User login
Erythematous and Ulcerated Plaque on the Left Temple
The Diagnosis: Primary Cutaneous Carcinosarcoma
The immunohistochemical findings supported an epithelial component consistent with moderately differentiated squamous cell carcinoma (SCC) and a mesenchymal component with features consistent with a sarcoma. Consequently, the lesion was diagnosed as a primary cutaneous carcinosarcoma (PCCS).
Primary cutaneous carcinosarcoma is a rare biphasic neoplasm consisting of malignant epithelial (carcinoma) and mesenchymal (sarcoma) components.1 Primary cutaneous carcinosarcomas are uncommon, poorly understood, primary cutaneous tumors.2,3 Characteristic of this tumor, cytokeratins highlight the epithelial component while vimentin highlights the mesenchymal component.4 Histologically, the sarcomatous components of PCCS often are highly variable, with an absence of transitional areas within the epithelial component, which frequently resembles basal cell carcinoma and/ or SCC.5-7 Primary cutaneous carcinosarcoma favors areas of chronic UV radiation exposure, particularly on the head and neck. Most tumors present with a slowly growing, polypoid, flesh-colored to erythematous nodule due to the infiltrative mesenchymal component.7 Primary cutaneous carcinosarcoma primarily is diagnosed in elderly patients, with the majority of cases diagnosed in the eighth or ninth decades of life (range, 32–98 years).1,8 Men appear to be twice as likely to be diagnosed with a PCCS compared to women.1 Primary cutaneous carcinosarcomas are recognized as aggressive tumors with a high propensity to metastasize and recur locally, necessitating early diagnosis and treatment.4 Accurate diagnosis of PCCSs can be challenging due to the biphasic nature of the neoplasm as well as poor differentiation or unequal proportions of the epithelial and mesenchymal components.5 Additionally, overlapping diagnostic criteria coupled with vague demarcation between soft-tissue sarcomas and distinct carcinomas also may contribute to a delay in diagnosis.9 Treatment is achieved surgically by complete wide resection, with no evidence to support the use of adjuvant or neoadjuvant external beam radiation therapy. Due to the small number of reported cases, no treatment recommendations currently exist.1
Surgical management with wide local excision has been disappointing, with recurrence rates reported as high as 33%.6 Primary cutaneous carcinosarcoma has an estimated overall recurrence rate of 19% and a 5-year disease-free rate of 50%.10 Risk factors associated with poorer prognosis include tumors with adnexal subtype, age less than 65 years, rapid tumor growth, a tumor greater than 20 mm at presentation, and a long-standing tumor lasting up to 30 years.2,4 Although wide local excision and Mohs micrographic surgery (MMS) both have been utilized successfully, MMS has been shown to result in a cure rate of greater than 98%.6
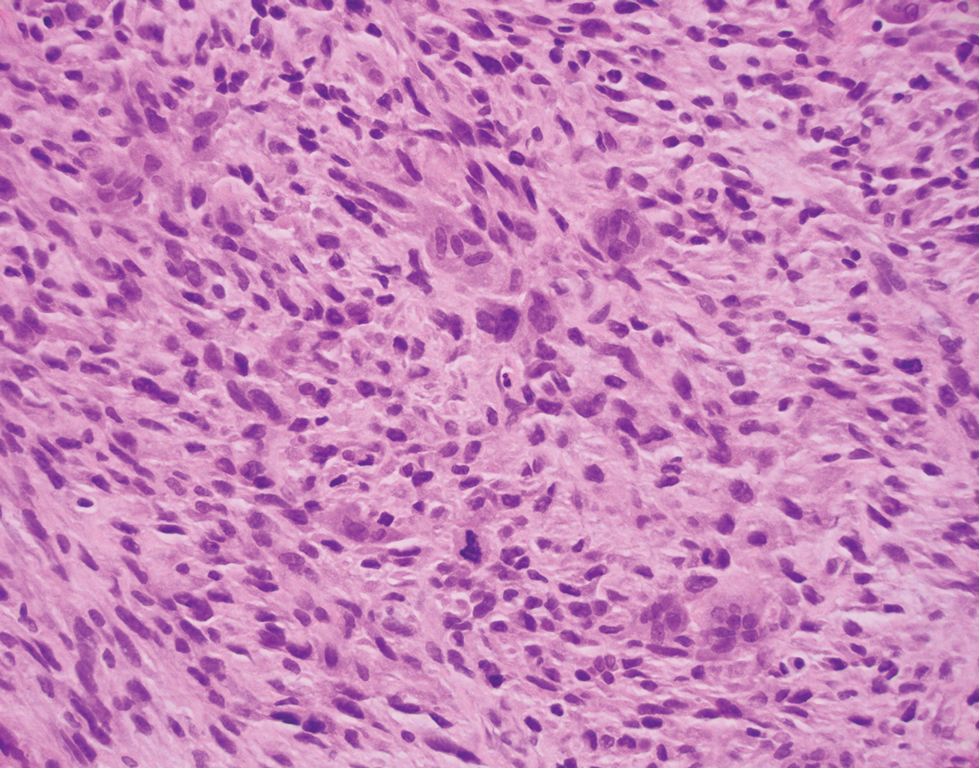
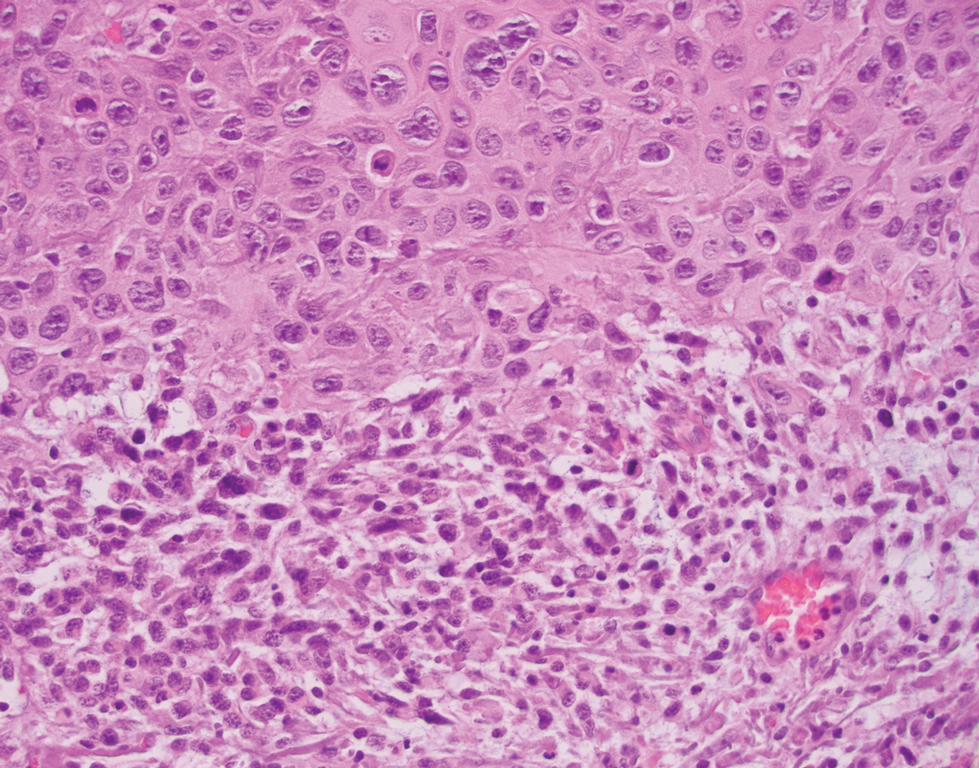
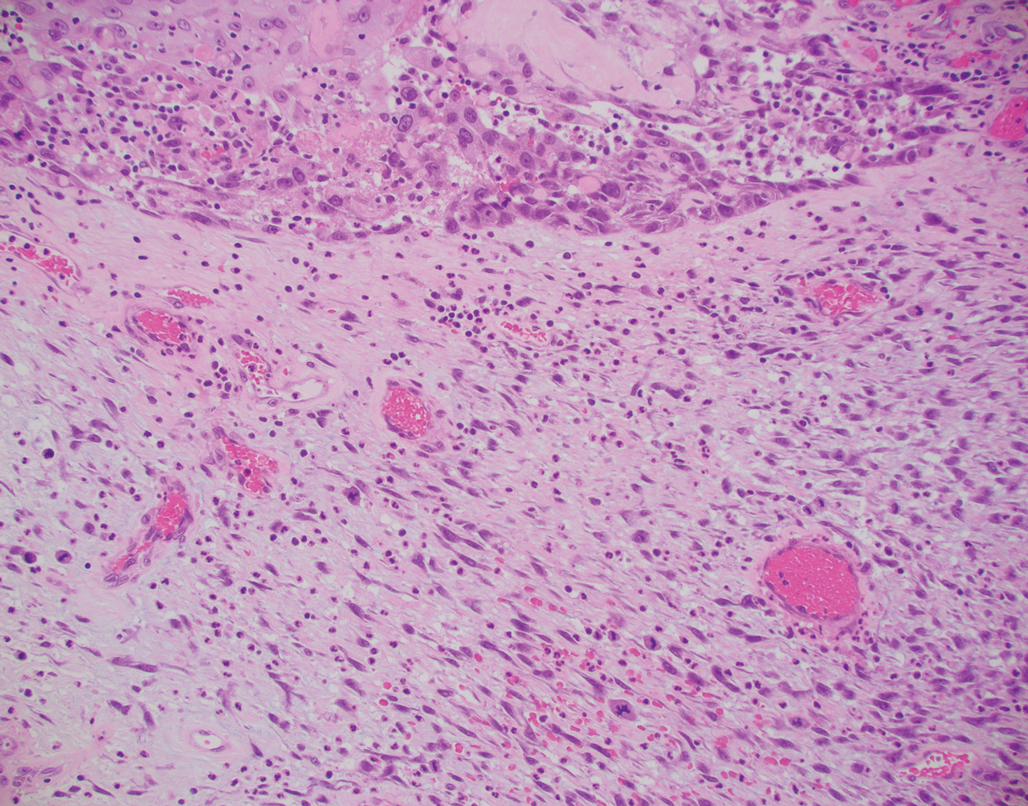
Atypical fibroxanthoma (AFX) is a cutaneous tumor of fibrohistiocytic mesenchymal origin that typically manifests on sun-damaged skin in elderly individuals. Clinically, it presents as a rapidly growing neoplasm that often ulcerates and bleeds. These heterogenous neoplasms have several distinct characteristics, including dense cellularity with disorganized, large, pleomorphic, and atypical-appearing spindle-shaped cells arising in the upper layers of the dermis, often disseminating into the reticular dermis and occasionally into the subcutaneous fat (Figure 1). The neoplastic cells often exhibit hyperchromic and irregular nuclei, multinucleated giant cells, and atypical mitotic figures. In most cases, negative immunohistochemical staining with SOX-10, S-100, cytokeratins, desmin, and caldesmon will allow pathologists to differentiate between AFX and other common tumors on the differential diagnosis, such as SCC, melanoma, and leiomyosarcoma. CD10 and procollagen type 1 are positive antigenic markers in AFX, but they are not specific. The standard treatment of AFX includes wide local excision or MMS for superior margin control.11
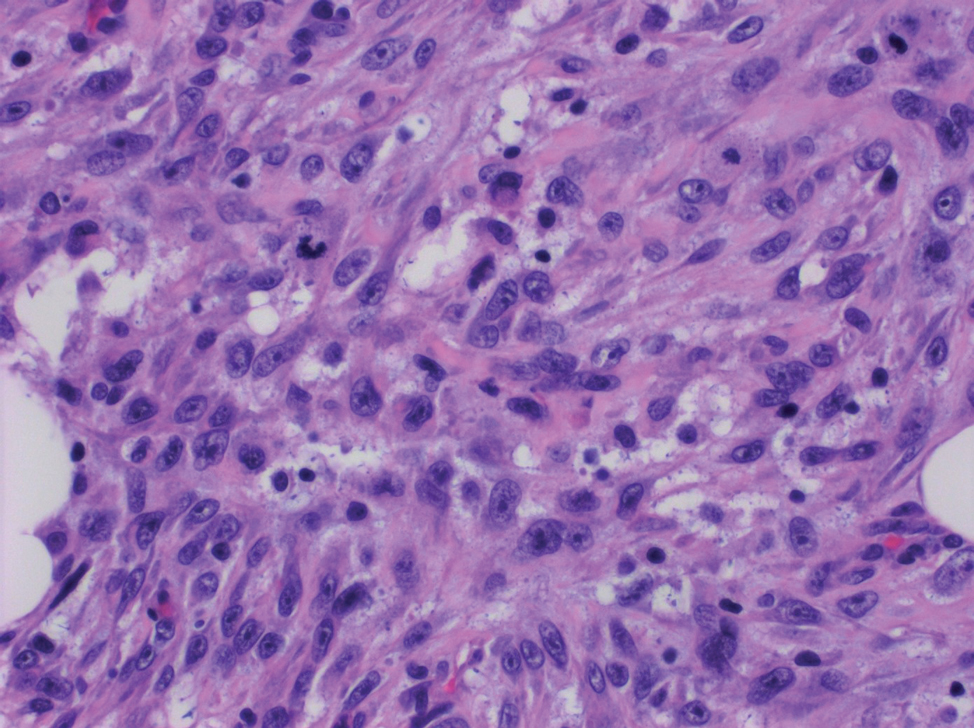
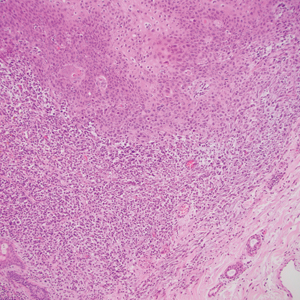
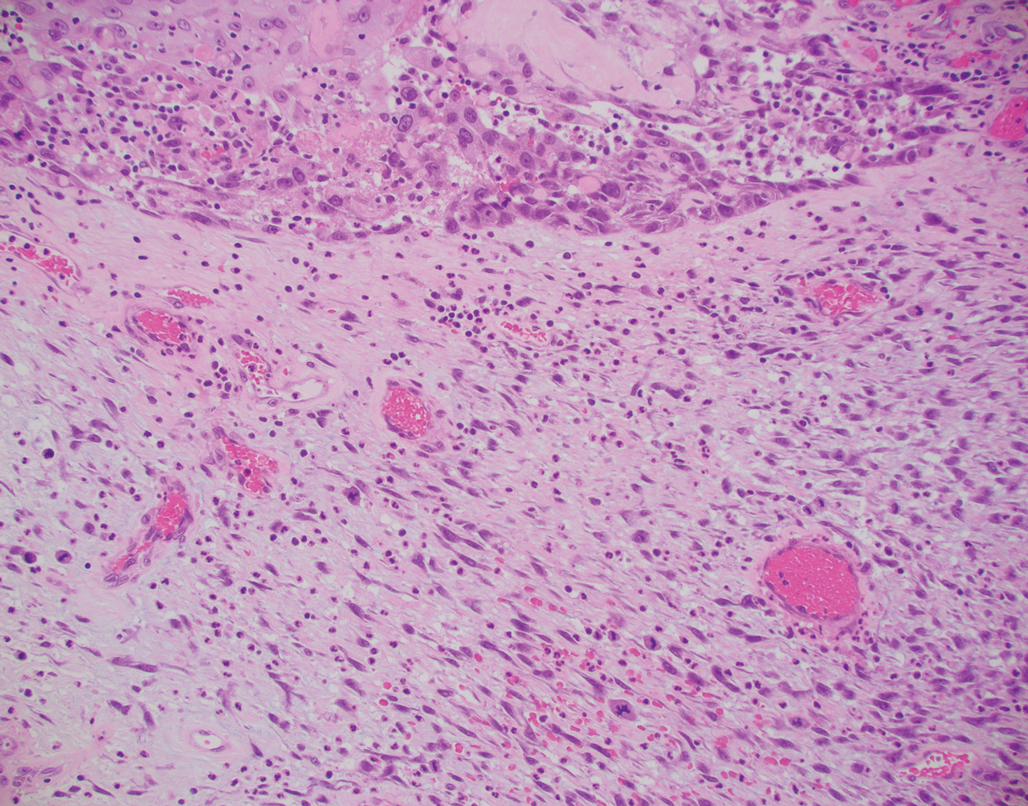
Spindle cell SCC presents as a raised or exophytic nodule, often with spontaneous bleeding and central ulceration. It usually presents on sun-damaged skin or in individuals with a history of ionizing radiation. Histologically, it is characterized by atypical spindleshaped keratinocytes in the dermis existing as single cells or cohesive nests along with keratin pearls (Figure 2). The atypical spindle cells may comprise the entire tumor or only a small portion. The use of immunohistochemical markers often is required to establish a definitive diagnosis. Spindle cell SCC stains positively, albeit frequently focally, for p63, p40, and high-molecular-weight cytokeratins such as cytokeratin 5/6, while S-100 protein, SOX-10, MART-1/Melan-A, and muscle-specific actin stains typically are negative. Wide local excision or MMS is recommended for treatment of these lesions.12
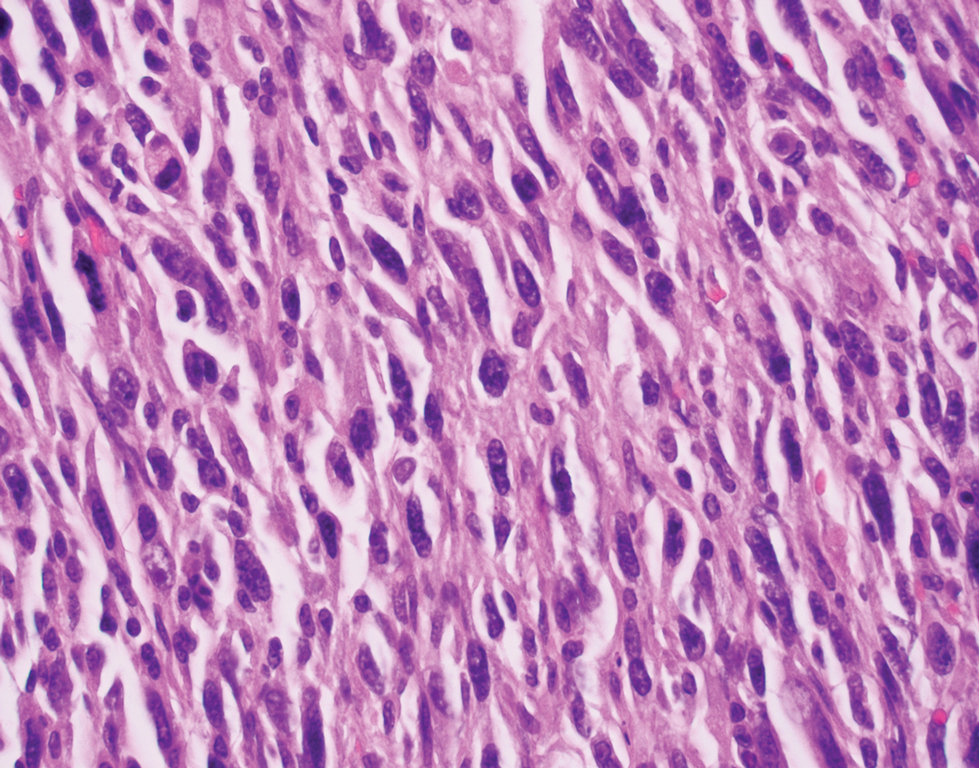
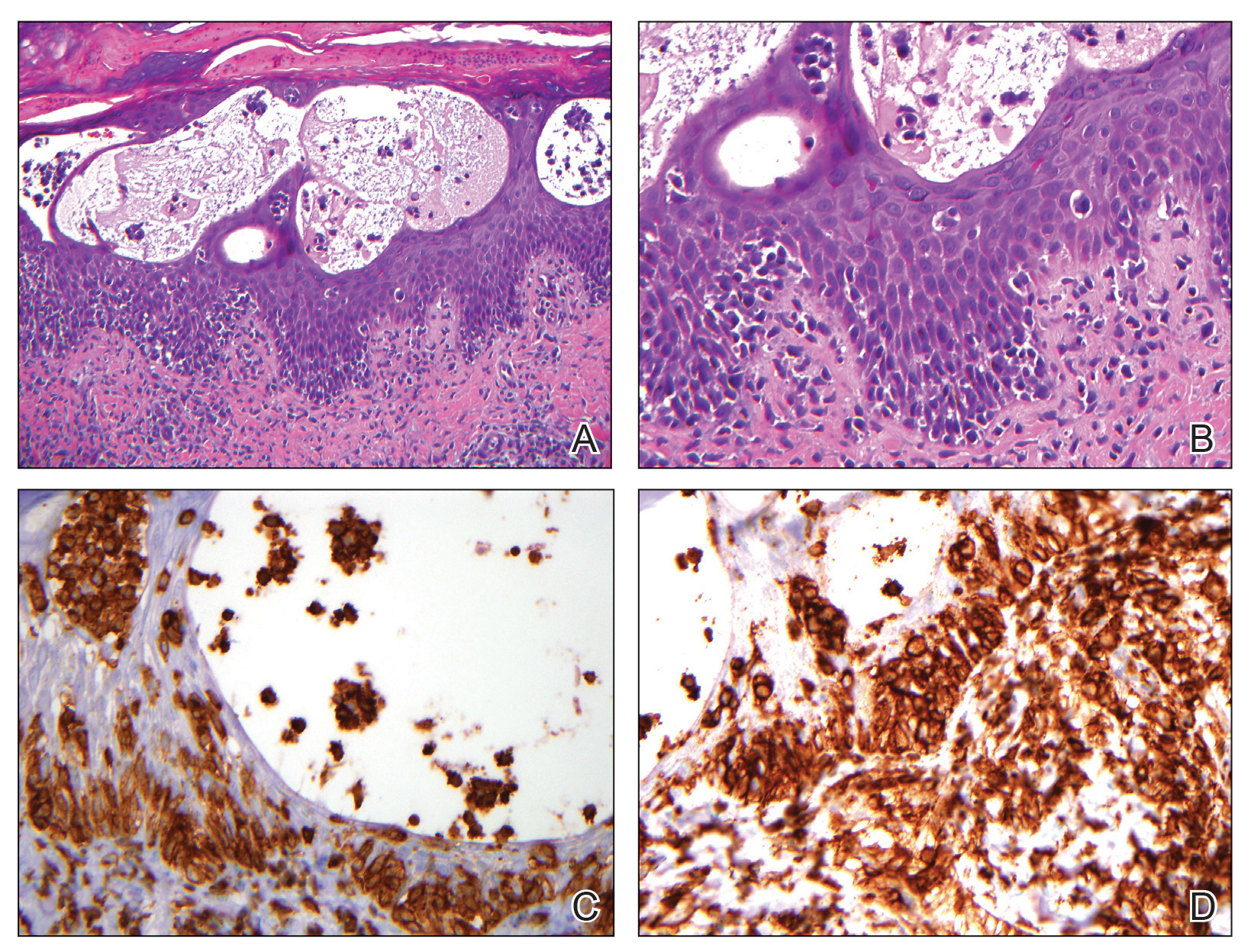
Primary cutaneous myoepithelial carcinomas are uncommon neoplasms of myoepithelial differentiation. Clinically, they often arise as soft nodular lesions on the head, neck, and lower extremities with a bimodal age distribution (50 years). Histologically cutaneous myoepithelial tumors are well-differentiated, dermal-based nodules without connection to the overlying epidermis (Figure 3). The myoepithelial cells can exhibit spindled, epithelioid, plasmacytoid, or clear cell morphologic features and show variability in cell growth patterns. One of the most common growth patterns is oval to round cells forming cords and chains in a chondromyxoid stroma. Most cases display an immunophenotyped co-expression of an epithelial cytokeratin and S-100 protein. Myoepithelial markers also may be present, including keratins, smooth muscle actin, calponin, glial fibrillary acidic protein, p63, and desmin. Surgical removal with wide local excision or MMS is essential.13
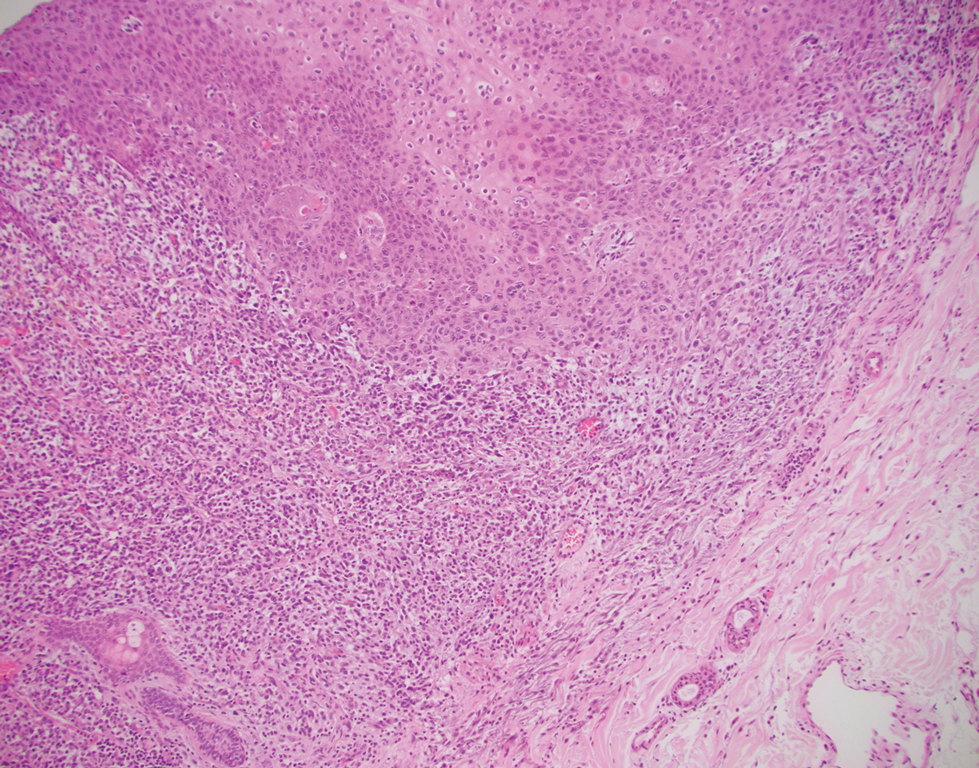
Leiomyosarcoma (LMS) is a tumor that originates from smooth muscle and rarely develops in the dermis.14 Pleomorphic LMS is a morphologic variant of LMS that has a low propensity to metastasize but commonly exhibits local recurrence.15 Leiomyosarcoma can present in any age group but most commonly manifests in individuals aged 50 to 70 years. Clinically, LMS presents as a firm solitary nodule with a smooth pink surface or a more exophytic tumor with a reddish or brown color on the extensor surface of the lower limbs; it is less common on the scalp and face.14 Histologically, most cases of pleomorphic LMS show small foci of fascicles consisting of smooth muscle tumor cells in addition to cellular pleomorphism (Figure 4).15 Many of these cells demonstrate a clear perinuclear vacuole that generally is appreciated in neoplastic smooth muscle cells.14 Pleomorphic LMS typically stains positively for at least one smooth muscle marker including desmin, h-caldesmon, muscle-specific actin, α-smooth muscle actin, or smooth muscle myosin in the leiomyosarcomatous fascicular areas.16 Complete surgical excision is the treatment of choice, and the best results are obtained with MMS.14
- Syme-Grant J, Syme-Grant NJ, Motta L, et al. Are primary cutaneous carcinosarcomas underdiagnosed? five cases and a review of the literature. J Plast Reconstr Aesthet Surg. 2006;59:1402-1408.
- Bourgeault E, Alain J, Gagne E. Primary cutaneous carcinosarcoma of the basal cell subtype should be treated as a high-risk basal cell carcinoma. J Cutan Med Surg. 2015;19:407-411.
- West L, Srivastava D. Cutaneous carcinosarcoma of the medial canthus discovered on Mohs debulk analysis. Dermatol Surg. 2019;45:1700-1702.
- Kwan JM, Satter EK. Carcinosarcoma: a primary cutaneous tumor with biphasic differentiation. Cutis. 2013;92:247-249.
- Suh KY, Lacouture M, Gerami P. p63 in primary cutaneous carcinosarcoma. Am J Dermatopathol. 2007;29:374‐377.
- Ruiz-Villaverde R, Aneiros-Fernandez J. Primary cutaneous carcinosarcoma: a cutaneous neoplasm with an exceptional presentation. Sultan Qaboos Univ Med J. 2018;18:E114-E115.
- Smart CN, Pucci RA, Binder SW, et al. Cutaneous carcinosarcoma with myoepithelial differentiation: immunohistochemical and cytogenetic analysis of a case presenting in an unusual location. Am J Dermatopathol. 2009;31:715‐717.
- Clark JJ, Bowen AR, Bowen GM, et al. Cutaneous carcinosarcoma: a series of six cases and a review of the literature. J Cutan Pathol. 2017;44:34‐44.
- Müller CS, Pföhler C, Schiekofer C, et al. Primary cutaneous carcinosarcomas: a morphological histogenetic concept revisited. Am J Dermatopathol. 2014;36:328‐339.
- Bellew S, Del Rosso JQ, Mobini N. Primary carcinosarcoma of the ear: case report and review of the literature. J Clin Aesthet Dermatol. 2009;2:33‐35.
- Hong SH, Hong SJ, Lee Y, et al. Primary cutaneous carcinosarcoma of the shoulder: case report with literature review. Dermatol Surg. 2013;39:338-340.
- Soleymani T, Aasi SZ, Novoa R, et al. Atypical fibroxanthoma and pleomorphic dermal sarcoma: updates on classification and management. Dermatol Clin. 2019;37:253-259.
- Parekh V, Seykora JT. Cutaneous squamous cell carcinoma. Clin Lab Med. 2017;37:503-525.
- Johnson GE, Stevens K, Morrison AO, et al. Cutaneous myoepithelial carcinoma with disseminated metastases. Cutis. 2017;99:E19-E26.
- Llombart B, Serra-Guillén C, Requena C, et al. Leiomyosarcoma and pleomorphic dermal sarcoma: guidelines for diagnosis and treatment. Actas Dermosifiliogr. 2019;110:4-11.
- Oda Y, Miyajima K, Kawaguchi K, et al. Pleomorphic leiomyosarcoma: clinicopathologic and immunohistochemical study with special emphasis on its distinction from ordinary leiomyosarcoma and malignant fibrous histiocytoma. Am J Surg Pathol. 2001;25:1030-1038.
The Diagnosis: Primary Cutaneous Carcinosarcoma
The immunohistochemical findings supported an epithelial component consistent with moderately differentiated squamous cell carcinoma (SCC) and a mesenchymal component with features consistent with a sarcoma. Consequently, the lesion was diagnosed as a primary cutaneous carcinosarcoma (PCCS).
Primary cutaneous carcinosarcoma is a rare biphasic neoplasm consisting of malignant epithelial (carcinoma) and mesenchymal (sarcoma) components.1 Primary cutaneous carcinosarcomas are uncommon, poorly understood, primary cutaneous tumors.2,3 Characteristic of this tumor, cytokeratins highlight the epithelial component while vimentin highlights the mesenchymal component.4 Histologically, the sarcomatous components of PCCS often are highly variable, with an absence of transitional areas within the epithelial component, which frequently resembles basal cell carcinoma and/ or SCC.5-7 Primary cutaneous carcinosarcoma favors areas of chronic UV radiation exposure, particularly on the head and neck. Most tumors present with a slowly growing, polypoid, flesh-colored to erythematous nodule due to the infiltrative mesenchymal component.7 Primary cutaneous carcinosarcoma primarily is diagnosed in elderly patients, with the majority of cases diagnosed in the eighth or ninth decades of life (range, 32–98 years).1,8 Men appear to be twice as likely to be diagnosed with a PCCS compared to women.1 Primary cutaneous carcinosarcomas are recognized as aggressive tumors with a high propensity to metastasize and recur locally, necessitating early diagnosis and treatment.4 Accurate diagnosis of PCCSs can be challenging due to the biphasic nature of the neoplasm as well as poor differentiation or unequal proportions of the epithelial and mesenchymal components.5 Additionally, overlapping diagnostic criteria coupled with vague demarcation between soft-tissue sarcomas and distinct carcinomas also may contribute to a delay in diagnosis.9 Treatment is achieved surgically by complete wide resection, with no evidence to support the use of adjuvant or neoadjuvant external beam radiation therapy. Due to the small number of reported cases, no treatment recommendations currently exist.1
Surgical management with wide local excision has been disappointing, with recurrence rates reported as high as 33%.6 Primary cutaneous carcinosarcoma has an estimated overall recurrence rate of 19% and a 5-year disease-free rate of 50%.10 Risk factors associated with poorer prognosis include tumors with adnexal subtype, age less than 65 years, rapid tumor growth, a tumor greater than 20 mm at presentation, and a long-standing tumor lasting up to 30 years.2,4 Although wide local excision and Mohs micrographic surgery (MMS) both have been utilized successfully, MMS has been shown to result in a cure rate of greater than 98%.6
Atypical fibroxanthoma (AFX) is a cutaneous tumor of fibrohistiocytic mesenchymal origin that typically manifests on sun-damaged skin in elderly individuals. Clinically, it presents as a rapidly growing neoplasm that often ulcerates and bleeds. These heterogenous neoplasms have several distinct characteristics, including dense cellularity with disorganized, large, pleomorphic, and atypical-appearing spindle-shaped cells arising in the upper layers of the dermis, often disseminating into the reticular dermis and occasionally into the subcutaneous fat (Figure 1). The neoplastic cells often exhibit hyperchromic and irregular nuclei, multinucleated giant cells, and atypical mitotic figures. In most cases, negative immunohistochemical staining with SOX-10, S-100, cytokeratins, desmin, and caldesmon will allow pathologists to differentiate between AFX and other common tumors on the differential diagnosis, such as SCC, melanoma, and leiomyosarcoma. CD10 and procollagen type 1 are positive antigenic markers in AFX, but they are not specific. The standard treatment of AFX includes wide local excision or MMS for superior margin control.11
Spindle cell SCC presents as a raised or exophytic nodule, often with spontaneous bleeding and central ulceration. It usually presents on sun-damaged skin or in individuals with a history of ionizing radiation. Histologically, it is characterized by atypical spindleshaped keratinocytes in the dermis existing as single cells or cohesive nests along with keratin pearls (Figure 2). The atypical spindle cells may comprise the entire tumor or only a small portion. The use of immunohistochemical markers often is required to establish a definitive diagnosis. Spindle cell SCC stains positively, albeit frequently focally, for p63, p40, and high-molecular-weight cytokeratins such as cytokeratin 5/6, while S-100 protein, SOX-10, MART-1/Melan-A, and muscle-specific actin stains typically are negative. Wide local excision or MMS is recommended for treatment of these lesions.12
Primary cutaneous myoepithelial carcinomas are uncommon neoplasms of myoepithelial differentiation. Clinically, they often arise as soft nodular lesions on the head, neck, and lower extremities with a bimodal age distribution (50 years). Histologically cutaneous myoepithelial tumors are well-differentiated, dermal-based nodules without connection to the overlying epidermis (Figure 3). The myoepithelial cells can exhibit spindled, epithelioid, plasmacytoid, or clear cell morphologic features and show variability in cell growth patterns. One of the most common growth patterns is oval to round cells forming cords and chains in a chondromyxoid stroma. Most cases display an immunophenotyped co-expression of an epithelial cytokeratin and S-100 protein. Myoepithelial markers also may be present, including keratins, smooth muscle actin, calponin, glial fibrillary acidic protein, p63, and desmin. Surgical removal with wide local excision or MMS is essential.13
Leiomyosarcoma (LMS) is a tumor that originates from smooth muscle and rarely develops in the dermis.14 Pleomorphic LMS is a morphologic variant of LMS that has a low propensity to metastasize but commonly exhibits local recurrence.15 Leiomyosarcoma can present in any age group but most commonly manifests in individuals aged 50 to 70 years. Clinically, LMS presents as a firm solitary nodule with a smooth pink surface or a more exophytic tumor with a reddish or brown color on the extensor surface of the lower limbs; it is less common on the scalp and face.14 Histologically, most cases of pleomorphic LMS show small foci of fascicles consisting of smooth muscle tumor cells in addition to cellular pleomorphism (Figure 4).15 Many of these cells demonstrate a clear perinuclear vacuole that generally is appreciated in neoplastic smooth muscle cells.14 Pleomorphic LMS typically stains positively for at least one smooth muscle marker including desmin, h-caldesmon, muscle-specific actin, α-smooth muscle actin, or smooth muscle myosin in the leiomyosarcomatous fascicular areas.16 Complete surgical excision is the treatment of choice, and the best results are obtained with MMS.14
The Diagnosis: Primary Cutaneous Carcinosarcoma
The immunohistochemical findings supported an epithelial component consistent with moderately differentiated squamous cell carcinoma (SCC) and a mesenchymal component with features consistent with a sarcoma. Consequently, the lesion was diagnosed as a primary cutaneous carcinosarcoma (PCCS).
Primary cutaneous carcinosarcoma is a rare biphasic neoplasm consisting of malignant epithelial (carcinoma) and mesenchymal (sarcoma) components.1 Primary cutaneous carcinosarcomas are uncommon, poorly understood, primary cutaneous tumors.2,3 Characteristic of this tumor, cytokeratins highlight the epithelial component while vimentin highlights the mesenchymal component.4 Histologically, the sarcomatous components of PCCS often are highly variable, with an absence of transitional areas within the epithelial component, which frequently resembles basal cell carcinoma and/ or SCC.5-7 Primary cutaneous carcinosarcoma favors areas of chronic UV radiation exposure, particularly on the head and neck. Most tumors present with a slowly growing, polypoid, flesh-colored to erythematous nodule due to the infiltrative mesenchymal component.7 Primary cutaneous carcinosarcoma primarily is diagnosed in elderly patients, with the majority of cases diagnosed in the eighth or ninth decades of life (range, 32–98 years).1,8 Men appear to be twice as likely to be diagnosed with a PCCS compared to women.1 Primary cutaneous carcinosarcomas are recognized as aggressive tumors with a high propensity to metastasize and recur locally, necessitating early diagnosis and treatment.4 Accurate diagnosis of PCCSs can be challenging due to the biphasic nature of the neoplasm as well as poor differentiation or unequal proportions of the epithelial and mesenchymal components.5 Additionally, overlapping diagnostic criteria coupled with vague demarcation between soft-tissue sarcomas and distinct carcinomas also may contribute to a delay in diagnosis.9 Treatment is achieved surgically by complete wide resection, with no evidence to support the use of adjuvant or neoadjuvant external beam radiation therapy. Due to the small number of reported cases, no treatment recommendations currently exist.1
Surgical management with wide local excision has been disappointing, with recurrence rates reported as high as 33%.6 Primary cutaneous carcinosarcoma has an estimated overall recurrence rate of 19% and a 5-year disease-free rate of 50%.10 Risk factors associated with poorer prognosis include tumors with adnexal subtype, age less than 65 years, rapid tumor growth, a tumor greater than 20 mm at presentation, and a long-standing tumor lasting up to 30 years.2,4 Although wide local excision and Mohs micrographic surgery (MMS) both have been utilized successfully, MMS has been shown to result in a cure rate of greater than 98%.6
Atypical fibroxanthoma (AFX) is a cutaneous tumor of fibrohistiocytic mesenchymal origin that typically manifests on sun-damaged skin in elderly individuals. Clinically, it presents as a rapidly growing neoplasm that often ulcerates and bleeds. These heterogenous neoplasms have several distinct characteristics, including dense cellularity with disorganized, large, pleomorphic, and atypical-appearing spindle-shaped cells arising in the upper layers of the dermis, often disseminating into the reticular dermis and occasionally into the subcutaneous fat (Figure 1). The neoplastic cells often exhibit hyperchromic and irregular nuclei, multinucleated giant cells, and atypical mitotic figures. In most cases, negative immunohistochemical staining with SOX-10, S-100, cytokeratins, desmin, and caldesmon will allow pathologists to differentiate between AFX and other common tumors on the differential diagnosis, such as SCC, melanoma, and leiomyosarcoma. CD10 and procollagen type 1 are positive antigenic markers in AFX, but they are not specific. The standard treatment of AFX includes wide local excision or MMS for superior margin control.11
Spindle cell SCC presents as a raised or exophytic nodule, often with spontaneous bleeding and central ulceration. It usually presents on sun-damaged skin or in individuals with a history of ionizing radiation. Histologically, it is characterized by atypical spindleshaped keratinocytes in the dermis existing as single cells or cohesive nests along with keratin pearls (Figure 2). The atypical spindle cells may comprise the entire tumor or only a small portion. The use of immunohistochemical markers often is required to establish a definitive diagnosis. Spindle cell SCC stains positively, albeit frequently focally, for p63, p40, and high-molecular-weight cytokeratins such as cytokeratin 5/6, while S-100 protein, SOX-10, MART-1/Melan-A, and muscle-specific actin stains typically are negative. Wide local excision or MMS is recommended for treatment of these lesions.12
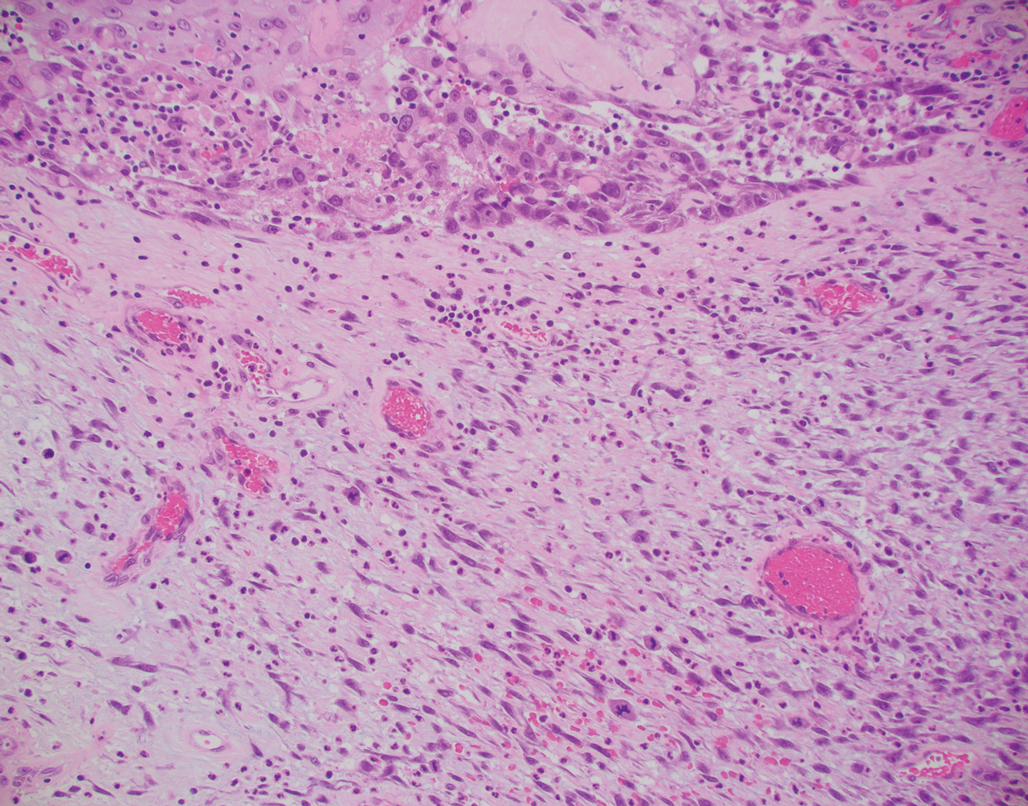
Primary cutaneous myoepithelial carcinomas are uncommon neoplasms of myoepithelial differentiation. Clinically, they often arise as soft nodular lesions on the head, neck, and lower extremities with a bimodal age distribution (50 years). Histologically cutaneous myoepithelial tumors are well-differentiated, dermal-based nodules without connection to the overlying epidermis (Figure 3). The myoepithelial cells can exhibit spindled, epithelioid, plasmacytoid, or clear cell morphologic features and show variability in cell growth patterns. One of the most common growth patterns is oval to round cells forming cords and chains in a chondromyxoid stroma. Most cases display an immunophenotyped co-expression of an epithelial cytokeratin and S-100 protein. Myoepithelial markers also may be present, including keratins, smooth muscle actin, calponin, glial fibrillary acidic protein, p63, and desmin. Surgical removal with wide local excision or MMS is essential.13
Leiomyosarcoma (LMS) is a tumor that originates from smooth muscle and rarely develops in the dermis.14 Pleomorphic LMS is a morphologic variant of LMS that has a low propensity to metastasize but commonly exhibits local recurrence.15 Leiomyosarcoma can present in any age group but most commonly manifests in individuals aged 50 to 70 years. Clinically, LMS presents as a firm solitary nodule with a smooth pink surface or a more exophytic tumor with a reddish or brown color on the extensor surface of the lower limbs; it is less common on the scalp and face.14 Histologically, most cases of pleomorphic LMS show small foci of fascicles consisting of smooth muscle tumor cells in addition to cellular pleomorphism (Figure 4).15 Many of these cells demonstrate a clear perinuclear vacuole that generally is appreciated in neoplastic smooth muscle cells.14 Pleomorphic LMS typically stains positively for at least one smooth muscle marker including desmin, h-caldesmon, muscle-specific actin, α-smooth muscle actin, or smooth muscle myosin in the leiomyosarcomatous fascicular areas.16 Complete surgical excision is the treatment of choice, and the best results are obtained with MMS.14
- Syme-Grant J, Syme-Grant NJ, Motta L, et al. Are primary cutaneous carcinosarcomas underdiagnosed? five cases and a review of the literature. J Plast Reconstr Aesthet Surg. 2006;59:1402-1408.
- Bourgeault E, Alain J, Gagne E. Primary cutaneous carcinosarcoma of the basal cell subtype should be treated as a high-risk basal cell carcinoma. J Cutan Med Surg. 2015;19:407-411.
- West L, Srivastava D. Cutaneous carcinosarcoma of the medial canthus discovered on Mohs debulk analysis. Dermatol Surg. 2019;45:1700-1702.
- Kwan JM, Satter EK. Carcinosarcoma: a primary cutaneous tumor with biphasic differentiation. Cutis. 2013;92:247-249.
- Suh KY, Lacouture M, Gerami P. p63 in primary cutaneous carcinosarcoma. Am J Dermatopathol. 2007;29:374‐377.
- Ruiz-Villaverde R, Aneiros-Fernandez J. Primary cutaneous carcinosarcoma: a cutaneous neoplasm with an exceptional presentation. Sultan Qaboos Univ Med J. 2018;18:E114-E115.
- Smart CN, Pucci RA, Binder SW, et al. Cutaneous carcinosarcoma with myoepithelial differentiation: immunohistochemical and cytogenetic analysis of a case presenting in an unusual location. Am J Dermatopathol. 2009;31:715‐717.
- Clark JJ, Bowen AR, Bowen GM, et al. Cutaneous carcinosarcoma: a series of six cases and a review of the literature. J Cutan Pathol. 2017;44:34‐44.
- Müller CS, Pföhler C, Schiekofer C, et al. Primary cutaneous carcinosarcomas: a morphological histogenetic concept revisited. Am J Dermatopathol. 2014;36:328‐339.
- Bellew S, Del Rosso JQ, Mobini N. Primary carcinosarcoma of the ear: case report and review of the literature. J Clin Aesthet Dermatol. 2009;2:33‐35.
- Hong SH, Hong SJ, Lee Y, et al. Primary cutaneous carcinosarcoma of the shoulder: case report with literature review. Dermatol Surg. 2013;39:338-340.
- Soleymani T, Aasi SZ, Novoa R, et al. Atypical fibroxanthoma and pleomorphic dermal sarcoma: updates on classification and management. Dermatol Clin. 2019;37:253-259.
- Parekh V, Seykora JT. Cutaneous squamous cell carcinoma. Clin Lab Med. 2017;37:503-525.
- Johnson GE, Stevens K, Morrison AO, et al. Cutaneous myoepithelial carcinoma with disseminated metastases. Cutis. 2017;99:E19-E26.
- Llombart B, Serra-Guillén C, Requena C, et al. Leiomyosarcoma and pleomorphic dermal sarcoma: guidelines for diagnosis and treatment. Actas Dermosifiliogr. 2019;110:4-11.
- Oda Y, Miyajima K, Kawaguchi K, et al. Pleomorphic leiomyosarcoma: clinicopathologic and immunohistochemical study with special emphasis on its distinction from ordinary leiomyosarcoma and malignant fibrous histiocytoma. Am J Surg Pathol. 2001;25:1030-1038.
- Syme-Grant J, Syme-Grant NJ, Motta L, et al. Are primary cutaneous carcinosarcomas underdiagnosed? five cases and a review of the literature. J Plast Reconstr Aesthet Surg. 2006;59:1402-1408.
- Bourgeault E, Alain J, Gagne E. Primary cutaneous carcinosarcoma of the basal cell subtype should be treated as a high-risk basal cell carcinoma. J Cutan Med Surg. 2015;19:407-411.
- West L, Srivastava D. Cutaneous carcinosarcoma of the medial canthus discovered on Mohs debulk analysis. Dermatol Surg. 2019;45:1700-1702.
- Kwan JM, Satter EK. Carcinosarcoma: a primary cutaneous tumor with biphasic differentiation. Cutis. 2013;92:247-249.
- Suh KY, Lacouture M, Gerami P. p63 in primary cutaneous carcinosarcoma. Am J Dermatopathol. 2007;29:374‐377.
- Ruiz-Villaverde R, Aneiros-Fernandez J. Primary cutaneous carcinosarcoma: a cutaneous neoplasm with an exceptional presentation. Sultan Qaboos Univ Med J. 2018;18:E114-E115.
- Smart CN, Pucci RA, Binder SW, et al. Cutaneous carcinosarcoma with myoepithelial differentiation: immunohistochemical and cytogenetic analysis of a case presenting in an unusual location. Am J Dermatopathol. 2009;31:715‐717.
- Clark JJ, Bowen AR, Bowen GM, et al. Cutaneous carcinosarcoma: a series of six cases and a review of the literature. J Cutan Pathol. 2017;44:34‐44.
- Müller CS, Pföhler C, Schiekofer C, et al. Primary cutaneous carcinosarcomas: a morphological histogenetic concept revisited. Am J Dermatopathol. 2014;36:328‐339.
- Bellew S, Del Rosso JQ, Mobini N. Primary carcinosarcoma of the ear: case report and review of the literature. J Clin Aesthet Dermatol. 2009;2:33‐35.
- Hong SH, Hong SJ, Lee Y, et al. Primary cutaneous carcinosarcoma of the shoulder: case report with literature review. Dermatol Surg. 2013;39:338-340.
- Soleymani T, Aasi SZ, Novoa R, et al. Atypical fibroxanthoma and pleomorphic dermal sarcoma: updates on classification and management. Dermatol Clin. 2019;37:253-259.
- Parekh V, Seykora JT. Cutaneous squamous cell carcinoma. Clin Lab Med. 2017;37:503-525.
- Johnson GE, Stevens K, Morrison AO, et al. Cutaneous myoepithelial carcinoma with disseminated metastases. Cutis. 2017;99:E19-E26.
- Llombart B, Serra-Guillén C, Requena C, et al. Leiomyosarcoma and pleomorphic dermal sarcoma: guidelines for diagnosis and treatment. Actas Dermosifiliogr. 2019;110:4-11.
- Oda Y, Miyajima K, Kawaguchi K, et al. Pleomorphic leiomyosarcoma: clinicopathologic and immunohistochemical study with special emphasis on its distinction from ordinary leiomyosarcoma and malignant fibrous histiocytoma. Am J Surg Pathol. 2001;25:1030-1038.
A 72-year-old man with a history of nonmelanoma skin cancer and lung transplant maintained on stable doses of prednisone and tacrolimus presented with a 1.3×1.8-cm, slow-growing, well-demarcated, ulcerated, erythematous plaque with overlying serous crust on the left temple of 6 months’ duration. No cervical or axillary lymphadenopathy was appreciated on physical examination. A biopsy was performed followed by Mohs micrographic surgery. Microscopic examination of the debulking specimen revealed atypical spindle cells in the papillary and reticular dermis radiating from a central focus of a moderately differentiated squamous cell carcinoma. The squamous cells stained positive for cytokeratin 5/6, pankeratin, and p40, while the spindle cells stained positive only for vimentin.
Atopic dermatitis subtype worsens into midlife, predicting poor health
giving reason to observe patients beyond the pediatric stage, according to a cohort study of more than 30,000 patients.
Early-life environmental factors, such as tobacco smoke exposure, were not reliable predictors of increasing AD into mid-adulthood, suggesting that a patient’s contemporaneous environment may impact disease course throughout life, reported lead author Katrina Abuabara, MD, associate professor of dermatology at the University of California, San Francisco, and colleagues.
“There is a lack of studies that prospectively examine the course of atopic eczema beyond adolescence/early adulthood, and a more comprehensive understanding of disease activity across the life span is needed,” the investigators wrote in JAMA Dermatology. “Data on long-term disease course may offer insight into mechanisms for disease onset and persistence, are important when counseling patients, and would establish baseline trajectories for future studies of whether new treatments can modify disease course and development of comorbidities.”
The present study included 30,905 patients from two population-based birth cohorts: the 1958 National Childhood Development Study (NCDS) and the 1970 British Cohort Study (BCS70). Follow-up data were collected between 1958 and 2016 via nine waves of standardized questionnaires, and subtypes of atopic eczema patterns were identified “based on parent-reported or self-reported atopic eczema period prevalence.”
This measure “was previously shown to coincide with standardized clinical examinations among children in the NCDS, and a similar questionnaire demonstrated high sensitivity and specificity for physician-diagnosed atopic eczema in U.S. populations,” the investigators noted.
Latent class analysis identified four disease subtypes based on probability of reporting prevalent AD into midlife: low (88%-91%), decreasing (4%), increasing (2%-6%), and persistently high (2%-3%) probability.
Next, the investigators looked for associations between these subtypes and established early-life risk factors, such as history of breastfeeding and childhood smoke exposure. None of the childhood environmental factors differentiated between high versus decreasing disease in adulthood, or increasing versus decreasing disease in adulthood. In contrast, female sex predicted the high versus decreasing adult subtype (odds ratio, 1.99; 95% confidence interval, 1.66-2.38), and the increasing versus decreasing adult subtype (OR, 1.99; 95% CI, 1.69-2.35).
These findings suggest that “disease trajectory is modifiable and may be influenced by environmental factors throughout life,” the investigators wrote.
Further analysis uncovered associations between adult AD subtypes and other health outcomes. For example, compared with adults in the low probability group, those in the high probability group were significantly more likely to report rhinitis (OR, 2.70; 95% CI, 2.24-3.26) and asthma (OR, 3.45; 95% CI, 2.82-4.21). Adults with the increasing subtype also had elevated rates of asthma and rhinitis, along with worse self-reported mental health at age 42 (OR, 1.45; 95% CI, 1.23-1.72) and poor general health at age 46/50 (OR, 1.29; 95% CI, 1.09-1.53).
“When extending the window of observation beyond childhood, clear subtypes of atopic eczema based on patterns of disease activity emerged,” the investigators concluded. “In particular, a newly identified subtype with increasing probability of activity in adulthood warrants additional attention given associations with poor self-reported physical and mental health in midlife.”
Commenting on these results, Robert Sidbury, MD, professor of dermatology at the University of Washington, Seattle, said that this is an “important study” because it adds to our understanding of natural disease course over time.
This knowledge, as a pediatric dermatologist, will help Dr. Sidbury answer one of the most common questions he hears from parents: When is it going to stop?
“Trying to put a little bit more evidence-based heft behind the answer ... is really important,” he said in an interview.
Based on available data, up to 10% of children with AD may have disease activity into adulthood, according to Dr. Sidbury, who is also chief of dermatology at Seattle Children’s Hospital.
“I would hazard to guess that most of those adults who have atopic dermatitis – at least the ones who had it in childhood – were told that they would grow out of it,” he said. “And so I think awareness is important – that [resolution with age] does not always happen.”
The findings also support the possibility that AD is a systemic disease, and that underlying immune dysregulation may be linked with serious health consequences later in life, Dr. Sidbury said, noting that “the stakes get higher and higher when you start speculating in that way.”
According to Dr. Sidbury, the reported link between childhood AD and poor midlife health raises questions about how modifiable the disease course may be, particularly in response to earlier intervention with emerging AD medications, which “seem to be much more effective and potent.”
“Will the advent of these medications and their adoption and use in treatment perhaps have a significant impact, not just on the prevention of atopic dermatitis itself, but maybe other comorbidities?” he asked.
For the time being, this question remains unanswered.
The study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Wellcome Trust. Dr. Abuabara received grants from the National Institutes of Health during the study, as well as personal fees from Target RWE and Pfizer outside of this study. One author reported receiving NIH grants during the study, another reported receiving grants from the Wellcome Trust and the Innovative Medicine Initiative Horizon 2020 (BIOMAP project) during the study; there were no other disclosures. Dr. Sidbury disclosed relationships with Galderma, Regeneron, and Pfizer.
giving reason to observe patients beyond the pediatric stage, according to a cohort study of more than 30,000 patients.
Early-life environmental factors, such as tobacco smoke exposure, were not reliable predictors of increasing AD into mid-adulthood, suggesting that a patient’s contemporaneous environment may impact disease course throughout life, reported lead author Katrina Abuabara, MD, associate professor of dermatology at the University of California, San Francisco, and colleagues.
“There is a lack of studies that prospectively examine the course of atopic eczema beyond adolescence/early adulthood, and a more comprehensive understanding of disease activity across the life span is needed,” the investigators wrote in JAMA Dermatology. “Data on long-term disease course may offer insight into mechanisms for disease onset and persistence, are important when counseling patients, and would establish baseline trajectories for future studies of whether new treatments can modify disease course and development of comorbidities.”
The present study included 30,905 patients from two population-based birth cohorts: the 1958 National Childhood Development Study (NCDS) and the 1970 British Cohort Study (BCS70). Follow-up data were collected between 1958 and 2016 via nine waves of standardized questionnaires, and subtypes of atopic eczema patterns were identified “based on parent-reported or self-reported atopic eczema period prevalence.”
This measure “was previously shown to coincide with standardized clinical examinations among children in the NCDS, and a similar questionnaire demonstrated high sensitivity and specificity for physician-diagnosed atopic eczema in U.S. populations,” the investigators noted.
Latent class analysis identified four disease subtypes based on probability of reporting prevalent AD into midlife: low (88%-91%), decreasing (4%), increasing (2%-6%), and persistently high (2%-3%) probability.
Next, the investigators looked for associations between these subtypes and established early-life risk factors, such as history of breastfeeding and childhood smoke exposure. None of the childhood environmental factors differentiated between high versus decreasing disease in adulthood, or increasing versus decreasing disease in adulthood. In contrast, female sex predicted the high versus decreasing adult subtype (odds ratio, 1.99; 95% confidence interval, 1.66-2.38), and the increasing versus decreasing adult subtype (OR, 1.99; 95% CI, 1.69-2.35).
These findings suggest that “disease trajectory is modifiable and may be influenced by environmental factors throughout life,” the investigators wrote.
Further analysis uncovered associations between adult AD subtypes and other health outcomes. For example, compared with adults in the low probability group, those in the high probability group were significantly more likely to report rhinitis (OR, 2.70; 95% CI, 2.24-3.26) and asthma (OR, 3.45; 95% CI, 2.82-4.21). Adults with the increasing subtype also had elevated rates of asthma and rhinitis, along with worse self-reported mental health at age 42 (OR, 1.45; 95% CI, 1.23-1.72) and poor general health at age 46/50 (OR, 1.29; 95% CI, 1.09-1.53).
“When extending the window of observation beyond childhood, clear subtypes of atopic eczema based on patterns of disease activity emerged,” the investigators concluded. “In particular, a newly identified subtype with increasing probability of activity in adulthood warrants additional attention given associations with poor self-reported physical and mental health in midlife.”
Commenting on these results, Robert Sidbury, MD, professor of dermatology at the University of Washington, Seattle, said that this is an “important study” because it adds to our understanding of natural disease course over time.
This knowledge, as a pediatric dermatologist, will help Dr. Sidbury answer one of the most common questions he hears from parents: When is it going to stop?
“Trying to put a little bit more evidence-based heft behind the answer ... is really important,” he said in an interview.
Based on available data, up to 10% of children with AD may have disease activity into adulthood, according to Dr. Sidbury, who is also chief of dermatology at Seattle Children’s Hospital.
“I would hazard to guess that most of those adults who have atopic dermatitis – at least the ones who had it in childhood – were told that they would grow out of it,” he said. “And so I think awareness is important – that [resolution with age] does not always happen.”
The findings also support the possibility that AD is a systemic disease, and that underlying immune dysregulation may be linked with serious health consequences later in life, Dr. Sidbury said, noting that “the stakes get higher and higher when you start speculating in that way.”
According to Dr. Sidbury, the reported link between childhood AD and poor midlife health raises questions about how modifiable the disease course may be, particularly in response to earlier intervention with emerging AD medications, which “seem to be much more effective and potent.”
“Will the advent of these medications and their adoption and use in treatment perhaps have a significant impact, not just on the prevention of atopic dermatitis itself, but maybe other comorbidities?” he asked.
For the time being, this question remains unanswered.
The study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Wellcome Trust. Dr. Abuabara received grants from the National Institutes of Health during the study, as well as personal fees from Target RWE and Pfizer outside of this study. One author reported receiving NIH grants during the study, another reported receiving grants from the Wellcome Trust and the Innovative Medicine Initiative Horizon 2020 (BIOMAP project) during the study; there were no other disclosures. Dr. Sidbury disclosed relationships with Galderma, Regeneron, and Pfizer.
giving reason to observe patients beyond the pediatric stage, according to a cohort study of more than 30,000 patients.
Early-life environmental factors, such as tobacco smoke exposure, were not reliable predictors of increasing AD into mid-adulthood, suggesting that a patient’s contemporaneous environment may impact disease course throughout life, reported lead author Katrina Abuabara, MD, associate professor of dermatology at the University of California, San Francisco, and colleagues.
“There is a lack of studies that prospectively examine the course of atopic eczema beyond adolescence/early adulthood, and a more comprehensive understanding of disease activity across the life span is needed,” the investigators wrote in JAMA Dermatology. “Data on long-term disease course may offer insight into mechanisms for disease onset and persistence, are important when counseling patients, and would establish baseline trajectories for future studies of whether new treatments can modify disease course and development of comorbidities.”
The present study included 30,905 patients from two population-based birth cohorts: the 1958 National Childhood Development Study (NCDS) and the 1970 British Cohort Study (BCS70). Follow-up data were collected between 1958 and 2016 via nine waves of standardized questionnaires, and subtypes of atopic eczema patterns were identified “based on parent-reported or self-reported atopic eczema period prevalence.”
This measure “was previously shown to coincide with standardized clinical examinations among children in the NCDS, and a similar questionnaire demonstrated high sensitivity and specificity for physician-diagnosed atopic eczema in U.S. populations,” the investigators noted.
Latent class analysis identified four disease subtypes based on probability of reporting prevalent AD into midlife: low (88%-91%), decreasing (4%), increasing (2%-6%), and persistently high (2%-3%) probability.
Next, the investigators looked for associations between these subtypes and established early-life risk factors, such as history of breastfeeding and childhood smoke exposure. None of the childhood environmental factors differentiated between high versus decreasing disease in adulthood, or increasing versus decreasing disease in adulthood. In contrast, female sex predicted the high versus decreasing adult subtype (odds ratio, 1.99; 95% confidence interval, 1.66-2.38), and the increasing versus decreasing adult subtype (OR, 1.99; 95% CI, 1.69-2.35).
These findings suggest that “disease trajectory is modifiable and may be influenced by environmental factors throughout life,” the investigators wrote.
Further analysis uncovered associations between adult AD subtypes and other health outcomes. For example, compared with adults in the low probability group, those in the high probability group were significantly more likely to report rhinitis (OR, 2.70; 95% CI, 2.24-3.26) and asthma (OR, 3.45; 95% CI, 2.82-4.21). Adults with the increasing subtype also had elevated rates of asthma and rhinitis, along with worse self-reported mental health at age 42 (OR, 1.45; 95% CI, 1.23-1.72) and poor general health at age 46/50 (OR, 1.29; 95% CI, 1.09-1.53).
“When extending the window of observation beyond childhood, clear subtypes of atopic eczema based on patterns of disease activity emerged,” the investigators concluded. “In particular, a newly identified subtype with increasing probability of activity in adulthood warrants additional attention given associations with poor self-reported physical and mental health in midlife.”
Commenting on these results, Robert Sidbury, MD, professor of dermatology at the University of Washington, Seattle, said that this is an “important study” because it adds to our understanding of natural disease course over time.
This knowledge, as a pediatric dermatologist, will help Dr. Sidbury answer one of the most common questions he hears from parents: When is it going to stop?
“Trying to put a little bit more evidence-based heft behind the answer ... is really important,” he said in an interview.
Based on available data, up to 10% of children with AD may have disease activity into adulthood, according to Dr. Sidbury, who is also chief of dermatology at Seattle Children’s Hospital.
“I would hazard to guess that most of those adults who have atopic dermatitis – at least the ones who had it in childhood – were told that they would grow out of it,” he said. “And so I think awareness is important – that [resolution with age] does not always happen.”
The findings also support the possibility that AD is a systemic disease, and that underlying immune dysregulation may be linked with serious health consequences later in life, Dr. Sidbury said, noting that “the stakes get higher and higher when you start speculating in that way.”
According to Dr. Sidbury, the reported link between childhood AD and poor midlife health raises questions about how modifiable the disease course may be, particularly in response to earlier intervention with emerging AD medications, which “seem to be much more effective and potent.”
“Will the advent of these medications and their adoption and use in treatment perhaps have a significant impact, not just on the prevention of atopic dermatitis itself, but maybe other comorbidities?” he asked.
For the time being, this question remains unanswered.
The study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Wellcome Trust. Dr. Abuabara received grants from the National Institutes of Health during the study, as well as personal fees from Target RWE and Pfizer outside of this study. One author reported receiving NIH grants during the study, another reported receiving grants from the Wellcome Trust and the Innovative Medicine Initiative Horizon 2020 (BIOMAP project) during the study; there were no other disclosures. Dr. Sidbury disclosed relationships with Galderma, Regeneron, and Pfizer.
FROM JAMA DERMATOLOGY
Growing proportion of cardiac arrests in U.S. considered opioid related
Observational data indicate that the number of hospitalizations for cardiac arrests linked to opioid use roughly doubled from 2012 to 2018.
“This was an observational study, so we cannot conclude that all of the arrests were caused by opioids, but the findings do suggest the opioid epidemic is a contributor to increasing rates,” Senada S. Malik, of the University of New England, Portland, Maine, reported at the virtual annual congress of the European Society of Cardiology.
The data were drawn from the Nationwide Inpatient Sample (NIS) from 2012 to 2018, the most recent period available. Cardiac arrests were considered opioid related if there was a secondary diagnosis of opioid disease. The rates of opioid-associated hospitalizations for these types of cardiac arrests climbed from about 800 per year in 2012 to 1,500 per year in 2018, a trend that was statistically significant (P < .05).
The profile of patients with an opioid-associated cardiac arrest was different from those without secondary diagnosis of opioid disease. This included a younger age and lower rates of comorbidities: heart failure (21.2% vs. 40.6%; P < .05), renal failure (14.3% vs. 30.2%; P < .05), diabetes (19.5% vs. 35.4%; P < .05), and hypertension (43.4% vs. 64.9%; P < .05).
Mortality from opioid-associated cardiac arrest is lower
These features might explain the lower rate of in-hospital mortality for opioid-associated cardiac arrests (56.7% vs. 61.2%), according to Ms. Malik, who performed this research in collaboration with Wilbert S. Aronow, MD, director of cardiology research, Westchester Medical Center, Valhalla, N.Y.
When compared to those without a history of opioid use on admission, those with opioid-associated cardiac arrest were more likely to be depressed (18.8% vs. 9.0%), to smoke (37.0% vs. 21.8%) and to abuse alcohol (16.9% vs. 7.1%), according to the NIS data.
While these findings are based on cardiac arrests brought to a hospital, some opioid-induced cardiac arrests never result in hospital admission, according to data included in a recently issued scientific statement from the American Heart Association.
Rate of opioid-associated cardiac arrests underestimated
In that statement, which was focused on opioid-associated out-of-hospital cardiac arrests (OA-OHCA), numerous studies were cited to support the conclusion that these events are common and underestimated. One problem is that opioid-induced cardiac arrests are not always accurately differentiated from cardiac arrests induced by use of other substances, such as barbiturates, cocaine, or alcohol.
For this and other reasons, the data are inconsistent. One study based on emergency medical service (EMS) response data concluded that 9% of all out-of-hospital cardiac arrests are opioid associated.
In another study using potentially more accurate autopsy data, 60% of the non–cardiac-associated cardiac arrests were found to occur in individuals with potentially lethal serum concentrations of opioids. As 40% of out-of-hospital cardiac arrests were considered non–cardiac related, this suggested that 15% of all out-of-hospital cardiac arrests are opioid related.
In the NIS data, the incident curves of opioid-related cardiac arrests appeared to be flattening in 2018, the last year of data collection, but there was no indication they were declining.
Patterns of opioid-induced cardiac arrests evolving
The patterns of opioid-induced cardiac arrest have changed and are likely to continue to change in response to the evolving opioid epidemic, according to the AHA scientific statement. The authors described three waves of opioid abuse. The first, which was related to the promotion of prescription opioids to treat chronic pain that ultimately led to high rates of opioid addiction, peaked in 2012 when rates of these prescriptions began to fall. At that time a second wave, attributed to patients switching to less expensive nonprescription heroin, was already underway. A third wave, attributed to growth in the use of synthetic opioids, such as fentanyl, began in 2013 and is ongoing, according to data cited in the AHA statement.
Recognizing the role of opioids in rising rates of cardiac arrest is important for promoting strategies of effective treatment and prevention, according to Cameron Dezfulian, MD, medical director of the adult congenital heart disease program at Texas Children’s Hospital, Houston. Dr. Dezfulian was vice chair and leader of the writing committee for the AHA scientific statement on OA-OHCA. He said there are plenty of data to support the need for greater attention to the role of opioids in cardiac arrest.
“The recent data affirms the trends many of us have observed without our emergency rooms and ICUs: a steady increase in the proportion of OA-OHCA, primarily in young and otherwise healthy individuals,” he said.
He calls not only for more awareness at the front lines of health are but also for a more comprehensive approach.
“Public health policies and community- and hospital-based interventions are needed to reduce the mortality due to OA-OHCA, which is distinct from the traditional cardiac etiology,” Dr. Dezfulian said.
In opioid-induced cardiac arrest, as in other types of cardiac arrest, prompt initiation of cardiopulmonary resuscitation is essential, but early administration of the opioid antagonist naloxone can also be lifesaving, according to treatment strategies outlined in the AHA scientific statement. The fact that OA-OHCA typically occur in patients with structurally and electrophysiologically normal hearts is emphasized in the AHA statement. So is the enormous public health toll of OA-OHCA.
Death due to opioid overdose, which includes cardiac arrests, is now the leading cause of mortality in the U.S. among individuals between the ages of 25 and 64 years, according to the statement.
Ms. Malik reports no potential conflicts of interest. Dr. Dezfulian reports a financial relationship with Mallinckrodt.
Observational data indicate that the number of hospitalizations for cardiac arrests linked to opioid use roughly doubled from 2012 to 2018.
“This was an observational study, so we cannot conclude that all of the arrests were caused by opioids, but the findings do suggest the opioid epidemic is a contributor to increasing rates,” Senada S. Malik, of the University of New England, Portland, Maine, reported at the virtual annual congress of the European Society of Cardiology.
The data were drawn from the Nationwide Inpatient Sample (NIS) from 2012 to 2018, the most recent period available. Cardiac arrests were considered opioid related if there was a secondary diagnosis of opioid disease. The rates of opioid-associated hospitalizations for these types of cardiac arrests climbed from about 800 per year in 2012 to 1,500 per year in 2018, a trend that was statistically significant (P < .05).
The profile of patients with an opioid-associated cardiac arrest was different from those without secondary diagnosis of opioid disease. This included a younger age and lower rates of comorbidities: heart failure (21.2% vs. 40.6%; P < .05), renal failure (14.3% vs. 30.2%; P < .05), diabetes (19.5% vs. 35.4%; P < .05), and hypertension (43.4% vs. 64.9%; P < .05).
Mortality from opioid-associated cardiac arrest is lower
These features might explain the lower rate of in-hospital mortality for opioid-associated cardiac arrests (56.7% vs. 61.2%), according to Ms. Malik, who performed this research in collaboration with Wilbert S. Aronow, MD, director of cardiology research, Westchester Medical Center, Valhalla, N.Y.
When compared to those without a history of opioid use on admission, those with opioid-associated cardiac arrest were more likely to be depressed (18.8% vs. 9.0%), to smoke (37.0% vs. 21.8%) and to abuse alcohol (16.9% vs. 7.1%), according to the NIS data.
While these findings are based on cardiac arrests brought to a hospital, some opioid-induced cardiac arrests never result in hospital admission, according to data included in a recently issued scientific statement from the American Heart Association.
Rate of opioid-associated cardiac arrests underestimated
In that statement, which was focused on opioid-associated out-of-hospital cardiac arrests (OA-OHCA), numerous studies were cited to support the conclusion that these events are common and underestimated. One problem is that opioid-induced cardiac arrests are not always accurately differentiated from cardiac arrests induced by use of other substances, such as barbiturates, cocaine, or alcohol.
For this and other reasons, the data are inconsistent. One study based on emergency medical service (EMS) response data concluded that 9% of all out-of-hospital cardiac arrests are opioid associated.
In another study using potentially more accurate autopsy data, 60% of the non–cardiac-associated cardiac arrests were found to occur in individuals with potentially lethal serum concentrations of opioids. As 40% of out-of-hospital cardiac arrests were considered non–cardiac related, this suggested that 15% of all out-of-hospital cardiac arrests are opioid related.
In the NIS data, the incident curves of opioid-related cardiac arrests appeared to be flattening in 2018, the last year of data collection, but there was no indication they were declining.
Patterns of opioid-induced cardiac arrests evolving
The patterns of opioid-induced cardiac arrest have changed and are likely to continue to change in response to the evolving opioid epidemic, according to the AHA scientific statement. The authors described three waves of opioid abuse. The first, which was related to the promotion of prescription opioids to treat chronic pain that ultimately led to high rates of opioid addiction, peaked in 2012 when rates of these prescriptions began to fall. At that time a second wave, attributed to patients switching to less expensive nonprescription heroin, was already underway. A third wave, attributed to growth in the use of synthetic opioids, such as fentanyl, began in 2013 and is ongoing, according to data cited in the AHA statement.
Recognizing the role of opioids in rising rates of cardiac arrest is important for promoting strategies of effective treatment and prevention, according to Cameron Dezfulian, MD, medical director of the adult congenital heart disease program at Texas Children’s Hospital, Houston. Dr. Dezfulian was vice chair and leader of the writing committee for the AHA scientific statement on OA-OHCA. He said there are plenty of data to support the need for greater attention to the role of opioids in cardiac arrest.
“The recent data affirms the trends many of us have observed without our emergency rooms and ICUs: a steady increase in the proportion of OA-OHCA, primarily in young and otherwise healthy individuals,” he said.
He calls not only for more awareness at the front lines of health are but also for a more comprehensive approach.
“Public health policies and community- and hospital-based interventions are needed to reduce the mortality due to OA-OHCA, which is distinct from the traditional cardiac etiology,” Dr. Dezfulian said.
In opioid-induced cardiac arrest, as in other types of cardiac arrest, prompt initiation of cardiopulmonary resuscitation is essential, but early administration of the opioid antagonist naloxone can also be lifesaving, according to treatment strategies outlined in the AHA scientific statement. The fact that OA-OHCA typically occur in patients with structurally and electrophysiologically normal hearts is emphasized in the AHA statement. So is the enormous public health toll of OA-OHCA.
Death due to opioid overdose, which includes cardiac arrests, is now the leading cause of mortality in the U.S. among individuals between the ages of 25 and 64 years, according to the statement.
Ms. Malik reports no potential conflicts of interest. Dr. Dezfulian reports a financial relationship with Mallinckrodt.
Observational data indicate that the number of hospitalizations for cardiac arrests linked to opioid use roughly doubled from 2012 to 2018.
“This was an observational study, so we cannot conclude that all of the arrests were caused by opioids, but the findings do suggest the opioid epidemic is a contributor to increasing rates,” Senada S. Malik, of the University of New England, Portland, Maine, reported at the virtual annual congress of the European Society of Cardiology.
The data were drawn from the Nationwide Inpatient Sample (NIS) from 2012 to 2018, the most recent period available. Cardiac arrests were considered opioid related if there was a secondary diagnosis of opioid disease. The rates of opioid-associated hospitalizations for these types of cardiac arrests climbed from about 800 per year in 2012 to 1,500 per year in 2018, a trend that was statistically significant (P < .05).
The profile of patients with an opioid-associated cardiac arrest was different from those without secondary diagnosis of opioid disease. This included a younger age and lower rates of comorbidities: heart failure (21.2% vs. 40.6%; P < .05), renal failure (14.3% vs. 30.2%; P < .05), diabetes (19.5% vs. 35.4%; P < .05), and hypertension (43.4% vs. 64.9%; P < .05).
Mortality from opioid-associated cardiac arrest is lower
These features might explain the lower rate of in-hospital mortality for opioid-associated cardiac arrests (56.7% vs. 61.2%), according to Ms. Malik, who performed this research in collaboration with Wilbert S. Aronow, MD, director of cardiology research, Westchester Medical Center, Valhalla, N.Y.
When compared to those without a history of opioid use on admission, those with opioid-associated cardiac arrest were more likely to be depressed (18.8% vs. 9.0%), to smoke (37.0% vs. 21.8%) and to abuse alcohol (16.9% vs. 7.1%), according to the NIS data.
While these findings are based on cardiac arrests brought to a hospital, some opioid-induced cardiac arrests never result in hospital admission, according to data included in a recently issued scientific statement from the American Heart Association.
Rate of opioid-associated cardiac arrests underestimated
In that statement, which was focused on opioid-associated out-of-hospital cardiac arrests (OA-OHCA), numerous studies were cited to support the conclusion that these events are common and underestimated. One problem is that opioid-induced cardiac arrests are not always accurately differentiated from cardiac arrests induced by use of other substances, such as barbiturates, cocaine, or alcohol.
For this and other reasons, the data are inconsistent. One study based on emergency medical service (EMS) response data concluded that 9% of all out-of-hospital cardiac arrests are opioid associated.
In another study using potentially more accurate autopsy data, 60% of the non–cardiac-associated cardiac arrests were found to occur in individuals with potentially lethal serum concentrations of opioids. As 40% of out-of-hospital cardiac arrests were considered non–cardiac related, this suggested that 15% of all out-of-hospital cardiac arrests are opioid related.
In the NIS data, the incident curves of opioid-related cardiac arrests appeared to be flattening in 2018, the last year of data collection, but there was no indication they were declining.
Patterns of opioid-induced cardiac arrests evolving
The patterns of opioid-induced cardiac arrest have changed and are likely to continue to change in response to the evolving opioid epidemic, according to the AHA scientific statement. The authors described three waves of opioid abuse. The first, which was related to the promotion of prescription opioids to treat chronic pain that ultimately led to high rates of opioid addiction, peaked in 2012 when rates of these prescriptions began to fall. At that time a second wave, attributed to patients switching to less expensive nonprescription heroin, was already underway. A third wave, attributed to growth in the use of synthetic opioids, such as fentanyl, began in 2013 and is ongoing, according to data cited in the AHA statement.
Recognizing the role of opioids in rising rates of cardiac arrest is important for promoting strategies of effective treatment and prevention, according to Cameron Dezfulian, MD, medical director of the adult congenital heart disease program at Texas Children’s Hospital, Houston. Dr. Dezfulian was vice chair and leader of the writing committee for the AHA scientific statement on OA-OHCA. He said there are plenty of data to support the need for greater attention to the role of opioids in cardiac arrest.
“The recent data affirms the trends many of us have observed without our emergency rooms and ICUs: a steady increase in the proportion of OA-OHCA, primarily in young and otherwise healthy individuals,” he said.
He calls not only for more awareness at the front lines of health are but also for a more comprehensive approach.
“Public health policies and community- and hospital-based interventions are needed to reduce the mortality due to OA-OHCA, which is distinct from the traditional cardiac etiology,” Dr. Dezfulian said.
In opioid-induced cardiac arrest, as in other types of cardiac arrest, prompt initiation of cardiopulmonary resuscitation is essential, but early administration of the opioid antagonist naloxone can also be lifesaving, according to treatment strategies outlined in the AHA scientific statement. The fact that OA-OHCA typically occur in patients with structurally and electrophysiologically normal hearts is emphasized in the AHA statement. So is the enormous public health toll of OA-OHCA.
Death due to opioid overdose, which includes cardiac arrests, is now the leading cause of mortality in the U.S. among individuals between the ages of 25 and 64 years, according to the statement.
Ms. Malik reports no potential conflicts of interest. Dr. Dezfulian reports a financial relationship with Mallinckrodt.
FROM ESC 2021
Sweeping new vaccine mandates will impact most U.S. workers
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
Korean siblings face high familial IBD risk
Among Asian-Pacific populations, the first-degree relatives (FDRs) of individuals with inflammatory bowel disease (IBD) have a significantly increased risk for IBD themselves, according to a large analysis of data from South Korea. The greatest risk was found in siblings and for Crohn’s disease (CD).
The analysis of the South Korean Health Insurance Database included a cohort of 21,940,795 individuals from about 12 million families, with data collected between 2002 and 2017.
Previous studies have examined risk of IBD and familial relationships with existing IBD patients, but they have been subject to biases and have been heterogeneous in design, according to the authors, led by co–first authors Hyun Jung Kim, MD, of Korea University in Seoul, South Korea, and Shailja C. Shah, MD, of Vanderbilt University in Nashville, Tenn. There are few true population-based studies that quantify specific risks for family members of IBD patients, and none that were conducted in non-Western populations.
There are concerns about extrapolating familial IBD risk estimates from Western European populations to Asian populations because new data suggest that there are both genetic and nongenetic disease risk factors that reflect geography and ethnicity, the authors noted.
The researchers identified 45,717 individuals with ulcerative colitis (UC) and 17,848 with CD. Mean annual incidence rates were 4.6 cases of UC and 3.2 cases of CD per 100,000 person-years, which was relatively stable across the study period.
In all, 3.8% of UC and 3.1% of CD diagnoses occurred in FDR’s of existing patients. Among those with an FDR with IBD, the incidence of UC and CD was 54.5 and 99.2 per 100,000 person-years, respectively. When compared with individuals who had no FDRs with IBD, subjects who had an FDR with CD were at a more than 20-fold increased risk of CD (incident rate ratio, 22.2; 95% confidence interval, 20.5-24.5), whereas individuals with an FDR with UC were at a little more than a 10-fold risk for UC (IRR, 10.2; 95% CI, 9.39-11.1).
Subjects with an FDR with CD were at higher risk of UC (IRR, 3.56; 95% CI, 2.77-4.50), and those with an FDR with UC were at higher risk of CD (IRR, 2.94; 95% CI, 2.45-3.49). After adjustment for smoking, having an FDR with IBD was associated with an almost eightfold increased risk of UC (IRR, 7.94; 95% CI, 6.98-9.03) and a nearly 20-fold increased risk of CD (IRR, 19.03; 95% CI, 15.58-23.25).
The investigators also performed an analysis based on type of relative, with matching relations with unaffected relatives as the reference for each comparison. The highest risk for incident CD was with twin siblings (IRR, 336.2; 95% CI, 235.0-481.1) followed by nontwin siblings (IRR, 27.6; 95% CI, 24.6-30.9). The risk of CD among offspring of an affected father was 9.40 (95% CI, 6.81-13.0) and 6.54 (95% CI, 4.17-10.3) for offspring of affected mothers. There was a similar pattern for UC, although the magnitude was smaller: 163.7 for twin siblings (95% CI, 105.6-253.9), 13.1 for nontwin siblings (95% CI, 11.4-15.0), 7.11 for offspring of affected fathers (95% CI, 6.10-8.29), and 8.77 for offspring of affected mothers (95% CI, 7.46-10.3).
The researchers found no evidence of a birth cohort effect. Family history and IBD risk is a complicated relationship. Family history includes shared genetics as well as similar environmental exposures, and gene-environment interactions can add another layer of uncertainty. Previous studies have found that asymptomatic family members of IBD patients sometimes have preclinical signs such as changes in intestinal permeability, immune function, the microbiome, and biomarker levels.
IBD has emerged recently among Asian-Pacific populations as a serious health concern, with a recent rapid increase. This may reflect a shift in potentially modifiable environmental triggers. “Precisely quantifying familial risk and patterns might enable more accurate risk counseling and better-targeted clinical surveillance for earlier diagnosis and treatment among FDRs. Moreover, an accurate definition of familial IBD risk across populations also might inform subsequent investigations untangling the various shared environmental and genetic contributions,” the authors wrote.
Although genetic susceptibility is generally accepted as the predominant driver in familial trends for IBD, the authors noted their “study was not designed to determine the contribution of genetic vs. nongenetic determinants to familial IBD risk, and future well-designed dedicated investigations are needed to provide this clarity.”
The study is limited by the relatively short follow-up period, which may not have captured all IBD cases within patients’ families.
The authors have no relevant financial disclosures.
Among Asian-Pacific populations, the first-degree relatives (FDRs) of individuals with inflammatory bowel disease (IBD) have a significantly increased risk for IBD themselves, according to a large analysis of data from South Korea. The greatest risk was found in siblings and for Crohn’s disease (CD).
The analysis of the South Korean Health Insurance Database included a cohort of 21,940,795 individuals from about 12 million families, with data collected between 2002 and 2017.
Previous studies have examined risk of IBD and familial relationships with existing IBD patients, but they have been subject to biases and have been heterogeneous in design, according to the authors, led by co–first authors Hyun Jung Kim, MD, of Korea University in Seoul, South Korea, and Shailja C. Shah, MD, of Vanderbilt University in Nashville, Tenn. There are few true population-based studies that quantify specific risks for family members of IBD patients, and none that were conducted in non-Western populations.
There are concerns about extrapolating familial IBD risk estimates from Western European populations to Asian populations because new data suggest that there are both genetic and nongenetic disease risk factors that reflect geography and ethnicity, the authors noted.
The researchers identified 45,717 individuals with ulcerative colitis (UC) and 17,848 with CD. Mean annual incidence rates were 4.6 cases of UC and 3.2 cases of CD per 100,000 person-years, which was relatively stable across the study period.
In all, 3.8% of UC and 3.1% of CD diagnoses occurred in FDR’s of existing patients. Among those with an FDR with IBD, the incidence of UC and CD was 54.5 and 99.2 per 100,000 person-years, respectively. When compared with individuals who had no FDRs with IBD, subjects who had an FDR with CD were at a more than 20-fold increased risk of CD (incident rate ratio, 22.2; 95% confidence interval, 20.5-24.5), whereas individuals with an FDR with UC were at a little more than a 10-fold risk for UC (IRR, 10.2; 95% CI, 9.39-11.1).
Subjects with an FDR with CD were at higher risk of UC (IRR, 3.56; 95% CI, 2.77-4.50), and those with an FDR with UC were at higher risk of CD (IRR, 2.94; 95% CI, 2.45-3.49). After adjustment for smoking, having an FDR with IBD was associated with an almost eightfold increased risk of UC (IRR, 7.94; 95% CI, 6.98-9.03) and a nearly 20-fold increased risk of CD (IRR, 19.03; 95% CI, 15.58-23.25).
The investigators also performed an analysis based on type of relative, with matching relations with unaffected relatives as the reference for each comparison. The highest risk for incident CD was with twin siblings (IRR, 336.2; 95% CI, 235.0-481.1) followed by nontwin siblings (IRR, 27.6; 95% CI, 24.6-30.9). The risk of CD among offspring of an affected father was 9.40 (95% CI, 6.81-13.0) and 6.54 (95% CI, 4.17-10.3) for offspring of affected mothers. There was a similar pattern for UC, although the magnitude was smaller: 163.7 for twin siblings (95% CI, 105.6-253.9), 13.1 for nontwin siblings (95% CI, 11.4-15.0), 7.11 for offspring of affected fathers (95% CI, 6.10-8.29), and 8.77 for offspring of affected mothers (95% CI, 7.46-10.3).
The researchers found no evidence of a birth cohort effect. Family history and IBD risk is a complicated relationship. Family history includes shared genetics as well as similar environmental exposures, and gene-environment interactions can add another layer of uncertainty. Previous studies have found that asymptomatic family members of IBD patients sometimes have preclinical signs such as changes in intestinal permeability, immune function, the microbiome, and biomarker levels.
IBD has emerged recently among Asian-Pacific populations as a serious health concern, with a recent rapid increase. This may reflect a shift in potentially modifiable environmental triggers. “Precisely quantifying familial risk and patterns might enable more accurate risk counseling and better-targeted clinical surveillance for earlier diagnosis and treatment among FDRs. Moreover, an accurate definition of familial IBD risk across populations also might inform subsequent investigations untangling the various shared environmental and genetic contributions,” the authors wrote.
Although genetic susceptibility is generally accepted as the predominant driver in familial trends for IBD, the authors noted their “study was not designed to determine the contribution of genetic vs. nongenetic determinants to familial IBD risk, and future well-designed dedicated investigations are needed to provide this clarity.”
The study is limited by the relatively short follow-up period, which may not have captured all IBD cases within patients’ families.
The authors have no relevant financial disclosures.
Among Asian-Pacific populations, the first-degree relatives (FDRs) of individuals with inflammatory bowel disease (IBD) have a significantly increased risk for IBD themselves, according to a large analysis of data from South Korea. The greatest risk was found in siblings and for Crohn’s disease (CD).
The analysis of the South Korean Health Insurance Database included a cohort of 21,940,795 individuals from about 12 million families, with data collected between 2002 and 2017.
Previous studies have examined risk of IBD and familial relationships with existing IBD patients, but they have been subject to biases and have been heterogeneous in design, according to the authors, led by co–first authors Hyun Jung Kim, MD, of Korea University in Seoul, South Korea, and Shailja C. Shah, MD, of Vanderbilt University in Nashville, Tenn. There are few true population-based studies that quantify specific risks for family members of IBD patients, and none that were conducted in non-Western populations.
There are concerns about extrapolating familial IBD risk estimates from Western European populations to Asian populations because new data suggest that there are both genetic and nongenetic disease risk factors that reflect geography and ethnicity, the authors noted.
The researchers identified 45,717 individuals with ulcerative colitis (UC) and 17,848 with CD. Mean annual incidence rates were 4.6 cases of UC and 3.2 cases of CD per 100,000 person-years, which was relatively stable across the study period.
In all, 3.8% of UC and 3.1% of CD diagnoses occurred in FDR’s of existing patients. Among those with an FDR with IBD, the incidence of UC and CD was 54.5 and 99.2 per 100,000 person-years, respectively. When compared with individuals who had no FDRs with IBD, subjects who had an FDR with CD were at a more than 20-fold increased risk of CD (incident rate ratio, 22.2; 95% confidence interval, 20.5-24.5), whereas individuals with an FDR with UC were at a little more than a 10-fold risk for UC (IRR, 10.2; 95% CI, 9.39-11.1).
Subjects with an FDR with CD were at higher risk of UC (IRR, 3.56; 95% CI, 2.77-4.50), and those with an FDR with UC were at higher risk of CD (IRR, 2.94; 95% CI, 2.45-3.49). After adjustment for smoking, having an FDR with IBD was associated with an almost eightfold increased risk of UC (IRR, 7.94; 95% CI, 6.98-9.03) and a nearly 20-fold increased risk of CD (IRR, 19.03; 95% CI, 15.58-23.25).
The investigators also performed an analysis based on type of relative, with matching relations with unaffected relatives as the reference for each comparison. The highest risk for incident CD was with twin siblings (IRR, 336.2; 95% CI, 235.0-481.1) followed by nontwin siblings (IRR, 27.6; 95% CI, 24.6-30.9). The risk of CD among offspring of an affected father was 9.40 (95% CI, 6.81-13.0) and 6.54 (95% CI, 4.17-10.3) for offspring of affected mothers. There was a similar pattern for UC, although the magnitude was smaller: 163.7 for twin siblings (95% CI, 105.6-253.9), 13.1 for nontwin siblings (95% CI, 11.4-15.0), 7.11 for offspring of affected fathers (95% CI, 6.10-8.29), and 8.77 for offspring of affected mothers (95% CI, 7.46-10.3).
The researchers found no evidence of a birth cohort effect. Family history and IBD risk is a complicated relationship. Family history includes shared genetics as well as similar environmental exposures, and gene-environment interactions can add another layer of uncertainty. Previous studies have found that asymptomatic family members of IBD patients sometimes have preclinical signs such as changes in intestinal permeability, immune function, the microbiome, and biomarker levels.
IBD has emerged recently among Asian-Pacific populations as a serious health concern, with a recent rapid increase. This may reflect a shift in potentially modifiable environmental triggers. “Precisely quantifying familial risk and patterns might enable more accurate risk counseling and better-targeted clinical surveillance for earlier diagnosis and treatment among FDRs. Moreover, an accurate definition of familial IBD risk across populations also might inform subsequent investigations untangling the various shared environmental and genetic contributions,” the authors wrote.
Although genetic susceptibility is generally accepted as the predominant driver in familial trends for IBD, the authors noted their “study was not designed to determine the contribution of genetic vs. nongenetic determinants to familial IBD risk, and future well-designed dedicated investigations are needed to provide this clarity.”
The study is limited by the relatively short follow-up period, which may not have captured all IBD cases within patients’ families.
The authors have no relevant financial disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Spiral Plaque on the Left Ankle
The Diagnosis: Recurrent Cutaneous T-Cell Lymphoma
The skin biopsy revealed alternating orthokeratosis and parakeratosis with mild to moderate spongiosis and intraepidermal vesiculation as well as individual and nested atypical mononuclear cells with moderately enlarged hyperchromatic nuclei in the epidermis. There was a superficial interstitial lymphocytic infiltrate with occasional enlarged cells (Figure, A and B), and atypical cells in the epidermis and dermis stained with antibodies against CD3 and CD4 (Figure, C and D) but not against CD20 or CD8. These histopathologic findings were consistent with cutaneous T-cell lymphoma (CTCL), mycosis fungoides (MF) type. Additional application of bexarotene gel on days the patient received narrowband UVB was recommended with noted improvement of the skin.
Cutaneous T-cell lymphomas are a heterogenous group of diseases with monoclonal proliferation of T lymphocytes that largely are confined to the skin at the time of diagnosis.1 The incidence of CTCL rose steadily for more than 25 years, with an annual age-adjusted incidence of 6.4 to 9.6 cases per million individuals in the United States from 1973 to 2002.2 Mycosis fungoides is the most common classification of CTCL. It usually is characterized by patches or plaques of scaly erythema or poikiloderma; however, it also can present with annular, arcuate, concentrative, annular and linear morphologies. Mycosis fungoides tumor cells typically express a mature memory T helper cell phenotype of CD3+, CD4+, and CD8−, but there are different variants that have been discovered.3 Mycosis fungoides distributed in a spiral pattern is a distinctly unusual manifestation. Mechanisms of such dynamic morphologies are unknown but may represent an interplay between malignant cell proliferation and lost immune responses in temporospatial relationships.
The presence of keratotic gyrate lesions on acral surfaces should raise the possibility of pagetoid reticulosis. However, our patient had a history of MF involving areas of the body beyond the extremities, making this diagnosis less likely. Pagetoid reticulosis is categorized as an MF variant under the current World Health Organization– European Organization for Research and Treatment of Cancer classification for cutaneous lymphomas.4 Pagetoid reticulosis clinically presents as a solitary psoriasiform or hyperkeratotic patch or plaque that affects the distal extremities. Variable immunophenotypes have been shown in pagetoid reticulosis, such as CD4−/CD8+ and CD4−/CD8−, while classic MF typically shows CD4+/CD8−, as in our case.5
Tinea pedis is a superficial fungal infection usually caused by anthropophilic dermatophytes, with Trichophyton rubrum being the most common organism. Four common clinical presentations of tinea pedis have been identified: interdigital, moccasin, vesicular, and acute ulcerative. Clinical presentation ranges from macerations, ulcerations, and erosions in the toe web spaces to dry hyperkeratotic scaling and fissures on the plantar foot.6 Tinea pedis primarily affects the plantar and interdigital spaces, sparing the dorsal foot and ankle. Treatment is recommended to alleviate symptoms and limit the spread of infection; topical antifungals for 4 weeks is the treatment of choice. However, recurrence is common, and maintenance therapy often is indicated. Oral antifungals or a combination of both topical and oral medications may be needed in certain cases.7
Erythema annulare centrifugum (EAC) is a rare dermatologic disease described as erythematous or urticarial papules that can enlarge centrifugally to form annular lesions that clear centrally. Thought to be a hypersensitivity reaction to an underlying condition, EAC has been associated with fungal infections, various cutaneous diseases, and even internal malignancies. Clinically, EAC can be divided into 2 forms: deep and superficial. Deep gyrate erythema is characterized by a firm indurated border with rare scaling and pruritus that histologically shows perivascular lymphocytic infiltration in the upper and deep dermis. Superficial gyrate erythema has minimally elevated lesions with an indistinct border and trailing scales and pruritus; histopathologic findings present a dense, perivascular, lymphocytic infiltration restricted to the upper dermis.8 Therapy for EAC is directed at relieving symptoms and treating the underlying condition if there is one associated.
Granuloma annulare (GA) is a common skin disorder classically characterized by ringed erythematous plaques, though many variants have been identified. Localized GA is the most common variant and presents with pink-red, nonscaly, annular patches or plaques, typically affecting the hands and feet. Generalized GA is characterized as diffuse annular patches or plaques classically affecting the trunk and extremities. Histology is notable for mucin with a palisading or interstitial pattern of granulomatous inflammation, which was not evident in our patient.9 Topical or intralesional corticosteroids are the first-line treatment of localized GA; however, localized GA generally is self-limited, and treatment often is not necessary. Treatment with cryosurgery, laser therapy, and topical dapsone and tacrolimus also has been described, but evidence of the efficacy of these agents is limited. For generalized GA, phototherapy currently is the most reliable therapy. Systemic therapies include antimalarials, fumaric acid esters, biologics, antimicrobials, and isotretinoin.10
Erythema gyratum repens (EGR) is a rare dermatologic disease described as erythematous concentric bands arranged in parallel rings that can be annular, figurate, or gyrate, with a fine scale trailing the leading edge. Histopathologic features of EGR are nonspecific but are characterized by a perivascular, superficial, mononuclear dermatitis. Diagnosis is based on its characteristic clinical presentation. Although EGR commonly is associated with internal malignancies such as bronchial carcinoma, it also may be associated with benign conditions.11 Improvement often is seen with successful therapy of the underlying associated malignancy.12
Treatment of MF is based on tumor-node-metastasisblood classification, prognostic factors, and clinical stage at the time of diagnosis. Early-stage MF (IA–IIA) commonly is treated with skin-directed therapies such as topical corticosteroids, topical mechlorethamine, topical retinoids, UV phototherapy, and localized radiotherapy. In late stages (IIB–IV), systemic therapy is indicated and includes systemic retinoids, interferon alfa, chemotherapy, monoclonal antibodies, and psoralen plus UVA.13 In many cases, patients may require combination therapy to achieve remission or better control of their condition, as in our patient.
The Diagnosis: Recurrent Cutaneous T-Cell Lymphoma
The skin biopsy revealed alternating orthokeratosis and parakeratosis with mild to moderate spongiosis and intraepidermal vesiculation as well as individual and nested atypical mononuclear cells with moderately enlarged hyperchromatic nuclei in the epidermis. There was a superficial interstitial lymphocytic infiltrate with occasional enlarged cells (Figure, A and B), and atypical cells in the epidermis and dermis stained with antibodies against CD3 and CD4 (Figure, C and D) but not against CD20 or CD8. These histopathologic findings were consistent with cutaneous T-cell lymphoma (CTCL), mycosis fungoides (MF) type. Additional application of bexarotene gel on days the patient received narrowband UVB was recommended with noted improvement of the skin.
Cutaneous T-cell lymphomas are a heterogenous group of diseases with monoclonal proliferation of T lymphocytes that largely are confined to the skin at the time of diagnosis.1 The incidence of CTCL rose steadily for more than 25 years, with an annual age-adjusted incidence of 6.4 to 9.6 cases per million individuals in the United States from 1973 to 2002.2 Mycosis fungoides is the most common classification of CTCL. It usually is characterized by patches or plaques of scaly erythema or poikiloderma; however, it also can present with annular, arcuate, concentrative, annular and linear morphologies. Mycosis fungoides tumor cells typically express a mature memory T helper cell phenotype of CD3+, CD4+, and CD8−, but there are different variants that have been discovered.3 Mycosis fungoides distributed in a spiral pattern is a distinctly unusual manifestation. Mechanisms of such dynamic morphologies are unknown but may represent an interplay between malignant cell proliferation and lost immune responses in temporospatial relationships.
The presence of keratotic gyrate lesions on acral surfaces should raise the possibility of pagetoid reticulosis. However, our patient had a history of MF involving areas of the body beyond the extremities, making this diagnosis less likely. Pagetoid reticulosis is categorized as an MF variant under the current World Health Organization– European Organization for Research and Treatment of Cancer classification for cutaneous lymphomas.4 Pagetoid reticulosis clinically presents as a solitary psoriasiform or hyperkeratotic patch or plaque that affects the distal extremities. Variable immunophenotypes have been shown in pagetoid reticulosis, such as CD4−/CD8+ and CD4−/CD8−, while classic MF typically shows CD4+/CD8−, as in our case.5
Tinea pedis is a superficial fungal infection usually caused by anthropophilic dermatophytes, with Trichophyton rubrum being the most common organism. Four common clinical presentations of tinea pedis have been identified: interdigital, moccasin, vesicular, and acute ulcerative. Clinical presentation ranges from macerations, ulcerations, and erosions in the toe web spaces to dry hyperkeratotic scaling and fissures on the plantar foot.6 Tinea pedis primarily affects the plantar and interdigital spaces, sparing the dorsal foot and ankle. Treatment is recommended to alleviate symptoms and limit the spread of infection; topical antifungals for 4 weeks is the treatment of choice. However, recurrence is common, and maintenance therapy often is indicated. Oral antifungals or a combination of both topical and oral medications may be needed in certain cases.7
Erythema annulare centrifugum (EAC) is a rare dermatologic disease described as erythematous or urticarial papules that can enlarge centrifugally to form annular lesions that clear centrally. Thought to be a hypersensitivity reaction to an underlying condition, EAC has been associated with fungal infections, various cutaneous diseases, and even internal malignancies. Clinically, EAC can be divided into 2 forms: deep and superficial. Deep gyrate erythema is characterized by a firm indurated border with rare scaling and pruritus that histologically shows perivascular lymphocytic infiltration in the upper and deep dermis. Superficial gyrate erythema has minimally elevated lesions with an indistinct border and trailing scales and pruritus; histopathologic findings present a dense, perivascular, lymphocytic infiltration restricted to the upper dermis.8 Therapy for EAC is directed at relieving symptoms and treating the underlying condition if there is one associated.
Granuloma annulare (GA) is a common skin disorder classically characterized by ringed erythematous plaques, though many variants have been identified. Localized GA is the most common variant and presents with pink-red, nonscaly, annular patches or plaques, typically affecting the hands and feet. Generalized GA is characterized as diffuse annular patches or plaques classically affecting the trunk and extremities. Histology is notable for mucin with a palisading or interstitial pattern of granulomatous inflammation, which was not evident in our patient.9 Topical or intralesional corticosteroids are the first-line treatment of localized GA; however, localized GA generally is self-limited, and treatment often is not necessary. Treatment with cryosurgery, laser therapy, and topical dapsone and tacrolimus also has been described, but evidence of the efficacy of these agents is limited. For generalized GA, phototherapy currently is the most reliable therapy. Systemic therapies include antimalarials, fumaric acid esters, biologics, antimicrobials, and isotretinoin.10
Erythema gyratum repens (EGR) is a rare dermatologic disease described as erythematous concentric bands arranged in parallel rings that can be annular, figurate, or gyrate, with a fine scale trailing the leading edge. Histopathologic features of EGR are nonspecific but are characterized by a perivascular, superficial, mononuclear dermatitis. Diagnosis is based on its characteristic clinical presentation. Although EGR commonly is associated with internal malignancies such as bronchial carcinoma, it also may be associated with benign conditions.11 Improvement often is seen with successful therapy of the underlying associated malignancy.12
Treatment of MF is based on tumor-node-metastasisblood classification, prognostic factors, and clinical stage at the time of diagnosis. Early-stage MF (IA–IIA) commonly is treated with skin-directed therapies such as topical corticosteroids, topical mechlorethamine, topical retinoids, UV phototherapy, and localized radiotherapy. In late stages (IIB–IV), systemic therapy is indicated and includes systemic retinoids, interferon alfa, chemotherapy, monoclonal antibodies, and psoralen plus UVA.13 In many cases, patients may require combination therapy to achieve remission or better control of their condition, as in our patient.
The Diagnosis: Recurrent Cutaneous T-Cell Lymphoma
The skin biopsy revealed alternating orthokeratosis and parakeratosis with mild to moderate spongiosis and intraepidermal vesiculation as well as individual and nested atypical mononuclear cells with moderately enlarged hyperchromatic nuclei in the epidermis. There was a superficial interstitial lymphocytic infiltrate with occasional enlarged cells (Figure, A and B), and atypical cells in the epidermis and dermis stained with antibodies against CD3 and CD4 (Figure, C and D) but not against CD20 or CD8. These histopathologic findings were consistent with cutaneous T-cell lymphoma (CTCL), mycosis fungoides (MF) type. Additional application of bexarotene gel on days the patient received narrowband UVB was recommended with noted improvement of the skin.
Cutaneous T-cell lymphomas are a heterogenous group of diseases with monoclonal proliferation of T lymphocytes that largely are confined to the skin at the time of diagnosis.1 The incidence of CTCL rose steadily for more than 25 years, with an annual age-adjusted incidence of 6.4 to 9.6 cases per million individuals in the United States from 1973 to 2002.2 Mycosis fungoides is the most common classification of CTCL. It usually is characterized by patches or plaques of scaly erythema or poikiloderma; however, it also can present with annular, arcuate, concentrative, annular and linear morphologies. Mycosis fungoides tumor cells typically express a mature memory T helper cell phenotype of CD3+, CD4+, and CD8−, but there are different variants that have been discovered.3 Mycosis fungoides distributed in a spiral pattern is a distinctly unusual manifestation. Mechanisms of such dynamic morphologies are unknown but may represent an interplay between malignant cell proliferation and lost immune responses in temporospatial relationships.
The presence of keratotic gyrate lesions on acral surfaces should raise the possibility of pagetoid reticulosis. However, our patient had a history of MF involving areas of the body beyond the extremities, making this diagnosis less likely. Pagetoid reticulosis is categorized as an MF variant under the current World Health Organization– European Organization for Research and Treatment of Cancer classification for cutaneous lymphomas.4 Pagetoid reticulosis clinically presents as a solitary psoriasiform or hyperkeratotic patch or plaque that affects the distal extremities. Variable immunophenotypes have been shown in pagetoid reticulosis, such as CD4−/CD8+ and CD4−/CD8−, while classic MF typically shows CD4+/CD8−, as in our case.5
Tinea pedis is a superficial fungal infection usually caused by anthropophilic dermatophytes, with Trichophyton rubrum being the most common organism. Four common clinical presentations of tinea pedis have been identified: interdigital, moccasin, vesicular, and acute ulcerative. Clinical presentation ranges from macerations, ulcerations, and erosions in the toe web spaces to dry hyperkeratotic scaling and fissures on the plantar foot.6 Tinea pedis primarily affects the plantar and interdigital spaces, sparing the dorsal foot and ankle. Treatment is recommended to alleviate symptoms and limit the spread of infection; topical antifungals for 4 weeks is the treatment of choice. However, recurrence is common, and maintenance therapy often is indicated. Oral antifungals or a combination of both topical and oral medications may be needed in certain cases.7
Erythema annulare centrifugum (EAC) is a rare dermatologic disease described as erythematous or urticarial papules that can enlarge centrifugally to form annular lesions that clear centrally. Thought to be a hypersensitivity reaction to an underlying condition, EAC has been associated with fungal infections, various cutaneous diseases, and even internal malignancies. Clinically, EAC can be divided into 2 forms: deep and superficial. Deep gyrate erythema is characterized by a firm indurated border with rare scaling and pruritus that histologically shows perivascular lymphocytic infiltration in the upper and deep dermis. Superficial gyrate erythema has minimally elevated lesions with an indistinct border and trailing scales and pruritus; histopathologic findings present a dense, perivascular, lymphocytic infiltration restricted to the upper dermis.8 Therapy for EAC is directed at relieving symptoms and treating the underlying condition if there is one associated.
Granuloma annulare (GA) is a common skin disorder classically characterized by ringed erythematous plaques, though many variants have been identified. Localized GA is the most common variant and presents with pink-red, nonscaly, annular patches or plaques, typically affecting the hands and feet. Generalized GA is characterized as diffuse annular patches or plaques classically affecting the trunk and extremities. Histology is notable for mucin with a palisading or interstitial pattern of granulomatous inflammation, which was not evident in our patient.9 Topical or intralesional corticosteroids are the first-line treatment of localized GA; however, localized GA generally is self-limited, and treatment often is not necessary. Treatment with cryosurgery, laser therapy, and topical dapsone and tacrolimus also has been described, but evidence of the efficacy of these agents is limited. For generalized GA, phototherapy currently is the most reliable therapy. Systemic therapies include antimalarials, fumaric acid esters, biologics, antimicrobials, and isotretinoin.10
Erythema gyratum repens (EGR) is a rare dermatologic disease described as erythematous concentric bands arranged in parallel rings that can be annular, figurate, or gyrate, with a fine scale trailing the leading edge. Histopathologic features of EGR are nonspecific but are characterized by a perivascular, superficial, mononuclear dermatitis. Diagnosis is based on its characteristic clinical presentation. Although EGR commonly is associated with internal malignancies such as bronchial carcinoma, it also may be associated with benign conditions.11 Improvement often is seen with successful therapy of the underlying associated malignancy.12
Treatment of MF is based on tumor-node-metastasisblood classification, prognostic factors, and clinical stage at the time of diagnosis. Early-stage MF (IA–IIA) commonly is treated with skin-directed therapies such as topical corticosteroids, topical mechlorethamine, topical retinoids, UV phototherapy, and localized radiotherapy. In late stages (IIB–IV), systemic therapy is indicated and includes systemic retinoids, interferon alfa, chemotherapy, monoclonal antibodies, and psoralen plus UVA.13 In many cases, patients may require combination therapy to achieve remission or better control of their condition, as in our patient.
A 60-year-old man presented with a whorl-like plaque on the left ankle that he had noticed while undergoing treatment with narrowband UVB every other week and nitrogen mustard gel daily for stage IB cutaneous T-cell lymphoma, mycosis fungoides type. He denied pain, pruritus, and any other associated symptoms at the site. He denied recent illness, new medications, or changes in diet. His medical history included multiple sclerosis, vascular disease, and stroke. Physical examination revealed an 8×6-cm, welldemarcated, slightly scaly, erythematous plaque with a spiral appearance and peripheral hyperpigmentation involving the left ankle. The remainder of the examination was notable for well-controlled mycosis fungoides with several hyperpigmented patches at sites of prior involvement on the trunk and upper and lower extremities. No cervical, axillary, or inguinal lymphadenopathy was noted. A 4-mm punch biopsy was performed and sent for histopathologic examination.
Pandemic-related school closures tied to mental health inequities
Back-to-school jitters are heightened this year, as children head back to the risk of COVID transmission in class, but one upside to the return of in-person school may be better mental health for students.
New research shows that virtual schooling, which dominated in many districts last year, was associated with worse mental health outcomes for students – especially older ones – and youth from Black, Hispanic, or lower-income families were hit hardest because they experienced the most closures.
“Schools with lower funding may have had more difficulty meeting guidelines for safe reopening, including updates to ventilation systems and finding the physical space to create safe distancing between children,” explained lead author Matt Hawrilenko, PhD, of the department of psychiatry and behavioral sciences at the University of Washington, Seattle, in an interview.
“In the context of complex school reopening decisions that balance competing risks and benefits, these findings suggest that allocating funding to support safe in-person instruction may reduce mental health inequities associated with race/ethnicity and income,” he and his coauthors noted in the study, published in JAMA Network Open. “Ensuring that all students have access to additional educational and mental health resources must be an important public health priority, met with appropriate funding and work force augmentation, during and beyond the COVID-19 pandemic.”
The study used a cross-sectional population-based survey of 2,324 parents of school-age children in the United States. It was administered in English and Spanish via web and telephone between Dec. 2 and Dec. 21, 2020, and used the parent-report version of the Strengths and Difficulties Questionnaire (SDQ) to assess mental health difficulties of one child per family in four domains: emotional problems, peer problems, conduct, and hyperactivity. Parents were also asked about what kind of schooling their child had received in the last year (remote, in-person, or hybrid) and about demographic information such as child age, gender, household income, parent race and ethnicity, and parent education.
The results showed that, during the 2020 school year, 58.0% of children attended school remotely, 24% attended fully in person, and 18.0% attended in a hybrid format. “Fully remote schooling was strongly patterned along lines of parent race and ethnicity as well as income,” the authors noted. “Parents of 336 children attending school in person (65.8%) but of 597 children attending school fully remotely (44.5%) were White, whereas all other racial/ethnic groups had larger proportions of children attending school fully remotely (P < .001).”
In terms of mental health, the findings showed that older children who attended school remotely had more difficulties, compared with those who attended in-person – but among younger children, remote learning was comparable or slightly better for mental health.
Specifically, “a child aged 17 years attending school remotely would be expected to have a total difficulty score 2.4 points higher than a child of the same age attending school in person, corresponding to a small effect size in favor of in-person schooling,” the authors wrote. “Conversely, a child aged 4 years attending school remotely would be expected to have a total difficulty score 0.5 points lower than a child of the same age attending school in person, corresponding to a very small effect size in favor of remote schooling.”
Age of child proves critical
“Our best estimate is that remote schooling was associated with no difference in mental health difficulties at age 6, and with slightly more difficulties with each year of age after that, with differences most clearly apparent for high school–aged kids,” explained Dr. Hawrilenko, adding the finding suggests that school reopenings should prioritize older children.
However, “what kids are doing at home matters,” he added. “In the youngest age group, the biggest work kids are doing in school and childcare settings is social and emotional development. … Finding opportunities for regular, safe social interactions with peers – perhaps during outdoor playdates – can help them build those skills.”
He emphasized with the anticipated starts and stutters of the new school year there is an important role that doctors can play.
“First, they can help families assess their own risk profile, and whether it makes sense for their children to attend school in person or remotely [to the extent that is an option]. Second, they can help families think through how school closures might impact their child specifically. For those kids who wind up with long chunks of remote schooling, scheduling in regular interactions with other kids in safe ways could make a big difference. Another driver of child anxiety might be learning loss, and this is a good place to reinforce that not every mental health problem needs a mental health solution.
“A lot of kids might be rightfully anxious about having fallen behind over the pandemic. These kids are preparing to transition to college or to the workforce and may be feeling increasingly behind while approaching these moments of transition. Pointing families toward the resources to help them navigate these issues could go a long way to helping quell child anxiety.”
Research helps fill vacuum
Elizabeth A. Stuart, PhD, who was not involved in the study, said in an interview that this research is particularly valuable because there have been very few data on this topic, especially on a large-scale national sample.
“Sadly, many of the results are not surprising,” said Dr. Stuart, a statistician and professor of mental health at Johns Hopkins University, Baltimore. “Data have shown significant mental health challenges for adults during the pandemic, and it is not surprising that children and youth would experience that as well, especially for those whose daily routines and structures changed dramatically and who were not able to be interacting in-person with teachers, staff, and classmates. This is an important reminder that schools provide not just academic instruction for students, but that the social interactions and other services (such as behavioral health supports, meals, and connections with other social services) students might receive in school are crucial.
“It has been heartening to see a stronger commitment to getting students safely back into school this fall across the country, and that the Centers for Disease Control and Prevention highlighted the benefits of in-person schooling in their COVID-19–related guidance for schools.”
Dr. Stuart added that, as students return to classes, it will be important for schools to tackle ongoing mental health challenges.
“Some students may be struggling in obvious ways; for others it may be harder to identify. It will also be important to continue to monitor children’s and youth mental health … as returning to in-person school may bring its own challenges. ”
Dr. Hawrilenko agreed.
“From a policy perspective, I am quite frankly terrified about how these inequities – in particular, learning loss – might play out long after school closures are a distant memory,” he said. “It is critical to provide schools the resources not just to minimize risk when reopening, but additional funding for workforce augmentation – both for mental health staffing and for additional educational support – to help students navigate the months and years over which they transition back into the classroom.”
Dr. Hawrilenko and Dr. Stuart had no disclosures.
Back-to-school jitters are heightened this year, as children head back to the risk of COVID transmission in class, but one upside to the return of in-person school may be better mental health for students.
New research shows that virtual schooling, which dominated in many districts last year, was associated with worse mental health outcomes for students – especially older ones – and youth from Black, Hispanic, or lower-income families were hit hardest because they experienced the most closures.
“Schools with lower funding may have had more difficulty meeting guidelines for safe reopening, including updates to ventilation systems and finding the physical space to create safe distancing between children,” explained lead author Matt Hawrilenko, PhD, of the department of psychiatry and behavioral sciences at the University of Washington, Seattle, in an interview.
“In the context of complex school reopening decisions that balance competing risks and benefits, these findings suggest that allocating funding to support safe in-person instruction may reduce mental health inequities associated with race/ethnicity and income,” he and his coauthors noted in the study, published in JAMA Network Open. “Ensuring that all students have access to additional educational and mental health resources must be an important public health priority, met with appropriate funding and work force augmentation, during and beyond the COVID-19 pandemic.”
The study used a cross-sectional population-based survey of 2,324 parents of school-age children in the United States. It was administered in English and Spanish via web and telephone between Dec. 2 and Dec. 21, 2020, and used the parent-report version of the Strengths and Difficulties Questionnaire (SDQ) to assess mental health difficulties of one child per family in four domains: emotional problems, peer problems, conduct, and hyperactivity. Parents were also asked about what kind of schooling their child had received in the last year (remote, in-person, or hybrid) and about demographic information such as child age, gender, household income, parent race and ethnicity, and parent education.
The results showed that, during the 2020 school year, 58.0% of children attended school remotely, 24% attended fully in person, and 18.0% attended in a hybrid format. “Fully remote schooling was strongly patterned along lines of parent race and ethnicity as well as income,” the authors noted. “Parents of 336 children attending school in person (65.8%) but of 597 children attending school fully remotely (44.5%) were White, whereas all other racial/ethnic groups had larger proportions of children attending school fully remotely (P < .001).”
In terms of mental health, the findings showed that older children who attended school remotely had more difficulties, compared with those who attended in-person – but among younger children, remote learning was comparable or slightly better for mental health.
Specifically, “a child aged 17 years attending school remotely would be expected to have a total difficulty score 2.4 points higher than a child of the same age attending school in person, corresponding to a small effect size in favor of in-person schooling,” the authors wrote. “Conversely, a child aged 4 years attending school remotely would be expected to have a total difficulty score 0.5 points lower than a child of the same age attending school in person, corresponding to a very small effect size in favor of remote schooling.”
Age of child proves critical
“Our best estimate is that remote schooling was associated with no difference in mental health difficulties at age 6, and with slightly more difficulties with each year of age after that, with differences most clearly apparent for high school–aged kids,” explained Dr. Hawrilenko, adding the finding suggests that school reopenings should prioritize older children.
However, “what kids are doing at home matters,” he added. “In the youngest age group, the biggest work kids are doing in school and childcare settings is social and emotional development. … Finding opportunities for regular, safe social interactions with peers – perhaps during outdoor playdates – can help them build those skills.”
He emphasized with the anticipated starts and stutters of the new school year there is an important role that doctors can play.
“First, they can help families assess their own risk profile, and whether it makes sense for their children to attend school in person or remotely [to the extent that is an option]. Second, they can help families think through how school closures might impact their child specifically. For those kids who wind up with long chunks of remote schooling, scheduling in regular interactions with other kids in safe ways could make a big difference. Another driver of child anxiety might be learning loss, and this is a good place to reinforce that not every mental health problem needs a mental health solution.
“A lot of kids might be rightfully anxious about having fallen behind over the pandemic. These kids are preparing to transition to college or to the workforce and may be feeling increasingly behind while approaching these moments of transition. Pointing families toward the resources to help them navigate these issues could go a long way to helping quell child anxiety.”
Research helps fill vacuum
Elizabeth A. Stuart, PhD, who was not involved in the study, said in an interview that this research is particularly valuable because there have been very few data on this topic, especially on a large-scale national sample.
“Sadly, many of the results are not surprising,” said Dr. Stuart, a statistician and professor of mental health at Johns Hopkins University, Baltimore. “Data have shown significant mental health challenges for adults during the pandemic, and it is not surprising that children and youth would experience that as well, especially for those whose daily routines and structures changed dramatically and who were not able to be interacting in-person with teachers, staff, and classmates. This is an important reminder that schools provide not just academic instruction for students, but that the social interactions and other services (such as behavioral health supports, meals, and connections with other social services) students might receive in school are crucial.
“It has been heartening to see a stronger commitment to getting students safely back into school this fall across the country, and that the Centers for Disease Control and Prevention highlighted the benefits of in-person schooling in their COVID-19–related guidance for schools.”
Dr. Stuart added that, as students return to classes, it will be important for schools to tackle ongoing mental health challenges.
“Some students may be struggling in obvious ways; for others it may be harder to identify. It will also be important to continue to monitor children’s and youth mental health … as returning to in-person school may bring its own challenges. ”
Dr. Hawrilenko agreed.
“From a policy perspective, I am quite frankly terrified about how these inequities – in particular, learning loss – might play out long after school closures are a distant memory,” he said. “It is critical to provide schools the resources not just to minimize risk when reopening, but additional funding for workforce augmentation – both for mental health staffing and for additional educational support – to help students navigate the months and years over which they transition back into the classroom.”
Dr. Hawrilenko and Dr. Stuart had no disclosures.
Back-to-school jitters are heightened this year, as children head back to the risk of COVID transmission in class, but one upside to the return of in-person school may be better mental health for students.
New research shows that virtual schooling, which dominated in many districts last year, was associated with worse mental health outcomes for students – especially older ones – and youth from Black, Hispanic, or lower-income families were hit hardest because they experienced the most closures.
“Schools with lower funding may have had more difficulty meeting guidelines for safe reopening, including updates to ventilation systems and finding the physical space to create safe distancing between children,” explained lead author Matt Hawrilenko, PhD, of the department of psychiatry and behavioral sciences at the University of Washington, Seattle, in an interview.
“In the context of complex school reopening decisions that balance competing risks and benefits, these findings suggest that allocating funding to support safe in-person instruction may reduce mental health inequities associated with race/ethnicity and income,” he and his coauthors noted in the study, published in JAMA Network Open. “Ensuring that all students have access to additional educational and mental health resources must be an important public health priority, met with appropriate funding and work force augmentation, during and beyond the COVID-19 pandemic.”
The study used a cross-sectional population-based survey of 2,324 parents of school-age children in the United States. It was administered in English and Spanish via web and telephone between Dec. 2 and Dec. 21, 2020, and used the parent-report version of the Strengths and Difficulties Questionnaire (SDQ) to assess mental health difficulties of one child per family in four domains: emotional problems, peer problems, conduct, and hyperactivity. Parents were also asked about what kind of schooling their child had received in the last year (remote, in-person, or hybrid) and about demographic information such as child age, gender, household income, parent race and ethnicity, and parent education.
The results showed that, during the 2020 school year, 58.0% of children attended school remotely, 24% attended fully in person, and 18.0% attended in a hybrid format. “Fully remote schooling was strongly patterned along lines of parent race and ethnicity as well as income,” the authors noted. “Parents of 336 children attending school in person (65.8%) but of 597 children attending school fully remotely (44.5%) were White, whereas all other racial/ethnic groups had larger proportions of children attending school fully remotely (P < .001).”
In terms of mental health, the findings showed that older children who attended school remotely had more difficulties, compared with those who attended in-person – but among younger children, remote learning was comparable or slightly better for mental health.
Specifically, “a child aged 17 years attending school remotely would be expected to have a total difficulty score 2.4 points higher than a child of the same age attending school in person, corresponding to a small effect size in favor of in-person schooling,” the authors wrote. “Conversely, a child aged 4 years attending school remotely would be expected to have a total difficulty score 0.5 points lower than a child of the same age attending school in person, corresponding to a very small effect size in favor of remote schooling.”
Age of child proves critical
“Our best estimate is that remote schooling was associated with no difference in mental health difficulties at age 6, and with slightly more difficulties with each year of age after that, with differences most clearly apparent for high school–aged kids,” explained Dr. Hawrilenko, adding the finding suggests that school reopenings should prioritize older children.
However, “what kids are doing at home matters,” he added. “In the youngest age group, the biggest work kids are doing in school and childcare settings is social and emotional development. … Finding opportunities for regular, safe social interactions with peers – perhaps during outdoor playdates – can help them build those skills.”
He emphasized with the anticipated starts and stutters of the new school year there is an important role that doctors can play.
“First, they can help families assess their own risk profile, and whether it makes sense for their children to attend school in person or remotely [to the extent that is an option]. Second, they can help families think through how school closures might impact their child specifically. For those kids who wind up with long chunks of remote schooling, scheduling in regular interactions with other kids in safe ways could make a big difference. Another driver of child anxiety might be learning loss, and this is a good place to reinforce that not every mental health problem needs a mental health solution.
“A lot of kids might be rightfully anxious about having fallen behind over the pandemic. These kids are preparing to transition to college or to the workforce and may be feeling increasingly behind while approaching these moments of transition. Pointing families toward the resources to help them navigate these issues could go a long way to helping quell child anxiety.”
Research helps fill vacuum
Elizabeth A. Stuart, PhD, who was not involved in the study, said in an interview that this research is particularly valuable because there have been very few data on this topic, especially on a large-scale national sample.
“Sadly, many of the results are not surprising,” said Dr. Stuart, a statistician and professor of mental health at Johns Hopkins University, Baltimore. “Data have shown significant mental health challenges for adults during the pandemic, and it is not surprising that children and youth would experience that as well, especially for those whose daily routines and structures changed dramatically and who were not able to be interacting in-person with teachers, staff, and classmates. This is an important reminder that schools provide not just academic instruction for students, but that the social interactions and other services (such as behavioral health supports, meals, and connections with other social services) students might receive in school are crucial.
“It has been heartening to see a stronger commitment to getting students safely back into school this fall across the country, and that the Centers for Disease Control and Prevention highlighted the benefits of in-person schooling in their COVID-19–related guidance for schools.”
Dr. Stuart added that, as students return to classes, it will be important for schools to tackle ongoing mental health challenges.
“Some students may be struggling in obvious ways; for others it may be harder to identify. It will also be important to continue to monitor children’s and youth mental health … as returning to in-person school may bring its own challenges. ”
Dr. Hawrilenko agreed.
“From a policy perspective, I am quite frankly terrified about how these inequities – in particular, learning loss – might play out long after school closures are a distant memory,” he said. “It is critical to provide schools the resources not just to minimize risk when reopening, but additional funding for workforce augmentation – both for mental health staffing and for additional educational support – to help students navigate the months and years over which they transition back into the classroom.”
Dr. Hawrilenko and Dr. Stuart had no disclosures.
FROM JAMA NETWORK OPEN
Transgender individuals twice as likely to die as general population
Mortality is consistently twice as high in transgender people receiving hormone treatment, compared with cisgender individuals in the general population and has not decreased over time, results of a 5 decades–long study from the Netherlands indicate.
Particularly concerning is that trans women (male to female) had a mortality risk nearly double that of cis men (born and remain male) in the general Dutch population (standardized mortality ratio, 1.8), while it was nearly triple that of cis women (SMR, 2.8).
Compared with cisgender women, transgender women were more than twice as likely to die from heart disease, three times more likely to die from lung cancer, and almost nine times more likely to die from infection. HIV-related disease mortality risk was nearly 50 times higher for trans women than cis women, and the risk of suicide was almost seven times greater.
Suicide and other nonnatural causes of death were more common in trans men, compared with cis women.
The report, by Christel J.M. de Blok, MD, of Amsterdam University Medical Center and colleagues, was published online Sept. 2 in The Lancet Diabetes & Endocrinology.
The study included trans men who received testosterone to transition from female to male and trans women who received estrogen plus an antiandrogen to transition from male to female.
Is gender-affirming hormone therapy associated with increased mortality?
Senior author Martin den Heijer, MD, also of Amsterdam University Medical Center, said: “The findings of our large, nationwide study highlight a substantially increased mortality risk among transgender people that has persisted for decades.”
But he pointed out that, overall, the data do not appear to suggest the premature deaths were related to gender-affirming hormone treatment.
However, he conceded that more work is needed on this aspect of care. “There is insufficient evidence at present to determine long-term safety of [gender-affirming hormone treatment]. More research is needed to fully establish whether it in any way affects mortality risk for transgender people,” said Dr. den Heijer.
Endocrinologist Will Malone, MD, of Twin Falls, Idaho, told this news organization, “The study confirms, like others before it, that individuals taking cross-sex hormones are more likely to die prematurely from a number of causes.”
“While the authors speculate that this higher mortality rate is not connected to cross-sex hormones, the study was not designed to be able to make such a claim,” he said, pointing to limited follow-up times.
In an accompanying commentary, Vin Tangpricha, MD, PhD, an endocrinologist from Emory University, Atlanta, noted: “Transgender men do not appear to have as significantly increased comorbidity following receipt of gender-affirming hormone therapy when compared with transgender women.”
Dr. Tangpricha added future studies should examine which factors – hormone regimen, hormone concentrations, access to health care, or other biological factors – explain the higher increased risk of morbidity and mortality observed in trans women as opposed to trans men.
However, Dr. de Blok and colleagues note that, as there were relatively few deaths among transgender men in the cohort, analysis on cause of death in this group is limited.
Transgender individuals more likely to die younger
For their study, Dutch researchers retrospectively examined data from 4,568 transgender people attending their clinic (2,927 transgender women and 1,641 transgender men) treated in 1972-2018. People were excluded if they started treatment before the age of 17 or if they had received puberty-blocking drugs.
Data on age at start of hormone treatment, type of treatment, smoking habits, medical history, and last date of follow-up were gathered from medical records. Where possible, SMRs were determined for deaths among trans men and trans women, compared with rates for the adult Dutch general population.
Median age at the start of cross-sex hormone treatment was 30 years in transgender women and 23 years in transgender men. But the median follow-up time was only 11 years in transgender women and 5 years in transgender men.
A total of 317 (10.8%) trans women died, and 44 (2.7%) trans men died. The findings were higher than expected, compared with the general population of cisgender women (SMR, 1.8) but not cisgender men (SMR 1.2).
Mortality risk did increase more in transgender people who started gender-affirming hormone treatment in the past 2 decades compared with earlier, a fact that Dr. de Blok said was surprising.
Trans men, for example, compared with cis women, had an SMR of 2.1-2.4 in 2000-2018 (compared with 1.8 overall).
“This may be due to changes in clinical practice. ... In the past, health care providers were reluctant to provide hormone treatment to people with a history of comorbidities such as cardiovascular disease. However, because of the many benefits of enabling people to access hormone therapy, nowadays this rarely results in treatment being denied,” Dr. de Blok noted.
More research needed, especially in trans-identifying youth
Dr. Malone remarked that previous studies have shown associations between taking cross-sex hormones and elevated mortality, while also “not designed to detect causality,” have “generally accepted that natal males who take estrogen have estrogen-related increases in the rates of heart disease, stroke, and deep venous thrombosis.”
He added that the risks of testosterone use in natal females were less well established, “but testosterone is also felt to increase their risk of heart disease.”
He stressed the limited follow-up times in the study by Dr. de Blok and colleagues.
This “strongly suggests that the rate of elevated mortality far exceeds the doubling measured by the study, especially for natal females.”
Dr. Malone is one of several clinicians and researchers who has formed the Society for Evidence-Based Gender Medicine, a nonprofit organization that now has at least 100 physician members. SEGM is concerned about the lack of quality evidence for the use of hormonal and surgical interventions as first-line treatment, especially for young people with gender dysphoria.
Dr. Tangpricha also highlighted that the findings do not apply to transgender people who began treatment before age 17 years or those who had taken puberty blockers before gender-affirming hormone treatment.
There are no long-term data on transgender individuals who have received gender-affirming hormone therapies close to the time of puberty.
These data, such as those from the Trans Youth Care study, should be available in the future, he added.
The authors have reported no relevant financial relationships. Dr. Tangpricha has reported receiving funding from the National Institutes of Health and served as past president of the World Professional Association for Transgender Health. He is editor-in-chief of Endocrine Practice and has provided expert testimony for Kirkland and Ellis.
A version of this article first appeared on Medscape.com.
Mortality is consistently twice as high in transgender people receiving hormone treatment, compared with cisgender individuals in the general population and has not decreased over time, results of a 5 decades–long study from the Netherlands indicate.
Particularly concerning is that trans women (male to female) had a mortality risk nearly double that of cis men (born and remain male) in the general Dutch population (standardized mortality ratio, 1.8), while it was nearly triple that of cis women (SMR, 2.8).
Compared with cisgender women, transgender women were more than twice as likely to die from heart disease, three times more likely to die from lung cancer, and almost nine times more likely to die from infection. HIV-related disease mortality risk was nearly 50 times higher for trans women than cis women, and the risk of suicide was almost seven times greater.
Suicide and other nonnatural causes of death were more common in trans men, compared with cis women.
The report, by Christel J.M. de Blok, MD, of Amsterdam University Medical Center and colleagues, was published online Sept. 2 in The Lancet Diabetes & Endocrinology.
The study included trans men who received testosterone to transition from female to male and trans women who received estrogen plus an antiandrogen to transition from male to female.
Is gender-affirming hormone therapy associated with increased mortality?
Senior author Martin den Heijer, MD, also of Amsterdam University Medical Center, said: “The findings of our large, nationwide study highlight a substantially increased mortality risk among transgender people that has persisted for decades.”
But he pointed out that, overall, the data do not appear to suggest the premature deaths were related to gender-affirming hormone treatment.
However, he conceded that more work is needed on this aspect of care. “There is insufficient evidence at present to determine long-term safety of [gender-affirming hormone treatment]. More research is needed to fully establish whether it in any way affects mortality risk for transgender people,” said Dr. den Heijer.
Endocrinologist Will Malone, MD, of Twin Falls, Idaho, told this news organization, “The study confirms, like others before it, that individuals taking cross-sex hormones are more likely to die prematurely from a number of causes.”
“While the authors speculate that this higher mortality rate is not connected to cross-sex hormones, the study was not designed to be able to make such a claim,” he said, pointing to limited follow-up times.
In an accompanying commentary, Vin Tangpricha, MD, PhD, an endocrinologist from Emory University, Atlanta, noted: “Transgender men do not appear to have as significantly increased comorbidity following receipt of gender-affirming hormone therapy when compared with transgender women.”
Dr. Tangpricha added future studies should examine which factors – hormone regimen, hormone concentrations, access to health care, or other biological factors – explain the higher increased risk of morbidity and mortality observed in trans women as opposed to trans men.
However, Dr. de Blok and colleagues note that, as there were relatively few deaths among transgender men in the cohort, analysis on cause of death in this group is limited.
Transgender individuals more likely to die younger
For their study, Dutch researchers retrospectively examined data from 4,568 transgender people attending their clinic (2,927 transgender women and 1,641 transgender men) treated in 1972-2018. People were excluded if they started treatment before the age of 17 or if they had received puberty-blocking drugs.
Data on age at start of hormone treatment, type of treatment, smoking habits, medical history, and last date of follow-up were gathered from medical records. Where possible, SMRs were determined for deaths among trans men and trans women, compared with rates for the adult Dutch general population.
Median age at the start of cross-sex hormone treatment was 30 years in transgender women and 23 years in transgender men. But the median follow-up time was only 11 years in transgender women and 5 years in transgender men.
A total of 317 (10.8%) trans women died, and 44 (2.7%) trans men died. The findings were higher than expected, compared with the general population of cisgender women (SMR, 1.8) but not cisgender men (SMR 1.2).
Mortality risk did increase more in transgender people who started gender-affirming hormone treatment in the past 2 decades compared with earlier, a fact that Dr. de Blok said was surprising.
Trans men, for example, compared with cis women, had an SMR of 2.1-2.4 in 2000-2018 (compared with 1.8 overall).
“This may be due to changes in clinical practice. ... In the past, health care providers were reluctant to provide hormone treatment to people with a history of comorbidities such as cardiovascular disease. However, because of the many benefits of enabling people to access hormone therapy, nowadays this rarely results in treatment being denied,” Dr. de Blok noted.
More research needed, especially in trans-identifying youth
Dr. Malone remarked that previous studies have shown associations between taking cross-sex hormones and elevated mortality, while also “not designed to detect causality,” have “generally accepted that natal males who take estrogen have estrogen-related increases in the rates of heart disease, stroke, and deep venous thrombosis.”
He added that the risks of testosterone use in natal females were less well established, “but testosterone is also felt to increase their risk of heart disease.”
He stressed the limited follow-up times in the study by Dr. de Blok and colleagues.
This “strongly suggests that the rate of elevated mortality far exceeds the doubling measured by the study, especially for natal females.”
Dr. Malone is one of several clinicians and researchers who has formed the Society for Evidence-Based Gender Medicine, a nonprofit organization that now has at least 100 physician members. SEGM is concerned about the lack of quality evidence for the use of hormonal and surgical interventions as first-line treatment, especially for young people with gender dysphoria.
Dr. Tangpricha also highlighted that the findings do not apply to transgender people who began treatment before age 17 years or those who had taken puberty blockers before gender-affirming hormone treatment.
There are no long-term data on transgender individuals who have received gender-affirming hormone therapies close to the time of puberty.
These data, such as those from the Trans Youth Care study, should be available in the future, he added.
The authors have reported no relevant financial relationships. Dr. Tangpricha has reported receiving funding from the National Institutes of Health and served as past president of the World Professional Association for Transgender Health. He is editor-in-chief of Endocrine Practice and has provided expert testimony for Kirkland and Ellis.
A version of this article first appeared on Medscape.com.
Mortality is consistently twice as high in transgender people receiving hormone treatment, compared with cisgender individuals in the general population and has not decreased over time, results of a 5 decades–long study from the Netherlands indicate.
Particularly concerning is that trans women (male to female) had a mortality risk nearly double that of cis men (born and remain male) in the general Dutch population (standardized mortality ratio, 1.8), while it was nearly triple that of cis women (SMR, 2.8).
Compared with cisgender women, transgender women were more than twice as likely to die from heart disease, three times more likely to die from lung cancer, and almost nine times more likely to die from infection. HIV-related disease mortality risk was nearly 50 times higher for trans women than cis women, and the risk of suicide was almost seven times greater.
Suicide and other nonnatural causes of death were more common in trans men, compared with cis women.
The report, by Christel J.M. de Blok, MD, of Amsterdam University Medical Center and colleagues, was published online Sept. 2 in The Lancet Diabetes & Endocrinology.
The study included trans men who received testosterone to transition from female to male and trans women who received estrogen plus an antiandrogen to transition from male to female.
Is gender-affirming hormone therapy associated with increased mortality?
Senior author Martin den Heijer, MD, also of Amsterdam University Medical Center, said: “The findings of our large, nationwide study highlight a substantially increased mortality risk among transgender people that has persisted for decades.”
But he pointed out that, overall, the data do not appear to suggest the premature deaths were related to gender-affirming hormone treatment.
However, he conceded that more work is needed on this aspect of care. “There is insufficient evidence at present to determine long-term safety of [gender-affirming hormone treatment]. More research is needed to fully establish whether it in any way affects mortality risk for transgender people,” said Dr. den Heijer.
Endocrinologist Will Malone, MD, of Twin Falls, Idaho, told this news organization, “The study confirms, like others before it, that individuals taking cross-sex hormones are more likely to die prematurely from a number of causes.”
“While the authors speculate that this higher mortality rate is not connected to cross-sex hormones, the study was not designed to be able to make such a claim,” he said, pointing to limited follow-up times.
In an accompanying commentary, Vin Tangpricha, MD, PhD, an endocrinologist from Emory University, Atlanta, noted: “Transgender men do not appear to have as significantly increased comorbidity following receipt of gender-affirming hormone therapy when compared with transgender women.”
Dr. Tangpricha added future studies should examine which factors – hormone regimen, hormone concentrations, access to health care, or other biological factors – explain the higher increased risk of morbidity and mortality observed in trans women as opposed to trans men.
However, Dr. de Blok and colleagues note that, as there were relatively few deaths among transgender men in the cohort, analysis on cause of death in this group is limited.
Transgender individuals more likely to die younger
For their study, Dutch researchers retrospectively examined data from 4,568 transgender people attending their clinic (2,927 transgender women and 1,641 transgender men) treated in 1972-2018. People were excluded if they started treatment before the age of 17 or if they had received puberty-blocking drugs.
Data on age at start of hormone treatment, type of treatment, smoking habits, medical history, and last date of follow-up were gathered from medical records. Where possible, SMRs were determined for deaths among trans men and trans women, compared with rates for the adult Dutch general population.
Median age at the start of cross-sex hormone treatment was 30 years in transgender women and 23 years in transgender men. But the median follow-up time was only 11 years in transgender women and 5 years in transgender men.
A total of 317 (10.8%) trans women died, and 44 (2.7%) trans men died. The findings were higher than expected, compared with the general population of cisgender women (SMR, 1.8) but not cisgender men (SMR 1.2).
Mortality risk did increase more in transgender people who started gender-affirming hormone treatment in the past 2 decades compared with earlier, a fact that Dr. de Blok said was surprising.
Trans men, for example, compared with cis women, had an SMR of 2.1-2.4 in 2000-2018 (compared with 1.8 overall).
“This may be due to changes in clinical practice. ... In the past, health care providers were reluctant to provide hormone treatment to people with a history of comorbidities such as cardiovascular disease. However, because of the many benefits of enabling people to access hormone therapy, nowadays this rarely results in treatment being denied,” Dr. de Blok noted.
More research needed, especially in trans-identifying youth
Dr. Malone remarked that previous studies have shown associations between taking cross-sex hormones and elevated mortality, while also “not designed to detect causality,” have “generally accepted that natal males who take estrogen have estrogen-related increases in the rates of heart disease, stroke, and deep venous thrombosis.”
He added that the risks of testosterone use in natal females were less well established, “but testosterone is also felt to increase their risk of heart disease.”
He stressed the limited follow-up times in the study by Dr. de Blok and colleagues.
This “strongly suggests that the rate of elevated mortality far exceeds the doubling measured by the study, especially for natal females.”
Dr. Malone is one of several clinicians and researchers who has formed the Society for Evidence-Based Gender Medicine, a nonprofit organization that now has at least 100 physician members. SEGM is concerned about the lack of quality evidence for the use of hormonal and surgical interventions as first-line treatment, especially for young people with gender dysphoria.
Dr. Tangpricha also highlighted that the findings do not apply to transgender people who began treatment before age 17 years or those who had taken puberty blockers before gender-affirming hormone treatment.
There are no long-term data on transgender individuals who have received gender-affirming hormone therapies close to the time of puberty.
These data, such as those from the Trans Youth Care study, should be available in the future, he added.
The authors have reported no relevant financial relationships. Dr. Tangpricha has reported receiving funding from the National Institutes of Health and served as past president of the World Professional Association for Transgender Health. He is editor-in-chief of Endocrine Practice and has provided expert testimony for Kirkland and Ellis.
A version of this article first appeared on Medscape.com.
2021 Update on pelvic floor disorders
With the increasing prevalence of pelvic floor disorders among our aging population, women’s health clinicians should be prepared to counsel patients on treatment options and posttreatment expectations. In this Update, we will review recent literature on surgical treatments for pelvic organ prolapse (POP) and stress urinary incontinence (SUI). We also include our review of an award-winning and practice-changing study on office-based pessary care. Lastly, we will finish with a summary of a recent Society of Gynecologic Surgeons collaborative systematic review on sexual function after surgery.
5-year RCT data on hysteropexy vs hysterectomy for POP
Nager CW, Visco AG, Richter HE, et al; National Institute of Child Health and Human Development Pelvic Floor Disorders Network. Effect of sacrospinous hysteropexy with graft vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with uterovaginal prolapse: 5-year results of a randomized clinical trial. Am J Obstet Gynecol. 2021;225:153. e1-153.e31. doi: 10.1016/j.ajog.2021.03.012.
The Pelvic Floor Disorders Network conducted a multisite randomized superiority trial comparing sacrospinous hysteropexy with mesh graft to vaginal hysterectomy with uterosacral ligament suspension for POP.
Study details
Postmenopausal women who desired surgery for symptomatic uterovaginal prolapse were randomly assigned to sacrospinous hysteropexy with polypropylene mesh graft using the Uphold-LITE device (Boston Scientific) versus vaginal hysterectomy with uterosacral ligament suspension. Participants were masked to treatment allocation and completed study visits at 6-month intervals through 60 months. Quantitative prolapse POP-Q exams were performed and patients completed multiple validated questionnaires regarding the presence; severity; and impact of prolapse, urinary, bowel, and pelvic pain symptoms.
Results
A total of 183 postmenopausal women were randomized, and 156 (81 hysteropexy and 75 hysterectomy) patients completed 5-year follow up with no demographic differences between the 2 intervention groups. Operative time was statistically less in the hysteropexy group (111.5 min vs 156.7 min). There were fewer treatment failures (a composite including retreatment for prolapse, prolapse beyond the hymen, and/or bothersome bulge symptoms) in the hysteropexy than in the hysterectomy group (37% vs 54%, respectively) at 5 years of follow up. However, most patients with treatment failure were classified as an intermittent failure, with only 16% of hysteropexy patients and 22% of hysterectomy patients classified as persistent failures. There were no meaningful differences between patient-reported outcomes. Hysteropexy had an 8% mesh exposure risk, with none requiring surgical management.
This study represents the highest quality randomized trial design and boasts high patient retention rates and 5-year follow up. Findings support further investigation on the use of polypropylene mesh for POP. In April of 2019, the US Food and Drug Administration halted the selling and distribution of vaginal mesh products for prolapse repair given the lack of safety outcomes, concerns about mesh exposure rates, and possible increased rates of pelvic pain and adverse events. This study invites pelvic reconstructive surgeons to revisit the debate of hysteropexy versus hysterectomy and synthetic mesh versus native tissue repairs. The 8% mesh exposure rate represents a challenge for the future design and development of vaginal implant materials, weighing the balancing of improved long-term efficacy with the safety and complication concerns.
Continue to: Preliminary 12-month data for a single-incision sling for surgical management of SUI...
Preliminary 12-month data for a single-incision sling for surgical management of SUI
Erickson T, Roovers JP, Gheiler E, et al. A multicenter prospective study evaluating efficacy and safety of a single-incision sling procedure for stress urinary incontinence. J Minim Invasive Gynecol. 2021;28:93-99. doi: 10.1016/j.jmig.2020.04.014.
In this industry-sponsored study, researchers compared a novel single-incision sling to currently available midurethral slings for SUI with 12-month outcomes and adverse event details. However, results are primarily descriptive with no statistical testing.
Study details
Patients were eligible for inclusion in this prospective, nonrandomized cohort study if SUI was their primary incontinence symptom, with confirmatory office testing. Exclusion criteria included POP greater than stage 2, prior SUI surgery, plans for future pregnancy, elevated postvoid residuals, or concomitant surgical procedures. The single-incision Altis (Coloplast) sling was compared to all commercially available transobturator and retropubic midurethral slings. The primary outcome of this study was reduction in 24-hour pad weights, and secondary outcomes included negative cough-stress test and subjective patient-reported outcomes via validated questionnaires.
Results
A total of 184 women were enrolled in the Altis group and 171 in the comparator other sling group. Symptom severity was similar between groups, but more patients in the comparator group had mixed urinary incontinence, and more patients in the Altis group had intrinsic sphincter deficiency. The Altis group had a higher proportion of “dry patients,” but otherwise the outcomes were similar between the 2 groups, including negative cough-stress test and patientreported outcomes. Two patients in the Altis group and 7 patients in the comparator group underwent device revisions. Again, statistical analysis was not performed.
Single-incision slings may reduce the risk of groin pain associated with transobturator slings and may be a good option for patients who desire less mesh burden than the traditional retropubic slings or who are not good candidates. This trial suggests that the Altis single-incision sling may be similar in outcomes and adverse events to currently available midurethral slings, but further, more rigorous trials are underway to fully evaluate this—including a US-based multicenter randomized trial of Altis single-incision slings versus retropubic slings (ClinicalTrials.gov Identifier: NCT03520114).
Office-based pessary care can be safely spaced out to 24 weeks without an increase in erosions
Propst K, Mellen C, O’Sullivan DM, et al. Timing of office-based pessary care: a randomized controlled trial. Obstet Gynecol. 2020;135:100-105. doi: 10.1097 /AOG.0000000000003580.
For women already using a pessary without issues, extending office visits to every 6 months does not increase rates of vaginal epithelial abnormalities, according to results of this randomized controlled trial.
Study details
Women already using a Gelhorn, ring, or incontinence dish pessary for POP, SUI, or both were randomized to continue routine care with office evaluation every 12 weeks versus the extended-care cohort (with office evaluation every 24 weeks). Women were excluded if they removed and replaced the pessary themselves or if there was a presence of vaginal epithelial abnormalities, such as erosion or granulation tissue.
Results
The rate of vaginal epithelium erosion was 7.4% in the routine arm and 1.7% in the extended-care arm, meeting criteria for noninferiority of extended care. The majority of patients with office visits every 24 weeks preferred the less frequent examinations, and there was no difference in degree of bother due to vaginal discharge. There was also no difference in the percentage of patients with unscheduled visits. The only factors associated with vaginal epithelium abnormalities were prior abnormalities and lifetime duration of pessary use.
As there are currently no evidenced-based guidelines for pessary care, this study contributes data to support extended office-based care up to 24 weeks, a common practice in the United Kingdom. During the COVID-19 pandemic, with reduced health care access, these findings should be reassuring to clinicians and patients.
Continue to: How can we counsel patients regarding changes in sexual activity and function after surgery for POP?...
How can we counsel patients regarding changes in sexual activity and function after surgery for POP?
Antosh DD, Dieter AA, Balk EM, et al. Sexual function after pelvic organ prolapse surgery: a systematic review comparing different approaches to pelvic floor repair. Am J Obstet Gynecol. 2021;2:S0002-9378(21)00610-4. doi: 10.1016/j.ajog.2021.05.042.
A secondary analysis of a recent systematic review found overall moderate- to high-quality evidence that were no differences in total dyspareunia, de novo dyspareunia, and scores on a validated sexual function questionnaire (PISQ12) when comparing postoperative sexual function outcomes of native tissue repair to sacrocolpopexy, transvaginal mesh, or biologic graft. Rates of postoperative dyspareunia were higher for transvaginal mesh than for sacrocolpopexy.
Study details
The Society of Gynecologic Surgeons Systematic Review Group identified 43 original prospective, comparative studies of reconstructive prolapse surgery that reported sexual function outcomes when comparing 2 different types of POP procedures. Thirty-seven of those studies were randomized controlled trials. Specifically, they looked at data comparing outcomes for native tissue versus sacrocolpopexy, native tissue versus transvaginal mesh, native tissue versus biologic graft, and transvaginal mesh versus sacrocolpopexy.
Results
Overall, the prevalence of postoperative dyspareunia was lower than preoperatively after all surgery types. The only statistical difference in this review demonstrated higher postoperative prevalence of dyspareunia after transvaginal mesh than sacrocolpopexy, based on 2 studies. When comparing native tissue prolapse repair to transvaginal mesh, sacrocolpopexy, or biologic grafts, there were no significant differences in sexual activity, baseline, or postoperative total dyspareunia, de-novo dyspareunia, or sexual function changes as measured by the PISQ12 validated questionnaire. ●
This systematic review further contributes to the growing evidence that, regardless of surgical approach to POP, sexual function generally improves and dyspareunia rates generally decrease postoperatively, with overall low rates of de novo dyspareunia. This will help patients and providers select the best-fit surgical approach without concern for worsened sexual function. It also underscores the need for inclusion of standardized sexual function terminology use and sexual health outcomes in future prolapse surgery research.
With the increasing prevalence of pelvic floor disorders among our aging population, women’s health clinicians should be prepared to counsel patients on treatment options and posttreatment expectations. In this Update, we will review recent literature on surgical treatments for pelvic organ prolapse (POP) and stress urinary incontinence (SUI). We also include our review of an award-winning and practice-changing study on office-based pessary care. Lastly, we will finish with a summary of a recent Society of Gynecologic Surgeons collaborative systematic review on sexual function after surgery.
5-year RCT data on hysteropexy vs hysterectomy for POP
Nager CW, Visco AG, Richter HE, et al; National Institute of Child Health and Human Development Pelvic Floor Disorders Network. Effect of sacrospinous hysteropexy with graft vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with uterovaginal prolapse: 5-year results of a randomized clinical trial. Am J Obstet Gynecol. 2021;225:153. e1-153.e31. doi: 10.1016/j.ajog.2021.03.012.
The Pelvic Floor Disorders Network conducted a multisite randomized superiority trial comparing sacrospinous hysteropexy with mesh graft to vaginal hysterectomy with uterosacral ligament suspension for POP.
Study details
Postmenopausal women who desired surgery for symptomatic uterovaginal prolapse were randomly assigned to sacrospinous hysteropexy with polypropylene mesh graft using the Uphold-LITE device (Boston Scientific) versus vaginal hysterectomy with uterosacral ligament suspension. Participants were masked to treatment allocation and completed study visits at 6-month intervals through 60 months. Quantitative prolapse POP-Q exams were performed and patients completed multiple validated questionnaires regarding the presence; severity; and impact of prolapse, urinary, bowel, and pelvic pain symptoms.
Results
A total of 183 postmenopausal women were randomized, and 156 (81 hysteropexy and 75 hysterectomy) patients completed 5-year follow up with no demographic differences between the 2 intervention groups. Operative time was statistically less in the hysteropexy group (111.5 min vs 156.7 min). There were fewer treatment failures (a composite including retreatment for prolapse, prolapse beyond the hymen, and/or bothersome bulge symptoms) in the hysteropexy than in the hysterectomy group (37% vs 54%, respectively) at 5 years of follow up. However, most patients with treatment failure were classified as an intermittent failure, with only 16% of hysteropexy patients and 22% of hysterectomy patients classified as persistent failures. There were no meaningful differences between patient-reported outcomes. Hysteropexy had an 8% mesh exposure risk, with none requiring surgical management.
This study represents the highest quality randomized trial design and boasts high patient retention rates and 5-year follow up. Findings support further investigation on the use of polypropylene mesh for POP. In April of 2019, the US Food and Drug Administration halted the selling and distribution of vaginal mesh products for prolapse repair given the lack of safety outcomes, concerns about mesh exposure rates, and possible increased rates of pelvic pain and adverse events. This study invites pelvic reconstructive surgeons to revisit the debate of hysteropexy versus hysterectomy and synthetic mesh versus native tissue repairs. The 8% mesh exposure rate represents a challenge for the future design and development of vaginal implant materials, weighing the balancing of improved long-term efficacy with the safety and complication concerns.
Continue to: Preliminary 12-month data for a single-incision sling for surgical management of SUI...
Preliminary 12-month data for a single-incision sling for surgical management of SUI
Erickson T, Roovers JP, Gheiler E, et al. A multicenter prospective study evaluating efficacy and safety of a single-incision sling procedure for stress urinary incontinence. J Minim Invasive Gynecol. 2021;28:93-99. doi: 10.1016/j.jmig.2020.04.014.
In this industry-sponsored study, researchers compared a novel single-incision sling to currently available midurethral slings for SUI with 12-month outcomes and adverse event details. However, results are primarily descriptive with no statistical testing.
Study details
Patients were eligible for inclusion in this prospective, nonrandomized cohort study if SUI was their primary incontinence symptom, with confirmatory office testing. Exclusion criteria included POP greater than stage 2, prior SUI surgery, plans for future pregnancy, elevated postvoid residuals, or concomitant surgical procedures. The single-incision Altis (Coloplast) sling was compared to all commercially available transobturator and retropubic midurethral slings. The primary outcome of this study was reduction in 24-hour pad weights, and secondary outcomes included negative cough-stress test and subjective patient-reported outcomes via validated questionnaires.
Results
A total of 184 women were enrolled in the Altis group and 171 in the comparator other sling group. Symptom severity was similar between groups, but more patients in the comparator group had mixed urinary incontinence, and more patients in the Altis group had intrinsic sphincter deficiency. The Altis group had a higher proportion of “dry patients,” but otherwise the outcomes were similar between the 2 groups, including negative cough-stress test and patientreported outcomes. Two patients in the Altis group and 7 patients in the comparator group underwent device revisions. Again, statistical analysis was not performed.
Single-incision slings may reduce the risk of groin pain associated with transobturator slings and may be a good option for patients who desire less mesh burden than the traditional retropubic slings or who are not good candidates. This trial suggests that the Altis single-incision sling may be similar in outcomes and adverse events to currently available midurethral slings, but further, more rigorous trials are underway to fully evaluate this—including a US-based multicenter randomized trial of Altis single-incision slings versus retropubic slings (ClinicalTrials.gov Identifier: NCT03520114).
Office-based pessary care can be safely spaced out to 24 weeks without an increase in erosions
Propst K, Mellen C, O’Sullivan DM, et al. Timing of office-based pessary care: a randomized controlled trial. Obstet Gynecol. 2020;135:100-105. doi: 10.1097 /AOG.0000000000003580.
For women already using a pessary without issues, extending office visits to every 6 months does not increase rates of vaginal epithelial abnormalities, according to results of this randomized controlled trial.
Study details
Women already using a Gelhorn, ring, or incontinence dish pessary for POP, SUI, or both were randomized to continue routine care with office evaluation every 12 weeks versus the extended-care cohort (with office evaluation every 24 weeks). Women were excluded if they removed and replaced the pessary themselves or if there was a presence of vaginal epithelial abnormalities, such as erosion or granulation tissue.
Results
The rate of vaginal epithelium erosion was 7.4% in the routine arm and 1.7% in the extended-care arm, meeting criteria for noninferiority of extended care. The majority of patients with office visits every 24 weeks preferred the less frequent examinations, and there was no difference in degree of bother due to vaginal discharge. There was also no difference in the percentage of patients with unscheduled visits. The only factors associated with vaginal epithelium abnormalities were prior abnormalities and lifetime duration of pessary use.
As there are currently no evidenced-based guidelines for pessary care, this study contributes data to support extended office-based care up to 24 weeks, a common practice in the United Kingdom. During the COVID-19 pandemic, with reduced health care access, these findings should be reassuring to clinicians and patients.
Continue to: How can we counsel patients regarding changes in sexual activity and function after surgery for POP?...
How can we counsel patients regarding changes in sexual activity and function after surgery for POP?
Antosh DD, Dieter AA, Balk EM, et al. Sexual function after pelvic organ prolapse surgery: a systematic review comparing different approaches to pelvic floor repair. Am J Obstet Gynecol. 2021;2:S0002-9378(21)00610-4. doi: 10.1016/j.ajog.2021.05.042.
A secondary analysis of a recent systematic review found overall moderate- to high-quality evidence that were no differences in total dyspareunia, de novo dyspareunia, and scores on a validated sexual function questionnaire (PISQ12) when comparing postoperative sexual function outcomes of native tissue repair to sacrocolpopexy, transvaginal mesh, or biologic graft. Rates of postoperative dyspareunia were higher for transvaginal mesh than for sacrocolpopexy.
Study details
The Society of Gynecologic Surgeons Systematic Review Group identified 43 original prospective, comparative studies of reconstructive prolapse surgery that reported sexual function outcomes when comparing 2 different types of POP procedures. Thirty-seven of those studies were randomized controlled trials. Specifically, they looked at data comparing outcomes for native tissue versus sacrocolpopexy, native tissue versus transvaginal mesh, native tissue versus biologic graft, and transvaginal mesh versus sacrocolpopexy.
Results
Overall, the prevalence of postoperative dyspareunia was lower than preoperatively after all surgery types. The only statistical difference in this review demonstrated higher postoperative prevalence of dyspareunia after transvaginal mesh than sacrocolpopexy, based on 2 studies. When comparing native tissue prolapse repair to transvaginal mesh, sacrocolpopexy, or biologic grafts, there were no significant differences in sexual activity, baseline, or postoperative total dyspareunia, de-novo dyspareunia, or sexual function changes as measured by the PISQ12 validated questionnaire. ●
This systematic review further contributes to the growing evidence that, regardless of surgical approach to POP, sexual function generally improves and dyspareunia rates generally decrease postoperatively, with overall low rates of de novo dyspareunia. This will help patients and providers select the best-fit surgical approach without concern for worsened sexual function. It also underscores the need for inclusion of standardized sexual function terminology use and sexual health outcomes in future prolapse surgery research.
With the increasing prevalence of pelvic floor disorders among our aging population, women’s health clinicians should be prepared to counsel patients on treatment options and posttreatment expectations. In this Update, we will review recent literature on surgical treatments for pelvic organ prolapse (POP) and stress urinary incontinence (SUI). We also include our review of an award-winning and practice-changing study on office-based pessary care. Lastly, we will finish with a summary of a recent Society of Gynecologic Surgeons collaborative systematic review on sexual function after surgery.
5-year RCT data on hysteropexy vs hysterectomy for POP
Nager CW, Visco AG, Richter HE, et al; National Institute of Child Health and Human Development Pelvic Floor Disorders Network. Effect of sacrospinous hysteropexy with graft vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with uterovaginal prolapse: 5-year results of a randomized clinical trial. Am J Obstet Gynecol. 2021;225:153. e1-153.e31. doi: 10.1016/j.ajog.2021.03.012.
The Pelvic Floor Disorders Network conducted a multisite randomized superiority trial comparing sacrospinous hysteropexy with mesh graft to vaginal hysterectomy with uterosacral ligament suspension for POP.
Study details
Postmenopausal women who desired surgery for symptomatic uterovaginal prolapse were randomly assigned to sacrospinous hysteropexy with polypropylene mesh graft using the Uphold-LITE device (Boston Scientific) versus vaginal hysterectomy with uterosacral ligament suspension. Participants were masked to treatment allocation and completed study visits at 6-month intervals through 60 months. Quantitative prolapse POP-Q exams were performed and patients completed multiple validated questionnaires regarding the presence; severity; and impact of prolapse, urinary, bowel, and pelvic pain symptoms.
Results
A total of 183 postmenopausal women were randomized, and 156 (81 hysteropexy and 75 hysterectomy) patients completed 5-year follow up with no demographic differences between the 2 intervention groups. Operative time was statistically less in the hysteropexy group (111.5 min vs 156.7 min). There were fewer treatment failures (a composite including retreatment for prolapse, prolapse beyond the hymen, and/or bothersome bulge symptoms) in the hysteropexy than in the hysterectomy group (37% vs 54%, respectively) at 5 years of follow up. However, most patients with treatment failure were classified as an intermittent failure, with only 16% of hysteropexy patients and 22% of hysterectomy patients classified as persistent failures. There were no meaningful differences between patient-reported outcomes. Hysteropexy had an 8% mesh exposure risk, with none requiring surgical management.
This study represents the highest quality randomized trial design and boasts high patient retention rates and 5-year follow up. Findings support further investigation on the use of polypropylene mesh for POP. In April of 2019, the US Food and Drug Administration halted the selling and distribution of vaginal mesh products for prolapse repair given the lack of safety outcomes, concerns about mesh exposure rates, and possible increased rates of pelvic pain and adverse events. This study invites pelvic reconstructive surgeons to revisit the debate of hysteropexy versus hysterectomy and synthetic mesh versus native tissue repairs. The 8% mesh exposure rate represents a challenge for the future design and development of vaginal implant materials, weighing the balancing of improved long-term efficacy with the safety and complication concerns.
Continue to: Preliminary 12-month data for a single-incision sling for surgical management of SUI...
Preliminary 12-month data for a single-incision sling for surgical management of SUI
Erickson T, Roovers JP, Gheiler E, et al. A multicenter prospective study evaluating efficacy and safety of a single-incision sling procedure for stress urinary incontinence. J Minim Invasive Gynecol. 2021;28:93-99. doi: 10.1016/j.jmig.2020.04.014.
In this industry-sponsored study, researchers compared a novel single-incision sling to currently available midurethral slings for SUI with 12-month outcomes and adverse event details. However, results are primarily descriptive with no statistical testing.
Study details
Patients were eligible for inclusion in this prospective, nonrandomized cohort study if SUI was their primary incontinence symptom, with confirmatory office testing. Exclusion criteria included POP greater than stage 2, prior SUI surgery, plans for future pregnancy, elevated postvoid residuals, or concomitant surgical procedures. The single-incision Altis (Coloplast) sling was compared to all commercially available transobturator and retropubic midurethral slings. The primary outcome of this study was reduction in 24-hour pad weights, and secondary outcomes included negative cough-stress test and subjective patient-reported outcomes via validated questionnaires.
Results
A total of 184 women were enrolled in the Altis group and 171 in the comparator other sling group. Symptom severity was similar between groups, but more patients in the comparator group had mixed urinary incontinence, and more patients in the Altis group had intrinsic sphincter deficiency. The Altis group had a higher proportion of “dry patients,” but otherwise the outcomes were similar between the 2 groups, including negative cough-stress test and patientreported outcomes. Two patients in the Altis group and 7 patients in the comparator group underwent device revisions. Again, statistical analysis was not performed.
Single-incision slings may reduce the risk of groin pain associated with transobturator slings and may be a good option for patients who desire less mesh burden than the traditional retropubic slings or who are not good candidates. This trial suggests that the Altis single-incision sling may be similar in outcomes and adverse events to currently available midurethral slings, but further, more rigorous trials are underway to fully evaluate this—including a US-based multicenter randomized trial of Altis single-incision slings versus retropubic slings (ClinicalTrials.gov Identifier: NCT03520114).
Office-based pessary care can be safely spaced out to 24 weeks without an increase in erosions
Propst K, Mellen C, O’Sullivan DM, et al. Timing of office-based pessary care: a randomized controlled trial. Obstet Gynecol. 2020;135:100-105. doi: 10.1097 /AOG.0000000000003580.
For women already using a pessary without issues, extending office visits to every 6 months does not increase rates of vaginal epithelial abnormalities, according to results of this randomized controlled trial.
Study details
Women already using a Gelhorn, ring, or incontinence dish pessary for POP, SUI, or both were randomized to continue routine care with office evaluation every 12 weeks versus the extended-care cohort (with office evaluation every 24 weeks). Women were excluded if they removed and replaced the pessary themselves or if there was a presence of vaginal epithelial abnormalities, such as erosion or granulation tissue.
Results
The rate of vaginal epithelium erosion was 7.4% in the routine arm and 1.7% in the extended-care arm, meeting criteria for noninferiority of extended care. The majority of patients with office visits every 24 weeks preferred the less frequent examinations, and there was no difference in degree of bother due to vaginal discharge. There was also no difference in the percentage of patients with unscheduled visits. The only factors associated with vaginal epithelium abnormalities were prior abnormalities and lifetime duration of pessary use.
As there are currently no evidenced-based guidelines for pessary care, this study contributes data to support extended office-based care up to 24 weeks, a common practice in the United Kingdom. During the COVID-19 pandemic, with reduced health care access, these findings should be reassuring to clinicians and patients.
Continue to: How can we counsel patients regarding changes in sexual activity and function after surgery for POP?...
How can we counsel patients regarding changes in sexual activity and function after surgery for POP?
Antosh DD, Dieter AA, Balk EM, et al. Sexual function after pelvic organ prolapse surgery: a systematic review comparing different approaches to pelvic floor repair. Am J Obstet Gynecol. 2021;2:S0002-9378(21)00610-4. doi: 10.1016/j.ajog.2021.05.042.
A secondary analysis of a recent systematic review found overall moderate- to high-quality evidence that were no differences in total dyspareunia, de novo dyspareunia, and scores on a validated sexual function questionnaire (PISQ12) when comparing postoperative sexual function outcomes of native tissue repair to sacrocolpopexy, transvaginal mesh, or biologic graft. Rates of postoperative dyspareunia were higher for transvaginal mesh than for sacrocolpopexy.
Study details
The Society of Gynecologic Surgeons Systematic Review Group identified 43 original prospective, comparative studies of reconstructive prolapse surgery that reported sexual function outcomes when comparing 2 different types of POP procedures. Thirty-seven of those studies were randomized controlled trials. Specifically, they looked at data comparing outcomes for native tissue versus sacrocolpopexy, native tissue versus transvaginal mesh, native tissue versus biologic graft, and transvaginal mesh versus sacrocolpopexy.
Results
Overall, the prevalence of postoperative dyspareunia was lower than preoperatively after all surgery types. The only statistical difference in this review demonstrated higher postoperative prevalence of dyspareunia after transvaginal mesh than sacrocolpopexy, based on 2 studies. When comparing native tissue prolapse repair to transvaginal mesh, sacrocolpopexy, or biologic grafts, there were no significant differences in sexual activity, baseline, or postoperative total dyspareunia, de-novo dyspareunia, or sexual function changes as measured by the PISQ12 validated questionnaire. ●
This systematic review further contributes to the growing evidence that, regardless of surgical approach to POP, sexual function generally improves and dyspareunia rates generally decrease postoperatively, with overall low rates of de novo dyspareunia. This will help patients and providers select the best-fit surgical approach without concern for worsened sexual function. It also underscores the need for inclusion of standardized sexual function terminology use and sexual health outcomes in future prolapse surgery research.
Innovative therapies in gynecology: The evidence and your practice
As more and more gynecologic therapies move to the outpatient setting, keeping up on the latest data regarding emerging options can be challenging. Furthermore, it can be difficult to justify purchasing expensive equipment for the office when a therapy is not covered by medical insurance plans. However, if a therapy is efficacious and patients are willing to pay out of pocket, clinicians may want to have these options available for their patients.
In an effort to work through these complex issues, a panel of experts was convened at the 47th Annual Scientific Meeting of the Society of Gynecologic Surgeons in Palm Springs, California, on June 29, 2021. This article includes the salient points from that panel discussion.
Fractionated CO2 laser therapy
Fractionated CO2 laser therapy is considered second-line therapy for the treatment of genitourinary syndrome of menopause (GSM). In 2018, the US Food and Drug Administration (FDA) issued a safety warning about the use of CO2 laser therapy and warned patients and clinicians that the FDA had not approved the treatment for vaginal rejuvenation or treatment of vaginal symptoms related to menopause, urinary incontinence, or sexual function. Despite this warning, laser treatments are still performed in many practices.
In 2019, the International Continence Society (ICS) and the International Society for the Study of Vulvovaginal Disease (ISSVD) put out a joint practice consensus statement that essentially did not recommend the routine use of laser treatment for GSM, urinary incontinence, or lichen sclerosus.1 Conversely, the 2020 American Urogynecologic Society (AUGS) published a clinical consensus statement that spoke to the promising results of laser therapy for the treatment of vulvovaginal atrophy, vaginal dryness, and menopausal dyspareunia, with benefits lasting up to 1 year.2 This statement also suggested that the short-term safety profile of the CO2 laser device was favorable.
How CO2 lasers work
Fractionated CO2 laser therapy differs from unfractionated treatment (which often is used in the treatment of condyloma) in that it is not ablative. The laser works by using fractionated beams of light to penetrate the affected tissue to create small wounds in the epithelium and underlying lamina propria, which leads to collagen remodeling and regeneration that then results in the restoration of the superficial epithelium, vaginal rugae, and lubrication.3 Most clinicians perform 3 applications of the laser treatment 6 weeks apart, a recommendation that is based on manufacturer-sponsored studies in menopausal women.
Study results of patient outcomes with laser therapy
GSM. Several retrospective4,5 and prospective studies6-10 have looked at short- and longer-term outcomes in patients undergoing treatment with the CO2 laser. All of these studies showed improvement in patient symptoms related to GSM.
The VeLVET trial, conducted by Paraiso and colleagues, was a randomized trial that compared CO2 laser treatment with vaginal estrogen in women with GSM.11 While the study was underpowered due to cessation of enrollment once the FDA safety warning was issued, the authors reported that at 6 months, both the fractionated CO2 laser therapy group and the vaginal estrogen group had similar improvements, with 70% to 80% of participants reporting satisfaction with treatment. The authors concluded that laser therapy is likely to be as efficacious as vaginal estrogen and may be a good option for patients who cannot use vaginal estrogen to treat GSM.11
Lichen sclerosus. Some data exist on the efficacy of laser therapy for the treatment of lichen sclerosus. One recently published randomized trial showed that at 6 months, fractionated CO2 laser treatment and prior treatment with high potency topical corticosteroids was associated with higher improvement in subjective symptoms and objective measures compared with clobetasol propionate treatment.12 Another trial, however, revealed that laser treatment was not an effective monotherapy treatment for lichen sclerosus when compared with placebo.13 Fewer studies have examined the effect of laser therapy on urinary incontinence.
More prospective data are emerging, evidenced by trials currently registered in ClinicalTrials.gov. While some studies provide evidence that laser therapy may be efficacious in the treatment of vulvovaginal atrophy, additional data are needed to confirm the favorable outcomes observed with laser therapy for the treatment of lichen sclerosus, and a significant amount of data are needed to evaluate the efficacy of laser treatment for urinary incontinence.
Until such evidence is available, fractionated CO2 vaginal laser therapy will remain a fee-for-service treatment option and will be inaccessible to patients who cannot afford the cost of treatment.
Continue to: Hydrogel urethral bulking...
Hydrogel urethral bulking
Urethral bulking agents have been used for 5 decades in the treatment of stress urinary incontinence (SUI) in women. Unlike midurethral slings, in which many medical device companies use the same implant material (microporous, monofilament polypropylene mesh), the material for bulking agents has varied greatly. A 2017 Cochrane review of urethral bulking listed these agents used for this indication: autologous fat, carbon beads, calcium hydroxylapatite, ethylene vinyl alcohol copolymer, glutaraldehyde cross-linked bovine collagen, hyaluronic acid with dextranomer, porcine dermal implant, polytetrafluoroethylene, and silicone particles.14 These agents can be injected through a transurethral or periurethral technique. The review failed to find superiority of one material or injection technique over another.
New bulking agent available
In January 2020, the FDA approved the premarket application for a new bulking agent. This new agent is a permanently implanted, nonresorbable hydrogel that consists of cross-linked polyacrylamide (2.5%) and water (97.5%). It is intended to be used with a transurethral bulking system that includes a rotatable sheath and two 23-guage needles; a total of 1.5 to 2.0 mL of the hydrogel is injected in 3 locations in the proximal urethra per session. Patients may undergo an additional 2 sessions, if needed, at least 4 weeks after the previous session.
Polyacrylamide hydrogel has been used as a bulking agent in cosmetic and ophthalmic surgery for many years, and it was first approved for medical use in Europe in 2001. The initial European data on its use as a urethral bulking agent was published in 2006.15 The first North American data came in 2014 from a multicenter, randomized trial that compared polyacrylamide hydrogel with collagen gel.16 This investigation followed 345 women for 12 months and concluded that the safety and efficacy of polyacrylamide hydrogel was not inferior to collagen, with a little over half of both cohorts demonstrating a 50% or greater decrease in incontinence episodes.
Since these initial studies, 3-year17 and 7-year safety and efficacy data18 have been reported, with reassuring findings, but both studies experienced significant attrition of the original group of patients. The most commonly reported adverse events associated with the procedure are pain at the injection site (4%–14%) and urinary tract infection (3%–7%); transient urinary retention rates range in incidence from 1.5% to 15%.19
Short procedure, long-term results
Given that a urethral bulking procedure can be done in less than 10 minutes in the office under local analgesia, this treatment may lend itself to use in more brittle patient populations. One study of women aged 80 or older showed a greater than 50% decrease in the number of daily pads used for up to 2 years after initial injection.20 Another study found the greatest treatment success in women aged 60 years or older with fewer than 2.5 episodes of SUI per day.21
Platelet-rich plasma therapy
Platelet-rich plasma (PRP) therapy has been used in multiple disciplines for more than 2 decades as a treatment to regenerate damaged tissue, particularly in sports medicine for treating tendonitis as well as in plastic surgery, gynecology, urology, and ophthalmology, and good outcomes have been demonstrated with no serious adverse effects. PRP is a natural product in which high levels of platelets are concentrated through centrifugation with bioactive growth factors, including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), fibroblast growth factor (FGF), and insulin growth factor (IGF).22 The activated platelets are then injected autologously back into the patient’s tissue. This process releases activated growth factors that accelerate tissue healing by stimulating the number of reparative cells to create collagen production, angiogenesis, and neurogenesis while fighting infection and downregulating the autoimmune system.
Continue to: Uses for PRP in gynecology...
Uses for PRP in gynecology
In gynecology, dating back to 2007 PRP was shown to facilitate wound healing, when Fanning and colleagues reported PRP applications in gynecologic operative wounds, such as hysterectomies and urogynecologic procedures, to reduce postoperative pain.23 In the last decade, there has been a dramatic increasing trend in the application of PRP injections as an alternative therapy in gynecology to improve intimate health. PRP has been used to treat lichen sclerosus, atrophic vaginitis, SUI, and female sexual dysfunction; however, there is a dearth of studies that compare PRP with traditional therapies.
Runels and colleagues described the effects of localized injections of autologous PRP for the treatment of sexual dysfunction early in 2014.24 Those authors pioneered PRP use in women with dyspareunia and other symptoms related to sexual dysfunction. Women were offered PRP injections into the periurethral area of the Skene glands and the clitoris. Sexual satisfaction and pain were improved but results did not reach statistical significance. The results of this pilot study of 11 patients suggested that PRP injections could perhaps be an effective method to treat certain types of female sexual dysfunction, including desire, arousal, lubrication, and orgasm.
In another pilot study, Long and colleagues looked at the effectiveness of local injection of PRP for treating women with SUI.25 In that study, younger patients with mild severity of SUI had promising results, with up to 75% cured or improved. Results in the older group, with 50% cured or improved, did not reach statistical significance. Other small, limited studies have been conducted under the hypothesis that PRP as an “O-shot” may be a promising treatment that is a safe, effective, nonsurgical, and nonhormonal option for women with dyspareunia from lack of lubrication and related sexual dysfunction, such as decreased libido or arousal.26-29 A pilot study by Behnia-Willison and colleagues demonstrated clinical improvement in PRP use as an alternative to topical steroids for lichen sclerosus.30 Several other studies also have shown efficacy for the treatment of lichen sclerosus.31-34
More evidence of efficacy needed
To date, preliminary studies suggest that PRP holds promise for a host of gynecologic conditions. Since PRP is autologous, there are no significant contraindications, and thus far there have been no known serious adverse effects. However, most health insurers still do not cover this therapy, so for now patients must pay out-of-pocket fees for these treatments.
As we continue to investigate therapies in regenerative medicine, the continued efforts of our discipline are required to conduct well-designed prospective, randomized controlled studies. While initial series suggest that PRP is safe, it is unlikely that this therapy will be embraced widely in the paradigm as an alternative treatment option for many genitourinary symptoms of menopause and vulvar disorders until efficacy is better established.
Radiofrequency therapy
For the past 20 years, radiofrequency (RF) energy has been used through the vagina, urethra, and periurethral tissues for the treatment of genitourinary symptoms, with limited success. More recently, because some patients hesitate to receive mesh implants for treatment of urinary incontinence,35 there has been gravitation to office-based procedures.
In contrast to lasers, which transmit energy through light, RF waves (measured in hertz) transform the kinetic energy of the intracellular atoms, which move and collide, generating thermal energy.36,37 RF therapy has been shown to increase the proportion of smooth muscle and connective tissue; stimulate proliferation of the epithelium, neovascularization, and collagen formation in the lamina propria; and improve natural lubrication.36,38 In addition, RF is:
- ablative when the heat is capable of generating ablation and/or necrosis of the epidermis and dermis
- microablative when energy fractionation produces microscopic columns of ablative thermal lesions in the epidermis and upper dermis, resulting in microscopic columns of treated tissue interspersed with areas of untreated skin,39 and
- nonablative when trauma occurs only in the dermis by heating without causing ablation of the epidermis.39
The RF devices discussed below are used with settings for microablation in the treatment of SUI and sexual health/vaginal laxity, and with nonablative settings in the treatment of GSM.
RF for the treatment of urinary incontinence
Studies with RF have shown its benefits in urinary symptoms as secondary outcomes, such as improvement of SUI.38,40 One theory that favors energy devices as a treatment for SUI is that the treatment strengthens suburethral and pubocervical support, thereby decreasing urethral mobility.41
In 2016, the Viveve system (Viveve) received FDA 510(k) clearance for “use in general surgical procedures for electrocoagulation and hemostasis.” A single-site, randomized, nonblinded pilot study compared 1 treatment (group 1) versus 2 treatments (group 2) with the Viveve system for SUI in 35 participants.42 At 12 months, only for group 2 did mean scores on the Incontinence Impact Questionnaire Short Form (IIQ-7) and the International Consultation on Incontinence Modular Questionnaire-Urinary Incontinence-Short Form (ICIQ-UI-SF) decrease by the minimum clinically important difference of 16 and 2.52 points, respectively, compared with baseline.
The ThermiVa device (ThermiGen, LLC) received FDA clearance for “use in dermatological and general surgical procedures for electrocoagulation and hemostasis” in 2017. A single-site, prospective, double-blind, randomized controlled pilot trial evaluated the efficacy of this device for the treatment of SUI in 20 participants randomly assigned in a 1:1 fashion to active and sham groups.43 At 12 weeks, mean scores of the Urogenital Distress Inventory (UDI-6) and the ICIQ-UI-SF decreased by the minimal clinically important difference only in the treatment group arm. Additionally, 70% of treatment group participants had a negative stress test at 12 weeks compared with 0% of control group participants.43 In another study of 48 patients who were followed longitudinally for 5 months, a substantial improvement in genital appearance was observed.44 Assessment based on validated instruments demonstrated significant improvements in sexual function and SUI.44
A microablative RF device (Wavetronic 6000 Touch Device, Megapulse HF FRAXX system; Loktal Medical Electronics) consists of a vaginal probe with 64 microneedles at the tip, each capable of penetrating to a depth of 1 mm. During activation, delivery of RF energy, which results in vaporization of tissue at 100 °C, occurs in a preset sequence of 8 needles at a time, preventing the overheating of intervening tissue between adjacent needles.
Slongo and colleagues conducted a 3-arm randomized clinical trial that included 117 climacteric women with SUI.45 In group 1, treatment consisted of 3 monthly sessions of RF; group 2 received 12 weekly sessions of pelvic floor muscle training (PFMT); and group 3 received RF treatment plus PFMT simultaneously. Assessments were conducted at baseline and 30 days after the end of therapy using validated questionnaires and scales for urinary, vaginal, and sexual functions, and cytology was used to assess vaginal atrophy. The association between RF and PFMT showed significant improvement in the SUI symptoms assessed by questionnaire. The vaginal symptoms and dryness showed more substantial improvement with the RF treatment, and vaginal laxity showed similar improvement in the 3 treatment groups.45
Continue to: RF for the treatment of GSM...
RF for the treatment of GSM
For women who are not candidates for localized hormone therapy, as well as others who simply do not wish to use hormones, nonablative RF laser therapy may be an alternative for the management of GSM.
The VIVEVE I trial was one of the largest randomized, sham-controlled trials performed to determine the efficacy of vaginal rejuvenation using surface-cooled RF; 174 women received either RF treatment (90 J/cm2) or sham treatment (1 J/cm2).46 Treated participants had a significant improvement in perception of vaginal laxity/looseness and sexual function up to 6 months posttreatment.46 Overall, participants were satisfied with the treatment (77.8%–100%) and reported significant improvements in vaginal laxity and symptoms of atrophy. RF was well tolerated with minimal adverse effects, such as procedure-related erythema and edema of treated tissue, and vaginal discharge. One patient discontinued treatment because of procedural pain.47,48
The ThermiVa system also was evaluated for efficacy in the treatment of GSM in a single-site, double-blind randomized controlled pilot study, the methods of which were previously described above.43 GSM symptoms were evaluated at baseline and 12 weeks using the Vaginal Health Index (VHI) and visual analog scale (VAS). At the 12-week follow-up, compared with baseline scores, VHI scores were unchanged in the control group and improved in the treatment group. Additionally, VAS scores for dyspareunia decreased in the treatment group compared with baseline while VAS for dyspareunia in the sham group did not change from baseline to 12 weeks.
RF treatment for sexual health
The efficacy of the Viveve RF system for female sexual dysfunction was evaluated in an international, randomized, controlled, single-blinded study (n = 154) that compared 6-month outcomes of RF treatment versus sham treatment.46 Although there was a statistically significant improvement in patient-reported sexual dysfunction on validated instruments, it is essential to note that the study was powered for the primary outcome of vaginal laxity. In addition, the study was not adequately powered to evaluate safety; however, the adverse events reported were mild, and the most frequently reported adverse event was vaginal discharge.
Microablative monopolar RF treatment for GSM has been evaluated in 2 single-arm clinical trials that included a total of 70 patients.39,49 Pre- and posttreatment outcomes were analyzed after delivery of 3 treatment sessions 28 to 40 days apart. Although the only significant improvement in quality of life was in the health domain of the World Health Organization Quality of Life Adapted Questionnaire (P = .04), significant improvements in sexual functioning were seen in terms of the desire (P = .002), lubrication (P = .001), satisfaction (P = .003), and pain (P = .007) domains of the Female Sexual Function Index (FSFI) questionnaire except for excitation and orgasm.39 Overall, 100% of participants reported being satisfied or very satisfied with treatments, and 13 of 14 women felt “cured” or “much better.”39 After treatment, significant increases in vaginal Lactobacillus (P<.001), decreases in vaginal pH (P<.001), improvements in maturation of vaginal cellularity (decreased parabasal cells, P<.001; increased superficial cells, P<.001), and increased VHI score (P<.001) alone occurred.49 No adverse events beyond self-limited vaginal burning and redness were reported.39,49 In another study mentioned above, the combination of RF and PFMT in sexual function does not offer benefits superior to those achieved by the therapies alone.45
Evidence on RF treatment does not support marketing efforts
Radiofrequency devices have been marketed for a variety of genitourinary problems in women, with limited high-quality, randomized, comparative evidence of efficacy and durability in the literature. It is unfortunate that RF treatment continues to be promoted by practitioners around the world who cite small, short-term studies that lack biostatistical rigor in their reporting of protocols and results. Statements from both AUGS and the International Urogynecological Association have heeded caution on the use of lasers but they could not even evaluate RF devices due to lack of evidence.2,41
Informed counseling and shared decision making remain the bottom line
By the year 2025, all members of the Baby Boom generation will be aged 60 or older. While in the past there has been a reluctance to discuss women’s sexual health, urinary incontinence, and GSM, the need for open discussion and a variety of treatment options for these conditions has never been more critical.
Many patients prefer office-based therapies over hospital-based procedures, and others are leery of synthetic implants. These concerns are leading toward great interest in the types of treatments covered in this article. However, it is paramount that clinicians are aware of the evidence-based data behind these emerging options so that we can openly and accurately counsel our patients.
As we have shown, the quality of the data behind these officed-based therapies varies significantly. Until a greater body of research data is available, we must carefully balance our desire to meet patient wishes with solid, informed counseling and shared decision making. ●
- Preti M, Viera-Baptista P, Digesu GA, et al. The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: an ICS/ISSVD best practice consensus document. J Lower Genital Tract Dis. 2019;23:151-160.
- Alshiek J, Garcia B, Minassian V, et al. Vaginal energy-based devices: AUGS clinical consensus statement. Female Pelvic Med Reconstr Surg. 2020;26:287-298.
- Streicher LF. Vulvar and vaginal fractional CO2 laser treatments for genitourinary syndrome of menopause: NAMS practice pearl. Menopause. 2018;25:571-573.
- Gardner AN, Aschkenazi SO. The short-term efficacy and safety of fractional CO2 laser therapy for vulvovaginal symptoms in menopause, breast cancer, and lichen sclerosus. Menopause. 2021; 28:511-516.
- Balchander D, Nyirjesy P. Fractionated CO2 laser therapy in recalcitrant lichen sclerosus. J Lower Genital Tract Disease. 2020;24:225-228.
- Pieralli A, Fallani MG, Becorpi A, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294:841-846.
- Pieralli A, Bianchi C, Longinotti M, et al. Long-term reliability of fractionated CO2 laser as a treatment of vulvovaginal atrophy (VVA) symptoms. Arch Gynecol Obstet. 2017; 296:973-978.
- Sokol ER, Karram MM. Use of novel fractional CO2 laser for the treatment of genitourinary syndrome of menopause: 1-year outcomes. Menopause. 2017;24: 810-814.
- Pagano T, Conforti A, Buonfantino C, et al. Effect of rescue fractional microablative CO2 laser on symptoms and sexual dysfunction in women affected by vulvar lichen sclerosus resistant to long-term use of topic corticosteroid: a prospective longitudinal study. Menopause. 2020;27:418-422.
- Sindou-Faurie T, Louis-Vahdat C, Oueld Es Cheikh E, et al. Evaluation of the efficacy of fractional CO2 laser in the treatment of vulvar and vaginal menopausal symptoms. Arch Gynecol Obstet. 2021;303:955-963.
- Paraiso MFR, Ferrando CA, Sokol ER, at al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: the VeLVET trial. Menopause. 2019;27:50-56.
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978.
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;136:979-987.
- Kirchin V, Page T, Keegan PE, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD003881.
- Lose G, Mouritsen L, Nielson JB. A new bulking agent (polyacrylamide hydrogel) for treating stress urinary incontinence in women. BJU Int. 2006;98:100-104.
- Sokol ER, Karram MM, Dmochowski R. Efficacy and safety of polyacrylamide hydrogel for the treatment of female stress incontinence: a randomized, prospective, multicenter North American study. J Urol. 2014;192:843-849.
- Pai A, Al-Singary W. Durability, safety and efficacy of polyacrylamide hydrogel (Bulkamid) in the management of stress and mixed urinary incontinence: three year follow up outcomes. Cent European J Urol. 2015;68:428-433.
- Brosche T, Kuhn A, Lobodasch K, et al. Seven-year efficacy and safety outcomes of Bulkamid for the treatment of stress urinary incontinence. Neurourol Urodyn. 2021;40:502-508.
- Kasi AD, Pergialiotis V, Perrea DN, et al. Polyacrylamide hydrogel (Bulkamid) for stress urinary incontinence in women: a systematic review of the literature. Int Urogynecol J. 2016;27:367-375.
- Vecchioli-Scaldazza CV, Smaali C, Morosetti C, et al. Polyacrylamide hydrogel (Bulkamid) in female patients of 80 or more years with urinary incontinence. Int Braz J Urol. 2014;40:37-43.
- Elmelund M, Sokol ER, Darram MM, et al. Patient characteristics that may influence the effect of urethral injection therapy for female stress urinary incontinence. J Urol. 2019;202:125-131.
- Sanoulis V, Nikolettos N, Vlahos N. The use of platelet-rich plasma in the gynecological clinical setting: a review. HJOG. 2019;18:55-65.
- Fanning J, Murrain L, Flora R, et al. Phase I/II prospective trial of autologous platelet tissue graft in gynecologic surgery. J Minim Invasive Gynecol. 2007;14:633-637.
- Runels CE, Melnick H, DeBourbon E, et al. A pilot study of the effect of localized injections of autologous platelet rich plasma (PRP) for the treatment of female sexual dysfunction. J Womens Health Care. 2014;3:4.
- Long CY, Lin KL, Shen CR, et al. A pilot study: effectiveness of local injection of autologous platelet-rich plasma in treating women with stress urinary incontinence. Sci Rep. 2021;11:1584.
- Matz EJ, Pearlman AM, Terlecki RP. Safety and feasibility of platelet rich fibrin matrix injections for treatment of common urologic conditions. Investig Clin Urol. 2018;59:61-65.
- Neto JB. O-Shot: platelets rich plasma in intimate female treatment. J Womens Health Care. 2017;6:5.
- Nikolopoulos KI, Pergialiotis V, Perrea D, et al. Restoration of the pubourethral ligament with platelet rich plasma for the treatment of stress urinary incontinence. Med Hypotheses. 2016;90:29-31.
- Hersant B, SidAhmed-Mezi M, Belkacemi Y, et al. Efficacy of injecting platelet concentrate combined with hyaluronic acid for the treatment of vulvovaginal atrophy in postmenopausal women with a history of breast cancer: a phase 2 pilot study. Menopause. 2018;25:1124-1130.
- Behnia-Willison F, Pour NR, Mohamadi B, et al. Use of platelet-rich plasma for vulvovaginal autoimmune conditions like lichen sclerosus. Plast Reconstr Surg Glob Open. 2016;4:e1124.
- Goldstein AT, King M, Runels C, et al. Intradermal injection of autologous platelet-rich plasma for the treatment of vulvar lichen sclerosus. J Am Acad Dermatol. 2017;76:158-160.
- Casabona F, Priano V, Vallerino V, et al. New surgical approach to lichen sclerosus of the vulva: the role of adipose-derived mesenchymal cells and platelet-rich plasma in tissue regeneration. Plast Reconstr Surg. 2010;126:210e-211e.
- Franic D, Iternica Z, Franic-Ivanisevic M. Platelet-rich plasma (PRP) for the treatment of vulvar lichen sclerosus in a premenopausal woman: a case report. Case Rep Womens Health. 2018;18: e0062.
- Posey LK, Runels C. In office surgery and use of platelet rich plasma for the treatment of vulvar lichen sclerosus to alleviate painful sexual intercourse. J Lower Genital Tract Dis. 2017;21(4S):S14.
- Stachowicz AM, Hoover ML, Karram MM. Clinical utility of radiofrequency energy for female genitourinary dysfunction: past, present, and future. Int Urogynecol J. 2021;32:1345-1350.
- Tadir Y, Gaspar A, Lev-Sagie A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med. 2017;49:137-159.
- US Food and Drug Administration. Statement from FDA Commissioner Scott Gottlieb, MD, on efforts to safeguard women’s health from deceptive health claims and significant risks related to devices marketed for use in medical procedures for “vaginal rejuvenation.” https://www.fda.gov/news-events/pressannouncements/statement-fda-commissioner-scott-gottlieb-mdefforts-safeguard-womens-health-deceptive-health-claims. Updated August 2, 2018. Accessed August 13, 2021.
- Vicariotto F, Raichi M. Technological evolution in the radiofrequency treatment of vaginal laxity and menopausal vulvo-vaginal atrophy and other genitourinary symptoms: first experiences with a novel dynamic quadripolar device. Minerva Ginecol. 2016;68:225-236.
- Kamilos MF, Borrelli CL. New therapeutic option in genitourinary syndrome of menopause: pilot study using microablative fractional radiofrequency. Einstein (Sao Paulo). 2017;15:445-551.
- Caruth JC. Evaluation of the safety and efficacy of a novel radiofrequency device for vaginal treatment. Surg Technol Int. 2018;32:145-149.
- Shobeiri SA, Kerkhof MH, Minassian VA, et al. IUGA committee opinion: laser-based vaginal devices for treatment of stress urinary incontinence, genitourinary syndrome of menopause, and vaginal laxity. Int Urogynecol J. 2019;30:371-376.
- Allan BB, Bell S, Husarek K. Early feasibility study to evaluate the Viveve system for female stress urinary incontinence: interim 6-month report. J Womens Health (Larchmt). 2020;29:383-389.
- Leibaschoff G, Izasa PG, Cardona JL, et al. Transcutaneous temperature controlled radiofrequency (TTCRF) for the treatment of menopausal vaginal/genitourinary symptoms. Surg Technol Int. 2016;29:149-159.
- Desai SA, Vakil Z, Kroumpouzos G. Transcutaneous temperature-controlled radiofrequency treatment: improvement in female genital appearance, sexual dysfunction, and stress urinary incontinence. Aesthet Surg J. 2021;sjab174. doi: 10.1093/asj/sjab174.
- Slongo H, Lunardi AL, Riccetto CL, et al. Microablative radiofrequency versus pelvic floor muscle training for stress urinary incontinence: a randomized controlled trial. Int Urogynecol J. 2021. doi: 10.1007 /s00192-021-04758-2.
- Krychman M, Rowan CG, Allan BB, et al. Effect of single-treatment, surface-cooled radiofrequency therapy on vaginal laxity and female sexual function: the VIVEVE I randomized controlled trial. J Sex Med. 2017;14:215-225.
- Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015;30: 429-436.
- Juhasz ML, Korta DZ, Mesinkovska NA. Vaginal rejuvenation: a retrospective review of lasers and radiofrequency devices. Dermatol Surg. 2021;47:489-494.
- Sarmento AC, Fernandes FS, Marconi C, et al. Impact of microablative fractional radiofrequency on the vaginal health, microbiota, and cellularity of postmenopausal women. Clinics (Sao Paulo). 2020;75:e1750.
As more and more gynecologic therapies move to the outpatient setting, keeping up on the latest data regarding emerging options can be challenging. Furthermore, it can be difficult to justify purchasing expensive equipment for the office when a therapy is not covered by medical insurance plans. However, if a therapy is efficacious and patients are willing to pay out of pocket, clinicians may want to have these options available for their patients.
In an effort to work through these complex issues, a panel of experts was convened at the 47th Annual Scientific Meeting of the Society of Gynecologic Surgeons in Palm Springs, California, on June 29, 2021. This article includes the salient points from that panel discussion.
Fractionated CO2 laser therapy
Fractionated CO2 laser therapy is considered second-line therapy for the treatment of genitourinary syndrome of menopause (GSM). In 2018, the US Food and Drug Administration (FDA) issued a safety warning about the use of CO2 laser therapy and warned patients and clinicians that the FDA had not approved the treatment for vaginal rejuvenation or treatment of vaginal symptoms related to menopause, urinary incontinence, or sexual function. Despite this warning, laser treatments are still performed in many practices.
In 2019, the International Continence Society (ICS) and the International Society for the Study of Vulvovaginal Disease (ISSVD) put out a joint practice consensus statement that essentially did not recommend the routine use of laser treatment for GSM, urinary incontinence, or lichen sclerosus.1 Conversely, the 2020 American Urogynecologic Society (AUGS) published a clinical consensus statement that spoke to the promising results of laser therapy for the treatment of vulvovaginal atrophy, vaginal dryness, and menopausal dyspareunia, with benefits lasting up to 1 year.2 This statement also suggested that the short-term safety profile of the CO2 laser device was favorable.
How CO2 lasers work
Fractionated CO2 laser therapy differs from unfractionated treatment (which often is used in the treatment of condyloma) in that it is not ablative. The laser works by using fractionated beams of light to penetrate the affected tissue to create small wounds in the epithelium and underlying lamina propria, which leads to collagen remodeling and regeneration that then results in the restoration of the superficial epithelium, vaginal rugae, and lubrication.3 Most clinicians perform 3 applications of the laser treatment 6 weeks apart, a recommendation that is based on manufacturer-sponsored studies in menopausal women.
Study results of patient outcomes with laser therapy
GSM. Several retrospective4,5 and prospective studies6-10 have looked at short- and longer-term outcomes in patients undergoing treatment with the CO2 laser. All of these studies showed improvement in patient symptoms related to GSM.
The VeLVET trial, conducted by Paraiso and colleagues, was a randomized trial that compared CO2 laser treatment with vaginal estrogen in women with GSM.11 While the study was underpowered due to cessation of enrollment once the FDA safety warning was issued, the authors reported that at 6 months, both the fractionated CO2 laser therapy group and the vaginal estrogen group had similar improvements, with 70% to 80% of participants reporting satisfaction with treatment. The authors concluded that laser therapy is likely to be as efficacious as vaginal estrogen and may be a good option for patients who cannot use vaginal estrogen to treat GSM.11
Lichen sclerosus. Some data exist on the efficacy of laser therapy for the treatment of lichen sclerosus. One recently published randomized trial showed that at 6 months, fractionated CO2 laser treatment and prior treatment with high potency topical corticosteroids was associated with higher improvement in subjective symptoms and objective measures compared with clobetasol propionate treatment.12 Another trial, however, revealed that laser treatment was not an effective monotherapy treatment for lichen sclerosus when compared with placebo.13 Fewer studies have examined the effect of laser therapy on urinary incontinence.
More prospective data are emerging, evidenced by trials currently registered in ClinicalTrials.gov. While some studies provide evidence that laser therapy may be efficacious in the treatment of vulvovaginal atrophy, additional data are needed to confirm the favorable outcomes observed with laser therapy for the treatment of lichen sclerosus, and a significant amount of data are needed to evaluate the efficacy of laser treatment for urinary incontinence.
Until such evidence is available, fractionated CO2 vaginal laser therapy will remain a fee-for-service treatment option and will be inaccessible to patients who cannot afford the cost of treatment.
Continue to: Hydrogel urethral bulking...
Hydrogel urethral bulking
Urethral bulking agents have been used for 5 decades in the treatment of stress urinary incontinence (SUI) in women. Unlike midurethral slings, in which many medical device companies use the same implant material (microporous, monofilament polypropylene mesh), the material for bulking agents has varied greatly. A 2017 Cochrane review of urethral bulking listed these agents used for this indication: autologous fat, carbon beads, calcium hydroxylapatite, ethylene vinyl alcohol copolymer, glutaraldehyde cross-linked bovine collagen, hyaluronic acid with dextranomer, porcine dermal implant, polytetrafluoroethylene, and silicone particles.14 These agents can be injected through a transurethral or periurethral technique. The review failed to find superiority of one material or injection technique over another.
New bulking agent available
In January 2020, the FDA approved the premarket application for a new bulking agent. This new agent is a permanently implanted, nonresorbable hydrogel that consists of cross-linked polyacrylamide (2.5%) and water (97.5%). It is intended to be used with a transurethral bulking system that includes a rotatable sheath and two 23-guage needles; a total of 1.5 to 2.0 mL of the hydrogel is injected in 3 locations in the proximal urethra per session. Patients may undergo an additional 2 sessions, if needed, at least 4 weeks after the previous session.
Polyacrylamide hydrogel has been used as a bulking agent in cosmetic and ophthalmic surgery for many years, and it was first approved for medical use in Europe in 2001. The initial European data on its use as a urethral bulking agent was published in 2006.15 The first North American data came in 2014 from a multicenter, randomized trial that compared polyacrylamide hydrogel with collagen gel.16 This investigation followed 345 women for 12 months and concluded that the safety and efficacy of polyacrylamide hydrogel was not inferior to collagen, with a little over half of both cohorts demonstrating a 50% or greater decrease in incontinence episodes.
Since these initial studies, 3-year17 and 7-year safety and efficacy data18 have been reported, with reassuring findings, but both studies experienced significant attrition of the original group of patients. The most commonly reported adverse events associated with the procedure are pain at the injection site (4%–14%) and urinary tract infection (3%–7%); transient urinary retention rates range in incidence from 1.5% to 15%.19
Short procedure, long-term results
Given that a urethral bulking procedure can be done in less than 10 minutes in the office under local analgesia, this treatment may lend itself to use in more brittle patient populations. One study of women aged 80 or older showed a greater than 50% decrease in the number of daily pads used for up to 2 years after initial injection.20 Another study found the greatest treatment success in women aged 60 years or older with fewer than 2.5 episodes of SUI per day.21
Platelet-rich plasma therapy
Platelet-rich plasma (PRP) therapy has been used in multiple disciplines for more than 2 decades as a treatment to regenerate damaged tissue, particularly in sports medicine for treating tendonitis as well as in plastic surgery, gynecology, urology, and ophthalmology, and good outcomes have been demonstrated with no serious adverse effects. PRP is a natural product in which high levels of platelets are concentrated through centrifugation with bioactive growth factors, including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), fibroblast growth factor (FGF), and insulin growth factor (IGF).22 The activated platelets are then injected autologously back into the patient’s tissue. This process releases activated growth factors that accelerate tissue healing by stimulating the number of reparative cells to create collagen production, angiogenesis, and neurogenesis while fighting infection and downregulating the autoimmune system.
Continue to: Uses for PRP in gynecology...
Uses for PRP in gynecology
In gynecology, dating back to 2007 PRP was shown to facilitate wound healing, when Fanning and colleagues reported PRP applications in gynecologic operative wounds, such as hysterectomies and urogynecologic procedures, to reduce postoperative pain.23 In the last decade, there has been a dramatic increasing trend in the application of PRP injections as an alternative therapy in gynecology to improve intimate health. PRP has been used to treat lichen sclerosus, atrophic vaginitis, SUI, and female sexual dysfunction; however, there is a dearth of studies that compare PRP with traditional therapies.
Runels and colleagues described the effects of localized injections of autologous PRP for the treatment of sexual dysfunction early in 2014.24 Those authors pioneered PRP use in women with dyspareunia and other symptoms related to sexual dysfunction. Women were offered PRP injections into the periurethral area of the Skene glands and the clitoris. Sexual satisfaction and pain were improved but results did not reach statistical significance. The results of this pilot study of 11 patients suggested that PRP injections could perhaps be an effective method to treat certain types of female sexual dysfunction, including desire, arousal, lubrication, and orgasm.
In another pilot study, Long and colleagues looked at the effectiveness of local injection of PRP for treating women with SUI.25 In that study, younger patients with mild severity of SUI had promising results, with up to 75% cured or improved. Results in the older group, with 50% cured or improved, did not reach statistical significance. Other small, limited studies have been conducted under the hypothesis that PRP as an “O-shot” may be a promising treatment that is a safe, effective, nonsurgical, and nonhormonal option for women with dyspareunia from lack of lubrication and related sexual dysfunction, such as decreased libido or arousal.26-29 A pilot study by Behnia-Willison and colleagues demonstrated clinical improvement in PRP use as an alternative to topical steroids for lichen sclerosus.30 Several other studies also have shown efficacy for the treatment of lichen sclerosus.31-34
More evidence of efficacy needed
To date, preliminary studies suggest that PRP holds promise for a host of gynecologic conditions. Since PRP is autologous, there are no significant contraindications, and thus far there have been no known serious adverse effects. However, most health insurers still do not cover this therapy, so for now patients must pay out-of-pocket fees for these treatments.
As we continue to investigate therapies in regenerative medicine, the continued efforts of our discipline are required to conduct well-designed prospective, randomized controlled studies. While initial series suggest that PRP is safe, it is unlikely that this therapy will be embraced widely in the paradigm as an alternative treatment option for many genitourinary symptoms of menopause and vulvar disorders until efficacy is better established.
Radiofrequency therapy
For the past 20 years, radiofrequency (RF) energy has been used through the vagina, urethra, and periurethral tissues for the treatment of genitourinary symptoms, with limited success. More recently, because some patients hesitate to receive mesh implants for treatment of urinary incontinence,35 there has been gravitation to office-based procedures.
In contrast to lasers, which transmit energy through light, RF waves (measured in hertz) transform the kinetic energy of the intracellular atoms, which move and collide, generating thermal energy.36,37 RF therapy has been shown to increase the proportion of smooth muscle and connective tissue; stimulate proliferation of the epithelium, neovascularization, and collagen formation in the lamina propria; and improve natural lubrication.36,38 In addition, RF is:
- ablative when the heat is capable of generating ablation and/or necrosis of the epidermis and dermis
- microablative when energy fractionation produces microscopic columns of ablative thermal lesions in the epidermis and upper dermis, resulting in microscopic columns of treated tissue interspersed with areas of untreated skin,39 and
- nonablative when trauma occurs only in the dermis by heating without causing ablation of the epidermis.39
The RF devices discussed below are used with settings for microablation in the treatment of SUI and sexual health/vaginal laxity, and with nonablative settings in the treatment of GSM.
RF for the treatment of urinary incontinence
Studies with RF have shown its benefits in urinary symptoms as secondary outcomes, such as improvement of SUI.38,40 One theory that favors energy devices as a treatment for SUI is that the treatment strengthens suburethral and pubocervical support, thereby decreasing urethral mobility.41
In 2016, the Viveve system (Viveve) received FDA 510(k) clearance for “use in general surgical procedures for electrocoagulation and hemostasis.” A single-site, randomized, nonblinded pilot study compared 1 treatment (group 1) versus 2 treatments (group 2) with the Viveve system for SUI in 35 participants.42 At 12 months, only for group 2 did mean scores on the Incontinence Impact Questionnaire Short Form (IIQ-7) and the International Consultation on Incontinence Modular Questionnaire-Urinary Incontinence-Short Form (ICIQ-UI-SF) decrease by the minimum clinically important difference of 16 and 2.52 points, respectively, compared with baseline.
The ThermiVa device (ThermiGen, LLC) received FDA clearance for “use in dermatological and general surgical procedures for electrocoagulation and hemostasis” in 2017. A single-site, prospective, double-blind, randomized controlled pilot trial evaluated the efficacy of this device for the treatment of SUI in 20 participants randomly assigned in a 1:1 fashion to active and sham groups.43 At 12 weeks, mean scores of the Urogenital Distress Inventory (UDI-6) and the ICIQ-UI-SF decreased by the minimal clinically important difference only in the treatment group arm. Additionally, 70% of treatment group participants had a negative stress test at 12 weeks compared with 0% of control group participants.43 In another study of 48 patients who were followed longitudinally for 5 months, a substantial improvement in genital appearance was observed.44 Assessment based on validated instruments demonstrated significant improvements in sexual function and SUI.44
A microablative RF device (Wavetronic 6000 Touch Device, Megapulse HF FRAXX system; Loktal Medical Electronics) consists of a vaginal probe with 64 microneedles at the tip, each capable of penetrating to a depth of 1 mm. During activation, delivery of RF energy, which results in vaporization of tissue at 100 °C, occurs in a preset sequence of 8 needles at a time, preventing the overheating of intervening tissue between adjacent needles.
Slongo and colleagues conducted a 3-arm randomized clinical trial that included 117 climacteric women with SUI.45 In group 1, treatment consisted of 3 monthly sessions of RF; group 2 received 12 weekly sessions of pelvic floor muscle training (PFMT); and group 3 received RF treatment plus PFMT simultaneously. Assessments were conducted at baseline and 30 days after the end of therapy using validated questionnaires and scales for urinary, vaginal, and sexual functions, and cytology was used to assess vaginal atrophy. The association between RF and PFMT showed significant improvement in the SUI symptoms assessed by questionnaire. The vaginal symptoms and dryness showed more substantial improvement with the RF treatment, and vaginal laxity showed similar improvement in the 3 treatment groups.45
Continue to: RF for the treatment of GSM...
RF for the treatment of GSM
For women who are not candidates for localized hormone therapy, as well as others who simply do not wish to use hormones, nonablative RF laser therapy may be an alternative for the management of GSM.
The VIVEVE I trial was one of the largest randomized, sham-controlled trials performed to determine the efficacy of vaginal rejuvenation using surface-cooled RF; 174 women received either RF treatment (90 J/cm2) or sham treatment (1 J/cm2).46 Treated participants had a significant improvement in perception of vaginal laxity/looseness and sexual function up to 6 months posttreatment.46 Overall, participants were satisfied with the treatment (77.8%–100%) and reported significant improvements in vaginal laxity and symptoms of atrophy. RF was well tolerated with minimal adverse effects, such as procedure-related erythema and edema of treated tissue, and vaginal discharge. One patient discontinued treatment because of procedural pain.47,48
The ThermiVa system also was evaluated for efficacy in the treatment of GSM in a single-site, double-blind randomized controlled pilot study, the methods of which were previously described above.43 GSM symptoms were evaluated at baseline and 12 weeks using the Vaginal Health Index (VHI) and visual analog scale (VAS). At the 12-week follow-up, compared with baseline scores, VHI scores were unchanged in the control group and improved in the treatment group. Additionally, VAS scores for dyspareunia decreased in the treatment group compared with baseline while VAS for dyspareunia in the sham group did not change from baseline to 12 weeks.
RF treatment for sexual health
The efficacy of the Viveve RF system for female sexual dysfunction was evaluated in an international, randomized, controlled, single-blinded study (n = 154) that compared 6-month outcomes of RF treatment versus sham treatment.46 Although there was a statistically significant improvement in patient-reported sexual dysfunction on validated instruments, it is essential to note that the study was powered for the primary outcome of vaginal laxity. In addition, the study was not adequately powered to evaluate safety; however, the adverse events reported were mild, and the most frequently reported adverse event was vaginal discharge.
Microablative monopolar RF treatment for GSM has been evaluated in 2 single-arm clinical trials that included a total of 70 patients.39,49 Pre- and posttreatment outcomes were analyzed after delivery of 3 treatment sessions 28 to 40 days apart. Although the only significant improvement in quality of life was in the health domain of the World Health Organization Quality of Life Adapted Questionnaire (P = .04), significant improvements in sexual functioning were seen in terms of the desire (P = .002), lubrication (P = .001), satisfaction (P = .003), and pain (P = .007) domains of the Female Sexual Function Index (FSFI) questionnaire except for excitation and orgasm.39 Overall, 100% of participants reported being satisfied or very satisfied with treatments, and 13 of 14 women felt “cured” or “much better.”39 After treatment, significant increases in vaginal Lactobacillus (P<.001), decreases in vaginal pH (P<.001), improvements in maturation of vaginal cellularity (decreased parabasal cells, P<.001; increased superficial cells, P<.001), and increased VHI score (P<.001) alone occurred.49 No adverse events beyond self-limited vaginal burning and redness were reported.39,49 In another study mentioned above, the combination of RF and PFMT in sexual function does not offer benefits superior to those achieved by the therapies alone.45
Evidence on RF treatment does not support marketing efforts
Radiofrequency devices have been marketed for a variety of genitourinary problems in women, with limited high-quality, randomized, comparative evidence of efficacy and durability in the literature. It is unfortunate that RF treatment continues to be promoted by practitioners around the world who cite small, short-term studies that lack biostatistical rigor in their reporting of protocols and results. Statements from both AUGS and the International Urogynecological Association have heeded caution on the use of lasers but they could not even evaluate RF devices due to lack of evidence.2,41
Informed counseling and shared decision making remain the bottom line
By the year 2025, all members of the Baby Boom generation will be aged 60 or older. While in the past there has been a reluctance to discuss women’s sexual health, urinary incontinence, and GSM, the need for open discussion and a variety of treatment options for these conditions has never been more critical.
Many patients prefer office-based therapies over hospital-based procedures, and others are leery of synthetic implants. These concerns are leading toward great interest in the types of treatments covered in this article. However, it is paramount that clinicians are aware of the evidence-based data behind these emerging options so that we can openly and accurately counsel our patients.
As we have shown, the quality of the data behind these officed-based therapies varies significantly. Until a greater body of research data is available, we must carefully balance our desire to meet patient wishes with solid, informed counseling and shared decision making. ●
As more and more gynecologic therapies move to the outpatient setting, keeping up on the latest data regarding emerging options can be challenging. Furthermore, it can be difficult to justify purchasing expensive equipment for the office when a therapy is not covered by medical insurance plans. However, if a therapy is efficacious and patients are willing to pay out of pocket, clinicians may want to have these options available for their patients.
In an effort to work through these complex issues, a panel of experts was convened at the 47th Annual Scientific Meeting of the Society of Gynecologic Surgeons in Palm Springs, California, on June 29, 2021. This article includes the salient points from that panel discussion.
Fractionated CO2 laser therapy
Fractionated CO2 laser therapy is considered second-line therapy for the treatment of genitourinary syndrome of menopause (GSM). In 2018, the US Food and Drug Administration (FDA) issued a safety warning about the use of CO2 laser therapy and warned patients and clinicians that the FDA had not approved the treatment for vaginal rejuvenation or treatment of vaginal symptoms related to menopause, urinary incontinence, or sexual function. Despite this warning, laser treatments are still performed in many practices.
In 2019, the International Continence Society (ICS) and the International Society for the Study of Vulvovaginal Disease (ISSVD) put out a joint practice consensus statement that essentially did not recommend the routine use of laser treatment for GSM, urinary incontinence, or lichen sclerosus.1 Conversely, the 2020 American Urogynecologic Society (AUGS) published a clinical consensus statement that spoke to the promising results of laser therapy for the treatment of vulvovaginal atrophy, vaginal dryness, and menopausal dyspareunia, with benefits lasting up to 1 year.2 This statement also suggested that the short-term safety profile of the CO2 laser device was favorable.
How CO2 lasers work
Fractionated CO2 laser therapy differs from unfractionated treatment (which often is used in the treatment of condyloma) in that it is not ablative. The laser works by using fractionated beams of light to penetrate the affected tissue to create small wounds in the epithelium and underlying lamina propria, which leads to collagen remodeling and regeneration that then results in the restoration of the superficial epithelium, vaginal rugae, and lubrication.3 Most clinicians perform 3 applications of the laser treatment 6 weeks apart, a recommendation that is based on manufacturer-sponsored studies in menopausal women.
Study results of patient outcomes with laser therapy
GSM. Several retrospective4,5 and prospective studies6-10 have looked at short- and longer-term outcomes in patients undergoing treatment with the CO2 laser. All of these studies showed improvement in patient symptoms related to GSM.
The VeLVET trial, conducted by Paraiso and colleagues, was a randomized trial that compared CO2 laser treatment with vaginal estrogen in women with GSM.11 While the study was underpowered due to cessation of enrollment once the FDA safety warning was issued, the authors reported that at 6 months, both the fractionated CO2 laser therapy group and the vaginal estrogen group had similar improvements, with 70% to 80% of participants reporting satisfaction with treatment. The authors concluded that laser therapy is likely to be as efficacious as vaginal estrogen and may be a good option for patients who cannot use vaginal estrogen to treat GSM.11
Lichen sclerosus. Some data exist on the efficacy of laser therapy for the treatment of lichen sclerosus. One recently published randomized trial showed that at 6 months, fractionated CO2 laser treatment and prior treatment with high potency topical corticosteroids was associated with higher improvement in subjective symptoms and objective measures compared with clobetasol propionate treatment.12 Another trial, however, revealed that laser treatment was not an effective monotherapy treatment for lichen sclerosus when compared with placebo.13 Fewer studies have examined the effect of laser therapy on urinary incontinence.
More prospective data are emerging, evidenced by trials currently registered in ClinicalTrials.gov. While some studies provide evidence that laser therapy may be efficacious in the treatment of vulvovaginal atrophy, additional data are needed to confirm the favorable outcomes observed with laser therapy for the treatment of lichen sclerosus, and a significant amount of data are needed to evaluate the efficacy of laser treatment for urinary incontinence.
Until such evidence is available, fractionated CO2 vaginal laser therapy will remain a fee-for-service treatment option and will be inaccessible to patients who cannot afford the cost of treatment.
Continue to: Hydrogel urethral bulking...
Hydrogel urethral bulking
Urethral bulking agents have been used for 5 decades in the treatment of stress urinary incontinence (SUI) in women. Unlike midurethral slings, in which many medical device companies use the same implant material (microporous, monofilament polypropylene mesh), the material for bulking agents has varied greatly. A 2017 Cochrane review of urethral bulking listed these agents used for this indication: autologous fat, carbon beads, calcium hydroxylapatite, ethylene vinyl alcohol copolymer, glutaraldehyde cross-linked bovine collagen, hyaluronic acid with dextranomer, porcine dermal implant, polytetrafluoroethylene, and silicone particles.14 These agents can be injected through a transurethral or periurethral technique. The review failed to find superiority of one material or injection technique over another.
New bulking agent available
In January 2020, the FDA approved the premarket application for a new bulking agent. This new agent is a permanently implanted, nonresorbable hydrogel that consists of cross-linked polyacrylamide (2.5%) and water (97.5%). It is intended to be used with a transurethral bulking system that includes a rotatable sheath and two 23-guage needles; a total of 1.5 to 2.0 mL of the hydrogel is injected in 3 locations in the proximal urethra per session. Patients may undergo an additional 2 sessions, if needed, at least 4 weeks after the previous session.
Polyacrylamide hydrogel has been used as a bulking agent in cosmetic and ophthalmic surgery for many years, and it was first approved for medical use in Europe in 2001. The initial European data on its use as a urethral bulking agent was published in 2006.15 The first North American data came in 2014 from a multicenter, randomized trial that compared polyacrylamide hydrogel with collagen gel.16 This investigation followed 345 women for 12 months and concluded that the safety and efficacy of polyacrylamide hydrogel was not inferior to collagen, with a little over half of both cohorts demonstrating a 50% or greater decrease in incontinence episodes.
Since these initial studies, 3-year17 and 7-year safety and efficacy data18 have been reported, with reassuring findings, but both studies experienced significant attrition of the original group of patients. The most commonly reported adverse events associated with the procedure are pain at the injection site (4%–14%) and urinary tract infection (3%–7%); transient urinary retention rates range in incidence from 1.5% to 15%.19
Short procedure, long-term results
Given that a urethral bulking procedure can be done in less than 10 minutes in the office under local analgesia, this treatment may lend itself to use in more brittle patient populations. One study of women aged 80 or older showed a greater than 50% decrease in the number of daily pads used for up to 2 years after initial injection.20 Another study found the greatest treatment success in women aged 60 years or older with fewer than 2.5 episodes of SUI per day.21
Platelet-rich plasma therapy
Platelet-rich plasma (PRP) therapy has been used in multiple disciplines for more than 2 decades as a treatment to regenerate damaged tissue, particularly in sports medicine for treating tendonitis as well as in plastic surgery, gynecology, urology, and ophthalmology, and good outcomes have been demonstrated with no serious adverse effects. PRP is a natural product in which high levels of platelets are concentrated through centrifugation with bioactive growth factors, including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), fibroblast growth factor (FGF), and insulin growth factor (IGF).22 The activated platelets are then injected autologously back into the patient’s tissue. This process releases activated growth factors that accelerate tissue healing by stimulating the number of reparative cells to create collagen production, angiogenesis, and neurogenesis while fighting infection and downregulating the autoimmune system.
Continue to: Uses for PRP in gynecology...
Uses for PRP in gynecology
In gynecology, dating back to 2007 PRP was shown to facilitate wound healing, when Fanning and colleagues reported PRP applications in gynecologic operative wounds, such as hysterectomies and urogynecologic procedures, to reduce postoperative pain.23 In the last decade, there has been a dramatic increasing trend in the application of PRP injections as an alternative therapy in gynecology to improve intimate health. PRP has been used to treat lichen sclerosus, atrophic vaginitis, SUI, and female sexual dysfunction; however, there is a dearth of studies that compare PRP with traditional therapies.
Runels and colleagues described the effects of localized injections of autologous PRP for the treatment of sexual dysfunction early in 2014.24 Those authors pioneered PRP use in women with dyspareunia and other symptoms related to sexual dysfunction. Women were offered PRP injections into the periurethral area of the Skene glands and the clitoris. Sexual satisfaction and pain were improved but results did not reach statistical significance. The results of this pilot study of 11 patients suggested that PRP injections could perhaps be an effective method to treat certain types of female sexual dysfunction, including desire, arousal, lubrication, and orgasm.
In another pilot study, Long and colleagues looked at the effectiveness of local injection of PRP for treating women with SUI.25 In that study, younger patients with mild severity of SUI had promising results, with up to 75% cured or improved. Results in the older group, with 50% cured or improved, did not reach statistical significance. Other small, limited studies have been conducted under the hypothesis that PRP as an “O-shot” may be a promising treatment that is a safe, effective, nonsurgical, and nonhormonal option for women with dyspareunia from lack of lubrication and related sexual dysfunction, such as decreased libido or arousal.26-29 A pilot study by Behnia-Willison and colleagues demonstrated clinical improvement in PRP use as an alternative to topical steroids for lichen sclerosus.30 Several other studies also have shown efficacy for the treatment of lichen sclerosus.31-34
More evidence of efficacy needed
To date, preliminary studies suggest that PRP holds promise for a host of gynecologic conditions. Since PRP is autologous, there are no significant contraindications, and thus far there have been no known serious adverse effects. However, most health insurers still do not cover this therapy, so for now patients must pay out-of-pocket fees for these treatments.
As we continue to investigate therapies in regenerative medicine, the continued efforts of our discipline are required to conduct well-designed prospective, randomized controlled studies. While initial series suggest that PRP is safe, it is unlikely that this therapy will be embraced widely in the paradigm as an alternative treatment option for many genitourinary symptoms of menopause and vulvar disorders until efficacy is better established.
Radiofrequency therapy
For the past 20 years, radiofrequency (RF) energy has been used through the vagina, urethra, and periurethral tissues for the treatment of genitourinary symptoms, with limited success. More recently, because some patients hesitate to receive mesh implants for treatment of urinary incontinence,35 there has been gravitation to office-based procedures.
In contrast to lasers, which transmit energy through light, RF waves (measured in hertz) transform the kinetic energy of the intracellular atoms, which move and collide, generating thermal energy.36,37 RF therapy has been shown to increase the proportion of smooth muscle and connective tissue; stimulate proliferation of the epithelium, neovascularization, and collagen formation in the lamina propria; and improve natural lubrication.36,38 In addition, RF is:
- ablative when the heat is capable of generating ablation and/or necrosis of the epidermis and dermis
- microablative when energy fractionation produces microscopic columns of ablative thermal lesions in the epidermis and upper dermis, resulting in microscopic columns of treated tissue interspersed with areas of untreated skin,39 and
- nonablative when trauma occurs only in the dermis by heating without causing ablation of the epidermis.39
The RF devices discussed below are used with settings for microablation in the treatment of SUI and sexual health/vaginal laxity, and with nonablative settings in the treatment of GSM.
RF for the treatment of urinary incontinence
Studies with RF have shown its benefits in urinary symptoms as secondary outcomes, such as improvement of SUI.38,40 One theory that favors energy devices as a treatment for SUI is that the treatment strengthens suburethral and pubocervical support, thereby decreasing urethral mobility.41
In 2016, the Viveve system (Viveve) received FDA 510(k) clearance for “use in general surgical procedures for electrocoagulation and hemostasis.” A single-site, randomized, nonblinded pilot study compared 1 treatment (group 1) versus 2 treatments (group 2) with the Viveve system for SUI in 35 participants.42 At 12 months, only for group 2 did mean scores on the Incontinence Impact Questionnaire Short Form (IIQ-7) and the International Consultation on Incontinence Modular Questionnaire-Urinary Incontinence-Short Form (ICIQ-UI-SF) decrease by the minimum clinically important difference of 16 and 2.52 points, respectively, compared with baseline.
The ThermiVa device (ThermiGen, LLC) received FDA clearance for “use in dermatological and general surgical procedures for electrocoagulation and hemostasis” in 2017. A single-site, prospective, double-blind, randomized controlled pilot trial evaluated the efficacy of this device for the treatment of SUI in 20 participants randomly assigned in a 1:1 fashion to active and sham groups.43 At 12 weeks, mean scores of the Urogenital Distress Inventory (UDI-6) and the ICIQ-UI-SF decreased by the minimal clinically important difference only in the treatment group arm. Additionally, 70% of treatment group participants had a negative stress test at 12 weeks compared with 0% of control group participants.43 In another study of 48 patients who were followed longitudinally for 5 months, a substantial improvement in genital appearance was observed.44 Assessment based on validated instruments demonstrated significant improvements in sexual function and SUI.44
A microablative RF device (Wavetronic 6000 Touch Device, Megapulse HF FRAXX system; Loktal Medical Electronics) consists of a vaginal probe with 64 microneedles at the tip, each capable of penetrating to a depth of 1 mm. During activation, delivery of RF energy, which results in vaporization of tissue at 100 °C, occurs in a preset sequence of 8 needles at a time, preventing the overheating of intervening tissue between adjacent needles.
Slongo and colleagues conducted a 3-arm randomized clinical trial that included 117 climacteric women with SUI.45 In group 1, treatment consisted of 3 monthly sessions of RF; group 2 received 12 weekly sessions of pelvic floor muscle training (PFMT); and group 3 received RF treatment plus PFMT simultaneously. Assessments were conducted at baseline and 30 days after the end of therapy using validated questionnaires and scales for urinary, vaginal, and sexual functions, and cytology was used to assess vaginal atrophy. The association between RF and PFMT showed significant improvement in the SUI symptoms assessed by questionnaire. The vaginal symptoms and dryness showed more substantial improvement with the RF treatment, and vaginal laxity showed similar improvement in the 3 treatment groups.45
Continue to: RF for the treatment of GSM...
RF for the treatment of GSM
For women who are not candidates for localized hormone therapy, as well as others who simply do not wish to use hormones, nonablative RF laser therapy may be an alternative for the management of GSM.
The VIVEVE I trial was one of the largest randomized, sham-controlled trials performed to determine the efficacy of vaginal rejuvenation using surface-cooled RF; 174 women received either RF treatment (90 J/cm2) or sham treatment (1 J/cm2).46 Treated participants had a significant improvement in perception of vaginal laxity/looseness and sexual function up to 6 months posttreatment.46 Overall, participants were satisfied with the treatment (77.8%–100%) and reported significant improvements in vaginal laxity and symptoms of atrophy. RF was well tolerated with minimal adverse effects, such as procedure-related erythema and edema of treated tissue, and vaginal discharge. One patient discontinued treatment because of procedural pain.47,48
The ThermiVa system also was evaluated for efficacy in the treatment of GSM in a single-site, double-blind randomized controlled pilot study, the methods of which were previously described above.43 GSM symptoms were evaluated at baseline and 12 weeks using the Vaginal Health Index (VHI) and visual analog scale (VAS). At the 12-week follow-up, compared with baseline scores, VHI scores were unchanged in the control group and improved in the treatment group. Additionally, VAS scores for dyspareunia decreased in the treatment group compared with baseline while VAS for dyspareunia in the sham group did not change from baseline to 12 weeks.
RF treatment for sexual health
The efficacy of the Viveve RF system for female sexual dysfunction was evaluated in an international, randomized, controlled, single-blinded study (n = 154) that compared 6-month outcomes of RF treatment versus sham treatment.46 Although there was a statistically significant improvement in patient-reported sexual dysfunction on validated instruments, it is essential to note that the study was powered for the primary outcome of vaginal laxity. In addition, the study was not adequately powered to evaluate safety; however, the adverse events reported were mild, and the most frequently reported adverse event was vaginal discharge.
Microablative monopolar RF treatment for GSM has been evaluated in 2 single-arm clinical trials that included a total of 70 patients.39,49 Pre- and posttreatment outcomes were analyzed after delivery of 3 treatment sessions 28 to 40 days apart. Although the only significant improvement in quality of life was in the health domain of the World Health Organization Quality of Life Adapted Questionnaire (P = .04), significant improvements in sexual functioning were seen in terms of the desire (P = .002), lubrication (P = .001), satisfaction (P = .003), and pain (P = .007) domains of the Female Sexual Function Index (FSFI) questionnaire except for excitation and orgasm.39 Overall, 100% of participants reported being satisfied or very satisfied with treatments, and 13 of 14 women felt “cured” or “much better.”39 After treatment, significant increases in vaginal Lactobacillus (P<.001), decreases in vaginal pH (P<.001), improvements in maturation of vaginal cellularity (decreased parabasal cells, P<.001; increased superficial cells, P<.001), and increased VHI score (P<.001) alone occurred.49 No adverse events beyond self-limited vaginal burning and redness were reported.39,49 In another study mentioned above, the combination of RF and PFMT in sexual function does not offer benefits superior to those achieved by the therapies alone.45
Evidence on RF treatment does not support marketing efforts
Radiofrequency devices have been marketed for a variety of genitourinary problems in women, with limited high-quality, randomized, comparative evidence of efficacy and durability in the literature. It is unfortunate that RF treatment continues to be promoted by practitioners around the world who cite small, short-term studies that lack biostatistical rigor in their reporting of protocols and results. Statements from both AUGS and the International Urogynecological Association have heeded caution on the use of lasers but they could not even evaluate RF devices due to lack of evidence.2,41
Informed counseling and shared decision making remain the bottom line
By the year 2025, all members of the Baby Boom generation will be aged 60 or older. While in the past there has been a reluctance to discuss women’s sexual health, urinary incontinence, and GSM, the need for open discussion and a variety of treatment options for these conditions has never been more critical.
Many patients prefer office-based therapies over hospital-based procedures, and others are leery of synthetic implants. These concerns are leading toward great interest in the types of treatments covered in this article. However, it is paramount that clinicians are aware of the evidence-based data behind these emerging options so that we can openly and accurately counsel our patients.
As we have shown, the quality of the data behind these officed-based therapies varies significantly. Until a greater body of research data is available, we must carefully balance our desire to meet patient wishes with solid, informed counseling and shared decision making. ●
- Preti M, Viera-Baptista P, Digesu GA, et al. The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: an ICS/ISSVD best practice consensus document. J Lower Genital Tract Dis. 2019;23:151-160.
- Alshiek J, Garcia B, Minassian V, et al. Vaginal energy-based devices: AUGS clinical consensus statement. Female Pelvic Med Reconstr Surg. 2020;26:287-298.
- Streicher LF. Vulvar and vaginal fractional CO2 laser treatments for genitourinary syndrome of menopause: NAMS practice pearl. Menopause. 2018;25:571-573.
- Gardner AN, Aschkenazi SO. The short-term efficacy and safety of fractional CO2 laser therapy for vulvovaginal symptoms in menopause, breast cancer, and lichen sclerosus. Menopause. 2021; 28:511-516.
- Balchander D, Nyirjesy P. Fractionated CO2 laser therapy in recalcitrant lichen sclerosus. J Lower Genital Tract Disease. 2020;24:225-228.
- Pieralli A, Fallani MG, Becorpi A, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294:841-846.
- Pieralli A, Bianchi C, Longinotti M, et al. Long-term reliability of fractionated CO2 laser as a treatment of vulvovaginal atrophy (VVA) symptoms. Arch Gynecol Obstet. 2017; 296:973-978.
- Sokol ER, Karram MM. Use of novel fractional CO2 laser for the treatment of genitourinary syndrome of menopause: 1-year outcomes. Menopause. 2017;24: 810-814.
- Pagano T, Conforti A, Buonfantino C, et al. Effect of rescue fractional microablative CO2 laser on symptoms and sexual dysfunction in women affected by vulvar lichen sclerosus resistant to long-term use of topic corticosteroid: a prospective longitudinal study. Menopause. 2020;27:418-422.
- Sindou-Faurie T, Louis-Vahdat C, Oueld Es Cheikh E, et al. Evaluation of the efficacy of fractional CO2 laser in the treatment of vulvar and vaginal menopausal symptoms. Arch Gynecol Obstet. 2021;303:955-963.
- Paraiso MFR, Ferrando CA, Sokol ER, at al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: the VeLVET trial. Menopause. 2019;27:50-56.
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978.
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;136:979-987.
- Kirchin V, Page T, Keegan PE, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD003881.
- Lose G, Mouritsen L, Nielson JB. A new bulking agent (polyacrylamide hydrogel) for treating stress urinary incontinence in women. BJU Int. 2006;98:100-104.
- Sokol ER, Karram MM, Dmochowski R. Efficacy and safety of polyacrylamide hydrogel for the treatment of female stress incontinence: a randomized, prospective, multicenter North American study. J Urol. 2014;192:843-849.
- Pai A, Al-Singary W. Durability, safety and efficacy of polyacrylamide hydrogel (Bulkamid) in the management of stress and mixed urinary incontinence: three year follow up outcomes. Cent European J Urol. 2015;68:428-433.
- Brosche T, Kuhn A, Lobodasch K, et al. Seven-year efficacy and safety outcomes of Bulkamid for the treatment of stress urinary incontinence. Neurourol Urodyn. 2021;40:502-508.
- Kasi AD, Pergialiotis V, Perrea DN, et al. Polyacrylamide hydrogel (Bulkamid) for stress urinary incontinence in women: a systematic review of the literature. Int Urogynecol J. 2016;27:367-375.
- Vecchioli-Scaldazza CV, Smaali C, Morosetti C, et al. Polyacrylamide hydrogel (Bulkamid) in female patients of 80 or more years with urinary incontinence. Int Braz J Urol. 2014;40:37-43.
- Elmelund M, Sokol ER, Darram MM, et al. Patient characteristics that may influence the effect of urethral injection therapy for female stress urinary incontinence. J Urol. 2019;202:125-131.
- Sanoulis V, Nikolettos N, Vlahos N. The use of platelet-rich plasma in the gynecological clinical setting: a review. HJOG. 2019;18:55-65.
- Fanning J, Murrain L, Flora R, et al. Phase I/II prospective trial of autologous platelet tissue graft in gynecologic surgery. J Minim Invasive Gynecol. 2007;14:633-637.
- Runels CE, Melnick H, DeBourbon E, et al. A pilot study of the effect of localized injections of autologous platelet rich plasma (PRP) for the treatment of female sexual dysfunction. J Womens Health Care. 2014;3:4.
- Long CY, Lin KL, Shen CR, et al. A pilot study: effectiveness of local injection of autologous platelet-rich plasma in treating women with stress urinary incontinence. Sci Rep. 2021;11:1584.
- Matz EJ, Pearlman AM, Terlecki RP. Safety and feasibility of platelet rich fibrin matrix injections for treatment of common urologic conditions. Investig Clin Urol. 2018;59:61-65.
- Neto JB. O-Shot: platelets rich plasma in intimate female treatment. J Womens Health Care. 2017;6:5.
- Nikolopoulos KI, Pergialiotis V, Perrea D, et al. Restoration of the pubourethral ligament with platelet rich plasma for the treatment of stress urinary incontinence. Med Hypotheses. 2016;90:29-31.
- Hersant B, SidAhmed-Mezi M, Belkacemi Y, et al. Efficacy of injecting platelet concentrate combined with hyaluronic acid for the treatment of vulvovaginal atrophy in postmenopausal women with a history of breast cancer: a phase 2 pilot study. Menopause. 2018;25:1124-1130.
- Behnia-Willison F, Pour NR, Mohamadi B, et al. Use of platelet-rich plasma for vulvovaginal autoimmune conditions like lichen sclerosus. Plast Reconstr Surg Glob Open. 2016;4:e1124.
- Goldstein AT, King M, Runels C, et al. Intradermal injection of autologous platelet-rich plasma for the treatment of vulvar lichen sclerosus. J Am Acad Dermatol. 2017;76:158-160.
- Casabona F, Priano V, Vallerino V, et al. New surgical approach to lichen sclerosus of the vulva: the role of adipose-derived mesenchymal cells and platelet-rich plasma in tissue regeneration. Plast Reconstr Surg. 2010;126:210e-211e.
- Franic D, Iternica Z, Franic-Ivanisevic M. Platelet-rich plasma (PRP) for the treatment of vulvar lichen sclerosus in a premenopausal woman: a case report. Case Rep Womens Health. 2018;18: e0062.
- Posey LK, Runels C. In office surgery and use of platelet rich plasma for the treatment of vulvar lichen sclerosus to alleviate painful sexual intercourse. J Lower Genital Tract Dis. 2017;21(4S):S14.
- Stachowicz AM, Hoover ML, Karram MM. Clinical utility of radiofrequency energy for female genitourinary dysfunction: past, present, and future. Int Urogynecol J. 2021;32:1345-1350.
- Tadir Y, Gaspar A, Lev-Sagie A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med. 2017;49:137-159.
- US Food and Drug Administration. Statement from FDA Commissioner Scott Gottlieb, MD, on efforts to safeguard women’s health from deceptive health claims and significant risks related to devices marketed for use in medical procedures for “vaginal rejuvenation.” https://www.fda.gov/news-events/pressannouncements/statement-fda-commissioner-scott-gottlieb-mdefforts-safeguard-womens-health-deceptive-health-claims. Updated August 2, 2018. Accessed August 13, 2021.
- Vicariotto F, Raichi M. Technological evolution in the radiofrequency treatment of vaginal laxity and menopausal vulvo-vaginal atrophy and other genitourinary symptoms: first experiences with a novel dynamic quadripolar device. Minerva Ginecol. 2016;68:225-236.
- Kamilos MF, Borrelli CL. New therapeutic option in genitourinary syndrome of menopause: pilot study using microablative fractional radiofrequency. Einstein (Sao Paulo). 2017;15:445-551.
- Caruth JC. Evaluation of the safety and efficacy of a novel radiofrequency device for vaginal treatment. Surg Technol Int. 2018;32:145-149.
- Shobeiri SA, Kerkhof MH, Minassian VA, et al. IUGA committee opinion: laser-based vaginal devices for treatment of stress urinary incontinence, genitourinary syndrome of menopause, and vaginal laxity. Int Urogynecol J. 2019;30:371-376.
- Allan BB, Bell S, Husarek K. Early feasibility study to evaluate the Viveve system for female stress urinary incontinence: interim 6-month report. J Womens Health (Larchmt). 2020;29:383-389.
- Leibaschoff G, Izasa PG, Cardona JL, et al. Transcutaneous temperature controlled radiofrequency (TTCRF) for the treatment of menopausal vaginal/genitourinary symptoms. Surg Technol Int. 2016;29:149-159.
- Desai SA, Vakil Z, Kroumpouzos G. Transcutaneous temperature-controlled radiofrequency treatment: improvement in female genital appearance, sexual dysfunction, and stress urinary incontinence. Aesthet Surg J. 2021;sjab174. doi: 10.1093/asj/sjab174.
- Slongo H, Lunardi AL, Riccetto CL, et al. Microablative radiofrequency versus pelvic floor muscle training for stress urinary incontinence: a randomized controlled trial. Int Urogynecol J. 2021. doi: 10.1007 /s00192-021-04758-2.
- Krychman M, Rowan CG, Allan BB, et al. Effect of single-treatment, surface-cooled radiofrequency therapy on vaginal laxity and female sexual function: the VIVEVE I randomized controlled trial. J Sex Med. 2017;14:215-225.
- Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015;30: 429-436.
- Juhasz ML, Korta DZ, Mesinkovska NA. Vaginal rejuvenation: a retrospective review of lasers and radiofrequency devices. Dermatol Surg. 2021;47:489-494.
- Sarmento AC, Fernandes FS, Marconi C, et al. Impact of microablative fractional radiofrequency on the vaginal health, microbiota, and cellularity of postmenopausal women. Clinics (Sao Paulo). 2020;75:e1750.
- Preti M, Viera-Baptista P, Digesu GA, et al. The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: an ICS/ISSVD best practice consensus document. J Lower Genital Tract Dis. 2019;23:151-160.
- Alshiek J, Garcia B, Minassian V, et al. Vaginal energy-based devices: AUGS clinical consensus statement. Female Pelvic Med Reconstr Surg. 2020;26:287-298.
- Streicher LF. Vulvar and vaginal fractional CO2 laser treatments for genitourinary syndrome of menopause: NAMS practice pearl. Menopause. 2018;25:571-573.
- Gardner AN, Aschkenazi SO. The short-term efficacy and safety of fractional CO2 laser therapy for vulvovaginal symptoms in menopause, breast cancer, and lichen sclerosus. Menopause. 2021; 28:511-516.
- Balchander D, Nyirjesy P. Fractionated CO2 laser therapy in recalcitrant lichen sclerosus. J Lower Genital Tract Disease. 2020;24:225-228.
- Pieralli A, Fallani MG, Becorpi A, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294:841-846.
- Pieralli A, Bianchi C, Longinotti M, et al. Long-term reliability of fractionated CO2 laser as a treatment of vulvovaginal atrophy (VVA) symptoms. Arch Gynecol Obstet. 2017; 296:973-978.
- Sokol ER, Karram MM. Use of novel fractional CO2 laser for the treatment of genitourinary syndrome of menopause: 1-year outcomes. Menopause. 2017;24: 810-814.
- Pagano T, Conforti A, Buonfantino C, et al. Effect of rescue fractional microablative CO2 laser on symptoms and sexual dysfunction in women affected by vulvar lichen sclerosus resistant to long-term use of topic corticosteroid: a prospective longitudinal study. Menopause. 2020;27:418-422.
- Sindou-Faurie T, Louis-Vahdat C, Oueld Es Cheikh E, et al. Evaluation of the efficacy of fractional CO2 laser in the treatment of vulvar and vaginal menopausal symptoms. Arch Gynecol Obstet. 2021;303:955-963.
- Paraiso MFR, Ferrando CA, Sokol ER, at al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: the VeLVET trial. Menopause. 2019;27:50-56.
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978.
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;136:979-987.
- Kirchin V, Page T, Keegan PE, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD003881.
- Lose G, Mouritsen L, Nielson JB. A new bulking agent (polyacrylamide hydrogel) for treating stress urinary incontinence in women. BJU Int. 2006;98:100-104.
- Sokol ER, Karram MM, Dmochowski R. Efficacy and safety of polyacrylamide hydrogel for the treatment of female stress incontinence: a randomized, prospective, multicenter North American study. J Urol. 2014;192:843-849.
- Pai A, Al-Singary W. Durability, safety and efficacy of polyacrylamide hydrogel (Bulkamid) in the management of stress and mixed urinary incontinence: three year follow up outcomes. Cent European J Urol. 2015;68:428-433.
- Brosche T, Kuhn A, Lobodasch K, et al. Seven-year efficacy and safety outcomes of Bulkamid for the treatment of stress urinary incontinence. Neurourol Urodyn. 2021;40:502-508.
- Kasi AD, Pergialiotis V, Perrea DN, et al. Polyacrylamide hydrogel (Bulkamid) for stress urinary incontinence in women: a systematic review of the literature. Int Urogynecol J. 2016;27:367-375.
- Vecchioli-Scaldazza CV, Smaali C, Morosetti C, et al. Polyacrylamide hydrogel (Bulkamid) in female patients of 80 or more years with urinary incontinence. Int Braz J Urol. 2014;40:37-43.
- Elmelund M, Sokol ER, Darram MM, et al. Patient characteristics that may influence the effect of urethral injection therapy for female stress urinary incontinence. J Urol. 2019;202:125-131.
- Sanoulis V, Nikolettos N, Vlahos N. The use of platelet-rich plasma in the gynecological clinical setting: a review. HJOG. 2019;18:55-65.
- Fanning J, Murrain L, Flora R, et al. Phase I/II prospective trial of autologous platelet tissue graft in gynecologic surgery. J Minim Invasive Gynecol. 2007;14:633-637.
- Runels CE, Melnick H, DeBourbon E, et al. A pilot study of the effect of localized injections of autologous platelet rich plasma (PRP) for the treatment of female sexual dysfunction. J Womens Health Care. 2014;3:4.
- Long CY, Lin KL, Shen CR, et al. A pilot study: effectiveness of local injection of autologous platelet-rich plasma in treating women with stress urinary incontinence. Sci Rep. 2021;11:1584.
- Matz EJ, Pearlman AM, Terlecki RP. Safety and feasibility of platelet rich fibrin matrix injections for treatment of common urologic conditions. Investig Clin Urol. 2018;59:61-65.
- Neto JB. O-Shot: platelets rich plasma in intimate female treatment. J Womens Health Care. 2017;6:5.
- Nikolopoulos KI, Pergialiotis V, Perrea D, et al. Restoration of the pubourethral ligament with platelet rich plasma for the treatment of stress urinary incontinence. Med Hypotheses. 2016;90:29-31.
- Hersant B, SidAhmed-Mezi M, Belkacemi Y, et al. Efficacy of injecting platelet concentrate combined with hyaluronic acid for the treatment of vulvovaginal atrophy in postmenopausal women with a history of breast cancer: a phase 2 pilot study. Menopause. 2018;25:1124-1130.
- Behnia-Willison F, Pour NR, Mohamadi B, et al. Use of platelet-rich plasma for vulvovaginal autoimmune conditions like lichen sclerosus. Plast Reconstr Surg Glob Open. 2016;4:e1124.
- Goldstein AT, King M, Runels C, et al. Intradermal injection of autologous platelet-rich plasma for the treatment of vulvar lichen sclerosus. J Am Acad Dermatol. 2017;76:158-160.
- Casabona F, Priano V, Vallerino V, et al. New surgical approach to lichen sclerosus of the vulva: the role of adipose-derived mesenchymal cells and platelet-rich plasma in tissue regeneration. Plast Reconstr Surg. 2010;126:210e-211e.
- Franic D, Iternica Z, Franic-Ivanisevic M. Platelet-rich plasma (PRP) for the treatment of vulvar lichen sclerosus in a premenopausal woman: a case report. Case Rep Womens Health. 2018;18: e0062.
- Posey LK, Runels C. In office surgery and use of platelet rich plasma for the treatment of vulvar lichen sclerosus to alleviate painful sexual intercourse. J Lower Genital Tract Dis. 2017;21(4S):S14.
- Stachowicz AM, Hoover ML, Karram MM. Clinical utility of radiofrequency energy for female genitourinary dysfunction: past, present, and future. Int Urogynecol J. 2021;32:1345-1350.
- Tadir Y, Gaspar A, Lev-Sagie A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med. 2017;49:137-159.
- US Food and Drug Administration. Statement from FDA Commissioner Scott Gottlieb, MD, on efforts to safeguard women’s health from deceptive health claims and significant risks related to devices marketed for use in medical procedures for “vaginal rejuvenation.” https://www.fda.gov/news-events/pressannouncements/statement-fda-commissioner-scott-gottlieb-mdefforts-safeguard-womens-health-deceptive-health-claims. Updated August 2, 2018. Accessed August 13, 2021.
- Vicariotto F, Raichi M. Technological evolution in the radiofrequency treatment of vaginal laxity and menopausal vulvo-vaginal atrophy and other genitourinary symptoms: first experiences with a novel dynamic quadripolar device. Minerva Ginecol. 2016;68:225-236.
- Kamilos MF, Borrelli CL. New therapeutic option in genitourinary syndrome of menopause: pilot study using microablative fractional radiofrequency. Einstein (Sao Paulo). 2017;15:445-551.
- Caruth JC. Evaluation of the safety and efficacy of a novel radiofrequency device for vaginal treatment. Surg Technol Int. 2018;32:145-149.
- Shobeiri SA, Kerkhof MH, Minassian VA, et al. IUGA committee opinion: laser-based vaginal devices for treatment of stress urinary incontinence, genitourinary syndrome of menopause, and vaginal laxity. Int Urogynecol J. 2019;30:371-376.
- Allan BB, Bell S, Husarek K. Early feasibility study to evaluate the Viveve system for female stress urinary incontinence: interim 6-month report. J Womens Health (Larchmt). 2020;29:383-389.
- Leibaschoff G, Izasa PG, Cardona JL, et al. Transcutaneous temperature controlled radiofrequency (TTCRF) for the treatment of menopausal vaginal/genitourinary symptoms. Surg Technol Int. 2016;29:149-159.
- Desai SA, Vakil Z, Kroumpouzos G. Transcutaneous temperature-controlled radiofrequency treatment: improvement in female genital appearance, sexual dysfunction, and stress urinary incontinence. Aesthet Surg J. 2021;sjab174. doi: 10.1093/asj/sjab174.
- Slongo H, Lunardi AL, Riccetto CL, et al. Microablative radiofrequency versus pelvic floor muscle training for stress urinary incontinence: a randomized controlled trial. Int Urogynecol J. 2021. doi: 10.1007 /s00192-021-04758-2.
- Krychman M, Rowan CG, Allan BB, et al. Effect of single-treatment, surface-cooled radiofrequency therapy on vaginal laxity and female sexual function: the VIVEVE I randomized controlled trial. J Sex Med. 2017;14:215-225.
- Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015;30: 429-436.
- Juhasz ML, Korta DZ, Mesinkovska NA. Vaginal rejuvenation: a retrospective review of lasers and radiofrequency devices. Dermatol Surg. 2021;47:489-494.
- Sarmento AC, Fernandes FS, Marconi C, et al. Impact of microablative fractional radiofrequency on the vaginal health, microbiota, and cellularity of postmenopausal women. Clinics (Sao Paulo). 2020;75:e1750.