User login
Flexible Bronchoscopic Removal of 3 Foreign Objects
Consider flexible bronchoscopy as an option to retrieve aspirated foreign bodies in the airway.
Airway foreign-body aspiration may cause no symptoms, although it can produce acute and life-threatening central airway obstruction.1 In the US, at least 2,700 people, including more than 300 children, die of foreign-body aspiration each year.2 Most foreign-body aspirations occur in children and elderly patients.3 In adults, dementia, drug intoxication, strokes, seizures, and neurologic disorders may predispose patients to aspiration.3 Some of the consequences of an aspirated object are complete or partial airway obstruction, respiratory distress and failure, pneumothorax, and hemorrhage.2 In addition, inadvertent aspiration of foreign objects in asymptomatic patients may not be evident for months, resulting in late complications as postobstructive pneumonia, bronchiectasis, or lung abscess.2
We present a case of a patient with documented schizophrenia with nonadherence to his antipsychotic medications who aspirated different objects. Flexible bronchoscopy was performed since rigid bronchoscopy is not available at our institution. Several bronchoscopy tools were required to successfully remove the objects and avoid further invasive interventions, such as cardiothoracic surgery.
Case Presentation
A 55-year-old man with schizophrenia on antipsychotics developed cough, shortness of breath, and dysphagia of 1-month of evolution. Because his symptoms worsened, his mother brought him to the emergency department. Peripheral oxygen saturation was 97% at room air. Lung auscultation was remarkable for bilateral scattered rhonchi and wheezes.
Laboratory results showed leukocytosis with neutrophilia and hypotonic hypovolemic hyponatremia.
The patient stated that he did not remember swallowing any objects, although his mother confirmed that he was not adherent with his antipsychotic medications, which could have predisposed him to aspiration secondary to possible psychotic episodes.
Piperacillin/tazobactam 4.5 g every 8 hours was started to cover anaerobic bacterial organisms causing abscess, and IV fluids were given for hypovolemia. Flexible bronchoscopy (rigid bronchoscopy is superior although not available at our institution) was planned to be performed in the operating room (OR) because we predicted a difficult and prolonged retrieval in view of multiple and different-sized objects.
A bronchoscopy was performed, showing a disk-shaped metallic foreign body at the right main stem bronchus. After multiple attempts using the tripod retrieval tool, a coin was removed (Figures 3A and 3B).
The patient was reintubated without any complications. A postprocedure chest radiograph showed the absence of foreign bodies and no pneumothorax. The patient completed IV antibiotic with piperacillin/tazobactam and supportive therapy with clinical improvement and successful extubation within 2 days. Cardiothoracic surgery was not required. Psychiatry service recommended to continue the same antipsychotic medications, administered only by his mother to assure adherence and to avoid similar future events. The patient was discharged home without any immediate complications despite having had a coin, nail, and screw aspiration (Figure 6).
Discussion
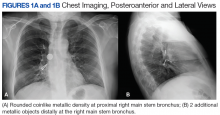
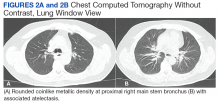
More than 50% of foreign bodies lodge at the right main stem bronchus due to the trachea’s anatomical position.2,4 In adults, foreign-body aspiration may present with nonspecific symptoms, such as cough and dyspnea.4 Other symptoms might include wheezes, chest discomfort, and sputum production. A chest radiograph is helpful as part of the initial diagnostic workup. A chest CT scan without contrast should be performed to confirm the diagnosis and to plan possible foreign-body retrieval.
Bronchoscopy is the gold standard for diagnosis and management of foreign-body aspiration.1 Rigid bronchoscopy is superior to flexible bronchoscopy in removal of large airway foreign bodies.1 The rigid bronchoscopy provides the ability to function as an endotracheal tube, thus allowing control of the airway and a conduit through which foreign bodies can be removed.1 Nonetheless, sometimes retrieval of foreign bodies deeper into the subsegmental bronchi cannot be achieved.1 Moreover, the required equipment or knowledgeable staff is not always available.1 Therefore, flexible bronchoscopy is an option to retrieve airway foreign bodies especially those located distal in the airway and for those medical centers without rigid bronchoscopy as is the case in our institution.
In our case, flexible bronchoscopy was performed in the OR because we predicted a difficult and prolonged retrieval in view of multiple and different-sized objects. Anesthesia Service assistance was requested anticipating need for patient sedation and intubation. We used the tripod and snare retrieval tools to remove 3 foreign objects located at the right main stem bronchus. Even though multiple attempts were made and endotracheal intubation was required, a successful retrieval with flexible bronchoscopy was performed. Moreover, cardiothoracic surgery was not required avoiding more invasive interventions with subsequent morbidity and mortality.
Conclusion
Flexible bronchoscopy is an important tool within the arsenal of the Pulmonology Service. The management of the underlying etiology also should be performed. In our case, the Psychiatry Service recommended that the patient’s medications should be administered by his mother to avoid similar events in the future. Flexible bronchoscopy can be a valuable option for foreign objects removal, especially those distally located in the lung segments as well as in those medical centers where rigid bronchoscopy is not available.
1. Mehta D, Mehta C, Bansal S, Singla S, Tangri N. Flexible bronchoscopic removal of a three piece foreign body from a child’s bronchus. Australas Med J. 2012;5(4):227-230.
2. Mercado JA, Rodríguez W. Occult aspiration of a chicken wishbone as a cause of hemoptysis. P R Health Sci J. 1999;18(1):71-73.
3. Robles-Arias CM, Campos-Santiago Z, Vega MT, Rosa-Cruz F, Rodríguez-Cintrón W. Aspiration of a dental tool during a crown placement procedure. Fed Pract. 2014;31(6):12-14.
4. Blanco-Ramos M, Botana-Rial M, García-Fontán E, Fernández-Villar A, Gallas-Torreira M. Update in the extraction of airway foreign bodies in adults. J Thorac Dis. 2016;8(11):3452-3456.
Consider flexible bronchoscopy as an option to retrieve aspirated foreign bodies in the airway.
Consider flexible bronchoscopy as an option to retrieve aspirated foreign bodies in the airway.
Airway foreign-body aspiration may cause no symptoms, although it can produce acute and life-threatening central airway obstruction.1 In the US, at least 2,700 people, including more than 300 children, die of foreign-body aspiration each year.2 Most foreign-body aspirations occur in children and elderly patients.3 In adults, dementia, drug intoxication, strokes, seizures, and neurologic disorders may predispose patients to aspiration.3 Some of the consequences of an aspirated object are complete or partial airway obstruction, respiratory distress and failure, pneumothorax, and hemorrhage.2 In addition, inadvertent aspiration of foreign objects in asymptomatic patients may not be evident for months, resulting in late complications as postobstructive pneumonia, bronchiectasis, or lung abscess.2
We present a case of a patient with documented schizophrenia with nonadherence to his antipsychotic medications who aspirated different objects. Flexible bronchoscopy was performed since rigid bronchoscopy is not available at our institution. Several bronchoscopy tools were required to successfully remove the objects and avoid further invasive interventions, such as cardiothoracic surgery.
Case Presentation
A 55-year-old man with schizophrenia on antipsychotics developed cough, shortness of breath, and dysphagia of 1-month of evolution. Because his symptoms worsened, his mother brought him to the emergency department. Peripheral oxygen saturation was 97% at room air. Lung auscultation was remarkable for bilateral scattered rhonchi and wheezes.
Laboratory results showed leukocytosis with neutrophilia and hypotonic hypovolemic hyponatremia.
The patient stated that he did not remember swallowing any objects, although his mother confirmed that he was not adherent with his antipsychotic medications, which could have predisposed him to aspiration secondary to possible psychotic episodes.
Piperacillin/tazobactam 4.5 g every 8 hours was started to cover anaerobic bacterial organisms causing abscess, and IV fluids were given for hypovolemia. Flexible bronchoscopy (rigid bronchoscopy is superior although not available at our institution) was planned to be performed in the operating room (OR) because we predicted a difficult and prolonged retrieval in view of multiple and different-sized objects.
A bronchoscopy was performed, showing a disk-shaped metallic foreign body at the right main stem bronchus. After multiple attempts using the tripod retrieval tool, a coin was removed (Figures 3A and 3B).
The patient was reintubated without any complications. A postprocedure chest radiograph showed the absence of foreign bodies and no pneumothorax. The patient completed IV antibiotic with piperacillin/tazobactam and supportive therapy with clinical improvement and successful extubation within 2 days. Cardiothoracic surgery was not required. Psychiatry service recommended to continue the same antipsychotic medications, administered only by his mother to assure adherence and to avoid similar future events. The patient was discharged home without any immediate complications despite having had a coin, nail, and screw aspiration (Figure 6).
Discussion
More than 50% of foreign bodies lodge at the right main stem bronchus due to the trachea’s anatomical position.2,4 In adults, foreign-body aspiration may present with nonspecific symptoms, such as cough and dyspnea.4 Other symptoms might include wheezes, chest discomfort, and sputum production. A chest radiograph is helpful as part of the initial diagnostic workup. A chest CT scan without contrast should be performed to confirm the diagnosis and to plan possible foreign-body retrieval.
Bronchoscopy is the gold standard for diagnosis and management of foreign-body aspiration.1 Rigid bronchoscopy is superior to flexible bronchoscopy in removal of large airway foreign bodies.1 The rigid bronchoscopy provides the ability to function as an endotracheal tube, thus allowing control of the airway and a conduit through which foreign bodies can be removed.1 Nonetheless, sometimes retrieval of foreign bodies deeper into the subsegmental bronchi cannot be achieved.1 Moreover, the required equipment or knowledgeable staff is not always available.1 Therefore, flexible bronchoscopy is an option to retrieve airway foreign bodies especially those located distal in the airway and for those medical centers without rigid bronchoscopy as is the case in our institution.
In our case, flexible bronchoscopy was performed in the OR because we predicted a difficult and prolonged retrieval in view of multiple and different-sized objects. Anesthesia Service assistance was requested anticipating need for patient sedation and intubation. We used the tripod and snare retrieval tools to remove 3 foreign objects located at the right main stem bronchus. Even though multiple attempts were made and endotracheal intubation was required, a successful retrieval with flexible bronchoscopy was performed. Moreover, cardiothoracic surgery was not required avoiding more invasive interventions with subsequent morbidity and mortality.
Conclusion
Flexible bronchoscopy is an important tool within the arsenal of the Pulmonology Service. The management of the underlying etiology also should be performed. In our case, the Psychiatry Service recommended that the patient’s medications should be administered by his mother to avoid similar events in the future. Flexible bronchoscopy can be a valuable option for foreign objects removal, especially those distally located in the lung segments as well as in those medical centers where rigid bronchoscopy is not available.
Airway foreign-body aspiration may cause no symptoms, although it can produce acute and life-threatening central airway obstruction.1 In the US, at least 2,700 people, including more than 300 children, die of foreign-body aspiration each year.2 Most foreign-body aspirations occur in children and elderly patients.3 In adults, dementia, drug intoxication, strokes, seizures, and neurologic disorders may predispose patients to aspiration.3 Some of the consequences of an aspirated object are complete or partial airway obstruction, respiratory distress and failure, pneumothorax, and hemorrhage.2 In addition, inadvertent aspiration of foreign objects in asymptomatic patients may not be evident for months, resulting in late complications as postobstructive pneumonia, bronchiectasis, or lung abscess.2
We present a case of a patient with documented schizophrenia with nonadherence to his antipsychotic medications who aspirated different objects. Flexible bronchoscopy was performed since rigid bronchoscopy is not available at our institution. Several bronchoscopy tools were required to successfully remove the objects and avoid further invasive interventions, such as cardiothoracic surgery.
Case Presentation
A 55-year-old man with schizophrenia on antipsychotics developed cough, shortness of breath, and dysphagia of 1-month of evolution. Because his symptoms worsened, his mother brought him to the emergency department. Peripheral oxygen saturation was 97% at room air. Lung auscultation was remarkable for bilateral scattered rhonchi and wheezes.
Laboratory results showed leukocytosis with neutrophilia and hypotonic hypovolemic hyponatremia.
The patient stated that he did not remember swallowing any objects, although his mother confirmed that he was not adherent with his antipsychotic medications, which could have predisposed him to aspiration secondary to possible psychotic episodes.
Piperacillin/tazobactam 4.5 g every 8 hours was started to cover anaerobic bacterial organisms causing abscess, and IV fluids were given for hypovolemia. Flexible bronchoscopy (rigid bronchoscopy is superior although not available at our institution) was planned to be performed in the operating room (OR) because we predicted a difficult and prolonged retrieval in view of multiple and different-sized objects.
A bronchoscopy was performed, showing a disk-shaped metallic foreign body at the right main stem bronchus. After multiple attempts using the tripod retrieval tool, a coin was removed (Figures 3A and 3B).
The patient was reintubated without any complications. A postprocedure chest radiograph showed the absence of foreign bodies and no pneumothorax. The patient completed IV antibiotic with piperacillin/tazobactam and supportive therapy with clinical improvement and successful extubation within 2 days. Cardiothoracic surgery was not required. Psychiatry service recommended to continue the same antipsychotic medications, administered only by his mother to assure adherence and to avoid similar future events. The patient was discharged home without any immediate complications despite having had a coin, nail, and screw aspiration (Figure 6).
Discussion
More than 50% of foreign bodies lodge at the right main stem bronchus due to the trachea’s anatomical position.2,4 In adults, foreign-body aspiration may present with nonspecific symptoms, such as cough and dyspnea.4 Other symptoms might include wheezes, chest discomfort, and sputum production. A chest radiograph is helpful as part of the initial diagnostic workup. A chest CT scan without contrast should be performed to confirm the diagnosis and to plan possible foreign-body retrieval.
Bronchoscopy is the gold standard for diagnosis and management of foreign-body aspiration.1 Rigid bronchoscopy is superior to flexible bronchoscopy in removal of large airway foreign bodies.1 The rigid bronchoscopy provides the ability to function as an endotracheal tube, thus allowing control of the airway and a conduit through which foreign bodies can be removed.1 Nonetheless, sometimes retrieval of foreign bodies deeper into the subsegmental bronchi cannot be achieved.1 Moreover, the required equipment or knowledgeable staff is not always available.1 Therefore, flexible bronchoscopy is an option to retrieve airway foreign bodies especially those located distal in the airway and for those medical centers without rigid bronchoscopy as is the case in our institution.
In our case, flexible bronchoscopy was performed in the OR because we predicted a difficult and prolonged retrieval in view of multiple and different-sized objects. Anesthesia Service assistance was requested anticipating need for patient sedation and intubation. We used the tripod and snare retrieval tools to remove 3 foreign objects located at the right main stem bronchus. Even though multiple attempts were made and endotracheal intubation was required, a successful retrieval with flexible bronchoscopy was performed. Moreover, cardiothoracic surgery was not required avoiding more invasive interventions with subsequent morbidity and mortality.
Conclusion
Flexible bronchoscopy is an important tool within the arsenal of the Pulmonology Service. The management of the underlying etiology also should be performed. In our case, the Psychiatry Service recommended that the patient’s medications should be administered by his mother to avoid similar events in the future. Flexible bronchoscopy can be a valuable option for foreign objects removal, especially those distally located in the lung segments as well as in those medical centers where rigid bronchoscopy is not available.
1. Mehta D, Mehta C, Bansal S, Singla S, Tangri N. Flexible bronchoscopic removal of a three piece foreign body from a child’s bronchus. Australas Med J. 2012;5(4):227-230.
2. Mercado JA, Rodríguez W. Occult aspiration of a chicken wishbone as a cause of hemoptysis. P R Health Sci J. 1999;18(1):71-73.
3. Robles-Arias CM, Campos-Santiago Z, Vega MT, Rosa-Cruz F, Rodríguez-Cintrón W. Aspiration of a dental tool during a crown placement procedure. Fed Pract. 2014;31(6):12-14.
4. Blanco-Ramos M, Botana-Rial M, García-Fontán E, Fernández-Villar A, Gallas-Torreira M. Update in the extraction of airway foreign bodies in adults. J Thorac Dis. 2016;8(11):3452-3456.
1. Mehta D, Mehta C, Bansal S, Singla S, Tangri N. Flexible bronchoscopic removal of a three piece foreign body from a child’s bronchus. Australas Med J. 2012;5(4):227-230.
2. Mercado JA, Rodríguez W. Occult aspiration of a chicken wishbone as a cause of hemoptysis. P R Health Sci J. 1999;18(1):71-73.
3. Robles-Arias CM, Campos-Santiago Z, Vega MT, Rosa-Cruz F, Rodríguez-Cintrón W. Aspiration of a dental tool during a crown placement procedure. Fed Pract. 2014;31(6):12-14.
4. Blanco-Ramos M, Botana-Rial M, García-Fontán E, Fernández-Villar A, Gallas-Torreira M. Update in the extraction of airway foreign bodies in adults. J Thorac Dis. 2016;8(11):3452-3456.
What’s The Impact of Occult HBV in Chronic HCV?
The reported prevalence of occult hepatitis B infection (OBI) varies widely: from < 1% to as high as 89.5% in HIV patients. Among patients with chronic hepatitis, the prevalence—again—ranges widely, from 0% to 52% but is highest in patients with chronic hepatitis C (CHC).
The clinical impact of OBI on patients with CHC has been extensively investigated, say researchers from the Institute of Liver and Biliary Sciences in New Delhi, India, but the available data are conflicting. In fact, when they conducted their study to assess the prevalence of OBI and evaluate its impact on clinical outcomes and response to antiviral therapy in CHC, the findings were “largely inconclusive.”
The study included 80 patients, of whom 32 (40%) had seropositive OBI. Hepatitis C virus genotype information was available for 59 patients, revealing that genotype 3 was most common.
However, analysis of clinical, biochemical, histopathologic and treatment response based on seropositivity and semiquantitative estimate of anti-HBc did not yield statistically significant results. Plasma samples of 14 were reactive for anti-HBc, 12 for anti-HBs, and 6 for both antibodies. Hepatitis B virus DNA (34 IU/mL) was detected in the plasma sample of only 1 patient by quantitative polymerase chain reaction. Therefore, the researchers say, the prevalence of OBI was 1.25%.
Anti-HBc total antibody levels did not influence clinical outcomes and response to directly acting antiviral therapy. Nor did genotype make a significant difference: 90.7% of genotype 3 patients and 92.8% of genotype 1 patients attained sustained virologic response.
More prospective studies should be conducted, the researchers urge, to further explore “this seemingly enigmatic issue.”
Source:
Bhatia M, Gupta E, Choudhary MC, Jindal A, Sarin SK. J Lab Physicians. 2018;10(3):304-308.
doi: 10.4103/JLP.JLP_12_18.
The reported prevalence of occult hepatitis B infection (OBI) varies widely: from < 1% to as high as 89.5% in HIV patients. Among patients with chronic hepatitis, the prevalence—again—ranges widely, from 0% to 52% but is highest in patients with chronic hepatitis C (CHC).
The clinical impact of OBI on patients with CHC has been extensively investigated, say researchers from the Institute of Liver and Biliary Sciences in New Delhi, India, but the available data are conflicting. In fact, when they conducted their study to assess the prevalence of OBI and evaluate its impact on clinical outcomes and response to antiviral therapy in CHC, the findings were “largely inconclusive.”
The study included 80 patients, of whom 32 (40%) had seropositive OBI. Hepatitis C virus genotype information was available for 59 patients, revealing that genotype 3 was most common.
However, analysis of clinical, biochemical, histopathologic and treatment response based on seropositivity and semiquantitative estimate of anti-HBc did not yield statistically significant results. Plasma samples of 14 were reactive for anti-HBc, 12 for anti-HBs, and 6 for both antibodies. Hepatitis B virus DNA (34 IU/mL) was detected in the plasma sample of only 1 patient by quantitative polymerase chain reaction. Therefore, the researchers say, the prevalence of OBI was 1.25%.
Anti-HBc total antibody levels did not influence clinical outcomes and response to directly acting antiviral therapy. Nor did genotype make a significant difference: 90.7% of genotype 3 patients and 92.8% of genotype 1 patients attained sustained virologic response.
More prospective studies should be conducted, the researchers urge, to further explore “this seemingly enigmatic issue.”
Source:
Bhatia M, Gupta E, Choudhary MC, Jindal A, Sarin SK. J Lab Physicians. 2018;10(3):304-308.
doi: 10.4103/JLP.JLP_12_18.
The reported prevalence of occult hepatitis B infection (OBI) varies widely: from < 1% to as high as 89.5% in HIV patients. Among patients with chronic hepatitis, the prevalence—again—ranges widely, from 0% to 52% but is highest in patients with chronic hepatitis C (CHC).
The clinical impact of OBI on patients with CHC has been extensively investigated, say researchers from the Institute of Liver and Biliary Sciences in New Delhi, India, but the available data are conflicting. In fact, when they conducted their study to assess the prevalence of OBI and evaluate its impact on clinical outcomes and response to antiviral therapy in CHC, the findings were “largely inconclusive.”
The study included 80 patients, of whom 32 (40%) had seropositive OBI. Hepatitis C virus genotype information was available for 59 patients, revealing that genotype 3 was most common.
However, analysis of clinical, biochemical, histopathologic and treatment response based on seropositivity and semiquantitative estimate of anti-HBc did not yield statistically significant results. Plasma samples of 14 were reactive for anti-HBc, 12 for anti-HBs, and 6 for both antibodies. Hepatitis B virus DNA (34 IU/mL) was detected in the plasma sample of only 1 patient by quantitative polymerase chain reaction. Therefore, the researchers say, the prevalence of OBI was 1.25%.
Anti-HBc total antibody levels did not influence clinical outcomes and response to directly acting antiviral therapy. Nor did genotype make a significant difference: 90.7% of genotype 3 patients and 92.8% of genotype 1 patients attained sustained virologic response.
More prospective studies should be conducted, the researchers urge, to further explore “this seemingly enigmatic issue.”
Source:
Bhatia M, Gupta E, Choudhary MC, Jindal A, Sarin SK. J Lab Physicians. 2018;10(3):304-308.
doi: 10.4103/JLP.JLP_12_18.
Team identifies potential immunotherapy target for AML
New research could aid the development of immunotherapies tailored to patients with acute myeloid leukemia (AML) who are undergoing stem cell transplant (SCT).
Researchers found they could use genetic sequencing and computer software to identify minor histocompatibility antigens (mHAs) known to occur in AML.
The team used this method to predict novel graft-versus-leukemia (GVL) mHAs and demonstrated that one of these mHAs could be a “potentially useful” therapeutic target.
Ben Vincent, MD, of the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill, and his colleagues reported these findings in Blood Advances.
In their retrospective study, the researchers tested whether their software could predict antigenic targets in 101 SCT donor-recipient pairs.
The researchers found they could correctly identify 14 of 18 mHAs known to occur in AML, but they were also able to predict 102 new GVL mHAs.
The researchers then confirmed one of these GVL mHAs, called UNC-GRK4-V, as a potential target for immunotherapy. The team observed immune responses to UNC-GRK4-V in four of nine AML patients who had undergone SCT.
Looking ahead, the researchers want to optimize their software to predict the most common AML-associated mHAs present in the U.S. population and confirm these predicted antigens as valid immunotherapy targets.
The team believes they could potentially use their predictions to engineer donor immune cells to specifically target the cancer cell antigens while preventing graft-versus-host disease.
“We’ve developed a software package that predicts leukemia-specific immune targets in any leukemia patient undergoing a stem cell transplant based on DNA and RNA sequencing and demonstrated that these data can lead to actual targets expressed on leukemia cells,” Dr. Vincent said.
“The next step of our work is to use that information for patient-specific therapies to try to improve cure rates without making graft-versus-host disease worse.”
The current research was supported by a National Cancer Institute grant, an ASCO Young Investigator Award, the North Carolina University Cancer Research Fund, and the Scott Neil Schwirck Fellowship.
New research could aid the development of immunotherapies tailored to patients with acute myeloid leukemia (AML) who are undergoing stem cell transplant (SCT).
Researchers found they could use genetic sequencing and computer software to identify minor histocompatibility antigens (mHAs) known to occur in AML.
The team used this method to predict novel graft-versus-leukemia (GVL) mHAs and demonstrated that one of these mHAs could be a “potentially useful” therapeutic target.
Ben Vincent, MD, of the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill, and his colleagues reported these findings in Blood Advances.
In their retrospective study, the researchers tested whether their software could predict antigenic targets in 101 SCT donor-recipient pairs.
The researchers found they could correctly identify 14 of 18 mHAs known to occur in AML, but they were also able to predict 102 new GVL mHAs.
The researchers then confirmed one of these GVL mHAs, called UNC-GRK4-V, as a potential target for immunotherapy. The team observed immune responses to UNC-GRK4-V in four of nine AML patients who had undergone SCT.
Looking ahead, the researchers want to optimize their software to predict the most common AML-associated mHAs present in the U.S. population and confirm these predicted antigens as valid immunotherapy targets.
The team believes they could potentially use their predictions to engineer donor immune cells to specifically target the cancer cell antigens while preventing graft-versus-host disease.
“We’ve developed a software package that predicts leukemia-specific immune targets in any leukemia patient undergoing a stem cell transplant based on DNA and RNA sequencing and demonstrated that these data can lead to actual targets expressed on leukemia cells,” Dr. Vincent said.
“The next step of our work is to use that information for patient-specific therapies to try to improve cure rates without making graft-versus-host disease worse.”
The current research was supported by a National Cancer Institute grant, an ASCO Young Investigator Award, the North Carolina University Cancer Research Fund, and the Scott Neil Schwirck Fellowship.
New research could aid the development of immunotherapies tailored to patients with acute myeloid leukemia (AML) who are undergoing stem cell transplant (SCT).
Researchers found they could use genetic sequencing and computer software to identify minor histocompatibility antigens (mHAs) known to occur in AML.
The team used this method to predict novel graft-versus-leukemia (GVL) mHAs and demonstrated that one of these mHAs could be a “potentially useful” therapeutic target.
Ben Vincent, MD, of the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill, and his colleagues reported these findings in Blood Advances.
In their retrospective study, the researchers tested whether their software could predict antigenic targets in 101 SCT donor-recipient pairs.
The researchers found they could correctly identify 14 of 18 mHAs known to occur in AML, but they were also able to predict 102 new GVL mHAs.
The researchers then confirmed one of these GVL mHAs, called UNC-GRK4-V, as a potential target for immunotherapy. The team observed immune responses to UNC-GRK4-V in four of nine AML patients who had undergone SCT.
Looking ahead, the researchers want to optimize their software to predict the most common AML-associated mHAs present in the U.S. population and confirm these predicted antigens as valid immunotherapy targets.
The team believes they could potentially use their predictions to engineer donor immune cells to specifically target the cancer cell antigens while preventing graft-versus-host disease.
“We’ve developed a software package that predicts leukemia-specific immune targets in any leukemia patient undergoing a stem cell transplant based on DNA and RNA sequencing and demonstrated that these data can lead to actual targets expressed on leukemia cells,” Dr. Vincent said.
“The next step of our work is to use that information for patient-specific therapies to try to improve cure rates without making graft-versus-host disease worse.”
The current research was supported by a National Cancer Institute grant, an ASCO Young Investigator Award, the North Carolina University Cancer Research Fund, and the Scott Neil Schwirck Fellowship.
Taking a Stab in the Dark
ANSWER
The radiograph shows an obvious metallic foreign body that appears to be lodged within the first and second lumbar disc space. This is likely the tip of the knife, which presumably broke off when the patient was stabbed.
The patient was promptly transferred to a trauma center with neurosurgery coverage. Subsequent CT showed that the blade had penetrated the spinal canal, but remarkably, the patient remained neurologically intact. He underwent successful removal without any neurologic compromise.
This case highlights several points for clinicians: First, provider-to-provider sign-out of patients should be complete and detailed. Second, obtaining a thorough history is essential. And third, you should maintain a low threshold for obtaining radiographs of wounds, to rule out a foreign body.
ANSWER
The radiograph shows an obvious metallic foreign body that appears to be lodged within the first and second lumbar disc space. This is likely the tip of the knife, which presumably broke off when the patient was stabbed.
The patient was promptly transferred to a trauma center with neurosurgery coverage. Subsequent CT showed that the blade had penetrated the spinal canal, but remarkably, the patient remained neurologically intact. He underwent successful removal without any neurologic compromise.
This case highlights several points for clinicians: First, provider-to-provider sign-out of patients should be complete and detailed. Second, obtaining a thorough history is essential. And third, you should maintain a low threshold for obtaining radiographs of wounds, to rule out a foreign body.
ANSWER
The radiograph shows an obvious metallic foreign body that appears to be lodged within the first and second lumbar disc space. This is likely the tip of the knife, which presumably broke off when the patient was stabbed.
The patient was promptly transferred to a trauma center with neurosurgery coverage. Subsequent CT showed that the blade had penetrated the spinal canal, but remarkably, the patient remained neurologically intact. He underwent successful removal without any neurologic compromise.
This case highlights several points for clinicians: First, provider-to-provider sign-out of patients should be complete and detailed. Second, obtaining a thorough history is essential. And third, you should maintain a low threshold for obtaining radiographs of wounds, to rule out a foreign body.
As you arrive for your shift in the emergency department, the outgoing provider asks if you would mind checking a laceration that his student is stapling. “The discharge paperwork is all done,” he says, as he waves goodbye and walks out the door.
You find that the student has just about completed his task: sterilely stapling a 2.5-cm laceration on the left lumbar area of a man in his early 40s.
You ask the student for the basic history, and he informs you that the patient was drinking with friends and “accidentally got cut” when they started roughhousing. You turn your attention to the patient, who appears intoxicated but in no obvious distress; he confirms the story as presented.
A quick review of the chart shows no significant medial history, stable vital signs, and up-to-date tetanus status. The patient can move all extremities well and appears neurovascularly intact. But some instinct prompts you to probe further.
On additional questioning, the patient reveals that he was accidentally stabbed. When you inquire about the object he was stabbed with, he describes it as a knife, “pretty long, sort of like a dagger.”
With this information, you decide to order some laboratory studies and abdominal radiographs (lateral view shown). What is your impression?
Expert provides antibiotic stewardship tips for dermatologists
LAKE TAHOE, CALIF. – Dermatologists prescribe more antibiotics than any other physician group, a statistic that George G. Zhanel, PhD, would like to see go by the wayside.
After all, the World Health Organization projects that the number of annual deaths in North America attributable to antibiotic resistance will reach 317,000 by the year 2050.
Dr. Zhanel, a microbiologist at the College of Medicine, University of Manitoba, Winnipeg, Canada, said at the annual meeting of the Society for Pediatric Dermatology. “Many of us are very concerned about this. Countries have put together an optimal action plan. What are we going to do about this? The plans are quite similar from country to country. They talk about surveillance, finding where these pathogens are. They talk about infection control such as washing your hands in the clinic so you’re not moving antibiotic-resistant organisms around. They talk about diagnostic and treatment guidelines, new antibiotic therapies, probiotics, and vaccination strategies. My own group is doing research on all of these areas, but today I’m going to focus on antibiotic stewardship: Using antibiotics wisely, trying to optimize efficacy while trying to minimize the development of resistant organisms.”
Dr. Zhanel, who is also director of the Canadian Antimicrobial Resistance Alliance (CARA) at the College of Medicine, University of Manitoba, described dermatologists as “big players” when it comes to antibiotic use. According to a 2016 report from the Scientific Panel on Antibiotic Use in Dermatology, dermatologists order 8.2 million oral antibiotic prescriptions each year, which is more common than any other physician group based on the prescribing rate per clinician (J Clin Aesthet Dermatol. 2016;9[4]:18-24). In addition, the prescribed duration of antibiotic therapy is often markedly longer with therapies treated by dermatologists, especially acne and rosacea. One study of general practitioners in the United Kingdom found that the mean duration of oral antibiotic use for treating acne was 175 days (J Am Acad Dermatol 2016;75:1142-50). “For some patients it went on much longer,” said Dr. Zhanel, who was not affiliated with the study.
“You are important players when it comes to antibiotics. How you use them and if you use them wisely impacts not only your patients, but the world.”
The correlation between antibiotic use and resistance is widely established, he continued. “We have known for 30 to 40 years that if you treat patients with tetracyclines, the Staphylococcus epidermidis that we all have on our skin develop tetracycline resistance,” he said. “The tetracycline resistance genes from S. epidermidis can then transfer to putative pathogens such as Staphylococcus aureus, and potentially [methicillin-resistant S. aureus]. That’s why we need to try to minimize oral tetracycline exposure on the normal microbiome.” In addition, tetracycline use can help create multidrug resistant organisms.
Next, Dr. Zhanel discussed potential solutions to antimicrobial usage/resistance in dermatology. According to recent guidelines on the care for the management of acne vulgaris, systemic antibiotic use should be limited to the shortest possible duration, typically 90 days (J Am Acad Dermatol. 2016;74[5]:945-73). A common treatment for moderate to-severe acne is to combine a topical retinoid with an oral or topical antimicrobial (J Am Acad Dermatol. 2009;60(5 suppl):S1-S50). If the addition of an oral antibiotic is required, limit its use to 3 or 4 months and co-prescribe with a product that contains benzoyl peroxide (BPO), or use as a washout. “Ideally, that’s your exit strategy,” he said. “Once you finish the oral antibiotic, in about 3 months if possible, continue with the topical retinoids plus BPO to maintain that particular remission.”
Why add benzoyl peroxide to topical retinoids for maintenance therapy? “Benzoyl peroxide and topical retinoids affect multiple targets in your acne strategy, and when you use them together they are powerful,” Dr. Zhanel said. He advises dermatologists not to prescribe oral or topical clindamycin unless they have to, because that drug is one of the main drivers of Clostridium difficile infection.
Dr. Zhanel’s stewardship tips for topical antibiotics involve not using topical tetracyclines/clindamycin/macrolides, in favor of using a topical antimicrobial such as BPO. “We think that benzoyl peroxide is less likely to drive resistance than are the traditional topical antibiotics like tetracyclines and clindamycin,” he said. “Use topical retinoids and benzoyl peroxide, if possible.”
Subtherapeutic oral doses of tetracyclines such as doxycycline 40 mg modified release “look very powerful for treating rosacea and do not affect the normal microbiome or select for resistance,” he said. In the meantime, Dr. Zhanel and other researchers are working to develop narrow spectrum tetracyclines with less impact on the GI flora, such as sarecycline. “So there is the potential for more eco-friendly tetracyclines,” he said.
Going forward, many questions remain about optimal antibiotic stewardship in dermatology, Dr. Zhanel said. For example, if you combine a topical antibiotic with benzoyl peroxide, are you less likely to get resistance to that topical antibiotic? “I think the answer is yes, but the literature isn’t very strong on that,” he said. “Also, is benzoyl peroxide plus a topical retinoid better than benzoyl peroxide plus a topical antibiotic in terms of resistance? I think the answer is yes, but again there is very little data on this.”
Dr. Zhanel disclosed having numerous financial ties to the pharmaceutical industry.
LAKE TAHOE, CALIF. – Dermatologists prescribe more antibiotics than any other physician group, a statistic that George G. Zhanel, PhD, would like to see go by the wayside.
After all, the World Health Organization projects that the number of annual deaths in North America attributable to antibiotic resistance will reach 317,000 by the year 2050.
Dr. Zhanel, a microbiologist at the College of Medicine, University of Manitoba, Winnipeg, Canada, said at the annual meeting of the Society for Pediatric Dermatology. “Many of us are very concerned about this. Countries have put together an optimal action plan. What are we going to do about this? The plans are quite similar from country to country. They talk about surveillance, finding where these pathogens are. They talk about infection control such as washing your hands in the clinic so you’re not moving antibiotic-resistant organisms around. They talk about diagnostic and treatment guidelines, new antibiotic therapies, probiotics, and vaccination strategies. My own group is doing research on all of these areas, but today I’m going to focus on antibiotic stewardship: Using antibiotics wisely, trying to optimize efficacy while trying to minimize the development of resistant organisms.”
Dr. Zhanel, who is also director of the Canadian Antimicrobial Resistance Alliance (CARA) at the College of Medicine, University of Manitoba, described dermatologists as “big players” when it comes to antibiotic use. According to a 2016 report from the Scientific Panel on Antibiotic Use in Dermatology, dermatologists order 8.2 million oral antibiotic prescriptions each year, which is more common than any other physician group based on the prescribing rate per clinician (J Clin Aesthet Dermatol. 2016;9[4]:18-24). In addition, the prescribed duration of antibiotic therapy is often markedly longer with therapies treated by dermatologists, especially acne and rosacea. One study of general practitioners in the United Kingdom found that the mean duration of oral antibiotic use for treating acne was 175 days (J Am Acad Dermatol 2016;75:1142-50). “For some patients it went on much longer,” said Dr. Zhanel, who was not affiliated with the study.
“You are important players when it comes to antibiotics. How you use them and if you use them wisely impacts not only your patients, but the world.”
The correlation between antibiotic use and resistance is widely established, he continued. “We have known for 30 to 40 years that if you treat patients with tetracyclines, the Staphylococcus epidermidis that we all have on our skin develop tetracycline resistance,” he said. “The tetracycline resistance genes from S. epidermidis can then transfer to putative pathogens such as Staphylococcus aureus, and potentially [methicillin-resistant S. aureus]. That’s why we need to try to minimize oral tetracycline exposure on the normal microbiome.” In addition, tetracycline use can help create multidrug resistant organisms.
Next, Dr. Zhanel discussed potential solutions to antimicrobial usage/resistance in dermatology. According to recent guidelines on the care for the management of acne vulgaris, systemic antibiotic use should be limited to the shortest possible duration, typically 90 days (J Am Acad Dermatol. 2016;74[5]:945-73). A common treatment for moderate to-severe acne is to combine a topical retinoid with an oral or topical antimicrobial (J Am Acad Dermatol. 2009;60(5 suppl):S1-S50). If the addition of an oral antibiotic is required, limit its use to 3 or 4 months and co-prescribe with a product that contains benzoyl peroxide (BPO), or use as a washout. “Ideally, that’s your exit strategy,” he said. “Once you finish the oral antibiotic, in about 3 months if possible, continue with the topical retinoids plus BPO to maintain that particular remission.”
Why add benzoyl peroxide to topical retinoids for maintenance therapy? “Benzoyl peroxide and topical retinoids affect multiple targets in your acne strategy, and when you use them together they are powerful,” Dr. Zhanel said. He advises dermatologists not to prescribe oral or topical clindamycin unless they have to, because that drug is one of the main drivers of Clostridium difficile infection.
Dr. Zhanel’s stewardship tips for topical antibiotics involve not using topical tetracyclines/clindamycin/macrolides, in favor of using a topical antimicrobial such as BPO. “We think that benzoyl peroxide is less likely to drive resistance than are the traditional topical antibiotics like tetracyclines and clindamycin,” he said. “Use topical retinoids and benzoyl peroxide, if possible.”
Subtherapeutic oral doses of tetracyclines such as doxycycline 40 mg modified release “look very powerful for treating rosacea and do not affect the normal microbiome or select for resistance,” he said. In the meantime, Dr. Zhanel and other researchers are working to develop narrow spectrum tetracyclines with less impact on the GI flora, such as sarecycline. “So there is the potential for more eco-friendly tetracyclines,” he said.
Going forward, many questions remain about optimal antibiotic stewardship in dermatology, Dr. Zhanel said. For example, if you combine a topical antibiotic with benzoyl peroxide, are you less likely to get resistance to that topical antibiotic? “I think the answer is yes, but the literature isn’t very strong on that,” he said. “Also, is benzoyl peroxide plus a topical retinoid better than benzoyl peroxide plus a topical antibiotic in terms of resistance? I think the answer is yes, but again there is very little data on this.”
Dr. Zhanel disclosed having numerous financial ties to the pharmaceutical industry.
LAKE TAHOE, CALIF. – Dermatologists prescribe more antibiotics than any other physician group, a statistic that George G. Zhanel, PhD, would like to see go by the wayside.
After all, the World Health Organization projects that the number of annual deaths in North America attributable to antibiotic resistance will reach 317,000 by the year 2050.
Dr. Zhanel, a microbiologist at the College of Medicine, University of Manitoba, Winnipeg, Canada, said at the annual meeting of the Society for Pediatric Dermatology. “Many of us are very concerned about this. Countries have put together an optimal action plan. What are we going to do about this? The plans are quite similar from country to country. They talk about surveillance, finding where these pathogens are. They talk about infection control such as washing your hands in the clinic so you’re not moving antibiotic-resistant organisms around. They talk about diagnostic and treatment guidelines, new antibiotic therapies, probiotics, and vaccination strategies. My own group is doing research on all of these areas, but today I’m going to focus on antibiotic stewardship: Using antibiotics wisely, trying to optimize efficacy while trying to minimize the development of resistant organisms.”
Dr. Zhanel, who is also director of the Canadian Antimicrobial Resistance Alliance (CARA) at the College of Medicine, University of Manitoba, described dermatologists as “big players” when it comes to antibiotic use. According to a 2016 report from the Scientific Panel on Antibiotic Use in Dermatology, dermatologists order 8.2 million oral antibiotic prescriptions each year, which is more common than any other physician group based on the prescribing rate per clinician (J Clin Aesthet Dermatol. 2016;9[4]:18-24). In addition, the prescribed duration of antibiotic therapy is often markedly longer with therapies treated by dermatologists, especially acne and rosacea. One study of general practitioners in the United Kingdom found that the mean duration of oral antibiotic use for treating acne was 175 days (J Am Acad Dermatol 2016;75:1142-50). “For some patients it went on much longer,” said Dr. Zhanel, who was not affiliated with the study.
“You are important players when it comes to antibiotics. How you use them and if you use them wisely impacts not only your patients, but the world.”
The correlation between antibiotic use and resistance is widely established, he continued. “We have known for 30 to 40 years that if you treat patients with tetracyclines, the Staphylococcus epidermidis that we all have on our skin develop tetracycline resistance,” he said. “The tetracycline resistance genes from S. epidermidis can then transfer to putative pathogens such as Staphylococcus aureus, and potentially [methicillin-resistant S. aureus]. That’s why we need to try to minimize oral tetracycline exposure on the normal microbiome.” In addition, tetracycline use can help create multidrug resistant organisms.
Next, Dr. Zhanel discussed potential solutions to antimicrobial usage/resistance in dermatology. According to recent guidelines on the care for the management of acne vulgaris, systemic antibiotic use should be limited to the shortest possible duration, typically 90 days (J Am Acad Dermatol. 2016;74[5]:945-73). A common treatment for moderate to-severe acne is to combine a topical retinoid with an oral or topical antimicrobial (J Am Acad Dermatol. 2009;60(5 suppl):S1-S50). If the addition of an oral antibiotic is required, limit its use to 3 or 4 months and co-prescribe with a product that contains benzoyl peroxide (BPO), or use as a washout. “Ideally, that’s your exit strategy,” he said. “Once you finish the oral antibiotic, in about 3 months if possible, continue with the topical retinoids plus BPO to maintain that particular remission.”
Why add benzoyl peroxide to topical retinoids for maintenance therapy? “Benzoyl peroxide and topical retinoids affect multiple targets in your acne strategy, and when you use them together they are powerful,” Dr. Zhanel said. He advises dermatologists not to prescribe oral or topical clindamycin unless they have to, because that drug is one of the main drivers of Clostridium difficile infection.
Dr. Zhanel’s stewardship tips for topical antibiotics involve not using topical tetracyclines/clindamycin/macrolides, in favor of using a topical antimicrobial such as BPO. “We think that benzoyl peroxide is less likely to drive resistance than are the traditional topical antibiotics like tetracyclines and clindamycin,” he said. “Use topical retinoids and benzoyl peroxide, if possible.”
Subtherapeutic oral doses of tetracyclines such as doxycycline 40 mg modified release “look very powerful for treating rosacea and do not affect the normal microbiome or select for resistance,” he said. In the meantime, Dr. Zhanel and other researchers are working to develop narrow spectrum tetracyclines with less impact on the GI flora, such as sarecycline. “So there is the potential for more eco-friendly tetracyclines,” he said.
Going forward, many questions remain about optimal antibiotic stewardship in dermatology, Dr. Zhanel said. For example, if you combine a topical antibiotic with benzoyl peroxide, are you less likely to get resistance to that topical antibiotic? “I think the answer is yes, but the literature isn’t very strong on that,” he said. “Also, is benzoyl peroxide plus a topical retinoid better than benzoyl peroxide plus a topical antibiotic in terms of resistance? I think the answer is yes, but again there is very little data on this.”
Dr. Zhanel disclosed having numerous financial ties to the pharmaceutical industry.
EXPERT ANALYSIS FROM THE SPD ANNUAL MEETING
Certain skin conditions signal potential overgrowth disorder
LAKE TAHOE, CALIF. – and during human development, Leslie G. Biesecker, MD said at the annual meeting of the Society for Pediatric Dermatology.
Dr. Biesecker, senior investigator and head of the clinical genomics section of the National Human Genome Research Institute’s Medical Genomics and Metabolic Genetics Branch, discussed mosaicism and a number of overgrowth syndromes that he and his associates have been studying that have clinical relevance for pediatric dermatologists. He noted that mosaicism can affect any tissue, anywhere, in any pattern. “If an affected cell cannot survive gametogenesis, fertilization, or survive early development, this generates Happle-type mosaicism,” explained Dr. Biesecker, who is trained in pediatrics and in clinical and molecular genetics.
“This is characterized by patchy manifestations, and no parent-to-child transmission or recurrence. You must always be careful here, though, because Mother Nature does what she wants to. Mosaic mutations can happen more than once, but it’s a very unlikely outcome. Happle-type mosaicism is also characterized by discordant monozygotic twins,” he noted.
The prototype for Happle-type mosaicism is Proteus syndrome, formerly known as Elephant Man disease, which is caused by a mutation in the AKT1 gene. Patients with Proteus syndrome undergo severe, relentless overgrowth, and about 25% of them die during childhood. “If you see one of these patients, you have a serious clinical problem on your hands,” he said. “There is enormous individual variability, but it is ultra rare.”
Dermatologic lesions that are characteristic of Proteus syndrome include cerebriform connective tissue nevus, which typically presents on the hands and feet. “A wide range of vascular malformations have also been associated with this, even patients with arteriovenous malformations,” Dr. Biesecker said. “They are a serious problem.” Linear verrucous epidermal nevus is another characteristic lesion of Proteus syndrome. It can present in a number of ways and in various body sites. “The natural history of these lesions is important,” he commented. “Over time, are they stable, or do they spread and expand over time? These lesions do not ever spontaneously regress. This does enable molecular diagnosis, but don’t bother sampling their blood, because it will be negative. You have to have a biopsy sample.”
Overgrowth syndromes that do not meet criteria for Proteus syndrome fall into a category known as PIK3CA-related overgrowth spectrum, which Dr. Biesecker characterized as “a bunch of clinical designations all caused by the same underlying somatic mutation in a gene called PIK3CA. There is an enormous variability in these patients, ranging from those who have profound overgrowth, including malformations, truncal overgrowth, and vascular malformations, and digital overgrowth in all sorts of patterns. We designate this as PIK3CA-related overgrowth spectrum (PROS), because we can’t clinically separate these things from one another.”
These conditions include what used to be called CLOVES syndrome (congenital lipomatous overgrowth, vascular malformations, epidermal nevi, and scoliosis/skeletal/spinal anomalies), facial infiltrating lipomatosis, and megalencephaly-capillary malformation syndrome. PROS is about 100 times more common than Proteus syndrome. “There are no rational boundaries to distinguish these entities,” Dr. Biesecker said. “They are rationalized under a combined clinical-molecular PROS framework, meaning that the molecular diagnosis is absolutely key to correctly diagnosing these patients.”
In this way, mosaicism challenges the traditional concept of diagnosing overgrowth disorders. “What we thought were separate disorders are in fact many manifestations of a single disorder,” he continued. “When I was doing my genetics training, we were taught that it would turn out that there was one gene for every disease, and one disease for every gene. That is completely wrong; it’s much more complicated than that. Mosaicism is also important for us as biologists, because it gives us a window into biology we otherwise would not see. Without a mosaicism, Proteus syndrome cannot exist biologically. So if I want to understand that gene product, I have to study patients who are mosaics. Mosaicism can happen in any tissue, whether it’s visible or not.”
Dr. Biesecker, who has been elected to serve as president of the American Society of Human Genetics for 2019, noted that most of the gene mutations that cause overgrowth disorders are the same ones implicated in cancer. “It makes sense, because cancer is a disorder of uncontrolled proliferation and differentiation,” he said. “These overgrowth disorders are similar but less severe manifestations of the same problem. It turns out that these mosaic patients are single gene model systems of cancer biology.” Therefore, when a drug company develops an anti-cancer drug, he continued, it also can be useful for PROS or Proteus syndrome. It’s much easier to inhibit a protein that’s overactive than it is to replace the activity of a gene that has lost its function.
But in PROS and Proteus, “we have very different treatment objectives than oncologists do,” he said. “Our goal is to reduce the signaling caused by these mutations; we do not want to kill the cells. Some of my patients with these disorders have pretty close to 50% of cells in their body carrying these mutations. If I were thinking like an oncologist, the oncologist wants to kill cancer cells; that’s their objective. If I were to kill all of the mutant cells in my patients, I’m certain that would kill them.”
One promising development is the investigational oral agent ARQ 092, which is an inhibitor of AKT1. Dr. Biesecker and his colleagues at the NIH have been working to figure out what dosing should be used in humans based on mouse data, lab data, and data from cancer patients. They started with about one-twelvth the dose that oncologists use. After treating the first patient with overgrowth syndrome, on day 15 that person’s AKT1 level dropped to about 20% of normal, while on day 75 it moved to around 60% of normal. “We are right in that zone where we want to drive the activity of that protein to about half of what it should be,” Dr. Biesecker said. He and his colleagues also have observed regression of lesions in a patient with cerebriform connective tissue nevus who was treated with ARQ 092. “We’ve never seen this before.”
Dr. Biesecker disclosed that he is a member of the Illumina medical ethics board. He has received royalties from Genentech and in-kind research support from ArQule and Pfizer.
dbrunk@mdedge.com
LAKE TAHOE, CALIF. – and during human development, Leslie G. Biesecker, MD said at the annual meeting of the Society for Pediatric Dermatology.
Dr. Biesecker, senior investigator and head of the clinical genomics section of the National Human Genome Research Institute’s Medical Genomics and Metabolic Genetics Branch, discussed mosaicism and a number of overgrowth syndromes that he and his associates have been studying that have clinical relevance for pediatric dermatologists. He noted that mosaicism can affect any tissue, anywhere, in any pattern. “If an affected cell cannot survive gametogenesis, fertilization, or survive early development, this generates Happle-type mosaicism,” explained Dr. Biesecker, who is trained in pediatrics and in clinical and molecular genetics.
“This is characterized by patchy manifestations, and no parent-to-child transmission or recurrence. You must always be careful here, though, because Mother Nature does what she wants to. Mosaic mutations can happen more than once, but it’s a very unlikely outcome. Happle-type mosaicism is also characterized by discordant monozygotic twins,” he noted.
The prototype for Happle-type mosaicism is Proteus syndrome, formerly known as Elephant Man disease, which is caused by a mutation in the AKT1 gene. Patients with Proteus syndrome undergo severe, relentless overgrowth, and about 25% of them die during childhood. “If you see one of these patients, you have a serious clinical problem on your hands,” he said. “There is enormous individual variability, but it is ultra rare.”
Dermatologic lesions that are characteristic of Proteus syndrome include cerebriform connective tissue nevus, which typically presents on the hands and feet. “A wide range of vascular malformations have also been associated with this, even patients with arteriovenous malformations,” Dr. Biesecker said. “They are a serious problem.” Linear verrucous epidermal nevus is another characteristic lesion of Proteus syndrome. It can present in a number of ways and in various body sites. “The natural history of these lesions is important,” he commented. “Over time, are they stable, or do they spread and expand over time? These lesions do not ever spontaneously regress. This does enable molecular diagnosis, but don’t bother sampling their blood, because it will be negative. You have to have a biopsy sample.”
Overgrowth syndromes that do not meet criteria for Proteus syndrome fall into a category known as PIK3CA-related overgrowth spectrum, which Dr. Biesecker characterized as “a bunch of clinical designations all caused by the same underlying somatic mutation in a gene called PIK3CA. There is an enormous variability in these patients, ranging from those who have profound overgrowth, including malformations, truncal overgrowth, and vascular malformations, and digital overgrowth in all sorts of patterns. We designate this as PIK3CA-related overgrowth spectrum (PROS), because we can’t clinically separate these things from one another.”
These conditions include what used to be called CLOVES syndrome (congenital lipomatous overgrowth, vascular malformations, epidermal nevi, and scoliosis/skeletal/spinal anomalies), facial infiltrating lipomatosis, and megalencephaly-capillary malformation syndrome. PROS is about 100 times more common than Proteus syndrome. “There are no rational boundaries to distinguish these entities,” Dr. Biesecker said. “They are rationalized under a combined clinical-molecular PROS framework, meaning that the molecular diagnosis is absolutely key to correctly diagnosing these patients.”
In this way, mosaicism challenges the traditional concept of diagnosing overgrowth disorders. “What we thought were separate disorders are in fact many manifestations of a single disorder,” he continued. “When I was doing my genetics training, we were taught that it would turn out that there was one gene for every disease, and one disease for every gene. That is completely wrong; it’s much more complicated than that. Mosaicism is also important for us as biologists, because it gives us a window into biology we otherwise would not see. Without a mosaicism, Proteus syndrome cannot exist biologically. So if I want to understand that gene product, I have to study patients who are mosaics. Mosaicism can happen in any tissue, whether it’s visible or not.”
Dr. Biesecker, who has been elected to serve as president of the American Society of Human Genetics for 2019, noted that most of the gene mutations that cause overgrowth disorders are the same ones implicated in cancer. “It makes sense, because cancer is a disorder of uncontrolled proliferation and differentiation,” he said. “These overgrowth disorders are similar but less severe manifestations of the same problem. It turns out that these mosaic patients are single gene model systems of cancer biology.” Therefore, when a drug company develops an anti-cancer drug, he continued, it also can be useful for PROS or Proteus syndrome. It’s much easier to inhibit a protein that’s overactive than it is to replace the activity of a gene that has lost its function.
But in PROS and Proteus, “we have very different treatment objectives than oncologists do,” he said. “Our goal is to reduce the signaling caused by these mutations; we do not want to kill the cells. Some of my patients with these disorders have pretty close to 50% of cells in their body carrying these mutations. If I were thinking like an oncologist, the oncologist wants to kill cancer cells; that’s their objective. If I were to kill all of the mutant cells in my patients, I’m certain that would kill them.”
One promising development is the investigational oral agent ARQ 092, which is an inhibitor of AKT1. Dr. Biesecker and his colleagues at the NIH have been working to figure out what dosing should be used in humans based on mouse data, lab data, and data from cancer patients. They started with about one-twelvth the dose that oncologists use. After treating the first patient with overgrowth syndrome, on day 15 that person’s AKT1 level dropped to about 20% of normal, while on day 75 it moved to around 60% of normal. “We are right in that zone where we want to drive the activity of that protein to about half of what it should be,” Dr. Biesecker said. He and his colleagues also have observed regression of lesions in a patient with cerebriform connective tissue nevus who was treated with ARQ 092. “We’ve never seen this before.”
Dr. Biesecker disclosed that he is a member of the Illumina medical ethics board. He has received royalties from Genentech and in-kind research support from ArQule and Pfizer.
dbrunk@mdedge.com
LAKE TAHOE, CALIF. – and during human development, Leslie G. Biesecker, MD said at the annual meeting of the Society for Pediatric Dermatology.
Dr. Biesecker, senior investigator and head of the clinical genomics section of the National Human Genome Research Institute’s Medical Genomics and Metabolic Genetics Branch, discussed mosaicism and a number of overgrowth syndromes that he and his associates have been studying that have clinical relevance for pediatric dermatologists. He noted that mosaicism can affect any tissue, anywhere, in any pattern. “If an affected cell cannot survive gametogenesis, fertilization, or survive early development, this generates Happle-type mosaicism,” explained Dr. Biesecker, who is trained in pediatrics and in clinical and molecular genetics.
“This is characterized by patchy manifestations, and no parent-to-child transmission or recurrence. You must always be careful here, though, because Mother Nature does what she wants to. Mosaic mutations can happen more than once, but it’s a very unlikely outcome. Happle-type mosaicism is also characterized by discordant monozygotic twins,” he noted.
The prototype for Happle-type mosaicism is Proteus syndrome, formerly known as Elephant Man disease, which is caused by a mutation in the AKT1 gene. Patients with Proteus syndrome undergo severe, relentless overgrowth, and about 25% of them die during childhood. “If you see one of these patients, you have a serious clinical problem on your hands,” he said. “There is enormous individual variability, but it is ultra rare.”
Dermatologic lesions that are characteristic of Proteus syndrome include cerebriform connective tissue nevus, which typically presents on the hands and feet. “A wide range of vascular malformations have also been associated with this, even patients with arteriovenous malformations,” Dr. Biesecker said. “They are a serious problem.” Linear verrucous epidermal nevus is another characteristic lesion of Proteus syndrome. It can present in a number of ways and in various body sites. “The natural history of these lesions is important,” he commented. “Over time, are they stable, or do they spread and expand over time? These lesions do not ever spontaneously regress. This does enable molecular diagnosis, but don’t bother sampling their blood, because it will be negative. You have to have a biopsy sample.”
Overgrowth syndromes that do not meet criteria for Proteus syndrome fall into a category known as PIK3CA-related overgrowth spectrum, which Dr. Biesecker characterized as “a bunch of clinical designations all caused by the same underlying somatic mutation in a gene called PIK3CA. There is an enormous variability in these patients, ranging from those who have profound overgrowth, including malformations, truncal overgrowth, and vascular malformations, and digital overgrowth in all sorts of patterns. We designate this as PIK3CA-related overgrowth spectrum (PROS), because we can’t clinically separate these things from one another.”
These conditions include what used to be called CLOVES syndrome (congenital lipomatous overgrowth, vascular malformations, epidermal nevi, and scoliosis/skeletal/spinal anomalies), facial infiltrating lipomatosis, and megalencephaly-capillary malformation syndrome. PROS is about 100 times more common than Proteus syndrome. “There are no rational boundaries to distinguish these entities,” Dr. Biesecker said. “They are rationalized under a combined clinical-molecular PROS framework, meaning that the molecular diagnosis is absolutely key to correctly diagnosing these patients.”
In this way, mosaicism challenges the traditional concept of diagnosing overgrowth disorders. “What we thought were separate disorders are in fact many manifestations of a single disorder,” he continued. “When I was doing my genetics training, we were taught that it would turn out that there was one gene for every disease, and one disease for every gene. That is completely wrong; it’s much more complicated than that. Mosaicism is also important for us as biologists, because it gives us a window into biology we otherwise would not see. Without a mosaicism, Proteus syndrome cannot exist biologically. So if I want to understand that gene product, I have to study patients who are mosaics. Mosaicism can happen in any tissue, whether it’s visible or not.”
Dr. Biesecker, who has been elected to serve as president of the American Society of Human Genetics for 2019, noted that most of the gene mutations that cause overgrowth disorders are the same ones implicated in cancer. “It makes sense, because cancer is a disorder of uncontrolled proliferation and differentiation,” he said. “These overgrowth disorders are similar but less severe manifestations of the same problem. It turns out that these mosaic patients are single gene model systems of cancer biology.” Therefore, when a drug company develops an anti-cancer drug, he continued, it also can be useful for PROS or Proteus syndrome. It’s much easier to inhibit a protein that’s overactive than it is to replace the activity of a gene that has lost its function.
But in PROS and Proteus, “we have very different treatment objectives than oncologists do,” he said. “Our goal is to reduce the signaling caused by these mutations; we do not want to kill the cells. Some of my patients with these disorders have pretty close to 50% of cells in their body carrying these mutations. If I were thinking like an oncologist, the oncologist wants to kill cancer cells; that’s their objective. If I were to kill all of the mutant cells in my patients, I’m certain that would kill them.”
One promising development is the investigational oral agent ARQ 092, which is an inhibitor of AKT1. Dr. Biesecker and his colleagues at the NIH have been working to figure out what dosing should be used in humans based on mouse data, lab data, and data from cancer patients. They started with about one-twelvth the dose that oncologists use. After treating the first patient with overgrowth syndrome, on day 15 that person’s AKT1 level dropped to about 20% of normal, while on day 75 it moved to around 60% of normal. “We are right in that zone where we want to drive the activity of that protein to about half of what it should be,” Dr. Biesecker said. He and his colleagues also have observed regression of lesions in a patient with cerebriform connective tissue nevus who was treated with ARQ 092. “We’ve never seen this before.”
Dr. Biesecker disclosed that he is a member of the Illumina medical ethics board. He has received royalties from Genentech and in-kind research support from ArQule and Pfizer.
dbrunk@mdedge.com
EXPERT ANALYSIS FROM THE SPD ANNUAL MEETING
JAK inhibitors emerge as promising alopecia treatment
LAKE TAHOE, CALIF. – After Brett King, MD, PhD, and his wife and collaborator, Brittany G. Craiglow, MD, published an index case of oral tofacitinib reversing alopecia universalis in a 25-year-old male patient back in 2014 (J Invest Dermatol. 2014;134:2988-90), they received hundreds of e-mails and phone calls from clinicians and patients.
“We also received quite a bit of media attention from around the world,” Dr. King recalled at the annual meeting of the Society for Pediatric Dermatology.
After all, alopecia areata and its variants affect 1%-2% of the population and have a marked impact on health-related quality of life, with high rates of concomitant generalized anxiety disorder and major depressive disorder. “The health-related quality of life is similar to that of atopic dermatitis and psoriasis, and there are no reliably effective therapies, especially for severe disease,” he said. “”
Currently available Janus kinase (JAK) inhibitors include tofacitinib (Xeljanz), ruxolitinib (Jakafi), and baricitinib (Olumiant). “These medicines are not [Food and Drug Administration] approved for alopecia areata, though tofacitinib was recently approved for psoriatic arthritis, and so we have formal entry of this medicine into dermatology for the first time,” said Dr. King, who is a dermatologist at Yale University, New Haven, Conn.
Potential adverse effects of JAKs include nasopharyngitis, headache, diarrhea, elevated cholesterol, uncommonly herpes zoster, cytopenias, transaminitis, and rarely non-melanoma skin cancer, solid organ malignancy and lymphoma, and GI perforation. Tofacitinib has an FDA black box warning regarding serious infections and malignancies, and baricitinib has these plus an additional warning about thrombosis.
In an open label, two-center trial that followed the index patient report, Dr. King and his associates enrolled 66 patients aged 19-35 years who had greater than 50% scalp hair loss for at least 6 months to receive tofacitinib 5 mg twice daily for 3 months (JCI Insight. 2016; 1[15]:e89776). A primary outcome of interest was regrowth of hair as measured by the percent change in Severity of Alopecia Tool (SALT) score. A SALT score of 100 indicates baldness, while a score of zero indicates no hair loss. Following 3 months of treatment, 32% of patients had a greater than 50% change in their SALT score, 32% had a change in the range of 5%-50%, while 36% had a change that was less than 5%.
“One of the interesting findings was that long duration of current episode of complete scalp hair loss was a negative predictor of treatment response, especially for those who have had hair loss greater than 10 years,” Dr. King said. Adverse events were “pretty bland,” with the most common being upper respiratory infection (17%), headache (8%), abdominal pain (8%), and acne (8%). Weight gain occurred in 1.5% of patients.
Next, Dr. King and colleagues reviewed the records of 90 patients aged 18 years or older who were treated with tofacitinib for at least 4 months (J Am Acad Dermatol. 2017;76[1]:22-8). Patients had greater than 40% scalp hair loss, and the tofacitinib dose was up to 10 mg per day at the discretion of the physician. “About 43% of patients were treated with tofacitinib 5 mg” twice daily, Dr. King said. “Other patients had higher doses or the addition of prednisone for three doses to see if that would help.”
After treatment, 20% of patients had a greater than 90% change in their SALT score (complete scalp hair regrowth), while 38.4% had a change that ranged from 51%-90%. At the same time, 18% had a change in their SALT score that ranged from 6%-50%, while 23% had a change that was 5% or less. As observed in the earlier trial, researchers saw a negative correlation between duration of current episode of hair loss and latest percent change in SALT score.
“We believe that you have to catch people before they get to more than 10 years of complete scalp hair loss,” Dr. King said. “This is important for the pediatric age group. I just saw somebody who’s 13, and they’ve been bald for 8 years. You might make the argument that this person deserves treatment, at least for a period of time long enough to regrow their hair in order to reset the clock.”
The most common adverse events were acne and weight gain.
In a separate analysis, Dr. King, Dr. Craiglow, and Lucy Y. Liu, evaluated the use of tofacitinib for at least 2 months in 13 alopecia areata patients aged 12-17 years (J Am Acad Dermatol. 2017;76[1]:29-32). They limited the analysis to those who had greater than 20% scalp hair loss, alopecia totalis, or alopecia universalis that was stable or worsening for 6 months or longer. Of the 13 patients, 9 (69%) were responders. Of the four non-responders, one had a very long duration of baldness. The percent change in SALT score was 93% overall, including 100% in the responder group over a median of 5 months and just 1% in the non-responder group over a median of 4 months. “This does not work every time,” Dr. King said.
While some preliminary studies of topical JAK inhibitors for alopecia areata show promise, it remains unclear if this approach will translate in a clinically meaningful way, he said. Clinical trials are currently under way.
Dr. King disclosed that he has received honoraria or consulting fees from Aclaris Therapeutics, Celgene, Concert Pharmaceuticals, Eli Lilly, Pfizer, Regeneron Pharmaceuticals, and Dermavant Sciences. He has also received funding support from The Ranjini and Ajay Poddar Resource Fund for Dermatologic Diseases Research.
dbrunk@mdedge.com
LAKE TAHOE, CALIF. – After Brett King, MD, PhD, and his wife and collaborator, Brittany G. Craiglow, MD, published an index case of oral tofacitinib reversing alopecia universalis in a 25-year-old male patient back in 2014 (J Invest Dermatol. 2014;134:2988-90), they received hundreds of e-mails and phone calls from clinicians and patients.
“We also received quite a bit of media attention from around the world,” Dr. King recalled at the annual meeting of the Society for Pediatric Dermatology.
After all, alopecia areata and its variants affect 1%-2% of the population and have a marked impact on health-related quality of life, with high rates of concomitant generalized anxiety disorder and major depressive disorder. “The health-related quality of life is similar to that of atopic dermatitis and psoriasis, and there are no reliably effective therapies, especially for severe disease,” he said. “”
Currently available Janus kinase (JAK) inhibitors include tofacitinib (Xeljanz), ruxolitinib (Jakafi), and baricitinib (Olumiant). “These medicines are not [Food and Drug Administration] approved for alopecia areata, though tofacitinib was recently approved for psoriatic arthritis, and so we have formal entry of this medicine into dermatology for the first time,” said Dr. King, who is a dermatologist at Yale University, New Haven, Conn.
Potential adverse effects of JAKs include nasopharyngitis, headache, diarrhea, elevated cholesterol, uncommonly herpes zoster, cytopenias, transaminitis, and rarely non-melanoma skin cancer, solid organ malignancy and lymphoma, and GI perforation. Tofacitinib has an FDA black box warning regarding serious infections and malignancies, and baricitinib has these plus an additional warning about thrombosis.
In an open label, two-center trial that followed the index patient report, Dr. King and his associates enrolled 66 patients aged 19-35 years who had greater than 50% scalp hair loss for at least 6 months to receive tofacitinib 5 mg twice daily for 3 months (JCI Insight. 2016; 1[15]:e89776). A primary outcome of interest was regrowth of hair as measured by the percent change in Severity of Alopecia Tool (SALT) score. A SALT score of 100 indicates baldness, while a score of zero indicates no hair loss. Following 3 months of treatment, 32% of patients had a greater than 50% change in their SALT score, 32% had a change in the range of 5%-50%, while 36% had a change that was less than 5%.
“One of the interesting findings was that long duration of current episode of complete scalp hair loss was a negative predictor of treatment response, especially for those who have had hair loss greater than 10 years,” Dr. King said. Adverse events were “pretty bland,” with the most common being upper respiratory infection (17%), headache (8%), abdominal pain (8%), and acne (8%). Weight gain occurred in 1.5% of patients.
Next, Dr. King and colleagues reviewed the records of 90 patients aged 18 years or older who were treated with tofacitinib for at least 4 months (J Am Acad Dermatol. 2017;76[1]:22-8). Patients had greater than 40% scalp hair loss, and the tofacitinib dose was up to 10 mg per day at the discretion of the physician. “About 43% of patients were treated with tofacitinib 5 mg” twice daily, Dr. King said. “Other patients had higher doses or the addition of prednisone for three doses to see if that would help.”
After treatment, 20% of patients had a greater than 90% change in their SALT score (complete scalp hair regrowth), while 38.4% had a change that ranged from 51%-90%. At the same time, 18% had a change in their SALT score that ranged from 6%-50%, while 23% had a change that was 5% or less. As observed in the earlier trial, researchers saw a negative correlation between duration of current episode of hair loss and latest percent change in SALT score.
“We believe that you have to catch people before they get to more than 10 years of complete scalp hair loss,” Dr. King said. “This is important for the pediatric age group. I just saw somebody who’s 13, and they’ve been bald for 8 years. You might make the argument that this person deserves treatment, at least for a period of time long enough to regrow their hair in order to reset the clock.”
The most common adverse events were acne and weight gain.
In a separate analysis, Dr. King, Dr. Craiglow, and Lucy Y. Liu, evaluated the use of tofacitinib for at least 2 months in 13 alopecia areata patients aged 12-17 years (J Am Acad Dermatol. 2017;76[1]:29-32). They limited the analysis to those who had greater than 20% scalp hair loss, alopecia totalis, or alopecia universalis that was stable or worsening for 6 months or longer. Of the 13 patients, 9 (69%) were responders. Of the four non-responders, one had a very long duration of baldness. The percent change in SALT score was 93% overall, including 100% in the responder group over a median of 5 months and just 1% in the non-responder group over a median of 4 months. “This does not work every time,” Dr. King said.
While some preliminary studies of topical JAK inhibitors for alopecia areata show promise, it remains unclear if this approach will translate in a clinically meaningful way, he said. Clinical trials are currently under way.
Dr. King disclosed that he has received honoraria or consulting fees from Aclaris Therapeutics, Celgene, Concert Pharmaceuticals, Eli Lilly, Pfizer, Regeneron Pharmaceuticals, and Dermavant Sciences. He has also received funding support from The Ranjini and Ajay Poddar Resource Fund for Dermatologic Diseases Research.
dbrunk@mdedge.com
LAKE TAHOE, CALIF. – After Brett King, MD, PhD, and his wife and collaborator, Brittany G. Craiglow, MD, published an index case of oral tofacitinib reversing alopecia universalis in a 25-year-old male patient back in 2014 (J Invest Dermatol. 2014;134:2988-90), they received hundreds of e-mails and phone calls from clinicians and patients.
“We also received quite a bit of media attention from around the world,” Dr. King recalled at the annual meeting of the Society for Pediatric Dermatology.
After all, alopecia areata and its variants affect 1%-2% of the population and have a marked impact on health-related quality of life, with high rates of concomitant generalized anxiety disorder and major depressive disorder. “The health-related quality of life is similar to that of atopic dermatitis and psoriasis, and there are no reliably effective therapies, especially for severe disease,” he said. “”
Currently available Janus kinase (JAK) inhibitors include tofacitinib (Xeljanz), ruxolitinib (Jakafi), and baricitinib (Olumiant). “These medicines are not [Food and Drug Administration] approved for alopecia areata, though tofacitinib was recently approved for psoriatic arthritis, and so we have formal entry of this medicine into dermatology for the first time,” said Dr. King, who is a dermatologist at Yale University, New Haven, Conn.
Potential adverse effects of JAKs include nasopharyngitis, headache, diarrhea, elevated cholesterol, uncommonly herpes zoster, cytopenias, transaminitis, and rarely non-melanoma skin cancer, solid organ malignancy and lymphoma, and GI perforation. Tofacitinib has an FDA black box warning regarding serious infections and malignancies, and baricitinib has these plus an additional warning about thrombosis.
In an open label, two-center trial that followed the index patient report, Dr. King and his associates enrolled 66 patients aged 19-35 years who had greater than 50% scalp hair loss for at least 6 months to receive tofacitinib 5 mg twice daily for 3 months (JCI Insight. 2016; 1[15]:e89776). A primary outcome of interest was regrowth of hair as measured by the percent change in Severity of Alopecia Tool (SALT) score. A SALT score of 100 indicates baldness, while a score of zero indicates no hair loss. Following 3 months of treatment, 32% of patients had a greater than 50% change in their SALT score, 32% had a change in the range of 5%-50%, while 36% had a change that was less than 5%.
“One of the interesting findings was that long duration of current episode of complete scalp hair loss was a negative predictor of treatment response, especially for those who have had hair loss greater than 10 years,” Dr. King said. Adverse events were “pretty bland,” with the most common being upper respiratory infection (17%), headache (8%), abdominal pain (8%), and acne (8%). Weight gain occurred in 1.5% of patients.
Next, Dr. King and colleagues reviewed the records of 90 patients aged 18 years or older who were treated with tofacitinib for at least 4 months (J Am Acad Dermatol. 2017;76[1]:22-8). Patients had greater than 40% scalp hair loss, and the tofacitinib dose was up to 10 mg per day at the discretion of the physician. “About 43% of patients were treated with tofacitinib 5 mg” twice daily, Dr. King said. “Other patients had higher doses or the addition of prednisone for three doses to see if that would help.”
After treatment, 20% of patients had a greater than 90% change in their SALT score (complete scalp hair regrowth), while 38.4% had a change that ranged from 51%-90%. At the same time, 18% had a change in their SALT score that ranged from 6%-50%, while 23% had a change that was 5% or less. As observed in the earlier trial, researchers saw a negative correlation between duration of current episode of hair loss and latest percent change in SALT score.
“We believe that you have to catch people before they get to more than 10 years of complete scalp hair loss,” Dr. King said. “This is important for the pediatric age group. I just saw somebody who’s 13, and they’ve been bald for 8 years. You might make the argument that this person deserves treatment, at least for a period of time long enough to regrow their hair in order to reset the clock.”
The most common adverse events were acne and weight gain.
In a separate analysis, Dr. King, Dr. Craiglow, and Lucy Y. Liu, evaluated the use of tofacitinib for at least 2 months in 13 alopecia areata patients aged 12-17 years (J Am Acad Dermatol. 2017;76[1]:29-32). They limited the analysis to those who had greater than 20% scalp hair loss, alopecia totalis, or alopecia universalis that was stable or worsening for 6 months or longer. Of the 13 patients, 9 (69%) were responders. Of the four non-responders, one had a very long duration of baldness. The percent change in SALT score was 93% overall, including 100% in the responder group over a median of 5 months and just 1% in the non-responder group over a median of 4 months. “This does not work every time,” Dr. King said.
While some preliminary studies of topical JAK inhibitors for alopecia areata show promise, it remains unclear if this approach will translate in a clinically meaningful way, he said. Clinical trials are currently under way.
Dr. King disclosed that he has received honoraria or consulting fees from Aclaris Therapeutics, Celgene, Concert Pharmaceuticals, Eli Lilly, Pfizer, Regeneron Pharmaceuticals, and Dermavant Sciences. He has also received funding support from The Ranjini and Ajay Poddar Resource Fund for Dermatologic Diseases Research.
dbrunk@mdedge.com
EXPERT ANALYSIS FROM THE SPD ANNUAL MEETING
Poor gut health tied to increased systemic disease risk
LAKE TAHOE, CALIF. – according to Mark A. Underwood, MD.
“Antibiotic exposure changes the composition of the intestinal microbiota,” he said at the annual meeting of the Society for Pediatric Dermatology. “That clearly causes both antibiotic-associated diarrhea and Clostridium difficile colitis. The bigger question is, is it possible that intestinal dysbiosis is related to a whole bunch of other systemic diseases? In other words, does an insult during a critical window of development cause changes in the intestinal microbiota that can lead to systemic diseases in the brain, the lung, the liver, or the immune system?”
According Dr. Underwood, a pediatrician who is chief of the division of neonatology at the University of California, Davis, the prevalence of dysbiosis is increasing worldwide, particularly in developed countries, where Bifidobacteria are decreasing and Enterobacteriaceae are increasing. “Those changes are associated with gut permeability and alterations in both local and systemic inflammation, and the risk for a number of diseases, including atopic dermatitis,” he said. Key reasons for the increasing prevalence of dysbiosis, he continued, include the use of antibiotics, cesarean section delivery, formula feeding, changes in hygiene that alter the intestinal biota, the high-fat, high-sugar Western diet, and a loss of vertical and horizontal transmission over generations.
In an effort to evaluate the association between early childhood antibiotic use with allergic diseases in later childhood, Japanese researchers followed 1,200 infants to the age of 5 years (Ann Allergy Asthma Immunol. 2017;119:54-8). They found that antibiotic exposure within the first 2 years of life was associated with an increased risk of asthma (adjusted odds ratio 1.72), allergic rhinitis (adjusted OR 1.65), and atopic dermatitis (adjusted OR 1.40). In a more recent, smaller prospective study, 436 Dutch infants were followed to 1 year of age (Pediatr Allergy Immunol. 2018;29[2]:151-8). The researchers found that antibiotic exposure within the first week of life was associated with allergic sensitization (adjusted OR 3.26), colic (adjusted OR 1.66), and wheezing (adjusted OR 1.56).
In a study of 44 term infants with a family history of allergy, changes in the fecal microbiota, especially colonization with Ruminococcus gnavus, preceded the onset of allergic symptoms (Gastroenterol. 2018;154[1]:154-67). The same researchers observed similar findings in an animal model.
One potential mechanism by which intestinal dysbiosis causes systemic disease is stimulation of toll-like receptor 4 (TLR4), “which is a receptor on a variety of mucosal cells that senses the presence of a microbial pathogen-associated patterns, particularly those of Gram-negative Enterobacteriaceae,” Dr. Underwood explained. Other potential mechanisms include increased intestinal permeability, an increase in the pH and decreases in short-chain fatty acids within the gut lumen, and a loss of intraluminal hypoxia. “Think of the colon as an anaerobic chamber,” he said. “The colon lumen should be very low in oxygen. It should be dominated by obligate anaerobes.”
Efforts to prevent or treat dysbiosis-related diseases include the use of probiotics and fecal transplantation. A recent Cochrane review of 8,672 patients found “moderate certainty evidence” that probiotics are effective for preventing C. difficile-associated diarrhea. The analysis included 31 randomized, controlled trials of adults who were treated either with a probiotic or with a placebo. When pooled, the risk ratio was 0.40, which represented a significant protection. In addition, a summary of 7 randomized controlled trials and 30 case series suggests that fecal microbial transplantation is superior to vancomycin for adults with recurrent C. difficile colitis (relative risk 0.23) (Aliment Pharmacol Ther. 2017;46[5]:470-93).
To date, the effect of giving probiotics to pregnant women who have a family history of allergy is less clear. One pooled analysis of such studies put the overall risk ratio at 0.74 (Mil Med. 2014;179[6]:580-92). “While I think the jury’s still out on how to best prevent atopic dermatitis in these families, it looks like there is some potential benefit in treating these moms during pregnancy with probiotics and treating the infant during the first few months of life,” Dr. Underwood said. The most effective were mixtures including one or more Lactobacillus species or L. rhamnosus, mixtures including one or more Bifidobacterium species, or B. lactis by itself. The use of probiotics also has been found to prevent necrotizing enterocolitis, sepsis, and death in premature infants (Semin Pediatr Surg. 2018;27[1]:39-46).
Dr. Underwood disclosed that he has received honoraria from Abbott and that he was a member of the scientific review board for Avexegen. He also chaired the data safety and monitoring board for Infant Bacterial Therapeutics and has received support from Evolve BioSystems to perform a clinical trial.
dbrunk@mdedge.com
LAKE TAHOE, CALIF. – according to Mark A. Underwood, MD.
“Antibiotic exposure changes the composition of the intestinal microbiota,” he said at the annual meeting of the Society for Pediatric Dermatology. “That clearly causes both antibiotic-associated diarrhea and Clostridium difficile colitis. The bigger question is, is it possible that intestinal dysbiosis is related to a whole bunch of other systemic diseases? In other words, does an insult during a critical window of development cause changes in the intestinal microbiota that can lead to systemic diseases in the brain, the lung, the liver, or the immune system?”
According Dr. Underwood, a pediatrician who is chief of the division of neonatology at the University of California, Davis, the prevalence of dysbiosis is increasing worldwide, particularly in developed countries, where Bifidobacteria are decreasing and Enterobacteriaceae are increasing. “Those changes are associated with gut permeability and alterations in both local and systemic inflammation, and the risk for a number of diseases, including atopic dermatitis,” he said. Key reasons for the increasing prevalence of dysbiosis, he continued, include the use of antibiotics, cesarean section delivery, formula feeding, changes in hygiene that alter the intestinal biota, the high-fat, high-sugar Western diet, and a loss of vertical and horizontal transmission over generations.
In an effort to evaluate the association between early childhood antibiotic use with allergic diseases in later childhood, Japanese researchers followed 1,200 infants to the age of 5 years (Ann Allergy Asthma Immunol. 2017;119:54-8). They found that antibiotic exposure within the first 2 years of life was associated with an increased risk of asthma (adjusted odds ratio 1.72), allergic rhinitis (adjusted OR 1.65), and atopic dermatitis (adjusted OR 1.40). In a more recent, smaller prospective study, 436 Dutch infants were followed to 1 year of age (Pediatr Allergy Immunol. 2018;29[2]:151-8). The researchers found that antibiotic exposure within the first week of life was associated with allergic sensitization (adjusted OR 3.26), colic (adjusted OR 1.66), and wheezing (adjusted OR 1.56).
In a study of 44 term infants with a family history of allergy, changes in the fecal microbiota, especially colonization with Ruminococcus gnavus, preceded the onset of allergic symptoms (Gastroenterol. 2018;154[1]:154-67). The same researchers observed similar findings in an animal model.
One potential mechanism by which intestinal dysbiosis causes systemic disease is stimulation of toll-like receptor 4 (TLR4), “which is a receptor on a variety of mucosal cells that senses the presence of a microbial pathogen-associated patterns, particularly those of Gram-negative Enterobacteriaceae,” Dr. Underwood explained. Other potential mechanisms include increased intestinal permeability, an increase in the pH and decreases in short-chain fatty acids within the gut lumen, and a loss of intraluminal hypoxia. “Think of the colon as an anaerobic chamber,” he said. “The colon lumen should be very low in oxygen. It should be dominated by obligate anaerobes.”
Efforts to prevent or treat dysbiosis-related diseases include the use of probiotics and fecal transplantation. A recent Cochrane review of 8,672 patients found “moderate certainty evidence” that probiotics are effective for preventing C. difficile-associated diarrhea. The analysis included 31 randomized, controlled trials of adults who were treated either with a probiotic or with a placebo. When pooled, the risk ratio was 0.40, which represented a significant protection. In addition, a summary of 7 randomized controlled trials and 30 case series suggests that fecal microbial transplantation is superior to vancomycin for adults with recurrent C. difficile colitis (relative risk 0.23) (Aliment Pharmacol Ther. 2017;46[5]:470-93).
To date, the effect of giving probiotics to pregnant women who have a family history of allergy is less clear. One pooled analysis of such studies put the overall risk ratio at 0.74 (Mil Med. 2014;179[6]:580-92). “While I think the jury’s still out on how to best prevent atopic dermatitis in these families, it looks like there is some potential benefit in treating these moms during pregnancy with probiotics and treating the infant during the first few months of life,” Dr. Underwood said. The most effective were mixtures including one or more Lactobacillus species or L. rhamnosus, mixtures including one or more Bifidobacterium species, or B. lactis by itself. The use of probiotics also has been found to prevent necrotizing enterocolitis, sepsis, and death in premature infants (Semin Pediatr Surg. 2018;27[1]:39-46).
Dr. Underwood disclosed that he has received honoraria from Abbott and that he was a member of the scientific review board for Avexegen. He also chaired the data safety and monitoring board for Infant Bacterial Therapeutics and has received support from Evolve BioSystems to perform a clinical trial.
dbrunk@mdedge.com
LAKE TAHOE, CALIF. – according to Mark A. Underwood, MD.
“Antibiotic exposure changes the composition of the intestinal microbiota,” he said at the annual meeting of the Society for Pediatric Dermatology. “That clearly causes both antibiotic-associated diarrhea and Clostridium difficile colitis. The bigger question is, is it possible that intestinal dysbiosis is related to a whole bunch of other systemic diseases? In other words, does an insult during a critical window of development cause changes in the intestinal microbiota that can lead to systemic diseases in the brain, the lung, the liver, or the immune system?”
According Dr. Underwood, a pediatrician who is chief of the division of neonatology at the University of California, Davis, the prevalence of dysbiosis is increasing worldwide, particularly in developed countries, where Bifidobacteria are decreasing and Enterobacteriaceae are increasing. “Those changes are associated with gut permeability and alterations in both local and systemic inflammation, and the risk for a number of diseases, including atopic dermatitis,” he said. Key reasons for the increasing prevalence of dysbiosis, he continued, include the use of antibiotics, cesarean section delivery, formula feeding, changes in hygiene that alter the intestinal biota, the high-fat, high-sugar Western diet, and a loss of vertical and horizontal transmission over generations.
In an effort to evaluate the association between early childhood antibiotic use with allergic diseases in later childhood, Japanese researchers followed 1,200 infants to the age of 5 years (Ann Allergy Asthma Immunol. 2017;119:54-8). They found that antibiotic exposure within the first 2 years of life was associated with an increased risk of asthma (adjusted odds ratio 1.72), allergic rhinitis (adjusted OR 1.65), and atopic dermatitis (adjusted OR 1.40). In a more recent, smaller prospective study, 436 Dutch infants were followed to 1 year of age (Pediatr Allergy Immunol. 2018;29[2]:151-8). The researchers found that antibiotic exposure within the first week of life was associated with allergic sensitization (adjusted OR 3.26), colic (adjusted OR 1.66), and wheezing (adjusted OR 1.56).
In a study of 44 term infants with a family history of allergy, changes in the fecal microbiota, especially colonization with Ruminococcus gnavus, preceded the onset of allergic symptoms (Gastroenterol. 2018;154[1]:154-67). The same researchers observed similar findings in an animal model.
One potential mechanism by which intestinal dysbiosis causes systemic disease is stimulation of toll-like receptor 4 (TLR4), “which is a receptor on a variety of mucosal cells that senses the presence of a microbial pathogen-associated patterns, particularly those of Gram-negative Enterobacteriaceae,” Dr. Underwood explained. Other potential mechanisms include increased intestinal permeability, an increase in the pH and decreases in short-chain fatty acids within the gut lumen, and a loss of intraluminal hypoxia. “Think of the colon as an anaerobic chamber,” he said. “The colon lumen should be very low in oxygen. It should be dominated by obligate anaerobes.”
Efforts to prevent or treat dysbiosis-related diseases include the use of probiotics and fecal transplantation. A recent Cochrane review of 8,672 patients found “moderate certainty evidence” that probiotics are effective for preventing C. difficile-associated diarrhea. The analysis included 31 randomized, controlled trials of adults who were treated either with a probiotic or with a placebo. When pooled, the risk ratio was 0.40, which represented a significant protection. In addition, a summary of 7 randomized controlled trials and 30 case series suggests that fecal microbial transplantation is superior to vancomycin for adults with recurrent C. difficile colitis (relative risk 0.23) (Aliment Pharmacol Ther. 2017;46[5]:470-93).
To date, the effect of giving probiotics to pregnant women who have a family history of allergy is less clear. One pooled analysis of such studies put the overall risk ratio at 0.74 (Mil Med. 2014;179[6]:580-92). “While I think the jury’s still out on how to best prevent atopic dermatitis in these families, it looks like there is some potential benefit in treating these moms during pregnancy with probiotics and treating the infant during the first few months of life,” Dr. Underwood said. The most effective were mixtures including one or more Lactobacillus species or L. rhamnosus, mixtures including one or more Bifidobacterium species, or B. lactis by itself. The use of probiotics also has been found to prevent necrotizing enterocolitis, sepsis, and death in premature infants (Semin Pediatr Surg. 2018;27[1]:39-46).
Dr. Underwood disclosed that he has received honoraria from Abbott and that he was a member of the scientific review board for Avexegen. He also chaired the data safety and monitoring board for Infant Bacterial Therapeutics and has received support from Evolve BioSystems to perform a clinical trial.
dbrunk@mdedge.com
EXPERT ANALYSIS FROM THE SPD ANNUAL MEETING
So it’s pediatric onychomycosis. Now what?
CHICAGO – Though research shows that nail fungus occurs in just 0.3% of pediatric patients in the United States, that’s not what Sheila Friedlander, MD, is seeing in her southern California practice, where it’s not uncommon to see children whose nails, toe nails in particular, have fungal involvement.
said Dr. Friedlander during a nail-focused session at the annual summer meeting of the American Academy of Dermatology. Dr. Friedlander, professor of dermatology and pediatrics at the University of California San Diego and Rady Children’s Hospital, said that she suspects that more participation in organized sports at a young age may be contributing to the increase, with occlusive sports footwear replacing bare feet or sandals for more hours of the day, presenting more opportunities for toenail trauma in sports such as soccer.
When making the clinical call about a nail problem, bear in mind that the younger the child, the less likely a nail problem is fungal, Dr. Friedlander noted. “Little children are much less likely than older children to have nail fungus. Pediatric nails are thinner, and they are faster growing, with better blood supply to the matrix.”
And if frank onychomadesis is observed, think about the time of year, and ask about recent fevers and rashes, because coxsackievirus may be the culprit. “Be not afraid, and look everywhere if the nail is confusing to you,” she said. In all ages, the diagnosis is primarily clinical, “but I culture them, I ‘PAS’ [periodic acid-Schiff stain] them, too. If you do both, you’ll increase your yield,” Dr. Friedlander said, adding, “the beauty of PAS is you can use it to give your families an answer very soon.”
Once you’ve established that fungus is to blame for a nail problem, there’s a conundrum: There are no Food and Drug Administration-approved therapies, either topical or systemic, for pediatric onychomycosis, Dr. Friedlander said. She, along with coauthors and first author Aditya Gupta, MD, of Mediprobe Research, London, Ontario, Canada, recently published an article reviewing the safety and efficacy of antifungal agents in this age group (Pediatr Dermatol. 2018 Jun 26. doi: 10.1111/pde.13561).
Reviewing information available in the United States and Canada, Dr. Friedlander and her coauthors came up with three topical and four oral options for children, along with recommendations for dosage and duration.
In response to an audience question about the use of topical antifungal treatment for nail involvement, Dr. Friedlander responded, “I think topicals would be great for kids, but it’s for kids where there is no nail matrix involvement. Also, cost is a problem. Nobody will cover it. But some families are willing to do this to avoid systemic therapy,” and if the family budget can accommodate a topical choice, it’s a logical option, she said, noting that partial reimbursement via a coupon system is available from some pharmaceutical companies.
Where appropriate, ciclopirox 8%, efinaconazole 10%, and tavaborole 5% can each be considered. Dr. Friedlander cited one study she coauthored, which reported that 70% of pediatric participants with nonmatrix onychomycosis saw effective treatment, with a 71% mycological cure rate (P = .03), after 32 weeks of treatment with ciclopirox lacquer versus vehicle (Pediatr Dermatol. 2013 May-Jun;30[3]:316-22).
Systemic therapies – which, when studied, have been given at tinea capitis doses – could include griseofulvin, terbinafine, itraconazole, and fluconazole.
In terms of oral options, Dr. Friedlander said, griseofulvin has some practical limitations. While prolonged treatment is required in any case, terbinafine may produce results in about 3 months, whereas griseofulvin may require up to 9 months of therapy. “I always try to use terbinafine … griseofulvin takes a year and a day,” she said.
She also shared some tips to improve pediatric adherence with oral antifungals: “You can tell parents to crush terbinafine tablets and mix in peanut butter or applesauce to improve adherence. Griseofulvin can be flavored by the pharmacy, but volumes are big with griseofulvin, so it’s a challenge to get kids to take it all,” she said.
Dr. Friedlander reported that she had no relevant financial disclosures.
koakes@mdedge.com
CHICAGO – Though research shows that nail fungus occurs in just 0.3% of pediatric patients in the United States, that’s not what Sheila Friedlander, MD, is seeing in her southern California practice, where it’s not uncommon to see children whose nails, toe nails in particular, have fungal involvement.
said Dr. Friedlander during a nail-focused session at the annual summer meeting of the American Academy of Dermatology. Dr. Friedlander, professor of dermatology and pediatrics at the University of California San Diego and Rady Children’s Hospital, said that she suspects that more participation in organized sports at a young age may be contributing to the increase, with occlusive sports footwear replacing bare feet or sandals for more hours of the day, presenting more opportunities for toenail trauma in sports such as soccer.
When making the clinical call about a nail problem, bear in mind that the younger the child, the less likely a nail problem is fungal, Dr. Friedlander noted. “Little children are much less likely than older children to have nail fungus. Pediatric nails are thinner, and they are faster growing, with better blood supply to the matrix.”
And if frank onychomadesis is observed, think about the time of year, and ask about recent fevers and rashes, because coxsackievirus may be the culprit. “Be not afraid, and look everywhere if the nail is confusing to you,” she said. In all ages, the diagnosis is primarily clinical, “but I culture them, I ‘PAS’ [periodic acid-Schiff stain] them, too. If you do both, you’ll increase your yield,” Dr. Friedlander said, adding, “the beauty of PAS is you can use it to give your families an answer very soon.”
Once you’ve established that fungus is to blame for a nail problem, there’s a conundrum: There are no Food and Drug Administration-approved therapies, either topical or systemic, for pediatric onychomycosis, Dr. Friedlander said. She, along with coauthors and first author Aditya Gupta, MD, of Mediprobe Research, London, Ontario, Canada, recently published an article reviewing the safety and efficacy of antifungal agents in this age group (Pediatr Dermatol. 2018 Jun 26. doi: 10.1111/pde.13561).
Reviewing information available in the United States and Canada, Dr. Friedlander and her coauthors came up with three topical and four oral options for children, along with recommendations for dosage and duration.
In response to an audience question about the use of topical antifungal treatment for nail involvement, Dr. Friedlander responded, “I think topicals would be great for kids, but it’s for kids where there is no nail matrix involvement. Also, cost is a problem. Nobody will cover it. But some families are willing to do this to avoid systemic therapy,” and if the family budget can accommodate a topical choice, it’s a logical option, she said, noting that partial reimbursement via a coupon system is available from some pharmaceutical companies.
Where appropriate, ciclopirox 8%, efinaconazole 10%, and tavaborole 5% can each be considered. Dr. Friedlander cited one study she coauthored, which reported that 70% of pediatric participants with nonmatrix onychomycosis saw effective treatment, with a 71% mycological cure rate (P = .03), after 32 weeks of treatment with ciclopirox lacquer versus vehicle (Pediatr Dermatol. 2013 May-Jun;30[3]:316-22).
Systemic therapies – which, when studied, have been given at tinea capitis doses – could include griseofulvin, terbinafine, itraconazole, and fluconazole.
In terms of oral options, Dr. Friedlander said, griseofulvin has some practical limitations. While prolonged treatment is required in any case, terbinafine may produce results in about 3 months, whereas griseofulvin may require up to 9 months of therapy. “I always try to use terbinafine … griseofulvin takes a year and a day,” she said.
She also shared some tips to improve pediatric adherence with oral antifungals: “You can tell parents to crush terbinafine tablets and mix in peanut butter or applesauce to improve adherence. Griseofulvin can be flavored by the pharmacy, but volumes are big with griseofulvin, so it’s a challenge to get kids to take it all,” she said.
Dr. Friedlander reported that she had no relevant financial disclosures.
koakes@mdedge.com
CHICAGO – Though research shows that nail fungus occurs in just 0.3% of pediatric patients in the United States, that’s not what Sheila Friedlander, MD, is seeing in her southern California practice, where it’s not uncommon to see children whose nails, toe nails in particular, have fungal involvement.
said Dr. Friedlander during a nail-focused session at the annual summer meeting of the American Academy of Dermatology. Dr. Friedlander, professor of dermatology and pediatrics at the University of California San Diego and Rady Children’s Hospital, said that she suspects that more participation in organized sports at a young age may be contributing to the increase, with occlusive sports footwear replacing bare feet or sandals for more hours of the day, presenting more opportunities for toenail trauma in sports such as soccer.
When making the clinical call about a nail problem, bear in mind that the younger the child, the less likely a nail problem is fungal, Dr. Friedlander noted. “Little children are much less likely than older children to have nail fungus. Pediatric nails are thinner, and they are faster growing, with better blood supply to the matrix.”
And if frank onychomadesis is observed, think about the time of year, and ask about recent fevers and rashes, because coxsackievirus may be the culprit. “Be not afraid, and look everywhere if the nail is confusing to you,” she said. In all ages, the diagnosis is primarily clinical, “but I culture them, I ‘PAS’ [periodic acid-Schiff stain] them, too. If you do both, you’ll increase your yield,” Dr. Friedlander said, adding, “the beauty of PAS is you can use it to give your families an answer very soon.”
Once you’ve established that fungus is to blame for a nail problem, there’s a conundrum: There are no Food and Drug Administration-approved therapies, either topical or systemic, for pediatric onychomycosis, Dr. Friedlander said. She, along with coauthors and first author Aditya Gupta, MD, of Mediprobe Research, London, Ontario, Canada, recently published an article reviewing the safety and efficacy of antifungal agents in this age group (Pediatr Dermatol. 2018 Jun 26. doi: 10.1111/pde.13561).
Reviewing information available in the United States and Canada, Dr. Friedlander and her coauthors came up with three topical and four oral options for children, along with recommendations for dosage and duration.
In response to an audience question about the use of topical antifungal treatment for nail involvement, Dr. Friedlander responded, “I think topicals would be great for kids, but it’s for kids where there is no nail matrix involvement. Also, cost is a problem. Nobody will cover it. But some families are willing to do this to avoid systemic therapy,” and if the family budget can accommodate a topical choice, it’s a logical option, she said, noting that partial reimbursement via a coupon system is available from some pharmaceutical companies.
Where appropriate, ciclopirox 8%, efinaconazole 10%, and tavaborole 5% can each be considered. Dr. Friedlander cited one study she coauthored, which reported that 70% of pediatric participants with nonmatrix onychomycosis saw effective treatment, with a 71% mycological cure rate (P = .03), after 32 weeks of treatment with ciclopirox lacquer versus vehicle (Pediatr Dermatol. 2013 May-Jun;30[3]:316-22).
Systemic therapies – which, when studied, have been given at tinea capitis doses – could include griseofulvin, terbinafine, itraconazole, and fluconazole.
In terms of oral options, Dr. Friedlander said, griseofulvin has some practical limitations. While prolonged treatment is required in any case, terbinafine may produce results in about 3 months, whereas griseofulvin may require up to 9 months of therapy. “I always try to use terbinafine … griseofulvin takes a year and a day,” she said.
She also shared some tips to improve pediatric adherence with oral antifungals: “You can tell parents to crush terbinafine tablets and mix in peanut butter or applesauce to improve adherence. Griseofulvin can be flavored by the pharmacy, but volumes are big with griseofulvin, so it’s a challenge to get kids to take it all,” she said.
Dr. Friedlander reported that she had no relevant financial disclosures.
koakes@mdedge.com
EXPERT ANALYSIS FROM SUMMER AAD 2018
New guidelines on antimicrobial prophylaxis
Experts have published updated guidelines on antimicrobial prophylaxis for adults with cancer-related immunosuppression.
The guidelines include antibacterial, antifungal, and antiviral prophylaxis recommendations, along with additional precautions, such as hand hygiene, that may reduce infection risk.
The guidelines were developed by the American Society of Clinical Oncology (ASCO) with the Infectious Diseases Society of America (IDSA) and published in the Journal of Clinical Oncology.
For the most part, the expert panel that created these guidelines endorsed the previous ASCO recommendations, published in 2013.
However, the panel considered six new studies and six new or updated meta-analyses to make modifications and add some new recommendations.
Recommendations
The ASCO/IDSA guidelines say health care providers should systematically assess the risk of febrile neutropenia, taking into account patient-, cancer-, and treatment-related factors.
Fluoroquinolone prophylaxis is recommended for patients at high risk of febrile neutropenia or profound, protracted neutropenia. This includes most patients with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) and patients undergoing hematopoietic stem cell transplant (HSCT) who are treated with myeloablative conditioning regimens.
Antifungal prophylaxis with an oral triazole or parenteral echinocandin is recommended for patients at risk of profound, protracted neutropenia, which includes HSCT recipients and most patients with AML/MDS.
However, neither antifungal nor antibiotic prophylaxis are routinely recommended for patients with solid tumors.
Prophylaxis with a nucleoside analog, such as acyclovir, is recommended in patients who are herpes simplex virus–seropositive and are undergoing allogeneic HSCT or leukemia induction.
Pneumocystis jirovecii prophylaxis, such as trimethoprim-sulfamethoxazole, is recommended for patients receiving chemotherapy regimens associated with a greater than 3.5% risk for pneumonia from P jirovecii.
Treatment with a nucleoside reverse transcription inhibitor, such as entecavir or tenofovir, is recommended for patients at high risk of hepatitis B virus reactivation.
Yearly influenza vaccination with an inactivated quadrivalent vaccine is recommended for all patients undergoing chemotherapy for malignancy as well as their family members, household contacts, and health care providers.
Health care workers should follow hand hygiene and respiratory hygiene/cough etiquette to reduce the risk of pathogen transmission, according to the guidelines.
The guidelines also note that outpatients who develop neutropenia following cancer therapy should avoid prolonged contact with environments that have high concentrations of airborne fungal spores.
The guidelines do not recommend interventions such as neutropenic diet, footwear exchange, nutritional supplements, and surgical masks. “Evidence of clinical benefit is lacking” for those interventions, the expert panel said.
Members of the expert panel disclosed potential conflicts of interest related to Merck, Chimerix, GlyPharma Therapeutic, Pfizer, Cidara Therapeutics, Celgene, Astellas Pharma, Gilead Sciences, and Allergan, among other entities.
Experts have published updated guidelines on antimicrobial prophylaxis for adults with cancer-related immunosuppression.
The guidelines include antibacterial, antifungal, and antiviral prophylaxis recommendations, along with additional precautions, such as hand hygiene, that may reduce infection risk.
The guidelines were developed by the American Society of Clinical Oncology (ASCO) with the Infectious Diseases Society of America (IDSA) and published in the Journal of Clinical Oncology.
For the most part, the expert panel that created these guidelines endorsed the previous ASCO recommendations, published in 2013.
However, the panel considered six new studies and six new or updated meta-analyses to make modifications and add some new recommendations.
Recommendations
The ASCO/IDSA guidelines say health care providers should systematically assess the risk of febrile neutropenia, taking into account patient-, cancer-, and treatment-related factors.
Fluoroquinolone prophylaxis is recommended for patients at high risk of febrile neutropenia or profound, protracted neutropenia. This includes most patients with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) and patients undergoing hematopoietic stem cell transplant (HSCT) who are treated with myeloablative conditioning regimens.
Antifungal prophylaxis with an oral triazole or parenteral echinocandin is recommended for patients at risk of profound, protracted neutropenia, which includes HSCT recipients and most patients with AML/MDS.
However, neither antifungal nor antibiotic prophylaxis are routinely recommended for patients with solid tumors.
Prophylaxis with a nucleoside analog, such as acyclovir, is recommended in patients who are herpes simplex virus–seropositive and are undergoing allogeneic HSCT or leukemia induction.
Pneumocystis jirovecii prophylaxis, such as trimethoprim-sulfamethoxazole, is recommended for patients receiving chemotherapy regimens associated with a greater than 3.5% risk for pneumonia from P jirovecii.
Treatment with a nucleoside reverse transcription inhibitor, such as entecavir or tenofovir, is recommended for patients at high risk of hepatitis B virus reactivation.
Yearly influenza vaccination with an inactivated quadrivalent vaccine is recommended for all patients undergoing chemotherapy for malignancy as well as their family members, household contacts, and health care providers.
Health care workers should follow hand hygiene and respiratory hygiene/cough etiquette to reduce the risk of pathogen transmission, according to the guidelines.
The guidelines also note that outpatients who develop neutropenia following cancer therapy should avoid prolonged contact with environments that have high concentrations of airborne fungal spores.
The guidelines do not recommend interventions such as neutropenic diet, footwear exchange, nutritional supplements, and surgical masks. “Evidence of clinical benefit is lacking” for those interventions, the expert panel said.
Members of the expert panel disclosed potential conflicts of interest related to Merck, Chimerix, GlyPharma Therapeutic, Pfizer, Cidara Therapeutics, Celgene, Astellas Pharma, Gilead Sciences, and Allergan, among other entities.
Experts have published updated guidelines on antimicrobial prophylaxis for adults with cancer-related immunosuppression.
The guidelines include antibacterial, antifungal, and antiviral prophylaxis recommendations, along with additional precautions, such as hand hygiene, that may reduce infection risk.
The guidelines were developed by the American Society of Clinical Oncology (ASCO) with the Infectious Diseases Society of America (IDSA) and published in the Journal of Clinical Oncology.
For the most part, the expert panel that created these guidelines endorsed the previous ASCO recommendations, published in 2013.
However, the panel considered six new studies and six new or updated meta-analyses to make modifications and add some new recommendations.
Recommendations
The ASCO/IDSA guidelines say health care providers should systematically assess the risk of febrile neutropenia, taking into account patient-, cancer-, and treatment-related factors.
Fluoroquinolone prophylaxis is recommended for patients at high risk of febrile neutropenia or profound, protracted neutropenia. This includes most patients with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) and patients undergoing hematopoietic stem cell transplant (HSCT) who are treated with myeloablative conditioning regimens.
Antifungal prophylaxis with an oral triazole or parenteral echinocandin is recommended for patients at risk of profound, protracted neutropenia, which includes HSCT recipients and most patients with AML/MDS.
However, neither antifungal nor antibiotic prophylaxis are routinely recommended for patients with solid tumors.
Prophylaxis with a nucleoside analog, such as acyclovir, is recommended in patients who are herpes simplex virus–seropositive and are undergoing allogeneic HSCT or leukemia induction.
Pneumocystis jirovecii prophylaxis, such as trimethoprim-sulfamethoxazole, is recommended for patients receiving chemotherapy regimens associated with a greater than 3.5% risk for pneumonia from P jirovecii.
Treatment with a nucleoside reverse transcription inhibitor, such as entecavir or tenofovir, is recommended for patients at high risk of hepatitis B virus reactivation.
Yearly influenza vaccination with an inactivated quadrivalent vaccine is recommended for all patients undergoing chemotherapy for malignancy as well as their family members, household contacts, and health care providers.
Health care workers should follow hand hygiene and respiratory hygiene/cough etiquette to reduce the risk of pathogen transmission, according to the guidelines.
The guidelines also note that outpatients who develop neutropenia following cancer therapy should avoid prolonged contact with environments that have high concentrations of airborne fungal spores.
The guidelines do not recommend interventions such as neutropenic diet, footwear exchange, nutritional supplements, and surgical masks. “Evidence of clinical benefit is lacking” for those interventions, the expert panel said.
Members of the expert panel disclosed potential conflicts of interest related to Merck, Chimerix, GlyPharma Therapeutic, Pfizer, Cidara Therapeutics, Celgene, Astellas Pharma, Gilead Sciences, and Allergan, among other entities.