User login
More than half of urine drug screens showed improper medication use
LAS VEGAS –
Of almost 4 million urine screens examined, 52% were discordant for the screen-ordered drugs, Jeffrey Gudin, MD, said at the annual PAINWeek. Most common was the combination of opioids and benzodiazepines, which accounted for 21% of the discordant samples – and, in 64% of these cases, at least one of the drugs was not prescribed.
“Drug testing is a standard of care in pain management, and it’s the only objective way to know what patients are really taking,” said Dr. Gudin, director of pain and palliative care at Englewood (N.J.) Hospital and Medical Center. “What this tells us is that, if we just ask our patients, half the time they won’t tell you the whole story. More than 50% of the time things don’t match up. To me this is just unbelievable.”
Quest Diagnostics compiled these data, and many more, in its “Health Trends Report: Drug Misuse in America 2018.”
The report examines 3.9 million routine drug screens ordered by primary care and pain physicians during 2011-2017. It not only looks at prescription drug use and misuse but also tracks illicit drugs in both general and substance abuse patient populations. The findings reported at PAINWeek were based on 456,675 screens from 276,953 patients conducted in 2017. These results were included in the Quest Diagnostics medMATCH reports, which indicated what tested drugs were prescribed and whether these drugs were detected in the specimen.
The following were found among the discordant screens identified in 2017:
- 45% were positive for nonprescribed or illicit drugs in addition to all the prescribed drugs.
- 34% did not show all the drugs they had been prescribed, or any other tested drug.
- 22% did not show all the drugs they had been prescribed but were positive for other illicit or nonprescribed drugs.
The tests were ordered as a part of routine care – an important point, Dr. Gudin said in an interview. “These are not ‘gotcha tests,’ ” intended to catch patients unawares. “These are regularly ordered screens that are standard of care in pain management.”
The report found that men and women were equally likely to misuse medications (52% each). There were some age-related differences, with misuse peaking in young adulthood: 60% of 18- to 24-year-olds and 56% of 25- to 45-year-olds. Misuse dropped off in those aged 55-64 years (52%) and in those 65 years and older (43%). But even children showed evidence of medication misuse, with about 41% of samples from children aged 10 years and younger being discordant.
The rates of misuse were about 50% in Medicare and private pay patients, but around 65% in Medicaid patients.
There was some good news: In the general patient population, opioid use was down by 12% from 2016 – the largest annual decrease Quest has noted since 2012. Several factors probably contributed to that decline, including shifts in clinical care and payer reimbursement, as well as regulatory and legislative restrictions.
“This shows that we’re doing better on the pain management front,” Dr. Gudin said. “But in substance use disorder settings, we saw 400% increases for both fentanyl and heroin. The addiction front it out of control.”
More than 27% of all specimens that came from substance abuse treatment centers were positive for nonprescribed fentanyl and 10% were positive for heroin. “We also saw that, in 2016, 45% of those heroin-positive samples had fentanyl in them, and in 2017, 83% did.”
Although not discussed at PAINWeek, the report also noted a rise in gabapentin misuse. The antiepileptic is now the 10th most commonly prescribed drug in the United States, the report noted, with 68 million prescriptions dispensed last year. The report found that 9.5% of tests showed nonprescription gabapentin. In the subset of samples obtained from substance abuse treatment centers, gabapentin misuse increased by 800% from 2016 – the most dramatic increase of any of the tracked drugs.
The combination of gabapentin and opioids is risky, the report noted. Opioid-related deaths are 49% more common among those taking both than those taking opioids only.
SOURCE: Gudin J et al. PAINWeek 2018, abstract 44.
LAS VEGAS –
Of almost 4 million urine screens examined, 52% were discordant for the screen-ordered drugs, Jeffrey Gudin, MD, said at the annual PAINWeek. Most common was the combination of opioids and benzodiazepines, which accounted for 21% of the discordant samples – and, in 64% of these cases, at least one of the drugs was not prescribed.
“Drug testing is a standard of care in pain management, and it’s the only objective way to know what patients are really taking,” said Dr. Gudin, director of pain and palliative care at Englewood (N.J.) Hospital and Medical Center. “What this tells us is that, if we just ask our patients, half the time they won’t tell you the whole story. More than 50% of the time things don’t match up. To me this is just unbelievable.”
Quest Diagnostics compiled these data, and many more, in its “Health Trends Report: Drug Misuse in America 2018.”
The report examines 3.9 million routine drug screens ordered by primary care and pain physicians during 2011-2017. It not only looks at prescription drug use and misuse but also tracks illicit drugs in both general and substance abuse patient populations. The findings reported at PAINWeek were based on 456,675 screens from 276,953 patients conducted in 2017. These results were included in the Quest Diagnostics medMATCH reports, which indicated what tested drugs were prescribed and whether these drugs were detected in the specimen.
The following were found among the discordant screens identified in 2017:
- 45% were positive for nonprescribed or illicit drugs in addition to all the prescribed drugs.
- 34% did not show all the drugs they had been prescribed, or any other tested drug.
- 22% did not show all the drugs they had been prescribed but were positive for other illicit or nonprescribed drugs.
The tests were ordered as a part of routine care – an important point, Dr. Gudin said in an interview. “These are not ‘gotcha tests,’ ” intended to catch patients unawares. “These are regularly ordered screens that are standard of care in pain management.”
The report found that men and women were equally likely to misuse medications (52% each). There were some age-related differences, with misuse peaking in young adulthood: 60% of 18- to 24-year-olds and 56% of 25- to 45-year-olds. Misuse dropped off in those aged 55-64 years (52%) and in those 65 years and older (43%). But even children showed evidence of medication misuse, with about 41% of samples from children aged 10 years and younger being discordant.
The rates of misuse were about 50% in Medicare and private pay patients, but around 65% in Medicaid patients.
There was some good news: In the general patient population, opioid use was down by 12% from 2016 – the largest annual decrease Quest has noted since 2012. Several factors probably contributed to that decline, including shifts in clinical care and payer reimbursement, as well as regulatory and legislative restrictions.
“This shows that we’re doing better on the pain management front,” Dr. Gudin said. “But in substance use disorder settings, we saw 400% increases for both fentanyl and heroin. The addiction front it out of control.”
More than 27% of all specimens that came from substance abuse treatment centers were positive for nonprescribed fentanyl and 10% were positive for heroin. “We also saw that, in 2016, 45% of those heroin-positive samples had fentanyl in them, and in 2017, 83% did.”
Although not discussed at PAINWeek, the report also noted a rise in gabapentin misuse. The antiepileptic is now the 10th most commonly prescribed drug in the United States, the report noted, with 68 million prescriptions dispensed last year. The report found that 9.5% of tests showed nonprescription gabapentin. In the subset of samples obtained from substance abuse treatment centers, gabapentin misuse increased by 800% from 2016 – the most dramatic increase of any of the tracked drugs.
The combination of gabapentin and opioids is risky, the report noted. Opioid-related deaths are 49% more common among those taking both than those taking opioids only.
SOURCE: Gudin J et al. PAINWeek 2018, abstract 44.
LAS VEGAS –
Of almost 4 million urine screens examined, 52% were discordant for the screen-ordered drugs, Jeffrey Gudin, MD, said at the annual PAINWeek. Most common was the combination of opioids and benzodiazepines, which accounted for 21% of the discordant samples – and, in 64% of these cases, at least one of the drugs was not prescribed.
“Drug testing is a standard of care in pain management, and it’s the only objective way to know what patients are really taking,” said Dr. Gudin, director of pain and palliative care at Englewood (N.J.) Hospital and Medical Center. “What this tells us is that, if we just ask our patients, half the time they won’t tell you the whole story. More than 50% of the time things don’t match up. To me this is just unbelievable.”
Quest Diagnostics compiled these data, and many more, in its “Health Trends Report: Drug Misuse in America 2018.”
The report examines 3.9 million routine drug screens ordered by primary care and pain physicians during 2011-2017. It not only looks at prescription drug use and misuse but also tracks illicit drugs in both general and substance abuse patient populations. The findings reported at PAINWeek were based on 456,675 screens from 276,953 patients conducted in 2017. These results were included in the Quest Diagnostics medMATCH reports, which indicated what tested drugs were prescribed and whether these drugs were detected in the specimen.
The following were found among the discordant screens identified in 2017:
- 45% were positive for nonprescribed or illicit drugs in addition to all the prescribed drugs.
- 34% did not show all the drugs they had been prescribed, or any other tested drug.
- 22% did not show all the drugs they had been prescribed but were positive for other illicit or nonprescribed drugs.
The tests were ordered as a part of routine care – an important point, Dr. Gudin said in an interview. “These are not ‘gotcha tests,’ ” intended to catch patients unawares. “These are regularly ordered screens that are standard of care in pain management.”
The report found that men and women were equally likely to misuse medications (52% each). There were some age-related differences, with misuse peaking in young adulthood: 60% of 18- to 24-year-olds and 56% of 25- to 45-year-olds. Misuse dropped off in those aged 55-64 years (52%) and in those 65 years and older (43%). But even children showed evidence of medication misuse, with about 41% of samples from children aged 10 years and younger being discordant.
The rates of misuse were about 50% in Medicare and private pay patients, but around 65% in Medicaid patients.
There was some good news: In the general patient population, opioid use was down by 12% from 2016 – the largest annual decrease Quest has noted since 2012. Several factors probably contributed to that decline, including shifts in clinical care and payer reimbursement, as well as regulatory and legislative restrictions.
“This shows that we’re doing better on the pain management front,” Dr. Gudin said. “But in substance use disorder settings, we saw 400% increases for both fentanyl and heroin. The addiction front it out of control.”
More than 27% of all specimens that came from substance abuse treatment centers were positive for nonprescribed fentanyl and 10% were positive for heroin. “We also saw that, in 2016, 45% of those heroin-positive samples had fentanyl in them, and in 2017, 83% did.”
Although not discussed at PAINWeek, the report also noted a rise in gabapentin misuse. The antiepileptic is now the 10th most commonly prescribed drug in the United States, the report noted, with 68 million prescriptions dispensed last year. The report found that 9.5% of tests showed nonprescription gabapentin. In the subset of samples obtained from substance abuse treatment centers, gabapentin misuse increased by 800% from 2016 – the most dramatic increase of any of the tracked drugs.
The combination of gabapentin and opioids is risky, the report noted. Opioid-related deaths are 49% more common among those taking both than those taking opioids only.
SOURCE: Gudin J et al. PAINWeek 2018, abstract 44.
REPORTING FROM PAINWEEK 2018
Key clinical point: More than half of patients undergoing urine drug screens were misusing medications.
Major finding: The samples were discordant for the queried drug in 52% of samples.
Study details: The study was based on 3.9 million drug screens ordered during 2011-2017.
Disclosures: The findings were included in Quest Diagnostics’ “Health Trends Report: Drug Misuse in America 2018.”
Source: Gudin J et al. PAINWeek, Abstract 44.
FDA grants praliciguat Fast Track Designation for HFpEF
fraction (HFpEF), according to its developer Ironwood.
A phase 2, randomized, double-blind, placebo-controlled trial is currently enrolling patients to evaluate praliciguat as a treatment for HFpEF. The trial aims to enroll about 175 patients and intends to evaluate safety and efficacy, and topline data is expected later in 2019.
Praliciguat is an oral, once-daily, soluble guanylate cyclase (sGC) stimulator. It is being studied in patients with diabetic nephropathy and in patients with HFpEF. The condition affects an estimated 3 million Americans, but there are no approved therapies at this time to treat it; however, praliciguat may have the potential to treat the underlying causes by improving nitric oxide signaling, according to the press release from Ironwood.
fraction (HFpEF), according to its developer Ironwood.
A phase 2, randomized, double-blind, placebo-controlled trial is currently enrolling patients to evaluate praliciguat as a treatment for HFpEF. The trial aims to enroll about 175 patients and intends to evaluate safety and efficacy, and topline data is expected later in 2019.
Praliciguat is an oral, once-daily, soluble guanylate cyclase (sGC) stimulator. It is being studied in patients with diabetic nephropathy and in patients with HFpEF. The condition affects an estimated 3 million Americans, but there are no approved therapies at this time to treat it; however, praliciguat may have the potential to treat the underlying causes by improving nitric oxide signaling, according to the press release from Ironwood.
fraction (HFpEF), according to its developer Ironwood.
A phase 2, randomized, double-blind, placebo-controlled trial is currently enrolling patients to evaluate praliciguat as a treatment for HFpEF. The trial aims to enroll about 175 patients and intends to evaluate safety and efficacy, and topline data is expected later in 2019.
Praliciguat is an oral, once-daily, soluble guanylate cyclase (sGC) stimulator. It is being studied in patients with diabetic nephropathy and in patients with HFpEF. The condition affects an estimated 3 million Americans, but there are no approved therapies at this time to treat it; however, praliciguat may have the potential to treat the underlying causes by improving nitric oxide signaling, according to the press release from Ironwood.
Zika virus infection: Novel assay extends diagnostic window
ATLANTA – A novel pyrosequencing (PSQ)–based reverse-transcription polymerase chain reaction (RT-PCR) assay improves and expands diagnostic capabilities for Zika virus infection, according to findings in 60 patients diagnosed with the virus in 2016 and 2017.
The PSQ assay provides rapid, specific, and cost-effective detection of the virus in tissues of congenital and pregnancy-associated infections, and, compared with serum-based assays, extends the time frame for Zika virus detection, Julu Bhatnagar, PhD, reported in a presentation at the International Conference on Emerging Infectious Diseases.
Dr. Bhatnagar and her colleagues from the Centers for Disease Control and Prevention in Atlanta developed the assay and evaluated it using RNA extracted from formalin-fixed, paraffin-embedded placental/fetal tissues from 53 women with varying pregnancy outcomes, and brain tissues from seven infants with microcephaly who died. In all of the tissue samples, which were received between January 2016 and August 2017, Zika virus was previously identified by conventional RT-PCR and Sanger sequencing.
The PSQ assay detected and sequence confirmed Zika virus in tissues from all 60 patients, whereas 40 negative control samples, including tissues from dengue- and chikungunya virus–confirmed cases, all tested negative.
In addition, the PSQ assay detected Zika virus in placental tissues from three other cases that were previously negative by the conventional tissue-based RT-PCR, thereby demonstrating better sensitivity of the PSQ assay in comparison to conventional tissue RT-PCR, said Dr. Bhatnagar, who is molecular pathology team leader in the Infectious Diseases Pathology Branch, Division of High-Consequence Pathogens and Pathology at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
“Importantly, PSQ results can be obtained in 1 day and at half the cost of Sanger sequencing,” she said.
The findings are important because Zika virus infection during pregnancy can cause microcephaly and is associated with pregnancy loss. Laboratory diagnosis of the virus is challenging for pregnancy-associated infections because of the short duration of viremia, she explained.
However, prolonged detection of Zika virus RNA in placental, fetal, and neonatal brain tissue has been reported.
Dr. Bhatnagar was the first author on a 2016 study published in Emerging Infectious Diseases that provided confirmation of the linkage of Zika virus with microcephaly and that suggested its association with adverse pregnancy outcomes and provided evidence of Zika virus replication and persistence in fetal brain and placenta.
“This article highlights the value of tissue analysis to expand opportunities to diagnose Zika virus congenital and pregnancy-associated infections and to enhance the understanding of mechanism of Zika virus intrauterine transmission and pathogenesis,” she and her colleagues wrote in that article. “In addition, the tissue-based RT-PCRs extend the time frame for Zika virus detection and particularly help to establish a diagnosis retrospectively, enabling pregnant women and their health care providers to identify the cause of severe microcephaly or fetal loss.”
Those findings led to the hypothesis that the PSQ assay evaluated in the current study would provide better opportunities for detection, particularly in cases where serum RT-PCR or serologic testing is negative because of testing performed outside the optimal testing window, she said.
Indeed, the novel assay not only allows for an extended time frame for Zika virus detection, it also provides insights into viral tissue tropism and persistence, she noted.
According to the CDC, no local mosquito-borne Zika virus transmissions have been reported in the continental United States in 2018, but transmission is still a threat internationally, and those traveling outside of the continental United States should find out if they are traveling to an area with risk of Zika.
Dr. Bhatnagar reported having no disclosures.
SOURCE: Bhatnagar J et al. ICEID 2018, Abstract O1.
ATLANTA – A novel pyrosequencing (PSQ)–based reverse-transcription polymerase chain reaction (RT-PCR) assay improves and expands diagnostic capabilities for Zika virus infection, according to findings in 60 patients diagnosed with the virus in 2016 and 2017.
The PSQ assay provides rapid, specific, and cost-effective detection of the virus in tissues of congenital and pregnancy-associated infections, and, compared with serum-based assays, extends the time frame for Zika virus detection, Julu Bhatnagar, PhD, reported in a presentation at the International Conference on Emerging Infectious Diseases.
Dr. Bhatnagar and her colleagues from the Centers for Disease Control and Prevention in Atlanta developed the assay and evaluated it using RNA extracted from formalin-fixed, paraffin-embedded placental/fetal tissues from 53 women with varying pregnancy outcomes, and brain tissues from seven infants with microcephaly who died. In all of the tissue samples, which were received between January 2016 and August 2017, Zika virus was previously identified by conventional RT-PCR and Sanger sequencing.
The PSQ assay detected and sequence confirmed Zika virus in tissues from all 60 patients, whereas 40 negative control samples, including tissues from dengue- and chikungunya virus–confirmed cases, all tested negative.
In addition, the PSQ assay detected Zika virus in placental tissues from three other cases that were previously negative by the conventional tissue-based RT-PCR, thereby demonstrating better sensitivity of the PSQ assay in comparison to conventional tissue RT-PCR, said Dr. Bhatnagar, who is molecular pathology team leader in the Infectious Diseases Pathology Branch, Division of High-Consequence Pathogens and Pathology at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
“Importantly, PSQ results can be obtained in 1 day and at half the cost of Sanger sequencing,” she said.
The findings are important because Zika virus infection during pregnancy can cause microcephaly and is associated with pregnancy loss. Laboratory diagnosis of the virus is challenging for pregnancy-associated infections because of the short duration of viremia, she explained.
However, prolonged detection of Zika virus RNA in placental, fetal, and neonatal brain tissue has been reported.
Dr. Bhatnagar was the first author on a 2016 study published in Emerging Infectious Diseases that provided confirmation of the linkage of Zika virus with microcephaly and that suggested its association with adverse pregnancy outcomes and provided evidence of Zika virus replication and persistence in fetal brain and placenta.
“This article highlights the value of tissue analysis to expand opportunities to diagnose Zika virus congenital and pregnancy-associated infections and to enhance the understanding of mechanism of Zika virus intrauterine transmission and pathogenesis,” she and her colleagues wrote in that article. “In addition, the tissue-based RT-PCRs extend the time frame for Zika virus detection and particularly help to establish a diagnosis retrospectively, enabling pregnant women and their health care providers to identify the cause of severe microcephaly or fetal loss.”
Those findings led to the hypothesis that the PSQ assay evaluated in the current study would provide better opportunities for detection, particularly in cases where serum RT-PCR or serologic testing is negative because of testing performed outside the optimal testing window, she said.
Indeed, the novel assay not only allows for an extended time frame for Zika virus detection, it also provides insights into viral tissue tropism and persistence, she noted.
According to the CDC, no local mosquito-borne Zika virus transmissions have been reported in the continental United States in 2018, but transmission is still a threat internationally, and those traveling outside of the continental United States should find out if they are traveling to an area with risk of Zika.
Dr. Bhatnagar reported having no disclosures.
SOURCE: Bhatnagar J et al. ICEID 2018, Abstract O1.
ATLANTA – A novel pyrosequencing (PSQ)–based reverse-transcription polymerase chain reaction (RT-PCR) assay improves and expands diagnostic capabilities for Zika virus infection, according to findings in 60 patients diagnosed with the virus in 2016 and 2017.
The PSQ assay provides rapid, specific, and cost-effective detection of the virus in tissues of congenital and pregnancy-associated infections, and, compared with serum-based assays, extends the time frame for Zika virus detection, Julu Bhatnagar, PhD, reported in a presentation at the International Conference on Emerging Infectious Diseases.
Dr. Bhatnagar and her colleagues from the Centers for Disease Control and Prevention in Atlanta developed the assay and evaluated it using RNA extracted from formalin-fixed, paraffin-embedded placental/fetal tissues from 53 women with varying pregnancy outcomes, and brain tissues from seven infants with microcephaly who died. In all of the tissue samples, which were received between January 2016 and August 2017, Zika virus was previously identified by conventional RT-PCR and Sanger sequencing.
The PSQ assay detected and sequence confirmed Zika virus in tissues from all 60 patients, whereas 40 negative control samples, including tissues from dengue- and chikungunya virus–confirmed cases, all tested negative.
In addition, the PSQ assay detected Zika virus in placental tissues from three other cases that were previously negative by the conventional tissue-based RT-PCR, thereby demonstrating better sensitivity of the PSQ assay in comparison to conventional tissue RT-PCR, said Dr. Bhatnagar, who is molecular pathology team leader in the Infectious Diseases Pathology Branch, Division of High-Consequence Pathogens and Pathology at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
“Importantly, PSQ results can be obtained in 1 day and at half the cost of Sanger sequencing,” she said.
The findings are important because Zika virus infection during pregnancy can cause microcephaly and is associated with pregnancy loss. Laboratory diagnosis of the virus is challenging for pregnancy-associated infections because of the short duration of viremia, she explained.
However, prolonged detection of Zika virus RNA in placental, fetal, and neonatal brain tissue has been reported.
Dr. Bhatnagar was the first author on a 2016 study published in Emerging Infectious Diseases that provided confirmation of the linkage of Zika virus with microcephaly and that suggested its association with adverse pregnancy outcomes and provided evidence of Zika virus replication and persistence in fetal brain and placenta.
“This article highlights the value of tissue analysis to expand opportunities to diagnose Zika virus congenital and pregnancy-associated infections and to enhance the understanding of mechanism of Zika virus intrauterine transmission and pathogenesis,” she and her colleagues wrote in that article. “In addition, the tissue-based RT-PCRs extend the time frame for Zika virus detection and particularly help to establish a diagnosis retrospectively, enabling pregnant women and their health care providers to identify the cause of severe microcephaly or fetal loss.”
Those findings led to the hypothesis that the PSQ assay evaluated in the current study would provide better opportunities for detection, particularly in cases where serum RT-PCR or serologic testing is negative because of testing performed outside the optimal testing window, she said.
Indeed, the novel assay not only allows for an extended time frame for Zika virus detection, it also provides insights into viral tissue tropism and persistence, she noted.
According to the CDC, no local mosquito-borne Zika virus transmissions have been reported in the continental United States in 2018, but transmission is still a threat internationally, and those traveling outside of the continental United States should find out if they are traveling to an area with risk of Zika.
Dr. Bhatnagar reported having no disclosures.
SOURCE: Bhatnagar J et al. ICEID 2018, Abstract O1.
REPORTING FROM ICEID 2018
Key clinical point: A novel assay extends the time frame for diagnosing Zika virus infection.
Major finding: The PSQ assay detected and sequence confirmed Zika virus in all 60 samples; 40 negative control samples all tested negative.
Study details: An analysis of 60 tissue samples using a novel assay.
Disclosures: Dr. Bhatnagar reported having no disclosures.
Source: Bhatnagar J et al. ICEID 2018, Abstract O1.
Subcutaneous Actemra approved for systemic JIA
The Food and Drug Administration has approved the subcutaneous formulation of Actemra (tocilizumab) for systemic juvenile idiopathic arthritis (SJIA) for patients aged 2 years and older, according to a press release from its developer, Genentech. The intravenous formulation was approved in 2011 for this indication.
The approval is based on data the JIGSAW-118 study. This 52-week, open-label, multicenter, phase 1b pharmacokinetic/pharmacodynamic bridging study was designed to determine the appropriate dosing regimen by treating 51 patients with SJIA according to body weight.
The safety profile of subcutaneous tocilizumab was similar to that seen with intravenous tocilizumab, although there were more injection-site reactions seen with the subcutaneous formulation. Its efficacy was extrapolated based on the drug’s pharmacokinetic profile seen with IV tocilizumab in SJIA patients and with subcutaneous tocilizumab in patients with rheumatoid arthritis.
SJIA is a rare disease with limited treatment options, according to the press release. In general, JIA affects almost 300,000 children in the United States, and about 10% of those cases are SJIA.
The Food and Drug Administration has approved the subcutaneous formulation of Actemra (tocilizumab) for systemic juvenile idiopathic arthritis (SJIA) for patients aged 2 years and older, according to a press release from its developer, Genentech. The intravenous formulation was approved in 2011 for this indication.
The approval is based on data the JIGSAW-118 study. This 52-week, open-label, multicenter, phase 1b pharmacokinetic/pharmacodynamic bridging study was designed to determine the appropriate dosing regimen by treating 51 patients with SJIA according to body weight.
The safety profile of subcutaneous tocilizumab was similar to that seen with intravenous tocilizumab, although there were more injection-site reactions seen with the subcutaneous formulation. Its efficacy was extrapolated based on the drug’s pharmacokinetic profile seen with IV tocilizumab in SJIA patients and with subcutaneous tocilizumab in patients with rheumatoid arthritis.
SJIA is a rare disease with limited treatment options, according to the press release. In general, JIA affects almost 300,000 children in the United States, and about 10% of those cases are SJIA.
The Food and Drug Administration has approved the subcutaneous formulation of Actemra (tocilizumab) for systemic juvenile idiopathic arthritis (SJIA) for patients aged 2 years and older, according to a press release from its developer, Genentech. The intravenous formulation was approved in 2011 for this indication.
The approval is based on data the JIGSAW-118 study. This 52-week, open-label, multicenter, phase 1b pharmacokinetic/pharmacodynamic bridging study was designed to determine the appropriate dosing regimen by treating 51 patients with SJIA according to body weight.
The safety profile of subcutaneous tocilizumab was similar to that seen with intravenous tocilizumab, although there were more injection-site reactions seen with the subcutaneous formulation. Its efficacy was extrapolated based on the drug’s pharmacokinetic profile seen with IV tocilizumab in SJIA patients and with subcutaneous tocilizumab in patients with rheumatoid arthritis.
SJIA is a rare disease with limited treatment options, according to the press release. In general, JIA affects almost 300,000 children in the United States, and about 10% of those cases are SJIA.
FDA approves new hairy cell leukemia drug
The Food and Drug Administration (FDA) has approved moxetumomab pasudotox-tdfk (Lumoxiti), a CD22-directed cytotoxin, to treat hairy cell leukemia (HCL).
Moxetumomab pasudotox is approved to treat adults with relapsed or refractory HCL who have received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
The prescribing information for moxetumomab pasudotox includes a boxed warning noting that the drug poses risks of capillary leak syndrome and hemolytic uremic syndrome. Other serious warnings include the risk of decreased renal function, infusion-related reactions, and electrolyte abnormalities.
The FDA granted the application for moxetumomab pasudotox fast track, priority review, and an orphan drug designation.
The agency approved AstraZeneca’s moxetumomab pasudotox based on results from a phase 3 trial (NCT01829711). Data from this study were presented at the 2018 annual meeting of the American Society of Clinical Oncology (abstract 7004).
The trial included 80 patients with relapsed or refractory HCL who had received at least two prior lines of therapy.
At a median of 16.7 months of follow-up, the objective response rate was 75%, the complete response (CR) rate was 41%, and the durable CR rate was 30%. Durable CR was defined as CR with hematologic remission for more than 180 days.
Most patients with a CR achieved minimal residual disease negativity (82%; 27/33).
The median duration of response was not reached, nor was the median progression-free survival.
The most common treatment-related adverse events (AEs) were nausea, peripheral edema, headache, and pyrexia. Other treatment-related AEs included infections and neutropenia.
Treatment-related AEs that led to discontinuation included capillary leak syndrome, hemolytic uremic syndrome, and increased blood creatinine.
There were three deaths in this trial, but none of them were considered treatment related.
The Food and Drug Administration (FDA) has approved moxetumomab pasudotox-tdfk (Lumoxiti), a CD22-directed cytotoxin, to treat hairy cell leukemia (HCL).
Moxetumomab pasudotox is approved to treat adults with relapsed or refractory HCL who have received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
The prescribing information for moxetumomab pasudotox includes a boxed warning noting that the drug poses risks of capillary leak syndrome and hemolytic uremic syndrome. Other serious warnings include the risk of decreased renal function, infusion-related reactions, and electrolyte abnormalities.
The FDA granted the application for moxetumomab pasudotox fast track, priority review, and an orphan drug designation.
The agency approved AstraZeneca’s moxetumomab pasudotox based on results from a phase 3 trial (NCT01829711). Data from this study were presented at the 2018 annual meeting of the American Society of Clinical Oncology (abstract 7004).
The trial included 80 patients with relapsed or refractory HCL who had received at least two prior lines of therapy.
At a median of 16.7 months of follow-up, the objective response rate was 75%, the complete response (CR) rate was 41%, and the durable CR rate was 30%. Durable CR was defined as CR with hematologic remission for more than 180 days.
Most patients with a CR achieved minimal residual disease negativity (82%; 27/33).
The median duration of response was not reached, nor was the median progression-free survival.
The most common treatment-related adverse events (AEs) were nausea, peripheral edema, headache, and pyrexia. Other treatment-related AEs included infections and neutropenia.
Treatment-related AEs that led to discontinuation included capillary leak syndrome, hemolytic uremic syndrome, and increased blood creatinine.
There were three deaths in this trial, but none of them were considered treatment related.
The Food and Drug Administration (FDA) has approved moxetumomab pasudotox-tdfk (Lumoxiti), a CD22-directed cytotoxin, to treat hairy cell leukemia (HCL).
Moxetumomab pasudotox is approved to treat adults with relapsed or refractory HCL who have received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
The prescribing information for moxetumomab pasudotox includes a boxed warning noting that the drug poses risks of capillary leak syndrome and hemolytic uremic syndrome. Other serious warnings include the risk of decreased renal function, infusion-related reactions, and electrolyte abnormalities.
The FDA granted the application for moxetumomab pasudotox fast track, priority review, and an orphan drug designation.
The agency approved AstraZeneca’s moxetumomab pasudotox based on results from a phase 3 trial (NCT01829711). Data from this study were presented at the 2018 annual meeting of the American Society of Clinical Oncology (abstract 7004).
The trial included 80 patients with relapsed or refractory HCL who had received at least two prior lines of therapy.
At a median of 16.7 months of follow-up, the objective response rate was 75%, the complete response (CR) rate was 41%, and the durable CR rate was 30%. Durable CR was defined as CR with hematologic remission for more than 180 days.
Most patients with a CR achieved minimal residual disease negativity (82%; 27/33).
The median duration of response was not reached, nor was the median progression-free survival.
The most common treatment-related adverse events (AEs) were nausea, peripheral edema, headache, and pyrexia. Other treatment-related AEs included infections and neutropenia.
Treatment-related AEs that led to discontinuation included capillary leak syndrome, hemolytic uremic syndrome, and increased blood creatinine.
There were three deaths in this trial, but none of them were considered treatment related.
Does nurse-physician rounding matter?
Advancing the Quadruple Aim
Inadequate and fragmented communication between physicians and nurses can lead to unwelcome events for the hospitalized patient and clinicians. Missing orders, medication errors, patient misidentification, and lack of physician awareness of significant changes in patient status are just some examples of how deficits in formal communication can affect health outcomes during acute stays.
A 2000 Institute of Medicine report showed that bad systems, not bad people, account for the majority of errors and injuries caused by complexity, professional fragmentation, and barriers in communication. Their recommendation was to train physicians, nurses, and other professionals in teamwork.1,2 However, as Milisa Manojlovich, PhD, RN, found, there are significant differences in how physicians and nurses perceive collaboration and communication.3
Nurse-physician rounding was historically standard for patient care during hospitalization. When physicians split time between inpatient and outpatient care, nurses had to maximize their time to collaborate and communicate with physicians whenever the physicians left their outpatient offices to come and round on their patients. Today most inpatient care is delivered by hospitalists on a 24-hour basis. This continuous availability of physicians reduces the perceived need to have joint rounds.
However, health care teams in acute care facilities now face higher and sicker patient volumes, different productivity models and demands, new compliance standards, changing work flows, and increased complexity of treatment and management of patients. This has led to gaps in timely communication and partnership.4-6 Erosion of the traditional nurse-physician relationships affects the quality of patient care, the patient’s experience, and patient safety.8-10 Poor communication among health care team members is one of the most common causes of patient care errors.4 Poor nurse-physician communication can also lead to medical errors, poor outcomes caused by lack of coordination within the treatment team, increased use of unnecessary resources with inefficiency, and increases in the complexity of communication among team members, and time wastage.5,7,11 All these lead to poor work flows and directly affect patient safety.7
At Lee Health System in Lee County, Fla., we saw an opportunity in this changing health care environment to promote nurse-physician rounding. We created a structured, standardized process for morning rounding and engaged unit clerks, nursing leadership, and hospitalist service line leaders. We envisioned improvement of the patient experience, nurse-physician relationship, quality of care, the discharge planning process, and efficiency, as well as decreasing length of stay, improving communication, and bringing the patient and the treatment team closer, as demonstrated by Bradley Monash, MD, et al.12
Some data suggest that patient-centered bedside rounds on hospitalized patients have no effect on patient perceptions or their satisfaction with care.13 However, we felt that collaboration among a multidisciplinary team would help us achieve better outcomes. For example, our patients would perceive the care team (MD-RN) as a cohesive unit, and in turn gain trust in the members of the treatment team, as found by Nathalie McIntosh, PhD, et al and by Jason Ramirez, MD.7,16 Our vision was to empower nurses to be advocates for patients and their family members as they navigated their acute care admission. Nurses could also support physicians by communicating the physicians’ care plans to families and patients. After rounding with the physician, the nurse would be part of the decision-making process and care planning.17
Every rounding session had discharge planning and hospital stay expectations that were shared with the patient and nurse, who could then partner with case managers and social workers, which would streamline and reduce length of stay.14 We hoped rounding would also decrease the number of nurse pages to clarify or question orders. This would, in turn, improve daily work flow for the physicians and the nursing team with improvements in employee satisfaction scores.15 A study also has demonstrated a reduction in readmission rates from nurse-physician rounding.19
A disconnect in communication and trust between physicians and the nursing staff was reflected in low patient experience scores and perceived quality of care received during in-hospital stay. Gwendolyn Lancaster, EdD, MSN, RN, CCRN, et al, as well as a Joint Commission report, demonstrated how a lack of communication and poor team dynamics can translate to poor patient experience and be a major cause for sentinel events.6,20 Artificial, forced hierarchies and role perception among health care team members led to frustration, hostility, and distrust, which compromises quality and patient safety.1
One of our biggest challenges when we started this project was explaining the “Why” to the hospitalist group and nursing staff. Physicians were used to being the dominant partner in the team. Partnering with and engaging nurses in shared decision making and care planning was a seismic shift in culture and work flow within the care team. Early gains helped skeptical team members begin to understand the value in nurse-physician rounding. Near universal adoption of the rounding process at Lee Health has caused improvements in the working relationship and trust among the health care professionals. We have seen improvements in utilization management, as well as appropriateness and timeliness of resource use, because of better communication and understanding of care plans by nursing and physicians. Collaboration with specialists and alignment in care planning are other gains. Hospitalists and nurses are both very satisfied with the decrease in the number of pages during the day, and this has lowered stressors on health care teams.
How we did it
Nurse-physician rounding is a proven method to improve collaboration, communication, and relationships among health care team members in acute care facilities. In the complex health care challenges faced today, this improved work flow for taking care of patients can help advance the Quadruple Aim of high quality, low cost, improved patient experience, physician, and staff satisfaction.21
Lee Health System includes four facilities in Lee County, with a total of 1,216 licensed adult acute care beds. The pilot project was started in 2014.
Initially the vice president of nursing and the hospitalist medical director met to create an education plan for nurses and physicians. We chose one adult medicine unit to pilot the project because there already existed a closely knit nursing and hospitalist team. In our facility there is no strict geographical rounding; each hospitalist carries between three and six patients in the unit. As a first step, a nurse floor assignment sheet was faxed in the morning to the hospitalist office with the direct phone numbers of the nurses. The unit clerk, using physician assignments in the EHR, teamed up the physician and nurses for rounding. Once the physician arrived at the unit, he or she checked in with the unit clerk, who alerted nurses that the hospitalist was available on the floor to commence rounding. If the primary nurse was unavailable because of other duties or breaks, the charge nurse rounded with the physician.
Once in the room with the patient, the duo introduced themselves as members of the treatment team and acknowledged the patient’s needs. During the visit, care plans and treatment were reviewed, the patient’s questions were answered, a physical exam was completed, and lab and imaging results were discussed; the nurse also helped raise questions he or she had received from family members so answers could be communicated to the family later. Patients appreciated knowing that their physicians and nurses were working together as a team for their safety and recovery. During the visit, care was taken to focus specially on the course of hospitalization and discharge planning.
We tracked the rounding with a manual paper process maintained by the charge nurse. Our initial rounding rates were 30%-40%, and we continued to promote this initiative to the team, and eventually the importance and value of these rounds caught on with both nurses and physicians, and now our current average rounding rate is 90%. We then decided to scale this to all units in the hospital.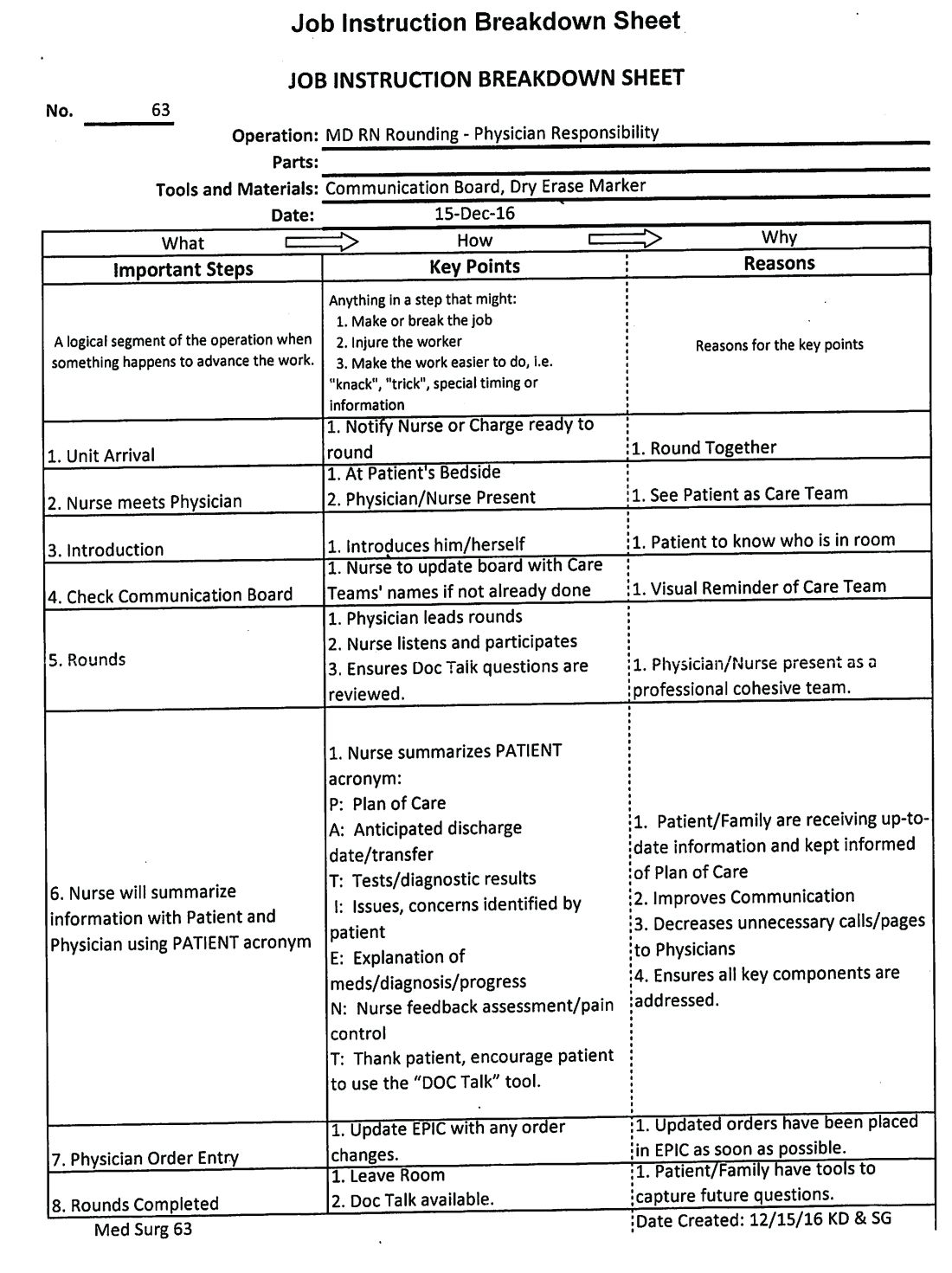
This process was repeated at other hospitals in the system once a standardized work flow was created (See Image 1). This initiative was next presented to the health system board of directors, who agreed that nurse-physician rounding should be the standard of care across our health system. Through partnership and collaboration with the IT department, we developed a tool to track nurse-physician rounding through our EHR system, which gave accountability to both physicians and nurses.
In conclusion, improved communication by timely nurse-physician rounding can lead to better outcomes for patients and also reduce costs and improve patient and staff experience, advancing the Quadruple Aim. Moving forward to build and sustain this work flow, we plan to continue nurse-physician collaboration across the health system consistently and for all areas of acute care operations.
Explaining the “Why,” sharing data on the benefits of the model, and reinforcing documentation of the rounding in our EHR are some steps we have put into action at leadership and staff meetings to sustain the activity. We are soliciting feedback, as well as monitoring and identifying any unaddressed barriers during rounding. Addition of this process measure to our quality improvement bonus opportunity also has helped to sustain performance from our teams.
Dr. Laufer is system medical director of hospital medicine and transitional care at Lee Health in Ft. Myers, Fla. Dr. Prasad is chief medical officer of Lee Physician Group, Ft. Myers, Fla.
References
1. Leape LL et al. Five years after to err is human: What we have learned? JAMA. 2005;293(19):2384-90.
2. Sutcliffe KM et al. Communication failures: An insidious contributor to medical mishaps. Acad Med. 2004;79(2):186-94.
3. Manojlovich M. Reframing communication with physicians as sensemaking. J Nurs Care Qual. 2013 Oct-Dec;28(4):295-303.
4. Siegele P. Enhancing outcomes in a surgical intensive care unit by implementing daily goals. Crit Care Nurse. 2009 Dec;29(6):58-69.
5. Asthon J et al. Qualitative evaluation of regular morning meeting aimed at improving interdisciplinary communication and patient outcomes. Int J Nurs Pract. 2005 Oct;11(5):206-13.
6. Lancaster G et al. Interdisciplinary Communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015 May;47(3):275-84.
7. McIntosh N et al. Impact of provider coordination on nurse and physician perception of patient care quality. J Nurs Care Qual. 2014 Jul-Sep;29(3):269-79.
8. Jo M et al. An organizational assessment of disruptive clinical behavior. J Nurs Care Qual. 2013 Apr-Jun;28(2):110-21.
9. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, 2010.
10. O’Connor P et al. A mixed-methods study of the causes and impact of poor teamwork between junior doctors and nurses. Int J Qual Health Care. 2016 Jun;28(3):339-45.
11. Manojlovich M. Nurse/Physician communication through a sense making lens. Med Care. 2010 Nov;48(11):941-6.
12. Monash B et al. Standardized attending rounds to improve the patient experience: A pragmatic cluster randomized controlled trial. J Hosp Med. 2017 Mar;12(3):143-9.
13. O’Leary KJ et al. Effect of patient-centered bedside rounds on hospitalized patients decision control, activation and satisfaction with care. BMJ Qual Saf. 2016 Dec;25(12):921-8.
14. Dutton RP et al. Daily multidisciplinary rounds shorten length of stay for trauma patients. J Trauma. 2003 Nov;55(5):913-9.
15. Manojlovich M et al. Healthy work environments, nurse-physician communication, and patients’ outcomes. Am J Crit Care. 2007 Nov;16(6):536-43.
16. Ramirez J et al. Patient satisfaction with bedside teaching rounds compared with nonbedside rounds. South Med J. 2016 Feb;109(2):112-5.
17. Sollami A et al. Nurse-Physician collaboration: A meta-analytical investigation of survey scores. J Interprof Care. 2015 May;29(3):223-9.
18. House S et al. Nurses and physicians perceptions of nurse-physician collaboration. J Nurs Adm. 2017 Mar;47(3):165-71.
19. Townsend-Gervis M et al. Interdisciplinary rounds and structured communications reduce re-admissions and improve some patients’ outcomes. West J Nurs Res. 2014 Aug;36(7):917-28.
20. The Joint Commission. Sentinel Events. http://www.jointcommission.org/sentinel_event.aspx. Accessed Oct 2017.
21. Bodenheimer T et al. From Triple to Quadruple Aim: Care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6.
Advancing the Quadruple Aim
Advancing the Quadruple Aim
Inadequate and fragmented communication between physicians and nurses can lead to unwelcome events for the hospitalized patient and clinicians. Missing orders, medication errors, patient misidentification, and lack of physician awareness of significant changes in patient status are just some examples of how deficits in formal communication can affect health outcomes during acute stays.
A 2000 Institute of Medicine report showed that bad systems, not bad people, account for the majority of errors and injuries caused by complexity, professional fragmentation, and barriers in communication. Their recommendation was to train physicians, nurses, and other professionals in teamwork.1,2 However, as Milisa Manojlovich, PhD, RN, found, there are significant differences in how physicians and nurses perceive collaboration and communication.3
Nurse-physician rounding was historically standard for patient care during hospitalization. When physicians split time between inpatient and outpatient care, nurses had to maximize their time to collaborate and communicate with physicians whenever the physicians left their outpatient offices to come and round on their patients. Today most inpatient care is delivered by hospitalists on a 24-hour basis. This continuous availability of physicians reduces the perceived need to have joint rounds.
However, health care teams in acute care facilities now face higher and sicker patient volumes, different productivity models and demands, new compliance standards, changing work flows, and increased complexity of treatment and management of patients. This has led to gaps in timely communication and partnership.4-6 Erosion of the traditional nurse-physician relationships affects the quality of patient care, the patient’s experience, and patient safety.8-10 Poor communication among health care team members is one of the most common causes of patient care errors.4 Poor nurse-physician communication can also lead to medical errors, poor outcomes caused by lack of coordination within the treatment team, increased use of unnecessary resources with inefficiency, and increases in the complexity of communication among team members, and time wastage.5,7,11 All these lead to poor work flows and directly affect patient safety.7
At Lee Health System in Lee County, Fla., we saw an opportunity in this changing health care environment to promote nurse-physician rounding. We created a structured, standardized process for morning rounding and engaged unit clerks, nursing leadership, and hospitalist service line leaders. We envisioned improvement of the patient experience, nurse-physician relationship, quality of care, the discharge planning process, and efficiency, as well as decreasing length of stay, improving communication, and bringing the patient and the treatment team closer, as demonstrated by Bradley Monash, MD, et al.12
Some data suggest that patient-centered bedside rounds on hospitalized patients have no effect on patient perceptions or their satisfaction with care.13 However, we felt that collaboration among a multidisciplinary team would help us achieve better outcomes. For example, our patients would perceive the care team (MD-RN) as a cohesive unit, and in turn gain trust in the members of the treatment team, as found by Nathalie McIntosh, PhD, et al and by Jason Ramirez, MD.7,16 Our vision was to empower nurses to be advocates for patients and their family members as they navigated their acute care admission. Nurses could also support physicians by communicating the physicians’ care plans to families and patients. After rounding with the physician, the nurse would be part of the decision-making process and care planning.17
Every rounding session had discharge planning and hospital stay expectations that were shared with the patient and nurse, who could then partner with case managers and social workers, which would streamline and reduce length of stay.14 We hoped rounding would also decrease the number of nurse pages to clarify or question orders. This would, in turn, improve daily work flow for the physicians and the nursing team with improvements in employee satisfaction scores.15 A study also has demonstrated a reduction in readmission rates from nurse-physician rounding.19
A disconnect in communication and trust between physicians and the nursing staff was reflected in low patient experience scores and perceived quality of care received during in-hospital stay. Gwendolyn Lancaster, EdD, MSN, RN, CCRN, et al, as well as a Joint Commission report, demonstrated how a lack of communication and poor team dynamics can translate to poor patient experience and be a major cause for sentinel events.6,20 Artificial, forced hierarchies and role perception among health care team members led to frustration, hostility, and distrust, which compromises quality and patient safety.1
One of our biggest challenges when we started this project was explaining the “Why” to the hospitalist group and nursing staff. Physicians were used to being the dominant partner in the team. Partnering with and engaging nurses in shared decision making and care planning was a seismic shift in culture and work flow within the care team. Early gains helped skeptical team members begin to understand the value in nurse-physician rounding. Near universal adoption of the rounding process at Lee Health has caused improvements in the working relationship and trust among the health care professionals. We have seen improvements in utilization management, as well as appropriateness and timeliness of resource use, because of better communication and understanding of care plans by nursing and physicians. Collaboration with specialists and alignment in care planning are other gains. Hospitalists and nurses are both very satisfied with the decrease in the number of pages during the day, and this has lowered stressors on health care teams.
How we did it
Nurse-physician rounding is a proven method to improve collaboration, communication, and relationships among health care team members in acute care facilities. In the complex health care challenges faced today, this improved work flow for taking care of patients can help advance the Quadruple Aim of high quality, low cost, improved patient experience, physician, and staff satisfaction.21
Lee Health System includes four facilities in Lee County, with a total of 1,216 licensed adult acute care beds. The pilot project was started in 2014.
Initially the vice president of nursing and the hospitalist medical director met to create an education plan for nurses and physicians. We chose one adult medicine unit to pilot the project because there already existed a closely knit nursing and hospitalist team. In our facility there is no strict geographical rounding; each hospitalist carries between three and six patients in the unit. As a first step, a nurse floor assignment sheet was faxed in the morning to the hospitalist office with the direct phone numbers of the nurses. The unit clerk, using physician assignments in the EHR, teamed up the physician and nurses for rounding. Once the physician arrived at the unit, he or she checked in with the unit clerk, who alerted nurses that the hospitalist was available on the floor to commence rounding. If the primary nurse was unavailable because of other duties or breaks, the charge nurse rounded with the physician.
Once in the room with the patient, the duo introduced themselves as members of the treatment team and acknowledged the patient’s needs. During the visit, care plans and treatment were reviewed, the patient’s questions were answered, a physical exam was completed, and lab and imaging results were discussed; the nurse also helped raise questions he or she had received from family members so answers could be communicated to the family later. Patients appreciated knowing that their physicians and nurses were working together as a team for their safety and recovery. During the visit, care was taken to focus specially on the course of hospitalization and discharge planning.
We tracked the rounding with a manual paper process maintained by the charge nurse. Our initial rounding rates were 30%-40%, and we continued to promote this initiative to the team, and eventually the importance and value of these rounds caught on with both nurses and physicians, and now our current average rounding rate is 90%. We then decided to scale this to all units in the hospital.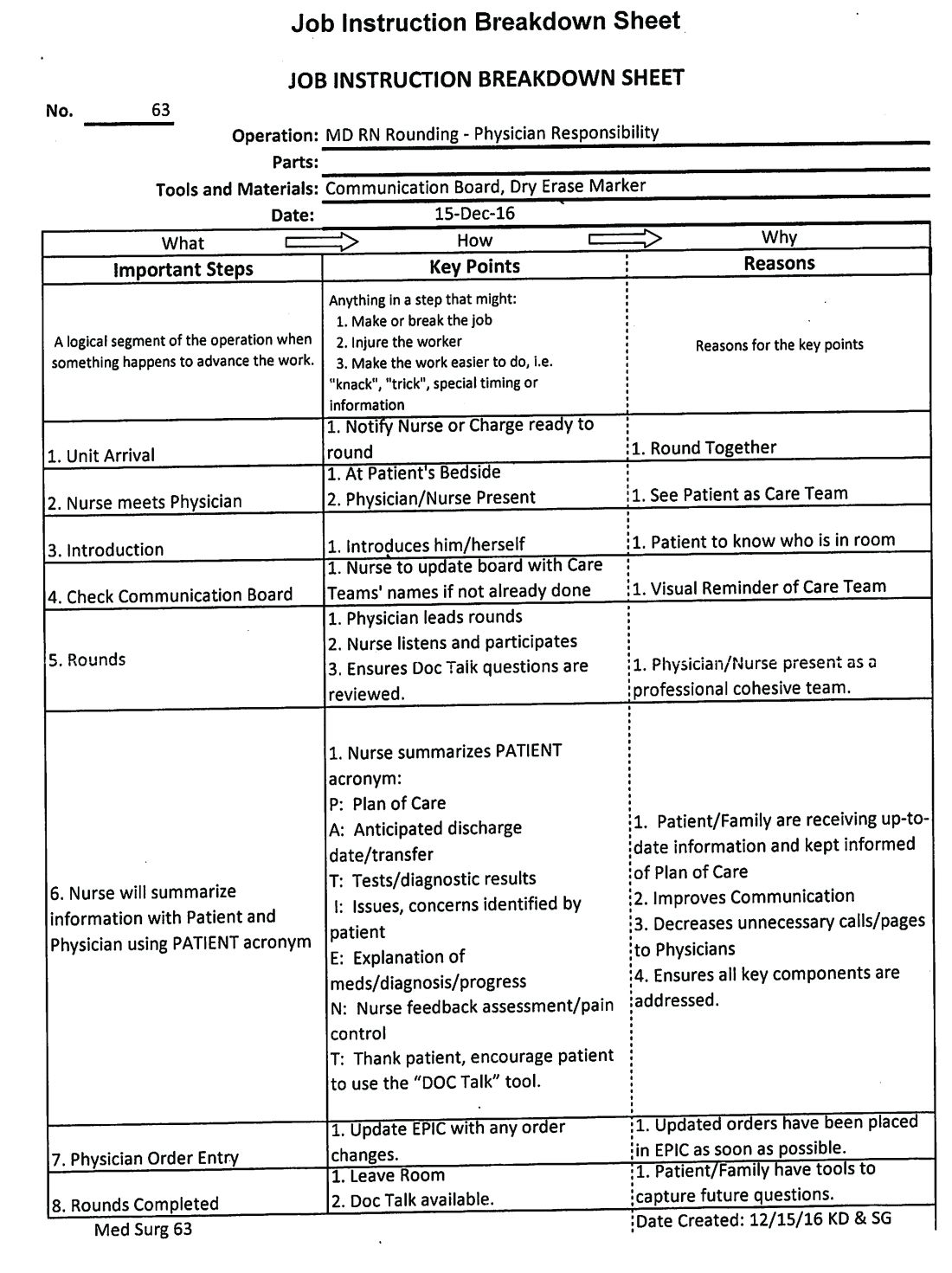
This process was repeated at other hospitals in the system once a standardized work flow was created (See Image 1). This initiative was next presented to the health system board of directors, who agreed that nurse-physician rounding should be the standard of care across our health system. Through partnership and collaboration with the IT department, we developed a tool to track nurse-physician rounding through our EHR system, which gave accountability to both physicians and nurses.
In conclusion, improved communication by timely nurse-physician rounding can lead to better outcomes for patients and also reduce costs and improve patient and staff experience, advancing the Quadruple Aim. Moving forward to build and sustain this work flow, we plan to continue nurse-physician collaboration across the health system consistently and for all areas of acute care operations.
Explaining the “Why,” sharing data on the benefits of the model, and reinforcing documentation of the rounding in our EHR are some steps we have put into action at leadership and staff meetings to sustain the activity. We are soliciting feedback, as well as monitoring and identifying any unaddressed barriers during rounding. Addition of this process measure to our quality improvement bonus opportunity also has helped to sustain performance from our teams.
Dr. Laufer is system medical director of hospital medicine and transitional care at Lee Health in Ft. Myers, Fla. Dr. Prasad is chief medical officer of Lee Physician Group, Ft. Myers, Fla.
References
1. Leape LL et al. Five years after to err is human: What we have learned? JAMA. 2005;293(19):2384-90.
2. Sutcliffe KM et al. Communication failures: An insidious contributor to medical mishaps. Acad Med. 2004;79(2):186-94.
3. Manojlovich M. Reframing communication with physicians as sensemaking. J Nurs Care Qual. 2013 Oct-Dec;28(4):295-303.
4. Siegele P. Enhancing outcomes in a surgical intensive care unit by implementing daily goals. Crit Care Nurse. 2009 Dec;29(6):58-69.
5. Asthon J et al. Qualitative evaluation of regular morning meeting aimed at improving interdisciplinary communication and patient outcomes. Int J Nurs Pract. 2005 Oct;11(5):206-13.
6. Lancaster G et al. Interdisciplinary Communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015 May;47(3):275-84.
7. McIntosh N et al. Impact of provider coordination on nurse and physician perception of patient care quality. J Nurs Care Qual. 2014 Jul-Sep;29(3):269-79.
8. Jo M et al. An organizational assessment of disruptive clinical behavior. J Nurs Care Qual. 2013 Apr-Jun;28(2):110-21.
9. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, 2010.
10. O’Connor P et al. A mixed-methods study of the causes and impact of poor teamwork between junior doctors and nurses. Int J Qual Health Care. 2016 Jun;28(3):339-45.
11. Manojlovich M. Nurse/Physician communication through a sense making lens. Med Care. 2010 Nov;48(11):941-6.
12. Monash B et al. Standardized attending rounds to improve the patient experience: A pragmatic cluster randomized controlled trial. J Hosp Med. 2017 Mar;12(3):143-9.
13. O’Leary KJ et al. Effect of patient-centered bedside rounds on hospitalized patients decision control, activation and satisfaction with care. BMJ Qual Saf. 2016 Dec;25(12):921-8.
14. Dutton RP et al. Daily multidisciplinary rounds shorten length of stay for trauma patients. J Trauma. 2003 Nov;55(5):913-9.
15. Manojlovich M et al. Healthy work environments, nurse-physician communication, and patients’ outcomes. Am J Crit Care. 2007 Nov;16(6):536-43.
16. Ramirez J et al. Patient satisfaction with bedside teaching rounds compared with nonbedside rounds. South Med J. 2016 Feb;109(2):112-5.
17. Sollami A et al. Nurse-Physician collaboration: A meta-analytical investigation of survey scores. J Interprof Care. 2015 May;29(3):223-9.
18. House S et al. Nurses and physicians perceptions of nurse-physician collaboration. J Nurs Adm. 2017 Mar;47(3):165-71.
19. Townsend-Gervis M et al. Interdisciplinary rounds and structured communications reduce re-admissions and improve some patients’ outcomes. West J Nurs Res. 2014 Aug;36(7):917-28.
20. The Joint Commission. Sentinel Events. http://www.jointcommission.org/sentinel_event.aspx. Accessed Oct 2017.
21. Bodenheimer T et al. From Triple to Quadruple Aim: Care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6.
Inadequate and fragmented communication between physicians and nurses can lead to unwelcome events for the hospitalized patient and clinicians. Missing orders, medication errors, patient misidentification, and lack of physician awareness of significant changes in patient status are just some examples of how deficits in formal communication can affect health outcomes during acute stays.
A 2000 Institute of Medicine report showed that bad systems, not bad people, account for the majority of errors and injuries caused by complexity, professional fragmentation, and barriers in communication. Their recommendation was to train physicians, nurses, and other professionals in teamwork.1,2 However, as Milisa Manojlovich, PhD, RN, found, there are significant differences in how physicians and nurses perceive collaboration and communication.3
Nurse-physician rounding was historically standard for patient care during hospitalization. When physicians split time between inpatient and outpatient care, nurses had to maximize their time to collaborate and communicate with physicians whenever the physicians left their outpatient offices to come and round on their patients. Today most inpatient care is delivered by hospitalists on a 24-hour basis. This continuous availability of physicians reduces the perceived need to have joint rounds.
However, health care teams in acute care facilities now face higher and sicker patient volumes, different productivity models and demands, new compliance standards, changing work flows, and increased complexity of treatment and management of patients. This has led to gaps in timely communication and partnership.4-6 Erosion of the traditional nurse-physician relationships affects the quality of patient care, the patient’s experience, and patient safety.8-10 Poor communication among health care team members is one of the most common causes of patient care errors.4 Poor nurse-physician communication can also lead to medical errors, poor outcomes caused by lack of coordination within the treatment team, increased use of unnecessary resources with inefficiency, and increases in the complexity of communication among team members, and time wastage.5,7,11 All these lead to poor work flows and directly affect patient safety.7
At Lee Health System in Lee County, Fla., we saw an opportunity in this changing health care environment to promote nurse-physician rounding. We created a structured, standardized process for morning rounding and engaged unit clerks, nursing leadership, and hospitalist service line leaders. We envisioned improvement of the patient experience, nurse-physician relationship, quality of care, the discharge planning process, and efficiency, as well as decreasing length of stay, improving communication, and bringing the patient and the treatment team closer, as demonstrated by Bradley Monash, MD, et al.12
Some data suggest that patient-centered bedside rounds on hospitalized patients have no effect on patient perceptions or their satisfaction with care.13 However, we felt that collaboration among a multidisciplinary team would help us achieve better outcomes. For example, our patients would perceive the care team (MD-RN) as a cohesive unit, and in turn gain trust in the members of the treatment team, as found by Nathalie McIntosh, PhD, et al and by Jason Ramirez, MD.7,16 Our vision was to empower nurses to be advocates for patients and their family members as they navigated their acute care admission. Nurses could also support physicians by communicating the physicians’ care plans to families and patients. After rounding with the physician, the nurse would be part of the decision-making process and care planning.17
Every rounding session had discharge planning and hospital stay expectations that were shared with the patient and nurse, who could then partner with case managers and social workers, which would streamline and reduce length of stay.14 We hoped rounding would also decrease the number of nurse pages to clarify or question orders. This would, in turn, improve daily work flow for the physicians and the nursing team with improvements in employee satisfaction scores.15 A study also has demonstrated a reduction in readmission rates from nurse-physician rounding.19
A disconnect in communication and trust between physicians and the nursing staff was reflected in low patient experience scores and perceived quality of care received during in-hospital stay. Gwendolyn Lancaster, EdD, MSN, RN, CCRN, et al, as well as a Joint Commission report, demonstrated how a lack of communication and poor team dynamics can translate to poor patient experience and be a major cause for sentinel events.6,20 Artificial, forced hierarchies and role perception among health care team members led to frustration, hostility, and distrust, which compromises quality and patient safety.1
One of our biggest challenges when we started this project was explaining the “Why” to the hospitalist group and nursing staff. Physicians were used to being the dominant partner in the team. Partnering with and engaging nurses in shared decision making and care planning was a seismic shift in culture and work flow within the care team. Early gains helped skeptical team members begin to understand the value in nurse-physician rounding. Near universal adoption of the rounding process at Lee Health has caused improvements in the working relationship and trust among the health care professionals. We have seen improvements in utilization management, as well as appropriateness and timeliness of resource use, because of better communication and understanding of care plans by nursing and physicians. Collaboration with specialists and alignment in care planning are other gains. Hospitalists and nurses are both very satisfied with the decrease in the number of pages during the day, and this has lowered stressors on health care teams.
How we did it
Nurse-physician rounding is a proven method to improve collaboration, communication, and relationships among health care team members in acute care facilities. In the complex health care challenges faced today, this improved work flow for taking care of patients can help advance the Quadruple Aim of high quality, low cost, improved patient experience, physician, and staff satisfaction.21
Lee Health System includes four facilities in Lee County, with a total of 1,216 licensed adult acute care beds. The pilot project was started in 2014.
Initially the vice president of nursing and the hospitalist medical director met to create an education plan for nurses and physicians. We chose one adult medicine unit to pilot the project because there already existed a closely knit nursing and hospitalist team. In our facility there is no strict geographical rounding; each hospitalist carries between three and six patients in the unit. As a first step, a nurse floor assignment sheet was faxed in the morning to the hospitalist office with the direct phone numbers of the nurses. The unit clerk, using physician assignments in the EHR, teamed up the physician and nurses for rounding. Once the physician arrived at the unit, he or she checked in with the unit clerk, who alerted nurses that the hospitalist was available on the floor to commence rounding. If the primary nurse was unavailable because of other duties or breaks, the charge nurse rounded with the physician.
Once in the room with the patient, the duo introduced themselves as members of the treatment team and acknowledged the patient’s needs. During the visit, care plans and treatment were reviewed, the patient’s questions were answered, a physical exam was completed, and lab and imaging results were discussed; the nurse also helped raise questions he or she had received from family members so answers could be communicated to the family later. Patients appreciated knowing that their physicians and nurses were working together as a team for their safety and recovery. During the visit, care was taken to focus specially on the course of hospitalization and discharge planning.
We tracked the rounding with a manual paper process maintained by the charge nurse. Our initial rounding rates were 30%-40%, and we continued to promote this initiative to the team, and eventually the importance and value of these rounds caught on with both nurses and physicians, and now our current average rounding rate is 90%. We then decided to scale this to all units in the hospital.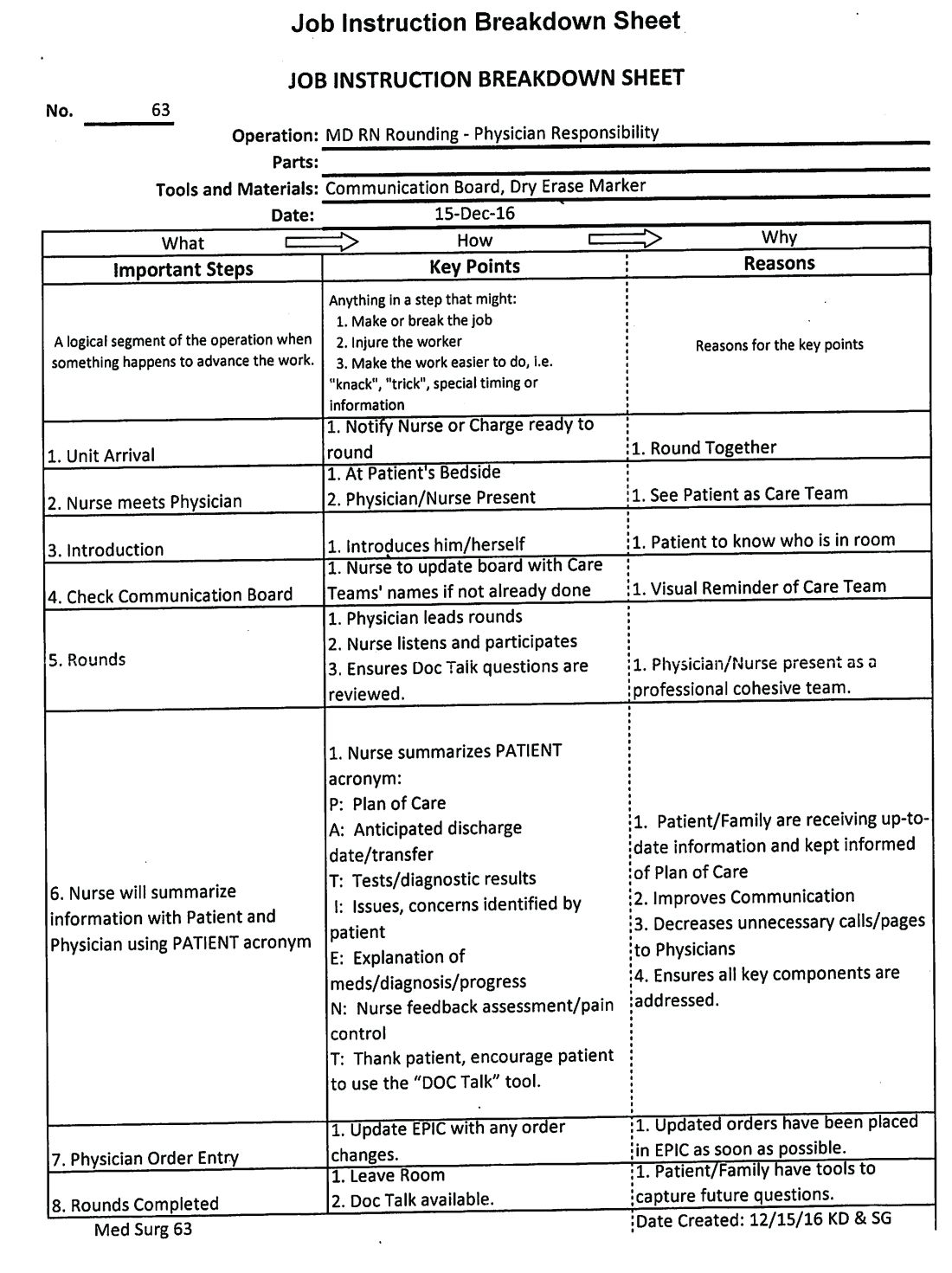
This process was repeated at other hospitals in the system once a standardized work flow was created (See Image 1). This initiative was next presented to the health system board of directors, who agreed that nurse-physician rounding should be the standard of care across our health system. Through partnership and collaboration with the IT department, we developed a tool to track nurse-physician rounding through our EHR system, which gave accountability to both physicians and nurses.
In conclusion, improved communication by timely nurse-physician rounding can lead to better outcomes for patients and also reduce costs and improve patient and staff experience, advancing the Quadruple Aim. Moving forward to build and sustain this work flow, we plan to continue nurse-physician collaboration across the health system consistently and for all areas of acute care operations.
Explaining the “Why,” sharing data on the benefits of the model, and reinforcing documentation of the rounding in our EHR are some steps we have put into action at leadership and staff meetings to sustain the activity. We are soliciting feedback, as well as monitoring and identifying any unaddressed barriers during rounding. Addition of this process measure to our quality improvement bonus opportunity also has helped to sustain performance from our teams.
Dr. Laufer is system medical director of hospital medicine and transitional care at Lee Health in Ft. Myers, Fla. Dr. Prasad is chief medical officer of Lee Physician Group, Ft. Myers, Fla.
References
1. Leape LL et al. Five years after to err is human: What we have learned? JAMA. 2005;293(19):2384-90.
2. Sutcliffe KM et al. Communication failures: An insidious contributor to medical mishaps. Acad Med. 2004;79(2):186-94.
3. Manojlovich M. Reframing communication with physicians as sensemaking. J Nurs Care Qual. 2013 Oct-Dec;28(4):295-303.
4. Siegele P. Enhancing outcomes in a surgical intensive care unit by implementing daily goals. Crit Care Nurse. 2009 Dec;29(6):58-69.
5. Asthon J et al. Qualitative evaluation of regular morning meeting aimed at improving interdisciplinary communication and patient outcomes. Int J Nurs Pract. 2005 Oct;11(5):206-13.
6. Lancaster G et al. Interdisciplinary Communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015 May;47(3):275-84.
7. McIntosh N et al. Impact of provider coordination on nurse and physician perception of patient care quality. J Nurs Care Qual. 2014 Jul-Sep;29(3):269-79.
8. Jo M et al. An organizational assessment of disruptive clinical behavior. J Nurs Care Qual. 2013 Apr-Jun;28(2):110-21.
9. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, 2010.
10. O’Connor P et al. A mixed-methods study of the causes and impact of poor teamwork between junior doctors and nurses. Int J Qual Health Care. 2016 Jun;28(3):339-45.
11. Manojlovich M. Nurse/Physician communication through a sense making lens. Med Care. 2010 Nov;48(11):941-6.
12. Monash B et al. Standardized attending rounds to improve the patient experience: A pragmatic cluster randomized controlled trial. J Hosp Med. 2017 Mar;12(3):143-9.
13. O’Leary KJ et al. Effect of patient-centered bedside rounds on hospitalized patients decision control, activation and satisfaction with care. BMJ Qual Saf. 2016 Dec;25(12):921-8.
14. Dutton RP et al. Daily multidisciplinary rounds shorten length of stay for trauma patients. J Trauma. 2003 Nov;55(5):913-9.
15. Manojlovich M et al. Healthy work environments, nurse-physician communication, and patients’ outcomes. Am J Crit Care. 2007 Nov;16(6):536-43.
16. Ramirez J et al. Patient satisfaction with bedside teaching rounds compared with nonbedside rounds. South Med J. 2016 Feb;109(2):112-5.
17. Sollami A et al. Nurse-Physician collaboration: A meta-analytical investigation of survey scores. J Interprof Care. 2015 May;29(3):223-9.
18. House S et al. Nurses and physicians perceptions of nurse-physician collaboration. J Nurs Adm. 2017 Mar;47(3):165-71.
19. Townsend-Gervis M et al. Interdisciplinary rounds and structured communications reduce re-admissions and improve some patients’ outcomes. West J Nurs Res. 2014 Aug;36(7):917-28.
20. The Joint Commission. Sentinel Events. http://www.jointcommission.org/sentinel_event.aspx. Accessed Oct 2017.
21. Bodenheimer T et al. From Triple to Quadruple Aim: Care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6.
Skin signs may be good omens during cancer therapy
Signs of efficacy of anti-cancer therapies may be only skin deep, results of a retrospective review indicate.
Cutaneous toxicities such as vitiligo, rash, alopecia, and nail toxicities may be early signs of efficacy of targeted therapies, immunotherapy, or cytotoxic chemotherapy, according to Alexandra K. Rzepecki, of the University of Michigan, and her coauthors from Albert Einstein Medical College in the Bronx, New York.
“Because cutaneous toxicities are a clinically visible parameter, they may alert clinicians to the possibility of treatment success or failure in a rapid, cost-effective, and noninvasive manner,” they wrote. The report is in the Journal of the American Academy of Dermatology.
The investigators reviewed the medical literature for clinical studies of three major classes of anti-cancer therapies that included data on associations between cutaneous toxicities and clinical outcomes such progression-free survival (PFS) overall survival (OS).
The drug classes and their associations with cutaneous toxicities and clinical outcomes were as follows:
- Targeted therapies, including tyrosine kinase inhibitors targeting the epidermal growth factor receptor (EGFR) such as cetuximab (Erbitux) and erlotinib (Tarceva), and multikinase targeted agents such as sorafenib (Nexavar) and sunitinib (Sutent). Toxicities associated with clinical benefit from EGFR inhibitors include rash, xerosis, leukocytoclastic vasculitis, paronychia, and pruritus, whereas skin toxicities associated with the multikinase inhibitors trended toward the hand-foot syndrome and hand-foot skin reaction.
- Immunotherapies included blockers of cytotoxic T-lymphocyte associated protein 4 (CTLA4) such as ipilimumab (Yervoy) and inhibitors of programmed death 1 protein (PD-1) and its ligand 1 (PD-L1) such as nivolumab (Opdivo), pembrolizumab (Keytruda), and atezolizumab (Tecentriq). In studies of pembrolizumab for various malignancies, rash or vitiligo was an independent prognostic factor for longer OS, a higher proportion of objective responses, and longer PFS. Similar associations were seen with nivolumab, with the additional association of hair repigmentation among patients with non–small-cell lung cancer being associated with stable disease responses or better. Among patients with melanoma treated with ipilimumab, hair depigmentation correlated with durable responses.
- Cytotoxic chemotherapy agents included the anthracycline doxorubicin, taxanes such as paclitaxel and docetaxel, platinum agents (cisplatin and carboplatin), and fluoropyrimidines such as capecitabine. Patients treated for various cancers with doxorubicin who had alopecia were significantly more likely to have clinical remissions than were patients who did not lose their hair, and patients treated with this agent who developed hand-foot syndrome had significantly longer PFS. For patients treated with docetaxel, severity of nail changes and/or development of nail alterations were associated with both improved OS and PFS. Patients treated with the combination of paclitaxel and a platinum agent who developed grade 2 or greater alopecia up to cycle 3 had significantly longer OS than did patients who had hair loss later in the course of therapy. Patients treated with capecitabine who developed had hand-foot skin reactions had improved progression-free and disease-free survival.
“Although further studies are needed to better evaluate these promising associations, vigilant monitoring of cutaneous toxicities should be a priority, as their development may indicate a favorable response to treatment. Dermatologists have a unique opportunity to collaborate with oncologists to help identify and manage these toxicities, thereby allowing patients to receive life-prolonging anticancer therapy while minimizing dose reduction or interruption of their treatment,” the authors wrote.
They reported no study funding source and no conflicts of interest.
SOURCE: Rzepecki A, et al. J Am Acad Dermatol. 2018;79:545-555.
Signs of efficacy of anti-cancer therapies may be only skin deep, results of a retrospective review indicate.
Cutaneous toxicities such as vitiligo, rash, alopecia, and nail toxicities may be early signs of efficacy of targeted therapies, immunotherapy, or cytotoxic chemotherapy, according to Alexandra K. Rzepecki, of the University of Michigan, and her coauthors from Albert Einstein Medical College in the Bronx, New York.
“Because cutaneous toxicities are a clinically visible parameter, they may alert clinicians to the possibility of treatment success or failure in a rapid, cost-effective, and noninvasive manner,” they wrote. The report is in the Journal of the American Academy of Dermatology.
The investigators reviewed the medical literature for clinical studies of three major classes of anti-cancer therapies that included data on associations between cutaneous toxicities and clinical outcomes such progression-free survival (PFS) overall survival (OS).
The drug classes and their associations with cutaneous toxicities and clinical outcomes were as follows:
- Targeted therapies, including tyrosine kinase inhibitors targeting the epidermal growth factor receptor (EGFR) such as cetuximab (Erbitux) and erlotinib (Tarceva), and multikinase targeted agents such as sorafenib (Nexavar) and sunitinib (Sutent). Toxicities associated with clinical benefit from EGFR inhibitors include rash, xerosis, leukocytoclastic vasculitis, paronychia, and pruritus, whereas skin toxicities associated with the multikinase inhibitors trended toward the hand-foot syndrome and hand-foot skin reaction.
- Immunotherapies included blockers of cytotoxic T-lymphocyte associated protein 4 (CTLA4) such as ipilimumab (Yervoy) and inhibitors of programmed death 1 protein (PD-1) and its ligand 1 (PD-L1) such as nivolumab (Opdivo), pembrolizumab (Keytruda), and atezolizumab (Tecentriq). In studies of pembrolizumab for various malignancies, rash or vitiligo was an independent prognostic factor for longer OS, a higher proportion of objective responses, and longer PFS. Similar associations were seen with nivolumab, with the additional association of hair repigmentation among patients with non–small-cell lung cancer being associated with stable disease responses or better. Among patients with melanoma treated with ipilimumab, hair depigmentation correlated with durable responses.
- Cytotoxic chemotherapy agents included the anthracycline doxorubicin, taxanes such as paclitaxel and docetaxel, platinum agents (cisplatin and carboplatin), and fluoropyrimidines such as capecitabine. Patients treated for various cancers with doxorubicin who had alopecia were significantly more likely to have clinical remissions than were patients who did not lose their hair, and patients treated with this agent who developed hand-foot syndrome had significantly longer PFS. For patients treated with docetaxel, severity of nail changes and/or development of nail alterations were associated with both improved OS and PFS. Patients treated with the combination of paclitaxel and a platinum agent who developed grade 2 or greater alopecia up to cycle 3 had significantly longer OS than did patients who had hair loss later in the course of therapy. Patients treated with capecitabine who developed had hand-foot skin reactions had improved progression-free and disease-free survival.
“Although further studies are needed to better evaluate these promising associations, vigilant monitoring of cutaneous toxicities should be a priority, as their development may indicate a favorable response to treatment. Dermatologists have a unique opportunity to collaborate with oncologists to help identify and manage these toxicities, thereby allowing patients to receive life-prolonging anticancer therapy while minimizing dose reduction or interruption of their treatment,” the authors wrote.
They reported no study funding source and no conflicts of interest.
SOURCE: Rzepecki A, et al. J Am Acad Dermatol. 2018;79:545-555.
Signs of efficacy of anti-cancer therapies may be only skin deep, results of a retrospective review indicate.
Cutaneous toxicities such as vitiligo, rash, alopecia, and nail toxicities may be early signs of efficacy of targeted therapies, immunotherapy, or cytotoxic chemotherapy, according to Alexandra K. Rzepecki, of the University of Michigan, and her coauthors from Albert Einstein Medical College in the Bronx, New York.
“Because cutaneous toxicities are a clinically visible parameter, they may alert clinicians to the possibility of treatment success or failure in a rapid, cost-effective, and noninvasive manner,” they wrote. The report is in the Journal of the American Academy of Dermatology.
The investigators reviewed the medical literature for clinical studies of three major classes of anti-cancer therapies that included data on associations between cutaneous toxicities and clinical outcomes such progression-free survival (PFS) overall survival (OS).
The drug classes and their associations with cutaneous toxicities and clinical outcomes were as follows:
- Targeted therapies, including tyrosine kinase inhibitors targeting the epidermal growth factor receptor (EGFR) such as cetuximab (Erbitux) and erlotinib (Tarceva), and multikinase targeted agents such as sorafenib (Nexavar) and sunitinib (Sutent). Toxicities associated with clinical benefit from EGFR inhibitors include rash, xerosis, leukocytoclastic vasculitis, paronychia, and pruritus, whereas skin toxicities associated with the multikinase inhibitors trended toward the hand-foot syndrome and hand-foot skin reaction.
- Immunotherapies included blockers of cytotoxic T-lymphocyte associated protein 4 (CTLA4) such as ipilimumab (Yervoy) and inhibitors of programmed death 1 protein (PD-1) and its ligand 1 (PD-L1) such as nivolumab (Opdivo), pembrolizumab (Keytruda), and atezolizumab (Tecentriq). In studies of pembrolizumab for various malignancies, rash or vitiligo was an independent prognostic factor for longer OS, a higher proportion of objective responses, and longer PFS. Similar associations were seen with nivolumab, with the additional association of hair repigmentation among patients with non–small-cell lung cancer being associated with stable disease responses or better. Among patients with melanoma treated with ipilimumab, hair depigmentation correlated with durable responses.
- Cytotoxic chemotherapy agents included the anthracycline doxorubicin, taxanes such as paclitaxel and docetaxel, platinum agents (cisplatin and carboplatin), and fluoropyrimidines such as capecitabine. Patients treated for various cancers with doxorubicin who had alopecia were significantly more likely to have clinical remissions than were patients who did not lose their hair, and patients treated with this agent who developed hand-foot syndrome had significantly longer PFS. For patients treated with docetaxel, severity of nail changes and/or development of nail alterations were associated with both improved OS and PFS. Patients treated with the combination of paclitaxel and a platinum agent who developed grade 2 or greater alopecia up to cycle 3 had significantly longer OS than did patients who had hair loss later in the course of therapy. Patients treated with capecitabine who developed had hand-foot skin reactions had improved progression-free and disease-free survival.
“Although further studies are needed to better evaluate these promising associations, vigilant monitoring of cutaneous toxicities should be a priority, as their development may indicate a favorable response to treatment. Dermatologists have a unique opportunity to collaborate with oncologists to help identify and manage these toxicities, thereby allowing patients to receive life-prolonging anticancer therapy while minimizing dose reduction or interruption of their treatment,” the authors wrote.
They reported no study funding source and no conflicts of interest.
SOURCE: Rzepecki A, et al. J Am Acad Dermatol. 2018;79:545-555.
FROM JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point: Cutaneous adverse events may be early signs of drug efficacy in patients treated for various cancers.
Major finding: Cutaneous toxicities with targeted therapies, immunotherapy, and cytotoxic drugs were associated in multiple studies with improved outcomes, including progression-free and overall survival.
Study details: Retrospective review of medical literature for clinical studies reporting associations between cutaneous toxicities and clinical outcomes of cancer therapy.
Disclosures: The authors reported no study funding source and no conflicts of interest.
Source: Rzepecki A et al. J Am Acad Dermatol. 2018 Sep;79[3]:545-55.
Dr. Hal C. Lawrence III retires from ACOG
The American College of Obstetricians and Gynecologists has announced that, after 11 years with ACOG, Hal C. Lawrence III, MD, is retiring from his positions as executive vice president and chief executive officer.
“It has been an honor to lead the association and our dedicated team of employees to support members and advance women’s health,” Dr. Lawrence said in a statement from ACOG. “I am proud of all that we have achieved together.”
Under his leadership, ACOG has seen the creation of the Council on Patient Safety in Women’s Health Care and the Alliance for Innovation on Maternal Health, development of ACOG’s Global Operations Advisory Group and immunization expert work group, and creation of the Women’s Preventive Services Initiative. He also helped to restructure and revitalize the ACOG annual meeting, which has been credited for increased member attendance and improved attendee satisfaction.
His retirement becomes effective Oct. 31, 2018.
Prior to his leadership roles at ACOG, Dr. Lawrence was a practicing ob.gyn. in Asheville, N.C., from 1979 to 2007 and was a member of the Ob.Gyn. News editorial advisory board.
The American College of Obstetricians and Gynecologists has announced that, after 11 years with ACOG, Hal C. Lawrence III, MD, is retiring from his positions as executive vice president and chief executive officer.
“It has been an honor to lead the association and our dedicated team of employees to support members and advance women’s health,” Dr. Lawrence said in a statement from ACOG. “I am proud of all that we have achieved together.”
Under his leadership, ACOG has seen the creation of the Council on Patient Safety in Women’s Health Care and the Alliance for Innovation on Maternal Health, development of ACOG’s Global Operations Advisory Group and immunization expert work group, and creation of the Women’s Preventive Services Initiative. He also helped to restructure and revitalize the ACOG annual meeting, which has been credited for increased member attendance and improved attendee satisfaction.
His retirement becomes effective Oct. 31, 2018.
Prior to his leadership roles at ACOG, Dr. Lawrence was a practicing ob.gyn. in Asheville, N.C., from 1979 to 2007 and was a member of the Ob.Gyn. News editorial advisory board.
The American College of Obstetricians and Gynecologists has announced that, after 11 years with ACOG, Hal C. Lawrence III, MD, is retiring from his positions as executive vice president and chief executive officer.
“It has been an honor to lead the association and our dedicated team of employees to support members and advance women’s health,” Dr. Lawrence said in a statement from ACOG. “I am proud of all that we have achieved together.”
Under his leadership, ACOG has seen the creation of the Council on Patient Safety in Women’s Health Care and the Alliance for Innovation on Maternal Health, development of ACOG’s Global Operations Advisory Group and immunization expert work group, and creation of the Women’s Preventive Services Initiative. He also helped to restructure and revitalize the ACOG annual meeting, which has been credited for increased member attendance and improved attendee satisfaction.
His retirement becomes effective Oct. 31, 2018.
Prior to his leadership roles at ACOG, Dr. Lawrence was a practicing ob.gyn. in Asheville, N.C., from 1979 to 2007 and was a member of the Ob.Gyn. News editorial advisory board.
Slowing down
This past Labor Day weekend, I did something radical. I slowed down. Way down. My wife slowed down with me, which helped. We spent the weekend close to home walking, talking, reading, contemplating, planning, assessing, doing puzzles and crosswords, and imbibing a craft beer or two, slowly, of course. Why? Because of Adam Grant, PhD, the organizational psychologist at the University of Pennsylvania’s Wharton School of Business, Philadelphia. I had recently reread his 2016 book I’m a big fan; he’s one of those professors who makes you fervently wish you were a student again, someone who will provoke you and challenge your way of thinking.
Dr. Grant’s basic premise, which he has proved through research, is that procrastination boosts productivity. Here’s how: Let’s say you’re facing a challenge or difficult task. He says to start working on it immediately, then take some time away for reflection. This “quick to start and slow to finish” method allows your brain to continually percolate on the problem. An incomplete task stays partially active in your brain. When you come back to it you often see it with fresh eyes. You will experience your highest productivity when you are toggling between these two modes.
This makes sense, and Dr. Grant cites numerous examples from Leonardo da Vinci to the founders of Warby-Parker, as examples of success. But how can it benefit physicians? Many of us are “precrastinators,” people who tend to complete or at least begin tasks as soon as possible, even when it’s unnecessary or not urgent. Unlike some jobs in which it’s easier to take a break from a project and return to it with more creative solutions, we often are racing against a clock to see more patients, read more slides, answer more emails, and make more phone calls. We are perpetually frenetic, which is not conducive to original thinking.
If this sounds like you, then you are likely to benefit from deliberate procrastination. Here are a few ways to slow down:
- Put it on your calendar. Yes, I see the irony, but it works. Start by scheduling one hour a week where you are to accomplish nothing. You can fill this time with whatever your mind wants to do at that moment.
- When faced with a diagnostic dilemma or treatment failure, resist the urge to solve that problem in that moment. Save that note for later, tell the patient you will call him back or bring him back for a visit later. Even if you’re not actively working on it, it will incubate somewhere in your brain, allowing more divergent thought processes to take over. It’s a little like trying to solve a crossword that seems impossible in the moment and then answers suddenly appear without effort.
- Take up a hobby: Play the guitar, learn to make pasta, climb a big rock. When you are fully engaged in such pursuits it requires complete mental focus. When you revisit the difficult problem you’re working on, you will likely see it from different perspectives.
- Meditate: Meditation requires our brains and bodies to slow down. It can help reduce self-doubt and criticism which stifle problem solving.
- Watch Slow TV. Slow TV is a Scandinavian phenomenon where you sit and watch meditative video such as a 7-hour train cam from Bergen, Norway, to Oslo. There’s no dialogue, no plot, no commercials. It’s just 7 hours of track and train and is weirdly comforting.
If you want to learn more, then when you get a chance, Google “slow living” and explore. Of course, some of you precrastinators probably have already started before finishing this column.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
This past Labor Day weekend, I did something radical. I slowed down. Way down. My wife slowed down with me, which helped. We spent the weekend close to home walking, talking, reading, contemplating, planning, assessing, doing puzzles and crosswords, and imbibing a craft beer or two, slowly, of course. Why? Because of Adam Grant, PhD, the organizational psychologist at the University of Pennsylvania’s Wharton School of Business, Philadelphia. I had recently reread his 2016 book I’m a big fan; he’s one of those professors who makes you fervently wish you were a student again, someone who will provoke you and challenge your way of thinking.
Dr. Grant’s basic premise, which he has proved through research, is that procrastination boosts productivity. Here’s how: Let’s say you’re facing a challenge or difficult task. He says to start working on it immediately, then take some time away for reflection. This “quick to start and slow to finish” method allows your brain to continually percolate on the problem. An incomplete task stays partially active in your brain. When you come back to it you often see it with fresh eyes. You will experience your highest productivity when you are toggling between these two modes.
This makes sense, and Dr. Grant cites numerous examples from Leonardo da Vinci to the founders of Warby-Parker, as examples of success. But how can it benefit physicians? Many of us are “precrastinators,” people who tend to complete or at least begin tasks as soon as possible, even when it’s unnecessary or not urgent. Unlike some jobs in which it’s easier to take a break from a project and return to it with more creative solutions, we often are racing against a clock to see more patients, read more slides, answer more emails, and make more phone calls. We are perpetually frenetic, which is not conducive to original thinking.
If this sounds like you, then you are likely to benefit from deliberate procrastination. Here are a few ways to slow down:
- Put it on your calendar. Yes, I see the irony, but it works. Start by scheduling one hour a week where you are to accomplish nothing. You can fill this time with whatever your mind wants to do at that moment.
- When faced with a diagnostic dilemma or treatment failure, resist the urge to solve that problem in that moment. Save that note for later, tell the patient you will call him back or bring him back for a visit later. Even if you’re not actively working on it, it will incubate somewhere in your brain, allowing more divergent thought processes to take over. It’s a little like trying to solve a crossword that seems impossible in the moment and then answers suddenly appear without effort.
- Take up a hobby: Play the guitar, learn to make pasta, climb a big rock. When you are fully engaged in such pursuits it requires complete mental focus. When you revisit the difficult problem you’re working on, you will likely see it from different perspectives.
- Meditate: Meditation requires our brains and bodies to slow down. It can help reduce self-doubt and criticism which stifle problem solving.
- Watch Slow TV. Slow TV is a Scandinavian phenomenon where you sit and watch meditative video such as a 7-hour train cam from Bergen, Norway, to Oslo. There’s no dialogue, no plot, no commercials. It’s just 7 hours of track and train and is weirdly comforting.
If you want to learn more, then when you get a chance, Google “slow living” and explore. Of course, some of you precrastinators probably have already started before finishing this column.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
This past Labor Day weekend, I did something radical. I slowed down. Way down. My wife slowed down with me, which helped. We spent the weekend close to home walking, talking, reading, contemplating, planning, assessing, doing puzzles and crosswords, and imbibing a craft beer or two, slowly, of course. Why? Because of Adam Grant, PhD, the organizational psychologist at the University of Pennsylvania’s Wharton School of Business, Philadelphia. I had recently reread his 2016 book I’m a big fan; he’s one of those professors who makes you fervently wish you were a student again, someone who will provoke you and challenge your way of thinking.
Dr. Grant’s basic premise, which he has proved through research, is that procrastination boosts productivity. Here’s how: Let’s say you’re facing a challenge or difficult task. He says to start working on it immediately, then take some time away for reflection. This “quick to start and slow to finish” method allows your brain to continually percolate on the problem. An incomplete task stays partially active in your brain. When you come back to it you often see it with fresh eyes. You will experience your highest productivity when you are toggling between these two modes.
This makes sense, and Dr. Grant cites numerous examples from Leonardo da Vinci to the founders of Warby-Parker, as examples of success. But how can it benefit physicians? Many of us are “precrastinators,” people who tend to complete or at least begin tasks as soon as possible, even when it’s unnecessary or not urgent. Unlike some jobs in which it’s easier to take a break from a project and return to it with more creative solutions, we often are racing against a clock to see more patients, read more slides, answer more emails, and make more phone calls. We are perpetually frenetic, which is not conducive to original thinking.
If this sounds like you, then you are likely to benefit from deliberate procrastination. Here are a few ways to slow down:
- Put it on your calendar. Yes, I see the irony, but it works. Start by scheduling one hour a week where you are to accomplish nothing. You can fill this time with whatever your mind wants to do at that moment.
- When faced with a diagnostic dilemma or treatment failure, resist the urge to solve that problem in that moment. Save that note for later, tell the patient you will call him back or bring him back for a visit later. Even if you’re not actively working on it, it will incubate somewhere in your brain, allowing more divergent thought processes to take over. It’s a little like trying to solve a crossword that seems impossible in the moment and then answers suddenly appear without effort.
- Take up a hobby: Play the guitar, learn to make pasta, climb a big rock. When you are fully engaged in such pursuits it requires complete mental focus. When you revisit the difficult problem you’re working on, you will likely see it from different perspectives.
- Meditate: Meditation requires our brains and bodies to slow down. It can help reduce self-doubt and criticism which stifle problem solving.
- Watch Slow TV. Slow TV is a Scandinavian phenomenon where you sit and watch meditative video such as a 7-hour train cam from Bergen, Norway, to Oslo. There’s no dialogue, no plot, no commercials. It’s just 7 hours of track and train and is weirdly comforting.
If you want to learn more, then when you get a chance, Google “slow living” and explore. Of course, some of you precrastinators probably have already started before finishing this column.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
How to screen for, manage FASD in a medical home
providing early intervention and accessing community resources, according to a clinical report from the American Academy of Pediatrics.
After the AAP released its guidelines on fetal alcohol spectrum disorder (FASD) in 2015, some pediatricians asked for further guidance on how to care for patients with FASD within the medical home, as many had a knowledge gap on how to best manage these patients.
“For some pediatricians, it can seem like a daunting task to care for an individual with an FASD, but there are aspects of integrated care and providing a medical home that can be instituted as with all children with complex medical diagnoses,” wrote Renee M. Turchi, MD, MPH, of the department of pediatrics at St. Christopher’s Hospital for Children and Drexel Dornsife School of Public Health in Philadelphia, and her colleagues on the AAP Committee on Substance Abuse and the Council on Children with Disabilities. Their report is in Pediatrics. “In addition, not recognizing an FASD can lead to inadequate treatment and less-than-optimal outcomes for the patient and family.”
Dr. Turchi and her colleagues released the FASD clinical report with “strategies to support families who are interacting with early intervention services, the educational system, the behavioral and/or mental health system, other community resources, and the transition to adult-oriented heath care systems when appropriate.” They noted the prevalence of FASD is increasing, with 1 in 10 pregnant women using alcohol within the past 30 days and 1 in 33 pregnant women reporting binge drinking in the past 30 days. They reaffirmed the AAP’s endorsement from the 2015 clinical report on FASD regarding abstinence of alcohol for pregnant women, emphasizing that there is no amount or kind of alcohol that is risk free during pregnancy, nor is there a time in pregnancy when drinking alcohol is risk free.
Providers in a medical home should communicate any prenatal alcohol exposure (PAE) to obstetric providers so they can review risk factors, optimize screening, and monitor children, Dr. Turchi and her colleagues said. They also should understand the diagnostic criteria and classifications for FASDs, including physical features such as low weight, short palpebral features, smooth philtrum, a thin upper lip, abnormalities in the central nervous system, and any alcohol use during pregnancy. Any child – regardless of age – is a candidate for universal PAE screening at initial visits or when “additional cognitive and behavioral concerns arise.”
The federal Child Abuse Prevention and Treatment Act “does not require clinicians to report to child protective services if a child has been exposed prenatally to alcohol (i.e., for a positive PAE screening result). Referral to child protective services is required if the child has been diagnosed with an FASD in the period between birth and 3 years. The intent of this referral is to develop safe care and possible treatment plans for the infant and caregiver if needed, not to initiate punitive actions,” according to the report. States have their own definitions about child abuse and neglect, so the report encourages providers to know the mandates and reporting laws in the states where they practice.
Monitoring children in a medical home for the signs and symptoms of FASD is important, the authors said, because research has shown an increased chance at reducing adverse life outcomes if a child is diagnosed before age 6 and is in a stable home with access to support services.
Management of children with FASD is individual, as symptoms for each child will uniquely present not just in terms of physical issues such as growth or congenital defects affecting the heart, eyes, kidneys, or bones, but also as developmental, cognitive, and behavioral problems. Children with FASD also may receive a concomitant diagnosis when evaluated, such as ADHD or depression, that will require additional accommodation. The use of evidence-based diagnostic and standard screening approaches and referring when necessary will help reevaluate whether a child has a condition such as ADHD, oppositional defiant disorder, or another diagnosis, or is displaying symptoms of FASD such as a receptive or expressive language disorder.
Pediatricians must work together with the families, educational professionals, the mental health community, and therapists to help manage FASD in children. In cases where a child is in foster care, partnering with the foster care partners and child welfare agencies to gain access to the medical information of the biological parents is important to determine whether there is parental history of substance abuse and to provide appropriate treatment and interventions.
“Given the complex array of systems and services requiring navigation and coordination for children with an FASD and their families, a high-quality primary care medical home with partnerships with families, specialists, therapists, mental and/or behavioral health professionals, and community partners is critical, as it is for all children with special health care needs,” Dr. Turchi and her colleagues said.
The authors reported no relevant conflicts of interest.
SOURCE: Turchi RM et al. Pediatrics. 2018 Sept 10. doi:10.1542/peds.2018-2333.
providing early intervention and accessing community resources, according to a clinical report from the American Academy of Pediatrics.
After the AAP released its guidelines on fetal alcohol spectrum disorder (FASD) in 2015, some pediatricians asked for further guidance on how to care for patients with FASD within the medical home, as many had a knowledge gap on how to best manage these patients.
“For some pediatricians, it can seem like a daunting task to care for an individual with an FASD, but there are aspects of integrated care and providing a medical home that can be instituted as with all children with complex medical diagnoses,” wrote Renee M. Turchi, MD, MPH, of the department of pediatrics at St. Christopher’s Hospital for Children and Drexel Dornsife School of Public Health in Philadelphia, and her colleagues on the AAP Committee on Substance Abuse and the Council on Children with Disabilities. Their report is in Pediatrics. “In addition, not recognizing an FASD can lead to inadequate treatment and less-than-optimal outcomes for the patient and family.”
Dr. Turchi and her colleagues released the FASD clinical report with “strategies to support families who are interacting with early intervention services, the educational system, the behavioral and/or mental health system, other community resources, and the transition to adult-oriented heath care systems when appropriate.” They noted the prevalence of FASD is increasing, with 1 in 10 pregnant women using alcohol within the past 30 days and 1 in 33 pregnant women reporting binge drinking in the past 30 days. They reaffirmed the AAP’s endorsement from the 2015 clinical report on FASD regarding abstinence of alcohol for pregnant women, emphasizing that there is no amount or kind of alcohol that is risk free during pregnancy, nor is there a time in pregnancy when drinking alcohol is risk free.
Providers in a medical home should communicate any prenatal alcohol exposure (PAE) to obstetric providers so they can review risk factors, optimize screening, and monitor children, Dr. Turchi and her colleagues said. They also should understand the diagnostic criteria and classifications for FASDs, including physical features such as low weight, short palpebral features, smooth philtrum, a thin upper lip, abnormalities in the central nervous system, and any alcohol use during pregnancy. Any child – regardless of age – is a candidate for universal PAE screening at initial visits or when “additional cognitive and behavioral concerns arise.”
The federal Child Abuse Prevention and Treatment Act “does not require clinicians to report to child protective services if a child has been exposed prenatally to alcohol (i.e., for a positive PAE screening result). Referral to child protective services is required if the child has been diagnosed with an FASD in the period between birth and 3 years. The intent of this referral is to develop safe care and possible treatment plans for the infant and caregiver if needed, not to initiate punitive actions,” according to the report. States have their own definitions about child abuse and neglect, so the report encourages providers to know the mandates and reporting laws in the states where they practice.
Monitoring children in a medical home for the signs and symptoms of FASD is important, the authors said, because research has shown an increased chance at reducing adverse life outcomes if a child is diagnosed before age 6 and is in a stable home with access to support services.
Management of children with FASD is individual, as symptoms for each child will uniquely present not just in terms of physical issues such as growth or congenital defects affecting the heart, eyes, kidneys, or bones, but also as developmental, cognitive, and behavioral problems. Children with FASD also may receive a concomitant diagnosis when evaluated, such as ADHD or depression, that will require additional accommodation. The use of evidence-based diagnostic and standard screening approaches and referring when necessary will help reevaluate whether a child has a condition such as ADHD, oppositional defiant disorder, or another diagnosis, or is displaying symptoms of FASD such as a receptive or expressive language disorder.
Pediatricians must work together with the families, educational professionals, the mental health community, and therapists to help manage FASD in children. In cases where a child is in foster care, partnering with the foster care partners and child welfare agencies to gain access to the medical information of the biological parents is important to determine whether there is parental history of substance abuse and to provide appropriate treatment and interventions.
“Given the complex array of systems and services requiring navigation and coordination for children with an FASD and their families, a high-quality primary care medical home with partnerships with families, specialists, therapists, mental and/or behavioral health professionals, and community partners is critical, as it is for all children with special health care needs,” Dr. Turchi and her colleagues said.
The authors reported no relevant conflicts of interest.
SOURCE: Turchi RM et al. Pediatrics. 2018 Sept 10. doi:10.1542/peds.2018-2333.
providing early intervention and accessing community resources, according to a clinical report from the American Academy of Pediatrics.
After the AAP released its guidelines on fetal alcohol spectrum disorder (FASD) in 2015, some pediatricians asked for further guidance on how to care for patients with FASD within the medical home, as many had a knowledge gap on how to best manage these patients.
“For some pediatricians, it can seem like a daunting task to care for an individual with an FASD, but there are aspects of integrated care and providing a medical home that can be instituted as with all children with complex medical diagnoses,” wrote Renee M. Turchi, MD, MPH, of the department of pediatrics at St. Christopher’s Hospital for Children and Drexel Dornsife School of Public Health in Philadelphia, and her colleagues on the AAP Committee on Substance Abuse and the Council on Children with Disabilities. Their report is in Pediatrics. “In addition, not recognizing an FASD can lead to inadequate treatment and less-than-optimal outcomes for the patient and family.”
Dr. Turchi and her colleagues released the FASD clinical report with “strategies to support families who are interacting with early intervention services, the educational system, the behavioral and/or mental health system, other community resources, and the transition to adult-oriented heath care systems when appropriate.” They noted the prevalence of FASD is increasing, with 1 in 10 pregnant women using alcohol within the past 30 days and 1 in 33 pregnant women reporting binge drinking in the past 30 days. They reaffirmed the AAP’s endorsement from the 2015 clinical report on FASD regarding abstinence of alcohol for pregnant women, emphasizing that there is no amount or kind of alcohol that is risk free during pregnancy, nor is there a time in pregnancy when drinking alcohol is risk free.
Providers in a medical home should communicate any prenatal alcohol exposure (PAE) to obstetric providers so they can review risk factors, optimize screening, and monitor children, Dr. Turchi and her colleagues said. They also should understand the diagnostic criteria and classifications for FASDs, including physical features such as low weight, short palpebral features, smooth philtrum, a thin upper lip, abnormalities in the central nervous system, and any alcohol use during pregnancy. Any child – regardless of age – is a candidate for universal PAE screening at initial visits or when “additional cognitive and behavioral concerns arise.”
The federal Child Abuse Prevention and Treatment Act “does not require clinicians to report to child protective services if a child has been exposed prenatally to alcohol (i.e., for a positive PAE screening result). Referral to child protective services is required if the child has been diagnosed with an FASD in the period between birth and 3 years. The intent of this referral is to develop safe care and possible treatment plans for the infant and caregiver if needed, not to initiate punitive actions,” according to the report. States have their own definitions about child abuse and neglect, so the report encourages providers to know the mandates and reporting laws in the states where they practice.
Monitoring children in a medical home for the signs and symptoms of FASD is important, the authors said, because research has shown an increased chance at reducing adverse life outcomes if a child is diagnosed before age 6 and is in a stable home with access to support services.
Management of children with FASD is individual, as symptoms for each child will uniquely present not just in terms of physical issues such as growth or congenital defects affecting the heart, eyes, kidneys, or bones, but also as developmental, cognitive, and behavioral problems. Children with FASD also may receive a concomitant diagnosis when evaluated, such as ADHD or depression, that will require additional accommodation. The use of evidence-based diagnostic and standard screening approaches and referring when necessary will help reevaluate whether a child has a condition such as ADHD, oppositional defiant disorder, or another diagnosis, or is displaying symptoms of FASD such as a receptive or expressive language disorder.
Pediatricians must work together with the families, educational professionals, the mental health community, and therapists to help manage FASD in children. In cases where a child is in foster care, partnering with the foster care partners and child welfare agencies to gain access to the medical information of the biological parents is important to determine whether there is parental history of substance abuse and to provide appropriate treatment and interventions.
“Given the complex array of systems and services requiring navigation and coordination for children with an FASD and their families, a high-quality primary care medical home with partnerships with families, specialists, therapists, mental and/or behavioral health professionals, and community partners is critical, as it is for all children with special health care needs,” Dr. Turchi and her colleagues said.
The authors reported no relevant conflicts of interest.
SOURCE: Turchi RM et al. Pediatrics. 2018 Sept 10. doi:10.1542/peds.2018-2333.
FROM PEDIATRICS