User login
State of Confusion: Should All Children Get Lipid Labs for High Cholesterol?
Clinicians receive conflicting advice on whether to order blood tests to screen for lipids in children. A new study could add to the confusion. Researchers found that a combination of physical proxy measures such as hypertension and body mass index (BMI) predicted the risk for future cardiovascular events as well as the physical model plus lipid labs, questioning the value of those blood tests.
Some medical organizations advise screening only for high-risk children because more research is needed to define the harms and benefits of universal screening. Diet and behavioral changes are sufficient for most children, and universal screening could lead to false positives and unnecessary further testing, they said.
Groups that favor lipid tests for all children say these measurements detect familial hypercholesterolemia (FH) that would not otherwise be diagnosed, leading to treatment with drugs like statins and a greater chance of preventing cardiovascular disease (CVD) in adulthood.
Researchers from the new study said their findings do not address screenings for FH, which affects 1 in 250 US children and puts them at a risk for atherosclerotic CVD.
Recommending Blood Tests in Age Groups
One of the seminal guidelines on screening lipids in children came from the National Heart, Lung, and Blood Institute (NHLBI), which in 2011 recommended children undergo dyslipidemia screening between the ages of 9 and 11 years and again between 17 and 21 years. Children should receive a screening starting at age 2 years if they have a family history of CVD or dyslipidemia or have diabetes, an elevated BMI, or hypertension. The American Academy of Pediatrics shortly followed suit, issuing similar recommendations.
Screening for the two subsets of ages was an expansion from the original 1992 guidelines from the National Cholesterol Education Program, which recommended screening only for children with either a family history of early CVD or elevated total cholesterol levels.
A 2011 panel for the NHLBI said the older approach identified significantly fewer children with abnormal levels of low-density lipoprotein cholesterol (LDL-C) than the addition of two age groups for screening, adding that many children do not have a complete family history. The American College of Cardiology and American Heart Association later supported NHLBI’s stance in their joint guidelines on the management of cholesterol.
Mark Corkins, MD, chair of the AAP’s Committee on Nutrition, told Medscape Medical News that if children are screened only because they have obesity or a family history of FH, some with elevated lipid levels will be missed. For instance, studies indicate caregiver recall of FH often is inaccurate, and the genetic disorder that causes the condition is not related to obesity.
“The screening is to find familial hypercholesterolemia, to try to find the ones that need therapy,” that would not be caught by the risk-based screening earlier on in childhood, Corkins said.
Only Screen Children With Risk Factors
But other groups do not agree. The US Preventive Services Task Force (USPSTF) found insufficient evidence to recommend for or against screening for lipid disorders in asymptomatic children and teens.
The group also said it found inadequate evidence that lipid-lowering interventions in the general pediatric population lead to reductions in cardiovascular events or all-cause mortality once they reached adulthood. USPSTF also raised questions about the safety of lipid-lowering drugs in children.
“The current evidence is insufficient to assess the balance of benefits and harms of screening for lipid disorders in children and adolescents 20 years or younger,” the panel wrote.
The American Academy of Family Physicians supports USPSTF’s recommendations.
Low Rate of Screening
While the uncertainty over screening in children continues, the practice has been adopted by a minority of clinicians.
A study published in JAMA Network Open in July found 9% of 700,000 9- to 11-year-olds had a documented result from a lipid screening. Among more than 1.3 million 17- to 21-year-olds, 13% had received a screening.
As BMI went up, so did screening rates. A little over 9% children and teens with a healthy weight were screened compared with 14.7% of those with moderate obesity and 21.9% of those with severe obesity.
Among those screened, 32.3% of 9- to 11-year-olds and 30.2% of 17- to 21-year-olds had abnormal lipid levels, defined as having one elevated measure out of five, including total cholesterol of 200 mg/dL or higher or LDL-C levels of 130 mg/dL or higher.
Justin Zachariah, MD, MPH, an associate professor of pediatrics-cardiology at Baylor College of Medicine in Houston, spoke about physicians screening children based only on factors like obesity during a presentation at the recent annual meeting of the American Academy of Pediatrics. He cited research showing roughly one in four children with abnormal lipids had a normal weight.
If a clinician is reserving a lipid screening for a child who is overweight or has obesity, “you’re missing nearly half the problem,” Zachariah said during his presentation.
One reason for the low rate of universal screening may be inattention to FH by clinicians, according to Samuel S. Gidding, MD, a professor in the Department of Genomic Health at Geisinger College of Health Sciences in Bridgewater Corners, Vermont.
For instance, a clinician has only a set amount of time during a well-child visit and other issues may take precedence, “so it doesn’t make sense to broach preventive screening for something that could happen 30 or 40 years from now, vs this [other] very immediate problem,” he said.
Clinicians “are triggered to act on the LDL level, but don’t think about FH as a possible diagnosis,” Gidding told Medscape Medical News.
Another barrier is that in some settings, caregivers must take children and teens to another facility on a different day to fulfill an order for a lipid test.
“It’s reluctance of doctors to order it, knowing patients won’t go through with it,” Gidding said.
Gidding is a consultant for Esperion Therapeutics. Other sources in this story reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
Clinicians receive conflicting advice on whether to order blood tests to screen for lipids in children. A new study could add to the confusion. Researchers found that a combination of physical proxy measures such as hypertension and body mass index (BMI) predicted the risk for future cardiovascular events as well as the physical model plus lipid labs, questioning the value of those blood tests.
Some medical organizations advise screening only for high-risk children because more research is needed to define the harms and benefits of universal screening. Diet and behavioral changes are sufficient for most children, and universal screening could lead to false positives and unnecessary further testing, they said.
Groups that favor lipid tests for all children say these measurements detect familial hypercholesterolemia (FH) that would not otherwise be diagnosed, leading to treatment with drugs like statins and a greater chance of preventing cardiovascular disease (CVD) in adulthood.
Researchers from the new study said their findings do not address screenings for FH, which affects 1 in 250 US children and puts them at a risk for atherosclerotic CVD.
Recommending Blood Tests in Age Groups
One of the seminal guidelines on screening lipids in children came from the National Heart, Lung, and Blood Institute (NHLBI), which in 2011 recommended children undergo dyslipidemia screening between the ages of 9 and 11 years and again between 17 and 21 years. Children should receive a screening starting at age 2 years if they have a family history of CVD or dyslipidemia or have diabetes, an elevated BMI, or hypertension. The American Academy of Pediatrics shortly followed suit, issuing similar recommendations.
Screening for the two subsets of ages was an expansion from the original 1992 guidelines from the National Cholesterol Education Program, which recommended screening only for children with either a family history of early CVD or elevated total cholesterol levels.
A 2011 panel for the NHLBI said the older approach identified significantly fewer children with abnormal levels of low-density lipoprotein cholesterol (LDL-C) than the addition of two age groups for screening, adding that many children do not have a complete family history. The American College of Cardiology and American Heart Association later supported NHLBI’s stance in their joint guidelines on the management of cholesterol.
Mark Corkins, MD, chair of the AAP’s Committee on Nutrition, told Medscape Medical News that if children are screened only because they have obesity or a family history of FH, some with elevated lipid levels will be missed. For instance, studies indicate caregiver recall of FH often is inaccurate, and the genetic disorder that causes the condition is not related to obesity.
“The screening is to find familial hypercholesterolemia, to try to find the ones that need therapy,” that would not be caught by the risk-based screening earlier on in childhood, Corkins said.
Only Screen Children With Risk Factors
But other groups do not agree. The US Preventive Services Task Force (USPSTF) found insufficient evidence to recommend for or against screening for lipid disorders in asymptomatic children and teens.
The group also said it found inadequate evidence that lipid-lowering interventions in the general pediatric population lead to reductions in cardiovascular events or all-cause mortality once they reached adulthood. USPSTF also raised questions about the safety of lipid-lowering drugs in children.
“The current evidence is insufficient to assess the balance of benefits and harms of screening for lipid disorders in children and adolescents 20 years or younger,” the panel wrote.
The American Academy of Family Physicians supports USPSTF’s recommendations.
Low Rate of Screening
While the uncertainty over screening in children continues, the practice has been adopted by a minority of clinicians.
A study published in JAMA Network Open in July found 9% of 700,000 9- to 11-year-olds had a documented result from a lipid screening. Among more than 1.3 million 17- to 21-year-olds, 13% had received a screening.
As BMI went up, so did screening rates. A little over 9% children and teens with a healthy weight were screened compared with 14.7% of those with moderate obesity and 21.9% of those with severe obesity.
Among those screened, 32.3% of 9- to 11-year-olds and 30.2% of 17- to 21-year-olds had abnormal lipid levels, defined as having one elevated measure out of five, including total cholesterol of 200 mg/dL or higher or LDL-C levels of 130 mg/dL or higher.
Justin Zachariah, MD, MPH, an associate professor of pediatrics-cardiology at Baylor College of Medicine in Houston, spoke about physicians screening children based only on factors like obesity during a presentation at the recent annual meeting of the American Academy of Pediatrics. He cited research showing roughly one in four children with abnormal lipids had a normal weight.
If a clinician is reserving a lipid screening for a child who is overweight or has obesity, “you’re missing nearly half the problem,” Zachariah said during his presentation.
One reason for the low rate of universal screening may be inattention to FH by clinicians, according to Samuel S. Gidding, MD, a professor in the Department of Genomic Health at Geisinger College of Health Sciences in Bridgewater Corners, Vermont.
For instance, a clinician has only a set amount of time during a well-child visit and other issues may take precedence, “so it doesn’t make sense to broach preventive screening for something that could happen 30 or 40 years from now, vs this [other] very immediate problem,” he said.
Clinicians “are triggered to act on the LDL level, but don’t think about FH as a possible diagnosis,” Gidding told Medscape Medical News.
Another barrier is that in some settings, caregivers must take children and teens to another facility on a different day to fulfill an order for a lipid test.
“It’s reluctance of doctors to order it, knowing patients won’t go through with it,” Gidding said.
Gidding is a consultant for Esperion Therapeutics. Other sources in this story reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
Clinicians receive conflicting advice on whether to order blood tests to screen for lipids in children. A new study could add to the confusion. Researchers found that a combination of physical proxy measures such as hypertension and body mass index (BMI) predicted the risk for future cardiovascular events as well as the physical model plus lipid labs, questioning the value of those blood tests.
Some medical organizations advise screening only for high-risk children because more research is needed to define the harms and benefits of universal screening. Diet and behavioral changes are sufficient for most children, and universal screening could lead to false positives and unnecessary further testing, they said.
Groups that favor lipid tests for all children say these measurements detect familial hypercholesterolemia (FH) that would not otherwise be diagnosed, leading to treatment with drugs like statins and a greater chance of preventing cardiovascular disease (CVD) in adulthood.
Researchers from the new study said their findings do not address screenings for FH, which affects 1 in 250 US children and puts them at a risk for atherosclerotic CVD.
Recommending Blood Tests in Age Groups
One of the seminal guidelines on screening lipids in children came from the National Heart, Lung, and Blood Institute (NHLBI), which in 2011 recommended children undergo dyslipidemia screening between the ages of 9 and 11 years and again between 17 and 21 years. Children should receive a screening starting at age 2 years if they have a family history of CVD or dyslipidemia or have diabetes, an elevated BMI, or hypertension. The American Academy of Pediatrics shortly followed suit, issuing similar recommendations.
Screening for the two subsets of ages was an expansion from the original 1992 guidelines from the National Cholesterol Education Program, which recommended screening only for children with either a family history of early CVD or elevated total cholesterol levels.
A 2011 panel for the NHLBI said the older approach identified significantly fewer children with abnormal levels of low-density lipoprotein cholesterol (LDL-C) than the addition of two age groups for screening, adding that many children do not have a complete family history. The American College of Cardiology and American Heart Association later supported NHLBI’s stance in their joint guidelines on the management of cholesterol.
Mark Corkins, MD, chair of the AAP’s Committee on Nutrition, told Medscape Medical News that if children are screened only because they have obesity or a family history of FH, some with elevated lipid levels will be missed. For instance, studies indicate caregiver recall of FH often is inaccurate, and the genetic disorder that causes the condition is not related to obesity.
“The screening is to find familial hypercholesterolemia, to try to find the ones that need therapy,” that would not be caught by the risk-based screening earlier on in childhood, Corkins said.
Only Screen Children With Risk Factors
But other groups do not agree. The US Preventive Services Task Force (USPSTF) found insufficient evidence to recommend for or against screening for lipid disorders in asymptomatic children and teens.
The group also said it found inadequate evidence that lipid-lowering interventions in the general pediatric population lead to reductions in cardiovascular events or all-cause mortality once they reached adulthood. USPSTF also raised questions about the safety of lipid-lowering drugs in children.
“The current evidence is insufficient to assess the balance of benefits and harms of screening for lipid disorders in children and adolescents 20 years or younger,” the panel wrote.
The American Academy of Family Physicians supports USPSTF’s recommendations.
Low Rate of Screening
While the uncertainty over screening in children continues, the practice has been adopted by a minority of clinicians.
A study published in JAMA Network Open in July found 9% of 700,000 9- to 11-year-olds had a documented result from a lipid screening. Among more than 1.3 million 17- to 21-year-olds, 13% had received a screening.
As BMI went up, so did screening rates. A little over 9% children and teens with a healthy weight were screened compared with 14.7% of those with moderate obesity and 21.9% of those with severe obesity.
Among those screened, 32.3% of 9- to 11-year-olds and 30.2% of 17- to 21-year-olds had abnormal lipid levels, defined as having one elevated measure out of five, including total cholesterol of 200 mg/dL or higher or LDL-C levels of 130 mg/dL or higher.
Justin Zachariah, MD, MPH, an associate professor of pediatrics-cardiology at Baylor College of Medicine in Houston, spoke about physicians screening children based only on factors like obesity during a presentation at the recent annual meeting of the American Academy of Pediatrics. He cited research showing roughly one in four children with abnormal lipids had a normal weight.
If a clinician is reserving a lipid screening for a child who is overweight or has obesity, “you’re missing nearly half the problem,” Zachariah said during his presentation.
One reason for the low rate of universal screening may be inattention to FH by clinicians, according to Samuel S. Gidding, MD, a professor in the Department of Genomic Health at Geisinger College of Health Sciences in Bridgewater Corners, Vermont.
For instance, a clinician has only a set amount of time during a well-child visit and other issues may take precedence, “so it doesn’t make sense to broach preventive screening for something that could happen 30 or 40 years from now, vs this [other] very immediate problem,” he said.
Clinicians “are triggered to act on the LDL level, but don’t think about FH as a possible diagnosis,” Gidding told Medscape Medical News.
Another barrier is that in some settings, caregivers must take children and teens to another facility on a different day to fulfill an order for a lipid test.
“It’s reluctance of doctors to order it, knowing patients won’t go through with it,” Gidding said.
Gidding is a consultant for Esperion Therapeutics. Other sources in this story reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
AHA Scientific Statement Links Three Common Cardiovascular Diseases to Cognitive Decline, Dementia
The statement includes an extensive research review and offers compelling evidence of the inextricable link between heart health and brain health, which investigators said underscores the benefit of early intervention.
The cumulative evidence “confirms that the trajectories of cardiac health and brain health are inextricably intertwined through modifiable and nonmodifiable factors,” the authors wrote.
Investigators say the findings reinforce the message that addressing cardiovascular health early in life may deter the onset or progression of cognitive impairment later on.
And the earlier this is done, the better, said lead author Fernando D. Testai, MD, PhD, a professor of neurology and the vascular neurology section head, Department of Neurology and Rehabilitation, University of Illinois, Chicago.
The statement was published online in Stroke.
Bridging the Research Gap
It’s well known that there’s a bidirectional relationship between heart and brain function. For example, heart failure can lead to decreased blood flow that can damage the brain, and stroke in some areas of the brain can affect the heart.
However, that’s only part of the puzzle and doesn’t address all the gaps in the understanding of how cardiovascular disease contributes to cognition, said Testai.
“What we’re trying to do here is to go one step further and describe other connections between the heart and the brain,” he said.
Investigators carried out an extensive PubMed search for heart failure, atrial fibrillation, and coronary heart disease. Researchers detailed the frequency of each condition, mechanisms by which they might cause cognitive impairment, and prospects for prevention and treatment to maintain brain health.
A recurring theme in the paper is the role of inflammation. Evidence shows there are “remarkable similarities in the inflammatory response that takes place,” with both cardiac disease and cognitive decline, said Testai.
Another potential shared mechanism relates to biomarkers, particularly amyloid, which is strongly linked to Alzheimer’s disease.
“But some studies show amyloid can also be present in the heart, especially in patients who have decreased ejection fraction,” said Testai.
Robust Heart-Brain Connection
The statement’s authors collected a substantial amount of evidence showing vascular risk factors such as hypertension and diabetes “can change how the brain processes and clears up amyloid,” Testai added.
The paper also provides a compilation of evidence of shared genetic predispositions when it comes to heart and brain disorders.
“We noticed that some genetic signatures that have historically been associated with heart disease seem to also correlate with structural changes in the brain. That means that at the end of the day, some patients may be born with a genetic predisposition to developing both conditions,” said Testai.
This indicates that the link between the two organs “begins as early as conception” and underscores the importance of adopting healthy lifestyle habits as early as possible, he added.
“That means you can avoid bad habits that eventually lead to hypertension, diabetes, and cholesterol, that eventually will lead to cardiac disease, which eventually will lead to stroke, which eventually will lead to cognitive decline,” Testai noted.
However, cardiovascular health is more complicated than having good genes and adhering to a healthy lifestyle. It’s not clear, for example, why some people who should be predisposed to developing heart disease do not develop it, something Testai refers to as enhanced “resilience.”
For example, Hispanic or Latino patients, who have relatively poor cardiovascular risk factor profiles, seem to be less susceptible to developing cardiac disease.
More Research Needed
While genetics may partly explain the paradox, Testai believes other protective factors are at play, including strong social support networks.
Testai referred to the AHA’s “Life’s Essential 8” — the eight components of cardiovascular health. These include a healthy diet, participation in physical activity, nicotine avoidance, healthy sleep, healthy weight, and healthy levels of blood lipids, blood glucose, and blood pressure.
More evidence is needed to show that effective management of cardiac disease positively affects cognition. Currently, cognitive measures are rarely included in studies examining various heart disease treatments, said Testai.
“There should probably be an effort to include brain health outcomes in some of the cardiac literature to make sure we can also measure whether the intervention in the heart leads to an advantage for the brain,” he said.
More research is also needed to determine whether immunomodulation has a beneficial effect on the cognitive trajectory, the statement’s authors noted.
They point out that the interpretation and generalizability of the studies described in the statement are confounded by disparate methodologies, including small sample sizes, cross-sectional designs, and underrepresentation of Black and Hispanic individuals.
‘An Important Step’
Reached for a comment, Natalia S. Rost, MD, Chief of the Stroke Division at Massachusetts General Hospital and professor of neurology at Harvard Medical School, both in Boston, said this paper “is an important step” in terms of pulling together pertinent information on the topic of heart-brain health.
She praised the authors for gathering evidence on risk factors related to atrial fibrillation, heart failure, and coronary heart disease, which is “the part of the puzzle that is controllable.”
This helps reinforce the message that controlling vascular risk factors helps with brain health, said Rost.
But brain health is “much more complex than just vascular health,” she said. It includes other elements such as freedom from epilepsy, migraine, traumatic brain injury, and adult learning disabilities.
No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
The statement includes an extensive research review and offers compelling evidence of the inextricable link between heart health and brain health, which investigators said underscores the benefit of early intervention.
The cumulative evidence “confirms that the trajectories of cardiac health and brain health are inextricably intertwined through modifiable and nonmodifiable factors,” the authors wrote.
Investigators say the findings reinforce the message that addressing cardiovascular health early in life may deter the onset or progression of cognitive impairment later on.
And the earlier this is done, the better, said lead author Fernando D. Testai, MD, PhD, a professor of neurology and the vascular neurology section head, Department of Neurology and Rehabilitation, University of Illinois, Chicago.
The statement was published online in Stroke.
Bridging the Research Gap
It’s well known that there’s a bidirectional relationship between heart and brain function. For example, heart failure can lead to decreased blood flow that can damage the brain, and stroke in some areas of the brain can affect the heart.
However, that’s only part of the puzzle and doesn’t address all the gaps in the understanding of how cardiovascular disease contributes to cognition, said Testai.
“What we’re trying to do here is to go one step further and describe other connections between the heart and the brain,” he said.
Investigators carried out an extensive PubMed search for heart failure, atrial fibrillation, and coronary heart disease. Researchers detailed the frequency of each condition, mechanisms by which they might cause cognitive impairment, and prospects for prevention and treatment to maintain brain health.
A recurring theme in the paper is the role of inflammation. Evidence shows there are “remarkable similarities in the inflammatory response that takes place,” with both cardiac disease and cognitive decline, said Testai.
Another potential shared mechanism relates to biomarkers, particularly amyloid, which is strongly linked to Alzheimer’s disease.
“But some studies show amyloid can also be present in the heart, especially in patients who have decreased ejection fraction,” said Testai.
Robust Heart-Brain Connection
The statement’s authors collected a substantial amount of evidence showing vascular risk factors such as hypertension and diabetes “can change how the brain processes and clears up amyloid,” Testai added.
The paper also provides a compilation of evidence of shared genetic predispositions when it comes to heart and brain disorders.
“We noticed that some genetic signatures that have historically been associated with heart disease seem to also correlate with structural changes in the brain. That means that at the end of the day, some patients may be born with a genetic predisposition to developing both conditions,” said Testai.
This indicates that the link between the two organs “begins as early as conception” and underscores the importance of adopting healthy lifestyle habits as early as possible, he added.
“That means you can avoid bad habits that eventually lead to hypertension, diabetes, and cholesterol, that eventually will lead to cardiac disease, which eventually will lead to stroke, which eventually will lead to cognitive decline,” Testai noted.
However, cardiovascular health is more complicated than having good genes and adhering to a healthy lifestyle. It’s not clear, for example, why some people who should be predisposed to developing heart disease do not develop it, something Testai refers to as enhanced “resilience.”
For example, Hispanic or Latino patients, who have relatively poor cardiovascular risk factor profiles, seem to be less susceptible to developing cardiac disease.
More Research Needed
While genetics may partly explain the paradox, Testai believes other protective factors are at play, including strong social support networks.
Testai referred to the AHA’s “Life’s Essential 8” — the eight components of cardiovascular health. These include a healthy diet, participation in physical activity, nicotine avoidance, healthy sleep, healthy weight, and healthy levels of blood lipids, blood glucose, and blood pressure.
More evidence is needed to show that effective management of cardiac disease positively affects cognition. Currently, cognitive measures are rarely included in studies examining various heart disease treatments, said Testai.
“There should probably be an effort to include brain health outcomes in some of the cardiac literature to make sure we can also measure whether the intervention in the heart leads to an advantage for the brain,” he said.
More research is also needed to determine whether immunomodulation has a beneficial effect on the cognitive trajectory, the statement’s authors noted.
They point out that the interpretation and generalizability of the studies described in the statement are confounded by disparate methodologies, including small sample sizes, cross-sectional designs, and underrepresentation of Black and Hispanic individuals.
‘An Important Step’
Reached for a comment, Natalia S. Rost, MD, Chief of the Stroke Division at Massachusetts General Hospital and professor of neurology at Harvard Medical School, both in Boston, said this paper “is an important step” in terms of pulling together pertinent information on the topic of heart-brain health.
She praised the authors for gathering evidence on risk factors related to atrial fibrillation, heart failure, and coronary heart disease, which is “the part of the puzzle that is controllable.”
This helps reinforce the message that controlling vascular risk factors helps with brain health, said Rost.
But brain health is “much more complex than just vascular health,” she said. It includes other elements such as freedom from epilepsy, migraine, traumatic brain injury, and adult learning disabilities.
No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
The statement includes an extensive research review and offers compelling evidence of the inextricable link between heart health and brain health, which investigators said underscores the benefit of early intervention.
The cumulative evidence “confirms that the trajectories of cardiac health and brain health are inextricably intertwined through modifiable and nonmodifiable factors,” the authors wrote.
Investigators say the findings reinforce the message that addressing cardiovascular health early in life may deter the onset or progression of cognitive impairment later on.
And the earlier this is done, the better, said lead author Fernando D. Testai, MD, PhD, a professor of neurology and the vascular neurology section head, Department of Neurology and Rehabilitation, University of Illinois, Chicago.
The statement was published online in Stroke.
Bridging the Research Gap
It’s well known that there’s a bidirectional relationship between heart and brain function. For example, heart failure can lead to decreased blood flow that can damage the brain, and stroke in some areas of the brain can affect the heart.
However, that’s only part of the puzzle and doesn’t address all the gaps in the understanding of how cardiovascular disease contributes to cognition, said Testai.
“What we’re trying to do here is to go one step further and describe other connections between the heart and the brain,” he said.
Investigators carried out an extensive PubMed search for heart failure, atrial fibrillation, and coronary heart disease. Researchers detailed the frequency of each condition, mechanisms by which they might cause cognitive impairment, and prospects for prevention and treatment to maintain brain health.
A recurring theme in the paper is the role of inflammation. Evidence shows there are “remarkable similarities in the inflammatory response that takes place,” with both cardiac disease and cognitive decline, said Testai.
Another potential shared mechanism relates to biomarkers, particularly amyloid, which is strongly linked to Alzheimer’s disease.
“But some studies show amyloid can also be present in the heart, especially in patients who have decreased ejection fraction,” said Testai.
Robust Heart-Brain Connection
The statement’s authors collected a substantial amount of evidence showing vascular risk factors such as hypertension and diabetes “can change how the brain processes and clears up amyloid,” Testai added.
The paper also provides a compilation of evidence of shared genetic predispositions when it comes to heart and brain disorders.
“We noticed that some genetic signatures that have historically been associated with heart disease seem to also correlate with structural changes in the brain. That means that at the end of the day, some patients may be born with a genetic predisposition to developing both conditions,” said Testai.
This indicates that the link between the two organs “begins as early as conception” and underscores the importance of adopting healthy lifestyle habits as early as possible, he added.
“That means you can avoid bad habits that eventually lead to hypertension, diabetes, and cholesterol, that eventually will lead to cardiac disease, which eventually will lead to stroke, which eventually will lead to cognitive decline,” Testai noted.
However, cardiovascular health is more complicated than having good genes and adhering to a healthy lifestyle. It’s not clear, for example, why some people who should be predisposed to developing heart disease do not develop it, something Testai refers to as enhanced “resilience.”
For example, Hispanic or Latino patients, who have relatively poor cardiovascular risk factor profiles, seem to be less susceptible to developing cardiac disease.
More Research Needed
While genetics may partly explain the paradox, Testai believes other protective factors are at play, including strong social support networks.
Testai referred to the AHA’s “Life’s Essential 8” — the eight components of cardiovascular health. These include a healthy diet, participation in physical activity, nicotine avoidance, healthy sleep, healthy weight, and healthy levels of blood lipids, blood glucose, and blood pressure.
More evidence is needed to show that effective management of cardiac disease positively affects cognition. Currently, cognitive measures are rarely included in studies examining various heart disease treatments, said Testai.
“There should probably be an effort to include brain health outcomes in some of the cardiac literature to make sure we can also measure whether the intervention in the heart leads to an advantage for the brain,” he said.
More research is also needed to determine whether immunomodulation has a beneficial effect on the cognitive trajectory, the statement’s authors noted.
They point out that the interpretation and generalizability of the studies described in the statement are confounded by disparate methodologies, including small sample sizes, cross-sectional designs, and underrepresentation of Black and Hispanic individuals.
‘An Important Step’
Reached for a comment, Natalia S. Rost, MD, Chief of the Stroke Division at Massachusetts General Hospital and professor of neurology at Harvard Medical School, both in Boston, said this paper “is an important step” in terms of pulling together pertinent information on the topic of heart-brain health.
She praised the authors for gathering evidence on risk factors related to atrial fibrillation, heart failure, and coronary heart disease, which is “the part of the puzzle that is controllable.”
This helps reinforce the message that controlling vascular risk factors helps with brain health, said Rost.
But brain health is “much more complex than just vascular health,” she said. It includes other elements such as freedom from epilepsy, migraine, traumatic brain injury, and adult learning disabilities.
No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
FROM STROKE
Ultraprocessed Foods and CVD: Myths vs Facts
I’d like to talk with you about ultraprocessed foods (UPFs) and risk for cardiovascular disease (CVD) and try to separate some of the facts from the myths. I’d like to discuss a recent report in The Lancet Regional Health that looks at this topic comprehensively and in detail.
This report includes three large-scale prospective cohort studies of US female and male health professionals, more than 200,000 participants in total. It also includes a meta-analysis of 22 international cohorts with about 1.2 million participants. I’d like to acknowledge that I’m a co-author of this study.
What are UPFs, and why are they important? Why do we care, and what are the knowledge gaps? UPFs are generally packaged foods that contain ingredients to extend shelf life and improve taste and palatability. It’s important because 60%-70% of the US diet, if not more, is made up of UPFs. So, the relationship between UPFs and CVD and other health outcomes is actually very important.
And the research to date on this subject has been quite limited.
In other studies, these UPFs have been linked to weight gain and dyslipidemia; some tissue glycation has been found, and some changes in the microbiome. Some studies have linked higher UPF intake with type 2 diabetes. A few have looked at certain selected UPF foods and found a higher risk for CVD, but a really comprehensive look at this question hasn’t been done.
So, that’s what we did in this paper and in the meta-analysis with the 22 cohorts, and we saw a very clear and distinct significant increase in coronary heart disease by 23%, total CVD by 17%, and stroke by 9% when comparing the highest vs the lowest category [of UPF intake]. When we drilled down deeply into the types of UPFs in the US health professional cohorts, we saw that there were some major differences in the relationship with CVD depending on the type of UPF.
In comparing the highest quintile vs the lowest quintile [of total UPF intake], we saw that some of the UPFs were associated with significant elevations in risk for CVD. These included sugar-sweetened beverages and processed meats. But some UPFs were linked with a lower risk for CVD. These included breakfast cereals, yogurt, some dairy desserts, and whole grains.
Overall, it seemed that UPFs are actually quite diverse in their association with health. It’s not one size fits all. They’re not all created equal, and some of these differences matter. Although overall we would recommend that our diets be focused on whole foods, primarily plant based, lots of fruits and vegetables, whole grains, fish, and other whole foods, it seems from this report and the meta-analysis that certain types of UPFs can be incorporated into a healthy diet and don’t need to be avoided entirely.
Dr. Manson is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School, and Chief of the Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston, Massachusetts. She reported receiving donations and infrastructure support from Mars Symbioscience.
A version of this article first appeared on Medscape.com.
I’d like to talk with you about ultraprocessed foods (UPFs) and risk for cardiovascular disease (CVD) and try to separate some of the facts from the myths. I’d like to discuss a recent report in The Lancet Regional Health that looks at this topic comprehensively and in detail.
This report includes three large-scale prospective cohort studies of US female and male health professionals, more than 200,000 participants in total. It also includes a meta-analysis of 22 international cohorts with about 1.2 million participants. I’d like to acknowledge that I’m a co-author of this study.
What are UPFs, and why are they important? Why do we care, and what are the knowledge gaps? UPFs are generally packaged foods that contain ingredients to extend shelf life and improve taste and palatability. It’s important because 60%-70% of the US diet, if not more, is made up of UPFs. So, the relationship between UPFs and CVD and other health outcomes is actually very important.
And the research to date on this subject has been quite limited.
In other studies, these UPFs have been linked to weight gain and dyslipidemia; some tissue glycation has been found, and some changes in the microbiome. Some studies have linked higher UPF intake with type 2 diabetes. A few have looked at certain selected UPF foods and found a higher risk for CVD, but a really comprehensive look at this question hasn’t been done.
So, that’s what we did in this paper and in the meta-analysis with the 22 cohorts, and we saw a very clear and distinct significant increase in coronary heart disease by 23%, total CVD by 17%, and stroke by 9% when comparing the highest vs the lowest category [of UPF intake]. When we drilled down deeply into the types of UPFs in the US health professional cohorts, we saw that there were some major differences in the relationship with CVD depending on the type of UPF.
In comparing the highest quintile vs the lowest quintile [of total UPF intake], we saw that some of the UPFs were associated with significant elevations in risk for CVD. These included sugar-sweetened beverages and processed meats. But some UPFs were linked with a lower risk for CVD. These included breakfast cereals, yogurt, some dairy desserts, and whole grains.
Overall, it seemed that UPFs are actually quite diverse in their association with health. It’s not one size fits all. They’re not all created equal, and some of these differences matter. Although overall we would recommend that our diets be focused on whole foods, primarily plant based, lots of fruits and vegetables, whole grains, fish, and other whole foods, it seems from this report and the meta-analysis that certain types of UPFs can be incorporated into a healthy diet and don’t need to be avoided entirely.
Dr. Manson is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School, and Chief of the Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston, Massachusetts. She reported receiving donations and infrastructure support from Mars Symbioscience.
A version of this article first appeared on Medscape.com.
I’d like to talk with you about ultraprocessed foods (UPFs) and risk for cardiovascular disease (CVD) and try to separate some of the facts from the myths. I’d like to discuss a recent report in The Lancet Regional Health that looks at this topic comprehensively and in detail.
This report includes three large-scale prospective cohort studies of US female and male health professionals, more than 200,000 participants in total. It also includes a meta-analysis of 22 international cohorts with about 1.2 million participants. I’d like to acknowledge that I’m a co-author of this study.
What are UPFs, and why are they important? Why do we care, and what are the knowledge gaps? UPFs are generally packaged foods that contain ingredients to extend shelf life and improve taste and palatability. It’s important because 60%-70% of the US diet, if not more, is made up of UPFs. So, the relationship between UPFs and CVD and other health outcomes is actually very important.
And the research to date on this subject has been quite limited.
In other studies, these UPFs have been linked to weight gain and dyslipidemia; some tissue glycation has been found, and some changes in the microbiome. Some studies have linked higher UPF intake with type 2 diabetes. A few have looked at certain selected UPF foods and found a higher risk for CVD, but a really comprehensive look at this question hasn’t been done.
So, that’s what we did in this paper and in the meta-analysis with the 22 cohorts, and we saw a very clear and distinct significant increase in coronary heart disease by 23%, total CVD by 17%, and stroke by 9% when comparing the highest vs the lowest category [of UPF intake]. When we drilled down deeply into the types of UPFs in the US health professional cohorts, we saw that there were some major differences in the relationship with CVD depending on the type of UPF.
In comparing the highest quintile vs the lowest quintile [of total UPF intake], we saw that some of the UPFs were associated with significant elevations in risk for CVD. These included sugar-sweetened beverages and processed meats. But some UPFs were linked with a lower risk for CVD. These included breakfast cereals, yogurt, some dairy desserts, and whole grains.
Overall, it seemed that UPFs are actually quite diverse in their association with health. It’s not one size fits all. They’re not all created equal, and some of these differences matter. Although overall we would recommend that our diets be focused on whole foods, primarily plant based, lots of fruits and vegetables, whole grains, fish, and other whole foods, it seems from this report and the meta-analysis that certain types of UPFs can be incorporated into a healthy diet and don’t need to be avoided entirely.
Dr. Manson is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School, and Chief of the Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston, Massachusetts. She reported receiving donations and infrastructure support from Mars Symbioscience.
A version of this article first appeared on Medscape.com.
Heard of ApoB Testing? New Guidelines
This transcript has been edited for clarity.
I've been hearing a lot about apolipoprotein B (apoB) lately. It keeps popping up, but I've not been sure where it fits in or what I should do about it. The new Expert Clinical Consensus from the National Lipid Association now finally gives us clear guidance.
ApoB is the main protein that is found on all atherogenic lipoproteins. It is found on low-density lipoprotein (LDL) but also on other atherogenic lipoprotein particles. Because it is a part of all atherogenic particles, it predicts cardiovascular (CV) risk more accurately than does LDL cholesterol (LDL-C).
ApoB and LDL-C tend to run together, but not always. While they are correlated fairly well on a population level, for a given individual they can diverge; and when they do, apoB is the better predictor of future CV outcomes. This divergence occurs frequently, and it can occur even more frequently after treatment with statins. When LDL decreases to reach the LDL threshold for treatment, but apoB remains elevated, there is the potential for misclassification of CV risk and essentially the risk for undertreatment of someone whose CV risk is actually higher than it appears to be if we only look at their LDL-C. The consensus statement says, "Where there is discordance between apoB and LDL-C, risk follows apoB."
This understanding leads to the places where measurement of apoB may be helpful:
In patients with borderline atherosclerotic cardiovascular disease risk in whom a shared decision about statin therapy is being determined and the patient prefers not to start a statin, apoB can be useful for further risk stratification. If apoB suggests low risk, then statin therapy could be withheld, and if apoB is high, that would favor starting statin therapy. Certain common conditions, such as obesity and insulin resistance, can lead to smaller cholesterol-depleted LDL particles that result in lower LDL-C, but elevated apoB levels in this circumstance may drive the decision to treat with a statin.
In patients already treated with statins, but a decision must be made about whether treatment intensification is warranted. If the LDL-C is to goal and apoB is above threshold, treatment intensification may be considered. In patients who are not yet to goal, based on an elevated apoB, the first step is intensification of statin therapy. After that, intensification would be the same as has already been addressed in my review of the 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering.
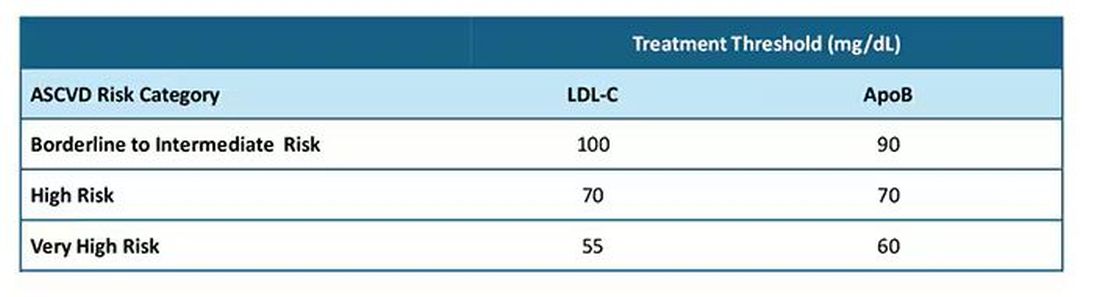
After clarifying the importance of apoB in providing additional discrimination of CV risk, the consensus statement clarifies the treatment thresholds, or goals for treatment, for apoB that correlate with established LDL-C thresholds, as shown in this table:
Let me be really clear: The consensus statement does not say that we need to measure apoB in all patients or that such measurement is the standard of care. It is not. It says, and I'll quote, "At present, the use of apoB to assess the effectiveness of lipid-lowering therapies remains a matter of clinical judgment." This guideline is helpful in pointing out the patients most likely to benefit from this additional measurement, including those with hypertriglyceridemia, diabetes, visceral adiposity, insulin resistance/metabolic syndrome, low HDL-C, or very low LDL-C levels.
In summary, measurement of apoB can be helpful for further risk stratification in patients with borderline or intermediate LDL-C levels, and for deciding whether further intensification of lipid-lowering therapy may be warranted when the LDL threshold has been reached.
Lipid management is something that we do every day in the office. This is new information, or at least clarifying information, for most of us. Hopefully it is helpful. I'm interested in your thoughts on this topic, including whether and how you plan to use apoB measurements.
Dr. Skolnik, Professor, Department of Family Medicine, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia; Associate Director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I've been hearing a lot about apolipoprotein B (apoB) lately. It keeps popping up, but I've not been sure where it fits in or what I should do about it. The new Expert Clinical Consensus from the National Lipid Association now finally gives us clear guidance.
ApoB is the main protein that is found on all atherogenic lipoproteins. It is found on low-density lipoprotein (LDL) but also on other atherogenic lipoprotein particles. Because it is a part of all atherogenic particles, it predicts cardiovascular (CV) risk more accurately than does LDL cholesterol (LDL-C).
ApoB and LDL-C tend to run together, but not always. While they are correlated fairly well on a population level, for a given individual they can diverge; and when they do, apoB is the better predictor of future CV outcomes. This divergence occurs frequently, and it can occur even more frequently after treatment with statins. When LDL decreases to reach the LDL threshold for treatment, but apoB remains elevated, there is the potential for misclassification of CV risk and essentially the risk for undertreatment of someone whose CV risk is actually higher than it appears to be if we only look at their LDL-C. The consensus statement says, "Where there is discordance between apoB and LDL-C, risk follows apoB."
This understanding leads to the places where measurement of apoB may be helpful:
In patients with borderline atherosclerotic cardiovascular disease risk in whom a shared decision about statin therapy is being determined and the patient prefers not to start a statin, apoB can be useful for further risk stratification. If apoB suggests low risk, then statin therapy could be withheld, and if apoB is high, that would favor starting statin therapy. Certain common conditions, such as obesity and insulin resistance, can lead to smaller cholesterol-depleted LDL particles that result in lower LDL-C, but elevated apoB levels in this circumstance may drive the decision to treat with a statin.
In patients already treated with statins, but a decision must be made about whether treatment intensification is warranted. If the LDL-C is to goal and apoB is above threshold, treatment intensification may be considered. In patients who are not yet to goal, based on an elevated apoB, the first step is intensification of statin therapy. After that, intensification would be the same as has already been addressed in my review of the 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering.
After clarifying the importance of apoB in providing additional discrimination of CV risk, the consensus statement clarifies the treatment thresholds, or goals for treatment, for apoB that correlate with established LDL-C thresholds, as shown in this table:
Let me be really clear: The consensus statement does not say that we need to measure apoB in all patients or that such measurement is the standard of care. It is not. It says, and I'll quote, "At present, the use of apoB to assess the effectiveness of lipid-lowering therapies remains a matter of clinical judgment." This guideline is helpful in pointing out the patients most likely to benefit from this additional measurement, including those with hypertriglyceridemia, diabetes, visceral adiposity, insulin resistance/metabolic syndrome, low HDL-C, or very low LDL-C levels.
In summary, measurement of apoB can be helpful for further risk stratification in patients with borderline or intermediate LDL-C levels, and for deciding whether further intensification of lipid-lowering therapy may be warranted when the LDL threshold has been reached.
Lipid management is something that we do every day in the office. This is new information, or at least clarifying information, for most of us. Hopefully it is helpful. I'm interested in your thoughts on this topic, including whether and how you plan to use apoB measurements.
Dr. Skolnik, Professor, Department of Family Medicine, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia; Associate Director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I've been hearing a lot about apolipoprotein B (apoB) lately. It keeps popping up, but I've not been sure where it fits in or what I should do about it. The new Expert Clinical Consensus from the National Lipid Association now finally gives us clear guidance.
ApoB is the main protein that is found on all atherogenic lipoproteins. It is found on low-density lipoprotein (LDL) but also on other atherogenic lipoprotein particles. Because it is a part of all atherogenic particles, it predicts cardiovascular (CV) risk more accurately than does LDL cholesterol (LDL-C).
ApoB and LDL-C tend to run together, but not always. While they are correlated fairly well on a population level, for a given individual they can diverge; and when they do, apoB is the better predictor of future CV outcomes. This divergence occurs frequently, and it can occur even more frequently after treatment with statins. When LDL decreases to reach the LDL threshold for treatment, but apoB remains elevated, there is the potential for misclassification of CV risk and essentially the risk for undertreatment of someone whose CV risk is actually higher than it appears to be if we only look at their LDL-C. The consensus statement says, "Where there is discordance between apoB and LDL-C, risk follows apoB."
This understanding leads to the places where measurement of apoB may be helpful:
In patients with borderline atherosclerotic cardiovascular disease risk in whom a shared decision about statin therapy is being determined and the patient prefers not to start a statin, apoB can be useful for further risk stratification. If apoB suggests low risk, then statin therapy could be withheld, and if apoB is high, that would favor starting statin therapy. Certain common conditions, such as obesity and insulin resistance, can lead to smaller cholesterol-depleted LDL particles that result in lower LDL-C, but elevated apoB levels in this circumstance may drive the decision to treat with a statin.
In patients already treated with statins, but a decision must be made about whether treatment intensification is warranted. If the LDL-C is to goal and apoB is above threshold, treatment intensification may be considered. In patients who are not yet to goal, based on an elevated apoB, the first step is intensification of statin therapy. After that, intensification would be the same as has already been addressed in my review of the 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering.
After clarifying the importance of apoB in providing additional discrimination of CV risk, the consensus statement clarifies the treatment thresholds, or goals for treatment, for apoB that correlate with established LDL-C thresholds, as shown in this table:
Let me be really clear: The consensus statement does not say that we need to measure apoB in all patients or that such measurement is the standard of care. It is not. It says, and I'll quote, "At present, the use of apoB to assess the effectiveness of lipid-lowering therapies remains a matter of clinical judgment." This guideline is helpful in pointing out the patients most likely to benefit from this additional measurement, including those with hypertriglyceridemia, diabetes, visceral adiposity, insulin resistance/metabolic syndrome, low HDL-C, or very low LDL-C levels.
In summary, measurement of apoB can be helpful for further risk stratification in patients with borderline or intermediate LDL-C levels, and for deciding whether further intensification of lipid-lowering therapy may be warranted when the LDL threshold has been reached.
Lipid management is something that we do every day in the office. This is new information, or at least clarifying information, for most of us. Hopefully it is helpful. I'm interested in your thoughts on this topic, including whether and how you plan to use apoB measurements.
Dr. Skolnik, Professor, Department of Family Medicine, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia; Associate Director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer.
A version of this article first appeared on Medscape.com.
Heart Attack, Stroke Survivors at High Risk for Long COVID
Primary care doctors and specialists should advise patients who have already experienced a heart attack or stroke that they are at a higher risk for long COVID and need to take steps to avoid contracting the virus, according to new research.
The study, led by researchers at Columbia University, New York City, suggests that anyone with cardiovascular disease (CVD) — defined as having experienced a heart attack or stroke — should consider getting the updated COVID vaccine boosters. They also suggest patients with CVD take other steps to avoid an acute infection, such as avoiding crowded indoor spaces.
There is no specific test or treatment for long COVID, which can become disabling and chronic. Long COVID is defined by the failure to recover from acute COVID-19 in 90 days.
The scientists used data from nearly 5000 people enrolled in 14 established, ongoing research programs, including the 76-year-old Framingham Heart Study. The results of the analysis of the “mega-cohort” were published in JAMA Network Open.
Most of the 14 studies already had 10-20 years of data on the cardiac health of thousands of enrollees, said Norrina B. Allen, one of the authors and a cardiac epidemiologist at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
“This is a particularly strong study that looked at risk factors — or individual health — prior to developing COVID and their impact on the likely of recovering from COVID,” she said.
In addition to those with CVD, women and adults with preexisting chronic illnesses took longer to recover.
More than 20% of those in the large, racially and ethnically diverse US population–based study did not recover from COVID in 90 days. The researchers found that the median self-reported time to recovery from acute infection was 20 days.
While women and those with chronic illness had a higher risk for long COVID, vaccination and infection with the Omicron variant wave were associated with shorter recovery times.
These findings make sense, said Ziyad Al-Aly, MD, chief of research at Veterans Affairs St. Louis Health Care System and clinical epidemiologist at Washington University in St. Louis, Missouri.
“We also see that COVID-19 can lead to new-onset cardiovascular disease,” said Al-Aly, who was not involved in the study. “There is clearly a (link) between COVID and cardiovascular disease. These two seem to be intimately intertwined. In my view, this emphasizes the importance of targeting these individuals for vaccination and potentially antivirals (when they get infected) to help reduce their risk of adverse events and ameliorate their chance of full and fast recovery.”
The study used data from the Collaborative Cohort of Cohorts for COVID-19 Research. The long list of researchers contributing to this study includes epidemiologists, biostatisticians, neurologists, pulmonologists, and cardiologists. The data come from a list of cohorts like the Framingham Heart Study, which identified key risk factors for CVD, including cholesterol levels. Other studies include the Atherosclerosis Risk in Communities study, which began in the mid-1980s. Researchers there recruited a cohort of 15,792 men and women in rural North Carolina and Mississippi and suburban Minneapolis. They enrolled a high number of African American participants, who have been underrepresented in past studies. Other cohorts focused on young adults with CVD and Hispanics, while another focused on people with chronic obstructive pulmonary disease.
Lead author Elizabeth C. Oelsner, MD, of Columbia University Irving Medical Center in New York City, said she was not surprised by the CVD-long COVID link.
“We were aware that individuals with CVD were at higher risk of a more severe acute infection,” she said. “We were also seeing evidence that long and severe infection led to persistent symptoms.”
Oelsner noted that many patients still take more than 3 months to recover, even during the Omicron wave.
“While that has improved over the course of the pandemic, many individuals are taking a very long time to recover, and that can have a huge burden on the patient,” she said.
She encourages healthcare providers to tell patients at higher risk to take steps to avoid the virus, including vaccination and boosters.
A version of this article first appeared on Medscape.com.
Primary care doctors and specialists should advise patients who have already experienced a heart attack or stroke that they are at a higher risk for long COVID and need to take steps to avoid contracting the virus, according to new research.
The study, led by researchers at Columbia University, New York City, suggests that anyone with cardiovascular disease (CVD) — defined as having experienced a heart attack or stroke — should consider getting the updated COVID vaccine boosters. They also suggest patients with CVD take other steps to avoid an acute infection, such as avoiding crowded indoor spaces.
There is no specific test or treatment for long COVID, which can become disabling and chronic. Long COVID is defined by the failure to recover from acute COVID-19 in 90 days.
The scientists used data from nearly 5000 people enrolled in 14 established, ongoing research programs, including the 76-year-old Framingham Heart Study. The results of the analysis of the “mega-cohort” were published in JAMA Network Open.
Most of the 14 studies already had 10-20 years of data on the cardiac health of thousands of enrollees, said Norrina B. Allen, one of the authors and a cardiac epidemiologist at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
“This is a particularly strong study that looked at risk factors — or individual health — prior to developing COVID and their impact on the likely of recovering from COVID,” she said.
In addition to those with CVD, women and adults with preexisting chronic illnesses took longer to recover.
More than 20% of those in the large, racially and ethnically diverse US population–based study did not recover from COVID in 90 days. The researchers found that the median self-reported time to recovery from acute infection was 20 days.
While women and those with chronic illness had a higher risk for long COVID, vaccination and infection with the Omicron variant wave were associated with shorter recovery times.
These findings make sense, said Ziyad Al-Aly, MD, chief of research at Veterans Affairs St. Louis Health Care System and clinical epidemiologist at Washington University in St. Louis, Missouri.
“We also see that COVID-19 can lead to new-onset cardiovascular disease,” said Al-Aly, who was not involved in the study. “There is clearly a (link) between COVID and cardiovascular disease. These two seem to be intimately intertwined. In my view, this emphasizes the importance of targeting these individuals for vaccination and potentially antivirals (when they get infected) to help reduce their risk of adverse events and ameliorate their chance of full and fast recovery.”
The study used data from the Collaborative Cohort of Cohorts for COVID-19 Research. The long list of researchers contributing to this study includes epidemiologists, biostatisticians, neurologists, pulmonologists, and cardiologists. The data come from a list of cohorts like the Framingham Heart Study, which identified key risk factors for CVD, including cholesterol levels. Other studies include the Atherosclerosis Risk in Communities study, which began in the mid-1980s. Researchers there recruited a cohort of 15,792 men and women in rural North Carolina and Mississippi and suburban Minneapolis. They enrolled a high number of African American participants, who have been underrepresented in past studies. Other cohorts focused on young adults with CVD and Hispanics, while another focused on people with chronic obstructive pulmonary disease.
Lead author Elizabeth C. Oelsner, MD, of Columbia University Irving Medical Center in New York City, said she was not surprised by the CVD-long COVID link.
“We were aware that individuals with CVD were at higher risk of a more severe acute infection,” she said. “We were also seeing evidence that long and severe infection led to persistent symptoms.”
Oelsner noted that many patients still take more than 3 months to recover, even during the Omicron wave.
“While that has improved over the course of the pandemic, many individuals are taking a very long time to recover, and that can have a huge burden on the patient,” she said.
She encourages healthcare providers to tell patients at higher risk to take steps to avoid the virus, including vaccination and boosters.
A version of this article first appeared on Medscape.com.
Primary care doctors and specialists should advise patients who have already experienced a heart attack or stroke that they are at a higher risk for long COVID and need to take steps to avoid contracting the virus, according to new research.
The study, led by researchers at Columbia University, New York City, suggests that anyone with cardiovascular disease (CVD) — defined as having experienced a heart attack or stroke — should consider getting the updated COVID vaccine boosters. They also suggest patients with CVD take other steps to avoid an acute infection, such as avoiding crowded indoor spaces.
There is no specific test or treatment for long COVID, which can become disabling and chronic. Long COVID is defined by the failure to recover from acute COVID-19 in 90 days.
The scientists used data from nearly 5000 people enrolled in 14 established, ongoing research programs, including the 76-year-old Framingham Heart Study. The results of the analysis of the “mega-cohort” were published in JAMA Network Open.
Most of the 14 studies already had 10-20 years of data on the cardiac health of thousands of enrollees, said Norrina B. Allen, one of the authors and a cardiac epidemiologist at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
“This is a particularly strong study that looked at risk factors — or individual health — prior to developing COVID and their impact on the likely of recovering from COVID,” she said.
In addition to those with CVD, women and adults with preexisting chronic illnesses took longer to recover.
More than 20% of those in the large, racially and ethnically diverse US population–based study did not recover from COVID in 90 days. The researchers found that the median self-reported time to recovery from acute infection was 20 days.
While women and those with chronic illness had a higher risk for long COVID, vaccination and infection with the Omicron variant wave were associated with shorter recovery times.
These findings make sense, said Ziyad Al-Aly, MD, chief of research at Veterans Affairs St. Louis Health Care System and clinical epidemiologist at Washington University in St. Louis, Missouri.
“We also see that COVID-19 can lead to new-onset cardiovascular disease,” said Al-Aly, who was not involved in the study. “There is clearly a (link) between COVID and cardiovascular disease. These two seem to be intimately intertwined. In my view, this emphasizes the importance of targeting these individuals for vaccination and potentially antivirals (when they get infected) to help reduce their risk of adverse events and ameliorate their chance of full and fast recovery.”
The study used data from the Collaborative Cohort of Cohorts for COVID-19 Research. The long list of researchers contributing to this study includes epidemiologists, biostatisticians, neurologists, pulmonologists, and cardiologists. The data come from a list of cohorts like the Framingham Heart Study, which identified key risk factors for CVD, including cholesterol levels. Other studies include the Atherosclerosis Risk in Communities study, which began in the mid-1980s. Researchers there recruited a cohort of 15,792 men and women in rural North Carolina and Mississippi and suburban Minneapolis. They enrolled a high number of African American participants, who have been underrepresented in past studies. Other cohorts focused on young adults with CVD and Hispanics, while another focused on people with chronic obstructive pulmonary disease.
Lead author Elizabeth C. Oelsner, MD, of Columbia University Irving Medical Center in New York City, said she was not surprised by the CVD-long COVID link.
“We were aware that individuals with CVD were at higher risk of a more severe acute infection,” she said. “We were also seeing evidence that long and severe infection led to persistent symptoms.”
Oelsner noted that many patients still take more than 3 months to recover, even during the Omicron wave.
“While that has improved over the course of the pandemic, many individuals are taking a very long time to recover, and that can have a huge burden on the patient,” she said.
She encourages healthcare providers to tell patients at higher risk to take steps to avoid the virus, including vaccination and boosters.
A version of this article first appeared on Medscape.com.
Genetic Risk for Gout Raises Risk for Cardiovascular Disease Independent of Urate Level
TOPLINE:
Genetic predisposition to gout, unfavorable lifestyle habits, and poor metabolic health are associated with an increased risk for cardiovascular disease (CVD); however, adherence to a healthy lifestyle can reduce this risk by up to 62%, even in individuals with high genetic risk.
METHODOLOGY:
- Researchers investigated the association between genetic predisposition to gout, combined with lifestyle habits, and the risk for CVD in two diverse prospective cohorts from different ancestral backgrounds.
- They analyzed the data of 224,689 participants of European descent from the UK Biobank (mean age, 57.0 years; 56.1% women) and 50,364 participants of East Asian descent from the Korean Genome and Epidemiology Study (KoGES; mean age, 53.7 years; 66.0% women).
- The genetic predisposition to gout was evaluated using a polygenic risk score (PRS) derived from a metagenome-wide association study, and the participants were categorized into low, intermediate, and high genetic risk groups based on their PRS for gout.
- A favorable lifestyle was defined as having ≥ 3 healthy lifestyle factors, and 0-1 metabolic syndrome factor defined the ideal metabolic health status.
- The incident CVD risk was evaluated according to genetic risk, lifestyle habits, and metabolic syndrome.
TAKEAWAY:
- Individuals in the high genetic risk group had a higher risk for CVD than those in the low genetic risk group in both the UK Biobank (adjusted hazard ratio [aHR], 1.10; P < .001) and KoGES (aHR, 1.31; P = .024) cohorts.
- In the UK Biobank cohort, individuals with a high genetic risk for gout and unfavorable lifestyle choices had a 1.99 times higher risk for incident CVD than those with low genetic risk (aHR, 1.99; P < .001); similar outcomes were observed in the KoGES cohort.
- Similarly, individuals with a high genetic risk for gout and poor metabolic health in the UK Biobank cohort had a 2.16 times higher risk for CVD than those with low genetic risk (aHR, 2.16; P < .001 for both); outcomes were no different in the KoGES cohort.
- Improving metabolic health and adhering to a healthy lifestyle reduced the risk for CVD by 62% in individuals with high genetic risk and by 46% in those with low genetic risk (P < .001 for both).
IN PRACTICE:
“PRS for gout can be used for preventing not only gout but also CVD. It is possible to identify individuals with high genetic risk for gout and strongly recommend modifying lifestyle habits. Weight reduction, smoking cessation, regular exercise, and eating healthy food are effective strategies to prevent gout and CVD,” the authors wrote.
SOURCE:
This study was led by Ki Won Moon, MD, PhD, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Republic of Korea, and SangHyuk Jung, PhD, University of Pennsylvania, Philadelphia, and was published online on October 8, 2024, in RMD Open.
LIMITATIONS:
The definitions of lifestyle and metabolic syndrome were different in each cohort, which may have affected the findings. Data on lifestyle behaviors and metabolic health statuses were collected at enrollment, but these variables may have changed during the follow-up period, which potentially introduced bias into the results. This study was not able to establish causality between genetic predisposition to gout and the incident risk for CVD.
DISCLOSURES:
This study was supported by the National Institute of General Medical Sciences and the National Research Foundation of Korea. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Genetic predisposition to gout, unfavorable lifestyle habits, and poor metabolic health are associated with an increased risk for cardiovascular disease (CVD); however, adherence to a healthy lifestyle can reduce this risk by up to 62%, even in individuals with high genetic risk.
METHODOLOGY:
- Researchers investigated the association between genetic predisposition to gout, combined with lifestyle habits, and the risk for CVD in two diverse prospective cohorts from different ancestral backgrounds.
- They analyzed the data of 224,689 participants of European descent from the UK Biobank (mean age, 57.0 years; 56.1% women) and 50,364 participants of East Asian descent from the Korean Genome and Epidemiology Study (KoGES; mean age, 53.7 years; 66.0% women).
- The genetic predisposition to gout was evaluated using a polygenic risk score (PRS) derived from a metagenome-wide association study, and the participants were categorized into low, intermediate, and high genetic risk groups based on their PRS for gout.
- A favorable lifestyle was defined as having ≥ 3 healthy lifestyle factors, and 0-1 metabolic syndrome factor defined the ideal metabolic health status.
- The incident CVD risk was evaluated according to genetic risk, lifestyle habits, and metabolic syndrome.
TAKEAWAY:
- Individuals in the high genetic risk group had a higher risk for CVD than those in the low genetic risk group in both the UK Biobank (adjusted hazard ratio [aHR], 1.10; P < .001) and KoGES (aHR, 1.31; P = .024) cohorts.
- In the UK Biobank cohort, individuals with a high genetic risk for gout and unfavorable lifestyle choices had a 1.99 times higher risk for incident CVD than those with low genetic risk (aHR, 1.99; P < .001); similar outcomes were observed in the KoGES cohort.
- Similarly, individuals with a high genetic risk for gout and poor metabolic health in the UK Biobank cohort had a 2.16 times higher risk for CVD than those with low genetic risk (aHR, 2.16; P < .001 for both); outcomes were no different in the KoGES cohort.
- Improving metabolic health and adhering to a healthy lifestyle reduced the risk for CVD by 62% in individuals with high genetic risk and by 46% in those with low genetic risk (P < .001 for both).
IN PRACTICE:
“PRS for gout can be used for preventing not only gout but also CVD. It is possible to identify individuals with high genetic risk for gout and strongly recommend modifying lifestyle habits. Weight reduction, smoking cessation, regular exercise, and eating healthy food are effective strategies to prevent gout and CVD,” the authors wrote.
SOURCE:
This study was led by Ki Won Moon, MD, PhD, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Republic of Korea, and SangHyuk Jung, PhD, University of Pennsylvania, Philadelphia, and was published online on October 8, 2024, in RMD Open.
LIMITATIONS:
The definitions of lifestyle and metabolic syndrome were different in each cohort, which may have affected the findings. Data on lifestyle behaviors and metabolic health statuses were collected at enrollment, but these variables may have changed during the follow-up period, which potentially introduced bias into the results. This study was not able to establish causality between genetic predisposition to gout and the incident risk for CVD.
DISCLOSURES:
This study was supported by the National Institute of General Medical Sciences and the National Research Foundation of Korea. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Genetic predisposition to gout, unfavorable lifestyle habits, and poor metabolic health are associated with an increased risk for cardiovascular disease (CVD); however, adherence to a healthy lifestyle can reduce this risk by up to 62%, even in individuals with high genetic risk.
METHODOLOGY:
- Researchers investigated the association between genetic predisposition to gout, combined with lifestyle habits, and the risk for CVD in two diverse prospective cohorts from different ancestral backgrounds.
- They analyzed the data of 224,689 participants of European descent from the UK Biobank (mean age, 57.0 years; 56.1% women) and 50,364 participants of East Asian descent from the Korean Genome and Epidemiology Study (KoGES; mean age, 53.7 years; 66.0% women).
- The genetic predisposition to gout was evaluated using a polygenic risk score (PRS) derived from a metagenome-wide association study, and the participants were categorized into low, intermediate, and high genetic risk groups based on their PRS for gout.
- A favorable lifestyle was defined as having ≥ 3 healthy lifestyle factors, and 0-1 metabolic syndrome factor defined the ideal metabolic health status.
- The incident CVD risk was evaluated according to genetic risk, lifestyle habits, and metabolic syndrome.
TAKEAWAY:
- Individuals in the high genetic risk group had a higher risk for CVD than those in the low genetic risk group in both the UK Biobank (adjusted hazard ratio [aHR], 1.10; P < .001) and KoGES (aHR, 1.31; P = .024) cohorts.
- In the UK Biobank cohort, individuals with a high genetic risk for gout and unfavorable lifestyle choices had a 1.99 times higher risk for incident CVD than those with low genetic risk (aHR, 1.99; P < .001); similar outcomes were observed in the KoGES cohort.
- Similarly, individuals with a high genetic risk for gout and poor metabolic health in the UK Biobank cohort had a 2.16 times higher risk for CVD than those with low genetic risk (aHR, 2.16; P < .001 for both); outcomes were no different in the KoGES cohort.
- Improving metabolic health and adhering to a healthy lifestyle reduced the risk for CVD by 62% in individuals with high genetic risk and by 46% in those with low genetic risk (P < .001 for both).
IN PRACTICE:
“PRS for gout can be used for preventing not only gout but also CVD. It is possible to identify individuals with high genetic risk for gout and strongly recommend modifying lifestyle habits. Weight reduction, smoking cessation, regular exercise, and eating healthy food are effective strategies to prevent gout and CVD,” the authors wrote.
SOURCE:
This study was led by Ki Won Moon, MD, PhD, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Republic of Korea, and SangHyuk Jung, PhD, University of Pennsylvania, Philadelphia, and was published online on October 8, 2024, in RMD Open.
LIMITATIONS:
The definitions of lifestyle and metabolic syndrome were different in each cohort, which may have affected the findings. Data on lifestyle behaviors and metabolic health statuses were collected at enrollment, but these variables may have changed during the follow-up period, which potentially introduced bias into the results. This study was not able to establish causality between genetic predisposition to gout and the incident risk for CVD.
DISCLOSURES:
This study was supported by the National Institute of General Medical Sciences and the National Research Foundation of Korea. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Group Aims to Better Define ‘Extraordinarily Heterogeneous’ Mast Cell Activation Syndrome
Depending on one’s perspective, “mast cell activation syndrome (MCAS)” is either a relatively rare, narrowly defined severe allergic condition or a vastly underrecognized underlying cause of multiple chronic inflammatory conditions that affect roughly 17% of the entire population.
Inappropriate activation of mast cells — now termed mast cell activation disease (MCAD) — has long been known to underlie allergic symptoms and inflammation, and far less commonly, neoplasias such as mastocytosis. The concept of chronic, persistent MCAS associated with aberrant growth and dystrophism is more recent, emerging only in the last couple of decades as a separate entity under the MCAD heading.
Observational studies and clinical experience have linked signs and symptoms of MCAS with other inflammatory chronic conditions such as hypermobile Ehlers-Danlos Syndrome (EDS), postural orthostatic tachycardia syndrome (POTS), myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), and recently, long COVID. However, those conditions themselves are diagnostically challenging, and as yet there is no proof of causation.
The idea that MCAS is the entity — or at least, a key one — at the center of “a confoundingly, extraordinarily heterogeneous chronic multisystem polymorbidity” was the theme of a recent 4-day meeting of a professional group informally dubbed “Masterminds.” Since their first meeting in 2018, the group has grown from about 35 to nearly 650 multidisciplinary professionals.
Stephanie L. Grach, MD, assistant professor of medicine at the Mayo Clinic, Rochester, Minnesota, gave an introductory talk about the importance of changing “the medical paradigm around complex chronic illness.” Much of the rest of the meeting was devoted to sharing approaches for managing MCAS comorbidities, including dysautonomia, hypermobility, and associated craniocervical dysfunction, and various other multi-system conditions characterized by chronic pain and/or fatigue. Several talks covered the use of agents that block mast cell activity as potential treatment.
In an interview, Grach said “the meeting was an exciting example of how not only research, but also medicine, is moving forward, and it’s really cool to see that people are independently coming to very similar conclusions about shared pathologies, and because of that, the importance of overlap amongst complex medical conditions that historically have really been poorly addressed.”
She added, “mast cell activation, or mast cell hyperactivity, is one part of the greater picture. What’s important about the mast cell component is that of the multiple different targetable pathologies, it’s one that currently has potential available therapies that can be explored, some of them relatively easily.”
But Christopher Chang, MD, PhD, chief of the Pediatric Allergy and Immunology program, Joe DiMaggio Children’s Hospital, Hollywood, Florida, sees it differently. In an interview, he noted that the reason for disagreement over what constitutes MCAS is that “it doesn’t have a lot of objective findings that we can identify. ... We know that mast cells are important immune cells, just like all immune cells are important. It seems like whenever someone has unexplained symptoms, people try to blame it on mast cells. But it’s very hard to prove that.”
Two Definitions Characterize the Illness Differently
One proposed “consensus” MCAS definition was first published in 2011 by a group led by hematologist Peter Valent, MD, of the Medical University of Vienna in Austria. It has been revised since, and similar versions adopted by medical societies, including the American Academy of Allergy, Asthma & Immunology (AAAAI). The most recent versions propose three core MCAS criteria:
- Typical clinical signs of severe, recurrent (episodic) systemic (at least two organ systems) MCA are present (often in the form of anaphylaxis).
- The involvement of mast cells (MCs) is documented by biochemical studies, preferably an increase in serum tryptase levels from the individual’s baseline to plus 20% + 2 ng/mL.
- Response of symptoms to therapy with MC-stabilizing agents, drugs directed against MC mediator production, or drugs blocking mediator release or effects of MC-derived mediators.
The following year, a separate publication authored by Gerhard J. Molderings, MD, University of Bonn in Germany, and colleagues proposed a much broader MCAS definition. Also revised since, the latest “consensus-2” was published in 2020. This definition consists of one major criterion: “A constellation of clinical complaints attributable to pathologically increased MC activity, ie, MC mediator release syndrome.” This “constellation” involves conditions of nearly every organ system that, taken together, are estimated to affect up to 17% of the entire population. These are just a few examples:
- Constitutional: Chronic fatigue, flushing, or sweats
- Dermatologic: Rashes or lesions
- Ophthalmologic: dry eyes
- Oral: Burning or itching in mouth
- Pulmonary: Airway inflammation at any/all levels
- Cardiovascular: Blood pressure lability or codiagnosis of POTS is common
- Gastrointestinal: Reflux, dysphagia, or malabsorption
- Genitourinary: Endometriosis, dysmenorrhea, or dyspareunia
- Musculoskeletal/connective tissue: Fibromyalgia or diagnosis of hypermobile EDS is common
- Neurologic: Headaches or sensory neuropathies
- Psychiatric: Depression or anxiety
- Endocrinologic: Thyroid disease or dyslipidemia
- Hematologic: Polycythemia or anemia (after ruling out other causes)
The diagnosis is made by fulfilling that major criterion, plus at least one objective assessment of pathologically increased release of MC mediators, including infiltrates, abnormal MC morphology, or MC genetic changes shown to increase MC activity. Other alternatives include evidence of above-normal levels of MC mediators, including tryptase, histamine or its metabolites, heparin, or chromatin A, in whole blood, serum, plasma, or urine. Symptomatic response to MC activation inhibitors can also be used but isn’t required as it is in the other definition.
Underdiagnosis vs Overdiagnosis
Lawrence B. Afrin, MD, senior consultant in hematology/oncology at the AIM Center for Personalized Medicine, Westchester, New York, and lead author of the 2020 update of the broader “consensus-2” criteria, said in an interview, “we now know MCAS exists, and it’s prevalent, even though, for understandable and forgivable reasons, we’ve been missing it all along. ... If you see a patient who has this chronic, multisystem unwellness with general themes of inflammation plus or minus allergic issues and you can’t find some other rational explanation that better accounts for what’s going on ... then it’s reasonable to think to include MCAS in the differential diagnosis. If the patient happens not to fit the diagnostic criteria being advanced by one group, that doesn’t necessarily rule out the possibility that this is still going on.”
Afrin, along with his coauthors, faulted the narrower “consensus-1” definition for lacking data to support the “20% + 2” criteria for requiring the difficult determination of a patient’s “baseline” and for requiring evidence of response to treatment prior to making the diagnosis. Not all patients will respond to a given histamine blocker, he noted.
But Lawrence B. Schwartz, MD, PhD, an author on both the Valent and AAAAI criteria, disagreed, noting that the narrower criteria “appear to have a high degree of specificity and sensitivity when the reaction is systemic and involves hypotension. Less severe clinical events, particularly involving the gastrointestinal or central nervous systems, do not have precise clinical or biomarker criteria for identifying mast cell involvement.”
Added Schwartz, who is professor of medicine and chair of the Division of Rheumatology, Allergy, and Immunology and program director of Allergy and Immunology, Virginia Commonwealth University (VCU), Richmond, “when mast cell activation events occur only in the skin, we refer to it as chronic urticaria and in the airways or conjunctiva of allergic individuals as allergic asthma, rhinitis, and/or conjunctivitis. The absence of specific criteria for mast cell activation in the GI [gastrointestinal] tract or CNS [central nervous system] neither rules in mast cell involvement nor does it rule out mast cell involvement. Thus, more research is needed to find better diagnostic criteria.”
Schwartz also pointed to a recent paper reporting the use of artificial intelligence models to “quantify diagnostic precision and specificity” of “alternative” MCAS definitions. The conclusion was a “lack of specificity is pronounced in relation to multiple control criteria, raising the concern that alternative criteria could disproportionately contribute to MCAS overdiagnosis, to the exclusion of more appropriate diagnoses.”
During the meeting, Afrin acknowledged that the broader view risks overdiagnosis of MCAS. However, he also referenced Occam’s razor, the principle that the simplest explanation is probably the best one. “Which scenario is more likely? Multiple diagnoses and problems that are all independent of each other vs one diagnosis that’s biologically capable of causing most or all of the findings, ie, the simplest solution even if it’s not the most immediately obvious solution?”
He said in an interview: “Do we have any proof that MCAS is what’s underlying hypermobile Ehlers-Danlos or POTS or chronic fatigue? No, we don’t have any proof, not because anybody has done studies that have shown there to be no connection but simply because we’re so early in our awareness that the disease even exists that the necessary studies haven’t even been done yet.”
At the meeting, Afrin introduced proposals to turn the “Masterminds” group into a formal professional society and to launch a journal. He also gave an update on progress in developing a symptom assessment tool both for clinical use and to enable clinical trials of new drugs to target mast cells or their mediators. The plan is to field test the tool in 2025 and publish those results in 2026.
Grach, Afrin, and Chang had no disclosures. Schwartz discovered tryptase and invented the Thermo Fisher tryptase assay, for which his institution (VCU) receives royalties that are shared with him. He also invented monoclonal antibodies used for detecting mast cells or basophils, for which VCU receives royalties from several companies, including Millipore, Santa Cruz, BioLegend, and Hycult Biotech, that are also shared with him. He is a paid consultant for Blueprint Medicines, Celldex Therapeutics, Invea, Third Harmonic Bio, HYCOR Biomedical, Jasper, TerSera Therapeutics, and GLG. He also serves on an AstraZeneca data safety monitoring board for a clinical trial involving benralizumab treatment of hypereosinophilic syndrome and receives royalties from UpToDate (biomarkers for anaphylaxis) and Goldman-Cecil Medicine (anaphylaxis).
A version of this article first appeared on Medscape.com.
Depending on one’s perspective, “mast cell activation syndrome (MCAS)” is either a relatively rare, narrowly defined severe allergic condition or a vastly underrecognized underlying cause of multiple chronic inflammatory conditions that affect roughly 17% of the entire population.
Inappropriate activation of mast cells — now termed mast cell activation disease (MCAD) — has long been known to underlie allergic symptoms and inflammation, and far less commonly, neoplasias such as mastocytosis. The concept of chronic, persistent MCAS associated with aberrant growth and dystrophism is more recent, emerging only in the last couple of decades as a separate entity under the MCAD heading.
Observational studies and clinical experience have linked signs and symptoms of MCAS with other inflammatory chronic conditions such as hypermobile Ehlers-Danlos Syndrome (EDS), postural orthostatic tachycardia syndrome (POTS), myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), and recently, long COVID. However, those conditions themselves are diagnostically challenging, and as yet there is no proof of causation.
The idea that MCAS is the entity — or at least, a key one — at the center of “a confoundingly, extraordinarily heterogeneous chronic multisystem polymorbidity” was the theme of a recent 4-day meeting of a professional group informally dubbed “Masterminds.” Since their first meeting in 2018, the group has grown from about 35 to nearly 650 multidisciplinary professionals.
Stephanie L. Grach, MD, assistant professor of medicine at the Mayo Clinic, Rochester, Minnesota, gave an introductory talk about the importance of changing “the medical paradigm around complex chronic illness.” Much of the rest of the meeting was devoted to sharing approaches for managing MCAS comorbidities, including dysautonomia, hypermobility, and associated craniocervical dysfunction, and various other multi-system conditions characterized by chronic pain and/or fatigue. Several talks covered the use of agents that block mast cell activity as potential treatment.
In an interview, Grach said “the meeting was an exciting example of how not only research, but also medicine, is moving forward, and it’s really cool to see that people are independently coming to very similar conclusions about shared pathologies, and because of that, the importance of overlap amongst complex medical conditions that historically have really been poorly addressed.”
She added, “mast cell activation, or mast cell hyperactivity, is one part of the greater picture. What’s important about the mast cell component is that of the multiple different targetable pathologies, it’s one that currently has potential available therapies that can be explored, some of them relatively easily.”
But Christopher Chang, MD, PhD, chief of the Pediatric Allergy and Immunology program, Joe DiMaggio Children’s Hospital, Hollywood, Florida, sees it differently. In an interview, he noted that the reason for disagreement over what constitutes MCAS is that “it doesn’t have a lot of objective findings that we can identify. ... We know that mast cells are important immune cells, just like all immune cells are important. It seems like whenever someone has unexplained symptoms, people try to blame it on mast cells. But it’s very hard to prove that.”
Two Definitions Characterize the Illness Differently
One proposed “consensus” MCAS definition was first published in 2011 by a group led by hematologist Peter Valent, MD, of the Medical University of Vienna in Austria. It has been revised since, and similar versions adopted by medical societies, including the American Academy of Allergy, Asthma & Immunology (AAAAI). The most recent versions propose three core MCAS criteria:
- Typical clinical signs of severe, recurrent (episodic) systemic (at least two organ systems) MCA are present (often in the form of anaphylaxis).
- The involvement of mast cells (MCs) is documented by biochemical studies, preferably an increase in serum tryptase levels from the individual’s baseline to plus 20% + 2 ng/mL.
- Response of symptoms to therapy with MC-stabilizing agents, drugs directed against MC mediator production, or drugs blocking mediator release or effects of MC-derived mediators.
The following year, a separate publication authored by Gerhard J. Molderings, MD, University of Bonn in Germany, and colleagues proposed a much broader MCAS definition. Also revised since, the latest “consensus-2” was published in 2020. This definition consists of one major criterion: “A constellation of clinical complaints attributable to pathologically increased MC activity, ie, MC mediator release syndrome.” This “constellation” involves conditions of nearly every organ system that, taken together, are estimated to affect up to 17% of the entire population. These are just a few examples:
- Constitutional: Chronic fatigue, flushing, or sweats
- Dermatologic: Rashes or lesions
- Ophthalmologic: dry eyes
- Oral: Burning or itching in mouth
- Pulmonary: Airway inflammation at any/all levels
- Cardiovascular: Blood pressure lability or codiagnosis of POTS is common
- Gastrointestinal: Reflux, dysphagia, or malabsorption
- Genitourinary: Endometriosis, dysmenorrhea, or dyspareunia
- Musculoskeletal/connective tissue: Fibromyalgia or diagnosis of hypermobile EDS is common
- Neurologic: Headaches or sensory neuropathies
- Psychiatric: Depression or anxiety
- Endocrinologic: Thyroid disease or dyslipidemia
- Hematologic: Polycythemia or anemia (after ruling out other causes)
The diagnosis is made by fulfilling that major criterion, plus at least one objective assessment of pathologically increased release of MC mediators, including infiltrates, abnormal MC morphology, or MC genetic changes shown to increase MC activity. Other alternatives include evidence of above-normal levels of MC mediators, including tryptase, histamine or its metabolites, heparin, or chromatin A, in whole blood, serum, plasma, or urine. Symptomatic response to MC activation inhibitors can also be used but isn’t required as it is in the other definition.
Underdiagnosis vs Overdiagnosis
Lawrence B. Afrin, MD, senior consultant in hematology/oncology at the AIM Center for Personalized Medicine, Westchester, New York, and lead author of the 2020 update of the broader “consensus-2” criteria, said in an interview, “we now know MCAS exists, and it’s prevalent, even though, for understandable and forgivable reasons, we’ve been missing it all along. ... If you see a patient who has this chronic, multisystem unwellness with general themes of inflammation plus or minus allergic issues and you can’t find some other rational explanation that better accounts for what’s going on ... then it’s reasonable to think to include MCAS in the differential diagnosis. If the patient happens not to fit the diagnostic criteria being advanced by one group, that doesn’t necessarily rule out the possibility that this is still going on.”
Afrin, along with his coauthors, faulted the narrower “consensus-1” definition for lacking data to support the “20% + 2” criteria for requiring the difficult determination of a patient’s “baseline” and for requiring evidence of response to treatment prior to making the diagnosis. Not all patients will respond to a given histamine blocker, he noted.
But Lawrence B. Schwartz, MD, PhD, an author on both the Valent and AAAAI criteria, disagreed, noting that the narrower criteria “appear to have a high degree of specificity and sensitivity when the reaction is systemic and involves hypotension. Less severe clinical events, particularly involving the gastrointestinal or central nervous systems, do not have precise clinical or biomarker criteria for identifying mast cell involvement.”
Added Schwartz, who is professor of medicine and chair of the Division of Rheumatology, Allergy, and Immunology and program director of Allergy and Immunology, Virginia Commonwealth University (VCU), Richmond, “when mast cell activation events occur only in the skin, we refer to it as chronic urticaria and in the airways or conjunctiva of allergic individuals as allergic asthma, rhinitis, and/or conjunctivitis. The absence of specific criteria for mast cell activation in the GI [gastrointestinal] tract or CNS [central nervous system] neither rules in mast cell involvement nor does it rule out mast cell involvement. Thus, more research is needed to find better diagnostic criteria.”
Schwartz also pointed to a recent paper reporting the use of artificial intelligence models to “quantify diagnostic precision and specificity” of “alternative” MCAS definitions. The conclusion was a “lack of specificity is pronounced in relation to multiple control criteria, raising the concern that alternative criteria could disproportionately contribute to MCAS overdiagnosis, to the exclusion of more appropriate diagnoses.”
During the meeting, Afrin acknowledged that the broader view risks overdiagnosis of MCAS. However, he also referenced Occam’s razor, the principle that the simplest explanation is probably the best one. “Which scenario is more likely? Multiple diagnoses and problems that are all independent of each other vs one diagnosis that’s biologically capable of causing most or all of the findings, ie, the simplest solution even if it’s not the most immediately obvious solution?”
He said in an interview: “Do we have any proof that MCAS is what’s underlying hypermobile Ehlers-Danlos or POTS or chronic fatigue? No, we don’t have any proof, not because anybody has done studies that have shown there to be no connection but simply because we’re so early in our awareness that the disease even exists that the necessary studies haven’t even been done yet.”
At the meeting, Afrin introduced proposals to turn the “Masterminds” group into a formal professional society and to launch a journal. He also gave an update on progress in developing a symptom assessment tool both for clinical use and to enable clinical trials of new drugs to target mast cells or their mediators. The plan is to field test the tool in 2025 and publish those results in 2026.
Grach, Afrin, and Chang had no disclosures. Schwartz discovered tryptase and invented the Thermo Fisher tryptase assay, for which his institution (VCU) receives royalties that are shared with him. He also invented monoclonal antibodies used for detecting mast cells or basophils, for which VCU receives royalties from several companies, including Millipore, Santa Cruz, BioLegend, and Hycult Biotech, that are also shared with him. He is a paid consultant for Blueprint Medicines, Celldex Therapeutics, Invea, Third Harmonic Bio, HYCOR Biomedical, Jasper, TerSera Therapeutics, and GLG. He also serves on an AstraZeneca data safety monitoring board for a clinical trial involving benralizumab treatment of hypereosinophilic syndrome and receives royalties from UpToDate (biomarkers for anaphylaxis) and Goldman-Cecil Medicine (anaphylaxis).
A version of this article first appeared on Medscape.com.
Depending on one’s perspective, “mast cell activation syndrome (MCAS)” is either a relatively rare, narrowly defined severe allergic condition or a vastly underrecognized underlying cause of multiple chronic inflammatory conditions that affect roughly 17% of the entire population.
Inappropriate activation of mast cells — now termed mast cell activation disease (MCAD) — has long been known to underlie allergic symptoms and inflammation, and far less commonly, neoplasias such as mastocytosis. The concept of chronic, persistent MCAS associated with aberrant growth and dystrophism is more recent, emerging only in the last couple of decades as a separate entity under the MCAD heading.
Observational studies and clinical experience have linked signs and symptoms of MCAS with other inflammatory chronic conditions such as hypermobile Ehlers-Danlos Syndrome (EDS), postural orthostatic tachycardia syndrome (POTS), myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), and recently, long COVID. However, those conditions themselves are diagnostically challenging, and as yet there is no proof of causation.
The idea that MCAS is the entity — or at least, a key one — at the center of “a confoundingly, extraordinarily heterogeneous chronic multisystem polymorbidity” was the theme of a recent 4-day meeting of a professional group informally dubbed “Masterminds.” Since their first meeting in 2018, the group has grown from about 35 to nearly 650 multidisciplinary professionals.
Stephanie L. Grach, MD, assistant professor of medicine at the Mayo Clinic, Rochester, Minnesota, gave an introductory talk about the importance of changing “the medical paradigm around complex chronic illness.” Much of the rest of the meeting was devoted to sharing approaches for managing MCAS comorbidities, including dysautonomia, hypermobility, and associated craniocervical dysfunction, and various other multi-system conditions characterized by chronic pain and/or fatigue. Several talks covered the use of agents that block mast cell activity as potential treatment.
In an interview, Grach said “the meeting was an exciting example of how not only research, but also medicine, is moving forward, and it’s really cool to see that people are independently coming to very similar conclusions about shared pathologies, and because of that, the importance of overlap amongst complex medical conditions that historically have really been poorly addressed.”
She added, “mast cell activation, or mast cell hyperactivity, is one part of the greater picture. What’s important about the mast cell component is that of the multiple different targetable pathologies, it’s one that currently has potential available therapies that can be explored, some of them relatively easily.”
But Christopher Chang, MD, PhD, chief of the Pediatric Allergy and Immunology program, Joe DiMaggio Children’s Hospital, Hollywood, Florida, sees it differently. In an interview, he noted that the reason for disagreement over what constitutes MCAS is that “it doesn’t have a lot of objective findings that we can identify. ... We know that mast cells are important immune cells, just like all immune cells are important. It seems like whenever someone has unexplained symptoms, people try to blame it on mast cells. But it’s very hard to prove that.”
Two Definitions Characterize the Illness Differently
One proposed “consensus” MCAS definition was first published in 2011 by a group led by hematologist Peter Valent, MD, of the Medical University of Vienna in Austria. It has been revised since, and similar versions adopted by medical societies, including the American Academy of Allergy, Asthma & Immunology (AAAAI). The most recent versions propose three core MCAS criteria:
- Typical clinical signs of severe, recurrent (episodic) systemic (at least two organ systems) MCA are present (often in the form of anaphylaxis).
- The involvement of mast cells (MCs) is documented by biochemical studies, preferably an increase in serum tryptase levels from the individual’s baseline to plus 20% + 2 ng/mL.
- Response of symptoms to therapy with MC-stabilizing agents, drugs directed against MC mediator production, or drugs blocking mediator release or effects of MC-derived mediators.
The following year, a separate publication authored by Gerhard J. Molderings, MD, University of Bonn in Germany, and colleagues proposed a much broader MCAS definition. Also revised since, the latest “consensus-2” was published in 2020. This definition consists of one major criterion: “A constellation of clinical complaints attributable to pathologically increased MC activity, ie, MC mediator release syndrome.” This “constellation” involves conditions of nearly every organ system that, taken together, are estimated to affect up to 17% of the entire population. These are just a few examples:
- Constitutional: Chronic fatigue, flushing, or sweats
- Dermatologic: Rashes or lesions
- Ophthalmologic: dry eyes
- Oral: Burning or itching in mouth
- Pulmonary: Airway inflammation at any/all levels
- Cardiovascular: Blood pressure lability or codiagnosis of POTS is common
- Gastrointestinal: Reflux, dysphagia, or malabsorption
- Genitourinary: Endometriosis, dysmenorrhea, or dyspareunia
- Musculoskeletal/connective tissue: Fibromyalgia or diagnosis of hypermobile EDS is common
- Neurologic: Headaches or sensory neuropathies
- Psychiatric: Depression or anxiety
- Endocrinologic: Thyroid disease or dyslipidemia
- Hematologic: Polycythemia or anemia (after ruling out other causes)
The diagnosis is made by fulfilling that major criterion, plus at least one objective assessment of pathologically increased release of MC mediators, including infiltrates, abnormal MC morphology, or MC genetic changes shown to increase MC activity. Other alternatives include evidence of above-normal levels of MC mediators, including tryptase, histamine or its metabolites, heparin, or chromatin A, in whole blood, serum, plasma, or urine. Symptomatic response to MC activation inhibitors can also be used but isn’t required as it is in the other definition.
Underdiagnosis vs Overdiagnosis
Lawrence B. Afrin, MD, senior consultant in hematology/oncology at the AIM Center for Personalized Medicine, Westchester, New York, and lead author of the 2020 update of the broader “consensus-2” criteria, said in an interview, “we now know MCAS exists, and it’s prevalent, even though, for understandable and forgivable reasons, we’ve been missing it all along. ... If you see a patient who has this chronic, multisystem unwellness with general themes of inflammation plus or minus allergic issues and you can’t find some other rational explanation that better accounts for what’s going on ... then it’s reasonable to think to include MCAS in the differential diagnosis. If the patient happens not to fit the diagnostic criteria being advanced by one group, that doesn’t necessarily rule out the possibility that this is still going on.”
Afrin, along with his coauthors, faulted the narrower “consensus-1” definition for lacking data to support the “20% + 2” criteria for requiring the difficult determination of a patient’s “baseline” and for requiring evidence of response to treatment prior to making the diagnosis. Not all patients will respond to a given histamine blocker, he noted.
But Lawrence B. Schwartz, MD, PhD, an author on both the Valent and AAAAI criteria, disagreed, noting that the narrower criteria “appear to have a high degree of specificity and sensitivity when the reaction is systemic and involves hypotension. Less severe clinical events, particularly involving the gastrointestinal or central nervous systems, do not have precise clinical or biomarker criteria for identifying mast cell involvement.”
Added Schwartz, who is professor of medicine and chair of the Division of Rheumatology, Allergy, and Immunology and program director of Allergy and Immunology, Virginia Commonwealth University (VCU), Richmond, “when mast cell activation events occur only in the skin, we refer to it as chronic urticaria and in the airways or conjunctiva of allergic individuals as allergic asthma, rhinitis, and/or conjunctivitis. The absence of specific criteria for mast cell activation in the GI [gastrointestinal] tract or CNS [central nervous system] neither rules in mast cell involvement nor does it rule out mast cell involvement. Thus, more research is needed to find better diagnostic criteria.”
Schwartz also pointed to a recent paper reporting the use of artificial intelligence models to “quantify diagnostic precision and specificity” of “alternative” MCAS definitions. The conclusion was a “lack of specificity is pronounced in relation to multiple control criteria, raising the concern that alternative criteria could disproportionately contribute to MCAS overdiagnosis, to the exclusion of more appropriate diagnoses.”
During the meeting, Afrin acknowledged that the broader view risks overdiagnosis of MCAS. However, he also referenced Occam’s razor, the principle that the simplest explanation is probably the best one. “Which scenario is more likely? Multiple diagnoses and problems that are all independent of each other vs one diagnosis that’s biologically capable of causing most or all of the findings, ie, the simplest solution even if it’s not the most immediately obvious solution?”
He said in an interview: “Do we have any proof that MCAS is what’s underlying hypermobile Ehlers-Danlos or POTS or chronic fatigue? No, we don’t have any proof, not because anybody has done studies that have shown there to be no connection but simply because we’re so early in our awareness that the disease even exists that the necessary studies haven’t even been done yet.”
At the meeting, Afrin introduced proposals to turn the “Masterminds” group into a formal professional society and to launch a journal. He also gave an update on progress in developing a symptom assessment tool both for clinical use and to enable clinical trials of new drugs to target mast cells or their mediators. The plan is to field test the tool in 2025 and publish those results in 2026.
Grach, Afrin, and Chang had no disclosures. Schwartz discovered tryptase and invented the Thermo Fisher tryptase assay, for which his institution (VCU) receives royalties that are shared with him. He also invented monoclonal antibodies used for detecting mast cells or basophils, for which VCU receives royalties from several companies, including Millipore, Santa Cruz, BioLegend, and Hycult Biotech, that are also shared with him. He is a paid consultant for Blueprint Medicines, Celldex Therapeutics, Invea, Third Harmonic Bio, HYCOR Biomedical, Jasper, TerSera Therapeutics, and GLG. He also serves on an AstraZeneca data safety monitoring board for a clinical trial involving benralizumab treatment of hypereosinophilic syndrome and receives royalties from UpToDate (biomarkers for anaphylaxis) and Goldman-Cecil Medicine (anaphylaxis).
A version of this article first appeared on Medscape.com.
Cognitive Decline and Antihypertensive Use: New Data
TOPLINE:
a new study suggests. The association was strongest among those with dementia.
METHODOLOGY:
- The cohort study included 12,644 long-term care residents (mean age, 77.7 years; 97% men; 17.5% Black) with stays of at least 12 weeks from 2006 to 2019.
- Residents who experienced either a reduction in the total number of antihypertensive medications or a sustained 30% decrease in dosage for at least 2 weeks were classified as deprescribing users (n = 1290). Those with no medication changes were considered stable users (n = 11,354).
- The primary outcome was cognitive impairment assessed using the four-point Cognitive Function Scale (CFS), with the score proportional to the severity of impairment.
- The median follow-up duration was 23 weeks for the deprescribing users and 21 weeks for the stable users.
TAKEAWAY:
- Deprescribing antihypertensives was associated with a 12% lower likelihood of progressing to a worse CFS score per 12-week period (odds ratio [OR], 0.88; 95% CI, 0.78-0.99), compared with stable users.
- Among residents with dementia, deprescribing was associated with a 16% reduced likelihood of cognitive decline per 12-week period (OR, 0.84; 95% CI, 0.72-0.98).
- At the end of follow-up, 12% of residents had a higher CFS score and 7.7% had a lower CFS score.
- In the intention-to-treat analysis, the association between deprescribing antihypertensive medications and reduced cognitive decline remained consistent (OR, 0.94; 95% CI, 0.90-0.98).
IN PRACTICE:
“This work highlights the need for patient-centered approaches to deprescribing, ensuring that medication regimens for older adults are optimized to preserve cognitive function and minimize potential harms,” the study authors wrote.
SOURCE:
The study was led by Bocheng Jing, MS, Department of Medicine, University of California, San Francisco. It was published online in JAMA Internal Medicine.
LIMITATIONS:
The study population included predominantly men and White individuals, limiting the generalizability of the results to women and other racial and ethnic groups. The findings may not be applicable to patients with heart failure owing to their noninclusion. The specificity of dementia diagnosis was limited, as this study combined various forms of dementia, making it challenging to differentiate the impacts among subgroups.
DISCLOSURES:
This study was supported by the US National Institute on Aging. Two authors reported receiving grants, honoraria, consulting fees, or royalties from various sources. Details are provided in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
a new study suggests. The association was strongest among those with dementia.
METHODOLOGY:
- The cohort study included 12,644 long-term care residents (mean age, 77.7 years; 97% men; 17.5% Black) with stays of at least 12 weeks from 2006 to 2019.
- Residents who experienced either a reduction in the total number of antihypertensive medications or a sustained 30% decrease in dosage for at least 2 weeks were classified as deprescribing users (n = 1290). Those with no medication changes were considered stable users (n = 11,354).
- The primary outcome was cognitive impairment assessed using the four-point Cognitive Function Scale (CFS), with the score proportional to the severity of impairment.
- The median follow-up duration was 23 weeks for the deprescribing users and 21 weeks for the stable users.
TAKEAWAY:
- Deprescribing antihypertensives was associated with a 12% lower likelihood of progressing to a worse CFS score per 12-week period (odds ratio [OR], 0.88; 95% CI, 0.78-0.99), compared with stable users.
- Among residents with dementia, deprescribing was associated with a 16% reduced likelihood of cognitive decline per 12-week period (OR, 0.84; 95% CI, 0.72-0.98).
- At the end of follow-up, 12% of residents had a higher CFS score and 7.7% had a lower CFS score.
- In the intention-to-treat analysis, the association between deprescribing antihypertensive medications and reduced cognitive decline remained consistent (OR, 0.94; 95% CI, 0.90-0.98).
IN PRACTICE:
“This work highlights the need for patient-centered approaches to deprescribing, ensuring that medication regimens for older adults are optimized to preserve cognitive function and minimize potential harms,” the study authors wrote.
SOURCE:
The study was led by Bocheng Jing, MS, Department of Medicine, University of California, San Francisco. It was published online in JAMA Internal Medicine.
LIMITATIONS:
The study population included predominantly men and White individuals, limiting the generalizability of the results to women and other racial and ethnic groups. The findings may not be applicable to patients with heart failure owing to their noninclusion. The specificity of dementia diagnosis was limited, as this study combined various forms of dementia, making it challenging to differentiate the impacts among subgroups.
DISCLOSURES:
This study was supported by the US National Institute on Aging. Two authors reported receiving grants, honoraria, consulting fees, or royalties from various sources. Details are provided in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
a new study suggests. The association was strongest among those with dementia.
METHODOLOGY:
- The cohort study included 12,644 long-term care residents (mean age, 77.7 years; 97% men; 17.5% Black) with stays of at least 12 weeks from 2006 to 2019.
- Residents who experienced either a reduction in the total number of antihypertensive medications or a sustained 30% decrease in dosage for at least 2 weeks were classified as deprescribing users (n = 1290). Those with no medication changes were considered stable users (n = 11,354).
- The primary outcome was cognitive impairment assessed using the four-point Cognitive Function Scale (CFS), with the score proportional to the severity of impairment.
- The median follow-up duration was 23 weeks for the deprescribing users and 21 weeks for the stable users.
TAKEAWAY:
- Deprescribing antihypertensives was associated with a 12% lower likelihood of progressing to a worse CFS score per 12-week period (odds ratio [OR], 0.88; 95% CI, 0.78-0.99), compared with stable users.
- Among residents with dementia, deprescribing was associated with a 16% reduced likelihood of cognitive decline per 12-week period (OR, 0.84; 95% CI, 0.72-0.98).
- At the end of follow-up, 12% of residents had a higher CFS score and 7.7% had a lower CFS score.
- In the intention-to-treat analysis, the association between deprescribing antihypertensive medications and reduced cognitive decline remained consistent (OR, 0.94; 95% CI, 0.90-0.98).
IN PRACTICE:
“This work highlights the need for patient-centered approaches to deprescribing, ensuring that medication regimens for older adults are optimized to preserve cognitive function and minimize potential harms,” the study authors wrote.
SOURCE:
The study was led by Bocheng Jing, MS, Department of Medicine, University of California, San Francisco. It was published online in JAMA Internal Medicine.
LIMITATIONS:
The study population included predominantly men and White individuals, limiting the generalizability of the results to women and other racial and ethnic groups. The findings may not be applicable to patients with heart failure owing to their noninclusion. The specificity of dementia diagnosis was limited, as this study combined various forms of dementia, making it challenging to differentiate the impacts among subgroups.
DISCLOSURES:
This study was supported by the US National Institute on Aging. Two authors reported receiving grants, honoraria, consulting fees, or royalties from various sources. Details are provided in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
GPs Urged to Embed Lifestyle Medicine into Primary Care
LIVERPOOL — “Healthy doctors make healthy patients”, stated a GP during a workshop at the Royal College of General Practitioners (RCGP) annual meeting. The session aimed to encourage GPs to embed lifestyle medicine into primary care through collaborative action.
Callum Leese from Aberfeldy Medical Practice in Scotland, who is also a lecturer at the University of Dundee for the Scottish Clinical Research Excellence Development Scheme (SCREDS), discussed the benefits of lifestyle medicine services in addressing lifestyle-related diseases, reducing their contribution towards the prevalence of chronic conditions, and helping prevent premature mortality.
Leese is leading a project to make Aberfeldy the healthiest town in Scotland by promoting physical activities, such as the 2-km, 5-km, and 7-km Santa Stride walking group in November, and a recent food festival to encourage healthy cooking and eating. “There’s loads of things that can be done to try and inspire change,” he said. “The research is fairly unequivocal in that healthy doctors make healthy patients,” Leese asserted. “The most important thing we can do is target our doctors and our nurses and make them advocates for what we want to see with our patients.”
Speaking to this news organization, he emphasized that, “if the doctors are moving, they’re much more likely to promote it, and if they’re eating well, they’re much more likely to be able to be evangelistic.”
Physical Activity Advice Shows High Return
About one-third of the population in the United Kingdom are physically inactive, which costs the economy £7.2 billion, with £1 billion attributed directly to the NHS, he informed the workshop.
As an honorary support fellow in physical activity and lifestyle medicine at the RCGP, Leese specializes in integrating physical activity into primary care settings. “We know it’s cost effective. If we compare it to smoking cessation advice, we know that we need to give advice to one person about 50 times for one person to stop smoking in primary care. But for physical activity, you need to give advice to 12 people for one person to increase their physical activity levels to meet the guidance,” he noted.
Leese stressed the importance of short but effective discussions between GPs and patients. He gave examples of online resources to recommend to patients, such as Moving Medicine, which aims to help healthcare professionals integrate physical activity into routine clinical conversations, or the RCGP toolkit (the Physical Activity Hub). “It really takes 1 minute of asking if the patient has ever considered being more active, and briefly explaining that being more active might have really significant outcomes for their condition,” he said.
In primary care, most patients who need to be more physically activity are directed toward 12-week exercise referral schemes, and sometimes we use social prescribing, for example, inviting patients to walk in groups, Leese explained. “However, despite the best intentions, about 78% of GPs aren’t doing it [advising on physical activity] regularly,” he noted. He cited four main challenges: lack of time, knowledge, resources, and financial support.
Geographical Variation in Social Prescribing
Social prescribing, which links patients with non–medical community support, also varies widely across the United Kingdom. “Social prescribing is a real example of that because it’s really well established in some places and not in others,” Leese remarked. He noted that inner-city and rural areas often have different needs. Contrary to some expectations, city dwellers are sometimes more active than those living in rural areas because despite having lots of green space for physical activity, “they tend to park the car outside the front door and park again right outside their place of work, whereas in London, for example, you can persuade people to get off a stop early on the Tube or a stop early in the bus.”
MAN v FAT 5-a-side Football
Leese also emphasized the importance of innovation in implementing lifestyle medicine, pointing out that nonmedical personnel, social prescribers, and health coaches can alleviate time pressures on GPs.
Citing an example of a physical activity-related intervention, he described a UK-wide organization developed for men in the 40s-50s age group, called MAN v FAT, which involves a novel weight-related way of playing five-a-side football. Players have a weigh-in before each game and teams are rewarded with points on the pitch for every pound lost as a team since their last match.
However, Leese acknowledged the need to tailor physical activity advice to different age groups. For example, “in an 80-year-old, physical activity might improve their balance and they’re less likely to fall and break something.”
Lifestyle Clinics
Leese cited the PCN Lifestyle Clinics, originating from the Leamington Primary Care Network (PCN), as an example of successful lifestyle medicine integration to help address the needs of people living with chronic conditions. “We don’t want to prescribe a model, but we can draw on a program run by the Leamington Spa PCN, that involves four group sessions of 6-10 people focused on lifestyle,” he said.
The weekly group-based sessions are run by a GP, a health and wellbeing coach, a dietitian, and a psychiatrist. Together, they cover four aspects of lifestyle and health comprising individual challenges, how community influences behavior and vice versa, food and nutrition, and physical activity for health and wellbeing.
“We try to debunk some of those myths around nutrition, compared with diet, and physical activity, compared with exercise. So, for example, the idea that exercise is usually considered to be using an elliptical cross-trainer whereas physical activity, which might be just dancing in your kitchen while you’re making dinner, is something that can be done more easily,” explained Leese.
Physical activities include running and swimming in collaboration with a leisure center. “It’s an amazing program,” he remarked.
Outcomes from 142 patients who attended the Lifestyle Clinic at a North Leamington GP practice over 14 months showed that 53% gained confidence in making lifestyle changes, 60% noticed a positive impact on their physical health, and 77% reported positive impacts on their mental health.
GP Embraces Lifestyle Medicine
Rachel Burnett, a GP from Park Medical Practice in Derby, a delegate who attended the session, commented on the central idea of incorporating lifestyle medicine into primary care practice. She told this news organization that, “I think it could prevent a lot of ill health and therefore a lot of health inequalities just by embedding lifestyle medicine into our work. To hear about the Leamington Spa project and how it›s been a success was really inspiring.”
Referring to her own practice, Burnett said: “My patients are familiar with the way I go on and on about lifestyle measures, but I believe the way forward is with group sessions because we need to give the same advice to a large number of patients, for example, with prediabetes. This could save time and resource, and I think patients who are more likely to make the changes will actually attend the sessions so we’re not wasting our breath.”
Neither Leese nor Burnett declared any relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
LIVERPOOL — “Healthy doctors make healthy patients”, stated a GP during a workshop at the Royal College of General Practitioners (RCGP) annual meeting. The session aimed to encourage GPs to embed lifestyle medicine into primary care through collaborative action.
Callum Leese from Aberfeldy Medical Practice in Scotland, who is also a lecturer at the University of Dundee for the Scottish Clinical Research Excellence Development Scheme (SCREDS), discussed the benefits of lifestyle medicine services in addressing lifestyle-related diseases, reducing their contribution towards the prevalence of chronic conditions, and helping prevent premature mortality.
Leese is leading a project to make Aberfeldy the healthiest town in Scotland by promoting physical activities, such as the 2-km, 5-km, and 7-km Santa Stride walking group in November, and a recent food festival to encourage healthy cooking and eating. “There’s loads of things that can be done to try and inspire change,” he said. “The research is fairly unequivocal in that healthy doctors make healthy patients,” Leese asserted. “The most important thing we can do is target our doctors and our nurses and make them advocates for what we want to see with our patients.”
Speaking to this news organization, he emphasized that, “if the doctors are moving, they’re much more likely to promote it, and if they’re eating well, they’re much more likely to be able to be evangelistic.”
Physical Activity Advice Shows High Return
About one-third of the population in the United Kingdom are physically inactive, which costs the economy £7.2 billion, with £1 billion attributed directly to the NHS, he informed the workshop.
As an honorary support fellow in physical activity and lifestyle medicine at the RCGP, Leese specializes in integrating physical activity into primary care settings. “We know it’s cost effective. If we compare it to smoking cessation advice, we know that we need to give advice to one person about 50 times for one person to stop smoking in primary care. But for physical activity, you need to give advice to 12 people for one person to increase their physical activity levels to meet the guidance,” he noted.
Leese stressed the importance of short but effective discussions between GPs and patients. He gave examples of online resources to recommend to patients, such as Moving Medicine, which aims to help healthcare professionals integrate physical activity into routine clinical conversations, or the RCGP toolkit (the Physical Activity Hub). “It really takes 1 minute of asking if the patient has ever considered being more active, and briefly explaining that being more active might have really significant outcomes for their condition,” he said.
In primary care, most patients who need to be more physically activity are directed toward 12-week exercise referral schemes, and sometimes we use social prescribing, for example, inviting patients to walk in groups, Leese explained. “However, despite the best intentions, about 78% of GPs aren’t doing it [advising on physical activity] regularly,” he noted. He cited four main challenges: lack of time, knowledge, resources, and financial support.
Geographical Variation in Social Prescribing
Social prescribing, which links patients with non–medical community support, also varies widely across the United Kingdom. “Social prescribing is a real example of that because it’s really well established in some places and not in others,” Leese remarked. He noted that inner-city and rural areas often have different needs. Contrary to some expectations, city dwellers are sometimes more active than those living in rural areas because despite having lots of green space for physical activity, “they tend to park the car outside the front door and park again right outside their place of work, whereas in London, for example, you can persuade people to get off a stop early on the Tube or a stop early in the bus.”
MAN v FAT 5-a-side Football
Leese also emphasized the importance of innovation in implementing lifestyle medicine, pointing out that nonmedical personnel, social prescribers, and health coaches can alleviate time pressures on GPs.
Citing an example of a physical activity-related intervention, he described a UK-wide organization developed for men in the 40s-50s age group, called MAN v FAT, which involves a novel weight-related way of playing five-a-side football. Players have a weigh-in before each game and teams are rewarded with points on the pitch for every pound lost as a team since their last match.
However, Leese acknowledged the need to tailor physical activity advice to different age groups. For example, “in an 80-year-old, physical activity might improve their balance and they’re less likely to fall and break something.”
Lifestyle Clinics
Leese cited the PCN Lifestyle Clinics, originating from the Leamington Primary Care Network (PCN), as an example of successful lifestyle medicine integration to help address the needs of people living with chronic conditions. “We don’t want to prescribe a model, but we can draw on a program run by the Leamington Spa PCN, that involves four group sessions of 6-10 people focused on lifestyle,” he said.
The weekly group-based sessions are run by a GP, a health and wellbeing coach, a dietitian, and a psychiatrist. Together, they cover four aspects of lifestyle and health comprising individual challenges, how community influences behavior and vice versa, food and nutrition, and physical activity for health and wellbeing.
“We try to debunk some of those myths around nutrition, compared with diet, and physical activity, compared with exercise. So, for example, the idea that exercise is usually considered to be using an elliptical cross-trainer whereas physical activity, which might be just dancing in your kitchen while you’re making dinner, is something that can be done more easily,” explained Leese.
Physical activities include running and swimming in collaboration with a leisure center. “It’s an amazing program,” he remarked.
Outcomes from 142 patients who attended the Lifestyle Clinic at a North Leamington GP practice over 14 months showed that 53% gained confidence in making lifestyle changes, 60% noticed a positive impact on their physical health, and 77% reported positive impacts on their mental health.
GP Embraces Lifestyle Medicine
Rachel Burnett, a GP from Park Medical Practice in Derby, a delegate who attended the session, commented on the central idea of incorporating lifestyle medicine into primary care practice. She told this news organization that, “I think it could prevent a lot of ill health and therefore a lot of health inequalities just by embedding lifestyle medicine into our work. To hear about the Leamington Spa project and how it›s been a success was really inspiring.”
Referring to her own practice, Burnett said: “My patients are familiar with the way I go on and on about lifestyle measures, but I believe the way forward is with group sessions because we need to give the same advice to a large number of patients, for example, with prediabetes. This could save time and resource, and I think patients who are more likely to make the changes will actually attend the sessions so we’re not wasting our breath.”
Neither Leese nor Burnett declared any relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
LIVERPOOL — “Healthy doctors make healthy patients”, stated a GP during a workshop at the Royal College of General Practitioners (RCGP) annual meeting. The session aimed to encourage GPs to embed lifestyle medicine into primary care through collaborative action.
Callum Leese from Aberfeldy Medical Practice in Scotland, who is also a lecturer at the University of Dundee for the Scottish Clinical Research Excellence Development Scheme (SCREDS), discussed the benefits of lifestyle medicine services in addressing lifestyle-related diseases, reducing their contribution towards the prevalence of chronic conditions, and helping prevent premature mortality.
Leese is leading a project to make Aberfeldy the healthiest town in Scotland by promoting physical activities, such as the 2-km, 5-km, and 7-km Santa Stride walking group in November, and a recent food festival to encourage healthy cooking and eating. “There’s loads of things that can be done to try and inspire change,” he said. “The research is fairly unequivocal in that healthy doctors make healthy patients,” Leese asserted. “The most important thing we can do is target our doctors and our nurses and make them advocates for what we want to see with our patients.”
Speaking to this news organization, he emphasized that, “if the doctors are moving, they’re much more likely to promote it, and if they’re eating well, they’re much more likely to be able to be evangelistic.”
Physical Activity Advice Shows High Return
About one-third of the population in the United Kingdom are physically inactive, which costs the economy £7.2 billion, with £1 billion attributed directly to the NHS, he informed the workshop.
As an honorary support fellow in physical activity and lifestyle medicine at the RCGP, Leese specializes in integrating physical activity into primary care settings. “We know it’s cost effective. If we compare it to smoking cessation advice, we know that we need to give advice to one person about 50 times for one person to stop smoking in primary care. But for physical activity, you need to give advice to 12 people for one person to increase their physical activity levels to meet the guidance,” he noted.
Leese stressed the importance of short but effective discussions between GPs and patients. He gave examples of online resources to recommend to patients, such as Moving Medicine, which aims to help healthcare professionals integrate physical activity into routine clinical conversations, or the RCGP toolkit (the Physical Activity Hub). “It really takes 1 minute of asking if the patient has ever considered being more active, and briefly explaining that being more active might have really significant outcomes for their condition,” he said.
In primary care, most patients who need to be more physically activity are directed toward 12-week exercise referral schemes, and sometimes we use social prescribing, for example, inviting patients to walk in groups, Leese explained. “However, despite the best intentions, about 78% of GPs aren’t doing it [advising on physical activity] regularly,” he noted. He cited four main challenges: lack of time, knowledge, resources, and financial support.
Geographical Variation in Social Prescribing
Social prescribing, which links patients with non–medical community support, also varies widely across the United Kingdom. “Social prescribing is a real example of that because it’s really well established in some places and not in others,” Leese remarked. He noted that inner-city and rural areas often have different needs. Contrary to some expectations, city dwellers are sometimes more active than those living in rural areas because despite having lots of green space for physical activity, “they tend to park the car outside the front door and park again right outside their place of work, whereas in London, for example, you can persuade people to get off a stop early on the Tube or a stop early in the bus.”
MAN v FAT 5-a-side Football
Leese also emphasized the importance of innovation in implementing lifestyle medicine, pointing out that nonmedical personnel, social prescribers, and health coaches can alleviate time pressures on GPs.
Citing an example of a physical activity-related intervention, he described a UK-wide organization developed for men in the 40s-50s age group, called MAN v FAT, which involves a novel weight-related way of playing five-a-side football. Players have a weigh-in before each game and teams are rewarded with points on the pitch for every pound lost as a team since their last match.
However, Leese acknowledged the need to tailor physical activity advice to different age groups. For example, “in an 80-year-old, physical activity might improve their balance and they’re less likely to fall and break something.”
Lifestyle Clinics
Leese cited the PCN Lifestyle Clinics, originating from the Leamington Primary Care Network (PCN), as an example of successful lifestyle medicine integration to help address the needs of people living with chronic conditions. “We don’t want to prescribe a model, but we can draw on a program run by the Leamington Spa PCN, that involves four group sessions of 6-10 people focused on lifestyle,” he said.
The weekly group-based sessions are run by a GP, a health and wellbeing coach, a dietitian, and a psychiatrist. Together, they cover four aspects of lifestyle and health comprising individual challenges, how community influences behavior and vice versa, food and nutrition, and physical activity for health and wellbeing.
“We try to debunk some of those myths around nutrition, compared with diet, and physical activity, compared with exercise. So, for example, the idea that exercise is usually considered to be using an elliptical cross-trainer whereas physical activity, which might be just dancing in your kitchen while you’re making dinner, is something that can be done more easily,” explained Leese.
Physical activities include running and swimming in collaboration with a leisure center. “It’s an amazing program,” he remarked.
Outcomes from 142 patients who attended the Lifestyle Clinic at a North Leamington GP practice over 14 months showed that 53% gained confidence in making lifestyle changes, 60% noticed a positive impact on their physical health, and 77% reported positive impacts on their mental health.
GP Embraces Lifestyle Medicine
Rachel Burnett, a GP from Park Medical Practice in Derby, a delegate who attended the session, commented on the central idea of incorporating lifestyle medicine into primary care practice. She told this news organization that, “I think it could prevent a lot of ill health and therefore a lot of health inequalities just by embedding lifestyle medicine into our work. To hear about the Leamington Spa project and how it›s been a success was really inspiring.”
Referring to her own practice, Burnett said: “My patients are familiar with the way I go on and on about lifestyle measures, but I believe the way forward is with group sessions because we need to give the same advice to a large number of patients, for example, with prediabetes. This could save time and resource, and I think patients who are more likely to make the changes will actually attend the sessions so we’re not wasting our breath.”
Neither Leese nor Burnett declared any relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Caffeine Brings Benefits and Risks
Coffee and tea are among the plants that are highest in caffeine. Their use as beverages makes caffeine the most consumed psychoactive agent in the world. Coffee is commonly used to increase alertness and work productivity. Synthetic caffeine is added to soft drinks, energy drinks, and products intended to reduce fatigue or promote weight loss.
The caffeine content varies with the type of drink: It is high in coffee, energy drinks, and caffeine tablets; intermediate in tea; and low in soft drinks. Coffee is the predominant source of the caffeine ingested by adults. The evidence for caffeine’s effects on people is ambiguous, and some risks and benefits deserve special attention because of the impact they may have on our health.
Characteristics of Caffeine
The half-life of caffeine varies according to age. In adults, it is 2.5-4.5 hours; in newborns, 80 hours; in children older than 6 months, it remains stable over time with respect to weight. Smoking accelerates caffeine metabolism by reducing the half-life by 50%. Oral contraceptives, however, double caffeine’s half-life. Caffeine metabolism is reduced during pregnancy (it is greater in the first trimester), with a half-life of more than 15 hours. Caffeine clearance can be slowed by several classes of drugs (eg, quinolones, cardiovascular drugs, bronchodilators, and antidepressants) that increase its half-life because they are metabolized by the same liver enzymes.
Caffeine passes the blood-brain barrier and, having an adenosine-like structure, inhibits adenosine’s effects by binding to adenosine receptors. In the brain, caffeine reduces fatigue, increases alertness, reduces reaction times, may reduce the risk for depression, and increases the effectiveness of nonsteroidal anti-inflammatory drugs in treating headaches and other types of pain.
Caffeine and Chronic Diseases
The evidence available on the relationship between caffeine and health has several methodological limitations. Observations of the acute effects of caffeine may not reflect long-term effects because tolerance to caffeine’s effects may develop over time. Smoking and unhealthy lifestyles are confounding factors in epidemiological studies of caffeine intake. In addition, the estimate of the amount and frequency of caffeine intake is often inaccurate because it is mainly based on self-assessment systems. Finally, prospective studies of caffeine consumption are mainly based on coffee and tea consumption, but it is unclear how much the observed outcomes can be translated to intake of other beverages such as energy drinks.
Considering the very high prevalence of arterial hypertension worldwide (31.1% of adults), many questions have been raised about the influence of coffee consumption on blood pressure (BP) and the risk for arterial hypertension. Administration of 200-300 mg caffeine is shown to induce a mean increase of 8.1 mm Hg systolic BP and 5.7 mm Hg diastolic BP. The increase is observed in the first hour after caffeine intake and lasts no longer than 3 hours.
Yet, the moderate and usual consumption of coffee does not increase, but may even reduce, the risk of developing high BP. In contrast, occasional coffee consumption can have hypertensive effects, and moderate and usual consumption in patients with high BP does not appear to increase the risk for uncontrolled BP and can reduce the risk for death from any cause. The inverse association between coffee consumption and hypertension risk was confirmed in a review and meta-analysis of cross-sectional and cohort studies.
With respect to lipid metabolism, cholesterol levels may increase after caffeine consumption because of cafestol. Concentrations of cafestol are high in unfiltered coffee, intermediate in espresso and moka pot coffee, and negligible in instant or filtered coffee. Studies on the impact of coffee on lipid levels have led to inconsistent results, however. Data have shown that people who drink more coffee have higher triglycerides, total cholesterol, and low-density lipoprotein cholesterol (LDL-C) levels. Other data have shown that caffeine promotes LDL receptor expression and clearance of LDL cholesterol.
Experimental and cohort studies have not shown an association between coffee consumption and atrial fibrillation (AF). In fact, evidence suggests that coffee consumption tends to reduce the risk for AF in a dose-response relationship. Similarly, coffee consumption is not associated with increased risk for cardiovascular events in the general population or among patients with a history of hypertension, diabetes, or cardiovascular disease.
The Coffee and Real-Time Atrial and Ventricular Ectopy study evaluated the acute effects of coffee consumption on cardiac ectopy using wearable sensors with continuous recording. It did not demonstrate any increase in daily premature atrial contractions with coffee consumption, compared with abstaining from caffeine.
In patients with type 2 diabetes, a study performed in Japan showed that coffee consumption was associated with reduced all-cause mortality. The results suggested a dose-response relationship, and drinking coffee and green tea appeared to reduce mortality risk further. The results were not generalizable, however, because of the study population’s ethnic homogeneity.
Dose and Toxicity
Caffeine at high doses (> 400 mg daily) and in susceptible patients can induce anxiety, but the effects of caffeine on sleep and anxiety can differ from patient to patient. This variation reflects differences in caffeine metabolism rate and adenosine receptor gene variants.
High caffeine intake can stimulate diuresis, but without causing damaging effects on hydration when taking moderate doses of caffeine (≤ 400 mg daily) for long periods. Stopping caffeine suddenly, in a regular consumer, can lead to withdrawal symptoms such as headache, asthenia, decreased attention, depressed mood, and flu-like symptoms.
The toxic effects of caffeine occur with intake > 1.2 g. A dose of 10-14 g is considered fatal. Caffeine overdose is rare when considering traditional methods of intake (coffee and tea) because 70-100 cups of coffee should be sufficient for caffeine poisoning. Severe events can occur following the use of caffeine tablets or as energy drinks for the following reasons:
- The episodic consumption of caffeine does not allow for tolerance to develop.
- Young people are more vulnerable to the effects of caffeine.
- Caffeine has a synergistic effect in combination with other components in energy drinks.
- Taking caffeine in combination with alcohol or intense exertion causes serious, even fatal, outcomes.
Products Containing Caffeine
Evidence supports the relationship between high consumption (approximately 1 L) of energy drinks with a caffeine content of 320 mg and short-term cardiovascular adverse events, such as increased BP, QT-segment prolongation corrected for heart rate, and palpitations. These tests prompt the recommendation to avoid consuming these beverages in high quantities and in association with alcohol.
Weight loss products generally contain caffeine coupled with herbal extracts that are expected to improve fat metabolism, lipolysis, and oxidation. These products, because of their easy availability, presumed benefits, and high caffeine concentration, may be more susceptible to misuse because they can be taken in larger portions than recommended. The combination of multiple ingredients, concentrated amounts of caffeine, and excessive consumption increases the likelihood of adverse effects.
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Coffee and tea are among the plants that are highest in caffeine. Their use as beverages makes caffeine the most consumed psychoactive agent in the world. Coffee is commonly used to increase alertness and work productivity. Synthetic caffeine is added to soft drinks, energy drinks, and products intended to reduce fatigue or promote weight loss.
The caffeine content varies with the type of drink: It is high in coffee, energy drinks, and caffeine tablets; intermediate in tea; and low in soft drinks. Coffee is the predominant source of the caffeine ingested by adults. The evidence for caffeine’s effects on people is ambiguous, and some risks and benefits deserve special attention because of the impact they may have on our health.
Characteristics of Caffeine
The half-life of caffeine varies according to age. In adults, it is 2.5-4.5 hours; in newborns, 80 hours; in children older than 6 months, it remains stable over time with respect to weight. Smoking accelerates caffeine metabolism by reducing the half-life by 50%. Oral contraceptives, however, double caffeine’s half-life. Caffeine metabolism is reduced during pregnancy (it is greater in the first trimester), with a half-life of more than 15 hours. Caffeine clearance can be slowed by several classes of drugs (eg, quinolones, cardiovascular drugs, bronchodilators, and antidepressants) that increase its half-life because they are metabolized by the same liver enzymes.
Caffeine passes the blood-brain barrier and, having an adenosine-like structure, inhibits adenosine’s effects by binding to adenosine receptors. In the brain, caffeine reduces fatigue, increases alertness, reduces reaction times, may reduce the risk for depression, and increases the effectiveness of nonsteroidal anti-inflammatory drugs in treating headaches and other types of pain.
Caffeine and Chronic Diseases
The evidence available on the relationship between caffeine and health has several methodological limitations. Observations of the acute effects of caffeine may not reflect long-term effects because tolerance to caffeine’s effects may develop over time. Smoking and unhealthy lifestyles are confounding factors in epidemiological studies of caffeine intake. In addition, the estimate of the amount and frequency of caffeine intake is often inaccurate because it is mainly based on self-assessment systems. Finally, prospective studies of caffeine consumption are mainly based on coffee and tea consumption, but it is unclear how much the observed outcomes can be translated to intake of other beverages such as energy drinks.
Considering the very high prevalence of arterial hypertension worldwide (31.1% of adults), many questions have been raised about the influence of coffee consumption on blood pressure (BP) and the risk for arterial hypertension. Administration of 200-300 mg caffeine is shown to induce a mean increase of 8.1 mm Hg systolic BP and 5.7 mm Hg diastolic BP. The increase is observed in the first hour after caffeine intake and lasts no longer than 3 hours.
Yet, the moderate and usual consumption of coffee does not increase, but may even reduce, the risk of developing high BP. In contrast, occasional coffee consumption can have hypertensive effects, and moderate and usual consumption in patients with high BP does not appear to increase the risk for uncontrolled BP and can reduce the risk for death from any cause. The inverse association between coffee consumption and hypertension risk was confirmed in a review and meta-analysis of cross-sectional and cohort studies.
With respect to lipid metabolism, cholesterol levels may increase after caffeine consumption because of cafestol. Concentrations of cafestol are high in unfiltered coffee, intermediate in espresso and moka pot coffee, and negligible in instant or filtered coffee. Studies on the impact of coffee on lipid levels have led to inconsistent results, however. Data have shown that people who drink more coffee have higher triglycerides, total cholesterol, and low-density lipoprotein cholesterol (LDL-C) levels. Other data have shown that caffeine promotes LDL receptor expression and clearance of LDL cholesterol.
Experimental and cohort studies have not shown an association between coffee consumption and atrial fibrillation (AF). In fact, evidence suggests that coffee consumption tends to reduce the risk for AF in a dose-response relationship. Similarly, coffee consumption is not associated with increased risk for cardiovascular events in the general population or among patients with a history of hypertension, diabetes, or cardiovascular disease.
The Coffee and Real-Time Atrial and Ventricular Ectopy study evaluated the acute effects of coffee consumption on cardiac ectopy using wearable sensors with continuous recording. It did not demonstrate any increase in daily premature atrial contractions with coffee consumption, compared with abstaining from caffeine.
In patients with type 2 diabetes, a study performed in Japan showed that coffee consumption was associated with reduced all-cause mortality. The results suggested a dose-response relationship, and drinking coffee and green tea appeared to reduce mortality risk further. The results were not generalizable, however, because of the study population’s ethnic homogeneity.
Dose and Toxicity
Caffeine at high doses (> 400 mg daily) and in susceptible patients can induce anxiety, but the effects of caffeine on sleep and anxiety can differ from patient to patient. This variation reflects differences in caffeine metabolism rate and adenosine receptor gene variants.
High caffeine intake can stimulate diuresis, but without causing damaging effects on hydration when taking moderate doses of caffeine (≤ 400 mg daily) for long periods. Stopping caffeine suddenly, in a regular consumer, can lead to withdrawal symptoms such as headache, asthenia, decreased attention, depressed mood, and flu-like symptoms.
The toxic effects of caffeine occur with intake > 1.2 g. A dose of 10-14 g is considered fatal. Caffeine overdose is rare when considering traditional methods of intake (coffee and tea) because 70-100 cups of coffee should be sufficient for caffeine poisoning. Severe events can occur following the use of caffeine tablets or as energy drinks for the following reasons:
- The episodic consumption of caffeine does not allow for tolerance to develop.
- Young people are more vulnerable to the effects of caffeine.
- Caffeine has a synergistic effect in combination with other components in energy drinks.
- Taking caffeine in combination with alcohol or intense exertion causes serious, even fatal, outcomes.
Products Containing Caffeine
Evidence supports the relationship between high consumption (approximately 1 L) of energy drinks with a caffeine content of 320 mg and short-term cardiovascular adverse events, such as increased BP, QT-segment prolongation corrected for heart rate, and palpitations. These tests prompt the recommendation to avoid consuming these beverages in high quantities and in association with alcohol.
Weight loss products generally contain caffeine coupled with herbal extracts that are expected to improve fat metabolism, lipolysis, and oxidation. These products, because of their easy availability, presumed benefits, and high caffeine concentration, may be more susceptible to misuse because they can be taken in larger portions than recommended. The combination of multiple ingredients, concentrated amounts of caffeine, and excessive consumption increases the likelihood of adverse effects.
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Coffee and tea are among the plants that are highest in caffeine. Their use as beverages makes caffeine the most consumed psychoactive agent in the world. Coffee is commonly used to increase alertness and work productivity. Synthetic caffeine is added to soft drinks, energy drinks, and products intended to reduce fatigue or promote weight loss.
The caffeine content varies with the type of drink: It is high in coffee, energy drinks, and caffeine tablets; intermediate in tea; and low in soft drinks. Coffee is the predominant source of the caffeine ingested by adults. The evidence for caffeine’s effects on people is ambiguous, and some risks and benefits deserve special attention because of the impact they may have on our health.
Characteristics of Caffeine
The half-life of caffeine varies according to age. In adults, it is 2.5-4.5 hours; in newborns, 80 hours; in children older than 6 months, it remains stable over time with respect to weight. Smoking accelerates caffeine metabolism by reducing the half-life by 50%. Oral contraceptives, however, double caffeine’s half-life. Caffeine metabolism is reduced during pregnancy (it is greater in the first trimester), with a half-life of more than 15 hours. Caffeine clearance can be slowed by several classes of drugs (eg, quinolones, cardiovascular drugs, bronchodilators, and antidepressants) that increase its half-life because they are metabolized by the same liver enzymes.
Caffeine passes the blood-brain barrier and, having an adenosine-like structure, inhibits adenosine’s effects by binding to adenosine receptors. In the brain, caffeine reduces fatigue, increases alertness, reduces reaction times, may reduce the risk for depression, and increases the effectiveness of nonsteroidal anti-inflammatory drugs in treating headaches and other types of pain.
Caffeine and Chronic Diseases
The evidence available on the relationship between caffeine and health has several methodological limitations. Observations of the acute effects of caffeine may not reflect long-term effects because tolerance to caffeine’s effects may develop over time. Smoking and unhealthy lifestyles are confounding factors in epidemiological studies of caffeine intake. In addition, the estimate of the amount and frequency of caffeine intake is often inaccurate because it is mainly based on self-assessment systems. Finally, prospective studies of caffeine consumption are mainly based on coffee and tea consumption, but it is unclear how much the observed outcomes can be translated to intake of other beverages such as energy drinks.
Considering the very high prevalence of arterial hypertension worldwide (31.1% of adults), many questions have been raised about the influence of coffee consumption on blood pressure (BP) and the risk for arterial hypertension. Administration of 200-300 mg caffeine is shown to induce a mean increase of 8.1 mm Hg systolic BP and 5.7 mm Hg diastolic BP. The increase is observed in the first hour after caffeine intake and lasts no longer than 3 hours.
Yet, the moderate and usual consumption of coffee does not increase, but may even reduce, the risk of developing high BP. In contrast, occasional coffee consumption can have hypertensive effects, and moderate and usual consumption in patients with high BP does not appear to increase the risk for uncontrolled BP and can reduce the risk for death from any cause. The inverse association between coffee consumption and hypertension risk was confirmed in a review and meta-analysis of cross-sectional and cohort studies.
With respect to lipid metabolism, cholesterol levels may increase after caffeine consumption because of cafestol. Concentrations of cafestol are high in unfiltered coffee, intermediate in espresso and moka pot coffee, and negligible in instant or filtered coffee. Studies on the impact of coffee on lipid levels have led to inconsistent results, however. Data have shown that people who drink more coffee have higher triglycerides, total cholesterol, and low-density lipoprotein cholesterol (LDL-C) levels. Other data have shown that caffeine promotes LDL receptor expression and clearance of LDL cholesterol.
Experimental and cohort studies have not shown an association between coffee consumption and atrial fibrillation (AF). In fact, evidence suggests that coffee consumption tends to reduce the risk for AF in a dose-response relationship. Similarly, coffee consumption is not associated with increased risk for cardiovascular events in the general population or among patients with a history of hypertension, diabetes, or cardiovascular disease.
The Coffee and Real-Time Atrial and Ventricular Ectopy study evaluated the acute effects of coffee consumption on cardiac ectopy using wearable sensors with continuous recording. It did not demonstrate any increase in daily premature atrial contractions with coffee consumption, compared with abstaining from caffeine.
In patients with type 2 diabetes, a study performed in Japan showed that coffee consumption was associated with reduced all-cause mortality. The results suggested a dose-response relationship, and drinking coffee and green tea appeared to reduce mortality risk further. The results were not generalizable, however, because of the study population’s ethnic homogeneity.
Dose and Toxicity
Caffeine at high doses (> 400 mg daily) and in susceptible patients can induce anxiety, but the effects of caffeine on sleep and anxiety can differ from patient to patient. This variation reflects differences in caffeine metabolism rate and adenosine receptor gene variants.
High caffeine intake can stimulate diuresis, but without causing damaging effects on hydration when taking moderate doses of caffeine (≤ 400 mg daily) for long periods. Stopping caffeine suddenly, in a regular consumer, can lead to withdrawal symptoms such as headache, asthenia, decreased attention, depressed mood, and flu-like symptoms.
The toxic effects of caffeine occur with intake > 1.2 g. A dose of 10-14 g is considered fatal. Caffeine overdose is rare when considering traditional methods of intake (coffee and tea) because 70-100 cups of coffee should be sufficient for caffeine poisoning. Severe events can occur following the use of caffeine tablets or as energy drinks for the following reasons:
- The episodic consumption of caffeine does not allow for tolerance to develop.
- Young people are more vulnerable to the effects of caffeine.
- Caffeine has a synergistic effect in combination with other components in energy drinks.
- Taking caffeine in combination with alcohol or intense exertion causes serious, even fatal, outcomes.
Products Containing Caffeine
Evidence supports the relationship between high consumption (approximately 1 L) of energy drinks with a caffeine content of 320 mg and short-term cardiovascular adverse events, such as increased BP, QT-segment prolongation corrected for heart rate, and palpitations. These tests prompt the recommendation to avoid consuming these beverages in high quantities and in association with alcohol.
Weight loss products generally contain caffeine coupled with herbal extracts that are expected to improve fat metabolism, lipolysis, and oxidation. These products, because of their easy availability, presumed benefits, and high caffeine concentration, may be more susceptible to misuse because they can be taken in larger portions than recommended. The combination of multiple ingredients, concentrated amounts of caffeine, and excessive consumption increases the likelihood of adverse effects.
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.