User login
LAA closure device shown safe in groups omitted in trials
WASHINGTON – Left atrial appendage closure can be performed safely and effectively in older patients, those with end-stage renal disease, and likely others not included in the pivotal clinical trials, according to a series of new studies, including a late-breaker, presented on the both older and newer Watchman devices at the Cardiovascular Research Technologies conference.
In the case of the late-breaking clinical trial report, which included more than 60,000 patients, the goal was to look at the safety of the Watchman FLX, which is the newest of the devices in real-world practice, according to Samir R. Kapadia, MD, chairman of the department of cardiovascular medicine at the Cleveland Clinic.
In the SURPASS registry, the number of patients discharged on the Watchman FLX climbed from zero in August 2020, when data accrual began, to 66,894 by March 2022. For the current analysis, 45-day follow-up was available for 61,963 patients and 1-year follow-up was available for 18,233.
Based on this number of patients treated by more than 2,300 clinicians at more than 740 sites, the SURPASS registry establishes that Watchman FLX “can be accomplished safely with clinical outcomes similar to pivotal trials at 45 days and 1 year,” Dr. Kapadia reported.
No surprises found in real-world outcome
At 7 days or hospital discharge (whichever came last), the rate of all-cause death was 0.18%, the rate of ischemic stroke was 0.13%, and there were no systemic emboli. By 45 days, the rate of all-cause death (0.84%) and stroke of any kind (0.32%) remained less than 1% and there were still no systemic emboli. Major bleeding events, of which about one-third occurred during hospitalization, had reached 3.34% by day 45.
By 1 year, all-cause mortality had risen to 8.3%, the stroke rate was 1.6%, and major bleeding reached 6.7%. The rate of systemic emboli remained very low (0.1%). The rates of death and stroke rose at a slow but steady rate throughout the 1-year follow-up. In contrast, major bleeding events rose steeply in the first 90 days and were followed by a much slower accrual subsequently.
At 1 year, 84.4% of patients had a complete seal. Leaks ≤ 3 mm were observed in 12.1%. The remaining leaks were larger, but just 0.7% had a leak > 5 mm.
Relative to the first-generation Watchman, the Watchman FLX has numerous design changes, including a shorter profile, more struts, and a reduced metal exposure. Most of these changes were performed to make the device easier to deploy.
When the SURPASS data are compared to the pivotal trials with Watchman FLX or to the Ewolution and National Cardiovascular Data (NCD) registries, which were created to monitor efficacy and safety with the earlier generation Watchman, the outcomes are similar or, in many cases, numerically favorable for such outcomes as bleeding and rates of stroke.
In addition to providing reassurance for the real-world safety of Watchman FLX, Dr. Kapadia said that these data establish reasonable benchmarks for centers tracking in-hospital and 1-year outcomes.
Dr. Kapadia also reported that outcomes overall in SURPASS were similar in women and men with the exception of major bleeding, a finding common to other interventional studies.
The late-breaker panelists generally agreed that SURPASS provides a robust set of data by which to be reassured, but David J. Cohen, MD, director of Clinical and Outcomes Research at the Cardiovascular Research Foundation in New York, said that he thinks the rate of bleeding is unnecessarily high.
“You really need to figure out a way to get the rate of bleeding at 45 days down,” Dr. Cohen said. He called for studies of anticoagulation in the post-procedural period that offer a better benefit-to-risk ratio.
Elderly patients benefit equally from Watchman
Yet, Watchman devices are generally regarded as a success story, and this has led investigators to evaluate safety in patients not well represented or explicitly excluded from clinical trials, such as the elderly and those with end-stage renal disease (ESRD). New data derived from experience in both of these groups were presented at the conference, which was sponsored by MedStar Heart & Vascular Institute.
To tease out the relative safety of Watchman in octogenarians, Samian Sulaiman, MD, a cardiology fellow at West Virginia University Heart and Vascular Institute, Morgantown, performed a competing risk analysis to study the relative benefit of Watchman devices after controlling for the greater overall risk of complications in the elderly.
In raw data comparisons of those 80 years of age or older to those younger in published trials, the not-surprising result is that overall rates of death and ischemic events are far higher in the elderly, according to Dr. Sulaiman, but it’s an “unfair comparison,” he said.
“It is easy to mistakenly conclude that left atrial appendage closure is associated with worse outcomes, but older patients have far higher rates of these events independent of other factors,” Dr. Sulaiman noted.
In fact, in his comparison of 472 older patients to 1,404 younger patients, the seal rates at 45 days, 6 months, and 12 months are almost identical. Moreover, after the extensive adjustments performed for competing risk analysis, the rates of death, stroke, and bleeding were also almost identical for those 80 years or older whether or not they received a Watchman.
Although he acknowledged the risk for residual confounding, Dr. Sulaiman concluded that elderly patients derive about the same benefits as younger patients from the Watchman. He concluded age alone should not be a factor in selecting candidates for this device.
ESRD is not Watchman contraindication
A similar point was made about ESRD based on analysis of 237 patients who received either an earlier generation Watchman or the Watchman FLX. Initiated in Spain, the study was amended to collect data from centers elsewhere in Europe, the United States, and Australia.
Successful implantation was achieved in 99.2% of the patients, reported Armando Perez de Prado, MD, PhD, head of interventional cardiology at the University of Leon, Spain.
After a median follow-up of 480 days, stroke or transient ischemic attacks were observed in 3.1%, leaks > 5 mm were observed in 1.4%, and systemic emboli were observed in 0.9%. Major bleeding (BARC > 2) occurred in 13.3%.
Although the all-cause mortality over the period of follow-up was high (37.4%), most of the deaths (61.2%) were of noncardiovascular origin, according to Dr. Sulaiman. He said mortality and adverse events linked to the Watchman appeared to be roughly comparable to those seen in patients with ESRD.
“The Watchman device for patients on hemodialysis with nonvalvular atrial fibrillation is an effective and safe intervention to prevent embolic events,” he said. However, he also cautioned these the ESRD and the accompanying comorbidities place these patients at high risk of a limited life expectancy.
“Given the high mortality rate of this population, proper selection of candidates is paramount to ensure the optimal clinical benefit,” he cautioned.
Dr. Samir reported no potential conflicts of interest but stated that this study was funded by Boston Scientific. Dr. Cohen reported financial ties with Abbott Vascular, Boston Scientific, Corvia Medical, Edwards Lifesciences, Impulse Dynamics, MyoKardia, Phillips, Svelte, V-Wave, and Zoll. Dr. Sulaiman reported no potential conflicts of interest. Dr. Perez de Prado reported no potential conflicts of interest but stated that this study was funded by Boston Scientific.
WASHINGTON – Left atrial appendage closure can be performed safely and effectively in older patients, those with end-stage renal disease, and likely others not included in the pivotal clinical trials, according to a series of new studies, including a late-breaker, presented on the both older and newer Watchman devices at the Cardiovascular Research Technologies conference.
In the case of the late-breaking clinical trial report, which included more than 60,000 patients, the goal was to look at the safety of the Watchman FLX, which is the newest of the devices in real-world practice, according to Samir R. Kapadia, MD, chairman of the department of cardiovascular medicine at the Cleveland Clinic.
In the SURPASS registry, the number of patients discharged on the Watchman FLX climbed from zero in August 2020, when data accrual began, to 66,894 by March 2022. For the current analysis, 45-day follow-up was available for 61,963 patients and 1-year follow-up was available for 18,233.
Based on this number of patients treated by more than 2,300 clinicians at more than 740 sites, the SURPASS registry establishes that Watchman FLX “can be accomplished safely with clinical outcomes similar to pivotal trials at 45 days and 1 year,” Dr. Kapadia reported.
No surprises found in real-world outcome
At 7 days or hospital discharge (whichever came last), the rate of all-cause death was 0.18%, the rate of ischemic stroke was 0.13%, and there were no systemic emboli. By 45 days, the rate of all-cause death (0.84%) and stroke of any kind (0.32%) remained less than 1% and there were still no systemic emboli. Major bleeding events, of which about one-third occurred during hospitalization, had reached 3.34% by day 45.
By 1 year, all-cause mortality had risen to 8.3%, the stroke rate was 1.6%, and major bleeding reached 6.7%. The rate of systemic emboli remained very low (0.1%). The rates of death and stroke rose at a slow but steady rate throughout the 1-year follow-up. In contrast, major bleeding events rose steeply in the first 90 days and were followed by a much slower accrual subsequently.
At 1 year, 84.4% of patients had a complete seal. Leaks ≤ 3 mm were observed in 12.1%. The remaining leaks were larger, but just 0.7% had a leak > 5 mm.
Relative to the first-generation Watchman, the Watchman FLX has numerous design changes, including a shorter profile, more struts, and a reduced metal exposure. Most of these changes were performed to make the device easier to deploy.
When the SURPASS data are compared to the pivotal trials with Watchman FLX or to the Ewolution and National Cardiovascular Data (NCD) registries, which were created to monitor efficacy and safety with the earlier generation Watchman, the outcomes are similar or, in many cases, numerically favorable for such outcomes as bleeding and rates of stroke.
In addition to providing reassurance for the real-world safety of Watchman FLX, Dr. Kapadia said that these data establish reasonable benchmarks for centers tracking in-hospital and 1-year outcomes.
Dr. Kapadia also reported that outcomes overall in SURPASS were similar in women and men with the exception of major bleeding, a finding common to other interventional studies.
The late-breaker panelists generally agreed that SURPASS provides a robust set of data by which to be reassured, but David J. Cohen, MD, director of Clinical and Outcomes Research at the Cardiovascular Research Foundation in New York, said that he thinks the rate of bleeding is unnecessarily high.
“You really need to figure out a way to get the rate of bleeding at 45 days down,” Dr. Cohen said. He called for studies of anticoagulation in the post-procedural period that offer a better benefit-to-risk ratio.
Elderly patients benefit equally from Watchman
Yet, Watchman devices are generally regarded as a success story, and this has led investigators to evaluate safety in patients not well represented or explicitly excluded from clinical trials, such as the elderly and those with end-stage renal disease (ESRD). New data derived from experience in both of these groups were presented at the conference, which was sponsored by MedStar Heart & Vascular Institute.
To tease out the relative safety of Watchman in octogenarians, Samian Sulaiman, MD, a cardiology fellow at West Virginia University Heart and Vascular Institute, Morgantown, performed a competing risk analysis to study the relative benefit of Watchman devices after controlling for the greater overall risk of complications in the elderly.
In raw data comparisons of those 80 years of age or older to those younger in published trials, the not-surprising result is that overall rates of death and ischemic events are far higher in the elderly, according to Dr. Sulaiman, but it’s an “unfair comparison,” he said.
“It is easy to mistakenly conclude that left atrial appendage closure is associated with worse outcomes, but older patients have far higher rates of these events independent of other factors,” Dr. Sulaiman noted.
In fact, in his comparison of 472 older patients to 1,404 younger patients, the seal rates at 45 days, 6 months, and 12 months are almost identical. Moreover, after the extensive adjustments performed for competing risk analysis, the rates of death, stroke, and bleeding were also almost identical for those 80 years or older whether or not they received a Watchman.
Although he acknowledged the risk for residual confounding, Dr. Sulaiman concluded that elderly patients derive about the same benefits as younger patients from the Watchman. He concluded age alone should not be a factor in selecting candidates for this device.
ESRD is not Watchman contraindication
A similar point was made about ESRD based on analysis of 237 patients who received either an earlier generation Watchman or the Watchman FLX. Initiated in Spain, the study was amended to collect data from centers elsewhere in Europe, the United States, and Australia.
Successful implantation was achieved in 99.2% of the patients, reported Armando Perez de Prado, MD, PhD, head of interventional cardiology at the University of Leon, Spain.
After a median follow-up of 480 days, stroke or transient ischemic attacks were observed in 3.1%, leaks > 5 mm were observed in 1.4%, and systemic emboli were observed in 0.9%. Major bleeding (BARC > 2) occurred in 13.3%.
Although the all-cause mortality over the period of follow-up was high (37.4%), most of the deaths (61.2%) were of noncardiovascular origin, according to Dr. Sulaiman. He said mortality and adverse events linked to the Watchman appeared to be roughly comparable to those seen in patients with ESRD.
“The Watchman device for patients on hemodialysis with nonvalvular atrial fibrillation is an effective and safe intervention to prevent embolic events,” he said. However, he also cautioned these the ESRD and the accompanying comorbidities place these patients at high risk of a limited life expectancy.
“Given the high mortality rate of this population, proper selection of candidates is paramount to ensure the optimal clinical benefit,” he cautioned.
Dr. Samir reported no potential conflicts of interest but stated that this study was funded by Boston Scientific. Dr. Cohen reported financial ties with Abbott Vascular, Boston Scientific, Corvia Medical, Edwards Lifesciences, Impulse Dynamics, MyoKardia, Phillips, Svelte, V-Wave, and Zoll. Dr. Sulaiman reported no potential conflicts of interest. Dr. Perez de Prado reported no potential conflicts of interest but stated that this study was funded by Boston Scientific.
WASHINGTON – Left atrial appendage closure can be performed safely and effectively in older patients, those with end-stage renal disease, and likely others not included in the pivotal clinical trials, according to a series of new studies, including a late-breaker, presented on the both older and newer Watchman devices at the Cardiovascular Research Technologies conference.
In the case of the late-breaking clinical trial report, which included more than 60,000 patients, the goal was to look at the safety of the Watchman FLX, which is the newest of the devices in real-world practice, according to Samir R. Kapadia, MD, chairman of the department of cardiovascular medicine at the Cleveland Clinic.
In the SURPASS registry, the number of patients discharged on the Watchman FLX climbed from zero in August 2020, when data accrual began, to 66,894 by March 2022. For the current analysis, 45-day follow-up was available for 61,963 patients and 1-year follow-up was available for 18,233.
Based on this number of patients treated by more than 2,300 clinicians at more than 740 sites, the SURPASS registry establishes that Watchman FLX “can be accomplished safely with clinical outcomes similar to pivotal trials at 45 days and 1 year,” Dr. Kapadia reported.
No surprises found in real-world outcome
At 7 days or hospital discharge (whichever came last), the rate of all-cause death was 0.18%, the rate of ischemic stroke was 0.13%, and there were no systemic emboli. By 45 days, the rate of all-cause death (0.84%) and stroke of any kind (0.32%) remained less than 1% and there were still no systemic emboli. Major bleeding events, of which about one-third occurred during hospitalization, had reached 3.34% by day 45.
By 1 year, all-cause mortality had risen to 8.3%, the stroke rate was 1.6%, and major bleeding reached 6.7%. The rate of systemic emboli remained very low (0.1%). The rates of death and stroke rose at a slow but steady rate throughout the 1-year follow-up. In contrast, major bleeding events rose steeply in the first 90 days and were followed by a much slower accrual subsequently.
At 1 year, 84.4% of patients had a complete seal. Leaks ≤ 3 mm were observed in 12.1%. The remaining leaks were larger, but just 0.7% had a leak > 5 mm.
Relative to the first-generation Watchman, the Watchman FLX has numerous design changes, including a shorter profile, more struts, and a reduced metal exposure. Most of these changes were performed to make the device easier to deploy.
When the SURPASS data are compared to the pivotal trials with Watchman FLX or to the Ewolution and National Cardiovascular Data (NCD) registries, which were created to monitor efficacy and safety with the earlier generation Watchman, the outcomes are similar or, in many cases, numerically favorable for such outcomes as bleeding and rates of stroke.
In addition to providing reassurance for the real-world safety of Watchman FLX, Dr. Kapadia said that these data establish reasonable benchmarks for centers tracking in-hospital and 1-year outcomes.
Dr. Kapadia also reported that outcomes overall in SURPASS were similar in women and men with the exception of major bleeding, a finding common to other interventional studies.
The late-breaker panelists generally agreed that SURPASS provides a robust set of data by which to be reassured, but David J. Cohen, MD, director of Clinical and Outcomes Research at the Cardiovascular Research Foundation in New York, said that he thinks the rate of bleeding is unnecessarily high.
“You really need to figure out a way to get the rate of bleeding at 45 days down,” Dr. Cohen said. He called for studies of anticoagulation in the post-procedural period that offer a better benefit-to-risk ratio.
Elderly patients benefit equally from Watchman
Yet, Watchman devices are generally regarded as a success story, and this has led investigators to evaluate safety in patients not well represented or explicitly excluded from clinical trials, such as the elderly and those with end-stage renal disease (ESRD). New data derived from experience in both of these groups were presented at the conference, which was sponsored by MedStar Heart & Vascular Institute.
To tease out the relative safety of Watchman in octogenarians, Samian Sulaiman, MD, a cardiology fellow at West Virginia University Heart and Vascular Institute, Morgantown, performed a competing risk analysis to study the relative benefit of Watchman devices after controlling for the greater overall risk of complications in the elderly.
In raw data comparisons of those 80 years of age or older to those younger in published trials, the not-surprising result is that overall rates of death and ischemic events are far higher in the elderly, according to Dr. Sulaiman, but it’s an “unfair comparison,” he said.
“It is easy to mistakenly conclude that left atrial appendage closure is associated with worse outcomes, but older patients have far higher rates of these events independent of other factors,” Dr. Sulaiman noted.
In fact, in his comparison of 472 older patients to 1,404 younger patients, the seal rates at 45 days, 6 months, and 12 months are almost identical. Moreover, after the extensive adjustments performed for competing risk analysis, the rates of death, stroke, and bleeding were also almost identical for those 80 years or older whether or not they received a Watchman.
Although he acknowledged the risk for residual confounding, Dr. Sulaiman concluded that elderly patients derive about the same benefits as younger patients from the Watchman. He concluded age alone should not be a factor in selecting candidates for this device.
ESRD is not Watchman contraindication
A similar point was made about ESRD based on analysis of 237 patients who received either an earlier generation Watchman or the Watchman FLX. Initiated in Spain, the study was amended to collect data from centers elsewhere in Europe, the United States, and Australia.
Successful implantation was achieved in 99.2% of the patients, reported Armando Perez de Prado, MD, PhD, head of interventional cardiology at the University of Leon, Spain.
After a median follow-up of 480 days, stroke or transient ischemic attacks were observed in 3.1%, leaks > 5 mm were observed in 1.4%, and systemic emboli were observed in 0.9%. Major bleeding (BARC > 2) occurred in 13.3%.
Although the all-cause mortality over the period of follow-up was high (37.4%), most of the deaths (61.2%) were of noncardiovascular origin, according to Dr. Sulaiman. He said mortality and adverse events linked to the Watchman appeared to be roughly comparable to those seen in patients with ESRD.
“The Watchman device for patients on hemodialysis with nonvalvular atrial fibrillation is an effective and safe intervention to prevent embolic events,” he said. However, he also cautioned these the ESRD and the accompanying comorbidities place these patients at high risk of a limited life expectancy.
“Given the high mortality rate of this population, proper selection of candidates is paramount to ensure the optimal clinical benefit,” he cautioned.
Dr. Samir reported no potential conflicts of interest but stated that this study was funded by Boston Scientific. Dr. Cohen reported financial ties with Abbott Vascular, Boston Scientific, Corvia Medical, Edwards Lifesciences, Impulse Dynamics, MyoKardia, Phillips, Svelte, V-Wave, and Zoll. Dr. Sulaiman reported no potential conflicts of interest. Dr. Perez de Prado reported no potential conflicts of interest but stated that this study was funded by Boston Scientific.
AT CRT 2023
Risk of expulsion low after early postpartum IUD placement
Intrauterine device (IUD) placement at 2-4 weeks postpartum was noninferior to placement at 6-8 weeks postpartum for complete expulsion, and carried only a slightly higher risk of partial expulsion. A randomized study of expulsion rates reports the risk of expulsion at these points may help patients and clinicians make informed choices about the timing of IUD insertion, wrote the study authors, led by Sarah H. Averbach, MD, MAS, an obstetrician-gynecologist at the University of California, San Diego. “We found that the risk of complete IUD expulsion was low at 2% after early IUD placement 2-4 weeks after delivery, and was noninferior to interval placement 6-8 weeks after delivery at 0%,” Dr. Averbach said in an interview.
Although the risks of partial expulsion and malposition were modestly greater after early placement, “the possibility of a small increase in the risk of IUD expulsion or malposition with early IUD placement should be weighed against the risk of undesired pregnancy and short-interval pregnancy by delaying placement.”
The timing of IUD placement in the postpartum period should be guided by patients’ goals and preferences, she added. The early postpartum period 2-4 weeks after birth has the advantage of convenience since it coincides with early-postpartum or well-baby visits. The absolute risk differences observed between early and interval placement were small for both complete or partial expulsion at 3.8%, and the rate for complete expulsion after early placement was much lower than historical expulsion rates for immediate postpartum placement within in few days of delivery.
Last year, a large study showed an increase in expulsion risk with IUD insertion within 3 days of delivery. Current guidelines, however, support immediate insertion as a safe practice.
The study
Enrolling 404 participants from diverse settings during the period of 2018 to July 2021, researchers for the noninferiority trial randomly assigned 203 to early IUD placement 14-28 days postpartum and 201 to standard-interval placement at 42-56 days. Patients had a mean age of 29.9 years, 11.4% were Black, 56.4% were White, and 43.3% were Hispanic (some Hispanic participants self-identified as White and some as Black). By 6 months postpartum, 73% of the cohort had received an IUD and completed 6-months of follow-up, while 13% had never received an IUD and 14% were lost to follow-up. Complete expulsion rates were 3 of 149, or 2.0% (95% confidence interval [CI], 0.4-5.8) in the early group and 0 of 145, or 0% (95% CI, 0.0-2.5) in the standard group, for a between-group difference of 2.0 percentage points (95% CI, −0.5 to 5.7, P = .04). Two women chose to replace their IUDs.
Partial expulsion occurred in 14, or 9.4% (95% CI, 5.2-15.3) of patients in the early group and 11, or 7.6% (95% CI, 3.9-13.2) in the standard-interval group, for a between-group difference of 1.8 (95% CI, −4.8 to 8.6) percentage points (P = .22).
The small absolute increase in risk of partial expulsion in the early arm did not meet the prespecified criterion for noninferiority of 6%. Three pelvic infections occurred in the early placement arm.
There were 42 IUD removals: 25 in the early placement group and 17 in the standard interval group. Thirteen participants had their IUDs removed for symptoms such as cramping and bothersome vaginal bleeding.
No perforations were identified in either group at 6 months, suggesting that the rate of uterine perforations is low when IUDs are placed in the early and standard-interval postpartum periods. IUD use at 6 months remained comparable between arms: 69.5% in the early group vs. 67.2% in the standard-interval group.
Commenting on the trial but not involved in it, Maureen K. Baldwin, MD, MPH, associate professor of obstetrics and gynecology at Oregon Health & Science University in Portland, said it provides further data on the prevalence of expulsion and malposition after placements using ultrasonography as needed. While two failures occurred with asymptomatic malposition, she added, “It should be noted that IUD position can change as a result of pregnancy, so it was not determined that malposition occurred prior to contraceptive failure.”
According to Dr. Baldwin, one strategy to reduce concerns is to use transvaginal ultrasonography at a later time or in the presence of unusual symptoms.
Overall, the study establishes that postpartum placement is an option equivalent to standard timing and it should be incorporated into patient preferences, she said. “Pain may be lowest at early placement compared to other timings, particularly for those who had vaginal birth.”
The study was supported by the Society of Family Planning research fund and the National Institutes of Health - National Institute of Child Health and Human Development. Dr. Averbach reported personal fees from Bayer Pharmaceuticals for advice on postpartum IUD placement as well as grants from the NIH outside of the submitted work. Dr. Baldwin disclosed no potential conflicts of interest with regard to her comments.
Intrauterine device (IUD) placement at 2-4 weeks postpartum was noninferior to placement at 6-8 weeks postpartum for complete expulsion, and carried only a slightly higher risk of partial expulsion. A randomized study of expulsion rates reports the risk of expulsion at these points may help patients and clinicians make informed choices about the timing of IUD insertion, wrote the study authors, led by Sarah H. Averbach, MD, MAS, an obstetrician-gynecologist at the University of California, San Diego. “We found that the risk of complete IUD expulsion was low at 2% after early IUD placement 2-4 weeks after delivery, and was noninferior to interval placement 6-8 weeks after delivery at 0%,” Dr. Averbach said in an interview.
Although the risks of partial expulsion and malposition were modestly greater after early placement, “the possibility of a small increase in the risk of IUD expulsion or malposition with early IUD placement should be weighed against the risk of undesired pregnancy and short-interval pregnancy by delaying placement.”
The timing of IUD placement in the postpartum period should be guided by patients’ goals and preferences, she added. The early postpartum period 2-4 weeks after birth has the advantage of convenience since it coincides with early-postpartum or well-baby visits. The absolute risk differences observed between early and interval placement were small for both complete or partial expulsion at 3.8%, and the rate for complete expulsion after early placement was much lower than historical expulsion rates for immediate postpartum placement within in few days of delivery.
Last year, a large study showed an increase in expulsion risk with IUD insertion within 3 days of delivery. Current guidelines, however, support immediate insertion as a safe practice.
The study
Enrolling 404 participants from diverse settings during the period of 2018 to July 2021, researchers for the noninferiority trial randomly assigned 203 to early IUD placement 14-28 days postpartum and 201 to standard-interval placement at 42-56 days. Patients had a mean age of 29.9 years, 11.4% were Black, 56.4% were White, and 43.3% were Hispanic (some Hispanic participants self-identified as White and some as Black). By 6 months postpartum, 73% of the cohort had received an IUD and completed 6-months of follow-up, while 13% had never received an IUD and 14% were lost to follow-up. Complete expulsion rates were 3 of 149, or 2.0% (95% confidence interval [CI], 0.4-5.8) in the early group and 0 of 145, or 0% (95% CI, 0.0-2.5) in the standard group, for a between-group difference of 2.0 percentage points (95% CI, −0.5 to 5.7, P = .04). Two women chose to replace their IUDs.
Partial expulsion occurred in 14, or 9.4% (95% CI, 5.2-15.3) of patients in the early group and 11, or 7.6% (95% CI, 3.9-13.2) in the standard-interval group, for a between-group difference of 1.8 (95% CI, −4.8 to 8.6) percentage points (P = .22).
The small absolute increase in risk of partial expulsion in the early arm did not meet the prespecified criterion for noninferiority of 6%. Three pelvic infections occurred in the early placement arm.
There were 42 IUD removals: 25 in the early placement group and 17 in the standard interval group. Thirteen participants had their IUDs removed for symptoms such as cramping and bothersome vaginal bleeding.
No perforations were identified in either group at 6 months, suggesting that the rate of uterine perforations is low when IUDs are placed in the early and standard-interval postpartum periods. IUD use at 6 months remained comparable between arms: 69.5% in the early group vs. 67.2% in the standard-interval group.
Commenting on the trial but not involved in it, Maureen K. Baldwin, MD, MPH, associate professor of obstetrics and gynecology at Oregon Health & Science University in Portland, said it provides further data on the prevalence of expulsion and malposition after placements using ultrasonography as needed. While two failures occurred with asymptomatic malposition, she added, “It should be noted that IUD position can change as a result of pregnancy, so it was not determined that malposition occurred prior to contraceptive failure.”
According to Dr. Baldwin, one strategy to reduce concerns is to use transvaginal ultrasonography at a later time or in the presence of unusual symptoms.
Overall, the study establishes that postpartum placement is an option equivalent to standard timing and it should be incorporated into patient preferences, she said. “Pain may be lowest at early placement compared to other timings, particularly for those who had vaginal birth.”
The study was supported by the Society of Family Planning research fund and the National Institutes of Health - National Institute of Child Health and Human Development. Dr. Averbach reported personal fees from Bayer Pharmaceuticals for advice on postpartum IUD placement as well as grants from the NIH outside of the submitted work. Dr. Baldwin disclosed no potential conflicts of interest with regard to her comments.
Intrauterine device (IUD) placement at 2-4 weeks postpartum was noninferior to placement at 6-8 weeks postpartum for complete expulsion, and carried only a slightly higher risk of partial expulsion. A randomized study of expulsion rates reports the risk of expulsion at these points may help patients and clinicians make informed choices about the timing of IUD insertion, wrote the study authors, led by Sarah H. Averbach, MD, MAS, an obstetrician-gynecologist at the University of California, San Diego. “We found that the risk of complete IUD expulsion was low at 2% after early IUD placement 2-4 weeks after delivery, and was noninferior to interval placement 6-8 weeks after delivery at 0%,” Dr. Averbach said in an interview.
Although the risks of partial expulsion and malposition were modestly greater after early placement, “the possibility of a small increase in the risk of IUD expulsion or malposition with early IUD placement should be weighed against the risk of undesired pregnancy and short-interval pregnancy by delaying placement.”
The timing of IUD placement in the postpartum period should be guided by patients’ goals and preferences, she added. The early postpartum period 2-4 weeks after birth has the advantage of convenience since it coincides with early-postpartum or well-baby visits. The absolute risk differences observed between early and interval placement were small for both complete or partial expulsion at 3.8%, and the rate for complete expulsion after early placement was much lower than historical expulsion rates for immediate postpartum placement within in few days of delivery.
Last year, a large study showed an increase in expulsion risk with IUD insertion within 3 days of delivery. Current guidelines, however, support immediate insertion as a safe practice.
The study
Enrolling 404 participants from diverse settings during the period of 2018 to July 2021, researchers for the noninferiority trial randomly assigned 203 to early IUD placement 14-28 days postpartum and 201 to standard-interval placement at 42-56 days. Patients had a mean age of 29.9 years, 11.4% were Black, 56.4% were White, and 43.3% were Hispanic (some Hispanic participants self-identified as White and some as Black). By 6 months postpartum, 73% of the cohort had received an IUD and completed 6-months of follow-up, while 13% had never received an IUD and 14% were lost to follow-up. Complete expulsion rates were 3 of 149, or 2.0% (95% confidence interval [CI], 0.4-5.8) in the early group and 0 of 145, or 0% (95% CI, 0.0-2.5) in the standard group, for a between-group difference of 2.0 percentage points (95% CI, −0.5 to 5.7, P = .04). Two women chose to replace their IUDs.
Partial expulsion occurred in 14, or 9.4% (95% CI, 5.2-15.3) of patients in the early group and 11, or 7.6% (95% CI, 3.9-13.2) in the standard-interval group, for a between-group difference of 1.8 (95% CI, −4.8 to 8.6) percentage points (P = .22).
The small absolute increase in risk of partial expulsion in the early arm did not meet the prespecified criterion for noninferiority of 6%. Three pelvic infections occurred in the early placement arm.
There were 42 IUD removals: 25 in the early placement group and 17 in the standard interval group. Thirteen participants had their IUDs removed for symptoms such as cramping and bothersome vaginal bleeding.
No perforations were identified in either group at 6 months, suggesting that the rate of uterine perforations is low when IUDs are placed in the early and standard-interval postpartum periods. IUD use at 6 months remained comparable between arms: 69.5% in the early group vs. 67.2% in the standard-interval group.
Commenting on the trial but not involved in it, Maureen K. Baldwin, MD, MPH, associate professor of obstetrics and gynecology at Oregon Health & Science University in Portland, said it provides further data on the prevalence of expulsion and malposition after placements using ultrasonography as needed. While two failures occurred with asymptomatic malposition, she added, “It should be noted that IUD position can change as a result of pregnancy, so it was not determined that malposition occurred prior to contraceptive failure.”
According to Dr. Baldwin, one strategy to reduce concerns is to use transvaginal ultrasonography at a later time or in the presence of unusual symptoms.
Overall, the study establishes that postpartum placement is an option equivalent to standard timing and it should be incorporated into patient preferences, she said. “Pain may be lowest at early placement compared to other timings, particularly for those who had vaginal birth.”
The study was supported by the Society of Family Planning research fund and the National Institutes of Health - National Institute of Child Health and Human Development. Dr. Averbach reported personal fees from Bayer Pharmaceuticals for advice on postpartum IUD placement as well as grants from the NIH outside of the submitted work. Dr. Baldwin disclosed no potential conflicts of interest with regard to her comments.
FROM JAMA
Fast, cheap ... or accurate?
A recent study on the JAMA Network found that, .
Does this surprise anyone?
One of my friends, a pharmacist, has a sign in his home office: “Fast. Accurate. Cheap. You can’t have all 3.” A true statement. I’ve also seen it at car repair places, but they’re doctors in their own way.
The problem here is that physicians are increasingly squeezed for time. If your only revenue stream is seeing patients, and your expenses are going up (and whose aren’t?) then your options are to either raise your prices or see more patients.
Of course, raising prices in medicine can’t happen for most of us. We’re all tied into insurance contracts, which themselves are pegged to Medicare, as to how much we get paid. I mean, yes, you can raise your prices, but that doesn’t matter. The insurance company will still pay a predetermined amount set years ago, in better economic times, no matter what you charge.
So the only real option for most is to see more patients. Which means less time with each one. Which, inevitably, leads to more snap judgments, inappropriate prescriptions, and mistakes.
Patients may get Fast and Cheap, but Accurate gets sidelined. This is the nature of things. If you don’t have enough time to gather and process data, then you’re less likely to reach the right answer.
There’s also the fact that sometimes it’s easier for anyone to just take the path of least resistance. The patient wants an antibiotic, and you realize it’s going to take less time to hand them a script for one than to explain why they don’t need it for what’s probably a viral infection. Not only that, but then you run the risk of their giving you a bad Yelp review (“incompetent, refused to give me antibiotics when I obviously needed them, 1 star”) and who needs that? If you’re employed by a large health care system a bad online review will get you a talking-to by some nonmedical admin from marketing, saying you’re hurting the practice’s “brand.”
Years ago the satire site The Onion had an article about a doctor who specialized in “giving a shit” - assumedly where Accurate dominates. While none of us may intentionally rush through patients or do half-assed jobs, we also have to deal with pressures of time. There never seems to be enough in a workday.
Nowhere is this more true than in primary care, where the pressures of time, overhead, and a large patient volume intersect. There are patients to see, labs to review, phone calls to return, forms to complete, meetings to attend, samples to sign for ... and probably many other things I’ve left out.
The fact that this situation exists shouldn’t surprise anyone. People talk about “burnout” and “making health care better” but that just seems to be lip service. They give you a free subscription to a meditation app, phone access to a counselor, and a mandatory early morning meeting to discuss stress reduction. Of course, these things take time away from seeing patients, which sort of defeats the whole purpose. Unless you want to do them at home – taking time away from your family, or doing the taxes, or other things you have to do besides your day job.
This is not sustainable for patients, doctors, or the health care system as a whole. But right now the situation is only getting worse, and there aren’t any easy answers.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A recent study on the JAMA Network found that, .
Does this surprise anyone?
One of my friends, a pharmacist, has a sign in his home office: “Fast. Accurate. Cheap. You can’t have all 3.” A true statement. I’ve also seen it at car repair places, but they’re doctors in their own way.
The problem here is that physicians are increasingly squeezed for time. If your only revenue stream is seeing patients, and your expenses are going up (and whose aren’t?) then your options are to either raise your prices or see more patients.
Of course, raising prices in medicine can’t happen for most of us. We’re all tied into insurance contracts, which themselves are pegged to Medicare, as to how much we get paid. I mean, yes, you can raise your prices, but that doesn’t matter. The insurance company will still pay a predetermined amount set years ago, in better economic times, no matter what you charge.
So the only real option for most is to see more patients. Which means less time with each one. Which, inevitably, leads to more snap judgments, inappropriate prescriptions, and mistakes.
Patients may get Fast and Cheap, but Accurate gets sidelined. This is the nature of things. If you don’t have enough time to gather and process data, then you’re less likely to reach the right answer.
There’s also the fact that sometimes it’s easier for anyone to just take the path of least resistance. The patient wants an antibiotic, and you realize it’s going to take less time to hand them a script for one than to explain why they don’t need it for what’s probably a viral infection. Not only that, but then you run the risk of their giving you a bad Yelp review (“incompetent, refused to give me antibiotics when I obviously needed them, 1 star”) and who needs that? If you’re employed by a large health care system a bad online review will get you a talking-to by some nonmedical admin from marketing, saying you’re hurting the practice’s “brand.”
Years ago the satire site The Onion had an article about a doctor who specialized in “giving a shit” - assumedly where Accurate dominates. While none of us may intentionally rush through patients or do half-assed jobs, we also have to deal with pressures of time. There never seems to be enough in a workday.
Nowhere is this more true than in primary care, where the pressures of time, overhead, and a large patient volume intersect. There are patients to see, labs to review, phone calls to return, forms to complete, meetings to attend, samples to sign for ... and probably many other things I’ve left out.
The fact that this situation exists shouldn’t surprise anyone. People talk about “burnout” and “making health care better” but that just seems to be lip service. They give you a free subscription to a meditation app, phone access to a counselor, and a mandatory early morning meeting to discuss stress reduction. Of course, these things take time away from seeing patients, which sort of defeats the whole purpose. Unless you want to do them at home – taking time away from your family, or doing the taxes, or other things you have to do besides your day job.
This is not sustainable for patients, doctors, or the health care system as a whole. But right now the situation is only getting worse, and there aren’t any easy answers.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A recent study on the JAMA Network found that, .
Does this surprise anyone?
One of my friends, a pharmacist, has a sign in his home office: “Fast. Accurate. Cheap. You can’t have all 3.” A true statement. I’ve also seen it at car repair places, but they’re doctors in their own way.
The problem here is that physicians are increasingly squeezed for time. If your only revenue stream is seeing patients, and your expenses are going up (and whose aren’t?) then your options are to either raise your prices or see more patients.
Of course, raising prices in medicine can’t happen for most of us. We’re all tied into insurance contracts, which themselves are pegged to Medicare, as to how much we get paid. I mean, yes, you can raise your prices, but that doesn’t matter. The insurance company will still pay a predetermined amount set years ago, in better economic times, no matter what you charge.
So the only real option for most is to see more patients. Which means less time with each one. Which, inevitably, leads to more snap judgments, inappropriate prescriptions, and mistakes.
Patients may get Fast and Cheap, but Accurate gets sidelined. This is the nature of things. If you don’t have enough time to gather and process data, then you’re less likely to reach the right answer.
There’s also the fact that sometimes it’s easier for anyone to just take the path of least resistance. The patient wants an antibiotic, and you realize it’s going to take less time to hand them a script for one than to explain why they don’t need it for what’s probably a viral infection. Not only that, but then you run the risk of their giving you a bad Yelp review (“incompetent, refused to give me antibiotics when I obviously needed them, 1 star”) and who needs that? If you’re employed by a large health care system a bad online review will get you a talking-to by some nonmedical admin from marketing, saying you’re hurting the practice’s “brand.”
Years ago the satire site The Onion had an article about a doctor who specialized in “giving a shit” - assumedly where Accurate dominates. While none of us may intentionally rush through patients or do half-assed jobs, we also have to deal with pressures of time. There never seems to be enough in a workday.
Nowhere is this more true than in primary care, where the pressures of time, overhead, and a large patient volume intersect. There are patients to see, labs to review, phone calls to return, forms to complete, meetings to attend, samples to sign for ... and probably many other things I’ve left out.
The fact that this situation exists shouldn’t surprise anyone. People talk about “burnout” and “making health care better” but that just seems to be lip service. They give you a free subscription to a meditation app, phone access to a counselor, and a mandatory early morning meeting to discuss stress reduction. Of course, these things take time away from seeing patients, which sort of defeats the whole purpose. Unless you want to do them at home – taking time away from your family, or doing the taxes, or other things you have to do besides your day job.
This is not sustainable for patients, doctors, or the health care system as a whole. But right now the situation is only getting worse, and there aren’t any easy answers.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Surgery for early breast cancer can worsen frailty in older women
according to a new study.
About 1 in 5 experienced clinically significant deterioration in frailty status after treatment, the study team found. Women at highest risk for declines in frailty following treatment had “robust” baseline frailty status at diagnosis and underwent more invasive mastectomy compared with lumpectomy.
The fact that “robust” older women were more likely to become frail after locoregional therapy suggests that “thoughtful treatment decisions should be undertaken in all older women, not simply those who have frailty at diagnosis,” said the investigators, led by Christina Minami, MD, of Dana-Farber/Brigham and Women’s Cancer Center in Boston.
The study findings emphasize that there is no one-size-fits-all approach to breast cancer treatment in the elderly, said Sarah P. Cate, MD, director, Breast Surgery Quality Program, Mount Sinai Health System, New York, who wasn’t involved in the research. “Some patients will sail through a surgery, and others are severely affected by it.”
The study was published online in JAMA Surgery.
Given the growing number of older adults with breast cancer, understanding how age-related syndromes, such as frailty, may alter cancer outcomes and how cancer treatments change aging trajectories remains important.
To investigate, Dr. Minami and colleagues used Surveillance, Epidemiology, and End Results Medicare data to identify 31,084 women (mean age, 73) who had been diagnosed with ductal carcinoma in situ (DCIS) or stage I HR-positive, ERBB2-positive breast cancer and who underwent surgery (23% mastectomy, 77% lumpectomy) and radiation therapy.
Worsening frailty status was defined as a decline of 0.03 or greater in a validated frailty index from the time of diagnosis to 1 year. This level of change has been linked to greater mortality risk and greater cost of care.
Frailty status at diagnosis was “robust” in 56% of the women, prefrail in 40%, mildly frail in 4%, and moderately to severely frail in 0.3%.
According to the researchers, 21.4% of the women experienced clinically significant declines in their frailty status after treatment. These declines occurred in 25% of women who underwent mastectomy and 20% of those who underwent lumpectomy.
After adjusting for covariates, there was a higher likelihood of worsening frailty among women who were robustly frail at baseline, in comparison with those who were moderately to severely frail at baseline (odds ratio, 6.12), and in those who underwent mastectomy vs. lumpectomy (OR, 1.31).
Older age and race were also linked to worsening frailty status following treatment. Compared with younger women (aged 65-74 years), older women were more likely to experience worsening frailty (OR, 1.21 for women aged 75-79; OR, 1.53 for those aged 80-84; OR, 1.94 for those aged 85 and older). In addition, Black women were more likely than non-Hispanic White women to experience worsening frailty after treatment (OR, 1.12).
“Previous studies have documented lasting declines in functional status after surgery in older patients with breast cancer, but breast cancer treatment has not been implicated in worsening frailty to date,” Dr. Minami and colleagues explain. But “given the substantial proportion of women experiencing worsening frailty and the significant difference by breast surgery type, frailty status as a cancer therapy outcome should be further explored.” In addition, “tailoring locoregional therapy intensity in this population is important,” they write.
Dr. Cate explained that randomized clinical trials such as COMET and LORIS, which explore the monitoring of patients with DCIS in lieu of active treatment, “will likely make a big impact on this population, as we currently do not have randomized controlled data for observation of breast cancer.”
Dr. Cate added as well that assessing a patient’s ECOG [Eastern Cooperative Oncology Group] performance status is vital “to determine who can really tolerate a breast cancer surgery” and that opting for antiestrogens, such as aromatase inhibitors, which can keep cancer at bay for years, “may be preferable for many older patients.”
The study was funded by Brigham and Women’s Hospital’s Department of Surgery’s Beal Fellowship. Dr. Minami and Dr. Cate have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study.
About 1 in 5 experienced clinically significant deterioration in frailty status after treatment, the study team found. Women at highest risk for declines in frailty following treatment had “robust” baseline frailty status at diagnosis and underwent more invasive mastectomy compared with lumpectomy.
The fact that “robust” older women were more likely to become frail after locoregional therapy suggests that “thoughtful treatment decisions should be undertaken in all older women, not simply those who have frailty at diagnosis,” said the investigators, led by Christina Minami, MD, of Dana-Farber/Brigham and Women’s Cancer Center in Boston.
The study findings emphasize that there is no one-size-fits-all approach to breast cancer treatment in the elderly, said Sarah P. Cate, MD, director, Breast Surgery Quality Program, Mount Sinai Health System, New York, who wasn’t involved in the research. “Some patients will sail through a surgery, and others are severely affected by it.”
The study was published online in JAMA Surgery.
Given the growing number of older adults with breast cancer, understanding how age-related syndromes, such as frailty, may alter cancer outcomes and how cancer treatments change aging trajectories remains important.
To investigate, Dr. Minami and colleagues used Surveillance, Epidemiology, and End Results Medicare data to identify 31,084 women (mean age, 73) who had been diagnosed with ductal carcinoma in situ (DCIS) or stage I HR-positive, ERBB2-positive breast cancer and who underwent surgery (23% mastectomy, 77% lumpectomy) and radiation therapy.
Worsening frailty status was defined as a decline of 0.03 or greater in a validated frailty index from the time of diagnosis to 1 year. This level of change has been linked to greater mortality risk and greater cost of care.
Frailty status at diagnosis was “robust” in 56% of the women, prefrail in 40%, mildly frail in 4%, and moderately to severely frail in 0.3%.
According to the researchers, 21.4% of the women experienced clinically significant declines in their frailty status after treatment. These declines occurred in 25% of women who underwent mastectomy and 20% of those who underwent lumpectomy.
After adjusting for covariates, there was a higher likelihood of worsening frailty among women who were robustly frail at baseline, in comparison with those who were moderately to severely frail at baseline (odds ratio, 6.12), and in those who underwent mastectomy vs. lumpectomy (OR, 1.31).
Older age and race were also linked to worsening frailty status following treatment. Compared with younger women (aged 65-74 years), older women were more likely to experience worsening frailty (OR, 1.21 for women aged 75-79; OR, 1.53 for those aged 80-84; OR, 1.94 for those aged 85 and older). In addition, Black women were more likely than non-Hispanic White women to experience worsening frailty after treatment (OR, 1.12).
“Previous studies have documented lasting declines in functional status after surgery in older patients with breast cancer, but breast cancer treatment has not been implicated in worsening frailty to date,” Dr. Minami and colleagues explain. But “given the substantial proportion of women experiencing worsening frailty and the significant difference by breast surgery type, frailty status as a cancer therapy outcome should be further explored.” In addition, “tailoring locoregional therapy intensity in this population is important,” they write.
Dr. Cate explained that randomized clinical trials such as COMET and LORIS, which explore the monitoring of patients with DCIS in lieu of active treatment, “will likely make a big impact on this population, as we currently do not have randomized controlled data for observation of breast cancer.”
Dr. Cate added as well that assessing a patient’s ECOG [Eastern Cooperative Oncology Group] performance status is vital “to determine who can really tolerate a breast cancer surgery” and that opting for antiestrogens, such as aromatase inhibitors, which can keep cancer at bay for years, “may be preferable for many older patients.”
The study was funded by Brigham and Women’s Hospital’s Department of Surgery’s Beal Fellowship. Dr. Minami and Dr. Cate have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study.
About 1 in 5 experienced clinically significant deterioration in frailty status after treatment, the study team found. Women at highest risk for declines in frailty following treatment had “robust” baseline frailty status at diagnosis and underwent more invasive mastectomy compared with lumpectomy.
The fact that “robust” older women were more likely to become frail after locoregional therapy suggests that “thoughtful treatment decisions should be undertaken in all older women, not simply those who have frailty at diagnosis,” said the investigators, led by Christina Minami, MD, of Dana-Farber/Brigham and Women’s Cancer Center in Boston.
The study findings emphasize that there is no one-size-fits-all approach to breast cancer treatment in the elderly, said Sarah P. Cate, MD, director, Breast Surgery Quality Program, Mount Sinai Health System, New York, who wasn’t involved in the research. “Some patients will sail through a surgery, and others are severely affected by it.”
The study was published online in JAMA Surgery.
Given the growing number of older adults with breast cancer, understanding how age-related syndromes, such as frailty, may alter cancer outcomes and how cancer treatments change aging trajectories remains important.
To investigate, Dr. Minami and colleagues used Surveillance, Epidemiology, and End Results Medicare data to identify 31,084 women (mean age, 73) who had been diagnosed with ductal carcinoma in situ (DCIS) or stage I HR-positive, ERBB2-positive breast cancer and who underwent surgery (23% mastectomy, 77% lumpectomy) and radiation therapy.
Worsening frailty status was defined as a decline of 0.03 or greater in a validated frailty index from the time of diagnosis to 1 year. This level of change has been linked to greater mortality risk and greater cost of care.
Frailty status at diagnosis was “robust” in 56% of the women, prefrail in 40%, mildly frail in 4%, and moderately to severely frail in 0.3%.
According to the researchers, 21.4% of the women experienced clinically significant declines in their frailty status after treatment. These declines occurred in 25% of women who underwent mastectomy and 20% of those who underwent lumpectomy.
After adjusting for covariates, there was a higher likelihood of worsening frailty among women who were robustly frail at baseline, in comparison with those who were moderately to severely frail at baseline (odds ratio, 6.12), and in those who underwent mastectomy vs. lumpectomy (OR, 1.31).
Older age and race were also linked to worsening frailty status following treatment. Compared with younger women (aged 65-74 years), older women were more likely to experience worsening frailty (OR, 1.21 for women aged 75-79; OR, 1.53 for those aged 80-84; OR, 1.94 for those aged 85 and older). In addition, Black women were more likely than non-Hispanic White women to experience worsening frailty after treatment (OR, 1.12).
“Previous studies have documented lasting declines in functional status after surgery in older patients with breast cancer, but breast cancer treatment has not been implicated in worsening frailty to date,” Dr. Minami and colleagues explain. But “given the substantial proportion of women experiencing worsening frailty and the significant difference by breast surgery type, frailty status as a cancer therapy outcome should be further explored.” In addition, “tailoring locoregional therapy intensity in this population is important,” they write.
Dr. Cate explained that randomized clinical trials such as COMET and LORIS, which explore the monitoring of patients with DCIS in lieu of active treatment, “will likely make a big impact on this population, as we currently do not have randomized controlled data for observation of breast cancer.”
Dr. Cate added as well that assessing a patient’s ECOG [Eastern Cooperative Oncology Group] performance status is vital “to determine who can really tolerate a breast cancer surgery” and that opting for antiestrogens, such as aromatase inhibitors, which can keep cancer at bay for years, “may be preferable for many older patients.”
The study was funded by Brigham and Women’s Hospital’s Department of Surgery’s Beal Fellowship. Dr. Minami and Dr. Cate have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA SURGERY
Prostate cancer drug shortage leaves some with uncertainty
according to the Food and Drug Administration.
The therapy lutetium Lu 177 vipivotide tetraxetan (Pluvicto), approved in March 2022, will remain in limited supply until the drug’s manufacturer, Novartis, can ramp up production of the drug over the next 12 months.
In a letter in February, Novartis said it is giving priority to patients who have already started the regimen so they can “appropriately complete their course of therapy.” The manufacturer will not be taking any orders for new patients over the next 4-6 months, as they work to increase supply.
“We are operating our production site at full capacity to treat as many patients as possible, as quickly as possible,” Novartis said. “However, with a nuclear medicine like Pluvicto, there is no backup supply that we can draw from when we experience a delay.”
Pluvicto is currently made in small batches in the company’s manufacturing facility in Italy. The drug only has a 5-day window to reach its intended patient, after which time it cannot be used. Any disruption in the production or shipping process can create a delay.
Novartis said the facility in Italy is currently operating at full capacity and the company is “working to increase production capacity and supply” of the drug over the next 12 months at two new manufacturing sites in the United States.
The company also encountered supply problems with Pluvicto in 2022 after quality issues were discovered in the manufacturing process.
Currently, patients who are waiting for their first dose of Pluvicto will need to be rescheduled. The manufacturer will be reaching out to health care professionals with options for rescheduling.
Jonathan McConathy, MD, PhD, told The Wall Street Journal that “people will die from this shortage, for sure.”
Dr. McConathy, a radiologist at the University of Alabama at Birmingham who has consulted for Novartis, explained that some patients who would have benefited from the drug likely won’t receive it in time.
A version of this article first appeared on Medscape.com.
according to the Food and Drug Administration.
The therapy lutetium Lu 177 vipivotide tetraxetan (Pluvicto), approved in March 2022, will remain in limited supply until the drug’s manufacturer, Novartis, can ramp up production of the drug over the next 12 months.
In a letter in February, Novartis said it is giving priority to patients who have already started the regimen so they can “appropriately complete their course of therapy.” The manufacturer will not be taking any orders for new patients over the next 4-6 months, as they work to increase supply.
“We are operating our production site at full capacity to treat as many patients as possible, as quickly as possible,” Novartis said. “However, with a nuclear medicine like Pluvicto, there is no backup supply that we can draw from when we experience a delay.”
Pluvicto is currently made in small batches in the company’s manufacturing facility in Italy. The drug only has a 5-day window to reach its intended patient, after which time it cannot be used. Any disruption in the production or shipping process can create a delay.
Novartis said the facility in Italy is currently operating at full capacity and the company is “working to increase production capacity and supply” of the drug over the next 12 months at two new manufacturing sites in the United States.
The company also encountered supply problems with Pluvicto in 2022 after quality issues were discovered in the manufacturing process.
Currently, patients who are waiting for their first dose of Pluvicto will need to be rescheduled. The manufacturer will be reaching out to health care professionals with options for rescheduling.
Jonathan McConathy, MD, PhD, told The Wall Street Journal that “people will die from this shortage, for sure.”
Dr. McConathy, a radiologist at the University of Alabama at Birmingham who has consulted for Novartis, explained that some patients who would have benefited from the drug likely won’t receive it in time.
A version of this article first appeared on Medscape.com.
according to the Food and Drug Administration.
The therapy lutetium Lu 177 vipivotide tetraxetan (Pluvicto), approved in March 2022, will remain in limited supply until the drug’s manufacturer, Novartis, can ramp up production of the drug over the next 12 months.
In a letter in February, Novartis said it is giving priority to patients who have already started the regimen so they can “appropriately complete their course of therapy.” The manufacturer will not be taking any orders for new patients over the next 4-6 months, as they work to increase supply.
“We are operating our production site at full capacity to treat as many patients as possible, as quickly as possible,” Novartis said. “However, with a nuclear medicine like Pluvicto, there is no backup supply that we can draw from when we experience a delay.”
Pluvicto is currently made in small batches in the company’s manufacturing facility in Italy. The drug only has a 5-day window to reach its intended patient, after which time it cannot be used. Any disruption in the production or shipping process can create a delay.
Novartis said the facility in Italy is currently operating at full capacity and the company is “working to increase production capacity and supply” of the drug over the next 12 months at two new manufacturing sites in the United States.
The company also encountered supply problems with Pluvicto in 2022 after quality issues were discovered in the manufacturing process.
Currently, patients who are waiting for their first dose of Pluvicto will need to be rescheduled. The manufacturer will be reaching out to health care professionals with options for rescheduling.
Jonathan McConathy, MD, PhD, told The Wall Street Journal that “people will die from this shortage, for sure.”
Dr. McConathy, a radiologist at the University of Alabama at Birmingham who has consulted for Novartis, explained that some patients who would have benefited from the drug likely won’t receive it in time.
A version of this article first appeared on Medscape.com.
Restless legs a new modifiable risk factor for dementia?
suggesting the disorder may be a risk factor for dementia or a very early noncognitive sign of dementia, researchers say.
In a large population-based cohort study, adults with RLS were significantly more likely to develop dementia over more than a decade than were their peers without RLS.
If confirmed in future studies, “regular check-ups for cognitive decline in older patients with RLS may facilitate earlier detection and intervention for those with dementia risk,” wrote investigators led by Eosu Kim, MD, PhD, with Yonsei University, Seoul, Republic of Korea.
The study was published online in Alzheimer’s Research and Therapy.
Sleep disorders and dementia
RLS is associated with poor sleep, depression/anxiety, poor diet, microvasculopathy, and hypoxia – all of which are known risk factors for dementia. However, the relationship between RLS and incident dementia has been unclear.
The researchers compared risk for all-cause dementia, Alzheimer’s disease (AD), and vascular dementia (VaD) among 2,501 adults with newly diagnosed RLS and 9,977 matched control persons participating in the Korean National Health Insurance Service–Elderly Cohort, a nationwide population-based cohort of adults aged 60 and older.
The mean age of the cohort was 73 years; most of the participants were women (65%). Among all 12,478 participants, 874 (7%) developed all-cause dementia during follow-up – 475 (54%) developed AD, and 194 (22%) developed VaD.
The incidence of all-cause dementia was significantly higher among the RLS group than among the control group (10.4% vs. 6.2%). Incidence rates of AD and VaD (5.6% and 2.6%, respectively) were also higher in the RLS group than in the control group (3.4% and 1.3%, respectively).
In Cox regression analysis, RLS was significantly associated with an increased risk of all-cause dementia (adjusted hazard ratio [aHR], 1.46; 95% confidence interval [CI], 1.24-1.72), AD (aHR 1.38; 95% CI, 1.11-1.72) and VaD (aHR, 1.81; 95% CI, 1.30-2.53).
The researchers noted that RLS may precede deterioration of cognitive function, leading to dementia, and they suggest that RLS could be regarded as a “newly identified” risk factor or prodromal sign of dementia.
Modifiable risk factor
Reached for comment, Thanh Dang-Vu, MD, PhD, professor and research chair in sleep, neuroimaging, and cognitive health at Concordia University in Montreal, said there is now “increasing literature that shows sleep as a modifiable risk factor for cognitive decline.
“Previous evidence indicates that both sleep apnea and insomnia disorder increase the risk for cognitive decline and possibly dementia. Here the study adds to this body of evidence linking sleep disorders to dementia, suggesting that RLS should also be considered as a sleep-related risk factor,” Dr. Dang-Vu told this news organization.
“More evidence is needed, though, as here, all diagnoses were based on national health insurance diagnostic codes, and it is likely there were missed diagnoses for RLS but also for other sleep disorders, as there was no systematic screening for them,” Dr. Dang-Vu cautioned.
Support for the study was provided by the Ministry of Health and Welfare, the Korean government, and Yonsei University. Dr. Kim and Dr. Dang-Vu reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
suggesting the disorder may be a risk factor for dementia or a very early noncognitive sign of dementia, researchers say.
In a large population-based cohort study, adults with RLS were significantly more likely to develop dementia over more than a decade than were their peers without RLS.
If confirmed in future studies, “regular check-ups for cognitive decline in older patients with RLS may facilitate earlier detection and intervention for those with dementia risk,” wrote investigators led by Eosu Kim, MD, PhD, with Yonsei University, Seoul, Republic of Korea.
The study was published online in Alzheimer’s Research and Therapy.
Sleep disorders and dementia
RLS is associated with poor sleep, depression/anxiety, poor diet, microvasculopathy, and hypoxia – all of which are known risk factors for dementia. However, the relationship between RLS and incident dementia has been unclear.
The researchers compared risk for all-cause dementia, Alzheimer’s disease (AD), and vascular dementia (VaD) among 2,501 adults with newly diagnosed RLS and 9,977 matched control persons participating in the Korean National Health Insurance Service–Elderly Cohort, a nationwide population-based cohort of adults aged 60 and older.
The mean age of the cohort was 73 years; most of the participants were women (65%). Among all 12,478 participants, 874 (7%) developed all-cause dementia during follow-up – 475 (54%) developed AD, and 194 (22%) developed VaD.
The incidence of all-cause dementia was significantly higher among the RLS group than among the control group (10.4% vs. 6.2%). Incidence rates of AD and VaD (5.6% and 2.6%, respectively) were also higher in the RLS group than in the control group (3.4% and 1.3%, respectively).
In Cox regression analysis, RLS was significantly associated with an increased risk of all-cause dementia (adjusted hazard ratio [aHR], 1.46; 95% confidence interval [CI], 1.24-1.72), AD (aHR 1.38; 95% CI, 1.11-1.72) and VaD (aHR, 1.81; 95% CI, 1.30-2.53).
The researchers noted that RLS may precede deterioration of cognitive function, leading to dementia, and they suggest that RLS could be regarded as a “newly identified” risk factor or prodromal sign of dementia.
Modifiable risk factor
Reached for comment, Thanh Dang-Vu, MD, PhD, professor and research chair in sleep, neuroimaging, and cognitive health at Concordia University in Montreal, said there is now “increasing literature that shows sleep as a modifiable risk factor for cognitive decline.
“Previous evidence indicates that both sleep apnea and insomnia disorder increase the risk for cognitive decline and possibly dementia. Here the study adds to this body of evidence linking sleep disorders to dementia, suggesting that RLS should also be considered as a sleep-related risk factor,” Dr. Dang-Vu told this news organization.
“More evidence is needed, though, as here, all diagnoses were based on national health insurance diagnostic codes, and it is likely there were missed diagnoses for RLS but also for other sleep disorders, as there was no systematic screening for them,” Dr. Dang-Vu cautioned.
Support for the study was provided by the Ministry of Health and Welfare, the Korean government, and Yonsei University. Dr. Kim and Dr. Dang-Vu reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
suggesting the disorder may be a risk factor for dementia or a very early noncognitive sign of dementia, researchers say.
In a large population-based cohort study, adults with RLS were significantly more likely to develop dementia over more than a decade than were their peers without RLS.
If confirmed in future studies, “regular check-ups for cognitive decline in older patients with RLS may facilitate earlier detection and intervention for those with dementia risk,” wrote investigators led by Eosu Kim, MD, PhD, with Yonsei University, Seoul, Republic of Korea.
The study was published online in Alzheimer’s Research and Therapy.
Sleep disorders and dementia
RLS is associated with poor sleep, depression/anxiety, poor diet, microvasculopathy, and hypoxia – all of which are known risk factors for dementia. However, the relationship between RLS and incident dementia has been unclear.
The researchers compared risk for all-cause dementia, Alzheimer’s disease (AD), and vascular dementia (VaD) among 2,501 adults with newly diagnosed RLS and 9,977 matched control persons participating in the Korean National Health Insurance Service–Elderly Cohort, a nationwide population-based cohort of adults aged 60 and older.
The mean age of the cohort was 73 years; most of the participants were women (65%). Among all 12,478 participants, 874 (7%) developed all-cause dementia during follow-up – 475 (54%) developed AD, and 194 (22%) developed VaD.
The incidence of all-cause dementia was significantly higher among the RLS group than among the control group (10.4% vs. 6.2%). Incidence rates of AD and VaD (5.6% and 2.6%, respectively) were also higher in the RLS group than in the control group (3.4% and 1.3%, respectively).
In Cox regression analysis, RLS was significantly associated with an increased risk of all-cause dementia (adjusted hazard ratio [aHR], 1.46; 95% confidence interval [CI], 1.24-1.72), AD (aHR 1.38; 95% CI, 1.11-1.72) and VaD (aHR, 1.81; 95% CI, 1.30-2.53).
The researchers noted that RLS may precede deterioration of cognitive function, leading to dementia, and they suggest that RLS could be regarded as a “newly identified” risk factor or prodromal sign of dementia.
Modifiable risk factor
Reached for comment, Thanh Dang-Vu, MD, PhD, professor and research chair in sleep, neuroimaging, and cognitive health at Concordia University in Montreal, said there is now “increasing literature that shows sleep as a modifiable risk factor for cognitive decline.
“Previous evidence indicates that both sleep apnea and insomnia disorder increase the risk for cognitive decline and possibly dementia. Here the study adds to this body of evidence linking sleep disorders to dementia, suggesting that RLS should also be considered as a sleep-related risk factor,” Dr. Dang-Vu told this news organization.
“More evidence is needed, though, as here, all diagnoses were based on national health insurance diagnostic codes, and it is likely there were missed diagnoses for RLS but also for other sleep disorders, as there was no systematic screening for them,” Dr. Dang-Vu cautioned.
Support for the study was provided by the Ministry of Health and Welfare, the Korean government, and Yonsei University. Dr. Kim and Dr. Dang-Vu reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ALZHEIMER’S RESEARCH AND THERAPY
Cases of potentially deadly fungus jump 200%: CDC
prompting the Centers for Disease Control and Prevention to issue a warning to health care facilities about the rising threat.
C. auris is a yeast that spreads easily from touching it on a surface like a countertop. It can also spread from person to person. It isn’t a threat to healthy people, but people in hospitals and nursing homes are at a heightened risk because they might have weakened immune systems or be using invasive medical devices that can introduce the fungus inside their bodies. When C. auris progresses to causing an infection that reaches the brain, blood, or lungs, more than one in three people die.
The worrying increase was detailed in the journal Annals of Internal Medicine. In 2021, cases reached a count of 3,270 with an active infection, and 7,413 cases showed the fungus was present but hadn’t caused an infection. Infection counts were up 95% over the previous year, and the fungus showed up on screenings three times as often. The number of cases resistant to medication also tripled.
The CDC called the figures “alarming,” noting that the fungus was only detected in the United States in 2016.
“The timing of this increase and findings from public health investigations suggest C. auris spread may have worsened due to strain on health care and public health systems during the COVID-19 pandemic,” the CDC explained in a news release.
Another potential reason for the jump could be that screening for C. auris has simply increased and it’s being found more often because it’s being looked for more often. But researchers believe that, even with the increase in testing, the reported counts are underestimated. That’s because even though screening has increased, health care providers still aren’t looking for the presence of the fungus as often as the CDC would like.
“The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control,” said study author Meghan Lyman, MD, a CDC epidemiologist in Atlanta, in a statement.
Cases of C. auris continued to rise in 2022, the CDC said. A map on the agency’s website of reported cases from 2022 shows it was found in more than half of U.S. states, with the highest counts occurring in California, Florida, Illinois, Nevada, New York, and Texas. The fungus is a problem worldwide and is listed among the most threatening treatment-resistant fungi by the World Health Organization.
The study authors concluded that screening capacity for the fungus needs to be expanded nationwide so that when C. auris is detected, measures can be taken to prevent its spread.
A version of this article originally appeared on WebMD.com.
prompting the Centers for Disease Control and Prevention to issue a warning to health care facilities about the rising threat.
C. auris is a yeast that spreads easily from touching it on a surface like a countertop. It can also spread from person to person. It isn’t a threat to healthy people, but people in hospitals and nursing homes are at a heightened risk because they might have weakened immune systems or be using invasive medical devices that can introduce the fungus inside their bodies. When C. auris progresses to causing an infection that reaches the brain, blood, or lungs, more than one in three people die.
The worrying increase was detailed in the journal Annals of Internal Medicine. In 2021, cases reached a count of 3,270 with an active infection, and 7,413 cases showed the fungus was present but hadn’t caused an infection. Infection counts were up 95% over the previous year, and the fungus showed up on screenings three times as often. The number of cases resistant to medication also tripled.
The CDC called the figures “alarming,” noting that the fungus was only detected in the United States in 2016.
“The timing of this increase and findings from public health investigations suggest C. auris spread may have worsened due to strain on health care and public health systems during the COVID-19 pandemic,” the CDC explained in a news release.
Another potential reason for the jump could be that screening for C. auris has simply increased and it’s being found more often because it’s being looked for more often. But researchers believe that, even with the increase in testing, the reported counts are underestimated. That’s because even though screening has increased, health care providers still aren’t looking for the presence of the fungus as often as the CDC would like.
“The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control,” said study author Meghan Lyman, MD, a CDC epidemiologist in Atlanta, in a statement.
Cases of C. auris continued to rise in 2022, the CDC said. A map on the agency’s website of reported cases from 2022 shows it was found in more than half of U.S. states, with the highest counts occurring in California, Florida, Illinois, Nevada, New York, and Texas. The fungus is a problem worldwide and is listed among the most threatening treatment-resistant fungi by the World Health Organization.
The study authors concluded that screening capacity for the fungus needs to be expanded nationwide so that when C. auris is detected, measures can be taken to prevent its spread.
A version of this article originally appeared on WebMD.com.
prompting the Centers for Disease Control and Prevention to issue a warning to health care facilities about the rising threat.
C. auris is a yeast that spreads easily from touching it on a surface like a countertop. It can also spread from person to person. It isn’t a threat to healthy people, but people in hospitals and nursing homes are at a heightened risk because they might have weakened immune systems or be using invasive medical devices that can introduce the fungus inside their bodies. When C. auris progresses to causing an infection that reaches the brain, blood, or lungs, more than one in three people die.
The worrying increase was detailed in the journal Annals of Internal Medicine. In 2021, cases reached a count of 3,270 with an active infection, and 7,413 cases showed the fungus was present but hadn’t caused an infection. Infection counts were up 95% over the previous year, and the fungus showed up on screenings three times as often. The number of cases resistant to medication also tripled.
The CDC called the figures “alarming,” noting that the fungus was only detected in the United States in 2016.
“The timing of this increase and findings from public health investigations suggest C. auris spread may have worsened due to strain on health care and public health systems during the COVID-19 pandemic,” the CDC explained in a news release.
Another potential reason for the jump could be that screening for C. auris has simply increased and it’s being found more often because it’s being looked for more often. But researchers believe that, even with the increase in testing, the reported counts are underestimated. That’s because even though screening has increased, health care providers still aren’t looking for the presence of the fungus as often as the CDC would like.
“The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control,” said study author Meghan Lyman, MD, a CDC epidemiologist in Atlanta, in a statement.
Cases of C. auris continued to rise in 2022, the CDC said. A map on the agency’s website of reported cases from 2022 shows it was found in more than half of U.S. states, with the highest counts occurring in California, Florida, Illinois, Nevada, New York, and Texas. The fungus is a problem worldwide and is listed among the most threatening treatment-resistant fungi by the World Health Organization.
The study authors concluded that screening capacity for the fungus needs to be expanded nationwide so that when C. auris is detected, measures can be taken to prevent its spread.
A version of this article originally appeared on WebMD.com.
After the Match: Next steps for new residents, unmatched
Medical school graduates around the US took to social media after last week's Match Day to share their joy ― or explore their options if they did not match.
Take this post March 19 on Twitter: “I went unmatched this year; looking for research position at any institute for internal medicine.”
including an international medical graduate who matched into his chosen specialty after multiple disappointments.
“I’ve waited for this email for 8 years,” Sahil Bawa, MD, posted on Twitter on March 13. A few days later, when he learned about his residency position, he posted: “I’m beyond grateful. Will be moving to Alabama soon #familymedicine.”
Dr. Bawa, who matched into UAB Medicine Selma (Ala.), graduated from medical school in India in 2014. He said in an interview that he has visited the United States periodically since then to pass medical tests, obtain letters of recommendation, and participate in research.
Over the years he watched his Indian colleagues give up on becoming American doctors, find alternative careers, or resolve to practice in their native country. But he held onto the few success stories he saw on social media. “There were always one to two every year. It kept me going. If they can do it, I can do it.”
International medical graduates (IMGs) like Dr. Bawa applied in record numbers to Match2023, according to the National Resident Matching Program (NRMP), which announced the results on March 13 of its main residency match and the Supplemental Offer and Acceptance Program (SOAP) for unfilled positions or unmatched applicants.
Overall, 48,156 total applicants registered for the match, which was driven by the increase of non-U.S. IMG applicants and U.S. DO seniors over the past year, NRMP stated in its release. U.S. MD seniors had a match rate of nearly 94%, and U.S. DO seniors, nearly 92%. U.S. IMGs had a match rate of nearly 68%, an “all-time high,” and non-U.S. IMGs, nearly 60%, NRMP stated.
Three specialties that filled all of their 30 or more available positions were orthopedic surgery, plastic surgery (integrated), radiology – diagnostic, and thoracic surgery. Specialties with 30 or more positions that filled with the highest percentage of U.S. MD and DO seniors were plastic surgery (integrated), internal medicine-pediatrics, ob.gyn., and orthopedic surgery.
The number of available primary care positions increased slightly, NRMP reported. Considering “a serious and growing shortage of primary care physicians across the U.S.,” there were 571 more primary care positions than 2022. That’s an increase of about 3% over last year and 17% over the past 5 years. Primary care positions filled at a rate of 94%, which remained steady from 2022.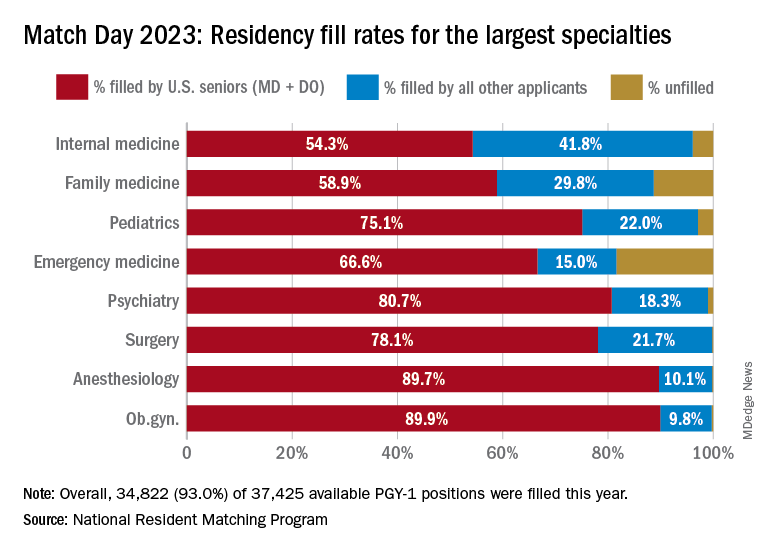
NRMP also pointed out specialties with increases in the number of positions filled by U.S. MD seniors of more than 10% and 10 positions in the past 5 years: anesthesiology, child neurology, interventional radiology, neurology, pathology, physical medicine and rehabilitation, plastic surgery (integrated), psychiatry, radiology-diagnostic, transitional year, and vascular surgery.
Bryan Carmody, MD, MPH, a pediatric nephrologist known for his medical school commentaries, said in an interview that the most competitive specialties he noted in 2023 were radiology, pathology, and neurology.
“The surgical specialties are always competitive, so it wasn’t a surprise that orthopedics, plastic surgery, and thoracic surgery filled all of their positions. But I was surprised to see diagnostic radiology fill every single one of their positions in the match. And although pathology and neurology aren’t typically considered extremely competitive specialties, they filled over 99% of their positions in the Match this year.”
On Dr. Carmody’s blog about the winners and losers of Match Day, he said that despite the record number of primary care positions offered, family medicine programs suffered. “Only 89% of family medicine programs filled in the Match, and graduating U.S. MD and DO students only filled a little more than half of all the available positions,” he wrote.
For a record number of applicants that match each year, and “the most favorable ratio in the past 2 decades” of applicants-to-positions in 2023, there are still a lot unmatched, Dr. Carmody said. “It’s a tough thing to talk about. The reality is the number of residency positions should be determined by the number of physicians needed.”
One student, Asim Ansari, didn’t match into a traditional residency or through SOAP. It was his fifth attempt. He was serving a transitional-year residency at Merit Health Wesley in Hattiesburg, Miss., and when he didn’t match, he accepted a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City.
He said he was “relieved and excited” to have found a program in his chosen specialty. Still, in 2 years, Mr. Ansari must again try to match into a traditional psychiatry residency.
Meanwhile, Dr. Bawa will prepare for his 3-year residency in Alabama after completing his interim research year in the surgery department at Wayne State University, Detroit, in May.
Despite his years in limbo, Dr. Bawa said, “I have no regrets, no complaints. I am still very happy.”
A version of this article originally appeared on Medscape.com.
Medical school graduates around the US took to social media after last week's Match Day to share their joy ― or explore their options if they did not match.
Take this post March 19 on Twitter: “I went unmatched this year; looking for research position at any institute for internal medicine.”
including an international medical graduate who matched into his chosen specialty after multiple disappointments.
“I’ve waited for this email for 8 years,” Sahil Bawa, MD, posted on Twitter on March 13. A few days later, when he learned about his residency position, he posted: “I’m beyond grateful. Will be moving to Alabama soon #familymedicine.”
Dr. Bawa, who matched into UAB Medicine Selma (Ala.), graduated from medical school in India in 2014. He said in an interview that he has visited the United States periodically since then to pass medical tests, obtain letters of recommendation, and participate in research.
Over the years he watched his Indian colleagues give up on becoming American doctors, find alternative careers, or resolve to practice in their native country. But he held onto the few success stories he saw on social media. “There were always one to two every year. It kept me going. If they can do it, I can do it.”
International medical graduates (IMGs) like Dr. Bawa applied in record numbers to Match2023, according to the National Resident Matching Program (NRMP), which announced the results on March 13 of its main residency match and the Supplemental Offer and Acceptance Program (SOAP) for unfilled positions or unmatched applicants.
Overall, 48,156 total applicants registered for the match, which was driven by the increase of non-U.S. IMG applicants and U.S. DO seniors over the past year, NRMP stated in its release. U.S. MD seniors had a match rate of nearly 94%, and U.S. DO seniors, nearly 92%. U.S. IMGs had a match rate of nearly 68%, an “all-time high,” and non-U.S. IMGs, nearly 60%, NRMP stated.
Three specialties that filled all of their 30 or more available positions were orthopedic surgery, plastic surgery (integrated), radiology – diagnostic, and thoracic surgery. Specialties with 30 or more positions that filled with the highest percentage of U.S. MD and DO seniors were plastic surgery (integrated), internal medicine-pediatrics, ob.gyn., and orthopedic surgery.
The number of available primary care positions increased slightly, NRMP reported. Considering “a serious and growing shortage of primary care physicians across the U.S.,” there were 571 more primary care positions than 2022. That’s an increase of about 3% over last year and 17% over the past 5 years. Primary care positions filled at a rate of 94%, which remained steady from 2022.
NRMP also pointed out specialties with increases in the number of positions filled by U.S. MD seniors of more than 10% and 10 positions in the past 5 years: anesthesiology, child neurology, interventional radiology, neurology, pathology, physical medicine and rehabilitation, plastic surgery (integrated), psychiatry, radiology-diagnostic, transitional year, and vascular surgery.
Bryan Carmody, MD, MPH, a pediatric nephrologist known for his medical school commentaries, said in an interview that the most competitive specialties he noted in 2023 were radiology, pathology, and neurology.
“The surgical specialties are always competitive, so it wasn’t a surprise that orthopedics, plastic surgery, and thoracic surgery filled all of their positions. But I was surprised to see diagnostic radiology fill every single one of their positions in the match. And although pathology and neurology aren’t typically considered extremely competitive specialties, they filled over 99% of their positions in the Match this year.”
On Dr. Carmody’s blog about the winners and losers of Match Day, he said that despite the record number of primary care positions offered, family medicine programs suffered. “Only 89% of family medicine programs filled in the Match, and graduating U.S. MD and DO students only filled a little more than half of all the available positions,” he wrote.
For a record number of applicants that match each year, and “the most favorable ratio in the past 2 decades” of applicants-to-positions in 2023, there are still a lot unmatched, Dr. Carmody said. “It’s a tough thing to talk about. The reality is the number of residency positions should be determined by the number of physicians needed.”
One student, Asim Ansari, didn’t match into a traditional residency or through SOAP. It was his fifth attempt. He was serving a transitional-year residency at Merit Health Wesley in Hattiesburg, Miss., and when he didn’t match, he accepted a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City.
He said he was “relieved and excited” to have found a program in his chosen specialty. Still, in 2 years, Mr. Ansari must again try to match into a traditional psychiatry residency.
Meanwhile, Dr. Bawa will prepare for his 3-year residency in Alabama after completing his interim research year in the surgery department at Wayne State University, Detroit, in May.
Despite his years in limbo, Dr. Bawa said, “I have no regrets, no complaints. I am still very happy.”
A version of this article originally appeared on Medscape.com.
Medical school graduates around the US took to social media after last week's Match Day to share their joy ― or explore their options if they did not match.
Take this post March 19 on Twitter: “I went unmatched this year; looking for research position at any institute for internal medicine.”
including an international medical graduate who matched into his chosen specialty after multiple disappointments.
“I’ve waited for this email for 8 years,” Sahil Bawa, MD, posted on Twitter on March 13. A few days later, when he learned about his residency position, he posted: “I’m beyond grateful. Will be moving to Alabama soon #familymedicine.”
Dr. Bawa, who matched into UAB Medicine Selma (Ala.), graduated from medical school in India in 2014. He said in an interview that he has visited the United States periodically since then to pass medical tests, obtain letters of recommendation, and participate in research.
Over the years he watched his Indian colleagues give up on becoming American doctors, find alternative careers, or resolve to practice in their native country. But he held onto the few success stories he saw on social media. “There were always one to two every year. It kept me going. If they can do it, I can do it.”
International medical graduates (IMGs) like Dr. Bawa applied in record numbers to Match2023, according to the National Resident Matching Program (NRMP), which announced the results on March 13 of its main residency match and the Supplemental Offer and Acceptance Program (SOAP) for unfilled positions or unmatched applicants.
Overall, 48,156 total applicants registered for the match, which was driven by the increase of non-U.S. IMG applicants and U.S. DO seniors over the past year, NRMP stated in its release. U.S. MD seniors had a match rate of nearly 94%, and U.S. DO seniors, nearly 92%. U.S. IMGs had a match rate of nearly 68%, an “all-time high,” and non-U.S. IMGs, nearly 60%, NRMP stated.
Three specialties that filled all of their 30 or more available positions were orthopedic surgery, plastic surgery (integrated), radiology – diagnostic, and thoracic surgery. Specialties with 30 or more positions that filled with the highest percentage of U.S. MD and DO seniors were plastic surgery (integrated), internal medicine-pediatrics, ob.gyn., and orthopedic surgery.
The number of available primary care positions increased slightly, NRMP reported. Considering “a serious and growing shortage of primary care physicians across the U.S.,” there were 571 more primary care positions than 2022. That’s an increase of about 3% over last year and 17% over the past 5 years. Primary care positions filled at a rate of 94%, which remained steady from 2022.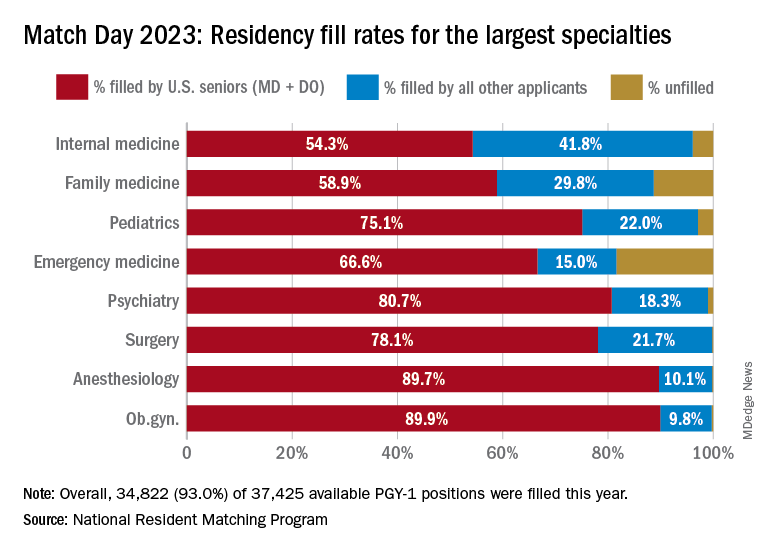
NRMP also pointed out specialties with increases in the number of positions filled by U.S. MD seniors of more than 10% and 10 positions in the past 5 years: anesthesiology, child neurology, interventional radiology, neurology, pathology, physical medicine and rehabilitation, plastic surgery (integrated), psychiatry, radiology-diagnostic, transitional year, and vascular surgery.
Bryan Carmody, MD, MPH, a pediatric nephrologist known for his medical school commentaries, said in an interview that the most competitive specialties he noted in 2023 were radiology, pathology, and neurology.
“The surgical specialties are always competitive, so it wasn’t a surprise that orthopedics, plastic surgery, and thoracic surgery filled all of their positions. But I was surprised to see diagnostic radiology fill every single one of their positions in the match. And although pathology and neurology aren’t typically considered extremely competitive specialties, they filled over 99% of their positions in the Match this year.”
On Dr. Carmody’s blog about the winners and losers of Match Day, he said that despite the record number of primary care positions offered, family medicine programs suffered. “Only 89% of family medicine programs filled in the Match, and graduating U.S. MD and DO students only filled a little more than half of all the available positions,” he wrote.
For a record number of applicants that match each year, and “the most favorable ratio in the past 2 decades” of applicants-to-positions in 2023, there are still a lot unmatched, Dr. Carmody said. “It’s a tough thing to talk about. The reality is the number of residency positions should be determined by the number of physicians needed.”
One student, Asim Ansari, didn’t match into a traditional residency or through SOAP. It was his fifth attempt. He was serving a transitional-year residency at Merit Health Wesley in Hattiesburg, Miss., and when he didn’t match, he accepted a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City.
He said he was “relieved and excited” to have found a program in his chosen specialty. Still, in 2 years, Mr. Ansari must again try to match into a traditional psychiatry residency.
Meanwhile, Dr. Bawa will prepare for his 3-year residency in Alabama after completing his interim research year in the surgery department at Wayne State University, Detroit, in May.
Despite his years in limbo, Dr. Bawa said, “I have no regrets, no complaints. I am still very happy.”
A version of this article originally appeared on Medscape.com.
Old-school printer helps scientists quickly spot bacteria in blood
When a bacterial infection reaches the bloodstream, every second is critical. The person’s life is on the line. Yet blood tests to identify bacteria take hours to days. While waiting, doctors often prescribe broad-spectrum antibiotics in hopes of killing whatever bug may be at fault.
Someday soon, that wait time could shrink significantly, allowing health care providers to more quickly zero in on the best antibiotic for each infection – thanks to an innovation from Stanford (Calif.) University that identifies bacteria in seconds.
The cutting-edge method relies on old-school tech: an inkjet printer similar the kind you might have at home – except this one has been modified to print blood instead of ink.
The very small sample size – each drop is two trillionths of a liter, or about a billion times smaller than a raindrop – make spotting bacteria easier. Smaller samples mean fewer cells, so lab techs can more swiftly separate the bacterial spectra from other components, like red blood cells and white blood cells.
To boost efficiency even more, the researchers added gold nanoparticles, which attach to the bacteria, serving like antennas to focus the light. Machine learning – a type of artificial intelligence – helps interpret the spectrum of light and identify which fingerprint goes with which bacteria.
“It kind of wound up being this really interesting historical period where we could put the pieces together from different technologies, including nanophotonics, printing, and artificial intelligence, to help accelerate identification of bacteria in these complex samples,” says study author Jennifer Dionne, PhD, associate professor of materials science and engineering at Stanford.
Compare that to blood culture testing in hospitals, where it takes days for bacterial cells to grow and multiply inside a large machine that looks like a refrigerator. For some bacteria, like the kinds that cause tuberculosis, cultures take weeks.
Then further testing is needed to identify which antibiotics will quell the infection. The new technology from Stanford could accelerate this process, too.
“The promise of our technique is that you don’t need to have a culture of cells to put the antibiotic on top,” says Dr. Dionne. “What we’re finding is that from the Raman scattering, we can use that to identify – even without incubating with antibiotics – which drug the bacteria would respond to, and that’s really exciting.”
If patients can receive the antibiotic best suited for their infection, they will likely have better outcomes.
“Blood cultures can typically take 48-72 hours to come back, and then you base your clinical decisions and adjusting antibiotics based on those blood cultures,” says Richard Watkins, MD, an infectious disease physician and professor of medicine at the Northeastern Ohio Universities, Rootstown. Dr. Watkins was not involved in the study.
“Sometimes, despite your best guess, you’re wrong,” Dr. Watkins says, “and obviously, the patient could have an adverse outcome. So, if you can diagnose the pathogen sooner, that is ideal. Whatever technology enables clinicians to do that is definitely progress and a step forward.”
On a global scale, this technology could help reduce the overuse of broad-spectrum antibiotics, which contributes to antimicrobial resistance, an emerging health threat, says Dr. Dionne.
The team is working to develop the technology further into an instrument the size of a shoebox and, with further testing, commercialize the product. That could take a few years.
This technology has potential beyond bloodstream infections, too. It could be used to identify bacteria in other fluids, such as in wastewater or contaminated food.
A version of this article originally appeared on WebMD.com.
When a bacterial infection reaches the bloodstream, every second is critical. The person’s life is on the line. Yet blood tests to identify bacteria take hours to days. While waiting, doctors often prescribe broad-spectrum antibiotics in hopes of killing whatever bug may be at fault.
Someday soon, that wait time could shrink significantly, allowing health care providers to more quickly zero in on the best antibiotic for each infection – thanks to an innovation from Stanford (Calif.) University that identifies bacteria in seconds.
The cutting-edge method relies on old-school tech: an inkjet printer similar the kind you might have at home – except this one has been modified to print blood instead of ink.
The very small sample size – each drop is two trillionths of a liter, or about a billion times smaller than a raindrop – make spotting bacteria easier. Smaller samples mean fewer cells, so lab techs can more swiftly separate the bacterial spectra from other components, like red blood cells and white blood cells.
To boost efficiency even more, the researchers added gold nanoparticles, which attach to the bacteria, serving like antennas to focus the light. Machine learning – a type of artificial intelligence – helps interpret the spectrum of light and identify which fingerprint goes with which bacteria.
“It kind of wound up being this really interesting historical period where we could put the pieces together from different technologies, including nanophotonics, printing, and artificial intelligence, to help accelerate identification of bacteria in these complex samples,” says study author Jennifer Dionne, PhD, associate professor of materials science and engineering at Stanford.
Compare that to blood culture testing in hospitals, where it takes days for bacterial cells to grow and multiply inside a large machine that looks like a refrigerator. For some bacteria, like the kinds that cause tuberculosis, cultures take weeks.
Then further testing is needed to identify which antibiotics will quell the infection. The new technology from Stanford could accelerate this process, too.
“The promise of our technique is that you don’t need to have a culture of cells to put the antibiotic on top,” says Dr. Dionne. “What we’re finding is that from the Raman scattering, we can use that to identify – even without incubating with antibiotics – which drug the bacteria would respond to, and that’s really exciting.”
If patients can receive the antibiotic best suited for their infection, they will likely have better outcomes.
“Blood cultures can typically take 48-72 hours to come back, and then you base your clinical decisions and adjusting antibiotics based on those blood cultures,” says Richard Watkins, MD, an infectious disease physician and professor of medicine at the Northeastern Ohio Universities, Rootstown. Dr. Watkins was not involved in the study.
“Sometimes, despite your best guess, you’re wrong,” Dr. Watkins says, “and obviously, the patient could have an adverse outcome. So, if you can diagnose the pathogen sooner, that is ideal. Whatever technology enables clinicians to do that is definitely progress and a step forward.”
On a global scale, this technology could help reduce the overuse of broad-spectrum antibiotics, which contributes to antimicrobial resistance, an emerging health threat, says Dr. Dionne.
The team is working to develop the technology further into an instrument the size of a shoebox and, with further testing, commercialize the product. That could take a few years.
This technology has potential beyond bloodstream infections, too. It could be used to identify bacteria in other fluids, such as in wastewater or contaminated food.
A version of this article originally appeared on WebMD.com.
When a bacterial infection reaches the bloodstream, every second is critical. The person’s life is on the line. Yet blood tests to identify bacteria take hours to days. While waiting, doctors often prescribe broad-spectrum antibiotics in hopes of killing whatever bug may be at fault.
Someday soon, that wait time could shrink significantly, allowing health care providers to more quickly zero in on the best antibiotic for each infection – thanks to an innovation from Stanford (Calif.) University that identifies bacteria in seconds.
The cutting-edge method relies on old-school tech: an inkjet printer similar the kind you might have at home – except this one has been modified to print blood instead of ink.
The very small sample size – each drop is two trillionths of a liter, or about a billion times smaller than a raindrop – make spotting bacteria easier. Smaller samples mean fewer cells, so lab techs can more swiftly separate the bacterial spectra from other components, like red blood cells and white blood cells.
To boost efficiency even more, the researchers added gold nanoparticles, which attach to the bacteria, serving like antennas to focus the light. Machine learning – a type of artificial intelligence – helps interpret the spectrum of light and identify which fingerprint goes with which bacteria.
“It kind of wound up being this really interesting historical period where we could put the pieces together from different technologies, including nanophotonics, printing, and artificial intelligence, to help accelerate identification of bacteria in these complex samples,” says study author Jennifer Dionne, PhD, associate professor of materials science and engineering at Stanford.
Compare that to blood culture testing in hospitals, where it takes days for bacterial cells to grow and multiply inside a large machine that looks like a refrigerator. For some bacteria, like the kinds that cause tuberculosis, cultures take weeks.
Then further testing is needed to identify which antibiotics will quell the infection. The new technology from Stanford could accelerate this process, too.
“The promise of our technique is that you don’t need to have a culture of cells to put the antibiotic on top,” says Dr. Dionne. “What we’re finding is that from the Raman scattering, we can use that to identify – even without incubating with antibiotics – which drug the bacteria would respond to, and that’s really exciting.”
If patients can receive the antibiotic best suited for their infection, they will likely have better outcomes.
“Blood cultures can typically take 48-72 hours to come back, and then you base your clinical decisions and adjusting antibiotics based on those blood cultures,” says Richard Watkins, MD, an infectious disease physician and professor of medicine at the Northeastern Ohio Universities, Rootstown. Dr. Watkins was not involved in the study.
“Sometimes, despite your best guess, you’re wrong,” Dr. Watkins says, “and obviously, the patient could have an adverse outcome. So, if you can diagnose the pathogen sooner, that is ideal. Whatever technology enables clinicians to do that is definitely progress and a step forward.”
On a global scale, this technology could help reduce the overuse of broad-spectrum antibiotics, which contributes to antimicrobial resistance, an emerging health threat, says Dr. Dionne.
The team is working to develop the technology further into an instrument the size of a shoebox and, with further testing, commercialize the product. That could take a few years.
This technology has potential beyond bloodstream infections, too. It could be used to identify bacteria in other fluids, such as in wastewater or contaminated food.
A version of this article originally appeared on WebMD.com.
Ectopic pregnancy risk and levonorgestrel-releasing IUDs
Researchers report that use of any levonorgestrel-releasing intrauterine system was associated with a significantly increased risk of ectopic pregnancy, compared with other hormonal contraceptives, in a study published in JAMA.
A national health database analysis headed by Amani Meaidi, MD, PhD, of the Danish Cancer Society Research Center, Cancer Surveillance and Pharmacoepidemiology, in Copenhagen, compared the 13.5-mg with the 19.5-mg and 52-mg dosages of levonorgestrel-releasing intrauterine systems (IUSs).
The hormone content in levonorgestrel-releasing IUSs must be high enough to maintain optimal contraceptive effect but sufficiently low to minimize progestin-related adverse events, Dr. Meaidi and colleagues noted; they advised using the middle dosage of 19.5 mg. All dosages are recommended for contraception, with the highest dosage also recommended for heavy menstrual bleeding.
“If 10,000 women using the hormonal IUD for 1 year were given the 19.5-mg hormonal IUD instead of the 13.5-mg hormonal IUD, around nine ectopic pregnancies would be avoided,” Dr. Meaidi said in an interview.
“Ectopic pregnancy is an acknowledged adverse event of hormonal IUD use. Although a rare event, it is a serious one, and a difference in ectopic pregnancy safety between the two low-dose hormonal IUDs would impact my recommendations to women.”
The study
Dr. Meaidi’s group followed 963,964 women for 7.8 million person-years. For users of levonorgestrel IUS dosages 52 mg, 19.5 mg, and 13.5 mg, and other hormonal contraceptives, the median ages were 24, 22, 22, and 21 years, respectively.
Eligible women were nulliparous with no previous ectopic pregnancy, abdominal or pelvic surgery, infertility treatment, endometriosis, or use of a levonorgestrel IUS. They were followed from Jan. 1, 2001, or their 15th birthday, until July 1, 2021, age 35, pregnancy, death, emigration, or the occurrence of any exclusion criterion.
During the study period, the cohort registered 2,925 ectopic pregnancies, including 35 at 52 mg, 32 at 19.5 mg, and 80 at 13.5 mg of levonorgestrel. For all other types of hormonal contraception, there were 763 ectopic pregnancies.
In terms of adjusted absolute rates of ectopic pregnancy per 10,000 person-years, compared with other hormonal contraceptives (rate = 2.4), these were 7.7 with 52 mg levonorgestrel IUS, 7.1 with 19.5 mg, and 15.7 with 13.5 mg. They translated to comparative differences of 5.3 (95% confidence interval, 1.9-8.7), 4.8 (95% CI, 1.5-8.0), and 13.4 (95% CI, 8.8-18.1), respectively.
Corresponding adjusted relative rate ratios were 3.4, 4.1, and 7.9. For each levonorgestrel IUS dosage; the ectopic pregnancy rate increased with duration of use.
The adjusted ectopic pregnancy rate difference per 10,000 person-years between the 19.5-mg and 52-mg levonorgestrel dosages was −0.6 , and between the 13.5-mg and 52-mg doses, 8.0, with a rate ratio of 2.3. The rate difference between the 13.5-mg and 19.5-mg levonorgestrel IUS was 8.6, with a rate ratio of 1.9.
An outsider’s perspective
Offering an outsider’s perspective on the study, Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital in New York, said these data should spark further evaluation of risk of ectopic pregnancy with levonorgestrel-releasing IUDs. “The best advice for clinicians is to individualize the choice of which contraceptive to use, and when levonorgestrel IUD is selected, to individualize the appropriate dose and timing of placement,” he said in an interview.
Several additional factors may determine the best choice, Dr. Bornstein added, including medical conditions that contraindicate other contraceptives and those conditions that justify avoidance of pregnancy, as well as uterine myomas or malformation, the ability of the patient to comply with other options, and informed patient choice. “It is important to remember the potential risk for expulsion and ectopic pregnancy, maintain alertness, and use ultrasound to exclude these potential complications if suspected,” he said.
Dr. Meaidi said the mechanism of ectopic pregnancy with hormonal IUDs is unclear, but in vitro and animal studies have observed that levonorgestrel reduces the ciliary beat frequency in the fallopian tubes. “Thus, it could be hypothesized that if a woman was unfortunate enough to become pregnant using a hormonal IUD, the hormone could inhibit or slow down the movement of the zygote into the uterus for rightful intrauterine implantation and thereby increase the risk of ectopic pregnancy.”
Two coauthors of the study reported financial support from private-sector companies. Dr. Meaidi had no conflicts of interest. Dr. Bornstein disclosed no competing interests.
Researchers report that use of any levonorgestrel-releasing intrauterine system was associated with a significantly increased risk of ectopic pregnancy, compared with other hormonal contraceptives, in a study published in JAMA.
A national health database analysis headed by Amani Meaidi, MD, PhD, of the Danish Cancer Society Research Center, Cancer Surveillance and Pharmacoepidemiology, in Copenhagen, compared the 13.5-mg with the 19.5-mg and 52-mg dosages of levonorgestrel-releasing intrauterine systems (IUSs).
The hormone content in levonorgestrel-releasing IUSs must be high enough to maintain optimal contraceptive effect but sufficiently low to minimize progestin-related adverse events, Dr. Meaidi and colleagues noted; they advised using the middle dosage of 19.5 mg. All dosages are recommended for contraception, with the highest dosage also recommended for heavy menstrual bleeding.
“If 10,000 women using the hormonal IUD for 1 year were given the 19.5-mg hormonal IUD instead of the 13.5-mg hormonal IUD, around nine ectopic pregnancies would be avoided,” Dr. Meaidi said in an interview.
“Ectopic pregnancy is an acknowledged adverse event of hormonal IUD use. Although a rare event, it is a serious one, and a difference in ectopic pregnancy safety between the two low-dose hormonal IUDs would impact my recommendations to women.”
The study
Dr. Meaidi’s group followed 963,964 women for 7.8 million person-years. For users of levonorgestrel IUS dosages 52 mg, 19.5 mg, and 13.5 mg, and other hormonal contraceptives, the median ages were 24, 22, 22, and 21 years, respectively.
Eligible women were nulliparous with no previous ectopic pregnancy, abdominal or pelvic surgery, infertility treatment, endometriosis, or use of a levonorgestrel IUS. They were followed from Jan. 1, 2001, or their 15th birthday, until July 1, 2021, age 35, pregnancy, death, emigration, or the occurrence of any exclusion criterion.
During the study period, the cohort registered 2,925 ectopic pregnancies, including 35 at 52 mg, 32 at 19.5 mg, and 80 at 13.5 mg of levonorgestrel. For all other types of hormonal contraception, there were 763 ectopic pregnancies.
In terms of adjusted absolute rates of ectopic pregnancy per 10,000 person-years, compared with other hormonal contraceptives (rate = 2.4), these were 7.7 with 52 mg levonorgestrel IUS, 7.1 with 19.5 mg, and 15.7 with 13.5 mg. They translated to comparative differences of 5.3 (95% confidence interval, 1.9-8.7), 4.8 (95% CI, 1.5-8.0), and 13.4 (95% CI, 8.8-18.1), respectively.
Corresponding adjusted relative rate ratios were 3.4, 4.1, and 7.9. For each levonorgestrel IUS dosage; the ectopic pregnancy rate increased with duration of use.
The adjusted ectopic pregnancy rate difference per 10,000 person-years between the 19.5-mg and 52-mg levonorgestrel dosages was −0.6 , and between the 13.5-mg and 52-mg doses, 8.0, with a rate ratio of 2.3. The rate difference between the 13.5-mg and 19.5-mg levonorgestrel IUS was 8.6, with a rate ratio of 1.9.
An outsider’s perspective
Offering an outsider’s perspective on the study, Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital in New York, said these data should spark further evaluation of risk of ectopic pregnancy with levonorgestrel-releasing IUDs. “The best advice for clinicians is to individualize the choice of which contraceptive to use, and when levonorgestrel IUD is selected, to individualize the appropriate dose and timing of placement,” he said in an interview.
Several additional factors may determine the best choice, Dr. Bornstein added, including medical conditions that contraindicate other contraceptives and those conditions that justify avoidance of pregnancy, as well as uterine myomas or malformation, the ability of the patient to comply with other options, and informed patient choice. “It is important to remember the potential risk for expulsion and ectopic pregnancy, maintain alertness, and use ultrasound to exclude these potential complications if suspected,” he said.
Dr. Meaidi said the mechanism of ectopic pregnancy with hormonal IUDs is unclear, but in vitro and animal studies have observed that levonorgestrel reduces the ciliary beat frequency in the fallopian tubes. “Thus, it could be hypothesized that if a woman was unfortunate enough to become pregnant using a hormonal IUD, the hormone could inhibit or slow down the movement of the zygote into the uterus for rightful intrauterine implantation and thereby increase the risk of ectopic pregnancy.”
Two coauthors of the study reported financial support from private-sector companies. Dr. Meaidi had no conflicts of interest. Dr. Bornstein disclosed no competing interests.
Researchers report that use of any levonorgestrel-releasing intrauterine system was associated with a significantly increased risk of ectopic pregnancy, compared with other hormonal contraceptives, in a study published in JAMA.
A national health database analysis headed by Amani Meaidi, MD, PhD, of the Danish Cancer Society Research Center, Cancer Surveillance and Pharmacoepidemiology, in Copenhagen, compared the 13.5-mg with the 19.5-mg and 52-mg dosages of levonorgestrel-releasing intrauterine systems (IUSs).
The hormone content in levonorgestrel-releasing IUSs must be high enough to maintain optimal contraceptive effect but sufficiently low to minimize progestin-related adverse events, Dr. Meaidi and colleagues noted; they advised using the middle dosage of 19.5 mg. All dosages are recommended for contraception, with the highest dosage also recommended for heavy menstrual bleeding.
“If 10,000 women using the hormonal IUD for 1 year were given the 19.5-mg hormonal IUD instead of the 13.5-mg hormonal IUD, around nine ectopic pregnancies would be avoided,” Dr. Meaidi said in an interview.
“Ectopic pregnancy is an acknowledged adverse event of hormonal IUD use. Although a rare event, it is a serious one, and a difference in ectopic pregnancy safety between the two low-dose hormonal IUDs would impact my recommendations to women.”
The study
Dr. Meaidi’s group followed 963,964 women for 7.8 million person-years. For users of levonorgestrel IUS dosages 52 mg, 19.5 mg, and 13.5 mg, and other hormonal contraceptives, the median ages were 24, 22, 22, and 21 years, respectively.
Eligible women were nulliparous with no previous ectopic pregnancy, abdominal or pelvic surgery, infertility treatment, endometriosis, or use of a levonorgestrel IUS. They were followed from Jan. 1, 2001, or their 15th birthday, until July 1, 2021, age 35, pregnancy, death, emigration, or the occurrence of any exclusion criterion.
During the study period, the cohort registered 2,925 ectopic pregnancies, including 35 at 52 mg, 32 at 19.5 mg, and 80 at 13.5 mg of levonorgestrel. For all other types of hormonal contraception, there were 763 ectopic pregnancies.
In terms of adjusted absolute rates of ectopic pregnancy per 10,000 person-years, compared with other hormonal contraceptives (rate = 2.4), these were 7.7 with 52 mg levonorgestrel IUS, 7.1 with 19.5 mg, and 15.7 with 13.5 mg. They translated to comparative differences of 5.3 (95% confidence interval, 1.9-8.7), 4.8 (95% CI, 1.5-8.0), and 13.4 (95% CI, 8.8-18.1), respectively.
Corresponding adjusted relative rate ratios were 3.4, 4.1, and 7.9. For each levonorgestrel IUS dosage; the ectopic pregnancy rate increased with duration of use.
The adjusted ectopic pregnancy rate difference per 10,000 person-years between the 19.5-mg and 52-mg levonorgestrel dosages was −0.6 , and between the 13.5-mg and 52-mg doses, 8.0, with a rate ratio of 2.3. The rate difference between the 13.5-mg and 19.5-mg levonorgestrel IUS was 8.6, with a rate ratio of 1.9.
An outsider’s perspective
Offering an outsider’s perspective on the study, Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital in New York, said these data should spark further evaluation of risk of ectopic pregnancy with levonorgestrel-releasing IUDs. “The best advice for clinicians is to individualize the choice of which contraceptive to use, and when levonorgestrel IUD is selected, to individualize the appropriate dose and timing of placement,” he said in an interview.
Several additional factors may determine the best choice, Dr. Bornstein added, including medical conditions that contraindicate other contraceptives and those conditions that justify avoidance of pregnancy, as well as uterine myomas or malformation, the ability of the patient to comply with other options, and informed patient choice. “It is important to remember the potential risk for expulsion and ectopic pregnancy, maintain alertness, and use ultrasound to exclude these potential complications if suspected,” he said.
Dr. Meaidi said the mechanism of ectopic pregnancy with hormonal IUDs is unclear, but in vitro and animal studies have observed that levonorgestrel reduces the ciliary beat frequency in the fallopian tubes. “Thus, it could be hypothesized that if a woman was unfortunate enough to become pregnant using a hormonal IUD, the hormone could inhibit or slow down the movement of the zygote into the uterus for rightful intrauterine implantation and thereby increase the risk of ectopic pregnancy.”
Two coauthors of the study reported financial support from private-sector companies. Dr. Meaidi had no conflicts of interest. Dr. Bornstein disclosed no competing interests.
FROM JAMA