User login
For MD-IQ use only
Six healthy lifestyle habits linked to slowed memory decline
Investigators found that a healthy diet, cognitive activity, regular physical exercise, not smoking, and abstaining from alcohol were significantly linked to slowed cognitive decline irrespective of APOE4 status.
After adjusting for health and socioeconomic factors, investigators found that each individual healthy behavior was associated with a slower-than-average decline in memory over a decade. A healthy diet emerged as the strongest deterrent, followed by cognitive activity and physical exercise.
“A healthy lifestyle is associated with slower memory decline, even in the presence of the APOE4 allele,” study investigators led by Jianping Jia, MD, PhD, of the Innovation Center for Neurological Disorders and the department of neurology, Xuan Wu Hospital, Capital Medical University, Beijing, write.
“This study might offer important information to protect older adults against memory decline,” they add.
The study was published online in the BMJ.
Preventing memory decline
Memory “continuously declines as people age,” but age-related memory decline is not necessarily a prodrome of dementia and can “merely be senescent forgetfulness,” the investigators note. This can be “reversed or [can] become stable,” instead of progressing to a pathologic state.
Factors affecting memory include aging, APOE4 genotype, chronic diseases, and lifestyle patterns, with lifestyle “receiving increasing attention as a modifiable behavior.”
Nevertheless, few studies have focused on the impact of lifestyle on memory, and those that have are mostly cross-sectional and also “did not consider the interaction between a healthy lifestyle and genetic risk,” the researchers note.
To investigate, the researchers conducted a longitudinal study, known as the China Cognition and Aging Study, that considered genetic risk as well as lifestyle factors.
The study began in 2009 and concluded in 2019. Participants were evaluated and underwent neuropsychological testing in 2012, 2014, 2016, and at the study’s conclusion.
Participants (n = 29,072; mean [SD] age, 72.23 [6.61] years; 48.54% women; 20.43% APOE4 carriers) were required to have normal cognitive function at baseline. Data on those whose condition progressed to mild cognitive impairment (MCI) or dementia during the follow-up period were excluded after their diagnosis.
The Mini–Mental State Examination was used to assess global cognitive function. Memory function was assessed using the World Health Organization/University of California, Los Angeles Auditory Verbal Learning Test.
“Lifestyle” consisted of six modifiable factors: physical exercise (weekly frequency and total time), smoking (current, former, or never-smokers), alcohol consumption (never drank, drank occasionally, low to excess drinking, and heavy drinking), diet (daily intake of 12 food items: fruits, vegetables, fish, meat, dairy products, salt, oil, eggs, cereals, legumes, nuts, tea), cognitive activity (writing, reading, playing cards, mahjong, other games), and social contact (participating in meetings, attending parties, visiting friends/relatives, traveling, chatting online).
Participants’ lifestyles were scored on the basis of the number of healthy factors they engaged in.
Participants were also stratified by APOE genotype into APOE4 carriers and noncarriers.
Demographic and other items of health information, including the presence of medical illness, were used as covariates. The researchers also included the “learning effect of each participant as a covariate, due to repeated cognitive assessments.”
Important for public health
During the 10-year period, 7,164 participants died, and 3,567 stopped participating.
Participants in the favorable and average groups showed slower memory decline per increased year of age (0.007 [0.005-0.009], P < .001; and 0.002 [0 .000-0.003], P = .033 points higher, respectively), compared with those in the unfavorable group.
Healthy diet had the strongest protective effect on memory.
Memory decline occurred faster in APOE4 vesus non-APOE4 carriers (0.002 points/year [95% confidence interval, 0.001-0.003]; P = .007).
But APOE4 carriers with favorable and average lifestyles showed slower memory decline (0.027 [0.023-0.031] and 0.014 [0.010-0.019], respectively), compared with those with unfavorable lifestyles. Similar findings were obtained in non-APOE4 carriers.
Those with favorable or average lifestyle were respectively almost 90% and 30% less likely to develop dementia or MCI, compared with those with an unfavorable lifestyle.
The authors acknowledge the study’s limitations, including its observational design and the potential for measurement errors, owing to self-reporting of lifestyle factors. Additionally, some participants did not return for follow-up evaluations, leading to potential selection bias.
Nevertheless, the findings “might offer important information for public health to protect older [people] against memory decline,” they note – especially since the study “provides evidence that these effects also include individuals with the APOE4 allele.”
‘Important, encouraging’ research
In a comment, Severine Sabia, PhD, a senior researcher at the Université Paris Cité, INSERM Institut National de la Santé et de la Recherche Medicalé, France, called the findings “important and encouraging.”
However, said Dr. Sabia, who was not involved with the study, “there remain important research questions that need to be investigated in order to identify key behaviors: which combination, the cutoff of risk, and when to intervene.”
Future research on prevention “should examine a wider range of possible risk factors” and should also “identify specific exposures associated with the greatest risk, while also considering the risk threshold and age at exposure for each one.”
In an accompanying editorial, Dr. Sabia and co-author Archana Singh-Manoux, PhD, note that the risk of cognitive decline and dementia are probably determined by multiple factors.
They liken it to the “multifactorial risk paradigm introduced by the Framingham study,” which has “led to a substantial reduction in cardiovascular disease.” A similar approach could be used with dementia prevention, they suggest.
The authors received support from the Xuanwu Hospital of Capital Medical University for the submitted work. One of the authors received a grant from the French National Research Agency. The other authors have disclosed no relevant financial relationships. Dr. Sabia received grant funding from the French National Research Agency. Dr. Singh-Manoux received grants from the National Institute on Aging of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Investigators found that a healthy diet, cognitive activity, regular physical exercise, not smoking, and abstaining from alcohol were significantly linked to slowed cognitive decline irrespective of APOE4 status.
After adjusting for health and socioeconomic factors, investigators found that each individual healthy behavior was associated with a slower-than-average decline in memory over a decade. A healthy diet emerged as the strongest deterrent, followed by cognitive activity and physical exercise.
“A healthy lifestyle is associated with slower memory decline, even in the presence of the APOE4 allele,” study investigators led by Jianping Jia, MD, PhD, of the Innovation Center for Neurological Disorders and the department of neurology, Xuan Wu Hospital, Capital Medical University, Beijing, write.
“This study might offer important information to protect older adults against memory decline,” they add.
The study was published online in the BMJ.
Preventing memory decline
Memory “continuously declines as people age,” but age-related memory decline is not necessarily a prodrome of dementia and can “merely be senescent forgetfulness,” the investigators note. This can be “reversed or [can] become stable,” instead of progressing to a pathologic state.
Factors affecting memory include aging, APOE4 genotype, chronic diseases, and lifestyle patterns, with lifestyle “receiving increasing attention as a modifiable behavior.”
Nevertheless, few studies have focused on the impact of lifestyle on memory, and those that have are mostly cross-sectional and also “did not consider the interaction between a healthy lifestyle and genetic risk,” the researchers note.
To investigate, the researchers conducted a longitudinal study, known as the China Cognition and Aging Study, that considered genetic risk as well as lifestyle factors.
The study began in 2009 and concluded in 2019. Participants were evaluated and underwent neuropsychological testing in 2012, 2014, 2016, and at the study’s conclusion.
Participants (n = 29,072; mean [SD] age, 72.23 [6.61] years; 48.54% women; 20.43% APOE4 carriers) were required to have normal cognitive function at baseline. Data on those whose condition progressed to mild cognitive impairment (MCI) or dementia during the follow-up period were excluded after their diagnosis.
The Mini–Mental State Examination was used to assess global cognitive function. Memory function was assessed using the World Health Organization/University of California, Los Angeles Auditory Verbal Learning Test.
“Lifestyle” consisted of six modifiable factors: physical exercise (weekly frequency and total time), smoking (current, former, or never-smokers), alcohol consumption (never drank, drank occasionally, low to excess drinking, and heavy drinking), diet (daily intake of 12 food items: fruits, vegetables, fish, meat, dairy products, salt, oil, eggs, cereals, legumes, nuts, tea), cognitive activity (writing, reading, playing cards, mahjong, other games), and social contact (participating in meetings, attending parties, visiting friends/relatives, traveling, chatting online).
Participants’ lifestyles were scored on the basis of the number of healthy factors they engaged in.
Participants were also stratified by APOE genotype into APOE4 carriers and noncarriers.
Demographic and other items of health information, including the presence of medical illness, were used as covariates. The researchers also included the “learning effect of each participant as a covariate, due to repeated cognitive assessments.”
Important for public health
During the 10-year period, 7,164 participants died, and 3,567 stopped participating.
Participants in the favorable and average groups showed slower memory decline per increased year of age (0.007 [0.005-0.009], P < .001; and 0.002 [0 .000-0.003], P = .033 points higher, respectively), compared with those in the unfavorable group.
Healthy diet had the strongest protective effect on memory.
Memory decline occurred faster in APOE4 vesus non-APOE4 carriers (0.002 points/year [95% confidence interval, 0.001-0.003]; P = .007).
But APOE4 carriers with favorable and average lifestyles showed slower memory decline (0.027 [0.023-0.031] and 0.014 [0.010-0.019], respectively), compared with those with unfavorable lifestyles. Similar findings were obtained in non-APOE4 carriers.
Those with favorable or average lifestyle were respectively almost 90% and 30% less likely to develop dementia or MCI, compared with those with an unfavorable lifestyle.
The authors acknowledge the study’s limitations, including its observational design and the potential for measurement errors, owing to self-reporting of lifestyle factors. Additionally, some participants did not return for follow-up evaluations, leading to potential selection bias.
Nevertheless, the findings “might offer important information for public health to protect older [people] against memory decline,” they note – especially since the study “provides evidence that these effects also include individuals with the APOE4 allele.”
‘Important, encouraging’ research
In a comment, Severine Sabia, PhD, a senior researcher at the Université Paris Cité, INSERM Institut National de la Santé et de la Recherche Medicalé, France, called the findings “important and encouraging.”
However, said Dr. Sabia, who was not involved with the study, “there remain important research questions that need to be investigated in order to identify key behaviors: which combination, the cutoff of risk, and when to intervene.”
Future research on prevention “should examine a wider range of possible risk factors” and should also “identify specific exposures associated with the greatest risk, while also considering the risk threshold and age at exposure for each one.”
In an accompanying editorial, Dr. Sabia and co-author Archana Singh-Manoux, PhD, note that the risk of cognitive decline and dementia are probably determined by multiple factors.
They liken it to the “multifactorial risk paradigm introduced by the Framingham study,” which has “led to a substantial reduction in cardiovascular disease.” A similar approach could be used with dementia prevention, they suggest.
The authors received support from the Xuanwu Hospital of Capital Medical University for the submitted work. One of the authors received a grant from the French National Research Agency. The other authors have disclosed no relevant financial relationships. Dr. Sabia received grant funding from the French National Research Agency. Dr. Singh-Manoux received grants from the National Institute on Aging of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Investigators found that a healthy diet, cognitive activity, regular physical exercise, not smoking, and abstaining from alcohol were significantly linked to slowed cognitive decline irrespective of APOE4 status.
After adjusting for health and socioeconomic factors, investigators found that each individual healthy behavior was associated with a slower-than-average decline in memory over a decade. A healthy diet emerged as the strongest deterrent, followed by cognitive activity and physical exercise.
“A healthy lifestyle is associated with slower memory decline, even in the presence of the APOE4 allele,” study investigators led by Jianping Jia, MD, PhD, of the Innovation Center for Neurological Disorders and the department of neurology, Xuan Wu Hospital, Capital Medical University, Beijing, write.
“This study might offer important information to protect older adults against memory decline,” they add.
The study was published online in the BMJ.
Preventing memory decline
Memory “continuously declines as people age,” but age-related memory decline is not necessarily a prodrome of dementia and can “merely be senescent forgetfulness,” the investigators note. This can be “reversed or [can] become stable,” instead of progressing to a pathologic state.
Factors affecting memory include aging, APOE4 genotype, chronic diseases, and lifestyle patterns, with lifestyle “receiving increasing attention as a modifiable behavior.”
Nevertheless, few studies have focused on the impact of lifestyle on memory, and those that have are mostly cross-sectional and also “did not consider the interaction between a healthy lifestyle and genetic risk,” the researchers note.
To investigate, the researchers conducted a longitudinal study, known as the China Cognition and Aging Study, that considered genetic risk as well as lifestyle factors.
The study began in 2009 and concluded in 2019. Participants were evaluated and underwent neuropsychological testing in 2012, 2014, 2016, and at the study’s conclusion.
Participants (n = 29,072; mean [SD] age, 72.23 [6.61] years; 48.54% women; 20.43% APOE4 carriers) were required to have normal cognitive function at baseline. Data on those whose condition progressed to mild cognitive impairment (MCI) or dementia during the follow-up period were excluded after their diagnosis.
The Mini–Mental State Examination was used to assess global cognitive function. Memory function was assessed using the World Health Organization/University of California, Los Angeles Auditory Verbal Learning Test.
“Lifestyle” consisted of six modifiable factors: physical exercise (weekly frequency and total time), smoking (current, former, or never-smokers), alcohol consumption (never drank, drank occasionally, low to excess drinking, and heavy drinking), diet (daily intake of 12 food items: fruits, vegetables, fish, meat, dairy products, salt, oil, eggs, cereals, legumes, nuts, tea), cognitive activity (writing, reading, playing cards, mahjong, other games), and social contact (participating in meetings, attending parties, visiting friends/relatives, traveling, chatting online).
Participants’ lifestyles were scored on the basis of the number of healthy factors they engaged in.
Participants were also stratified by APOE genotype into APOE4 carriers and noncarriers.
Demographic and other items of health information, including the presence of medical illness, were used as covariates. The researchers also included the “learning effect of each participant as a covariate, due to repeated cognitive assessments.”
Important for public health
During the 10-year period, 7,164 participants died, and 3,567 stopped participating.
Participants in the favorable and average groups showed slower memory decline per increased year of age (0.007 [0.005-0.009], P < .001; and 0.002 [0 .000-0.003], P = .033 points higher, respectively), compared with those in the unfavorable group.
Healthy diet had the strongest protective effect on memory.
Memory decline occurred faster in APOE4 vesus non-APOE4 carriers (0.002 points/year [95% confidence interval, 0.001-0.003]; P = .007).
But APOE4 carriers with favorable and average lifestyles showed slower memory decline (0.027 [0.023-0.031] and 0.014 [0.010-0.019], respectively), compared with those with unfavorable lifestyles. Similar findings were obtained in non-APOE4 carriers.
Those with favorable or average lifestyle were respectively almost 90% and 30% less likely to develop dementia or MCI, compared with those with an unfavorable lifestyle.
The authors acknowledge the study’s limitations, including its observational design and the potential for measurement errors, owing to self-reporting of lifestyle factors. Additionally, some participants did not return for follow-up evaluations, leading to potential selection bias.
Nevertheless, the findings “might offer important information for public health to protect older [people] against memory decline,” they note – especially since the study “provides evidence that these effects also include individuals with the APOE4 allele.”
‘Important, encouraging’ research
In a comment, Severine Sabia, PhD, a senior researcher at the Université Paris Cité, INSERM Institut National de la Santé et de la Recherche Medicalé, France, called the findings “important and encouraging.”
However, said Dr. Sabia, who was not involved with the study, “there remain important research questions that need to be investigated in order to identify key behaviors: which combination, the cutoff of risk, and when to intervene.”
Future research on prevention “should examine a wider range of possible risk factors” and should also “identify specific exposures associated with the greatest risk, while also considering the risk threshold and age at exposure for each one.”
In an accompanying editorial, Dr. Sabia and co-author Archana Singh-Manoux, PhD, note that the risk of cognitive decline and dementia are probably determined by multiple factors.
They liken it to the “multifactorial risk paradigm introduced by the Framingham study,” which has “led to a substantial reduction in cardiovascular disease.” A similar approach could be used with dementia prevention, they suggest.
The authors received support from the Xuanwu Hospital of Capital Medical University for the submitted work. One of the authors received a grant from the French National Research Agency. The other authors have disclosed no relevant financial relationships. Dr. Sabia received grant funding from the French National Research Agency. Dr. Singh-Manoux received grants from the National Institute on Aging of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
FROM THE BMJ
What's your diagnosis?
Answer: Blue rubber bleb nevus syndrome.
According to an American College of Gastroenterology Clinical Guideline,1 for patients with recurrence of small bowel bleeding, endoscopic management could be considered depending on the patient’s clinical course and response to prior therapy. Consequently, injections of lauromacrogol with SBE (single-balloon enteroscopy) were given (Figure D). Lesions that ranged from 1 to 2 cm were injected with 1-2 mL lauromacrogol until the mucosa turned white. Three SBEs had been performed in a 5-month period. A total of 20 lesions were successfully treated with lauromacrogol. The treated hemangiomas became small, and the site healed 5 months after treatment (Figures E and F). The patient has been followed for 1 year, and he remains in good clinical condition with his latest hemoglobin level at 110 g/L. No further blood transfusion is needed.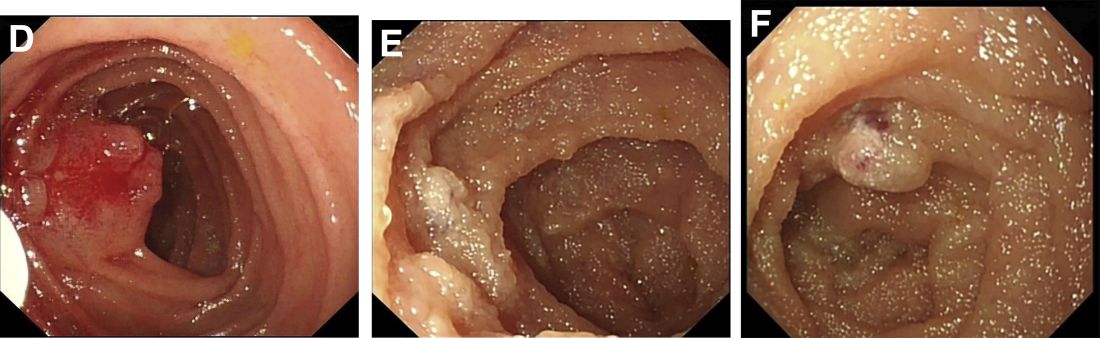
BRBNS is a rare disorder characterized by discrete venous malformations of varying size and appearance that are present on the skin and within the gastrointestinal tract.2With wider application of video capsule endoscopy (VCE) and the increase of image resolution, the detection rate and diagnostic accuracy of BRBNS are significantly improved. Treatment of BRBNS varies depending on the site, size, and number of lesions. Medication, surgery, and endoscopic therapy are currently clinically applied. The successful use of sirolimus was recently reported in the treatment of vascular lesions.3Sirolimus has potential adverse effects on renal function, bone marrow, and cholesterol metabolism, however. In consideration of the patient’s young age, we did not adopt this method. Surgical resection is more suitable for limited or life-threatening lesions. The lesions in this patient were mild and sporadic. Consequently, in this case, endoscopic injection of lauromacrogol was performed. This was the most complicated case of endoscopic treatment of BRBNS in our center and proved lauromacrogol injection was a feasible approach. According to a literature review, lauromacrogol has been used to treat vascular lesions for decades, but there is still no standard instruction for the dosage of lauromacrogol. We hope that our experience can be a reference for the endoscopic treatment of BRBNS.
References (add links)
1. Gerson LB et al. ACG clinical guideline: Diagnosis and management of small bowel bleeding. Am J Gastroenterol.
2. Felton SJ and Ferguson JE. Multiple cutaneous swellings associated with sudden collapse. JAMA.
3. Yuksekkaya H et al. Blue rubber bleb nevus syndrome: Successful treatment with sirolimus. Pediatrics.
Answer: Blue rubber bleb nevus syndrome.
According to an American College of Gastroenterology Clinical Guideline,1 for patients with recurrence of small bowel bleeding, endoscopic management could be considered depending on the patient’s clinical course and response to prior therapy. Consequently, injections of lauromacrogol with SBE (single-balloon enteroscopy) were given (Figure D). Lesions that ranged from 1 to 2 cm were injected with 1-2 mL lauromacrogol until the mucosa turned white. Three SBEs had been performed in a 5-month period. A total of 20 lesions were successfully treated with lauromacrogol. The treated hemangiomas became small, and the site healed 5 months after treatment (Figures E and F). The patient has been followed for 1 year, and he remains in good clinical condition with his latest hemoglobin level at 110 g/L. No further blood transfusion is needed.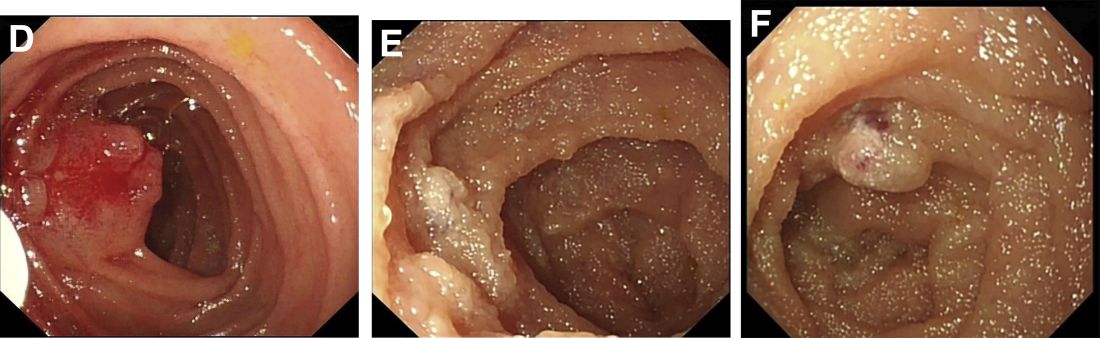
BRBNS is a rare disorder characterized by discrete venous malformations of varying size and appearance that are present on the skin and within the gastrointestinal tract.2With wider application of video capsule endoscopy (VCE) and the increase of image resolution, the detection rate and diagnostic accuracy of BRBNS are significantly improved. Treatment of BRBNS varies depending on the site, size, and number of lesions. Medication, surgery, and endoscopic therapy are currently clinically applied. The successful use of sirolimus was recently reported in the treatment of vascular lesions.3Sirolimus has potential adverse effects on renal function, bone marrow, and cholesterol metabolism, however. In consideration of the patient’s young age, we did not adopt this method. Surgical resection is more suitable for limited or life-threatening lesions. The lesions in this patient were mild and sporadic. Consequently, in this case, endoscopic injection of lauromacrogol was performed. This was the most complicated case of endoscopic treatment of BRBNS in our center and proved lauromacrogol injection was a feasible approach. According to a literature review, lauromacrogol has been used to treat vascular lesions for decades, but there is still no standard instruction for the dosage of lauromacrogol. We hope that our experience can be a reference for the endoscopic treatment of BRBNS.
References (add links)
1. Gerson LB et al. ACG clinical guideline: Diagnosis and management of small bowel bleeding. Am J Gastroenterol.
2. Felton SJ and Ferguson JE. Multiple cutaneous swellings associated with sudden collapse. JAMA.
3. Yuksekkaya H et al. Blue rubber bleb nevus syndrome: Successful treatment with sirolimus. Pediatrics.
Answer: Blue rubber bleb nevus syndrome.
According to an American College of Gastroenterology Clinical Guideline,1 for patients with recurrence of small bowel bleeding, endoscopic management could be considered depending on the patient’s clinical course and response to prior therapy. Consequently, injections of lauromacrogol with SBE (single-balloon enteroscopy) were given (Figure D). Lesions that ranged from 1 to 2 cm were injected with 1-2 mL lauromacrogol until the mucosa turned white. Three SBEs had been performed in a 5-month period. A total of 20 lesions were successfully treated with lauromacrogol. The treated hemangiomas became small, and the site healed 5 months after treatment (Figures E and F). The patient has been followed for 1 year, and he remains in good clinical condition with his latest hemoglobin level at 110 g/L. No further blood transfusion is needed.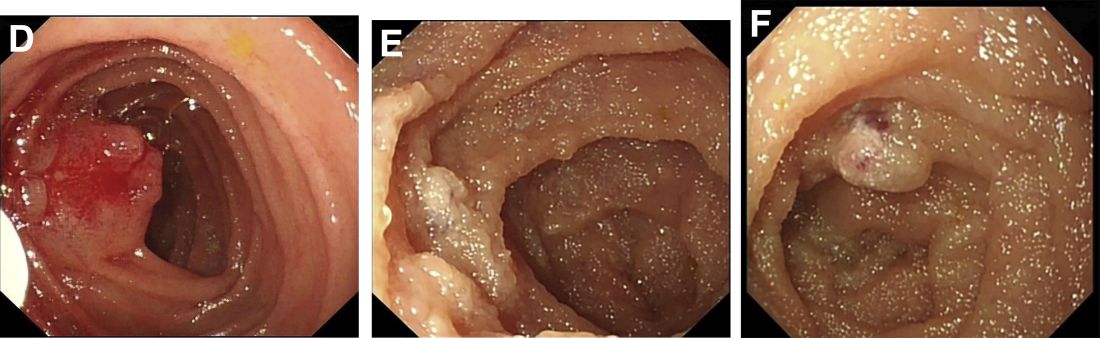
BRBNS is a rare disorder characterized by discrete venous malformations of varying size and appearance that are present on the skin and within the gastrointestinal tract.2With wider application of video capsule endoscopy (VCE) and the increase of image resolution, the detection rate and diagnostic accuracy of BRBNS are significantly improved. Treatment of BRBNS varies depending on the site, size, and number of lesions. Medication, surgery, and endoscopic therapy are currently clinically applied. The successful use of sirolimus was recently reported in the treatment of vascular lesions.3Sirolimus has potential adverse effects on renal function, bone marrow, and cholesterol metabolism, however. In consideration of the patient’s young age, we did not adopt this method. Surgical resection is more suitable for limited or life-threatening lesions. The lesions in this patient were mild and sporadic. Consequently, in this case, endoscopic injection of lauromacrogol was performed. This was the most complicated case of endoscopic treatment of BRBNS in our center and proved lauromacrogol injection was a feasible approach. According to a literature review, lauromacrogol has been used to treat vascular lesions for decades, but there is still no standard instruction for the dosage of lauromacrogol. We hope that our experience can be a reference for the endoscopic treatment of BRBNS.
References (add links)
1. Gerson LB et al. ACG clinical guideline: Diagnosis and management of small bowel bleeding. Am J Gastroenterol.
2. Felton SJ and Ferguson JE. Multiple cutaneous swellings associated with sudden collapse. JAMA.
3. Yuksekkaya H et al. Blue rubber bleb nevus syndrome: Successful treatment with sirolimus. Pediatrics.
A 13-year-old boy presented with recurrent melena for 10 years accompanied with dizziness and fatigue. This patient had no history of nonsteroidal anti-inflammatory drug use, peptic ulcer, or chronic liver disease, and no family history of gastrointestinal bleeding. He was born with a right foot hemangioma that was resected when he was 2 years old. Additionally, he had received multiple blood transfusions for iron deficiency anemia since childhood. The body mass index was 16.5 kg/m2 and physical examination revealed active bowel sounds.
Laboratory examinations showed severe iron deficiency anemia (the lowest hemoglobin available was 36 g/L) and positive stool occult blood. Gastroscopy unveiled superficial gastritis and colonoscopy was normal. Second-look examinations showed the same results. No clinically important signs were observed on computed tomography scan. Given these results, small intestinal bleeding was considered. Therefore, a video capsule endoscopy (VCE) was carried out and revealed multifocal hemangioma-like purplish blue lesions in jejunum and ileum (Figure A). Then a single-balloon enteroscopy (SBE) was performed, which showed multifocal vascular lesions ranging between 1.0 and 2.0 cm in the jejunum and ileum (Figure B, C).
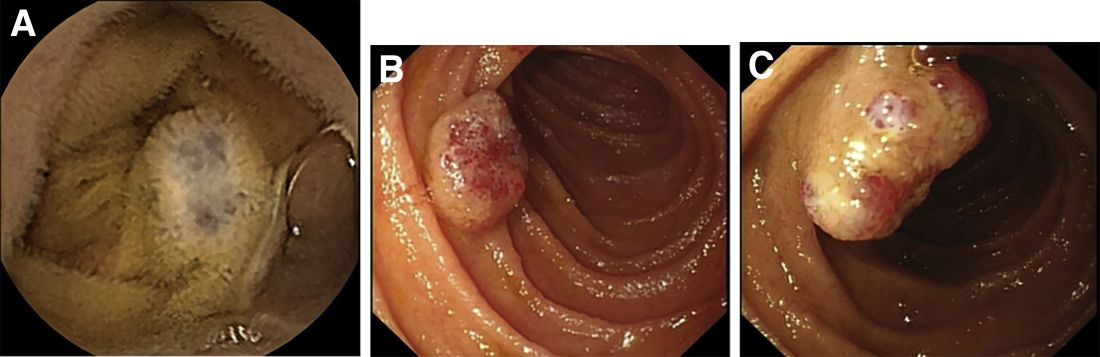
Based on these findings, what is your diagnosis? What is the next step in management for this patient?
Flu, other common viruses linked to neurologic disease
People hospitalized with viral infections like the flu are more likely to have disorders that degrade the nervous system, like Alzheimer’s or Parkinson’s, later in life, a new analysis shows.
The viruses included influenza, encephalitis, herpes, hepatitis, pneumonia, meningitis, and shingles. Those viruses were linked to one or more of these conditions: Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis (ALS), dementia, and multiple sclerosis.
The authors of the study, which was published this month in the journal Neuron, cautioned that their findings stopped short of saying the viruses caused the disorders.
“Neurodegenerative disorders are a collection of diseases for which there are very few effective treatments and many risk factors,” study author and National Institutes of Health researcher Andrew B. Singleton, PhD, said in a news release from the NIH. “Our results support the idea that viral infections and related inflammation in the nervous system may be common – and possibly avoidable – risk factors for these types of disorders.”
For the study, two data sets were analyzed with a combined 800,000 medical records for people in Finland and the United Kingdom. People who were hospitalized with COVID-19 were excluded from the study.
Generalized dementia was the condition linked to the most viruses. People exposed to viral encephalitis, which causes brain inflammation, were 20 times more likely to be diagnosed with Alzheimer’s, compared with those who were not diagnosed with that virus.
Both influenza and pneumonia were also associated with all of the neurodegenerative disorder diagnoses studied, with the exception of multiple sclerosis. The researchers found that severe flu cases were linked to the most risks.
“Keep in mind that the individuals we studied did not have the common cold. Their infections made them so sick that they had to go to the hospital,” said study author and NIH researcher Michael Nalls, PhD. “Nevertheless, the fact that commonly used vaccines reduce the risk or severity of many of the viral illnesses observed in this study raises the possibility that the risks of neurodegenerative disorders might also be mitigated.”
The researchers examined the time from when someone was infected with a virus to the time when they were diagnosed with one of the neurodegenerative disorders. They found that most had a high risk within 1 year of infection. But in six scenarios, there were significant links that showed up after 5-15 years.
The authors wrote that vaccines that are available for some of the viruses studied may be a way to reduce the risk of getting diseases that degrade the nervous system.
A version of this article first appeared on WebMD.com.
People hospitalized with viral infections like the flu are more likely to have disorders that degrade the nervous system, like Alzheimer’s or Parkinson’s, later in life, a new analysis shows.
The viruses included influenza, encephalitis, herpes, hepatitis, pneumonia, meningitis, and shingles. Those viruses were linked to one or more of these conditions: Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis (ALS), dementia, and multiple sclerosis.
The authors of the study, which was published this month in the journal Neuron, cautioned that their findings stopped short of saying the viruses caused the disorders.
“Neurodegenerative disorders are a collection of diseases for which there are very few effective treatments and many risk factors,” study author and National Institutes of Health researcher Andrew B. Singleton, PhD, said in a news release from the NIH. “Our results support the idea that viral infections and related inflammation in the nervous system may be common – and possibly avoidable – risk factors for these types of disorders.”
For the study, two data sets were analyzed with a combined 800,000 medical records for people in Finland and the United Kingdom. People who were hospitalized with COVID-19 were excluded from the study.
Generalized dementia was the condition linked to the most viruses. People exposed to viral encephalitis, which causes brain inflammation, were 20 times more likely to be diagnosed with Alzheimer’s, compared with those who were not diagnosed with that virus.
Both influenza and pneumonia were also associated with all of the neurodegenerative disorder diagnoses studied, with the exception of multiple sclerosis. The researchers found that severe flu cases were linked to the most risks.
“Keep in mind that the individuals we studied did not have the common cold. Their infections made them so sick that they had to go to the hospital,” said study author and NIH researcher Michael Nalls, PhD. “Nevertheless, the fact that commonly used vaccines reduce the risk or severity of many of the viral illnesses observed in this study raises the possibility that the risks of neurodegenerative disorders might also be mitigated.”
The researchers examined the time from when someone was infected with a virus to the time when they were diagnosed with one of the neurodegenerative disorders. They found that most had a high risk within 1 year of infection. But in six scenarios, there were significant links that showed up after 5-15 years.
The authors wrote that vaccines that are available for some of the viruses studied may be a way to reduce the risk of getting diseases that degrade the nervous system.
A version of this article first appeared on WebMD.com.
People hospitalized with viral infections like the flu are more likely to have disorders that degrade the nervous system, like Alzheimer’s or Parkinson’s, later in life, a new analysis shows.
The viruses included influenza, encephalitis, herpes, hepatitis, pneumonia, meningitis, and shingles. Those viruses were linked to one or more of these conditions: Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis (ALS), dementia, and multiple sclerosis.
The authors of the study, which was published this month in the journal Neuron, cautioned that their findings stopped short of saying the viruses caused the disorders.
“Neurodegenerative disorders are a collection of diseases for which there are very few effective treatments and many risk factors,” study author and National Institutes of Health researcher Andrew B. Singleton, PhD, said in a news release from the NIH. “Our results support the idea that viral infections and related inflammation in the nervous system may be common – and possibly avoidable – risk factors for these types of disorders.”
For the study, two data sets were analyzed with a combined 800,000 medical records for people in Finland and the United Kingdom. People who were hospitalized with COVID-19 were excluded from the study.
Generalized dementia was the condition linked to the most viruses. People exposed to viral encephalitis, which causes brain inflammation, were 20 times more likely to be diagnosed with Alzheimer’s, compared with those who were not diagnosed with that virus.
Both influenza and pneumonia were also associated with all of the neurodegenerative disorder diagnoses studied, with the exception of multiple sclerosis. The researchers found that severe flu cases were linked to the most risks.
“Keep in mind that the individuals we studied did not have the common cold. Their infections made them so sick that they had to go to the hospital,” said study author and NIH researcher Michael Nalls, PhD. “Nevertheless, the fact that commonly used vaccines reduce the risk or severity of many of the viral illnesses observed in this study raises the possibility that the risks of neurodegenerative disorders might also be mitigated.”
The researchers examined the time from when someone was infected with a virus to the time when they were diagnosed with one of the neurodegenerative disorders. They found that most had a high risk within 1 year of infection. But in six scenarios, there were significant links that showed up after 5-15 years.
The authors wrote that vaccines that are available for some of the viruses studied may be a way to reduce the risk of getting diseases that degrade the nervous system.
A version of this article first appeared on WebMD.com.
FROM NEURON
If we care about cancer patients, we must care about climate change
Because we care about our patients, we need to get involved in the climate change movement. If we want to help prevent cancer and deliver the best possible care to our patients, we need to stop burning fossil fuels. As addressed in an earlier version of this column, burning fossil fuels results in the release of particulate matter and particles measuring 2.5 micrometers in diameter (PM2.5), are classified as group 1 carcinogens by the International Association of Research and Cancer.
Fossil fuels also release greenhouse gases (carbon dioxide, methane, nitrous oxide, and fluorinated gases) which trap solar radiation that would otherwise have been reflected back into space after hitting the earth’s surface. Instead, it is redirected back to earth as infrared radiation warming the planet by 1.1° C since preindustrial times.
Climate change has a number of consequences, including more extreme weather events, rising sea levels, warming seas, environmental degradation, and affects water and food quality, supply, and production. A global increase of 1.5° C above the preindustrial average risks catastrophic harm to health that will be impossible to reverse, prompting the editors of over 260 health journals to call for emergency action to limit global temperature increases, restore biodiversity, and protect health.
In October, the 2022 version of the Lancet Countdown on health and climate change was issued and the findings are not good. “After 30 years of UNFCCC negotiations, the Lancet Countdown indicators show that countries and companies continue to make choices that threaten the health and survival of people in every part of the world. As countries devise ways to recover from the coexisting crises, the evidence is unequivocal. At this critical juncture, an immediate, health-centered response can still secure a future in which world populations can not only survive, but thrive,” the authors wrote. Governments and companies continue to prioritize fossil fuels over people’s health.
Among the key findings from the report, Marina Romanello, PhD, of the Institute for Global Health at University College London, and her colleagues, call for “A health-centered response to the coexisting climate, energy, and cost-of-living crises provides an opportunity to deliver a healthy, low-carbon future. The associated reduction in the burden of disease will in turn reduce the strain on overwhelmed health care providers, and enable better care.”
The authors also state that “Well-prepared health systems are essential to protect populations from the health impacts of climate change. However, global health systems have been drastically weakened by the effects of the COVID-19 pandemic, and the funds available for climate action decreased in 239 (30%) of 798 cities, with health systems increasingly being affected by extreme weather events and supply chain disruptions.”
And, the authors are concerned that health systems have left themselves vulnerable to climate change–related health hazards because they have not adapted their operations for climate-related changes. “Only 48 of 95 countries have assessed their climate change adaptation needs and only 63% of countries reported high to very high implementation status for health emergency management in 2021. Increasing adaptation to climate change has the potential to simultaneously improve the capacity of health systems to manage both future infectious disease outbreaks and other health emergencies.”
There is roughly a 50% chance that the 1.5° C threshold proposed in the Paris Agreement will be exceeded within 5 years. The carbon intensity of the global energy system has been reduced by less than 1% from 1992 levels, when the United Nations Framework Convention on Climate Change was adopted. At our current pace, global emissions could be 13.7% above 2010 levels by 2030 and fully decarbonizing the energy system would take 150 years. Clearly, we are nowhere near meeting the goals of the Paris Agreement signed in 2015 by 192 countries and the European Union. Participants pledged to decrease their carbon footprint by 50% by 2030, and net zero by the end of the century.
The effect of increasing greenhouse gases in our atmosphere will have a massive impact on the prevention and care of cancer patients. Air pollution is responsible for about 14% of lung cancer deaths throughout the world. Rising temperatures lead to extreme weather events which disrupts infrastructure and the ability to access health care, leading to delays in treatment, increased morbidity, and death. Screening rates for cancer go down, which leads to more patients presenting with advanced cancer in the future.
As oncologists who care deeply about their patients, we need to get actively involved. It is our responsibility to our current and future patients to do whatever we can to prevent cancer and reduce its complications.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Because we care about our patients, we need to get involved in the climate change movement. If we want to help prevent cancer and deliver the best possible care to our patients, we need to stop burning fossil fuels. As addressed in an earlier version of this column, burning fossil fuels results in the release of particulate matter and particles measuring 2.5 micrometers in diameter (PM2.5), are classified as group 1 carcinogens by the International Association of Research and Cancer.
Fossil fuels also release greenhouse gases (carbon dioxide, methane, nitrous oxide, and fluorinated gases) which trap solar radiation that would otherwise have been reflected back into space after hitting the earth’s surface. Instead, it is redirected back to earth as infrared radiation warming the planet by 1.1° C since preindustrial times.
Climate change has a number of consequences, including more extreme weather events, rising sea levels, warming seas, environmental degradation, and affects water and food quality, supply, and production. A global increase of 1.5° C above the preindustrial average risks catastrophic harm to health that will be impossible to reverse, prompting the editors of over 260 health journals to call for emergency action to limit global temperature increases, restore biodiversity, and protect health.
In October, the 2022 version of the Lancet Countdown on health and climate change was issued and the findings are not good. “After 30 years of UNFCCC negotiations, the Lancet Countdown indicators show that countries and companies continue to make choices that threaten the health and survival of people in every part of the world. As countries devise ways to recover from the coexisting crises, the evidence is unequivocal. At this critical juncture, an immediate, health-centered response can still secure a future in which world populations can not only survive, but thrive,” the authors wrote. Governments and companies continue to prioritize fossil fuels over people’s health.
Among the key findings from the report, Marina Romanello, PhD, of the Institute for Global Health at University College London, and her colleagues, call for “A health-centered response to the coexisting climate, energy, and cost-of-living crises provides an opportunity to deliver a healthy, low-carbon future. The associated reduction in the burden of disease will in turn reduce the strain on overwhelmed health care providers, and enable better care.”
The authors also state that “Well-prepared health systems are essential to protect populations from the health impacts of climate change. However, global health systems have been drastically weakened by the effects of the COVID-19 pandemic, and the funds available for climate action decreased in 239 (30%) of 798 cities, with health systems increasingly being affected by extreme weather events and supply chain disruptions.”
And, the authors are concerned that health systems have left themselves vulnerable to climate change–related health hazards because they have not adapted their operations for climate-related changes. “Only 48 of 95 countries have assessed their climate change adaptation needs and only 63% of countries reported high to very high implementation status for health emergency management in 2021. Increasing adaptation to climate change has the potential to simultaneously improve the capacity of health systems to manage both future infectious disease outbreaks and other health emergencies.”
There is roughly a 50% chance that the 1.5° C threshold proposed in the Paris Agreement will be exceeded within 5 years. The carbon intensity of the global energy system has been reduced by less than 1% from 1992 levels, when the United Nations Framework Convention on Climate Change was adopted. At our current pace, global emissions could be 13.7% above 2010 levels by 2030 and fully decarbonizing the energy system would take 150 years. Clearly, we are nowhere near meeting the goals of the Paris Agreement signed in 2015 by 192 countries and the European Union. Participants pledged to decrease their carbon footprint by 50% by 2030, and net zero by the end of the century.
The effect of increasing greenhouse gases in our atmosphere will have a massive impact on the prevention and care of cancer patients. Air pollution is responsible for about 14% of lung cancer deaths throughout the world. Rising temperatures lead to extreme weather events which disrupts infrastructure and the ability to access health care, leading to delays in treatment, increased morbidity, and death. Screening rates for cancer go down, which leads to more patients presenting with advanced cancer in the future.
As oncologists who care deeply about their patients, we need to get actively involved. It is our responsibility to our current and future patients to do whatever we can to prevent cancer and reduce its complications.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Because we care about our patients, we need to get involved in the climate change movement. If we want to help prevent cancer and deliver the best possible care to our patients, we need to stop burning fossil fuels. As addressed in an earlier version of this column, burning fossil fuels results in the release of particulate matter and particles measuring 2.5 micrometers in diameter (PM2.5), are classified as group 1 carcinogens by the International Association of Research and Cancer.
Fossil fuels also release greenhouse gases (carbon dioxide, methane, nitrous oxide, and fluorinated gases) which trap solar radiation that would otherwise have been reflected back into space after hitting the earth’s surface. Instead, it is redirected back to earth as infrared radiation warming the planet by 1.1° C since preindustrial times.
Climate change has a number of consequences, including more extreme weather events, rising sea levels, warming seas, environmental degradation, and affects water and food quality, supply, and production. A global increase of 1.5° C above the preindustrial average risks catastrophic harm to health that will be impossible to reverse, prompting the editors of over 260 health journals to call for emergency action to limit global temperature increases, restore biodiversity, and protect health.
In October, the 2022 version of the Lancet Countdown on health and climate change was issued and the findings are not good. “After 30 years of UNFCCC negotiations, the Lancet Countdown indicators show that countries and companies continue to make choices that threaten the health and survival of people in every part of the world. As countries devise ways to recover from the coexisting crises, the evidence is unequivocal. At this critical juncture, an immediate, health-centered response can still secure a future in which world populations can not only survive, but thrive,” the authors wrote. Governments and companies continue to prioritize fossil fuels over people’s health.
Among the key findings from the report, Marina Romanello, PhD, of the Institute for Global Health at University College London, and her colleagues, call for “A health-centered response to the coexisting climate, energy, and cost-of-living crises provides an opportunity to deliver a healthy, low-carbon future. The associated reduction in the burden of disease will in turn reduce the strain on overwhelmed health care providers, and enable better care.”
The authors also state that “Well-prepared health systems are essential to protect populations from the health impacts of climate change. However, global health systems have been drastically weakened by the effects of the COVID-19 pandemic, and the funds available for climate action decreased in 239 (30%) of 798 cities, with health systems increasingly being affected by extreme weather events and supply chain disruptions.”
And, the authors are concerned that health systems have left themselves vulnerable to climate change–related health hazards because they have not adapted their operations for climate-related changes. “Only 48 of 95 countries have assessed their climate change adaptation needs and only 63% of countries reported high to very high implementation status for health emergency management in 2021. Increasing adaptation to climate change has the potential to simultaneously improve the capacity of health systems to manage both future infectious disease outbreaks and other health emergencies.”
There is roughly a 50% chance that the 1.5° C threshold proposed in the Paris Agreement will be exceeded within 5 years. The carbon intensity of the global energy system has been reduced by less than 1% from 1992 levels, when the United Nations Framework Convention on Climate Change was adopted. At our current pace, global emissions could be 13.7% above 2010 levels by 2030 and fully decarbonizing the energy system would take 150 years. Clearly, we are nowhere near meeting the goals of the Paris Agreement signed in 2015 by 192 countries and the European Union. Participants pledged to decrease their carbon footprint by 50% by 2030, and net zero by the end of the century.
The effect of increasing greenhouse gases in our atmosphere will have a massive impact on the prevention and care of cancer patients. Air pollution is responsible for about 14% of lung cancer deaths throughout the world. Rising temperatures lead to extreme weather events which disrupts infrastructure and the ability to access health care, leading to delays in treatment, increased morbidity, and death. Screening rates for cancer go down, which leads to more patients presenting with advanced cancer in the future.
As oncologists who care deeply about their patients, we need to get actively involved. It is our responsibility to our current and future patients to do whatever we can to prevent cancer and reduce its complications.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Severe health diagnoses drive suicide risk
Individuals diagnosed with a severe physical health condition were significantly more likely to commit suicide at 6 months and at 1 year later, based on data from more than 47 million individuals in a national database.
Previous smaller studies have shown a link between increased risk for suicide and a range of health conditions including cancer, coronary heart disease, neurologic conditions, diabetes, and osteoporosis, Vahé Nafilyan, PhD, of the Office for National Statistics, Newport, England, and colleagues wrote.
However, large-scale population-level studies of the association between specific diagnoses and suicide are lacking, they said.
In a study published in The Lancet Regional Health–Europe, the researchers reviewed a dataset that combined the 2011 Census, death registration records, and the Hospital Episode Statistics. The study population included 47,354,696 individuals aged 6 years and older living in England in 2017. The mean age of the study population was 39.6 years, and 52% were female. The researchers examined deaths that occurred between Jan. 1, 2017, and Dec. 31, 2021.
The health conditions included in the analysis were low-survival cancers, chronic ischemic heart disease, chronic obstructive pulmonary disease, and degenerative neurological disease.
The diagnosis of any of these conditions significantly increased the risk for suicide compared with controls. The highest risk appeared within 6 months of a diagnosis or first treatment, but the increased risk persisted at 1 year.
The suicide rate among low-survival cancer patients was 16.6 per 100,000 patients, compared with 5.7 per 100,000 controls; at 1 year, these rates were 21.6 and 9.5 per 100,000 patients and controls, respectively.
For COPD patients, the suicide rate at 6 months after diagnosis was 13.7 per 100,000 patients versus 5.6 per 100,000 matched controls; the suicide rates at 1 year were 22.4 per 100,000 patients and 10.6 per 100,000 matched controls.
The suicide rate at 6 months for individuals diagnosed with chronic ischemic heart disease was 11.0 per 100,000 patients and 4.2 per 100,000 matched controls; at 1 year, the suicide rates were 16.1 per 100,000 patients and 8.8 per 100,000 matched controls.
The 1-year suicide rate was especially high among patients with degenerative neurological conditions (114.5 per 100,000 patients); however, the estimate was considered imprecise because of the rarity of these diseases and subsequent low number of suicides, the researchers noted.
The results support data from previous studies showing links between increased risk of suicide and severe physical conditions, the researchers wrote. Patterns of suicide were similar between men and women and after adjusting for sociodemographic factors.
The findings were limited by the inability to fully control for a history of depression or self-harm, and by the imprecise estimates given the rare occurrence of suicide overall, the researchers noted. Other limitations included the late registration of deaths from external causes and the focus only on suicides that occurred in England and Wales, meaning that individuals who traveled abroad for assisted suicide were not captured in the dataset.
“Further research is needed to understand the mechanisms driving the elevated risk of suicide and help provide the best support to these patients,” the researchers concluded.
However, the current results enhance the literature with a large, population-based review of the elevated suicide risk among individuals newly diagnosed with severe health conditions, and reflect the need for better support for these patients to help with coping, they said.
The study was funded by the Office for National Statistics. The researchers reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Individuals diagnosed with a severe physical health condition were significantly more likely to commit suicide at 6 months and at 1 year later, based on data from more than 47 million individuals in a national database.
Previous smaller studies have shown a link between increased risk for suicide and a range of health conditions including cancer, coronary heart disease, neurologic conditions, diabetes, and osteoporosis, Vahé Nafilyan, PhD, of the Office for National Statistics, Newport, England, and colleagues wrote.
However, large-scale population-level studies of the association between specific diagnoses and suicide are lacking, they said.
In a study published in The Lancet Regional Health–Europe, the researchers reviewed a dataset that combined the 2011 Census, death registration records, and the Hospital Episode Statistics. The study population included 47,354,696 individuals aged 6 years and older living in England in 2017. The mean age of the study population was 39.6 years, and 52% were female. The researchers examined deaths that occurred between Jan. 1, 2017, and Dec. 31, 2021.
The health conditions included in the analysis were low-survival cancers, chronic ischemic heart disease, chronic obstructive pulmonary disease, and degenerative neurological disease.
The diagnosis of any of these conditions significantly increased the risk for suicide compared with controls. The highest risk appeared within 6 months of a diagnosis or first treatment, but the increased risk persisted at 1 year.
The suicide rate among low-survival cancer patients was 16.6 per 100,000 patients, compared with 5.7 per 100,000 controls; at 1 year, these rates were 21.6 and 9.5 per 100,000 patients and controls, respectively.
For COPD patients, the suicide rate at 6 months after diagnosis was 13.7 per 100,000 patients versus 5.6 per 100,000 matched controls; the suicide rates at 1 year were 22.4 per 100,000 patients and 10.6 per 100,000 matched controls.
The suicide rate at 6 months for individuals diagnosed with chronic ischemic heart disease was 11.0 per 100,000 patients and 4.2 per 100,000 matched controls; at 1 year, the suicide rates were 16.1 per 100,000 patients and 8.8 per 100,000 matched controls.
The 1-year suicide rate was especially high among patients with degenerative neurological conditions (114.5 per 100,000 patients); however, the estimate was considered imprecise because of the rarity of these diseases and subsequent low number of suicides, the researchers noted.
The results support data from previous studies showing links between increased risk of suicide and severe physical conditions, the researchers wrote. Patterns of suicide were similar between men and women and after adjusting for sociodemographic factors.
The findings were limited by the inability to fully control for a history of depression or self-harm, and by the imprecise estimates given the rare occurrence of suicide overall, the researchers noted. Other limitations included the late registration of deaths from external causes and the focus only on suicides that occurred in England and Wales, meaning that individuals who traveled abroad for assisted suicide were not captured in the dataset.
“Further research is needed to understand the mechanisms driving the elevated risk of suicide and help provide the best support to these patients,” the researchers concluded.
However, the current results enhance the literature with a large, population-based review of the elevated suicide risk among individuals newly diagnosed with severe health conditions, and reflect the need for better support for these patients to help with coping, they said.
The study was funded by the Office for National Statistics. The researchers reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Individuals diagnosed with a severe physical health condition were significantly more likely to commit suicide at 6 months and at 1 year later, based on data from more than 47 million individuals in a national database.
Previous smaller studies have shown a link between increased risk for suicide and a range of health conditions including cancer, coronary heart disease, neurologic conditions, diabetes, and osteoporosis, Vahé Nafilyan, PhD, of the Office for National Statistics, Newport, England, and colleagues wrote.
However, large-scale population-level studies of the association between specific diagnoses and suicide are lacking, they said.
In a study published in The Lancet Regional Health–Europe, the researchers reviewed a dataset that combined the 2011 Census, death registration records, and the Hospital Episode Statistics. The study population included 47,354,696 individuals aged 6 years and older living in England in 2017. The mean age of the study population was 39.6 years, and 52% were female. The researchers examined deaths that occurred between Jan. 1, 2017, and Dec. 31, 2021.
The health conditions included in the analysis were low-survival cancers, chronic ischemic heart disease, chronic obstructive pulmonary disease, and degenerative neurological disease.
The diagnosis of any of these conditions significantly increased the risk for suicide compared with controls. The highest risk appeared within 6 months of a diagnosis or first treatment, but the increased risk persisted at 1 year.
The suicide rate among low-survival cancer patients was 16.6 per 100,000 patients, compared with 5.7 per 100,000 controls; at 1 year, these rates were 21.6 and 9.5 per 100,000 patients and controls, respectively.
For COPD patients, the suicide rate at 6 months after diagnosis was 13.7 per 100,000 patients versus 5.6 per 100,000 matched controls; the suicide rates at 1 year were 22.4 per 100,000 patients and 10.6 per 100,000 matched controls.
The suicide rate at 6 months for individuals diagnosed with chronic ischemic heart disease was 11.0 per 100,000 patients and 4.2 per 100,000 matched controls; at 1 year, the suicide rates were 16.1 per 100,000 patients and 8.8 per 100,000 matched controls.
The 1-year suicide rate was especially high among patients with degenerative neurological conditions (114.5 per 100,000 patients); however, the estimate was considered imprecise because of the rarity of these diseases and subsequent low number of suicides, the researchers noted.
The results support data from previous studies showing links between increased risk of suicide and severe physical conditions, the researchers wrote. Patterns of suicide were similar between men and women and after adjusting for sociodemographic factors.
The findings were limited by the inability to fully control for a history of depression or self-harm, and by the imprecise estimates given the rare occurrence of suicide overall, the researchers noted. Other limitations included the late registration of deaths from external causes and the focus only on suicides that occurred in England and Wales, meaning that individuals who traveled abroad for assisted suicide were not captured in the dataset.
“Further research is needed to understand the mechanisms driving the elevated risk of suicide and help provide the best support to these patients,” the researchers concluded.
However, the current results enhance the literature with a large, population-based review of the elevated suicide risk among individuals newly diagnosed with severe health conditions, and reflect the need for better support for these patients to help with coping, they said.
The study was funded by the Office for National Statistics. The researchers reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM THE LANCET REGIONAL HEALTH–EUROPE
The longevity gene: Healthy mutant reverses heart aging
Everybody wants a younger heart
As more people live well past 90, scientists have been taking a closer look at how they’ve been doing it. Mostly it boiled down to genetics. You either had it or you didn’t. Well, a recent study suggests that doesn’t have to be true anymore, at least for the heart.
Scientists from the United Kingdom and Italy found an antiaging gene in some centenarians that has shown possible antiaging effects in mice and in human heart cells. A single administration of the mutant antiaging gene, they found, stopped heart function decay in middle-aged mice and even reversed the biological clock by the human equivalent of 10 years in elderly mice.
When the researchers applied the antiaging gene to samples of human heart cells from elderly people with heart problems, the cells “resumed functioning properly, proving to be more efficient in building new blood vessels,” they said in a written statement. It all kind of sounds like something out of Dr. Frankenstein’s lab.
I want to believe … in better sleep
The “X-Files” theme song plays. Mulder and Scully are sitting in a diner, breakfast laid out around them. The diner is quiet, with only a few people inside.
Mulder: I’m telling you, Scully, there’s something spooky going on here.
Scully: You mean other than the fact that this town in Georgia looks suspiciously like Vancouver?
Mulder: Not one person we spoke to yesterday has gotten a full night’s sleep since the UFO sighting last month. I’m telling you, they’re here, they’re experimenting.
Scully: Do you really want me to do this to you again?
Mulder: Do what again?
Scully: There’s nothing going on here that can’t be explained by the current research. Why, in January 2023 a study was published revealing a link between poor sleep and belief in paranormal phenomena like UFOS, demons, or ghosts. Which probably explains why you’re on your third cup of coffee for the morning.
Mulder: Scully, you’ve literally been abducted by aliens. Do we have to play this game every time?
Scully: Look, it’s simple. In a sample of nearly 9,000 people, nearly two-thirds of those who reported experiencing sleep paralysis or exploding head syndrome reported believing in UFOs and aliens walking amongst humanity, despite making up just 3% of the overall sample.
Furthermore, about 60% of those reporting sleep paralysis also reported believing near-death experiences prove the soul lingers on after death, and those with stronger insomnia symptoms were more likely to believe in the devil.
Mulder: Aha!
Scully: Aha what?
Mulder: You’re a devout Christian. You believe in the devil and the soul.
Scully: Yes, but I don’t let it interfere with a good night’s sleep, Mulder. These people saw something strange, convinced themselves it was a UFO, and now they can’t sleep. It’s a vicious cycle. The study authors even said that people experiencing strange nighttime phenomena could interpret this as evidence of aliens or other paranormal beings, thus making them even more susceptible to further sleep disruption and deepening beliefs. Look who I’m talking to.
Mulder: Always with the facts, eh?
Scully: I am a doctor, after all. And if you want more research into how paranormal belief and poor sleep quality are linked, I’d be happy to dig out the literature, because the truth is out there, Mulder.
Mulder: I hate you sometimes.
It’s ChatGPT’s world. We’re just living in it
Have you heard about ChatGPT? The artificial intelligence chatbot was just launched in November and it’s already more important to the Internet than either Vladimir Putin or “Rick and Morty.”
What’s that? You’re wondering why you should care? Well, excuuuuuse us, but we thought you might want to know that ChatGPT is in the process of taking over the world. Let’s take a quick look at what it’s been up to.
“ChatGPT bot passes law school exam”
“ChatGPT passes MBA exam given by a Wharton professor”
“A freelance writer says ChatGPT wrote a $600 article in just 30 seconds”
And here’s one that might be of interest to those of the health care persuasion: “ChatGPT can pass part of the U.S. Medical Licensing Exam.” See? It’s coming for you, too.
The artificial intelligence known as ChatGPT “performed at >50% accuracy across [the three USMLE] examinations, exceeding 60% in most analyses,” a group of researchers wrote on the preprint server medRxiv, noting that 60% is usually the pass threshold for humans taking the exam in any given year.
ChatGPT was not given any special medical training before the exam, but the investigators pointed out that another AI, PubMedGPT, which is trained exclusively on biomedical domain literature, was only 50.8% accurate on the USMLE. Its reliance on “ongoing academic discourse that tends to be inconclusive, contradictory, or highly conservative or noncommittal in its language” was its undoing, the team suggested.
To top it off, ChatGPT is listed as one of the authors at the top of the medRxiv report, with an acknowledgment at the end saying that “ChatGPT contributed to the writing of several sections of this manuscript.”
We’ve said it before, and no doubt we’ll say it again: We’re doomed.
Everybody wants a younger heart
As more people live well past 90, scientists have been taking a closer look at how they’ve been doing it. Mostly it boiled down to genetics. You either had it or you didn’t. Well, a recent study suggests that doesn’t have to be true anymore, at least for the heart.
Scientists from the United Kingdom and Italy found an antiaging gene in some centenarians that has shown possible antiaging effects in mice and in human heart cells. A single administration of the mutant antiaging gene, they found, stopped heart function decay in middle-aged mice and even reversed the biological clock by the human equivalent of 10 years in elderly mice.
When the researchers applied the antiaging gene to samples of human heart cells from elderly people with heart problems, the cells “resumed functioning properly, proving to be more efficient in building new blood vessels,” they said in a written statement. It all kind of sounds like something out of Dr. Frankenstein’s lab.
I want to believe … in better sleep
The “X-Files” theme song plays. Mulder and Scully are sitting in a diner, breakfast laid out around them. The diner is quiet, with only a few people inside.
Mulder: I’m telling you, Scully, there’s something spooky going on here.
Scully: You mean other than the fact that this town in Georgia looks suspiciously like Vancouver?
Mulder: Not one person we spoke to yesterday has gotten a full night’s sleep since the UFO sighting last month. I’m telling you, they’re here, they’re experimenting.
Scully: Do you really want me to do this to you again?
Mulder: Do what again?
Scully: There’s nothing going on here that can’t be explained by the current research. Why, in January 2023 a study was published revealing a link between poor sleep and belief in paranormal phenomena like UFOS, demons, or ghosts. Which probably explains why you’re on your third cup of coffee for the morning.
Mulder: Scully, you’ve literally been abducted by aliens. Do we have to play this game every time?
Scully: Look, it’s simple. In a sample of nearly 9,000 people, nearly two-thirds of those who reported experiencing sleep paralysis or exploding head syndrome reported believing in UFOs and aliens walking amongst humanity, despite making up just 3% of the overall sample.
Furthermore, about 60% of those reporting sleep paralysis also reported believing near-death experiences prove the soul lingers on after death, and those with stronger insomnia symptoms were more likely to believe in the devil.
Mulder: Aha!
Scully: Aha what?
Mulder: You’re a devout Christian. You believe in the devil and the soul.
Scully: Yes, but I don’t let it interfere with a good night’s sleep, Mulder. These people saw something strange, convinced themselves it was a UFO, and now they can’t sleep. It’s a vicious cycle. The study authors even said that people experiencing strange nighttime phenomena could interpret this as evidence of aliens or other paranormal beings, thus making them even more susceptible to further sleep disruption and deepening beliefs. Look who I’m talking to.
Mulder: Always with the facts, eh?
Scully: I am a doctor, after all. And if you want more research into how paranormal belief and poor sleep quality are linked, I’d be happy to dig out the literature, because the truth is out there, Mulder.
Mulder: I hate you sometimes.
It’s ChatGPT’s world. We’re just living in it
Have you heard about ChatGPT? The artificial intelligence chatbot was just launched in November and it’s already more important to the Internet than either Vladimir Putin or “Rick and Morty.”
What’s that? You’re wondering why you should care? Well, excuuuuuse us, but we thought you might want to know that ChatGPT is in the process of taking over the world. Let’s take a quick look at what it’s been up to.
“ChatGPT bot passes law school exam”
“ChatGPT passes MBA exam given by a Wharton professor”
“A freelance writer says ChatGPT wrote a $600 article in just 30 seconds”
And here’s one that might be of interest to those of the health care persuasion: “ChatGPT can pass part of the U.S. Medical Licensing Exam.” See? It’s coming for you, too.
The artificial intelligence known as ChatGPT “performed at >50% accuracy across [the three USMLE] examinations, exceeding 60% in most analyses,” a group of researchers wrote on the preprint server medRxiv, noting that 60% is usually the pass threshold for humans taking the exam in any given year.
ChatGPT was not given any special medical training before the exam, but the investigators pointed out that another AI, PubMedGPT, which is trained exclusively on biomedical domain literature, was only 50.8% accurate on the USMLE. Its reliance on “ongoing academic discourse that tends to be inconclusive, contradictory, or highly conservative or noncommittal in its language” was its undoing, the team suggested.
To top it off, ChatGPT is listed as one of the authors at the top of the medRxiv report, with an acknowledgment at the end saying that “ChatGPT contributed to the writing of several sections of this manuscript.”
We’ve said it before, and no doubt we’ll say it again: We’re doomed.
Everybody wants a younger heart
As more people live well past 90, scientists have been taking a closer look at how they’ve been doing it. Mostly it boiled down to genetics. You either had it or you didn’t. Well, a recent study suggests that doesn’t have to be true anymore, at least for the heart.
Scientists from the United Kingdom and Italy found an antiaging gene in some centenarians that has shown possible antiaging effects in mice and in human heart cells. A single administration of the mutant antiaging gene, they found, stopped heart function decay in middle-aged mice and even reversed the biological clock by the human equivalent of 10 years in elderly mice.
When the researchers applied the antiaging gene to samples of human heart cells from elderly people with heart problems, the cells “resumed functioning properly, proving to be more efficient in building new blood vessels,” they said in a written statement. It all kind of sounds like something out of Dr. Frankenstein’s lab.
I want to believe … in better sleep
The “X-Files” theme song plays. Mulder and Scully are sitting in a diner, breakfast laid out around them. The diner is quiet, with only a few people inside.
Mulder: I’m telling you, Scully, there’s something spooky going on here.
Scully: You mean other than the fact that this town in Georgia looks suspiciously like Vancouver?
Mulder: Not one person we spoke to yesterday has gotten a full night’s sleep since the UFO sighting last month. I’m telling you, they’re here, they’re experimenting.
Scully: Do you really want me to do this to you again?
Mulder: Do what again?
Scully: There’s nothing going on here that can’t be explained by the current research. Why, in January 2023 a study was published revealing a link between poor sleep and belief in paranormal phenomena like UFOS, demons, or ghosts. Which probably explains why you’re on your third cup of coffee for the morning.
Mulder: Scully, you’ve literally been abducted by aliens. Do we have to play this game every time?
Scully: Look, it’s simple. In a sample of nearly 9,000 people, nearly two-thirds of those who reported experiencing sleep paralysis or exploding head syndrome reported believing in UFOs and aliens walking amongst humanity, despite making up just 3% of the overall sample.
Furthermore, about 60% of those reporting sleep paralysis also reported believing near-death experiences prove the soul lingers on after death, and those with stronger insomnia symptoms were more likely to believe in the devil.
Mulder: Aha!
Scully: Aha what?
Mulder: You’re a devout Christian. You believe in the devil and the soul.
Scully: Yes, but I don’t let it interfere with a good night’s sleep, Mulder. These people saw something strange, convinced themselves it was a UFO, and now they can’t sleep. It’s a vicious cycle. The study authors even said that people experiencing strange nighttime phenomena could interpret this as evidence of aliens or other paranormal beings, thus making them even more susceptible to further sleep disruption and deepening beliefs. Look who I’m talking to.
Mulder: Always with the facts, eh?
Scully: I am a doctor, after all. And if you want more research into how paranormal belief and poor sleep quality are linked, I’d be happy to dig out the literature, because the truth is out there, Mulder.
Mulder: I hate you sometimes.
It’s ChatGPT’s world. We’re just living in it
Have you heard about ChatGPT? The artificial intelligence chatbot was just launched in November and it’s already more important to the Internet than either Vladimir Putin or “Rick and Morty.”
What’s that? You’re wondering why you should care? Well, excuuuuuse us, but we thought you might want to know that ChatGPT is in the process of taking over the world. Let’s take a quick look at what it’s been up to.
“ChatGPT bot passes law school exam”
“ChatGPT passes MBA exam given by a Wharton professor”
“A freelance writer says ChatGPT wrote a $600 article in just 30 seconds”
And here’s one that might be of interest to those of the health care persuasion: “ChatGPT can pass part of the U.S. Medical Licensing Exam.” See? It’s coming for you, too.
The artificial intelligence known as ChatGPT “performed at >50% accuracy across [the three USMLE] examinations, exceeding 60% in most analyses,” a group of researchers wrote on the preprint server medRxiv, noting that 60% is usually the pass threshold for humans taking the exam in any given year.
ChatGPT was not given any special medical training before the exam, but the investigators pointed out that another AI, PubMedGPT, which is trained exclusively on biomedical domain literature, was only 50.8% accurate on the USMLE. Its reliance on “ongoing academic discourse that tends to be inconclusive, contradictory, or highly conservative or noncommittal in its language” was its undoing, the team suggested.
To top it off, ChatGPT is listed as one of the authors at the top of the medRxiv report, with an acknowledgment at the end saying that “ChatGPT contributed to the writing of several sections of this manuscript.”
We’ve said it before, and no doubt we’ll say it again: We’re doomed.
Patients with COPD at higher risk of death 1 year after surgery
Patients with chronic obstructive pulmonary disease (COPD) are more likely to die within a year of undergoing elective surgery and to incur higher health care costs than are similar patients without COPD, data suggest.
An analysis of close to a million patient records found that, after adjustment for sociodemographic factors, procedure type, and comorbidities, patients with COPD were 26% more likely to die in the year after surgery than were those without COPD. Moreover, COPD was associated with a 4.6% increase in health care costs.
Previous studies have evaluated outcomes for the first 30 days after surgery. Those data “may not adequately capture the overall burden of surgery and how long it may take patients to recover,” study author Ashwin Sankar, MD, a clinician-investigator at St. Michael’s Hospital and assistant professor of anesthesia at the University of Toronto, told this news organization.
“We found that COPD often coexists with other conditions, like diabetes, coronary artery disease, and frailty,” Dr. Sankar added.
The study was published online in the Canadian Medical Association Journal.
Additional recovery support
The authors analyzed data from 932,616 patients who underwent intermediate-risk to high-risk elective noncardiac surgeries from 2005 to 2019 in Ontario. Procedures included carotid endarterectomy, open or endovascular abdominal aortic aneurysm repair, peripheral arterial bypass, total hip replacement, total knee replacement, shoulder surgery, large-bowel surgery, partial liver resection, pancreaticoduodenectomy, gastrectomy, esophagectomy, nephrectomy, cystectomy, prostatectomy, and hysterectomy.
The researchers quantified the associations of COPD with survival and costs. Their analyses included partial adjustment for sociodemographic factors and procedure type and full adjustment, which included comorbidities.
The primary outcome was all-cause death in the year after surgery; the secondary outcome was total health care costs in that year.
The mean age of the population was 65 years, and 60% of patients were women. A total of 170,482 (18%) patients had COPD. Compared with those without COPD, the patients with COPD were older and were more likely to be male, to be in a lower income quintile, to be residents of long-term care facilities, and to have been admitted to the hospital before surgery. They were also more likely to have comorbidities, including coronary artery disease, heart failure, and lung cancer.
A larger proportion of patients with COPD had frailty and medium to high comorbidity. They also more frequently underwent orthopedic, open upper abdominal, and vascular surgery.
During the year after surgery, 52,021 (5.6%) patients died, including 18,007 (10.6%) with COPD and 34,014 (4.5%) without. Those with COPD were more likely to die within 30 days of surgery (3.4% vs 1.2%).
For patients with COPD, the partially adjusted hazard ratio (HR) was 1.61 for risk of death; the fully adjusted HR was 1.26. COPD also was associated with a partially adjusted relative increase of 13.1% in health care costs and an increase of 4.6% with full adjustment.
Frailty, cancer, and procedure type were factors that modified the association between COPD and outcomes. “Procedures such as open aortic and upper abdominal surgery are associated with higher postoperative risks irrespective of COPD status, whereas others, such as orthopedic and lower abdominal surgery, may be of significantly greater risk for patients with COPD,” the authors wrote. “Our results suggest that perioperative management of patients with COPD requires careful consideration of the multiple domains that contribute to their elevated perioperative risk.
“Our finding that patients with COPD are at risk beyond 30 days after surgery suggests that it may be worthwhile to additionally support these patients’ recovery well beyond the first month after the procedure,” said Dr. Sankar.
Shared decision-making
Commenting on the study, William Whalen, MD, a pulmonary critical care specialist at Weill Cornell Medicine in New York, said, “I echo the authors’ sentiments that these findings highlight how chronically ill COPD patients are, which may be playing a role in the elevated mortality seen in this study.”
One caveat is in regard to the interpretation of the interaction effects of the study, he said. “Clinicians are unlikely to send patients who are frail or have multiple comorbidities to overly complex surgeries. Therefore, these effects may be misestimated due to selection bias.”
Two questions remain after reading the study, he added. “The first is how the degree of obstruction (i.e., the severity of COPD) impacts long-term mortality. Previous observational studies in nonsurgical COPD patients have shown increased mortality as the severity of obstruction increases. The second is how much of the long-term mortality observed in this study is related to respiratory disease from COPD. Patients with COPD are complex, and many die from nonrespiratory-related causes.”
Dr. Whalen suggests that discussion be held with the surgical team about the long-term morbidity and mortality with and without surgical intervention. Such a discussion could inform a shared decision-making process with the patient.
“Some procedures may be necessary to reduce immediate mortality, such as aortic aneurysmal repair, so [the risk of] longer-term mortality may be more acceptable in this setting,” he said. “Less straightforward are procedures that may improve quality of life. Would a patient accept an increased long-term mortality [risk] if that meant living without orthopedic-related pain?”
The study was funded by the Government of Ontario. Dr. Sankar and Dr. Whalen have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with chronic obstructive pulmonary disease (COPD) are more likely to die within a year of undergoing elective surgery and to incur higher health care costs than are similar patients without COPD, data suggest.
An analysis of close to a million patient records found that, after adjustment for sociodemographic factors, procedure type, and comorbidities, patients with COPD were 26% more likely to die in the year after surgery than were those without COPD. Moreover, COPD was associated with a 4.6% increase in health care costs.
Previous studies have evaluated outcomes for the first 30 days after surgery. Those data “may not adequately capture the overall burden of surgery and how long it may take patients to recover,” study author Ashwin Sankar, MD, a clinician-investigator at St. Michael’s Hospital and assistant professor of anesthesia at the University of Toronto, told this news organization.
“We found that COPD often coexists with other conditions, like diabetes, coronary artery disease, and frailty,” Dr. Sankar added.
The study was published online in the Canadian Medical Association Journal.
Additional recovery support
The authors analyzed data from 932,616 patients who underwent intermediate-risk to high-risk elective noncardiac surgeries from 2005 to 2019 in Ontario. Procedures included carotid endarterectomy, open or endovascular abdominal aortic aneurysm repair, peripheral arterial bypass, total hip replacement, total knee replacement, shoulder surgery, large-bowel surgery, partial liver resection, pancreaticoduodenectomy, gastrectomy, esophagectomy, nephrectomy, cystectomy, prostatectomy, and hysterectomy.
The researchers quantified the associations of COPD with survival and costs. Their analyses included partial adjustment for sociodemographic factors and procedure type and full adjustment, which included comorbidities.
The primary outcome was all-cause death in the year after surgery; the secondary outcome was total health care costs in that year.
The mean age of the population was 65 years, and 60% of patients were women. A total of 170,482 (18%) patients had COPD. Compared with those without COPD, the patients with COPD were older and were more likely to be male, to be in a lower income quintile, to be residents of long-term care facilities, and to have been admitted to the hospital before surgery. They were also more likely to have comorbidities, including coronary artery disease, heart failure, and lung cancer.
A larger proportion of patients with COPD had frailty and medium to high comorbidity. They also more frequently underwent orthopedic, open upper abdominal, and vascular surgery.
During the year after surgery, 52,021 (5.6%) patients died, including 18,007 (10.6%) with COPD and 34,014 (4.5%) without. Those with COPD were more likely to die within 30 days of surgery (3.4% vs 1.2%).
For patients with COPD, the partially adjusted hazard ratio (HR) was 1.61 for risk of death; the fully adjusted HR was 1.26. COPD also was associated with a partially adjusted relative increase of 13.1% in health care costs and an increase of 4.6% with full adjustment.
Frailty, cancer, and procedure type were factors that modified the association between COPD and outcomes. “Procedures such as open aortic and upper abdominal surgery are associated with higher postoperative risks irrespective of COPD status, whereas others, such as orthopedic and lower abdominal surgery, may be of significantly greater risk for patients with COPD,” the authors wrote. “Our results suggest that perioperative management of patients with COPD requires careful consideration of the multiple domains that contribute to their elevated perioperative risk.
“Our finding that patients with COPD are at risk beyond 30 days after surgery suggests that it may be worthwhile to additionally support these patients’ recovery well beyond the first month after the procedure,” said Dr. Sankar.
Shared decision-making
Commenting on the study, William Whalen, MD, a pulmonary critical care specialist at Weill Cornell Medicine in New York, said, “I echo the authors’ sentiments that these findings highlight how chronically ill COPD patients are, which may be playing a role in the elevated mortality seen in this study.”
One caveat is in regard to the interpretation of the interaction effects of the study, he said. “Clinicians are unlikely to send patients who are frail or have multiple comorbidities to overly complex surgeries. Therefore, these effects may be misestimated due to selection bias.”
Two questions remain after reading the study, he added. “The first is how the degree of obstruction (i.e., the severity of COPD) impacts long-term mortality. Previous observational studies in nonsurgical COPD patients have shown increased mortality as the severity of obstruction increases. The second is how much of the long-term mortality observed in this study is related to respiratory disease from COPD. Patients with COPD are complex, and many die from nonrespiratory-related causes.”
Dr. Whalen suggests that discussion be held with the surgical team about the long-term morbidity and mortality with and without surgical intervention. Such a discussion could inform a shared decision-making process with the patient.
“Some procedures may be necessary to reduce immediate mortality, such as aortic aneurysmal repair, so [the risk of] longer-term mortality may be more acceptable in this setting,” he said. “Less straightforward are procedures that may improve quality of life. Would a patient accept an increased long-term mortality [risk] if that meant living without orthopedic-related pain?”
The study was funded by the Government of Ontario. Dr. Sankar and Dr. Whalen have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with chronic obstructive pulmonary disease (COPD) are more likely to die within a year of undergoing elective surgery and to incur higher health care costs than are similar patients without COPD, data suggest.
An analysis of close to a million patient records found that, after adjustment for sociodemographic factors, procedure type, and comorbidities, patients with COPD were 26% more likely to die in the year after surgery than were those without COPD. Moreover, COPD was associated with a 4.6% increase in health care costs.
Previous studies have evaluated outcomes for the first 30 days after surgery. Those data “may not adequately capture the overall burden of surgery and how long it may take patients to recover,” study author Ashwin Sankar, MD, a clinician-investigator at St. Michael’s Hospital and assistant professor of anesthesia at the University of Toronto, told this news organization.
“We found that COPD often coexists with other conditions, like diabetes, coronary artery disease, and frailty,” Dr. Sankar added.
The study was published online in the Canadian Medical Association Journal.
Additional recovery support
The authors analyzed data from 932,616 patients who underwent intermediate-risk to high-risk elective noncardiac surgeries from 2005 to 2019 in Ontario. Procedures included carotid endarterectomy, open or endovascular abdominal aortic aneurysm repair, peripheral arterial bypass, total hip replacement, total knee replacement, shoulder surgery, large-bowel surgery, partial liver resection, pancreaticoduodenectomy, gastrectomy, esophagectomy, nephrectomy, cystectomy, prostatectomy, and hysterectomy.
The researchers quantified the associations of COPD with survival and costs. Their analyses included partial adjustment for sociodemographic factors and procedure type and full adjustment, which included comorbidities.
The primary outcome was all-cause death in the year after surgery; the secondary outcome was total health care costs in that year.
The mean age of the population was 65 years, and 60% of patients were women. A total of 170,482 (18%) patients had COPD. Compared with those without COPD, the patients with COPD were older and were more likely to be male, to be in a lower income quintile, to be residents of long-term care facilities, and to have been admitted to the hospital before surgery. They were also more likely to have comorbidities, including coronary artery disease, heart failure, and lung cancer.
A larger proportion of patients with COPD had frailty and medium to high comorbidity. They also more frequently underwent orthopedic, open upper abdominal, and vascular surgery.
During the year after surgery, 52,021 (5.6%) patients died, including 18,007 (10.6%) with COPD and 34,014 (4.5%) without. Those with COPD were more likely to die within 30 days of surgery (3.4% vs 1.2%).
For patients with COPD, the partially adjusted hazard ratio (HR) was 1.61 for risk of death; the fully adjusted HR was 1.26. COPD also was associated with a partially adjusted relative increase of 13.1% in health care costs and an increase of 4.6% with full adjustment.
Frailty, cancer, and procedure type were factors that modified the association between COPD and outcomes. “Procedures such as open aortic and upper abdominal surgery are associated with higher postoperative risks irrespective of COPD status, whereas others, such as orthopedic and lower abdominal surgery, may be of significantly greater risk for patients with COPD,” the authors wrote. “Our results suggest that perioperative management of patients with COPD requires careful consideration of the multiple domains that contribute to their elevated perioperative risk.
“Our finding that patients with COPD are at risk beyond 30 days after surgery suggests that it may be worthwhile to additionally support these patients’ recovery well beyond the first month after the procedure,” said Dr. Sankar.
Shared decision-making
Commenting on the study, William Whalen, MD, a pulmonary critical care specialist at Weill Cornell Medicine in New York, said, “I echo the authors’ sentiments that these findings highlight how chronically ill COPD patients are, which may be playing a role in the elevated mortality seen in this study.”
One caveat is in regard to the interpretation of the interaction effects of the study, he said. “Clinicians are unlikely to send patients who are frail or have multiple comorbidities to overly complex surgeries. Therefore, these effects may be misestimated due to selection bias.”
Two questions remain after reading the study, he added. “The first is how the degree of obstruction (i.e., the severity of COPD) impacts long-term mortality. Previous observational studies in nonsurgical COPD patients have shown increased mortality as the severity of obstruction increases. The second is how much of the long-term mortality observed in this study is related to respiratory disease from COPD. Patients with COPD are complex, and many die from nonrespiratory-related causes.”
Dr. Whalen suggests that discussion be held with the surgical team about the long-term morbidity and mortality with and without surgical intervention. Such a discussion could inform a shared decision-making process with the patient.
“Some procedures may be necessary to reduce immediate mortality, such as aortic aneurysmal repair, so [the risk of] longer-term mortality may be more acceptable in this setting,” he said. “Less straightforward are procedures that may improve quality of life. Would a patient accept an increased long-term mortality [risk] if that meant living without orthopedic-related pain?”
The study was funded by the Government of Ontario. Dr. Sankar and Dr. Whalen have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Canadian guidance recommends reducing alcohol consumption
“Drinking less is better,” says the guidance, which replaces Canada’s 2011 Low-Risk Drinking Guidelines (LRDGs).
Developed in consultation with an executive committee from federal, provincial, and territorial governments; national organizations; three scientific expert panels; and an internal evidence review working group, the guidance presents the following findings:
- Consuming no drinks per week has benefits, such as better health and better sleep, and it’s the only safe option during pregnancy.
- Consuming one or two standard drinks weekly will likely not have alcohol-related consequences.
- Three to six drinks raise the risk of developing breast, colon, and other cancers.
- Seven or more increase the risk of heart disease or stroke.
- Each additional drink “radically increases” the risk of these health consequences.
“Alcohol is more harmful than was previously thought and is a key component of the health of your patients,” Adam Sherk, PhD, a scientist at the Canadian Institute for Substance Use Research at the University of Victoria (B.C.), and a member of the scientific expert panel that contributed to the guidance, said in an interview. “Display and discuss the new guidance with your patients with the main message that drinking less is better.”
Peter Butt, MD, a clinical associate professor at the University of Saskatchewan, Saskatoon, and cochair of the guidance project, said in an interview: “The World Health Organization has identified over 200 ICD-coded conditions associated with alcohol use. This creates many opportunities to inquire into quantity and frequency of alcohol use, relate it to the patient’s health and well-being, and provide advice on reduction.”
“Canada’s Guidance on Alcohol and Health: Final Report” and a related infographic were published online Jan. 17.
Continuum of risk
The impetus for the new guidance came from the fact that “our 2011 LRDGs were no longer current, and there was emerging evidence that people drinking within those levels were coming to harm,” said Dr. Butt.
That evidence indicates that alcohol causes at least seven types of cancer, mostly of the breast or colon; is a risk factor for most types of heart disease; and is a main cause of liver disease. Evidence also indicates that avoiding drinking to the point of intoxication will reduce people’s risk of perpetrating alcohol-related violence.
Responding to the need to accurately quantify the risk, the guidance defines a “standard” drink as 12 oz of beer, cooler, or cider (5% alcohol); 5 oz of wine (12% alcohol); and 1.5 oz of spirits such as whiskey, vodka, or gin (40% alcohol).
Using different mortality risk thresholds, the project’s experts developed the following continuum of risk:
- Low for individuals who consume two standard drinks or fewer per week
- Moderate for those who consume from three to six standard drinks per week
- Increasingly high for those who consume seven standard drinks or more per week
The guidance makes the following observations:
- Consuming more than two standard drinks per drinking occasion is associated with an increased risk of harms to self and others, including injuries and violence.
- When pregnant or trying to get pregnant, no amount of alcohol is safe.
- When breastfeeding, not drinking is safest.
- Above the upper limit of the moderate risk zone, health risks increase more steeply for females than males.
- Far more injuries, violence, and deaths result from men’s alcohol use, especially for per occasion drinking, than from women’s alcohol use.
- Young people should delay alcohol use for as long as possible.
- Individuals should not start to use alcohol or increase their alcohol use for health benefits.
- Any reduction in alcohol use is beneficial.
Other national guidelines
“Countries that haven’t updated their alcohol use guidelines recently should do so, as the evidence regarding alcohol and health has advanced considerably in the past 10 years,” said Dr. Sherk. He acknowledged that “any time health guidance changes substantially, it’s reasonable to expect a period of readjustment.”
“Some will be resistant,” Dr. Butt agreed. “Some professionals will need more education than others on the health effects of alcohol. Some patients will also be more invested in drinking than others. The harm-reduction, risk-zone approach should assist in the process of engaging patients and helping them reduce over time.
“Just as we benefited from the updates done in the United Kingdom, France, and especially Australia, so also researchers elsewhere will critique our work and our approach and make their own decisions on how best to communicate with their public,” Dr. Butt said. He noted that Canada’s contributions regarding the association between alcohol and violence, as well as their sex/gender approach to the evidence, “may influence the next country’s review.”
Commenting on whether the United States should consider changing its guidance, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York, said in an interview, “A lot of people will be surprised at the recommended limits on alcohol. Most think that they can have one or two glasses of alcohol per day and not have any increased risk to their health. I think the Canadians deserve credit for putting themselves out there.”
Dr. Brennan said there will “certainly be pushback by the drinking lobby, which is very strong both in the U.S. and in Canada.” In fact, the national trade group Beer Canada was recently quoted as stating that it still supports the 2011 guidelines and that the updating process lacked full transparency and expert technical peer review.
Nevertheless, Dr. Brennan said, “it’s overwhelmingly clear that alcohol affects a ton of different parts of our body, so limiting the amount of alcohol we take in is always going to be a good thing. The Canadian graphic is great because it color-codes the risk. I recommend that clinicians put it up in their offices and begin quantifying the units of alcohol that are going into a patient’s body each day.”
A version of this article originally appeared on Medscape.com.
“Drinking less is better,” says the guidance, which replaces Canada’s 2011 Low-Risk Drinking Guidelines (LRDGs).
Developed in consultation with an executive committee from federal, provincial, and territorial governments; national organizations; three scientific expert panels; and an internal evidence review working group, the guidance presents the following findings:
- Consuming no drinks per week has benefits, such as better health and better sleep, and it’s the only safe option during pregnancy.
- Consuming one or two standard drinks weekly will likely not have alcohol-related consequences.
- Three to six drinks raise the risk of developing breast, colon, and other cancers.
- Seven or more increase the risk of heart disease or stroke.
- Each additional drink “radically increases” the risk of these health consequences.
“Alcohol is more harmful than was previously thought and is a key component of the health of your patients,” Adam Sherk, PhD, a scientist at the Canadian Institute for Substance Use Research at the University of Victoria (B.C.), and a member of the scientific expert panel that contributed to the guidance, said in an interview. “Display and discuss the new guidance with your patients with the main message that drinking less is better.”
Peter Butt, MD, a clinical associate professor at the University of Saskatchewan, Saskatoon, and cochair of the guidance project, said in an interview: “The World Health Organization has identified over 200 ICD-coded conditions associated with alcohol use. This creates many opportunities to inquire into quantity and frequency of alcohol use, relate it to the patient’s health and well-being, and provide advice on reduction.”
“Canada’s Guidance on Alcohol and Health: Final Report” and a related infographic were published online Jan. 17.
Continuum of risk
The impetus for the new guidance came from the fact that “our 2011 LRDGs were no longer current, and there was emerging evidence that people drinking within those levels were coming to harm,” said Dr. Butt.
That evidence indicates that alcohol causes at least seven types of cancer, mostly of the breast or colon; is a risk factor for most types of heart disease; and is a main cause of liver disease. Evidence also indicates that avoiding drinking to the point of intoxication will reduce people’s risk of perpetrating alcohol-related violence.
Responding to the need to accurately quantify the risk, the guidance defines a “standard” drink as 12 oz of beer, cooler, or cider (5% alcohol); 5 oz of wine (12% alcohol); and 1.5 oz of spirits such as whiskey, vodka, or gin (40% alcohol).
Using different mortality risk thresholds, the project’s experts developed the following continuum of risk:
- Low for individuals who consume two standard drinks or fewer per week
- Moderate for those who consume from three to six standard drinks per week
- Increasingly high for those who consume seven standard drinks or more per week
The guidance makes the following observations:
- Consuming more than two standard drinks per drinking occasion is associated with an increased risk of harms to self and others, including injuries and violence.
- When pregnant or trying to get pregnant, no amount of alcohol is safe.
- When breastfeeding, not drinking is safest.
- Above the upper limit of the moderate risk zone, health risks increase more steeply for females than males.
- Far more injuries, violence, and deaths result from men’s alcohol use, especially for per occasion drinking, than from women’s alcohol use.
- Young people should delay alcohol use for as long as possible.
- Individuals should not start to use alcohol or increase their alcohol use for health benefits.
- Any reduction in alcohol use is beneficial.
Other national guidelines
“Countries that haven’t updated their alcohol use guidelines recently should do so, as the evidence regarding alcohol and health has advanced considerably in the past 10 years,” said Dr. Sherk. He acknowledged that “any time health guidance changes substantially, it’s reasonable to expect a period of readjustment.”
“Some will be resistant,” Dr. Butt agreed. “Some professionals will need more education than others on the health effects of alcohol. Some patients will also be more invested in drinking than others. The harm-reduction, risk-zone approach should assist in the process of engaging patients and helping them reduce over time.
“Just as we benefited from the updates done in the United Kingdom, France, and especially Australia, so also researchers elsewhere will critique our work and our approach and make their own decisions on how best to communicate with their public,” Dr. Butt said. He noted that Canada’s contributions regarding the association between alcohol and violence, as well as their sex/gender approach to the evidence, “may influence the next country’s review.”
Commenting on whether the United States should consider changing its guidance, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York, said in an interview, “A lot of people will be surprised at the recommended limits on alcohol. Most think that they can have one or two glasses of alcohol per day and not have any increased risk to their health. I think the Canadians deserve credit for putting themselves out there.”
Dr. Brennan said there will “certainly be pushback by the drinking lobby, which is very strong both in the U.S. and in Canada.” In fact, the national trade group Beer Canada was recently quoted as stating that it still supports the 2011 guidelines and that the updating process lacked full transparency and expert technical peer review.
Nevertheless, Dr. Brennan said, “it’s overwhelmingly clear that alcohol affects a ton of different parts of our body, so limiting the amount of alcohol we take in is always going to be a good thing. The Canadian graphic is great because it color-codes the risk. I recommend that clinicians put it up in their offices and begin quantifying the units of alcohol that are going into a patient’s body each day.”
A version of this article originally appeared on Medscape.com.
“Drinking less is better,” says the guidance, which replaces Canada’s 2011 Low-Risk Drinking Guidelines (LRDGs).
Developed in consultation with an executive committee from federal, provincial, and territorial governments; national organizations; three scientific expert panels; and an internal evidence review working group, the guidance presents the following findings:
- Consuming no drinks per week has benefits, such as better health and better sleep, and it’s the only safe option during pregnancy.
- Consuming one or two standard drinks weekly will likely not have alcohol-related consequences.
- Three to six drinks raise the risk of developing breast, colon, and other cancers.
- Seven or more increase the risk of heart disease or stroke.
- Each additional drink “radically increases” the risk of these health consequences.
“Alcohol is more harmful than was previously thought and is a key component of the health of your patients,” Adam Sherk, PhD, a scientist at the Canadian Institute for Substance Use Research at the University of Victoria (B.C.), and a member of the scientific expert panel that contributed to the guidance, said in an interview. “Display and discuss the new guidance with your patients with the main message that drinking less is better.”
Peter Butt, MD, a clinical associate professor at the University of Saskatchewan, Saskatoon, and cochair of the guidance project, said in an interview: “The World Health Organization has identified over 200 ICD-coded conditions associated with alcohol use. This creates many opportunities to inquire into quantity and frequency of alcohol use, relate it to the patient’s health and well-being, and provide advice on reduction.”
“Canada’s Guidance on Alcohol and Health: Final Report” and a related infographic were published online Jan. 17.
Continuum of risk
The impetus for the new guidance came from the fact that “our 2011 LRDGs were no longer current, and there was emerging evidence that people drinking within those levels were coming to harm,” said Dr. Butt.
That evidence indicates that alcohol causes at least seven types of cancer, mostly of the breast or colon; is a risk factor for most types of heart disease; and is a main cause of liver disease. Evidence also indicates that avoiding drinking to the point of intoxication will reduce people’s risk of perpetrating alcohol-related violence.
Responding to the need to accurately quantify the risk, the guidance defines a “standard” drink as 12 oz of beer, cooler, or cider (5% alcohol); 5 oz of wine (12% alcohol); and 1.5 oz of spirits such as whiskey, vodka, or gin (40% alcohol).
Using different mortality risk thresholds, the project’s experts developed the following continuum of risk:
- Low for individuals who consume two standard drinks or fewer per week
- Moderate for those who consume from three to six standard drinks per week
- Increasingly high for those who consume seven standard drinks or more per week
The guidance makes the following observations:
- Consuming more than two standard drinks per drinking occasion is associated with an increased risk of harms to self and others, including injuries and violence.
- When pregnant or trying to get pregnant, no amount of alcohol is safe.
- When breastfeeding, not drinking is safest.
- Above the upper limit of the moderate risk zone, health risks increase more steeply for females than males.
- Far more injuries, violence, and deaths result from men’s alcohol use, especially for per occasion drinking, than from women’s alcohol use.
- Young people should delay alcohol use for as long as possible.
- Individuals should not start to use alcohol or increase their alcohol use for health benefits.
- Any reduction in alcohol use is beneficial.
Other national guidelines
“Countries that haven’t updated their alcohol use guidelines recently should do so, as the evidence regarding alcohol and health has advanced considerably in the past 10 years,” said Dr. Sherk. He acknowledged that “any time health guidance changes substantially, it’s reasonable to expect a period of readjustment.”
“Some will be resistant,” Dr. Butt agreed. “Some professionals will need more education than others on the health effects of alcohol. Some patients will also be more invested in drinking than others. The harm-reduction, risk-zone approach should assist in the process of engaging patients and helping them reduce over time.
“Just as we benefited from the updates done in the United Kingdom, France, and especially Australia, so also researchers elsewhere will critique our work and our approach and make their own decisions on how best to communicate with their public,” Dr. Butt said. He noted that Canada’s contributions regarding the association between alcohol and violence, as well as their sex/gender approach to the evidence, “may influence the next country’s review.”
Commenting on whether the United States should consider changing its guidance, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York, said in an interview, “A lot of people will be surprised at the recommended limits on alcohol. Most think that they can have one or two glasses of alcohol per day and not have any increased risk to their health. I think the Canadians deserve credit for putting themselves out there.”
Dr. Brennan said there will “certainly be pushback by the drinking lobby, which is very strong both in the U.S. and in Canada.” In fact, the national trade group Beer Canada was recently quoted as stating that it still supports the 2011 guidelines and that the updating process lacked full transparency and expert technical peer review.
Nevertheless, Dr. Brennan said, “it’s overwhelmingly clear that alcohol affects a ton of different parts of our body, so limiting the amount of alcohol we take in is always going to be a good thing. The Canadian graphic is great because it color-codes the risk. I recommend that clinicians put it up in their offices and begin quantifying the units of alcohol that are going into a patient’s body each day.”
A version of this article originally appeared on Medscape.com.
Tips for getting involved with industry
Introduction
The professional activity of physicians has traditionally consisted of patient care, teaching/education, and research in varying proportions. These aims, especially education and research, have traditionally been achieved in academic health settings. However, involvement with industry can afford all physicians an opportunity to increase patient referrals, gain exposure to colleagues through a variety of educational opportunities, and participate in meaningful research projects they could not initiate independently.
How to initiate relationships with industry
Here are several ways to initiate a collaboration with industry. A few of the most common ways are to become a site investigator of a multicenter device or pharmaceutical trial, participate as a member of a speaker’s bureau, or obtain training on a new technology and subsequently incorporate it into your clinical practice. To find out what trials are enrolling and looking for additional sites or new studies that are being planned, I would suggest contacting the company’s local representative and have them put you in touch the appropriate personnel in the clinical trials division. For individuals who become involved in trials, this can be a great way to improve your understanding of how to design and conduct clinical trials as well as gain exposure to colleagues with similar clinical and research interests. Some of my closest long-term collaborators and friends have been individuals who I initially met as part of industry trials at investigator meetings. Another approach is to participate in a speaker’s bureau, which can be an excellent way to improve one’s presentation skills as well as gain knowledge with respect to a specific disease state. It is also a great way to network, meet colleagues, and develop a local and regional reputation as a content expert on a specific topic. Methods to find out about such opportunities include touring the exhibit halls during educational meetings and reading scientific journals to identify new products that are launching. I have found these sorts of opportunities can significantly increase topic-based referrals. Finally, obtaining training on a new diagnostic or therapeutic technology (usually through an industry-sponsored course) can allow individuals an opportunity to offer a unique or distinctive service to their community. In addition, as further clinical expertise is gained, the relationship can be expanded to offer local, regional, or even national training courses to colleagues via either on-site or virtual courses. Similarly, opportunities to speak about or demonstrate the technology/technique at educational courses may also follow.
Navigating and expanding the relationship
Once an individual establishes a relationship with a company or has established a reputation as a key opinion leader, additional opportunities for engagement may become available. These include serving as a consultant, becoming a member of an advisory board, participating or directing educational courses for trainees/practitioners, or serving as the principal investigator of a future clinical trial. Serving as a consultant can be quite rewarding as it can highlight clinical needs, identify where product improvement can be achieved, and focus where research and development funds should be directed. Serving on the advisory board can afford an even higher level of influence where corporate strategy can be influenced. Such input is particularly impactful with smaller companies looking to enter a new field or expand a limited market share. There are also a variety of educational opportunities offered by industry including local, regional, and national courses that focus on utilizing a new technology or education concerning a specific disease state. These courses can be held locally at the physician’s clinical site or off site to attract the desired target audience. Finally, being involved in research studies, especially early-stage projects, can be critical as many small companies have limited capital, and it is essential for them to design studies with appropriate endpoints that will ideally achieve both regulatory approval as well as payor coverage. Of note, in addition to relationships directly involving industry, the American Gastroenterological Association Center for GI Innovation and Technology (CGIT) also offers the opportunity to be part of key opinion leader meetings arranged and organized by the AGA. This may allow for some individuals to participate who may be restricted from direct relationships with industry partners. The industry services offered by the CGIT also include clinical trial design and registry management services.
Entrepreneurship/intellectual property
A less commonly explored opportunity with industry involves the development of one’s own intellectual property. Some of the most impactful technologies in my advanced endoscopy clinical practice have been developed from the ideas of gastroenterology colleagues that have been successfully commercialized. These include radiofrequency ablation technology to treat Barrett’s esophagus and the development of lumen-apposing stents. There are several options for physicians with an idea for an innovation. These can include working with a university technology transfer department if they are in an academic setting, creation of their own company, or collaborating with industry to develop the device through a licensing/royalty agreement. The AGA CGIT offers extensive resources to physicians with new ideas on how to secure their intellectual property as well as to evaluate the feasibility of the aforementioned options to choose which may be most appropriate for them.
Important caveats
It is important that physicians with industry relations be aware of their local institutional policies. Some institutions may prohibit such activities while others may limit the types of relationships or the amount of income that can be received. It is the physician’s responsibility to be aware of their institution’s guidelines prior to formalizing industry agreements. If intellectual property is involved, it is essential to know the specific rules regarding physician remuneration, especially pertaining to royalty or equity agreements. Furthermore, with regard to presentations and publications, it is required to acknowledge industry relations and potential conflicts of interest. Failure to do so may adversely affect an individual’s reputation as well as lead to additional consequences such as the potential for retraction of publications or restrictions regarding future educational speaking opportunities. In addition, key opinion leaders often consult for several companies that may be in competition with each other. Therefore, it is essential that there is no disclosure of confidential proprietary information among companies. Finally, the financial incentives resulting from industry collaboration should never influence physician judgment when interpreting or speaking about data regarding product efficacy or safety.
Conclusions
In summary, there are numerous opportunities for physicians to collaborate with industry. These relationships can be very rewarding and can serve to expedite the introduction of new diagnostic or treatment modalities and provide the opportunity to network and interact with colleagues as well as to participate in important research that improves clinical practice. The nature of these relationships should always be transparent, and it is the physician’s responsibility to ensure that the types of relationships that are engaged in are permitted by their employer. Over the course of my career, I have participated in nearly all forms of these relationships and have seen that participation lead to important publications, changes in corporate strategy, the fostering of acquisitions, and the rapid development and utilization of new endoscopic technologies. It is my personal belief than industry relationships can improve professional satisfaction, enhance one’s brand, and most importantly, expedite clinical innovation to improve patient care.
Dr. Muthusamy is professor of clinical medicine at the University of California, Los Angeles, and medical director of endoscopy, UCLA Health System. He disclosed ties with Medtronic, Boston Scientific, Motus GI, Endogastric Solutions, and Capsovision.
Introduction
The professional activity of physicians has traditionally consisted of patient care, teaching/education, and research in varying proportions. These aims, especially education and research, have traditionally been achieved in academic health settings. However, involvement with industry can afford all physicians an opportunity to increase patient referrals, gain exposure to colleagues through a variety of educational opportunities, and participate in meaningful research projects they could not initiate independently.
How to initiate relationships with industry
Here are several ways to initiate a collaboration with industry. A few of the most common ways are to become a site investigator of a multicenter device or pharmaceutical trial, participate as a member of a speaker’s bureau, or obtain training on a new technology and subsequently incorporate it into your clinical practice. To find out what trials are enrolling and looking for additional sites or new studies that are being planned, I would suggest contacting the company’s local representative and have them put you in touch the appropriate personnel in the clinical trials division. For individuals who become involved in trials, this can be a great way to improve your understanding of how to design and conduct clinical trials as well as gain exposure to colleagues with similar clinical and research interests. Some of my closest long-term collaborators and friends have been individuals who I initially met as part of industry trials at investigator meetings. Another approach is to participate in a speaker’s bureau, which can be an excellent way to improve one’s presentation skills as well as gain knowledge with respect to a specific disease state. It is also a great way to network, meet colleagues, and develop a local and regional reputation as a content expert on a specific topic. Methods to find out about such opportunities include touring the exhibit halls during educational meetings and reading scientific journals to identify new products that are launching. I have found these sorts of opportunities can significantly increase topic-based referrals. Finally, obtaining training on a new diagnostic or therapeutic technology (usually through an industry-sponsored course) can allow individuals an opportunity to offer a unique or distinctive service to their community. In addition, as further clinical expertise is gained, the relationship can be expanded to offer local, regional, or even national training courses to colleagues via either on-site or virtual courses. Similarly, opportunities to speak about or demonstrate the technology/technique at educational courses may also follow.
Navigating and expanding the relationship
Once an individual establishes a relationship with a company or has established a reputation as a key opinion leader, additional opportunities for engagement may become available. These include serving as a consultant, becoming a member of an advisory board, participating or directing educational courses for trainees/practitioners, or serving as the principal investigator of a future clinical trial. Serving as a consultant can be quite rewarding as it can highlight clinical needs, identify where product improvement can be achieved, and focus where research and development funds should be directed. Serving on the advisory board can afford an even higher level of influence where corporate strategy can be influenced. Such input is particularly impactful with smaller companies looking to enter a new field or expand a limited market share. There are also a variety of educational opportunities offered by industry including local, regional, and national courses that focus on utilizing a new technology or education concerning a specific disease state. These courses can be held locally at the physician’s clinical site or off site to attract the desired target audience. Finally, being involved in research studies, especially early-stage projects, can be critical as many small companies have limited capital, and it is essential for them to design studies with appropriate endpoints that will ideally achieve both regulatory approval as well as payor coverage. Of note, in addition to relationships directly involving industry, the American Gastroenterological Association Center for GI Innovation and Technology (CGIT) also offers the opportunity to be part of key opinion leader meetings arranged and organized by the AGA. This may allow for some individuals to participate who may be restricted from direct relationships with industry partners. The industry services offered by the CGIT also include clinical trial design and registry management services.
Entrepreneurship/intellectual property
A less commonly explored opportunity with industry involves the development of one’s own intellectual property. Some of the most impactful technologies in my advanced endoscopy clinical practice have been developed from the ideas of gastroenterology colleagues that have been successfully commercialized. These include radiofrequency ablation technology to treat Barrett’s esophagus and the development of lumen-apposing stents. There are several options for physicians with an idea for an innovation. These can include working with a university technology transfer department if they are in an academic setting, creation of their own company, or collaborating with industry to develop the device through a licensing/royalty agreement. The AGA CGIT offers extensive resources to physicians with new ideas on how to secure their intellectual property as well as to evaluate the feasibility of the aforementioned options to choose which may be most appropriate for them.
Important caveats
It is important that physicians with industry relations be aware of their local institutional policies. Some institutions may prohibit such activities while others may limit the types of relationships or the amount of income that can be received. It is the physician’s responsibility to be aware of their institution’s guidelines prior to formalizing industry agreements. If intellectual property is involved, it is essential to know the specific rules regarding physician remuneration, especially pertaining to royalty or equity agreements. Furthermore, with regard to presentations and publications, it is required to acknowledge industry relations and potential conflicts of interest. Failure to do so may adversely affect an individual’s reputation as well as lead to additional consequences such as the potential for retraction of publications or restrictions regarding future educational speaking opportunities. In addition, key opinion leaders often consult for several companies that may be in competition with each other. Therefore, it is essential that there is no disclosure of confidential proprietary information among companies. Finally, the financial incentives resulting from industry collaboration should never influence physician judgment when interpreting or speaking about data regarding product efficacy or safety.
Conclusions
In summary, there are numerous opportunities for physicians to collaborate with industry. These relationships can be very rewarding and can serve to expedite the introduction of new diagnostic or treatment modalities and provide the opportunity to network and interact with colleagues as well as to participate in important research that improves clinical practice. The nature of these relationships should always be transparent, and it is the physician’s responsibility to ensure that the types of relationships that are engaged in are permitted by their employer. Over the course of my career, I have participated in nearly all forms of these relationships and have seen that participation lead to important publications, changes in corporate strategy, the fostering of acquisitions, and the rapid development and utilization of new endoscopic technologies. It is my personal belief than industry relationships can improve professional satisfaction, enhance one’s brand, and most importantly, expedite clinical innovation to improve patient care.
Dr. Muthusamy is professor of clinical medicine at the University of California, Los Angeles, and medical director of endoscopy, UCLA Health System. He disclosed ties with Medtronic, Boston Scientific, Motus GI, Endogastric Solutions, and Capsovision.
Introduction
The professional activity of physicians has traditionally consisted of patient care, teaching/education, and research in varying proportions. These aims, especially education and research, have traditionally been achieved in academic health settings. However, involvement with industry can afford all physicians an opportunity to increase patient referrals, gain exposure to colleagues through a variety of educational opportunities, and participate in meaningful research projects they could not initiate independently.
How to initiate relationships with industry
Here are several ways to initiate a collaboration with industry. A few of the most common ways are to become a site investigator of a multicenter device or pharmaceutical trial, participate as a member of a speaker’s bureau, or obtain training on a new technology and subsequently incorporate it into your clinical practice. To find out what trials are enrolling and looking for additional sites or new studies that are being planned, I would suggest contacting the company’s local representative and have them put you in touch the appropriate personnel in the clinical trials division. For individuals who become involved in trials, this can be a great way to improve your understanding of how to design and conduct clinical trials as well as gain exposure to colleagues with similar clinical and research interests. Some of my closest long-term collaborators and friends have been individuals who I initially met as part of industry trials at investigator meetings. Another approach is to participate in a speaker’s bureau, which can be an excellent way to improve one’s presentation skills as well as gain knowledge with respect to a specific disease state. It is also a great way to network, meet colleagues, and develop a local and regional reputation as a content expert on a specific topic. Methods to find out about such opportunities include touring the exhibit halls during educational meetings and reading scientific journals to identify new products that are launching. I have found these sorts of opportunities can significantly increase topic-based referrals. Finally, obtaining training on a new diagnostic or therapeutic technology (usually through an industry-sponsored course) can allow individuals an opportunity to offer a unique or distinctive service to their community. In addition, as further clinical expertise is gained, the relationship can be expanded to offer local, regional, or even national training courses to colleagues via either on-site or virtual courses. Similarly, opportunities to speak about or demonstrate the technology/technique at educational courses may also follow.
Navigating and expanding the relationship
Once an individual establishes a relationship with a company or has established a reputation as a key opinion leader, additional opportunities for engagement may become available. These include serving as a consultant, becoming a member of an advisory board, participating or directing educational courses for trainees/practitioners, or serving as the principal investigator of a future clinical trial. Serving as a consultant can be quite rewarding as it can highlight clinical needs, identify where product improvement can be achieved, and focus where research and development funds should be directed. Serving on the advisory board can afford an even higher level of influence where corporate strategy can be influenced. Such input is particularly impactful with smaller companies looking to enter a new field or expand a limited market share. There are also a variety of educational opportunities offered by industry including local, regional, and national courses that focus on utilizing a new technology or education concerning a specific disease state. These courses can be held locally at the physician’s clinical site or off site to attract the desired target audience. Finally, being involved in research studies, especially early-stage projects, can be critical as many small companies have limited capital, and it is essential for them to design studies with appropriate endpoints that will ideally achieve both regulatory approval as well as payor coverage. Of note, in addition to relationships directly involving industry, the American Gastroenterological Association Center for GI Innovation and Technology (CGIT) also offers the opportunity to be part of key opinion leader meetings arranged and organized by the AGA. This may allow for some individuals to participate who may be restricted from direct relationships with industry partners. The industry services offered by the CGIT also include clinical trial design and registry management services.
Entrepreneurship/intellectual property
A less commonly explored opportunity with industry involves the development of one’s own intellectual property. Some of the most impactful technologies in my advanced endoscopy clinical practice have been developed from the ideas of gastroenterology colleagues that have been successfully commercialized. These include radiofrequency ablation technology to treat Barrett’s esophagus and the development of lumen-apposing stents. There are several options for physicians with an idea for an innovation. These can include working with a university technology transfer department if they are in an academic setting, creation of their own company, or collaborating with industry to develop the device through a licensing/royalty agreement. The AGA CGIT offers extensive resources to physicians with new ideas on how to secure their intellectual property as well as to evaluate the feasibility of the aforementioned options to choose which may be most appropriate for them.
Important caveats
It is important that physicians with industry relations be aware of their local institutional policies. Some institutions may prohibit such activities while others may limit the types of relationships or the amount of income that can be received. It is the physician’s responsibility to be aware of their institution’s guidelines prior to formalizing industry agreements. If intellectual property is involved, it is essential to know the specific rules regarding physician remuneration, especially pertaining to royalty or equity agreements. Furthermore, with regard to presentations and publications, it is required to acknowledge industry relations and potential conflicts of interest. Failure to do so may adversely affect an individual’s reputation as well as lead to additional consequences such as the potential for retraction of publications or restrictions regarding future educational speaking opportunities. In addition, key opinion leaders often consult for several companies that may be in competition with each other. Therefore, it is essential that there is no disclosure of confidential proprietary information among companies. Finally, the financial incentives resulting from industry collaboration should never influence physician judgment when interpreting or speaking about data regarding product efficacy or safety.
Conclusions
In summary, there are numerous opportunities for physicians to collaborate with industry. These relationships can be very rewarding and can serve to expedite the introduction of new diagnostic or treatment modalities and provide the opportunity to network and interact with colleagues as well as to participate in important research that improves clinical practice. The nature of these relationships should always be transparent, and it is the physician’s responsibility to ensure that the types of relationships that are engaged in are permitted by their employer. Over the course of my career, I have participated in nearly all forms of these relationships and have seen that participation lead to important publications, changes in corporate strategy, the fostering of acquisitions, and the rapid development and utilization of new endoscopic technologies. It is my personal belief than industry relationships can improve professional satisfaction, enhance one’s brand, and most importantly, expedite clinical innovation to improve patient care.
Dr. Muthusamy is professor of clinical medicine at the University of California, Los Angeles, and medical director of endoscopy, UCLA Health System. He disclosed ties with Medtronic, Boston Scientific, Motus GI, Endogastric Solutions, and Capsovision.
Over half of ED visits from cancer patients could be prevented
Overall, researchers found that 18.3 million (52%) ED visits among patients with cancer between 2012 and 2019 were potentially avoidable. Pain was the most common reason for such a visit. Notably, the number of potentially preventable ED visits documented each year increased over the study period.
“These findings highlight the need for cancer care programs to implement evidence-based interventions to better manage cancer treatment complications, such as uncontrolled pain, in outpatient and ambulatory settings,” said the authors, led by Amir Alishahi Tabriz, MD, PhD, MPH, department of health outcomes and behavior, Moffitt Cancer Center, Tampa.
Authors of an accompanying editorial agree, noting that “patients at risk for having uncontrolled pain could potentially be identified earlier, and steps could be taken that would address their pain and help prevent acute care visits.”
The study and the editorial were published online Jan. 19, 2022, in JAMA Network Open.
Patients with cancer experience a range of side effects from their cancer and treatment. Many such problems can be managed in the ambulatory setting but are often managed in the ED, which is far from optimal for patients with cancer from both a complications and cost perspective. Still, little is known about whether ED visits among patients with cancer are avoidable.
To better understand unnecessary emergency care use by these patients, Dr. Tabriz and colleagues evaluated trends and characteristics of potentially preventable ED visits among adults with cancer who had an ED visit between 2012 and 2019. The authors used the Centers for Medicare & Medicaid Services definition for a potentially preventable ED visit among patients receiving chemotherapy.
Among the 35.5 million ED visits made by patients with cancer during the study period, 18.3 million (52%) were identified as potentially preventable. Nearly 5.8 million of these visits (21%) were classified as being of “high acuity,” and almost 30% resulted in unplanned hospitalizations.
Pain was the most common reason for potentially preventable ED visits, accounting for 37% of these visits.
The absolute number of potentially preventable ED visits among cancer patients increased from about 1.8 million in 2012 to 3.2 million in 2019. The number of patients who visited the ED because of pain more than doubled, from roughly 1.2 million in 2012 to 2.4 million in 2019.
“The disproportionate increase in the number of ED visits by patients with cancer has put a substantial burden on EDs that are already operating at peak capacity” and “reinforces the need for cancer care programs to devise innovative ways to manage complications associated with cancer treatment in the outpatient and ambulatory settings,” Dr. Tabriz and coauthors wrote.
The increase could be an “unintended” consequence of efforts to decrease overall opioid administration in response to the opioid epidemic, Dr. Tabriz and colleagues noted. For example, the authors point to a recent study that found that about half of patients with cancer who had severe pain did not receive outpatient opioids in the week before visiting the ED.
“Even access to outpatient care does not mean patients can get the care they need outside an ED,” wrote editorialists Erek Majka, MD, with Summerlin Hospital, Las Vegas, and N. Seth Trueger, MD, MPH, with Northwestern University, Chicago. Thus, “it is no surprise that patients are sent to the ED if the alternatives do not have the staff or diagnostic and therapeutic capabilities the patients need.”
Overall, however, the “goal is not to eliminate ED visits for their own sake; rather, the goal is better care of patients with cancer, and secondarily, in a manner that is cost-effective,” Dr. Majka and Dr. Trueger explained.
No specific funding for the study was reported. The authors disclosed no relevant financial relationships. Dr. Trueger is digital media editor of JAMA Network Open, but he was not involved in decisions regarding review of the manuscript or its acceptance.
A version of this article first appeared on Medscape.com.
Overall, researchers found that 18.3 million (52%) ED visits among patients with cancer between 2012 and 2019 were potentially avoidable. Pain was the most common reason for such a visit. Notably, the number of potentially preventable ED visits documented each year increased over the study period.
“These findings highlight the need for cancer care programs to implement evidence-based interventions to better manage cancer treatment complications, such as uncontrolled pain, in outpatient and ambulatory settings,” said the authors, led by Amir Alishahi Tabriz, MD, PhD, MPH, department of health outcomes and behavior, Moffitt Cancer Center, Tampa.
Authors of an accompanying editorial agree, noting that “patients at risk for having uncontrolled pain could potentially be identified earlier, and steps could be taken that would address their pain and help prevent acute care visits.”
The study and the editorial were published online Jan. 19, 2022, in JAMA Network Open.
Patients with cancer experience a range of side effects from their cancer and treatment. Many such problems can be managed in the ambulatory setting but are often managed in the ED, which is far from optimal for patients with cancer from both a complications and cost perspective. Still, little is known about whether ED visits among patients with cancer are avoidable.
To better understand unnecessary emergency care use by these patients, Dr. Tabriz and colleagues evaluated trends and characteristics of potentially preventable ED visits among adults with cancer who had an ED visit between 2012 and 2019. The authors used the Centers for Medicare & Medicaid Services definition for a potentially preventable ED visit among patients receiving chemotherapy.
Among the 35.5 million ED visits made by patients with cancer during the study period, 18.3 million (52%) were identified as potentially preventable. Nearly 5.8 million of these visits (21%) were classified as being of “high acuity,” and almost 30% resulted in unplanned hospitalizations.
Pain was the most common reason for potentially preventable ED visits, accounting for 37% of these visits.
The absolute number of potentially preventable ED visits among cancer patients increased from about 1.8 million in 2012 to 3.2 million in 2019. The number of patients who visited the ED because of pain more than doubled, from roughly 1.2 million in 2012 to 2.4 million in 2019.
“The disproportionate increase in the number of ED visits by patients with cancer has put a substantial burden on EDs that are already operating at peak capacity” and “reinforces the need for cancer care programs to devise innovative ways to manage complications associated with cancer treatment in the outpatient and ambulatory settings,” Dr. Tabriz and coauthors wrote.
The increase could be an “unintended” consequence of efforts to decrease overall opioid administration in response to the opioid epidemic, Dr. Tabriz and colleagues noted. For example, the authors point to a recent study that found that about half of patients with cancer who had severe pain did not receive outpatient opioids in the week before visiting the ED.
“Even access to outpatient care does not mean patients can get the care they need outside an ED,” wrote editorialists Erek Majka, MD, with Summerlin Hospital, Las Vegas, and N. Seth Trueger, MD, MPH, with Northwestern University, Chicago. Thus, “it is no surprise that patients are sent to the ED if the alternatives do not have the staff or diagnostic and therapeutic capabilities the patients need.”
Overall, however, the “goal is not to eliminate ED visits for their own sake; rather, the goal is better care of patients with cancer, and secondarily, in a manner that is cost-effective,” Dr. Majka and Dr. Trueger explained.
No specific funding for the study was reported. The authors disclosed no relevant financial relationships. Dr. Trueger is digital media editor of JAMA Network Open, but he was not involved in decisions regarding review of the manuscript or its acceptance.
A version of this article first appeared on Medscape.com.
Overall, researchers found that 18.3 million (52%) ED visits among patients with cancer between 2012 and 2019 were potentially avoidable. Pain was the most common reason for such a visit. Notably, the number of potentially preventable ED visits documented each year increased over the study period.
“These findings highlight the need for cancer care programs to implement evidence-based interventions to better manage cancer treatment complications, such as uncontrolled pain, in outpatient and ambulatory settings,” said the authors, led by Amir Alishahi Tabriz, MD, PhD, MPH, department of health outcomes and behavior, Moffitt Cancer Center, Tampa.
Authors of an accompanying editorial agree, noting that “patients at risk for having uncontrolled pain could potentially be identified earlier, and steps could be taken that would address their pain and help prevent acute care visits.”
The study and the editorial were published online Jan. 19, 2022, in JAMA Network Open.
Patients with cancer experience a range of side effects from their cancer and treatment. Many such problems can be managed in the ambulatory setting but are often managed in the ED, which is far from optimal for patients with cancer from both a complications and cost perspective. Still, little is known about whether ED visits among patients with cancer are avoidable.
To better understand unnecessary emergency care use by these patients, Dr. Tabriz and colleagues evaluated trends and characteristics of potentially preventable ED visits among adults with cancer who had an ED visit between 2012 and 2019. The authors used the Centers for Medicare & Medicaid Services definition for a potentially preventable ED visit among patients receiving chemotherapy.
Among the 35.5 million ED visits made by patients with cancer during the study period, 18.3 million (52%) were identified as potentially preventable. Nearly 5.8 million of these visits (21%) were classified as being of “high acuity,” and almost 30% resulted in unplanned hospitalizations.
Pain was the most common reason for potentially preventable ED visits, accounting for 37% of these visits.
The absolute number of potentially preventable ED visits among cancer patients increased from about 1.8 million in 2012 to 3.2 million in 2019. The number of patients who visited the ED because of pain more than doubled, from roughly 1.2 million in 2012 to 2.4 million in 2019.
“The disproportionate increase in the number of ED visits by patients with cancer has put a substantial burden on EDs that are already operating at peak capacity” and “reinforces the need for cancer care programs to devise innovative ways to manage complications associated with cancer treatment in the outpatient and ambulatory settings,” Dr. Tabriz and coauthors wrote.
The increase could be an “unintended” consequence of efforts to decrease overall opioid administration in response to the opioid epidemic, Dr. Tabriz and colleagues noted. For example, the authors point to a recent study that found that about half of patients with cancer who had severe pain did not receive outpatient opioids in the week before visiting the ED.
“Even access to outpatient care does not mean patients can get the care they need outside an ED,” wrote editorialists Erek Majka, MD, with Summerlin Hospital, Las Vegas, and N. Seth Trueger, MD, MPH, with Northwestern University, Chicago. Thus, “it is no surprise that patients are sent to the ED if the alternatives do not have the staff or diagnostic and therapeutic capabilities the patients need.”
Overall, however, the “goal is not to eliminate ED visits for their own sake; rather, the goal is better care of patients with cancer, and secondarily, in a manner that is cost-effective,” Dr. Majka and Dr. Trueger explained.
No specific funding for the study was reported. The authors disclosed no relevant financial relationships. Dr. Trueger is digital media editor of JAMA Network Open, but he was not involved in decisions regarding review of the manuscript or its acceptance.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN







