User login
Bile spillage during lap cholecystectomy comes with a price
Bile spillage that happens during laparoscopic gallbladder removal is a known problem, but a large study has put some numbers to quantify the risks to patients.
A research team at Massachusetts General Hospital, Boston, conducted a prospective study of 1,001 such operations to look at the impact of bile spillage. They found that wound infection rates in cases involving bile spillage were almost three times higher than were those without spillage and resulting hospital stays were 50% longer, according to an article in the Journal of the American College of Surgeons.
The study involved adults who had laparoscopic and laparoscopic converted to open cholecystectomy at the academic hospital during May 2010-March 2017. The latter category accounted for 95 patients, a 9.5% conversion rate. Overall, bile was spilled in 591 patients (59%), with empyema in 86 (8.6%), hydrops in 62 (6.2%), and clear bile spillage in the remainder. Bile spillage along with gallstone spillage occurred in 202 patients (20.2%), with recovery of all spilled gallstones in 145 (71.8%) of those cases.
Overall, the surgical site infection (SSI) rate was 2.4% (n = 8) in patients with no bile spillage vs. 7.1% (n = 30) for those with bile spillage. Median hospital length of stay was 2 days for the nonspillage patients vs. 3 days for those with spillage. The 30-day readmission rates were 5.9% for the nonspillage group vs. 9.6% for the spillage group.
The bile spillage rate in this study was considerably higher than previous studies had reported, the researchers noted. A retrospective study of 1,127 patients reported a spillage rate of 11.6% (World J Surg. 1999;23:1186-90). “One needs to notice that a retrospective review of medical records almost certainly underappreciates the rate of bile spillage,” the investigators wrote. A Mayo Clinic study reported a bile spillage rate of 29% and an increased risk of intra-abdominal abscesses (J Gastrointest Surg. 1997;1:85-90). The complex and acute nature of the cases at Mass General may explain their higher spillage rates, the researchers suggested.
This study identifies bile spillage, along with conversion to open surgery and patient ASA class 2 or higher as the only independent predictors of SSI. The study also found no link between empyema and hydrops with SSI, although the small number of cases may preclude an representative sample.
Nonetheless, surgeons must face the question of how to decrease SSI in laparoscopic cholecystectomy with bile spillage, study authors wrote. “First, surgeons should acknowledge that gallbladder perforations and bile spillage come at a price,” they said, “and thus should be cautious and try to avoid them.”
When bile is spilled, liberal peritoneal irrigation may be futile; this study showed similar SSI rates after bile spillage, regardless of peritoneal irrigation. “We could consider modifying perioperative antibiotic coverage,” the investigators wrote, but they acknowledged a need for more research to validate its benefit.
The investigators reported having no financial disclosures.
SOURCE: Peponis T et al. J Am Coll Surg. 2018 Mar 1. doi: 10.1016/j.jamcollsurg.2017.11.025.
Bile spillage that happens during laparoscopic gallbladder removal is a known problem, but a large study has put some numbers to quantify the risks to patients.
A research team at Massachusetts General Hospital, Boston, conducted a prospective study of 1,001 such operations to look at the impact of bile spillage. They found that wound infection rates in cases involving bile spillage were almost three times higher than were those without spillage and resulting hospital stays were 50% longer, according to an article in the Journal of the American College of Surgeons.
The study involved adults who had laparoscopic and laparoscopic converted to open cholecystectomy at the academic hospital during May 2010-March 2017. The latter category accounted for 95 patients, a 9.5% conversion rate. Overall, bile was spilled in 591 patients (59%), with empyema in 86 (8.6%), hydrops in 62 (6.2%), and clear bile spillage in the remainder. Bile spillage along with gallstone spillage occurred in 202 patients (20.2%), with recovery of all spilled gallstones in 145 (71.8%) of those cases.
Overall, the surgical site infection (SSI) rate was 2.4% (n = 8) in patients with no bile spillage vs. 7.1% (n = 30) for those with bile spillage. Median hospital length of stay was 2 days for the nonspillage patients vs. 3 days for those with spillage. The 30-day readmission rates were 5.9% for the nonspillage group vs. 9.6% for the spillage group.
The bile spillage rate in this study was considerably higher than previous studies had reported, the researchers noted. A retrospective study of 1,127 patients reported a spillage rate of 11.6% (World J Surg. 1999;23:1186-90). “One needs to notice that a retrospective review of medical records almost certainly underappreciates the rate of bile spillage,” the investigators wrote. A Mayo Clinic study reported a bile spillage rate of 29% and an increased risk of intra-abdominal abscesses (J Gastrointest Surg. 1997;1:85-90). The complex and acute nature of the cases at Mass General may explain their higher spillage rates, the researchers suggested.
This study identifies bile spillage, along with conversion to open surgery and patient ASA class 2 or higher as the only independent predictors of SSI. The study also found no link between empyema and hydrops with SSI, although the small number of cases may preclude an representative sample.
Nonetheless, surgeons must face the question of how to decrease SSI in laparoscopic cholecystectomy with bile spillage, study authors wrote. “First, surgeons should acknowledge that gallbladder perforations and bile spillage come at a price,” they said, “and thus should be cautious and try to avoid them.”
When bile is spilled, liberal peritoneal irrigation may be futile; this study showed similar SSI rates after bile spillage, regardless of peritoneal irrigation. “We could consider modifying perioperative antibiotic coverage,” the investigators wrote, but they acknowledged a need for more research to validate its benefit.
The investigators reported having no financial disclosures.
SOURCE: Peponis T et al. J Am Coll Surg. 2018 Mar 1. doi: 10.1016/j.jamcollsurg.2017.11.025.
Bile spillage that happens during laparoscopic gallbladder removal is a known problem, but a large study has put some numbers to quantify the risks to patients.
A research team at Massachusetts General Hospital, Boston, conducted a prospective study of 1,001 such operations to look at the impact of bile spillage. They found that wound infection rates in cases involving bile spillage were almost three times higher than were those without spillage and resulting hospital stays were 50% longer, according to an article in the Journal of the American College of Surgeons.
The study involved adults who had laparoscopic and laparoscopic converted to open cholecystectomy at the academic hospital during May 2010-March 2017. The latter category accounted for 95 patients, a 9.5% conversion rate. Overall, bile was spilled in 591 patients (59%), with empyema in 86 (8.6%), hydrops in 62 (6.2%), and clear bile spillage in the remainder. Bile spillage along with gallstone spillage occurred in 202 patients (20.2%), with recovery of all spilled gallstones in 145 (71.8%) of those cases.
Overall, the surgical site infection (SSI) rate was 2.4% (n = 8) in patients with no bile spillage vs. 7.1% (n = 30) for those with bile spillage. Median hospital length of stay was 2 days for the nonspillage patients vs. 3 days for those with spillage. The 30-day readmission rates were 5.9% for the nonspillage group vs. 9.6% for the spillage group.
The bile spillage rate in this study was considerably higher than previous studies had reported, the researchers noted. A retrospective study of 1,127 patients reported a spillage rate of 11.6% (World J Surg. 1999;23:1186-90). “One needs to notice that a retrospective review of medical records almost certainly underappreciates the rate of bile spillage,” the investigators wrote. A Mayo Clinic study reported a bile spillage rate of 29% and an increased risk of intra-abdominal abscesses (J Gastrointest Surg. 1997;1:85-90). The complex and acute nature of the cases at Mass General may explain their higher spillage rates, the researchers suggested.
This study identifies bile spillage, along with conversion to open surgery and patient ASA class 2 or higher as the only independent predictors of SSI. The study also found no link between empyema and hydrops with SSI, although the small number of cases may preclude an representative sample.
Nonetheless, surgeons must face the question of how to decrease SSI in laparoscopic cholecystectomy with bile spillage, study authors wrote. “First, surgeons should acknowledge that gallbladder perforations and bile spillage come at a price,” they said, “and thus should be cautious and try to avoid them.”
When bile is spilled, liberal peritoneal irrigation may be futile; this study showed similar SSI rates after bile spillage, regardless of peritoneal irrigation. “We could consider modifying perioperative antibiotic coverage,” the investigators wrote, but they acknowledged a need for more research to validate its benefit.
The investigators reported having no financial disclosures.
SOURCE: Peponis T et al. J Am Coll Surg. 2018 Mar 1. doi: 10.1016/j.jamcollsurg.2017.11.025.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Bile spillage during laparoscopic cholecystectomy increases the patient’s risk for surgical site infection.
Major finding: Surgical site infection rates were 7.1% in cases in which bile spillage occurred vs. 2.4% in cases that had no bile spillage.
Data source: Prospective analysis of 1,001 laparoscopic or laparoscopic converted to open operations in adults during May 2010-March 2017.
Disclosures: Dr. Velmahos and coauthors reported having no financial disclosures.
Source: Peponis T et al. J Am Coll Surg. 2018 Mar 1. doi: 10.1016/j.jamcollsurg.2017.11.025.
Migraine and Dysfunction of Discrete Cell Types
Both familial and common migraine may arise from dysfunction of discrete cell types within the neurovascular unit, and localization of the affected cell type(s) in an individual patient may provide insight into to their susceptibility to migraine, according to a recent study. The cell-type specific expression of both familial and common migraine-associated genes was determined bioinformatically using data from 2039 individual human brain cells across 2 published single-cell RNA sequencing datasets. Enrichment of migraine-associated genes was determined for each brain cell type. Researchers found:
- Analysis of single-brain cell RNA sequencing data from 5 major subtypes of cells in the human cortex (neurons, oligodendrocytes, astrocytes, microglia, and endothelial cells) indicates that greater than 40% of known migraine-associated genes are enriched in the expression profiles of a specific brain cell type.
- Further analysis of neuronal migraine-associated genes demonstrated that approximately 70% were significantly enriched in inhibitory neurons and 30% in excitatory neurons.
Localization of migraine susceptibility genes in human brain by single-cell RNA sequencing. [Published online ahead of print March 2, 2018]. Cephalalgia. doi:10.1177/0333102418762476.
Both familial and common migraine may arise from dysfunction of discrete cell types within the neurovascular unit, and localization of the affected cell type(s) in an individual patient may provide insight into to their susceptibility to migraine, according to a recent study. The cell-type specific expression of both familial and common migraine-associated genes was determined bioinformatically using data from 2039 individual human brain cells across 2 published single-cell RNA sequencing datasets. Enrichment of migraine-associated genes was determined for each brain cell type. Researchers found:
- Analysis of single-brain cell RNA sequencing data from 5 major subtypes of cells in the human cortex (neurons, oligodendrocytes, astrocytes, microglia, and endothelial cells) indicates that greater than 40% of known migraine-associated genes are enriched in the expression profiles of a specific brain cell type.
- Further analysis of neuronal migraine-associated genes demonstrated that approximately 70% were significantly enriched in inhibitory neurons and 30% in excitatory neurons.
Localization of migraine susceptibility genes in human brain by single-cell RNA sequencing. [Published online ahead of print March 2, 2018]. Cephalalgia. doi:10.1177/0333102418762476.
Both familial and common migraine may arise from dysfunction of discrete cell types within the neurovascular unit, and localization of the affected cell type(s) in an individual patient may provide insight into to their susceptibility to migraine, according to a recent study. The cell-type specific expression of both familial and common migraine-associated genes was determined bioinformatically using data from 2039 individual human brain cells across 2 published single-cell RNA sequencing datasets. Enrichment of migraine-associated genes was determined for each brain cell type. Researchers found:
- Analysis of single-brain cell RNA sequencing data from 5 major subtypes of cells in the human cortex (neurons, oligodendrocytes, astrocytes, microglia, and endothelial cells) indicates that greater than 40% of known migraine-associated genes are enriched in the expression profiles of a specific brain cell type.
- Further analysis of neuronal migraine-associated genes demonstrated that approximately 70% were significantly enriched in inhibitory neurons and 30% in excitatory neurons.
Localization of migraine susceptibility genes in human brain by single-cell RNA sequencing. [Published online ahead of print March 2, 2018]. Cephalalgia. doi:10.1177/0333102418762476.
sTMS: Well-Tolerated and Effective for Migraine
Single pulse transcranial magnetic stimulation (sTMS) may be an effective, well-tolerated treatment option for migraine prevention, according to a recent study. Researchers conducted the eNeura Spring TMS Post-Market Observational US Study of Migraine (ESPOUSE), a multicenter, prospective, open label, observational study. Of the total subjects (n=263), 229 completed a baseline diary, and 220 were found to be eligible based on the number of headache days. The treatment protocol consisted of preventive (4 pulses twice daily) and acute (3 pulses repeated up to 3 times for each attack) treatment. Researchers found:
- The device was assigned to 217 subjects (Safety Data Set) and 132 were included in the intention to treat Full Analysis Set.
- For the primary endpoint, there was a −2.75 ± 0.40 mean reduction of headache days from baseline compared to the performance goal (-0.63 days).
- There was a reduction of −2.93 (5.24) days of acute medication use, headache impact measured by HIT-6, −3.1 (6.4), and total headache days of any intensity −3.16 days (5.21) compared to the performance goal (−0.63 days).
- The most common adverse events were lightheadedness, tingling, and tinnitus; there were no serious adverse events.
A multicenter, prospective, single arm, open label, observational study of sTMS for migraine prevention (ESPOUSE study). [Published online ahead of print March 4, 2018]. Cephalalgia. doi:10.1177/0333102418762525.
Single pulse transcranial magnetic stimulation (sTMS) may be an effective, well-tolerated treatment option for migraine prevention, according to a recent study. Researchers conducted the eNeura Spring TMS Post-Market Observational US Study of Migraine (ESPOUSE), a multicenter, prospective, open label, observational study. Of the total subjects (n=263), 229 completed a baseline diary, and 220 were found to be eligible based on the number of headache days. The treatment protocol consisted of preventive (4 pulses twice daily) and acute (3 pulses repeated up to 3 times for each attack) treatment. Researchers found:
- The device was assigned to 217 subjects (Safety Data Set) and 132 were included in the intention to treat Full Analysis Set.
- For the primary endpoint, there was a −2.75 ± 0.40 mean reduction of headache days from baseline compared to the performance goal (-0.63 days).
- There was a reduction of −2.93 (5.24) days of acute medication use, headache impact measured by HIT-6, −3.1 (6.4), and total headache days of any intensity −3.16 days (5.21) compared to the performance goal (−0.63 days).
- The most common adverse events were lightheadedness, tingling, and tinnitus; there were no serious adverse events.
A multicenter, prospective, single arm, open label, observational study of sTMS for migraine prevention (ESPOUSE study). [Published online ahead of print March 4, 2018]. Cephalalgia. doi:10.1177/0333102418762525.
Single pulse transcranial magnetic stimulation (sTMS) may be an effective, well-tolerated treatment option for migraine prevention, according to a recent study. Researchers conducted the eNeura Spring TMS Post-Market Observational US Study of Migraine (ESPOUSE), a multicenter, prospective, open label, observational study. Of the total subjects (n=263), 229 completed a baseline diary, and 220 were found to be eligible based on the number of headache days. The treatment protocol consisted of preventive (4 pulses twice daily) and acute (3 pulses repeated up to 3 times for each attack) treatment. Researchers found:
- The device was assigned to 217 subjects (Safety Data Set) and 132 were included in the intention to treat Full Analysis Set.
- For the primary endpoint, there was a −2.75 ± 0.40 mean reduction of headache days from baseline compared to the performance goal (-0.63 days).
- There was a reduction of −2.93 (5.24) days of acute medication use, headache impact measured by HIT-6, −3.1 (6.4), and total headache days of any intensity −3.16 days (5.21) compared to the performance goal (−0.63 days).
- The most common adverse events were lightheadedness, tingling, and tinnitus; there were no serious adverse events.
A multicenter, prospective, single arm, open label, observational study of sTMS for migraine prevention (ESPOUSE study). [Published online ahead of print March 4, 2018]. Cephalalgia. doi:10.1177/0333102418762525.
Migraine More Common and Burdensome for Women
Severe headache and migraine remain important public health problems that are more common and burdensome for women, particularly women of childbearing age, and other historically disadvantaged segments of the population, according to a recent study. Researchers searched for the most current publicly available summary statistics from the National Health Interview Survey (NHIS), the National Hospital Ambulatory Medical Care Survey (NHAMCS), and the National Ambulatory Medical Care Survey (NAMCS). They found:
- The prevalence and burden of self-reported migraine and severe headache in the US adult population is high, affecting roughly 1 out of every 6 Americans and 1 in 5 women over a 3-month period (15.3% overall, 9.7% of males, and 20.7% of females).
- The prevalence of migraine or severe headache in 2015 was highest in American Indians or Alaska Natives (18.4%) compared with whites, blacks, or Hispanics, with the lowest prevalence in Asians (11.3%).
- There is a higher burden of migraine in those aged 18-44 (17.9%), people who are unemployed (21.4%), those with family income less than $35,000 per year (19.9%), and the elderly and disabled (16.4%).
The prevalence and impact of migraine and severe headache in the United States: Figures and trends from government health studies. [Published online ahead of print March 12, 2018]. Headache. doi:10.1111/head.13281.
Severe headache and migraine remain important public health problems that are more common and burdensome for women, particularly women of childbearing age, and other historically disadvantaged segments of the population, according to a recent study. Researchers searched for the most current publicly available summary statistics from the National Health Interview Survey (NHIS), the National Hospital Ambulatory Medical Care Survey (NHAMCS), and the National Ambulatory Medical Care Survey (NAMCS). They found:
- The prevalence and burden of self-reported migraine and severe headache in the US adult population is high, affecting roughly 1 out of every 6 Americans and 1 in 5 women over a 3-month period (15.3% overall, 9.7% of males, and 20.7% of females).
- The prevalence of migraine or severe headache in 2015 was highest in American Indians or Alaska Natives (18.4%) compared with whites, blacks, or Hispanics, with the lowest prevalence in Asians (11.3%).
- There is a higher burden of migraine in those aged 18-44 (17.9%), people who are unemployed (21.4%), those with family income less than $35,000 per year (19.9%), and the elderly and disabled (16.4%).
The prevalence and impact of migraine and severe headache in the United States: Figures and trends from government health studies. [Published online ahead of print March 12, 2018]. Headache. doi:10.1111/head.13281.
Severe headache and migraine remain important public health problems that are more common and burdensome for women, particularly women of childbearing age, and other historically disadvantaged segments of the population, according to a recent study. Researchers searched for the most current publicly available summary statistics from the National Health Interview Survey (NHIS), the National Hospital Ambulatory Medical Care Survey (NHAMCS), and the National Ambulatory Medical Care Survey (NAMCS). They found:
- The prevalence and burden of self-reported migraine and severe headache in the US adult population is high, affecting roughly 1 out of every 6 Americans and 1 in 5 women over a 3-month period (15.3% overall, 9.7% of males, and 20.7% of females).
- The prevalence of migraine or severe headache in 2015 was highest in American Indians or Alaska Natives (18.4%) compared with whites, blacks, or Hispanics, with the lowest prevalence in Asians (11.3%).
- There is a higher burden of migraine in those aged 18-44 (17.9%), people who are unemployed (21.4%), those with family income less than $35,000 per year (19.9%), and the elderly and disabled (16.4%).
The prevalence and impact of migraine and severe headache in the United States: Figures and trends from government health studies. [Published online ahead of print March 12, 2018]. Headache. doi:10.1111/head.13281.
MedPAC to Congress: Eliminate MIPS
The Medicare Payment Advisory Commission has formally recommended to Congress that it repeal the Merit-based Incentive Payment System track of Medicare’s Quality Payment Program.
MedPAC “has concluded that ... the Merit-based Incentive Payment System (MIPS) will not fulfill its goals and therefore should be eliminated,” the commission said in its March 15 report to Congress. MedPAC added that the “basic design of MIPS is fundamentally incompatible with the goals of a beneficiary-focused approach to quality measurement.”
MedPAC adds that, by the Centers for Medicare & Medicaid Services’ own estimates, more than half of clinicians will be exempt from reporting on MIPS, based on the low-volume threshold that exempts providers who bill for $90,000 or less in Medicare claims or see 200 or fewer Medicare patients.
The advisory panel also highlighted other flaws. Those include MIPS’ onerous reporting burden; measures that do not allow for meaningful comparisons among clinicians; differing rules for clinicians depending on location, practice size, and other factors; and payment adjustments that could vary wildly from year to year, creating financial uncertainty for physicians.
The commission, which voted 14-2 in favor of eliminating MIPS, also recommended it be replaced with a “voluntary value program.” But it has offered Congress only a conceptual direction for that replacement program.
“This voluntary value program (VVP) is based on the premise that patient outcomes rely on the combined contributions of clinicians and emphasizes that quality improvement is a collective effort,” according to the report.
The VVP would measure all clinicians based on the same set of measures: clinical quality, patient experience, and value. And it would do so on a population level, rather than the individual patient level.
MedPAC sees the VVP not as an end goal in the transition to paying for value, but rather a stepping stone to get clinicians more comfortable with value-based payments en route to moving into the QPP’s advanced alternative payment model (A-APM) track.
“A VVP’s penalties and rewards might not be significant enough to meaningfully change clinician behavior,” the report stated. “However, the intent is to get clinicians comfortable with being measured in a manner similar to the way they would be in A-APMs. With that experience, clinicians would be poised to form or join robust A-APMs, under which the risk and reward are more meaningful, and the potential for true delivery system reform is within reach.”
There was a near unanimous consensus among MedPAC commissioners that MIPS is flawed, but not all commissioners were ready to give up on it – especially considering how much clinicians have already invested in the program.
MedPAC also heard from the American Medical Association, which voiced opposition to the idea of ending MIPS. In addition, the commission received written feedback from physicians against its proposal.
Other experts support preserving MIPS. Gail R. Wilensky, PhD, economist and senior fellow at Project Hope and a former top health aide to President George H.W. Bush, wrote in the New England Journal of Medicine that MIPS should be fixed rather than scrapped.
The Medicare Payment Advisory Commission has formally recommended to Congress that it repeal the Merit-based Incentive Payment System track of Medicare’s Quality Payment Program.
MedPAC “has concluded that ... the Merit-based Incentive Payment System (MIPS) will not fulfill its goals and therefore should be eliminated,” the commission said in its March 15 report to Congress. MedPAC added that the “basic design of MIPS is fundamentally incompatible with the goals of a beneficiary-focused approach to quality measurement.”
MedPAC adds that, by the Centers for Medicare & Medicaid Services’ own estimates, more than half of clinicians will be exempt from reporting on MIPS, based on the low-volume threshold that exempts providers who bill for $90,000 or less in Medicare claims or see 200 or fewer Medicare patients.
The advisory panel also highlighted other flaws. Those include MIPS’ onerous reporting burden; measures that do not allow for meaningful comparisons among clinicians; differing rules for clinicians depending on location, practice size, and other factors; and payment adjustments that could vary wildly from year to year, creating financial uncertainty for physicians.
The commission, which voted 14-2 in favor of eliminating MIPS, also recommended it be replaced with a “voluntary value program.” But it has offered Congress only a conceptual direction for that replacement program.
“This voluntary value program (VVP) is based on the premise that patient outcomes rely on the combined contributions of clinicians and emphasizes that quality improvement is a collective effort,” according to the report.
The VVP would measure all clinicians based on the same set of measures: clinical quality, patient experience, and value. And it would do so on a population level, rather than the individual patient level.
MedPAC sees the VVP not as an end goal in the transition to paying for value, but rather a stepping stone to get clinicians more comfortable with value-based payments en route to moving into the QPP’s advanced alternative payment model (A-APM) track.
“A VVP’s penalties and rewards might not be significant enough to meaningfully change clinician behavior,” the report stated. “However, the intent is to get clinicians comfortable with being measured in a manner similar to the way they would be in A-APMs. With that experience, clinicians would be poised to form or join robust A-APMs, under which the risk and reward are more meaningful, and the potential for true delivery system reform is within reach.”
There was a near unanimous consensus among MedPAC commissioners that MIPS is flawed, but not all commissioners were ready to give up on it – especially considering how much clinicians have already invested in the program.
MedPAC also heard from the American Medical Association, which voiced opposition to the idea of ending MIPS. In addition, the commission received written feedback from physicians against its proposal.
Other experts support preserving MIPS. Gail R. Wilensky, PhD, economist and senior fellow at Project Hope and a former top health aide to President George H.W. Bush, wrote in the New England Journal of Medicine that MIPS should be fixed rather than scrapped.
The Medicare Payment Advisory Commission has formally recommended to Congress that it repeal the Merit-based Incentive Payment System track of Medicare’s Quality Payment Program.
MedPAC “has concluded that ... the Merit-based Incentive Payment System (MIPS) will not fulfill its goals and therefore should be eliminated,” the commission said in its March 15 report to Congress. MedPAC added that the “basic design of MIPS is fundamentally incompatible with the goals of a beneficiary-focused approach to quality measurement.”
MedPAC adds that, by the Centers for Medicare & Medicaid Services’ own estimates, more than half of clinicians will be exempt from reporting on MIPS, based on the low-volume threshold that exempts providers who bill for $90,000 or less in Medicare claims or see 200 or fewer Medicare patients.
The advisory panel also highlighted other flaws. Those include MIPS’ onerous reporting burden; measures that do not allow for meaningful comparisons among clinicians; differing rules for clinicians depending on location, practice size, and other factors; and payment adjustments that could vary wildly from year to year, creating financial uncertainty for physicians.
The commission, which voted 14-2 in favor of eliminating MIPS, also recommended it be replaced with a “voluntary value program.” But it has offered Congress only a conceptual direction for that replacement program.
“This voluntary value program (VVP) is based on the premise that patient outcomes rely on the combined contributions of clinicians and emphasizes that quality improvement is a collective effort,” according to the report.
The VVP would measure all clinicians based on the same set of measures: clinical quality, patient experience, and value. And it would do so on a population level, rather than the individual patient level.
MedPAC sees the VVP not as an end goal in the transition to paying for value, but rather a stepping stone to get clinicians more comfortable with value-based payments en route to moving into the QPP’s advanced alternative payment model (A-APM) track.
“A VVP’s penalties and rewards might not be significant enough to meaningfully change clinician behavior,” the report stated. “However, the intent is to get clinicians comfortable with being measured in a manner similar to the way they would be in A-APMs. With that experience, clinicians would be poised to form or join robust A-APMs, under which the risk and reward are more meaningful, and the potential for true delivery system reform is within reach.”
There was a near unanimous consensus among MedPAC commissioners that MIPS is flawed, but not all commissioners were ready to give up on it – especially considering how much clinicians have already invested in the program.
MedPAC also heard from the American Medical Association, which voiced opposition to the idea of ending MIPS. In addition, the commission received written feedback from physicians against its proposal.
Other experts support preserving MIPS. Gail R. Wilensky, PhD, economist and senior fellow at Project Hope and a former top health aide to President George H.W. Bush, wrote in the New England Journal of Medicine that MIPS should be fixed rather than scrapped.
CDC: Beware Brazil yellow fever outbreak
The Centers for Disease Control and Prevention recommends that travelers who haven’t been vaccinated against yellow fever should avoid travel to Brazil, according to a media teleconference by CDC officials.
“The most important new recommendation ... is that travelers should not go to these yellow fever hot spots in Brazil, unless they are vaccinated,” stated Martin Cetron, MD, director of the Division of Global Migration and Quarantine at the CDC. “Health officials in Brazil recently confirmed more than 920 cases of yellow fever, including more than 300 deaths, during this outbreak” he added.
Since the beginning of 2018, 10 travel-related cases of yellow fever have been reported among international travelers returning from Brazil. Four of these travelers died. All 10 travelers had not received the yellow fever vaccine. Of these 10 travelers, 8 acquired the disease on Ilha Grande, an island off the coast of Rio De Janeiro that is popular among tourists.
The CDC is urging travelers to get vaccinated because of the potentially fatal effects of yellow fever. Vaccinations are recommended for any eligible person 9 months of age or older traveling to Brazil, specifically Espírito Santo, São Paulo, and Rio de Janeiro states, and certain cities in Bahia state, as well as Ilha Grande in particular.
Individuals heading to Brazil should receive the vaccination at least 10 days before travel. If a traveler is unvaccinated and cannot get the vaccination in the appropriate amount of time, areas where vaccination is recommended should be avoided.
The Food and Drug Administration–approved yellow fever vaccine, YF-VAX, is not currently available because of manufacturing issues. Stamaril, another yellow fever vaccine, is available at a limited number of yellow fever vaccination clinics in the United States.
In light of these supply issues, the CDC has provided resources to locate yellow fever vaccination clinics.
Dr. Cetron reemphasized that unvaccinated individuals planning to vacation in Brazil may want to reconsider their travel plans.
“People who have never been vaccinated against yellow fever should not travel to the areas in Brazil affected by the outbreak. Particularly the hot spot of Ilha Grande.”
Information for clinicians and travelers is available on the travel notice portion of the CDC site. The travel notice for Brazil includes a map of the yellow fever–affected areas in Brazil, as well as other informational resources.
The related CDC Morbidity and Mortality Weekly Report is available online.
The Centers for Disease Control and Prevention recommends that travelers who haven’t been vaccinated against yellow fever should avoid travel to Brazil, according to a media teleconference by CDC officials.
“The most important new recommendation ... is that travelers should not go to these yellow fever hot spots in Brazil, unless they are vaccinated,” stated Martin Cetron, MD, director of the Division of Global Migration and Quarantine at the CDC. “Health officials in Brazil recently confirmed more than 920 cases of yellow fever, including more than 300 deaths, during this outbreak” he added.
Since the beginning of 2018, 10 travel-related cases of yellow fever have been reported among international travelers returning from Brazil. Four of these travelers died. All 10 travelers had not received the yellow fever vaccine. Of these 10 travelers, 8 acquired the disease on Ilha Grande, an island off the coast of Rio De Janeiro that is popular among tourists.
The CDC is urging travelers to get vaccinated because of the potentially fatal effects of yellow fever. Vaccinations are recommended for any eligible person 9 months of age or older traveling to Brazil, specifically Espírito Santo, São Paulo, and Rio de Janeiro states, and certain cities in Bahia state, as well as Ilha Grande in particular.
Individuals heading to Brazil should receive the vaccination at least 10 days before travel. If a traveler is unvaccinated and cannot get the vaccination in the appropriate amount of time, areas where vaccination is recommended should be avoided.
The Food and Drug Administration–approved yellow fever vaccine, YF-VAX, is not currently available because of manufacturing issues. Stamaril, another yellow fever vaccine, is available at a limited number of yellow fever vaccination clinics in the United States.
In light of these supply issues, the CDC has provided resources to locate yellow fever vaccination clinics.
Dr. Cetron reemphasized that unvaccinated individuals planning to vacation in Brazil may want to reconsider their travel plans.
“People who have never been vaccinated against yellow fever should not travel to the areas in Brazil affected by the outbreak. Particularly the hot spot of Ilha Grande.”
Information for clinicians and travelers is available on the travel notice portion of the CDC site. The travel notice for Brazil includes a map of the yellow fever–affected areas in Brazil, as well as other informational resources.
The related CDC Morbidity and Mortality Weekly Report is available online.
The Centers for Disease Control and Prevention recommends that travelers who haven’t been vaccinated against yellow fever should avoid travel to Brazil, according to a media teleconference by CDC officials.
“The most important new recommendation ... is that travelers should not go to these yellow fever hot spots in Brazil, unless they are vaccinated,” stated Martin Cetron, MD, director of the Division of Global Migration and Quarantine at the CDC. “Health officials in Brazil recently confirmed more than 920 cases of yellow fever, including more than 300 deaths, during this outbreak” he added.
Since the beginning of 2018, 10 travel-related cases of yellow fever have been reported among international travelers returning from Brazil. Four of these travelers died. All 10 travelers had not received the yellow fever vaccine. Of these 10 travelers, 8 acquired the disease on Ilha Grande, an island off the coast of Rio De Janeiro that is popular among tourists.
The CDC is urging travelers to get vaccinated because of the potentially fatal effects of yellow fever. Vaccinations are recommended for any eligible person 9 months of age or older traveling to Brazil, specifically Espírito Santo, São Paulo, and Rio de Janeiro states, and certain cities in Bahia state, as well as Ilha Grande in particular.
Individuals heading to Brazil should receive the vaccination at least 10 days before travel. If a traveler is unvaccinated and cannot get the vaccination in the appropriate amount of time, areas where vaccination is recommended should be avoided.
The Food and Drug Administration–approved yellow fever vaccine, YF-VAX, is not currently available because of manufacturing issues. Stamaril, another yellow fever vaccine, is available at a limited number of yellow fever vaccination clinics in the United States.
In light of these supply issues, the CDC has provided resources to locate yellow fever vaccination clinics.
Dr. Cetron reemphasized that unvaccinated individuals planning to vacation in Brazil may want to reconsider their travel plans.
“People who have never been vaccinated against yellow fever should not travel to the areas in Brazil affected by the outbreak. Particularly the hot spot of Ilha Grande.”
Information for clinicians and travelers is available on the travel notice portion of the CDC site. The travel notice for Brazil includes a map of the yellow fever–affected areas in Brazil, as well as other informational resources.
The related CDC Morbidity and Mortality Weekly Report is available online.
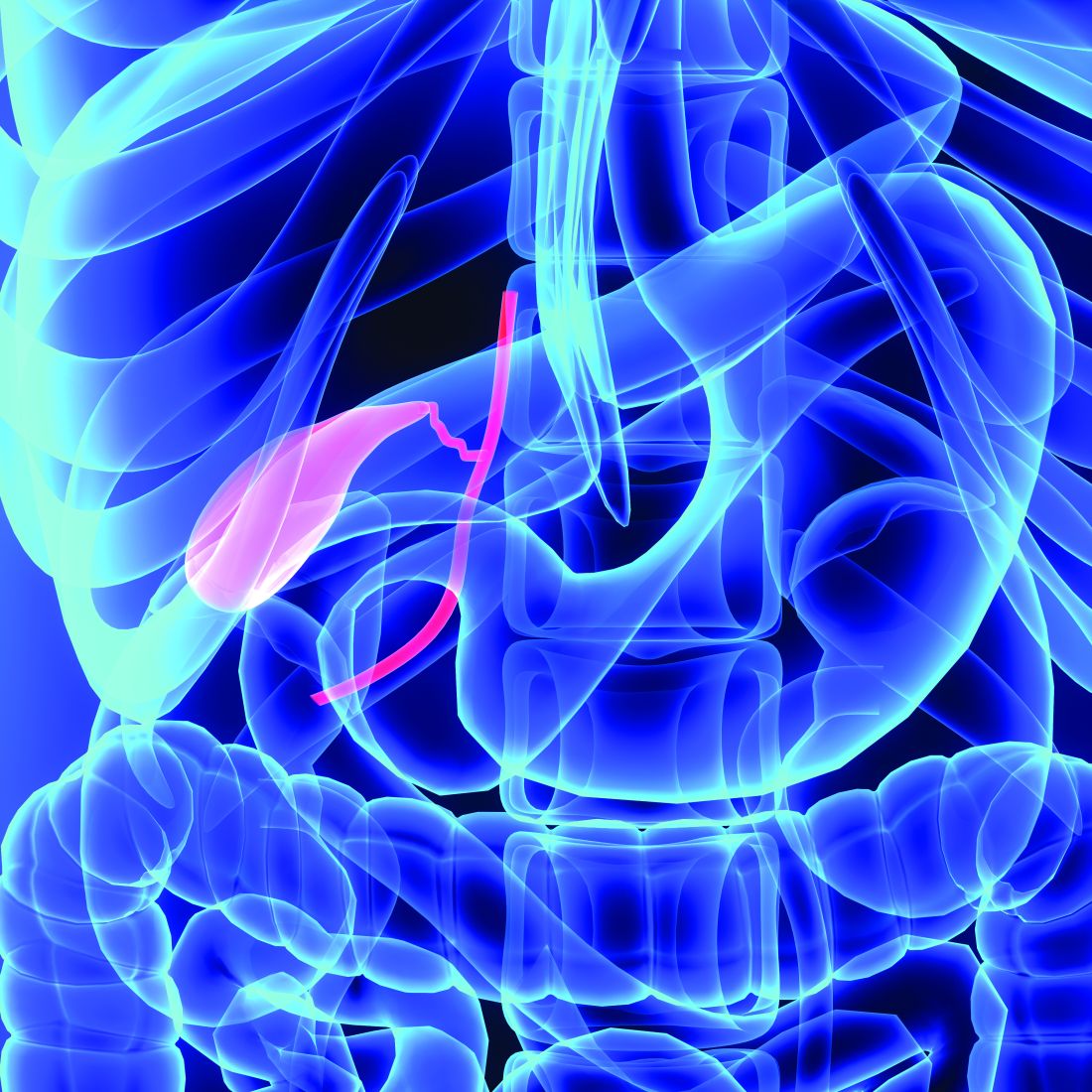
Match Day 2018: A slow year for dermatology
according to the National Resident Matching Program (NRMP).
The 2018 Match also set new highs for total positions offered (up 4.4% over last year), total positions filled (up 4.7%), PGY-1 positions (up 4.9%) filled, and total applicants (up 1.7%). “The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
according to the National Resident Matching Program (NRMP).
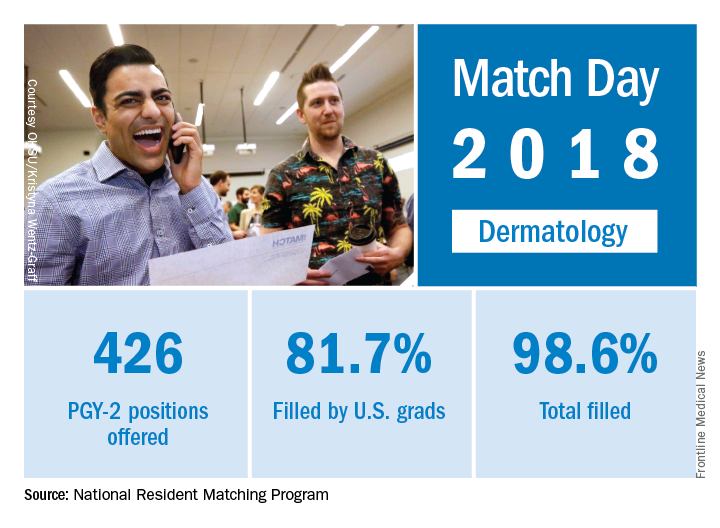
The 2018 Match also set new highs for total positions offered (up 4.4% over last year), total positions filled (up 4.7%), PGY-1 positions (up 4.9%) filled, and total applicants (up 1.7%). “The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
according to the National Resident Matching Program (NRMP).
The 2018 Match also set new highs for total positions offered (up 4.4% over last year), total positions filled (up 4.7%), PGY-1 positions (up 4.9%) filled, and total applicants (up 1.7%). “The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
CT angiography boosts success in chronic total occlusion revascularization
WASHINGTON – When performed prior to revascularization, CT angiography almost doubles the likelihood of successful revascularization of chronic total occlusion relative to no CT angiography, according to a meta-analysis.
Because the meta-analysis relied primarily on retrospective data, the conclusion was characterized as hypothesis-generating. But the author, Wael Abuzeid, MD, an interventional cardiologist and assistant professor at Queen’s University, Kingston, Ont., suggested that there are several arguments to be made for pursuing a randomized trial.
This is not a new idea, according to results of a systematic review of the literature. Although only four articles met prespecified criteria for entry into the meta-analysis that was eventually conducted, Dr. Abuzeid and his coauthors found 424 articles on this subject in a search of three literature databases.
Only one of the four studies entered into the meta-analysis involved prospective data collection, but three of the four found a significant advantage for preprocedural CTA when compared with no CTA for procedural success, meaning restoration of blood flow in the target CTO. The fourth study also associated preprocedural CTA with improved procedural success, but the advantage did not reach statistical significance.
When the data were combined for a meta-analysis, the odds ratio for procedural success for conducting a preprocedural CTA relative to no preprocedural CTA was 1.89 with a significant 95% confidence interval (1.18-3.04; P less than .05).
The four studies were published during 2012-2015. Two of them used CTA with only a 64-slice capacity, raising the possibility that an even greater improvement in results would have been achieved with CTA using the greater resolutions now available.
There were several important limitations of the study, particularly the potential for selection bias from the nonrandomized designs in the studies evaluated, Dr. Abuzeid acknowledged. However, the most likely selection bias would be funneling of more challenging cases to preprocedural CTA, a potential disadvantage for CTA if this resulted in a patient population likely to have a poor outcome.
Currently, few centers employ preprocedural CTA in routine management of CTO, according to Dr. Abuzeid.
“CTA prior to revascularization in CTO is not a standard approach even in complex patients,” Dr. Abuzeid said. However, he believes an argument can already be made for preprocedural CTA in some types of challenging patients, such as those with particularly long target lesions. In such cases, CTA could provide advance information about negative distal remodeling and the likelihood that a retrograde approach might be needed.
“For the junior operator, I think the information provided by preprocedural CTA could be very useful in planning,” Dr. Abuzeid said.
The arguments against preprocedural CTA include higher radiation exposure and a delay in the time to procedure by adding the extra step of first conducting the imaging study. In addition to verifying that procedural success is achieved with preprocedural CTA, these issues are among those that deserve evaluation in a prospective study.
“The appropriate randomized trial would be conducted at high-volume centers with all comers, not just complex patients, randomized to undergo a preprocedural CTA or no preprocedural imaging,” Dr. Abuzeid suggested. He said the appropriate primary outcome is relative success at restoring Thrombolysis in Myocardial Infarction grade 2 flow, but suggested that other endpoints, such as procedure time and rate of complications, would be useful for determining the value of this approach.
Dr. Abuzeid reports having no financial relationships.
SOURCE: Abuzeid W. CRT 18.
WASHINGTON – When performed prior to revascularization, CT angiography almost doubles the likelihood of successful revascularization of chronic total occlusion relative to no CT angiography, according to a meta-analysis.
Because the meta-analysis relied primarily on retrospective data, the conclusion was characterized as hypothesis-generating. But the author, Wael Abuzeid, MD, an interventional cardiologist and assistant professor at Queen’s University, Kingston, Ont., suggested that there are several arguments to be made for pursuing a randomized trial.
This is not a new idea, according to results of a systematic review of the literature. Although only four articles met prespecified criteria for entry into the meta-analysis that was eventually conducted, Dr. Abuzeid and his coauthors found 424 articles on this subject in a search of three literature databases.
Only one of the four studies entered into the meta-analysis involved prospective data collection, but three of the four found a significant advantage for preprocedural CTA when compared with no CTA for procedural success, meaning restoration of blood flow in the target CTO. The fourth study also associated preprocedural CTA with improved procedural success, but the advantage did not reach statistical significance.
When the data were combined for a meta-analysis, the odds ratio for procedural success for conducting a preprocedural CTA relative to no preprocedural CTA was 1.89 with a significant 95% confidence interval (1.18-3.04; P less than .05).
The four studies were published during 2012-2015. Two of them used CTA with only a 64-slice capacity, raising the possibility that an even greater improvement in results would have been achieved with CTA using the greater resolutions now available.
There were several important limitations of the study, particularly the potential for selection bias from the nonrandomized designs in the studies evaluated, Dr. Abuzeid acknowledged. However, the most likely selection bias would be funneling of more challenging cases to preprocedural CTA, a potential disadvantage for CTA if this resulted in a patient population likely to have a poor outcome.
Currently, few centers employ preprocedural CTA in routine management of CTO, according to Dr. Abuzeid.
“CTA prior to revascularization in CTO is not a standard approach even in complex patients,” Dr. Abuzeid said. However, he believes an argument can already be made for preprocedural CTA in some types of challenging patients, such as those with particularly long target lesions. In such cases, CTA could provide advance information about negative distal remodeling and the likelihood that a retrograde approach might be needed.
“For the junior operator, I think the information provided by preprocedural CTA could be very useful in planning,” Dr. Abuzeid said.
The arguments against preprocedural CTA include higher radiation exposure and a delay in the time to procedure by adding the extra step of first conducting the imaging study. In addition to verifying that procedural success is achieved with preprocedural CTA, these issues are among those that deserve evaluation in a prospective study.
“The appropriate randomized trial would be conducted at high-volume centers with all comers, not just complex patients, randomized to undergo a preprocedural CTA or no preprocedural imaging,” Dr. Abuzeid suggested. He said the appropriate primary outcome is relative success at restoring Thrombolysis in Myocardial Infarction grade 2 flow, but suggested that other endpoints, such as procedure time and rate of complications, would be useful for determining the value of this approach.
Dr. Abuzeid reports having no financial relationships.
SOURCE: Abuzeid W. CRT 18.
WASHINGTON – When performed prior to revascularization, CT angiography almost doubles the likelihood of successful revascularization of chronic total occlusion relative to no CT angiography, according to a meta-analysis.
Because the meta-analysis relied primarily on retrospective data, the conclusion was characterized as hypothesis-generating. But the author, Wael Abuzeid, MD, an interventional cardiologist and assistant professor at Queen’s University, Kingston, Ont., suggested that there are several arguments to be made for pursuing a randomized trial.
This is not a new idea, according to results of a systematic review of the literature. Although only four articles met prespecified criteria for entry into the meta-analysis that was eventually conducted, Dr. Abuzeid and his coauthors found 424 articles on this subject in a search of three literature databases.
Only one of the four studies entered into the meta-analysis involved prospective data collection, but three of the four found a significant advantage for preprocedural CTA when compared with no CTA for procedural success, meaning restoration of blood flow in the target CTO. The fourth study also associated preprocedural CTA with improved procedural success, but the advantage did not reach statistical significance.
When the data were combined for a meta-analysis, the odds ratio for procedural success for conducting a preprocedural CTA relative to no preprocedural CTA was 1.89 with a significant 95% confidence interval (1.18-3.04; P less than .05).
The four studies were published during 2012-2015. Two of them used CTA with only a 64-slice capacity, raising the possibility that an even greater improvement in results would have been achieved with CTA using the greater resolutions now available.
There were several important limitations of the study, particularly the potential for selection bias from the nonrandomized designs in the studies evaluated, Dr. Abuzeid acknowledged. However, the most likely selection bias would be funneling of more challenging cases to preprocedural CTA, a potential disadvantage for CTA if this resulted in a patient population likely to have a poor outcome.
Currently, few centers employ preprocedural CTA in routine management of CTO, according to Dr. Abuzeid.
“CTA prior to revascularization in CTO is not a standard approach even in complex patients,” Dr. Abuzeid said. However, he believes an argument can already be made for preprocedural CTA in some types of challenging patients, such as those with particularly long target lesions. In such cases, CTA could provide advance information about negative distal remodeling and the likelihood that a retrograde approach might be needed.
“For the junior operator, I think the information provided by preprocedural CTA could be very useful in planning,” Dr. Abuzeid said.
The arguments against preprocedural CTA include higher radiation exposure and a delay in the time to procedure by adding the extra step of first conducting the imaging study. In addition to verifying that procedural success is achieved with preprocedural CTA, these issues are among those that deserve evaluation in a prospective study.
“The appropriate randomized trial would be conducted at high-volume centers with all comers, not just complex patients, randomized to undergo a preprocedural CTA or no preprocedural imaging,” Dr. Abuzeid suggested. He said the appropriate primary outcome is relative success at restoring Thrombolysis in Myocardial Infarction grade 2 flow, but suggested that other endpoints, such as procedure time and rate of complications, would be useful for determining the value of this approach.
Dr. Abuzeid reports having no financial relationships.
SOURCE: Abuzeid W. CRT 18.
REPORTING FROM CRT 2018
Key clinical point:
Major finding: In a meta-analysis of data from four studies, CT angiography almost doubled the likelihood of procedural success (OR 1.89; P less than .05).
Study details: A systematic review and meta-analysis of four studies.
Disclosures: Dr. Abuzeid reports having no financial relationships.
Source: Abuzaid W. CRT 18.
Match Day 2018: Internal medicine increases positions, matches
Internal medicine helped to make the 2018 Main Residency Match the largest ever as the specialty offered and filled about 4% more residency slots than in 2017, according to the National Resident Matching Program (NRMP).
Internal medicine brought 7,542 PGY-1 positions – more than any other specialty – to the Match Day party this year and filled 44.9% of them with U.S. graduates and 96.7% overall. Despite the increase in IM residency slots, however, the number and percentage of U.S. seniors matching declined, as it has done each year since 2015. For all specialties, U.S. graduates filled 58.7% of the record-high 30,232 available spots, and the overall fill rate was 96.1%, the NRMP said in its 2018 Main Residency Match report.
The 2018 Match also set new highs for total positions offered (up 4.4% over last year), total (up 4.7%) and PGY-1 positions (up 4.9%) filled, and total applicants (up 1.7%). “The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
Internal medicine helped to make the 2018 Main Residency Match the largest ever as the specialty offered and filled about 4% more residency slots than in 2017, according to the National Resident Matching Program (NRMP).
Internal medicine brought 7,542 PGY-1 positions – more than any other specialty – to the Match Day party this year and filled 44.9% of them with U.S. graduates and 96.7% overall. Despite the increase in IM residency slots, however, the number and percentage of U.S. seniors matching declined, as it has done each year since 2015. For all specialties, U.S. graduates filled 58.7% of the record-high 30,232 available spots, and the overall fill rate was 96.1%, the NRMP said in its 2018 Main Residency Match report.
The 2018 Match also set new highs for total positions offered (up 4.4% over last year), total (up 4.7%) and PGY-1 positions (up 4.9%) filled, and total applicants (up 1.7%). “The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
Internal medicine helped to make the 2018 Main Residency Match the largest ever as the specialty offered and filled about 4% more residency slots than in 2017, according to the National Resident Matching Program (NRMP).
Internal medicine brought 7,542 PGY-1 positions – more than any other specialty – to the Match Day party this year and filled 44.9% of them with U.S. graduates and 96.7% overall. Despite the increase in IM residency slots, however, the number and percentage of U.S. seniors matching declined, as it has done each year since 2015. For all specialties, U.S. graduates filled 58.7% of the record-high 30,232 available spots, and the overall fill rate was 96.1%, the NRMP said in its 2018 Main Residency Match report.
The 2018 Match also set new highs for total positions offered (up 4.4% over last year), total (up 4.7%) and PGY-1 positions (up 4.9%) filled, and total applicants (up 1.7%). “The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
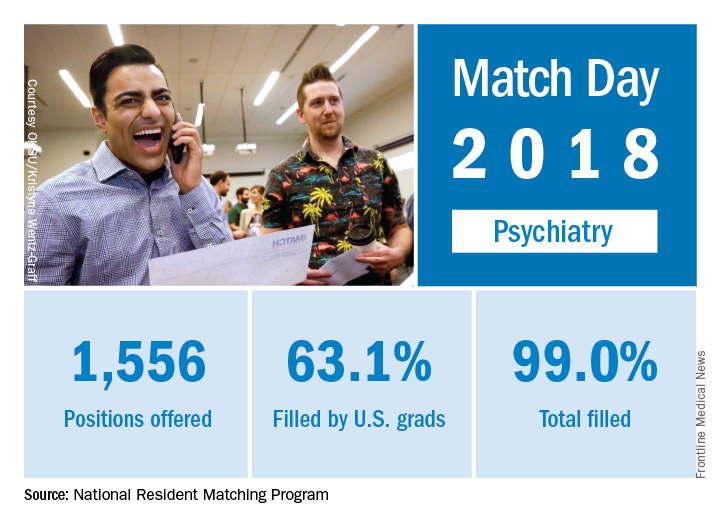
Match Day 2018: Psychiatry increases positions and matches
as the specialty increased residency slots by 4.1% and accepted 3.3% more applicants, compared with 2017, according to the National Resident Matching Program.
Psychiatry brought 1,556 PGY-1 positions to the Match Day table this year and filled 63.1% of them with U.S. graduates – up for the fourth consecutive year – and 99.0% overall. For all specialties, U.S. graduates filled 58.7% of the record-high 30,232 available spots, and the overall fill rate was 96.1%, the NRMP said in its 2018 Main Residency Match report.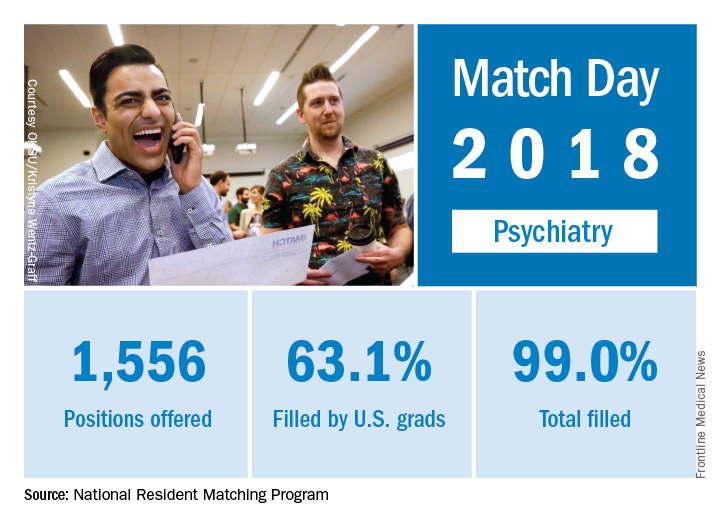
as the specialty increased residency slots by 4.1% and accepted 3.3% more applicants, compared with 2017, according to the National Resident Matching Program.
Psychiatry brought 1,556 PGY-1 positions to the Match Day table this year and filled 63.1% of them with U.S. graduates – up for the fourth consecutive year – and 99.0% overall. For all specialties, U.S. graduates filled 58.7% of the record-high 30,232 available spots, and the overall fill rate was 96.1%, the NRMP said in its 2018 Main Residency Match report.
as the specialty increased residency slots by 4.1% and accepted 3.3% more applicants, compared with 2017, according to the National Resident Matching Program.
Psychiatry brought 1,556 PGY-1 positions to the Match Day table this year and filled 63.1% of them with U.S. graduates – up for the fourth consecutive year – and 99.0% overall. For all specialties, U.S. graduates filled 58.7% of the record-high 30,232 available spots, and the overall fill rate was 96.1%, the NRMP said in its 2018 Main Residency Match report.