User login
The SHOW UP Act Threatens VA Telehealth
In February, the US House of Representatives hurriedly passed the Stopping Home Office Work’s Unproductive Problems (SHOW UP) Act, H.R. 139, a bill that calls into question the contributions of federal employees allowed to work from home and resets telework policies to those in place in 2019. Its author, House Oversight Committee Chairman James Comer (R, Kentucky) claimed that this change was necessary because the expansion of federal telework during the COVID-19 pandemic “has crippled the ability of agencies to get their jobs done and created backlogs.” His targets included the US Department of Veterans Affairs (VA), where, he charged, “veterans have been unable…to obtain care they have earned.” He added, “it’s hard to argue that teleworking has helped the VA.”
While oversight of government programs is an authority of Congress, the SHOW UP Act is based on unsubstantiated assumptions of dereliction. It also disregards the devastating impact the proposed changes will have on veterans’ ability to receive care and inaccurately implies improving it. As the Senate considers the bill, they should take heed of these and other facts involving this often misunderstood form of labor.
COVID-19 irrevocably transformed the use of virtual care within the VA and across the world. Even as the pandemic subsides, public and private health care systems have continued to use telework-centered telehealth far above prepandemic levels, especially for mental health and primary care. Employers, including the VA, capitalize on telework for its benefits to both consumers and the workforce. For consumers, research supports the clinical effectiveness of telemental health service, as well as its cost-effectiveness and consumer satisfaction. On the workforce side, research has documented heightened productivity, lower distractibility, and higher job satisfaction among counselors who shifted to remote work.
Remote work also serves as a key tool in attracting and retaining a qualified workforce. As one VA service chief explained, “I am having enough trouble competing with the private sector, where extensive telework is now the norm. If telework options were rolled back, the private sector will have a field day picking off my best staff.” These comments are consistent with the data. McKinsey’s American Opportunity Survey shows that Americans have embraced remote work and want more of it. Recent data from Gallup show that 6 of 10 currently exclusively remote employees would be extremely likely to change companies if they lost their remote flexibility. Further, Gallup data show that when an employee’s location preference does not match their current work location, burnout rises, and engagement drops.
Between 2019 and 2023, the VA’s telework expansion is what has enabled it to meet the growing demand for mental health services. VA is keeping pace by having 2 or more clinicians rotate between home and a shared VA office. Forcing these hybrid practitioners to work full time at VA facilities would drastically reduce the number of patients they can care for. There simply are not enough offices on crammed VA grounds to house staff who telework today. The net result would be that fewer appointments would be available, creating longer wait times. And that is just for existing patients. It does not factor in the expected influx due to new veteran eligibility made possible by the toxic exposures PACT Act.
Here is another good example of crucial VA telework: With the advent of the 988 Suicide & Crisis Lifeline, VA is adding more than 1000 new Veterans Crisis Line responders. All these new positions are remote. The SHOW UP Act would inhibit this expansion of lifesaving programs.
Veterans want more, not fewer, telehealth options. At a House Committee on Veterans’ Affairs hearing this past September, the VA reported that most veterans would prefer to receive mental health services virtually than to have to commute to a VA medical center or clinic. Telehealth benefits veterans in meaningful ways, including that it reduces their travel time, travel expense, depletion of sick leave, and need for childcare. Veterans with posttraumatic stress disorder, military sexual trauma, those with mobility issues, or those who struggle with the stigma of mental health treatment may prefer the familiarity of their own homes for care. Virtual options also relieve a patient’s need to enter a hospital and be unnecessarily exposed to contagious viruses. That’s safer not only for veterans but also for VA staff.
Finally, virtual care improves treatment. Research has revealed that the likelihood of missing telehealth appointments is lower than for in-person appointments. When patients miss appointments, continuity of care is disrupted, and health care outcomes are diminished.
The pandemic is receding, but the advantages of telework-centered virtual care are greater than ever. Political representatives who want to show up for veterans should do everything in their power to expand—not cut—VA’s ability to authorize working from home.
In February, the US House of Representatives hurriedly passed the Stopping Home Office Work’s Unproductive Problems (SHOW UP) Act, H.R. 139, a bill that calls into question the contributions of federal employees allowed to work from home and resets telework policies to those in place in 2019. Its author, House Oversight Committee Chairman James Comer (R, Kentucky) claimed that this change was necessary because the expansion of federal telework during the COVID-19 pandemic “has crippled the ability of agencies to get their jobs done and created backlogs.” His targets included the US Department of Veterans Affairs (VA), where, he charged, “veterans have been unable…to obtain care they have earned.” He added, “it’s hard to argue that teleworking has helped the VA.”
While oversight of government programs is an authority of Congress, the SHOW UP Act is based on unsubstantiated assumptions of dereliction. It also disregards the devastating impact the proposed changes will have on veterans’ ability to receive care and inaccurately implies improving it. As the Senate considers the bill, they should take heed of these and other facts involving this often misunderstood form of labor.
COVID-19 irrevocably transformed the use of virtual care within the VA and across the world. Even as the pandemic subsides, public and private health care systems have continued to use telework-centered telehealth far above prepandemic levels, especially for mental health and primary care. Employers, including the VA, capitalize on telework for its benefits to both consumers and the workforce. For consumers, research supports the clinical effectiveness of telemental health service, as well as its cost-effectiveness and consumer satisfaction. On the workforce side, research has documented heightened productivity, lower distractibility, and higher job satisfaction among counselors who shifted to remote work.
Remote work also serves as a key tool in attracting and retaining a qualified workforce. As one VA service chief explained, “I am having enough trouble competing with the private sector, where extensive telework is now the norm. If telework options were rolled back, the private sector will have a field day picking off my best staff.” These comments are consistent with the data. McKinsey’s American Opportunity Survey shows that Americans have embraced remote work and want more of it. Recent data from Gallup show that 6 of 10 currently exclusively remote employees would be extremely likely to change companies if they lost their remote flexibility. Further, Gallup data show that when an employee’s location preference does not match their current work location, burnout rises, and engagement drops.
Between 2019 and 2023, the VA’s telework expansion is what has enabled it to meet the growing demand for mental health services. VA is keeping pace by having 2 or more clinicians rotate between home and a shared VA office. Forcing these hybrid practitioners to work full time at VA facilities would drastically reduce the number of patients they can care for. There simply are not enough offices on crammed VA grounds to house staff who telework today. The net result would be that fewer appointments would be available, creating longer wait times. And that is just for existing patients. It does not factor in the expected influx due to new veteran eligibility made possible by the toxic exposures PACT Act.
Here is another good example of crucial VA telework: With the advent of the 988 Suicide & Crisis Lifeline, VA is adding more than 1000 new Veterans Crisis Line responders. All these new positions are remote. The SHOW UP Act would inhibit this expansion of lifesaving programs.
Veterans want more, not fewer, telehealth options. At a House Committee on Veterans’ Affairs hearing this past September, the VA reported that most veterans would prefer to receive mental health services virtually than to have to commute to a VA medical center or clinic. Telehealth benefits veterans in meaningful ways, including that it reduces their travel time, travel expense, depletion of sick leave, and need for childcare. Veterans with posttraumatic stress disorder, military sexual trauma, those with mobility issues, or those who struggle with the stigma of mental health treatment may prefer the familiarity of their own homes for care. Virtual options also relieve a patient’s need to enter a hospital and be unnecessarily exposed to contagious viruses. That’s safer not only for veterans but also for VA staff.
Finally, virtual care improves treatment. Research has revealed that the likelihood of missing telehealth appointments is lower than for in-person appointments. When patients miss appointments, continuity of care is disrupted, and health care outcomes are diminished.
The pandemic is receding, but the advantages of telework-centered virtual care are greater than ever. Political representatives who want to show up for veterans should do everything in their power to expand—not cut—VA’s ability to authorize working from home.
In February, the US House of Representatives hurriedly passed the Stopping Home Office Work’s Unproductive Problems (SHOW UP) Act, H.R. 139, a bill that calls into question the contributions of federal employees allowed to work from home and resets telework policies to those in place in 2019. Its author, House Oversight Committee Chairman James Comer (R, Kentucky) claimed that this change was necessary because the expansion of federal telework during the COVID-19 pandemic “has crippled the ability of agencies to get their jobs done and created backlogs.” His targets included the US Department of Veterans Affairs (VA), where, he charged, “veterans have been unable…to obtain care they have earned.” He added, “it’s hard to argue that teleworking has helped the VA.”
While oversight of government programs is an authority of Congress, the SHOW UP Act is based on unsubstantiated assumptions of dereliction. It also disregards the devastating impact the proposed changes will have on veterans’ ability to receive care and inaccurately implies improving it. As the Senate considers the bill, they should take heed of these and other facts involving this often misunderstood form of labor.
COVID-19 irrevocably transformed the use of virtual care within the VA and across the world. Even as the pandemic subsides, public and private health care systems have continued to use telework-centered telehealth far above prepandemic levels, especially for mental health and primary care. Employers, including the VA, capitalize on telework for its benefits to both consumers and the workforce. For consumers, research supports the clinical effectiveness of telemental health service, as well as its cost-effectiveness and consumer satisfaction. On the workforce side, research has documented heightened productivity, lower distractibility, and higher job satisfaction among counselors who shifted to remote work.
Remote work also serves as a key tool in attracting and retaining a qualified workforce. As one VA service chief explained, “I am having enough trouble competing with the private sector, where extensive telework is now the norm. If telework options were rolled back, the private sector will have a field day picking off my best staff.” These comments are consistent with the data. McKinsey’s American Opportunity Survey shows that Americans have embraced remote work and want more of it. Recent data from Gallup show that 6 of 10 currently exclusively remote employees would be extremely likely to change companies if they lost their remote flexibility. Further, Gallup data show that when an employee’s location preference does not match their current work location, burnout rises, and engagement drops.
Between 2019 and 2023, the VA’s telework expansion is what has enabled it to meet the growing demand for mental health services. VA is keeping pace by having 2 or more clinicians rotate between home and a shared VA office. Forcing these hybrid practitioners to work full time at VA facilities would drastically reduce the number of patients they can care for. There simply are not enough offices on crammed VA grounds to house staff who telework today. The net result would be that fewer appointments would be available, creating longer wait times. And that is just for existing patients. It does not factor in the expected influx due to new veteran eligibility made possible by the toxic exposures PACT Act.
Here is another good example of crucial VA telework: With the advent of the 988 Suicide & Crisis Lifeline, VA is adding more than 1000 new Veterans Crisis Line responders. All these new positions are remote. The SHOW UP Act would inhibit this expansion of lifesaving programs.
Veterans want more, not fewer, telehealth options. At a House Committee on Veterans’ Affairs hearing this past September, the VA reported that most veterans would prefer to receive mental health services virtually than to have to commute to a VA medical center or clinic. Telehealth benefits veterans in meaningful ways, including that it reduces their travel time, travel expense, depletion of sick leave, and need for childcare. Veterans with posttraumatic stress disorder, military sexual trauma, those with mobility issues, or those who struggle with the stigma of mental health treatment may prefer the familiarity of their own homes for care. Virtual options also relieve a patient’s need to enter a hospital and be unnecessarily exposed to contagious viruses. That’s safer not only for veterans but also for VA staff.
Finally, virtual care improves treatment. Research has revealed that the likelihood of missing telehealth appointments is lower than for in-person appointments. When patients miss appointments, continuity of care is disrupted, and health care outcomes are diminished.
The pandemic is receding, but the advantages of telework-centered virtual care are greater than ever. Political representatives who want to show up for veterans should do everything in their power to expand—not cut—VA’s ability to authorize working from home.
COORDINATEd effort boosts optimal therapy in patients with T2D and ASCVD
NEW ORLEANS – Twenty cardiology clinics successfully intensified the medical care they gave patients with type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD) after receiving a simple and scalable investigational intervention that gave the clinics’ staffs guidance on best prescribing practices and implementation and also provided quality-improvement feedback.
Within a year, these clinics quadrupled optimal medical management of these patients, compared with control clinics, in a randomized trial involving a total of 43 clinics and 1,049 patients.
“This multifaceted intervention is effective in increasing the prescription of evidence-based therapies in adults with T2D and ASCVD,” Neha J. Pagidipati, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
“The next step is to scale this intervention across cardiology practices” interested in improving the quality of care they deliver to these patients, added Dr. Pagidipati, a cardiologist specializing in cardiometabolic disease prevention at Duke University in Durham, N.C.
The goal is getting patients on triple therapy
The primary outcome of the COORDINATE-Diabetes trial was the change in the number of patients with T2D and ASCVD who received prescriptions for agents from three recommended medication classes and at recommended dosages: a high-intensity statin, a renin-angiotensin system inhibitor (RASi), and at least one agent from either of two classes that have both cardiovascular-protective and antihyperglycemic effects: the sodium-glucose cotransporter 2 (SGLT2) inhibitors, or the glucagonlike peptide 1 (GLP-1)–receptor agonists.
Among the 457 patients treated at the 20 cardiology clinics who received the quality-improvement intervention, 37.9% were on the promoted triple therapy after 12 months, compared with 14.5% of the 588 patients treated at the 23 clinics that continued with their usual care approach. This 23.4–percentage point increase in triple-class prescribing at recommended dosages represented a significant 4.4-fold increase in the goal prescribing endpoint after adjustment for possible confounders, Dr. Pagidipati reported.
Simultaneously with her report, the findings also appeared online in JAMA.
At baseline, 41%-50% of the patients were on both a high-intensity statin and a RASi, with a total of about 58%-67% on a high-intensity statin and about 70%-75% on a RASi. Fewer than 1% of patients were on SGLT2 inhibitors or GLP-1–receptor agonists at baseline. By design, no patient could be on all three categories of medication at baseline.
At their last follow-up visit (after 12 months for 97% of patients, or after 6 months for the remainder) 71% of the patients at practices that received the intervention were on a high-intensity statin, 81% were taking a RASi, and 60% were on an SGLT2 inhibitor or GLP-1–receptor agonist. Among the control patients, 58% were on a high-intensity statin, 68% on a RASi, and 36% were on one of the antihyperglycemic agents.
Effective interventions and the need for a champion
The clinics randomized to the active arm received instruction from a three-member team, either from an in-person or virtual one-time visit, on an intervention comprising several initiatives:
- Analysis of the barriers to evidence-based care at each clinic.
- Development of local interdisciplinary care pathways to address the identified barriers.
- Facilitation of care coordination among clinicians – particularly among cardiology, endocrinology, and primary care clinicians.
- Education of the clinic staff, including provision of educational materials.
- Auditing of clinic performance using specified metrics and feedback on the findings.
Clinics in the usual care group were given current clinical practice guidelines.
The investigational intervention was, by design, “low-tech and designed to be scalable,” explained Dr. Pagidipati, and once the COVID pandemic started the intervention team shifted to a virtual consultation with participating practices that was mostly front-loaded, followed by monthly phone calls to give clinics feedback on their progress.
Among the most helpful aspects of the intervention was involving the entire clinic staff, including pharmacists, nurses, and advanced care practitioners; boosting familiarity with the relevant medications and their appropriate use; and advice on navigating insurance-coverage barriers such as prior authorizations.
“What was most critical was having a local champion who took on making this effort an important part” of what the clinic was trying to do, she explained. “All it takes is passion, and the tenacity of a bulldog,” Dr. Pagidipati said.
Research advances often don’t translate into management changes
“We don’t do a great job of translating findings from trials to patient care, so any method we can use to improve that will improve practice,” commented Kristen B. Campbell, PharmD, a clinical pharmacist at Duke who was not involved in the study.
“Although the trial was not powered to look at patient outcomes, we think that patients will benefit” because all the recommended medication uses have been proven to help patients in prior trials, Dr. Campbell noted.
“A particular strength of this study was its simple design. All the interventions are low-tech and scalable.”
The low level of use of guideline-directed medical therapy in American adults with type 2 diabetes and atherosclerotic cardiovascular disease is “incredible,” said Christopher B. Granger, MD, a senior investigator on the study and a cardiologist and professor at Duke.
The researchers who ran the study are now focused on evaluating which cardiology clinics and patients had the most success from the intervention and are using that information to further refine implementation. They are also planning to encourage cardiology practices as well as other relevant medical groups to incorporate the intervention and implementation model used in the trial. The intervention program is detailed and available at no charge on the COORDINATE-Diabetes website.
COORDINATE-Diabetes received funding from Boehringer Ingelheim and Eli Lilly. Dr. Pagidipati has received personal fees from Boehringer Ingelheim, Lilly, AstraZeneca, Novartis, Novo Nordisk, Merck, and CRISPR Therapeutics, and she has received research grants from Amgen, Novartis, Novo Nordisk, and Eggland’s Best. Dr. Campbell had no disclosures. Dr. Granger has received personal fees and research funding from numerous companies.
NEW ORLEANS – Twenty cardiology clinics successfully intensified the medical care they gave patients with type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD) after receiving a simple and scalable investigational intervention that gave the clinics’ staffs guidance on best prescribing practices and implementation and also provided quality-improvement feedback.
Within a year, these clinics quadrupled optimal medical management of these patients, compared with control clinics, in a randomized trial involving a total of 43 clinics and 1,049 patients.
“This multifaceted intervention is effective in increasing the prescription of evidence-based therapies in adults with T2D and ASCVD,” Neha J. Pagidipati, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
“The next step is to scale this intervention across cardiology practices” interested in improving the quality of care they deliver to these patients, added Dr. Pagidipati, a cardiologist specializing in cardiometabolic disease prevention at Duke University in Durham, N.C.
The goal is getting patients on triple therapy
The primary outcome of the COORDINATE-Diabetes trial was the change in the number of patients with T2D and ASCVD who received prescriptions for agents from three recommended medication classes and at recommended dosages: a high-intensity statin, a renin-angiotensin system inhibitor (RASi), and at least one agent from either of two classes that have both cardiovascular-protective and antihyperglycemic effects: the sodium-glucose cotransporter 2 (SGLT2) inhibitors, or the glucagonlike peptide 1 (GLP-1)–receptor agonists.
Among the 457 patients treated at the 20 cardiology clinics who received the quality-improvement intervention, 37.9% were on the promoted triple therapy after 12 months, compared with 14.5% of the 588 patients treated at the 23 clinics that continued with their usual care approach. This 23.4–percentage point increase in triple-class prescribing at recommended dosages represented a significant 4.4-fold increase in the goal prescribing endpoint after adjustment for possible confounders, Dr. Pagidipati reported.
Simultaneously with her report, the findings also appeared online in JAMA.
At baseline, 41%-50% of the patients were on both a high-intensity statin and a RASi, with a total of about 58%-67% on a high-intensity statin and about 70%-75% on a RASi. Fewer than 1% of patients were on SGLT2 inhibitors or GLP-1–receptor agonists at baseline. By design, no patient could be on all three categories of medication at baseline.
At their last follow-up visit (after 12 months for 97% of patients, or after 6 months for the remainder) 71% of the patients at practices that received the intervention were on a high-intensity statin, 81% were taking a RASi, and 60% were on an SGLT2 inhibitor or GLP-1–receptor agonist. Among the control patients, 58% were on a high-intensity statin, 68% on a RASi, and 36% were on one of the antihyperglycemic agents.
Effective interventions and the need for a champion
The clinics randomized to the active arm received instruction from a three-member team, either from an in-person or virtual one-time visit, on an intervention comprising several initiatives:
- Analysis of the barriers to evidence-based care at each clinic.
- Development of local interdisciplinary care pathways to address the identified barriers.
- Facilitation of care coordination among clinicians – particularly among cardiology, endocrinology, and primary care clinicians.
- Education of the clinic staff, including provision of educational materials.
- Auditing of clinic performance using specified metrics and feedback on the findings.
Clinics in the usual care group were given current clinical practice guidelines.
The investigational intervention was, by design, “low-tech and designed to be scalable,” explained Dr. Pagidipati, and once the COVID pandemic started the intervention team shifted to a virtual consultation with participating practices that was mostly front-loaded, followed by monthly phone calls to give clinics feedback on their progress.
Among the most helpful aspects of the intervention was involving the entire clinic staff, including pharmacists, nurses, and advanced care practitioners; boosting familiarity with the relevant medications and their appropriate use; and advice on navigating insurance-coverage barriers such as prior authorizations.
“What was most critical was having a local champion who took on making this effort an important part” of what the clinic was trying to do, she explained. “All it takes is passion, and the tenacity of a bulldog,” Dr. Pagidipati said.
Research advances often don’t translate into management changes
“We don’t do a great job of translating findings from trials to patient care, so any method we can use to improve that will improve practice,” commented Kristen B. Campbell, PharmD, a clinical pharmacist at Duke who was not involved in the study.
“Although the trial was not powered to look at patient outcomes, we think that patients will benefit” because all the recommended medication uses have been proven to help patients in prior trials, Dr. Campbell noted.
“A particular strength of this study was its simple design. All the interventions are low-tech and scalable.”
The low level of use of guideline-directed medical therapy in American adults with type 2 diabetes and atherosclerotic cardiovascular disease is “incredible,” said Christopher B. Granger, MD, a senior investigator on the study and a cardiologist and professor at Duke.
The researchers who ran the study are now focused on evaluating which cardiology clinics and patients had the most success from the intervention and are using that information to further refine implementation. They are also planning to encourage cardiology practices as well as other relevant medical groups to incorporate the intervention and implementation model used in the trial. The intervention program is detailed and available at no charge on the COORDINATE-Diabetes website.
COORDINATE-Diabetes received funding from Boehringer Ingelheim and Eli Lilly. Dr. Pagidipati has received personal fees from Boehringer Ingelheim, Lilly, AstraZeneca, Novartis, Novo Nordisk, Merck, and CRISPR Therapeutics, and she has received research grants from Amgen, Novartis, Novo Nordisk, and Eggland’s Best. Dr. Campbell had no disclosures. Dr. Granger has received personal fees and research funding from numerous companies.
NEW ORLEANS – Twenty cardiology clinics successfully intensified the medical care they gave patients with type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD) after receiving a simple and scalable investigational intervention that gave the clinics’ staffs guidance on best prescribing practices and implementation and also provided quality-improvement feedback.
Within a year, these clinics quadrupled optimal medical management of these patients, compared with control clinics, in a randomized trial involving a total of 43 clinics and 1,049 patients.
“This multifaceted intervention is effective in increasing the prescription of evidence-based therapies in adults with T2D and ASCVD,” Neha J. Pagidipati, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
“The next step is to scale this intervention across cardiology practices” interested in improving the quality of care they deliver to these patients, added Dr. Pagidipati, a cardiologist specializing in cardiometabolic disease prevention at Duke University in Durham, N.C.
The goal is getting patients on triple therapy
The primary outcome of the COORDINATE-Diabetes trial was the change in the number of patients with T2D and ASCVD who received prescriptions for agents from three recommended medication classes and at recommended dosages: a high-intensity statin, a renin-angiotensin system inhibitor (RASi), and at least one agent from either of two classes that have both cardiovascular-protective and antihyperglycemic effects: the sodium-glucose cotransporter 2 (SGLT2) inhibitors, or the glucagonlike peptide 1 (GLP-1)–receptor agonists.
Among the 457 patients treated at the 20 cardiology clinics who received the quality-improvement intervention, 37.9% were on the promoted triple therapy after 12 months, compared with 14.5% of the 588 patients treated at the 23 clinics that continued with their usual care approach. This 23.4–percentage point increase in triple-class prescribing at recommended dosages represented a significant 4.4-fold increase in the goal prescribing endpoint after adjustment for possible confounders, Dr. Pagidipati reported.
Simultaneously with her report, the findings also appeared online in JAMA.
At baseline, 41%-50% of the patients were on both a high-intensity statin and a RASi, with a total of about 58%-67% on a high-intensity statin and about 70%-75% on a RASi. Fewer than 1% of patients were on SGLT2 inhibitors or GLP-1–receptor agonists at baseline. By design, no patient could be on all three categories of medication at baseline.
At their last follow-up visit (after 12 months for 97% of patients, or after 6 months for the remainder) 71% of the patients at practices that received the intervention were on a high-intensity statin, 81% were taking a RASi, and 60% were on an SGLT2 inhibitor or GLP-1–receptor agonist. Among the control patients, 58% were on a high-intensity statin, 68% on a RASi, and 36% were on one of the antihyperglycemic agents.
Effective interventions and the need for a champion
The clinics randomized to the active arm received instruction from a three-member team, either from an in-person or virtual one-time visit, on an intervention comprising several initiatives:
- Analysis of the barriers to evidence-based care at each clinic.
- Development of local interdisciplinary care pathways to address the identified barriers.
- Facilitation of care coordination among clinicians – particularly among cardiology, endocrinology, and primary care clinicians.
- Education of the clinic staff, including provision of educational materials.
- Auditing of clinic performance using specified metrics and feedback on the findings.
Clinics in the usual care group were given current clinical practice guidelines.
The investigational intervention was, by design, “low-tech and designed to be scalable,” explained Dr. Pagidipati, and once the COVID pandemic started the intervention team shifted to a virtual consultation with participating practices that was mostly front-loaded, followed by monthly phone calls to give clinics feedback on their progress.
Among the most helpful aspects of the intervention was involving the entire clinic staff, including pharmacists, nurses, and advanced care practitioners; boosting familiarity with the relevant medications and their appropriate use; and advice on navigating insurance-coverage barriers such as prior authorizations.
“What was most critical was having a local champion who took on making this effort an important part” of what the clinic was trying to do, she explained. “All it takes is passion, and the tenacity of a bulldog,” Dr. Pagidipati said.
Research advances often don’t translate into management changes
“We don’t do a great job of translating findings from trials to patient care, so any method we can use to improve that will improve practice,” commented Kristen B. Campbell, PharmD, a clinical pharmacist at Duke who was not involved in the study.
“Although the trial was not powered to look at patient outcomes, we think that patients will benefit” because all the recommended medication uses have been proven to help patients in prior trials, Dr. Campbell noted.
“A particular strength of this study was its simple design. All the interventions are low-tech and scalable.”
The low level of use of guideline-directed medical therapy in American adults with type 2 diabetes and atherosclerotic cardiovascular disease is “incredible,” said Christopher B. Granger, MD, a senior investigator on the study and a cardiologist and professor at Duke.
The researchers who ran the study are now focused on evaluating which cardiology clinics and patients had the most success from the intervention and are using that information to further refine implementation. They are also planning to encourage cardiology practices as well as other relevant medical groups to incorporate the intervention and implementation model used in the trial. The intervention program is detailed and available at no charge on the COORDINATE-Diabetes website.
COORDINATE-Diabetes received funding from Boehringer Ingelheim and Eli Lilly. Dr. Pagidipati has received personal fees from Boehringer Ingelheim, Lilly, AstraZeneca, Novartis, Novo Nordisk, Merck, and CRISPR Therapeutics, and she has received research grants from Amgen, Novartis, Novo Nordisk, and Eggland’s Best. Dr. Campbell had no disclosures. Dr. Granger has received personal fees and research funding from numerous companies.
AT ACC 2023
Shaved costs, high risk, maximum profits: Regulators worry about Florida’s butt lift boom
The office in Miami where she scheduled what’s known as a Brazilian butt lift had closed and transferred her records to a different facility, she said. The price she was quoted – and paid upfront – increased the day of the procedure, and she said she did not meet her surgeon until she was about to be placed under general anesthesia.
“I was ready to walk out,” said Ms. Ruston, 44, of Lake Alfred in Central Florida. “But I had paid everything.”
A few days after the July procedure, Ms. Ruston was hospitalized because of infection, blood loss, and nausea, her medical records show.
“I went cheap. That’s what I did,” Ms. Ruston recalled recently. “I looked for the lowest price, and I found him on Instagram.”
People like Ms. Ruston are commonly lured to office-based surgery centers in South Florida through social media marketing that makes Brazilian butt lifts and other cosmetic surgery look deceptively painless, safe, and affordable, say researchers, patient advocates, and surgeon groups.
Unlike ambulatory surgery centers and hospitals, where a patient might stay overnight for observation after treatment, office-based surgery centers offer procedures that don’t typically require an inpatient stay and are regulated as an extension of a doctor’s private practice.
But such surgical offices are often owned by corporations that can offer discount prices by contracting with surgeons who are incentivized to work on as many patients per day as possible, in as little time as possible, according to state regulators and physicians critical of the facilities.
After a rash of deaths, and in the absence of national standards, Florida regulators were the first in the nation to enact rules in 2019 meant to make the procedures safer. More than 3 years later, data shows deaths still occur.
Patient advocates and some surgeons – including those who perform the procedure themselves – anticipate the problem will only get worse. Emergency restrictions imposed by the state’s medical board in June expired in September, and the corporate business model popularized in Miami is spreading to other cities.
“We’re seeing entities that have a strong footprint in low-cost, high-volume cosmetic surgery, based in South Florida, manifesting in other parts of the country,” said Bob Basu, MD, MPH, a vice president of the American Society of Plastic Surgeons and a practicing physician in Houston.
During a Brazilian butt lift, fat is taken via liposuction from other areas of the body – such as the torso, back, or thighs – and injected into the buttocks. More than 61,000 buttock augmentation procedures, both butt lifts and implants, were performed nationwide in 2021, a 37% increase from the previous year, according to data from the Aesthetic Society, a trade group of plastic surgeons.
As with all surgery, complications can occur. Miami-Dade County’s medical examiner has documented nearly three dozen cosmetic surgery patient deaths since 2009, of which 26 resulted from a Brazilian butt lift. In each case, the person died from a pulmonary fat embolism, when fat entered the bloodstream through veins in the gluteal muscles and stopped blood from flowing to the lungs.
No national reporting system or insurance code tracks outcomes and patient demographics for a Brazilian butt lift. About 3% of surgeons worldwide had a patient die as a result of the procedure, according to a 2017 report from an Aesthetic Surgery Education and Research Foundation task force.
Medical experts said the problem is driven, in part, by having medical professionals like physician assistants and nurse practitioners perform key parts of the butt lift instead of doctors. It’s also driven by a business model that is motivated by profit, not safety, and incentivizes surgeons to exceed the number of surgeries outlined in their contracts.
In May, after a fifth patient in as many months died of complications in Miami-Dade County, Kevin Cairns, MD, proposed the state’s emergency rule to limit the number of butt lifts a surgeon could perform each day.
“I was getting sick of reading about women dying and seeing cases come before the board,” said Dr. Cairns, a physician and former member of the Florida Board of Medicine.
Some doctors performed as many as seven, according to disciplinary cases against surgeons prosecuted by the Florida Department of Health. The emergency rule limited them to no more than three, and required the use of an ultrasound to help surgeons lower the risk of a pulmonary fat clot.
But a group of physicians who perform Brazilian butt lifts in South Florida clapped back and formed Surgeons for Safety. They argued the new requirements would make the situation worse. Qualified doctors would have to do fewer procedures, they said, thus driving patients to dangerous medical professionals who don’t follow rules.
The group has since donated more than $350,000 to the state’s Republican Party, Republican candidates, and Republican political action committees, according to campaign contribution data from the Florida Department of State.
Surgeons for Safety declined KHN’s repeated interview requests. Although the group’s president, Constantino Mendieta, MD, wrote in an August editorial that he agreed not all surgeons have followed the standard of care, he called the limits put on surgeons “arbitrary.” The rule sets “a historic precedent of controlling surgeons,” he said during a meeting with Florida’s medical board.
In January, Florida state Sen. Ileana Garcia, a Republican, filed a draft bill with the state legislature that proposes no limit on the number of Brazilian butt lifts a surgeon can perform in a day. Instead, it requires office surgery centers where the procedures are performed to staff one physician per patient and prohibits surgeons from working on more than one person at a time.
The bill would also allow surgeons to delegate some parts of the procedure to other clinicians under their direct supervision.
Florida’s legislature convenes on March 7.
Consumers considering cosmetic procedures are urged to be cautious. Like Ms. Ruston, many people base their expectations on before-and-after photos and marketing videos posted on social media platforms such as Facebook, Snapchat, and Instagram.
“That’s very dangerous,” said Dr. Basu, of the American Society of Plastic Surgeons. “They’re excited about a low price and they forget about doing their homework,” he said.
The average price of a buttocks augmentation in 2021 was $4,000, according to data from the Aesthetic Society. But that’s only for the physician’s fee and does not cover anesthesia, operating room fees, prescriptions, or other expenses. A “safe” Brazilian butt lift, performed in an accredited facility and with proper aftercare, costs between $12,000 and $18,000, according to a recent article on the American Society of Plastic Surgeons’ website.
Although Florida requires a physician’s license to perform liposuction on patients who are under general anesthesia, it’s common in the medical field for midlevel medical practitioners, such as physician assistants and nurse practitioners, to do the procedure in office settings, according to Mark Mofid, MD, who coauthored the 2017 Aesthetic Surgery Education and Research Foundation task force study.
By relying on staffers who don’t have the same specialty training and get paid less, office-based surgeons can complete more butt lifts per day and charge a lower price.
“They’re doing all of them simultaneously in three or four different rooms, and it’s being staffed by one surgeon,” said Dr. Mofid, a plastic surgeon in San Diego, who added that he does not perform more than one Brazilian butt lift in a day. “The surgeon isn’t doing the actual case. It’s assistants.”
Dr. Basu said patients should ask whether their doctor holds privileges to perform the same procedure at a hospital or ambulatory surgery center, which have stricter rules than office surgery centers in terms of who can perform butt lifts and how they should be done.
People in search of bargains are reminded that cosmetic surgery can have other serious risks beyond the deadly fat clots, such as infection and organ puncture, plus problems with the kidneys, heart, and lungs.
Ms. Ruston’s surgery was performed by a board-certified plastic surgeon she said she found on Instagram. She was originally quoted $4,995, which she said she paid in full before surgery. But when she arrived in Miami, she said, the clinic tacked on fees for liposuction and for postsurgical garments and devices.
“I ended up having to pay, like, $8,000,” Ms. Ruston said. A few days after Ms. Ruston returned home to Lake Alfred, she said, she started to feel dizzy and weak and called 911.
Paramedics took her to an emergency room, where doctors diagnosed her with anemia due to blood loss, and blood and abdominal infections, her medical records show.
“If I could go back in time,” she said, “I wouldn’t have had it done.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The office in Miami where she scheduled what’s known as a Brazilian butt lift had closed and transferred her records to a different facility, she said. The price she was quoted – and paid upfront – increased the day of the procedure, and she said she did not meet her surgeon until she was about to be placed under general anesthesia.
“I was ready to walk out,” said Ms. Ruston, 44, of Lake Alfred in Central Florida. “But I had paid everything.”
A few days after the July procedure, Ms. Ruston was hospitalized because of infection, blood loss, and nausea, her medical records show.
“I went cheap. That’s what I did,” Ms. Ruston recalled recently. “I looked for the lowest price, and I found him on Instagram.”
People like Ms. Ruston are commonly lured to office-based surgery centers in South Florida through social media marketing that makes Brazilian butt lifts and other cosmetic surgery look deceptively painless, safe, and affordable, say researchers, patient advocates, and surgeon groups.
Unlike ambulatory surgery centers and hospitals, where a patient might stay overnight for observation after treatment, office-based surgery centers offer procedures that don’t typically require an inpatient stay and are regulated as an extension of a doctor’s private practice.
But such surgical offices are often owned by corporations that can offer discount prices by contracting with surgeons who are incentivized to work on as many patients per day as possible, in as little time as possible, according to state regulators and physicians critical of the facilities.
After a rash of deaths, and in the absence of national standards, Florida regulators were the first in the nation to enact rules in 2019 meant to make the procedures safer. More than 3 years later, data shows deaths still occur.
Patient advocates and some surgeons – including those who perform the procedure themselves – anticipate the problem will only get worse. Emergency restrictions imposed by the state’s medical board in June expired in September, and the corporate business model popularized in Miami is spreading to other cities.
“We’re seeing entities that have a strong footprint in low-cost, high-volume cosmetic surgery, based in South Florida, manifesting in other parts of the country,” said Bob Basu, MD, MPH, a vice president of the American Society of Plastic Surgeons and a practicing physician in Houston.
During a Brazilian butt lift, fat is taken via liposuction from other areas of the body – such as the torso, back, or thighs – and injected into the buttocks. More than 61,000 buttock augmentation procedures, both butt lifts and implants, were performed nationwide in 2021, a 37% increase from the previous year, according to data from the Aesthetic Society, a trade group of plastic surgeons.
As with all surgery, complications can occur. Miami-Dade County’s medical examiner has documented nearly three dozen cosmetic surgery patient deaths since 2009, of which 26 resulted from a Brazilian butt lift. In each case, the person died from a pulmonary fat embolism, when fat entered the bloodstream through veins in the gluteal muscles and stopped blood from flowing to the lungs.
No national reporting system or insurance code tracks outcomes and patient demographics for a Brazilian butt lift. About 3% of surgeons worldwide had a patient die as a result of the procedure, according to a 2017 report from an Aesthetic Surgery Education and Research Foundation task force.
Medical experts said the problem is driven, in part, by having medical professionals like physician assistants and nurse practitioners perform key parts of the butt lift instead of doctors. It’s also driven by a business model that is motivated by profit, not safety, and incentivizes surgeons to exceed the number of surgeries outlined in their contracts.
In May, after a fifth patient in as many months died of complications in Miami-Dade County, Kevin Cairns, MD, proposed the state’s emergency rule to limit the number of butt lifts a surgeon could perform each day.
“I was getting sick of reading about women dying and seeing cases come before the board,” said Dr. Cairns, a physician and former member of the Florida Board of Medicine.
Some doctors performed as many as seven, according to disciplinary cases against surgeons prosecuted by the Florida Department of Health. The emergency rule limited them to no more than three, and required the use of an ultrasound to help surgeons lower the risk of a pulmonary fat clot.
But a group of physicians who perform Brazilian butt lifts in South Florida clapped back and formed Surgeons for Safety. They argued the new requirements would make the situation worse. Qualified doctors would have to do fewer procedures, they said, thus driving patients to dangerous medical professionals who don’t follow rules.
The group has since donated more than $350,000 to the state’s Republican Party, Republican candidates, and Republican political action committees, according to campaign contribution data from the Florida Department of State.
Surgeons for Safety declined KHN’s repeated interview requests. Although the group’s president, Constantino Mendieta, MD, wrote in an August editorial that he agreed not all surgeons have followed the standard of care, he called the limits put on surgeons “arbitrary.” The rule sets “a historic precedent of controlling surgeons,” he said during a meeting with Florida’s medical board.
In January, Florida state Sen. Ileana Garcia, a Republican, filed a draft bill with the state legislature that proposes no limit on the number of Brazilian butt lifts a surgeon can perform in a day. Instead, it requires office surgery centers where the procedures are performed to staff one physician per patient and prohibits surgeons from working on more than one person at a time.
The bill would also allow surgeons to delegate some parts of the procedure to other clinicians under their direct supervision.
Florida’s legislature convenes on March 7.
Consumers considering cosmetic procedures are urged to be cautious. Like Ms. Ruston, many people base their expectations on before-and-after photos and marketing videos posted on social media platforms such as Facebook, Snapchat, and Instagram.
“That’s very dangerous,” said Dr. Basu, of the American Society of Plastic Surgeons. “They’re excited about a low price and they forget about doing their homework,” he said.
The average price of a buttocks augmentation in 2021 was $4,000, according to data from the Aesthetic Society. But that’s only for the physician’s fee and does not cover anesthesia, operating room fees, prescriptions, or other expenses. A “safe” Brazilian butt lift, performed in an accredited facility and with proper aftercare, costs between $12,000 and $18,000, according to a recent article on the American Society of Plastic Surgeons’ website.
Although Florida requires a physician’s license to perform liposuction on patients who are under general anesthesia, it’s common in the medical field for midlevel medical practitioners, such as physician assistants and nurse practitioners, to do the procedure in office settings, according to Mark Mofid, MD, who coauthored the 2017 Aesthetic Surgery Education and Research Foundation task force study.
By relying on staffers who don’t have the same specialty training and get paid less, office-based surgeons can complete more butt lifts per day and charge a lower price.
“They’re doing all of them simultaneously in three or four different rooms, and it’s being staffed by one surgeon,” said Dr. Mofid, a plastic surgeon in San Diego, who added that he does not perform more than one Brazilian butt lift in a day. “The surgeon isn’t doing the actual case. It’s assistants.”
Dr. Basu said patients should ask whether their doctor holds privileges to perform the same procedure at a hospital or ambulatory surgery center, which have stricter rules than office surgery centers in terms of who can perform butt lifts and how they should be done.
People in search of bargains are reminded that cosmetic surgery can have other serious risks beyond the deadly fat clots, such as infection and organ puncture, plus problems with the kidneys, heart, and lungs.
Ms. Ruston’s surgery was performed by a board-certified plastic surgeon she said she found on Instagram. She was originally quoted $4,995, which she said she paid in full before surgery. But when she arrived in Miami, she said, the clinic tacked on fees for liposuction and for postsurgical garments and devices.
“I ended up having to pay, like, $8,000,” Ms. Ruston said. A few days after Ms. Ruston returned home to Lake Alfred, she said, she started to feel dizzy and weak and called 911.
Paramedics took her to an emergency room, where doctors diagnosed her with anemia due to blood loss, and blood and abdominal infections, her medical records show.
“If I could go back in time,” she said, “I wouldn’t have had it done.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The office in Miami where she scheduled what’s known as a Brazilian butt lift had closed and transferred her records to a different facility, she said. The price she was quoted – and paid upfront – increased the day of the procedure, and she said she did not meet her surgeon until she was about to be placed under general anesthesia.
“I was ready to walk out,” said Ms. Ruston, 44, of Lake Alfred in Central Florida. “But I had paid everything.”
A few days after the July procedure, Ms. Ruston was hospitalized because of infection, blood loss, and nausea, her medical records show.
“I went cheap. That’s what I did,” Ms. Ruston recalled recently. “I looked for the lowest price, and I found him on Instagram.”
People like Ms. Ruston are commonly lured to office-based surgery centers in South Florida through social media marketing that makes Brazilian butt lifts and other cosmetic surgery look deceptively painless, safe, and affordable, say researchers, patient advocates, and surgeon groups.
Unlike ambulatory surgery centers and hospitals, where a patient might stay overnight for observation after treatment, office-based surgery centers offer procedures that don’t typically require an inpatient stay and are regulated as an extension of a doctor’s private practice.
But such surgical offices are often owned by corporations that can offer discount prices by contracting with surgeons who are incentivized to work on as many patients per day as possible, in as little time as possible, according to state regulators and physicians critical of the facilities.
After a rash of deaths, and in the absence of national standards, Florida regulators were the first in the nation to enact rules in 2019 meant to make the procedures safer. More than 3 years later, data shows deaths still occur.
Patient advocates and some surgeons – including those who perform the procedure themselves – anticipate the problem will only get worse. Emergency restrictions imposed by the state’s medical board in June expired in September, and the corporate business model popularized in Miami is spreading to other cities.
“We’re seeing entities that have a strong footprint in low-cost, high-volume cosmetic surgery, based in South Florida, manifesting in other parts of the country,” said Bob Basu, MD, MPH, a vice president of the American Society of Plastic Surgeons and a practicing physician in Houston.
During a Brazilian butt lift, fat is taken via liposuction from other areas of the body – such as the torso, back, or thighs – and injected into the buttocks. More than 61,000 buttock augmentation procedures, both butt lifts and implants, were performed nationwide in 2021, a 37% increase from the previous year, according to data from the Aesthetic Society, a trade group of plastic surgeons.
As with all surgery, complications can occur. Miami-Dade County’s medical examiner has documented nearly three dozen cosmetic surgery patient deaths since 2009, of which 26 resulted from a Brazilian butt lift. In each case, the person died from a pulmonary fat embolism, when fat entered the bloodstream through veins in the gluteal muscles and stopped blood from flowing to the lungs.
No national reporting system or insurance code tracks outcomes and patient demographics for a Brazilian butt lift. About 3% of surgeons worldwide had a patient die as a result of the procedure, according to a 2017 report from an Aesthetic Surgery Education and Research Foundation task force.
Medical experts said the problem is driven, in part, by having medical professionals like physician assistants and nurse practitioners perform key parts of the butt lift instead of doctors. It’s also driven by a business model that is motivated by profit, not safety, and incentivizes surgeons to exceed the number of surgeries outlined in their contracts.
In May, after a fifth patient in as many months died of complications in Miami-Dade County, Kevin Cairns, MD, proposed the state’s emergency rule to limit the number of butt lifts a surgeon could perform each day.
“I was getting sick of reading about women dying and seeing cases come before the board,” said Dr. Cairns, a physician and former member of the Florida Board of Medicine.
Some doctors performed as many as seven, according to disciplinary cases against surgeons prosecuted by the Florida Department of Health. The emergency rule limited them to no more than three, and required the use of an ultrasound to help surgeons lower the risk of a pulmonary fat clot.
But a group of physicians who perform Brazilian butt lifts in South Florida clapped back and formed Surgeons for Safety. They argued the new requirements would make the situation worse. Qualified doctors would have to do fewer procedures, they said, thus driving patients to dangerous medical professionals who don’t follow rules.
The group has since donated more than $350,000 to the state’s Republican Party, Republican candidates, and Republican political action committees, according to campaign contribution data from the Florida Department of State.
Surgeons for Safety declined KHN’s repeated interview requests. Although the group’s president, Constantino Mendieta, MD, wrote in an August editorial that he agreed not all surgeons have followed the standard of care, he called the limits put on surgeons “arbitrary.” The rule sets “a historic precedent of controlling surgeons,” he said during a meeting with Florida’s medical board.
In January, Florida state Sen. Ileana Garcia, a Republican, filed a draft bill with the state legislature that proposes no limit on the number of Brazilian butt lifts a surgeon can perform in a day. Instead, it requires office surgery centers where the procedures are performed to staff one physician per patient and prohibits surgeons from working on more than one person at a time.
The bill would also allow surgeons to delegate some parts of the procedure to other clinicians under their direct supervision.
Florida’s legislature convenes on March 7.
Consumers considering cosmetic procedures are urged to be cautious. Like Ms. Ruston, many people base their expectations on before-and-after photos and marketing videos posted on social media platforms such as Facebook, Snapchat, and Instagram.
“That’s very dangerous,” said Dr. Basu, of the American Society of Plastic Surgeons. “They’re excited about a low price and they forget about doing their homework,” he said.
The average price of a buttocks augmentation in 2021 was $4,000, according to data from the Aesthetic Society. But that’s only for the physician’s fee and does not cover anesthesia, operating room fees, prescriptions, or other expenses. A “safe” Brazilian butt lift, performed in an accredited facility and with proper aftercare, costs between $12,000 and $18,000, according to a recent article on the American Society of Plastic Surgeons’ website.
Although Florida requires a physician’s license to perform liposuction on patients who are under general anesthesia, it’s common in the medical field for midlevel medical practitioners, such as physician assistants and nurse practitioners, to do the procedure in office settings, according to Mark Mofid, MD, who coauthored the 2017 Aesthetic Surgery Education and Research Foundation task force study.
By relying on staffers who don’t have the same specialty training and get paid less, office-based surgeons can complete more butt lifts per day and charge a lower price.
“They’re doing all of them simultaneously in three or four different rooms, and it’s being staffed by one surgeon,” said Dr. Mofid, a plastic surgeon in San Diego, who added that he does not perform more than one Brazilian butt lift in a day. “The surgeon isn’t doing the actual case. It’s assistants.”
Dr. Basu said patients should ask whether their doctor holds privileges to perform the same procedure at a hospital or ambulatory surgery center, which have stricter rules than office surgery centers in terms of who can perform butt lifts and how they should be done.
People in search of bargains are reminded that cosmetic surgery can have other serious risks beyond the deadly fat clots, such as infection and organ puncture, plus problems with the kidneys, heart, and lungs.
Ms. Ruston’s surgery was performed by a board-certified plastic surgeon she said she found on Instagram. She was originally quoted $4,995, which she said she paid in full before surgery. But when she arrived in Miami, she said, the clinic tacked on fees for liposuction and for postsurgical garments and devices.
“I ended up having to pay, like, $8,000,” Ms. Ruston said. A few days after Ms. Ruston returned home to Lake Alfred, she said, she started to feel dizzy and weak and called 911.
Paramedics took her to an emergency room, where doctors diagnosed her with anemia due to blood loss, and blood and abdominal infections, her medical records show.
“If I could go back in time,” she said, “I wouldn’t have had it done.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Nicotinamide does not prevent skin cancer after organ transplant
published in the New England Journal of Medicine.
“No signal of efficacy was observed,” said investigators led by Nicholas Allen, MPH, of the University of Sydney department of dermatology.
These results fill an “important gap in our understanding” and “will probably change the practice of many skin-cancer physicians,” two experts on the topic commented in a related editorial.
The editorialists are David Miller, MD, PhD, a dermatologist and medical oncologist at Massachusetts General Hospital, and Kevin Emerick, MD, a head and neck surgeon as Massachusetts Eye and Ear, both in Boston.
Transplant patients have 50 times the risk of nonmelanoma skin cancers – also known as keratinocyte cancers – than the general public, owing to immunosuppression, and their lesions are more aggressive and are more likely to metastasize, they explain.
Nicotinamide (vitamin B3) has been shown to prevent nonmelanoma skin cancers in healthy, immunocompetent people, so physicians routinely prescribe it to transplant patients on the assumption that it will do the same for them, they comment.
The Australian investigators decided to put the assumption to the test.
The team randomly assigned 79 patients who had undergone solid-organ transplant to receive nicotinamide 500 mg twice a day and 79 other patients to receive twice-daily placebo for a year. Participants underwent dermatology exams every 3 months to check for new lesions.
The participants were at high risk for new lesions; some had had more than 40 in the previous 5 years. The two groups were well balanced; kidney transplants were the most common.
At 12 months, there was virtually no difference in the incidence of new nonmelanoma skin cancers: 207 in the nicotinamide group and 210 in the placebo group (P = .96).
There was also no significant difference in squamous cell and basal cell carcinoma counts or actinic keratosis counts.
“The interpretation of the results is straightforward: nicotinamide lacks clinical usefulness in preventing the development of keratinocyte carcinomas in solid-organ transplant recipients,” the team concludes.
As for why nicotinamide didn’t work in the trial, the investigators say it could be because it is not potent enough to overcome the stifling of antitumor immunity and DNA-repair enzymes with immunosuppression.
Fewer than half of participants in the trial reported using sunscreen at any point during the study, which is in line with past reports that transplant patients don’t routinely use sunscreen.
Two other strategies for preventing squamous cell carcinoma after transplant – use of oral retinoids and mTOR inhibitors – are problematic for various reasons, and use was low in both study arms.
Editorialists Dr. Miller and Dr. Emerick suggest a possible new approach: immune checkpoint inhibitors before transplant to reduce the risk of nonmelanoma skin cancer afterward. They say the strategy should be explored and that ongoing efforts to minimize or eliminate the need for immunosuppression after transplant are promising.
The investigators originally planned to enroll 254 persons, but the trial was stopped early because of poor recruitment. Potential participants may already have been taking nicotinamide, which is commonly used, and that may have affected recruitment, the investigators say.
The work was funded by Australia’s National Health and Medical Research Council. Dr. Allen has disclosed no relevant financial relationships. One investigator has received speaker’s fees from BMS. Another is a consultant for many companies, including Amgen, BMS, GlaxoSmithKline, and Merck. Dr. Emerick is an advisor for Regeneron, Sanofi, and Castle Biosciences. Dr. Miller is a researcher or consultant for those companies as well as Pfizer and others and has stock options in Avstera.
A version of this article first appeared on Medscape.com.
published in the New England Journal of Medicine.
“No signal of efficacy was observed,” said investigators led by Nicholas Allen, MPH, of the University of Sydney department of dermatology.
These results fill an “important gap in our understanding” and “will probably change the practice of many skin-cancer physicians,” two experts on the topic commented in a related editorial.
The editorialists are David Miller, MD, PhD, a dermatologist and medical oncologist at Massachusetts General Hospital, and Kevin Emerick, MD, a head and neck surgeon as Massachusetts Eye and Ear, both in Boston.
Transplant patients have 50 times the risk of nonmelanoma skin cancers – also known as keratinocyte cancers – than the general public, owing to immunosuppression, and their lesions are more aggressive and are more likely to metastasize, they explain.
Nicotinamide (vitamin B3) has been shown to prevent nonmelanoma skin cancers in healthy, immunocompetent people, so physicians routinely prescribe it to transplant patients on the assumption that it will do the same for them, they comment.
The Australian investigators decided to put the assumption to the test.
The team randomly assigned 79 patients who had undergone solid-organ transplant to receive nicotinamide 500 mg twice a day and 79 other patients to receive twice-daily placebo for a year. Participants underwent dermatology exams every 3 months to check for new lesions.
The participants were at high risk for new lesions; some had had more than 40 in the previous 5 years. The two groups were well balanced; kidney transplants were the most common.
At 12 months, there was virtually no difference in the incidence of new nonmelanoma skin cancers: 207 in the nicotinamide group and 210 in the placebo group (P = .96).
There was also no significant difference in squamous cell and basal cell carcinoma counts or actinic keratosis counts.
“The interpretation of the results is straightforward: nicotinamide lacks clinical usefulness in preventing the development of keratinocyte carcinomas in solid-organ transplant recipients,” the team concludes.
As for why nicotinamide didn’t work in the trial, the investigators say it could be because it is not potent enough to overcome the stifling of antitumor immunity and DNA-repair enzymes with immunosuppression.
Fewer than half of participants in the trial reported using sunscreen at any point during the study, which is in line with past reports that transplant patients don’t routinely use sunscreen.
Two other strategies for preventing squamous cell carcinoma after transplant – use of oral retinoids and mTOR inhibitors – are problematic for various reasons, and use was low in both study arms.
Editorialists Dr. Miller and Dr. Emerick suggest a possible new approach: immune checkpoint inhibitors before transplant to reduce the risk of nonmelanoma skin cancer afterward. They say the strategy should be explored and that ongoing efforts to minimize or eliminate the need for immunosuppression after transplant are promising.
The investigators originally planned to enroll 254 persons, but the trial was stopped early because of poor recruitment. Potential participants may already have been taking nicotinamide, which is commonly used, and that may have affected recruitment, the investigators say.
The work was funded by Australia’s National Health and Medical Research Council. Dr. Allen has disclosed no relevant financial relationships. One investigator has received speaker’s fees from BMS. Another is a consultant for many companies, including Amgen, BMS, GlaxoSmithKline, and Merck. Dr. Emerick is an advisor for Regeneron, Sanofi, and Castle Biosciences. Dr. Miller is a researcher or consultant for those companies as well as Pfizer and others and has stock options in Avstera.
A version of this article first appeared on Medscape.com.
published in the New England Journal of Medicine.
“No signal of efficacy was observed,” said investigators led by Nicholas Allen, MPH, of the University of Sydney department of dermatology.
These results fill an “important gap in our understanding” and “will probably change the practice of many skin-cancer physicians,” two experts on the topic commented in a related editorial.
The editorialists are David Miller, MD, PhD, a dermatologist and medical oncologist at Massachusetts General Hospital, and Kevin Emerick, MD, a head and neck surgeon as Massachusetts Eye and Ear, both in Boston.
Transplant patients have 50 times the risk of nonmelanoma skin cancers – also known as keratinocyte cancers – than the general public, owing to immunosuppression, and their lesions are more aggressive and are more likely to metastasize, they explain.
Nicotinamide (vitamin B3) has been shown to prevent nonmelanoma skin cancers in healthy, immunocompetent people, so physicians routinely prescribe it to transplant patients on the assumption that it will do the same for them, they comment.
The Australian investigators decided to put the assumption to the test.
The team randomly assigned 79 patients who had undergone solid-organ transplant to receive nicotinamide 500 mg twice a day and 79 other patients to receive twice-daily placebo for a year. Participants underwent dermatology exams every 3 months to check for new lesions.
The participants were at high risk for new lesions; some had had more than 40 in the previous 5 years. The two groups were well balanced; kidney transplants were the most common.
At 12 months, there was virtually no difference in the incidence of new nonmelanoma skin cancers: 207 in the nicotinamide group and 210 in the placebo group (P = .96).
There was also no significant difference in squamous cell and basal cell carcinoma counts or actinic keratosis counts.
“The interpretation of the results is straightforward: nicotinamide lacks clinical usefulness in preventing the development of keratinocyte carcinomas in solid-organ transplant recipients,” the team concludes.
As for why nicotinamide didn’t work in the trial, the investigators say it could be because it is not potent enough to overcome the stifling of antitumor immunity and DNA-repair enzymes with immunosuppression.
Fewer than half of participants in the trial reported using sunscreen at any point during the study, which is in line with past reports that transplant patients don’t routinely use sunscreen.
Two other strategies for preventing squamous cell carcinoma after transplant – use of oral retinoids and mTOR inhibitors – are problematic for various reasons, and use was low in both study arms.
Editorialists Dr. Miller and Dr. Emerick suggest a possible new approach: immune checkpoint inhibitors before transplant to reduce the risk of nonmelanoma skin cancer afterward. They say the strategy should be explored and that ongoing efforts to minimize or eliminate the need for immunosuppression after transplant are promising.
The investigators originally planned to enroll 254 persons, but the trial was stopped early because of poor recruitment. Potential participants may already have been taking nicotinamide, which is commonly used, and that may have affected recruitment, the investigators say.
The work was funded by Australia’s National Health and Medical Research Council. Dr. Allen has disclosed no relevant financial relationships. One investigator has received speaker’s fees from BMS. Another is a consultant for many companies, including Amgen, BMS, GlaxoSmithKline, and Merck. Dr. Emerick is an advisor for Regeneron, Sanofi, and Castle Biosciences. Dr. Miller is a researcher or consultant for those companies as well as Pfizer and others and has stock options in Avstera.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
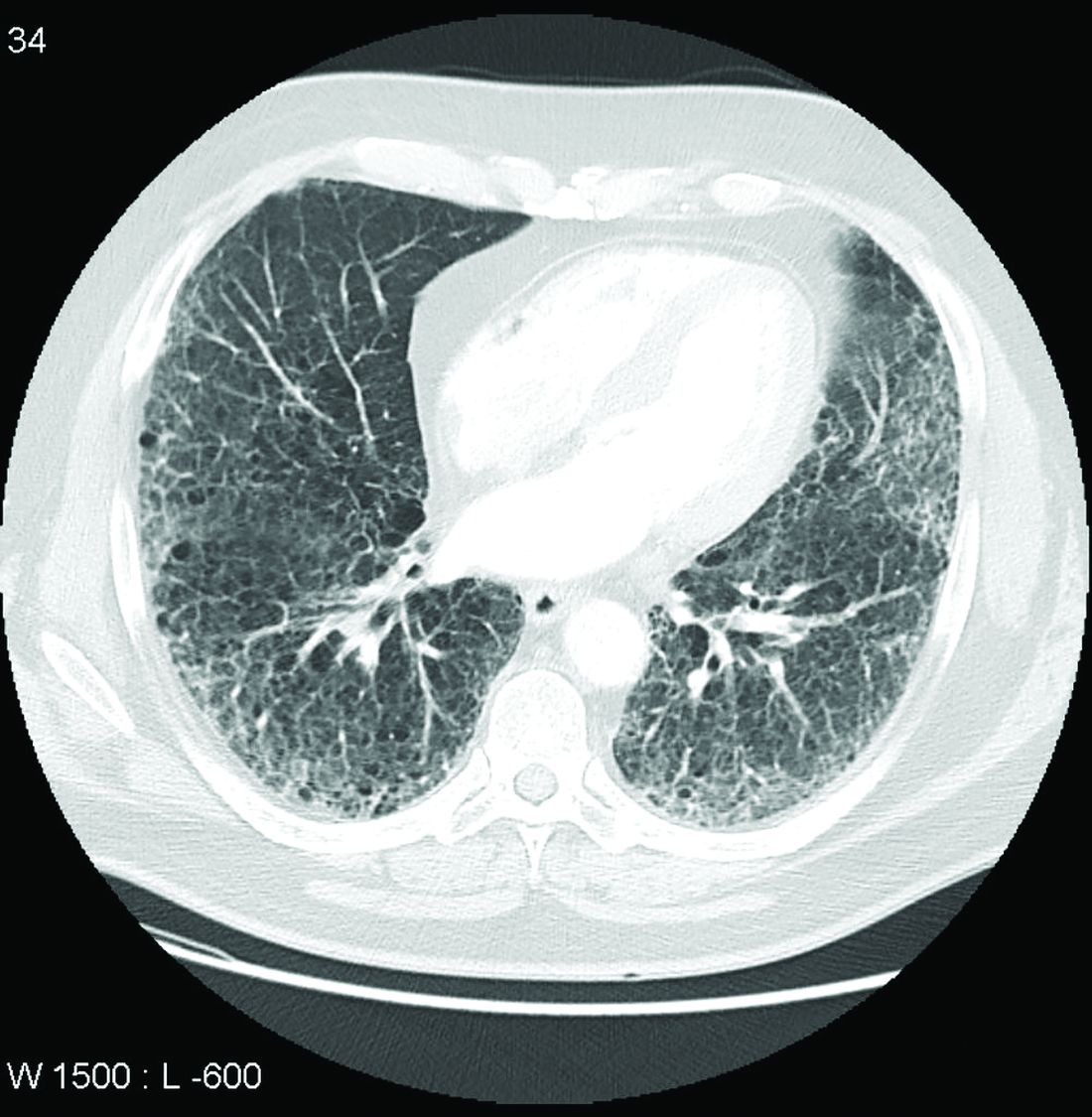
Call it preclinical or subclinical, ILD in RA needs to be tracked
More clinical guidance is needed for monitoring interstitial lung disease (ILD) in patients with rheumatoid arthritis, according to a new commentary.
Though ILD is a leading cause of death among patients with RA, these patients are not routinely screened for ILD, the authors say, and there are currently no guidelines on how to monitor ILD progression in patients with RA.
“ILD associated with rheumatoid arthritis is a disease for which there’s been very little research done, so it’s an area of rheumatology where there are many unknowns,” lead author Elizabeth R. Volkmann, MD, who codirects the connective tissue disease–related interstitial lung disease (CTD-ILD) program at University of California, Los Angeles, told this news organization.
The commentary was published in The Lancet Rheumatology.
Defining disease
One of the major unknowns is how to define the disease, she said. RA patients sometimes undergo imaging for other medical reasons, and interstitial lung abnormalities are incidentally detected. These patients can be classified as having “preclinical” or “subclinical” ILD, as they do not yet have symptoms; however, there is no consensus as to what these terms mean, the commentary authors write. “The other problem that we have with these terms is that it sometimes creates the perception that this is a nonworrisome feature of rheumatoid arthritis,” Dr. Volkmann said, although the condition should be followed closely.
“We know we can detect imaging features of ILD in people who may not yet have symptoms, and we need to know when to define a clinically important informality that requires follow-up or treatment,” added John M. Davis III, MD, a rheumatologist at the Mayo Clinic, Rochester, Minn. He was not involved with the work.
Dr. Volkmann proposed eliminating the prefixes “pre” and “sub” when referring to ILD. “In other connective tissue diseases, like systemic sclerosis, for example, we can use the term ‘limited’ or ‘extensive’ ILD, based on the extent of involvement of the ILD on high-resolution computed tomography (HRCT) imaging,” she said. “This could potentially be something that is applied to how we classify patients with RA-ILD.”
Tracking ILD progression
Once ILD is identified, monitoring its progression poses challenges, as respiratory symptoms may be difficult to detect. RA patients may already be avoiding exercise because of joint pain, so they may not notice shortness of breath during physical activity, noted Jessica K. Gordon, MD, of the Hospital for Special Surgery, New York, in an interview with this news organization. She was not involved with the commentary. Cough is a potential symptom of ILD, but cough can also be the result of allergies, postnasal drip, or reflux, she said. Making the distinction between “preclinical” and symptomatic disease can be “complicated,” she added; “you may have to really dig.”
Additionally, there has been little research on the outcomes of patients with preclinical or subclinical ILD and clinical ILD, the commentary authors write. “It is therefore conceivable that some patients with rheumatoid arthritis diagnosed with preclinical or subclinical ILD could potentially have worse outcomes if both the rheumatoid arthritis and ILD are not monitored closely,” they note.
To better track RA-associated ILD for patients with and those without symptoms, the authors advocate for monitoring patients using pulmonary testing and CT scanning, as well as evaluating symptoms. How often these assessments should be conducted depends on the individual, they note. In her own practice, Dr. Volkmann sees patients every 3 months to evaluate their symptoms and conduct pulmonary function tests (PFTs). For patients early in the course of ILD, she orders HRCT imaging once per year.
For Dr. Davis, the frequency of follow-up depends on the severity of ILD. “For minimally symptomatic patients without compromised lung function, we would generally follow annually. For patients with symptomatic ILD on stable therapy, we may monitor every 6 months. For patients with active/progressive ILD, we would generally be following at least every 1-3 months,” he said.
Screening and future research
While there is no evidence to recommend screening patients for ILD using CT, there are certain risk factors for ILD in RA patients, including a history of smoking, male sex, and high RA disease activity despite antirheumatic treatment, Dr. Volkmann said. In both of their practices, Dr. Davis and Dr. Volkmann screen with RA via HRCT and PFTs for ILD for patients with known risk factors that predispose them to the lung condition and/or for patients who report respiratory symptoms.
“We still don’t have an algorithm [for screening patients], and that is a desperate need in this field,” added Joshua J. Solomon, MD, a pulmonologist at National Jewish Health, Denver, whose research focuses on RA-associated ILD. While recommendations state that all patients with scleroderma should be screened with CT, ILD incidence is lower among patients with RA, and thus these screening recommendations need to be narrowed, he said. But more research is needed to better fine tune recommendations, he said; “The only thing you can do is give some expert consensus until there are good data.”
Dr. Volkmann has received consulting and speaking fees from Boehringer Ingelheim and institutional support for performing studies on systemic sclerosis for Kadmon, Forbius, Boehringer Ingelheim, Horizon, and Prometheus. Dr. Gordon, Dr. Davis, and Dr. Solomon report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
More clinical guidance is needed for monitoring interstitial lung disease (ILD) in patients with rheumatoid arthritis, according to a new commentary.
Though ILD is a leading cause of death among patients with RA, these patients are not routinely screened for ILD, the authors say, and there are currently no guidelines on how to monitor ILD progression in patients with RA.
“ILD associated with rheumatoid arthritis is a disease for which there’s been very little research done, so it’s an area of rheumatology where there are many unknowns,” lead author Elizabeth R. Volkmann, MD, who codirects the connective tissue disease–related interstitial lung disease (CTD-ILD) program at University of California, Los Angeles, told this news organization.
The commentary was published in The Lancet Rheumatology.
Defining disease
One of the major unknowns is how to define the disease, she said. RA patients sometimes undergo imaging for other medical reasons, and interstitial lung abnormalities are incidentally detected. These patients can be classified as having “preclinical” or “subclinical” ILD, as they do not yet have symptoms; however, there is no consensus as to what these terms mean, the commentary authors write. “The other problem that we have with these terms is that it sometimes creates the perception that this is a nonworrisome feature of rheumatoid arthritis,” Dr. Volkmann said, although the condition should be followed closely.
“We know we can detect imaging features of ILD in people who may not yet have symptoms, and we need to know when to define a clinically important informality that requires follow-up or treatment,” added John M. Davis III, MD, a rheumatologist at the Mayo Clinic, Rochester, Minn. He was not involved with the work.
Dr. Volkmann proposed eliminating the prefixes “pre” and “sub” when referring to ILD. “In other connective tissue diseases, like systemic sclerosis, for example, we can use the term ‘limited’ or ‘extensive’ ILD, based on the extent of involvement of the ILD on high-resolution computed tomography (HRCT) imaging,” she said. “This could potentially be something that is applied to how we classify patients with RA-ILD.”
Tracking ILD progression
Once ILD is identified, monitoring its progression poses challenges, as respiratory symptoms may be difficult to detect. RA patients may already be avoiding exercise because of joint pain, so they may not notice shortness of breath during physical activity, noted Jessica K. Gordon, MD, of the Hospital for Special Surgery, New York, in an interview with this news organization. She was not involved with the commentary. Cough is a potential symptom of ILD, but cough can also be the result of allergies, postnasal drip, or reflux, she said. Making the distinction between “preclinical” and symptomatic disease can be “complicated,” she added; “you may have to really dig.”
Additionally, there has been little research on the outcomes of patients with preclinical or subclinical ILD and clinical ILD, the commentary authors write. “It is therefore conceivable that some patients with rheumatoid arthritis diagnosed with preclinical or subclinical ILD could potentially have worse outcomes if both the rheumatoid arthritis and ILD are not monitored closely,” they note.
To better track RA-associated ILD for patients with and those without symptoms, the authors advocate for monitoring patients using pulmonary testing and CT scanning, as well as evaluating symptoms. How often these assessments should be conducted depends on the individual, they note. In her own practice, Dr. Volkmann sees patients every 3 months to evaluate their symptoms and conduct pulmonary function tests (PFTs). For patients early in the course of ILD, she orders HRCT imaging once per year.
For Dr. Davis, the frequency of follow-up depends on the severity of ILD. “For minimally symptomatic patients without compromised lung function, we would generally follow annually. For patients with symptomatic ILD on stable therapy, we may monitor every 6 months. For patients with active/progressive ILD, we would generally be following at least every 1-3 months,” he said.
Screening and future research
While there is no evidence to recommend screening patients for ILD using CT, there are certain risk factors for ILD in RA patients, including a history of smoking, male sex, and high RA disease activity despite antirheumatic treatment, Dr. Volkmann said. In both of their practices, Dr. Davis and Dr. Volkmann screen with RA via HRCT and PFTs for ILD for patients with known risk factors that predispose them to the lung condition and/or for patients who report respiratory symptoms.
“We still don’t have an algorithm [for screening patients], and that is a desperate need in this field,” added Joshua J. Solomon, MD, a pulmonologist at National Jewish Health, Denver, whose research focuses on RA-associated ILD. While recommendations state that all patients with scleroderma should be screened with CT, ILD incidence is lower among patients with RA, and thus these screening recommendations need to be narrowed, he said. But more research is needed to better fine tune recommendations, he said; “The only thing you can do is give some expert consensus until there are good data.”
Dr. Volkmann has received consulting and speaking fees from Boehringer Ingelheim and institutional support for performing studies on systemic sclerosis for Kadmon, Forbius, Boehringer Ingelheim, Horizon, and Prometheus. Dr. Gordon, Dr. Davis, and Dr. Solomon report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
More clinical guidance is needed for monitoring interstitial lung disease (ILD) in patients with rheumatoid arthritis, according to a new commentary.
Though ILD is a leading cause of death among patients with RA, these patients are not routinely screened for ILD, the authors say, and there are currently no guidelines on how to monitor ILD progression in patients with RA.
“ILD associated with rheumatoid arthritis is a disease for which there’s been very little research done, so it’s an area of rheumatology where there are many unknowns,” lead author Elizabeth R. Volkmann, MD, who codirects the connective tissue disease–related interstitial lung disease (CTD-ILD) program at University of California, Los Angeles, told this news organization.
The commentary was published in The Lancet Rheumatology.
Defining disease
One of the major unknowns is how to define the disease, she said. RA patients sometimes undergo imaging for other medical reasons, and interstitial lung abnormalities are incidentally detected. These patients can be classified as having “preclinical” or “subclinical” ILD, as they do not yet have symptoms; however, there is no consensus as to what these terms mean, the commentary authors write. “The other problem that we have with these terms is that it sometimes creates the perception that this is a nonworrisome feature of rheumatoid arthritis,” Dr. Volkmann said, although the condition should be followed closely.
“We know we can detect imaging features of ILD in people who may not yet have symptoms, and we need to know when to define a clinically important informality that requires follow-up or treatment,” added John M. Davis III, MD, a rheumatologist at the Mayo Clinic, Rochester, Minn. He was not involved with the work.
Dr. Volkmann proposed eliminating the prefixes “pre” and “sub” when referring to ILD. “In other connective tissue diseases, like systemic sclerosis, for example, we can use the term ‘limited’ or ‘extensive’ ILD, based on the extent of involvement of the ILD on high-resolution computed tomography (HRCT) imaging,” she said. “This could potentially be something that is applied to how we classify patients with RA-ILD.”
Tracking ILD progression
Once ILD is identified, monitoring its progression poses challenges, as respiratory symptoms may be difficult to detect. RA patients may already be avoiding exercise because of joint pain, so they may not notice shortness of breath during physical activity, noted Jessica K. Gordon, MD, of the Hospital for Special Surgery, New York, in an interview with this news organization. She was not involved with the commentary. Cough is a potential symptom of ILD, but cough can also be the result of allergies, postnasal drip, or reflux, she said. Making the distinction between “preclinical” and symptomatic disease can be “complicated,” she added; “you may have to really dig.”
Additionally, there has been little research on the outcomes of patients with preclinical or subclinical ILD and clinical ILD, the commentary authors write. “It is therefore conceivable that some patients with rheumatoid arthritis diagnosed with preclinical or subclinical ILD could potentially have worse outcomes if both the rheumatoid arthritis and ILD are not monitored closely,” they note.
To better track RA-associated ILD for patients with and those without symptoms, the authors advocate for monitoring patients using pulmonary testing and CT scanning, as well as evaluating symptoms. How often these assessments should be conducted depends on the individual, they note. In her own practice, Dr. Volkmann sees patients every 3 months to evaluate their symptoms and conduct pulmonary function tests (PFTs). For patients early in the course of ILD, she orders HRCT imaging once per year.
For Dr. Davis, the frequency of follow-up depends on the severity of ILD. “For minimally symptomatic patients without compromised lung function, we would generally follow annually. For patients with symptomatic ILD on stable therapy, we may monitor every 6 months. For patients with active/progressive ILD, we would generally be following at least every 1-3 months,” he said.
Screening and future research
While there is no evidence to recommend screening patients for ILD using CT, there are certain risk factors for ILD in RA patients, including a history of smoking, male sex, and high RA disease activity despite antirheumatic treatment, Dr. Volkmann said. In both of their practices, Dr. Davis and Dr. Volkmann screen with RA via HRCT and PFTs for ILD for patients with known risk factors that predispose them to the lung condition and/or for patients who report respiratory symptoms.
“We still don’t have an algorithm [for screening patients], and that is a desperate need in this field,” added Joshua J. Solomon, MD, a pulmonologist at National Jewish Health, Denver, whose research focuses on RA-associated ILD. While recommendations state that all patients with scleroderma should be screened with CT, ILD incidence is lower among patients with RA, and thus these screening recommendations need to be narrowed, he said. But more research is needed to better fine tune recommendations, he said; “The only thing you can do is give some expert consensus until there are good data.”
Dr. Volkmann has received consulting and speaking fees from Boehringer Ingelheim and institutional support for performing studies on systemic sclerosis for Kadmon, Forbius, Boehringer Ingelheim, Horizon, and Prometheus. Dr. Gordon, Dr. Davis, and Dr. Solomon report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CLL treatment: More infections among real-world patients
For example, “the rate of severe infection for ibrutinib in clinical trials ranged from 12.8% to 45% with median follow-up ranging from 27 to 65 months. In our study, the rate of severe infection was 45.3% within a shorter median follow-up period of 23.3 months,” said study lead author Amanda Tey, MPharm, a hematology pharmacist with Monash Health in Clayton, Australia, in an interview.
The results suggest that “real-world severe infection risk is higher than previously appreciated,” said Ms. Tey, whose findings were published in the European Journal of Hematology. “Poor performance status and a high comorbidity burden further increase this risk.”
According to the study, there are limited data about real-world infection rates for patients with CLL or B-cell lymphoma who take the three drugs.
Both the underlying blood cancer and the drugs themselves may disrupt the immune system in these patients, Ms. Tey noted. “Ibrutinib inhibits interleukin-2-inducible T-cell kinase, which has a role in T-cell maturation. Idelalisib reduces regulatory T-cell activity and natural killer cell and neutrophil inflammatory responses. Venetoclax is associated with a high rate of neutropenia.”
For the new retrospective, single-center study, researchers tracked adult patients who’d received the drugs from 2014 to 2021 in a hospital network serving 1.5 million people in the Australian state of Victoria. The primary outcome was severe infection of grade 3 or higher. Patients were excluded for such factors as having been primarily treated at other facilities, receiving less than 30 days of treatment, or having been treated for other indications such as primary central nervous system lymphoma.
Of the 67 patients in the study, the numbers taking the drugs were 53 (ibrutinib), 8 (idelalisib), and 6 (venetoclax). Eleven patients took more than one drug. Median age was 73 years, and 73% of patients were male.
Patients spent a median 23.3, 4.8, and 3.5 months taking ibrutinib, idelalisib, and venetoclax, respectively, before treatment stopped or data were collected. Patients were commonly prescribed antimicrobials to prevent pneumocystis jirovecii pneumonia and herpes simplex virus (HSV)/varicella zoster virus (VZV) infection.
Researchers found that 48% of the patients had at least one serious infection: 45% of those on ibrutinib, 63% of those on idelalisib, and 50% of those on venetoclax. Seven patients died of infections.
In comparison, the researchers reported, a systematic review of idelalisib in blood cancer clinical trials reported an overall infection rate of 28%, while clinical trials reported an infection rate of 17.5%-22% in patients taking venetoclax for CLL.
Poor performance status and higher levels of comorbidity were linked to higher risk of infection, and infections occurred at a median of 5.4 months.
Lead author Ms. Tey highlighted the fact that most of the patients in the new study had relapsed/refractory disease. The infection risk in the real-world first-line setting is unknown, she said. “Furthermore, due to the size of our study and high uptake of antimicrobial prophylaxis, the optimal prophylaxis strategy for these patients remains unclear.”
In an interview, infectious disease physician Gemma Reynolds, MChD, MPH, of Austin Health and Peter MacCallum Cancer Center in Melbourne, said the study findings reflect “a lot of what we know from other observational studies and clinical practice. There is a risk of infection, and serious infection, associated with these agents. Sometimes the pathogen is classically opportunistic, but often it is bacterial, and respiratory sites are common. Infections often occur early into a course of therapy.”
Dr. Reynolds, who didn’t take part in the study, urged colleagues to cast a wide net if a patient appears to have an infection but doesn’t respond to conventional therapies such as antibiotics. “Unusual infections are possible,” she said, and aggressive early workups may be advisable via blood cultures, viral swabs, sputum culture, early imaging, bronchoscopy, and preemptive monitoring in patients with a prior infection history with a disease such as CMV.
Alessandra Ferrajoli, MD, a hematologist/oncologist at MD Anderson Cancer Center who also didn’t take part in the study, agreed in an interview that the findings reflect those found in other reports. “It should be highlighted that the population studied is at particular high risk for infections given the high proportion of patients with recurrent disease (85%), many patients with concurrent hypogammaglobulinemia (64%), and the patient median age of 73 years and a high comorbidities burden,” she said. “In my view, this explains the higher rate of infections reported in this study, when compared to other case series.”
Dr. Ferrajoli added that there’s no standard antimicrobial prophylaxis for patients with B-cell malignancies receiving targeted therapies. “Anti-HSV/VZV prophylaxis is commonly implemented. Additional antiviral, antimicrobial, and antifungal prophylaxis should be used based on patients’ absolute neutrophil and T-cell count and individual risk factors, including prior history of infections such as CMV, prior splenectomy, and history of invasive fungal infections.”
The study was funded by Monash Health, the National Health and Medical Research Council (Australia), and the Society of Hospital Pharmacists of Australia. Ms. Tey reported no disclosures. Some of the study authors reported multiple disclosures. Dr. Reynolds discloses a PhD scholarship from the National Health and Medical Research Council. Dr. Ferrajoli reported no disclosures.
For example, “the rate of severe infection for ibrutinib in clinical trials ranged from 12.8% to 45% with median follow-up ranging from 27 to 65 months. In our study, the rate of severe infection was 45.3% within a shorter median follow-up period of 23.3 months,” said study lead author Amanda Tey, MPharm, a hematology pharmacist with Monash Health in Clayton, Australia, in an interview.
The results suggest that “real-world severe infection risk is higher than previously appreciated,” said Ms. Tey, whose findings were published in the European Journal of Hematology. “Poor performance status and a high comorbidity burden further increase this risk.”
According to the study, there are limited data about real-world infection rates for patients with CLL or B-cell lymphoma who take the three drugs.
Both the underlying blood cancer and the drugs themselves may disrupt the immune system in these patients, Ms. Tey noted. “Ibrutinib inhibits interleukin-2-inducible T-cell kinase, which has a role in T-cell maturation. Idelalisib reduces regulatory T-cell activity and natural killer cell and neutrophil inflammatory responses. Venetoclax is associated with a high rate of neutropenia.”
For the new retrospective, single-center study, researchers tracked adult patients who’d received the drugs from 2014 to 2021 in a hospital network serving 1.5 million people in the Australian state of Victoria. The primary outcome was severe infection of grade 3 or higher. Patients were excluded for such factors as having been primarily treated at other facilities, receiving less than 30 days of treatment, or having been treated for other indications such as primary central nervous system lymphoma.
Of the 67 patients in the study, the numbers taking the drugs were 53 (ibrutinib), 8 (idelalisib), and 6 (venetoclax). Eleven patients took more than one drug. Median age was 73 years, and 73% of patients were male.
Patients spent a median 23.3, 4.8, and 3.5 months taking ibrutinib, idelalisib, and venetoclax, respectively, before treatment stopped or data were collected. Patients were commonly prescribed antimicrobials to prevent pneumocystis jirovecii pneumonia and herpes simplex virus (HSV)/varicella zoster virus (VZV) infection.
Researchers found that 48% of the patients had at least one serious infection: 45% of those on ibrutinib, 63% of those on idelalisib, and 50% of those on venetoclax. Seven patients died of infections.
In comparison, the researchers reported, a systematic review of idelalisib in blood cancer clinical trials reported an overall infection rate of 28%, while clinical trials reported an infection rate of 17.5%-22% in patients taking venetoclax for CLL.
Poor performance status and higher levels of comorbidity were linked to higher risk of infection, and infections occurred at a median of 5.4 months.
Lead author Ms. Tey highlighted the fact that most of the patients in the new study had relapsed/refractory disease. The infection risk in the real-world first-line setting is unknown, she said. “Furthermore, due to the size of our study and high uptake of antimicrobial prophylaxis, the optimal prophylaxis strategy for these patients remains unclear.”
In an interview, infectious disease physician Gemma Reynolds, MChD, MPH, of Austin Health and Peter MacCallum Cancer Center in Melbourne, said the study findings reflect “a lot of what we know from other observational studies and clinical practice. There is a risk of infection, and serious infection, associated with these agents. Sometimes the pathogen is classically opportunistic, but often it is bacterial, and respiratory sites are common. Infections often occur early into a course of therapy.”
Dr. Reynolds, who didn’t take part in the study, urged colleagues to cast a wide net if a patient appears to have an infection but doesn’t respond to conventional therapies such as antibiotics. “Unusual infections are possible,” she said, and aggressive early workups may be advisable via blood cultures, viral swabs, sputum culture, early imaging, bronchoscopy, and preemptive monitoring in patients with a prior infection history with a disease such as CMV.
Alessandra Ferrajoli, MD, a hematologist/oncologist at MD Anderson Cancer Center who also didn’t take part in the study, agreed in an interview that the findings reflect those found in other reports. “It should be highlighted that the population studied is at particular high risk for infections given the high proportion of patients with recurrent disease (85%), many patients with concurrent hypogammaglobulinemia (64%), and the patient median age of 73 years and a high comorbidities burden,” she said. “In my view, this explains the higher rate of infections reported in this study, when compared to other case series.”
Dr. Ferrajoli added that there’s no standard antimicrobial prophylaxis for patients with B-cell malignancies receiving targeted therapies. “Anti-HSV/VZV prophylaxis is commonly implemented. Additional antiviral, antimicrobial, and antifungal prophylaxis should be used based on patients’ absolute neutrophil and T-cell count and individual risk factors, including prior history of infections such as CMV, prior splenectomy, and history of invasive fungal infections.”
The study was funded by Monash Health, the National Health and Medical Research Council (Australia), and the Society of Hospital Pharmacists of Australia. Ms. Tey reported no disclosures. Some of the study authors reported multiple disclosures. Dr. Reynolds discloses a PhD scholarship from the National Health and Medical Research Council. Dr. Ferrajoli reported no disclosures.
For example, “the rate of severe infection for ibrutinib in clinical trials ranged from 12.8% to 45% with median follow-up ranging from 27 to 65 months. In our study, the rate of severe infection was 45.3% within a shorter median follow-up period of 23.3 months,” said study lead author Amanda Tey, MPharm, a hematology pharmacist with Monash Health in Clayton, Australia, in an interview.
The results suggest that “real-world severe infection risk is higher than previously appreciated,” said Ms. Tey, whose findings were published in the European Journal of Hematology. “Poor performance status and a high comorbidity burden further increase this risk.”
According to the study, there are limited data about real-world infection rates for patients with CLL or B-cell lymphoma who take the three drugs.
Both the underlying blood cancer and the drugs themselves may disrupt the immune system in these patients, Ms. Tey noted. “Ibrutinib inhibits interleukin-2-inducible T-cell kinase, which has a role in T-cell maturation. Idelalisib reduces regulatory T-cell activity and natural killer cell and neutrophil inflammatory responses. Venetoclax is associated with a high rate of neutropenia.”
For the new retrospective, single-center study, researchers tracked adult patients who’d received the drugs from 2014 to 2021 in a hospital network serving 1.5 million people in the Australian state of Victoria. The primary outcome was severe infection of grade 3 or higher. Patients were excluded for such factors as having been primarily treated at other facilities, receiving less than 30 days of treatment, or having been treated for other indications such as primary central nervous system lymphoma.
Of the 67 patients in the study, the numbers taking the drugs were 53 (ibrutinib), 8 (idelalisib), and 6 (venetoclax). Eleven patients took more than one drug. Median age was 73 years, and 73% of patients were male.
Patients spent a median 23.3, 4.8, and 3.5 months taking ibrutinib, idelalisib, and venetoclax, respectively, before treatment stopped or data were collected. Patients were commonly prescribed antimicrobials to prevent pneumocystis jirovecii pneumonia and herpes simplex virus (HSV)/varicella zoster virus (VZV) infection.
Researchers found that 48% of the patients had at least one serious infection: 45% of those on ibrutinib, 63% of those on idelalisib, and 50% of those on venetoclax. Seven patients died of infections.
In comparison, the researchers reported, a systematic review of idelalisib in blood cancer clinical trials reported an overall infection rate of 28%, while clinical trials reported an infection rate of 17.5%-22% in patients taking venetoclax for CLL.
Poor performance status and higher levels of comorbidity were linked to higher risk of infection, and infections occurred at a median of 5.4 months.
Lead author Ms. Tey highlighted the fact that most of the patients in the new study had relapsed/refractory disease. The infection risk in the real-world first-line setting is unknown, she said. “Furthermore, due to the size of our study and high uptake of antimicrobial prophylaxis, the optimal prophylaxis strategy for these patients remains unclear.”
In an interview, infectious disease physician Gemma Reynolds, MChD, MPH, of Austin Health and Peter MacCallum Cancer Center in Melbourne, said the study findings reflect “a lot of what we know from other observational studies and clinical practice. There is a risk of infection, and serious infection, associated with these agents. Sometimes the pathogen is classically opportunistic, but often it is bacterial, and respiratory sites are common. Infections often occur early into a course of therapy.”
Dr. Reynolds, who didn’t take part in the study, urged colleagues to cast a wide net if a patient appears to have an infection but doesn’t respond to conventional therapies such as antibiotics. “Unusual infections are possible,” she said, and aggressive early workups may be advisable via blood cultures, viral swabs, sputum culture, early imaging, bronchoscopy, and preemptive monitoring in patients with a prior infection history with a disease such as CMV.
Alessandra Ferrajoli, MD, a hematologist/oncologist at MD Anderson Cancer Center who also didn’t take part in the study, agreed in an interview that the findings reflect those found in other reports. “It should be highlighted that the population studied is at particular high risk for infections given the high proportion of patients with recurrent disease (85%), many patients with concurrent hypogammaglobulinemia (64%), and the patient median age of 73 years and a high comorbidities burden,” she said. “In my view, this explains the higher rate of infections reported in this study, when compared to other case series.”
Dr. Ferrajoli added that there’s no standard antimicrobial prophylaxis for patients with B-cell malignancies receiving targeted therapies. “Anti-HSV/VZV prophylaxis is commonly implemented. Additional antiviral, antimicrobial, and antifungal prophylaxis should be used based on patients’ absolute neutrophil and T-cell count and individual risk factors, including prior history of infections such as CMV, prior splenectomy, and history of invasive fungal infections.”
The study was funded by Monash Health, the National Health and Medical Research Council (Australia), and the Society of Hospital Pharmacists of Australia. Ms. Tey reported no disclosures. Some of the study authors reported multiple disclosures. Dr. Reynolds discloses a PhD scholarship from the National Health and Medical Research Council. Dr. Ferrajoli reported no disclosures.
FROM THE EUROPEAN JOURNAL OF HEMATOLOGY
Med center and top cardio surgeon must pay $8.5 million for fraud, concurrent surgeries
the Department of Justice (DOJ) announced.
The lawsuit alleges that James L. Luketich, MD, the longtime chair of the school’s cardiothoracic surgery department, regularly performed up to three complex surgical procedures simultaneously, moving among multiple operating rooms and attending to matters other than patient care. The investigation began after Jonathan D’Cunha, MD, a former UPMC surgeon, raised concerns about his colleague’s surgical scheduling and billing practices.
Dr. Luketich’s overbooking of procedures led to patients enduring hours of medically unnecessary anesthesia time and risking surgical complications, according to court documents.
In addition, the complaint states that these practices violated the False Claims Act, which prohibits “teaching physicians” like Dr. Luketich from billing Medicare and other government health plans for “concurrent surgeries” – regulations federal authorities say UPMC leadership were aware of and the University of Pittsburgh Physicians (UPP), also named in the suit, permitted Dr. Luketich to skirt.
The whistleblower provision of the False Claims Act allows private parties to file an action on behalf of the United States and receive a portion of the recovery to help deter health care fraud, says the DOJ.
The defendants previously asked the court to dismiss the case, but a judge denied the request in June 2022.
Paul Wood, vice president and chief communications officer for UPMC, told this news organization that the lawsuit pertained to Dr. Luketich’s “most complicated, team-based surgical procedures.”
“At issue was compliance with the Centers for Medicare & Medicaid Services’ (CMS’s) Teaching Physician Regulation and related billing guidance as well as with UPMC’s internal surgical policies,” he said.
“While UPMC continues to believe Dr. Luketich’s surgical practice complies with CMS requirements, it has agreed to [the settlement] to avoid the distraction and expense of further litigation,” said Mr. Wood, adding that all parties agree that UPMC can seek clarity from CMS regarding future billing of these surgeries.
Efrem Grail, JD, Dr. Luketich’s attorney, said in an interview that he and Dr. Luketich are pleased that the settlement puts an end to the case and that he hopes the United States will issue “authoritative guidance” on billing regulations for teaching physicians, something medical schools and hospitals have sought for years.
Dr. Luketich, UPMC, and UPP face more legal challenges from a separate medical malpractice lawsuit. In March 2018, Bernadette Fedorka underwent a lung transplant at UPMC. Although Dr. Luketich did not perform the surgery, Ms. Fedorka alleges that his poor leadership caused understaffing of the lung transplant program and contributed to surgical complications, including a 4-inch piece of wire left in her neck.
Ms. Fedorka claims that suboxone impaired Dr. Luketich’s decision-making. He began taking the drug in 2008 to manage the pain from a slipped disc injury after a history of prescription drug abuse. Both UPMC and Dr. Luketich have denied the validity of Ms. Fedorka’s claims.
The malpractice suit centers on a recording of a conversation between Dr. Luketich and David Wilson, MD, who prescribed the suboxone and treated the surgeon’s opioid use disorder for several years. Dr. Luketich has accused former colleagues, Dr. D’Cunha and Lara Schaheen, MD, of illegally recording the private conversation that discussed Dr. Luketich’s suboxone prescription – something both physicians deny.
For the billing fraud case, Dr. Luketich has agreed to complete a corrective action plan and submit to a third-party audit of his Medicare billings for 1 year.
“This is an important settlement and a just conclusion to the United States’ investigation into Dr. Luketich’s surgical and billing practices and UPMC and UPP’s acceptance of those practices,” Acting U.S. Attorney Troy Rivetti said in a statement that, “no medical provider – however renowned – is excepted from scrutiny or above the law.”
A version of this article first appeared on Medscape.com.
the Department of Justice (DOJ) announced.
The lawsuit alleges that James L. Luketich, MD, the longtime chair of the school’s cardiothoracic surgery department, regularly performed up to three complex surgical procedures simultaneously, moving among multiple operating rooms and attending to matters other than patient care. The investigation began after Jonathan D’Cunha, MD, a former UPMC surgeon, raised concerns about his colleague’s surgical scheduling and billing practices.
Dr. Luketich’s overbooking of procedures led to patients enduring hours of medically unnecessary anesthesia time and risking surgical complications, according to court documents.
In addition, the complaint states that these practices violated the False Claims Act, which prohibits “teaching physicians” like Dr. Luketich from billing Medicare and other government health plans for “concurrent surgeries” – regulations federal authorities say UPMC leadership were aware of and the University of Pittsburgh Physicians (UPP), also named in the suit, permitted Dr. Luketich to skirt.
The whistleblower provision of the False Claims Act allows private parties to file an action on behalf of the United States and receive a portion of the recovery to help deter health care fraud, says the DOJ.
The defendants previously asked the court to dismiss the case, but a judge denied the request in June 2022.
Paul Wood, vice president and chief communications officer for UPMC, told this news organization that the lawsuit pertained to Dr. Luketich’s “most complicated, team-based surgical procedures.”
“At issue was compliance with the Centers for Medicare & Medicaid Services’ (CMS’s) Teaching Physician Regulation and related billing guidance as well as with UPMC’s internal surgical policies,” he said.
“While UPMC continues to believe Dr. Luketich’s surgical practice complies with CMS requirements, it has agreed to [the settlement] to avoid the distraction and expense of further litigation,” said Mr. Wood, adding that all parties agree that UPMC can seek clarity from CMS regarding future billing of these surgeries.
Efrem Grail, JD, Dr. Luketich’s attorney, said in an interview that he and Dr. Luketich are pleased that the settlement puts an end to the case and that he hopes the United States will issue “authoritative guidance” on billing regulations for teaching physicians, something medical schools and hospitals have sought for years.
Dr. Luketich, UPMC, and UPP face more legal challenges from a separate medical malpractice lawsuit. In March 2018, Bernadette Fedorka underwent a lung transplant at UPMC. Although Dr. Luketich did not perform the surgery, Ms. Fedorka alleges that his poor leadership caused understaffing of the lung transplant program and contributed to surgical complications, including a 4-inch piece of wire left in her neck.
Ms. Fedorka claims that suboxone impaired Dr. Luketich’s decision-making. He began taking the drug in 2008 to manage the pain from a slipped disc injury after a history of prescription drug abuse. Both UPMC and Dr. Luketich have denied the validity of Ms. Fedorka’s claims.
The malpractice suit centers on a recording of a conversation between Dr. Luketich and David Wilson, MD, who prescribed the suboxone and treated the surgeon’s opioid use disorder for several years. Dr. Luketich has accused former colleagues, Dr. D’Cunha and Lara Schaheen, MD, of illegally recording the private conversation that discussed Dr. Luketich’s suboxone prescription – something both physicians deny.
For the billing fraud case, Dr. Luketich has agreed to complete a corrective action plan and submit to a third-party audit of his Medicare billings for 1 year.
“This is an important settlement and a just conclusion to the United States’ investigation into Dr. Luketich’s surgical and billing practices and UPMC and UPP’s acceptance of those practices,” Acting U.S. Attorney Troy Rivetti said in a statement that, “no medical provider – however renowned – is excepted from scrutiny or above the law.”
A version of this article first appeared on Medscape.com.
the Department of Justice (DOJ) announced.
The lawsuit alleges that James L. Luketich, MD, the longtime chair of the school’s cardiothoracic surgery department, regularly performed up to three complex surgical procedures simultaneously, moving among multiple operating rooms and attending to matters other than patient care. The investigation began after Jonathan D’Cunha, MD, a former UPMC surgeon, raised concerns about his colleague’s surgical scheduling and billing practices.
Dr. Luketich’s overbooking of procedures led to patients enduring hours of medically unnecessary anesthesia time and risking surgical complications, according to court documents.
In addition, the complaint states that these practices violated the False Claims Act, which prohibits “teaching physicians” like Dr. Luketich from billing Medicare and other government health plans for “concurrent surgeries” – regulations federal authorities say UPMC leadership were aware of and the University of Pittsburgh Physicians (UPP), also named in the suit, permitted Dr. Luketich to skirt.
The whistleblower provision of the False Claims Act allows private parties to file an action on behalf of the United States and receive a portion of the recovery to help deter health care fraud, says the DOJ.
The defendants previously asked the court to dismiss the case, but a judge denied the request in June 2022.
Paul Wood, vice president and chief communications officer for UPMC, told this news organization that the lawsuit pertained to Dr. Luketich’s “most complicated, team-based surgical procedures.”
“At issue was compliance with the Centers for Medicare & Medicaid Services’ (CMS’s) Teaching Physician Regulation and related billing guidance as well as with UPMC’s internal surgical policies,” he said.
“While UPMC continues to believe Dr. Luketich’s surgical practice complies with CMS requirements, it has agreed to [the settlement] to avoid the distraction and expense of further litigation,” said Mr. Wood, adding that all parties agree that UPMC can seek clarity from CMS regarding future billing of these surgeries.
Efrem Grail, JD, Dr. Luketich’s attorney, said in an interview that he and Dr. Luketich are pleased that the settlement puts an end to the case and that he hopes the United States will issue “authoritative guidance” on billing regulations for teaching physicians, something medical schools and hospitals have sought for years.
Dr. Luketich, UPMC, and UPP face more legal challenges from a separate medical malpractice lawsuit. In March 2018, Bernadette Fedorka underwent a lung transplant at UPMC. Although Dr. Luketich did not perform the surgery, Ms. Fedorka alleges that his poor leadership caused understaffing of the lung transplant program and contributed to surgical complications, including a 4-inch piece of wire left in her neck.
Ms. Fedorka claims that suboxone impaired Dr. Luketich’s decision-making. He began taking the drug in 2008 to manage the pain from a slipped disc injury after a history of prescription drug abuse. Both UPMC and Dr. Luketich have denied the validity of Ms. Fedorka’s claims.
The malpractice suit centers on a recording of a conversation between Dr. Luketich and David Wilson, MD, who prescribed the suboxone and treated the surgeon’s opioid use disorder for several years. Dr. Luketich has accused former colleagues, Dr. D’Cunha and Lara Schaheen, MD, of illegally recording the private conversation that discussed Dr. Luketich’s suboxone prescription – something both physicians deny.
For the billing fraud case, Dr. Luketich has agreed to complete a corrective action plan and submit to a third-party audit of his Medicare billings for 1 year.
“This is an important settlement and a just conclusion to the United States’ investigation into Dr. Luketich’s surgical and billing practices and UPMC and UPP’s acceptance of those practices,” Acting U.S. Attorney Troy Rivetti said in a statement that, “no medical provider – however renowned – is excepted from scrutiny or above the law.”
A version of this article first appeared on Medscape.com.
What happens if we sit for more than 8 hours per day?
according to a recent Latin American study published in BMC Public Health.
These data come from almost 8,000 people aged 20-65 years (half of whom are women) who participated in the Latin American Study on Nutrition and Health (ELANS). The cross-sectional survey included representative samples from urban populations in Argentina, Brazil, Chile, Colombia, Costa Rica, Ecuador, Peru, and Venezuela. The average time spent sitting was 420 min/d. Ecuador had the lowest time (300 min/day), and Argentina and Peru had the highest (480 min/day).
No amount of sitting time has been associated with a greater health risk, but the World Health Organization recommends that sitting time be minimal.
“We used to believe that any intense physical exercise could compensate for a sedentary life. But now we know that a sedentary lifestyle in general and sitting time in particular have a direct effect and are an independent risk factor for chronic diseases,” said study author Irina Kovalskys, PhD, a pediatric specialist in nutrition and a professor of nutrition at the Catholic University of Argentina, Buenos Aires, and a principal investigator of ELANS.
Dr. Kovalskys stated that the 420-min average sitting time is worrying in a population such as the one studied, in which 60% of adults are obese and there are high rates of cardiometabolic risk factors. She affirmed that it is important to raise awareness among the population and focus on adolescents.
Felipe Lobelo, PhD, is a Colombian physician, an associate professor of global health at Emory University and director of epidemiology at Kaiser Permanente Georgia, both in Atlanta. He did not participate in this study but promotes the concept of exercise in medicine. The activity of the patient must be included in a clinical setting, and improving the level of physical activity can have a positive impact on health prognosis, he said.
“To make public health recommendations or even advise patients, a cutoff point is needed. Guidelines recommend 150 minutes per week of moderate to vigorous physical activity, and some countries have started to indicate that we should be concerned about people’s sitting time. There is still no equivalent to the 150 minutes, therefore, these studies are important, especially in the Latin American population,” said Dr. Lobelo.
He explained that the concept of an increased risk of death or chronic disease because of a lack of physical activity arose in the past 50 years, but only in the past 2 decades have we started thinking about sitting time.
“Spending more than 8 hours sitting per day clearly causes a much higher risk of chronic diseases, including obesity and diabetes. It may be a continuous and progressive association, and the point at which this increase becomes exponential is clearly between 6 and 8 hours of sitting time,” Dr. Lobelo added.
The authors expected to find a linear association with risk for being overweight or obese after 4 hours, but they did not find one. “This study has limitations. Among them was that other indicators were not considered, such as health indicators. Collaborations are starting with other research groups, and other studies are being designed,” said study author Gerson Ferrari, PhD, an associate professor at Santiago de Chile University.
Comparing indicators
The Latin American study tried to establish a sitting cutoff time after which the risk of becoming overweight or obese increases. It used three indicators of excess weight: body mass index (BMI), waist circumference, and neck circumference.
Sitting for more than 8 hours increased the chances of excess weight by 10% when measured by BMI and by 13% when neck circumference was used.
Dr. Ferrari stated that the result obtained measuring BMI is the one that should be considered, because it is used in public policy. Neck circumference is a more recent measurement of detection and it is less studied, but it is a valid indicator, with good sensitivity and advantages over others, such as ease of measurement and lack of variation over time.
According to the results of this study, measuring neck circumference may be the most sensitive method of the three. Neck circumference was proportionally greater in people who sat for at least 4, at least 6, and at least 8 hours/day than in those who sat for less than 4, less than 6, and less than 8 hours/day. This relationship was not observed with the other indicators.
Broaching the topic
“What is important is uninterrupted sitting time. The recommendation is to break up those sitting times with active periods. Health professionals have already incorporated the concept of moderate to vigorous physical exercise, but nonintense activities are sufficient to reduce sitting time. Yoga may not be vigorous, but it is valuable at reducing sitting time,” said Dr. Kovalskys.
Dr. Ferrari recommended giving patients concrete messages so that they spend as little time possible sitting. “It is better to stand on the bus or the subway even when there is a place to sit. Are you going to talk on the phone? It is better to do it while walking or at least standing instead of sitting.”
A recent literature review conducted by investigators of the University of Birmingham (England) studied the possible molecular and physiologic mechanisms of inactivity time, health consequences, and protection strategies. It offers an evaluation of interventions that can compensate for the immediate negative consequences of inactivity.
Physical activity
Some studies suggest that more than 60 min/day of moderate-intensity exercise or more than 150 min/week of moderate to vigorous exercise may be effective at mitigating the increased risk for mortality associated with sitting time, but reduced intensity may not be enough.
Active pauses
Interrupting sitting every 30-60 min to walk or cycle (2-10 min), performing 3 minutes of simple resistance activities every 30 minutes, such as calf or knee lifts, performing intermittent leg movements (1 minute of activity for every 4 minutes of inactivity during a 3-hour protocol session), or pausing to climb stairs (5 minutes every hour) may be beneficial for vascular health. However, not all studies have demonstrated these positive effects, therefore, some populations may need exercise of greater intensity or duration to counteract the negative vascular effects of acute inactivity periods.
Standing workstations
Standing workstations are effective at reducing sitting time in offices but may be ineffective at reducing vascular alterations related to sitting time. Although some experimental studies indicate vascular benefits, epidemiologic studies suggest that long periods of standing can be harmful to vascular health, especially for venous diseases. Recommendations for use should be accompanied by specific regimens on the frequency and duration of the position to attain the maximum benefits and minimize other vascular complications.
One problem that Dr. Lobelo noted is that some doctors ask their patients how active they are, but they do so in a nonstandardized manner. This observation led him to publish, together with the American Heart Association, an article on the importance for health systems of considering physical activity as a vital sign and including it in records in a standardized manner.
He said that “one advantage of having physical activity as a vital sign in patient medical records is that it allows us to identify individuals who are at greater risk.”
Kaiser Permanente asks the following questions: how many minutes of physical activity do you perform regularly per week, and what is the average intensity of that activity? Patients can be classified into the following three groups: those who follow the recommendations, those with almost no activity, and those who perform some physical activity but do not meet the recommended 150 min/week of moderate to vigorous activity.
Recording sitting time is more difficult. Dr. Lobelo indicated that “it is easier for a person to remember how much time they spent running than how long they were sitting.” Regarding the use of technology, he commented that most watches provide a good estimate. Without technology, it can be estimated by asking how much time is spent in the car, on the bus, or in front of the computer or television and then adding up these times.
Dr. Lobelo emphasized that the two behaviors, lack of physical activity and excessive sitting time, have independent associations with health outcomes. But if both are combined, the risk of obesity, diabetes, and cardiovascular diseases is not just added but rather is multiplied. These behaviors contribute to the epidemic of obesity and diabetes, since most people do not follow either of the two recommendations.
“Studies show that of the two behaviors, the more negative for health would be not following the physical activity recommendations,” said Dr. Lobelo. “If the recommendation of 150 min/week of moderate to vigorous physical activity is followed, the associated risk of sitting too much declines by 80%-90%. Additionally, we can prevent, help to manage, and decrease the risk of complications in more than 100 diseases, including infections. During the pandemic, it was observed that more active people had a lower risk of dying or of being hospitalized due to COVID-19 than less active people, independently of other factors, such as hypertension, diabetes, and obesity.”
Moreover, Dr. Lobelo believes in “practicing what you preach” and advocates that doctors become healthy models.
Dr. Lobelo, Dr. Ferrari, and Dr. Kovalskys disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish edition. A version appeared on Medscape.com.
according to a recent Latin American study published in BMC Public Health.
These data come from almost 8,000 people aged 20-65 years (half of whom are women) who participated in the Latin American Study on Nutrition and Health (ELANS). The cross-sectional survey included representative samples from urban populations in Argentina, Brazil, Chile, Colombia, Costa Rica, Ecuador, Peru, and Venezuela. The average time spent sitting was 420 min/d. Ecuador had the lowest time (300 min/day), and Argentina and Peru had the highest (480 min/day).
No amount of sitting time has been associated with a greater health risk, but the World Health Organization recommends that sitting time be minimal.
“We used to believe that any intense physical exercise could compensate for a sedentary life. But now we know that a sedentary lifestyle in general and sitting time in particular have a direct effect and are an independent risk factor for chronic diseases,” said study author Irina Kovalskys, PhD, a pediatric specialist in nutrition and a professor of nutrition at the Catholic University of Argentina, Buenos Aires, and a principal investigator of ELANS.
Dr. Kovalskys stated that the 420-min average sitting time is worrying in a population such as the one studied, in which 60% of adults are obese and there are high rates of cardiometabolic risk factors. She affirmed that it is important to raise awareness among the population and focus on adolescents.
Felipe Lobelo, PhD, is a Colombian physician, an associate professor of global health at Emory University and director of epidemiology at Kaiser Permanente Georgia, both in Atlanta. He did not participate in this study but promotes the concept of exercise in medicine. The activity of the patient must be included in a clinical setting, and improving the level of physical activity can have a positive impact on health prognosis, he said.
“To make public health recommendations or even advise patients, a cutoff point is needed. Guidelines recommend 150 minutes per week of moderate to vigorous physical activity, and some countries have started to indicate that we should be concerned about people’s sitting time. There is still no equivalent to the 150 minutes, therefore, these studies are important, especially in the Latin American population,” said Dr. Lobelo.
He explained that the concept of an increased risk of death or chronic disease because of a lack of physical activity arose in the past 50 years, but only in the past 2 decades have we started thinking about sitting time.
“Spending more than 8 hours sitting per day clearly causes a much higher risk of chronic diseases, including obesity and diabetes. It may be a continuous and progressive association, and the point at which this increase becomes exponential is clearly between 6 and 8 hours of sitting time,” Dr. Lobelo added.
The authors expected to find a linear association with risk for being overweight or obese after 4 hours, but they did not find one. “This study has limitations. Among them was that other indicators were not considered, such as health indicators. Collaborations are starting with other research groups, and other studies are being designed,” said study author Gerson Ferrari, PhD, an associate professor at Santiago de Chile University.
Comparing indicators
The Latin American study tried to establish a sitting cutoff time after which the risk of becoming overweight or obese increases. It used three indicators of excess weight: body mass index (BMI), waist circumference, and neck circumference.
Sitting for more than 8 hours increased the chances of excess weight by 10% when measured by BMI and by 13% when neck circumference was used.
Dr. Ferrari stated that the result obtained measuring BMI is the one that should be considered, because it is used in public policy. Neck circumference is a more recent measurement of detection and it is less studied, but it is a valid indicator, with good sensitivity and advantages over others, such as ease of measurement and lack of variation over time.
According to the results of this study, measuring neck circumference may be the most sensitive method of the three. Neck circumference was proportionally greater in people who sat for at least 4, at least 6, and at least 8 hours/day than in those who sat for less than 4, less than 6, and less than 8 hours/day. This relationship was not observed with the other indicators.
Broaching the topic
“What is important is uninterrupted sitting time. The recommendation is to break up those sitting times with active periods. Health professionals have already incorporated the concept of moderate to vigorous physical exercise, but nonintense activities are sufficient to reduce sitting time. Yoga may not be vigorous, but it is valuable at reducing sitting time,” said Dr. Kovalskys.
Dr. Ferrari recommended giving patients concrete messages so that they spend as little time possible sitting. “It is better to stand on the bus or the subway even when there is a place to sit. Are you going to talk on the phone? It is better to do it while walking or at least standing instead of sitting.”
A recent literature review conducted by investigators of the University of Birmingham (England) studied the possible molecular and physiologic mechanisms of inactivity time, health consequences, and protection strategies. It offers an evaluation of interventions that can compensate for the immediate negative consequences of inactivity.
Physical activity
Some studies suggest that more than 60 min/day of moderate-intensity exercise or more than 150 min/week of moderate to vigorous exercise may be effective at mitigating the increased risk for mortality associated with sitting time, but reduced intensity may not be enough.
Active pauses
Interrupting sitting every 30-60 min to walk or cycle (2-10 min), performing 3 minutes of simple resistance activities every 30 minutes, such as calf or knee lifts, performing intermittent leg movements (1 minute of activity for every 4 minutes of inactivity during a 3-hour protocol session), or pausing to climb stairs (5 minutes every hour) may be beneficial for vascular health. However, not all studies have demonstrated these positive effects, therefore, some populations may need exercise of greater intensity or duration to counteract the negative vascular effects of acute inactivity periods.
Standing workstations
Standing workstations are effective at reducing sitting time in offices but may be ineffective at reducing vascular alterations related to sitting time. Although some experimental studies indicate vascular benefits, epidemiologic studies suggest that long periods of standing can be harmful to vascular health, especially for venous diseases. Recommendations for use should be accompanied by specific regimens on the frequency and duration of the position to attain the maximum benefits and minimize other vascular complications.
One problem that Dr. Lobelo noted is that some doctors ask their patients how active they are, but they do so in a nonstandardized manner. This observation led him to publish, together with the American Heart Association, an article on the importance for health systems of considering physical activity as a vital sign and including it in records in a standardized manner.
He said that “one advantage of having physical activity as a vital sign in patient medical records is that it allows us to identify individuals who are at greater risk.”
Kaiser Permanente asks the following questions: how many minutes of physical activity do you perform regularly per week, and what is the average intensity of that activity? Patients can be classified into the following three groups: those who follow the recommendations, those with almost no activity, and those who perform some physical activity but do not meet the recommended 150 min/week of moderate to vigorous activity.
Recording sitting time is more difficult. Dr. Lobelo indicated that “it is easier for a person to remember how much time they spent running than how long they were sitting.” Regarding the use of technology, he commented that most watches provide a good estimate. Without technology, it can be estimated by asking how much time is spent in the car, on the bus, or in front of the computer or television and then adding up these times.
Dr. Lobelo emphasized that the two behaviors, lack of physical activity and excessive sitting time, have independent associations with health outcomes. But if both are combined, the risk of obesity, diabetes, and cardiovascular diseases is not just added but rather is multiplied. These behaviors contribute to the epidemic of obesity and diabetes, since most people do not follow either of the two recommendations.
“Studies show that of the two behaviors, the more negative for health would be not following the physical activity recommendations,” said Dr. Lobelo. “If the recommendation of 150 min/week of moderate to vigorous physical activity is followed, the associated risk of sitting too much declines by 80%-90%. Additionally, we can prevent, help to manage, and decrease the risk of complications in more than 100 diseases, including infections. During the pandemic, it was observed that more active people had a lower risk of dying or of being hospitalized due to COVID-19 than less active people, independently of other factors, such as hypertension, diabetes, and obesity.”
Moreover, Dr. Lobelo believes in “practicing what you preach” and advocates that doctors become healthy models.
Dr. Lobelo, Dr. Ferrari, and Dr. Kovalskys disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish edition. A version appeared on Medscape.com.
according to a recent Latin American study published in BMC Public Health.
These data come from almost 8,000 people aged 20-65 years (half of whom are women) who participated in the Latin American Study on Nutrition and Health (ELANS). The cross-sectional survey included representative samples from urban populations in Argentina, Brazil, Chile, Colombia, Costa Rica, Ecuador, Peru, and Venezuela. The average time spent sitting was 420 min/d. Ecuador had the lowest time (300 min/day), and Argentina and Peru had the highest (480 min/day).
No amount of sitting time has been associated with a greater health risk, but the World Health Organization recommends that sitting time be minimal.
“We used to believe that any intense physical exercise could compensate for a sedentary life. But now we know that a sedentary lifestyle in general and sitting time in particular have a direct effect and are an independent risk factor for chronic diseases,” said study author Irina Kovalskys, PhD, a pediatric specialist in nutrition and a professor of nutrition at the Catholic University of Argentina, Buenos Aires, and a principal investigator of ELANS.
Dr. Kovalskys stated that the 420-min average sitting time is worrying in a population such as the one studied, in which 60% of adults are obese and there are high rates of cardiometabolic risk factors. She affirmed that it is important to raise awareness among the population and focus on adolescents.
Felipe Lobelo, PhD, is a Colombian physician, an associate professor of global health at Emory University and director of epidemiology at Kaiser Permanente Georgia, both in Atlanta. He did not participate in this study but promotes the concept of exercise in medicine. The activity of the patient must be included in a clinical setting, and improving the level of physical activity can have a positive impact on health prognosis, he said.
“To make public health recommendations or even advise patients, a cutoff point is needed. Guidelines recommend 150 minutes per week of moderate to vigorous physical activity, and some countries have started to indicate that we should be concerned about people’s sitting time. There is still no equivalent to the 150 minutes, therefore, these studies are important, especially in the Latin American population,” said Dr. Lobelo.
He explained that the concept of an increased risk of death or chronic disease because of a lack of physical activity arose in the past 50 years, but only in the past 2 decades have we started thinking about sitting time.
“Spending more than 8 hours sitting per day clearly causes a much higher risk of chronic diseases, including obesity and diabetes. It may be a continuous and progressive association, and the point at which this increase becomes exponential is clearly between 6 and 8 hours of sitting time,” Dr. Lobelo added.
The authors expected to find a linear association with risk for being overweight or obese after 4 hours, but they did not find one. “This study has limitations. Among them was that other indicators were not considered, such as health indicators. Collaborations are starting with other research groups, and other studies are being designed,” said study author Gerson Ferrari, PhD, an associate professor at Santiago de Chile University.
Comparing indicators
The Latin American study tried to establish a sitting cutoff time after which the risk of becoming overweight or obese increases. It used three indicators of excess weight: body mass index (BMI), waist circumference, and neck circumference.
Sitting for more than 8 hours increased the chances of excess weight by 10% when measured by BMI and by 13% when neck circumference was used.
Dr. Ferrari stated that the result obtained measuring BMI is the one that should be considered, because it is used in public policy. Neck circumference is a more recent measurement of detection and it is less studied, but it is a valid indicator, with good sensitivity and advantages over others, such as ease of measurement and lack of variation over time.
According to the results of this study, measuring neck circumference may be the most sensitive method of the three. Neck circumference was proportionally greater in people who sat for at least 4, at least 6, and at least 8 hours/day than in those who sat for less than 4, less than 6, and less than 8 hours/day. This relationship was not observed with the other indicators.
Broaching the topic
“What is important is uninterrupted sitting time. The recommendation is to break up those sitting times with active periods. Health professionals have already incorporated the concept of moderate to vigorous physical exercise, but nonintense activities are sufficient to reduce sitting time. Yoga may not be vigorous, but it is valuable at reducing sitting time,” said Dr. Kovalskys.
Dr. Ferrari recommended giving patients concrete messages so that they spend as little time possible sitting. “It is better to stand on the bus or the subway even when there is a place to sit. Are you going to talk on the phone? It is better to do it while walking or at least standing instead of sitting.”
A recent literature review conducted by investigators of the University of Birmingham (England) studied the possible molecular and physiologic mechanisms of inactivity time, health consequences, and protection strategies. It offers an evaluation of interventions that can compensate for the immediate negative consequences of inactivity.
Physical activity
Some studies suggest that more than 60 min/day of moderate-intensity exercise or more than 150 min/week of moderate to vigorous exercise may be effective at mitigating the increased risk for mortality associated with sitting time, but reduced intensity may not be enough.
Active pauses
Interrupting sitting every 30-60 min to walk or cycle (2-10 min), performing 3 minutes of simple resistance activities every 30 minutes, such as calf or knee lifts, performing intermittent leg movements (1 minute of activity for every 4 minutes of inactivity during a 3-hour protocol session), or pausing to climb stairs (5 minutes every hour) may be beneficial for vascular health. However, not all studies have demonstrated these positive effects, therefore, some populations may need exercise of greater intensity or duration to counteract the negative vascular effects of acute inactivity periods.
Standing workstations
Standing workstations are effective at reducing sitting time in offices but may be ineffective at reducing vascular alterations related to sitting time. Although some experimental studies indicate vascular benefits, epidemiologic studies suggest that long periods of standing can be harmful to vascular health, especially for venous diseases. Recommendations for use should be accompanied by specific regimens on the frequency and duration of the position to attain the maximum benefits and minimize other vascular complications.
One problem that Dr. Lobelo noted is that some doctors ask their patients how active they are, but they do so in a nonstandardized manner. This observation led him to publish, together with the American Heart Association, an article on the importance for health systems of considering physical activity as a vital sign and including it in records in a standardized manner.
He said that “one advantage of having physical activity as a vital sign in patient medical records is that it allows us to identify individuals who are at greater risk.”
Kaiser Permanente asks the following questions: how many minutes of physical activity do you perform regularly per week, and what is the average intensity of that activity? Patients can be classified into the following three groups: those who follow the recommendations, those with almost no activity, and those who perform some physical activity but do not meet the recommended 150 min/week of moderate to vigorous activity.
Recording sitting time is more difficult. Dr. Lobelo indicated that “it is easier for a person to remember how much time they spent running than how long they were sitting.” Regarding the use of technology, he commented that most watches provide a good estimate. Without technology, it can be estimated by asking how much time is spent in the car, on the bus, or in front of the computer or television and then adding up these times.
Dr. Lobelo emphasized that the two behaviors, lack of physical activity and excessive sitting time, have independent associations with health outcomes. But if both are combined, the risk of obesity, diabetes, and cardiovascular diseases is not just added but rather is multiplied. These behaviors contribute to the epidemic of obesity and diabetes, since most people do not follow either of the two recommendations.
“Studies show that of the two behaviors, the more negative for health would be not following the physical activity recommendations,” said Dr. Lobelo. “If the recommendation of 150 min/week of moderate to vigorous physical activity is followed, the associated risk of sitting too much declines by 80%-90%. Additionally, we can prevent, help to manage, and decrease the risk of complications in more than 100 diseases, including infections. During the pandemic, it was observed that more active people had a lower risk of dying or of being hospitalized due to COVID-19 than less active people, independently of other factors, such as hypertension, diabetes, and obesity.”
Moreover, Dr. Lobelo believes in “practicing what you preach” and advocates that doctors become healthy models.
Dr. Lobelo, Dr. Ferrari, and Dr. Kovalskys disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish edition. A version appeared on Medscape.com.
FROM BMC PUBLIC HEALTH
Ileocecal resection possible first-line option in early Crohn’s disease
COPENHAGEN – Half of patients with ileocecal Crohn’s disease who undergo ileocecal resection within a year of diagnosis remain off drug treatment 5 years post procedure, challenging the current paradigm of reserving surgery for complicated Crohn’s disease, show real-world data comparing outcomes of surgery with anti–tumor necrosis factor inhibitor (TNFi) therapy.
“These data show that resection of inflamed bowel in early ileocecal Crohn’s disease effectively resets the clock,” said Manasi Agrawal, MD, of the department of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York, and a research associate with the Center for Molecular Prediction of Inflammatory Bowel Disease, Aalborg University, Copenhagen, who presented the findings at the annual congress of the European Crohn’s and Colitis Organisation. “These data are in accordance with the LIR!C study data and suggest that ileocecal resection could be a first-line therapeutic option in early ileal or ileocecal Crohn’s disease that could be discussed with our patients.”
While ileocecal resection is accepted as a therapeutic option in early Crohn’s disease, most clinicians reserve it for complicated disease that is refractory or intolerant to medication.
A radical shift in approach might be justified, said Jean-Frederic Colombel, MD, a study coinvestigator and gastroenterologist at Mount Sinai Hospital.
“These data can be transforming. It confirms that there may be a subset of patients with limited ileal Crohn’s disease that is uncomplicated and in whom surgery may be almost ‘curative’ because after follow-up there was no need for drug therapy. We need to reposition surgery as one possible option at diagnosis in patients with limited Crohn’s disease,” he said.
The 2017 LIR!C trial demonstrated comparable 1-year outcomes with ileocecal resection and anti-TNFi therapy in limited, nonstricturing ileocecal Crohn’s disease. A retrospective analysis of 5-year data from this trial, further reinforced ileocecal resection as a first-line option for limited Crohn’s disease, such that of those patients who underwent resection, 26% continued on anti-TNFi therapy, compared with 38% in those patients who took anti-TNFi therapy only. In addition, no patient in the resection group underwent subsequent surgery, whereas 48% of patients on anti-TNF underwent surgery.
Dr. Agrawal and coinvestigators decided that more conclusive, real-world data were needed and would help to determine whether ileocecal resection offered better patient outcomes than staying on anti-TNFi therapy.
The new findings are based on an analysis of 16,443 adults living with ileal Crohn’s disease and were diagnosed between 2003 and 2018. The data is based on an analysis of nationwide Danish registries. It included individuals who underwent
Ileocecal resection or received anti-TNF drugs within 1 year of diagnosis. Of the 16,443 patients diagnosed with Crohn’s disease over the study period, 1,279 had ileal or ileocecal disease and were included with 581 (3.5%) undergoing resection and 698 (4.2%) anti-TNFi index therapy.
Outcomes were compared between the two groups, and the proportions of individuals initiated on immunomodulator, anti-TNFi therapy, or no therapy at 5 years after their ileocecal resection were determined.
The primary outcome was CD-related hospitalization, systemic corticosteroid exposure, CD-related surgery, and perianal CD diagnosis. Crohn’s disease–related hospitalization, systemic corticosteroid use, Crohn’s disease–related surgery or perianal Crohn’s disease occurred in 273 versus 318 people in the ileocecal resection and anti-TNFi therapy groups respectively, equating to a 33% lower risk in the resection group. Of those patients who underwent ileocecal resection, 50.3% were on no treatment 5 years later; 47.5% and 17.1% were on immunomodulators and on anti-TNFi therapy respectively.
Resection was found to be associated with a statistically significant reduced risk of systemic corticosteroid use with an adjusted hazard ratio of 0.71 (95% confidence interval, 0.54-0.92). No statistically significant reduced risk was found for Crohn’s disease-related hospitalization (aHR, 0.79; 95% CI, 0.61-1.01) or perianal Crohn’s disease diagnosis (aHR, 0.70; 95% CI, 0.38-1.30). Adjustments were made for demographic and clinical variables, for example, age, sex, year of treatment, number of hospital contacts for an indication all in the year prior to index treatment.
In comparison with the proportion of resection patients at 5 years who were on no treatment, immunomodulators or anti-TNFi therapy, there are no data on the 5-year outcomes of those patients who began on anti-TNFi therapy, but patients typically continue unless they become intolerant or response starts to fail, Dr. Agrawal said.
Willem Bemelmen, MD, a colorectal surgeon from the University of Amsterdam who served as a moderator after the presentation said: “These results could lead to a paradigm shift in the management of patients with Crohn’s disease. Prior studies gave us early signals that surgery in Crohn’s disease might benefit the patients, but now with these larger scale data, with many patients, we might finally convince gastroenterologists to send patients in for early surgery.”
Dr. Agrawal, Dr. Bemelmen, and Dr. Colombel declared no relevant conflicts of interest.
This article was updated 3/7/23.
COPENHAGEN – Half of patients with ileocecal Crohn’s disease who undergo ileocecal resection within a year of diagnosis remain off drug treatment 5 years post procedure, challenging the current paradigm of reserving surgery for complicated Crohn’s disease, show real-world data comparing outcomes of surgery with anti–tumor necrosis factor inhibitor (TNFi) therapy.
“These data show that resection of inflamed bowel in early ileocecal Crohn’s disease effectively resets the clock,” said Manasi Agrawal, MD, of the department of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York, and a research associate with the Center for Molecular Prediction of Inflammatory Bowel Disease, Aalborg University, Copenhagen, who presented the findings at the annual congress of the European Crohn’s and Colitis Organisation. “These data are in accordance with the LIR!C study data and suggest that ileocecal resection could be a first-line therapeutic option in early ileal or ileocecal Crohn’s disease that could be discussed with our patients.”
While ileocecal resection is accepted as a therapeutic option in early Crohn’s disease, most clinicians reserve it for complicated disease that is refractory or intolerant to medication.
A radical shift in approach might be justified, said Jean-Frederic Colombel, MD, a study coinvestigator and gastroenterologist at Mount Sinai Hospital.
“These data can be transforming. It confirms that there may be a subset of patients with limited ileal Crohn’s disease that is uncomplicated and in whom surgery may be almost ‘curative’ because after follow-up there was no need for drug therapy. We need to reposition surgery as one possible option at diagnosis in patients with limited Crohn’s disease,” he said.
The 2017 LIR!C trial demonstrated comparable 1-year outcomes with ileocecal resection and anti-TNFi therapy in limited, nonstricturing ileocecal Crohn’s disease. A retrospective analysis of 5-year data from this trial, further reinforced ileocecal resection as a first-line option for limited Crohn’s disease, such that of those patients who underwent resection, 26% continued on anti-TNFi therapy, compared with 38% in those patients who took anti-TNFi therapy only. In addition, no patient in the resection group underwent subsequent surgery, whereas 48% of patients on anti-TNF underwent surgery.
Dr. Agrawal and coinvestigators decided that more conclusive, real-world data were needed and would help to determine whether ileocecal resection offered better patient outcomes than staying on anti-TNFi therapy.
The new findings are based on an analysis of 16,443 adults living with ileal Crohn’s disease and were diagnosed between 2003 and 2018. The data is based on an analysis of nationwide Danish registries. It included individuals who underwent
Ileocecal resection or received anti-TNF drugs within 1 year of diagnosis. Of the 16,443 patients diagnosed with Crohn’s disease over the study period, 1,279 had ileal or ileocecal disease and were included with 581 (3.5%) undergoing resection and 698 (4.2%) anti-TNFi index therapy.
Outcomes were compared between the two groups, and the proportions of individuals initiated on immunomodulator, anti-TNFi therapy, or no therapy at 5 years after their ileocecal resection were determined.
The primary outcome was CD-related hospitalization, systemic corticosteroid exposure, CD-related surgery, and perianal CD diagnosis. Crohn’s disease–related hospitalization, systemic corticosteroid use, Crohn’s disease–related surgery or perianal Crohn’s disease occurred in 273 versus 318 people in the ileocecal resection and anti-TNFi therapy groups respectively, equating to a 33% lower risk in the resection group. Of those patients who underwent ileocecal resection, 50.3% were on no treatment 5 years later; 47.5% and 17.1% were on immunomodulators and on anti-TNFi therapy respectively.
Resection was found to be associated with a statistically significant reduced risk of systemic corticosteroid use with an adjusted hazard ratio of 0.71 (95% confidence interval, 0.54-0.92). No statistically significant reduced risk was found for Crohn’s disease-related hospitalization (aHR, 0.79; 95% CI, 0.61-1.01) or perianal Crohn’s disease diagnosis (aHR, 0.70; 95% CI, 0.38-1.30). Adjustments were made for demographic and clinical variables, for example, age, sex, year of treatment, number of hospital contacts for an indication all in the year prior to index treatment.
In comparison with the proportion of resection patients at 5 years who were on no treatment, immunomodulators or anti-TNFi therapy, there are no data on the 5-year outcomes of those patients who began on anti-TNFi therapy, but patients typically continue unless they become intolerant or response starts to fail, Dr. Agrawal said.
Willem Bemelmen, MD, a colorectal surgeon from the University of Amsterdam who served as a moderator after the presentation said: “These results could lead to a paradigm shift in the management of patients with Crohn’s disease. Prior studies gave us early signals that surgery in Crohn’s disease might benefit the patients, but now with these larger scale data, with many patients, we might finally convince gastroenterologists to send patients in for early surgery.”
Dr. Agrawal, Dr. Bemelmen, and Dr. Colombel declared no relevant conflicts of interest.
This article was updated 3/7/23.
COPENHAGEN – Half of patients with ileocecal Crohn’s disease who undergo ileocecal resection within a year of diagnosis remain off drug treatment 5 years post procedure, challenging the current paradigm of reserving surgery for complicated Crohn’s disease, show real-world data comparing outcomes of surgery with anti–tumor necrosis factor inhibitor (TNFi) therapy.
“These data show that resection of inflamed bowel in early ileocecal Crohn’s disease effectively resets the clock,” said Manasi Agrawal, MD, of the department of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York, and a research associate with the Center for Molecular Prediction of Inflammatory Bowel Disease, Aalborg University, Copenhagen, who presented the findings at the annual congress of the European Crohn’s and Colitis Organisation. “These data are in accordance with the LIR!C study data and suggest that ileocecal resection could be a first-line therapeutic option in early ileal or ileocecal Crohn’s disease that could be discussed with our patients.”
While ileocecal resection is accepted as a therapeutic option in early Crohn’s disease, most clinicians reserve it for complicated disease that is refractory or intolerant to medication.
A radical shift in approach might be justified, said Jean-Frederic Colombel, MD, a study coinvestigator and gastroenterologist at Mount Sinai Hospital.
“These data can be transforming. It confirms that there may be a subset of patients with limited ileal Crohn’s disease that is uncomplicated and in whom surgery may be almost ‘curative’ because after follow-up there was no need for drug therapy. We need to reposition surgery as one possible option at diagnosis in patients with limited Crohn’s disease,” he said.
The 2017 LIR!C trial demonstrated comparable 1-year outcomes with ileocecal resection and anti-TNFi therapy in limited, nonstricturing ileocecal Crohn’s disease. A retrospective analysis of 5-year data from this trial, further reinforced ileocecal resection as a first-line option for limited Crohn’s disease, such that of those patients who underwent resection, 26% continued on anti-TNFi therapy, compared with 38% in those patients who took anti-TNFi therapy only. In addition, no patient in the resection group underwent subsequent surgery, whereas 48% of patients on anti-TNF underwent surgery.
Dr. Agrawal and coinvestigators decided that more conclusive, real-world data were needed and would help to determine whether ileocecal resection offered better patient outcomes than staying on anti-TNFi therapy.
The new findings are based on an analysis of 16,443 adults living with ileal Crohn’s disease and were diagnosed between 2003 and 2018. The data is based on an analysis of nationwide Danish registries. It included individuals who underwent
Ileocecal resection or received anti-TNF drugs within 1 year of diagnosis. Of the 16,443 patients diagnosed with Crohn’s disease over the study period, 1,279 had ileal or ileocecal disease and were included with 581 (3.5%) undergoing resection and 698 (4.2%) anti-TNFi index therapy.
Outcomes were compared between the two groups, and the proportions of individuals initiated on immunomodulator, anti-TNFi therapy, or no therapy at 5 years after their ileocecal resection were determined.
The primary outcome was CD-related hospitalization, systemic corticosteroid exposure, CD-related surgery, and perianal CD diagnosis. Crohn’s disease–related hospitalization, systemic corticosteroid use, Crohn’s disease–related surgery or perianal Crohn’s disease occurred in 273 versus 318 people in the ileocecal resection and anti-TNFi therapy groups respectively, equating to a 33% lower risk in the resection group. Of those patients who underwent ileocecal resection, 50.3% were on no treatment 5 years later; 47.5% and 17.1% were on immunomodulators and on anti-TNFi therapy respectively.
Resection was found to be associated with a statistically significant reduced risk of systemic corticosteroid use with an adjusted hazard ratio of 0.71 (95% confidence interval, 0.54-0.92). No statistically significant reduced risk was found for Crohn’s disease-related hospitalization (aHR, 0.79; 95% CI, 0.61-1.01) or perianal Crohn’s disease diagnosis (aHR, 0.70; 95% CI, 0.38-1.30). Adjustments were made for demographic and clinical variables, for example, age, sex, year of treatment, number of hospital contacts for an indication all in the year prior to index treatment.
In comparison with the proportion of resection patients at 5 years who were on no treatment, immunomodulators or anti-TNFi therapy, there are no data on the 5-year outcomes of those patients who began on anti-TNFi therapy, but patients typically continue unless they become intolerant or response starts to fail, Dr. Agrawal said.
Willem Bemelmen, MD, a colorectal surgeon from the University of Amsterdam who served as a moderator after the presentation said: “These results could lead to a paradigm shift in the management of patients with Crohn’s disease. Prior studies gave us early signals that surgery in Crohn’s disease might benefit the patients, but now with these larger scale data, with many patients, we might finally convince gastroenterologists to send patients in for early surgery.”
Dr. Agrawal, Dr. Bemelmen, and Dr. Colombel declared no relevant conflicts of interest.
This article was updated 3/7/23.
AT ECCO 2023
Pediatric IBD patients wrestle with lingering gut pain
COPENHAGEN –
“A major finding of our small study was the impact of chronic pain on well-being and emotional health which was particularly significant in vulnerable children moving through adolescence towards adulthood,” said Dhamyanthi Thangarajah, MD, a consultant pediatric gastroenterologist at Chelsea and Westminster Hospital, London, in a presentation at the annual congress of the European Crohn’s and Colitis Organisation.
In the study of 41 children between 10 and 17 years old, chronic pain was found in 80% of participants who had established and extensive disease. Most participants had markers for fecal calprotectin, a sensitive marker for inflammation in the gastrointestinal tract, and others had Crohn’s disease and were prescribed biologics.
No relationship was found between chronic pain and IBD activity, but quality of life scores were negatively impacted in children with chronic pain.
“Moving forward, strategies should target screening for chronic pain in children with IBD and provide psychosocial interventions early on,” Dr. Thangarajah said. “We also need to understand more about internalizing pain and explore mood disorders.”
Many children with IBD also present with chronic abdominal pain, which was the impetus for conducting the study. “Essentially, we wondered whether this was a symptom of active disease, or were we missing something? In adult patients, chronic pain is prevalent, but in children we don’t necessarily screen for chronic pain, although it is part of active disease,” she said.
There is considerable patient and parental anxiety around the nature and origins of the chronic pain, Dr. Thangarajah said.
“We need to understand the prevalence and impact of chronic pain in children and adolescents, and as such we wanted to understand and characterize our cohort,” she said.
Dr. Thangarajah said clinicians tend to be very focused on disease activity and that screening for chronic pain is not usually carried out. “When we look at their clinical indices, the patients seem better, but the fact that it affects emotional health, and we don’t screen for it, means we need psychological help for these pediatric patients,” she said. “Patients need to be able to talk about their pain, and we need to understand if these children are having IBD-type symptoms, and this just isn’t asked about. It would be good to extend this study with a psychologist to understand more about this pain.”
How the study was conducted
The findings are based on the IMPACT III quality of life questionnaire for IBD. Chronic pain was defined as mild, moderate, or severe according to the van Korff scale.
“Patients had extensive and established disease, as expected in a pediatric cohort, the majority of whom were on immunosuppressant biologic drugs [64%-89%]. Among these patients, analgesic use was low, which is part of the education we give parents, and there was no opiate use in children, which differs from adults with IBD,” Dr. Thangarajah said.
A total of 33/41 (80%) of patients had chronic pain, and of these, abdominal chronic pain was most common in 30/33 (90%), joint pain was present in 2/33 (6%), and headache in 1/33, (3%). The majority 26/33 (79%) were on biologic agents, and analgesia use was low at 15/33 (45%). A total of 42% of children across the spectrum of chronic pain severity were on immunomodulators. Comorbidities were present in 42%-57% of patients with mild, and moderate-severe chronic pain respectively.
IBD disease activity in children with chronic pain was compared with those without chronic pain, as defined by Pediatric Crohn’s Disease Activity Index (PCDAI), Pediatric Ulcerative Colitis Activity Index (PUCAI), C-reactive protein (CRP), and faecal calprotectin. No difference was found.
Dr. Thangarajah highlighted the significantly lower quality of life score in children with chronic pain (69 and 51 in mild, and moderate-severe pain subgroups respectively, compared with 81 in those children without chronic pain, P < .05). Specifically, body image showed no difference between children with and without chronic pain (59-65 points across no pain, mild, moderate and severe chronic pain).
Chronic pain patients also commonly reported sleep disturbance with around 66% of patients with chronic pain, compared with around 11% in those without. Anemia was reported in 30% versus 21% respectively. However, nearly half of children with chronic pain had comorbidities 16/33 (48%), and 5/16 (31%) had diagnoses that may be associated with comorbid pain.
Psychosocial support within gastroenterology unavailable
Christine Norton, PhD, professor of nursing at Kings College London, also spoke at the conference on abdominal pain and the well-being of patients with IBD. She said that pain can still be a problem for some patients in remission from IBD.
“In adults we find pain is related to disease activity, however, 40%-50% of patients with IBD remission still report pain. Abdominal pain is dominant but it can be anywhere in the body. This is really poorly addressed in clinical consultations. It’s a ‘don’t ask, don’t tell’ situation where the nurse or doctor would do something if they could, but they just don’t ask the patients,” she said.
If patients volunteer the information that they still have pain during remission, it might get dismissed as irritable bowel syndrome (IBS), Dr. Norton said. “Some patients do fulfill these criteria for IBS, but it still needs to be managed. Here at ECCO, the focus is on getting patients into deep remission and inflammation under tight control, but what do we do with the jangling pain nerves although there’s nothing apparently triggering them, the gut-brain sensitivity – it’s so hard to live with it. They need support,” she said.
Dr. Norton said clinicians need a better way to validate chronic pain. “Sometimes people don’t feel believed, but even if the doctor believes them, they don’t know what to do anyway. There’s very few places with psychological support within the field of gastroenterology. Do we educate the gastroenterologist in this aspect? Do we develop the skills of IBD nurses?”
Dr. Thangarajah and Dr. Norton have no disclosures to declare.
COPENHAGEN –
“A major finding of our small study was the impact of chronic pain on well-being and emotional health which was particularly significant in vulnerable children moving through adolescence towards adulthood,” said Dhamyanthi Thangarajah, MD, a consultant pediatric gastroenterologist at Chelsea and Westminster Hospital, London, in a presentation at the annual congress of the European Crohn’s and Colitis Organisation.
In the study of 41 children between 10 and 17 years old, chronic pain was found in 80% of participants who had established and extensive disease. Most participants had markers for fecal calprotectin, a sensitive marker for inflammation in the gastrointestinal tract, and others had Crohn’s disease and were prescribed biologics.
No relationship was found between chronic pain and IBD activity, but quality of life scores were negatively impacted in children with chronic pain.
“Moving forward, strategies should target screening for chronic pain in children with IBD and provide psychosocial interventions early on,” Dr. Thangarajah said. “We also need to understand more about internalizing pain and explore mood disorders.”
Many children with IBD also present with chronic abdominal pain, which was the impetus for conducting the study. “Essentially, we wondered whether this was a symptom of active disease, or were we missing something? In adult patients, chronic pain is prevalent, but in children we don’t necessarily screen for chronic pain, although it is part of active disease,” she said.
There is considerable patient and parental anxiety around the nature and origins of the chronic pain, Dr. Thangarajah said.
“We need to understand the prevalence and impact of chronic pain in children and adolescents, and as such we wanted to understand and characterize our cohort,” she said.
Dr. Thangarajah said clinicians tend to be very focused on disease activity and that screening for chronic pain is not usually carried out. “When we look at their clinical indices, the patients seem better, but the fact that it affects emotional health, and we don’t screen for it, means we need psychological help for these pediatric patients,” she said. “Patients need to be able to talk about their pain, and we need to understand if these children are having IBD-type symptoms, and this just isn’t asked about. It would be good to extend this study with a psychologist to understand more about this pain.”
How the study was conducted
The findings are based on the IMPACT III quality of life questionnaire for IBD. Chronic pain was defined as mild, moderate, or severe according to the van Korff scale.
“Patients had extensive and established disease, as expected in a pediatric cohort, the majority of whom were on immunosuppressant biologic drugs [64%-89%]. Among these patients, analgesic use was low, which is part of the education we give parents, and there was no opiate use in children, which differs from adults with IBD,” Dr. Thangarajah said.
A total of 33/41 (80%) of patients had chronic pain, and of these, abdominal chronic pain was most common in 30/33 (90%), joint pain was present in 2/33 (6%), and headache in 1/33, (3%). The majority 26/33 (79%) were on biologic agents, and analgesia use was low at 15/33 (45%). A total of 42% of children across the spectrum of chronic pain severity were on immunomodulators. Comorbidities were present in 42%-57% of patients with mild, and moderate-severe chronic pain respectively.
IBD disease activity in children with chronic pain was compared with those without chronic pain, as defined by Pediatric Crohn’s Disease Activity Index (PCDAI), Pediatric Ulcerative Colitis Activity Index (PUCAI), C-reactive protein (CRP), and faecal calprotectin. No difference was found.
Dr. Thangarajah highlighted the significantly lower quality of life score in children with chronic pain (69 and 51 in mild, and moderate-severe pain subgroups respectively, compared with 81 in those children without chronic pain, P < .05). Specifically, body image showed no difference between children with and without chronic pain (59-65 points across no pain, mild, moderate and severe chronic pain).
Chronic pain patients also commonly reported sleep disturbance with around 66% of patients with chronic pain, compared with around 11% in those without. Anemia was reported in 30% versus 21% respectively. However, nearly half of children with chronic pain had comorbidities 16/33 (48%), and 5/16 (31%) had diagnoses that may be associated with comorbid pain.
Psychosocial support within gastroenterology unavailable
Christine Norton, PhD, professor of nursing at Kings College London, also spoke at the conference on abdominal pain and the well-being of patients with IBD. She said that pain can still be a problem for some patients in remission from IBD.
“In adults we find pain is related to disease activity, however, 40%-50% of patients with IBD remission still report pain. Abdominal pain is dominant but it can be anywhere in the body. This is really poorly addressed in clinical consultations. It’s a ‘don’t ask, don’t tell’ situation where the nurse or doctor would do something if they could, but they just don’t ask the patients,” she said.
If patients volunteer the information that they still have pain during remission, it might get dismissed as irritable bowel syndrome (IBS), Dr. Norton said. “Some patients do fulfill these criteria for IBS, but it still needs to be managed. Here at ECCO, the focus is on getting patients into deep remission and inflammation under tight control, but what do we do with the jangling pain nerves although there’s nothing apparently triggering them, the gut-brain sensitivity – it’s so hard to live with it. They need support,” she said.
Dr. Norton said clinicians need a better way to validate chronic pain. “Sometimes people don’t feel believed, but even if the doctor believes them, they don’t know what to do anyway. There’s very few places with psychological support within the field of gastroenterology. Do we educate the gastroenterologist in this aspect? Do we develop the skills of IBD nurses?”
Dr. Thangarajah and Dr. Norton have no disclosures to declare.
COPENHAGEN –
“A major finding of our small study was the impact of chronic pain on well-being and emotional health which was particularly significant in vulnerable children moving through adolescence towards adulthood,” said Dhamyanthi Thangarajah, MD, a consultant pediatric gastroenterologist at Chelsea and Westminster Hospital, London, in a presentation at the annual congress of the European Crohn’s and Colitis Organisation.
In the study of 41 children between 10 and 17 years old, chronic pain was found in 80% of participants who had established and extensive disease. Most participants had markers for fecal calprotectin, a sensitive marker for inflammation in the gastrointestinal tract, and others had Crohn’s disease and were prescribed biologics.
No relationship was found between chronic pain and IBD activity, but quality of life scores were negatively impacted in children with chronic pain.
“Moving forward, strategies should target screening for chronic pain in children with IBD and provide psychosocial interventions early on,” Dr. Thangarajah said. “We also need to understand more about internalizing pain and explore mood disorders.”
Many children with IBD also present with chronic abdominal pain, which was the impetus for conducting the study. “Essentially, we wondered whether this was a symptom of active disease, or were we missing something? In adult patients, chronic pain is prevalent, but in children we don’t necessarily screen for chronic pain, although it is part of active disease,” she said.
There is considerable patient and parental anxiety around the nature and origins of the chronic pain, Dr. Thangarajah said.
“We need to understand the prevalence and impact of chronic pain in children and adolescents, and as such we wanted to understand and characterize our cohort,” she said.
Dr. Thangarajah said clinicians tend to be very focused on disease activity and that screening for chronic pain is not usually carried out. “When we look at their clinical indices, the patients seem better, but the fact that it affects emotional health, and we don’t screen for it, means we need psychological help for these pediatric patients,” she said. “Patients need to be able to talk about their pain, and we need to understand if these children are having IBD-type symptoms, and this just isn’t asked about. It would be good to extend this study with a psychologist to understand more about this pain.”
How the study was conducted
The findings are based on the IMPACT III quality of life questionnaire for IBD. Chronic pain was defined as mild, moderate, or severe according to the van Korff scale.
“Patients had extensive and established disease, as expected in a pediatric cohort, the majority of whom were on immunosuppressant biologic drugs [64%-89%]. Among these patients, analgesic use was low, which is part of the education we give parents, and there was no opiate use in children, which differs from adults with IBD,” Dr. Thangarajah said.
A total of 33/41 (80%) of patients had chronic pain, and of these, abdominal chronic pain was most common in 30/33 (90%), joint pain was present in 2/33 (6%), and headache in 1/33, (3%). The majority 26/33 (79%) were on biologic agents, and analgesia use was low at 15/33 (45%). A total of 42% of children across the spectrum of chronic pain severity were on immunomodulators. Comorbidities were present in 42%-57% of patients with mild, and moderate-severe chronic pain respectively.
IBD disease activity in children with chronic pain was compared with those without chronic pain, as defined by Pediatric Crohn’s Disease Activity Index (PCDAI), Pediatric Ulcerative Colitis Activity Index (PUCAI), C-reactive protein (CRP), and faecal calprotectin. No difference was found.
Dr. Thangarajah highlighted the significantly lower quality of life score in children with chronic pain (69 and 51 in mild, and moderate-severe pain subgroups respectively, compared with 81 in those children without chronic pain, P < .05). Specifically, body image showed no difference between children with and without chronic pain (59-65 points across no pain, mild, moderate and severe chronic pain).
Chronic pain patients also commonly reported sleep disturbance with around 66% of patients with chronic pain, compared with around 11% in those without. Anemia was reported in 30% versus 21% respectively. However, nearly half of children with chronic pain had comorbidities 16/33 (48%), and 5/16 (31%) had diagnoses that may be associated with comorbid pain.
Psychosocial support within gastroenterology unavailable
Christine Norton, PhD, professor of nursing at Kings College London, also spoke at the conference on abdominal pain and the well-being of patients with IBD. She said that pain can still be a problem for some patients in remission from IBD.
“In adults we find pain is related to disease activity, however, 40%-50% of patients with IBD remission still report pain. Abdominal pain is dominant but it can be anywhere in the body. This is really poorly addressed in clinical consultations. It’s a ‘don’t ask, don’t tell’ situation where the nurse or doctor would do something if they could, but they just don’t ask the patients,” she said.
If patients volunteer the information that they still have pain during remission, it might get dismissed as irritable bowel syndrome (IBS), Dr. Norton said. “Some patients do fulfill these criteria for IBS, but it still needs to be managed. Here at ECCO, the focus is on getting patients into deep remission and inflammation under tight control, but what do we do with the jangling pain nerves although there’s nothing apparently triggering them, the gut-brain sensitivity – it’s so hard to live with it. They need support,” she said.
Dr. Norton said clinicians need a better way to validate chronic pain. “Sometimes people don’t feel believed, but even if the doctor believes them, they don’t know what to do anyway. There’s very few places with psychological support within the field of gastroenterology. Do we educate the gastroenterologist in this aspect? Do we develop the skills of IBD nurses?”
Dr. Thangarajah and Dr. Norton have no disclosures to declare.
AT ECCO 2023