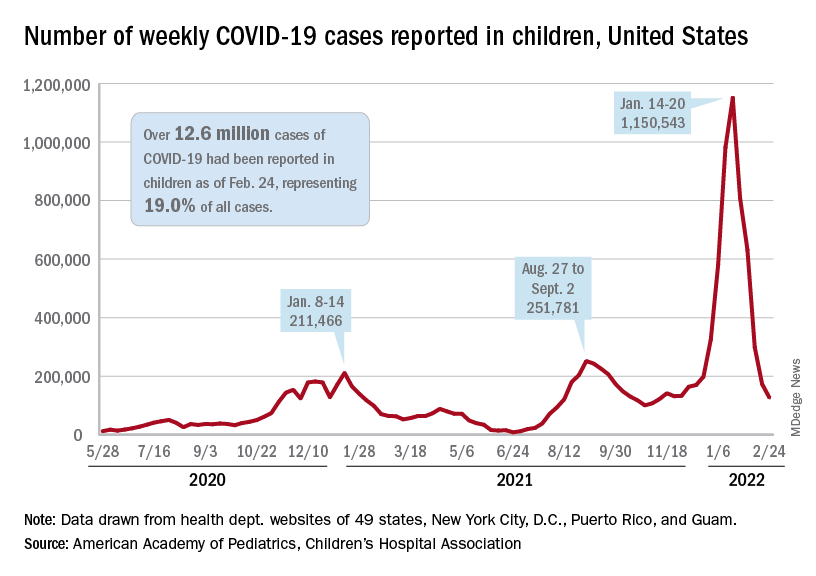
Over 12.6 million pediatric cases have been reported by those jurisdictions since the start of the pandemic, representing 19.0% of all cases in the United States, the AAP and CHA said in their weekly COVID report.
The highest cumulative rate among the states, 27.5%, can be found in Vermont, followed by New Hampshire (26.7%) and Alaska (26.6%). Alabama’s 12.1% is lower than any other jurisdiction, but the state stopped reporting during the summer of 2021, just as the Delta surge was beginning. The next two lowest states, Florida (12.8%) and Utah (13.9%), both define children as those aged 0-14 years, so the state with the lowest rate and no qualifiers is Idaho at 14.3%, the AAP/CHA data show.
The downward trend in new cases is reflected in other national measures. The daily rate of new hospital admissions for children aged 0-17 years was 0.32 per 100,000 population on Feb. 26, which is a drop of 75% since admissions peaked at 1.25 per 100,000 on Jan. 15, according to the Centers for Disease Control and Prevention.
The most recent 7-day average (Feb. 20-26) for child admissions with confirmed COVID-19 was 237 per day, compared with 914 per day during the peak week of Jan. 10-16. Emergency department visits with diagnosed COVID, measured as a percentage of all ED visits by age group, are down even more. The 7-day average was 1.2% on Feb. 25 for children aged 0-11 years, compared with a peak of 13.9% in mid-January, the CDC said on its COVID Data Tracker. The current rates for older children are even lower.
The decline of the Omicron surge over the last few weeks is allowing states to end mask mandates in schools around the country. The governors of California, Oregon, and Washington just announced that their states will be lifting their mask requirements on March 11, and New York State will end its mandate on March 2, while New York City is scheduled to go mask-free as of March 7, according to District Administration.
Those types of government moves, however, do not seem to be entirely supported by the public. In a survey conducted Feb. 9-21 by the Kaiser Family Foundation, 43% of the 1,502 respondents said that all students and staff should be required to wear masks in schools, while 40% said that there should be no mask requirements at all.
New cases of COVID-19 in U.S. children dropped for the fifth consecutive week, but the rate of decline slowed considerably, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The national count of new cases has now fallen for five straight weeks since peaking Jan. 14-20, and this week’s figure is the lowest since the pre-Omicron days of mid-November, based on data collected by the AAP and CHA from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.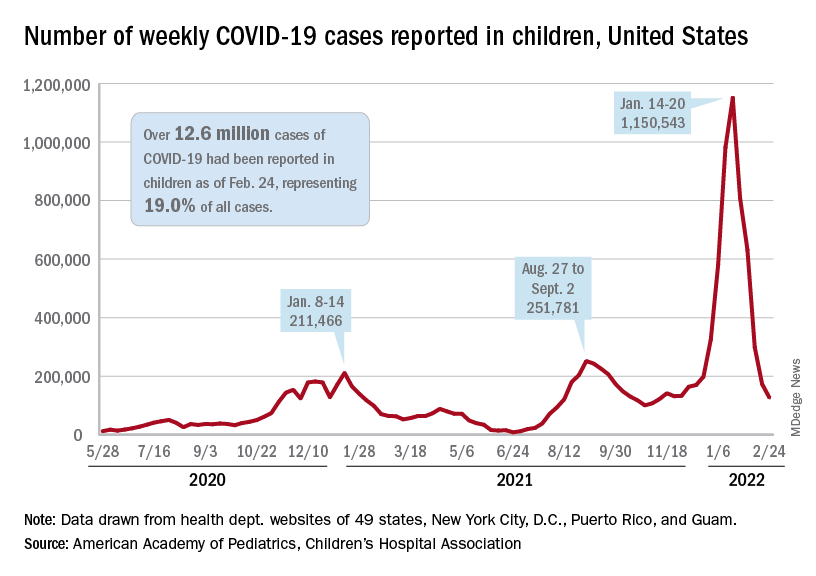
Over 12.6 million pediatric cases have been reported by those jurisdictions since the start of the pandemic, representing 19.0% of all cases in the United States, the AAP and CHA said in their weekly COVID report.
The highest cumulative rate among the states, 27.5%, can be found in Vermont, followed by New Hampshire (26.7%) and Alaska (26.6%). Alabama’s 12.1% is lower than any other jurisdiction, but the state stopped reporting during the summer of 2021, just as the Delta surge was beginning. The next two lowest states, Florida (12.8%) and Utah (13.9%), both define children as those aged 0-14 years, so the state with the lowest rate and no qualifiers is Idaho at 14.3%, the AAP/CHA data show.
The downward trend in new cases is reflected in other national measures. The daily rate of new hospital admissions for children aged 0-17 years was 0.32 per 100,000 population on Feb. 26, which is a drop of 75% since admissions peaked at 1.25 per 100,000 on Jan. 15, according to the Centers for Disease Control and Prevention.
The most recent 7-day average (Feb. 20-26) for child admissions with confirmed COVID-19 was 237 per day, compared with 914 per day during the peak week of Jan. 10-16. Emergency department visits with diagnosed COVID, measured as a percentage of all ED visits by age group, are down even more. The 7-day average was 1.2% on Feb. 25 for children aged 0-11 years, compared with a peak of 13.9% in mid-January, the CDC said on its COVID Data Tracker. The current rates for older children are even lower.
The decline of the Omicron surge over the last few weeks is allowing states to end mask mandates in schools around the country. The governors of California, Oregon, and Washington just announced that their states will be lifting their mask requirements on March 11, and New York State will end its mandate on March 2, while New York City is scheduled to go mask-free as of March 7, according to District Administration.
Those types of government moves, however, do not seem to be entirely supported by the public. In a survey conducted Feb. 9-21 by the Kaiser Family Foundation, 43% of the 1,502 respondents said that all students and staff should be required to wear masks in schools, while 40% said that there should be no mask requirements at all.
Columbia names interim chair of psychiatry after Twitter controversy
Helen Blair Simpson, MD, PhD, will take over for Jeffrey Lieberman, MD, who was suspended over a tweet he sent that was widely condemned as both racist and sexist.
She will also serve as interim director of the New York State Psychiatric Institute and interim psychiatrist-in-chief at New York–Presbyterian/Columbia University Irving Medical Center, the email stated.
All appointments were effective on Feb. 28.
Latest response
Dr. Simpson, who joined the faculty at Columbia in 1999, previously served as a professor and vice chair of research for the psychiatry department, director of Columbia’s Center for Obsessive-Compulsive and Related Disorders, and director of psychiatry research at the New York State Psychiatric Institute. Dr. Simpson is associate editor of JAMA Psychiatry and is president-elect of the Anxiety and Depression Association of America.
Her research has been continuously funded by the National Institute of Mental Health since 1999, and she has advised both the World Health Organization and the American Psychiatric Association on the diagnosis and treatment of OCD.
Dr. Simpson has a bachelor’s degree in biology from Yale University and completed an MD-PhD program at The Rockefeller University and Weill Cornell Medicine, New York. She did her residency in psychiatry at New York–Presbyterian.
The announcement is Columbia’s latest response to the furor that erupted on social media following Dr. Lieberman’s tweet about Sudanese model Nyakim Gatwech, in which he wrote, “Whether a work of art or a freak of nature she’s a beautiful sight to behold.”
Twitter reacted immediately and negatively to the tweet, which even Dr. Lieberman later acknowledged was “racist and sexist” in an email apology he sent Feb. 22 to faculty and staff in the department of psychiatry.
As reported by this news organization, Columbia suspended Dr. Lieberman from his chair position on Feb. 23 and permanently removed him from the post of psychiatrist-in-chief at New York–Presbyterian Hospital/Columbia University Irving Medical Center. Lieberman also resigned as executive director of the New York State Psychiatric Institute.
The email announcing Simpson’s appointment was signed by Katrina Armstrong, MD, incoming CEO, Columbia University Irving Medical Center and dean of the Faculties of Health Sciences and the Vagelos College of Physicians and Surgeons; Anil K. Rustgi, MD, interim executive vice president and dean of the Faculties of Health Sciences and Medicine; Steven J. Corwin, MD; president and CEO, New York–Presbyterian; and Ann Marie Sullivan, MD, commissioner of the New York State Office of Mental Health.
This is a developing story.
A version of this article first appeared on Medscape.com.
Helen Blair Simpson, MD, PhD, will take over for Jeffrey Lieberman, MD, who was suspended over a tweet he sent that was widely condemned as both racist and sexist.
She will also serve as interim director of the New York State Psychiatric Institute and interim psychiatrist-in-chief at New York–Presbyterian/Columbia University Irving Medical Center, the email stated.
All appointments were effective on Feb. 28.
Latest response
Dr. Simpson, who joined the faculty at Columbia in 1999, previously served as a professor and vice chair of research for the psychiatry department, director of Columbia’s Center for Obsessive-Compulsive and Related Disorders, and director of psychiatry research at the New York State Psychiatric Institute. Dr. Simpson is associate editor of JAMA Psychiatry and is president-elect of the Anxiety and Depression Association of America.
Her research has been continuously funded by the National Institute of Mental Health since 1999, and she has advised both the World Health Organization and the American Psychiatric Association on the diagnosis and treatment of OCD.
Dr. Simpson has a bachelor’s degree in biology from Yale University and completed an MD-PhD program at The Rockefeller University and Weill Cornell Medicine, New York. She did her residency in psychiatry at New York–Presbyterian.
The announcement is Columbia’s latest response to the furor that erupted on social media following Dr. Lieberman’s tweet about Sudanese model Nyakim Gatwech, in which he wrote, “Whether a work of art or a freak of nature she’s a beautiful sight to behold.”
Twitter reacted immediately and negatively to the tweet, which even Dr. Lieberman later acknowledged was “racist and sexist” in an email apology he sent Feb. 22 to faculty and staff in the department of psychiatry.
As reported by this news organization, Columbia suspended Dr. Lieberman from his chair position on Feb. 23 and permanently removed him from the post of psychiatrist-in-chief at New York–Presbyterian Hospital/Columbia University Irving Medical Center. Lieberman also resigned as executive director of the New York State Psychiatric Institute.
The email announcing Simpson’s appointment was signed by Katrina Armstrong, MD, incoming CEO, Columbia University Irving Medical Center and dean of the Faculties of Health Sciences and the Vagelos College of Physicians and Surgeons; Anil K. Rustgi, MD, interim executive vice president and dean of the Faculties of Health Sciences and Medicine; Steven J. Corwin, MD; president and CEO, New York–Presbyterian; and Ann Marie Sullivan, MD, commissioner of the New York State Office of Mental Health.
This is a developing story.
A version of this article first appeared on Medscape.com.
Helen Blair Simpson, MD, PhD, will take over for Jeffrey Lieberman, MD, who was suspended over a tweet he sent that was widely condemned as both racist and sexist.
She will also serve as interim director of the New York State Psychiatric Institute and interim psychiatrist-in-chief at New York–Presbyterian/Columbia University Irving Medical Center, the email stated.
All appointments were effective on Feb. 28.
Latest response
Dr. Simpson, who joined the faculty at Columbia in 1999, previously served as a professor and vice chair of research for the psychiatry department, director of Columbia’s Center for Obsessive-Compulsive and Related Disorders, and director of psychiatry research at the New York State Psychiatric Institute. Dr. Simpson is associate editor of JAMA Psychiatry and is president-elect of the Anxiety and Depression Association of America.
Her research has been continuously funded by the National Institute of Mental Health since 1999, and she has advised both the World Health Organization and the American Psychiatric Association on the diagnosis and treatment of OCD.
Dr. Simpson has a bachelor’s degree in biology from Yale University and completed an MD-PhD program at The Rockefeller University and Weill Cornell Medicine, New York. She did her residency in psychiatry at New York–Presbyterian.
The announcement is Columbia’s latest response to the furor that erupted on social media following Dr. Lieberman’s tweet about Sudanese model Nyakim Gatwech, in which he wrote, “Whether a work of art or a freak of nature she’s a beautiful sight to behold.”
Twitter reacted immediately and negatively to the tweet, which even Dr. Lieberman later acknowledged was “racist and sexist” in an email apology he sent Feb. 22 to faculty and staff in the department of psychiatry.
As reported by this news organization, Columbia suspended Dr. Lieberman from his chair position on Feb. 23 and permanently removed him from the post of psychiatrist-in-chief at New York–Presbyterian Hospital/Columbia University Irving Medical Center. Lieberman also resigned as executive director of the New York State Psychiatric Institute.
The email announcing Simpson’s appointment was signed by Katrina Armstrong, MD, incoming CEO, Columbia University Irving Medical Center and dean of the Faculties of Health Sciences and the Vagelos College of Physicians and Surgeons; Anil K. Rustgi, MD, interim executive vice president and dean of the Faculties of Health Sciences and Medicine; Steven J. Corwin, MD; president and CEO, New York–Presbyterian; and Ann Marie Sullivan, MD, commissioner of the New York State Office of Mental Health.
This is a developing story.
A version of this article first appeared on Medscape.com.

