User login
Clinical genetic testing for skin disorders continues to advance
and families of pediatric patients to navigate the landscape.
“Testing options range from targeted variant testing and single-gene testing to exome and genome sequencing,” Gabriele Richard, MD, said at the annual meeting of the Society for Pediatric Dermatology. “It is not always easy to determine which testing is right.”
Increasingly, clinical genomic tests, including exome and genome sequencing, are used for patients with complex phenotypes, and possibly multiple disorders, who might have no diagnosis despite extensive prior testing, said Dr. Richard, medical director at Gaithersburg, Md.–based GeneDx., a molecular diagnostic laboratory that performs comprehensive testing for rare genetic disorders. These tests are also being used more for first-line testing in critically ill patients in the neonatal and pediatric intensive care units, and “have heralded a whole new era of gene and disease discovery,” she added.
Targeted variant testing is used for known familial variants, to test family members for carrier status and segregation, and to make a prenatal diagnosis, she said. Single-gene testing is available for most genes and has its place for conditions that can be clinically well-recognized, such as ichthyosis vulgaris, Darier disease, or Papillon-Lefèvre syndrome.
Specific tests for identifying gene deletions or duplications are exon-level microarrays, multiplex ligation-dependent probe amplification (MLPA), and chromosomal microarray analysis. “The latter has been successful in identifying diseases causing chromosomal abnormalities in over 10% of cases overall,” Dr. Richard said. An example of a skin disorder is X-linked ichthyosis caused by a deletion of the steroid sulfatase locus in more than 95% of affected males, she said.
“However, the current staple of molecular diagnostic testing is multigene next-generation sequencing (NGS) panels, which allow you to interrogate two to hundreds of genes concurrently, including sequencing and deletion duplication testing.” These tests are the most cost effective, she said, and are available for almost any genodermatosis or group of disorders with overlapping phenotypes, such as albinism or ichthyosis, epidermolysis bullosa and skin fragility, ectodermal dysplasia, or porphyria. According to Dr. Richard, the diagnostic outcomes of NGS panels mainly depend on test indication, panel size and gene curation, age of onset, and prevailing inheritance pattern of disorders.
Her recommended criteria for distinguishing the myriad of available NGS panels include checking gene content, technical sensitivity of sequencing and deletion/duplication analysis, quality of variant interpretation and reporting, turn-around time, and available familial follow-up testing. “If a family might consider future prenatal diagnosis, choose the lab that performs prenatal and diagnostic testing,” Dr. Richard said. “Equally important are client services such as ease of ordering, insurance coverage, and the ability to determine out-of-pocket cost to patients.”
Resources that enable consumers to compare panel content, methodology, turnaround time, and other parameters include the Genetic Testing Registry (GTR) operated by the National Center for Biotechnology Information, and Concert Genetics, a genetic testing company. The National Society of Genetic Counselors also offers a searchable database for finding a genetic counselor.
Exome sequencing includes the coding sequences of about 20,000 genes and has an average depth of 50 to about 150 reads. “It is a phenotype-driven test where only select variants are being reported fitting the phenotype,” Dr. Richard said. “The outcome of exome and genome sequencing much depends on optimization of bioinformatic pipelines and tools.” Besides small sequence variants, exome sequencing is able to identify a variety of different types of disease-causing variants, such as gene copy number variants seen in about 6% of positive cases, mosaicism, regions of homozygosity, uniparental disomy, and other unusual events and is cost effective.
Whole-genome sequencing, meanwhile, includes the entire genome, particularly noncoding regions, and has an average depth of more than 30 reads. “It’s based on single-molecule sequencing, has longer reads and more uniform coverage, compared to exome sequencing,” she said. “Higher cost, variant interpretation, and lack of coverage by payers are still presenting challenges for genome sequencing.” Genome sequencing can be done in a day or less.
According to diagnostic outcomes based on 280,000 individuals including 125,000 probands from GeneDx data, a definitive diagnosis was made in 26% of probands, of which 2.8% had more than one diagnostic finding and 1.8% had actionable secondary findings. In addition, 7% of the variants were found in candidate genes; 31% of probands had variants of uncertain significance, while 36% tested negative. “Nevertheless, the diagnostic yield of exome sequencing depends on the phenotype and cohort studied,” Dr. Richard continued.
At her company, she said, the highest positive rate is for multiple congenital anomalies (34%), skeletal system abnormalities (30%), and nervous system abnormalities (29%). Trio testing – the concurrent analysis of both biological parents and proband for all genes – “is a critical factor for success,” she added. “It not only improves the variant calling because we have three times the data and increases test sensitivity, it also provides more certain results, determines inheritance and allows for detection of parental mosaicism.”
According to Dr. Richard, trio testing has a one-third higher diagnostic rate than sequencing of the proband alone. Citing a published prospective study that compiled data from eight different exome- and genome-sequencing studies in critically ill neonates and children, trio testing made it possible to make a genetic diagnosis in up to 58% of children.
Whole-genome sequencing is estimated to have a 5%-10% higher diagnostic rate than exome sequencing. “However, we are still a ways away from using it as a routine diagnostic test for all test indications,” Dr. Richard said. “Automation, special bioinformatics algorithms and databases, and combination of genome sequencing with mRNA sequencing are being explored and built to further improve the diagnostic yield.”
Dr. Richard had no disclosures other than being an employee of GeneDx.
and families of pediatric patients to navigate the landscape.
“Testing options range from targeted variant testing and single-gene testing to exome and genome sequencing,” Gabriele Richard, MD, said at the annual meeting of the Society for Pediatric Dermatology. “It is not always easy to determine which testing is right.”
Increasingly, clinical genomic tests, including exome and genome sequencing, are used for patients with complex phenotypes, and possibly multiple disorders, who might have no diagnosis despite extensive prior testing, said Dr. Richard, medical director at Gaithersburg, Md.–based GeneDx., a molecular diagnostic laboratory that performs comprehensive testing for rare genetic disorders. These tests are also being used more for first-line testing in critically ill patients in the neonatal and pediatric intensive care units, and “have heralded a whole new era of gene and disease discovery,” she added.
Targeted variant testing is used for known familial variants, to test family members for carrier status and segregation, and to make a prenatal diagnosis, she said. Single-gene testing is available for most genes and has its place for conditions that can be clinically well-recognized, such as ichthyosis vulgaris, Darier disease, or Papillon-Lefèvre syndrome.
Specific tests for identifying gene deletions or duplications are exon-level microarrays, multiplex ligation-dependent probe amplification (MLPA), and chromosomal microarray analysis. “The latter has been successful in identifying diseases causing chromosomal abnormalities in over 10% of cases overall,” Dr. Richard said. An example of a skin disorder is X-linked ichthyosis caused by a deletion of the steroid sulfatase locus in more than 95% of affected males, she said.
“However, the current staple of molecular diagnostic testing is multigene next-generation sequencing (NGS) panels, which allow you to interrogate two to hundreds of genes concurrently, including sequencing and deletion duplication testing.” These tests are the most cost effective, she said, and are available for almost any genodermatosis or group of disorders with overlapping phenotypes, such as albinism or ichthyosis, epidermolysis bullosa and skin fragility, ectodermal dysplasia, or porphyria. According to Dr. Richard, the diagnostic outcomes of NGS panels mainly depend on test indication, panel size and gene curation, age of onset, and prevailing inheritance pattern of disorders.
Her recommended criteria for distinguishing the myriad of available NGS panels include checking gene content, technical sensitivity of sequencing and deletion/duplication analysis, quality of variant interpretation and reporting, turn-around time, and available familial follow-up testing. “If a family might consider future prenatal diagnosis, choose the lab that performs prenatal and diagnostic testing,” Dr. Richard said. “Equally important are client services such as ease of ordering, insurance coverage, and the ability to determine out-of-pocket cost to patients.”
Resources that enable consumers to compare panel content, methodology, turnaround time, and other parameters include the Genetic Testing Registry (GTR) operated by the National Center for Biotechnology Information, and Concert Genetics, a genetic testing company. The National Society of Genetic Counselors also offers a searchable database for finding a genetic counselor.
Exome sequencing includes the coding sequences of about 20,000 genes and has an average depth of 50 to about 150 reads. “It is a phenotype-driven test where only select variants are being reported fitting the phenotype,” Dr. Richard said. “The outcome of exome and genome sequencing much depends on optimization of bioinformatic pipelines and tools.” Besides small sequence variants, exome sequencing is able to identify a variety of different types of disease-causing variants, such as gene copy number variants seen in about 6% of positive cases, mosaicism, regions of homozygosity, uniparental disomy, and other unusual events and is cost effective.
Whole-genome sequencing, meanwhile, includes the entire genome, particularly noncoding regions, and has an average depth of more than 30 reads. “It’s based on single-molecule sequencing, has longer reads and more uniform coverage, compared to exome sequencing,” she said. “Higher cost, variant interpretation, and lack of coverage by payers are still presenting challenges for genome sequencing.” Genome sequencing can be done in a day or less.
According to diagnostic outcomes based on 280,000 individuals including 125,000 probands from GeneDx data, a definitive diagnosis was made in 26% of probands, of which 2.8% had more than one diagnostic finding and 1.8% had actionable secondary findings. In addition, 7% of the variants were found in candidate genes; 31% of probands had variants of uncertain significance, while 36% tested negative. “Nevertheless, the diagnostic yield of exome sequencing depends on the phenotype and cohort studied,” Dr. Richard continued.
At her company, she said, the highest positive rate is for multiple congenital anomalies (34%), skeletal system abnormalities (30%), and nervous system abnormalities (29%). Trio testing – the concurrent analysis of both biological parents and proband for all genes – “is a critical factor for success,” she added. “It not only improves the variant calling because we have three times the data and increases test sensitivity, it also provides more certain results, determines inheritance and allows for detection of parental mosaicism.”
According to Dr. Richard, trio testing has a one-third higher diagnostic rate than sequencing of the proband alone. Citing a published prospective study that compiled data from eight different exome- and genome-sequencing studies in critically ill neonates and children, trio testing made it possible to make a genetic diagnosis in up to 58% of children.
Whole-genome sequencing is estimated to have a 5%-10% higher diagnostic rate than exome sequencing. “However, we are still a ways away from using it as a routine diagnostic test for all test indications,” Dr. Richard said. “Automation, special bioinformatics algorithms and databases, and combination of genome sequencing with mRNA sequencing are being explored and built to further improve the diagnostic yield.”
Dr. Richard had no disclosures other than being an employee of GeneDx.
and families of pediatric patients to navigate the landscape.
“Testing options range from targeted variant testing and single-gene testing to exome and genome sequencing,” Gabriele Richard, MD, said at the annual meeting of the Society for Pediatric Dermatology. “It is not always easy to determine which testing is right.”
Increasingly, clinical genomic tests, including exome and genome sequencing, are used for patients with complex phenotypes, and possibly multiple disorders, who might have no diagnosis despite extensive prior testing, said Dr. Richard, medical director at Gaithersburg, Md.–based GeneDx., a molecular diagnostic laboratory that performs comprehensive testing for rare genetic disorders. These tests are also being used more for first-line testing in critically ill patients in the neonatal and pediatric intensive care units, and “have heralded a whole new era of gene and disease discovery,” she added.
Targeted variant testing is used for known familial variants, to test family members for carrier status and segregation, and to make a prenatal diagnosis, she said. Single-gene testing is available for most genes and has its place for conditions that can be clinically well-recognized, such as ichthyosis vulgaris, Darier disease, or Papillon-Lefèvre syndrome.
Specific tests for identifying gene deletions or duplications are exon-level microarrays, multiplex ligation-dependent probe amplification (MLPA), and chromosomal microarray analysis. “The latter has been successful in identifying diseases causing chromosomal abnormalities in over 10% of cases overall,” Dr. Richard said. An example of a skin disorder is X-linked ichthyosis caused by a deletion of the steroid sulfatase locus in more than 95% of affected males, she said.
“However, the current staple of molecular diagnostic testing is multigene next-generation sequencing (NGS) panels, which allow you to interrogate two to hundreds of genes concurrently, including sequencing and deletion duplication testing.” These tests are the most cost effective, she said, and are available for almost any genodermatosis or group of disorders with overlapping phenotypes, such as albinism or ichthyosis, epidermolysis bullosa and skin fragility, ectodermal dysplasia, or porphyria. According to Dr. Richard, the diagnostic outcomes of NGS panels mainly depend on test indication, panel size and gene curation, age of onset, and prevailing inheritance pattern of disorders.
Her recommended criteria for distinguishing the myriad of available NGS panels include checking gene content, technical sensitivity of sequencing and deletion/duplication analysis, quality of variant interpretation and reporting, turn-around time, and available familial follow-up testing. “If a family might consider future prenatal diagnosis, choose the lab that performs prenatal and diagnostic testing,” Dr. Richard said. “Equally important are client services such as ease of ordering, insurance coverage, and the ability to determine out-of-pocket cost to patients.”
Resources that enable consumers to compare panel content, methodology, turnaround time, and other parameters include the Genetic Testing Registry (GTR) operated by the National Center for Biotechnology Information, and Concert Genetics, a genetic testing company. The National Society of Genetic Counselors also offers a searchable database for finding a genetic counselor.
Exome sequencing includes the coding sequences of about 20,000 genes and has an average depth of 50 to about 150 reads. “It is a phenotype-driven test where only select variants are being reported fitting the phenotype,” Dr. Richard said. “The outcome of exome and genome sequencing much depends on optimization of bioinformatic pipelines and tools.” Besides small sequence variants, exome sequencing is able to identify a variety of different types of disease-causing variants, such as gene copy number variants seen in about 6% of positive cases, mosaicism, regions of homozygosity, uniparental disomy, and other unusual events and is cost effective.
Whole-genome sequencing, meanwhile, includes the entire genome, particularly noncoding regions, and has an average depth of more than 30 reads. “It’s based on single-molecule sequencing, has longer reads and more uniform coverage, compared to exome sequencing,” she said. “Higher cost, variant interpretation, and lack of coverage by payers are still presenting challenges for genome sequencing.” Genome sequencing can be done in a day or less.
According to diagnostic outcomes based on 280,000 individuals including 125,000 probands from GeneDx data, a definitive diagnosis was made in 26% of probands, of which 2.8% had more than one diagnostic finding and 1.8% had actionable secondary findings. In addition, 7% of the variants were found in candidate genes; 31% of probands had variants of uncertain significance, while 36% tested negative. “Nevertheless, the diagnostic yield of exome sequencing depends on the phenotype and cohort studied,” Dr. Richard continued.
At her company, she said, the highest positive rate is for multiple congenital anomalies (34%), skeletal system abnormalities (30%), and nervous system abnormalities (29%). Trio testing – the concurrent analysis of both biological parents and proband for all genes – “is a critical factor for success,” she added. “It not only improves the variant calling because we have three times the data and increases test sensitivity, it also provides more certain results, determines inheritance and allows for detection of parental mosaicism.”
According to Dr. Richard, trio testing has a one-third higher diagnostic rate than sequencing of the proband alone. Citing a published prospective study that compiled data from eight different exome- and genome-sequencing studies in critically ill neonates and children, trio testing made it possible to make a genetic diagnosis in up to 58% of children.
Whole-genome sequencing is estimated to have a 5%-10% higher diagnostic rate than exome sequencing. “However, we are still a ways away from using it as a routine diagnostic test for all test indications,” Dr. Richard said. “Automation, special bioinformatics algorithms and databases, and combination of genome sequencing with mRNA sequencing are being explored and built to further improve the diagnostic yield.”
Dr. Richard had no disclosures other than being an employee of GeneDx.
FROM SPD 2021
New gene variant found for hereditary bleeding disorder
Clinical symptoms in a 19-year-old Vietnamese woman who experienced several life-threatening bleeding events, including ovarian hemorrhage, led to the discovery of a novel gene variant causing her bleeding disorder.
Blood analysis of the patients showed decreased fibrinogen level with “markedly elevated fibrinogen/fibrin degradation products and D-dimer levels.” Attempts to treat the patient with hemostatic surgery, administration of several medications, including nafamostat mesylate, tranexamic acid, and unfractionated heparin, produced no correction of her coagulation abnormalities, and the patient experienced repeated hemorrhagic events, according to researchers from the Tokyo Saiseikai Central Hospital, Japan, and colleagues.
However, the researchers found that treatment with recombinant human thrombomodulin (rhTM) remarkably improved the patient’s pathophysiology, according to the results of a case study reported in Blood Advances.
Genetic analysis
Upon screening and sequencing of the patient’s thrombomodulin gene, a previously unreported homozygous variation, c.793T>A (p.Cys265Ser) was discovered. Under normal circumstances, the Cys265 residue forms one of three disulfide bonds in the epidermal growth factor (EGF)-like domain 1 of thrombomoduliin (TM), according to the researchers.
However, transient expression analysis of the patient’s mutation using COS-1 cells demonstrated markedly reduced expression of TM-Cys265Ser on the plasma membrane relative to wild-type TM. The TM-Cys265Ser mutant was intracellularly degraded, probably due to EGF-like domain 1 misfolding, according to the researchers and the reduced expression of TM on the endothelial cell membrane may be responsible for the disseminated intravascular coagulation-like symptoms observed in the patient, the speculated.
“The clinical symptoms of the patient in this study were characterized by recurrent hemorrhage, indicating that TM-C265S mainly causes hyperfibrinolysis rather than hypercoagulation. The C265S mutation may disrupt the timely and delicate balance between coagulation and fibrinolysis,” the researchers suggested.
The authors reported that they had no conflicts of interest.
Clinical symptoms in a 19-year-old Vietnamese woman who experienced several life-threatening bleeding events, including ovarian hemorrhage, led to the discovery of a novel gene variant causing her bleeding disorder.
Blood analysis of the patients showed decreased fibrinogen level with “markedly elevated fibrinogen/fibrin degradation products and D-dimer levels.” Attempts to treat the patient with hemostatic surgery, administration of several medications, including nafamostat mesylate, tranexamic acid, and unfractionated heparin, produced no correction of her coagulation abnormalities, and the patient experienced repeated hemorrhagic events, according to researchers from the Tokyo Saiseikai Central Hospital, Japan, and colleagues.
However, the researchers found that treatment with recombinant human thrombomodulin (rhTM) remarkably improved the patient’s pathophysiology, according to the results of a case study reported in Blood Advances.
Genetic analysis
Upon screening and sequencing of the patient’s thrombomodulin gene, a previously unreported homozygous variation, c.793T>A (p.Cys265Ser) was discovered. Under normal circumstances, the Cys265 residue forms one of three disulfide bonds in the epidermal growth factor (EGF)-like domain 1 of thrombomoduliin (TM), according to the researchers.
However, transient expression analysis of the patient’s mutation using COS-1 cells demonstrated markedly reduced expression of TM-Cys265Ser on the plasma membrane relative to wild-type TM. The TM-Cys265Ser mutant was intracellularly degraded, probably due to EGF-like domain 1 misfolding, according to the researchers and the reduced expression of TM on the endothelial cell membrane may be responsible for the disseminated intravascular coagulation-like symptoms observed in the patient, the speculated.
“The clinical symptoms of the patient in this study were characterized by recurrent hemorrhage, indicating that TM-C265S mainly causes hyperfibrinolysis rather than hypercoagulation. The C265S mutation may disrupt the timely and delicate balance between coagulation and fibrinolysis,” the researchers suggested.
The authors reported that they had no conflicts of interest.
Clinical symptoms in a 19-year-old Vietnamese woman who experienced several life-threatening bleeding events, including ovarian hemorrhage, led to the discovery of a novel gene variant causing her bleeding disorder.
Blood analysis of the patients showed decreased fibrinogen level with “markedly elevated fibrinogen/fibrin degradation products and D-dimer levels.” Attempts to treat the patient with hemostatic surgery, administration of several medications, including nafamostat mesylate, tranexamic acid, and unfractionated heparin, produced no correction of her coagulation abnormalities, and the patient experienced repeated hemorrhagic events, according to researchers from the Tokyo Saiseikai Central Hospital, Japan, and colleagues.
However, the researchers found that treatment with recombinant human thrombomodulin (rhTM) remarkably improved the patient’s pathophysiology, according to the results of a case study reported in Blood Advances.
Genetic analysis
Upon screening and sequencing of the patient’s thrombomodulin gene, a previously unreported homozygous variation, c.793T>A (p.Cys265Ser) was discovered. Under normal circumstances, the Cys265 residue forms one of three disulfide bonds in the epidermal growth factor (EGF)-like domain 1 of thrombomoduliin (TM), according to the researchers.
However, transient expression analysis of the patient’s mutation using COS-1 cells demonstrated markedly reduced expression of TM-Cys265Ser on the plasma membrane relative to wild-type TM. The TM-Cys265Ser mutant was intracellularly degraded, probably due to EGF-like domain 1 misfolding, according to the researchers and the reduced expression of TM on the endothelial cell membrane may be responsible for the disseminated intravascular coagulation-like symptoms observed in the patient, the speculated.
“The clinical symptoms of the patient in this study were characterized by recurrent hemorrhage, indicating that TM-C265S mainly causes hyperfibrinolysis rather than hypercoagulation. The C265S mutation may disrupt the timely and delicate balance between coagulation and fibrinolysis,” the researchers suggested.
The authors reported that they had no conflicts of interest.
FROM BLOOD ADVANCES
Autoeczematization: A Strange Id Reaction of the Skin
Autoeczematization (AE), or id reaction, is a disseminated eczematous reaction that occurs days or weeks after exposure to a primary stimulus, resulting from a release of antigen(s). Whitfield1 first described AE in 1921, when he postulated that the id reaction was due to sensitization of the skin after a primary stimulus. He called it “a form of auto-intoxication derived from changes in the patient’s own tissues.”1 The exact prevalence of id reactions is unknown; one study showed that 17% of patients with dermatophyte infections developed an id reaction, typically tinea pedis linked with vesicles on the palms.2 Tinea capitis is one of the most common causes of AE in children, which is frequently misdiagnosed as a drug reaction. Approximately 37% of patients diagnosed with stasis dermatitis develop an id reaction (Figure 1). A history of contact dermatitis is common in patients presenting with AE.2-6
Pathophysiology of Id Reactions
An abnormal immune response against autologous skin antigens may be responsible for the development of AE. Shelley5 postulated that hair follicles play an important role in id reactions, as Sharquie et al6 recently emphasized for many skin disorders. The pathogenesis of AE is uncertain, but circulating T lymphocytes play a role in this reaction. Normally, T cells are activated by a release of antigens after a primary exposure to a stimulus. However, overactivation of these T cells induces autoimmune reactions such as AE.7 Activated T lymphocytes express HLA-DR and IL-2 receptor, markers elevated in the peripheral blood of patients undergoing id reactions. After treatment, the levels of activated T lymphocytes decline. An increase in the number of CD25+ T cells and a decrease in the number of suppressor T cells in the blood may occur during an id reaction.7-9 Keratinocytes produce proinflammatory cytokines, such as thymic stromal erythropoietin, IL-25, and IL-33, that activate T cells.10-12 Therefore, the most likely pathogenesis of an id reaction is that T lymphocytes are activated at the primary reaction site due to proinflammatory cytokines released by keratinocytes. These activated T cells then travel systemically via hematogenous dissemination. The spread of activated T lymphocytes produces an eczematous reaction at secondary locations distant to the primary site.9
Clinical and Histopathological Features of Id Reactions
Clinically, AE is first evident as a vesicular dissemination that groups to form papules or nummular patches and usually is present on the legs, feet, arms, and/or trunk (Figure 2). The primary dermatitis is localized to the area that was the site of contact to the offending stimuli. This localized eczematous eruption begins with an acute or subacute onset. It has the appearance of small crusted vesicles with erythema (Figure 1). The first sign of AE is vesicles presenting near the primary site on flexural surfaces or on the hands and feet. A classic example is tinea pedis linked with vesicles on the palms and sides of the fingers, resembling dyshidrotic eczema. Sites of prior cutaneous trauma, such as dermatoses, scars, and burns, are common locations for early AE. In later stages, vesicles disseminate to the legs, arms, and trunk, where they group to form papules and nummular patches in a symmetrical pattern.5,13-15 These lesions may be extremely pruritic. The pruritus may be so intense that it interrupts daily activities and disrupts the ability to fall or stay asleep.16
Histologically, biopsy specimens show psoriasiform spongiotic dermatitis with mononuclear cells contained in the vesicles. Interstitial edema and perivascular lymphohistiocytic infiltrates are evident. Eosinophils also may be present. This pattern is not unique toid reactions.17-19 Although AE is a reaction pattern that may be due to a fungal or bacterial infection, the etiologic agent is not evident microscopically within the eczema itself.
Etiology of Id Reactions
Id reactions most commonly occur from either stasis dermatitis or tinea pedis, although a wide variety of other causes should be considered. Evaluation of the primary site rather than the id reaction may identify an infectious or parasitic agent. Sometimes the AE reaction is specifically named: dermatophytid with dermatophytosis, bacterid with a bacterial infectious process, and tuberculid with tuberculosis. Similarly, there may be reactions to underlying candidiasis, sporotrichosis, histoplasmosis, and other fungal infections that can cause a cutaneous id reaction.18,20-22Mycobacterium species, Pseudomonas, Staphylococcus, and Streptococcus are bacterial causes of AE.15,23-26 Viral infections that can cause an id reaction are herpes simplex virus and molluscum contagiosum.27-29 Scabies, leishmaniasis, and pediculosis capitis are parasitic infections that may be etiologic.14,30,31 In addition, noninfectious stimuli besides stasis dermatitis that can produce id reactions include medications, topical creams, tattoo ink, sutures, radiotherapy, and dyshidrotic eczema. The primary reaction to these agents is a localized dermatitis followed by the immunological response that induces a secondary reaction distant from the primary site.17,18,32-38
Differential Diagnoses
Differential diagnoses include other types of eczema and some vesicular eruptions. Irritant contact dermatitis is another dermatosis that presents as a widespread vesicular eruption due to repetitive exposure to toxic irritants. The rash is erythematous with pustules, blisters, and crusts. It is only found in areas directly exposed to irritants, as opposed to AE, which spreads to areas distant to the primary reaction site. Irritant contact dermatitis presents with more of a burning sensation, whereas AE is more pruritic.39,40 Allergic contact dermatitis presents with erythematous vesicles and papules and sometimes with bullae. There is edema and crust formation, which often can spread past the point of contact in later stages. Similar to AE, there is intense pruritus. However, allergic contact dermatitis most commonly is caused by exposure to metals, cosmetics, and fragrances, whereas infectious agents and stasis dermatitis are the most common causes of AE.40,41 It may be challenging to distinguish AE from other causes of widespread eczematous dissemination. Vesicular eruptions sometimes require distinction from AE, including herpetic infections, insect bite reactions, and drug eruptions.18,42
Treatment
The underlying condition should be treated to mitigate the inflammatory response causing the id reaction. If not skillfully orchestrated, the id reaction can reoccur. For infectious causes of AE, an antifungal, antibacterial, antiviral, or antiparasitic should be given. If stasis dermatitis is responsible for the id reaction, compression stockings and leg elevation are indicated. The id reaction itself is treated with systemic or topical corticosteroids and wet compresses if acute. The goal of these treatments is to reduce patient discomfort caused by the inflammation and pruritus.18,43
Conclusion
Id reactions are an unusual phenomenon that commonly occurs after fungal skin infections and stasis dermatitis. T lymphocytes and keratinocytes may play a key role in this reaction, with newer research further delineating the process and possibly providing enhanced treatment options. Therapy focuses on treating the underlying condition, supplemented with corticosteroids for the autoeczema.
- Whitfield A. Lumleian Lectures on Some Points in the Aetiology of Skin Diseases. Delivered before the Royal College of Physicians of London on March 10th, 15th, and 17th, 1921. Lecture II. Lancet. 1921;2:122-127.
- Cheng N, Rucker Wright D, Cohen BA. Dermatophytid in tinea capitis: rarely reported common phenomenon with clinical implications. Pediatrics. 2011;128:E453-E457.
- Schrom KP, Kobs A, Nedorost S. Clinical psoriasiform dermatitis following dupilumab use for autoeczematization secondary to chronic stasis dermatitis. Cureus. 2020;12:e7831. doi:10.7759/cureus.7831
- Templeton HJ, Lunsford CJ, Allington HV. Autosensitization dermatitis; report of five cases and protocol of an experiment. Arch Derm Syphilol. 1949;59:68-77.
- Shelley WB. Id reaction. In: Consultations in Dermatology. Saunders; 1972:262-267.
- Sharquie KE, Noaimi AA, Flayih RA. Clinical and histopathological findings in patients with follicular dermatoses: all skin diseases starts in the hair follicles as new hypothesis. Am J Clin Res Rev. 2020;4:17.
- Kasteler JS, Petersen MJ, Vance JE, et al. Circulating activated T lymphocytes in autoeczematization. Arch Dermatol. 1992;128:795-798.
- González-Amaro R, Baranda L, Abud-Mendoza C, et al. Autoeczematization is associated with abnormal immune recognition of autologous skin antigens. J Am Acad Dermatol. 1993;28:56-60.
- Cunningham MJ, Zone JJ, Petersen MJ, et al. Circulating activated (DR-positive) T lymphocytes in a patient with autoeczematization. J Am Acad Dermatol. 1986;14:1039-1041.
- Furue M, Ulzii D, Vu YH, et al. Pathogenesis of atopic dermatitis: current paradigm. Iran J Immunol. 2019;16:97-107.
- Uchi H, Terao H, Koga T, et al. Cytokines and chemokines in the epidermis. J Dermatol Sci. 2000;24(suppl 1):S29-S38.
- Bos JD, Kapsenberg ML. The skin immune system: progress in cutaneous biology. Immunol Today. 1993;14:75-78.
- Young AW Jr. Dynamics of autosensitization dermatitis; a clinical and microscopic concept of autoeczematization. AMA Arch Derm. 1958;77:495-502.
- Brenner S, Wolf R, Landau M. Scabid: an unusual id reaction to scabies. Int J Dermatol. 1993;32:128-129.
- Yamany T, Schwartz RA. Infectious eczematoid dermatitis: a comprehensive review. J Eur Acad Dermatol Venereol. 2015;29:203-208.
- Wang X, Li L, Shi X, et al. Itching and its related factors in subtypes of eczema: a cross-sectional multicenter study in tertiary hospitals of China. Sci Rep. 2018;8:10754.
- Price A, Tavazoie M, Meehan SA, et al. Id reaction associated with red tattoo ink. Cutis. 2018;102:E32-E34.
- Ilkit M, Durdu M, Karaks¸ M. Cutaneous id reactions: a comprehensive review of clinical manifestations, epidemiology, etiology, and management. Crit Rev Microbiol. 2012;38:191-202.
- Kaner SR. Dermatitis venenata of the feet with a generalized “id” reaction. J Am Podiatry Assoc. 1970;60:199-204.
- Jordan L, Jackson NA, Carter-Snell B, et al. Pustular tinea id reaction. Cutis. 2019;103:E3-E4.
- Crum N, Hardaway C, Graham B. Development of an idlike reaction during treatment for acute pulmonary histoplasmosis: a new cutaneous manifestation in histoplasmosis. J Am Acad Dermatol. 2003;48(2 suppl):S5-S6.
- Chirac A, Brzezinski P, Chiriac AE, et al. Autosensitisation (autoeczematisation) reactions in a case of diaper dermatitis candidiasis. Niger Med J. 2014;55:274-275.
- Singh PY, Sinha P, Baveja S, et al. Immune-mediated tuberculous uveitis—a rare association with papulonecrotic tuberculid. Indian J Ophthalmol. 2019;67:1207-1209.
- Urso B, Georgesen C, Harp J. Papulonecrotic tuberculid secondary to Mycobacterium avium complex. Cutis. 2019;104:E11-E13.
- Choudhri SH, Magro CM, Crowson AN, et al. An id reaction to Mycobacterium leprae: first documented case. Cutis. 1994;54:282-286.
- Park JW, Jeong GJ, Seo SJ, et al. Pseudomonas toe web infection and autosensitisation dermatitis: diagnostic and therapeutic challenge. Int Wound J. 2020;17:1543-1544. doi:10.1111/iwj.13386
- Netchiporouk E, Cohen BA. Recognizing and managing eczematous id reactions to molluscum contagiosum virus in children. Pediatrics. 2012;129:E1072-E1075.
- Aurelian L, Ono F, Burnett J. Herpes simplex virus (HSV)-associated erythema multiforme (HAEM): a viral disease with an autoimmune component. Dermatol Online J. 2003;9:1.
- Rocamora V, Romaní J, Puig L, et al. Id reaction to molluscum contagiosum. Pediatr Dermatol. 1996;13:349-350.
- Yes¸ilova Y, Özbilgin A, Turan E, et al. Clinical exacerbation developing during treatment of cutaneous leishmaniasis: an id reaction? Turkiye Parazitol Derg. 2014;38:281-282.
- Connor CJ, Selby JC, Wanat KA. Severe pediculosis capitus: a case of “crusted lice” with autoeczematization. Dermatol Online J. 2016;22:13030/qt7c91z913.
- Shelley WB. The autoimmune mechanism in clinical dermatology. Arch Dermatol. 1962;86:27-34.
- Bosworth A, Hull PR. Disseminated eczema following radiotherapy: a case report. J Cutan Med Surg. 2018;22:353-355.
- Lowther C, Miedler JD, Cockerell CJ. Id-like reaction to BCG therapy for bladder cancer. Cutis. 2013;91:145-151.
- Huerth KA, Glick PL, Glick ZR. Cutaneous id reaction after using cyanoacrylate for wound closure. Cutis. 2020;105:E11-E13.
- Amini S, Burdick AE, Janniger CK. Dyshidrotic eczema (pompholyx). Updated April 22, 2020. Accessed August 23, 2021. https://emedicine.medscape.com/article/1122527-overview
- Sundaresan S, Migden MR, Silapunt S. Stasis dermatitis: pathophysiology, evaluation, and management. Am J Clin Dermatol. 2017;18:383-390.
- Hughes JDM, Pratt MD. Allergic contact dermatitis and autoeczematization to proctosedyl® cream and proctomyxin® cream. Case Rep Dermatol. 2018;10:238-246.
- Bains SN, Nash P, Fonacier L. Irritant contact dermatitis. Clin Rev Allergy Immunol. 2019;56:99-109.
- Novak-Bilic´ G, Vucˇic´ M, Japundžic´ I, et al. Irritant and allergic contact dermatitis—skin lesion characteristics. Acta Clin Croat. 2018;57:713-720.
- Nassau S, Fonacier L. Allergic contact dermatitis. Med Clin North Am. 2020;104:61-76.
- Lewis DJ, Schlichte MJ, Dao H Jr. Atypical disseminated herpes zoster: management guidelines in immunocompromised patients. Cutis. 2017;100:321-330.
- Nedorost S, White S, Rowland DY, et al. Development and implementation of an order set to improve value of care for patients with severe stasis dermatitis. J Am Acad Dermatol. 2019;80:815-817.
Autoeczematization (AE), or id reaction, is a disseminated eczematous reaction that occurs days or weeks after exposure to a primary stimulus, resulting from a release of antigen(s). Whitfield1 first described AE in 1921, when he postulated that the id reaction was due to sensitization of the skin after a primary stimulus. He called it “a form of auto-intoxication derived from changes in the patient’s own tissues.”1 The exact prevalence of id reactions is unknown; one study showed that 17% of patients with dermatophyte infections developed an id reaction, typically tinea pedis linked with vesicles on the palms.2 Tinea capitis is one of the most common causes of AE in children, which is frequently misdiagnosed as a drug reaction. Approximately 37% of patients diagnosed with stasis dermatitis develop an id reaction (Figure 1). A history of contact dermatitis is common in patients presenting with AE.2-6
Pathophysiology of Id Reactions
An abnormal immune response against autologous skin antigens may be responsible for the development of AE. Shelley5 postulated that hair follicles play an important role in id reactions, as Sharquie et al6 recently emphasized for many skin disorders. The pathogenesis of AE is uncertain, but circulating T lymphocytes play a role in this reaction. Normally, T cells are activated by a release of antigens after a primary exposure to a stimulus. However, overactivation of these T cells induces autoimmune reactions such as AE.7 Activated T lymphocytes express HLA-DR and IL-2 receptor, markers elevated in the peripheral blood of patients undergoing id reactions. After treatment, the levels of activated T lymphocytes decline. An increase in the number of CD25+ T cells and a decrease in the number of suppressor T cells in the blood may occur during an id reaction.7-9 Keratinocytes produce proinflammatory cytokines, such as thymic stromal erythropoietin, IL-25, and IL-33, that activate T cells.10-12 Therefore, the most likely pathogenesis of an id reaction is that T lymphocytes are activated at the primary reaction site due to proinflammatory cytokines released by keratinocytes. These activated T cells then travel systemically via hematogenous dissemination. The spread of activated T lymphocytes produces an eczematous reaction at secondary locations distant to the primary site.9
Clinical and Histopathological Features of Id Reactions
Clinically, AE is first evident as a vesicular dissemination that groups to form papules or nummular patches and usually is present on the legs, feet, arms, and/or trunk (Figure 2). The primary dermatitis is localized to the area that was the site of contact to the offending stimuli. This localized eczematous eruption begins with an acute or subacute onset. It has the appearance of small crusted vesicles with erythema (Figure 1). The first sign of AE is vesicles presenting near the primary site on flexural surfaces or on the hands and feet. A classic example is tinea pedis linked with vesicles on the palms and sides of the fingers, resembling dyshidrotic eczema. Sites of prior cutaneous trauma, such as dermatoses, scars, and burns, are common locations for early AE. In later stages, vesicles disseminate to the legs, arms, and trunk, where they group to form papules and nummular patches in a symmetrical pattern.5,13-15 These lesions may be extremely pruritic. The pruritus may be so intense that it interrupts daily activities and disrupts the ability to fall or stay asleep.16
Histologically, biopsy specimens show psoriasiform spongiotic dermatitis with mononuclear cells contained in the vesicles. Interstitial edema and perivascular lymphohistiocytic infiltrates are evident. Eosinophils also may be present. This pattern is not unique toid reactions.17-19 Although AE is a reaction pattern that may be due to a fungal or bacterial infection, the etiologic agent is not evident microscopically within the eczema itself.
Etiology of Id Reactions
Id reactions most commonly occur from either stasis dermatitis or tinea pedis, although a wide variety of other causes should be considered. Evaluation of the primary site rather than the id reaction may identify an infectious or parasitic agent. Sometimes the AE reaction is specifically named: dermatophytid with dermatophytosis, bacterid with a bacterial infectious process, and tuberculid with tuberculosis. Similarly, there may be reactions to underlying candidiasis, sporotrichosis, histoplasmosis, and other fungal infections that can cause a cutaneous id reaction.18,20-22Mycobacterium species, Pseudomonas, Staphylococcus, and Streptococcus are bacterial causes of AE.15,23-26 Viral infections that can cause an id reaction are herpes simplex virus and molluscum contagiosum.27-29 Scabies, leishmaniasis, and pediculosis capitis are parasitic infections that may be etiologic.14,30,31 In addition, noninfectious stimuli besides stasis dermatitis that can produce id reactions include medications, topical creams, tattoo ink, sutures, radiotherapy, and dyshidrotic eczema. The primary reaction to these agents is a localized dermatitis followed by the immunological response that induces a secondary reaction distant from the primary site.17,18,32-38
Differential Diagnoses
Differential diagnoses include other types of eczema and some vesicular eruptions. Irritant contact dermatitis is another dermatosis that presents as a widespread vesicular eruption due to repetitive exposure to toxic irritants. The rash is erythematous with pustules, blisters, and crusts. It is only found in areas directly exposed to irritants, as opposed to AE, which spreads to areas distant to the primary reaction site. Irritant contact dermatitis presents with more of a burning sensation, whereas AE is more pruritic.39,40 Allergic contact dermatitis presents with erythematous vesicles and papules and sometimes with bullae. There is edema and crust formation, which often can spread past the point of contact in later stages. Similar to AE, there is intense pruritus. However, allergic contact dermatitis most commonly is caused by exposure to metals, cosmetics, and fragrances, whereas infectious agents and stasis dermatitis are the most common causes of AE.40,41 It may be challenging to distinguish AE from other causes of widespread eczematous dissemination. Vesicular eruptions sometimes require distinction from AE, including herpetic infections, insect bite reactions, and drug eruptions.18,42
Treatment
The underlying condition should be treated to mitigate the inflammatory response causing the id reaction. If not skillfully orchestrated, the id reaction can reoccur. For infectious causes of AE, an antifungal, antibacterial, antiviral, or antiparasitic should be given. If stasis dermatitis is responsible for the id reaction, compression stockings and leg elevation are indicated. The id reaction itself is treated with systemic or topical corticosteroids and wet compresses if acute. The goal of these treatments is to reduce patient discomfort caused by the inflammation and pruritus.18,43
Conclusion
Id reactions are an unusual phenomenon that commonly occurs after fungal skin infections and stasis dermatitis. T lymphocytes and keratinocytes may play a key role in this reaction, with newer research further delineating the process and possibly providing enhanced treatment options. Therapy focuses on treating the underlying condition, supplemented with corticosteroids for the autoeczema.
Autoeczematization (AE), or id reaction, is a disseminated eczematous reaction that occurs days or weeks after exposure to a primary stimulus, resulting from a release of antigen(s). Whitfield1 first described AE in 1921, when he postulated that the id reaction was due to sensitization of the skin after a primary stimulus. He called it “a form of auto-intoxication derived from changes in the patient’s own tissues.”1 The exact prevalence of id reactions is unknown; one study showed that 17% of patients with dermatophyte infections developed an id reaction, typically tinea pedis linked with vesicles on the palms.2 Tinea capitis is one of the most common causes of AE in children, which is frequently misdiagnosed as a drug reaction. Approximately 37% of patients diagnosed with stasis dermatitis develop an id reaction (Figure 1). A history of contact dermatitis is common in patients presenting with AE.2-6
Pathophysiology of Id Reactions
An abnormal immune response against autologous skin antigens may be responsible for the development of AE. Shelley5 postulated that hair follicles play an important role in id reactions, as Sharquie et al6 recently emphasized for many skin disorders. The pathogenesis of AE is uncertain, but circulating T lymphocytes play a role in this reaction. Normally, T cells are activated by a release of antigens after a primary exposure to a stimulus. However, overactivation of these T cells induces autoimmune reactions such as AE.7 Activated T lymphocytes express HLA-DR and IL-2 receptor, markers elevated in the peripheral blood of patients undergoing id reactions. After treatment, the levels of activated T lymphocytes decline. An increase in the number of CD25+ T cells and a decrease in the number of suppressor T cells in the blood may occur during an id reaction.7-9 Keratinocytes produce proinflammatory cytokines, such as thymic stromal erythropoietin, IL-25, and IL-33, that activate T cells.10-12 Therefore, the most likely pathogenesis of an id reaction is that T lymphocytes are activated at the primary reaction site due to proinflammatory cytokines released by keratinocytes. These activated T cells then travel systemically via hematogenous dissemination. The spread of activated T lymphocytes produces an eczematous reaction at secondary locations distant to the primary site.9
Clinical and Histopathological Features of Id Reactions
Clinically, AE is first evident as a vesicular dissemination that groups to form papules or nummular patches and usually is present on the legs, feet, arms, and/or trunk (Figure 2). The primary dermatitis is localized to the area that was the site of contact to the offending stimuli. This localized eczematous eruption begins with an acute or subacute onset. It has the appearance of small crusted vesicles with erythema (Figure 1). The first sign of AE is vesicles presenting near the primary site on flexural surfaces or on the hands and feet. A classic example is tinea pedis linked with vesicles on the palms and sides of the fingers, resembling dyshidrotic eczema. Sites of prior cutaneous trauma, such as dermatoses, scars, and burns, are common locations for early AE. In later stages, vesicles disseminate to the legs, arms, and trunk, where they group to form papules and nummular patches in a symmetrical pattern.5,13-15 These lesions may be extremely pruritic. The pruritus may be so intense that it interrupts daily activities and disrupts the ability to fall or stay asleep.16
Histologically, biopsy specimens show psoriasiform spongiotic dermatitis with mononuclear cells contained in the vesicles. Interstitial edema and perivascular lymphohistiocytic infiltrates are evident. Eosinophils also may be present. This pattern is not unique toid reactions.17-19 Although AE is a reaction pattern that may be due to a fungal or bacterial infection, the etiologic agent is not evident microscopically within the eczema itself.
Etiology of Id Reactions
Id reactions most commonly occur from either stasis dermatitis or tinea pedis, although a wide variety of other causes should be considered. Evaluation of the primary site rather than the id reaction may identify an infectious or parasitic agent. Sometimes the AE reaction is specifically named: dermatophytid with dermatophytosis, bacterid with a bacterial infectious process, and tuberculid with tuberculosis. Similarly, there may be reactions to underlying candidiasis, sporotrichosis, histoplasmosis, and other fungal infections that can cause a cutaneous id reaction.18,20-22Mycobacterium species, Pseudomonas, Staphylococcus, and Streptococcus are bacterial causes of AE.15,23-26 Viral infections that can cause an id reaction are herpes simplex virus and molluscum contagiosum.27-29 Scabies, leishmaniasis, and pediculosis capitis are parasitic infections that may be etiologic.14,30,31 In addition, noninfectious stimuli besides stasis dermatitis that can produce id reactions include medications, topical creams, tattoo ink, sutures, radiotherapy, and dyshidrotic eczema. The primary reaction to these agents is a localized dermatitis followed by the immunological response that induces a secondary reaction distant from the primary site.17,18,32-38
Differential Diagnoses
Differential diagnoses include other types of eczema and some vesicular eruptions. Irritant contact dermatitis is another dermatosis that presents as a widespread vesicular eruption due to repetitive exposure to toxic irritants. The rash is erythematous with pustules, blisters, and crusts. It is only found in areas directly exposed to irritants, as opposed to AE, which spreads to areas distant to the primary reaction site. Irritant contact dermatitis presents with more of a burning sensation, whereas AE is more pruritic.39,40 Allergic contact dermatitis presents with erythematous vesicles and papules and sometimes with bullae. There is edema and crust formation, which often can spread past the point of contact in later stages. Similar to AE, there is intense pruritus. However, allergic contact dermatitis most commonly is caused by exposure to metals, cosmetics, and fragrances, whereas infectious agents and stasis dermatitis are the most common causes of AE.40,41 It may be challenging to distinguish AE from other causes of widespread eczematous dissemination. Vesicular eruptions sometimes require distinction from AE, including herpetic infections, insect bite reactions, and drug eruptions.18,42
Treatment
The underlying condition should be treated to mitigate the inflammatory response causing the id reaction. If not skillfully orchestrated, the id reaction can reoccur. For infectious causes of AE, an antifungal, antibacterial, antiviral, or antiparasitic should be given. If stasis dermatitis is responsible for the id reaction, compression stockings and leg elevation are indicated. The id reaction itself is treated with systemic or topical corticosteroids and wet compresses if acute. The goal of these treatments is to reduce patient discomfort caused by the inflammation and pruritus.18,43
Conclusion
Id reactions are an unusual phenomenon that commonly occurs after fungal skin infections and stasis dermatitis. T lymphocytes and keratinocytes may play a key role in this reaction, with newer research further delineating the process and possibly providing enhanced treatment options. Therapy focuses on treating the underlying condition, supplemented with corticosteroids for the autoeczema.
- Whitfield A. Lumleian Lectures on Some Points in the Aetiology of Skin Diseases. Delivered before the Royal College of Physicians of London on March 10th, 15th, and 17th, 1921. Lecture II. Lancet. 1921;2:122-127.
- Cheng N, Rucker Wright D, Cohen BA. Dermatophytid in tinea capitis: rarely reported common phenomenon with clinical implications. Pediatrics. 2011;128:E453-E457.
- Schrom KP, Kobs A, Nedorost S. Clinical psoriasiform dermatitis following dupilumab use for autoeczematization secondary to chronic stasis dermatitis. Cureus. 2020;12:e7831. doi:10.7759/cureus.7831
- Templeton HJ, Lunsford CJ, Allington HV. Autosensitization dermatitis; report of five cases and protocol of an experiment. Arch Derm Syphilol. 1949;59:68-77.
- Shelley WB. Id reaction. In: Consultations in Dermatology. Saunders; 1972:262-267.
- Sharquie KE, Noaimi AA, Flayih RA. Clinical and histopathological findings in patients with follicular dermatoses: all skin diseases starts in the hair follicles as new hypothesis. Am J Clin Res Rev. 2020;4:17.
- Kasteler JS, Petersen MJ, Vance JE, et al. Circulating activated T lymphocytes in autoeczematization. Arch Dermatol. 1992;128:795-798.
- González-Amaro R, Baranda L, Abud-Mendoza C, et al. Autoeczematization is associated with abnormal immune recognition of autologous skin antigens. J Am Acad Dermatol. 1993;28:56-60.
- Cunningham MJ, Zone JJ, Petersen MJ, et al. Circulating activated (DR-positive) T lymphocytes in a patient with autoeczematization. J Am Acad Dermatol. 1986;14:1039-1041.
- Furue M, Ulzii D, Vu YH, et al. Pathogenesis of atopic dermatitis: current paradigm. Iran J Immunol. 2019;16:97-107.
- Uchi H, Terao H, Koga T, et al. Cytokines and chemokines in the epidermis. J Dermatol Sci. 2000;24(suppl 1):S29-S38.
- Bos JD, Kapsenberg ML. The skin immune system: progress in cutaneous biology. Immunol Today. 1993;14:75-78.
- Young AW Jr. Dynamics of autosensitization dermatitis; a clinical and microscopic concept of autoeczematization. AMA Arch Derm. 1958;77:495-502.
- Brenner S, Wolf R, Landau M. Scabid: an unusual id reaction to scabies. Int J Dermatol. 1993;32:128-129.
- Yamany T, Schwartz RA. Infectious eczematoid dermatitis: a comprehensive review. J Eur Acad Dermatol Venereol. 2015;29:203-208.
- Wang X, Li L, Shi X, et al. Itching and its related factors in subtypes of eczema: a cross-sectional multicenter study in tertiary hospitals of China. Sci Rep. 2018;8:10754.
- Price A, Tavazoie M, Meehan SA, et al. Id reaction associated with red tattoo ink. Cutis. 2018;102:E32-E34.
- Ilkit M, Durdu M, Karaks¸ M. Cutaneous id reactions: a comprehensive review of clinical manifestations, epidemiology, etiology, and management. Crit Rev Microbiol. 2012;38:191-202.
- Kaner SR. Dermatitis venenata of the feet with a generalized “id” reaction. J Am Podiatry Assoc. 1970;60:199-204.
- Jordan L, Jackson NA, Carter-Snell B, et al. Pustular tinea id reaction. Cutis. 2019;103:E3-E4.
- Crum N, Hardaway C, Graham B. Development of an idlike reaction during treatment for acute pulmonary histoplasmosis: a new cutaneous manifestation in histoplasmosis. J Am Acad Dermatol. 2003;48(2 suppl):S5-S6.
- Chirac A, Brzezinski P, Chiriac AE, et al. Autosensitisation (autoeczematisation) reactions in a case of diaper dermatitis candidiasis. Niger Med J. 2014;55:274-275.
- Singh PY, Sinha P, Baveja S, et al. Immune-mediated tuberculous uveitis—a rare association with papulonecrotic tuberculid. Indian J Ophthalmol. 2019;67:1207-1209.
- Urso B, Georgesen C, Harp J. Papulonecrotic tuberculid secondary to Mycobacterium avium complex. Cutis. 2019;104:E11-E13.
- Choudhri SH, Magro CM, Crowson AN, et al. An id reaction to Mycobacterium leprae: first documented case. Cutis. 1994;54:282-286.
- Park JW, Jeong GJ, Seo SJ, et al. Pseudomonas toe web infection and autosensitisation dermatitis: diagnostic and therapeutic challenge. Int Wound J. 2020;17:1543-1544. doi:10.1111/iwj.13386
- Netchiporouk E, Cohen BA. Recognizing and managing eczematous id reactions to molluscum contagiosum virus in children. Pediatrics. 2012;129:E1072-E1075.
- Aurelian L, Ono F, Burnett J. Herpes simplex virus (HSV)-associated erythema multiforme (HAEM): a viral disease with an autoimmune component. Dermatol Online J. 2003;9:1.
- Rocamora V, Romaní J, Puig L, et al. Id reaction to molluscum contagiosum. Pediatr Dermatol. 1996;13:349-350.
- Yes¸ilova Y, Özbilgin A, Turan E, et al. Clinical exacerbation developing during treatment of cutaneous leishmaniasis: an id reaction? Turkiye Parazitol Derg. 2014;38:281-282.
- Connor CJ, Selby JC, Wanat KA. Severe pediculosis capitus: a case of “crusted lice” with autoeczematization. Dermatol Online J. 2016;22:13030/qt7c91z913.
- Shelley WB. The autoimmune mechanism in clinical dermatology. Arch Dermatol. 1962;86:27-34.
- Bosworth A, Hull PR. Disseminated eczema following radiotherapy: a case report. J Cutan Med Surg. 2018;22:353-355.
- Lowther C, Miedler JD, Cockerell CJ. Id-like reaction to BCG therapy for bladder cancer. Cutis. 2013;91:145-151.
- Huerth KA, Glick PL, Glick ZR. Cutaneous id reaction after using cyanoacrylate for wound closure. Cutis. 2020;105:E11-E13.
- Amini S, Burdick AE, Janniger CK. Dyshidrotic eczema (pompholyx). Updated April 22, 2020. Accessed August 23, 2021. https://emedicine.medscape.com/article/1122527-overview
- Sundaresan S, Migden MR, Silapunt S. Stasis dermatitis: pathophysiology, evaluation, and management. Am J Clin Dermatol. 2017;18:383-390.
- Hughes JDM, Pratt MD. Allergic contact dermatitis and autoeczematization to proctosedyl® cream and proctomyxin® cream. Case Rep Dermatol. 2018;10:238-246.
- Bains SN, Nash P, Fonacier L. Irritant contact dermatitis. Clin Rev Allergy Immunol. 2019;56:99-109.
- Novak-Bilic´ G, Vucˇic´ M, Japundžic´ I, et al. Irritant and allergic contact dermatitis—skin lesion characteristics. Acta Clin Croat. 2018;57:713-720.
- Nassau S, Fonacier L. Allergic contact dermatitis. Med Clin North Am. 2020;104:61-76.
- Lewis DJ, Schlichte MJ, Dao H Jr. Atypical disseminated herpes zoster: management guidelines in immunocompromised patients. Cutis. 2017;100:321-330.
- Nedorost S, White S, Rowland DY, et al. Development and implementation of an order set to improve value of care for patients with severe stasis dermatitis. J Am Acad Dermatol. 2019;80:815-817.
- Whitfield A. Lumleian Lectures on Some Points in the Aetiology of Skin Diseases. Delivered before the Royal College of Physicians of London on March 10th, 15th, and 17th, 1921. Lecture II. Lancet. 1921;2:122-127.
- Cheng N, Rucker Wright D, Cohen BA. Dermatophytid in tinea capitis: rarely reported common phenomenon with clinical implications. Pediatrics. 2011;128:E453-E457.
- Schrom KP, Kobs A, Nedorost S. Clinical psoriasiform dermatitis following dupilumab use for autoeczematization secondary to chronic stasis dermatitis. Cureus. 2020;12:e7831. doi:10.7759/cureus.7831
- Templeton HJ, Lunsford CJ, Allington HV. Autosensitization dermatitis; report of five cases and protocol of an experiment. Arch Derm Syphilol. 1949;59:68-77.
- Shelley WB. Id reaction. In: Consultations in Dermatology. Saunders; 1972:262-267.
- Sharquie KE, Noaimi AA, Flayih RA. Clinical and histopathological findings in patients with follicular dermatoses: all skin diseases starts in the hair follicles as new hypothesis. Am J Clin Res Rev. 2020;4:17.
- Kasteler JS, Petersen MJ, Vance JE, et al. Circulating activated T lymphocytes in autoeczematization. Arch Dermatol. 1992;128:795-798.
- González-Amaro R, Baranda L, Abud-Mendoza C, et al. Autoeczematization is associated with abnormal immune recognition of autologous skin antigens. J Am Acad Dermatol. 1993;28:56-60.
- Cunningham MJ, Zone JJ, Petersen MJ, et al. Circulating activated (DR-positive) T lymphocytes in a patient with autoeczematization. J Am Acad Dermatol. 1986;14:1039-1041.
- Furue M, Ulzii D, Vu YH, et al. Pathogenesis of atopic dermatitis: current paradigm. Iran J Immunol. 2019;16:97-107.
- Uchi H, Terao H, Koga T, et al. Cytokines and chemokines in the epidermis. J Dermatol Sci. 2000;24(suppl 1):S29-S38.
- Bos JD, Kapsenberg ML. The skin immune system: progress in cutaneous biology. Immunol Today. 1993;14:75-78.
- Young AW Jr. Dynamics of autosensitization dermatitis; a clinical and microscopic concept of autoeczematization. AMA Arch Derm. 1958;77:495-502.
- Brenner S, Wolf R, Landau M. Scabid: an unusual id reaction to scabies. Int J Dermatol. 1993;32:128-129.
- Yamany T, Schwartz RA. Infectious eczematoid dermatitis: a comprehensive review. J Eur Acad Dermatol Venereol. 2015;29:203-208.
- Wang X, Li L, Shi X, et al. Itching and its related factors in subtypes of eczema: a cross-sectional multicenter study in tertiary hospitals of China. Sci Rep. 2018;8:10754.
- Price A, Tavazoie M, Meehan SA, et al. Id reaction associated with red tattoo ink. Cutis. 2018;102:E32-E34.
- Ilkit M, Durdu M, Karaks¸ M. Cutaneous id reactions: a comprehensive review of clinical manifestations, epidemiology, etiology, and management. Crit Rev Microbiol. 2012;38:191-202.
- Kaner SR. Dermatitis venenata of the feet with a generalized “id” reaction. J Am Podiatry Assoc. 1970;60:199-204.
- Jordan L, Jackson NA, Carter-Snell B, et al. Pustular tinea id reaction. Cutis. 2019;103:E3-E4.
- Crum N, Hardaway C, Graham B. Development of an idlike reaction during treatment for acute pulmonary histoplasmosis: a new cutaneous manifestation in histoplasmosis. J Am Acad Dermatol. 2003;48(2 suppl):S5-S6.
- Chirac A, Brzezinski P, Chiriac AE, et al. Autosensitisation (autoeczematisation) reactions in a case of diaper dermatitis candidiasis. Niger Med J. 2014;55:274-275.
- Singh PY, Sinha P, Baveja S, et al. Immune-mediated tuberculous uveitis—a rare association with papulonecrotic tuberculid. Indian J Ophthalmol. 2019;67:1207-1209.
- Urso B, Georgesen C, Harp J. Papulonecrotic tuberculid secondary to Mycobacterium avium complex. Cutis. 2019;104:E11-E13.
- Choudhri SH, Magro CM, Crowson AN, et al. An id reaction to Mycobacterium leprae: first documented case. Cutis. 1994;54:282-286.
- Park JW, Jeong GJ, Seo SJ, et al. Pseudomonas toe web infection and autosensitisation dermatitis: diagnostic and therapeutic challenge. Int Wound J. 2020;17:1543-1544. doi:10.1111/iwj.13386
- Netchiporouk E, Cohen BA. Recognizing and managing eczematous id reactions to molluscum contagiosum virus in children. Pediatrics. 2012;129:E1072-E1075.
- Aurelian L, Ono F, Burnett J. Herpes simplex virus (HSV)-associated erythema multiforme (HAEM): a viral disease with an autoimmune component. Dermatol Online J. 2003;9:1.
- Rocamora V, Romaní J, Puig L, et al. Id reaction to molluscum contagiosum. Pediatr Dermatol. 1996;13:349-350.
- Yes¸ilova Y, Özbilgin A, Turan E, et al. Clinical exacerbation developing during treatment of cutaneous leishmaniasis: an id reaction? Turkiye Parazitol Derg. 2014;38:281-282.
- Connor CJ, Selby JC, Wanat KA. Severe pediculosis capitus: a case of “crusted lice” with autoeczematization. Dermatol Online J. 2016;22:13030/qt7c91z913.
- Shelley WB. The autoimmune mechanism in clinical dermatology. Arch Dermatol. 1962;86:27-34.
- Bosworth A, Hull PR. Disseminated eczema following radiotherapy: a case report. J Cutan Med Surg. 2018;22:353-355.
- Lowther C, Miedler JD, Cockerell CJ. Id-like reaction to BCG therapy for bladder cancer. Cutis. 2013;91:145-151.
- Huerth KA, Glick PL, Glick ZR. Cutaneous id reaction after using cyanoacrylate for wound closure. Cutis. 2020;105:E11-E13.
- Amini S, Burdick AE, Janniger CK. Dyshidrotic eczema (pompholyx). Updated April 22, 2020. Accessed August 23, 2021. https://emedicine.medscape.com/article/1122527-overview
- Sundaresan S, Migden MR, Silapunt S. Stasis dermatitis: pathophysiology, evaluation, and management. Am J Clin Dermatol. 2017;18:383-390.
- Hughes JDM, Pratt MD. Allergic contact dermatitis and autoeczematization to proctosedyl® cream and proctomyxin® cream. Case Rep Dermatol. 2018;10:238-246.
- Bains SN, Nash P, Fonacier L. Irritant contact dermatitis. Clin Rev Allergy Immunol. 2019;56:99-109.
- Novak-Bilic´ G, Vucˇic´ M, Japundžic´ I, et al. Irritant and allergic contact dermatitis—skin lesion characteristics. Acta Clin Croat. 2018;57:713-720.
- Nassau S, Fonacier L. Allergic contact dermatitis. Med Clin North Am. 2020;104:61-76.
- Lewis DJ, Schlichte MJ, Dao H Jr. Atypical disseminated herpes zoster: management guidelines in immunocompromised patients. Cutis. 2017;100:321-330.
- Nedorost S, White S, Rowland DY, et al. Development and implementation of an order set to improve value of care for patients with severe stasis dermatitis. J Am Acad Dermatol. 2019;80:815-817.
Practice Points
- Autoeczematization, or id reaction, is a disseminated reaction of the skin occurring at a site distant to a primary cutaneous infection or stimulus.
- T lymphocytes and keratinocytes are postulated to be involved in the pathogenesis of id reactions.
- Therapy includes treating the underlying pathology while providing topical corticosteroids for the autoeczematous lesions.
Atopic Dermatitis Oral Therapies: What Are Patients Learning on YouTube?
To the Editor:
Oral immunosuppressive therapies are prescribed for moderate to severe atopic dermatitis. Patients often consult YouTube to make informed decisions about these therapies. In the United States, most health-related online searches are initiated through a search engine, which frequently leads to social media sites such as YouTube. Recent studies have examined the reasons why users turn to the Internet for health-related information, indicating that users typically seek specific information regarding health concerns.1,2 Furthermore, social media platforms such as YouTube are a popular means of sharing health information with the public.3-5 Currently, YouTube has more than 1 billion registered users, and 30 million health-related videos are watched each day.6 Almost one-third of US consumers use YouTube, Facebook, and Twitter to obtain medical information.7 YouTube is a versatile tool because of its video-discovery mechanisms such as a keyword-based search engine, video-recommendation system, highlight feature for videos on home pages, and the capacity to embed YouTube videos on various web pages.8 Searchers use videos that are short, fast paced, emotion evoking, from credible sources, recently uploaded, and relevant to the searcher for aiding in health decisions.9 Furthermore, studies have demonstrated YouTube’s capacity to support a change in attitude and increase users’ knowledge. In fact, YouTube had higher impact on recall, attitudes, and behaviors when compared with written materials on other social media platforms, such as Facebook and Twitter.9 We conducted a cross-sectional study to examine the quality of YouTube videos on oral therapies for atopic dermatitis, such as cyclosporine, methotrexate, azathioprine, and mycophenolate mofetil.
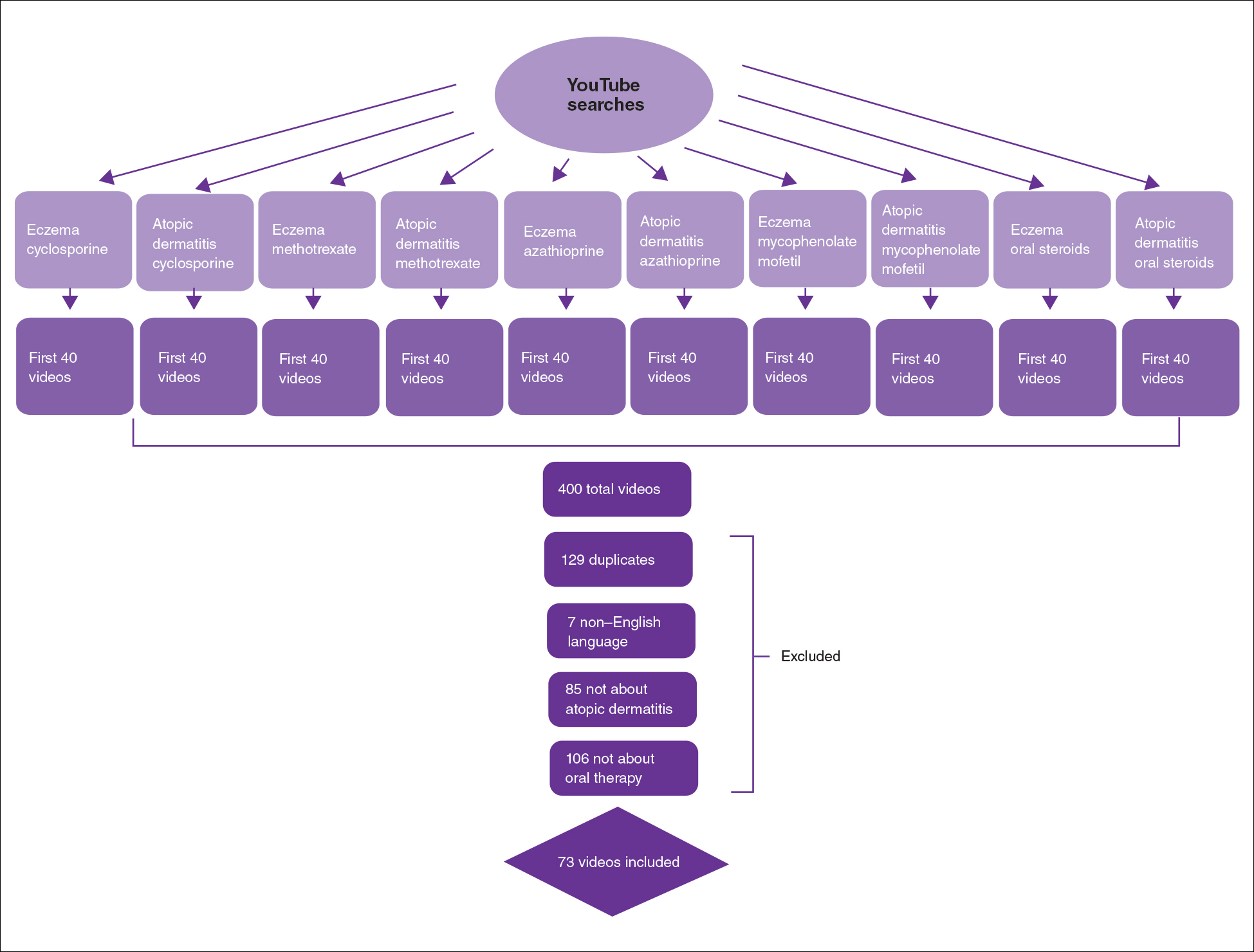
On April 23, 2020, we performed 8 searches using a private browser with default filters on YouTube (Figure). Injectables were not included in the analysis, as the YouTube experience on dupilumab previously has been investigated.10 The top 40 videos from each search were screened by 3 researchers. Duplicates, non–English-language videos, and videos that did not discuss atopic dermatitis or oral therapies were excluded, resulting in 73 videos included in this analysis. Testimonials generated by patients made up 39 of 73 (53.4%) videos. Health care professionals created 23 of 73 (31.5%) videos, and educators with financial interest created 11 of 73 (15.1%) videos. The dates of production for the videos spanned from 2008 to 2020.
The major topics addressed in the videos were symptomatic changes (63 [68.8% of all topics discussed]), adverse effects (52 [67.5%]), and quality-of-life changes (37 [48.1%]). Of the videos included, the majority (42/73 [57.5%]) contained a neutral tone about the medication, citing advantages and disadvantages with therapy, while 22 of 73 (30.1%) had an encouraging tone, and 9 of 73 (12.3%) had a discouraging tone. Regarding videos with positive tones, there were 17 videos on cyclosporine, 9 on azathioprine, 7 on methotrexate, 4 on oral steroids, and 2 on mycophenolate mofetil. Regarding videos with negative tones, there were 4 on cyclosporine, 3 on azathioprine, 2 on methotrexate, and 2 on mycophenolate mofetil.
Of the videos made with financial interest, the majority (28/34 [77.8%]) were more suitable for informing health care providers rather than patients, containing jargon as well as complex information on clinical trials, dosing, and mechanisms of action. From the videos discussing clinical recommendations, there were 9 of 73 (12.3%) Grade A recommendations (eg, citing evidence-based information and clinical trials) and 64 of 73 (87.7%) Grade B recommendations (eg, anecdotal information on patient experience). Thirty-seven of 73 (50.7%) videos were evidence based, and 36 of 73 (49.3%) were non–evidence based. Six videos were patient-oriented news broadcasts.
Patient-generated testimonials had the most views (mean, 9238.4) and highest interaction ratio (the sum of likes, dislikes, and comments divided by the number of views)(mean, 0.027), while health care provider–generated videos had fewer views (mean, 9218.7) and a lower interaction ratio (mean, 0.011). Financial-based videos had 4233.4 views on average, with an average interaction ratio of 0.014. Based on these results, biased, patient-generated content comprised greater than 50% of YouTube videos about oral therapies for atopic dermatitis and was quite likely to be engaged with by users. Thus, these patient testimonials have great potential to affect decision-making.
The high number of patient-generated videos about oral therapies was consistent with prior studies of YouTube videos about therapies for numerous conditions.11-13 Dermatologists should consider utilizing YouTube for providing evidence-based, patient-oriented information about novel therapeutics. They may consider collaborating with patients to assist with their creation of YouTube videos and directing patients to credible resources by the American Academy of Dermatology and Canadian Dermatology Association for decision-making.
Importantly, this analysis is limited by its lack of quality-assessment tools for video-based resources such as JAMA score and DISCERN score.14,15 However, these metrics have limited ability to evaluate audiovisual elements, indicating the need for novel tools to score their validity.
- Fox S, Duggan M. Health online 2013. January 15, 2013. Accessed August 15, 2021. https://www.pewresearch.org/internet/2013/01/15/health-online-2013/
- Ní Ríordáin R, McCreary C. Dental patients’ use of the Internet. Br Dent J. 2009;207:583-586, 575.
- Fergie G, Hilton S, Hunt K. Young adults’ experiences of seeking online information about diabetes and mental health in the age of social media. Health Expect. 2016;19:1324-1335.
- Antheunis ML, Tates K, Nieboer TE. Patients’ and health professionals’ use of social media in health care: motives, barriers and expectations. Patient Educ Couns. 2013;92:426-431.
- McGregor F, Somner JE, Bourne RR, et al. Social media use by patients with glaucoma: what can we learn? Ophthalmic Physiol Opt. 2014;34:46-52.
- YouTube Statistics—15 Amazing Stats for 2015. Published April 30, 2015. Accessed August 27, 2021. YouTube.com/watch?v=9ZLBSPzY7GQ
- Health Research Institute. Social media “likes” healthcare: from marketing to social business. April 2012. Accessed August 15, 2021. https://www.pwc.com/us/en/health-industries/health-research-institute/publications/pdf/health-care-social-media-report.pdf
- Zhou R, Khemmarat S, Gao L, et al. How YouTube videos are discovered and its impact on videos views. Multimed Tools Appl. 2016;75:6035-6058.
- Haslam K, Doucette H, Hachey S, et al. YouTube videos as health decision aids for the public: an integrative review. Can J Dent Hyg. 2019;53:53-66.
- Pithadia D, Reynolds K, Lee E, et al. Dupilumab for atopic dermatitis: what are patients learning on YouTube [published online ahead of print April 16,2020]? J Dermatolog Treat. doi: 10.1080/09546634.2020.1755418
- Tolu S, Yurdakul OV, Basaran B, et al. English-language videos on YouTube as a source of information on self-administer subcutaneous anti-tumour necrosis factor agent injections. Rheumatol Int. 2018;38:1285-1292.
- Reynolds KA, Pithadia DJ, Lee EB, et al. A cross-sectional study of YouTube videos about psoriasis biologics. Int J Dermatol. 2019;58:E61-E62.
- Kocyigit BF, Akaltun MS. Does YouTube provide high quality information? assessment of secukinumab videos. Rheumatol Int. 2019;39:1263-1268.
- Qi J, Trang T, Doong J, et al. Misinformation is prevalent in psoriasis-related YouTube videos. Dermatol Online J. 2016;22:13030/qt7qc9z2m5
- Gokcen HB, Gumussuyu G. A quality analysis of disc herniation videos on YouTube. World Neurosurg. 2019;124:E799-E804.
To the Editor:
Oral immunosuppressive therapies are prescribed for moderate to severe atopic dermatitis. Patients often consult YouTube to make informed decisions about these therapies. In the United States, most health-related online searches are initiated through a search engine, which frequently leads to social media sites such as YouTube. Recent studies have examined the reasons why users turn to the Internet for health-related information, indicating that users typically seek specific information regarding health concerns.1,2 Furthermore, social media platforms such as YouTube are a popular means of sharing health information with the public.3-5 Currently, YouTube has more than 1 billion registered users, and 30 million health-related videos are watched each day.6 Almost one-third of US consumers use YouTube, Facebook, and Twitter to obtain medical information.7 YouTube is a versatile tool because of its video-discovery mechanisms such as a keyword-based search engine, video-recommendation system, highlight feature for videos on home pages, and the capacity to embed YouTube videos on various web pages.8 Searchers use videos that are short, fast paced, emotion evoking, from credible sources, recently uploaded, and relevant to the searcher for aiding in health decisions.9 Furthermore, studies have demonstrated YouTube’s capacity to support a change in attitude and increase users’ knowledge. In fact, YouTube had higher impact on recall, attitudes, and behaviors when compared with written materials on other social media platforms, such as Facebook and Twitter.9 We conducted a cross-sectional study to examine the quality of YouTube videos on oral therapies for atopic dermatitis, such as cyclosporine, methotrexate, azathioprine, and mycophenolate mofetil.
On April 23, 2020, we performed 8 searches using a private browser with default filters on YouTube (Figure). Injectables were not included in the analysis, as the YouTube experience on dupilumab previously has been investigated.10 The top 40 videos from each search were screened by 3 researchers. Duplicates, non–English-language videos, and videos that did not discuss atopic dermatitis or oral therapies were excluded, resulting in 73 videos included in this analysis. Testimonials generated by patients made up 39 of 73 (53.4%) videos. Health care professionals created 23 of 73 (31.5%) videos, and educators with financial interest created 11 of 73 (15.1%) videos. The dates of production for the videos spanned from 2008 to 2020.
The major topics addressed in the videos were symptomatic changes (63 [68.8% of all topics discussed]), adverse effects (52 [67.5%]), and quality-of-life changes (37 [48.1%]). Of the videos included, the majority (42/73 [57.5%]) contained a neutral tone about the medication, citing advantages and disadvantages with therapy, while 22 of 73 (30.1%) had an encouraging tone, and 9 of 73 (12.3%) had a discouraging tone. Regarding videos with positive tones, there were 17 videos on cyclosporine, 9 on azathioprine, 7 on methotrexate, 4 on oral steroids, and 2 on mycophenolate mofetil. Regarding videos with negative tones, there were 4 on cyclosporine, 3 on azathioprine, 2 on methotrexate, and 2 on mycophenolate mofetil.
Of the videos made with financial interest, the majority (28/34 [77.8%]) were more suitable for informing health care providers rather than patients, containing jargon as well as complex information on clinical trials, dosing, and mechanisms of action. From the videos discussing clinical recommendations, there were 9 of 73 (12.3%) Grade A recommendations (eg, citing evidence-based information and clinical trials) and 64 of 73 (87.7%) Grade B recommendations (eg, anecdotal information on patient experience). Thirty-seven of 73 (50.7%) videos were evidence based, and 36 of 73 (49.3%) were non–evidence based. Six videos were patient-oriented news broadcasts.
Patient-generated testimonials had the most views (mean, 9238.4) and highest interaction ratio (the sum of likes, dislikes, and comments divided by the number of views)(mean, 0.027), while health care provider–generated videos had fewer views (mean, 9218.7) and a lower interaction ratio (mean, 0.011). Financial-based videos had 4233.4 views on average, with an average interaction ratio of 0.014. Based on these results, biased, patient-generated content comprised greater than 50% of YouTube videos about oral therapies for atopic dermatitis and was quite likely to be engaged with by users. Thus, these patient testimonials have great potential to affect decision-making.
The high number of patient-generated videos about oral therapies was consistent with prior studies of YouTube videos about therapies for numerous conditions.11-13 Dermatologists should consider utilizing YouTube for providing evidence-based, patient-oriented information about novel therapeutics. They may consider collaborating with patients to assist with their creation of YouTube videos and directing patients to credible resources by the American Academy of Dermatology and Canadian Dermatology Association for decision-making.
Importantly, this analysis is limited by its lack of quality-assessment tools for video-based resources such as JAMA score and DISCERN score.14,15 However, these metrics have limited ability to evaluate audiovisual elements, indicating the need for novel tools to score their validity.
To the Editor:
Oral immunosuppressive therapies are prescribed for moderate to severe atopic dermatitis. Patients often consult YouTube to make informed decisions about these therapies. In the United States, most health-related online searches are initiated through a search engine, which frequently leads to social media sites such as YouTube. Recent studies have examined the reasons why users turn to the Internet for health-related information, indicating that users typically seek specific information regarding health concerns.1,2 Furthermore, social media platforms such as YouTube are a popular means of sharing health information with the public.3-5 Currently, YouTube has more than 1 billion registered users, and 30 million health-related videos are watched each day.6 Almost one-third of US consumers use YouTube, Facebook, and Twitter to obtain medical information.7 YouTube is a versatile tool because of its video-discovery mechanisms such as a keyword-based search engine, video-recommendation system, highlight feature for videos on home pages, and the capacity to embed YouTube videos on various web pages.8 Searchers use videos that are short, fast paced, emotion evoking, from credible sources, recently uploaded, and relevant to the searcher for aiding in health decisions.9 Furthermore, studies have demonstrated YouTube’s capacity to support a change in attitude and increase users’ knowledge. In fact, YouTube had higher impact on recall, attitudes, and behaviors when compared with written materials on other social media platforms, such as Facebook and Twitter.9 We conducted a cross-sectional study to examine the quality of YouTube videos on oral therapies for atopic dermatitis, such as cyclosporine, methotrexate, azathioprine, and mycophenolate mofetil.
On April 23, 2020, we performed 8 searches using a private browser with default filters on YouTube (Figure). Injectables were not included in the analysis, as the YouTube experience on dupilumab previously has been investigated.10 The top 40 videos from each search were screened by 3 researchers. Duplicates, non–English-language videos, and videos that did not discuss atopic dermatitis or oral therapies were excluded, resulting in 73 videos included in this analysis. Testimonials generated by patients made up 39 of 73 (53.4%) videos. Health care professionals created 23 of 73 (31.5%) videos, and educators with financial interest created 11 of 73 (15.1%) videos. The dates of production for the videos spanned from 2008 to 2020.
The major topics addressed in the videos were symptomatic changes (63 [68.8% of all topics discussed]), adverse effects (52 [67.5%]), and quality-of-life changes (37 [48.1%]). Of the videos included, the majority (42/73 [57.5%]) contained a neutral tone about the medication, citing advantages and disadvantages with therapy, while 22 of 73 (30.1%) had an encouraging tone, and 9 of 73 (12.3%) had a discouraging tone. Regarding videos with positive tones, there were 17 videos on cyclosporine, 9 on azathioprine, 7 on methotrexate, 4 on oral steroids, and 2 on mycophenolate mofetil. Regarding videos with negative tones, there were 4 on cyclosporine, 3 on azathioprine, 2 on methotrexate, and 2 on mycophenolate mofetil.
Of the videos made with financial interest, the majority (28/34 [77.8%]) were more suitable for informing health care providers rather than patients, containing jargon as well as complex information on clinical trials, dosing, and mechanisms of action. From the videos discussing clinical recommendations, there were 9 of 73 (12.3%) Grade A recommendations (eg, citing evidence-based information and clinical trials) and 64 of 73 (87.7%) Grade B recommendations (eg, anecdotal information on patient experience). Thirty-seven of 73 (50.7%) videos were evidence based, and 36 of 73 (49.3%) were non–evidence based. Six videos were patient-oriented news broadcasts.
Patient-generated testimonials had the most views (mean, 9238.4) and highest interaction ratio (the sum of likes, dislikes, and comments divided by the number of views)(mean, 0.027), while health care provider–generated videos had fewer views (mean, 9218.7) and a lower interaction ratio (mean, 0.011). Financial-based videos had 4233.4 views on average, with an average interaction ratio of 0.014. Based on these results, biased, patient-generated content comprised greater than 50% of YouTube videos about oral therapies for atopic dermatitis and was quite likely to be engaged with by users. Thus, these patient testimonials have great potential to affect decision-making.
The high number of patient-generated videos about oral therapies was consistent with prior studies of YouTube videos about therapies for numerous conditions.11-13 Dermatologists should consider utilizing YouTube for providing evidence-based, patient-oriented information about novel therapeutics. They may consider collaborating with patients to assist with their creation of YouTube videos and directing patients to credible resources by the American Academy of Dermatology and Canadian Dermatology Association for decision-making.
Importantly, this analysis is limited by its lack of quality-assessment tools for video-based resources such as JAMA score and DISCERN score.14,15 However, these metrics have limited ability to evaluate audiovisual elements, indicating the need for novel tools to score their validity.
- Fox S, Duggan M. Health online 2013. January 15, 2013. Accessed August 15, 2021. https://www.pewresearch.org/internet/2013/01/15/health-online-2013/
- Ní Ríordáin R, McCreary C. Dental patients’ use of the Internet. Br Dent J. 2009;207:583-586, 575.
- Fergie G, Hilton S, Hunt K. Young adults’ experiences of seeking online information about diabetes and mental health in the age of social media. Health Expect. 2016;19:1324-1335.
- Antheunis ML, Tates K, Nieboer TE. Patients’ and health professionals’ use of social media in health care: motives, barriers and expectations. Patient Educ Couns. 2013;92:426-431.
- McGregor F, Somner JE, Bourne RR, et al. Social media use by patients with glaucoma: what can we learn? Ophthalmic Physiol Opt. 2014;34:46-52.
- YouTube Statistics—15 Amazing Stats for 2015. Published April 30, 2015. Accessed August 27, 2021. YouTube.com/watch?v=9ZLBSPzY7GQ
- Health Research Institute. Social media “likes” healthcare: from marketing to social business. April 2012. Accessed August 15, 2021. https://www.pwc.com/us/en/health-industries/health-research-institute/publications/pdf/health-care-social-media-report.pdf
- Zhou R, Khemmarat S, Gao L, et al. How YouTube videos are discovered and its impact on videos views. Multimed Tools Appl. 2016;75:6035-6058.
- Haslam K, Doucette H, Hachey S, et al. YouTube videos as health decision aids for the public: an integrative review. Can J Dent Hyg. 2019;53:53-66.
- Pithadia D, Reynolds K, Lee E, et al. Dupilumab for atopic dermatitis: what are patients learning on YouTube [published online ahead of print April 16,2020]? J Dermatolog Treat. doi: 10.1080/09546634.2020.1755418
- Tolu S, Yurdakul OV, Basaran B, et al. English-language videos on YouTube as a source of information on self-administer subcutaneous anti-tumour necrosis factor agent injections. Rheumatol Int. 2018;38:1285-1292.
- Reynolds KA, Pithadia DJ, Lee EB, et al. A cross-sectional study of YouTube videos about psoriasis biologics. Int J Dermatol. 2019;58:E61-E62.
- Kocyigit BF, Akaltun MS. Does YouTube provide high quality information? assessment of secukinumab videos. Rheumatol Int. 2019;39:1263-1268.
- Qi J, Trang T, Doong J, et al. Misinformation is prevalent in psoriasis-related YouTube videos. Dermatol Online J. 2016;22:13030/qt7qc9z2m5
- Gokcen HB, Gumussuyu G. A quality analysis of disc herniation videos on YouTube. World Neurosurg. 2019;124:E799-E804.
- Fox S, Duggan M. Health online 2013. January 15, 2013. Accessed August 15, 2021. https://www.pewresearch.org/internet/2013/01/15/health-online-2013/
- Ní Ríordáin R, McCreary C. Dental patients’ use of the Internet. Br Dent J. 2009;207:583-586, 575.
- Fergie G, Hilton S, Hunt K. Young adults’ experiences of seeking online information about diabetes and mental health in the age of social media. Health Expect. 2016;19:1324-1335.
- Antheunis ML, Tates K, Nieboer TE. Patients’ and health professionals’ use of social media in health care: motives, barriers and expectations. Patient Educ Couns. 2013;92:426-431.
- McGregor F, Somner JE, Bourne RR, et al. Social media use by patients with glaucoma: what can we learn? Ophthalmic Physiol Opt. 2014;34:46-52.
- YouTube Statistics—15 Amazing Stats for 2015. Published April 30, 2015. Accessed August 27, 2021. YouTube.com/watch?v=9ZLBSPzY7GQ
- Health Research Institute. Social media “likes” healthcare: from marketing to social business. April 2012. Accessed August 15, 2021. https://www.pwc.com/us/en/health-industries/health-research-institute/publications/pdf/health-care-social-media-report.pdf
- Zhou R, Khemmarat S, Gao L, et al. How YouTube videos are discovered and its impact on videos views. Multimed Tools Appl. 2016;75:6035-6058.
- Haslam K, Doucette H, Hachey S, et al. YouTube videos as health decision aids for the public: an integrative review. Can J Dent Hyg. 2019;53:53-66.
- Pithadia D, Reynolds K, Lee E, et al. Dupilumab for atopic dermatitis: what are patients learning on YouTube [published online ahead of print April 16,2020]? J Dermatolog Treat. doi: 10.1080/09546634.2020.1755418
- Tolu S, Yurdakul OV, Basaran B, et al. English-language videos on YouTube as a source of information on self-administer subcutaneous anti-tumour necrosis factor agent injections. Rheumatol Int. 2018;38:1285-1292.
- Reynolds KA, Pithadia DJ, Lee EB, et al. A cross-sectional study of YouTube videos about psoriasis biologics. Int J Dermatol. 2019;58:E61-E62.
- Kocyigit BF, Akaltun MS. Does YouTube provide high quality information? assessment of secukinumab videos. Rheumatol Int. 2019;39:1263-1268.
- Qi J, Trang T, Doong J, et al. Misinformation is prevalent in psoriasis-related YouTube videos. Dermatol Online J. 2016;22:13030/qt7qc9z2m5
- Gokcen HB, Gumussuyu G. A quality analysis of disc herniation videos on YouTube. World Neurosurg. 2019;124:E799-E804.
Practice Points
- Patient-based YouTube videos comprised the majority of videos on oral therapies for atopic dermatitis, with the greatest views and interaction ratio.
- Most YouTube videos on this topic contained a neutral tone and Grade B recommendations, thus meriting production of more evidence-based videos in collaboration with patients on the YouTube platform.
Atopic Dermatitis Topical Therapies: Study of YouTube Videos as a Source of Patient Information
To the Editor:
Atopic dermatitis (eczema) affects approximately 20% of children worldwide.1 In atopic dermatitis management, patient education is crucial for optimal outcomes.2 The COVID-19 pandemic has impacted patient-physician interactions. To ensure safety of patients and physicians, visits may have been canceled, postponed, or conducted virtually, leaving less time for discussion and questions.3 As a consequence, patients may seek information about atopic dermatitis from alternative sources, including YouTube videos. We performed a cross-sectional study to analyze YouTube videos about topical treatments for atopic dermatitis.
During the week of July 16, 2020, we performed 4 private browser YouTube searches with default filters using the following terms: eczema topicals, eczema topical treatments, atopic dermatitis topicals, and atopic dermatitis topical treatments. For video selection, we defined topical treatments as topical corticosteroids, topical calcineurin inhibitors, crisaborole, emollients, wet wraps, and any prospective treatment topically administered. For each of the 4 searches, 2 researchers (A.M. and A.T.) independently examined the top 75 videos, yielding a total of 300 videos. Of them, 98 videos were duplicates, 19 videos were not about atopic dermatitis, and 91 videos were not about topical treatments, leaving a total of 92 videos for analysis (Figure 1).
For the 92 included videos, the length; upload year; number of views, likes, dislikes, and comments; interaction ratio (IR)(the sum of likes, dislikes, and comments divided by the number of views); and video content were determined. The videos were placed into mutually exclusive categories as follows: (1) patient experience, defined as a video about patient perspective; (2) professional source, defined as a video featuring a physician, physician extender, pharmacist, or scientist, or produced by a formal organization; or (3) other. The DISCERN Instrument was used for grading the reliability and quality of the 92 included videos. This instrument consists of 16 questions with the responses rated on a scale of 1 to 5.4 For analysis of DISCERN scores, patient experience and other videos were grouped together as nonprofessional source videos. A 2-sample t-test was used to compare DISCERN scores between professional source and nonprofessional source videos.
Most videos were uploaded in 2017 (n=19), 2018 (n=23), and 2019 (n=25), but 20 were uploaded in 2012-2016 and 5 were uploaded in 2020. The 92 videos had a mean length of 8 minutes and 35 seconds (range, 30 seconds to 62 minutes and 23 seconds).
Patient experience videos accounted for 23.9% (n=22) of videos. These videos discussed topical steroid withdrawal (TSW)(n=16), instructions for making emollients (n=2), and treatment successes (n=4). Professional source videos represented 67.4% (n=62) of videos. Of them, 40.3% (n=25) were physician oriented, defined as having extensive medical terminology or qualifying for continuing medical education credit. Three (4.8%) of the professional source videos were sponsored by a drug company. Other constituted the remaining 8.7% (n=8) of videos. Patient experience videos had more views (median views [interquartile range], 6865 [10,307]) and higher engagement (median IR [interquartile range], 0.038 [0.022]) than professional source videos (views: median views [interquartile range], 1052.5 [10,610.5]; engagement: median IR [interquartile range], 0.006 [0.008]).
Although less popular, professional source videos had a significantly higher DISCERN overall quality rating score (question 16) compared to those categorized as nonprofessional source (3.92 vs 1.53; P<.001). In contrast, nonprofessional source videos scored significantly higher on the quality-of-life question (question 13) compared to professional source videos (3.90 vs 2.56; P<.001)(eTable). (Three professional source videos were removed from YouTube before DISCERN scores could be assigned.)
Notably, 20.7% (n=19) of the 92 videos discussed TSW, and most of them were patient experiences (n=16). Other categories included topical steroids excluding TSW (n=11), steroid phobia (n=2), topical calcineurin inhibitors (n=2), crisaborole (n=6), news broadcast (n=7), wet wraps (n=5), product advertisement (n=7), and research (n=11)(Figure 2). Interestingly, there were no videos focusing on the calcineurin inhibitor black box warning.
Similar to prior studies, our results indicate preference for patient-generated videos over videos produced by or including a professional source.5 Additionally, only 3 of 19 videos about TSW were from a professional source, increasing the potential for patient misconceptions about topical corticosteroids. Future studies should examine the educational impact of patient-generated videos as well as features that make the patient experience videos more desirable for viewing.
- Mueller SM, Hongler VNS, Jungo P, et al. Fiction, falsehoods, and few facts: cross-sectional study on the content-related quality of atopic eczema-related videos on YouTube. J Med Internet Res. 2020;22:e15599. doi:10.2196/15599
- Torres T, Ferreira EO, Gonçalo M, et al. Update on atopic dermatitis. Acta Med Port. 2019;32:606-613. doi:10.20344/amp.11963
- Vogler SA, Lightner AL. Rethinking how we care for our patients in a time of social distancing during the COVID-19 pandemic. Br J Surg. 2020;107:937-939. doi:10.1002/bjs.11636
- The DISCERN Instrument. discern online. Accessed January 22, 2021. http://www.discern.org.uk/discern_instrument.php
- Pithadia DJ, Reynolds KA, Lee EB, et al. Dupilumab for atopic dermatitis: what are patients learning on YouTube? [published online April 16, 2020]. J Dermatolog Treat. doi:10.1080/09546634.2020.1755418
To the Editor:
Atopic dermatitis (eczema) affects approximately 20% of children worldwide.1 In atopic dermatitis management, patient education is crucial for optimal outcomes.2 The COVID-19 pandemic has impacted patient-physician interactions. To ensure safety of patients and physicians, visits may have been canceled, postponed, or conducted virtually, leaving less time for discussion and questions.3 As a consequence, patients may seek information about atopic dermatitis from alternative sources, including YouTube videos. We performed a cross-sectional study to analyze YouTube videos about topical treatments for atopic dermatitis.
During the week of July 16, 2020, we performed 4 private browser YouTube searches with default filters using the following terms: eczema topicals, eczema topical treatments, atopic dermatitis topicals, and atopic dermatitis topical treatments. For video selection, we defined topical treatments as topical corticosteroids, topical calcineurin inhibitors, crisaborole, emollients, wet wraps, and any prospective treatment topically administered. For each of the 4 searches, 2 researchers (A.M. and A.T.) independently examined the top 75 videos, yielding a total of 300 videos. Of them, 98 videos were duplicates, 19 videos were not about atopic dermatitis, and 91 videos were not about topical treatments, leaving a total of 92 videos for analysis (Figure 1).
For the 92 included videos, the length; upload year; number of views, likes, dislikes, and comments; interaction ratio (IR)(the sum of likes, dislikes, and comments divided by the number of views); and video content were determined. The videos were placed into mutually exclusive categories as follows: (1) patient experience, defined as a video about patient perspective; (2) professional source, defined as a video featuring a physician, physician extender, pharmacist, or scientist, or produced by a formal organization; or (3) other. The DISCERN Instrument was used for grading the reliability and quality of the 92 included videos. This instrument consists of 16 questions with the responses rated on a scale of 1 to 5.4 For analysis of DISCERN scores, patient experience and other videos were grouped together as nonprofessional source videos. A 2-sample t-test was used to compare DISCERN scores between professional source and nonprofessional source videos.
Most videos were uploaded in 2017 (n=19), 2018 (n=23), and 2019 (n=25), but 20 were uploaded in 2012-2016 and 5 were uploaded in 2020. The 92 videos had a mean length of 8 minutes and 35 seconds (range, 30 seconds to 62 minutes and 23 seconds).
Patient experience videos accounted for 23.9% (n=22) of videos. These videos discussed topical steroid withdrawal (TSW)(n=16), instructions for making emollients (n=2), and treatment successes (n=4). Professional source videos represented 67.4% (n=62) of videos. Of them, 40.3% (n=25) were physician oriented, defined as having extensive medical terminology or qualifying for continuing medical education credit. Three (4.8%) of the professional source videos were sponsored by a drug company. Other constituted the remaining 8.7% (n=8) of videos. Patient experience videos had more views (median views [interquartile range], 6865 [10,307]) and higher engagement (median IR [interquartile range], 0.038 [0.022]) than professional source videos (views: median views [interquartile range], 1052.5 [10,610.5]; engagement: median IR [interquartile range], 0.006 [0.008]).
Although less popular, professional source videos had a significantly higher DISCERN overall quality rating score (question 16) compared to those categorized as nonprofessional source (3.92 vs 1.53; P<.001). In contrast, nonprofessional source videos scored significantly higher on the quality-of-life question (question 13) compared to professional source videos (3.90 vs 2.56; P<.001)(eTable). (Three professional source videos were removed from YouTube before DISCERN scores could be assigned.)
Notably, 20.7% (n=19) of the 92 videos discussed TSW, and most of them were patient experiences (n=16). Other categories included topical steroids excluding TSW (n=11), steroid phobia (n=2), topical calcineurin inhibitors (n=2), crisaborole (n=6), news broadcast (n=7), wet wraps (n=5), product advertisement (n=7), and research (n=11)(Figure 2). Interestingly, there were no videos focusing on the calcineurin inhibitor black box warning.
Similar to prior studies, our results indicate preference for patient-generated videos over videos produced by or including a professional source.5 Additionally, only 3 of 19 videos about TSW were from a professional source, increasing the potential for patient misconceptions about topical corticosteroids. Future studies should examine the educational impact of patient-generated videos as well as features that make the patient experience videos more desirable for viewing.
To the Editor:
Atopic dermatitis (eczema) affects approximately 20% of children worldwide.1 In atopic dermatitis management, patient education is crucial for optimal outcomes.2 The COVID-19 pandemic has impacted patient-physician interactions. To ensure safety of patients and physicians, visits may have been canceled, postponed, or conducted virtually, leaving less time for discussion and questions.3 As a consequence, patients may seek information about atopic dermatitis from alternative sources, including YouTube videos. We performed a cross-sectional study to analyze YouTube videos about topical treatments for atopic dermatitis.
During the week of July 16, 2020, we performed 4 private browser YouTube searches with default filters using the following terms: eczema topicals, eczema topical treatments, atopic dermatitis topicals, and atopic dermatitis topical treatments. For video selection, we defined topical treatments as topical corticosteroids, topical calcineurin inhibitors, crisaborole, emollients, wet wraps, and any prospective treatment topically administered. For each of the 4 searches, 2 researchers (A.M. and A.T.) independently examined the top 75 videos, yielding a total of 300 videos. Of them, 98 videos were duplicates, 19 videos were not about atopic dermatitis, and 91 videos were not about topical treatments, leaving a total of 92 videos for analysis (Figure 1).
For the 92 included videos, the length; upload year; number of views, likes, dislikes, and comments; interaction ratio (IR)(the sum of likes, dislikes, and comments divided by the number of views); and video content were determined. The videos were placed into mutually exclusive categories as follows: (1) patient experience, defined as a video about patient perspective; (2) professional source, defined as a video featuring a physician, physician extender, pharmacist, or scientist, or produced by a formal organization; or (3) other. The DISCERN Instrument was used for grading the reliability and quality of the 92 included videos. This instrument consists of 16 questions with the responses rated on a scale of 1 to 5.4 For analysis of DISCERN scores, patient experience and other videos were grouped together as nonprofessional source videos. A 2-sample t-test was used to compare DISCERN scores between professional source and nonprofessional source videos.
Most videos were uploaded in 2017 (n=19), 2018 (n=23), and 2019 (n=25), but 20 were uploaded in 2012-2016 and 5 were uploaded in 2020. The 92 videos had a mean length of 8 minutes and 35 seconds (range, 30 seconds to 62 minutes and 23 seconds).
Patient experience videos accounted for 23.9% (n=22) of videos. These videos discussed topical steroid withdrawal (TSW)(n=16), instructions for making emollients (n=2), and treatment successes (n=4). Professional source videos represented 67.4% (n=62) of videos. Of them, 40.3% (n=25) were physician oriented, defined as having extensive medical terminology or qualifying for continuing medical education credit. Three (4.8%) of the professional source videos were sponsored by a drug company. Other constituted the remaining 8.7% (n=8) of videos. Patient experience videos had more views (median views [interquartile range], 6865 [10,307]) and higher engagement (median IR [interquartile range], 0.038 [0.022]) than professional source videos (views: median views [interquartile range], 1052.5 [10,610.5]; engagement: median IR [interquartile range], 0.006 [0.008]).
Although less popular, professional source videos had a significantly higher DISCERN overall quality rating score (question 16) compared to those categorized as nonprofessional source (3.92 vs 1.53; P<.001). In contrast, nonprofessional source videos scored significantly higher on the quality-of-life question (question 13) compared to professional source videos (3.90 vs 2.56; P<.001)(eTable). (Three professional source videos were removed from YouTube before DISCERN scores could be assigned.)
Notably, 20.7% (n=19) of the 92 videos discussed TSW, and most of them were patient experiences (n=16). Other categories included topical steroids excluding TSW (n=11), steroid phobia (n=2), topical calcineurin inhibitors (n=2), crisaborole (n=6), news broadcast (n=7), wet wraps (n=5), product advertisement (n=7), and research (n=11)(Figure 2). Interestingly, there were no videos focusing on the calcineurin inhibitor black box warning.
Similar to prior studies, our results indicate preference for patient-generated videos over videos produced by or including a professional source.5 Additionally, only 3 of 19 videos about TSW were from a professional source, increasing the potential for patient misconceptions about topical corticosteroids. Future studies should examine the educational impact of patient-generated videos as well as features that make the patient experience videos more desirable for viewing.
- Mueller SM, Hongler VNS, Jungo P, et al. Fiction, falsehoods, and few facts: cross-sectional study on the content-related quality of atopic eczema-related videos on YouTube. J Med Internet Res. 2020;22:e15599. doi:10.2196/15599
- Torres T, Ferreira EO, Gonçalo M, et al. Update on atopic dermatitis. Acta Med Port. 2019;32:606-613. doi:10.20344/amp.11963
- Vogler SA, Lightner AL. Rethinking how we care for our patients in a time of social distancing during the COVID-19 pandemic. Br J Surg. 2020;107:937-939. doi:10.1002/bjs.11636
- The DISCERN Instrument. discern online. Accessed January 22, 2021. http://www.discern.org.uk/discern_instrument.php
- Pithadia DJ, Reynolds KA, Lee EB, et al. Dupilumab for atopic dermatitis: what are patients learning on YouTube? [published online April 16, 2020]. J Dermatolog Treat. doi:10.1080/09546634.2020.1755418
- Mueller SM, Hongler VNS, Jungo P, et al. Fiction, falsehoods, and few facts: cross-sectional study on the content-related quality of atopic eczema-related videos on YouTube. J Med Internet Res. 2020;22:e15599. doi:10.2196/15599
- Torres T, Ferreira EO, Gonçalo M, et al. Update on atopic dermatitis. Acta Med Port. 2019;32:606-613. doi:10.20344/amp.11963
- Vogler SA, Lightner AL. Rethinking how we care for our patients in a time of social distancing during the COVID-19 pandemic. Br J Surg. 2020;107:937-939. doi:10.1002/bjs.11636
- The DISCERN Instrument. discern online. Accessed January 22, 2021. http://www.discern.org.uk/discern_instrument.php
- Pithadia DJ, Reynolds KA, Lee EB, et al. Dupilumab for atopic dermatitis: what are patients learning on YouTube? [published online April 16, 2020]. J Dermatolog Treat. doi:10.1080/09546634.2020.1755418
Practice Points
- YouTube is a readily accessible resource for educating patients about topical treatments for atopic dermatitis.
- Although professional source videos comprised a larger percentage of the videos included within our study, patient experience videos had a higher number of views and engagement.
- Twenty-one percent (19/92) of the videos examined in our study discussed topical steroid withdrawal, and the majority of them were patient experience videos.
Plant Dermatitis: More Than Just Poison Ivy
Plants can contribute to a variety of dermatoses. The Toxicodendron genus, which includes poison ivy, poison oak, and poison sumac, is a well-known and common cause of allergic contact dermatitis (ACD), but many other plants can cause direct or airborne contact dermatitis, especially in gardeners, florists, and farmers. This article provides an overview of different plant-related dermatoses and culprit plants as well as how these dermatoses should be diagnosed and treated.
Epidemiology
Plant dermatoses affect more than 50 million individuals each year.1,2 In the United States, the Toxicodendron genus causes ACD in more than 70% of exposed individuals, leading to medical visits.3 An urgent care visit for a plant-related dermatitis is estimated to cost $168, while an emergency department visit can cost 3 times as much.4 Although less common, Compositae plants are another important culprit of plant dermatitis, particularly in gardeners, florists, and farmers. Data from the 2017-2018 North American Contact Dermatitis Group screening series (N=4947) showed sesquiterpene lactones and Compositae to be positive in 0.5% of patch-tested patients.5
Plant Dermatitis Classifications
Plant dermatitis can be classified into 5 main categories: ACD, mechanical irritant contact dermatitis, chemical irritant contact dermatitis, light-mediated dermatitis, and pseudophytodermatitis.6
Allergic contact dermatitis is an immune-mediated type IV delayed hypersensitivity reaction. The common molecular allergens in plants include phenols, α-methylene-γ-butyrolactones, quinones, terpenes, disulfides, isothiocyanates, and polyacetylenic derivatives.6
Plant contact dermatitis due to mechanical and chemical irritants is precipitated by multiple mechanisms, including disruption of the epidermal barrier and subsequent cytokine release from keratinocytes.7 Nonimmunologic contact urticaria from plants is thought to be a type of irritant reaction precipitated by mechanical or chemical trauma.8
Light-mediated dermatitis includes phytophotodermatitis and photoallergic contact dermatitis. Phytophotodermatitis is a phototoxic reaction triggered by exposure to both plant-derived furanocoumarin and UVA light.9 By contrast, photoallergic contact dermatitis is a delayed hypersensitivity reaction from prior sensitization to a light-activated antigen.10
Pseudophytodermatitis, as its name implies, is not truly mediated by an allergen or irritant intrinsic to the plant but rather by dyes, waxes, insecticides, or arthropods that inhabit the plant or are secondarily applied.6
Common Plant Allergens
Anacardiaceae Family
Most of the allergenic plants within the Anacardiaceae family belong to the Toxicodendron genus, which encompasses poison ivy (Toxicodendron radicans), poison oak (Toxicodendron pubescens,Toxicodendron quercifolium, Toxicodendron diversiloum), and poison sumac (Toxicodendron vernix). Poison ivy is the celebrity of the Anacardiaceae family and contributes to most cases of plant-related ACD. It is found in every state in the continental United States. Poison oak is another common culprit found in the western and southeastern United States.11 Plants within the Anacardiaceae family contain an oleoresin called urushiol, which is the primary sensitizing substance. Although poison ivy and poison oak grow well in full sun to partial shade, poison sumac typically is found in damp swampy areas east of the Rocky Mountains. Most cases of ACD related to Anacardiaceae species are due to direct contact with urushiol from a Toxicodendron plant, but burning of brush containing Toxicodendron can cause airborne exposure when urushiol oil is carried by smoke particles.12 Sensitization to Toxicodendron can cause ACD to other Anacardiaceae species such as the Japanese lacquer tree (Toxicodendron vernicifluum), mango tree (Mangifera indica), cashew tree (Anacardium occidentale), and Indian marking nut tree (Semecarpus anacardium).6 Cross-reactions to components of the ginkgo tree (Ginkgo biloba) also are possible.
Toxicodendron plants can be more easily identified and avoided with knowledge of their characteristic leaf patterns. The most dependable way to identify poison ivy and poison oak species is to look for plants with 3 leaves, giving rise to the common saying, “Leaves of three, leave them be.” Poison sumac plants have groups of 7 to 13 leaves arranged as pairs along a central rib. Another helpful finding is a black deposit that Toxicodendron species leave behind following trauma to the leaves. Urushiol oxidizes when exposed to air and turns into a black deposit that can be seen on damaged leaves themselves or can be demonstrated in a black spot test to verify if a plant is a Toxicodendron species. The test is performed by gathering (carefully, without direct contact) a few leaves in a paper towel and crushing them to release sap. Within minutes, the sap will turn black if the plant is indeed a Toxicodendron species.13Pruritic, edematous, erythematous papules, plaques, and eventual vesicles in a linear distribution are suspicious for Toxicodendron exposure. Although your pet will not develop Toxicodendron ACD, oleoresin-contaminated pets can transfer the oils to their owners after coming into contact with these plants. Toxicodendron dermatitis also can be acquired from oleoresin-contaminated fomites such as clothing and shoes worn in the garden or when hiking. Toxicodendron dermatitis can appear at different sites on the body at different times depending on the amount of oleoresin exposure as well as epidermal thickness. For example, the oleoresin can be transferred from the hands to body areas with a thinner stratum corneum (eg, genitalia) and cause subsequent dermatitis.1
Compositae Family
The Compositae family (also known as Asteraceae) is a large plant family with more than 20,000 species, including numerous weeds, wildflowers, and vegetables. The flowers, leaves, stems, and pollens of the Compositae family are coated by cyclic esters called sesquiterpene lactones. Mitchell and Dupuis14 showed that sesquiterpene lactones are the allergens responsible for ACD to various Compositae plants, including ragweed (Ambrosia), sneezeweed (Helenium), and chrysanthemums (Chrysanthemum). Common Compositae vegetables such as lettuce (Lactuca sativa) have been reported to cause ACD in chefs, grocery store produce handlers, gardeners, and even owners of lettuce-eating pet guinea pigs and turtles.15 Similarly, artichokes (Cynara scolymus) can cause ACD in gardeners.16 Exposure to Compositae species also has been implicated in photoallergic reactions, and studies have demonstrated that some patients with chronic actinic dermatitis also have positive patch test reactions to Compositae species and/or sesquiterpene lactones.17,18
In addition to direct contact with Compositae plants, airborne exposure to sesquiterpene lactones can cause ACD.14 The pattern of airborne contact dermatitis typically involves exposed areas such as the eyelids, central face, and/or neck. The beak sign also can be a clue to airborne contact dermatitis, which involves dermatitis of the face that spares the nasal tip and/or nasal ridge. It is thought that the beak sign may result from increased sebaceous gland concentration on the nose, which prevents penetration of allergens and irritants.19 Unlike photoallergic contact dermatitis, which also can involve the face, airborne ACD frequently involves photoprotected areas such as the submandibular chin and the upper lip. Davies and Kersey20 reported the case of a groundsman who was cutting grass with dandelions (Taraxacum officinale) and was found to have associated airborne ACD of the face, neck, and forearms due to Compositae allergy. In a different setting, the aromas of chamomile (Matricaria chamomilla) have been reported to cause airborne ACD in a tea drinker.21 Paulsen22 found that ingestion of chamomile tea can induce systemic ACD in sensitized individuals.
Alstroemeriaceae, Liliaceae, and Primulaceae
Florists are exposed to many plant species and have a high prevalence of ACD. Thiboutot et al23 found that 15 of 57 (26%) floral workers experienced hand dermatitis that cleared with time away from work. The Peruvian lily (Alstroemeria, Alstroemeriaceae family), which contains tuliposide A, was found to be the leading cause of sensitization.23 Tulips (Tulipa, Liliaceae family), as the flower name suggests, also contain tuliposide A, which along with mechanical irritation from the course tecta fibers on the bulbs lead to a dermatitis known as tulip fingers.24,25 Poison primrose (Primula obconica, Primulaceae family), cultivated for its highly colorful flowers, contains the contact allergen primin.6 A common clinical presentation of ACD for any of these culprit flowers is localized dermatitis of the thumb and index finger in a florist or gardener.
Plants That Cause Irritant Reactions
Cactuses
Although the long spines of the Cactaceae family of cactuses is a warning for passersby, it is the small and nearly invisible barbed hairs (glochids) that inflict a more dramatic cutaneous reaction. The prickly pear cactus (Opuntia species) is a good example of such a plant, as its glochids cause mechanical irritation but also can become embedded in the skin and result in subcutaneous granulomas known as sabra dermatitis.26
Stinging Nettle
The dermatologic term urticaria owes its namesake to the stinging nettle plant, which comes from the family Urticaceae. The stinging nettle has small hairs on its leaves, referred to as stinging trichomes, which have needlelike tips that pierce the skin and inject a mix of histamine, formic acid, and acetylcholine, causing a pruritic dermatitis that may last up to 12 hours.27 The plant is found worldwide and is a common weed in North America.
Phytophotodermatitis
Lemons and limes (Rutaceae family) are common culprits of phytophotodermatitis, often causing what is known as a margarita burn after outdoor consumption or preparation of this tasty citrus beverage.28 An accidental spray of lime juice on the skin while adding it to a beer, guacamole, salsa, or any other food or beverage also can cause phytophotodermatitis.29-31 Although the juice of lemons and limes contains psoralens, the rind can contain a 6- to 186-fold increased concentration.32 Psoralen is the photoactive agent in Rutaceae plants that intercalates in double-stranded DNA and promotes intrastrand cross-links when exposed to UVA light, which ultimately leads to dermatitis.9 Phytophotodermatitis commonly causes erythema, edema, and painful bullae on sun-exposed areas and classically heals with hyperpigmentation.
Pseudophytodermatitis can occur in grain farmers and harvesters who handle wheat and/or barley and incidentally come in contact with insects and chemicals on the plant material. Pseudophytodermatitis from mites in the wheat and/or barley plant can occur at harvest time when contact with the plant material is high. Insects such as the North American itch mite (Pediculoides ventricosus) can cause petechiae, wheals, and pustules. In addition, insecticides such as malathion and arsenical sprays that are applied to plant leaves can cause pseudophytodermatitis, which may be initially diagnosed as dermatitis to the plant itself.6
Patch Testing to Plants
When a patient presents with recurrent or persistent dermatitis and a plant contact allergen is suspected, patch testing is indicated. Most comprehensive patch test series contain various plant allergens, such as sesquiterpene lactones, Compositae mix, and limonene hydroperoxides, and patch testing to a specialized plant series may be necessary. Poison ivy/oak/sumac allergens typically are not included in patch test series because of the high prevalence of allergic reactions to these chemicals and the likelihood of sensitization when patch testing with urushiol. Compositae contact sensitization can be difficult to diagnose because neither sesquiterpene lactone mix 0.1% nor parthenolide 0.1% are sensitive enough to pick up all Compositae allergies.33,34 Paulsen and Andersen34 proposed that if Compositae sensitization is suspected, testing should include sesquiterpene lactone, parthenolide, and Compositae mix II 2.5%, as well as other potential Compositae allergens based on the patient’s history.34
Because plants can have geographic variability and contain potentially unknown allergens,35 testing to plant components may increase the diagnostic yield of patch testing. Dividing the plant into component parts (ie, stem, bulb, leaf, flower) is helpful, as different components have different allergen concentrations. It is important to consult expert resources before proceeding with plant component patch testing because irritant reactions are frequent and may confound the testing.36
Prevention and Treatment
For all plant dermatoses, the mainstay of prevention is to avoid contact with the offending plant material. Gloves can be an important protective tool for plant dermatitis prevention; the correct material depends on the plant species being handled. Rubber gloves should not be worn to protect against Toxicodendron plants since the catechols in urushiol are soluble in rubber; vinyl gloves should be worn instead.6 Marks37 found that tuliposide A, the allergen in the Peruvian lily (Alstroemeria), penetrates both vinyl and latex gloves; it does not penetrate nitrile gloves. If exposed, the risk of dermatitis can be decreased if the allergen is washed away with soap and water as soon as possible. Some allergens such as Toxicodendron are absorbed quickly and need to be washed off within 10 minutes of exposure.6 Importantly, exposed gardening gloves may continue to perpetuate ACD if the allergen is not also washed off the gloves themselves.
For light-mediated dermatoses, sun avoidance or use of an effective sunscreen can reduce symptoms in an individual who has already been exposed.10 UVA light activates psoralen-mediated dermatitis but not until 30 to 120 minutes after absorption into the skin.38
Barrier creams are thought to be protective against plant ACD through a variety of mechanisms. The cream itself is meant to reduce skin contact to an allergen or irritant. Additionally, barrier creams contain active ingredients such as silicone, hydrocarbons, and aluminum chlorohydrate, which are thought to trap or transform offending agents before contacting the skin. When contact with a Toxicodendron species is anticipated, Marks et al39 found that dermatitis was absent or significantly reduced when 144 patients were pretreated with quaternium-18 bentonite lotion 5% (P<.0001).
Although allergen avoidance and use of gloves and barrier creams are the mainstays of preventing plant dermatoses, treatment often is required to control postexposure symptoms. For all plant dermatoses, topical corticosteroids can be used to reduce inflammation and pruritus. In some cases, systemic steroids may be necessary. To prevent rebound of dermatitis, patients often require a 3-week or longer course of oral steroids to quell the reaction, particularly if the dermatitis is vigorous or an id reaction is present.40 Antihistamines and cold compresses also can provide symptomatic relief.
Final Interpretation
Plants can cause a variety of dermatoses. Although Toxicodendron plants are the most frequent cause of ACD, it is important to keep in mind that florists, gardeners, and farmers are exposed to a large variety of allergens, irritants, and phototoxic agents that cause dermatoses as well. Confirmation of plant-induced ACD involves patch testing against suspected species. Prevention involves use of appropriate barriers and avoidance of implicated plants. Treatment includes topical steroids, antihistamines, and prednisone.
- Gladman AC. Toxicodendron dermatitis: poison ivy, oak, and sumac. Wilderness Environ Med. 2006;17:120-128.
- Pariser D, Ceilley R, Lefkovits A, et al. Poison ivy, oak and sumac. Derm Insights. 2003;4:26-28.
- Wolff K, Johnson R. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 6th ed. McGraw Hill Education; 2009.
- Zomorodi N, Butt M, Maczuga S, et al. Cost and diagnostic characteristics of Toxicodendron dermatitis in the USA: a retrospective cross-sectional analysis. Br J Dermatol. 2020;183:772-773.
- DeKoven JG, Silverberg JI, Warshaw EM, et al. North American Contact Dermatitis Group patch test results: 2017-2018. Dermatitis. 2021;32:111-123.
- Fowler JF, Zirwas MJ. Fisher’s Contact Dermatitis. 7th ed. Contact Dermatitis Institute; 2019.
- Smith HR, Basketter DA, McFadden JP. Irritant dermatitis, irritancy and its role in allergic contact dermatitis. Clin Exp Dermatol. 2002;27:138-146.
- Wakelin SH. Contact urticaria. Clin Exp Dermatol. 2001;26:132-136.
- Ellis CR, Elston DM. Psoralen-induced phytophotodermatitis. Dermatitis. 2021;32:140-143.
- Deleo VA. Photocontact dermatitis. Dermatol Ther. 2004;17:279-288.
- National Institute for Occupational Safety and Health. Poisonous plants. Centers for Disease Control and Prevention website. Updated June 1, 2018. Accessed August 10, 2021. https://www.cdc.gov/niosh/topics/plants/geographic.html
- Schloemer JA, Zirwas MJ, Burkhart CG. Airborne contact dermatitis: common causes in the USA. Int J Dermatol. 2015;54:271-274.
- Guin JD. The black spot test for recognizing poison ivy and related species. J Am Acad Dermatol. 1980;2:332-333.
- Mitchell J, Dupuis G. Allergic contact dermatitis from sesquiterpenoids of the Compositae family of plants. Br J Dermatol. 1971;84:139-150.
- Paulsen E, Andersen KE. Lettuce contact allergy. Contact Dermatitis. 2016;74:67-75.
- Samaran Q, Clark E, Dereure O, et al. Airborne allergic contact dermatitis caused by artichoke. Contact Dermatitis. 2020;82:395-397.
- Du H, Ross JS, Norris PG, et al. Contact and photocontact sensitization in chronic actinic dermatitis: sesquiterpene lactone mix is an important allergen. Br J Dermatol. 1995;132:543-547.
- Wrangsjo K, Marie Ros A, Walhberg JE. Contact allergy to Compositae plants in patients with summer-exacerbated dermatitis. Contact Dermatitis. 1990;22:148-154.
- Staser K, Ezra N, Sheehan MP, et al. The beak sign: a clinical clue to airborne contact dermatitis. Dermatitis. 2014;25:97-98.
- Davies M, Kersey J. Contact allergy to yarrow and dandelion. Contact Dermatitis. 1986;14:256-257.
- Anzai A, Vázquez Herrera NE, Tosti A. Airborne allergic contact dermatitis caused by chamomile tea. Contact Dermatitis. 2015;72:254-255.
- Paulsen E. Systemic allergic dermatitis caused by sesquiterpene lactones. Contact Dermatitis. 2017;76:1-10.
- Thiboutot DM, Hamory BH, Marks JG. Dermatoses among floral shop workers. J Am Acad Dermatol. 1990;22:54-58.
- Hjorth N, Wilkinson DS. Contact dermatitis IV. tulip fingers, hyacinth itch and lily rash. Br J Dermatol. 1968;80:696-698.
- Guin JD, Franks H. Fingertip dermatitis in a retail florist. Cutis. 2001;67:328-330.
- Magro C, Lipner S. Sabra dermatitis: combined features of delayed hypersensitivity and foreign body reaction to implanted glochidia. Dermatol Online J. 2020;26:13030/qt2157f9g0.
- Cummings AJ, Olsen M. Mechanism of action of stinging nettles. Wilderness Environ Med. 2011;22:136-139.
- Maniam G, Light KML, Wilson J. Margarita burn: recognition and treatment of phytophotodermatitis. J Am Board Fam Med. 2021;34:398-401.
- Flugman SL. Mexican beer dermatitis: a unique variant of lime phytophotodermatitis attributable to contemporary beer-drinking practices. Arch Dermatol. 2010;146:1194-1195.
- Kung AC, Stephens MB, Darling T. Phytophotodermatitis: bulla formation and hyperpigmentation during spring break. Mil Med. 2009;174:657-661.
- Smith LG. Phytophotodermatitis. Images Emerg Med. 2017;1:146-147.
- Wagner AM, Wu JJ, Hansen RC, et al. Bullous phytophotodermatitis associated with high natural concentrations of furanocoumarins in limes. Am J Contact Dermat. 2002;13:10-14.
- Green C, Ferguson J. Sesquiterpene lactone mix is not an adequate screen for Compositae allergy. Contact Dermatitis. 1994;31:151-153.
- Paulsen E, Andersen KE. Screening for Compositae contact sensitization with sesquiterpene lactones and Compositae mix 2.5% pet. Contact Dermatitis. 2019;81:368-373.
- Paulsen E, Andersen KE. Patch testing with constituents of Compositae mixes. Contact Dermatitis. 2012;66:241-246.
- Frosch PJ, Geier J, Uter W, et al. Patch testing with the patients’ own products. Contact Dermatitis. 2011:929-941.
- Marks JG. Allergic contact dermatitis to Alstroemeria. Arch Dermatol. 1988;124:914-916.
- Moreau JF, English JC, Gehris RP. Phytophotodermatitis. J Pediatr Adolesc Gynecol. 2014;27:93-94.
- Marks JG, Fowler JF, Sherertz EF, et al. Prevention of poison ivy and poison oak allergic contact dermatitis by quaternium-18 bentonite. J Am Acad Dermatol. 1995;33:212-216.
- Craig K, Meadows SE. What is the best duration of steroid therapy for contact dermatitis (rhus)? J Fam Pract. 2006;55:166-167.
Plants can contribute to a variety of dermatoses. The Toxicodendron genus, which includes poison ivy, poison oak, and poison sumac, is a well-known and common cause of allergic contact dermatitis (ACD), but many other plants can cause direct or airborne contact dermatitis, especially in gardeners, florists, and farmers. This article provides an overview of different plant-related dermatoses and culprit plants as well as how these dermatoses should be diagnosed and treated.
Epidemiology
Plant dermatoses affect more than 50 million individuals each year.1,2 In the United States, the Toxicodendron genus causes ACD in more than 70% of exposed individuals, leading to medical visits.3 An urgent care visit for a plant-related dermatitis is estimated to cost $168, while an emergency department visit can cost 3 times as much.4 Although less common, Compositae plants are another important culprit of plant dermatitis, particularly in gardeners, florists, and farmers. Data from the 2017-2018 North American Contact Dermatitis Group screening series (N=4947) showed sesquiterpene lactones and Compositae to be positive in 0.5% of patch-tested patients.5
Plant Dermatitis Classifications
Plant dermatitis can be classified into 5 main categories: ACD, mechanical irritant contact dermatitis, chemical irritant contact dermatitis, light-mediated dermatitis, and pseudophytodermatitis.6
Allergic contact dermatitis is an immune-mediated type IV delayed hypersensitivity reaction. The common molecular allergens in plants include phenols, α-methylene-γ-butyrolactones, quinones, terpenes, disulfides, isothiocyanates, and polyacetylenic derivatives.6
Plant contact dermatitis due to mechanical and chemical irritants is precipitated by multiple mechanisms, including disruption of the epidermal barrier and subsequent cytokine release from keratinocytes.7 Nonimmunologic contact urticaria from plants is thought to be a type of irritant reaction precipitated by mechanical or chemical trauma.8
Light-mediated dermatitis includes phytophotodermatitis and photoallergic contact dermatitis. Phytophotodermatitis is a phototoxic reaction triggered by exposure to both plant-derived furanocoumarin and UVA light.9 By contrast, photoallergic contact dermatitis is a delayed hypersensitivity reaction from prior sensitization to a light-activated antigen.10
Pseudophytodermatitis, as its name implies, is not truly mediated by an allergen or irritant intrinsic to the plant but rather by dyes, waxes, insecticides, or arthropods that inhabit the plant or are secondarily applied.6
Common Plant Allergens
Anacardiaceae Family
Most of the allergenic plants within the Anacardiaceae family belong to the Toxicodendron genus, which encompasses poison ivy (Toxicodendron radicans), poison oak (Toxicodendron pubescens,Toxicodendron quercifolium, Toxicodendron diversiloum), and poison sumac (Toxicodendron vernix). Poison ivy is the celebrity of the Anacardiaceae family and contributes to most cases of plant-related ACD. It is found in every state in the continental United States. Poison oak is another common culprit found in the western and southeastern United States.11 Plants within the Anacardiaceae family contain an oleoresin called urushiol, which is the primary sensitizing substance. Although poison ivy and poison oak grow well in full sun to partial shade, poison sumac typically is found in damp swampy areas east of the Rocky Mountains. Most cases of ACD related to Anacardiaceae species are due to direct contact with urushiol from a Toxicodendron plant, but burning of brush containing Toxicodendron can cause airborne exposure when urushiol oil is carried by smoke particles.12 Sensitization to Toxicodendron can cause ACD to other Anacardiaceae species such as the Japanese lacquer tree (Toxicodendron vernicifluum), mango tree (Mangifera indica), cashew tree (Anacardium occidentale), and Indian marking nut tree (Semecarpus anacardium).6 Cross-reactions to components of the ginkgo tree (Ginkgo biloba) also are possible.
Toxicodendron plants can be more easily identified and avoided with knowledge of their characteristic leaf patterns. The most dependable way to identify poison ivy and poison oak species is to look for plants with 3 leaves, giving rise to the common saying, “Leaves of three, leave them be.” Poison sumac plants have groups of 7 to 13 leaves arranged as pairs along a central rib. Another helpful finding is a black deposit that Toxicodendron species leave behind following trauma to the leaves. Urushiol oxidizes when exposed to air and turns into a black deposit that can be seen on damaged leaves themselves or can be demonstrated in a black spot test to verify if a plant is a Toxicodendron species. The test is performed by gathering (carefully, without direct contact) a few leaves in a paper towel and crushing them to release sap. Within minutes, the sap will turn black if the plant is indeed a Toxicodendron species.13Pruritic, edematous, erythematous papules, plaques, and eventual vesicles in a linear distribution are suspicious for Toxicodendron exposure. Although your pet will not develop Toxicodendron ACD, oleoresin-contaminated pets can transfer the oils to their owners after coming into contact with these plants. Toxicodendron dermatitis also can be acquired from oleoresin-contaminated fomites such as clothing and shoes worn in the garden or when hiking. Toxicodendron dermatitis can appear at different sites on the body at different times depending on the amount of oleoresin exposure as well as epidermal thickness. For example, the oleoresin can be transferred from the hands to body areas with a thinner stratum corneum (eg, genitalia) and cause subsequent dermatitis.1
Compositae Family
The Compositae family (also known as Asteraceae) is a large plant family with more than 20,000 species, including numerous weeds, wildflowers, and vegetables. The flowers, leaves, stems, and pollens of the Compositae family are coated by cyclic esters called sesquiterpene lactones. Mitchell and Dupuis14 showed that sesquiterpene lactones are the allergens responsible for ACD to various Compositae plants, including ragweed (Ambrosia), sneezeweed (Helenium), and chrysanthemums (Chrysanthemum). Common Compositae vegetables such as lettuce (Lactuca sativa) have been reported to cause ACD in chefs, grocery store produce handlers, gardeners, and even owners of lettuce-eating pet guinea pigs and turtles.15 Similarly, artichokes (Cynara scolymus) can cause ACD in gardeners.16 Exposure to Compositae species also has been implicated in photoallergic reactions, and studies have demonstrated that some patients with chronic actinic dermatitis also have positive patch test reactions to Compositae species and/or sesquiterpene lactones.17,18
In addition to direct contact with Compositae plants, airborne exposure to sesquiterpene lactones can cause ACD.14 The pattern of airborne contact dermatitis typically involves exposed areas such as the eyelids, central face, and/or neck. The beak sign also can be a clue to airborne contact dermatitis, which involves dermatitis of the face that spares the nasal tip and/or nasal ridge. It is thought that the beak sign may result from increased sebaceous gland concentration on the nose, which prevents penetration of allergens and irritants.19 Unlike photoallergic contact dermatitis, which also can involve the face, airborne ACD frequently involves photoprotected areas such as the submandibular chin and the upper lip. Davies and Kersey20 reported the case of a groundsman who was cutting grass with dandelions (Taraxacum officinale) and was found to have associated airborne ACD of the face, neck, and forearms due to Compositae allergy. In a different setting, the aromas of chamomile (Matricaria chamomilla) have been reported to cause airborne ACD in a tea drinker.21 Paulsen22 found that ingestion of chamomile tea can induce systemic ACD in sensitized individuals.
Alstroemeriaceae, Liliaceae, and Primulaceae
Florists are exposed to many plant species and have a high prevalence of ACD. Thiboutot et al23 found that 15 of 57 (26%) floral workers experienced hand dermatitis that cleared with time away from work. The Peruvian lily (Alstroemeria, Alstroemeriaceae family), which contains tuliposide A, was found to be the leading cause of sensitization.23 Tulips (Tulipa, Liliaceae family), as the flower name suggests, also contain tuliposide A, which along with mechanical irritation from the course tecta fibers on the bulbs lead to a dermatitis known as tulip fingers.24,25 Poison primrose (Primula obconica, Primulaceae family), cultivated for its highly colorful flowers, contains the contact allergen primin.6 A common clinical presentation of ACD for any of these culprit flowers is localized dermatitis of the thumb and index finger in a florist or gardener.
Plants That Cause Irritant Reactions
Cactuses
Although the long spines of the Cactaceae family of cactuses is a warning for passersby, it is the small and nearly invisible barbed hairs (glochids) that inflict a more dramatic cutaneous reaction. The prickly pear cactus (Opuntia species) is a good example of such a plant, as its glochids cause mechanical irritation but also can become embedded in the skin and result in subcutaneous granulomas known as sabra dermatitis.26
Stinging Nettle
The dermatologic term urticaria owes its namesake to the stinging nettle plant, which comes from the family Urticaceae. The stinging nettle has small hairs on its leaves, referred to as stinging trichomes, which have needlelike tips that pierce the skin and inject a mix of histamine, formic acid, and acetylcholine, causing a pruritic dermatitis that may last up to 12 hours.27 The plant is found worldwide and is a common weed in North America.
Phytophotodermatitis
Lemons and limes (Rutaceae family) are common culprits of phytophotodermatitis, often causing what is known as a margarita burn after outdoor consumption or preparation of this tasty citrus beverage.28 An accidental spray of lime juice on the skin while adding it to a beer, guacamole, salsa, or any other food or beverage also can cause phytophotodermatitis.29-31 Although the juice of lemons and limes contains psoralens, the rind can contain a 6- to 186-fold increased concentration.32 Psoralen is the photoactive agent in Rutaceae plants that intercalates in double-stranded DNA and promotes intrastrand cross-links when exposed to UVA light, which ultimately leads to dermatitis.9 Phytophotodermatitis commonly causes erythema, edema, and painful bullae on sun-exposed areas and classically heals with hyperpigmentation.
Pseudophytodermatitis can occur in grain farmers and harvesters who handle wheat and/or barley and incidentally come in contact with insects and chemicals on the plant material. Pseudophytodermatitis from mites in the wheat and/or barley plant can occur at harvest time when contact with the plant material is high. Insects such as the North American itch mite (Pediculoides ventricosus) can cause petechiae, wheals, and pustules. In addition, insecticides such as malathion and arsenical sprays that are applied to plant leaves can cause pseudophytodermatitis, which may be initially diagnosed as dermatitis to the plant itself.6
Patch Testing to Plants
When a patient presents with recurrent or persistent dermatitis and a plant contact allergen is suspected, patch testing is indicated. Most comprehensive patch test series contain various plant allergens, such as sesquiterpene lactones, Compositae mix, and limonene hydroperoxides, and patch testing to a specialized plant series may be necessary. Poison ivy/oak/sumac allergens typically are not included in patch test series because of the high prevalence of allergic reactions to these chemicals and the likelihood of sensitization when patch testing with urushiol. Compositae contact sensitization can be difficult to diagnose because neither sesquiterpene lactone mix 0.1% nor parthenolide 0.1% are sensitive enough to pick up all Compositae allergies.33,34 Paulsen and Andersen34 proposed that if Compositae sensitization is suspected, testing should include sesquiterpene lactone, parthenolide, and Compositae mix II 2.5%, as well as other potential Compositae allergens based on the patient’s history.34
Because plants can have geographic variability and contain potentially unknown allergens,35 testing to plant components may increase the diagnostic yield of patch testing. Dividing the plant into component parts (ie, stem, bulb, leaf, flower) is helpful, as different components have different allergen concentrations. It is important to consult expert resources before proceeding with plant component patch testing because irritant reactions are frequent and may confound the testing.36
Prevention and Treatment
For all plant dermatoses, the mainstay of prevention is to avoid contact with the offending plant material. Gloves can be an important protective tool for plant dermatitis prevention; the correct material depends on the plant species being handled. Rubber gloves should not be worn to protect against Toxicodendron plants since the catechols in urushiol are soluble in rubber; vinyl gloves should be worn instead.6 Marks37 found that tuliposide A, the allergen in the Peruvian lily (Alstroemeria), penetrates both vinyl and latex gloves; it does not penetrate nitrile gloves. If exposed, the risk of dermatitis can be decreased if the allergen is washed away with soap and water as soon as possible. Some allergens such as Toxicodendron are absorbed quickly and need to be washed off within 10 minutes of exposure.6 Importantly, exposed gardening gloves may continue to perpetuate ACD if the allergen is not also washed off the gloves themselves.
For light-mediated dermatoses, sun avoidance or use of an effective sunscreen can reduce symptoms in an individual who has already been exposed.10 UVA light activates psoralen-mediated dermatitis but not until 30 to 120 minutes after absorption into the skin.38
Barrier creams are thought to be protective against plant ACD through a variety of mechanisms. The cream itself is meant to reduce skin contact to an allergen or irritant. Additionally, barrier creams contain active ingredients such as silicone, hydrocarbons, and aluminum chlorohydrate, which are thought to trap or transform offending agents before contacting the skin. When contact with a Toxicodendron species is anticipated, Marks et al39 found that dermatitis was absent or significantly reduced when 144 patients were pretreated with quaternium-18 bentonite lotion 5% (P<.0001).
Although allergen avoidance and use of gloves and barrier creams are the mainstays of preventing plant dermatoses, treatment often is required to control postexposure symptoms. For all plant dermatoses, topical corticosteroids can be used to reduce inflammation and pruritus. In some cases, systemic steroids may be necessary. To prevent rebound of dermatitis, patients often require a 3-week or longer course of oral steroids to quell the reaction, particularly if the dermatitis is vigorous or an id reaction is present.40 Antihistamines and cold compresses also can provide symptomatic relief.
Final Interpretation
Plants can cause a variety of dermatoses. Although Toxicodendron plants are the most frequent cause of ACD, it is important to keep in mind that florists, gardeners, and farmers are exposed to a large variety of allergens, irritants, and phototoxic agents that cause dermatoses as well. Confirmation of plant-induced ACD involves patch testing against suspected species. Prevention involves use of appropriate barriers and avoidance of implicated plants. Treatment includes topical steroids, antihistamines, and prednisone.
Plants can contribute to a variety of dermatoses. The Toxicodendron genus, which includes poison ivy, poison oak, and poison sumac, is a well-known and common cause of allergic contact dermatitis (ACD), but many other plants can cause direct or airborne contact dermatitis, especially in gardeners, florists, and farmers. This article provides an overview of different plant-related dermatoses and culprit plants as well as how these dermatoses should be diagnosed and treated.
Epidemiology
Plant dermatoses affect more than 50 million individuals each year.1,2 In the United States, the Toxicodendron genus causes ACD in more than 70% of exposed individuals, leading to medical visits.3 An urgent care visit for a plant-related dermatitis is estimated to cost $168, while an emergency department visit can cost 3 times as much.4 Although less common, Compositae plants are another important culprit of plant dermatitis, particularly in gardeners, florists, and farmers. Data from the 2017-2018 North American Contact Dermatitis Group screening series (N=4947) showed sesquiterpene lactones and Compositae to be positive in 0.5% of patch-tested patients.5
Plant Dermatitis Classifications
Plant dermatitis can be classified into 5 main categories: ACD, mechanical irritant contact dermatitis, chemical irritant contact dermatitis, light-mediated dermatitis, and pseudophytodermatitis.6
Allergic contact dermatitis is an immune-mediated type IV delayed hypersensitivity reaction. The common molecular allergens in plants include phenols, α-methylene-γ-butyrolactones, quinones, terpenes, disulfides, isothiocyanates, and polyacetylenic derivatives.6
Plant contact dermatitis due to mechanical and chemical irritants is precipitated by multiple mechanisms, including disruption of the epidermal barrier and subsequent cytokine release from keratinocytes.7 Nonimmunologic contact urticaria from plants is thought to be a type of irritant reaction precipitated by mechanical or chemical trauma.8
Light-mediated dermatitis includes phytophotodermatitis and photoallergic contact dermatitis. Phytophotodermatitis is a phototoxic reaction triggered by exposure to both plant-derived furanocoumarin and UVA light.9 By contrast, photoallergic contact dermatitis is a delayed hypersensitivity reaction from prior sensitization to a light-activated antigen.10
Pseudophytodermatitis, as its name implies, is not truly mediated by an allergen or irritant intrinsic to the plant but rather by dyes, waxes, insecticides, or arthropods that inhabit the plant or are secondarily applied.6
Common Plant Allergens
Anacardiaceae Family
Most of the allergenic plants within the Anacardiaceae family belong to the Toxicodendron genus, which encompasses poison ivy (Toxicodendron radicans), poison oak (Toxicodendron pubescens,Toxicodendron quercifolium, Toxicodendron diversiloum), and poison sumac (Toxicodendron vernix). Poison ivy is the celebrity of the Anacardiaceae family and contributes to most cases of plant-related ACD. It is found in every state in the continental United States. Poison oak is another common culprit found in the western and southeastern United States.11 Plants within the Anacardiaceae family contain an oleoresin called urushiol, which is the primary sensitizing substance. Although poison ivy and poison oak grow well in full sun to partial shade, poison sumac typically is found in damp swampy areas east of the Rocky Mountains. Most cases of ACD related to Anacardiaceae species are due to direct contact with urushiol from a Toxicodendron plant, but burning of brush containing Toxicodendron can cause airborne exposure when urushiol oil is carried by smoke particles.12 Sensitization to Toxicodendron can cause ACD to other Anacardiaceae species such as the Japanese lacquer tree (Toxicodendron vernicifluum), mango tree (Mangifera indica), cashew tree (Anacardium occidentale), and Indian marking nut tree (Semecarpus anacardium).6 Cross-reactions to components of the ginkgo tree (Ginkgo biloba) also are possible.
Toxicodendron plants can be more easily identified and avoided with knowledge of their characteristic leaf patterns. The most dependable way to identify poison ivy and poison oak species is to look for plants with 3 leaves, giving rise to the common saying, “Leaves of three, leave them be.” Poison sumac plants have groups of 7 to 13 leaves arranged as pairs along a central rib. Another helpful finding is a black deposit that Toxicodendron species leave behind following trauma to the leaves. Urushiol oxidizes when exposed to air and turns into a black deposit that can be seen on damaged leaves themselves or can be demonstrated in a black spot test to verify if a plant is a Toxicodendron species. The test is performed by gathering (carefully, without direct contact) a few leaves in a paper towel and crushing them to release sap. Within minutes, the sap will turn black if the plant is indeed a Toxicodendron species.13Pruritic, edematous, erythematous papules, plaques, and eventual vesicles in a linear distribution are suspicious for Toxicodendron exposure. Although your pet will not develop Toxicodendron ACD, oleoresin-contaminated pets can transfer the oils to their owners after coming into contact with these plants. Toxicodendron dermatitis also can be acquired from oleoresin-contaminated fomites such as clothing and shoes worn in the garden or when hiking. Toxicodendron dermatitis can appear at different sites on the body at different times depending on the amount of oleoresin exposure as well as epidermal thickness. For example, the oleoresin can be transferred from the hands to body areas with a thinner stratum corneum (eg, genitalia) and cause subsequent dermatitis.1
Compositae Family
The Compositae family (also known as Asteraceae) is a large plant family with more than 20,000 species, including numerous weeds, wildflowers, and vegetables. The flowers, leaves, stems, and pollens of the Compositae family are coated by cyclic esters called sesquiterpene lactones. Mitchell and Dupuis14 showed that sesquiterpene lactones are the allergens responsible for ACD to various Compositae plants, including ragweed (Ambrosia), sneezeweed (Helenium), and chrysanthemums (Chrysanthemum). Common Compositae vegetables such as lettuce (Lactuca sativa) have been reported to cause ACD in chefs, grocery store produce handlers, gardeners, and even owners of lettuce-eating pet guinea pigs and turtles.15 Similarly, artichokes (Cynara scolymus) can cause ACD in gardeners.16 Exposure to Compositae species also has been implicated in photoallergic reactions, and studies have demonstrated that some patients with chronic actinic dermatitis also have positive patch test reactions to Compositae species and/or sesquiterpene lactones.17,18
In addition to direct contact with Compositae plants, airborne exposure to sesquiterpene lactones can cause ACD.14 The pattern of airborne contact dermatitis typically involves exposed areas such as the eyelids, central face, and/or neck. The beak sign also can be a clue to airborne contact dermatitis, which involves dermatitis of the face that spares the nasal tip and/or nasal ridge. It is thought that the beak sign may result from increased sebaceous gland concentration on the nose, which prevents penetration of allergens and irritants.19 Unlike photoallergic contact dermatitis, which also can involve the face, airborne ACD frequently involves photoprotected areas such as the submandibular chin and the upper lip. Davies and Kersey20 reported the case of a groundsman who was cutting grass with dandelions (Taraxacum officinale) and was found to have associated airborne ACD of the face, neck, and forearms due to Compositae allergy. In a different setting, the aromas of chamomile (Matricaria chamomilla) have been reported to cause airborne ACD in a tea drinker.21 Paulsen22 found that ingestion of chamomile tea can induce systemic ACD in sensitized individuals.
Alstroemeriaceae, Liliaceae, and Primulaceae
Florists are exposed to many plant species and have a high prevalence of ACD. Thiboutot et al23 found that 15 of 57 (26%) floral workers experienced hand dermatitis that cleared with time away from work. The Peruvian lily (Alstroemeria, Alstroemeriaceae family), which contains tuliposide A, was found to be the leading cause of sensitization.23 Tulips (Tulipa, Liliaceae family), as the flower name suggests, also contain tuliposide A, which along with mechanical irritation from the course tecta fibers on the bulbs lead to a dermatitis known as tulip fingers.24,25 Poison primrose (Primula obconica, Primulaceae family), cultivated for its highly colorful flowers, contains the contact allergen primin.6 A common clinical presentation of ACD for any of these culprit flowers is localized dermatitis of the thumb and index finger in a florist or gardener.
Plants That Cause Irritant Reactions
Cactuses
Although the long spines of the Cactaceae family of cactuses is a warning for passersby, it is the small and nearly invisible barbed hairs (glochids) that inflict a more dramatic cutaneous reaction. The prickly pear cactus (Opuntia species) is a good example of such a plant, as its glochids cause mechanical irritation but also can become embedded in the skin and result in subcutaneous granulomas known as sabra dermatitis.26
Stinging Nettle
The dermatologic term urticaria owes its namesake to the stinging nettle plant, which comes from the family Urticaceae. The stinging nettle has small hairs on its leaves, referred to as stinging trichomes, which have needlelike tips that pierce the skin and inject a mix of histamine, formic acid, and acetylcholine, causing a pruritic dermatitis that may last up to 12 hours.27 The plant is found worldwide and is a common weed in North America.
Phytophotodermatitis
Lemons and limes (Rutaceae family) are common culprits of phytophotodermatitis, often causing what is known as a margarita burn after outdoor consumption or preparation of this tasty citrus beverage.28 An accidental spray of lime juice on the skin while adding it to a beer, guacamole, salsa, or any other food or beverage also can cause phytophotodermatitis.29-31 Although the juice of lemons and limes contains psoralens, the rind can contain a 6- to 186-fold increased concentration.32 Psoralen is the photoactive agent in Rutaceae plants that intercalates in double-stranded DNA and promotes intrastrand cross-links when exposed to UVA light, which ultimately leads to dermatitis.9 Phytophotodermatitis commonly causes erythema, edema, and painful bullae on sun-exposed areas and classically heals with hyperpigmentation.
Pseudophytodermatitis can occur in grain farmers and harvesters who handle wheat and/or barley and incidentally come in contact with insects and chemicals on the plant material. Pseudophytodermatitis from mites in the wheat and/or barley plant can occur at harvest time when contact with the plant material is high. Insects such as the North American itch mite (Pediculoides ventricosus) can cause petechiae, wheals, and pustules. In addition, insecticides such as malathion and arsenical sprays that are applied to plant leaves can cause pseudophytodermatitis, which may be initially diagnosed as dermatitis to the plant itself.6
Patch Testing to Plants
When a patient presents with recurrent or persistent dermatitis and a plant contact allergen is suspected, patch testing is indicated. Most comprehensive patch test series contain various plant allergens, such as sesquiterpene lactones, Compositae mix, and limonene hydroperoxides, and patch testing to a specialized plant series may be necessary. Poison ivy/oak/sumac allergens typically are not included in patch test series because of the high prevalence of allergic reactions to these chemicals and the likelihood of sensitization when patch testing with urushiol. Compositae contact sensitization can be difficult to diagnose because neither sesquiterpene lactone mix 0.1% nor parthenolide 0.1% are sensitive enough to pick up all Compositae allergies.33,34 Paulsen and Andersen34 proposed that if Compositae sensitization is suspected, testing should include sesquiterpene lactone, parthenolide, and Compositae mix II 2.5%, as well as other potential Compositae allergens based on the patient’s history.34
Because plants can have geographic variability and contain potentially unknown allergens,35 testing to plant components may increase the diagnostic yield of patch testing. Dividing the plant into component parts (ie, stem, bulb, leaf, flower) is helpful, as different components have different allergen concentrations. It is important to consult expert resources before proceeding with plant component patch testing because irritant reactions are frequent and may confound the testing.36
Prevention and Treatment
For all plant dermatoses, the mainstay of prevention is to avoid contact with the offending plant material. Gloves can be an important protective tool for plant dermatitis prevention; the correct material depends on the plant species being handled. Rubber gloves should not be worn to protect against Toxicodendron plants since the catechols in urushiol are soluble in rubber; vinyl gloves should be worn instead.6 Marks37 found that tuliposide A, the allergen in the Peruvian lily (Alstroemeria), penetrates both vinyl and latex gloves; it does not penetrate nitrile gloves. If exposed, the risk of dermatitis can be decreased if the allergen is washed away with soap and water as soon as possible. Some allergens such as Toxicodendron are absorbed quickly and need to be washed off within 10 minutes of exposure.6 Importantly, exposed gardening gloves may continue to perpetuate ACD if the allergen is not also washed off the gloves themselves.
For light-mediated dermatoses, sun avoidance or use of an effective sunscreen can reduce symptoms in an individual who has already been exposed.10 UVA light activates psoralen-mediated dermatitis but not until 30 to 120 minutes after absorption into the skin.38
Barrier creams are thought to be protective against plant ACD through a variety of mechanisms. The cream itself is meant to reduce skin contact to an allergen or irritant. Additionally, barrier creams contain active ingredients such as silicone, hydrocarbons, and aluminum chlorohydrate, which are thought to trap or transform offending agents before contacting the skin. When contact with a Toxicodendron species is anticipated, Marks et al39 found that dermatitis was absent or significantly reduced when 144 patients were pretreated with quaternium-18 bentonite lotion 5% (P<.0001).
Although allergen avoidance and use of gloves and barrier creams are the mainstays of preventing plant dermatoses, treatment often is required to control postexposure symptoms. For all plant dermatoses, topical corticosteroids can be used to reduce inflammation and pruritus. In some cases, systemic steroids may be necessary. To prevent rebound of dermatitis, patients often require a 3-week or longer course of oral steroids to quell the reaction, particularly if the dermatitis is vigorous or an id reaction is present.40 Antihistamines and cold compresses also can provide symptomatic relief.
Final Interpretation
Plants can cause a variety of dermatoses. Although Toxicodendron plants are the most frequent cause of ACD, it is important to keep in mind that florists, gardeners, and farmers are exposed to a large variety of allergens, irritants, and phototoxic agents that cause dermatoses as well. Confirmation of plant-induced ACD involves patch testing against suspected species. Prevention involves use of appropriate barriers and avoidance of implicated plants. Treatment includes topical steroids, antihistamines, and prednisone.
- Gladman AC. Toxicodendron dermatitis: poison ivy, oak, and sumac. Wilderness Environ Med. 2006;17:120-128.
- Pariser D, Ceilley R, Lefkovits A, et al. Poison ivy, oak and sumac. Derm Insights. 2003;4:26-28.
- Wolff K, Johnson R. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 6th ed. McGraw Hill Education; 2009.
- Zomorodi N, Butt M, Maczuga S, et al. Cost and diagnostic characteristics of Toxicodendron dermatitis in the USA: a retrospective cross-sectional analysis. Br J Dermatol. 2020;183:772-773.
- DeKoven JG, Silverberg JI, Warshaw EM, et al. North American Contact Dermatitis Group patch test results: 2017-2018. Dermatitis. 2021;32:111-123.
- Fowler JF, Zirwas MJ. Fisher’s Contact Dermatitis. 7th ed. Contact Dermatitis Institute; 2019.
- Smith HR, Basketter DA, McFadden JP. Irritant dermatitis, irritancy and its role in allergic contact dermatitis. Clin Exp Dermatol. 2002;27:138-146.
- Wakelin SH. Contact urticaria. Clin Exp Dermatol. 2001;26:132-136.
- Ellis CR, Elston DM. Psoralen-induced phytophotodermatitis. Dermatitis. 2021;32:140-143.
- Deleo VA. Photocontact dermatitis. Dermatol Ther. 2004;17:279-288.
- National Institute for Occupational Safety and Health. Poisonous plants. Centers for Disease Control and Prevention website. Updated June 1, 2018. Accessed August 10, 2021. https://www.cdc.gov/niosh/topics/plants/geographic.html
- Schloemer JA, Zirwas MJ, Burkhart CG. Airborne contact dermatitis: common causes in the USA. Int J Dermatol. 2015;54:271-274.
- Guin JD. The black spot test for recognizing poison ivy and related species. J Am Acad Dermatol. 1980;2:332-333.
- Mitchell J, Dupuis G. Allergic contact dermatitis from sesquiterpenoids of the Compositae family of plants. Br J Dermatol. 1971;84:139-150.
- Paulsen E, Andersen KE. Lettuce contact allergy. Contact Dermatitis. 2016;74:67-75.
- Samaran Q, Clark E, Dereure O, et al. Airborne allergic contact dermatitis caused by artichoke. Contact Dermatitis. 2020;82:395-397.
- Du H, Ross JS, Norris PG, et al. Contact and photocontact sensitization in chronic actinic dermatitis: sesquiterpene lactone mix is an important allergen. Br J Dermatol. 1995;132:543-547.
- Wrangsjo K, Marie Ros A, Walhberg JE. Contact allergy to Compositae plants in patients with summer-exacerbated dermatitis. Contact Dermatitis. 1990;22:148-154.
- Staser K, Ezra N, Sheehan MP, et al. The beak sign: a clinical clue to airborne contact dermatitis. Dermatitis. 2014;25:97-98.
- Davies M, Kersey J. Contact allergy to yarrow and dandelion. Contact Dermatitis. 1986;14:256-257.
- Anzai A, Vázquez Herrera NE, Tosti A. Airborne allergic contact dermatitis caused by chamomile tea. Contact Dermatitis. 2015;72:254-255.
- Paulsen E. Systemic allergic dermatitis caused by sesquiterpene lactones. Contact Dermatitis. 2017;76:1-10.
- Thiboutot DM, Hamory BH, Marks JG. Dermatoses among floral shop workers. J Am Acad Dermatol. 1990;22:54-58.
- Hjorth N, Wilkinson DS. Contact dermatitis IV. tulip fingers, hyacinth itch and lily rash. Br J Dermatol. 1968;80:696-698.
- Guin JD, Franks H. Fingertip dermatitis in a retail florist. Cutis. 2001;67:328-330.
- Magro C, Lipner S. Sabra dermatitis: combined features of delayed hypersensitivity and foreign body reaction to implanted glochidia. Dermatol Online J. 2020;26:13030/qt2157f9g0.
- Cummings AJ, Olsen M. Mechanism of action of stinging nettles. Wilderness Environ Med. 2011;22:136-139.
- Maniam G, Light KML, Wilson J. Margarita burn: recognition and treatment of phytophotodermatitis. J Am Board Fam Med. 2021;34:398-401.
- Flugman SL. Mexican beer dermatitis: a unique variant of lime phytophotodermatitis attributable to contemporary beer-drinking practices. Arch Dermatol. 2010;146:1194-1195.
- Kung AC, Stephens MB, Darling T. Phytophotodermatitis: bulla formation and hyperpigmentation during spring break. Mil Med. 2009;174:657-661.
- Smith LG. Phytophotodermatitis. Images Emerg Med. 2017;1:146-147.
- Wagner AM, Wu JJ, Hansen RC, et al. Bullous phytophotodermatitis associated with high natural concentrations of furanocoumarins in limes. Am J Contact Dermat. 2002;13:10-14.
- Green C, Ferguson J. Sesquiterpene lactone mix is not an adequate screen for Compositae allergy. Contact Dermatitis. 1994;31:151-153.
- Paulsen E, Andersen KE. Screening for Compositae contact sensitization with sesquiterpene lactones and Compositae mix 2.5% pet. Contact Dermatitis. 2019;81:368-373.
- Paulsen E, Andersen KE. Patch testing with constituents of Compositae mixes. Contact Dermatitis. 2012;66:241-246.
- Frosch PJ, Geier J, Uter W, et al. Patch testing with the patients’ own products. Contact Dermatitis. 2011:929-941.
- Marks JG. Allergic contact dermatitis to Alstroemeria. Arch Dermatol. 1988;124:914-916.
- Moreau JF, English JC, Gehris RP. Phytophotodermatitis. J Pediatr Adolesc Gynecol. 2014;27:93-94.
- Marks JG, Fowler JF, Sherertz EF, et al. Prevention of poison ivy and poison oak allergic contact dermatitis by quaternium-18 bentonite. J Am Acad Dermatol. 1995;33:212-216.
- Craig K, Meadows SE. What is the best duration of steroid therapy for contact dermatitis (rhus)? J Fam Pract. 2006;55:166-167.
- Gladman AC. Toxicodendron dermatitis: poison ivy, oak, and sumac. Wilderness Environ Med. 2006;17:120-128.
- Pariser D, Ceilley R, Lefkovits A, et al. Poison ivy, oak and sumac. Derm Insights. 2003;4:26-28.
- Wolff K, Johnson R. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 6th ed. McGraw Hill Education; 2009.
- Zomorodi N, Butt M, Maczuga S, et al. Cost and diagnostic characteristics of Toxicodendron dermatitis in the USA: a retrospective cross-sectional analysis. Br J Dermatol. 2020;183:772-773.
- DeKoven JG, Silverberg JI, Warshaw EM, et al. North American Contact Dermatitis Group patch test results: 2017-2018. Dermatitis. 2021;32:111-123.
- Fowler JF, Zirwas MJ. Fisher’s Contact Dermatitis. 7th ed. Contact Dermatitis Institute; 2019.
- Smith HR, Basketter DA, McFadden JP. Irritant dermatitis, irritancy and its role in allergic contact dermatitis. Clin Exp Dermatol. 2002;27:138-146.
- Wakelin SH. Contact urticaria. Clin Exp Dermatol. 2001;26:132-136.
- Ellis CR, Elston DM. Psoralen-induced phytophotodermatitis. Dermatitis. 2021;32:140-143.
- Deleo VA. Photocontact dermatitis. Dermatol Ther. 2004;17:279-288.
- National Institute for Occupational Safety and Health. Poisonous plants. Centers for Disease Control and Prevention website. Updated June 1, 2018. Accessed August 10, 2021. https://www.cdc.gov/niosh/topics/plants/geographic.html
- Schloemer JA, Zirwas MJ, Burkhart CG. Airborne contact dermatitis: common causes in the USA. Int J Dermatol. 2015;54:271-274.
- Guin JD. The black spot test for recognizing poison ivy and related species. J Am Acad Dermatol. 1980;2:332-333.
- Mitchell J, Dupuis G. Allergic contact dermatitis from sesquiterpenoids of the Compositae family of plants. Br J Dermatol. 1971;84:139-150.
- Paulsen E, Andersen KE. Lettuce contact allergy. Contact Dermatitis. 2016;74:67-75.
- Samaran Q, Clark E, Dereure O, et al. Airborne allergic contact dermatitis caused by artichoke. Contact Dermatitis. 2020;82:395-397.
- Du H, Ross JS, Norris PG, et al. Contact and photocontact sensitization in chronic actinic dermatitis: sesquiterpene lactone mix is an important allergen. Br J Dermatol. 1995;132:543-547.
- Wrangsjo K, Marie Ros A, Walhberg JE. Contact allergy to Compositae plants in patients with summer-exacerbated dermatitis. Contact Dermatitis. 1990;22:148-154.
- Staser K, Ezra N, Sheehan MP, et al. The beak sign: a clinical clue to airborne contact dermatitis. Dermatitis. 2014;25:97-98.
- Davies M, Kersey J. Contact allergy to yarrow and dandelion. Contact Dermatitis. 1986;14:256-257.
- Anzai A, Vázquez Herrera NE, Tosti A. Airborne allergic contact dermatitis caused by chamomile tea. Contact Dermatitis. 2015;72:254-255.
- Paulsen E. Systemic allergic dermatitis caused by sesquiterpene lactones. Contact Dermatitis. 2017;76:1-10.
- Thiboutot DM, Hamory BH, Marks JG. Dermatoses among floral shop workers. J Am Acad Dermatol. 1990;22:54-58.
- Hjorth N, Wilkinson DS. Contact dermatitis IV. tulip fingers, hyacinth itch and lily rash. Br J Dermatol. 1968;80:696-698.
- Guin JD, Franks H. Fingertip dermatitis in a retail florist. Cutis. 2001;67:328-330.
- Magro C, Lipner S. Sabra dermatitis: combined features of delayed hypersensitivity and foreign body reaction to implanted glochidia. Dermatol Online J. 2020;26:13030/qt2157f9g0.
- Cummings AJ, Olsen M. Mechanism of action of stinging nettles. Wilderness Environ Med. 2011;22:136-139.
- Maniam G, Light KML, Wilson J. Margarita burn: recognition and treatment of phytophotodermatitis. J Am Board Fam Med. 2021;34:398-401.
- Flugman SL. Mexican beer dermatitis: a unique variant of lime phytophotodermatitis attributable to contemporary beer-drinking practices. Arch Dermatol. 2010;146:1194-1195.
- Kung AC, Stephens MB, Darling T. Phytophotodermatitis: bulla formation and hyperpigmentation during spring break. Mil Med. 2009;174:657-661.
- Smith LG. Phytophotodermatitis. Images Emerg Med. 2017;1:146-147.
- Wagner AM, Wu JJ, Hansen RC, et al. Bullous phytophotodermatitis associated with high natural concentrations of furanocoumarins in limes. Am J Contact Dermat. 2002;13:10-14.
- Green C, Ferguson J. Sesquiterpene lactone mix is not an adequate screen for Compositae allergy. Contact Dermatitis. 1994;31:151-153.
- Paulsen E, Andersen KE. Screening for Compositae contact sensitization with sesquiterpene lactones and Compositae mix 2.5% pet. Contact Dermatitis. 2019;81:368-373.
- Paulsen E, Andersen KE. Patch testing with constituents of Compositae mixes. Contact Dermatitis. 2012;66:241-246.
- Frosch PJ, Geier J, Uter W, et al. Patch testing with the patients’ own products. Contact Dermatitis. 2011:929-941.
- Marks JG. Allergic contact dermatitis to Alstroemeria. Arch Dermatol. 1988;124:914-916.
- Moreau JF, English JC, Gehris RP. Phytophotodermatitis. J Pediatr Adolesc Gynecol. 2014;27:93-94.
- Marks JG, Fowler JF, Sherertz EF, et al. Prevention of poison ivy and poison oak allergic contact dermatitis by quaternium-18 bentonite. J Am Acad Dermatol. 1995;33:212-216.
- Craig K, Meadows SE. What is the best duration of steroid therapy for contact dermatitis (rhus)? J Fam Pract. 2006;55:166-167.
Practice Points
- Gardeners, florists, farmers, and outdoor enthusiasts are at risk for various plant dermatoses, which can be classified into 5 main categories: allergic contact dermatitis (ACD), mechanical irritant contact dermatitis, chemical irritant contact dermatitis, light-mediated dermatitis, and pseudophytodermatitis.
- Poison ivy, from the Toxicodendron genus, is the leading cause of plant ACD; however, a myriad of other plants also can cause dermatoses.
- Patch testing can be used to identify the source of immune-mediated type IV delayed hypersensitivity reactions to various plant species in individuals with recurrent or persistent dermatitis.
- Treatment options for all plant dermatoses can include topical steroids, antihistamines, and oral prednisone. Prevention involves avoidance or use of an effective barrier.
No gender gap seen in ankylosing spondylitis prevalence, study finds
A new study rebuts the conventional rheumatology wisdom about ankylosing spondylitis (AS) by reporting that actually there’s no gender gap in the prevalence of the disease. Researchers found no statistically significant difference in rates between men and women based on an analysis of military medical records.
“Our findings challenge the widely held belief that AS in the U.S. occurs substantially more frequently in males than females,” the study authors, led by data scientist D. Alan Nelson, PhD, of Stanford (Calif.) University, wrote in a study published Aug. 30 in Arthritis Care & Research.
The researchers launched the study to fill a gap in knowledge regarding case rates by gender. “The incidence of AS in the U.S. has been understudied and incompletely characterized,” they wrote.
Even though AS is fairly common, affecting an estimated 1% of the American adult population (2.5 million people), only one published population study has examined rates by gender in the United States. That study tracked cases in Minnesota’s Olmsted County during 1980-2009 and found that the ratio of cases in men vs. women was 3.8:1, which was “consistent with more recent estimates” at the time.
However, the population in that study in 1980 was 100% White, the authors of the new study note. A Canadian study that tracked an Ontario population from 1995 to 2010, meanwhile, suggested that AS rates among women were rising and the gender gap was shrinking. AS rates as a whole also nearly tripled, possibly because of more awareness.
For the new study, researchers retrospectively tracked 728,556 members of the U.S. military who underwent guideline-directed screening for back pain during 2014-2017. The study population was about 68% White, 22% Black, 5% Asian or Pacific Islander, and the remainder were other races or unknown. About 85% were male.
The subjects were monitored for a mean of 2.21 years, and 438 (0.06%) were diagnosed with AS at least once over that period.
The researchers found that the AS rates among males vs. females were similar (incidence rate ratio, 1.16; P = .23; adjusted odds ratio, 0.79; 95% confidence interval, 0.61-1.02; P = .072).
The researchers also found that Whites were more likely to develop AS than Blacks (aOR, 1.39; 95% CI, 1.01-1.66; P = .04).
The risk of AS increased with age, the researchers reported, with the odds growing sevenfold in the 45-and-older population vs. the under-24 population (aOR, 7.3; 95% CI, 5.7-10.3; P < .001).
The researchers noted that their study examined a more diverse population than the earlier Minnesota study. It’s also possible that the results of the two studies differed because of differences in definitions of AS diagnosis or imprecision in diagnosis codes, they wrote.
The researchers added that “the finding of a 1.21 male-female prevalence ratio of AS in the Canadian Ontario study was also generally consistent with our findings. Similar to our study population, the Canadian population was racially more diverse than the Olmsted study population at the times of both studies.”
Some limitations of the study include the fact that the military population is not a random sample and may have low rates of AS. “It is highly likely that most clinically evident cases of AS would have been screened out prior to enrollment in the military service,” they wrote. “Differences between military service members and the general population may explain why we observed a different association between AS incidence and age in comparison to that reported by prior studies. The increasing risk of AS with adult age that we observed could reflect selective discharge patterns related to very early symptoms of AS in this population.”
The study was funded in part by a grant from the Spondylitis Association of America. No information about potential conflicts of interest was provided in the manuscript.
A new study rebuts the conventional rheumatology wisdom about ankylosing spondylitis (AS) by reporting that actually there’s no gender gap in the prevalence of the disease. Researchers found no statistically significant difference in rates between men and women based on an analysis of military medical records.
“Our findings challenge the widely held belief that AS in the U.S. occurs substantially more frequently in males than females,” the study authors, led by data scientist D. Alan Nelson, PhD, of Stanford (Calif.) University, wrote in a study published Aug. 30 in Arthritis Care & Research.
The researchers launched the study to fill a gap in knowledge regarding case rates by gender. “The incidence of AS in the U.S. has been understudied and incompletely characterized,” they wrote.
Even though AS is fairly common, affecting an estimated 1% of the American adult population (2.5 million people), only one published population study has examined rates by gender in the United States. That study tracked cases in Minnesota’s Olmsted County during 1980-2009 and found that the ratio of cases in men vs. women was 3.8:1, which was “consistent with more recent estimates” at the time.
However, the population in that study in 1980 was 100% White, the authors of the new study note. A Canadian study that tracked an Ontario population from 1995 to 2010, meanwhile, suggested that AS rates among women were rising and the gender gap was shrinking. AS rates as a whole also nearly tripled, possibly because of more awareness.
For the new study, researchers retrospectively tracked 728,556 members of the U.S. military who underwent guideline-directed screening for back pain during 2014-2017. The study population was about 68% White, 22% Black, 5% Asian or Pacific Islander, and the remainder were other races or unknown. About 85% were male.
The subjects were monitored for a mean of 2.21 years, and 438 (0.06%) were diagnosed with AS at least once over that period.
The researchers found that the AS rates among males vs. females were similar (incidence rate ratio, 1.16; P = .23; adjusted odds ratio, 0.79; 95% confidence interval, 0.61-1.02; P = .072).
The researchers also found that Whites were more likely to develop AS than Blacks (aOR, 1.39; 95% CI, 1.01-1.66; P = .04).
The risk of AS increased with age, the researchers reported, with the odds growing sevenfold in the 45-and-older population vs. the under-24 population (aOR, 7.3; 95% CI, 5.7-10.3; P < .001).
The researchers noted that their study examined a more diverse population than the earlier Minnesota study. It’s also possible that the results of the two studies differed because of differences in definitions of AS diagnosis or imprecision in diagnosis codes, they wrote.
The researchers added that “the finding of a 1.21 male-female prevalence ratio of AS in the Canadian Ontario study was also generally consistent with our findings. Similar to our study population, the Canadian population was racially more diverse than the Olmsted study population at the times of both studies.”
Some limitations of the study include the fact that the military population is not a random sample and may have low rates of AS. “It is highly likely that most clinically evident cases of AS would have been screened out prior to enrollment in the military service,” they wrote. “Differences between military service members and the general population may explain why we observed a different association between AS incidence and age in comparison to that reported by prior studies. The increasing risk of AS with adult age that we observed could reflect selective discharge patterns related to very early symptoms of AS in this population.”
The study was funded in part by a grant from the Spondylitis Association of America. No information about potential conflicts of interest was provided in the manuscript.
A new study rebuts the conventional rheumatology wisdom about ankylosing spondylitis (AS) by reporting that actually there’s no gender gap in the prevalence of the disease. Researchers found no statistically significant difference in rates between men and women based on an analysis of military medical records.
“Our findings challenge the widely held belief that AS in the U.S. occurs substantially more frequently in males than females,” the study authors, led by data scientist D. Alan Nelson, PhD, of Stanford (Calif.) University, wrote in a study published Aug. 30 in Arthritis Care & Research.
The researchers launched the study to fill a gap in knowledge regarding case rates by gender. “The incidence of AS in the U.S. has been understudied and incompletely characterized,” they wrote.
Even though AS is fairly common, affecting an estimated 1% of the American adult population (2.5 million people), only one published population study has examined rates by gender in the United States. That study tracked cases in Minnesota’s Olmsted County during 1980-2009 and found that the ratio of cases in men vs. women was 3.8:1, which was “consistent with more recent estimates” at the time.
However, the population in that study in 1980 was 100% White, the authors of the new study note. A Canadian study that tracked an Ontario population from 1995 to 2010, meanwhile, suggested that AS rates among women were rising and the gender gap was shrinking. AS rates as a whole also nearly tripled, possibly because of more awareness.
For the new study, researchers retrospectively tracked 728,556 members of the U.S. military who underwent guideline-directed screening for back pain during 2014-2017. The study population was about 68% White, 22% Black, 5% Asian or Pacific Islander, and the remainder were other races or unknown. About 85% were male.
The subjects were monitored for a mean of 2.21 years, and 438 (0.06%) were diagnosed with AS at least once over that period.
The researchers found that the AS rates among males vs. females were similar (incidence rate ratio, 1.16; P = .23; adjusted odds ratio, 0.79; 95% confidence interval, 0.61-1.02; P = .072).
The researchers also found that Whites were more likely to develop AS than Blacks (aOR, 1.39; 95% CI, 1.01-1.66; P = .04).
The risk of AS increased with age, the researchers reported, with the odds growing sevenfold in the 45-and-older population vs. the under-24 population (aOR, 7.3; 95% CI, 5.7-10.3; P < .001).
The researchers noted that their study examined a more diverse population than the earlier Minnesota study. It’s also possible that the results of the two studies differed because of differences in definitions of AS diagnosis or imprecision in diagnosis codes, they wrote.
The researchers added that “the finding of a 1.21 male-female prevalence ratio of AS in the Canadian Ontario study was also generally consistent with our findings. Similar to our study population, the Canadian population was racially more diverse than the Olmsted study population at the times of both studies.”
Some limitations of the study include the fact that the military population is not a random sample and may have low rates of AS. “It is highly likely that most clinically evident cases of AS would have been screened out prior to enrollment in the military service,” they wrote. “Differences between military service members and the general population may explain why we observed a different association between AS incidence and age in comparison to that reported by prior studies. The increasing risk of AS with adult age that we observed could reflect selective discharge patterns related to very early symptoms of AS in this population.”
The study was funded in part by a grant from the Spondylitis Association of America. No information about potential conflicts of interest was provided in the manuscript.
FROM ARTHRITIS CARE & RESEARCH
Anakinra improved survival in hospitalized COVID-19 patients
Hospitalized COVID-19 patients at increased risk for respiratory failure showed significant improvement after treatment with anakinra, compared with placebo, based on data from a phase 3, randomized trial of nearly 600 patients who also received standard of care treatment.
Anakinra, a recombinant interleukin (IL)-1 receptor antagonist that blocks activity for both IL-1 alpha and beta, showed a 70% decrease in the risk of progression to severe respiratory failure in a prior open-label, phase 2, proof-of-concept study, wrote Evdoxia Kyriazopoulou, MD, PhD, of National and Kapodistrian University of Athens, and colleagues.
Previous research has shown that soluble urokinase plasminogen activator receptor (suPAR) serum levels can signal increased risk of progression to severe disease and respiratory failure in COVID-19 patients, they noted.
Supported by these early findings, “the SAVE-MORE study (suPAR-guided anakinra treatment for validation of the risk and early management of severe respiratory failure by COVID-19) is a pivotal, confirmatory, phase 3, double-blind, randomized controlled trial that evaluated the efficacy and safety of early initiation of anakinra treatment in hospitalized patients with moderate or severe COVID-19,” the researchers said.
In the SAVE-MORE study published Sept. 3 in Nature Medicine, the researchers identified 594 adults with COVID-19 who were hospitalized at 37 centers in Greece and Italy and at risk of progressing to respiratory failure based on plasma suPAR levels of at least 6 ng/mL.
The primary objective was to assess the impact of early anakinra treatment on the clinical status of COVID-19 patients at risk for severe disease according to the 11-point, ordinal World Health Organization Clinical Progression Scale (WHO-CPS) at 28 days after starting treatment. All patients received standard of care, which consisted of regular monitoring of physical signs, oximetry, and anticoagulation. Patients with severe disease by the WHO definition were also received 6 mg of dexamethasone intravenously daily for 10 days. A total of 405 were randomized to anakinra and 189 to placebo. Approximately 92% of the study participants had severe pneumonia according to the WHO classification for COVID-19. The average age of the patients was 62 years, 58% were male, and the average body mass index was 29.5 kg/m2.
At 28 days, 204 (50.4%) of the anakinra-treated patients had fully recovered, with no detectable viral RNA, compared with 50 (26.5%) of the placebo-treated patients (P < .0001). In addition, significantly fewer patients in the anakinra group had died by 28 days (13 patients, 3.2%), compared with patients in the placebo group (13 patients, 6.9%).
The median decrease in WHO-CPS scores from baseline to 28 days was 4 points in the anakinra group and 3 points in the placebo group, a statistically significant difference (P < .0001).
“Overall, the unadjusted proportional odds of having a worse score on the 11-point WHO-CPS at day 28 with anakinra was 0.36 versus placebo,” and this number remained the same in adjusted analysis, the researchers wrote.
All five secondary endpoints on the WHO-CPS showed significant benefits of anakinra, compared with placebo. These included an absolute decrease of WHO-CPS at day 28 and day 14 from baseline; an absolute decrease of Sequential Organ Failure Assessment scores at day 7 from baseline; and a significantly shorter mean time to both hospital and ICU discharge (1 day and 4 days, respectively) with anakinra versus placebo.
Follow-up laboratory data showed a significant increase in absolute lymphocyte count at 7 days, a significant decrease in circulating IL-6 levels at 4 and 7 days, and significantly decreased plasma C-reactive protein (CRP) levels at 7 days.
Serious treatment-emergent adverse events were reported in 16% with anakinra and in 21.7% with placebo; the most common of these events were infections (8.4% with anakinra and 15.9% with placebo). The next most common serious treatment-emergent adverse events were ventilator-associated pneumonia, septic shock and multiple organ dysfunction, bloodstream infections, and pulmonary embolism. The most common nonserious treatment-emergent adverse events were an increase of liver function tests and hyperglycemia (similar in anakinra and placebo groups) and nonserious anemia (lower in the anakinra group).
The study findings were limited by several factors, including the lack of patients with critical COVID-19 disease and the challenge of application of suPAR in all hospital settings, the researchers noted. However, “the results validate the findings of the previous SAVE open-label phase 2 trial,” they said. The results suggest “that suPAR should be measured upon admission of all patients with COVID-19 who do not need oxygen or who need nasal or mask oxygen, and that, if suPAR levels are 6 ng/mL or higher, anakinra treatment might be a suitable therapy,” they concluded.
Cytokine storm syndrome remains a treatment challenge
“Many who die from COVID-19 suffer hyperinflammation with features of cytokine storm syndrome (CSS) and associated acute respiratory distress syndrome,” wrote Randy Q. Cron, MD, and W. Winn Chatham, MD, of the University of Alabama at Birmingham, and Roberto Caricchio, MD, of Temple University, Philadelphia, in an accompanying editorial. They noted that the SAVE-MORE trial results contrast with another recent randomized trial of canakinumab, which failed to show notable benefits, compared with placebo, in treating hospitalized patients with COVID-19 pneumonia.
“There are some key differences between these trials, one being that anakinra blocks signaling of both IL-1 alpha and IL-1 beta, whereas canakinumab binds only IL-1 beta,” the editorialists explained. “SARS-CoV-2–infected endothelium may be a particularly important source of IL-1 alpha that is not targeted by canakinumab,” they noted.
Additional studies have examined IL-6 inhibition to treat COVID-19 patients, but data have been inconsistent, the editorialists said.
“One thing that is clearly emerging from this pandemic is that the CSS associated with COVID-19 is relatively unique, with only modestly elevated levels of IL-6, CRP, and ferritin, for example,” they noted. However, the SAVE-MORE study suggests that more targeted approaches, such as anakinra, “may allow earlier introduction of anticytokine treatment” and support the use of IL-1 blockade with anakinra for cases of severe COVID-19 pneumonia.
Predicting risk for severe disease
“One of the major challenges in the management of patients with COVID-19 is identifying patients at risk of severe disease who would warrant early intervention with anti-inflammatory therapy,” said Salim Hayek, MD, medical director of the University of Michigan’s Frankel Cardiovascular Center Clinics, in an interview. “We and others had found that soluble urokinase plasminogen activator receptor (suPAR) levels are the strongest predictor of severe disease amongst biomarkers of inflammation,” he said. “In this study, patients with high suPAR levels derived benefit from anakinra, compared to those with placebo. This study is a great example of how suPAR levels could be used to identify high-risk patients that would benefit from therapies targeting inflammation,” Dr. Hayek emphasized.
“The findings are in line with the hypothesis that patients with the highest degrees of inflammation would benefit the best from targeting the hyperinflammatory cascade using anakinra or other interleukin antagonists,” Dr. Hayek said. “Given suPAR levels are the best predictors of high-risk disease, it is not surprising to see that patients with high levels benefit from targeting inflammation,” he noted.
The take-home message for clinicians at this time is that anakinra effectively improves outcomes in COVID-19 patients with high suPAR levels, Dr. Hayek said. “SuPAR can be measured easily at the point of care. Thus, a targeted strategy using suPAR to identify patients who would benefit from anakinra appears to be viable,” he explained.
However, “Whether anakinra is effective in patients with lower suPAR levels (<6 ng/mL) is unclear and was not answered by this study,” he said. “We eagerly await results of other trials to make that determination. Whether suPAR levels can also help guide the use of other therapies for COVID-19 should be explored and would enhance the personalization of treatment for COVID-19 according to the underlying inflammatory state,” he added.
The SAVE-MORE study was funded by the Hellenic Institute for the Study of Sepsis and Sobi, which manufactures anakinra. Some of the study authors reported financial relationships with Sobi and other pharmaceutical companies.
Dr. Cron disclosed serving as a consultant to Sobi, Novartis, Pfizer, and Sironax. Dr. Cron and Dr. Chatham disclosed having received grant support from Sobi for investigator-initiated clinical trials, and Dr. Caricchio disclosed serving as a consultant to GlaxoSmithKline, Johnson & Johnson, Aurinia, and Bristol-Myers Squibb. Dr. Hayek had no relevant financial conflicts to disclose.
Hospitalized COVID-19 patients at increased risk for respiratory failure showed significant improvement after treatment with anakinra, compared with placebo, based on data from a phase 3, randomized trial of nearly 600 patients who also received standard of care treatment.
Anakinra, a recombinant interleukin (IL)-1 receptor antagonist that blocks activity for both IL-1 alpha and beta, showed a 70% decrease in the risk of progression to severe respiratory failure in a prior open-label, phase 2, proof-of-concept study, wrote Evdoxia Kyriazopoulou, MD, PhD, of National and Kapodistrian University of Athens, and colleagues.
Previous research has shown that soluble urokinase plasminogen activator receptor (suPAR) serum levels can signal increased risk of progression to severe disease and respiratory failure in COVID-19 patients, they noted.
Supported by these early findings, “the SAVE-MORE study (suPAR-guided anakinra treatment for validation of the risk and early management of severe respiratory failure by COVID-19) is a pivotal, confirmatory, phase 3, double-blind, randomized controlled trial that evaluated the efficacy and safety of early initiation of anakinra treatment in hospitalized patients with moderate or severe COVID-19,” the researchers said.
In the SAVE-MORE study published Sept. 3 in Nature Medicine, the researchers identified 594 adults with COVID-19 who were hospitalized at 37 centers in Greece and Italy and at risk of progressing to respiratory failure based on plasma suPAR levels of at least 6 ng/mL.
The primary objective was to assess the impact of early anakinra treatment on the clinical status of COVID-19 patients at risk for severe disease according to the 11-point, ordinal World Health Organization Clinical Progression Scale (WHO-CPS) at 28 days after starting treatment. All patients received standard of care, which consisted of regular monitoring of physical signs, oximetry, and anticoagulation. Patients with severe disease by the WHO definition were also received 6 mg of dexamethasone intravenously daily for 10 days. A total of 405 were randomized to anakinra and 189 to placebo. Approximately 92% of the study participants had severe pneumonia according to the WHO classification for COVID-19. The average age of the patients was 62 years, 58% were male, and the average body mass index was 29.5 kg/m2.
At 28 days, 204 (50.4%) of the anakinra-treated patients had fully recovered, with no detectable viral RNA, compared with 50 (26.5%) of the placebo-treated patients (P < .0001). In addition, significantly fewer patients in the anakinra group had died by 28 days (13 patients, 3.2%), compared with patients in the placebo group (13 patients, 6.9%).
The median decrease in WHO-CPS scores from baseline to 28 days was 4 points in the anakinra group and 3 points in the placebo group, a statistically significant difference (P < .0001).
“Overall, the unadjusted proportional odds of having a worse score on the 11-point WHO-CPS at day 28 with anakinra was 0.36 versus placebo,” and this number remained the same in adjusted analysis, the researchers wrote.
All five secondary endpoints on the WHO-CPS showed significant benefits of anakinra, compared with placebo. These included an absolute decrease of WHO-CPS at day 28 and day 14 from baseline; an absolute decrease of Sequential Organ Failure Assessment scores at day 7 from baseline; and a significantly shorter mean time to both hospital and ICU discharge (1 day and 4 days, respectively) with anakinra versus placebo.
Follow-up laboratory data showed a significant increase in absolute lymphocyte count at 7 days, a significant decrease in circulating IL-6 levels at 4 and 7 days, and significantly decreased plasma C-reactive protein (CRP) levels at 7 days.
Serious treatment-emergent adverse events were reported in 16% with anakinra and in 21.7% with placebo; the most common of these events were infections (8.4% with anakinra and 15.9% with placebo). The next most common serious treatment-emergent adverse events were ventilator-associated pneumonia, septic shock and multiple organ dysfunction, bloodstream infections, and pulmonary embolism. The most common nonserious treatment-emergent adverse events were an increase of liver function tests and hyperglycemia (similar in anakinra and placebo groups) and nonserious anemia (lower in the anakinra group).
The study findings were limited by several factors, including the lack of patients with critical COVID-19 disease and the challenge of application of suPAR in all hospital settings, the researchers noted. However, “the results validate the findings of the previous SAVE open-label phase 2 trial,” they said. The results suggest “that suPAR should be measured upon admission of all patients with COVID-19 who do not need oxygen or who need nasal or mask oxygen, and that, if suPAR levels are 6 ng/mL or higher, anakinra treatment might be a suitable therapy,” they concluded.
Cytokine storm syndrome remains a treatment challenge
“Many who die from COVID-19 suffer hyperinflammation with features of cytokine storm syndrome (CSS) and associated acute respiratory distress syndrome,” wrote Randy Q. Cron, MD, and W. Winn Chatham, MD, of the University of Alabama at Birmingham, and Roberto Caricchio, MD, of Temple University, Philadelphia, in an accompanying editorial. They noted that the SAVE-MORE trial results contrast with another recent randomized trial of canakinumab, which failed to show notable benefits, compared with placebo, in treating hospitalized patients with COVID-19 pneumonia.
“There are some key differences between these trials, one being that anakinra blocks signaling of both IL-1 alpha and IL-1 beta, whereas canakinumab binds only IL-1 beta,” the editorialists explained. “SARS-CoV-2–infected endothelium may be a particularly important source of IL-1 alpha that is not targeted by canakinumab,” they noted.
Additional studies have examined IL-6 inhibition to treat COVID-19 patients, but data have been inconsistent, the editorialists said.
“One thing that is clearly emerging from this pandemic is that the CSS associated with COVID-19 is relatively unique, with only modestly elevated levels of IL-6, CRP, and ferritin, for example,” they noted. However, the SAVE-MORE study suggests that more targeted approaches, such as anakinra, “may allow earlier introduction of anticytokine treatment” and support the use of IL-1 blockade with anakinra for cases of severe COVID-19 pneumonia.
Predicting risk for severe disease
“One of the major challenges in the management of patients with COVID-19 is identifying patients at risk of severe disease who would warrant early intervention with anti-inflammatory therapy,” said Salim Hayek, MD, medical director of the University of Michigan’s Frankel Cardiovascular Center Clinics, in an interview. “We and others had found that soluble urokinase plasminogen activator receptor (suPAR) levels are the strongest predictor of severe disease amongst biomarkers of inflammation,” he said. “In this study, patients with high suPAR levels derived benefit from anakinra, compared to those with placebo. This study is a great example of how suPAR levels could be used to identify high-risk patients that would benefit from therapies targeting inflammation,” Dr. Hayek emphasized.
“The findings are in line with the hypothesis that patients with the highest degrees of inflammation would benefit the best from targeting the hyperinflammatory cascade using anakinra or other interleukin antagonists,” Dr. Hayek said. “Given suPAR levels are the best predictors of high-risk disease, it is not surprising to see that patients with high levels benefit from targeting inflammation,” he noted.
The take-home message for clinicians at this time is that anakinra effectively improves outcomes in COVID-19 patients with high suPAR levels, Dr. Hayek said. “SuPAR can be measured easily at the point of care. Thus, a targeted strategy using suPAR to identify patients who would benefit from anakinra appears to be viable,” he explained.
However, “Whether anakinra is effective in patients with lower suPAR levels (<6 ng/mL) is unclear and was not answered by this study,” he said. “We eagerly await results of other trials to make that determination. Whether suPAR levels can also help guide the use of other therapies for COVID-19 should be explored and would enhance the personalization of treatment for COVID-19 according to the underlying inflammatory state,” he added.
The SAVE-MORE study was funded by the Hellenic Institute for the Study of Sepsis and Sobi, which manufactures anakinra. Some of the study authors reported financial relationships with Sobi and other pharmaceutical companies.
Dr. Cron disclosed serving as a consultant to Sobi, Novartis, Pfizer, and Sironax. Dr. Cron and Dr. Chatham disclosed having received grant support from Sobi for investigator-initiated clinical trials, and Dr. Caricchio disclosed serving as a consultant to GlaxoSmithKline, Johnson & Johnson, Aurinia, and Bristol-Myers Squibb. Dr. Hayek had no relevant financial conflicts to disclose.
Hospitalized COVID-19 patients at increased risk for respiratory failure showed significant improvement after treatment with anakinra, compared with placebo, based on data from a phase 3, randomized trial of nearly 600 patients who also received standard of care treatment.
Anakinra, a recombinant interleukin (IL)-1 receptor antagonist that blocks activity for both IL-1 alpha and beta, showed a 70% decrease in the risk of progression to severe respiratory failure in a prior open-label, phase 2, proof-of-concept study, wrote Evdoxia Kyriazopoulou, MD, PhD, of National and Kapodistrian University of Athens, and colleagues.
Previous research has shown that soluble urokinase plasminogen activator receptor (suPAR) serum levels can signal increased risk of progression to severe disease and respiratory failure in COVID-19 patients, they noted.
Supported by these early findings, “the SAVE-MORE study (suPAR-guided anakinra treatment for validation of the risk and early management of severe respiratory failure by COVID-19) is a pivotal, confirmatory, phase 3, double-blind, randomized controlled trial that evaluated the efficacy and safety of early initiation of anakinra treatment in hospitalized patients with moderate or severe COVID-19,” the researchers said.
In the SAVE-MORE study published Sept. 3 in Nature Medicine, the researchers identified 594 adults with COVID-19 who were hospitalized at 37 centers in Greece and Italy and at risk of progressing to respiratory failure based on plasma suPAR levels of at least 6 ng/mL.
The primary objective was to assess the impact of early anakinra treatment on the clinical status of COVID-19 patients at risk for severe disease according to the 11-point, ordinal World Health Organization Clinical Progression Scale (WHO-CPS) at 28 days after starting treatment. All patients received standard of care, which consisted of regular monitoring of physical signs, oximetry, and anticoagulation. Patients with severe disease by the WHO definition were also received 6 mg of dexamethasone intravenously daily for 10 days. A total of 405 were randomized to anakinra and 189 to placebo. Approximately 92% of the study participants had severe pneumonia according to the WHO classification for COVID-19. The average age of the patients was 62 years, 58% were male, and the average body mass index was 29.5 kg/m2.
At 28 days, 204 (50.4%) of the anakinra-treated patients had fully recovered, with no detectable viral RNA, compared with 50 (26.5%) of the placebo-treated patients (P < .0001). In addition, significantly fewer patients in the anakinra group had died by 28 days (13 patients, 3.2%), compared with patients in the placebo group (13 patients, 6.9%).
The median decrease in WHO-CPS scores from baseline to 28 days was 4 points in the anakinra group and 3 points in the placebo group, a statistically significant difference (P < .0001).
“Overall, the unadjusted proportional odds of having a worse score on the 11-point WHO-CPS at day 28 with anakinra was 0.36 versus placebo,” and this number remained the same in adjusted analysis, the researchers wrote.
All five secondary endpoints on the WHO-CPS showed significant benefits of anakinra, compared with placebo. These included an absolute decrease of WHO-CPS at day 28 and day 14 from baseline; an absolute decrease of Sequential Organ Failure Assessment scores at day 7 from baseline; and a significantly shorter mean time to both hospital and ICU discharge (1 day and 4 days, respectively) with anakinra versus placebo.
Follow-up laboratory data showed a significant increase in absolute lymphocyte count at 7 days, a significant decrease in circulating IL-6 levels at 4 and 7 days, and significantly decreased plasma C-reactive protein (CRP) levels at 7 days.
Serious treatment-emergent adverse events were reported in 16% with anakinra and in 21.7% with placebo; the most common of these events were infections (8.4% with anakinra and 15.9% with placebo). The next most common serious treatment-emergent adverse events were ventilator-associated pneumonia, septic shock and multiple organ dysfunction, bloodstream infections, and pulmonary embolism. The most common nonserious treatment-emergent adverse events were an increase of liver function tests and hyperglycemia (similar in anakinra and placebo groups) and nonserious anemia (lower in the anakinra group).
The study findings were limited by several factors, including the lack of patients with critical COVID-19 disease and the challenge of application of suPAR in all hospital settings, the researchers noted. However, “the results validate the findings of the previous SAVE open-label phase 2 trial,” they said. The results suggest “that suPAR should be measured upon admission of all patients with COVID-19 who do not need oxygen or who need nasal or mask oxygen, and that, if suPAR levels are 6 ng/mL or higher, anakinra treatment might be a suitable therapy,” they concluded.
Cytokine storm syndrome remains a treatment challenge
“Many who die from COVID-19 suffer hyperinflammation with features of cytokine storm syndrome (CSS) and associated acute respiratory distress syndrome,” wrote Randy Q. Cron, MD, and W. Winn Chatham, MD, of the University of Alabama at Birmingham, and Roberto Caricchio, MD, of Temple University, Philadelphia, in an accompanying editorial. They noted that the SAVE-MORE trial results contrast with another recent randomized trial of canakinumab, which failed to show notable benefits, compared with placebo, in treating hospitalized patients with COVID-19 pneumonia.
“There are some key differences between these trials, one being that anakinra blocks signaling of both IL-1 alpha and IL-1 beta, whereas canakinumab binds only IL-1 beta,” the editorialists explained. “SARS-CoV-2–infected endothelium may be a particularly important source of IL-1 alpha that is not targeted by canakinumab,” they noted.
Additional studies have examined IL-6 inhibition to treat COVID-19 patients, but data have been inconsistent, the editorialists said.
“One thing that is clearly emerging from this pandemic is that the CSS associated with COVID-19 is relatively unique, with only modestly elevated levels of IL-6, CRP, and ferritin, for example,” they noted. However, the SAVE-MORE study suggests that more targeted approaches, such as anakinra, “may allow earlier introduction of anticytokine treatment” and support the use of IL-1 blockade with anakinra for cases of severe COVID-19 pneumonia.
Predicting risk for severe disease
“One of the major challenges in the management of patients with COVID-19 is identifying patients at risk of severe disease who would warrant early intervention with anti-inflammatory therapy,” said Salim Hayek, MD, medical director of the University of Michigan’s Frankel Cardiovascular Center Clinics, in an interview. “We and others had found that soluble urokinase plasminogen activator receptor (suPAR) levels are the strongest predictor of severe disease amongst biomarkers of inflammation,” he said. “In this study, patients with high suPAR levels derived benefit from anakinra, compared to those with placebo. This study is a great example of how suPAR levels could be used to identify high-risk patients that would benefit from therapies targeting inflammation,” Dr. Hayek emphasized.
“The findings are in line with the hypothesis that patients with the highest degrees of inflammation would benefit the best from targeting the hyperinflammatory cascade using anakinra or other interleukin antagonists,” Dr. Hayek said. “Given suPAR levels are the best predictors of high-risk disease, it is not surprising to see that patients with high levels benefit from targeting inflammation,” he noted.
The take-home message for clinicians at this time is that anakinra effectively improves outcomes in COVID-19 patients with high suPAR levels, Dr. Hayek said. “SuPAR can be measured easily at the point of care. Thus, a targeted strategy using suPAR to identify patients who would benefit from anakinra appears to be viable,” he explained.
However, “Whether anakinra is effective in patients with lower suPAR levels (<6 ng/mL) is unclear and was not answered by this study,” he said. “We eagerly await results of other trials to make that determination. Whether suPAR levels can also help guide the use of other therapies for COVID-19 should be explored and would enhance the personalization of treatment for COVID-19 according to the underlying inflammatory state,” he added.
The SAVE-MORE study was funded by the Hellenic Institute for the Study of Sepsis and Sobi, which manufactures anakinra. Some of the study authors reported financial relationships with Sobi and other pharmaceutical companies.
Dr. Cron disclosed serving as a consultant to Sobi, Novartis, Pfizer, and Sironax. Dr. Cron and Dr. Chatham disclosed having received grant support from Sobi for investigator-initiated clinical trials, and Dr. Caricchio disclosed serving as a consultant to GlaxoSmithKline, Johnson & Johnson, Aurinia, and Bristol-Myers Squibb. Dr. Hayek had no relevant financial conflicts to disclose.
FROM NATURE MEDICINE
Addressing vaccine hesitancy with patients
Breakthrough with empathy and compassion
The COVID-19 pandemic is a worldwide tragedy. In the beginning there was a lack of testing, personal protective equipment, COVID tests, and support for health care workers and patients. As 2020 came to a close, the world was given a glimpse of hope with the development of a vaccine against the deadly virus. Many world citizens celebrated the scientific accomplishment and began to breathe a sigh of relief that there was an end in sight. However, the development and distribution of the COVID-19 vaccine revealed a new challenge, vaccine hesitancy.
Community members, young healthy people, and even critically ill hospitalized patients who have the fortune of surviving acute illness are hesitant to the COVID-19 vaccine. I recently cared for a critically ill young patient who was intubated for days with status asthmaticus, one of the worst cases I’d ever seen. She was extubated and made a full recovery. Prior to discharge I asked if she wanted the first dose of the COVID-19 vaccine and she said, “No.” I was shocked. This was an otherwise healthy 30-something-year-old who was lucky enough to survive without any underlying infection in the setting of severe obstructive lung disease. A co-infection with COVID-19 would be disastrous and increase her mortality. I had a long talk at the bedside and asked the reason for her hesitancy. Her answer left me speechless, “I don’t know, I just don’t want to.” I ultimately convinced her that contracting COVID-19 would be a fate worse than she could imagine, and she agreed to the vaccine prior to discharge. This interaction made me ponder – “why are our patients, friends, and family members hesitant about receiving a lifesaving vaccine, especially when they are aware of how sick they or others can become without it?”
According to the World Health Organization, vaccine hesitancy refers to a delay in acceptance or refusal of vaccines despite availability of vaccine services. Vaccine hesitancy is complex and context specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience, and confidence.1 No vaccine is 100% effective. However, throughout history, the work of scientists and doctors to create vaccines saved millions of lives and revolutionized global health. Arguably, the single most life-saving innovation in the history of medicine, vaccines have eradicated smallpox, protected against whooping cough (1914), diphtheria (1926), tetanus (1938), influenza (1945) and mumps (1948), polio (1955), measles (1963), and rubella (1969), and worldwide vaccination rates increased dramatically thanks to successful global health campaigns.2 However, there was a paradox of vaccine success. As terrifying diseases decreased in prevalence, so did the fear of these diseases and their effects – paralysis, brain damage, blindness, and death. This gave birth to a new challenge in modern medicine, vaccine hesitancy – a privilege of first world nations.
Vaccines saved countless lives and improved health and wellbeing around the world for decades. However, to prevent the morbidity and mortality associated with vaccine-preventable diseases and their complications, and optimize control of vaccine-preventable diseases in communities, high vaccination rates must be achieved. Enter the COVID-19 pandemic, the creation of the COVID-19 vaccine, and vaccine hesitancy.
The question we ask ourselves as health care providers is ‘how do we convince the skeptics and those opposed to vaccination to take the vaccine?’ The answer is complicated. If you are like me, you’ve had many conversations with people – friends, patients, family members, who are resistant to the vaccine. Very often the facts are not well received, and those discussions end in argument, high emotions, and broken relationships. With the delta variant of COVID-19 on the rise, spreading aggressively among the unvaccinated, and increased hospitalizations, we foresee the reoccurrence of overwhelmed health systems and a continued death toll.
The new paradox we are faced with is that people choose to believe fiction versus fact, despite the real life evidence of the severe health effects and increased deaths related to COVID-19. Do these skeptics simply have a cavalier attitude towards not only their own life, but the lives of others? Or, is there something deeper? It is not enough to tell people that the vaccines are proven safe3 and are more widely available than ever. It is not enough to tell people that they can die of COVID-19 – they already know that. Emotional pleas to family members are falling on deaf ears. This past month, when asking patients why they don’t want the vaccine, many have no real legitimate health-related reason and respond with a simple, “I don’t want to.” So, how do we get through to the unvaccinated?
A compassionate approach
We navigate these difficult conversations over time with the approach of compassion and empathy, not hostility or bullying. As health care providers, we start by being good empathic listeners. Similar to when we have advance care planning and code status conversations, we cannot enter the dialogue with our intention, beliefs, or formulated goals for that person. We have to listen without judgement to the wide range of reasons why others are reluctant or unwilling to get the vaccine – historical mistrust, political identity, religious reasons, short-term side effects that may cause them to lose a day or two of work – and understand that for each person their reasons are different. The point is to not assume that you know or understand what barriers and beliefs they have towards vaccination, but to meet them at their point of view and listen while keeping your own emotions level and steady.
Identifying the reason for vaccine hesitancy is the first step to getting the unvaccinated closer to vaccination. Ask open ended questions: “Can you help me understand, what is your hesitancy to the vaccine?”; “What about the vaccine worries you?”; “What have you heard about/know about the COVID-19 vaccine?”; or “Can you tell me more about why you feel that way?” As meticulous as it sounds, we have to go back to the basics of patient interviewing.
It is important to remember that this is not a debate and escalation to arguments will certainly backfire. Think about any time you disagreed with someone on a topic. Did criticizing, blaming, and shaming ever convince you to change your beliefs or behaviors? The likely answer is, “No.” Avoid the “backfire effect”– which is when giving people facts disproving their “incorrect” beliefs can actually reinforce those beliefs. The more people are confronted with facts at odds with their opinions, the stronger they cling to those opinions. If you want them to change their mind, you cannot approach the conversation as a debate. You are having this vaccine discussion to try to meet the other person where they are, understand their position, and talk with them, and not at them, about their concerns.
As leaders in health care, we have to be willing to give up control and lead with empathy. We have to show others that we hear them, believe their concerns, and acknowledge that their beliefs are valid to them as individuals. Even if you disagree, this is not the place to let anger, disappointment, or resentment take a front seat. This is about balance, and highlighting the autonomy in decision making that the other person has to make a choice. Be humble in these conversations and avoid condescending tones or statements.
We already know that you are a caring health care provider. As hospitalists, we are frontline providers who have seen unnecessary deaths and illness due to COVID-19. You are passionate and motivated because you are committed to your oath to save lives. However, you have to check your own feelings and remember that you are not speaking with an unvaccinated person to make them get vaccinated, but rather to understand their cognitive process and hopefully walk with them down a path that provides them with a clarity of options they truly have. Extend empathy and they will see your motivation is rooted in good-heartedness and a concern for their wellbeing.
If someone admits to reasons for avoiding vaccination that are not rooted in any fact, then guide them to the best resources. Our health care system recently released a COVID-19 fact versus myth handout called Trust the Facts. This could be the kind of vetted resource you offer. Guide them to accredited websites, such as the World Health Organization, the Center for Disease Control, or their local and state departments of health to help debunk fiction by reviewing it with them. Discuss myths such as, ‘the vaccine will cause infertility,’ ‘the vaccine will give me COVID,’ ‘the vaccine was rushed and is not safe,’ ‘the vaccine is not needed if I am young and healthy,’ ‘the vaccine has a microchip,’ etc. Knowledge is power and disinformation is deadly, but how facts are presented will make the biggest difference in how others receive them, so remember your role is not to argue with these statements, but rather to provide perspective without agreeing or disagreeing.
Respond to their concerns with statements such as, “I hear you…it sounds like you are worried/fearful/mistrusting about the side effects/safety/efficacy of the vaccine…can we talk more about that?” Ask them where these concerns come from – the news, social media, an article, word of mouth, friends, or family. Ask them about the information they have and show genuine interest that you want to see it from their perspective. This is the key to compassionate and empathic dialogue – you relinquish your intentions.
Once you know or unveil their reasons for hesitancy, ask them what they would like to see with regards to COVID-19 and ending the pandemic. Would they like to get back to a new normal, to visit family members, to travel once again, to not have to wear masks and quarantine? What do they want for themselves, their families, communities, the country, or even the world? The goal is to find something in our shared humanity, to connect on a deeper level so they start to open up and let down walls, and find something you both see eye-to-eye on. Know your audience and speak to what serves them. To effectively persuade someone to come around to your point of view starts with recognizing the root of the disagreement and trying to overcome it before trying to change the person’s mind, understanding both the logic and the emotion that’s driving their decision making.4
Building trust
Reminding patients, friends or family members that their health and well-being means a lot to you can also be a strategy to keeping the conversation open and friendly. Sharing stories as hospitalists caring for many critically ill COVID patients or patients who died alone due to COVID-19, and the trauma you experienced as a health care provider feeling paralyzed by the limitations of modern medicine against the deadly virus, will only serve to humanize you in such an interaction.
Building trust will also increase vaccine willingness. This will require a concerted effort by scientists, doctors, and health care systems to engage with community leaders and members. To address hesitancy, the people we serve have to hear those local, personal, and relatable stories about vaccinations, and how it benefits not just themselves, but others around them in their community. As part of the #VaxUp campaign in Virginia, community and physician leaders shared their stories of hesitancy and motivation surrounding the vaccine. These are real people in the community discussing why getting vaccinated is so important and what helped them make an informed decision. I discussed my own hesitancy and concerns and also tackled a few vaccine myths.
As vaccinated health care workers or community leaders, you are living proof of the benefits of getting the COVID vaccine. Focus on the positives but also be honest. If your second shot gave you fevers, chills, or myalgias, then admit it and share how you overcame these expected reactions. Refocus on the safety of the vaccine and the fact that it is freely available to all people. Maybe the person you are speaking with doesn’t know where or how to get an appointment to get vaccinated. Help them find the nearest place to get an appointment and identify barriers they may have in transportation, child, or senior care to leave home safely to get vaccinated, or physical conditions that are preventing them from receiving the vaccine. Share that being vaccinated protects you from contracting the virus and spreading it to loved ones. Focus on how a fully vaccinated community and country can open up opportunities to heal and connect as a society, spend time with family/friends in another county or state, hold a newborn grandchild, or even travel outside the U.S.
There is no guarantee that you will be able to persuade someone to get vaccinated. It’s possible the outcome of your conversation will not result in the other person changing their mind in that moment. That doesn’t mean that you failed, because you started the dialogue and planted the seed. If you are a vaccinated health care provider, your words have influence and power, and we are obliged by our positions to have responsibility for the health of our communities. Don’t be discouraged, as it is through caring, compassionate, respectful, and empathic conversations that your influence will make the most difference in these relationships as you continue to advocate for all human life.
Dr. Williams is vice president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as vice president of the Medical Executive Committee.
References
1. World Health Organization. Report of the SAGE working group on vaccine hesitancy. Oct 2014. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf
2. Hsu JL. A brief history of vaccines: Smallpox to the present. S D Med. 2013;Spec no:33-7. PMID: 23444589.
3. Chiu A, Bever L. Are they experimental? Can they alter DNA? Experts tackle lingering coronavirus vaccine fears. The Washington Post. 2021 May 14. https://www.washingtonpost.com/lifestyle/2021/05/14/safe-fast-vaccine-fear-infertility-dna/
4. Huang L. Edge: Turning Adversity into Advantage. New York: Portfolio/Penguin, 2020.
Breakthrough with empathy and compassion
Breakthrough with empathy and compassion
The COVID-19 pandemic is a worldwide tragedy. In the beginning there was a lack of testing, personal protective equipment, COVID tests, and support for health care workers and patients. As 2020 came to a close, the world was given a glimpse of hope with the development of a vaccine against the deadly virus. Many world citizens celebrated the scientific accomplishment and began to breathe a sigh of relief that there was an end in sight. However, the development and distribution of the COVID-19 vaccine revealed a new challenge, vaccine hesitancy.
Community members, young healthy people, and even critically ill hospitalized patients who have the fortune of surviving acute illness are hesitant to the COVID-19 vaccine. I recently cared for a critically ill young patient who was intubated for days with status asthmaticus, one of the worst cases I’d ever seen. She was extubated and made a full recovery. Prior to discharge I asked if she wanted the first dose of the COVID-19 vaccine and she said, “No.” I was shocked. This was an otherwise healthy 30-something-year-old who was lucky enough to survive without any underlying infection in the setting of severe obstructive lung disease. A co-infection with COVID-19 would be disastrous and increase her mortality. I had a long talk at the bedside and asked the reason for her hesitancy. Her answer left me speechless, “I don’t know, I just don’t want to.” I ultimately convinced her that contracting COVID-19 would be a fate worse than she could imagine, and she agreed to the vaccine prior to discharge. This interaction made me ponder – “why are our patients, friends, and family members hesitant about receiving a lifesaving vaccine, especially when they are aware of how sick they or others can become without it?”
According to the World Health Organization, vaccine hesitancy refers to a delay in acceptance or refusal of vaccines despite availability of vaccine services. Vaccine hesitancy is complex and context specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience, and confidence.1 No vaccine is 100% effective. However, throughout history, the work of scientists and doctors to create vaccines saved millions of lives and revolutionized global health. Arguably, the single most life-saving innovation in the history of medicine, vaccines have eradicated smallpox, protected against whooping cough (1914), diphtheria (1926), tetanus (1938), influenza (1945) and mumps (1948), polio (1955), measles (1963), and rubella (1969), and worldwide vaccination rates increased dramatically thanks to successful global health campaigns.2 However, there was a paradox of vaccine success. As terrifying diseases decreased in prevalence, so did the fear of these diseases and their effects – paralysis, brain damage, blindness, and death. This gave birth to a new challenge in modern medicine, vaccine hesitancy – a privilege of first world nations.
Vaccines saved countless lives and improved health and wellbeing around the world for decades. However, to prevent the morbidity and mortality associated with vaccine-preventable diseases and their complications, and optimize control of vaccine-preventable diseases in communities, high vaccination rates must be achieved. Enter the COVID-19 pandemic, the creation of the COVID-19 vaccine, and vaccine hesitancy.
The question we ask ourselves as health care providers is ‘how do we convince the skeptics and those opposed to vaccination to take the vaccine?’ The answer is complicated. If you are like me, you’ve had many conversations with people – friends, patients, family members, who are resistant to the vaccine. Very often the facts are not well received, and those discussions end in argument, high emotions, and broken relationships. With the delta variant of COVID-19 on the rise, spreading aggressively among the unvaccinated, and increased hospitalizations, we foresee the reoccurrence of overwhelmed health systems and a continued death toll.
The new paradox we are faced with is that people choose to believe fiction versus fact, despite the real life evidence of the severe health effects and increased deaths related to COVID-19. Do these skeptics simply have a cavalier attitude towards not only their own life, but the lives of others? Or, is there something deeper? It is not enough to tell people that the vaccines are proven safe3 and are more widely available than ever. It is not enough to tell people that they can die of COVID-19 – they already know that. Emotional pleas to family members are falling on deaf ears. This past month, when asking patients why they don’t want the vaccine, many have no real legitimate health-related reason and respond with a simple, “I don’t want to.” So, how do we get through to the unvaccinated?
A compassionate approach
We navigate these difficult conversations over time with the approach of compassion and empathy, not hostility or bullying. As health care providers, we start by being good empathic listeners. Similar to when we have advance care planning and code status conversations, we cannot enter the dialogue with our intention, beliefs, or formulated goals for that person. We have to listen without judgement to the wide range of reasons why others are reluctant or unwilling to get the vaccine – historical mistrust, political identity, religious reasons, short-term side effects that may cause them to lose a day or two of work – and understand that for each person their reasons are different. The point is to not assume that you know or understand what barriers and beliefs they have towards vaccination, but to meet them at their point of view and listen while keeping your own emotions level and steady.
Identifying the reason for vaccine hesitancy is the first step to getting the unvaccinated closer to vaccination. Ask open ended questions: “Can you help me understand, what is your hesitancy to the vaccine?”; “What about the vaccine worries you?”; “What have you heard about/know about the COVID-19 vaccine?”; or “Can you tell me more about why you feel that way?” As meticulous as it sounds, we have to go back to the basics of patient interviewing.
It is important to remember that this is not a debate and escalation to arguments will certainly backfire. Think about any time you disagreed with someone on a topic. Did criticizing, blaming, and shaming ever convince you to change your beliefs or behaviors? The likely answer is, “No.” Avoid the “backfire effect”– which is when giving people facts disproving their “incorrect” beliefs can actually reinforce those beliefs. The more people are confronted with facts at odds with their opinions, the stronger they cling to those opinions. If you want them to change their mind, you cannot approach the conversation as a debate. You are having this vaccine discussion to try to meet the other person where they are, understand their position, and talk with them, and not at them, about their concerns.
As leaders in health care, we have to be willing to give up control and lead with empathy. We have to show others that we hear them, believe their concerns, and acknowledge that their beliefs are valid to them as individuals. Even if you disagree, this is not the place to let anger, disappointment, or resentment take a front seat. This is about balance, and highlighting the autonomy in decision making that the other person has to make a choice. Be humble in these conversations and avoid condescending tones or statements.
We already know that you are a caring health care provider. As hospitalists, we are frontline providers who have seen unnecessary deaths and illness due to COVID-19. You are passionate and motivated because you are committed to your oath to save lives. However, you have to check your own feelings and remember that you are not speaking with an unvaccinated person to make them get vaccinated, but rather to understand their cognitive process and hopefully walk with them down a path that provides them with a clarity of options they truly have. Extend empathy and they will see your motivation is rooted in good-heartedness and a concern for their wellbeing.
If someone admits to reasons for avoiding vaccination that are not rooted in any fact, then guide them to the best resources. Our health care system recently released a COVID-19 fact versus myth handout called Trust the Facts. This could be the kind of vetted resource you offer. Guide them to accredited websites, such as the World Health Organization, the Center for Disease Control, or their local and state departments of health to help debunk fiction by reviewing it with them. Discuss myths such as, ‘the vaccine will cause infertility,’ ‘the vaccine will give me COVID,’ ‘the vaccine was rushed and is not safe,’ ‘the vaccine is not needed if I am young and healthy,’ ‘the vaccine has a microchip,’ etc. Knowledge is power and disinformation is deadly, but how facts are presented will make the biggest difference in how others receive them, so remember your role is not to argue with these statements, but rather to provide perspective without agreeing or disagreeing.
Respond to their concerns with statements such as, “I hear you…it sounds like you are worried/fearful/mistrusting about the side effects/safety/efficacy of the vaccine…can we talk more about that?” Ask them where these concerns come from – the news, social media, an article, word of mouth, friends, or family. Ask them about the information they have and show genuine interest that you want to see it from their perspective. This is the key to compassionate and empathic dialogue – you relinquish your intentions.
Once you know or unveil their reasons for hesitancy, ask them what they would like to see with regards to COVID-19 and ending the pandemic. Would they like to get back to a new normal, to visit family members, to travel once again, to not have to wear masks and quarantine? What do they want for themselves, their families, communities, the country, or even the world? The goal is to find something in our shared humanity, to connect on a deeper level so they start to open up and let down walls, and find something you both see eye-to-eye on. Know your audience and speak to what serves them. To effectively persuade someone to come around to your point of view starts with recognizing the root of the disagreement and trying to overcome it before trying to change the person’s mind, understanding both the logic and the emotion that’s driving their decision making.4
Building trust
Reminding patients, friends or family members that their health and well-being means a lot to you can also be a strategy to keeping the conversation open and friendly. Sharing stories as hospitalists caring for many critically ill COVID patients or patients who died alone due to COVID-19, and the trauma you experienced as a health care provider feeling paralyzed by the limitations of modern medicine against the deadly virus, will only serve to humanize you in such an interaction.
Building trust will also increase vaccine willingness. This will require a concerted effort by scientists, doctors, and health care systems to engage with community leaders and members. To address hesitancy, the people we serve have to hear those local, personal, and relatable stories about vaccinations, and how it benefits not just themselves, but others around them in their community. As part of the #VaxUp campaign in Virginia, community and physician leaders shared their stories of hesitancy and motivation surrounding the vaccine. These are real people in the community discussing why getting vaccinated is so important and what helped them make an informed decision. I discussed my own hesitancy and concerns and also tackled a few vaccine myths.
As vaccinated health care workers or community leaders, you are living proof of the benefits of getting the COVID vaccine. Focus on the positives but also be honest. If your second shot gave you fevers, chills, or myalgias, then admit it and share how you overcame these expected reactions. Refocus on the safety of the vaccine and the fact that it is freely available to all people. Maybe the person you are speaking with doesn’t know where or how to get an appointment to get vaccinated. Help them find the nearest place to get an appointment and identify barriers they may have in transportation, child, or senior care to leave home safely to get vaccinated, or physical conditions that are preventing them from receiving the vaccine. Share that being vaccinated protects you from contracting the virus and spreading it to loved ones. Focus on how a fully vaccinated community and country can open up opportunities to heal and connect as a society, spend time with family/friends in another county or state, hold a newborn grandchild, or even travel outside the U.S.
There is no guarantee that you will be able to persuade someone to get vaccinated. It’s possible the outcome of your conversation will not result in the other person changing their mind in that moment. That doesn’t mean that you failed, because you started the dialogue and planted the seed. If you are a vaccinated health care provider, your words have influence and power, and we are obliged by our positions to have responsibility for the health of our communities. Don’t be discouraged, as it is through caring, compassionate, respectful, and empathic conversations that your influence will make the most difference in these relationships as you continue to advocate for all human life.
Dr. Williams is vice president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as vice president of the Medical Executive Committee.
References
1. World Health Organization. Report of the SAGE working group on vaccine hesitancy. Oct 2014. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf
2. Hsu JL. A brief history of vaccines: Smallpox to the present. S D Med. 2013;Spec no:33-7. PMID: 23444589.
3. Chiu A, Bever L. Are they experimental? Can they alter DNA? Experts tackle lingering coronavirus vaccine fears. The Washington Post. 2021 May 14. https://www.washingtonpost.com/lifestyle/2021/05/14/safe-fast-vaccine-fear-infertility-dna/
4. Huang L. Edge: Turning Adversity into Advantage. New York: Portfolio/Penguin, 2020.
The COVID-19 pandemic is a worldwide tragedy. In the beginning there was a lack of testing, personal protective equipment, COVID tests, and support for health care workers and patients. As 2020 came to a close, the world was given a glimpse of hope with the development of a vaccine against the deadly virus. Many world citizens celebrated the scientific accomplishment and began to breathe a sigh of relief that there was an end in sight. However, the development and distribution of the COVID-19 vaccine revealed a new challenge, vaccine hesitancy.
Community members, young healthy people, and even critically ill hospitalized patients who have the fortune of surviving acute illness are hesitant to the COVID-19 vaccine. I recently cared for a critically ill young patient who was intubated for days with status asthmaticus, one of the worst cases I’d ever seen. She was extubated and made a full recovery. Prior to discharge I asked if she wanted the first dose of the COVID-19 vaccine and she said, “No.” I was shocked. This was an otherwise healthy 30-something-year-old who was lucky enough to survive without any underlying infection in the setting of severe obstructive lung disease. A co-infection with COVID-19 would be disastrous and increase her mortality. I had a long talk at the bedside and asked the reason for her hesitancy. Her answer left me speechless, “I don’t know, I just don’t want to.” I ultimately convinced her that contracting COVID-19 would be a fate worse than she could imagine, and she agreed to the vaccine prior to discharge. This interaction made me ponder – “why are our patients, friends, and family members hesitant about receiving a lifesaving vaccine, especially when they are aware of how sick they or others can become without it?”
According to the World Health Organization, vaccine hesitancy refers to a delay in acceptance or refusal of vaccines despite availability of vaccine services. Vaccine hesitancy is complex and context specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience, and confidence.1 No vaccine is 100% effective. However, throughout history, the work of scientists and doctors to create vaccines saved millions of lives and revolutionized global health. Arguably, the single most life-saving innovation in the history of medicine, vaccines have eradicated smallpox, protected against whooping cough (1914), diphtheria (1926), tetanus (1938), influenza (1945) and mumps (1948), polio (1955), measles (1963), and rubella (1969), and worldwide vaccination rates increased dramatically thanks to successful global health campaigns.2 However, there was a paradox of vaccine success. As terrifying diseases decreased in prevalence, so did the fear of these diseases and their effects – paralysis, brain damage, blindness, and death. This gave birth to a new challenge in modern medicine, vaccine hesitancy – a privilege of first world nations.
Vaccines saved countless lives and improved health and wellbeing around the world for decades. However, to prevent the morbidity and mortality associated with vaccine-preventable diseases and their complications, and optimize control of vaccine-preventable diseases in communities, high vaccination rates must be achieved. Enter the COVID-19 pandemic, the creation of the COVID-19 vaccine, and vaccine hesitancy.
The question we ask ourselves as health care providers is ‘how do we convince the skeptics and those opposed to vaccination to take the vaccine?’ The answer is complicated. If you are like me, you’ve had many conversations with people – friends, patients, family members, who are resistant to the vaccine. Very often the facts are not well received, and those discussions end in argument, high emotions, and broken relationships. With the delta variant of COVID-19 on the rise, spreading aggressively among the unvaccinated, and increased hospitalizations, we foresee the reoccurrence of overwhelmed health systems and a continued death toll.
The new paradox we are faced with is that people choose to believe fiction versus fact, despite the real life evidence of the severe health effects and increased deaths related to COVID-19. Do these skeptics simply have a cavalier attitude towards not only their own life, but the lives of others? Or, is there something deeper? It is not enough to tell people that the vaccines are proven safe3 and are more widely available than ever. It is not enough to tell people that they can die of COVID-19 – they already know that. Emotional pleas to family members are falling on deaf ears. This past month, when asking patients why they don’t want the vaccine, many have no real legitimate health-related reason and respond with a simple, “I don’t want to.” So, how do we get through to the unvaccinated?
A compassionate approach
We navigate these difficult conversations over time with the approach of compassion and empathy, not hostility or bullying. As health care providers, we start by being good empathic listeners. Similar to when we have advance care planning and code status conversations, we cannot enter the dialogue with our intention, beliefs, or formulated goals for that person. We have to listen without judgement to the wide range of reasons why others are reluctant or unwilling to get the vaccine – historical mistrust, political identity, religious reasons, short-term side effects that may cause them to lose a day or two of work – and understand that for each person their reasons are different. The point is to not assume that you know or understand what barriers and beliefs they have towards vaccination, but to meet them at their point of view and listen while keeping your own emotions level and steady.
Identifying the reason for vaccine hesitancy is the first step to getting the unvaccinated closer to vaccination. Ask open ended questions: “Can you help me understand, what is your hesitancy to the vaccine?”; “What about the vaccine worries you?”; “What have you heard about/know about the COVID-19 vaccine?”; or “Can you tell me more about why you feel that way?” As meticulous as it sounds, we have to go back to the basics of patient interviewing.
It is important to remember that this is not a debate and escalation to arguments will certainly backfire. Think about any time you disagreed with someone on a topic. Did criticizing, blaming, and shaming ever convince you to change your beliefs or behaviors? The likely answer is, “No.” Avoid the “backfire effect”– which is when giving people facts disproving their “incorrect” beliefs can actually reinforce those beliefs. The more people are confronted with facts at odds with their opinions, the stronger they cling to those opinions. If you want them to change their mind, you cannot approach the conversation as a debate. You are having this vaccine discussion to try to meet the other person where they are, understand their position, and talk with them, and not at them, about their concerns.
As leaders in health care, we have to be willing to give up control and lead with empathy. We have to show others that we hear them, believe their concerns, and acknowledge that their beliefs are valid to them as individuals. Even if you disagree, this is not the place to let anger, disappointment, or resentment take a front seat. This is about balance, and highlighting the autonomy in decision making that the other person has to make a choice. Be humble in these conversations and avoid condescending tones or statements.
We already know that you are a caring health care provider. As hospitalists, we are frontline providers who have seen unnecessary deaths and illness due to COVID-19. You are passionate and motivated because you are committed to your oath to save lives. However, you have to check your own feelings and remember that you are not speaking with an unvaccinated person to make them get vaccinated, but rather to understand their cognitive process and hopefully walk with them down a path that provides them with a clarity of options they truly have. Extend empathy and they will see your motivation is rooted in good-heartedness and a concern for their wellbeing.
If someone admits to reasons for avoiding vaccination that are not rooted in any fact, then guide them to the best resources. Our health care system recently released a COVID-19 fact versus myth handout called Trust the Facts. This could be the kind of vetted resource you offer. Guide them to accredited websites, such as the World Health Organization, the Center for Disease Control, or their local and state departments of health to help debunk fiction by reviewing it with them. Discuss myths such as, ‘the vaccine will cause infertility,’ ‘the vaccine will give me COVID,’ ‘the vaccine was rushed and is not safe,’ ‘the vaccine is not needed if I am young and healthy,’ ‘the vaccine has a microchip,’ etc. Knowledge is power and disinformation is deadly, but how facts are presented will make the biggest difference in how others receive them, so remember your role is not to argue with these statements, but rather to provide perspective without agreeing or disagreeing.
Respond to their concerns with statements such as, “I hear you…it sounds like you are worried/fearful/mistrusting about the side effects/safety/efficacy of the vaccine…can we talk more about that?” Ask them where these concerns come from – the news, social media, an article, word of mouth, friends, or family. Ask them about the information they have and show genuine interest that you want to see it from their perspective. This is the key to compassionate and empathic dialogue – you relinquish your intentions.
Once you know or unveil their reasons for hesitancy, ask them what they would like to see with regards to COVID-19 and ending the pandemic. Would they like to get back to a new normal, to visit family members, to travel once again, to not have to wear masks and quarantine? What do they want for themselves, their families, communities, the country, or even the world? The goal is to find something in our shared humanity, to connect on a deeper level so they start to open up and let down walls, and find something you both see eye-to-eye on. Know your audience and speak to what serves them. To effectively persuade someone to come around to your point of view starts with recognizing the root of the disagreement and trying to overcome it before trying to change the person’s mind, understanding both the logic and the emotion that’s driving their decision making.4
Building trust
Reminding patients, friends or family members that their health and well-being means a lot to you can also be a strategy to keeping the conversation open and friendly. Sharing stories as hospitalists caring for many critically ill COVID patients or patients who died alone due to COVID-19, and the trauma you experienced as a health care provider feeling paralyzed by the limitations of modern medicine against the deadly virus, will only serve to humanize you in such an interaction.
Building trust will also increase vaccine willingness. This will require a concerted effort by scientists, doctors, and health care systems to engage with community leaders and members. To address hesitancy, the people we serve have to hear those local, personal, and relatable stories about vaccinations, and how it benefits not just themselves, but others around them in their community. As part of the #VaxUp campaign in Virginia, community and physician leaders shared their stories of hesitancy and motivation surrounding the vaccine. These are real people in the community discussing why getting vaccinated is so important and what helped them make an informed decision. I discussed my own hesitancy and concerns and also tackled a few vaccine myths.
As vaccinated health care workers or community leaders, you are living proof of the benefits of getting the COVID vaccine. Focus on the positives but also be honest. If your second shot gave you fevers, chills, or myalgias, then admit it and share how you overcame these expected reactions. Refocus on the safety of the vaccine and the fact that it is freely available to all people. Maybe the person you are speaking with doesn’t know where or how to get an appointment to get vaccinated. Help them find the nearest place to get an appointment and identify barriers they may have in transportation, child, or senior care to leave home safely to get vaccinated, or physical conditions that are preventing them from receiving the vaccine. Share that being vaccinated protects you from contracting the virus and spreading it to loved ones. Focus on how a fully vaccinated community and country can open up opportunities to heal and connect as a society, spend time with family/friends in another county or state, hold a newborn grandchild, or even travel outside the U.S.
There is no guarantee that you will be able to persuade someone to get vaccinated. It’s possible the outcome of your conversation will not result in the other person changing their mind in that moment. That doesn’t mean that you failed, because you started the dialogue and planted the seed. If you are a vaccinated health care provider, your words have influence and power, and we are obliged by our positions to have responsibility for the health of our communities. Don’t be discouraged, as it is through caring, compassionate, respectful, and empathic conversations that your influence will make the most difference in these relationships as you continue to advocate for all human life.
Dr. Williams is vice president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as vice president of the Medical Executive Committee.
References
1. World Health Organization. Report of the SAGE working group on vaccine hesitancy. Oct 2014. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf
2. Hsu JL. A brief history of vaccines: Smallpox to the present. S D Med. 2013;Spec no:33-7. PMID: 23444589.
3. Chiu A, Bever L. Are they experimental? Can they alter DNA? Experts tackle lingering coronavirus vaccine fears. The Washington Post. 2021 May 14. https://www.washingtonpost.com/lifestyle/2021/05/14/safe-fast-vaccine-fear-infertility-dna/
4. Huang L. Edge: Turning Adversity into Advantage. New York: Portfolio/Penguin, 2020.
Old saying about prostate cancer not true when it’s metastatic
.
The findings fill an information gap because, remarkably, “data are lacking” on causes of death among men whose prostate cancer has spread to other sites, say lead author Ahmed Elmehrath, MD, of Cairo University, Egypt, and colleagues.
“It was an important realization by our team that prostate cancer was the cause of death in 78% of patients,” said senior author Omar Alhalabi, MD, of University of Texas MD Anderson Cancer Center, Houston, in an email.
“Most patients with metastatic prostate cancer die from it, rather than other possible causes of death,” confirm Samuel Merriel, MSc, Tanimola Martins, PhD, and Sarah Bailey, PhD, University of Exeter, United Kingdom, in an accompanying editorial. The study was published last month in JAMA Network Open.
The findings represent the near opposite of a commonly held – and comforting – belief about early-stage disease: “You die with prostate cancer, not from it.”
That old saying is articulated in various ways, such as this from the Prostate Cancer Foundation: “We can confirm that there are those prostate cancers a man may die with and not of, while others are very aggressive.” The American Cancer Society says this: “Prostate cancer can be a serious disease, but most men diagnosed with prostate cancer do not die from it.”
However, these commonplace comments do not cover metastatic disease, which is what the authors of the new study decided to focus on.
The team used data from the Surveillance, Epidemiology, and End Results Program (SEER) database to gather a sample of 26,168 U.S. men who received a diagnosis of metastatic prostate cancer from January 2000 to December 2016. They then analyzed the data in 2020 and found that 16,732 men (64%) had died during the follow-up period.
The majority of these deaths (77.8%) were from prostate cancer, 5.5% were from other cancers, and 16.7% were from noncancer causes, including cardiovascular diseases, chronic obstructive pulmonary disease, and cerebrovascular diseases.
Senior author Dr. Alhalabi acknowledged a limitation in these findings – that the SEER database relies on causes of death extracted from death certificates. “Death certificates have limited granularity in terms of the details they can contain about the cause of death and also have reporting bias,” he said.
Most of the prostate cancer deaths (59%) occurred within 2 years. The 5-year overall survival rate in the study group was 26%.
The deadliness of metastatic disease “reinforces the need for innovations to promote early-stage diagnosis,” comment the editorialists. Striking a hopeful note, they also say that “new tests for prostate cancer detection may reduce the proportion of patients who receive a diagnosis at a late stage.”
Death from other causes
The mean age at metastatic prostate cancer diagnosis in the study was roughly 71 years. Most of the cohort was White (74.5%) and had a diagnosis of stage M1b metastatic prostate cancer (72.7%), which means the cancer had spread to the bones.
Among men in the cohort, the rates of death from septicemia, suicide, accidents, COPD, and cerebrovascular diseases were significantly increased compared with the general U.S. male population, the team observes.
Thus, the study authors were concerned with not only with death from metastatic prostate cancer but death from other causes.
That concern is rooted in the established fact that there is now improved survival among patients with prostate cancer in the U.S., including among men with advanced disease. “Patients tend to live long enough after a prostate cancer diagnosis for non–cancer-related comorbidities to be associated with their overall survival,” they write.
The editorialists agree: Prostate cancer “has a high long-term survival rate compared with almost all other cancer types and signals the need for greater holistic care for patients.”
As noted above, cardiovascular diseases were the most common cause of nonprostate cancer–related deaths in the new study.
As in the management of other cancers, there is concern among clinicians and researchers about the cardiotoxic effects of prostate cancer treatments.
The study authors point to a 2017 analysis that showed that men with prostate cancer and no prior cardiac disease had greater risk of heart failure after taking androgen deprivation therapy (ADT), a common treatment used when the disease recurs after definitive treatment. Another study suggested an association between cardiotoxic effects of ADT and myocardial infarction regardless of medical history in general.
The authors of the current study say that such findings highlight “the importance of multidisciplinary care for such patients and the role of primary care physicians in optimizing cardiovascular risk prevention and providing early referrals to cardiologists.”
Further, the team says that tailoring “ADT to each patient’s needs may be associated with improved survival, especially for patients with factors associated with cardiovascular disease.”
Who should lead the way in multidisciplinary care? “The answer probably is case-by-case,” said Dr. Alhalabi, adding that it might depend on the presence of underlying morbidities such as cardiovascular disease and COPD.
“It is also important for the oncologist (‘the gatekeeper’) to try to mitigate the potential metabolic effects of hormonal deprivation therapy such as weight gain, decreased muscle mass, hyperlipidemia, etc.,” he added.
The study had no specific funding. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
.
The findings fill an information gap because, remarkably, “data are lacking” on causes of death among men whose prostate cancer has spread to other sites, say lead author Ahmed Elmehrath, MD, of Cairo University, Egypt, and colleagues.
“It was an important realization by our team that prostate cancer was the cause of death in 78% of patients,” said senior author Omar Alhalabi, MD, of University of Texas MD Anderson Cancer Center, Houston, in an email.
“Most patients with metastatic prostate cancer die from it, rather than other possible causes of death,” confirm Samuel Merriel, MSc, Tanimola Martins, PhD, and Sarah Bailey, PhD, University of Exeter, United Kingdom, in an accompanying editorial. The study was published last month in JAMA Network Open.
The findings represent the near opposite of a commonly held – and comforting – belief about early-stage disease: “You die with prostate cancer, not from it.”
That old saying is articulated in various ways, such as this from the Prostate Cancer Foundation: “We can confirm that there are those prostate cancers a man may die with and not of, while others are very aggressive.” The American Cancer Society says this: “Prostate cancer can be a serious disease, but most men diagnosed with prostate cancer do not die from it.”
However, these commonplace comments do not cover metastatic disease, which is what the authors of the new study decided to focus on.
The team used data from the Surveillance, Epidemiology, and End Results Program (SEER) database to gather a sample of 26,168 U.S. men who received a diagnosis of metastatic prostate cancer from January 2000 to December 2016. They then analyzed the data in 2020 and found that 16,732 men (64%) had died during the follow-up period.
The majority of these deaths (77.8%) were from prostate cancer, 5.5% were from other cancers, and 16.7% were from noncancer causes, including cardiovascular diseases, chronic obstructive pulmonary disease, and cerebrovascular diseases.
Senior author Dr. Alhalabi acknowledged a limitation in these findings – that the SEER database relies on causes of death extracted from death certificates. “Death certificates have limited granularity in terms of the details they can contain about the cause of death and also have reporting bias,” he said.
Most of the prostate cancer deaths (59%) occurred within 2 years. The 5-year overall survival rate in the study group was 26%.
The deadliness of metastatic disease “reinforces the need for innovations to promote early-stage diagnosis,” comment the editorialists. Striking a hopeful note, they also say that “new tests for prostate cancer detection may reduce the proportion of patients who receive a diagnosis at a late stage.”
Death from other causes
The mean age at metastatic prostate cancer diagnosis in the study was roughly 71 years. Most of the cohort was White (74.5%) and had a diagnosis of stage M1b metastatic prostate cancer (72.7%), which means the cancer had spread to the bones.
Among men in the cohort, the rates of death from septicemia, suicide, accidents, COPD, and cerebrovascular diseases were significantly increased compared with the general U.S. male population, the team observes.
Thus, the study authors were concerned with not only with death from metastatic prostate cancer but death from other causes.
That concern is rooted in the established fact that there is now improved survival among patients with prostate cancer in the U.S., including among men with advanced disease. “Patients tend to live long enough after a prostate cancer diagnosis for non–cancer-related comorbidities to be associated with their overall survival,” they write.
The editorialists agree: Prostate cancer “has a high long-term survival rate compared with almost all other cancer types and signals the need for greater holistic care for patients.”
As noted above, cardiovascular diseases were the most common cause of nonprostate cancer–related deaths in the new study.
As in the management of other cancers, there is concern among clinicians and researchers about the cardiotoxic effects of prostate cancer treatments.
The study authors point to a 2017 analysis that showed that men with prostate cancer and no prior cardiac disease had greater risk of heart failure after taking androgen deprivation therapy (ADT), a common treatment used when the disease recurs after definitive treatment. Another study suggested an association between cardiotoxic effects of ADT and myocardial infarction regardless of medical history in general.
The authors of the current study say that such findings highlight “the importance of multidisciplinary care for such patients and the role of primary care physicians in optimizing cardiovascular risk prevention and providing early referrals to cardiologists.”
Further, the team says that tailoring “ADT to each patient’s needs may be associated with improved survival, especially for patients with factors associated with cardiovascular disease.”
Who should lead the way in multidisciplinary care? “The answer probably is case-by-case,” said Dr. Alhalabi, adding that it might depend on the presence of underlying morbidities such as cardiovascular disease and COPD.
“It is also important for the oncologist (‘the gatekeeper’) to try to mitigate the potential metabolic effects of hormonal deprivation therapy such as weight gain, decreased muscle mass, hyperlipidemia, etc.,” he added.
The study had no specific funding. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
.
The findings fill an information gap because, remarkably, “data are lacking” on causes of death among men whose prostate cancer has spread to other sites, say lead author Ahmed Elmehrath, MD, of Cairo University, Egypt, and colleagues.
“It was an important realization by our team that prostate cancer was the cause of death in 78% of patients,” said senior author Omar Alhalabi, MD, of University of Texas MD Anderson Cancer Center, Houston, in an email.
“Most patients with metastatic prostate cancer die from it, rather than other possible causes of death,” confirm Samuel Merriel, MSc, Tanimola Martins, PhD, and Sarah Bailey, PhD, University of Exeter, United Kingdom, in an accompanying editorial. The study was published last month in JAMA Network Open.
The findings represent the near opposite of a commonly held – and comforting – belief about early-stage disease: “You die with prostate cancer, not from it.”
That old saying is articulated in various ways, such as this from the Prostate Cancer Foundation: “We can confirm that there are those prostate cancers a man may die with and not of, while others are very aggressive.” The American Cancer Society says this: “Prostate cancer can be a serious disease, but most men diagnosed with prostate cancer do not die from it.”
However, these commonplace comments do not cover metastatic disease, which is what the authors of the new study decided to focus on.
The team used data from the Surveillance, Epidemiology, and End Results Program (SEER) database to gather a sample of 26,168 U.S. men who received a diagnosis of metastatic prostate cancer from January 2000 to December 2016. They then analyzed the data in 2020 and found that 16,732 men (64%) had died during the follow-up period.
The majority of these deaths (77.8%) were from prostate cancer, 5.5% were from other cancers, and 16.7% were from noncancer causes, including cardiovascular diseases, chronic obstructive pulmonary disease, and cerebrovascular diseases.
Senior author Dr. Alhalabi acknowledged a limitation in these findings – that the SEER database relies on causes of death extracted from death certificates. “Death certificates have limited granularity in terms of the details they can contain about the cause of death and also have reporting bias,” he said.
Most of the prostate cancer deaths (59%) occurred within 2 years. The 5-year overall survival rate in the study group was 26%.
The deadliness of metastatic disease “reinforces the need for innovations to promote early-stage diagnosis,” comment the editorialists. Striking a hopeful note, they also say that “new tests for prostate cancer detection may reduce the proportion of patients who receive a diagnosis at a late stage.”
Death from other causes
The mean age at metastatic prostate cancer diagnosis in the study was roughly 71 years. Most of the cohort was White (74.5%) and had a diagnosis of stage M1b metastatic prostate cancer (72.7%), which means the cancer had spread to the bones.
Among men in the cohort, the rates of death from septicemia, suicide, accidents, COPD, and cerebrovascular diseases were significantly increased compared with the general U.S. male population, the team observes.
Thus, the study authors were concerned with not only with death from metastatic prostate cancer but death from other causes.
That concern is rooted in the established fact that there is now improved survival among patients with prostate cancer in the U.S., including among men with advanced disease. “Patients tend to live long enough after a prostate cancer diagnosis for non–cancer-related comorbidities to be associated with their overall survival,” they write.
The editorialists agree: Prostate cancer “has a high long-term survival rate compared with almost all other cancer types and signals the need for greater holistic care for patients.”
As noted above, cardiovascular diseases were the most common cause of nonprostate cancer–related deaths in the new study.
As in the management of other cancers, there is concern among clinicians and researchers about the cardiotoxic effects of prostate cancer treatments.
The study authors point to a 2017 analysis that showed that men with prostate cancer and no prior cardiac disease had greater risk of heart failure after taking androgen deprivation therapy (ADT), a common treatment used when the disease recurs after definitive treatment. Another study suggested an association between cardiotoxic effects of ADT and myocardial infarction regardless of medical history in general.
The authors of the current study say that such findings highlight “the importance of multidisciplinary care for such patients and the role of primary care physicians in optimizing cardiovascular risk prevention and providing early referrals to cardiologists.”
Further, the team says that tailoring “ADT to each patient’s needs may be associated with improved survival, especially for patients with factors associated with cardiovascular disease.”
Who should lead the way in multidisciplinary care? “The answer probably is case-by-case,” said Dr. Alhalabi, adding that it might depend on the presence of underlying morbidities such as cardiovascular disease and COPD.
“It is also important for the oncologist (‘the gatekeeper’) to try to mitigate the potential metabolic effects of hormonal deprivation therapy such as weight gain, decreased muscle mass, hyperlipidemia, etc.,” he added.
The study had no specific funding. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.