User login
Is MS caused by one-two punch of pinworm and Epstein-Barr virus?
SAN DIEGO – What causes multiple sclerosis (MS)? A team of Scottish researchers offers a new theory that it’s triggered in part by a one-two punch of infection with pinworm – a common condition in the United States, especially among children – and the Epstein-Barr virus (EBV).
The theory identifies pinworm as the prime suspect to be the “missing link” that explains why EBV and MS are so tightly connected, said Patrick Kearns, MBChB, a graduate student at Harvard T.H. Chan School of Public Health in Boston.
Dr. Kearns is the lead author of two reports about the possible role of pinworm that were presented at ACTRIMS Forum 2018, which is held by the Americas Committee for Treatment and Research in Multiple Sclerosis. He spoke in an interview.
Dr. Kearns and his colleagues focused on a well-known cluster of MS cases that began to appear in the Faroe Islands – a Danish possession in the North Atlantic – during World War II. The cases began to appear after British troops occupied the islands.
“Many of the occupation soldiers were from the Scottish Highlands, where the MS prevalence is quite high: 90 cases per 100,000, comparable to the northern U.S.,” according to a National MS Society summary about MS clusters.
In a theory that spawned controversy, the late neurologist John Kurtzke, MD, speculated that the British soldiers brought a transmissible agent to the islands, which triggered MS cases.
Could the agent be EBV alone? The authors of the new studies don’t think so, although they note that EBV is “robustly linked” to MS. Indeed, a 2012 meta-analysis reported that the virus “appears to be present in 100% of MS patients,” based on studies considered to be the strongest (Mult Scler. 2013 Feb;19[2]:162-6).
The authors of the new reports note that, while EBV infection “appears necessary,” it is “clearly not sufficient” to cause the disease on its own.
“Certainly almost everyone gets EBV eventually,” Dr. Kearns said. “So mere presence of the virus is certainly not sufficient for causing the disease. But it seems still to be necessary, and timing of infection might be everything.”
So what’s the missing piece of the puzzle?
Dr. Kearns began to think it might be the lowly pinworm after helping a colleague by analyzing data from appendicitis samples in children. He noted that uninflamed samples often had pinworms in them, but the inflamed samples often didn’t, which suggested that “the rate of pinworms in normal appendices must be very high in the healthy pediatric population at any given time.”
More data confirmed this to be true, and medical literature told Dr. Kearns that pinworms were common in high latitudes – places where people often are especially prone to MS.
“Most remarkably, they are known to have very little migration and stay spatially stable in populations over long periods of time,” Dr. Kearns said, “and typically everyone in an affected population will encounter them because their eggs are transmitted in household dust.”
And, he said, “they are known to be common in soldiers who live in military accommodation.”
According to the Centers for Disease Control and Prevention, pinworm prevalence can be as high as 50% in at-risk groups – children, caregivers of infected children, and people who live in institutions. Pinworms, which are spread through ingestion, are often asymptomatic but may cause anal itching and trigger bacterial infections.
The researchers suggest that pinworm infection comes first, followed by EBV infection. This makes sense because “late EBV infection in the form of infectious mononucleosis is known to be a risk factor for MS,” Dr. Kearns said.
The one-two punch of pinworm and then EBV is a plausible theory “because EBV lives in memory B cells, which are known to be important in MS and could be specific for the previous exposure to pinworm,” Dr. Kearns said. “However, this is very speculative and some researchers will argue this is very unlikely to be the case. But I think there is a chance it could explain some of the epidemiology, so I’m keen to try and test the theory if I can.”
What’s next? Dr. Kearns wants to explore data from Scotland in search of areas of high and low MS incidence that could offer insight into environmental triggers.
He added that the development of a serological blood test to prove a history of pinworm infection would be “the most effective way to prove or disprove this theory.”
“I have approached an investigator who has a track record of doing this for other infections and have been encouraged that he thinks that it would be achievable,” he said. “But this will definitely take time and funding.”
No specific funding was reported. The study authors reported no relevant disclosures.
SOURCE: Kearns P et al. ACTRIMS Forum 2018, Abstracts LB257 and LB264.
SAN DIEGO – What causes multiple sclerosis (MS)? A team of Scottish researchers offers a new theory that it’s triggered in part by a one-two punch of infection with pinworm – a common condition in the United States, especially among children – and the Epstein-Barr virus (EBV).
The theory identifies pinworm as the prime suspect to be the “missing link” that explains why EBV and MS are so tightly connected, said Patrick Kearns, MBChB, a graduate student at Harvard T.H. Chan School of Public Health in Boston.
Dr. Kearns is the lead author of two reports about the possible role of pinworm that were presented at ACTRIMS Forum 2018, which is held by the Americas Committee for Treatment and Research in Multiple Sclerosis. He spoke in an interview.
Dr. Kearns and his colleagues focused on a well-known cluster of MS cases that began to appear in the Faroe Islands – a Danish possession in the North Atlantic – during World War II. The cases began to appear after British troops occupied the islands.
“Many of the occupation soldiers were from the Scottish Highlands, where the MS prevalence is quite high: 90 cases per 100,000, comparable to the northern U.S.,” according to a National MS Society summary about MS clusters.
In a theory that spawned controversy, the late neurologist John Kurtzke, MD, speculated that the British soldiers brought a transmissible agent to the islands, which triggered MS cases.
Could the agent be EBV alone? The authors of the new studies don’t think so, although they note that EBV is “robustly linked” to MS. Indeed, a 2012 meta-analysis reported that the virus “appears to be present in 100% of MS patients,” based on studies considered to be the strongest (Mult Scler. 2013 Feb;19[2]:162-6).
The authors of the new reports note that, while EBV infection “appears necessary,” it is “clearly not sufficient” to cause the disease on its own.
“Certainly almost everyone gets EBV eventually,” Dr. Kearns said. “So mere presence of the virus is certainly not sufficient for causing the disease. But it seems still to be necessary, and timing of infection might be everything.”
So what’s the missing piece of the puzzle?
Dr. Kearns began to think it might be the lowly pinworm after helping a colleague by analyzing data from appendicitis samples in children. He noted that uninflamed samples often had pinworms in them, but the inflamed samples often didn’t, which suggested that “the rate of pinworms in normal appendices must be very high in the healthy pediatric population at any given time.”
More data confirmed this to be true, and medical literature told Dr. Kearns that pinworms were common in high latitudes – places where people often are especially prone to MS.
“Most remarkably, they are known to have very little migration and stay spatially stable in populations over long periods of time,” Dr. Kearns said, “and typically everyone in an affected population will encounter them because their eggs are transmitted in household dust.”
And, he said, “they are known to be common in soldiers who live in military accommodation.”
According to the Centers for Disease Control and Prevention, pinworm prevalence can be as high as 50% in at-risk groups – children, caregivers of infected children, and people who live in institutions. Pinworms, which are spread through ingestion, are often asymptomatic but may cause anal itching and trigger bacterial infections.
The researchers suggest that pinworm infection comes first, followed by EBV infection. This makes sense because “late EBV infection in the form of infectious mononucleosis is known to be a risk factor for MS,” Dr. Kearns said.
The one-two punch of pinworm and then EBV is a plausible theory “because EBV lives in memory B cells, which are known to be important in MS and could be specific for the previous exposure to pinworm,” Dr. Kearns said. “However, this is very speculative and some researchers will argue this is very unlikely to be the case. But I think there is a chance it could explain some of the epidemiology, so I’m keen to try and test the theory if I can.”
What’s next? Dr. Kearns wants to explore data from Scotland in search of areas of high and low MS incidence that could offer insight into environmental triggers.
He added that the development of a serological blood test to prove a history of pinworm infection would be “the most effective way to prove or disprove this theory.”
“I have approached an investigator who has a track record of doing this for other infections and have been encouraged that he thinks that it would be achievable,” he said. “But this will definitely take time and funding.”
No specific funding was reported. The study authors reported no relevant disclosures.
SOURCE: Kearns P et al. ACTRIMS Forum 2018, Abstracts LB257 and LB264.
SAN DIEGO – What causes multiple sclerosis (MS)? A team of Scottish researchers offers a new theory that it’s triggered in part by a one-two punch of infection with pinworm – a common condition in the United States, especially among children – and the Epstein-Barr virus (EBV).
The theory identifies pinworm as the prime suspect to be the “missing link” that explains why EBV and MS are so tightly connected, said Patrick Kearns, MBChB, a graduate student at Harvard T.H. Chan School of Public Health in Boston.
Dr. Kearns is the lead author of two reports about the possible role of pinworm that were presented at ACTRIMS Forum 2018, which is held by the Americas Committee for Treatment and Research in Multiple Sclerosis. He spoke in an interview.
Dr. Kearns and his colleagues focused on a well-known cluster of MS cases that began to appear in the Faroe Islands – a Danish possession in the North Atlantic – during World War II. The cases began to appear after British troops occupied the islands.
“Many of the occupation soldiers were from the Scottish Highlands, where the MS prevalence is quite high: 90 cases per 100,000, comparable to the northern U.S.,” according to a National MS Society summary about MS clusters.
In a theory that spawned controversy, the late neurologist John Kurtzke, MD, speculated that the British soldiers brought a transmissible agent to the islands, which triggered MS cases.
Could the agent be EBV alone? The authors of the new studies don’t think so, although they note that EBV is “robustly linked” to MS. Indeed, a 2012 meta-analysis reported that the virus “appears to be present in 100% of MS patients,” based on studies considered to be the strongest (Mult Scler. 2013 Feb;19[2]:162-6).
The authors of the new reports note that, while EBV infection “appears necessary,” it is “clearly not sufficient” to cause the disease on its own.
“Certainly almost everyone gets EBV eventually,” Dr. Kearns said. “So mere presence of the virus is certainly not sufficient for causing the disease. But it seems still to be necessary, and timing of infection might be everything.”
So what’s the missing piece of the puzzle?
Dr. Kearns began to think it might be the lowly pinworm after helping a colleague by analyzing data from appendicitis samples in children. He noted that uninflamed samples often had pinworms in them, but the inflamed samples often didn’t, which suggested that “the rate of pinworms in normal appendices must be very high in the healthy pediatric population at any given time.”
More data confirmed this to be true, and medical literature told Dr. Kearns that pinworms were common in high latitudes – places where people often are especially prone to MS.
“Most remarkably, they are known to have very little migration and stay spatially stable in populations over long periods of time,” Dr. Kearns said, “and typically everyone in an affected population will encounter them because their eggs are transmitted in household dust.”
And, he said, “they are known to be common in soldiers who live in military accommodation.”
According to the Centers for Disease Control and Prevention, pinworm prevalence can be as high as 50% in at-risk groups – children, caregivers of infected children, and people who live in institutions. Pinworms, which are spread through ingestion, are often asymptomatic but may cause anal itching and trigger bacterial infections.
The researchers suggest that pinworm infection comes first, followed by EBV infection. This makes sense because “late EBV infection in the form of infectious mononucleosis is known to be a risk factor for MS,” Dr. Kearns said.
The one-two punch of pinworm and then EBV is a plausible theory “because EBV lives in memory B cells, which are known to be important in MS and could be specific for the previous exposure to pinworm,” Dr. Kearns said. “However, this is very speculative and some researchers will argue this is very unlikely to be the case. But I think there is a chance it could explain some of the epidemiology, so I’m keen to try and test the theory if I can.”
What’s next? Dr. Kearns wants to explore data from Scotland in search of areas of high and low MS incidence that could offer insight into environmental triggers.
He added that the development of a serological blood test to prove a history of pinworm infection would be “the most effective way to prove or disprove this theory.”
“I have approached an investigator who has a track record of doing this for other infections and have been encouraged that he thinks that it would be achievable,” he said. “But this will definitely take time and funding.”
No specific funding was reported. The study authors reported no relevant disclosures.
SOURCE: Kearns P et al. ACTRIMS Forum 2018, Abstracts LB257 and LB264.
REPORTING FROM ACTRIMS FORUM 2018
Asymptomatic Erythematous Plaques on the Scalp and Face
The Diagnosis: Granuloma Faciale
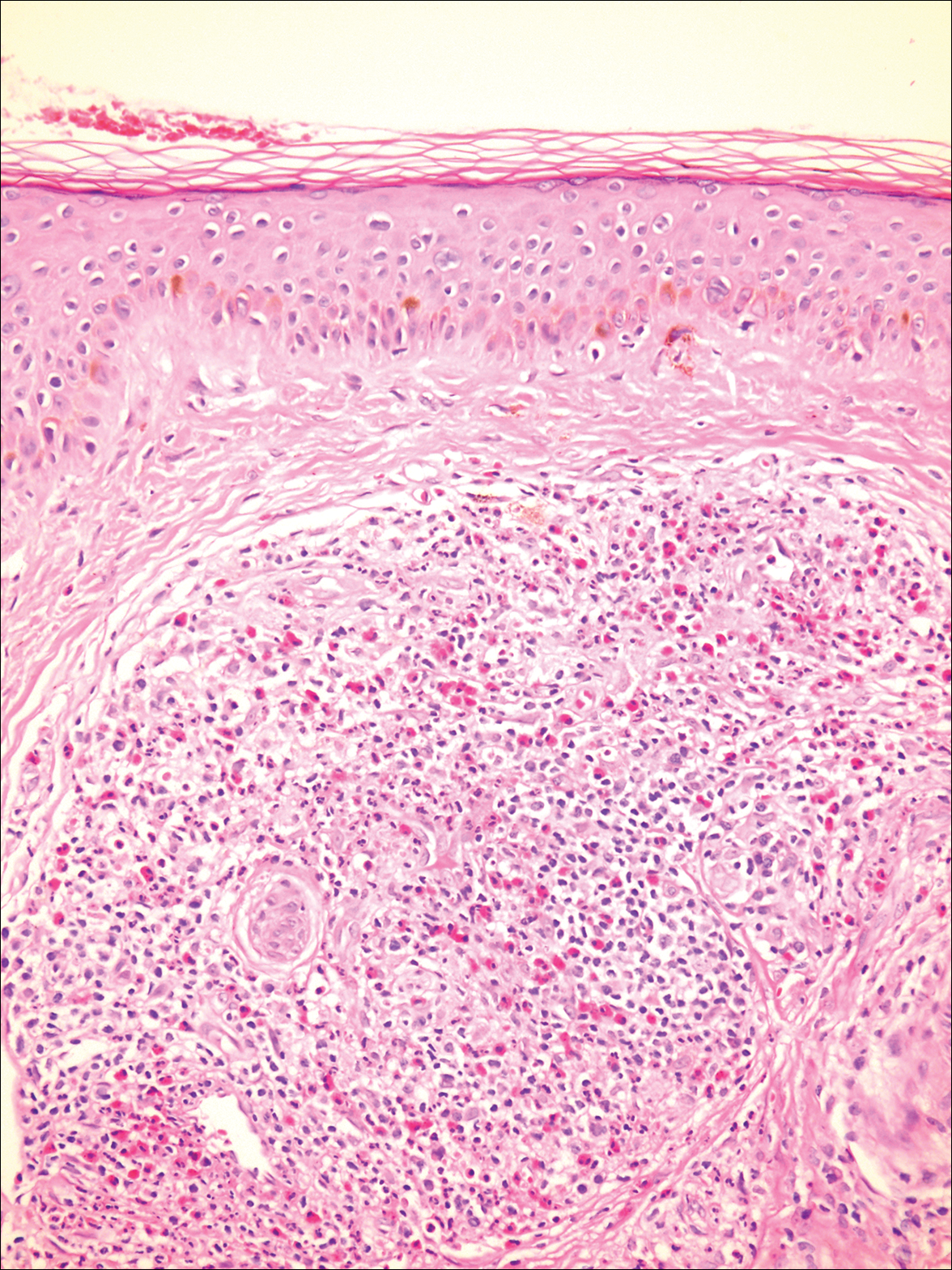
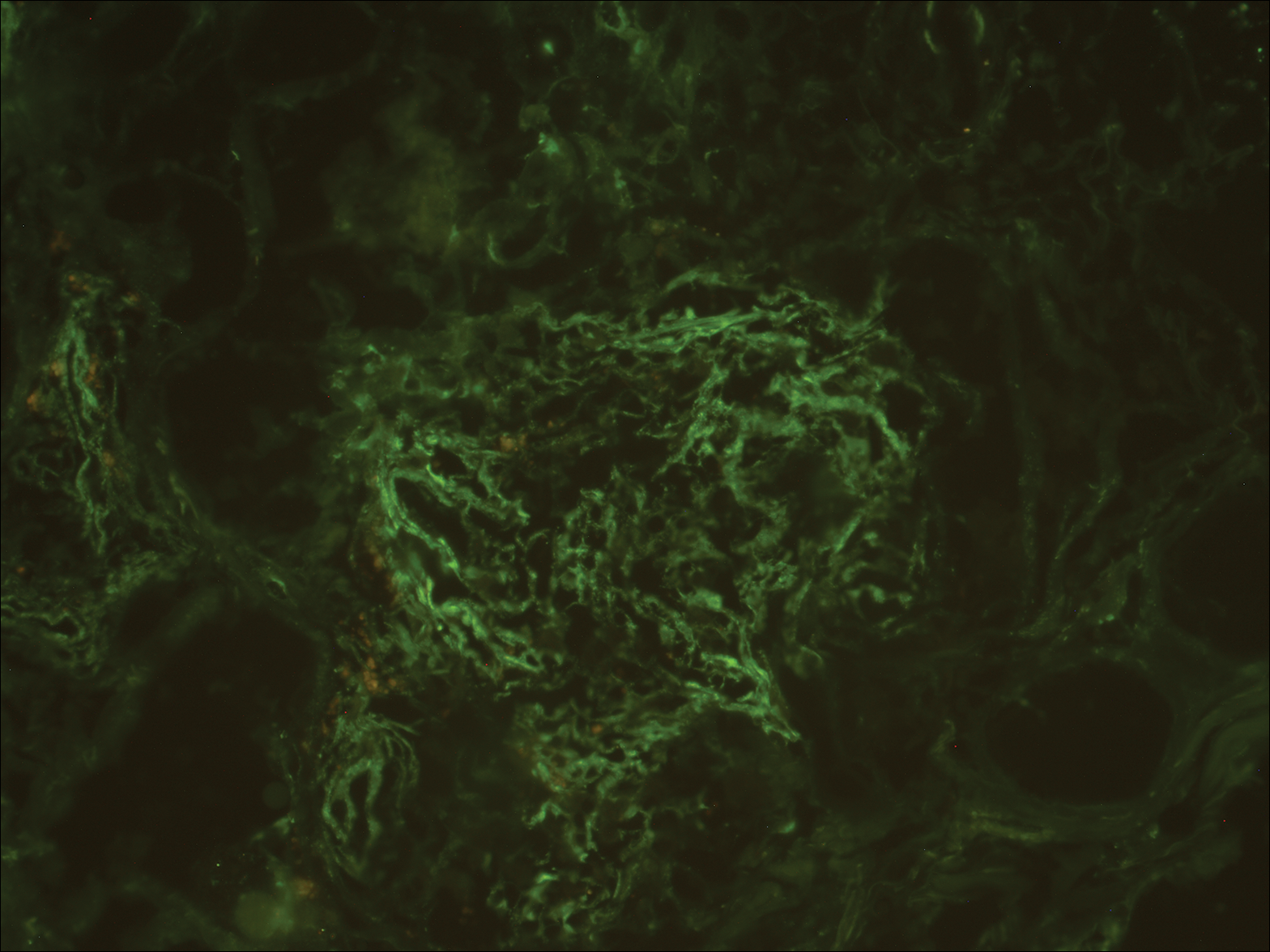
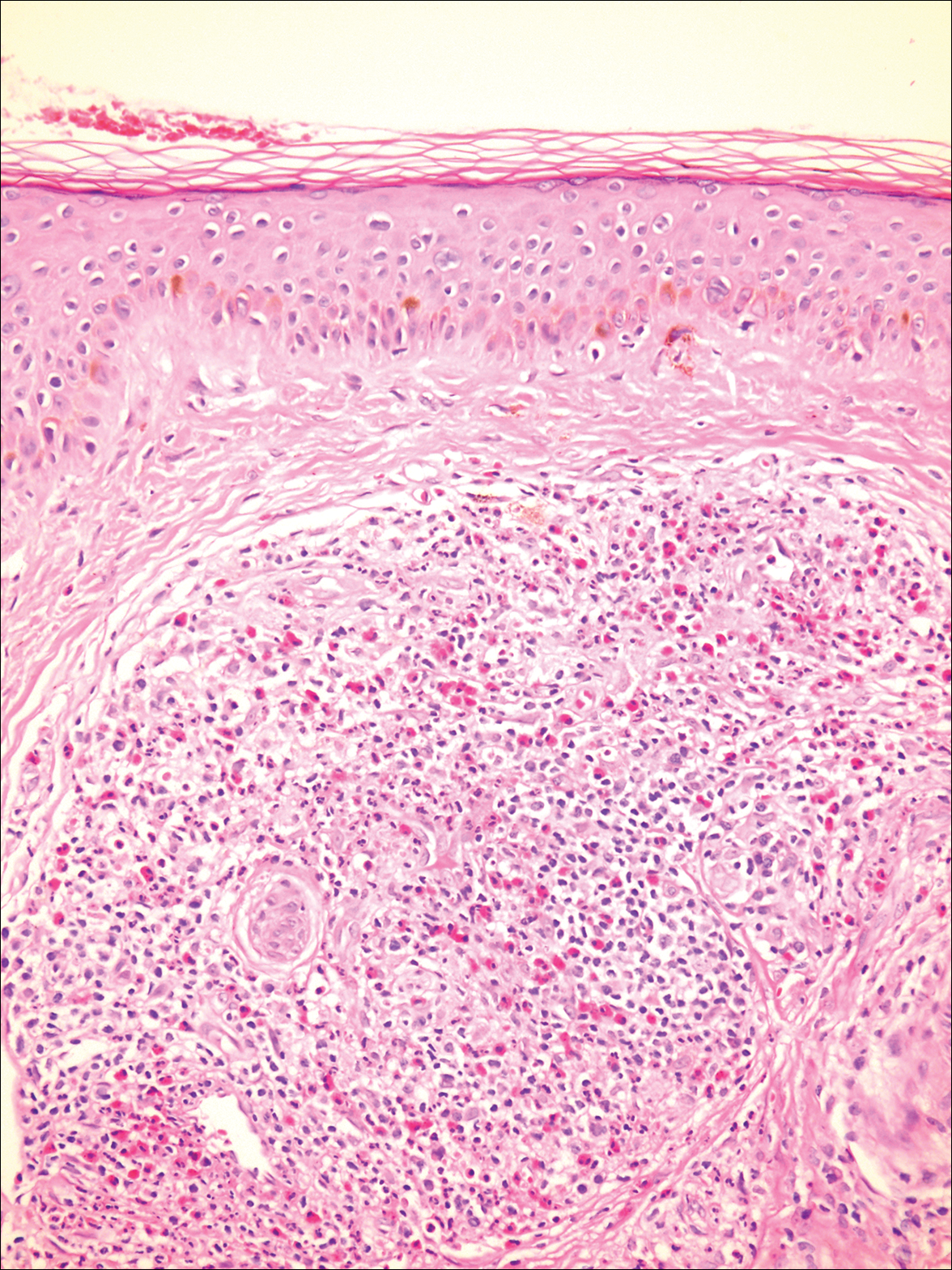
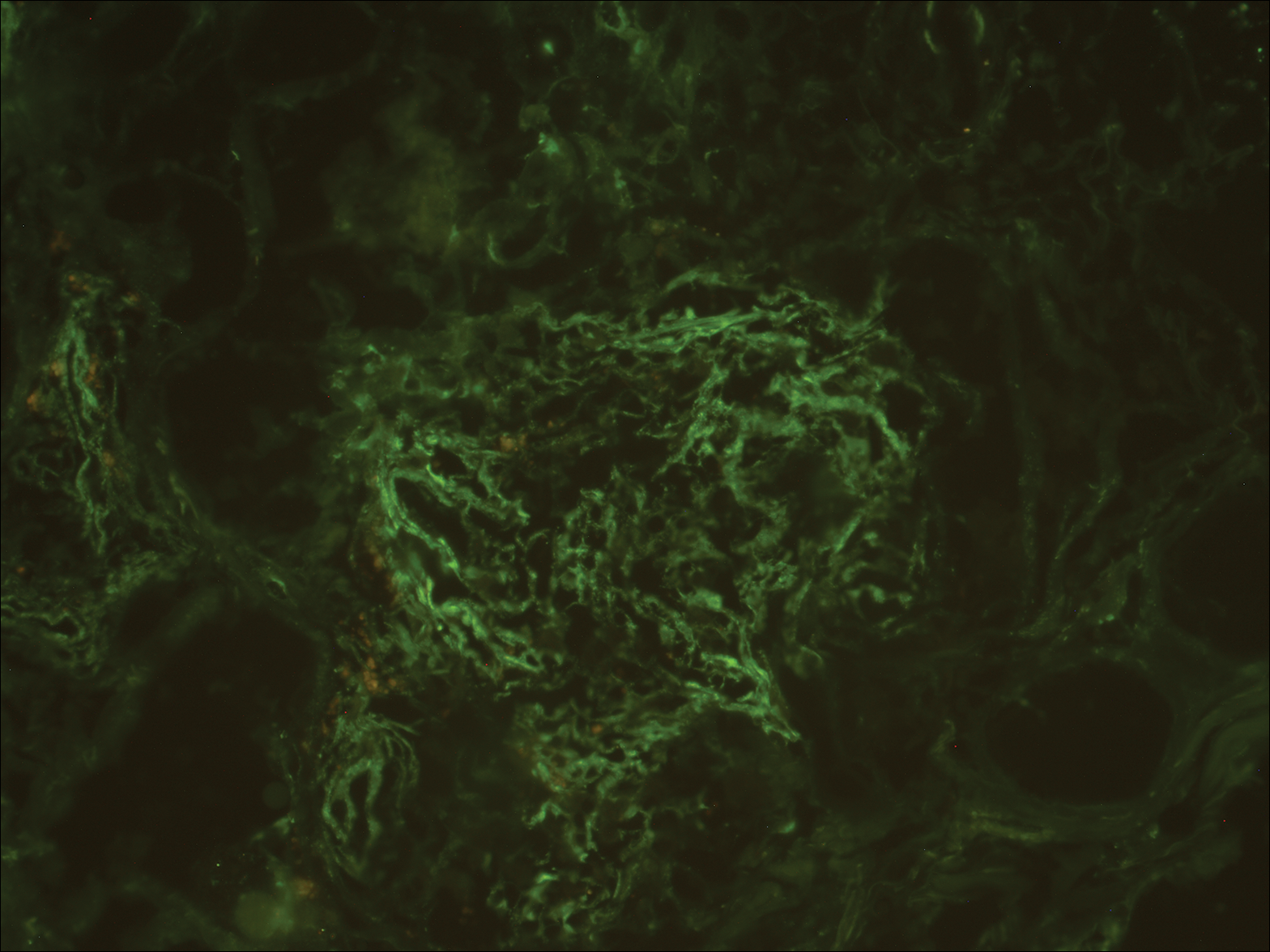
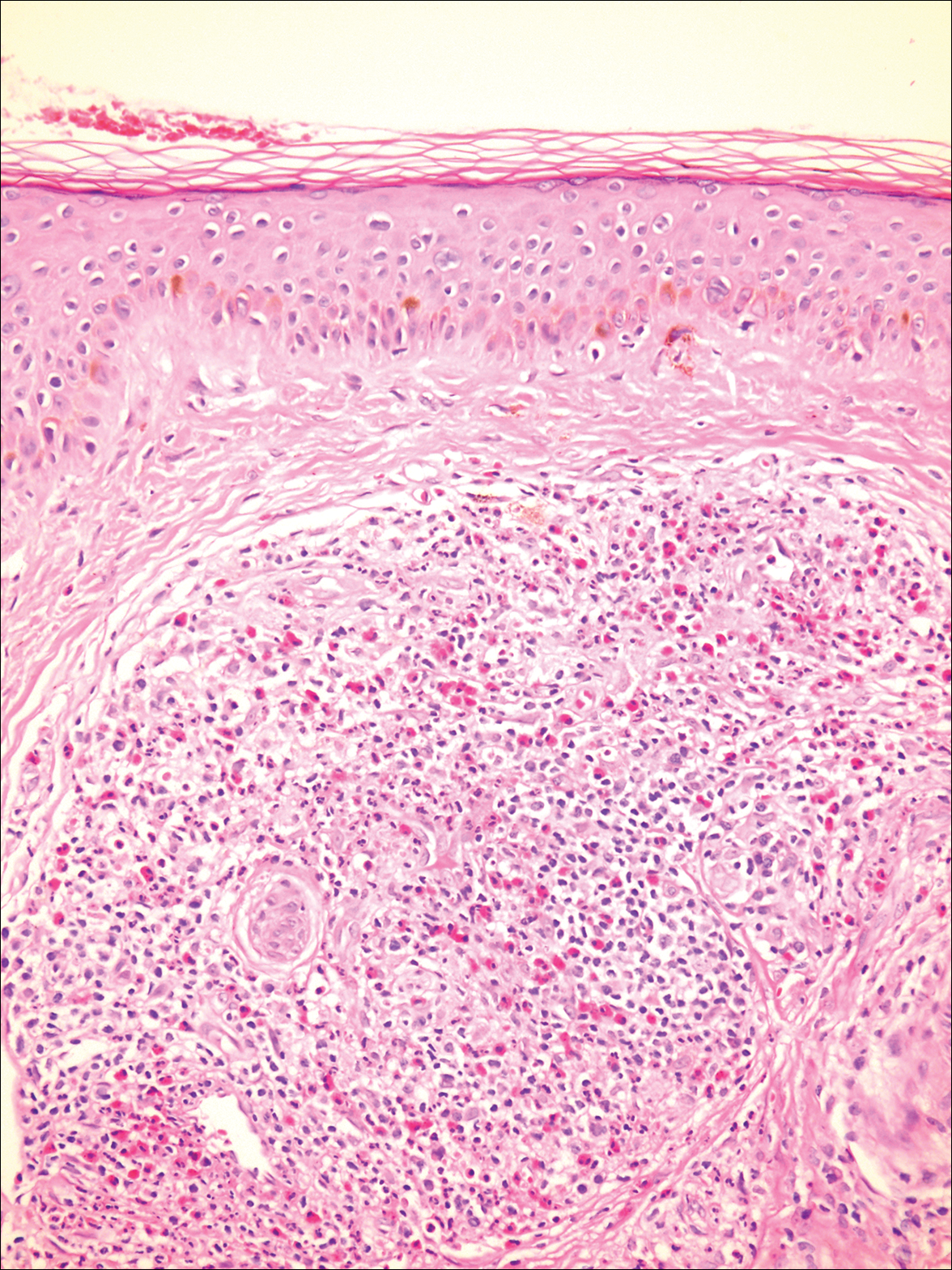
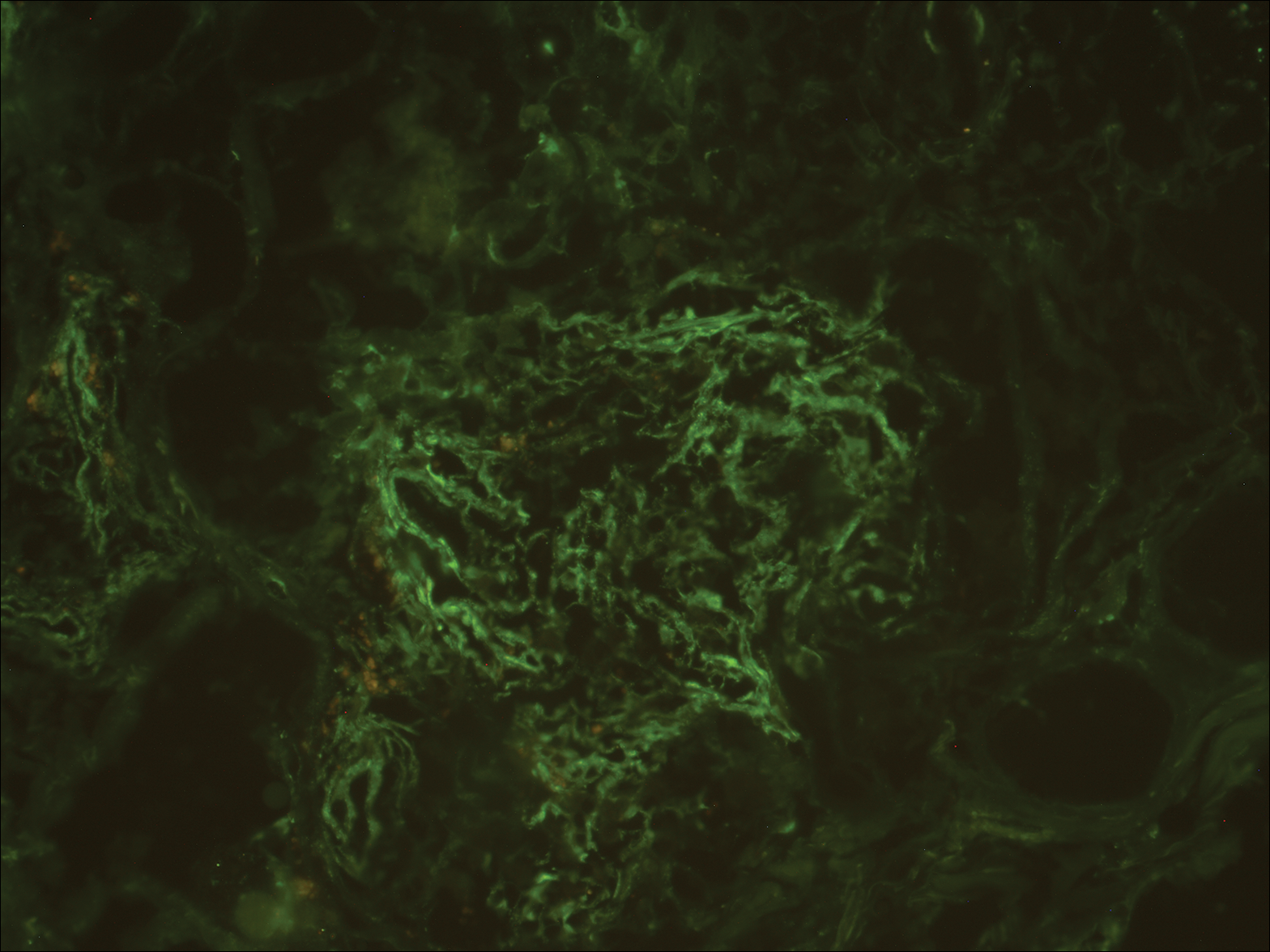
A biopsy from a scalp lesion showed an intense mixed inflammatory infiltrate mainly consisting of eosinophils, but lymphocytes, histiocytes, neutrophils, and plasma cells also were present. A grenz zone was observed between the dermal infiltrate and epidermis. Perivascular infiltrates were penetrating vessel walls, and hyalinization of the vessel walls also was seen (Figure 1). Direct immunofluorescence demonstrated IgG positivity on vessel walls (Figure 2). A diagnosis of granuloma faciale with extrafacial lesions was made. Twice daily application of tacrolimus ointment 0.1% was started, but after a 10-month course of treatment, there was no notable difference in the lesions.
Granuloma faciale (GF) is an uncommon benign dermatosis of unknown pathogenesis characterized by erythematous, brown, or violaceous papules, plaques, or nodules. Granuloma faciale lesions can be solitary or multiple as well as disseminated and most often occur on the face. Predilection sites include the nose, periauricular area, cheeks, forehead, eyelids, and ears; however, lesions also have been reported to occur in extrafacial areas such as the trunk, arms, and legs.1-4 In our patient, multiple plaques were seen on the scalp. Facial lesions usually precede extrafacial lesions, which may present months to several years after the appearance of facial disease; however, according to our patient's history his scalp lesions appeared before the facial lesions.
The differential diagnoses for GF mainly include erythema elevatum diutinum, cutaneous sarcoidosis, cutaneous lymphoma, lupus, basal cell carcinoma, and cutaneous pseudolymphoma.5 Diagnosis may be established based on a combination of clinical features and skin biopsy results. On histopathologic examination, small-vessel vasculitis usually is present with an infiltrate predominantly consisting of neutrophils and eosinophils.6
It has been suggested that actinic damage plays a role in the etiology of GF.7 The pathogenesis is uncertain, but it is thought that immunophenotypic and molecular analysis of the dermal infiltrate in GF reveals that most lymphocytes are clonally expanded and the process is mediated by interferon gamma.7 Tacrolimus acts by binding and inactivating calcineurin and thus blocking T-cell activation and proliferation, so it is not surprising that topical tacrolimus has been shown to be useful in the management of this condition.8
- Leite I, Moreira A, Guedes R, et al. Granuloma faciale of the scalp. Dermatol Online J. 2011;17:6.
- De D, Kanwar AJ, Radotra BD, et al. Extrafacial granuloma faciale: report of a case. J Eur Acad Dermatol Venereol. 2007;21:1284-1286.
- Castellano-Howard L, Fairbee SI, Hogan DJ, et al. Extrafacial granuloma faciale: report of a case and response to treatment. Cutis. 2001;67:413-415.
- Inanir I, Alvur Y. Granuloma faciale with extrafacial lesions. Br J Dermatol. 2001;145:360-362.
- Ortonne N, Wechsler J, Bagot M, et al. Granuloma faciale: a clinicopathologic study of 66 patients. J Am Acad Dermatol. 2005;53:1002-1009.
- LeBoit PE. Granuloma faciale: a diagnosis deserving of dignity. Am J Dermatopathol. 2002;24:440-443.
- Koplon BS, Wood MG. Granuloma faciale. first reported case in a Negro. Arch Dermatol. 1967;96:188-192.
- Ludwig E, Allam JP, Bieber T, et al. New treatment modalities for granuloma faciale. Br J Dermatol. 2003;149:634-637.
The Diagnosis: Granuloma Faciale
A biopsy from a scalp lesion showed an intense mixed inflammatory infiltrate mainly consisting of eosinophils, but lymphocytes, histiocytes, neutrophils, and plasma cells also were present. A grenz zone was observed between the dermal infiltrate and epidermis. Perivascular infiltrates were penetrating vessel walls, and hyalinization of the vessel walls also was seen (Figure 1). Direct immunofluorescence demonstrated IgG positivity on vessel walls (Figure 2). A diagnosis of granuloma faciale with extrafacial lesions was made. Twice daily application of tacrolimus ointment 0.1% was started, but after a 10-month course of treatment, there was no notable difference in the lesions.
Granuloma faciale (GF) is an uncommon benign dermatosis of unknown pathogenesis characterized by erythematous, brown, or violaceous papules, plaques, or nodules. Granuloma faciale lesions can be solitary or multiple as well as disseminated and most often occur on the face. Predilection sites include the nose, periauricular area, cheeks, forehead, eyelids, and ears; however, lesions also have been reported to occur in extrafacial areas such as the trunk, arms, and legs.1-4 In our patient, multiple plaques were seen on the scalp. Facial lesions usually precede extrafacial lesions, which may present months to several years after the appearance of facial disease; however, according to our patient's history his scalp lesions appeared before the facial lesions.
The differential diagnoses for GF mainly include erythema elevatum diutinum, cutaneous sarcoidosis, cutaneous lymphoma, lupus, basal cell carcinoma, and cutaneous pseudolymphoma.5 Diagnosis may be established based on a combination of clinical features and skin biopsy results. On histopathologic examination, small-vessel vasculitis usually is present with an infiltrate predominantly consisting of neutrophils and eosinophils.6
It has been suggested that actinic damage plays a role in the etiology of GF.7 The pathogenesis is uncertain, but it is thought that immunophenotypic and molecular analysis of the dermal infiltrate in GF reveals that most lymphocytes are clonally expanded and the process is mediated by interferon gamma.7 Tacrolimus acts by binding and inactivating calcineurin and thus blocking T-cell activation and proliferation, so it is not surprising that topical tacrolimus has been shown to be useful in the management of this condition.8
The Diagnosis: Granuloma Faciale
A biopsy from a scalp lesion showed an intense mixed inflammatory infiltrate mainly consisting of eosinophils, but lymphocytes, histiocytes, neutrophils, and plasma cells also were present. A grenz zone was observed between the dermal infiltrate and epidermis. Perivascular infiltrates were penetrating vessel walls, and hyalinization of the vessel walls also was seen (Figure 1). Direct immunofluorescence demonstrated IgG positivity on vessel walls (Figure 2). A diagnosis of granuloma faciale with extrafacial lesions was made. Twice daily application of tacrolimus ointment 0.1% was started, but after a 10-month course of treatment, there was no notable difference in the lesions.
Granuloma faciale (GF) is an uncommon benign dermatosis of unknown pathogenesis characterized by erythematous, brown, or violaceous papules, plaques, or nodules. Granuloma faciale lesions can be solitary or multiple as well as disseminated and most often occur on the face. Predilection sites include the nose, periauricular area, cheeks, forehead, eyelids, and ears; however, lesions also have been reported to occur in extrafacial areas such as the trunk, arms, and legs.1-4 In our patient, multiple plaques were seen on the scalp. Facial lesions usually precede extrafacial lesions, which may present months to several years after the appearance of facial disease; however, according to our patient's history his scalp lesions appeared before the facial lesions.
The differential diagnoses for GF mainly include erythema elevatum diutinum, cutaneous sarcoidosis, cutaneous lymphoma, lupus, basal cell carcinoma, and cutaneous pseudolymphoma.5 Diagnosis may be established based on a combination of clinical features and skin biopsy results. On histopathologic examination, small-vessel vasculitis usually is present with an infiltrate predominantly consisting of neutrophils and eosinophils.6
It has been suggested that actinic damage plays a role in the etiology of GF.7 The pathogenesis is uncertain, but it is thought that immunophenotypic and molecular analysis of the dermal infiltrate in GF reveals that most lymphocytes are clonally expanded and the process is mediated by interferon gamma.7 Tacrolimus acts by binding and inactivating calcineurin and thus blocking T-cell activation and proliferation, so it is not surprising that topical tacrolimus has been shown to be useful in the management of this condition.8
- Leite I, Moreira A, Guedes R, et al. Granuloma faciale of the scalp. Dermatol Online J. 2011;17:6.
- De D, Kanwar AJ, Radotra BD, et al. Extrafacial granuloma faciale: report of a case. J Eur Acad Dermatol Venereol. 2007;21:1284-1286.
- Castellano-Howard L, Fairbee SI, Hogan DJ, et al. Extrafacial granuloma faciale: report of a case and response to treatment. Cutis. 2001;67:413-415.
- Inanir I, Alvur Y. Granuloma faciale with extrafacial lesions. Br J Dermatol. 2001;145:360-362.
- Ortonne N, Wechsler J, Bagot M, et al. Granuloma faciale: a clinicopathologic study of 66 patients. J Am Acad Dermatol. 2005;53:1002-1009.
- LeBoit PE. Granuloma faciale: a diagnosis deserving of dignity. Am J Dermatopathol. 2002;24:440-443.
- Koplon BS, Wood MG. Granuloma faciale. first reported case in a Negro. Arch Dermatol. 1967;96:188-192.
- Ludwig E, Allam JP, Bieber T, et al. New treatment modalities for granuloma faciale. Br J Dermatol. 2003;149:634-637.
- Leite I, Moreira A, Guedes R, et al. Granuloma faciale of the scalp. Dermatol Online J. 2011;17:6.
- De D, Kanwar AJ, Radotra BD, et al. Extrafacial granuloma faciale: report of a case. J Eur Acad Dermatol Venereol. 2007;21:1284-1286.
- Castellano-Howard L, Fairbee SI, Hogan DJ, et al. Extrafacial granuloma faciale: report of a case and response to treatment. Cutis. 2001;67:413-415.
- Inanir I, Alvur Y. Granuloma faciale with extrafacial lesions. Br J Dermatol. 2001;145:360-362.
- Ortonne N, Wechsler J, Bagot M, et al. Granuloma faciale: a clinicopathologic study of 66 patients. J Am Acad Dermatol. 2005;53:1002-1009.
- LeBoit PE. Granuloma faciale: a diagnosis deserving of dignity. Am J Dermatopathol. 2002;24:440-443.
- Koplon BS, Wood MG. Granuloma faciale. first reported case in a Negro. Arch Dermatol. 1967;96:188-192.
- Ludwig E, Allam JP, Bieber T, et al. New treatment modalities for granuloma faciale. Br J Dermatol. 2003;149:634-637.
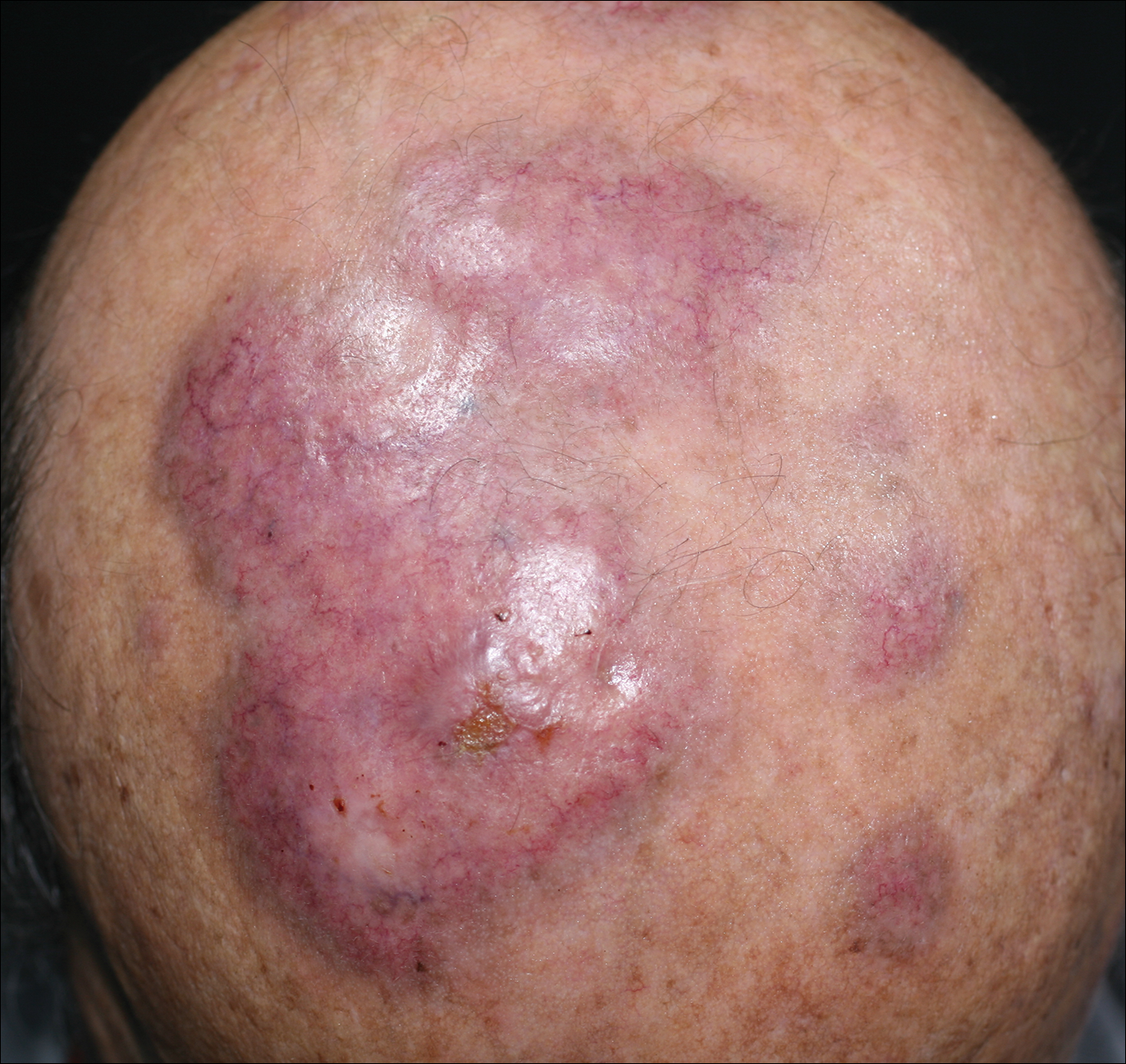
An 84-year-old man presented with gradually enlarging, asymptomatic, erythematous to violaceous plaques on the face and scalp of 11 years' duration ranging in size from 0.5×0.5 cm to 10×8 cm. The plaques were unresponsive to treatment with topical steroids. The lesions were nontender with no associated bleeding, burning, or pruritus. The patient denied any trauma to the sites or systemic symptoms. He had a history of essential hypertension and benign prostatic hyperplasia and had been taking ramipril, tamsulosin, and dutasteride for 5 years. His medical history was otherwise unremarkable, and routine laboratory findings were within normal range.
Guidelines update best practices for hemorrhoid treatment
Each year, more than 2.2 million patients in the United States undergo evaluations for symptoms of hemorrhoids, according to updated guidelines on the management of hemorrhoids issued by the American Society of Colon and Rectal Surgeons.
“As a result, it is important to identify symptomatic hemorrhoids as the underlying source of the anorectal symptom and to have a clear understanding of the evaluation and management of this disease process,” wrote Bradley R. Davis, MD, FACS, chief of colon and rectal surgery at the Carolinas Medical Center, Charlotte, N.C., and the fellow members of the Clinical Practice Guidelines Committee of the ASCRS.
The guidelines recommend evaluation of hemorrhoids based on a disease-specific history, and a physical that emphasizes the degree and duration of symptoms and identifies risk factors. But the guideline writers note that the recommendation is a grade 1C because the supporting data mainly come from observational or case studies.
“The cardinal signs of internal hemorrhoids are painless bleeding with bowel movements with intermittent protrusion,” the committee said, also emphasizing that patients should be evaluated for fecal incontinence, which could inform surgical decision making.
In addition, the guidelines call for a complete endoscopic evaluation of the colon for patients who present with symptomatic hemorrhoids and rectal bleeding; this recommendation is based on moderately strong evidence, and presented with a grade of 1B.
Medical management of hemorrhoids may include office-based procedures or surgery, according to the guidelines.
“Most patients with grade I and II and select patients with grade III internal hemorrhoidal disease who fail medical treatment can be effectively treated with office-based procedures, such as banding, sclerotherapy, and infrared coagulation,” the committee wrote, and medical office treatment received a strong grade 1A recommendation based on high-quality evidence. Although office procedures are generally well tolerated, the condition can recur. Bleeding is the most common complication, and it is more likely after rubber-band ligation than other office-based options, the guidelines state.
The guidelines offer a weak recommendation of 2C, based on the lack of quality evidence, for the use of early surgical excision to treat patients with thrombosed external hemorrhoids. “Although most patients treated nonoperatively will experience eventual resolution of their symptoms, excision of thrombosed external hemorrhoids may result in more rapid symptom resolution, lower incidence of recurrence, and longer remission intervals,” the committee noted.
Surgical hemorrhoidectomy received the strongest possible recommendation (1A, based on high-quality evidence) for the treatment of patients with external hemorrhoids or a combination of internal and external hemorrhoids with prolapse.
Surgical options described in the recommendations include surgical excision (hemorrhoidectomy), hemorrhoidopexy, and Doppler-guided hemorrhoidectomy, with citations of studies on each procedure. Data from a meta-analysis of 18 randomized prospective studies comparing hemorrhoidectomy with office-based procedures showed that hemorrhoidectomy was “the most effective treatment for patients with grade III hemorrhoids,” but it was associated with greater pain and complication rates, according to the guidelines.
However, complications in general are low after surgical hemorrhoidectomy, with reported complication rates of 1%-2% for the most common complication of postprocedure hemorrhage, the guidelines state. After surgery, the guidelines recommend with a 1B grade (moderate quality evidence) that patients use “a multimodality pain regimen to reduce narcotic usage and promote a faster recovery.”
The committee members had no financial conflicts to disclose.
acssurgerynews@frontlinemedcom.com
SOURCE: Davis BR et al. Dis Colon Rectum. 2018; 61:284-92.
Each year, more than 2.2 million patients in the United States undergo evaluations for symptoms of hemorrhoids, according to updated guidelines on the management of hemorrhoids issued by the American Society of Colon and Rectal Surgeons.
“As a result, it is important to identify symptomatic hemorrhoids as the underlying source of the anorectal symptom and to have a clear understanding of the evaluation and management of this disease process,” wrote Bradley R. Davis, MD, FACS, chief of colon and rectal surgery at the Carolinas Medical Center, Charlotte, N.C., and the fellow members of the Clinical Practice Guidelines Committee of the ASCRS.
The guidelines recommend evaluation of hemorrhoids based on a disease-specific history, and a physical that emphasizes the degree and duration of symptoms and identifies risk factors. But the guideline writers note that the recommendation is a grade 1C because the supporting data mainly come from observational or case studies.
“The cardinal signs of internal hemorrhoids are painless bleeding with bowel movements with intermittent protrusion,” the committee said, also emphasizing that patients should be evaluated for fecal incontinence, which could inform surgical decision making.
In addition, the guidelines call for a complete endoscopic evaluation of the colon for patients who present with symptomatic hemorrhoids and rectal bleeding; this recommendation is based on moderately strong evidence, and presented with a grade of 1B.
Medical management of hemorrhoids may include office-based procedures or surgery, according to the guidelines.
“Most patients with grade I and II and select patients with grade III internal hemorrhoidal disease who fail medical treatment can be effectively treated with office-based procedures, such as banding, sclerotherapy, and infrared coagulation,” the committee wrote, and medical office treatment received a strong grade 1A recommendation based on high-quality evidence. Although office procedures are generally well tolerated, the condition can recur. Bleeding is the most common complication, and it is more likely after rubber-band ligation than other office-based options, the guidelines state.
The guidelines offer a weak recommendation of 2C, based on the lack of quality evidence, for the use of early surgical excision to treat patients with thrombosed external hemorrhoids. “Although most patients treated nonoperatively will experience eventual resolution of their symptoms, excision of thrombosed external hemorrhoids may result in more rapid symptom resolution, lower incidence of recurrence, and longer remission intervals,” the committee noted.
Surgical hemorrhoidectomy received the strongest possible recommendation (1A, based on high-quality evidence) for the treatment of patients with external hemorrhoids or a combination of internal and external hemorrhoids with prolapse.
Surgical options described in the recommendations include surgical excision (hemorrhoidectomy), hemorrhoidopexy, and Doppler-guided hemorrhoidectomy, with citations of studies on each procedure. Data from a meta-analysis of 18 randomized prospective studies comparing hemorrhoidectomy with office-based procedures showed that hemorrhoidectomy was “the most effective treatment for patients with grade III hemorrhoids,” but it was associated with greater pain and complication rates, according to the guidelines.
However, complications in general are low after surgical hemorrhoidectomy, with reported complication rates of 1%-2% for the most common complication of postprocedure hemorrhage, the guidelines state. After surgery, the guidelines recommend with a 1B grade (moderate quality evidence) that patients use “a multimodality pain regimen to reduce narcotic usage and promote a faster recovery.”
The committee members had no financial conflicts to disclose.
acssurgerynews@frontlinemedcom.com
SOURCE: Davis BR et al. Dis Colon Rectum. 2018; 61:284-92.
Each year, more than 2.2 million patients in the United States undergo evaluations for symptoms of hemorrhoids, according to updated guidelines on the management of hemorrhoids issued by the American Society of Colon and Rectal Surgeons.
“As a result, it is important to identify symptomatic hemorrhoids as the underlying source of the anorectal symptom and to have a clear understanding of the evaluation and management of this disease process,” wrote Bradley R. Davis, MD, FACS, chief of colon and rectal surgery at the Carolinas Medical Center, Charlotte, N.C., and the fellow members of the Clinical Practice Guidelines Committee of the ASCRS.
The guidelines recommend evaluation of hemorrhoids based on a disease-specific history, and a physical that emphasizes the degree and duration of symptoms and identifies risk factors. But the guideline writers note that the recommendation is a grade 1C because the supporting data mainly come from observational or case studies.
“The cardinal signs of internal hemorrhoids are painless bleeding with bowel movements with intermittent protrusion,” the committee said, also emphasizing that patients should be evaluated for fecal incontinence, which could inform surgical decision making.
In addition, the guidelines call for a complete endoscopic evaluation of the colon for patients who present with symptomatic hemorrhoids and rectal bleeding; this recommendation is based on moderately strong evidence, and presented with a grade of 1B.
Medical management of hemorrhoids may include office-based procedures or surgery, according to the guidelines.
“Most patients with grade I and II and select patients with grade III internal hemorrhoidal disease who fail medical treatment can be effectively treated with office-based procedures, such as banding, sclerotherapy, and infrared coagulation,” the committee wrote, and medical office treatment received a strong grade 1A recommendation based on high-quality evidence. Although office procedures are generally well tolerated, the condition can recur. Bleeding is the most common complication, and it is more likely after rubber-band ligation than other office-based options, the guidelines state.
The guidelines offer a weak recommendation of 2C, based on the lack of quality evidence, for the use of early surgical excision to treat patients with thrombosed external hemorrhoids. “Although most patients treated nonoperatively will experience eventual resolution of their symptoms, excision of thrombosed external hemorrhoids may result in more rapid symptom resolution, lower incidence of recurrence, and longer remission intervals,” the committee noted.
Surgical hemorrhoidectomy received the strongest possible recommendation (1A, based on high-quality evidence) for the treatment of patients with external hemorrhoids or a combination of internal and external hemorrhoids with prolapse.
Surgical options described in the recommendations include surgical excision (hemorrhoidectomy), hemorrhoidopexy, and Doppler-guided hemorrhoidectomy, with citations of studies on each procedure. Data from a meta-analysis of 18 randomized prospective studies comparing hemorrhoidectomy with office-based procedures showed that hemorrhoidectomy was “the most effective treatment for patients with grade III hemorrhoids,” but it was associated with greater pain and complication rates, according to the guidelines.
However, complications in general are low after surgical hemorrhoidectomy, with reported complication rates of 1%-2% for the most common complication of postprocedure hemorrhage, the guidelines state. After surgery, the guidelines recommend with a 1B grade (moderate quality evidence) that patients use “a multimodality pain regimen to reduce narcotic usage and promote a faster recovery.”
The committee members had no financial conflicts to disclose.
acssurgerynews@frontlinemedcom.com
SOURCE: Davis BR et al. Dis Colon Rectum. 2018; 61:284-92.
FROM DISEASES OF THE COLON & RECTUM
VIDEO: Bioimpedance provides accurate assessment of Mohs surgical margins
SAN DIEGO – In assessing tumor-free margins during Mohs micrographic surgery for skin cancer, of histologic sections, in a single-center, pilot study of bioimpedance in 151 specimens from 50 consecutive patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
If the finding of high diagnostic accuracy using bioimpedance spectroscopy is confirmed in larger numbers of patients and specimens run at multiple sites, this approach could “potentially revolutionize what happens with the way Mohs sections are processed in the future” by potentially shaving many minutes off the duration of a standard procedure, Darrell S. Rigel, MD, said in a video interview during the annual meeting of the American Academy of Dermatology.
Usually, it takes 10-20 minutes to process and examine Mohs specimens at each stage of the surgical procedure to determine whether additional excision must remove residual cancer cells, said Dr. Rigel, a dermatologist at New York University. In contrast, assessment for residual cancer cells in the surgical field takes less than a minute using bioimpedance spectroscopy, which relies on differences in electrical conductivity between benign and cancerous cells to identify cancer cells remaining at the surgical margins.
The results of the study were presented in a poster at the meeting, by a research associate of Dr. Rigel’s, Ryan Svoboda, MD, of the National Society for Cutaneous Medicine, New York.
The researchers used a bioimpedance spectroscopy device made by NovaScan to assess 151 histology slides prepared during Mohs micrographic surgery on patients with nonmelanoma skin cancer, and compared the findings against the gold standard of histological slide examination. By this criterion, bioimpedance spectroscopy identified 105 true negatives and 2 false negatives, and 43 true positives and 1 false positive. Calculations showed that this equated to 95.6% sensitivity, 99.1% specificity, a 97.7% positive predictive value, and a 98.1% negative predictive value.
These may be underestimates of the accuracy of bioimpedance spectroscopy because the calculations presume that conventional histology is always correct, but Dr. Rigel noted that sometimes the histological diagnosis is wrong.
SOURCE: Svoboda R et al. Poster 7304.
SAN DIEGO – In assessing tumor-free margins during Mohs micrographic surgery for skin cancer, of histologic sections, in a single-center, pilot study of bioimpedance in 151 specimens from 50 consecutive patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
If the finding of high diagnostic accuracy using bioimpedance spectroscopy is confirmed in larger numbers of patients and specimens run at multiple sites, this approach could “potentially revolutionize what happens with the way Mohs sections are processed in the future” by potentially shaving many minutes off the duration of a standard procedure, Darrell S. Rigel, MD, said in a video interview during the annual meeting of the American Academy of Dermatology.
Usually, it takes 10-20 minutes to process and examine Mohs specimens at each stage of the surgical procedure to determine whether additional excision must remove residual cancer cells, said Dr. Rigel, a dermatologist at New York University. In contrast, assessment for residual cancer cells in the surgical field takes less than a minute using bioimpedance spectroscopy, which relies on differences in electrical conductivity between benign and cancerous cells to identify cancer cells remaining at the surgical margins.
The results of the study were presented in a poster at the meeting, by a research associate of Dr. Rigel’s, Ryan Svoboda, MD, of the National Society for Cutaneous Medicine, New York.
The researchers used a bioimpedance spectroscopy device made by NovaScan to assess 151 histology slides prepared during Mohs micrographic surgery on patients with nonmelanoma skin cancer, and compared the findings against the gold standard of histological slide examination. By this criterion, bioimpedance spectroscopy identified 105 true negatives and 2 false negatives, and 43 true positives and 1 false positive. Calculations showed that this equated to 95.6% sensitivity, 99.1% specificity, a 97.7% positive predictive value, and a 98.1% negative predictive value.
These may be underestimates of the accuracy of bioimpedance spectroscopy because the calculations presume that conventional histology is always correct, but Dr. Rigel noted that sometimes the histological diagnosis is wrong.
SOURCE: Svoboda R et al. Poster 7304.
SAN DIEGO – In assessing tumor-free margins during Mohs micrographic surgery for skin cancer, of histologic sections, in a single-center, pilot study of bioimpedance in 151 specimens from 50 consecutive patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
If the finding of high diagnostic accuracy using bioimpedance spectroscopy is confirmed in larger numbers of patients and specimens run at multiple sites, this approach could “potentially revolutionize what happens with the way Mohs sections are processed in the future” by potentially shaving many minutes off the duration of a standard procedure, Darrell S. Rigel, MD, said in a video interview during the annual meeting of the American Academy of Dermatology.
Usually, it takes 10-20 minutes to process and examine Mohs specimens at each stage of the surgical procedure to determine whether additional excision must remove residual cancer cells, said Dr. Rigel, a dermatologist at New York University. In contrast, assessment for residual cancer cells in the surgical field takes less than a minute using bioimpedance spectroscopy, which relies on differences in electrical conductivity between benign and cancerous cells to identify cancer cells remaining at the surgical margins.
The results of the study were presented in a poster at the meeting, by a research associate of Dr. Rigel’s, Ryan Svoboda, MD, of the National Society for Cutaneous Medicine, New York.
The researchers used a bioimpedance spectroscopy device made by NovaScan to assess 151 histology slides prepared during Mohs micrographic surgery on patients with nonmelanoma skin cancer, and compared the findings against the gold standard of histological slide examination. By this criterion, bioimpedance spectroscopy identified 105 true negatives and 2 false negatives, and 43 true positives and 1 false positive. Calculations showed that this equated to 95.6% sensitivity, 99.1% specificity, a 97.7% positive predictive value, and a 98.1% negative predictive value.
These may be underestimates of the accuracy of bioimpedance spectroscopy because the calculations presume that conventional histology is always correct, but Dr. Rigel noted that sometimes the histological diagnosis is wrong.
SOURCE: Svoboda R et al. Poster 7304.
REPORTING FROM AAD 18
Key clinical point: Bioimpedance spectroscopy showed excellent diagnostic accuracy for cancer cells on Mohs surgical margins.
Major finding: Bioimpedance spectroscopy had a sensitivity of 95.6% and specificity of 99.1% compared with Mohs histology.
Study details: A single-center pilot study with 151 Mohs surgical specimens taken from 50 patients.
Disclosures: The study was funded by NovaScan, the company developing the device tested in the study. Dr. Rigel has been a consultant to NovaScan and to Castle Biosciences, DermTech, Ferndale, Myriad, and Neutrogena, and has received research support from Castle and Neutrogena.
Source: Svoboda R et al. Poster 7304.
Anti–IL-33 antibody stakes a first-in-class claim on moderate to severe atopic dermatitis
SAN DIEGO – and will proceed along its developmental pathway.
All 12 patients who received one intravenous infusion of ANB020 achieved at least a 50% reduction in their Eczema Area and Severity Index (EASI) by day 29, Graham Ogg, MD, said at the annual meeting of the American Academy of Dermatology. Most of the improvement occurred in the first 2 weeks, was largely sustained for 2 months, then gradually began to fade, said Dr. Ogg, professor of dermatology at Oxford University, England.
The EASI improvement, along with improvements in itch and clinical assessment, are enough to propel ANB020 into a phase 2b, placebo-controlled, randomized trial, which Dr. Ogg said would recruit 200 to 300 adults with moderate to severe atomic dermatitis (AD).
ANB020 is a selective inhibitor of interleukin-33 (IL-33), which is highly expressed in the lesions of AD, Dr. Ogg said. “IL-33 is produced by a number of cells, including keratinocytes and epithelial cells. It’s an alarm molecule predominately produced after damage to keratinocytes; for example, after an allergenic challenge to the skin.”
The antibody has already passed its phase 1 trials, which included both a fixed and ascending dose study of 10 mg to 750 mg in healthy adults. ANB020 has a long half-life of 16 days after IV infusion or subcutaneous injection, inhibits IL-33 for up to 85 days, and has no apparent dose-limiting toxicities.
The phase 2a study comprised 12 adults (mean age 40 years) with a mean EASI score of 32, Dr. Ogg reported. The mean Investigator’s Global Assessment score was 4, and the mean Severity Scoring of Atopic Dermatitis almost 65. Patients had high itch scores and scored a mean of 13 on the Dermatology Life Quality Index. All were inadequately controlled on topical corticosteroids, and about half had failed at least one systemic immunomodulator.
Following a washout period, all subjects received an initial placebo infusion, and 1 week later received a single 300-mg infusion of ANB020. The primary endpoint – at least a 50% reduction in EASI score (EASI-50) – was assessed at day 29, with close follow-up until day 140.
By day 15, nine patients (75%) had achieved EASI-50, and three (25%) had achieved a 75% reduction in EASI score (EASI-75). The average EASI score reduction was 58% at that point. By day 29, 10 (83%) had achieved EASI-50, and 4 (33%), EASI-75. This benefit was largely maintained until day 78, when it began to tail off somewhat. By day 140, five patients (42%) still had an EASI-50 and three (25%), an EASI-75.
Three patients (25%) achieved an Investigator’s Global Assessment score of 0 or 1, indicating clear or almost clear skin. On day 29, the average pruritus decrease was 32%, which dropped to 21% by day 140. The average Severity Scoring of Atopic Dermatitis reduction was 40% on day 29 and 32% on day 140. The average Dermatology Life Quality Index reduction was 45% on day 29 and 43% on day 140.
ANB020 was well tolerated with no drug-related safety signals. Dizziness occurred in 17% of subjects, and mild headache in 25%. There was one serious adverse event, a case of major depression that occurred on day 140. This was consistent with the patient’s baseline health history and deemed unrelated to the study drug.
According to an AnaptysBio press release, ANB020 is also being investigated in a double-blind, placebo-controlled study of 20 adults with severe peanut allergy. The company also is enrolling a 24-patient randomized, double-blind, placebo-controlled, phase 2a trial in adults with severe eosinophilic asthma.
Topline data from both of these studies are expected soon, the website noted.
AnaptysBio funded Dr. Ogg’s travel and registration fees for the meeting. He said he had no other financial disclosures relevant to ANB020.
SOURCE: Ogg G et al. AAD 2018. Abstract 6658.
SAN DIEGO – and will proceed along its developmental pathway.
All 12 patients who received one intravenous infusion of ANB020 achieved at least a 50% reduction in their Eczema Area and Severity Index (EASI) by day 29, Graham Ogg, MD, said at the annual meeting of the American Academy of Dermatology. Most of the improvement occurred in the first 2 weeks, was largely sustained for 2 months, then gradually began to fade, said Dr. Ogg, professor of dermatology at Oxford University, England.
The EASI improvement, along with improvements in itch and clinical assessment, are enough to propel ANB020 into a phase 2b, placebo-controlled, randomized trial, which Dr. Ogg said would recruit 200 to 300 adults with moderate to severe atomic dermatitis (AD).
ANB020 is a selective inhibitor of interleukin-33 (IL-33), which is highly expressed in the lesions of AD, Dr. Ogg said. “IL-33 is produced by a number of cells, including keratinocytes and epithelial cells. It’s an alarm molecule predominately produced after damage to keratinocytes; for example, after an allergenic challenge to the skin.”
The antibody has already passed its phase 1 trials, which included both a fixed and ascending dose study of 10 mg to 750 mg in healthy adults. ANB020 has a long half-life of 16 days after IV infusion or subcutaneous injection, inhibits IL-33 for up to 85 days, and has no apparent dose-limiting toxicities.
The phase 2a study comprised 12 adults (mean age 40 years) with a mean EASI score of 32, Dr. Ogg reported. The mean Investigator’s Global Assessment score was 4, and the mean Severity Scoring of Atopic Dermatitis almost 65. Patients had high itch scores and scored a mean of 13 on the Dermatology Life Quality Index. All were inadequately controlled on topical corticosteroids, and about half had failed at least one systemic immunomodulator.
Following a washout period, all subjects received an initial placebo infusion, and 1 week later received a single 300-mg infusion of ANB020. The primary endpoint – at least a 50% reduction in EASI score (EASI-50) – was assessed at day 29, with close follow-up until day 140.
By day 15, nine patients (75%) had achieved EASI-50, and three (25%) had achieved a 75% reduction in EASI score (EASI-75). The average EASI score reduction was 58% at that point. By day 29, 10 (83%) had achieved EASI-50, and 4 (33%), EASI-75. This benefit was largely maintained until day 78, when it began to tail off somewhat. By day 140, five patients (42%) still had an EASI-50 and three (25%), an EASI-75.
Three patients (25%) achieved an Investigator’s Global Assessment score of 0 or 1, indicating clear or almost clear skin. On day 29, the average pruritus decrease was 32%, which dropped to 21% by day 140. The average Severity Scoring of Atopic Dermatitis reduction was 40% on day 29 and 32% on day 140. The average Dermatology Life Quality Index reduction was 45% on day 29 and 43% on day 140.
ANB020 was well tolerated with no drug-related safety signals. Dizziness occurred in 17% of subjects, and mild headache in 25%. There was one serious adverse event, a case of major depression that occurred on day 140. This was consistent with the patient’s baseline health history and deemed unrelated to the study drug.
According to an AnaptysBio press release, ANB020 is also being investigated in a double-blind, placebo-controlled study of 20 adults with severe peanut allergy. The company also is enrolling a 24-patient randomized, double-blind, placebo-controlled, phase 2a trial in adults with severe eosinophilic asthma.
Topline data from both of these studies are expected soon, the website noted.
AnaptysBio funded Dr. Ogg’s travel and registration fees for the meeting. He said he had no other financial disclosures relevant to ANB020.
SOURCE: Ogg G et al. AAD 2018. Abstract 6658.
SAN DIEGO – and will proceed along its developmental pathway.
All 12 patients who received one intravenous infusion of ANB020 achieved at least a 50% reduction in their Eczema Area and Severity Index (EASI) by day 29, Graham Ogg, MD, said at the annual meeting of the American Academy of Dermatology. Most of the improvement occurred in the first 2 weeks, was largely sustained for 2 months, then gradually began to fade, said Dr. Ogg, professor of dermatology at Oxford University, England.
The EASI improvement, along with improvements in itch and clinical assessment, are enough to propel ANB020 into a phase 2b, placebo-controlled, randomized trial, which Dr. Ogg said would recruit 200 to 300 adults with moderate to severe atomic dermatitis (AD).
ANB020 is a selective inhibitor of interleukin-33 (IL-33), which is highly expressed in the lesions of AD, Dr. Ogg said. “IL-33 is produced by a number of cells, including keratinocytes and epithelial cells. It’s an alarm molecule predominately produced after damage to keratinocytes; for example, after an allergenic challenge to the skin.”
The antibody has already passed its phase 1 trials, which included both a fixed and ascending dose study of 10 mg to 750 mg in healthy adults. ANB020 has a long half-life of 16 days after IV infusion or subcutaneous injection, inhibits IL-33 for up to 85 days, and has no apparent dose-limiting toxicities.
The phase 2a study comprised 12 adults (mean age 40 years) with a mean EASI score of 32, Dr. Ogg reported. The mean Investigator’s Global Assessment score was 4, and the mean Severity Scoring of Atopic Dermatitis almost 65. Patients had high itch scores and scored a mean of 13 on the Dermatology Life Quality Index. All were inadequately controlled on topical corticosteroids, and about half had failed at least one systemic immunomodulator.
Following a washout period, all subjects received an initial placebo infusion, and 1 week later received a single 300-mg infusion of ANB020. The primary endpoint – at least a 50% reduction in EASI score (EASI-50) – was assessed at day 29, with close follow-up until day 140.
By day 15, nine patients (75%) had achieved EASI-50, and three (25%) had achieved a 75% reduction in EASI score (EASI-75). The average EASI score reduction was 58% at that point. By day 29, 10 (83%) had achieved EASI-50, and 4 (33%), EASI-75. This benefit was largely maintained until day 78, when it began to tail off somewhat. By day 140, five patients (42%) still had an EASI-50 and three (25%), an EASI-75.
Three patients (25%) achieved an Investigator’s Global Assessment score of 0 or 1, indicating clear or almost clear skin. On day 29, the average pruritus decrease was 32%, which dropped to 21% by day 140. The average Severity Scoring of Atopic Dermatitis reduction was 40% on day 29 and 32% on day 140. The average Dermatology Life Quality Index reduction was 45% on day 29 and 43% on day 140.
ANB020 was well tolerated with no drug-related safety signals. Dizziness occurred in 17% of subjects, and mild headache in 25%. There was one serious adverse event, a case of major depression that occurred on day 140. This was consistent with the patient’s baseline health history and deemed unrelated to the study drug.
According to an AnaptysBio press release, ANB020 is also being investigated in a double-blind, placebo-controlled study of 20 adults with severe peanut allergy. The company also is enrolling a 24-patient randomized, double-blind, placebo-controlled, phase 2a trial in adults with severe eosinophilic asthma.
Topline data from both of these studies are expected soon, the website noted.
AnaptysBio funded Dr. Ogg’s travel and registration fees for the meeting. He said he had no other financial disclosures relevant to ANB020.
SOURCE: Ogg G et al. AAD 2018. Abstract 6658.
REPORTING FROM AAD 2018
Key clinical point: ANB020 improved skin involvement and itch in a small phase 2 study.
Major finding: All patients who received one infusion achieved at least a 50% reduction in their EASI scores by day 29.
Study details: The phase 2a study comprised 12 patients with moderate to severe AD.
Disclosures: AnaptysBio is developing the molecule. The company paid Dr. Ogg’s travel and meeting registration fees.
Source: Ogg G et al. AAD 2018. Abstract 6658.
Defining incisional hernia risk in IBD surgery
Open surgery for inflammatory bowel disease (IBD) has been known to carry a high risk of incisional hernia, but the risk factors have not been well understood.
A review of 1,000 operations performed over nearly 40 years at a high-volume, nationally recognized center has identified five patient factors that can raise the risk of incisional hernia in these operations by 50% or more, according to a study published in the Annals of Surgery.
The study followed the patients for an average of 8 years after their operations, which were performed between January 1976 and December 2014 at Mount Sinai Medical Center in New York. The overall incidence of incisional hernia was 20%-21% for patients with ulcerative colitis and 20% for those with Crohn’s disease.
Half of these patients developed an incisional hernia less than 2 years after the index surgery and 75% in less than 4 years.
The researchers identified the following statistically significant risk factors for incisional hernia: wound infection (hazard ratio, 3.66; P less than .001); hypoalbuminemia (HR, 2.02; P = .002); previous bowel resection (HR, 1.6; P = .003); ileostomy created at time of procedure (HR, 1.53; P = .01); and a history of smoking (HR, 1.52; P less than .013). Other risk factors to lesser degrees are body mass index at time of surgery (HR, 1.036; P = .009); age at time of surgery (HR, 1.021; P less than .001), and age at disease onset (HR, 1.018; P less than .001).
Lead author Tomas Heimann, MD, and his coauthors pointed out that this study population had severe levels of disease. Almost half of the patients had severe intractable disease that had resisted medical treatment. More than a quarter of these patients had received preoperative steroid therapy within 6 weeks, and 15% had received recent immunosuppressive therapy. Almost 80% were either anemic or had hypoalbuminemia or both. The average duration of disease was 12 years. More than half had undergone previous bowel surgery – “often lengthy and difficult” – with many patients suffering from fistulae, abscesses, and dense adhesions. “These factors were more likely to predispose patients to develop wound infections and delayed healing resulting in incisional hernia in one-fifth of our patients,” Dr. Heimann and his coauthors noted.
A somewhat unexpected finding was that immunosuppressive therapy and steroids were not linked to incisional hernia in these patients.
Prophylactic mesh placement in patients with IBD is impractical because of the risk of infection it carries, Dr. Heimann and his coauthors said.
Dr. Heimann and his coauthors reported having no financial disclosures.
SOURCE: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
Open surgery for inflammatory bowel disease (IBD) has been known to carry a high risk of incisional hernia, but the risk factors have not been well understood.
A review of 1,000 operations performed over nearly 40 years at a high-volume, nationally recognized center has identified five patient factors that can raise the risk of incisional hernia in these operations by 50% or more, according to a study published in the Annals of Surgery.
The study followed the patients for an average of 8 years after their operations, which were performed between January 1976 and December 2014 at Mount Sinai Medical Center in New York. The overall incidence of incisional hernia was 20%-21% for patients with ulcerative colitis and 20% for those with Crohn’s disease.
Half of these patients developed an incisional hernia less than 2 years after the index surgery and 75% in less than 4 years.
The researchers identified the following statistically significant risk factors for incisional hernia: wound infection (hazard ratio, 3.66; P less than .001); hypoalbuminemia (HR, 2.02; P = .002); previous bowel resection (HR, 1.6; P = .003); ileostomy created at time of procedure (HR, 1.53; P = .01); and a history of smoking (HR, 1.52; P less than .013). Other risk factors to lesser degrees are body mass index at time of surgery (HR, 1.036; P = .009); age at time of surgery (HR, 1.021; P less than .001), and age at disease onset (HR, 1.018; P less than .001).
Lead author Tomas Heimann, MD, and his coauthors pointed out that this study population had severe levels of disease. Almost half of the patients had severe intractable disease that had resisted medical treatment. More than a quarter of these patients had received preoperative steroid therapy within 6 weeks, and 15% had received recent immunosuppressive therapy. Almost 80% were either anemic or had hypoalbuminemia or both. The average duration of disease was 12 years. More than half had undergone previous bowel surgery – “often lengthy and difficult” – with many patients suffering from fistulae, abscesses, and dense adhesions. “These factors were more likely to predispose patients to develop wound infections and delayed healing resulting in incisional hernia in one-fifth of our patients,” Dr. Heimann and his coauthors noted.
A somewhat unexpected finding was that immunosuppressive therapy and steroids were not linked to incisional hernia in these patients.
Prophylactic mesh placement in patients with IBD is impractical because of the risk of infection it carries, Dr. Heimann and his coauthors said.
Dr. Heimann and his coauthors reported having no financial disclosures.
SOURCE: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
Open surgery for inflammatory bowel disease (IBD) has been known to carry a high risk of incisional hernia, but the risk factors have not been well understood.
A review of 1,000 operations performed over nearly 40 years at a high-volume, nationally recognized center has identified five patient factors that can raise the risk of incisional hernia in these operations by 50% or more, according to a study published in the Annals of Surgery.
The study followed the patients for an average of 8 years after their operations, which were performed between January 1976 and December 2014 at Mount Sinai Medical Center in New York. The overall incidence of incisional hernia was 20%-21% for patients with ulcerative colitis and 20% for those with Crohn’s disease.
Half of these patients developed an incisional hernia less than 2 years after the index surgery and 75% in less than 4 years.
The researchers identified the following statistically significant risk factors for incisional hernia: wound infection (hazard ratio, 3.66; P less than .001); hypoalbuminemia (HR, 2.02; P = .002); previous bowel resection (HR, 1.6; P = .003); ileostomy created at time of procedure (HR, 1.53; P = .01); and a history of smoking (HR, 1.52; P less than .013). Other risk factors to lesser degrees are body mass index at time of surgery (HR, 1.036; P = .009); age at time of surgery (HR, 1.021; P less than .001), and age at disease onset (HR, 1.018; P less than .001).
Lead author Tomas Heimann, MD, and his coauthors pointed out that this study population had severe levels of disease. Almost half of the patients had severe intractable disease that had resisted medical treatment. More than a quarter of these patients had received preoperative steroid therapy within 6 weeks, and 15% had received recent immunosuppressive therapy. Almost 80% were either anemic or had hypoalbuminemia or both. The average duration of disease was 12 years. More than half had undergone previous bowel surgery – “often lengthy and difficult” – with many patients suffering from fistulae, abscesses, and dense adhesions. “These factors were more likely to predispose patients to develop wound infections and delayed healing resulting in incisional hernia in one-fifth of our patients,” Dr. Heimann and his coauthors noted.
A somewhat unexpected finding was that immunosuppressive therapy and steroids were not linked to incisional hernia in these patients.
Prophylactic mesh placement in patients with IBD is impractical because of the risk of infection it carries, Dr. Heimann and his coauthors said.
Dr. Heimann and his coauthors reported having no financial disclosures.
SOURCE: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
FROM ANNALS OF SURGERY
Key clinical point: Patients with IBD have a high incidence of incisional hernia after open bowel resection.
Major finding: The overall incidence of incisional hernia after open bowel resection was 20%.
Data source: One thousand patients who had undergone open bowel surgery for IBD at Mount Sinai Medical Center, New York, between January 1976 and December 2014.
Disclosures: Dr. Heimann and his coauthors reported having no financial disclosures.
Source: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
Social recovery therapy, early intervention ‘superior’ in first-episode psychosis
Adding social recovery therapy to early intervention services significantly improved social function, compared with early intervention alone for young first-episode psychosis patients with extreme social withdrawal, according to data from 155 patients.
“New interventions targeting functional and social recovery are needed in people with first-episode psychosis,” wrote David Fowler of the psychology department at the University of Sussex, Brighton, England, and his colleagues.
In a study known as SUPEREDEN3, published in The Lancet Psychiatry, the researchers randomized 76 patients aged 16-35 years to social recovery therapy plus early intervention and 79 to early intervention alone. The study participants were selected between Oct. 1, 2012, and June 20, 2014, and suffered from extreme social withdrawal as well as complex comorbidities, including anxiety and depression, hopelessness, and residual and treatment-resistant positive psychotic symptoms.
The social recovery therapy, delivered in three stages, included working with the patients to identify new activities and to get them engaged in those pursuits. “Therapists adopt an assertive outreach style of contact, most frequently visiting people at home or in community settings,” the researchers wrote. “Therapists are also encouraged to work systematically with family members, employers, and educational providers to discuss and overcome potential problems that could impede social recovery.”
. Structured activity was defined as time spent over the previous month on activities, including work, education, volunteering, leisure activities, sports, housework or other chores, and child care. No adverse events related to the intervention were reported.
“Our findings show that social recovery therapy plus early intervention services is superior to early intervention services alone on the primary outcome of time spent in structured activity,” Mr. Fowler and his colleagues wrote.
The findings were limited by the lack of data from secondary outcomes, in part because of the challenges of following up with a withdrawn study population, the researchers said. However, they said, the study is the first to show benefits of social recovery therapy in this challenging group.
The results offer “encouragement for practitioners in early intervention services to focus on this subgroup who are often neglected. Our results also suggest that social recovery therapy techniques could be a useful addition in this group,” the researchers said.
The National Institute for Health Research funded the study. The researchers had no financial conflicts to disclose.
SOURCE: Fowler D et al. Lancet Psychiatry. 2018 Jan;5(1):41-50.
Helping patients with first-episode psychosis improve their social function remains a challenge, Nikolai Albert, MD, and his coauthors wrote in an accompanying editorial. Social recovery therapy could help those patients but must be approached respectfully, they noted.
“The focus on everyday life in social recovery therapy has some promising elements, and seemingly can serve as a supplement to other established forms of individual support,” they wrote.
Social recovery therapy could be a tool to help guide patients with severe social withdrawal back to community living, said Dr. Albert and his coauthors. Despite the small sample size and absence of adequate 15-month follow-up data to show whether the effects of the therapy persist, the findings remain statistically significant and clinically relevant – and offer a promising option for a severely debilitated group of patients, they added (Lancet Psychiatry. 2018 Jan;5[1]:3-4).
Dr. Albert is affiliated with Mental Health Centre Copenhagen at the University of Copenhagen. The authors had no financial conflicts to disclose.
Helping patients with first-episode psychosis improve their social function remains a challenge, Nikolai Albert, MD, and his coauthors wrote in an accompanying editorial. Social recovery therapy could help those patients but must be approached respectfully, they noted.
“The focus on everyday life in social recovery therapy has some promising elements, and seemingly can serve as a supplement to other established forms of individual support,” they wrote.
Social recovery therapy could be a tool to help guide patients with severe social withdrawal back to community living, said Dr. Albert and his coauthors. Despite the small sample size and absence of adequate 15-month follow-up data to show whether the effects of the therapy persist, the findings remain statistically significant and clinically relevant – and offer a promising option for a severely debilitated group of patients, they added (Lancet Psychiatry. 2018 Jan;5[1]:3-4).
Dr. Albert is affiliated with Mental Health Centre Copenhagen at the University of Copenhagen. The authors had no financial conflicts to disclose.
Helping patients with first-episode psychosis improve their social function remains a challenge, Nikolai Albert, MD, and his coauthors wrote in an accompanying editorial. Social recovery therapy could help those patients but must be approached respectfully, they noted.
“The focus on everyday life in social recovery therapy has some promising elements, and seemingly can serve as a supplement to other established forms of individual support,” they wrote.
Social recovery therapy could be a tool to help guide patients with severe social withdrawal back to community living, said Dr. Albert and his coauthors. Despite the small sample size and absence of adequate 15-month follow-up data to show whether the effects of the therapy persist, the findings remain statistically significant and clinically relevant – and offer a promising option for a severely debilitated group of patients, they added (Lancet Psychiatry. 2018 Jan;5[1]:3-4).
Dr. Albert is affiliated with Mental Health Centre Copenhagen at the University of Copenhagen. The authors had no financial conflicts to disclose.
Adding social recovery therapy to early intervention services significantly improved social function, compared with early intervention alone for young first-episode psychosis patients with extreme social withdrawal, according to data from 155 patients.
“New interventions targeting functional and social recovery are needed in people with first-episode psychosis,” wrote David Fowler of the psychology department at the University of Sussex, Brighton, England, and his colleagues.
In a study known as SUPEREDEN3, published in The Lancet Psychiatry, the researchers randomized 76 patients aged 16-35 years to social recovery therapy plus early intervention and 79 to early intervention alone. The study participants were selected between Oct. 1, 2012, and June 20, 2014, and suffered from extreme social withdrawal as well as complex comorbidities, including anxiety and depression, hopelessness, and residual and treatment-resistant positive psychotic symptoms.
The social recovery therapy, delivered in three stages, included working with the patients to identify new activities and to get them engaged in those pursuits. “Therapists adopt an assertive outreach style of contact, most frequently visiting people at home or in community settings,” the researchers wrote. “Therapists are also encouraged to work systematically with family members, employers, and educational providers to discuss and overcome potential problems that could impede social recovery.”
. Structured activity was defined as time spent over the previous month on activities, including work, education, volunteering, leisure activities, sports, housework or other chores, and child care. No adverse events related to the intervention were reported.
“Our findings show that social recovery therapy plus early intervention services is superior to early intervention services alone on the primary outcome of time spent in structured activity,” Mr. Fowler and his colleagues wrote.
The findings were limited by the lack of data from secondary outcomes, in part because of the challenges of following up with a withdrawn study population, the researchers said. However, they said, the study is the first to show benefits of social recovery therapy in this challenging group.
The results offer “encouragement for practitioners in early intervention services to focus on this subgroup who are often neglected. Our results also suggest that social recovery therapy techniques could be a useful addition in this group,” the researchers said.
The National Institute for Health Research funded the study. The researchers had no financial conflicts to disclose.
SOURCE: Fowler D et al. Lancet Psychiatry. 2018 Jan;5(1):41-50.
Adding social recovery therapy to early intervention services significantly improved social function, compared with early intervention alone for young first-episode psychosis patients with extreme social withdrawal, according to data from 155 patients.
“New interventions targeting functional and social recovery are needed in people with first-episode psychosis,” wrote David Fowler of the psychology department at the University of Sussex, Brighton, England, and his colleagues.
In a study known as SUPEREDEN3, published in The Lancet Psychiatry, the researchers randomized 76 patients aged 16-35 years to social recovery therapy plus early intervention and 79 to early intervention alone. The study participants were selected between Oct. 1, 2012, and June 20, 2014, and suffered from extreme social withdrawal as well as complex comorbidities, including anxiety and depression, hopelessness, and residual and treatment-resistant positive psychotic symptoms.
The social recovery therapy, delivered in three stages, included working with the patients to identify new activities and to get them engaged in those pursuits. “Therapists adopt an assertive outreach style of contact, most frequently visiting people at home or in community settings,” the researchers wrote. “Therapists are also encouraged to work systematically with family members, employers, and educational providers to discuss and overcome potential problems that could impede social recovery.”
. Structured activity was defined as time spent over the previous month on activities, including work, education, volunteering, leisure activities, sports, housework or other chores, and child care. No adverse events related to the intervention were reported.
“Our findings show that social recovery therapy plus early intervention services is superior to early intervention services alone on the primary outcome of time spent in structured activity,” Mr. Fowler and his colleagues wrote.
The findings were limited by the lack of data from secondary outcomes, in part because of the challenges of following up with a withdrawn study population, the researchers said. However, they said, the study is the first to show benefits of social recovery therapy in this challenging group.
The results offer “encouragement for practitioners in early intervention services to focus on this subgroup who are often neglected. Our results also suggest that social recovery therapy techniques could be a useful addition in this group,” the researchers said.
The National Institute for Health Research funded the study. The researchers had no financial conflicts to disclose.
SOURCE: Fowler D et al. Lancet Psychiatry. 2018 Jan;5(1):41-50.
FROM THE LANCET PSYCHIATRY
Key clinical point: Adding social recovery therapy significantly improved function in first-episode psychosis patients, compared with early intervention alone.
Major finding: After 9 months, the intervention group averaged 8 more hours of structured activity compared with controls.
Study details: A randomized trial of 155 patients aged 16-35 years.
Disclosures: The National Institute for Health Research funded the study. The investigators had no financial conflicts to disclose.
Source: Fowler D et al. Lancet Psychiatry 2018 Jan;5:41-50.
Pre–bariatric surgery weight loss improves outcomes
Preoperative weight loss improves bariatric surgery outcomes, according to findings from a single-institution retrospective analysis. The weight loss came from following a 4-week low-calorie diet (LCD) and was of greatest benefit to patients who lost 8% or more of their excess weight. These patients had a greater loss of excess weight in the 12 months following surgery, as well as shorter average hospital length of stay.
The results appeared online in the Journal of the American College of Surgeons.
Preliminary studies indicated that short-term weight loss before surgery might reduce surgical complexity by reducing the size of the liver and intra-abdominal fat mass, but it remained uncertain what effect weight loss might have on long-term outcomes.
The LCD included 1,200 kcal/day (45% carbohydrates, 35% protein, 20% fat), which were consumed through five meal-replacement products and one food-based meal. Liquids included at least 80 ounces of calorie-free, caffeine-free, carbonation-free beverages per day. Patients were also instructed to conduct 30 minutes of moderate to vigorous activity per day.
Deborah A. Hutcheon, DCN, and her fellow researchers analyzed data from their own institution, where a presurgical 4-week LCD with a target loss of 8% or more of excess weight had been standard policy already. The population included 355 patients who underwent sleeve gastrectomy (n = 167) or Roux-en-Y gastric bypass (n = 188) between January 2014 and January 2016.
Almost two-thirds (63.3%) of patients achieved the target weight loss before surgery. There were some differences between the two groups. The group that achieved the target contained a greater proportion of men than did the other group (25.5% vs. 13.7%, respectively; P = .013), a higher proportion of white patients (84.8% vs. 74.1%; P = .011), and a higher proportion of patients taking antihypertensive medications (68.3% vs. 57.3%; P = .048). The two groups had similar rates of preoperative comorbidities and surgery types.
Those who achieved the target weight loss had a shorter hospital length of stay (1.8 days vs. 2.1 days; P = .006). They also had a higher percentage loss of excess weight at 3 months (42.3% vs. 36.1%; P less than .001), 6 months (56.0% vs. 47.5%; P less than .001), and at 12 months (65.1% vs. 55.7%; P = .003).
After controlling for patient characteristics, insurance status, 12-month diet compliance, and surgery type, successful presurgery weight loss was associated with greater weight loss at 12 months.
The AGA Obesity Practice Guide was created to provide a comprehensive, multidisciplinary process to personalize innovative obesity care for safe and effective weight management, including nonsurgical and endoscopic management of obesity. Learn more at www.gastro.org/obesity.
SOURCE: Hutcheon DA et al. J Am Coll Surgeons. 2018 Jan 31. doi: 10.1016/j.jamcollsurg.2017.12.032.
Preoperative weight loss improves bariatric surgery outcomes, according to findings from a single-institution retrospective analysis. The weight loss came from following a 4-week low-calorie diet (LCD) and was of greatest benefit to patients who lost 8% or more of their excess weight. These patients had a greater loss of excess weight in the 12 months following surgery, as well as shorter average hospital length of stay.
The results appeared online in the Journal of the American College of Surgeons.
Preliminary studies indicated that short-term weight loss before surgery might reduce surgical complexity by reducing the size of the liver and intra-abdominal fat mass, but it remained uncertain what effect weight loss might have on long-term outcomes.
The LCD included 1,200 kcal/day (45% carbohydrates, 35% protein, 20% fat), which were consumed through five meal-replacement products and one food-based meal. Liquids included at least 80 ounces of calorie-free, caffeine-free, carbonation-free beverages per day. Patients were also instructed to conduct 30 minutes of moderate to vigorous activity per day.
Deborah A. Hutcheon, DCN, and her fellow researchers analyzed data from their own institution, where a presurgical 4-week LCD with a target loss of 8% or more of excess weight had been standard policy already. The population included 355 patients who underwent sleeve gastrectomy (n = 167) or Roux-en-Y gastric bypass (n = 188) between January 2014 and January 2016.
Almost two-thirds (63.3%) of patients achieved the target weight loss before surgery. There were some differences between the two groups. The group that achieved the target contained a greater proportion of men than did the other group (25.5% vs. 13.7%, respectively; P = .013), a higher proportion of white patients (84.8% vs. 74.1%; P = .011), and a higher proportion of patients taking antihypertensive medications (68.3% vs. 57.3%; P = .048). The two groups had similar rates of preoperative comorbidities and surgery types.
Those who achieved the target weight loss had a shorter hospital length of stay (1.8 days vs. 2.1 days; P = .006). They also had a higher percentage loss of excess weight at 3 months (42.3% vs. 36.1%; P less than .001), 6 months (56.0% vs. 47.5%; P less than .001), and at 12 months (65.1% vs. 55.7%; P = .003).
After controlling for patient characteristics, insurance status, 12-month diet compliance, and surgery type, successful presurgery weight loss was associated with greater weight loss at 12 months.
The AGA Obesity Practice Guide was created to provide a comprehensive, multidisciplinary process to personalize innovative obesity care for safe and effective weight management, including nonsurgical and endoscopic management of obesity. Learn more at www.gastro.org/obesity.
SOURCE: Hutcheon DA et al. J Am Coll Surgeons. 2018 Jan 31. doi: 10.1016/j.jamcollsurg.2017.12.032.
Preoperative weight loss improves bariatric surgery outcomes, according to findings from a single-institution retrospective analysis. The weight loss came from following a 4-week low-calorie diet (LCD) and was of greatest benefit to patients who lost 8% or more of their excess weight. These patients had a greater loss of excess weight in the 12 months following surgery, as well as shorter average hospital length of stay.
The results appeared online in the Journal of the American College of Surgeons.
Preliminary studies indicated that short-term weight loss before surgery might reduce surgical complexity by reducing the size of the liver and intra-abdominal fat mass, but it remained uncertain what effect weight loss might have on long-term outcomes.
The LCD included 1,200 kcal/day (45% carbohydrates, 35% protein, 20% fat), which were consumed through five meal-replacement products and one food-based meal. Liquids included at least 80 ounces of calorie-free, caffeine-free, carbonation-free beverages per day. Patients were also instructed to conduct 30 minutes of moderate to vigorous activity per day.
Deborah A. Hutcheon, DCN, and her fellow researchers analyzed data from their own institution, where a presurgical 4-week LCD with a target loss of 8% or more of excess weight had been standard policy already. The population included 355 patients who underwent sleeve gastrectomy (n = 167) or Roux-en-Y gastric bypass (n = 188) between January 2014 and January 2016.
Almost two-thirds (63.3%) of patients achieved the target weight loss before surgery. There were some differences between the two groups. The group that achieved the target contained a greater proportion of men than did the other group (25.5% vs. 13.7%, respectively; P = .013), a higher proportion of white patients (84.8% vs. 74.1%; P = .011), and a higher proportion of patients taking antihypertensive medications (68.3% vs. 57.3%; P = .048). The two groups had similar rates of preoperative comorbidities and surgery types.
Those who achieved the target weight loss had a shorter hospital length of stay (1.8 days vs. 2.1 days; P = .006). They also had a higher percentage loss of excess weight at 3 months (42.3% vs. 36.1%; P less than .001), 6 months (56.0% vs. 47.5%; P less than .001), and at 12 months (65.1% vs. 55.7%; P = .003).
After controlling for patient characteristics, insurance status, 12-month diet compliance, and surgery type, successful presurgery weight loss was associated with greater weight loss at 12 months.
The AGA Obesity Practice Guide was created to provide a comprehensive, multidisciplinary process to personalize innovative obesity care for safe and effective weight management, including nonsurgical and endoscopic management of obesity. Learn more at www.gastro.org/obesity.
SOURCE: Hutcheon DA et al. J Am Coll Surgeons. 2018 Jan 31. doi: 10.1016/j.jamcollsurg.2017.12.032.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Weight loss before bariatric surgery boosts results.
Major finding: Patients who lost at least 8% of excess body weight had an average of 65.1% loss of excess weight at 12 months, compared with the 55.7% seen in those who did not.
Data source: Retrospective, single-center analysis (n = 355).
Disclosures: No source of funding was disclosed.
Source: Hutcheon DA et al. J Am Coll Surgeons. 2018 Jan 31. doi: 10.1016/j.jamcollsurg.2017.12.032.
Transfusion threshold and bleeding risk in malignancy-related thrombocytopenia
Background: The association between platelet counts, risk of bleeding, and transfusions in patients with thrombocytopenia related to stem cell transplant (SCT) or chemotherapy is not clear, except at very low platelet counts.
Study design: Secondary analysis of a multicenter, randomized controlled trial, stratified by cause of thrombocytopenia: autologous or syngeneic SCT (AUTO), allogeneic SCT (ALLO), or chemotherapy for hematologic malignancy without SCT (CHEMO).
Setting: Twenty-six hospitals from 2004 to 2007.
Synopsis: The PLADO trial enrolled more than 1,200 patients aged 18 years and older expected to experience a period of hypoproliferative thrombocytopenia as a result of chemotherapy or SCT, and randomized them to low, medium, or high doses of prophylactic platelets. This secondary analysis assessed laboratory predictors of bleeding, and the effect of transfusion.
Of 1,077 patients who received platelet transfusions, there were no differences between dose groups for any bleeding outcomes. Over a wide range of platelet counts, the ALLO stratum had a higher risk of bleeding than other strata, with clinically significant bleeding on 21% of patient-days in the ALLO stratum, compared with 19% in the AUTO stratum and 11% in the CHEMO stratum (P less than .001). Risk for bleeding was significantly higher at platelet counts of equal to or less than 5x109/L compared with platelet counts greater than or equal to 81x109/L. Higher aPTT and INR were also associated with higher risk of clinically significant bleeding. In a multipredictor model, only hematocrit was significantly associated with more severe bleeding. Neither platelet transfusion nor RBC transfusion reduced the risk of bleeding on the following day, although the authors note some possibility of confounding by indication.
Bottom line: Predictors of overall increased risk for bleeding in patients with secondary hypoproliferative thrombocytopenia were treatment stratum, platelet counts less than or equal to 5x109/L, hematocrit less than 25%, INR greater than 1.2, and aPTT greater than 30 seconds. This study challenges the conventional wisdom that transfusions reduce bleeding risk in patients with secondary hypoproliferative thrombocytopenia.
Citation: Uhl L, Assmann SF, Hamza TH, et al. Laboratory predictors of bleeding and the effect of platelet and RBC transfusions on bleeding outcomes in the PLADO trial. Blood. 2017;130(10):1247-58.
Background: The association between platelet counts, risk of bleeding, and transfusions in patients with thrombocytopenia related to stem cell transplant (SCT) or chemotherapy is not clear, except at very low platelet counts.
Study design: Secondary analysis of a multicenter, randomized controlled trial, stratified by cause of thrombocytopenia: autologous or syngeneic SCT (AUTO), allogeneic SCT (ALLO), or chemotherapy for hematologic malignancy without SCT (CHEMO).
Setting: Twenty-six hospitals from 2004 to 2007.
Synopsis: The PLADO trial enrolled more than 1,200 patients aged 18 years and older expected to experience a period of hypoproliferative thrombocytopenia as a result of chemotherapy or SCT, and randomized them to low, medium, or high doses of prophylactic platelets. This secondary analysis assessed laboratory predictors of bleeding, and the effect of transfusion.
Of 1,077 patients who received platelet transfusions, there were no differences between dose groups for any bleeding outcomes. Over a wide range of platelet counts, the ALLO stratum had a higher risk of bleeding than other strata, with clinically significant bleeding on 21% of patient-days in the ALLO stratum, compared with 19% in the AUTO stratum and 11% in the CHEMO stratum (P less than .001). Risk for bleeding was significantly higher at platelet counts of equal to or less than 5x109/L compared with platelet counts greater than or equal to 81x109/L. Higher aPTT and INR were also associated with higher risk of clinically significant bleeding. In a multipredictor model, only hematocrit was significantly associated with more severe bleeding. Neither platelet transfusion nor RBC transfusion reduced the risk of bleeding on the following day, although the authors note some possibility of confounding by indication.
Bottom line: Predictors of overall increased risk for bleeding in patients with secondary hypoproliferative thrombocytopenia were treatment stratum, platelet counts less than or equal to 5x109/L, hematocrit less than 25%, INR greater than 1.2, and aPTT greater than 30 seconds. This study challenges the conventional wisdom that transfusions reduce bleeding risk in patients with secondary hypoproliferative thrombocytopenia.
Citation: Uhl L, Assmann SF, Hamza TH, et al. Laboratory predictors of bleeding and the effect of platelet and RBC transfusions on bleeding outcomes in the PLADO trial. Blood. 2017;130(10):1247-58.
Background: The association between platelet counts, risk of bleeding, and transfusions in patients with thrombocytopenia related to stem cell transplant (SCT) or chemotherapy is not clear, except at very low platelet counts.
Study design: Secondary analysis of a multicenter, randomized controlled trial, stratified by cause of thrombocytopenia: autologous or syngeneic SCT (AUTO), allogeneic SCT (ALLO), or chemotherapy for hematologic malignancy without SCT (CHEMO).
Setting: Twenty-six hospitals from 2004 to 2007.
Synopsis: The PLADO trial enrolled more than 1,200 patients aged 18 years and older expected to experience a period of hypoproliferative thrombocytopenia as a result of chemotherapy or SCT, and randomized them to low, medium, or high doses of prophylactic platelets. This secondary analysis assessed laboratory predictors of bleeding, and the effect of transfusion.
Of 1,077 patients who received platelet transfusions, there were no differences between dose groups for any bleeding outcomes. Over a wide range of platelet counts, the ALLO stratum had a higher risk of bleeding than other strata, with clinically significant bleeding on 21% of patient-days in the ALLO stratum, compared with 19% in the AUTO stratum and 11% in the CHEMO stratum (P less than .001). Risk for bleeding was significantly higher at platelet counts of equal to or less than 5x109/L compared with platelet counts greater than or equal to 81x109/L. Higher aPTT and INR were also associated with higher risk of clinically significant bleeding. In a multipredictor model, only hematocrit was significantly associated with more severe bleeding. Neither platelet transfusion nor RBC transfusion reduced the risk of bleeding on the following day, although the authors note some possibility of confounding by indication.
Bottom line: Predictors of overall increased risk for bleeding in patients with secondary hypoproliferative thrombocytopenia were treatment stratum, platelet counts less than or equal to 5x109/L, hematocrit less than 25%, INR greater than 1.2, and aPTT greater than 30 seconds. This study challenges the conventional wisdom that transfusions reduce bleeding risk in patients with secondary hypoproliferative thrombocytopenia.
Citation: Uhl L, Assmann SF, Hamza TH, et al. Laboratory predictors of bleeding and the effect of platelet and RBC transfusions on bleeding outcomes in the PLADO trial. Blood. 2017;130(10):1247-58.
Is 17-OHPC effective for reducing risk of preterm birth?
In 2003, the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Maternal-Fetal Medicine Units (MFMU) Network reported on a placebo-controlled randomized study of 17–alpha hydroxyprogesterone caproate (17-OHPC) in women with a history of spontaneous preterm delivery. The study demonstrated a 33% reduction in recurrent preterm birth after weekly treatment with 17-OHPC, which was initiated at 16-20 weeks of gestation.
This landmark study, led by Paul Meis, MD, validated what had been suggested in an earlier meta-analysis (1990) by Mark Keirse, MD – and it quickly altered clinical practice. It set into motion a string of studies on the use of 17-OHPC and other progestational compounds in women with a variety of conditions associated with an increased risk for preterm birth.
It is not surprising, then, that the literature has become muddied and full of contradictory findings since publication of the Meis study and the initial studies on vaginal progesterone in women with a midtrimester short cervix. Further confounding our ability to judge a treatment’s effectiveness is the fact that spontaneous preterm birth is increasingly understood to be a multifactorial, highly heterogeneous condition. We cannot, with a broad stroke, say that all women with a prior preterm birth, for instance, will respond to progestogens in a similar manner or are at the same level of risk of recurrent spontaneous preterm birth (sPTB).
The number of large, randomized clinical trials evaluating progestins is actually quite small but opinions abound about the data from these studies. Below, I have categorized these treatments according to my view at this time of the currently available data.
Consensus
One area in which there is agreement concerns the use of 17-OHPC intramuscular injections in multifetal gestations. Two randomized clinical trials undertaken by the MFMU Network – one in twins and one in triplets – concluded that 17-OHPC is ineffective in reducing the rate of preterm birth. Moreover, in another, more recent MFMU Network study, there was a negative linear relationship between concentrations of 17-OHPC and gestational age at delivery. Women with twin gestations who had higher concentrations of 17-OHPC delivered at earlier gestational ages than women with lower concentrations (Am J Obstet Gynecol. 2012;207[5]:396.e1-8).
Other investigators have similarly shown in clinical trials that the preterm birth rate actually seems to be worsened in multifetal gestations when 17-OHPC is used. There is now widespread agreement that the compound should not be used in these patients.
In addition, an MFMU Network study led by William A. Grobman, MD, demonstrated that 17-OHPC (250-mg injections) does not provide any benefit to nulliparous women with a sonographic cervical length less than 30 mm (Am J Obstet Gynecol. 2012;207[5]:390.e1-8). Other studies utilizing higher doses of 17-OHPC similarly found no benefit. There is also agreement that 17-OHPC has no benefit in treating women with preterm premature rupture of the membranes, preterm labor, or as a maintenance treatment after an episode of preterm labor.
General agreement without consensus
There is general agreement that women with a singleton gestation and a prior spontaneous preterm birth should be offered 17-OHPC, and that women with a singleton gestation and a midtrimester shortened cervical length should be offered vaginal progesterone and not 17-OHPC. However, even in these populations, there are questions about efficacy, dosing, and other issues.
In the Meis study (N Engl J Med. 2003;348:2379-85), treatment with 17-OHPC in women with a singleton gestation and a prior preterm delivery significantly reduced the risk of another preterm birth at less than 37 weeks’ gestation (36.3% in the progesterone group vs. 54.9% in the placebo group; relative risk, 0.66), at less than 35 weeks’ gestation (RR, 0.67), and at less than 32 weeks’ gestation (RR, 0.58). The exceptionally high rate of preterm delivery in the placebo group, however, prompted other investigators to express concern in published correspondence that the study was potentially flawed.
We reported an inverse relationship between 17-OHPC concentration and spontaneous preterm birth as part of a study conducted with the MFMU Network and the Obstetrical-Fetal Pharmacology Research Units Network. All women in the study had singleton gestations and received 250 mg weekly 17-OHPC (the broader study was designed to evaluate the benefit of omega-3 supplementation). We measured plasma concentrations of 17-OHPC and found that women with concentrations in the lowest quartile had a significantly higher risk of preterm birth and delivered at significantly earlier gestational ages than did women in the second through fourth quartiles (Am J Obstet Gynecol. 2014;210[2]:128.e1-6).
Other studies/abstracts similarly evaluating the relationship between 17-OHPC concentrations and preterm birth have reported mixed results, with both validation and refutation of our findings.
Research underway may help settle the controversy. In an ongoing, open-label pharmacology study being conducted by the Obstetrical-Fetal Pharmacology Research Units Network, women with singleton pregnancies and a history of prior preterm birth are being randomly assigned to receive either 250 mg (the empirically chosen, currently recommended dose) or 500 mg 17-OHPC. A relationship between the plasma concentration of 17-OHPC at 26-30 weeks’ gestation and the incidence of preterm birth would offer proof of efficacy and could help elucidate the therapeutic dosing; if there is no relationship, we revert to the question of whether the agent really works. Based on current evidence, both the Society for Maternal-Fetal Medicine (SMFM) and the American College of Obstetricians and Gynecologists (ACOG) support the use of 17-OHPC for prevention of sPTB in women with a prior sPTB.
Questions about vaginal progesterone have also been somewhat unsettled. Eduardo B. Fonseca, MD, reported in 2007 that asymptomatic women with a short cervix (defined as 15 mm or less) who were randomized to receive vaginal progesterone at a median of 22 weeks’ gestation had a significantly lower rate of preterm birth before 34 weeks’ gestation than those who received placebo (RR, 0.56; N Engl J Med. 2007;357[5]:462-9). Research that followed offered mixed conclusions, with a study by Sonia S. Hassan, MD, showing benefit and a study by Jane E. Norman, MD, showing no benefit. Notably, in 2012, the Food and Drug Administration voted against approval of a sustained-release progesterone vaginal gel, citing research results that were not sufficiently compelling.
Still, vaginal progesterone has been endorsed by both ACOG and by the SMFM for women with a short cervical length in the midtrimester. This is supported by a new review and meta-analysis of individual patient data by Roberto Romero, MD, in which vaginal progesterone was found to significantly decrease the risk of preterm birth in singleton gestations with a midtrimester cervical length of 25 mm or less. The reduction occurred over a wide range of gestational ages, including at less than 33 weeks of gestation (RR, 0.62; Am J Obstet Gynecol. 2018 Feb;218[2]:161-80).
Disagreement
Some have argued that vaginal progesterone should be offered to women with a history of prior spontaneous preterm birth, but the largest study to look at this application – a randomized multinational trial reported by John M. O’Brien, MD, and his colleagues in 2007 – found that use of the compound did not reduce the frequency of recurrent preterm birth at or before 32 weeks. Others have argued that vaginal progesterone is of benefit in this group of women based on a combination of multiple subgroup analyses. There is disagreement between ACOG and SMFM on this issue. ACOG supports the use of vaginal progesterone for women with a prior preterm birth but the SMFM strongly rejects this treatment and only endorses 17-OHPC for this indication.
Unresolved
The value of vaginal progesterone supplementation in reducing preterm births in women with twin gestations is under continuing investigation, including a study of women with twin gestation and a short cervix. This MFMU Network randomized trial, now underway, is evaluating the effectiveness of vaginal progesterone or pessary, compared with placebo, in preventing early preterm birth in women carrying twins who have a cervical length less than 30 mm.
Another question about the use of progesterone concerns the woman who delivered preterm during a twin gestation and is now pregnant with a singleton gestation. Should anything be offered to her? This is a question that has not yet been addressed in the literature.
What does seem clear is that spontaneous preterm birth is a multifactorial condition with numerous causes, and quite possibly an interaction between genetics, maternal characteristics, and the environment surrounding each pregnancy (Semin Perinatol. 2016;40[5]:273-80). Certainly, there are different pathways and mechanisms at play in patients who deliver at 35-36 weeks, for instance, compared with those who deliver at 25-26 weeks.
We recently obtained cervical fluid from pregnant women with prior preterm births and analyzed the samples for concentrations of cytokines and matrix metalloproteinases. Women with a prior early preterm delivery at less than 26 weeks had elevations in five cervical cytokines – an inflammatory signature, in essence – while those whose prior preterm birth occurred at a later gestational age had no elevations of these cytokines (Am J Perinatol. 2017 Nov 15. doi: 10.1055/s-0037-1608631).
Hopefully, we soon will be able to identify subpopulations of pregnant women who will benefit more from progesterone supplementation. More research needs to be done at a granular level, with more narrowly defined populations – and with consideration of various pharmacologic, genetic and environmental factors – in order to develop a more specific treatment approach. In the meantime, it is important to appreciate the unknowns that underlie the highly variable clinical responses and outcomes seen in our clinical trials.
Dr. Caritis is professor of obstetrics, gynecology, and reproductive sciences at Magee-Womens Hospital, University of Pittsburgh. He has no disclosures relevant to this Master Class.
In 2003, the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Maternal-Fetal Medicine Units (MFMU) Network reported on a placebo-controlled randomized study of 17–alpha hydroxyprogesterone caproate (17-OHPC) in women with a history of spontaneous preterm delivery. The study demonstrated a 33% reduction in recurrent preterm birth after weekly treatment with 17-OHPC, which was initiated at 16-20 weeks of gestation.
This landmark study, led by Paul Meis, MD, validated what had been suggested in an earlier meta-analysis (1990) by Mark Keirse, MD – and it quickly altered clinical practice. It set into motion a string of studies on the use of 17-OHPC and other progestational compounds in women with a variety of conditions associated with an increased risk for preterm birth.
It is not surprising, then, that the literature has become muddied and full of contradictory findings since publication of the Meis study and the initial studies on vaginal progesterone in women with a midtrimester short cervix. Further confounding our ability to judge a treatment’s effectiveness is the fact that spontaneous preterm birth is increasingly understood to be a multifactorial, highly heterogeneous condition. We cannot, with a broad stroke, say that all women with a prior preterm birth, for instance, will respond to progestogens in a similar manner or are at the same level of risk of recurrent spontaneous preterm birth (sPTB).
The number of large, randomized clinical trials evaluating progestins is actually quite small but opinions abound about the data from these studies. Below, I have categorized these treatments according to my view at this time of the currently available data.
Consensus
One area in which there is agreement concerns the use of 17-OHPC intramuscular injections in multifetal gestations. Two randomized clinical trials undertaken by the MFMU Network – one in twins and one in triplets – concluded that 17-OHPC is ineffective in reducing the rate of preterm birth. Moreover, in another, more recent MFMU Network study, there was a negative linear relationship between concentrations of 17-OHPC and gestational age at delivery. Women with twin gestations who had higher concentrations of 17-OHPC delivered at earlier gestational ages than women with lower concentrations (Am J Obstet Gynecol. 2012;207[5]:396.e1-8).
Other investigators have similarly shown in clinical trials that the preterm birth rate actually seems to be worsened in multifetal gestations when 17-OHPC is used. There is now widespread agreement that the compound should not be used in these patients.
In addition, an MFMU Network study led by William A. Grobman, MD, demonstrated that 17-OHPC (250-mg injections) does not provide any benefit to nulliparous women with a sonographic cervical length less than 30 mm (Am J Obstet Gynecol. 2012;207[5]:390.e1-8). Other studies utilizing higher doses of 17-OHPC similarly found no benefit. There is also agreement that 17-OHPC has no benefit in treating women with preterm premature rupture of the membranes, preterm labor, or as a maintenance treatment after an episode of preterm labor.
General agreement without consensus
There is general agreement that women with a singleton gestation and a prior spontaneous preterm birth should be offered 17-OHPC, and that women with a singleton gestation and a midtrimester shortened cervical length should be offered vaginal progesterone and not 17-OHPC. However, even in these populations, there are questions about efficacy, dosing, and other issues.
In the Meis study (N Engl J Med. 2003;348:2379-85), treatment with 17-OHPC in women with a singleton gestation and a prior preterm delivery significantly reduced the risk of another preterm birth at less than 37 weeks’ gestation (36.3% in the progesterone group vs. 54.9% in the placebo group; relative risk, 0.66), at less than 35 weeks’ gestation (RR, 0.67), and at less than 32 weeks’ gestation (RR, 0.58). The exceptionally high rate of preterm delivery in the placebo group, however, prompted other investigators to express concern in published correspondence that the study was potentially flawed.
We reported an inverse relationship between 17-OHPC concentration and spontaneous preterm birth as part of a study conducted with the MFMU Network and the Obstetrical-Fetal Pharmacology Research Units Network. All women in the study had singleton gestations and received 250 mg weekly 17-OHPC (the broader study was designed to evaluate the benefit of omega-3 supplementation). We measured plasma concentrations of 17-OHPC and found that women with concentrations in the lowest quartile had a significantly higher risk of preterm birth and delivered at significantly earlier gestational ages than did women in the second through fourth quartiles (Am J Obstet Gynecol. 2014;210[2]:128.e1-6).
Other studies/abstracts similarly evaluating the relationship between 17-OHPC concentrations and preterm birth have reported mixed results, with both validation and refutation of our findings.
Research underway may help settle the controversy. In an ongoing, open-label pharmacology study being conducted by the Obstetrical-Fetal Pharmacology Research Units Network, women with singleton pregnancies and a history of prior preterm birth are being randomly assigned to receive either 250 mg (the empirically chosen, currently recommended dose) or 500 mg 17-OHPC. A relationship between the plasma concentration of 17-OHPC at 26-30 weeks’ gestation and the incidence of preterm birth would offer proof of efficacy and could help elucidate the therapeutic dosing; if there is no relationship, we revert to the question of whether the agent really works. Based on current evidence, both the Society for Maternal-Fetal Medicine (SMFM) and the American College of Obstetricians and Gynecologists (ACOG) support the use of 17-OHPC for prevention of sPTB in women with a prior sPTB.
Questions about vaginal progesterone have also been somewhat unsettled. Eduardo B. Fonseca, MD, reported in 2007 that asymptomatic women with a short cervix (defined as 15 mm or less) who were randomized to receive vaginal progesterone at a median of 22 weeks’ gestation had a significantly lower rate of preterm birth before 34 weeks’ gestation than those who received placebo (RR, 0.56; N Engl J Med. 2007;357[5]:462-9). Research that followed offered mixed conclusions, with a study by Sonia S. Hassan, MD, showing benefit and a study by Jane E. Norman, MD, showing no benefit. Notably, in 2012, the Food and Drug Administration voted against approval of a sustained-release progesterone vaginal gel, citing research results that were not sufficiently compelling.
Still, vaginal progesterone has been endorsed by both ACOG and by the SMFM for women with a short cervical length in the midtrimester. This is supported by a new review and meta-analysis of individual patient data by Roberto Romero, MD, in which vaginal progesterone was found to significantly decrease the risk of preterm birth in singleton gestations with a midtrimester cervical length of 25 mm or less. The reduction occurred over a wide range of gestational ages, including at less than 33 weeks of gestation (RR, 0.62; Am J Obstet Gynecol. 2018 Feb;218[2]:161-80).
Disagreement
Some have argued that vaginal progesterone should be offered to women with a history of prior spontaneous preterm birth, but the largest study to look at this application – a randomized multinational trial reported by John M. O’Brien, MD, and his colleagues in 2007 – found that use of the compound did not reduce the frequency of recurrent preterm birth at or before 32 weeks. Others have argued that vaginal progesterone is of benefit in this group of women based on a combination of multiple subgroup analyses. There is disagreement between ACOG and SMFM on this issue. ACOG supports the use of vaginal progesterone for women with a prior preterm birth but the SMFM strongly rejects this treatment and only endorses 17-OHPC for this indication.
Unresolved
The value of vaginal progesterone supplementation in reducing preterm births in women with twin gestations is under continuing investigation, including a study of women with twin gestation and a short cervix. This MFMU Network randomized trial, now underway, is evaluating the effectiveness of vaginal progesterone or pessary, compared with placebo, in preventing early preterm birth in women carrying twins who have a cervical length less than 30 mm.
Another question about the use of progesterone concerns the woman who delivered preterm during a twin gestation and is now pregnant with a singleton gestation. Should anything be offered to her? This is a question that has not yet been addressed in the literature.
What does seem clear is that spontaneous preterm birth is a multifactorial condition with numerous causes, and quite possibly an interaction between genetics, maternal characteristics, and the environment surrounding each pregnancy (Semin Perinatol. 2016;40[5]:273-80). Certainly, there are different pathways and mechanisms at play in patients who deliver at 35-36 weeks, for instance, compared with those who deliver at 25-26 weeks.
We recently obtained cervical fluid from pregnant women with prior preterm births and analyzed the samples for concentrations of cytokines and matrix metalloproteinases. Women with a prior early preterm delivery at less than 26 weeks had elevations in five cervical cytokines – an inflammatory signature, in essence – while those whose prior preterm birth occurred at a later gestational age had no elevations of these cytokines (Am J Perinatol. 2017 Nov 15. doi: 10.1055/s-0037-1608631).
Hopefully, we soon will be able to identify subpopulations of pregnant women who will benefit more from progesterone supplementation. More research needs to be done at a granular level, with more narrowly defined populations – and with consideration of various pharmacologic, genetic and environmental factors – in order to develop a more specific treatment approach. In the meantime, it is important to appreciate the unknowns that underlie the highly variable clinical responses and outcomes seen in our clinical trials.
Dr. Caritis is professor of obstetrics, gynecology, and reproductive sciences at Magee-Womens Hospital, University of Pittsburgh. He has no disclosures relevant to this Master Class.
In 2003, the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Maternal-Fetal Medicine Units (MFMU) Network reported on a placebo-controlled randomized study of 17–alpha hydroxyprogesterone caproate (17-OHPC) in women with a history of spontaneous preterm delivery. The study demonstrated a 33% reduction in recurrent preterm birth after weekly treatment with 17-OHPC, which was initiated at 16-20 weeks of gestation.
This landmark study, led by Paul Meis, MD, validated what had been suggested in an earlier meta-analysis (1990) by Mark Keirse, MD – and it quickly altered clinical practice. It set into motion a string of studies on the use of 17-OHPC and other progestational compounds in women with a variety of conditions associated with an increased risk for preterm birth.
It is not surprising, then, that the literature has become muddied and full of contradictory findings since publication of the Meis study and the initial studies on vaginal progesterone in women with a midtrimester short cervix. Further confounding our ability to judge a treatment’s effectiveness is the fact that spontaneous preterm birth is increasingly understood to be a multifactorial, highly heterogeneous condition. We cannot, with a broad stroke, say that all women with a prior preterm birth, for instance, will respond to progestogens in a similar manner or are at the same level of risk of recurrent spontaneous preterm birth (sPTB).
The number of large, randomized clinical trials evaluating progestins is actually quite small but opinions abound about the data from these studies. Below, I have categorized these treatments according to my view at this time of the currently available data.
Consensus
One area in which there is agreement concerns the use of 17-OHPC intramuscular injections in multifetal gestations. Two randomized clinical trials undertaken by the MFMU Network – one in twins and one in triplets – concluded that 17-OHPC is ineffective in reducing the rate of preterm birth. Moreover, in another, more recent MFMU Network study, there was a negative linear relationship between concentrations of 17-OHPC and gestational age at delivery. Women with twin gestations who had higher concentrations of 17-OHPC delivered at earlier gestational ages than women with lower concentrations (Am J Obstet Gynecol. 2012;207[5]:396.e1-8).
Other investigators have similarly shown in clinical trials that the preterm birth rate actually seems to be worsened in multifetal gestations when 17-OHPC is used. There is now widespread agreement that the compound should not be used in these patients.
In addition, an MFMU Network study led by William A. Grobman, MD, demonstrated that 17-OHPC (250-mg injections) does not provide any benefit to nulliparous women with a sonographic cervical length less than 30 mm (Am J Obstet Gynecol. 2012;207[5]:390.e1-8). Other studies utilizing higher doses of 17-OHPC similarly found no benefit. There is also agreement that 17-OHPC has no benefit in treating women with preterm premature rupture of the membranes, preterm labor, or as a maintenance treatment after an episode of preterm labor.
General agreement without consensus
There is general agreement that women with a singleton gestation and a prior spontaneous preterm birth should be offered 17-OHPC, and that women with a singleton gestation and a midtrimester shortened cervical length should be offered vaginal progesterone and not 17-OHPC. However, even in these populations, there are questions about efficacy, dosing, and other issues.
In the Meis study (N Engl J Med. 2003;348:2379-85), treatment with 17-OHPC in women with a singleton gestation and a prior preterm delivery significantly reduced the risk of another preterm birth at less than 37 weeks’ gestation (36.3% in the progesterone group vs. 54.9% in the placebo group; relative risk, 0.66), at less than 35 weeks’ gestation (RR, 0.67), and at less than 32 weeks’ gestation (RR, 0.58). The exceptionally high rate of preterm delivery in the placebo group, however, prompted other investigators to express concern in published correspondence that the study was potentially flawed.
We reported an inverse relationship between 17-OHPC concentration and spontaneous preterm birth as part of a study conducted with the MFMU Network and the Obstetrical-Fetal Pharmacology Research Units Network. All women in the study had singleton gestations and received 250 mg weekly 17-OHPC (the broader study was designed to evaluate the benefit of omega-3 supplementation). We measured plasma concentrations of 17-OHPC and found that women with concentrations in the lowest quartile had a significantly higher risk of preterm birth and delivered at significantly earlier gestational ages than did women in the second through fourth quartiles (Am J Obstet Gynecol. 2014;210[2]:128.e1-6).
Other studies/abstracts similarly evaluating the relationship between 17-OHPC concentrations and preterm birth have reported mixed results, with both validation and refutation of our findings.
Research underway may help settle the controversy. In an ongoing, open-label pharmacology study being conducted by the Obstetrical-Fetal Pharmacology Research Units Network, women with singleton pregnancies and a history of prior preterm birth are being randomly assigned to receive either 250 mg (the empirically chosen, currently recommended dose) or 500 mg 17-OHPC. A relationship between the plasma concentration of 17-OHPC at 26-30 weeks’ gestation and the incidence of preterm birth would offer proof of efficacy and could help elucidate the therapeutic dosing; if there is no relationship, we revert to the question of whether the agent really works. Based on current evidence, both the Society for Maternal-Fetal Medicine (SMFM) and the American College of Obstetricians and Gynecologists (ACOG) support the use of 17-OHPC for prevention of sPTB in women with a prior sPTB.
Questions about vaginal progesterone have also been somewhat unsettled. Eduardo B. Fonseca, MD, reported in 2007 that asymptomatic women with a short cervix (defined as 15 mm or less) who were randomized to receive vaginal progesterone at a median of 22 weeks’ gestation had a significantly lower rate of preterm birth before 34 weeks’ gestation than those who received placebo (RR, 0.56; N Engl J Med. 2007;357[5]:462-9). Research that followed offered mixed conclusions, with a study by Sonia S. Hassan, MD, showing benefit and a study by Jane E. Norman, MD, showing no benefit. Notably, in 2012, the Food and Drug Administration voted against approval of a sustained-release progesterone vaginal gel, citing research results that were not sufficiently compelling.
Still, vaginal progesterone has been endorsed by both ACOG and by the SMFM for women with a short cervical length in the midtrimester. This is supported by a new review and meta-analysis of individual patient data by Roberto Romero, MD, in which vaginal progesterone was found to significantly decrease the risk of preterm birth in singleton gestations with a midtrimester cervical length of 25 mm or less. The reduction occurred over a wide range of gestational ages, including at less than 33 weeks of gestation (RR, 0.62; Am J Obstet Gynecol. 2018 Feb;218[2]:161-80).
Disagreement
Some have argued that vaginal progesterone should be offered to women with a history of prior spontaneous preterm birth, but the largest study to look at this application – a randomized multinational trial reported by John M. O’Brien, MD, and his colleagues in 2007 – found that use of the compound did not reduce the frequency of recurrent preterm birth at or before 32 weeks. Others have argued that vaginal progesterone is of benefit in this group of women based on a combination of multiple subgroup analyses. There is disagreement between ACOG and SMFM on this issue. ACOG supports the use of vaginal progesterone for women with a prior preterm birth but the SMFM strongly rejects this treatment and only endorses 17-OHPC for this indication.
Unresolved
The value of vaginal progesterone supplementation in reducing preterm births in women with twin gestations is under continuing investigation, including a study of women with twin gestation and a short cervix. This MFMU Network randomized trial, now underway, is evaluating the effectiveness of vaginal progesterone or pessary, compared with placebo, in preventing early preterm birth in women carrying twins who have a cervical length less than 30 mm.
Another question about the use of progesterone concerns the woman who delivered preterm during a twin gestation and is now pregnant with a singleton gestation. Should anything be offered to her? This is a question that has not yet been addressed in the literature.
What does seem clear is that spontaneous preterm birth is a multifactorial condition with numerous causes, and quite possibly an interaction between genetics, maternal characteristics, and the environment surrounding each pregnancy (Semin Perinatol. 2016;40[5]:273-80). Certainly, there are different pathways and mechanisms at play in patients who deliver at 35-36 weeks, for instance, compared with those who deliver at 25-26 weeks.
We recently obtained cervical fluid from pregnant women with prior preterm births and analyzed the samples for concentrations of cytokines and matrix metalloproteinases. Women with a prior early preterm delivery at less than 26 weeks had elevations in five cervical cytokines – an inflammatory signature, in essence – while those whose prior preterm birth occurred at a later gestational age had no elevations of these cytokines (Am J Perinatol. 2017 Nov 15. doi: 10.1055/s-0037-1608631).
Hopefully, we soon will be able to identify subpopulations of pregnant women who will benefit more from progesterone supplementation. More research needs to be done at a granular level, with more narrowly defined populations – and with consideration of various pharmacologic, genetic and environmental factors – in order to develop a more specific treatment approach. In the meantime, it is important to appreciate the unknowns that underlie the highly variable clinical responses and outcomes seen in our clinical trials.
Dr. Caritis is professor of obstetrics, gynecology, and reproductive sciences at Magee-Womens Hospital, University of Pittsburgh. He has no disclosures relevant to this Master Class.










