User login
Upadacitinib calms itch, clears skin in moderate to severe atopic dermatitis
SAN DIEGO – Upadacitinib, a selective inhibitor of the Janus kinase 1 enzyme, affected up to 90% skin clearance in a phase 2 study in patients with moderate to severe atopic dermatitis (AD).
The molecule significantly outperformed placebo with all three of the doses tested, with patients experiencing improvement in itch and skin are involved in the first week of use. During the 16-week trial, there were none of the thromboembolic events that have proven a concern with other inhibitors of the Janus kinase family of enzymes, Emma Guttman, MD, PhD, said at the annual meeting of the American Academy of Dermatology.
The study enrolled adults (mean age, 40 years) with moderate to severe atopic dermatitis of about 30 years’ duration. Their mean Eczema Area and Severity Index (EASI) score at baseline was about 30, and mean Body Surface Area score ranged from 42-50. The mean pruritus numerical rating scale score was about 6.5.
After a month-long washout period that excluded all medications except a topical emollient, patients were randomized to placebo (40 patients) or to daily upadacitinib at 7.5-mg, 15-mg, or 30-mg doses, taken orally (42 in each group). The 16-week placebo-controlled period is being followed by a 72-week blinded extension study in which the placebo patients will be switched to upadacitinib 30 mg, and half of each upadacitinib group will be switched to placebo. Dr. Guttman reported only the 16-week results.
The study’s primary endpoint was the mean percent EASI improvement from baseline. Dr. Guttman reported several of the key secondary endpoints as well.
On the primary endpoint, all three doses of upadacitinib separated from placebo quickly and dramatically. Patients began to see some skin clearance after 1 week; by 2 weeks, the 7.5-mg group had achieved a 39% improvement and the 15- and 30-mg groups, 56% and 59% improvement, respectively.
Efficacy in the 7.5-mg group peaked at a 50% improvement by week 4, and then trailed off somewhat, with a mean 39% improvement by week 16.
Efficacy in the two higher dose groups also peaked around 4 weeks, with a 66% improvement in the 15-mg group and a 78% improvement in the 30-mg group. There was some tailing off of effect in each of these groups as well. By 16 weeks, the mean EASI improvement was 61.7% in the 15-mg group and 74.4% in the 30-mg group.
A good number of patients in each dosing group even achieved 90% skin clearance, Dr. Guttman noted.
“We generally say that we like to see an EASI 50, but now we are talking about EASI 75 and even 90. More than 60% on the highest dose achieved an EASI 75 and 60% an EASI 90. Even the 15-mg group achieved a nice EASI 90 response, at around 26%.”
Itching also responded well to upadacitinib, Dr. Guttman said. Within 1 week, all three active groups had separated significantly from the placebo group. By 2 weeks, the 7.5-mg group had a mean 29% improvement on the pruritus numerical rating scale. The improvement was 46% in the 15-mg group and 57.6% in the 30-mg group. By 16 weeks, the improvements were 39.6%, 48%, and 68.9%, respectively, compared with 9.7% among those on placebo.
The most common treatment-emergent adverse event was upper respiratory infection, which Dr. Guttman noted has been seen with JAK inhibitors. This occurred in 10% of those taking placebo and in 16.7% of the 7.5-mg group and 11.9% of both the 15-mg and 30-mg groups. A few patients experienced exacerbation of their AD on the medication (16.7%, 7% and 11.9% of the active groups, compared with 7.5% of those on placebo). New acne developed in 2.5% of placebo patients and in 9.5%, 4.8%, and 14.3% of those taking upadacitinib. The acne was on the body, considered mild, and resolved, Dr. Guttman said.
Two patients taking 7.5 mg and one taking 15 mg developed a serious infection, although she did not elaborate on the illnesses. Two taking 15 mg developed a liver disorder. There were four cases of neutropenia and one lymphopenia, all among the active groups. Creatine phosphokinase elevations occurred in one taking placebo and seven taking the study drug.
There were no pulmonary or deep vein thromboses; no opportunistic infections or malignancies; and no cases of herpes zoster, tuberculosis, or renal dysfunction. There were no deaths during the trial.
Phase 3 studies of upadacitinib in patients with rheumatoid arthritis, psoriatic arthritis, and Crohn’s disease are underway, according to AbbVie.
AbbVie sponsored the AD study. Dr. Guttman is a consultant for the company.
SOURCE: Guttman E et al. AAD late-breaking clinical trials, Abstract 6533
SAN DIEGO – Upadacitinib, a selective inhibitor of the Janus kinase 1 enzyme, affected up to 90% skin clearance in a phase 2 study in patients with moderate to severe atopic dermatitis (AD).
The molecule significantly outperformed placebo with all three of the doses tested, with patients experiencing improvement in itch and skin are involved in the first week of use. During the 16-week trial, there were none of the thromboembolic events that have proven a concern with other inhibitors of the Janus kinase family of enzymes, Emma Guttman, MD, PhD, said at the annual meeting of the American Academy of Dermatology.
The study enrolled adults (mean age, 40 years) with moderate to severe atopic dermatitis of about 30 years’ duration. Their mean Eczema Area and Severity Index (EASI) score at baseline was about 30, and mean Body Surface Area score ranged from 42-50. The mean pruritus numerical rating scale score was about 6.5.
After a month-long washout period that excluded all medications except a topical emollient, patients were randomized to placebo (40 patients) or to daily upadacitinib at 7.5-mg, 15-mg, or 30-mg doses, taken orally (42 in each group). The 16-week placebo-controlled period is being followed by a 72-week blinded extension study in which the placebo patients will be switched to upadacitinib 30 mg, and half of each upadacitinib group will be switched to placebo. Dr. Guttman reported only the 16-week results.
The study’s primary endpoint was the mean percent EASI improvement from baseline. Dr. Guttman reported several of the key secondary endpoints as well.
On the primary endpoint, all three doses of upadacitinib separated from placebo quickly and dramatically. Patients began to see some skin clearance after 1 week; by 2 weeks, the 7.5-mg group had achieved a 39% improvement and the 15- and 30-mg groups, 56% and 59% improvement, respectively.
Efficacy in the 7.5-mg group peaked at a 50% improvement by week 4, and then trailed off somewhat, with a mean 39% improvement by week 16.
Efficacy in the two higher dose groups also peaked around 4 weeks, with a 66% improvement in the 15-mg group and a 78% improvement in the 30-mg group. There was some tailing off of effect in each of these groups as well. By 16 weeks, the mean EASI improvement was 61.7% in the 15-mg group and 74.4% in the 30-mg group.
A good number of patients in each dosing group even achieved 90% skin clearance, Dr. Guttman noted.
“We generally say that we like to see an EASI 50, but now we are talking about EASI 75 and even 90. More than 60% on the highest dose achieved an EASI 75 and 60% an EASI 90. Even the 15-mg group achieved a nice EASI 90 response, at around 26%.”
Itching also responded well to upadacitinib, Dr. Guttman said. Within 1 week, all three active groups had separated significantly from the placebo group. By 2 weeks, the 7.5-mg group had a mean 29% improvement on the pruritus numerical rating scale. The improvement was 46% in the 15-mg group and 57.6% in the 30-mg group. By 16 weeks, the improvements were 39.6%, 48%, and 68.9%, respectively, compared with 9.7% among those on placebo.
The most common treatment-emergent adverse event was upper respiratory infection, which Dr. Guttman noted has been seen with JAK inhibitors. This occurred in 10% of those taking placebo and in 16.7% of the 7.5-mg group and 11.9% of both the 15-mg and 30-mg groups. A few patients experienced exacerbation of their AD on the medication (16.7%, 7% and 11.9% of the active groups, compared with 7.5% of those on placebo). New acne developed in 2.5% of placebo patients and in 9.5%, 4.8%, and 14.3% of those taking upadacitinib. The acne was on the body, considered mild, and resolved, Dr. Guttman said.
Two patients taking 7.5 mg and one taking 15 mg developed a serious infection, although she did not elaborate on the illnesses. Two taking 15 mg developed a liver disorder. There were four cases of neutropenia and one lymphopenia, all among the active groups. Creatine phosphokinase elevations occurred in one taking placebo and seven taking the study drug.
There were no pulmonary or deep vein thromboses; no opportunistic infections or malignancies; and no cases of herpes zoster, tuberculosis, or renal dysfunction. There were no deaths during the trial.
Phase 3 studies of upadacitinib in patients with rheumatoid arthritis, psoriatic arthritis, and Crohn’s disease are underway, according to AbbVie.
AbbVie sponsored the AD study. Dr. Guttman is a consultant for the company.
SOURCE: Guttman E et al. AAD late-breaking clinical trials, Abstract 6533
SAN DIEGO – Upadacitinib, a selective inhibitor of the Janus kinase 1 enzyme, affected up to 90% skin clearance in a phase 2 study in patients with moderate to severe atopic dermatitis (AD).
The molecule significantly outperformed placebo with all three of the doses tested, with patients experiencing improvement in itch and skin are involved in the first week of use. During the 16-week trial, there were none of the thromboembolic events that have proven a concern with other inhibitors of the Janus kinase family of enzymes, Emma Guttman, MD, PhD, said at the annual meeting of the American Academy of Dermatology.
The study enrolled adults (mean age, 40 years) with moderate to severe atopic dermatitis of about 30 years’ duration. Their mean Eczema Area and Severity Index (EASI) score at baseline was about 30, and mean Body Surface Area score ranged from 42-50. The mean pruritus numerical rating scale score was about 6.5.
After a month-long washout period that excluded all medications except a topical emollient, patients were randomized to placebo (40 patients) or to daily upadacitinib at 7.5-mg, 15-mg, or 30-mg doses, taken orally (42 in each group). The 16-week placebo-controlled period is being followed by a 72-week blinded extension study in which the placebo patients will be switched to upadacitinib 30 mg, and half of each upadacitinib group will be switched to placebo. Dr. Guttman reported only the 16-week results.
The study’s primary endpoint was the mean percent EASI improvement from baseline. Dr. Guttman reported several of the key secondary endpoints as well.
On the primary endpoint, all three doses of upadacitinib separated from placebo quickly and dramatically. Patients began to see some skin clearance after 1 week; by 2 weeks, the 7.5-mg group had achieved a 39% improvement and the 15- and 30-mg groups, 56% and 59% improvement, respectively.
Efficacy in the 7.5-mg group peaked at a 50% improvement by week 4, and then trailed off somewhat, with a mean 39% improvement by week 16.
Efficacy in the two higher dose groups also peaked around 4 weeks, with a 66% improvement in the 15-mg group and a 78% improvement in the 30-mg group. There was some tailing off of effect in each of these groups as well. By 16 weeks, the mean EASI improvement was 61.7% in the 15-mg group and 74.4% in the 30-mg group.
A good number of patients in each dosing group even achieved 90% skin clearance, Dr. Guttman noted.
“We generally say that we like to see an EASI 50, but now we are talking about EASI 75 and even 90. More than 60% on the highest dose achieved an EASI 75 and 60% an EASI 90. Even the 15-mg group achieved a nice EASI 90 response, at around 26%.”
Itching also responded well to upadacitinib, Dr. Guttman said. Within 1 week, all three active groups had separated significantly from the placebo group. By 2 weeks, the 7.5-mg group had a mean 29% improvement on the pruritus numerical rating scale. The improvement was 46% in the 15-mg group and 57.6% in the 30-mg group. By 16 weeks, the improvements were 39.6%, 48%, and 68.9%, respectively, compared with 9.7% among those on placebo.
The most common treatment-emergent adverse event was upper respiratory infection, which Dr. Guttman noted has been seen with JAK inhibitors. This occurred in 10% of those taking placebo and in 16.7% of the 7.5-mg group and 11.9% of both the 15-mg and 30-mg groups. A few patients experienced exacerbation of their AD on the medication (16.7%, 7% and 11.9% of the active groups, compared with 7.5% of those on placebo). New acne developed in 2.5% of placebo patients and in 9.5%, 4.8%, and 14.3% of those taking upadacitinib. The acne was on the body, considered mild, and resolved, Dr. Guttman said.
Two patients taking 7.5 mg and one taking 15 mg developed a serious infection, although she did not elaborate on the illnesses. Two taking 15 mg developed a liver disorder. There were four cases of neutropenia and one lymphopenia, all among the active groups. Creatine phosphokinase elevations occurred in one taking placebo and seven taking the study drug.
There were no pulmonary or deep vein thromboses; no opportunistic infections or malignancies; and no cases of herpes zoster, tuberculosis, or renal dysfunction. There were no deaths during the trial.
Phase 3 studies of upadacitinib in patients with rheumatoid arthritis, psoriatic arthritis, and Crohn’s disease are underway, according to AbbVie.
AbbVie sponsored the AD study. Dr. Guttman is a consultant for the company.
SOURCE: Guttman E et al. AAD late-breaking clinical trials, Abstract 6533
REPORTING FROM AAD 2018
Key clinical point: Upadacitinib had significant effects on reducing itch and clearing skin in patients with moderate to severe atopic dermatitis
Major finding: By 16 weeks, the mean EASI improvement was 61.7% in the 15-mg group and 74.4% in the 30-mg group.
Study details: In the dose-ranging, phase 2b randomized, placebo-controlled study, 126 patients with moderate to severe AD were treated with one of 3 upadacitinib doses, and 40 received placebo for 16 weeks.
Disclosures: AbbVie sponsored the study. Dr. Guttman is a consultant for the company.
Source: Guttman E et al. AAD late-breaking clinical trials, Abstract 6533
CPAP adherence linked to reduced readmissions
Hospitalized patients with obstructive sleep apnea (OSA) who were nonadherent to continuous positive airway pressure (CPAP) treatment were more than three times as likely to be readmitted for complications, according to a study.
Since preventable causes of readmission like congestive heart failure, obstructive lung disease, and diabetes are connected to OSA, boosting adherence rates to sleep apnea treatment could be an effective way to mitigate these risks.
Investigators gathered data for 345 hospitalized patients with OSA who were admitted to the VA Long Beach (Calif.) Healthcare System between January 2007 and December 2015.
Both the adherent and nonadherent groups were mostly white males. The 183 adherent patients were, on average, slightly older than the patients in the nonadherent group (66.3 vs. 62.3 years), while the nonadherent group had a larger proportion of African Americans (19.1%) than did the adherent group (10.4%).
In an analysis of both groups, 28% of nonadherent patients were readmitted within 30 days of discharge, compared with 10.2% of those in the adherent group (P less than .001). Readmission rates were significantly higher for nonadherent patients brought in for all-causes (adjusted odds ratio, 3.52; P less than .001), as were their rates of cardiovascular-related readmission (AOR, 2.31; P = .02).
The cardiovascular-related readmissions were most often caused by atrial fibrillation (29%), myocardial ischemia (22.5%), and congestive heart failure (19.3%) in the group who were not using CPAP. In this same group, urologic problems (10.7%), infections (8.0%), and psychiatric issues (5.3%) were the most common causes for hospital readmissions.
Investigators were surprised to find that the rate of pulmonary-related readmissions was not higher among nonadherent patients, considering the shared characteristics of OSA and COPD.
While nonadherent patients had an adjusted rate of pulmonary-related readmissions of 3.66, the difference between nonadherent and adherent patients was not significant.
“Those with OSA and COPD are considered to have overlap syndrome and, without CPAP therapy, are at higher risk for COPD exacerbation requiring hospitalization, pulmonary hypertension, and mortality,” according to Dr. Truong and her colleagues. “However, the number of patients with pulmonary readmissions was very small, and analysis did not reach statistical or clinical significance.”
Given the single-center nature of the study, these findings have limited generalizability. The study may also have been underpowered to uncover certain differences between the two groups because of the small population size.
Investigators reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: K. Truong et al. J Clin Sleep Med. 2018;14(2):183–9.
The comorbidities associated with obstructive sleep apnea (OSA), such as heart failure, coronary artery disease, diabetes, and stroke, can be detrimental to patients’ care and commonly lead to hospitalization. Not only are these diseases interfering with successful treatment, but financial penalties linked to 30-day readmissions have economic implications for hospitals as well. Increasing CPAP adherence, therefore, may be a low-cost tool to improve hospital outcomes. Dr. Truong and her colleagues find compelling data showing the association of CPAP adherence and reduced 30-day readmissions. However, more work is needed before we can fully back the idea that CPAP adherence will prevent readmissions. While many studies have shown associations between OSA and cardiovascular events, there are no large, randomized trials that show the cardiovascular benefit of CPAP. The current theory is that patients who are adherent to CPAP are more likely to be healthier individuals, which makes them less likely to exhibit the comorbidities that would cause readmissions. A large randomized trial is the next logical step, and with OSA costs estimated at $2,000 annually per patient, it is a step worth pursuing.
Lucas M. Donovan, MD, is a pulmonologist at the University of Washington, Seattle. Martha E. Billings, MD, is an assistant professor in the division of pulmonary and critical care medicine at the University of Washington, Seattle. They reported no conflicts of interest.
The comorbidities associated with obstructive sleep apnea (OSA), such as heart failure, coronary artery disease, diabetes, and stroke, can be detrimental to patients’ care and commonly lead to hospitalization. Not only are these diseases interfering with successful treatment, but financial penalties linked to 30-day readmissions have economic implications for hospitals as well. Increasing CPAP adherence, therefore, may be a low-cost tool to improve hospital outcomes. Dr. Truong and her colleagues find compelling data showing the association of CPAP adherence and reduced 30-day readmissions. However, more work is needed before we can fully back the idea that CPAP adherence will prevent readmissions. While many studies have shown associations between OSA and cardiovascular events, there are no large, randomized trials that show the cardiovascular benefit of CPAP. The current theory is that patients who are adherent to CPAP are more likely to be healthier individuals, which makes them less likely to exhibit the comorbidities that would cause readmissions. A large randomized trial is the next logical step, and with OSA costs estimated at $2,000 annually per patient, it is a step worth pursuing.
Lucas M. Donovan, MD, is a pulmonologist at the University of Washington, Seattle. Martha E. Billings, MD, is an assistant professor in the division of pulmonary and critical care medicine at the University of Washington, Seattle. They reported no conflicts of interest.
The comorbidities associated with obstructive sleep apnea (OSA), such as heart failure, coronary artery disease, diabetes, and stroke, can be detrimental to patients’ care and commonly lead to hospitalization. Not only are these diseases interfering with successful treatment, but financial penalties linked to 30-day readmissions have economic implications for hospitals as well. Increasing CPAP adherence, therefore, may be a low-cost tool to improve hospital outcomes. Dr. Truong and her colleagues find compelling data showing the association of CPAP adherence and reduced 30-day readmissions. However, more work is needed before we can fully back the idea that CPAP adherence will prevent readmissions. While many studies have shown associations between OSA and cardiovascular events, there are no large, randomized trials that show the cardiovascular benefit of CPAP. The current theory is that patients who are adherent to CPAP are more likely to be healthier individuals, which makes them less likely to exhibit the comorbidities that would cause readmissions. A large randomized trial is the next logical step, and with OSA costs estimated at $2,000 annually per patient, it is a step worth pursuing.
Lucas M. Donovan, MD, is a pulmonologist at the University of Washington, Seattle. Martha E. Billings, MD, is an assistant professor in the division of pulmonary and critical care medicine at the University of Washington, Seattle. They reported no conflicts of interest.
Hospitalized patients with obstructive sleep apnea (OSA) who were nonadherent to continuous positive airway pressure (CPAP) treatment were more than three times as likely to be readmitted for complications, according to a study.
Since preventable causes of readmission like congestive heart failure, obstructive lung disease, and diabetes are connected to OSA, boosting adherence rates to sleep apnea treatment could be an effective way to mitigate these risks.
Investigators gathered data for 345 hospitalized patients with OSA who were admitted to the VA Long Beach (Calif.) Healthcare System between January 2007 and December 2015.
Both the adherent and nonadherent groups were mostly white males. The 183 adherent patients were, on average, slightly older than the patients in the nonadherent group (66.3 vs. 62.3 years), while the nonadherent group had a larger proportion of African Americans (19.1%) than did the adherent group (10.4%).
In an analysis of both groups, 28% of nonadherent patients were readmitted within 30 days of discharge, compared with 10.2% of those in the adherent group (P less than .001). Readmission rates were significantly higher for nonadherent patients brought in for all-causes (adjusted odds ratio, 3.52; P less than .001), as were their rates of cardiovascular-related readmission (AOR, 2.31; P = .02).
The cardiovascular-related readmissions were most often caused by atrial fibrillation (29%), myocardial ischemia (22.5%), and congestive heart failure (19.3%) in the group who were not using CPAP. In this same group, urologic problems (10.7%), infections (8.0%), and psychiatric issues (5.3%) were the most common causes for hospital readmissions.
Investigators were surprised to find that the rate of pulmonary-related readmissions was not higher among nonadherent patients, considering the shared characteristics of OSA and COPD.
While nonadherent patients had an adjusted rate of pulmonary-related readmissions of 3.66, the difference between nonadherent and adherent patients was not significant.
“Those with OSA and COPD are considered to have overlap syndrome and, without CPAP therapy, are at higher risk for COPD exacerbation requiring hospitalization, pulmonary hypertension, and mortality,” according to Dr. Truong and her colleagues. “However, the number of patients with pulmonary readmissions was very small, and analysis did not reach statistical or clinical significance.”
Given the single-center nature of the study, these findings have limited generalizability. The study may also have been underpowered to uncover certain differences between the two groups because of the small population size.
Investigators reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: K. Truong et al. J Clin Sleep Med. 2018;14(2):183–9.
Hospitalized patients with obstructive sleep apnea (OSA) who were nonadherent to continuous positive airway pressure (CPAP) treatment were more than three times as likely to be readmitted for complications, according to a study.
Since preventable causes of readmission like congestive heart failure, obstructive lung disease, and diabetes are connected to OSA, boosting adherence rates to sleep apnea treatment could be an effective way to mitigate these risks.
Investigators gathered data for 345 hospitalized patients with OSA who were admitted to the VA Long Beach (Calif.) Healthcare System between January 2007 and December 2015.
Both the adherent and nonadherent groups were mostly white males. The 183 adherent patients were, on average, slightly older than the patients in the nonadherent group (66.3 vs. 62.3 years), while the nonadherent group had a larger proportion of African Americans (19.1%) than did the adherent group (10.4%).
In an analysis of both groups, 28% of nonadherent patients were readmitted within 30 days of discharge, compared with 10.2% of those in the adherent group (P less than .001). Readmission rates were significantly higher for nonadherent patients brought in for all-causes (adjusted odds ratio, 3.52; P less than .001), as were their rates of cardiovascular-related readmission (AOR, 2.31; P = .02).
The cardiovascular-related readmissions were most often caused by atrial fibrillation (29%), myocardial ischemia (22.5%), and congestive heart failure (19.3%) in the group who were not using CPAP. In this same group, urologic problems (10.7%), infections (8.0%), and psychiatric issues (5.3%) were the most common causes for hospital readmissions.
Investigators were surprised to find that the rate of pulmonary-related readmissions was not higher among nonadherent patients, considering the shared characteristics of OSA and COPD.
While nonadherent patients had an adjusted rate of pulmonary-related readmissions of 3.66, the difference between nonadherent and adherent patients was not significant.
“Those with OSA and COPD are considered to have overlap syndrome and, without CPAP therapy, are at higher risk for COPD exacerbation requiring hospitalization, pulmonary hypertension, and mortality,” according to Dr. Truong and her colleagues. “However, the number of patients with pulmonary readmissions was very small, and analysis did not reach statistical or clinical significance.”
Given the single-center nature of the study, these findings have limited generalizability. The study may also have been underpowered to uncover certain differences between the two groups because of the small population size.
Investigators reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: K. Truong et al. J Clin Sleep Med. 2018;14(2):183–9.
FROM THE JOURNAL OF CLINICAL SLEEP MEDICINE
Key clinical point:
Major finding: CPAP-nonadherent patients were 3.5 times more likely to be readmitted within 30 days.
Study details: A retrospective study of 345 patients with obstructive sleep apnea who were hospitalized at a Veterans Affairs hospital between Jan. 1, 2007, and Dec. 31, 2015.
Disclosures: Investigators reported no relevant financial disclosures.
Source: K. Truong et al. J Clin Sleep Med. 2018;14(2):183-9.
Learning from the 2017 Oscar fiasco
It was a “never event.” At the very end of the 2017 Academy Awards presentation, the winner for Best Picture was announced. It was wrong. Two and a half minutes later it was corrected. The true winner was “Moonlight,” not “La La Land.” But by then much damage had been done.
I watched it happen live on TV and reviewed it again on YouTube. Several news agencies investigated and reported on what happened. I don’t have any inside information beyond that, but my engineering perspective can illuminate how to reduce mistakes.
The first lesson is how quickly people seek to assign blame after something goes wrong. I saw various online news agencies say Warren Beatty had announced the wrong winner. While he opened the envelope, it was Faye Dunaway who actually made the announcement of “La La Land.” Furthermore, Warren and Faye were merely reading the card. Warren had been given the wrong envelope, as high resolution photographs prove. The envelope was a duplicate for the prize announced just before them for the Best Actress award. The card said Emma Stone and in a smaller font “La La Land,” the film in which she starred. Warren hesitated because of how this was written on the card. Faye thought he was trying to pause as a shtick to increase suspense so she glanced at the card and blurted out “La La Land.”
Experts in quality improvement have learned that the best way to reduce errors is to resist this tendency to assign blame. A better approach is to assume, absent evidence to the contrary, that everyone is acting responsibly and sincerely to help the patient. Hear both sides of the story before jumping to any conclusions. Find systemic factors that contributed to a human error. Then focus on ameliorating systemic weaknesses.
One contributing factor for the error at the Oscars was that there were two copies of the set of award envelopes, with one set available on each side of the stage. This way the presenters can enter from either side of the stage. They are handed an envelope by one of the two auditors from PricewaterhouseCoopers, who are the only ones who know the contents.
A key component of safety is having check backs. The envelopes have the name of the award on the outside. One might hope the presenter would double check that they are being given the correct envelope by the auditor. But backstage is a very nervous and hectic place for the presenters. Actors are not professionals dedicated to safety.
Medical care is different. Before giving a transfusion, one nurse reads the number on the bag of blood to another nurse, who confirms that it matches a paper form. That simple act can prevent mistakes. Perhaps the auditor handing the envelope to the Oscar presenter should ask the presenter, who knows which award s/he is scheduled to announce, to read out loud the award title on the front of the envelope.
Clearly, Warren Beatty was confused by the contents of the envelope. He was expecting a card to have the name of a film, not the name of an actress with the film’s name in small print below it. He didn’t know what action to take and hesitated. Faye Dunaway plunged forward and misinterpreted the card. A key component of quality is making it safe for anyone, if they are not confident in what is happening, to stop the proceeding, ask questions, and challenge plans. For example, there are time-outs prior to surgery. A second component is presenting information in a form less likely to be misinterpreted. Medicine has a problem with many sound-alike and look-alike drug names, so sometimes these words are spelled with particular letters capitalized, to distinguish them. I wish EHRs would present lab results in large, bold font.
Another contributing factor here was that Faye misinterpreted Warren’s behaviors as a joke. Major airlines utilize the “sterile cockpit.” During the few minutes that they are running through the preflight checklist, the pilot and copilot do not discuss last night’s football game, crack jokes, or engage in any other extraneous conversations. They avoid interruptions and distractions, focusing solely on the task. Sign outs in medicine need to adopt this habit.
There is a concern that one of the auditors tweeted a picture of Emma Stone backstage holding her Oscar at the same time the fiasco was happening on stage. In the modern world, cell phones and selfies are a key source of distraction, errors, and car accidents.
Per the Army, “Prior planning prevents poor performance.” A couple days before the Oscar fiasco, the auditors were interviewed and they revealed that they didn’t have an action plan to deal with the situation of a mistaken announcement. They figured it was extremely unlikely and that the circumstances would determine the best response.
Experience has shown that in the hours leading up to a pediatric code, there may be several opportunities to recognize the risk and intervene so that blame cannot be assigned to a single person or action. Mock codes prepare people to think on their feet. And it is important to have a clearly designated person in charge of a code. Leadership matters.
In the Oscar fiasco, the damage was quickly limited by the gracious words of a “La La Land” producer He assessed the situation, announced the mistake, beckoned the “Moonlight” cast and crew to the stage, graciously complimented them, showed the correct award envelope and card to the camera, and offered the statue to the correct producer. Then he hastened his team off the stage. These actions of responsibility, truthfulness, transparency, and grace staunched the bleeding, minimized the damage, and as best as possible, remediated the error. Movie producers are experts at dealing with crises and catastrophes. Medical staff, when revealing errors to patients, can learn from this role model.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@frontlinemedcom.com.
It was a “never event.” At the very end of the 2017 Academy Awards presentation, the winner for Best Picture was announced. It was wrong. Two and a half minutes later it was corrected. The true winner was “Moonlight,” not “La La Land.” But by then much damage had been done.
I watched it happen live on TV and reviewed it again on YouTube. Several news agencies investigated and reported on what happened. I don’t have any inside information beyond that, but my engineering perspective can illuminate how to reduce mistakes.
The first lesson is how quickly people seek to assign blame after something goes wrong. I saw various online news agencies say Warren Beatty had announced the wrong winner. While he opened the envelope, it was Faye Dunaway who actually made the announcement of “La La Land.” Furthermore, Warren and Faye were merely reading the card. Warren had been given the wrong envelope, as high resolution photographs prove. The envelope was a duplicate for the prize announced just before them for the Best Actress award. The card said Emma Stone and in a smaller font “La La Land,” the film in which she starred. Warren hesitated because of how this was written on the card. Faye thought he was trying to pause as a shtick to increase suspense so she glanced at the card and blurted out “La La Land.”
Experts in quality improvement have learned that the best way to reduce errors is to resist this tendency to assign blame. A better approach is to assume, absent evidence to the contrary, that everyone is acting responsibly and sincerely to help the patient. Hear both sides of the story before jumping to any conclusions. Find systemic factors that contributed to a human error. Then focus on ameliorating systemic weaknesses.
One contributing factor for the error at the Oscars was that there were two copies of the set of award envelopes, with one set available on each side of the stage. This way the presenters can enter from either side of the stage. They are handed an envelope by one of the two auditors from PricewaterhouseCoopers, who are the only ones who know the contents.
A key component of safety is having check backs. The envelopes have the name of the award on the outside. One might hope the presenter would double check that they are being given the correct envelope by the auditor. But backstage is a very nervous and hectic place for the presenters. Actors are not professionals dedicated to safety.
Medical care is different. Before giving a transfusion, one nurse reads the number on the bag of blood to another nurse, who confirms that it matches a paper form. That simple act can prevent mistakes. Perhaps the auditor handing the envelope to the Oscar presenter should ask the presenter, who knows which award s/he is scheduled to announce, to read out loud the award title on the front of the envelope.
Clearly, Warren Beatty was confused by the contents of the envelope. He was expecting a card to have the name of a film, not the name of an actress with the film’s name in small print below it. He didn’t know what action to take and hesitated. Faye Dunaway plunged forward and misinterpreted the card. A key component of quality is making it safe for anyone, if they are not confident in what is happening, to stop the proceeding, ask questions, and challenge plans. For example, there are time-outs prior to surgery. A second component is presenting information in a form less likely to be misinterpreted. Medicine has a problem with many sound-alike and look-alike drug names, so sometimes these words are spelled with particular letters capitalized, to distinguish them. I wish EHRs would present lab results in large, bold font.
Another contributing factor here was that Faye misinterpreted Warren’s behaviors as a joke. Major airlines utilize the “sterile cockpit.” During the few minutes that they are running through the preflight checklist, the pilot and copilot do not discuss last night’s football game, crack jokes, or engage in any other extraneous conversations. They avoid interruptions and distractions, focusing solely on the task. Sign outs in medicine need to adopt this habit.
There is a concern that one of the auditors tweeted a picture of Emma Stone backstage holding her Oscar at the same time the fiasco was happening on stage. In the modern world, cell phones and selfies are a key source of distraction, errors, and car accidents.
Per the Army, “Prior planning prevents poor performance.” A couple days before the Oscar fiasco, the auditors were interviewed and they revealed that they didn’t have an action plan to deal with the situation of a mistaken announcement. They figured it was extremely unlikely and that the circumstances would determine the best response.
Experience has shown that in the hours leading up to a pediatric code, there may be several opportunities to recognize the risk and intervene so that blame cannot be assigned to a single person or action. Mock codes prepare people to think on their feet. And it is important to have a clearly designated person in charge of a code. Leadership matters.
In the Oscar fiasco, the damage was quickly limited by the gracious words of a “La La Land” producer He assessed the situation, announced the mistake, beckoned the “Moonlight” cast and crew to the stage, graciously complimented them, showed the correct award envelope and card to the camera, and offered the statue to the correct producer. Then he hastened his team off the stage. These actions of responsibility, truthfulness, transparency, and grace staunched the bleeding, minimized the damage, and as best as possible, remediated the error. Movie producers are experts at dealing with crises and catastrophes. Medical staff, when revealing errors to patients, can learn from this role model.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@frontlinemedcom.com.
It was a “never event.” At the very end of the 2017 Academy Awards presentation, the winner for Best Picture was announced. It was wrong. Two and a half minutes later it was corrected. The true winner was “Moonlight,” not “La La Land.” But by then much damage had been done.
I watched it happen live on TV and reviewed it again on YouTube. Several news agencies investigated and reported on what happened. I don’t have any inside information beyond that, but my engineering perspective can illuminate how to reduce mistakes.
The first lesson is how quickly people seek to assign blame after something goes wrong. I saw various online news agencies say Warren Beatty had announced the wrong winner. While he opened the envelope, it was Faye Dunaway who actually made the announcement of “La La Land.” Furthermore, Warren and Faye were merely reading the card. Warren had been given the wrong envelope, as high resolution photographs prove. The envelope was a duplicate for the prize announced just before them for the Best Actress award. The card said Emma Stone and in a smaller font “La La Land,” the film in which she starred. Warren hesitated because of how this was written on the card. Faye thought he was trying to pause as a shtick to increase suspense so she glanced at the card and blurted out “La La Land.”
Experts in quality improvement have learned that the best way to reduce errors is to resist this tendency to assign blame. A better approach is to assume, absent evidence to the contrary, that everyone is acting responsibly and sincerely to help the patient. Hear both sides of the story before jumping to any conclusions. Find systemic factors that contributed to a human error. Then focus on ameliorating systemic weaknesses.
One contributing factor for the error at the Oscars was that there were two copies of the set of award envelopes, with one set available on each side of the stage. This way the presenters can enter from either side of the stage. They are handed an envelope by one of the two auditors from PricewaterhouseCoopers, who are the only ones who know the contents.
A key component of safety is having check backs. The envelopes have the name of the award on the outside. One might hope the presenter would double check that they are being given the correct envelope by the auditor. But backstage is a very nervous and hectic place for the presenters. Actors are not professionals dedicated to safety.
Medical care is different. Before giving a transfusion, one nurse reads the number on the bag of blood to another nurse, who confirms that it matches a paper form. That simple act can prevent mistakes. Perhaps the auditor handing the envelope to the Oscar presenter should ask the presenter, who knows which award s/he is scheduled to announce, to read out loud the award title on the front of the envelope.
Clearly, Warren Beatty was confused by the contents of the envelope. He was expecting a card to have the name of a film, not the name of an actress with the film’s name in small print below it. He didn’t know what action to take and hesitated. Faye Dunaway plunged forward and misinterpreted the card. A key component of quality is making it safe for anyone, if they are not confident in what is happening, to stop the proceeding, ask questions, and challenge plans. For example, there are time-outs prior to surgery. A second component is presenting information in a form less likely to be misinterpreted. Medicine has a problem with many sound-alike and look-alike drug names, so sometimes these words are spelled with particular letters capitalized, to distinguish them. I wish EHRs would present lab results in large, bold font.
Another contributing factor here was that Faye misinterpreted Warren’s behaviors as a joke. Major airlines utilize the “sterile cockpit.” During the few minutes that they are running through the preflight checklist, the pilot and copilot do not discuss last night’s football game, crack jokes, or engage in any other extraneous conversations. They avoid interruptions and distractions, focusing solely on the task. Sign outs in medicine need to adopt this habit.
There is a concern that one of the auditors tweeted a picture of Emma Stone backstage holding her Oscar at the same time the fiasco was happening on stage. In the modern world, cell phones and selfies are a key source of distraction, errors, and car accidents.
Per the Army, “Prior planning prevents poor performance.” A couple days before the Oscar fiasco, the auditors were interviewed and they revealed that they didn’t have an action plan to deal with the situation of a mistaken announcement. They figured it was extremely unlikely and that the circumstances would determine the best response.
Experience has shown that in the hours leading up to a pediatric code, there may be several opportunities to recognize the risk and intervene so that blame cannot be assigned to a single person or action. Mock codes prepare people to think on their feet. And it is important to have a clearly designated person in charge of a code. Leadership matters.
In the Oscar fiasco, the damage was quickly limited by the gracious words of a “La La Land” producer He assessed the situation, announced the mistake, beckoned the “Moonlight” cast and crew to the stage, graciously complimented them, showed the correct award envelope and card to the camera, and offered the statue to the correct producer. Then he hastened his team off the stage. These actions of responsibility, truthfulness, transparency, and grace staunched the bleeding, minimized the damage, and as best as possible, remediated the error. Movie producers are experts at dealing with crises and catastrophes. Medical staff, when revealing errors to patients, can learn from this role model.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@frontlinemedcom.com.
Delayed treatment for psychosis can have ‘deleterious’ effects
The longer that patients with schizophrenia go without treatment for a psychotic episode, the more their hippocampus atrophies, suggests a study published Feb. 21 in JAMA Psychiatry.
To conduct the study, researchers studied 71 patients between March 5, 2013, and Oct. 8, 2014, who were experiencing their first psychotic episode and were antipsychotic naive. The research team matched those patients with 73 healthy controls, treated the patients with antipsychotics, and performed MRIs on members of both groups at baseline and 8 weeks later. The primary outcome measure was change in left and right hippocampal volume integrity, which is inversely associated with hippocampal atrophy.
Results showed that many patients with psychosis had lower median hippocampal volume integrity. Furthermore, those . The duration of untreated psychosis was correlated with both decreases, but this association was only significant with left hippocampal volume integrity.
This relationship is “consistent with a persistent, possibly deleterious, effect of untreated psychosis on brain structure,” wrote Donald C. Goff, MD, of the psychiatry department at New York University, and his associates. “Larger longitudinal studies of longer duration are needed to examine the association between [duration of untreated psychosis], hippocampal volume, and clinical outcomes.”
Dr. Goff reported receiving research support from the National Institute of Mental Health, the Stanley Medical Research Institute, and Avanir Pharmaceuticals. Another author reported receiving support from numerous entities and honoraria for serving on an advisory board for Allergan. No other disclosures were reported.
Read more at JAMA Psychiatry.
The longer that patients with schizophrenia go without treatment for a psychotic episode, the more their hippocampus atrophies, suggests a study published Feb. 21 in JAMA Psychiatry.
To conduct the study, researchers studied 71 patients between March 5, 2013, and Oct. 8, 2014, who were experiencing their first psychotic episode and were antipsychotic naive. The research team matched those patients with 73 healthy controls, treated the patients with antipsychotics, and performed MRIs on members of both groups at baseline and 8 weeks later. The primary outcome measure was change in left and right hippocampal volume integrity, which is inversely associated with hippocampal atrophy.
Results showed that many patients with psychosis had lower median hippocampal volume integrity. Furthermore, those . The duration of untreated psychosis was correlated with both decreases, but this association was only significant with left hippocampal volume integrity.
This relationship is “consistent with a persistent, possibly deleterious, effect of untreated psychosis on brain structure,” wrote Donald C. Goff, MD, of the psychiatry department at New York University, and his associates. “Larger longitudinal studies of longer duration are needed to examine the association between [duration of untreated psychosis], hippocampal volume, and clinical outcomes.”
Dr. Goff reported receiving research support from the National Institute of Mental Health, the Stanley Medical Research Institute, and Avanir Pharmaceuticals. Another author reported receiving support from numerous entities and honoraria for serving on an advisory board for Allergan. No other disclosures were reported.
Read more at JAMA Psychiatry.
The longer that patients with schizophrenia go without treatment for a psychotic episode, the more their hippocampus atrophies, suggests a study published Feb. 21 in JAMA Psychiatry.
To conduct the study, researchers studied 71 patients between March 5, 2013, and Oct. 8, 2014, who were experiencing their first psychotic episode and were antipsychotic naive. The research team matched those patients with 73 healthy controls, treated the patients with antipsychotics, and performed MRIs on members of both groups at baseline and 8 weeks later. The primary outcome measure was change in left and right hippocampal volume integrity, which is inversely associated with hippocampal atrophy.
Results showed that many patients with psychosis had lower median hippocampal volume integrity. Furthermore, those . The duration of untreated psychosis was correlated with both decreases, but this association was only significant with left hippocampal volume integrity.
This relationship is “consistent with a persistent, possibly deleterious, effect of untreated psychosis on brain structure,” wrote Donald C. Goff, MD, of the psychiatry department at New York University, and his associates. “Larger longitudinal studies of longer duration are needed to examine the association between [duration of untreated psychosis], hippocampal volume, and clinical outcomes.”
Dr. Goff reported receiving research support from the National Institute of Mental Health, the Stanley Medical Research Institute, and Avanir Pharmaceuticals. Another author reported receiving support from numerous entities and honoraria for serving on an advisory board for Allergan. No other disclosures were reported.
Read more at JAMA Psychiatry.
FROM JAMA PSYCHIATRY
Lung scan often not requested for new SSc patients
Only half of American general rheumatologists and two-thirds of global systemic sclerosis experts routinely request high-resolution CT chest scans for all their newly diagnosed systemic sclerosis patients despite their increased risk of interstitial lung disease, according to survey data from approximately 200 clinicians.
The researchers, led by Elana J. Bernstein, MD, of Columbia University, New York, conducted the survey because of a lack of data on how often rheumatologists order high-resolution CT for their newly diagnosed patients and the absence of clinical practice guidelines that recommend screening for interstitial lung disease (ILD) in systemic sclerosis (SSc).
In a study published in Arthritis & Rheumatology, the researchers surveyed 676 American College of Rheumatology members and 356 global experts on systemic sclerosis; of these, 76 ACR general rheumatologists and 135 SSc experts responded. The use of high-resolution CT varied widely by country or region: 0 of 5 respondents from Australia, 2 of 6 from Canada, 28 of 47 from the United States, 45 of 57 from Europe, 4 of 5 from Asia, and 7 of 7 from Latin America.
The researchers also found little consensus on indications for high-resolution CT in SSc patients. Among the SSc experts who do not routinely obtain screening high-resolution CTs in their SSc patients, 81% said they would request one for dyspnea on exertion, 74% would request one for an abnormal forced vital capacity less than 80% of predicted, and 52% would request one for an abnormal diffusion capacity for carbon monoxide less than 80% predicted.
A significant limitation of the study was the low response rate, and more research is needed on the clinical impact of high-resolution CT screening for ILD in SSc patients, the researchers noted. However, the results highlight the need for a clinical practice guideline to create a more consistent approach to identifying ILD in these patients, they said.
The researchers had no financial conflicts to disclose. Dr. Bernstein was supported by a Rheumatology Research Foundation Scientist Development Award, and two of her colleagues were funded in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Heart, Lung, and Blood Institute.
SOURCE: Bernstein E et al. Arthritis Rheumatol. 2018 Feb 9. doi: 10.1002/art.40441.
Only half of American general rheumatologists and two-thirds of global systemic sclerosis experts routinely request high-resolution CT chest scans for all their newly diagnosed systemic sclerosis patients despite their increased risk of interstitial lung disease, according to survey data from approximately 200 clinicians.
The researchers, led by Elana J. Bernstein, MD, of Columbia University, New York, conducted the survey because of a lack of data on how often rheumatologists order high-resolution CT for their newly diagnosed patients and the absence of clinical practice guidelines that recommend screening for interstitial lung disease (ILD) in systemic sclerosis (SSc).
In a study published in Arthritis & Rheumatology, the researchers surveyed 676 American College of Rheumatology members and 356 global experts on systemic sclerosis; of these, 76 ACR general rheumatologists and 135 SSc experts responded. The use of high-resolution CT varied widely by country or region: 0 of 5 respondents from Australia, 2 of 6 from Canada, 28 of 47 from the United States, 45 of 57 from Europe, 4 of 5 from Asia, and 7 of 7 from Latin America.
The researchers also found little consensus on indications for high-resolution CT in SSc patients. Among the SSc experts who do not routinely obtain screening high-resolution CTs in their SSc patients, 81% said they would request one for dyspnea on exertion, 74% would request one for an abnormal forced vital capacity less than 80% of predicted, and 52% would request one for an abnormal diffusion capacity for carbon monoxide less than 80% predicted.
A significant limitation of the study was the low response rate, and more research is needed on the clinical impact of high-resolution CT screening for ILD in SSc patients, the researchers noted. However, the results highlight the need for a clinical practice guideline to create a more consistent approach to identifying ILD in these patients, they said.
The researchers had no financial conflicts to disclose. Dr. Bernstein was supported by a Rheumatology Research Foundation Scientist Development Award, and two of her colleagues were funded in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Heart, Lung, and Blood Institute.
SOURCE: Bernstein E et al. Arthritis Rheumatol. 2018 Feb 9. doi: 10.1002/art.40441.
Only half of American general rheumatologists and two-thirds of global systemic sclerosis experts routinely request high-resolution CT chest scans for all their newly diagnosed systemic sclerosis patients despite their increased risk of interstitial lung disease, according to survey data from approximately 200 clinicians.
The researchers, led by Elana J. Bernstein, MD, of Columbia University, New York, conducted the survey because of a lack of data on how often rheumatologists order high-resolution CT for their newly diagnosed patients and the absence of clinical practice guidelines that recommend screening for interstitial lung disease (ILD) in systemic sclerosis (SSc).
In a study published in Arthritis & Rheumatology, the researchers surveyed 676 American College of Rheumatology members and 356 global experts on systemic sclerosis; of these, 76 ACR general rheumatologists and 135 SSc experts responded. The use of high-resolution CT varied widely by country or region: 0 of 5 respondents from Australia, 2 of 6 from Canada, 28 of 47 from the United States, 45 of 57 from Europe, 4 of 5 from Asia, and 7 of 7 from Latin America.
The researchers also found little consensus on indications for high-resolution CT in SSc patients. Among the SSc experts who do not routinely obtain screening high-resolution CTs in their SSc patients, 81% said they would request one for dyspnea on exertion, 74% would request one for an abnormal forced vital capacity less than 80% of predicted, and 52% would request one for an abnormal diffusion capacity for carbon monoxide less than 80% predicted.
A significant limitation of the study was the low response rate, and more research is needed on the clinical impact of high-resolution CT screening for ILD in SSc patients, the researchers noted. However, the results highlight the need for a clinical practice guideline to create a more consistent approach to identifying ILD in these patients, they said.
The researchers had no financial conflicts to disclose. Dr. Bernstein was supported by a Rheumatology Research Foundation Scientist Development Award, and two of her colleagues were funded in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Heart, Lung, and Blood Institute.
SOURCE: Bernstein E et al. Arthritis Rheumatol. 2018 Feb 9. doi: 10.1002/art.40441.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Despite the risk of interstitial lung disease in systemic sclerosis patients, the use of high-resolution CT scans of the chest is inconsistent.
Major finding: Overall, 51% of ACR general rheumatologists and 66% of global systemic sclerosis experts ordered high-resolution CTs for new SSc patients.
Study details: The data come from surveys completed by 76 ACR general rheumatologists and 135 SSc experts worldwide.
Disclosures: The researchers had no financial conflicts to disclose. Dr. Bernstein was supported by a Rheumatology Research Foundation Scientist Development Award, and two of her colleagues were funded in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Heart, Lung, and Blood Institute.
Source: Bernstein E et al. Arthritis Rheumatol. 2018 Feb 9. doi: 10.1002/art.40441.
Viremic suppression linked to decreased MACE rate in patients with HCV-cirrhosis
Hepatitis C viremic suppression was associated with a lower rate of cardiovascular events in patients with compensated HCV-related cirrhosis, compared with control patients who did not achieve a sustained virological response. In addition, predictive factors for major adverse cardiovascular events (MACEs) in compensated HCV-related cirrhosis were Asian ethnic origin, hypertension, smoking, and low serum albumin, according to a report in American Heart Journal.
A total of 878 patients with HCV-related cirrhosis were enrolled at 35 French centers. Upon enrollment, all patients received HCV treatment and were followed for MACEs, including stroke, myocardial infarction, ischemic heart disease, heart failure, peripheral arterial disease, cardiac arrest, and cardiovascular-related death, according to Patrice Cacoub, MD, of Sorbonne Universités, Paris, and his colleagues.
Five-year survival for patients presenting with a MACE was 60% vs. 88% in patients who did not have an event.
“[Our] results strengthen the systemic nature of HCV infection, a chronic disease in which cardiovascular risk must be carefully assessed. The decreased rate of MACEs after [sustained virological response] in this population should be taken into account to enable wider access to new [direct-acting antivirals]. Further studies are warranted to evaluate whether a similar benefit can be obtained in less severe patients, such as noncirrhotic HCV-infected patients,” the researchers concluded.
The authors reported having no conflicts of interest.
SOURCE: Cacoub, P et al. Am Heart J. 2018;198:4-17.
Hepatitis C viremic suppression was associated with a lower rate of cardiovascular events in patients with compensated HCV-related cirrhosis, compared with control patients who did not achieve a sustained virological response. In addition, predictive factors for major adverse cardiovascular events (MACEs) in compensated HCV-related cirrhosis were Asian ethnic origin, hypertension, smoking, and low serum albumin, according to a report in American Heart Journal.
A total of 878 patients with HCV-related cirrhosis were enrolled at 35 French centers. Upon enrollment, all patients received HCV treatment and were followed for MACEs, including stroke, myocardial infarction, ischemic heart disease, heart failure, peripheral arterial disease, cardiac arrest, and cardiovascular-related death, according to Patrice Cacoub, MD, of Sorbonne Universités, Paris, and his colleagues.
Five-year survival for patients presenting with a MACE was 60% vs. 88% in patients who did not have an event.
“[Our] results strengthen the systemic nature of HCV infection, a chronic disease in which cardiovascular risk must be carefully assessed. The decreased rate of MACEs after [sustained virological response] in this population should be taken into account to enable wider access to new [direct-acting antivirals]. Further studies are warranted to evaluate whether a similar benefit can be obtained in less severe patients, such as noncirrhotic HCV-infected patients,” the researchers concluded.
The authors reported having no conflicts of interest.
SOURCE: Cacoub, P et al. Am Heart J. 2018;198:4-17.
Hepatitis C viremic suppression was associated with a lower rate of cardiovascular events in patients with compensated HCV-related cirrhosis, compared with control patients who did not achieve a sustained virological response. In addition, predictive factors for major adverse cardiovascular events (MACEs) in compensated HCV-related cirrhosis were Asian ethnic origin, hypertension, smoking, and low serum albumin, according to a report in American Heart Journal.
A total of 878 patients with HCV-related cirrhosis were enrolled at 35 French centers. Upon enrollment, all patients received HCV treatment and were followed for MACEs, including stroke, myocardial infarction, ischemic heart disease, heart failure, peripheral arterial disease, cardiac arrest, and cardiovascular-related death, according to Patrice Cacoub, MD, of Sorbonne Universités, Paris, and his colleagues.
Five-year survival for patients presenting with a MACE was 60% vs. 88% in patients who did not have an event.
“[Our] results strengthen the systemic nature of HCV infection, a chronic disease in which cardiovascular risk must be carefully assessed. The decreased rate of MACEs after [sustained virological response] in this population should be taken into account to enable wider access to new [direct-acting antivirals]. Further studies are warranted to evaluate whether a similar benefit can be obtained in less severe patients, such as noncirrhotic HCV-infected patients,” the researchers concluded.
The authors reported having no conflicts of interest.
SOURCE: Cacoub, P et al. Am Heart J. 2018;198:4-17.
FROM AMERICAN HEART JOURNAL
Key clinical point: Predictive factors for MACE in compensated HCV-related cirrhosis were Asian ethnic origin, hypertension, smoking, and low serum albumin.
Major finding: Achieving viremic suppression was associated with a lower rate of cardiovascular events in patients with compensated HCV-related cirrhosis.
Study details: A study at 35 French centers of 878 patients with HCV-related cirrhosis.
Disclosures: The authors reported having no conflicts of interest.
Source: Cacoub, P et al. Am Heart J. 2018;198:4-17.
A simplified risk prediction model for patients presenting with acute pulmonary embolism
Clinical question: Is there a simplified risk prediction model to identify those with low risk pulmonary embolism (PE) who can be treated as outpatients?
Background: Existing prognostic models for patients with acute PE are dependent on comorbidities, which can be challenging to use in a scoring system. Models that make use of acute clinical variables to predict morbidity or mortality may be of greater clinical utility.
Study design: Retrospective chart review with derivation and validation analysis.
Setting: Tertiary care hospital in Chennai, India.
Synopsis: The authors identified 400 patients with acute PE who met inclusion criteria. Using logistic regression and readily accessible clinical variables previously shown to be associated with acute PE mortality, the authors created the HOPPE prediction score: heart rate, PaO2, systolic blood pressure, diastolic blood pressure, and ECG score. Each variable was classified into three groups and assigned a point value that could be summed to a cumulative 30-day mortality risk score. In the derivation and validation cohorts, the low, intermediate, and high HOPPE scores were associated with a 30-day mortality of 0%, 7.5-8.5%, and 18.2-18.8%, respectively, with similar trends for secondary outcomes including right ventricular dysfunction, nonfatal cardiogenic shock, and cardiorespiratory arrest.
In comparison with the previously validated PESI score, the HOPPE score had significantly higher sensitivity, specificity, and discriminative power. The conclusions from this study were limited by its single institutional design.
Bottom line: The HOPPE score provides a risk assessment tool to identify those patients with acute PE who are at lowest and highest risk for morbidity and mortality.
Citation: Subramanian M et al. Derivation and validation of a novel prediction model to identify low-risk patients with acute pulmonary embolism. Am J Cardiol. 2017;120(4):676-81.
Dr. Pizza is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Clinical question: Is there a simplified risk prediction model to identify those with low risk pulmonary embolism (PE) who can be treated as outpatients?
Background: Existing prognostic models for patients with acute PE are dependent on comorbidities, which can be challenging to use in a scoring system. Models that make use of acute clinical variables to predict morbidity or mortality may be of greater clinical utility.
Study design: Retrospective chart review with derivation and validation analysis.
Setting: Tertiary care hospital in Chennai, India.
Synopsis: The authors identified 400 patients with acute PE who met inclusion criteria. Using logistic regression and readily accessible clinical variables previously shown to be associated with acute PE mortality, the authors created the HOPPE prediction score: heart rate, PaO2, systolic blood pressure, diastolic blood pressure, and ECG score. Each variable was classified into three groups and assigned a point value that could be summed to a cumulative 30-day mortality risk score. In the derivation and validation cohorts, the low, intermediate, and high HOPPE scores were associated with a 30-day mortality of 0%, 7.5-8.5%, and 18.2-18.8%, respectively, with similar trends for secondary outcomes including right ventricular dysfunction, nonfatal cardiogenic shock, and cardiorespiratory arrest.
In comparison with the previously validated PESI score, the HOPPE score had significantly higher sensitivity, specificity, and discriminative power. The conclusions from this study were limited by its single institutional design.
Bottom line: The HOPPE score provides a risk assessment tool to identify those patients with acute PE who are at lowest and highest risk for morbidity and mortality.
Citation: Subramanian M et al. Derivation and validation of a novel prediction model to identify low-risk patients with acute pulmonary embolism. Am J Cardiol. 2017;120(4):676-81.
Dr. Pizza is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Clinical question: Is there a simplified risk prediction model to identify those with low risk pulmonary embolism (PE) who can be treated as outpatients?
Background: Existing prognostic models for patients with acute PE are dependent on comorbidities, which can be challenging to use in a scoring system. Models that make use of acute clinical variables to predict morbidity or mortality may be of greater clinical utility.
Study design: Retrospective chart review with derivation and validation analysis.
Setting: Tertiary care hospital in Chennai, India.
Synopsis: The authors identified 400 patients with acute PE who met inclusion criteria. Using logistic regression and readily accessible clinical variables previously shown to be associated with acute PE mortality, the authors created the HOPPE prediction score: heart rate, PaO2, systolic blood pressure, diastolic blood pressure, and ECG score. Each variable was classified into three groups and assigned a point value that could be summed to a cumulative 30-day mortality risk score. In the derivation and validation cohorts, the low, intermediate, and high HOPPE scores were associated with a 30-day mortality of 0%, 7.5-8.5%, and 18.2-18.8%, respectively, with similar trends for secondary outcomes including right ventricular dysfunction, nonfatal cardiogenic shock, and cardiorespiratory arrest.
In comparison with the previously validated PESI score, the HOPPE score had significantly higher sensitivity, specificity, and discriminative power. The conclusions from this study were limited by its single institutional design.
Bottom line: The HOPPE score provides a risk assessment tool to identify those patients with acute PE who are at lowest and highest risk for morbidity and mortality.
Citation: Subramanian M et al. Derivation and validation of a novel prediction model to identify low-risk patients with acute pulmonary embolism. Am J Cardiol. 2017;120(4):676-81.
Dr. Pizza is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
RA associated with higher risk of psychiatric disorders
The incidence and prevalence of anxiety disorder, depression, and bipolar disorder are higher among patients with rheumatoid arthritis than individuals from the general population, according to findings from a Canadian retrospective matched cohort study.
In the study of 10,206 rheumatoid arthritis (RA) patients and 50,960 individuals matched from the general population of Manitoba between 1989 and 2012, depression incidence was higher in the RA group, compared with the matched group, when adjusted for factors including age, sex, year, region of residence, and socioeconomic status (incidence rate ratio = 1.46; 95% confidence interval, 1.35-1.58). Incidence of anxiety disorder (IRR = 1.24; 95% CI, 1.15-1.34) and bipolar disorder (IRR = 1.21; 95% CI, 1.00-1.47) were also higher in the RA group. The incidence of schizophrenia did not differ between groups (IRR = 0.96; 95% CI, 0.61-1.50), Ruth Ann Marrie, MD, PhD, of the University of Manitoba, Winnipeg, and her coauthors reported in Arthritis Care & Research.
To estimate psychiatric disorder incidence after RA diagnosis (or the index date in the matched population), the first claim had to occur after the index date, and had to be preceded by a 5-year period with no claims for that psychiatric disorder. To estimate lifetime prevalence, once a patient met the case definition for a disorder, he or she was considered affected in all subsequent years if alive and a Manitoba resident. To account for varying periods of remission, however, annual period prevalence was defined as a patient having one or more hospital claims or two or more physician claims for the disorder in that year, Dr. Marrie and her colleagues wrote.
The adjusted lifetime prevalence was also higher in the RA group for both depression (PR = 1.35; 95% CI, 1.26-1.45) and anxiety disorder (PR = 1.20; 95% CI, 1.13-1.27), as was the annual period prevalence of depression (PR = 1.36; 95% CI, 1.26-1.47) and anxiety disorder (PR = 1.30; 95% CI, 1.19-1.41). Neither lifetime prevalence of bipolar disorder (PR = 1.13; 95% CI, 0.95-1.36) and schizophrenia (PR = 1.02; 95% CI, 0.72-1.43) nor annual period prevalence of bipolar disorder (PR = 1.06; 95% CI, 0.86-1.31) and schizophrenia (PR = 0.68; 95% CI, 0.40-1.15) differed between the RA and matched cohorts, the authors reported.
Female sex was associated with risk of psychiatric disease, as was lower socioeconomic status and living in an urban area, the authors reported.
Although the study had strengths including a large study population and use of population-based data, it did not evaluate psychiatric multimorbidity, a “common and clinically relevant issue which may affect outcomes,” Dr. Marrie and her coauthors said in the report. Additionally, the use of administrative data makes it difficult to account for care provided by nonphysician providers, such as psychologists, and for conditions that cause symptoms but do not meet diagnostic criteria, the authors noted.
“Future studies should explore these issues in population-based clinical cohorts which comprehensively evaluate multiple psychiatric disorders,” they concluded.
The study was funded by the Canadian Institutes of Health Research and the Waugh Family Chair in Multiple Sclerosis. Dr. Marrie has conducted clinical trials for Sanofi Aventis. Two other authors disclosed financial ties to pharmaceutical companies.
SOURCE: Marrie R et al. Arthritis Care Res. 2018 Feb 13. doi: 10.1002/acr.23539.
The incidence and prevalence of anxiety disorder, depression, and bipolar disorder are higher among patients with rheumatoid arthritis than individuals from the general population, according to findings from a Canadian retrospective matched cohort study.
In the study of 10,206 rheumatoid arthritis (RA) patients and 50,960 individuals matched from the general population of Manitoba between 1989 and 2012, depression incidence was higher in the RA group, compared with the matched group, when adjusted for factors including age, sex, year, region of residence, and socioeconomic status (incidence rate ratio = 1.46; 95% confidence interval, 1.35-1.58). Incidence of anxiety disorder (IRR = 1.24; 95% CI, 1.15-1.34) and bipolar disorder (IRR = 1.21; 95% CI, 1.00-1.47) were also higher in the RA group. The incidence of schizophrenia did not differ between groups (IRR = 0.96; 95% CI, 0.61-1.50), Ruth Ann Marrie, MD, PhD, of the University of Manitoba, Winnipeg, and her coauthors reported in Arthritis Care & Research.
To estimate psychiatric disorder incidence after RA diagnosis (or the index date in the matched population), the first claim had to occur after the index date, and had to be preceded by a 5-year period with no claims for that psychiatric disorder. To estimate lifetime prevalence, once a patient met the case definition for a disorder, he or she was considered affected in all subsequent years if alive and a Manitoba resident. To account for varying periods of remission, however, annual period prevalence was defined as a patient having one or more hospital claims or two or more physician claims for the disorder in that year, Dr. Marrie and her colleagues wrote.
The adjusted lifetime prevalence was also higher in the RA group for both depression (PR = 1.35; 95% CI, 1.26-1.45) and anxiety disorder (PR = 1.20; 95% CI, 1.13-1.27), as was the annual period prevalence of depression (PR = 1.36; 95% CI, 1.26-1.47) and anxiety disorder (PR = 1.30; 95% CI, 1.19-1.41). Neither lifetime prevalence of bipolar disorder (PR = 1.13; 95% CI, 0.95-1.36) and schizophrenia (PR = 1.02; 95% CI, 0.72-1.43) nor annual period prevalence of bipolar disorder (PR = 1.06; 95% CI, 0.86-1.31) and schizophrenia (PR = 0.68; 95% CI, 0.40-1.15) differed between the RA and matched cohorts, the authors reported.
Female sex was associated with risk of psychiatric disease, as was lower socioeconomic status and living in an urban area, the authors reported.
Although the study had strengths including a large study population and use of population-based data, it did not evaluate psychiatric multimorbidity, a “common and clinically relevant issue which may affect outcomes,” Dr. Marrie and her coauthors said in the report. Additionally, the use of administrative data makes it difficult to account for care provided by nonphysician providers, such as psychologists, and for conditions that cause symptoms but do not meet diagnostic criteria, the authors noted.
“Future studies should explore these issues in population-based clinical cohorts which comprehensively evaluate multiple psychiatric disorders,” they concluded.
The study was funded by the Canadian Institutes of Health Research and the Waugh Family Chair in Multiple Sclerosis. Dr. Marrie has conducted clinical trials for Sanofi Aventis. Two other authors disclosed financial ties to pharmaceutical companies.
SOURCE: Marrie R et al. Arthritis Care Res. 2018 Feb 13. doi: 10.1002/acr.23539.
The incidence and prevalence of anxiety disorder, depression, and bipolar disorder are higher among patients with rheumatoid arthritis than individuals from the general population, according to findings from a Canadian retrospective matched cohort study.
In the study of 10,206 rheumatoid arthritis (RA) patients and 50,960 individuals matched from the general population of Manitoba between 1989 and 2012, depression incidence was higher in the RA group, compared with the matched group, when adjusted for factors including age, sex, year, region of residence, and socioeconomic status (incidence rate ratio = 1.46; 95% confidence interval, 1.35-1.58). Incidence of anxiety disorder (IRR = 1.24; 95% CI, 1.15-1.34) and bipolar disorder (IRR = 1.21; 95% CI, 1.00-1.47) were also higher in the RA group. The incidence of schizophrenia did not differ between groups (IRR = 0.96; 95% CI, 0.61-1.50), Ruth Ann Marrie, MD, PhD, of the University of Manitoba, Winnipeg, and her coauthors reported in Arthritis Care & Research.
To estimate psychiatric disorder incidence after RA diagnosis (or the index date in the matched population), the first claim had to occur after the index date, and had to be preceded by a 5-year period with no claims for that psychiatric disorder. To estimate lifetime prevalence, once a patient met the case definition for a disorder, he or she was considered affected in all subsequent years if alive and a Manitoba resident. To account for varying periods of remission, however, annual period prevalence was defined as a patient having one or more hospital claims or two or more physician claims for the disorder in that year, Dr. Marrie and her colleagues wrote.
The adjusted lifetime prevalence was also higher in the RA group for both depression (PR = 1.35; 95% CI, 1.26-1.45) and anxiety disorder (PR = 1.20; 95% CI, 1.13-1.27), as was the annual period prevalence of depression (PR = 1.36; 95% CI, 1.26-1.47) and anxiety disorder (PR = 1.30; 95% CI, 1.19-1.41). Neither lifetime prevalence of bipolar disorder (PR = 1.13; 95% CI, 0.95-1.36) and schizophrenia (PR = 1.02; 95% CI, 0.72-1.43) nor annual period prevalence of bipolar disorder (PR = 1.06; 95% CI, 0.86-1.31) and schizophrenia (PR = 0.68; 95% CI, 0.40-1.15) differed between the RA and matched cohorts, the authors reported.
Female sex was associated with risk of psychiatric disease, as was lower socioeconomic status and living in an urban area, the authors reported.
Although the study had strengths including a large study population and use of population-based data, it did not evaluate psychiatric multimorbidity, a “common and clinically relevant issue which may affect outcomes,” Dr. Marrie and her coauthors said in the report. Additionally, the use of administrative data makes it difficult to account for care provided by nonphysician providers, such as psychologists, and for conditions that cause symptoms but do not meet diagnostic criteria, the authors noted.
“Future studies should explore these issues in population-based clinical cohorts which comprehensively evaluate multiple psychiatric disorders,” they concluded.
The study was funded by the Canadian Institutes of Health Research and the Waugh Family Chair in Multiple Sclerosis. Dr. Marrie has conducted clinical trials for Sanofi Aventis. Two other authors disclosed financial ties to pharmaceutical companies.
SOURCE: Marrie R et al. Arthritis Care Res. 2018 Feb 13. doi: 10.1002/acr.23539.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point:
Major finding: Incidence of depression (IRR = 1.46; 95% CI, 1.35-1.58), anxiety disorder (IRR = 1.24; 95% CI, 1.15-1.34), and bipolar disorder (IRR = 1.21; 95% CI, 1.00-1.47) were higher in the RA group than in the matched group.
Data source: A retrospective matched cohort study of 10,206 RA patients and 50,960 matched individuals from the general population between 1989 and 2012.
Disclosures: The study was funded by the Canadian Institutes of Health Research and the Waugh Family Chair in Multiple Sclerosis. Dr. Marrie has conducted clinical trials for Sanofi Aventis. Two other authors disclosed financial ties to pharmaceutical companies.
Source: Marrie R et al. Arthritis Care Res. 2018 Feb 13. doi: 10.1002/acr.23539
Inflammatory markers predict vaccine response in HCV, HIV
In patients with chronic hepatitis C (HCV) and HIV infection, blood protein markers showing evidence of systemic inflammation were associated with a poor immune response to hepatitis A/hepatitis B vaccination, according to a study of blood samples obtained in two small clinical trials.
Prevaccination plasma levels of inflammatory proteins IP10, IL-6, and sCD14 were elevated in both HCV- and HIV-infected patients, while sCD163 was also elevated in HCV-infected patients, according to the report in Vaccine.
Fifteen HCV-infected, 24 HIV-infected, and 10 uninfected control patients followed an appropriate vaccination course for a combined hepatitis A–hepatitis B vaccine. Antibody levels against the challenging vaccine proteins were assessed and quantified by ELISA, according to Carey L. Shive, PhD, of Louis Stokes Cleveland VA Medical Center, and her colleagues.
After HAV/HBV vaccination, HCV- and HIV-infected patients had lower and less durable HAV and HBV antibody responses than those of uninfected control patients. This was inversely correlated with the level of the inflammatory proteins seen in HCV-infected patients. The level of the HAV/HBV antibody response was too low in the HIV-infected patients to assess correlations with the inflammatory protein levels.
The researchers speculated that the elevated blood inflammatory markers indicated similar elevation in lymph node tissues, where high levels of the proteins may effect the survival and function of T follicular helper cells that may influence the generation of B cell antibody response and B cell memory activation to vaccination.
“Understanding mechanisms underlying immune impairment during chronic viral infection is needed to guide strategies to improve immune health during these morbid infections,” the researchers concluded.
The authors reported having no conflicts. The study was funded by U.S. government grants.
Source: Shive, CL et al. Vaccine 2018;38:453-60.
In patients with chronic hepatitis C (HCV) and HIV infection, blood protein markers showing evidence of systemic inflammation were associated with a poor immune response to hepatitis A/hepatitis B vaccination, according to a study of blood samples obtained in two small clinical trials.
Prevaccination plasma levels of inflammatory proteins IP10, IL-6, and sCD14 were elevated in both HCV- and HIV-infected patients, while sCD163 was also elevated in HCV-infected patients, according to the report in Vaccine.
Fifteen HCV-infected, 24 HIV-infected, and 10 uninfected control patients followed an appropriate vaccination course for a combined hepatitis A–hepatitis B vaccine. Antibody levels against the challenging vaccine proteins were assessed and quantified by ELISA, according to Carey L. Shive, PhD, of Louis Stokes Cleveland VA Medical Center, and her colleagues.
After HAV/HBV vaccination, HCV- and HIV-infected patients had lower and less durable HAV and HBV antibody responses than those of uninfected control patients. This was inversely correlated with the level of the inflammatory proteins seen in HCV-infected patients. The level of the HAV/HBV antibody response was too low in the HIV-infected patients to assess correlations with the inflammatory protein levels.
The researchers speculated that the elevated blood inflammatory markers indicated similar elevation in lymph node tissues, where high levels of the proteins may effect the survival and function of T follicular helper cells that may influence the generation of B cell antibody response and B cell memory activation to vaccination.
“Understanding mechanisms underlying immune impairment during chronic viral infection is needed to guide strategies to improve immune health during these morbid infections,” the researchers concluded.
The authors reported having no conflicts. The study was funded by U.S. government grants.
Source: Shive, CL et al. Vaccine 2018;38:453-60.
In patients with chronic hepatitis C (HCV) and HIV infection, blood protein markers showing evidence of systemic inflammation were associated with a poor immune response to hepatitis A/hepatitis B vaccination, according to a study of blood samples obtained in two small clinical trials.
Prevaccination plasma levels of inflammatory proteins IP10, IL-6, and sCD14 were elevated in both HCV- and HIV-infected patients, while sCD163 was also elevated in HCV-infected patients, according to the report in Vaccine.
Fifteen HCV-infected, 24 HIV-infected, and 10 uninfected control patients followed an appropriate vaccination course for a combined hepatitis A–hepatitis B vaccine. Antibody levels against the challenging vaccine proteins were assessed and quantified by ELISA, according to Carey L. Shive, PhD, of Louis Stokes Cleveland VA Medical Center, and her colleagues.
After HAV/HBV vaccination, HCV- and HIV-infected patients had lower and less durable HAV and HBV antibody responses than those of uninfected control patients. This was inversely correlated with the level of the inflammatory proteins seen in HCV-infected patients. The level of the HAV/HBV antibody response was too low in the HIV-infected patients to assess correlations with the inflammatory protein levels.
The researchers speculated that the elevated blood inflammatory markers indicated similar elevation in lymph node tissues, where high levels of the proteins may effect the survival and function of T follicular helper cells that may influence the generation of B cell antibody response and B cell memory activation to vaccination.
“Understanding mechanisms underlying immune impairment during chronic viral infection is needed to guide strategies to improve immune health during these morbid infections,” the researchers concluded.
The authors reported having no conflicts. The study was funded by U.S. government grants.
Source: Shive, CL et al. Vaccine 2018;38:453-60.
FROM VACCINE
Key clinical point:
Major finding: HCV/HIV-associated inflammatory markers reflect immune dysfunction and poor performance of subsequent vaccinations.
Study details: Clinical trials comparing 15 HCV-infected, 24 HIV-infected, and 10 uninfected control patients.
Disclosures: The authors reported having no conflicts. The study was funded by U.S. government grants.
Source: Shive, CL et al. Vaccine 2018;38:453-60.
Telling her she has cancer: A patient-centered approach to breaking bad news
Hearing a diagnosis of cancer is one of the most significant moments of a patient’s life and informing a patient of her diagnosis is an emotionally and technically challenging task for an obstetrician gynecologist who is frequently on the front line of making this diagnosis. In this column, we will explore some patient-centered strategies to perform this difficult task well so that patients come away informed but with the highest chance for positive emotional adjustment.
Fewer than 10% of physicians report receiving formal training in techniques of breaking bad news. For the majority of clinicians concerns are centered on being honest and not taking away hope, and in responding to a patient’s emotions.1 The SPIKES approach was developed to arm physicians with strategies to discuss a cancer diagnosis with their patients. This approach includes six key elements to incorporate during the encounter. These strategies are not meant to be formulaic but rather consistent principles that can be adjusted for individual patient needs.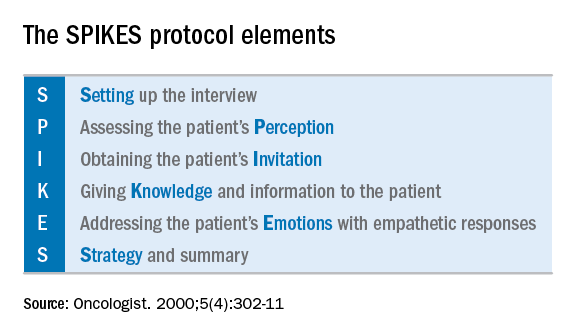
Setting up the discussion
Breaking bad news should not be a one-size-fits-all approach. Age, educational level, culture, religion, race and ethnicity, and socioeconomic opportunities each affects what and how patients may want to have this kind of information communicated to them. So how do you know how best to deliver a patient-centered approach for your patient? I recommend this simple strategy: Ask her. When ordering a test or performing a biopsy, let the patient know then why you are ordering the test and inform her of the possibility that the results may show cancer. Ask her how she would like for you to communicate that result. Would she like to be called by phone, the benefit of which is quick dissemination of information? Or would she like to receive the information face to face in the office? Research supports that most patients prefer to learn the result in the office.2 If so, I recommend scheduling a follow-up appointment in advance to prevent delays. Ask her if she would like a family member or a supportive friend to be present for the conveying of results so that she will have time to make these arrangements. Ask her if she would prefer for an alternate person to be provided with the results on her behalf.
When preparing to speak with the patient, it is valuable to mentally rehearse the words that you’ll use. Arrange for privacy and manage time constraints and interruptions (silence pagers and phones, ensure there is adequate time allocated in the schedule). Sit down to deliver the news and make a connection with eye contact and, if appropriate, touch.
Assessing the patient’s perception. Before you tell, ask. For example, “what is your understanding about why we did the biopsy?” This will guide you in where her head and heart are and can ensure you meet her wherever she is.
Obtaining the patient’s invitation. Ask the patient what she would like to be told and how much information. What would she like you to focus on? What does she not want to hear?
Giving knowledge and information to the patient. Especially now, it is important to avoid jargon and use nontechnical terms. However, do not shy away from using specific words like “cancer” by substituting them for more vague and confusing terms such as “malignancy” or “tumor.” It is important to find the balance between expressing information without being overly emotive, while avoiding excessive bluntness. Word choice is critical. Communication styles in the breaking of bad news can be separated broadly into three styles: disease centered, emotion centered, and patient-centered.3 The patient-centered approach is achieved by balancing emotional connection, information sharing, nondominance, and conveying hope. (For example, “I have some disappointing news to share. Shall we talk about the next steps in treatment? I understand this is that this is difficult for you.”) In general, this approach is most valued by patients and is associated with better information recall.
Addressing the patient’s emotions with empathetic responses. It is important that physicians take a moment to pause after communicating the test result. Even if prepared, most patients will still have a moment of shock, and their minds will likely spin through a multitude of thoughts preventing them from being able to “hear” and focus on the subsequent information. This is a moment to reflect on her reactions, her body language, and nonverbal communications to guide you on how to approach the rest of the encounter. Offer her your comfort and condolence in whichever way feels appropriate for you and her.
Beware of your own inclinations to “soften the blow.” It is a natural, compassionate instinct to follow-up giving a bad piece of information by balancing a good piece of information. For example, after just telling a woman that she has endometrial cancer, following with a statement such as “but it’s just stage 1 and is curable with surgery.” While this certainly may have immediate comforting effects, it has a couple of unintended consequences. First, it can result in difficulties later adjusting to a change in diagnosis when more information comes in (for example, upstaging after surgery or imaging). It is better to be honest and tell patients only what you know for sure in these immediate first moments of diagnosis when complete information is lacking. A more general statement such as “for most women, this is found at an early stage and is highly treatable” may be more appropriate and still provide some comfort. Second, attempts to soften the blow with a qualifying statement of positivity, such as “this is a good kind of cancer to have” might be interpreted by some patients as failing to acknowledge their devastation. She may feel that you are minimizing her condition and not allowing her to grieve or be distressed.
Strategy and summary. Patients who leave the encounter with some kind of plan for the future feel less distressed and anxious. The direction at this point of the encounter should be led by the patient. What are her greatest concerns (such as mortality, loss of fertility, time off work for treatment), and what does she want to know right now? Most patients express a desire to know more about treatment or prognosis.2,4 Unfortunately, it often is not possible to furnish this yet, particularly if this falls into the realm of a subspecialist, and prognostication typically requires more information than a provider has at initial diagnosis. However, leaving these questions unanswered is likely to result in a patient feeling helpless. For example, if an ob.gyn. discovers an apparent advanced ovarian cancer on a CT scan, tell her that, despite its apparent advanced case, it is usually treatable and that a gynecologic oncologist will discuss those best treatment options with her. Assure her that you will expeditiously refer her to a specialist who will provide her with those specifics.
The aftermath
That interval between initial diagnosis and specialist consultation is extraordinarily difficult and a high anxiety time. It is not unreasonable, in such cases, to recommend the patient to reputable online information sources, such as the Society of Gynecologic Oncology or American Cancer Society websites so that she and her family can do some research prior to that visit in order to prepare them better and give them a sense of understanding in their disease.
It is a particularly compassionate touch to reach out to the patient in the days following her cancer diagnosis, even if she has moved on to a specialist. Patients often tell me that they felt enormous reassurance and appreciation when their ob.gyn. reached out to them to “check on how they are doing.” This can usually reasonably be done by phone. This second contact serves another critical purpose: it allows for repetition of the diagnosis and initial plan, and the ability to fill in the blanks of what the patient may have missed during the prior visit, if her mind was, naturally, elsewhere. It also, quite simply, shows that you care.
Ultimately, none of us can break bad news perfectly every time. We all need to be insightful with each of these encounters as to what we did well, what we did not, and how we can adjust in the future. With respect to the SPIKES approach, patients report that physicians struggle most with the “perception,” “invitation,” and “strategy and summary” components.5 Our objective should be keeping the patient’s needs in mind, rather than our own, to maximize the chance of doing a good job. If this task is done well, not only are patients more likely to have positive emotional adjustments to their diagnosis but also more adherence with future therapies.4 In the end, it is the patient who has the final say on whether it was done well or not.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She reports no relevant financial disclosures.
References
1. Baile WF et al. Oncologist. 2000;5(4):302-11.
2. Girgis A et al. Behav Med. 1999 Summer;25(2):69-77.
3. Schmid MM et al. Patient Educ Couns. 2005 Sep;58(3):244-51.
4. Girgis A et al. J Clin Oncol. 1995 Sep;13(9):2449-56.
5. Marscholiek P et al. J Cancer Educ. 2018 Feb 5. doi: 10.1007/s13187-017-1315-3.
Hearing a diagnosis of cancer is one of the most significant moments of a patient’s life and informing a patient of her diagnosis is an emotionally and technically challenging task for an obstetrician gynecologist who is frequently on the front line of making this diagnosis. In this column, we will explore some patient-centered strategies to perform this difficult task well so that patients come away informed but with the highest chance for positive emotional adjustment.
Fewer than 10% of physicians report receiving formal training in techniques of breaking bad news. For the majority of clinicians concerns are centered on being honest and not taking away hope, and in responding to a patient’s emotions.1 The SPIKES approach was developed to arm physicians with strategies to discuss a cancer diagnosis with their patients. This approach includes six key elements to incorporate during the encounter. These strategies are not meant to be formulaic but rather consistent principles that can be adjusted for individual patient needs.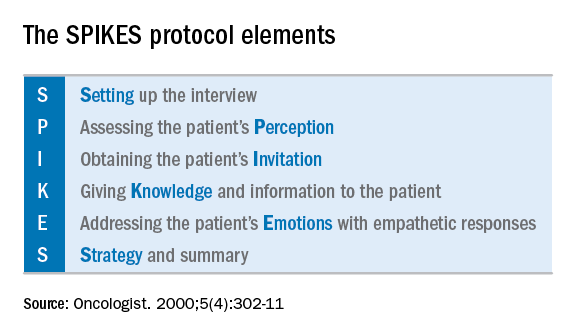
Setting up the discussion
Breaking bad news should not be a one-size-fits-all approach. Age, educational level, culture, religion, race and ethnicity, and socioeconomic opportunities each affects what and how patients may want to have this kind of information communicated to them. So how do you know how best to deliver a patient-centered approach for your patient? I recommend this simple strategy: Ask her. When ordering a test or performing a biopsy, let the patient know then why you are ordering the test and inform her of the possibility that the results may show cancer. Ask her how she would like for you to communicate that result. Would she like to be called by phone, the benefit of which is quick dissemination of information? Or would she like to receive the information face to face in the office? Research supports that most patients prefer to learn the result in the office.2 If so, I recommend scheduling a follow-up appointment in advance to prevent delays. Ask her if she would like a family member or a supportive friend to be present for the conveying of results so that she will have time to make these arrangements. Ask her if she would prefer for an alternate person to be provided with the results on her behalf.
When preparing to speak with the patient, it is valuable to mentally rehearse the words that you’ll use. Arrange for privacy and manage time constraints and interruptions (silence pagers and phones, ensure there is adequate time allocated in the schedule). Sit down to deliver the news and make a connection with eye contact and, if appropriate, touch.
Assessing the patient’s perception. Before you tell, ask. For example, “what is your understanding about why we did the biopsy?” This will guide you in where her head and heart are and can ensure you meet her wherever she is.
Obtaining the patient’s invitation. Ask the patient what she would like to be told and how much information. What would she like you to focus on? What does she not want to hear?
Giving knowledge and information to the patient. Especially now, it is important to avoid jargon and use nontechnical terms. However, do not shy away from using specific words like “cancer” by substituting them for more vague and confusing terms such as “malignancy” or “tumor.” It is important to find the balance between expressing information without being overly emotive, while avoiding excessive bluntness. Word choice is critical. Communication styles in the breaking of bad news can be separated broadly into three styles: disease centered, emotion centered, and patient-centered.3 The patient-centered approach is achieved by balancing emotional connection, information sharing, nondominance, and conveying hope. (For example, “I have some disappointing news to share. Shall we talk about the next steps in treatment? I understand this is that this is difficult for you.”) In general, this approach is most valued by patients and is associated with better information recall.
Addressing the patient’s emotions with empathetic responses. It is important that physicians take a moment to pause after communicating the test result. Even if prepared, most patients will still have a moment of shock, and their minds will likely spin through a multitude of thoughts preventing them from being able to “hear” and focus on the subsequent information. This is a moment to reflect on her reactions, her body language, and nonverbal communications to guide you on how to approach the rest of the encounter. Offer her your comfort and condolence in whichever way feels appropriate for you and her.
Beware of your own inclinations to “soften the blow.” It is a natural, compassionate instinct to follow-up giving a bad piece of information by balancing a good piece of information. For example, after just telling a woman that she has endometrial cancer, following with a statement such as “but it’s just stage 1 and is curable with surgery.” While this certainly may have immediate comforting effects, it has a couple of unintended consequences. First, it can result in difficulties later adjusting to a change in diagnosis when more information comes in (for example, upstaging after surgery or imaging). It is better to be honest and tell patients only what you know for sure in these immediate first moments of diagnosis when complete information is lacking. A more general statement such as “for most women, this is found at an early stage and is highly treatable” may be more appropriate and still provide some comfort. Second, attempts to soften the blow with a qualifying statement of positivity, such as “this is a good kind of cancer to have” might be interpreted by some patients as failing to acknowledge their devastation. She may feel that you are minimizing her condition and not allowing her to grieve or be distressed.
Strategy and summary. Patients who leave the encounter with some kind of plan for the future feel less distressed and anxious. The direction at this point of the encounter should be led by the patient. What are her greatest concerns (such as mortality, loss of fertility, time off work for treatment), and what does she want to know right now? Most patients express a desire to know more about treatment or prognosis.2,4 Unfortunately, it often is not possible to furnish this yet, particularly if this falls into the realm of a subspecialist, and prognostication typically requires more information than a provider has at initial diagnosis. However, leaving these questions unanswered is likely to result in a patient feeling helpless. For example, if an ob.gyn. discovers an apparent advanced ovarian cancer on a CT scan, tell her that, despite its apparent advanced case, it is usually treatable and that a gynecologic oncologist will discuss those best treatment options with her. Assure her that you will expeditiously refer her to a specialist who will provide her with those specifics.
The aftermath
That interval between initial diagnosis and specialist consultation is extraordinarily difficult and a high anxiety time. It is not unreasonable, in such cases, to recommend the patient to reputable online information sources, such as the Society of Gynecologic Oncology or American Cancer Society websites so that she and her family can do some research prior to that visit in order to prepare them better and give them a sense of understanding in their disease.
It is a particularly compassionate touch to reach out to the patient in the days following her cancer diagnosis, even if she has moved on to a specialist. Patients often tell me that they felt enormous reassurance and appreciation when their ob.gyn. reached out to them to “check on how they are doing.” This can usually reasonably be done by phone. This second contact serves another critical purpose: it allows for repetition of the diagnosis and initial plan, and the ability to fill in the blanks of what the patient may have missed during the prior visit, if her mind was, naturally, elsewhere. It also, quite simply, shows that you care.
Ultimately, none of us can break bad news perfectly every time. We all need to be insightful with each of these encounters as to what we did well, what we did not, and how we can adjust in the future. With respect to the SPIKES approach, patients report that physicians struggle most with the “perception,” “invitation,” and “strategy and summary” components.5 Our objective should be keeping the patient’s needs in mind, rather than our own, to maximize the chance of doing a good job. If this task is done well, not only are patients more likely to have positive emotional adjustments to their diagnosis but also more adherence with future therapies.4 In the end, it is the patient who has the final say on whether it was done well or not.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She reports no relevant financial disclosures.
References
1. Baile WF et al. Oncologist. 2000;5(4):302-11.
2. Girgis A et al. Behav Med. 1999 Summer;25(2):69-77.
3. Schmid MM et al. Patient Educ Couns. 2005 Sep;58(3):244-51.
4. Girgis A et al. J Clin Oncol. 1995 Sep;13(9):2449-56.
5. Marscholiek P et al. J Cancer Educ. 2018 Feb 5. doi: 10.1007/s13187-017-1315-3.
Hearing a diagnosis of cancer is one of the most significant moments of a patient’s life and informing a patient of her diagnosis is an emotionally and technically challenging task for an obstetrician gynecologist who is frequently on the front line of making this diagnosis. In this column, we will explore some patient-centered strategies to perform this difficult task well so that patients come away informed but with the highest chance for positive emotional adjustment.
Fewer than 10% of physicians report receiving formal training in techniques of breaking bad news. For the majority of clinicians concerns are centered on being honest and not taking away hope, and in responding to a patient’s emotions.1 The SPIKES approach was developed to arm physicians with strategies to discuss a cancer diagnosis with their patients. This approach includes six key elements to incorporate during the encounter. These strategies are not meant to be formulaic but rather consistent principles that can be adjusted for individual patient needs.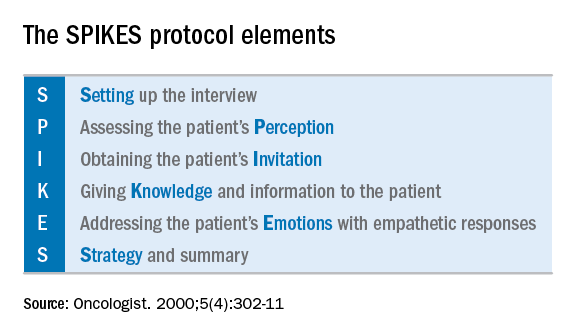
Setting up the discussion
Breaking bad news should not be a one-size-fits-all approach. Age, educational level, culture, religion, race and ethnicity, and socioeconomic opportunities each affects what and how patients may want to have this kind of information communicated to them. So how do you know how best to deliver a patient-centered approach for your patient? I recommend this simple strategy: Ask her. When ordering a test or performing a biopsy, let the patient know then why you are ordering the test and inform her of the possibility that the results may show cancer. Ask her how she would like for you to communicate that result. Would she like to be called by phone, the benefit of which is quick dissemination of information? Or would she like to receive the information face to face in the office? Research supports that most patients prefer to learn the result in the office.2 If so, I recommend scheduling a follow-up appointment in advance to prevent delays. Ask her if she would like a family member or a supportive friend to be present for the conveying of results so that she will have time to make these arrangements. Ask her if she would prefer for an alternate person to be provided with the results on her behalf.
When preparing to speak with the patient, it is valuable to mentally rehearse the words that you’ll use. Arrange for privacy and manage time constraints and interruptions (silence pagers and phones, ensure there is adequate time allocated in the schedule). Sit down to deliver the news and make a connection with eye contact and, if appropriate, touch.
Assessing the patient’s perception. Before you tell, ask. For example, “what is your understanding about why we did the biopsy?” This will guide you in where her head and heart are and can ensure you meet her wherever she is.
Obtaining the patient’s invitation. Ask the patient what she would like to be told and how much information. What would she like you to focus on? What does she not want to hear?
Giving knowledge and information to the patient. Especially now, it is important to avoid jargon and use nontechnical terms. However, do not shy away from using specific words like “cancer” by substituting them for more vague and confusing terms such as “malignancy” or “tumor.” It is important to find the balance between expressing information without being overly emotive, while avoiding excessive bluntness. Word choice is critical. Communication styles in the breaking of bad news can be separated broadly into three styles: disease centered, emotion centered, and patient-centered.3 The patient-centered approach is achieved by balancing emotional connection, information sharing, nondominance, and conveying hope. (For example, “I have some disappointing news to share. Shall we talk about the next steps in treatment? I understand this is that this is difficult for you.”) In general, this approach is most valued by patients and is associated with better information recall.
Addressing the patient’s emotions with empathetic responses. It is important that physicians take a moment to pause after communicating the test result. Even if prepared, most patients will still have a moment of shock, and their minds will likely spin through a multitude of thoughts preventing them from being able to “hear” and focus on the subsequent information. This is a moment to reflect on her reactions, her body language, and nonverbal communications to guide you on how to approach the rest of the encounter. Offer her your comfort and condolence in whichever way feels appropriate for you and her.
Beware of your own inclinations to “soften the blow.” It is a natural, compassionate instinct to follow-up giving a bad piece of information by balancing a good piece of information. For example, after just telling a woman that she has endometrial cancer, following with a statement such as “but it’s just stage 1 and is curable with surgery.” While this certainly may have immediate comforting effects, it has a couple of unintended consequences. First, it can result in difficulties later adjusting to a change in diagnosis when more information comes in (for example, upstaging after surgery or imaging). It is better to be honest and tell patients only what you know for sure in these immediate first moments of diagnosis when complete information is lacking. A more general statement such as “for most women, this is found at an early stage and is highly treatable” may be more appropriate and still provide some comfort. Second, attempts to soften the blow with a qualifying statement of positivity, such as “this is a good kind of cancer to have” might be interpreted by some patients as failing to acknowledge their devastation. She may feel that you are minimizing her condition and not allowing her to grieve or be distressed.
Strategy and summary. Patients who leave the encounter with some kind of plan for the future feel less distressed and anxious. The direction at this point of the encounter should be led by the patient. What are her greatest concerns (such as mortality, loss of fertility, time off work for treatment), and what does she want to know right now? Most patients express a desire to know more about treatment or prognosis.2,4 Unfortunately, it often is not possible to furnish this yet, particularly if this falls into the realm of a subspecialist, and prognostication typically requires more information than a provider has at initial diagnosis. However, leaving these questions unanswered is likely to result in a patient feeling helpless. For example, if an ob.gyn. discovers an apparent advanced ovarian cancer on a CT scan, tell her that, despite its apparent advanced case, it is usually treatable and that a gynecologic oncologist will discuss those best treatment options with her. Assure her that you will expeditiously refer her to a specialist who will provide her with those specifics.
The aftermath
That interval between initial diagnosis and specialist consultation is extraordinarily difficult and a high anxiety time. It is not unreasonable, in such cases, to recommend the patient to reputable online information sources, such as the Society of Gynecologic Oncology or American Cancer Society websites so that she and her family can do some research prior to that visit in order to prepare them better and give them a sense of understanding in their disease.
It is a particularly compassionate touch to reach out to the patient in the days following her cancer diagnosis, even if she has moved on to a specialist. Patients often tell me that they felt enormous reassurance and appreciation when their ob.gyn. reached out to them to “check on how they are doing.” This can usually reasonably be done by phone. This second contact serves another critical purpose: it allows for repetition of the diagnosis and initial plan, and the ability to fill in the blanks of what the patient may have missed during the prior visit, if her mind was, naturally, elsewhere. It also, quite simply, shows that you care.
Ultimately, none of us can break bad news perfectly every time. We all need to be insightful with each of these encounters as to what we did well, what we did not, and how we can adjust in the future. With respect to the SPIKES approach, patients report that physicians struggle most with the “perception,” “invitation,” and “strategy and summary” components.5 Our objective should be keeping the patient’s needs in mind, rather than our own, to maximize the chance of doing a good job. If this task is done well, not only are patients more likely to have positive emotional adjustments to their diagnosis but also more adherence with future therapies.4 In the end, it is the patient who has the final say on whether it was done well or not.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She reports no relevant financial disclosures.
References
1. Baile WF et al. Oncologist. 2000;5(4):302-11.
2. Girgis A et al. Behav Med. 1999 Summer;25(2):69-77.
3. Schmid MM et al. Patient Educ Couns. 2005 Sep;58(3):244-51.
4. Girgis A et al. J Clin Oncol. 1995 Sep;13(9):2449-56.
5. Marscholiek P et al. J Cancer Educ. 2018 Feb 5. doi: 10.1007/s13187-017-1315-3.












