User login
Dearth of Hospitalist Investigators in Academic Medicine: A Call to Action
In their report celebrating the increase in the number of hospitalists from a few hundred in the 1990s to more than 50,000 in 2016, Drs Robert Wachter and Lee Goldman also noted the stunted growth of productive hospital medicine research programs, which presents a challenge to academic credibility in hospital medicine.1 Given the substantial increase in the number of hospitalists over the past two decades, we surveyed adult academic hospital medicine groups to quantify the number of hospitalist clinician investigators and identify gaps in resources for researchers. The number of clinician investigators supported at academic medical centers (AMCs) remains disturbingly low despite the rapid growth of our specialty. Some programs also reported a lack of access to fundamental research services. We report selected results from our survey and provide recommendations to support and facilitate the development of clinician investigators in hospital medicine.
DEARTH OF CLINICIAN INVESTIGATORS IN HOSPITAL MEDICINE
We performed a survey of hospital medicine programs at AMCs in the United States through the Hospital Medicine Reengineering Network (HOMERuN), a hospital medicine research collaborative that facilitates and conducts multisite research studies.2 The purpose of this survey was to obtain a profile of adult academic hospital medicine groups. Surveys were distributed via email to directors and/or senior leaders of each hospital medicine group between January and August 2019. In the survey, a clinician investigator was defined as “faculty whose primary nonclinical focus is scientific papers and grant writing.”
We received responses from 43 of the 86 invitees (50%), each of whom represented a unique hospital medicine group; 41 of the representatives responded to the questions concerning available research services. Collectively, these 43 programs represented 2,503 hospitalists. There were 79 clinician investigators reported among all surveyed hospital medicine groups (3.1% of all hospitalists). The median number of clinician investigators per hospital medicine group was 0 (range 0-12) (Appendix Figure 1), and 22 of 43 (51.2%) hospital medicine groups reported having no clinician investigators. Two of the hospital medicine groups, however, reported having 12 clinician investigators at their respective institutions, comprising nearly one third of the total number of clinician investigators reported in the survey.
Many of the programs reported lack of access to resources such as research assistants (56.1%) and dedicated research fellowships (53.7%) (Appendix Figure 2). A number of groups reported a need for more support for various junior faculty development activities, including research mentoring (53.5%), networking with other researchers (60.5%), and access to clinical data from multiple sites (62.8%).
One of the limitations of this survey was the manner in which the participating hospital medicine groups were chosen. Selection was based on groups affiliated with HOMERuN; among those chosen were highly visible US AMCs, including 70% of the top 20 AMCs based on National Institutes of Health (NIH) funding.3 Therefore, our results likely overestimate the research presence of hospital medicine across all AMCs in the United States.
LACK OF GROWTH OVER TIME: CONTEXTUALIZATION AND IMPLICATIONS
Despite the substantial growth of hospital medicine over the past 2 decades, there has been no proportional increase in the number of hospitalist clinician investigators, with earlier surveys also demonstrating low numbers.4,5 Along with the survey by Chopra and colleagues published in 2019,6 our survey provides an additional contemporary appraisal of research activities for adult academic hospital medicine groups. In the survey by Chopra et al, only 54% (15 of 28) of responding programs reported having any faculty with research as their major activity (ie, >50% effort), and 3% of total faculty reported having funding for >50% effort toward research.6 Our study expands upon these findings by providing more detailed data on the number of clinician investigators per hospital medicine group. Results of our survey showed a concentration of hospitalists within a small number of programs, which may have contributed to the observed lack of growth. We also expand on prior work by identifying a lack of resources and services to support hospitalist researchers.
The findings of our survey have important implications for the field of hospital medicine. Without a critical mass of hospitalist clinician investigators, the quality of research that addresses important questions in our field will suffer. It will also limit academic credibility of the field, as well as individual academic achievement; previous studies have consistently demonstrated that few hospitalists at AMCs achieve the rank of associate or full professor.5-9
POTENTIAL EXPLANATIONS FOR LACK OF RESEARCH GROWTH
The results of our study additionally offer possible explanations for the dearth of clinician investigators in hospital medicine. The limited access to research resources and fellowship training identified in our survey are critical domains that must be addressed in order to develop successful academic hospital medicine programs.4,6,8,10
Regarding dedicated hospital medicine research fellowships, there are only a handful across the country. The small number of existing research fellowships only have one or two fellows per year, and these positions often go unfilled because of a lack of applicants and lower salaries compared to full-time clinical positions.11 The lack of applicants for adult hospital medicine fellowship positions is also integrally linked to board certification requirements. Unlike pediatric hospital medicine where additional fellowship training is required to become board-certified, no such fellowship is required in adult hospital medicine. In pediatrics, this requirement has led to a rapid increase in the number of fellowships with scholarly work requirements (more than 60 fellowships, plus additional programs in development) and greater standardization among training experiences.12,13
The lack of fellowship applicants may also stem from the fact that many trainees are not aware of a potential career as a hospitalist clinician investigator due to limited exposure to this career at most AMCs. Our results revealed that nearly half of sites in our survey had zero clinician investigators, depriving trainees at these programs of role models and thus perpetuating a negative feedback loop. Lastly, although unfilled fellowship positions may indicate that demand is a larger problem than supply, it is also true that fellowship programs generate their own demand through recruitment efforts and the gradual establishment of a positive reputation.
Another potential explanation could relate to the development of hospital medicine in response to rising clinical demands at hospitals: compared with other medical specialties, AMCs may regard hospitalists as being clinicians first and academicians second.1,7,10 Also, hospitalists may be perceived as being beholden to hospitals and less engaged with their surrounding communities than other general medicine fields. With a small footprint in health equity research, academic hospital medicine may be less of a draw to generalists interested in pursuing this area of research. Further, there are very few underrepresented in medicine (URiM) hospital medicine research faculty.5
Another challenge to the career development of hospitalist researchers is the lack of available funding for the type of research typically conducted by hospitalists (eg, rigorous quality improvement implementation and evaluation, optimizing best evidence-based care delivery models, evaluation of patient safety in the hospital setting). As hospitalists tend to be system-level thinkers, this lack of funding may steer potential researchers away from externally funded research careers and into hospital operations and quality improvement positions. Also, unlike other medical specialties, there is no dedicated NIH funding source for hospital medicine research (eg, cardiology and the National Heart, Lung, and Blood Institute), placing hospitalists at a disadvantage in seeking funding compared to subspecialists.
STRATEGIES TO ENHANCE RESEARCH PRESENCE
We recommend several approaches—ones that should be pursued simultaneously—to increase the number of clinician investigators in hospital medicine. First, hospital medicine groups and their respective divisions, departments, and hospitals should allocate funding to support research resources; this includes investing in research assistants, data analysts, statisticians, and administrative support. Through the funding of such research infrastructure programs, AMCs could incentivize hospitalists to research best approaches to improve the value of healthcare delivery, ultimately leading to cost savings.
With 60% of respondents identifying the need for improved access to data across multiple sites, our survey also emphasizes the requirement for further collaboration among hospital medicine groups. Such collaboration could lead to high-powered observational studies and the evaluation of interventions across multiple sites, thus improving the generalizability of study findings.
The Society of Hospital Medicine (SHM) and its research committee can continue to expand the research footprint of hospital medicine. To date, the committee has achieved this by highlighting hospitalist research activity at the SHM Annual Conference Scientific Abstract and Poster Competition and developing a visiting professorship exchange program. In addition to these efforts, SHM could foster collaboration and networking between institutions, as well as take advantage of the current political push for expanded Medicare access by lobbying for robust funding for the Agency for Healthcare Research and Quality, which could provide more opportunities for hospitalists to study the effects of healthcare policy reform on the delivery of inpatient care.
Another strategy to increase the number of hospitalist clinician investigators is to expand hospital medicine research fellowships and recruit trainees for these programs. Fellowships could be internally funded wherein a fellow’s clinical productivity is used to offset the costs associated with obtaining advanced degrees. As an incentive to encourage applicants to temporarily forego a full-time clinical salary during fellowship, hospital medicine groups could offer expanded moonlighting opportunities and contribute to repayment of medical school loans. Hospital medicine groups should also advocate for NIH-funded T32 or K12 training grants for hospital medicine. (There are, however, challenges with this approach because the number of T32 spots per NIH institute is usually fixed). The success of academic emergency medicine offers a precedent for such efforts: After the development of a K12 research training program in emergency medicine, the number of NIH-sponsored principal investigators in this specialty increased by 40% in 6 years.14 Additionally, now that fellowships are required for the pediatric hospital medicine clinician investigators, it would be revealing to track the growth of this workforce.12,13
Structured and formalized mentorship is an essential part of the development of clinician investigators in hospital medicine.4,7,8,10 One successful strategy for mentorship has been the partnering of hospital medicine groups with faculty of general internal medicine and other subspecialty divisions with robust research programs.7,8,15 In addition to developing sustainable mentorship programs, hospital medicine researchers must increase their visibility to trainees. Therefore, it is essential that the majority of academic hospital medicine groups not only hire clinician investigators but also invest in their development, rather than rely on the few programs that have several such faculty members. With this strategy, we could dramatically increase the number of hospitalist clinician investigators from a diverse background of training institutions.
SHM could also play a greater role in organizing events for networking and mentoring for trainees and medical students interested in pursuing a career in hospital medicine research. It is also critically important that hospital medicine groups actively recruit, retain, and develop URiM hospital medicine research faculty in order to attract talented researchers and actively participate in the necessary effort to mitigate the inequities prevalent throughout our healthcare system.
CONCLUSION
Despite the growth of hospital medicine over the past decade, there remains a dearth of hospitalist clinician investigators at major AMCs in the United States. This may be due in part to lack of research resources and mentorship within hospital medicine groups. We believe that investment in these resources, expanded funding opportunities, mentorship development, research fellowship programs, and greater exposure of trainees to hospitalist researchers are solutions that should be strongly considered to develop hospitalist clinician investigators.
Acknowledgments
The authors thank HOMERuN executive committee members, including Grant Fletcher, MD, James Harrison, PhD, BSC, MPH, Peter K. Lindenauer, MD, Melissa Mattison, MD, David Meltzer, MD, PhD, Joshua Metlay, MD, PhD, Jennifer Myers, MD, Sumant Ranji, MD, Gregory Ruhnke, MD, MPH, Edmondo Robinson, MD, MBA, and Neil Sehgal, MPH PhD, for their assistance in developing the survey. They also thank Tiffany Lee, MA, for her project management assistance for HOMERuN.
1. Wachter RM, Goldman L. Zero to 50,000 – The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958
2. Auerbach AD, Patel MS, Metlay JP, et al. The Hospital Medicine Reengineering Network (HOMERuN): a learning organization focused on improving hospital care. Acad Med. 2014;89(3):415-420. https://doi.org/10.1097/acm.0000000000000139
3. Roskoski R Jr, Parslow TG. Ranking Tables of NIH funding to US medical schools in 2019. Blue Ridge Institute for Medical Research. Published 2020. Updated July 14, 2020. Accessed July 30, 2020. http://www.brimr.org/NIH_Awards/2019/NIH_Awards_2019.htm
4. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5
5. Miller CS, Fogerty RL, Gann J, Bruti CP, Klein R; The Society of General Internal Medicine Membership Committee. The growth of hospitalists and the future of the society of general internal medicine: results from the 2014 membership survey. J Gen Intern Med. 2017;32(11):1179-1185. https://doi.org/10.1007/s11606-017-4126-7
6. Chopra V, Burden M, Jones CD, et al; Society of Hospital Medicine Research Committee. State of research in adult hospital medicine: results of a national survey. J Hosp Med. 2019;14(4):207-211. https://doi.org/10.12788/jhm.3136
7. Seymann GB, Southern W, Burger A, et al. Features of successful academic hospitalist programs: insights from the SCHOLAR (SuCcessful HOspitaLists in academics and research) project. J Hosp Med. 2016;11(10):708-713. https://doi.org/10.1002/jhm.2603
8. Harrison R, Hunter AJ, Sharpe B, Auerbach AD. Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5-9. https://doi.org/10.1002/jhm.836
9. Dang Do AN, Munchhof AM, Terry C, Emmett T, Kara A. Research and publication trends in hospital medicine. J Hosp Med. 2014;9(3):148-154. https://doi.org/10.1002/jhm.2148
10. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845
11. Ranji SR, Rosenman DJ, Amin AN, Kripalani S. Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1-72.e7. https://doi.org/10.1016/j.amjmed.2005.07.061
12. Shah NH, Rhim HJ, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: a survey of program directors. J Hosp Med. 2016;11(5):324-328. https://doi.org/10.1002/jhm.2571
13. Jerardi KE, Fisher E, Rassbach C, et al; Council of Pediatric Hospital Medicine Fellowship Directors. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698
14. Lewis RJ, Neumar RW. Research in emergency medicine: building the investigator pipeline. Ann Emerg Med. 2018;72(6):691-695. https://doi.org/10.1016/j.annemergmed.2018.10.019
15. Flanders SA, Kaufman SR, Nallamothu BK, Saint S. The University of Michigan Specialist-Hospitalist Allied Research Program: jumpstarting hospital medicine research. J Hosp Med. 2008;3(4):308-313. https://doi.org/10.1002/jhm.342
In their report celebrating the increase in the number of hospitalists from a few hundred in the 1990s to more than 50,000 in 2016, Drs Robert Wachter and Lee Goldman also noted the stunted growth of productive hospital medicine research programs, which presents a challenge to academic credibility in hospital medicine.1 Given the substantial increase in the number of hospitalists over the past two decades, we surveyed adult academic hospital medicine groups to quantify the number of hospitalist clinician investigators and identify gaps in resources for researchers. The number of clinician investigators supported at academic medical centers (AMCs) remains disturbingly low despite the rapid growth of our specialty. Some programs also reported a lack of access to fundamental research services. We report selected results from our survey and provide recommendations to support and facilitate the development of clinician investigators in hospital medicine.
DEARTH OF CLINICIAN INVESTIGATORS IN HOSPITAL MEDICINE
We performed a survey of hospital medicine programs at AMCs in the United States through the Hospital Medicine Reengineering Network (HOMERuN), a hospital medicine research collaborative that facilitates and conducts multisite research studies.2 The purpose of this survey was to obtain a profile of adult academic hospital medicine groups. Surveys were distributed via email to directors and/or senior leaders of each hospital medicine group between January and August 2019. In the survey, a clinician investigator was defined as “faculty whose primary nonclinical focus is scientific papers and grant writing.”
We received responses from 43 of the 86 invitees (50%), each of whom represented a unique hospital medicine group; 41 of the representatives responded to the questions concerning available research services. Collectively, these 43 programs represented 2,503 hospitalists. There were 79 clinician investigators reported among all surveyed hospital medicine groups (3.1% of all hospitalists). The median number of clinician investigators per hospital medicine group was 0 (range 0-12) (Appendix Figure 1), and 22 of 43 (51.2%) hospital medicine groups reported having no clinician investigators. Two of the hospital medicine groups, however, reported having 12 clinician investigators at their respective institutions, comprising nearly one third of the total number of clinician investigators reported in the survey.
Many of the programs reported lack of access to resources such as research assistants (56.1%) and dedicated research fellowships (53.7%) (Appendix Figure 2). A number of groups reported a need for more support for various junior faculty development activities, including research mentoring (53.5%), networking with other researchers (60.5%), and access to clinical data from multiple sites (62.8%).
One of the limitations of this survey was the manner in which the participating hospital medicine groups were chosen. Selection was based on groups affiliated with HOMERuN; among those chosen were highly visible US AMCs, including 70% of the top 20 AMCs based on National Institutes of Health (NIH) funding.3 Therefore, our results likely overestimate the research presence of hospital medicine across all AMCs in the United States.
LACK OF GROWTH OVER TIME: CONTEXTUALIZATION AND IMPLICATIONS
Despite the substantial growth of hospital medicine over the past 2 decades, there has been no proportional increase in the number of hospitalist clinician investigators, with earlier surveys also demonstrating low numbers.4,5 Along with the survey by Chopra and colleagues published in 2019,6 our survey provides an additional contemporary appraisal of research activities for adult academic hospital medicine groups. In the survey by Chopra et al, only 54% (15 of 28) of responding programs reported having any faculty with research as their major activity (ie, >50% effort), and 3% of total faculty reported having funding for >50% effort toward research.6 Our study expands upon these findings by providing more detailed data on the number of clinician investigators per hospital medicine group. Results of our survey showed a concentration of hospitalists within a small number of programs, which may have contributed to the observed lack of growth. We also expand on prior work by identifying a lack of resources and services to support hospitalist researchers.
The findings of our survey have important implications for the field of hospital medicine. Without a critical mass of hospitalist clinician investigators, the quality of research that addresses important questions in our field will suffer. It will also limit academic credibility of the field, as well as individual academic achievement; previous studies have consistently demonstrated that few hospitalists at AMCs achieve the rank of associate or full professor.5-9
POTENTIAL EXPLANATIONS FOR LACK OF RESEARCH GROWTH
The results of our study additionally offer possible explanations for the dearth of clinician investigators in hospital medicine. The limited access to research resources and fellowship training identified in our survey are critical domains that must be addressed in order to develop successful academic hospital medicine programs.4,6,8,10
Regarding dedicated hospital medicine research fellowships, there are only a handful across the country. The small number of existing research fellowships only have one or two fellows per year, and these positions often go unfilled because of a lack of applicants and lower salaries compared to full-time clinical positions.11 The lack of applicants for adult hospital medicine fellowship positions is also integrally linked to board certification requirements. Unlike pediatric hospital medicine where additional fellowship training is required to become board-certified, no such fellowship is required in adult hospital medicine. In pediatrics, this requirement has led to a rapid increase in the number of fellowships with scholarly work requirements (more than 60 fellowships, plus additional programs in development) and greater standardization among training experiences.12,13
The lack of fellowship applicants may also stem from the fact that many trainees are not aware of a potential career as a hospitalist clinician investigator due to limited exposure to this career at most AMCs. Our results revealed that nearly half of sites in our survey had zero clinician investigators, depriving trainees at these programs of role models and thus perpetuating a negative feedback loop. Lastly, although unfilled fellowship positions may indicate that demand is a larger problem than supply, it is also true that fellowship programs generate their own demand through recruitment efforts and the gradual establishment of a positive reputation.
Another potential explanation could relate to the development of hospital medicine in response to rising clinical demands at hospitals: compared with other medical specialties, AMCs may regard hospitalists as being clinicians first and academicians second.1,7,10 Also, hospitalists may be perceived as being beholden to hospitals and less engaged with their surrounding communities than other general medicine fields. With a small footprint in health equity research, academic hospital medicine may be less of a draw to generalists interested in pursuing this area of research. Further, there are very few underrepresented in medicine (URiM) hospital medicine research faculty.5
Another challenge to the career development of hospitalist researchers is the lack of available funding for the type of research typically conducted by hospitalists (eg, rigorous quality improvement implementation and evaluation, optimizing best evidence-based care delivery models, evaluation of patient safety in the hospital setting). As hospitalists tend to be system-level thinkers, this lack of funding may steer potential researchers away from externally funded research careers and into hospital operations and quality improvement positions. Also, unlike other medical specialties, there is no dedicated NIH funding source for hospital medicine research (eg, cardiology and the National Heart, Lung, and Blood Institute), placing hospitalists at a disadvantage in seeking funding compared to subspecialists.
STRATEGIES TO ENHANCE RESEARCH PRESENCE
We recommend several approaches—ones that should be pursued simultaneously—to increase the number of clinician investigators in hospital medicine. First, hospital medicine groups and their respective divisions, departments, and hospitals should allocate funding to support research resources; this includes investing in research assistants, data analysts, statisticians, and administrative support. Through the funding of such research infrastructure programs, AMCs could incentivize hospitalists to research best approaches to improve the value of healthcare delivery, ultimately leading to cost savings.
With 60% of respondents identifying the need for improved access to data across multiple sites, our survey also emphasizes the requirement for further collaboration among hospital medicine groups. Such collaboration could lead to high-powered observational studies and the evaluation of interventions across multiple sites, thus improving the generalizability of study findings.
The Society of Hospital Medicine (SHM) and its research committee can continue to expand the research footprint of hospital medicine. To date, the committee has achieved this by highlighting hospitalist research activity at the SHM Annual Conference Scientific Abstract and Poster Competition and developing a visiting professorship exchange program. In addition to these efforts, SHM could foster collaboration and networking between institutions, as well as take advantage of the current political push for expanded Medicare access by lobbying for robust funding for the Agency for Healthcare Research and Quality, which could provide more opportunities for hospitalists to study the effects of healthcare policy reform on the delivery of inpatient care.
Another strategy to increase the number of hospitalist clinician investigators is to expand hospital medicine research fellowships and recruit trainees for these programs. Fellowships could be internally funded wherein a fellow’s clinical productivity is used to offset the costs associated with obtaining advanced degrees. As an incentive to encourage applicants to temporarily forego a full-time clinical salary during fellowship, hospital medicine groups could offer expanded moonlighting opportunities and contribute to repayment of medical school loans. Hospital medicine groups should also advocate for NIH-funded T32 or K12 training grants for hospital medicine. (There are, however, challenges with this approach because the number of T32 spots per NIH institute is usually fixed). The success of academic emergency medicine offers a precedent for such efforts: After the development of a K12 research training program in emergency medicine, the number of NIH-sponsored principal investigators in this specialty increased by 40% in 6 years.14 Additionally, now that fellowships are required for the pediatric hospital medicine clinician investigators, it would be revealing to track the growth of this workforce.12,13
Structured and formalized mentorship is an essential part of the development of clinician investigators in hospital medicine.4,7,8,10 One successful strategy for mentorship has been the partnering of hospital medicine groups with faculty of general internal medicine and other subspecialty divisions with robust research programs.7,8,15 In addition to developing sustainable mentorship programs, hospital medicine researchers must increase their visibility to trainees. Therefore, it is essential that the majority of academic hospital medicine groups not only hire clinician investigators but also invest in their development, rather than rely on the few programs that have several such faculty members. With this strategy, we could dramatically increase the number of hospitalist clinician investigators from a diverse background of training institutions.
SHM could also play a greater role in organizing events for networking and mentoring for trainees and medical students interested in pursuing a career in hospital medicine research. It is also critically important that hospital medicine groups actively recruit, retain, and develop URiM hospital medicine research faculty in order to attract talented researchers and actively participate in the necessary effort to mitigate the inequities prevalent throughout our healthcare system.
CONCLUSION
Despite the growth of hospital medicine over the past decade, there remains a dearth of hospitalist clinician investigators at major AMCs in the United States. This may be due in part to lack of research resources and mentorship within hospital medicine groups. We believe that investment in these resources, expanded funding opportunities, mentorship development, research fellowship programs, and greater exposure of trainees to hospitalist researchers are solutions that should be strongly considered to develop hospitalist clinician investigators.
Acknowledgments
The authors thank HOMERuN executive committee members, including Grant Fletcher, MD, James Harrison, PhD, BSC, MPH, Peter K. Lindenauer, MD, Melissa Mattison, MD, David Meltzer, MD, PhD, Joshua Metlay, MD, PhD, Jennifer Myers, MD, Sumant Ranji, MD, Gregory Ruhnke, MD, MPH, Edmondo Robinson, MD, MBA, and Neil Sehgal, MPH PhD, for their assistance in developing the survey. They also thank Tiffany Lee, MA, for her project management assistance for HOMERuN.
In their report celebrating the increase in the number of hospitalists from a few hundred in the 1990s to more than 50,000 in 2016, Drs Robert Wachter and Lee Goldman also noted the stunted growth of productive hospital medicine research programs, which presents a challenge to academic credibility in hospital medicine.1 Given the substantial increase in the number of hospitalists over the past two decades, we surveyed adult academic hospital medicine groups to quantify the number of hospitalist clinician investigators and identify gaps in resources for researchers. The number of clinician investigators supported at academic medical centers (AMCs) remains disturbingly low despite the rapid growth of our specialty. Some programs also reported a lack of access to fundamental research services. We report selected results from our survey and provide recommendations to support and facilitate the development of clinician investigators in hospital medicine.
DEARTH OF CLINICIAN INVESTIGATORS IN HOSPITAL MEDICINE
We performed a survey of hospital medicine programs at AMCs in the United States through the Hospital Medicine Reengineering Network (HOMERuN), a hospital medicine research collaborative that facilitates and conducts multisite research studies.2 The purpose of this survey was to obtain a profile of adult academic hospital medicine groups. Surveys were distributed via email to directors and/or senior leaders of each hospital medicine group between January and August 2019. In the survey, a clinician investigator was defined as “faculty whose primary nonclinical focus is scientific papers and grant writing.”
We received responses from 43 of the 86 invitees (50%), each of whom represented a unique hospital medicine group; 41 of the representatives responded to the questions concerning available research services. Collectively, these 43 programs represented 2,503 hospitalists. There were 79 clinician investigators reported among all surveyed hospital medicine groups (3.1% of all hospitalists). The median number of clinician investigators per hospital medicine group was 0 (range 0-12) (Appendix Figure 1), and 22 of 43 (51.2%) hospital medicine groups reported having no clinician investigators. Two of the hospital medicine groups, however, reported having 12 clinician investigators at their respective institutions, comprising nearly one third of the total number of clinician investigators reported in the survey.
Many of the programs reported lack of access to resources such as research assistants (56.1%) and dedicated research fellowships (53.7%) (Appendix Figure 2). A number of groups reported a need for more support for various junior faculty development activities, including research mentoring (53.5%), networking with other researchers (60.5%), and access to clinical data from multiple sites (62.8%).
One of the limitations of this survey was the manner in which the participating hospital medicine groups were chosen. Selection was based on groups affiliated with HOMERuN; among those chosen were highly visible US AMCs, including 70% of the top 20 AMCs based on National Institutes of Health (NIH) funding.3 Therefore, our results likely overestimate the research presence of hospital medicine across all AMCs in the United States.
LACK OF GROWTH OVER TIME: CONTEXTUALIZATION AND IMPLICATIONS
Despite the substantial growth of hospital medicine over the past 2 decades, there has been no proportional increase in the number of hospitalist clinician investigators, with earlier surveys also demonstrating low numbers.4,5 Along with the survey by Chopra and colleagues published in 2019,6 our survey provides an additional contemporary appraisal of research activities for adult academic hospital medicine groups. In the survey by Chopra et al, only 54% (15 of 28) of responding programs reported having any faculty with research as their major activity (ie, >50% effort), and 3% of total faculty reported having funding for >50% effort toward research.6 Our study expands upon these findings by providing more detailed data on the number of clinician investigators per hospital medicine group. Results of our survey showed a concentration of hospitalists within a small number of programs, which may have contributed to the observed lack of growth. We also expand on prior work by identifying a lack of resources and services to support hospitalist researchers.
The findings of our survey have important implications for the field of hospital medicine. Without a critical mass of hospitalist clinician investigators, the quality of research that addresses important questions in our field will suffer. It will also limit academic credibility of the field, as well as individual academic achievement; previous studies have consistently demonstrated that few hospitalists at AMCs achieve the rank of associate or full professor.5-9
POTENTIAL EXPLANATIONS FOR LACK OF RESEARCH GROWTH
The results of our study additionally offer possible explanations for the dearth of clinician investigators in hospital medicine. The limited access to research resources and fellowship training identified in our survey are critical domains that must be addressed in order to develop successful academic hospital medicine programs.4,6,8,10
Regarding dedicated hospital medicine research fellowships, there are only a handful across the country. The small number of existing research fellowships only have one or two fellows per year, and these positions often go unfilled because of a lack of applicants and lower salaries compared to full-time clinical positions.11 The lack of applicants for adult hospital medicine fellowship positions is also integrally linked to board certification requirements. Unlike pediatric hospital medicine where additional fellowship training is required to become board-certified, no such fellowship is required in adult hospital medicine. In pediatrics, this requirement has led to a rapid increase in the number of fellowships with scholarly work requirements (more than 60 fellowships, plus additional programs in development) and greater standardization among training experiences.12,13
The lack of fellowship applicants may also stem from the fact that many trainees are not aware of a potential career as a hospitalist clinician investigator due to limited exposure to this career at most AMCs. Our results revealed that nearly half of sites in our survey had zero clinician investigators, depriving trainees at these programs of role models and thus perpetuating a negative feedback loop. Lastly, although unfilled fellowship positions may indicate that demand is a larger problem than supply, it is also true that fellowship programs generate their own demand through recruitment efforts and the gradual establishment of a positive reputation.
Another potential explanation could relate to the development of hospital medicine in response to rising clinical demands at hospitals: compared with other medical specialties, AMCs may regard hospitalists as being clinicians first and academicians second.1,7,10 Also, hospitalists may be perceived as being beholden to hospitals and less engaged with their surrounding communities than other general medicine fields. With a small footprint in health equity research, academic hospital medicine may be less of a draw to generalists interested in pursuing this area of research. Further, there are very few underrepresented in medicine (URiM) hospital medicine research faculty.5
Another challenge to the career development of hospitalist researchers is the lack of available funding for the type of research typically conducted by hospitalists (eg, rigorous quality improvement implementation and evaluation, optimizing best evidence-based care delivery models, evaluation of patient safety in the hospital setting). As hospitalists tend to be system-level thinkers, this lack of funding may steer potential researchers away from externally funded research careers and into hospital operations and quality improvement positions. Also, unlike other medical specialties, there is no dedicated NIH funding source for hospital medicine research (eg, cardiology and the National Heart, Lung, and Blood Institute), placing hospitalists at a disadvantage in seeking funding compared to subspecialists.
STRATEGIES TO ENHANCE RESEARCH PRESENCE
We recommend several approaches—ones that should be pursued simultaneously—to increase the number of clinician investigators in hospital medicine. First, hospital medicine groups and their respective divisions, departments, and hospitals should allocate funding to support research resources; this includes investing in research assistants, data analysts, statisticians, and administrative support. Through the funding of such research infrastructure programs, AMCs could incentivize hospitalists to research best approaches to improve the value of healthcare delivery, ultimately leading to cost savings.
With 60% of respondents identifying the need for improved access to data across multiple sites, our survey also emphasizes the requirement for further collaboration among hospital medicine groups. Such collaboration could lead to high-powered observational studies and the evaluation of interventions across multiple sites, thus improving the generalizability of study findings.
The Society of Hospital Medicine (SHM) and its research committee can continue to expand the research footprint of hospital medicine. To date, the committee has achieved this by highlighting hospitalist research activity at the SHM Annual Conference Scientific Abstract and Poster Competition and developing a visiting professorship exchange program. In addition to these efforts, SHM could foster collaboration and networking between institutions, as well as take advantage of the current political push for expanded Medicare access by lobbying for robust funding for the Agency for Healthcare Research and Quality, which could provide more opportunities for hospitalists to study the effects of healthcare policy reform on the delivery of inpatient care.
Another strategy to increase the number of hospitalist clinician investigators is to expand hospital medicine research fellowships and recruit trainees for these programs. Fellowships could be internally funded wherein a fellow’s clinical productivity is used to offset the costs associated with obtaining advanced degrees. As an incentive to encourage applicants to temporarily forego a full-time clinical salary during fellowship, hospital medicine groups could offer expanded moonlighting opportunities and contribute to repayment of medical school loans. Hospital medicine groups should also advocate for NIH-funded T32 or K12 training grants for hospital medicine. (There are, however, challenges with this approach because the number of T32 spots per NIH institute is usually fixed). The success of academic emergency medicine offers a precedent for such efforts: After the development of a K12 research training program in emergency medicine, the number of NIH-sponsored principal investigators in this specialty increased by 40% in 6 years.14 Additionally, now that fellowships are required for the pediatric hospital medicine clinician investigators, it would be revealing to track the growth of this workforce.12,13
Structured and formalized mentorship is an essential part of the development of clinician investigators in hospital medicine.4,7,8,10 One successful strategy for mentorship has been the partnering of hospital medicine groups with faculty of general internal medicine and other subspecialty divisions with robust research programs.7,8,15 In addition to developing sustainable mentorship programs, hospital medicine researchers must increase their visibility to trainees. Therefore, it is essential that the majority of academic hospital medicine groups not only hire clinician investigators but also invest in their development, rather than rely on the few programs that have several such faculty members. With this strategy, we could dramatically increase the number of hospitalist clinician investigators from a diverse background of training institutions.
SHM could also play a greater role in organizing events for networking and mentoring for trainees and medical students interested in pursuing a career in hospital medicine research. It is also critically important that hospital medicine groups actively recruit, retain, and develop URiM hospital medicine research faculty in order to attract talented researchers and actively participate in the necessary effort to mitigate the inequities prevalent throughout our healthcare system.
CONCLUSION
Despite the growth of hospital medicine over the past decade, there remains a dearth of hospitalist clinician investigators at major AMCs in the United States. This may be due in part to lack of research resources and mentorship within hospital medicine groups. We believe that investment in these resources, expanded funding opportunities, mentorship development, research fellowship programs, and greater exposure of trainees to hospitalist researchers are solutions that should be strongly considered to develop hospitalist clinician investigators.
Acknowledgments
The authors thank HOMERuN executive committee members, including Grant Fletcher, MD, James Harrison, PhD, BSC, MPH, Peter K. Lindenauer, MD, Melissa Mattison, MD, David Meltzer, MD, PhD, Joshua Metlay, MD, PhD, Jennifer Myers, MD, Sumant Ranji, MD, Gregory Ruhnke, MD, MPH, Edmondo Robinson, MD, MBA, and Neil Sehgal, MPH PhD, for their assistance in developing the survey. They also thank Tiffany Lee, MA, for her project management assistance for HOMERuN.
1. Wachter RM, Goldman L. Zero to 50,000 – The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958
2. Auerbach AD, Patel MS, Metlay JP, et al. The Hospital Medicine Reengineering Network (HOMERuN): a learning organization focused on improving hospital care. Acad Med. 2014;89(3):415-420. https://doi.org/10.1097/acm.0000000000000139
3. Roskoski R Jr, Parslow TG. Ranking Tables of NIH funding to US medical schools in 2019. Blue Ridge Institute for Medical Research. Published 2020. Updated July 14, 2020. Accessed July 30, 2020. http://www.brimr.org/NIH_Awards/2019/NIH_Awards_2019.htm
4. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5
5. Miller CS, Fogerty RL, Gann J, Bruti CP, Klein R; The Society of General Internal Medicine Membership Committee. The growth of hospitalists and the future of the society of general internal medicine: results from the 2014 membership survey. J Gen Intern Med. 2017;32(11):1179-1185. https://doi.org/10.1007/s11606-017-4126-7
6. Chopra V, Burden M, Jones CD, et al; Society of Hospital Medicine Research Committee. State of research in adult hospital medicine: results of a national survey. J Hosp Med. 2019;14(4):207-211. https://doi.org/10.12788/jhm.3136
7. Seymann GB, Southern W, Burger A, et al. Features of successful academic hospitalist programs: insights from the SCHOLAR (SuCcessful HOspitaLists in academics and research) project. J Hosp Med. 2016;11(10):708-713. https://doi.org/10.1002/jhm.2603
8. Harrison R, Hunter AJ, Sharpe B, Auerbach AD. Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5-9. https://doi.org/10.1002/jhm.836
9. Dang Do AN, Munchhof AM, Terry C, Emmett T, Kara A. Research and publication trends in hospital medicine. J Hosp Med. 2014;9(3):148-154. https://doi.org/10.1002/jhm.2148
10. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845
11. Ranji SR, Rosenman DJ, Amin AN, Kripalani S. Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1-72.e7. https://doi.org/10.1016/j.amjmed.2005.07.061
12. Shah NH, Rhim HJ, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: a survey of program directors. J Hosp Med. 2016;11(5):324-328. https://doi.org/10.1002/jhm.2571
13. Jerardi KE, Fisher E, Rassbach C, et al; Council of Pediatric Hospital Medicine Fellowship Directors. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698
14. Lewis RJ, Neumar RW. Research in emergency medicine: building the investigator pipeline. Ann Emerg Med. 2018;72(6):691-695. https://doi.org/10.1016/j.annemergmed.2018.10.019
15. Flanders SA, Kaufman SR, Nallamothu BK, Saint S. The University of Michigan Specialist-Hospitalist Allied Research Program: jumpstarting hospital medicine research. J Hosp Med. 2008;3(4):308-313. https://doi.org/10.1002/jhm.342
1. Wachter RM, Goldman L. Zero to 50,000 – The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958
2. Auerbach AD, Patel MS, Metlay JP, et al. The Hospital Medicine Reengineering Network (HOMERuN): a learning organization focused on improving hospital care. Acad Med. 2014;89(3):415-420. https://doi.org/10.1097/acm.0000000000000139
3. Roskoski R Jr, Parslow TG. Ranking Tables of NIH funding to US medical schools in 2019. Blue Ridge Institute for Medical Research. Published 2020. Updated July 14, 2020. Accessed July 30, 2020. http://www.brimr.org/NIH_Awards/2019/NIH_Awards_2019.htm
4. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5
5. Miller CS, Fogerty RL, Gann J, Bruti CP, Klein R; The Society of General Internal Medicine Membership Committee. The growth of hospitalists and the future of the society of general internal medicine: results from the 2014 membership survey. J Gen Intern Med. 2017;32(11):1179-1185. https://doi.org/10.1007/s11606-017-4126-7
6. Chopra V, Burden M, Jones CD, et al; Society of Hospital Medicine Research Committee. State of research in adult hospital medicine: results of a national survey. J Hosp Med. 2019;14(4):207-211. https://doi.org/10.12788/jhm.3136
7. Seymann GB, Southern W, Burger A, et al. Features of successful academic hospitalist programs: insights from the SCHOLAR (SuCcessful HOspitaLists in academics and research) project. J Hosp Med. 2016;11(10):708-713. https://doi.org/10.1002/jhm.2603
8. Harrison R, Hunter AJ, Sharpe B, Auerbach AD. Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5-9. https://doi.org/10.1002/jhm.836
9. Dang Do AN, Munchhof AM, Terry C, Emmett T, Kara A. Research and publication trends in hospital medicine. J Hosp Med. 2014;9(3):148-154. https://doi.org/10.1002/jhm.2148
10. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845
11. Ranji SR, Rosenman DJ, Amin AN, Kripalani S. Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1-72.e7. https://doi.org/10.1016/j.amjmed.2005.07.061
12. Shah NH, Rhim HJ, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: a survey of program directors. J Hosp Med. 2016;11(5):324-328. https://doi.org/10.1002/jhm.2571
13. Jerardi KE, Fisher E, Rassbach C, et al; Council of Pediatric Hospital Medicine Fellowship Directors. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698
14. Lewis RJ, Neumar RW. Research in emergency medicine: building the investigator pipeline. Ann Emerg Med. 2018;72(6):691-695. https://doi.org/10.1016/j.annemergmed.2018.10.019
15. Flanders SA, Kaufman SR, Nallamothu BK, Saint S. The University of Michigan Specialist-Hospitalist Allied Research Program: jumpstarting hospital medicine research. J Hosp Med. 2008;3(4):308-313. https://doi.org/10.1002/jhm.342
© 2021 Society of Hospital Medicine
Unmasked: How the COVID-19 Pandemic Exacerbates Disparities for People With Communication-Based Disabilities
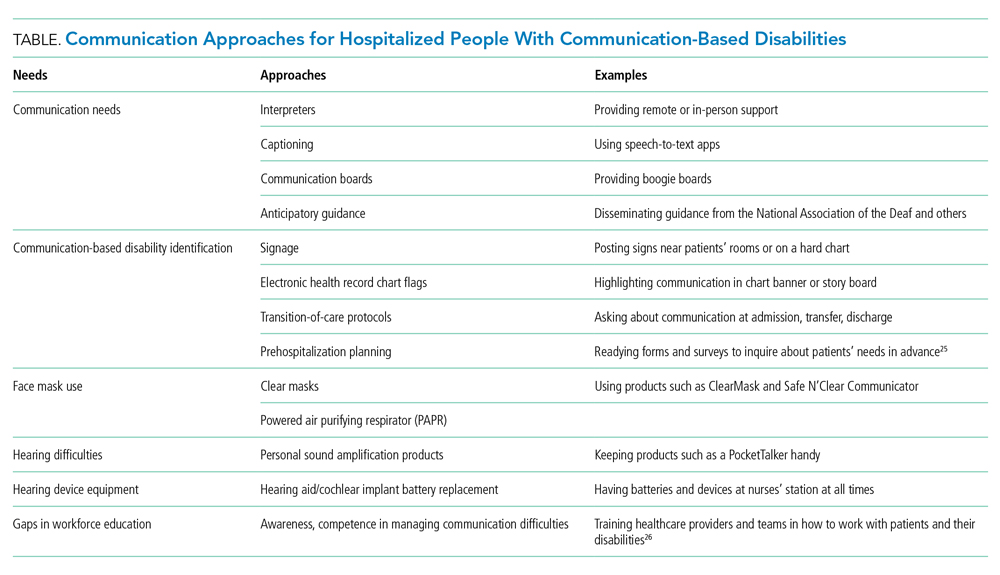
Adults with communication-based disabilities struggle with healthcare inequities,1-4 largely secondary to poor healthcare provider-patient communication. The prevalence of communication-based disabilities, which include speech, language, voice, and/or hearing disabilities, is relatively high yet difficult to ascertain. Ten percent of adults in the United States report having had a speech, language, or voice disability within the past year,5 and hearing loss also affects 17% of the US population.6 These individuals’ collective communication difficulties have been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic, with healthcare systems mandating personal protective equipment (PPE), including face masks, to ensure the safety of workers and patients. This change has placed patients with communication-based disabilities at even greater risk for communication breakdowns.7,8
Hospitals pose challenging communicative environments due to multiple factors (eg, noisy equipment alarms, harried healthcare teams spending less time with patients, PPE use obstructing faces and muffling sounds). Adverse communication among those with communication-based disabilities results in poorer healthcare outcomes, including higher rates of readmission and preventable adverse medical events, as well as lower healthcare satisfaction.7,9,10 Ineffective communication leads to reduced adherence, longer hospitalizations, and worse health outcomes in general.11-13 This is problematic because those with communication-based disabilities are more likely to require hospitalization due to higher rates of associated comorbidities, including frailty, cardiovascular disease, cognitive decline, and falls.4,14-16 Yet hospitals rarely screen and implement best practices to ensure effective and accessible communication for those with communication-based disabilities. The COVID-19 pandemic has exacerbated existing barriers, despite feasible solutions. Importantly, the Americans with Disabilities Act (ADA) remains in effect despite the pandemic. Therefore, hospitals should review existing policies and approaches to ensure adherence to ADA mandates. We address commonly encountered COVID-19-related communication barriers and recommend potential solutions.17
KEY COMMUNICATION BARRIERS
Limited Time or Support
Patients with communication-based disabilities may need more time than others to communicate their needs, values, and preferences effectively, whether due to slower articulation (eg, movement disorders) or communicating via an intermediary (eg, family member who understands them well) or an interpreter. Due to capacity or patient acuity issues, or even concerns about minimizing time in the room of a patient infected with COVID-19, hospital staff may inadvertently spend less time than needed to develop the necessary therapeutic relationships. This concern is magnified when restrictive visitor policies limit the availability of caregivers, such as loved ones, who assist at the bedside with communication.18
Universal Masking and Face Shields
Standard face masks, now required for all in-person encounters regardless of the patient’s COVID-19 status, obstruct the view of the lips and many facial expressions. Facial cues are an important form of nonverbal communication and are critical to conveying meaning in sign language. Face masks, particularly N95 respirators, substantially degrade speech perception.19 Masking increases the difficulty of acoustically and visually understanding patients who have disorders that decrease speech intelligibility, such as dysphonia, dysarthria, or
Interpreters
For deaf and hard-of-hearing people who use American Sign Language (ASL) as their preferred healthcare communication method, interpreters play a critical role in ensuring accessible healthcare communication. Signed language interpretation can occur in person or remotely by video. For in-person interpretation, interpreters must likewise wear PPE. The use of PPE, including face masks, can obscure many of the facial cues important to ASL grammar. Similarly, patients’ face masks can make it more challenging for interpreters to interpret effectively. With remote video interpretation, technological difficulties (eg, dropped WiFi connections) and the loss of environmental cues (eg, interpreter at a remote location unable to see or hear patient surroundings) often mar opportunities for accessible and effective communication. For the DeafBlind community, the use of remote video interpretation is not feasible. DeafBlind people rely on tactile forms of ASL, requiring interpreters’ physical touch throughout the communication encounter. This potentially increases COVID-19 transmission risk.
POTENTIAL OR IMPLEMENTED SOLUTIONS
While some of the solutions listed below also apply to communication in nonpandemic times, identifying high-risk patients and anticipatory planning for communication has become even more important during the COVID-19 outbreak.
Identification and Assessment of
Hospital staff should systematically review admission and transfer protocols to ensure every patient is asked about their communication preferences, necessary accommodations, and specific needs. Any communication needs or accommodation requests (eg, interpreters, communication boards) should be documented and flagged in highly visible areas of the electronic health record. These patients should be assessed regularly to ensure their communication needs are being met and documented throughout their hospital stay.
Assistive Communication Steps
Some steps can be performed in advance. Careful consideration should be given to healthcare providers’ ability to spend additional time with patients with communication-based disabilities. Even if providers are limited physically in the room, they can still work to optimize mindful, high-quality communication by calling into the patient’s room by phone or video. The additional time is important especially when establishing rapport with patients and identifying their preferred communication approaches, as well as engaging their support networks. Patients with communication-based disabilities and their support team often have expertise on their ideal communication strategies. Healthcare providers and staff should inquire about communication preferences. Patients should also be oriented to hospital team structure and members, which could include simple solutions such as legible name tags. Hearing aids, batteries, and other assistive technology should have designated places to prevent loss and ensure ongoing working status. In addition, nurse stations should have a communication toolbox that includes replacement batteries for hearing aids along with other assistive technology devices, such as a personal sound amplification product.
Communication Strategies
Healthcare teams should be trained and reminded to use patient-centered communication strategies, including assessing their comprehension of shared health information through teach-back principles. Strategies vary by patient and may require teams’ flexibility in meeting the patient’s needs and preferences. Examples include ensuring one has the patient’s attention and uses good eye contact. Using a projected “radio voice,” which emphasizes clarity and articulation rather than volume, is helpful for those with hearing loss. For some, meaningful gestures (eg, pointing to one’s own head when asking about headaches) can aid communication. Another strategy when having difficulty understanding patients with decreased speech intelligibility is to repeat the audible speech so that the patient only needs to repeat the inaudible portions that were missed. Patients should have secure access to personal assistive devices, such as hearing aids and even smartphones with communication apps (eg, speech-to-text apps) to facilitate interpersonal communication.
Clear Face Masks
Face masks with transparent windows have been developed. Deaf and hard of hearing people’s speech perception increases when speakers use transparent versus conventional masks. The Food and Drug Administration has approved two clear face masks as American Society for Testing Materials Level 1 (Table). These two masks have limited utility for high-risk situations, such as aerosolizing procedures; in such cases, a powered air purifying respirator with a clear viewing window will be needed instead. Notably, clear mask supply has lagged behind demand, creating limited mask availability during the pandemic; their use may need to be restricted to those working with patients with communication-based disabilities.
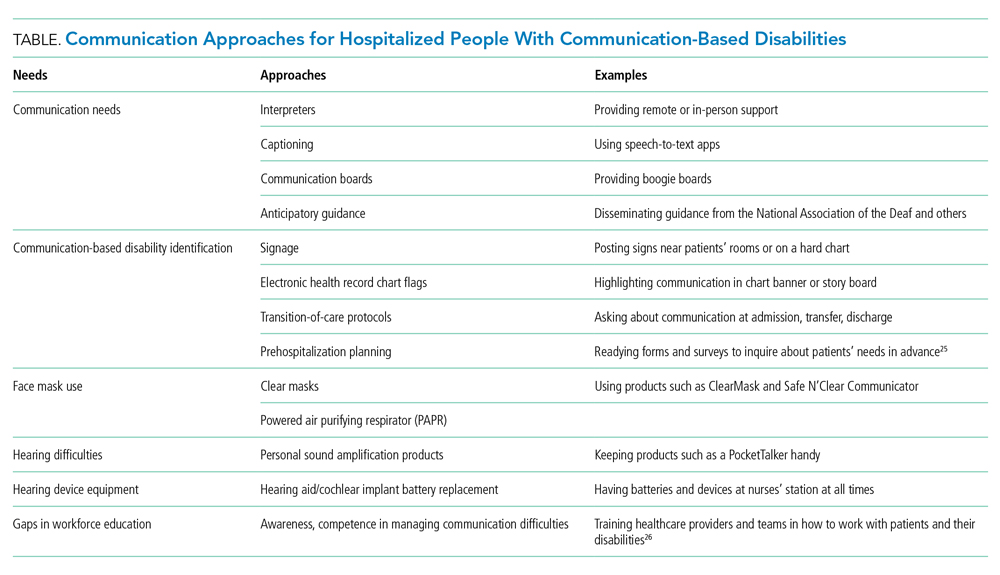
Tools for Communicating Within the Patient’s Room
Erasable whiteboards and communication boards are useful tools for simple exchanges as long as patients’ literacy and fluency are adequate. “PocketTalkers” or personalized sound amplification products may allow providers to speak into a microphone, providing amplified speech via a patient’s headphones. These amplification products are typically useful for those with mild to moderate hearing loss who are not using a hearing aid. Automatic speech recognition apps are device-based apps for converting speech to text. Speakers hold the device near the mouth to maximize accuracy while the patient reads the captions on their screen. With social distancing, lavalier microphones can increase text accuracy, but higher rates of error may still occur due to background noises or accents. For increased reliability and accuracy, Computer Access Realtime Translation stenographers can provide live speech to text on a computer screen from off-site via a computer or smartphone.
Tools for Isolation-Limited Communication
Team members can call an intermediary service to communicate with the patient via the patient’s smartphone or hospital-provided remote video interpreting service, depending on the patient’s preferred communication modality. For oral and spoken language, some services (Table) use remote stenographers to convert speech to text or sign language interpreters for those who use sign language. For both communication modes, smartphone-based videoconferencing may be beneficial while maintaining isolation precautions.
Interpreter Accessibility
Conceptualize interpreters as consulting healthcare team members. They should receive the same PPE training and monitoring as other healthcare workers. For patients using remote video interpretation, this technology needs to be optimized for best results. The room should be in a location with a strong Wi-Fi signal. Equipment should be consistently charged when not in use and rapidly accessible, even remaining in the patients’ room if possible. Healthcare teams need training to appropriately locate and set up the equipment with appropriate support from information technology staff.
Signage
Signage is useful to remind healthcare teams of the patients’ and/or caregivers’ communication-based disability. The most commonly used disability signage shows a line across an ear to indicate hearing loss (Appendix Figure).22 Appropriate signage use, even simple printed sheets documenting a communication issue, can remind healthcare team members of patients’ needs to ensure that communication is accessible and avoid misconceptions toward the patient (eg, noncompliance or cognitive issues). Chart banners, patient room doorways, and over the patients’ beds are good signage locations.
Systematic Noise Reduction
Consistent with previous calls to reduce inpatient noise,23 hospitals should systematically review and monitor protocols to reduce noise pollution. If intra-unit noise varies, patients relying on acoustic-based communication due to hearing loss or speech, language, or voice disability should be placed in quieter rooms.
Communication Concordance
Healthcare professionals and staff with disabilities are an increasingly recognized workforce segment,24 and often are experienced innovators in communicating effectively with patients with communication-based disabilities. Healthcare systems can explore whether they have healthcare team members, employees, disability resource professionals, and/or trainees with these backgrounds and, if they are available, recruit them into developing effective inpatient communication policies and processes.
CONCLUSION
People with communication disabilities experience significant healthcare disparities, now further exacerbated by COVID-19. As clinicians, staff and hospitals work to fuse safety with high-quality communication and care, we should capitalize on multipronged opportunities at the system and individual levels to identify barriers and ensure accessible and effective communication with patients who have communication-based disabilities.
1. McKee MM, Moreland C, Atcherson SR, Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP Essent. 2015;434:24-28.
2. Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disabil Rehabil Assist Technol. 2013;8(6):472-481. https://doi.org/10.3109/17483107.2012.746398
3. Steinberg AG, Barnett S, Meador HE, Wiggins EA, Zazove P. Health care system accessibility. experiences and perceptions of deaf people. J Gen Intern Med. 2006;21(3):260-266. https://doi.org/10.1111/j.1525-1497.2006.00340.x
4. Stransky ML, Jensen KM, Morris MA. Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. J Gen Intern Med. 2018;33(12):2147-2155. https://doi.org/10.1007/s11606-018-4625-1
5. Morris MA, Meier SK, Griffin JM, Branda ME, Phelan SM. Prevalence and etiologies of adult communication disabilities in the United States: results from the 2012 National Health Interview Survey. Disabil Health J. 2016;9(1):140-144. https://doi.org/10.1016/j.dhjo.2015.07.004
6. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital Health Stat. 2014(260):1-161.
7. Chang JE, Weinstein B, Chodosh J, Blustein J. Hospital readmission risk for patients with self-reported hearing loss and communication trouble. J Am Geriatr Soc. 2018;66(11):2227-2228. https://doi.org/10.1111/jgs.15545
8. McKee M, Moran C, Zazove P. Overcoming additional barriers to care for deaf and hard of hearing patients during COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;146(9):781-782. https://doi.org/10.1001/jamaoto.2020.1705
9. Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. https://doi.org/10.1503/cmaj.070690
10. Hoffman JM, Yorkston KM, Shumway-Cook A, Ciol MA, Dudgeon BJ, Chan L. Effect of communication disability on satisfaction with health care: a survey of medicare beneficiaries. Am J Speech Lang Pathol. 2005;14(3):221-228. https://doi.org/10.1044/1058-0360(2005/022)
11. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(4):e94207. https://doi.org/10.1371/journal.pone.0094207
12. Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315-318. https://doi.org/10.1016/j.pec.2007.03.005
13. Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295-301. https://doi.org/10.1016/j.pec.2008.11.015
14. Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322-2324. https://doi.org/10.1001/jama.2013.5912
15. Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293-299. https://doi.org/10.1001/jamainternmed.2013.1868
16. McKee MM, Stransky ML, Reichard A. Hearing loss and associated medical conditions among individuals 65 years and older. Disabil Health J. 2018;11(1):122-125. https://doi.org/10.1016/j.dhjo.2017.05.007
17. ADA requirements: effective communication. U.S. Department of Justice. January 31, 2014. Accessed February 12, 2021. https://www.ada.gov/effective-comm.htm
18. OCR resolves complaints after State of Connecticut and private hospital safeguard the rights of persons with disabilities to have reasonable access to support persons in hospital settings during COVID-19. Press Release. US Department of Health and Human Services; June 9, 2020. Accessed September 19, 2020. https://www.hhs.gov/about/news/2020/06/09/ocr-resolves-complaints-after-state-connecticut-private-hospital-safeguard-rights-persons.html
19. Goldin A, Weinstein B, Shiman N. How do medical masks degrade speech perception? The Hearing Review. April 1, 2020. Accessed September 30, 2020. https://www.hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception
20. Mendel LL, Gardino JA, Atcherson SR. Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol. 2008;19(9):686-695. https://doi.org/10.3766/jaaa.19.9.4
21. Atcherson SR, Finley ET, McDowell BR, Watson C. More speech degradations and considerations in the search for transparent face coverings during the COVID-19 pandemic. American Academy of Audiology. November/December 2020. Accessed September 19, 2020. https://www.audiology.org/audiology-today-julyaugust-2020/online-feature-more-speech-degradations-and-considerations-search
22. Hearing Loss. Wikipedia. Accessed October 28, 2020. https://en.wikipedia.org/wiki/Hearing_loss
23. Kamdar BB, Martin JL, Needham DM. Noise and light pollution in the hospital: a call for action. J Hosp Med. 2017;12(10):861-862. https://doi.org/10.12788/jhm.2838
24. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med. 2018;93(4):540-543. https://doi.org/10.1097/acm.0000000000002112
25. Communication Access Plan (CAP): Instructions for Patients and Providers. Hearing Loss Association of America (HLAA). Accessed September 30, 2020. https://www.hearingloss.org/wp-content/uploads/HLAA_HC_CAP_Form_and_Instructions.pdf
26. How Do I Communicate with Doctors, Nurses, and Staff at the Hospital During COVID-19? Hearing Loss Association of America (HLAA). May 8, 2020. Accessed September 30, 2020. https://www.hearingloss.org/communication-access-recommendations-hospitals-covid-19/
Adults with communication-based disabilities struggle with healthcare inequities,1-4 largely secondary to poor healthcare provider-patient communication. The prevalence of communication-based disabilities, which include speech, language, voice, and/or hearing disabilities, is relatively high yet difficult to ascertain. Ten percent of adults in the United States report having had a speech, language, or voice disability within the past year,5 and hearing loss also affects 17% of the US population.6 These individuals’ collective communication difficulties have been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic, with healthcare systems mandating personal protective equipment (PPE), including face masks, to ensure the safety of workers and patients. This change has placed patients with communication-based disabilities at even greater risk for communication breakdowns.7,8
Hospitals pose challenging communicative environments due to multiple factors (eg, noisy equipment alarms, harried healthcare teams spending less time with patients, PPE use obstructing faces and muffling sounds). Adverse communication among those with communication-based disabilities results in poorer healthcare outcomes, including higher rates of readmission and preventable adverse medical events, as well as lower healthcare satisfaction.7,9,10 Ineffective communication leads to reduced adherence, longer hospitalizations, and worse health outcomes in general.11-13 This is problematic because those with communication-based disabilities are more likely to require hospitalization due to higher rates of associated comorbidities, including frailty, cardiovascular disease, cognitive decline, and falls.4,14-16 Yet hospitals rarely screen and implement best practices to ensure effective and accessible communication for those with communication-based disabilities. The COVID-19 pandemic has exacerbated existing barriers, despite feasible solutions. Importantly, the Americans with Disabilities Act (ADA) remains in effect despite the pandemic. Therefore, hospitals should review existing policies and approaches to ensure adherence to ADA mandates. We address commonly encountered COVID-19-related communication barriers and recommend potential solutions.17
KEY COMMUNICATION BARRIERS
Limited Time or Support
Patients with communication-based disabilities may need more time than others to communicate their needs, values, and preferences effectively, whether due to slower articulation (eg, movement disorders) or communicating via an intermediary (eg, family member who understands them well) or an interpreter. Due to capacity or patient acuity issues, or even concerns about minimizing time in the room of a patient infected with COVID-19, hospital staff may inadvertently spend less time than needed to develop the necessary therapeutic relationships. This concern is magnified when restrictive visitor policies limit the availability of caregivers, such as loved ones, who assist at the bedside with communication.18
Universal Masking and Face Shields
Standard face masks, now required for all in-person encounters regardless of the patient’s COVID-19 status, obstruct the view of the lips and many facial expressions. Facial cues are an important form of nonverbal communication and are critical to conveying meaning in sign language. Face masks, particularly N95 respirators, substantially degrade speech perception.19 Masking increases the difficulty of acoustically and visually understanding patients who have disorders that decrease speech intelligibility, such as dysphonia, dysarthria, or
Interpreters
For deaf and hard-of-hearing people who use American Sign Language (ASL) as their preferred healthcare communication method, interpreters play a critical role in ensuring accessible healthcare communication. Signed language interpretation can occur in person or remotely by video. For in-person interpretation, interpreters must likewise wear PPE. The use of PPE, including face masks, can obscure many of the facial cues important to ASL grammar. Similarly, patients’ face masks can make it more challenging for interpreters to interpret effectively. With remote video interpretation, technological difficulties (eg, dropped WiFi connections) and the loss of environmental cues (eg, interpreter at a remote location unable to see or hear patient surroundings) often mar opportunities for accessible and effective communication. For the DeafBlind community, the use of remote video interpretation is not feasible. DeafBlind people rely on tactile forms of ASL, requiring interpreters’ physical touch throughout the communication encounter. This potentially increases COVID-19 transmission risk.
POTENTIAL OR IMPLEMENTED SOLUTIONS
While some of the solutions listed below also apply to communication in nonpandemic times, identifying high-risk patients and anticipatory planning for communication has become even more important during the COVID-19 outbreak.
Identification and Assessment of
Hospital staff should systematically review admission and transfer protocols to ensure every patient is asked about their communication preferences, necessary accommodations, and specific needs. Any communication needs or accommodation requests (eg, interpreters, communication boards) should be documented and flagged in highly visible areas of the electronic health record. These patients should be assessed regularly to ensure their communication needs are being met and documented throughout their hospital stay.
Assistive Communication Steps
Some steps can be performed in advance. Careful consideration should be given to healthcare providers’ ability to spend additional time with patients with communication-based disabilities. Even if providers are limited physically in the room, they can still work to optimize mindful, high-quality communication by calling into the patient’s room by phone or video. The additional time is important especially when establishing rapport with patients and identifying their preferred communication approaches, as well as engaging their support networks. Patients with communication-based disabilities and their support team often have expertise on their ideal communication strategies. Healthcare providers and staff should inquire about communication preferences. Patients should also be oriented to hospital team structure and members, which could include simple solutions such as legible name tags. Hearing aids, batteries, and other assistive technology should have designated places to prevent loss and ensure ongoing working status. In addition, nurse stations should have a communication toolbox that includes replacement batteries for hearing aids along with other assistive technology devices, such as a personal sound amplification product.
Communication Strategies
Healthcare teams should be trained and reminded to use patient-centered communication strategies, including assessing their comprehension of shared health information through teach-back principles. Strategies vary by patient and may require teams’ flexibility in meeting the patient’s needs and preferences. Examples include ensuring one has the patient’s attention and uses good eye contact. Using a projected “radio voice,” which emphasizes clarity and articulation rather than volume, is helpful for those with hearing loss. For some, meaningful gestures (eg, pointing to one’s own head when asking about headaches) can aid communication. Another strategy when having difficulty understanding patients with decreased speech intelligibility is to repeat the audible speech so that the patient only needs to repeat the inaudible portions that were missed. Patients should have secure access to personal assistive devices, such as hearing aids and even smartphones with communication apps (eg, speech-to-text apps) to facilitate interpersonal communication.
Clear Face Masks
Face masks with transparent windows have been developed. Deaf and hard of hearing people’s speech perception increases when speakers use transparent versus conventional masks. The Food and Drug Administration has approved two clear face masks as American Society for Testing Materials Level 1 (Table). These two masks have limited utility for high-risk situations, such as aerosolizing procedures; in such cases, a powered air purifying respirator with a clear viewing window will be needed instead. Notably, clear mask supply has lagged behind demand, creating limited mask availability during the pandemic; their use may need to be restricted to those working with patients with communication-based disabilities.
Tools for Communicating Within the Patient’s Room
Erasable whiteboards and communication boards are useful tools for simple exchanges as long as patients’ literacy and fluency are adequate. “PocketTalkers” or personalized sound amplification products may allow providers to speak into a microphone, providing amplified speech via a patient’s headphones. These amplification products are typically useful for those with mild to moderate hearing loss who are not using a hearing aid. Automatic speech recognition apps are device-based apps for converting speech to text. Speakers hold the device near the mouth to maximize accuracy while the patient reads the captions on their screen. With social distancing, lavalier microphones can increase text accuracy, but higher rates of error may still occur due to background noises or accents. For increased reliability and accuracy, Computer Access Realtime Translation stenographers can provide live speech to text on a computer screen from off-site via a computer or smartphone.
Tools for Isolation-Limited Communication
Team members can call an intermediary service to communicate with the patient via the patient’s smartphone or hospital-provided remote video interpreting service, depending on the patient’s preferred communication modality. For oral and spoken language, some services (Table) use remote stenographers to convert speech to text or sign language interpreters for those who use sign language. For both communication modes, smartphone-based videoconferencing may be beneficial while maintaining isolation precautions.
Interpreter Accessibility
Conceptualize interpreters as consulting healthcare team members. They should receive the same PPE training and monitoring as other healthcare workers. For patients using remote video interpretation, this technology needs to be optimized for best results. The room should be in a location with a strong Wi-Fi signal. Equipment should be consistently charged when not in use and rapidly accessible, even remaining in the patients’ room if possible. Healthcare teams need training to appropriately locate and set up the equipment with appropriate support from information technology staff.
Signage
Signage is useful to remind healthcare teams of the patients’ and/or caregivers’ communication-based disability. The most commonly used disability signage shows a line across an ear to indicate hearing loss (Appendix Figure).22 Appropriate signage use, even simple printed sheets documenting a communication issue, can remind healthcare team members of patients’ needs to ensure that communication is accessible and avoid misconceptions toward the patient (eg, noncompliance or cognitive issues). Chart banners, patient room doorways, and over the patients’ beds are good signage locations.
Systematic Noise Reduction
Consistent with previous calls to reduce inpatient noise,23 hospitals should systematically review and monitor protocols to reduce noise pollution. If intra-unit noise varies, patients relying on acoustic-based communication due to hearing loss or speech, language, or voice disability should be placed in quieter rooms.
Communication Concordance
Healthcare professionals and staff with disabilities are an increasingly recognized workforce segment,24 and often are experienced innovators in communicating effectively with patients with communication-based disabilities. Healthcare systems can explore whether they have healthcare team members, employees, disability resource professionals, and/or trainees with these backgrounds and, if they are available, recruit them into developing effective inpatient communication policies and processes.
CONCLUSION
People with communication disabilities experience significant healthcare disparities, now further exacerbated by COVID-19. As clinicians, staff and hospitals work to fuse safety with high-quality communication and care, we should capitalize on multipronged opportunities at the system and individual levels to identify barriers and ensure accessible and effective communication with patients who have communication-based disabilities.
Adults with communication-based disabilities struggle with healthcare inequities,1-4 largely secondary to poor healthcare provider-patient communication. The prevalence of communication-based disabilities, which include speech, language, voice, and/or hearing disabilities, is relatively high yet difficult to ascertain. Ten percent of adults in the United States report having had a speech, language, or voice disability within the past year,5 and hearing loss also affects 17% of the US population.6 These individuals’ collective communication difficulties have been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic, with healthcare systems mandating personal protective equipment (PPE), including face masks, to ensure the safety of workers and patients. This change has placed patients with communication-based disabilities at even greater risk for communication breakdowns.7,8
Hospitals pose challenging communicative environments due to multiple factors (eg, noisy equipment alarms, harried healthcare teams spending less time with patients, PPE use obstructing faces and muffling sounds). Adverse communication among those with communication-based disabilities results in poorer healthcare outcomes, including higher rates of readmission and preventable adverse medical events, as well as lower healthcare satisfaction.7,9,10 Ineffective communication leads to reduced adherence, longer hospitalizations, and worse health outcomes in general.11-13 This is problematic because those with communication-based disabilities are more likely to require hospitalization due to higher rates of associated comorbidities, including frailty, cardiovascular disease, cognitive decline, and falls.4,14-16 Yet hospitals rarely screen and implement best practices to ensure effective and accessible communication for those with communication-based disabilities. The COVID-19 pandemic has exacerbated existing barriers, despite feasible solutions. Importantly, the Americans with Disabilities Act (ADA) remains in effect despite the pandemic. Therefore, hospitals should review existing policies and approaches to ensure adherence to ADA mandates. We address commonly encountered COVID-19-related communication barriers and recommend potential solutions.17
KEY COMMUNICATION BARRIERS
Limited Time or Support
Patients with communication-based disabilities may need more time than others to communicate their needs, values, and preferences effectively, whether due to slower articulation (eg, movement disorders) or communicating via an intermediary (eg, family member who understands them well) or an interpreter. Due to capacity or patient acuity issues, or even concerns about minimizing time in the room of a patient infected with COVID-19, hospital staff may inadvertently spend less time than needed to develop the necessary therapeutic relationships. This concern is magnified when restrictive visitor policies limit the availability of caregivers, such as loved ones, who assist at the bedside with communication.18
Universal Masking and Face Shields
Standard face masks, now required for all in-person encounters regardless of the patient’s COVID-19 status, obstruct the view of the lips and many facial expressions. Facial cues are an important form of nonverbal communication and are critical to conveying meaning in sign language. Face masks, particularly N95 respirators, substantially degrade speech perception.19 Masking increases the difficulty of acoustically and visually understanding patients who have disorders that decrease speech intelligibility, such as dysphonia, dysarthria, or
Interpreters
For deaf and hard-of-hearing people who use American Sign Language (ASL) as their preferred healthcare communication method, interpreters play a critical role in ensuring accessible healthcare communication. Signed language interpretation can occur in person or remotely by video. For in-person interpretation, interpreters must likewise wear PPE. The use of PPE, including face masks, can obscure many of the facial cues important to ASL grammar. Similarly, patients’ face masks can make it more challenging for interpreters to interpret effectively. With remote video interpretation, technological difficulties (eg, dropped WiFi connections) and the loss of environmental cues (eg, interpreter at a remote location unable to see or hear patient surroundings) often mar opportunities for accessible and effective communication. For the DeafBlind community, the use of remote video interpretation is not feasible. DeafBlind people rely on tactile forms of ASL, requiring interpreters’ physical touch throughout the communication encounter. This potentially increases COVID-19 transmission risk.
POTENTIAL OR IMPLEMENTED SOLUTIONS
While some of the solutions listed below also apply to communication in nonpandemic times, identifying high-risk patients and anticipatory planning for communication has become even more important during the COVID-19 outbreak.
Identification and Assessment of
Hospital staff should systematically review admission and transfer protocols to ensure every patient is asked about their communication preferences, necessary accommodations, and specific needs. Any communication needs or accommodation requests (eg, interpreters, communication boards) should be documented and flagged in highly visible areas of the electronic health record. These patients should be assessed regularly to ensure their communication needs are being met and documented throughout their hospital stay.
Assistive Communication Steps
Some steps can be performed in advance. Careful consideration should be given to healthcare providers’ ability to spend additional time with patients with communication-based disabilities. Even if providers are limited physically in the room, they can still work to optimize mindful, high-quality communication by calling into the patient’s room by phone or video. The additional time is important especially when establishing rapport with patients and identifying their preferred communication approaches, as well as engaging their support networks. Patients with communication-based disabilities and their support team often have expertise on their ideal communication strategies. Healthcare providers and staff should inquire about communication preferences. Patients should also be oriented to hospital team structure and members, which could include simple solutions such as legible name tags. Hearing aids, batteries, and other assistive technology should have designated places to prevent loss and ensure ongoing working status. In addition, nurse stations should have a communication toolbox that includes replacement batteries for hearing aids along with other assistive technology devices, such as a personal sound amplification product.
Communication Strategies
Healthcare teams should be trained and reminded to use patient-centered communication strategies, including assessing their comprehension of shared health information through teach-back principles. Strategies vary by patient and may require teams’ flexibility in meeting the patient’s needs and preferences. Examples include ensuring one has the patient’s attention and uses good eye contact. Using a projected “radio voice,” which emphasizes clarity and articulation rather than volume, is helpful for those with hearing loss. For some, meaningful gestures (eg, pointing to one’s own head when asking about headaches) can aid communication. Another strategy when having difficulty understanding patients with decreased speech intelligibility is to repeat the audible speech so that the patient only needs to repeat the inaudible portions that were missed. Patients should have secure access to personal assistive devices, such as hearing aids and even smartphones with communication apps (eg, speech-to-text apps) to facilitate interpersonal communication.
Clear Face Masks
Face masks with transparent windows have been developed. Deaf and hard of hearing people’s speech perception increases when speakers use transparent versus conventional masks. The Food and Drug Administration has approved two clear face masks as American Society for Testing Materials Level 1 (Table). These two masks have limited utility for high-risk situations, such as aerosolizing procedures; in such cases, a powered air purifying respirator with a clear viewing window will be needed instead. Notably, clear mask supply has lagged behind demand, creating limited mask availability during the pandemic; their use may need to be restricted to those working with patients with communication-based disabilities.
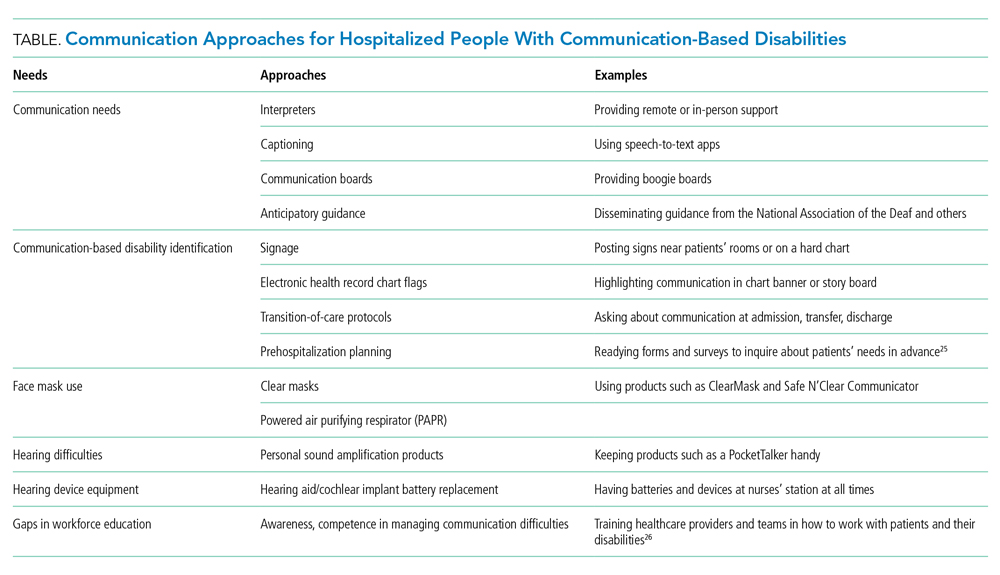
Tools for Communicating Within the Patient’s Room
Erasable whiteboards and communication boards are useful tools for simple exchanges as long as patients’ literacy and fluency are adequate. “PocketTalkers” or personalized sound amplification products may allow providers to speak into a microphone, providing amplified speech via a patient’s headphones. These amplification products are typically useful for those with mild to moderate hearing loss who are not using a hearing aid. Automatic speech recognition apps are device-based apps for converting speech to text. Speakers hold the device near the mouth to maximize accuracy while the patient reads the captions on their screen. With social distancing, lavalier microphones can increase text accuracy, but higher rates of error may still occur due to background noises or accents. For increased reliability and accuracy, Computer Access Realtime Translation stenographers can provide live speech to text on a computer screen from off-site via a computer or smartphone.
Tools for Isolation-Limited Communication
Team members can call an intermediary service to communicate with the patient via the patient’s smartphone or hospital-provided remote video interpreting service, depending on the patient’s preferred communication modality. For oral and spoken language, some services (Table) use remote stenographers to convert speech to text or sign language interpreters for those who use sign language. For both communication modes, smartphone-based videoconferencing may be beneficial while maintaining isolation precautions.
Interpreter Accessibility
Conceptualize interpreters as consulting healthcare team members. They should receive the same PPE training and monitoring as other healthcare workers. For patients using remote video interpretation, this technology needs to be optimized for best results. The room should be in a location with a strong Wi-Fi signal. Equipment should be consistently charged when not in use and rapidly accessible, even remaining in the patients’ room if possible. Healthcare teams need training to appropriately locate and set up the equipment with appropriate support from information technology staff.
Signage
Signage is useful to remind healthcare teams of the patients’ and/or caregivers’ communication-based disability. The most commonly used disability signage shows a line across an ear to indicate hearing loss (Appendix Figure).22 Appropriate signage use, even simple printed sheets documenting a communication issue, can remind healthcare team members of patients’ needs to ensure that communication is accessible and avoid misconceptions toward the patient (eg, noncompliance or cognitive issues). Chart banners, patient room doorways, and over the patients’ beds are good signage locations.
Systematic Noise Reduction
Consistent with previous calls to reduce inpatient noise,23 hospitals should systematically review and monitor protocols to reduce noise pollution. If intra-unit noise varies, patients relying on acoustic-based communication due to hearing loss or speech, language, or voice disability should be placed in quieter rooms.
Communication Concordance
Healthcare professionals and staff with disabilities are an increasingly recognized workforce segment,24 and often are experienced innovators in communicating effectively with patients with communication-based disabilities. Healthcare systems can explore whether they have healthcare team members, employees, disability resource professionals, and/or trainees with these backgrounds and, if they are available, recruit them into developing effective inpatient communication policies and processes.
CONCLUSION
People with communication disabilities experience significant healthcare disparities, now further exacerbated by COVID-19. As clinicians, staff and hospitals work to fuse safety with high-quality communication and care, we should capitalize on multipronged opportunities at the system and individual levels to identify barriers and ensure accessible and effective communication with patients who have communication-based disabilities.
1. McKee MM, Moreland C, Atcherson SR, Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP Essent. 2015;434:24-28.
2. Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disabil Rehabil Assist Technol. 2013;8(6):472-481. https://doi.org/10.3109/17483107.2012.746398
3. Steinberg AG, Barnett S, Meador HE, Wiggins EA, Zazove P. Health care system accessibility. experiences and perceptions of deaf people. J Gen Intern Med. 2006;21(3):260-266. https://doi.org/10.1111/j.1525-1497.2006.00340.x
4. Stransky ML, Jensen KM, Morris MA. Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. J Gen Intern Med. 2018;33(12):2147-2155. https://doi.org/10.1007/s11606-018-4625-1
5. Morris MA, Meier SK, Griffin JM, Branda ME, Phelan SM. Prevalence and etiologies of adult communication disabilities in the United States: results from the 2012 National Health Interview Survey. Disabil Health J. 2016;9(1):140-144. https://doi.org/10.1016/j.dhjo.2015.07.004
6. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital Health Stat. 2014(260):1-161.
7. Chang JE, Weinstein B, Chodosh J, Blustein J. Hospital readmission risk for patients with self-reported hearing loss and communication trouble. J Am Geriatr Soc. 2018;66(11):2227-2228. https://doi.org/10.1111/jgs.15545
8. McKee M, Moran C, Zazove P. Overcoming additional barriers to care for deaf and hard of hearing patients during COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;146(9):781-782. https://doi.org/10.1001/jamaoto.2020.1705
9. Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. https://doi.org/10.1503/cmaj.070690
10. Hoffman JM, Yorkston KM, Shumway-Cook A, Ciol MA, Dudgeon BJ, Chan L. Effect of communication disability on satisfaction with health care: a survey of medicare beneficiaries. Am J Speech Lang Pathol. 2005;14(3):221-228. https://doi.org/10.1044/1058-0360(2005/022)
11. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(4):e94207. https://doi.org/10.1371/journal.pone.0094207
12. Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315-318. https://doi.org/10.1016/j.pec.2007.03.005
13. Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295-301. https://doi.org/10.1016/j.pec.2008.11.015
14. Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322-2324. https://doi.org/10.1001/jama.2013.5912
15. Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293-299. https://doi.org/10.1001/jamainternmed.2013.1868
16. McKee MM, Stransky ML, Reichard A. Hearing loss and associated medical conditions among individuals 65 years and older. Disabil Health J. 2018;11(1):122-125. https://doi.org/10.1016/j.dhjo.2017.05.007
17. ADA requirements: effective communication. U.S. Department of Justice. January 31, 2014. Accessed February 12, 2021. https://www.ada.gov/effective-comm.htm
18. OCR resolves complaints after State of Connecticut and private hospital safeguard the rights of persons with disabilities to have reasonable access to support persons in hospital settings during COVID-19. Press Release. US Department of Health and Human Services; June 9, 2020. Accessed September 19, 2020. https://www.hhs.gov/about/news/2020/06/09/ocr-resolves-complaints-after-state-connecticut-private-hospital-safeguard-rights-persons.html
19. Goldin A, Weinstein B, Shiman N. How do medical masks degrade speech perception? The Hearing Review. April 1, 2020. Accessed September 30, 2020. https://www.hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception
20. Mendel LL, Gardino JA, Atcherson SR. Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol. 2008;19(9):686-695. https://doi.org/10.3766/jaaa.19.9.4
21. Atcherson SR, Finley ET, McDowell BR, Watson C. More speech degradations and considerations in the search for transparent face coverings during the COVID-19 pandemic. American Academy of Audiology. November/December 2020. Accessed September 19, 2020. https://www.audiology.org/audiology-today-julyaugust-2020/online-feature-more-speech-degradations-and-considerations-search
22. Hearing Loss. Wikipedia. Accessed October 28, 2020. https://en.wikipedia.org/wiki/Hearing_loss
23. Kamdar BB, Martin JL, Needham DM. Noise and light pollution in the hospital: a call for action. J Hosp Med. 2017;12(10):861-862. https://doi.org/10.12788/jhm.2838
24. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med. 2018;93(4):540-543. https://doi.org/10.1097/acm.0000000000002112
25. Communication Access Plan (CAP): Instructions for Patients and Providers. Hearing Loss Association of America (HLAA). Accessed September 30, 2020. https://www.hearingloss.org/wp-content/uploads/HLAA_HC_CAP_Form_and_Instructions.pdf
26. How Do I Communicate with Doctors, Nurses, and Staff at the Hospital During COVID-19? Hearing Loss Association of America (HLAA). May 8, 2020. Accessed September 30, 2020. https://www.hearingloss.org/communication-access-recommendations-hospitals-covid-19/
1. McKee MM, Moreland C, Atcherson SR, Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP Essent. 2015;434:24-28.
2. Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disabil Rehabil Assist Technol. 2013;8(6):472-481. https://doi.org/10.3109/17483107.2012.746398
3. Steinberg AG, Barnett S, Meador HE, Wiggins EA, Zazove P. Health care system accessibility. experiences and perceptions of deaf people. J Gen Intern Med. 2006;21(3):260-266. https://doi.org/10.1111/j.1525-1497.2006.00340.x
4. Stransky ML, Jensen KM, Morris MA. Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. J Gen Intern Med. 2018;33(12):2147-2155. https://doi.org/10.1007/s11606-018-4625-1
5. Morris MA, Meier SK, Griffin JM, Branda ME, Phelan SM. Prevalence and etiologies of adult communication disabilities in the United States: results from the 2012 National Health Interview Survey. Disabil Health J. 2016;9(1):140-144. https://doi.org/10.1016/j.dhjo.2015.07.004
6. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital Health Stat. 2014(260):1-161.
7. Chang JE, Weinstein B, Chodosh J, Blustein J. Hospital readmission risk for patients with self-reported hearing loss and communication trouble. J Am Geriatr Soc. 2018;66(11):2227-2228. https://doi.org/10.1111/jgs.15545
8. McKee M, Moran C, Zazove P. Overcoming additional barriers to care for deaf and hard of hearing patients during COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;146(9):781-782. https://doi.org/10.1001/jamaoto.2020.1705
9. Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. https://doi.org/10.1503/cmaj.070690
10. Hoffman JM, Yorkston KM, Shumway-Cook A, Ciol MA, Dudgeon BJ, Chan L. Effect of communication disability on satisfaction with health care: a survey of medicare beneficiaries. Am J Speech Lang Pathol. 2005;14(3):221-228. https://doi.org/10.1044/1058-0360(2005/022)
11. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(4):e94207. https://doi.org/10.1371/journal.pone.0094207
12. Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315-318. https://doi.org/10.1016/j.pec.2007.03.005
13. Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295-301. https://doi.org/10.1016/j.pec.2008.11.015
14. Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322-2324. https://doi.org/10.1001/jama.2013.5912
15. Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293-299. https://doi.org/10.1001/jamainternmed.2013.1868
16. McKee MM, Stransky ML, Reichard A. Hearing loss and associated medical conditions among individuals 65 years and older. Disabil Health J. 2018;11(1):122-125. https://doi.org/10.1016/j.dhjo.2017.05.007
17. ADA requirements: effective communication. U.S. Department of Justice. January 31, 2014. Accessed February 12, 2021. https://www.ada.gov/effective-comm.htm
18. OCR resolves complaints after State of Connecticut and private hospital safeguard the rights of persons with disabilities to have reasonable access to support persons in hospital settings during COVID-19. Press Release. US Department of Health and Human Services; June 9, 2020. Accessed September 19, 2020. https://www.hhs.gov/about/news/2020/06/09/ocr-resolves-complaints-after-state-connecticut-private-hospital-safeguard-rights-persons.html
19. Goldin A, Weinstein B, Shiman N. How do medical masks degrade speech perception? The Hearing Review. April 1, 2020. Accessed September 30, 2020. https://www.hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception
20. Mendel LL, Gardino JA, Atcherson SR. Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol. 2008;19(9):686-695. https://doi.org/10.3766/jaaa.19.9.4
21. Atcherson SR, Finley ET, McDowell BR, Watson C. More speech degradations and considerations in the search for transparent face coverings during the COVID-19 pandemic. American Academy of Audiology. November/December 2020. Accessed September 19, 2020. https://www.audiology.org/audiology-today-julyaugust-2020/online-feature-more-speech-degradations-and-considerations-search
22. Hearing Loss. Wikipedia. Accessed October 28, 2020. https://en.wikipedia.org/wiki/Hearing_loss
23. Kamdar BB, Martin JL, Needham DM. Noise and light pollution in the hospital: a call for action. J Hosp Med. 2017;12(10):861-862. https://doi.org/10.12788/jhm.2838
24. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med. 2018;93(4):540-543. https://doi.org/10.1097/acm.0000000000002112
25. Communication Access Plan (CAP): Instructions for Patients and Providers. Hearing Loss Association of America (HLAA). Accessed September 30, 2020. https://www.hearingloss.org/wp-content/uploads/HLAA_HC_CAP_Form_and_Instructions.pdf
26. How Do I Communicate with Doctors, Nurses, and Staff at the Hospital During COVID-19? Hearing Loss Association of America (HLAA). May 8, 2020. Accessed September 30, 2020. https://www.hearingloss.org/communication-access-recommendations-hospitals-covid-19/
© 2021 Society of Hospital Medicine
What to do if an employee tests positive for COVID-19
An increasingly common question I’m receiving is:
As always, it depends, but here is some general advice: The specifics will vary depending on state/local laws, or your particular situation.
First, you need to determine the level of exposure, and whether it requires action. According to the Centers for Disease Control and Prevention, actionable exposure occurs 2 days prior to the onset of illness, and lasts 10 days after onset.
If action is required, you’ll need to determine who needs to quarantine and who needs to be tested. Vaccinated employees who have been exposed to suspected or confirmed COVID-19 are not required to quarantine or be tested if they are fully vaccinated and have remained asymptomatic since the exposure. Those employees should, however, follow all the usual precautions (masks, social distancing, handwashing, etc.) with increased diligence. Remind them that no vaccine is 100% effective, and suggest they self-monitor for symptoms (fever, cough, shortness of breath, etc.)
All other exposed employees should be tested. A negative test means an individual was not infected at the time the sample was collected, but that does not mean an individual will not get sick later. Some providers are retesting on days 5 and 7 post exposure.
Some experts advise that you monitor exposed employees (vaccinated or not) yourself, with daily temperature readings and inquiries regarding symptoms, and perhaps a daily pulse oximetry check, for 14 days following exposure. Document these screenings in writing. Anyone testing positive or developing a fever or other symptoms should, of course, be sent home and seek medical treatment as necessary.
Employees who develop symptoms or test positive for COVID-19 should remain out of work until all CDC “return-to-work” criteria are met. At this writing, the basic criteria include:
- At least 10 days pass after symptoms first appeared
- At least 24 hours pass after last fever without the use of fever-reducing medications
- Cough, shortness of breath, and any other symptoms improve
Anyone who is significantly immunocompromised may need more time at home, and probably consultation with an infectious disease specialist.
Your facility should be thoroughly cleaned after the exposure. Close off all areas used by the sick individual, and clean and disinfect all areas such as offices, doorknobs, bathrooms, common areas, and shared electronic equipment. Of course, the cleaners should wear gowns, gloves, masks, and goggles. Some practices are hiring cleaning crews to professionally disinfect their offices. Once the area has been disinfected, it can be reopened for use. Workers without close contact with the person who is sick can return to work immediately after disinfection.
If the potential infected area is widespread and cannot be isolated to a room or rooms where doors can be shut, it may be prudent to temporarily close your office, send staff home, and divert patients to other locations if they cannot be rescheduled. Once your facility is cleaned and disinfected and staff have been cleared, your office may reopen.
Use enhanced precautions for any staff or patients who are immunocompromised, or otherwise fall into the high-risk category, to keep them out of the path of potential exposure areas and allow them to self-quarantine if they desire.
You should continue following existing leave policies (paid time off, vacation, sick, short-term disability, leave of absence, Family and Medical Leave Act, and Americans with Disabilities Act). If the employee was exposed at work, contact your workers’ compensation carrier regarding lost wages. Unless your state laws specify otherwise, you are under no obligation to pay beyond your policies, but you may do so if you choose.
Of course, you can take proactive steps to prevent unnecessary exposure and avoid closures in the first place; for example:
- Call patients prior to their visit, or question them upon arrival, regarding fever, shortness of breath, and other COVID-19 symptoms.
- Check employees’ temperatures every morning.
- Check patients’ temperatures as they enter the office.
- Require everyone, patients and employees alike, to wear face coverings.
- Ask patients to leave friends and family members at home.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
An increasingly common question I’m receiving is:
As always, it depends, but here is some general advice: The specifics will vary depending on state/local laws, or your particular situation.
First, you need to determine the level of exposure, and whether it requires action. According to the Centers for Disease Control and Prevention, actionable exposure occurs 2 days prior to the onset of illness, and lasts 10 days after onset.
If action is required, you’ll need to determine who needs to quarantine and who needs to be tested. Vaccinated employees who have been exposed to suspected or confirmed COVID-19 are not required to quarantine or be tested if they are fully vaccinated and have remained asymptomatic since the exposure. Those employees should, however, follow all the usual precautions (masks, social distancing, handwashing, etc.) with increased diligence. Remind them that no vaccine is 100% effective, and suggest they self-monitor for symptoms (fever, cough, shortness of breath, etc.)
All other exposed employees should be tested. A negative test means an individual was not infected at the time the sample was collected, but that does not mean an individual will not get sick later. Some providers are retesting on days 5 and 7 post exposure.
Some experts advise that you monitor exposed employees (vaccinated or not) yourself, with daily temperature readings and inquiries regarding symptoms, and perhaps a daily pulse oximetry check, for 14 days following exposure. Document these screenings in writing. Anyone testing positive or developing a fever or other symptoms should, of course, be sent home and seek medical treatment as necessary.
Employees who develop symptoms or test positive for COVID-19 should remain out of work until all CDC “return-to-work” criteria are met. At this writing, the basic criteria include:
- At least 10 days pass after symptoms first appeared
- At least 24 hours pass after last fever without the use of fever-reducing medications
- Cough, shortness of breath, and any other symptoms improve
Anyone who is significantly immunocompromised may need more time at home, and probably consultation with an infectious disease specialist.
Your facility should be thoroughly cleaned after the exposure. Close off all areas used by the sick individual, and clean and disinfect all areas such as offices, doorknobs, bathrooms, common areas, and shared electronic equipment. Of course, the cleaners should wear gowns, gloves, masks, and goggles. Some practices are hiring cleaning crews to professionally disinfect their offices. Once the area has been disinfected, it can be reopened for use. Workers without close contact with the person who is sick can return to work immediately after disinfection.
If the potential infected area is widespread and cannot be isolated to a room or rooms where doors can be shut, it may be prudent to temporarily close your office, send staff home, and divert patients to other locations if they cannot be rescheduled. Once your facility is cleaned and disinfected and staff have been cleared, your office may reopen.
Use enhanced precautions for any staff or patients who are immunocompromised, or otherwise fall into the high-risk category, to keep them out of the path of potential exposure areas and allow them to self-quarantine if they desire.
You should continue following existing leave policies (paid time off, vacation, sick, short-term disability, leave of absence, Family and Medical Leave Act, and Americans with Disabilities Act). If the employee was exposed at work, contact your workers’ compensation carrier regarding lost wages. Unless your state laws specify otherwise, you are under no obligation to pay beyond your policies, but you may do so if you choose.
Of course, you can take proactive steps to prevent unnecessary exposure and avoid closures in the first place; for example:
- Call patients prior to their visit, or question them upon arrival, regarding fever, shortness of breath, and other COVID-19 symptoms.
- Check employees’ temperatures every morning.
- Check patients’ temperatures as they enter the office.
- Require everyone, patients and employees alike, to wear face coverings.
- Ask patients to leave friends and family members at home.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
An increasingly common question I’m receiving is:
As always, it depends, but here is some general advice: The specifics will vary depending on state/local laws, or your particular situation.
First, you need to determine the level of exposure, and whether it requires action. According to the Centers for Disease Control and Prevention, actionable exposure occurs 2 days prior to the onset of illness, and lasts 10 days after onset.
If action is required, you’ll need to determine who needs to quarantine and who needs to be tested. Vaccinated employees who have been exposed to suspected or confirmed COVID-19 are not required to quarantine or be tested if they are fully vaccinated and have remained asymptomatic since the exposure. Those employees should, however, follow all the usual precautions (masks, social distancing, handwashing, etc.) with increased diligence. Remind them that no vaccine is 100% effective, and suggest they self-monitor for symptoms (fever, cough, shortness of breath, etc.)
All other exposed employees should be tested. A negative test means an individual was not infected at the time the sample was collected, but that does not mean an individual will not get sick later. Some providers are retesting on days 5 and 7 post exposure.
Some experts advise that you monitor exposed employees (vaccinated or not) yourself, with daily temperature readings and inquiries regarding symptoms, and perhaps a daily pulse oximetry check, for 14 days following exposure. Document these screenings in writing. Anyone testing positive or developing a fever or other symptoms should, of course, be sent home and seek medical treatment as necessary.
Employees who develop symptoms or test positive for COVID-19 should remain out of work until all CDC “return-to-work” criteria are met. At this writing, the basic criteria include:
- At least 10 days pass after symptoms first appeared
- At least 24 hours pass after last fever without the use of fever-reducing medications
- Cough, shortness of breath, and any other symptoms improve
Anyone who is significantly immunocompromised may need more time at home, and probably consultation with an infectious disease specialist.
Your facility should be thoroughly cleaned after the exposure. Close off all areas used by the sick individual, and clean and disinfect all areas such as offices, doorknobs, bathrooms, common areas, and shared electronic equipment. Of course, the cleaners should wear gowns, gloves, masks, and goggles. Some practices are hiring cleaning crews to professionally disinfect their offices. Once the area has been disinfected, it can be reopened for use. Workers without close contact with the person who is sick can return to work immediately after disinfection.
If the potential infected area is widespread and cannot be isolated to a room or rooms where doors can be shut, it may be prudent to temporarily close your office, send staff home, and divert patients to other locations if they cannot be rescheduled. Once your facility is cleaned and disinfected and staff have been cleared, your office may reopen.
Use enhanced precautions for any staff or patients who are immunocompromised, or otherwise fall into the high-risk category, to keep them out of the path of potential exposure areas and allow them to self-quarantine if they desire.
You should continue following existing leave policies (paid time off, vacation, sick, short-term disability, leave of absence, Family and Medical Leave Act, and Americans with Disabilities Act). If the employee was exposed at work, contact your workers’ compensation carrier regarding lost wages. Unless your state laws specify otherwise, you are under no obligation to pay beyond your policies, but you may do so if you choose.
Of course, you can take proactive steps to prevent unnecessary exposure and avoid closures in the first place; for example:
- Call patients prior to their visit, or question them upon arrival, regarding fever, shortness of breath, and other COVID-19 symptoms.
- Check employees’ temperatures every morning.
- Check patients’ temperatures as they enter the office.
- Require everyone, patients and employees alike, to wear face coverings.
- Ask patients to leave friends and family members at home.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
One-third of health care workers leery of getting COVID-19 vaccine, survey shows
Moreover, 54% of direct care providers indicated that they would take the vaccine if offered, compared with 60% of noncare providers.
The findings come from what is believed to be the largest survey of health care provider attitudes toward COVID-19 vaccination, published online Jan. 25 in Clinical Infectious Diseases.
“We have shown that self-reported willingness to receive vaccination against COVID-19 differs by age, gender, race and hospital role, with physicians and research scientists showing the highest acceptance,” Jana Shaw, MD, MPH, State University of New York, Syracuse, N.Y, the study’s corresponding author, told this news organization. “Building trust in authorities and confidence in vaccines is a complex and time-consuming process that requires commitment and resources. We have to make those investments as hesitancy can severely undermine vaccination coverage. Because health care providers are members of our communities, it is possible that their views are shared by the public at large. Our findings can assist public health professionals as a starting point of discussion and engagement with communities to ensure that we vaccinate at least 80% of the public to end the pandemic.”
For the study, Dr. Shaw and her colleagues emailed an anonymous survey to 9,565 employees of State University of New York Upstate Medical University, Syracuse, an academic medical center that cares for an estimated 1.8 million people. The survey, which contained questions intended to evaluate attitudes, belief, and willingness to get vaccinated, took place between Nov. 23 and Dec. 5, about a week before the U.S. Food and Drug Administration granted the first emergency use authorization for the Pfizer-BioNTech BNT162b2 mRNA vaccine.
Survey recipients included physicians, nurse practitioners, physician assistants, nurses, pharmacists, medical and nursing students, allied health professionals, and nonclinical ancillary staff.
Of the 9,565 surveys sent, 5,287 responses were collected and used in the final analysis, for a response rate of 55%. The mean age of respondents was 43, 73% were female, 85% were White, 6% were Asian, 5% were Black/African American, and the rest were Native American, Native Hawaiian/Pacific Islander, or from other races. More than half of respondents (59%) reported that they provided direct patient care, and 32% said they provided care for patients with COVID-19.
Of all survey respondents, 58% expressed their intent to receive a COVID-19 vaccine, but this varied by their role in the health care system. For example, in response to the statement, “If a vaccine were offered free of charge, I would take it,” 80% of scientists and physicians agreed that they would, while colleagues in other roles were unsure whether they would take the vaccine, including 34% of registered nurses, 32% of allied health professionals, and 32% of master’s-level clinicians. These differences across roles were significant (P less than .001).
The researchers also found that direct patient care or care for COVID-19 patients was associated with lower vaccination intent. For example, 54% of direct care providers and 62% of non-care providers indicated they would take the vaccine if offered, compared with 52% of those who had provided care for COVID-19 patients vs. 61% of those who had not (P less than .001).
“This was a really surprising finding,” said Dr. Shaw, who is a pediatric infectious diseases physician at SUNY Upstate. “In general, one would expect that perceived severity of disease would lead to a greater desire to get vaccinated. Because our question did not address severity of disease, it is possible that we oversampled respondents who took care of patients with mild disease (i.e., in an outpatient setting). This could have led to an underestimation of disease severity and resulted in lower vaccination intent.”
A focus on rebuilding trust
Survey respondents who agreed or strongly agreed that they would accept a vaccine were older (a mean age of 44 years), compared with those who were not sure or who disagreed (a mean age of 42 vs. 38 years, respectively; P less than .001). In addition, fewer females agreed or strongly agreed that they would accept a vaccine (54% vs. 73% of males), whereas those who self-identified as Black/African American were least likely to want to get vaccinated, compared with those from other ethnic groups (31%, compared with 74% of Asians, 58% of Whites, and 39% of American Indians or Alaska Natives).
“We are deeply aware of the poor decisions scientists made in the past, which led to a prevailing skepticism and ‘feeling like guinea pigs’ among people of color, especially Black adults,” Dr. Shaw said. “Black adults are less likely, compared [with] White adults, to have confidence that scientists act in the public interest. Rebuilding trust will take time and has to start with addressing health care disparities. In addition, we need to acknowledge contributions of Black researchers to science. For example, until recently very few knew that the Moderna vaccine was developed [with the help of] Dr. Kizzmekia Corbett, who is Black.”
The top five main areas of unease that all respondents expressed about a COVID-19 vaccine were concern about adverse events/side effects (47%), efficacy (15%), rushed release (11%), safety (11%), and the research and authorization process (3%).
“I think it is important that fellow clinicians recognize that, in order to boost vaccine confidence we will need careful, individually tailored communication strategies,” Dr. Shaw said. “A consideration should be given to those [strategies] that utilize interpersonal channels that deliver leadership by example and leverage influencers in the institution to encourage wider adoption of vaccination.”
Aaron M. Milstone, MD, MHS, asked to comment on the research, recommended that health care workers advocate for the vaccine and encourage their patients, friends, and loved ones to get vaccinated. “Soon, COVID-19 will have taken more than half a million lives in the U.S.,” said Dr. Milstone, a pediatric epidemiologist at Johns Hopkins University, Baltimore. “Although vaccines can have side effects like fever and muscle aches, and very, very rare more serious side effects, the risks of dying from COVID are much greater than the risk of a serious vaccine reaction. The study’s authors shed light on the ongoing need for leaders of all communities to support the COVID vaccines, not just the scientific community, but religious leaders, political leaders, and community leaders.”
Addressing vaccine hesitancy
Informed by their own survey, Dr. Shaw and her colleagues have developed a plan to address vaccine hesitancy to ensure high vaccine uptake at SUNY Upstate. Those strategies include, but aren’t limited to, institution-wide forums for all employees on COVID-19 vaccine safety, risks, and benefits followed by Q&A sessions, grand rounds for providers summarizing clinical trial data on mRNA vaccines, development of an Ask COVID email line for staff to ask vaccine-related questions, and a detailed vaccine-specific FAQ document.
In addition, SUNY Upstate experts have engaged in numerous media interviews to provide education and updates on the benefits of vaccination to public and staff, stationary vaccine locations, and mobile COVID-19 vaccine carts. “To date, the COVID-19 vaccination process has been well received, and we anticipate strong vaccine uptake,” she said.
Dr. Shaw acknowledged certain limitations of the survey, including its cross-sectional design and the fact that it was conducted in a single health care system in the northeastern United States. “Thus, generalizability to other regions of the U.S. and other countries may be limited,” Dr. Shaw said. “The study was also conducted before EUA [emergency use authorization] was granted to either the Moderna or Pfizer-BioNTech vaccines. It is therefore likely that vaccine acceptance will change over time as more people get vaccinated.”
The authors have disclosed no relevant financial relationships. Dr. Milstone disclosed that he has received a research grant from Merck, but it is not related to vaccines.
A version of this article first appeared on Medscape.com.
Moreover, 54% of direct care providers indicated that they would take the vaccine if offered, compared with 60% of noncare providers.
The findings come from what is believed to be the largest survey of health care provider attitudes toward COVID-19 vaccination, published online Jan. 25 in Clinical Infectious Diseases.
“We have shown that self-reported willingness to receive vaccination against COVID-19 differs by age, gender, race and hospital role, with physicians and research scientists showing the highest acceptance,” Jana Shaw, MD, MPH, State University of New York, Syracuse, N.Y, the study’s corresponding author, told this news organization. “Building trust in authorities and confidence in vaccines is a complex and time-consuming process that requires commitment and resources. We have to make those investments as hesitancy can severely undermine vaccination coverage. Because health care providers are members of our communities, it is possible that their views are shared by the public at large. Our findings can assist public health professionals as a starting point of discussion and engagement with communities to ensure that we vaccinate at least 80% of the public to end the pandemic.”
For the study, Dr. Shaw and her colleagues emailed an anonymous survey to 9,565 employees of State University of New York Upstate Medical University, Syracuse, an academic medical center that cares for an estimated 1.8 million people. The survey, which contained questions intended to evaluate attitudes, belief, and willingness to get vaccinated, took place between Nov. 23 and Dec. 5, about a week before the U.S. Food and Drug Administration granted the first emergency use authorization for the Pfizer-BioNTech BNT162b2 mRNA vaccine.
Survey recipients included physicians, nurse practitioners, physician assistants, nurses, pharmacists, medical and nursing students, allied health professionals, and nonclinical ancillary staff.
Of the 9,565 surveys sent, 5,287 responses were collected and used in the final analysis, for a response rate of 55%. The mean age of respondents was 43, 73% were female, 85% were White, 6% were Asian, 5% were Black/African American, and the rest were Native American, Native Hawaiian/Pacific Islander, or from other races. More than half of respondents (59%) reported that they provided direct patient care, and 32% said they provided care for patients with COVID-19.
Of all survey respondents, 58% expressed their intent to receive a COVID-19 vaccine, but this varied by their role in the health care system. For example, in response to the statement, “If a vaccine were offered free of charge, I would take it,” 80% of scientists and physicians agreed that they would, while colleagues in other roles were unsure whether they would take the vaccine, including 34% of registered nurses, 32% of allied health professionals, and 32% of master’s-level clinicians. These differences across roles were significant (P less than .001).
The researchers also found that direct patient care or care for COVID-19 patients was associated with lower vaccination intent. For example, 54% of direct care providers and 62% of non-care providers indicated they would take the vaccine if offered, compared with 52% of those who had provided care for COVID-19 patients vs. 61% of those who had not (P less than .001).
“This was a really surprising finding,” said Dr. Shaw, who is a pediatric infectious diseases physician at SUNY Upstate. “In general, one would expect that perceived severity of disease would lead to a greater desire to get vaccinated. Because our question did not address severity of disease, it is possible that we oversampled respondents who took care of patients with mild disease (i.e., in an outpatient setting). This could have led to an underestimation of disease severity and resulted in lower vaccination intent.”
A focus on rebuilding trust
Survey respondents who agreed or strongly agreed that they would accept a vaccine were older (a mean age of 44 years), compared with those who were not sure or who disagreed (a mean age of 42 vs. 38 years, respectively; P less than .001). In addition, fewer females agreed or strongly agreed that they would accept a vaccine (54% vs. 73% of males), whereas those who self-identified as Black/African American were least likely to want to get vaccinated, compared with those from other ethnic groups (31%, compared with 74% of Asians, 58% of Whites, and 39% of American Indians or Alaska Natives).
“We are deeply aware of the poor decisions scientists made in the past, which led to a prevailing skepticism and ‘feeling like guinea pigs’ among people of color, especially Black adults,” Dr. Shaw said. “Black adults are less likely, compared [with] White adults, to have confidence that scientists act in the public interest. Rebuilding trust will take time and has to start with addressing health care disparities. In addition, we need to acknowledge contributions of Black researchers to science. For example, until recently very few knew that the Moderna vaccine was developed [with the help of] Dr. Kizzmekia Corbett, who is Black.”
The top five main areas of unease that all respondents expressed about a COVID-19 vaccine were concern about adverse events/side effects (47%), efficacy (15%), rushed release (11%), safety (11%), and the research and authorization process (3%).
“I think it is important that fellow clinicians recognize that, in order to boost vaccine confidence we will need careful, individually tailored communication strategies,” Dr. Shaw said. “A consideration should be given to those [strategies] that utilize interpersonal channels that deliver leadership by example and leverage influencers in the institution to encourage wider adoption of vaccination.”
Aaron M. Milstone, MD, MHS, asked to comment on the research, recommended that health care workers advocate for the vaccine and encourage their patients, friends, and loved ones to get vaccinated. “Soon, COVID-19 will have taken more than half a million lives in the U.S.,” said Dr. Milstone, a pediatric epidemiologist at Johns Hopkins University, Baltimore. “Although vaccines can have side effects like fever and muscle aches, and very, very rare more serious side effects, the risks of dying from COVID are much greater than the risk of a serious vaccine reaction. The study’s authors shed light on the ongoing need for leaders of all communities to support the COVID vaccines, not just the scientific community, but religious leaders, political leaders, and community leaders.”
Addressing vaccine hesitancy
Informed by their own survey, Dr. Shaw and her colleagues have developed a plan to address vaccine hesitancy to ensure high vaccine uptake at SUNY Upstate. Those strategies include, but aren’t limited to, institution-wide forums for all employees on COVID-19 vaccine safety, risks, and benefits followed by Q&A sessions, grand rounds for providers summarizing clinical trial data on mRNA vaccines, development of an Ask COVID email line for staff to ask vaccine-related questions, and a detailed vaccine-specific FAQ document.
In addition, SUNY Upstate experts have engaged in numerous media interviews to provide education and updates on the benefits of vaccination to public and staff, stationary vaccine locations, and mobile COVID-19 vaccine carts. “To date, the COVID-19 vaccination process has been well received, and we anticipate strong vaccine uptake,” she said.
Dr. Shaw acknowledged certain limitations of the survey, including its cross-sectional design and the fact that it was conducted in a single health care system in the northeastern United States. “Thus, generalizability to other regions of the U.S. and other countries may be limited,” Dr. Shaw said. “The study was also conducted before EUA [emergency use authorization] was granted to either the Moderna or Pfizer-BioNTech vaccines. It is therefore likely that vaccine acceptance will change over time as more people get vaccinated.”
The authors have disclosed no relevant financial relationships. Dr. Milstone disclosed that he has received a research grant from Merck, but it is not related to vaccines.
A version of this article first appeared on Medscape.com.
Moreover, 54% of direct care providers indicated that they would take the vaccine if offered, compared with 60% of noncare providers.
The findings come from what is believed to be the largest survey of health care provider attitudes toward COVID-19 vaccination, published online Jan. 25 in Clinical Infectious Diseases.
“We have shown that self-reported willingness to receive vaccination against COVID-19 differs by age, gender, race and hospital role, with physicians and research scientists showing the highest acceptance,” Jana Shaw, MD, MPH, State University of New York, Syracuse, N.Y, the study’s corresponding author, told this news organization. “Building trust in authorities and confidence in vaccines is a complex and time-consuming process that requires commitment and resources. We have to make those investments as hesitancy can severely undermine vaccination coverage. Because health care providers are members of our communities, it is possible that their views are shared by the public at large. Our findings can assist public health professionals as a starting point of discussion and engagement with communities to ensure that we vaccinate at least 80% of the public to end the pandemic.”
For the study, Dr. Shaw and her colleagues emailed an anonymous survey to 9,565 employees of State University of New York Upstate Medical University, Syracuse, an academic medical center that cares for an estimated 1.8 million people. The survey, which contained questions intended to evaluate attitudes, belief, and willingness to get vaccinated, took place between Nov. 23 and Dec. 5, about a week before the U.S. Food and Drug Administration granted the first emergency use authorization for the Pfizer-BioNTech BNT162b2 mRNA vaccine.
Survey recipients included physicians, nurse practitioners, physician assistants, nurses, pharmacists, medical and nursing students, allied health professionals, and nonclinical ancillary staff.
Of the 9,565 surveys sent, 5,287 responses were collected and used in the final analysis, for a response rate of 55%. The mean age of respondents was 43, 73% were female, 85% were White, 6% were Asian, 5% were Black/African American, and the rest were Native American, Native Hawaiian/Pacific Islander, or from other races. More than half of respondents (59%) reported that they provided direct patient care, and 32% said they provided care for patients with COVID-19.
Of all survey respondents, 58% expressed their intent to receive a COVID-19 vaccine, but this varied by their role in the health care system. For example, in response to the statement, “If a vaccine were offered free of charge, I would take it,” 80% of scientists and physicians agreed that they would, while colleagues in other roles were unsure whether they would take the vaccine, including 34% of registered nurses, 32% of allied health professionals, and 32% of master’s-level clinicians. These differences across roles were significant (P less than .001).
The researchers also found that direct patient care or care for COVID-19 patients was associated with lower vaccination intent. For example, 54% of direct care providers and 62% of non-care providers indicated they would take the vaccine if offered, compared with 52% of those who had provided care for COVID-19 patients vs. 61% of those who had not (P less than .001).
“This was a really surprising finding,” said Dr. Shaw, who is a pediatric infectious diseases physician at SUNY Upstate. “In general, one would expect that perceived severity of disease would lead to a greater desire to get vaccinated. Because our question did not address severity of disease, it is possible that we oversampled respondents who took care of patients with mild disease (i.e., in an outpatient setting). This could have led to an underestimation of disease severity and resulted in lower vaccination intent.”
A focus on rebuilding trust
Survey respondents who agreed or strongly agreed that they would accept a vaccine were older (a mean age of 44 years), compared with those who were not sure or who disagreed (a mean age of 42 vs. 38 years, respectively; P less than .001). In addition, fewer females agreed or strongly agreed that they would accept a vaccine (54% vs. 73% of males), whereas those who self-identified as Black/African American were least likely to want to get vaccinated, compared with those from other ethnic groups (31%, compared with 74% of Asians, 58% of Whites, and 39% of American Indians or Alaska Natives).
“We are deeply aware of the poor decisions scientists made in the past, which led to a prevailing skepticism and ‘feeling like guinea pigs’ among people of color, especially Black adults,” Dr. Shaw said. “Black adults are less likely, compared [with] White adults, to have confidence that scientists act in the public interest. Rebuilding trust will take time and has to start with addressing health care disparities. In addition, we need to acknowledge contributions of Black researchers to science. For example, until recently very few knew that the Moderna vaccine was developed [with the help of] Dr. Kizzmekia Corbett, who is Black.”
The top five main areas of unease that all respondents expressed about a COVID-19 vaccine were concern about adverse events/side effects (47%), efficacy (15%), rushed release (11%), safety (11%), and the research and authorization process (3%).
“I think it is important that fellow clinicians recognize that, in order to boost vaccine confidence we will need careful, individually tailored communication strategies,” Dr. Shaw said. “A consideration should be given to those [strategies] that utilize interpersonal channels that deliver leadership by example and leverage influencers in the institution to encourage wider adoption of vaccination.”
Aaron M. Milstone, MD, MHS, asked to comment on the research, recommended that health care workers advocate for the vaccine and encourage their patients, friends, and loved ones to get vaccinated. “Soon, COVID-19 will have taken more than half a million lives in the U.S.,” said Dr. Milstone, a pediatric epidemiologist at Johns Hopkins University, Baltimore. “Although vaccines can have side effects like fever and muscle aches, and very, very rare more serious side effects, the risks of dying from COVID are much greater than the risk of a serious vaccine reaction. The study’s authors shed light on the ongoing need for leaders of all communities to support the COVID vaccines, not just the scientific community, but religious leaders, political leaders, and community leaders.”
Addressing vaccine hesitancy
Informed by their own survey, Dr. Shaw and her colleagues have developed a plan to address vaccine hesitancy to ensure high vaccine uptake at SUNY Upstate. Those strategies include, but aren’t limited to, institution-wide forums for all employees on COVID-19 vaccine safety, risks, and benefits followed by Q&A sessions, grand rounds for providers summarizing clinical trial data on mRNA vaccines, development of an Ask COVID email line for staff to ask vaccine-related questions, and a detailed vaccine-specific FAQ document.
In addition, SUNY Upstate experts have engaged in numerous media interviews to provide education and updates on the benefits of vaccination to public and staff, stationary vaccine locations, and mobile COVID-19 vaccine carts. “To date, the COVID-19 vaccination process has been well received, and we anticipate strong vaccine uptake,” she said.
Dr. Shaw acknowledged certain limitations of the survey, including its cross-sectional design and the fact that it was conducted in a single health care system in the northeastern United States. “Thus, generalizability to other regions of the U.S. and other countries may be limited,” Dr. Shaw said. “The study was also conducted before EUA [emergency use authorization] was granted to either the Moderna or Pfizer-BioNTech vaccines. It is therefore likely that vaccine acceptance will change over time as more people get vaccinated.”
The authors have disclosed no relevant financial relationships. Dr. Milstone disclosed that he has received a research grant from Merck, but it is not related to vaccines.
A version of this article first appeared on Medscape.com.
Cabozantinib could be new standard for papillary RCC
Compared with the VEGFR-2 inhibitor sunitinib, the MET inhibitor cabozantinib improved both response rate and progression-free survival. Two other MET inhibitors, crizotinib and savolitinib, were not more efficacious than sunitinib.
“To date, there have been no randomized data specifically in papillary RCC showing an advantage of one systemic therapy over another,” said Sumanta K. Pal, MD, of City of Hope National Medical Center, Duarte, Calif., when presenting results from SWOG 1500.
Dr. Pal presented the results at the 2021 Genitourinary Cancers Symposium (Abstract 270), and they were published simultaneously in The Lancet.
The SWOG 1500 trial, also known as the PAPMET trial, was undertaken given evidence that signaling in the MET pathway is a driver in a sizable proportion of papillary RCCs, Dr. Pal explained.
Compared with sunitinib, cabozantinib reduced the risk of progression-free survival events by 40% and netted a response rate that was almost six times higher. On the other hand, the crizotinib and savolitinib arms of the trial were stopped early because of futility.
“Cabozantinib should be considered the new reference standard for systemic therapy in patients with metastatic papillary RCC,” Dr. Pal recommended. At present, VEGF-directed therapy is used as standard of care.
Dr. Pal noted that current evidence supports only monotherapy in papillary disease.
“There may be a temptation to put a patient on a combination of cabozantinib with immunotherapy, and certainly there is data in the context of clear-cell disease to support that. But we have to stop and think. We don’t know yet if that actually results in benefit for our patients, and obviously, it could extend the spectrum of toxicities that they incur,” he added.
Dr. Pal therefore encouraged oncologists and their patients with papillary RCC to consider the planned PAPMET-2 trial, which will explore the benefits and risks of adding immunotherapy to cabozantinib for this patient population.
SWOG 1500 details
The phase 2 SWOG 1500 trial was conducted in 65 U.S. and Canadian centers. It enrolled 152 patients with metastatic papillary RCC who had received up to one prior systemic therapy, excluding sunitinib. The trial is the first exclusively in this patient population to complete accrual, Dr. Pal noted.
Patients were randomized evenly to sunitinib, cabozantinib, crizotinib, or savolitinib.
The investigators stopped accrual to the savolitinib and crizotinib arms early based on a prespecified futility analysis showing that the hazard ratios for progression-free survival, compared with sunitinib, exceeded 1.
For the remaining arms, the median progression-free survival was 9.0 months with cabozantinib and 5.6 months with sunitinib (hazard ratio for events, 0.60; one-sided P = .019), meeting the trial’s primary endpoint. Subgroup analyses numerically favored cabozantinib in both type I and type II disease.
The confirmed overall response rate was 23% with cabozantinib and 4% with sunitinib (two-sided P = .010). Respective rates of complete response were 5% and 0%.
The median overall survival was 20.0 months with cabozantinib and 16.4 months with sunitinib, a nonsignificant difference.
The investigators are conducting exploratory analyses of MET mutational status and MET expression, and their associations with outcomes, according to Dr. Pal. Findings of other studies are suggesting that MET-altered papillary RCC may be a distinct entity, which would support genomically driven studies, he noted.
The rate of grade 3-4 toxicity was 68% in the sunitinib group, 74% in the cabozantinib group, 37% in the crizotinib group, and 39% in the savolitinib group. The types of toxicities seen were similar to those observed with each agent in larger trials, Dr. Pal observed.
There was a single grade 5 event, a death secondary to thromboembolism in the cabozantinib arm.
MET alterations may be key
“We should consider cabozantinib as another first-line option for papillary kidney cancer,” said invited discussant Stephanie A. Berg, DO, of Loyola University Medical Center in Maywood, Ill.
Dr. Berg noted that the phase 3 SAVOIR trial, recently published in JAMA Oncology, compared savolitinib against sunitinib in MET-driven papillary RCC and stopped recruitment early. Although the trial did not meet its primary endpoint of progression-free survival, it did show numerically better results with the MET inhibitor.
“I question if the savolitinib arm in SWOG 1500 may have fared better if tumors were exclusively MET driven, especially as type II papillary patients represented almost half of the total patient population, and typically, 40% express alterations in MET,” Dr. Berg commented. “We will have to wait for further exploratory analysis regarding MET mutational status to tease out these differences.”
SWOG 1500 was sponsored by the National Cancer Institute. Dr. Pal disclosed a consulting or advisory role with Astellas Pharma, Aveo, Bristol-Myers Squibb, Eisai, Exelixis, Genentech, Ipsen, Myriad Pharmaceuticals, Novartis, and Pfizer. Dr. Berg disclosed a consulting or advisory role with Bristol-Myers Squibb.
Compared with the VEGFR-2 inhibitor sunitinib, the MET inhibitor cabozantinib improved both response rate and progression-free survival. Two other MET inhibitors, crizotinib and savolitinib, were not more efficacious than sunitinib.
“To date, there have been no randomized data specifically in papillary RCC showing an advantage of one systemic therapy over another,” said Sumanta K. Pal, MD, of City of Hope National Medical Center, Duarte, Calif., when presenting results from SWOG 1500.
Dr. Pal presented the results at the 2021 Genitourinary Cancers Symposium (Abstract 270), and they were published simultaneously in The Lancet.
The SWOG 1500 trial, also known as the PAPMET trial, was undertaken given evidence that signaling in the MET pathway is a driver in a sizable proportion of papillary RCCs, Dr. Pal explained.
Compared with sunitinib, cabozantinib reduced the risk of progression-free survival events by 40% and netted a response rate that was almost six times higher. On the other hand, the crizotinib and savolitinib arms of the trial were stopped early because of futility.
“Cabozantinib should be considered the new reference standard for systemic therapy in patients with metastatic papillary RCC,” Dr. Pal recommended. At present, VEGF-directed therapy is used as standard of care.
Dr. Pal noted that current evidence supports only monotherapy in papillary disease.
“There may be a temptation to put a patient on a combination of cabozantinib with immunotherapy, and certainly there is data in the context of clear-cell disease to support that. But we have to stop and think. We don’t know yet if that actually results in benefit for our patients, and obviously, it could extend the spectrum of toxicities that they incur,” he added.
Dr. Pal therefore encouraged oncologists and their patients with papillary RCC to consider the planned PAPMET-2 trial, which will explore the benefits and risks of adding immunotherapy to cabozantinib for this patient population.
SWOG 1500 details
The phase 2 SWOG 1500 trial was conducted in 65 U.S. and Canadian centers. It enrolled 152 patients with metastatic papillary RCC who had received up to one prior systemic therapy, excluding sunitinib. The trial is the first exclusively in this patient population to complete accrual, Dr. Pal noted.
Patients were randomized evenly to sunitinib, cabozantinib, crizotinib, or savolitinib.
The investigators stopped accrual to the savolitinib and crizotinib arms early based on a prespecified futility analysis showing that the hazard ratios for progression-free survival, compared with sunitinib, exceeded 1.
For the remaining arms, the median progression-free survival was 9.0 months with cabozantinib and 5.6 months with sunitinib (hazard ratio for events, 0.60; one-sided P = .019), meeting the trial’s primary endpoint. Subgroup analyses numerically favored cabozantinib in both type I and type II disease.
The confirmed overall response rate was 23% with cabozantinib and 4% with sunitinib (two-sided P = .010). Respective rates of complete response were 5% and 0%.
The median overall survival was 20.0 months with cabozantinib and 16.4 months with sunitinib, a nonsignificant difference.
The investigators are conducting exploratory analyses of MET mutational status and MET expression, and their associations with outcomes, according to Dr. Pal. Findings of other studies are suggesting that MET-altered papillary RCC may be a distinct entity, which would support genomically driven studies, he noted.
The rate of grade 3-4 toxicity was 68% in the sunitinib group, 74% in the cabozantinib group, 37% in the crizotinib group, and 39% in the savolitinib group. The types of toxicities seen were similar to those observed with each agent in larger trials, Dr. Pal observed.
There was a single grade 5 event, a death secondary to thromboembolism in the cabozantinib arm.
MET alterations may be key
“We should consider cabozantinib as another first-line option for papillary kidney cancer,” said invited discussant Stephanie A. Berg, DO, of Loyola University Medical Center in Maywood, Ill.
Dr. Berg noted that the phase 3 SAVOIR trial, recently published in JAMA Oncology, compared savolitinib against sunitinib in MET-driven papillary RCC and stopped recruitment early. Although the trial did not meet its primary endpoint of progression-free survival, it did show numerically better results with the MET inhibitor.
“I question if the savolitinib arm in SWOG 1500 may have fared better if tumors were exclusively MET driven, especially as type II papillary patients represented almost half of the total patient population, and typically, 40% express alterations in MET,” Dr. Berg commented. “We will have to wait for further exploratory analysis regarding MET mutational status to tease out these differences.”
SWOG 1500 was sponsored by the National Cancer Institute. Dr. Pal disclosed a consulting or advisory role with Astellas Pharma, Aveo, Bristol-Myers Squibb, Eisai, Exelixis, Genentech, Ipsen, Myriad Pharmaceuticals, Novartis, and Pfizer. Dr. Berg disclosed a consulting or advisory role with Bristol-Myers Squibb.
Compared with the VEGFR-2 inhibitor sunitinib, the MET inhibitor cabozantinib improved both response rate and progression-free survival. Two other MET inhibitors, crizotinib and savolitinib, were not more efficacious than sunitinib.
“To date, there have been no randomized data specifically in papillary RCC showing an advantage of one systemic therapy over another,” said Sumanta K. Pal, MD, of City of Hope National Medical Center, Duarte, Calif., when presenting results from SWOG 1500.
Dr. Pal presented the results at the 2021 Genitourinary Cancers Symposium (Abstract 270), and they were published simultaneously in The Lancet.
The SWOG 1500 trial, also known as the PAPMET trial, was undertaken given evidence that signaling in the MET pathway is a driver in a sizable proportion of papillary RCCs, Dr. Pal explained.
Compared with sunitinib, cabozantinib reduced the risk of progression-free survival events by 40% and netted a response rate that was almost six times higher. On the other hand, the crizotinib and savolitinib arms of the trial were stopped early because of futility.
“Cabozantinib should be considered the new reference standard for systemic therapy in patients with metastatic papillary RCC,” Dr. Pal recommended. At present, VEGF-directed therapy is used as standard of care.
Dr. Pal noted that current evidence supports only monotherapy in papillary disease.
“There may be a temptation to put a patient on a combination of cabozantinib with immunotherapy, and certainly there is data in the context of clear-cell disease to support that. But we have to stop and think. We don’t know yet if that actually results in benefit for our patients, and obviously, it could extend the spectrum of toxicities that they incur,” he added.
Dr. Pal therefore encouraged oncologists and their patients with papillary RCC to consider the planned PAPMET-2 trial, which will explore the benefits and risks of adding immunotherapy to cabozantinib for this patient population.
SWOG 1500 details
The phase 2 SWOG 1500 trial was conducted in 65 U.S. and Canadian centers. It enrolled 152 patients with metastatic papillary RCC who had received up to one prior systemic therapy, excluding sunitinib. The trial is the first exclusively in this patient population to complete accrual, Dr. Pal noted.
Patients were randomized evenly to sunitinib, cabozantinib, crizotinib, or savolitinib.
The investigators stopped accrual to the savolitinib and crizotinib arms early based on a prespecified futility analysis showing that the hazard ratios for progression-free survival, compared with sunitinib, exceeded 1.
For the remaining arms, the median progression-free survival was 9.0 months with cabozantinib and 5.6 months with sunitinib (hazard ratio for events, 0.60; one-sided P = .019), meeting the trial’s primary endpoint. Subgroup analyses numerically favored cabozantinib in both type I and type II disease.
The confirmed overall response rate was 23% with cabozantinib and 4% with sunitinib (two-sided P = .010). Respective rates of complete response were 5% and 0%.
The median overall survival was 20.0 months with cabozantinib and 16.4 months with sunitinib, a nonsignificant difference.
The investigators are conducting exploratory analyses of MET mutational status and MET expression, and their associations with outcomes, according to Dr. Pal. Findings of other studies are suggesting that MET-altered papillary RCC may be a distinct entity, which would support genomically driven studies, he noted.
The rate of grade 3-4 toxicity was 68% in the sunitinib group, 74% in the cabozantinib group, 37% in the crizotinib group, and 39% in the savolitinib group. The types of toxicities seen were similar to those observed with each agent in larger trials, Dr. Pal observed.
There was a single grade 5 event, a death secondary to thromboembolism in the cabozantinib arm.
MET alterations may be key
“We should consider cabozantinib as another first-line option for papillary kidney cancer,” said invited discussant Stephanie A. Berg, DO, of Loyola University Medical Center in Maywood, Ill.
Dr. Berg noted that the phase 3 SAVOIR trial, recently published in JAMA Oncology, compared savolitinib against sunitinib in MET-driven papillary RCC and stopped recruitment early. Although the trial did not meet its primary endpoint of progression-free survival, it did show numerically better results with the MET inhibitor.
“I question if the savolitinib arm in SWOG 1500 may have fared better if tumors were exclusively MET driven, especially as type II papillary patients represented almost half of the total patient population, and typically, 40% express alterations in MET,” Dr. Berg commented. “We will have to wait for further exploratory analysis regarding MET mutational status to tease out these differences.”
SWOG 1500 was sponsored by the National Cancer Institute. Dr. Pal disclosed a consulting or advisory role with Astellas Pharma, Aveo, Bristol-Myers Squibb, Eisai, Exelixis, Genentech, Ipsen, Myriad Pharmaceuticals, Novartis, and Pfizer. Dr. Berg disclosed a consulting or advisory role with Bristol-Myers Squibb.
FROM GUCS 2021
X-ray vision: Using AI to maximize the value of radiographic images
Artificial intelligence (AI) is expected to one day affect the entire continuum of cancer care – from screening and risk prediction to diagnosis, risk stratification, treatment selection, and follow-up, according to an expert in the field.
Hugo J.W.L. Aerts, PhD, director of the AI in Medicine Program at Brigham and Women’s Hospital in Boston, described studies using AI for some of these purposes during a presentation at the AACR Virtual Special Conference: Artificial Intelligence, Diagnosis, and Imaging (Abstract IA-06).
In one study, Dr. Aerts and colleagues set out to determine whether a convolutional neural network (CNN) could extract prognostic information from chest radiographs. The researchers tested this theory using patients from two trials – the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial and the National Lung Screening Trial (NLST).
The team developed a CNN, called CXR-risk, and tested whether it could predict the longevity and prognosis of patients in the PLCO (n = 52,320) and NLST (n = 5,493) trials over a 12-year time period, based only on chest radiographs. No clinical information, demographics, radiographic interpretations, duration of follow-up, or censoring were provided to the deep-learning system.
CXR-risk output was stratified into five categories of radiographic risk scores for probability of death, from 0 (very low likelihood of mortality) to 1 (very high likelihood of mortality).
The investigators found a graded association between radiographic risk score and mortality. The very-high-risk group had mortality rates of 53.0% (PLCO) and 33.9% (NLST). In both trials, this was significantly higher than for the very-low-risk group. The unadjusted hazard ratio was 18.3 in the PCLO data set and 15.2 in the NLST data set (P < .001 for both).
This association was maintained after adjustment for radiologists’ findings (e.g., a lung nodule) and risk factors such as age, gender, and comorbid illnesses like diabetes. The adjusted HR was 4.8 in the PCLO data set and 7.0 in the NLST data set (P < .001 for both).
In both data sets, individuals in the very-high-risk group were significantly more likely to die of lung cancer. The aHR was 11.1 in the PCLO data set and 8.4 in the NSLT data set (P < .001 for both).
This might be expected for people who were interested in being screened for lung cancer. However, patients in the very-high-risk group were also more likely to die of cardiovascular illness (aHR, 3.6 for PLCO and 47.8 for NSLT; P < .001 for both) and respiratory illness (aHR, 27.5 for PLCO and 31.9 for NLST; P ≤ .001 for both).
With this information, a clinician could initiate additional testing and/or utilize more aggressive surveillance measures. If an oncologist considered therapy for a patient with newly diagnosed cancer, treatment choices and stratification for adverse events would be more intelligently planned.
Using AI to predict the risk of lung cancer
In another study, Dr. Aerts and colleagues developed and validated a CNN called CXR-LC, which was based on CXR-risk. The goal of this study was to see if CXR-LC could predict long-term incident lung cancer using data available in the EHR, including chest radiographs, age, sex, and smoking status.
The CXR-LC model was developed using data from the PLCO trial (n = 41,856) and was validated in smokers from the PLCO trial (n = 5,615; 12-year follow-up) as well as heavy smokers from the NLST trial (n = 5,493; 6-year follow-up).
Results showed that CXR-LC was able to predict which patients were at highest risk for developing lung cancer.
CXR-LC had better discrimination for incident lung cancer than did Medicare eligibility in the PLCO data set (area under the curve, 0.755 vs. 0.634; P < .001). And the performance of CXR-LC was similar to that of the PLCOM2012 risk score in both the PLCO data set (AUC, 0.755 vs. 0.751) and the NLST data set (AUC, 0.659 vs. 0.650).
When they were compared in screening populations of equal size, CXR-LC was more sensitive than Medicare eligibility criteria in the PLCO data set (74.9% vs. 63.8%; P = .012) and missed 30.7% fewer incident lung cancer diagnoses.
AI as a substitute for specialized testing and consultation
In a third study, Dr. Aerts and colleagues used a CNN to predict cardiovascular risk by assessing coronary artery calcium (CAC) from clinically obtained, readily available CT scans.
Ordinarily, identifying CAC – an accurate predictor of cardiovascular events – requires specialized expertise (manual measurement and cardiologist interpretation), time (estimated at 20 minutes/scan), and equipment (ECG-gated cardiac CT scan and special software).
In this study, the researchers used a fully end-to-end automated system with analytic time measured in less than 2 seconds.
The team trained and tuned their CNN using the Framingham Heart Study Offspring and Third Generation cohorts (n = 1,636), which included asymptomatic patients with high-quality, cardiac-gated CT scans for CAC quantification.
The researchers then tested the CNN on two asymptomatic and two symptomatic cohorts:
- Asymptomatic Framingham Heart Study participants (n = 663) in whom the outcome measures were cardiovascular disease and death.
- Asymptomatic NLST participants (n = 14,959) in whom the outcome measure was atherosclerotic cardiovascular death.
- Symptomatic PROMISE study participants with stable chest pain (n = 4,021) in whom the outcome measures were all-cause mortality, MI, and hospitalization for unstable angina.
- Symptomatic ROMICAT-II study patients with acute chest pain (n = 441) in whom the outcome measure was acute coronary syndrome at 28 days.
Among 5,521 subjects across all testing cohorts with cardiac-gated and nongated chest CT scans, the CNN and expert reader interpretations agreed on the CAC risk scores with a high level of concordance (kappa, 0.71; concordance rate, 0.79).
There was a very high Spearman’s correlation of 0.92 (P < .0001) and substantial agreement between automatically and manually calculated CAC risk groups, substantiating robust risk prediction for cardiovascular disease across multiple clinical scenarios.
Dr. Aerts commented that, among the NLST participants who had the highest risk of developing lung cancer, the risk of cardiovascular death was as high as the risk of death from lung cancer.
Using AI to assess patient outcomes
In an unpublished study, Dr. Aerts and colleagues used AI in an attempt to determine whether changes in measurements of subcutaneous adipose tissue (SAT), visceral adipose tissue (VAT), and skeletal muscle mass would provide clues about treatment outcomes in lung cancer patients.
The researchers developed a deep learning model using data from 1,129 patients at Massachusetts General and Brigham and Women’s Hospitals, measuring SAT, VAT, and muscle mass. The team applied the measurement system to a population of 12,128 outpatients and calculated z scores for SAT, VAT, and muscle mass to determine “normal” values.
When they applied the norms to surgical lung cancer data sets from the Boston Lung Cancer Study (n = 437) and TRACERx study (n = 394), the researchers found that smokers had lower adiposity and lower muscle mass than never-smokers.
More importantly, over time, among lung cancer patients who lost greater than 5% of VAT, SAT, and muscle mass, those patients with the greatest SAT loss (P < .0001) or VAT loss (P = .0015) had the lowest lung cancer–specific survival in the TRACERx study. There was no significant impairment of lung cancer-specific survival for patients who experienced skeletal muscle loss (P = .23).
The same observation was made for overall survival among patients enrolled in the Boston Lung Cancer Study, using the 5% threshold. Overall survival was significantly worse with increasing VAT loss (P = .0023) and SAT loss (P = .0082) but not with increasing skeletal muscle loss (P = .3).
The investigators speculated about whether the correlation between body composition and clinical outcome could yield clues about tumor biology. To test this, the researchers used the RNA sequencing–based ORACLE risk score in lung cancer patients from TRACERx. There was a high correlation between higher ORACLE risk scores and lower VAT and SAT, suggesting that measures of adiposity on CT were reflected in tumor biology patterns on an RNA level in lung cancer patients. There was no such correlation between ORACLE risk scores and skeletal muscle mass.
Wonderment ... tempered by concern and challenges
AI has awe-inspiring potential to yield actionable and prognostically important information from data mining the EHR and extracting the vast quantities of information from images. In some cases (like CAC), it is information that is “hiding in plain sight.” However, Dr. Aerts expressed several cautions, some of which have already plagued AI.
He referenced the Gartner Hype Cycle, which provides a graphic representation of five phases in the life cycle of emerging technologies. The “innovation trigger” is followed by a “peak of inflated expectations,” a “trough of disillusionment,” a “slope of enlightenment,” and a “plateau of productivity.”
Dr. Aerts noted that, in recent years, AI has seemed to fall into the trough of disillusionment, but it may be entering the slope of enlightenment on the way to the plateau of productivity.
His research highlighted several examples of productivity in radiomics in cancer patients and those who are at high risk of developing cancer.
In Dr. Aerts’s opinion, a second concern is replication of AI research results. He noted that, among 400 published studies, only 6% of authors shared the codes that would enable their findings to be corroborated. About 30% shared test data, and 54% shared “pseudocodes,” but transparency and reproducibility are problems for the acceptance and broad implementation of AI.
Dr. Aerts endorsed the Modelhub initiative (www.modelhub.ai), a multi-institutional initiative to advance reproducibility in the AI field and advance its full potential.
However, there are additional concerns about the implementation of radiomics and, more generally, data mining from clinicians’ EHRs to personalize care.
Firstly, it may be laborious and difficult to explain complex, computer-based risk stratification models to patients. Hereditary cancer testing is an example of a risk assessment test that requires complicated explanations that many clinicians relegate to genetics counselors – when patients elect to see them. When a model is not explainable, it undermines the confidence of patients and their care providers, according to an editorial related to the CXR-LC study.
Another issue is that uptake of lung cancer screening, in practice, has been underutilized by individuals who meet current, relatively straightforward Medicare criteria. Despite the apparently better accuracy of the CXR-LC deep-learning model, its complexity and limited access could constitute an additional barrier for the at-risk individuals who should avail themselves of screening.
Furthermore, although age and gender are accurate in most circumstances, there is legitimate concern about the accuracy of, for example, smoking history data and comorbid conditions in current EHRs. Who performs the laborious curation of the input in an AI model to assure its accuracy for individual patients?
Finally, it is unclear how scalable and applicable AI will be to medically underserved populations (e.g., smaller, community-based, free-standing, socioeconomically disadvantaged or rural health care institutions). There are substantial initial and maintenance costs that may limit AI’s availability to some academic institutions and large health maintenance organizations.
As the concerns and challenges are addressed, it will be interesting to see where and when the plateau of productivity for AI in cancer care occurs. When it does, many cancer patients will benefit from enhanced care along the continuum of the complex disease they and their caregivers seek to master.
Dr. Aerts disclosed relationships with Onc.AI outside the presented work.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Artificial intelligence (AI) is expected to one day affect the entire continuum of cancer care – from screening and risk prediction to diagnosis, risk stratification, treatment selection, and follow-up, according to an expert in the field.
Hugo J.W.L. Aerts, PhD, director of the AI in Medicine Program at Brigham and Women’s Hospital in Boston, described studies using AI for some of these purposes during a presentation at the AACR Virtual Special Conference: Artificial Intelligence, Diagnosis, and Imaging (Abstract IA-06).
In one study, Dr. Aerts and colleagues set out to determine whether a convolutional neural network (CNN) could extract prognostic information from chest radiographs. The researchers tested this theory using patients from two trials – the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial and the National Lung Screening Trial (NLST).
The team developed a CNN, called CXR-risk, and tested whether it could predict the longevity and prognosis of patients in the PLCO (n = 52,320) and NLST (n = 5,493) trials over a 12-year time period, based only on chest radiographs. No clinical information, demographics, radiographic interpretations, duration of follow-up, or censoring were provided to the deep-learning system.
CXR-risk output was stratified into five categories of radiographic risk scores for probability of death, from 0 (very low likelihood of mortality) to 1 (very high likelihood of mortality).
The investigators found a graded association between radiographic risk score and mortality. The very-high-risk group had mortality rates of 53.0% (PLCO) and 33.9% (NLST). In both trials, this was significantly higher than for the very-low-risk group. The unadjusted hazard ratio was 18.3 in the PCLO data set and 15.2 in the NLST data set (P < .001 for both).
This association was maintained after adjustment for radiologists’ findings (e.g., a lung nodule) and risk factors such as age, gender, and comorbid illnesses like diabetes. The adjusted HR was 4.8 in the PCLO data set and 7.0 in the NLST data set (P < .001 for both).
In both data sets, individuals in the very-high-risk group were significantly more likely to die of lung cancer. The aHR was 11.1 in the PCLO data set and 8.4 in the NSLT data set (P < .001 for both).
This might be expected for people who were interested in being screened for lung cancer. However, patients in the very-high-risk group were also more likely to die of cardiovascular illness (aHR, 3.6 for PLCO and 47.8 for NSLT; P < .001 for both) and respiratory illness (aHR, 27.5 for PLCO and 31.9 for NLST; P ≤ .001 for both).
With this information, a clinician could initiate additional testing and/or utilize more aggressive surveillance measures. If an oncologist considered therapy for a patient with newly diagnosed cancer, treatment choices and stratification for adverse events would be more intelligently planned.
Using AI to predict the risk of lung cancer
In another study, Dr. Aerts and colleagues developed and validated a CNN called CXR-LC, which was based on CXR-risk. The goal of this study was to see if CXR-LC could predict long-term incident lung cancer using data available in the EHR, including chest radiographs, age, sex, and smoking status.
The CXR-LC model was developed using data from the PLCO trial (n = 41,856) and was validated in smokers from the PLCO trial (n = 5,615; 12-year follow-up) as well as heavy smokers from the NLST trial (n = 5,493; 6-year follow-up).
Results showed that CXR-LC was able to predict which patients were at highest risk for developing lung cancer.
CXR-LC had better discrimination for incident lung cancer than did Medicare eligibility in the PLCO data set (area under the curve, 0.755 vs. 0.634; P < .001). And the performance of CXR-LC was similar to that of the PLCOM2012 risk score in both the PLCO data set (AUC, 0.755 vs. 0.751) and the NLST data set (AUC, 0.659 vs. 0.650).
When they were compared in screening populations of equal size, CXR-LC was more sensitive than Medicare eligibility criteria in the PLCO data set (74.9% vs. 63.8%; P = .012) and missed 30.7% fewer incident lung cancer diagnoses.
AI as a substitute for specialized testing and consultation
In a third study, Dr. Aerts and colleagues used a CNN to predict cardiovascular risk by assessing coronary artery calcium (CAC) from clinically obtained, readily available CT scans.
Ordinarily, identifying CAC – an accurate predictor of cardiovascular events – requires specialized expertise (manual measurement and cardiologist interpretation), time (estimated at 20 minutes/scan), and equipment (ECG-gated cardiac CT scan and special software).
In this study, the researchers used a fully end-to-end automated system with analytic time measured in less than 2 seconds.
The team trained and tuned their CNN using the Framingham Heart Study Offspring and Third Generation cohorts (n = 1,636), which included asymptomatic patients with high-quality, cardiac-gated CT scans for CAC quantification.
The researchers then tested the CNN on two asymptomatic and two symptomatic cohorts:
- Asymptomatic Framingham Heart Study participants (n = 663) in whom the outcome measures were cardiovascular disease and death.
- Asymptomatic NLST participants (n = 14,959) in whom the outcome measure was atherosclerotic cardiovascular death.
- Symptomatic PROMISE study participants with stable chest pain (n = 4,021) in whom the outcome measures were all-cause mortality, MI, and hospitalization for unstable angina.
- Symptomatic ROMICAT-II study patients with acute chest pain (n = 441) in whom the outcome measure was acute coronary syndrome at 28 days.
Among 5,521 subjects across all testing cohorts with cardiac-gated and nongated chest CT scans, the CNN and expert reader interpretations agreed on the CAC risk scores with a high level of concordance (kappa, 0.71; concordance rate, 0.79).
There was a very high Spearman’s correlation of 0.92 (P < .0001) and substantial agreement between automatically and manually calculated CAC risk groups, substantiating robust risk prediction for cardiovascular disease across multiple clinical scenarios.
Dr. Aerts commented that, among the NLST participants who had the highest risk of developing lung cancer, the risk of cardiovascular death was as high as the risk of death from lung cancer.
Using AI to assess patient outcomes
In an unpublished study, Dr. Aerts and colleagues used AI in an attempt to determine whether changes in measurements of subcutaneous adipose tissue (SAT), visceral adipose tissue (VAT), and skeletal muscle mass would provide clues about treatment outcomes in lung cancer patients.
The researchers developed a deep learning model using data from 1,129 patients at Massachusetts General and Brigham and Women’s Hospitals, measuring SAT, VAT, and muscle mass. The team applied the measurement system to a population of 12,128 outpatients and calculated z scores for SAT, VAT, and muscle mass to determine “normal” values.
When they applied the norms to surgical lung cancer data sets from the Boston Lung Cancer Study (n = 437) and TRACERx study (n = 394), the researchers found that smokers had lower adiposity and lower muscle mass than never-smokers.
More importantly, over time, among lung cancer patients who lost greater than 5% of VAT, SAT, and muscle mass, those patients with the greatest SAT loss (P < .0001) or VAT loss (P = .0015) had the lowest lung cancer–specific survival in the TRACERx study. There was no significant impairment of lung cancer-specific survival for patients who experienced skeletal muscle loss (P = .23).
The same observation was made for overall survival among patients enrolled in the Boston Lung Cancer Study, using the 5% threshold. Overall survival was significantly worse with increasing VAT loss (P = .0023) and SAT loss (P = .0082) but not with increasing skeletal muscle loss (P = .3).
The investigators speculated about whether the correlation between body composition and clinical outcome could yield clues about tumor biology. To test this, the researchers used the RNA sequencing–based ORACLE risk score in lung cancer patients from TRACERx. There was a high correlation between higher ORACLE risk scores and lower VAT and SAT, suggesting that measures of adiposity on CT were reflected in tumor biology patterns on an RNA level in lung cancer patients. There was no such correlation between ORACLE risk scores and skeletal muscle mass.
Wonderment ... tempered by concern and challenges
AI has awe-inspiring potential to yield actionable and prognostically important information from data mining the EHR and extracting the vast quantities of information from images. In some cases (like CAC), it is information that is “hiding in plain sight.” However, Dr. Aerts expressed several cautions, some of which have already plagued AI.
He referenced the Gartner Hype Cycle, which provides a graphic representation of five phases in the life cycle of emerging technologies. The “innovation trigger” is followed by a “peak of inflated expectations,” a “trough of disillusionment,” a “slope of enlightenment,” and a “plateau of productivity.”
Dr. Aerts noted that, in recent years, AI has seemed to fall into the trough of disillusionment, but it may be entering the slope of enlightenment on the way to the plateau of productivity.
His research highlighted several examples of productivity in radiomics in cancer patients and those who are at high risk of developing cancer.
In Dr. Aerts’s opinion, a second concern is replication of AI research results. He noted that, among 400 published studies, only 6% of authors shared the codes that would enable their findings to be corroborated. About 30% shared test data, and 54% shared “pseudocodes,” but transparency and reproducibility are problems for the acceptance and broad implementation of AI.
Dr. Aerts endorsed the Modelhub initiative (www.modelhub.ai), a multi-institutional initiative to advance reproducibility in the AI field and advance its full potential.
However, there are additional concerns about the implementation of radiomics and, more generally, data mining from clinicians’ EHRs to personalize care.
Firstly, it may be laborious and difficult to explain complex, computer-based risk stratification models to patients. Hereditary cancer testing is an example of a risk assessment test that requires complicated explanations that many clinicians relegate to genetics counselors – when patients elect to see them. When a model is not explainable, it undermines the confidence of patients and their care providers, according to an editorial related to the CXR-LC study.
Another issue is that uptake of lung cancer screening, in practice, has been underutilized by individuals who meet current, relatively straightforward Medicare criteria. Despite the apparently better accuracy of the CXR-LC deep-learning model, its complexity and limited access could constitute an additional barrier for the at-risk individuals who should avail themselves of screening.
Furthermore, although age and gender are accurate in most circumstances, there is legitimate concern about the accuracy of, for example, smoking history data and comorbid conditions in current EHRs. Who performs the laborious curation of the input in an AI model to assure its accuracy for individual patients?
Finally, it is unclear how scalable and applicable AI will be to medically underserved populations (e.g., smaller, community-based, free-standing, socioeconomically disadvantaged or rural health care institutions). There are substantial initial and maintenance costs that may limit AI’s availability to some academic institutions and large health maintenance organizations.
As the concerns and challenges are addressed, it will be interesting to see where and when the plateau of productivity for AI in cancer care occurs. When it does, many cancer patients will benefit from enhanced care along the continuum of the complex disease they and their caregivers seek to master.
Dr. Aerts disclosed relationships with Onc.AI outside the presented work.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Artificial intelligence (AI) is expected to one day affect the entire continuum of cancer care – from screening and risk prediction to diagnosis, risk stratification, treatment selection, and follow-up, according to an expert in the field.
Hugo J.W.L. Aerts, PhD, director of the AI in Medicine Program at Brigham and Women’s Hospital in Boston, described studies using AI for some of these purposes during a presentation at the AACR Virtual Special Conference: Artificial Intelligence, Diagnosis, and Imaging (Abstract IA-06).
In one study, Dr. Aerts and colleagues set out to determine whether a convolutional neural network (CNN) could extract prognostic information from chest radiographs. The researchers tested this theory using patients from two trials – the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial and the National Lung Screening Trial (NLST).
The team developed a CNN, called CXR-risk, and tested whether it could predict the longevity and prognosis of patients in the PLCO (n = 52,320) and NLST (n = 5,493) trials over a 12-year time period, based only on chest radiographs. No clinical information, demographics, radiographic interpretations, duration of follow-up, or censoring were provided to the deep-learning system.
CXR-risk output was stratified into five categories of radiographic risk scores for probability of death, from 0 (very low likelihood of mortality) to 1 (very high likelihood of mortality).
The investigators found a graded association between radiographic risk score and mortality. The very-high-risk group had mortality rates of 53.0% (PLCO) and 33.9% (NLST). In both trials, this was significantly higher than for the very-low-risk group. The unadjusted hazard ratio was 18.3 in the PCLO data set and 15.2 in the NLST data set (P < .001 for both).
This association was maintained after adjustment for radiologists’ findings (e.g., a lung nodule) and risk factors such as age, gender, and comorbid illnesses like diabetes. The adjusted HR was 4.8 in the PCLO data set and 7.0 in the NLST data set (P < .001 for both).
In both data sets, individuals in the very-high-risk group were significantly more likely to die of lung cancer. The aHR was 11.1 in the PCLO data set and 8.4 in the NSLT data set (P < .001 for both).
This might be expected for people who were interested in being screened for lung cancer. However, patients in the very-high-risk group were also more likely to die of cardiovascular illness (aHR, 3.6 for PLCO and 47.8 for NSLT; P < .001 for both) and respiratory illness (aHR, 27.5 for PLCO and 31.9 for NLST; P ≤ .001 for both).
With this information, a clinician could initiate additional testing and/or utilize more aggressive surveillance measures. If an oncologist considered therapy for a patient with newly diagnosed cancer, treatment choices and stratification for adverse events would be more intelligently planned.
Using AI to predict the risk of lung cancer
In another study, Dr. Aerts and colleagues developed and validated a CNN called CXR-LC, which was based on CXR-risk. The goal of this study was to see if CXR-LC could predict long-term incident lung cancer using data available in the EHR, including chest radiographs, age, sex, and smoking status.
The CXR-LC model was developed using data from the PLCO trial (n = 41,856) and was validated in smokers from the PLCO trial (n = 5,615; 12-year follow-up) as well as heavy smokers from the NLST trial (n = 5,493; 6-year follow-up).
Results showed that CXR-LC was able to predict which patients were at highest risk for developing lung cancer.
CXR-LC had better discrimination for incident lung cancer than did Medicare eligibility in the PLCO data set (area under the curve, 0.755 vs. 0.634; P < .001). And the performance of CXR-LC was similar to that of the PLCOM2012 risk score in both the PLCO data set (AUC, 0.755 vs. 0.751) and the NLST data set (AUC, 0.659 vs. 0.650).
When they were compared in screening populations of equal size, CXR-LC was more sensitive than Medicare eligibility criteria in the PLCO data set (74.9% vs. 63.8%; P = .012) and missed 30.7% fewer incident lung cancer diagnoses.
AI as a substitute for specialized testing and consultation
In a third study, Dr. Aerts and colleagues used a CNN to predict cardiovascular risk by assessing coronary artery calcium (CAC) from clinically obtained, readily available CT scans.
Ordinarily, identifying CAC – an accurate predictor of cardiovascular events – requires specialized expertise (manual measurement and cardiologist interpretation), time (estimated at 20 minutes/scan), and equipment (ECG-gated cardiac CT scan and special software).
In this study, the researchers used a fully end-to-end automated system with analytic time measured in less than 2 seconds.
The team trained and tuned their CNN using the Framingham Heart Study Offspring and Third Generation cohorts (n = 1,636), which included asymptomatic patients with high-quality, cardiac-gated CT scans for CAC quantification.
The researchers then tested the CNN on two asymptomatic and two symptomatic cohorts:
- Asymptomatic Framingham Heart Study participants (n = 663) in whom the outcome measures were cardiovascular disease and death.
- Asymptomatic NLST participants (n = 14,959) in whom the outcome measure was atherosclerotic cardiovascular death.
- Symptomatic PROMISE study participants with stable chest pain (n = 4,021) in whom the outcome measures were all-cause mortality, MI, and hospitalization for unstable angina.
- Symptomatic ROMICAT-II study patients with acute chest pain (n = 441) in whom the outcome measure was acute coronary syndrome at 28 days.
Among 5,521 subjects across all testing cohorts with cardiac-gated and nongated chest CT scans, the CNN and expert reader interpretations agreed on the CAC risk scores with a high level of concordance (kappa, 0.71; concordance rate, 0.79).
There was a very high Spearman’s correlation of 0.92 (P < .0001) and substantial agreement between automatically and manually calculated CAC risk groups, substantiating robust risk prediction for cardiovascular disease across multiple clinical scenarios.
Dr. Aerts commented that, among the NLST participants who had the highest risk of developing lung cancer, the risk of cardiovascular death was as high as the risk of death from lung cancer.
Using AI to assess patient outcomes
In an unpublished study, Dr. Aerts and colleagues used AI in an attempt to determine whether changes in measurements of subcutaneous adipose tissue (SAT), visceral adipose tissue (VAT), and skeletal muscle mass would provide clues about treatment outcomes in lung cancer patients.
The researchers developed a deep learning model using data from 1,129 patients at Massachusetts General and Brigham and Women’s Hospitals, measuring SAT, VAT, and muscle mass. The team applied the measurement system to a population of 12,128 outpatients and calculated z scores for SAT, VAT, and muscle mass to determine “normal” values.
When they applied the norms to surgical lung cancer data sets from the Boston Lung Cancer Study (n = 437) and TRACERx study (n = 394), the researchers found that smokers had lower adiposity and lower muscle mass than never-smokers.
More importantly, over time, among lung cancer patients who lost greater than 5% of VAT, SAT, and muscle mass, those patients with the greatest SAT loss (P < .0001) or VAT loss (P = .0015) had the lowest lung cancer–specific survival in the TRACERx study. There was no significant impairment of lung cancer-specific survival for patients who experienced skeletal muscle loss (P = .23).
The same observation was made for overall survival among patients enrolled in the Boston Lung Cancer Study, using the 5% threshold. Overall survival was significantly worse with increasing VAT loss (P = .0023) and SAT loss (P = .0082) but not with increasing skeletal muscle loss (P = .3).
The investigators speculated about whether the correlation between body composition and clinical outcome could yield clues about tumor biology. To test this, the researchers used the RNA sequencing–based ORACLE risk score in lung cancer patients from TRACERx. There was a high correlation between higher ORACLE risk scores and lower VAT and SAT, suggesting that measures of adiposity on CT were reflected in tumor biology patterns on an RNA level in lung cancer patients. There was no such correlation between ORACLE risk scores and skeletal muscle mass.
Wonderment ... tempered by concern and challenges
AI has awe-inspiring potential to yield actionable and prognostically important information from data mining the EHR and extracting the vast quantities of information from images. In some cases (like CAC), it is information that is “hiding in plain sight.” However, Dr. Aerts expressed several cautions, some of which have already plagued AI.
He referenced the Gartner Hype Cycle, which provides a graphic representation of five phases in the life cycle of emerging technologies. The “innovation trigger” is followed by a “peak of inflated expectations,” a “trough of disillusionment,” a “slope of enlightenment,” and a “plateau of productivity.”
Dr. Aerts noted that, in recent years, AI has seemed to fall into the trough of disillusionment, but it may be entering the slope of enlightenment on the way to the plateau of productivity.
His research highlighted several examples of productivity in radiomics in cancer patients and those who are at high risk of developing cancer.
In Dr. Aerts’s opinion, a second concern is replication of AI research results. He noted that, among 400 published studies, only 6% of authors shared the codes that would enable their findings to be corroborated. About 30% shared test data, and 54% shared “pseudocodes,” but transparency and reproducibility are problems for the acceptance and broad implementation of AI.
Dr. Aerts endorsed the Modelhub initiative (www.modelhub.ai), a multi-institutional initiative to advance reproducibility in the AI field and advance its full potential.
However, there are additional concerns about the implementation of radiomics and, more generally, data mining from clinicians’ EHRs to personalize care.
Firstly, it may be laborious and difficult to explain complex, computer-based risk stratification models to patients. Hereditary cancer testing is an example of a risk assessment test that requires complicated explanations that many clinicians relegate to genetics counselors – when patients elect to see them. When a model is not explainable, it undermines the confidence of patients and their care providers, according to an editorial related to the CXR-LC study.
Another issue is that uptake of lung cancer screening, in practice, has been underutilized by individuals who meet current, relatively straightforward Medicare criteria. Despite the apparently better accuracy of the CXR-LC deep-learning model, its complexity and limited access could constitute an additional barrier for the at-risk individuals who should avail themselves of screening.
Furthermore, although age and gender are accurate in most circumstances, there is legitimate concern about the accuracy of, for example, smoking history data and comorbid conditions in current EHRs. Who performs the laborious curation of the input in an AI model to assure its accuracy for individual patients?
Finally, it is unclear how scalable and applicable AI will be to medically underserved populations (e.g., smaller, community-based, free-standing, socioeconomically disadvantaged or rural health care institutions). There are substantial initial and maintenance costs that may limit AI’s availability to some academic institutions and large health maintenance organizations.
As the concerns and challenges are addressed, it will be interesting to see where and when the plateau of productivity for AI in cancer care occurs. When it does, many cancer patients will benefit from enhanced care along the continuum of the complex disease they and their caregivers seek to master.
Dr. Aerts disclosed relationships with Onc.AI outside the presented work.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM AACR: AI, DIAGNOSIS, AND IMAGING 2021
Prospective data support delaying antibiotics for pediatric respiratory infections
For pediatric patients with respiratory tract infections (RTIs), immediately prescribing antibiotics may do more harm than good, based on prospective data from 436 children treated by primary care pediatricians in Spain.
In the largest trial of its kind to date, children who were immediately prescribed antibiotics showed no significant difference in symptom severity or duration from those who received a delayed prescription for antibiotics, or no prescription at all; yet those in the immediate-prescription group had a higher rate of gastrointestinal adverse events, reported lead author Gemma Mas-Dalmau, MD, of the Sant Pau Institute for Biomedical Research, Barcelona, and colleagues.
“Most RTIs are self-limiting, and antibiotics hardly alter the course of the condition, yet antibiotics are frequently prescribed for these conditions,” the investigators wrote in Pediatrics. “Antibiotic prescription for RTIs in children is especially considered to be inappropriately high.”
This clinical behavior is driven by several factors, according to Dr. Mas-Dalmau and colleagues, including limited diagnostics in primary care, pressure to meet parental expectations, and concern for possible complications if antibiotics are withheld or delayed.
In an accompanying editorial, Jeffrey S. Gerber, MD, PhD and Bonnie F. Offit, MD, of Children’s Hospital of Philadelphia, noted that “children in the United States receive more than one antibiotic prescription per year, driven largely by acute RTIs.”
Dr. Gerber and Dr. Offit noted that some RTIs are indeed caused by bacteria, and therefore benefit from antibiotics, but it’s “not always easy” to identify these cases.
“Primary care, urgent care, and emergency medicine clinicians have a hard job,” they wrote.
According to the Centers for Disease Control and Prevention, delayed prescription of antibiotics, in which a prescription is filled upon persistence or worsening of symptoms, can balance clinical caution and antibiotic stewardship.
“An example of this approach is acute otitis media, in which delayed prescribing has been shown to safely reduce antibiotic exposure,” wrote Dr. Gerber and Dr. Offit.
In a 2017 Cochrane systematic review of both adults and children with RTIs, antibiotic prescriptions, whether immediate, delayed, or not given at all, had no significant effect on most symptoms or complications. Although several randomized trials have evaluated delayed antibiotic prescriptions in children, Dr. Mas-Dalmau and colleagues described the current body of evidence as “scant.”
The present study built upon this knowledge base by prospectively following 436 children treated at 39 primary care centers in Spain from 2012 to 2016. Patients were between 2 and 14 years of age and presented for rhinosinusitis, pharyngitis, acute otitis media, or acute bronchitis. Inclusion in the study required the pediatrician to have “reasonable doubts about the need to prescribe an antibiotic.” Clinics with access to rapid streptococcal testing did not enroll patients with pharyngitis.
Patients were randomized in approximately equal groups to receive either immediate prescription of antibiotics, delayed prescription, or no prescription. In the delayed group, caregivers were advised to fill prescriptions if any of following three events occurred:
- No symptom improvement after a certain amount of days, depending on presenting complaint (acute otitis media, 4 days; pharyngitis, 7 days; acute rhinosinusitis, 15 days; acute bronchitis, 20 days).
- Temperature of at least 39° C after 24 hours, or at least 38° C but less than 39° C after 48 hours.
- Patient feeling “much worse.”
Primary outcomes were severity and duration of symptoms over 30 days, while secondary outcomes included antibiotic use over 30 days, additional unscheduled visits to primary care over 30 days, and parental satisfaction and beliefs regarding antibiotic efficacy.
In the final dataset, 148 patients received immediate antibiotic prescriptions, while 146 received delayed prescriptions, and 142 received no prescription. Rate of antibiotic use was highest in the immediate prescription group, at 96%, versus 25.3% in the delayed group and 12% among those who received no prescription upon first presentation (P < .001).
Although the mean duration of severe symptoms was longest in the delayed-prescription group, at 12.4 days, versus 10.9 days in the no-prescription group and 10.1 days in the immediate-prescription group, these differences were not statistically significant (P = .539). Median score for greatest severity of any symptom was also similar across groups. Secondary outcomes echoed this pattern, in which reconsultation rates and caregiver satisfaction were statistically similar regardless of treatment type.
In contrast, patients who received immediate antibiotic prescriptions had a significantly higher rate of gastrointestinal adverse events (8.8%) than those who received a delayed prescription (3.4%) or no prescription (2.8%; P = .037).
“Delayed antibiotic prescription is an efficacious and safe strategy for reducing inappropriate antibiotic treatment of uncomplicated RTIs in children when the doctor has reasonable doubts regarding the indication,” the investigators concluded. “[It] is therefore a useful tool for addressing the public health issue of bacterial resistance. However, no antibiotic prescription remains the recommended strategy when it is clear that antibiotics are not indicated, like in most cases of acute bronchitis.”
“These data are reassuring,” wrote Dr. Gerber and Dr. Offit; however, they went on to suggest that the data “might not substantially move the needle.”
“With rare exceptions, children with acute pharyngitis should first receive a group A streptococcal test,” they wrote. “If results are positive, all patients should get antibiotics; if results are negative, no one gets them. Acute bronchitis (whatever that is in children) is viral. Acute sinusitis with persistent symptoms (the most commonly diagnosed variety) already has a delayed option, and the current study ... was not powered for this outcome. We are left with acute otitis media, which dominated enrollment but already has an evidence-based guideline.”
Still, Dr. Gerber and Dr. Offit suggested that the findings should further encourage pediatricians to prescribe antibiotics judiciously, and when elected, to choose the shortest duration and narrowest spectrum possible.
In a joint comment, Rana El Feghaly, MD, MSCI, director of outpatient antibiotic stewardship at Children’s Mercy, Kansas City, and her colleague, Mary Anne Jackson, MD, noted that the findings are “in accordance” with the 2017 Cochrane review.
Dr. Feghaly and Dr. Jackson said that these new data provide greater support for conservative use of antibiotics, which is badly needed, considering approximately 50% of outpatient prescriptions are unnecessary or inappropriate .
Delayed antibiotic prescription is part of a multifaceted approach to the issue, they said, joining “communication skills training, antibiotic justification documentation, audit and feedback reporting with peer comparison, diagnostic stewardship, [and] the use of clinician education on practice-based guidelines.”
“Leveraging delayed antibiotic prescription may be an excellent way to combat antibiotic overuse in the outpatient setting, while avoiding provider and parental fear of the ‘no antibiotic’ approach,” Dr. Feghaly and Dr. Jackson said.
Karlyn Kinsella, MD, of Pediatric Associates of Cheshire, Conn., suggested that clinicians discuss these findings with parents who request antibiotics for “otitis, pharyngitis, bronchitis, or sinusitis.”
“We can cite this study that antibiotics have no effect on symptom duration or severity for these illnesses,” Dr. Kinsella said. “Of course, our clinical opinion in each case takes precedent.”
According to Dr. Kinsella, conversations with parents also need to cover reasonable expectations, as the study did, with clear time frames for each condition in which children should start to get better.
“I think this is really key in our anticipatory guidance so that patients know what to expect,” she said.
The study was funded by Instituto de Salud Carlos III, the European Union, and the Spanish Ministry of Health, Social Services, and Equality. The investigators and interviewees reported no conflicts of interest.
For pediatric patients with respiratory tract infections (RTIs), immediately prescribing antibiotics may do more harm than good, based on prospective data from 436 children treated by primary care pediatricians in Spain.
In the largest trial of its kind to date, children who were immediately prescribed antibiotics showed no significant difference in symptom severity or duration from those who received a delayed prescription for antibiotics, or no prescription at all; yet those in the immediate-prescription group had a higher rate of gastrointestinal adverse events, reported lead author Gemma Mas-Dalmau, MD, of the Sant Pau Institute for Biomedical Research, Barcelona, and colleagues.
“Most RTIs are self-limiting, and antibiotics hardly alter the course of the condition, yet antibiotics are frequently prescribed for these conditions,” the investigators wrote in Pediatrics. “Antibiotic prescription for RTIs in children is especially considered to be inappropriately high.”
This clinical behavior is driven by several factors, according to Dr. Mas-Dalmau and colleagues, including limited diagnostics in primary care, pressure to meet parental expectations, and concern for possible complications if antibiotics are withheld or delayed.
In an accompanying editorial, Jeffrey S. Gerber, MD, PhD and Bonnie F. Offit, MD, of Children’s Hospital of Philadelphia, noted that “children in the United States receive more than one antibiotic prescription per year, driven largely by acute RTIs.”
Dr. Gerber and Dr. Offit noted that some RTIs are indeed caused by bacteria, and therefore benefit from antibiotics, but it’s “not always easy” to identify these cases.
“Primary care, urgent care, and emergency medicine clinicians have a hard job,” they wrote.
According to the Centers for Disease Control and Prevention, delayed prescription of antibiotics, in which a prescription is filled upon persistence or worsening of symptoms, can balance clinical caution and antibiotic stewardship.
“An example of this approach is acute otitis media, in which delayed prescribing has been shown to safely reduce antibiotic exposure,” wrote Dr. Gerber and Dr. Offit.
In a 2017 Cochrane systematic review of both adults and children with RTIs, antibiotic prescriptions, whether immediate, delayed, or not given at all, had no significant effect on most symptoms or complications. Although several randomized trials have evaluated delayed antibiotic prescriptions in children, Dr. Mas-Dalmau and colleagues described the current body of evidence as “scant.”
The present study built upon this knowledge base by prospectively following 436 children treated at 39 primary care centers in Spain from 2012 to 2016. Patients were between 2 and 14 years of age and presented for rhinosinusitis, pharyngitis, acute otitis media, or acute bronchitis. Inclusion in the study required the pediatrician to have “reasonable doubts about the need to prescribe an antibiotic.” Clinics with access to rapid streptococcal testing did not enroll patients with pharyngitis.
Patients were randomized in approximately equal groups to receive either immediate prescription of antibiotics, delayed prescription, or no prescription. In the delayed group, caregivers were advised to fill prescriptions if any of following three events occurred:
- No symptom improvement after a certain amount of days, depending on presenting complaint (acute otitis media, 4 days; pharyngitis, 7 days; acute rhinosinusitis, 15 days; acute bronchitis, 20 days).
- Temperature of at least 39° C after 24 hours, or at least 38° C but less than 39° C after 48 hours.
- Patient feeling “much worse.”
Primary outcomes were severity and duration of symptoms over 30 days, while secondary outcomes included antibiotic use over 30 days, additional unscheduled visits to primary care over 30 days, and parental satisfaction and beliefs regarding antibiotic efficacy.
In the final dataset, 148 patients received immediate antibiotic prescriptions, while 146 received delayed prescriptions, and 142 received no prescription. Rate of antibiotic use was highest in the immediate prescription group, at 96%, versus 25.3% in the delayed group and 12% among those who received no prescription upon first presentation (P < .001).
Although the mean duration of severe symptoms was longest in the delayed-prescription group, at 12.4 days, versus 10.9 days in the no-prescription group and 10.1 days in the immediate-prescription group, these differences were not statistically significant (P = .539). Median score for greatest severity of any symptom was also similar across groups. Secondary outcomes echoed this pattern, in which reconsultation rates and caregiver satisfaction were statistically similar regardless of treatment type.
In contrast, patients who received immediate antibiotic prescriptions had a significantly higher rate of gastrointestinal adverse events (8.8%) than those who received a delayed prescription (3.4%) or no prescription (2.8%; P = .037).
“Delayed antibiotic prescription is an efficacious and safe strategy for reducing inappropriate antibiotic treatment of uncomplicated RTIs in children when the doctor has reasonable doubts regarding the indication,” the investigators concluded. “[It] is therefore a useful tool for addressing the public health issue of bacterial resistance. However, no antibiotic prescription remains the recommended strategy when it is clear that antibiotics are not indicated, like in most cases of acute bronchitis.”
“These data are reassuring,” wrote Dr. Gerber and Dr. Offit; however, they went on to suggest that the data “might not substantially move the needle.”
“With rare exceptions, children with acute pharyngitis should first receive a group A streptococcal test,” they wrote. “If results are positive, all patients should get antibiotics; if results are negative, no one gets them. Acute bronchitis (whatever that is in children) is viral. Acute sinusitis with persistent symptoms (the most commonly diagnosed variety) already has a delayed option, and the current study ... was not powered for this outcome. We are left with acute otitis media, which dominated enrollment but already has an evidence-based guideline.”
Still, Dr. Gerber and Dr. Offit suggested that the findings should further encourage pediatricians to prescribe antibiotics judiciously, and when elected, to choose the shortest duration and narrowest spectrum possible.
In a joint comment, Rana El Feghaly, MD, MSCI, director of outpatient antibiotic stewardship at Children’s Mercy, Kansas City, and her colleague, Mary Anne Jackson, MD, noted that the findings are “in accordance” with the 2017 Cochrane review.
Dr. Feghaly and Dr. Jackson said that these new data provide greater support for conservative use of antibiotics, which is badly needed, considering approximately 50% of outpatient prescriptions are unnecessary or inappropriate .
Delayed antibiotic prescription is part of a multifaceted approach to the issue, they said, joining “communication skills training, antibiotic justification documentation, audit and feedback reporting with peer comparison, diagnostic stewardship, [and] the use of clinician education on practice-based guidelines.”
“Leveraging delayed antibiotic prescription may be an excellent way to combat antibiotic overuse in the outpatient setting, while avoiding provider and parental fear of the ‘no antibiotic’ approach,” Dr. Feghaly and Dr. Jackson said.
Karlyn Kinsella, MD, of Pediatric Associates of Cheshire, Conn., suggested that clinicians discuss these findings with parents who request antibiotics for “otitis, pharyngitis, bronchitis, or sinusitis.”
“We can cite this study that antibiotics have no effect on symptom duration or severity for these illnesses,” Dr. Kinsella said. “Of course, our clinical opinion in each case takes precedent.”
According to Dr. Kinsella, conversations with parents also need to cover reasonable expectations, as the study did, with clear time frames for each condition in which children should start to get better.
“I think this is really key in our anticipatory guidance so that patients know what to expect,” she said.
The study was funded by Instituto de Salud Carlos III, the European Union, and the Spanish Ministry of Health, Social Services, and Equality. The investigators and interviewees reported no conflicts of interest.
For pediatric patients with respiratory tract infections (RTIs), immediately prescribing antibiotics may do more harm than good, based on prospective data from 436 children treated by primary care pediatricians in Spain.
In the largest trial of its kind to date, children who were immediately prescribed antibiotics showed no significant difference in symptom severity or duration from those who received a delayed prescription for antibiotics, or no prescription at all; yet those in the immediate-prescription group had a higher rate of gastrointestinal adverse events, reported lead author Gemma Mas-Dalmau, MD, of the Sant Pau Institute for Biomedical Research, Barcelona, and colleagues.
“Most RTIs are self-limiting, and antibiotics hardly alter the course of the condition, yet antibiotics are frequently prescribed for these conditions,” the investigators wrote in Pediatrics. “Antibiotic prescription for RTIs in children is especially considered to be inappropriately high.”
This clinical behavior is driven by several factors, according to Dr. Mas-Dalmau and colleagues, including limited diagnostics in primary care, pressure to meet parental expectations, and concern for possible complications if antibiotics are withheld or delayed.
In an accompanying editorial, Jeffrey S. Gerber, MD, PhD and Bonnie F. Offit, MD, of Children’s Hospital of Philadelphia, noted that “children in the United States receive more than one antibiotic prescription per year, driven largely by acute RTIs.”
Dr. Gerber and Dr. Offit noted that some RTIs are indeed caused by bacteria, and therefore benefit from antibiotics, but it’s “not always easy” to identify these cases.
“Primary care, urgent care, and emergency medicine clinicians have a hard job,” they wrote.
According to the Centers for Disease Control and Prevention, delayed prescription of antibiotics, in which a prescription is filled upon persistence or worsening of symptoms, can balance clinical caution and antibiotic stewardship.
“An example of this approach is acute otitis media, in which delayed prescribing has been shown to safely reduce antibiotic exposure,” wrote Dr. Gerber and Dr. Offit.
In a 2017 Cochrane systematic review of both adults and children with RTIs, antibiotic prescriptions, whether immediate, delayed, or not given at all, had no significant effect on most symptoms or complications. Although several randomized trials have evaluated delayed antibiotic prescriptions in children, Dr. Mas-Dalmau and colleagues described the current body of evidence as “scant.”
The present study built upon this knowledge base by prospectively following 436 children treated at 39 primary care centers in Spain from 2012 to 2016. Patients were between 2 and 14 years of age and presented for rhinosinusitis, pharyngitis, acute otitis media, or acute bronchitis. Inclusion in the study required the pediatrician to have “reasonable doubts about the need to prescribe an antibiotic.” Clinics with access to rapid streptococcal testing did not enroll patients with pharyngitis.
Patients were randomized in approximately equal groups to receive either immediate prescription of antibiotics, delayed prescription, or no prescription. In the delayed group, caregivers were advised to fill prescriptions if any of following three events occurred:
- No symptom improvement after a certain amount of days, depending on presenting complaint (acute otitis media, 4 days; pharyngitis, 7 days; acute rhinosinusitis, 15 days; acute bronchitis, 20 days).
- Temperature of at least 39° C after 24 hours, or at least 38° C but less than 39° C after 48 hours.
- Patient feeling “much worse.”
Primary outcomes were severity and duration of symptoms over 30 days, while secondary outcomes included antibiotic use over 30 days, additional unscheduled visits to primary care over 30 days, and parental satisfaction and beliefs regarding antibiotic efficacy.
In the final dataset, 148 patients received immediate antibiotic prescriptions, while 146 received delayed prescriptions, and 142 received no prescription. Rate of antibiotic use was highest in the immediate prescription group, at 96%, versus 25.3% in the delayed group and 12% among those who received no prescription upon first presentation (P < .001).
Although the mean duration of severe symptoms was longest in the delayed-prescription group, at 12.4 days, versus 10.9 days in the no-prescription group and 10.1 days in the immediate-prescription group, these differences were not statistically significant (P = .539). Median score for greatest severity of any symptom was also similar across groups. Secondary outcomes echoed this pattern, in which reconsultation rates and caregiver satisfaction were statistically similar regardless of treatment type.
In contrast, patients who received immediate antibiotic prescriptions had a significantly higher rate of gastrointestinal adverse events (8.8%) than those who received a delayed prescription (3.4%) or no prescription (2.8%; P = .037).
“Delayed antibiotic prescription is an efficacious and safe strategy for reducing inappropriate antibiotic treatment of uncomplicated RTIs in children when the doctor has reasonable doubts regarding the indication,” the investigators concluded. “[It] is therefore a useful tool for addressing the public health issue of bacterial resistance. However, no antibiotic prescription remains the recommended strategy when it is clear that antibiotics are not indicated, like in most cases of acute bronchitis.”
“These data are reassuring,” wrote Dr. Gerber and Dr. Offit; however, they went on to suggest that the data “might not substantially move the needle.”
“With rare exceptions, children with acute pharyngitis should first receive a group A streptococcal test,” they wrote. “If results are positive, all patients should get antibiotics; if results are negative, no one gets them. Acute bronchitis (whatever that is in children) is viral. Acute sinusitis with persistent symptoms (the most commonly diagnosed variety) already has a delayed option, and the current study ... was not powered for this outcome. We are left with acute otitis media, which dominated enrollment but already has an evidence-based guideline.”
Still, Dr. Gerber and Dr. Offit suggested that the findings should further encourage pediatricians to prescribe antibiotics judiciously, and when elected, to choose the shortest duration and narrowest spectrum possible.
In a joint comment, Rana El Feghaly, MD, MSCI, director of outpatient antibiotic stewardship at Children’s Mercy, Kansas City, and her colleague, Mary Anne Jackson, MD, noted that the findings are “in accordance” with the 2017 Cochrane review.
Dr. Feghaly and Dr. Jackson said that these new data provide greater support for conservative use of antibiotics, which is badly needed, considering approximately 50% of outpatient prescriptions are unnecessary or inappropriate .
Delayed antibiotic prescription is part of a multifaceted approach to the issue, they said, joining “communication skills training, antibiotic justification documentation, audit and feedback reporting with peer comparison, diagnostic stewardship, [and] the use of clinician education on practice-based guidelines.”
“Leveraging delayed antibiotic prescription may be an excellent way to combat antibiotic overuse in the outpatient setting, while avoiding provider and parental fear of the ‘no antibiotic’ approach,” Dr. Feghaly and Dr. Jackson said.
Karlyn Kinsella, MD, of Pediatric Associates of Cheshire, Conn., suggested that clinicians discuss these findings with parents who request antibiotics for “otitis, pharyngitis, bronchitis, or sinusitis.”
“We can cite this study that antibiotics have no effect on symptom duration or severity for these illnesses,” Dr. Kinsella said. “Of course, our clinical opinion in each case takes precedent.”
According to Dr. Kinsella, conversations with parents also need to cover reasonable expectations, as the study did, with clear time frames for each condition in which children should start to get better.
“I think this is really key in our anticipatory guidance so that patients know what to expect,” she said.
The study was funded by Instituto de Salud Carlos III, the European Union, and the Spanish Ministry of Health, Social Services, and Equality. The investigators and interviewees reported no conflicts of interest.
FROM PEDIATRICS
Zika vaccine candidate shows promise in phase 1 trial
in a phase 1 study.
Although Zika cases have declined in recent years, “geographic expansion of the Aedes aegypti mosquito to areas where population-level immunity is low poses a substantial risk for future epidemics,” wrote Nadine C. Salisch, PhD, of Janssen Vaccines and Prevention, Leiden, the Netherlands, and colleagues in a paper published in Annals of Internal Medicine.
No vaccine against Zika is yet available, although more than 10 candidates have been studied in preclinical trials to date, they said.
The researchers randomized 100 healthy adult volunteers to an experimental Zika vaccine candidate known as Ad26.ZIKV.001 in either one-dose or two-dose regimens of 5x1010 viral particles (low dose) or 1x1011 viral particles (high dose) or placebo. Approximately half (55%) of the participants were women, and 72% were White.
Approximately 80% of patients in both two-dose groups showed antibody responses for a year after vaccination. Geometric mean titers (GMTs) reached peak of 823.4 in the low-dose/low-dose group and 961.5 in the high-dose/high-dose group. At day 365, the GMTs for these groups were 68.7 and 87.0, respectively.
A single high-dose vaccine achieved a similar level of neutralizing antibody titers, but lower peak neutralizing responses than the two-dose strategies, the researchers noted.
Most of the reported adverse events were mild to moderate, and short lived; the most common were injection site pain or tenderness, headache, and fatigue, the researchers said. After the first vaccination, 75% of participants in the low-dose groups, 88% of participants in high-dose groups, and 45% of participants receiving placebo reported local adverse events. In addition, 73%, 83%, and 40% of the participants in the low-dose, high-dose, and placebo groups, respectively, reported systemic adverse events. Reports were similar after the second vaccination. Two serious adverse events not related to vaccination were reported; one case of right lower lobe pneumonia and one case of incomplete spontaneous abortion.
The researchers also explored protective efficacy through a nonlethal mouse challenge model. “Transfer of 6 mg of IgG from Ad26.ZIKV.001 vaccines conferred complete protection from viremia in most recipient animals, with statistically significantly decreased breakthrough rates and cumulative viral loads per group compared with placebo,” they said.
The study findings were limited by the inability to assess safety and immunogenicity in an endemic area, the researchers noted. However, “Ad26.ZIKV.001 induces potent ZIKV-specific neutralizing responses with durability of at least 1 year, which supports further clinical development if an unmet medical need reemerges,” they said. “In addition, these data underscore the performance of the Ad26 vaccine platform, which Janssen is using for different infectious diseases, including COVID-19,” they noted.
Ad26 vector platform shows consistency
“Development of the investigational Janssen Zika vaccine candidate was initiated in 2015, and while the incidence of Zika virus has declined since the 2015-2016 outbreak, spread of the ‘carrier’ Aedes aegypti mosquito to areas where population-level immunity is low poses a substantial risk for future epidemics,” lead author Dr. Salisch said in an interview. For this reason, researchers say the vaccine warrants further development should the need reemerge, she said.
“Our research has found that while a single higher-dose regimen had lower peak neutralizing responses than a two-dose regimen, it achieved a similar level of neutralizing antibody responses at 1 year, an encouraging finding that shows our vaccine may be a useful tool to curb Zika epidemics,” Dr. Salisch noted. “Previous experience with the Ad26 vector platform across our investigational vaccine programs have yielded similarly promising results, most recently with our investigational Janssen COVID-19 vaccine program, for which phase 3 data show a single-dose vaccine met all primary and key secondary endpoints,” she said.
“The biggest barrier [to further development of the candidate vaccine] is one that we actually consider ourselves fortunate to have: The very low incidence of reported Zika cases currently reported worldwide,” Dr. Salisch said. “However, the current Zika case rate can change at any time, and in the event the situation demands it, we are open to alternative regulatory pathways to help us glean the necessary insights on vaccine safety and efficacy to further advance the development of this candidate,” she emphasized.
As for additional research, “there are still questions surrounding Zika transmission and the pathomechanism of congenital Zika syndrome,” said Dr. Salisch. “Our hope is that a correlate of protection against Zika disease, and in particular against congenital Zika syndrome, can be identified,” she said.
Consider pregnant women in next phase of research
“A major hurdle in ZIKV vaccine development is the inability to conduct large efficacy studies in the absence of a current outbreak,” Ann Chahroudi, MD, of Emory University, Atlanta, and Sallie Permar, MD, of Weill Cornell Medicine, New York, wrote in an accompanying editorial.
The current study provided some efficacy data using a mouse model, but “these data are obviously not conclusive for human protection,” they said.
“A further challenge for ZIKV vaccine efficacy trials will be to demonstrate fetal protection from [congenital Zika syndrome] after adult immunization. There should be a clear plan to readily deploy phase 3 trials for the most promising vaccines to emerge from phase 1 and 2 in the event of an outbreak, as was implemented for Ebola, including infant follow-up,” they emphasized.
The editorialists noted that the study did not include pregnant women, who represent a major target for immunization, but they said that vaccination of pregnant women against other neonatal pathogens such as influenza and tetanus has been effective. “Candidate ZIKV vaccines proven safe in phase 1 trials should immediately be assessed for safety and efficacy in pregnant women,” they said. Although Zika infections are not at epidemic levels currently, resurgence remains a possibility and the coronavirus pandemic “has taught us that preparedness for emerging infections is crucial,” they said.
Zika vaccine research is a challenge worth pursuing
“It is important to continue Zika vaccine research because of the unpredictable nature of that infection,” Kevin Ault, MD, of the University of Kansas, Kansas City, said in an interview. “Several times Zika has gained a foothold in unexposed and vulnerable populations,” Dr. Ault said. “Additionally, there are some data about using this vector during pregnancy, and eventually this vaccine may prevent the birth defects associated with Zika infections during pregnancy, he noted.
Dr. Ault said he was not surprised by the study findings. “This is a promising early phase vaccine candidate, and this adenovirus vector has been used in other similar trials,” he said. Potential barriers to vaccine development include the challenge of conducting late phase clinical trials in pregnant women, he noted. “The relevant endpoint is going to be clinical disease, and one of the most critical populations is pregnant women,” he said. In addition, “later phase 3 trials would be conducted in a population where there is an ongoing Zika outbreak,” Dr. Ault emphasized.
The study was supported by Janssen Vaccines and Infectious Diseases.
Dr. Chahroudi had no financial conflicts to disclose. Dr. Permar disclosed grants from Merck and Moderna unrelated to the current study. Dr. Ault had no relevant financial conflicts to disclose; he has served as an adviser to the Centers for Disease Control and Prevention, the World Medical Association, the National Vaccine Program Office, and the National Institute for Allergy and Infectious Diseases. He is a fellow of the Infectious Disease Society of American and a fellow of ACOG.
in a phase 1 study.
Although Zika cases have declined in recent years, “geographic expansion of the Aedes aegypti mosquito to areas where population-level immunity is low poses a substantial risk for future epidemics,” wrote Nadine C. Salisch, PhD, of Janssen Vaccines and Prevention, Leiden, the Netherlands, and colleagues in a paper published in Annals of Internal Medicine.
No vaccine against Zika is yet available, although more than 10 candidates have been studied in preclinical trials to date, they said.
The researchers randomized 100 healthy adult volunteers to an experimental Zika vaccine candidate known as Ad26.ZIKV.001 in either one-dose or two-dose regimens of 5x1010 viral particles (low dose) or 1x1011 viral particles (high dose) or placebo. Approximately half (55%) of the participants were women, and 72% were White.
Approximately 80% of patients in both two-dose groups showed antibody responses for a year after vaccination. Geometric mean titers (GMTs) reached peak of 823.4 in the low-dose/low-dose group and 961.5 in the high-dose/high-dose group. At day 365, the GMTs for these groups were 68.7 and 87.0, respectively.
A single high-dose vaccine achieved a similar level of neutralizing antibody titers, but lower peak neutralizing responses than the two-dose strategies, the researchers noted.
Most of the reported adverse events were mild to moderate, and short lived; the most common were injection site pain or tenderness, headache, and fatigue, the researchers said. After the first vaccination, 75% of participants in the low-dose groups, 88% of participants in high-dose groups, and 45% of participants receiving placebo reported local adverse events. In addition, 73%, 83%, and 40% of the participants in the low-dose, high-dose, and placebo groups, respectively, reported systemic adverse events. Reports were similar after the second vaccination. Two serious adverse events not related to vaccination were reported; one case of right lower lobe pneumonia and one case of incomplete spontaneous abortion.
The researchers also explored protective efficacy through a nonlethal mouse challenge model. “Transfer of 6 mg of IgG from Ad26.ZIKV.001 vaccines conferred complete protection from viremia in most recipient animals, with statistically significantly decreased breakthrough rates and cumulative viral loads per group compared with placebo,” they said.
The study findings were limited by the inability to assess safety and immunogenicity in an endemic area, the researchers noted. However, “Ad26.ZIKV.001 induces potent ZIKV-specific neutralizing responses with durability of at least 1 year, which supports further clinical development if an unmet medical need reemerges,” they said. “In addition, these data underscore the performance of the Ad26 vaccine platform, which Janssen is using for different infectious diseases, including COVID-19,” they noted.
Ad26 vector platform shows consistency
“Development of the investigational Janssen Zika vaccine candidate was initiated in 2015, and while the incidence of Zika virus has declined since the 2015-2016 outbreak, spread of the ‘carrier’ Aedes aegypti mosquito to areas where population-level immunity is low poses a substantial risk for future epidemics,” lead author Dr. Salisch said in an interview. For this reason, researchers say the vaccine warrants further development should the need reemerge, she said.
“Our research has found that while a single higher-dose regimen had lower peak neutralizing responses than a two-dose regimen, it achieved a similar level of neutralizing antibody responses at 1 year, an encouraging finding that shows our vaccine may be a useful tool to curb Zika epidemics,” Dr. Salisch noted. “Previous experience with the Ad26 vector platform across our investigational vaccine programs have yielded similarly promising results, most recently with our investigational Janssen COVID-19 vaccine program, for which phase 3 data show a single-dose vaccine met all primary and key secondary endpoints,” she said.
“The biggest barrier [to further development of the candidate vaccine] is one that we actually consider ourselves fortunate to have: The very low incidence of reported Zika cases currently reported worldwide,” Dr. Salisch said. “However, the current Zika case rate can change at any time, and in the event the situation demands it, we are open to alternative regulatory pathways to help us glean the necessary insights on vaccine safety and efficacy to further advance the development of this candidate,” she emphasized.
As for additional research, “there are still questions surrounding Zika transmission and the pathomechanism of congenital Zika syndrome,” said Dr. Salisch. “Our hope is that a correlate of protection against Zika disease, and in particular against congenital Zika syndrome, can be identified,” she said.
Consider pregnant women in next phase of research
“A major hurdle in ZIKV vaccine development is the inability to conduct large efficacy studies in the absence of a current outbreak,” Ann Chahroudi, MD, of Emory University, Atlanta, and Sallie Permar, MD, of Weill Cornell Medicine, New York, wrote in an accompanying editorial.
The current study provided some efficacy data using a mouse model, but “these data are obviously not conclusive for human protection,” they said.
“A further challenge for ZIKV vaccine efficacy trials will be to demonstrate fetal protection from [congenital Zika syndrome] after adult immunization. There should be a clear plan to readily deploy phase 3 trials for the most promising vaccines to emerge from phase 1 and 2 in the event of an outbreak, as was implemented for Ebola, including infant follow-up,” they emphasized.
The editorialists noted that the study did not include pregnant women, who represent a major target for immunization, but they said that vaccination of pregnant women against other neonatal pathogens such as influenza and tetanus has been effective. “Candidate ZIKV vaccines proven safe in phase 1 trials should immediately be assessed for safety and efficacy in pregnant women,” they said. Although Zika infections are not at epidemic levels currently, resurgence remains a possibility and the coronavirus pandemic “has taught us that preparedness for emerging infections is crucial,” they said.
Zika vaccine research is a challenge worth pursuing
“It is important to continue Zika vaccine research because of the unpredictable nature of that infection,” Kevin Ault, MD, of the University of Kansas, Kansas City, said in an interview. “Several times Zika has gained a foothold in unexposed and vulnerable populations,” Dr. Ault said. “Additionally, there are some data about using this vector during pregnancy, and eventually this vaccine may prevent the birth defects associated with Zika infections during pregnancy, he noted.
Dr. Ault said he was not surprised by the study findings. “This is a promising early phase vaccine candidate, and this adenovirus vector has been used in other similar trials,” he said. Potential barriers to vaccine development include the challenge of conducting late phase clinical trials in pregnant women, he noted. “The relevant endpoint is going to be clinical disease, and one of the most critical populations is pregnant women,” he said. In addition, “later phase 3 trials would be conducted in a population where there is an ongoing Zika outbreak,” Dr. Ault emphasized.
The study was supported by Janssen Vaccines and Infectious Diseases.
Dr. Chahroudi had no financial conflicts to disclose. Dr. Permar disclosed grants from Merck and Moderna unrelated to the current study. Dr. Ault had no relevant financial conflicts to disclose; he has served as an adviser to the Centers for Disease Control and Prevention, the World Medical Association, the National Vaccine Program Office, and the National Institute for Allergy and Infectious Diseases. He is a fellow of the Infectious Disease Society of American and a fellow of ACOG.
in a phase 1 study.
Although Zika cases have declined in recent years, “geographic expansion of the Aedes aegypti mosquito to areas where population-level immunity is low poses a substantial risk for future epidemics,” wrote Nadine C. Salisch, PhD, of Janssen Vaccines and Prevention, Leiden, the Netherlands, and colleagues in a paper published in Annals of Internal Medicine.
No vaccine against Zika is yet available, although more than 10 candidates have been studied in preclinical trials to date, they said.
The researchers randomized 100 healthy adult volunteers to an experimental Zika vaccine candidate known as Ad26.ZIKV.001 in either one-dose or two-dose regimens of 5x1010 viral particles (low dose) or 1x1011 viral particles (high dose) or placebo. Approximately half (55%) of the participants were women, and 72% were White.
Approximately 80% of patients in both two-dose groups showed antibody responses for a year after vaccination. Geometric mean titers (GMTs) reached peak of 823.4 in the low-dose/low-dose group and 961.5 in the high-dose/high-dose group. At day 365, the GMTs for these groups were 68.7 and 87.0, respectively.
A single high-dose vaccine achieved a similar level of neutralizing antibody titers, but lower peak neutralizing responses than the two-dose strategies, the researchers noted.
Most of the reported adverse events were mild to moderate, and short lived; the most common were injection site pain or tenderness, headache, and fatigue, the researchers said. After the first vaccination, 75% of participants in the low-dose groups, 88% of participants in high-dose groups, and 45% of participants receiving placebo reported local adverse events. In addition, 73%, 83%, and 40% of the participants in the low-dose, high-dose, and placebo groups, respectively, reported systemic adverse events. Reports were similar after the second vaccination. Two serious adverse events not related to vaccination were reported; one case of right lower lobe pneumonia and one case of incomplete spontaneous abortion.
The researchers also explored protective efficacy through a nonlethal mouse challenge model. “Transfer of 6 mg of IgG from Ad26.ZIKV.001 vaccines conferred complete protection from viremia in most recipient animals, with statistically significantly decreased breakthrough rates and cumulative viral loads per group compared with placebo,” they said.
The study findings were limited by the inability to assess safety and immunogenicity in an endemic area, the researchers noted. However, “Ad26.ZIKV.001 induces potent ZIKV-specific neutralizing responses with durability of at least 1 year, which supports further clinical development if an unmet medical need reemerges,” they said. “In addition, these data underscore the performance of the Ad26 vaccine platform, which Janssen is using for different infectious diseases, including COVID-19,” they noted.
Ad26 vector platform shows consistency
“Development of the investigational Janssen Zika vaccine candidate was initiated in 2015, and while the incidence of Zika virus has declined since the 2015-2016 outbreak, spread of the ‘carrier’ Aedes aegypti mosquito to areas where population-level immunity is low poses a substantial risk for future epidemics,” lead author Dr. Salisch said in an interview. For this reason, researchers say the vaccine warrants further development should the need reemerge, she said.
“Our research has found that while a single higher-dose regimen had lower peak neutralizing responses than a two-dose regimen, it achieved a similar level of neutralizing antibody responses at 1 year, an encouraging finding that shows our vaccine may be a useful tool to curb Zika epidemics,” Dr. Salisch noted. “Previous experience with the Ad26 vector platform across our investigational vaccine programs have yielded similarly promising results, most recently with our investigational Janssen COVID-19 vaccine program, for which phase 3 data show a single-dose vaccine met all primary and key secondary endpoints,” she said.
“The biggest barrier [to further development of the candidate vaccine] is one that we actually consider ourselves fortunate to have: The very low incidence of reported Zika cases currently reported worldwide,” Dr. Salisch said. “However, the current Zika case rate can change at any time, and in the event the situation demands it, we are open to alternative regulatory pathways to help us glean the necessary insights on vaccine safety and efficacy to further advance the development of this candidate,” she emphasized.
As for additional research, “there are still questions surrounding Zika transmission and the pathomechanism of congenital Zika syndrome,” said Dr. Salisch. “Our hope is that a correlate of protection against Zika disease, and in particular against congenital Zika syndrome, can be identified,” she said.
Consider pregnant women in next phase of research
“A major hurdle in ZIKV vaccine development is the inability to conduct large efficacy studies in the absence of a current outbreak,” Ann Chahroudi, MD, of Emory University, Atlanta, and Sallie Permar, MD, of Weill Cornell Medicine, New York, wrote in an accompanying editorial.
The current study provided some efficacy data using a mouse model, but “these data are obviously not conclusive for human protection,” they said.
“A further challenge for ZIKV vaccine efficacy trials will be to demonstrate fetal protection from [congenital Zika syndrome] after adult immunization. There should be a clear plan to readily deploy phase 3 trials for the most promising vaccines to emerge from phase 1 and 2 in the event of an outbreak, as was implemented for Ebola, including infant follow-up,” they emphasized.
The editorialists noted that the study did not include pregnant women, who represent a major target for immunization, but they said that vaccination of pregnant women against other neonatal pathogens such as influenza and tetanus has been effective. “Candidate ZIKV vaccines proven safe in phase 1 trials should immediately be assessed for safety and efficacy in pregnant women,” they said. Although Zika infections are not at epidemic levels currently, resurgence remains a possibility and the coronavirus pandemic “has taught us that preparedness for emerging infections is crucial,” they said.
Zika vaccine research is a challenge worth pursuing
“It is important to continue Zika vaccine research because of the unpredictable nature of that infection,” Kevin Ault, MD, of the University of Kansas, Kansas City, said in an interview. “Several times Zika has gained a foothold in unexposed and vulnerable populations,” Dr. Ault said. “Additionally, there are some data about using this vector during pregnancy, and eventually this vaccine may prevent the birth defects associated with Zika infections during pregnancy, he noted.
Dr. Ault said he was not surprised by the study findings. “This is a promising early phase vaccine candidate, and this adenovirus vector has been used in other similar trials,” he said. Potential barriers to vaccine development include the challenge of conducting late phase clinical trials in pregnant women, he noted. “The relevant endpoint is going to be clinical disease, and one of the most critical populations is pregnant women,” he said. In addition, “later phase 3 trials would be conducted in a population where there is an ongoing Zika outbreak,” Dr. Ault emphasized.
The study was supported by Janssen Vaccines and Infectious Diseases.
Dr. Chahroudi had no financial conflicts to disclose. Dr. Permar disclosed grants from Merck and Moderna unrelated to the current study. Dr. Ault had no relevant financial conflicts to disclose; he has served as an adviser to the Centers for Disease Control and Prevention, the World Medical Association, the National Vaccine Program Office, and the National Institute for Allergy and Infectious Diseases. He is a fellow of the Infectious Disease Society of American and a fellow of ACOG.
FROM ANNALS OF INTERNAL MEDICINE
The importance of family acceptance for LGBTQ youth
It is well established that LGBTQ individuals experience more health disparities compared with their cisgender, heterosexual counterparts. In general, LGBTQ adolescents and young adults have higher levels of depression, suicide attempts, and substance use than those of their heterosexual peers. However, a key protective factor is family acceptance and support. By encouraging families to modify and change behaviors that are experienced by their LGBTQ children as rejecting and to engage in supportive and affirming behaviors, providers can help families to decrease risk and promote healthy outcomes for LGBTQ youth and young adults. 
We all know that a supportive family can make a difference for any child, but this is especially true for LGBTQ youth and is critical during a pandemic when young people are confined with families and separated from peers and supportive adults outside the home. Several research studies show that family support can improve outcomes related to suicide, depression, homelessness, drug use, and HIV in LGBTQ young people. Family acceptance improves health outcomes, while rejection undermines family relationships and worsens both health and other serious outcomes such as homelessness and placement in custodial care. Pediatricians can help their patients by educating parents and caregivers with LGBTQ children about the critical role of family support – both those who see themselves as accepting and those who believe that being gay or transgender is wrong and are struggling with parenting a child who identifies as LGBTQ or who is gender diverse.
The Family Acceptance Project (FAP) at San Francisco State University conducted the first research on LGBTQ youth and families, developed the first evidence-informed family support model, and has published a range of studies and evidence-based resources that demonstrate the harm caused by family rejection, validate the importance of family acceptance, and provide guidance to increase family support. FAP’s research found that parents and caregivers that engage in rejecting behaviors are typically motivated by care and concern and by trying to protect their children from harm. They believe such behaviors will help their LGBTQ children fit in, have a good life, meet cultural and religious expectations, and be respected by others.1 FAP’s research identified and measured more than 50 rejecting behaviors that parents and caregivers use to respond to their LGBTQ children. Some of these commonly expressed rejecting behaviors include ridiculing and making disparaging comments about their child and other LGBTQ people; excluding them from family activities; blaming their child when others mistreat them because they are LGBTQ; blocking access to LGBTQ resources including friends, support groups, and activities; and trying to change their child’s sexual orientation and gender identity.2 LGBTQ youth experience these and other such behaviors as hurtful, harmful, and traumatic and may feel that they need to hide or repress their identity which can affect their self-esteem, increase isolation, depression, and risky behaviors.3 Providers working with families of LGBTQ youth should focus on shared goals, such as reducing risk and having a happy, healthy child. Most parents love their children and fear for their well-being. However, many are uninformed about their child’s gender identity and sexual orientation and don’t know how to nurture and support them.
In FAP’s initial study, LGB young people who reported higher levels of family rejection had substantially higher rates of attempted suicide, depression, illegal drug use, and unprotected sex.4 These rates were even more significant among Latino gay and bisexual men.4 Those who are rejected by family are less likely to want to have a family or to be parents themselves5 and have lower educational and income levels.6
To reduce risk, pediatricians should ask LGBTQ patients about family rejecting behaviors and help parents and caregivers to identify and understand the effect of such behaviors to reduce health risks and conflict that can lead to running away, expulsion, and removal from the home. Even decreasing rejecting behaviors to moderate levels can significantly improve negative outcomes.5
Caitlin Ryan, PhD, and her team also identified and measured more than 50 family accepting behaviors that help protect against risk and promote well-being. They found that young adults who experience high levels of family acceptance during adolescence report significantly higher levels of self-esteem, social support, and general health with much lower levels of depression, suicidality, and substance abuse.7 Family accepting and supportive behaviors include talking with the child about their LGBTQ identity; advocating for their LGBTQ child when others mistreat them; requiring other family members to treat their LGBTQ child with respect; and supporting their child’s gender identity.5 FAP has developed an evidence-informed family support model and multilingual educational resources for families, providers, youth and religious leaders to decrease rejection and increase family support. These are available in print copies and for download at familyproject.sfsu.edu.
In addition, Dr. Ryan and colleagues1,4,8 recommend the following guidance for providers:
- Ask LGBTQ adolescents about family reactions to their sexual orientation, gender identity, and expression, and refer to LGBTQ community support programs and for supportive counseling, as needed.
- Identify LGBTQ community support programs and online resources to educate parents about how to help their children. Parents need culturally relevant peer support to help decrease rejection and increase family support.
- Advise parents that negative reactions to their adolescent’s LGBTQ identity may negatively impact their child’s health and mental health while supportive and affirming reactions promote well-being.
- Advise parents and caregivers to modify and change family rejecting behaviors that increase their child’s risk for suicide, depression, substance abuse ,and risky sexual behaviors.
- Expand anticipatory guidance to include information on the need for support and the link between family rejection and negative health problems.
- Provide guidance on sexual orientation and gender identity as part of normative child development during well-baby and early childhood care.
- Use FAP’s multilingual family education booklets and Healthy Futures poster series in family and patient education and provide these materials in clinical and community settings. FAP’s Healthy Futures posters include a poster guidance, a version on family acceptance, a version on family rejection and a family acceptance version for conservative families and settings. They are available in camera-ready art in four sizes in English and Spanish and are forthcoming in five Asian languages: familyproject.sfsu.edu/poster.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures.
Resources
• Family Acceptance Project – consultation and training; evidence-based educational materials for families, providers, religious leaders and youth.
• PFLAG – peer support for parents and friends with LGBTQ children in all states and several other countries.
References
1. Ryan C. Generating a revolution in prevention, wellness & care for LGBT children & youth. Temple Political & Civil Rights Law Review. 2014;23(2):331-44.
2. Ryan C. Healthy Futures Poster Series – Family Accepting & Rejecting Behaviors That Impact LGBTQ Children’s Health & Well-Being. In: Family Acceptance Project Marian Wright Edelman Institute SFSU, ed. San Francisco, CA2019.
3. Ryan C. Family Acceptance Project: Culturally grounded framework for supporting LGBTQ children and youth. J Am Acad Child Adolesc Psychiatr. 2019;58(10):S58-9.
4. Ryan C et al. Family rejection as a predictor of negative health outcomes in White and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123(1):346-52.
5. Ryan C. Supportive families, healthy children: Helping families with lesbian, gay, bisexual & transgender children. In: Family Acceptance Project Marian Wright Edelman Institute SFSU, ed. San Francisco, CA2009.
6. Ryan C et al. Parent-initiated sexual orientation change efforts with LGBT adolescents: Implications for young adult mental health and adjustment. J Homosexuality. 2020;67(2):159-73.
7. Ryan C et al. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nursing. 2010;23(4):205-13. 8. Substance Abuse and Mental Health Services Administration. A Practitioner’s Guide: Helping Families to Support Their LGBT Children. In: Administration SAaMhS, ed. Vol PEP14-LGBTKIDS. Rockville, MD: HHS Publication; 2014.
It is well established that LGBTQ individuals experience more health disparities compared with their cisgender, heterosexual counterparts. In general, LGBTQ adolescents and young adults have higher levels of depression, suicide attempts, and substance use than those of their heterosexual peers. However, a key protective factor is family acceptance and support. By encouraging families to modify and change behaviors that are experienced by their LGBTQ children as rejecting and to engage in supportive and affirming behaviors, providers can help families to decrease risk and promote healthy outcomes for LGBTQ youth and young adults. 
We all know that a supportive family can make a difference for any child, but this is especially true for LGBTQ youth and is critical during a pandemic when young people are confined with families and separated from peers and supportive adults outside the home. Several research studies show that family support can improve outcomes related to suicide, depression, homelessness, drug use, and HIV in LGBTQ young people. Family acceptance improves health outcomes, while rejection undermines family relationships and worsens both health and other serious outcomes such as homelessness and placement in custodial care. Pediatricians can help their patients by educating parents and caregivers with LGBTQ children about the critical role of family support – both those who see themselves as accepting and those who believe that being gay or transgender is wrong and are struggling with parenting a child who identifies as LGBTQ or who is gender diverse.
The Family Acceptance Project (FAP) at San Francisco State University conducted the first research on LGBTQ youth and families, developed the first evidence-informed family support model, and has published a range of studies and evidence-based resources that demonstrate the harm caused by family rejection, validate the importance of family acceptance, and provide guidance to increase family support. FAP’s research found that parents and caregivers that engage in rejecting behaviors are typically motivated by care and concern and by trying to protect their children from harm. They believe such behaviors will help their LGBTQ children fit in, have a good life, meet cultural and religious expectations, and be respected by others.1 FAP’s research identified and measured more than 50 rejecting behaviors that parents and caregivers use to respond to their LGBTQ children. Some of these commonly expressed rejecting behaviors include ridiculing and making disparaging comments about their child and other LGBTQ people; excluding them from family activities; blaming their child when others mistreat them because they are LGBTQ; blocking access to LGBTQ resources including friends, support groups, and activities; and trying to change their child’s sexual orientation and gender identity.2 LGBTQ youth experience these and other such behaviors as hurtful, harmful, and traumatic and may feel that they need to hide or repress their identity which can affect their self-esteem, increase isolation, depression, and risky behaviors.3 Providers working with families of LGBTQ youth should focus on shared goals, such as reducing risk and having a happy, healthy child. Most parents love their children and fear for their well-being. However, many are uninformed about their child’s gender identity and sexual orientation and don’t know how to nurture and support them.
In FAP’s initial study, LGB young people who reported higher levels of family rejection had substantially higher rates of attempted suicide, depression, illegal drug use, and unprotected sex.4 These rates were even more significant among Latino gay and bisexual men.4 Those who are rejected by family are less likely to want to have a family or to be parents themselves5 and have lower educational and income levels.6
To reduce risk, pediatricians should ask LGBTQ patients about family rejecting behaviors and help parents and caregivers to identify and understand the effect of such behaviors to reduce health risks and conflict that can lead to running away, expulsion, and removal from the home. Even decreasing rejecting behaviors to moderate levels can significantly improve negative outcomes.5
Caitlin Ryan, PhD, and her team also identified and measured more than 50 family accepting behaviors that help protect against risk and promote well-being. They found that young adults who experience high levels of family acceptance during adolescence report significantly higher levels of self-esteem, social support, and general health with much lower levels of depression, suicidality, and substance abuse.7 Family accepting and supportive behaviors include talking with the child about their LGBTQ identity; advocating for their LGBTQ child when others mistreat them; requiring other family members to treat their LGBTQ child with respect; and supporting their child’s gender identity.5 FAP has developed an evidence-informed family support model and multilingual educational resources for families, providers, youth and religious leaders to decrease rejection and increase family support. These are available in print copies and for download at familyproject.sfsu.edu.
In addition, Dr. Ryan and colleagues1,4,8 recommend the following guidance for providers:
- Ask LGBTQ adolescents about family reactions to their sexual orientation, gender identity, and expression, and refer to LGBTQ community support programs and for supportive counseling, as needed.
- Identify LGBTQ community support programs and online resources to educate parents about how to help their children. Parents need culturally relevant peer support to help decrease rejection and increase family support.
- Advise parents that negative reactions to their adolescent’s LGBTQ identity may negatively impact their child’s health and mental health while supportive and affirming reactions promote well-being.
- Advise parents and caregivers to modify and change family rejecting behaviors that increase their child’s risk for suicide, depression, substance abuse ,and risky sexual behaviors.
- Expand anticipatory guidance to include information on the need for support and the link between family rejection and negative health problems.
- Provide guidance on sexual orientation and gender identity as part of normative child development during well-baby and early childhood care.
- Use FAP’s multilingual family education booklets and Healthy Futures poster series in family and patient education and provide these materials in clinical and community settings. FAP’s Healthy Futures posters include a poster guidance, a version on family acceptance, a version on family rejection and a family acceptance version for conservative families and settings. They are available in camera-ready art in four sizes in English and Spanish and are forthcoming in five Asian languages: familyproject.sfsu.edu/poster.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures.
Resources
• Family Acceptance Project – consultation and training; evidence-based educational materials for families, providers, religious leaders and youth.
• PFLAG – peer support for parents and friends with LGBTQ children in all states and several other countries.
References
1. Ryan C. Generating a revolution in prevention, wellness & care for LGBT children & youth. Temple Political & Civil Rights Law Review. 2014;23(2):331-44.
2. Ryan C. Healthy Futures Poster Series – Family Accepting & Rejecting Behaviors That Impact LGBTQ Children’s Health & Well-Being. In: Family Acceptance Project Marian Wright Edelman Institute SFSU, ed. San Francisco, CA2019.
3. Ryan C. Family Acceptance Project: Culturally grounded framework for supporting LGBTQ children and youth. J Am Acad Child Adolesc Psychiatr. 2019;58(10):S58-9.
4. Ryan C et al. Family rejection as a predictor of negative health outcomes in White and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123(1):346-52.
5. Ryan C. Supportive families, healthy children: Helping families with lesbian, gay, bisexual & transgender children. In: Family Acceptance Project Marian Wright Edelman Institute SFSU, ed. San Francisco, CA2009.
6. Ryan C et al. Parent-initiated sexual orientation change efforts with LGBT adolescents: Implications for young adult mental health and adjustment. J Homosexuality. 2020;67(2):159-73.
7. Ryan C et al. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nursing. 2010;23(4):205-13. 8. Substance Abuse and Mental Health Services Administration. A Practitioner’s Guide: Helping Families to Support Their LGBT Children. In: Administration SAaMhS, ed. Vol PEP14-LGBTKIDS. Rockville, MD: HHS Publication; 2014.
It is well established that LGBTQ individuals experience more health disparities compared with their cisgender, heterosexual counterparts. In general, LGBTQ adolescents and young adults have higher levels of depression, suicide attempts, and substance use than those of their heterosexual peers. However, a key protective factor is family acceptance and support. By encouraging families to modify and change behaviors that are experienced by their LGBTQ children as rejecting and to engage in supportive and affirming behaviors, providers can help families to decrease risk and promote healthy outcomes for LGBTQ youth and young adults. 
We all know that a supportive family can make a difference for any child, but this is especially true for LGBTQ youth and is critical during a pandemic when young people are confined with families and separated from peers and supportive adults outside the home. Several research studies show that family support can improve outcomes related to suicide, depression, homelessness, drug use, and HIV in LGBTQ young people. Family acceptance improves health outcomes, while rejection undermines family relationships and worsens both health and other serious outcomes such as homelessness and placement in custodial care. Pediatricians can help their patients by educating parents and caregivers with LGBTQ children about the critical role of family support – both those who see themselves as accepting and those who believe that being gay or transgender is wrong and are struggling with parenting a child who identifies as LGBTQ or who is gender diverse.
The Family Acceptance Project (FAP) at San Francisco State University conducted the first research on LGBTQ youth and families, developed the first evidence-informed family support model, and has published a range of studies and evidence-based resources that demonstrate the harm caused by family rejection, validate the importance of family acceptance, and provide guidance to increase family support. FAP’s research found that parents and caregivers that engage in rejecting behaviors are typically motivated by care and concern and by trying to protect their children from harm. They believe such behaviors will help their LGBTQ children fit in, have a good life, meet cultural and religious expectations, and be respected by others.1 FAP’s research identified and measured more than 50 rejecting behaviors that parents and caregivers use to respond to their LGBTQ children. Some of these commonly expressed rejecting behaviors include ridiculing and making disparaging comments about their child and other LGBTQ people; excluding them from family activities; blaming their child when others mistreat them because they are LGBTQ; blocking access to LGBTQ resources including friends, support groups, and activities; and trying to change their child’s sexual orientation and gender identity.2 LGBTQ youth experience these and other such behaviors as hurtful, harmful, and traumatic and may feel that they need to hide or repress their identity which can affect their self-esteem, increase isolation, depression, and risky behaviors.3 Providers working with families of LGBTQ youth should focus on shared goals, such as reducing risk and having a happy, healthy child. Most parents love their children and fear for their well-being. However, many are uninformed about their child’s gender identity and sexual orientation and don’t know how to nurture and support them.
In FAP’s initial study, LGB young people who reported higher levels of family rejection had substantially higher rates of attempted suicide, depression, illegal drug use, and unprotected sex.4 These rates were even more significant among Latino gay and bisexual men.4 Those who are rejected by family are less likely to want to have a family or to be parents themselves5 and have lower educational and income levels.6
To reduce risk, pediatricians should ask LGBTQ patients about family rejecting behaviors and help parents and caregivers to identify and understand the effect of such behaviors to reduce health risks and conflict that can lead to running away, expulsion, and removal from the home. Even decreasing rejecting behaviors to moderate levels can significantly improve negative outcomes.5
Caitlin Ryan, PhD, and her team also identified and measured more than 50 family accepting behaviors that help protect against risk and promote well-being. They found that young adults who experience high levels of family acceptance during adolescence report significantly higher levels of self-esteem, social support, and general health with much lower levels of depression, suicidality, and substance abuse.7 Family accepting and supportive behaviors include talking with the child about their LGBTQ identity; advocating for their LGBTQ child when others mistreat them; requiring other family members to treat their LGBTQ child with respect; and supporting their child’s gender identity.5 FAP has developed an evidence-informed family support model and multilingual educational resources for families, providers, youth and religious leaders to decrease rejection and increase family support. These are available in print copies and for download at familyproject.sfsu.edu.
In addition, Dr. Ryan and colleagues1,4,8 recommend the following guidance for providers:
- Ask LGBTQ adolescents about family reactions to their sexual orientation, gender identity, and expression, and refer to LGBTQ community support programs and for supportive counseling, as needed.
- Identify LGBTQ community support programs and online resources to educate parents about how to help their children. Parents need culturally relevant peer support to help decrease rejection and increase family support.
- Advise parents that negative reactions to their adolescent’s LGBTQ identity may negatively impact their child’s health and mental health while supportive and affirming reactions promote well-being.
- Advise parents and caregivers to modify and change family rejecting behaviors that increase their child’s risk for suicide, depression, substance abuse ,and risky sexual behaviors.
- Expand anticipatory guidance to include information on the need for support and the link between family rejection and negative health problems.
- Provide guidance on sexual orientation and gender identity as part of normative child development during well-baby and early childhood care.
- Use FAP’s multilingual family education booklets and Healthy Futures poster series in family and patient education and provide these materials in clinical and community settings. FAP’s Healthy Futures posters include a poster guidance, a version on family acceptance, a version on family rejection and a family acceptance version for conservative families and settings. They are available in camera-ready art in four sizes in English and Spanish and are forthcoming in five Asian languages: familyproject.sfsu.edu/poster.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures.
Resources
• Family Acceptance Project – consultation and training; evidence-based educational materials for families, providers, religious leaders and youth.
• PFLAG – peer support for parents and friends with LGBTQ children in all states and several other countries.
References
1. Ryan C. Generating a revolution in prevention, wellness & care for LGBT children & youth. Temple Political & Civil Rights Law Review. 2014;23(2):331-44.
2. Ryan C. Healthy Futures Poster Series – Family Accepting & Rejecting Behaviors That Impact LGBTQ Children’s Health & Well-Being. In: Family Acceptance Project Marian Wright Edelman Institute SFSU, ed. San Francisco, CA2019.
3. Ryan C. Family Acceptance Project: Culturally grounded framework for supporting LGBTQ children and youth. J Am Acad Child Adolesc Psychiatr. 2019;58(10):S58-9.
4. Ryan C et al. Family rejection as a predictor of negative health outcomes in White and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123(1):346-52.
5. Ryan C. Supportive families, healthy children: Helping families with lesbian, gay, bisexual & transgender children. In: Family Acceptance Project Marian Wright Edelman Institute SFSU, ed. San Francisco, CA2009.
6. Ryan C et al. Parent-initiated sexual orientation change efforts with LGBT adolescents: Implications for young adult mental health and adjustment. J Homosexuality. 2020;67(2):159-73.
7. Ryan C et al. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nursing. 2010;23(4):205-13. 8. Substance Abuse and Mental Health Services Administration. A Practitioner’s Guide: Helping Families to Support Their LGBT Children. In: Administration SAaMhS, ed. Vol PEP14-LGBTKIDS. Rockville, MD: HHS Publication; 2014.
Checkpoint inhibitors’ ‘big picture’ safety shown with preexisting autoimmune diseases
Patients with advanced melanoma and preexisting autoimmune diseases (AIDs) who were treated with immune checkpoint inhibitors (ICIs) responded well and did not suffer more grade 3 or higher immune-related adverse events than patients without an AID, a new study finds, although some concerns were raised regarding patients with inflammatory bowel disease (IBD).
“To our knowledge, this is the first study to bridge this knowledge gap by presenting ‘real-world’ data on the safety and efficacy of ICI on a national scale,” wrote Monique K. van der Kooij, MD, of Leiden (the Netherlands) University Medical Center and coauthors. The study was published online in Annals of Internal Medicine.
To investigate ICI use and response among this specific subset of melanoma patients, the researchers launched a nationwide cohort study set in the Netherlands. Data were gathered via the Dutch Melanoma Treatment Registry (DMTR), in which 4,367 patients with advanced melanoma were enrolled between July 2013 and July 2018.
Within that cohort, 415 (9.5%) had preexisting AIDs. Nearly 55% had rheumatologic AIDs (n = 227) – which included RA, systemic lupus erythematosus, scleroderma, sarcoidosis, and vasculitis – with the next most frequent being endocrine AID (n = 143) and IBD (n = 55). Patients with AID were older than patients without (67 vs. 63 years) and were more likely to be female (53% vs. 41%).
The ICIs used in the study included anti-CTLA4 (ipilimumab), anti–programmed death 1 (PD-1) (nivolumab or pembrolizumab), or a combination of nivolumab and ipilimumab. Of the patients with AID, 55% (n = 228) were treated with ICI, compared with 58% of patients without AID. A total of 87 AID patients were treated with anti-CTLA4, 187 received anti-PD-1, and 34 received the combination. The combination was not readily available in the Netherlands until 2017, the authors stated, acknowledging that it may be wise to revisit its effects in the coming years.
Incidence of immune-related adverse events
The incidence of immune-related adverse events (irAEs) grade 3 and above for patients with and without AID who were given anti-CTLA4 was 30%. The incidence rate of irAEs was also similar for patients with (17%; 95% confidence interval, 12%-23%) and without (13%; 95% CI, 12%-15%) AID on anti-PD-1. Patients with AIDs who took anti-PD-1 therapy discontinued it more often because of toxicity than did the patients without AIDs.
The combination group had irAE incidence rates of 44% (95% CI, 27%-62%) for patients with AID, compared with 48% (95% CI, 43%-53%) for patients without AIDs. Overall, no patients with AIDs on ICIs died of toxicity, compared with three deaths among patients without AID on anti-CTLA4, five deaths among patients on anti-PD-1, and one patient on the combination.
Patients with IBD had a notably higher risk of anti-PD-1–induced colitis (19%; 95% CI, 7%-37%), compared with patients with other AIDs (3%; 95% CI, 0%-6%) and patients without AIDs (2%; 95% CI, 2%-3%). IBD patients were also more likely than all other groups on ICIs to stop treatment because of toxicity, leading the researchers to note that “close monitoring in patients with IBD is advised.”
Overall survival after diagnosis was similar in patients with AIDs (median, 13 months; 95% CI, 10-16 months) and without (median, 14 months; 95% CI, 13-15 months), as was the objective response rate to anti-CTLA4 treatment (10% vs. 16%), anti-PD-1 treatment (40% vs. 44%), and combination therapy (39% vs. 43%).
Study largely bypasses the effects of checkpoint inhibitors on RA patients
“For detail, you can’t look to this study,” Anne R. Bass, MD, of the division of rheumatology at the Hospital for Special Surgery in New York, said in an interview. “But for a big-picture look at ‘how safe are checkpoint inhibitors,’ I think it’s an important one.”
Dr. Bass noted that the investigators lumped certain elements together and bypassed others, including their focus on grade 3 or higher adverse events. That was a decision the authors themselves recognized as a potential limitation of their research.
“Understandably, they were worried about life-threatening adverse events, and that’s fine,” she said. But for patients with arthritis who flare, their events are usually grade 2 or even grade 1 and therefore not captured or analyzed in the study. “This does not really address the risk of flare in an RA patient.”
She also questioned their grouping of AIDs, with a bevy of rheumatic diseases categorized as one cluster and the “other” group being particularly broad in its inclusion of “all AIDs not listed” – though only eight patients were placed into that group.
That said, the researchers relied on an oncology database, not one aimed at AID or adverse events. “The numbers are so much bigger than any other study in this area that’s been done,” she said. “It’s both a strength and a weakness of this kind of database.”
Indeed, the authors considered their use of nationwide, population-based data from the DMTR a benefit, calling it “a strength of our approach.”
The DMTR was funded by a grant from the Netherlands Organization for Health Research and Development and sponsored by Bristol-Myers Squibb, Novartis, Roche Nederland, Merck Sharp & Dohme, and Pierre Fabre via the Dutch Institute for Clinical Auditing.
Patients with advanced melanoma and preexisting autoimmune diseases (AIDs) who were treated with immune checkpoint inhibitors (ICIs) responded well and did not suffer more grade 3 or higher immune-related adverse events than patients without an AID, a new study finds, although some concerns were raised regarding patients with inflammatory bowel disease (IBD).
“To our knowledge, this is the first study to bridge this knowledge gap by presenting ‘real-world’ data on the safety and efficacy of ICI on a national scale,” wrote Monique K. van der Kooij, MD, of Leiden (the Netherlands) University Medical Center and coauthors. The study was published online in Annals of Internal Medicine.
To investigate ICI use and response among this specific subset of melanoma patients, the researchers launched a nationwide cohort study set in the Netherlands. Data were gathered via the Dutch Melanoma Treatment Registry (DMTR), in which 4,367 patients with advanced melanoma were enrolled between July 2013 and July 2018.
Within that cohort, 415 (9.5%) had preexisting AIDs. Nearly 55% had rheumatologic AIDs (n = 227) – which included RA, systemic lupus erythematosus, scleroderma, sarcoidosis, and vasculitis – with the next most frequent being endocrine AID (n = 143) and IBD (n = 55). Patients with AID were older than patients without (67 vs. 63 years) and were more likely to be female (53% vs. 41%).
The ICIs used in the study included anti-CTLA4 (ipilimumab), anti–programmed death 1 (PD-1) (nivolumab or pembrolizumab), or a combination of nivolumab and ipilimumab. Of the patients with AID, 55% (n = 228) were treated with ICI, compared with 58% of patients without AID. A total of 87 AID patients were treated with anti-CTLA4, 187 received anti-PD-1, and 34 received the combination. The combination was not readily available in the Netherlands until 2017, the authors stated, acknowledging that it may be wise to revisit its effects in the coming years.
Incidence of immune-related adverse events
The incidence of immune-related adverse events (irAEs) grade 3 and above for patients with and without AID who were given anti-CTLA4 was 30%. The incidence rate of irAEs was also similar for patients with (17%; 95% confidence interval, 12%-23%) and without (13%; 95% CI, 12%-15%) AID on anti-PD-1. Patients with AIDs who took anti-PD-1 therapy discontinued it more often because of toxicity than did the patients without AIDs.
The combination group had irAE incidence rates of 44% (95% CI, 27%-62%) for patients with AID, compared with 48% (95% CI, 43%-53%) for patients without AIDs. Overall, no patients with AIDs on ICIs died of toxicity, compared with three deaths among patients without AID on anti-CTLA4, five deaths among patients on anti-PD-1, and one patient on the combination.
Patients with IBD had a notably higher risk of anti-PD-1–induced colitis (19%; 95% CI, 7%-37%), compared with patients with other AIDs (3%; 95% CI, 0%-6%) and patients without AIDs (2%; 95% CI, 2%-3%). IBD patients were also more likely than all other groups on ICIs to stop treatment because of toxicity, leading the researchers to note that “close monitoring in patients with IBD is advised.”
Overall survival after diagnosis was similar in patients with AIDs (median, 13 months; 95% CI, 10-16 months) and without (median, 14 months; 95% CI, 13-15 months), as was the objective response rate to anti-CTLA4 treatment (10% vs. 16%), anti-PD-1 treatment (40% vs. 44%), and combination therapy (39% vs. 43%).
Study largely bypasses the effects of checkpoint inhibitors on RA patients
“For detail, you can’t look to this study,” Anne R. Bass, MD, of the division of rheumatology at the Hospital for Special Surgery in New York, said in an interview. “But for a big-picture look at ‘how safe are checkpoint inhibitors,’ I think it’s an important one.”
Dr. Bass noted that the investigators lumped certain elements together and bypassed others, including their focus on grade 3 or higher adverse events. That was a decision the authors themselves recognized as a potential limitation of their research.
“Understandably, they were worried about life-threatening adverse events, and that’s fine,” she said. But for patients with arthritis who flare, their events are usually grade 2 or even grade 1 and therefore not captured or analyzed in the study. “This does not really address the risk of flare in an RA patient.”
She also questioned their grouping of AIDs, with a bevy of rheumatic diseases categorized as one cluster and the “other” group being particularly broad in its inclusion of “all AIDs not listed” – though only eight patients were placed into that group.
That said, the researchers relied on an oncology database, not one aimed at AID or adverse events. “The numbers are so much bigger than any other study in this area that’s been done,” she said. “It’s both a strength and a weakness of this kind of database.”
Indeed, the authors considered their use of nationwide, population-based data from the DMTR a benefit, calling it “a strength of our approach.”
The DMTR was funded by a grant from the Netherlands Organization for Health Research and Development and sponsored by Bristol-Myers Squibb, Novartis, Roche Nederland, Merck Sharp & Dohme, and Pierre Fabre via the Dutch Institute for Clinical Auditing.
Patients with advanced melanoma and preexisting autoimmune diseases (AIDs) who were treated with immune checkpoint inhibitors (ICIs) responded well and did not suffer more grade 3 or higher immune-related adverse events than patients without an AID, a new study finds, although some concerns were raised regarding patients with inflammatory bowel disease (IBD).
“To our knowledge, this is the first study to bridge this knowledge gap by presenting ‘real-world’ data on the safety and efficacy of ICI on a national scale,” wrote Monique K. van der Kooij, MD, of Leiden (the Netherlands) University Medical Center and coauthors. The study was published online in Annals of Internal Medicine.
To investigate ICI use and response among this specific subset of melanoma patients, the researchers launched a nationwide cohort study set in the Netherlands. Data were gathered via the Dutch Melanoma Treatment Registry (DMTR), in which 4,367 patients with advanced melanoma were enrolled between July 2013 and July 2018.
Within that cohort, 415 (9.5%) had preexisting AIDs. Nearly 55% had rheumatologic AIDs (n = 227) – which included RA, systemic lupus erythematosus, scleroderma, sarcoidosis, and vasculitis – with the next most frequent being endocrine AID (n = 143) and IBD (n = 55). Patients with AID were older than patients without (67 vs. 63 years) and were more likely to be female (53% vs. 41%).
The ICIs used in the study included anti-CTLA4 (ipilimumab), anti–programmed death 1 (PD-1) (nivolumab or pembrolizumab), or a combination of nivolumab and ipilimumab. Of the patients with AID, 55% (n = 228) were treated with ICI, compared with 58% of patients without AID. A total of 87 AID patients were treated with anti-CTLA4, 187 received anti-PD-1, and 34 received the combination. The combination was not readily available in the Netherlands until 2017, the authors stated, acknowledging that it may be wise to revisit its effects in the coming years.
Incidence of immune-related adverse events
The incidence of immune-related adverse events (irAEs) grade 3 and above for patients with and without AID who were given anti-CTLA4 was 30%. The incidence rate of irAEs was also similar for patients with (17%; 95% confidence interval, 12%-23%) and without (13%; 95% CI, 12%-15%) AID on anti-PD-1. Patients with AIDs who took anti-PD-1 therapy discontinued it more often because of toxicity than did the patients without AIDs.
The combination group had irAE incidence rates of 44% (95% CI, 27%-62%) for patients with AID, compared with 48% (95% CI, 43%-53%) for patients without AIDs. Overall, no patients with AIDs on ICIs died of toxicity, compared with three deaths among patients without AID on anti-CTLA4, five deaths among patients on anti-PD-1, and one patient on the combination.
Patients with IBD had a notably higher risk of anti-PD-1–induced colitis (19%; 95% CI, 7%-37%), compared with patients with other AIDs (3%; 95% CI, 0%-6%) and patients without AIDs (2%; 95% CI, 2%-3%). IBD patients were also more likely than all other groups on ICIs to stop treatment because of toxicity, leading the researchers to note that “close monitoring in patients with IBD is advised.”
Overall survival after diagnosis was similar in patients with AIDs (median, 13 months; 95% CI, 10-16 months) and without (median, 14 months; 95% CI, 13-15 months), as was the objective response rate to anti-CTLA4 treatment (10% vs. 16%), anti-PD-1 treatment (40% vs. 44%), and combination therapy (39% vs. 43%).
Study largely bypasses the effects of checkpoint inhibitors on RA patients
“For detail, you can’t look to this study,” Anne R. Bass, MD, of the division of rheumatology at the Hospital for Special Surgery in New York, said in an interview. “But for a big-picture look at ‘how safe are checkpoint inhibitors,’ I think it’s an important one.”
Dr. Bass noted that the investigators lumped certain elements together and bypassed others, including their focus on grade 3 or higher adverse events. That was a decision the authors themselves recognized as a potential limitation of their research.
“Understandably, they were worried about life-threatening adverse events, and that’s fine,” she said. But for patients with arthritis who flare, their events are usually grade 2 or even grade 1 and therefore not captured or analyzed in the study. “This does not really address the risk of flare in an RA patient.”
She also questioned their grouping of AIDs, with a bevy of rheumatic diseases categorized as one cluster and the “other” group being particularly broad in its inclusion of “all AIDs not listed” – though only eight patients were placed into that group.
That said, the researchers relied on an oncology database, not one aimed at AID or adverse events. “The numbers are so much bigger than any other study in this area that’s been done,” she said. “It’s both a strength and a weakness of this kind of database.”
Indeed, the authors considered their use of nationwide, population-based data from the DMTR a benefit, calling it “a strength of our approach.”
The DMTR was funded by a grant from the Netherlands Organization for Health Research and Development and sponsored by Bristol-Myers Squibb, Novartis, Roche Nederland, Merck Sharp & Dohme, and Pierre Fabre via the Dutch Institute for Clinical Auditing.
FROM ANNALS OF INTERNAL MEDICINE