User login
Community service grants bedrock of support for communities in need
Community service grants are one way the Foundation strives to make a tangible, lasting impact on the lives of the patients we serve – they’re not just one-off projects with limited effects. But how do we really know that we’re making a difference?
For Dr. Roberta Kato, it’s when she gets to witness an “Aha!” moment – a time when everything clicks and a parent finally understands how to better care for their child. For Marina Lima, MD, MSc, it’s knowing that one more teen isn’t gasping for air. And for Dr. Joseph Huang, it’s seeing a country of 100 million people gain access to 14 pulmonologists when there was previously only one.
Whether it’s hosting family workshops in children’s museums across Los Angeles, developing a gaming app to help children in Brazil control their asthma symptoms, or establishing a pulmonary and critical care training program in Uganda, the Foundation community service grants all focus on the same goal: to enable our underserved patients gain access to the resources and care they need when they need it most.
Why community service grants?
The Foundation began giving community service grants in 1997 under the leadership of CHEST President D. Robert McCaffree, MD, Master FCCP. He believed the program would be the best way to support his colleagues in achieving their community service endeavors .To date, over $2 million has been given specifically to community service projects. “
Our physicians experience the limitations of our health care system first-hand – a system that isn’t built to assist the people who need help the most. Finding solutions requires a willingness to think and operate creatively. The funding the Foundation provides through our community service grants supplies the resources to do just that – implement real-world solutions that will help patients gain better access to care.
Cases in point
Marina Lima, MD, MSc, was seeing an inordinate number of children and teens with uncontrolled asthma symptoms in Brazil. She applied for and was awarded a grant to make Asthmaland, the first gamified pediatric asthma educational program in Portuguese.
Besides her “Aha!” moments, Dr. Roberta Kato revealed a way she knows her work is making a difference: the funding is helping to shift the nonprofit landscape in her community.
“Sometimes there is a rift between different organizations. When I ask them to collaborate or advertise together, I get resistance. However, when I’ve reached out and said that I’ve received funding for an initiative, all of a sudden, there is forward movement. That is how I am hoping to make the biggest difference,” explained Dr. Kato.
Dr. Joseph Huang, who received a grant to fund the East Africa Training Initiative (EATI), is faced with a different obstacle. “We’ve been awarded the grant many times, and I know the Foundation is focused on supporting new, up-and-coming programs. Therefore, I’m committed to ensuring that my program can continue even after we stop receiving funding.”
How is Dr. Huang going to do that? Besides procuring ICU equipment, EATI focuses on training pulmonology fellows in east Africa. The fellows who graduate will train other physicians and care team members across the continent, both in hospitals and rural clinics, safeguarding the future of his program.
A clear vision for the future
While the Foundation is ready to tackle new problems, community service grants will remain the constant thread woven throughout the work, and it’s obvious why. As Dr. Huang emphasized, his grant “will ensure that the people living in Africa have a better chance at getting access to the care they need.”
When you strip away everything else, community service grants boil down to one thing: helping people live healthier, more fulfilled lives. What can be more worthwhile?
Help us continue this important work
While we are privileged to award numerous grants over the past 2 decades, our community service grants have always held a special place in the hearts and minds of everyone involved with the CHEST Foundation. We hope they hold a special place in your heart too.
Please consider donating so that we can continue this work together.
Community service grants are one way the Foundation strives to make a tangible, lasting impact on the lives of the patients we serve – they’re not just one-off projects with limited effects. But how do we really know that we’re making a difference?
For Dr. Roberta Kato, it’s when she gets to witness an “Aha!” moment – a time when everything clicks and a parent finally understands how to better care for their child. For Marina Lima, MD, MSc, it’s knowing that one more teen isn’t gasping for air. And for Dr. Joseph Huang, it’s seeing a country of 100 million people gain access to 14 pulmonologists when there was previously only one.
Whether it’s hosting family workshops in children’s museums across Los Angeles, developing a gaming app to help children in Brazil control their asthma symptoms, or establishing a pulmonary and critical care training program in Uganda, the Foundation community service grants all focus on the same goal: to enable our underserved patients gain access to the resources and care they need when they need it most.
Why community service grants?
The Foundation began giving community service grants in 1997 under the leadership of CHEST President D. Robert McCaffree, MD, Master FCCP. He believed the program would be the best way to support his colleagues in achieving their community service endeavors .To date, over $2 million has been given specifically to community service projects. “
Our physicians experience the limitations of our health care system first-hand – a system that isn’t built to assist the people who need help the most. Finding solutions requires a willingness to think and operate creatively. The funding the Foundation provides through our community service grants supplies the resources to do just that – implement real-world solutions that will help patients gain better access to care.
Cases in point
Marina Lima, MD, MSc, was seeing an inordinate number of children and teens with uncontrolled asthma symptoms in Brazil. She applied for and was awarded a grant to make Asthmaland, the first gamified pediatric asthma educational program in Portuguese.
Besides her “Aha!” moments, Dr. Roberta Kato revealed a way she knows her work is making a difference: the funding is helping to shift the nonprofit landscape in her community.
“Sometimes there is a rift between different organizations. When I ask them to collaborate or advertise together, I get resistance. However, when I’ve reached out and said that I’ve received funding for an initiative, all of a sudden, there is forward movement. That is how I am hoping to make the biggest difference,” explained Dr. Kato.
Dr. Joseph Huang, who received a grant to fund the East Africa Training Initiative (EATI), is faced with a different obstacle. “We’ve been awarded the grant many times, and I know the Foundation is focused on supporting new, up-and-coming programs. Therefore, I’m committed to ensuring that my program can continue even after we stop receiving funding.”
How is Dr. Huang going to do that? Besides procuring ICU equipment, EATI focuses on training pulmonology fellows in east Africa. The fellows who graduate will train other physicians and care team members across the continent, both in hospitals and rural clinics, safeguarding the future of his program.
A clear vision for the future
While the Foundation is ready to tackle new problems, community service grants will remain the constant thread woven throughout the work, and it’s obvious why. As Dr. Huang emphasized, his grant “will ensure that the people living in Africa have a better chance at getting access to the care they need.”
When you strip away everything else, community service grants boil down to one thing: helping people live healthier, more fulfilled lives. What can be more worthwhile?
Help us continue this important work
While we are privileged to award numerous grants over the past 2 decades, our community service grants have always held a special place in the hearts and minds of everyone involved with the CHEST Foundation. We hope they hold a special place in your heart too.
Please consider donating so that we can continue this work together.
Community service grants are one way the Foundation strives to make a tangible, lasting impact on the lives of the patients we serve – they’re not just one-off projects with limited effects. But how do we really know that we’re making a difference?
For Dr. Roberta Kato, it’s when she gets to witness an “Aha!” moment – a time when everything clicks and a parent finally understands how to better care for their child. For Marina Lima, MD, MSc, it’s knowing that one more teen isn’t gasping for air. And for Dr. Joseph Huang, it’s seeing a country of 100 million people gain access to 14 pulmonologists when there was previously only one.
Whether it’s hosting family workshops in children’s museums across Los Angeles, developing a gaming app to help children in Brazil control their asthma symptoms, or establishing a pulmonary and critical care training program in Uganda, the Foundation community service grants all focus on the same goal: to enable our underserved patients gain access to the resources and care they need when they need it most.
Why community service grants?
The Foundation began giving community service grants in 1997 under the leadership of CHEST President D. Robert McCaffree, MD, Master FCCP. He believed the program would be the best way to support his colleagues in achieving their community service endeavors .To date, over $2 million has been given specifically to community service projects. “
Our physicians experience the limitations of our health care system first-hand – a system that isn’t built to assist the people who need help the most. Finding solutions requires a willingness to think and operate creatively. The funding the Foundation provides through our community service grants supplies the resources to do just that – implement real-world solutions that will help patients gain better access to care.
Cases in point
Marina Lima, MD, MSc, was seeing an inordinate number of children and teens with uncontrolled asthma symptoms in Brazil. She applied for and was awarded a grant to make Asthmaland, the first gamified pediatric asthma educational program in Portuguese.
Besides her “Aha!” moments, Dr. Roberta Kato revealed a way she knows her work is making a difference: the funding is helping to shift the nonprofit landscape in her community.
“Sometimes there is a rift between different organizations. When I ask them to collaborate or advertise together, I get resistance. However, when I’ve reached out and said that I’ve received funding for an initiative, all of a sudden, there is forward movement. That is how I am hoping to make the biggest difference,” explained Dr. Kato.
Dr. Joseph Huang, who received a grant to fund the East Africa Training Initiative (EATI), is faced with a different obstacle. “We’ve been awarded the grant many times, and I know the Foundation is focused on supporting new, up-and-coming programs. Therefore, I’m committed to ensuring that my program can continue even after we stop receiving funding.”
How is Dr. Huang going to do that? Besides procuring ICU equipment, EATI focuses on training pulmonology fellows in east Africa. The fellows who graduate will train other physicians and care team members across the continent, both in hospitals and rural clinics, safeguarding the future of his program.
A clear vision for the future
While the Foundation is ready to tackle new problems, community service grants will remain the constant thread woven throughout the work, and it’s obvious why. As Dr. Huang emphasized, his grant “will ensure that the people living in Africa have a better chance at getting access to the care they need.”
When you strip away everything else, community service grants boil down to one thing: helping people live healthier, more fulfilled lives. What can be more worthwhile?
Help us continue this important work
While we are privileged to award numerous grants over the past 2 decades, our community service grants have always held a special place in the hearts and minds of everyone involved with the CHEST Foundation. We hope they hold a special place in your heart too.
Please consider donating so that we can continue this work together.
Update – CHEST clinical practice guidelines
CHEST has a long history of developing high quality clinical practice guidelines based on rigorous methodology, particularly in Thoracic Oncology, Pulmonary Vascular/Venous Thromboembolic Disease, and Clinical Pulmonary Medicine/Cough. Using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach, CHEST guidelines aim to optimize patient care by providing evidence-based recommendations that are transparent and free from bias.
Recently, CHEST invested in reassessing how we could further enhance the relevance, timeliness, and impact of guidelines on patient care and outcomes. We re-evaluated how we prioritize guideline topics to ensure we identify conditions in which patient care might be significantly improved by the application of evidence-based recommendations. In addition to re-committing to the rigorous GRADE approach, we also committed to timelier guideline development that would cover a broader scope of clinical topics, better mirroring the needs of our membership.
Since resuming our guideline process last year, we completed four Expert Panel Reports covering COVID-19–related topics, as well as several CHEST clinical practice guidelines. This includes publications on the management of cough in various conditions and populations – chronic bronchitis, acute bronchitis in the immunocompromised adult, asthma and nonasthmatic eosinophilic bronchitis, and in children. We also published Diagnosis and Evaluation of Hypersensitivity Pneumonitis earlier this year. This guideline outlines a patient-centered and interdisciplinary diagnostic approach to aid clinicians and patients in navigating many of the uncertainties in the evaluation of this condition.
Updates from two of our guidelines following our ‘living guideline’ model were also recently published – Screening for Lung Cancer and Antithrombic Therapy for VTE Disease. The Screening for Lung Cancer update provides guidance on patient selection for lung cancer screening, updating the age and smoking history criteria based on new evidence published since the original CHEST guideline. The updated guideline also provides recommendations for implementing high-quality lung cancer screening programs to optimize the overall benefits of screening.
In Antithrombotic Therapy for VTE, the structure of recommendations follows the chronology of VTE management: ‘Whether to treat,’ ‘Interventional and adjunctive treatments,’ ‘Initiation phase,’ ‘Treatment phase,’ ‘Extended phase,’ and ‘Complications of VTE.’ This guideline was designed to provide a comprehensive reference for VTE management in patients at any stage of the disease. Several recommendations are new from prior versions of the guideline, including whether patients with cerebral venous sinus thrombosis should be treated with anticoagulation and the choice of anticoagulant therapy for patients with antiphospholipid syndrome and thrombosis.
As we look toward the future of guideline development at CHEST, we are excited by the opportunity to expand the CHEST guideline portfolio. Starting in 2022, we will be broadening the scope of CHEST guidelines to include topics in nine clinical domains: Airway Disorders, Chest Infections, Clinical Pulmonary Medicine, Critical Care, Interstitial Lung Disease, Interventional Pulmonology, Pulmonary Vascular Disease (including venous thromboembolic disease), Thoracic Oncology, and Sleep. We anticipate issuing a Request for Proposals in select areas from these domains in the Spring of 2022, allowing CHEST members the opportunity to propose topics for which clinical guidance is needed.
As we recommit to the rigorous guideline methodology for which CHEST is known and broaden our impact across the spectrum of chest disease, we seek to ensure CHEST remains the leading resource for evidence-based guidelines in the field of chest medicine.
CHEST has a long history of developing high quality clinical practice guidelines based on rigorous methodology, particularly in Thoracic Oncology, Pulmonary Vascular/Venous Thromboembolic Disease, and Clinical Pulmonary Medicine/Cough. Using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach, CHEST guidelines aim to optimize patient care by providing evidence-based recommendations that are transparent and free from bias.
Recently, CHEST invested in reassessing how we could further enhance the relevance, timeliness, and impact of guidelines on patient care and outcomes. We re-evaluated how we prioritize guideline topics to ensure we identify conditions in which patient care might be significantly improved by the application of evidence-based recommendations. In addition to re-committing to the rigorous GRADE approach, we also committed to timelier guideline development that would cover a broader scope of clinical topics, better mirroring the needs of our membership.
Since resuming our guideline process last year, we completed four Expert Panel Reports covering COVID-19–related topics, as well as several CHEST clinical practice guidelines. This includes publications on the management of cough in various conditions and populations – chronic bronchitis, acute bronchitis in the immunocompromised adult, asthma and nonasthmatic eosinophilic bronchitis, and in children. We also published Diagnosis and Evaluation of Hypersensitivity Pneumonitis earlier this year. This guideline outlines a patient-centered and interdisciplinary diagnostic approach to aid clinicians and patients in navigating many of the uncertainties in the evaluation of this condition.
Updates from two of our guidelines following our ‘living guideline’ model were also recently published – Screening for Lung Cancer and Antithrombic Therapy for VTE Disease. The Screening for Lung Cancer update provides guidance on patient selection for lung cancer screening, updating the age and smoking history criteria based on new evidence published since the original CHEST guideline. The updated guideline also provides recommendations for implementing high-quality lung cancer screening programs to optimize the overall benefits of screening.
In Antithrombotic Therapy for VTE, the structure of recommendations follows the chronology of VTE management: ‘Whether to treat,’ ‘Interventional and adjunctive treatments,’ ‘Initiation phase,’ ‘Treatment phase,’ ‘Extended phase,’ and ‘Complications of VTE.’ This guideline was designed to provide a comprehensive reference for VTE management in patients at any stage of the disease. Several recommendations are new from prior versions of the guideline, including whether patients with cerebral venous sinus thrombosis should be treated with anticoagulation and the choice of anticoagulant therapy for patients with antiphospholipid syndrome and thrombosis.
As we look toward the future of guideline development at CHEST, we are excited by the opportunity to expand the CHEST guideline portfolio. Starting in 2022, we will be broadening the scope of CHEST guidelines to include topics in nine clinical domains: Airway Disorders, Chest Infections, Clinical Pulmonary Medicine, Critical Care, Interstitial Lung Disease, Interventional Pulmonology, Pulmonary Vascular Disease (including venous thromboembolic disease), Thoracic Oncology, and Sleep. We anticipate issuing a Request for Proposals in select areas from these domains in the Spring of 2022, allowing CHEST members the opportunity to propose topics for which clinical guidance is needed.
As we recommit to the rigorous guideline methodology for which CHEST is known and broaden our impact across the spectrum of chest disease, we seek to ensure CHEST remains the leading resource for evidence-based guidelines in the field of chest medicine.
CHEST has a long history of developing high quality clinical practice guidelines based on rigorous methodology, particularly in Thoracic Oncology, Pulmonary Vascular/Venous Thromboembolic Disease, and Clinical Pulmonary Medicine/Cough. Using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach, CHEST guidelines aim to optimize patient care by providing evidence-based recommendations that are transparent and free from bias.
Recently, CHEST invested in reassessing how we could further enhance the relevance, timeliness, and impact of guidelines on patient care and outcomes. We re-evaluated how we prioritize guideline topics to ensure we identify conditions in which patient care might be significantly improved by the application of evidence-based recommendations. In addition to re-committing to the rigorous GRADE approach, we also committed to timelier guideline development that would cover a broader scope of clinical topics, better mirroring the needs of our membership.
Since resuming our guideline process last year, we completed four Expert Panel Reports covering COVID-19–related topics, as well as several CHEST clinical practice guidelines. This includes publications on the management of cough in various conditions and populations – chronic bronchitis, acute bronchitis in the immunocompromised adult, asthma and nonasthmatic eosinophilic bronchitis, and in children. We also published Diagnosis and Evaluation of Hypersensitivity Pneumonitis earlier this year. This guideline outlines a patient-centered and interdisciplinary diagnostic approach to aid clinicians and patients in navigating many of the uncertainties in the evaluation of this condition.
Updates from two of our guidelines following our ‘living guideline’ model were also recently published – Screening for Lung Cancer and Antithrombic Therapy for VTE Disease. The Screening for Lung Cancer update provides guidance on patient selection for lung cancer screening, updating the age and smoking history criteria based on new evidence published since the original CHEST guideline. The updated guideline also provides recommendations for implementing high-quality lung cancer screening programs to optimize the overall benefits of screening.
In Antithrombotic Therapy for VTE, the structure of recommendations follows the chronology of VTE management: ‘Whether to treat,’ ‘Interventional and adjunctive treatments,’ ‘Initiation phase,’ ‘Treatment phase,’ ‘Extended phase,’ and ‘Complications of VTE.’ This guideline was designed to provide a comprehensive reference for VTE management in patients at any stage of the disease. Several recommendations are new from prior versions of the guideline, including whether patients with cerebral venous sinus thrombosis should be treated with anticoagulation and the choice of anticoagulant therapy for patients with antiphospholipid syndrome and thrombosis.
As we look toward the future of guideline development at CHEST, we are excited by the opportunity to expand the CHEST guideline portfolio. Starting in 2022, we will be broadening the scope of CHEST guidelines to include topics in nine clinical domains: Airway Disorders, Chest Infections, Clinical Pulmonary Medicine, Critical Care, Interstitial Lung Disease, Interventional Pulmonology, Pulmonary Vascular Disease (including venous thromboembolic disease), Thoracic Oncology, and Sleep. We anticipate issuing a Request for Proposals in select areas from these domains in the Spring of 2022, allowing CHEST members the opportunity to propose topics for which clinical guidance is needed.
As we recommit to the rigorous guideline methodology for which CHEST is known and broaden our impact across the spectrum of chest disease, we seek to ensure CHEST remains the leading resource for evidence-based guidelines in the field of chest medicine.
New guidance on preventing cutaneous SCC in solid organ transplant patients
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.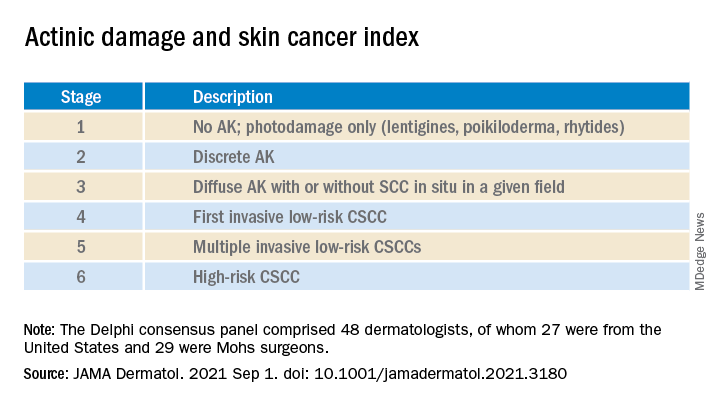
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.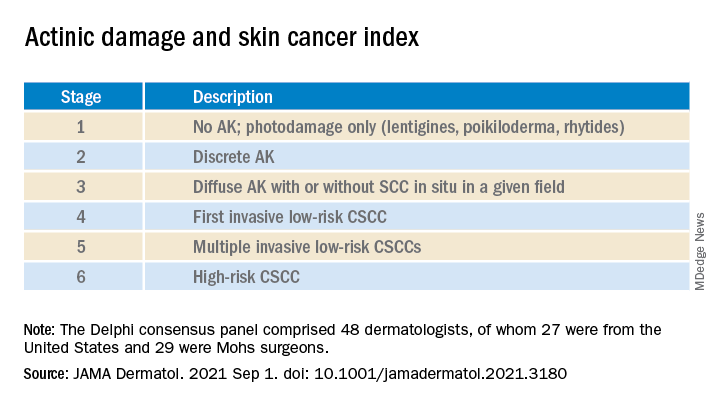
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.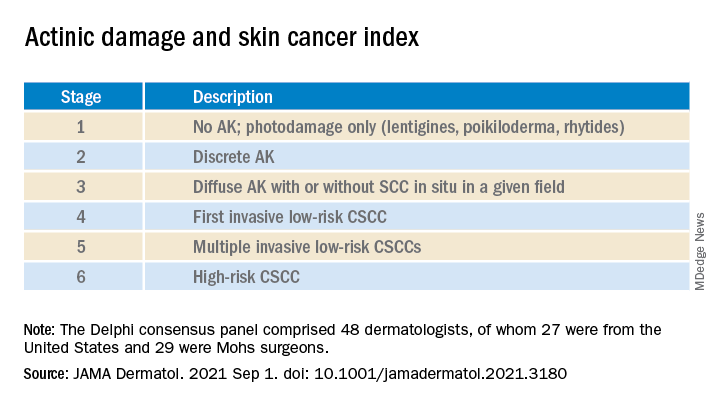
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
Even those who just test positive at more risk for long COVID: CDC
Long-term symptoms, like those linked with COVID-19, were common in people who had even just a single positive test, new Centers for Disease Control and Prevention data show.
The data show that symptoms in this group – including fatigue, cough, and headache – tended to last for more than a month.
Frequency of symptoms in people with a positive test was 1.5 times higher, compared with people whose tests had always been negative, according to the research published in the CDC’s latest Morbidity and Mortality Weekly Report.
Lead author Valentine Wanga, PhD, with the CDC’s COVID-19 response team, and colleagues conducted a non–probability-based internet panel survey of about 6,000 U.S. adults to assess long-term symptoms often associated with COVID-19 among those who had ever tested positive or always tested negative for COVID-19 between January 2020 and April 2021.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., said in an interview that this research “establishes more securely than before that you don’t have to be hospitalized with COVID in order to develop long COVID symptoms.”
That’s better known among infectious disease experts, he said, but added that “this survey really gives a firm database for that.”
Study results
The study’s results showed that, compared with respondents who had a negative test result, those who received a positive result reported a significantly higher prevalence of any long-term symptom (65.9% vs. 42.9%), fatigue (22.5% vs. 12.0%), change in sense of smell or taste (17.3% vs. 1.7%), shortness of breath (15.5% vs. 5.2%), cough (14.5% vs. 4.9%), and headache (13.8% vs. 9.9%).
More people who had a positive test result (76.2%) reported persistence for more than a month of at least one initially occurring symptom, compared with those whose test results were always negative (69.6%).
The numbers are further proof, Dr. Schaffner said, that COVID not only will be an acute stressor on the health care system but patients with long COVID will need help with managing care for the long term.
“We still don’t know what the COVID virus does that results in these long COVID symptoms,” he said. Vanderbilt and many other institutions have developed “long COVID” centers as a testament to how important the problem is.
Long COVID symptoms are not well understood and most studies have looked at the effects from patients who had been hospitalized with COVID-19.
In this survey, respondents self-reported whether they had ever had a positive SARS-CoV-2 test result (698), always received a negative test result (2,437), or never were tested for SARS-CoV-2 (2,750).
Compared with those who always tested negative, a larger proportion of those who tested positive (28.7% vs. 15.7%) reported believing that receiving a COVID-19 vaccine made their long-term symptoms better. No difference was found in reported beliefs that a vaccine made long-term symptoms worse.
Dr. Schaffner said he found that survey result interesting, but said that is not backed up by current data and would need further study.
“I would treat that with great caution,” he said. “I’m not dismissing it, but you can’t take that at face value. All of us who get sick and those of us who care for people who are sick – if there’s an intervention, we all hope for the best. We’re being optimistic. It’s when you do a randomized, double-blind, placebo-controlled study that you can find out whether your instincts or hopes were correct.”
The authors said that findings can inform public health preparedness, help guide care for people with post-COVID conditions, and help make the case for vaccines.
The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term symptoms, like those linked with COVID-19, were common in people who had even just a single positive test, new Centers for Disease Control and Prevention data show.
The data show that symptoms in this group – including fatigue, cough, and headache – tended to last for more than a month.
Frequency of symptoms in people with a positive test was 1.5 times higher, compared with people whose tests had always been negative, according to the research published in the CDC’s latest Morbidity and Mortality Weekly Report.
Lead author Valentine Wanga, PhD, with the CDC’s COVID-19 response team, and colleagues conducted a non–probability-based internet panel survey of about 6,000 U.S. adults to assess long-term symptoms often associated with COVID-19 among those who had ever tested positive or always tested negative for COVID-19 between January 2020 and April 2021.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., said in an interview that this research “establishes more securely than before that you don’t have to be hospitalized with COVID in order to develop long COVID symptoms.”
That’s better known among infectious disease experts, he said, but added that “this survey really gives a firm database for that.”
Study results
The study’s results showed that, compared with respondents who had a negative test result, those who received a positive result reported a significantly higher prevalence of any long-term symptom (65.9% vs. 42.9%), fatigue (22.5% vs. 12.0%), change in sense of smell or taste (17.3% vs. 1.7%), shortness of breath (15.5% vs. 5.2%), cough (14.5% vs. 4.9%), and headache (13.8% vs. 9.9%).
More people who had a positive test result (76.2%) reported persistence for more than a month of at least one initially occurring symptom, compared with those whose test results were always negative (69.6%).
The numbers are further proof, Dr. Schaffner said, that COVID not only will be an acute stressor on the health care system but patients with long COVID will need help with managing care for the long term.
“We still don’t know what the COVID virus does that results in these long COVID symptoms,” he said. Vanderbilt and many other institutions have developed “long COVID” centers as a testament to how important the problem is.
Long COVID symptoms are not well understood and most studies have looked at the effects from patients who had been hospitalized with COVID-19.
In this survey, respondents self-reported whether they had ever had a positive SARS-CoV-2 test result (698), always received a negative test result (2,437), or never were tested for SARS-CoV-2 (2,750).
Compared with those who always tested negative, a larger proportion of those who tested positive (28.7% vs. 15.7%) reported believing that receiving a COVID-19 vaccine made their long-term symptoms better. No difference was found in reported beliefs that a vaccine made long-term symptoms worse.
Dr. Schaffner said he found that survey result interesting, but said that is not backed up by current data and would need further study.
“I would treat that with great caution,” he said. “I’m not dismissing it, but you can’t take that at face value. All of us who get sick and those of us who care for people who are sick – if there’s an intervention, we all hope for the best. We’re being optimistic. It’s when you do a randomized, double-blind, placebo-controlled study that you can find out whether your instincts or hopes were correct.”
The authors said that findings can inform public health preparedness, help guide care for people with post-COVID conditions, and help make the case for vaccines.
The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term symptoms, like those linked with COVID-19, were common in people who had even just a single positive test, new Centers for Disease Control and Prevention data show.
The data show that symptoms in this group – including fatigue, cough, and headache – tended to last for more than a month.
Frequency of symptoms in people with a positive test was 1.5 times higher, compared with people whose tests had always been negative, according to the research published in the CDC’s latest Morbidity and Mortality Weekly Report.
Lead author Valentine Wanga, PhD, with the CDC’s COVID-19 response team, and colleagues conducted a non–probability-based internet panel survey of about 6,000 U.S. adults to assess long-term symptoms often associated with COVID-19 among those who had ever tested positive or always tested negative for COVID-19 between January 2020 and April 2021.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., said in an interview that this research “establishes more securely than before that you don’t have to be hospitalized with COVID in order to develop long COVID symptoms.”
That’s better known among infectious disease experts, he said, but added that “this survey really gives a firm database for that.”
Study results
The study’s results showed that, compared with respondents who had a negative test result, those who received a positive result reported a significantly higher prevalence of any long-term symptom (65.9% vs. 42.9%), fatigue (22.5% vs. 12.0%), change in sense of smell or taste (17.3% vs. 1.7%), shortness of breath (15.5% vs. 5.2%), cough (14.5% vs. 4.9%), and headache (13.8% vs. 9.9%).
More people who had a positive test result (76.2%) reported persistence for more than a month of at least one initially occurring symptom, compared with those whose test results were always negative (69.6%).
The numbers are further proof, Dr. Schaffner said, that COVID not only will be an acute stressor on the health care system but patients with long COVID will need help with managing care for the long term.
“We still don’t know what the COVID virus does that results in these long COVID symptoms,” he said. Vanderbilt and many other institutions have developed “long COVID” centers as a testament to how important the problem is.
Long COVID symptoms are not well understood and most studies have looked at the effects from patients who had been hospitalized with COVID-19.
In this survey, respondents self-reported whether they had ever had a positive SARS-CoV-2 test result (698), always received a negative test result (2,437), or never were tested for SARS-CoV-2 (2,750).
Compared with those who always tested negative, a larger proportion of those who tested positive (28.7% vs. 15.7%) reported believing that receiving a COVID-19 vaccine made their long-term symptoms better. No difference was found in reported beliefs that a vaccine made long-term symptoms worse.
Dr. Schaffner said he found that survey result interesting, but said that is not backed up by current data and would need further study.
“I would treat that with great caution,” he said. “I’m not dismissing it, but you can’t take that at face value. All of us who get sick and those of us who care for people who are sick – if there’s an intervention, we all hope for the best. We’re being optimistic. It’s when you do a randomized, double-blind, placebo-controlled study that you can find out whether your instincts or hopes were correct.”
The authors said that findings can inform public health preparedness, help guide care for people with post-COVID conditions, and help make the case for vaccines.
The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Seizure a first sign of COVID in kids?
Unlike in adults, seizures, including status epilepticus (SE), may be the first and main manifestation of COVID-19 in children, new research suggests.
Seizures may occur even in children with no history of epilepsy and in the absence of fever or severe COVID-19 illness, necessitating a “high index” of suspicion for the virus to make an early diagnosis and allow for appropriate infection control measures, say the researchers.
“We hope to increase physicians’ awareness of noninfluenza-like presentations of COVID in children. In areas with a high prevalence of COVID, we suggest that children with seizures be tested for COVID,” Tal Gilboa, MD, director of the child neurology unit and codirector of epilepsy, Hadassah Medical Center, Jerusalem, told this news organization.
The study was published online August 27 in the journal Seizure.
Presenting symptom
Among 175 children diagnosed with acute SARS-CoV-2 infection in the emergency department over 10 months in 2020, 11 (6%) presented with seizures. Studies in adults with COVID-19 have reported seizures in 0% to 2% of cases, the investigators note.
The 11 children with seizures (seven boys) ranged in age from 6 months to 17 years (median age, 11.5 years). All of them had seizures as the presenting sign of infection and none had severe COVID-19 requiring ventilatory or hemodynamic support. Six of the 11 children presented with fever.
Seven of the children had a prior history of neurological disorder: Five had epilepsy, one had a single unprovoked seizure 3 years before admission, and one had an intellectual disability. Three of the children had uncontrolled seizures despite appropriate treatment with antiseizure medication.
Nine of the 11 children presented with generalized tonic-clonic seizures. One child with a prior history of uncontrolled epilepsy with multiple seizure types had a focal tonic seizure. The youngest patient, a 5-month-old infant, presented with bilateral asymmetrical tonic-clonic seizure.
Of note, say the investigators, five of the 11 children presented with convulsive SE; none had a history of prior SE, and one had no history of seizures.
Although young age, especially under 12 months, is a known risk factor for SE, four of the five patients with SE were between 5 and 17 years old. All five children with SE responded to treatment with antiseizure medications.
All 11 children made a full recovery while in hospital, although further follow-up is essential to determine long-term outcomes, the researchers report.
“Children with no prior history of epilepsy and those with well-controlled epilepsy who present with breakthrough seizures, regardless of their body temperature, should be considered as potentially infected by SARS-CoV-2,” said Dr. Gilboa.
“It is possible, however unlikely, that a child, especially with prior epilepsy, may have an unprovoked seizure while being asymptomatically infected by SARS-CoV-2; in any case, infection control measures should be taken,” Dr. Gilboa added.
Need for replication
Weighing in on the study, Carl E. Stafstrom, MD, PhD, professor of neurology and pediatrics, Johns Hopkins University, Baltimore, said it’s important to note that “about half of the children had had epilepsy already, and for whatever reason, had a seizure, which required an ED visit, and then they found COVID.”
“Nevertheless, this article is interesting and surprising in what they found because nobody else has found nearly as frequent a seizure presentation,” said Dr. Stafstrom, director of the John M. Freeman Pediatric Epilepsy Center, Johns Hopkins Medicine.
“We would want to see some replication from other institutions and other populations,” he added.
The study had no specific funding. Dr. Gilboa and Dr. Stafstrom have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Unlike in adults, seizures, including status epilepticus (SE), may be the first and main manifestation of COVID-19 in children, new research suggests.
Seizures may occur even in children with no history of epilepsy and in the absence of fever or severe COVID-19 illness, necessitating a “high index” of suspicion for the virus to make an early diagnosis and allow for appropriate infection control measures, say the researchers.
“We hope to increase physicians’ awareness of noninfluenza-like presentations of COVID in children. In areas with a high prevalence of COVID, we suggest that children with seizures be tested for COVID,” Tal Gilboa, MD, director of the child neurology unit and codirector of epilepsy, Hadassah Medical Center, Jerusalem, told this news organization.
The study was published online August 27 in the journal Seizure.
Presenting symptom
Among 175 children diagnosed with acute SARS-CoV-2 infection in the emergency department over 10 months in 2020, 11 (6%) presented with seizures. Studies in adults with COVID-19 have reported seizures in 0% to 2% of cases, the investigators note.
The 11 children with seizures (seven boys) ranged in age from 6 months to 17 years (median age, 11.5 years). All of them had seizures as the presenting sign of infection and none had severe COVID-19 requiring ventilatory or hemodynamic support. Six of the 11 children presented with fever.
Seven of the children had a prior history of neurological disorder: Five had epilepsy, one had a single unprovoked seizure 3 years before admission, and one had an intellectual disability. Three of the children had uncontrolled seizures despite appropriate treatment with antiseizure medication.
Nine of the 11 children presented with generalized tonic-clonic seizures. One child with a prior history of uncontrolled epilepsy with multiple seizure types had a focal tonic seizure. The youngest patient, a 5-month-old infant, presented with bilateral asymmetrical tonic-clonic seizure.
Of note, say the investigators, five of the 11 children presented with convulsive SE; none had a history of prior SE, and one had no history of seizures.
Although young age, especially under 12 months, is a known risk factor for SE, four of the five patients with SE were between 5 and 17 years old. All five children with SE responded to treatment with antiseizure medications.
All 11 children made a full recovery while in hospital, although further follow-up is essential to determine long-term outcomes, the researchers report.
“Children with no prior history of epilepsy and those with well-controlled epilepsy who present with breakthrough seizures, regardless of their body temperature, should be considered as potentially infected by SARS-CoV-2,” said Dr. Gilboa.
“It is possible, however unlikely, that a child, especially with prior epilepsy, may have an unprovoked seizure while being asymptomatically infected by SARS-CoV-2; in any case, infection control measures should be taken,” Dr. Gilboa added.
Need for replication
Weighing in on the study, Carl E. Stafstrom, MD, PhD, professor of neurology and pediatrics, Johns Hopkins University, Baltimore, said it’s important to note that “about half of the children had had epilepsy already, and for whatever reason, had a seizure, which required an ED visit, and then they found COVID.”
“Nevertheless, this article is interesting and surprising in what they found because nobody else has found nearly as frequent a seizure presentation,” said Dr. Stafstrom, director of the John M. Freeman Pediatric Epilepsy Center, Johns Hopkins Medicine.
“We would want to see some replication from other institutions and other populations,” he added.
The study had no specific funding. Dr. Gilboa and Dr. Stafstrom have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Unlike in adults, seizures, including status epilepticus (SE), may be the first and main manifestation of COVID-19 in children, new research suggests.
Seizures may occur even in children with no history of epilepsy and in the absence of fever or severe COVID-19 illness, necessitating a “high index” of suspicion for the virus to make an early diagnosis and allow for appropriate infection control measures, say the researchers.
“We hope to increase physicians’ awareness of noninfluenza-like presentations of COVID in children. In areas with a high prevalence of COVID, we suggest that children with seizures be tested for COVID,” Tal Gilboa, MD, director of the child neurology unit and codirector of epilepsy, Hadassah Medical Center, Jerusalem, told this news organization.
The study was published online August 27 in the journal Seizure.
Presenting symptom
Among 175 children diagnosed with acute SARS-CoV-2 infection in the emergency department over 10 months in 2020, 11 (6%) presented with seizures. Studies in adults with COVID-19 have reported seizures in 0% to 2% of cases, the investigators note.
The 11 children with seizures (seven boys) ranged in age from 6 months to 17 years (median age, 11.5 years). All of them had seizures as the presenting sign of infection and none had severe COVID-19 requiring ventilatory or hemodynamic support. Six of the 11 children presented with fever.
Seven of the children had a prior history of neurological disorder: Five had epilepsy, one had a single unprovoked seizure 3 years before admission, and one had an intellectual disability. Three of the children had uncontrolled seizures despite appropriate treatment with antiseizure medication.
Nine of the 11 children presented with generalized tonic-clonic seizures. One child with a prior history of uncontrolled epilepsy with multiple seizure types had a focal tonic seizure. The youngest patient, a 5-month-old infant, presented with bilateral asymmetrical tonic-clonic seizure.
Of note, say the investigators, five of the 11 children presented with convulsive SE; none had a history of prior SE, and one had no history of seizures.
Although young age, especially under 12 months, is a known risk factor for SE, four of the five patients with SE were between 5 and 17 years old. All five children with SE responded to treatment with antiseizure medications.
All 11 children made a full recovery while in hospital, although further follow-up is essential to determine long-term outcomes, the researchers report.
“Children with no prior history of epilepsy and those with well-controlled epilepsy who present with breakthrough seizures, regardless of their body temperature, should be considered as potentially infected by SARS-CoV-2,” said Dr. Gilboa.
“It is possible, however unlikely, that a child, especially with prior epilepsy, may have an unprovoked seizure while being asymptomatically infected by SARS-CoV-2; in any case, infection control measures should be taken,” Dr. Gilboa added.
Need for replication
Weighing in on the study, Carl E. Stafstrom, MD, PhD, professor of neurology and pediatrics, Johns Hopkins University, Baltimore, said it’s important to note that “about half of the children had had epilepsy already, and for whatever reason, had a seizure, which required an ED visit, and then they found COVID.”
“Nevertheless, this article is interesting and surprising in what they found because nobody else has found nearly as frequent a seizure presentation,” said Dr. Stafstrom, director of the John M. Freeman Pediatric Epilepsy Center, Johns Hopkins Medicine.
“We would want to see some replication from other institutions and other populations,” he added.
The study had no specific funding. Dr. Gilboa and Dr. Stafstrom have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Medical power couple launch robot that helps in the labor room
Medical Power Couples is a new series highlighting spouses or domestic partners prominent in health care. Both have achieved high-level professional success and have made significant contributions to their respective fields.
Julie Shah, PhD, and Neel Shah, MD
Ob.gyn. Neel Shah was telling his wife how challenging it was for labor and delivery nurses to make room assignments: to delegate available beds, predict the timing of patient progression from one room to another, and pair patients with staff nurses, equipment, and resources.
Julie Shah, a roboticist with Massachusetts Institute of Technology, Cambridge, compared the head nurses to air traffic controllers, but without near the decision support. Julie had previously worked for aerospace giant Boeing, where she helped design a set of algorithmic techniques to give decision support to manufacturing personnel and embed robots to aid their work.
Suddenly the Shahs had an idea.
The robot, tested in 2018 at a Boston tertiary care center, produced high-quality recommendations accepted by nurses and physicians 90% of the time. The android was taught to observe actual performances of human tasks – what was done and not done in certain situations – and develop a scheduling policy. The Shahs and their team were the first to field a robotic system on a labor and delivery unit to aid in the coordination of resources required for patient care.
“For the first time, we were able to develop a novel machine-learning technique that could learn from demonstration or observation, heuristics, or strategies for solving resource allocation and scheduling problems, which was really exciting,” Julie said. “We were able to show also how that system could be embedded to offer decision support to reduce the cognitive burden of nurses.”
Neel and Julie joke that their first collaboration dates back to middle school when they sang together in chorus. The Shahs grew up in the same small New Jersey town and met as 14-year-olds.
Though the Shahs have known each other more than half their lives, they haven’t always lived side by side. After they married, Julie accepted an opportunity in Seattle, while Neel remained 3,000 miles away in Boston.
“He does all the cooking, so I did not eat well,” Julie recalled with a laugh. “It was not great.”
“I don’t self-regulate well,” Neel adds. “I just worked 24/7. I started a nonprofit that year, so externally, it looked like I was crushing it, but …”
“He was lonely,” Julie says.
Now back in the same city, the Shahs are doting parents to two toddlers aged 2 and 4, and also serve as heads of house at an MIT graduate dorm.
Julie, 39, is an associate professor in the department of aeronautics and astronautics at MIT and leads the Interactive Robotics Group of the Computer Science and Artificial Intelligence Laboratory. She is renowned for her innovative methods for enabling fluid human-robot teamwork in time- and safety-critical environments such as surgery, manufacturing, and space exploration. In 2014, she was recognized by the MIT Technology Review as one of the world’s top innovators under 35, and her work on industrial human-robot collaboration was recognized as one of the 10 breakthrough technologies of 2013.
Neel, 39, is an assistant professor of obstetrics, gynecology and reproductive biology at Harvard Medical School in Boston and chief medical officer of Maven Clinic, a virtual clinic for women’s and family health. A scientist and entrepreneur, Neel is globally recognized for designing solutions to improve health care. He is founder of Costs of Care, an NGO that curates insights from clinicians and patients to help delivery systems provide better care.
He also cofounded the March for Moms Association, a coalition of organizations that works to raise public and private investment in mothers’ well-being. Most recently, Neel and his team designed TeamBirth, an intrapartum care process that aims to improve the safety and dignity of childbirth care and promote communication and teamwork.
The Shahs say their personalities are sometimes opposite, but that they balance each other well.
“Julie thinks in lists, which sometimes drives me crazy, and I think in exploding clouds, which I think drives her crazy, but the combination usually works out,” Neel said. “We seem to be good complements for each other.”
In their own words
What is one food that your spouse eats that you can’t stand?
Neel: She eats raisins, and I hate raisins. Raisins are a crime against humanity. They’re wrong. The chocolate-covered raisins are even grosser.
What is one parenting difference you have?
Julie: Safety. I hover around the kids around safety hazards, and Neel is very relaxed.
What’s one quirky thing about your partner?
Neel: She has a parrot that predates our marriage. He started out as an illegal dorm bird. He just screeches and poops. If you’re developing a character in a book or a movie and you want to make them seem slightly off, you make them a bird owner. Think about it.
Julie: He’s 19 and his name is Bolivar, after the South American revolutionary. He’s very sweet.
Neel: I live in a Hitchcock movie.
If you weren’t a physician/scientist, what is a dream job you might have?
Julie: I would be a dolphin trainer. That was my childhood dream.
Neel: I’d want to do something creative. I’ve always wanted to be a better musician. I play the guitar and piano.
A version of this article first appeared on Medscape.com.
Medical Power Couples is a new series highlighting spouses or domestic partners prominent in health care. Both have achieved high-level professional success and have made significant contributions to their respective fields.
Julie Shah, PhD, and Neel Shah, MD
Ob.gyn. Neel Shah was telling his wife how challenging it was for labor and delivery nurses to make room assignments: to delegate available beds, predict the timing of patient progression from one room to another, and pair patients with staff nurses, equipment, and resources.
Julie Shah, a roboticist with Massachusetts Institute of Technology, Cambridge, compared the head nurses to air traffic controllers, but without near the decision support. Julie had previously worked for aerospace giant Boeing, where she helped design a set of algorithmic techniques to give decision support to manufacturing personnel and embed robots to aid their work.
Suddenly the Shahs had an idea.
The robot, tested in 2018 at a Boston tertiary care center, produced high-quality recommendations accepted by nurses and physicians 90% of the time. The android was taught to observe actual performances of human tasks – what was done and not done in certain situations – and develop a scheduling policy. The Shahs and their team were the first to field a robotic system on a labor and delivery unit to aid in the coordination of resources required for patient care.
“For the first time, we were able to develop a novel machine-learning technique that could learn from demonstration or observation, heuristics, or strategies for solving resource allocation and scheduling problems, which was really exciting,” Julie said. “We were able to show also how that system could be embedded to offer decision support to reduce the cognitive burden of nurses.”
Neel and Julie joke that their first collaboration dates back to middle school when they sang together in chorus. The Shahs grew up in the same small New Jersey town and met as 14-year-olds.
Though the Shahs have known each other more than half their lives, they haven’t always lived side by side. After they married, Julie accepted an opportunity in Seattle, while Neel remained 3,000 miles away in Boston.
“He does all the cooking, so I did not eat well,” Julie recalled with a laugh. “It was not great.”
“I don’t self-regulate well,” Neel adds. “I just worked 24/7. I started a nonprofit that year, so externally, it looked like I was crushing it, but …”
“He was lonely,” Julie says.
Now back in the same city, the Shahs are doting parents to two toddlers aged 2 and 4, and also serve as heads of house at an MIT graduate dorm.
Julie, 39, is an associate professor in the department of aeronautics and astronautics at MIT and leads the Interactive Robotics Group of the Computer Science and Artificial Intelligence Laboratory. She is renowned for her innovative methods for enabling fluid human-robot teamwork in time- and safety-critical environments such as surgery, manufacturing, and space exploration. In 2014, she was recognized by the MIT Technology Review as one of the world’s top innovators under 35, and her work on industrial human-robot collaboration was recognized as one of the 10 breakthrough technologies of 2013.
Neel, 39, is an assistant professor of obstetrics, gynecology and reproductive biology at Harvard Medical School in Boston and chief medical officer of Maven Clinic, a virtual clinic for women’s and family health. A scientist and entrepreneur, Neel is globally recognized for designing solutions to improve health care. He is founder of Costs of Care, an NGO that curates insights from clinicians and patients to help delivery systems provide better care.
He also cofounded the March for Moms Association, a coalition of organizations that works to raise public and private investment in mothers’ well-being. Most recently, Neel and his team designed TeamBirth, an intrapartum care process that aims to improve the safety and dignity of childbirth care and promote communication and teamwork.
The Shahs say their personalities are sometimes opposite, but that they balance each other well.
“Julie thinks in lists, which sometimes drives me crazy, and I think in exploding clouds, which I think drives her crazy, but the combination usually works out,” Neel said. “We seem to be good complements for each other.”
In their own words
What is one food that your spouse eats that you can’t stand?
Neel: She eats raisins, and I hate raisins. Raisins are a crime against humanity. They’re wrong. The chocolate-covered raisins are even grosser.
What is one parenting difference you have?
Julie: Safety. I hover around the kids around safety hazards, and Neel is very relaxed.
What’s one quirky thing about your partner?
Neel: She has a parrot that predates our marriage. He started out as an illegal dorm bird. He just screeches and poops. If you’re developing a character in a book or a movie and you want to make them seem slightly off, you make them a bird owner. Think about it.
Julie: He’s 19 and his name is Bolivar, after the South American revolutionary. He’s very sweet.
Neel: I live in a Hitchcock movie.
If you weren’t a physician/scientist, what is a dream job you might have?
Julie: I would be a dolphin trainer. That was my childhood dream.
Neel: I’d want to do something creative. I’ve always wanted to be a better musician. I play the guitar and piano.
A version of this article first appeared on Medscape.com.
Medical Power Couples is a new series highlighting spouses or domestic partners prominent in health care. Both have achieved high-level professional success and have made significant contributions to their respective fields.
Julie Shah, PhD, and Neel Shah, MD
Ob.gyn. Neel Shah was telling his wife how challenging it was for labor and delivery nurses to make room assignments: to delegate available beds, predict the timing of patient progression from one room to another, and pair patients with staff nurses, equipment, and resources.
Julie Shah, a roboticist with Massachusetts Institute of Technology, Cambridge, compared the head nurses to air traffic controllers, but without near the decision support. Julie had previously worked for aerospace giant Boeing, where she helped design a set of algorithmic techniques to give decision support to manufacturing personnel and embed robots to aid their work.
Suddenly the Shahs had an idea.
The robot, tested in 2018 at a Boston tertiary care center, produced high-quality recommendations accepted by nurses and physicians 90% of the time. The android was taught to observe actual performances of human tasks – what was done and not done in certain situations – and develop a scheduling policy. The Shahs and their team were the first to field a robotic system on a labor and delivery unit to aid in the coordination of resources required for patient care.
“For the first time, we were able to develop a novel machine-learning technique that could learn from demonstration or observation, heuristics, or strategies for solving resource allocation and scheduling problems, which was really exciting,” Julie said. “We were able to show also how that system could be embedded to offer decision support to reduce the cognitive burden of nurses.”
Neel and Julie joke that their first collaboration dates back to middle school when they sang together in chorus. The Shahs grew up in the same small New Jersey town and met as 14-year-olds.
Though the Shahs have known each other more than half their lives, they haven’t always lived side by side. After they married, Julie accepted an opportunity in Seattle, while Neel remained 3,000 miles away in Boston.
“He does all the cooking, so I did not eat well,” Julie recalled with a laugh. “It was not great.”
“I don’t self-regulate well,” Neel adds. “I just worked 24/7. I started a nonprofit that year, so externally, it looked like I was crushing it, but …”
“He was lonely,” Julie says.
Now back in the same city, the Shahs are doting parents to two toddlers aged 2 and 4, and also serve as heads of house at an MIT graduate dorm.
Julie, 39, is an associate professor in the department of aeronautics and astronautics at MIT and leads the Interactive Robotics Group of the Computer Science and Artificial Intelligence Laboratory. She is renowned for her innovative methods for enabling fluid human-robot teamwork in time- and safety-critical environments such as surgery, manufacturing, and space exploration. In 2014, she was recognized by the MIT Technology Review as one of the world’s top innovators under 35, and her work on industrial human-robot collaboration was recognized as one of the 10 breakthrough technologies of 2013.
Neel, 39, is an assistant professor of obstetrics, gynecology and reproductive biology at Harvard Medical School in Boston and chief medical officer of Maven Clinic, a virtual clinic for women’s and family health. A scientist and entrepreneur, Neel is globally recognized for designing solutions to improve health care. He is founder of Costs of Care, an NGO that curates insights from clinicians and patients to help delivery systems provide better care.
He also cofounded the March for Moms Association, a coalition of organizations that works to raise public and private investment in mothers’ well-being. Most recently, Neel and his team designed TeamBirth, an intrapartum care process that aims to improve the safety and dignity of childbirth care and promote communication and teamwork.
The Shahs say their personalities are sometimes opposite, but that they balance each other well.
“Julie thinks in lists, which sometimes drives me crazy, and I think in exploding clouds, which I think drives her crazy, but the combination usually works out,” Neel said. “We seem to be good complements for each other.”
In their own words
What is one food that your spouse eats that you can’t stand?
Neel: She eats raisins, and I hate raisins. Raisins are a crime against humanity. They’re wrong. The chocolate-covered raisins are even grosser.
What is one parenting difference you have?
Julie: Safety. I hover around the kids around safety hazards, and Neel is very relaxed.
What’s one quirky thing about your partner?
Neel: She has a parrot that predates our marriage. He started out as an illegal dorm bird. He just screeches and poops. If you’re developing a character in a book or a movie and you want to make them seem slightly off, you make them a bird owner. Think about it.
Julie: He’s 19 and his name is Bolivar, after the South American revolutionary. He’s very sweet.
Neel: I live in a Hitchcock movie.
If you weren’t a physician/scientist, what is a dream job you might have?
Julie: I would be a dolphin trainer. That was my childhood dream.
Neel: I’d want to do something creative. I’ve always wanted to be a better musician. I play the guitar and piano.
A version of this article first appeared on Medscape.com.
Unequal resource distribution underlies lung cancer disparities
Lung cancer disparities are reversible, but it will take changes at the social policy and organizational levels to do it, according to Ray Osarogiagbon, MBBS, a medical oncologist in the thoracic oncology program at Baptist Cancer Center, Memphis.
Much of the issue comes down to unequal distribution of services across the country, with less high-end care available in areas hardest hit by lung cancer, which are often areas with higher percentages of Black people, Dr. Osarogiagbon said. He addressed the issues – which he conceptualizes as “avoidable differences” – in a plenary presentation at the virtual 2021 World Conference on Lung Cancer.
He said that much of disparity research has focused on patient-level issues, but it has the least potential to effect change and also has “the unpleasant side effect of stigmatizing the victims of disparate health care delivery.”
Better to look at the big picture. “We have to focus on the areas where we are most likely to be successful, the social policy level, next the organizational level, and then providers,” he said.
Kentucky, followed by Mississippi, Arkansas, Tennessee, West Virginia, and Alabama, has the highest lung cancer burden in the United States. While lung cancer has been on the decline for decades nationwide, some counties in those states in particular continue to struggle with rising lung cancer mortality.
Dr. Osarogiagbon’s own health care system, which serves western Tennessee as well as eastern Arkansas and northern Mississippi, sees about 1,300 lung cancer cases annually, more than many states in the United States.
Regional disparities in lung cancer care span the entirety of available services, from unequal access to tobacco cessation and other preventive measures straight through to access to leading-edge systemic therapies. Disparities are particularly acute with more recent advances such as immunotherapy and low-dose CT screening.
One recent study, for instance, found that several southern states with high lung cancer burdens had screening rates below 4%, while several New England states had rates ranging to over 15%.
“There is a mismatch between the places were lung cancer kills and the places where we have invested in low-dose CT scan facilities,” Dr. Osarogiagbon said. As a side effect, White patients have better access,
It’s not, he said, that Black people are more likely to refuse such services, as least as far as clinical trials go.
Black patients are significantly underrepresented in pharmaceutical industry trials. Part of the issues is that areas hardest hit by lung cancer are often also ones less likely to have the infrastructure to support trials.
But on an equal playing field, Black patients are at least as eager as White patients to sign up for a trial. Dr. Osarogiagbon and colleagues found that, if offered the chance, almost 60% of Black patients said they would participate in a trial versus 53.4% of White patients. If access were equal, there would be “no race-based disparities” in trial participation, he said.
It’s also emerging that Black patients might benefit more from innovations such as immune checkpoint inhibitors treatment and low-dose CT screening, which means that, if they were included in more trials, companies would likely have stronger study results.
It’s something they should pay attention to, if for no other reason than it would help their bottom line, Dr. Osarogiagbon said.
Curative surgery for early-stage lung tumors is another issue. At the county level in the United States, he and his team found that it’s offered to anywhere from 13% to 92% of patients who qualify.
“Counties in the lowest quartile for receipt of surgery were those with a high proportion of non-Hispanic Black subjects, high poverty and uninsured rates, low surgeon-to-population ratio, and nonmetropolitan status,” they found.
Dr. Osarogiagbon is a consultant for and/or has stock in a number of companies, including AstraZeneca, Eli Lilly, and Genentech.
Lung cancer disparities are reversible, but it will take changes at the social policy and organizational levels to do it, according to Ray Osarogiagbon, MBBS, a medical oncologist in the thoracic oncology program at Baptist Cancer Center, Memphis.
Much of the issue comes down to unequal distribution of services across the country, with less high-end care available in areas hardest hit by lung cancer, which are often areas with higher percentages of Black people, Dr. Osarogiagbon said. He addressed the issues – which he conceptualizes as “avoidable differences” – in a plenary presentation at the virtual 2021 World Conference on Lung Cancer.
He said that much of disparity research has focused on patient-level issues, but it has the least potential to effect change and also has “the unpleasant side effect of stigmatizing the victims of disparate health care delivery.”
Better to look at the big picture. “We have to focus on the areas where we are most likely to be successful, the social policy level, next the organizational level, and then providers,” he said.
Kentucky, followed by Mississippi, Arkansas, Tennessee, West Virginia, and Alabama, has the highest lung cancer burden in the United States. While lung cancer has been on the decline for decades nationwide, some counties in those states in particular continue to struggle with rising lung cancer mortality.
Dr. Osarogiagbon’s own health care system, which serves western Tennessee as well as eastern Arkansas and northern Mississippi, sees about 1,300 lung cancer cases annually, more than many states in the United States.
Regional disparities in lung cancer care span the entirety of available services, from unequal access to tobacco cessation and other preventive measures straight through to access to leading-edge systemic therapies. Disparities are particularly acute with more recent advances such as immunotherapy and low-dose CT screening.
One recent study, for instance, found that several southern states with high lung cancer burdens had screening rates below 4%, while several New England states had rates ranging to over 15%.
“There is a mismatch between the places were lung cancer kills and the places where we have invested in low-dose CT scan facilities,” Dr. Osarogiagbon said. As a side effect, White patients have better access,
It’s not, he said, that Black people are more likely to refuse such services, as least as far as clinical trials go.
Black patients are significantly underrepresented in pharmaceutical industry trials. Part of the issues is that areas hardest hit by lung cancer are often also ones less likely to have the infrastructure to support trials.
But on an equal playing field, Black patients are at least as eager as White patients to sign up for a trial. Dr. Osarogiagbon and colleagues found that, if offered the chance, almost 60% of Black patients said they would participate in a trial versus 53.4% of White patients. If access were equal, there would be “no race-based disparities” in trial participation, he said.
It’s also emerging that Black patients might benefit more from innovations such as immune checkpoint inhibitors treatment and low-dose CT screening, which means that, if they were included in more trials, companies would likely have stronger study results.
It’s something they should pay attention to, if for no other reason than it would help their bottom line, Dr. Osarogiagbon said.
Curative surgery for early-stage lung tumors is another issue. At the county level in the United States, he and his team found that it’s offered to anywhere from 13% to 92% of patients who qualify.
“Counties in the lowest quartile for receipt of surgery were those with a high proportion of non-Hispanic Black subjects, high poverty and uninsured rates, low surgeon-to-population ratio, and nonmetropolitan status,” they found.
Dr. Osarogiagbon is a consultant for and/or has stock in a number of companies, including AstraZeneca, Eli Lilly, and Genentech.
Lung cancer disparities are reversible, but it will take changes at the social policy and organizational levels to do it, according to Ray Osarogiagbon, MBBS, a medical oncologist in the thoracic oncology program at Baptist Cancer Center, Memphis.
Much of the issue comes down to unequal distribution of services across the country, with less high-end care available in areas hardest hit by lung cancer, which are often areas with higher percentages of Black people, Dr. Osarogiagbon said. He addressed the issues – which he conceptualizes as “avoidable differences” – in a plenary presentation at the virtual 2021 World Conference on Lung Cancer.
He said that much of disparity research has focused on patient-level issues, but it has the least potential to effect change and also has “the unpleasant side effect of stigmatizing the victims of disparate health care delivery.”
Better to look at the big picture. “We have to focus on the areas where we are most likely to be successful, the social policy level, next the organizational level, and then providers,” he said.
Kentucky, followed by Mississippi, Arkansas, Tennessee, West Virginia, and Alabama, has the highest lung cancer burden in the United States. While lung cancer has been on the decline for decades nationwide, some counties in those states in particular continue to struggle with rising lung cancer mortality.
Dr. Osarogiagbon’s own health care system, which serves western Tennessee as well as eastern Arkansas and northern Mississippi, sees about 1,300 lung cancer cases annually, more than many states in the United States.
Regional disparities in lung cancer care span the entirety of available services, from unequal access to tobacco cessation and other preventive measures straight through to access to leading-edge systemic therapies. Disparities are particularly acute with more recent advances such as immunotherapy and low-dose CT screening.
One recent study, for instance, found that several southern states with high lung cancer burdens had screening rates below 4%, while several New England states had rates ranging to over 15%.
“There is a mismatch between the places were lung cancer kills and the places where we have invested in low-dose CT scan facilities,” Dr. Osarogiagbon said. As a side effect, White patients have better access,
It’s not, he said, that Black people are more likely to refuse such services, as least as far as clinical trials go.
Black patients are significantly underrepresented in pharmaceutical industry trials. Part of the issues is that areas hardest hit by lung cancer are often also ones less likely to have the infrastructure to support trials.
But on an equal playing field, Black patients are at least as eager as White patients to sign up for a trial. Dr. Osarogiagbon and colleagues found that, if offered the chance, almost 60% of Black patients said they would participate in a trial versus 53.4% of White patients. If access were equal, there would be “no race-based disparities” in trial participation, he said.
It’s also emerging that Black patients might benefit more from innovations such as immune checkpoint inhibitors treatment and low-dose CT screening, which means that, if they were included in more trials, companies would likely have stronger study results.
It’s something they should pay attention to, if for no other reason than it would help their bottom line, Dr. Osarogiagbon said.
Curative surgery for early-stage lung tumors is another issue. At the county level in the United States, he and his team found that it’s offered to anywhere from 13% to 92% of patients who qualify.
“Counties in the lowest quartile for receipt of surgery were those with a high proportion of non-Hispanic Black subjects, high poverty and uninsured rates, low surgeon-to-population ratio, and nonmetropolitan status,” they found.
Dr. Osarogiagbon is a consultant for and/or has stock in a number of companies, including AstraZeneca, Eli Lilly, and Genentech.
FROM WCLC 2021
Finding the most bang for the buck with adjuvant atezolizumab for NSCLC
Investigators are zeroing in on the stage II-IIIa non–small cell lung cancer patients most likely to benefit from adjuvant atezolizumab (Tecentriq) following resection and chemotherapy.
It seems that PD-L1 positive patients, those who undergo lobectomy, those who have nodal involvement, and those treated with all common platinum doublets, with the possible exception of cisplatin-gemcitabine, are most likely to benefit from adjuvant treatment, according to a report at the virtual 2021 World Congress on Lung Cancer.
Results come for an analysis of IMpower010, which randomized 1,005 patients equally to either best supportive care or atezolizumab every 21 days for 16 cycles following resection and chemotherapy.
The topline results, reported recently, found a 34% improvement in disease-free survival (DFS) in stage II-IIIa patients expressing PD-L1 and a 21% improvement across all patients regardless of PD-L1 expression.
It was the first positive phase 3 trial for adjuvant immunotherapy in NSCLC. Maker Hoffman-La Roche subsequently applied to the U.S. Food and Drug Administration for an indication for adjuvant treatment following surgery and platinum-based chemotherapy for NSCLC with PD-L1 expression of at least 1%.
At the WCLC meeting, investigators took a closer look at IMpower010 to gauge the impact of different surgery and chemotherapy types on outcomes.
“Improved DFS was observed with adjuvant atezolizumab” for II-IIIa disease across most stages in patients “with nodal involvement, and across most surgery resection types and chemotherapy regimens,” said lead investigator Nasser Altorki, MD, director of the division of thoracic surgery at New York Presbyterian-Weill Cornell Medical Center in New York.
Study discussant Ichiro Yoshino, MD, PhD, a thoracic surgeon at Chiba University, in Japan, expanded on the “most” part of the assertion.
“Patients who underwent lobectomy [78%] had more evident benefit. … Patients who had a pneumonectomy [16%] did not benefit from atezolizumab,” he said (DFS hazard ratio, 0.91, 95% confidence interval, 0.56-1.47).
The reasons are unclear. It could be because patients who have pneumonectomies are less tolerant of adjuvant chemotherapy, so might have not gotten complete courses, but whatever the cause, Dr. Yoshino said it’s an important finding that needs further investigation.
Also, there was no DFS benefit in the 16% of patients who received cisplatin-gemcitabine for chemotherapy instead of other platinum doublets (HR, 0.94, 95% CI, 0.56-1.57).
It might have to do with the fact that under 80% of cisplatin-gemcitabine patients completed all four cycles of chemotherapy versus completion rates of up to more than 90% with other platinum doublets. It might also, however, have something to do with the way gemcitabine works or its interaction with atezolizumab.
The issue is another one that needs “to be examined,” Dr. Yoshino said.
The trial was funded by Hoffman-La Roche. Dr. Altorki is an advisor and/or researcher for AstraZeneca, Merck, and Johnson & Johnson. Among various company ties, Dr. Yoshino is an advisor and speaker for AstraZeneca and Johnson & Johnson and a researcher for Pfizer.
Investigators are zeroing in on the stage II-IIIa non–small cell lung cancer patients most likely to benefit from adjuvant atezolizumab (Tecentriq) following resection and chemotherapy.
It seems that PD-L1 positive patients, those who undergo lobectomy, those who have nodal involvement, and those treated with all common platinum doublets, with the possible exception of cisplatin-gemcitabine, are most likely to benefit from adjuvant treatment, according to a report at the virtual 2021 World Congress on Lung Cancer.
Results come for an analysis of IMpower010, which randomized 1,005 patients equally to either best supportive care or atezolizumab every 21 days for 16 cycles following resection and chemotherapy.
The topline results, reported recently, found a 34% improvement in disease-free survival (DFS) in stage II-IIIa patients expressing PD-L1 and a 21% improvement across all patients regardless of PD-L1 expression.
It was the first positive phase 3 trial for adjuvant immunotherapy in NSCLC. Maker Hoffman-La Roche subsequently applied to the U.S. Food and Drug Administration for an indication for adjuvant treatment following surgery and platinum-based chemotherapy for NSCLC with PD-L1 expression of at least 1%.
At the WCLC meeting, investigators took a closer look at IMpower010 to gauge the impact of different surgery and chemotherapy types on outcomes.
“Improved DFS was observed with adjuvant atezolizumab” for II-IIIa disease across most stages in patients “with nodal involvement, and across most surgery resection types and chemotherapy regimens,” said lead investigator Nasser Altorki, MD, director of the division of thoracic surgery at New York Presbyterian-Weill Cornell Medical Center in New York.
Study discussant Ichiro Yoshino, MD, PhD, a thoracic surgeon at Chiba University, in Japan, expanded on the “most” part of the assertion.
“Patients who underwent lobectomy [78%] had more evident benefit. … Patients who had a pneumonectomy [16%] did not benefit from atezolizumab,” he said (DFS hazard ratio, 0.91, 95% confidence interval, 0.56-1.47).
The reasons are unclear. It could be because patients who have pneumonectomies are less tolerant of adjuvant chemotherapy, so might have not gotten complete courses, but whatever the cause, Dr. Yoshino said it’s an important finding that needs further investigation.
Also, there was no DFS benefit in the 16% of patients who received cisplatin-gemcitabine for chemotherapy instead of other platinum doublets (HR, 0.94, 95% CI, 0.56-1.57).
It might have to do with the fact that under 80% of cisplatin-gemcitabine patients completed all four cycles of chemotherapy versus completion rates of up to more than 90% with other platinum doublets. It might also, however, have something to do with the way gemcitabine works or its interaction with atezolizumab.
The issue is another one that needs “to be examined,” Dr. Yoshino said.
The trial was funded by Hoffman-La Roche. Dr. Altorki is an advisor and/or researcher for AstraZeneca, Merck, and Johnson & Johnson. Among various company ties, Dr. Yoshino is an advisor and speaker for AstraZeneca and Johnson & Johnson and a researcher for Pfizer.
Investigators are zeroing in on the stage II-IIIa non–small cell lung cancer patients most likely to benefit from adjuvant atezolizumab (Tecentriq) following resection and chemotherapy.
It seems that PD-L1 positive patients, those who undergo lobectomy, those who have nodal involvement, and those treated with all common platinum doublets, with the possible exception of cisplatin-gemcitabine, are most likely to benefit from adjuvant treatment, according to a report at the virtual 2021 World Congress on Lung Cancer.
Results come for an analysis of IMpower010, which randomized 1,005 patients equally to either best supportive care or atezolizumab every 21 days for 16 cycles following resection and chemotherapy.
The topline results, reported recently, found a 34% improvement in disease-free survival (DFS) in stage II-IIIa patients expressing PD-L1 and a 21% improvement across all patients regardless of PD-L1 expression.
It was the first positive phase 3 trial for adjuvant immunotherapy in NSCLC. Maker Hoffman-La Roche subsequently applied to the U.S. Food and Drug Administration for an indication for adjuvant treatment following surgery and platinum-based chemotherapy for NSCLC with PD-L1 expression of at least 1%.
At the WCLC meeting, investigators took a closer look at IMpower010 to gauge the impact of different surgery and chemotherapy types on outcomes.
“Improved DFS was observed with adjuvant atezolizumab” for II-IIIa disease across most stages in patients “with nodal involvement, and across most surgery resection types and chemotherapy regimens,” said lead investigator Nasser Altorki, MD, director of the division of thoracic surgery at New York Presbyterian-Weill Cornell Medical Center in New York.
Study discussant Ichiro Yoshino, MD, PhD, a thoracic surgeon at Chiba University, in Japan, expanded on the “most” part of the assertion.
“Patients who underwent lobectomy [78%] had more evident benefit. … Patients who had a pneumonectomy [16%] did not benefit from atezolizumab,” he said (DFS hazard ratio, 0.91, 95% confidence interval, 0.56-1.47).
The reasons are unclear. It could be because patients who have pneumonectomies are less tolerant of adjuvant chemotherapy, so might have not gotten complete courses, but whatever the cause, Dr. Yoshino said it’s an important finding that needs further investigation.
Also, there was no DFS benefit in the 16% of patients who received cisplatin-gemcitabine for chemotherapy instead of other platinum doublets (HR, 0.94, 95% CI, 0.56-1.57).
It might have to do with the fact that under 80% of cisplatin-gemcitabine patients completed all four cycles of chemotherapy versus completion rates of up to more than 90% with other platinum doublets. It might also, however, have something to do with the way gemcitabine works or its interaction with atezolizumab.
The issue is another one that needs “to be examined,” Dr. Yoshino said.
The trial was funded by Hoffman-La Roche. Dr. Altorki is an advisor and/or researcher for AstraZeneca, Merck, and Johnson & Johnson. Among various company ties, Dr. Yoshino is an advisor and speaker for AstraZeneca and Johnson & Johnson and a researcher for Pfizer.
FROM WCLC 2021
Gluten-free diet may reduce cancer risk in celiac disease
Overall cancer risk is slightly increased in patients older than 40 years within their first year of a celiac disease diagnosis, but the risk drops within a year of diagnosis, shows a Swedish study of 47,000 people with celiac disease.
“Celiac disease is associated with an increased risk of types of cancer, and we believe that this is due to the longstanding inflammation that is induced by gluten,” said first author Benjamin Lebwohl, MD, director of clinical research at the Columbia University Celiac Disease Center in New York.
Writing in Clinical Gastroenterology and Hepatology, the authors explained that most studies investigating cancer risk in patients with celiac disease were done before both the widespread use of serologic testing for celiac disease and access to gluten-free food was widely available. Earlier studies linked celiac disease to gastrointestinal malignancies, such as small intestinal adenocarcinoma, and lymphomas.
A prior analysis of this Swedish cohort found that the risk of small intestinal adenocarcinoma, while low, continued for up to 10 years after diagnosis with celiac disease. In the study, which was published in Gastroenterology, the authors found the risks of small-bowel adenocarcinoma and adenomas were significantly increased in people with celiac disease, compared with those without this disease.
“We have known from prior studies that people with celiac disease are at increased risk of developing certain cancers, but there has been limited study of this risk in celiac disease in the 21st century, where there is increased recognition (leading to more prompt diagnosis) and increased access to gluten-free food options (which may allow for more effective treatment),” said Dr. Lebwohl, who is also the director of quality improvement in the division of digestive and liver diseases at Columbia University. “We aimed to determine whether there is still an increased risk of cancer in this modern era, and we found that there still is an increased risk, but this increase is small and that it diminishes beyond the first year after the diagnosis of celiac disease.”
This nationwide cohort study in Sweden included 47,241 patients with celiac disease (62% female; mean age, 24 years), of which 64% were diagnosed since 2000. Each patient was age and sex matched to up to five controls. After a median follow-up of 11.5 years, a 1.11-fold increased risk of cancer overall was found in patients with celiac disease, compared with controls. The respective incidences of cancer were 6.5 and 5.7 per 1,000 person-years, and most of the excess risk was caused by gastrointestinal and hematologic cancer.
The overall risk of cancer was increased in the first year after celiac disease diagnosis (HR, 2.47; 95% CI, 2.22-2.74) but not afterwards (HR, 1.01; 95% CI, 0.97-1.05).
“It appears that the increased risk of cancer in people with celiac disease decreased over time, and this may be related to the beneficial effect of the gluten-free diet in the long term,” Dr. Lebwohl said.
The authors suggest that cancer risk, followed by a decline to no risk, may alternatively be due to the increased monitoring and medical examinations among patients with celiac disease. Also, symptoms of cancer, such as weight loss, may lead to broad testing that identifies celiac disease, the authors wrote.
For cancer subtypes, the strongest association between celiac disease and cancer was found for hematologic, lymphoproliferative and gastrointestinal cancers. Among gastrointestinal cancer subtypes, elevated risks were found for hepatobiliary and pancreatic cancer, but not for gastric or colorectal cancer. The cancer risk in celiac disease decreased in breast and lung cancer, which the authors suggested may be attributed to lower body mass index and smoking rates, respectively, observed in individuals with celiac disease.
Certain cancer types persist after 1 year
Although there was no overall cancer risk for more than 1 year after celiac disease diagnosis, the risks of hematologic and lymphoproliferative cancers persisted. While the increased risk of gastrointestinal cancers collectively was no longer significant beyond 1 year after celiac disease diagnosis, the risk persisted for hepatobiliary and pancreatic cancer.
“We found that the risk of gastrointestinal cancers is increased in people with celiac disease, compared to the general population, but these risks vary according to the cancer type,” Dr. Lebwohl said. “For instance, the risk of pancreatic cancer is increased in people with celiac disease, compared to the general population, while the risk of colon cancer in people with celiac disease is not increased, compared to the general population.
“But pancreatic cancer is far less common than colon cancer. We found that pancreatic cancer occurs in 1 in 5,000 people with celiac disease per year, whereas colorectal cancer occurred in 1 in 1,400 people per year. Taken all together, the risk of any gastrointestinal cancer was around 1 in 700 per year among people with celiac disease,” Dr. Lebwohl said.
The overall cancer risk was highest in patients diagnosed with celiac disease after age 60 and was not increased in those diagnosed with celiac disease before age 40. The authors noted that, in recent years, there has been a pronounced increase in the diagnosis of celiac disease in people aged over 60, an age group with a higher risk of developing severe outcomes related to refractory celiac disease. The cancer risk was similar among patients diagnosed with celiac disease before or after 2000.
Since this is an observational study, causality cannot be proven, and the authors suggested that the findings may not be applicable to settings outside of the relatively homogeneous ethnic population of Sweden.
Carol E. Semrad, MD, professor of medicine and director of clinical research in the Celiac Center at the University of Chicago Medicine, said: “This is an observational study and therefore cannot answer whether celiac disease is the cause of cancer or merely an association.” She added that “it is unknown why the risk for some cancers is higher in celiac disease.
“This paper argues against delayed diagnosis and low detection rate to explain the increase in cancer risk as those diagnosed with celiac disease prior to 2000 had the same cancer risk as those diagnosed after 2000 when diagnostic testing, earlier diagnosis, and access to a gluten-free diet were better,” Dr. Semrad said.
Link to mortality data
The authors said increased cancer risk being restricted to the first year of diagnosis is consistent with prior celiac disease studies of morbidity and mortality.
A study published in 2019 in United European Gastroenterology looked at mortality risk in 602 patients with celiac disease from Lothian, Scotland, identified between 1979 and 1983 and followed up from 1970 to 2016. All-cause mortality was 43% higher than in the general population, mainly from hematologic malignancies, and this risk was greatest during the first few years of diagnosis.
An analysis of cause-specific mortality in the Swedish cohort, published in 2020 in JAMA, found that celiac disease was associated with a small but statistically significant increased mortality risk. After a median follow-up of 12.5 years of 49,829 patients with celiac disease, the mortality rate was 9.7 and 8.6 deaths per 1000 person-years, compared with the general population, respectively. Individuals with celiac disease were at increased risk of death from cancer, cardiovascular disease and respiratory disease. The overall mortality risk was greatest in the first year after diagnosis with celiac disease, after which the risk diminished with the establishment of the gluten-free diet but remained modestly elevated in the long term.
However, a Finnish population-based study, published in the American Journal of Gastroenterology, found no increase in overall mortality in patients with celiac disease. The study included 12,803 adults diagnosed with celiac disease between 2005 and 2014. Participants were followed for an average of 7.7 years and mortality from all malignancies, gastrointestinal tract malignancies or cardiovascular diseases were not increased among patients with celiac disease, compared with the general population. Mortality from lymphoproliferative diseases was increased in patients with celiac disease but was lower than previously reported.
Dr. Lebwohl and colleagues noted that the incidences of cancer types vary by the age and geographical region of the study population, as does the diagnosis of celiac disease, which may explain why increased risk for cancer or cancer related-mortality in patients with celiac disease has not always been reported.
Dr Ludvigsson coordinates a study on behalf of the Swedish IBD quality register. This study has received funding from Janssen. The remaining authors disclosed no conflicts.
Overall cancer risk is slightly increased in patients older than 40 years within their first year of a celiac disease diagnosis, but the risk drops within a year of diagnosis, shows a Swedish study of 47,000 people with celiac disease.
“Celiac disease is associated with an increased risk of types of cancer, and we believe that this is due to the longstanding inflammation that is induced by gluten,” said first author Benjamin Lebwohl, MD, director of clinical research at the Columbia University Celiac Disease Center in New York.
Writing in Clinical Gastroenterology and Hepatology, the authors explained that most studies investigating cancer risk in patients with celiac disease were done before both the widespread use of serologic testing for celiac disease and access to gluten-free food was widely available. Earlier studies linked celiac disease to gastrointestinal malignancies, such as small intestinal adenocarcinoma, and lymphomas.
A prior analysis of this Swedish cohort found that the risk of small intestinal adenocarcinoma, while low, continued for up to 10 years after diagnosis with celiac disease. In the study, which was published in Gastroenterology, the authors found the risks of small-bowel adenocarcinoma and adenomas were significantly increased in people with celiac disease, compared with those without this disease.
“We have known from prior studies that people with celiac disease are at increased risk of developing certain cancers, but there has been limited study of this risk in celiac disease in the 21st century, where there is increased recognition (leading to more prompt diagnosis) and increased access to gluten-free food options (which may allow for more effective treatment),” said Dr. Lebwohl, who is also the director of quality improvement in the division of digestive and liver diseases at Columbia University. “We aimed to determine whether there is still an increased risk of cancer in this modern era, and we found that there still is an increased risk, but this increase is small and that it diminishes beyond the first year after the diagnosis of celiac disease.”
This nationwide cohort study in Sweden included 47,241 patients with celiac disease (62% female; mean age, 24 years), of which 64% were diagnosed since 2000. Each patient was age and sex matched to up to five controls. After a median follow-up of 11.5 years, a 1.11-fold increased risk of cancer overall was found in patients with celiac disease, compared with controls. The respective incidences of cancer were 6.5 and 5.7 per 1,000 person-years, and most of the excess risk was caused by gastrointestinal and hematologic cancer.
The overall risk of cancer was increased in the first year after celiac disease diagnosis (HR, 2.47; 95% CI, 2.22-2.74) but not afterwards (HR, 1.01; 95% CI, 0.97-1.05).
“It appears that the increased risk of cancer in people with celiac disease decreased over time, and this may be related to the beneficial effect of the gluten-free diet in the long term,” Dr. Lebwohl said.
The authors suggest that cancer risk, followed by a decline to no risk, may alternatively be due to the increased monitoring and medical examinations among patients with celiac disease. Also, symptoms of cancer, such as weight loss, may lead to broad testing that identifies celiac disease, the authors wrote.
For cancer subtypes, the strongest association between celiac disease and cancer was found for hematologic, lymphoproliferative and gastrointestinal cancers. Among gastrointestinal cancer subtypes, elevated risks were found for hepatobiliary and pancreatic cancer, but not for gastric or colorectal cancer. The cancer risk in celiac disease decreased in breast and lung cancer, which the authors suggested may be attributed to lower body mass index and smoking rates, respectively, observed in individuals with celiac disease.
Certain cancer types persist after 1 year
Although there was no overall cancer risk for more than 1 year after celiac disease diagnosis, the risks of hematologic and lymphoproliferative cancers persisted. While the increased risk of gastrointestinal cancers collectively was no longer significant beyond 1 year after celiac disease diagnosis, the risk persisted for hepatobiliary and pancreatic cancer.
“We found that the risk of gastrointestinal cancers is increased in people with celiac disease, compared to the general population, but these risks vary according to the cancer type,” Dr. Lebwohl said. “For instance, the risk of pancreatic cancer is increased in people with celiac disease, compared to the general population, while the risk of colon cancer in people with celiac disease is not increased, compared to the general population.
“But pancreatic cancer is far less common than colon cancer. We found that pancreatic cancer occurs in 1 in 5,000 people with celiac disease per year, whereas colorectal cancer occurred in 1 in 1,400 people per year. Taken all together, the risk of any gastrointestinal cancer was around 1 in 700 per year among people with celiac disease,” Dr. Lebwohl said.
The overall cancer risk was highest in patients diagnosed with celiac disease after age 60 and was not increased in those diagnosed with celiac disease before age 40. The authors noted that, in recent years, there has been a pronounced increase in the diagnosis of celiac disease in people aged over 60, an age group with a higher risk of developing severe outcomes related to refractory celiac disease. The cancer risk was similar among patients diagnosed with celiac disease before or after 2000.
Since this is an observational study, causality cannot be proven, and the authors suggested that the findings may not be applicable to settings outside of the relatively homogeneous ethnic population of Sweden.
Carol E. Semrad, MD, professor of medicine and director of clinical research in the Celiac Center at the University of Chicago Medicine, said: “This is an observational study and therefore cannot answer whether celiac disease is the cause of cancer or merely an association.” She added that “it is unknown why the risk for some cancers is higher in celiac disease.
“This paper argues against delayed diagnosis and low detection rate to explain the increase in cancer risk as those diagnosed with celiac disease prior to 2000 had the same cancer risk as those diagnosed after 2000 when diagnostic testing, earlier diagnosis, and access to a gluten-free diet were better,” Dr. Semrad said.
Link to mortality data
The authors said increased cancer risk being restricted to the first year of diagnosis is consistent with prior celiac disease studies of morbidity and mortality.
A study published in 2019 in United European Gastroenterology looked at mortality risk in 602 patients with celiac disease from Lothian, Scotland, identified between 1979 and 1983 and followed up from 1970 to 2016. All-cause mortality was 43% higher than in the general population, mainly from hematologic malignancies, and this risk was greatest during the first few years of diagnosis.
An analysis of cause-specific mortality in the Swedish cohort, published in 2020 in JAMA, found that celiac disease was associated with a small but statistically significant increased mortality risk. After a median follow-up of 12.5 years of 49,829 patients with celiac disease, the mortality rate was 9.7 and 8.6 deaths per 1000 person-years, compared with the general population, respectively. Individuals with celiac disease were at increased risk of death from cancer, cardiovascular disease and respiratory disease. The overall mortality risk was greatest in the first year after diagnosis with celiac disease, after which the risk diminished with the establishment of the gluten-free diet but remained modestly elevated in the long term.
However, a Finnish population-based study, published in the American Journal of Gastroenterology, found no increase in overall mortality in patients with celiac disease. The study included 12,803 adults diagnosed with celiac disease between 2005 and 2014. Participants were followed for an average of 7.7 years and mortality from all malignancies, gastrointestinal tract malignancies or cardiovascular diseases were not increased among patients with celiac disease, compared with the general population. Mortality from lymphoproliferative diseases was increased in patients with celiac disease but was lower than previously reported.
Dr. Lebwohl and colleagues noted that the incidences of cancer types vary by the age and geographical region of the study population, as does the diagnosis of celiac disease, which may explain why increased risk for cancer or cancer related-mortality in patients with celiac disease has not always been reported.
Dr Ludvigsson coordinates a study on behalf of the Swedish IBD quality register. This study has received funding from Janssen. The remaining authors disclosed no conflicts.
Overall cancer risk is slightly increased in patients older than 40 years within their first year of a celiac disease diagnosis, but the risk drops within a year of diagnosis, shows a Swedish study of 47,000 people with celiac disease.
“Celiac disease is associated with an increased risk of types of cancer, and we believe that this is due to the longstanding inflammation that is induced by gluten,” said first author Benjamin Lebwohl, MD, director of clinical research at the Columbia University Celiac Disease Center in New York.
Writing in Clinical Gastroenterology and Hepatology, the authors explained that most studies investigating cancer risk in patients with celiac disease were done before both the widespread use of serologic testing for celiac disease and access to gluten-free food was widely available. Earlier studies linked celiac disease to gastrointestinal malignancies, such as small intestinal adenocarcinoma, and lymphomas.
A prior analysis of this Swedish cohort found that the risk of small intestinal adenocarcinoma, while low, continued for up to 10 years after diagnosis with celiac disease. In the study, which was published in Gastroenterology, the authors found the risks of small-bowel adenocarcinoma and adenomas were significantly increased in people with celiac disease, compared with those without this disease.
“We have known from prior studies that people with celiac disease are at increased risk of developing certain cancers, but there has been limited study of this risk in celiac disease in the 21st century, where there is increased recognition (leading to more prompt diagnosis) and increased access to gluten-free food options (which may allow for more effective treatment),” said Dr. Lebwohl, who is also the director of quality improvement in the division of digestive and liver diseases at Columbia University. “We aimed to determine whether there is still an increased risk of cancer in this modern era, and we found that there still is an increased risk, but this increase is small and that it diminishes beyond the first year after the diagnosis of celiac disease.”
This nationwide cohort study in Sweden included 47,241 patients with celiac disease (62% female; mean age, 24 years), of which 64% were diagnosed since 2000. Each patient was age and sex matched to up to five controls. After a median follow-up of 11.5 years, a 1.11-fold increased risk of cancer overall was found in patients with celiac disease, compared with controls. The respective incidences of cancer were 6.5 and 5.7 per 1,000 person-years, and most of the excess risk was caused by gastrointestinal and hematologic cancer.
The overall risk of cancer was increased in the first year after celiac disease diagnosis (HR, 2.47; 95% CI, 2.22-2.74) but not afterwards (HR, 1.01; 95% CI, 0.97-1.05).
“It appears that the increased risk of cancer in people with celiac disease decreased over time, and this may be related to the beneficial effect of the gluten-free diet in the long term,” Dr. Lebwohl said.
The authors suggest that cancer risk, followed by a decline to no risk, may alternatively be due to the increased monitoring and medical examinations among patients with celiac disease. Also, symptoms of cancer, such as weight loss, may lead to broad testing that identifies celiac disease, the authors wrote.
For cancer subtypes, the strongest association between celiac disease and cancer was found for hematologic, lymphoproliferative and gastrointestinal cancers. Among gastrointestinal cancer subtypes, elevated risks were found for hepatobiliary and pancreatic cancer, but not for gastric or colorectal cancer. The cancer risk in celiac disease decreased in breast and lung cancer, which the authors suggested may be attributed to lower body mass index and smoking rates, respectively, observed in individuals with celiac disease.
Certain cancer types persist after 1 year
Although there was no overall cancer risk for more than 1 year after celiac disease diagnosis, the risks of hematologic and lymphoproliferative cancers persisted. While the increased risk of gastrointestinal cancers collectively was no longer significant beyond 1 year after celiac disease diagnosis, the risk persisted for hepatobiliary and pancreatic cancer.
“We found that the risk of gastrointestinal cancers is increased in people with celiac disease, compared to the general population, but these risks vary according to the cancer type,” Dr. Lebwohl said. “For instance, the risk of pancreatic cancer is increased in people with celiac disease, compared to the general population, while the risk of colon cancer in people with celiac disease is not increased, compared to the general population.
“But pancreatic cancer is far less common than colon cancer. We found that pancreatic cancer occurs in 1 in 5,000 people with celiac disease per year, whereas colorectal cancer occurred in 1 in 1,400 people per year. Taken all together, the risk of any gastrointestinal cancer was around 1 in 700 per year among people with celiac disease,” Dr. Lebwohl said.
The overall cancer risk was highest in patients diagnosed with celiac disease after age 60 and was not increased in those diagnosed with celiac disease before age 40. The authors noted that, in recent years, there has been a pronounced increase in the diagnosis of celiac disease in people aged over 60, an age group with a higher risk of developing severe outcomes related to refractory celiac disease. The cancer risk was similar among patients diagnosed with celiac disease before or after 2000.
Since this is an observational study, causality cannot be proven, and the authors suggested that the findings may not be applicable to settings outside of the relatively homogeneous ethnic population of Sweden.
Carol E. Semrad, MD, professor of medicine and director of clinical research in the Celiac Center at the University of Chicago Medicine, said: “This is an observational study and therefore cannot answer whether celiac disease is the cause of cancer or merely an association.” She added that “it is unknown why the risk for some cancers is higher in celiac disease.
“This paper argues against delayed diagnosis and low detection rate to explain the increase in cancer risk as those diagnosed with celiac disease prior to 2000 had the same cancer risk as those diagnosed after 2000 when diagnostic testing, earlier diagnosis, and access to a gluten-free diet were better,” Dr. Semrad said.
Link to mortality data
The authors said increased cancer risk being restricted to the first year of diagnosis is consistent with prior celiac disease studies of morbidity and mortality.
A study published in 2019 in United European Gastroenterology looked at mortality risk in 602 patients with celiac disease from Lothian, Scotland, identified between 1979 and 1983 and followed up from 1970 to 2016. All-cause mortality was 43% higher than in the general population, mainly from hematologic malignancies, and this risk was greatest during the first few years of diagnosis.
An analysis of cause-specific mortality in the Swedish cohort, published in 2020 in JAMA, found that celiac disease was associated with a small but statistically significant increased mortality risk. After a median follow-up of 12.5 years of 49,829 patients with celiac disease, the mortality rate was 9.7 and 8.6 deaths per 1000 person-years, compared with the general population, respectively. Individuals with celiac disease were at increased risk of death from cancer, cardiovascular disease and respiratory disease. The overall mortality risk was greatest in the first year after diagnosis with celiac disease, after which the risk diminished with the establishment of the gluten-free diet but remained modestly elevated in the long term.
However, a Finnish population-based study, published in the American Journal of Gastroenterology, found no increase in overall mortality in patients with celiac disease. The study included 12,803 adults diagnosed with celiac disease between 2005 and 2014. Participants were followed for an average of 7.7 years and mortality from all malignancies, gastrointestinal tract malignancies or cardiovascular diseases were not increased among patients with celiac disease, compared with the general population. Mortality from lymphoproliferative diseases was increased in patients with celiac disease but was lower than previously reported.
Dr. Lebwohl and colleagues noted that the incidences of cancer types vary by the age and geographical region of the study population, as does the diagnosis of celiac disease, which may explain why increased risk for cancer or cancer related-mortality in patients with celiac disease has not always been reported.
Dr Ludvigsson coordinates a study on behalf of the Swedish IBD quality register. This study has received funding from Janssen. The remaining authors disclosed no conflicts.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Medical boards: Docs who spread COVID misinformation put license at risk
Leaders of the American Board of Family Medicine, the American Board of Internal Medicine, and the American Board of Pediatrics said Sept. 9 that they support FSMB’s position.
“We also want all physicians certified by our boards to know that such unethical or unprofessional conduct may prompt their respective Board to take action that could put their certification at risk,” a statement read.
“Expertise matters, and board-certified physicians have demonstrated that they have stayed current in their field. Spreading misinformation or falsehoods to the public during a time of a public health emergency goes against everything our boards and our community of board-certified physicians stand for,” the leaders wrote.
“The evidence that we have safe, effective, and widely available vaccines against COVID-19 is overwhelming. We are particularly concerned about physicians who use their authority to denigrate vaccination at a time when vaccines continue to demonstrate excellent effectiveness against severe illness, hospitalization, and death.”
Small number spread false information
However, a small number of doctors continue to spread misinformation against the vaccines and communicate other false information surrounding COVID-19.
Some of the misinformation spreaders have had ultra-viral reach.
Among them is Daniel Stock, MD, a family physician in Indiana who has come out against COVID-19 vaccines. At a recent meeting of the Mt. Vernon Community School board in Indiana, he gave a speech urging the board to ignore the prevailing recommendations around COVID-19, such as test-and-trace measures.
Forbes reported in August that versions of the video of Stock›s speech on Facebook “have collected a total of 90 million engagements – a metric encompassing things such as comments, likes and shares – according to data collected by Media Matters for America, a liberal tech-watchdog group.”
This news organization published a story in August asking whether physicians who spread such information should lose their license and the question drew rapid-fire comments.
Commenters who argued with potential disciplinary actions raised questions about where the line will be drawn between misinformation and deeply held beliefs in terms of care.
Several comments centered on ivermectin, which is not approved by the Food and Drug Administration to treat COVID-19 but is enthusiastically supported as a COVID-19 treatment by a group of physicians called the Front Line COVID-19 Critical Care Alliance, whose website includes requests for donations.
Some cited free speech protections.
‘Not consistent with standards’
As for ivermectin, David G. Nichols, MD, president and CEO of the American Board of Pediatrics, gave this news organization an example: “Spreading the notion that one would not need to get vaccinated because if you get sick you could take ivermectin is a very dangerous statement. That is not consistent with the standards of professionalism required for certification or licensure.”
Ivermectin, he noted, is not an approved treatment for COVID-19.
“To say that it is or has any benefit is a false statement. We’re not willing to allow individuals who make false statements to devalue the terrific work of tens of thousands of physicians across the United States doing work under very difficult circumstances,” Dr. Nichols said.
He continued: “To suggest treatments that are known not to be effective in exchange for treatment that is known to be effective is dangerous – and ivermectin falls under that category.”
Asked whether such suggestions could result in suspension or revocation of a physician’s license, Dr. Nichols said, “It’s the kind of thing that would certainly trigger a review.”
He said the standard for separating misinformation from personal beliefs is based on whether there is scientific evidence to support the belief.
The boards are not, with this statement, attempting to referee legitimate scientific debate, he said.
The misinformation the boards are referring to, Dr. Nichols said, is “where the evidence is 100% on one side and zero on another. And the zero is not only that the opinions or beliefs are unsupported or unsubstantiated, they are indeed harmful if followed. That’s the distinction we’re trying to make here.”
As for free-speech arguments, he said, “Free speech is a constitutional right. You can say whatever you want. The issue here is you do not have the right to expect continued professional sanction of a board certificate if you are lying to the public.”
The board statement also said: “We all look to board-certified physicians to provide outstanding care and guidance; providing misinformation about a lethal disease is unethical, unprofessional, and dangerous. In times of medical emergency, the community of expert physicians committed to science and evidence collectively shares a responsibility for giving the public the most accurate and timely health information available, so they can make decisions that work best for themselves and their families.”
In addition to Dr. Nichols, the statement was signed by Warren Newton, MD, MPH, president and CEO of the American Board of Family Medicine, and Richard J. Baron, MD, president and CEO of the American Board of Internal Medicine.
A version of this article first appeared on Medscape.com.
Leaders of the American Board of Family Medicine, the American Board of Internal Medicine, and the American Board of Pediatrics said Sept. 9 that they support FSMB’s position.
“We also want all physicians certified by our boards to know that such unethical or unprofessional conduct may prompt their respective Board to take action that could put their certification at risk,” a statement read.
“Expertise matters, and board-certified physicians have demonstrated that they have stayed current in their field. Spreading misinformation or falsehoods to the public during a time of a public health emergency goes against everything our boards and our community of board-certified physicians stand for,” the leaders wrote.
“The evidence that we have safe, effective, and widely available vaccines against COVID-19 is overwhelming. We are particularly concerned about physicians who use their authority to denigrate vaccination at a time when vaccines continue to demonstrate excellent effectiveness against severe illness, hospitalization, and death.”
Small number spread false information
However, a small number of doctors continue to spread misinformation against the vaccines and communicate other false information surrounding COVID-19.
Some of the misinformation spreaders have had ultra-viral reach.
Among them is Daniel Stock, MD, a family physician in Indiana who has come out against COVID-19 vaccines. At a recent meeting of the Mt. Vernon Community School board in Indiana, he gave a speech urging the board to ignore the prevailing recommendations around COVID-19, such as test-and-trace measures.
Forbes reported in August that versions of the video of Stock›s speech on Facebook “have collected a total of 90 million engagements – a metric encompassing things such as comments, likes and shares – according to data collected by Media Matters for America, a liberal tech-watchdog group.”
This news organization published a story in August asking whether physicians who spread such information should lose their license and the question drew rapid-fire comments.
Commenters who argued with potential disciplinary actions raised questions about where the line will be drawn between misinformation and deeply held beliefs in terms of care.
Several comments centered on ivermectin, which is not approved by the Food and Drug Administration to treat COVID-19 but is enthusiastically supported as a COVID-19 treatment by a group of physicians called the Front Line COVID-19 Critical Care Alliance, whose website includes requests for donations.
Some cited free speech protections.
‘Not consistent with standards’
As for ivermectin, David G. Nichols, MD, president and CEO of the American Board of Pediatrics, gave this news organization an example: “Spreading the notion that one would not need to get vaccinated because if you get sick you could take ivermectin is a very dangerous statement. That is not consistent with the standards of professionalism required for certification or licensure.”
Ivermectin, he noted, is not an approved treatment for COVID-19.
“To say that it is or has any benefit is a false statement. We’re not willing to allow individuals who make false statements to devalue the terrific work of tens of thousands of physicians across the United States doing work under very difficult circumstances,” Dr. Nichols said.
He continued: “To suggest treatments that are known not to be effective in exchange for treatment that is known to be effective is dangerous – and ivermectin falls under that category.”
Asked whether such suggestions could result in suspension or revocation of a physician’s license, Dr. Nichols said, “It’s the kind of thing that would certainly trigger a review.”
He said the standard for separating misinformation from personal beliefs is based on whether there is scientific evidence to support the belief.
The boards are not, with this statement, attempting to referee legitimate scientific debate, he said.
The misinformation the boards are referring to, Dr. Nichols said, is “where the evidence is 100% on one side and zero on another. And the zero is not only that the opinions or beliefs are unsupported or unsubstantiated, they are indeed harmful if followed. That’s the distinction we’re trying to make here.”
As for free-speech arguments, he said, “Free speech is a constitutional right. You can say whatever you want. The issue here is you do not have the right to expect continued professional sanction of a board certificate if you are lying to the public.”
The board statement also said: “We all look to board-certified physicians to provide outstanding care and guidance; providing misinformation about a lethal disease is unethical, unprofessional, and dangerous. In times of medical emergency, the community of expert physicians committed to science and evidence collectively shares a responsibility for giving the public the most accurate and timely health information available, so they can make decisions that work best for themselves and their families.”
In addition to Dr. Nichols, the statement was signed by Warren Newton, MD, MPH, president and CEO of the American Board of Family Medicine, and Richard J. Baron, MD, president and CEO of the American Board of Internal Medicine.
A version of this article first appeared on Medscape.com.
Leaders of the American Board of Family Medicine, the American Board of Internal Medicine, and the American Board of Pediatrics said Sept. 9 that they support FSMB’s position.
“We also want all physicians certified by our boards to know that such unethical or unprofessional conduct may prompt their respective Board to take action that could put their certification at risk,” a statement read.
“Expertise matters, and board-certified physicians have demonstrated that they have stayed current in their field. Spreading misinformation or falsehoods to the public during a time of a public health emergency goes against everything our boards and our community of board-certified physicians stand for,” the leaders wrote.
“The evidence that we have safe, effective, and widely available vaccines against COVID-19 is overwhelming. We are particularly concerned about physicians who use their authority to denigrate vaccination at a time when vaccines continue to demonstrate excellent effectiveness against severe illness, hospitalization, and death.”
Small number spread false information
However, a small number of doctors continue to spread misinformation against the vaccines and communicate other false information surrounding COVID-19.
Some of the misinformation spreaders have had ultra-viral reach.
Among them is Daniel Stock, MD, a family physician in Indiana who has come out against COVID-19 vaccines. At a recent meeting of the Mt. Vernon Community School board in Indiana, he gave a speech urging the board to ignore the prevailing recommendations around COVID-19, such as test-and-trace measures.
Forbes reported in August that versions of the video of Stock›s speech on Facebook “have collected a total of 90 million engagements – a metric encompassing things such as comments, likes and shares – according to data collected by Media Matters for America, a liberal tech-watchdog group.”
This news organization published a story in August asking whether physicians who spread such information should lose their license and the question drew rapid-fire comments.
Commenters who argued with potential disciplinary actions raised questions about where the line will be drawn between misinformation and deeply held beliefs in terms of care.
Several comments centered on ivermectin, which is not approved by the Food and Drug Administration to treat COVID-19 but is enthusiastically supported as a COVID-19 treatment by a group of physicians called the Front Line COVID-19 Critical Care Alliance, whose website includes requests for donations.
Some cited free speech protections.
‘Not consistent with standards’
As for ivermectin, David G. Nichols, MD, president and CEO of the American Board of Pediatrics, gave this news organization an example: “Spreading the notion that one would not need to get vaccinated because if you get sick you could take ivermectin is a very dangerous statement. That is not consistent with the standards of professionalism required for certification or licensure.”
Ivermectin, he noted, is not an approved treatment for COVID-19.
“To say that it is or has any benefit is a false statement. We’re not willing to allow individuals who make false statements to devalue the terrific work of tens of thousands of physicians across the United States doing work under very difficult circumstances,” Dr. Nichols said.
He continued: “To suggest treatments that are known not to be effective in exchange for treatment that is known to be effective is dangerous – and ivermectin falls under that category.”
Asked whether such suggestions could result in suspension or revocation of a physician’s license, Dr. Nichols said, “It’s the kind of thing that would certainly trigger a review.”
He said the standard for separating misinformation from personal beliefs is based on whether there is scientific evidence to support the belief.
The boards are not, with this statement, attempting to referee legitimate scientific debate, he said.
The misinformation the boards are referring to, Dr. Nichols said, is “where the evidence is 100% on one side and zero on another. And the zero is not only that the opinions or beliefs are unsupported or unsubstantiated, they are indeed harmful if followed. That’s the distinction we’re trying to make here.”
As for free-speech arguments, he said, “Free speech is a constitutional right. You can say whatever you want. The issue here is you do not have the right to expect continued professional sanction of a board certificate if you are lying to the public.”
The board statement also said: “We all look to board-certified physicians to provide outstanding care and guidance; providing misinformation about a lethal disease is unethical, unprofessional, and dangerous. In times of medical emergency, the community of expert physicians committed to science and evidence collectively shares a responsibility for giving the public the most accurate and timely health information available, so they can make decisions that work best for themselves and their families.”
In addition to Dr. Nichols, the statement was signed by Warren Newton, MD, MPH, president and CEO of the American Board of Family Medicine, and Richard J. Baron, MD, president and CEO of the American Board of Internal Medicine.
A version of this article first appeared on Medscape.com.