User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Employed physicians: A survival guide
The strike by health care workers at Kaiser Permanente may not involve physicians (yet). But as more doctors in the United States are finding themselves working as salaried employees, physicians can – and probably will – become a powerful force for change in a health care system that has shown itself to be increasingly hostile to employee concerns over issues involving patient care, wages and benefits, safety, and well-being.
Salaried employment has its challenges. Physician-employees may have less autonomy and voice in decision-making that affects patients. They may splinter into fragmented work groups; feel isolated; and have different imperatives based on who they are, what they want, and where they work. They may feel more removed from their patients and struggle to build strong relationships, with their employers in the way.
Yet important opportunities exist for doctors when embracing their employee side. Examples of these interests include adequate compensation, wellness, job security, patient and worker safety, health care quality, reasonable workloads and schedules, and fair treatment by employers, including the need to exhibit a strong collective voice in organizational decision-making.
Some believe that physician-employees must be unionized to maximize their rights and power as employees. Many expect physician unionization to take hold more fully over time. Medical residents, the doctors of tomorrow, are already considering unionization in greater numbers. Some are also doing it in the same employment setting alongside other health professionals, such as nurses.
Having studied doctors and their employment situations for years, I am convinced that whether through unionization or another approach, physicians must also change how they think about control; train and learn alongside other health care workers who share similar interests; and elevate at an early career stage their knowledge of the business side of health care.
Adopt a more pragmatic definition of autonomy
Doctors must embrace an updated definition of autonomy – one that matches their status as highly paid labor.
When I have spoken to physicians in my research about what autonomy means to them, many seem unable to reconceptualize it from a vague and absolute form of their profession’s strategic control over their economic fates and technical skills toward an individualized control that is situation-specific, one centered on winning the daily fights about workplace bread-and-butter issues such as those mentioned above.
But a more pragmatic definition of autonomy could get doctors focused on influencing important issues of the patient-care day and enhance their negotiating power with employers. It would allow physicians to break out of what often seems a paralysis of inaction – waiting for employers, insurers, or the government to reinstate the profession’s idealized version of control by handing it back the keys to the health care system through major regulatory, structural, and reimbursement-related changes. This fantasy is unlikely to become reality.
Physician-employees I’ve talked to over the years understand their everyday challenges. But when it comes to engaging in localized and sustained action to overcome them, they often perform less well, leading to feelings of helplessness and burnout. Valuing tactical control over their jobs and work setting will yield smaller but more impactful wins as employees intent on making their everyday work lives better.
Train alongside other health care professionals
Physicians must accept that how they are trained no longer prepares them for the employee world into which most are dropped. For instance, unless doctors are trained collaboratively alongside other health care professionals – such as nurses – they are less likely to identify closely with these colleagues once in practice. There is strength in numbers, so this mutual identification empowers both groups of employees. Yet, medical education remains largely the same: training young medical students in isolation for the first couple of years, then placing them into clerkships and residencies where true interprofessional care opportunities remain stunted and secondary to the “physician as captain of the team” mantra.
Unfortunately, the “hidden curriculum” of medicine helps convince medical students and residents early in their careers that they are the unquestioned leaders in patient care settings. This hierarchy encourages some doctors to keep their psychological distance from other members of the health care team and to resist sharing power, concerns, or insights with less skilled health care workers. This socialization harms the ability of physicians to act in a unified fashion alongside these other workers. Having physicians learn and train alongside other health professionals yields positive benefits for collective advocacy, including a shared sense of purpose, positive views on collaboration with others in the health setting, and greater development of bonds with nonphysician coworkers.
Integrate business with medical training in real time
Medical students and residents generally lack exposure to the everyday business realities of the U.S. health care system. This gap hinders their ability to understand the employee world and push for the types of changes and work conditions that benefit all health care workers. Formal business and management training should be a required part of every U.S. medical school and residency curriculum from day one. If you see it at all in medical schools now, it is mostly by accident, or given separate treatment in the form of standalone MBA or MPH degrees that rarely integrate organically and in real time with actual medical training. Not every doctor needs an MBA or MPH degree. However, all of them require a stronger contextual understanding of how the medicine they wish to practice is shaped by the economic and fiscal circumstances surrounding it – circumstances they do not control.
This is another reason why young doctors are unhappy and burned out. They cannot push for specific changes or properly critique the pros and cons of how their work is structured because they have not been made aware, in real time as they learn clinical practice, how their jobs are shaped by realities such as insurance coverage and reimbursement, the fragmentation of the care delivery system, their employer’s financial health , and the socioeconomic circumstances of their patients. They aren’t given the methods and tools related to process and quality improvement, budgeting, negotiation, risk management, leadership, and talent management that might help them navigate these undermining forces. They also get little advance exposure in their training to important workplace “soft” skills in such areas as how to work in teams, networking, communication and listening, empathy, and problem-solving – all necessary foci for bringing them closer to other health care workers and advocating alongside them effectively with health care employers.
Now is the time for physicians to embrace their identity as employees. Doing so is in their own best interest as professionals. It will help others in the health care workforce as well as patients. Moreover, it provides a needed counterbalance to the powerful corporate ethos now ascendant in U.S. health care.
Timothy Hoff, PhD, is a professor of management and healthcare systems at Northeastern University, Boston, and an associate fellow at the University of Oxford, England. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The strike by health care workers at Kaiser Permanente may not involve physicians (yet). But as more doctors in the United States are finding themselves working as salaried employees, physicians can – and probably will – become a powerful force for change in a health care system that has shown itself to be increasingly hostile to employee concerns over issues involving patient care, wages and benefits, safety, and well-being.
Salaried employment has its challenges. Physician-employees may have less autonomy and voice in decision-making that affects patients. They may splinter into fragmented work groups; feel isolated; and have different imperatives based on who they are, what they want, and where they work. They may feel more removed from their patients and struggle to build strong relationships, with their employers in the way.
Yet important opportunities exist for doctors when embracing their employee side. Examples of these interests include adequate compensation, wellness, job security, patient and worker safety, health care quality, reasonable workloads and schedules, and fair treatment by employers, including the need to exhibit a strong collective voice in organizational decision-making.
Some believe that physician-employees must be unionized to maximize their rights and power as employees. Many expect physician unionization to take hold more fully over time. Medical residents, the doctors of tomorrow, are already considering unionization in greater numbers. Some are also doing it in the same employment setting alongside other health professionals, such as nurses.
Having studied doctors and their employment situations for years, I am convinced that whether through unionization or another approach, physicians must also change how they think about control; train and learn alongside other health care workers who share similar interests; and elevate at an early career stage their knowledge of the business side of health care.
Adopt a more pragmatic definition of autonomy
Doctors must embrace an updated definition of autonomy – one that matches their status as highly paid labor.
When I have spoken to physicians in my research about what autonomy means to them, many seem unable to reconceptualize it from a vague and absolute form of their profession’s strategic control over their economic fates and technical skills toward an individualized control that is situation-specific, one centered on winning the daily fights about workplace bread-and-butter issues such as those mentioned above.
But a more pragmatic definition of autonomy could get doctors focused on influencing important issues of the patient-care day and enhance their negotiating power with employers. It would allow physicians to break out of what often seems a paralysis of inaction – waiting for employers, insurers, or the government to reinstate the profession’s idealized version of control by handing it back the keys to the health care system through major regulatory, structural, and reimbursement-related changes. This fantasy is unlikely to become reality.
Physician-employees I’ve talked to over the years understand their everyday challenges. But when it comes to engaging in localized and sustained action to overcome them, they often perform less well, leading to feelings of helplessness and burnout. Valuing tactical control over their jobs and work setting will yield smaller but more impactful wins as employees intent on making their everyday work lives better.
Train alongside other health care professionals
Physicians must accept that how they are trained no longer prepares them for the employee world into which most are dropped. For instance, unless doctors are trained collaboratively alongside other health care professionals – such as nurses – they are less likely to identify closely with these colleagues once in practice. There is strength in numbers, so this mutual identification empowers both groups of employees. Yet, medical education remains largely the same: training young medical students in isolation for the first couple of years, then placing them into clerkships and residencies where true interprofessional care opportunities remain stunted and secondary to the “physician as captain of the team” mantra.
Unfortunately, the “hidden curriculum” of medicine helps convince medical students and residents early in their careers that they are the unquestioned leaders in patient care settings. This hierarchy encourages some doctors to keep their psychological distance from other members of the health care team and to resist sharing power, concerns, or insights with less skilled health care workers. This socialization harms the ability of physicians to act in a unified fashion alongside these other workers. Having physicians learn and train alongside other health professionals yields positive benefits for collective advocacy, including a shared sense of purpose, positive views on collaboration with others in the health setting, and greater development of bonds with nonphysician coworkers.
Integrate business with medical training in real time
Medical students and residents generally lack exposure to the everyday business realities of the U.S. health care system. This gap hinders their ability to understand the employee world and push for the types of changes and work conditions that benefit all health care workers. Formal business and management training should be a required part of every U.S. medical school and residency curriculum from day one. If you see it at all in medical schools now, it is mostly by accident, or given separate treatment in the form of standalone MBA or MPH degrees that rarely integrate organically and in real time with actual medical training. Not every doctor needs an MBA or MPH degree. However, all of them require a stronger contextual understanding of how the medicine they wish to practice is shaped by the economic and fiscal circumstances surrounding it – circumstances they do not control.
This is another reason why young doctors are unhappy and burned out. They cannot push for specific changes or properly critique the pros and cons of how their work is structured because they have not been made aware, in real time as they learn clinical practice, how their jobs are shaped by realities such as insurance coverage and reimbursement, the fragmentation of the care delivery system, their employer’s financial health , and the socioeconomic circumstances of their patients. They aren’t given the methods and tools related to process and quality improvement, budgeting, negotiation, risk management, leadership, and talent management that might help them navigate these undermining forces. They also get little advance exposure in their training to important workplace “soft” skills in such areas as how to work in teams, networking, communication and listening, empathy, and problem-solving – all necessary foci for bringing them closer to other health care workers and advocating alongside them effectively with health care employers.
Now is the time for physicians to embrace their identity as employees. Doing so is in their own best interest as professionals. It will help others in the health care workforce as well as patients. Moreover, it provides a needed counterbalance to the powerful corporate ethos now ascendant in U.S. health care.
Timothy Hoff, PhD, is a professor of management and healthcare systems at Northeastern University, Boston, and an associate fellow at the University of Oxford, England. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The strike by health care workers at Kaiser Permanente may not involve physicians (yet). But as more doctors in the United States are finding themselves working as salaried employees, physicians can – and probably will – become a powerful force for change in a health care system that has shown itself to be increasingly hostile to employee concerns over issues involving patient care, wages and benefits, safety, and well-being.
Salaried employment has its challenges. Physician-employees may have less autonomy and voice in decision-making that affects patients. They may splinter into fragmented work groups; feel isolated; and have different imperatives based on who they are, what they want, and where they work. They may feel more removed from their patients and struggle to build strong relationships, with their employers in the way.
Yet important opportunities exist for doctors when embracing their employee side. Examples of these interests include adequate compensation, wellness, job security, patient and worker safety, health care quality, reasonable workloads and schedules, and fair treatment by employers, including the need to exhibit a strong collective voice in organizational decision-making.
Some believe that physician-employees must be unionized to maximize their rights and power as employees. Many expect physician unionization to take hold more fully over time. Medical residents, the doctors of tomorrow, are already considering unionization in greater numbers. Some are also doing it in the same employment setting alongside other health professionals, such as nurses.
Having studied doctors and their employment situations for years, I am convinced that whether through unionization or another approach, physicians must also change how they think about control; train and learn alongside other health care workers who share similar interests; and elevate at an early career stage their knowledge of the business side of health care.
Adopt a more pragmatic definition of autonomy
Doctors must embrace an updated definition of autonomy – one that matches their status as highly paid labor.
When I have spoken to physicians in my research about what autonomy means to them, many seem unable to reconceptualize it from a vague and absolute form of their profession’s strategic control over their economic fates and technical skills toward an individualized control that is situation-specific, one centered on winning the daily fights about workplace bread-and-butter issues such as those mentioned above.
But a more pragmatic definition of autonomy could get doctors focused on influencing important issues of the patient-care day and enhance their negotiating power with employers. It would allow physicians to break out of what often seems a paralysis of inaction – waiting for employers, insurers, or the government to reinstate the profession’s idealized version of control by handing it back the keys to the health care system through major regulatory, structural, and reimbursement-related changes. This fantasy is unlikely to become reality.
Physician-employees I’ve talked to over the years understand their everyday challenges. But when it comes to engaging in localized and sustained action to overcome them, they often perform less well, leading to feelings of helplessness and burnout. Valuing tactical control over their jobs and work setting will yield smaller but more impactful wins as employees intent on making their everyday work lives better.
Train alongside other health care professionals
Physicians must accept that how they are trained no longer prepares them for the employee world into which most are dropped. For instance, unless doctors are trained collaboratively alongside other health care professionals – such as nurses – they are less likely to identify closely with these colleagues once in practice. There is strength in numbers, so this mutual identification empowers both groups of employees. Yet, medical education remains largely the same: training young medical students in isolation for the first couple of years, then placing them into clerkships and residencies where true interprofessional care opportunities remain stunted and secondary to the “physician as captain of the team” mantra.
Unfortunately, the “hidden curriculum” of medicine helps convince medical students and residents early in their careers that they are the unquestioned leaders in patient care settings. This hierarchy encourages some doctors to keep their psychological distance from other members of the health care team and to resist sharing power, concerns, or insights with less skilled health care workers. This socialization harms the ability of physicians to act in a unified fashion alongside these other workers. Having physicians learn and train alongside other health professionals yields positive benefits for collective advocacy, including a shared sense of purpose, positive views on collaboration with others in the health setting, and greater development of bonds with nonphysician coworkers.
Integrate business with medical training in real time
Medical students and residents generally lack exposure to the everyday business realities of the U.S. health care system. This gap hinders their ability to understand the employee world and push for the types of changes and work conditions that benefit all health care workers. Formal business and management training should be a required part of every U.S. medical school and residency curriculum from day one. If you see it at all in medical schools now, it is mostly by accident, or given separate treatment in the form of standalone MBA or MPH degrees that rarely integrate organically and in real time with actual medical training. Not every doctor needs an MBA or MPH degree. However, all of them require a stronger contextual understanding of how the medicine they wish to practice is shaped by the economic and fiscal circumstances surrounding it – circumstances they do not control.
This is another reason why young doctors are unhappy and burned out. They cannot push for specific changes or properly critique the pros and cons of how their work is structured because they have not been made aware, in real time as they learn clinical practice, how their jobs are shaped by realities such as insurance coverage and reimbursement, the fragmentation of the care delivery system, their employer’s financial health , and the socioeconomic circumstances of their patients. They aren’t given the methods and tools related to process and quality improvement, budgeting, negotiation, risk management, leadership, and talent management that might help them navigate these undermining forces. They also get little advance exposure in their training to important workplace “soft” skills in such areas as how to work in teams, networking, communication and listening, empathy, and problem-solving – all necessary foci for bringing them closer to other health care workers and advocating alongside them effectively with health care employers.
Now is the time for physicians to embrace their identity as employees. Doing so is in their own best interest as professionals. It will help others in the health care workforce as well as patients. Moreover, it provides a needed counterbalance to the powerful corporate ethos now ascendant in U.S. health care.
Timothy Hoff, PhD, is a professor of management and healthcare systems at Northeastern University, Boston, and an associate fellow at the University of Oxford, England. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Why legal pot makes this physician sick
Last year, my husband and I took a 16-day road trip from Kentucky through Massachusetts to Maine. On our first morning in Boston, we exited the Park Street Station en route to Boston Common, but instead of being greeted by the aroma of molasses, we were hit full-on with a pungent, repulsive odor. “That’s skunk weed,” my husband chuckled as we stepped right into the middle of the Boston Freedom Rally, a celebration of all things cannabis.
As we boarded a hop-on-hop-off bus, we learned that this was the one week of the year that the city skips testing tour bus drivers for tetrahydrocannabinol (THC), “because we all test positive,” the driver quipped. As our open-air bus circled the Common, a crowd of pot enthusiasts displayed signs in support of relaxed regulation for public consumption.
The 34-year-old Boston Freedom Rally is a sign that U.S. culture has transformed forever. Mary Jane is no friend of emergency physicians nor of staff on hospital wards and offices.
Toking boomers and millennials
Researchers at the University of California, San Diego, looked at cannabis-related emergency department visits from all acute-care hospitals in the state from 2005 to 2019 and found an 1,808% increase in patients aged 65 or older (that is not a typo) who were there for complications from cannabis use.
The lead author said in an interview that, “older patients taking marijuana or related products may have dizziness and falls, heart palpitations, panic attacks, confusion, anxiety or worsening of underlying lung diseases, such as asthma or [chronic obstructive pulmonary disease].”
A recent study from Canada suggests that commercialization has been associated with an increase in related hospitalizations, including cannabis-induced psychosis.
According to a National Study of Drug Use and Health, marijuana use in young adults reached an all-time high (pun intended) in 2021. Nearly 10% of eighth graders and 20% of 10th graders reported using marijuana this past year.
The full downside of any drug, legal or illegal, is largely unknown until it infiltrates the mainstream market, but these are the typical cases we see:
Let’s start with the demotivated high school honors student who dropped out of college to work at the local cinema. He stumbled and broke his clavicle outside a bar at 2 AM, but he wasn’t sure if he passed out, so a cardiology consult was requested to “rule out” arrhythmia associated with syncope. He related that his plan to become a railway conductor had been upended because he knew he would be drug tested and just couldn’t give up pot. After a normal cardiac exam, ECG, labs, a Holter, and an echocardiogram were also requested and normal at a significant cost.
Cannabinoid hyperemesis syndrome
One of my Midwest colleagues related her encounter with two middle-aged pot users with ventricular tachycardia (VT). These episodes coincided with potassium levels less than 3.0 mEq/L in the setting of repetitive vomiting. The QTc interval didn’t normalize despite a corrected potassium level in one patient. They were both informed that they should never smoke pot because vomiting would predictably drop their K+ levels again and prolong their QTc intervals. Then began “the circular argument,” as my friend described it. The patient claims, “I smoke pot to relieve my nausea,” to which she explains that “in many folks, pot use induces nausea.” Of course, the classic reply is, “Not me.” Predictably one of these stoners soon returned with more VT, more puking, and more hypokalemia. “Consider yourself ‘allergic’ to pot smoke,” my friend advised, but “was met with no meaningful hint of understanding or hope for transformative change,” she told me.
I’ve seen cannabinoid hyperemesis syndrome several times in the past few years. It occurs in daily to weekly pot users. Very rarely, it can cause cerebral edema, but it is also associated with seizures and dehydration that can lead to hypovolemic shock and kidney failure.
Heart and brain harm
Then there are the young patients who for various reasons have developed heart failure. Unfortunately, some are repetitively tox screen positive with varying trifectas of methamphetamine (meth), cocaine, and THC; opiates, meth, and THC; alcohol, meth, and THC; or heroin, meth, and THC. THC, the ever present and essential third leg of the stool of stupor. These unfortunate patients often need heart failure medications that they can’t afford or won’t take because illicit drug use is expensive and dulls their ability to prioritize their health. Some desperately need a heart transplant, but the necessary negative drug screen is a pipe dream.
And it’s not just the heart that is affected. There are data linking cannabis use to a higher risk for both ischemic and hemorrhagic stroke. A retrospective study published in Stroke, of more than 1,000 people diagnosed with an aneurysmal subarachnoid hemorrhage, found that more than half of the 46 who tested positive for THC at admission developed delayed cerebral ischemia (DCI), which increases the risk for disability or early death. This was after adjusting for several patient characteristics as well as recent exposure to other illicit substances; cocaine, meth, and tobacco use were not associated with DCI.
Natural my ...
I’m certain my anti-cannabis stance will strike a nerve with those who love their recreational THC and push for its legal sale; after all, “It’s perfectly natural.” But I counter with the fact that tornadoes, earthquakes, cyanide, and appendicitis are all natural but certainly not optimal. And what we are seeing in the vascular specialties is completely unnatural. We are treating a different mix of complications than before pot was readily accessible across several states.
Our most effective action is to educate our patients. We should encourage those who don’t currently smoke cannabis to never start and those who do to quit. People who require marijuana for improved quality of life for terminal care or true (not supposed) disorders that mainstream medicine fails should be approached with empathy and caution.
A good rule of thumb is to never breathe anything you can see. Never put anything in your body that comes off the street: Drug dealers who sell cannabis cut with fentanyl will be ecstatic to take someone’s money then merely keep scrolling when their obituary comes up.
Let’s try to reverse the rise of vascular complications, orthopedic injuries, and vomiting across America. We can start by encouraging our patients to avoid “skunk weed” and get back to the sweet smells of nature in our cities and parks.
Some details have been changed to protect the patients’ identities, but the essence of their diagnoses has been preserved.
Dr. Walton-Shirley is a retired clinical cardiologist from Nashville, Tenn. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Last year, my husband and I took a 16-day road trip from Kentucky through Massachusetts to Maine. On our first morning in Boston, we exited the Park Street Station en route to Boston Common, but instead of being greeted by the aroma of molasses, we were hit full-on with a pungent, repulsive odor. “That’s skunk weed,” my husband chuckled as we stepped right into the middle of the Boston Freedom Rally, a celebration of all things cannabis.
As we boarded a hop-on-hop-off bus, we learned that this was the one week of the year that the city skips testing tour bus drivers for tetrahydrocannabinol (THC), “because we all test positive,” the driver quipped. As our open-air bus circled the Common, a crowd of pot enthusiasts displayed signs in support of relaxed regulation for public consumption.
The 34-year-old Boston Freedom Rally is a sign that U.S. culture has transformed forever. Mary Jane is no friend of emergency physicians nor of staff on hospital wards and offices.
Toking boomers and millennials
Researchers at the University of California, San Diego, looked at cannabis-related emergency department visits from all acute-care hospitals in the state from 2005 to 2019 and found an 1,808% increase in patients aged 65 or older (that is not a typo) who were there for complications from cannabis use.
The lead author said in an interview that, “older patients taking marijuana or related products may have dizziness and falls, heart palpitations, panic attacks, confusion, anxiety or worsening of underlying lung diseases, such as asthma or [chronic obstructive pulmonary disease].”
A recent study from Canada suggests that commercialization has been associated with an increase in related hospitalizations, including cannabis-induced psychosis.
According to a National Study of Drug Use and Health, marijuana use in young adults reached an all-time high (pun intended) in 2021. Nearly 10% of eighth graders and 20% of 10th graders reported using marijuana this past year.
The full downside of any drug, legal or illegal, is largely unknown until it infiltrates the mainstream market, but these are the typical cases we see:
Let’s start with the demotivated high school honors student who dropped out of college to work at the local cinema. He stumbled and broke his clavicle outside a bar at 2 AM, but he wasn’t sure if he passed out, so a cardiology consult was requested to “rule out” arrhythmia associated with syncope. He related that his plan to become a railway conductor had been upended because he knew he would be drug tested and just couldn’t give up pot. After a normal cardiac exam, ECG, labs, a Holter, and an echocardiogram were also requested and normal at a significant cost.
Cannabinoid hyperemesis syndrome
One of my Midwest colleagues related her encounter with two middle-aged pot users with ventricular tachycardia (VT). These episodes coincided with potassium levels less than 3.0 mEq/L in the setting of repetitive vomiting. The QTc interval didn’t normalize despite a corrected potassium level in one patient. They were both informed that they should never smoke pot because vomiting would predictably drop their K+ levels again and prolong their QTc intervals. Then began “the circular argument,” as my friend described it. The patient claims, “I smoke pot to relieve my nausea,” to which she explains that “in many folks, pot use induces nausea.” Of course, the classic reply is, “Not me.” Predictably one of these stoners soon returned with more VT, more puking, and more hypokalemia. “Consider yourself ‘allergic’ to pot smoke,” my friend advised, but “was met with no meaningful hint of understanding or hope for transformative change,” she told me.
I’ve seen cannabinoid hyperemesis syndrome several times in the past few years. It occurs in daily to weekly pot users. Very rarely, it can cause cerebral edema, but it is also associated with seizures and dehydration that can lead to hypovolemic shock and kidney failure.
Heart and brain harm
Then there are the young patients who for various reasons have developed heart failure. Unfortunately, some are repetitively tox screen positive with varying trifectas of methamphetamine (meth), cocaine, and THC; opiates, meth, and THC; alcohol, meth, and THC; or heroin, meth, and THC. THC, the ever present and essential third leg of the stool of stupor. These unfortunate patients often need heart failure medications that they can’t afford or won’t take because illicit drug use is expensive and dulls their ability to prioritize their health. Some desperately need a heart transplant, but the necessary negative drug screen is a pipe dream.
And it’s not just the heart that is affected. There are data linking cannabis use to a higher risk for both ischemic and hemorrhagic stroke. A retrospective study published in Stroke, of more than 1,000 people diagnosed with an aneurysmal subarachnoid hemorrhage, found that more than half of the 46 who tested positive for THC at admission developed delayed cerebral ischemia (DCI), which increases the risk for disability or early death. This was after adjusting for several patient characteristics as well as recent exposure to other illicit substances; cocaine, meth, and tobacco use were not associated with DCI.
Natural my ...
I’m certain my anti-cannabis stance will strike a nerve with those who love their recreational THC and push for its legal sale; after all, “It’s perfectly natural.” But I counter with the fact that tornadoes, earthquakes, cyanide, and appendicitis are all natural but certainly not optimal. And what we are seeing in the vascular specialties is completely unnatural. We are treating a different mix of complications than before pot was readily accessible across several states.
Our most effective action is to educate our patients. We should encourage those who don’t currently smoke cannabis to never start and those who do to quit. People who require marijuana for improved quality of life for terminal care or true (not supposed) disorders that mainstream medicine fails should be approached with empathy and caution.
A good rule of thumb is to never breathe anything you can see. Never put anything in your body that comes off the street: Drug dealers who sell cannabis cut with fentanyl will be ecstatic to take someone’s money then merely keep scrolling when their obituary comes up.
Let’s try to reverse the rise of vascular complications, orthopedic injuries, and vomiting across America. We can start by encouraging our patients to avoid “skunk weed” and get back to the sweet smells of nature in our cities and parks.
Some details have been changed to protect the patients’ identities, but the essence of their diagnoses has been preserved.
Dr. Walton-Shirley is a retired clinical cardiologist from Nashville, Tenn. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Last year, my husband and I took a 16-day road trip from Kentucky through Massachusetts to Maine. On our first morning in Boston, we exited the Park Street Station en route to Boston Common, but instead of being greeted by the aroma of molasses, we were hit full-on with a pungent, repulsive odor. “That’s skunk weed,” my husband chuckled as we stepped right into the middle of the Boston Freedom Rally, a celebration of all things cannabis.
As we boarded a hop-on-hop-off bus, we learned that this was the one week of the year that the city skips testing tour bus drivers for tetrahydrocannabinol (THC), “because we all test positive,” the driver quipped. As our open-air bus circled the Common, a crowd of pot enthusiasts displayed signs in support of relaxed regulation for public consumption.
The 34-year-old Boston Freedom Rally is a sign that U.S. culture has transformed forever. Mary Jane is no friend of emergency physicians nor of staff on hospital wards and offices.
Toking boomers and millennials
Researchers at the University of California, San Diego, looked at cannabis-related emergency department visits from all acute-care hospitals in the state from 2005 to 2019 and found an 1,808% increase in patients aged 65 or older (that is not a typo) who were there for complications from cannabis use.
The lead author said in an interview that, “older patients taking marijuana or related products may have dizziness and falls, heart palpitations, panic attacks, confusion, anxiety or worsening of underlying lung diseases, such as asthma or [chronic obstructive pulmonary disease].”
A recent study from Canada suggests that commercialization has been associated with an increase in related hospitalizations, including cannabis-induced psychosis.
According to a National Study of Drug Use and Health, marijuana use in young adults reached an all-time high (pun intended) in 2021. Nearly 10% of eighth graders and 20% of 10th graders reported using marijuana this past year.
The full downside of any drug, legal or illegal, is largely unknown until it infiltrates the mainstream market, but these are the typical cases we see:
Let’s start with the demotivated high school honors student who dropped out of college to work at the local cinema. He stumbled and broke his clavicle outside a bar at 2 AM, but he wasn’t sure if he passed out, so a cardiology consult was requested to “rule out” arrhythmia associated with syncope. He related that his plan to become a railway conductor had been upended because he knew he would be drug tested and just couldn’t give up pot. After a normal cardiac exam, ECG, labs, a Holter, and an echocardiogram were also requested and normal at a significant cost.
Cannabinoid hyperemesis syndrome
One of my Midwest colleagues related her encounter with two middle-aged pot users with ventricular tachycardia (VT). These episodes coincided with potassium levels less than 3.0 mEq/L in the setting of repetitive vomiting. The QTc interval didn’t normalize despite a corrected potassium level in one patient. They were both informed that they should never smoke pot because vomiting would predictably drop their K+ levels again and prolong their QTc intervals. Then began “the circular argument,” as my friend described it. The patient claims, “I smoke pot to relieve my nausea,” to which she explains that “in many folks, pot use induces nausea.” Of course, the classic reply is, “Not me.” Predictably one of these stoners soon returned with more VT, more puking, and more hypokalemia. “Consider yourself ‘allergic’ to pot smoke,” my friend advised, but “was met with no meaningful hint of understanding or hope for transformative change,” she told me.
I’ve seen cannabinoid hyperemesis syndrome several times in the past few years. It occurs in daily to weekly pot users. Very rarely, it can cause cerebral edema, but it is also associated with seizures and dehydration that can lead to hypovolemic shock and kidney failure.
Heart and brain harm
Then there are the young patients who for various reasons have developed heart failure. Unfortunately, some are repetitively tox screen positive with varying trifectas of methamphetamine (meth), cocaine, and THC; opiates, meth, and THC; alcohol, meth, and THC; or heroin, meth, and THC. THC, the ever present and essential third leg of the stool of stupor. These unfortunate patients often need heart failure medications that they can’t afford or won’t take because illicit drug use is expensive and dulls their ability to prioritize their health. Some desperately need a heart transplant, but the necessary negative drug screen is a pipe dream.
And it’s not just the heart that is affected. There are data linking cannabis use to a higher risk for both ischemic and hemorrhagic stroke. A retrospective study published in Stroke, of more than 1,000 people diagnosed with an aneurysmal subarachnoid hemorrhage, found that more than half of the 46 who tested positive for THC at admission developed delayed cerebral ischemia (DCI), which increases the risk for disability or early death. This was after adjusting for several patient characteristics as well as recent exposure to other illicit substances; cocaine, meth, and tobacco use were not associated with DCI.
Natural my ...
I’m certain my anti-cannabis stance will strike a nerve with those who love their recreational THC and push for its legal sale; after all, “It’s perfectly natural.” But I counter with the fact that tornadoes, earthquakes, cyanide, and appendicitis are all natural but certainly not optimal. And what we are seeing in the vascular specialties is completely unnatural. We are treating a different mix of complications than before pot was readily accessible across several states.
Our most effective action is to educate our patients. We should encourage those who don’t currently smoke cannabis to never start and those who do to quit. People who require marijuana for improved quality of life for terminal care or true (not supposed) disorders that mainstream medicine fails should be approached with empathy and caution.
A good rule of thumb is to never breathe anything you can see. Never put anything in your body that comes off the street: Drug dealers who sell cannabis cut with fentanyl will be ecstatic to take someone’s money then merely keep scrolling when their obituary comes up.
Let’s try to reverse the rise of vascular complications, orthopedic injuries, and vomiting across America. We can start by encouraging our patients to avoid “skunk weed” and get back to the sweet smells of nature in our cities and parks.
Some details have been changed to protect the patients’ identities, but the essence of their diagnoses has been preserved.
Dr. Walton-Shirley is a retired clinical cardiologist from Nashville, Tenn. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Artificial intelligence in the office: Part 2
In the year since generative artificial intelligence (AI) software first began to emerge for use, the staggering pace and breadth of development has condensed years of growth and change into months and weeks. Among the settings where these tools may find the greatest straight-line relevance is private medical practice.
. A multitude of generative AI products with potential medical applications are now available, with new ones appearing almost weekly. (As always, I have no financial interest in any product or service mentioned in this column.)
Last month, I discussed ChatGPT, the best-known AI algorithm, and some of its applications in clinical practice, such as generating website, video, and blog content. ChatGPT can also provide rapid and concise answers to general medical questions, like a search engine – but with more natural language processing and contextual understanding. Additionally, the algorithm can draft generic medical documents, including templates for after-visit summaries, postprocedure instructions, referrals, prior authorization appeal letters, and educational handouts.
Another useful feature of ChatGPT is its ability to provide accurate and conversational language translations, thus serving as an interpreter during clinic visits in situations where a human translator is not available. It also has potential uses in clinical research by finding resources, formulating hypotheses, drafting study protocols, and collecting large amounts of data in short periods of time. Other possibilities include survey administration, clinical trial recruitment, and automatic medication monitoring.
GPT-4, the latest version of ChatGPT, is reported to have greater problem-solving abilities and an even broader knowledge base. Among its claimed skills are the ability to find the latest literature in a given area, write a discharge summary for a patient following an uncomplicated surgery, and an image analysis feature to identify objects in photos. GPT-4 has been praised as having “the potential to help drive medical innovation, from aiding with patient discharge notes, summarizing recent clinical trials, providing information on ethical guidelines, and much more.”
Bard, an AI “chat bot” introduced by Google earlier this year, intends to leverage Google’s enormous database to compete with ChatGPT in providing answers to medical questions. Bard also hopes to play a pivotal role in expanding telemedicine and remote care via Google’s secure connections and access to patient records and medical history, and “facilitate seamless communication through appointment scheduling, messaging, and sharing medical images,” according to PackT, a website for IT professionals. The company claims that Bard’s integration of AI and machine learning capabilities will serve to elevate health care efficiency and patient outcomes, PackT says, and “the platform’s AI system quickly and accurately analyzes patient records, identifies patterns and trends, and aids medical professionals in developing effective treatment plans.”
Doximity has introduced an AI engine called DocsGPT, an encrypted, HIPAA-compliant writing assistant that, the company says, can draft any form of professional correspondence, including prior authorization letters, insurance appeals, patient support letters, and patient education materials. The service is available at no charge to all U.S. physicians and medical students through their Doximity accounts.
Microsoft has introduced several AI products. BioGPT is a language model specifically designed for health care. Compared with GPT models that are trained on more general text data, BioGPT is purported to have a deeper understanding of the language used in biomedical research and can generate more accurate and relevant outputs for biomedical tasks, such as drug discovery, disease classification, and clinical decision support. Fabric is another health care–specific data and analytics platform the company described in an announcement in May. It can combine data from sources such as electronic health records, images, lab systems, medical devices, and claims systems so hospitals and offices can standardize it and access it in the same place. Microsoft said the new tools will help eliminate the “time-consuming” process of searching through these sources one by one. Microsoft will also offer a new generative AI chatbot called the Azure Health Bot, which can pull information from a health organization’s own internal data as well as reputable external sources such as the Food and Drug Administration and the National Institutes of Health.
Several other AI products are available for clinicians. Tana served as an administrative aid and a clinical helper during the height of the COVID-19 pandemic, answering frequently asked questions, facilitating appointment management, and gathering preliminary medical information prior to teleconsultations. Dougall GPT is another AI chatbot tailored for health care professionals. It provides clinicians with AI-tuned answers to their queries, augmented by links to relevant, up-to-date, authoritative resources. It also assists in drafting patient instructions, consultation summaries, speeches, and professional correspondence. Wang has created Clinical Camel, an open-source health care–focused chatbot that assembles medical data with a combination of user-shared conversations and synthetic conversations derived from curated clinical articles. The Chinese company Baidu has rolled out Ernie as a potential rival to ChatGPT. You get the idea.
Of course, the inherent drawbacks of AI, such as producing false or biased information, perpetuating harmful stereotypes, and presenting information that has since been proven inaccurate or out-of-date, must always be kept in mind. All AI algorithms have been criticized for giving wrong answers, as their datasets are generally culled from information published in 2021 or earlier. Several of them have been shown to fabricate information – a phenomenon labeled “artificial hallucinations” in one article. “The scientific community must be vigilant in verifying the accuracy and reliability of the information provided by AI tools,” wrote the authors of that paper. “Researchers should use AI as an aid rather than a replacement for critical thinking and fact-checking.”
In the year since generative artificial intelligence (AI) software first began to emerge for use, the staggering pace and breadth of development has condensed years of growth and change into months and weeks. Among the settings where these tools may find the greatest straight-line relevance is private medical practice.
. A multitude of generative AI products with potential medical applications are now available, with new ones appearing almost weekly. (As always, I have no financial interest in any product or service mentioned in this column.)
Last month, I discussed ChatGPT, the best-known AI algorithm, and some of its applications in clinical practice, such as generating website, video, and blog content. ChatGPT can also provide rapid and concise answers to general medical questions, like a search engine – but with more natural language processing and contextual understanding. Additionally, the algorithm can draft generic medical documents, including templates for after-visit summaries, postprocedure instructions, referrals, prior authorization appeal letters, and educational handouts.
Another useful feature of ChatGPT is its ability to provide accurate and conversational language translations, thus serving as an interpreter during clinic visits in situations where a human translator is not available. It also has potential uses in clinical research by finding resources, formulating hypotheses, drafting study protocols, and collecting large amounts of data in short periods of time. Other possibilities include survey administration, clinical trial recruitment, and automatic medication monitoring.
GPT-4, the latest version of ChatGPT, is reported to have greater problem-solving abilities and an even broader knowledge base. Among its claimed skills are the ability to find the latest literature in a given area, write a discharge summary for a patient following an uncomplicated surgery, and an image analysis feature to identify objects in photos. GPT-4 has been praised as having “the potential to help drive medical innovation, from aiding with patient discharge notes, summarizing recent clinical trials, providing information on ethical guidelines, and much more.”
Bard, an AI “chat bot” introduced by Google earlier this year, intends to leverage Google’s enormous database to compete with ChatGPT in providing answers to medical questions. Bard also hopes to play a pivotal role in expanding telemedicine and remote care via Google’s secure connections and access to patient records and medical history, and “facilitate seamless communication through appointment scheduling, messaging, and sharing medical images,” according to PackT, a website for IT professionals. The company claims that Bard’s integration of AI and machine learning capabilities will serve to elevate health care efficiency and patient outcomes, PackT says, and “the platform’s AI system quickly and accurately analyzes patient records, identifies patterns and trends, and aids medical professionals in developing effective treatment plans.”
Doximity has introduced an AI engine called DocsGPT, an encrypted, HIPAA-compliant writing assistant that, the company says, can draft any form of professional correspondence, including prior authorization letters, insurance appeals, patient support letters, and patient education materials. The service is available at no charge to all U.S. physicians and medical students through their Doximity accounts.
Microsoft has introduced several AI products. BioGPT is a language model specifically designed for health care. Compared with GPT models that are trained on more general text data, BioGPT is purported to have a deeper understanding of the language used in biomedical research and can generate more accurate and relevant outputs for biomedical tasks, such as drug discovery, disease classification, and clinical decision support. Fabric is another health care–specific data and analytics platform the company described in an announcement in May. It can combine data from sources such as electronic health records, images, lab systems, medical devices, and claims systems so hospitals and offices can standardize it and access it in the same place. Microsoft said the new tools will help eliminate the “time-consuming” process of searching through these sources one by one. Microsoft will also offer a new generative AI chatbot called the Azure Health Bot, which can pull information from a health organization’s own internal data as well as reputable external sources such as the Food and Drug Administration and the National Institutes of Health.
Several other AI products are available for clinicians. Tana served as an administrative aid and a clinical helper during the height of the COVID-19 pandemic, answering frequently asked questions, facilitating appointment management, and gathering preliminary medical information prior to teleconsultations. Dougall GPT is another AI chatbot tailored for health care professionals. It provides clinicians with AI-tuned answers to their queries, augmented by links to relevant, up-to-date, authoritative resources. It also assists in drafting patient instructions, consultation summaries, speeches, and professional correspondence. Wang has created Clinical Camel, an open-source health care–focused chatbot that assembles medical data with a combination of user-shared conversations and synthetic conversations derived from curated clinical articles. The Chinese company Baidu has rolled out Ernie as a potential rival to ChatGPT. You get the idea.
Of course, the inherent drawbacks of AI, such as producing false or biased information, perpetuating harmful stereotypes, and presenting information that has since been proven inaccurate or out-of-date, must always be kept in mind. All AI algorithms have been criticized for giving wrong answers, as their datasets are generally culled from information published in 2021 or earlier. Several of them have been shown to fabricate information – a phenomenon labeled “artificial hallucinations” in one article. “The scientific community must be vigilant in verifying the accuracy and reliability of the information provided by AI tools,” wrote the authors of that paper. “Researchers should use AI as an aid rather than a replacement for critical thinking and fact-checking.”
In the year since generative artificial intelligence (AI) software first began to emerge for use, the staggering pace and breadth of development has condensed years of growth and change into months and weeks. Among the settings where these tools may find the greatest straight-line relevance is private medical practice.
. A multitude of generative AI products with potential medical applications are now available, with new ones appearing almost weekly. (As always, I have no financial interest in any product or service mentioned in this column.)
Last month, I discussed ChatGPT, the best-known AI algorithm, and some of its applications in clinical practice, such as generating website, video, and blog content. ChatGPT can also provide rapid and concise answers to general medical questions, like a search engine – but with more natural language processing and contextual understanding. Additionally, the algorithm can draft generic medical documents, including templates for after-visit summaries, postprocedure instructions, referrals, prior authorization appeal letters, and educational handouts.
Another useful feature of ChatGPT is its ability to provide accurate and conversational language translations, thus serving as an interpreter during clinic visits in situations where a human translator is not available. It also has potential uses in clinical research by finding resources, formulating hypotheses, drafting study protocols, and collecting large amounts of data in short periods of time. Other possibilities include survey administration, clinical trial recruitment, and automatic medication monitoring.
GPT-4, the latest version of ChatGPT, is reported to have greater problem-solving abilities and an even broader knowledge base. Among its claimed skills are the ability to find the latest literature in a given area, write a discharge summary for a patient following an uncomplicated surgery, and an image analysis feature to identify objects in photos. GPT-4 has been praised as having “the potential to help drive medical innovation, from aiding with patient discharge notes, summarizing recent clinical trials, providing information on ethical guidelines, and much more.”
Bard, an AI “chat bot” introduced by Google earlier this year, intends to leverage Google’s enormous database to compete with ChatGPT in providing answers to medical questions. Bard also hopes to play a pivotal role in expanding telemedicine and remote care via Google’s secure connections and access to patient records and medical history, and “facilitate seamless communication through appointment scheduling, messaging, and sharing medical images,” according to PackT, a website for IT professionals. The company claims that Bard’s integration of AI and machine learning capabilities will serve to elevate health care efficiency and patient outcomes, PackT says, and “the platform’s AI system quickly and accurately analyzes patient records, identifies patterns and trends, and aids medical professionals in developing effective treatment plans.”
Doximity has introduced an AI engine called DocsGPT, an encrypted, HIPAA-compliant writing assistant that, the company says, can draft any form of professional correspondence, including prior authorization letters, insurance appeals, patient support letters, and patient education materials. The service is available at no charge to all U.S. physicians and medical students through their Doximity accounts.
Microsoft has introduced several AI products. BioGPT is a language model specifically designed for health care. Compared with GPT models that are trained on more general text data, BioGPT is purported to have a deeper understanding of the language used in biomedical research and can generate more accurate and relevant outputs for biomedical tasks, such as drug discovery, disease classification, and clinical decision support. Fabric is another health care–specific data and analytics platform the company described in an announcement in May. It can combine data from sources such as electronic health records, images, lab systems, medical devices, and claims systems so hospitals and offices can standardize it and access it in the same place. Microsoft said the new tools will help eliminate the “time-consuming” process of searching through these sources one by one. Microsoft will also offer a new generative AI chatbot called the Azure Health Bot, which can pull information from a health organization’s own internal data as well as reputable external sources such as the Food and Drug Administration and the National Institutes of Health.
Several other AI products are available for clinicians. Tana served as an administrative aid and a clinical helper during the height of the COVID-19 pandemic, answering frequently asked questions, facilitating appointment management, and gathering preliminary medical information prior to teleconsultations. Dougall GPT is another AI chatbot tailored for health care professionals. It provides clinicians with AI-tuned answers to their queries, augmented by links to relevant, up-to-date, authoritative resources. It also assists in drafting patient instructions, consultation summaries, speeches, and professional correspondence. Wang has created Clinical Camel, an open-source health care–focused chatbot that assembles medical data with a combination of user-shared conversations and synthetic conversations derived from curated clinical articles. The Chinese company Baidu has rolled out Ernie as a potential rival to ChatGPT. You get the idea.
Of course, the inherent drawbacks of AI, such as producing false or biased information, perpetuating harmful stereotypes, and presenting information that has since been proven inaccurate or out-of-date, must always be kept in mind. All AI algorithms have been criticized for giving wrong answers, as their datasets are generally culled from information published in 2021 or earlier. Several of them have been shown to fabricate information – a phenomenon labeled “artificial hallucinations” in one article. “The scientific community must be vigilant in verifying the accuracy and reliability of the information provided by AI tools,” wrote the authors of that paper. “Researchers should use AI as an aid rather than a replacement for critical thinking and fact-checking.”
Prior authorization software: Saves time but hurdles remain
New England Baptist Hospital has been grappling with a serious problem facing health care today: insurers demanding prior authorizations for services ordered by physicians. Meeting payers’ requirements eats up time, delays treatment, and can be a costly drain on doctors’ practices.
To deal with this problem, the Boston orthopedic hospital has opted to automate submission of prior authorization requests on behalf of more than 100 mostly orthopedic surgeons on staff.
After 5 years using this system, “we can say that automation definitely works,” said Lidiya Hadzhieva, director of patient access at the hospital. The software has reduced write-offs by 30% and staff costs by 25%. Prior authorization gets approved 3 days after scheduling, compared with 11 days previously, she said.
“This software not only saves staff time, but it can also more accurately predict when prior authorization is needed,” she added.
For practices deluged with required prior authorizations by insurers, automation is emerging as a way for practices to make the process less time-consuming and save money. However, the software can be costly and may not be adoptable to many practices, and many physicians are not even aware it exists.
So far, the software is mainly used at large organizations like hospital systems. But as word gets out and the software becomes easier to use, private practices and other smaller entities may join the automation trend.
There is definitely a need to automate prior authorization. The American Medical Association reports that physicians spend 16 hours per week on prior authorizations. In a recent AMA survey, more than 60% of physicians indicated that it’s difficult to know when prior authorization is needed. And 93% of physicians reported care delays while waiting for authorization, the AMA said.
Experts estimate that 80% of prior authorization work could be automated, but most practices still use the phone or fax, even as numbers of prior authorizations continue to increase.
How it works
Automation software connects directly to the practice’s electronic health record (EHR). “When the doctor places an order in the EHR, the process starts automatically,” Ms. Hadzhieva said. “The doctor may not even notice it.”
In addition to using an EHR connection, many software products can communicate with the payer through its portal or by fax or phone, while still automating other parts of the process.
The software’s first step is to decide whether prior authorization is needed. This requires having an updated list of the rules that each payer uses for prior authorization. Manually keeping track of payer rules is very time-consuming, but automation uses bots to visit each payer site to look for rules changes. One vendor, Infinitus, uses a voice-based bot called Eva that calls up each payer and speaks with a representative.
“Automatically updating payer rules is not a new technology,” said YiDing Yu, MD, chief product officer at Olive, the automation vendor for New England Baptist. “What is new in the last 5 years is extracting the information needed for the prior authorization out of the clinical notes.”
This is challenging because each doctor has different ways to describe each step of clinical work. To identify this shorthand, Dr. Yu said Olive uses natural language processing, which is a form of artificial intelligence that learns how each doctor describes things.
Dr. Yu asserts that Olive is actually better than a practice’s staff at digging out clinical information. She said staff without much clinical training may miss terms that the software can catch, and they don’t have the time to go back many months into the record to find valuable information. But automation can do that.
In some instances, however, the software may not be able to find the information, in which case it alerts staff through a prompt in the EHR and the information is retrieved manually, Dr. Yu said.
Next, the Olive software puts the information it found into the request form and sends it to the payer. After submission, the software constantly checks on the status of each request, again visiting payer sites with a bot.
At New England Baptist, the software is used mainly by physicians in fairly small private practices who are on staff. They are using the software on the hospital’s dime, but it only works inside the hospital, Ms. Hadzhieva said. For their work outside of the hospital, they would have to purchase the Olive software on their own, she said.
Automation hasn’t spread to practices yet
Despite the promising outcomes for products like Olive, automation software is still primarily used by large organizations. Vendors say very few private practices have bought it yet. “The technology works, but it is still in the early-adopter phase,” Dr. Yu said.
For one thing, the software can be expensive. Very few vendors reveal their prices, but Dr. Yu did so. She said Olive normally costs about $50,000 a year for even a small organization. She insisted, however, that the savings from avoiding just one denial each month for a hip surgery would justify the expense.
On the other hand, some automation software is free, such as the Surescripts product for prior authorization of prescriptions. But it is unclear whether Surescripts does as much as Olive. Vendors’ descriptions of their products tend to be vague.
Also, Surescripts and Olive have entirely separate functions. Dr. Yu said Olive is limited to procedures, so it benefits specialties like oncology, neurosurgery, colorectal surgery, vascular surgery, and cardiology. Olive does not cover prescriptions, because they operate on a different technology.
Dr. Yu said another hurdle for adopting the software is the kind of EHR systems that doctors use. At this point, only a few EHR systems – such as Epic, Cerner, and Athena – are compatible with Olive. Large organizations tend to use Epic and Cerner, while many practices often use Athena or a variety of other systems, she said.
Despite stunted demand, there is no shortage of companies offering automation software for medical (that is, non-prescription) prior authorization. One compilation lists 25 such vendors, including companies like Myndshft, Rhyme, Infinitus, Infinx, and Waystar. As with any start-up technology, companies occasionally buy each other out.
In addition to issues like cost, specialty, and EHR compatibility, another hurdle is that few doctors even know the technology exists. Vendors say marketing focuses on larger provider organizations, not smaller practices.
Even many tech-savvy doctors, like Adam Bruggeman, MD, an orthopedist and CEO of Texas Spine Care Center in San Antonio, say they know little about the technology. “There is definitely a need to automate prior authorization,” he said. “But I don’t know of any colleagues who use it.” He has only just begun to explore vendors, he said.
Many medical practice consultants also have not yet explored the technology. “Automation makes a lot of sense, because there are a lot of repetitive tasks in prior authorization,” said Jill Arena, CEO of Portland, Ore.–based Health e Practices. “But I haven’t looked into it yet, and none of my clients has even asked about it.”
“I could see how it could be an easier sell for large organizations,” she added. “They have an IT person and a CFO who can explore the issue. Smaller practices usually don’t have that kind of expertise.”
Where does automation go from here?
Until now, clinicians who want to fully automate prior authorizations would have to buy two products – one for medical procedures and one for prescriptions. This has to do with incompatible electronic transmission standards, which are used to digitize information, said Susan Lawson-Dawson, content marketing strategist for the vendor Myndshft Health.
Myndshft has long been selling automation software for medical prior authorizations, but now it is introducing a product for prescriptions, Ms. Lawson-Dawson said. She said Myndshft will then be the only vendor to automate both kinds of prior authorizations.
Ms. Lawson-Dawson said Myndshft has 685 customers to date and is looking for more business. Recently the company entered the Google Cloud Marketplace. Google Cloud customers can now direct their committed spend with Google to purchasing Myndshft, meaning they could get it at a discount.
Software like Olive and Myndshft can operate independently of payers, but a vendor called Rhyme depends on payers for its software to function, said Rhyme CEO Joe Anstine. He said more than 300 payers have agreed to install the Rhyme system, and Rhyme has signed up a number of large health systems to use the product. Initially, he said, clinicians paid for the service, but now Rhyme is beginning to find payers to foot the costs and to let clinicians use it for free, which would open Rhyme up to smaller practices.
EHR companies themselves are beginning to offer automation, too. Epic, for example, has created a tool for prior authorization as part of its Epic Payer Platform. Like Rhyme, it requires payer cooperation, because information goes back and forth between clinician and payer in what is called bi-directional exchange.
The Epic product is still in its pilot phase. Epic reported that several large health systems were using its product in conjunction with a specific payer – for instance, Mayo Clinic with Blue Cross and Blue Shield of Minnesota and Ochsner Health with Humana. According to Epic, the arrangement reduced Mayo’s denials due to additional documentation requests by 63% for professional billing.
Automating with just one payer still means the clinician has to deal with manual processes at other payers, but a large clinician could have sufficient volume with that one payer to make the arrangement useful.
Will payers automate prior authorization?
Ultimately, payers may take the automation business away from vendors, offering a free product to all clinicians. But don’t hold your breath. Payers first have to rebuild their electronic systems to accommodate an electronic connection with providers. Even then, some payers might hold back from automating, forcing practices to continue manually processing some prior authorizations.
Efforts are underway, however, to mandate payers to support prior authorization automation. For this to happen, payers would have to revamp their data so that it could be easily read by practices’ EHRs. This would mean adopting a specific interoperability standard called Health Level 7 Fast Healthcare Interoperability Resources (FHIR).
Toward this goal, the Centers for Medicare & Medicaid Services proposes to require payers to adopt FHIR by January 2026. (CMS still has to finalize the rule.) Experts say the two-year ramp-up time is needed because it takes extensive work for payers to translate their data into FHIR.
The only payer so far to switch to FHIR for prior authorization is Regence in Washington state. In a pilot project, it has automated prior authorization with just one provider, MultiCare Connected Care, an accountable care organization (ACO), also in Washington state.
Anna Taylor, associate vice president of population health and value-based care at MultiCare, explained how the arrangement works. “Two separate entities are sharing one operational process,” she told this news organization. “That means they can have a digital conversation back and forth, so it is much easier to resolve prior authorization issues.”
Unlike many vendor products, the Regence service is free. And while the vendors market only to large organizations, most doctors in the MultiCare arrangement are in independent practices. Ms. Taylor said these doctors have been “enthusiastic” about the arrangement.
The results of the pilot are impressive. Ms. Taylor said automation has resulted in a 233% productivity gain for MultiCare clinicians, and 89% of submissions to Regence get an immediate response.
There is a potential downside, however, to working directly with payers. A direct connection to clinicians allows payers to access the doctor’s clinical notes, which could make many doctors uneasy. But Ms. Taylor said Regence only has access to the “discrete data fields” on MultiCare’s EHR dashboard, not to the notes themselves.
The ultimate goal of the Regence-Multicare project is to include more payers and clinicians. Ms. Taylor said two of the 27 other payers that MultiCare works with are “highly interested,” but it would take a lot of work for them to get connected with practices and other clinicians.
Ultimately, payers could offer automation and third-party vendors might then fade away. However, physicians may resist working directly with payers if the arrangement requires full access to their medical records.
A version of this article first appeared on Medscape.com.
New England Baptist Hospital has been grappling with a serious problem facing health care today: insurers demanding prior authorizations for services ordered by physicians. Meeting payers’ requirements eats up time, delays treatment, and can be a costly drain on doctors’ practices.
To deal with this problem, the Boston orthopedic hospital has opted to automate submission of prior authorization requests on behalf of more than 100 mostly orthopedic surgeons on staff.
After 5 years using this system, “we can say that automation definitely works,” said Lidiya Hadzhieva, director of patient access at the hospital. The software has reduced write-offs by 30% and staff costs by 25%. Prior authorization gets approved 3 days after scheduling, compared with 11 days previously, she said.
“This software not only saves staff time, but it can also more accurately predict when prior authorization is needed,” she added.
For practices deluged with required prior authorizations by insurers, automation is emerging as a way for practices to make the process less time-consuming and save money. However, the software can be costly and may not be adoptable to many practices, and many physicians are not even aware it exists.
So far, the software is mainly used at large organizations like hospital systems. But as word gets out and the software becomes easier to use, private practices and other smaller entities may join the automation trend.
There is definitely a need to automate prior authorization. The American Medical Association reports that physicians spend 16 hours per week on prior authorizations. In a recent AMA survey, more than 60% of physicians indicated that it’s difficult to know when prior authorization is needed. And 93% of physicians reported care delays while waiting for authorization, the AMA said.
Experts estimate that 80% of prior authorization work could be automated, but most practices still use the phone or fax, even as numbers of prior authorizations continue to increase.
How it works
Automation software connects directly to the practice’s electronic health record (EHR). “When the doctor places an order in the EHR, the process starts automatically,” Ms. Hadzhieva said. “The doctor may not even notice it.”
In addition to using an EHR connection, many software products can communicate with the payer through its portal or by fax or phone, while still automating other parts of the process.
The software’s first step is to decide whether prior authorization is needed. This requires having an updated list of the rules that each payer uses for prior authorization. Manually keeping track of payer rules is very time-consuming, but automation uses bots to visit each payer site to look for rules changes. One vendor, Infinitus, uses a voice-based bot called Eva that calls up each payer and speaks with a representative.
“Automatically updating payer rules is not a new technology,” said YiDing Yu, MD, chief product officer at Olive, the automation vendor for New England Baptist. “What is new in the last 5 years is extracting the information needed for the prior authorization out of the clinical notes.”
This is challenging because each doctor has different ways to describe each step of clinical work. To identify this shorthand, Dr. Yu said Olive uses natural language processing, which is a form of artificial intelligence that learns how each doctor describes things.
Dr. Yu asserts that Olive is actually better than a practice’s staff at digging out clinical information. She said staff without much clinical training may miss terms that the software can catch, and they don’t have the time to go back many months into the record to find valuable information. But automation can do that.
In some instances, however, the software may not be able to find the information, in which case it alerts staff through a prompt in the EHR and the information is retrieved manually, Dr. Yu said.
Next, the Olive software puts the information it found into the request form and sends it to the payer. After submission, the software constantly checks on the status of each request, again visiting payer sites with a bot.
At New England Baptist, the software is used mainly by physicians in fairly small private practices who are on staff. They are using the software on the hospital’s dime, but it only works inside the hospital, Ms. Hadzhieva said. For their work outside of the hospital, they would have to purchase the Olive software on their own, she said.
Automation hasn’t spread to practices yet
Despite the promising outcomes for products like Olive, automation software is still primarily used by large organizations. Vendors say very few private practices have bought it yet. “The technology works, but it is still in the early-adopter phase,” Dr. Yu said.
For one thing, the software can be expensive. Very few vendors reveal their prices, but Dr. Yu did so. She said Olive normally costs about $50,000 a year for even a small organization. She insisted, however, that the savings from avoiding just one denial each month for a hip surgery would justify the expense.
On the other hand, some automation software is free, such as the Surescripts product for prior authorization of prescriptions. But it is unclear whether Surescripts does as much as Olive. Vendors’ descriptions of their products tend to be vague.
Also, Surescripts and Olive have entirely separate functions. Dr. Yu said Olive is limited to procedures, so it benefits specialties like oncology, neurosurgery, colorectal surgery, vascular surgery, and cardiology. Olive does not cover prescriptions, because they operate on a different technology.
Dr. Yu said another hurdle for adopting the software is the kind of EHR systems that doctors use. At this point, only a few EHR systems – such as Epic, Cerner, and Athena – are compatible with Olive. Large organizations tend to use Epic and Cerner, while many practices often use Athena or a variety of other systems, she said.
Despite stunted demand, there is no shortage of companies offering automation software for medical (that is, non-prescription) prior authorization. One compilation lists 25 such vendors, including companies like Myndshft, Rhyme, Infinitus, Infinx, and Waystar. As with any start-up technology, companies occasionally buy each other out.
In addition to issues like cost, specialty, and EHR compatibility, another hurdle is that few doctors even know the technology exists. Vendors say marketing focuses on larger provider organizations, not smaller practices.
Even many tech-savvy doctors, like Adam Bruggeman, MD, an orthopedist and CEO of Texas Spine Care Center in San Antonio, say they know little about the technology. “There is definitely a need to automate prior authorization,” he said. “But I don’t know of any colleagues who use it.” He has only just begun to explore vendors, he said.
Many medical practice consultants also have not yet explored the technology. “Automation makes a lot of sense, because there are a lot of repetitive tasks in prior authorization,” said Jill Arena, CEO of Portland, Ore.–based Health e Practices. “But I haven’t looked into it yet, and none of my clients has even asked about it.”
“I could see how it could be an easier sell for large organizations,” she added. “They have an IT person and a CFO who can explore the issue. Smaller practices usually don’t have that kind of expertise.”
Where does automation go from here?
Until now, clinicians who want to fully automate prior authorizations would have to buy two products – one for medical procedures and one for prescriptions. This has to do with incompatible electronic transmission standards, which are used to digitize information, said Susan Lawson-Dawson, content marketing strategist for the vendor Myndshft Health.
Myndshft has long been selling automation software for medical prior authorizations, but now it is introducing a product for prescriptions, Ms. Lawson-Dawson said. She said Myndshft will then be the only vendor to automate both kinds of prior authorizations.
Ms. Lawson-Dawson said Myndshft has 685 customers to date and is looking for more business. Recently the company entered the Google Cloud Marketplace. Google Cloud customers can now direct their committed spend with Google to purchasing Myndshft, meaning they could get it at a discount.
Software like Olive and Myndshft can operate independently of payers, but a vendor called Rhyme depends on payers for its software to function, said Rhyme CEO Joe Anstine. He said more than 300 payers have agreed to install the Rhyme system, and Rhyme has signed up a number of large health systems to use the product. Initially, he said, clinicians paid for the service, but now Rhyme is beginning to find payers to foot the costs and to let clinicians use it for free, which would open Rhyme up to smaller practices.
EHR companies themselves are beginning to offer automation, too. Epic, for example, has created a tool for prior authorization as part of its Epic Payer Platform. Like Rhyme, it requires payer cooperation, because information goes back and forth between clinician and payer in what is called bi-directional exchange.
The Epic product is still in its pilot phase. Epic reported that several large health systems were using its product in conjunction with a specific payer – for instance, Mayo Clinic with Blue Cross and Blue Shield of Minnesota and Ochsner Health with Humana. According to Epic, the arrangement reduced Mayo’s denials due to additional documentation requests by 63% for professional billing.
Automating with just one payer still means the clinician has to deal with manual processes at other payers, but a large clinician could have sufficient volume with that one payer to make the arrangement useful.
Will payers automate prior authorization?
Ultimately, payers may take the automation business away from vendors, offering a free product to all clinicians. But don’t hold your breath. Payers first have to rebuild their electronic systems to accommodate an electronic connection with providers. Even then, some payers might hold back from automating, forcing practices to continue manually processing some prior authorizations.
Efforts are underway, however, to mandate payers to support prior authorization automation. For this to happen, payers would have to revamp their data so that it could be easily read by practices’ EHRs. This would mean adopting a specific interoperability standard called Health Level 7 Fast Healthcare Interoperability Resources (FHIR).
Toward this goal, the Centers for Medicare & Medicaid Services proposes to require payers to adopt FHIR by January 2026. (CMS still has to finalize the rule.) Experts say the two-year ramp-up time is needed because it takes extensive work for payers to translate their data into FHIR.
The only payer so far to switch to FHIR for prior authorization is Regence in Washington state. In a pilot project, it has automated prior authorization with just one provider, MultiCare Connected Care, an accountable care organization (ACO), also in Washington state.
Anna Taylor, associate vice president of population health and value-based care at MultiCare, explained how the arrangement works. “Two separate entities are sharing one operational process,” she told this news organization. “That means they can have a digital conversation back and forth, so it is much easier to resolve prior authorization issues.”
Unlike many vendor products, the Regence service is free. And while the vendors market only to large organizations, most doctors in the MultiCare arrangement are in independent practices. Ms. Taylor said these doctors have been “enthusiastic” about the arrangement.
The results of the pilot are impressive. Ms. Taylor said automation has resulted in a 233% productivity gain for MultiCare clinicians, and 89% of submissions to Regence get an immediate response.
There is a potential downside, however, to working directly with payers. A direct connection to clinicians allows payers to access the doctor’s clinical notes, which could make many doctors uneasy. But Ms. Taylor said Regence only has access to the “discrete data fields” on MultiCare’s EHR dashboard, not to the notes themselves.
The ultimate goal of the Regence-Multicare project is to include more payers and clinicians. Ms. Taylor said two of the 27 other payers that MultiCare works with are “highly interested,” but it would take a lot of work for them to get connected with practices and other clinicians.
Ultimately, payers could offer automation and third-party vendors might then fade away. However, physicians may resist working directly with payers if the arrangement requires full access to their medical records.
A version of this article first appeared on Medscape.com.
New England Baptist Hospital has been grappling with a serious problem facing health care today: insurers demanding prior authorizations for services ordered by physicians. Meeting payers’ requirements eats up time, delays treatment, and can be a costly drain on doctors’ practices.
To deal with this problem, the Boston orthopedic hospital has opted to automate submission of prior authorization requests on behalf of more than 100 mostly orthopedic surgeons on staff.
After 5 years using this system, “we can say that automation definitely works,” said Lidiya Hadzhieva, director of patient access at the hospital. The software has reduced write-offs by 30% and staff costs by 25%. Prior authorization gets approved 3 days after scheduling, compared with 11 days previously, she said.
“This software not only saves staff time, but it can also more accurately predict when prior authorization is needed,” she added.
For practices deluged with required prior authorizations by insurers, automation is emerging as a way for practices to make the process less time-consuming and save money. However, the software can be costly and may not be adoptable to many practices, and many physicians are not even aware it exists.
So far, the software is mainly used at large organizations like hospital systems. But as word gets out and the software becomes easier to use, private practices and other smaller entities may join the automation trend.
There is definitely a need to automate prior authorization. The American Medical Association reports that physicians spend 16 hours per week on prior authorizations. In a recent AMA survey, more than 60% of physicians indicated that it’s difficult to know when prior authorization is needed. And 93% of physicians reported care delays while waiting for authorization, the AMA said.
Experts estimate that 80% of prior authorization work could be automated, but most practices still use the phone or fax, even as numbers of prior authorizations continue to increase.
How it works
Automation software connects directly to the practice’s electronic health record (EHR). “When the doctor places an order in the EHR, the process starts automatically,” Ms. Hadzhieva said. “The doctor may not even notice it.”
In addition to using an EHR connection, many software products can communicate with the payer through its portal or by fax or phone, while still automating other parts of the process.
The software’s first step is to decide whether prior authorization is needed. This requires having an updated list of the rules that each payer uses for prior authorization. Manually keeping track of payer rules is very time-consuming, but automation uses bots to visit each payer site to look for rules changes. One vendor, Infinitus, uses a voice-based bot called Eva that calls up each payer and speaks with a representative.
“Automatically updating payer rules is not a new technology,” said YiDing Yu, MD, chief product officer at Olive, the automation vendor for New England Baptist. “What is new in the last 5 years is extracting the information needed for the prior authorization out of the clinical notes.”
This is challenging because each doctor has different ways to describe each step of clinical work. To identify this shorthand, Dr. Yu said Olive uses natural language processing, which is a form of artificial intelligence that learns how each doctor describes things.
Dr. Yu asserts that Olive is actually better than a practice’s staff at digging out clinical information. She said staff without much clinical training may miss terms that the software can catch, and they don’t have the time to go back many months into the record to find valuable information. But automation can do that.
In some instances, however, the software may not be able to find the information, in which case it alerts staff through a prompt in the EHR and the information is retrieved manually, Dr. Yu said.
Next, the Olive software puts the information it found into the request form and sends it to the payer. After submission, the software constantly checks on the status of each request, again visiting payer sites with a bot.
At New England Baptist, the software is used mainly by physicians in fairly small private practices who are on staff. They are using the software on the hospital’s dime, but it only works inside the hospital, Ms. Hadzhieva said. For their work outside of the hospital, they would have to purchase the Olive software on their own, she said.
Automation hasn’t spread to practices yet
Despite the promising outcomes for products like Olive, automation software is still primarily used by large organizations. Vendors say very few private practices have bought it yet. “The technology works, but it is still in the early-adopter phase,” Dr. Yu said.
For one thing, the software can be expensive. Very few vendors reveal their prices, but Dr. Yu did so. She said Olive normally costs about $50,000 a year for even a small organization. She insisted, however, that the savings from avoiding just one denial each month for a hip surgery would justify the expense.
On the other hand, some automation software is free, such as the Surescripts product for prior authorization of prescriptions. But it is unclear whether Surescripts does as much as Olive. Vendors’ descriptions of their products tend to be vague.
Also, Surescripts and Olive have entirely separate functions. Dr. Yu said Olive is limited to procedures, so it benefits specialties like oncology, neurosurgery, colorectal surgery, vascular surgery, and cardiology. Olive does not cover prescriptions, because they operate on a different technology.
Dr. Yu said another hurdle for adopting the software is the kind of EHR systems that doctors use. At this point, only a few EHR systems – such as Epic, Cerner, and Athena – are compatible with Olive. Large organizations tend to use Epic and Cerner, while many practices often use Athena or a variety of other systems, she said.
Despite stunted demand, there is no shortage of companies offering automation software for medical (that is, non-prescription) prior authorization. One compilation lists 25 such vendors, including companies like Myndshft, Rhyme, Infinitus, Infinx, and Waystar. As with any start-up technology, companies occasionally buy each other out.
In addition to issues like cost, specialty, and EHR compatibility, another hurdle is that few doctors even know the technology exists. Vendors say marketing focuses on larger provider organizations, not smaller practices.
Even many tech-savvy doctors, like Adam Bruggeman, MD, an orthopedist and CEO of Texas Spine Care Center in San Antonio, say they know little about the technology. “There is definitely a need to automate prior authorization,” he said. “But I don’t know of any colleagues who use it.” He has only just begun to explore vendors, he said.
Many medical practice consultants also have not yet explored the technology. “Automation makes a lot of sense, because there are a lot of repetitive tasks in prior authorization,” said Jill Arena, CEO of Portland, Ore.–based Health e Practices. “But I haven’t looked into it yet, and none of my clients has even asked about it.”
“I could see how it could be an easier sell for large organizations,” she added. “They have an IT person and a CFO who can explore the issue. Smaller practices usually don’t have that kind of expertise.”
Where does automation go from here?
Until now, clinicians who want to fully automate prior authorizations would have to buy two products – one for medical procedures and one for prescriptions. This has to do with incompatible electronic transmission standards, which are used to digitize information, said Susan Lawson-Dawson, content marketing strategist for the vendor Myndshft Health.
Myndshft has long been selling automation software for medical prior authorizations, but now it is introducing a product for prescriptions, Ms. Lawson-Dawson said. She said Myndshft will then be the only vendor to automate both kinds of prior authorizations.
Ms. Lawson-Dawson said Myndshft has 685 customers to date and is looking for more business. Recently the company entered the Google Cloud Marketplace. Google Cloud customers can now direct their committed spend with Google to purchasing Myndshft, meaning they could get it at a discount.
Software like Olive and Myndshft can operate independently of payers, but a vendor called Rhyme depends on payers for its software to function, said Rhyme CEO Joe Anstine. He said more than 300 payers have agreed to install the Rhyme system, and Rhyme has signed up a number of large health systems to use the product. Initially, he said, clinicians paid for the service, but now Rhyme is beginning to find payers to foot the costs and to let clinicians use it for free, which would open Rhyme up to smaller practices.
EHR companies themselves are beginning to offer automation, too. Epic, for example, has created a tool for prior authorization as part of its Epic Payer Platform. Like Rhyme, it requires payer cooperation, because information goes back and forth between clinician and payer in what is called bi-directional exchange.
The Epic product is still in its pilot phase. Epic reported that several large health systems were using its product in conjunction with a specific payer – for instance, Mayo Clinic with Blue Cross and Blue Shield of Minnesota and Ochsner Health with Humana. According to Epic, the arrangement reduced Mayo’s denials due to additional documentation requests by 63% for professional billing.
Automating with just one payer still means the clinician has to deal with manual processes at other payers, but a large clinician could have sufficient volume with that one payer to make the arrangement useful.
Will payers automate prior authorization?
Ultimately, payers may take the automation business away from vendors, offering a free product to all clinicians. But don’t hold your breath. Payers first have to rebuild their electronic systems to accommodate an electronic connection with providers. Even then, some payers might hold back from automating, forcing practices to continue manually processing some prior authorizations.
Efforts are underway, however, to mandate payers to support prior authorization automation. For this to happen, payers would have to revamp their data so that it could be easily read by practices’ EHRs. This would mean adopting a specific interoperability standard called Health Level 7 Fast Healthcare Interoperability Resources (FHIR).
Toward this goal, the Centers for Medicare & Medicaid Services proposes to require payers to adopt FHIR by January 2026. (CMS still has to finalize the rule.) Experts say the two-year ramp-up time is needed because it takes extensive work for payers to translate their data into FHIR.
The only payer so far to switch to FHIR for prior authorization is Regence in Washington state. In a pilot project, it has automated prior authorization with just one provider, MultiCare Connected Care, an accountable care organization (ACO), also in Washington state.
Anna Taylor, associate vice president of population health and value-based care at MultiCare, explained how the arrangement works. “Two separate entities are sharing one operational process,” she told this news organization. “That means they can have a digital conversation back and forth, so it is much easier to resolve prior authorization issues.”
Unlike many vendor products, the Regence service is free. And while the vendors market only to large organizations, most doctors in the MultiCare arrangement are in independent practices. Ms. Taylor said these doctors have been “enthusiastic” about the arrangement.
The results of the pilot are impressive. Ms. Taylor said automation has resulted in a 233% productivity gain for MultiCare clinicians, and 89% of submissions to Regence get an immediate response.
There is a potential downside, however, to working directly with payers. A direct connection to clinicians allows payers to access the doctor’s clinical notes, which could make many doctors uneasy. But Ms. Taylor said Regence only has access to the “discrete data fields” on MultiCare’s EHR dashboard, not to the notes themselves.
The ultimate goal of the Regence-Multicare project is to include more payers and clinicians. Ms. Taylor said two of the 27 other payers that MultiCare works with are “highly interested,” but it would take a lot of work for them to get connected with practices and other clinicians.
Ultimately, payers could offer automation and third-party vendors might then fade away. However, physicians may resist working directly with payers if the arrangement requires full access to their medical records.
A version of this article first appeared on Medscape.com.
‘Diagnosis creep’: Are some AFib patients overtreated?
without those treatments having been validated in those particular groups.
This concern has been highlighted recently in the atrial fibrillation (AF) field, with the recent change in the definition of hypertension in the United States at lower levels of blood pressure causing a lot more patients to become eligible for oral anticoagulation at an earlier stage in their AF course.
U.S. researchers analyzed data from 316,388 patients with AF from the National Cardiovascular Data Registry Practice Innovation and Clinical Excellence outpatient quality improvement registry, and found that at 36 months’ follow-up, 83.5% of patients met the new 130/80 mm Hg definition of hypertension, while only 53.3% met the previous 140/90 mm Hg definition.
The diagnosis of hypertension gives 1 point in the CHA2DS2-VASc score, which is used to determine risk in AF patients, those with scores of 2 or more being eligible for oral anticoagulation.
The researchers report that in patients with an index CHA2DS2-VASc score of 1 (before the hypertension diagnosis), at 36 months, 83% fulfilled the 130/80 mm Hg definition of hypertension while the 140/90 mm Hg definition was met by only 50%, giving a large increase in the number of patients who could qualify for oral anticoagulation therapy.
“While the definition of hypertension has changed in response to landmark clinical trials, CHA2DS2-VASc was validated using an older hypertension definition, with limited ambulatory blood pressure monitoring and higher blood pressure goals for treatment,” the authors state.
“Now, patients with AF will meet the CHA2DS2-VASc threshold for oral anticoagulation earlier in their disease course. However, it is not known if patients with scores of 1 or 2 using the new hypertension definition have sufficient stroke risk to offset the bleeding risk of oral anticoagulation and will receive net clinical benefit,” they point out.
This study was published online as a research letter in JAMA Network Open.
Senior author of the report, Mintu Turakhia, MD, Stanford (Calif.) University/iRhythm Technologies Inc., said AF is a good example of how “diagnosis creep” may lead to patients receiving inappropriate treatment.
“Risk scores derived when risk variables were described in one way are starting to be applied based on a diagnosis made in a totally different way,” he said in an interview. “Diagnosis creep is a problem everywhere in medicine. The goal of this study was to quantify what this means for the new definition of hypertension in the context of risk scoring AF patients for anticoagulation treatment. We are calling attention to this issue so clinicians are aware of possible implications.”
Dr. Turakhia explained that the CHA2DS2-VASc score was formulated based on claims data so there was a record of hypertension on the clinical encounter. That hypertension diagnosis would have been based on the old definition of 140/90 mm Hg.
“But now we apply a label of hypertension in the office every time someone has a measurement of elevated blood pressure – treated or untreated – and the blood pressure threshold for a hypertension diagnosis has changed to 130/80 mm Hg,” he said. “We are asking what this means for risk stratification scores such as CHA2DS2-VASc, and how do we quantify what that means for anticoagulation eligibility?”
He said that while identifying hypertension at lower blood pressures may be beneficial with regard to starting antihypertensive treatment earlier with a consequent reduction in cardiovascular outcomes, when this also affects risk scores that determine treatment for other conditions, as is the case for AF, the case is not so clear.
Dr. Turakhia pointed out that with AF, there are additional factors causing diagnosis creep, including earlier detection of AF and identification of shorter episodes due to the use of higher sensitivity tools to detect abnormal rhythms.
“What about the patient who has been identified as having AF based on just a few seconds found on monitoring and who is aged 65 (so just over the age threshold for 1 point on the CHA2DS2-VASc score)?” he asked. “Now we’re going to throw in hypertension with a blood pressure measurement just over 130/80 mm Hg, and they will be eligible for anticoagulation.”
Dr. Turakhia noted that in addition to earlier classification of hypertension, other conditions contributing to the CHA2DS2-VASc score are also being detected earlier, including diabetes and reduced ejection fractions that are considered heart failure.
“I worry about the sum of the parts. We don’t know if the risk score performs equally well when we’re using these different thresholds. We have to be careful that we are not exposing patients to the bleeding risks of anticoagulation unnecessarily. There is a clear issue here,” he said.
What should clinicians do?
In a comment, Gregory Lip, MD, chair of cardiovascular medicine at the University of Liverpool, England, who helped develop the CHA2DS2-VASc score, said clinicians needed to think more broadly when considering hypertension as a risk factor for the score.
He points out that if a patient had a history of hypertension but is now controlled to below 130/80 mm Hg, they would still be considered to be at risk per the CHA2DS2-VASc score.
And for patients without a history of hypertension, and who have a current blood pressure measurement of around 130/80 mm Hg, Dr. Lip advises that it would be premature to diagnose hypertension immediately.
“Hypertension is not a yes/no diagnosis. If you look at the relationship between blood pressure and risk of stroke, it is like a continual dose-response. It doesn’t mean that at 129/79 there is no stroke risk but that at 130/80 there is a stroke risk. It’s not like that,” he said.
“I wouldn’t make a diagnosis on a one-off blood pressure measurement. I would want to monitor that patient and get them to do home measurements,” he commented. “If someone constantly has levels around that 130/80 mm Hg, I don’t necessarily rush in with a definite diagnosis of hypertension and start drug treatment. I would look at lifestyle first. And in such patients, I wouldn’t give them the 1 point for hypertension on the CHA2DS2-VASc score.”
Dr. Lip points out that a hypertension diagnosis is not just about blood pressure numbers. “We have to assess the patients much more completely before giving them a diagnosis and consider factors such as whether there is evidence of hypertension-related end-organ damage, and if lifestyle issues have been addressed.”
Are new risk scores needed?
Dr. Turakhia agreed that clinicians need to look at the bigger picture, but he also suggested that new risk scores may need to be developed.
“All of us in the medical community need to think about whether we should be recalibrating risk prediction with more contemporary evidence – based on our ability to detect disease now,” he commented.
“This could even be a different risk score altogether, possibly incorporating a wider range of parameters or perhaps incorporating machine learning. That’s really the question we need to be asking ourselves,” Dr. Turakhia added.
Dr. Lip noted that there are many stroke risk factors and only those that are most common and have been well validated go into clinical risk scores such as CHA2DS2-VASc.
“These risks scores are by design simplifications, and only have modest predictive value for identifying patients at high risk of stroke. You can always improve on clinical risk scores by adding in other variables,” he said. “There are some risk scores in AF with 26 variables. But the practical application of these more complex scores can be difficult in clinical practice. These risks scores are meant to be simple so that they can be used by busy clinicians in the outpatient clinic or on a ward round. It is not easy to input 26 different variables.”
He also noted that many guidelines are now veering away from categorizing patients at high, medium, or low risk of stroke, which he refers to as “artificial” classifications. “There is now more of a default position that patients should receive stroke prevention normally with a DOAC [direct oral anticoagulant] unless they are low risk.”
Dr. Turakhia agreed that it is imperative to look at the bigger picture when identifying AF patients for anticoagulation. “We have to be careful not to take things at face value. It is more important than ever to use clinical judgment to avoid overtreatment in borderline situations,” he concluded.
This study was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry. Dr. Turakhia reported employment from iRhythm Technologies; equity from AliveCor, Connect America, Evidently, and Forward; grants from U.S. Food and Drug Administration, American Heart Association, Bayer, Sanofi, Gilead, and Bristol Myers Squibb; and personal fees from Pfizer and JAMA Cardiology (prior associate editor) outside the submitted work. Dr. Lip has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
without those treatments having been validated in those particular groups.
This concern has been highlighted recently in the atrial fibrillation (AF) field, with the recent change in the definition of hypertension in the United States at lower levels of blood pressure causing a lot more patients to become eligible for oral anticoagulation at an earlier stage in their AF course.
U.S. researchers analyzed data from 316,388 patients with AF from the National Cardiovascular Data Registry Practice Innovation and Clinical Excellence outpatient quality improvement registry, and found that at 36 months’ follow-up, 83.5% of patients met the new 130/80 mm Hg definition of hypertension, while only 53.3% met the previous 140/90 mm Hg definition.
The diagnosis of hypertension gives 1 point in the CHA2DS2-VASc score, which is used to determine risk in AF patients, those with scores of 2 or more being eligible for oral anticoagulation.
The researchers report that in patients with an index CHA2DS2-VASc score of 1 (before the hypertension diagnosis), at 36 months, 83% fulfilled the 130/80 mm Hg definition of hypertension while the 140/90 mm Hg definition was met by only 50%, giving a large increase in the number of patients who could qualify for oral anticoagulation therapy.
“While the definition of hypertension has changed in response to landmark clinical trials, CHA2DS2-VASc was validated using an older hypertension definition, with limited ambulatory blood pressure monitoring and higher blood pressure goals for treatment,” the authors state.
“Now, patients with AF will meet the CHA2DS2-VASc threshold for oral anticoagulation earlier in their disease course. However, it is not known if patients with scores of 1 or 2 using the new hypertension definition have sufficient stroke risk to offset the bleeding risk of oral anticoagulation and will receive net clinical benefit,” they point out.
This study was published online as a research letter in JAMA Network Open.
Senior author of the report, Mintu Turakhia, MD, Stanford (Calif.) University/iRhythm Technologies Inc., said AF is a good example of how “diagnosis creep” may lead to patients receiving inappropriate treatment.
“Risk scores derived when risk variables were described in one way are starting to be applied based on a diagnosis made in a totally different way,” he said in an interview. “Diagnosis creep is a problem everywhere in medicine. The goal of this study was to quantify what this means for the new definition of hypertension in the context of risk scoring AF patients for anticoagulation treatment. We are calling attention to this issue so clinicians are aware of possible implications.”
Dr. Turakhia explained that the CHA2DS2-VASc score was formulated based on claims data so there was a record of hypertension on the clinical encounter. That hypertension diagnosis would have been based on the old definition of 140/90 mm Hg.
“But now we apply a label of hypertension in the office every time someone has a measurement of elevated blood pressure – treated or untreated – and the blood pressure threshold for a hypertension diagnosis has changed to 130/80 mm Hg,” he said. “We are asking what this means for risk stratification scores such as CHA2DS2-VASc, and how do we quantify what that means for anticoagulation eligibility?”
He said that while identifying hypertension at lower blood pressures may be beneficial with regard to starting antihypertensive treatment earlier with a consequent reduction in cardiovascular outcomes, when this also affects risk scores that determine treatment for other conditions, as is the case for AF, the case is not so clear.
Dr. Turakhia pointed out that with AF, there are additional factors causing diagnosis creep, including earlier detection of AF and identification of shorter episodes due to the use of higher sensitivity tools to detect abnormal rhythms.
“What about the patient who has been identified as having AF based on just a few seconds found on monitoring and who is aged 65 (so just over the age threshold for 1 point on the CHA2DS2-VASc score)?” he asked. “Now we’re going to throw in hypertension with a blood pressure measurement just over 130/80 mm Hg, and they will be eligible for anticoagulation.”
Dr. Turakhia noted that in addition to earlier classification of hypertension, other conditions contributing to the CHA2DS2-VASc score are also being detected earlier, including diabetes and reduced ejection fractions that are considered heart failure.
“I worry about the sum of the parts. We don’t know if the risk score performs equally well when we’re using these different thresholds. We have to be careful that we are not exposing patients to the bleeding risks of anticoagulation unnecessarily. There is a clear issue here,” he said.
What should clinicians do?
In a comment, Gregory Lip, MD, chair of cardiovascular medicine at the University of Liverpool, England, who helped develop the CHA2DS2-VASc score, said clinicians needed to think more broadly when considering hypertension as a risk factor for the score.
He points out that if a patient had a history of hypertension but is now controlled to below 130/80 mm Hg, they would still be considered to be at risk per the CHA2DS2-VASc score.
And for patients without a history of hypertension, and who have a current blood pressure measurement of around 130/80 mm Hg, Dr. Lip advises that it would be premature to diagnose hypertension immediately.
“Hypertension is not a yes/no diagnosis. If you look at the relationship between blood pressure and risk of stroke, it is like a continual dose-response. It doesn’t mean that at 129/79 there is no stroke risk but that at 130/80 there is a stroke risk. It’s not like that,” he said.
“I wouldn’t make a diagnosis on a one-off blood pressure measurement. I would want to monitor that patient and get them to do home measurements,” he commented. “If someone constantly has levels around that 130/80 mm Hg, I don’t necessarily rush in with a definite diagnosis of hypertension and start drug treatment. I would look at lifestyle first. And in such patients, I wouldn’t give them the 1 point for hypertension on the CHA2DS2-VASc score.”
Dr. Lip points out that a hypertension diagnosis is not just about blood pressure numbers. “We have to assess the patients much more completely before giving them a diagnosis and consider factors such as whether there is evidence of hypertension-related end-organ damage, and if lifestyle issues have been addressed.”
Are new risk scores needed?
Dr. Turakhia agreed that clinicians need to look at the bigger picture, but he also suggested that new risk scores may need to be developed.
“All of us in the medical community need to think about whether we should be recalibrating risk prediction with more contemporary evidence – based on our ability to detect disease now,” he commented.
“This could even be a different risk score altogether, possibly incorporating a wider range of parameters or perhaps incorporating machine learning. That’s really the question we need to be asking ourselves,” Dr. Turakhia added.
Dr. Lip noted that there are many stroke risk factors and only those that are most common and have been well validated go into clinical risk scores such as CHA2DS2-VASc.
“These risks scores are by design simplifications, and only have modest predictive value for identifying patients at high risk of stroke. You can always improve on clinical risk scores by adding in other variables,” he said. “There are some risk scores in AF with 26 variables. But the practical application of these more complex scores can be difficult in clinical practice. These risks scores are meant to be simple so that they can be used by busy clinicians in the outpatient clinic or on a ward round. It is not easy to input 26 different variables.”
He also noted that many guidelines are now veering away from categorizing patients at high, medium, or low risk of stroke, which he refers to as “artificial” classifications. “There is now more of a default position that patients should receive stroke prevention normally with a DOAC [direct oral anticoagulant] unless they are low risk.”
Dr. Turakhia agreed that it is imperative to look at the bigger picture when identifying AF patients for anticoagulation. “We have to be careful not to take things at face value. It is more important than ever to use clinical judgment to avoid overtreatment in borderline situations,” he concluded.
This study was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry. Dr. Turakhia reported employment from iRhythm Technologies; equity from AliveCor, Connect America, Evidently, and Forward; grants from U.S. Food and Drug Administration, American Heart Association, Bayer, Sanofi, Gilead, and Bristol Myers Squibb; and personal fees from Pfizer and JAMA Cardiology (prior associate editor) outside the submitted work. Dr. Lip has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
without those treatments having been validated in those particular groups.
This concern has been highlighted recently in the atrial fibrillation (AF) field, with the recent change in the definition of hypertension in the United States at lower levels of blood pressure causing a lot more patients to become eligible for oral anticoagulation at an earlier stage in their AF course.
U.S. researchers analyzed data from 316,388 patients with AF from the National Cardiovascular Data Registry Practice Innovation and Clinical Excellence outpatient quality improvement registry, and found that at 36 months’ follow-up, 83.5% of patients met the new 130/80 mm Hg definition of hypertension, while only 53.3% met the previous 140/90 mm Hg definition.
The diagnosis of hypertension gives 1 point in the CHA2DS2-VASc score, which is used to determine risk in AF patients, those with scores of 2 or more being eligible for oral anticoagulation.
The researchers report that in patients with an index CHA2DS2-VASc score of 1 (before the hypertension diagnosis), at 36 months, 83% fulfilled the 130/80 mm Hg definition of hypertension while the 140/90 mm Hg definition was met by only 50%, giving a large increase in the number of patients who could qualify for oral anticoagulation therapy.
“While the definition of hypertension has changed in response to landmark clinical trials, CHA2DS2-VASc was validated using an older hypertension definition, with limited ambulatory blood pressure monitoring and higher blood pressure goals for treatment,” the authors state.
“Now, patients with AF will meet the CHA2DS2-VASc threshold for oral anticoagulation earlier in their disease course. However, it is not known if patients with scores of 1 or 2 using the new hypertension definition have sufficient stroke risk to offset the bleeding risk of oral anticoagulation and will receive net clinical benefit,” they point out.
This study was published online as a research letter in JAMA Network Open.
Senior author of the report, Mintu Turakhia, MD, Stanford (Calif.) University/iRhythm Technologies Inc., said AF is a good example of how “diagnosis creep” may lead to patients receiving inappropriate treatment.
“Risk scores derived when risk variables were described in one way are starting to be applied based on a diagnosis made in a totally different way,” he said in an interview. “Diagnosis creep is a problem everywhere in medicine. The goal of this study was to quantify what this means for the new definition of hypertension in the context of risk scoring AF patients for anticoagulation treatment. We are calling attention to this issue so clinicians are aware of possible implications.”
Dr. Turakhia explained that the CHA2DS2-VASc score was formulated based on claims data so there was a record of hypertension on the clinical encounter. That hypertension diagnosis would have been based on the old definition of 140/90 mm Hg.
“But now we apply a label of hypertension in the office every time someone has a measurement of elevated blood pressure – treated or untreated – and the blood pressure threshold for a hypertension diagnosis has changed to 130/80 mm Hg,” he said. “We are asking what this means for risk stratification scores such as CHA2DS2-VASc, and how do we quantify what that means for anticoagulation eligibility?”
He said that while identifying hypertension at lower blood pressures may be beneficial with regard to starting antihypertensive treatment earlier with a consequent reduction in cardiovascular outcomes, when this also affects risk scores that determine treatment for other conditions, as is the case for AF, the case is not so clear.
Dr. Turakhia pointed out that with AF, there are additional factors causing diagnosis creep, including earlier detection of AF and identification of shorter episodes due to the use of higher sensitivity tools to detect abnormal rhythms.
“What about the patient who has been identified as having AF based on just a few seconds found on monitoring and who is aged 65 (so just over the age threshold for 1 point on the CHA2DS2-VASc score)?” he asked. “Now we’re going to throw in hypertension with a blood pressure measurement just over 130/80 mm Hg, and they will be eligible for anticoagulation.”
Dr. Turakhia noted that in addition to earlier classification of hypertension, other conditions contributing to the CHA2DS2-VASc score are also being detected earlier, including diabetes and reduced ejection fractions that are considered heart failure.
“I worry about the sum of the parts. We don’t know if the risk score performs equally well when we’re using these different thresholds. We have to be careful that we are not exposing patients to the bleeding risks of anticoagulation unnecessarily. There is a clear issue here,” he said.
What should clinicians do?
In a comment, Gregory Lip, MD, chair of cardiovascular medicine at the University of Liverpool, England, who helped develop the CHA2DS2-VASc score, said clinicians needed to think more broadly when considering hypertension as a risk factor for the score.
He points out that if a patient had a history of hypertension but is now controlled to below 130/80 mm Hg, they would still be considered to be at risk per the CHA2DS2-VASc score.
And for patients without a history of hypertension, and who have a current blood pressure measurement of around 130/80 mm Hg, Dr. Lip advises that it would be premature to diagnose hypertension immediately.
“Hypertension is not a yes/no diagnosis. If you look at the relationship between blood pressure and risk of stroke, it is like a continual dose-response. It doesn’t mean that at 129/79 there is no stroke risk but that at 130/80 there is a stroke risk. It’s not like that,” he said.
“I wouldn’t make a diagnosis on a one-off blood pressure measurement. I would want to monitor that patient and get them to do home measurements,” he commented. “If someone constantly has levels around that 130/80 mm Hg, I don’t necessarily rush in with a definite diagnosis of hypertension and start drug treatment. I would look at lifestyle first. And in such patients, I wouldn’t give them the 1 point for hypertension on the CHA2DS2-VASc score.”
Dr. Lip points out that a hypertension diagnosis is not just about blood pressure numbers. “We have to assess the patients much more completely before giving them a diagnosis and consider factors such as whether there is evidence of hypertension-related end-organ damage, and if lifestyle issues have been addressed.”
Are new risk scores needed?
Dr. Turakhia agreed that clinicians need to look at the bigger picture, but he also suggested that new risk scores may need to be developed.
“All of us in the medical community need to think about whether we should be recalibrating risk prediction with more contemporary evidence – based on our ability to detect disease now,” he commented.
“This could even be a different risk score altogether, possibly incorporating a wider range of parameters or perhaps incorporating machine learning. That’s really the question we need to be asking ourselves,” Dr. Turakhia added.
Dr. Lip noted that there are many stroke risk factors and only those that are most common and have been well validated go into clinical risk scores such as CHA2DS2-VASc.
“These risks scores are by design simplifications, and only have modest predictive value for identifying patients at high risk of stroke. You can always improve on clinical risk scores by adding in other variables,” he said. “There are some risk scores in AF with 26 variables. But the practical application of these more complex scores can be difficult in clinical practice. These risks scores are meant to be simple so that they can be used by busy clinicians in the outpatient clinic or on a ward round. It is not easy to input 26 different variables.”
He also noted that many guidelines are now veering away from categorizing patients at high, medium, or low risk of stroke, which he refers to as “artificial” classifications. “There is now more of a default position that patients should receive stroke prevention normally with a DOAC [direct oral anticoagulant] unless they are low risk.”
Dr. Turakhia agreed that it is imperative to look at the bigger picture when identifying AF patients for anticoagulation. “We have to be careful not to take things at face value. It is more important than ever to use clinical judgment to avoid overtreatment in borderline situations,” he concluded.
This study was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry. Dr. Turakhia reported employment from iRhythm Technologies; equity from AliveCor, Connect America, Evidently, and Forward; grants from U.S. Food and Drug Administration, American Heart Association, Bayer, Sanofi, Gilead, and Bristol Myers Squibb; and personal fees from Pfizer and JAMA Cardiology (prior associate editor) outside the submitted work. Dr. Lip has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
CKD linked to cardiac arrest in Hispanic, Latinx patients
TOPLINE:
new data show, suggesting early identification of CKD may provide an opportunity to reduce the risk in these groups. Other predictors included heavy drinking, atrial fibrillation, coronary artery disease, heart failure and diabetes.
METHODOLOGY:
- The study included 295 Hispanic or Latinx patients with out-of-hospital SCA from the PRESTO study in Ventura County, California, and 590 frequency-matched controls from the San Diego site of the population-based HCHS/SOL (Hispanic Community Health Survey/Study of Latinos); in both cohorts, men made up 70% of participants, and the median age was about 63 years.
- Researchers collected data on demographics, medical history, and current health conditions. Of note, 51.2% of SCA cases and 8.8% of control participants had CKD, and 20.0% of cases and 0.7% of the control group were on dialysis.
- Pre-SCA echocardiograms were available for 48% of SCA cases and baseline echocardiograms for more than 99% of control participants.
TAKEAWAY:
- In analyses adjusted for age, sex, and clinical variables, predictors significantly associated with higher odds of SCA included: CKD (odds ratio, 7.3; 95% confidence interval, 3.8-14.3; P < .001), heavy drinking (OR, 4.5), stroke (OR, 3.1), atrial fibrillation (OR, 3.7), coronary artery disease (OR, 2.9), heart failure (OR, 2.5), and diabetes (OR, 1.5).
- Hypertension, hyperlipemia, body mass index, and current smoking status were not significantly associated with SCA.
- In adjusted analyses, heart rate (OR, 1.8 per one standard deviation [1-SD] increase), QTc interval (OR, 2.5 per 1-SD increase) and left ventricular ejection fraction (OR, 4.4 per 1-SD decrease) were significantly associated with SCA, suggesting echocardiogram evaluations could help identify Hispanic or Latinx individuals at increased risk for SCA, wrote the authors.
IN PRACTICE:
“Our study, the first to include feasible numbers of Hispanic or Latino individuals, highlights the importance of renal dysfunction as a risk factor for SCA in the community,” the authors wrote, adding that early identification and management of chronic kidney disease could reduce risk for SCA in this population.
SOURCE:
The study was conducted by Kyndaron Reinier, PhD, MPH, Cedars-Sinai Health System, Los Angeles, and colleagues. It was published online in the Journal of the American Heart Association.
LIMITATIONS:
Most participants from the HCHS/SOL study were born outside the United States, compared with about half the SCA cases, which could have influenced cardiovascular disease risk, although results did not change considerably when models were adjusted for place of birth. Study participants were predominantly of Mexican heritage, so results may not be generalizable to Hispanic or Latinx individuals from other regions. As medical history was assessed differently in the two studies, there could be some error in estimating the strength of associations. Results from echocardiographic data should be viewed as hypothesis generating because of the potential for residual bias.
DISCLOSURES:
The Ventura PRESTO study was funded, in part, by the National Institutes of Health, and National Heart, Lung, and Blood Institute. The HCHS/SOL was carried out as a collaborative study supported by contracts from the NHLBI.
A version of this article first appeared on Medscape.com.
TOPLINE:
new data show, suggesting early identification of CKD may provide an opportunity to reduce the risk in these groups. Other predictors included heavy drinking, atrial fibrillation, coronary artery disease, heart failure and diabetes.
METHODOLOGY:
- The study included 295 Hispanic or Latinx patients with out-of-hospital SCA from the PRESTO study in Ventura County, California, and 590 frequency-matched controls from the San Diego site of the population-based HCHS/SOL (Hispanic Community Health Survey/Study of Latinos); in both cohorts, men made up 70% of participants, and the median age was about 63 years.
- Researchers collected data on demographics, medical history, and current health conditions. Of note, 51.2% of SCA cases and 8.8% of control participants had CKD, and 20.0% of cases and 0.7% of the control group were on dialysis.
- Pre-SCA echocardiograms were available for 48% of SCA cases and baseline echocardiograms for more than 99% of control participants.
TAKEAWAY:
- In analyses adjusted for age, sex, and clinical variables, predictors significantly associated with higher odds of SCA included: CKD (odds ratio, 7.3; 95% confidence interval, 3.8-14.3; P < .001), heavy drinking (OR, 4.5), stroke (OR, 3.1), atrial fibrillation (OR, 3.7), coronary artery disease (OR, 2.9), heart failure (OR, 2.5), and diabetes (OR, 1.5).
- Hypertension, hyperlipemia, body mass index, and current smoking status were not significantly associated with SCA.
- In adjusted analyses, heart rate (OR, 1.8 per one standard deviation [1-SD] increase), QTc interval (OR, 2.5 per 1-SD increase) and left ventricular ejection fraction (OR, 4.4 per 1-SD decrease) were significantly associated with SCA, suggesting echocardiogram evaluations could help identify Hispanic or Latinx individuals at increased risk for SCA, wrote the authors.
IN PRACTICE:
“Our study, the first to include feasible numbers of Hispanic or Latino individuals, highlights the importance of renal dysfunction as a risk factor for SCA in the community,” the authors wrote, adding that early identification and management of chronic kidney disease could reduce risk for SCA in this population.
SOURCE:
The study was conducted by Kyndaron Reinier, PhD, MPH, Cedars-Sinai Health System, Los Angeles, and colleagues. It was published online in the Journal of the American Heart Association.
LIMITATIONS:
Most participants from the HCHS/SOL study were born outside the United States, compared with about half the SCA cases, which could have influenced cardiovascular disease risk, although results did not change considerably when models were adjusted for place of birth. Study participants were predominantly of Mexican heritage, so results may not be generalizable to Hispanic or Latinx individuals from other regions. As medical history was assessed differently in the two studies, there could be some error in estimating the strength of associations. Results from echocardiographic data should be viewed as hypothesis generating because of the potential for residual bias.
DISCLOSURES:
The Ventura PRESTO study was funded, in part, by the National Institutes of Health, and National Heart, Lung, and Blood Institute. The HCHS/SOL was carried out as a collaborative study supported by contracts from the NHLBI.
A version of this article first appeared on Medscape.com.
TOPLINE:
new data show, suggesting early identification of CKD may provide an opportunity to reduce the risk in these groups. Other predictors included heavy drinking, atrial fibrillation, coronary artery disease, heart failure and diabetes.
METHODOLOGY:
- The study included 295 Hispanic or Latinx patients with out-of-hospital SCA from the PRESTO study in Ventura County, California, and 590 frequency-matched controls from the San Diego site of the population-based HCHS/SOL (Hispanic Community Health Survey/Study of Latinos); in both cohorts, men made up 70% of participants, and the median age was about 63 years.
- Researchers collected data on demographics, medical history, and current health conditions. Of note, 51.2% of SCA cases and 8.8% of control participants had CKD, and 20.0% of cases and 0.7% of the control group were on dialysis.
- Pre-SCA echocardiograms were available for 48% of SCA cases and baseline echocardiograms for more than 99% of control participants.
TAKEAWAY:
- In analyses adjusted for age, sex, and clinical variables, predictors significantly associated with higher odds of SCA included: CKD (odds ratio, 7.3; 95% confidence interval, 3.8-14.3; P < .001), heavy drinking (OR, 4.5), stroke (OR, 3.1), atrial fibrillation (OR, 3.7), coronary artery disease (OR, 2.9), heart failure (OR, 2.5), and diabetes (OR, 1.5).
- Hypertension, hyperlipemia, body mass index, and current smoking status were not significantly associated with SCA.
- In adjusted analyses, heart rate (OR, 1.8 per one standard deviation [1-SD] increase), QTc interval (OR, 2.5 per 1-SD increase) and left ventricular ejection fraction (OR, 4.4 per 1-SD decrease) were significantly associated with SCA, suggesting echocardiogram evaluations could help identify Hispanic or Latinx individuals at increased risk for SCA, wrote the authors.
IN PRACTICE:
“Our study, the first to include feasible numbers of Hispanic or Latino individuals, highlights the importance of renal dysfunction as a risk factor for SCA in the community,” the authors wrote, adding that early identification and management of chronic kidney disease could reduce risk for SCA in this population.
SOURCE:
The study was conducted by Kyndaron Reinier, PhD, MPH, Cedars-Sinai Health System, Los Angeles, and colleagues. It was published online in the Journal of the American Heart Association.
LIMITATIONS:
Most participants from the HCHS/SOL study were born outside the United States, compared with about half the SCA cases, which could have influenced cardiovascular disease risk, although results did not change considerably when models were adjusted for place of birth. Study participants were predominantly of Mexican heritage, so results may not be generalizable to Hispanic or Latinx individuals from other regions. As medical history was assessed differently in the two studies, there could be some error in estimating the strength of associations. Results from echocardiographic data should be viewed as hypothesis generating because of the potential for residual bias.
DISCLOSURES:
The Ventura PRESTO study was funded, in part, by the National Institutes of Health, and National Heart, Lung, and Blood Institute. The HCHS/SOL was carried out as a collaborative study supported by contracts from the NHLBI.
A version of this article first appeared on Medscape.com.
Suits or joggers? A doctor’s dress code
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
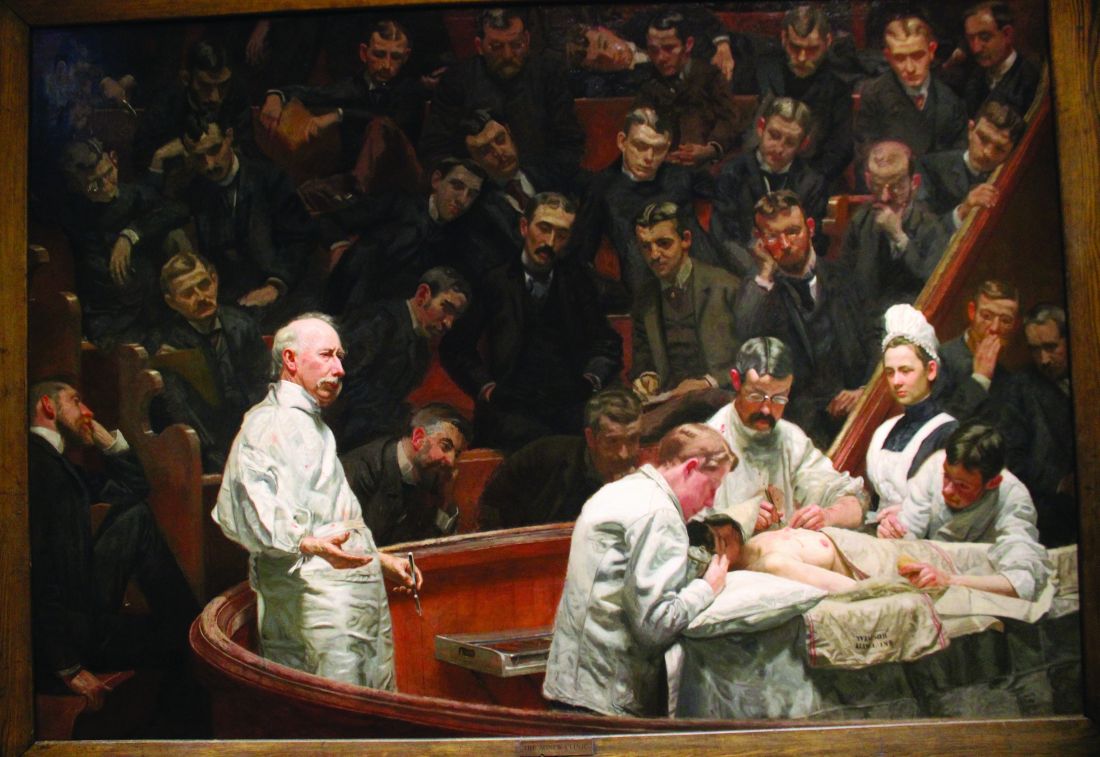
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
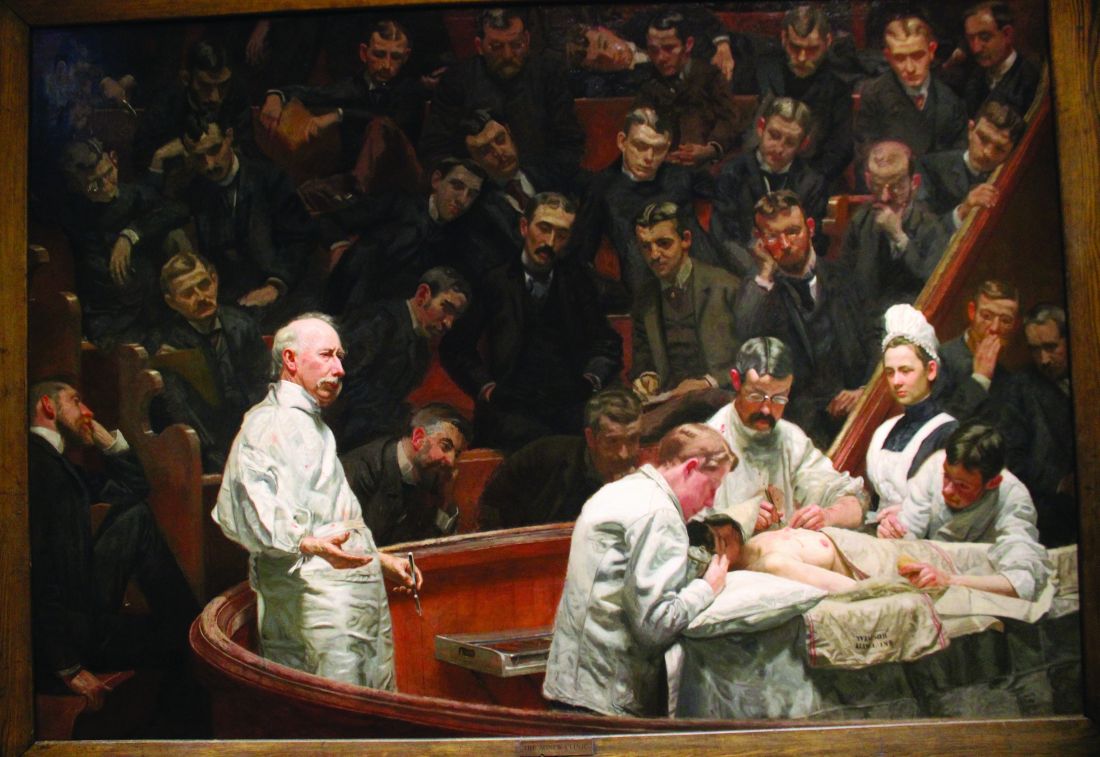
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
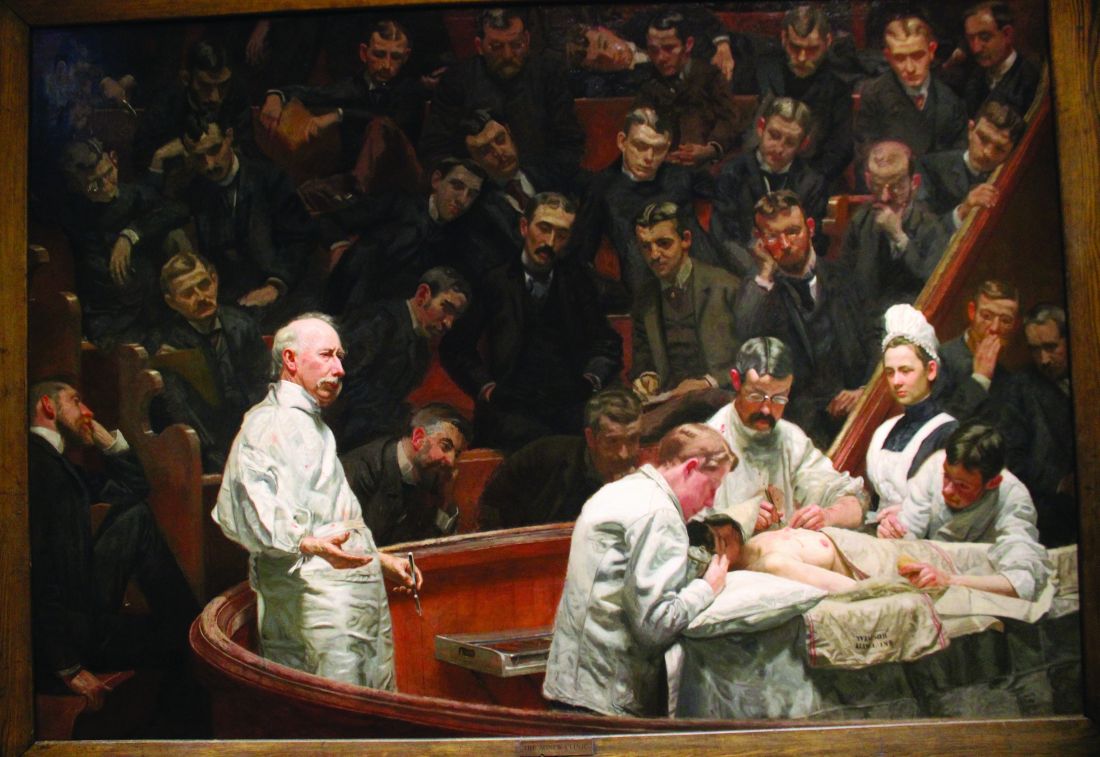
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Trials say start sacubitril-valsartan in hospital in HF with ‘below normal’ LVEF
CLEVELAND – suggests a combined analysis of two major studies.
Short-term risk for cardiovascular (CV) death or HF hospitalization fell 30% for such patients put on the angiotensin-receptor/neprilysin inhibitor (ARNI) at that early stage, compared with those assigned to receive an ACE inhibitor or angiotensin receptor blocker (ARB).
Of note, the risk-reduction benefit reached 41% among the overwhelming majority of patients with a left ventricular ejection fraction (LVEF) of 60% or lower across the two trials, PIONEER-HF and PARAGLIDE-HF. No such significant benefit was seen in patients with higher LVEF.
The prespecified analysis of 1,347 patients medically stabilized after a “worsening-HF event” was reported by Robert J. Mentz, MD, Duke Clinical Research Institute, Durham, N.C., at the annual scientific meeting of the Heart Failure Society of America.
Across both studies, levels of the prognostically telling biomarker NT-proBNP dropped further in the ARNI group, by almost a fourth, compared with those getting an ACE inhibitor or ARB. The difference emerged within a week and was “similar and consistent” throughout at least 8 weeks of follow-up, Dr. Mentz said.
Sacubitril-valsartan is approved in the United States for chronic HF, broadly but with labeling suggesting clearer efficacy at lower LVEF levels, based on the PARADIGM-HF and PARAGON-HF trials.
The PIONEER-HF and PARAGLIDE-HF trials lending patients to the current analysis demonstrated superiority for the drug vs. an ACE inhibitor or ARB when started in hospital in stabilized patients with HF.
Cautions about starting sacubitril-valsartan
In the pooled analysis, patients on sacubitril-valsartan were more likely to experience symptomatic hypotension, with a relative risk for drug’s known potential side effect reaching 1.35 (95% confidence interval, 1.05-1.72), compared with ACE inhibitor or ARB recipients.
But the hypotension risk when starting the drug is manageable to some extent, observed Dr. Mentz. “We can safely start sacubitril-valsartan in the hospital or early post discharge, but we need to make sure their volume status is okay” and keep track of their blood pressure trajectory, he told this news organization.
Those with initially low BP, unsurprisingly, seem more susceptible to the problem, Dr. Mentz said. In such patients “on antihypertensives or other therapies that aren’t going to give them a clinical outcome benefit,” those meds can be withdrawn or their dosages reduced before sacubitril-valsartan is added.
Such cautions are an “important take-home message” of the analysis, observed invited discussant Carolyn S. P. Lam, MBBS, PhD, National Heart Centre, Singapore, after the Dr. Mentz presentation.
Sacubitril-valsartan should be started only in stabilized patients, she emphasized. It should be delayed in those “with ongoing adjustments of antihypertensives, diuretics, and so on,” in whom premature initiation of the drug may promote symptomatic hypotension. Should that happen, Dr. Lam cautioned, there’s a risk that such patients would be “mislabeled as intolerant” of the ARNI and so wouldn’t be started on it later.
The pooled PIONEER-HF and PARAGLIDE-HF analysis, Dr. Lam proposed, might also help overcome the “clinical inertia and fear” that is slowing the uptake of early guideline-directed drug therapy initiation in patients hospitalized with HF.
LVEF spectrum across two studies
As Dr. Mentz reported, the analysis included 881 and 466 patients from PIONEER-HF and PARAGLIDE-HF, respectively. Of the total, 673 were assigned to receive valsartan and 674 to receive either enalapril or valsartan. Overall, 36% of the population were women.
Patients in PIONEER-HF, with an LVEF 40% or lower, were started on their assigned drug during an acute-HF hospitalization and followed a median of 8 weeks. PARAGLIDE-HF patients, with LVEF higher than 40%, started therapy either in hospital (in 70% of cases) or within 30 days of their HF event; they were followed a median of 6 months.
Hazard ratios for outcomes in the sacubitril-valsartan group vs. those on ACE inhibitors or ARBs were 0.76; 95% CI, 0.69-0.83; P < .0001 for change in NT-proBNP levels. For the composite of CV death or HF hospitalization, HRs were as follows:
- 0.70 (95% CI, 0.54-0.91; P = .0077) overall.
- 0.59 (95% CI, 0.44-0.79) for LVEF < 60%.
- 1.53 (95% CI, 0.80-2.91) for LVEF > 60%.
Current guidelines, Dr. Mentz noted, recommend that sacubitril-valsartan “be initiated de novo” predischarge in patients without contraindications who are hospitalized with acute HF with reduced LVEF. The combined analysis of PIONEER-HF and PARAGLIDE-HF, he said, potentially extends the recommendation “across the ejection fraction spectrum.”
Dr. Mentz has received research support and honoraria from Abbott, American Regent, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Boston Scientific, Cytokinetics, Fast BioMedical, Gilead, Innolife, Eli Lilly, Medtronic, Medable, Merck, Novartis, Novo Nordisk, Pfizer, Pharmacosmos, Relypsa, Respicardia, Roche, Sanofi, Vifor, Windtree Therapeutics, and Zoll. Dr. Lam has reported financial relationships “with more than 25 pharmaceutical or device manufacturers, many of which produce therapies for heart failure,” as well as with Medscape/WebMD Global LLC.
A version of this article first appeared on Medscape.com.
CLEVELAND – suggests a combined analysis of two major studies.
Short-term risk for cardiovascular (CV) death or HF hospitalization fell 30% for such patients put on the angiotensin-receptor/neprilysin inhibitor (ARNI) at that early stage, compared with those assigned to receive an ACE inhibitor or angiotensin receptor blocker (ARB).
Of note, the risk-reduction benefit reached 41% among the overwhelming majority of patients with a left ventricular ejection fraction (LVEF) of 60% or lower across the two trials, PIONEER-HF and PARAGLIDE-HF. No such significant benefit was seen in patients with higher LVEF.
The prespecified analysis of 1,347 patients medically stabilized after a “worsening-HF event” was reported by Robert J. Mentz, MD, Duke Clinical Research Institute, Durham, N.C., at the annual scientific meeting of the Heart Failure Society of America.
Across both studies, levels of the prognostically telling biomarker NT-proBNP dropped further in the ARNI group, by almost a fourth, compared with those getting an ACE inhibitor or ARB. The difference emerged within a week and was “similar and consistent” throughout at least 8 weeks of follow-up, Dr. Mentz said.
Sacubitril-valsartan is approved in the United States for chronic HF, broadly but with labeling suggesting clearer efficacy at lower LVEF levels, based on the PARADIGM-HF and PARAGON-HF trials.
The PIONEER-HF and PARAGLIDE-HF trials lending patients to the current analysis demonstrated superiority for the drug vs. an ACE inhibitor or ARB when started in hospital in stabilized patients with HF.
Cautions about starting sacubitril-valsartan
In the pooled analysis, patients on sacubitril-valsartan were more likely to experience symptomatic hypotension, with a relative risk for drug’s known potential side effect reaching 1.35 (95% confidence interval, 1.05-1.72), compared with ACE inhibitor or ARB recipients.
But the hypotension risk when starting the drug is manageable to some extent, observed Dr. Mentz. “We can safely start sacubitril-valsartan in the hospital or early post discharge, but we need to make sure their volume status is okay” and keep track of their blood pressure trajectory, he told this news organization.
Those with initially low BP, unsurprisingly, seem more susceptible to the problem, Dr. Mentz said. In such patients “on antihypertensives or other therapies that aren’t going to give them a clinical outcome benefit,” those meds can be withdrawn or their dosages reduced before sacubitril-valsartan is added.
Such cautions are an “important take-home message” of the analysis, observed invited discussant Carolyn S. P. Lam, MBBS, PhD, National Heart Centre, Singapore, after the Dr. Mentz presentation.
Sacubitril-valsartan should be started only in stabilized patients, she emphasized. It should be delayed in those “with ongoing adjustments of antihypertensives, diuretics, and so on,” in whom premature initiation of the drug may promote symptomatic hypotension. Should that happen, Dr. Lam cautioned, there’s a risk that such patients would be “mislabeled as intolerant” of the ARNI and so wouldn’t be started on it later.
The pooled PIONEER-HF and PARAGLIDE-HF analysis, Dr. Lam proposed, might also help overcome the “clinical inertia and fear” that is slowing the uptake of early guideline-directed drug therapy initiation in patients hospitalized with HF.
LVEF spectrum across two studies
As Dr. Mentz reported, the analysis included 881 and 466 patients from PIONEER-HF and PARAGLIDE-HF, respectively. Of the total, 673 were assigned to receive valsartan and 674 to receive either enalapril or valsartan. Overall, 36% of the population were women.
Patients in PIONEER-HF, with an LVEF 40% or lower, were started on their assigned drug during an acute-HF hospitalization and followed a median of 8 weeks. PARAGLIDE-HF patients, with LVEF higher than 40%, started therapy either in hospital (in 70% of cases) or within 30 days of their HF event; they were followed a median of 6 months.
Hazard ratios for outcomes in the sacubitril-valsartan group vs. those on ACE inhibitors or ARBs were 0.76; 95% CI, 0.69-0.83; P < .0001 for change in NT-proBNP levels. For the composite of CV death or HF hospitalization, HRs were as follows:
- 0.70 (95% CI, 0.54-0.91; P = .0077) overall.
- 0.59 (95% CI, 0.44-0.79) for LVEF < 60%.
- 1.53 (95% CI, 0.80-2.91) for LVEF > 60%.
Current guidelines, Dr. Mentz noted, recommend that sacubitril-valsartan “be initiated de novo” predischarge in patients without contraindications who are hospitalized with acute HF with reduced LVEF. The combined analysis of PIONEER-HF and PARAGLIDE-HF, he said, potentially extends the recommendation “across the ejection fraction spectrum.”
Dr. Mentz has received research support and honoraria from Abbott, American Regent, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Boston Scientific, Cytokinetics, Fast BioMedical, Gilead, Innolife, Eli Lilly, Medtronic, Medable, Merck, Novartis, Novo Nordisk, Pfizer, Pharmacosmos, Relypsa, Respicardia, Roche, Sanofi, Vifor, Windtree Therapeutics, and Zoll. Dr. Lam has reported financial relationships “with more than 25 pharmaceutical or device manufacturers, many of which produce therapies for heart failure,” as well as with Medscape/WebMD Global LLC.
A version of this article first appeared on Medscape.com.
CLEVELAND – suggests a combined analysis of two major studies.
Short-term risk for cardiovascular (CV) death or HF hospitalization fell 30% for such patients put on the angiotensin-receptor/neprilysin inhibitor (ARNI) at that early stage, compared with those assigned to receive an ACE inhibitor or angiotensin receptor blocker (ARB).
Of note, the risk-reduction benefit reached 41% among the overwhelming majority of patients with a left ventricular ejection fraction (LVEF) of 60% or lower across the two trials, PIONEER-HF and PARAGLIDE-HF. No such significant benefit was seen in patients with higher LVEF.
The prespecified analysis of 1,347 patients medically stabilized after a “worsening-HF event” was reported by Robert J. Mentz, MD, Duke Clinical Research Institute, Durham, N.C., at the annual scientific meeting of the Heart Failure Society of America.
Across both studies, levels of the prognostically telling biomarker NT-proBNP dropped further in the ARNI group, by almost a fourth, compared with those getting an ACE inhibitor or ARB. The difference emerged within a week and was “similar and consistent” throughout at least 8 weeks of follow-up, Dr. Mentz said.
Sacubitril-valsartan is approved in the United States for chronic HF, broadly but with labeling suggesting clearer efficacy at lower LVEF levels, based on the PARADIGM-HF and PARAGON-HF trials.
The PIONEER-HF and PARAGLIDE-HF trials lending patients to the current analysis demonstrated superiority for the drug vs. an ACE inhibitor or ARB when started in hospital in stabilized patients with HF.
Cautions about starting sacubitril-valsartan
In the pooled analysis, patients on sacubitril-valsartan were more likely to experience symptomatic hypotension, with a relative risk for drug’s known potential side effect reaching 1.35 (95% confidence interval, 1.05-1.72), compared with ACE inhibitor or ARB recipients.
But the hypotension risk when starting the drug is manageable to some extent, observed Dr. Mentz. “We can safely start sacubitril-valsartan in the hospital or early post discharge, but we need to make sure their volume status is okay” and keep track of their blood pressure trajectory, he told this news organization.
Those with initially low BP, unsurprisingly, seem more susceptible to the problem, Dr. Mentz said. In such patients “on antihypertensives or other therapies that aren’t going to give them a clinical outcome benefit,” those meds can be withdrawn or their dosages reduced before sacubitril-valsartan is added.
Such cautions are an “important take-home message” of the analysis, observed invited discussant Carolyn S. P. Lam, MBBS, PhD, National Heart Centre, Singapore, after the Dr. Mentz presentation.
Sacubitril-valsartan should be started only in stabilized patients, she emphasized. It should be delayed in those “with ongoing adjustments of antihypertensives, diuretics, and so on,” in whom premature initiation of the drug may promote symptomatic hypotension. Should that happen, Dr. Lam cautioned, there’s a risk that such patients would be “mislabeled as intolerant” of the ARNI and so wouldn’t be started on it later.
The pooled PIONEER-HF and PARAGLIDE-HF analysis, Dr. Lam proposed, might also help overcome the “clinical inertia and fear” that is slowing the uptake of early guideline-directed drug therapy initiation in patients hospitalized with HF.
LVEF spectrum across two studies
As Dr. Mentz reported, the analysis included 881 and 466 patients from PIONEER-HF and PARAGLIDE-HF, respectively. Of the total, 673 were assigned to receive valsartan and 674 to receive either enalapril or valsartan. Overall, 36% of the population were women.
Patients in PIONEER-HF, with an LVEF 40% or lower, were started on their assigned drug during an acute-HF hospitalization and followed a median of 8 weeks. PARAGLIDE-HF patients, with LVEF higher than 40%, started therapy either in hospital (in 70% of cases) or within 30 days of their HF event; they were followed a median of 6 months.
Hazard ratios for outcomes in the sacubitril-valsartan group vs. those on ACE inhibitors or ARBs were 0.76; 95% CI, 0.69-0.83; P < .0001 for change in NT-proBNP levels. For the composite of CV death or HF hospitalization, HRs were as follows:
- 0.70 (95% CI, 0.54-0.91; P = .0077) overall.
- 0.59 (95% CI, 0.44-0.79) for LVEF < 60%.
- 1.53 (95% CI, 0.80-2.91) for LVEF > 60%.
Current guidelines, Dr. Mentz noted, recommend that sacubitril-valsartan “be initiated de novo” predischarge in patients without contraindications who are hospitalized with acute HF with reduced LVEF. The combined analysis of PIONEER-HF and PARAGLIDE-HF, he said, potentially extends the recommendation “across the ejection fraction spectrum.”
Dr. Mentz has received research support and honoraria from Abbott, American Regent, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Boston Scientific, Cytokinetics, Fast BioMedical, Gilead, Innolife, Eli Lilly, Medtronic, Medable, Merck, Novartis, Novo Nordisk, Pfizer, Pharmacosmos, Relypsa, Respicardia, Roche, Sanofi, Vifor, Windtree Therapeutics, and Zoll. Dr. Lam has reported financial relationships “with more than 25 pharmaceutical or device manufacturers, many of which produce therapies for heart failure,” as well as with Medscape/WebMD Global LLC.
A version of this article first appeared on Medscape.com.
AT HFSA 2023
New tool to guide transcatheter aortic valve replacement
TOPLINE:
, results of a new study suggest.
Researchers developed TJ-ICE–guided TAVR to facilitate implanting a heart valve at an optimal depth, guided by direct visualization of the membranous septum (MS) during the procedure.
METHODOLOGY:
- The single-center study included 163 patients with severe aortic stenosis (AS) from an ongoing registry, mean age 85 years, 71% women, and median Society of Thoracic Surgeons score of 6.3%, who underwent TAVR.
- The primary endpoint was the incidence at 30 days of PPMI; secondary endpoints included the feasibility of TJ-ICE–guided TAVR and safety, including complications related to TJ-ICE.
TAKEAWAY:
- Although all patients underwent valve placement in the proper anatomical location, moderate paravalvular leakage (PVL) occurred in four patients, and a second valve was required in two patients, resulting in a device success of 96.3%.
- New PPMI within 30 days was required in 11 patients (6.7%), all because of complete atrioventricular block; patients with baseline right bundle branch block (RBBB) had a higher incidence of new PPMI than did those without RBBB (23.8% vs. 4.2%; P < .001).
- Patients whose device was implanted inside the MS had a significantly lower incidence of new PPMI (overall 2.1% vs. 13.4%; P = .005); this finding was consistent in patients with baseline RBBB (6.7% vs. 66.7%; P = .004) or without RBBB (1.2% vs. 8.2%; P = .041).
- By 30 days, there was one death, which occurred as a result of bleeding in a patient with liver cirrhosis after a successful TAVR procedure; four patients experienced disabling strokes, and vascular complications developed in 16 patients.
IN PRACTICE:
The study demonstrated the “notable feasibility and safety” of TJ-ICE–guided TAVR, the authors write. They point to the “strong association of TAV position with new PPMI rate, which was clearly visualized by ICE during the procedure.”
In an accompanying editorial, Thomas Bartel, MD, PHD, Flexdoc Inc., Düsseldorf, Germany, noted that the study is the first to report a clinical benefit using a TJ-ICE approach, although barriers such as cost and lack of expertise could prevent interventional cardiologists from taking full advantage of ICE monitoring during TAVR, and further research is warranted.
Randomized and prospective trials comparing the accuracy, reproducibility, and outcomes of ICE guidance vs. guidance by transesophageal echocardiography, and pure fluoroscopy and angiography, “need to be performed before ICE imaging is adopted as the primary nonradiographic imaging modality for TAVR.”
SOURCE:
The study was carried out by Tsutomu Murakami, MD, department of cardiology, Tokai University, Isehara, Japan, and colleagues. It was published online in JACC: Asia.
LIMITATIONS:
The retrospective nonrandomized design has inherent limitations. The choice of intraprocedural imaging modality was decided based on heart team discussion, which may have introduced selection bias. Operators’ implantation skills could have influenced the results although most cases involved highly experienced board-certified operators. The limited number of subjects and the relatively low event rates preclude definitive conclusions.
DISCLOSURES:
Dr. Murakami has no relevant conflicts of interest; see paper for disclosures of other study authors. Dr. Bartel has no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
, results of a new study suggest.
Researchers developed TJ-ICE–guided TAVR to facilitate implanting a heart valve at an optimal depth, guided by direct visualization of the membranous septum (MS) during the procedure.
METHODOLOGY:
- The single-center study included 163 patients with severe aortic stenosis (AS) from an ongoing registry, mean age 85 years, 71% women, and median Society of Thoracic Surgeons score of 6.3%, who underwent TAVR.
- The primary endpoint was the incidence at 30 days of PPMI; secondary endpoints included the feasibility of TJ-ICE–guided TAVR and safety, including complications related to TJ-ICE.
TAKEAWAY:
- Although all patients underwent valve placement in the proper anatomical location, moderate paravalvular leakage (PVL) occurred in four patients, and a second valve was required in two patients, resulting in a device success of 96.3%.
- New PPMI within 30 days was required in 11 patients (6.7%), all because of complete atrioventricular block; patients with baseline right bundle branch block (RBBB) had a higher incidence of new PPMI than did those without RBBB (23.8% vs. 4.2%; P < .001).
- Patients whose device was implanted inside the MS had a significantly lower incidence of new PPMI (overall 2.1% vs. 13.4%; P = .005); this finding was consistent in patients with baseline RBBB (6.7% vs. 66.7%; P = .004) or without RBBB (1.2% vs. 8.2%; P = .041).
- By 30 days, there was one death, which occurred as a result of bleeding in a patient with liver cirrhosis after a successful TAVR procedure; four patients experienced disabling strokes, and vascular complications developed in 16 patients.
IN PRACTICE:
The study demonstrated the “notable feasibility and safety” of TJ-ICE–guided TAVR, the authors write. They point to the “strong association of TAV position with new PPMI rate, which was clearly visualized by ICE during the procedure.”
In an accompanying editorial, Thomas Bartel, MD, PHD, Flexdoc Inc., Düsseldorf, Germany, noted that the study is the first to report a clinical benefit using a TJ-ICE approach, although barriers such as cost and lack of expertise could prevent interventional cardiologists from taking full advantage of ICE monitoring during TAVR, and further research is warranted.
Randomized and prospective trials comparing the accuracy, reproducibility, and outcomes of ICE guidance vs. guidance by transesophageal echocardiography, and pure fluoroscopy and angiography, “need to be performed before ICE imaging is adopted as the primary nonradiographic imaging modality for TAVR.”
SOURCE:
The study was carried out by Tsutomu Murakami, MD, department of cardiology, Tokai University, Isehara, Japan, and colleagues. It was published online in JACC: Asia.
LIMITATIONS:
The retrospective nonrandomized design has inherent limitations. The choice of intraprocedural imaging modality was decided based on heart team discussion, which may have introduced selection bias. Operators’ implantation skills could have influenced the results although most cases involved highly experienced board-certified operators. The limited number of subjects and the relatively low event rates preclude definitive conclusions.
DISCLOSURES:
Dr. Murakami has no relevant conflicts of interest; see paper for disclosures of other study authors. Dr. Bartel has no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
, results of a new study suggest.
Researchers developed TJ-ICE–guided TAVR to facilitate implanting a heart valve at an optimal depth, guided by direct visualization of the membranous septum (MS) during the procedure.
METHODOLOGY:
- The single-center study included 163 patients with severe aortic stenosis (AS) from an ongoing registry, mean age 85 years, 71% women, and median Society of Thoracic Surgeons score of 6.3%, who underwent TAVR.
- The primary endpoint was the incidence at 30 days of PPMI; secondary endpoints included the feasibility of TJ-ICE–guided TAVR and safety, including complications related to TJ-ICE.
TAKEAWAY:
- Although all patients underwent valve placement in the proper anatomical location, moderate paravalvular leakage (PVL) occurred in four patients, and a second valve was required in two patients, resulting in a device success of 96.3%.
- New PPMI within 30 days was required in 11 patients (6.7%), all because of complete atrioventricular block; patients with baseline right bundle branch block (RBBB) had a higher incidence of new PPMI than did those without RBBB (23.8% vs. 4.2%; P < .001).
- Patients whose device was implanted inside the MS had a significantly lower incidence of new PPMI (overall 2.1% vs. 13.4%; P = .005); this finding was consistent in patients with baseline RBBB (6.7% vs. 66.7%; P = .004) or without RBBB (1.2% vs. 8.2%; P = .041).
- By 30 days, there was one death, which occurred as a result of bleeding in a patient with liver cirrhosis after a successful TAVR procedure; four patients experienced disabling strokes, and vascular complications developed in 16 patients.
IN PRACTICE:
The study demonstrated the “notable feasibility and safety” of TJ-ICE–guided TAVR, the authors write. They point to the “strong association of TAV position with new PPMI rate, which was clearly visualized by ICE during the procedure.”
In an accompanying editorial, Thomas Bartel, MD, PHD, Flexdoc Inc., Düsseldorf, Germany, noted that the study is the first to report a clinical benefit using a TJ-ICE approach, although barriers such as cost and lack of expertise could prevent interventional cardiologists from taking full advantage of ICE monitoring during TAVR, and further research is warranted.
Randomized and prospective trials comparing the accuracy, reproducibility, and outcomes of ICE guidance vs. guidance by transesophageal echocardiography, and pure fluoroscopy and angiography, “need to be performed before ICE imaging is adopted as the primary nonradiographic imaging modality for TAVR.”
SOURCE:
The study was carried out by Tsutomu Murakami, MD, department of cardiology, Tokai University, Isehara, Japan, and colleagues. It was published online in JACC: Asia.
LIMITATIONS:
The retrospective nonrandomized design has inherent limitations. The choice of intraprocedural imaging modality was decided based on heart team discussion, which may have introduced selection bias. Operators’ implantation skills could have influenced the results although most cases involved highly experienced board-certified operators. The limited number of subjects and the relatively low event rates preclude definitive conclusions.
DISCLOSURES:
Dr. Murakami has no relevant conflicts of interest; see paper for disclosures of other study authors. Dr. Bartel has no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
EMA warns that omega-3-acid ethyl esters may cause AFib
In its September meeting, the Should atrial fibrillation develop, intake of the medication must be stopped permanently.
Omega-3-acid ethyl esters are used to treat hypertriglyceridemia if lifestyle changes, particularly those related to nutrition, have not been sufficient to lower the blood triglyceride level. Hypertriglyceridemia is a risk factor for coronary heart disease.
During a Periodic Safety Update Single Assessment Procedure, the EMA safety committee analyzed systematic overviews and meta-analyses of randomized, controlled clinical studies. Experts found a dose-dependent increase in the risk for atrial fibrillation in patients with cardiovascular diseases or cardiovascular risk factors who were being treated with omega-3-acid ethyl esters, compared with those treated with placebo. The observed risk was at its highest at a dose of 4 g/d.
The PRAC will recommend an update to the Summary of Product Characteristics for preparations that contain omega-3-acid ethyl esters. The aim is to inform physicians, pharmacists, and patients of the risk for atrial fibrillation. A notification will be sent to health care professionals soon to inform them of further details.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
In its September meeting, the Should atrial fibrillation develop, intake of the medication must be stopped permanently.
Omega-3-acid ethyl esters are used to treat hypertriglyceridemia if lifestyle changes, particularly those related to nutrition, have not been sufficient to lower the blood triglyceride level. Hypertriglyceridemia is a risk factor for coronary heart disease.
During a Periodic Safety Update Single Assessment Procedure, the EMA safety committee analyzed systematic overviews and meta-analyses of randomized, controlled clinical studies. Experts found a dose-dependent increase in the risk for atrial fibrillation in patients with cardiovascular diseases or cardiovascular risk factors who were being treated with omega-3-acid ethyl esters, compared with those treated with placebo. The observed risk was at its highest at a dose of 4 g/d.
The PRAC will recommend an update to the Summary of Product Characteristics for preparations that contain omega-3-acid ethyl esters. The aim is to inform physicians, pharmacists, and patients of the risk for atrial fibrillation. A notification will be sent to health care professionals soon to inform them of further details.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
In its September meeting, the Should atrial fibrillation develop, intake of the medication must be stopped permanently.
Omega-3-acid ethyl esters are used to treat hypertriglyceridemia if lifestyle changes, particularly those related to nutrition, have not been sufficient to lower the blood triglyceride level. Hypertriglyceridemia is a risk factor for coronary heart disease.
During a Periodic Safety Update Single Assessment Procedure, the EMA safety committee analyzed systematic overviews and meta-analyses of randomized, controlled clinical studies. Experts found a dose-dependent increase in the risk for atrial fibrillation in patients with cardiovascular diseases or cardiovascular risk factors who were being treated with omega-3-acid ethyl esters, compared with those treated with placebo. The observed risk was at its highest at a dose of 4 g/d.
The PRAC will recommend an update to the Summary of Product Characteristics for preparations that contain omega-3-acid ethyl esters. The aim is to inform physicians, pharmacists, and patients of the risk for atrial fibrillation. A notification will be sent to health care professionals soon to inform them of further details.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.



