User login
PCOS Linked to Hypertensive Blood Pressure in Teens
TOPLINE:
Adolescent girls with polycystic ovary syndrome (PCOS) have an increased risk for hypertension, according to a new study which underscores the importance of blood pressure surveillance in this population.
METHODOLOGY:
- The retrospective cohort study examined the association between PCOS and hypertension in adolescent girls within a diverse community-based US healthcare population.
- The researchers analyzed data from 224,418 adolescent girls (mean age at index visit, 14.9 years; 15.8% classified as having obesity) who had a well-child visit between 2013 and 2019, during which their systolic blood pressure and diastolic blood pressure were measured.
- Blood pressure in the hypertensive range was classified using the 2017 American Academy of Pediatrics Practice Guideline, with thresholds of 130/80 mm Hg or greater.
TAKEAWAY:
- The proportion of adolescent girls with high blood pressure was significantly greater among those with PCOS than among those without the condition (18.2% vs 7.1%; P < .001).
- Adolescent girls with PCOS had a 25% higher risk for hypertension than those without the disorder (adjusted odds ratio [aOR], 1.25; 95% CI, 1.10-1.42).
- Similarly, adolescent girls with obesity and PCOS had a 23% higher risk for high blood pressure than those without PCOS (aOR, 1.23; 95% CI, 1.06-1.42).
IN PRACTICE:
“The high prevalence of [hypertension] associated with PCOS emphasizes the key role of early [blood pressure] monitoring in this high-risk group,” the authors of the study wrote.
SOURCE:
The study was led by Sherry Zhang, MD, Kaiser Permanente Oakland Medical Center, Oakland, California, and was published online in the American Journal of Preventive Medicine.
LIMITATIONS:
The study relied on coded diagnoses of PCOS from clinical settings, which may have led to detection and referral biases. The findings may not be generalizable to an unselected population in which adolescent girls are systematically screened for both PCOS and hypertension.
DISCLOSURES:
This study was funded by the Cardiovascular and Metabolic Conditions Research Section and the Biostatistical Consulting Unit at the Division of Research, Kaiser Permanente Northern California and by the Kaiser Permanente Northern California Community Health Program. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Adolescent girls with polycystic ovary syndrome (PCOS) have an increased risk for hypertension, according to a new study which underscores the importance of blood pressure surveillance in this population.
METHODOLOGY:
- The retrospective cohort study examined the association between PCOS and hypertension in adolescent girls within a diverse community-based US healthcare population.
- The researchers analyzed data from 224,418 adolescent girls (mean age at index visit, 14.9 years; 15.8% classified as having obesity) who had a well-child visit between 2013 and 2019, during which their systolic blood pressure and diastolic blood pressure were measured.
- Blood pressure in the hypertensive range was classified using the 2017 American Academy of Pediatrics Practice Guideline, with thresholds of 130/80 mm Hg or greater.
TAKEAWAY:
- The proportion of adolescent girls with high blood pressure was significantly greater among those with PCOS than among those without the condition (18.2% vs 7.1%; P < .001).
- Adolescent girls with PCOS had a 25% higher risk for hypertension than those without the disorder (adjusted odds ratio [aOR], 1.25; 95% CI, 1.10-1.42).
- Similarly, adolescent girls with obesity and PCOS had a 23% higher risk for high blood pressure than those without PCOS (aOR, 1.23; 95% CI, 1.06-1.42).
IN PRACTICE:
“The high prevalence of [hypertension] associated with PCOS emphasizes the key role of early [blood pressure] monitoring in this high-risk group,” the authors of the study wrote.
SOURCE:
The study was led by Sherry Zhang, MD, Kaiser Permanente Oakland Medical Center, Oakland, California, and was published online in the American Journal of Preventive Medicine.
LIMITATIONS:
The study relied on coded diagnoses of PCOS from clinical settings, which may have led to detection and referral biases. The findings may not be generalizable to an unselected population in which adolescent girls are systematically screened for both PCOS and hypertension.
DISCLOSURES:
This study was funded by the Cardiovascular and Metabolic Conditions Research Section and the Biostatistical Consulting Unit at the Division of Research, Kaiser Permanente Northern California and by the Kaiser Permanente Northern California Community Health Program. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Adolescent girls with polycystic ovary syndrome (PCOS) have an increased risk for hypertension, according to a new study which underscores the importance of blood pressure surveillance in this population.
METHODOLOGY:
- The retrospective cohort study examined the association between PCOS and hypertension in adolescent girls within a diverse community-based US healthcare population.
- The researchers analyzed data from 224,418 adolescent girls (mean age at index visit, 14.9 years; 15.8% classified as having obesity) who had a well-child visit between 2013 and 2019, during which their systolic blood pressure and diastolic blood pressure were measured.
- Blood pressure in the hypertensive range was classified using the 2017 American Academy of Pediatrics Practice Guideline, with thresholds of 130/80 mm Hg or greater.
TAKEAWAY:
- The proportion of adolescent girls with high blood pressure was significantly greater among those with PCOS than among those without the condition (18.2% vs 7.1%; P < .001).
- Adolescent girls with PCOS had a 25% higher risk for hypertension than those without the disorder (adjusted odds ratio [aOR], 1.25; 95% CI, 1.10-1.42).
- Similarly, adolescent girls with obesity and PCOS had a 23% higher risk for high blood pressure than those without PCOS (aOR, 1.23; 95% CI, 1.06-1.42).
IN PRACTICE:
“The high prevalence of [hypertension] associated with PCOS emphasizes the key role of early [blood pressure] monitoring in this high-risk group,” the authors of the study wrote.
SOURCE:
The study was led by Sherry Zhang, MD, Kaiser Permanente Oakland Medical Center, Oakland, California, and was published online in the American Journal of Preventive Medicine.
LIMITATIONS:
The study relied on coded diagnoses of PCOS from clinical settings, which may have led to detection and referral biases. The findings may not be generalizable to an unselected population in which adolescent girls are systematically screened for both PCOS and hypertension.
DISCLOSURES:
This study was funded by the Cardiovascular and Metabolic Conditions Research Section and the Biostatistical Consulting Unit at the Division of Research, Kaiser Permanente Northern California and by the Kaiser Permanente Northern California Community Health Program. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Dry Eye Linked to Increased Risk for Mental Health Disorders
TOPLINE:
Patients with dry eye disease are more than three times as likely to have mental health conditions, such as depression and anxiety, as those without the condition.
METHODOLOGY:
- Researchers used a database from the National Institutes of Health to investigate the association between dry eye disease and mental health disorders in a large and diverse nationwide population of American adults.
- They identified 18,257 patients (mean age, 64.9 years; 67% women) with dry eye disease who were propensity score–matched with 54,765 participants without the condition.
- The cases of dry eye disease were identified using Systematized Nomenclature of Medicine codes for dry eyes, meibomian gland dysfunction, and tear film insufficiency.
- The outcome measures for mental health conditions were clinical diagnoses of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders.
TAKEAWAY:
- Patients with dry eye disease had more than triple the risk for mental health conditions than participants without the condition (adjusted odds ratio [aOR], 3.21; P < .001).
- Patients with dry eye disease had a higher risk for a depressive disorder (aOR, 3.47), anxiety-related disorder (aOR, 2.74), bipolar disorder (aOR, 2.23), and schizophrenia spectrum disorder (aOR, 2.48; P < .001 for all) than participants without the condition.
- The associations between dry eye disease and mental health conditions were significantly stronger among Black individuals than among White individuals, except for bipolar disorder.
- Dry eye disease was associated with two- to threefold higher odds of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders even in participants who never used medications for mental health (P < .001 for all).
IN PRACTICE:
“Greater efforts should be undertaken to screen patients with DED [dry eye disease] for mental health conditions, particularly in historically medically underserved populations,” the authors of the study wrote.
SOURCE:
This study was led by Aaron T. Zhao, of the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, and was published online on October 15, 2024, in the American Journal of Ophthalmology.
LIMITATIONS:
This study relied on electronic health record data, which may have led to the inclusion of participants with undiagnosed dry eye disease as control participants. Moreover, the study did not evaluate the severity of dry eye disease or the severity and duration of mental health conditions, which may have affected the results. The database analyzed in this study may not have fully captured the complete demographic profile of the nationwide population, which may have affected the generalizability of the findings.
DISCLOSURES:
This study was supported by funding from the National Institutes of Health and Research to Prevent Blindness. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Patients with dry eye disease are more than three times as likely to have mental health conditions, such as depression and anxiety, as those without the condition.
METHODOLOGY:
- Researchers used a database from the National Institutes of Health to investigate the association between dry eye disease and mental health disorders in a large and diverse nationwide population of American adults.
- They identified 18,257 patients (mean age, 64.9 years; 67% women) with dry eye disease who were propensity score–matched with 54,765 participants without the condition.
- The cases of dry eye disease were identified using Systematized Nomenclature of Medicine codes for dry eyes, meibomian gland dysfunction, and tear film insufficiency.
- The outcome measures for mental health conditions were clinical diagnoses of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders.
TAKEAWAY:
- Patients with dry eye disease had more than triple the risk for mental health conditions than participants without the condition (adjusted odds ratio [aOR], 3.21; P < .001).
- Patients with dry eye disease had a higher risk for a depressive disorder (aOR, 3.47), anxiety-related disorder (aOR, 2.74), bipolar disorder (aOR, 2.23), and schizophrenia spectrum disorder (aOR, 2.48; P < .001 for all) than participants without the condition.
- The associations between dry eye disease and mental health conditions were significantly stronger among Black individuals than among White individuals, except for bipolar disorder.
- Dry eye disease was associated with two- to threefold higher odds of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders even in participants who never used medications for mental health (P < .001 for all).
IN PRACTICE:
“Greater efforts should be undertaken to screen patients with DED [dry eye disease] for mental health conditions, particularly in historically medically underserved populations,” the authors of the study wrote.
SOURCE:
This study was led by Aaron T. Zhao, of the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, and was published online on October 15, 2024, in the American Journal of Ophthalmology.
LIMITATIONS:
This study relied on electronic health record data, which may have led to the inclusion of participants with undiagnosed dry eye disease as control participants. Moreover, the study did not evaluate the severity of dry eye disease or the severity and duration of mental health conditions, which may have affected the results. The database analyzed in this study may not have fully captured the complete demographic profile of the nationwide population, which may have affected the generalizability of the findings.
DISCLOSURES:
This study was supported by funding from the National Institutes of Health and Research to Prevent Blindness. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Patients with dry eye disease are more than three times as likely to have mental health conditions, such as depression and anxiety, as those without the condition.
METHODOLOGY:
- Researchers used a database from the National Institutes of Health to investigate the association between dry eye disease and mental health disorders in a large and diverse nationwide population of American adults.
- They identified 18,257 patients (mean age, 64.9 years; 67% women) with dry eye disease who were propensity score–matched with 54,765 participants without the condition.
- The cases of dry eye disease were identified using Systematized Nomenclature of Medicine codes for dry eyes, meibomian gland dysfunction, and tear film insufficiency.
- The outcome measures for mental health conditions were clinical diagnoses of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders.
TAKEAWAY:
- Patients with dry eye disease had more than triple the risk for mental health conditions than participants without the condition (adjusted odds ratio [aOR], 3.21; P < .001).
- Patients with dry eye disease had a higher risk for a depressive disorder (aOR, 3.47), anxiety-related disorder (aOR, 2.74), bipolar disorder (aOR, 2.23), and schizophrenia spectrum disorder (aOR, 2.48; P < .001 for all) than participants without the condition.
- The associations between dry eye disease and mental health conditions were significantly stronger among Black individuals than among White individuals, except for bipolar disorder.
- Dry eye disease was associated with two- to threefold higher odds of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders even in participants who never used medications for mental health (P < .001 for all).
IN PRACTICE:
“Greater efforts should be undertaken to screen patients with DED [dry eye disease] for mental health conditions, particularly in historically medically underserved populations,” the authors of the study wrote.
SOURCE:
This study was led by Aaron T. Zhao, of the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, and was published online on October 15, 2024, in the American Journal of Ophthalmology.
LIMITATIONS:
This study relied on electronic health record data, which may have led to the inclusion of participants with undiagnosed dry eye disease as control participants. Moreover, the study did not evaluate the severity of dry eye disease or the severity and duration of mental health conditions, which may have affected the results. The database analyzed in this study may not have fully captured the complete demographic profile of the nationwide population, which may have affected the generalizability of the findings.
DISCLOSURES:
This study was supported by funding from the National Institutes of Health and Research to Prevent Blindness. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Higher Doses of Vitamin D3 Do Not Reduce Cardiac Biomarkers in Older Adults
TOPLINE:
Higher doses of vitamin D3 supplementation did not significantly reduce cardiac biomarkers in older adults with low serum vitamin D levels. The STURDY trial found no significant differences in high-sensitivity cardiac troponin I (hs-cTnI) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) between low- and high-dose groups.
METHODOLOGY:
- A total of 688 participants aged 70 years or older with low serum 25-hydroxy vitamin D levels (10-29 ng/mL) were included in the STURDY trial.
- Participants were randomized to receive one of four doses of vitamin D3 supplementation: 200, 1000, 2000, or 4000 IU/d, with 200 IU/d as the reference dose.
- Cardiac biomarkers, including hs-cTnI and NT-proBNP, were measured at baseline, 3 months, 12 months, and 24 months.
- The trial was conducted at two community-based research institutions in the United States between July 2015 and March 2019.
- The effects of vitamin D3 dose on biomarkers were assessed via mixed-effects tobit models, with participants followed up to 24 months or until study termination.
TAKEAWAY:
- Higher doses of vitamin D3 supplementation did not significantly affect hs-cTnI levels compared with the low-dose group (1.6% difference; 95% CI, −5.3 to 8.9).
- No significant differences were observed in NT-proBNP levels between the high-dose and low-dose groups (−1.8% difference; 95% CI, −9.3 to 6.3).
- Both hs-cTnI and NT-proBNP levels increased in both low- and high-dose groups over time, with hs-cTnI increasing by 5.2% and 7.0%, respectively, and NT-proBNP increasing by 11.3% and 9.3%, respectively.
- The findings suggest that higher doses of vitamin D3 supplementation do not reduce markers of subclinical cardiovascular disease in older adults with low serum vitamin D levels.
IN PRACTICE:
“We can speculate that the systemic effects of vitamin D deficiency are more profound among the very old, and there may be an inverse relationship between supplementation and inflammation. It is also possible that serum vitamin D level is a risk marker but not a risk factor for CVD risk and related underlying mechanisms,” wrote the authors of the study.
SOURCE:
The study was led by Katharine W. Rainer, MD, Beth Israel Deaconess Medical Center in Boston. It was published online in the Journal of the American College of Cardiology.
LIMITATIONS:
The study’s community-based population may limit the generalizability of the findings to populations at higher risk for cardiovascular disease. Additionally, the baseline cardiac biomarkers were lower than those in some high-risk populations, which may affect the precision of the assay performance. The study may not have had adequate power for cross-sectional and subgroup analyses. Both groups received some vitamin D3 supplementation, making it difficult to determine the impact of lower-dose supplementation vs no supplementation.
DISCLOSURES:
The study was supported by grants from the National Institute on Aging, the Office of Dietary Supplements, the Mid-Atlantic Nutrition Obesity Research Center, and the Johns Hopkins Institute for Clinical and Translational Research. Rainer disclosed receiving grants from these organizations.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Higher doses of vitamin D3 supplementation did not significantly reduce cardiac biomarkers in older adults with low serum vitamin D levels. The STURDY trial found no significant differences in high-sensitivity cardiac troponin I (hs-cTnI) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) between low- and high-dose groups.
METHODOLOGY:
- A total of 688 participants aged 70 years or older with low serum 25-hydroxy vitamin D levels (10-29 ng/mL) were included in the STURDY trial.
- Participants were randomized to receive one of four doses of vitamin D3 supplementation: 200, 1000, 2000, or 4000 IU/d, with 200 IU/d as the reference dose.
- Cardiac biomarkers, including hs-cTnI and NT-proBNP, were measured at baseline, 3 months, 12 months, and 24 months.
- The trial was conducted at two community-based research institutions in the United States between July 2015 and March 2019.
- The effects of vitamin D3 dose on biomarkers were assessed via mixed-effects tobit models, with participants followed up to 24 months or until study termination.
TAKEAWAY:
- Higher doses of vitamin D3 supplementation did not significantly affect hs-cTnI levels compared with the low-dose group (1.6% difference; 95% CI, −5.3 to 8.9).
- No significant differences were observed in NT-proBNP levels between the high-dose and low-dose groups (−1.8% difference; 95% CI, −9.3 to 6.3).
- Both hs-cTnI and NT-proBNP levels increased in both low- and high-dose groups over time, with hs-cTnI increasing by 5.2% and 7.0%, respectively, and NT-proBNP increasing by 11.3% and 9.3%, respectively.
- The findings suggest that higher doses of vitamin D3 supplementation do not reduce markers of subclinical cardiovascular disease in older adults with low serum vitamin D levels.
IN PRACTICE:
“We can speculate that the systemic effects of vitamin D deficiency are more profound among the very old, and there may be an inverse relationship between supplementation and inflammation. It is also possible that serum vitamin D level is a risk marker but not a risk factor for CVD risk and related underlying mechanisms,” wrote the authors of the study.
SOURCE:
The study was led by Katharine W. Rainer, MD, Beth Israel Deaconess Medical Center in Boston. It was published online in the Journal of the American College of Cardiology.
LIMITATIONS:
The study’s community-based population may limit the generalizability of the findings to populations at higher risk for cardiovascular disease. Additionally, the baseline cardiac biomarkers were lower than those in some high-risk populations, which may affect the precision of the assay performance. The study may not have had adequate power for cross-sectional and subgroup analyses. Both groups received some vitamin D3 supplementation, making it difficult to determine the impact of lower-dose supplementation vs no supplementation.
DISCLOSURES:
The study was supported by grants from the National Institute on Aging, the Office of Dietary Supplements, the Mid-Atlantic Nutrition Obesity Research Center, and the Johns Hopkins Institute for Clinical and Translational Research. Rainer disclosed receiving grants from these organizations.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Higher doses of vitamin D3 supplementation did not significantly reduce cardiac biomarkers in older adults with low serum vitamin D levels. The STURDY trial found no significant differences in high-sensitivity cardiac troponin I (hs-cTnI) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) between low- and high-dose groups.
METHODOLOGY:
- A total of 688 participants aged 70 years or older with low serum 25-hydroxy vitamin D levels (10-29 ng/mL) were included in the STURDY trial.
- Participants were randomized to receive one of four doses of vitamin D3 supplementation: 200, 1000, 2000, or 4000 IU/d, with 200 IU/d as the reference dose.
- Cardiac biomarkers, including hs-cTnI and NT-proBNP, were measured at baseline, 3 months, 12 months, and 24 months.
- The trial was conducted at two community-based research institutions in the United States between July 2015 and March 2019.
- The effects of vitamin D3 dose on biomarkers were assessed via mixed-effects tobit models, with participants followed up to 24 months or until study termination.
TAKEAWAY:
- Higher doses of vitamin D3 supplementation did not significantly affect hs-cTnI levels compared with the low-dose group (1.6% difference; 95% CI, −5.3 to 8.9).
- No significant differences were observed in NT-proBNP levels between the high-dose and low-dose groups (−1.8% difference; 95% CI, −9.3 to 6.3).
- Both hs-cTnI and NT-proBNP levels increased in both low- and high-dose groups over time, with hs-cTnI increasing by 5.2% and 7.0%, respectively, and NT-proBNP increasing by 11.3% and 9.3%, respectively.
- The findings suggest that higher doses of vitamin D3 supplementation do not reduce markers of subclinical cardiovascular disease in older adults with low serum vitamin D levels.
IN PRACTICE:
“We can speculate that the systemic effects of vitamin D deficiency are more profound among the very old, and there may be an inverse relationship between supplementation and inflammation. It is also possible that serum vitamin D level is a risk marker but not a risk factor for CVD risk and related underlying mechanisms,” wrote the authors of the study.
SOURCE:
The study was led by Katharine W. Rainer, MD, Beth Israel Deaconess Medical Center in Boston. It was published online in the Journal of the American College of Cardiology.
LIMITATIONS:
The study’s community-based population may limit the generalizability of the findings to populations at higher risk for cardiovascular disease. Additionally, the baseline cardiac biomarkers were lower than those in some high-risk populations, which may affect the precision of the assay performance. The study may not have had adequate power for cross-sectional and subgroup analyses. Both groups received some vitamin D3 supplementation, making it difficult to determine the impact of lower-dose supplementation vs no supplementation.
DISCLOSURES:
The study was supported by grants from the National Institute on Aging, the Office of Dietary Supplements, the Mid-Atlantic Nutrition Obesity Research Center, and the Johns Hopkins Institute for Clinical and Translational Research. Rainer disclosed receiving grants from these organizations.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Projected 2023 Cost Reduction From Tumor Necrosis Factor α Inhibitor Biosimilars in Dermatology: A National Medicare Analysis
To the Editor:
Although biologics provide major therapeutic benefits for dermatologic conditions, they also come with a substantial cost, making them among the most expensive medications available. Medicare and Medicaid spending on biologics for dermatologic conditions increased by 320% from 2012 to 2018, reaching a staggering $10.6 billion in 2018 alone.1 Biosimilars show promise in reducing health care spending for dermatologic conditions; however, their utilization has been limited due to multiple factors, including delayed market entry from patent thickets, exclusionary formulary contracts, and prescriber skepticism regarding their safety and efficacy.2 For instance, a national survey of 1201 US physicians in specialties that are high prescribers of biologics reported that 55% doubted the safety and appropriateness of biosimilars.3
US Food and Drug Administration approval of biosimilars for adalimumab and etanercept offers the potential to reduce health care spending for dermatologic conditions. However, this cost reduction is dependent on utilization rates among dermatologists. In this national cross-sectional review of Medicare data, we predicted the impact of these biosimilars on dermatologic Medicare costs and demonstrated how differing utilization rates among dermatologists can influence potential savings.
To model 2023 utilization and cost reduction from biosimilars, we analyzed Medicare Part D data from 2020 on existing biosimilars, including granulocyte colony–stimulating factors, erythropoiesis-stimulating agents, and tumor necrosis factor α inhibitors.4 Methods in line with a 2021 report from the US Department of Health and Human Services5 as well as those of Yazdany et al6 were used. For each class, we calculated the 2020 distribution of biosimilar and originator drug claims as well as biosimilar cost reduction per 30-day claim. We utilized 2018-2021 annual growth rates for branded adalimumab and etanercept to estimate 30-day claims for 2023 and the cost of these branded agents in the absence of biosimilars. The hypothetical 2023 cost reduction from adalimumab and etanercept biosimilars was estimated by assuming 2020 biosimilar utilization rates and mean cost reduction per claim. This study utilized publicly available or aggregate summary data (not attributable to specific patients) and did not qualify as human subject research; therefore, institutional review board approval was not required.
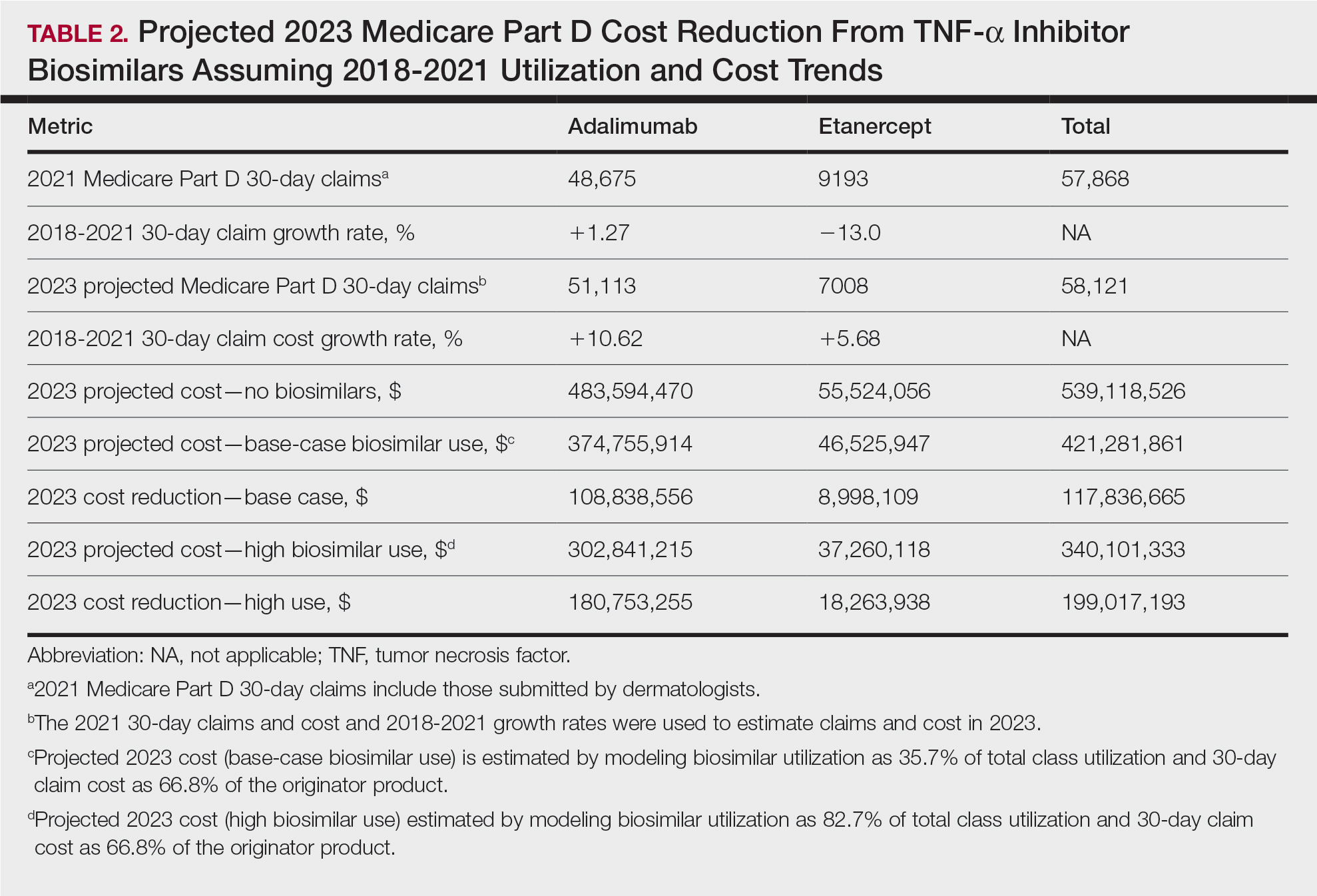
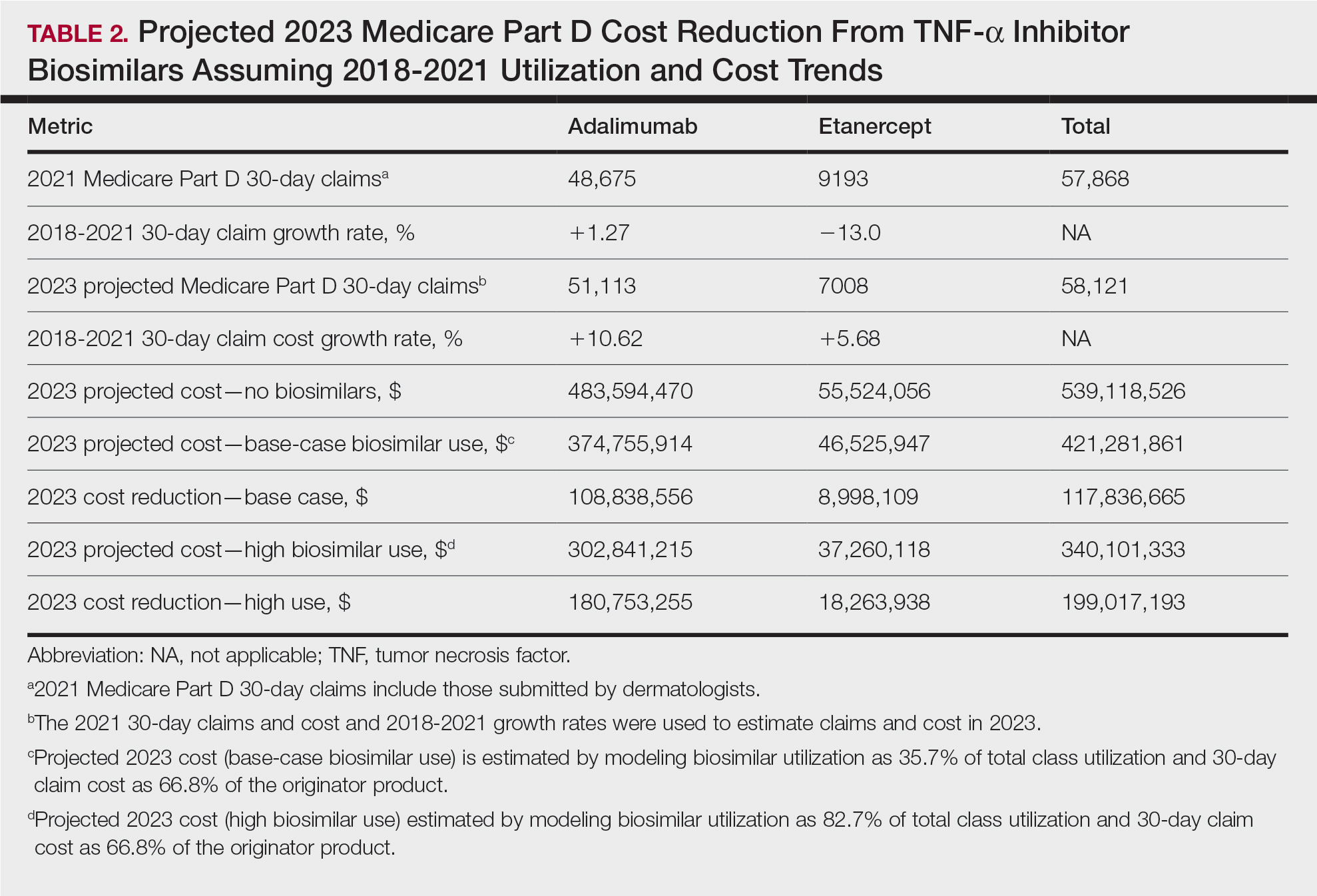
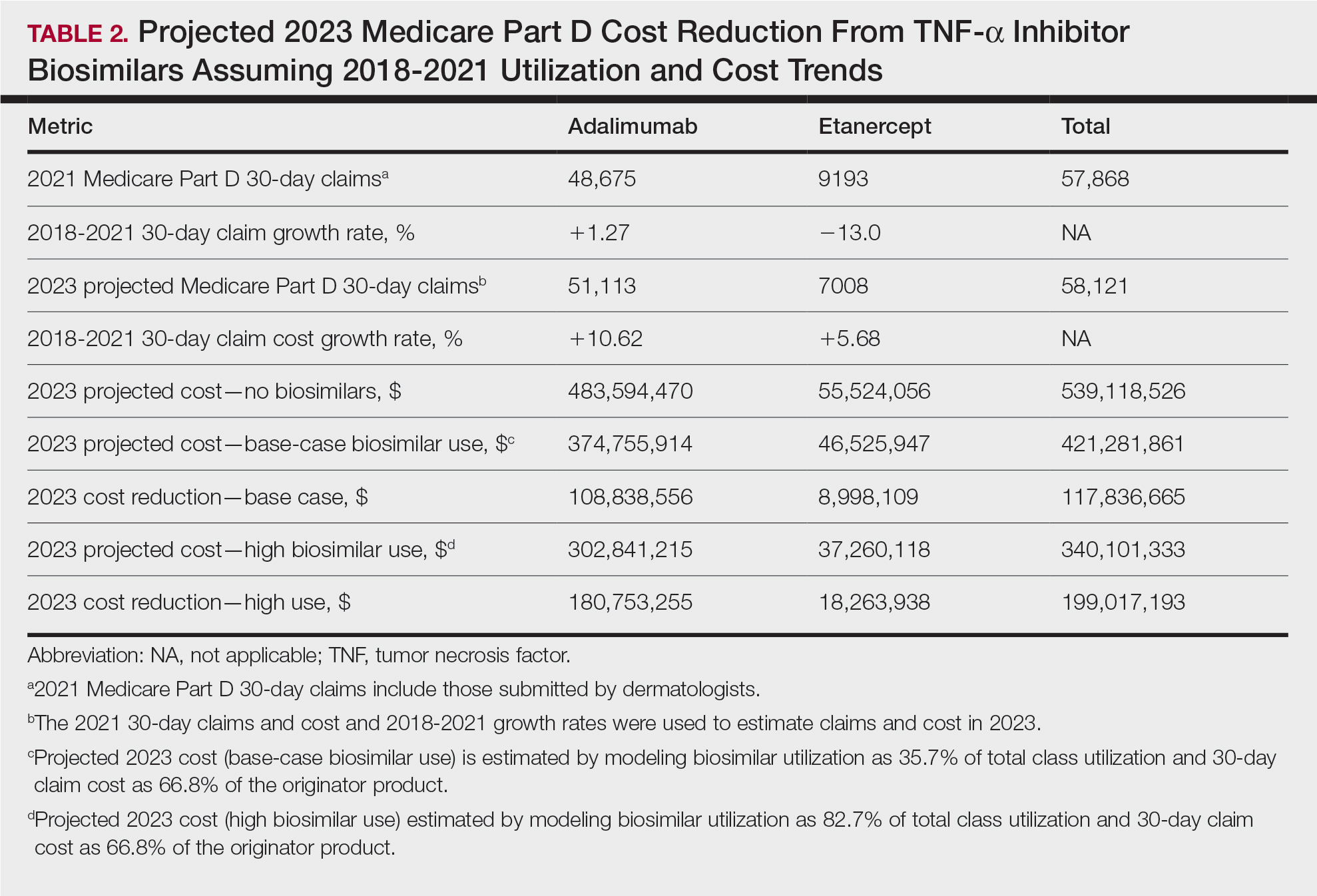
In 2020, biosimilar utilization proportions ranged from 6.4% (tumor necrosis factor α inhibitors) to 82.7% (granulocyte colony–stimulating factors), with a mean across all classes of 35.7%. On average, the cost per 30-day claim of biosimilars was 66.8% of originator agents (Table 1). In 2021, we identified 57,868 30-day claims for branded adalimumab and etanercept submitted by dermatologists. From 2018 to 2021, 30-day branded adalimumab claims increased by 1.27% annually (cost + 10.62% annually), while claims for branded etanercept decreased by 13.0% annually (cost + 5.68% annually). Assuming these trends, the cost of branded adalimumab and etanercept was estimated to be $539 million in 2023. Applying the aforementioned 35.7% utilization, the introduction of biosimilars in dermatology would yield a cost reduction of approximately $118 million (21.9%). A high utilization rate (82.7%) of biosimilars among dermatologists would increase cost savings to $199 million (36.9%)(Table 2).

Our study demonstrates that the introduction of 2 biosimilars into dermatology may result in a notable reduction in Medicare expenditures. The savings observed are likely to translate to substantial cost savings for patients. A cross-sectional analysis of 2020 Medicare data indicated that coverage for psoriasis medications was 10.0% to 99.8% across different products and Medicare Part D plans. Consequently, patients faced considerable out-of-pocket expenses, amounting to $5653 and $5714 per year for adalimumab and etanercept, respectively.7
We found that the extent of savings from biosimilars was dependent on the utilization rates among dermatologists, with the highest utilization rate almost doubling the total savings of average utilization rates. Given the impact of high utilization and the wide variation observed, understanding the factors that have influenced uptake of biosimilars is important to increasing utilization as these medications become integrated into dermatology. For instance, limited uptake of infliximab initially may have been influenced by concerns about efficacy and increased adverse events.8,9 In contrast, the high utilization of filgrastim biosimilars (82.7%) may be attributed to its longevity in the market and familiarity to prescribers, as filgrastim was the first biosimilar to be approved in the United States.10
Promoting reasonable utilization of biosimilars may require prescriber education on their safety and approval processes, which could foster increased utilization and reduce skepticism.4 Under the Biologics Price Competition and Innovation Act, the US Food and Drug Administration approves biosimilars only when they exhibit “high similarity” and show no “clinically meaningful differences” compared to the reference biologic, with no added safety risks or reduced efficacy.11 Moreover, a 2023 systematic review of 17 studies found no major difference in efficacy and safety between biosimilars and originators of etanercept, infliximab, and other biologics.12 Understanding these findings may reassure dermatologists and patients about the reliability and safety of biosimilars.
A limitation of our study is that it solely assesses Medicare data and estimates derived from existing (separate) biologic classes. It also does not account for potential expenditure shifts to newer biologic agents (eg, IL-12/17/23 inhibitors) or changes in manufacturer behavior or promotions. Nevertheless, it indicates notable financial savings from new biosimilar agents in dermatology; along with their compelling efficacy and safety profiles, this could represent a substantial benefit to patients and the health care system.
- Price KN, Atluri S, Hsiao JL, et al. Medicare and medicaid spending trends for immunomodulators prescribed for dermatologic conditions. J Dermatolog Treat. 2020;33:575-579.
- Zhai MZ, Sarpatwari A, Kesselheim AS. Why are biosimilars not living up to their promise in the US? AMA J Ethics. 2019;21:E668-E678. doi:10.1001/amajethics.2019.668
- Cohen H, Beydoun D, Chien D, et al. Awareness, knowledge, and perceptions of biosimilars among specialty physicians. Adv Ther. 2017;33:2160-2172.
- Centers for Medicare & Medicaid Services. Medicare Part D prescribers— by provider and drug. Accessed September 11, 2024. https://data.cms.gov/provider-summary-by-type-of-service/medicare-part-d-prescribers/medicare-part-d-prescribers-by-provider-and-drug/data
- US Department of Health and Human Services. Office of Inspector General. Medicare Part D and beneficiaries could realize significant spending reductions with increased biosimilar use. Accessed September 11, 2024. https://oig.hhs.gov/oei/reports/OEI-05-20-00480.pdf
- Yazdany J, Dudley RA, Lin GA, et al. Out-of-pocket costs for infliximab and its biosimilar for rheumatoid arthritis under Medicare Part D. JAMA. 2018;320:931-933. doi:10.1001/jama.2018.7316
- Pourali SP, Nshuti L, Dusetzina SB. Out-of-pocket costs of specialty medications for psoriasis and psoriatic arthritis treatment in the medicare population. JAMA Dermatol. 2021;157:1239-1241. doi:10.1001/ jamadermatol.2021.3616
- Lebwohl M. Biosimilars in dermatology. JAMA Dermatol. 2021; 157:641-642. doi:10.1001/jamadermatol.2021.0219
- Westerkam LL, Tackett KJ, Sayed CJ. Comparing the effectiveness and safety associated with infliximab vs infliximab-abda therapy for patients with hidradenitis suppurativa. JAMA Dermatol. 2021;157:708-711. doi:10.1001/jamadermatol.2021.0220
- Awad M, Singh P, Hilas O. Zarxio (Filgrastim-sndz): the first biosimilar approved by the FDA. P T. 2017;42:19-23.
- Development of therapeutic protein biosimilars: comparative analytical assessment and other quality-related considerations guidance for industry. US Department of Health and Human Services website. Updated June 15, 2022. Accessed October 21, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-therapeutic-protein-biosimilars-comparative-analyticalassessment-and-other-quality
- Phan DB, Elyoussfi S, Stevenson M, et al. Biosimilars for the treatment of psoriasis: a systematic review of clinical trials and observational studies. JAMA Dermatol. 2023;159:763-771. doi:10.1001/jamadermatol.2023.1338
To the Editor:
Although biologics provide major therapeutic benefits for dermatologic conditions, they also come with a substantial cost, making them among the most expensive medications available. Medicare and Medicaid spending on biologics for dermatologic conditions increased by 320% from 2012 to 2018, reaching a staggering $10.6 billion in 2018 alone.1 Biosimilars show promise in reducing health care spending for dermatologic conditions; however, their utilization has been limited due to multiple factors, including delayed market entry from patent thickets, exclusionary formulary contracts, and prescriber skepticism regarding their safety and efficacy.2 For instance, a national survey of 1201 US physicians in specialties that are high prescribers of biologics reported that 55% doubted the safety and appropriateness of biosimilars.3
US Food and Drug Administration approval of biosimilars for adalimumab and etanercept offers the potential to reduce health care spending for dermatologic conditions. However, this cost reduction is dependent on utilization rates among dermatologists. In this national cross-sectional review of Medicare data, we predicted the impact of these biosimilars on dermatologic Medicare costs and demonstrated how differing utilization rates among dermatologists can influence potential savings.
To model 2023 utilization and cost reduction from biosimilars, we analyzed Medicare Part D data from 2020 on existing biosimilars, including granulocyte colony–stimulating factors, erythropoiesis-stimulating agents, and tumor necrosis factor α inhibitors.4 Methods in line with a 2021 report from the US Department of Health and Human Services5 as well as those of Yazdany et al6 were used. For each class, we calculated the 2020 distribution of biosimilar and originator drug claims as well as biosimilar cost reduction per 30-day claim. We utilized 2018-2021 annual growth rates for branded adalimumab and etanercept to estimate 30-day claims for 2023 and the cost of these branded agents in the absence of biosimilars. The hypothetical 2023 cost reduction from adalimumab and etanercept biosimilars was estimated by assuming 2020 biosimilar utilization rates and mean cost reduction per claim. This study utilized publicly available or aggregate summary data (not attributable to specific patients) and did not qualify as human subject research; therefore, institutional review board approval was not required.
In 2020, biosimilar utilization proportions ranged from 6.4% (tumor necrosis factor α inhibitors) to 82.7% (granulocyte colony–stimulating factors), with a mean across all classes of 35.7%. On average, the cost per 30-day claim of biosimilars was 66.8% of originator agents (Table 1). In 2021, we identified 57,868 30-day claims for branded adalimumab and etanercept submitted by dermatologists. From 2018 to 2021, 30-day branded adalimumab claims increased by 1.27% annually (cost + 10.62% annually), while claims for branded etanercept decreased by 13.0% annually (cost + 5.68% annually). Assuming these trends, the cost of branded adalimumab and etanercept was estimated to be $539 million in 2023. Applying the aforementioned 35.7% utilization, the introduction of biosimilars in dermatology would yield a cost reduction of approximately $118 million (21.9%). A high utilization rate (82.7%) of biosimilars among dermatologists would increase cost savings to $199 million (36.9%)(Table 2).

Our study demonstrates that the introduction of 2 biosimilars into dermatology may result in a notable reduction in Medicare expenditures. The savings observed are likely to translate to substantial cost savings for patients. A cross-sectional analysis of 2020 Medicare data indicated that coverage for psoriasis medications was 10.0% to 99.8% across different products and Medicare Part D plans. Consequently, patients faced considerable out-of-pocket expenses, amounting to $5653 and $5714 per year for adalimumab and etanercept, respectively.7
We found that the extent of savings from biosimilars was dependent on the utilization rates among dermatologists, with the highest utilization rate almost doubling the total savings of average utilization rates. Given the impact of high utilization and the wide variation observed, understanding the factors that have influenced uptake of biosimilars is important to increasing utilization as these medications become integrated into dermatology. For instance, limited uptake of infliximab initially may have been influenced by concerns about efficacy and increased adverse events.8,9 In contrast, the high utilization of filgrastim biosimilars (82.7%) may be attributed to its longevity in the market and familiarity to prescribers, as filgrastim was the first biosimilar to be approved in the United States.10
Promoting reasonable utilization of biosimilars may require prescriber education on their safety and approval processes, which could foster increased utilization and reduce skepticism.4 Under the Biologics Price Competition and Innovation Act, the US Food and Drug Administration approves biosimilars only when they exhibit “high similarity” and show no “clinically meaningful differences” compared to the reference biologic, with no added safety risks or reduced efficacy.11 Moreover, a 2023 systematic review of 17 studies found no major difference in efficacy and safety between biosimilars and originators of etanercept, infliximab, and other biologics.12 Understanding these findings may reassure dermatologists and patients about the reliability and safety of biosimilars.
A limitation of our study is that it solely assesses Medicare data and estimates derived from existing (separate) biologic classes. It also does not account for potential expenditure shifts to newer biologic agents (eg, IL-12/17/23 inhibitors) or changes in manufacturer behavior or promotions. Nevertheless, it indicates notable financial savings from new biosimilar agents in dermatology; along with their compelling efficacy and safety profiles, this could represent a substantial benefit to patients and the health care system.
To the Editor:
Although biologics provide major therapeutic benefits for dermatologic conditions, they also come with a substantial cost, making them among the most expensive medications available. Medicare and Medicaid spending on biologics for dermatologic conditions increased by 320% from 2012 to 2018, reaching a staggering $10.6 billion in 2018 alone.1 Biosimilars show promise in reducing health care spending for dermatologic conditions; however, their utilization has been limited due to multiple factors, including delayed market entry from patent thickets, exclusionary formulary contracts, and prescriber skepticism regarding their safety and efficacy.2 For instance, a national survey of 1201 US physicians in specialties that are high prescribers of biologics reported that 55% doubted the safety and appropriateness of biosimilars.3
US Food and Drug Administration approval of biosimilars for adalimumab and etanercept offers the potential to reduce health care spending for dermatologic conditions. However, this cost reduction is dependent on utilization rates among dermatologists. In this national cross-sectional review of Medicare data, we predicted the impact of these biosimilars on dermatologic Medicare costs and demonstrated how differing utilization rates among dermatologists can influence potential savings.
To model 2023 utilization and cost reduction from biosimilars, we analyzed Medicare Part D data from 2020 on existing biosimilars, including granulocyte colony–stimulating factors, erythropoiesis-stimulating agents, and tumor necrosis factor α inhibitors.4 Methods in line with a 2021 report from the US Department of Health and Human Services5 as well as those of Yazdany et al6 were used. For each class, we calculated the 2020 distribution of biosimilar and originator drug claims as well as biosimilar cost reduction per 30-day claim. We utilized 2018-2021 annual growth rates for branded adalimumab and etanercept to estimate 30-day claims for 2023 and the cost of these branded agents in the absence of biosimilars. The hypothetical 2023 cost reduction from adalimumab and etanercept biosimilars was estimated by assuming 2020 biosimilar utilization rates and mean cost reduction per claim. This study utilized publicly available or aggregate summary data (not attributable to specific patients) and did not qualify as human subject research; therefore, institutional review board approval was not required.
In 2020, biosimilar utilization proportions ranged from 6.4% (tumor necrosis factor α inhibitors) to 82.7% (granulocyte colony–stimulating factors), with a mean across all classes of 35.7%. On average, the cost per 30-day claim of biosimilars was 66.8% of originator agents (Table 1). In 2021, we identified 57,868 30-day claims for branded adalimumab and etanercept submitted by dermatologists. From 2018 to 2021, 30-day branded adalimumab claims increased by 1.27% annually (cost + 10.62% annually), while claims for branded etanercept decreased by 13.0% annually (cost + 5.68% annually). Assuming these trends, the cost of branded adalimumab and etanercept was estimated to be $539 million in 2023. Applying the aforementioned 35.7% utilization, the introduction of biosimilars in dermatology would yield a cost reduction of approximately $118 million (21.9%). A high utilization rate (82.7%) of biosimilars among dermatologists would increase cost savings to $199 million (36.9%)(Table 2).

Our study demonstrates that the introduction of 2 biosimilars into dermatology may result in a notable reduction in Medicare expenditures. The savings observed are likely to translate to substantial cost savings for patients. A cross-sectional analysis of 2020 Medicare data indicated that coverage for psoriasis medications was 10.0% to 99.8% across different products and Medicare Part D plans. Consequently, patients faced considerable out-of-pocket expenses, amounting to $5653 and $5714 per year for adalimumab and etanercept, respectively.7
We found that the extent of savings from biosimilars was dependent on the utilization rates among dermatologists, with the highest utilization rate almost doubling the total savings of average utilization rates. Given the impact of high utilization and the wide variation observed, understanding the factors that have influenced uptake of biosimilars is important to increasing utilization as these medications become integrated into dermatology. For instance, limited uptake of infliximab initially may have been influenced by concerns about efficacy and increased adverse events.8,9 In contrast, the high utilization of filgrastim biosimilars (82.7%) may be attributed to its longevity in the market and familiarity to prescribers, as filgrastim was the first biosimilar to be approved in the United States.10
Promoting reasonable utilization of biosimilars may require prescriber education on their safety and approval processes, which could foster increased utilization and reduce skepticism.4 Under the Biologics Price Competition and Innovation Act, the US Food and Drug Administration approves biosimilars only when they exhibit “high similarity” and show no “clinically meaningful differences” compared to the reference biologic, with no added safety risks or reduced efficacy.11 Moreover, a 2023 systematic review of 17 studies found no major difference in efficacy and safety between biosimilars and originators of etanercept, infliximab, and other biologics.12 Understanding these findings may reassure dermatologists and patients about the reliability and safety of biosimilars.
A limitation of our study is that it solely assesses Medicare data and estimates derived from existing (separate) biologic classes. It also does not account for potential expenditure shifts to newer biologic agents (eg, IL-12/17/23 inhibitors) or changes in manufacturer behavior or promotions. Nevertheless, it indicates notable financial savings from new biosimilar agents in dermatology; along with their compelling efficacy and safety profiles, this could represent a substantial benefit to patients and the health care system.
- Price KN, Atluri S, Hsiao JL, et al. Medicare and medicaid spending trends for immunomodulators prescribed for dermatologic conditions. J Dermatolog Treat. 2020;33:575-579.
- Zhai MZ, Sarpatwari A, Kesselheim AS. Why are biosimilars not living up to their promise in the US? AMA J Ethics. 2019;21:E668-E678. doi:10.1001/amajethics.2019.668
- Cohen H, Beydoun D, Chien D, et al. Awareness, knowledge, and perceptions of biosimilars among specialty physicians. Adv Ther. 2017;33:2160-2172.
- Centers for Medicare & Medicaid Services. Medicare Part D prescribers— by provider and drug. Accessed September 11, 2024. https://data.cms.gov/provider-summary-by-type-of-service/medicare-part-d-prescribers/medicare-part-d-prescribers-by-provider-and-drug/data
- US Department of Health and Human Services. Office of Inspector General. Medicare Part D and beneficiaries could realize significant spending reductions with increased biosimilar use. Accessed September 11, 2024. https://oig.hhs.gov/oei/reports/OEI-05-20-00480.pdf
- Yazdany J, Dudley RA, Lin GA, et al. Out-of-pocket costs for infliximab and its biosimilar for rheumatoid arthritis under Medicare Part D. JAMA. 2018;320:931-933. doi:10.1001/jama.2018.7316
- Pourali SP, Nshuti L, Dusetzina SB. Out-of-pocket costs of specialty medications for psoriasis and psoriatic arthritis treatment in the medicare population. JAMA Dermatol. 2021;157:1239-1241. doi:10.1001/ jamadermatol.2021.3616
- Lebwohl M. Biosimilars in dermatology. JAMA Dermatol. 2021; 157:641-642. doi:10.1001/jamadermatol.2021.0219
- Westerkam LL, Tackett KJ, Sayed CJ. Comparing the effectiveness and safety associated with infliximab vs infliximab-abda therapy for patients with hidradenitis suppurativa. JAMA Dermatol. 2021;157:708-711. doi:10.1001/jamadermatol.2021.0220
- Awad M, Singh P, Hilas O. Zarxio (Filgrastim-sndz): the first biosimilar approved by the FDA. P T. 2017;42:19-23.
- Development of therapeutic protein biosimilars: comparative analytical assessment and other quality-related considerations guidance for industry. US Department of Health and Human Services website. Updated June 15, 2022. Accessed October 21, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-therapeutic-protein-biosimilars-comparative-analyticalassessment-and-other-quality
- Phan DB, Elyoussfi S, Stevenson M, et al. Biosimilars for the treatment of psoriasis: a systematic review of clinical trials and observational studies. JAMA Dermatol. 2023;159:763-771. doi:10.1001/jamadermatol.2023.1338
- Price KN, Atluri S, Hsiao JL, et al. Medicare and medicaid spending trends for immunomodulators prescribed for dermatologic conditions. J Dermatolog Treat. 2020;33:575-579.
- Zhai MZ, Sarpatwari A, Kesselheim AS. Why are biosimilars not living up to their promise in the US? AMA J Ethics. 2019;21:E668-E678. doi:10.1001/amajethics.2019.668
- Cohen H, Beydoun D, Chien D, et al. Awareness, knowledge, and perceptions of biosimilars among specialty physicians. Adv Ther. 2017;33:2160-2172.
- Centers for Medicare & Medicaid Services. Medicare Part D prescribers— by provider and drug. Accessed September 11, 2024. https://data.cms.gov/provider-summary-by-type-of-service/medicare-part-d-prescribers/medicare-part-d-prescribers-by-provider-and-drug/data
- US Department of Health and Human Services. Office of Inspector General. Medicare Part D and beneficiaries could realize significant spending reductions with increased biosimilar use. Accessed September 11, 2024. https://oig.hhs.gov/oei/reports/OEI-05-20-00480.pdf
- Yazdany J, Dudley RA, Lin GA, et al. Out-of-pocket costs for infliximab and its biosimilar for rheumatoid arthritis under Medicare Part D. JAMA. 2018;320:931-933. doi:10.1001/jama.2018.7316
- Pourali SP, Nshuti L, Dusetzina SB. Out-of-pocket costs of specialty medications for psoriasis and psoriatic arthritis treatment in the medicare population. JAMA Dermatol. 2021;157:1239-1241. doi:10.1001/ jamadermatol.2021.3616
- Lebwohl M. Biosimilars in dermatology. JAMA Dermatol. 2021; 157:641-642. doi:10.1001/jamadermatol.2021.0219
- Westerkam LL, Tackett KJ, Sayed CJ. Comparing the effectiveness and safety associated with infliximab vs infliximab-abda therapy for patients with hidradenitis suppurativa. JAMA Dermatol. 2021;157:708-711. doi:10.1001/jamadermatol.2021.0220
- Awad M, Singh P, Hilas O. Zarxio (Filgrastim-sndz): the first biosimilar approved by the FDA. P T. 2017;42:19-23.
- Development of therapeutic protein biosimilars: comparative analytical assessment and other quality-related considerations guidance for industry. US Department of Health and Human Services website. Updated June 15, 2022. Accessed October 21, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-therapeutic-protein-biosimilars-comparative-analyticalassessment-and-other-quality
- Phan DB, Elyoussfi S, Stevenson M, et al. Biosimilars for the treatment of psoriasis: a systematic review of clinical trials and observational studies. JAMA Dermatol. 2023;159:763-771. doi:10.1001/jamadermatol.2023.1338
Practice Points
- Biosimilars for adalimumab and etanercept are safe and effective alternatives with the potential to reduce health care costs in dermatology by approximately $118 million.
- A high utilization rate of biosimilars by dermatologists would increase cost savings even further.
Phenytoin-Induced DRESS Syndrome: Clinical and Laboratory Characteristics
To the Editor:
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome—a severe cutaneous adverse drug reaction—is characterized by a cutaneous rash and systemic upset in the form of various internal organ and hematologic disturbances. This delayed and idiosyncratic syndrome went by several names, including anticonvulsant hypersensitivity syndrome, before Bocquet et al1 proposed the term DRESS syndrome.
Phenytoin, a hydantoin derivative used in neurology, was implicated in 41% of cases of DRESS syndrome in a study of 100 patients conducted in southern India.2,3 While DRESS syndrome is a newer name, the clinical picture of DRESS secondary to phenytoin use remains similar in that it manifests with a morbilliform rash and systemic upset. We sought to describe the clinical and laboratory characteristics of phenytoin-induced DRESS syndrome in this case series.
The analysis included 23 patients with DRESS syndrome secondary to phenytoin use who presented to a tertiary care institution in North India between July 2021 and December 2022, satisfied the European Registry of Severe Cutaneous Adverse Reaction (RegiSCAR) criteria,4 and achieved a DRESS diagnostic score of more than 1. The mean age of the patients was 44 years (range, 14–74 years). There was a slight female predominance with a male to female ratio of 0.9:1. More than half of the patients (52.2% [12/23]) presented directly to the dermatology outpatient department; the remaining patients were referred from other departments (47.8% [11/23]). Patients primarily were receiving phenytoin for neurologic indications. Specific reasons included antiseizure prophylaxis following a traffic accident (34.8% [8/23]); epilepsy (26.1% [6/23]); and neoplastic (17.4% [4/23]), vascular (17.4% [4/23]), and infectious (4.3% [1/23]) causes. The mean latency period from drug intake to symptom onset was 29 days (range, 6–62 days), and the mean illness duration was 9 days (range, 1–45 days).
The majority of patients experienced pruritus (91.3% [21/23]) and fever (74.0% [17/23]), and all initially had a rash. Maculopapular morphology was seen in all patients. Erythema multiforme–like (17.4% [4/23]), erythrodermic (17.4% [4/23]), and vesicular (13.0% [3/23]) rashes also were documented (Figure 1). The trunk (100% [23/23]) and extremities (95.7% [22/23]) were involved most often, followed by the palms and soles (56.5% [13/23]). The mean total body surface area affected was 73.65%. Only 7 patients (30.4%) had mucosal involvement; nonhemorrhagic cheilitis was the most common manifestation.

Facial edema, a hallmark feature of DRESS syndrome, was noted in 69.6% (16/23) of patients (Figure 2). Lymphadenopathy was present in 43.5% (10/23) of patients; of those cases, the inguinal (40.0%; n=4) and cervical (30%; n=3) nodes most commonly were involved. Although DRESS syndrome can affect internal organs, this was an issue for only 2 (8.7%) patients who experienced mild hepatomegaly.

Laboratory investigations revealed a mean differential eosinophil percentage of 10.3% (reference range, 1%–4%), while the mean absolute eosinophil count was 1.0634×109/L (reference range, 0.02–0.5×109/L). Other hematologic findings included the mean percentages of neutrophils (60%; reference range, 50%–60%), lymphocytes (19.95%; reference range, 20%–50%), and monocytes (8.70%; reference range, 2%–8%).
Liver function tests revealed transaminitis5 as the most common finding, with mean aspartate aminotransferase levels of 109 U/L (reference range, 8–33 U/L), mean alanine aminotransferase of 97.9 U/L (reference range, 7–56 U/L), and mean alkaline phosphatase levels of 211.35 U/L (reference range, 44–147 U/L). Half of the patients had notable (>2 times the upper limit of normal) transaminitis.
Renal blood workup revealed slightly elevated blood urea nitrogen levels with a mean value of 28.4 mg/dL (reference range, 6–24 mg/dL), and mean serum creatinine was 0.78 mg/dL (reference range for men, 0.7–1.3 mg/dL; for women, 0.6–1.1 mg/dL).
All patients were treated with oral steroids (prednisolone 1 mg/kg/d) before tapering slowly over the following 6 to 8 weeks. The culprit drug (phenytoin) was stopped on the day of presentation. Resolution of rash and itching was seen in all patients by 3 weeks after presentation without any relapse by follow-up at 6 weeks from presentation to the hospital.
Our case series seeks to discuss the clinical and laboratory features of phenytoin-induced DRESS syndrome. Our patients had more erythrodermic and erythema multiforme–like morphologies, less mucosal involvement, more hepatic involvement, and earlier resolution.
- Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (drug rash with eosinophilia and systemic symptoms: DRESS). Semin Cutan Med Surg. 1996;15:250-257. doi:10.1016/s1085-5629(96)80038-1
- Patocka J, Wu Q, Nepovimova E, et al. Phenytoin—an anti-seizure drug: overview of its chemistry, pharmacology and toxicology. Food Chem Toxicol. 2020;142:111393. doi:10.1016/j.fct.2020.111393
- Sasidharanpillai S, Chathoth AT, Khader A, et al. Predictors of disease severity in drug reaction with eosinophilia and systemic symptoms. Indian J Dermatol Venereol Leprol. 2019;85:266-275. doi:10.4103/ijdvl.IJDVL_482_17
- Kardaun SH, Sekula P, Valeyrie-Allanore L, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Brit J Dermatol. 2013;169:1071-1080.
- Morán-Mariños C, Alva-Diaz C, De la Cruz Ramirez W, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS) induced by phenytoin re-exposure: case report and systematic review. Acta Clin Belg. 2022;77:177-185. doi:10.1080/17843286.2020.1767459
To the Editor:
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome—a severe cutaneous adverse drug reaction—is characterized by a cutaneous rash and systemic upset in the form of various internal organ and hematologic disturbances. This delayed and idiosyncratic syndrome went by several names, including anticonvulsant hypersensitivity syndrome, before Bocquet et al1 proposed the term DRESS syndrome.
Phenytoin, a hydantoin derivative used in neurology, was implicated in 41% of cases of DRESS syndrome in a study of 100 patients conducted in southern India.2,3 While DRESS syndrome is a newer name, the clinical picture of DRESS secondary to phenytoin use remains similar in that it manifests with a morbilliform rash and systemic upset. We sought to describe the clinical and laboratory characteristics of phenytoin-induced DRESS syndrome in this case series.
The analysis included 23 patients with DRESS syndrome secondary to phenytoin use who presented to a tertiary care institution in North India between July 2021 and December 2022, satisfied the European Registry of Severe Cutaneous Adverse Reaction (RegiSCAR) criteria,4 and achieved a DRESS diagnostic score of more than 1. The mean age of the patients was 44 years (range, 14–74 years). There was a slight female predominance with a male to female ratio of 0.9:1. More than half of the patients (52.2% [12/23]) presented directly to the dermatology outpatient department; the remaining patients were referred from other departments (47.8% [11/23]). Patients primarily were receiving phenytoin for neurologic indications. Specific reasons included antiseizure prophylaxis following a traffic accident (34.8% [8/23]); epilepsy (26.1% [6/23]); and neoplastic (17.4% [4/23]), vascular (17.4% [4/23]), and infectious (4.3% [1/23]) causes. The mean latency period from drug intake to symptom onset was 29 days (range, 6–62 days), and the mean illness duration was 9 days (range, 1–45 days).
The majority of patients experienced pruritus (91.3% [21/23]) and fever (74.0% [17/23]), and all initially had a rash. Maculopapular morphology was seen in all patients. Erythema multiforme–like (17.4% [4/23]), erythrodermic (17.4% [4/23]), and vesicular (13.0% [3/23]) rashes also were documented (Figure 1). The trunk (100% [23/23]) and extremities (95.7% [22/23]) were involved most often, followed by the palms and soles (56.5% [13/23]). The mean total body surface area affected was 73.65%. Only 7 patients (30.4%) had mucosal involvement; nonhemorrhagic cheilitis was the most common manifestation.

Facial edema, a hallmark feature of DRESS syndrome, was noted in 69.6% (16/23) of patients (Figure 2). Lymphadenopathy was present in 43.5% (10/23) of patients; of those cases, the inguinal (40.0%; n=4) and cervical (30%; n=3) nodes most commonly were involved. Although DRESS syndrome can affect internal organs, this was an issue for only 2 (8.7%) patients who experienced mild hepatomegaly.

Laboratory investigations revealed a mean differential eosinophil percentage of 10.3% (reference range, 1%–4%), while the mean absolute eosinophil count was 1.0634×109/L (reference range, 0.02–0.5×109/L). Other hematologic findings included the mean percentages of neutrophils (60%; reference range, 50%–60%), lymphocytes (19.95%; reference range, 20%–50%), and monocytes (8.70%; reference range, 2%–8%).
Liver function tests revealed transaminitis5 as the most common finding, with mean aspartate aminotransferase levels of 109 U/L (reference range, 8–33 U/L), mean alanine aminotransferase of 97.9 U/L (reference range, 7–56 U/L), and mean alkaline phosphatase levels of 211.35 U/L (reference range, 44–147 U/L). Half of the patients had notable (>2 times the upper limit of normal) transaminitis.
Renal blood workup revealed slightly elevated blood urea nitrogen levels with a mean value of 28.4 mg/dL (reference range, 6–24 mg/dL), and mean serum creatinine was 0.78 mg/dL (reference range for men, 0.7–1.3 mg/dL; for women, 0.6–1.1 mg/dL).
All patients were treated with oral steroids (prednisolone 1 mg/kg/d) before tapering slowly over the following 6 to 8 weeks. The culprit drug (phenytoin) was stopped on the day of presentation. Resolution of rash and itching was seen in all patients by 3 weeks after presentation without any relapse by follow-up at 6 weeks from presentation to the hospital.
Our case series seeks to discuss the clinical and laboratory features of phenytoin-induced DRESS syndrome. Our patients had more erythrodermic and erythema multiforme–like morphologies, less mucosal involvement, more hepatic involvement, and earlier resolution.
To the Editor:
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome—a severe cutaneous adverse drug reaction—is characterized by a cutaneous rash and systemic upset in the form of various internal organ and hematologic disturbances. This delayed and idiosyncratic syndrome went by several names, including anticonvulsant hypersensitivity syndrome, before Bocquet et al1 proposed the term DRESS syndrome.
Phenytoin, a hydantoin derivative used in neurology, was implicated in 41% of cases of DRESS syndrome in a study of 100 patients conducted in southern India.2,3 While DRESS syndrome is a newer name, the clinical picture of DRESS secondary to phenytoin use remains similar in that it manifests with a morbilliform rash and systemic upset. We sought to describe the clinical and laboratory characteristics of phenytoin-induced DRESS syndrome in this case series.
The analysis included 23 patients with DRESS syndrome secondary to phenytoin use who presented to a tertiary care institution in North India between July 2021 and December 2022, satisfied the European Registry of Severe Cutaneous Adverse Reaction (RegiSCAR) criteria,4 and achieved a DRESS diagnostic score of more than 1. The mean age of the patients was 44 years (range, 14–74 years). There was a slight female predominance with a male to female ratio of 0.9:1. More than half of the patients (52.2% [12/23]) presented directly to the dermatology outpatient department; the remaining patients were referred from other departments (47.8% [11/23]). Patients primarily were receiving phenytoin for neurologic indications. Specific reasons included antiseizure prophylaxis following a traffic accident (34.8% [8/23]); epilepsy (26.1% [6/23]); and neoplastic (17.4% [4/23]), vascular (17.4% [4/23]), and infectious (4.3% [1/23]) causes. The mean latency period from drug intake to symptom onset was 29 days (range, 6–62 days), and the mean illness duration was 9 days (range, 1–45 days).
The majority of patients experienced pruritus (91.3% [21/23]) and fever (74.0% [17/23]), and all initially had a rash. Maculopapular morphology was seen in all patients. Erythema multiforme–like (17.4% [4/23]), erythrodermic (17.4% [4/23]), and vesicular (13.0% [3/23]) rashes also were documented (Figure 1). The trunk (100% [23/23]) and extremities (95.7% [22/23]) were involved most often, followed by the palms and soles (56.5% [13/23]). The mean total body surface area affected was 73.65%. Only 7 patients (30.4%) had mucosal involvement; nonhemorrhagic cheilitis was the most common manifestation.

Facial edema, a hallmark feature of DRESS syndrome, was noted in 69.6% (16/23) of patients (Figure 2). Lymphadenopathy was present in 43.5% (10/23) of patients; of those cases, the inguinal (40.0%; n=4) and cervical (30%; n=3) nodes most commonly were involved. Although DRESS syndrome can affect internal organs, this was an issue for only 2 (8.7%) patients who experienced mild hepatomegaly.

Laboratory investigations revealed a mean differential eosinophil percentage of 10.3% (reference range, 1%–4%), while the mean absolute eosinophil count was 1.0634×109/L (reference range, 0.02–0.5×109/L). Other hematologic findings included the mean percentages of neutrophils (60%; reference range, 50%–60%), lymphocytes (19.95%; reference range, 20%–50%), and monocytes (8.70%; reference range, 2%–8%).
Liver function tests revealed transaminitis5 as the most common finding, with mean aspartate aminotransferase levels of 109 U/L (reference range, 8–33 U/L), mean alanine aminotransferase of 97.9 U/L (reference range, 7–56 U/L), and mean alkaline phosphatase levels of 211.35 U/L (reference range, 44–147 U/L). Half of the patients had notable (>2 times the upper limit of normal) transaminitis.
Renal blood workup revealed slightly elevated blood urea nitrogen levels with a mean value of 28.4 mg/dL (reference range, 6–24 mg/dL), and mean serum creatinine was 0.78 mg/dL (reference range for men, 0.7–1.3 mg/dL; for women, 0.6–1.1 mg/dL).
All patients were treated with oral steroids (prednisolone 1 mg/kg/d) before tapering slowly over the following 6 to 8 weeks. The culprit drug (phenytoin) was stopped on the day of presentation. Resolution of rash and itching was seen in all patients by 3 weeks after presentation without any relapse by follow-up at 6 weeks from presentation to the hospital.
Our case series seeks to discuss the clinical and laboratory features of phenytoin-induced DRESS syndrome. Our patients had more erythrodermic and erythema multiforme–like morphologies, less mucosal involvement, more hepatic involvement, and earlier resolution.
- Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (drug rash with eosinophilia and systemic symptoms: DRESS). Semin Cutan Med Surg. 1996;15:250-257. doi:10.1016/s1085-5629(96)80038-1
- Patocka J, Wu Q, Nepovimova E, et al. Phenytoin—an anti-seizure drug: overview of its chemistry, pharmacology and toxicology. Food Chem Toxicol. 2020;142:111393. doi:10.1016/j.fct.2020.111393
- Sasidharanpillai S, Chathoth AT, Khader A, et al. Predictors of disease severity in drug reaction with eosinophilia and systemic symptoms. Indian J Dermatol Venereol Leprol. 2019;85:266-275. doi:10.4103/ijdvl.IJDVL_482_17
- Kardaun SH, Sekula P, Valeyrie-Allanore L, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Brit J Dermatol. 2013;169:1071-1080.
- Morán-Mariños C, Alva-Diaz C, De la Cruz Ramirez W, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS) induced by phenytoin re-exposure: case report and systematic review. Acta Clin Belg. 2022;77:177-185. doi:10.1080/17843286.2020.1767459
- Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (drug rash with eosinophilia and systemic symptoms: DRESS). Semin Cutan Med Surg. 1996;15:250-257. doi:10.1016/s1085-5629(96)80038-1
- Patocka J, Wu Q, Nepovimova E, et al. Phenytoin—an anti-seizure drug: overview of its chemistry, pharmacology and toxicology. Food Chem Toxicol. 2020;142:111393. doi:10.1016/j.fct.2020.111393
- Sasidharanpillai S, Chathoth AT, Khader A, et al. Predictors of disease severity in drug reaction with eosinophilia and systemic symptoms. Indian J Dermatol Venereol Leprol. 2019;85:266-275. doi:10.4103/ijdvl.IJDVL_482_17
- Kardaun SH, Sekula P, Valeyrie-Allanore L, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Brit J Dermatol. 2013;169:1071-1080.
- Morán-Mariños C, Alva-Diaz C, De la Cruz Ramirez W, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS) induced by phenytoin re-exposure: case report and systematic review. Acta Clin Belg. 2022;77:177-185. doi:10.1080/17843286.2020.1767459
Practice Points
- Phenytoin has been implicated in drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, and common symptoms include rash, pruritus, and fever.
- Transaminitis may occur in patients with DRESS syndrome secondary to phenytoin use.
Cardiac Monitoring Is Crucial in Neuromuscular Disorder Care
SAVANNAH, GEORGIA — , a neurologist told an audience of nerve/muscle specialists.
The cardiac conditions can range from asymptomatic to potentially lethal, Nicholas J. Silvestri, MD, professor of neurology at the Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, in New York, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. “It’s really important to know when to do tests and refer to cardiology, and it’s really important to find a cardiologist who can work in concert in taking care of these patients.”
Protein Alterations May Disrupt Heart Muscles
In muscular dystrophies, a prevailing theory suggests that alterations to proteins such as dystrophin disrupt structural integrity in both muscle and cardiac cells, he said.
In Duchenne muscular dystrophy (DMD), cardiomyopathy, cardiac conduction abnormalities, or both usually appear in patients by age 10. “It’s important to know that it’s probably present to some degree before that, and it’s not going to get better over time,” he said.
Cardiac problems are universal in DMD by age 18, he said. “Men and boys are living longer, so they have the opportunity to develop the cardiac abnormalities that accrue with time.” Conduction abnormalities typically appear first. “In a lot of these boys, you’ll typically see persistent sinus tachycardia. But they can also develop atrial arrhythmias and bundle branch blocks.”
Sudden cardiac death is responsible for mortality in an estimated 15% patients with DMD. “Very sadly, I lost a patient this way just a few months ago,” Silvestri said.
ECGs and Echos Are Recommended
Screening is crucial. “Make sure that patients get that referral and get these tests done,” he said. “You need an ECG and echo by diagnosis or age 6. This is usually repeated annually or biannually, typically by the cardiologist you’re working with.”
The good news is that there’s evidence of survival benefits from treatment with angiotensin-converting enzyme inhibitors for dilated cardiomyopathy. “Some cardiac experts feel treatment with angiotensin receptor blockers (ARBs) is equivalent.”
Most boys will get echocardiograms, he said, “but there’s a lot of evidence showing that cardiac MRI is probably preferable for a number of reasons,” including better visualization. But the need for sedation limits access, he said, and cardiac MRI may not be available at some facilities.
Worse Outcomes in Becker Muscular Dystrophy (BMD)
Cardiac involvement is more common and more severe in BMD than in DMD. About 50% of deaths in BMD are attributed to malignant arrhythmias or congestive heart failure, he said.
Screening requirements and treatment options in BMD are similar to those in DMD, with the added option of heart transplantation.
Silvestri cautioned that up to 40% of female carriers of dystrophin mutations can develop cardiac dysfunction similar to that seen in DMD and BMD. Cardiac assessments are recommended every 5 years. “It’s important to genotype Mom,” he said, especially in light of the fact that two thirds of DMD cases may be inherited.
“When I send genetic testing on the mother and find her to be a carrier, I send her to a cardiologist so she has the appropriate screening done,” he said.
Pacemakers May Be Considered in Type 1 Myotonic Dystrophy
In type 1 myotonic dystrophy, cardiac conduction abnormalities are seen in two thirds of patients, and sudden cardiac death in up to 30% of patients. “When it is diagnosed, patients do need an ECG at that time, as well as annually,” he said.
Holter monitoring or implantable loop recorders may be recommended, and permanent pacing via an implantable cardioverter-defibrillator might be appropriate.
“Based on the literature to date, the exact timing is not is not clear,” Silvestri said. “The electrophysiologists in my area tend to be very aggressive, thankfully, and treat them fairly soon with pacemakers when we see the first sign of trouble.”
Silvestri disclosed consultant/advisory relationships with argenx, Alexion, Amgen, UCB, Immunovant, and Janssen.
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA — , a neurologist told an audience of nerve/muscle specialists.
The cardiac conditions can range from asymptomatic to potentially lethal, Nicholas J. Silvestri, MD, professor of neurology at the Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, in New York, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. “It’s really important to know when to do tests and refer to cardiology, and it’s really important to find a cardiologist who can work in concert in taking care of these patients.”
Protein Alterations May Disrupt Heart Muscles
In muscular dystrophies, a prevailing theory suggests that alterations to proteins such as dystrophin disrupt structural integrity in both muscle and cardiac cells, he said.
In Duchenne muscular dystrophy (DMD), cardiomyopathy, cardiac conduction abnormalities, or both usually appear in patients by age 10. “It’s important to know that it’s probably present to some degree before that, and it’s not going to get better over time,” he said.
Cardiac problems are universal in DMD by age 18, he said. “Men and boys are living longer, so they have the opportunity to develop the cardiac abnormalities that accrue with time.” Conduction abnormalities typically appear first. “In a lot of these boys, you’ll typically see persistent sinus tachycardia. But they can also develop atrial arrhythmias and bundle branch blocks.”
Sudden cardiac death is responsible for mortality in an estimated 15% patients with DMD. “Very sadly, I lost a patient this way just a few months ago,” Silvestri said.
ECGs and Echos Are Recommended
Screening is crucial. “Make sure that patients get that referral and get these tests done,” he said. “You need an ECG and echo by diagnosis or age 6. This is usually repeated annually or biannually, typically by the cardiologist you’re working with.”
The good news is that there’s evidence of survival benefits from treatment with angiotensin-converting enzyme inhibitors for dilated cardiomyopathy. “Some cardiac experts feel treatment with angiotensin receptor blockers (ARBs) is equivalent.”
Most boys will get echocardiograms, he said, “but there’s a lot of evidence showing that cardiac MRI is probably preferable for a number of reasons,” including better visualization. But the need for sedation limits access, he said, and cardiac MRI may not be available at some facilities.
Worse Outcomes in Becker Muscular Dystrophy (BMD)
Cardiac involvement is more common and more severe in BMD than in DMD. About 50% of deaths in BMD are attributed to malignant arrhythmias or congestive heart failure, he said.
Screening requirements and treatment options in BMD are similar to those in DMD, with the added option of heart transplantation.
Silvestri cautioned that up to 40% of female carriers of dystrophin mutations can develop cardiac dysfunction similar to that seen in DMD and BMD. Cardiac assessments are recommended every 5 years. “It’s important to genotype Mom,” he said, especially in light of the fact that two thirds of DMD cases may be inherited.
“When I send genetic testing on the mother and find her to be a carrier, I send her to a cardiologist so she has the appropriate screening done,” he said.
Pacemakers May Be Considered in Type 1 Myotonic Dystrophy
In type 1 myotonic dystrophy, cardiac conduction abnormalities are seen in two thirds of patients, and sudden cardiac death in up to 30% of patients. “When it is diagnosed, patients do need an ECG at that time, as well as annually,” he said.
Holter monitoring or implantable loop recorders may be recommended, and permanent pacing via an implantable cardioverter-defibrillator might be appropriate.
“Based on the literature to date, the exact timing is not is not clear,” Silvestri said. “The electrophysiologists in my area tend to be very aggressive, thankfully, and treat them fairly soon with pacemakers when we see the first sign of trouble.”
Silvestri disclosed consultant/advisory relationships with argenx, Alexion, Amgen, UCB, Immunovant, and Janssen.
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA — , a neurologist told an audience of nerve/muscle specialists.
The cardiac conditions can range from asymptomatic to potentially lethal, Nicholas J. Silvestri, MD, professor of neurology at the Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, in New York, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. “It’s really important to know when to do tests and refer to cardiology, and it’s really important to find a cardiologist who can work in concert in taking care of these patients.”
Protein Alterations May Disrupt Heart Muscles
In muscular dystrophies, a prevailing theory suggests that alterations to proteins such as dystrophin disrupt structural integrity in both muscle and cardiac cells, he said.
In Duchenne muscular dystrophy (DMD), cardiomyopathy, cardiac conduction abnormalities, or both usually appear in patients by age 10. “It’s important to know that it’s probably present to some degree before that, and it’s not going to get better over time,” he said.
Cardiac problems are universal in DMD by age 18, he said. “Men and boys are living longer, so they have the opportunity to develop the cardiac abnormalities that accrue with time.” Conduction abnormalities typically appear first. “In a lot of these boys, you’ll typically see persistent sinus tachycardia. But they can also develop atrial arrhythmias and bundle branch blocks.”
Sudden cardiac death is responsible for mortality in an estimated 15% patients with DMD. “Very sadly, I lost a patient this way just a few months ago,” Silvestri said.
ECGs and Echos Are Recommended
Screening is crucial. “Make sure that patients get that referral and get these tests done,” he said. “You need an ECG and echo by diagnosis or age 6. This is usually repeated annually or biannually, typically by the cardiologist you’re working with.”
The good news is that there’s evidence of survival benefits from treatment with angiotensin-converting enzyme inhibitors for dilated cardiomyopathy. “Some cardiac experts feel treatment with angiotensin receptor blockers (ARBs) is equivalent.”
Most boys will get echocardiograms, he said, “but there’s a lot of evidence showing that cardiac MRI is probably preferable for a number of reasons,” including better visualization. But the need for sedation limits access, he said, and cardiac MRI may not be available at some facilities.
Worse Outcomes in Becker Muscular Dystrophy (BMD)
Cardiac involvement is more common and more severe in BMD than in DMD. About 50% of deaths in BMD are attributed to malignant arrhythmias or congestive heart failure, he said.
Screening requirements and treatment options in BMD are similar to those in DMD, with the added option of heart transplantation.
Silvestri cautioned that up to 40% of female carriers of dystrophin mutations can develop cardiac dysfunction similar to that seen in DMD and BMD. Cardiac assessments are recommended every 5 years. “It’s important to genotype Mom,” he said, especially in light of the fact that two thirds of DMD cases may be inherited.
“When I send genetic testing on the mother and find her to be a carrier, I send her to a cardiologist so she has the appropriate screening done,” he said.
Pacemakers May Be Considered in Type 1 Myotonic Dystrophy
In type 1 myotonic dystrophy, cardiac conduction abnormalities are seen in two thirds of patients, and sudden cardiac death in up to 30% of patients. “When it is diagnosed, patients do need an ECG at that time, as well as annually,” he said.
Holter monitoring or implantable loop recorders may be recommended, and permanent pacing via an implantable cardioverter-defibrillator might be appropriate.
“Based on the literature to date, the exact timing is not is not clear,” Silvestri said. “The electrophysiologists in my area tend to be very aggressive, thankfully, and treat them fairly soon with pacemakers when we see the first sign of trouble.”
Silvestri disclosed consultant/advisory relationships with argenx, Alexion, Amgen, UCB, Immunovant, and Janssen.
A version of this article appeared on Medscape.com.
FROM AANEM 2024
ALS Update: Drug Therapy Continues to Offer Little Benefit
SAVANNAH, GEORGIA — , nerve specialists learned.
The glutamate blocker riluzole (Rilutek), which became the first ALS drug to receive US Food and Drug Administration (FDA) approval in 1995, continues to be used, Michael D. Weiss, MD, professor of neurology at University of Washington School of Medicine, Seattle, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Weiss highlighted a 2012 Cochrane Library review that examined research and found the drug is “reasonably safe” and prolongs median survival by about 2-3 months. “About 12% develop liver disease. It’s pretty rare that we stop the medicine due to liver toxicity.”
Earlier Treatment Could Pay Dividends
A recent study “suggests we might be able to get more bang for our buck from riluzole” by initiating treatment earlier, Weiss said.
Researchers tracked 4778 patients with ALS, including 3446 (72.1%) who took riluzole. Those who took the drug survived a median 2 extra months (22.6 vs 20.2 months; P < .001). The data suggested that delaying riluzole initiation by 1 year (from 6 months to 18 months after diagnosis) reduced the median survival by 1.9 months (from 40.1 to 38.2 months).
There’s “a relatively significant additional benefit” to earlier treatment, Weiss said, although patients will vary on whether they think it’s meaningful. As for limitations, “there’s no clear impact on disease progression, and there’s a need for periodic monitoring of liver function profile.”
He added that there’s an out-of-pocket co-pay. “Even as a generic, it’s not that cheap. Depending on the source, it could cost anywhere from $1800 to $8400 a year.”
Edaravone Could Lack Relevant Benefit
No other ALS treatment appeared until 2017, when the FDA approved the novel antioxidant edaravone (Radicava). In 2022, the agency approved an oral suspension version, but a study published that year suggested there may not be a clinically relevant benefit.
The University of Washington, where Weiss works, offered the drug to 144 patients, according to an analysis. Eighty percent of the patients wanted it, but insurers refused to cover it for more than 20%. The average time to treatment with the drug was 28 days after patients said they wanted it.
That’s a “substantial delay,” Weiss said.
The cost is about $171,000 a year, he said, and assistance is limited for underinsured patients.*
Other Options
As Weiss noted, another drug, AMX0035 (Relyvrio), received FDA approval in 2022, but its manufacturer pulled it from the US/Canada market in April 2024 following poor phase 3 trial findings.
In 2023, the FDA approved another drug, the antisense oligonucleotide tofersen (Qalsody), in patients with ALS associated with a mutation in the superoxide dismutase 1 gene. According to the FDA, reductions in plasma neurofilament light concentration were “reasonably likely to predict a clinical benefit in patients.”
Only 1%-2% of patients with ALS fit the criteria to get the drug, Weiss said. He noted other limitations such as the cost ($180,000 a year), the need for lifelong monthly intrathecal injections, and serious neurological side effects in 7% of patients per a 2022 trial.
Weiss disclosed advisory board (Alexion, Ra [now UCB], argenx, Biogen, Mitsubishi Tanabe Pharma, Amylyx), data safety monitoring board (Sanofi, AI), consulting (Cytokinetics, CSL Behring), and speaker (Soleo) relationships.
*Correction, 10/23/2024: This story originally quoted Weiss as saying the maker of edaravone provides no assistance to underinsured patients. Weiss has clarified that he should have said this coverage is “limited.”
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA — , nerve specialists learned.
The glutamate blocker riluzole (Rilutek), which became the first ALS drug to receive US Food and Drug Administration (FDA) approval in 1995, continues to be used, Michael D. Weiss, MD, professor of neurology at University of Washington School of Medicine, Seattle, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Weiss highlighted a 2012 Cochrane Library review that examined research and found the drug is “reasonably safe” and prolongs median survival by about 2-3 months. “About 12% develop liver disease. It’s pretty rare that we stop the medicine due to liver toxicity.”
Earlier Treatment Could Pay Dividends
A recent study “suggests we might be able to get more bang for our buck from riluzole” by initiating treatment earlier, Weiss said.
Researchers tracked 4778 patients with ALS, including 3446 (72.1%) who took riluzole. Those who took the drug survived a median 2 extra months (22.6 vs 20.2 months; P < .001). The data suggested that delaying riluzole initiation by 1 year (from 6 months to 18 months after diagnosis) reduced the median survival by 1.9 months (from 40.1 to 38.2 months).
There’s “a relatively significant additional benefit” to earlier treatment, Weiss said, although patients will vary on whether they think it’s meaningful. As for limitations, “there’s no clear impact on disease progression, and there’s a need for periodic monitoring of liver function profile.”
He added that there’s an out-of-pocket co-pay. “Even as a generic, it’s not that cheap. Depending on the source, it could cost anywhere from $1800 to $8400 a year.”
Edaravone Could Lack Relevant Benefit
No other ALS treatment appeared until 2017, when the FDA approved the novel antioxidant edaravone (Radicava). In 2022, the agency approved an oral suspension version, but a study published that year suggested there may not be a clinically relevant benefit.
The University of Washington, where Weiss works, offered the drug to 144 patients, according to an analysis. Eighty percent of the patients wanted it, but insurers refused to cover it for more than 20%. The average time to treatment with the drug was 28 days after patients said they wanted it.
That’s a “substantial delay,” Weiss said.
The cost is about $171,000 a year, he said, and assistance is limited for underinsured patients.*
Other Options
As Weiss noted, another drug, AMX0035 (Relyvrio), received FDA approval in 2022, but its manufacturer pulled it from the US/Canada market in April 2024 following poor phase 3 trial findings.
In 2023, the FDA approved another drug, the antisense oligonucleotide tofersen (Qalsody), in patients with ALS associated with a mutation in the superoxide dismutase 1 gene. According to the FDA, reductions in plasma neurofilament light concentration were “reasonably likely to predict a clinical benefit in patients.”
Only 1%-2% of patients with ALS fit the criteria to get the drug, Weiss said. He noted other limitations such as the cost ($180,000 a year), the need for lifelong monthly intrathecal injections, and serious neurological side effects in 7% of patients per a 2022 trial.
Weiss disclosed advisory board (Alexion, Ra [now UCB], argenx, Biogen, Mitsubishi Tanabe Pharma, Amylyx), data safety monitoring board (Sanofi, AI), consulting (Cytokinetics, CSL Behring), and speaker (Soleo) relationships.
*Correction, 10/23/2024: This story originally quoted Weiss as saying the maker of edaravone provides no assistance to underinsured patients. Weiss has clarified that he should have said this coverage is “limited.”
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA — , nerve specialists learned.
The glutamate blocker riluzole (Rilutek), which became the first ALS drug to receive US Food and Drug Administration (FDA) approval in 1995, continues to be used, Michael D. Weiss, MD, professor of neurology at University of Washington School of Medicine, Seattle, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Weiss highlighted a 2012 Cochrane Library review that examined research and found the drug is “reasonably safe” and prolongs median survival by about 2-3 months. “About 12% develop liver disease. It’s pretty rare that we stop the medicine due to liver toxicity.”
Earlier Treatment Could Pay Dividends
A recent study “suggests we might be able to get more bang for our buck from riluzole” by initiating treatment earlier, Weiss said.
Researchers tracked 4778 patients with ALS, including 3446 (72.1%) who took riluzole. Those who took the drug survived a median 2 extra months (22.6 vs 20.2 months; P < .001). The data suggested that delaying riluzole initiation by 1 year (from 6 months to 18 months after diagnosis) reduced the median survival by 1.9 months (from 40.1 to 38.2 months).
There’s “a relatively significant additional benefit” to earlier treatment, Weiss said, although patients will vary on whether they think it’s meaningful. As for limitations, “there’s no clear impact on disease progression, and there’s a need for periodic monitoring of liver function profile.”
He added that there’s an out-of-pocket co-pay. “Even as a generic, it’s not that cheap. Depending on the source, it could cost anywhere from $1800 to $8400 a year.”
Edaravone Could Lack Relevant Benefit
No other ALS treatment appeared until 2017, when the FDA approved the novel antioxidant edaravone (Radicava). In 2022, the agency approved an oral suspension version, but a study published that year suggested there may not be a clinically relevant benefit.
The University of Washington, where Weiss works, offered the drug to 144 patients, according to an analysis. Eighty percent of the patients wanted it, but insurers refused to cover it for more than 20%. The average time to treatment with the drug was 28 days after patients said they wanted it.
That’s a “substantial delay,” Weiss said.
The cost is about $171,000 a year, he said, and assistance is limited for underinsured patients.*
Other Options
As Weiss noted, another drug, AMX0035 (Relyvrio), received FDA approval in 2022, but its manufacturer pulled it from the US/Canada market in April 2024 following poor phase 3 trial findings.
In 2023, the FDA approved another drug, the antisense oligonucleotide tofersen (Qalsody), in patients with ALS associated with a mutation in the superoxide dismutase 1 gene. According to the FDA, reductions in plasma neurofilament light concentration were “reasonably likely to predict a clinical benefit in patients.”
Only 1%-2% of patients with ALS fit the criteria to get the drug, Weiss said. He noted other limitations such as the cost ($180,000 a year), the need for lifelong monthly intrathecal injections, and serious neurological side effects in 7% of patients per a 2022 trial.
Weiss disclosed advisory board (Alexion, Ra [now UCB], argenx, Biogen, Mitsubishi Tanabe Pharma, Amylyx), data safety monitoring board (Sanofi, AI), consulting (Cytokinetics, CSL Behring), and speaker (Soleo) relationships.
*Correction, 10/23/2024: This story originally quoted Weiss as saying the maker of edaravone provides no assistance to underinsured patients. Weiss has clarified that he should have said this coverage is “limited.”
A version of this article appeared on Medscape.com.
FROM AANEM 2024
A Brief Glimpse Into 80,000 Years of Human History
Like millions of other modern humans, my daughter and I stood in the backyard recently and watched comet C/2023 A3 (Tsuchinshan–ATLAS) with binoculars. It took a few minutes to locate, but once you see it is unmistakable.
It’s got a long (at least in human terms) orbit, roughly 80,000 years. So what was going on here, on our pale blue dot, the last time it graced our skies?
Well, here in Phoenix, the people were ... not here. Nor were they in Arizona, or North America, or pretty much the entire Western Hemisphere.
In fact, Homo sapiens were confined to Africa. The hardier Neanderthals had successfully moved into Eurasia, but our lineage was just starting to migrate there. There’s some evidence that we numbered maybe 10,000-15,000 at that point. Far more people saw the comet that night in the United States than our entire population count last time it swung by.
But we were moving up in the world. Our ancestors at the time had developed the first forms of jewelry, using seashells. There’s evidence that we’d learned to trade with other, distant, communities. We were using spears to put dinner on the table with less risk to ourselves than clubs posed.
And, in what’s now Kenya, in the same time frame, a pair of grieving parents carefully buried their 3-year-old child, wrapped in a covering and gently placed on a pillow.
Sadly, this isn’t a scene we’re unfamiliar with. Possibly the most famous painting of a physician is “The Doctor” (1891) by Luke Fildes, showing a physician trying to treat a seriously ill child while the parents look on helplessly.

What did the Kenyan child die from? We’ll probably never know. Did they try to treat it? Most likely.
Humans, by nature, form societies. The size varies, but everyone has a role. There was probably some ancestor of Fildes’ doctor in the group who tried to help. Perhaps with prayers in an unknown tongue, or a preparation of certain leaves, or placing the child near a fire. When whatever they tried failed, the same person likely consoled the parents. Maybe they were involved in the burial, too.
The child would be found in 2017, giving us the first clear evidence of a ritual human burial in Africa. Just like today, we let go of our lost ones with ceremony. Perhaps the parents noticed the comet and thought it was their child’s spirit departing.
Now the comet is back. The planet hasn’t changed dramatically in 80,000 years (which isn’t much in geological time), but we have.
Would today’s doctors have been able to save the child? No idea, though we probably have a better chance than our professional ancestor did.
But our job hasn’t changed. Like us, the ancient practitioner probably tried to figure out why the child was sick and what could be done about it. When it was over they, and others, grieved with the parents.
The comet will be back in 80,000 years. On our scale, that’s a long time. The entire recorded history of our species is only 5,000 to 8,000 years. We’ve come a long way, but where we’re going in 80,000 years is anyone’s guess.
Will doctors in the year 82024 even know what we do now to care for people? Will they still be practicing on the third rock from the sun, or spread out across the galaxy? Will there even be doctors? (Probably, in one form or another.)
But We do our best to care, heal, and hope now, as we did then, and as our descendants will.
And, like my daughter and I did, no matter where we are, we will still look up at the sky with wonder.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Like millions of other modern humans, my daughter and I stood in the backyard recently and watched comet C/2023 A3 (Tsuchinshan–ATLAS) with binoculars. It took a few minutes to locate, but once you see it is unmistakable.
It’s got a long (at least in human terms) orbit, roughly 80,000 years. So what was going on here, on our pale blue dot, the last time it graced our skies?
Well, here in Phoenix, the people were ... not here. Nor were they in Arizona, or North America, or pretty much the entire Western Hemisphere.
In fact, Homo sapiens were confined to Africa. The hardier Neanderthals had successfully moved into Eurasia, but our lineage was just starting to migrate there. There’s some evidence that we numbered maybe 10,000-15,000 at that point. Far more people saw the comet that night in the United States than our entire population count last time it swung by.
But we were moving up in the world. Our ancestors at the time had developed the first forms of jewelry, using seashells. There’s evidence that we’d learned to trade with other, distant, communities. We were using spears to put dinner on the table with less risk to ourselves than clubs posed.
And, in what’s now Kenya, in the same time frame, a pair of grieving parents carefully buried their 3-year-old child, wrapped in a covering and gently placed on a pillow.
Sadly, this isn’t a scene we’re unfamiliar with. Possibly the most famous painting of a physician is “The Doctor” (1891) by Luke Fildes, showing a physician trying to treat a seriously ill child while the parents look on helplessly.

What did the Kenyan child die from? We’ll probably never know. Did they try to treat it? Most likely.
Humans, by nature, form societies. The size varies, but everyone has a role. There was probably some ancestor of Fildes’ doctor in the group who tried to help. Perhaps with prayers in an unknown tongue, or a preparation of certain leaves, or placing the child near a fire. When whatever they tried failed, the same person likely consoled the parents. Maybe they were involved in the burial, too.
The child would be found in 2017, giving us the first clear evidence of a ritual human burial in Africa. Just like today, we let go of our lost ones with ceremony. Perhaps the parents noticed the comet and thought it was their child’s spirit departing.
Now the comet is back. The planet hasn’t changed dramatically in 80,000 years (which isn’t much in geological time), but we have.
Would today’s doctors have been able to save the child? No idea, though we probably have a better chance than our professional ancestor did.
But our job hasn’t changed. Like us, the ancient practitioner probably tried to figure out why the child was sick and what could be done about it. When it was over they, and others, grieved with the parents.
The comet will be back in 80,000 years. On our scale, that’s a long time. The entire recorded history of our species is only 5,000 to 8,000 years. We’ve come a long way, but where we’re going in 80,000 years is anyone’s guess.
Will doctors in the year 82024 even know what we do now to care for people? Will they still be practicing on the third rock from the sun, or spread out across the galaxy? Will there even be doctors? (Probably, in one form or another.)
But We do our best to care, heal, and hope now, as we did then, and as our descendants will.
And, like my daughter and I did, no matter where we are, we will still look up at the sky with wonder.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Like millions of other modern humans, my daughter and I stood in the backyard recently and watched comet C/2023 A3 (Tsuchinshan–ATLAS) with binoculars. It took a few minutes to locate, but once you see it is unmistakable.
It’s got a long (at least in human terms) orbit, roughly 80,000 years. So what was going on here, on our pale blue dot, the last time it graced our skies?
Well, here in Phoenix, the people were ... not here. Nor were they in Arizona, or North America, or pretty much the entire Western Hemisphere.
In fact, Homo sapiens were confined to Africa. The hardier Neanderthals had successfully moved into Eurasia, but our lineage was just starting to migrate there. There’s some evidence that we numbered maybe 10,000-15,000 at that point. Far more people saw the comet that night in the United States than our entire population count last time it swung by.
But we were moving up in the world. Our ancestors at the time had developed the first forms of jewelry, using seashells. There’s evidence that we’d learned to trade with other, distant, communities. We were using spears to put dinner on the table with less risk to ourselves than clubs posed.
And, in what’s now Kenya, in the same time frame, a pair of grieving parents carefully buried their 3-year-old child, wrapped in a covering and gently placed on a pillow.
Sadly, this isn’t a scene we’re unfamiliar with. Possibly the most famous painting of a physician is “The Doctor” (1891) by Luke Fildes, showing a physician trying to treat a seriously ill child while the parents look on helplessly.

What did the Kenyan child die from? We’ll probably never know. Did they try to treat it? Most likely.
Humans, by nature, form societies. The size varies, but everyone has a role. There was probably some ancestor of Fildes’ doctor in the group who tried to help. Perhaps with prayers in an unknown tongue, or a preparation of certain leaves, or placing the child near a fire. When whatever they tried failed, the same person likely consoled the parents. Maybe they were involved in the burial, too.
The child would be found in 2017, giving us the first clear evidence of a ritual human burial in Africa. Just like today, we let go of our lost ones with ceremony. Perhaps the parents noticed the comet and thought it was their child’s spirit departing.
Now the comet is back. The planet hasn’t changed dramatically in 80,000 years (which isn’t much in geological time), but we have.
Would today’s doctors have been able to save the child? No idea, though we probably have a better chance than our professional ancestor did.
But our job hasn’t changed. Like us, the ancient practitioner probably tried to figure out why the child was sick and what could be done about it. When it was over they, and others, grieved with the parents.
The comet will be back in 80,000 years. On our scale, that’s a long time. The entire recorded history of our species is only 5,000 to 8,000 years. We’ve come a long way, but where we’re going in 80,000 years is anyone’s guess.
Will doctors in the year 82024 even know what we do now to care for people? Will they still be practicing on the third rock from the sun, or spread out across the galaxy? Will there even be doctors? (Probably, in one form or another.)
But We do our best to care, heal, and hope now, as we did then, and as our descendants will.
And, like my daughter and I did, no matter where we are, we will still look up at the sky with wonder.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Spontaneously Draining Axillary Tumors in a Young Woman
THE DIAGNOSIS: Ectopic (Accessory) Breast Tissue
Ectopic (accessory) breast tissue (EBT) is a phenomenon caused by failed regression of one or more components of the embryonic mammary ridges— paired ectodermal thickenings that eventually develop into definitive breast tissue including the nipples, areolae, and parenchyma. Ectopic breast tissue is more common in women than men and is believed to be sporadic, although an autosomal-dominant inheritance mechanism with incomplete penetrance has been proposed for some cases.1 The reported incidence of EBT varies greatly among racial and ethnic groups but is most common in individuals of Asian descent. The incidence across all types of EBT is estimated at 0.25% to 6% in the general population.2
Observed clinical variations of EBT range from simple polythelia (additional nipple[s] without associated parenchyma) to complete polymastia (organized and differentiated accessory breasts). Some types of EBT are rarer than others: One report of gynecologic cancer screenings in 1660 patients found polymastia and polythelia incidences of 0.12% and 5.48%, respectively.3 Of the symptomatic variations, isolated parenchymal EBT without a nipple or areolar complex is the most common and may manifest clinically as unilateral or bilateral tender, mildly erythematous nodules or masses often located in the axillae. Ectopic breast tissue generally is observed along the milk line, a developmental regional designation corresponding to the embryologic mammary ridge and extending linearly from the anterior axilla to the inguinal fold on both sides of the body; however, there have been rare reports of EBT manifesting in areas outside the milk line, such as the face, neck, back, vulva, and extremities.2,3
Given that the underlying elements of EBT usually are hormone responsive (as with normal breast tissue), the initial symptom onset and subsequent manifestation frequently coincide with pubertal milestones, pregnancy, or lactation. Furthermore, some patients with EBT may experience symptom fluctuations in concordance with monthly menstrual phases. Many cases of EBT are selflimited and resolve within weeks to months after the end of a pregnancy or lactation, but some cases may persist. Continued observation and follow-up are advisable in all patients, as EBT symptoms often recur and the tissue is susceptible to the same disease processes that affect normal breasts, the most concerning of which is malignancy.4 Although the true incidence is limited by available data, primary ectopic breast malignancy has been estimated to account for 0.3% to 3.8% of diagnosed breast malignancies.2 Cases of malignancy arising from EBT often are of higher grade and poorer prognosis, a finding that may be attributable to diagnostic delays caused by oversight or misdiagnosis of EBT rather than inherent differences in the biologic profile of the tumors.2,4 Patients with a documented history of EBT may benefit from having their routine breast cancer screenings expanded to include areas with EBT foci.
Potential misdiagnoses for EBT include subcutaneous lipoma, axillary lymphadenopathy, abscess, hidradenitis suppurativa, or malignancy. Features that are suggestive of EBT include symptom association with hormone fluctuations (eg, menstrual phases), absence of fever, and lactescent rather than purulent drainage. Among reported EBT cases, spontaneous lactation rarely is described and, if present, often is associated with a history of prior trauma (eg, core needle biopsy or local abscess formation).5 This trauma creates an aberrant connection known as a milk fistula between the underlying parenchyma and the skin surface. Interestingly, our patient denied any history of axillary trauma, but she was noted to be lactating from an apparent milk fistula rather than an organized secretory duct system.
Though a patient history and clinical examination may be sufficient to diagnose EBT cases that are more physically apparent and well correlated with hormone fluctuations, many cases require additional diagnostic studies for confirmation. Of the tools available, ultrasonography generally is considered first-line due to its noninvasive nature, low cost, minimal risk, and high diagnostic value.2 Ultrasonography quickly differentiates between abscesses and cystlike processes, which may appear as discrete areas of decreased echogenicity, and breast tissue, which manifests with fibroglandular tissue and lobules of fat.2,6 Additionally, ultrasonography may demonstrate the secretion of milk through ducts or fistulae, if present. Should examination with ultrasonography prove inconclusive, follow-up studies using conventional radiographic mammography or magnetic resonance imaging may be warranted. Biopsy of EBT foci generally is not indicated unless first-line noninvasive studies fail to yield a conclusive diagnosis; however, biopsy also may be warranted if initial imaging is suggestive of malignancy arising from EBT.2
Management of EBT generally is conservative, and symptoms often resolve without intervention.4 Symptomatic relief may be achieved through techniques such as application of warm/cold compresses, avoidance of mechanical stimulation, and use of over-the-counter pain medicine. In cases that are persistent, frequently recurrent, or associated with severe symptoms or that cause considerable cosmetic impact, management with surgical excision and/or liposuction may be warranted.7 In our patient, the symptoms were not bothersome enough to warrant surgical intervention, so she was managed conservatively and did not return for follow-up.
- Leung AK. Familial supernumerary nipples. Am J Med Genet. 1988;31:631-635. doi:10.1002/ajmg.1320310318
- Visconti G, Eltahir Y, Van Ginkel RJ, et al. Approach and management of primary ectopic breast carcinoma in the axilla: where are we? a comprehensive historical literature review. J Plast Reconstr Aesthet Surg. 2011;64:E1-E11. doi:10.1016/j.bjps.2010.08.015
- Göttlicher S. Incidence and location of polythelias, polymastias and mammae aberratae. a prospective one year study of 1,660 patients of a gynecologic practice. Article in German. Geburtshilfe Frauenheilkd. 1986;46:697-699. doi:10.1055/s-2008-1035944
- Ghosn SH, Khatri KA, Bhawan J. Bilateral aberrant axillary breast tissue mimicking lipomas: report of a case and review of the literature. J Cutan Pathol. 2007;34(suppl 1):9-13. doi:10.1111/j.1600-0560.2006.00713.x
- Firat D, Idiz O, Isik A, et al. Spontaneous milk fistula from an accessory breast: an extremely rare case. Breast J. 2015;21:554-555. doi:10.1111/tbj.12452
- Lim HS, Kim SJ, Baek JM, et al. Sonographic findings of accessory breast tissue in axilla and related diseases. J Ultrasound Med. 2017;36:1469-1478. doi:10.7863/ultra.16.06056
- Gentile P, Izzo V, Cervelli V. Fibroadenoma in the bilateral accessory axillary breast. Aesthetic Plast Surg. 2010;34:657-659. doi:10.1007/ s00266-010-9505-y
THE DIAGNOSIS: Ectopic (Accessory) Breast Tissue
Ectopic (accessory) breast tissue (EBT) is a phenomenon caused by failed regression of one or more components of the embryonic mammary ridges— paired ectodermal thickenings that eventually develop into definitive breast tissue including the nipples, areolae, and parenchyma. Ectopic breast tissue is more common in women than men and is believed to be sporadic, although an autosomal-dominant inheritance mechanism with incomplete penetrance has been proposed for some cases.1 The reported incidence of EBT varies greatly among racial and ethnic groups but is most common in individuals of Asian descent. The incidence across all types of EBT is estimated at 0.25% to 6% in the general population.2
Observed clinical variations of EBT range from simple polythelia (additional nipple[s] without associated parenchyma) to complete polymastia (organized and differentiated accessory breasts). Some types of EBT are rarer than others: One report of gynecologic cancer screenings in 1660 patients found polymastia and polythelia incidences of 0.12% and 5.48%, respectively.3 Of the symptomatic variations, isolated parenchymal EBT without a nipple or areolar complex is the most common and may manifest clinically as unilateral or bilateral tender, mildly erythematous nodules or masses often located in the axillae. Ectopic breast tissue generally is observed along the milk line, a developmental regional designation corresponding to the embryologic mammary ridge and extending linearly from the anterior axilla to the inguinal fold on both sides of the body; however, there have been rare reports of EBT manifesting in areas outside the milk line, such as the face, neck, back, vulva, and extremities.2,3
Given that the underlying elements of EBT usually are hormone responsive (as with normal breast tissue), the initial symptom onset and subsequent manifestation frequently coincide with pubertal milestones, pregnancy, or lactation. Furthermore, some patients with EBT may experience symptom fluctuations in concordance with monthly menstrual phases. Many cases of EBT are selflimited and resolve within weeks to months after the end of a pregnancy or lactation, but some cases may persist. Continued observation and follow-up are advisable in all patients, as EBT symptoms often recur and the tissue is susceptible to the same disease processes that affect normal breasts, the most concerning of which is malignancy.4 Although the true incidence is limited by available data, primary ectopic breast malignancy has been estimated to account for 0.3% to 3.8% of diagnosed breast malignancies.2 Cases of malignancy arising from EBT often are of higher grade and poorer prognosis, a finding that may be attributable to diagnostic delays caused by oversight or misdiagnosis of EBT rather than inherent differences in the biologic profile of the tumors.2,4 Patients with a documented history of EBT may benefit from having their routine breast cancer screenings expanded to include areas with EBT foci.
Potential misdiagnoses for EBT include subcutaneous lipoma, axillary lymphadenopathy, abscess, hidradenitis suppurativa, or malignancy. Features that are suggestive of EBT include symptom association with hormone fluctuations (eg, menstrual phases), absence of fever, and lactescent rather than purulent drainage. Among reported EBT cases, spontaneous lactation rarely is described and, if present, often is associated with a history of prior trauma (eg, core needle biopsy or local abscess formation).5 This trauma creates an aberrant connection known as a milk fistula between the underlying parenchyma and the skin surface. Interestingly, our patient denied any history of axillary trauma, but she was noted to be lactating from an apparent milk fistula rather than an organized secretory duct system.
Though a patient history and clinical examination may be sufficient to diagnose EBT cases that are more physically apparent and well correlated with hormone fluctuations, many cases require additional diagnostic studies for confirmation. Of the tools available, ultrasonography generally is considered first-line due to its noninvasive nature, low cost, minimal risk, and high diagnostic value.2 Ultrasonography quickly differentiates between abscesses and cystlike processes, which may appear as discrete areas of decreased echogenicity, and breast tissue, which manifests with fibroglandular tissue and lobules of fat.2,6 Additionally, ultrasonography may demonstrate the secretion of milk through ducts or fistulae, if present. Should examination with ultrasonography prove inconclusive, follow-up studies using conventional radiographic mammography or magnetic resonance imaging may be warranted. Biopsy of EBT foci generally is not indicated unless first-line noninvasive studies fail to yield a conclusive diagnosis; however, biopsy also may be warranted if initial imaging is suggestive of malignancy arising from EBT.2
Management of EBT generally is conservative, and symptoms often resolve without intervention.4 Symptomatic relief may be achieved through techniques such as application of warm/cold compresses, avoidance of mechanical stimulation, and use of over-the-counter pain medicine. In cases that are persistent, frequently recurrent, or associated with severe symptoms or that cause considerable cosmetic impact, management with surgical excision and/or liposuction may be warranted.7 In our patient, the symptoms were not bothersome enough to warrant surgical intervention, so she was managed conservatively and did not return for follow-up.
THE DIAGNOSIS: Ectopic (Accessory) Breast Tissue
Ectopic (accessory) breast tissue (EBT) is a phenomenon caused by failed regression of one or more components of the embryonic mammary ridges— paired ectodermal thickenings that eventually develop into definitive breast tissue including the nipples, areolae, and parenchyma. Ectopic breast tissue is more common in women than men and is believed to be sporadic, although an autosomal-dominant inheritance mechanism with incomplete penetrance has been proposed for some cases.1 The reported incidence of EBT varies greatly among racial and ethnic groups but is most common in individuals of Asian descent. The incidence across all types of EBT is estimated at 0.25% to 6% in the general population.2
Observed clinical variations of EBT range from simple polythelia (additional nipple[s] without associated parenchyma) to complete polymastia (organized and differentiated accessory breasts). Some types of EBT are rarer than others: One report of gynecologic cancer screenings in 1660 patients found polymastia and polythelia incidences of 0.12% and 5.48%, respectively.3 Of the symptomatic variations, isolated parenchymal EBT without a nipple or areolar complex is the most common and may manifest clinically as unilateral or bilateral tender, mildly erythematous nodules or masses often located in the axillae. Ectopic breast tissue generally is observed along the milk line, a developmental regional designation corresponding to the embryologic mammary ridge and extending linearly from the anterior axilla to the inguinal fold on both sides of the body; however, there have been rare reports of EBT manifesting in areas outside the milk line, such as the face, neck, back, vulva, and extremities.2,3
Given that the underlying elements of EBT usually are hormone responsive (as with normal breast tissue), the initial symptom onset and subsequent manifestation frequently coincide with pubertal milestones, pregnancy, or lactation. Furthermore, some patients with EBT may experience symptom fluctuations in concordance with monthly menstrual phases. Many cases of EBT are selflimited and resolve within weeks to months after the end of a pregnancy or lactation, but some cases may persist. Continued observation and follow-up are advisable in all patients, as EBT symptoms often recur and the tissue is susceptible to the same disease processes that affect normal breasts, the most concerning of which is malignancy.4 Although the true incidence is limited by available data, primary ectopic breast malignancy has been estimated to account for 0.3% to 3.8% of diagnosed breast malignancies.2 Cases of malignancy arising from EBT often are of higher grade and poorer prognosis, a finding that may be attributable to diagnostic delays caused by oversight or misdiagnosis of EBT rather than inherent differences in the biologic profile of the tumors.2,4 Patients with a documented history of EBT may benefit from having their routine breast cancer screenings expanded to include areas with EBT foci.
Potential misdiagnoses for EBT include subcutaneous lipoma, axillary lymphadenopathy, abscess, hidradenitis suppurativa, or malignancy. Features that are suggestive of EBT include symptom association with hormone fluctuations (eg, menstrual phases), absence of fever, and lactescent rather than purulent drainage. Among reported EBT cases, spontaneous lactation rarely is described and, if present, often is associated with a history of prior trauma (eg, core needle biopsy or local abscess formation).5 This trauma creates an aberrant connection known as a milk fistula between the underlying parenchyma and the skin surface. Interestingly, our patient denied any history of axillary trauma, but she was noted to be lactating from an apparent milk fistula rather than an organized secretory duct system.
Though a patient history and clinical examination may be sufficient to diagnose EBT cases that are more physically apparent and well correlated with hormone fluctuations, many cases require additional diagnostic studies for confirmation. Of the tools available, ultrasonography generally is considered first-line due to its noninvasive nature, low cost, minimal risk, and high diagnostic value.2 Ultrasonography quickly differentiates between abscesses and cystlike processes, which may appear as discrete areas of decreased echogenicity, and breast tissue, which manifests with fibroglandular tissue and lobules of fat.2,6 Additionally, ultrasonography may demonstrate the secretion of milk through ducts or fistulae, if present. Should examination with ultrasonography prove inconclusive, follow-up studies using conventional radiographic mammography or magnetic resonance imaging may be warranted. Biopsy of EBT foci generally is not indicated unless first-line noninvasive studies fail to yield a conclusive diagnosis; however, biopsy also may be warranted if initial imaging is suggestive of malignancy arising from EBT.2
Management of EBT generally is conservative, and symptoms often resolve without intervention.4 Symptomatic relief may be achieved through techniques such as application of warm/cold compresses, avoidance of mechanical stimulation, and use of over-the-counter pain medicine. In cases that are persistent, frequently recurrent, or associated with severe symptoms or that cause considerable cosmetic impact, management with surgical excision and/or liposuction may be warranted.7 In our patient, the symptoms were not bothersome enough to warrant surgical intervention, so she was managed conservatively and did not return for follow-up.
- Leung AK. Familial supernumerary nipples. Am J Med Genet. 1988;31:631-635. doi:10.1002/ajmg.1320310318
- Visconti G, Eltahir Y, Van Ginkel RJ, et al. Approach and management of primary ectopic breast carcinoma in the axilla: where are we? a comprehensive historical literature review. J Plast Reconstr Aesthet Surg. 2011;64:E1-E11. doi:10.1016/j.bjps.2010.08.015
- Göttlicher S. Incidence and location of polythelias, polymastias and mammae aberratae. a prospective one year study of 1,660 patients of a gynecologic practice. Article in German. Geburtshilfe Frauenheilkd. 1986;46:697-699. doi:10.1055/s-2008-1035944
- Ghosn SH, Khatri KA, Bhawan J. Bilateral aberrant axillary breast tissue mimicking lipomas: report of a case and review of the literature. J Cutan Pathol. 2007;34(suppl 1):9-13. doi:10.1111/j.1600-0560.2006.00713.x
- Firat D, Idiz O, Isik A, et al. Spontaneous milk fistula from an accessory breast: an extremely rare case. Breast J. 2015;21:554-555. doi:10.1111/tbj.12452
- Lim HS, Kim SJ, Baek JM, et al. Sonographic findings of accessory breast tissue in axilla and related diseases. J Ultrasound Med. 2017;36:1469-1478. doi:10.7863/ultra.16.06056
- Gentile P, Izzo V, Cervelli V. Fibroadenoma in the bilateral accessory axillary breast. Aesthetic Plast Surg. 2010;34:657-659. doi:10.1007/ s00266-010-9505-y
- Leung AK. Familial supernumerary nipples. Am J Med Genet. 1988;31:631-635. doi:10.1002/ajmg.1320310318
- Visconti G, Eltahir Y, Van Ginkel RJ, et al. Approach and management of primary ectopic breast carcinoma in the axilla: where are we? a comprehensive historical literature review. J Plast Reconstr Aesthet Surg. 2011;64:E1-E11. doi:10.1016/j.bjps.2010.08.015
- Göttlicher S. Incidence and location of polythelias, polymastias and mammae aberratae. a prospective one year study of 1,660 patients of a gynecologic practice. Article in German. Geburtshilfe Frauenheilkd. 1986;46:697-699. doi:10.1055/s-2008-1035944
- Ghosn SH, Khatri KA, Bhawan J. Bilateral aberrant axillary breast tissue mimicking lipomas: report of a case and review of the literature. J Cutan Pathol. 2007;34(suppl 1):9-13. doi:10.1111/j.1600-0560.2006.00713.x
- Firat D, Idiz O, Isik A, et al. Spontaneous milk fistula from an accessory breast: an extremely rare case. Breast J. 2015;21:554-555. doi:10.1111/tbj.12452
- Lim HS, Kim SJ, Baek JM, et al. Sonographic findings of accessory breast tissue in axilla and related diseases. J Ultrasound Med. 2017;36:1469-1478. doi:10.7863/ultra.16.06056
- Gentile P, Izzo V, Cervelli V. Fibroadenoma in the bilateral accessory axillary breast. Aesthetic Plast Surg. 2010;34:657-659. doi:10.1007/ s00266-010-9505-y
A 19-year-old G1P1A0 woman presented to the dermatology clinic for evaluation of bilateral axillary swelling, pain, and spontaneous drainage of approximately 2 weeks’ duration. The patient, who was 2 weeks postpartum, reported that the symptoms were associated with lactation when breastfeeding. She denied any personal or family history of hidradenitis suppurativa or other formally diagnosed dermatologic condition. Physical examination revealed a soft, mildly tender, well-circumscribed, nonfluctuant mobile mass in each axilla. Both lesions had a single central sinus tract with thin lactescent discharge that spontaneously drained and was expressible. A single thin hyperpigmented papule was noted on the anterior aspect of each mass.

EHR Prompt Helped Cut Acute Otitis Media Antibiotic Use by Half
LOS ANGELES — Embedding a new discharge order set into electronic health records (EHRs) with a preselected 5-day antibiotic course for children aged 2 years or older diagnosed with acute otitis media (AOM) cut antibiotic duration sharply, according to new data presented at the Infectious Disease Week (IDWeek) 2024 Annual Meeting.
“We were effectively able to cut antibiotic use in half by shortening the duration of treatment,” said lead author Joana Dimo, DO, a Pediatric Infectious Diseases fellow at the University of Colorado Denver/Children’s Hospital Colorado.
In the United States, 80% of children will experience otitis media during their lifetime. Untreated ear infections can lead to symptoms ranging from mild ear discharge to life-threatening conditions such as mastoiditis and intracranial abscesses.
Most Cases Resolve Without Antibiotics
Ear infections “are the leading reason for antibiotic prescriptions in kids,” Dimo noted, adding that 24% of all pediatric antibiotic prescriptions are for AOM. Amoxicillin is the preferred first-line treatment. “Research supports that 75% of children get better on their own without antibiotics, and when needed, short courses of just 5 days are safe and effective.”
Antibiotics can cause side effects such as diarrhea and rashes. “Each additional day of antibiotics that are not needed leads to more side effects,” Dimo said, as well as contributing to antibiotic resistance.
Dimo’s team implemented new EHR order sets across the University of Colorado/Children’s Hospital Colorado health network’s four emergency departments and four urgent care centers and included 31,929 patients in the study.
Then they conducted a retrospective review of patients 61 days to 18 years old who entered those settings and had confirmed AOM between January 2019 through December 2023, before and after the April 2021 intervention. The researchers also developed a guideline on managing ear infections to support clinicians as part of the intervention in December 2022.
Compliance Grew From 3% to 83%
Dimo said they found very few clinicians in their study had been prescribing according to current guidelines. Their results showed a jump from 3% to 83% in providers prescribing 5-day durations of antibiotics for children aged 2 years or older after their intervention.
The intervention did not lead to increased treatment failures or complications, she added. The team looked for diagnostic codes for mastoiditis, subperiosteal abscess, petrositis, labyrinthitis, meningitis, and intracranial abscess, and “none of our patients” developed any of those complications, Dimo said.
Dimo said the overall rate of prescribing, however, increased. Finding out why prescribing rates remained high throughout the study, before and after their intervention, is a question they are investigating in future work, she said.
Cost-Effective and Scalable
“The benefit of this strategy to other institutions is that it’s not labor-intensive. It’s cost-effective, and it can result in dramatic changes in antibiotic use,” Dimo said.
“In the outpatient setting, there’s still a lot of antibiotics being given unnecessarily to children with acute otitis media,” said William Schaffner, MD, infectious disease specialist at Vanderbilt University School of Medicine in Nashville, Tennessee, who was not part of the research. “The American Academy of Pediatrics has been working on that for about a decade — to get pediatricians attuned to when you use them. Most of these episodes of acute otitis media — it’s now well-established — are due to viral infections.”
He said that some physicians may still be defaulting to the longer doses — up to 10 days — that they may have learned in medical school or residency.
“The data would indicate that 5 days of treatment — when treatment is appropriate — is, in the vast majority of instances, sufficient,” Schaffner said.
The researchers “were remarkably successful,” he said, adding that another question is ripe for research. “They still have to get to this issue of whether all of these antibiotic starts were necessary.”
Not knowing whether antibiotic prescriptions in this study were warranted is a limitation of the study, Dimo said, as was not being able to track whether patients presented to institutions outside their own for a return visit or for complications.
She said she thinks one of the reasons for such a sharp increase in compliance was that clinicians in their system routinely use order sets, so using the new order sets easily became part of their workflow.
Dimo and Schaffner reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LOS ANGELES — Embedding a new discharge order set into electronic health records (EHRs) with a preselected 5-day antibiotic course for children aged 2 years or older diagnosed with acute otitis media (AOM) cut antibiotic duration sharply, according to new data presented at the Infectious Disease Week (IDWeek) 2024 Annual Meeting.
“We were effectively able to cut antibiotic use in half by shortening the duration of treatment,” said lead author Joana Dimo, DO, a Pediatric Infectious Diseases fellow at the University of Colorado Denver/Children’s Hospital Colorado.
In the United States, 80% of children will experience otitis media during their lifetime. Untreated ear infections can lead to symptoms ranging from mild ear discharge to life-threatening conditions such as mastoiditis and intracranial abscesses.
Most Cases Resolve Without Antibiotics
Ear infections “are the leading reason for antibiotic prescriptions in kids,” Dimo noted, adding that 24% of all pediatric antibiotic prescriptions are for AOM. Amoxicillin is the preferred first-line treatment. “Research supports that 75% of children get better on their own without antibiotics, and when needed, short courses of just 5 days are safe and effective.”
Antibiotics can cause side effects such as diarrhea and rashes. “Each additional day of antibiotics that are not needed leads to more side effects,” Dimo said, as well as contributing to antibiotic resistance.
Dimo’s team implemented new EHR order sets across the University of Colorado/Children’s Hospital Colorado health network’s four emergency departments and four urgent care centers and included 31,929 patients in the study.
Then they conducted a retrospective review of patients 61 days to 18 years old who entered those settings and had confirmed AOM between January 2019 through December 2023, before and after the April 2021 intervention. The researchers also developed a guideline on managing ear infections to support clinicians as part of the intervention in December 2022.
Compliance Grew From 3% to 83%
Dimo said they found very few clinicians in their study had been prescribing according to current guidelines. Their results showed a jump from 3% to 83% in providers prescribing 5-day durations of antibiotics for children aged 2 years or older after their intervention.
The intervention did not lead to increased treatment failures or complications, she added. The team looked for diagnostic codes for mastoiditis, subperiosteal abscess, petrositis, labyrinthitis, meningitis, and intracranial abscess, and “none of our patients” developed any of those complications, Dimo said.
Dimo said the overall rate of prescribing, however, increased. Finding out why prescribing rates remained high throughout the study, before and after their intervention, is a question they are investigating in future work, she said.
Cost-Effective and Scalable
“The benefit of this strategy to other institutions is that it’s not labor-intensive. It’s cost-effective, and it can result in dramatic changes in antibiotic use,” Dimo said.
“In the outpatient setting, there’s still a lot of antibiotics being given unnecessarily to children with acute otitis media,” said William Schaffner, MD, infectious disease specialist at Vanderbilt University School of Medicine in Nashville, Tennessee, who was not part of the research. “The American Academy of Pediatrics has been working on that for about a decade — to get pediatricians attuned to when you use them. Most of these episodes of acute otitis media — it’s now well-established — are due to viral infections.”
He said that some physicians may still be defaulting to the longer doses — up to 10 days — that they may have learned in medical school or residency.
“The data would indicate that 5 days of treatment — when treatment is appropriate — is, in the vast majority of instances, sufficient,” Schaffner said.
The researchers “were remarkably successful,” he said, adding that another question is ripe for research. “They still have to get to this issue of whether all of these antibiotic starts were necessary.”
Not knowing whether antibiotic prescriptions in this study were warranted is a limitation of the study, Dimo said, as was not being able to track whether patients presented to institutions outside their own for a return visit or for complications.
She said she thinks one of the reasons for such a sharp increase in compliance was that clinicians in their system routinely use order sets, so using the new order sets easily became part of their workflow.
Dimo and Schaffner reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LOS ANGELES — Embedding a new discharge order set into electronic health records (EHRs) with a preselected 5-day antibiotic course for children aged 2 years or older diagnosed with acute otitis media (AOM) cut antibiotic duration sharply, according to new data presented at the Infectious Disease Week (IDWeek) 2024 Annual Meeting.
“We were effectively able to cut antibiotic use in half by shortening the duration of treatment,” said lead author Joana Dimo, DO, a Pediatric Infectious Diseases fellow at the University of Colorado Denver/Children’s Hospital Colorado.
In the United States, 80% of children will experience otitis media during their lifetime. Untreated ear infections can lead to symptoms ranging from mild ear discharge to life-threatening conditions such as mastoiditis and intracranial abscesses.
Most Cases Resolve Without Antibiotics
Ear infections “are the leading reason for antibiotic prescriptions in kids,” Dimo noted, adding that 24% of all pediatric antibiotic prescriptions are for AOM. Amoxicillin is the preferred first-line treatment. “Research supports that 75% of children get better on their own without antibiotics, and when needed, short courses of just 5 days are safe and effective.”
Antibiotics can cause side effects such as diarrhea and rashes. “Each additional day of antibiotics that are not needed leads to more side effects,” Dimo said, as well as contributing to antibiotic resistance.
Dimo’s team implemented new EHR order sets across the University of Colorado/Children’s Hospital Colorado health network’s four emergency departments and four urgent care centers and included 31,929 patients in the study.
Then they conducted a retrospective review of patients 61 days to 18 years old who entered those settings and had confirmed AOM between January 2019 through December 2023, before and after the April 2021 intervention. The researchers also developed a guideline on managing ear infections to support clinicians as part of the intervention in December 2022.
Compliance Grew From 3% to 83%
Dimo said they found very few clinicians in their study had been prescribing according to current guidelines. Their results showed a jump from 3% to 83% in providers prescribing 5-day durations of antibiotics for children aged 2 years or older after their intervention.
The intervention did not lead to increased treatment failures or complications, she added. The team looked for diagnostic codes for mastoiditis, subperiosteal abscess, petrositis, labyrinthitis, meningitis, and intracranial abscess, and “none of our patients” developed any of those complications, Dimo said.
Dimo said the overall rate of prescribing, however, increased. Finding out why prescribing rates remained high throughout the study, before and after their intervention, is a question they are investigating in future work, she said.
Cost-Effective and Scalable
“The benefit of this strategy to other institutions is that it’s not labor-intensive. It’s cost-effective, and it can result in dramatic changes in antibiotic use,” Dimo said.
“In the outpatient setting, there’s still a lot of antibiotics being given unnecessarily to children with acute otitis media,” said William Schaffner, MD, infectious disease specialist at Vanderbilt University School of Medicine in Nashville, Tennessee, who was not part of the research. “The American Academy of Pediatrics has been working on that for about a decade — to get pediatricians attuned to when you use them. Most of these episodes of acute otitis media — it’s now well-established — are due to viral infections.”
He said that some physicians may still be defaulting to the longer doses — up to 10 days — that they may have learned in medical school or residency.
“The data would indicate that 5 days of treatment — when treatment is appropriate — is, in the vast majority of instances, sufficient,” Schaffner said.
The researchers “were remarkably successful,” he said, adding that another question is ripe for research. “They still have to get to this issue of whether all of these antibiotic starts were necessary.”
Not knowing whether antibiotic prescriptions in this study were warranted is a limitation of the study, Dimo said, as was not being able to track whether patients presented to institutions outside their own for a return visit or for complications.
She said she thinks one of the reasons for such a sharp increase in compliance was that clinicians in their system routinely use order sets, so using the new order sets easily became part of their workflow.
Dimo and Schaffner reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM IDWEEK 2024


