User login
Tryptophan depletion may explain high rate of eating disorders in women
TAMPA, FLA. – The far higher rate of eating disorders in women than men appears to be explained at least in part by a greater acute depletion of tryptophan, which is essential for the formation of serotonin, a key mediator of risk, according to a research review presented at the annual meeting of the American College of Psychiatrists.
“The specific vulnerability of women to eating disorders relates to the fact that women’s brains are much more sensitive to dietary intake of tryptophan than are men’s brains,” explained Allan S. Kaplan, MD, senior scientist at the Center for Addiction and Mental Health at the University of Toronto.
“Women are more likely than men to be dieting,” said Dr. Kaplan, walking through the evidence. “Low-calorie diets tend to be high in protein and low in cholesterol and fat. Such diets lead to tryptophan depletion and decreased serotonin synthesis in the brain. Because of lower levels of central serotonin, women are more vulnerable to mood and eating disorders than men.”
Not all women who diet may be vulnerable to this sequence of events. Genetics are likely to be a factor, according to Dr. Kaplan, who said, “Genes load the gun; the environment pulls the trigger.”
However, women do appear to be more susceptible for a number of reasons. For one, the mean rate of serotonin synthesis is 52% higher in normal males than normal females, giving them a greater buffer when dietary intake of tryptophan is low. For another, there is evidence that intake of nutrients most rich in tryptophan, particularly proteins, is typically lower in women than men.
The ratio of females to males for both anorexia nervosa and bulimia nervosa is about 10:1. Although the female-to-male ratio of binge eating is lower at 2:1, women dominate these psychiatric diagnoses. Several environmental factors associated with eating disorders are more closely associated with women than men, including a history of sexual or physical abuse and female preoccupation with body image, but acute tryptophan depletion may be an important factor participating in the translation of risk to an active disease, according to Dr. Kaplan.
Acute tryptophan deficiency may also explain why treatment of eating disorders with SSRIs has been disappointing. With low levels of tryptophan leading to serotonin depletion, “there is no substrate” for drugs administered to increase serotonin-mediated signaling, Dr. Kaplan explained.
Ensuring adequate dietary intake of tryptophan, which is “found mainly in high-protein animal foods,” may be important, even though Dr. Kaplan warned that achieving optimal levels of serotonin “can be challenging from food alone.” Nevertheless, behavioral therapies are commonly effective for eating disorders, presumably at least partially as a result of their ability to normalize diet.
Overall, the tryptophan hypothesis has provided a major shift in the understanding of eating disorders, according to Dr. Kaplan. Further studies are needed, but he said that the key message is that, “For women’s brains, you are what you eat.”
Dr. Kaplan reported no conflicts of interest relevant to this topic.
This story was updated on 2/25/2018.
TAMPA, FLA. – The far higher rate of eating disorders in women than men appears to be explained at least in part by a greater acute depletion of tryptophan, which is essential for the formation of serotonin, a key mediator of risk, according to a research review presented at the annual meeting of the American College of Psychiatrists.
“The specific vulnerability of women to eating disorders relates to the fact that women’s brains are much more sensitive to dietary intake of tryptophan than are men’s brains,” explained Allan S. Kaplan, MD, senior scientist at the Center for Addiction and Mental Health at the University of Toronto.
“Women are more likely than men to be dieting,” said Dr. Kaplan, walking through the evidence. “Low-calorie diets tend to be high in protein and low in cholesterol and fat. Such diets lead to tryptophan depletion and decreased serotonin synthesis in the brain. Because of lower levels of central serotonin, women are more vulnerable to mood and eating disorders than men.”
Not all women who diet may be vulnerable to this sequence of events. Genetics are likely to be a factor, according to Dr. Kaplan, who said, “Genes load the gun; the environment pulls the trigger.”
However, women do appear to be more susceptible for a number of reasons. For one, the mean rate of serotonin synthesis is 52% higher in normal males than normal females, giving them a greater buffer when dietary intake of tryptophan is low. For another, there is evidence that intake of nutrients most rich in tryptophan, particularly proteins, is typically lower in women than men.
The ratio of females to males for both anorexia nervosa and bulimia nervosa is about 10:1. Although the female-to-male ratio of binge eating is lower at 2:1, women dominate these psychiatric diagnoses. Several environmental factors associated with eating disorders are more closely associated with women than men, including a history of sexual or physical abuse and female preoccupation with body image, but acute tryptophan depletion may be an important factor participating in the translation of risk to an active disease, according to Dr. Kaplan.
Acute tryptophan deficiency may also explain why treatment of eating disorders with SSRIs has been disappointing. With low levels of tryptophan leading to serotonin depletion, “there is no substrate” for drugs administered to increase serotonin-mediated signaling, Dr. Kaplan explained.
Ensuring adequate dietary intake of tryptophan, which is “found mainly in high-protein animal foods,” may be important, even though Dr. Kaplan warned that achieving optimal levels of serotonin “can be challenging from food alone.” Nevertheless, behavioral therapies are commonly effective for eating disorders, presumably at least partially as a result of their ability to normalize diet.
Overall, the tryptophan hypothesis has provided a major shift in the understanding of eating disorders, according to Dr. Kaplan. Further studies are needed, but he said that the key message is that, “For women’s brains, you are what you eat.”
Dr. Kaplan reported no conflicts of interest relevant to this topic.
This story was updated on 2/25/2018.
TAMPA, FLA. – The far higher rate of eating disorders in women than men appears to be explained at least in part by a greater acute depletion of tryptophan, which is essential for the formation of serotonin, a key mediator of risk, according to a research review presented at the annual meeting of the American College of Psychiatrists.
“The specific vulnerability of women to eating disorders relates to the fact that women’s brains are much more sensitive to dietary intake of tryptophan than are men’s brains,” explained Allan S. Kaplan, MD, senior scientist at the Center for Addiction and Mental Health at the University of Toronto.
“Women are more likely than men to be dieting,” said Dr. Kaplan, walking through the evidence. “Low-calorie diets tend to be high in protein and low in cholesterol and fat. Such diets lead to tryptophan depletion and decreased serotonin synthesis in the brain. Because of lower levels of central serotonin, women are more vulnerable to mood and eating disorders than men.”
Not all women who diet may be vulnerable to this sequence of events. Genetics are likely to be a factor, according to Dr. Kaplan, who said, “Genes load the gun; the environment pulls the trigger.”
However, women do appear to be more susceptible for a number of reasons. For one, the mean rate of serotonin synthesis is 52% higher in normal males than normal females, giving them a greater buffer when dietary intake of tryptophan is low. For another, there is evidence that intake of nutrients most rich in tryptophan, particularly proteins, is typically lower in women than men.
The ratio of females to males for both anorexia nervosa and bulimia nervosa is about 10:1. Although the female-to-male ratio of binge eating is lower at 2:1, women dominate these psychiatric diagnoses. Several environmental factors associated with eating disorders are more closely associated with women than men, including a history of sexual or physical abuse and female preoccupation with body image, but acute tryptophan depletion may be an important factor participating in the translation of risk to an active disease, according to Dr. Kaplan.
Acute tryptophan deficiency may also explain why treatment of eating disorders with SSRIs has been disappointing. With low levels of tryptophan leading to serotonin depletion, “there is no substrate” for drugs administered to increase serotonin-mediated signaling, Dr. Kaplan explained.
Ensuring adequate dietary intake of tryptophan, which is “found mainly in high-protein animal foods,” may be important, even though Dr. Kaplan warned that achieving optimal levels of serotonin “can be challenging from food alone.” Nevertheless, behavioral therapies are commonly effective for eating disorders, presumably at least partially as a result of their ability to normalize diet.
Overall, the tryptophan hypothesis has provided a major shift in the understanding of eating disorders, according to Dr. Kaplan. Further studies are needed, but he said that the key message is that, “For women’s brains, you are what you eat.”
Dr. Kaplan reported no conflicts of interest relevant to this topic.
This story was updated on 2/25/2018.
EXPERT ANALYSIS FROM THE COLLEGE 2018
Flu season shows signs of slowing
Flu-related outpatient activity dropped for the second week in a row as the cumulative hospitalization rate continues to rise, according to data from the Centers for Disease Control and Prevention.
For the week ending Feb. 17, the proportion of outpatient visits for influenza-like illness (ILI) was 6.4%, which was down from 7.4% the previous week (Feb. 10) and down from the seasonal high of 7.5% set 2 weeks earlier, the CDC said in its weekly flu surveillance report. The rate for the week ending Feb. 10 was reported last week as 7.5%, but it has been revised downward.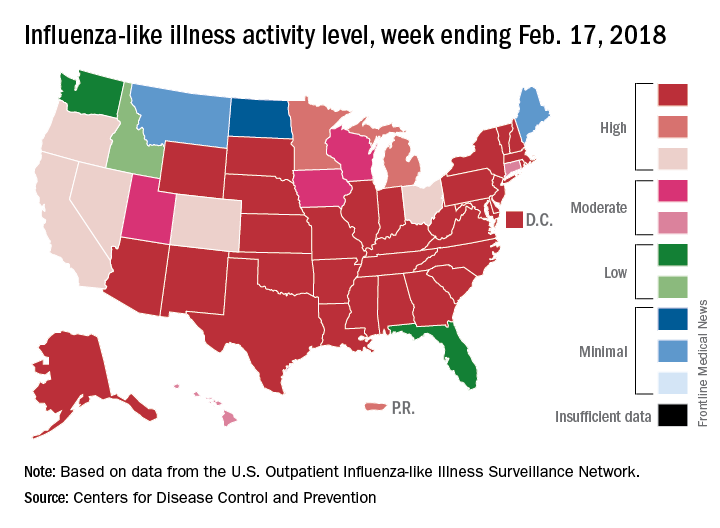
State reports of ILI activity support the decreases seen in the national outpatient rate. There were 33 states at level 10 on the CDC’s 1-10 scale for the week ending Feb. 17 – down from 39 the week before – and a total of 41 states in the “high” range from levels 8-10, compared with 45 the previous week, CDC’s FluView website shows.
Reports of flu-related pediatric deaths continued: 13 deaths were reported during the week, although 9 occurred in previous weeks. The total for the 2017-2018 season is now 97. There were 110 pediatric deaths in the entire 2016-2017 season, 93 during the 2015-2016 season, and 149 in 2014-2015, the CDC said.
Flu-related outpatient activity dropped for the second week in a row as the cumulative hospitalization rate continues to rise, according to data from the Centers for Disease Control and Prevention.
For the week ending Feb. 17, the proportion of outpatient visits for influenza-like illness (ILI) was 6.4%, which was down from 7.4% the previous week (Feb. 10) and down from the seasonal high of 7.5% set 2 weeks earlier, the CDC said in its weekly flu surveillance report. The rate for the week ending Feb. 10 was reported last week as 7.5%, but it has been revised downward.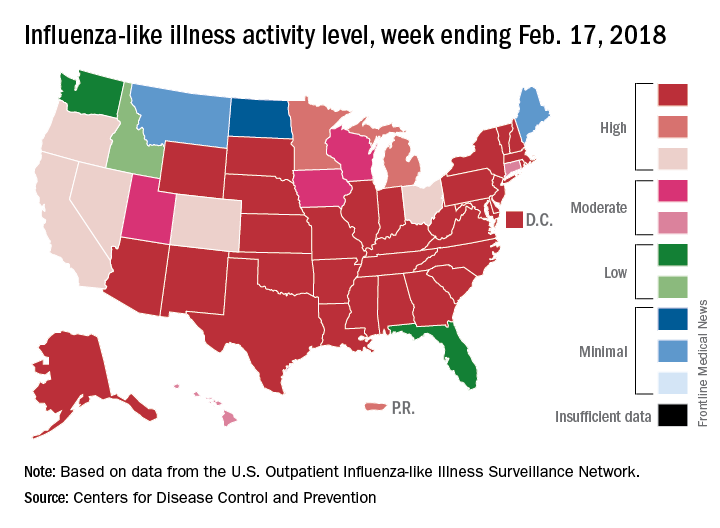
State reports of ILI activity support the decreases seen in the national outpatient rate. There were 33 states at level 10 on the CDC’s 1-10 scale for the week ending Feb. 17 – down from 39 the week before – and a total of 41 states in the “high” range from levels 8-10, compared with 45 the previous week, CDC’s FluView website shows.
Reports of flu-related pediatric deaths continued: 13 deaths were reported during the week, although 9 occurred in previous weeks. The total for the 2017-2018 season is now 97. There were 110 pediatric deaths in the entire 2016-2017 season, 93 during the 2015-2016 season, and 149 in 2014-2015, the CDC said.
Flu-related outpatient activity dropped for the second week in a row as the cumulative hospitalization rate continues to rise, according to data from the Centers for Disease Control and Prevention.
For the week ending Feb. 17, the proportion of outpatient visits for influenza-like illness (ILI) was 6.4%, which was down from 7.4% the previous week (Feb. 10) and down from the seasonal high of 7.5% set 2 weeks earlier, the CDC said in its weekly flu surveillance report. The rate for the week ending Feb. 10 was reported last week as 7.5%, but it has been revised downward.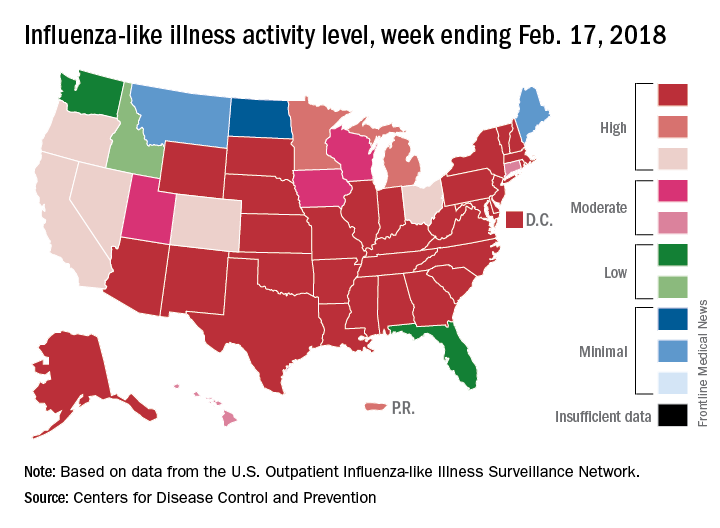
State reports of ILI activity support the decreases seen in the national outpatient rate. There were 33 states at level 10 on the CDC’s 1-10 scale for the week ending Feb. 17 – down from 39 the week before – and a total of 41 states in the “high” range from levels 8-10, compared with 45 the previous week, CDC’s FluView website shows.
Reports of flu-related pediatric deaths continued: 13 deaths were reported during the week, although 9 occurred in previous weeks. The total for the 2017-2018 season is now 97. There were 110 pediatric deaths in the entire 2016-2017 season, 93 during the 2015-2016 season, and 149 in 2014-2015, the CDC said.
Sleep disturbance not linked to age or IQ in early ASD
Sleep disturbance is not associated with age and IQ in young children with autism spectrum disorder (ASD) and disruptive behaviors, according to Cynthia R. Johnson, PhD, and her associates.
They assessed 177 children aged 3-7 who were participating in the Research Units on Behavioral Intervention study, a 24-week trial. All of the children had a diagnosis of autism spectrum disorder, based on DSM-IV criteria. The diagnoses were corroborated by the Autism Diagnostic Observation Schedule and the Autism Diagnostic Interview–Revised.
The children were randomized into a parent training group or a parent education group. After getting parents to complete several forms, including the Children’s Sleep Habits Questionnaire, Dr. Johnson and her associates found no age differences between children who fell into the category of “good sleepers” (n = 52), and those characterized as “poor sleepers” (n = 46) (P = .57). In both sleep groups, more than 70% of the children had an IQ of 70 or above, and no significant difference was found in good sleepers, compared with poor sleepers, in IQ variable (P = .87) (Sleep Med. 2018. 44:61-6).
In addition, the researchers found that poor sleepers had significantly higher scores on the Aberrant Behavior Checklist subscales of irritability, hyperactivity, stereotypic behavior, and social withdrawal/lethargy, compared with good sleepers. All subscales of the parenting stress index and the PSI total score also were significantly higher in the poor sleepers group, compared with children in the good sleepers group, reported Dr. Johnson of the University of Florida, Gainesville, and her associates.
Additional studies are needed within a “comprehensive biopsychosocial model” to advance the understanding of why some children with autism experience disrupted sleep patterns and others do not. “, regardless of age and cognitive level,” Dr. Johnson and her associates concluded. “With improved sleep, better outcomes for children with ASD could be expected.”
Read the full study in Sleep Medicine
Sleep disturbance is not associated with age and IQ in young children with autism spectrum disorder (ASD) and disruptive behaviors, according to Cynthia R. Johnson, PhD, and her associates.
They assessed 177 children aged 3-7 who were participating in the Research Units on Behavioral Intervention study, a 24-week trial. All of the children had a diagnosis of autism spectrum disorder, based on DSM-IV criteria. The diagnoses were corroborated by the Autism Diagnostic Observation Schedule and the Autism Diagnostic Interview–Revised.
The children were randomized into a parent training group or a parent education group. After getting parents to complete several forms, including the Children’s Sleep Habits Questionnaire, Dr. Johnson and her associates found no age differences between children who fell into the category of “good sleepers” (n = 52), and those characterized as “poor sleepers” (n = 46) (P = .57). In both sleep groups, more than 70% of the children had an IQ of 70 or above, and no significant difference was found in good sleepers, compared with poor sleepers, in IQ variable (P = .87) (Sleep Med. 2018. 44:61-6).
In addition, the researchers found that poor sleepers had significantly higher scores on the Aberrant Behavior Checklist subscales of irritability, hyperactivity, stereotypic behavior, and social withdrawal/lethargy, compared with good sleepers. All subscales of the parenting stress index and the PSI total score also were significantly higher in the poor sleepers group, compared with children in the good sleepers group, reported Dr. Johnson of the University of Florida, Gainesville, and her associates.
Additional studies are needed within a “comprehensive biopsychosocial model” to advance the understanding of why some children with autism experience disrupted sleep patterns and others do not. “, regardless of age and cognitive level,” Dr. Johnson and her associates concluded. “With improved sleep, better outcomes for children with ASD could be expected.”
Read the full study in Sleep Medicine
Sleep disturbance is not associated with age and IQ in young children with autism spectrum disorder (ASD) and disruptive behaviors, according to Cynthia R. Johnson, PhD, and her associates.
They assessed 177 children aged 3-7 who were participating in the Research Units on Behavioral Intervention study, a 24-week trial. All of the children had a diagnosis of autism spectrum disorder, based on DSM-IV criteria. The diagnoses were corroborated by the Autism Diagnostic Observation Schedule and the Autism Diagnostic Interview–Revised.
The children were randomized into a parent training group or a parent education group. After getting parents to complete several forms, including the Children’s Sleep Habits Questionnaire, Dr. Johnson and her associates found no age differences between children who fell into the category of “good sleepers” (n = 52), and those characterized as “poor sleepers” (n = 46) (P = .57). In both sleep groups, more than 70% of the children had an IQ of 70 or above, and no significant difference was found in good sleepers, compared with poor sleepers, in IQ variable (P = .87) (Sleep Med. 2018. 44:61-6).
In addition, the researchers found that poor sleepers had significantly higher scores on the Aberrant Behavior Checklist subscales of irritability, hyperactivity, stereotypic behavior, and social withdrawal/lethargy, compared with good sleepers. All subscales of the parenting stress index and the PSI total score also were significantly higher in the poor sleepers group, compared with children in the good sleepers group, reported Dr. Johnson of the University of Florida, Gainesville, and her associates.
Additional studies are needed within a “comprehensive biopsychosocial model” to advance the understanding of why some children with autism experience disrupted sleep patterns and others do not. “, regardless of age and cognitive level,” Dr. Johnson and her associates concluded. “With improved sleep, better outcomes for children with ASD could be expected.”
Read the full study in Sleep Medicine
FROM SLEEP MEDICINE
Suicidal behaviors are associated with discordant sexual orientation in teens
Teenagers with discordant sexual orientation are more likely to experience nonfatal suicidal behaviors, according to results of a study published in the American Journal of Preventative Medicine.
“In this study, discordance refers to reporting sexual contact that is inconsistent with a respondent’s sexual identity. ... Discrimination, stigma, prejudice, rejection, and societal norms may put pressure on sexual minorities to present a sexual identity inconsistent with their true sexual identity or to act in a manner inconsistent with their sexual identity,” said Francis Annor, PhD, of the Centers for Disease Control and Prevention, and fellow investigators.
“In considering the health and well-being of youth, sexual identity and sexual behavior and their intersection should be considered for their association with the mental health and well-being of adolescents,” according to Dr. Annor and his colleagues. “Some adolescents reporting discordance may have needs that should be considered when developing and implementing suicide prevention programs.”
For this study, investigators analyzed survey questions from 6,790 high school students queried during the 2015 national Youth Risk Behavior Survey.
Sexual discordance was measured by asking students their sexual orientation and the gender of any sexual partners they may have had. Students who responded as being bisexual or who had not experienced sexual contact before were excluded from final analysis.
Students were majority male (56% vs. 44%), white (54.8%), and heterosexual (97.8%), and sexually concordant (96.1%).
When analyzing suicidal tendencies among students, teens who were sexually discordant were 70% more likely to report thinking about, or planning, suicide. High risk for nonfatal suicidal behaviors was significantly more common among discordant students, compared with concordant students (46.3% vs .22.4%, P less than .0001). Students who were gay or lesbian were significantly more likely to report sexual orientation discordance than heterosexual students (32% vs. 3%, P less than .001).
Sexual discordance also was common among students who were female, black, bullied on school property, used marijuana, or physically forced to have sexual intercourse.
Dr. Annor and fellow investigators theorized that the association between discordance and suicidal ideation may stem from self-discrepancy, which can lead to increased anxiety, stress, or depression.
Another theory was that the stress was induced from being a minority, which is supported by the increased number of nonfatal suicidal behaviors in students who were discordant, female, or gay or lesbian, according to investigators. “The minority stress theory suggests that stigma experienced by sexual minorities may cause chronic, cumulative stress that may negatively impact both mental and physical health,” Dr. Francis and associates explained. “Minority stress has been associated with increased depression, overall poor physical health, and increased risk of chronic disease diagnosis.”
To help prevent these suicidal tendencies, Dr. Annor and colleagues suggested using a multipronged public health approach, including using CDC suicide prevention materials, creating safe spaces for kids to understand their developing sexual identities, and further studies to examine risk among discordant teens and nonfatal suicidal behaviors.
The findings of this study are limited by the use of only high school students, which excludes what may be a significant part of the population. Certain aspects of the survey, including no specific definition of sexual contact, as well as the self-reported nature of the information, might have affected findings. Finally, some of those involved in the study may not have been fully aware of their sexual preference at this age and may have experimented with those of the opposite sex as their reported sexual preference, and this may not have been associated with distress, the researchers said.
Dr. Annor and associates reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: Annor F et al. Am J Prev Med. 2018. doi: 10.1016/j.amepre.2018.01.013
Teenagers with discordant sexual orientation are more likely to experience nonfatal suicidal behaviors, according to results of a study published in the American Journal of Preventative Medicine.
“In this study, discordance refers to reporting sexual contact that is inconsistent with a respondent’s sexual identity. ... Discrimination, stigma, prejudice, rejection, and societal norms may put pressure on sexual minorities to present a sexual identity inconsistent with their true sexual identity or to act in a manner inconsistent with their sexual identity,” said Francis Annor, PhD, of the Centers for Disease Control and Prevention, and fellow investigators.
“In considering the health and well-being of youth, sexual identity and sexual behavior and their intersection should be considered for their association with the mental health and well-being of adolescents,” according to Dr. Annor and his colleagues. “Some adolescents reporting discordance may have needs that should be considered when developing and implementing suicide prevention programs.”
For this study, investigators analyzed survey questions from 6,790 high school students queried during the 2015 national Youth Risk Behavior Survey.
Sexual discordance was measured by asking students their sexual orientation and the gender of any sexual partners they may have had. Students who responded as being bisexual or who had not experienced sexual contact before were excluded from final analysis.
Students were majority male (56% vs. 44%), white (54.8%), and heterosexual (97.8%), and sexually concordant (96.1%).
When analyzing suicidal tendencies among students, teens who were sexually discordant were 70% more likely to report thinking about, or planning, suicide. High risk for nonfatal suicidal behaviors was significantly more common among discordant students, compared with concordant students (46.3% vs .22.4%, P less than .0001). Students who were gay or lesbian were significantly more likely to report sexual orientation discordance than heterosexual students (32% vs. 3%, P less than .001).
Sexual discordance also was common among students who were female, black, bullied on school property, used marijuana, or physically forced to have sexual intercourse.
Dr. Annor and fellow investigators theorized that the association between discordance and suicidal ideation may stem from self-discrepancy, which can lead to increased anxiety, stress, or depression.
Another theory was that the stress was induced from being a minority, which is supported by the increased number of nonfatal suicidal behaviors in students who were discordant, female, or gay or lesbian, according to investigators. “The minority stress theory suggests that stigma experienced by sexual minorities may cause chronic, cumulative stress that may negatively impact both mental and physical health,” Dr. Francis and associates explained. “Minority stress has been associated with increased depression, overall poor physical health, and increased risk of chronic disease diagnosis.”
To help prevent these suicidal tendencies, Dr. Annor and colleagues suggested using a multipronged public health approach, including using CDC suicide prevention materials, creating safe spaces for kids to understand their developing sexual identities, and further studies to examine risk among discordant teens and nonfatal suicidal behaviors.
The findings of this study are limited by the use of only high school students, which excludes what may be a significant part of the population. Certain aspects of the survey, including no specific definition of sexual contact, as well as the self-reported nature of the information, might have affected findings. Finally, some of those involved in the study may not have been fully aware of their sexual preference at this age and may have experimented with those of the opposite sex as their reported sexual preference, and this may not have been associated with distress, the researchers said.
Dr. Annor and associates reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: Annor F et al. Am J Prev Med. 2018. doi: 10.1016/j.amepre.2018.01.013
Teenagers with discordant sexual orientation are more likely to experience nonfatal suicidal behaviors, according to results of a study published in the American Journal of Preventative Medicine.
“In this study, discordance refers to reporting sexual contact that is inconsistent with a respondent’s sexual identity. ... Discrimination, stigma, prejudice, rejection, and societal norms may put pressure on sexual minorities to present a sexual identity inconsistent with their true sexual identity or to act in a manner inconsistent with their sexual identity,” said Francis Annor, PhD, of the Centers for Disease Control and Prevention, and fellow investigators.
“In considering the health and well-being of youth, sexual identity and sexual behavior and their intersection should be considered for their association with the mental health and well-being of adolescents,” according to Dr. Annor and his colleagues. “Some adolescents reporting discordance may have needs that should be considered when developing and implementing suicide prevention programs.”
For this study, investigators analyzed survey questions from 6,790 high school students queried during the 2015 national Youth Risk Behavior Survey.
Sexual discordance was measured by asking students their sexual orientation and the gender of any sexual partners they may have had. Students who responded as being bisexual or who had not experienced sexual contact before were excluded from final analysis.
Students were majority male (56% vs. 44%), white (54.8%), and heterosexual (97.8%), and sexually concordant (96.1%).
When analyzing suicidal tendencies among students, teens who were sexually discordant were 70% more likely to report thinking about, or planning, suicide. High risk for nonfatal suicidal behaviors was significantly more common among discordant students, compared with concordant students (46.3% vs .22.4%, P less than .0001). Students who were gay or lesbian were significantly more likely to report sexual orientation discordance than heterosexual students (32% vs. 3%, P less than .001).
Sexual discordance also was common among students who were female, black, bullied on school property, used marijuana, or physically forced to have sexual intercourse.
Dr. Annor and fellow investigators theorized that the association between discordance and suicidal ideation may stem from self-discrepancy, which can lead to increased anxiety, stress, or depression.
Another theory was that the stress was induced from being a minority, which is supported by the increased number of nonfatal suicidal behaviors in students who were discordant, female, or gay or lesbian, according to investigators. “The minority stress theory suggests that stigma experienced by sexual minorities may cause chronic, cumulative stress that may negatively impact both mental and physical health,” Dr. Francis and associates explained. “Minority stress has been associated with increased depression, overall poor physical health, and increased risk of chronic disease diagnosis.”
To help prevent these suicidal tendencies, Dr. Annor and colleagues suggested using a multipronged public health approach, including using CDC suicide prevention materials, creating safe spaces for kids to understand their developing sexual identities, and further studies to examine risk among discordant teens and nonfatal suicidal behaviors.
The findings of this study are limited by the use of only high school students, which excludes what may be a significant part of the population. Certain aspects of the survey, including no specific definition of sexual contact, as well as the self-reported nature of the information, might have affected findings. Finally, some of those involved in the study may not have been fully aware of their sexual preference at this age and may have experimented with those of the opposite sex as their reported sexual preference, and this may not have been associated with distress, the researchers said.
Dr. Annor and associates reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: Annor F et al. Am J Prev Med. 2018. doi: 10.1016/j.amepre.2018.01.013
FROM THE AMERICAN JOURNAL OF PREVENTIVE MEDICINE
Key clinical point:
Major finding: Teens with conflicting answers about sexual preference were 70% more likely to report suicidal ideation than their concordant counterparts.
Study details: Retrospective study of 6,790 high school students surveyed in the 2015 national Youth Risk Behavior Survey.
Disclosures: Dr. Annor and associates reported no relevant financial disclosures.
Source: Annor F et al. Am J Prev Med. 2018. doi: 10.1016/j.amepre.2018.01.013.
Pediatric Dermatology Consult - February 2018
The patient was diagnosed with pityriasis rosea (PR) on the basis of the clinical findings; a biopsy was not performed. The patient’s pruritus was treated with oral hydroxyzine and topical 1% triamcinolone ointment. She experienced itch relief with these treatments. On follow-up at 3 months, the patient’s lesions had mostly resolved with some postinflammatory hyperpigmentation.
In some patients, flu-like symptoms precede the onset of skin lesions; this has led to speculation regarding a viral etiology for PR. This prodrome, which is present in as many as half of all cases,can include mild headache, low-grade fever, joint aches, or malaise.2 Pityriasis rosea is thought to occur secondary to a systemic activation of human herpesviruses (HHV) 6 and/or HHV-7. Three cases of PR have been reported in the setting of H1N1 influenza virus infection.3 In one small study, HHV-8 was detected by polymerase chain reaction in approximately 20% of biopsy samples of lesional skin in patients with PR.4 However, most research on a viral etiology for pityriasis rosea has focused on HHV-6 and to a lesser extent HHV-7. DNA from both viruses has been isolated from PR lesions, but at varying detection rates.5,6 Furthermore, HHV-7 DNA has been isolated in as many as 14% of normal individuals without pityriasis rosea, suggesting that the presence of this virus on the skin is fairly common.7
Pityriasis rosea occurs in males and females of all ethnicities, with a slight female predominance. It is rare in young children and older adults. Most cases occur in adolescents and in adults in their twenties and early thirties. Cases occur most frequently in fall and spring.8
The herald patch of pityriasis rosea is typically solitary, but cases with multiple herald patches have been described. The herald patch can range in size from 1-10 cm and usually contains the best example of trailing scale – scale seen on the inside edge of the annular lesion. The satellite lesions of pityriasis rosea are typically papules or plaques with a collarette of scale. These lesions usually are oriented along the Langer cleavage lines, giving them a “Christmas tree” configuration when they appear on the posterior trunk.
Mimics
The herald patch of pityriasis rosea can resemble tinea corporis, and if there is any doubt as to the diagnosis, potassium hydroxide examination (also known as a KOH test) and/or fungal culture should be done to rule out a fungal etiology. However, certain features of this case, particularly the subsequent development of satellite lesions, are more consistent with pityriasis rosea.
Secondary syphilis should be considered in patients who are sexually active. The lesions of secondary syphilis are not typically pruritic, and involvement of the palms and soles is common (whereas such involvement is rare in pityriasis rosea).
Like pityriasis rosea, pityriasis lichenoides et varioliformis acuta (PLEVA) is characterized by papular lesions that resolve spontaneously; the lesions of PLEVA usually evolve to vesicular, necrotic, and purpuric papules that take longer to resolve than PR lesions. The lesions of PLEVA are more erythematous, pustular, and crusting than the lesions of pityriasis rosea.
Guttate psoriasis, which occurs following streptococcal pharyngitis in over 50% of patients, does not present with a herald lesion or distribution along Langer’s lines.10 If guttate psoriasis is suspected, rapid streptococcal testing of the throat or perianal area may be considered.
Nummular eczema presents as papules that enlarge to form erythematous, lichenified plaques that measure 1-2 cm in diameter. A relatively sudden eruption, such as this patient’s, would be unusual for nummular eczema. Also, nummular eczema typically occurs on xerotic skin, more often on the extremities than the trunk.
Diagnostic tests, treatment
Most patients do not require specific therapy for pityriasis rosea. Patients should be reassured that PR is typically a self-limited disease without long-term sequelae. Pregnant patients who develop pityriasis rosea in the first trimester may be at higher risk for spontaneous abortion,although data on the subject are sorely lacking.11 Oral antihistamines are useful in reducing pruritus associated with PR, and some patients experience relief by applying a low-potency topical corticosteroid.
In more severe cases, or in cases in which the patient is greatly distressed by the lesions, both broadband and narrowband UVB phototherapy effectively improve severity of lesions and reduces symptoms.12 These observations suggest that moderate sun exposure can help to reduce severity of PR lesions and hasten their resolution, but no studies assessing the effect of sun exposure on pityriasis rosea symptoms have been performed.
Furthermore, the possible role of the HHV-6 in PR has led some investigators to explore the utility of acyclovir in managing pityriasis rosea.13 One group recently found that 400 mg of acyclovir three times per day for 7 days decreased the number of lesions and pruritus associated with pityriasis rosea, compared those seen in controls, at 1-month follow-up.13
Timely recognition of the diagnosis, consideration of mimics, and ample reassurance are appropriate when approaching this disease.
Mr. Kusari is with the division of pediatric and adolescent dermatology at Rady Children’s Hospital, San Diego, and the departments of dermatology and pediatrics, University of California, San Diego. Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. They have no relevant financial disclosures. Email them at pdnews@frontlinemedcom.com.
References
1. Dermatology. 2015;231(1):9-14.
2. World J Clin Cases. 2017 Jun 16;5(6):203-11.
3. Pediatr Dermatol. 2011 May-Jun;28(3):341-2.
4. J Eur Acad Dermatol Venereol. 2006 Jul;20(6):667-71.
5. Dermatology. 1997;195(4):374-8.
6. J Invest Dermatol. 2005 Jun;124(6):1234-40.
7. Arch Dermatol. 1999 Sep;135(9):1070-2.
8. J Am Acad Dermatol. 1982 Jul;7(1):80-9.
9. Iran J Pediatr. 2010 Jun;20(2):237-41.
10. J Pediatr. 1988 Dec;113(6):1037-9.
11. J Am Acad Dermatol. 2008 May;58(5 Suppl 1):S78-83.
12. J Am Acad Dermatol. 1995 Dec;33(6):996-9.
13. Indian Dermatol Online J. 2015 May-Jun;6(3):181-4.
The patient was diagnosed with pityriasis rosea (PR) on the basis of the clinical findings; a biopsy was not performed. The patient’s pruritus was treated with oral hydroxyzine and topical 1% triamcinolone ointment. She experienced itch relief with these treatments. On follow-up at 3 months, the patient’s lesions had mostly resolved with some postinflammatory hyperpigmentation.
In some patients, flu-like symptoms precede the onset of skin lesions; this has led to speculation regarding a viral etiology for PR. This prodrome, which is present in as many as half of all cases,can include mild headache, low-grade fever, joint aches, or malaise.2 Pityriasis rosea is thought to occur secondary to a systemic activation of human herpesviruses (HHV) 6 and/or HHV-7. Three cases of PR have been reported in the setting of H1N1 influenza virus infection.3 In one small study, HHV-8 was detected by polymerase chain reaction in approximately 20% of biopsy samples of lesional skin in patients with PR.4 However, most research on a viral etiology for pityriasis rosea has focused on HHV-6 and to a lesser extent HHV-7. DNA from both viruses has been isolated from PR lesions, but at varying detection rates.5,6 Furthermore, HHV-7 DNA has been isolated in as many as 14% of normal individuals without pityriasis rosea, suggesting that the presence of this virus on the skin is fairly common.7
Pityriasis rosea occurs in males and females of all ethnicities, with a slight female predominance. It is rare in young children and older adults. Most cases occur in adolescents and in adults in their twenties and early thirties. Cases occur most frequently in fall and spring.8
The herald patch of pityriasis rosea is typically solitary, but cases with multiple herald patches have been described. The herald patch can range in size from 1-10 cm and usually contains the best example of trailing scale – scale seen on the inside edge of the annular lesion. The satellite lesions of pityriasis rosea are typically papules or plaques with a collarette of scale. These lesions usually are oriented along the Langer cleavage lines, giving them a “Christmas tree” configuration when they appear on the posterior trunk.
Mimics
The herald patch of pityriasis rosea can resemble tinea corporis, and if there is any doubt as to the diagnosis, potassium hydroxide examination (also known as a KOH test) and/or fungal culture should be done to rule out a fungal etiology. However, certain features of this case, particularly the subsequent development of satellite lesions, are more consistent with pityriasis rosea.
Secondary syphilis should be considered in patients who are sexually active. The lesions of secondary syphilis are not typically pruritic, and involvement of the palms and soles is common (whereas such involvement is rare in pityriasis rosea).
Like pityriasis rosea, pityriasis lichenoides et varioliformis acuta (PLEVA) is characterized by papular lesions that resolve spontaneously; the lesions of PLEVA usually evolve to vesicular, necrotic, and purpuric papules that take longer to resolve than PR lesions. The lesions of PLEVA are more erythematous, pustular, and crusting than the lesions of pityriasis rosea.
Guttate psoriasis, which occurs following streptococcal pharyngitis in over 50% of patients, does not present with a herald lesion or distribution along Langer’s lines.10 If guttate psoriasis is suspected, rapid streptococcal testing of the throat or perianal area may be considered.
Nummular eczema presents as papules that enlarge to form erythematous, lichenified plaques that measure 1-2 cm in diameter. A relatively sudden eruption, such as this patient’s, would be unusual for nummular eczema. Also, nummular eczema typically occurs on xerotic skin, more often on the extremities than the trunk.
Diagnostic tests, treatment
Most patients do not require specific therapy for pityriasis rosea. Patients should be reassured that PR is typically a self-limited disease without long-term sequelae. Pregnant patients who develop pityriasis rosea in the first trimester may be at higher risk for spontaneous abortion,although data on the subject are sorely lacking.11 Oral antihistamines are useful in reducing pruritus associated with PR, and some patients experience relief by applying a low-potency topical corticosteroid.
In more severe cases, or in cases in which the patient is greatly distressed by the lesions, both broadband and narrowband UVB phototherapy effectively improve severity of lesions and reduces symptoms.12 These observations suggest that moderate sun exposure can help to reduce severity of PR lesions and hasten their resolution, but no studies assessing the effect of sun exposure on pityriasis rosea symptoms have been performed.
Furthermore, the possible role of the HHV-6 in PR has led some investigators to explore the utility of acyclovir in managing pityriasis rosea.13 One group recently found that 400 mg of acyclovir three times per day for 7 days decreased the number of lesions and pruritus associated with pityriasis rosea, compared those seen in controls, at 1-month follow-up.13
Timely recognition of the diagnosis, consideration of mimics, and ample reassurance are appropriate when approaching this disease.
Mr. Kusari is with the division of pediatric and adolescent dermatology at Rady Children’s Hospital, San Diego, and the departments of dermatology and pediatrics, University of California, San Diego. Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. They have no relevant financial disclosures. Email them at pdnews@frontlinemedcom.com.
References
1. Dermatology. 2015;231(1):9-14.
2. World J Clin Cases. 2017 Jun 16;5(6):203-11.
3. Pediatr Dermatol. 2011 May-Jun;28(3):341-2.
4. J Eur Acad Dermatol Venereol. 2006 Jul;20(6):667-71.
5. Dermatology. 1997;195(4):374-8.
6. J Invest Dermatol. 2005 Jun;124(6):1234-40.
7. Arch Dermatol. 1999 Sep;135(9):1070-2.
8. J Am Acad Dermatol. 1982 Jul;7(1):80-9.
9. Iran J Pediatr. 2010 Jun;20(2):237-41.
10. J Pediatr. 1988 Dec;113(6):1037-9.
11. J Am Acad Dermatol. 2008 May;58(5 Suppl 1):S78-83.
12. J Am Acad Dermatol. 1995 Dec;33(6):996-9.
13. Indian Dermatol Online J. 2015 May-Jun;6(3):181-4.
The patient was diagnosed with pityriasis rosea (PR) on the basis of the clinical findings; a biopsy was not performed. The patient’s pruritus was treated with oral hydroxyzine and topical 1% triamcinolone ointment. She experienced itch relief with these treatments. On follow-up at 3 months, the patient’s lesions had mostly resolved with some postinflammatory hyperpigmentation.
In some patients, flu-like symptoms precede the onset of skin lesions; this has led to speculation regarding a viral etiology for PR. This prodrome, which is present in as many as half of all cases,can include mild headache, low-grade fever, joint aches, or malaise.2 Pityriasis rosea is thought to occur secondary to a systemic activation of human herpesviruses (HHV) 6 and/or HHV-7. Three cases of PR have been reported in the setting of H1N1 influenza virus infection.3 In one small study, HHV-8 was detected by polymerase chain reaction in approximately 20% of biopsy samples of lesional skin in patients with PR.4 However, most research on a viral etiology for pityriasis rosea has focused on HHV-6 and to a lesser extent HHV-7. DNA from both viruses has been isolated from PR lesions, but at varying detection rates.5,6 Furthermore, HHV-7 DNA has been isolated in as many as 14% of normal individuals without pityriasis rosea, suggesting that the presence of this virus on the skin is fairly common.7
Pityriasis rosea occurs in males and females of all ethnicities, with a slight female predominance. It is rare in young children and older adults. Most cases occur in adolescents and in adults in their twenties and early thirties. Cases occur most frequently in fall and spring.8
The herald patch of pityriasis rosea is typically solitary, but cases with multiple herald patches have been described. The herald patch can range in size from 1-10 cm and usually contains the best example of trailing scale – scale seen on the inside edge of the annular lesion. The satellite lesions of pityriasis rosea are typically papules or plaques with a collarette of scale. These lesions usually are oriented along the Langer cleavage lines, giving them a “Christmas tree” configuration when they appear on the posterior trunk.
Mimics
The herald patch of pityriasis rosea can resemble tinea corporis, and if there is any doubt as to the diagnosis, potassium hydroxide examination (also known as a KOH test) and/or fungal culture should be done to rule out a fungal etiology. However, certain features of this case, particularly the subsequent development of satellite lesions, are more consistent with pityriasis rosea.
Secondary syphilis should be considered in patients who are sexually active. The lesions of secondary syphilis are not typically pruritic, and involvement of the palms and soles is common (whereas such involvement is rare in pityriasis rosea).
Like pityriasis rosea, pityriasis lichenoides et varioliformis acuta (PLEVA) is characterized by papular lesions that resolve spontaneously; the lesions of PLEVA usually evolve to vesicular, necrotic, and purpuric papules that take longer to resolve than PR lesions. The lesions of PLEVA are more erythematous, pustular, and crusting than the lesions of pityriasis rosea.
Guttate psoriasis, which occurs following streptococcal pharyngitis in over 50% of patients, does not present with a herald lesion or distribution along Langer’s lines.10 If guttate psoriasis is suspected, rapid streptococcal testing of the throat or perianal area may be considered.
Nummular eczema presents as papules that enlarge to form erythematous, lichenified plaques that measure 1-2 cm in diameter. A relatively sudden eruption, such as this patient’s, would be unusual for nummular eczema. Also, nummular eczema typically occurs on xerotic skin, more often on the extremities than the trunk.
Diagnostic tests, treatment
Most patients do not require specific therapy for pityriasis rosea. Patients should be reassured that PR is typically a self-limited disease without long-term sequelae. Pregnant patients who develop pityriasis rosea in the first trimester may be at higher risk for spontaneous abortion,although data on the subject are sorely lacking.11 Oral antihistamines are useful in reducing pruritus associated with PR, and some patients experience relief by applying a low-potency topical corticosteroid.
In more severe cases, or in cases in which the patient is greatly distressed by the lesions, both broadband and narrowband UVB phototherapy effectively improve severity of lesions and reduces symptoms.12 These observations suggest that moderate sun exposure can help to reduce severity of PR lesions and hasten their resolution, but no studies assessing the effect of sun exposure on pityriasis rosea symptoms have been performed.
Furthermore, the possible role of the HHV-6 in PR has led some investigators to explore the utility of acyclovir in managing pityriasis rosea.13 One group recently found that 400 mg of acyclovir three times per day for 7 days decreased the number of lesions and pruritus associated with pityriasis rosea, compared those seen in controls, at 1-month follow-up.13
Timely recognition of the diagnosis, consideration of mimics, and ample reassurance are appropriate when approaching this disease.
Mr. Kusari is with the division of pediatric and adolescent dermatology at Rady Children’s Hospital, San Diego, and the departments of dermatology and pediatrics, University of California, San Diego. Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. They have no relevant financial disclosures. Email them at pdnews@frontlinemedcom.com.
References
1. Dermatology. 2015;231(1):9-14.
2. World J Clin Cases. 2017 Jun 16;5(6):203-11.
3. Pediatr Dermatol. 2011 May-Jun;28(3):341-2.
4. J Eur Acad Dermatol Venereol. 2006 Jul;20(6):667-71.
5. Dermatology. 1997;195(4):374-8.
6. J Invest Dermatol. 2005 Jun;124(6):1234-40.
7. Arch Dermatol. 1999 Sep;135(9):1070-2.
8. J Am Acad Dermatol. 1982 Jul;7(1):80-9.
9. Iran J Pediatr. 2010 Jun;20(2):237-41.
10. J Pediatr. 1988 Dec;113(6):1037-9.
11. J Am Acad Dermatol. 2008 May;58(5 Suppl 1):S78-83.
12. J Am Acad Dermatol. 1995 Dec;33(6):996-9.
13. Indian Dermatol Online J. 2015 May-Jun;6(3):181-4.
A 6-year-old female presents to the pediatric dermatology office with a 2-day history of a slightly itchy skin lesion on her back. Her birthday was a week prior, and her mother gave her a new kitten, and since then she has been playing with the kitten daily. She has tried some over-the-counter antifungal cream since the lesion first appeared, but there hasn’t been much improvement. The night prior to presenting to the office, the mother noticed more lesions developing on the child’s torso, and because of this, she became worried.
On physical exam, the patient is well appearing, and vital signs are normal. She has multiple scaly, pink, oval plaques and papules on her torso. There are no oral lesions, and her palms and soles are spared.
Study: Natpara slightly boosts health-related QoL in hypoparathyroidism
A new industry-funded analysis suggests that recombinant human parathyroid hormone, an extraordinarily expensive treatment for hypoparathyroidism, produces slight improvement in some health-related quality of life (HRQoL) domains.
While researchers didn’t find any statistically significant between-group differences vs. a placebo, the study lead author said the positive findings about within-group differences reflect her experiences with some patients. “They’re telling me they feel much better, and they don’t have emergency room visits,” endocrinologist Tamara J. Vokes, MD, of the University of Chicago, said in an interview.
And, she said, as reflected in the findings, she’s seen that those with the lowest HRQoL levels at baseline especially show signs of improvement.
The treatment, known as rhPTH(1-84) or Natpara, was approved by the Food and Drug Administration as a treatment for hypoparathyroidism in 2015. The FDA stated that the drug “is only for people who do not respond well to treatment with calcium and active forms of vitamin D alone, because it may increase the possible risk of bone cancer, known as osteosarcoma.”
Pharmacies list the drug as costing $9,500-$9,900 per month with a coupon or discount. According to the new study, research has shown that quality of life is often impaired in patients who have tried the traditional hypoparathyroidism treatments of calcium supplements and vitamin D. Dr. Vokes and her colleagues aimed to expand upon previous studies of HRQoL that did not reach conclusions or failed to include controls.
They examined findings of a previous multinational, randomized, placebo-controlled study of 122 adults with hypoparathyroidism. Average age was 48 years, and roughly 80% of the patients were women.
After their serum calcium levels were adjusted through medication, the patients were randomly assigned to placebo (n = 39) or rhPTH(1-84) (n = 83, starting dose of 50 mg/d that could be raised to 100 mg/d).
The study, which appears in the Journal of Clinical Endocrinology and Metabolism, analyzes the changes in HRQoL from baseline to 24 weeks per the 36-Item Short-Form Health Survey (SF-36).
The researchers found no significant between-group differences. However, those who took the drug did see statistically significant improvements in 4 of 10 domains: physical component summary score (P = .004), body pain (P = .05), general health (P = .05), and vitality (P less than .001). The changes were small, with the vitality score improving the most, from a mean SF-36 score of 49.5 to 53.
In some cases, she said, she’s seen QoL improve in patients whom she normally wouldn’t consider candidates for the medication. “I would have not have recommended PTH for them, but they insisted on taking it, and they report feeling better.”
This may be a placebo effect, she said. Even so, “if someone doesn’t feel well, it’s worth it at least to try to use PTH and see whether they improve.”
She added that lack of well-being is a preexisting condition for some hypoparathyroidism patients. “I’ve seen quite a number of them who have what we call premorbid personality disorder. They didn’t feel well and weren’t happy, and when you get hypoparathyroidism, you’re more unwell and unhappy.”
With medication, however, “you’re a bit less unhappy but you’re still miserable,” she said.
Carol Greenlee, MD, an endocrinologist in Grand Junction, Colo., said in an interview that she saw a patient in a clinical study who had experienced a marked improvement in QoL. However, she said, “it will be the cost of the PTH that is the burden.”
For her part, Dr. Vokes cautioned that it’s important to take special care with patients taking Natpara. “You can’t just give this injection and say, ‘Goodbye, you will be better.’ It requires following certain protocol, frequent monitoring of the blood levels. Be sure the patient has access to the lab, and insurance that covers the test.”
Dr. Greenlee reported no relevant disclosures. The study was funded by Shire Human Genetic Therapies, and the initial clinical trial was funded by NPS Pharmaceuticals, a wholly owned indirect subsidiary. Dr. Vokes reported consulting for Shire and serving as an investigator for the initial clinical trial. Other study authors reported serving as clinical investigators and/or consulting for Shire, and three authors are employees of Shire.
SOURCE: Vokes, TJ et al. J Clin Endocrinol Metab. 2018 Feb 1;103(2):722-31
A new industry-funded analysis suggests that recombinant human parathyroid hormone, an extraordinarily expensive treatment for hypoparathyroidism, produces slight improvement in some health-related quality of life (HRQoL) domains.
While researchers didn’t find any statistically significant between-group differences vs. a placebo, the study lead author said the positive findings about within-group differences reflect her experiences with some patients. “They’re telling me they feel much better, and they don’t have emergency room visits,” endocrinologist Tamara J. Vokes, MD, of the University of Chicago, said in an interview.
And, she said, as reflected in the findings, she’s seen that those with the lowest HRQoL levels at baseline especially show signs of improvement.
The treatment, known as rhPTH(1-84) or Natpara, was approved by the Food and Drug Administration as a treatment for hypoparathyroidism in 2015. The FDA stated that the drug “is only for people who do not respond well to treatment with calcium and active forms of vitamin D alone, because it may increase the possible risk of bone cancer, known as osteosarcoma.”
Pharmacies list the drug as costing $9,500-$9,900 per month with a coupon or discount. According to the new study, research has shown that quality of life is often impaired in patients who have tried the traditional hypoparathyroidism treatments of calcium supplements and vitamin D. Dr. Vokes and her colleagues aimed to expand upon previous studies of HRQoL that did not reach conclusions or failed to include controls.
They examined findings of a previous multinational, randomized, placebo-controlled study of 122 adults with hypoparathyroidism. Average age was 48 years, and roughly 80% of the patients were women.
After their serum calcium levels were adjusted through medication, the patients were randomly assigned to placebo (n = 39) or rhPTH(1-84) (n = 83, starting dose of 50 mg/d that could be raised to 100 mg/d).
The study, which appears in the Journal of Clinical Endocrinology and Metabolism, analyzes the changes in HRQoL from baseline to 24 weeks per the 36-Item Short-Form Health Survey (SF-36).
The researchers found no significant between-group differences. However, those who took the drug did see statistically significant improvements in 4 of 10 domains: physical component summary score (P = .004), body pain (P = .05), general health (P = .05), and vitality (P less than .001). The changes were small, with the vitality score improving the most, from a mean SF-36 score of 49.5 to 53.
In some cases, she said, she’s seen QoL improve in patients whom she normally wouldn’t consider candidates for the medication. “I would have not have recommended PTH for them, but they insisted on taking it, and they report feeling better.”
This may be a placebo effect, she said. Even so, “if someone doesn’t feel well, it’s worth it at least to try to use PTH and see whether they improve.”
She added that lack of well-being is a preexisting condition for some hypoparathyroidism patients. “I’ve seen quite a number of them who have what we call premorbid personality disorder. They didn’t feel well and weren’t happy, and when you get hypoparathyroidism, you’re more unwell and unhappy.”
With medication, however, “you’re a bit less unhappy but you’re still miserable,” she said.
Carol Greenlee, MD, an endocrinologist in Grand Junction, Colo., said in an interview that she saw a patient in a clinical study who had experienced a marked improvement in QoL. However, she said, “it will be the cost of the PTH that is the burden.”
For her part, Dr. Vokes cautioned that it’s important to take special care with patients taking Natpara. “You can’t just give this injection and say, ‘Goodbye, you will be better.’ It requires following certain protocol, frequent monitoring of the blood levels. Be sure the patient has access to the lab, and insurance that covers the test.”
Dr. Greenlee reported no relevant disclosures. The study was funded by Shire Human Genetic Therapies, and the initial clinical trial was funded by NPS Pharmaceuticals, a wholly owned indirect subsidiary. Dr. Vokes reported consulting for Shire and serving as an investigator for the initial clinical trial. Other study authors reported serving as clinical investigators and/or consulting for Shire, and three authors are employees of Shire.
SOURCE: Vokes, TJ et al. J Clin Endocrinol Metab. 2018 Feb 1;103(2):722-31
A new industry-funded analysis suggests that recombinant human parathyroid hormone, an extraordinarily expensive treatment for hypoparathyroidism, produces slight improvement in some health-related quality of life (HRQoL) domains.
While researchers didn’t find any statistically significant between-group differences vs. a placebo, the study lead author said the positive findings about within-group differences reflect her experiences with some patients. “They’re telling me they feel much better, and they don’t have emergency room visits,” endocrinologist Tamara J. Vokes, MD, of the University of Chicago, said in an interview.
And, she said, as reflected in the findings, she’s seen that those with the lowest HRQoL levels at baseline especially show signs of improvement.
The treatment, known as rhPTH(1-84) or Natpara, was approved by the Food and Drug Administration as a treatment for hypoparathyroidism in 2015. The FDA stated that the drug “is only for people who do not respond well to treatment with calcium and active forms of vitamin D alone, because it may increase the possible risk of bone cancer, known as osteosarcoma.”
Pharmacies list the drug as costing $9,500-$9,900 per month with a coupon or discount. According to the new study, research has shown that quality of life is often impaired in patients who have tried the traditional hypoparathyroidism treatments of calcium supplements and vitamin D. Dr. Vokes and her colleagues aimed to expand upon previous studies of HRQoL that did not reach conclusions or failed to include controls.
They examined findings of a previous multinational, randomized, placebo-controlled study of 122 adults with hypoparathyroidism. Average age was 48 years, and roughly 80% of the patients were women.
After their serum calcium levels were adjusted through medication, the patients were randomly assigned to placebo (n = 39) or rhPTH(1-84) (n = 83, starting dose of 50 mg/d that could be raised to 100 mg/d).
The study, which appears in the Journal of Clinical Endocrinology and Metabolism, analyzes the changes in HRQoL from baseline to 24 weeks per the 36-Item Short-Form Health Survey (SF-36).
The researchers found no significant between-group differences. However, those who took the drug did see statistically significant improvements in 4 of 10 domains: physical component summary score (P = .004), body pain (P = .05), general health (P = .05), and vitality (P less than .001). The changes were small, with the vitality score improving the most, from a mean SF-36 score of 49.5 to 53.
In some cases, she said, she’s seen QoL improve in patients whom she normally wouldn’t consider candidates for the medication. “I would have not have recommended PTH for them, but they insisted on taking it, and they report feeling better.”
This may be a placebo effect, she said. Even so, “if someone doesn’t feel well, it’s worth it at least to try to use PTH and see whether they improve.”
She added that lack of well-being is a preexisting condition for some hypoparathyroidism patients. “I’ve seen quite a number of them who have what we call premorbid personality disorder. They didn’t feel well and weren’t happy, and when you get hypoparathyroidism, you’re more unwell and unhappy.”
With medication, however, “you’re a bit less unhappy but you’re still miserable,” she said.
Carol Greenlee, MD, an endocrinologist in Grand Junction, Colo., said in an interview that she saw a patient in a clinical study who had experienced a marked improvement in QoL. However, she said, “it will be the cost of the PTH that is the burden.”
For her part, Dr. Vokes cautioned that it’s important to take special care with patients taking Natpara. “You can’t just give this injection and say, ‘Goodbye, you will be better.’ It requires following certain protocol, frequent monitoring of the blood levels. Be sure the patient has access to the lab, and insurance that covers the test.”
Dr. Greenlee reported no relevant disclosures. The study was funded by Shire Human Genetic Therapies, and the initial clinical trial was funded by NPS Pharmaceuticals, a wholly owned indirect subsidiary. Dr. Vokes reported consulting for Shire and serving as an investigator for the initial clinical trial. Other study authors reported serving as clinical investigators and/or consulting for Shire, and three authors are employees of Shire.
SOURCE: Vokes, TJ et al. J Clin Endocrinol Metab. 2018 Feb 1;103(2):722-31
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
Key clinical point: Health-related quality of life (HRQoL) may improve slightly in patients on recombinant human parathyroid hormone for hypoparathyroidism.
Major finding: In 4 of 10 SF-36 domains, HRQoL improved in within-group analysis. There was no statistically significant improvement vs. placebo.
Study details: A 24-week analysis of previous drug vs. placebo clinical trial of 122 adults with hypoparathyroidism.
Disclosures: Shire Human Genetic Therapies funded the study, and the initial clinical trial was funded by NPS Pharmaceuticals, a wholly owned indirect subsidiary. The researchers reported various relationships to Shire, including employment.
Source: Vokes TJ et al. J Clin Endocrinol Metab. 2018 Feb 1;103(2):722-31.
Evaluations of Medicaid experiments by states, CMS are weak, GAO says
With federal spending on Medicaid experiments soaring in recent years, a congressional watchdog said state and federal governments fail to adequately evaluate if the efforts improve care and save money.
A study by the Government Accountability Office released Feb. 20 found that some states don’t complete evaluation reports for up to 7 years after an experiment begins and often fail to answer vital questions to determine effectiveness. The GAO also slammed the federal Centers for Medicare & Medicaid Services for failing to make results from Medicaid evaluation reports public in a timely manner.
“CMS is missing an opportunity to inform federal and state policy discussions,” the GAO report said.
Joan Alker, executive director of the Georgetown University Center for Children and Families, called the report’s findings “troubling but not surprising.”
“It has been clear for some time that evaluations of Section 1115 waivers are not adequate,” she said. “There is some good work going on in this space at the state level, for example in Michigan and Iowa, but as the report makes clear state’s evaluations are often incomplete and not rigorous enough.”
These experiments are often called “demonstration projects” or “1115 demonstration waivers” – based on the section of the law that allows the federal government to authorize them. They allow federal officials to approve states’ requests to test new approaches to providing coverage. They are used for a wide variety of purposes, including efforts to extend Medicaid to people or services not generally covered or to change payment systems to improve care.
Medicaid demonstration programs often run for a decade or more. Several states that expanded Medicaid eligibility under the Affordable Care Act did so through a demonstration program, including Indiana, Iowa, Arkansas and New Hampshire.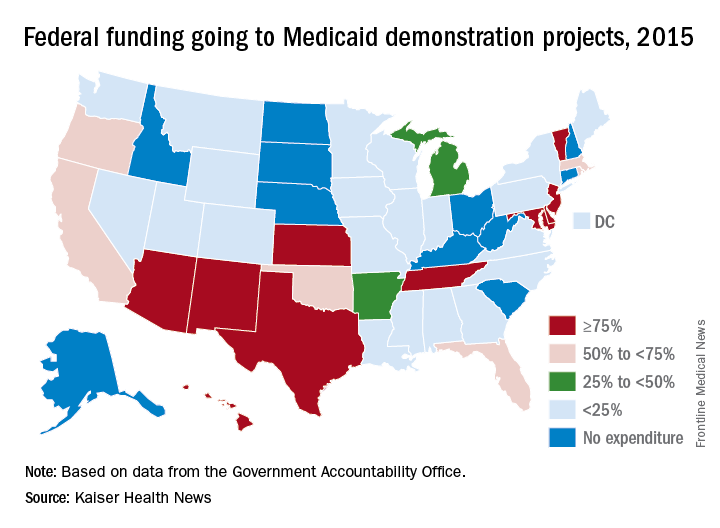
The study, requested by top GOP lawmakers including Sen. Orrin Hatch (R-Utah), reviewed demonstration programs in eight states – Arizona, Arkansas, California, Indiana, Kansas, Maryland, Massachusetts, and New York.
In five of these states, money from their Medicaid demonstration program makes up more than half their total federal Medicaid budgets. Nearly all of Arizona’s funding – 99.7% – is through a demonstration program.
The use of Medicaid demonstration programs accelerated during the 1990s. But, in recent years, the experiments often have reflected the political leanings of state officials or the party controlling the White House. Under a demonstration program, the Trump administration this year approved requests from Indiana and Kentucky to enact work requirements for some adult Medicaid enrollees.
The GAO report noted that states often do not complete their evaluation reports until after the federal government renews their demonstration program. For example, Indiana’s Medicaid expansion demonstration program, which charges premiums and locks some enrollees out of coverage for lack of payment, was renewed in February even though a final evaluation report is not yet complete.
GAO said Indiana’s evaluation of its Medicaid expansion won’t look at the effect of the state’s provision that locks out enrollees for six months if they fail to pay premiums.
“GAO found that selected states’ evaluations of these demonstrations often had significant limitations that affected their usefulness in informing policy decisions,” the report said.
Ms. Alker said that “more sunshine and data are needed” to assess waivers, “especially as they are clearly the vehicle the Trump administration is now using to pursue its ideological objectives for Medicaid.”
While states typically contract with independent groups to evaluate Medicaid demonstration programs, the federal government sometimes does its own review.
But the GAO investigators found Indiana’s Medicaid agency wasn’t willing to work with the federal contractor out of privacy concerns, which halted efforts for a federal review.
Joel Cantor, director of the Center for State Health Policy at Rutgers University in New Brunswick, N.J., said the demonstration programs often have shifted from their intended purpose because they are designed by lawmakers pushing an agenda rather than as a scientific experiment to find better ways to deliver care.
“Demonstration programs have been used since the 1990s to advance policy agenda for whoever holds power in Washington and not designed to test an innovative idea,” he said.
The evaluations often take several years to complete, he said, because of the difficulty of getting patient data from states. His center has done evaluations for New Jersey’s Medicaid program.
GAO recommended that CMS require states to submit a final evaluation report after the end of the waiver period, regardless of whether the experiment is being renewed, and that the federal agency publicly release findings from federal evaluations in a timely manner. Federal officials said they agreed with the recommendations.
Matt Salo, executive director of the National Association of Medicaid Directors, said the report highlighted a need to modernize the law dealing with Medicaid so that successful experiments are quickly incorporated into the overall program.
“The underlying problem is that the Medicaid statute has fundamentally failed to keep up with the changing reality of health care in the 21st century,” he said. “There’s no way to update the rules to make these changes” a permanent part of the program.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
With federal spending on Medicaid experiments soaring in recent years, a congressional watchdog said state and federal governments fail to adequately evaluate if the efforts improve care and save money.
A study by the Government Accountability Office released Feb. 20 found that some states don’t complete evaluation reports for up to 7 years after an experiment begins and often fail to answer vital questions to determine effectiveness. The GAO also slammed the federal Centers for Medicare & Medicaid Services for failing to make results from Medicaid evaluation reports public in a timely manner.
“CMS is missing an opportunity to inform federal and state policy discussions,” the GAO report said.
Joan Alker, executive director of the Georgetown University Center for Children and Families, called the report’s findings “troubling but not surprising.”
“It has been clear for some time that evaluations of Section 1115 waivers are not adequate,” she said. “There is some good work going on in this space at the state level, for example in Michigan and Iowa, but as the report makes clear state’s evaluations are often incomplete and not rigorous enough.”
These experiments are often called “demonstration projects” or “1115 demonstration waivers” – based on the section of the law that allows the federal government to authorize them. They allow federal officials to approve states’ requests to test new approaches to providing coverage. They are used for a wide variety of purposes, including efforts to extend Medicaid to people or services not generally covered or to change payment systems to improve care.
Medicaid demonstration programs often run for a decade or more. Several states that expanded Medicaid eligibility under the Affordable Care Act did so through a demonstration program, including Indiana, Iowa, Arkansas and New Hampshire.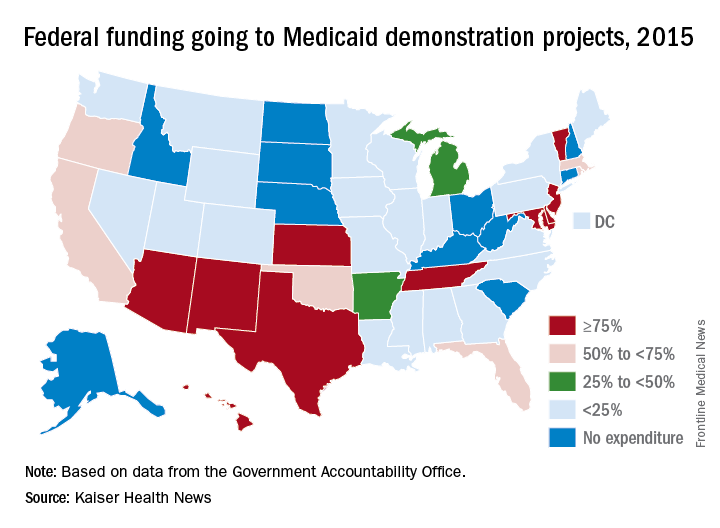
The study, requested by top GOP lawmakers including Sen. Orrin Hatch (R-Utah), reviewed demonstration programs in eight states – Arizona, Arkansas, California, Indiana, Kansas, Maryland, Massachusetts, and New York.
In five of these states, money from their Medicaid demonstration program makes up more than half their total federal Medicaid budgets. Nearly all of Arizona’s funding – 99.7% – is through a demonstration program.
The use of Medicaid demonstration programs accelerated during the 1990s. But, in recent years, the experiments often have reflected the political leanings of state officials or the party controlling the White House. Under a demonstration program, the Trump administration this year approved requests from Indiana and Kentucky to enact work requirements for some adult Medicaid enrollees.
The GAO report noted that states often do not complete their evaluation reports until after the federal government renews their demonstration program. For example, Indiana’s Medicaid expansion demonstration program, which charges premiums and locks some enrollees out of coverage for lack of payment, was renewed in February even though a final evaluation report is not yet complete.
GAO said Indiana’s evaluation of its Medicaid expansion won’t look at the effect of the state’s provision that locks out enrollees for six months if they fail to pay premiums.
“GAO found that selected states’ evaluations of these demonstrations often had significant limitations that affected their usefulness in informing policy decisions,” the report said.
Ms. Alker said that “more sunshine and data are needed” to assess waivers, “especially as they are clearly the vehicle the Trump administration is now using to pursue its ideological objectives for Medicaid.”
While states typically contract with independent groups to evaluate Medicaid demonstration programs, the federal government sometimes does its own review.
But the GAO investigators found Indiana’s Medicaid agency wasn’t willing to work with the federal contractor out of privacy concerns, which halted efforts for a federal review.
Joel Cantor, director of the Center for State Health Policy at Rutgers University in New Brunswick, N.J., said the demonstration programs often have shifted from their intended purpose because they are designed by lawmakers pushing an agenda rather than as a scientific experiment to find better ways to deliver care.
“Demonstration programs have been used since the 1990s to advance policy agenda for whoever holds power in Washington and not designed to test an innovative idea,” he said.
The evaluations often take several years to complete, he said, because of the difficulty of getting patient data from states. His center has done evaluations for New Jersey’s Medicaid program.
GAO recommended that CMS require states to submit a final evaluation report after the end of the waiver period, regardless of whether the experiment is being renewed, and that the federal agency publicly release findings from federal evaluations in a timely manner. Federal officials said they agreed with the recommendations.
Matt Salo, executive director of the National Association of Medicaid Directors, said the report highlighted a need to modernize the law dealing with Medicaid so that successful experiments are quickly incorporated into the overall program.
“The underlying problem is that the Medicaid statute has fundamentally failed to keep up with the changing reality of health care in the 21st century,” he said. “There’s no way to update the rules to make these changes” a permanent part of the program.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
With federal spending on Medicaid experiments soaring in recent years, a congressional watchdog said state and federal governments fail to adequately evaluate if the efforts improve care and save money.
A study by the Government Accountability Office released Feb. 20 found that some states don’t complete evaluation reports for up to 7 years after an experiment begins and often fail to answer vital questions to determine effectiveness. The GAO also slammed the federal Centers for Medicare & Medicaid Services for failing to make results from Medicaid evaluation reports public in a timely manner.
“CMS is missing an opportunity to inform federal and state policy discussions,” the GAO report said.
Joan Alker, executive director of the Georgetown University Center for Children and Families, called the report’s findings “troubling but not surprising.”
“It has been clear for some time that evaluations of Section 1115 waivers are not adequate,” she said. “There is some good work going on in this space at the state level, for example in Michigan and Iowa, but as the report makes clear state’s evaluations are often incomplete and not rigorous enough.”
These experiments are often called “demonstration projects” or “1115 demonstration waivers” – based on the section of the law that allows the federal government to authorize them. They allow federal officials to approve states’ requests to test new approaches to providing coverage. They are used for a wide variety of purposes, including efforts to extend Medicaid to people or services not generally covered or to change payment systems to improve care.
Medicaid demonstration programs often run for a decade or more. Several states that expanded Medicaid eligibility under the Affordable Care Act did so through a demonstration program, including Indiana, Iowa, Arkansas and New Hampshire.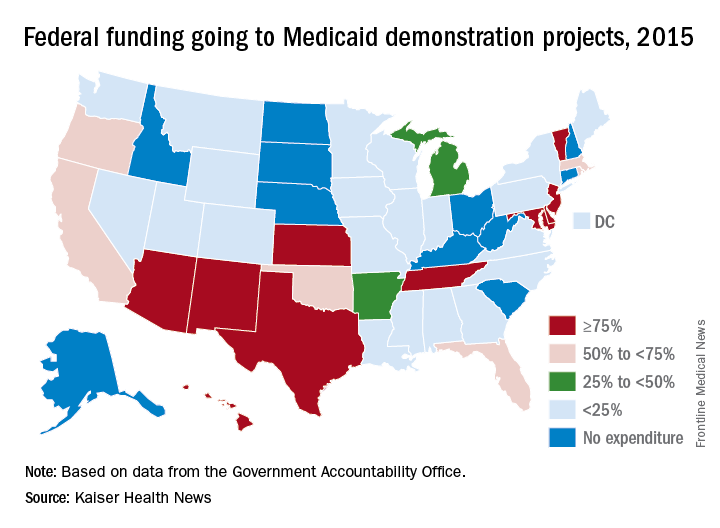
The study, requested by top GOP lawmakers including Sen. Orrin Hatch (R-Utah), reviewed demonstration programs in eight states – Arizona, Arkansas, California, Indiana, Kansas, Maryland, Massachusetts, and New York.
In five of these states, money from their Medicaid demonstration program makes up more than half their total federal Medicaid budgets. Nearly all of Arizona’s funding – 99.7% – is through a demonstration program.
The use of Medicaid demonstration programs accelerated during the 1990s. But, in recent years, the experiments often have reflected the political leanings of state officials or the party controlling the White House. Under a demonstration program, the Trump administration this year approved requests from Indiana and Kentucky to enact work requirements for some adult Medicaid enrollees.
The GAO report noted that states often do not complete their evaluation reports until after the federal government renews their demonstration program. For example, Indiana’s Medicaid expansion demonstration program, which charges premiums and locks some enrollees out of coverage for lack of payment, was renewed in February even though a final evaluation report is not yet complete.
GAO said Indiana’s evaluation of its Medicaid expansion won’t look at the effect of the state’s provision that locks out enrollees for six months if they fail to pay premiums.
“GAO found that selected states’ evaluations of these demonstrations often had significant limitations that affected their usefulness in informing policy decisions,” the report said.
Ms. Alker said that “more sunshine and data are needed” to assess waivers, “especially as they are clearly the vehicle the Trump administration is now using to pursue its ideological objectives for Medicaid.”
While states typically contract with independent groups to evaluate Medicaid demonstration programs, the federal government sometimes does its own review.
But the GAO investigators found Indiana’s Medicaid agency wasn’t willing to work with the federal contractor out of privacy concerns, which halted efforts for a federal review.
Joel Cantor, director of the Center for State Health Policy at Rutgers University in New Brunswick, N.J., said the demonstration programs often have shifted from their intended purpose because they are designed by lawmakers pushing an agenda rather than as a scientific experiment to find better ways to deliver care.
“Demonstration programs have been used since the 1990s to advance policy agenda for whoever holds power in Washington and not designed to test an innovative idea,” he said.
The evaluations often take several years to complete, he said, because of the difficulty of getting patient data from states. His center has done evaluations for New Jersey’s Medicaid program.
GAO recommended that CMS require states to submit a final evaluation report after the end of the waiver period, regardless of whether the experiment is being renewed, and that the federal agency publicly release findings from federal evaluations in a timely manner. Federal officials said they agreed with the recommendations.
Matt Salo, executive director of the National Association of Medicaid Directors, said the report highlighted a need to modernize the law dealing with Medicaid so that successful experiments are quickly incorporated into the overall program.
“The underlying problem is that the Medicaid statute has fundamentally failed to keep up with the changing reality of health care in the 21st century,” he said. “There’s no way to update the rules to make these changes” a permanent part of the program.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
FDA warns against clarithromycin use in patients with heart disease
The Food and Drug Administration has added a new warning for an increased risk of death in patients with heart disease who have used clarithromycin (Biaxin), on the basis of results of a 10-year follow-up from the CLARICOR trial.
The CLARICOR trial followed 4,372 randomized patients for at least 2 years after undergoing 14 days of treatment with daily doses of 500 mg clarithromycin. Among these patients, researchers observed an unexpected increase in deaths in patients with coronary heart disease. (The Feb. 22 FDA statement announcing the alert did not provide data from CLARICOR.) As of yet, there is no clear explanation of how clarithromycin would lead to more deaths, compared with a placebo, the agency said.
Regardless, two of the six observational studies published found a link between clarithromycin use and long-term risks; four did not. The CLARICOR trial provides the strongest evidence of increased health risks, the statement said.
The FDA is recommending that health care professionals be aware of the risks associated with clarithromycin use and consider the benefits and risks of use in patients with heart disease. If at all possible, the use of other antibiotics may be a better option. Doctors should advise patients to be aware of signs and symptoms associated with cardiovascular issues.
Patients are also an important piece of the puzzle and should communicate with their health care providers about heart disease, particularly when taking antibiotics to treat for an infection.
The FDA has added the results of the CLARICOR trial to the clarithromycin drug labels. The agency will continue to monitor the safety reports in patients using clarithromycin.
Serious adverse events associated with clarithromycin should be reported to the FDA’s MedWatch program at 800-332-1088 or www.fda.gov/medwatch/.
The Food and Drug Administration has added a new warning for an increased risk of death in patients with heart disease who have used clarithromycin (Biaxin), on the basis of results of a 10-year follow-up from the CLARICOR trial.
The CLARICOR trial followed 4,372 randomized patients for at least 2 years after undergoing 14 days of treatment with daily doses of 500 mg clarithromycin. Among these patients, researchers observed an unexpected increase in deaths in patients with coronary heart disease. (The Feb. 22 FDA statement announcing the alert did not provide data from CLARICOR.) As of yet, there is no clear explanation of how clarithromycin would lead to more deaths, compared with a placebo, the agency said.
Regardless, two of the six observational studies published found a link between clarithromycin use and long-term risks; four did not. The CLARICOR trial provides the strongest evidence of increased health risks, the statement said.
The FDA is recommending that health care professionals be aware of the risks associated with clarithromycin use and consider the benefits and risks of use in patients with heart disease. If at all possible, the use of other antibiotics may be a better option. Doctors should advise patients to be aware of signs and symptoms associated with cardiovascular issues.
Patients are also an important piece of the puzzle and should communicate with their health care providers about heart disease, particularly when taking antibiotics to treat for an infection.
The FDA has added the results of the CLARICOR trial to the clarithromycin drug labels. The agency will continue to monitor the safety reports in patients using clarithromycin.
Serious adverse events associated with clarithromycin should be reported to the FDA’s MedWatch program at 800-332-1088 or www.fda.gov/medwatch/.
The Food and Drug Administration has added a new warning for an increased risk of death in patients with heart disease who have used clarithromycin (Biaxin), on the basis of results of a 10-year follow-up from the CLARICOR trial.
The CLARICOR trial followed 4,372 randomized patients for at least 2 years after undergoing 14 days of treatment with daily doses of 500 mg clarithromycin. Among these patients, researchers observed an unexpected increase in deaths in patients with coronary heart disease. (The Feb. 22 FDA statement announcing the alert did not provide data from CLARICOR.) As of yet, there is no clear explanation of how clarithromycin would lead to more deaths, compared with a placebo, the agency said.
Regardless, two of the six observational studies published found a link between clarithromycin use and long-term risks; four did not. The CLARICOR trial provides the strongest evidence of increased health risks, the statement said.
The FDA is recommending that health care professionals be aware of the risks associated with clarithromycin use and consider the benefits and risks of use in patients with heart disease. If at all possible, the use of other antibiotics may be a better option. Doctors should advise patients to be aware of signs and symptoms associated with cardiovascular issues.
Patients are also an important piece of the puzzle and should communicate with their health care providers about heart disease, particularly when taking antibiotics to treat for an infection.
The FDA has added the results of the CLARICOR trial to the clarithromycin drug labels. The agency will continue to monitor the safety reports in patients using clarithromycin.
Serious adverse events associated with clarithromycin should be reported to the FDA’s MedWatch program at 800-332-1088 or www.fda.gov/medwatch/.
25 Years of Movement Disorders
Peter A. LeWitt, MD
Dr. LeWitt is the Director of the Parkinson Disease and Movement Disorder Program at Henry Ford Hospital, West Bloomfield, Michigan.
For most neurology subspecialties, the past quarter-century was only the latest chapter of a productive history extending through the mid-19th century, but for movement disorders, these years were formative. Before then, movement disorder specialists were few in number, and their medical literature was far more scanty than it is now, with multiple journals and texts now devoted to this topic. Twenty-five years ago, the international society devoted to Parkinson disease and other movement disorders was only a recent arrival. Fortunately, two charismatic and brilliant leaders—the American neurologist Stanley Fahn, MD, and the British neurologist C. David Marsden, MBBS—came forward to inspire a generation of trainees with their broad interests in bridging clinical neurology, experimental neuroscience, and patient advocacy. Today, the impact of these pioneers is still felt by a growing community of movement disorder clinicians and researchers who have transformed movement disorders from an earlier realm of descriptive neurology into a vibrant field exploring disease mechanisms and therapeutics, as well as an expanding array of clinical insights.
When Neurology Reviews was founded in 1993, the majority of significant developments in movement disorders concerned Parkinson’s disease. Strategies to improve upon dopaminergic therapy were being tested in clinical trials, along with ventures into pallidotomy as a neurosurgical treatment. Animal models of parkinsonism and neurochemical analysis of brain and putative biomarkers provided scientific guidance for trials of disease modification. Another milestone from the 1990s was discovery of the first gene leading to autosomal-dominant parkinsonism. This rare mutation in the structural protein alpha-synuclein had a much broader impact on Parkinson’s disease research in that it provided important information about the sporadic disorder’s final common pathway of pathogenesis. Today, alpha-synuclein is the focus of therapeutic intervention utilizing immunologic therapies to halt disease progression. Over the past quarter-century, more than two dozen additional gene mutations associated with parkinsonism have been discovered. These mutations provide additional insight into disease mechanisms. Beyond the science and clinical insights that have propelled advances in understanding Parkinson’s disease and its related disorders, the growth of the patient advocacy and caregiver movement has also been remarkable in expanding what is needed to improve daily life with this disorder.
Since 1993, other movement disorders have also profited from the tremendous growth of molecular neuroscience and its applications. Novel neuroimaging techniques like functional MRI, computation of neural pathways, and scanning using PET and SPECT have helped work out the brain mechanisms of several disorders. Genetic probing of familial disorders like dystonia and myoclonus have helped to unravel the neurochemistry of what has gone wrong to cause certain movement disorders. In turn, transgenic animal models using these human genetic mutations have allowed exploration of what might be done to fix the problems. These developments could have huge implications for making progress in the therapies of the future, since the most common categories of movement disorders—dystonia, myoclonus, ataxia, tremor, restless legs syndrome, Tourette syndrome, choreic disorders, and paroxysmal movement disorders—all can have hereditary patterns. Genetic testing can be valuable for choosing at-risk individuals for participation in trials of disease-modifying drugs for Huntington’s disease, for example, and this strategy may be the way of the future for other late-life emergent disorders. In the past decade, several gene therapy studies have been carried out in patients with Parkinson’s disease. The promise of this approach and the recent gene editing and RNA interference approaches, all part of the molecular biology revolution of the past 25 years, may further change the landscape of movement disorder therapeutics ahead.
Today, movement disorder specialists routinely use therapeutic approaches that were in their infancy in 1993. Botulinum toxin selective denervation has had a major impact by improving quality of life for patients affected with a wide range of movement disorders: dystonic necks, hands, and feet; involuntary facial movements and voice aberrations; tics; spasticity; and drooling. Deep brain stimulation is a routine option for many patients with tremor, Parkinson’s disease, and dystonia. Developments in this field have refined the choice of targets for stimulation and the possibility of treating other disorders with these techniques, like Tourette syndrome. A nonsurgical approach to abolishing tremor, MRI-guided focused ultrasound, recently was approved. In the background of these advances is the increasing knowledge of movement disorders that practitioners have to offer many patients with disorders that in the past were merely neurologic curiosities. Through clinical trial research and serendipity (the major treatment options for essential tremor arose this way), there is an expanding search for repurposing older medications and harnessing new biotechnology to target the mechanisms leading to various movement disorders.
It is impressive how much the neurologic discipline of movement disorders has changed in response to the new era of electronic communications and other technologies. In the past quarter-century, medical students, residents, and practicing neurologists have had instant access to a curriculum that includes resources such as video-recorded movement disorders. Clinical trials are being revolutionized by electronic technologies that record information in ways that improve upon human ratings. A patient with Parkinson’s disease, essential tremor, or restless legs syndrome can now have symptoms monitored remotely by wearable devices that offer a real-world view on how a new therapy is performing. But perhaps the greatest revolution in the recent past has been increasing confidence that progressive disabilities caused by movement disorders might be halted by emerging insights into disease mechanisms. There has been tremendous growth of interest among the basic neuroscience community in human diseases affecting motor control. More than half of research presentations at recent international Parkinson’s disease and movement disorder conferences reflect this trend. These efforts support an optimistic view that, over the nex
Peter A. LeWitt, MD
Dr. LeWitt is the Director of the Parkinson Disease and Movement Disorder Program at Henry Ford Hospital, West Bloomfield, Michigan.
For most neurology subspecialties, the past quarter-century was only the latest chapter of a productive history extending through the mid-19th century, but for movement disorders, these years were formative. Before then, movement disorder specialists were few in number, and their medical literature was far more scanty than it is now, with multiple journals and texts now devoted to this topic. Twenty-five years ago, the international society devoted to Parkinson disease and other movement disorders was only a recent arrival. Fortunately, two charismatic and brilliant leaders—the American neurologist Stanley Fahn, MD, and the British neurologist C. David Marsden, MBBS—came forward to inspire a generation of trainees with their broad interests in bridging clinical neurology, experimental neuroscience, and patient advocacy. Today, the impact of these pioneers is still felt by a growing community of movement disorder clinicians and researchers who have transformed movement disorders from an earlier realm of descriptive neurology into a vibrant field exploring disease mechanisms and therapeutics, as well as an expanding array of clinical insights.
When Neurology Reviews was founded in 1993, the majority of significant developments in movement disorders concerned Parkinson’s disease. Strategies to improve upon dopaminergic therapy were being tested in clinical trials, along with ventures into pallidotomy as a neurosurgical treatment. Animal models of parkinsonism and neurochemical analysis of brain and putative biomarkers provided scientific guidance for trials of disease modification. Another milestone from the 1990s was discovery of the first gene leading to autosomal-dominant parkinsonism. This rare mutation in the structural protein alpha-synuclein had a much broader impact on Parkinson’s disease research in that it provided important information about the sporadic disorder’s final common pathway of pathogenesis. Today, alpha-synuclein is the focus of therapeutic intervention utilizing immunologic therapies to halt disease progression. Over the past quarter-century, more than two dozen additional gene mutations associated with parkinsonism have been discovered. These mutations provide additional insight into disease mechanisms. Beyond the science and clinical insights that have propelled advances in understanding Parkinson’s disease and its related disorders, the growth of the patient advocacy and caregiver movement has also been remarkable in expanding what is needed to improve daily life with this disorder.
Since 1993, other movement disorders have also profited from the tremendous growth of molecular neuroscience and its applications. Novel neuroimaging techniques like functional MRI, computation of neural pathways, and scanning using PET and SPECT have helped work out the brain mechanisms of several disorders. Genetic probing of familial disorders like dystonia and myoclonus have helped to unravel the neurochemistry of what has gone wrong to cause certain movement disorders. In turn, transgenic animal models using these human genetic mutations have allowed exploration of what might be done to fix the problems. These developments could have huge implications for making progress in the therapies of the future, since the most common categories of movement disorders—dystonia, myoclonus, ataxia, tremor, restless legs syndrome, Tourette syndrome, choreic disorders, and paroxysmal movement disorders—all can have hereditary patterns. Genetic testing can be valuable for choosing at-risk individuals for participation in trials of disease-modifying drugs for Huntington’s disease, for example, and this strategy may be the way of the future for other late-life emergent disorders. In the past decade, several gene therapy studies have been carried out in patients with Parkinson’s disease. The promise of this approach and the recent gene editing and RNA interference approaches, all part of the molecular biology revolution of the past 25 years, may further change the landscape of movement disorder therapeutics ahead.
Today, movement disorder specialists routinely use therapeutic approaches that were in their infancy in 1993. Botulinum toxin selective denervation has had a major impact by improving quality of life for patients affected with a wide range of movement disorders: dystonic necks, hands, and feet; involuntary facial movements and voice aberrations; tics; spasticity; and drooling. Deep brain stimulation is a routine option for many patients with tremor, Parkinson’s disease, and dystonia. Developments in this field have refined the choice of targets for stimulation and the possibility of treating other disorders with these techniques, like Tourette syndrome. A nonsurgical approach to abolishing tremor, MRI-guided focused ultrasound, recently was approved. In the background of these advances is the increasing knowledge of movement disorders that practitioners have to offer many patients with disorders that in the past were merely neurologic curiosities. Through clinical trial research and serendipity (the major treatment options for essential tremor arose this way), there is an expanding search for repurposing older medications and harnessing new biotechnology to target the mechanisms leading to various movement disorders.
It is impressive how much the neurologic discipline of movement disorders has changed in response to the new era of electronic communications and other technologies. In the past quarter-century, medical students, residents, and practicing neurologists have had instant access to a curriculum that includes resources such as video-recorded movement disorders. Clinical trials are being revolutionized by electronic technologies that record information in ways that improve upon human ratings. A patient with Parkinson’s disease, essential tremor, or restless legs syndrome can now have symptoms monitored remotely by wearable devices that offer a real-world view on how a new therapy is performing. But perhaps the greatest revolution in the recent past has been increasing confidence that progressive disabilities caused by movement disorders might be halted by emerging insights into disease mechanisms. There has been tremendous growth of interest among the basic neuroscience community in human diseases affecting motor control. More than half of research presentations at recent international Parkinson’s disease and movement disorder conferences reflect this trend. These efforts support an optimistic view that, over the nex
Peter A. LeWitt, MD
Dr. LeWitt is the Director of the Parkinson Disease and Movement Disorder Program at Henry Ford Hospital, West Bloomfield, Michigan.
For most neurology subspecialties, the past quarter-century was only the latest chapter of a productive history extending through the mid-19th century, but for movement disorders, these years were formative. Before then, movement disorder specialists were few in number, and their medical literature was far more scanty than it is now, with multiple journals and texts now devoted to this topic. Twenty-five years ago, the international society devoted to Parkinson disease and other movement disorders was only a recent arrival. Fortunately, two charismatic and brilliant leaders—the American neurologist Stanley Fahn, MD, and the British neurologist C. David Marsden, MBBS—came forward to inspire a generation of trainees with their broad interests in bridging clinical neurology, experimental neuroscience, and patient advocacy. Today, the impact of these pioneers is still felt by a growing community of movement disorder clinicians and researchers who have transformed movement disorders from an earlier realm of descriptive neurology into a vibrant field exploring disease mechanisms and therapeutics, as well as an expanding array of clinical insights.
When Neurology Reviews was founded in 1993, the majority of significant developments in movement disorders concerned Parkinson’s disease. Strategies to improve upon dopaminergic therapy were being tested in clinical trials, along with ventures into pallidotomy as a neurosurgical treatment. Animal models of parkinsonism and neurochemical analysis of brain and putative biomarkers provided scientific guidance for trials of disease modification. Another milestone from the 1990s was discovery of the first gene leading to autosomal-dominant parkinsonism. This rare mutation in the structural protein alpha-synuclein had a much broader impact on Parkinson’s disease research in that it provided important information about the sporadic disorder’s final common pathway of pathogenesis. Today, alpha-synuclein is the focus of therapeutic intervention utilizing immunologic therapies to halt disease progression. Over the past quarter-century, more than two dozen additional gene mutations associated with parkinsonism have been discovered. These mutations provide additional insight into disease mechanisms. Beyond the science and clinical insights that have propelled advances in understanding Parkinson’s disease and its related disorders, the growth of the patient advocacy and caregiver movement has also been remarkable in expanding what is needed to improve daily life with this disorder.
Since 1993, other movement disorders have also profited from the tremendous growth of molecular neuroscience and its applications. Novel neuroimaging techniques like functional MRI, computation of neural pathways, and scanning using PET and SPECT have helped work out the brain mechanisms of several disorders. Genetic probing of familial disorders like dystonia and myoclonus have helped to unravel the neurochemistry of what has gone wrong to cause certain movement disorders. In turn, transgenic animal models using these human genetic mutations have allowed exploration of what might be done to fix the problems. These developments could have huge implications for making progress in the therapies of the future, since the most common categories of movement disorders—dystonia, myoclonus, ataxia, tremor, restless legs syndrome, Tourette syndrome, choreic disorders, and paroxysmal movement disorders—all can have hereditary patterns. Genetic testing can be valuable for choosing at-risk individuals for participation in trials of disease-modifying drugs for Huntington’s disease, for example, and this strategy may be the way of the future for other late-life emergent disorders. In the past decade, several gene therapy studies have been carried out in patients with Parkinson’s disease. The promise of this approach and the recent gene editing and RNA interference approaches, all part of the molecular biology revolution of the past 25 years, may further change the landscape of movement disorder therapeutics ahead.
Today, movement disorder specialists routinely use therapeutic approaches that were in their infancy in 1993. Botulinum toxin selective denervation has had a major impact by improving quality of life for patients affected with a wide range of movement disorders: dystonic necks, hands, and feet; involuntary facial movements and voice aberrations; tics; spasticity; and drooling. Deep brain stimulation is a routine option for many patients with tremor, Parkinson’s disease, and dystonia. Developments in this field have refined the choice of targets for stimulation and the possibility of treating other disorders with these techniques, like Tourette syndrome. A nonsurgical approach to abolishing tremor, MRI-guided focused ultrasound, recently was approved. In the background of these advances is the increasing knowledge of movement disorders that practitioners have to offer many patients with disorders that in the past were merely neurologic curiosities. Through clinical trial research and serendipity (the major treatment options for essential tremor arose this way), there is an expanding search for repurposing older medications and harnessing new biotechnology to target the mechanisms leading to various movement disorders.
It is impressive how much the neurologic discipline of movement disorders has changed in response to the new era of electronic communications and other technologies. In the past quarter-century, medical students, residents, and practicing neurologists have had instant access to a curriculum that includes resources such as video-recorded movement disorders. Clinical trials are being revolutionized by electronic technologies that record information in ways that improve upon human ratings. A patient with Parkinson’s disease, essential tremor, or restless legs syndrome can now have symptoms monitored remotely by wearable devices that offer a real-world view on how a new therapy is performing. But perhaps the greatest revolution in the recent past has been increasing confidence that progressive disabilities caused by movement disorders might be halted by emerging insights into disease mechanisms. There has been tremendous growth of interest among the basic neuroscience community in human diseases affecting motor control. More than half of research presentations at recent international Parkinson’s disease and movement disorder conferences reflect this trend. These efforts support an optimistic view that, over the nex
PFO closure reduces the risk of recurrent stroke compared to antiplatelet therapy alone
Background: Previous research on the use of PFO closure to prevent recurrent stroke has yielded mixed results.
Study design: Gore REDUCE, CLOSE, and RESPECT were all multicenter, randomized, open-label superiority trials, with blinded adjudication of endpoint events. RESPECT data reflected an exploratory analysis of an extended follow up period.
Setting: Gore REDUCE was a multinational study conducted at 63 sites in Europe and North America, from 2008-2015. CLOSE was conducted at 34 sites in France and Germany, from 2007 to 2016. RESPECT was conducted at 69 sites in the United States and Canada, from 2003 to 2011.
Synopsis: Three trials reexamined the impact of PFO closure with standard antiplatelet treatment, with a total of 2,307 patients between the ages of 16 and 60 years. CLOSE included only patients with a PFO and an associated atrial septal aneurysm or a large interatrial shunt. Gore REDUCE and RESPECT were both industry funded. All three trials found a statistically significant reduction in risk of recurrent ischemic stroke associated with PFO closure and antiplatelet therapy compared to antiplatelet therapy alone (CLOSE HR 0.03 [95% CI 0-0.26; P less than .001], RESPECT HR 0.55 [95% CI 0.31-0.999; P = .046], Gore REDUCE HR 0.23 [95% CI 0.09-0.62; P = .002]). Gore REDUCE and CLOSE identified increased rates of postprocedural atrial fibrillation or flutter (6.6% vs. 0.4% [P less than .001], 4.6% vs. 0.9% [P = .02], respectively). Serious adverse events related to the procedure or device ranged from 3.9-5.9%.
Bottom line: PFO closure combined with antiplatelet therapy in patients aged 60 years or younger, particularly in those with significant right-to-left shunts and atrial septal aneurysms, reduced the risk of recurrent ischemic stroke compared to antiplatelet therapy alone.
Citation: Mas JL. Derumeaux B. Guillon B, et al. Patent foramen ovale closure or anticoagulation vs. antiplatelets after stroke. N Engl J Med. 2017;377(11):1011-21.
Saver JL, Carroll JD, Thaler DE, et al. Long-term outcomes of patent foramen ovale closure or medical therapy after stroke. N Engl J Med. 2017;377(11):1022-32.
Søndergaard L, Kasner SE, Rhodes JF, et al. Patent foramen ovale closure or antiplatelet therapy for cryptogenic stroke. N Engl J Med. 2017;377(11):1033-42.
Background: Previous research on the use of PFO closure to prevent recurrent stroke has yielded mixed results.
Study design: Gore REDUCE, CLOSE, and RESPECT were all multicenter, randomized, open-label superiority trials, with blinded adjudication of endpoint events. RESPECT data reflected an exploratory analysis of an extended follow up period.
Setting: Gore REDUCE was a multinational study conducted at 63 sites in Europe and North America, from 2008-2015. CLOSE was conducted at 34 sites in France and Germany, from 2007 to 2016. RESPECT was conducted at 69 sites in the United States and Canada, from 2003 to 2011.
Synopsis: Three trials reexamined the impact of PFO closure with standard antiplatelet treatment, with a total of 2,307 patients between the ages of 16 and 60 years. CLOSE included only patients with a PFO and an associated atrial septal aneurysm or a large interatrial shunt. Gore REDUCE and RESPECT were both industry funded. All three trials found a statistically significant reduction in risk of recurrent ischemic stroke associated with PFO closure and antiplatelet therapy compared to antiplatelet therapy alone (CLOSE HR 0.03 [95% CI 0-0.26; P less than .001], RESPECT HR 0.55 [95% CI 0.31-0.999; P = .046], Gore REDUCE HR 0.23 [95% CI 0.09-0.62; P = .002]). Gore REDUCE and CLOSE identified increased rates of postprocedural atrial fibrillation or flutter (6.6% vs. 0.4% [P less than .001], 4.6% vs. 0.9% [P = .02], respectively). Serious adverse events related to the procedure or device ranged from 3.9-5.9%.
Bottom line: PFO closure combined with antiplatelet therapy in patients aged 60 years or younger, particularly in those with significant right-to-left shunts and atrial septal aneurysms, reduced the risk of recurrent ischemic stroke compared to antiplatelet therapy alone.
Citation: Mas JL. Derumeaux B. Guillon B, et al. Patent foramen ovale closure or anticoagulation vs. antiplatelets after stroke. N Engl J Med. 2017;377(11):1011-21.
Saver JL, Carroll JD, Thaler DE, et al. Long-term outcomes of patent foramen ovale closure or medical therapy after stroke. N Engl J Med. 2017;377(11):1022-32.
Søndergaard L, Kasner SE, Rhodes JF, et al. Patent foramen ovale closure or antiplatelet therapy for cryptogenic stroke. N Engl J Med. 2017;377(11):1033-42.
Background: Previous research on the use of PFO closure to prevent recurrent stroke has yielded mixed results.
Study design: Gore REDUCE, CLOSE, and RESPECT were all multicenter, randomized, open-label superiority trials, with blinded adjudication of endpoint events. RESPECT data reflected an exploratory analysis of an extended follow up period.
Setting: Gore REDUCE was a multinational study conducted at 63 sites in Europe and North America, from 2008-2015. CLOSE was conducted at 34 sites in France and Germany, from 2007 to 2016. RESPECT was conducted at 69 sites in the United States and Canada, from 2003 to 2011.
Synopsis: Three trials reexamined the impact of PFO closure with standard antiplatelet treatment, with a total of 2,307 patients between the ages of 16 and 60 years. CLOSE included only patients with a PFO and an associated atrial septal aneurysm or a large interatrial shunt. Gore REDUCE and RESPECT were both industry funded. All three trials found a statistically significant reduction in risk of recurrent ischemic stroke associated with PFO closure and antiplatelet therapy compared to antiplatelet therapy alone (CLOSE HR 0.03 [95% CI 0-0.26; P less than .001], RESPECT HR 0.55 [95% CI 0.31-0.999; P = .046], Gore REDUCE HR 0.23 [95% CI 0.09-0.62; P = .002]). Gore REDUCE and CLOSE identified increased rates of postprocedural atrial fibrillation or flutter (6.6% vs. 0.4% [P less than .001], 4.6% vs. 0.9% [P = .02], respectively). Serious adverse events related to the procedure or device ranged from 3.9-5.9%.
Bottom line: PFO closure combined with antiplatelet therapy in patients aged 60 years or younger, particularly in those with significant right-to-left shunts and atrial septal aneurysms, reduced the risk of recurrent ischemic stroke compared to antiplatelet therapy alone.
Citation: Mas JL. Derumeaux B. Guillon B, et al. Patent foramen ovale closure or anticoagulation vs. antiplatelets after stroke. N Engl J Med. 2017;377(11):1011-21.
Saver JL, Carroll JD, Thaler DE, et al. Long-term outcomes of patent foramen ovale closure or medical therapy after stroke. N Engl J Med. 2017;377(11):1022-32.
Søndergaard L, Kasner SE, Rhodes JF, et al. Patent foramen ovale closure or antiplatelet therapy for cryptogenic stroke. N Engl J Med. 2017;377(11):1033-42.