User login
Penile Paraffinoma: Dramatic Recurrence After Surgical Resection
To the Editor:
The term paraffinoma refers to a chronic granulomatous response to injection of paraffin, silicone, or other mineral oils into skin and soft tissue. Paraffinomas develop when the material is injected into the skin for cosmetic purposes to augment or enhance one’s appearance. Although they may occur in any location, the most common sites include the breasts and buttocks. The penis is a rare but emerging site for paraffinomas.1-3 We present a rare case of recurrence of a penile paraffinoma following surgical resection.
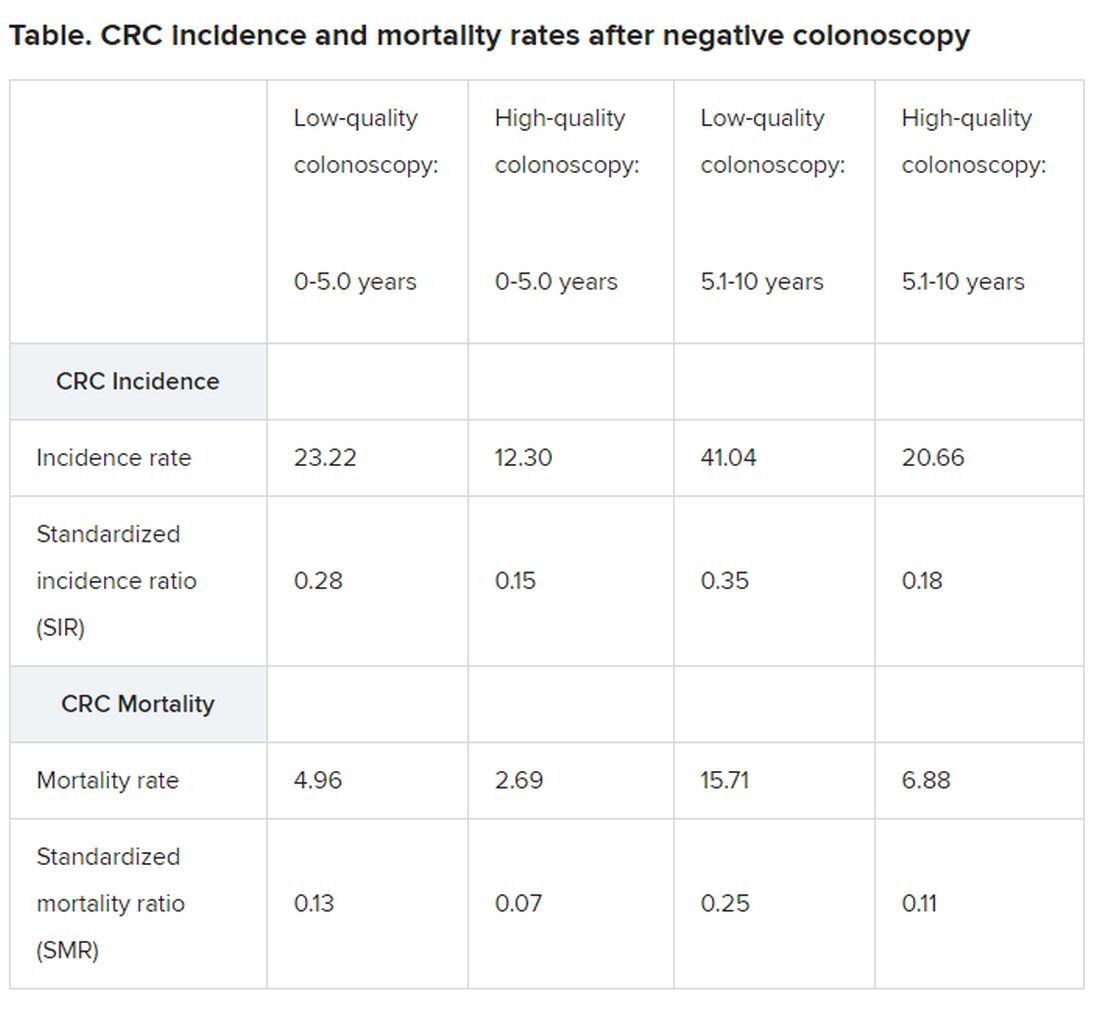
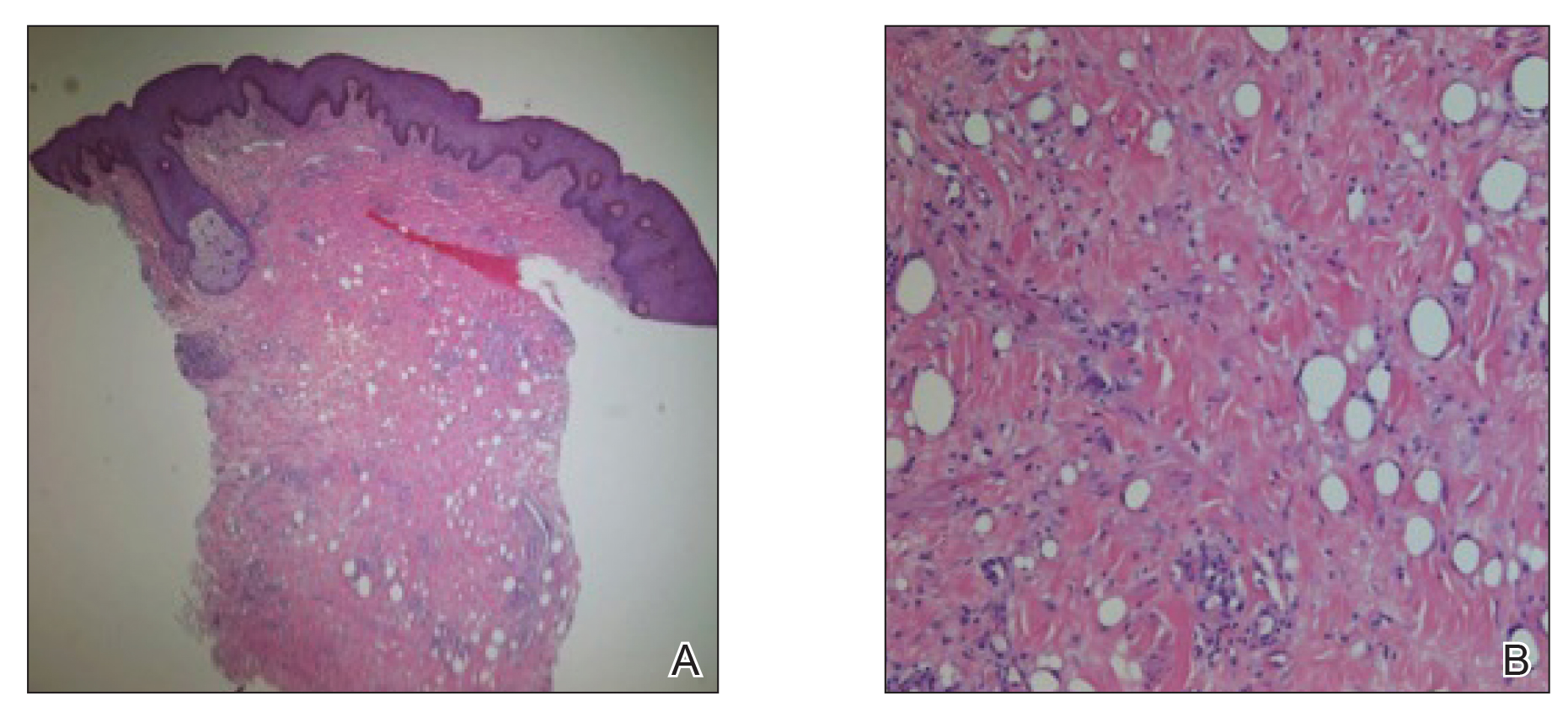
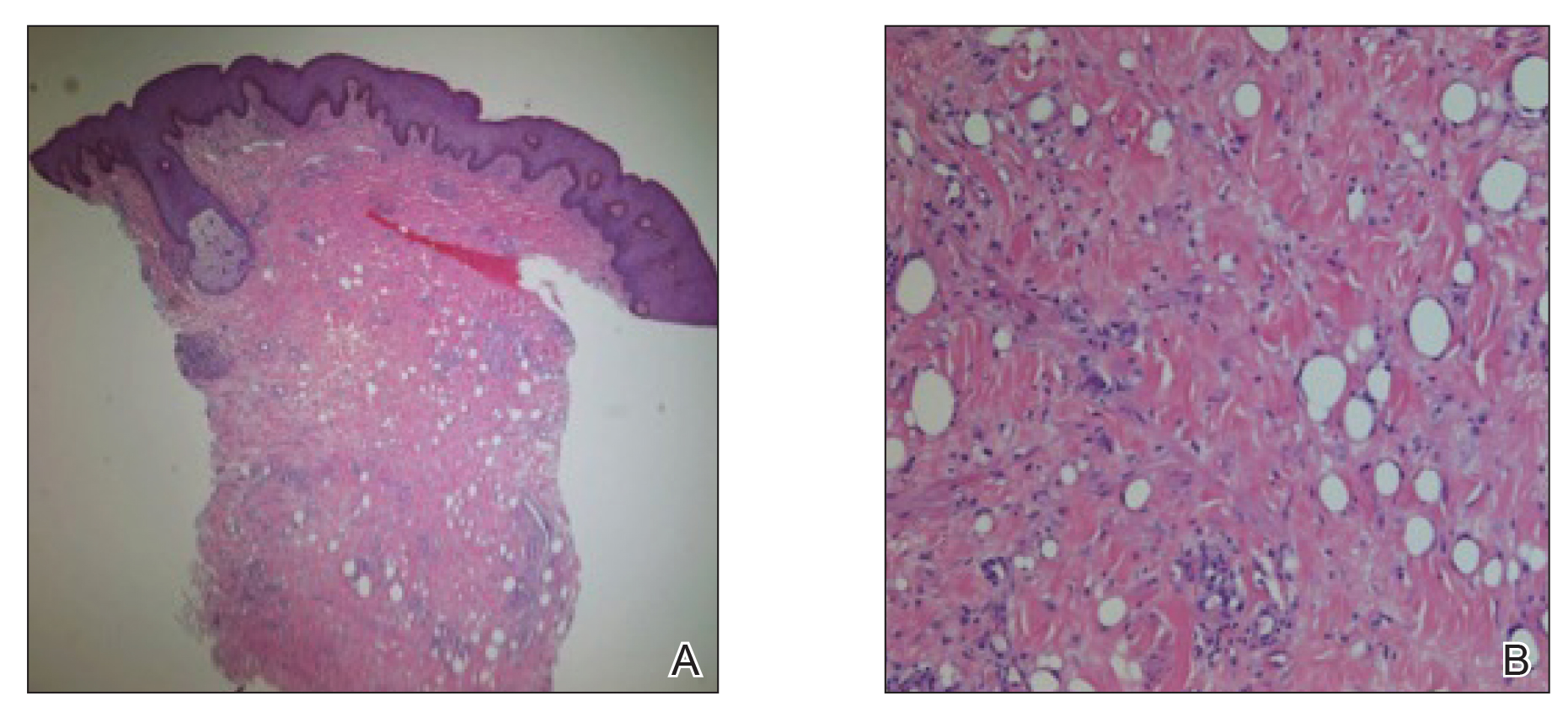
A 26-year-old uncircumcised Trinidadian man presented with a 5-cm, exquisitely tender tumor involving the penile shaft and median raphe that rapidly evolved over the course of 3 weeks (Figure 1). He presented with inability to urinate, attain an erection, or ambulate without notable tenderness. Additionally, he developed swelling of the penis and surrounding tissue. He had no other medical comorbidities; however, 1 year prior he presented to a urologist with a 1-cm nodule involving the median raphe that was surgically resected and required circumcision. Biopsy at the time of his surgical procedure revealed an exuberant foreign body giant cell reaction with surrounding empty spaces in the dermis resembling Swiss cheese, consistent with a paraffinoma (Figure 2). The recurrent tumor, which was 5 times the size of the initial nodule, was biopsied. Again, histopathologic findings were consistent with a paraffinoma with extensive dermal fibrosis and absence of polarizable material.

The patient underwent extensive reconstructive surgery requiring skin grafting to the penile shaft. Given the size and location of this recurrent tumor with the ability to destroy vital urologic and reproductive function, consideration for prevention of recurrent episodes included novel therapeutic treatment options to suppress inflammation and fibrosis with doxycycline and nicotinamide.
Paraffin injections are used for cosmetic enhancement and most often occur in a nonclinical setting without medical supervision, as they are not US Food and Drug Administration–approved medical injectable materials. Examples of oils injected include paraffin, camphorated oil, cottonseed or sesame oil, mineral oil, petroleum jelly, and beeswax. These oils are not hydrolyzed by tissue lipases but are instead treated as a foreign body substance with subsequent granuloma formation (also known as sclerosing lipogranuloma), which can occur many years after injection.4 The granulomatous response may be observed months to years after injection. The paraffinoma normally affects the injection site; however, regional lymphadenopathy and systemic disease has been reported.2 Histopathologic findings are characteristic and consist of a foreign body giant cell reaction, variably sized round to oval cavities within the dermis, and varying degrees of dermal fibrosis.5
In 1899, mineral oil was first injected into male genitalia to restore architecture in a patient’s testicles following bilateral orchiectomy. After the success of this endeavor, mineral oil injections were used as filler for other defects.3 However, by 1906 the complications of these injections became public knowledge when 2 patients developed subcutaneous nodules after receiving injections for facial wrinkles.2 Despite public knowledge of these complications, penile paraffin injections continued to occur both in medical and eventually nonmedical settings.
In 1947, Quérnu and Pérol6 described 6 penile paraffinoma cases outside the United States. Patients had petroleum jelly injections that eventuated in penile paraffinomas, and all of them lost the ability to attain an erection.6 Four years later, Bradley and Ehrgott7 described a case of penile paraffinoma likely caused by application of paraffin in association with occupational exposure. In 1956, May and Pickering8 cited a case of penile paraffinoma affecting the entire penile shaft in which the patient had undergone paraffin injection 7 years prior to treat premature ejaculation. Unfortunately, the injection resulted in a painful and unsatisfactory erection without resolution of premature ejaculation.8 Lee et al9 analyzed 26 cases of penile paraffinomas that occurred from 1981 to 1993. They found that all patients underwent injections of paraffin or petroleum jelly performed by nonmedical personnel with the predominant goal of enhancing penis size. Within 18.5 months of injection, 19 patients already experienced tenderness at the injection site. The remaining 7 patients experienced penile skin discoloration and abnormal contouring of the penis. Biopsy specimens revealed hyaline necrosis of subcutaneous adipose septa, cystlike spaces throughout involved tissue, and macrophages engulfing adipose tissue were found near blood vessels.9 In 2007, Eandi et al4 reported a case of penile paraffinoma with a 40-year delay of onset. Four years later, Manny et al10 reported penile paraffinomas in 3 Laotian men who injected a mineral oil.
Currently, paraffin injections are uncommon but still are being performed in some countries in Eastern Europe and the Far East11; they rarely are reported in the United States. Injections can occur in unusual sites such as the knee, and paraffinomas can develop many years after the procedure.12 Additionally, paraffinomas can obscure proper diagnosis of carcinomas, as described by Lee et al13 in a case in which a cervical paraffin injection confounded the diagnosis of a thyroid tumor. Furthermore, these injections usually are performed by nonmedical personnel and typically are repeated multiple times to reach cosmetic goals, rendering the patient vulnerable to early complications including allergic reactions, paraphimosis, infection, and inflammation.3
The clinical presentation of a penile paraffinoma may be a mimicker of several different entities, which are important to consider in the evaluation of a presenting patient. Infectious etiologies must be considered including lymphogranuloma venereum, granuloma inguinale, atypical mycobacteria, lupus vulgaris, and sexually transmitted infections. Importantly, neoplasms must be ruled out including squamous cell carcinoma, soft tissue sarcomas, melanoma, adenocarcinoma, or metastasis. Lymphedema, prior surgical procedures, trauma, and inflammatory etiologies also are in the differential diagnosis.14 Nonetheless, physicians must have a high clinical suspicion in the evaluation of a possible paraffinoma, as patients may not be forthcoming with relevant clinical history regarding a prior injection to the affected site, particularly if the injection occurred many years ago. As such, the patient may not consider this history relevant or may not even remember the event occurred, as was observed in our case. Furthermore, embarrassment, social taboo, and stigma may be associated with the behavior of undergoing injections in nonclinical settings without medical supervision.15
Patients may be motivated to undergo dangerous procedures to potentially alter their appearance due to perceived enhanced sexual ability, influence by loved ones, cultural rituals, and societal pressure.15,16 Furthermore, patients may not be aware of the material being injected or the volume. Given that these injections often are used with the goal of cosmetic enhancement, biopsies in cosmetically sensitive areas must be given careful consideration, and a thorough clinical history must support the decision to pursue a biopsy to obtain a definitive diagnosis.
The definitive diagnosis of a paraffinoma is determined by histopathology. However, the use of imaging modalities such as magnetic resonance imaging and computed tomography have been employed to delineate the extent of involvement. Imaging studies allow for surgical planning and may assist in narrowing a differential diagnosis.17 Currently, wide and complete surgical resection is the only definitive treatment of paraffinomas, including penile paraffinomas, as there is no evidence of spontaneous regression.3 A report of a reconstructive surgery involving penile resurfacing without T-style anastomosis has been found effective at preventing necrosis of the ventral penile skin. Not all paraffinomas behave similarly, and there is no reliable method to determine which paraffinoma may possess a more aggressive clinical course compared to those which have a more indolent course.18 As such, early detection is critical in the management of paraffinomas, especially in anatomic locations where tissue preservation is of utmost importance. In the case of a large penile paraffinoma with the ability to destroy vital urologic and reproductive function, physicians must consider prevention of recurrent episodes through suppression of inflammation and fibrosis with doxycycline and nicotinamide.19 Other medical treatments reported with varying success include corticosteroids, imiquimod, and isotretinoin.19-24 Employing adjunctive medical treatment may decrease the size of the mass, reducing the surgical defect size and preserving tissue vitality. Ultimately, the most crucial aspect in treatment is prevention, as injection of foreign materials elicits a foreign body response and can lead to notable morbidity.
- De Siati M, Selvaggio O, Di Fino G, et al. An unusual delayed complication of paraffin self-injection for penile girth augmentation. BMC Urol. 2013;13:66.
- Sejben I, Rácz A, Svébis M, et al. Petroleum jelly-induced penile paraffinoma with inguinal lymphadenitis mimicking incarcerated inguinal hernia. Can Urol Assoc J. 2012;6:E137-E139.
- Bayraktar N, Basar I. Penile paraffinoma [published online September 17, 2012]. Case Rep Urol. 2012;2012:202840.
- Eandi JA, Yao AP, Javidan J. Penile paraffinoma: the delayed presentation. Int Urol Nephrol. 2007;29:553-555.
- HirshBCJohnsonWC. Pathology of granulomatous diseases. foreign body granulomas. Int J Dermatol. 1984;23:531-538.
- Quérnu J, Pérol E. Paraffinomas of the penis. J Chir Par. 1947;63:345.
- Bradley, RH, Ehrgott WA. Paraffinoma of the penis: case report. J Urol. 1951;65:453.
- May JA, Pickering PP. Paraffinoma of the penis. Calif Med. 1956;85:42-44.
Yonsei Med J. 1994;35:344-348. - Lee T, Choi HR, Lee YT, et al. Paraffinoma of the penis.
- Manny T, Pettus J, Hemal A, et al. Penile sclerosing lipogranulomas and disfigurement from use of “1Super Extenze” among Laotian immigrants. J Sex Med. 2011;8:3505-3510.
- Akkus E Paraffinoma and ulcer of the external genitalia after self-injection of vaseline. J Sex Med. 2006;3:170-172.
- Grassetti L, Lazzeri D, Torresetti M, et al. Paraffinoma of the knee 60 years after primary infection. Arch Plast Surg. 2013;40:789-790.
- Lee YS, Son EJ, Kim BW, et al. Difficult evaluation of thyroid cancer due to cervical paraffin injection. J Korean Surg Soc. 2011;81(suppl 1):S17-S20.
- Gómez-Armayones S, Penín R, Marcoval J. Penile paraffinoma [in Spanish]. Actas Dermosifiliogr. 2014;105:957-959.
- Moon DG, Yoo JW, Bae JH, et al. Sexual function and psychological characteristics of penile paraffinoma. Asian J Androl. 2003;5:191-194.
- Pehlivanov G, Kavaklieva S, Kazandjieva J, et al. Foreign-body granuloma of the penis in sexually active individuals (penile paraffinoma). J Eur Acad Dermatol Venereol. 2008;22:845-851.
- Cormio L, Di Fino G, Scavone C, et al. Magnetic resonance imaging of penile paraffinoma: case report. BMC Med Imaging. 2014;14:39.
- Shin YS, Zhao C, Park JK. New reconstructive surgery for penile paraffinoma to prevent necrosis of ventral penile skin. Urology. 2013;81:437-441.
- Feldmann R, Harms M, Chavaz P, et al. Orbital and palpebral paraffinoma. J Am Acad Dermatol. 1992;26:833-835.
- MastruserioDNPesqueiraMJCobbMW. Severe granulomatous reaction and facial ulceration occurring after subcutaneous silicone injection. J Am Acad Dermatol. 1996;34:849-852.
- HoWS Management of paraffinoma of the breast. Br J Plast Surg. 2001;54:232-234.
- LloretPSuccessful treatment of granulomatous reactions secondary to injection of esthetic implants. Dermatol Surg. 2005;31:486-490.
- RosenbergEThree cases of penile paraffinoma. Urology. 2007;70:372.
- Baumann LS, Halem ML. Lip silicone granulomatous foreign body reaction treated with Aldara (imiquimod 5%). Dermatol Surg. 2003;29:429-432.
To the Editor:
The term paraffinoma refers to a chronic granulomatous response to injection of paraffin, silicone, or other mineral oils into skin and soft tissue. Paraffinomas develop when the material is injected into the skin for cosmetic purposes to augment or enhance one’s appearance. Although they may occur in any location, the most common sites include the breasts and buttocks. The penis is a rare but emerging site for paraffinomas.1-3 We present a rare case of recurrence of a penile paraffinoma following surgical resection.
A 26-year-old uncircumcised Trinidadian man presented with a 5-cm, exquisitely tender tumor involving the penile shaft and median raphe that rapidly evolved over the course of 3 weeks (Figure 1). He presented with inability to urinate, attain an erection, or ambulate without notable tenderness. Additionally, he developed swelling of the penis and surrounding tissue. He had no other medical comorbidities; however, 1 year prior he presented to a urologist with a 1-cm nodule involving the median raphe that was surgically resected and required circumcision. Biopsy at the time of his surgical procedure revealed an exuberant foreign body giant cell reaction with surrounding empty spaces in the dermis resembling Swiss cheese, consistent with a paraffinoma (Figure 2). The recurrent tumor, which was 5 times the size of the initial nodule, was biopsied. Again, histopathologic findings were consistent with a paraffinoma with extensive dermal fibrosis and absence of polarizable material.

The patient underwent extensive reconstructive surgery requiring skin grafting to the penile shaft. Given the size and location of this recurrent tumor with the ability to destroy vital urologic and reproductive function, consideration for prevention of recurrent episodes included novel therapeutic treatment options to suppress inflammation and fibrosis with doxycycline and nicotinamide.
Paraffin injections are used for cosmetic enhancement and most often occur in a nonclinical setting without medical supervision, as they are not US Food and Drug Administration–approved medical injectable materials. Examples of oils injected include paraffin, camphorated oil, cottonseed or sesame oil, mineral oil, petroleum jelly, and beeswax. These oils are not hydrolyzed by tissue lipases but are instead treated as a foreign body substance with subsequent granuloma formation (also known as sclerosing lipogranuloma), which can occur many years after injection.4 The granulomatous response may be observed months to years after injection. The paraffinoma normally affects the injection site; however, regional lymphadenopathy and systemic disease has been reported.2 Histopathologic findings are characteristic and consist of a foreign body giant cell reaction, variably sized round to oval cavities within the dermis, and varying degrees of dermal fibrosis.5
In 1899, mineral oil was first injected into male genitalia to restore architecture in a patient’s testicles following bilateral orchiectomy. After the success of this endeavor, mineral oil injections were used as filler for other defects.3 However, by 1906 the complications of these injections became public knowledge when 2 patients developed subcutaneous nodules after receiving injections for facial wrinkles.2 Despite public knowledge of these complications, penile paraffin injections continued to occur both in medical and eventually nonmedical settings.
In 1947, Quérnu and Pérol6 described 6 penile paraffinoma cases outside the United States. Patients had petroleum jelly injections that eventuated in penile paraffinomas, and all of them lost the ability to attain an erection.6 Four years later, Bradley and Ehrgott7 described a case of penile paraffinoma likely caused by application of paraffin in association with occupational exposure. In 1956, May and Pickering8 cited a case of penile paraffinoma affecting the entire penile shaft in which the patient had undergone paraffin injection 7 years prior to treat premature ejaculation. Unfortunately, the injection resulted in a painful and unsatisfactory erection without resolution of premature ejaculation.8 Lee et al9 analyzed 26 cases of penile paraffinomas that occurred from 1981 to 1993. They found that all patients underwent injections of paraffin or petroleum jelly performed by nonmedical personnel with the predominant goal of enhancing penis size. Within 18.5 months of injection, 19 patients already experienced tenderness at the injection site. The remaining 7 patients experienced penile skin discoloration and abnormal contouring of the penis. Biopsy specimens revealed hyaline necrosis of subcutaneous adipose septa, cystlike spaces throughout involved tissue, and macrophages engulfing adipose tissue were found near blood vessels.9 In 2007, Eandi et al4 reported a case of penile paraffinoma with a 40-year delay of onset. Four years later, Manny et al10 reported penile paraffinomas in 3 Laotian men who injected a mineral oil.
Currently, paraffin injections are uncommon but still are being performed in some countries in Eastern Europe and the Far East11; they rarely are reported in the United States. Injections can occur in unusual sites such as the knee, and paraffinomas can develop many years after the procedure.12 Additionally, paraffinomas can obscure proper diagnosis of carcinomas, as described by Lee et al13 in a case in which a cervical paraffin injection confounded the diagnosis of a thyroid tumor. Furthermore, these injections usually are performed by nonmedical personnel and typically are repeated multiple times to reach cosmetic goals, rendering the patient vulnerable to early complications including allergic reactions, paraphimosis, infection, and inflammation.3
The clinical presentation of a penile paraffinoma may be a mimicker of several different entities, which are important to consider in the evaluation of a presenting patient. Infectious etiologies must be considered including lymphogranuloma venereum, granuloma inguinale, atypical mycobacteria, lupus vulgaris, and sexually transmitted infections. Importantly, neoplasms must be ruled out including squamous cell carcinoma, soft tissue sarcomas, melanoma, adenocarcinoma, or metastasis. Lymphedema, prior surgical procedures, trauma, and inflammatory etiologies also are in the differential diagnosis.14 Nonetheless, physicians must have a high clinical suspicion in the evaluation of a possible paraffinoma, as patients may not be forthcoming with relevant clinical history regarding a prior injection to the affected site, particularly if the injection occurred many years ago. As such, the patient may not consider this history relevant or may not even remember the event occurred, as was observed in our case. Furthermore, embarrassment, social taboo, and stigma may be associated with the behavior of undergoing injections in nonclinical settings without medical supervision.15
Patients may be motivated to undergo dangerous procedures to potentially alter their appearance due to perceived enhanced sexual ability, influence by loved ones, cultural rituals, and societal pressure.15,16 Furthermore, patients may not be aware of the material being injected or the volume. Given that these injections often are used with the goal of cosmetic enhancement, biopsies in cosmetically sensitive areas must be given careful consideration, and a thorough clinical history must support the decision to pursue a biopsy to obtain a definitive diagnosis.
The definitive diagnosis of a paraffinoma is determined by histopathology. However, the use of imaging modalities such as magnetic resonance imaging and computed tomography have been employed to delineate the extent of involvement. Imaging studies allow for surgical planning and may assist in narrowing a differential diagnosis.17 Currently, wide and complete surgical resection is the only definitive treatment of paraffinomas, including penile paraffinomas, as there is no evidence of spontaneous regression.3 A report of a reconstructive surgery involving penile resurfacing without T-style anastomosis has been found effective at preventing necrosis of the ventral penile skin. Not all paraffinomas behave similarly, and there is no reliable method to determine which paraffinoma may possess a more aggressive clinical course compared to those which have a more indolent course.18 As such, early detection is critical in the management of paraffinomas, especially in anatomic locations where tissue preservation is of utmost importance. In the case of a large penile paraffinoma with the ability to destroy vital urologic and reproductive function, physicians must consider prevention of recurrent episodes through suppression of inflammation and fibrosis with doxycycline and nicotinamide.19 Other medical treatments reported with varying success include corticosteroids, imiquimod, and isotretinoin.19-24 Employing adjunctive medical treatment may decrease the size of the mass, reducing the surgical defect size and preserving tissue vitality. Ultimately, the most crucial aspect in treatment is prevention, as injection of foreign materials elicits a foreign body response and can lead to notable morbidity.
To the Editor:
The term paraffinoma refers to a chronic granulomatous response to injection of paraffin, silicone, or other mineral oils into skin and soft tissue. Paraffinomas develop when the material is injected into the skin for cosmetic purposes to augment or enhance one’s appearance. Although they may occur in any location, the most common sites include the breasts and buttocks. The penis is a rare but emerging site for paraffinomas.1-3 We present a rare case of recurrence of a penile paraffinoma following surgical resection.
A 26-year-old uncircumcised Trinidadian man presented with a 5-cm, exquisitely tender tumor involving the penile shaft and median raphe that rapidly evolved over the course of 3 weeks (Figure 1). He presented with inability to urinate, attain an erection, or ambulate without notable tenderness. Additionally, he developed swelling of the penis and surrounding tissue. He had no other medical comorbidities; however, 1 year prior he presented to a urologist with a 1-cm nodule involving the median raphe that was surgically resected and required circumcision. Biopsy at the time of his surgical procedure revealed an exuberant foreign body giant cell reaction with surrounding empty spaces in the dermis resembling Swiss cheese, consistent with a paraffinoma (Figure 2). The recurrent tumor, which was 5 times the size of the initial nodule, was biopsied. Again, histopathologic findings were consistent with a paraffinoma with extensive dermal fibrosis and absence of polarizable material.

The patient underwent extensive reconstructive surgery requiring skin grafting to the penile shaft. Given the size and location of this recurrent tumor with the ability to destroy vital urologic and reproductive function, consideration for prevention of recurrent episodes included novel therapeutic treatment options to suppress inflammation and fibrosis with doxycycline and nicotinamide.
Paraffin injections are used for cosmetic enhancement and most often occur in a nonclinical setting without medical supervision, as they are not US Food and Drug Administration–approved medical injectable materials. Examples of oils injected include paraffin, camphorated oil, cottonseed or sesame oil, mineral oil, petroleum jelly, and beeswax. These oils are not hydrolyzed by tissue lipases but are instead treated as a foreign body substance with subsequent granuloma formation (also known as sclerosing lipogranuloma), which can occur many years after injection.4 The granulomatous response may be observed months to years after injection. The paraffinoma normally affects the injection site; however, regional lymphadenopathy and systemic disease has been reported.2 Histopathologic findings are characteristic and consist of a foreign body giant cell reaction, variably sized round to oval cavities within the dermis, and varying degrees of dermal fibrosis.5
In 1899, mineral oil was first injected into male genitalia to restore architecture in a patient’s testicles following bilateral orchiectomy. After the success of this endeavor, mineral oil injections were used as filler for other defects.3 However, by 1906 the complications of these injections became public knowledge when 2 patients developed subcutaneous nodules after receiving injections for facial wrinkles.2 Despite public knowledge of these complications, penile paraffin injections continued to occur both in medical and eventually nonmedical settings.
In 1947, Quérnu and Pérol6 described 6 penile paraffinoma cases outside the United States. Patients had petroleum jelly injections that eventuated in penile paraffinomas, and all of them lost the ability to attain an erection.6 Four years later, Bradley and Ehrgott7 described a case of penile paraffinoma likely caused by application of paraffin in association with occupational exposure. In 1956, May and Pickering8 cited a case of penile paraffinoma affecting the entire penile shaft in which the patient had undergone paraffin injection 7 years prior to treat premature ejaculation. Unfortunately, the injection resulted in a painful and unsatisfactory erection without resolution of premature ejaculation.8 Lee et al9 analyzed 26 cases of penile paraffinomas that occurred from 1981 to 1993. They found that all patients underwent injections of paraffin or petroleum jelly performed by nonmedical personnel with the predominant goal of enhancing penis size. Within 18.5 months of injection, 19 patients already experienced tenderness at the injection site. The remaining 7 patients experienced penile skin discoloration and abnormal contouring of the penis. Biopsy specimens revealed hyaline necrosis of subcutaneous adipose septa, cystlike spaces throughout involved tissue, and macrophages engulfing adipose tissue were found near blood vessels.9 In 2007, Eandi et al4 reported a case of penile paraffinoma with a 40-year delay of onset. Four years later, Manny et al10 reported penile paraffinomas in 3 Laotian men who injected a mineral oil.
Currently, paraffin injections are uncommon but still are being performed in some countries in Eastern Europe and the Far East11; they rarely are reported in the United States. Injections can occur in unusual sites such as the knee, and paraffinomas can develop many years after the procedure.12 Additionally, paraffinomas can obscure proper diagnosis of carcinomas, as described by Lee et al13 in a case in which a cervical paraffin injection confounded the diagnosis of a thyroid tumor. Furthermore, these injections usually are performed by nonmedical personnel and typically are repeated multiple times to reach cosmetic goals, rendering the patient vulnerable to early complications including allergic reactions, paraphimosis, infection, and inflammation.3
The clinical presentation of a penile paraffinoma may be a mimicker of several different entities, which are important to consider in the evaluation of a presenting patient. Infectious etiologies must be considered including lymphogranuloma venereum, granuloma inguinale, atypical mycobacteria, lupus vulgaris, and sexually transmitted infections. Importantly, neoplasms must be ruled out including squamous cell carcinoma, soft tissue sarcomas, melanoma, adenocarcinoma, or metastasis. Lymphedema, prior surgical procedures, trauma, and inflammatory etiologies also are in the differential diagnosis.14 Nonetheless, physicians must have a high clinical suspicion in the evaluation of a possible paraffinoma, as patients may not be forthcoming with relevant clinical history regarding a prior injection to the affected site, particularly if the injection occurred many years ago. As such, the patient may not consider this history relevant or may not even remember the event occurred, as was observed in our case. Furthermore, embarrassment, social taboo, and stigma may be associated with the behavior of undergoing injections in nonclinical settings without medical supervision.15
Patients may be motivated to undergo dangerous procedures to potentially alter their appearance due to perceived enhanced sexual ability, influence by loved ones, cultural rituals, and societal pressure.15,16 Furthermore, patients may not be aware of the material being injected or the volume. Given that these injections often are used with the goal of cosmetic enhancement, biopsies in cosmetically sensitive areas must be given careful consideration, and a thorough clinical history must support the decision to pursue a biopsy to obtain a definitive diagnosis.
The definitive diagnosis of a paraffinoma is determined by histopathology. However, the use of imaging modalities such as magnetic resonance imaging and computed tomography have been employed to delineate the extent of involvement. Imaging studies allow for surgical planning and may assist in narrowing a differential diagnosis.17 Currently, wide and complete surgical resection is the only definitive treatment of paraffinomas, including penile paraffinomas, as there is no evidence of spontaneous regression.3 A report of a reconstructive surgery involving penile resurfacing without T-style anastomosis has been found effective at preventing necrosis of the ventral penile skin. Not all paraffinomas behave similarly, and there is no reliable method to determine which paraffinoma may possess a more aggressive clinical course compared to those which have a more indolent course.18 As such, early detection is critical in the management of paraffinomas, especially in anatomic locations where tissue preservation is of utmost importance. In the case of a large penile paraffinoma with the ability to destroy vital urologic and reproductive function, physicians must consider prevention of recurrent episodes through suppression of inflammation and fibrosis with doxycycline and nicotinamide.19 Other medical treatments reported with varying success include corticosteroids, imiquimod, and isotretinoin.19-24 Employing adjunctive medical treatment may decrease the size of the mass, reducing the surgical defect size and preserving tissue vitality. Ultimately, the most crucial aspect in treatment is prevention, as injection of foreign materials elicits a foreign body response and can lead to notable morbidity.
- De Siati M, Selvaggio O, Di Fino G, et al. An unusual delayed complication of paraffin self-injection for penile girth augmentation. BMC Urol. 2013;13:66.
- Sejben I, Rácz A, Svébis M, et al. Petroleum jelly-induced penile paraffinoma with inguinal lymphadenitis mimicking incarcerated inguinal hernia. Can Urol Assoc J. 2012;6:E137-E139.
- Bayraktar N, Basar I. Penile paraffinoma [published online September 17, 2012]. Case Rep Urol. 2012;2012:202840.
- Eandi JA, Yao AP, Javidan J. Penile paraffinoma: the delayed presentation. Int Urol Nephrol. 2007;29:553-555.
- HirshBCJohnsonWC. Pathology of granulomatous diseases. foreign body granulomas. Int J Dermatol. 1984;23:531-538.
- Quérnu J, Pérol E. Paraffinomas of the penis. J Chir Par. 1947;63:345.
- Bradley, RH, Ehrgott WA. Paraffinoma of the penis: case report. J Urol. 1951;65:453.
- May JA, Pickering PP. Paraffinoma of the penis. Calif Med. 1956;85:42-44.
Yonsei Med J. 1994;35:344-348. - Lee T, Choi HR, Lee YT, et al. Paraffinoma of the penis.
- Manny T, Pettus J, Hemal A, et al. Penile sclerosing lipogranulomas and disfigurement from use of “1Super Extenze” among Laotian immigrants. J Sex Med. 2011;8:3505-3510.
- Akkus E Paraffinoma and ulcer of the external genitalia after self-injection of vaseline. J Sex Med. 2006;3:170-172.
- Grassetti L, Lazzeri D, Torresetti M, et al. Paraffinoma of the knee 60 years after primary infection. Arch Plast Surg. 2013;40:789-790.
- Lee YS, Son EJ, Kim BW, et al. Difficult evaluation of thyroid cancer due to cervical paraffin injection. J Korean Surg Soc. 2011;81(suppl 1):S17-S20.
- Gómez-Armayones S, Penín R, Marcoval J. Penile paraffinoma [in Spanish]. Actas Dermosifiliogr. 2014;105:957-959.
- Moon DG, Yoo JW, Bae JH, et al. Sexual function and psychological characteristics of penile paraffinoma. Asian J Androl. 2003;5:191-194.
- Pehlivanov G, Kavaklieva S, Kazandjieva J, et al. Foreign-body granuloma of the penis in sexually active individuals (penile paraffinoma). J Eur Acad Dermatol Venereol. 2008;22:845-851.
- Cormio L, Di Fino G, Scavone C, et al. Magnetic resonance imaging of penile paraffinoma: case report. BMC Med Imaging. 2014;14:39.
- Shin YS, Zhao C, Park JK. New reconstructive surgery for penile paraffinoma to prevent necrosis of ventral penile skin. Urology. 2013;81:437-441.
- Feldmann R, Harms M, Chavaz P, et al. Orbital and palpebral paraffinoma. J Am Acad Dermatol. 1992;26:833-835.
- MastruserioDNPesqueiraMJCobbMW. Severe granulomatous reaction and facial ulceration occurring after subcutaneous silicone injection. J Am Acad Dermatol. 1996;34:849-852.
- HoWS Management of paraffinoma of the breast. Br J Plast Surg. 2001;54:232-234.
- LloretPSuccessful treatment of granulomatous reactions secondary to injection of esthetic implants. Dermatol Surg. 2005;31:486-490.
- RosenbergEThree cases of penile paraffinoma. Urology. 2007;70:372.
- Baumann LS, Halem ML. Lip silicone granulomatous foreign body reaction treated with Aldara (imiquimod 5%). Dermatol Surg. 2003;29:429-432.
- De Siati M, Selvaggio O, Di Fino G, et al. An unusual delayed complication of paraffin self-injection for penile girth augmentation. BMC Urol. 2013;13:66.
- Sejben I, Rácz A, Svébis M, et al. Petroleum jelly-induced penile paraffinoma with inguinal lymphadenitis mimicking incarcerated inguinal hernia. Can Urol Assoc J. 2012;6:E137-E139.
- Bayraktar N, Basar I. Penile paraffinoma [published online September 17, 2012]. Case Rep Urol. 2012;2012:202840.
- Eandi JA, Yao AP, Javidan J. Penile paraffinoma: the delayed presentation. Int Urol Nephrol. 2007;29:553-555.
- HirshBCJohnsonWC. Pathology of granulomatous diseases. foreign body granulomas. Int J Dermatol. 1984;23:531-538.
- Quérnu J, Pérol E. Paraffinomas of the penis. J Chir Par. 1947;63:345.
- Bradley, RH, Ehrgott WA. Paraffinoma of the penis: case report. J Urol. 1951;65:453.
- May JA, Pickering PP. Paraffinoma of the penis. Calif Med. 1956;85:42-44.
Yonsei Med J. 1994;35:344-348. - Lee T, Choi HR, Lee YT, et al. Paraffinoma of the penis.
- Manny T, Pettus J, Hemal A, et al. Penile sclerosing lipogranulomas and disfigurement from use of “1Super Extenze” among Laotian immigrants. J Sex Med. 2011;8:3505-3510.
- Akkus E Paraffinoma and ulcer of the external genitalia after self-injection of vaseline. J Sex Med. 2006;3:170-172.
- Grassetti L, Lazzeri D, Torresetti M, et al. Paraffinoma of the knee 60 years after primary infection. Arch Plast Surg. 2013;40:789-790.
- Lee YS, Son EJ, Kim BW, et al. Difficult evaluation of thyroid cancer due to cervical paraffin injection. J Korean Surg Soc. 2011;81(suppl 1):S17-S20.
- Gómez-Armayones S, Penín R, Marcoval J. Penile paraffinoma [in Spanish]. Actas Dermosifiliogr. 2014;105:957-959.
- Moon DG, Yoo JW, Bae JH, et al. Sexual function and psychological characteristics of penile paraffinoma. Asian J Androl. 2003;5:191-194.
- Pehlivanov G, Kavaklieva S, Kazandjieva J, et al. Foreign-body granuloma of the penis in sexually active individuals (penile paraffinoma). J Eur Acad Dermatol Venereol. 2008;22:845-851.
- Cormio L, Di Fino G, Scavone C, et al. Magnetic resonance imaging of penile paraffinoma: case report. BMC Med Imaging. 2014;14:39.
- Shin YS, Zhao C, Park JK. New reconstructive surgery for penile paraffinoma to prevent necrosis of ventral penile skin. Urology. 2013;81:437-441.
- Feldmann R, Harms M, Chavaz P, et al. Orbital and palpebral paraffinoma. J Am Acad Dermatol. 1992;26:833-835.
- MastruserioDNPesqueiraMJCobbMW. Severe granulomatous reaction and facial ulceration occurring after subcutaneous silicone injection. J Am Acad Dermatol. 1996;34:849-852.
- HoWS Management of paraffinoma of the breast. Br J Plast Surg. 2001;54:232-234.
- LloretPSuccessful treatment of granulomatous reactions secondary to injection of esthetic implants. Dermatol Surg. 2005;31:486-490.
- RosenbergEThree cases of penile paraffinoma. Urology. 2007;70:372.
- Baumann LS, Halem ML. Lip silicone granulomatous foreign body reaction treated with Aldara (imiquimod 5%). Dermatol Surg. 2003;29:429-432.
Practice Points
- Taking a thorough history in patients with possible paraffinomas is vital, including a history of injectables even in the genital region.
- Biopsies in cosmetically sensitive areas must be given careful consideration. Clinical history must support the decision to pursue a definitive diagnosis.
- Early detection is critical in the management of paraffinomas, especially in anatomic locations where tissue preservation is of utmost importance.
FDA approves apomorphine sublingual film for ‘off’ episodes in Parkinson’s disease
, the manufacturer has announced. This marks the first approval for a sublingual therapy for this indication, which is defined as the re-emergence or worsening of Parkinson’s disease symptoms that have otherwise been controlled with standard care of levodopa/carbidopa, Sunovion reports. Almost 60% of patients with Parkinson’s disease experience off episodes.
The approval “affords healthcare providers with a needed option that can be added to their patients’ medication regimen to adequately address off episodes as their Parkinson’s disease progresses,” Stewart Factor, DO, professor of neurology and director of the Movement Disorders Program at Emory University School of Medicine, Atlanta, Georgia, said in a press release from the manufacturer.
“We know from our research and discussion with the Parkinson’s community that off episodes can significantly disrupt a patient’s daily life,” Todd Sherer, PhD, CEO of the Michael J. Fox Foundation for Parkinson’s Research, said in the same release. He added that the Fox Foundation “supported early clinical development of sublingual apomorphine.”
The treatment is expected to be available in US pharmacies in September.
Disruptive symptoms
Off episodes can include periods of tremor, slowed movement, and stiffness and occur during daytime hours.
“Several years after a person is diagnosed with [Parkinson’s disease] they may notice problems such as having trouble getting out of bed in the morning or having difficulty getting out of a chair, or that they feel frozen while trying to walk as the effect of their maintenance medication diminishes,” Dr. Factor noted.
Subcutaneous infusion of the dopamine agonist apomorphine previously has shown benefit in treating persistent motor fluctuations in patients with Parkinson’s disease.
Apomorphine hydrochloride sublingual film is a novel formulation of apomorphine. It dissolves under the tongue to help improve off episode symptoms as needed up to five times per day.
A phase 3 study of 109 patients that was published in December in Lancet Neurology showed that those who received the sublingual film therapy had a mean reduction of 11.1 points on the Movement Disorder Society Unified Parkinson’s Disease Rating Scale Part III 30 minutes after dosing at the 12-week assessment. This was a significant improvement in motor symptoms versus those who received placebo (mean difference, -7.6 points; P = .0002).
In addition, initial clinical improvement was found 15 minutes after dosing.
The most frequently reported treatment-emergent adverse events in the study population were oropharyngeal reactions, followed by nausea, somnolence, and dizziness.
Long-term safety?
“The availability of this new apomorphine sublingual formulation, along with an inhaled formulation under development, will broaden the treatment options for off periods,” Angelo Antonini, MD, PhD, from University of Padua, Italy, wrote in an accompanying editorial in The Lancet Neurology.
Although the results were encouraging, he noted some caution should be heeded.
Because of “the high rate of oropharyngeal adverse events, long-term safety needs to be monitored once the product is registered and available for chronic use in patients with Parkinson’s disease,” Dr. Antonini wrote.
Other safety information issued by the manufacturer includes a warning that patients who take the 5HT3 antagonists ondansetron, dolasetron, palonosetron, granisetron, or alosetron for nausea should not also use apomorphine hydrochloride sublingual film.
“People taking ondansetron together with apomorphine, the active ingredient in Kynmobi, have had very low blood pressure and lost consciousness or ‘blacked out,’ “ the warning notes.
It also should not be taken by individuals who are allergic to the ingredients in the medication, including sodium metabisulfite.
This article first appeared on Medscape.com.
, the manufacturer has announced. This marks the first approval for a sublingual therapy for this indication, which is defined as the re-emergence or worsening of Parkinson’s disease symptoms that have otherwise been controlled with standard care of levodopa/carbidopa, Sunovion reports. Almost 60% of patients with Parkinson’s disease experience off episodes.
The approval “affords healthcare providers with a needed option that can be added to their patients’ medication regimen to adequately address off episodes as their Parkinson’s disease progresses,” Stewart Factor, DO, professor of neurology and director of the Movement Disorders Program at Emory University School of Medicine, Atlanta, Georgia, said in a press release from the manufacturer.
“We know from our research and discussion with the Parkinson’s community that off episodes can significantly disrupt a patient’s daily life,” Todd Sherer, PhD, CEO of the Michael J. Fox Foundation for Parkinson’s Research, said in the same release. He added that the Fox Foundation “supported early clinical development of sublingual apomorphine.”
The treatment is expected to be available in US pharmacies in September.
Disruptive symptoms
Off episodes can include periods of tremor, slowed movement, and stiffness and occur during daytime hours.
“Several years after a person is diagnosed with [Parkinson’s disease] they may notice problems such as having trouble getting out of bed in the morning or having difficulty getting out of a chair, or that they feel frozen while trying to walk as the effect of their maintenance medication diminishes,” Dr. Factor noted.
Subcutaneous infusion of the dopamine agonist apomorphine previously has shown benefit in treating persistent motor fluctuations in patients with Parkinson’s disease.
Apomorphine hydrochloride sublingual film is a novel formulation of apomorphine. It dissolves under the tongue to help improve off episode symptoms as needed up to five times per day.
A phase 3 study of 109 patients that was published in December in Lancet Neurology showed that those who received the sublingual film therapy had a mean reduction of 11.1 points on the Movement Disorder Society Unified Parkinson’s Disease Rating Scale Part III 30 minutes after dosing at the 12-week assessment. This was a significant improvement in motor symptoms versus those who received placebo (mean difference, -7.6 points; P = .0002).
In addition, initial clinical improvement was found 15 minutes after dosing.
The most frequently reported treatment-emergent adverse events in the study population were oropharyngeal reactions, followed by nausea, somnolence, and dizziness.
Long-term safety?
“The availability of this new apomorphine sublingual formulation, along with an inhaled formulation under development, will broaden the treatment options for off periods,” Angelo Antonini, MD, PhD, from University of Padua, Italy, wrote in an accompanying editorial in The Lancet Neurology.
Although the results were encouraging, he noted some caution should be heeded.
Because of “the high rate of oropharyngeal adverse events, long-term safety needs to be monitored once the product is registered and available for chronic use in patients with Parkinson’s disease,” Dr. Antonini wrote.
Other safety information issued by the manufacturer includes a warning that patients who take the 5HT3 antagonists ondansetron, dolasetron, palonosetron, granisetron, or alosetron for nausea should not also use apomorphine hydrochloride sublingual film.
“People taking ondansetron together with apomorphine, the active ingredient in Kynmobi, have had very low blood pressure and lost consciousness or ‘blacked out,’ “ the warning notes.
It also should not be taken by individuals who are allergic to the ingredients in the medication, including sodium metabisulfite.
This article first appeared on Medscape.com.
, the manufacturer has announced. This marks the first approval for a sublingual therapy for this indication, which is defined as the re-emergence or worsening of Parkinson’s disease symptoms that have otherwise been controlled with standard care of levodopa/carbidopa, Sunovion reports. Almost 60% of patients with Parkinson’s disease experience off episodes.
The approval “affords healthcare providers with a needed option that can be added to their patients’ medication regimen to adequately address off episodes as their Parkinson’s disease progresses,” Stewart Factor, DO, professor of neurology and director of the Movement Disorders Program at Emory University School of Medicine, Atlanta, Georgia, said in a press release from the manufacturer.
“We know from our research and discussion with the Parkinson’s community that off episodes can significantly disrupt a patient’s daily life,” Todd Sherer, PhD, CEO of the Michael J. Fox Foundation for Parkinson’s Research, said in the same release. He added that the Fox Foundation “supported early clinical development of sublingual apomorphine.”
The treatment is expected to be available in US pharmacies in September.
Disruptive symptoms
Off episodes can include periods of tremor, slowed movement, and stiffness and occur during daytime hours.
“Several years after a person is diagnosed with [Parkinson’s disease] they may notice problems such as having trouble getting out of bed in the morning or having difficulty getting out of a chair, or that they feel frozen while trying to walk as the effect of their maintenance medication diminishes,” Dr. Factor noted.
Subcutaneous infusion of the dopamine agonist apomorphine previously has shown benefit in treating persistent motor fluctuations in patients with Parkinson’s disease.
Apomorphine hydrochloride sublingual film is a novel formulation of apomorphine. It dissolves under the tongue to help improve off episode symptoms as needed up to five times per day.
A phase 3 study of 109 patients that was published in December in Lancet Neurology showed that those who received the sublingual film therapy had a mean reduction of 11.1 points on the Movement Disorder Society Unified Parkinson’s Disease Rating Scale Part III 30 minutes after dosing at the 12-week assessment. This was a significant improvement in motor symptoms versus those who received placebo (mean difference, -7.6 points; P = .0002).
In addition, initial clinical improvement was found 15 minutes after dosing.
The most frequently reported treatment-emergent adverse events in the study population were oropharyngeal reactions, followed by nausea, somnolence, and dizziness.
Long-term safety?
“The availability of this new apomorphine sublingual formulation, along with an inhaled formulation under development, will broaden the treatment options for off periods,” Angelo Antonini, MD, PhD, from University of Padua, Italy, wrote in an accompanying editorial in The Lancet Neurology.
Although the results were encouraging, he noted some caution should be heeded.
Because of “the high rate of oropharyngeal adverse events, long-term safety needs to be monitored once the product is registered and available for chronic use in patients with Parkinson’s disease,” Dr. Antonini wrote.
Other safety information issued by the manufacturer includes a warning that patients who take the 5HT3 antagonists ondansetron, dolasetron, palonosetron, granisetron, or alosetron for nausea should not also use apomorphine hydrochloride sublingual film.
“People taking ondansetron together with apomorphine, the active ingredient in Kynmobi, have had very low blood pressure and lost consciousness or ‘blacked out,’ “ the warning notes.
It also should not be taken by individuals who are allergic to the ingredients in the medication, including sodium metabisulfite.
This article first appeared on Medscape.com.
Complex Regional Pain Syndrome Type II After a Brachial Plexus and C6 Nerve Root Injury
To the Editor:
A 62-year-old man presented with an atrophied painful left arm of 17 years’ duration that began when he was hit by a car as a pedestrian. He sustained severe multisystem injuries from the accident, including left brachial plexus and C6 nerve root avulsion injury. When he regained consciousness after 6 weeks in the intensive care unit, he immediately noted diffuse pain throughout the body, especially in the left arm. Since the accident, the patient continued to have diminished sensation to touch and temperature in the left arm. He also had burning, throbbing, and electrical pain in the left arm with light touch as well as spontaneously. He was thoroughly evaluated by a neurologist and was diagnosed with complex regional pain syndrome (CRPS) type II. For the treatment of pain, dorsal column stimulation and hemilaminectomy with exploration of the avulsed nerve root were attempted, both of which had minimal effect. He was maintained on hydromorphone, methadone, and oxazepam. He reported that for many years he was unable move out of bed due to the unbearable pain. With pain medications, he was able to regain most of his independence in his daily life, though the pain and other clinical aspects of CRPS still completely limited his use of the left arm.
Physical examination revealed glossy, cold, hairless skin with hypohidrosis of the left arm, forearm, and hand (Figures 1 and 2A). The left arm was conspicuously atrophied, with the forearm and hand erythematous. The fingers were taut, contracted, and edematous (Figure 2B), and the skin was unable to be pinched. The fingernails on the left hand had dystrophic changes including yellow color and brittleness with longitudinal ridges (Figure 3). The patient could activate the left bicep and tricep muscles against gravity but had minimal function of the deltoid muscle. He also had minimal movement of the left index finger and was unable to move any other digits of the left hand. The patient was continued on pain management treatments and physical therapy for his condition.



Complex regional pain syndrome is a neuropathic disorder of the extremities characterized by pain and a variety of autonomic and motor disturbances such as local edema, limited active range of motion, and vasomotor and trophic skin changes. There are 2 types of CRPS: type II is marked by explicit nerve injury and type I is not. The pathophysiology of CRPS is unknown.1-3
There is no definite set of diagnostic criteria for CRPS. The lack of any gold-standard diagnostic test for CRPS has made arriving at one valid, widely accepted set of diagnostic criteria impossible.1 There are 4 widely used sets of diagnostic criteria. One is the International Association for the Study of Pain diagnostic criteria defined in 1994.4 However, the criteria rely entirely on subjective symptoms and have been under great scrutiny due to their questionable validity.2 Veldman et al5 presented other widely used CRPS diagnostic criteria in their prospective study of 829 reflex sympathetic dystrophy patients, which paid particular attention to the early clinical manifestations of CRPS. In 1999, Bruehl et al2 proposed their own modified diagnostic criteria, which required physician-assessed signs in 2 of 4 categories to avoid the practice of exclusively relying on subjective symptoms. In addition, during a consensus meeting in Budapest, Hungary, a modified version of the Bruehl criteria was proposed.6 All 4 criteria rely solely on detailed history and physical examination, and the choice of diagnostic criteria remains subjective.
The pathophysiology of CRPS also remains unclear. There are several proposed mechanisms such as sympathetic nervous system dysfunction, abnormal inflammatory response, and central nervous system involvement.1 Psychologic factors, sequelae of nerve injury, and genetic predisposition also have been implicated in the pathophysiology of CRPS.1 It is likely that several mechanisms variably contribute to each presentation of CRPS.
Many dermatologic findings, in addition to neuromuscular symptoms, accompany CRPS and serve as important clues to making the clinical diagnosis. Complex regional pain syndrome has been thought to have 3 distinct sequential stages of CRPS.1,3,7 Stage 1—the acute stage—is marked by hyperalgesia, allodynia, sudomotor disturbances, and prominent edema. Stage 2—the dystrophic stage—is characterized by more marked pain and sensory dysfunction, vasomotor dysfunction, development of motor dysfunction, soft tissue edema, skin and articular soft tissue thickening, and development of dystrophic nail changes. Stage 3—the atrophic stage—is marked by decreased pain and sensory disturbances, markedly increased motor dysfunction, waxy atrophic skin changes, progression of dystrophic nail changes, and skeletal cystic and subchondral erosions with diffuse osteoporosis.1,3,7
The staging model, however, has been called into question.3 In a cluster analysis, Bruehl et al3 arrived at 3 relatively consistent CRPS patient subgroups that did not have notably different pain duration, suggesting the existence of 3 CRPS subtypes, not stages. Their study found that one of the subgroups best represented the clinical presentation of CRPS type II. This subgroup had the greatest pain and sensory abnormalities and the least vasomotor dysfunction of all 3 subgroups. Nonetheless, this study has not settled the discussion, as it only included 113 patients.3 Thus, with future studies, our understanding of CRPS in stages may change, which likely will impact how the clinical diagnosis is made.
There is a lack of high-quality evidence for most treatment interventions for CRPS8; however, the current practice is to use an interdisciplinary approach.1,9,10 The main therapeutic arm of this approach is rehabilitation; physical and occupational therapy can help improve range of motion, contracture, and atrophy. The other 2 arms of the approach are psychologic therapy to improve quality of life and pain management with pharmacologic therapy and/or invasive interventions. The choice of therapy remains empirical; trial and error should be expected in developing an adequate treatment plan for each individual patient.
Many aspects of CRPS remain unclear, and even our current understanding of the disease will inevitably change over time. The syndrome can cause life-changing morbidities in patients, and late diagnosis and treatment are associated with poor prognosis. Because there are many dermatologic findings associated with the disorder, it is crucial for dermatologists to clinically recognize the disorder and to refer patients to appropriate channels so that treatment can be started as soon as possible.
- Borchers A, Gershwin M. Complex regional pain syndrome: a comprehensive and critical review. Autoimmun Rev. 2014;13:242-265.
- Bruehl S, Harden RN, Galer BS, et al. External validation of IASP diagnostic criteria for complex regional pain syndrome and proposed research diagnostic criteria. International Association for the Study of Pain. Pain. 1999;81:147-154.
- Bruehl S, Harden RN, Gaker BS, et al. Complex regional pain syndrome: are there distinct subtypes and sequential stages of the syndrome? Pain. 2002;95:119-124.
- Merskey H, Bogduk N. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. 2nd ed. Seattle, WA: IASP Press; 1994.
- Veldman PH, Reynen HM, Arntz IE, et al. Signs and symptoms of reflex sympathetic dystrophy: prospective study of 829 patients. Lancet. 1993;342:1012-1016.
- Harden RN, Bruehl S, Perez RS, et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for complex regional pain syndrome. Pain. 2010;150:268-274.
- Sebastin SJ. Complex regional pain syndrome. Indian J Plast Surg. 2011;44:298-307.
- O’Connell NE, Wand BM, McAuley J, et al. Interventions for treating pain and disability in adults with complex regional pain syndrome. Cochrane Database Syst Rev. 2013;4:CD009416.
- Hsu ES. Practical management of complex regional pain syndrome. Am J Ther. 2009;16:147-154.
- Stanton-Hicks MD, Burton AW, Bruehl SP, et al. An updated interdisciplinary clinical pathway for CRPS: report of an expert panel. Pain Pract. 2002;2:1-16.
To the Editor:
A 62-year-old man presented with an atrophied painful left arm of 17 years’ duration that began when he was hit by a car as a pedestrian. He sustained severe multisystem injuries from the accident, including left brachial plexus and C6 nerve root avulsion injury. When he regained consciousness after 6 weeks in the intensive care unit, he immediately noted diffuse pain throughout the body, especially in the left arm. Since the accident, the patient continued to have diminished sensation to touch and temperature in the left arm. He also had burning, throbbing, and electrical pain in the left arm with light touch as well as spontaneously. He was thoroughly evaluated by a neurologist and was diagnosed with complex regional pain syndrome (CRPS) type II. For the treatment of pain, dorsal column stimulation and hemilaminectomy with exploration of the avulsed nerve root were attempted, both of which had minimal effect. He was maintained on hydromorphone, methadone, and oxazepam. He reported that for many years he was unable move out of bed due to the unbearable pain. With pain medications, he was able to regain most of his independence in his daily life, though the pain and other clinical aspects of CRPS still completely limited his use of the left arm.
Physical examination revealed glossy, cold, hairless skin with hypohidrosis of the left arm, forearm, and hand (Figures 1 and 2A). The left arm was conspicuously atrophied, with the forearm and hand erythematous. The fingers were taut, contracted, and edematous (Figure 2B), and the skin was unable to be pinched. The fingernails on the left hand had dystrophic changes including yellow color and brittleness with longitudinal ridges (Figure 3). The patient could activate the left bicep and tricep muscles against gravity but had minimal function of the deltoid muscle. He also had minimal movement of the left index finger and was unable to move any other digits of the left hand. The patient was continued on pain management treatments and physical therapy for his condition.



Complex regional pain syndrome is a neuropathic disorder of the extremities characterized by pain and a variety of autonomic and motor disturbances such as local edema, limited active range of motion, and vasomotor and trophic skin changes. There are 2 types of CRPS: type II is marked by explicit nerve injury and type I is not. The pathophysiology of CRPS is unknown.1-3
There is no definite set of diagnostic criteria for CRPS. The lack of any gold-standard diagnostic test for CRPS has made arriving at one valid, widely accepted set of diagnostic criteria impossible.1 There are 4 widely used sets of diagnostic criteria. One is the International Association for the Study of Pain diagnostic criteria defined in 1994.4 However, the criteria rely entirely on subjective symptoms and have been under great scrutiny due to their questionable validity.2 Veldman et al5 presented other widely used CRPS diagnostic criteria in their prospective study of 829 reflex sympathetic dystrophy patients, which paid particular attention to the early clinical manifestations of CRPS. In 1999, Bruehl et al2 proposed their own modified diagnostic criteria, which required physician-assessed signs in 2 of 4 categories to avoid the practice of exclusively relying on subjective symptoms. In addition, during a consensus meeting in Budapest, Hungary, a modified version of the Bruehl criteria was proposed.6 All 4 criteria rely solely on detailed history and physical examination, and the choice of diagnostic criteria remains subjective.
The pathophysiology of CRPS also remains unclear. There are several proposed mechanisms such as sympathetic nervous system dysfunction, abnormal inflammatory response, and central nervous system involvement.1 Psychologic factors, sequelae of nerve injury, and genetic predisposition also have been implicated in the pathophysiology of CRPS.1 It is likely that several mechanisms variably contribute to each presentation of CRPS.
Many dermatologic findings, in addition to neuromuscular symptoms, accompany CRPS and serve as important clues to making the clinical diagnosis. Complex regional pain syndrome has been thought to have 3 distinct sequential stages of CRPS.1,3,7 Stage 1—the acute stage—is marked by hyperalgesia, allodynia, sudomotor disturbances, and prominent edema. Stage 2—the dystrophic stage—is characterized by more marked pain and sensory dysfunction, vasomotor dysfunction, development of motor dysfunction, soft tissue edema, skin and articular soft tissue thickening, and development of dystrophic nail changes. Stage 3—the atrophic stage—is marked by decreased pain and sensory disturbances, markedly increased motor dysfunction, waxy atrophic skin changes, progression of dystrophic nail changes, and skeletal cystic and subchondral erosions with diffuse osteoporosis.1,3,7
The staging model, however, has been called into question.3 In a cluster analysis, Bruehl et al3 arrived at 3 relatively consistent CRPS patient subgroups that did not have notably different pain duration, suggesting the existence of 3 CRPS subtypes, not stages. Their study found that one of the subgroups best represented the clinical presentation of CRPS type II. This subgroup had the greatest pain and sensory abnormalities and the least vasomotor dysfunction of all 3 subgroups. Nonetheless, this study has not settled the discussion, as it only included 113 patients.3 Thus, with future studies, our understanding of CRPS in stages may change, which likely will impact how the clinical diagnosis is made.
There is a lack of high-quality evidence for most treatment interventions for CRPS8; however, the current practice is to use an interdisciplinary approach.1,9,10 The main therapeutic arm of this approach is rehabilitation; physical and occupational therapy can help improve range of motion, contracture, and atrophy. The other 2 arms of the approach are psychologic therapy to improve quality of life and pain management with pharmacologic therapy and/or invasive interventions. The choice of therapy remains empirical; trial and error should be expected in developing an adequate treatment plan for each individual patient.
Many aspects of CRPS remain unclear, and even our current understanding of the disease will inevitably change over time. The syndrome can cause life-changing morbidities in patients, and late diagnosis and treatment are associated with poor prognosis. Because there are many dermatologic findings associated with the disorder, it is crucial for dermatologists to clinically recognize the disorder and to refer patients to appropriate channels so that treatment can be started as soon as possible.
To the Editor:
A 62-year-old man presented with an atrophied painful left arm of 17 years’ duration that began when he was hit by a car as a pedestrian. He sustained severe multisystem injuries from the accident, including left brachial plexus and C6 nerve root avulsion injury. When he regained consciousness after 6 weeks in the intensive care unit, he immediately noted diffuse pain throughout the body, especially in the left arm. Since the accident, the patient continued to have diminished sensation to touch and temperature in the left arm. He also had burning, throbbing, and electrical pain in the left arm with light touch as well as spontaneously. He was thoroughly evaluated by a neurologist and was diagnosed with complex regional pain syndrome (CRPS) type II. For the treatment of pain, dorsal column stimulation and hemilaminectomy with exploration of the avulsed nerve root were attempted, both of which had minimal effect. He was maintained on hydromorphone, methadone, and oxazepam. He reported that for many years he was unable move out of bed due to the unbearable pain. With pain medications, he was able to regain most of his independence in his daily life, though the pain and other clinical aspects of CRPS still completely limited his use of the left arm.
Physical examination revealed glossy, cold, hairless skin with hypohidrosis of the left arm, forearm, and hand (Figures 1 and 2A). The left arm was conspicuously atrophied, with the forearm and hand erythematous. The fingers were taut, contracted, and edematous (Figure 2B), and the skin was unable to be pinched. The fingernails on the left hand had dystrophic changes including yellow color and brittleness with longitudinal ridges (Figure 3). The patient could activate the left bicep and tricep muscles against gravity but had minimal function of the deltoid muscle. He also had minimal movement of the left index finger and was unable to move any other digits of the left hand. The patient was continued on pain management treatments and physical therapy for his condition.



Complex regional pain syndrome is a neuropathic disorder of the extremities characterized by pain and a variety of autonomic and motor disturbances such as local edema, limited active range of motion, and vasomotor and trophic skin changes. There are 2 types of CRPS: type II is marked by explicit nerve injury and type I is not. The pathophysiology of CRPS is unknown.1-3
There is no definite set of diagnostic criteria for CRPS. The lack of any gold-standard diagnostic test for CRPS has made arriving at one valid, widely accepted set of diagnostic criteria impossible.1 There are 4 widely used sets of diagnostic criteria. One is the International Association for the Study of Pain diagnostic criteria defined in 1994.4 However, the criteria rely entirely on subjective symptoms and have been under great scrutiny due to their questionable validity.2 Veldman et al5 presented other widely used CRPS diagnostic criteria in their prospective study of 829 reflex sympathetic dystrophy patients, which paid particular attention to the early clinical manifestations of CRPS. In 1999, Bruehl et al2 proposed their own modified diagnostic criteria, which required physician-assessed signs in 2 of 4 categories to avoid the practice of exclusively relying on subjective symptoms. In addition, during a consensus meeting in Budapest, Hungary, a modified version of the Bruehl criteria was proposed.6 All 4 criteria rely solely on detailed history and physical examination, and the choice of diagnostic criteria remains subjective.
The pathophysiology of CRPS also remains unclear. There are several proposed mechanisms such as sympathetic nervous system dysfunction, abnormal inflammatory response, and central nervous system involvement.1 Psychologic factors, sequelae of nerve injury, and genetic predisposition also have been implicated in the pathophysiology of CRPS.1 It is likely that several mechanisms variably contribute to each presentation of CRPS.
Many dermatologic findings, in addition to neuromuscular symptoms, accompany CRPS and serve as important clues to making the clinical diagnosis. Complex regional pain syndrome has been thought to have 3 distinct sequential stages of CRPS.1,3,7 Stage 1—the acute stage—is marked by hyperalgesia, allodynia, sudomotor disturbances, and prominent edema. Stage 2—the dystrophic stage—is characterized by more marked pain and sensory dysfunction, vasomotor dysfunction, development of motor dysfunction, soft tissue edema, skin and articular soft tissue thickening, and development of dystrophic nail changes. Stage 3—the atrophic stage—is marked by decreased pain and sensory disturbances, markedly increased motor dysfunction, waxy atrophic skin changes, progression of dystrophic nail changes, and skeletal cystic and subchondral erosions with diffuse osteoporosis.1,3,7
The staging model, however, has been called into question.3 In a cluster analysis, Bruehl et al3 arrived at 3 relatively consistent CRPS patient subgroups that did not have notably different pain duration, suggesting the existence of 3 CRPS subtypes, not stages. Their study found that one of the subgroups best represented the clinical presentation of CRPS type II. This subgroup had the greatest pain and sensory abnormalities and the least vasomotor dysfunction of all 3 subgroups. Nonetheless, this study has not settled the discussion, as it only included 113 patients.3 Thus, with future studies, our understanding of CRPS in stages may change, which likely will impact how the clinical diagnosis is made.
There is a lack of high-quality evidence for most treatment interventions for CRPS8; however, the current practice is to use an interdisciplinary approach.1,9,10 The main therapeutic arm of this approach is rehabilitation; physical and occupational therapy can help improve range of motion, contracture, and atrophy. The other 2 arms of the approach are psychologic therapy to improve quality of life and pain management with pharmacologic therapy and/or invasive interventions. The choice of therapy remains empirical; trial and error should be expected in developing an adequate treatment plan for each individual patient.
Many aspects of CRPS remain unclear, and even our current understanding of the disease will inevitably change over time. The syndrome can cause life-changing morbidities in patients, and late diagnosis and treatment are associated with poor prognosis. Because there are many dermatologic findings associated with the disorder, it is crucial for dermatologists to clinically recognize the disorder and to refer patients to appropriate channels so that treatment can be started as soon as possible.
- Borchers A, Gershwin M. Complex regional pain syndrome: a comprehensive and critical review. Autoimmun Rev. 2014;13:242-265.
- Bruehl S, Harden RN, Galer BS, et al. External validation of IASP diagnostic criteria for complex regional pain syndrome and proposed research diagnostic criteria. International Association for the Study of Pain. Pain. 1999;81:147-154.
- Bruehl S, Harden RN, Gaker BS, et al. Complex regional pain syndrome: are there distinct subtypes and sequential stages of the syndrome? Pain. 2002;95:119-124.
- Merskey H, Bogduk N. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. 2nd ed. Seattle, WA: IASP Press; 1994.
- Veldman PH, Reynen HM, Arntz IE, et al. Signs and symptoms of reflex sympathetic dystrophy: prospective study of 829 patients. Lancet. 1993;342:1012-1016.
- Harden RN, Bruehl S, Perez RS, et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for complex regional pain syndrome. Pain. 2010;150:268-274.
- Sebastin SJ. Complex regional pain syndrome. Indian J Plast Surg. 2011;44:298-307.
- O’Connell NE, Wand BM, McAuley J, et al. Interventions for treating pain and disability in adults with complex regional pain syndrome. Cochrane Database Syst Rev. 2013;4:CD009416.
- Hsu ES. Practical management of complex regional pain syndrome. Am J Ther. 2009;16:147-154.
- Stanton-Hicks MD, Burton AW, Bruehl SP, et al. An updated interdisciplinary clinical pathway for CRPS: report of an expert panel. Pain Pract. 2002;2:1-16.
- Borchers A, Gershwin M. Complex regional pain syndrome: a comprehensive and critical review. Autoimmun Rev. 2014;13:242-265.
- Bruehl S, Harden RN, Galer BS, et al. External validation of IASP diagnostic criteria for complex regional pain syndrome and proposed research diagnostic criteria. International Association for the Study of Pain. Pain. 1999;81:147-154.
- Bruehl S, Harden RN, Gaker BS, et al. Complex regional pain syndrome: are there distinct subtypes and sequential stages of the syndrome? Pain. 2002;95:119-124.
- Merskey H, Bogduk N. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. 2nd ed. Seattle, WA: IASP Press; 1994.
- Veldman PH, Reynen HM, Arntz IE, et al. Signs and symptoms of reflex sympathetic dystrophy: prospective study of 829 patients. Lancet. 1993;342:1012-1016.
- Harden RN, Bruehl S, Perez RS, et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for complex regional pain syndrome. Pain. 2010;150:268-274.
- Sebastin SJ. Complex regional pain syndrome. Indian J Plast Surg. 2011;44:298-307.
- O’Connell NE, Wand BM, McAuley J, et al. Interventions for treating pain and disability in adults with complex regional pain syndrome. Cochrane Database Syst Rev. 2013;4:CD009416.
- Hsu ES. Practical management of complex regional pain syndrome. Am J Ther. 2009;16:147-154.
- Stanton-Hicks MD, Burton AW, Bruehl SP, et al. An updated interdisciplinary clinical pathway for CRPS: report of an expert panel. Pain Pract. 2002;2:1-16.
Practice Points
- Complex regional pain syndrome (CRPS) is a neuropathic disorder of the extremities characterized by pain, a variety of autonomic and motor disturbances, and dermatologic findings.
- Early recognition of CRPS is critical, as it presents life-changing morbidities to patients.
- A multidisciplinary treatment approach with physical therapy, occupational therapy, psychological support, and pain control is needed for the management of CRPS.
Chronic migraine is associated with changes in the amygdala
, according to researchers. This increased connectivity is associated with clinical and affective measures. The data suggest that changes in the amygdala’s structure and function may play a role in the transformation to chronic migraine, according to the researchers. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Approximately 3% of patients with episodic migraine progress to chronic migraine each year. Chronic migraine is associated with increased headache frequency, greater disability, and increased psychiatric comorbidities. The pathophysiological mechanisms of the transformation from episodic to chronic migraine are not completely understood.
Danielle D. DeSouza, PhD, instructor in neurology at Stanford (Calif.) University, and colleagues sought to investigate the role of the amygdala in the transformation of migraine. The amygdala is involved in nociceptive processing, emotional responses, and affective states such as depression and anxiety. Researchers have suggested that alterations in the structure or function of the amygdala might contribute to the worsening of pain and mood that coincides with the transformation of migraine.
Dr. DeSouza and colleagues enrolled 88 patients with migraine, diagnosed according to International Classification of Headache Disorders–3 criteria, in their study. Forty-four patients (36 women; mean age, 37.8 years) had chronic migraine, and 44 patients (36 women; mean age, 37.5 years) had episodic migraine. Participants underwent 3T MRI scanning during which investigators acquired T1-weighted structural and resting-state images of the brain. Participants also completed self-report questionnaires to evaluate depression and somatization (Patient Health Questionnaire), anxiety (Generalized Anxiety Disorder 7-item scale), pain catastrophizing (Pain Catastrophizing Scale), headache frequency, and headache intensity.
The investigators examined resting-state functional connectivity between the amygdala and the following three brain networks: DMN, salience network (SN), and central executive network (CEN). They assessed amygdala volume with voxel-based morphometry.
Analyses indicated that connectivity between the left amygdala and the DMN (i.e., the medial prefrontal cortex and the precuneus/posterior cingulate cortex) was increased in patients with chronic migraine, compared with those with episodic migraine. In all patients, resting-state functional connectivity between the amygdala and the DMN was positively associated with headache frequency. Connectivity between the left amygdala and the SN was positively associated with headache intensity, and connectivity between the right amygdala and the CEN was positively associated with pain catastrophizing. Both of these findings held in all patients.
In addition, Dr. DeSouza and colleagues found that bilateral amygdala volumes, including the basolateral and superficial/corticoid nuclei, were increased in patients with chronic migraine, compared with those with episodic migraine. Headache intensity and depression predicted differences in right amygdala volume, and depression alone predicted differences in left amygdala volume.
Dr. DeSouza reported no disclosures. One of the investigators acts as an adviser to Alder, Allergan, Amgen, Biohaven, Curex, Teva, and Xoc about matters unrelated to this study.
SOURCE: DeSouza DD et al. AAN 2020, Abstract 46914.
, according to researchers. This increased connectivity is associated with clinical and affective measures. The data suggest that changes in the amygdala’s structure and function may play a role in the transformation to chronic migraine, according to the researchers. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Approximately 3% of patients with episodic migraine progress to chronic migraine each year. Chronic migraine is associated with increased headache frequency, greater disability, and increased psychiatric comorbidities. The pathophysiological mechanisms of the transformation from episodic to chronic migraine are not completely understood.
Danielle D. DeSouza, PhD, instructor in neurology at Stanford (Calif.) University, and colleagues sought to investigate the role of the amygdala in the transformation of migraine. The amygdala is involved in nociceptive processing, emotional responses, and affective states such as depression and anxiety. Researchers have suggested that alterations in the structure or function of the amygdala might contribute to the worsening of pain and mood that coincides with the transformation of migraine.
Dr. DeSouza and colleagues enrolled 88 patients with migraine, diagnosed according to International Classification of Headache Disorders–3 criteria, in their study. Forty-four patients (36 women; mean age, 37.8 years) had chronic migraine, and 44 patients (36 women; mean age, 37.5 years) had episodic migraine. Participants underwent 3T MRI scanning during which investigators acquired T1-weighted structural and resting-state images of the brain. Participants also completed self-report questionnaires to evaluate depression and somatization (Patient Health Questionnaire), anxiety (Generalized Anxiety Disorder 7-item scale), pain catastrophizing (Pain Catastrophizing Scale), headache frequency, and headache intensity.
The investigators examined resting-state functional connectivity between the amygdala and the following three brain networks: DMN, salience network (SN), and central executive network (CEN). They assessed amygdala volume with voxel-based morphometry.
Analyses indicated that connectivity between the left amygdala and the DMN (i.e., the medial prefrontal cortex and the precuneus/posterior cingulate cortex) was increased in patients with chronic migraine, compared with those with episodic migraine. In all patients, resting-state functional connectivity between the amygdala and the DMN was positively associated with headache frequency. Connectivity between the left amygdala and the SN was positively associated with headache intensity, and connectivity between the right amygdala and the CEN was positively associated with pain catastrophizing. Both of these findings held in all patients.
In addition, Dr. DeSouza and colleagues found that bilateral amygdala volumes, including the basolateral and superficial/corticoid nuclei, were increased in patients with chronic migraine, compared with those with episodic migraine. Headache intensity and depression predicted differences in right amygdala volume, and depression alone predicted differences in left amygdala volume.
Dr. DeSouza reported no disclosures. One of the investigators acts as an adviser to Alder, Allergan, Amgen, Biohaven, Curex, Teva, and Xoc about matters unrelated to this study.
SOURCE: DeSouza DD et al. AAN 2020, Abstract 46914.
, according to researchers. This increased connectivity is associated with clinical and affective measures. The data suggest that changes in the amygdala’s structure and function may play a role in the transformation to chronic migraine, according to the researchers. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Approximately 3% of patients with episodic migraine progress to chronic migraine each year. Chronic migraine is associated with increased headache frequency, greater disability, and increased psychiatric comorbidities. The pathophysiological mechanisms of the transformation from episodic to chronic migraine are not completely understood.
Danielle D. DeSouza, PhD, instructor in neurology at Stanford (Calif.) University, and colleagues sought to investigate the role of the amygdala in the transformation of migraine. The amygdala is involved in nociceptive processing, emotional responses, and affective states such as depression and anxiety. Researchers have suggested that alterations in the structure or function of the amygdala might contribute to the worsening of pain and mood that coincides with the transformation of migraine.
Dr. DeSouza and colleagues enrolled 88 patients with migraine, diagnosed according to International Classification of Headache Disorders–3 criteria, in their study. Forty-four patients (36 women; mean age, 37.8 years) had chronic migraine, and 44 patients (36 women; mean age, 37.5 years) had episodic migraine. Participants underwent 3T MRI scanning during which investigators acquired T1-weighted structural and resting-state images of the brain. Participants also completed self-report questionnaires to evaluate depression and somatization (Patient Health Questionnaire), anxiety (Generalized Anxiety Disorder 7-item scale), pain catastrophizing (Pain Catastrophizing Scale), headache frequency, and headache intensity.
The investigators examined resting-state functional connectivity between the amygdala and the following three brain networks: DMN, salience network (SN), and central executive network (CEN). They assessed amygdala volume with voxel-based morphometry.
Analyses indicated that connectivity between the left amygdala and the DMN (i.e., the medial prefrontal cortex and the precuneus/posterior cingulate cortex) was increased in patients with chronic migraine, compared with those with episodic migraine. In all patients, resting-state functional connectivity between the amygdala and the DMN was positively associated with headache frequency. Connectivity between the left amygdala and the SN was positively associated with headache intensity, and connectivity between the right amygdala and the CEN was positively associated with pain catastrophizing. Both of these findings held in all patients.
In addition, Dr. DeSouza and colleagues found that bilateral amygdala volumes, including the basolateral and superficial/corticoid nuclei, were increased in patients with chronic migraine, compared with those with episodic migraine. Headache intensity and depression predicted differences in right amygdala volume, and depression alone predicted differences in left amygdala volume.
Dr. DeSouza reported no disclosures. One of the investigators acts as an adviser to Alder, Allergan, Amgen, Biohaven, Curex, Teva, and Xoc about matters unrelated to this study.
SOURCE: DeSouza DD et al. AAN 2020, Abstract 46914.
FROM AAN 2020
Domestic abuse linked to cardiac disease, mortality in women
Adult female survivors of domestic abuse were at least one-third more likely to develop cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality over a short follow-up period, although they did not face a higher risk of hypertension, a new British study finds.
The study, published in the Journal of the American Heart Association, provides more evidence of a link between domestic abuse and poor health, even in younger women.
“The prevalence of domestic abuse is vast, so any increased risk in cardiometabolic disease may translate into a large burden of potentially preventable illness in society,” said study lead author Joht Singh Chandan, PhD, MBBS, of the University of Birmingham (England) and University of Warwick in Coventry, England, in an interview.
The researchers retrospectively tracked primary care patients in the United Kingdom from 1995-2017. They compared 18,547 adult female survivors of domestic abuse with a group of 72,231 other women who were matched to them at baseline by age, body mass index, smoking status, and a measure known as the Townsend deprivation score.
The average age of women in the groups was 37 years plus or minus 13 in the domestic abuse group and 37 years plus or minus 12 in the unexposed group. In both groups, 45% of women smoked; women in the domestic abuse group were more likely to drink excessively (10%), compared with those in the unexposed group (4%).
Researchers followed the women in the domestic abuse group for an average of 2 years and the unexposed group for 3 years. Those in the domestic abuse group were more likely to fall out of the study because they transferred to other medical practices.
Over the study period, 181 women in the domestic abuse group and 644 women in the unexposed group developed cardiovascular disease outcomes (adjusted incidence rate ratio, 1.31; 95% confidence interval, 1.11-1.55; P = .001). They were also more likely to develop type 2 diabetes (adjusted IRR, 1.51; 95% CI, 1.30-1.76; P less than .001) and all-cause mortality (adjusted IRR, 1.44; 95% CI, 1.24-1.67; P less than.001). But there was no increased risk of hypertension (adjusted IRR, 0.99; 95% CI, 0.88-1.12; P = 0.873).
Why might exposure to domestic abuse boost cardiovascular risk? “Although our study was not able to answer exactly why this relationship exists, Dr. Chandan said. “These can be broadly put into three categories: adoption of poor lifestyle behaviors due to difficult circumstances (physical inactivity, poor diet, disrupted sleep, substance misuse and smoking); associated development of mental ill health; and the alteration of the immune, metabolic, neuroendocrine, and autonomic nervous system due to the impact of stress on the body.”
It’s not clear why the risk of hypertension may be an outlier among cardiovascular outcomes, Dr. Chandan said. However, he pointed to a similar study whose results hinted that survivors of emotional abuse may be more susceptible to a negative impact on hypertension (Ann Epidemiol. 2012 Aug;22[8]:562-7). The new study does not provide information about the type of abuse suffered by subjects.
Adrienne O’Neil, PhD, a family violence practitioner and cardiovascular epidemiologist at Deakin University in Geelong, Australia, said in an interview that the study is “a very useful contribution to the literature.” However, she cautioned that the study might have missed cases of domestic abuse because it relies on reports from primary care practitioners.
As for the findings, she said they’re surprising because of the divergence of major cardiovascular outcomes such as ischemic heart disease and stroke in groups of women with an average age of 37. “These differential health outcomes were observed over a 2-3 period. You probably wouldn’t expect to see a divergence in cardiovascular outcomes for 5-10 years in this age group.”
Dr. O’Neil said that, moving forward, the research can be helpful to understanding the rise of cardiovascular disease in women aged 35-54, especially in the United States. “The way we assess an individual’s risk of having a heart attack in the future is largely guided by evidence based on men. For a long time, this has neglected female-specific risk factors like polycystic ovary syndrome and hypertensive disorders of pregnancy but also conditions and exposures to which young women are especially vulnerable like depression, anxiety and [domestic abuse],” she said.
“This research is important as it gives us clues about who may be at elevated risk to help us guide prevention efforts. Equally, there is some evidence that chest pain presentation may be a useful predictor of domestic abuse victimization so there could be multiple lines of further inquiry.”
Dr. Chandan, the other study authors, and Dr. O’Neil reported no relevant disclosures.
SOURCE: Chandan JS et al. J Am Heart Assoc. 2020. doi: 10.1161/JAHA.119.014580.
Adult female survivors of domestic abuse were at least one-third more likely to develop cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality over a short follow-up period, although they did not face a higher risk of hypertension, a new British study finds.
The study, published in the Journal of the American Heart Association, provides more evidence of a link between domestic abuse and poor health, even in younger women.
“The prevalence of domestic abuse is vast, so any increased risk in cardiometabolic disease may translate into a large burden of potentially preventable illness in society,” said study lead author Joht Singh Chandan, PhD, MBBS, of the University of Birmingham (England) and University of Warwick in Coventry, England, in an interview.
The researchers retrospectively tracked primary care patients in the United Kingdom from 1995-2017. They compared 18,547 adult female survivors of domestic abuse with a group of 72,231 other women who were matched to them at baseline by age, body mass index, smoking status, and a measure known as the Townsend deprivation score.
The average age of women in the groups was 37 years plus or minus 13 in the domestic abuse group and 37 years plus or minus 12 in the unexposed group. In both groups, 45% of women smoked; women in the domestic abuse group were more likely to drink excessively (10%), compared with those in the unexposed group (4%).
Researchers followed the women in the domestic abuse group for an average of 2 years and the unexposed group for 3 years. Those in the domestic abuse group were more likely to fall out of the study because they transferred to other medical practices.
Over the study period, 181 women in the domestic abuse group and 644 women in the unexposed group developed cardiovascular disease outcomes (adjusted incidence rate ratio, 1.31; 95% confidence interval, 1.11-1.55; P = .001). They were also more likely to develop type 2 diabetes (adjusted IRR, 1.51; 95% CI, 1.30-1.76; P less than .001) and all-cause mortality (adjusted IRR, 1.44; 95% CI, 1.24-1.67; P less than.001). But there was no increased risk of hypertension (adjusted IRR, 0.99; 95% CI, 0.88-1.12; P = 0.873).
Why might exposure to domestic abuse boost cardiovascular risk? “Although our study was not able to answer exactly why this relationship exists, Dr. Chandan said. “These can be broadly put into three categories: adoption of poor lifestyle behaviors due to difficult circumstances (physical inactivity, poor diet, disrupted sleep, substance misuse and smoking); associated development of mental ill health; and the alteration of the immune, metabolic, neuroendocrine, and autonomic nervous system due to the impact of stress on the body.”
It’s not clear why the risk of hypertension may be an outlier among cardiovascular outcomes, Dr. Chandan said. However, he pointed to a similar study whose results hinted that survivors of emotional abuse may be more susceptible to a negative impact on hypertension (Ann Epidemiol. 2012 Aug;22[8]:562-7). The new study does not provide information about the type of abuse suffered by subjects.
Adrienne O’Neil, PhD, a family violence practitioner and cardiovascular epidemiologist at Deakin University in Geelong, Australia, said in an interview that the study is “a very useful contribution to the literature.” However, she cautioned that the study might have missed cases of domestic abuse because it relies on reports from primary care practitioners.
As for the findings, she said they’re surprising because of the divergence of major cardiovascular outcomes such as ischemic heart disease and stroke in groups of women with an average age of 37. “These differential health outcomes were observed over a 2-3 period. You probably wouldn’t expect to see a divergence in cardiovascular outcomes for 5-10 years in this age group.”
Dr. O’Neil said that, moving forward, the research can be helpful to understanding the rise of cardiovascular disease in women aged 35-54, especially in the United States. “The way we assess an individual’s risk of having a heart attack in the future is largely guided by evidence based on men. For a long time, this has neglected female-specific risk factors like polycystic ovary syndrome and hypertensive disorders of pregnancy but also conditions and exposures to which young women are especially vulnerable like depression, anxiety and [domestic abuse],” she said.
“This research is important as it gives us clues about who may be at elevated risk to help us guide prevention efforts. Equally, there is some evidence that chest pain presentation may be a useful predictor of domestic abuse victimization so there could be multiple lines of further inquiry.”
Dr. Chandan, the other study authors, and Dr. O’Neil reported no relevant disclosures.
SOURCE: Chandan JS et al. J Am Heart Assoc. 2020. doi: 10.1161/JAHA.119.014580.
Adult female survivors of domestic abuse were at least one-third more likely to develop cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality over a short follow-up period, although they did not face a higher risk of hypertension, a new British study finds.
The study, published in the Journal of the American Heart Association, provides more evidence of a link between domestic abuse and poor health, even in younger women.
“The prevalence of domestic abuse is vast, so any increased risk in cardiometabolic disease may translate into a large burden of potentially preventable illness in society,” said study lead author Joht Singh Chandan, PhD, MBBS, of the University of Birmingham (England) and University of Warwick in Coventry, England, in an interview.
The researchers retrospectively tracked primary care patients in the United Kingdom from 1995-2017. They compared 18,547 adult female survivors of domestic abuse with a group of 72,231 other women who were matched to them at baseline by age, body mass index, smoking status, and a measure known as the Townsend deprivation score.
The average age of women in the groups was 37 years plus or minus 13 in the domestic abuse group and 37 years plus or minus 12 in the unexposed group. In both groups, 45% of women smoked; women in the domestic abuse group were more likely to drink excessively (10%), compared with those in the unexposed group (4%).
Researchers followed the women in the domestic abuse group for an average of 2 years and the unexposed group for 3 years. Those in the domestic abuse group were more likely to fall out of the study because they transferred to other medical practices.
Over the study period, 181 women in the domestic abuse group and 644 women in the unexposed group developed cardiovascular disease outcomes (adjusted incidence rate ratio, 1.31; 95% confidence interval, 1.11-1.55; P = .001). They were also more likely to develop type 2 diabetes (adjusted IRR, 1.51; 95% CI, 1.30-1.76; P less than .001) and all-cause mortality (adjusted IRR, 1.44; 95% CI, 1.24-1.67; P less than.001). But there was no increased risk of hypertension (adjusted IRR, 0.99; 95% CI, 0.88-1.12; P = 0.873).
Why might exposure to domestic abuse boost cardiovascular risk? “Although our study was not able to answer exactly why this relationship exists, Dr. Chandan said. “These can be broadly put into three categories: adoption of poor lifestyle behaviors due to difficult circumstances (physical inactivity, poor diet, disrupted sleep, substance misuse and smoking); associated development of mental ill health; and the alteration of the immune, metabolic, neuroendocrine, and autonomic nervous system due to the impact of stress on the body.”
It’s not clear why the risk of hypertension may be an outlier among cardiovascular outcomes, Dr. Chandan said. However, he pointed to a similar study whose results hinted that survivors of emotional abuse may be more susceptible to a negative impact on hypertension (Ann Epidemiol. 2012 Aug;22[8]:562-7). The new study does not provide information about the type of abuse suffered by subjects.
Adrienne O’Neil, PhD, a family violence practitioner and cardiovascular epidemiologist at Deakin University in Geelong, Australia, said in an interview that the study is “a very useful contribution to the literature.” However, she cautioned that the study might have missed cases of domestic abuse because it relies on reports from primary care practitioners.
As for the findings, she said they’re surprising because of the divergence of major cardiovascular outcomes such as ischemic heart disease and stroke in groups of women with an average age of 37. “These differential health outcomes were observed over a 2-3 period. You probably wouldn’t expect to see a divergence in cardiovascular outcomes for 5-10 years in this age group.”
Dr. O’Neil said that, moving forward, the research can be helpful to understanding the rise of cardiovascular disease in women aged 35-54, especially in the United States. “The way we assess an individual’s risk of having a heart attack in the future is largely guided by evidence based on men. For a long time, this has neglected female-specific risk factors like polycystic ovary syndrome and hypertensive disorders of pregnancy but also conditions and exposures to which young women are especially vulnerable like depression, anxiety and [domestic abuse],” she said.
“This research is important as it gives us clues about who may be at elevated risk to help us guide prevention efforts. Equally, there is some evidence that chest pain presentation may be a useful predictor of domestic abuse victimization so there could be multiple lines of further inquiry.”
Dr. Chandan, the other study authors, and Dr. O’Neil reported no relevant disclosures.
SOURCE: Chandan JS et al. J Am Heart Assoc. 2020. doi: 10.1161/JAHA.119.014580.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Single negative colonoscopy predicts low colorectal cancer risk
a new study concludes.
The population-based study showed a durable reduction in CRC risk over 17.4 years of follow-up.
“Our findings confirm that a 10-year interval between high-quality screening colonoscopies [as is currently recommended] is safe and that there is no benefit from more frequent screening,” lead author Nastazja Pilonis, MD, from the Maria Sklodowska-Curie National Research Institute of Oncology in Warsaw, Poland, told Medscape Medical News.
“Furthermore, our findings suggest that this interval could even be prolonged, provided the baseline colonoscopy is of high quality,” she added.
However, she emphasized that “only high-quality colonoscopy provided a durable reduction in mortality risk,” and noted that “low-quality colonoscopy was associated with a significantly increased risk of CRC death after the first 5 years following the examination.”
The study was published online May 25 in the Annals of Internal Medicine.
Polish Colonoscopy Screening Program
The study included 165,887 average-risk patients enrolled in the Polish Colonoscopy Screening Program who had a single negative screening colonoscopy between October 2000 and December 2011.
Negative colonoscopy was defined as an examination where no evidence of any neoplastic lesion was found.
A high-quality screening colonoscopy was defined by three key properties: cecal intubation, adequate bowel preparation, and an endoscopist’s adenoma detection rate (ADR) of 20% or greater calculated on a yearly basis.
A total of 505 different endoscopists performed the colonoscopies over a median follow-up of 10.1 years.
Compared with the general population, among individuals with a negative colonoscopy, the incidence of CRC was 72% lower and CRC mortality was 81% lower over a period of 5.1 to 10 years, Pilonis and colleagues report.
“This was mainly driven by long-lasting reductions in CRC incidence and mortality (by 84% and 90%, respectively) after high-quality screening colonoscopies,” the investigators emphasize.
Beyond 10 years of follow-up, reductions in CRC incidence and mortality were similar to those observed for the earlier period of 5.1 to 10 years but only for participants who had had a high-quality screening colonoscopy, they emphasize.
Subgroup analyses
In addition, subgroup analyses showed that high-quality colonoscopy – although not those of low-quality – effectively reduced the incidence of, and mortality from, CRC in women and in the proximal colon.
As Pilonis pointed out, previous studies have suggested that women may not benefit from screening colonoscopy to the same extent as men. Plus previous research suggests a reduced CRC risk in the proximal colon relative to that in the distal colon.
Overall, standardized incidence ratios (SIRs) and standardized mortality ratios (SMRs) significantly differed between men and women in the current study, but this difference was not observed after high-quality examinations, the investigators report.
“This is an extremely important finding because, for the first time, we showed that when you have high-quality colonoscopy, women benefit from screening colonoscopy as much as men,” Pilonis emphasized.
Similarly, high-quality screening colonoscopy was associated with a 50% reduction in mortality in the proximal colon throughout the 17.4-year follow-up, whereas there was no decrease in mortality from CRC in the proximal colon with low-quality colonoscopies.
As Pilonis noted, lesions in the proximal colon are more subtle and are harder to detect.”It’s also easier to achieve good bowel preparation in the distal colon than in the proximal colon,” she added.
Women are also more prone to develop lesions in the right (proximal) side of the colon and appear to have more pain with colonoscopy than men, all of which could have contributed to previous reports of colonoscopy not being very effective in women or for the detection of lesions in the proximal colon, as Pilonis suggested.
As the authors explain, current guidelines recommend a 10-year screening interval for the average-risk patient when colonoscopy results are negative.
This interval was partially based on the estimated time it was thought to take an adenoma to progress to a carcinoma and partially on the estimated sensitivity of screening colonoscopy.
“We showed that high-quality is a prerequisite for safe intervals between colonoscopies, Pilonis said. “So I would say that if, at a certain age, a patient has a negative colonoscopy of high-quality, a negative colonoscopy is highly predictive of a very low future risk of CRC,” she added.
The study was funded by the Polish Ministry of Health.
This article first appeared on Medscape.com.
a new study concludes.
The population-based study showed a durable reduction in CRC risk over 17.4 years of follow-up.
“Our findings confirm that a 10-year interval between high-quality screening colonoscopies [as is currently recommended] is safe and that there is no benefit from more frequent screening,” lead author Nastazja Pilonis, MD, from the Maria Sklodowska-Curie National Research Institute of Oncology in Warsaw, Poland, told Medscape Medical News.
“Furthermore, our findings suggest that this interval could even be prolonged, provided the baseline colonoscopy is of high quality,” she added.
However, she emphasized that “only high-quality colonoscopy provided a durable reduction in mortality risk,” and noted that “low-quality colonoscopy was associated with a significantly increased risk of CRC death after the first 5 years following the examination.”
The study was published online May 25 in the Annals of Internal Medicine.
Polish Colonoscopy Screening Program
The study included 165,887 average-risk patients enrolled in the Polish Colonoscopy Screening Program who had a single negative screening colonoscopy between October 2000 and December 2011.
Negative colonoscopy was defined as an examination where no evidence of any neoplastic lesion was found.
A high-quality screening colonoscopy was defined by three key properties: cecal intubation, adequate bowel preparation, and an endoscopist’s adenoma detection rate (ADR) of 20% or greater calculated on a yearly basis.
A total of 505 different endoscopists performed the colonoscopies over a median follow-up of 10.1 years.
Compared with the general population, among individuals with a negative colonoscopy, the incidence of CRC was 72% lower and CRC mortality was 81% lower over a period of 5.1 to 10 years, Pilonis and colleagues report.
“This was mainly driven by long-lasting reductions in CRC incidence and mortality (by 84% and 90%, respectively) after high-quality screening colonoscopies,” the investigators emphasize.
Beyond 10 years of follow-up, reductions in CRC incidence and mortality were similar to those observed for the earlier period of 5.1 to 10 years but only for participants who had had a high-quality screening colonoscopy, they emphasize.
Subgroup analyses
In addition, subgroup analyses showed that high-quality colonoscopy – although not those of low-quality – effectively reduced the incidence of, and mortality from, CRC in women and in the proximal colon.
As Pilonis pointed out, previous studies have suggested that women may not benefit from screening colonoscopy to the same extent as men. Plus previous research suggests a reduced CRC risk in the proximal colon relative to that in the distal colon.
Overall, standardized incidence ratios (SIRs) and standardized mortality ratios (SMRs) significantly differed between men and women in the current study, but this difference was not observed after high-quality examinations, the investigators report.
“This is an extremely important finding because, for the first time, we showed that when you have high-quality colonoscopy, women benefit from screening colonoscopy as much as men,” Pilonis emphasized.
Similarly, high-quality screening colonoscopy was associated with a 50% reduction in mortality in the proximal colon throughout the 17.4-year follow-up, whereas there was no decrease in mortality from CRC in the proximal colon with low-quality colonoscopies.
As Pilonis noted, lesions in the proximal colon are more subtle and are harder to detect.”It’s also easier to achieve good bowel preparation in the distal colon than in the proximal colon,” she added.
Women are also more prone to develop lesions in the right (proximal) side of the colon and appear to have more pain with colonoscopy than men, all of which could have contributed to previous reports of colonoscopy not being very effective in women or for the detection of lesions in the proximal colon, as Pilonis suggested.
As the authors explain, current guidelines recommend a 10-year screening interval for the average-risk patient when colonoscopy results are negative.
This interval was partially based on the estimated time it was thought to take an adenoma to progress to a carcinoma and partially on the estimated sensitivity of screening colonoscopy.
“We showed that high-quality is a prerequisite for safe intervals between colonoscopies, Pilonis said. “So I would say that if, at a certain age, a patient has a negative colonoscopy of high-quality, a negative colonoscopy is highly predictive of a very low future risk of CRC,” she added.
The study was funded by the Polish Ministry of Health.
This article first appeared on Medscape.com.
a new study concludes.
The population-based study showed a durable reduction in CRC risk over 17.4 years of follow-up.
“Our findings confirm that a 10-year interval between high-quality screening colonoscopies [as is currently recommended] is safe and that there is no benefit from more frequent screening,” lead author Nastazja Pilonis, MD, from the Maria Sklodowska-Curie National Research Institute of Oncology in Warsaw, Poland, told Medscape Medical News.
“Furthermore, our findings suggest that this interval could even be prolonged, provided the baseline colonoscopy is of high quality,” she added.
However, she emphasized that “only high-quality colonoscopy provided a durable reduction in mortality risk,” and noted that “low-quality colonoscopy was associated with a significantly increased risk of CRC death after the first 5 years following the examination.”
The study was published online May 25 in the Annals of Internal Medicine.
Polish Colonoscopy Screening Program
The study included 165,887 average-risk patients enrolled in the Polish Colonoscopy Screening Program who had a single negative screening colonoscopy between October 2000 and December 2011.
Negative colonoscopy was defined as an examination where no evidence of any neoplastic lesion was found.
A high-quality screening colonoscopy was defined by three key properties: cecal intubation, adequate bowel preparation, and an endoscopist’s adenoma detection rate (ADR) of 20% or greater calculated on a yearly basis.
A total of 505 different endoscopists performed the colonoscopies over a median follow-up of 10.1 years.
Compared with the general population, among individuals with a negative colonoscopy, the incidence of CRC was 72% lower and CRC mortality was 81% lower over a period of 5.1 to 10 years, Pilonis and colleagues report.
“This was mainly driven by long-lasting reductions in CRC incidence and mortality (by 84% and 90%, respectively) after high-quality screening colonoscopies,” the investigators emphasize.
Beyond 10 years of follow-up, reductions in CRC incidence and mortality were similar to those observed for the earlier period of 5.1 to 10 years but only for participants who had had a high-quality screening colonoscopy, they emphasize.
Subgroup analyses
In addition, subgroup analyses showed that high-quality colonoscopy – although not those of low-quality – effectively reduced the incidence of, and mortality from, CRC in women and in the proximal colon.
As Pilonis pointed out, previous studies have suggested that women may not benefit from screening colonoscopy to the same extent as men. Plus previous research suggests a reduced CRC risk in the proximal colon relative to that in the distal colon.
Overall, standardized incidence ratios (SIRs) and standardized mortality ratios (SMRs) significantly differed between men and women in the current study, but this difference was not observed after high-quality examinations, the investigators report.
“This is an extremely important finding because, for the first time, we showed that when you have high-quality colonoscopy, women benefit from screening colonoscopy as much as men,” Pilonis emphasized.
Similarly, high-quality screening colonoscopy was associated with a 50% reduction in mortality in the proximal colon throughout the 17.4-year follow-up, whereas there was no decrease in mortality from CRC in the proximal colon with low-quality colonoscopies.
As Pilonis noted, lesions in the proximal colon are more subtle and are harder to detect.”It’s also easier to achieve good bowel preparation in the distal colon than in the proximal colon,” she added.
Women are also more prone to develop lesions in the right (proximal) side of the colon and appear to have more pain with colonoscopy than men, all of which could have contributed to previous reports of colonoscopy not being very effective in women or for the detection of lesions in the proximal colon, as Pilonis suggested.
As the authors explain, current guidelines recommend a 10-year screening interval for the average-risk patient when colonoscopy results are negative.
This interval was partially based on the estimated time it was thought to take an adenoma to progress to a carcinoma and partially on the estimated sensitivity of screening colonoscopy.
“We showed that high-quality is a prerequisite for safe intervals between colonoscopies, Pilonis said. “So I would say that if, at a certain age, a patient has a negative colonoscopy of high-quality, a negative colonoscopy is highly predictive of a very low future risk of CRC,” she added.
The study was funded by the Polish Ministry of Health.
This article first appeared on Medscape.com.
Robotic and manual total knee arthroplasty found at least comparable
When results in a series of robotic-assisted total knee arthroplasties (TKA) were compared with a series of arthroplasties performed manually by the same surgeon, results were comparable even though the robotic procedures included a learning phase. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“Robotics appears to level the playing field for those who are less experienced, so that robotic total knee arthroplasty might be particularly well suited to low-volume surgeons,” reported Sridhar R. Rachala, MD, assistant professor of orthopaedic surgery, University of Buffalo (N.Y.).
In this retrospective cohort study, radiographic and clinical outcomes were evaluated in 164 total knee arthroplasties performed manually over an 8-month period and compared with 300 procedures performed robotically by the same experienced surgeon over the subsequent 15-month period.
There were no significant differences between patient groups for mean age or body mass index. Dr. Rachala, who performed both sets of procedures, reported inherent differences in technique. Specifically, the mechanical alignment was planned for a traditional neutral mechanical axis, while the robotic procedures were planned in kinematic alignment.
When evaluated at 1 year, the mean KOOS JR (Knee Injury and Osteoarthritis Outcome for Joint Replacement) scores were not significantly different for the robotic and manually performed procedures (76.0 vs. 73.9; P = .54). There were also no differences in the final extension (P = .64) or flexion (P = .59).
However, the difference in mean length of stay (2.0 vs. 2.4 days; P = .0002) favored the robotic approach, and the higher proportion of patients discharged to home after robotic surgery (73% vs. 66%; P = .11) suggested a favorable trend. Planned and postoperative alignment was within two degrees for both groups and not significantly different.
“The robotic series were at a disadvantage because it included cases that I performed when first switching to this approach,” reported Dr. Rachala in an interview.
Although a growing number of total hip arthroplasties are performed robotically, there have not so far been many comparisons of clinical outcomes among surgeons experienced with both approaches, according to Dr. Rachala. Acknowledging that a single-surgeon experience could be considered a limitation of this series, Dr. Rachala also considers it a potential strength. Dr. Rachala was highly experienced with manually instrumented total knee arthroplasty when he switched.
“Positioning and alignment are not just more accurate but easier to perform with robotic assistance,” he said, explaining why this approach is likely to offer a particular advantage to surgeons who perform these types of arthroplasties at low volume. He noted that robotic programming helps prevent errors and adopt alternative more personalized alignments.
Although Dr. Rachala acknowledged that long-term and controlled studies are needed, his experience suggests that robotic-assisted procedures are emerging as a viable alternative with advantages for the surgeon as well as the patient.
The principle that robotic assistance can add consistency to total joint arthroplasty is valid, according to Gwo-Chin Lee, MD, an associate professor of orthopaedic surgery, University of Pennsylvania, Philadelphia. “Robotic-assisted arthroplasty improves the accuracy and consistency of the procedure, which can potentially reduce the likelihood of failure. In knees, it is proven to be valuable in unicompartmental replacements in which results are correlated to a surgeon’s surgical volume. It has an equalizing effect relative to a surgeon with more extensive experience,” Dr. Lee said.
The senior author of a recent systematic review and meta-analysis of robotic-assisted unicompartmental knee arthroplasty (J Knee Surg. 2020 Jan 30; doi: 10.1055/s-0040-1701455), Dr. Lee said, “While the impact of robotics on other metrics including patient satisfaction and early recovery continues to be debated among surgeons who specialize in total knee arthroplasties, the technology can aid surgeons in component position, sizing, and ligament balance, particularly for the lower-volume surgeons and ultimately lead to more predictable outcomes.”
Dr. Rachala reports a financial relationship with Avanos and Stryker.
SOURCE: Rachala S et al. AAOS 2020. Abstract P0091.
When results in a series of robotic-assisted total knee arthroplasties (TKA) were compared with a series of arthroplasties performed manually by the same surgeon, results were comparable even though the robotic procedures included a learning phase. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“Robotics appears to level the playing field for those who are less experienced, so that robotic total knee arthroplasty might be particularly well suited to low-volume surgeons,” reported Sridhar R. Rachala, MD, assistant professor of orthopaedic surgery, University of Buffalo (N.Y.).
In this retrospective cohort study, radiographic and clinical outcomes were evaluated in 164 total knee arthroplasties performed manually over an 8-month period and compared with 300 procedures performed robotically by the same experienced surgeon over the subsequent 15-month period.
There were no significant differences between patient groups for mean age or body mass index. Dr. Rachala, who performed both sets of procedures, reported inherent differences in technique. Specifically, the mechanical alignment was planned for a traditional neutral mechanical axis, while the robotic procedures were planned in kinematic alignment.
When evaluated at 1 year, the mean KOOS JR (Knee Injury and Osteoarthritis Outcome for Joint Replacement) scores were not significantly different for the robotic and manually performed procedures (76.0 vs. 73.9; P = .54). There were also no differences in the final extension (P = .64) or flexion (P = .59).
However, the difference in mean length of stay (2.0 vs. 2.4 days; P = .0002) favored the robotic approach, and the higher proportion of patients discharged to home after robotic surgery (73% vs. 66%; P = .11) suggested a favorable trend. Planned and postoperative alignment was within two degrees for both groups and not significantly different.
“The robotic series were at a disadvantage because it included cases that I performed when first switching to this approach,” reported Dr. Rachala in an interview.
Although a growing number of total hip arthroplasties are performed robotically, there have not so far been many comparisons of clinical outcomes among surgeons experienced with both approaches, according to Dr. Rachala. Acknowledging that a single-surgeon experience could be considered a limitation of this series, Dr. Rachala also considers it a potential strength. Dr. Rachala was highly experienced with manually instrumented total knee arthroplasty when he switched.
“Positioning and alignment are not just more accurate but easier to perform with robotic assistance,” he said, explaining why this approach is likely to offer a particular advantage to surgeons who perform these types of arthroplasties at low volume. He noted that robotic programming helps prevent errors and adopt alternative more personalized alignments.
Although Dr. Rachala acknowledged that long-term and controlled studies are needed, his experience suggests that robotic-assisted procedures are emerging as a viable alternative with advantages for the surgeon as well as the patient.
The principle that robotic assistance can add consistency to total joint arthroplasty is valid, according to Gwo-Chin Lee, MD, an associate professor of orthopaedic surgery, University of Pennsylvania, Philadelphia. “Robotic-assisted arthroplasty improves the accuracy and consistency of the procedure, which can potentially reduce the likelihood of failure. In knees, it is proven to be valuable in unicompartmental replacements in which results are correlated to a surgeon’s surgical volume. It has an equalizing effect relative to a surgeon with more extensive experience,” Dr. Lee said.
The senior author of a recent systematic review and meta-analysis of robotic-assisted unicompartmental knee arthroplasty (J Knee Surg. 2020 Jan 30; doi: 10.1055/s-0040-1701455), Dr. Lee said, “While the impact of robotics on other metrics including patient satisfaction and early recovery continues to be debated among surgeons who specialize in total knee arthroplasties, the technology can aid surgeons in component position, sizing, and ligament balance, particularly for the lower-volume surgeons and ultimately lead to more predictable outcomes.”
Dr. Rachala reports a financial relationship with Avanos and Stryker.
SOURCE: Rachala S et al. AAOS 2020. Abstract P0091.
When results in a series of robotic-assisted total knee arthroplasties (TKA) were compared with a series of arthroplasties performed manually by the same surgeon, results were comparable even though the robotic procedures included a learning phase. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“Robotics appears to level the playing field for those who are less experienced, so that robotic total knee arthroplasty might be particularly well suited to low-volume surgeons,” reported Sridhar R. Rachala, MD, assistant professor of orthopaedic surgery, University of Buffalo (N.Y.).
In this retrospective cohort study, radiographic and clinical outcomes were evaluated in 164 total knee arthroplasties performed manually over an 8-month period and compared with 300 procedures performed robotically by the same experienced surgeon over the subsequent 15-month period.
There were no significant differences between patient groups for mean age or body mass index. Dr. Rachala, who performed both sets of procedures, reported inherent differences in technique. Specifically, the mechanical alignment was planned for a traditional neutral mechanical axis, while the robotic procedures were planned in kinematic alignment.
When evaluated at 1 year, the mean KOOS JR (Knee Injury and Osteoarthritis Outcome for Joint Replacement) scores were not significantly different for the robotic and manually performed procedures (76.0 vs. 73.9; P = .54). There were also no differences in the final extension (P = .64) or flexion (P = .59).
However, the difference in mean length of stay (2.0 vs. 2.4 days; P = .0002) favored the robotic approach, and the higher proportion of patients discharged to home after robotic surgery (73% vs. 66%; P = .11) suggested a favorable trend. Planned and postoperative alignment was within two degrees for both groups and not significantly different.
“The robotic series were at a disadvantage because it included cases that I performed when first switching to this approach,” reported Dr. Rachala in an interview.
Although a growing number of total hip arthroplasties are performed robotically, there have not so far been many comparisons of clinical outcomes among surgeons experienced with both approaches, according to Dr. Rachala. Acknowledging that a single-surgeon experience could be considered a limitation of this series, Dr. Rachala also considers it a potential strength. Dr. Rachala was highly experienced with manually instrumented total knee arthroplasty when he switched.
“Positioning and alignment are not just more accurate but easier to perform with robotic assistance,” he said, explaining why this approach is likely to offer a particular advantage to surgeons who perform these types of arthroplasties at low volume. He noted that robotic programming helps prevent errors and adopt alternative more personalized alignments.
Although Dr. Rachala acknowledged that long-term and controlled studies are needed, his experience suggests that robotic-assisted procedures are emerging as a viable alternative with advantages for the surgeon as well as the patient.
The principle that robotic assistance can add consistency to total joint arthroplasty is valid, according to Gwo-Chin Lee, MD, an associate professor of orthopaedic surgery, University of Pennsylvania, Philadelphia. “Robotic-assisted arthroplasty improves the accuracy and consistency of the procedure, which can potentially reduce the likelihood of failure. In knees, it is proven to be valuable in unicompartmental replacements in which results are correlated to a surgeon’s surgical volume. It has an equalizing effect relative to a surgeon with more extensive experience,” Dr. Lee said.
The senior author of a recent systematic review and meta-analysis of robotic-assisted unicompartmental knee arthroplasty (J Knee Surg. 2020 Jan 30; doi: 10.1055/s-0040-1701455), Dr. Lee said, “While the impact of robotics on other metrics including patient satisfaction and early recovery continues to be debated among surgeons who specialize in total knee arthroplasties, the technology can aid surgeons in component position, sizing, and ligament balance, particularly for the lower-volume surgeons and ultimately lead to more predictable outcomes.”
Dr. Rachala reports a financial relationship with Avanos and Stryker.
SOURCE: Rachala S et al. AAOS 2020. Abstract P0091.
FROM aaos 2020
Movement-based yoga ‘viable’ for depression in many mental disorders
Movement-based yoga appears to ease depressive symptoms in a wide range of mental health disorders, a new systematic review and meta-analysis suggest.
Results of the research, which included 19 studies and more than 1,000 patients with a variety of mental health diagnoses, showed that those who practiced yoga experienced greater reductions in depressive symptoms versus those undergoing no treatment, usual treatment, or attention-control exercises. In addition, there was a dose-dependent effect such that more weekly yoga sessions were associated with the greatest reduction in depressive symptoms.
“Once we reviewed all the existing science about the mental health benefits of movement-based yoga, we found that movement-based yoga – which is the same thing as postural yoga or asana – helped reduce symptoms of depression,” study investigator Jacinta Brinsley, BClinExPhys, of the University of South Australia, Adelaide, said in an interview.
“We also found those who practiced more frequently had bigger reductions. However, it didn’t matter how long the individual sessions were; what mattered was how many times per week people practiced,” she added.
The researchers noted that the study is the first to focus specifically on movement-based yoga.
“We excluded meditative forms of yoga, which have often been included in previous reviews, yielding mixed findings. The other thing we’ve done a bit differently is pool all the different diagnoses together and then look at depressive symptoms across them,” said Ms. Brinsley.
The study was published online May 18 in the British Journal of Sports Medicine.
Getting clarity
Depressive disorders are currently the world’s leading cause of disability, affecting more than 340 million people.
Most individuals who suffer from depressive disorders also experience a host of physical comorbidities including obesity, type 2 diabetes, metabolic syndrome, and cardiovascular disease.
Perhaps not surprisingly, physical inactivity is also associated with higher levels of depressive symptoms, which may be the reason some international organizations now recommend that physical activity be included as part of routine psychiatric care.
One potential form of exercise is yoga, which has become popular in Western culture, including among psychiatric patients. Although previous systematic reviews and meta-analyses have examined the effects of various yoga interventions on mental health, none has investigated the benefits of yoga across a range of psychiatric diagnoses.
What’s more, the authors of these reviews all urge caution when interpreting their results because of potential heterogeneity of the various yoga interventions, as well as poor methodological reporting.
“As an exercise physiologist, I prescribe evidence-based treatment,” said Ms. Brinsley. “I was interested in seeing if there’s evidence to support movement-based yoga in people who were struggling with mental health or who had a diagnosed mental illness.
“The [previous] findings are quite contradictory and there’s not a clear outcome in terms of intervention results, so we pooled the data and ran the meta-analysis, thinking it would be a great way to add some important evidence to the science,” she added.
To allow for a more comprehensive assessment of yoga’s potential mental health benefits, the investigators included a range of mental health diagnoses.
Dose-dependent effect
Studies were only included in the analysis if they were randomized, controlled trials with a yoga intervention that had a minimum of 50% physical activity during each session in adults with a recognized diagnosed mental disorder. Control conditions were defined as treatment as usual, wait list, or attention controls.
Two investigators independently scanned article titles and abstracts, and a final list of articles for the study was decided by consensus. Study quality was reported using the PEDro checklist; a random-effects meta-analysis was conducted using Comprehensive Meta-Analysis software.
A total of 3,880 records were identified and screened. The investigators assessed full-text versions of 80 articles, 19 of which (1,080 patients) were eligible for inclusion in the review.
Of these, nine studies included patients with a depressive disorder; five trials were in patients with a diagnosis of schizophrenia, three studies included patients with a diagnosis of PTSD, one study included patients diagnosed with alcohol dependence, and one study included patients with a range of psychiatric disorders.
Of the 1,080 patients included in the review, 578 were assigned to yoga and 502 to control conditions. Yoga practice involved a mixture of movement, breathing exercises, and/or mindfulness, but the movement component took up more than half of each session.
The yoga interventions lasted an average of 2.4 months (range, 1.5-2.5 months), with an average of 1.6 sessions per week (range, 1-3 sessions) that lasted an average of 60 minutes (range, 20-90 minutes).
Of the 19 studies (632 patients), 13 reported changes in depressive symptoms and were therefore included in the meta-analysis. The six studies excluded from the quantitative analysis did not report depression symptom scores.
With respect to primary outcomes, individuals who performed yoga showed a greater reduction in depressive symptoms, compared with the three control groups (standardized mean difference, –0.41; 95% CI, –0.65 to –0.17; P < .001).
Specific subgroup analyses showed a moderate effect of yoga on depressive symptoms, compared with wait-list controls (SMD, –0.58; P < .05), treatment as usual (SMD, –0.39; P = .31), and attention controls (SMD, –0.21; P = .22).
Subgroup analyses were also performed with respect to diagnostic category. These data showed a moderate effect of yoga on depressive symptoms in depressive disorders (SMD, –0.40; P < .01), no effect in PTSD (SMD, –0.01; P = .95), a nominal effect in alcohol use disorders (SMD, –0.24; P = .69), and a marked effect in schizophrenia (SMD, –0.90; P < .01).
Movement may be key
Researchers also performed a series of meta-regression analyses, which showed that the number of yoga sessions performed each week had a significant effect on depressive symptoms. Indeed, individuals with higher session frequencies demonstrated a greater improvement in symptoms (beta, –0.44; P < .001).
These findings, said Ms. Brinsley, suggest yoga may be a viable intervention for managing depressive symptoms in patients with a variety of mental disorders.
Based on these findings, along with other conventional forms of exercise.
Equally important was the finding that the number of weekly yoga sessions moderated the effect of depressive symptoms, as it may inform the future design of yoga interventions in patients with mental disorders.
With this in mind, the researchers recommended that such interventions should aim to increase the frequency or weekly sessions rather than the duration of each individual session or the overall duration of the intervention.
However, said Ms. Brinsley, these findings suggest it is the physical aspect of the yoga practice that may be key.
“Yoga comprises several different components, including the movement postures, the breathing component, and the mindfulness or meditative component, but in this meta-analysis we looked specifically at yoga that was at least 50% movement based. So it might have also included mindfulness and breathing, but it had to have the movement,” she said.
Don’t discount meditation
Commenting on the findings, Holger Cramer, MSc, PhD, DSc, who was not involved in the study, noted that the systematic review and meta-analysis builds on a number of previous reviews regarding the benefits of yoga for mental disorders.
“Surprisingly, the largest effect in this analysis was found in schizophrenia, even higher than in patients with depressive disorders,” said Dr. Cramer of the University of Duisburg-Essen (Germany). “This is in strong contradiction to what would otherwise be expected. As the authors point out, only about a quarter of all schizophrenia patients suffer from depression, so there should not be so much room for improvement.”
Dr. Cramer also advised against reducing yoga to simply a physical undertaking. “We have shown in our meta-analysis that those interventions focusing on meditation and/or breathing techniques are the most effective ones,” he added.
As such, he urged that breathing techniques be a part of yoga for treating depression in psychiatric disorders, though care should be taken in patients with PTSD, “since breath control might be perceived as unpleasant.”
For Ms. Brinsley, the findings help solidify yoga’s potential as a genuine treatment option for a variety of mental health patients suffering depressive symptoms.
“It’s about acknowledging that yoga can be a helpful part of treatment and can have a significant effect on mental health,” she noted.
At the same time, practitioners also need to acknowledge that patients suffering from mental health disorders may struggle with motivation when it comes to activities such as yoga.
“Engaging in a new activity can be particularly challenging if you’re struggling with mental health. Nevertheless, it’s important for people to have a choice and do something they enjoy. And yoga can be another tool in their toolbox for managing their mental health,” she said.
The study was funded by the U.K. National Institute for Health Research and Health Education England. Ms. Brinsley and Dr. Cramer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Movement-based yoga appears to ease depressive symptoms in a wide range of mental health disorders, a new systematic review and meta-analysis suggest.
Results of the research, which included 19 studies and more than 1,000 patients with a variety of mental health diagnoses, showed that those who practiced yoga experienced greater reductions in depressive symptoms versus those undergoing no treatment, usual treatment, or attention-control exercises. In addition, there was a dose-dependent effect such that more weekly yoga sessions were associated with the greatest reduction in depressive symptoms.
“Once we reviewed all the existing science about the mental health benefits of movement-based yoga, we found that movement-based yoga – which is the same thing as postural yoga or asana – helped reduce symptoms of depression,” study investigator Jacinta Brinsley, BClinExPhys, of the University of South Australia, Adelaide, said in an interview.
“We also found those who practiced more frequently had bigger reductions. However, it didn’t matter how long the individual sessions were; what mattered was how many times per week people practiced,” she added.
The researchers noted that the study is the first to focus specifically on movement-based yoga.
“We excluded meditative forms of yoga, which have often been included in previous reviews, yielding mixed findings. The other thing we’ve done a bit differently is pool all the different diagnoses together and then look at depressive symptoms across them,” said Ms. Brinsley.
The study was published online May 18 in the British Journal of Sports Medicine.
Getting clarity
Depressive disorders are currently the world’s leading cause of disability, affecting more than 340 million people.
Most individuals who suffer from depressive disorders also experience a host of physical comorbidities including obesity, type 2 diabetes, metabolic syndrome, and cardiovascular disease.
Perhaps not surprisingly, physical inactivity is also associated with higher levels of depressive symptoms, which may be the reason some international organizations now recommend that physical activity be included as part of routine psychiatric care.
One potential form of exercise is yoga, which has become popular in Western culture, including among psychiatric patients. Although previous systematic reviews and meta-analyses have examined the effects of various yoga interventions on mental health, none has investigated the benefits of yoga across a range of psychiatric diagnoses.
What’s more, the authors of these reviews all urge caution when interpreting their results because of potential heterogeneity of the various yoga interventions, as well as poor methodological reporting.
“As an exercise physiologist, I prescribe evidence-based treatment,” said Ms. Brinsley. “I was interested in seeing if there’s evidence to support movement-based yoga in people who were struggling with mental health or who had a diagnosed mental illness.
“The [previous] findings are quite contradictory and there’s not a clear outcome in terms of intervention results, so we pooled the data and ran the meta-analysis, thinking it would be a great way to add some important evidence to the science,” she added.
To allow for a more comprehensive assessment of yoga’s potential mental health benefits, the investigators included a range of mental health diagnoses.
Dose-dependent effect
Studies were only included in the analysis if they were randomized, controlled trials with a yoga intervention that had a minimum of 50% physical activity during each session in adults with a recognized diagnosed mental disorder. Control conditions were defined as treatment as usual, wait list, or attention controls.
Two investigators independently scanned article titles and abstracts, and a final list of articles for the study was decided by consensus. Study quality was reported using the PEDro checklist; a random-effects meta-analysis was conducted using Comprehensive Meta-Analysis software.
A total of 3,880 records were identified and screened. The investigators assessed full-text versions of 80 articles, 19 of which (1,080 patients) were eligible for inclusion in the review.
Of these, nine studies included patients with a depressive disorder; five trials were in patients with a diagnosis of schizophrenia, three studies included patients with a diagnosis of PTSD, one study included patients diagnosed with alcohol dependence, and one study included patients with a range of psychiatric disorders.
Of the 1,080 patients included in the review, 578 were assigned to yoga and 502 to control conditions. Yoga practice involved a mixture of movement, breathing exercises, and/or mindfulness, but the movement component took up more than half of each session.
The yoga interventions lasted an average of 2.4 months (range, 1.5-2.5 months), with an average of 1.6 sessions per week (range, 1-3 sessions) that lasted an average of 60 minutes (range, 20-90 minutes).
Of the 19 studies (632 patients), 13 reported changes in depressive symptoms and were therefore included in the meta-analysis. The six studies excluded from the quantitative analysis did not report depression symptom scores.
With respect to primary outcomes, individuals who performed yoga showed a greater reduction in depressive symptoms, compared with the three control groups (standardized mean difference, –0.41; 95% CI, –0.65 to –0.17; P < .001).
Specific subgroup analyses showed a moderate effect of yoga on depressive symptoms, compared with wait-list controls (SMD, –0.58; P < .05), treatment as usual (SMD, –0.39; P = .31), and attention controls (SMD, –0.21; P = .22).
Subgroup analyses were also performed with respect to diagnostic category. These data showed a moderate effect of yoga on depressive symptoms in depressive disorders (SMD, –0.40; P < .01), no effect in PTSD (SMD, –0.01; P = .95), a nominal effect in alcohol use disorders (SMD, –0.24; P = .69), and a marked effect in schizophrenia (SMD, –0.90; P < .01).
Movement may be key
Researchers also performed a series of meta-regression analyses, which showed that the number of yoga sessions performed each week had a significant effect on depressive symptoms. Indeed, individuals with higher session frequencies demonstrated a greater improvement in symptoms (beta, –0.44; P < .001).
These findings, said Ms. Brinsley, suggest yoga may be a viable intervention for managing depressive symptoms in patients with a variety of mental disorders.
Based on these findings, along with other conventional forms of exercise.
Equally important was the finding that the number of weekly yoga sessions moderated the effect of depressive symptoms, as it may inform the future design of yoga interventions in patients with mental disorders.
With this in mind, the researchers recommended that such interventions should aim to increase the frequency or weekly sessions rather than the duration of each individual session or the overall duration of the intervention.
However, said Ms. Brinsley, these findings suggest it is the physical aspect of the yoga practice that may be key.
“Yoga comprises several different components, including the movement postures, the breathing component, and the mindfulness or meditative component, but in this meta-analysis we looked specifically at yoga that was at least 50% movement based. So it might have also included mindfulness and breathing, but it had to have the movement,” she said.
Don’t discount meditation
Commenting on the findings, Holger Cramer, MSc, PhD, DSc, who was not involved in the study, noted that the systematic review and meta-analysis builds on a number of previous reviews regarding the benefits of yoga for mental disorders.
“Surprisingly, the largest effect in this analysis was found in schizophrenia, even higher than in patients with depressive disorders,” said Dr. Cramer of the University of Duisburg-Essen (Germany). “This is in strong contradiction to what would otherwise be expected. As the authors point out, only about a quarter of all schizophrenia patients suffer from depression, so there should not be so much room for improvement.”
Dr. Cramer also advised against reducing yoga to simply a physical undertaking. “We have shown in our meta-analysis that those interventions focusing on meditation and/or breathing techniques are the most effective ones,” he added.
As such, he urged that breathing techniques be a part of yoga for treating depression in psychiatric disorders, though care should be taken in patients with PTSD, “since breath control might be perceived as unpleasant.”
For Ms. Brinsley, the findings help solidify yoga’s potential as a genuine treatment option for a variety of mental health patients suffering depressive symptoms.
“It’s about acknowledging that yoga can be a helpful part of treatment and can have a significant effect on mental health,” she noted.
At the same time, practitioners also need to acknowledge that patients suffering from mental health disorders may struggle with motivation when it comes to activities such as yoga.
“Engaging in a new activity can be particularly challenging if you’re struggling with mental health. Nevertheless, it’s important for people to have a choice and do something they enjoy. And yoga can be another tool in their toolbox for managing their mental health,” she said.
The study was funded by the U.K. National Institute for Health Research and Health Education England. Ms. Brinsley and Dr. Cramer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Movement-based yoga appears to ease depressive symptoms in a wide range of mental health disorders, a new systematic review and meta-analysis suggest.
Results of the research, which included 19 studies and more than 1,000 patients with a variety of mental health diagnoses, showed that those who practiced yoga experienced greater reductions in depressive symptoms versus those undergoing no treatment, usual treatment, or attention-control exercises. In addition, there was a dose-dependent effect such that more weekly yoga sessions were associated with the greatest reduction in depressive symptoms.
“Once we reviewed all the existing science about the mental health benefits of movement-based yoga, we found that movement-based yoga – which is the same thing as postural yoga or asana – helped reduce symptoms of depression,” study investigator Jacinta Brinsley, BClinExPhys, of the University of South Australia, Adelaide, said in an interview.
“We also found those who practiced more frequently had bigger reductions. However, it didn’t matter how long the individual sessions were; what mattered was how many times per week people practiced,” she added.
The researchers noted that the study is the first to focus specifically on movement-based yoga.
“We excluded meditative forms of yoga, which have often been included in previous reviews, yielding mixed findings. The other thing we’ve done a bit differently is pool all the different diagnoses together and then look at depressive symptoms across them,” said Ms. Brinsley.
The study was published online May 18 in the British Journal of Sports Medicine.
Getting clarity
Depressive disorders are currently the world’s leading cause of disability, affecting more than 340 million people.
Most individuals who suffer from depressive disorders also experience a host of physical comorbidities including obesity, type 2 diabetes, metabolic syndrome, and cardiovascular disease.
Perhaps not surprisingly, physical inactivity is also associated with higher levels of depressive symptoms, which may be the reason some international organizations now recommend that physical activity be included as part of routine psychiatric care.
One potential form of exercise is yoga, which has become popular in Western culture, including among psychiatric patients. Although previous systematic reviews and meta-analyses have examined the effects of various yoga interventions on mental health, none has investigated the benefits of yoga across a range of psychiatric diagnoses.
What’s more, the authors of these reviews all urge caution when interpreting their results because of potential heterogeneity of the various yoga interventions, as well as poor methodological reporting.
“As an exercise physiologist, I prescribe evidence-based treatment,” said Ms. Brinsley. “I was interested in seeing if there’s evidence to support movement-based yoga in people who were struggling with mental health or who had a diagnosed mental illness.
“The [previous] findings are quite contradictory and there’s not a clear outcome in terms of intervention results, so we pooled the data and ran the meta-analysis, thinking it would be a great way to add some important evidence to the science,” she added.
To allow for a more comprehensive assessment of yoga’s potential mental health benefits, the investigators included a range of mental health diagnoses.
Dose-dependent effect
Studies were only included in the analysis if they were randomized, controlled trials with a yoga intervention that had a minimum of 50% physical activity during each session in adults with a recognized diagnosed mental disorder. Control conditions were defined as treatment as usual, wait list, or attention controls.
Two investigators independently scanned article titles and abstracts, and a final list of articles for the study was decided by consensus. Study quality was reported using the PEDro checklist; a random-effects meta-analysis was conducted using Comprehensive Meta-Analysis software.
A total of 3,880 records were identified and screened. The investigators assessed full-text versions of 80 articles, 19 of which (1,080 patients) were eligible for inclusion in the review.
Of these, nine studies included patients with a depressive disorder; five trials were in patients with a diagnosis of schizophrenia, three studies included patients with a diagnosis of PTSD, one study included patients diagnosed with alcohol dependence, and one study included patients with a range of psychiatric disorders.
Of the 1,080 patients included in the review, 578 were assigned to yoga and 502 to control conditions. Yoga practice involved a mixture of movement, breathing exercises, and/or mindfulness, but the movement component took up more than half of each session.
The yoga interventions lasted an average of 2.4 months (range, 1.5-2.5 months), with an average of 1.6 sessions per week (range, 1-3 sessions) that lasted an average of 60 minutes (range, 20-90 minutes).
Of the 19 studies (632 patients), 13 reported changes in depressive symptoms and were therefore included in the meta-analysis. The six studies excluded from the quantitative analysis did not report depression symptom scores.
With respect to primary outcomes, individuals who performed yoga showed a greater reduction in depressive symptoms, compared with the three control groups (standardized mean difference, –0.41; 95% CI, –0.65 to –0.17; P < .001).
Specific subgroup analyses showed a moderate effect of yoga on depressive symptoms, compared with wait-list controls (SMD, –0.58; P < .05), treatment as usual (SMD, –0.39; P = .31), and attention controls (SMD, –0.21; P = .22).
Subgroup analyses were also performed with respect to diagnostic category. These data showed a moderate effect of yoga on depressive symptoms in depressive disorders (SMD, –0.40; P < .01), no effect in PTSD (SMD, –0.01; P = .95), a nominal effect in alcohol use disorders (SMD, –0.24; P = .69), and a marked effect in schizophrenia (SMD, –0.90; P < .01).
Movement may be key
Researchers also performed a series of meta-regression analyses, which showed that the number of yoga sessions performed each week had a significant effect on depressive symptoms. Indeed, individuals with higher session frequencies demonstrated a greater improvement in symptoms (beta, –0.44; P < .001).
These findings, said Ms. Brinsley, suggest yoga may be a viable intervention for managing depressive symptoms in patients with a variety of mental disorders.
Based on these findings, along with other conventional forms of exercise.
Equally important was the finding that the number of weekly yoga sessions moderated the effect of depressive symptoms, as it may inform the future design of yoga interventions in patients with mental disorders.
With this in mind, the researchers recommended that such interventions should aim to increase the frequency or weekly sessions rather than the duration of each individual session or the overall duration of the intervention.
However, said Ms. Brinsley, these findings suggest it is the physical aspect of the yoga practice that may be key.
“Yoga comprises several different components, including the movement postures, the breathing component, and the mindfulness or meditative component, but in this meta-analysis we looked specifically at yoga that was at least 50% movement based. So it might have also included mindfulness and breathing, but it had to have the movement,” she said.
Don’t discount meditation
Commenting on the findings, Holger Cramer, MSc, PhD, DSc, who was not involved in the study, noted that the systematic review and meta-analysis builds on a number of previous reviews regarding the benefits of yoga for mental disorders.
“Surprisingly, the largest effect in this analysis was found in schizophrenia, even higher than in patients with depressive disorders,” said Dr. Cramer of the University of Duisburg-Essen (Germany). “This is in strong contradiction to what would otherwise be expected. As the authors point out, only about a quarter of all schizophrenia patients suffer from depression, so there should not be so much room for improvement.”
Dr. Cramer also advised against reducing yoga to simply a physical undertaking. “We have shown in our meta-analysis that those interventions focusing on meditation and/or breathing techniques are the most effective ones,” he added.
As such, he urged that breathing techniques be a part of yoga for treating depression in psychiatric disorders, though care should be taken in patients with PTSD, “since breath control might be perceived as unpleasant.”
For Ms. Brinsley, the findings help solidify yoga’s potential as a genuine treatment option for a variety of mental health patients suffering depressive symptoms.
“It’s about acknowledging that yoga can be a helpful part of treatment and can have a significant effect on mental health,” she noted.
At the same time, practitioners also need to acknowledge that patients suffering from mental health disorders may struggle with motivation when it comes to activities such as yoga.
“Engaging in a new activity can be particularly challenging if you’re struggling with mental health. Nevertheless, it’s important for people to have a choice and do something they enjoy. And yoga can be another tool in their toolbox for managing their mental health,” she said.
The study was funded by the U.K. National Institute for Health Research and Health Education England. Ms. Brinsley and Dr. Cramer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19: Psychiatrists assess geriatric harm from social distancing
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
Suicide often associated with bullying in LGBTQ youth
based on analysis of a national database.

Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
based on analysis of a national database.

Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
based on analysis of a national database.

Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
FROM JAMA PEDIATRICS