User login
Levosimendan does not improve 30-day mortality following cardiac surgery
Adding a low dose of levosimendan to the standard care for patients on perioperative hemodynamic support does not improve outcomes to any significant extent, according to the findings of a new study presented at the annual congress of the European Society of Intensive Care Medicine and published simultaneously online in the New England Journal of Medicine.
“Levosimendan (Simdax, Orion) is an inotropic agent that has been shown to be associated with a higher rate of survival than other inotropic agents in meta-analyses, especially those involving patients undergoing cardiac surgery,” wrote the authors of the study, led by Giovanni Landoni, MD, of Vita-Salute San Raffaele University in Milan, adding, “Considering the pharmacologic properties of levosimendan and the results of previous studies, we hypothesized that the administration of levosimendan, in addition to standard treatment, might result in lower mortality in this context.”
Dr. Landoni and his colleagues conducted the Levosimendan to Reduce Mortality in High Risk Cardiac Surgery Patients: A Multicenter Randomized Controlled Trial, known more commonly as CHEETAH. Written consent was given by 4,725 patients from 14 centers located in Italy, Russia, and Brazil between November 2009 and April 2016. The investigators recruited a total of 506 patients. All subjects included in the study underwent cardiac surgery and experienced a perioperative cardiovascular dysfunction (N Engl J Med. 2017 Mar 21. doi: 10.1056/NEJMoa1616325).
Subjects were then randomized into a cohort receiving either a placebo or a low dose of levosimendan, which varied between 0.025 to 0.2 mcg/kg of body weight per minute continuously for up to 48 hours. A total of 248 subjects received levosimendan and 258 received placebo. All patients were administered the treatment while in the ICU; patients were taken off their regimen prior to 48 hours if they were discharged from the ICU. Anyone screened for inclusion who already had experienced a negative reaction to levosimendan was excluded from the study.
“We collected preoperative data on baseline characteristics and coexisting conditions, intraoperative and postoperative treatment data, postoperative laboratory values, duration of mechanical ventilation, durations of ICU and hospital stays, and major outcomes,” the authors explained, adding that “telephone follow-up was performed at 30 days and 180 days after randomization by an investigator who was unaware of the trial group assignments.”
The primary outcome of the study was 30-day mortality. The levosimendan cohort experienced 32 deaths (12.9%), while the placebo cohort saw 33 (12.8%), a nonsignificant difference (P = .97) between the two groups. Similarly, the median time spent on mechanical ventilation was 19 hours for those on levosimendan, versus 21 hours for those on placebo (P = .48), and median length of hospital stay was 14 days in both groups (P = .39).
“Previous meta-analyses of randomized, controlled trials showed a higher rate of survival with levosimendan than with other treatment regimens among patients undergoing cardiac surgery,” Dr. Landoni and his coauthors noted. Previous studies also had a number of key differences, such as the number of subjects who underwent coronary artery bypass grafting, the dosing of levosimendan, and inclusion of patients who had reduced preoperative ejection fraction instead of ones with myocardial dysfunction who needed inotropic support, which the current study used.
The study was funded by the Italian Ministry of Health. Dr. Landoni reported receiving nonfinancial support from the Orion Corporation while the study was ongoing; several other coauthors reported similar disclosures.
Adding a low dose of levosimendan to the standard care for patients on perioperative hemodynamic support does not improve outcomes to any significant extent, according to the findings of a new study presented at the annual congress of the European Society of Intensive Care Medicine and published simultaneously online in the New England Journal of Medicine.
“Levosimendan (Simdax, Orion) is an inotropic agent that has been shown to be associated with a higher rate of survival than other inotropic agents in meta-analyses, especially those involving patients undergoing cardiac surgery,” wrote the authors of the study, led by Giovanni Landoni, MD, of Vita-Salute San Raffaele University in Milan, adding, “Considering the pharmacologic properties of levosimendan and the results of previous studies, we hypothesized that the administration of levosimendan, in addition to standard treatment, might result in lower mortality in this context.”
Dr. Landoni and his colleagues conducted the Levosimendan to Reduce Mortality in High Risk Cardiac Surgery Patients: A Multicenter Randomized Controlled Trial, known more commonly as CHEETAH. Written consent was given by 4,725 patients from 14 centers located in Italy, Russia, and Brazil between November 2009 and April 2016. The investigators recruited a total of 506 patients. All subjects included in the study underwent cardiac surgery and experienced a perioperative cardiovascular dysfunction (N Engl J Med. 2017 Mar 21. doi: 10.1056/NEJMoa1616325).
Subjects were then randomized into a cohort receiving either a placebo or a low dose of levosimendan, which varied between 0.025 to 0.2 mcg/kg of body weight per minute continuously for up to 48 hours. A total of 248 subjects received levosimendan and 258 received placebo. All patients were administered the treatment while in the ICU; patients were taken off their regimen prior to 48 hours if they were discharged from the ICU. Anyone screened for inclusion who already had experienced a negative reaction to levosimendan was excluded from the study.
“We collected preoperative data on baseline characteristics and coexisting conditions, intraoperative and postoperative treatment data, postoperative laboratory values, duration of mechanical ventilation, durations of ICU and hospital stays, and major outcomes,” the authors explained, adding that “telephone follow-up was performed at 30 days and 180 days after randomization by an investigator who was unaware of the trial group assignments.”
The primary outcome of the study was 30-day mortality. The levosimendan cohort experienced 32 deaths (12.9%), while the placebo cohort saw 33 (12.8%), a nonsignificant difference (P = .97) between the two groups. Similarly, the median time spent on mechanical ventilation was 19 hours for those on levosimendan, versus 21 hours for those on placebo (P = .48), and median length of hospital stay was 14 days in both groups (P = .39).
“Previous meta-analyses of randomized, controlled trials showed a higher rate of survival with levosimendan than with other treatment regimens among patients undergoing cardiac surgery,” Dr. Landoni and his coauthors noted. Previous studies also had a number of key differences, such as the number of subjects who underwent coronary artery bypass grafting, the dosing of levosimendan, and inclusion of patients who had reduced preoperative ejection fraction instead of ones with myocardial dysfunction who needed inotropic support, which the current study used.
The study was funded by the Italian Ministry of Health. Dr. Landoni reported receiving nonfinancial support from the Orion Corporation while the study was ongoing; several other coauthors reported similar disclosures.
Adding a low dose of levosimendan to the standard care for patients on perioperative hemodynamic support does not improve outcomes to any significant extent, according to the findings of a new study presented at the annual congress of the European Society of Intensive Care Medicine and published simultaneously online in the New England Journal of Medicine.
“Levosimendan (Simdax, Orion) is an inotropic agent that has been shown to be associated with a higher rate of survival than other inotropic agents in meta-analyses, especially those involving patients undergoing cardiac surgery,” wrote the authors of the study, led by Giovanni Landoni, MD, of Vita-Salute San Raffaele University in Milan, adding, “Considering the pharmacologic properties of levosimendan and the results of previous studies, we hypothesized that the administration of levosimendan, in addition to standard treatment, might result in lower mortality in this context.”
Dr. Landoni and his colleagues conducted the Levosimendan to Reduce Mortality in High Risk Cardiac Surgery Patients: A Multicenter Randomized Controlled Trial, known more commonly as CHEETAH. Written consent was given by 4,725 patients from 14 centers located in Italy, Russia, and Brazil between November 2009 and April 2016. The investigators recruited a total of 506 patients. All subjects included in the study underwent cardiac surgery and experienced a perioperative cardiovascular dysfunction (N Engl J Med. 2017 Mar 21. doi: 10.1056/NEJMoa1616325).
Subjects were then randomized into a cohort receiving either a placebo or a low dose of levosimendan, which varied between 0.025 to 0.2 mcg/kg of body weight per minute continuously for up to 48 hours. A total of 248 subjects received levosimendan and 258 received placebo. All patients were administered the treatment while in the ICU; patients were taken off their regimen prior to 48 hours if they were discharged from the ICU. Anyone screened for inclusion who already had experienced a negative reaction to levosimendan was excluded from the study.
“We collected preoperative data on baseline characteristics and coexisting conditions, intraoperative and postoperative treatment data, postoperative laboratory values, duration of mechanical ventilation, durations of ICU and hospital stays, and major outcomes,” the authors explained, adding that “telephone follow-up was performed at 30 days and 180 days after randomization by an investigator who was unaware of the trial group assignments.”
The primary outcome of the study was 30-day mortality. The levosimendan cohort experienced 32 deaths (12.9%), while the placebo cohort saw 33 (12.8%), a nonsignificant difference (P = .97) between the two groups. Similarly, the median time spent on mechanical ventilation was 19 hours for those on levosimendan, versus 21 hours for those on placebo (P = .48), and median length of hospital stay was 14 days in both groups (P = .39).
“Previous meta-analyses of randomized, controlled trials showed a higher rate of survival with levosimendan than with other treatment regimens among patients undergoing cardiac surgery,” Dr. Landoni and his coauthors noted. Previous studies also had a number of key differences, such as the number of subjects who underwent coronary artery bypass grafting, the dosing of levosimendan, and inclusion of patients who had reduced preoperative ejection fraction instead of ones with myocardial dysfunction who needed inotropic support, which the current study used.
The study was funded by the Italian Ministry of Health. Dr. Landoni reported receiving nonfinancial support from the Orion Corporation while the study was ongoing; several other coauthors reported similar disclosures.
Key clinical point:
Major finding: Among other things, 30-day mortality rates between levosimendan (12.9%) and placebo (12.8%) cohorts were not significantly different (P = .97).
Data source: The CHEETAH study is a multicenter, randomized, double-blind, placebo-controlled trial of 506 cardiac surgery patients recommended for perioperative hemodynamic support.
Disclosures: Funded by the Italian Ministry of Health. Several coauthors reported potentially relevant conflicts of interest.
Dexmedetomidine improves sedation in sepsis
Use of dexmedetomidine improved sedation among ventilated patients with sepsis, but did not significantly cut mortality rates or increase ventilator-free days in a multicenter, open-label randomized controlled trial.
Twenty-eight days after the start of mechanical ventilation, cumulative mortality rates were 23% among patients who received dexmedetomidine and 31% among those who did not (hazard ratio, 0.7; 95% confidence interval, 0.4 to 1.2; P = .2), Yu Kawazoe, MD, PhD, and his associates reported at the International Symposium on Intensive Care and Emergency Medicine. The report was simultaneously published in JAMA.
“The study may have identified a clinically important benefit of dexmedetomidine – an 8% reduction in 28-day mortality – that did not demonstrate statistical significance ... ” wrote Dr. Kawazoe of Tohoku University Graduate School of Medicine, Sendai, Japan. “Physicians may consider an 8% difference in 28-day mortality to be clinically significant, but this study was underpowered to detect this difference.”
Dexmedetomidine often is used for sedation during ventilation, but its effects on mortality and ventilator weaning are poorly understood, the researchers noted. However, this highly selective alpha2-adrenergic agonist has been found to suppress inflammation and to protect organs, and “can improve patients’ ability to communicate pain compared with midazolam and propofol,” the researchers wrote. Therefore, they randomly assigned 201 patients with sepsis at eight intensive care units in Japan to receive sedation with or without dexmedetomidine. Both arms received fentanyl, propofol, and midazolam, dosed to achieve Richmond Agitation-Sedation Scale (RASS) scores of 0 (calm) during the day and –2 (lightly sedated) at night (JAMA. 2017 March 21. doi: 10.1001/jama.2017.2088).
The dexmedetomidine group spent a median of 20 days off the ventilator, compared with 18 days for controls (P = .20), the investigators reported. However, dexmedetomidine led to significantly higher rates of well-controlled sedation. The highest rate of well-controlled sedation (defined as having a RASS scores between –3 and 1 throughout 1 day in the ICU) in treated patients was 58%, while the highest rate of well-controlled sedation in the control group was 39% (P = .01).
Rates of adverse events did not significantly differ between groups. Bradycardia was most common, affecting 7% of the intervention group and 2% of controls (P = .1) the researchers said.
Hospira Japan provided partial funding with a grant to Wakayama Medical University, and helped design the study but was otherwise not involved in the research project. Dr. Kawazoe disclosed ties to Hospira Japan and Pfizer Japan. Three coinvestigators disclosed ties to Pfizer Japan, AbbVie, AstraZeneca, Daiichi Sankyo, and several other pharmaceutical companies. The other coinvestigators had no disclosures.
Use of dexmedetomidine improved sedation among ventilated patients with sepsis, but did not significantly cut mortality rates or increase ventilator-free days in a multicenter, open-label randomized controlled trial.
Twenty-eight days after the start of mechanical ventilation, cumulative mortality rates were 23% among patients who received dexmedetomidine and 31% among those who did not (hazard ratio, 0.7; 95% confidence interval, 0.4 to 1.2; P = .2), Yu Kawazoe, MD, PhD, and his associates reported at the International Symposium on Intensive Care and Emergency Medicine. The report was simultaneously published in JAMA.
“The study may have identified a clinically important benefit of dexmedetomidine – an 8% reduction in 28-day mortality – that did not demonstrate statistical significance ... ” wrote Dr. Kawazoe of Tohoku University Graduate School of Medicine, Sendai, Japan. “Physicians may consider an 8% difference in 28-day mortality to be clinically significant, but this study was underpowered to detect this difference.”
Dexmedetomidine often is used for sedation during ventilation, but its effects on mortality and ventilator weaning are poorly understood, the researchers noted. However, this highly selective alpha2-adrenergic agonist has been found to suppress inflammation and to protect organs, and “can improve patients’ ability to communicate pain compared with midazolam and propofol,” the researchers wrote. Therefore, they randomly assigned 201 patients with sepsis at eight intensive care units in Japan to receive sedation with or without dexmedetomidine. Both arms received fentanyl, propofol, and midazolam, dosed to achieve Richmond Agitation-Sedation Scale (RASS) scores of 0 (calm) during the day and –2 (lightly sedated) at night (JAMA. 2017 March 21. doi: 10.1001/jama.2017.2088).
The dexmedetomidine group spent a median of 20 days off the ventilator, compared with 18 days for controls (P = .20), the investigators reported. However, dexmedetomidine led to significantly higher rates of well-controlled sedation. The highest rate of well-controlled sedation (defined as having a RASS scores between –3 and 1 throughout 1 day in the ICU) in treated patients was 58%, while the highest rate of well-controlled sedation in the control group was 39% (P = .01).
Rates of adverse events did not significantly differ between groups. Bradycardia was most common, affecting 7% of the intervention group and 2% of controls (P = .1) the researchers said.
Hospira Japan provided partial funding with a grant to Wakayama Medical University, and helped design the study but was otherwise not involved in the research project. Dr. Kawazoe disclosed ties to Hospira Japan and Pfizer Japan. Three coinvestigators disclosed ties to Pfizer Japan, AbbVie, AstraZeneca, Daiichi Sankyo, and several other pharmaceutical companies. The other coinvestigators had no disclosures.
Use of dexmedetomidine improved sedation among ventilated patients with sepsis, but did not significantly cut mortality rates or increase ventilator-free days in a multicenter, open-label randomized controlled trial.
Twenty-eight days after the start of mechanical ventilation, cumulative mortality rates were 23% among patients who received dexmedetomidine and 31% among those who did not (hazard ratio, 0.7; 95% confidence interval, 0.4 to 1.2; P = .2), Yu Kawazoe, MD, PhD, and his associates reported at the International Symposium on Intensive Care and Emergency Medicine. The report was simultaneously published in JAMA.
“The study may have identified a clinically important benefit of dexmedetomidine – an 8% reduction in 28-day mortality – that did not demonstrate statistical significance ... ” wrote Dr. Kawazoe of Tohoku University Graduate School of Medicine, Sendai, Japan. “Physicians may consider an 8% difference in 28-day mortality to be clinically significant, but this study was underpowered to detect this difference.”
Dexmedetomidine often is used for sedation during ventilation, but its effects on mortality and ventilator weaning are poorly understood, the researchers noted. However, this highly selective alpha2-adrenergic agonist has been found to suppress inflammation and to protect organs, and “can improve patients’ ability to communicate pain compared with midazolam and propofol,” the researchers wrote. Therefore, they randomly assigned 201 patients with sepsis at eight intensive care units in Japan to receive sedation with or without dexmedetomidine. Both arms received fentanyl, propofol, and midazolam, dosed to achieve Richmond Agitation-Sedation Scale (RASS) scores of 0 (calm) during the day and –2 (lightly sedated) at night (JAMA. 2017 March 21. doi: 10.1001/jama.2017.2088).
The dexmedetomidine group spent a median of 20 days off the ventilator, compared with 18 days for controls (P = .20), the investigators reported. However, dexmedetomidine led to significantly higher rates of well-controlled sedation. The highest rate of well-controlled sedation (defined as having a RASS scores between –3 and 1 throughout 1 day in the ICU) in treated patients was 58%, while the highest rate of well-controlled sedation in the control group was 39% (P = .01).
Rates of adverse events did not significantly differ between groups. Bradycardia was most common, affecting 7% of the intervention group and 2% of controls (P = .1) the researchers said.
Hospira Japan provided partial funding with a grant to Wakayama Medical University, and helped design the study but was otherwise not involved in the research project. Dr. Kawazoe disclosed ties to Hospira Japan and Pfizer Japan. Three coinvestigators disclosed ties to Pfizer Japan, AbbVie, AstraZeneca, Daiichi Sankyo, and several other pharmaceutical companies. The other coinvestigators had no disclosures.
Key clinical point. Use of dexmedetomidine improved sedation but did not significantly cut mortality rates or increase ventilator-free days among hospitalized patients with sepsis.
Major finding: Twenty-eight days after the start of mechanical ventilation, cumulative mortality rates were 23% among patients who received dexmedetomidine and 31% among those who did not (hazard ratio, 0.7; 95% confidence interval, 0.4 to 1.2; P = .2).
Data source: A multicenter, open-label randomized controlled trial of 201 ventilated patients with sepsis.
Disclosures: Hospira Japan provided partial funding with a grant to Wakayama Medical University, and helped design the study but was otherwise not involved. Dr. Kawazoe disclosed ties to Hospira Japan and Pfizer Japan. Three coinvestigators disclosed ties to Pfizer Japan, AbbVie, AstraZeneca, Daiichi Sankyo, and several other pharmaceutical companies. The other coinvestigators had no disclosures.
Osteoarthritis’ link to metabolic syndrome tied to body weight, BMI
The metabolic syndrome’s association with the development of osteoarthritis appears to occur primarily through the influence of factors related to body weight or body mass index, according to an analysis of data from the longitudinal Framingham osteoarthritis study.
Jingbo Niu, DSc, of the Clinical Epidemiology Research and Training Unit at Boston University, and her colleagues found that while the presence of the metabolic syndrome (MetS) and its individual components – central obesity, dyslipidemia, impaired fasting glucose, and hypertension – were associated with a risk of both radiographic osteoarthritis (ROA) and symptomatic OA (SxOA), all associations besides high blood pressure (particularly diastolic blood pressure) disappeared after they adjusted for body mass index (BMI) or body weight (Arthritis Rheumatol. 2017 Mar 3. doi: 10.1002/art.40087).
The research team analyzed 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline. Average age was 54.2 years; 55.1% were women. According to Adult Treatment Panel III criteria, 27% of the men and 23% of the women had MetS. Those who had MetS were older, had a higher BMI, and were less likely to drink alcohol or have a college education.
In 2002-2005, the cohort underwent follow-up for the presence of OA. The incidence of ROA in the cohort was 9.8% (78 of 800 knees) in men and 10.5% (105 of 1,003 knees) in women. ROA occurred when a knee without previous radiographic evidence of OA developed a Kellgren and Lawrence score of 2 or higher, and SxOA occurred when a knee developed ROA together with knee pain.
After adjusting for age, education, smoking status, alcohol consumption, and physical activity, the researchers found that MetS, abdominal obesity, and low high-density lipoprotein cholesterol were significantly associated with incident ROA among men. Among women, abdominal obesity and high blood pressure were associated with incident ROA, while MetS was not. However, after adjustment for body weight or BMI, none of the associations remained significant.
The incidence of SxOA was 6.3% (53 of 837 knees) in men and 7.2% (75 of 1,037 knees) in women. Incident SxOA was significantly associated with MetS in women and with the MetS components of abdominal obesity and high blood pressure in both men and women before adjustment for BMI or body weight. However, only an association between diastolic blood pressure and incident SxOA persisted in both sexes after adjustment for body weight, the study authors noted.
“High blood pressure is another MetS component associated with OA in previous studies before adjusting for BMI ... While we found [diastolic blood pressure] was related to incident SxOA even after adjustment for BMI, the relation of [systolic blood pressure] and incident SxOA was nearly significant also, suggesting that both might be related to SxOA,” the study authors wrote.
But a cross-sectional analysis of the relationship would be challenging to interpret, they said, since treatment for SxOA included NSAIDs, which are known to raise blood pressure.
The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
The OA incidence reported in the Framingham study is particularly noteworthy because it shows that preexisting MetS and its components are risk factors for subsequent symptomatic OA and not just radiographic OA, which seems to indicate the existence of common risk factors for both MetS and OA in a manner such that OA could be just a late-occurring component of MetS.
But it may be most appropriate to consider metabolic OA as a complication of MetS, similar to cardiovascular disease.
The fact that any component of MetS remained significantly associated with symptomatic OA after adjustment for BMI and body weight argued strongly for a metabolic driver of OA pathophysiology when considering the likely confounding of body weight between mechanical and metabolic processes.
Nevertheless, carefully designed studies are needed to determine the relative impact of increased body mass in MetS on joint loading versus metabolic derangements, including systemic inflammation, to rule in or out the effects of altered metabolism on incident OA risk independent of biomechanics.
This knowledge would help a great deal toward understanding metabolic OA and other phenotypes as well as for the development of rational treatment approaches.
Thomas Appleton, MD, PhD, of Western University in London, Ont., and his colleagues made these comments in an editorial (Arthritis Rheumatol. 2017 Mar 7. doi: 10.1002/art.40089). They declared having no conflicts of interest to relevant to their editorial.
The OA incidence reported in the Framingham study is particularly noteworthy because it shows that preexisting MetS and its components are risk factors for subsequent symptomatic OA and not just radiographic OA, which seems to indicate the existence of common risk factors for both MetS and OA in a manner such that OA could be just a late-occurring component of MetS.
But it may be most appropriate to consider metabolic OA as a complication of MetS, similar to cardiovascular disease.
The fact that any component of MetS remained significantly associated with symptomatic OA after adjustment for BMI and body weight argued strongly for a metabolic driver of OA pathophysiology when considering the likely confounding of body weight between mechanical and metabolic processes.
Nevertheless, carefully designed studies are needed to determine the relative impact of increased body mass in MetS on joint loading versus metabolic derangements, including systemic inflammation, to rule in or out the effects of altered metabolism on incident OA risk independent of biomechanics.
This knowledge would help a great deal toward understanding metabolic OA and other phenotypes as well as for the development of rational treatment approaches.
Thomas Appleton, MD, PhD, of Western University in London, Ont., and his colleagues made these comments in an editorial (Arthritis Rheumatol. 2017 Mar 7. doi: 10.1002/art.40089). They declared having no conflicts of interest to relevant to their editorial.
The OA incidence reported in the Framingham study is particularly noteworthy because it shows that preexisting MetS and its components are risk factors for subsequent symptomatic OA and not just radiographic OA, which seems to indicate the existence of common risk factors for both MetS and OA in a manner such that OA could be just a late-occurring component of MetS.
But it may be most appropriate to consider metabolic OA as a complication of MetS, similar to cardiovascular disease.
The fact that any component of MetS remained significantly associated with symptomatic OA after adjustment for BMI and body weight argued strongly for a metabolic driver of OA pathophysiology when considering the likely confounding of body weight between mechanical and metabolic processes.
Nevertheless, carefully designed studies are needed to determine the relative impact of increased body mass in MetS on joint loading versus metabolic derangements, including systemic inflammation, to rule in or out the effects of altered metabolism on incident OA risk independent of biomechanics.
This knowledge would help a great deal toward understanding metabolic OA and other phenotypes as well as for the development of rational treatment approaches.
Thomas Appleton, MD, PhD, of Western University in London, Ont., and his colleagues made these comments in an editorial (Arthritis Rheumatol. 2017 Mar 7. doi: 10.1002/art.40089). They declared having no conflicts of interest to relevant to their editorial.
The metabolic syndrome’s association with the development of osteoarthritis appears to occur primarily through the influence of factors related to body weight or body mass index, according to an analysis of data from the longitudinal Framingham osteoarthritis study.
Jingbo Niu, DSc, of the Clinical Epidemiology Research and Training Unit at Boston University, and her colleagues found that while the presence of the metabolic syndrome (MetS) and its individual components – central obesity, dyslipidemia, impaired fasting glucose, and hypertension – were associated with a risk of both radiographic osteoarthritis (ROA) and symptomatic OA (SxOA), all associations besides high blood pressure (particularly diastolic blood pressure) disappeared after they adjusted for body mass index (BMI) or body weight (Arthritis Rheumatol. 2017 Mar 3. doi: 10.1002/art.40087).
The research team analyzed 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline. Average age was 54.2 years; 55.1% were women. According to Adult Treatment Panel III criteria, 27% of the men and 23% of the women had MetS. Those who had MetS were older, had a higher BMI, and were less likely to drink alcohol or have a college education.
In 2002-2005, the cohort underwent follow-up for the presence of OA. The incidence of ROA in the cohort was 9.8% (78 of 800 knees) in men and 10.5% (105 of 1,003 knees) in women. ROA occurred when a knee without previous radiographic evidence of OA developed a Kellgren and Lawrence score of 2 or higher, and SxOA occurred when a knee developed ROA together with knee pain.
After adjusting for age, education, smoking status, alcohol consumption, and physical activity, the researchers found that MetS, abdominal obesity, and low high-density lipoprotein cholesterol were significantly associated with incident ROA among men. Among women, abdominal obesity and high blood pressure were associated with incident ROA, while MetS was not. However, after adjustment for body weight or BMI, none of the associations remained significant.
The incidence of SxOA was 6.3% (53 of 837 knees) in men and 7.2% (75 of 1,037 knees) in women. Incident SxOA was significantly associated with MetS in women and with the MetS components of abdominal obesity and high blood pressure in both men and women before adjustment for BMI or body weight. However, only an association between diastolic blood pressure and incident SxOA persisted in both sexes after adjustment for body weight, the study authors noted.
“High blood pressure is another MetS component associated with OA in previous studies before adjusting for BMI ... While we found [diastolic blood pressure] was related to incident SxOA even after adjustment for BMI, the relation of [systolic blood pressure] and incident SxOA was nearly significant also, suggesting that both might be related to SxOA,” the study authors wrote.
But a cross-sectional analysis of the relationship would be challenging to interpret, they said, since treatment for SxOA included NSAIDs, which are known to raise blood pressure.
The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
The metabolic syndrome’s association with the development of osteoarthritis appears to occur primarily through the influence of factors related to body weight or body mass index, according to an analysis of data from the longitudinal Framingham osteoarthritis study.
Jingbo Niu, DSc, of the Clinical Epidemiology Research and Training Unit at Boston University, and her colleagues found that while the presence of the metabolic syndrome (MetS) and its individual components – central obesity, dyslipidemia, impaired fasting glucose, and hypertension – were associated with a risk of both radiographic osteoarthritis (ROA) and symptomatic OA (SxOA), all associations besides high blood pressure (particularly diastolic blood pressure) disappeared after they adjusted for body mass index (BMI) or body weight (Arthritis Rheumatol. 2017 Mar 3. doi: 10.1002/art.40087).
The research team analyzed 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline. Average age was 54.2 years; 55.1% were women. According to Adult Treatment Panel III criteria, 27% of the men and 23% of the women had MetS. Those who had MetS were older, had a higher BMI, and were less likely to drink alcohol or have a college education.
In 2002-2005, the cohort underwent follow-up for the presence of OA. The incidence of ROA in the cohort was 9.8% (78 of 800 knees) in men and 10.5% (105 of 1,003 knees) in women. ROA occurred when a knee without previous radiographic evidence of OA developed a Kellgren and Lawrence score of 2 or higher, and SxOA occurred when a knee developed ROA together with knee pain.
After adjusting for age, education, smoking status, alcohol consumption, and physical activity, the researchers found that MetS, abdominal obesity, and low high-density lipoprotein cholesterol were significantly associated with incident ROA among men. Among women, abdominal obesity and high blood pressure were associated with incident ROA, while MetS was not. However, after adjustment for body weight or BMI, none of the associations remained significant.
The incidence of SxOA was 6.3% (53 of 837 knees) in men and 7.2% (75 of 1,037 knees) in women. Incident SxOA was significantly associated with MetS in women and with the MetS components of abdominal obesity and high blood pressure in both men and women before adjustment for BMI or body weight. However, only an association between diastolic blood pressure and incident SxOA persisted in both sexes after adjustment for body weight, the study authors noted.
“High blood pressure is another MetS component associated with OA in previous studies before adjusting for BMI ... While we found [diastolic blood pressure] was related to incident SxOA even after adjustment for BMI, the relation of [systolic blood pressure] and incident SxOA was nearly significant also, suggesting that both might be related to SxOA,” the study authors wrote.
But a cross-sectional analysis of the relationship would be challenging to interpret, they said, since treatment for SxOA included NSAIDs, which are known to raise blood pressure.
The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: There is no strong association between the metabolic syndrome (MetS) and OA after adjustment for BMI or body weight.
Major finding: Components of MetS were initially associated with incident radiographic and symptomatic OA, but after adjustment for BMI or body weight, most of the associations were weak and insignificant. However, an association between the MetS and high blood pressure persisted in both sexes.
Data source: An analysis of 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline and were followed for 10 years.
Disclosures: The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
The power of words in aesthetic procedures and healing patients
The words we choose to use prior to procedures can positively or negatively impact a patient’s experience during a procedure and their decision to have the procedure performed. A practical example would include using the word discomfort instead of pain to describe pain that may be associated with a procedure. The root word of discomfort is comfort, which the mind focuses on and creates less of an anxious state than pain.
Obviously, the need to provide proper and realistic expectations, as well as risks and benefits, is of utmost importance when obtaining informed consent. The words used can put a patient’s mind at ease or cause further anxiety about ideas of needles, scalpels, pain, risk of infection, and bleeding that are part of our everyday procedures.
Judith Thomas, DDS, a dentist in Virginia who is trained in clinical hypnosis, once described the power of the word but. People will often put more emphasis in their minds on what is said after the word but than on what is said before. For example, in a romantic relationship context, saying “I love you, but you drive me crazy” has a different impact than “You drive me crazy, but I love you.” The focus tends to stay on the “I love you” portion more when it is said last, after the “but.”
The same phenomenon can happen when we discuss procedures with our patients. When a medical assistant performs phlebotomy or when we as doctors are about to perform an injection, instead of saying this is going to hurt, another way to phrase it would be “In a moment you may feel something, but it doesn’t have to bother you” or “You may experience some discomfort, but it will resolve quickly.” Something I’ve said for years to patients before surgery is “You may feel a little stinging as the anesthetic goes in, after that you may feel me touching you, but nothing uncomfortable.” I guess I had been intuitively using this technique for years, without knowing the impact of the word “but.” Perhaps now that I am more mindful of it, I will be even more mindful of how I phrase these terms. We, in addition to our nurses and medical assistants, can use these techniques to enhance patient comfort and the patient’s experience.
According to the American Society of Clinical Hypnosis, physicians and dentists used the power of words through hypnosis as anesthesia before the first chemical general anesthetic agent, ether, was used for surgery in the 1840s, followed by chloroform. Prior to this time, British and Scottish physicians John Elliotson, James Esdaile, and James Braid performed over 3,000 procedures and surgeries with clinical hypnosis alone. Some may argue that the ancient Egyptians also used hypnosis for their well-described surgeries, as no other anesthetic has been documented. Moreover, there is evidence of “sleep temples” that the ancient Egyptians used for healing.1
This article is not to suggest that our words should replace anesthesia. Many advances in anesthesia and pain control have been made since the time of chloroform. However, being mindful of our words can aid and assist in our surgical and aesthetic procedures where less anesthesia is used: Patients feel more comfortable, they heal faster, and overall, they have a more positive outcome and pleasant physician-patient experience.2
For patients, the skill of the doctor and the outcome of the procedure are of the utmost importance, but, especially in aesthetic dermatology, where some of our procedures are repeated or performed periodically, the positive impact of the entire experience will entrust them with your care long term.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com. They had no relevant disclosures.
References
1. Mutter, C.B. (1998). History of Hypnosis. (pp. 10-12) “Hypnotic Induction and Suggestion.” Chicago: American Society of Clinical Hypnosis.
2. Burns. 2010 Aug;36(5):639-46.
The words we choose to use prior to procedures can positively or negatively impact a patient’s experience during a procedure and their decision to have the procedure performed. A practical example would include using the word discomfort instead of pain to describe pain that may be associated with a procedure. The root word of discomfort is comfort, which the mind focuses on and creates less of an anxious state than pain.
Obviously, the need to provide proper and realistic expectations, as well as risks and benefits, is of utmost importance when obtaining informed consent. The words used can put a patient’s mind at ease or cause further anxiety about ideas of needles, scalpels, pain, risk of infection, and bleeding that are part of our everyday procedures.
Judith Thomas, DDS, a dentist in Virginia who is trained in clinical hypnosis, once described the power of the word but. People will often put more emphasis in their minds on what is said after the word but than on what is said before. For example, in a romantic relationship context, saying “I love you, but you drive me crazy” has a different impact than “You drive me crazy, but I love you.” The focus tends to stay on the “I love you” portion more when it is said last, after the “but.”
The same phenomenon can happen when we discuss procedures with our patients. When a medical assistant performs phlebotomy or when we as doctors are about to perform an injection, instead of saying this is going to hurt, another way to phrase it would be “In a moment you may feel something, but it doesn’t have to bother you” or “You may experience some discomfort, but it will resolve quickly.” Something I’ve said for years to patients before surgery is “You may feel a little stinging as the anesthetic goes in, after that you may feel me touching you, but nothing uncomfortable.” I guess I had been intuitively using this technique for years, without knowing the impact of the word “but.” Perhaps now that I am more mindful of it, I will be even more mindful of how I phrase these terms. We, in addition to our nurses and medical assistants, can use these techniques to enhance patient comfort and the patient’s experience.
According to the American Society of Clinical Hypnosis, physicians and dentists used the power of words through hypnosis as anesthesia before the first chemical general anesthetic agent, ether, was used for surgery in the 1840s, followed by chloroform. Prior to this time, British and Scottish physicians John Elliotson, James Esdaile, and James Braid performed over 3,000 procedures and surgeries with clinical hypnosis alone. Some may argue that the ancient Egyptians also used hypnosis for their well-described surgeries, as no other anesthetic has been documented. Moreover, there is evidence of “sleep temples” that the ancient Egyptians used for healing.1
This article is not to suggest that our words should replace anesthesia. Many advances in anesthesia and pain control have been made since the time of chloroform. However, being mindful of our words can aid and assist in our surgical and aesthetic procedures where less anesthesia is used: Patients feel more comfortable, they heal faster, and overall, they have a more positive outcome and pleasant physician-patient experience.2
For patients, the skill of the doctor and the outcome of the procedure are of the utmost importance, but, especially in aesthetic dermatology, where some of our procedures are repeated or performed periodically, the positive impact of the entire experience will entrust them with your care long term.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com. They had no relevant disclosures.
References
1. Mutter, C.B. (1998). History of Hypnosis. (pp. 10-12) “Hypnotic Induction and Suggestion.” Chicago: American Society of Clinical Hypnosis.
2. Burns. 2010 Aug;36(5):639-46.
The words we choose to use prior to procedures can positively or negatively impact a patient’s experience during a procedure and their decision to have the procedure performed. A practical example would include using the word discomfort instead of pain to describe pain that may be associated with a procedure. The root word of discomfort is comfort, which the mind focuses on and creates less of an anxious state than pain.
Obviously, the need to provide proper and realistic expectations, as well as risks and benefits, is of utmost importance when obtaining informed consent. The words used can put a patient’s mind at ease or cause further anxiety about ideas of needles, scalpels, pain, risk of infection, and bleeding that are part of our everyday procedures.
Judith Thomas, DDS, a dentist in Virginia who is trained in clinical hypnosis, once described the power of the word but. People will often put more emphasis in their minds on what is said after the word but than on what is said before. For example, in a romantic relationship context, saying “I love you, but you drive me crazy” has a different impact than “You drive me crazy, but I love you.” The focus tends to stay on the “I love you” portion more when it is said last, after the “but.”
The same phenomenon can happen when we discuss procedures with our patients. When a medical assistant performs phlebotomy or when we as doctors are about to perform an injection, instead of saying this is going to hurt, another way to phrase it would be “In a moment you may feel something, but it doesn’t have to bother you” or “You may experience some discomfort, but it will resolve quickly.” Something I’ve said for years to patients before surgery is “You may feel a little stinging as the anesthetic goes in, after that you may feel me touching you, but nothing uncomfortable.” I guess I had been intuitively using this technique for years, without knowing the impact of the word “but.” Perhaps now that I am more mindful of it, I will be even more mindful of how I phrase these terms. We, in addition to our nurses and medical assistants, can use these techniques to enhance patient comfort and the patient’s experience.
According to the American Society of Clinical Hypnosis, physicians and dentists used the power of words through hypnosis as anesthesia before the first chemical general anesthetic agent, ether, was used for surgery in the 1840s, followed by chloroform. Prior to this time, British and Scottish physicians John Elliotson, James Esdaile, and James Braid performed over 3,000 procedures and surgeries with clinical hypnosis alone. Some may argue that the ancient Egyptians also used hypnosis for their well-described surgeries, as no other anesthetic has been documented. Moreover, there is evidence of “sleep temples” that the ancient Egyptians used for healing.1
This article is not to suggest that our words should replace anesthesia. Many advances in anesthesia and pain control have been made since the time of chloroform. However, being mindful of our words can aid and assist in our surgical and aesthetic procedures where less anesthesia is used: Patients feel more comfortable, they heal faster, and overall, they have a more positive outcome and pleasant physician-patient experience.2
For patients, the skill of the doctor and the outcome of the procedure are of the utmost importance, but, especially in aesthetic dermatology, where some of our procedures are repeated or performed periodically, the positive impact of the entire experience will entrust them with your care long term.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com. They had no relevant disclosures.
References
1. Mutter, C.B. (1998). History of Hypnosis. (pp. 10-12) “Hypnotic Induction and Suggestion.” Chicago: American Society of Clinical Hypnosis.
2. Burns. 2010 Aug;36(5):639-46.
Norepinephrine shortage linked to mortality in patients with septic shock
A national shortage of norepinephrine in the United States was associated with higher rates of mortality among patients hospitalized with septic shock, investigators reported.
Rates of in-hospital mortality in 2011 were 40% during quarters when hospitals were facing shortages and 36% when they were not, Emily Vail, MD, and her associates said at the International Symposium on Intensive Care and Emergency Medicine. The report was published simultaneously in JAMA.
The link between norepinephrine shortage and death from septic shock persisted even after the researchers accounted for numerous clinical and demographic factors (adjusted odds ratio, 1.2; 95% confidence interval, 1.01 to 1.30; P = .03), wrote Dr. Vail of Columbia University, New York (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2841).
Drug shortages are common in the United States, but few studies have explored their effects on patient outcomes. Investigators compared mortality rates among affected patients during 3-month intervals when hospitals were and were not using at least 20% less norepinephrine than baseline. The researchers used Premier Healthcare Database, which includes both standard claims and detailed, dated logs of all services billed to patients or insurance, with minimal missing data.
A total of 77% patients admitted with septic shock received norepinephrine before the shortage. During the lowest point of the shortage, 56% of patients received it, the researchers reported. Clinicians most often used phenylephrine instead, prescribing it to up to 54% of patients during the worst time of the shortage. The absolute increase in mortality during the quarters of shortage was 3.7% (95% CI, 1.5%-6.0%).
Several factors might explain the link between norepinephrine shortage and mortality, said the investigators. The vasopressors chosen to replace norepinephrine might result directly in worse outcomes, but a decrease in norepinephrine use also might be a proxy for relevant variables such as delayed use of vasopressors, lack of knowledge of how to optimally dose vasopressors besides norepinephrine, or the absence of a pharmacist dedicated to helping optimize the use of limited supplies.
The study did not uncover a dose-response association between greater decreases in norepinephrine use and increased mortality, the researchers noted. “This may be due to a threshold effect of vasopressor shortage on mortality, or lack of power due to relatively few hospital quarters at the extreme levels of vasopressor shortage,” they wrote.
Because the deaths captured included only those that occurred in-hospital, “the results may have underestimated mortality, particularly for hospitals that tend transfer patients early to other skilled care facilities,” the researchers noted.
The cohort of patients was limited to those who received vasopressors for 2 or more days and excluded patients who died on the first day of vasopressor treatment, the researchers said.
The Herbert and Florence Irving Scholars Program at Columbia University provided funding. One coinvestigator disclosed grant funding from the National Institutes of Health and personal fees from UpToDate. The other investigators reported having no conflicts of interest.
A national shortage of norepinephrine in the United States was associated with higher rates of mortality among patients hospitalized with septic shock, investigators reported.
Rates of in-hospital mortality in 2011 were 40% during quarters when hospitals were facing shortages and 36% when they were not, Emily Vail, MD, and her associates said at the International Symposium on Intensive Care and Emergency Medicine. The report was published simultaneously in JAMA.
The link between norepinephrine shortage and death from septic shock persisted even after the researchers accounted for numerous clinical and demographic factors (adjusted odds ratio, 1.2; 95% confidence interval, 1.01 to 1.30; P = .03), wrote Dr. Vail of Columbia University, New York (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2841).
Drug shortages are common in the United States, but few studies have explored their effects on patient outcomes. Investigators compared mortality rates among affected patients during 3-month intervals when hospitals were and were not using at least 20% less norepinephrine than baseline. The researchers used Premier Healthcare Database, which includes both standard claims and detailed, dated logs of all services billed to patients or insurance, with minimal missing data.
A total of 77% patients admitted with septic shock received norepinephrine before the shortage. During the lowest point of the shortage, 56% of patients received it, the researchers reported. Clinicians most often used phenylephrine instead, prescribing it to up to 54% of patients during the worst time of the shortage. The absolute increase in mortality during the quarters of shortage was 3.7% (95% CI, 1.5%-6.0%).
Several factors might explain the link between norepinephrine shortage and mortality, said the investigators. The vasopressors chosen to replace norepinephrine might result directly in worse outcomes, but a decrease in norepinephrine use also might be a proxy for relevant variables such as delayed use of vasopressors, lack of knowledge of how to optimally dose vasopressors besides norepinephrine, or the absence of a pharmacist dedicated to helping optimize the use of limited supplies.
The study did not uncover a dose-response association between greater decreases in norepinephrine use and increased mortality, the researchers noted. “This may be due to a threshold effect of vasopressor shortage on mortality, or lack of power due to relatively few hospital quarters at the extreme levels of vasopressor shortage,” they wrote.
Because the deaths captured included only those that occurred in-hospital, “the results may have underestimated mortality, particularly for hospitals that tend transfer patients early to other skilled care facilities,” the researchers noted.
The cohort of patients was limited to those who received vasopressors for 2 or more days and excluded patients who died on the first day of vasopressor treatment, the researchers said.
The Herbert and Florence Irving Scholars Program at Columbia University provided funding. One coinvestigator disclosed grant funding from the National Institutes of Health and personal fees from UpToDate. The other investigators reported having no conflicts of interest.
A national shortage of norepinephrine in the United States was associated with higher rates of mortality among patients hospitalized with septic shock, investigators reported.
Rates of in-hospital mortality in 2011 were 40% during quarters when hospitals were facing shortages and 36% when they were not, Emily Vail, MD, and her associates said at the International Symposium on Intensive Care and Emergency Medicine. The report was published simultaneously in JAMA.
The link between norepinephrine shortage and death from septic shock persisted even after the researchers accounted for numerous clinical and demographic factors (adjusted odds ratio, 1.2; 95% confidence interval, 1.01 to 1.30; P = .03), wrote Dr. Vail of Columbia University, New York (JAMA. 2017 Mar 21. doi: 10.1001/jama.2017.2841).
Drug shortages are common in the United States, but few studies have explored their effects on patient outcomes. Investigators compared mortality rates among affected patients during 3-month intervals when hospitals were and were not using at least 20% less norepinephrine than baseline. The researchers used Premier Healthcare Database, which includes both standard claims and detailed, dated logs of all services billed to patients or insurance, with minimal missing data.
A total of 77% patients admitted with septic shock received norepinephrine before the shortage. During the lowest point of the shortage, 56% of patients received it, the researchers reported. Clinicians most often used phenylephrine instead, prescribing it to up to 54% of patients during the worst time of the shortage. The absolute increase in mortality during the quarters of shortage was 3.7% (95% CI, 1.5%-6.0%).
Several factors might explain the link between norepinephrine shortage and mortality, said the investigators. The vasopressors chosen to replace norepinephrine might result directly in worse outcomes, but a decrease in norepinephrine use also might be a proxy for relevant variables such as delayed use of vasopressors, lack of knowledge of how to optimally dose vasopressors besides norepinephrine, or the absence of a pharmacist dedicated to helping optimize the use of limited supplies.
The study did not uncover a dose-response association between greater decreases in norepinephrine use and increased mortality, the researchers noted. “This may be due to a threshold effect of vasopressor shortage on mortality, or lack of power due to relatively few hospital quarters at the extreme levels of vasopressor shortage,” they wrote.
Because the deaths captured included only those that occurred in-hospital, “the results may have underestimated mortality, particularly for hospitals that tend transfer patients early to other skilled care facilities,” the researchers noted.
The cohort of patients was limited to those who received vasopressors for 2 or more days and excluded patients who died on the first day of vasopressor treatment, the researchers said.
The Herbert and Florence Irving Scholars Program at Columbia University provided funding. One coinvestigator disclosed grant funding from the National Institutes of Health and personal fees from UpToDate. The other investigators reported having no conflicts of interest.
FROM ISICEM
Key clinical point. The 2011 norepinephrine shortage was associated with mortality among patients hospitalized with septic shock.
Major finding: Rates of in-hospital mortality were 36% during quarters of normal norepinephrine use and 40% during quarters of decreased use (adjusted odds ratio, 1.2; P = .03).
Data source: A retrospective cohort study of 27,835 patients at 26 hospitals in the United States that were affected by the shortage.
Disclosures: The Herbert and Florence Irving Scholars Program at Columbia University provided funding. One coinvestigator disclosed grant funding from the National Institutes of Health and personal fees from UpToDate. The other investigators reported having no conflicts of interest.
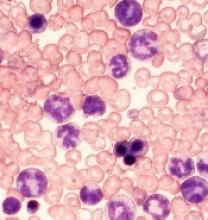
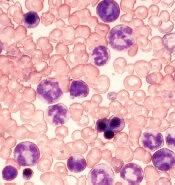
Pretreatment Imaging May Help Prevent Hodgkin Lymphoma Recurrence
Advances in radiation treatment have led to better targeting, minimizing the dose to healthy tissue. For patients with Hodgkin lymphoma (HL), pretreatment scanning with positron emission tomography and computed tomography (PET/CT) has become the gold standard, say researchers from University of Florida, in determining the extent of HL. Because HL may recur at the site of the original cancer, the scans are important to accurately capture the scope of the disease. Moreover, the researchers say pretreatment PET/CT may reduce disease progression.
Related: Study Points to Risk Factors for Lymphoma
In their study of 37 patients with stage I or II HL, 31 had PET/CT before chemotherapy. Two of the remaining 6 had PET/CT done within 5 days after chemotherapy was started. Median follow-up was 46 months.
The 4-year rate of relapse-free survival was 92%. Patients who did not receive pretreatment PET/CT were more likely to have a relapse (67%). Of 4 recurrences, 3 were within 12 months of follow-up; 1 developed 5 years after treatment.
Among the 6 patients who did not have a baseline PET/CT scan, all 3 recurrences were in lymph node regions outside of, but adjacent to, the radiation field. None of the 6 experienced an in-field treatment failure.
Related: Development and Implementation of a Veterans’ Cancer Survivorship Program
Long-term survivors of HL are vulnerable to late adverse effects, the researchers note, and that fact is “the impetus behind efforts to reduce radiation exposure to organs at risk.” They cite studies that have found that PET/CT scans, compared with using only pretreatment contrast-enhanced CT scans, can alter the staging in 10% to 30% of patients with HL. Their study, the researchers add, helps support the National Comprehensive Cancer Network guidelines that advise prechemotherapy PET/CT imaging in staging all HL patients. Not doing complete staging, the researchers say, puts patients at “unnecessary, and in some instances preventable, risk for recurrence.”
Source:
Figura N, Flampouri S, Mendenhall NP, et al. Adv Radiat Oncol. 2017;1-16.
Advances in radiation treatment have led to better targeting, minimizing the dose to healthy tissue. For patients with Hodgkin lymphoma (HL), pretreatment scanning with positron emission tomography and computed tomography (PET/CT) has become the gold standard, say researchers from University of Florida, in determining the extent of HL. Because HL may recur at the site of the original cancer, the scans are important to accurately capture the scope of the disease. Moreover, the researchers say pretreatment PET/CT may reduce disease progression.
Related: Study Points to Risk Factors for Lymphoma
In their study of 37 patients with stage I or II HL, 31 had PET/CT before chemotherapy. Two of the remaining 6 had PET/CT done within 5 days after chemotherapy was started. Median follow-up was 46 months.
The 4-year rate of relapse-free survival was 92%. Patients who did not receive pretreatment PET/CT were more likely to have a relapse (67%). Of 4 recurrences, 3 were within 12 months of follow-up; 1 developed 5 years after treatment.
Among the 6 patients who did not have a baseline PET/CT scan, all 3 recurrences were in lymph node regions outside of, but adjacent to, the radiation field. None of the 6 experienced an in-field treatment failure.
Related: Development and Implementation of a Veterans’ Cancer Survivorship Program
Long-term survivors of HL are vulnerable to late adverse effects, the researchers note, and that fact is “the impetus behind efforts to reduce radiation exposure to organs at risk.” They cite studies that have found that PET/CT scans, compared with using only pretreatment contrast-enhanced CT scans, can alter the staging in 10% to 30% of patients with HL. Their study, the researchers add, helps support the National Comprehensive Cancer Network guidelines that advise prechemotherapy PET/CT imaging in staging all HL patients. Not doing complete staging, the researchers say, puts patients at “unnecessary, and in some instances preventable, risk for recurrence.”
Source:
Figura N, Flampouri S, Mendenhall NP, et al. Adv Radiat Oncol. 2017;1-16.
Advances in radiation treatment have led to better targeting, minimizing the dose to healthy tissue. For patients with Hodgkin lymphoma (HL), pretreatment scanning with positron emission tomography and computed tomography (PET/CT) has become the gold standard, say researchers from University of Florida, in determining the extent of HL. Because HL may recur at the site of the original cancer, the scans are important to accurately capture the scope of the disease. Moreover, the researchers say pretreatment PET/CT may reduce disease progression.
Related: Study Points to Risk Factors for Lymphoma
In their study of 37 patients with stage I or II HL, 31 had PET/CT before chemotherapy. Two of the remaining 6 had PET/CT done within 5 days after chemotherapy was started. Median follow-up was 46 months.
The 4-year rate of relapse-free survival was 92%. Patients who did not receive pretreatment PET/CT were more likely to have a relapse (67%). Of 4 recurrences, 3 were within 12 months of follow-up; 1 developed 5 years after treatment.
Among the 6 patients who did not have a baseline PET/CT scan, all 3 recurrences were in lymph node regions outside of, but adjacent to, the radiation field. None of the 6 experienced an in-field treatment failure.
Related: Development and Implementation of a Veterans’ Cancer Survivorship Program
Long-term survivors of HL are vulnerable to late adverse effects, the researchers note, and that fact is “the impetus behind efforts to reduce radiation exposure to organs at risk.” They cite studies that have found that PET/CT scans, compared with using only pretreatment contrast-enhanced CT scans, can alter the staging in 10% to 30% of patients with HL. Their study, the researchers add, helps support the National Comprehensive Cancer Network guidelines that advise prechemotherapy PET/CT imaging in staging all HL patients. Not doing complete staging, the researchers say, puts patients at “unnecessary, and in some instances preventable, risk for recurrence.”
Source:
Figura N, Flampouri S, Mendenhall NP, et al. Adv Radiat Oncol. 2017;1-16.
Study supports use of rivaroxaban to prevent VTE recurrence
WASHINGTON, DC—Results of the EINSTEIN CHOICE study suggest rivaroxaban is more effective than, and just as safe as, aspirin for long-term anticoagulation in patients with venous thromboembolism (VTE).
In this phase 3 study, patients who had completed 6 to 12 months of anticoagulant therapy were randomized to receive rivaroxaban or aspirin.
Those who received rivaroxaban had a significantly lower risk of recurrent VTE, and the rates of major bleeding were similar between the treatment arms.
“How best to extend anticoagulant use beyond the initial treatment window has been a constant source of debate, with physicians carefully balancing patients’ risk of another VTE with the risk of anticoagulant-related bleeding,” said study investigator Philip S. Wells, MD, of The Ottawa Hospital in Ontario, Canada.
“With EINSTEIN CHOICE, for the first time, we have clinical evidence confirming rivaroxaban is superior to aspirin in reducing recurrent VTE, with no significant impact on safety. These important results have the potential to trigger a paradigm shift in how physicians manage their patients and protect them from VTE recurrence over the long term.”
These results were presented at the American College of Cardiology’s 66th Annual Scientific Session and published in NEJM. The research was funded by Bayer Pharmaceuticals.
The study enrolled 3365 patients with confirmed deep vein thrombosis or pulmonary embolism who were initially treated with anticoagulant therapy for 6 to 12 months.
Patients who required extended anticoagulation at therapeutic doses were not included in this trial, as the objective was to investigate those patients for whom the treating physician was uncertain about the need for continuing anticoagulant therapy.
Patients were randomized in a 1:1:1 ratio to receive a prophylactic dose of rivaroxaban (10 mg once daily), a treatment dose of rivaroxaban (20 mg once daily), or aspirin (100 mg once daily) for up to 12 months. Sixty percent of patients completed the full 12 months of treatment.
Efficacy
Both rivaroxaban doses were superior to aspirin in preventing fatal or non-fatal recurrent VTE, the study’s primary efficacy endpoint.
The rate of recurrent VTE was 1.2% in the 10 mg rivaroxaban arm (hazard ratio [HR]=0.26; 95% CI, 0.14 to 0.47; P<0.001), 1.5% in the 20 mg rivaroxaban arm (HR=0.34; 95% CI, 0.20 to 0.59; P<0.001), and 4.4% in the aspirin arm. Fatal VTE occurred in 0%, 0.2%, and 0.2%, respectively.
For the primary endpoint, the HR for the comparison between the 20 mg and 10 mg rivaroxaban arms was 1.34 (95% CI, 0.65 to 2.75, P=0.42). However, the researchers noted that the comparison of these 2 arms was not powered for significance.
The researchers also found that rivaroxaban reduced patients’ risk of experiencing one of the following events: recurrent VTE, heart attack, ischemic stroke, systemic embolism, or venous thrombosis in another location.
This endpoint occurred in 1.9% of patients in the 10 mg rivaroxaban group (HR=0.33; 95% CI, 0.20 to 0.54; P<0.001), 2.0% of patients in the 20 mg rivaroxaban group (HR=0.35; 95% CI, 0.22 to 0.57; P<0.001), and 5.6% of patients in the aspirin group.
Recurrent VTE or all-cause mortality occurred in 1.3% of patients in the 10 mg rivaroxaban group (HR=0.27; 95% CI, 0.15 to 0.47; P<0.001), 2.1% of patients in the 20 mg rivaroxaban group (HR=0.42; 95% CI, 0.26 to 0.68; P<0.001), and 4.9% of patients in the aspirin group.
Safety
The primary safety endpoint was major bleeding as defined by the International Society on Thrombosis and Haemostasis.
The rate of major bleeding was 0.4% for the 10 mg rivaroxaban group (HR=1.64; 95% CI, 0.39 to 6.84; P=0.50), 0.5% for the 20 mg rivaroxaban group (HR=2.01; 95% CI, 0.50 to 8.04; P=0.32), and 0.3% for the aspirin group.
Rates of clinically relevant non-major bleeding were 2.0%, 2.7%, and 1.8%, respectively (no significant difference).
“We know from previous studies that only about 40% of venous thromboembolism patients are actually on long-term blood thinners,” Dr Wells said.
“We hope that this study, which shows the blood thinner rivaroxaban is as safe as aspirin but much more effective at preventing future clots, will convince patients and their physicians to continue life-long medication that can prevent potentially dangerous blood clots.” ![]()
WASHINGTON, DC—Results of the EINSTEIN CHOICE study suggest rivaroxaban is more effective than, and just as safe as, aspirin for long-term anticoagulation in patients with venous thromboembolism (VTE).
In this phase 3 study, patients who had completed 6 to 12 months of anticoagulant therapy were randomized to receive rivaroxaban or aspirin.
Those who received rivaroxaban had a significantly lower risk of recurrent VTE, and the rates of major bleeding were similar between the treatment arms.
“How best to extend anticoagulant use beyond the initial treatment window has been a constant source of debate, with physicians carefully balancing patients’ risk of another VTE with the risk of anticoagulant-related bleeding,” said study investigator Philip S. Wells, MD, of The Ottawa Hospital in Ontario, Canada.
“With EINSTEIN CHOICE, for the first time, we have clinical evidence confirming rivaroxaban is superior to aspirin in reducing recurrent VTE, with no significant impact on safety. These important results have the potential to trigger a paradigm shift in how physicians manage their patients and protect them from VTE recurrence over the long term.”
These results were presented at the American College of Cardiology’s 66th Annual Scientific Session and published in NEJM. The research was funded by Bayer Pharmaceuticals.
The study enrolled 3365 patients with confirmed deep vein thrombosis or pulmonary embolism who were initially treated with anticoagulant therapy for 6 to 12 months.
Patients who required extended anticoagulation at therapeutic doses were not included in this trial, as the objective was to investigate those patients for whom the treating physician was uncertain about the need for continuing anticoagulant therapy.
Patients were randomized in a 1:1:1 ratio to receive a prophylactic dose of rivaroxaban (10 mg once daily), a treatment dose of rivaroxaban (20 mg once daily), or aspirin (100 mg once daily) for up to 12 months. Sixty percent of patients completed the full 12 months of treatment.
Efficacy
Both rivaroxaban doses were superior to aspirin in preventing fatal or non-fatal recurrent VTE, the study’s primary efficacy endpoint.
The rate of recurrent VTE was 1.2% in the 10 mg rivaroxaban arm (hazard ratio [HR]=0.26; 95% CI, 0.14 to 0.47; P<0.001), 1.5% in the 20 mg rivaroxaban arm (HR=0.34; 95% CI, 0.20 to 0.59; P<0.001), and 4.4% in the aspirin arm. Fatal VTE occurred in 0%, 0.2%, and 0.2%, respectively.
For the primary endpoint, the HR for the comparison between the 20 mg and 10 mg rivaroxaban arms was 1.34 (95% CI, 0.65 to 2.75, P=0.42). However, the researchers noted that the comparison of these 2 arms was not powered for significance.
The researchers also found that rivaroxaban reduced patients’ risk of experiencing one of the following events: recurrent VTE, heart attack, ischemic stroke, systemic embolism, or venous thrombosis in another location.
This endpoint occurred in 1.9% of patients in the 10 mg rivaroxaban group (HR=0.33; 95% CI, 0.20 to 0.54; P<0.001), 2.0% of patients in the 20 mg rivaroxaban group (HR=0.35; 95% CI, 0.22 to 0.57; P<0.001), and 5.6% of patients in the aspirin group.
Recurrent VTE or all-cause mortality occurred in 1.3% of patients in the 10 mg rivaroxaban group (HR=0.27; 95% CI, 0.15 to 0.47; P<0.001), 2.1% of patients in the 20 mg rivaroxaban group (HR=0.42; 95% CI, 0.26 to 0.68; P<0.001), and 4.9% of patients in the aspirin group.
Safety
The primary safety endpoint was major bleeding as defined by the International Society on Thrombosis and Haemostasis.
The rate of major bleeding was 0.4% for the 10 mg rivaroxaban group (HR=1.64; 95% CI, 0.39 to 6.84; P=0.50), 0.5% for the 20 mg rivaroxaban group (HR=2.01; 95% CI, 0.50 to 8.04; P=0.32), and 0.3% for the aspirin group.
Rates of clinically relevant non-major bleeding were 2.0%, 2.7%, and 1.8%, respectively (no significant difference).
“We know from previous studies that only about 40% of venous thromboembolism patients are actually on long-term blood thinners,” Dr Wells said.
“We hope that this study, which shows the blood thinner rivaroxaban is as safe as aspirin but much more effective at preventing future clots, will convince patients and their physicians to continue life-long medication that can prevent potentially dangerous blood clots.” ![]()
WASHINGTON, DC—Results of the EINSTEIN CHOICE study suggest rivaroxaban is more effective than, and just as safe as, aspirin for long-term anticoagulation in patients with venous thromboembolism (VTE).
In this phase 3 study, patients who had completed 6 to 12 months of anticoagulant therapy were randomized to receive rivaroxaban or aspirin.
Those who received rivaroxaban had a significantly lower risk of recurrent VTE, and the rates of major bleeding were similar between the treatment arms.
“How best to extend anticoagulant use beyond the initial treatment window has been a constant source of debate, with physicians carefully balancing patients’ risk of another VTE with the risk of anticoagulant-related bleeding,” said study investigator Philip S. Wells, MD, of The Ottawa Hospital in Ontario, Canada.
“With EINSTEIN CHOICE, for the first time, we have clinical evidence confirming rivaroxaban is superior to aspirin in reducing recurrent VTE, with no significant impact on safety. These important results have the potential to trigger a paradigm shift in how physicians manage their patients and protect them from VTE recurrence over the long term.”
These results were presented at the American College of Cardiology’s 66th Annual Scientific Session and published in NEJM. The research was funded by Bayer Pharmaceuticals.
The study enrolled 3365 patients with confirmed deep vein thrombosis or pulmonary embolism who were initially treated with anticoagulant therapy for 6 to 12 months.
Patients who required extended anticoagulation at therapeutic doses were not included in this trial, as the objective was to investigate those patients for whom the treating physician was uncertain about the need for continuing anticoagulant therapy.
Patients were randomized in a 1:1:1 ratio to receive a prophylactic dose of rivaroxaban (10 mg once daily), a treatment dose of rivaroxaban (20 mg once daily), or aspirin (100 mg once daily) for up to 12 months. Sixty percent of patients completed the full 12 months of treatment.
Efficacy
Both rivaroxaban doses were superior to aspirin in preventing fatal or non-fatal recurrent VTE, the study’s primary efficacy endpoint.
The rate of recurrent VTE was 1.2% in the 10 mg rivaroxaban arm (hazard ratio [HR]=0.26; 95% CI, 0.14 to 0.47; P<0.001), 1.5% in the 20 mg rivaroxaban arm (HR=0.34; 95% CI, 0.20 to 0.59; P<0.001), and 4.4% in the aspirin arm. Fatal VTE occurred in 0%, 0.2%, and 0.2%, respectively.
For the primary endpoint, the HR for the comparison between the 20 mg and 10 mg rivaroxaban arms was 1.34 (95% CI, 0.65 to 2.75, P=0.42). However, the researchers noted that the comparison of these 2 arms was not powered for significance.
The researchers also found that rivaroxaban reduced patients’ risk of experiencing one of the following events: recurrent VTE, heart attack, ischemic stroke, systemic embolism, or venous thrombosis in another location.
This endpoint occurred in 1.9% of patients in the 10 mg rivaroxaban group (HR=0.33; 95% CI, 0.20 to 0.54; P<0.001), 2.0% of patients in the 20 mg rivaroxaban group (HR=0.35; 95% CI, 0.22 to 0.57; P<0.001), and 5.6% of patients in the aspirin group.
Recurrent VTE or all-cause mortality occurred in 1.3% of patients in the 10 mg rivaroxaban group (HR=0.27; 95% CI, 0.15 to 0.47; P<0.001), 2.1% of patients in the 20 mg rivaroxaban group (HR=0.42; 95% CI, 0.26 to 0.68; P<0.001), and 4.9% of patients in the aspirin group.
Safety
The primary safety endpoint was major bleeding as defined by the International Society on Thrombosis and Haemostasis.
The rate of major bleeding was 0.4% for the 10 mg rivaroxaban group (HR=1.64; 95% CI, 0.39 to 6.84; P=0.50), 0.5% for the 20 mg rivaroxaban group (HR=2.01; 95% CI, 0.50 to 8.04; P=0.32), and 0.3% for the aspirin group.
Rates of clinically relevant non-major bleeding were 2.0%, 2.7%, and 1.8%, respectively (no significant difference).
“We know from previous studies that only about 40% of venous thromboembolism patients are actually on long-term blood thinners,” Dr Wells said.
“We hope that this study, which shows the blood thinner rivaroxaban is as safe as aspirin but much more effective at preventing future clots, will convince patients and their physicians to continue life-long medication that can prevent potentially dangerous blood clots.” ![]()
Proteins may be therapeutic targets for TKI-resistant CML, ALL
Researchers say they have identified 2 signaling proteins that enable resistance to tyrosine kinase inhibitors (TKIs) and could be therapeutic targets for acute lymphoblastic leukemia (ALL) and chronic myeloid leukemia (CML).
The team found that by deleting these proteins—c-Fos and Dusp1—they could eradicate BCR-ABL-induced B-cell ALL in mice.
And treatment combining c-Fos and Dusp1 inhibitors with the TKI imatinib was able to cure mice with BCR-ABL-driven CML.
The researchers reported these findings in Nature Medicine.
“We think that, within the next 5 years, our data will change the way people think about cancer development and targeted therapy,” said study author Mohammad Azam, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This study identifies a potential Achilles’ heel of kinase-driven cancers, and what we propose is intended to be curative, not just treatment.”
The potential Achilles’ heel is a common point of passage in cells—a signaling node—that appears to be required to generate cancer cells. The node is formed by the signaling proteins c-Fos and Dusp1, according to the researchers.
The team identified c-Fos and Dusp1 by conducting global gene-expression analysis of mouse leukemia cells and human CML cells. Analysis of the human cells revealed extremely high levels of c-FOS and DUSP1 in BCR-ABL-positive, TKI-resistant cells.
Dr Azam and his colleagues found that signaling from tyrosine kinase and growth factor proteins that support cell expansion (such as IL-3 and IL-6) converge to elevate c-Fos and Dusp1 levels in leukemia cells.
Working together, these molecules maintain the survival of leukemia stem cells (LSCs), which translates to minimal residual disease (MRD) after treatment.
Dr Azam said Dusp1 and c-Fos support the survival of LSCs by increasing the toxic threshold needed to kill them. This means imatinib and other TKIs cannot eliminate the residual LSCs.
After describing the roles of c-Fos and Dusp1, Dr Azam and his colleagues put their ideas to the test in mouse models of CML.
The team tested several treatments in these mice, including:
- monotherapy with imatinib
- inhibitors of c-Fos and Dusp1
- treatment with imatinib and inhibitors of c-Fos and Dusp1.
As suspected, treatment with imatinib alone initially stopped CML progression, but mice ultimately relapsed.
Treatment with c-Fos and Dusp1 inhibitors significantly slowed CML progression and prolonged survival in a majority of mice, but this treatment wasn’t curative.
However, a month of treatment with c-Fos and Dusp1 inhibitors as well as imatinib cured about 90% of mice with CML, and there were no signs of MRD.
The researchers also found that simply deleting c-Fos and Dusp1 was sufficient to block the development of B-cell ALL in mice.
The team said they are following up this study by testing c-Fos and Dusp1 as treatment targets for different kinase-fueled cancers. ![]()
Researchers say they have identified 2 signaling proteins that enable resistance to tyrosine kinase inhibitors (TKIs) and could be therapeutic targets for acute lymphoblastic leukemia (ALL) and chronic myeloid leukemia (CML).
The team found that by deleting these proteins—c-Fos and Dusp1—they could eradicate BCR-ABL-induced B-cell ALL in mice.
And treatment combining c-Fos and Dusp1 inhibitors with the TKI imatinib was able to cure mice with BCR-ABL-driven CML.
The researchers reported these findings in Nature Medicine.
“We think that, within the next 5 years, our data will change the way people think about cancer development and targeted therapy,” said study author Mohammad Azam, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This study identifies a potential Achilles’ heel of kinase-driven cancers, and what we propose is intended to be curative, not just treatment.”
The potential Achilles’ heel is a common point of passage in cells—a signaling node—that appears to be required to generate cancer cells. The node is formed by the signaling proteins c-Fos and Dusp1, according to the researchers.
The team identified c-Fos and Dusp1 by conducting global gene-expression analysis of mouse leukemia cells and human CML cells. Analysis of the human cells revealed extremely high levels of c-FOS and DUSP1 in BCR-ABL-positive, TKI-resistant cells.
Dr Azam and his colleagues found that signaling from tyrosine kinase and growth factor proteins that support cell expansion (such as IL-3 and IL-6) converge to elevate c-Fos and Dusp1 levels in leukemia cells.
Working together, these molecules maintain the survival of leukemia stem cells (LSCs), which translates to minimal residual disease (MRD) after treatment.
Dr Azam said Dusp1 and c-Fos support the survival of LSCs by increasing the toxic threshold needed to kill them. This means imatinib and other TKIs cannot eliminate the residual LSCs.
After describing the roles of c-Fos and Dusp1, Dr Azam and his colleagues put their ideas to the test in mouse models of CML.
The team tested several treatments in these mice, including:
- monotherapy with imatinib
- inhibitors of c-Fos and Dusp1
- treatment with imatinib and inhibitors of c-Fos and Dusp1.
As suspected, treatment with imatinib alone initially stopped CML progression, but mice ultimately relapsed.
Treatment with c-Fos and Dusp1 inhibitors significantly slowed CML progression and prolonged survival in a majority of mice, but this treatment wasn’t curative.
However, a month of treatment with c-Fos and Dusp1 inhibitors as well as imatinib cured about 90% of mice with CML, and there were no signs of MRD.
The researchers also found that simply deleting c-Fos and Dusp1 was sufficient to block the development of B-cell ALL in mice.
The team said they are following up this study by testing c-Fos and Dusp1 as treatment targets for different kinase-fueled cancers. ![]()
Researchers say they have identified 2 signaling proteins that enable resistance to tyrosine kinase inhibitors (TKIs) and could be therapeutic targets for acute lymphoblastic leukemia (ALL) and chronic myeloid leukemia (CML).
The team found that by deleting these proteins—c-Fos and Dusp1—they could eradicate BCR-ABL-induced B-cell ALL in mice.
And treatment combining c-Fos and Dusp1 inhibitors with the TKI imatinib was able to cure mice with BCR-ABL-driven CML.
The researchers reported these findings in Nature Medicine.
“We think that, within the next 5 years, our data will change the way people think about cancer development and targeted therapy,” said study author Mohammad Azam, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This study identifies a potential Achilles’ heel of kinase-driven cancers, and what we propose is intended to be curative, not just treatment.”
The potential Achilles’ heel is a common point of passage in cells—a signaling node—that appears to be required to generate cancer cells. The node is formed by the signaling proteins c-Fos and Dusp1, according to the researchers.
The team identified c-Fos and Dusp1 by conducting global gene-expression analysis of mouse leukemia cells and human CML cells. Analysis of the human cells revealed extremely high levels of c-FOS and DUSP1 in BCR-ABL-positive, TKI-resistant cells.
Dr Azam and his colleagues found that signaling from tyrosine kinase and growth factor proteins that support cell expansion (such as IL-3 and IL-6) converge to elevate c-Fos and Dusp1 levels in leukemia cells.
Working together, these molecules maintain the survival of leukemia stem cells (LSCs), which translates to minimal residual disease (MRD) after treatment.
Dr Azam said Dusp1 and c-Fos support the survival of LSCs by increasing the toxic threshold needed to kill them. This means imatinib and other TKIs cannot eliminate the residual LSCs.
After describing the roles of c-Fos and Dusp1, Dr Azam and his colleagues put their ideas to the test in mouse models of CML.
The team tested several treatments in these mice, including:
- monotherapy with imatinib
- inhibitors of c-Fos and Dusp1
- treatment with imatinib and inhibitors of c-Fos and Dusp1.
As suspected, treatment with imatinib alone initially stopped CML progression, but mice ultimately relapsed.
Treatment with c-Fos and Dusp1 inhibitors significantly slowed CML progression and prolonged survival in a majority of mice, but this treatment wasn’t curative.
However, a month of treatment with c-Fos and Dusp1 inhibitors as well as imatinib cured about 90% of mice with CML, and there were no signs of MRD.
The researchers also found that simply deleting c-Fos and Dusp1 was sufficient to block the development of B-cell ALL in mice.
The team said they are following up this study by testing c-Fos and Dusp1 as treatment targets for different kinase-fueled cancers. ![]()
Allo-HSCT cures adult with congenital dyserythropoietic anemia
Physicians have reported what they believe is the first case of an allogeneic hematopoietic stem cell transplant (allo-HSCT) curing an adult with congenital dyserythropoietic anemia (CDA).
The patient, David Levy, was previously transfusion-dependent and suffered from iron overload, severe pain, and other adverse effects of his illness.
Levy was denied a transplant for years, but, in 2014, he received a non-myeloablative allo-HSCT from a matched, unrelated donor.
Now, Levy no longer requires transfusions, iron chelation, or immunosuppression, and says he is able to live a normal life.
Damiano Rondelli, MD, of the University of Illinois at Chicago, and his colleagues described Levy’s case in a letter to Bone Marrow Transplantation.
Levy was diagnosed with CDA at 4 months of age and was treated with regular blood transfusions for most of his life. He was 24 when the pain from his illness became so severe that he had to withdraw from graduate school.
“I spent the following years doing nothing—no work, no school, no social contact—because all I could focus on was managing my pain and getting my health back on track,” Levy said.
By age 32, Levy required transfusions every 2 to 3 weeks, had undergone a splenectomy, had an enlarged liver, and was suffering from fatigue, heart palpitations, and iron overload.
“It was bad,” Levy said. “I had been through enough pain. I was angry and depressed, and I wanted a cure. That’s why I started emailing Dr Rondelli.”
Dr Rondelli said that because of Levy’s range of illnesses and inability to tolerate chemotherapy and radiation, several institutions had denied him the possibility of a transplant.
However, Dr Rondelli and his colleagues had reported success with chemotherapy-free allo-HSCT in patients with sickle cell disease. So Dr Rondelli performed Levy’s transplant in 2014.
Levy received a peripheral blood stem cell transplant from an unrelated donor who was a 10/10 HLA match but ABO incompatible. He received conditioning with rabbit anti-thymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
Levy also received graft-vs-host disease (GVHD) prophylaxis consisting of high-dose cyclophosphamide, mycophenolate mofetil, and sirolimus. And he received standard antibacterial, antifungal, antiviral, and anti-Pneumocystis jiroveci prophylaxis.
Levy experienced platelet engraftment on day 20 and neutrophil engraftment on day 21. Whole-blood donor-cell chimerism was 98.7% on day 30 and 100% on day 60 and beyond.
Levy did develop transient hemolytic anemia due to the ABO incompatibility. He was given a total of 10 units of packed red blood cells until day 78.
Levy was tapered off all immunosuppression at 12 months and has shown no signs of acute or chronic GVHD.
At 24 months after HSCT, Levy’s hemoglobin was 13.7 g/dL, and his ferritin was 376 ng/mL. He has had no iron chelation since the transplant.
“The transplant was hard, and I had some complications, but I am back to normal now,” said Levy, who is now 35.
“I still have some pain and some lingering issues from the years my condition was not properly managed, but I can be independent now. That is the most important thing to me.”
Levy is finishing his doctorate in psychology and running group therapy sessions at a behavioral health hospital.
Dr Rondelli said the potential of this treatment approach is promising.
“The use of this transplant protocol may represent a safe therapeutic strategy to treat adult patients with many types of congenital anemias—perhaps the only possible cure,” he said.
“For many adult patients with a blood disorder, treatment options have been limited because they are often not sick enough to qualify for a risky procedure, or they are too sick to tolerate the toxic drugs used alongside a standard transplant. This procedure gives some adults the option of a stem cell transplant, which was not previously available.” ![]()
Physicians have reported what they believe is the first case of an allogeneic hematopoietic stem cell transplant (allo-HSCT) curing an adult with congenital dyserythropoietic anemia (CDA).
The patient, David Levy, was previously transfusion-dependent and suffered from iron overload, severe pain, and other adverse effects of his illness.
Levy was denied a transplant for years, but, in 2014, he received a non-myeloablative allo-HSCT from a matched, unrelated donor.
Now, Levy no longer requires transfusions, iron chelation, or immunosuppression, and says he is able to live a normal life.
Damiano Rondelli, MD, of the University of Illinois at Chicago, and his colleagues described Levy’s case in a letter to Bone Marrow Transplantation.
Levy was diagnosed with CDA at 4 months of age and was treated with regular blood transfusions for most of his life. He was 24 when the pain from his illness became so severe that he had to withdraw from graduate school.
“I spent the following years doing nothing—no work, no school, no social contact—because all I could focus on was managing my pain and getting my health back on track,” Levy said.
By age 32, Levy required transfusions every 2 to 3 weeks, had undergone a splenectomy, had an enlarged liver, and was suffering from fatigue, heart palpitations, and iron overload.
“It was bad,” Levy said. “I had been through enough pain. I was angry and depressed, and I wanted a cure. That’s why I started emailing Dr Rondelli.”
Dr Rondelli said that because of Levy’s range of illnesses and inability to tolerate chemotherapy and radiation, several institutions had denied him the possibility of a transplant.
However, Dr Rondelli and his colleagues had reported success with chemotherapy-free allo-HSCT in patients with sickle cell disease. So Dr Rondelli performed Levy’s transplant in 2014.
Levy received a peripheral blood stem cell transplant from an unrelated donor who was a 10/10 HLA match but ABO incompatible. He received conditioning with rabbit anti-thymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
Levy also received graft-vs-host disease (GVHD) prophylaxis consisting of high-dose cyclophosphamide, mycophenolate mofetil, and sirolimus. And he received standard antibacterial, antifungal, antiviral, and anti-Pneumocystis jiroveci prophylaxis.
Levy experienced platelet engraftment on day 20 and neutrophil engraftment on day 21. Whole-blood donor-cell chimerism was 98.7% on day 30 and 100% on day 60 and beyond.
Levy did develop transient hemolytic anemia due to the ABO incompatibility. He was given a total of 10 units of packed red blood cells until day 78.
Levy was tapered off all immunosuppression at 12 months and has shown no signs of acute or chronic GVHD.
At 24 months after HSCT, Levy’s hemoglobin was 13.7 g/dL, and his ferritin was 376 ng/mL. He has had no iron chelation since the transplant.
“The transplant was hard, and I had some complications, but I am back to normal now,” said Levy, who is now 35.
“I still have some pain and some lingering issues from the years my condition was not properly managed, but I can be independent now. That is the most important thing to me.”
Levy is finishing his doctorate in psychology and running group therapy sessions at a behavioral health hospital.
Dr Rondelli said the potential of this treatment approach is promising.
“The use of this transplant protocol may represent a safe therapeutic strategy to treat adult patients with many types of congenital anemias—perhaps the only possible cure,” he said.
“For many adult patients with a blood disorder, treatment options have been limited because they are often not sick enough to qualify for a risky procedure, or they are too sick to tolerate the toxic drugs used alongside a standard transplant. This procedure gives some adults the option of a stem cell transplant, which was not previously available.” ![]()
Physicians have reported what they believe is the first case of an allogeneic hematopoietic stem cell transplant (allo-HSCT) curing an adult with congenital dyserythropoietic anemia (CDA).
The patient, David Levy, was previously transfusion-dependent and suffered from iron overload, severe pain, and other adverse effects of his illness.
Levy was denied a transplant for years, but, in 2014, he received a non-myeloablative allo-HSCT from a matched, unrelated donor.
Now, Levy no longer requires transfusions, iron chelation, or immunosuppression, and says he is able to live a normal life.
Damiano Rondelli, MD, of the University of Illinois at Chicago, and his colleagues described Levy’s case in a letter to Bone Marrow Transplantation.
Levy was diagnosed with CDA at 4 months of age and was treated with regular blood transfusions for most of his life. He was 24 when the pain from his illness became so severe that he had to withdraw from graduate school.
“I spent the following years doing nothing—no work, no school, no social contact—because all I could focus on was managing my pain and getting my health back on track,” Levy said.
By age 32, Levy required transfusions every 2 to 3 weeks, had undergone a splenectomy, had an enlarged liver, and was suffering from fatigue, heart palpitations, and iron overload.
“It was bad,” Levy said. “I had been through enough pain. I was angry and depressed, and I wanted a cure. That’s why I started emailing Dr Rondelli.”
Dr Rondelli said that because of Levy’s range of illnesses and inability to tolerate chemotherapy and radiation, several institutions had denied him the possibility of a transplant.
However, Dr Rondelli and his colleagues had reported success with chemotherapy-free allo-HSCT in patients with sickle cell disease. So Dr Rondelli performed Levy’s transplant in 2014.
Levy received a peripheral blood stem cell transplant from an unrelated donor who was a 10/10 HLA match but ABO incompatible. He received conditioning with rabbit anti-thymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
Levy also received graft-vs-host disease (GVHD) prophylaxis consisting of high-dose cyclophosphamide, mycophenolate mofetil, and sirolimus. And he received standard antibacterial, antifungal, antiviral, and anti-Pneumocystis jiroveci prophylaxis.
Levy experienced platelet engraftment on day 20 and neutrophil engraftment on day 21. Whole-blood donor-cell chimerism was 98.7% on day 30 and 100% on day 60 and beyond.
Levy did develop transient hemolytic anemia due to the ABO incompatibility. He was given a total of 10 units of packed red blood cells until day 78.
Levy was tapered off all immunosuppression at 12 months and has shown no signs of acute or chronic GVHD.
At 24 months after HSCT, Levy’s hemoglobin was 13.7 g/dL, and his ferritin was 376 ng/mL. He has had no iron chelation since the transplant.
“The transplant was hard, and I had some complications, but I am back to normal now,” said Levy, who is now 35.
“I still have some pain and some lingering issues from the years my condition was not properly managed, but I can be independent now. That is the most important thing to me.”
Levy is finishing his doctorate in psychology and running group therapy sessions at a behavioral health hospital.
Dr Rondelli said the potential of this treatment approach is promising.
“The use of this transplant protocol may represent a safe therapeutic strategy to treat adult patients with many types of congenital anemias—perhaps the only possible cure,” he said.
“For many adult patients with a blood disorder, treatment options have been limited because they are often not sick enough to qualify for a risky procedure, or they are too sick to tolerate the toxic drugs used alongside a standard transplant. This procedure gives some adults the option of a stem cell transplant, which was not previously available.” ![]()
New insight into high-hyperdiploid ALL
New research appears to explain how 10q21.2 influences the risk of high-hyperdiploid acute lymphoblastic leukemia (HD-ALL).
Previous research indicated that variation in the gene ARID5B at 10q21.2 is associated with HD-ALL.
Now, researchers have reported that the 10q21.2 risk locus for HD-ALL is mediated through the single nucleotide polymorphism (SNP) rs7090445, which disrupts RUNX3 transcription factor binding.
Specifically, the rs7090445-C allele confers an increased risk of HD-ALL through reduced RUNX3-mediated expression of ARID5B.
The researchers described these findings in Nature Communications.
“This study expands our understanding of how genetic risk factors can influence the development of acute lymphoblastic leukemia . . .,” said study author Richard Houlston, MD, PhD, of The Institute of Cancer Research in London, UK.
Dr Houlston and his colleagues focused this research on 10q21.2 because it had previously been implicated in HD-ALL, but it wasn’t clear how the region affects the risk of HD-ALL.
The team said they found that a SNP in the region, rs7090445, is “highly associated” with HD-ALL.
Further investigation revealed that variation at rs7090445 disrupts RUNX3 binding and reduces the expression of ARID5B, as RUNX3 regulates ARID5B expression.
The researchers also discovered that the rs7090445-C risk allele, which is associated with reduced ARID5B expression, is amplified in HD-ALL. The risk allele is “preferentially retained” on additional copies of chromosome 10 in HD-ALL blasts.
“We implicate reduced expression of a gene called ARID5B in the production and release of the immature ‘blast’ cells that characterize [HD-ALL],” Dr Houlston said. “Our study gives a new insight into the causes of the disease and may open up new strategies for prevention.” ![]()
New research appears to explain how 10q21.2 influences the risk of high-hyperdiploid acute lymphoblastic leukemia (HD-ALL).
Previous research indicated that variation in the gene ARID5B at 10q21.2 is associated with HD-ALL.
Now, researchers have reported that the 10q21.2 risk locus for HD-ALL is mediated through the single nucleotide polymorphism (SNP) rs7090445, which disrupts RUNX3 transcription factor binding.
Specifically, the rs7090445-C allele confers an increased risk of HD-ALL through reduced RUNX3-mediated expression of ARID5B.
The researchers described these findings in Nature Communications.
“This study expands our understanding of how genetic risk factors can influence the development of acute lymphoblastic leukemia . . .,” said study author Richard Houlston, MD, PhD, of The Institute of Cancer Research in London, UK.
Dr Houlston and his colleagues focused this research on 10q21.2 because it had previously been implicated in HD-ALL, but it wasn’t clear how the region affects the risk of HD-ALL.
The team said they found that a SNP in the region, rs7090445, is “highly associated” with HD-ALL.
Further investigation revealed that variation at rs7090445 disrupts RUNX3 binding and reduces the expression of ARID5B, as RUNX3 regulates ARID5B expression.
The researchers also discovered that the rs7090445-C risk allele, which is associated with reduced ARID5B expression, is amplified in HD-ALL. The risk allele is “preferentially retained” on additional copies of chromosome 10 in HD-ALL blasts.
“We implicate reduced expression of a gene called ARID5B in the production and release of the immature ‘blast’ cells that characterize [HD-ALL],” Dr Houlston said. “Our study gives a new insight into the causes of the disease and may open up new strategies for prevention.” ![]()
New research appears to explain how 10q21.2 influences the risk of high-hyperdiploid acute lymphoblastic leukemia (HD-ALL).
Previous research indicated that variation in the gene ARID5B at 10q21.2 is associated with HD-ALL.
Now, researchers have reported that the 10q21.2 risk locus for HD-ALL is mediated through the single nucleotide polymorphism (SNP) rs7090445, which disrupts RUNX3 transcription factor binding.
Specifically, the rs7090445-C allele confers an increased risk of HD-ALL through reduced RUNX3-mediated expression of ARID5B.
The researchers described these findings in Nature Communications.
“This study expands our understanding of how genetic risk factors can influence the development of acute lymphoblastic leukemia . . .,” said study author Richard Houlston, MD, PhD, of The Institute of Cancer Research in London, UK.
Dr Houlston and his colleagues focused this research on 10q21.2 because it had previously been implicated in HD-ALL, but it wasn’t clear how the region affects the risk of HD-ALL.
The team said they found that a SNP in the region, rs7090445, is “highly associated” with HD-ALL.
Further investigation revealed that variation at rs7090445 disrupts RUNX3 binding and reduces the expression of ARID5B, as RUNX3 regulates ARID5B expression.
The researchers also discovered that the rs7090445-C risk allele, which is associated with reduced ARID5B expression, is amplified in HD-ALL. The risk allele is “preferentially retained” on additional copies of chromosome 10 in HD-ALL blasts.
“We implicate reduced expression of a gene called ARID5B in the production and release of the immature ‘blast’ cells that characterize [HD-ALL],” Dr Houlston said. “Our study gives a new insight into the causes of the disease and may open up new strategies for prevention.” ![]()