User login
Half of deaths from homozygous FH occur before age 32 years
MANNHEIM, GERMANY –
The researchers looked at almost 40 patients from the HoFH International Clinical Collaborators (HICC) registry who had died before data entry, finding that they had a mean age of diagnosis of 12 years.
Even those who received treatment had high LDL cholesterol levels, and 70% developed atherosclerotic cardiovascular disease (ASCVD) at a median age of 28 years.
Worryingly, the results showed that the median age at death was 32 years. Results were presented at the annual congress of the European Atherosclerosis Society.
Patients with HoFH “have severe atherosclerotic cardiovascular disease risk,” said study presenter Janneke Mulder, a PhD candidate at the department of internal medicine, Erasmus University Medical Center, Rotterdam, the Netherlands.
“Therefore, early diagnosis and initiation of treatments, and also a combination of treatments, is really crucial,” she added.
Call to action
Approached for comment, Maciej Banach, MD, PhD, full professor of cardiology, Polish Mother’s Memorial Hospital Research Institute, Lodz, and Secretary of the EAS, described the results as “terrifying.”
He said in an interview that they are a “call to action,” especially given that so few patients in the study received intensive combination lipid-lowering therapy despite having a baseline LDL cholesterol level that was “very, very high.”
Banach underlined that patients who receive triple lipid-lowering therapy with a high-intensity statin, ezetimibe (Nustendi), and a proprotein convertase subtilisin/kexin type 9 inhibitor, could expect, based on current evidence, to see their LDL cholesterol levels reduced by 85% and be on target.
“Obviously, this is kind of academic,” because in the real-world “this 85% is not observed very often,” but it offers a target for steep reductions in cholesterol levels.
“This is something that we should focus on for these patients from the beginning,” said Dr. Banach, either with a stepwise approach “or for experts in pediatric HoFH, “maybe immediately.”
He emphasized that clinicians have everything at hand to “be both effective in the early diagnosis of HoFH, the earlier the better, and obviously to be effective with its treatment.”
“We should do something to prolong the lives of those people,” because the current results are “terrifying,” Dr. Banach added.
Rare genetic condition
Presenting her findings, Ms. Mulder began by highlighting that HoFH is a “rare genetic condition that occurs due to mutations in cholesterol metabolism.”
This, she continued, leads to “severely increased LDL cholesterol levels, and consequently to very premature cardiovascular disease,” with patients potentially experiencing their first cardiovascular event before age 20 years.
Ms. Mulder pointed out that, although there have been case series in the literature on HoFH, they have had “limited numbers” and patients have typically spent decades being treated at the same lipid management clinic.
To broaden the understanding of the clinical characteristics and management of patients dying with HoFH, the team examined data from the HICC registry, which is “the largest contemporary database of homozygous FH patients,” Ms. Mulder said.
It includes 751 patients with HoFH from 88 centers in 38 countries who were alive in 2010 or later. Data entry was between 2016 and 2020. The current analysis focused on 37 patients who had already died by the time they were included on the registry.
Of those, 49% were women, 38% were of White ethnicity, and 43% were from high-income countries.
The median age at diagnosis was 12 years, Ms. Mulder said, explaining that this is similar to that seen in other studies. The majority (86%) underwent genetic testing, and 92% presented with xanthomas.
Ms. Mulder also noted that, at their final clinical evaluation, which was conducted a median age of 18 years after their initial diagnosis, 43% of patients were recorded as current or former smokers.
In terms of their lipid-lowering therapy, 94% were taking a statin, whereas 68% were on ezetimibe, and 23% were undergoing apheresis.
Ms. Mulder said that the median number of lipid-lowering therapies per patient was two, and that “sadly ... 26% of the deceased patients had only one or no treatment.”
Therefore, perhaps unsurprisingly even those patients who were receiving treatment had LDL cholesterol levels that were “too high,” at 9.4 mmol/L versus 15.6 mmol/L among those who were untreated.
There was a high prevalence of ASCVD, at 70% overall, or 41% for aortic stenosis, 30% for myocardial infarction, 30% for angina pectoris, and 22% each for aortic valve replacement and coronary artery bypass grafting. In addition, 19% underwent percutaneous coronary intervention.
The median age of onset for ASCVD was 28 years. Ms. Mulder pointed out, however, that, as data were not available for all patients, “this might be an underestimation.” About 70% of patients experienced recurrent ASCVD.
There was a wide range in the age at which patients with HoFH died, although the median was, “strikingly,” 32 years, Ms. Mulder said. Death was confirmed as stemming from cardiovascular causes in 76% of cases.
During the postpresentation discussion, session chair Antonio J. Vallejo-Vaz, PhD, from the Research Group of Clinical Epidemiology and Vascular Risk, Institute of Biomedicine of Seville (Spain), highlighted that, if 38% of the patients were of White ethnicity, then the remainder must therefore be from other ethnic groups.
“There could be potential issues with accessibility to lipid centers” for these patients, which could affect the findings, noted Dr. Vallejo-Vaz, who is also chief scientist of the EAS Familial Hypercholesterolaemia Studies Collaboration.
Ms. Mulder agreed, replying that their results, though already striking, may be an underestimation because the patients were all from either high or middle-income countries, “so it would be good to have some data on low-income countries.”
She was also asked about two patients who died at a much older age than did the others, at ages 70 years and 86 years, respectively, and whether they had, for example, a protective genetic mutation.
Ms. Mulder said that they do not yet know, but they are planning an extended case series on these and other long-lived patients so that they can be investigated further.
No funding or relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
MANNHEIM, GERMANY –
The researchers looked at almost 40 patients from the HoFH International Clinical Collaborators (HICC) registry who had died before data entry, finding that they had a mean age of diagnosis of 12 years.
Even those who received treatment had high LDL cholesterol levels, and 70% developed atherosclerotic cardiovascular disease (ASCVD) at a median age of 28 years.
Worryingly, the results showed that the median age at death was 32 years. Results were presented at the annual congress of the European Atherosclerosis Society.
Patients with HoFH “have severe atherosclerotic cardiovascular disease risk,” said study presenter Janneke Mulder, a PhD candidate at the department of internal medicine, Erasmus University Medical Center, Rotterdam, the Netherlands.
“Therefore, early diagnosis and initiation of treatments, and also a combination of treatments, is really crucial,” she added.
Call to action
Approached for comment, Maciej Banach, MD, PhD, full professor of cardiology, Polish Mother’s Memorial Hospital Research Institute, Lodz, and Secretary of the EAS, described the results as “terrifying.”
He said in an interview that they are a “call to action,” especially given that so few patients in the study received intensive combination lipid-lowering therapy despite having a baseline LDL cholesterol level that was “very, very high.”
Banach underlined that patients who receive triple lipid-lowering therapy with a high-intensity statin, ezetimibe (Nustendi), and a proprotein convertase subtilisin/kexin type 9 inhibitor, could expect, based on current evidence, to see their LDL cholesterol levels reduced by 85% and be on target.
“Obviously, this is kind of academic,” because in the real-world “this 85% is not observed very often,” but it offers a target for steep reductions in cholesterol levels.
“This is something that we should focus on for these patients from the beginning,” said Dr. Banach, either with a stepwise approach “or for experts in pediatric HoFH, “maybe immediately.”
He emphasized that clinicians have everything at hand to “be both effective in the early diagnosis of HoFH, the earlier the better, and obviously to be effective with its treatment.”
“We should do something to prolong the lives of those people,” because the current results are “terrifying,” Dr. Banach added.
Rare genetic condition
Presenting her findings, Ms. Mulder began by highlighting that HoFH is a “rare genetic condition that occurs due to mutations in cholesterol metabolism.”
This, she continued, leads to “severely increased LDL cholesterol levels, and consequently to very premature cardiovascular disease,” with patients potentially experiencing their first cardiovascular event before age 20 years.
Ms. Mulder pointed out that, although there have been case series in the literature on HoFH, they have had “limited numbers” and patients have typically spent decades being treated at the same lipid management clinic.
To broaden the understanding of the clinical characteristics and management of patients dying with HoFH, the team examined data from the HICC registry, which is “the largest contemporary database of homozygous FH patients,” Ms. Mulder said.
It includes 751 patients with HoFH from 88 centers in 38 countries who were alive in 2010 or later. Data entry was between 2016 and 2020. The current analysis focused on 37 patients who had already died by the time they were included on the registry.
Of those, 49% were women, 38% were of White ethnicity, and 43% were from high-income countries.
The median age at diagnosis was 12 years, Ms. Mulder said, explaining that this is similar to that seen in other studies. The majority (86%) underwent genetic testing, and 92% presented with xanthomas.
Ms. Mulder also noted that, at their final clinical evaluation, which was conducted a median age of 18 years after their initial diagnosis, 43% of patients were recorded as current or former smokers.
In terms of their lipid-lowering therapy, 94% were taking a statin, whereas 68% were on ezetimibe, and 23% were undergoing apheresis.
Ms. Mulder said that the median number of lipid-lowering therapies per patient was two, and that “sadly ... 26% of the deceased patients had only one or no treatment.”
Therefore, perhaps unsurprisingly even those patients who were receiving treatment had LDL cholesterol levels that were “too high,” at 9.4 mmol/L versus 15.6 mmol/L among those who were untreated.
There was a high prevalence of ASCVD, at 70% overall, or 41% for aortic stenosis, 30% for myocardial infarction, 30% for angina pectoris, and 22% each for aortic valve replacement and coronary artery bypass grafting. In addition, 19% underwent percutaneous coronary intervention.
The median age of onset for ASCVD was 28 years. Ms. Mulder pointed out, however, that, as data were not available for all patients, “this might be an underestimation.” About 70% of patients experienced recurrent ASCVD.
There was a wide range in the age at which patients with HoFH died, although the median was, “strikingly,” 32 years, Ms. Mulder said. Death was confirmed as stemming from cardiovascular causes in 76% of cases.
During the postpresentation discussion, session chair Antonio J. Vallejo-Vaz, PhD, from the Research Group of Clinical Epidemiology and Vascular Risk, Institute of Biomedicine of Seville (Spain), highlighted that, if 38% of the patients were of White ethnicity, then the remainder must therefore be from other ethnic groups.
“There could be potential issues with accessibility to lipid centers” for these patients, which could affect the findings, noted Dr. Vallejo-Vaz, who is also chief scientist of the EAS Familial Hypercholesterolaemia Studies Collaboration.
Ms. Mulder agreed, replying that their results, though already striking, may be an underestimation because the patients were all from either high or middle-income countries, “so it would be good to have some data on low-income countries.”
She was also asked about two patients who died at a much older age than did the others, at ages 70 years and 86 years, respectively, and whether they had, for example, a protective genetic mutation.
Ms. Mulder said that they do not yet know, but they are planning an extended case series on these and other long-lived patients so that they can be investigated further.
No funding or relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
MANNHEIM, GERMANY –
The researchers looked at almost 40 patients from the HoFH International Clinical Collaborators (HICC) registry who had died before data entry, finding that they had a mean age of diagnosis of 12 years.
Even those who received treatment had high LDL cholesterol levels, and 70% developed atherosclerotic cardiovascular disease (ASCVD) at a median age of 28 years.
Worryingly, the results showed that the median age at death was 32 years. Results were presented at the annual congress of the European Atherosclerosis Society.
Patients with HoFH “have severe atherosclerotic cardiovascular disease risk,” said study presenter Janneke Mulder, a PhD candidate at the department of internal medicine, Erasmus University Medical Center, Rotterdam, the Netherlands.
“Therefore, early diagnosis and initiation of treatments, and also a combination of treatments, is really crucial,” she added.
Call to action
Approached for comment, Maciej Banach, MD, PhD, full professor of cardiology, Polish Mother’s Memorial Hospital Research Institute, Lodz, and Secretary of the EAS, described the results as “terrifying.”
He said in an interview that they are a “call to action,” especially given that so few patients in the study received intensive combination lipid-lowering therapy despite having a baseline LDL cholesterol level that was “very, very high.”
Banach underlined that patients who receive triple lipid-lowering therapy with a high-intensity statin, ezetimibe (Nustendi), and a proprotein convertase subtilisin/kexin type 9 inhibitor, could expect, based on current evidence, to see their LDL cholesterol levels reduced by 85% and be on target.
“Obviously, this is kind of academic,” because in the real-world “this 85% is not observed very often,” but it offers a target for steep reductions in cholesterol levels.
“This is something that we should focus on for these patients from the beginning,” said Dr. Banach, either with a stepwise approach “or for experts in pediatric HoFH, “maybe immediately.”
He emphasized that clinicians have everything at hand to “be both effective in the early diagnosis of HoFH, the earlier the better, and obviously to be effective with its treatment.”
“We should do something to prolong the lives of those people,” because the current results are “terrifying,” Dr. Banach added.
Rare genetic condition
Presenting her findings, Ms. Mulder began by highlighting that HoFH is a “rare genetic condition that occurs due to mutations in cholesterol metabolism.”
This, she continued, leads to “severely increased LDL cholesterol levels, and consequently to very premature cardiovascular disease,” with patients potentially experiencing their first cardiovascular event before age 20 years.
Ms. Mulder pointed out that, although there have been case series in the literature on HoFH, they have had “limited numbers” and patients have typically spent decades being treated at the same lipid management clinic.
To broaden the understanding of the clinical characteristics and management of patients dying with HoFH, the team examined data from the HICC registry, which is “the largest contemporary database of homozygous FH patients,” Ms. Mulder said.
It includes 751 patients with HoFH from 88 centers in 38 countries who were alive in 2010 or later. Data entry was between 2016 and 2020. The current analysis focused on 37 patients who had already died by the time they were included on the registry.
Of those, 49% were women, 38% were of White ethnicity, and 43% were from high-income countries.
The median age at diagnosis was 12 years, Ms. Mulder said, explaining that this is similar to that seen in other studies. The majority (86%) underwent genetic testing, and 92% presented with xanthomas.
Ms. Mulder also noted that, at their final clinical evaluation, which was conducted a median age of 18 years after their initial diagnosis, 43% of patients were recorded as current or former smokers.
In terms of their lipid-lowering therapy, 94% were taking a statin, whereas 68% were on ezetimibe, and 23% were undergoing apheresis.
Ms. Mulder said that the median number of lipid-lowering therapies per patient was two, and that “sadly ... 26% of the deceased patients had only one or no treatment.”
Therefore, perhaps unsurprisingly even those patients who were receiving treatment had LDL cholesterol levels that were “too high,” at 9.4 mmol/L versus 15.6 mmol/L among those who were untreated.
There was a high prevalence of ASCVD, at 70% overall, or 41% for aortic stenosis, 30% for myocardial infarction, 30% for angina pectoris, and 22% each for aortic valve replacement and coronary artery bypass grafting. In addition, 19% underwent percutaneous coronary intervention.
The median age of onset for ASCVD was 28 years. Ms. Mulder pointed out, however, that, as data were not available for all patients, “this might be an underestimation.” About 70% of patients experienced recurrent ASCVD.
There was a wide range in the age at which patients with HoFH died, although the median was, “strikingly,” 32 years, Ms. Mulder said. Death was confirmed as stemming from cardiovascular causes in 76% of cases.
During the postpresentation discussion, session chair Antonio J. Vallejo-Vaz, PhD, from the Research Group of Clinical Epidemiology and Vascular Risk, Institute of Biomedicine of Seville (Spain), highlighted that, if 38% of the patients were of White ethnicity, then the remainder must therefore be from other ethnic groups.
“There could be potential issues with accessibility to lipid centers” for these patients, which could affect the findings, noted Dr. Vallejo-Vaz, who is also chief scientist of the EAS Familial Hypercholesterolaemia Studies Collaboration.
Ms. Mulder agreed, replying that their results, though already striking, may be an underestimation because the patients were all from either high or middle-income countries, “so it would be good to have some data on low-income countries.”
She was also asked about two patients who died at a much older age than did the others, at ages 70 years and 86 years, respectively, and whether they had, for example, a protective genetic mutation.
Ms. Mulder said that they do not yet know, but they are planning an extended case series on these and other long-lived patients so that they can be investigated further.
No funding or relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
Maternal health clinic teams with legal services to aid patients
BALTIMORE – A novel partnership between a legal services program and a maternal health clinic is helping pregnant patients with issues such as housing or employment discrimination.
The Perinatal Legal Assistance and Well-being (P-LAW) program at Georgetown University, Washington, launched 2 years ago as a collaboration between GU’s Health Justice Alliance clinic and the Women’s and Infants Services division of nearby MedStar Washington Hospital Center, integrating attorneys into the health care team to offer no-cost legal aid for its diverse, urban population during the perinatal period. Since then, the effort has assisted more than 120 women.
“Our goal was to see how integrating a lawyer can help address some of those issues that, unfortunately, providers are not able to assist with because they go beyond the hospital or clinic walls,” said Roxana Richardson, JD, the project director and managing attorney for P-LAW, during a poster presentation at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “Our initial findings showed that there are issues that patients were facing that needed an intervention from an attorney. We trained the providers and social workers to identify these issues so that we could intervene.”
Improving health by tackling legal barriers
, Ms. Richardson said.
The program is one of few medical-legal partnerships specifically focused on the perinatal population. P-LAW is one component of a larger initiative at MedStar Health called DC Safe Babies Safe Moms. The initiative includes integrated mental health programming, treatment of health conditions that complicate pregnancy, assessments of social determinants of health, expanded support for lactation and nutrition, access to home visiting referrals, and extended postpartum follow-up. The work is supported through the A. James & Alice B. Clark Foundation.
Patients are evaluated for health-harming legal needs as part of a comprehensive social and behavioral health screening at their initial prenatal visit, 28-week appointment, and postpartum visit. Those who screen positive are contacted by a referral specialist on the health care team who confirms the patient has an active legal need and would like to be connected to the P-LAW team. The team then reaches out to conduct a legal intake and determine the appropriate course of action.
From March 2021 through February of this year, Ms. Richardson and others with the program have provided legal representation to 123 patients on 186 legal issues in areas such as public benefits, employment, and housing and family concerns. Services range from advising patients on steps they can take on their own (like reporting a housing condition issue to the Department of Buildings), to sending letters on patients’ behalf, to appearing in court. Most patients served were in their second and third trimesters of pregnancy. The majority were Black or African American, aged 20-34 years, and had incomes below 100% of the federal poverty level.
The most common legal issues were in the areas of public benefits (SNAP/food stamps, cash assistance), employment (parental leave, discrimination), housing (conditions, eviction), and family law (child support, domestic violence). Among the 186 issues, work has been completed on 106 concerns and 33 still have a case open; for 47, the client withdrew or ceased contact, Ms. Richardson reported.
Most times when obstetricians hear concerns like these, they wonder what to do, said Tamika Auguste, MD, chair of obstetrics and gynecology at MedStar Health. Having the P-LAW program as a resource is a huge help, she said. If patients express concerns, or if obstetricians uncover concerns during office visits, doctors can enter a referral directly in the electronic medical record.
Patients are “so relieved,” Dr. Auguste said in an interview, because they often wonder if their doctor can help. “Your doctor is only going to be able to help to a certain point. But to know they’re pregnant and they have this resource, and they’re going to get legal help, has been game-changing for so many patients.”
COVID ... or morning sickness?
In one rewarding case, Ms. Richardson said, a single mother of one child who was pregnant and experiencing hyperemesis explained that her employer would forbid her from working if she had any symptoms similar to COVID-19. The employer mistook her vomiting, nausea, and exhaustion as COVID symptoms and docked her pay. That started a cascade in which earning less meant she was facing eviction and car repossession – and, eventually, overdraft fees and withdrawals from her bank. She was so despondent she was thinking about self-harm, Ms. Richardson said.
With the aid of the P-LAW program, the woman had short-term disability approved within 72 hours, was referred to the hospital for inpatient mental health treatment, and received the care she needed. She ultimately delivered a healthy baby girl and found a new job.
Tiffany Moore Simas, MD, MPH, MEd, chair of the department of obstetrics and gynecology at the University of Massachusetts and UMass Memorial Health in Worcester, said she encounters similar concerns among her patients, with the vast majority having one or more issues with social determinants of health.
“I think it’s incredible, as we’re trying to address equity in perinatal health and maternal mortality and morbidity, to have a more holistic view of what health means, and all of the social determinants of health, and actually helping our patients address that in real time at their visits and connecting them,” said Dr. Simas, who also is professor of ob/gyn, pediatrics, psychiatry, and population and quantitative health sciences at UMass. “It has really opened my mind to the possibilities of things we need to explore and do differently.”
Ms. Richardson, Dr. Auguste, and Dr. Simas reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
BALTIMORE – A novel partnership between a legal services program and a maternal health clinic is helping pregnant patients with issues such as housing or employment discrimination.
The Perinatal Legal Assistance and Well-being (P-LAW) program at Georgetown University, Washington, launched 2 years ago as a collaboration between GU’s Health Justice Alliance clinic and the Women’s and Infants Services division of nearby MedStar Washington Hospital Center, integrating attorneys into the health care team to offer no-cost legal aid for its diverse, urban population during the perinatal period. Since then, the effort has assisted more than 120 women.
“Our goal was to see how integrating a lawyer can help address some of those issues that, unfortunately, providers are not able to assist with because they go beyond the hospital or clinic walls,” said Roxana Richardson, JD, the project director and managing attorney for P-LAW, during a poster presentation at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “Our initial findings showed that there are issues that patients were facing that needed an intervention from an attorney. We trained the providers and social workers to identify these issues so that we could intervene.”
Improving health by tackling legal barriers
, Ms. Richardson said.
The program is one of few medical-legal partnerships specifically focused on the perinatal population. P-LAW is one component of a larger initiative at MedStar Health called DC Safe Babies Safe Moms. The initiative includes integrated mental health programming, treatment of health conditions that complicate pregnancy, assessments of social determinants of health, expanded support for lactation and nutrition, access to home visiting referrals, and extended postpartum follow-up. The work is supported through the A. James & Alice B. Clark Foundation.
Patients are evaluated for health-harming legal needs as part of a comprehensive social and behavioral health screening at their initial prenatal visit, 28-week appointment, and postpartum visit. Those who screen positive are contacted by a referral specialist on the health care team who confirms the patient has an active legal need and would like to be connected to the P-LAW team. The team then reaches out to conduct a legal intake and determine the appropriate course of action.
From March 2021 through February of this year, Ms. Richardson and others with the program have provided legal representation to 123 patients on 186 legal issues in areas such as public benefits, employment, and housing and family concerns. Services range from advising patients on steps they can take on their own (like reporting a housing condition issue to the Department of Buildings), to sending letters on patients’ behalf, to appearing in court. Most patients served were in their second and third trimesters of pregnancy. The majority were Black or African American, aged 20-34 years, and had incomes below 100% of the federal poverty level.
The most common legal issues were in the areas of public benefits (SNAP/food stamps, cash assistance), employment (parental leave, discrimination), housing (conditions, eviction), and family law (child support, domestic violence). Among the 186 issues, work has been completed on 106 concerns and 33 still have a case open; for 47, the client withdrew or ceased contact, Ms. Richardson reported.
Most times when obstetricians hear concerns like these, they wonder what to do, said Tamika Auguste, MD, chair of obstetrics and gynecology at MedStar Health. Having the P-LAW program as a resource is a huge help, she said. If patients express concerns, or if obstetricians uncover concerns during office visits, doctors can enter a referral directly in the electronic medical record.
Patients are “so relieved,” Dr. Auguste said in an interview, because they often wonder if their doctor can help. “Your doctor is only going to be able to help to a certain point. But to know they’re pregnant and they have this resource, and they’re going to get legal help, has been game-changing for so many patients.”
COVID ... or morning sickness?
In one rewarding case, Ms. Richardson said, a single mother of one child who was pregnant and experiencing hyperemesis explained that her employer would forbid her from working if she had any symptoms similar to COVID-19. The employer mistook her vomiting, nausea, and exhaustion as COVID symptoms and docked her pay. That started a cascade in which earning less meant she was facing eviction and car repossession – and, eventually, overdraft fees and withdrawals from her bank. She was so despondent she was thinking about self-harm, Ms. Richardson said.
With the aid of the P-LAW program, the woman had short-term disability approved within 72 hours, was referred to the hospital for inpatient mental health treatment, and received the care she needed. She ultimately delivered a healthy baby girl and found a new job.
Tiffany Moore Simas, MD, MPH, MEd, chair of the department of obstetrics and gynecology at the University of Massachusetts and UMass Memorial Health in Worcester, said she encounters similar concerns among her patients, with the vast majority having one or more issues with social determinants of health.
“I think it’s incredible, as we’re trying to address equity in perinatal health and maternal mortality and morbidity, to have a more holistic view of what health means, and all of the social determinants of health, and actually helping our patients address that in real time at their visits and connecting them,” said Dr. Simas, who also is professor of ob/gyn, pediatrics, psychiatry, and population and quantitative health sciences at UMass. “It has really opened my mind to the possibilities of things we need to explore and do differently.”
Ms. Richardson, Dr. Auguste, and Dr. Simas reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
BALTIMORE – A novel partnership between a legal services program and a maternal health clinic is helping pregnant patients with issues such as housing or employment discrimination.
The Perinatal Legal Assistance and Well-being (P-LAW) program at Georgetown University, Washington, launched 2 years ago as a collaboration between GU’s Health Justice Alliance clinic and the Women’s and Infants Services division of nearby MedStar Washington Hospital Center, integrating attorneys into the health care team to offer no-cost legal aid for its diverse, urban population during the perinatal period. Since then, the effort has assisted more than 120 women.
“Our goal was to see how integrating a lawyer can help address some of those issues that, unfortunately, providers are not able to assist with because they go beyond the hospital or clinic walls,” said Roxana Richardson, JD, the project director and managing attorney for P-LAW, during a poster presentation at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “Our initial findings showed that there are issues that patients were facing that needed an intervention from an attorney. We trained the providers and social workers to identify these issues so that we could intervene.”
Improving health by tackling legal barriers
, Ms. Richardson said.
The program is one of few medical-legal partnerships specifically focused on the perinatal population. P-LAW is one component of a larger initiative at MedStar Health called DC Safe Babies Safe Moms. The initiative includes integrated mental health programming, treatment of health conditions that complicate pregnancy, assessments of social determinants of health, expanded support for lactation and nutrition, access to home visiting referrals, and extended postpartum follow-up. The work is supported through the A. James & Alice B. Clark Foundation.
Patients are evaluated for health-harming legal needs as part of a comprehensive social and behavioral health screening at their initial prenatal visit, 28-week appointment, and postpartum visit. Those who screen positive are contacted by a referral specialist on the health care team who confirms the patient has an active legal need and would like to be connected to the P-LAW team. The team then reaches out to conduct a legal intake and determine the appropriate course of action.
From March 2021 through February of this year, Ms. Richardson and others with the program have provided legal representation to 123 patients on 186 legal issues in areas such as public benefits, employment, and housing and family concerns. Services range from advising patients on steps they can take on their own (like reporting a housing condition issue to the Department of Buildings), to sending letters on patients’ behalf, to appearing in court. Most patients served were in their second and third trimesters of pregnancy. The majority were Black or African American, aged 20-34 years, and had incomes below 100% of the federal poverty level.
The most common legal issues were in the areas of public benefits (SNAP/food stamps, cash assistance), employment (parental leave, discrimination), housing (conditions, eviction), and family law (child support, domestic violence). Among the 186 issues, work has been completed on 106 concerns and 33 still have a case open; for 47, the client withdrew or ceased contact, Ms. Richardson reported.
Most times when obstetricians hear concerns like these, they wonder what to do, said Tamika Auguste, MD, chair of obstetrics and gynecology at MedStar Health. Having the P-LAW program as a resource is a huge help, she said. If patients express concerns, or if obstetricians uncover concerns during office visits, doctors can enter a referral directly in the electronic medical record.
Patients are “so relieved,” Dr. Auguste said in an interview, because they often wonder if their doctor can help. “Your doctor is only going to be able to help to a certain point. But to know they’re pregnant and they have this resource, and they’re going to get legal help, has been game-changing for so many patients.”
COVID ... or morning sickness?
In one rewarding case, Ms. Richardson said, a single mother of one child who was pregnant and experiencing hyperemesis explained that her employer would forbid her from working if she had any symptoms similar to COVID-19. The employer mistook her vomiting, nausea, and exhaustion as COVID symptoms and docked her pay. That started a cascade in which earning less meant she was facing eviction and car repossession – and, eventually, overdraft fees and withdrawals from her bank. She was so despondent she was thinking about self-harm, Ms. Richardson said.
With the aid of the P-LAW program, the woman had short-term disability approved within 72 hours, was referred to the hospital for inpatient mental health treatment, and received the care she needed. She ultimately delivered a healthy baby girl and found a new job.
Tiffany Moore Simas, MD, MPH, MEd, chair of the department of obstetrics and gynecology at the University of Massachusetts and UMass Memorial Health in Worcester, said she encounters similar concerns among her patients, with the vast majority having one or more issues with social determinants of health.
“I think it’s incredible, as we’re trying to address equity in perinatal health and maternal mortality and morbidity, to have a more holistic view of what health means, and all of the social determinants of health, and actually helping our patients address that in real time at their visits and connecting them,” said Dr. Simas, who also is professor of ob/gyn, pediatrics, psychiatry, and population and quantitative health sciences at UMass. “It has really opened my mind to the possibilities of things we need to explore and do differently.”
Ms. Richardson, Dr. Auguste, and Dr. Simas reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT ACOG 2023
Harmful emotional hit of antidepressants underappreciated
SAN FRANCISCO – , new research shows.
Emotional blunting can be described as feeling emotionally flat and incapable of finding pleasure. The patient may feel less sadness, guilt, or hopelessness, but that may come at the cost of feeling less joy, surprise, and happiness. Some people with SSRI-induced blunting even report caring less about important relationships.
It’s an issue that needs greater attention, study investigator Mujeeb U. Shad, MD, with Valley Health Services and University of Nevada, Las Vegas, said in an interview.
“Patients may come to the clinic and report feeling emotionally and cognitively flat and not be taken seriously by their provider, but they are genuinely reporting something that is happening to them and decreasing their quality of life,” Dr. Shad explained.
The study was presented at the annual meeting of the American Psychiatric Association.
Something ‘missing’
Dr. Shad said that the genesis for the study came from a resident who noticed that many patients receiving SSRIs reported feeling better and not as bothered by the depression, yet, at the same time, they felt something was “missing. Their families would say, ‘You’re better but you’re not the same person.’ ”
To investigate further, the researchers did a “scoping review” of 25 original studies that assessed antidepressant-related emotional blunting. Until now, there hasn’t been a systematic review of this issue, Dr. Shad said.
Ten of the studies looked at the role of SSRIs in emotional blunting, whereas the other 15 looked at serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and second-generation antipsychotic medications.
The results of the review show that emotional blunting is a significant patient-reported concern. It often presents as a subjective complaint of changed personality, feeling a lesser intensity of overall emotions, and the manifestation of not being oneself often attributed to antidepressant use, the researchers found. Emotional blunting was more commonly associated with SSRIs than with the other medications in the studies.
Common clinical strategies to manage antidepressant-induced emotional blunting reported in the literature include dose reduction or switching to a different antidepressant class; however, the literature did not make the distinction between emotional blunting as a primary symptom of depression or an adverse effect of antidepressants.
Dr. Shad said that there is a need to develop valid and reliable measures to assess emotional blunting related to antidepressants.
He noted that optimal patient care should include pre- and posttreatment assessment of emotional blunting. One useful tool is the Oxford Questionnaire on the Emotional Side-Effects of Antidepressants.
Can’t get to the top
Jacob Cross, MD, who wasn’t involved in the study, said that he has seen the impact of antidepressant-related emotional blunting first-hand.
“I’ve had multiple patients report emotional blunting on antidepressant therapy,” Dr. Cross, with the department of psychiatry, Rush Medical College, Chicago, said.
“These patients feel like their emotions are not as high and not as low; so they experience directional improvement, but they’re still not feeling like they can get that top peak emotion. It’s kind of similar to anhedonia. They’re just feeling like a little cut off, like they’re climbing a cliff and just can’t get to that top,” Dr. Cross said.
For a patient with emotional blunting, Dr. Cross said he might “switch to an antidepressant that’s more stimulating like an SNRI from an SSRI. You could also lower the dose and see if that helps, but I usually change the drug class.”
The study had no specific funding. Dr. Shad and Dr. Cross have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , new research shows.
Emotional blunting can be described as feeling emotionally flat and incapable of finding pleasure. The patient may feel less sadness, guilt, or hopelessness, but that may come at the cost of feeling less joy, surprise, and happiness. Some people with SSRI-induced blunting even report caring less about important relationships.
It’s an issue that needs greater attention, study investigator Mujeeb U. Shad, MD, with Valley Health Services and University of Nevada, Las Vegas, said in an interview.
“Patients may come to the clinic and report feeling emotionally and cognitively flat and not be taken seriously by their provider, but they are genuinely reporting something that is happening to them and decreasing their quality of life,” Dr. Shad explained.
The study was presented at the annual meeting of the American Psychiatric Association.
Something ‘missing’
Dr. Shad said that the genesis for the study came from a resident who noticed that many patients receiving SSRIs reported feeling better and not as bothered by the depression, yet, at the same time, they felt something was “missing. Their families would say, ‘You’re better but you’re not the same person.’ ”
To investigate further, the researchers did a “scoping review” of 25 original studies that assessed antidepressant-related emotional blunting. Until now, there hasn’t been a systematic review of this issue, Dr. Shad said.
Ten of the studies looked at the role of SSRIs in emotional blunting, whereas the other 15 looked at serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and second-generation antipsychotic medications.
The results of the review show that emotional blunting is a significant patient-reported concern. It often presents as a subjective complaint of changed personality, feeling a lesser intensity of overall emotions, and the manifestation of not being oneself often attributed to antidepressant use, the researchers found. Emotional blunting was more commonly associated with SSRIs than with the other medications in the studies.
Common clinical strategies to manage antidepressant-induced emotional blunting reported in the literature include dose reduction or switching to a different antidepressant class; however, the literature did not make the distinction between emotional blunting as a primary symptom of depression or an adverse effect of antidepressants.
Dr. Shad said that there is a need to develop valid and reliable measures to assess emotional blunting related to antidepressants.
He noted that optimal patient care should include pre- and posttreatment assessment of emotional blunting. One useful tool is the Oxford Questionnaire on the Emotional Side-Effects of Antidepressants.
Can’t get to the top
Jacob Cross, MD, who wasn’t involved in the study, said that he has seen the impact of antidepressant-related emotional blunting first-hand.
“I’ve had multiple patients report emotional blunting on antidepressant therapy,” Dr. Cross, with the department of psychiatry, Rush Medical College, Chicago, said.
“These patients feel like their emotions are not as high and not as low; so they experience directional improvement, but they’re still not feeling like they can get that top peak emotion. It’s kind of similar to anhedonia. They’re just feeling like a little cut off, like they’re climbing a cliff and just can’t get to that top,” Dr. Cross said.
For a patient with emotional blunting, Dr. Cross said he might “switch to an antidepressant that’s more stimulating like an SNRI from an SSRI. You could also lower the dose and see if that helps, but I usually change the drug class.”
The study had no specific funding. Dr. Shad and Dr. Cross have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , new research shows.
Emotional blunting can be described as feeling emotionally flat and incapable of finding pleasure. The patient may feel less sadness, guilt, or hopelessness, but that may come at the cost of feeling less joy, surprise, and happiness. Some people with SSRI-induced blunting even report caring less about important relationships.
It’s an issue that needs greater attention, study investigator Mujeeb U. Shad, MD, with Valley Health Services and University of Nevada, Las Vegas, said in an interview.
“Patients may come to the clinic and report feeling emotionally and cognitively flat and not be taken seriously by their provider, but they are genuinely reporting something that is happening to them and decreasing their quality of life,” Dr. Shad explained.
The study was presented at the annual meeting of the American Psychiatric Association.
Something ‘missing’
Dr. Shad said that the genesis for the study came from a resident who noticed that many patients receiving SSRIs reported feeling better and not as bothered by the depression, yet, at the same time, they felt something was “missing. Their families would say, ‘You’re better but you’re not the same person.’ ”
To investigate further, the researchers did a “scoping review” of 25 original studies that assessed antidepressant-related emotional blunting. Until now, there hasn’t been a systematic review of this issue, Dr. Shad said.
Ten of the studies looked at the role of SSRIs in emotional blunting, whereas the other 15 looked at serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and second-generation antipsychotic medications.
The results of the review show that emotional blunting is a significant patient-reported concern. It often presents as a subjective complaint of changed personality, feeling a lesser intensity of overall emotions, and the manifestation of not being oneself often attributed to antidepressant use, the researchers found. Emotional blunting was more commonly associated with SSRIs than with the other medications in the studies.
Common clinical strategies to manage antidepressant-induced emotional blunting reported in the literature include dose reduction or switching to a different antidepressant class; however, the literature did not make the distinction between emotional blunting as a primary symptom of depression or an adverse effect of antidepressants.
Dr. Shad said that there is a need to develop valid and reliable measures to assess emotional blunting related to antidepressants.
He noted that optimal patient care should include pre- and posttreatment assessment of emotional blunting. One useful tool is the Oxford Questionnaire on the Emotional Side-Effects of Antidepressants.
Can’t get to the top
Jacob Cross, MD, who wasn’t involved in the study, said that he has seen the impact of antidepressant-related emotional blunting first-hand.
“I’ve had multiple patients report emotional blunting on antidepressant therapy,” Dr. Cross, with the department of psychiatry, Rush Medical College, Chicago, said.
“These patients feel like their emotions are not as high and not as low; so they experience directional improvement, but they’re still not feeling like they can get that top peak emotion. It’s kind of similar to anhedonia. They’re just feeling like a little cut off, like they’re climbing a cliff and just can’t get to that top,” Dr. Cross said.
For a patient with emotional blunting, Dr. Cross said he might “switch to an antidepressant that’s more stimulating like an SNRI from an SSRI. You could also lower the dose and see if that helps, but I usually change the drug class.”
The study had no specific funding. Dr. Shad and Dr. Cross have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
AT APA 2023
People still want their medical intelligence in human form
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
AxSpA remission on TNFi seen in half of patients with comorbid IBD
CLEVELAND – About half (52%) of patients living with both axial spondyloarthritis and inflammatory bowel disease (IBD) reached clinical remission of axSpA at 12 months after starting a tumor necrosis factor inhibitor (TNFi), researchers have found.
The disease course for axSpA among patients with IBD who start anti-TNF agents is not well understood.
Rahul S. Dalal, MD, an advanced fellow in IBD with the division of gastroenterology, hepatology, and endoscopy at Brigham and Women’s Hospital, Boston, and colleagues studied whether certain clinical factors were associated with remission of axSpA after patients with axSpA, who also had Crohn’s disease (CD) or ulcerative colitis (UC), started anti-TNF therapy.
Short IBD duration, adalimumab linked with higher remission odds
They found that those who had IBD for less than 5 years and those taking the TNFi adalimumab (Humira and biosimilars), as opposed to another TNFi, had a higher likelihood of reaching axSpA remission at 1 year. The odds ratios calculated for those factors were statistically significant.
Dr. Dalal said that most of the patients in the study (70%) were prescribed adalimumab, and because the study didn’t compare TNFis head to head, it’s hard to say whether adalimumab should be the preferred treatment for these patients.
“But it’s an interesting question that should be addressed in a bigger study,” he said.
Other TNFis included infliximab (Remicade and biosimilars) in 27%, golimumab (Simponi) in 2%, and certolizumab pegol (Cimzia) in 1%.
He presented the results at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
Study details
Included in the retrospective cohort study were 82 adults with IBD and either ankylosing spondylitis or sacroiliitis who started anti-TNF agents approved for IBD between January 2012 and October 2021 at a large academic center.
Clinical remission of axSpA was the primary outcome, defined as the absence or adequate control of pain and/or stiffness related to axSpA as documented in the rheumatology note 1 year (+/– 2 months) after starting anti-TNF agents.
The secondary outcome was clinical remission of IBD, defined as 2 or less on the simple clinical colitis activity index, a score of less than 5 on the Harvey-Bradshaw Index, or provider assessment with no use of oral or intravenous glucocorticoids for 30 days. Dr. Dalal said 74% in the study reached that endpoint in the study period.
“Some patients had good response to anti-TNF treatments for their IBD but not necessarily for their spondyloarthritis,” he explained.
There were insufficient observations to calculate odds ratios for the variables, including Hispanic ethnicity, endoscopic inflammation, and prior history of using vedolizumab (Entyvio), secukinumab (Cosentyx), and ustekinumab (Stelara), the authors noted.
Dr. Dalal said it’s important to study this population because patients with IBD and axSpA take some of the same medications, but it’s not known how each medication acts in patients.
“We don’t have much data to tell us who’s going to respond to treatments from both diseases simultaneously,” he said.
Conclusions called ‘reassuring’
Jean Liew, MD, a spondyloarthritis specialist at Boston University, who was not part of the study, noted that the team reported univariate associations of clinical factors with achievement of clinical axSpA remission, but no multivariable analyses with adjustment for potential confounders.
She said the finding of half the patients achieving clinical remission is “reassuring, as anecdotally we may find that patients with IBD-associated spondyloarthritis tend to have more difficult-to-treat symptoms as well as more limited treatment options. For example, they cannot use [interleukin]-17 inhibitors.”
She noted the study is small and descriptive and further analyses are limited by the small number of patients.
“I think if a study of the same type could be performed at a larger scale with larger numbers, it could generate more data on which type of patient with IBD-associated spondyloarthritis is more likely to have a good response after starting a TNF inhibitor,” she said. “Of course, the other question is how long those patients would have good disease control while on the TNF inhibitor. What is the persistence of the medication? This study doesn’t ask or answer that question.”
Dr. Dalal added that in future research it will be important to look at response to medications beyond TNFis, especially Janus kinase inhibitors.
That will help show “whether there is a treatment algorithm that can be tailored to this population in terms of what agents to choose first,” he said. “I think we need multicenter studies to do this.”
Dr. Dalal has received grant funding from Pfizer and Janssen and has served as a consultant for Centaur Labs and Janssen. Dr. Liew has no relevant financial relationships.
CLEVELAND – About half (52%) of patients living with both axial spondyloarthritis and inflammatory bowel disease (IBD) reached clinical remission of axSpA at 12 months after starting a tumor necrosis factor inhibitor (TNFi), researchers have found.
The disease course for axSpA among patients with IBD who start anti-TNF agents is not well understood.
Rahul S. Dalal, MD, an advanced fellow in IBD with the division of gastroenterology, hepatology, and endoscopy at Brigham and Women’s Hospital, Boston, and colleagues studied whether certain clinical factors were associated with remission of axSpA after patients with axSpA, who also had Crohn’s disease (CD) or ulcerative colitis (UC), started anti-TNF therapy.
Short IBD duration, adalimumab linked with higher remission odds
They found that those who had IBD for less than 5 years and those taking the TNFi adalimumab (Humira and biosimilars), as opposed to another TNFi, had a higher likelihood of reaching axSpA remission at 1 year. The odds ratios calculated for those factors were statistically significant.
Dr. Dalal said that most of the patients in the study (70%) were prescribed adalimumab, and because the study didn’t compare TNFis head to head, it’s hard to say whether adalimumab should be the preferred treatment for these patients.
“But it’s an interesting question that should be addressed in a bigger study,” he said.
Other TNFis included infliximab (Remicade and biosimilars) in 27%, golimumab (Simponi) in 2%, and certolizumab pegol (Cimzia) in 1%.
He presented the results at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
Study details
Included in the retrospective cohort study were 82 adults with IBD and either ankylosing spondylitis or sacroiliitis who started anti-TNF agents approved for IBD between January 2012 and October 2021 at a large academic center.
Clinical remission of axSpA was the primary outcome, defined as the absence or adequate control of pain and/or stiffness related to axSpA as documented in the rheumatology note 1 year (+/– 2 months) after starting anti-TNF agents.
The secondary outcome was clinical remission of IBD, defined as 2 or less on the simple clinical colitis activity index, a score of less than 5 on the Harvey-Bradshaw Index, or provider assessment with no use of oral or intravenous glucocorticoids for 30 days. Dr. Dalal said 74% in the study reached that endpoint in the study period.
“Some patients had good response to anti-TNF treatments for their IBD but not necessarily for their spondyloarthritis,” he explained.
There were insufficient observations to calculate odds ratios for the variables, including Hispanic ethnicity, endoscopic inflammation, and prior history of using vedolizumab (Entyvio), secukinumab (Cosentyx), and ustekinumab (Stelara), the authors noted.
Dr. Dalal said it’s important to study this population because patients with IBD and axSpA take some of the same medications, but it’s not known how each medication acts in patients.
“We don’t have much data to tell us who’s going to respond to treatments from both diseases simultaneously,” he said.
Conclusions called ‘reassuring’
Jean Liew, MD, a spondyloarthritis specialist at Boston University, who was not part of the study, noted that the team reported univariate associations of clinical factors with achievement of clinical axSpA remission, but no multivariable analyses with adjustment for potential confounders.
She said the finding of half the patients achieving clinical remission is “reassuring, as anecdotally we may find that patients with IBD-associated spondyloarthritis tend to have more difficult-to-treat symptoms as well as more limited treatment options. For example, they cannot use [interleukin]-17 inhibitors.”
She noted the study is small and descriptive and further analyses are limited by the small number of patients.
“I think if a study of the same type could be performed at a larger scale with larger numbers, it could generate more data on which type of patient with IBD-associated spondyloarthritis is more likely to have a good response after starting a TNF inhibitor,” she said. “Of course, the other question is how long those patients would have good disease control while on the TNF inhibitor. What is the persistence of the medication? This study doesn’t ask or answer that question.”
Dr. Dalal added that in future research it will be important to look at response to medications beyond TNFis, especially Janus kinase inhibitors.
That will help show “whether there is a treatment algorithm that can be tailored to this population in terms of what agents to choose first,” he said. “I think we need multicenter studies to do this.”
Dr. Dalal has received grant funding from Pfizer and Janssen and has served as a consultant for Centaur Labs and Janssen. Dr. Liew has no relevant financial relationships.
CLEVELAND – About half (52%) of patients living with both axial spondyloarthritis and inflammatory bowel disease (IBD) reached clinical remission of axSpA at 12 months after starting a tumor necrosis factor inhibitor (TNFi), researchers have found.
The disease course for axSpA among patients with IBD who start anti-TNF agents is not well understood.
Rahul S. Dalal, MD, an advanced fellow in IBD with the division of gastroenterology, hepatology, and endoscopy at Brigham and Women’s Hospital, Boston, and colleagues studied whether certain clinical factors were associated with remission of axSpA after patients with axSpA, who also had Crohn’s disease (CD) or ulcerative colitis (UC), started anti-TNF therapy.
Short IBD duration, adalimumab linked with higher remission odds
They found that those who had IBD for less than 5 years and those taking the TNFi adalimumab (Humira and biosimilars), as opposed to another TNFi, had a higher likelihood of reaching axSpA remission at 1 year. The odds ratios calculated for those factors were statistically significant.
Dr. Dalal said that most of the patients in the study (70%) were prescribed adalimumab, and because the study didn’t compare TNFis head to head, it’s hard to say whether adalimumab should be the preferred treatment for these patients.
“But it’s an interesting question that should be addressed in a bigger study,” he said.
Other TNFis included infliximab (Remicade and biosimilars) in 27%, golimumab (Simponi) in 2%, and certolizumab pegol (Cimzia) in 1%.
He presented the results at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
Study details
Included in the retrospective cohort study were 82 adults with IBD and either ankylosing spondylitis or sacroiliitis who started anti-TNF agents approved for IBD between January 2012 and October 2021 at a large academic center.
Clinical remission of axSpA was the primary outcome, defined as the absence or adequate control of pain and/or stiffness related to axSpA as documented in the rheumatology note 1 year (+/– 2 months) after starting anti-TNF agents.
The secondary outcome was clinical remission of IBD, defined as 2 or less on the simple clinical colitis activity index, a score of less than 5 on the Harvey-Bradshaw Index, or provider assessment with no use of oral or intravenous glucocorticoids for 30 days. Dr. Dalal said 74% in the study reached that endpoint in the study period.
“Some patients had good response to anti-TNF treatments for their IBD but not necessarily for their spondyloarthritis,” he explained.
There were insufficient observations to calculate odds ratios for the variables, including Hispanic ethnicity, endoscopic inflammation, and prior history of using vedolizumab (Entyvio), secukinumab (Cosentyx), and ustekinumab (Stelara), the authors noted.
Dr. Dalal said it’s important to study this population because patients with IBD and axSpA take some of the same medications, but it’s not known how each medication acts in patients.
“We don’t have much data to tell us who’s going to respond to treatments from both diseases simultaneously,” he said.
Conclusions called ‘reassuring’
Jean Liew, MD, a spondyloarthritis specialist at Boston University, who was not part of the study, noted that the team reported univariate associations of clinical factors with achievement of clinical axSpA remission, but no multivariable analyses with adjustment for potential confounders.
She said the finding of half the patients achieving clinical remission is “reassuring, as anecdotally we may find that patients with IBD-associated spondyloarthritis tend to have more difficult-to-treat symptoms as well as more limited treatment options. For example, they cannot use [interleukin]-17 inhibitors.”
She noted the study is small and descriptive and further analyses are limited by the small number of patients.
“I think if a study of the same type could be performed at a larger scale with larger numbers, it could generate more data on which type of patient with IBD-associated spondyloarthritis is more likely to have a good response after starting a TNF inhibitor,” she said. “Of course, the other question is how long those patients would have good disease control while on the TNF inhibitor. What is the persistence of the medication? This study doesn’t ask or answer that question.”
Dr. Dalal added that in future research it will be important to look at response to medications beyond TNFis, especially Janus kinase inhibitors.
That will help show “whether there is a treatment algorithm that can be tailored to this population in terms of what agents to choose first,” he said. “I think we need multicenter studies to do this.”
Dr. Dalal has received grant funding from Pfizer and Janssen and has served as a consultant for Centaur Labs and Janssen. Dr. Liew has no relevant financial relationships.
AT SPARTAN 2023
Extracellular Matrix–Based Collagen Dressings for Scalp Repair Following Mohs Micrographic Surgery
To the Editor:
Squamous cell carcinoma (SCC) is the second most common cancer of the scalp.1 Mohs micrographic surgery is used to treat SCC, and it commonly generates a 2.5×2.5-cm open wound with exposed bone.2 Although Mohs micrographic surgery effectively treats cutaneous lesions, it carries a high risk for complications such as infection, wound dehiscence, and partial or full-thickness skin graft necrosis.3 Recommended therapies to decrease these complications include linear closures, flaps, and peripheral autograft tissue.4 However, these procedures do not come without risks and carry their own complications. Therefore, we suggest a safe, less-invasive initial approach using a synthetic extracellular matrix (ECM)–based collagen dressing for secondary wound closure.
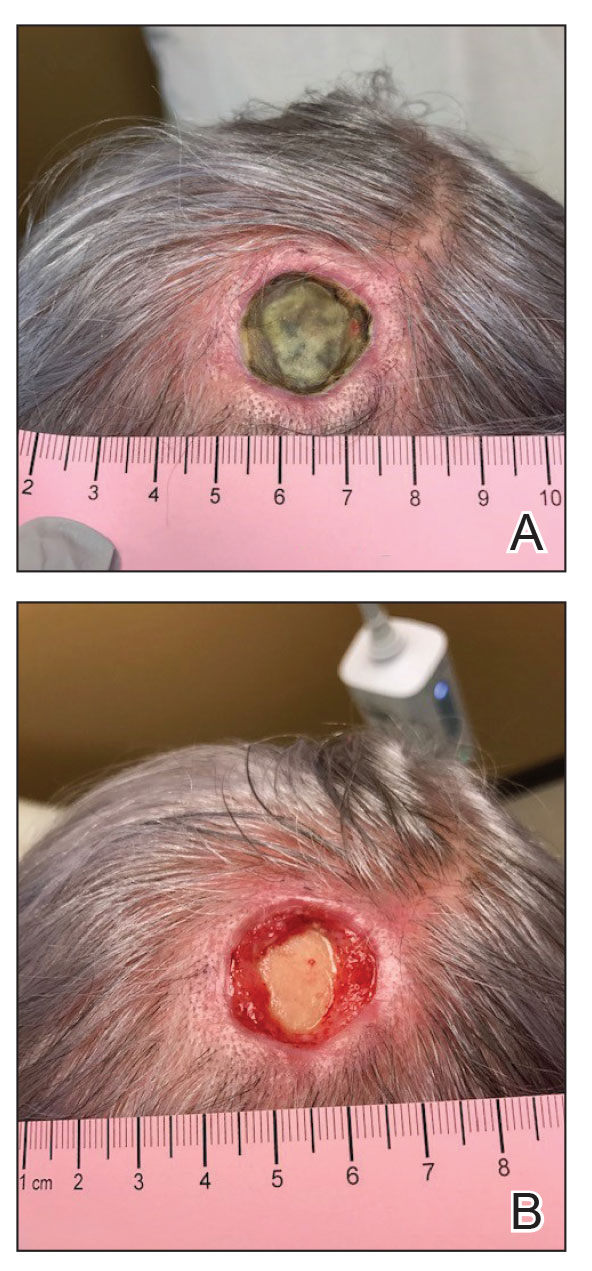
A 76-year-old woman presented to the infectious disease clinic at Monument Health Rapid City Clinic (Rapid City, South Dakota) for evaluation of a dehisced scalp wound 3 months following Mohs micrographic surgery for scalp SCC. The wound underwent primary closure following surgery and dehisced shortly after (Figure 1A). Various oral antimicrobials were used by the dermatologist to assist with wound closure but without success. The patient was referred to the wound clinic for management. At the first appointment, all necrotic tissue was debrided and the cranium was exposed in the wound base (Figure 1B). The wound measured 2.3×2.3×0.2 cm. An ECM-containing collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was used to provide a scaffold for wound closure (Figure 2A). It was dressed with the petroleum-based gauze Xeroform (Cardinal Health) and covered with dry gauze to prevent evaporation and provide moist wound healing. The wound developed some budding tissue islands 3 weeks after weekly ECM-based collagen dressing applications (Figure 3A). The wound continued to decrease in size and formed an isthmus by the second month of therapy (Figure 3B). The wound fully closed within 3 months and showed minimal scarring after 3 years (Figure 2B).
![A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure. A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure.](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig2_AB.jpg)
Chronic wounds usually get trapped in the inflammatory stage of wound healing due to destruction of growth factors and ECM by metalloproteases (MMPs), which creates a vicious cycle and wound stalling. Wound debridement converts a chronic wound back into an acute wound, which is the first step of healing. Following wound debridement, collagen-based dressings can assist with healing by binding the destructive MMPs, and ECM matrix promotes the building of new tissue. The 3 most commonly used ECM-based collagen dressings are Endoform, PuraPly AM (Organogenesis Inc), and Puracol Ultra ECM (Medline Industries, Inc).
![A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig3_AB.jpg)
Endoform is ovine-based collagen and provides a natural porous bioscaffold for rapid cell infiltration.5 It contains more than 150 ECM proteins along with residual vascular channels that help re-establish new vasculature. Ovine-based collagen contains collagen types I, III, and IV arranged as native fibers that retain the 3-dimensional architecture present in tissue ECM.5 Although MMPs are essential in normal healing, the elevated presence of MMPs has been linked to stalled wound healing. Clinical observation and assessment may not be sufficient to identify a wound with elevated protease activity that can break down ECM, affect wound fibroblasts, and impair growth factor response. Although collagen ECM itself does not contain any growth factors, it preserves the destruction of native ECM and growth factors by MMPs by functioning as a sacrificial substrate. The addition of 0.3% ionic silver to the ECM has been shown to decrease bacterial growth and prevent biofilm formation.6
PuraPly AM is a native, type I porcine collagen matrix embedded with the
Puracol Ultra ECM is made of porcine mesothelium and is comprised of types I, III, and IV collagens; elastin; fibronectin; laminin; and proteoglycans. It also contains fibroblast growth factors, contributing to angiogenesis in the wound.9
Application of ECM-based collagen dressings on debrided wounds requires moisture for absorption. Because cranium wounds lack sufficient exudate production, dermal templates need to be hydrated with sterile normal saline before application and covered with a moisture-retaining dressing. Extracellular matrix–based dressings are biodegradable and can be reapplied every 5 to 7 days. For chronic wounds, application of collagen dressings, such as Endoform, is essential and could be considered as the first step prior to switching to more advanced wound care modalities.6,10 Additional studies investigating ECM-containing may determine their comparative efficacy.
- Burton KA, Ashack KA, Khachemoune A. Cutaneous squamous cell carcinoma: a review of high-risk and metastatic disease. Am J Clin Dermatol. 2016;17:491-508. doi:10.1007/s40257-016-0207-3
- Kimyai-Asadi A, Goldberg LH, Peterson SR, et al. The incidence of major complications from Mohs micrographic surgery performed in office-based and hospital-based settings. J Am Acad Dermatol. 2005;53:628-634. doi:10.1016/j.jaad.2005.03.023
- Merritt BG, Lee NY, Brodland DG, et al. The safety of Mohs surgery: a prospective multicenter cohort study. J Am Acad Dermatol. 2012;67:1302-1309. doi:10.1016/j.jaad.2012.05.041
- Yu WY, Salmon P, Thuener J, et al. Mohs surgery for advanced tumors of the scalp. Dermatol Surg. 2019;45(suppl 2):S110-S117.
- Endoform. Aroa Biosurgery Limited website. Accessed May 22, 2023. https://aroa.com/product/endoform/
- Liden BA, May BC. Clinical outcomes following the use of ovine forestomach matrix (endoform dermal template) to treat chronic wounds. Adv Skin Wound Care. 2013;26:164-167. doi:10.1097/01.ASW.0000428862.34294.d4
- PuraPly AM. Organogenesis website. Accessed May 22, 2023. https://organogenesis.com/surgical-sports-medicine/puraplyam/
- Bain MA, Koullias GJ, Morse K, et al. Type I collagen matrix plus polyhexamethylene biguanide antimicrobial for the treatment of cutaneous wounds. J Comp Eff Res. 2020;9:691-703. doi:10.2217/cer-2020-0058
- Puracol Ultra ECM Collagen Wound Dressings. Medical Industries, LP website. May 22, 2023. https://punchout.medline.com/product/Puracol-Ultra-Extracellular-Matrix-ECM-Collagen-Wound-Dressing/Collagen-Dressings/Z05-PF188619?question=&index=P4&indexCount=4
- Raizman R, Hill R, Woo K. Prospective multicenter evaluation of an advanced extracellular matrix for wound management. Adv Skin Wound Care. 2020;33:437-444. doi:10.1097/01.ASW.0000667052.74087.d6
To the Editor:
Squamous cell carcinoma (SCC) is the second most common cancer of the scalp.1 Mohs micrographic surgery is used to treat SCC, and it commonly generates a 2.5×2.5-cm open wound with exposed bone.2 Although Mohs micrographic surgery effectively treats cutaneous lesions, it carries a high risk for complications such as infection, wound dehiscence, and partial or full-thickness skin graft necrosis.3 Recommended therapies to decrease these complications include linear closures, flaps, and peripheral autograft tissue.4 However, these procedures do not come without risks and carry their own complications. Therefore, we suggest a safe, less-invasive initial approach using a synthetic extracellular matrix (ECM)–based collagen dressing for secondary wound closure.
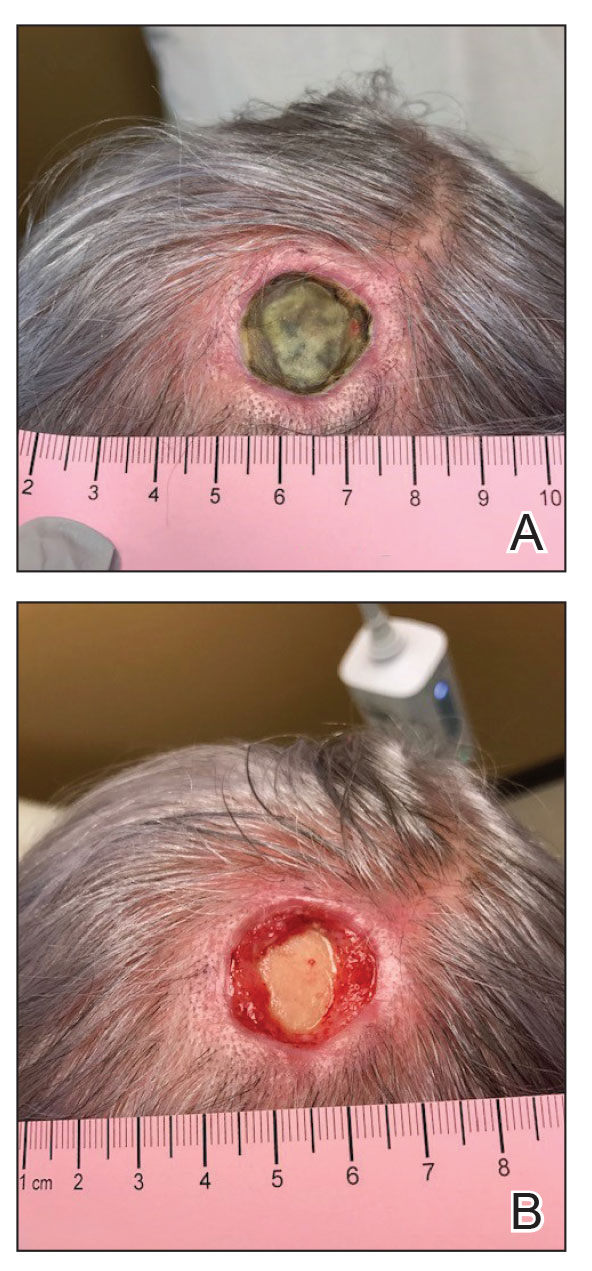
A 76-year-old woman presented to the infectious disease clinic at Monument Health Rapid City Clinic (Rapid City, South Dakota) for evaluation of a dehisced scalp wound 3 months following Mohs micrographic surgery for scalp SCC. The wound underwent primary closure following surgery and dehisced shortly after (Figure 1A). Various oral antimicrobials were used by the dermatologist to assist with wound closure but without success. The patient was referred to the wound clinic for management. At the first appointment, all necrotic tissue was debrided and the cranium was exposed in the wound base (Figure 1B). The wound measured 2.3×2.3×0.2 cm. An ECM-containing collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was used to provide a scaffold for wound closure (Figure 2A). It was dressed with the petroleum-based gauze Xeroform (Cardinal Health) and covered with dry gauze to prevent evaporation and provide moist wound healing. The wound developed some budding tissue islands 3 weeks after weekly ECM-based collagen dressing applications (Figure 3A). The wound continued to decrease in size and formed an isthmus by the second month of therapy (Figure 3B). The wound fully closed within 3 months and showed minimal scarring after 3 years (Figure 2B).
![A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure. A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure.](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig2_AB.jpg)
Chronic wounds usually get trapped in the inflammatory stage of wound healing due to destruction of growth factors and ECM by metalloproteases (MMPs), which creates a vicious cycle and wound stalling. Wound debridement converts a chronic wound back into an acute wound, which is the first step of healing. Following wound debridement, collagen-based dressings can assist with healing by binding the destructive MMPs, and ECM matrix promotes the building of new tissue. The 3 most commonly used ECM-based collagen dressings are Endoform, PuraPly AM (Organogenesis Inc), and Puracol Ultra ECM (Medline Industries, Inc).
![A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig3_AB.jpg)
Endoform is ovine-based collagen and provides a natural porous bioscaffold for rapid cell infiltration.5 It contains more than 150 ECM proteins along with residual vascular channels that help re-establish new vasculature. Ovine-based collagen contains collagen types I, III, and IV arranged as native fibers that retain the 3-dimensional architecture present in tissue ECM.5 Although MMPs are essential in normal healing, the elevated presence of MMPs has been linked to stalled wound healing. Clinical observation and assessment may not be sufficient to identify a wound with elevated protease activity that can break down ECM, affect wound fibroblasts, and impair growth factor response. Although collagen ECM itself does not contain any growth factors, it preserves the destruction of native ECM and growth factors by MMPs by functioning as a sacrificial substrate. The addition of 0.3% ionic silver to the ECM has been shown to decrease bacterial growth and prevent biofilm formation.6
PuraPly AM is a native, type I porcine collagen matrix embedded with the
Puracol Ultra ECM is made of porcine mesothelium and is comprised of types I, III, and IV collagens; elastin; fibronectin; laminin; and proteoglycans. It also contains fibroblast growth factors, contributing to angiogenesis in the wound.9
Application of ECM-based collagen dressings on debrided wounds requires moisture for absorption. Because cranium wounds lack sufficient exudate production, dermal templates need to be hydrated with sterile normal saline before application and covered with a moisture-retaining dressing. Extracellular matrix–based dressings are biodegradable and can be reapplied every 5 to 7 days. For chronic wounds, application of collagen dressings, such as Endoform, is essential and could be considered as the first step prior to switching to more advanced wound care modalities.6,10 Additional studies investigating ECM-containing may determine their comparative efficacy.
To the Editor:
Squamous cell carcinoma (SCC) is the second most common cancer of the scalp.1 Mohs micrographic surgery is used to treat SCC, and it commonly generates a 2.5×2.5-cm open wound with exposed bone.2 Although Mohs micrographic surgery effectively treats cutaneous lesions, it carries a high risk for complications such as infection, wound dehiscence, and partial or full-thickness skin graft necrosis.3 Recommended therapies to decrease these complications include linear closures, flaps, and peripheral autograft tissue.4 However, these procedures do not come without risks and carry their own complications. Therefore, we suggest a safe, less-invasive initial approach using a synthetic extracellular matrix (ECM)–based collagen dressing for secondary wound closure.
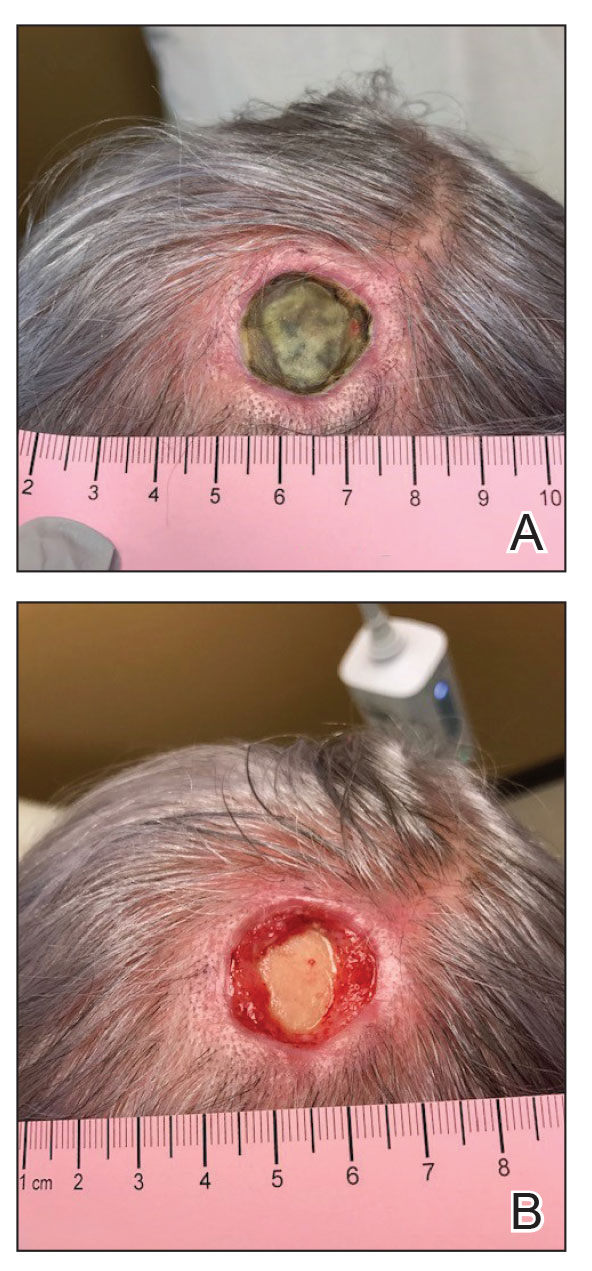
A 76-year-old woman presented to the infectious disease clinic at Monument Health Rapid City Clinic (Rapid City, South Dakota) for evaluation of a dehisced scalp wound 3 months following Mohs micrographic surgery for scalp SCC. The wound underwent primary closure following surgery and dehisced shortly after (Figure 1A). Various oral antimicrobials were used by the dermatologist to assist with wound closure but without success. The patient was referred to the wound clinic for management. At the first appointment, all necrotic tissue was debrided and the cranium was exposed in the wound base (Figure 1B). The wound measured 2.3×2.3×0.2 cm. An ECM-containing collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was used to provide a scaffold for wound closure (Figure 2A). It was dressed with the petroleum-based gauze Xeroform (Cardinal Health) and covered with dry gauze to prevent evaporation and provide moist wound healing. The wound developed some budding tissue islands 3 weeks after weekly ECM-based collagen dressing applications (Figure 3A). The wound continued to decrease in size and formed an isthmus by the second month of therapy (Figure 3B). The wound fully closed within 3 months and showed minimal scarring after 3 years (Figure 2B).
![A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure. A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure.](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig2_AB.jpg)
Chronic wounds usually get trapped in the inflammatory stage of wound healing due to destruction of growth factors and ECM by metalloproteases (MMPs), which creates a vicious cycle and wound stalling. Wound debridement converts a chronic wound back into an acute wound, which is the first step of healing. Following wound debridement, collagen-based dressings can assist with healing by binding the destructive MMPs, and ECM matrix promotes the building of new tissue. The 3 most commonly used ECM-based collagen dressings are Endoform, PuraPly AM (Organogenesis Inc), and Puracol Ultra ECM (Medline Industries, Inc).
![A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig3_AB.jpg)
Endoform is ovine-based collagen and provides a natural porous bioscaffold for rapid cell infiltration.5 It contains more than 150 ECM proteins along with residual vascular channels that help re-establish new vasculature. Ovine-based collagen contains collagen types I, III, and IV arranged as native fibers that retain the 3-dimensional architecture present in tissue ECM.5 Although MMPs are essential in normal healing, the elevated presence of MMPs has been linked to stalled wound healing. Clinical observation and assessment may not be sufficient to identify a wound with elevated protease activity that can break down ECM, affect wound fibroblasts, and impair growth factor response. Although collagen ECM itself does not contain any growth factors, it preserves the destruction of native ECM and growth factors by MMPs by functioning as a sacrificial substrate. The addition of 0.3% ionic silver to the ECM has been shown to decrease bacterial growth and prevent biofilm formation.6
PuraPly AM is a native, type I porcine collagen matrix embedded with the
Puracol Ultra ECM is made of porcine mesothelium and is comprised of types I, III, and IV collagens; elastin; fibronectin; laminin; and proteoglycans. It also contains fibroblast growth factors, contributing to angiogenesis in the wound.9
Application of ECM-based collagen dressings on debrided wounds requires moisture for absorption. Because cranium wounds lack sufficient exudate production, dermal templates need to be hydrated with sterile normal saline before application and covered with a moisture-retaining dressing. Extracellular matrix–based dressings are biodegradable and can be reapplied every 5 to 7 days. For chronic wounds, application of collagen dressings, such as Endoform, is essential and could be considered as the first step prior to switching to more advanced wound care modalities.6,10 Additional studies investigating ECM-containing may determine their comparative efficacy.
- Burton KA, Ashack KA, Khachemoune A. Cutaneous squamous cell carcinoma: a review of high-risk and metastatic disease. Am J Clin Dermatol. 2016;17:491-508. doi:10.1007/s40257-016-0207-3
- Kimyai-Asadi A, Goldberg LH, Peterson SR, et al. The incidence of major complications from Mohs micrographic surgery performed in office-based and hospital-based settings. J Am Acad Dermatol. 2005;53:628-634. doi:10.1016/j.jaad.2005.03.023
- Merritt BG, Lee NY, Brodland DG, et al. The safety of Mohs surgery: a prospective multicenter cohort study. J Am Acad Dermatol. 2012;67:1302-1309. doi:10.1016/j.jaad.2012.05.041
- Yu WY, Salmon P, Thuener J, et al. Mohs surgery for advanced tumors of the scalp. Dermatol Surg. 2019;45(suppl 2):S110-S117.
- Endoform. Aroa Biosurgery Limited website. Accessed May 22, 2023. https://aroa.com/product/endoform/
- Liden BA, May BC. Clinical outcomes following the use of ovine forestomach matrix (endoform dermal template) to treat chronic wounds. Adv Skin Wound Care. 2013;26:164-167. doi:10.1097/01.ASW.0000428862.34294.d4
- PuraPly AM. Organogenesis website. Accessed May 22, 2023. https://organogenesis.com/surgical-sports-medicine/puraplyam/
- Bain MA, Koullias GJ, Morse K, et al. Type I collagen matrix plus polyhexamethylene biguanide antimicrobial for the treatment of cutaneous wounds. J Comp Eff Res. 2020;9:691-703. doi:10.2217/cer-2020-0058
- Puracol Ultra ECM Collagen Wound Dressings. Medical Industries, LP website. May 22, 2023. https://punchout.medline.com/product/Puracol-Ultra-Extracellular-Matrix-ECM-Collagen-Wound-Dressing/Collagen-Dressings/Z05-PF188619?question=&index=P4&indexCount=4
- Raizman R, Hill R, Woo K. Prospective multicenter evaluation of an advanced extracellular matrix for wound management. Adv Skin Wound Care. 2020;33:437-444. doi:10.1097/01.ASW.0000667052.74087.d6
- Burton KA, Ashack KA, Khachemoune A. Cutaneous squamous cell carcinoma: a review of high-risk and metastatic disease. Am J Clin Dermatol. 2016;17:491-508. doi:10.1007/s40257-016-0207-3
- Kimyai-Asadi A, Goldberg LH, Peterson SR, et al. The incidence of major complications from Mohs micrographic surgery performed in office-based and hospital-based settings. J Am Acad Dermatol. 2005;53:628-634. doi:10.1016/j.jaad.2005.03.023
- Merritt BG, Lee NY, Brodland DG, et al. The safety of Mohs surgery: a prospective multicenter cohort study. J Am Acad Dermatol. 2012;67:1302-1309. doi:10.1016/j.jaad.2012.05.041
- Yu WY, Salmon P, Thuener J, et al. Mohs surgery for advanced tumors of the scalp. Dermatol Surg. 2019;45(suppl 2):S110-S117.
- Endoform. Aroa Biosurgery Limited website. Accessed May 22, 2023. https://aroa.com/product/endoform/
- Liden BA, May BC. Clinical outcomes following the use of ovine forestomach matrix (endoform dermal template) to treat chronic wounds. Adv Skin Wound Care. 2013;26:164-167. doi:10.1097/01.ASW.0000428862.34294.d4
- PuraPly AM. Organogenesis website. Accessed May 22, 2023. https://organogenesis.com/surgical-sports-medicine/puraplyam/
- Bain MA, Koullias GJ, Morse K, et al. Type I collagen matrix plus polyhexamethylene biguanide antimicrobial for the treatment of cutaneous wounds. J Comp Eff Res. 2020;9:691-703. doi:10.2217/cer-2020-0058
- Puracol Ultra ECM Collagen Wound Dressings. Medical Industries, LP website. May 22, 2023. https://punchout.medline.com/product/Puracol-Ultra-Extracellular-Matrix-ECM-Collagen-Wound-Dressing/Collagen-Dressings/Z05-PF188619?question=&index=P4&indexCount=4
- Raizman R, Hill R, Woo K. Prospective multicenter evaluation of an advanced extracellular matrix for wound management. Adv Skin Wound Care. 2020;33:437-444. doi:10.1097/01.ASW.0000667052.74087.d6
Practice Points
- Patients who undergo Mohs micrographic surgery on the scalp are prone to developing complications such as infection, wound dehiscence, and partial or full-thickness skin graft necrosis.
- Use of extracellular matrix–based dressings may assist with deep wound healing on the scalp.
Nevus Sebaceus With Novel HRAS Sequence Variant Mutation Misdiagnosed as Alopecia Areata
To the Editor:
A 12-year-old girl presented to the dermatology clinic for evaluation of a congenital scalp lesion. The patient was diagnosed with alopecia areata by a dermatologist at 4 years of age, and she was treated with topical corticosteroids and minoxidil, which failed to resolve her condition. Physical examination revealed an 8×10-cm, well-demarcated, yellowish-pink plaque located over the vertex and right parietal scalp (Figure 1A), extending down to the right preauricular cheek (Figure 1B) in a linear configuration with blaschkoid features. The scalp plaque appeared bald and completely lacking in terminal hairs but contained numerous fine vellus hairs (Figure 1A). A 6-mm, oval-appearing, pigmented papule was present in the plaque, and a few smaller, scattered, pigmented papules were noted in the vertex region (Figure 1A).
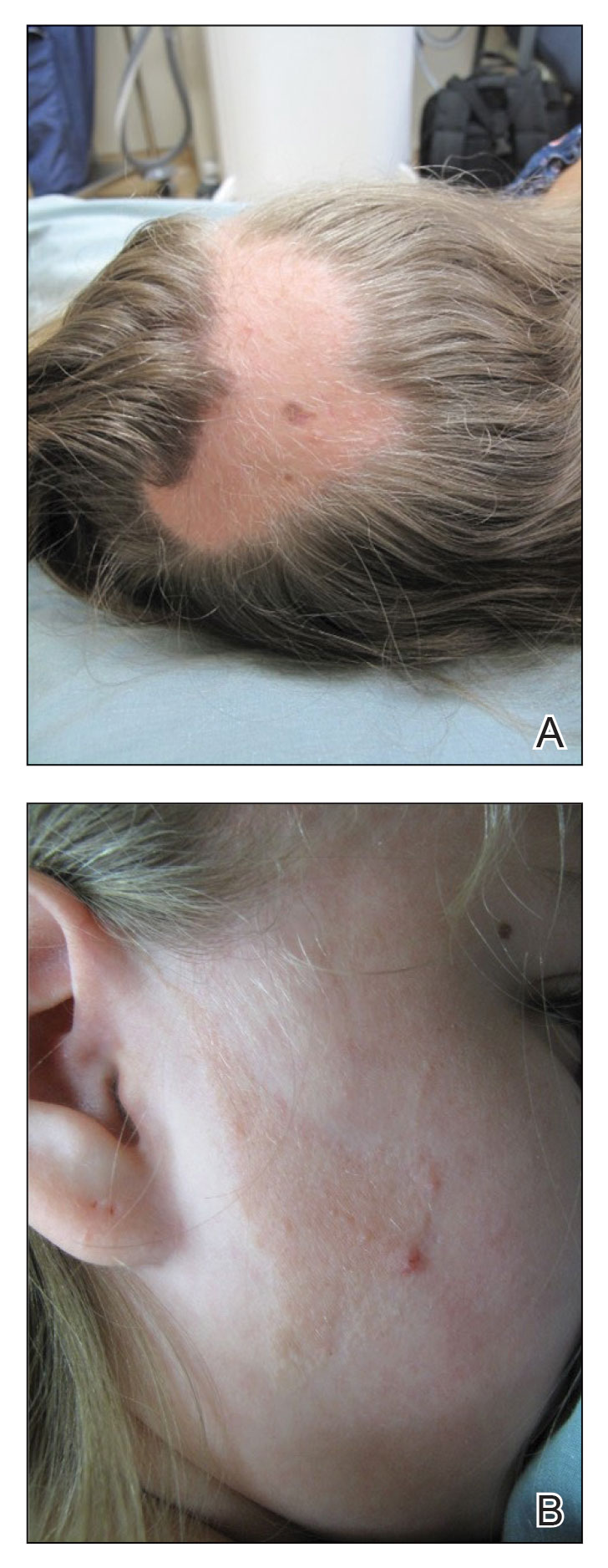
The cutaneous examination was otherwise unremarkable. A review of systems was negative, except for a history of attention-deficit/hyperactivity disorder. There was no history of seizures or other neurocognitive developmental abnormalities.
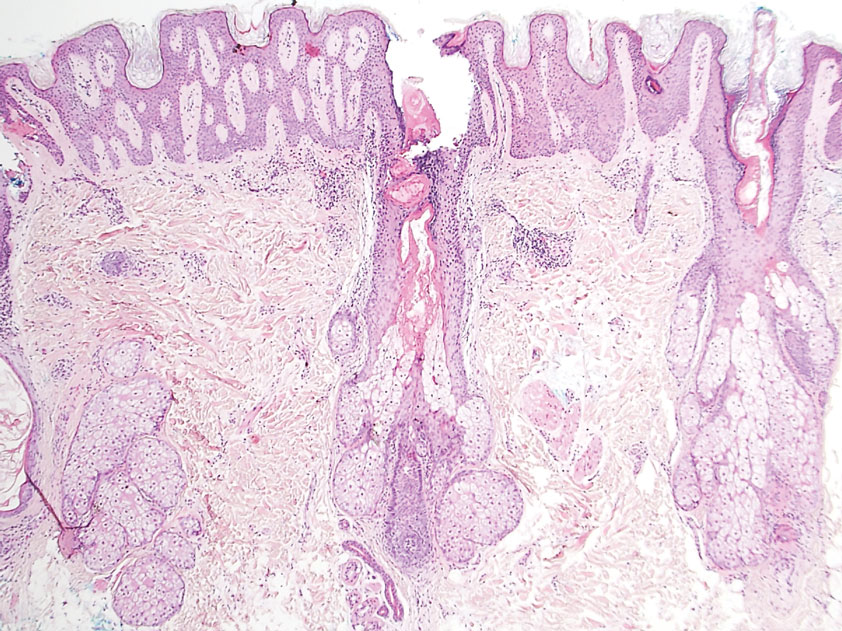
A 4-mm punch biopsy of the vertex scalp included the pigmented lesion but excluded an adnexal neoplasm. Epidermal acanthosis and mild papillomatosis were reported on microscopic examination. Multiple prominent sebaceous glands without associated hair follicles, which emptied directly onto the epidermal surface, were noted in the dermis (Figure 2). Several apocrine glands were observed (Figure 3). Epidermal and dermal melanocytic nests were highlighted with SOX-10 and Melan-A immunohistochemical stains, confirming the presence of a benign compound nevus. The punch biopsy analysis confirmed the diagnosis of a nevus sebaceus (NS) of Jadassohn (organoid nevus) with incidental compound nevus. Additional 4-mm punch biopsies were obtained for genetic testing, performed by the Genomics and Pathology Services at Washington University (St. Louis, Missouri). A missense HRAS p.G12V variant was observed in the tissue. A negative blood test result ruled out a germline mutation. The patient was managed with active observation of the lesion to evaluate for potential formation of neoplasms, as well as continuity of care with the dermatology clinic, considering the extent of the lesions, to monitor the development of any new medical conditions that would be concerning for syndromes associated with NS.
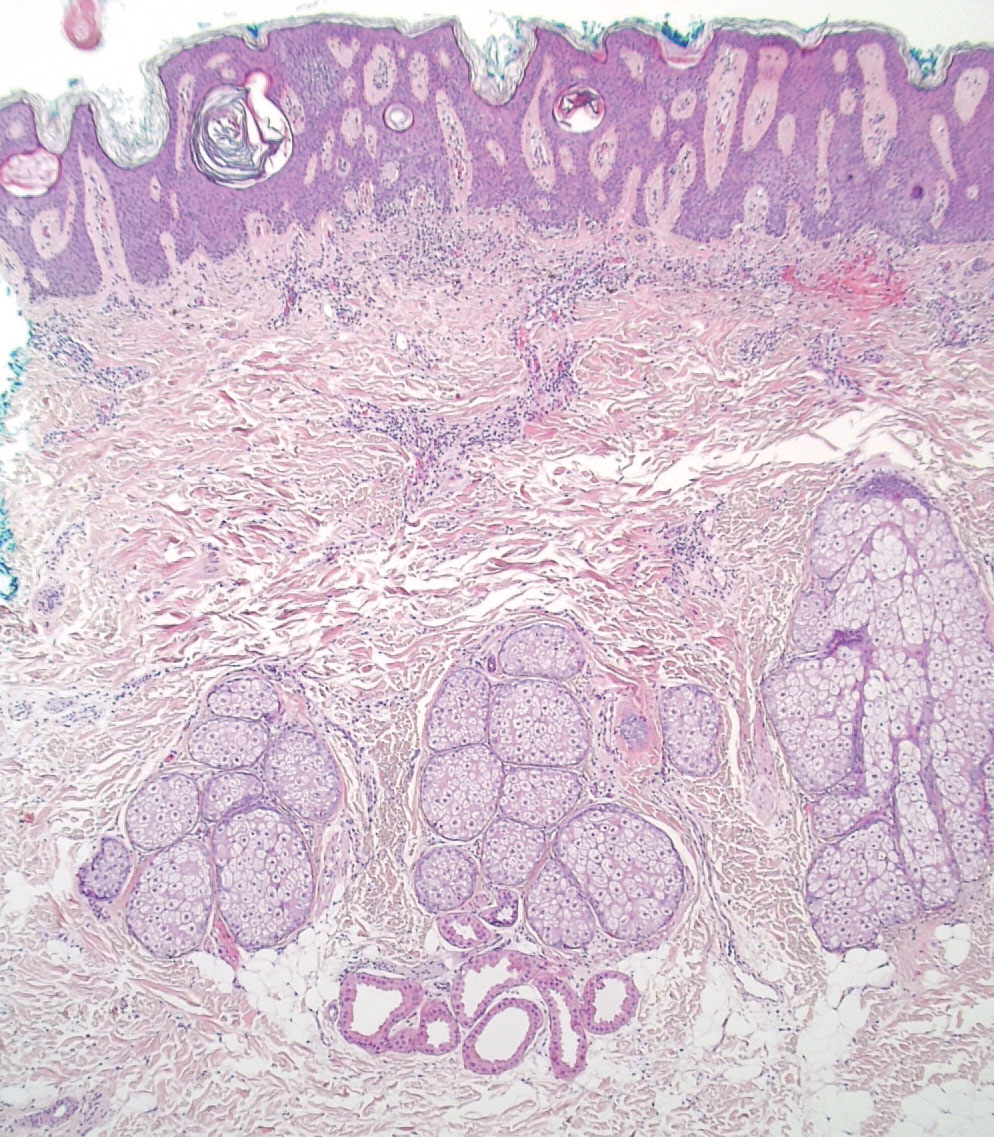
Nevus sebaceus is a benign skin hamartoma caused by a congenital defect in the pilosebaceous follicular unit and consists of epidermal, sebaceous, and apocrine elements.1,2 In dermatology patients, the prevalence of NS ranges from 0.05% to 1%.1 In 90% of cases, NS presents at birth as a 1- to 10-cm, round or linear, yellowish-orange, hairless plaque located on the scalp. It also may appear on the face, neck, trunk, oral mucosa, or labia minora.1,3 Although NS is a benign condition, secondary tumors may form within the lesion.3
The physical and histologic characteristics of NS evolve as the patient ages. In childhood, NS typically appears as a yellow-pink macule or patch with mild to moderate epidermal hyperplasia. Patients exhibit underdeveloped sebaceous glands, immature hair follicles, hyperkeratosis, and acanthosis.1,3,4 The development of early lesions can be quite subtle and can lead to diagnostic uncertainty, as described in our patient. During puberty, lesions thicken due to papillomatous hyperplasia in the epidermis, and the number and size of sebaceous and apocrine glands increase.4 In adults, the risk for secondary tumor formation increases. These physical and histologic transformations, including secondary tumor formation, are thought to be stimulated by the action of postpubertal androgens.1
Nevus sebaceus is associated with both benign and malignant secondary tumor formation; however, fewer than 1% of tumors are malignant.1 In a retrospective analysis, Idriss and Elston5 (N=707) reported that 21.4% of patients with NS had secondary neoplasms; 18.9% of the secondary neoplasms were benign, and 2.5% were malignant. Additionally, this study showed that secondary tumor formation can occur in children, though it typically occurs in adults. Benign neoplasms were reported in 5 children in the subset aged 0 to 10 years and 10 children in the subset aged 11 to 17 years; 1 child developed a malignant neoplasm in the latter subset.5 The most common NS-associated benign neoplasms include trichoblastoma and syringocystadenoma papilliferum. Others include trichilemmoma, apocrine/eccrine adenoma, and sebaceoma.1 Nevus sebaceus–associated malignant neoplasms include basal cell carcinoma, squamous cell carcinoma, adenocarcinoma, carcinosarcoma, and sebaceous carcinoma.3
Our patient was incorrectly diagnosed and treated for alopecia areata before an eventual diagnosis of NS was confirmed by biopsy. Additional genetic studies revealed a novel mutation in the HRAS gene, the most commonly affected gene in NS. The most common mutation location seen in more than 90% of NS lesions is HRAS c.37G>C (p.G13R), while KRAS mutations account for almost all the remaining cases.3 In our patient, a pathogenic missense HRAS p.G12V variant of somatic origin was detected with DNA extraction and sequencing from a fresh tissue sample acquired from two 4-mm punch biopsies performed on the lesion. The following genes were sequenced and found to be uninvolved: BRAF, FGFR1, FGFR2, FGFR3, GNA11, GNAQ, KRAS, MAP3K3, NRAS, PIK3CA, and TEK. The Sanger sequencing method for comparative analysis performed on peripheral blood was negative.
Nevus sebaceus typically is caused by a sporadic mutation, though familial cases have been reported.1 Additionally, germline HRAS mutations can lead to Costello syndrome, an autosomal-dominant disorder characterized by short stature; intellectual disabilities; coarse facial features; facial and perianal papillomata; cardiac defects; loose skin; joint hyperflexibility; and an increased risk for malignant tumors including rhabdomyosarcoma, neuroblastoma, and transitional cell carcinoma of the bladder.6
The diagnosis of NS often can be made clinically but can be difficult to confirm in underdeveloped lesions in young children. The differential diagnosis can include alopecia areata, aplasia cutis congenita, juvenile xanthogranuloma, epidermal nevus, de novo syringocystadenoma papilliferum, and solitary mastocytoma.1 Nevus sebaceus can be associated with 4 additional syndromes: Schimmelpenning syndrome; phacomatosis pigmentokeratotica; didymosis aplasticosebacea; and SCALP (sebaceus nevus, central nervous system malformations, aplasia cutis congenital, limbal dermoid, pigmented nevus) syndrome.1 Approximately 7% of NS cases may be associated with Schimmelpenning-Feuerstein-Mims (SFM) syndrome, a more severe condition that leads to systemic involvement and abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1,3 Phacomatosis pigmentokeratotica has speckled lentiginous nevi, as well as abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1 Didymosis aplasticosebacea is the concurrence of NS and aplasia cutis congenita.
The definitive treatment of NS is surgical excision. Alternative therapies include photodynamic therapy, fractional laser resurfacing, and dermabrasion; these are not definitive treatments, and patients must be monitored for the development of secondary neoplasms. Multiple variables must be considered when determining treatment, including patient age, risk potential for malignancy, and surgery-associated risks.1 In our patient, given the extent of the lesions, active observation and follow-up was agreed upon for management.
This case demonstrates the importance of considering NS as an alternative diagnosis when alopecia areata has been diagnosed in a child who is unresponsive to treatments. After the diagnosis of NS is confirmed, more serious associated syndromes should be ruled out, and treatment should be tailored to each case.
- Patel P, Malik K, Khachemoune A. Sebaceus and Becker’s nevus: overview of their presentation, pathogenesis, associations, and treatment. Am J Clin Dermatol. 2015;16:197-204. doi:10.1007/s40257-015-0123-y
- Azzam MJ, Beutler BD, Calame A, et al. Osteoma cutis associated with nevus sebaceus: case report and review of cutaneous osteoma-associated skin tumors (COASTs). Cureus. 2019;11:E4959. doi:10.7759/cureus.4959
- Aslam A, Salam A, Griffiths CEM, et al. Naevus sebaceus: a mosaic RASopathy. Clin Exp Dermatol. 2014;39:1-6. doi:10.1111/ced.12209
- Basu P, Erickson CP, Calame A, et al. Nevus sebaceus with syringocystadenoma papilliferum, prurigo nodularis, apocrine cystadenoma, basaloid follicular proliferation, and sebaceoma: case report and review of nevus sebaceus-associated conditions. Dermatol Online J. 2020;26:13030/qt85k968bk.
- Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332-337. doi:10.1016/j.jaad.2013.10.004
- Gripp KW, Rauen KA. Costello syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews [Internet]. University of Washington, Seattle; 1993-2020. August 29, 2006. Updated August 29, 2019. https://pubmed.ncbi.nlm.nih.gov/20301680
To the Editor:
A 12-year-old girl presented to the dermatology clinic for evaluation of a congenital scalp lesion. The patient was diagnosed with alopecia areata by a dermatologist at 4 years of age, and she was treated with topical corticosteroids and minoxidil, which failed to resolve her condition. Physical examination revealed an 8×10-cm, well-demarcated, yellowish-pink plaque located over the vertex and right parietal scalp (Figure 1A), extending down to the right preauricular cheek (Figure 1B) in a linear configuration with blaschkoid features. The scalp plaque appeared bald and completely lacking in terminal hairs but contained numerous fine vellus hairs (Figure 1A). A 6-mm, oval-appearing, pigmented papule was present in the plaque, and a few smaller, scattered, pigmented papules were noted in the vertex region (Figure 1A).
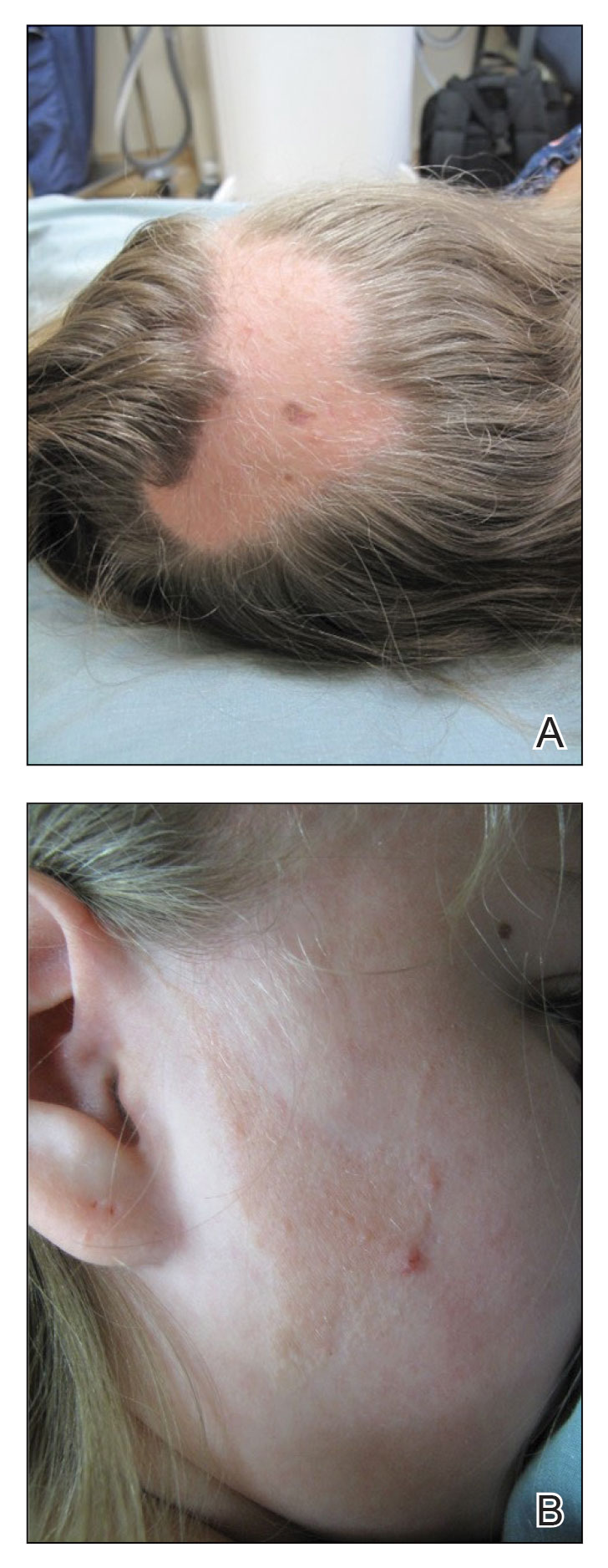
The cutaneous examination was otherwise unremarkable. A review of systems was negative, except for a history of attention-deficit/hyperactivity disorder. There was no history of seizures or other neurocognitive developmental abnormalities.
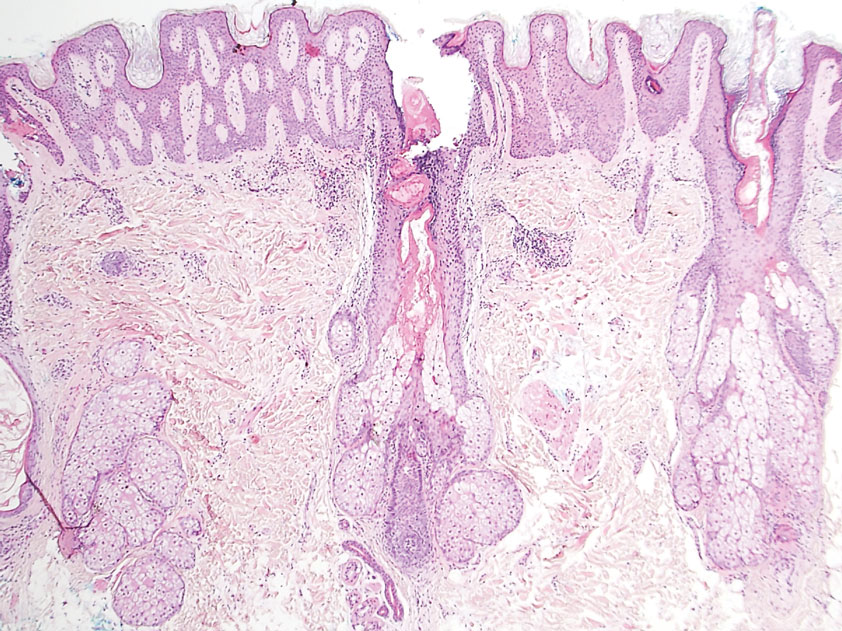
A 4-mm punch biopsy of the vertex scalp included the pigmented lesion but excluded an adnexal neoplasm. Epidermal acanthosis and mild papillomatosis were reported on microscopic examination. Multiple prominent sebaceous glands without associated hair follicles, which emptied directly onto the epidermal surface, were noted in the dermis (Figure 2). Several apocrine glands were observed (Figure 3). Epidermal and dermal melanocytic nests were highlighted with SOX-10 and Melan-A immunohistochemical stains, confirming the presence of a benign compound nevus. The punch biopsy analysis confirmed the diagnosis of a nevus sebaceus (NS) of Jadassohn (organoid nevus) with incidental compound nevus. Additional 4-mm punch biopsies were obtained for genetic testing, performed by the Genomics and Pathology Services at Washington University (St. Louis, Missouri). A missense HRAS p.G12V variant was observed in the tissue. A negative blood test result ruled out a germline mutation. The patient was managed with active observation of the lesion to evaluate for potential formation of neoplasms, as well as continuity of care with the dermatology clinic, considering the extent of the lesions, to monitor the development of any new medical conditions that would be concerning for syndromes associated with NS.
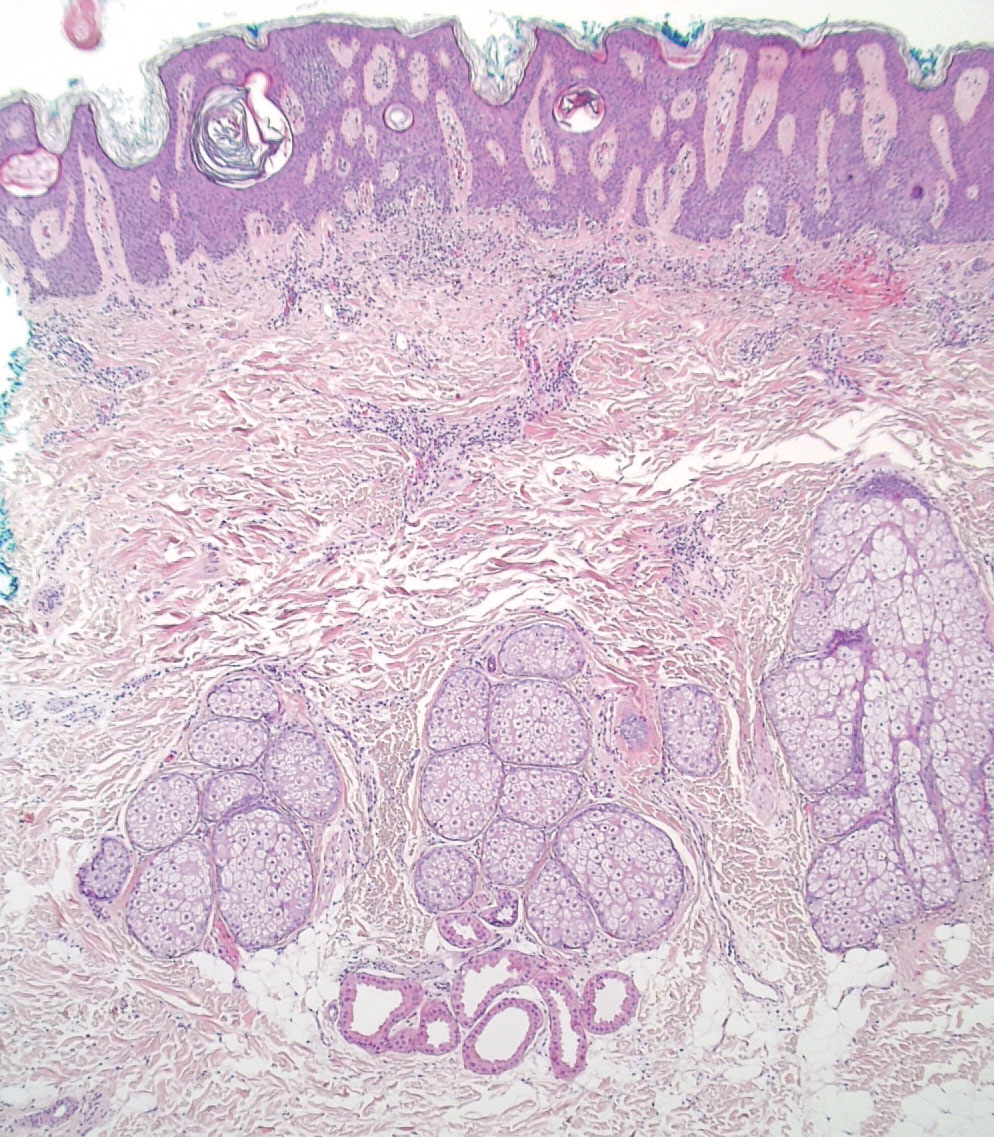
Nevus sebaceus is a benign skin hamartoma caused by a congenital defect in the pilosebaceous follicular unit and consists of epidermal, sebaceous, and apocrine elements.1,2 In dermatology patients, the prevalence of NS ranges from 0.05% to 1%.1 In 90% of cases, NS presents at birth as a 1- to 10-cm, round or linear, yellowish-orange, hairless plaque located on the scalp. It also may appear on the face, neck, trunk, oral mucosa, or labia minora.1,3 Although NS is a benign condition, secondary tumors may form within the lesion.3
The physical and histologic characteristics of NS evolve as the patient ages. In childhood, NS typically appears as a yellow-pink macule or patch with mild to moderate epidermal hyperplasia. Patients exhibit underdeveloped sebaceous glands, immature hair follicles, hyperkeratosis, and acanthosis.1,3,4 The development of early lesions can be quite subtle and can lead to diagnostic uncertainty, as described in our patient. During puberty, lesions thicken due to papillomatous hyperplasia in the epidermis, and the number and size of sebaceous and apocrine glands increase.4 In adults, the risk for secondary tumor formation increases. These physical and histologic transformations, including secondary tumor formation, are thought to be stimulated by the action of postpubertal androgens.1
Nevus sebaceus is associated with both benign and malignant secondary tumor formation; however, fewer than 1% of tumors are malignant.1 In a retrospective analysis, Idriss and Elston5 (N=707) reported that 21.4% of patients with NS had secondary neoplasms; 18.9% of the secondary neoplasms were benign, and 2.5% were malignant. Additionally, this study showed that secondary tumor formation can occur in children, though it typically occurs in adults. Benign neoplasms were reported in 5 children in the subset aged 0 to 10 years and 10 children in the subset aged 11 to 17 years; 1 child developed a malignant neoplasm in the latter subset.5 The most common NS-associated benign neoplasms include trichoblastoma and syringocystadenoma papilliferum. Others include trichilemmoma, apocrine/eccrine adenoma, and sebaceoma.1 Nevus sebaceus–associated malignant neoplasms include basal cell carcinoma, squamous cell carcinoma, adenocarcinoma, carcinosarcoma, and sebaceous carcinoma.3
Our patient was incorrectly diagnosed and treated for alopecia areata before an eventual diagnosis of NS was confirmed by biopsy. Additional genetic studies revealed a novel mutation in the HRAS gene, the most commonly affected gene in NS. The most common mutation location seen in more than 90% of NS lesions is HRAS c.37G>C (p.G13R), while KRAS mutations account for almost all the remaining cases.3 In our patient, a pathogenic missense HRAS p.G12V variant of somatic origin was detected with DNA extraction and sequencing from a fresh tissue sample acquired from two 4-mm punch biopsies performed on the lesion. The following genes were sequenced and found to be uninvolved: BRAF, FGFR1, FGFR2, FGFR3, GNA11, GNAQ, KRAS, MAP3K3, NRAS, PIK3CA, and TEK. The Sanger sequencing method for comparative analysis performed on peripheral blood was negative.
Nevus sebaceus typically is caused by a sporadic mutation, though familial cases have been reported.1 Additionally, germline HRAS mutations can lead to Costello syndrome, an autosomal-dominant disorder characterized by short stature; intellectual disabilities; coarse facial features; facial and perianal papillomata; cardiac defects; loose skin; joint hyperflexibility; and an increased risk for malignant tumors including rhabdomyosarcoma, neuroblastoma, and transitional cell carcinoma of the bladder.6
The diagnosis of NS often can be made clinically but can be difficult to confirm in underdeveloped lesions in young children. The differential diagnosis can include alopecia areata, aplasia cutis congenita, juvenile xanthogranuloma, epidermal nevus, de novo syringocystadenoma papilliferum, and solitary mastocytoma.1 Nevus sebaceus can be associated with 4 additional syndromes: Schimmelpenning syndrome; phacomatosis pigmentokeratotica; didymosis aplasticosebacea; and SCALP (sebaceus nevus, central nervous system malformations, aplasia cutis congenital, limbal dermoid, pigmented nevus) syndrome.1 Approximately 7% of NS cases may be associated with Schimmelpenning-Feuerstein-Mims (SFM) syndrome, a more severe condition that leads to systemic involvement and abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1,3 Phacomatosis pigmentokeratotica has speckled lentiginous nevi, as well as abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1 Didymosis aplasticosebacea is the concurrence of NS and aplasia cutis congenita.
The definitive treatment of NS is surgical excision. Alternative therapies include photodynamic therapy, fractional laser resurfacing, and dermabrasion; these are not definitive treatments, and patients must be monitored for the development of secondary neoplasms. Multiple variables must be considered when determining treatment, including patient age, risk potential for malignancy, and surgery-associated risks.1 In our patient, given the extent of the lesions, active observation and follow-up was agreed upon for management.
This case demonstrates the importance of considering NS as an alternative diagnosis when alopecia areata has been diagnosed in a child who is unresponsive to treatments. After the diagnosis of NS is confirmed, more serious associated syndromes should be ruled out, and treatment should be tailored to each case.
To the Editor:
A 12-year-old girl presented to the dermatology clinic for evaluation of a congenital scalp lesion. The patient was diagnosed with alopecia areata by a dermatologist at 4 years of age, and she was treated with topical corticosteroids and minoxidil, which failed to resolve her condition. Physical examination revealed an 8×10-cm, well-demarcated, yellowish-pink plaque located over the vertex and right parietal scalp (Figure 1A), extending down to the right preauricular cheek (Figure 1B) in a linear configuration with blaschkoid features. The scalp plaque appeared bald and completely lacking in terminal hairs but contained numerous fine vellus hairs (Figure 1A). A 6-mm, oval-appearing, pigmented papule was present in the plaque, and a few smaller, scattered, pigmented papules were noted in the vertex region (Figure 1A).
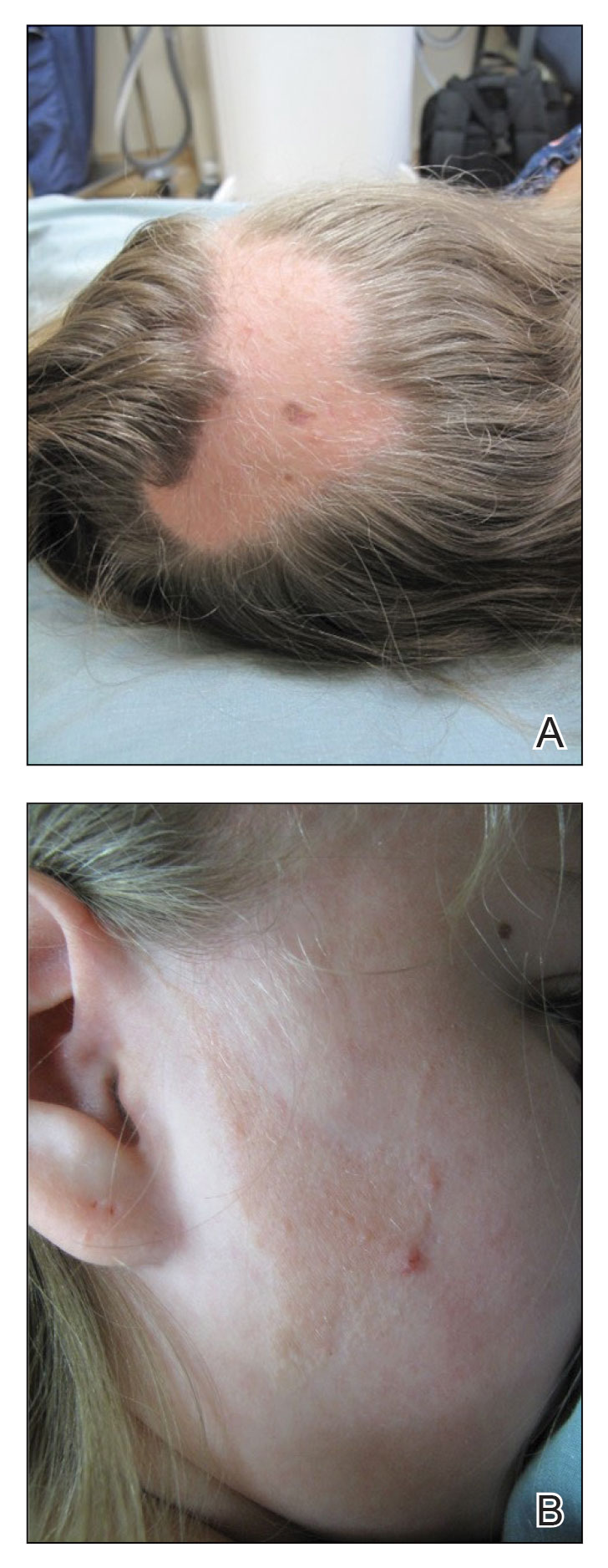
The cutaneous examination was otherwise unremarkable. A review of systems was negative, except for a history of attention-deficit/hyperactivity disorder. There was no history of seizures or other neurocognitive developmental abnormalities.
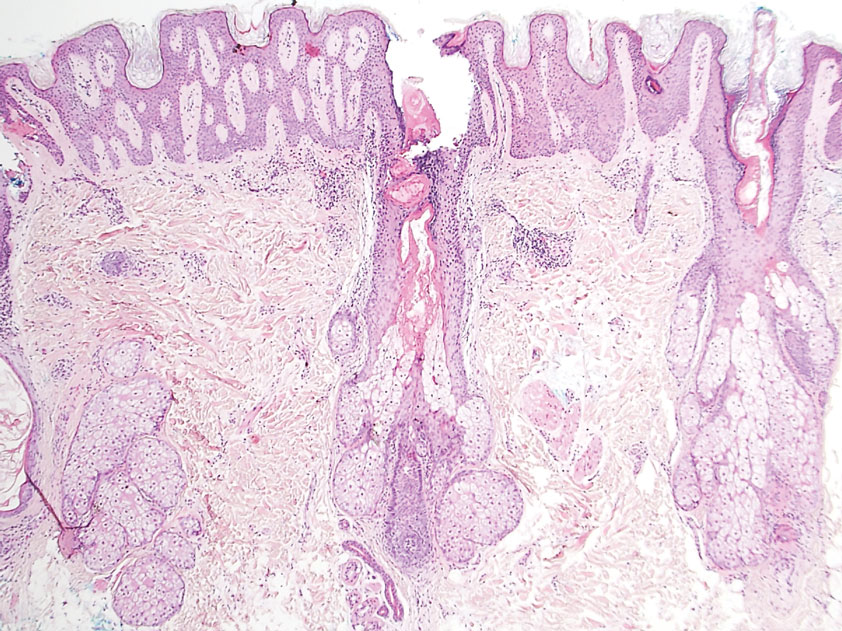
A 4-mm punch biopsy of the vertex scalp included the pigmented lesion but excluded an adnexal neoplasm. Epidermal acanthosis and mild papillomatosis were reported on microscopic examination. Multiple prominent sebaceous glands without associated hair follicles, which emptied directly onto the epidermal surface, were noted in the dermis (Figure 2). Several apocrine glands were observed (Figure 3). Epidermal and dermal melanocytic nests were highlighted with SOX-10 and Melan-A immunohistochemical stains, confirming the presence of a benign compound nevus. The punch biopsy analysis confirmed the diagnosis of a nevus sebaceus (NS) of Jadassohn (organoid nevus) with incidental compound nevus. Additional 4-mm punch biopsies were obtained for genetic testing, performed by the Genomics and Pathology Services at Washington University (St. Louis, Missouri). A missense HRAS p.G12V variant was observed in the tissue. A negative blood test result ruled out a germline mutation. The patient was managed with active observation of the lesion to evaluate for potential formation of neoplasms, as well as continuity of care with the dermatology clinic, considering the extent of the lesions, to monitor the development of any new medical conditions that would be concerning for syndromes associated with NS.
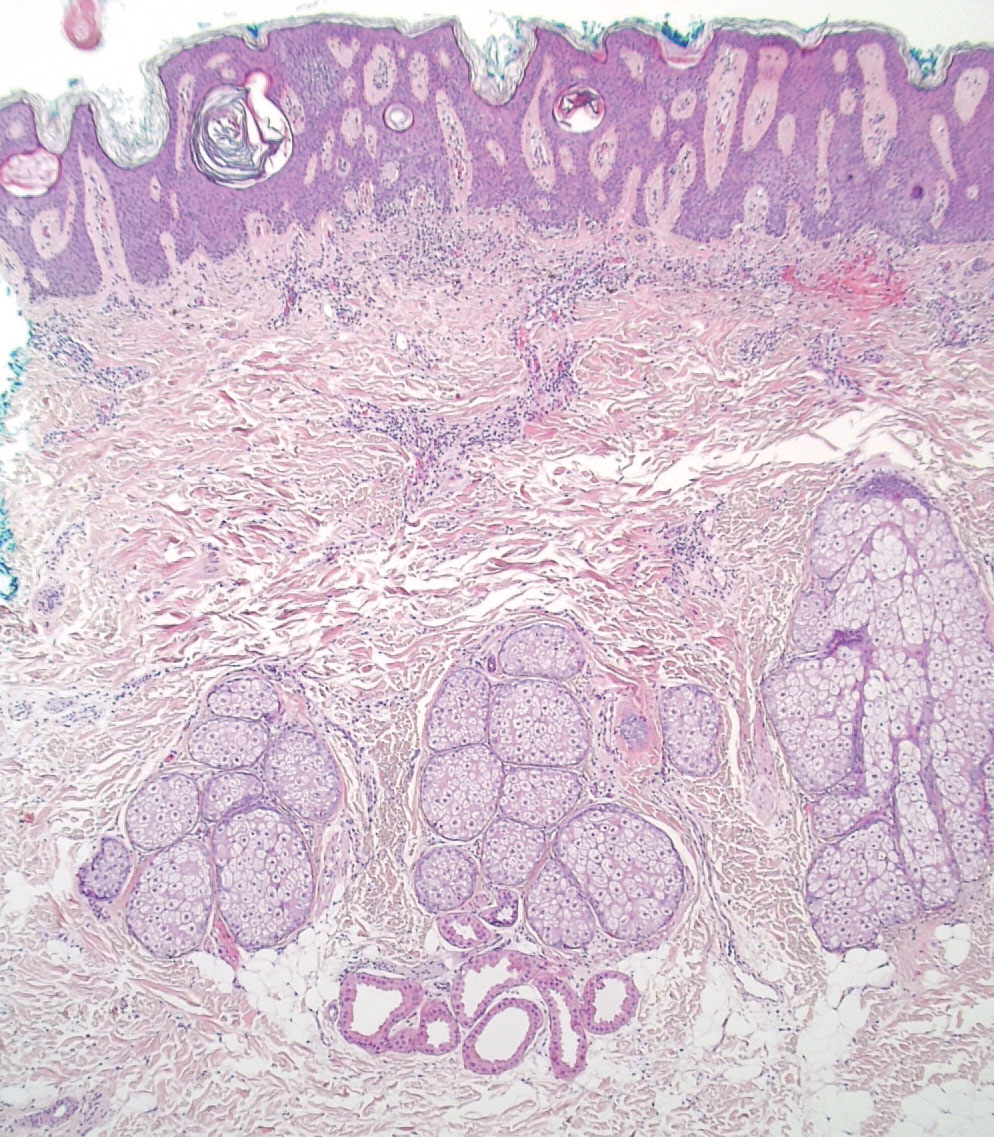
Nevus sebaceus is a benign skin hamartoma caused by a congenital defect in the pilosebaceous follicular unit and consists of epidermal, sebaceous, and apocrine elements.1,2 In dermatology patients, the prevalence of NS ranges from 0.05% to 1%.1 In 90% of cases, NS presents at birth as a 1- to 10-cm, round or linear, yellowish-orange, hairless plaque located on the scalp. It also may appear on the face, neck, trunk, oral mucosa, or labia minora.1,3 Although NS is a benign condition, secondary tumors may form within the lesion.3
The physical and histologic characteristics of NS evolve as the patient ages. In childhood, NS typically appears as a yellow-pink macule or patch with mild to moderate epidermal hyperplasia. Patients exhibit underdeveloped sebaceous glands, immature hair follicles, hyperkeratosis, and acanthosis.1,3,4 The development of early lesions can be quite subtle and can lead to diagnostic uncertainty, as described in our patient. During puberty, lesions thicken due to papillomatous hyperplasia in the epidermis, and the number and size of sebaceous and apocrine glands increase.4 In adults, the risk for secondary tumor formation increases. These physical and histologic transformations, including secondary tumor formation, are thought to be stimulated by the action of postpubertal androgens.1
Nevus sebaceus is associated with both benign and malignant secondary tumor formation; however, fewer than 1% of tumors are malignant.1 In a retrospective analysis, Idriss and Elston5 (N=707) reported that 21.4% of patients with NS had secondary neoplasms; 18.9% of the secondary neoplasms were benign, and 2.5% were malignant. Additionally, this study showed that secondary tumor formation can occur in children, though it typically occurs in adults. Benign neoplasms were reported in 5 children in the subset aged 0 to 10 years and 10 children in the subset aged 11 to 17 years; 1 child developed a malignant neoplasm in the latter subset.5 The most common NS-associated benign neoplasms include trichoblastoma and syringocystadenoma papilliferum. Others include trichilemmoma, apocrine/eccrine adenoma, and sebaceoma.1 Nevus sebaceus–associated malignant neoplasms include basal cell carcinoma, squamous cell carcinoma, adenocarcinoma, carcinosarcoma, and sebaceous carcinoma.3
Our patient was incorrectly diagnosed and treated for alopecia areata before an eventual diagnosis of NS was confirmed by biopsy. Additional genetic studies revealed a novel mutation in the HRAS gene, the most commonly affected gene in NS. The most common mutation location seen in more than 90% of NS lesions is HRAS c.37G>C (p.G13R), while KRAS mutations account for almost all the remaining cases.3 In our patient, a pathogenic missense HRAS p.G12V variant of somatic origin was detected with DNA extraction and sequencing from a fresh tissue sample acquired from two 4-mm punch biopsies performed on the lesion. The following genes were sequenced and found to be uninvolved: BRAF, FGFR1, FGFR2, FGFR3, GNA11, GNAQ, KRAS, MAP3K3, NRAS, PIK3CA, and TEK. The Sanger sequencing method for comparative analysis performed on peripheral blood was negative.
Nevus sebaceus typically is caused by a sporadic mutation, though familial cases have been reported.1 Additionally, germline HRAS mutations can lead to Costello syndrome, an autosomal-dominant disorder characterized by short stature; intellectual disabilities; coarse facial features; facial and perianal papillomata; cardiac defects; loose skin; joint hyperflexibility; and an increased risk for malignant tumors including rhabdomyosarcoma, neuroblastoma, and transitional cell carcinoma of the bladder.6
The diagnosis of NS often can be made clinically but can be difficult to confirm in underdeveloped lesions in young children. The differential diagnosis can include alopecia areata, aplasia cutis congenita, juvenile xanthogranuloma, epidermal nevus, de novo syringocystadenoma papilliferum, and solitary mastocytoma.1 Nevus sebaceus can be associated with 4 additional syndromes: Schimmelpenning syndrome; phacomatosis pigmentokeratotica; didymosis aplasticosebacea; and SCALP (sebaceus nevus, central nervous system malformations, aplasia cutis congenital, limbal dermoid, pigmented nevus) syndrome.1 Approximately 7% of NS cases may be associated with Schimmelpenning-Feuerstein-Mims (SFM) syndrome, a more severe condition that leads to systemic involvement and abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1,3 Phacomatosis pigmentokeratotica has speckled lentiginous nevi, as well as abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1 Didymosis aplasticosebacea is the concurrence of NS and aplasia cutis congenita.
The definitive treatment of NS is surgical excision. Alternative therapies include photodynamic therapy, fractional laser resurfacing, and dermabrasion; these are not definitive treatments, and patients must be monitored for the development of secondary neoplasms. Multiple variables must be considered when determining treatment, including patient age, risk potential for malignancy, and surgery-associated risks.1 In our patient, given the extent of the lesions, active observation and follow-up was agreed upon for management.
This case demonstrates the importance of considering NS as an alternative diagnosis when alopecia areata has been diagnosed in a child who is unresponsive to treatments. After the diagnosis of NS is confirmed, more serious associated syndromes should be ruled out, and treatment should be tailored to each case.
- Patel P, Malik K, Khachemoune A. Sebaceus and Becker’s nevus: overview of their presentation, pathogenesis, associations, and treatment. Am J Clin Dermatol. 2015;16:197-204. doi:10.1007/s40257-015-0123-y
- Azzam MJ, Beutler BD, Calame A, et al. Osteoma cutis associated with nevus sebaceus: case report and review of cutaneous osteoma-associated skin tumors (COASTs). Cureus. 2019;11:E4959. doi:10.7759/cureus.4959
- Aslam A, Salam A, Griffiths CEM, et al. Naevus sebaceus: a mosaic RASopathy. Clin Exp Dermatol. 2014;39:1-6. doi:10.1111/ced.12209
- Basu P, Erickson CP, Calame A, et al. Nevus sebaceus with syringocystadenoma papilliferum, prurigo nodularis, apocrine cystadenoma, basaloid follicular proliferation, and sebaceoma: case report and review of nevus sebaceus-associated conditions. Dermatol Online J. 2020;26:13030/qt85k968bk.
- Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332-337. doi:10.1016/j.jaad.2013.10.004
- Gripp KW, Rauen KA. Costello syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews [Internet]. University of Washington, Seattle; 1993-2020. August 29, 2006. Updated August 29, 2019. https://pubmed.ncbi.nlm.nih.gov/20301680
- Patel P, Malik K, Khachemoune A. Sebaceus and Becker’s nevus: overview of their presentation, pathogenesis, associations, and treatment. Am J Clin Dermatol. 2015;16:197-204. doi:10.1007/s40257-015-0123-y
- Azzam MJ, Beutler BD, Calame A, et al. Osteoma cutis associated with nevus sebaceus: case report and review of cutaneous osteoma-associated skin tumors (COASTs). Cureus. 2019;11:E4959. doi:10.7759/cureus.4959
- Aslam A, Salam A, Griffiths CEM, et al. Naevus sebaceus: a mosaic RASopathy. Clin Exp Dermatol. 2014;39:1-6. doi:10.1111/ced.12209
- Basu P, Erickson CP, Calame A, et al. Nevus sebaceus with syringocystadenoma papilliferum, prurigo nodularis, apocrine cystadenoma, basaloid follicular proliferation, and sebaceoma: case report and review of nevus sebaceus-associated conditions. Dermatol Online J. 2020;26:13030/qt85k968bk.
- Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332-337. doi:10.1016/j.jaad.2013.10.004
- Gripp KW, Rauen KA. Costello syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews [Internet]. University of Washington, Seattle; 1993-2020. August 29, 2006. Updated August 29, 2019. https://pubmed.ncbi.nlm.nih.gov/20301680
Practice Points
- Nevus sebaceus (NS), commonly referred to as NS of Jadassohn or organoid nevus, is a benign skin hamartoma that consists of epidermal, sebaceous, and apocrine elements and is caused by a congenital defect in the pilosebaceous follicular unit.
- Early stages of NS can be mistaken for alopecia areata.
- Once the diagnosis of NS is confirmed, the presence of associated syndromes should be evaluated.
- The definitive treatment of NS is surgical excision; however, multiple variables must be considered when determining treatment, including patient age, risk for developing malignancy, and surgery-associated risks.
FDA approves Yuflyma as ninth adalimumab biosimilar
The U.S. Food and Drug Administration has approved the biosimilar adalimumab-aaty (Yuflyma) in a citrate-free, high-concentration formulation, the manufacturer, Celltrion USA, announced today. It is the ninth biosimilar of adalimumab (Humira) to be approved in the United States.
Yuflyma is approved for the treatment of adult patients with rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis, plaque psoriasis, and hidradenitis suppurativa. It is also approved for polyarticular juvenile idiopathic arthritis for patients aged 2 years or older, as well as for Crohn’s disease in adults and in pediatric patients aged 6 years or older.
The formulation was approved on the basis of a comprehensive data package of analytic, preclinical, and clinical studies, according to Celltrion USA, “demonstrating that Yuflyma is comparable to the reference product Humira in terms of efficacy, safety, pharmacokinetics, and immunogenicity up to 24 weeks and 1 year following treatment.”
The company conducted a double-blind, randomized phase 3 trial that compared switching from reference adalimumab to Yuflyma with continuing either reference adalimumab or Yuflyma for patients with active rheumatoid arthritis. In that trial, the efficacy, pharmacokinetics, safety, and immunogenicity of Yuflyma and reference adalimumab were comparable after 1 year of treatment, including after switching from reference adalimumab to Yuflyma.
“Currently, more than 80% of patients treated with Humira in the United States rely on a high-concentration and citrate-free formulation of this medication. The availability of a high-concentration and citrate-free formulation adalimumab biosimilar provides an important treatment option for patients with inflammatory diseases who benefit from this effective therapy,” said Jonathan Kay, MD, of the University of Massachusetts, Worcester, in the press release.
The citrate-free formulation is thought to lead to less pain on injection.
Yuflyma will be available in prefilled syringe and autoinjector administration options.
Celltrion USA plans to market the drug in the United States in July 2023. Following the initial launch of 40 mg/0.4 mL, the company plans to launch dose forms of 80 mg/0.8 mL and 20 mg/0.2 mL.
Celltrion USA is also seeking an interchangeability designation from the FDA following the completion of an interchangeability trial of 366 patients with chronic plaque psoriasis. The interchangeability designation would mean that patients successfully switched from Humira to Yuflyma multiple times in the trial. The interchangeability designation would allow pharmacists to autosubstitute Humira with Yuflyma. In these cases, individual state laws control how and whether physicians will be notified of this switch.
If interchangeability is approved for Yuflyma, which the company tentatively expects in the fourth quarter of 2024, it would be just the third interchangeable biosimilar approved by the FDA overall and the second adalimumab biosimilar to be designated as such, after adalimumab-adbm (Cyltezo) in October 2021.
Yuflyma was approved in Canada in December 2021 for 10 indications: rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, adult Crohn’s disease, adult ulcerative colitis, hidradenitis suppurativa, plaque psoriasis, adult uveitis, and pediatric uveitis.
In February 2022, the European Commission granted marketing authorization for Yuflyma across those 10 indications, as well as for nonradiographic axial spondyloarthritis, pediatric plaque psoriasis, and pediatric Crohn’s disease.
In April 2022, Celltrion USA signed a licensing agreement with AbbVie, the manufacturer of Humira. Under that agreement, Celltrion will pay royalties to AbbVie on sales of their individual biosimilars, and AbbVie agreed to drop all patent litigation.
The full prescribing information for Yuflyma is available here.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved the biosimilar adalimumab-aaty (Yuflyma) in a citrate-free, high-concentration formulation, the manufacturer, Celltrion USA, announced today. It is the ninth biosimilar of adalimumab (Humira) to be approved in the United States.
Yuflyma is approved for the treatment of adult patients with rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis, plaque psoriasis, and hidradenitis suppurativa. It is also approved for polyarticular juvenile idiopathic arthritis for patients aged 2 years or older, as well as for Crohn’s disease in adults and in pediatric patients aged 6 years or older.
The formulation was approved on the basis of a comprehensive data package of analytic, preclinical, and clinical studies, according to Celltrion USA, “demonstrating that Yuflyma is comparable to the reference product Humira in terms of efficacy, safety, pharmacokinetics, and immunogenicity up to 24 weeks and 1 year following treatment.”
The company conducted a double-blind, randomized phase 3 trial that compared switching from reference adalimumab to Yuflyma with continuing either reference adalimumab or Yuflyma for patients with active rheumatoid arthritis. In that trial, the efficacy, pharmacokinetics, safety, and immunogenicity of Yuflyma and reference adalimumab were comparable after 1 year of treatment, including after switching from reference adalimumab to Yuflyma.
“Currently, more than 80% of patients treated with Humira in the United States rely on a high-concentration and citrate-free formulation of this medication. The availability of a high-concentration and citrate-free formulation adalimumab biosimilar provides an important treatment option for patients with inflammatory diseases who benefit from this effective therapy,” said Jonathan Kay, MD, of the University of Massachusetts, Worcester, in the press release.
The citrate-free formulation is thought to lead to less pain on injection.
Yuflyma will be available in prefilled syringe and autoinjector administration options.
Celltrion USA plans to market the drug in the United States in July 2023. Following the initial launch of 40 mg/0.4 mL, the company plans to launch dose forms of 80 mg/0.8 mL and 20 mg/0.2 mL.
Celltrion USA is also seeking an interchangeability designation from the FDA following the completion of an interchangeability trial of 366 patients with chronic plaque psoriasis. The interchangeability designation would mean that patients successfully switched from Humira to Yuflyma multiple times in the trial. The interchangeability designation would allow pharmacists to autosubstitute Humira with Yuflyma. In these cases, individual state laws control how and whether physicians will be notified of this switch.
If interchangeability is approved for Yuflyma, which the company tentatively expects in the fourth quarter of 2024, it would be just the third interchangeable biosimilar approved by the FDA overall and the second adalimumab biosimilar to be designated as such, after adalimumab-adbm (Cyltezo) in October 2021.
Yuflyma was approved in Canada in December 2021 for 10 indications: rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, adult Crohn’s disease, adult ulcerative colitis, hidradenitis suppurativa, plaque psoriasis, adult uveitis, and pediatric uveitis.
In February 2022, the European Commission granted marketing authorization for Yuflyma across those 10 indications, as well as for nonradiographic axial spondyloarthritis, pediatric plaque psoriasis, and pediatric Crohn’s disease.
In April 2022, Celltrion USA signed a licensing agreement with AbbVie, the manufacturer of Humira. Under that agreement, Celltrion will pay royalties to AbbVie on sales of their individual biosimilars, and AbbVie agreed to drop all patent litigation.
The full prescribing information for Yuflyma is available here.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved the biosimilar adalimumab-aaty (Yuflyma) in a citrate-free, high-concentration formulation, the manufacturer, Celltrion USA, announced today. It is the ninth biosimilar of adalimumab (Humira) to be approved in the United States.
Yuflyma is approved for the treatment of adult patients with rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis, plaque psoriasis, and hidradenitis suppurativa. It is also approved for polyarticular juvenile idiopathic arthritis for patients aged 2 years or older, as well as for Crohn’s disease in adults and in pediatric patients aged 6 years or older.
The formulation was approved on the basis of a comprehensive data package of analytic, preclinical, and clinical studies, according to Celltrion USA, “demonstrating that Yuflyma is comparable to the reference product Humira in terms of efficacy, safety, pharmacokinetics, and immunogenicity up to 24 weeks and 1 year following treatment.”
The company conducted a double-blind, randomized phase 3 trial that compared switching from reference adalimumab to Yuflyma with continuing either reference adalimumab or Yuflyma for patients with active rheumatoid arthritis. In that trial, the efficacy, pharmacokinetics, safety, and immunogenicity of Yuflyma and reference adalimumab were comparable after 1 year of treatment, including after switching from reference adalimumab to Yuflyma.
“Currently, more than 80% of patients treated with Humira in the United States rely on a high-concentration and citrate-free formulation of this medication. The availability of a high-concentration and citrate-free formulation adalimumab biosimilar provides an important treatment option for patients with inflammatory diseases who benefit from this effective therapy,” said Jonathan Kay, MD, of the University of Massachusetts, Worcester, in the press release.
The citrate-free formulation is thought to lead to less pain on injection.
Yuflyma will be available in prefilled syringe and autoinjector administration options.
Celltrion USA plans to market the drug in the United States in July 2023. Following the initial launch of 40 mg/0.4 mL, the company plans to launch dose forms of 80 mg/0.8 mL and 20 mg/0.2 mL.
Celltrion USA is also seeking an interchangeability designation from the FDA following the completion of an interchangeability trial of 366 patients with chronic plaque psoriasis. The interchangeability designation would mean that patients successfully switched from Humira to Yuflyma multiple times in the trial. The interchangeability designation would allow pharmacists to autosubstitute Humira with Yuflyma. In these cases, individual state laws control how and whether physicians will be notified of this switch.
If interchangeability is approved for Yuflyma, which the company tentatively expects in the fourth quarter of 2024, it would be just the third interchangeable biosimilar approved by the FDA overall and the second adalimumab biosimilar to be designated as such, after adalimumab-adbm (Cyltezo) in October 2021.
Yuflyma was approved in Canada in December 2021 for 10 indications: rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, adult Crohn’s disease, adult ulcerative colitis, hidradenitis suppurativa, plaque psoriasis, adult uveitis, and pediatric uveitis.
In February 2022, the European Commission granted marketing authorization for Yuflyma across those 10 indications, as well as for nonradiographic axial spondyloarthritis, pediatric plaque psoriasis, and pediatric Crohn’s disease.
In April 2022, Celltrion USA signed a licensing agreement with AbbVie, the manufacturer of Humira. Under that agreement, Celltrion will pay royalties to AbbVie on sales of their individual biosimilars, and AbbVie agreed to drop all patent litigation.
The full prescribing information for Yuflyma is available here.
A version of this article first appeared on Medscape.com.
Sublingual immunotherapy stops onset and worsening of asthma
PARIS – The EfficAPSI study showed with real-world data that sublingual immunotherapy (SLIT) reduces the risks for asthma onset and the worsening of asthma symptoms for patients with allergic rhinitis. The research was presented at the 18th French-language allergy conference.
These results confirm that allergen immunotherapy, or “desensitization,” is indeed an etiologic treatment of this allergic condition.
SLIT encompasses personalized solutions created for an individual specifically for allergies to dust mites, grass, birch, cats, and so on. These preparations are commonly used by allergy specialists when establishing an AIT treatment plan.
In 2017, the French Health Authority published a report indicating that there was insufficient clinical proof regarding the efficacy of SLIT. It subsequently removed injectable forms of these allergen extracts from the list of drugs reimbursed by the state and reduced state reimbursement of sublingual SLIT preparations from 30% to 15%, a step it confirmed in March 2018 and that led to outrage from allergy specialists. The chair of the French allergy society at the time, Jocelyne Just, MD, PhD, argued that conducting double-blind, placebo-controlled studies for all types (grass pollen, birch pollen, dust mites, asthma, allergic rhinitis, subcutaneous injections, sublingual treatments, tablets, liquid preparations) would take decades. Furthermore, meta-analyses on the subject, despite being heterogeneous and unable to answer all questions, are indeed pointing to the effectiveness of SLIT. To supplement existing data and to answer the queries raised by the HAS, several studies have been launched, including EfficAPSI.
The pharmacoepidemiologic EfficAPSI study is the largest retrospective, real-world, longitudinal cohort study ever carried out regarding liquid SLIT using data stored in the French National Health Data System (SNDS). The primary objective of the study was to evaluate the real-world impact of liquid SLIT on the onset and worsening of asthma for patients with allergic rhinitis and to evaluate the impact of sublingual treatments on public health.
A cohort analysis of patients treated with SLIT and control patients treated for allergic rhinitis with or without treatment for asthma was carried out. The patients treated with SLIT for at least 2 consecutive years were anonymously selected from the SNDS using the Stallergenes Greer prescription database.
In all, 99,538 patients who received SLIT were compared with 333,082 control patients (those who had received treatment for allergic rhinitis without taking SLIT). Participants were stratified according to their treatment history for asthma and were paired using a propensity score to minimize comparison bias.
The main definition of the onset of asthma included the first prescription of an asthma medication, hospital admission for asthma, or a diagnosis of chronic asthma. The secondary definition omitted the prescription of any treatment, and the third (sensitive and specific) took into consideration an initial prescription of omalizumab or a prescription of three inhaled corticosteroids (ICSs) associated with or without a long-acting beta-2 agonist (LABA) for a period of 1 year, admission to the hospital, or chronic asthma.
Asthma risk reduced
Among patients with allergic rhinitis without preexisting asthma, liquid SLIT was associated with a significantly lower risk of asthma onset in comparison with the control group (primary hazard ratio: 0.77; secondary HR: 0.66; and tertiary HR: 0.62).
The risk reductions were significant and were consistent regardless of the allergens analyzed (tertiary HR, dust mites: 0.57; grass: 0.52) for all age groups. These new results that were based on the tertiary definition corroborate the results from the primary and secondary definitions.
said study co-author Philippe Devillier, MD, PhD, research director at the respiratory tract diseases center of Foch Hospital, Paris. “These results are consistent with previous studies in the same French health care database, as well as in a German database with SLIT preparations in tablet form. This not only confirms the soundness of the methodology but also the benefit of liquid SLIT as an etiological treatment of respiratory allergies.”
Risk for worsening
Furthermore, in the same study, liquid SLIT treatment was associated with a 27% reduced risk for worsening asthma and a 36% reduced risk for severe asthma. Among patients with allergic rhinitis and preexisting asthma, liquid SLIT was associated with a significantly lower risk for worsening of asthma, compared with the control group (primary HR: 0.73; secondary HR: 0.61; and tertiary HR: 0.64). The primary definition was an initial prescription of an ICS-LABA combination in a patient treated with ICS alone, severe exacerbation of asthma symptoms, hospital admission, or a diagnosis of chronic asthma.
“The risk reductions were significant and consistent for the allergens analyzed,” said study co-author Pascal Demoly, MD, PhD, head of pulmonology at Montpellier University Hospital, France (tertiary HR, dust mites: 0.66; grass: 0.59; birch: 0.34; and cats: 0.77). “This was across all age groups,” he added.
“The results of the EfficAPSI real-world study on health data from the SNDS are consistent with outcomes from clinical trials, suggestive of a reduced risk of asthma onset in patients with allergic rhinitis receiving liquid SLIT, as well as a reduced risk of worsening of preexisting asthma,” said Devillier. “SLIT, in this case in the form of a liquid, thus appears to be an effective etiological treatment, since the use of symptomatic drugs, in particular preventer inhalers, but also reliever inhalers, is lower in patients treated with SLIT over at least two consecutive years, compared with paired control subjects. And it’s the same for the risk of treating asthma in nonasthmatic patients at the start of the study. EfficAPSI is the largest study using data from a comprehensive state drug reimbursement database, allowing us to assess the impact of liquid SLIT on public health. These results, also obtained with other allergen preparations, particularly in tablet form in French and German studies using data from health care databases, demonstrate the consistency of the data regarding the efficacy of SLIT.”
This article was translated from the Medscape French Edition. A version appeared on Medscape.com.
PARIS – The EfficAPSI study showed with real-world data that sublingual immunotherapy (SLIT) reduces the risks for asthma onset and the worsening of asthma symptoms for patients with allergic rhinitis. The research was presented at the 18th French-language allergy conference.
These results confirm that allergen immunotherapy, or “desensitization,” is indeed an etiologic treatment of this allergic condition.
SLIT encompasses personalized solutions created for an individual specifically for allergies to dust mites, grass, birch, cats, and so on. These preparations are commonly used by allergy specialists when establishing an AIT treatment plan.
In 2017, the French Health Authority published a report indicating that there was insufficient clinical proof regarding the efficacy of SLIT. It subsequently removed injectable forms of these allergen extracts from the list of drugs reimbursed by the state and reduced state reimbursement of sublingual SLIT preparations from 30% to 15%, a step it confirmed in March 2018 and that led to outrage from allergy specialists. The chair of the French allergy society at the time, Jocelyne Just, MD, PhD, argued that conducting double-blind, placebo-controlled studies for all types (grass pollen, birch pollen, dust mites, asthma, allergic rhinitis, subcutaneous injections, sublingual treatments, tablets, liquid preparations) would take decades. Furthermore, meta-analyses on the subject, despite being heterogeneous and unable to answer all questions, are indeed pointing to the effectiveness of SLIT. To supplement existing data and to answer the queries raised by the HAS, several studies have been launched, including EfficAPSI.
The pharmacoepidemiologic EfficAPSI study is the largest retrospective, real-world, longitudinal cohort study ever carried out regarding liquid SLIT using data stored in the French National Health Data System (SNDS). The primary objective of the study was to evaluate the real-world impact of liquid SLIT on the onset and worsening of asthma for patients with allergic rhinitis and to evaluate the impact of sublingual treatments on public health.
A cohort analysis of patients treated with SLIT and control patients treated for allergic rhinitis with or without treatment for asthma was carried out. The patients treated with SLIT for at least 2 consecutive years were anonymously selected from the SNDS using the Stallergenes Greer prescription database.
In all, 99,538 patients who received SLIT were compared with 333,082 control patients (those who had received treatment for allergic rhinitis without taking SLIT). Participants were stratified according to their treatment history for asthma and were paired using a propensity score to minimize comparison bias.
The main definition of the onset of asthma included the first prescription of an asthma medication, hospital admission for asthma, or a diagnosis of chronic asthma. The secondary definition omitted the prescription of any treatment, and the third (sensitive and specific) took into consideration an initial prescription of omalizumab or a prescription of three inhaled corticosteroids (ICSs) associated with or without a long-acting beta-2 agonist (LABA) for a period of 1 year, admission to the hospital, or chronic asthma.
Asthma risk reduced
Among patients with allergic rhinitis without preexisting asthma, liquid SLIT was associated with a significantly lower risk of asthma onset in comparison with the control group (primary hazard ratio: 0.77; secondary HR: 0.66; and tertiary HR: 0.62).
The risk reductions were significant and were consistent regardless of the allergens analyzed (tertiary HR, dust mites: 0.57; grass: 0.52) for all age groups. These new results that were based on the tertiary definition corroborate the results from the primary and secondary definitions.
said study co-author Philippe Devillier, MD, PhD, research director at the respiratory tract diseases center of Foch Hospital, Paris. “These results are consistent with previous studies in the same French health care database, as well as in a German database with SLIT preparations in tablet form. This not only confirms the soundness of the methodology but also the benefit of liquid SLIT as an etiological treatment of respiratory allergies.”
Risk for worsening
Furthermore, in the same study, liquid SLIT treatment was associated with a 27% reduced risk for worsening asthma and a 36% reduced risk for severe asthma. Among patients with allergic rhinitis and preexisting asthma, liquid SLIT was associated with a significantly lower risk for worsening of asthma, compared with the control group (primary HR: 0.73; secondary HR: 0.61; and tertiary HR: 0.64). The primary definition was an initial prescription of an ICS-LABA combination in a patient treated with ICS alone, severe exacerbation of asthma symptoms, hospital admission, or a diagnosis of chronic asthma.
“The risk reductions were significant and consistent for the allergens analyzed,” said study co-author Pascal Demoly, MD, PhD, head of pulmonology at Montpellier University Hospital, France (tertiary HR, dust mites: 0.66; grass: 0.59; birch: 0.34; and cats: 0.77). “This was across all age groups,” he added.
“The results of the EfficAPSI real-world study on health data from the SNDS are consistent with outcomes from clinical trials, suggestive of a reduced risk of asthma onset in patients with allergic rhinitis receiving liquid SLIT, as well as a reduced risk of worsening of preexisting asthma,” said Devillier. “SLIT, in this case in the form of a liquid, thus appears to be an effective etiological treatment, since the use of symptomatic drugs, in particular preventer inhalers, but also reliever inhalers, is lower in patients treated with SLIT over at least two consecutive years, compared with paired control subjects. And it’s the same for the risk of treating asthma in nonasthmatic patients at the start of the study. EfficAPSI is the largest study using data from a comprehensive state drug reimbursement database, allowing us to assess the impact of liquid SLIT on public health. These results, also obtained with other allergen preparations, particularly in tablet form in French and German studies using data from health care databases, demonstrate the consistency of the data regarding the efficacy of SLIT.”
This article was translated from the Medscape French Edition. A version appeared on Medscape.com.
PARIS – The EfficAPSI study showed with real-world data that sublingual immunotherapy (SLIT) reduces the risks for asthma onset and the worsening of asthma symptoms for patients with allergic rhinitis. The research was presented at the 18th French-language allergy conference.
These results confirm that allergen immunotherapy, or “desensitization,” is indeed an etiologic treatment of this allergic condition.
SLIT encompasses personalized solutions created for an individual specifically for allergies to dust mites, grass, birch, cats, and so on. These preparations are commonly used by allergy specialists when establishing an AIT treatment plan.
In 2017, the French Health Authority published a report indicating that there was insufficient clinical proof regarding the efficacy of SLIT. It subsequently removed injectable forms of these allergen extracts from the list of drugs reimbursed by the state and reduced state reimbursement of sublingual SLIT preparations from 30% to 15%, a step it confirmed in March 2018 and that led to outrage from allergy specialists. The chair of the French allergy society at the time, Jocelyne Just, MD, PhD, argued that conducting double-blind, placebo-controlled studies for all types (grass pollen, birch pollen, dust mites, asthma, allergic rhinitis, subcutaneous injections, sublingual treatments, tablets, liquid preparations) would take decades. Furthermore, meta-analyses on the subject, despite being heterogeneous and unable to answer all questions, are indeed pointing to the effectiveness of SLIT. To supplement existing data and to answer the queries raised by the HAS, several studies have been launched, including EfficAPSI.
The pharmacoepidemiologic EfficAPSI study is the largest retrospective, real-world, longitudinal cohort study ever carried out regarding liquid SLIT using data stored in the French National Health Data System (SNDS). The primary objective of the study was to evaluate the real-world impact of liquid SLIT on the onset and worsening of asthma for patients with allergic rhinitis and to evaluate the impact of sublingual treatments on public health.
A cohort analysis of patients treated with SLIT and control patients treated for allergic rhinitis with or without treatment for asthma was carried out. The patients treated with SLIT for at least 2 consecutive years were anonymously selected from the SNDS using the Stallergenes Greer prescription database.
In all, 99,538 patients who received SLIT were compared with 333,082 control patients (those who had received treatment for allergic rhinitis without taking SLIT). Participants were stratified according to their treatment history for asthma and were paired using a propensity score to minimize comparison bias.
The main definition of the onset of asthma included the first prescription of an asthma medication, hospital admission for asthma, or a diagnosis of chronic asthma. The secondary definition omitted the prescription of any treatment, and the third (sensitive and specific) took into consideration an initial prescription of omalizumab or a prescription of three inhaled corticosteroids (ICSs) associated with or without a long-acting beta-2 agonist (LABA) for a period of 1 year, admission to the hospital, or chronic asthma.
Asthma risk reduced
Among patients with allergic rhinitis without preexisting asthma, liquid SLIT was associated with a significantly lower risk of asthma onset in comparison with the control group (primary hazard ratio: 0.77; secondary HR: 0.66; and tertiary HR: 0.62).
The risk reductions were significant and were consistent regardless of the allergens analyzed (tertiary HR, dust mites: 0.57; grass: 0.52) for all age groups. These new results that were based on the tertiary definition corroborate the results from the primary and secondary definitions.
said study co-author Philippe Devillier, MD, PhD, research director at the respiratory tract diseases center of Foch Hospital, Paris. “These results are consistent with previous studies in the same French health care database, as well as in a German database with SLIT preparations in tablet form. This not only confirms the soundness of the methodology but also the benefit of liquid SLIT as an etiological treatment of respiratory allergies.”
Risk for worsening
Furthermore, in the same study, liquid SLIT treatment was associated with a 27% reduced risk for worsening asthma and a 36% reduced risk for severe asthma. Among patients with allergic rhinitis and preexisting asthma, liquid SLIT was associated with a significantly lower risk for worsening of asthma, compared with the control group (primary HR: 0.73; secondary HR: 0.61; and tertiary HR: 0.64). The primary definition was an initial prescription of an ICS-LABA combination in a patient treated with ICS alone, severe exacerbation of asthma symptoms, hospital admission, or a diagnosis of chronic asthma.
“The risk reductions were significant and consistent for the allergens analyzed,” said study co-author Pascal Demoly, MD, PhD, head of pulmonology at Montpellier University Hospital, France (tertiary HR, dust mites: 0.66; grass: 0.59; birch: 0.34; and cats: 0.77). “This was across all age groups,” he added.
“The results of the EfficAPSI real-world study on health data from the SNDS are consistent with outcomes from clinical trials, suggestive of a reduced risk of asthma onset in patients with allergic rhinitis receiving liquid SLIT, as well as a reduced risk of worsening of preexisting asthma,” said Devillier. “SLIT, in this case in the form of a liquid, thus appears to be an effective etiological treatment, since the use of symptomatic drugs, in particular preventer inhalers, but also reliever inhalers, is lower in patients treated with SLIT over at least two consecutive years, compared with paired control subjects. And it’s the same for the risk of treating asthma in nonasthmatic patients at the start of the study. EfficAPSI is the largest study using data from a comprehensive state drug reimbursement database, allowing us to assess the impact of liquid SLIT on public health. These results, also obtained with other allergen preparations, particularly in tablet form in French and German studies using data from health care databases, demonstrate the consistency of the data regarding the efficacy of SLIT.”
This article was translated from the Medscape French Edition. A version appeared on Medscape.com.
Circulating tumor DNA may predict poor prognosis in breast cancer
a new meta-analysis and systematic review found.
“Circulating tumor DNA (ctDNA) has been extensively studied as a prognostic biomarker in early breast cancer. However, there is a significant heterogeneity in the study results, which is probably related to the fact that each individual study included different patient populations, collected blood at different time points, and used different methods (assays) for ctDNA analysis,” said Guilherme Nader Marta, MD, of the Institut Jules Bordet, Anderlecht, Belgium, in an interview.
“The aim of our study was to summarize the available evidence that has been presented so far on this topic by performing a systematic review and meta-analysis including studies that reported the association between ctDNA detection and long-term outcomes,” said Dr. Nader Marta, who coauthored the new research, which was presented as a poster (Poster 26P) at the European Society for Medical Oncology (ESMO) Breast Cancer annual congress.
Methods and results
The authors identified 57 studies including data from 5,729 individuals with early breast cancer. The 44.5% for whom stages were reported consisted of 18.3% with stage I disease, 60.0% with stage II, and 21.5% with stage III. Patients’ ctDNA collection was divided into three groups: baseline, after neoadjuvant therapy (End-of-NAT), and during follow-up care; ctDNA assays were classified as tumor-informed or non–tumor-informed.
The detection of ctDNA at any time point during diagnosis and treatment was associated with worse disease-free survival (DFS) and overall survival (OS), compared with no ctDNA. The association was stronger in tumor-informed assays, the researchers said.
For disease-free survival, the overall multivariate hazard ratios were 2.5, 5.5, and 7.2 for ctDNA detection at baseline, End-of-NAT, and follow-up, respectively.
For overall survival, the overall multivariate hazard ratios were 3.0, 12.9, and 5.6, for ctDNA detection at baseline, End-of-NAT, and follow-up, respectively.
The pooled hazard ratios were numerically higher for both DFS and OS when ctDNA was detected at either End-of-NAT or follow-up.
In addition, detection of ctDNA was associated with a high degree of specificity (from 0.7 to 1.0) for breast cancer relapse; sensitivity ranged from 0.31 to 1.0, the researchers noted. The mean lead time from ctDNA detection to breast cancer recurrence in these cases was approximately 10 months.
Results show ctDNA detection is associated with worse survival
“Our study results demonstrate that ctDNA detection is associated with worse disease-free survival and overall survival in patients with early breast cancer, particularly when measured after treatment with tumor-informed assays,” Dr. Nader Marta said in an interview.
“As next steps, we need to build on this evidence to bring the potential benefits of this powerful prognostic tool to our patients,” said Dr. Nader Marta. “Ongoing studies exploring different management strategies based on serial ctDNA assessments will help us understand the exact role of this technology in our clinical practice.”
The study received no outside funding. Dr. Nader Marta disclosed relationships with companies including Roche and Bayer.
a new meta-analysis and systematic review found.
“Circulating tumor DNA (ctDNA) has been extensively studied as a prognostic biomarker in early breast cancer. However, there is a significant heterogeneity in the study results, which is probably related to the fact that each individual study included different patient populations, collected blood at different time points, and used different methods (assays) for ctDNA analysis,” said Guilherme Nader Marta, MD, of the Institut Jules Bordet, Anderlecht, Belgium, in an interview.
“The aim of our study was to summarize the available evidence that has been presented so far on this topic by performing a systematic review and meta-analysis including studies that reported the association between ctDNA detection and long-term outcomes,” said Dr. Nader Marta, who coauthored the new research, which was presented as a poster (Poster 26P) at the European Society for Medical Oncology (ESMO) Breast Cancer annual congress.
Methods and results
The authors identified 57 studies including data from 5,729 individuals with early breast cancer. The 44.5% for whom stages were reported consisted of 18.3% with stage I disease, 60.0% with stage II, and 21.5% with stage III. Patients’ ctDNA collection was divided into three groups: baseline, after neoadjuvant therapy (End-of-NAT), and during follow-up care; ctDNA assays were classified as tumor-informed or non–tumor-informed.
The detection of ctDNA at any time point during diagnosis and treatment was associated with worse disease-free survival (DFS) and overall survival (OS), compared with no ctDNA. The association was stronger in tumor-informed assays, the researchers said.
For disease-free survival, the overall multivariate hazard ratios were 2.5, 5.5, and 7.2 for ctDNA detection at baseline, End-of-NAT, and follow-up, respectively.
For overall survival, the overall multivariate hazard ratios were 3.0, 12.9, and 5.6, for ctDNA detection at baseline, End-of-NAT, and follow-up, respectively.
The pooled hazard ratios were numerically higher for both DFS and OS when ctDNA was detected at either End-of-NAT or follow-up.
In addition, detection of ctDNA was associated with a high degree of specificity (from 0.7 to 1.0) for breast cancer relapse; sensitivity ranged from 0.31 to 1.0, the researchers noted. The mean lead time from ctDNA detection to breast cancer recurrence in these cases was approximately 10 months.
Results show ctDNA detection is associated with worse survival
“Our study results demonstrate that ctDNA detection is associated with worse disease-free survival and overall survival in patients with early breast cancer, particularly when measured after treatment with tumor-informed assays,” Dr. Nader Marta said in an interview.
“As next steps, we need to build on this evidence to bring the potential benefits of this powerful prognostic tool to our patients,” said Dr. Nader Marta. “Ongoing studies exploring different management strategies based on serial ctDNA assessments will help us understand the exact role of this technology in our clinical practice.”
The study received no outside funding. Dr. Nader Marta disclosed relationships with companies including Roche and Bayer.
a new meta-analysis and systematic review found.
“Circulating tumor DNA (ctDNA) has been extensively studied as a prognostic biomarker in early breast cancer. However, there is a significant heterogeneity in the study results, which is probably related to the fact that each individual study included different patient populations, collected blood at different time points, and used different methods (assays) for ctDNA analysis,” said Guilherme Nader Marta, MD, of the Institut Jules Bordet, Anderlecht, Belgium, in an interview.
“The aim of our study was to summarize the available evidence that has been presented so far on this topic by performing a systematic review and meta-analysis including studies that reported the association between ctDNA detection and long-term outcomes,” said Dr. Nader Marta, who coauthored the new research, which was presented as a poster (Poster 26P) at the European Society for Medical Oncology (ESMO) Breast Cancer annual congress.
Methods and results
The authors identified 57 studies including data from 5,729 individuals with early breast cancer. The 44.5% for whom stages were reported consisted of 18.3% with stage I disease, 60.0% with stage II, and 21.5% with stage III. Patients’ ctDNA collection was divided into three groups: baseline, after neoadjuvant therapy (End-of-NAT), and during follow-up care; ctDNA assays were classified as tumor-informed or non–tumor-informed.
The detection of ctDNA at any time point during diagnosis and treatment was associated with worse disease-free survival (DFS) and overall survival (OS), compared with no ctDNA. The association was stronger in tumor-informed assays, the researchers said.
For disease-free survival, the overall multivariate hazard ratios were 2.5, 5.5, and 7.2 for ctDNA detection at baseline, End-of-NAT, and follow-up, respectively.
For overall survival, the overall multivariate hazard ratios were 3.0, 12.9, and 5.6, for ctDNA detection at baseline, End-of-NAT, and follow-up, respectively.
The pooled hazard ratios were numerically higher for both DFS and OS when ctDNA was detected at either End-of-NAT or follow-up.
In addition, detection of ctDNA was associated with a high degree of specificity (from 0.7 to 1.0) for breast cancer relapse; sensitivity ranged from 0.31 to 1.0, the researchers noted. The mean lead time from ctDNA detection to breast cancer recurrence in these cases was approximately 10 months.
Results show ctDNA detection is associated with worse survival
“Our study results demonstrate that ctDNA detection is associated with worse disease-free survival and overall survival in patients with early breast cancer, particularly when measured after treatment with tumor-informed assays,” Dr. Nader Marta said in an interview.
“As next steps, we need to build on this evidence to bring the potential benefits of this powerful prognostic tool to our patients,” said Dr. Nader Marta. “Ongoing studies exploring different management strategies based on serial ctDNA assessments will help us understand the exact role of this technology in our clinical practice.”
The study received no outside funding. Dr. Nader Marta disclosed relationships with companies including Roche and Bayer.
ESMO BREAST CANCER 2023









![An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound.](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_300x300.jpg)
