User login
Hospital leadership lessons in the era of COVID-19
The year 2020 has brought the COVID-19 pandemic and civil unrest and protests, which have resulted in unprecedented health care challenges to hospitals and clinics. The daunting prospect of a fall influenza season has hospital staff and administrators looking ahead to still greater challenges.
This year of crisis has put even greater emphasis on leadership in hospitals, as patients, clinicians, and staff look for direction in the face of uncertainty and stress. But hospital leaders often arrive at their positions unprepared for their roles, according to Leonard Marcus, PhD, director of the Program for Health Care Negotiation and Conflict Resolution at Harvard T.H. Chan School of Public Health, Boston.
“Many times what happens in medicine is that someone with the greatest technical skills or greatest clinical skills emerges to be leader of a department, or a group, or a hospital, without having really paid attention to how they can build their leadership skills,” Dr. Marcus said during the 2020 Society of Hospital Medicine Leadership Virtual Seminar, held online Sept. 16-17.
Over 2 days, Dr. Marcus discussed the complex environments faced by hospital leaders, and some of the tools and strategies that can be used to maintain calm, problem-solve, and chart a course ahead.
He emphasized that hospitals and medical systems are complex, nonlinear organizations, which could be swept up by change in the form of mergers, financial policies, patient surges due to local emergencies, or pandemics.
“Complexity has to be central to how you think about leadership. If you think you can control everything, that doesn’t work that well,” said Dr. Marcus.
Most think of leadership as hierarchical, with a boss on top and underlings below, though this is starting to change. Dr. Marcus suggested a different view. Instead of just “leading down” to those who report to them, leaders should consider “leading up” to their own bosses or oversight committees, and across to other departments or even beyond to interlinked organizations such as nursing homes.
“Being able to build that connectivity not only within your hospital, but beyond your hospital, lets you see the chain that goes through the experience of any patient. You are looking at the problem from a much wider lens. We call this meta-leadership,” Dr. Marcus said.
A key focus of meta-leadership is to create a culture where individuals are working together to help one another succeed. Leadership in hospitals is often dominated by egos, with individual leaders battling one another in a win-lose effort, and this gets in the way of incorporating different perspectives into problem-solving.
Dr. Marcus used an example from previous seminars in which he instructed participants to arm wrestle the person sitting next to them. The goal was to attain as many pins as possible in 30 seconds. About half would fight as hard as they could, and achieve a few victories. The other half worked cooperatively, letting one person win, then the other, so that they could have 30 or 40 wins each. Dr. Marcus told the story of a young nurse who was paired up with a much stronger surgeon. She let him win twice, and when he asked her why she wasn’t resisting, she took his arm and placed it in a winning position, then a losing position, and then a winning position again, and he instantly understood that the cooperative approach could be more effective. Why didn’t she just tell him? She told Dr. Marcus that she knew he wouldn’t take instruction, so she let him win and then demonstrated an alternative. “We nurses learned how to do that a long time ago,” she told Dr. Marcus.
The idea is collaborative problem-solving. “How do you orient people looking to you for leadership so that we’re in this together and we can accomplish a whole lot more in 30 seconds if we’re working together instead of always battling one another? If we’re always battling one another, we’re putting all of our effort into the contest,” said Dr. Marcus. This sort of approach is all the more important when facing the complexity experienced by hospital systems, especially during crises such as COVID-19.
A critical element of meta-leadership is emotional intelligence, which includes elements such as self-awareness, self-regulation, empathy, determining motivation of yourself and others, and the social skills to portray yourself as caring, open, and interested.
Emotional intelligence also can help recognize when you’ve entered survival mode in reaction to a crisis or incident, or something as simple as losing your car keys – what Dr. Marcus terms “going to the basement.” Responses revolve around freeze, fight, or flight. It’s helpful in the wake of a car accident, but not when trying to make managerial decisions or respond to a complex situation. It’s vital for leaders to quickly get themselves out of the basement, said Dr. Marcus, and that they help other members of the team get out as well.
He recommended protocols designed in advance, both to recognize when you’re in the basement, and to lift yourself out. Dr. Marcus uses a trigger script, telling himself “I can do this,” and then when he’s working with other people, “we can do this.” He also speaks slowly, measuring every word. Whatever you do, “it has to be a pivot you do to get yourself out of the basement,” he said. It can be helpful to predict the kinds of situations that send you “to the basement” to help recognize it when it has happened.
It’s very important not to lead, negotiate, or make important decisions while in the basement, according to Dr. Marcus. If one thinks about some of the things they’ve said to others while under duress, they are often some of the statements they regret most.
Practical leadership skills
On the second day of the Leadership Seminar, Dr. Marcus moved his focus to using leadership skills and techniques. One important technique is to incorporate multiple perspectives. He gave the example of an opaque cube with a cone inside it, with a window on the side and one on top. Viewers from the side see the cone in profile, and see it as a triangle. Viewers from the top see an aerial perspective that looks like the circular base of the cone. The two groups could argue about what’s inside the cube, but they can only identify the object if they work together.
“When dealing with complex reality, you oftentimes find there are different people with different perspectives on a problem. They may have different experiences of what the problem is, and what often happens is that people get into an adversarial fight. Looking at the problem from different perspectives actually allows a much richer and more comprehensive view,” said Dr. Marcus.
The metaphor comes from a study of the tragic events at the Twin Towers in Manhattan on Sept. 11, 2001. The New York Fire Department had a command center at the base of the building, while the police had a helicopter flying around the buildings. The helicopter could see the steel girders beginning to melt and predicted a collapse, and therefore ordered their personnel out of the buildings. But they were unable to convey that information to the firefighters, who continued to send personnel into the buildings. In all, 343 firefighters lost their lives. The police force lost 32.
To best understand a problem, a key element is the “unknown knowns.” That is, information that is available, that someone has, but is unknown to you. It takes some imagination to conceive of what “unknown knowns” might be out there, but it’s worth the effort to identify possible knowledge sources. It’s vital to seek out this information, because a common leadership mistake is to assume you know something when you really don’t.
“In many ways what you’re doing is looking for obstacles. It could be you don’t have access to the information, that it’s beyond some sort of curtain you need to overcome, or it could be people in your own department who have the information and they’re not sharing it with you,” Dr. Marcus said.
He outlined a tool called the POP-DOC loop, which is a 6-step exercise designed to analyze problems and implement solutions. Step 1 is Perceiving the situation, determining knowns and unknowns, and incorporating multiple perspectives, emotions, and politics. Step 2 is to Orient oneself: examine patterns and how they may replicate themselves as long as conditions don’t change. For example, during COVID-19, physicians have begun to learn how the virus transmits and how it affects the immune system. Step 3, based on those patterns is to make Predictions. With COVID-19, it’s predictable that people who assemble without wearing masks are vulnerable to transmission. Step 4 is to use the predictions to begin to make Decisions. Step 5 is to begin Operationalizing those decisions, and step 6 is to Communicate those decisions effectively.
Dr. Marcus emphasized that POP-DOC is not a one-time exercise. Once decisions have been made and implemented, if they aren’t having the planned effect, it’s important to incorporate the results of those actions and start right back at the beginning of the POP-DOC loop.
“The POP side of the loop is perceiving, analysis. You get out of the basement and understand the situation that surrounds you. On the DOC side, you lead down, lead up, lead across and lead beyond. You’re bringing people into the action to get things done,” Dr. Marcus said.
Another tool Dr. Marcus described, aimed at problem-solving and negotiation, is the “Walk in the Woods.” The idea is to bring two parties together to help each other succeed. The first step is Self-Interest, where both parties articulate their objectives, perspectives, and fears. The second step, Enlarged Interests, requires each party to list their points of agreement, and only then should they focus on and list their points of disagreement. During conflict, people tend to focus on their disagreements. The parties often find that they agree on more than they realize, and this can frame the disagreements as more manageable. The third step, Enlightened Interest, is a free thinking period where both parties come up with potential solutions that had not been previously considered. In step 4, Aligned Interests, the parties discuss some of those ideas that can be explored further.
The Walk in the Woods is applicable to a wide range of situations, and negotiation is central to being a leader. “Being a clinician is all about negotiating – with patients, family members, with other clinicians, with the institution,” Dr. Marcus said. “We all want the patient to have the best possible care, and in the course of those conversations if we can better understand people, have empathy, and if there are new ideas or ways we can individualize our care, let’s do it, and then at the end of the day combine our motivations so that we’re providing the best possible care.”
In the end, meta-leadership is about creating a culture where individuals strive to help each other succeed, said Dr. Marcus. “That’s the essence: involving people, making them part of the solution, and if it’s a solution they’ve created together, everyone wants to make that solution a success.”
For more information, see the book “You’re It,” coauthored by Dr. Marcus, and available on Amazon for $16.99 in hardback, or $3.99 in Kindle format.
The year 2020 has brought the COVID-19 pandemic and civil unrest and protests, which have resulted in unprecedented health care challenges to hospitals and clinics. The daunting prospect of a fall influenza season has hospital staff and administrators looking ahead to still greater challenges.
This year of crisis has put even greater emphasis on leadership in hospitals, as patients, clinicians, and staff look for direction in the face of uncertainty and stress. But hospital leaders often arrive at their positions unprepared for their roles, according to Leonard Marcus, PhD, director of the Program for Health Care Negotiation and Conflict Resolution at Harvard T.H. Chan School of Public Health, Boston.
“Many times what happens in medicine is that someone with the greatest technical skills or greatest clinical skills emerges to be leader of a department, or a group, or a hospital, without having really paid attention to how they can build their leadership skills,” Dr. Marcus said during the 2020 Society of Hospital Medicine Leadership Virtual Seminar, held online Sept. 16-17.
Over 2 days, Dr. Marcus discussed the complex environments faced by hospital leaders, and some of the tools and strategies that can be used to maintain calm, problem-solve, and chart a course ahead.
He emphasized that hospitals and medical systems are complex, nonlinear organizations, which could be swept up by change in the form of mergers, financial policies, patient surges due to local emergencies, or pandemics.
“Complexity has to be central to how you think about leadership. If you think you can control everything, that doesn’t work that well,” said Dr. Marcus.
Most think of leadership as hierarchical, with a boss on top and underlings below, though this is starting to change. Dr. Marcus suggested a different view. Instead of just “leading down” to those who report to them, leaders should consider “leading up” to their own bosses or oversight committees, and across to other departments or even beyond to interlinked organizations such as nursing homes.
“Being able to build that connectivity not only within your hospital, but beyond your hospital, lets you see the chain that goes through the experience of any patient. You are looking at the problem from a much wider lens. We call this meta-leadership,” Dr. Marcus said.
A key focus of meta-leadership is to create a culture where individuals are working together to help one another succeed. Leadership in hospitals is often dominated by egos, with individual leaders battling one another in a win-lose effort, and this gets in the way of incorporating different perspectives into problem-solving.
Dr. Marcus used an example from previous seminars in which he instructed participants to arm wrestle the person sitting next to them. The goal was to attain as many pins as possible in 30 seconds. About half would fight as hard as they could, and achieve a few victories. The other half worked cooperatively, letting one person win, then the other, so that they could have 30 or 40 wins each. Dr. Marcus told the story of a young nurse who was paired up with a much stronger surgeon. She let him win twice, and when he asked her why she wasn’t resisting, she took his arm and placed it in a winning position, then a losing position, and then a winning position again, and he instantly understood that the cooperative approach could be more effective. Why didn’t she just tell him? She told Dr. Marcus that she knew he wouldn’t take instruction, so she let him win and then demonstrated an alternative. “We nurses learned how to do that a long time ago,” she told Dr. Marcus.
The idea is collaborative problem-solving. “How do you orient people looking to you for leadership so that we’re in this together and we can accomplish a whole lot more in 30 seconds if we’re working together instead of always battling one another? If we’re always battling one another, we’re putting all of our effort into the contest,” said Dr. Marcus. This sort of approach is all the more important when facing the complexity experienced by hospital systems, especially during crises such as COVID-19.
A critical element of meta-leadership is emotional intelligence, which includes elements such as self-awareness, self-regulation, empathy, determining motivation of yourself and others, and the social skills to portray yourself as caring, open, and interested.
Emotional intelligence also can help recognize when you’ve entered survival mode in reaction to a crisis or incident, or something as simple as losing your car keys – what Dr. Marcus terms “going to the basement.” Responses revolve around freeze, fight, or flight. It’s helpful in the wake of a car accident, but not when trying to make managerial decisions or respond to a complex situation. It’s vital for leaders to quickly get themselves out of the basement, said Dr. Marcus, and that they help other members of the team get out as well.
He recommended protocols designed in advance, both to recognize when you’re in the basement, and to lift yourself out. Dr. Marcus uses a trigger script, telling himself “I can do this,” and then when he’s working with other people, “we can do this.” He also speaks slowly, measuring every word. Whatever you do, “it has to be a pivot you do to get yourself out of the basement,” he said. It can be helpful to predict the kinds of situations that send you “to the basement” to help recognize it when it has happened.
It’s very important not to lead, negotiate, or make important decisions while in the basement, according to Dr. Marcus. If one thinks about some of the things they’ve said to others while under duress, they are often some of the statements they regret most.
Practical leadership skills
On the second day of the Leadership Seminar, Dr. Marcus moved his focus to using leadership skills and techniques. One important technique is to incorporate multiple perspectives. He gave the example of an opaque cube with a cone inside it, with a window on the side and one on top. Viewers from the side see the cone in profile, and see it as a triangle. Viewers from the top see an aerial perspective that looks like the circular base of the cone. The two groups could argue about what’s inside the cube, but they can only identify the object if they work together.
“When dealing with complex reality, you oftentimes find there are different people with different perspectives on a problem. They may have different experiences of what the problem is, and what often happens is that people get into an adversarial fight. Looking at the problem from different perspectives actually allows a much richer and more comprehensive view,” said Dr. Marcus.
The metaphor comes from a study of the tragic events at the Twin Towers in Manhattan on Sept. 11, 2001. The New York Fire Department had a command center at the base of the building, while the police had a helicopter flying around the buildings. The helicopter could see the steel girders beginning to melt and predicted a collapse, and therefore ordered their personnel out of the buildings. But they were unable to convey that information to the firefighters, who continued to send personnel into the buildings. In all, 343 firefighters lost their lives. The police force lost 32.
To best understand a problem, a key element is the “unknown knowns.” That is, information that is available, that someone has, but is unknown to you. It takes some imagination to conceive of what “unknown knowns” might be out there, but it’s worth the effort to identify possible knowledge sources. It’s vital to seek out this information, because a common leadership mistake is to assume you know something when you really don’t.
“In many ways what you’re doing is looking for obstacles. It could be you don’t have access to the information, that it’s beyond some sort of curtain you need to overcome, or it could be people in your own department who have the information and they’re not sharing it with you,” Dr. Marcus said.
He outlined a tool called the POP-DOC loop, which is a 6-step exercise designed to analyze problems and implement solutions. Step 1 is Perceiving the situation, determining knowns and unknowns, and incorporating multiple perspectives, emotions, and politics. Step 2 is to Orient oneself: examine patterns and how they may replicate themselves as long as conditions don’t change. For example, during COVID-19, physicians have begun to learn how the virus transmits and how it affects the immune system. Step 3, based on those patterns is to make Predictions. With COVID-19, it’s predictable that people who assemble without wearing masks are vulnerable to transmission. Step 4 is to use the predictions to begin to make Decisions. Step 5 is to begin Operationalizing those decisions, and step 6 is to Communicate those decisions effectively.
Dr. Marcus emphasized that POP-DOC is not a one-time exercise. Once decisions have been made and implemented, if they aren’t having the planned effect, it’s important to incorporate the results of those actions and start right back at the beginning of the POP-DOC loop.
“The POP side of the loop is perceiving, analysis. You get out of the basement and understand the situation that surrounds you. On the DOC side, you lead down, lead up, lead across and lead beyond. You’re bringing people into the action to get things done,” Dr. Marcus said.
Another tool Dr. Marcus described, aimed at problem-solving and negotiation, is the “Walk in the Woods.” The idea is to bring two parties together to help each other succeed. The first step is Self-Interest, where both parties articulate their objectives, perspectives, and fears. The second step, Enlarged Interests, requires each party to list their points of agreement, and only then should they focus on and list their points of disagreement. During conflict, people tend to focus on their disagreements. The parties often find that they agree on more than they realize, and this can frame the disagreements as more manageable. The third step, Enlightened Interest, is a free thinking period where both parties come up with potential solutions that had not been previously considered. In step 4, Aligned Interests, the parties discuss some of those ideas that can be explored further.
The Walk in the Woods is applicable to a wide range of situations, and negotiation is central to being a leader. “Being a clinician is all about negotiating – with patients, family members, with other clinicians, with the institution,” Dr. Marcus said. “We all want the patient to have the best possible care, and in the course of those conversations if we can better understand people, have empathy, and if there are new ideas or ways we can individualize our care, let’s do it, and then at the end of the day combine our motivations so that we’re providing the best possible care.”
In the end, meta-leadership is about creating a culture where individuals strive to help each other succeed, said Dr. Marcus. “That’s the essence: involving people, making them part of the solution, and if it’s a solution they’ve created together, everyone wants to make that solution a success.”
For more information, see the book “You’re It,” coauthored by Dr. Marcus, and available on Amazon for $16.99 in hardback, or $3.99 in Kindle format.
The year 2020 has brought the COVID-19 pandemic and civil unrest and protests, which have resulted in unprecedented health care challenges to hospitals and clinics. The daunting prospect of a fall influenza season has hospital staff and administrators looking ahead to still greater challenges.
This year of crisis has put even greater emphasis on leadership in hospitals, as patients, clinicians, and staff look for direction in the face of uncertainty and stress. But hospital leaders often arrive at their positions unprepared for their roles, according to Leonard Marcus, PhD, director of the Program for Health Care Negotiation and Conflict Resolution at Harvard T.H. Chan School of Public Health, Boston.
“Many times what happens in medicine is that someone with the greatest technical skills or greatest clinical skills emerges to be leader of a department, or a group, or a hospital, without having really paid attention to how they can build their leadership skills,” Dr. Marcus said during the 2020 Society of Hospital Medicine Leadership Virtual Seminar, held online Sept. 16-17.
Over 2 days, Dr. Marcus discussed the complex environments faced by hospital leaders, and some of the tools and strategies that can be used to maintain calm, problem-solve, and chart a course ahead.
He emphasized that hospitals and medical systems are complex, nonlinear organizations, which could be swept up by change in the form of mergers, financial policies, patient surges due to local emergencies, or pandemics.
“Complexity has to be central to how you think about leadership. If you think you can control everything, that doesn’t work that well,” said Dr. Marcus.
Most think of leadership as hierarchical, with a boss on top and underlings below, though this is starting to change. Dr. Marcus suggested a different view. Instead of just “leading down” to those who report to them, leaders should consider “leading up” to their own bosses or oversight committees, and across to other departments or even beyond to interlinked organizations such as nursing homes.
“Being able to build that connectivity not only within your hospital, but beyond your hospital, lets you see the chain that goes through the experience of any patient. You are looking at the problem from a much wider lens. We call this meta-leadership,” Dr. Marcus said.
A key focus of meta-leadership is to create a culture where individuals are working together to help one another succeed. Leadership in hospitals is often dominated by egos, with individual leaders battling one another in a win-lose effort, and this gets in the way of incorporating different perspectives into problem-solving.
Dr. Marcus used an example from previous seminars in which he instructed participants to arm wrestle the person sitting next to them. The goal was to attain as many pins as possible in 30 seconds. About half would fight as hard as they could, and achieve a few victories. The other half worked cooperatively, letting one person win, then the other, so that they could have 30 or 40 wins each. Dr. Marcus told the story of a young nurse who was paired up with a much stronger surgeon. She let him win twice, and when he asked her why she wasn’t resisting, she took his arm and placed it in a winning position, then a losing position, and then a winning position again, and he instantly understood that the cooperative approach could be more effective. Why didn’t she just tell him? She told Dr. Marcus that she knew he wouldn’t take instruction, so she let him win and then demonstrated an alternative. “We nurses learned how to do that a long time ago,” she told Dr. Marcus.
The idea is collaborative problem-solving. “How do you orient people looking to you for leadership so that we’re in this together and we can accomplish a whole lot more in 30 seconds if we’re working together instead of always battling one another? If we’re always battling one another, we’re putting all of our effort into the contest,” said Dr. Marcus. This sort of approach is all the more important when facing the complexity experienced by hospital systems, especially during crises such as COVID-19.
A critical element of meta-leadership is emotional intelligence, which includes elements such as self-awareness, self-regulation, empathy, determining motivation of yourself and others, and the social skills to portray yourself as caring, open, and interested.
Emotional intelligence also can help recognize when you’ve entered survival mode in reaction to a crisis or incident, or something as simple as losing your car keys – what Dr. Marcus terms “going to the basement.” Responses revolve around freeze, fight, or flight. It’s helpful in the wake of a car accident, but not when trying to make managerial decisions or respond to a complex situation. It’s vital for leaders to quickly get themselves out of the basement, said Dr. Marcus, and that they help other members of the team get out as well.
He recommended protocols designed in advance, both to recognize when you’re in the basement, and to lift yourself out. Dr. Marcus uses a trigger script, telling himself “I can do this,” and then when he’s working with other people, “we can do this.” He also speaks slowly, measuring every word. Whatever you do, “it has to be a pivot you do to get yourself out of the basement,” he said. It can be helpful to predict the kinds of situations that send you “to the basement” to help recognize it when it has happened.
It’s very important not to lead, negotiate, or make important decisions while in the basement, according to Dr. Marcus. If one thinks about some of the things they’ve said to others while under duress, they are often some of the statements they regret most.
Practical leadership skills
On the second day of the Leadership Seminar, Dr. Marcus moved his focus to using leadership skills and techniques. One important technique is to incorporate multiple perspectives. He gave the example of an opaque cube with a cone inside it, with a window on the side and one on top. Viewers from the side see the cone in profile, and see it as a triangle. Viewers from the top see an aerial perspective that looks like the circular base of the cone. The two groups could argue about what’s inside the cube, but they can only identify the object if they work together.
“When dealing with complex reality, you oftentimes find there are different people with different perspectives on a problem. They may have different experiences of what the problem is, and what often happens is that people get into an adversarial fight. Looking at the problem from different perspectives actually allows a much richer and more comprehensive view,” said Dr. Marcus.
The metaphor comes from a study of the tragic events at the Twin Towers in Manhattan on Sept. 11, 2001. The New York Fire Department had a command center at the base of the building, while the police had a helicopter flying around the buildings. The helicopter could see the steel girders beginning to melt and predicted a collapse, and therefore ordered their personnel out of the buildings. But they were unable to convey that information to the firefighters, who continued to send personnel into the buildings. In all, 343 firefighters lost their lives. The police force lost 32.
To best understand a problem, a key element is the “unknown knowns.” That is, information that is available, that someone has, but is unknown to you. It takes some imagination to conceive of what “unknown knowns” might be out there, but it’s worth the effort to identify possible knowledge sources. It’s vital to seek out this information, because a common leadership mistake is to assume you know something when you really don’t.
“In many ways what you’re doing is looking for obstacles. It could be you don’t have access to the information, that it’s beyond some sort of curtain you need to overcome, or it could be people in your own department who have the information and they’re not sharing it with you,” Dr. Marcus said.
He outlined a tool called the POP-DOC loop, which is a 6-step exercise designed to analyze problems and implement solutions. Step 1 is Perceiving the situation, determining knowns and unknowns, and incorporating multiple perspectives, emotions, and politics. Step 2 is to Orient oneself: examine patterns and how they may replicate themselves as long as conditions don’t change. For example, during COVID-19, physicians have begun to learn how the virus transmits and how it affects the immune system. Step 3, based on those patterns is to make Predictions. With COVID-19, it’s predictable that people who assemble without wearing masks are vulnerable to transmission. Step 4 is to use the predictions to begin to make Decisions. Step 5 is to begin Operationalizing those decisions, and step 6 is to Communicate those decisions effectively.
Dr. Marcus emphasized that POP-DOC is not a one-time exercise. Once decisions have been made and implemented, if they aren’t having the planned effect, it’s important to incorporate the results of those actions and start right back at the beginning of the POP-DOC loop.
“The POP side of the loop is perceiving, analysis. You get out of the basement and understand the situation that surrounds you. On the DOC side, you lead down, lead up, lead across and lead beyond. You’re bringing people into the action to get things done,” Dr. Marcus said.
Another tool Dr. Marcus described, aimed at problem-solving and negotiation, is the “Walk in the Woods.” The idea is to bring two parties together to help each other succeed. The first step is Self-Interest, where both parties articulate their objectives, perspectives, and fears. The second step, Enlarged Interests, requires each party to list their points of agreement, and only then should they focus on and list their points of disagreement. During conflict, people tend to focus on their disagreements. The parties often find that they agree on more than they realize, and this can frame the disagreements as more manageable. The third step, Enlightened Interest, is a free thinking period where both parties come up with potential solutions that had not been previously considered. In step 4, Aligned Interests, the parties discuss some of those ideas that can be explored further.
The Walk in the Woods is applicable to a wide range of situations, and negotiation is central to being a leader. “Being a clinician is all about negotiating – with patients, family members, with other clinicians, with the institution,” Dr. Marcus said. “We all want the patient to have the best possible care, and in the course of those conversations if we can better understand people, have empathy, and if there are new ideas or ways we can individualize our care, let’s do it, and then at the end of the day combine our motivations so that we’re providing the best possible care.”
In the end, meta-leadership is about creating a culture where individuals strive to help each other succeed, said Dr. Marcus. “That’s the essence: involving people, making them part of the solution, and if it’s a solution they’ve created together, everyone wants to make that solution a success.”
For more information, see the book “You’re It,” coauthored by Dr. Marcus, and available on Amazon for $16.99 in hardback, or $3.99 in Kindle format.
FROM THE SHM LEADERSHIP SEMINAR
Neurodegeneration in MS: Association of cholesterol biomarkers with serum neurofilaments
Key clinical point: Increased high-density lipoprotein cholesterol (HDL-C) is associated with decreased gray matter and cortical atrophy in patients with multiple sclerosis (MS) after adjusting for baseline serum neurofilaments (sNfL).
Major finding: Gray matter volume and cortical volume had significant associations with percent change in HDL-C (P = .0024 and P less than .001, respectively) after adjusting for sNfL as a predictor.
Study details: This prospective longitudinal study assessed patients with relapsing-remitting MS (n = 75) and progressive multiple sclerosis (n = 37) over a 5-year follow-up period.
Disclosures: The study was funded by the National Center for Advancing Translational Sciences of the National Institutes of Health. B Weinstock-Guttman, J Kuhle, R Zivadinov and M Ramanathan reported ties with multiple pharmaceutical companies. The remaining authors declared no conflicts of interest.
Citation: McComb M et al. Mult Scler Relat Disord. 2020 Jul 11. doi: 10.1016/j.msard.2020.102389.
Key clinical point: Increased high-density lipoprotein cholesterol (HDL-C) is associated with decreased gray matter and cortical atrophy in patients with multiple sclerosis (MS) after adjusting for baseline serum neurofilaments (sNfL).
Major finding: Gray matter volume and cortical volume had significant associations with percent change in HDL-C (P = .0024 and P less than .001, respectively) after adjusting for sNfL as a predictor.
Study details: This prospective longitudinal study assessed patients with relapsing-remitting MS (n = 75) and progressive multiple sclerosis (n = 37) over a 5-year follow-up period.
Disclosures: The study was funded by the National Center for Advancing Translational Sciences of the National Institutes of Health. B Weinstock-Guttman, J Kuhle, R Zivadinov and M Ramanathan reported ties with multiple pharmaceutical companies. The remaining authors declared no conflicts of interest.
Citation: McComb M et al. Mult Scler Relat Disord. 2020 Jul 11. doi: 10.1016/j.msard.2020.102389.
Key clinical point: Increased high-density lipoprotein cholesterol (HDL-C) is associated with decreased gray matter and cortical atrophy in patients with multiple sclerosis (MS) after adjusting for baseline serum neurofilaments (sNfL).
Major finding: Gray matter volume and cortical volume had significant associations with percent change in HDL-C (P = .0024 and P less than .001, respectively) after adjusting for sNfL as a predictor.
Study details: This prospective longitudinal study assessed patients with relapsing-remitting MS (n = 75) and progressive multiple sclerosis (n = 37) over a 5-year follow-up period.
Disclosures: The study was funded by the National Center for Advancing Translational Sciences of the National Institutes of Health. B Weinstock-Guttman, J Kuhle, R Zivadinov and M Ramanathan reported ties with multiple pharmaceutical companies. The remaining authors declared no conflicts of interest.
Citation: McComb M et al. Mult Scler Relat Disord. 2020 Jul 11. doi: 10.1016/j.msard.2020.102389.
Long-term outcomes of early and continuous ocrelizumab treatment in relapsing MS
Key clinical point: Early and continuous ocrelizumab treatment can provide sustained benefit on clinical and magnetic resonance imaging measures for disease progression in patients with relapsing multiple sclerosis (MS).
Major finding: At 5 years, the cumulative proportion of patients with 24-week confirmed disability progression was lower among those who continued ocrelizumab vs those who switched from interferon (IFN) β-1a to ocrelizumab (16.1% vs 21.3%; P = .014). Similarly, brain atrophy was significantly lower among those who continued ocrelizumab than in those who switched to ocrelizumab (P less than .01).
Study details: The OPERA open label extension study evaluated long-term efficacy and safety (5 years follow-up) of ocrelizumab (600 mg) in adults with relapsing MS. Patients previously assigned to INF β-1a (n = 829) and ocrelizumab (n = 827) entered the open-label extension phase in this study, of which 623 switched to ocrelizumab and 702 continued ocrelizumab, respectively
Disclosures: This study was supported by F. Hoffmann-La Roche Ltd, Basel, Switzerland. The lead author reporting receiving travel reimbursement and writing assistance from F. Hoffmann-La Roche Ltd for CD20-related meetings and presentations. Some of his coinvestigators reported owning stock in, being an employee of, receiving support from, and/or serving on scientific advisory board for F. Hoffmann-La Roche Ltd.
Citation: Hauser SL et al. Neurology. 2020 Jul 20. doi: 10.1212/WNL.0000000000010376.
Key clinical point: Early and continuous ocrelizumab treatment can provide sustained benefit on clinical and magnetic resonance imaging measures for disease progression in patients with relapsing multiple sclerosis (MS).
Major finding: At 5 years, the cumulative proportion of patients with 24-week confirmed disability progression was lower among those who continued ocrelizumab vs those who switched from interferon (IFN) β-1a to ocrelizumab (16.1% vs 21.3%; P = .014). Similarly, brain atrophy was significantly lower among those who continued ocrelizumab than in those who switched to ocrelizumab (P less than .01).
Study details: The OPERA open label extension study evaluated long-term efficacy and safety (5 years follow-up) of ocrelizumab (600 mg) in adults with relapsing MS. Patients previously assigned to INF β-1a (n = 829) and ocrelizumab (n = 827) entered the open-label extension phase in this study, of which 623 switched to ocrelizumab and 702 continued ocrelizumab, respectively
Disclosures: This study was supported by F. Hoffmann-La Roche Ltd, Basel, Switzerland. The lead author reporting receiving travel reimbursement and writing assistance from F. Hoffmann-La Roche Ltd for CD20-related meetings and presentations. Some of his coinvestigators reported owning stock in, being an employee of, receiving support from, and/or serving on scientific advisory board for F. Hoffmann-La Roche Ltd.
Citation: Hauser SL et al. Neurology. 2020 Jul 20. doi: 10.1212/WNL.0000000000010376.
Key clinical point: Early and continuous ocrelizumab treatment can provide sustained benefit on clinical and magnetic resonance imaging measures for disease progression in patients with relapsing multiple sclerosis (MS).
Major finding: At 5 years, the cumulative proportion of patients with 24-week confirmed disability progression was lower among those who continued ocrelizumab vs those who switched from interferon (IFN) β-1a to ocrelizumab (16.1% vs 21.3%; P = .014). Similarly, brain atrophy was significantly lower among those who continued ocrelizumab than in those who switched to ocrelizumab (P less than .01).
Study details: The OPERA open label extension study evaluated long-term efficacy and safety (5 years follow-up) of ocrelizumab (600 mg) in adults with relapsing MS. Patients previously assigned to INF β-1a (n = 829) and ocrelizumab (n = 827) entered the open-label extension phase in this study, of which 623 switched to ocrelizumab and 702 continued ocrelizumab, respectively
Disclosures: This study was supported by F. Hoffmann-La Roche Ltd, Basel, Switzerland. The lead author reporting receiving travel reimbursement and writing assistance from F. Hoffmann-La Roche Ltd for CD20-related meetings and presentations. Some of his coinvestigators reported owning stock in, being an employee of, receiving support from, and/or serving on scientific advisory board for F. Hoffmann-La Roche Ltd.
Citation: Hauser SL et al. Neurology. 2020 Jul 20. doi: 10.1212/WNL.0000000000010376.
MS: Rituximab beneficial for long term treatment in a real-world setting
Key clinical point: Real-world data demonstrates effectiveness of rituximab in reducing disease activity and maintaining long-term treatment in patients with multiple sclerosis (MS).
Major finding: The odds for experiencing a clinical relapse, contrast-enhancing lesions (CEL), and/or new T2 lesions were greater with fingolimod (adjusted odds ratio [aOR], 3.17; P less than .001) and dimethyl fumarate (aOR, 2.68; P less than .001) compared with rituximab. Similarly, natalizimab vs rituximab showed higher odds for disease activity (aOR, 1.36; P = 0.216). The odds for discontinuation were higher for fingolimod (aOR, 2.02; P = .005) and dimethyl fumarate (aOR, 3.27; P less than .001) compared with rituximab.
Study details: A retrospective real-world study included MS patients who were initiated on rituximab (n = 182), natalizumab (n = 451), fingolimod (n = 271) or dimethyl fumarate (n = 342) and followed for 2 years.
Disclosures: This study received no funding. KV Nair, JR Corboy, T Vollmer and E Alvarez reported relationships with multiple pharmaceutical companies.
Citation: Vollmer BL et al. Ann Clin Transl Neurol. 2020 Aug 6. doi: 10.1002/acn3.51111.
Key clinical point: Real-world data demonstrates effectiveness of rituximab in reducing disease activity and maintaining long-term treatment in patients with multiple sclerosis (MS).
Major finding: The odds for experiencing a clinical relapse, contrast-enhancing lesions (CEL), and/or new T2 lesions were greater with fingolimod (adjusted odds ratio [aOR], 3.17; P less than .001) and dimethyl fumarate (aOR, 2.68; P less than .001) compared with rituximab. Similarly, natalizimab vs rituximab showed higher odds for disease activity (aOR, 1.36; P = 0.216). The odds for discontinuation were higher for fingolimod (aOR, 2.02; P = .005) and dimethyl fumarate (aOR, 3.27; P less than .001) compared with rituximab.
Study details: A retrospective real-world study included MS patients who were initiated on rituximab (n = 182), natalizumab (n = 451), fingolimod (n = 271) or dimethyl fumarate (n = 342) and followed for 2 years.
Disclosures: This study received no funding. KV Nair, JR Corboy, T Vollmer and E Alvarez reported relationships with multiple pharmaceutical companies.
Citation: Vollmer BL et al. Ann Clin Transl Neurol. 2020 Aug 6. doi: 10.1002/acn3.51111.
Key clinical point: Real-world data demonstrates effectiveness of rituximab in reducing disease activity and maintaining long-term treatment in patients with multiple sclerosis (MS).
Major finding: The odds for experiencing a clinical relapse, contrast-enhancing lesions (CEL), and/or new T2 lesions were greater with fingolimod (adjusted odds ratio [aOR], 3.17; P less than .001) and dimethyl fumarate (aOR, 2.68; P less than .001) compared with rituximab. Similarly, natalizimab vs rituximab showed higher odds for disease activity (aOR, 1.36; P = 0.216). The odds for discontinuation were higher for fingolimod (aOR, 2.02; P = .005) and dimethyl fumarate (aOR, 3.27; P less than .001) compared with rituximab.
Study details: A retrospective real-world study included MS patients who were initiated on rituximab (n = 182), natalizumab (n = 451), fingolimod (n = 271) or dimethyl fumarate (n = 342) and followed for 2 years.
Disclosures: This study received no funding. KV Nair, JR Corboy, T Vollmer and E Alvarez reported relationships with multiple pharmaceutical companies.
Citation: Vollmer BL et al. Ann Clin Transl Neurol. 2020 Aug 6. doi: 10.1002/acn3.51111.
Are lipid parameters linked to cognitive functions in MS?
Key clinical point: Elevated blood lipid parameters in patients with multiple sclerosis (MS) may harm cognitive functions.
Major finding: A negative correlation was observed between cholesterol and general cognitive functioning score after rehabilitation and the Expanded Disability Status Scale scores (Cronbach alpha, 0.60 and 0.65, respectively). Triglyceride scores also has a negative correlation with working memory scores before and after rehabilitation (Cronbach alpha, 0.36 and 0.40, respectively). Furthermore, body mass index scores had a negative correlation with the visuospatial ability (Cronbach alpha, 0.59)
Study details: The study included 90 inpatients with relapsing remitting, primary and secondary progressive MS who underwent intense neurorehabilitation training.
Disclosures: The study received no funding. The authors reported no conflicts of interest.
Citation: Andaloro A et al. Int J Neurosci. 2020 Aug 7. doi: 10.1080/00207454.2020.1807980.
Key clinical point: Elevated blood lipid parameters in patients with multiple sclerosis (MS) may harm cognitive functions.
Major finding: A negative correlation was observed between cholesterol and general cognitive functioning score after rehabilitation and the Expanded Disability Status Scale scores (Cronbach alpha, 0.60 and 0.65, respectively). Triglyceride scores also has a negative correlation with working memory scores before and after rehabilitation (Cronbach alpha, 0.36 and 0.40, respectively). Furthermore, body mass index scores had a negative correlation with the visuospatial ability (Cronbach alpha, 0.59)
Study details: The study included 90 inpatients with relapsing remitting, primary and secondary progressive MS who underwent intense neurorehabilitation training.
Disclosures: The study received no funding. The authors reported no conflicts of interest.
Citation: Andaloro A et al. Int J Neurosci. 2020 Aug 7. doi: 10.1080/00207454.2020.1807980.
Key clinical point: Elevated blood lipid parameters in patients with multiple sclerosis (MS) may harm cognitive functions.
Major finding: A negative correlation was observed between cholesterol and general cognitive functioning score after rehabilitation and the Expanded Disability Status Scale scores (Cronbach alpha, 0.60 and 0.65, respectively). Triglyceride scores also has a negative correlation with working memory scores before and after rehabilitation (Cronbach alpha, 0.36 and 0.40, respectively). Furthermore, body mass index scores had a negative correlation with the visuospatial ability (Cronbach alpha, 0.59)
Study details: The study included 90 inpatients with relapsing remitting, primary and secondary progressive MS who underwent intense neurorehabilitation training.
Disclosures: The study received no funding. The authors reported no conflicts of interest.
Citation: Andaloro A et al. Int J Neurosci. 2020 Aug 7. doi: 10.1080/00207454.2020.1807980.
Learning about “No”
To say that the pandemic has dropped us into uncharted territory is an understatement of unmeasurable proportions. Every day we learn more about it, and every day that new information brings us new challenges. COVID-19 is playing by its own set of rules. To keep pace with it societies have been forced to adapt to them, and members of those societies have had to realize that these new rules must be obeyed or be prepared to suffer the consequences.
I’m not sure exactly when it happened but gradually over my 7 and a half decades on this planet it appears that following the rules and understanding the value of “No” have become concepts to be ignored and left to gather dust in the attics and basements of our society. The tug of war between well-considered rules and the often misinterpreted concept of freedom has been ebbing and flowing since Eve plucked a forbidden apple off that tree.
In some parts of the world, the twin skills of saying and responding to “No” have become lost arts. I think it is not by chance that, of the four books I have written for parents, the one titled “How to Say No to Your Toddler” has become the most widely distributed, having been translated into Italian, Polish, and Russian. It is only slightly comforting to learn that at least some parents understand that creating rules can be important, but realize they aren’t quite sure how go about it.
As it has become clear that social distancing and mask wearing are associated with curtailing the spread of COVID-19, state and local governments have had to bone up on their long-forgotten No-saying skills. This relearning process has been particularly painful for school administrators who may have been warned that “You’ll never be able to get first and second graders to wear masks” or that “College students just won’t obey the rules.”
Both of these cautions are based on observations by educators with years of experience and certainly have a ring of truth to them. But could it be that these pessimistic predictions reflect a society in which parents and educators have lost the talent for crafting sensible rules and linking them to enforceable and rational consequences?
As colleges throughout the country have reopened using a variety of learning and residential strategies, there have been numerous incidents that validate the gloomy predictions of student misbehavior. Smaller schools seem to be having less difficulty, which is not surprising given their relative ease in fostering a sense of community. Many schools have been forced to rollback their plans for in-person learning because students have failed to follow some very simple but unpopular rules.
In a swift and decisive response to student misbehavior, Northeastern University in Boston dismissed 11 first-year students and will not refund their tuition when officials discovered a prohibited social gathering in one of the resident facilities (“Northeastern Dismisses 11 Students for Gathering in Violation of COVID-19 Policies,” by Ian Thomsen, News at Northwestern). This response seemed to have come as a surprise to many students and parents around the country who have become accustomed a diet of warnings and minor sanctions.
Whether this action by Northeastern will trigger similar responses by other universities remains to be seen. But we can hope that it sets an example of how learning about “No” can be an important part of one’s education.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
To say that the pandemic has dropped us into uncharted territory is an understatement of unmeasurable proportions. Every day we learn more about it, and every day that new information brings us new challenges. COVID-19 is playing by its own set of rules. To keep pace with it societies have been forced to adapt to them, and members of those societies have had to realize that these new rules must be obeyed or be prepared to suffer the consequences.
I’m not sure exactly when it happened but gradually over my 7 and a half decades on this planet it appears that following the rules and understanding the value of “No” have become concepts to be ignored and left to gather dust in the attics and basements of our society. The tug of war between well-considered rules and the often misinterpreted concept of freedom has been ebbing and flowing since Eve plucked a forbidden apple off that tree.
In some parts of the world, the twin skills of saying and responding to “No” have become lost arts. I think it is not by chance that, of the four books I have written for parents, the one titled “How to Say No to Your Toddler” has become the most widely distributed, having been translated into Italian, Polish, and Russian. It is only slightly comforting to learn that at least some parents understand that creating rules can be important, but realize they aren’t quite sure how go about it.
As it has become clear that social distancing and mask wearing are associated with curtailing the spread of COVID-19, state and local governments have had to bone up on their long-forgotten No-saying skills. This relearning process has been particularly painful for school administrators who may have been warned that “You’ll never be able to get first and second graders to wear masks” or that “College students just won’t obey the rules.”
Both of these cautions are based on observations by educators with years of experience and certainly have a ring of truth to them. But could it be that these pessimistic predictions reflect a society in which parents and educators have lost the talent for crafting sensible rules and linking them to enforceable and rational consequences?
As colleges throughout the country have reopened using a variety of learning and residential strategies, there have been numerous incidents that validate the gloomy predictions of student misbehavior. Smaller schools seem to be having less difficulty, which is not surprising given their relative ease in fostering a sense of community. Many schools have been forced to rollback their plans for in-person learning because students have failed to follow some very simple but unpopular rules.
In a swift and decisive response to student misbehavior, Northeastern University in Boston dismissed 11 first-year students and will not refund their tuition when officials discovered a prohibited social gathering in one of the resident facilities (“Northeastern Dismisses 11 Students for Gathering in Violation of COVID-19 Policies,” by Ian Thomsen, News at Northwestern). This response seemed to have come as a surprise to many students and parents around the country who have become accustomed a diet of warnings and minor sanctions.
Whether this action by Northeastern will trigger similar responses by other universities remains to be seen. But we can hope that it sets an example of how learning about “No” can be an important part of one’s education.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
To say that the pandemic has dropped us into uncharted territory is an understatement of unmeasurable proportions. Every day we learn more about it, and every day that new information brings us new challenges. COVID-19 is playing by its own set of rules. To keep pace with it societies have been forced to adapt to them, and members of those societies have had to realize that these new rules must be obeyed or be prepared to suffer the consequences.
I’m not sure exactly when it happened but gradually over my 7 and a half decades on this planet it appears that following the rules and understanding the value of “No” have become concepts to be ignored and left to gather dust in the attics and basements of our society. The tug of war between well-considered rules and the often misinterpreted concept of freedom has been ebbing and flowing since Eve plucked a forbidden apple off that tree.
In some parts of the world, the twin skills of saying and responding to “No” have become lost arts. I think it is not by chance that, of the four books I have written for parents, the one titled “How to Say No to Your Toddler” has become the most widely distributed, having been translated into Italian, Polish, and Russian. It is only slightly comforting to learn that at least some parents understand that creating rules can be important, but realize they aren’t quite sure how go about it.
As it has become clear that social distancing and mask wearing are associated with curtailing the spread of COVID-19, state and local governments have had to bone up on their long-forgotten No-saying skills. This relearning process has been particularly painful for school administrators who may have been warned that “You’ll never be able to get first and second graders to wear masks” or that “College students just won’t obey the rules.”
Both of these cautions are based on observations by educators with years of experience and certainly have a ring of truth to them. But could it be that these pessimistic predictions reflect a society in which parents and educators have lost the talent for crafting sensible rules and linking them to enforceable and rational consequences?
As colleges throughout the country have reopened using a variety of learning and residential strategies, there have been numerous incidents that validate the gloomy predictions of student misbehavior. Smaller schools seem to be having less difficulty, which is not surprising given their relative ease in fostering a sense of community. Many schools have been forced to rollback their plans for in-person learning because students have failed to follow some very simple but unpopular rules.
In a swift and decisive response to student misbehavior, Northeastern University in Boston dismissed 11 first-year students and will not refund their tuition when officials discovered a prohibited social gathering in one of the resident facilities (“Northeastern Dismisses 11 Students for Gathering in Violation of COVID-19 Policies,” by Ian Thomsen, News at Northwestern). This response seemed to have come as a surprise to many students and parents around the country who have become accustomed a diet of warnings and minor sanctions.
Whether this action by Northeastern will trigger similar responses by other universities remains to be seen. But we can hope that it sets an example of how learning about “No” can be an important part of one’s education.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
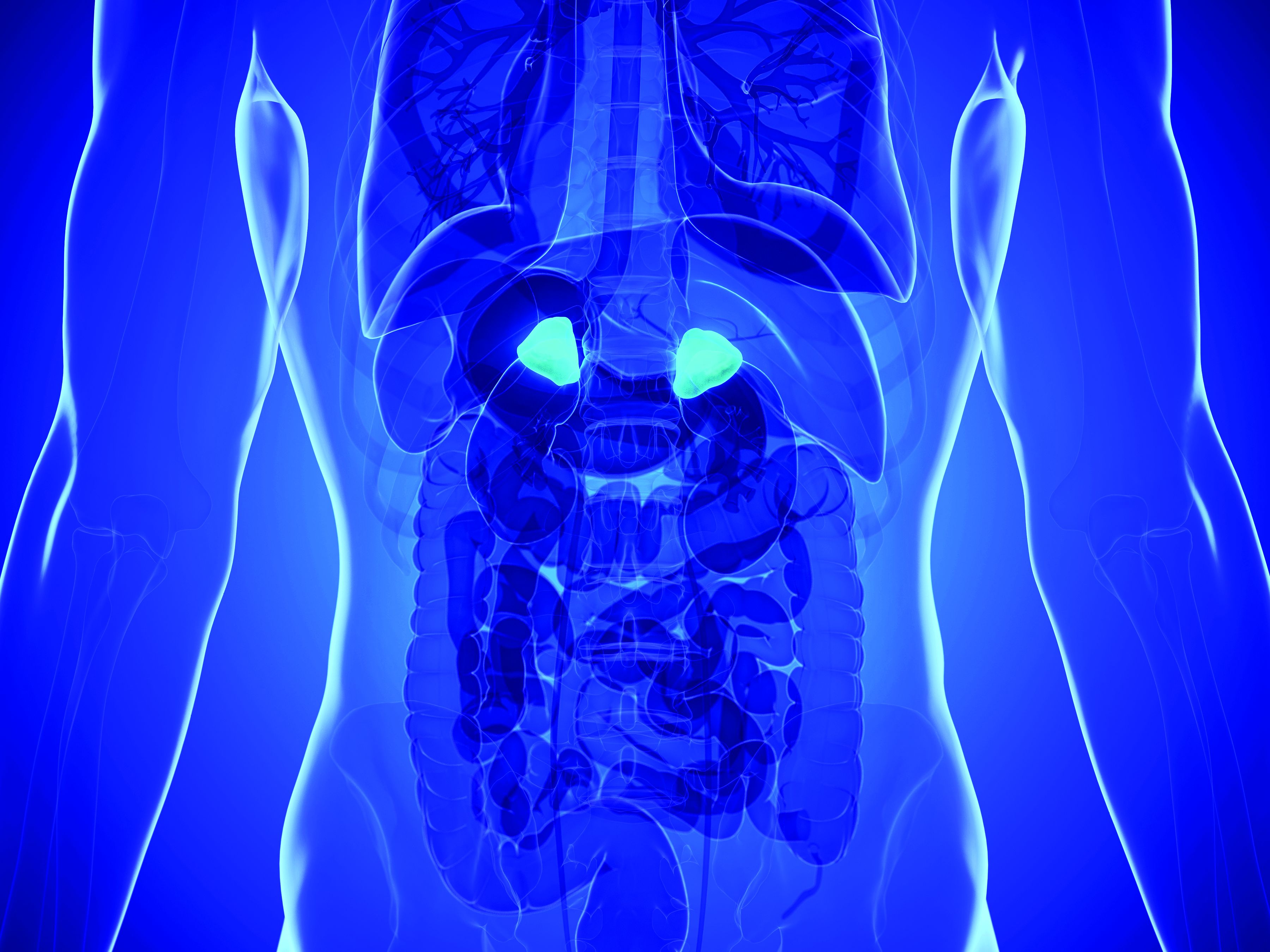
Adrenal vein sampling looms as choke point for aldosteronism assessment of hypertensives
At a time when new evidence strongly suggests that roughly a fifth of patents with hypertension have primary aldosteronism as the cause, other recent findings suggest that many of these possibly tens of millions of patients with aldosterone-driven high blood pressure may as a consequence need an expensive and not-widely-available diagnostic test – adrenal vein sampling – to determine whether they are candidates for a definitive surgical cure to their aldosteronism.
Some endocrinologists worry the worldwide infrastructure for running adrenal vein sampling (AVS) isn’t close to being in place to deliver on this looming need for patients with primary aldosteronism (PA), especially given the burgeoning numbers now being cited for PA prevalence.
“The system could be overwhelmed,” warned Robert M. Carey, MD, a cardiovascular endocrinologist and professor of medicine at the University of Virginia in Charlottesville. “Right now, adrenal vein sampling [AVS] is the gold standard,” for distinguishing unilateral and bilateral excess aldosterone secretion, “but not every radiologist can do AVS. Until we find a surrogate biomarker that can distinguish unilateral and bilateral PA” many patients will need AVS, Dr. Carey said in an interview.
“AVS is important for accurate lateralization of aldosterone excess in patients, but it may not be feasible for all patients with PA to undergo AVS. If the prevalence of PA truly is on the order of 15% [of all patients with hypertension] then health systems would be stretched to offer all of them AVS, which is technically challenging and requires dedicated training and is therefore limited to expert centers,” commented Jun Yang, MBBS, a cardiovascular endocrinologist at the Hudson Institute of Medical Research and a hypertension researcher at Monash University, both in Melbourne. “At Monash, our interventional radiologists have increased their [AVS] success rate from 40% to more than 90% during the past 10 years, and our waiting list for patients scheduled for AVS is now 3-4 months long,” Dr. Yang said in an interview.
Finding a unilateral adrenal nodule as the cause of PA means that surgical removal is an option, a step that often fully resolves the PA and normalizes blood pressure. Patients with a bilateral source of the aldosterone are not candidates for surgical cure and must be managed with medical treatment, usually a mineralocorticoid receptor antagonist such as spironolactone that can neutralize or at least reduce the impact of hyperaldosteronism.
AVS finds unilateral adenomas when imaging can’t
The evidence that raised concerns about the reliability of imaging as an easier and noninvasive means to identify hypertensive patients with PA and a unilateral adrenal nodule that makes them candidates for surgical removal to resolve their PA and hypertension came out in May 2020 in a review of 174 PA patients who underwent AVS at a single center in Calgary, Alta., during 2006-2018.
The review included 366 patients with PA referred to the University of Calgary for assessment, of whom 179 had no adrenal nodule visible with either CT or MRI imaging, with 174 of these patients also undergoing successful AVS. The procedure revealed 70 patients (40%) had unilateral aldosterone secretion (Can J Cardiol. 2020 May 16. doi: 10.1016/j.cjca.2020.05.013).
In an editorial about this report that appeared a few weeks later, Ross D. Feldman, MD, a hypertension-management researcher and professor of medicine at the University of Manitoba in Winnipeg, Man., said the finding was “amazing,” and “confirms that lateralization of aldosterone secretion in a patient with PA but without an identifiable mass on that side is not a zebra,” but instead a presentation that “occurs in almost half of patients with PA and no discernible adenoma on the side that lateralizes.” (Can J. Cardiol. 2020 Jul 3. doi: 10.1016/j.cjca.2020.06.022).
Although this was just one center’s experience, the authors are not alone in making this finding, although prior reports seem to have been largely forgotten or ignored until now.
“The discordance between AVS and adrenal imaging has been documented by numerous groups, and in our own experience [in Melbourne] around 40% of patients with unilateral aldosterone excess do not have a distinct unilateral adenoma on CT,” said Dr. Yang.
“Here’s the problem,” summed up Dr. Feldman in an interview. “Nearly half of patients with hyperaldosteronism don’t localize based on a CT or MRI, so you have to do AVS, but AVS is not generally available; it’s only at tertiary centers; and you have to do a lot of them,” to do them well. “It’s a half-day procedure, and you have to hit the correct adrenal vein.”
AVS for millions?
Compounding the challenge is the other bit of bombshell news recently dropped on the endocrinology and hypertension communities: PA may be much more prevalent that previously suspected, occurring in roughly 20% of patients with hypertension, according to study results that also came out in 2020 (Ann Int Med. 2020 Jul 7;173[1]:10-20).
The upshot, according to Dr. Feldman and others, is that researchers will need to find reliable criteria besides imaging for identifying PA patients with an increased likelihood of having a lateralized source for their excess aldosterone production. That’s “the only hope,” said Dr. Feldman, “so we won’t have to do AVS on 20 million Americans.”
Unfortunately, the path toward a successful screen to winnow down candidates for AVS has been long and not especially fruitful, with efforts dating back at least 50 years, and with one of the most recent efforts at stratifying PA patients by certain laboratory measures getting dismissed as producing a benefit that “might not be substantial,” wrote Michael Stowasser, MBBS, in a published commentary (J Hypertension. 2020 Jul;38[7]:1259-61).
In contrast to Dr. Feldman, Dr. Stowasser was more optimistic about the prospects for avoiding an immediate crisis in AVS assessment of PA patients, mostly because so few patients with PA are now identified by clinicians. Given the poor record clinicians have historically rung up diagnosing PA, “it would seem unlikely that we are going to be flooded with AVS requests any time soon,” he wrote. There is also reason to hope that increased demand for AVS will help broaden availability, and innovative testing methods promise to speed up the procedure, said Dr. Stowasser, a professor of medicine at the University of Queensland in Brisbane, Australia and director of the Endocrine Hypertension Research Centre at Greenslopes and Princess Alexandra Hospitals in Brisbane, in an interview.
But regardless of whether AVS testing becomes more available or streamlined, recent events suggest there will be little way to avoid eventually having to run millions of these diagnostic procedures.
Patients with PA “who decide they will not want surgery do not need AVS. For all other patients with PA, you need AVS. The medical system will just have to respond,” Dr. Carey concluded.
Dr. Carey, Dr. Yang, Dr. Feldman, and Dr. Stowasser had no relevant disclosures.
At a time when new evidence strongly suggests that roughly a fifth of patents with hypertension have primary aldosteronism as the cause, other recent findings suggest that many of these possibly tens of millions of patients with aldosterone-driven high blood pressure may as a consequence need an expensive and not-widely-available diagnostic test – adrenal vein sampling – to determine whether they are candidates for a definitive surgical cure to their aldosteronism.
Some endocrinologists worry the worldwide infrastructure for running adrenal vein sampling (AVS) isn’t close to being in place to deliver on this looming need for patients with primary aldosteronism (PA), especially given the burgeoning numbers now being cited for PA prevalence.
“The system could be overwhelmed,” warned Robert M. Carey, MD, a cardiovascular endocrinologist and professor of medicine at the University of Virginia in Charlottesville. “Right now, adrenal vein sampling [AVS] is the gold standard,” for distinguishing unilateral and bilateral excess aldosterone secretion, “but not every radiologist can do AVS. Until we find a surrogate biomarker that can distinguish unilateral and bilateral PA” many patients will need AVS, Dr. Carey said in an interview.
“AVS is important for accurate lateralization of aldosterone excess in patients, but it may not be feasible for all patients with PA to undergo AVS. If the prevalence of PA truly is on the order of 15% [of all patients with hypertension] then health systems would be stretched to offer all of them AVS, which is technically challenging and requires dedicated training and is therefore limited to expert centers,” commented Jun Yang, MBBS, a cardiovascular endocrinologist at the Hudson Institute of Medical Research and a hypertension researcher at Monash University, both in Melbourne. “At Monash, our interventional radiologists have increased their [AVS] success rate from 40% to more than 90% during the past 10 years, and our waiting list for patients scheduled for AVS is now 3-4 months long,” Dr. Yang said in an interview.
Finding a unilateral adrenal nodule as the cause of PA means that surgical removal is an option, a step that often fully resolves the PA and normalizes blood pressure. Patients with a bilateral source of the aldosterone are not candidates for surgical cure and must be managed with medical treatment, usually a mineralocorticoid receptor antagonist such as spironolactone that can neutralize or at least reduce the impact of hyperaldosteronism.
AVS finds unilateral adenomas when imaging can’t
The evidence that raised concerns about the reliability of imaging as an easier and noninvasive means to identify hypertensive patients with PA and a unilateral adrenal nodule that makes them candidates for surgical removal to resolve their PA and hypertension came out in May 2020 in a review of 174 PA patients who underwent AVS at a single center in Calgary, Alta., during 2006-2018.
The review included 366 patients with PA referred to the University of Calgary for assessment, of whom 179 had no adrenal nodule visible with either CT or MRI imaging, with 174 of these patients also undergoing successful AVS. The procedure revealed 70 patients (40%) had unilateral aldosterone secretion (Can J Cardiol. 2020 May 16. doi: 10.1016/j.cjca.2020.05.013).
In an editorial about this report that appeared a few weeks later, Ross D. Feldman, MD, a hypertension-management researcher and professor of medicine at the University of Manitoba in Winnipeg, Man., said the finding was “amazing,” and “confirms that lateralization of aldosterone secretion in a patient with PA but without an identifiable mass on that side is not a zebra,” but instead a presentation that “occurs in almost half of patients with PA and no discernible adenoma on the side that lateralizes.” (Can J. Cardiol. 2020 Jul 3. doi: 10.1016/j.cjca.2020.06.022).
Although this was just one center’s experience, the authors are not alone in making this finding, although prior reports seem to have been largely forgotten or ignored until now.
“The discordance between AVS and adrenal imaging has been documented by numerous groups, and in our own experience [in Melbourne] around 40% of patients with unilateral aldosterone excess do not have a distinct unilateral adenoma on CT,” said Dr. Yang.
“Here’s the problem,” summed up Dr. Feldman in an interview. “Nearly half of patients with hyperaldosteronism don’t localize based on a CT or MRI, so you have to do AVS, but AVS is not generally available; it’s only at tertiary centers; and you have to do a lot of them,” to do them well. “It’s a half-day procedure, and you have to hit the correct adrenal vein.”
AVS for millions?
Compounding the challenge is the other bit of bombshell news recently dropped on the endocrinology and hypertension communities: PA may be much more prevalent that previously suspected, occurring in roughly 20% of patients with hypertension, according to study results that also came out in 2020 (Ann Int Med. 2020 Jul 7;173[1]:10-20).
The upshot, according to Dr. Feldman and others, is that researchers will need to find reliable criteria besides imaging for identifying PA patients with an increased likelihood of having a lateralized source for their excess aldosterone production. That’s “the only hope,” said Dr. Feldman, “so we won’t have to do AVS on 20 million Americans.”
Unfortunately, the path toward a successful screen to winnow down candidates for AVS has been long and not especially fruitful, with efforts dating back at least 50 years, and with one of the most recent efforts at stratifying PA patients by certain laboratory measures getting dismissed as producing a benefit that “might not be substantial,” wrote Michael Stowasser, MBBS, in a published commentary (J Hypertension. 2020 Jul;38[7]:1259-61).
In contrast to Dr. Feldman, Dr. Stowasser was more optimistic about the prospects for avoiding an immediate crisis in AVS assessment of PA patients, mostly because so few patients with PA are now identified by clinicians. Given the poor record clinicians have historically rung up diagnosing PA, “it would seem unlikely that we are going to be flooded with AVS requests any time soon,” he wrote. There is also reason to hope that increased demand for AVS will help broaden availability, and innovative testing methods promise to speed up the procedure, said Dr. Stowasser, a professor of medicine at the University of Queensland in Brisbane, Australia and director of the Endocrine Hypertension Research Centre at Greenslopes and Princess Alexandra Hospitals in Brisbane, in an interview.
But regardless of whether AVS testing becomes more available or streamlined, recent events suggest there will be little way to avoid eventually having to run millions of these diagnostic procedures.
Patients with PA “who decide they will not want surgery do not need AVS. For all other patients with PA, you need AVS. The medical system will just have to respond,” Dr. Carey concluded.
Dr. Carey, Dr. Yang, Dr. Feldman, and Dr. Stowasser had no relevant disclosures.
At a time when new evidence strongly suggests that roughly a fifth of patents with hypertension have primary aldosteronism as the cause, other recent findings suggest that many of these possibly tens of millions of patients with aldosterone-driven high blood pressure may as a consequence need an expensive and not-widely-available diagnostic test – adrenal vein sampling – to determine whether they are candidates for a definitive surgical cure to their aldosteronism.
Some endocrinologists worry the worldwide infrastructure for running adrenal vein sampling (AVS) isn’t close to being in place to deliver on this looming need for patients with primary aldosteronism (PA), especially given the burgeoning numbers now being cited for PA prevalence.
“The system could be overwhelmed,” warned Robert M. Carey, MD, a cardiovascular endocrinologist and professor of medicine at the University of Virginia in Charlottesville. “Right now, adrenal vein sampling [AVS] is the gold standard,” for distinguishing unilateral and bilateral excess aldosterone secretion, “but not every radiologist can do AVS. Until we find a surrogate biomarker that can distinguish unilateral and bilateral PA” many patients will need AVS, Dr. Carey said in an interview.
“AVS is important for accurate lateralization of aldosterone excess in patients, but it may not be feasible for all patients with PA to undergo AVS. If the prevalence of PA truly is on the order of 15% [of all patients with hypertension] then health systems would be stretched to offer all of them AVS, which is technically challenging and requires dedicated training and is therefore limited to expert centers,” commented Jun Yang, MBBS, a cardiovascular endocrinologist at the Hudson Institute of Medical Research and a hypertension researcher at Monash University, both in Melbourne. “At Monash, our interventional radiologists have increased their [AVS] success rate from 40% to more than 90% during the past 10 years, and our waiting list for patients scheduled for AVS is now 3-4 months long,” Dr. Yang said in an interview.
Finding a unilateral adrenal nodule as the cause of PA means that surgical removal is an option, a step that often fully resolves the PA and normalizes blood pressure. Patients with a bilateral source of the aldosterone are not candidates for surgical cure and must be managed with medical treatment, usually a mineralocorticoid receptor antagonist such as spironolactone that can neutralize or at least reduce the impact of hyperaldosteronism.
AVS finds unilateral adenomas when imaging can’t
The evidence that raised concerns about the reliability of imaging as an easier and noninvasive means to identify hypertensive patients with PA and a unilateral adrenal nodule that makes them candidates for surgical removal to resolve their PA and hypertension came out in May 2020 in a review of 174 PA patients who underwent AVS at a single center in Calgary, Alta., during 2006-2018.
The review included 366 patients with PA referred to the University of Calgary for assessment, of whom 179 had no adrenal nodule visible with either CT or MRI imaging, with 174 of these patients also undergoing successful AVS. The procedure revealed 70 patients (40%) had unilateral aldosterone secretion (Can J Cardiol. 2020 May 16. doi: 10.1016/j.cjca.2020.05.013).
In an editorial about this report that appeared a few weeks later, Ross D. Feldman, MD, a hypertension-management researcher and professor of medicine at the University of Manitoba in Winnipeg, Man., said the finding was “amazing,” and “confirms that lateralization of aldosterone secretion in a patient with PA but without an identifiable mass on that side is not a zebra,” but instead a presentation that “occurs in almost half of patients with PA and no discernible adenoma on the side that lateralizes.” (Can J. Cardiol. 2020 Jul 3. doi: 10.1016/j.cjca.2020.06.022).
Although this was just one center’s experience, the authors are not alone in making this finding, although prior reports seem to have been largely forgotten or ignored until now.
“The discordance between AVS and adrenal imaging has been documented by numerous groups, and in our own experience [in Melbourne] around 40% of patients with unilateral aldosterone excess do not have a distinct unilateral adenoma on CT,” said Dr. Yang.
“Here’s the problem,” summed up Dr. Feldman in an interview. “Nearly half of patients with hyperaldosteronism don’t localize based on a CT or MRI, so you have to do AVS, but AVS is not generally available; it’s only at tertiary centers; and you have to do a lot of them,” to do them well. “It’s a half-day procedure, and you have to hit the correct adrenal vein.”
AVS for millions?
Compounding the challenge is the other bit of bombshell news recently dropped on the endocrinology and hypertension communities: PA may be much more prevalent that previously suspected, occurring in roughly 20% of patients with hypertension, according to study results that also came out in 2020 (Ann Int Med. 2020 Jul 7;173[1]:10-20).
The upshot, according to Dr. Feldman and others, is that researchers will need to find reliable criteria besides imaging for identifying PA patients with an increased likelihood of having a lateralized source for their excess aldosterone production. That’s “the only hope,” said Dr. Feldman, “so we won’t have to do AVS on 20 million Americans.”
Unfortunately, the path toward a successful screen to winnow down candidates for AVS has been long and not especially fruitful, with efforts dating back at least 50 years, and with one of the most recent efforts at stratifying PA patients by certain laboratory measures getting dismissed as producing a benefit that “might not be substantial,” wrote Michael Stowasser, MBBS, in a published commentary (J Hypertension. 2020 Jul;38[7]:1259-61).
In contrast to Dr. Feldman, Dr. Stowasser was more optimistic about the prospects for avoiding an immediate crisis in AVS assessment of PA patients, mostly because so few patients with PA are now identified by clinicians. Given the poor record clinicians have historically rung up diagnosing PA, “it would seem unlikely that we are going to be flooded with AVS requests any time soon,” he wrote. There is also reason to hope that increased demand for AVS will help broaden availability, and innovative testing methods promise to speed up the procedure, said Dr. Stowasser, a professor of medicine at the University of Queensland in Brisbane, Australia and director of the Endocrine Hypertension Research Centre at Greenslopes and Princess Alexandra Hospitals in Brisbane, in an interview.
But regardless of whether AVS testing becomes more available or streamlined, recent events suggest there will be little way to avoid eventually having to run millions of these diagnostic procedures.
Patients with PA “who decide they will not want surgery do not need AVS. For all other patients with PA, you need AVS. The medical system will just have to respond,” Dr. Carey concluded.
Dr. Carey, Dr. Yang, Dr. Feldman, and Dr. Stowasser had no relevant disclosures.
AHA issues new scientific statement on heart health for LGBTQ adults
Cardiovascular health should be routinely assessed and addressed in LGBTQ adults, the American Heart Association concluded in a new scientific statement.
“Among the most important takeaways from this scientific statement is the need for health care providers in clinical settings to routinely assess sexual orientation and gender identity,” Billy A. Caceres, PhD, RN, chair of the statement writing group, said in an interview.
“This will help health care providers engage LGBTQ patients in discussions about their heart health that account for the unique experiences of this population,” said Dr. Caceres, assistant professor at Columbia University, New York.
The statement was published online Oct. 8 in Circulation.
‘Invisible’ population
There are roughly 11 million LGBTQ adults in the United States, yet they are often “invisible in health care settings and cardiovascular research,” Dr. Caceres noted. The AHA scientific statement is the first from a national organization in the United States to comprehensively summarize the evidence on cardiovascular (CV) research in LGBTQ adults.
There is mounting evidence that LGBTQ adults experience worse CV health relative to their cisgender heterosexual peers. Disparities in CV health may be driven by unique psychosocial stressors in the LGBTQ individuals such as family rejection and anxiety of concealment of their sexual orientation or gender identity.
While there is limited information on the CV health of LGBTQ people, the writing group said providers should be aware of the following:
- LGBTQ adults are more likely to use tobacco than their cisgender heterosexual peers.
- Transgender adults may be less physically active than their cisgender counterparts. Gender-affirming care might play a role in promoting physical activity among transgender people.
- Transgender women may be at increased risk for heart disease because of behavioral and clinical factors (such as the use of gender-affirming hormones like estrogen).
- Transgender women and nonbinary persons are more likely to binge drink.
- Lesbian and bisexual women have a higher prevalence of obesity than heterosexual women do.
“We need to better understand how to support LGBTQ adults in optimizing their CV health. To do this, we will need rigorous research that examines potential explanations for the CV health disparities that have been observed in LGBTQ adults,” Dr. Caceres said.
He noted that research is also needed within the LGBTQ population among groups that might be at greater risk for heart disease, including racial- and ethnic-minority and low-income LGBTQ adults.
“Researchers should also design and test evidence-based interventions to promote the heart health of LGBTQ adults. This is an area that is greatly lacking within CV health research,” said Dr. Caceres.
Discrimination in health care
Discrimination against LGBTQ adults in health care settings also remains a problem, the authors noted.
The writing group cites data showing that nearly 56% of sexual-minority and 70% of gender-minority adults report having experienced some form of discrimination from clinicians, including the use of harsh/abusive language.
“Perhaps most alarming,” roughly 8% of sexual-minority and 25% of transgender individuals have been denied health care by clinicians, they noted.
“LGBTQ individuals are delaying primary care and preventative visits because there is a great fear of being treated differently. Being treated differently often means receiving inadequate or inferior care because of sexual orientation or gender identity,” Dr. Caceres said in a news release.
The writing group calls for greater emphasis on LGBTQ health issues in the education of all health care providers. Dr. Caceres said it’s “paramount to include content about LGBTQ health in clinical training and licensure requirements in order to address these cardiovascular health disparities.”
Traditionally, there has been very little LGBTQ-related content in health care professional education training. A 2018 online survey of students at 10 medical schools found that approximately 80% of students did not feel competent to provide care for transgender patients.
But that may soon change. In September 2020, the Accreditation Review Commission on Education for the Physician Assistant began requiring LGBTQ curricular content, the writing group notes.
The AHA scientific statement on LGBTQ was developed by the writing group on behalf of the AHA Council on Cardiovascular and Stroke Nursing, the Council on Hypertension, the Council on Lifestyle and Cardiometabolic Health, the Council on Peripheral Vascular Disease, and the Stroke Council.
A version of this article originally appeared on Medscape.com.
Cardiovascular health should be routinely assessed and addressed in LGBTQ adults, the American Heart Association concluded in a new scientific statement.
“Among the most important takeaways from this scientific statement is the need for health care providers in clinical settings to routinely assess sexual orientation and gender identity,” Billy A. Caceres, PhD, RN, chair of the statement writing group, said in an interview.
“This will help health care providers engage LGBTQ patients in discussions about their heart health that account for the unique experiences of this population,” said Dr. Caceres, assistant professor at Columbia University, New York.
The statement was published online Oct. 8 in Circulation.
‘Invisible’ population
There are roughly 11 million LGBTQ adults in the United States, yet they are often “invisible in health care settings and cardiovascular research,” Dr. Caceres noted. The AHA scientific statement is the first from a national organization in the United States to comprehensively summarize the evidence on cardiovascular (CV) research in LGBTQ adults.
There is mounting evidence that LGBTQ adults experience worse CV health relative to their cisgender heterosexual peers. Disparities in CV health may be driven by unique psychosocial stressors in the LGBTQ individuals such as family rejection and anxiety of concealment of their sexual orientation or gender identity.
While there is limited information on the CV health of LGBTQ people, the writing group said providers should be aware of the following:
- LGBTQ adults are more likely to use tobacco than their cisgender heterosexual peers.
- Transgender adults may be less physically active than their cisgender counterparts. Gender-affirming care might play a role in promoting physical activity among transgender people.
- Transgender women may be at increased risk for heart disease because of behavioral and clinical factors (such as the use of gender-affirming hormones like estrogen).
- Transgender women and nonbinary persons are more likely to binge drink.
- Lesbian and bisexual women have a higher prevalence of obesity than heterosexual women do.
“We need to better understand how to support LGBTQ adults in optimizing their CV health. To do this, we will need rigorous research that examines potential explanations for the CV health disparities that have been observed in LGBTQ adults,” Dr. Caceres said.
He noted that research is also needed within the LGBTQ population among groups that might be at greater risk for heart disease, including racial- and ethnic-minority and low-income LGBTQ adults.
“Researchers should also design and test evidence-based interventions to promote the heart health of LGBTQ adults. This is an area that is greatly lacking within CV health research,” said Dr. Caceres.
Discrimination in health care
Discrimination against LGBTQ adults in health care settings also remains a problem, the authors noted.
The writing group cites data showing that nearly 56% of sexual-minority and 70% of gender-minority adults report having experienced some form of discrimination from clinicians, including the use of harsh/abusive language.
“Perhaps most alarming,” roughly 8% of sexual-minority and 25% of transgender individuals have been denied health care by clinicians, they noted.
“LGBTQ individuals are delaying primary care and preventative visits because there is a great fear of being treated differently. Being treated differently often means receiving inadequate or inferior care because of sexual orientation or gender identity,” Dr. Caceres said in a news release.
The writing group calls for greater emphasis on LGBTQ health issues in the education of all health care providers. Dr. Caceres said it’s “paramount to include content about LGBTQ health in clinical training and licensure requirements in order to address these cardiovascular health disparities.”
Traditionally, there has been very little LGBTQ-related content in health care professional education training. A 2018 online survey of students at 10 medical schools found that approximately 80% of students did not feel competent to provide care for transgender patients.
But that may soon change. In September 2020, the Accreditation Review Commission on Education for the Physician Assistant began requiring LGBTQ curricular content, the writing group notes.
The AHA scientific statement on LGBTQ was developed by the writing group on behalf of the AHA Council on Cardiovascular and Stroke Nursing, the Council on Hypertension, the Council on Lifestyle and Cardiometabolic Health, the Council on Peripheral Vascular Disease, and the Stroke Council.
A version of this article originally appeared on Medscape.com.
Cardiovascular health should be routinely assessed and addressed in LGBTQ adults, the American Heart Association concluded in a new scientific statement.
“Among the most important takeaways from this scientific statement is the need for health care providers in clinical settings to routinely assess sexual orientation and gender identity,” Billy A. Caceres, PhD, RN, chair of the statement writing group, said in an interview.
“This will help health care providers engage LGBTQ patients in discussions about their heart health that account for the unique experiences of this population,” said Dr. Caceres, assistant professor at Columbia University, New York.
The statement was published online Oct. 8 in Circulation.
‘Invisible’ population
There are roughly 11 million LGBTQ adults in the United States, yet they are often “invisible in health care settings and cardiovascular research,” Dr. Caceres noted. The AHA scientific statement is the first from a national organization in the United States to comprehensively summarize the evidence on cardiovascular (CV) research in LGBTQ adults.
There is mounting evidence that LGBTQ adults experience worse CV health relative to their cisgender heterosexual peers. Disparities in CV health may be driven by unique psychosocial stressors in the LGBTQ individuals such as family rejection and anxiety of concealment of their sexual orientation or gender identity.
While there is limited information on the CV health of LGBTQ people, the writing group said providers should be aware of the following:
- LGBTQ adults are more likely to use tobacco than their cisgender heterosexual peers.
- Transgender adults may be less physically active than their cisgender counterparts. Gender-affirming care might play a role in promoting physical activity among transgender people.
- Transgender women may be at increased risk for heart disease because of behavioral and clinical factors (such as the use of gender-affirming hormones like estrogen).
- Transgender women and nonbinary persons are more likely to binge drink.
- Lesbian and bisexual women have a higher prevalence of obesity than heterosexual women do.
“We need to better understand how to support LGBTQ adults in optimizing their CV health. To do this, we will need rigorous research that examines potential explanations for the CV health disparities that have been observed in LGBTQ adults,” Dr. Caceres said.
He noted that research is also needed within the LGBTQ population among groups that might be at greater risk for heart disease, including racial- and ethnic-minority and low-income LGBTQ adults.
“Researchers should also design and test evidence-based interventions to promote the heart health of LGBTQ adults. This is an area that is greatly lacking within CV health research,” said Dr. Caceres.
Discrimination in health care
Discrimination against LGBTQ adults in health care settings also remains a problem, the authors noted.
The writing group cites data showing that nearly 56% of sexual-minority and 70% of gender-minority adults report having experienced some form of discrimination from clinicians, including the use of harsh/abusive language.
“Perhaps most alarming,” roughly 8% of sexual-minority and 25% of transgender individuals have been denied health care by clinicians, they noted.
“LGBTQ individuals are delaying primary care and preventative visits because there is a great fear of being treated differently. Being treated differently often means receiving inadequate or inferior care because of sexual orientation or gender identity,” Dr. Caceres said in a news release.
The writing group calls for greater emphasis on LGBTQ health issues in the education of all health care providers. Dr. Caceres said it’s “paramount to include content about LGBTQ health in clinical training and licensure requirements in order to address these cardiovascular health disparities.”
Traditionally, there has been very little LGBTQ-related content in health care professional education training. A 2018 online survey of students at 10 medical schools found that approximately 80% of students did not feel competent to provide care for transgender patients.
But that may soon change. In September 2020, the Accreditation Review Commission on Education for the Physician Assistant began requiring LGBTQ curricular content, the writing group notes.
The AHA scientific statement on LGBTQ was developed by the writing group on behalf of the AHA Council on Cardiovascular and Stroke Nursing, the Council on Hypertension, the Council on Lifestyle and Cardiometabolic Health, the Council on Peripheral Vascular Disease, and the Stroke Council.
A version of this article originally appeared on Medscape.com.
Repurposing cardiovascular drugs for serious mental illness
One of the hottest topics now in psychiatry is the possibility of repurposing long-established cardiovascular medications for treatment of patients with serious mental illness, Livia De Picker, MD, PhD, said at the virtual congress of the European College of Neuropsychopharmacology.

The appeal is multifold. A huge unmet need exists in psychiatry for new and better treatments with novel mechanisms of action. Many guideline-recommended cardiovascular medications have a long track record, including a well-established safety profile with no surprises, and are available in generic versions. They can be developed for a new indication at minimal cost, noted Dr. De Picker, a psychiatrist at the University of Antwerp (Belgium).
The idea of psychiatric repurposing of drugs originally developed for nonpsychiatric indications is nothing new, she added. Examples include lithium for gout, valproate for epilepsy, and ketamine for anesthesiology.
One hitch in efforts to repurpose cardiovascular medications is that, when psychiatric patients have been included in randomized trials of the drugs’ cardiovascular effects, the psychiatric outcomes often went untallied.
Indeed, the only high-quality randomized trial evidence of psychiatric benefits for any class of cardiovascular medications is for statins, where a modest-sized meta-analysis of six placebo-controlled trials in 339 patients with schizophrenia showed the lipid-lowering agents had benefit for both positive and negative symptoms (Psychiatry Res. 2018 Apr;262:84-93). But that’s not a body of data of sufficient size to be definitive, in Dr. De Picker’s view.
Much of the recent enthusiasm for exploring the potential of cardiovascular drugs for psychiatric conditions comes from hypothesis-generating big data analyses drawn from Scandinavian national patient registries. Danish investigators scrutinized all 1.6 million Danes exposed to six classes of drugs of interest during 2005-2015 and determined that those on long-term statins, low-dose aspirin, ACE inhibitors, angiotensin receptor blockers, or allopurinol were associated with a decreased rate of new-onset depression, while high-dose aspirin and non-aspirin NSAIDs were associated with an increased rate, compared with a 30% random sample of the country’s population (Acta Psychiatr Scand. 2019 Jan;1391:68-77).
Similarly, the Danish group found that continued use of statins, angiotensin agents, or low-dose aspirin was associated with a decreased rate of new-onset bipolar disorder, while high-dose aspirin and other NSAIDs were linked to increased risk (Bipolar Disord. 2019 Aug;[15]:410-8). What these agents have in common, the investigators observed, is that they act on inflammation and potentially on the stress response system.
Meanwhile, Swedish investigators examined the course of 142,691 Swedes with a diagnosis of bipolar disorder, schizophrenia, or nonaffective psychosis during 2005-2016. They determined that, during periods when those individuals were on a statin, calcium channel blocker, or metformin, they had reduced rates of psychiatric hospitalization and self-harm (JAMA Psychiatry. 2019 Apr 1;76[4]:382-90).
Scottish researchers analyzed the health records of 144,066 patients placed on monotherapy for hypertension and determined that the lowest risk for hospitalization for a mood disorder during follow-up was in those prescribed an ACE inhibitor or angiotensin receptor blocker. The risk was significantly higher in patients on a beta-blocker or calcium channel blocker, and intermediate in those on a thiazide diuretic (Hypertension. 2016 Nov;68[5:1132-8).
“Obviously, this is all at a very macro scale and we have no idea whatsoever what this means for individual patients, number needed to treat, or which type of patients would benefit, but it does provide us with some guidance for future research,” according to Dr. De Picker.
In the meantime, while physicians await definitive evidence of any impact of cardiovascular drugs might have on psychiatric outcomes, abundant data exist underscoring what she called “shockingly high levels” of inadequate management of cardiovascular risk factors in patients with serious mental illness. That problem needs to be addressed, and Dr. De Picker offered her personal recommendations for doing so in a manner consistent with the evidence to date suggestive of potential mental health benefits of some cardiovascular medications.
She advised that, for treatment of hypertension in patients with bipolar disorder or major depression, an ACE inhibitor or angiotensin-converting enzyme inhibitor is preferred as first-line. There is some evidence to suggest lipophilic beta-blockers, which cross the blood-brain barrier, improve anxiety symptoms and panic attacks, and prevent memory consolidation in patients with posttraumatic stress disorder. But the Scottish data suggest that they may worsen mood disorders.
“I would be careful in using beta-blockers as first-line treatment for hypertension. They’re not in the guidelines for anxiety disorders. British guidelines recommend them to prevent memory consolidation in PTSD, but do not use them as first-line in patients with major depressive disorder or bipolar disorder,” she said. As for calcium channel blockers, the jury is still out, with mixed and inconsistent evidence to date as to the impact of this drug class on mental illness outcomes.
She recommended a very low threshold for prescribing statin therapy in patients with serious mental illness in light of the superb risk/benefit ratio for this drug class. In her younger patients, she turns for guidance to an online calculator of an individual’s 10-year risk of a first acute MI or stroke.
Metformin has been shown to be beneficial for addressing the weight gain and other adverse metabolic effects caused by antipsychotic agents, and there is some preliminary evidence of improved psychiatric outcomes in patients with serious mental illness.
Christian Otte, MD, who also spoke at the session, noted that not only do emerging data point to the possibility that cardiovascular drugs might have benefit in terms of psychiatric outcomes, there is also some evidence, albeit mixed, that the converse is true: that is, psychiatric drugs may have cardiovascular benefits. He pointed to a South Korean trial in which 300 patients with a recent acute coronary syndrome and major depression were randomized to 24 weeks of escitalopram or placebo. At median 8.1 years of follow-up, the group that received the SSRI had a 31% relative risk reduction in the primary composite endpoint of all-cause mortality, acute MI, or percutaneous coronary intervention (JAMA. 2018 Jul 24; 320[4]:350–7).
“Potentially independent of their antidepressant effects, some SSRIs’ antiplatelet effects could be beneficial for patients with coronary heart disease, although the jury is still open regarding this question, with evidence in both directions,” said Dr. Otte, professor of psychiatry at Charite University Medical Center in Berlin.
Dr. De Picker offered an example as well: Finnish psychiatrists recently reported that cardiovascular mortality was reduced by an adjusted 38% during periods when 62,250 Finnish schizophrenia patients were on antipsychotic agents, compared with periods of nonuse of the drugs in a national study with a median 14.1 years of follow-up (World Psychiatry. 2020 Feb;19[1]:61-8).
“What they discovered – and this is quite contrary to what we are used to hearing about antipsychotic medication and cardiovascular risk – is that while the number of cardiovascular hospitalizations was not different in periods with or without antipsychotic use, the cardiovascular mortality was quite strikingly reduced when patients were on antipsychotic medication,” she said.
Asked by an audience member whether she personally prescribes metformin, Dr. De Picker replied: “Well, yes, why not? One of the very nice things about metformin is that it is actually a very safe drug, even in the hands of nonspecialists.
“I understand that maybe psychiatrists may not feel very comfortable in starting patients on metformin due to a lack of experience. But there are really only two things you need to take into account. About one-quarter of patients will experience GI side effects – nausea, vomiting, abdominal discomfort – and this can be reduced by gradually uptitrating the dose, dosing at mealtime, and using an extended-release formulation. And the second thing is that metformin can impair vitamin B12 absorption, so I think, especially in psychiatric patients, it would be good to do an annual measurement of vitamin B12 level and, if necessary, administer intramuscular supplements,” Dr. De Picker said.
She reported having no financial conflicts regarding her presentation.
SOURCE: De Picker L. ECNP 2020. Session EDU.05.
One of the hottest topics now in psychiatry is the possibility of repurposing long-established cardiovascular medications for treatment of patients with serious mental illness, Livia De Picker, MD, PhD, said at the virtual congress of the European College of Neuropsychopharmacology.

The appeal is multifold. A huge unmet need exists in psychiatry for new and better treatments with novel mechanisms of action. Many guideline-recommended cardiovascular medications have a long track record, including a well-established safety profile with no surprises, and are available in generic versions. They can be developed for a new indication at minimal cost, noted Dr. De Picker, a psychiatrist at the University of Antwerp (Belgium).
The idea of psychiatric repurposing of drugs originally developed for nonpsychiatric indications is nothing new, she added. Examples include lithium for gout, valproate for epilepsy, and ketamine for anesthesiology.
One hitch in efforts to repurpose cardiovascular medications is that, when psychiatric patients have been included in randomized trials of the drugs’ cardiovascular effects, the psychiatric outcomes often went untallied.
Indeed, the only high-quality randomized trial evidence of psychiatric benefits for any class of cardiovascular medications is for statins, where a modest-sized meta-analysis of six placebo-controlled trials in 339 patients with schizophrenia showed the lipid-lowering agents had benefit for both positive and negative symptoms (Psychiatry Res. 2018 Apr;262:84-93). But that’s not a body of data of sufficient size to be definitive, in Dr. De Picker’s view.
Much of the recent enthusiasm for exploring the potential of cardiovascular drugs for psychiatric conditions comes from hypothesis-generating big data analyses drawn from Scandinavian national patient registries. Danish investigators scrutinized all 1.6 million Danes exposed to six classes of drugs of interest during 2005-2015 and determined that those on long-term statins, low-dose aspirin, ACE inhibitors, angiotensin receptor blockers, or allopurinol were associated with a decreased rate of new-onset depression, while high-dose aspirin and non-aspirin NSAIDs were associated with an increased rate, compared with a 30% random sample of the country’s population (Acta Psychiatr Scand. 2019 Jan;1391:68-77).
Similarly, the Danish group found that continued use of statins, angiotensin agents, or low-dose aspirin was associated with a decreased rate of new-onset bipolar disorder, while high-dose aspirin and other NSAIDs were linked to increased risk (Bipolar Disord. 2019 Aug;[15]:410-8). What these agents have in common, the investigators observed, is that they act on inflammation and potentially on the stress response system.
Meanwhile, Swedish investigators examined the course of 142,691 Swedes with a diagnosis of bipolar disorder, schizophrenia, or nonaffective psychosis during 2005-2016. They determined that, during periods when those individuals were on a statin, calcium channel blocker, or metformin, they had reduced rates of psychiatric hospitalization and self-harm (JAMA Psychiatry. 2019 Apr 1;76[4]:382-90).
Scottish researchers analyzed the health records of 144,066 patients placed on monotherapy for hypertension and determined that the lowest risk for hospitalization for a mood disorder during follow-up was in those prescribed an ACE inhibitor or angiotensin receptor blocker. The risk was significantly higher in patients on a beta-blocker or calcium channel blocker, and intermediate in those on a thiazide diuretic (Hypertension. 2016 Nov;68[5:1132-8).
“Obviously, this is all at a very macro scale and we have no idea whatsoever what this means for individual patients, number needed to treat, or which type of patients would benefit, but it does provide us with some guidance for future research,” according to Dr. De Picker.
In the meantime, while physicians await definitive evidence of any impact of cardiovascular drugs might have on psychiatric outcomes, abundant data exist underscoring what she called “shockingly high levels” of inadequate management of cardiovascular risk factors in patients with serious mental illness. That problem needs to be addressed, and Dr. De Picker offered her personal recommendations for doing so in a manner consistent with the evidence to date suggestive of potential mental health benefits of some cardiovascular medications.
She advised that, for treatment of hypertension in patients with bipolar disorder or major depression, an ACE inhibitor or angiotensin-converting enzyme inhibitor is preferred as first-line. There is some evidence to suggest lipophilic beta-blockers, which cross the blood-brain barrier, improve anxiety symptoms and panic attacks, and prevent memory consolidation in patients with posttraumatic stress disorder. But the Scottish data suggest that they may worsen mood disorders.
“I would be careful in using beta-blockers as first-line treatment for hypertension. They’re not in the guidelines for anxiety disorders. British guidelines recommend them to prevent memory consolidation in PTSD, but do not use them as first-line in patients with major depressive disorder or bipolar disorder,” she said. As for calcium channel blockers, the jury is still out, with mixed and inconsistent evidence to date as to the impact of this drug class on mental illness outcomes.
She recommended a very low threshold for prescribing statin therapy in patients with serious mental illness in light of the superb risk/benefit ratio for this drug class. In her younger patients, she turns for guidance to an online calculator of an individual’s 10-year risk of a first acute MI or stroke.
Metformin has been shown to be beneficial for addressing the weight gain and other adverse metabolic effects caused by antipsychotic agents, and there is some preliminary evidence of improved psychiatric outcomes in patients with serious mental illness.
Christian Otte, MD, who also spoke at the session, noted that not only do emerging data point to the possibility that cardiovascular drugs might have benefit in terms of psychiatric outcomes, there is also some evidence, albeit mixed, that the converse is true: that is, psychiatric drugs may have cardiovascular benefits. He pointed to a South Korean trial in which 300 patients with a recent acute coronary syndrome and major depression were randomized to 24 weeks of escitalopram or placebo. At median 8.1 years of follow-up, the group that received the SSRI had a 31% relative risk reduction in the primary composite endpoint of all-cause mortality, acute MI, or percutaneous coronary intervention (JAMA. 2018 Jul 24; 320[4]:350–7).
“Potentially independent of their antidepressant effects, some SSRIs’ antiplatelet effects could be beneficial for patients with coronary heart disease, although the jury is still open regarding this question, with evidence in both directions,” said Dr. Otte, professor of psychiatry at Charite University Medical Center in Berlin.
Dr. De Picker offered an example as well: Finnish psychiatrists recently reported that cardiovascular mortality was reduced by an adjusted 38% during periods when 62,250 Finnish schizophrenia patients were on antipsychotic agents, compared with periods of nonuse of the drugs in a national study with a median 14.1 years of follow-up (World Psychiatry. 2020 Feb;19[1]:61-8).
“What they discovered – and this is quite contrary to what we are used to hearing about antipsychotic medication and cardiovascular risk – is that while the number of cardiovascular hospitalizations was not different in periods with or without antipsychotic use, the cardiovascular mortality was quite strikingly reduced when patients were on antipsychotic medication,” she said.
Asked by an audience member whether she personally prescribes metformin, Dr. De Picker replied: “Well, yes, why not? One of the very nice things about metformin is that it is actually a very safe drug, even in the hands of nonspecialists.
“I understand that maybe psychiatrists may not feel very comfortable in starting patients on metformin due to a lack of experience. But there are really only two things you need to take into account. About one-quarter of patients will experience GI side effects – nausea, vomiting, abdominal discomfort – and this can be reduced by gradually uptitrating the dose, dosing at mealtime, and using an extended-release formulation. And the second thing is that metformin can impair vitamin B12 absorption, so I think, especially in psychiatric patients, it would be good to do an annual measurement of vitamin B12 level and, if necessary, administer intramuscular supplements,” Dr. De Picker said.
She reported having no financial conflicts regarding her presentation.
SOURCE: De Picker L. ECNP 2020. Session EDU.05.
One of the hottest topics now in psychiatry is the possibility of repurposing long-established cardiovascular medications for treatment of patients with serious mental illness, Livia De Picker, MD, PhD, said at the virtual congress of the European College of Neuropsychopharmacology.

The appeal is multifold. A huge unmet need exists in psychiatry for new and better treatments with novel mechanisms of action. Many guideline-recommended cardiovascular medications have a long track record, including a well-established safety profile with no surprises, and are available in generic versions. They can be developed for a new indication at minimal cost, noted Dr. De Picker, a psychiatrist at the University of Antwerp (Belgium).
The idea of psychiatric repurposing of drugs originally developed for nonpsychiatric indications is nothing new, she added. Examples include lithium for gout, valproate for epilepsy, and ketamine for anesthesiology.
One hitch in efforts to repurpose cardiovascular medications is that, when psychiatric patients have been included in randomized trials of the drugs’ cardiovascular effects, the psychiatric outcomes often went untallied.
Indeed, the only high-quality randomized trial evidence of psychiatric benefits for any class of cardiovascular medications is for statins, where a modest-sized meta-analysis of six placebo-controlled trials in 339 patients with schizophrenia showed the lipid-lowering agents had benefit for both positive and negative symptoms (Psychiatry Res. 2018 Apr;262:84-93). But that’s not a body of data of sufficient size to be definitive, in Dr. De Picker’s view.
Much of the recent enthusiasm for exploring the potential of cardiovascular drugs for psychiatric conditions comes from hypothesis-generating big data analyses drawn from Scandinavian national patient registries. Danish investigators scrutinized all 1.6 million Danes exposed to six classes of drugs of interest during 2005-2015 and determined that those on long-term statins, low-dose aspirin, ACE inhibitors, angiotensin receptor blockers, or allopurinol were associated with a decreased rate of new-onset depression, while high-dose aspirin and non-aspirin NSAIDs were associated with an increased rate, compared with a 30% random sample of the country’s population (Acta Psychiatr Scand. 2019 Jan;1391:68-77).
Similarly, the Danish group found that continued use of statins, angiotensin agents, or low-dose aspirin was associated with a decreased rate of new-onset bipolar disorder, while high-dose aspirin and other NSAIDs were linked to increased risk (Bipolar Disord. 2019 Aug;[15]:410-8). What these agents have in common, the investigators observed, is that they act on inflammation and potentially on the stress response system.
Meanwhile, Swedish investigators examined the course of 142,691 Swedes with a diagnosis of bipolar disorder, schizophrenia, or nonaffective psychosis during 2005-2016. They determined that, during periods when those individuals were on a statin, calcium channel blocker, or metformin, they had reduced rates of psychiatric hospitalization and self-harm (JAMA Psychiatry. 2019 Apr 1;76[4]:382-90).
Scottish researchers analyzed the health records of 144,066 patients placed on monotherapy for hypertension and determined that the lowest risk for hospitalization for a mood disorder during follow-up was in those prescribed an ACE inhibitor or angiotensin receptor blocker. The risk was significantly higher in patients on a beta-blocker or calcium channel blocker, and intermediate in those on a thiazide diuretic (Hypertension. 2016 Nov;68[5:1132-8).
“Obviously, this is all at a very macro scale and we have no idea whatsoever what this means for individual patients, number needed to treat, or which type of patients would benefit, but it does provide us with some guidance for future research,” according to Dr. De Picker.
In the meantime, while physicians await definitive evidence of any impact of cardiovascular drugs might have on psychiatric outcomes, abundant data exist underscoring what she called “shockingly high levels” of inadequate management of cardiovascular risk factors in patients with serious mental illness. That problem needs to be addressed, and Dr. De Picker offered her personal recommendations for doing so in a manner consistent with the evidence to date suggestive of potential mental health benefits of some cardiovascular medications.
She advised that, for treatment of hypertension in patients with bipolar disorder or major depression, an ACE inhibitor or angiotensin-converting enzyme inhibitor is preferred as first-line. There is some evidence to suggest lipophilic beta-blockers, which cross the blood-brain barrier, improve anxiety symptoms and panic attacks, and prevent memory consolidation in patients with posttraumatic stress disorder. But the Scottish data suggest that they may worsen mood disorders.
“I would be careful in using beta-blockers as first-line treatment for hypertension. They’re not in the guidelines for anxiety disorders. British guidelines recommend them to prevent memory consolidation in PTSD, but do not use them as first-line in patients with major depressive disorder or bipolar disorder,” she said. As for calcium channel blockers, the jury is still out, with mixed and inconsistent evidence to date as to the impact of this drug class on mental illness outcomes.
She recommended a very low threshold for prescribing statin therapy in patients with serious mental illness in light of the superb risk/benefit ratio for this drug class. In her younger patients, she turns for guidance to an online calculator of an individual’s 10-year risk of a first acute MI or stroke.
Metformin has been shown to be beneficial for addressing the weight gain and other adverse metabolic effects caused by antipsychotic agents, and there is some preliminary evidence of improved psychiatric outcomes in patients with serious mental illness.
Christian Otte, MD, who also spoke at the session, noted that not only do emerging data point to the possibility that cardiovascular drugs might have benefit in terms of psychiatric outcomes, there is also some evidence, albeit mixed, that the converse is true: that is, psychiatric drugs may have cardiovascular benefits. He pointed to a South Korean trial in which 300 patients with a recent acute coronary syndrome and major depression were randomized to 24 weeks of escitalopram or placebo. At median 8.1 years of follow-up, the group that received the SSRI had a 31% relative risk reduction in the primary composite endpoint of all-cause mortality, acute MI, or percutaneous coronary intervention (JAMA. 2018 Jul 24; 320[4]:350–7).
“Potentially independent of their antidepressant effects, some SSRIs’ antiplatelet effects could be beneficial for patients with coronary heart disease, although the jury is still open regarding this question, with evidence in both directions,” said Dr. Otte, professor of psychiatry at Charite University Medical Center in Berlin.
Dr. De Picker offered an example as well: Finnish psychiatrists recently reported that cardiovascular mortality was reduced by an adjusted 38% during periods when 62,250 Finnish schizophrenia patients were on antipsychotic agents, compared with periods of nonuse of the drugs in a national study with a median 14.1 years of follow-up (World Psychiatry. 2020 Feb;19[1]:61-8).
“What they discovered – and this is quite contrary to what we are used to hearing about antipsychotic medication and cardiovascular risk – is that while the number of cardiovascular hospitalizations was not different in periods with or without antipsychotic use, the cardiovascular mortality was quite strikingly reduced when patients were on antipsychotic medication,” she said.
Asked by an audience member whether she personally prescribes metformin, Dr. De Picker replied: “Well, yes, why not? One of the very nice things about metformin is that it is actually a very safe drug, even in the hands of nonspecialists.
“I understand that maybe psychiatrists may not feel very comfortable in starting patients on metformin due to a lack of experience. But there are really only two things you need to take into account. About one-quarter of patients will experience GI side effects – nausea, vomiting, abdominal discomfort – and this can be reduced by gradually uptitrating the dose, dosing at mealtime, and using an extended-release formulation. And the second thing is that metformin can impair vitamin B12 absorption, so I think, especially in psychiatric patients, it would be good to do an annual measurement of vitamin B12 level and, if necessary, administer intramuscular supplements,” Dr. De Picker said.
She reported having no financial conflicts regarding her presentation.
SOURCE: De Picker L. ECNP 2020. Session EDU.05.
FROM ECNP 2020
Benefit of rivaroxaban after limb revascularization greatest in those with comorbid CAD
The absolute benefit of adding low-dose rivaroxaban to low-dose aspirin following revascularization for symptomatic lower-extremity peripheral artery disease (PAD) is significantly greater in patients with comorbid coronary artery disease (CAD), according to a new secondary analysis of the VOYAGER PAD trial.
“These findings suggest heterogeneity of prognostic risk for ischemic events in lower-extremity PAD patients, and may support shared decision-making with these patients,” William R. Hiatt, MD, observed in presenting the study results at the virtual annual congress of the European Society of Cardiology.
VOYAGER PAD was a 3-year, 34-country clinical trial in which 6,564 patients with symptomatic PAD who had recently undergone lower-limb revascularization were randomized in double-blind fashion to rivaroxaban (Xarelto) at 2.5 mg twice daily or placebo on top of background standard therapy with low-dose aspirin.
Among the 2,067 participants with baseline comorbid CAD, the primary outcome – a composite comprised of cardiovascular death, acute MI, ischemic stroke, acute limb ischemia, and major amputation – occurred in 18.9% of the rivaroxaban group at 3 years and 24.3% on placebo, for a highly significant 22% relative risk reduction.
In contrast, in the 4,497 patients with PAD only, the primary outcome occurred in 16.1% of those on rivaroxaban and 17.9% of controls, an 11% relative risk reduction which failed to reach statistical significance. The absolute risk reduction achieved with rivaroxaban was 5.4% in patients with PAD plus CAD versus 1.8% in those with PAD alone. Thus, the significant clinical benefit with rivaroxaban plus aspirin previously reported in the overall study population, with a number needed to treat for 3 years of 39 in order to prevent one primary outcome event, was largely driven by the superior outcomes in the dual-diagnosis subgroup, reported Dr. Hiatt, professor of medicine at the University of Colorado at Denver, Aurora.
“A strategy of rivaroxaban at 2.5 mg twice daily plus low-dose aspirin versus low-dose aspirin alone reduces ischemic events of the limb, brain, and heart, but also increases bleeding, with an overall net benefit,” the cardiologist said. “In particular, the benefits of this strategy for MI and ischemic stroke are robust, especially in patients with PAD and CAD.”
Indeed, the MI rate at 3 years in the dual diagnosis subgroup was 7.3% with rivaroxaban and 8.8% with placebo, for a 23% relative risk reduction, compared with rates of 3.3% and 3.7%, respectively, in patients with PAD only. Similarly, ischemic stroke occurred in 2.9% of patients with PAD and CAD in the rivaroxaban group, compared with 3.9% with placebo, whereas the rate in the PAD only group was identical at 2.6% regardless of whether patients were on rivaroxaban or placebo.
In patients without CAD, the clinical benefit of rivaroxaban was driven by reductions in severe limb events. Their rate of acute limb ischemia was 5.2% with rivaroxaban, compared with 8.3% with placebo, for a 37% relative risk reduction. In contrast, the reduction in acute limb ischemia with rivaroxaban in patients with PAD and CAD wasn’t significantly different from placebo.
Thrombolysis in Myocardial Infarction major bleeding occurred in 2.4% of patients with PAD and CAD on rivaroxaban, compared with 1.1% on placebo, and in 1.7% and 1.5% of patients with PAD alone. Of note, rates of ischemic stroke or fatal hemorrhage were low and similar at less than 1% in all four groups, Dr. Hiatt noted.
VOYAGER PAD was sponsored by Bayer and Janssen. Dr. Hiatt reported receiving research grant support from those two companies as well as Amgen.
The absolute benefit of adding low-dose rivaroxaban to low-dose aspirin following revascularization for symptomatic lower-extremity peripheral artery disease (PAD) is significantly greater in patients with comorbid coronary artery disease (CAD), according to a new secondary analysis of the VOYAGER PAD trial.
“These findings suggest heterogeneity of prognostic risk for ischemic events in lower-extremity PAD patients, and may support shared decision-making with these patients,” William R. Hiatt, MD, observed in presenting the study results at the virtual annual congress of the European Society of Cardiology.
VOYAGER PAD was a 3-year, 34-country clinical trial in which 6,564 patients with symptomatic PAD who had recently undergone lower-limb revascularization were randomized in double-blind fashion to rivaroxaban (Xarelto) at 2.5 mg twice daily or placebo on top of background standard therapy with low-dose aspirin.
Among the 2,067 participants with baseline comorbid CAD, the primary outcome – a composite comprised of cardiovascular death, acute MI, ischemic stroke, acute limb ischemia, and major amputation – occurred in 18.9% of the rivaroxaban group at 3 years and 24.3% on placebo, for a highly significant 22% relative risk reduction.
In contrast, in the 4,497 patients with PAD only, the primary outcome occurred in 16.1% of those on rivaroxaban and 17.9% of controls, an 11% relative risk reduction which failed to reach statistical significance. The absolute risk reduction achieved with rivaroxaban was 5.4% in patients with PAD plus CAD versus 1.8% in those with PAD alone. Thus, the significant clinical benefit with rivaroxaban plus aspirin previously reported in the overall study population, with a number needed to treat for 3 years of 39 in order to prevent one primary outcome event, was largely driven by the superior outcomes in the dual-diagnosis subgroup, reported Dr. Hiatt, professor of medicine at the University of Colorado at Denver, Aurora.
“A strategy of rivaroxaban at 2.5 mg twice daily plus low-dose aspirin versus low-dose aspirin alone reduces ischemic events of the limb, brain, and heart, but also increases bleeding, with an overall net benefit,” the cardiologist said. “In particular, the benefits of this strategy for MI and ischemic stroke are robust, especially in patients with PAD and CAD.”
Indeed, the MI rate at 3 years in the dual diagnosis subgroup was 7.3% with rivaroxaban and 8.8% with placebo, for a 23% relative risk reduction, compared with rates of 3.3% and 3.7%, respectively, in patients with PAD only. Similarly, ischemic stroke occurred in 2.9% of patients with PAD and CAD in the rivaroxaban group, compared with 3.9% with placebo, whereas the rate in the PAD only group was identical at 2.6% regardless of whether patients were on rivaroxaban or placebo.
In patients without CAD, the clinical benefit of rivaroxaban was driven by reductions in severe limb events. Their rate of acute limb ischemia was 5.2% with rivaroxaban, compared with 8.3% with placebo, for a 37% relative risk reduction. In contrast, the reduction in acute limb ischemia with rivaroxaban in patients with PAD and CAD wasn’t significantly different from placebo.
Thrombolysis in Myocardial Infarction major bleeding occurred in 2.4% of patients with PAD and CAD on rivaroxaban, compared with 1.1% on placebo, and in 1.7% and 1.5% of patients with PAD alone. Of note, rates of ischemic stroke or fatal hemorrhage were low and similar at less than 1% in all four groups, Dr. Hiatt noted.
VOYAGER PAD was sponsored by Bayer and Janssen. Dr. Hiatt reported receiving research grant support from those two companies as well as Amgen.
The absolute benefit of adding low-dose rivaroxaban to low-dose aspirin following revascularization for symptomatic lower-extremity peripheral artery disease (PAD) is significantly greater in patients with comorbid coronary artery disease (CAD), according to a new secondary analysis of the VOYAGER PAD trial.
“These findings suggest heterogeneity of prognostic risk for ischemic events in lower-extremity PAD patients, and may support shared decision-making with these patients,” William R. Hiatt, MD, observed in presenting the study results at the virtual annual congress of the European Society of Cardiology.
VOYAGER PAD was a 3-year, 34-country clinical trial in which 6,564 patients with symptomatic PAD who had recently undergone lower-limb revascularization were randomized in double-blind fashion to rivaroxaban (Xarelto) at 2.5 mg twice daily or placebo on top of background standard therapy with low-dose aspirin.
Among the 2,067 participants with baseline comorbid CAD, the primary outcome – a composite comprised of cardiovascular death, acute MI, ischemic stroke, acute limb ischemia, and major amputation – occurred in 18.9% of the rivaroxaban group at 3 years and 24.3% on placebo, for a highly significant 22% relative risk reduction.
In contrast, in the 4,497 patients with PAD only, the primary outcome occurred in 16.1% of those on rivaroxaban and 17.9% of controls, an 11% relative risk reduction which failed to reach statistical significance. The absolute risk reduction achieved with rivaroxaban was 5.4% in patients with PAD plus CAD versus 1.8% in those with PAD alone. Thus, the significant clinical benefit with rivaroxaban plus aspirin previously reported in the overall study population, with a number needed to treat for 3 years of 39 in order to prevent one primary outcome event, was largely driven by the superior outcomes in the dual-diagnosis subgroup, reported Dr. Hiatt, professor of medicine at the University of Colorado at Denver, Aurora.
“A strategy of rivaroxaban at 2.5 mg twice daily plus low-dose aspirin versus low-dose aspirin alone reduces ischemic events of the limb, brain, and heart, but also increases bleeding, with an overall net benefit,” the cardiologist said. “In particular, the benefits of this strategy for MI and ischemic stroke are robust, especially in patients with PAD and CAD.”
Indeed, the MI rate at 3 years in the dual diagnosis subgroup was 7.3% with rivaroxaban and 8.8% with placebo, for a 23% relative risk reduction, compared with rates of 3.3% and 3.7%, respectively, in patients with PAD only. Similarly, ischemic stroke occurred in 2.9% of patients with PAD and CAD in the rivaroxaban group, compared with 3.9% with placebo, whereas the rate in the PAD only group was identical at 2.6% regardless of whether patients were on rivaroxaban or placebo.
In patients without CAD, the clinical benefit of rivaroxaban was driven by reductions in severe limb events. Their rate of acute limb ischemia was 5.2% with rivaroxaban, compared with 8.3% with placebo, for a 37% relative risk reduction. In contrast, the reduction in acute limb ischemia with rivaroxaban in patients with PAD and CAD wasn’t significantly different from placebo.
Thrombolysis in Myocardial Infarction major bleeding occurred in 2.4% of patients with PAD and CAD on rivaroxaban, compared with 1.1% on placebo, and in 1.7% and 1.5% of patients with PAD alone. Of note, rates of ischemic stroke or fatal hemorrhage were low and similar at less than 1% in all four groups, Dr. Hiatt noted.
VOYAGER PAD was sponsored by Bayer and Janssen. Dr. Hiatt reported receiving research grant support from those two companies as well as Amgen.
FROM ESC CONGRESS 2020