User login
Bathing now more widely accepted as an eczema treatment strategy
According to Noreen Heer Nicol, PhD, RN, FNP, frustration still exists for patients, families, and health care providers regarding the lack of consensus that routine bathing is good for patients with atopic dermatitis.
During the Revolutionizing Atopic Dermatitis symposium, she said that conflicting and vague guidelines currently exist on the topic.
“This stems from the fact that we just don’t have good studies,” said Dr. Nicol, associate dean and associate professor of nursing at the University of Colorado at Denver, Aurora. “Particularly, we don’t have randomized, controlled trials on the effects of water and bathing. It’s not just parents that are frustrated, but health care providers are as well.”
In an observational analysis, researchers evaluated results from three online surveys of dermatologists, allergists, and immunologists, and primary care physicians regarding routine bathing frequency recommendations for children with AD. It found that PCPs recommended daily bathing less than 50% of the time, while specialists recommended daily bathing more than 50% of the time.
“It seems like the PCPs have embraced that old dermatology notion when bathing was avoided in patients with AD,” Dr. Nicol said. “This lack of consensus on the basic daily care steps in AD management causes a great deal of confusion amongst patients, families, and young health care providers, in particular,” she added.
She believes that this goes back to a century-long debate about the pros and cons of bathing in AD. “We used to say that bathing will dry the skin out if you take a bath or a shower without immediately applying something like a good moisturizer. That’s where the 3-minute rule came along from the National Eczema Association, meaning that bathing hydrates the stratum corneum if you take a bath or a shower and you immediately apply that good moisturizer within 3 minutes to retain that hydration and keep the barrier intact and flexible.”
Dr. Nicol presented a stepwise management model that she has published many times over the years (see Pediatr Nursing 2020;46[2]:92-8 and J Allergy Clin Immunol Pract 2019;7[1]:1-16).
Step 1 consists of basic care, including skin hydration/bathing, application of a daily moisturizer, avoiding irritants, and identifying and addressing specific triggers. “This is the foundation for every step as you go forward,” she explained. Soak and seal has been a mainstay of treatment at National Jewish Health, she noted. “By that, I mean taking a soaking 10-15 minute bath in warm water daily. Gently pat away excess water. Immediately apply skin medications or moisturizer within 3 minutes. Using a gentle fragrance-free, dye-free cleanser to clean skin is also important. Avoid scrubbing.”
A review article on bathing and associated treatments in AD was published in 2017 and includes 144 references to bathing studies. A separate recommendation known as the “AD Yardstick” published by Dr. Nicol’s colleague at National Jewish Health, Mark Boguniewicz, MD, and coauthors, elaborated on the definition of basic skin care for nonlesional AD. Besides recommending the liberal and frequent application of moisturizers, it suggests management with warm baths or showers using nonsoap cleansers, usually once per day, followed by application of a moisturizer, even on clear areas.
“This is now what people are thinking as the basis of skin care in patients with AD,” Dr. Nicol said. “Warm baths and showers don’t look so controversial anymore. This model nicely lays out what we want people to remember. In the past, many times we just skipped that important step of telling people about bathing.”
In a small 2009 study, researchers conducted a quantitative assessment of combination bathing and moisturizing regimens on skin hydration in AD. They found that bathing followed by application of a moisturizer provides modest hydration benefits, though less than that of simply applying moisturizer alone. “That has not been the case for most of us who are bathing advocates,” Dr. Nicol said. “We believe that there is an additional hydration that’s gained from bathing and moisturizers done properly.”
In an earlier retrospective study of 28 patients referred to a tertiary care center for refractory chronic pruritic eruptions, researchers found that a plain-water 20-minute soak followed by smearing of midstrength corticosteroid ointment led to clearing or dramatic improvement of the lesions (Arch Dermatol 2005;14:1556-9). The authors recommended prospective studies to confirm the findings.
In a separate review of medical literature, researchers explored the role of frequent bathing in the treatment of pediatric AD (Ann Allergy Asthma Immunol 2016;117[1]:9-13). They found that the weight of evidence suggests that the frequent soak and smear bathing is preferred to infrequent bathing in the management of AD. Frequent bathing was defined as bathing at least once a day, while infrequent bathing was defined as bathing less than once a day.
“Bleach baths have received much attention in recent years, and have been endorsed by multiple AD guidelines, though not to the same degree as regular bathing,” Dr. Nicol said. “Right now, you can find almost as much literature for this practice as against it. The populations that seem to value from beach baths the most, however, are those with frequent infections, particularly those who are methicillin resistant. Most people recommend a maximum of two to three times per week but only with an active infection. Care must be taken to avoid additional drying or irritation of the skin from bleach.”
Many bleach bath recipes call for adding one-eighth to one-half of a cup of bleach to a tub full or water.
Dr. Nicol disclosed that she has served as an advisory board member for Eli Lilly.
According to Noreen Heer Nicol, PhD, RN, FNP, frustration still exists for patients, families, and health care providers regarding the lack of consensus that routine bathing is good for patients with atopic dermatitis.
During the Revolutionizing Atopic Dermatitis symposium, she said that conflicting and vague guidelines currently exist on the topic.
“This stems from the fact that we just don’t have good studies,” said Dr. Nicol, associate dean and associate professor of nursing at the University of Colorado at Denver, Aurora. “Particularly, we don’t have randomized, controlled trials on the effects of water and bathing. It’s not just parents that are frustrated, but health care providers are as well.”
In an observational analysis, researchers evaluated results from three online surveys of dermatologists, allergists, and immunologists, and primary care physicians regarding routine bathing frequency recommendations for children with AD. It found that PCPs recommended daily bathing less than 50% of the time, while specialists recommended daily bathing more than 50% of the time.
“It seems like the PCPs have embraced that old dermatology notion when bathing was avoided in patients with AD,” Dr. Nicol said. “This lack of consensus on the basic daily care steps in AD management causes a great deal of confusion amongst patients, families, and young health care providers, in particular,” she added.
She believes that this goes back to a century-long debate about the pros and cons of bathing in AD. “We used to say that bathing will dry the skin out if you take a bath or a shower without immediately applying something like a good moisturizer. That’s where the 3-minute rule came along from the National Eczema Association, meaning that bathing hydrates the stratum corneum if you take a bath or a shower and you immediately apply that good moisturizer within 3 minutes to retain that hydration and keep the barrier intact and flexible.”
Dr. Nicol presented a stepwise management model that she has published many times over the years (see Pediatr Nursing 2020;46[2]:92-8 and J Allergy Clin Immunol Pract 2019;7[1]:1-16).
Step 1 consists of basic care, including skin hydration/bathing, application of a daily moisturizer, avoiding irritants, and identifying and addressing specific triggers. “This is the foundation for every step as you go forward,” she explained. Soak and seal has been a mainstay of treatment at National Jewish Health, she noted. “By that, I mean taking a soaking 10-15 minute bath in warm water daily. Gently pat away excess water. Immediately apply skin medications or moisturizer within 3 minutes. Using a gentle fragrance-free, dye-free cleanser to clean skin is also important. Avoid scrubbing.”
A review article on bathing and associated treatments in AD was published in 2017 and includes 144 references to bathing studies. A separate recommendation known as the “AD Yardstick” published by Dr. Nicol’s colleague at National Jewish Health, Mark Boguniewicz, MD, and coauthors, elaborated on the definition of basic skin care for nonlesional AD. Besides recommending the liberal and frequent application of moisturizers, it suggests management with warm baths or showers using nonsoap cleansers, usually once per day, followed by application of a moisturizer, even on clear areas.
“This is now what people are thinking as the basis of skin care in patients with AD,” Dr. Nicol said. “Warm baths and showers don’t look so controversial anymore. This model nicely lays out what we want people to remember. In the past, many times we just skipped that important step of telling people about bathing.”
In a small 2009 study, researchers conducted a quantitative assessment of combination bathing and moisturizing regimens on skin hydration in AD. They found that bathing followed by application of a moisturizer provides modest hydration benefits, though less than that of simply applying moisturizer alone. “That has not been the case for most of us who are bathing advocates,” Dr. Nicol said. “We believe that there is an additional hydration that’s gained from bathing and moisturizers done properly.”
In an earlier retrospective study of 28 patients referred to a tertiary care center for refractory chronic pruritic eruptions, researchers found that a plain-water 20-minute soak followed by smearing of midstrength corticosteroid ointment led to clearing or dramatic improvement of the lesions (Arch Dermatol 2005;14:1556-9). The authors recommended prospective studies to confirm the findings.
In a separate review of medical literature, researchers explored the role of frequent bathing in the treatment of pediatric AD (Ann Allergy Asthma Immunol 2016;117[1]:9-13). They found that the weight of evidence suggests that the frequent soak and smear bathing is preferred to infrequent bathing in the management of AD. Frequent bathing was defined as bathing at least once a day, while infrequent bathing was defined as bathing less than once a day.
“Bleach baths have received much attention in recent years, and have been endorsed by multiple AD guidelines, though not to the same degree as regular bathing,” Dr. Nicol said. “Right now, you can find almost as much literature for this practice as against it. The populations that seem to value from beach baths the most, however, are those with frequent infections, particularly those who are methicillin resistant. Most people recommend a maximum of two to three times per week but only with an active infection. Care must be taken to avoid additional drying or irritation of the skin from bleach.”
Many bleach bath recipes call for adding one-eighth to one-half of a cup of bleach to a tub full or water.
Dr. Nicol disclosed that she has served as an advisory board member for Eli Lilly.
According to Noreen Heer Nicol, PhD, RN, FNP, frustration still exists for patients, families, and health care providers regarding the lack of consensus that routine bathing is good for patients with atopic dermatitis.
During the Revolutionizing Atopic Dermatitis symposium, she said that conflicting and vague guidelines currently exist on the topic.
“This stems from the fact that we just don’t have good studies,” said Dr. Nicol, associate dean and associate professor of nursing at the University of Colorado at Denver, Aurora. “Particularly, we don’t have randomized, controlled trials on the effects of water and bathing. It’s not just parents that are frustrated, but health care providers are as well.”
In an observational analysis, researchers evaluated results from three online surveys of dermatologists, allergists, and immunologists, and primary care physicians regarding routine bathing frequency recommendations for children with AD. It found that PCPs recommended daily bathing less than 50% of the time, while specialists recommended daily bathing more than 50% of the time.
“It seems like the PCPs have embraced that old dermatology notion when bathing was avoided in patients with AD,” Dr. Nicol said. “This lack of consensus on the basic daily care steps in AD management causes a great deal of confusion amongst patients, families, and young health care providers, in particular,” she added.
She believes that this goes back to a century-long debate about the pros and cons of bathing in AD. “We used to say that bathing will dry the skin out if you take a bath or a shower without immediately applying something like a good moisturizer. That’s where the 3-minute rule came along from the National Eczema Association, meaning that bathing hydrates the stratum corneum if you take a bath or a shower and you immediately apply that good moisturizer within 3 minutes to retain that hydration and keep the barrier intact and flexible.”
Dr. Nicol presented a stepwise management model that she has published many times over the years (see Pediatr Nursing 2020;46[2]:92-8 and J Allergy Clin Immunol Pract 2019;7[1]:1-16).
Step 1 consists of basic care, including skin hydration/bathing, application of a daily moisturizer, avoiding irritants, and identifying and addressing specific triggers. “This is the foundation for every step as you go forward,” she explained. Soak and seal has been a mainstay of treatment at National Jewish Health, she noted. “By that, I mean taking a soaking 10-15 minute bath in warm water daily. Gently pat away excess water. Immediately apply skin medications or moisturizer within 3 minutes. Using a gentle fragrance-free, dye-free cleanser to clean skin is also important. Avoid scrubbing.”
A review article on bathing and associated treatments in AD was published in 2017 and includes 144 references to bathing studies. A separate recommendation known as the “AD Yardstick” published by Dr. Nicol’s colleague at National Jewish Health, Mark Boguniewicz, MD, and coauthors, elaborated on the definition of basic skin care for nonlesional AD. Besides recommending the liberal and frequent application of moisturizers, it suggests management with warm baths or showers using nonsoap cleansers, usually once per day, followed by application of a moisturizer, even on clear areas.
“This is now what people are thinking as the basis of skin care in patients with AD,” Dr. Nicol said. “Warm baths and showers don’t look so controversial anymore. This model nicely lays out what we want people to remember. In the past, many times we just skipped that important step of telling people about bathing.”
In a small 2009 study, researchers conducted a quantitative assessment of combination bathing and moisturizing regimens on skin hydration in AD. They found that bathing followed by application of a moisturizer provides modest hydration benefits, though less than that of simply applying moisturizer alone. “That has not been the case for most of us who are bathing advocates,” Dr. Nicol said. “We believe that there is an additional hydration that’s gained from bathing and moisturizers done properly.”
In an earlier retrospective study of 28 patients referred to a tertiary care center for refractory chronic pruritic eruptions, researchers found that a plain-water 20-minute soak followed by smearing of midstrength corticosteroid ointment led to clearing or dramatic improvement of the lesions (Arch Dermatol 2005;14:1556-9). The authors recommended prospective studies to confirm the findings.
In a separate review of medical literature, researchers explored the role of frequent bathing in the treatment of pediatric AD (Ann Allergy Asthma Immunol 2016;117[1]:9-13). They found that the weight of evidence suggests that the frequent soak and smear bathing is preferred to infrequent bathing in the management of AD. Frequent bathing was defined as bathing at least once a day, while infrequent bathing was defined as bathing less than once a day.
“Bleach baths have received much attention in recent years, and have been endorsed by multiple AD guidelines, though not to the same degree as regular bathing,” Dr. Nicol said. “Right now, you can find almost as much literature for this practice as against it. The populations that seem to value from beach baths the most, however, are those with frequent infections, particularly those who are methicillin resistant. Most people recommend a maximum of two to three times per week but only with an active infection. Care must be taken to avoid additional drying or irritation of the skin from bleach.”
Many bleach bath recipes call for adding one-eighth to one-half of a cup of bleach to a tub full or water.
Dr. Nicol disclosed that she has served as an advisory board member for Eli Lilly.
FROM REVOLUTIONIZING AD 2020
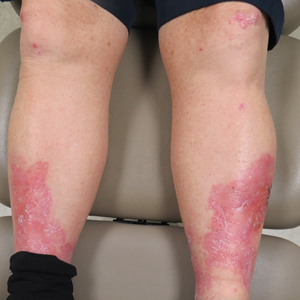
Erythema, Blisters, and Scars on the Elbows, Knees, and Legs
The Diagnosis: Epidermolysis Bullosa Acquisita
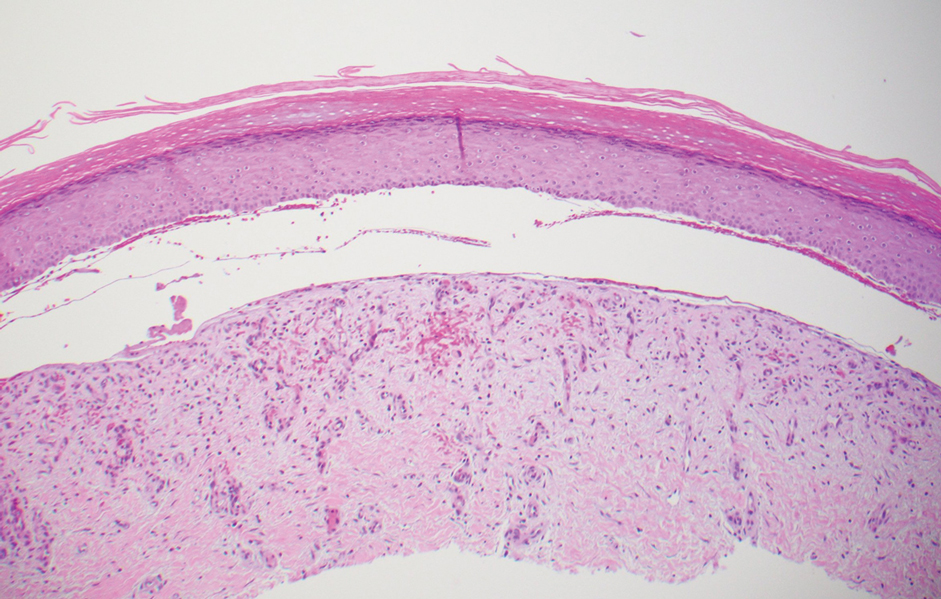
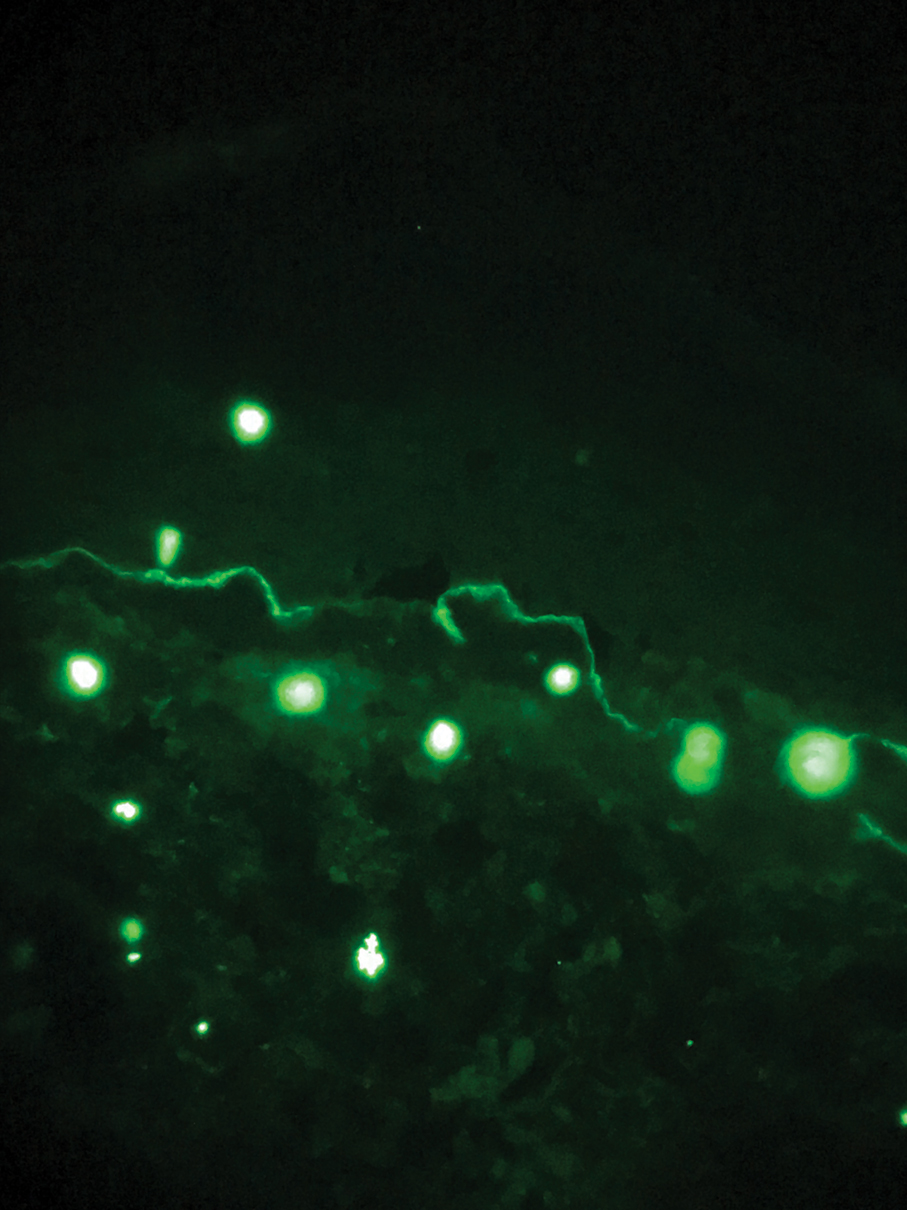
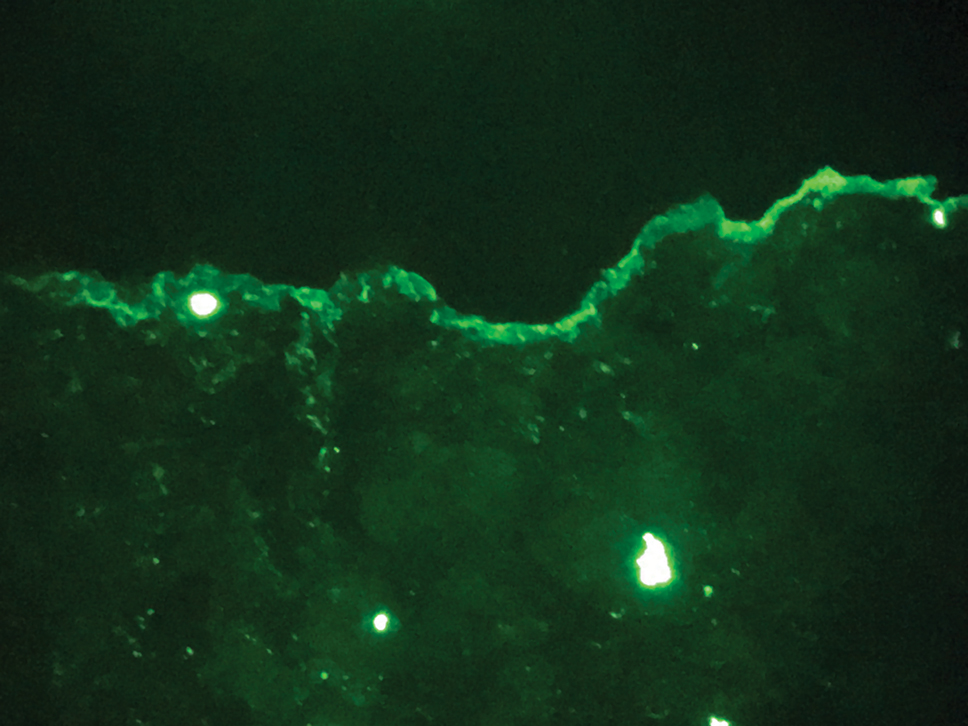
The diagnosis of epidermolysis bullosa acquisita (EBA) was made based on the clinical and pathologic findings. A blistering disorder that resolves with milia is characteristic of EBA. Hematoxylin and eosin staining demonstrated a pauci-inflammatory separation between the epidermis and dermis (Figure 1). Direct immunofluorescence studies showed linear IgG deposition along the basement membrane zone while C3 was negative (Figure 2). Salt-split skin was essential, as it revealed IgG deposition to the floor of the split (Figure 3), a pattern seen in EBA and not bullous pemphigoid (BP).1
Epidermolysis bullosa acquisita is an acquired autoimmune bullous disorder that results from antibodies to type VII collagen, an anchoring fibril that attaches the lamina densa to the dermis. The epidemiology and etiology of the trigger that leads to antibody production are not well known, but an association between EBA and inflammatory bowel disease has been described.2 Although this disease may present in childhood, EBA most commonly is a disorder seen in adults and the elderly. A classic noninflammatory mechanobullous form as well as an inflammatory BP-like form are the most commonly encountered presentations. Light microscopy demonstrates subepidermal cleavage without acantholysis. In the inflammatory BP-like subtype, an inflammatory infiltrate may be present. Direct immunofluorescence is remarkable for a linear band of IgG deposits along the basement membrane zone, with or without C3 deposition in a similar pattern.1
Bullous pemphigoid is within the differential of EBA. It can be difficult to differentiate clinically, especially when a patient has the BP-like variant of EBA because, as the name implies, it mimics BP. Patients with BP often will report a pruritic patch that will then develop into an urticarial plaque. Scarring and milia rarely are seen in BP but can be observed in the multiple presentations of EBA. Hematoxylin and eosin staining and direct immunofluorescence may be almost identical, and differentiating between the 2 disorders can be a challenge. Immunodeposition in EBA occurs in a U-shaped, serrated pattern, while the pattern in BP is N-shaped and serrated.3 Although the U-shaped, serrated pattern is relatively specific, it is not always easy to interpret and requires a high-quality biopsy specimen, which can be difficult to discern with certainty in suboptimal preparations. Another way to differentiate between the 2 entities is to utilize the salt-split skin technique, as performed in our patient. With salt-split skin, the biopsy is placed into a solution of 1 mol/L sodium chloride and incubated at 4 °C (39 °F) for 18 to 24 hours. A blister is then produced at the level of the lamina lucida, which allows for the staining of immunoreactants to occur either above or below that split (commonly referred to as staining on the roof or floor of the blister cavity). With EBA, there is immunoreactant deposition on the floor of the blister, while the opposite occurs in BP.4
Epidermolysis bullosa simplex is the most common type of epidermolysis bullosa, with keratin genes KRT5 and KRT14 as frequent mutations. Patients develop blisters, vesicles, bullae, and milia on traumatized areas of the body such as the hands, elbows, knees, and feet. This disease presents early in childhood. Histology exhibits a cell-poor subepidermal blister.5 With porphyria cutanea tarda, reduced activity of uroporphyrinogen decarboxylase, a major enzyme in the heme synthesis pathway, leads to blisters with erosions and milia on sun-exposed areas of the body. Histologic evaluation reveals a subepidermal pauci-inflammatory vesicle with festooning of the dermal papillae and amphophilic basement membrane within the epidermis. Direct immunofluorescence of porphyria cutanea tarda demonstrates IgM and C3 in the vessels.6 Sweet syndrome is a neutrophilic dermatosis that presents as erythematous, edematous, hot, and tender plaques along with fever and leukocytosis. It is associated with myeloproliferative disorders. Biopsy demonstrates papillary dermal edema along with diffuse neutrophilic infiltrate.7
Numerous medications have been recommended for the treatment of EBA, ranging from steroids to steroid-sparing drugs such as colchicine and dapsone.8,9 Our patient was educated on physical precautions and was started on dapsone alone due to comorbid diabetes mellitus and renal disease. Within a few weeks of initiating dapsone, he observed a reduction in erythema, and within months he experienced a decrease in blister eruption frequency.
- Vorobyev A, Ludwig RJ, Schmidt E. Clinical features and diagnosis of epidermolysis bullosa acquisita. Expert Rev Clin Immunol. 2017;13:157-169.
- Reddy H, Shipman AR, Wojnarowska F. Epidermolysis bullosa acquisita and inflammatory bowel disease: a review of the literature. Clin Exp Dermatol. 2013;38:225-230.
- Vodegel RM, Jonkman MF, Pas HH, et al. U-serrated immunodeposition pattern differentiates type VII collagen targeting bullous diseases from other subepidermal bullous autoimmune diseases. Br J Dermatol. 2004;151:112-118.
- Gardner KM, Crawford RI. Distinguishing epidermolysis bullosa acquisita from bullous pemphigoid without direct immunofluorescence. J Cutan Med Surg. 2018;22:22-24.
- Sprecher E. Epidermolysis bullosa simplex. Dermatol Clin. 2010;28:23-32.
- Maynard B, Peters MS. Histologic and immunofluorescence study of cutaneous porphyrias. J Cutan Pathol. 1992;19:40-47.
- Nelson CA, Stephen S, Ashchyan HJ, et al. Neutrophilic dermatoses: pathogenesis, Sweet syndrome, neutrophilic eccrine hidradenitis, and Behçet disease. J Am Acad Dermatol. 2018:79:987-1006.
- Kirtschig G, Murrell D, Wojnarowska F, et al. Interventions for mucous membrane pemphigoid and epidermolysis bullosa acquisita. Cochrane Database Syst Rev. 2003;1:CD004056
- Gürcan HM, Ahmed AR. Current concepts in the treatment of epidermolysis bullosa acquisita. Expert Opin Pharmacother. 2011;12:1259-1268.
The Diagnosis: Epidermolysis Bullosa Acquisita
The diagnosis of epidermolysis bullosa acquisita (EBA) was made based on the clinical and pathologic findings. A blistering disorder that resolves with milia is characteristic of EBA. Hematoxylin and eosin staining demonstrated a pauci-inflammatory separation between the epidermis and dermis (Figure 1). Direct immunofluorescence studies showed linear IgG deposition along the basement membrane zone while C3 was negative (Figure 2). Salt-split skin was essential, as it revealed IgG deposition to the floor of the split (Figure 3), a pattern seen in EBA and not bullous pemphigoid (BP).1
Epidermolysis bullosa acquisita is an acquired autoimmune bullous disorder that results from antibodies to type VII collagen, an anchoring fibril that attaches the lamina densa to the dermis. The epidemiology and etiology of the trigger that leads to antibody production are not well known, but an association between EBA and inflammatory bowel disease has been described.2 Although this disease may present in childhood, EBA most commonly is a disorder seen in adults and the elderly. A classic noninflammatory mechanobullous form as well as an inflammatory BP-like form are the most commonly encountered presentations. Light microscopy demonstrates subepidermal cleavage without acantholysis. In the inflammatory BP-like subtype, an inflammatory infiltrate may be present. Direct immunofluorescence is remarkable for a linear band of IgG deposits along the basement membrane zone, with or without C3 deposition in a similar pattern.1
Bullous pemphigoid is within the differential of EBA. It can be difficult to differentiate clinically, especially when a patient has the BP-like variant of EBA because, as the name implies, it mimics BP. Patients with BP often will report a pruritic patch that will then develop into an urticarial plaque. Scarring and milia rarely are seen in BP but can be observed in the multiple presentations of EBA. Hematoxylin and eosin staining and direct immunofluorescence may be almost identical, and differentiating between the 2 disorders can be a challenge. Immunodeposition in EBA occurs in a U-shaped, serrated pattern, while the pattern in BP is N-shaped and serrated.3 Although the U-shaped, serrated pattern is relatively specific, it is not always easy to interpret and requires a high-quality biopsy specimen, which can be difficult to discern with certainty in suboptimal preparations. Another way to differentiate between the 2 entities is to utilize the salt-split skin technique, as performed in our patient. With salt-split skin, the biopsy is placed into a solution of 1 mol/L sodium chloride and incubated at 4 °C (39 °F) for 18 to 24 hours. A blister is then produced at the level of the lamina lucida, which allows for the staining of immunoreactants to occur either above or below that split (commonly referred to as staining on the roof or floor of the blister cavity). With EBA, there is immunoreactant deposition on the floor of the blister, while the opposite occurs in BP.4
Epidermolysis bullosa simplex is the most common type of epidermolysis bullosa, with keratin genes KRT5 and KRT14 as frequent mutations. Patients develop blisters, vesicles, bullae, and milia on traumatized areas of the body such as the hands, elbows, knees, and feet. This disease presents early in childhood. Histology exhibits a cell-poor subepidermal blister.5 With porphyria cutanea tarda, reduced activity of uroporphyrinogen decarboxylase, a major enzyme in the heme synthesis pathway, leads to blisters with erosions and milia on sun-exposed areas of the body. Histologic evaluation reveals a subepidermal pauci-inflammatory vesicle with festooning of the dermal papillae and amphophilic basement membrane within the epidermis. Direct immunofluorescence of porphyria cutanea tarda demonstrates IgM and C3 in the vessels.6 Sweet syndrome is a neutrophilic dermatosis that presents as erythematous, edematous, hot, and tender plaques along with fever and leukocytosis. It is associated with myeloproliferative disorders. Biopsy demonstrates papillary dermal edema along with diffuse neutrophilic infiltrate.7
Numerous medications have been recommended for the treatment of EBA, ranging from steroids to steroid-sparing drugs such as colchicine and dapsone.8,9 Our patient was educated on physical precautions and was started on dapsone alone due to comorbid diabetes mellitus and renal disease. Within a few weeks of initiating dapsone, he observed a reduction in erythema, and within months he experienced a decrease in blister eruption frequency.
The Diagnosis: Epidermolysis Bullosa Acquisita
The diagnosis of epidermolysis bullosa acquisita (EBA) was made based on the clinical and pathologic findings. A blistering disorder that resolves with milia is characteristic of EBA. Hematoxylin and eosin staining demonstrated a pauci-inflammatory separation between the epidermis and dermis (Figure 1). Direct immunofluorescence studies showed linear IgG deposition along the basement membrane zone while C3 was negative (Figure 2). Salt-split skin was essential, as it revealed IgG deposition to the floor of the split (Figure 3), a pattern seen in EBA and not bullous pemphigoid (BP).1
Epidermolysis bullosa acquisita is an acquired autoimmune bullous disorder that results from antibodies to type VII collagen, an anchoring fibril that attaches the lamina densa to the dermis. The epidemiology and etiology of the trigger that leads to antibody production are not well known, but an association between EBA and inflammatory bowel disease has been described.2 Although this disease may present in childhood, EBA most commonly is a disorder seen in adults and the elderly. A classic noninflammatory mechanobullous form as well as an inflammatory BP-like form are the most commonly encountered presentations. Light microscopy demonstrates subepidermal cleavage without acantholysis. In the inflammatory BP-like subtype, an inflammatory infiltrate may be present. Direct immunofluorescence is remarkable for a linear band of IgG deposits along the basement membrane zone, with or without C3 deposition in a similar pattern.1
Bullous pemphigoid is within the differential of EBA. It can be difficult to differentiate clinically, especially when a patient has the BP-like variant of EBA because, as the name implies, it mimics BP. Patients with BP often will report a pruritic patch that will then develop into an urticarial plaque. Scarring and milia rarely are seen in BP but can be observed in the multiple presentations of EBA. Hematoxylin and eosin staining and direct immunofluorescence may be almost identical, and differentiating between the 2 disorders can be a challenge. Immunodeposition in EBA occurs in a U-shaped, serrated pattern, while the pattern in BP is N-shaped and serrated.3 Although the U-shaped, serrated pattern is relatively specific, it is not always easy to interpret and requires a high-quality biopsy specimen, which can be difficult to discern with certainty in suboptimal preparations. Another way to differentiate between the 2 entities is to utilize the salt-split skin technique, as performed in our patient. With salt-split skin, the biopsy is placed into a solution of 1 mol/L sodium chloride and incubated at 4 °C (39 °F) for 18 to 24 hours. A blister is then produced at the level of the lamina lucida, which allows for the staining of immunoreactants to occur either above or below that split (commonly referred to as staining on the roof or floor of the blister cavity). With EBA, there is immunoreactant deposition on the floor of the blister, while the opposite occurs in BP.4
Epidermolysis bullosa simplex is the most common type of epidermolysis bullosa, with keratin genes KRT5 and KRT14 as frequent mutations. Patients develop blisters, vesicles, bullae, and milia on traumatized areas of the body such as the hands, elbows, knees, and feet. This disease presents early in childhood. Histology exhibits a cell-poor subepidermal blister.5 With porphyria cutanea tarda, reduced activity of uroporphyrinogen decarboxylase, a major enzyme in the heme synthesis pathway, leads to blisters with erosions and milia on sun-exposed areas of the body. Histologic evaluation reveals a subepidermal pauci-inflammatory vesicle with festooning of the dermal papillae and amphophilic basement membrane within the epidermis. Direct immunofluorescence of porphyria cutanea tarda demonstrates IgM and C3 in the vessels.6 Sweet syndrome is a neutrophilic dermatosis that presents as erythematous, edematous, hot, and tender plaques along with fever and leukocytosis. It is associated with myeloproliferative disorders. Biopsy demonstrates papillary dermal edema along with diffuse neutrophilic infiltrate.7
Numerous medications have been recommended for the treatment of EBA, ranging from steroids to steroid-sparing drugs such as colchicine and dapsone.8,9 Our patient was educated on physical precautions and was started on dapsone alone due to comorbid diabetes mellitus and renal disease. Within a few weeks of initiating dapsone, he observed a reduction in erythema, and within months he experienced a decrease in blister eruption frequency.
- Vorobyev A, Ludwig RJ, Schmidt E. Clinical features and diagnosis of epidermolysis bullosa acquisita. Expert Rev Clin Immunol. 2017;13:157-169.
- Reddy H, Shipman AR, Wojnarowska F. Epidermolysis bullosa acquisita and inflammatory bowel disease: a review of the literature. Clin Exp Dermatol. 2013;38:225-230.
- Vodegel RM, Jonkman MF, Pas HH, et al. U-serrated immunodeposition pattern differentiates type VII collagen targeting bullous diseases from other subepidermal bullous autoimmune diseases. Br J Dermatol. 2004;151:112-118.
- Gardner KM, Crawford RI. Distinguishing epidermolysis bullosa acquisita from bullous pemphigoid without direct immunofluorescence. J Cutan Med Surg. 2018;22:22-24.
- Sprecher E. Epidermolysis bullosa simplex. Dermatol Clin. 2010;28:23-32.
- Maynard B, Peters MS. Histologic and immunofluorescence study of cutaneous porphyrias. J Cutan Pathol. 1992;19:40-47.
- Nelson CA, Stephen S, Ashchyan HJ, et al. Neutrophilic dermatoses: pathogenesis, Sweet syndrome, neutrophilic eccrine hidradenitis, and Behçet disease. J Am Acad Dermatol. 2018:79:987-1006.
- Kirtschig G, Murrell D, Wojnarowska F, et al. Interventions for mucous membrane pemphigoid and epidermolysis bullosa acquisita. Cochrane Database Syst Rev. 2003;1:CD004056
- Gürcan HM, Ahmed AR. Current concepts in the treatment of epidermolysis bullosa acquisita. Expert Opin Pharmacother. 2011;12:1259-1268.
- Vorobyev A, Ludwig RJ, Schmidt E. Clinical features and diagnosis of epidermolysis bullosa acquisita. Expert Rev Clin Immunol. 2017;13:157-169.
- Reddy H, Shipman AR, Wojnarowska F. Epidermolysis bullosa acquisita and inflammatory bowel disease: a review of the literature. Clin Exp Dermatol. 2013;38:225-230.
- Vodegel RM, Jonkman MF, Pas HH, et al. U-serrated immunodeposition pattern differentiates type VII collagen targeting bullous diseases from other subepidermal bullous autoimmune diseases. Br J Dermatol. 2004;151:112-118.
- Gardner KM, Crawford RI. Distinguishing epidermolysis bullosa acquisita from bullous pemphigoid without direct immunofluorescence. J Cutan Med Surg. 2018;22:22-24.
- Sprecher E. Epidermolysis bullosa simplex. Dermatol Clin. 2010;28:23-32.
- Maynard B, Peters MS. Histologic and immunofluorescence study of cutaneous porphyrias. J Cutan Pathol. 1992;19:40-47.
- Nelson CA, Stephen S, Ashchyan HJ, et al. Neutrophilic dermatoses: pathogenesis, Sweet syndrome, neutrophilic eccrine hidradenitis, and Behçet disease. J Am Acad Dermatol. 2018:79:987-1006.
- Kirtschig G, Murrell D, Wojnarowska F, et al. Interventions for mucous membrane pemphigoid and epidermolysis bullosa acquisita. Cochrane Database Syst Rev. 2003;1:CD004056
- Gürcan HM, Ahmed AR. Current concepts in the treatment of epidermolysis bullosa acquisita. Expert Opin Pharmacother. 2011;12:1259-1268.
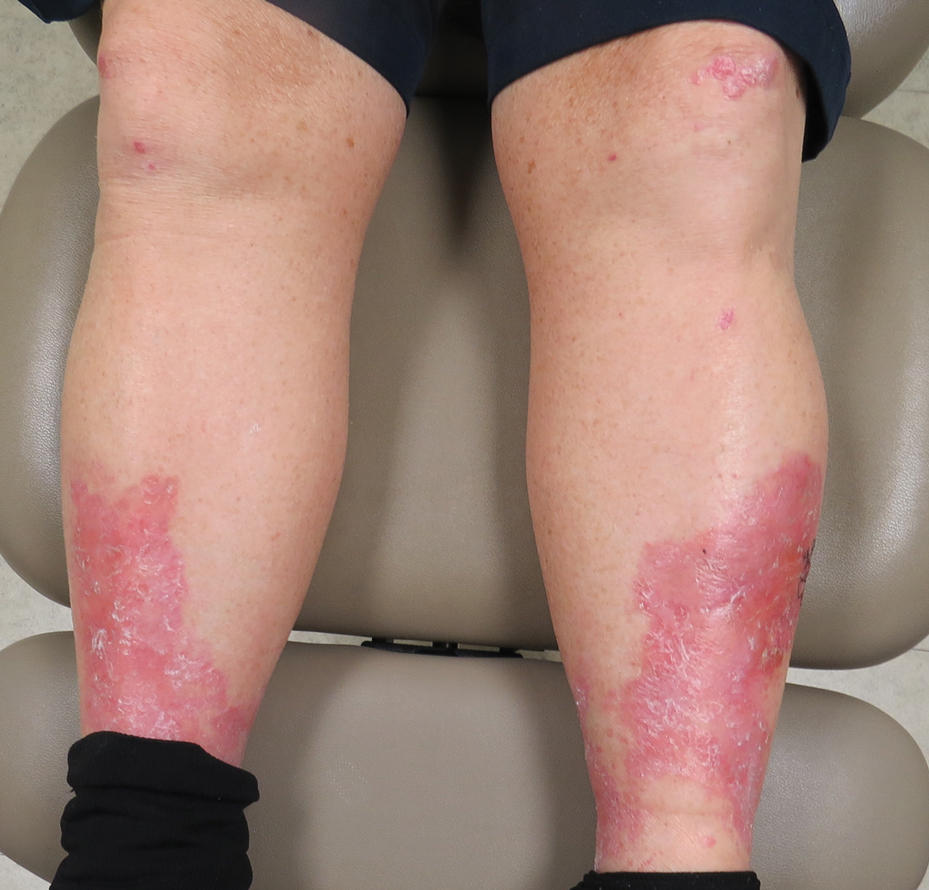
A 69-year-old man presented with an asymptomatic rash on the extensor surfaces of 2 years' duration. He reported recurrent blisters that would then scar over. The lesions did not occur in relation to any known trauma. The patient's medical history revealed dialysis-dependent end-stage renal disease secondary to type 2 diabetes mellitus. His medications were noncontributory, and there was no family history of blistering disorders. He had tried triamcinolone cream without any improvement. Physical examination was remarkable for erythematous blisters and bullae with scales and milia on the elbows, knees, and lower legs. The oral mucosa was unremarkable. Shave biopsies of the skin for direct immunofluorescence and salt-split skin studies were obtained.
Hospitalist movers and shakers: January 2021
Daniel Steinberg, MD, SFHM, recently was among 10 medical educators across the county to receive the Accreditation Council for Graduate Medical Education 2021 Parker J. Palmer Courage to Teach Award. Considered the most prestigious award given to graduate medical education program directors, it “recognizes program directors who have fostered innovation and improvement in their residency/fellowship program and served as exemplary role models for residents and fellows.”
Dr. Steinberg was program director for internal medicine residency at Mount Sinai Beth Israel, New York, for 11 years (2009-20) before becoming associate dean for quality and patient safety in graduate medical education in September. He is a professor of medicine and medical education at Icahn School of Medicine at Mount Sinai, New York.
Dr. Steinberg also is a leader within SHM, serving on the education, physicians-in-training, and annual conference committees. He is the course director for SHM Converge 2021.
Ann Sheehy, MD, SFHM, was honored in a virtual ceremony in December 2020 by the University of Wisconsin celebrating Physician Excellence Award winners. She was presented with the Physician Excellence Leadership Award.
Dr. Sheehy is division chief of the division of hospital medicine at the University of Wisconsin–Madison, and chair of the SHM Public Policy Committee.
Donald Schmidt, MD, has been named chief medical officer and vice president of medical affairs at Madonna Rehabilitation Hospitals in Omaha and Lincoln, Neb. He will replace Thomas Stalder, MD, who is retiring. Dr. Schmidt brings 20 years of experience to Madonna Rehabilitation Hospitals, including his most recent post as a hospitalist and medical director of the hospitalist program at Catholic Health Initiatives Health St. Elizabeth (Lincoln, Neb.).
Dr. Schmidt currently serves on the board of directors for OneHealth Nebraska, an independent physicians association.
Ezinne Nwude, MD, recently was presented with the SCP Health Excellence in Leadership Award during the organization’s Medical Leadership Conference. Dr. Nwude is chief of staff and hospitalist at the Medical Center of South Arkansas, El Dorado.
SCP Health coordinates staffing for more than 7,500 providers covering 30 states and is one of the nation’s largest clinical practice management companies. More than 420 medical leaders nationwide were eligible for the award. Dr. Nwude has focused on positive culture and health education since her start at MSCA in 2014. She has been chief of staff since October 2018.
RWJ Barnabas Health (West Orange, N.J.) recently named two new health system leaders from among its hospital medicine ranks, as Christopher Freer, MD, was tabbed as senior vice president for emergency and hospital medicine, and Maninder “Dolly” Abraham, MD, was picked as chief of hospital medicine. The moves were made as RWJBH takes over as the direct employer for Envision Physician Services in Nashville, Tenn.
Dr. Freer was elevated to his new role after spending the past 5 years as RWJBH’s system director for emergency services. He has nearly 3 decades of experience in hospital medicine.
Dr. Abraham comes to his new position after directing the hospitalist program at Saint Barnabas and serving as regional medical director with Envision.
Newman Regional Health (Emporia, Kan.) recently established a partnership with FreeState Healthcare (Wichita, Kan.). FreeState will be responsible for providing hospitalist services to adult inpatients and observation patients at Newman Regional Health during overnights.
Daniel Steinberg, MD, SFHM, recently was among 10 medical educators across the county to receive the Accreditation Council for Graduate Medical Education 2021 Parker J. Palmer Courage to Teach Award. Considered the most prestigious award given to graduate medical education program directors, it “recognizes program directors who have fostered innovation and improvement in their residency/fellowship program and served as exemplary role models for residents and fellows.”
Dr. Steinberg was program director for internal medicine residency at Mount Sinai Beth Israel, New York, for 11 years (2009-20) before becoming associate dean for quality and patient safety in graduate medical education in September. He is a professor of medicine and medical education at Icahn School of Medicine at Mount Sinai, New York.
Dr. Steinberg also is a leader within SHM, serving on the education, physicians-in-training, and annual conference committees. He is the course director for SHM Converge 2021.
Ann Sheehy, MD, SFHM, was honored in a virtual ceremony in December 2020 by the University of Wisconsin celebrating Physician Excellence Award winners. She was presented with the Physician Excellence Leadership Award.
Dr. Sheehy is division chief of the division of hospital medicine at the University of Wisconsin–Madison, and chair of the SHM Public Policy Committee.
Donald Schmidt, MD, has been named chief medical officer and vice president of medical affairs at Madonna Rehabilitation Hospitals in Omaha and Lincoln, Neb. He will replace Thomas Stalder, MD, who is retiring. Dr. Schmidt brings 20 years of experience to Madonna Rehabilitation Hospitals, including his most recent post as a hospitalist and medical director of the hospitalist program at Catholic Health Initiatives Health St. Elizabeth (Lincoln, Neb.).
Dr. Schmidt currently serves on the board of directors for OneHealth Nebraska, an independent physicians association.
Ezinne Nwude, MD, recently was presented with the SCP Health Excellence in Leadership Award during the organization’s Medical Leadership Conference. Dr. Nwude is chief of staff and hospitalist at the Medical Center of South Arkansas, El Dorado.
SCP Health coordinates staffing for more than 7,500 providers covering 30 states and is one of the nation’s largest clinical practice management companies. More than 420 medical leaders nationwide were eligible for the award. Dr. Nwude has focused on positive culture and health education since her start at MSCA in 2014. She has been chief of staff since October 2018.
RWJ Barnabas Health (West Orange, N.J.) recently named two new health system leaders from among its hospital medicine ranks, as Christopher Freer, MD, was tabbed as senior vice president for emergency and hospital medicine, and Maninder “Dolly” Abraham, MD, was picked as chief of hospital medicine. The moves were made as RWJBH takes over as the direct employer for Envision Physician Services in Nashville, Tenn.
Dr. Freer was elevated to his new role after spending the past 5 years as RWJBH’s system director for emergency services. He has nearly 3 decades of experience in hospital medicine.
Dr. Abraham comes to his new position after directing the hospitalist program at Saint Barnabas and serving as regional medical director with Envision.
Newman Regional Health (Emporia, Kan.) recently established a partnership with FreeState Healthcare (Wichita, Kan.). FreeState will be responsible for providing hospitalist services to adult inpatients and observation patients at Newman Regional Health during overnights.
Daniel Steinberg, MD, SFHM, recently was among 10 medical educators across the county to receive the Accreditation Council for Graduate Medical Education 2021 Parker J. Palmer Courage to Teach Award. Considered the most prestigious award given to graduate medical education program directors, it “recognizes program directors who have fostered innovation and improvement in their residency/fellowship program and served as exemplary role models for residents and fellows.”
Dr. Steinberg was program director for internal medicine residency at Mount Sinai Beth Israel, New York, for 11 years (2009-20) before becoming associate dean for quality and patient safety in graduate medical education in September. He is a professor of medicine and medical education at Icahn School of Medicine at Mount Sinai, New York.
Dr. Steinberg also is a leader within SHM, serving on the education, physicians-in-training, and annual conference committees. He is the course director for SHM Converge 2021.
Ann Sheehy, MD, SFHM, was honored in a virtual ceremony in December 2020 by the University of Wisconsin celebrating Physician Excellence Award winners. She was presented with the Physician Excellence Leadership Award.
Dr. Sheehy is division chief of the division of hospital medicine at the University of Wisconsin–Madison, and chair of the SHM Public Policy Committee.
Donald Schmidt, MD, has been named chief medical officer and vice president of medical affairs at Madonna Rehabilitation Hospitals in Omaha and Lincoln, Neb. He will replace Thomas Stalder, MD, who is retiring. Dr. Schmidt brings 20 years of experience to Madonna Rehabilitation Hospitals, including his most recent post as a hospitalist and medical director of the hospitalist program at Catholic Health Initiatives Health St. Elizabeth (Lincoln, Neb.).
Dr. Schmidt currently serves on the board of directors for OneHealth Nebraska, an independent physicians association.
Ezinne Nwude, MD, recently was presented with the SCP Health Excellence in Leadership Award during the organization’s Medical Leadership Conference. Dr. Nwude is chief of staff and hospitalist at the Medical Center of South Arkansas, El Dorado.
SCP Health coordinates staffing for more than 7,500 providers covering 30 states and is one of the nation’s largest clinical practice management companies. More than 420 medical leaders nationwide were eligible for the award. Dr. Nwude has focused on positive culture and health education since her start at MSCA in 2014. She has been chief of staff since October 2018.
RWJ Barnabas Health (West Orange, N.J.) recently named two new health system leaders from among its hospital medicine ranks, as Christopher Freer, MD, was tabbed as senior vice president for emergency and hospital medicine, and Maninder “Dolly” Abraham, MD, was picked as chief of hospital medicine. The moves were made as RWJBH takes over as the direct employer for Envision Physician Services in Nashville, Tenn.
Dr. Freer was elevated to his new role after spending the past 5 years as RWJBH’s system director for emergency services. He has nearly 3 decades of experience in hospital medicine.
Dr. Abraham comes to his new position after directing the hospitalist program at Saint Barnabas and serving as regional medical director with Envision.
Newman Regional Health (Emporia, Kan.) recently established a partnership with FreeState Healthcare (Wichita, Kan.). FreeState will be responsible for providing hospitalist services to adult inpatients and observation patients at Newman Regional Health during overnights.
Oral JAK1 inhibitor shows promise for hidradenitis suppurativa
A (HS) in a pair of small, randomized, phase 2 studies that established proof-of-concept for the novel agent, Afsaneh Alavi, MD, reported at the virtual annual congress of the European Academy of Dermatology and Venereology.
These favorable clinical findings were buttressed by a proteomic analysis demonstrating dose-dependent reductions in circulating inflammatory mediators, added Dr. Alavi, a dermatologist at the Mayo Clinic in Rochester, Minn.
The investigational oral small molecule, known for now as INCB54707, is 52 times more selective for JAK1 than JAK2.
Both multicenter studies entailed 8 weeks of active treatment with INCB54707 followed by a 4-week safety observation. In one study, 10 patients received 15 mg of the investigational agent once daily in open-label fashion. The other trial randomized 35 patients to the JAK1 inhibitor at 30 mg, 60 mg, or 90 mg per day or placebo. About 70% of participants in the studies had Hurley stage II HS; the rest were stage III.
Safety and tolerability were the primary outcomes in the two studies. One patient in the open-label study dropped out because of a flare of fibromyalgia. In the larger randomized trial, four patients – all in the group assigned to 90 mg/day of the JAK1 inhibitor – developed thrombocytopenia, resulting in temporary discontinuation of treatment for up to 2 weeks. In all four instances, the laboratory abnormality was reversed after temporary interruption of treatment, with no sequelae upon restarting the drug. There were no serious treatment-emergent adverse events in either study.
In the low-dose, open-label study, four of nine completers (44%) experienced a Hidradenitis Suppurativa Clinical Response (HiSCR) at week 8, defined as at least a 50% reduction in inflammatory lesion count with no increase in abscesses or draining fistulae compared to baseline. In the randomized trial, the week-8 HiSCR rate was 57% in placebo-treated controls, 56% in those on 30 mg/day or 60 mg/day of the JAK1 inhibitor, and significantly better at 88% in the group on 90 mg/day.
The rapidity of response to the JAK1 inhibitor was noteworthy. After just 1 week of treatment, an abscess and inflammatory nodule count of zero to two lesions was present in 22% of patients on INCB54707 at 60 mg/day and 29% of those on 90 mg/day, compared with none of the patients on 30 mg/day or placebo. At week 2, an abscess and nodule count of 0-2 was documented in 33% of participants on the JAK1 inhibitor at 30 mg/day, 58% at 60 mg/day, and 50% with 90 mg/day. At week 8, the rates were 57% with placebo, 44% with active treatment at 30 or 60 mg/day, and 63% in patients on 90 mg/day.
A dose-dependent significant improvement in Hidradenitis Suppurativa Quality of Life scores was documented in response to the JAK1 inhibitor.
There is an unmet need for effective therapies for HS, a chronic, extremely painful inflammatory condition with a large negative impact on quality of life. At present, the only Food and Drug Administration–approved medication for HS is the tumor necrosis factor inhibitor, adalimumab (Humira), noted Dr. Alavi. Ongoing studies are evaluating other JAK inhibitors, as well as TNF inhibitors and interleukin-17 and -23 blockers.
She reported receiving research funding from and serving as a consultant to Incyte, the studies’ sponsor, and more than a dozen other pharmaceutical companies.
A (HS) in a pair of small, randomized, phase 2 studies that established proof-of-concept for the novel agent, Afsaneh Alavi, MD, reported at the virtual annual congress of the European Academy of Dermatology and Venereology.
These favorable clinical findings were buttressed by a proteomic analysis demonstrating dose-dependent reductions in circulating inflammatory mediators, added Dr. Alavi, a dermatologist at the Mayo Clinic in Rochester, Minn.
The investigational oral small molecule, known for now as INCB54707, is 52 times more selective for JAK1 than JAK2.
Both multicenter studies entailed 8 weeks of active treatment with INCB54707 followed by a 4-week safety observation. In one study, 10 patients received 15 mg of the investigational agent once daily in open-label fashion. The other trial randomized 35 patients to the JAK1 inhibitor at 30 mg, 60 mg, or 90 mg per day or placebo. About 70% of participants in the studies had Hurley stage II HS; the rest were stage III.
Safety and tolerability were the primary outcomes in the two studies. One patient in the open-label study dropped out because of a flare of fibromyalgia. In the larger randomized trial, four patients – all in the group assigned to 90 mg/day of the JAK1 inhibitor – developed thrombocytopenia, resulting in temporary discontinuation of treatment for up to 2 weeks. In all four instances, the laboratory abnormality was reversed after temporary interruption of treatment, with no sequelae upon restarting the drug. There were no serious treatment-emergent adverse events in either study.
In the low-dose, open-label study, four of nine completers (44%) experienced a Hidradenitis Suppurativa Clinical Response (HiSCR) at week 8, defined as at least a 50% reduction in inflammatory lesion count with no increase in abscesses or draining fistulae compared to baseline. In the randomized trial, the week-8 HiSCR rate was 57% in placebo-treated controls, 56% in those on 30 mg/day or 60 mg/day of the JAK1 inhibitor, and significantly better at 88% in the group on 90 mg/day.
The rapidity of response to the JAK1 inhibitor was noteworthy. After just 1 week of treatment, an abscess and inflammatory nodule count of zero to two lesions was present in 22% of patients on INCB54707 at 60 mg/day and 29% of those on 90 mg/day, compared with none of the patients on 30 mg/day or placebo. At week 2, an abscess and nodule count of 0-2 was documented in 33% of participants on the JAK1 inhibitor at 30 mg/day, 58% at 60 mg/day, and 50% with 90 mg/day. At week 8, the rates were 57% with placebo, 44% with active treatment at 30 or 60 mg/day, and 63% in patients on 90 mg/day.
A dose-dependent significant improvement in Hidradenitis Suppurativa Quality of Life scores was documented in response to the JAK1 inhibitor.
There is an unmet need for effective therapies for HS, a chronic, extremely painful inflammatory condition with a large negative impact on quality of life. At present, the only Food and Drug Administration–approved medication for HS is the tumor necrosis factor inhibitor, adalimumab (Humira), noted Dr. Alavi. Ongoing studies are evaluating other JAK inhibitors, as well as TNF inhibitors and interleukin-17 and -23 blockers.
She reported receiving research funding from and serving as a consultant to Incyte, the studies’ sponsor, and more than a dozen other pharmaceutical companies.
A (HS) in a pair of small, randomized, phase 2 studies that established proof-of-concept for the novel agent, Afsaneh Alavi, MD, reported at the virtual annual congress of the European Academy of Dermatology and Venereology.
These favorable clinical findings were buttressed by a proteomic analysis demonstrating dose-dependent reductions in circulating inflammatory mediators, added Dr. Alavi, a dermatologist at the Mayo Clinic in Rochester, Minn.
The investigational oral small molecule, known for now as INCB54707, is 52 times more selective for JAK1 than JAK2.
Both multicenter studies entailed 8 weeks of active treatment with INCB54707 followed by a 4-week safety observation. In one study, 10 patients received 15 mg of the investigational agent once daily in open-label fashion. The other trial randomized 35 patients to the JAK1 inhibitor at 30 mg, 60 mg, or 90 mg per day or placebo. About 70% of participants in the studies had Hurley stage II HS; the rest were stage III.
Safety and tolerability were the primary outcomes in the two studies. One patient in the open-label study dropped out because of a flare of fibromyalgia. In the larger randomized trial, four patients – all in the group assigned to 90 mg/day of the JAK1 inhibitor – developed thrombocytopenia, resulting in temporary discontinuation of treatment for up to 2 weeks. In all four instances, the laboratory abnormality was reversed after temporary interruption of treatment, with no sequelae upon restarting the drug. There were no serious treatment-emergent adverse events in either study.
In the low-dose, open-label study, four of nine completers (44%) experienced a Hidradenitis Suppurativa Clinical Response (HiSCR) at week 8, defined as at least a 50% reduction in inflammatory lesion count with no increase in abscesses or draining fistulae compared to baseline. In the randomized trial, the week-8 HiSCR rate was 57% in placebo-treated controls, 56% in those on 30 mg/day or 60 mg/day of the JAK1 inhibitor, and significantly better at 88% in the group on 90 mg/day.
The rapidity of response to the JAK1 inhibitor was noteworthy. After just 1 week of treatment, an abscess and inflammatory nodule count of zero to two lesions was present in 22% of patients on INCB54707 at 60 mg/day and 29% of those on 90 mg/day, compared with none of the patients on 30 mg/day or placebo. At week 2, an abscess and nodule count of 0-2 was documented in 33% of participants on the JAK1 inhibitor at 30 mg/day, 58% at 60 mg/day, and 50% with 90 mg/day. At week 8, the rates were 57% with placebo, 44% with active treatment at 30 or 60 mg/day, and 63% in patients on 90 mg/day.
A dose-dependent significant improvement in Hidradenitis Suppurativa Quality of Life scores was documented in response to the JAK1 inhibitor.
There is an unmet need for effective therapies for HS, a chronic, extremely painful inflammatory condition with a large negative impact on quality of life. At present, the only Food and Drug Administration–approved medication for HS is the tumor necrosis factor inhibitor, adalimumab (Humira), noted Dr. Alavi. Ongoing studies are evaluating other JAK inhibitors, as well as TNF inhibitors and interleukin-17 and -23 blockers.
She reported receiving research funding from and serving as a consultant to Incyte, the studies’ sponsor, and more than a dozen other pharmaceutical companies.
FROM THE EADV CONGRESS
ctDNA outperforms CEA in colorectal cancer
Despite standard blood monitoring and routine imaging, patients with colorectal cancer (CRC) tend to have multiple, incurable metastases when relapse occurs.
A new study indicates that postsurgical circulating tumor DNA (ctDNA) testing may improve our ability to predict relapse in patients with stage I-III CRC.
ctDNA testing outperformed carcinoembryonic antigen (CEA) testing in predicting relapse-free survival, and ctDNA was detected about 8 months prior to relapse detection via CT.
Tenna V. Henriksen, of Aarhus University in Denmark, presented these results at the 2021 Gastrointestinal Cancers Symposium (abstract 11).
The multi-institutional study included 260 patients with CRC – 4 with stage I disease, 90 with stage II, and 166 with stage III disease.
Patients were monitored with plasma ctDNA testing within 2 months of primary surgery. Some patients were monitored with follow-up ctDNA sampling every 3 months for an additional 3 years.
Individual tumors and matched germline DNA were interrogated with whole-exome sequencing, and somatic single nucleotide variants were identified. Personalized multiplex PCR assays were developed to track tumor-specific single nucleotide variants via the Signatera® ctDNA assay.
The researchers retrospectively assessed ctDNA’s performance in:
- Stratifying the postoperative risk of relapse.
- Quantifying the benefit of adjuvant chemotherapy in patients who had or did not have ctDNA in plasma.
- Efficiently detecting relapse, in comparison with standard surveillance tests.
Surveillance CT scans were performed at 12 and 36 months but not at the frequency recommended in NCCN guidelines.
In all, 165 patients received adjuvant chemotherapy. The decision to give chemotherapy was made on a clinical basis by treating physicians who were blinded to the results of ctDNA testing.
Results
Of the 260 patients analyzed, 48 relapsed. The median follow-up was 28.4 months overall and 29.9 months in the nonrelapse cases.
The researchers assessed postoperative ctDNA status prior to adjuvant chemotherapy in 218 patients and after adjuvant chemotherapy in 108 patients.
In the prechemotherapy group, 20 patients were ctDNA positive, and 80% of them relapsed. In contrast, 13% of the 198 ctDNA-negative patients relapsed. The hazard ratio (HR) for relapse-free survival was 11 (95% confidence interval, 5.9-21; P < .0001).
After adjuvant chemotherapy, 12.5% of the ctDNA-negative patients relapsed, compared with 83.3% of the ctDNA-positive patients. The HR for relapse-free survival was 12 (95% CI, 4.9-27; P < .0001).
Results from longitudinal ctDNA testing in 202 patients suggested that serial sampling is more useful than sampling at a single point in time. The recurrence rate was 3.4% among patients who remained persistently ctDNA negative, compared with 89.3% in patients who were ctDNA positive. The HR for relapse-free survival was 51 (95% CI, 20-125; P < .0001).
In a subgroup of 29 patients with clinical recurrence detected by CT imaging, ctDNA detection occurred a median of 8.1 months earlier than radiologic relapse.
Among the 197 patients who had serial CEA and ctDNA measurements, longitudinal CEA testing correlated with relapse-free survival (HR, 4.9; 95% CI, 3.2-15, P < .0001) but not nearly as well as ctDNA testing (HR, 95.7; 95% CI, 28-322, P < .0001) in a univariable analysis.
In a multivariable analysis, the HR for relapse-free survival was 1.8 (95% CI, 0.77-4.0; P = .184) for longitudinal CEA and 80.55 (95% CI, 23.1-281; P < .0001) for longitudinal ctDNA.
“[W]hen we pit them against each other in a multivariable analysis, we can see that all the predictive power is in the ctDNA samples,” Ms. Henriksen said. “This indicates that ctDNA is a stronger biomarker compared to CEA, at least with relapse-free survival.”
Availability is not actionability
Study discussant Michael J. Overman, MD, of MD Anderson Cancer Center in Houston, acknowledged that this research substantiates the ability of postoperative ctDNA detection to risk stratify patients with stage III CRC, the predominant stage of participants in the study.
The current results reinforce the researchers’ previously published work (JAMA Oncol. 2019;5[8]:1124-31) and affirm similar findings by other groups (JAMA Oncol. 2019;5[12]:1710-17 and JAMA Oncol. 2019;5[8]:1118-23).
However, Dr. Overman cautioned that “availability is not the same as actionability.”
He also said the “tumor-informed mutation” approach utilized in the Signatera assay differs from the simpler “panel-based” approach, which is also undergoing clinical testing and offers the additional opportunity to test potentially actionable epigenetic targets such as DNA methylation.
Furthermore, the practicality of integrating the tumor-informed mutation approach into the time constraints required in clinical practice was not evaluated in the current analysis.
Dr. Overman pointed out that 16 of the 20 ctDNA-positive patients who received adjuvant chemotherapy sustained a recurrence, so the chemotherapy benefit was lower than expected.
Finally, although ctDNA outperformed CEA in detecting relapse, the greatest impact of ctDNA is its potential to inform the clinician’s decision to escalate and deescalate treatment with impact on survival – a potential that remains unfulfilled.
Next steps
Ms. Henriksen closed her presentation with the perspective that, for serial ctDNA monitoring to be implemented in clinical settings, testing in randomized clinical trials will be needed.
In Denmark, the IMPROVE-IT study is enrolling patients with stage I or low-risk stage II CRC. In this trial, ctDNA-positive patients will receive adjuvant chemotherapy, and ctDNA-negative patients will have longitudinal ctDNA testing but no adjuvant chemotherapy.
A second study, IMPROVE-IT2, will assess the value of ctDNA to direct intensified radiologic surveillance to improve the application of potentially curative treatment for patients with stage II (high-risk) or stage III CRC. Patients with negative ctDNA tests will be followed with longitudinal ctDNA testing only.
In his talk, Dr. Overman highlighted several prospective studies assessing the value of ctDNA testing.
One of these is the ongoing COBRA study (NRG-GI-005), which uses a ctDNA assay (Guardant Lunar-1) for patients with stage IIA CRC for whom standard adjuvant chemotherapy is not indicated.
The patients in COBRA are randomized to active surveillance or assay-directed therapy. Patients assigned to assay-directed therapy have samples analyzed for ctDNA, which would guide the decision about adjuvant chemotherapy. If the postoperative sample is ctDNA positive and the patient accepts adjuvant chemotherapy, the patient could receive one of two standard adjuvant chemotherapy regimens. If ctDNA negative, the patient would be followed with active surveillance alone.
Dr. Overman also highlighted the planned CIRCULATE US trial (NRG-GI008). The aim of this trial is to test intensified adjuvant treatment for stage III CRC patients with positive ctDNA tests. It will employ the Signatera assay.
Ideally, these ongoing trials will provide the evidence base needed for clinicians to optimize adjuvant therapy and surveillance using ctDNA technology.
The current study was sponsored by the Danish Council for Independent Research, The Novo Nordisk Foundation, The Danish Cancer Society, and Natera Inc. Ms. Henriksen disclosed no conflicts of interest. Dr. Overman disclosed relationships with Array BioPharma, Bristol-Myers Squibb, Gritstone Oncology, Janssen, MedImmune, Merck, Novartis, Pfizer, Promega, Roche/Genentech, and Spectrum Pharmaceuticals.
The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Despite standard blood monitoring and routine imaging, patients with colorectal cancer (CRC) tend to have multiple, incurable metastases when relapse occurs.
A new study indicates that postsurgical circulating tumor DNA (ctDNA) testing may improve our ability to predict relapse in patients with stage I-III CRC.
ctDNA testing outperformed carcinoembryonic antigen (CEA) testing in predicting relapse-free survival, and ctDNA was detected about 8 months prior to relapse detection via CT.
Tenna V. Henriksen, of Aarhus University in Denmark, presented these results at the 2021 Gastrointestinal Cancers Symposium (abstract 11).
The multi-institutional study included 260 patients with CRC – 4 with stage I disease, 90 with stage II, and 166 with stage III disease.
Patients were monitored with plasma ctDNA testing within 2 months of primary surgery. Some patients were monitored with follow-up ctDNA sampling every 3 months for an additional 3 years.
Individual tumors and matched germline DNA were interrogated with whole-exome sequencing, and somatic single nucleotide variants were identified. Personalized multiplex PCR assays were developed to track tumor-specific single nucleotide variants via the Signatera® ctDNA assay.
The researchers retrospectively assessed ctDNA’s performance in:
- Stratifying the postoperative risk of relapse.
- Quantifying the benefit of adjuvant chemotherapy in patients who had or did not have ctDNA in plasma.
- Efficiently detecting relapse, in comparison with standard surveillance tests.
Surveillance CT scans were performed at 12 and 36 months but not at the frequency recommended in NCCN guidelines.
In all, 165 patients received adjuvant chemotherapy. The decision to give chemotherapy was made on a clinical basis by treating physicians who were blinded to the results of ctDNA testing.
Results
Of the 260 patients analyzed, 48 relapsed. The median follow-up was 28.4 months overall and 29.9 months in the nonrelapse cases.
The researchers assessed postoperative ctDNA status prior to adjuvant chemotherapy in 218 patients and after adjuvant chemotherapy in 108 patients.
In the prechemotherapy group, 20 patients were ctDNA positive, and 80% of them relapsed. In contrast, 13% of the 198 ctDNA-negative patients relapsed. The hazard ratio (HR) for relapse-free survival was 11 (95% confidence interval, 5.9-21; P < .0001).
After adjuvant chemotherapy, 12.5% of the ctDNA-negative patients relapsed, compared with 83.3% of the ctDNA-positive patients. The HR for relapse-free survival was 12 (95% CI, 4.9-27; P < .0001).
Results from longitudinal ctDNA testing in 202 patients suggested that serial sampling is more useful than sampling at a single point in time. The recurrence rate was 3.4% among patients who remained persistently ctDNA negative, compared with 89.3% in patients who were ctDNA positive. The HR for relapse-free survival was 51 (95% CI, 20-125; P < .0001).
In a subgroup of 29 patients with clinical recurrence detected by CT imaging, ctDNA detection occurred a median of 8.1 months earlier than radiologic relapse.
Among the 197 patients who had serial CEA and ctDNA measurements, longitudinal CEA testing correlated with relapse-free survival (HR, 4.9; 95% CI, 3.2-15, P < .0001) but not nearly as well as ctDNA testing (HR, 95.7; 95% CI, 28-322, P < .0001) in a univariable analysis.
In a multivariable analysis, the HR for relapse-free survival was 1.8 (95% CI, 0.77-4.0; P = .184) for longitudinal CEA and 80.55 (95% CI, 23.1-281; P < .0001) for longitudinal ctDNA.
“[W]hen we pit them against each other in a multivariable analysis, we can see that all the predictive power is in the ctDNA samples,” Ms. Henriksen said. “This indicates that ctDNA is a stronger biomarker compared to CEA, at least with relapse-free survival.”
Availability is not actionability
Study discussant Michael J. Overman, MD, of MD Anderson Cancer Center in Houston, acknowledged that this research substantiates the ability of postoperative ctDNA detection to risk stratify patients with stage III CRC, the predominant stage of participants in the study.
The current results reinforce the researchers’ previously published work (JAMA Oncol. 2019;5[8]:1124-31) and affirm similar findings by other groups (JAMA Oncol. 2019;5[12]:1710-17 and JAMA Oncol. 2019;5[8]:1118-23).
However, Dr. Overman cautioned that “availability is not the same as actionability.”
He also said the “tumor-informed mutation” approach utilized in the Signatera assay differs from the simpler “panel-based” approach, which is also undergoing clinical testing and offers the additional opportunity to test potentially actionable epigenetic targets such as DNA methylation.
Furthermore, the practicality of integrating the tumor-informed mutation approach into the time constraints required in clinical practice was not evaluated in the current analysis.
Dr. Overman pointed out that 16 of the 20 ctDNA-positive patients who received adjuvant chemotherapy sustained a recurrence, so the chemotherapy benefit was lower than expected.
Finally, although ctDNA outperformed CEA in detecting relapse, the greatest impact of ctDNA is its potential to inform the clinician’s decision to escalate and deescalate treatment with impact on survival – a potential that remains unfulfilled.
Next steps
Ms. Henriksen closed her presentation with the perspective that, for serial ctDNA monitoring to be implemented in clinical settings, testing in randomized clinical trials will be needed.
In Denmark, the IMPROVE-IT study is enrolling patients with stage I or low-risk stage II CRC. In this trial, ctDNA-positive patients will receive adjuvant chemotherapy, and ctDNA-negative patients will have longitudinal ctDNA testing but no adjuvant chemotherapy.
A second study, IMPROVE-IT2, will assess the value of ctDNA to direct intensified radiologic surveillance to improve the application of potentially curative treatment for patients with stage II (high-risk) or stage III CRC. Patients with negative ctDNA tests will be followed with longitudinal ctDNA testing only.
In his talk, Dr. Overman highlighted several prospective studies assessing the value of ctDNA testing.
One of these is the ongoing COBRA study (NRG-GI-005), which uses a ctDNA assay (Guardant Lunar-1) for patients with stage IIA CRC for whom standard adjuvant chemotherapy is not indicated.
The patients in COBRA are randomized to active surveillance or assay-directed therapy. Patients assigned to assay-directed therapy have samples analyzed for ctDNA, which would guide the decision about adjuvant chemotherapy. If the postoperative sample is ctDNA positive and the patient accepts adjuvant chemotherapy, the patient could receive one of two standard adjuvant chemotherapy regimens. If ctDNA negative, the patient would be followed with active surveillance alone.
Dr. Overman also highlighted the planned CIRCULATE US trial (NRG-GI008). The aim of this trial is to test intensified adjuvant treatment for stage III CRC patients with positive ctDNA tests. It will employ the Signatera assay.
Ideally, these ongoing trials will provide the evidence base needed for clinicians to optimize adjuvant therapy and surveillance using ctDNA technology.
The current study was sponsored by the Danish Council for Independent Research, The Novo Nordisk Foundation, The Danish Cancer Society, and Natera Inc. Ms. Henriksen disclosed no conflicts of interest. Dr. Overman disclosed relationships with Array BioPharma, Bristol-Myers Squibb, Gritstone Oncology, Janssen, MedImmune, Merck, Novartis, Pfizer, Promega, Roche/Genentech, and Spectrum Pharmaceuticals.
The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Despite standard blood monitoring and routine imaging, patients with colorectal cancer (CRC) tend to have multiple, incurable metastases when relapse occurs.
A new study indicates that postsurgical circulating tumor DNA (ctDNA) testing may improve our ability to predict relapse in patients with stage I-III CRC.
ctDNA testing outperformed carcinoembryonic antigen (CEA) testing in predicting relapse-free survival, and ctDNA was detected about 8 months prior to relapse detection via CT.
Tenna V. Henriksen, of Aarhus University in Denmark, presented these results at the 2021 Gastrointestinal Cancers Symposium (abstract 11).
The multi-institutional study included 260 patients with CRC – 4 with stage I disease, 90 with stage II, and 166 with stage III disease.
Patients were monitored with plasma ctDNA testing within 2 months of primary surgery. Some patients were monitored with follow-up ctDNA sampling every 3 months for an additional 3 years.
Individual tumors and matched germline DNA were interrogated with whole-exome sequencing, and somatic single nucleotide variants were identified. Personalized multiplex PCR assays were developed to track tumor-specific single nucleotide variants via the Signatera® ctDNA assay.
The researchers retrospectively assessed ctDNA’s performance in:
- Stratifying the postoperative risk of relapse.
- Quantifying the benefit of adjuvant chemotherapy in patients who had or did not have ctDNA in plasma.
- Efficiently detecting relapse, in comparison with standard surveillance tests.
Surveillance CT scans were performed at 12 and 36 months but not at the frequency recommended in NCCN guidelines.
In all, 165 patients received adjuvant chemotherapy. The decision to give chemotherapy was made on a clinical basis by treating physicians who were blinded to the results of ctDNA testing.
Results
Of the 260 patients analyzed, 48 relapsed. The median follow-up was 28.4 months overall and 29.9 months in the nonrelapse cases.
The researchers assessed postoperative ctDNA status prior to adjuvant chemotherapy in 218 patients and after adjuvant chemotherapy in 108 patients.
In the prechemotherapy group, 20 patients were ctDNA positive, and 80% of them relapsed. In contrast, 13% of the 198 ctDNA-negative patients relapsed. The hazard ratio (HR) for relapse-free survival was 11 (95% confidence interval, 5.9-21; P < .0001).
After adjuvant chemotherapy, 12.5% of the ctDNA-negative patients relapsed, compared with 83.3% of the ctDNA-positive patients. The HR for relapse-free survival was 12 (95% CI, 4.9-27; P < .0001).
Results from longitudinal ctDNA testing in 202 patients suggested that serial sampling is more useful than sampling at a single point in time. The recurrence rate was 3.4% among patients who remained persistently ctDNA negative, compared with 89.3% in patients who were ctDNA positive. The HR for relapse-free survival was 51 (95% CI, 20-125; P < .0001).
In a subgroup of 29 patients with clinical recurrence detected by CT imaging, ctDNA detection occurred a median of 8.1 months earlier than radiologic relapse.
Among the 197 patients who had serial CEA and ctDNA measurements, longitudinal CEA testing correlated with relapse-free survival (HR, 4.9; 95% CI, 3.2-15, P < .0001) but not nearly as well as ctDNA testing (HR, 95.7; 95% CI, 28-322, P < .0001) in a univariable analysis.
In a multivariable analysis, the HR for relapse-free survival was 1.8 (95% CI, 0.77-4.0; P = .184) for longitudinal CEA and 80.55 (95% CI, 23.1-281; P < .0001) for longitudinal ctDNA.
“[W]hen we pit them against each other in a multivariable analysis, we can see that all the predictive power is in the ctDNA samples,” Ms. Henriksen said. “This indicates that ctDNA is a stronger biomarker compared to CEA, at least with relapse-free survival.”
Availability is not actionability
Study discussant Michael J. Overman, MD, of MD Anderson Cancer Center in Houston, acknowledged that this research substantiates the ability of postoperative ctDNA detection to risk stratify patients with stage III CRC, the predominant stage of participants in the study.
The current results reinforce the researchers’ previously published work (JAMA Oncol. 2019;5[8]:1124-31) and affirm similar findings by other groups (JAMA Oncol. 2019;5[12]:1710-17 and JAMA Oncol. 2019;5[8]:1118-23).
However, Dr. Overman cautioned that “availability is not the same as actionability.”
He also said the “tumor-informed mutation” approach utilized in the Signatera assay differs from the simpler “panel-based” approach, which is also undergoing clinical testing and offers the additional opportunity to test potentially actionable epigenetic targets such as DNA methylation.
Furthermore, the practicality of integrating the tumor-informed mutation approach into the time constraints required in clinical practice was not evaluated in the current analysis.
Dr. Overman pointed out that 16 of the 20 ctDNA-positive patients who received adjuvant chemotherapy sustained a recurrence, so the chemotherapy benefit was lower than expected.
Finally, although ctDNA outperformed CEA in detecting relapse, the greatest impact of ctDNA is its potential to inform the clinician’s decision to escalate and deescalate treatment with impact on survival – a potential that remains unfulfilled.
Next steps
Ms. Henriksen closed her presentation with the perspective that, for serial ctDNA monitoring to be implemented in clinical settings, testing in randomized clinical trials will be needed.
In Denmark, the IMPROVE-IT study is enrolling patients with stage I or low-risk stage II CRC. In this trial, ctDNA-positive patients will receive adjuvant chemotherapy, and ctDNA-negative patients will have longitudinal ctDNA testing but no adjuvant chemotherapy.
A second study, IMPROVE-IT2, will assess the value of ctDNA to direct intensified radiologic surveillance to improve the application of potentially curative treatment for patients with stage II (high-risk) or stage III CRC. Patients with negative ctDNA tests will be followed with longitudinal ctDNA testing only.
In his talk, Dr. Overman highlighted several prospective studies assessing the value of ctDNA testing.
One of these is the ongoing COBRA study (NRG-GI-005), which uses a ctDNA assay (Guardant Lunar-1) for patients with stage IIA CRC for whom standard adjuvant chemotherapy is not indicated.
The patients in COBRA are randomized to active surveillance or assay-directed therapy. Patients assigned to assay-directed therapy have samples analyzed for ctDNA, which would guide the decision about adjuvant chemotherapy. If the postoperative sample is ctDNA positive and the patient accepts adjuvant chemotherapy, the patient could receive one of two standard adjuvant chemotherapy regimens. If ctDNA negative, the patient would be followed with active surveillance alone.
Dr. Overman also highlighted the planned CIRCULATE US trial (NRG-GI008). The aim of this trial is to test intensified adjuvant treatment for stage III CRC patients with positive ctDNA tests. It will employ the Signatera assay.
Ideally, these ongoing trials will provide the evidence base needed for clinicians to optimize adjuvant therapy and surveillance using ctDNA technology.
The current study was sponsored by the Danish Council for Independent Research, The Novo Nordisk Foundation, The Danish Cancer Society, and Natera Inc. Ms. Henriksen disclosed no conflicts of interest. Dr. Overman disclosed relationships with Array BioPharma, Bristol-Myers Squibb, Gritstone Oncology, Janssen, MedImmune, Merck, Novartis, Pfizer, Promega, Roche/Genentech, and Spectrum Pharmaceuticals.
The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM GI Cancers Symposium 2021
Stem cell transplant shows long-term benefit in MS
The benefits of autologous hematopoietic stem cell transplant (AHSCT) for patients with multiple sclerosis (MS) persist for more than 10 years in the majority of patents, new data show. The study reports on 210 Italian patients who underwent AHSCT between 2007 and 2019. Among the entire study cohort, 79.5% of patients had not experienced worsening of disability at 5 years, and 65.5% had not experienced it at 10 years.
Patients with relapsing remitting MS had better results, with 85.5% experiencing no worsening of disability at 5 years, and 71.3% at 10 years. Among patients with progressive MS, 71.0% showed no worsening of disability at 5 years, and 57.2% at 10 years.
“This is the longest follow-up of AHSCT in MS patients so far to be reported,” said study author Matilde Inglese, MD, University of Genoa (Italy). “We have shown AHSCT to be highly effective to prevent long-term disability worsening in most treated patients.”
The study was published online Jan. 20 in Neurology.
“We suggest that AHSCT should be considered as a treatment strategy for MS not responding to conventional therapy,” the authors concluded.
The study had no control group, so a direct comparison is not possible. Nevertheless, Dr. Inglese said she believed these results are better than those that would be achieved with disease-modifying drug therapy for similar patients.
“The best patient candidates for this procedure are those with highly active multiple sclerosis who are not responsive to high-efficacy drugs, such as alemtuzumab or ocrelizumab,” Dr. Inglese commented. “Younger patients with an aggressive form of relapsing remitting MS tend to do the best, although patients with progressive forms of MS who still have active lesions on MRI also benefit.”
Renewing the immune system
The transplant procedure involves giving high-dose cyclophosphamide to stimulate mobilization of bone marrow stem cells, which are collected from peripheral blood. Patients then undergo intense immunosuppression with a cocktail of drugs to remove the autoreactive T cells, and the stem cells, which are not autoreactive, are reinfused.
“We are effectively renewing the immune system,” Dr. Inglese said. “While it is not correct to call it a cure, as we are not eliminating the etiology of the disease, it is the closest to complete suppression of the disease that we can get.”
Other results from the study show that among patients with relapsing remitting MS, rates of relapse-free survival were 78.1% at 5 years and 63.5% at 10 years.
Better results were achieved for patients who received the BEAM+ATG conditioning regimen for immunosuppression. That regimen includes carmustine, cytosine-arabinoside, etoposide, and melphalan, followed by rabbit antithymocyte globulin. Among patients with relapsing remitting disease who were treated with this protocol, rates of relapse-free survival were 86.4% at 5 years and 77.0% at 10 years.
For patients with relapsing remitting MS, the probability of achieving NEDA-3 status (no evidence of disease activity, including the absence of clinical relapses, disability worsening, and MRI inflammatory activity) was 62.2% at 5 years and 40.5% at 10 years.
Among those patients with relapsing remitting MS who received the BEAM+ATG conditioning protocol, NEDA-3 status was achieved in 67.7% at 5 years and in 54.9% at 10 years.
Three deaths occurred within 100 days following AHSCT (1.4% of the entire study population). One patient developed pulmonary thromboembolism, received fibrinolytic treatment, and died 48 hours later after intracranial hemorrhage. The second patient experienced engraftment failure and died 24 days after transplant because of an opportunistic infection. The third patient died 1 month after transplant from Wernicke-like encephalopathy. All the patients who died received the BEAM+ATG conditioning regimen. No transplant-related deaths occurred in patients who underwent transplant after 2007.
Dr. Inglese noted that the mortality rate associated with AHSCT has been greatly reduced in recent years. “We are seeing a very low mortality rate – about 0.3% – thanks to improvements in the procedure and better patient selection. This seems acceptable, given that we are treating patients with very aggressive disease who have a high risk of becoming significantly disabled relatively early in life,” she commented.
However, it is vitally important that the procedure be conducted in a specialized center with a highly experienced multidisciplinary team, she stressed.
In the Neurology article, the authors concluded: “Although patients with RRMS [relapsing remitting MS] are those who benefit the most from transplant, AHSCT has been also shown to prevent disability worsening in a large proportion of patients with active progressive MS.
“The BEAM+ATG conditioning protocol, although associated with a higher transplant mortality rate, was associated with a more pronounced suppression of clinical relapses and MRI inflammatory activity, allowing complete disease control in a higher proportion of patients,” they wrote.
Potent and durable efficacy, with caveats
Commenting on these latest findings, Jeffrey A. Cohen, MD, of the Mellen Center for Multiple Sclerosis at the Cleveland Clinic, said: “AHSCT appears to have potent and durable efficacy in MS but is associated with significant risk and cost.”
The patients who are most likely to benefit are young and have experienced the onset of disease relatively recently. They are still ambulatory with highly active MS and have experienced recent clinical relapses and/or MRI lesion activity, and such activity continues despite disease-modifying therapy, Dr. Cohen noted. He added that “AHSCT is a reasonable option for such patients who have essentially failed the available disease-modifying therapy options.”
He pointed out that the key question is where AHSCT belongs in the overall MS algorithm relative to other high-efficacy therapies. “We need to know whether it should be used more broadly rather than as a last resort.”
To address that question, several randomized trials comparing AHSCT with high-efficacy disease-modifying therapy are in progress, including the National Institutes of Health–sponsored BEAT-MS trial in the United States (for which Dr. Cohen is the lead investigator) and four European trials – NET-MS (for which Dr. Inglese is the lead investigator), STAR-MS, RAM-MS, and COAST-MS.
The current study was partially funded and supported by the Italian Multiple Sclerosis Foundation. Dr. Inglese disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The benefits of autologous hematopoietic stem cell transplant (AHSCT) for patients with multiple sclerosis (MS) persist for more than 10 years in the majority of patents, new data show. The study reports on 210 Italian patients who underwent AHSCT between 2007 and 2019. Among the entire study cohort, 79.5% of patients had not experienced worsening of disability at 5 years, and 65.5% had not experienced it at 10 years.
Patients with relapsing remitting MS had better results, with 85.5% experiencing no worsening of disability at 5 years, and 71.3% at 10 years. Among patients with progressive MS, 71.0% showed no worsening of disability at 5 years, and 57.2% at 10 years.
“This is the longest follow-up of AHSCT in MS patients so far to be reported,” said study author Matilde Inglese, MD, University of Genoa (Italy). “We have shown AHSCT to be highly effective to prevent long-term disability worsening in most treated patients.”
The study was published online Jan. 20 in Neurology.
“We suggest that AHSCT should be considered as a treatment strategy for MS not responding to conventional therapy,” the authors concluded.
The study had no control group, so a direct comparison is not possible. Nevertheless, Dr. Inglese said she believed these results are better than those that would be achieved with disease-modifying drug therapy for similar patients.
“The best patient candidates for this procedure are those with highly active multiple sclerosis who are not responsive to high-efficacy drugs, such as alemtuzumab or ocrelizumab,” Dr. Inglese commented. “Younger patients with an aggressive form of relapsing remitting MS tend to do the best, although patients with progressive forms of MS who still have active lesions on MRI also benefit.”
Renewing the immune system
The transplant procedure involves giving high-dose cyclophosphamide to stimulate mobilization of bone marrow stem cells, which are collected from peripheral blood. Patients then undergo intense immunosuppression with a cocktail of drugs to remove the autoreactive T cells, and the stem cells, which are not autoreactive, are reinfused.
“We are effectively renewing the immune system,” Dr. Inglese said. “While it is not correct to call it a cure, as we are not eliminating the etiology of the disease, it is the closest to complete suppression of the disease that we can get.”
Other results from the study show that among patients with relapsing remitting MS, rates of relapse-free survival were 78.1% at 5 years and 63.5% at 10 years.
Better results were achieved for patients who received the BEAM+ATG conditioning regimen for immunosuppression. That regimen includes carmustine, cytosine-arabinoside, etoposide, and melphalan, followed by rabbit antithymocyte globulin. Among patients with relapsing remitting disease who were treated with this protocol, rates of relapse-free survival were 86.4% at 5 years and 77.0% at 10 years.
For patients with relapsing remitting MS, the probability of achieving NEDA-3 status (no evidence of disease activity, including the absence of clinical relapses, disability worsening, and MRI inflammatory activity) was 62.2% at 5 years and 40.5% at 10 years.
Among those patients with relapsing remitting MS who received the BEAM+ATG conditioning protocol, NEDA-3 status was achieved in 67.7% at 5 years and in 54.9% at 10 years.
Three deaths occurred within 100 days following AHSCT (1.4% of the entire study population). One patient developed pulmonary thromboembolism, received fibrinolytic treatment, and died 48 hours later after intracranial hemorrhage. The second patient experienced engraftment failure and died 24 days after transplant because of an opportunistic infection. The third patient died 1 month after transplant from Wernicke-like encephalopathy. All the patients who died received the BEAM+ATG conditioning regimen. No transplant-related deaths occurred in patients who underwent transplant after 2007.
Dr. Inglese noted that the mortality rate associated with AHSCT has been greatly reduced in recent years. “We are seeing a very low mortality rate – about 0.3% – thanks to improvements in the procedure and better patient selection. This seems acceptable, given that we are treating patients with very aggressive disease who have a high risk of becoming significantly disabled relatively early in life,” she commented.
However, it is vitally important that the procedure be conducted in a specialized center with a highly experienced multidisciplinary team, she stressed.
In the Neurology article, the authors concluded: “Although patients with RRMS [relapsing remitting MS] are those who benefit the most from transplant, AHSCT has been also shown to prevent disability worsening in a large proportion of patients with active progressive MS.
“The BEAM+ATG conditioning protocol, although associated with a higher transplant mortality rate, was associated with a more pronounced suppression of clinical relapses and MRI inflammatory activity, allowing complete disease control in a higher proportion of patients,” they wrote.
Potent and durable efficacy, with caveats
Commenting on these latest findings, Jeffrey A. Cohen, MD, of the Mellen Center for Multiple Sclerosis at the Cleveland Clinic, said: “AHSCT appears to have potent and durable efficacy in MS but is associated with significant risk and cost.”
The patients who are most likely to benefit are young and have experienced the onset of disease relatively recently. They are still ambulatory with highly active MS and have experienced recent clinical relapses and/or MRI lesion activity, and such activity continues despite disease-modifying therapy, Dr. Cohen noted. He added that “AHSCT is a reasonable option for such patients who have essentially failed the available disease-modifying therapy options.”
He pointed out that the key question is where AHSCT belongs in the overall MS algorithm relative to other high-efficacy therapies. “We need to know whether it should be used more broadly rather than as a last resort.”
To address that question, several randomized trials comparing AHSCT with high-efficacy disease-modifying therapy are in progress, including the National Institutes of Health–sponsored BEAT-MS trial in the United States (for which Dr. Cohen is the lead investigator) and four European trials – NET-MS (for which Dr. Inglese is the lead investigator), STAR-MS, RAM-MS, and COAST-MS.
The current study was partially funded and supported by the Italian Multiple Sclerosis Foundation. Dr. Inglese disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The benefits of autologous hematopoietic stem cell transplant (AHSCT) for patients with multiple sclerosis (MS) persist for more than 10 years in the majority of patents, new data show. The study reports on 210 Italian patients who underwent AHSCT between 2007 and 2019. Among the entire study cohort, 79.5% of patients had not experienced worsening of disability at 5 years, and 65.5% had not experienced it at 10 years.
Patients with relapsing remitting MS had better results, with 85.5% experiencing no worsening of disability at 5 years, and 71.3% at 10 years. Among patients with progressive MS, 71.0% showed no worsening of disability at 5 years, and 57.2% at 10 years.
“This is the longest follow-up of AHSCT in MS patients so far to be reported,” said study author Matilde Inglese, MD, University of Genoa (Italy). “We have shown AHSCT to be highly effective to prevent long-term disability worsening in most treated patients.”
The study was published online Jan. 20 in Neurology.
“We suggest that AHSCT should be considered as a treatment strategy for MS not responding to conventional therapy,” the authors concluded.
The study had no control group, so a direct comparison is not possible. Nevertheless, Dr. Inglese said she believed these results are better than those that would be achieved with disease-modifying drug therapy for similar patients.
“The best patient candidates for this procedure are those with highly active multiple sclerosis who are not responsive to high-efficacy drugs, such as alemtuzumab or ocrelizumab,” Dr. Inglese commented. “Younger patients with an aggressive form of relapsing remitting MS tend to do the best, although patients with progressive forms of MS who still have active lesions on MRI also benefit.”
Renewing the immune system
The transplant procedure involves giving high-dose cyclophosphamide to stimulate mobilization of bone marrow stem cells, which are collected from peripheral blood. Patients then undergo intense immunosuppression with a cocktail of drugs to remove the autoreactive T cells, and the stem cells, which are not autoreactive, are reinfused.
“We are effectively renewing the immune system,” Dr. Inglese said. “While it is not correct to call it a cure, as we are not eliminating the etiology of the disease, it is the closest to complete suppression of the disease that we can get.”
Other results from the study show that among patients with relapsing remitting MS, rates of relapse-free survival were 78.1% at 5 years and 63.5% at 10 years.
Better results were achieved for patients who received the BEAM+ATG conditioning regimen for immunosuppression. That regimen includes carmustine, cytosine-arabinoside, etoposide, and melphalan, followed by rabbit antithymocyte globulin. Among patients with relapsing remitting disease who were treated with this protocol, rates of relapse-free survival were 86.4% at 5 years and 77.0% at 10 years.
For patients with relapsing remitting MS, the probability of achieving NEDA-3 status (no evidence of disease activity, including the absence of clinical relapses, disability worsening, and MRI inflammatory activity) was 62.2% at 5 years and 40.5% at 10 years.
Among those patients with relapsing remitting MS who received the BEAM+ATG conditioning protocol, NEDA-3 status was achieved in 67.7% at 5 years and in 54.9% at 10 years.
Three deaths occurred within 100 days following AHSCT (1.4% of the entire study population). One patient developed pulmonary thromboembolism, received fibrinolytic treatment, and died 48 hours later after intracranial hemorrhage. The second patient experienced engraftment failure and died 24 days after transplant because of an opportunistic infection. The third patient died 1 month after transplant from Wernicke-like encephalopathy. All the patients who died received the BEAM+ATG conditioning regimen. No transplant-related deaths occurred in patients who underwent transplant after 2007.
Dr. Inglese noted that the mortality rate associated with AHSCT has been greatly reduced in recent years. “We are seeing a very low mortality rate – about 0.3% – thanks to improvements in the procedure and better patient selection. This seems acceptable, given that we are treating patients with very aggressive disease who have a high risk of becoming significantly disabled relatively early in life,” she commented.
However, it is vitally important that the procedure be conducted in a specialized center with a highly experienced multidisciplinary team, she stressed.
In the Neurology article, the authors concluded: “Although patients with RRMS [relapsing remitting MS] are those who benefit the most from transplant, AHSCT has been also shown to prevent disability worsening in a large proportion of patients with active progressive MS.
“The BEAM+ATG conditioning protocol, although associated with a higher transplant mortality rate, was associated with a more pronounced suppression of clinical relapses and MRI inflammatory activity, allowing complete disease control in a higher proportion of patients,” they wrote.
Potent and durable efficacy, with caveats
Commenting on these latest findings, Jeffrey A. Cohen, MD, of the Mellen Center for Multiple Sclerosis at the Cleveland Clinic, said: “AHSCT appears to have potent and durable efficacy in MS but is associated with significant risk and cost.”
The patients who are most likely to benefit are young and have experienced the onset of disease relatively recently. They are still ambulatory with highly active MS and have experienced recent clinical relapses and/or MRI lesion activity, and such activity continues despite disease-modifying therapy, Dr. Cohen noted. He added that “AHSCT is a reasonable option for such patients who have essentially failed the available disease-modifying therapy options.”
He pointed out that the key question is where AHSCT belongs in the overall MS algorithm relative to other high-efficacy therapies. “We need to know whether it should be used more broadly rather than as a last resort.”
To address that question, several randomized trials comparing AHSCT with high-efficacy disease-modifying therapy are in progress, including the National Institutes of Health–sponsored BEAT-MS trial in the United States (for which Dr. Cohen is the lead investigator) and four European trials – NET-MS (for which Dr. Inglese is the lead investigator), STAR-MS, RAM-MS, and COAST-MS.
The current study was partially funded and supported by the Italian Multiple Sclerosis Foundation. Dr. Inglese disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
COVID-19 variants may prompt additional Moderna vaccine
As mutated strains of the coronavirus represent new threats in the pandemic, vaccine makers are racing to respond.
Moderna, whose two-dose vaccine has been authorized for use in the United States since Dec. 18, said on Jan. 25 that it is now investigating whether a third dose of the vaccine will better prevent the spread of a variant first seen in South Africa, while it also tests a new vaccine formula for the same purpose.
“Out of an abundance of caution and leveraging the flexibility of our mRNA platform, we are advancing an emerging variant booster candidate against the variant first identified in the Republic of South Africa into the clinic to determine if it will be more effective … against this and potentially future variants,” Moderna CEO Stéphane Bancel said in a statement. Pfizer and BioNTech, whose vaccine was also authorized in December, announced on Jan. 20 that their COVID-19 vaccine creates antibodies that could protect vaccine recipients from the U.K. variant B.1.1.7.
Moderna on Jan. 25 said laboratory tests have shown its COVID-19 vaccine could protect against the U.K. strain but that it is less effective – while still meeting efficacy benchmarks – against the strain identified in South Africa. Data from the study were submitted to a preprint server on Jan. 25 but have not yet been peer reviewed.
“This is not a problem yet,” Paul Offit, MD, director of the Vaccine Education Center at Children’s Hospital of Philadelphia, told CNBC.
“Prepare for it. Sequence these viruses,” he said. “Get ready just in case a variant emerges, which is resistant.”
There were at least 195 confirmed cases of patients infected with the U.K. variant, which is believed to be as much as 70% more transmissible, in the United States as of Jan. 22, according to the Centers for Disease Control and Prevention. No cases from the South African variant have been confirmed in the United States. To try to prevent the variant from entering the country, President Joe Biden plans to ban travel from South Africa, except for American citizens and permanent residents.
The U.S. has reported more than 25 million total COVID-19 cases, according to data from Johns Hopkins University, marking another major milestone during the pandemic.
That means about 1 in 13 people have contracted the virus, or about 7.6% of the U.S. population.
“Twenty-five million cases is an incredible scale of tragedy,” Caitlin Rivers, an epidemiologist at the Johns Hopkins Bloomberg School of Public Health, told The New York Times. She called the pandemic one of the worst public health crises in history.
After the first U.S. case was reported in January 2020, it took more than 9 months to reach 10 million cases in early November. Numbers rose during the holidays, and 10 million more cases were reported by the end of the year.
Following a major surge throughout January 2021, with a peak of more than 300,000 daily cases on some days, the U.S. reached 25 million in about 3 weeks.
Hospitalizations also peaked in early January, with more than 132,000 COVID-19 patients in hospitals across the country, according to the COVID Tracking Project. On Jan. 24, about 111,000 patients were hospitalized, which is the lowest since mid-December.
The U.S. has also reported nearly 420,000 deaths. As recently as the week starting Jan. 17, more than 4,400 deaths were reported in a single day, according to the COVID Tracking Project. Deaths are beginning to drop but still remain above 3,000 daily.
The University of Washington’s Institute for Health Metrics and Evaluation released a new projection Jan. 22 that said new cases would decline steadily in coming weeks. New COVID-19 cases had fallen about 21% in 2 weeks prior to Jan. 25, according to an analysis by The New York Times.
“We’ve been saying since summer that we thought we’d see a peak in January, and I think that, at the national level, we’re around the peak,” Christopher J.L. Murray, MD, director of the institute, told the newspaper.
At the same time, public health officials are concerned that new coronavirus variants could lead to an increase again. Dr. Murray said the variants could “totally change the story.” If the more transmissible strains spread quickly, cases and deaths will surge once more.
“We’re definitely on a downward slope, but I’m worried that the new variants will throw us a curveball in late February or March,” Ms. Rivers told the newspaper.
A version of this article first appeared on WebMD.com.
As mutated strains of the coronavirus represent new threats in the pandemic, vaccine makers are racing to respond.
Moderna, whose two-dose vaccine has been authorized for use in the United States since Dec. 18, said on Jan. 25 that it is now investigating whether a third dose of the vaccine will better prevent the spread of a variant first seen in South Africa, while it also tests a new vaccine formula for the same purpose.
“Out of an abundance of caution and leveraging the flexibility of our mRNA platform, we are advancing an emerging variant booster candidate against the variant first identified in the Republic of South Africa into the clinic to determine if it will be more effective … against this and potentially future variants,” Moderna CEO Stéphane Bancel said in a statement. Pfizer and BioNTech, whose vaccine was also authorized in December, announced on Jan. 20 that their COVID-19 vaccine creates antibodies that could protect vaccine recipients from the U.K. variant B.1.1.7.
Moderna on Jan. 25 said laboratory tests have shown its COVID-19 vaccine could protect against the U.K. strain but that it is less effective – while still meeting efficacy benchmarks – against the strain identified in South Africa. Data from the study were submitted to a preprint server on Jan. 25 but have not yet been peer reviewed.
“This is not a problem yet,” Paul Offit, MD, director of the Vaccine Education Center at Children’s Hospital of Philadelphia, told CNBC.
“Prepare for it. Sequence these viruses,” he said. “Get ready just in case a variant emerges, which is resistant.”
There were at least 195 confirmed cases of patients infected with the U.K. variant, which is believed to be as much as 70% more transmissible, in the United States as of Jan. 22, according to the Centers for Disease Control and Prevention. No cases from the South African variant have been confirmed in the United States. To try to prevent the variant from entering the country, President Joe Biden plans to ban travel from South Africa, except for American citizens and permanent residents.
The U.S. has reported more than 25 million total COVID-19 cases, according to data from Johns Hopkins University, marking another major milestone during the pandemic.
That means about 1 in 13 people have contracted the virus, or about 7.6% of the U.S. population.
“Twenty-five million cases is an incredible scale of tragedy,” Caitlin Rivers, an epidemiologist at the Johns Hopkins Bloomberg School of Public Health, told The New York Times. She called the pandemic one of the worst public health crises in history.
After the first U.S. case was reported in January 2020, it took more than 9 months to reach 10 million cases in early November. Numbers rose during the holidays, and 10 million more cases were reported by the end of the year.
Following a major surge throughout January 2021, with a peak of more than 300,000 daily cases on some days, the U.S. reached 25 million in about 3 weeks.
Hospitalizations also peaked in early January, with more than 132,000 COVID-19 patients in hospitals across the country, according to the COVID Tracking Project. On Jan. 24, about 111,000 patients were hospitalized, which is the lowest since mid-December.
The U.S. has also reported nearly 420,000 deaths. As recently as the week starting Jan. 17, more than 4,400 deaths were reported in a single day, according to the COVID Tracking Project. Deaths are beginning to drop but still remain above 3,000 daily.
The University of Washington’s Institute for Health Metrics and Evaluation released a new projection Jan. 22 that said new cases would decline steadily in coming weeks. New COVID-19 cases had fallen about 21% in 2 weeks prior to Jan. 25, according to an analysis by The New York Times.
“We’ve been saying since summer that we thought we’d see a peak in January, and I think that, at the national level, we’re around the peak,” Christopher J.L. Murray, MD, director of the institute, told the newspaper.
At the same time, public health officials are concerned that new coronavirus variants could lead to an increase again. Dr. Murray said the variants could “totally change the story.” If the more transmissible strains spread quickly, cases and deaths will surge once more.
“We’re definitely on a downward slope, but I’m worried that the new variants will throw us a curveball in late February or March,” Ms. Rivers told the newspaper.
A version of this article first appeared on WebMD.com.
As mutated strains of the coronavirus represent new threats in the pandemic, vaccine makers are racing to respond.
Moderna, whose two-dose vaccine has been authorized for use in the United States since Dec. 18, said on Jan. 25 that it is now investigating whether a third dose of the vaccine will better prevent the spread of a variant first seen in South Africa, while it also tests a new vaccine formula for the same purpose.
“Out of an abundance of caution and leveraging the flexibility of our mRNA platform, we are advancing an emerging variant booster candidate against the variant first identified in the Republic of South Africa into the clinic to determine if it will be more effective … against this and potentially future variants,” Moderna CEO Stéphane Bancel said in a statement. Pfizer and BioNTech, whose vaccine was also authorized in December, announced on Jan. 20 that their COVID-19 vaccine creates antibodies that could protect vaccine recipients from the U.K. variant B.1.1.7.
Moderna on Jan. 25 said laboratory tests have shown its COVID-19 vaccine could protect against the U.K. strain but that it is less effective – while still meeting efficacy benchmarks – against the strain identified in South Africa. Data from the study were submitted to a preprint server on Jan. 25 but have not yet been peer reviewed.
“This is not a problem yet,” Paul Offit, MD, director of the Vaccine Education Center at Children’s Hospital of Philadelphia, told CNBC.
“Prepare for it. Sequence these viruses,” he said. “Get ready just in case a variant emerges, which is resistant.”
There were at least 195 confirmed cases of patients infected with the U.K. variant, which is believed to be as much as 70% more transmissible, in the United States as of Jan. 22, according to the Centers for Disease Control and Prevention. No cases from the South African variant have been confirmed in the United States. To try to prevent the variant from entering the country, President Joe Biden plans to ban travel from South Africa, except for American citizens and permanent residents.
The U.S. has reported more than 25 million total COVID-19 cases, according to data from Johns Hopkins University, marking another major milestone during the pandemic.
That means about 1 in 13 people have contracted the virus, or about 7.6% of the U.S. population.
“Twenty-five million cases is an incredible scale of tragedy,” Caitlin Rivers, an epidemiologist at the Johns Hopkins Bloomberg School of Public Health, told The New York Times. She called the pandemic one of the worst public health crises in history.
After the first U.S. case was reported in January 2020, it took more than 9 months to reach 10 million cases in early November. Numbers rose during the holidays, and 10 million more cases were reported by the end of the year.
Following a major surge throughout January 2021, with a peak of more than 300,000 daily cases on some days, the U.S. reached 25 million in about 3 weeks.
Hospitalizations also peaked in early January, with more than 132,000 COVID-19 patients in hospitals across the country, according to the COVID Tracking Project. On Jan. 24, about 111,000 patients were hospitalized, which is the lowest since mid-December.
The U.S. has also reported nearly 420,000 deaths. As recently as the week starting Jan. 17, more than 4,400 deaths were reported in a single day, according to the COVID Tracking Project. Deaths are beginning to drop but still remain above 3,000 daily.
The University of Washington’s Institute for Health Metrics and Evaluation released a new projection Jan. 22 that said new cases would decline steadily in coming weeks. New COVID-19 cases had fallen about 21% in 2 weeks prior to Jan. 25, according to an analysis by The New York Times.
“We’ve been saying since summer that we thought we’d see a peak in January, and I think that, at the national level, we’re around the peak,” Christopher J.L. Murray, MD, director of the institute, told the newspaper.
At the same time, public health officials are concerned that new coronavirus variants could lead to an increase again. Dr. Murray said the variants could “totally change the story.” If the more transmissible strains spread quickly, cases and deaths will surge once more.
“We’re definitely on a downward slope, but I’m worried that the new variants will throw us a curveball in late February or March,” Ms. Rivers told the newspaper.
A version of this article first appeared on WebMD.com.
Even patients with cancer in remission at risk for severe COVID-19
It’s been shown that hospitalized cancer patients and those undergoing active treatment are at high risk for severe COVID-19 complications. A new study shows that patients with cancer in remission are at higher risk, too.
For the study, investigators from the University of Pennsylvania, Philadelphia, analyzed 323 patients with SARS-CoV-2 infection in a research database with more than 4,800 patients. About 20% of database patients were Black, but they accounted for almost 65% of the infections, reflecting previous reports of increased risk for COVID among Black people.
A total of 67 of the infected patients had cancer, including 18 patients with active cancer and 49 patients whose cancer was in remission. After adjusting for demographics, smoking status, and comorbidities, a diagnosis of cancer more than doubled the odds of hospitalization and increased the odds of 30-day mortality nearly sixfold.
Worse outcomes were more strongly associated with active cancer, but patients whose cancer was in remission were also at higher risk than patients who did not have cancer.
It’s not only “patients hospitalized or on treatment ... all oncology patients need to take significant precautions during the pandemic to protect themselves,” senior investigator Kara Maxwell, MD, PhD, hematologist/oncologist and assistant professor at the University of Pennsylvania, said in a press release.
The study was published online on Jan. 21 in JNCI Cancer Spectrum.
The good news is that steps to prevent SARS-CoV-2 infection work, suggests a second report from the University of Pennsylvania. Among 124 cancer patients who underwent outpatient infusions from May to October 2020, not a single one experienced seroconversion over a median of 13 clinical visits. That second study was published on Jan. 16 in medRxiv and is pending peer review.
The zero seroconversion rate likely reflects “the success of transmission mitigation measures within health care facilities,” wrote investigators led by Lova Sun, MD, a hematology/oncology fellow at the University of Pennsylvania.
Like many institutions, the University of Pennsylvania Health System (Penn Medicine) is aggressive in protecting outpatients against the virus, the authors wrote. Among other steps, patients are queried about symptoms and contacts before their office visit, and their temperature is taken when they come in. Masks are worn, check-in is contactless, the number of visitors is limited, and patients who test positive are treated in a separate space.
In addition, patients in the study also reported that they wore masks and practiced social distancing in their daily lives.
Approached for comment, hematologist/oncologist Charles Shapiro, MD, a professor at the Icahn School of Medicine at Mount Sinai and director of translational breast cancer research at Mount Sinai Hospital, both in New York, said he wasn’t surprised that the prevention measures followed at Penn Medicine work. They are very similar to the measures followed at Mount Sinai oncology clinics, and “there’ve been very few COVID cases in our shop,” he added.
The bigger take-home message from both studies is that cancer patients, regardless of their age or if they are in remission, should be prioritized for vaccination against COVID-19, which is the best way to mitigate risk. “I strongly urge my patients to get it” if they can, he said.
The problem in New York is that immunizations are largely limited to people aged 65 years and older. Younger cancer patients are left out, and access has been spotty for all patients. “Vaccine is available one day, then not the next. It’s disheartening,” Dr. Shapiro said in an interview. “Hopefully, with the new administration, this will smooth out,” and the age limit will drop.
The study was supported by the National Institutes of Health, among other organizations. Dr. Lova, Dr. Maxwell, and Dr. Shapiro have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s been shown that hospitalized cancer patients and those undergoing active treatment are at high risk for severe COVID-19 complications. A new study shows that patients with cancer in remission are at higher risk, too.
For the study, investigators from the University of Pennsylvania, Philadelphia, analyzed 323 patients with SARS-CoV-2 infection in a research database with more than 4,800 patients. About 20% of database patients were Black, but they accounted for almost 65% of the infections, reflecting previous reports of increased risk for COVID among Black people.
A total of 67 of the infected patients had cancer, including 18 patients with active cancer and 49 patients whose cancer was in remission. After adjusting for demographics, smoking status, and comorbidities, a diagnosis of cancer more than doubled the odds of hospitalization and increased the odds of 30-day mortality nearly sixfold.
Worse outcomes were more strongly associated with active cancer, but patients whose cancer was in remission were also at higher risk than patients who did not have cancer.
It’s not only “patients hospitalized or on treatment ... all oncology patients need to take significant precautions during the pandemic to protect themselves,” senior investigator Kara Maxwell, MD, PhD, hematologist/oncologist and assistant professor at the University of Pennsylvania, said in a press release.
The study was published online on Jan. 21 in JNCI Cancer Spectrum.
The good news is that steps to prevent SARS-CoV-2 infection work, suggests a second report from the University of Pennsylvania. Among 124 cancer patients who underwent outpatient infusions from May to October 2020, not a single one experienced seroconversion over a median of 13 clinical visits. That second study was published on Jan. 16 in medRxiv and is pending peer review.
The zero seroconversion rate likely reflects “the success of transmission mitigation measures within health care facilities,” wrote investigators led by Lova Sun, MD, a hematology/oncology fellow at the University of Pennsylvania.
Like many institutions, the University of Pennsylvania Health System (Penn Medicine) is aggressive in protecting outpatients against the virus, the authors wrote. Among other steps, patients are queried about symptoms and contacts before their office visit, and their temperature is taken when they come in. Masks are worn, check-in is contactless, the number of visitors is limited, and patients who test positive are treated in a separate space.
In addition, patients in the study also reported that they wore masks and practiced social distancing in their daily lives.
Approached for comment, hematologist/oncologist Charles Shapiro, MD, a professor at the Icahn School of Medicine at Mount Sinai and director of translational breast cancer research at Mount Sinai Hospital, both in New York, said he wasn’t surprised that the prevention measures followed at Penn Medicine work. They are very similar to the measures followed at Mount Sinai oncology clinics, and “there’ve been very few COVID cases in our shop,” he added.
The bigger take-home message from both studies is that cancer patients, regardless of their age or if they are in remission, should be prioritized for vaccination against COVID-19, which is the best way to mitigate risk. “I strongly urge my patients to get it” if they can, he said.
The problem in New York is that immunizations are largely limited to people aged 65 years and older. Younger cancer patients are left out, and access has been spotty for all patients. “Vaccine is available one day, then not the next. It’s disheartening,” Dr. Shapiro said in an interview. “Hopefully, with the new administration, this will smooth out,” and the age limit will drop.
The study was supported by the National Institutes of Health, among other organizations. Dr. Lova, Dr. Maxwell, and Dr. Shapiro have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s been shown that hospitalized cancer patients and those undergoing active treatment are at high risk for severe COVID-19 complications. A new study shows that patients with cancer in remission are at higher risk, too.
For the study, investigators from the University of Pennsylvania, Philadelphia, analyzed 323 patients with SARS-CoV-2 infection in a research database with more than 4,800 patients. About 20% of database patients were Black, but they accounted for almost 65% of the infections, reflecting previous reports of increased risk for COVID among Black people.
A total of 67 of the infected patients had cancer, including 18 patients with active cancer and 49 patients whose cancer was in remission. After adjusting for demographics, smoking status, and comorbidities, a diagnosis of cancer more than doubled the odds of hospitalization and increased the odds of 30-day mortality nearly sixfold.
Worse outcomes were more strongly associated with active cancer, but patients whose cancer was in remission were also at higher risk than patients who did not have cancer.
It’s not only “patients hospitalized or on treatment ... all oncology patients need to take significant precautions during the pandemic to protect themselves,” senior investigator Kara Maxwell, MD, PhD, hematologist/oncologist and assistant professor at the University of Pennsylvania, said in a press release.
The study was published online on Jan. 21 in JNCI Cancer Spectrum.
The good news is that steps to prevent SARS-CoV-2 infection work, suggests a second report from the University of Pennsylvania. Among 124 cancer patients who underwent outpatient infusions from May to October 2020, not a single one experienced seroconversion over a median of 13 clinical visits. That second study was published on Jan. 16 in medRxiv and is pending peer review.
The zero seroconversion rate likely reflects “the success of transmission mitigation measures within health care facilities,” wrote investigators led by Lova Sun, MD, a hematology/oncology fellow at the University of Pennsylvania.
Like many institutions, the University of Pennsylvania Health System (Penn Medicine) is aggressive in protecting outpatients against the virus, the authors wrote. Among other steps, patients are queried about symptoms and contacts before their office visit, and their temperature is taken when they come in. Masks are worn, check-in is contactless, the number of visitors is limited, and patients who test positive are treated in a separate space.
In addition, patients in the study also reported that they wore masks and practiced social distancing in their daily lives.
Approached for comment, hematologist/oncologist Charles Shapiro, MD, a professor at the Icahn School of Medicine at Mount Sinai and director of translational breast cancer research at Mount Sinai Hospital, both in New York, said he wasn’t surprised that the prevention measures followed at Penn Medicine work. They are very similar to the measures followed at Mount Sinai oncology clinics, and “there’ve been very few COVID cases in our shop,” he added.
The bigger take-home message from both studies is that cancer patients, regardless of their age or if they are in remission, should be prioritized for vaccination against COVID-19, which is the best way to mitigate risk. “I strongly urge my patients to get it” if they can, he said.
The problem in New York is that immunizations are largely limited to people aged 65 years and older. Younger cancer patients are left out, and access has been spotty for all patients. “Vaccine is available one day, then not the next. It’s disheartening,” Dr. Shapiro said in an interview. “Hopefully, with the new administration, this will smooth out,” and the age limit will drop.
The study was supported by the National Institutes of Health, among other organizations. Dr. Lova, Dr. Maxwell, and Dr. Shapiro have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
More than one-third of COVID-19 infections are asymptomatic: Review
A systematic review suggests at least one-third of SARS-CoV-2 infections occur in people who never develop symptoms, providing strong evidence for the prevalence of asymptomatic infections.
The finding that nearly one in three infected people remain symptom free suggests testing should be changed, the investigators noted.
“To reduce transmission from people who are presymptomatic or asymptomatic, we need to shift our testing focus to at-home screening,” lead author Daniel Oran, AM, said in an interview. “Inexpensive rapid antigen tests, provided to millions of people for frequent use, could help us significantly reduce the spread of the virus.”
The systematic review was published online Jan. 22 in Annals of Internal Medicine.
The findings come at a dire time when the official number of COVID-19 cases in the United States exceeds 25 million for the first time. Public health officials have raised concerns about more transmissible, and possibly more deadly, variants of SARS-CoV-2, while a new presidential administration tries to meet the challenge of improving vaccine distribution and acceptance rates.
The results also build on earlier findings from the same research team – Mr. Oran and senior author Eric Topol, MD – that published a review article looking at asymptomatic COVID-19 cases. Even though initial data were more limited, they likewise suggested a broader scope of testing is warranted, pointing out that asymptomatic individuals can transmit SARS-CoV-2 for up to 14 days. Dr. Topol is also editor in chief of Medscape.
In the current systematic review, the highest-quality evidence comes from large studies in England and Spain. The nationally representative evidence included serologic surveys from more than 365,000 people in England and more than 61,000 in Spain. When analyzed separately, about the same proportion of asymptomatic cases emerged: 32.4% in England and 33% in Spain.
“It was really remarkable to find that nationwide antibody testing studies in England and Spain – including hundreds of thousands of people – produced nearly identical results: About one-third of the SARS-CoV-2 infections were completely asymptomatic,” said Mr. Oran, a researcher at Scripps Research Translational Institute in La Jolla, Calif.
The systematic review included 43 studies with PCR testing for active SARS-CoV-2 infection and another 18 with antibody results that indicated present or previous infection. The studies were published up until Nov. 17, 2020.
An appreciation for asymptomatic transmission of SARS-CoV-2 infection has come a long way from initial dismissals about its importance, Dr. Topol noted via Twitter. “When Dr. @camilla_rothe reported an asymptomatic transmission a year ago, the @NEJM report was refuted and disparaged. She was later named a TIME 100 Person of the Year.”
Not symptomatic vs. never symptomatic
The term “asymptomatic” could be misleading because some people in this group do progress to develop signs of infection. This “presymptomatic” group of patients is likely a minority, the authors noted. Longitudinal studies indicate that about three-quarters of people who are asymptomatic with SARS-CoV-2 remain so.
Dr. Topol anticipated the one-third asymptomatic finding could draw some feedback about distinguishing asymptomatic from presymptomatic individuals. He tweeted, “Some will argue that there is admixture with presymptomatic cases, but review of all the data supports this estimate as being a conservative one.”
The heterogeneity of the settings, populations and other features of the studies prevented the authors from performing a meta-analysis of the findings.
Home is where the test is
Based on their findings, Mr. Oran and Dr. Topol believe “that COVID-19 control strategies must be altered, taking into account the prevalence and transmission risk of asymptomatic SARS-CoV-2 infection.” They suggested frequent use of inexpensive, rapid home tests to identify people who are asymptomatic or presymptomatic, along with programs and housing provided by the government to offer financial assistance and allow this group of people to isolate themselves.
Further research is warranted to determine if and how well vaccines for SARS-CoV-2 prevent asymptomatic infection.
Dr. Topol and Mr. Oran created a short video to highlight the findings from their systematic review.
The study was supported by a grant from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
A systematic review suggests at least one-third of SARS-CoV-2 infections occur in people who never develop symptoms, providing strong evidence for the prevalence of asymptomatic infections.
The finding that nearly one in three infected people remain symptom free suggests testing should be changed, the investigators noted.
“To reduce transmission from people who are presymptomatic or asymptomatic, we need to shift our testing focus to at-home screening,” lead author Daniel Oran, AM, said in an interview. “Inexpensive rapid antigen tests, provided to millions of people for frequent use, could help us significantly reduce the spread of the virus.”
The systematic review was published online Jan. 22 in Annals of Internal Medicine.
The findings come at a dire time when the official number of COVID-19 cases in the United States exceeds 25 million for the first time. Public health officials have raised concerns about more transmissible, and possibly more deadly, variants of SARS-CoV-2, while a new presidential administration tries to meet the challenge of improving vaccine distribution and acceptance rates.
The results also build on earlier findings from the same research team – Mr. Oran and senior author Eric Topol, MD – that published a review article looking at asymptomatic COVID-19 cases. Even though initial data were more limited, they likewise suggested a broader scope of testing is warranted, pointing out that asymptomatic individuals can transmit SARS-CoV-2 for up to 14 days. Dr. Topol is also editor in chief of Medscape.
In the current systematic review, the highest-quality evidence comes from large studies in England and Spain. The nationally representative evidence included serologic surveys from more than 365,000 people in England and more than 61,000 in Spain. When analyzed separately, about the same proportion of asymptomatic cases emerged: 32.4% in England and 33% in Spain.
“It was really remarkable to find that nationwide antibody testing studies in England and Spain – including hundreds of thousands of people – produced nearly identical results: About one-third of the SARS-CoV-2 infections were completely asymptomatic,” said Mr. Oran, a researcher at Scripps Research Translational Institute in La Jolla, Calif.
The systematic review included 43 studies with PCR testing for active SARS-CoV-2 infection and another 18 with antibody results that indicated present or previous infection. The studies were published up until Nov. 17, 2020.
An appreciation for asymptomatic transmission of SARS-CoV-2 infection has come a long way from initial dismissals about its importance, Dr. Topol noted via Twitter. “When Dr. @camilla_rothe reported an asymptomatic transmission a year ago, the @NEJM report was refuted and disparaged. She was later named a TIME 100 Person of the Year.”
Not symptomatic vs. never symptomatic
The term “asymptomatic” could be misleading because some people in this group do progress to develop signs of infection. This “presymptomatic” group of patients is likely a minority, the authors noted. Longitudinal studies indicate that about three-quarters of people who are asymptomatic with SARS-CoV-2 remain so.
Dr. Topol anticipated the one-third asymptomatic finding could draw some feedback about distinguishing asymptomatic from presymptomatic individuals. He tweeted, “Some will argue that there is admixture with presymptomatic cases, but review of all the data supports this estimate as being a conservative one.”
The heterogeneity of the settings, populations and other features of the studies prevented the authors from performing a meta-analysis of the findings.
Home is where the test is
Based on their findings, Mr. Oran and Dr. Topol believe “that COVID-19 control strategies must be altered, taking into account the prevalence and transmission risk of asymptomatic SARS-CoV-2 infection.” They suggested frequent use of inexpensive, rapid home tests to identify people who are asymptomatic or presymptomatic, along with programs and housing provided by the government to offer financial assistance and allow this group of people to isolate themselves.
Further research is warranted to determine if and how well vaccines for SARS-CoV-2 prevent asymptomatic infection.
Dr. Topol and Mr. Oran created a short video to highlight the findings from their systematic review.
The study was supported by a grant from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
A systematic review suggests at least one-third of SARS-CoV-2 infections occur in people who never develop symptoms, providing strong evidence for the prevalence of asymptomatic infections.
The finding that nearly one in three infected people remain symptom free suggests testing should be changed, the investigators noted.
“To reduce transmission from people who are presymptomatic or asymptomatic, we need to shift our testing focus to at-home screening,” lead author Daniel Oran, AM, said in an interview. “Inexpensive rapid antigen tests, provided to millions of people for frequent use, could help us significantly reduce the spread of the virus.”
The systematic review was published online Jan. 22 in Annals of Internal Medicine.
The findings come at a dire time when the official number of COVID-19 cases in the United States exceeds 25 million for the first time. Public health officials have raised concerns about more transmissible, and possibly more deadly, variants of SARS-CoV-2, while a new presidential administration tries to meet the challenge of improving vaccine distribution and acceptance rates.
The results also build on earlier findings from the same research team – Mr. Oran and senior author Eric Topol, MD – that published a review article looking at asymptomatic COVID-19 cases. Even though initial data were more limited, they likewise suggested a broader scope of testing is warranted, pointing out that asymptomatic individuals can transmit SARS-CoV-2 for up to 14 days. Dr. Topol is also editor in chief of Medscape.
In the current systematic review, the highest-quality evidence comes from large studies in England and Spain. The nationally representative evidence included serologic surveys from more than 365,000 people in England and more than 61,000 in Spain. When analyzed separately, about the same proportion of asymptomatic cases emerged: 32.4% in England and 33% in Spain.
“It was really remarkable to find that nationwide antibody testing studies in England and Spain – including hundreds of thousands of people – produced nearly identical results: About one-third of the SARS-CoV-2 infections were completely asymptomatic,” said Mr. Oran, a researcher at Scripps Research Translational Institute in La Jolla, Calif.
The systematic review included 43 studies with PCR testing for active SARS-CoV-2 infection and another 18 with antibody results that indicated present or previous infection. The studies were published up until Nov. 17, 2020.
An appreciation for asymptomatic transmission of SARS-CoV-2 infection has come a long way from initial dismissals about its importance, Dr. Topol noted via Twitter. “When Dr. @camilla_rothe reported an asymptomatic transmission a year ago, the @NEJM report was refuted and disparaged. She was later named a TIME 100 Person of the Year.”
Not symptomatic vs. never symptomatic
The term “asymptomatic” could be misleading because some people in this group do progress to develop signs of infection. This “presymptomatic” group of patients is likely a minority, the authors noted. Longitudinal studies indicate that about three-quarters of people who are asymptomatic with SARS-CoV-2 remain so.
Dr. Topol anticipated the one-third asymptomatic finding could draw some feedback about distinguishing asymptomatic from presymptomatic individuals. He tweeted, “Some will argue that there is admixture with presymptomatic cases, but review of all the data supports this estimate as being a conservative one.”
The heterogeneity of the settings, populations and other features of the studies prevented the authors from performing a meta-analysis of the findings.
Home is where the test is
Based on their findings, Mr. Oran and Dr. Topol believe “that COVID-19 control strategies must be altered, taking into account the prevalence and transmission risk of asymptomatic SARS-CoV-2 infection.” They suggested frequent use of inexpensive, rapid home tests to identify people who are asymptomatic or presymptomatic, along with programs and housing provided by the government to offer financial assistance and allow this group of people to isolate themselves.
Further research is warranted to determine if and how well vaccines for SARS-CoV-2 prevent asymptomatic infection.
Dr. Topol and Mr. Oran created a short video to highlight the findings from their systematic review.
The study was supported by a grant from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Palliative care underused in pulmonary arterial hypertension
of more than 30,000 hospital admissions has found.
“Specialty palliative care services (PCS) are present in the vast majority of hospitals with more than 300 beds, and PCS use for patients who are facing serious illness with potentially life-limiting prognoses increasingly is becoming the standard of care,” wrote Vidhu Anand, MD, of the Mayo Clinic, Rochester, Minn., and colleagues. But despite experts recommending PCS in pulmonary arterial hypertension (PAH), data on the use of palliative care referrals for PAH patients are limited, they added.
In a study published in Chest, the researchers used the National (Nationwide) Inpatient Sample to identify 30,495 admissions with a primary diagnosis of PAH between 2001 through 2017. The primary outcome was the use of PCS in these patients.
Overall, inpatient use of PCS was 2.2%, but that figure increased from 0.5% in 2001 to 7.6% in 2017, representing a fivefold increase over the study period, with a significant increase after 2009. The reason for this notable increase remains unclear; however, “it may be related to recognition of palliative care and hospice as a medical subspecialty with board certification in 2008 or identification of palliative care by the National Priorities Partnership as one of six priority areas in 2008,” the researchers said.
Incorporating palliative care in a treatment strategy
The perception of PCS as an element of treatment plans for patients with severe lung disease, and not only as end-of-life care, has certainly increased in recent years, Sachin Gupta, MD, FCCP, said in an interview.
Dr. Gupta is a pulmonologist practicing in the San Francisco Bay area, and he did not take part in the study. He recommended early integration of PCS treating patients with PAH. “I have frequently asked PCS to aid early on during inpatient admission with PAH patients for pain management, as well as for aiding in POLST [Physician Orders for Life-Sustaining Treatment] paperwork to be completed. Increased age and comorbidities are certainly risk factors themselves for a longer hospital course and worse outcomes; in addition, in center-based PAH care there are more means available by which to give a patient with right heart failure that ‘one last shot’ – an opportunity for a longer life. I truly think it is a relationship with the patient, built from the outpatient pulmonary hypertension clinic, that allows the treating physician to have a better sense of a patient’s quality of life longitudinally, and to have the candid conversation when things begin to decline.”
Which patients receive PCS?
The study found that socioeconomic factors, and the severity of illness, are the drivers of PCS referrals. In a multivariate analysis, independent predictors of PCS use included white race, private insurance, and higher socioeconomic status. Additional independent predictors of PCS use included increased comorbidities, admission to an urban hospital, admission to a small hospital, presence of heart failure and cardiogenic shock, acute noncardiac organ failure, and use of extracorporeal membrane oxygenation and noninvasive mechanical ventilation, the researchers noted.
Patients who received PCS consultation were significantly more likely than those not receiving PCS to have DNR status (46.2% vs. 1.8%), longer length of hospital stay (12.9 days vs. 7.2 days), higher hospitalization costs $130,434 vs. $56,499), and higher in-hospital mortality (52.8% vs. 6.4%; P < .001 for all).
Some patients refuse PCS and others are not offered PCS. Dr. Gupta noted that it should be no surprise that not all patients are comfortable with the idea of a PCS referral. “Fear, misunderstanding, and cultural beliefs may be individually or together at the root of resistance to PCS. Their reluctance may be due to a ‘false narrative’ of the purpose of palliative care. The conception of PCS being for end-of-life care may be the result of personal experiences or experience with loved ones. Occasionally, a patient equates PCS with access to narcotics (‘knock me out’), which they may or may not want. I try to reassure patients that there will be no coercion for anything they do not want, and at the end of the day, the medical team is the main driver of their care, not the palliative service.”
Actively drug-abusing PAH patients are a particular challenge, said Dr. Gupta. These patients often refuse palliative care referral both as inpatients and outpatients. “Such patients are an enigma for many PAH-treating physicians as they may survive to discharge, despite a terrible prognosis predicted by their testing.”
In addition, patients in whom organ transplantation is being pursued may not receive timely PCS, he said. “It can be an absolute challenge to bring such patients to the finish line (transplantation), and the timing of PCS referral is often deferred. Arguably, for better or worse, such patients refuse, or more often are not offered, PCS as inpatients while there is still a chance organ transplantation is a viable option for them.”
The use of PCS in less than 10% of PAH admissions is similar to previous studies showing low use of PCS for patients with acute myocardial infarction, heart failure, and COPD, the researchers noted. However, “Given the high morbidity and mortality associated with PAH even after hospitalization, hospital admissions without PCS use represent a missed opportunity,” the investigators wrote.
Early warning on the need for PCS
Increasing PCS referrals for PAH patients requires clinicians to be proactive, Dr. Gupta stressed. “Pulmonologists, especially those managing pulmonary hypertension outpatients without the aid of a PAH center, should remain vigilant at all routine visits to calculate a patient’s risk score (i.e. REVEAL 2.0 risk calculator) to stratify their risk of 1-year mortality. Based on this assessment, shared decision making can help guide next steps including early outpatient PCS involvement for those at high risk. I also calculate a patient’s risk score, based on the data I have, when PAH patients are admitted to the hospital. Occasionally, a patient who I initially think is moderate risk turns out to be high risk when I calculate their risk score. In such high-risk patients, PCS consultation should certainly be considered early on.”
The study findings were limited by several factors including the possible coding errors associated with use of discharge diagnosis, lack of data on medication and the cause of PAH, and lack of information on the reasons for PCS referrals, the researchers noted. However, the results “addressed an important knowledge gap highlighting the national use of PCS in PAH,” they said. Further research is needed to address disparities and the integration of PCS into PAH care protocols, they added.
The researchers had no financial conflicts to disclose. The study received no outside funding; one coauthor disclosed support from the National Center for Advancing Translational Sciences Clinical and Translational Science.
of more than 30,000 hospital admissions has found.
“Specialty palliative care services (PCS) are present in the vast majority of hospitals with more than 300 beds, and PCS use for patients who are facing serious illness with potentially life-limiting prognoses increasingly is becoming the standard of care,” wrote Vidhu Anand, MD, of the Mayo Clinic, Rochester, Minn., and colleagues. But despite experts recommending PCS in pulmonary arterial hypertension (PAH), data on the use of palliative care referrals for PAH patients are limited, they added.
In a study published in Chest, the researchers used the National (Nationwide) Inpatient Sample to identify 30,495 admissions with a primary diagnosis of PAH between 2001 through 2017. The primary outcome was the use of PCS in these patients.
Overall, inpatient use of PCS was 2.2%, but that figure increased from 0.5% in 2001 to 7.6% in 2017, representing a fivefold increase over the study period, with a significant increase after 2009. The reason for this notable increase remains unclear; however, “it may be related to recognition of palliative care and hospice as a medical subspecialty with board certification in 2008 or identification of palliative care by the National Priorities Partnership as one of six priority areas in 2008,” the researchers said.
Incorporating palliative care in a treatment strategy
The perception of PCS as an element of treatment plans for patients with severe lung disease, and not only as end-of-life care, has certainly increased in recent years, Sachin Gupta, MD, FCCP, said in an interview.
Dr. Gupta is a pulmonologist practicing in the San Francisco Bay area, and he did not take part in the study. He recommended early integration of PCS treating patients with PAH. “I have frequently asked PCS to aid early on during inpatient admission with PAH patients for pain management, as well as for aiding in POLST [Physician Orders for Life-Sustaining Treatment] paperwork to be completed. Increased age and comorbidities are certainly risk factors themselves for a longer hospital course and worse outcomes; in addition, in center-based PAH care there are more means available by which to give a patient with right heart failure that ‘one last shot’ – an opportunity for a longer life. I truly think it is a relationship with the patient, built from the outpatient pulmonary hypertension clinic, that allows the treating physician to have a better sense of a patient’s quality of life longitudinally, and to have the candid conversation when things begin to decline.”
Which patients receive PCS?
The study found that socioeconomic factors, and the severity of illness, are the drivers of PCS referrals. In a multivariate analysis, independent predictors of PCS use included white race, private insurance, and higher socioeconomic status. Additional independent predictors of PCS use included increased comorbidities, admission to an urban hospital, admission to a small hospital, presence of heart failure and cardiogenic shock, acute noncardiac organ failure, and use of extracorporeal membrane oxygenation and noninvasive mechanical ventilation, the researchers noted.
Patients who received PCS consultation were significantly more likely than those not receiving PCS to have DNR status (46.2% vs. 1.8%), longer length of hospital stay (12.9 days vs. 7.2 days), higher hospitalization costs $130,434 vs. $56,499), and higher in-hospital mortality (52.8% vs. 6.4%; P < .001 for all).
Some patients refuse PCS and others are not offered PCS. Dr. Gupta noted that it should be no surprise that not all patients are comfortable with the idea of a PCS referral. “Fear, misunderstanding, and cultural beliefs may be individually or together at the root of resistance to PCS. Their reluctance may be due to a ‘false narrative’ of the purpose of palliative care. The conception of PCS being for end-of-life care may be the result of personal experiences or experience with loved ones. Occasionally, a patient equates PCS with access to narcotics (‘knock me out’), which they may or may not want. I try to reassure patients that there will be no coercion for anything they do not want, and at the end of the day, the medical team is the main driver of their care, not the palliative service.”
Actively drug-abusing PAH patients are a particular challenge, said Dr. Gupta. These patients often refuse palliative care referral both as inpatients and outpatients. “Such patients are an enigma for many PAH-treating physicians as they may survive to discharge, despite a terrible prognosis predicted by their testing.”
In addition, patients in whom organ transplantation is being pursued may not receive timely PCS, he said. “It can be an absolute challenge to bring such patients to the finish line (transplantation), and the timing of PCS referral is often deferred. Arguably, for better or worse, such patients refuse, or more often are not offered, PCS as inpatients while there is still a chance organ transplantation is a viable option for them.”
The use of PCS in less than 10% of PAH admissions is similar to previous studies showing low use of PCS for patients with acute myocardial infarction, heart failure, and COPD, the researchers noted. However, “Given the high morbidity and mortality associated with PAH even after hospitalization, hospital admissions without PCS use represent a missed opportunity,” the investigators wrote.
Early warning on the need for PCS
Increasing PCS referrals for PAH patients requires clinicians to be proactive, Dr. Gupta stressed. “Pulmonologists, especially those managing pulmonary hypertension outpatients without the aid of a PAH center, should remain vigilant at all routine visits to calculate a patient’s risk score (i.e. REVEAL 2.0 risk calculator) to stratify their risk of 1-year mortality. Based on this assessment, shared decision making can help guide next steps including early outpatient PCS involvement for those at high risk. I also calculate a patient’s risk score, based on the data I have, when PAH patients are admitted to the hospital. Occasionally, a patient who I initially think is moderate risk turns out to be high risk when I calculate their risk score. In such high-risk patients, PCS consultation should certainly be considered early on.”
The study findings were limited by several factors including the possible coding errors associated with use of discharge diagnosis, lack of data on medication and the cause of PAH, and lack of information on the reasons for PCS referrals, the researchers noted. However, the results “addressed an important knowledge gap highlighting the national use of PCS in PAH,” they said. Further research is needed to address disparities and the integration of PCS into PAH care protocols, they added.
The researchers had no financial conflicts to disclose. The study received no outside funding; one coauthor disclosed support from the National Center for Advancing Translational Sciences Clinical and Translational Science.
of more than 30,000 hospital admissions has found.
“Specialty palliative care services (PCS) are present in the vast majority of hospitals with more than 300 beds, and PCS use for patients who are facing serious illness with potentially life-limiting prognoses increasingly is becoming the standard of care,” wrote Vidhu Anand, MD, of the Mayo Clinic, Rochester, Minn., and colleagues. But despite experts recommending PCS in pulmonary arterial hypertension (PAH), data on the use of palliative care referrals for PAH patients are limited, they added.
In a study published in Chest, the researchers used the National (Nationwide) Inpatient Sample to identify 30,495 admissions with a primary diagnosis of PAH between 2001 through 2017. The primary outcome was the use of PCS in these patients.
Overall, inpatient use of PCS was 2.2%, but that figure increased from 0.5% in 2001 to 7.6% in 2017, representing a fivefold increase over the study period, with a significant increase after 2009. The reason for this notable increase remains unclear; however, “it may be related to recognition of palliative care and hospice as a medical subspecialty with board certification in 2008 or identification of palliative care by the National Priorities Partnership as one of six priority areas in 2008,” the researchers said.
Incorporating palliative care in a treatment strategy
The perception of PCS as an element of treatment plans for patients with severe lung disease, and not only as end-of-life care, has certainly increased in recent years, Sachin Gupta, MD, FCCP, said in an interview.
Dr. Gupta is a pulmonologist practicing in the San Francisco Bay area, and he did not take part in the study. He recommended early integration of PCS treating patients with PAH. “I have frequently asked PCS to aid early on during inpatient admission with PAH patients for pain management, as well as for aiding in POLST [Physician Orders for Life-Sustaining Treatment] paperwork to be completed. Increased age and comorbidities are certainly risk factors themselves for a longer hospital course and worse outcomes; in addition, in center-based PAH care there are more means available by which to give a patient with right heart failure that ‘one last shot’ – an opportunity for a longer life. I truly think it is a relationship with the patient, built from the outpatient pulmonary hypertension clinic, that allows the treating physician to have a better sense of a patient’s quality of life longitudinally, and to have the candid conversation when things begin to decline.”
Which patients receive PCS?
The study found that socioeconomic factors, and the severity of illness, are the drivers of PCS referrals. In a multivariate analysis, independent predictors of PCS use included white race, private insurance, and higher socioeconomic status. Additional independent predictors of PCS use included increased comorbidities, admission to an urban hospital, admission to a small hospital, presence of heart failure and cardiogenic shock, acute noncardiac organ failure, and use of extracorporeal membrane oxygenation and noninvasive mechanical ventilation, the researchers noted.
Patients who received PCS consultation were significantly more likely than those not receiving PCS to have DNR status (46.2% vs. 1.8%), longer length of hospital stay (12.9 days vs. 7.2 days), higher hospitalization costs $130,434 vs. $56,499), and higher in-hospital mortality (52.8% vs. 6.4%; P < .001 for all).
Some patients refuse PCS and others are not offered PCS. Dr. Gupta noted that it should be no surprise that not all patients are comfortable with the idea of a PCS referral. “Fear, misunderstanding, and cultural beliefs may be individually or together at the root of resistance to PCS. Their reluctance may be due to a ‘false narrative’ of the purpose of palliative care. The conception of PCS being for end-of-life care may be the result of personal experiences or experience with loved ones. Occasionally, a patient equates PCS with access to narcotics (‘knock me out’), which they may or may not want. I try to reassure patients that there will be no coercion for anything they do not want, and at the end of the day, the medical team is the main driver of their care, not the palliative service.”
Actively drug-abusing PAH patients are a particular challenge, said Dr. Gupta. These patients often refuse palliative care referral both as inpatients and outpatients. “Such patients are an enigma for many PAH-treating physicians as they may survive to discharge, despite a terrible prognosis predicted by their testing.”
In addition, patients in whom organ transplantation is being pursued may not receive timely PCS, he said. “It can be an absolute challenge to bring such patients to the finish line (transplantation), and the timing of PCS referral is often deferred. Arguably, for better or worse, such patients refuse, or more often are not offered, PCS as inpatients while there is still a chance organ transplantation is a viable option for them.”
The use of PCS in less than 10% of PAH admissions is similar to previous studies showing low use of PCS for patients with acute myocardial infarction, heart failure, and COPD, the researchers noted. However, “Given the high morbidity and mortality associated with PAH even after hospitalization, hospital admissions without PCS use represent a missed opportunity,” the investigators wrote.
Early warning on the need for PCS
Increasing PCS referrals for PAH patients requires clinicians to be proactive, Dr. Gupta stressed. “Pulmonologists, especially those managing pulmonary hypertension outpatients without the aid of a PAH center, should remain vigilant at all routine visits to calculate a patient’s risk score (i.e. REVEAL 2.0 risk calculator) to stratify their risk of 1-year mortality. Based on this assessment, shared decision making can help guide next steps including early outpatient PCS involvement for those at high risk. I also calculate a patient’s risk score, based on the data I have, when PAH patients are admitted to the hospital. Occasionally, a patient who I initially think is moderate risk turns out to be high risk when I calculate their risk score. In such high-risk patients, PCS consultation should certainly be considered early on.”
The study findings were limited by several factors including the possible coding errors associated with use of discharge diagnosis, lack of data on medication and the cause of PAH, and lack of information on the reasons for PCS referrals, the researchers noted. However, the results “addressed an important knowledge gap highlighting the national use of PCS in PAH,” they said. Further research is needed to address disparities and the integration of PCS into PAH care protocols, they added.
The researchers had no financial conflicts to disclose. The study received no outside funding; one coauthor disclosed support from the National Center for Advancing Translational Sciences Clinical and Translational Science.
FROM CHEST