User login
Narcolepsy med shows early promise for adult ADHD
TOPLINE:
and clinical impression of ADHD severity in a pilot study of adults with ADHD.
METHODOLOGY:
- Solriamfetol is a dopamine and norepinephrine reuptake inhibitor that shares some of the properties of current ADHD medications.
- Researchers conducted a randomized, double-blind, placebo-controlled, dose-optimization trial of 75- or 150-mg solriamfetol in 60 adults with ADHD. For nearly all of the individuals who received solriamfetol, doses increased to 150 mg after the first week.
- The primary outcome was change in scores on the Adult ADHD Investigator Symptom Rating Scale (AISRS).
- Secondary outcomes included scores on the Clinical Global Impressions (CGI) scale and standard measures of executive function, behavior, and sleep.
TAKEAWAY:
- By week 6, total AISRS score improved 25% for 52% of individuals to took solriamfetol, vs. 17% of those who received placebo. Total AISRS score improved 50% by week 6 in 28% of those who took solriamfetol, vs. 3.4% of those who received placebo.
- By week 6, CGI ratings of “much improved” or “very much improved” occurred in significantly more individuals who received solriamfetol than those who took placebo (45% vs. 7%).
- Significantly more individuals who received solriamfetol than placebo self-reported improvements in executive function (69% vs. 34%). Improvement in wakefulness was noted with solriamfetol, but that did not moderate the change in ADHD symptom burden.
- Solriamfetol was well tolerated, with no significant effect on sleep quality or blood pressure. Adverse effects that occurred at a higher rate in the treatment group than in the placebo group were typical for solriamfetol and sympathomimetic agents used for ADHD.
IN PRACTICE:
“Solriamfetol may be a safe and effective treatment for ADHD in adults. Larger studies replicating these findings could confirm the strong evidence of benefit and the tolerability of this agent as a treatment,” lead author Craig B.H. Surman, MD, director of the clinical and research program in adult ADHD, Massachusetts General Hospital, Boston, said in a statement.
SOURCE:
The study was published online in The Journal of Clinical Psychiatry.
LIMITATIONS:
Limitations include the small sample size and short 6-week duration. More women than men received solriamfetol; it’s unclear how this could have affected the results.
DISCLOSURES:
The study was an investigator-initiated trial supported by Jazz Pharmaceuticals and Axsome Therapeutics. Dr. Surman has received consultant fees, research support, and royalties from multiple companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
and clinical impression of ADHD severity in a pilot study of adults with ADHD.
METHODOLOGY:
- Solriamfetol is a dopamine and norepinephrine reuptake inhibitor that shares some of the properties of current ADHD medications.
- Researchers conducted a randomized, double-blind, placebo-controlled, dose-optimization trial of 75- or 150-mg solriamfetol in 60 adults with ADHD. For nearly all of the individuals who received solriamfetol, doses increased to 150 mg after the first week.
- The primary outcome was change in scores on the Adult ADHD Investigator Symptom Rating Scale (AISRS).
- Secondary outcomes included scores on the Clinical Global Impressions (CGI) scale and standard measures of executive function, behavior, and sleep.
TAKEAWAY:
- By week 6, total AISRS score improved 25% for 52% of individuals to took solriamfetol, vs. 17% of those who received placebo. Total AISRS score improved 50% by week 6 in 28% of those who took solriamfetol, vs. 3.4% of those who received placebo.
- By week 6, CGI ratings of “much improved” or “very much improved” occurred in significantly more individuals who received solriamfetol than those who took placebo (45% vs. 7%).
- Significantly more individuals who received solriamfetol than placebo self-reported improvements in executive function (69% vs. 34%). Improvement in wakefulness was noted with solriamfetol, but that did not moderate the change in ADHD symptom burden.
- Solriamfetol was well tolerated, with no significant effect on sleep quality or blood pressure. Adverse effects that occurred at a higher rate in the treatment group than in the placebo group were typical for solriamfetol and sympathomimetic agents used for ADHD.
IN PRACTICE:
“Solriamfetol may be a safe and effective treatment for ADHD in adults. Larger studies replicating these findings could confirm the strong evidence of benefit and the tolerability of this agent as a treatment,” lead author Craig B.H. Surman, MD, director of the clinical and research program in adult ADHD, Massachusetts General Hospital, Boston, said in a statement.
SOURCE:
The study was published online in The Journal of Clinical Psychiatry.
LIMITATIONS:
Limitations include the small sample size and short 6-week duration. More women than men received solriamfetol; it’s unclear how this could have affected the results.
DISCLOSURES:
The study was an investigator-initiated trial supported by Jazz Pharmaceuticals and Axsome Therapeutics. Dr. Surman has received consultant fees, research support, and royalties from multiple companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
and clinical impression of ADHD severity in a pilot study of adults with ADHD.
METHODOLOGY:
- Solriamfetol is a dopamine and norepinephrine reuptake inhibitor that shares some of the properties of current ADHD medications.
- Researchers conducted a randomized, double-blind, placebo-controlled, dose-optimization trial of 75- or 150-mg solriamfetol in 60 adults with ADHD. For nearly all of the individuals who received solriamfetol, doses increased to 150 mg after the first week.
- The primary outcome was change in scores on the Adult ADHD Investigator Symptom Rating Scale (AISRS).
- Secondary outcomes included scores on the Clinical Global Impressions (CGI) scale and standard measures of executive function, behavior, and sleep.
TAKEAWAY:
- By week 6, total AISRS score improved 25% for 52% of individuals to took solriamfetol, vs. 17% of those who received placebo. Total AISRS score improved 50% by week 6 in 28% of those who took solriamfetol, vs. 3.4% of those who received placebo.
- By week 6, CGI ratings of “much improved” or “very much improved” occurred in significantly more individuals who received solriamfetol than those who took placebo (45% vs. 7%).
- Significantly more individuals who received solriamfetol than placebo self-reported improvements in executive function (69% vs. 34%). Improvement in wakefulness was noted with solriamfetol, but that did not moderate the change in ADHD symptom burden.
- Solriamfetol was well tolerated, with no significant effect on sleep quality or blood pressure. Adverse effects that occurred at a higher rate in the treatment group than in the placebo group were typical for solriamfetol and sympathomimetic agents used for ADHD.
IN PRACTICE:
“Solriamfetol may be a safe and effective treatment for ADHD in adults. Larger studies replicating these findings could confirm the strong evidence of benefit and the tolerability of this agent as a treatment,” lead author Craig B.H. Surman, MD, director of the clinical and research program in adult ADHD, Massachusetts General Hospital, Boston, said in a statement.
SOURCE:
The study was published online in The Journal of Clinical Psychiatry.
LIMITATIONS:
Limitations include the small sample size and short 6-week duration. More women than men received solriamfetol; it’s unclear how this could have affected the results.
DISCLOSURES:
The study was an investigator-initiated trial supported by Jazz Pharmaceuticals and Axsome Therapeutics. Dr. Surman has received consultant fees, research support, and royalties from multiple companies.
A version of this article first appeared on Medscape.com.
‘Diagnosis creep’: Are some AFib patients overtreated?
without those treatments having been validated in those particular groups.
This concern has been highlighted recently in the atrial fibrillation (AF) field, with the recent change in the definition of hypertension in the United States at lower levels of blood pressure causing a lot more patients to become eligible for oral anticoagulation at an earlier stage in their AF course.
U.S. researchers analyzed data from 316,388 patients with AF from the National Cardiovascular Data Registry Practice Innovation and Clinical Excellence outpatient quality improvement registry, and found that at 36 months’ follow-up, 83.5% of patients met the new 130/80 mm Hg definition of hypertension, while only 53.3% met the previous 140/90 mm Hg definition.
The diagnosis of hypertension gives 1 point in the CHA2DS2-VASc score, which is used to determine risk in AF patients, those with scores of 2 or more being eligible for oral anticoagulation.
The researchers report that in patients with an index CHA2DS2-VASc score of 1 (before the hypertension diagnosis), at 36 months, 83% fulfilled the 130/80 mm Hg definition of hypertension while the 140/90 mm Hg definition was met by only 50%, giving a large increase in the number of patients who could qualify for oral anticoagulation therapy.
“While the definition of hypertension has changed in response to landmark clinical trials, CHA2DS2-VASc was validated using an older hypertension definition, with limited ambulatory blood pressure monitoring and higher blood pressure goals for treatment,” the authors state.
“Now, patients with AF will meet the CHA2DS2-VASc threshold for oral anticoagulation earlier in their disease course. However, it is not known if patients with scores of 1 or 2 using the new hypertension definition have sufficient stroke risk to offset the bleeding risk of oral anticoagulation and will receive net clinical benefit,” they point out.
This study was published online as a research letter in JAMA Network Open.
Senior author of the report, Mintu Turakhia, MD, Stanford (Calif.) University/iRhythm Technologies Inc., said AF is a good example of how “diagnosis creep” may lead to patients receiving inappropriate treatment.
“Risk scores derived when risk variables were described in one way are starting to be applied based on a diagnosis made in a totally different way,” he said in an interview. “Diagnosis creep is a problem everywhere in medicine. The goal of this study was to quantify what this means for the new definition of hypertension in the context of risk scoring AF patients for anticoagulation treatment. We are calling attention to this issue so clinicians are aware of possible implications.”
Dr. Turakhia explained that the CHA2DS2-VASc score was formulated based on claims data so there was a record of hypertension on the clinical encounter. That hypertension diagnosis would have been based on the old definition of 140/90 mm Hg.
“But now we apply a label of hypertension in the office every time someone has a measurement of elevated blood pressure – treated or untreated – and the blood pressure threshold for a hypertension diagnosis has changed to 130/80 mm Hg,” he said. “We are asking what this means for risk stratification scores such as CHA2DS2-VASc, and how do we quantify what that means for anticoagulation eligibility?”
He said that while identifying hypertension at lower blood pressures may be beneficial with regard to starting antihypertensive treatment earlier with a consequent reduction in cardiovascular outcomes, when this also affects risk scores that determine treatment for other conditions, as is the case for AF, the case is not so clear.
Dr. Turakhia pointed out that with AF, there are additional factors causing diagnosis creep, including earlier detection of AF and identification of shorter episodes due to the use of higher sensitivity tools to detect abnormal rhythms.
“What about the patient who has been identified as having AF based on just a few seconds found on monitoring and who is aged 65 (so just over the age threshold for 1 point on the CHA2DS2-VASc score)?” he asked. “Now we’re going to throw in hypertension with a blood pressure measurement just over 130/80 mm Hg, and they will be eligible for anticoagulation.”
Dr. Turakhia noted that in addition to earlier classification of hypertension, other conditions contributing to the CHA2DS2-VASc score are also being detected earlier, including diabetes and reduced ejection fractions that are considered heart failure.
“I worry about the sum of the parts. We don’t know if the risk score performs equally well when we’re using these different thresholds. We have to be careful that we are not exposing patients to the bleeding risks of anticoagulation unnecessarily. There is a clear issue here,” he said.
What should clinicians do?
In a comment, Gregory Lip, MD, chair of cardiovascular medicine at the University of Liverpool, England, who helped develop the CHA2DS2-VASc score, said clinicians needed to think more broadly when considering hypertension as a risk factor for the score.
He points out that if a patient had a history of hypertension but is now controlled to below 130/80 mm Hg, they would still be considered to be at risk per the CHA2DS2-VASc score.
And for patients without a history of hypertension, and who have a current blood pressure measurement of around 130/80 mm Hg, Dr. Lip advises that it would be premature to diagnose hypertension immediately.
“Hypertension is not a yes/no diagnosis. If you look at the relationship between blood pressure and risk of stroke, it is like a continual dose-response. It doesn’t mean that at 129/79 there is no stroke risk but that at 130/80 there is a stroke risk. It’s not like that,” he said.
“I wouldn’t make a diagnosis on a one-off blood pressure measurement. I would want to monitor that patient and get them to do home measurements,” he commented. “If someone constantly has levels around that 130/80 mm Hg, I don’t necessarily rush in with a definite diagnosis of hypertension and start drug treatment. I would look at lifestyle first. And in such patients, I wouldn’t give them the 1 point for hypertension on the CHA2DS2-VASc score.”
Dr. Lip points out that a hypertension diagnosis is not just about blood pressure numbers. “We have to assess the patients much more completely before giving them a diagnosis and consider factors such as whether there is evidence of hypertension-related end-organ damage, and if lifestyle issues have been addressed.”
Are new risk scores needed?
Dr. Turakhia agreed that clinicians need to look at the bigger picture, but he also suggested that new risk scores may need to be developed.
“All of us in the medical community need to think about whether we should be recalibrating risk prediction with more contemporary evidence – based on our ability to detect disease now,” he commented.
“This could even be a different risk score altogether, possibly incorporating a wider range of parameters or perhaps incorporating machine learning. That’s really the question we need to be asking ourselves,” Dr. Turakhia added.
Dr. Lip noted that there are many stroke risk factors and only those that are most common and have been well validated go into clinical risk scores such as CHA2DS2-VASc.
“These risks scores are by design simplifications, and only have modest predictive value for identifying patients at high risk of stroke. You can always improve on clinical risk scores by adding in other variables,” he said. “There are some risk scores in AF with 26 variables. But the practical application of these more complex scores can be difficult in clinical practice. These risks scores are meant to be simple so that they can be used by busy clinicians in the outpatient clinic or on a ward round. It is not easy to input 26 different variables.”
He also noted that many guidelines are now veering away from categorizing patients at high, medium, or low risk of stroke, which he refers to as “artificial” classifications. “There is now more of a default position that patients should receive stroke prevention normally with a DOAC [direct oral anticoagulant] unless they are low risk.”
Dr. Turakhia agreed that it is imperative to look at the bigger picture when identifying AF patients for anticoagulation. “We have to be careful not to take things at face value. It is more important than ever to use clinical judgment to avoid overtreatment in borderline situations,” he concluded.
This study was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry. Dr. Turakhia reported employment from iRhythm Technologies; equity from AliveCor, Connect America, Evidently, and Forward; grants from U.S. Food and Drug Administration, American Heart Association, Bayer, Sanofi, Gilead, and Bristol Myers Squibb; and personal fees from Pfizer and JAMA Cardiology (prior associate editor) outside the submitted work. Dr. Lip has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
without those treatments having been validated in those particular groups.
This concern has been highlighted recently in the atrial fibrillation (AF) field, with the recent change in the definition of hypertension in the United States at lower levels of blood pressure causing a lot more patients to become eligible for oral anticoagulation at an earlier stage in their AF course.
U.S. researchers analyzed data from 316,388 patients with AF from the National Cardiovascular Data Registry Practice Innovation and Clinical Excellence outpatient quality improvement registry, and found that at 36 months’ follow-up, 83.5% of patients met the new 130/80 mm Hg definition of hypertension, while only 53.3% met the previous 140/90 mm Hg definition.
The diagnosis of hypertension gives 1 point in the CHA2DS2-VASc score, which is used to determine risk in AF patients, those with scores of 2 or more being eligible for oral anticoagulation.
The researchers report that in patients with an index CHA2DS2-VASc score of 1 (before the hypertension diagnosis), at 36 months, 83% fulfilled the 130/80 mm Hg definition of hypertension while the 140/90 mm Hg definition was met by only 50%, giving a large increase in the number of patients who could qualify for oral anticoagulation therapy.
“While the definition of hypertension has changed in response to landmark clinical trials, CHA2DS2-VASc was validated using an older hypertension definition, with limited ambulatory blood pressure monitoring and higher blood pressure goals for treatment,” the authors state.
“Now, patients with AF will meet the CHA2DS2-VASc threshold for oral anticoagulation earlier in their disease course. However, it is not known if patients with scores of 1 or 2 using the new hypertension definition have sufficient stroke risk to offset the bleeding risk of oral anticoagulation and will receive net clinical benefit,” they point out.
This study was published online as a research letter in JAMA Network Open.
Senior author of the report, Mintu Turakhia, MD, Stanford (Calif.) University/iRhythm Technologies Inc., said AF is a good example of how “diagnosis creep” may lead to patients receiving inappropriate treatment.
“Risk scores derived when risk variables were described in one way are starting to be applied based on a diagnosis made in a totally different way,” he said in an interview. “Diagnosis creep is a problem everywhere in medicine. The goal of this study was to quantify what this means for the new definition of hypertension in the context of risk scoring AF patients for anticoagulation treatment. We are calling attention to this issue so clinicians are aware of possible implications.”
Dr. Turakhia explained that the CHA2DS2-VASc score was formulated based on claims data so there was a record of hypertension on the clinical encounter. That hypertension diagnosis would have been based on the old definition of 140/90 mm Hg.
“But now we apply a label of hypertension in the office every time someone has a measurement of elevated blood pressure – treated or untreated – and the blood pressure threshold for a hypertension diagnosis has changed to 130/80 mm Hg,” he said. “We are asking what this means for risk stratification scores such as CHA2DS2-VASc, and how do we quantify what that means for anticoagulation eligibility?”
He said that while identifying hypertension at lower blood pressures may be beneficial with regard to starting antihypertensive treatment earlier with a consequent reduction in cardiovascular outcomes, when this also affects risk scores that determine treatment for other conditions, as is the case for AF, the case is not so clear.
Dr. Turakhia pointed out that with AF, there are additional factors causing diagnosis creep, including earlier detection of AF and identification of shorter episodes due to the use of higher sensitivity tools to detect abnormal rhythms.
“What about the patient who has been identified as having AF based on just a few seconds found on monitoring and who is aged 65 (so just over the age threshold for 1 point on the CHA2DS2-VASc score)?” he asked. “Now we’re going to throw in hypertension with a blood pressure measurement just over 130/80 mm Hg, and they will be eligible for anticoagulation.”
Dr. Turakhia noted that in addition to earlier classification of hypertension, other conditions contributing to the CHA2DS2-VASc score are also being detected earlier, including diabetes and reduced ejection fractions that are considered heart failure.
“I worry about the sum of the parts. We don’t know if the risk score performs equally well when we’re using these different thresholds. We have to be careful that we are not exposing patients to the bleeding risks of anticoagulation unnecessarily. There is a clear issue here,” he said.
What should clinicians do?
In a comment, Gregory Lip, MD, chair of cardiovascular medicine at the University of Liverpool, England, who helped develop the CHA2DS2-VASc score, said clinicians needed to think more broadly when considering hypertension as a risk factor for the score.
He points out that if a patient had a history of hypertension but is now controlled to below 130/80 mm Hg, they would still be considered to be at risk per the CHA2DS2-VASc score.
And for patients without a history of hypertension, and who have a current blood pressure measurement of around 130/80 mm Hg, Dr. Lip advises that it would be premature to diagnose hypertension immediately.
“Hypertension is not a yes/no diagnosis. If you look at the relationship between blood pressure and risk of stroke, it is like a continual dose-response. It doesn’t mean that at 129/79 there is no stroke risk but that at 130/80 there is a stroke risk. It’s not like that,” he said.
“I wouldn’t make a diagnosis on a one-off blood pressure measurement. I would want to monitor that patient and get them to do home measurements,” he commented. “If someone constantly has levels around that 130/80 mm Hg, I don’t necessarily rush in with a definite diagnosis of hypertension and start drug treatment. I would look at lifestyle first. And in such patients, I wouldn’t give them the 1 point for hypertension on the CHA2DS2-VASc score.”
Dr. Lip points out that a hypertension diagnosis is not just about blood pressure numbers. “We have to assess the patients much more completely before giving them a diagnosis and consider factors such as whether there is evidence of hypertension-related end-organ damage, and if lifestyle issues have been addressed.”
Are new risk scores needed?
Dr. Turakhia agreed that clinicians need to look at the bigger picture, but he also suggested that new risk scores may need to be developed.
“All of us in the medical community need to think about whether we should be recalibrating risk prediction with more contemporary evidence – based on our ability to detect disease now,” he commented.
“This could even be a different risk score altogether, possibly incorporating a wider range of parameters or perhaps incorporating machine learning. That’s really the question we need to be asking ourselves,” Dr. Turakhia added.
Dr. Lip noted that there are many stroke risk factors and only those that are most common and have been well validated go into clinical risk scores such as CHA2DS2-VASc.
“These risks scores are by design simplifications, and only have modest predictive value for identifying patients at high risk of stroke. You can always improve on clinical risk scores by adding in other variables,” he said. “There are some risk scores in AF with 26 variables. But the practical application of these more complex scores can be difficult in clinical practice. These risks scores are meant to be simple so that they can be used by busy clinicians in the outpatient clinic or on a ward round. It is not easy to input 26 different variables.”
He also noted that many guidelines are now veering away from categorizing patients at high, medium, or low risk of stroke, which he refers to as “artificial” classifications. “There is now more of a default position that patients should receive stroke prevention normally with a DOAC [direct oral anticoagulant] unless they are low risk.”
Dr. Turakhia agreed that it is imperative to look at the bigger picture when identifying AF patients for anticoagulation. “We have to be careful not to take things at face value. It is more important than ever to use clinical judgment to avoid overtreatment in borderline situations,” he concluded.
This study was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry. Dr. Turakhia reported employment from iRhythm Technologies; equity from AliveCor, Connect America, Evidently, and Forward; grants from U.S. Food and Drug Administration, American Heart Association, Bayer, Sanofi, Gilead, and Bristol Myers Squibb; and personal fees from Pfizer and JAMA Cardiology (prior associate editor) outside the submitted work. Dr. Lip has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
without those treatments having been validated in those particular groups.
This concern has been highlighted recently in the atrial fibrillation (AF) field, with the recent change in the definition of hypertension in the United States at lower levels of blood pressure causing a lot more patients to become eligible for oral anticoagulation at an earlier stage in their AF course.
U.S. researchers analyzed data from 316,388 patients with AF from the National Cardiovascular Data Registry Practice Innovation and Clinical Excellence outpatient quality improvement registry, and found that at 36 months’ follow-up, 83.5% of patients met the new 130/80 mm Hg definition of hypertension, while only 53.3% met the previous 140/90 mm Hg definition.
The diagnosis of hypertension gives 1 point in the CHA2DS2-VASc score, which is used to determine risk in AF patients, those with scores of 2 or more being eligible for oral anticoagulation.
The researchers report that in patients with an index CHA2DS2-VASc score of 1 (before the hypertension diagnosis), at 36 months, 83% fulfilled the 130/80 mm Hg definition of hypertension while the 140/90 mm Hg definition was met by only 50%, giving a large increase in the number of patients who could qualify for oral anticoagulation therapy.
“While the definition of hypertension has changed in response to landmark clinical trials, CHA2DS2-VASc was validated using an older hypertension definition, with limited ambulatory blood pressure monitoring and higher blood pressure goals for treatment,” the authors state.
“Now, patients with AF will meet the CHA2DS2-VASc threshold for oral anticoagulation earlier in their disease course. However, it is not known if patients with scores of 1 or 2 using the new hypertension definition have sufficient stroke risk to offset the bleeding risk of oral anticoagulation and will receive net clinical benefit,” they point out.
This study was published online as a research letter in JAMA Network Open.
Senior author of the report, Mintu Turakhia, MD, Stanford (Calif.) University/iRhythm Technologies Inc., said AF is a good example of how “diagnosis creep” may lead to patients receiving inappropriate treatment.
“Risk scores derived when risk variables were described in one way are starting to be applied based on a diagnosis made in a totally different way,” he said in an interview. “Diagnosis creep is a problem everywhere in medicine. The goal of this study was to quantify what this means for the new definition of hypertension in the context of risk scoring AF patients for anticoagulation treatment. We are calling attention to this issue so clinicians are aware of possible implications.”
Dr. Turakhia explained that the CHA2DS2-VASc score was formulated based on claims data so there was a record of hypertension on the clinical encounter. That hypertension diagnosis would have been based on the old definition of 140/90 mm Hg.
“But now we apply a label of hypertension in the office every time someone has a measurement of elevated blood pressure – treated or untreated – and the blood pressure threshold for a hypertension diagnosis has changed to 130/80 mm Hg,” he said. “We are asking what this means for risk stratification scores such as CHA2DS2-VASc, and how do we quantify what that means for anticoagulation eligibility?”
He said that while identifying hypertension at lower blood pressures may be beneficial with regard to starting antihypertensive treatment earlier with a consequent reduction in cardiovascular outcomes, when this also affects risk scores that determine treatment for other conditions, as is the case for AF, the case is not so clear.
Dr. Turakhia pointed out that with AF, there are additional factors causing diagnosis creep, including earlier detection of AF and identification of shorter episodes due to the use of higher sensitivity tools to detect abnormal rhythms.
“What about the patient who has been identified as having AF based on just a few seconds found on monitoring and who is aged 65 (so just over the age threshold for 1 point on the CHA2DS2-VASc score)?” he asked. “Now we’re going to throw in hypertension with a blood pressure measurement just over 130/80 mm Hg, and they will be eligible for anticoagulation.”
Dr. Turakhia noted that in addition to earlier classification of hypertension, other conditions contributing to the CHA2DS2-VASc score are also being detected earlier, including diabetes and reduced ejection fractions that are considered heart failure.
“I worry about the sum of the parts. We don’t know if the risk score performs equally well when we’re using these different thresholds. We have to be careful that we are not exposing patients to the bleeding risks of anticoagulation unnecessarily. There is a clear issue here,” he said.
What should clinicians do?
In a comment, Gregory Lip, MD, chair of cardiovascular medicine at the University of Liverpool, England, who helped develop the CHA2DS2-VASc score, said clinicians needed to think more broadly when considering hypertension as a risk factor for the score.
He points out that if a patient had a history of hypertension but is now controlled to below 130/80 mm Hg, they would still be considered to be at risk per the CHA2DS2-VASc score.
And for patients without a history of hypertension, and who have a current blood pressure measurement of around 130/80 mm Hg, Dr. Lip advises that it would be premature to diagnose hypertension immediately.
“Hypertension is not a yes/no diagnosis. If you look at the relationship between blood pressure and risk of stroke, it is like a continual dose-response. It doesn’t mean that at 129/79 there is no stroke risk but that at 130/80 there is a stroke risk. It’s not like that,” he said.
“I wouldn’t make a diagnosis on a one-off blood pressure measurement. I would want to monitor that patient and get them to do home measurements,” he commented. “If someone constantly has levels around that 130/80 mm Hg, I don’t necessarily rush in with a definite diagnosis of hypertension and start drug treatment. I would look at lifestyle first. And in such patients, I wouldn’t give them the 1 point for hypertension on the CHA2DS2-VASc score.”
Dr. Lip points out that a hypertension diagnosis is not just about blood pressure numbers. “We have to assess the patients much more completely before giving them a diagnosis and consider factors such as whether there is evidence of hypertension-related end-organ damage, and if lifestyle issues have been addressed.”
Are new risk scores needed?
Dr. Turakhia agreed that clinicians need to look at the bigger picture, but he also suggested that new risk scores may need to be developed.
“All of us in the medical community need to think about whether we should be recalibrating risk prediction with more contemporary evidence – based on our ability to detect disease now,” he commented.
“This could even be a different risk score altogether, possibly incorporating a wider range of parameters or perhaps incorporating machine learning. That’s really the question we need to be asking ourselves,” Dr. Turakhia added.
Dr. Lip noted that there are many stroke risk factors and only those that are most common and have been well validated go into clinical risk scores such as CHA2DS2-VASc.
“These risks scores are by design simplifications, and only have modest predictive value for identifying patients at high risk of stroke. You can always improve on clinical risk scores by adding in other variables,” he said. “There are some risk scores in AF with 26 variables. But the practical application of these more complex scores can be difficult in clinical practice. These risks scores are meant to be simple so that they can be used by busy clinicians in the outpatient clinic or on a ward round. It is not easy to input 26 different variables.”
He also noted that many guidelines are now veering away from categorizing patients at high, medium, or low risk of stroke, which he refers to as “artificial” classifications. “There is now more of a default position that patients should receive stroke prevention normally with a DOAC [direct oral anticoagulant] unless they are low risk.”
Dr. Turakhia agreed that it is imperative to look at the bigger picture when identifying AF patients for anticoagulation. “We have to be careful not to take things at face value. It is more important than ever to use clinical judgment to avoid overtreatment in borderline situations,” he concluded.
This study was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry. Dr. Turakhia reported employment from iRhythm Technologies; equity from AliveCor, Connect America, Evidently, and Forward; grants from U.S. Food and Drug Administration, American Heart Association, Bayer, Sanofi, Gilead, and Bristol Myers Squibb; and personal fees from Pfizer and JAMA Cardiology (prior associate editor) outside the submitted work. Dr. Lip has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Greater fracture risk reduction seen with denosumab vs. zoledronic acid in postmenopausal women
VANCOUVER –
A previous head-to-head comparison showed that denosumab increased bone mineral density at key skeletal sites compared with zoledronic acid, but only a single, small observational study has examined fracture risk, and it found no difference.
The new study, presented at the annual meeting of the American Society for Bone and Mineral Research, used a relatively new method of real-world comparative effectiveness analysis called negative control outcome (NCO) to analyze Medicare fee-for-service data.
NCO analysis takes extra pains to remove bias through data that might be linked to potential confounders but could not reasonably be attributed to a drug. For example, people who have greater contact with the health care system may be more likely to get one drug or another. The researchers used the frequency of receiving a flu or pneumonia vaccine as a proxy for this. If the two comparison groups had a significant difference in a proxy, it suggested a hidden bias and forced the researchers to abandon those groupings. Another example used car accidents as a proxy for cognitive impairment.
“If you find meaningful differences between the two groups, and you can say there’s no way a bone drug could account for these differences, then we shouldn’t do this analysis because these groups just aren’t comparable. They probably differ by that confounding factor we couldn’t measure,” said Jeffrey Curtis, MD, who presented the study. He is a professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham.
The study strongly suggests superiority for denosumab. “There was a significant difference in multiple different groupings of fractures – beginning at year 2, extending to year 3 and even out to year 5 – that showed that there is a significant reduction in fracture risk if you get treated with denosumab [that was greater] than if you get treated with zoledronic acid,” Dr. Curtis said.
The researchers weighed 118 covariates and ultimately identified a population of 90,805 women taking denosumab and 37,328 taking zoledronic acid that was equally balanced in all patient characteristics. The mean age was about 75 years in the denosumab group and 74 in the zoledronic acid group.
The researchers found a 34% lower risk for hip fracture in the denosumab group by 5 years (relative risk, 0.66; 95% confidence interval, 0.43-0.90).
Similar patterns in fracture risk reduction were observed at 5 years for nonvertebral fracture (RR, 0.67; 95% CI, 0.52-0.82), nonhip nonvertebral fracture (RR, 0.69; 95% CI, 0.50-0.88), and major osteoporotic fracture (RR, 0.74; 95% CI, 0.59-0.89).
During the Q&A session after the talk, one audience member commented that the study was limited because the researchers only followed patients who received zoledronic acid for 60 days, which could have missed potential long-term benefits of the drug, especially since bisphosphonates have a lengthy skeletal retention time. Dr. Curtis acknowledged the point but said, “Usually, that’s not something we do, but these are different enough mechanisms of action that it may be warranted at least as a sensitivity analysis,” he said.
The study and its methodology were impressive, according to Yumie Rhee, MD, who comoderated the session where the study was presented. “I think they did a really good job by doing the negative control analysis. We’re not going to have a head-to-head clinical trial, so we don’t know the real fracture reduction differences [between denosumab and zoledronic acid]. [The NCO analysis] is more than the propensity matching score that we do usually,” said Dr. Rhee, who is a professor of endocrinology at Yonsei University College of Medicine in Seoul, South Korea.
In particular, the study showed a significantly greater reduction in hip fractures with denosumab. “Even in the RCTs, it was really hard to see the reduction in hip fracture, so I think this is showing much stronger data for denosumab. Especially in patients who have more [general fracture] risk and patients with higher hip fracture risk, I would go with denosumab,” Dr. Rhee said.
Her comoderator, Maria Zanchetta, MD, agreed. “It can have clinical implication, because we think denosumab is better than [zoledronic acid] for higher-risk patients, but we didn’t have the evidence. So at least we have a new [study] to look at, and I think it’s very important for our practice,” said Dr. Zanchetta, who is a professor of osteology at the Institute of Diagnostics and Metabolic Research, Universidad del Salvador, Buenos Aires.
The study was funded by Amgen, which markets denosumab. Dr. Curtis has consulted for Amgen. Dr. Rhee and Dr. Zanchetta report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
VANCOUVER –
A previous head-to-head comparison showed that denosumab increased bone mineral density at key skeletal sites compared with zoledronic acid, but only a single, small observational study has examined fracture risk, and it found no difference.
The new study, presented at the annual meeting of the American Society for Bone and Mineral Research, used a relatively new method of real-world comparative effectiveness analysis called negative control outcome (NCO) to analyze Medicare fee-for-service data.
NCO analysis takes extra pains to remove bias through data that might be linked to potential confounders but could not reasonably be attributed to a drug. For example, people who have greater contact with the health care system may be more likely to get one drug or another. The researchers used the frequency of receiving a flu or pneumonia vaccine as a proxy for this. If the two comparison groups had a significant difference in a proxy, it suggested a hidden bias and forced the researchers to abandon those groupings. Another example used car accidents as a proxy for cognitive impairment.
“If you find meaningful differences between the two groups, and you can say there’s no way a bone drug could account for these differences, then we shouldn’t do this analysis because these groups just aren’t comparable. They probably differ by that confounding factor we couldn’t measure,” said Jeffrey Curtis, MD, who presented the study. He is a professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham.
The study strongly suggests superiority for denosumab. “There was a significant difference in multiple different groupings of fractures – beginning at year 2, extending to year 3 and even out to year 5 – that showed that there is a significant reduction in fracture risk if you get treated with denosumab [that was greater] than if you get treated with zoledronic acid,” Dr. Curtis said.
The researchers weighed 118 covariates and ultimately identified a population of 90,805 women taking denosumab and 37,328 taking zoledronic acid that was equally balanced in all patient characteristics. The mean age was about 75 years in the denosumab group and 74 in the zoledronic acid group.
The researchers found a 34% lower risk for hip fracture in the denosumab group by 5 years (relative risk, 0.66; 95% confidence interval, 0.43-0.90).
Similar patterns in fracture risk reduction were observed at 5 years for nonvertebral fracture (RR, 0.67; 95% CI, 0.52-0.82), nonhip nonvertebral fracture (RR, 0.69; 95% CI, 0.50-0.88), and major osteoporotic fracture (RR, 0.74; 95% CI, 0.59-0.89).
During the Q&A session after the talk, one audience member commented that the study was limited because the researchers only followed patients who received zoledronic acid for 60 days, which could have missed potential long-term benefits of the drug, especially since bisphosphonates have a lengthy skeletal retention time. Dr. Curtis acknowledged the point but said, “Usually, that’s not something we do, but these are different enough mechanisms of action that it may be warranted at least as a sensitivity analysis,” he said.
The study and its methodology were impressive, according to Yumie Rhee, MD, who comoderated the session where the study was presented. “I think they did a really good job by doing the negative control analysis. We’re not going to have a head-to-head clinical trial, so we don’t know the real fracture reduction differences [between denosumab and zoledronic acid]. [The NCO analysis] is more than the propensity matching score that we do usually,” said Dr. Rhee, who is a professor of endocrinology at Yonsei University College of Medicine in Seoul, South Korea.
In particular, the study showed a significantly greater reduction in hip fractures with denosumab. “Even in the RCTs, it was really hard to see the reduction in hip fracture, so I think this is showing much stronger data for denosumab. Especially in patients who have more [general fracture] risk and patients with higher hip fracture risk, I would go with denosumab,” Dr. Rhee said.
Her comoderator, Maria Zanchetta, MD, agreed. “It can have clinical implication, because we think denosumab is better than [zoledronic acid] for higher-risk patients, but we didn’t have the evidence. So at least we have a new [study] to look at, and I think it’s very important for our practice,” said Dr. Zanchetta, who is a professor of osteology at the Institute of Diagnostics and Metabolic Research, Universidad del Salvador, Buenos Aires.
The study was funded by Amgen, which markets denosumab. Dr. Curtis has consulted for Amgen. Dr. Rhee and Dr. Zanchetta report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
VANCOUVER –
A previous head-to-head comparison showed that denosumab increased bone mineral density at key skeletal sites compared with zoledronic acid, but only a single, small observational study has examined fracture risk, and it found no difference.
The new study, presented at the annual meeting of the American Society for Bone and Mineral Research, used a relatively new method of real-world comparative effectiveness analysis called negative control outcome (NCO) to analyze Medicare fee-for-service data.
NCO analysis takes extra pains to remove bias through data that might be linked to potential confounders but could not reasonably be attributed to a drug. For example, people who have greater contact with the health care system may be more likely to get one drug or another. The researchers used the frequency of receiving a flu or pneumonia vaccine as a proxy for this. If the two comparison groups had a significant difference in a proxy, it suggested a hidden bias and forced the researchers to abandon those groupings. Another example used car accidents as a proxy for cognitive impairment.
“If you find meaningful differences between the two groups, and you can say there’s no way a bone drug could account for these differences, then we shouldn’t do this analysis because these groups just aren’t comparable. They probably differ by that confounding factor we couldn’t measure,” said Jeffrey Curtis, MD, who presented the study. He is a professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham.
The study strongly suggests superiority for denosumab. “There was a significant difference in multiple different groupings of fractures – beginning at year 2, extending to year 3 and even out to year 5 – that showed that there is a significant reduction in fracture risk if you get treated with denosumab [that was greater] than if you get treated with zoledronic acid,” Dr. Curtis said.
The researchers weighed 118 covariates and ultimately identified a population of 90,805 women taking denosumab and 37,328 taking zoledronic acid that was equally balanced in all patient characteristics. The mean age was about 75 years in the denosumab group and 74 in the zoledronic acid group.
The researchers found a 34% lower risk for hip fracture in the denosumab group by 5 years (relative risk, 0.66; 95% confidence interval, 0.43-0.90).
Similar patterns in fracture risk reduction were observed at 5 years for nonvertebral fracture (RR, 0.67; 95% CI, 0.52-0.82), nonhip nonvertebral fracture (RR, 0.69; 95% CI, 0.50-0.88), and major osteoporotic fracture (RR, 0.74; 95% CI, 0.59-0.89).
During the Q&A session after the talk, one audience member commented that the study was limited because the researchers only followed patients who received zoledronic acid for 60 days, which could have missed potential long-term benefits of the drug, especially since bisphosphonates have a lengthy skeletal retention time. Dr. Curtis acknowledged the point but said, “Usually, that’s not something we do, but these are different enough mechanisms of action that it may be warranted at least as a sensitivity analysis,” he said.
The study and its methodology were impressive, according to Yumie Rhee, MD, who comoderated the session where the study was presented. “I think they did a really good job by doing the negative control analysis. We’re not going to have a head-to-head clinical trial, so we don’t know the real fracture reduction differences [between denosumab and zoledronic acid]. [The NCO analysis] is more than the propensity matching score that we do usually,” said Dr. Rhee, who is a professor of endocrinology at Yonsei University College of Medicine in Seoul, South Korea.
In particular, the study showed a significantly greater reduction in hip fractures with denosumab. “Even in the RCTs, it was really hard to see the reduction in hip fracture, so I think this is showing much stronger data for denosumab. Especially in patients who have more [general fracture] risk and patients with higher hip fracture risk, I would go with denosumab,” Dr. Rhee said.
Her comoderator, Maria Zanchetta, MD, agreed. “It can have clinical implication, because we think denosumab is better than [zoledronic acid] for higher-risk patients, but we didn’t have the evidence. So at least we have a new [study] to look at, and I think it’s very important for our practice,” said Dr. Zanchetta, who is a professor of osteology at the Institute of Diagnostics and Metabolic Research, Universidad del Salvador, Buenos Aires.
The study was funded by Amgen, which markets denosumab. Dr. Curtis has consulted for Amgen. Dr. Rhee and Dr. Zanchetta report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ASBMR 2023
CKD linked to cardiac arrest in Hispanic, Latinx patients
TOPLINE:
new data show, suggesting early identification of CKD may provide an opportunity to reduce the risk in these groups. Other predictors included heavy drinking, atrial fibrillation, coronary artery disease, heart failure and diabetes.
METHODOLOGY:
- The study included 295 Hispanic or Latinx patients with out-of-hospital SCA from the PRESTO study in Ventura County, California, and 590 frequency-matched controls from the San Diego site of the population-based HCHS/SOL (Hispanic Community Health Survey/Study of Latinos); in both cohorts, men made up 70% of participants, and the median age was about 63 years.
- Researchers collected data on demographics, medical history, and current health conditions. Of note, 51.2% of SCA cases and 8.8% of control participants had CKD, and 20.0% of cases and 0.7% of the control group were on dialysis.
- Pre-SCA echocardiograms were available for 48% of SCA cases and baseline echocardiograms for more than 99% of control participants.
TAKEAWAY:
- In analyses adjusted for age, sex, and clinical variables, predictors significantly associated with higher odds of SCA included: CKD (odds ratio, 7.3; 95% confidence interval, 3.8-14.3; P < .001), heavy drinking (OR, 4.5), stroke (OR, 3.1), atrial fibrillation (OR, 3.7), coronary artery disease (OR, 2.9), heart failure (OR, 2.5), and diabetes (OR, 1.5).
- Hypertension, hyperlipemia, body mass index, and current smoking status were not significantly associated with SCA.
- In adjusted analyses, heart rate (OR, 1.8 per one standard deviation [1-SD] increase), QTc interval (OR, 2.5 per 1-SD increase) and left ventricular ejection fraction (OR, 4.4 per 1-SD decrease) were significantly associated with SCA, suggesting echocardiogram evaluations could help identify Hispanic or Latinx individuals at increased risk for SCA, wrote the authors.
IN PRACTICE:
“Our study, the first to include feasible numbers of Hispanic or Latino individuals, highlights the importance of renal dysfunction as a risk factor for SCA in the community,” the authors wrote, adding that early identification and management of chronic kidney disease could reduce risk for SCA in this population.
SOURCE:
The study was conducted by Kyndaron Reinier, PhD, MPH, Cedars-Sinai Health System, Los Angeles, and colleagues. It was published online in the Journal of the American Heart Association.
LIMITATIONS:
Most participants from the HCHS/SOL study were born outside the United States, compared with about half the SCA cases, which could have influenced cardiovascular disease risk, although results did not change considerably when models were adjusted for place of birth. Study participants were predominantly of Mexican heritage, so results may not be generalizable to Hispanic or Latinx individuals from other regions. As medical history was assessed differently in the two studies, there could be some error in estimating the strength of associations. Results from echocardiographic data should be viewed as hypothesis generating because of the potential for residual bias.
DISCLOSURES:
The Ventura PRESTO study was funded, in part, by the National Institutes of Health, and National Heart, Lung, and Blood Institute. The HCHS/SOL was carried out as a collaborative study supported by contracts from the NHLBI.
A version of this article first appeared on Medscape.com.
TOPLINE:
new data show, suggesting early identification of CKD may provide an opportunity to reduce the risk in these groups. Other predictors included heavy drinking, atrial fibrillation, coronary artery disease, heart failure and diabetes.
METHODOLOGY:
- The study included 295 Hispanic or Latinx patients with out-of-hospital SCA from the PRESTO study in Ventura County, California, and 590 frequency-matched controls from the San Diego site of the population-based HCHS/SOL (Hispanic Community Health Survey/Study of Latinos); in both cohorts, men made up 70% of participants, and the median age was about 63 years.
- Researchers collected data on demographics, medical history, and current health conditions. Of note, 51.2% of SCA cases and 8.8% of control participants had CKD, and 20.0% of cases and 0.7% of the control group were on dialysis.
- Pre-SCA echocardiograms were available for 48% of SCA cases and baseline echocardiograms for more than 99% of control participants.
TAKEAWAY:
- In analyses adjusted for age, sex, and clinical variables, predictors significantly associated with higher odds of SCA included: CKD (odds ratio, 7.3; 95% confidence interval, 3.8-14.3; P < .001), heavy drinking (OR, 4.5), stroke (OR, 3.1), atrial fibrillation (OR, 3.7), coronary artery disease (OR, 2.9), heart failure (OR, 2.5), and diabetes (OR, 1.5).
- Hypertension, hyperlipemia, body mass index, and current smoking status were not significantly associated with SCA.
- In adjusted analyses, heart rate (OR, 1.8 per one standard deviation [1-SD] increase), QTc interval (OR, 2.5 per 1-SD increase) and left ventricular ejection fraction (OR, 4.4 per 1-SD decrease) were significantly associated with SCA, suggesting echocardiogram evaluations could help identify Hispanic or Latinx individuals at increased risk for SCA, wrote the authors.
IN PRACTICE:
“Our study, the first to include feasible numbers of Hispanic or Latino individuals, highlights the importance of renal dysfunction as a risk factor for SCA in the community,” the authors wrote, adding that early identification and management of chronic kidney disease could reduce risk for SCA in this population.
SOURCE:
The study was conducted by Kyndaron Reinier, PhD, MPH, Cedars-Sinai Health System, Los Angeles, and colleagues. It was published online in the Journal of the American Heart Association.
LIMITATIONS:
Most participants from the HCHS/SOL study were born outside the United States, compared with about half the SCA cases, which could have influenced cardiovascular disease risk, although results did not change considerably when models were adjusted for place of birth. Study participants were predominantly of Mexican heritage, so results may not be generalizable to Hispanic or Latinx individuals from other regions. As medical history was assessed differently in the two studies, there could be some error in estimating the strength of associations. Results from echocardiographic data should be viewed as hypothesis generating because of the potential for residual bias.
DISCLOSURES:
The Ventura PRESTO study was funded, in part, by the National Institutes of Health, and National Heart, Lung, and Blood Institute. The HCHS/SOL was carried out as a collaborative study supported by contracts from the NHLBI.
A version of this article first appeared on Medscape.com.
TOPLINE:
new data show, suggesting early identification of CKD may provide an opportunity to reduce the risk in these groups. Other predictors included heavy drinking, atrial fibrillation, coronary artery disease, heart failure and diabetes.
METHODOLOGY:
- The study included 295 Hispanic or Latinx patients with out-of-hospital SCA from the PRESTO study in Ventura County, California, and 590 frequency-matched controls from the San Diego site of the population-based HCHS/SOL (Hispanic Community Health Survey/Study of Latinos); in both cohorts, men made up 70% of participants, and the median age was about 63 years.
- Researchers collected data on demographics, medical history, and current health conditions. Of note, 51.2% of SCA cases and 8.8% of control participants had CKD, and 20.0% of cases and 0.7% of the control group were on dialysis.
- Pre-SCA echocardiograms were available for 48% of SCA cases and baseline echocardiograms for more than 99% of control participants.
TAKEAWAY:
- In analyses adjusted for age, sex, and clinical variables, predictors significantly associated with higher odds of SCA included: CKD (odds ratio, 7.3; 95% confidence interval, 3.8-14.3; P < .001), heavy drinking (OR, 4.5), stroke (OR, 3.1), atrial fibrillation (OR, 3.7), coronary artery disease (OR, 2.9), heart failure (OR, 2.5), and diabetes (OR, 1.5).
- Hypertension, hyperlipemia, body mass index, and current smoking status were not significantly associated with SCA.
- In adjusted analyses, heart rate (OR, 1.8 per one standard deviation [1-SD] increase), QTc interval (OR, 2.5 per 1-SD increase) and left ventricular ejection fraction (OR, 4.4 per 1-SD decrease) were significantly associated with SCA, suggesting echocardiogram evaluations could help identify Hispanic or Latinx individuals at increased risk for SCA, wrote the authors.
IN PRACTICE:
“Our study, the first to include feasible numbers of Hispanic or Latino individuals, highlights the importance of renal dysfunction as a risk factor for SCA in the community,” the authors wrote, adding that early identification and management of chronic kidney disease could reduce risk for SCA in this population.
SOURCE:
The study was conducted by Kyndaron Reinier, PhD, MPH, Cedars-Sinai Health System, Los Angeles, and colleagues. It was published online in the Journal of the American Heart Association.
LIMITATIONS:
Most participants from the HCHS/SOL study were born outside the United States, compared with about half the SCA cases, which could have influenced cardiovascular disease risk, although results did not change considerably when models were adjusted for place of birth. Study participants were predominantly of Mexican heritage, so results may not be generalizable to Hispanic or Latinx individuals from other regions. As medical history was assessed differently in the two studies, there could be some error in estimating the strength of associations. Results from echocardiographic data should be viewed as hypothesis generating because of the potential for residual bias.
DISCLOSURES:
The Ventura PRESTO study was funded, in part, by the National Institutes of Health, and National Heart, Lung, and Blood Institute. The HCHS/SOL was carried out as a collaborative study supported by contracts from the NHLBI.
A version of this article first appeared on Medscape.com.
Suits or joggers? A doctor’s dress code
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.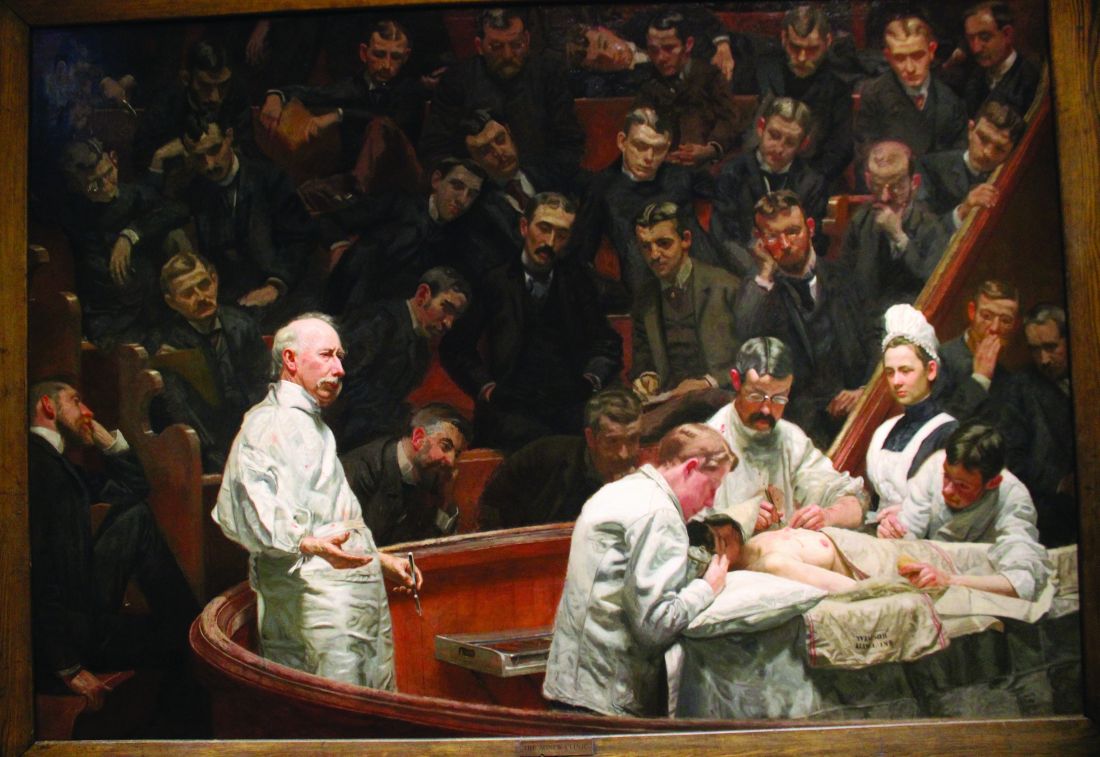
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.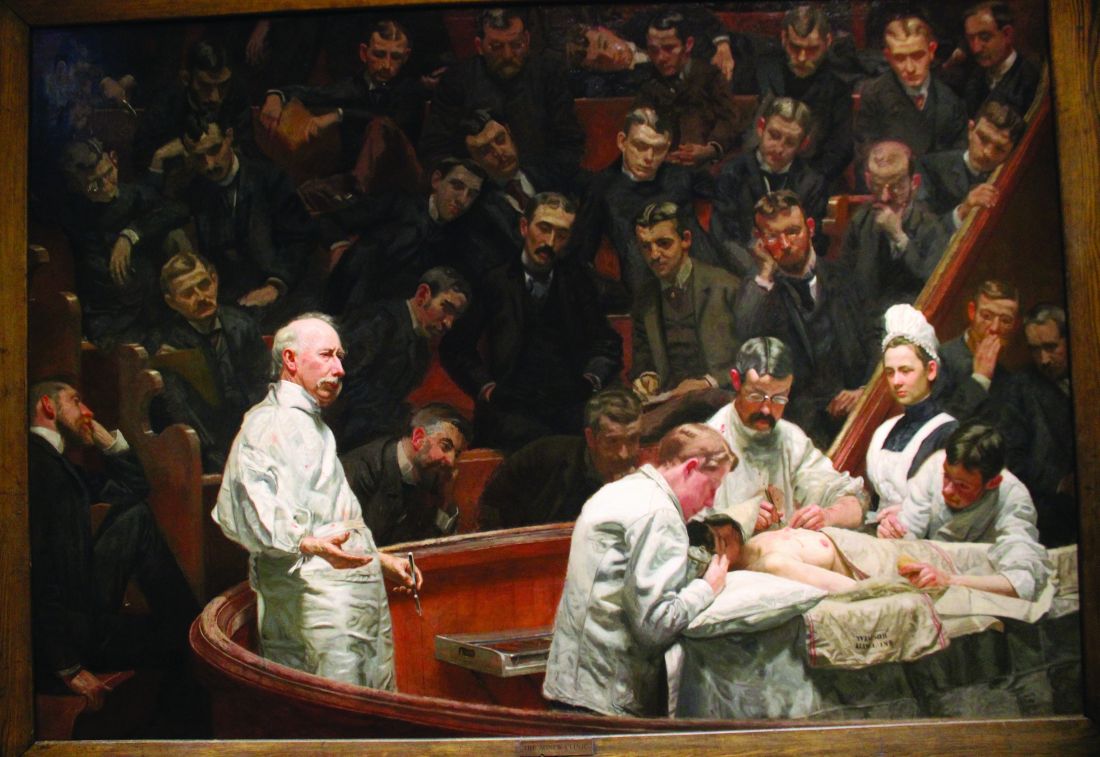
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.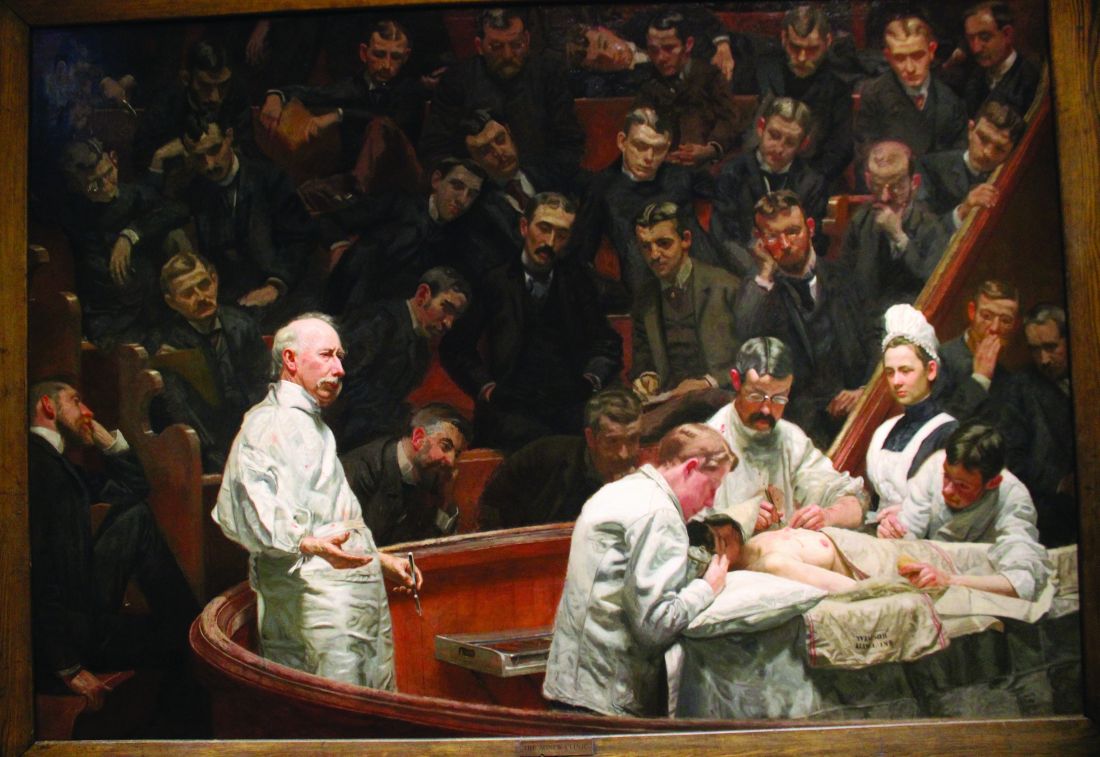
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Doublet therapy ups survival in metastatic prostate cancer
TOPLINE:
Swedish registry data show.
METHODOLOGY:
- The use of doublet therapy has increased significantly in Sweden in recent years given the growing body of evidence demonstrating that doublet therapy improves survival in individuals with de novo metastatic castration-sensitive prostate cancer.
- Investigators wanted to see whether the increasing use of doublet therapy in this patient population has improved survival when taking various other factors into consideration.
- The analysis, which included 11,382 men diagnosed with metastatic castration-sensitive prostate cancer in Sweden from 2008-2020 and registered in the country’s National Prostate Cancer Register, explored the use of doublet therapy over time and its association with survival, adjusting for age, comorbidities, and cancer characteristics.
- The researchers estimated average 5-year and 10-year survival over time using a survival model.
TAKEAWAY:
- During the study period, patients exhibited a shift toward less advanced prostate cancer, with median prostate-specific antigen (PSA) levels at diagnosis decreasing from 145 to 107 ng/mL in men with metastatic disease.
- Upfront treatment with doublet therapy in these men simultaneously increased from 1% in 2016 to 44% in 2020.
- Adjusted 5-year overall survival increased from 26% between 2008-2012 to 35% in the period 2017-2020; in the 5 years following diagnosis, patients’ mean survival increased by about 6 months between 2008-2012 and 2017-2020.
- The percentage of patients still alive at 10 years doubled from 9% in 2008 to 18% in 2020. Improvements were greater in men younger than 80 years old.
IN PRACTICE:
“A clinically meaningful increase in long-term survival was observed in men diagnosed with de novo [metastatic castration-sensitive prostate cancer] between 2008 and 2020 in Sweden. We argue that the main reason for this improvement was the increased upfront use of doublet therapy,” the authors concluded.
SOURCE:
The study, with first author Christian Corsini, MD, of Uppsala (Sweden) University, was published online in JAMA Network Open.
LIMITATIONS:
Although there were no substantial changes in the diagnostic workup, unmeasured and unknown changes over the years may have affected survival. The researchers lacked information on PSA levels during follow-up, and therefore could not assess progression-free survival. Some upfront docetaxel use was not captured before 2017.
DISCLOSURES:
The study received funding from the Swedish Cancer Society and Region Uppsala. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
Swedish registry data show.
METHODOLOGY:
- The use of doublet therapy has increased significantly in Sweden in recent years given the growing body of evidence demonstrating that doublet therapy improves survival in individuals with de novo metastatic castration-sensitive prostate cancer.
- Investigators wanted to see whether the increasing use of doublet therapy in this patient population has improved survival when taking various other factors into consideration.
- The analysis, which included 11,382 men diagnosed with metastatic castration-sensitive prostate cancer in Sweden from 2008-2020 and registered in the country’s National Prostate Cancer Register, explored the use of doublet therapy over time and its association with survival, adjusting for age, comorbidities, and cancer characteristics.
- The researchers estimated average 5-year and 10-year survival over time using a survival model.
TAKEAWAY:
- During the study period, patients exhibited a shift toward less advanced prostate cancer, with median prostate-specific antigen (PSA) levels at diagnosis decreasing from 145 to 107 ng/mL in men with metastatic disease.
- Upfront treatment with doublet therapy in these men simultaneously increased from 1% in 2016 to 44% in 2020.
- Adjusted 5-year overall survival increased from 26% between 2008-2012 to 35% in the period 2017-2020; in the 5 years following diagnosis, patients’ mean survival increased by about 6 months between 2008-2012 and 2017-2020.
- The percentage of patients still alive at 10 years doubled from 9% in 2008 to 18% in 2020. Improvements were greater in men younger than 80 years old.
IN PRACTICE:
“A clinically meaningful increase in long-term survival was observed in men diagnosed with de novo [metastatic castration-sensitive prostate cancer] between 2008 and 2020 in Sweden. We argue that the main reason for this improvement was the increased upfront use of doublet therapy,” the authors concluded.
SOURCE:
The study, with first author Christian Corsini, MD, of Uppsala (Sweden) University, was published online in JAMA Network Open.
LIMITATIONS:
Although there were no substantial changes in the diagnostic workup, unmeasured and unknown changes over the years may have affected survival. The researchers lacked information on PSA levels during follow-up, and therefore could not assess progression-free survival. Some upfront docetaxel use was not captured before 2017.
DISCLOSURES:
The study received funding from the Swedish Cancer Society and Region Uppsala. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
Swedish registry data show.
METHODOLOGY:
- The use of doublet therapy has increased significantly in Sweden in recent years given the growing body of evidence demonstrating that doublet therapy improves survival in individuals with de novo metastatic castration-sensitive prostate cancer.
- Investigators wanted to see whether the increasing use of doublet therapy in this patient population has improved survival when taking various other factors into consideration.
- The analysis, which included 11,382 men diagnosed with metastatic castration-sensitive prostate cancer in Sweden from 2008-2020 and registered in the country’s National Prostate Cancer Register, explored the use of doublet therapy over time and its association with survival, adjusting for age, comorbidities, and cancer characteristics.
- The researchers estimated average 5-year and 10-year survival over time using a survival model.
TAKEAWAY:
- During the study period, patients exhibited a shift toward less advanced prostate cancer, with median prostate-specific antigen (PSA) levels at diagnosis decreasing from 145 to 107 ng/mL in men with metastatic disease.
- Upfront treatment with doublet therapy in these men simultaneously increased from 1% in 2016 to 44% in 2020.
- Adjusted 5-year overall survival increased from 26% between 2008-2012 to 35% in the period 2017-2020; in the 5 years following diagnosis, patients’ mean survival increased by about 6 months between 2008-2012 and 2017-2020.
- The percentage of patients still alive at 10 years doubled from 9% in 2008 to 18% in 2020. Improvements were greater in men younger than 80 years old.
IN PRACTICE:
“A clinically meaningful increase in long-term survival was observed in men diagnosed with de novo [metastatic castration-sensitive prostate cancer] between 2008 and 2020 in Sweden. We argue that the main reason for this improvement was the increased upfront use of doublet therapy,” the authors concluded.
SOURCE:
The study, with first author Christian Corsini, MD, of Uppsala (Sweden) University, was published online in JAMA Network Open.
LIMITATIONS:
Although there were no substantial changes in the diagnostic workup, unmeasured and unknown changes over the years may have affected survival. The researchers lacked information on PSA levels during follow-up, and therefore could not assess progression-free survival. Some upfront docetaxel use was not captured before 2017.
DISCLOSURES:
The study received funding from the Swedish Cancer Society and Region Uppsala. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Metformin, weight management to stop type 2 diabetes in kids
TOPLINE:
Nearly one in five adolescents are living with prediabetes, a condition where blood glucose levels are elevated, but are not high enough for a type 2 diabetes (T2D) diagnosis. According to a new study, higher levels of nonfasting glucose and hemoglobin A1c, and worsening obesity are important predictors of progression to T2D. In addition, metformin and weight stabilization may prove to be important interventions for preventing T2D in kids.
METHODOLOGY:
- Researchers did a retrospective chart review of patient data from Vanderbilt University Medical Center Pediatric Prediabetes Clinic, Nashville, Tenn., from May 2015 to August 2022.
- The study included 552 children with prediabetes, defined as abnormal blood glucose (fasting plasma glucose [FPG] ≥ 100 mg/dL, random glucose ≥ 150 mg/dL), or hemoglobin A1c equal to or greater than 5.9%.
- Based on follow-up visits, patients were classified as having progressed to T2D, or nonprogression.
- Researchers analyzed the patients’ initial visit A1c, fasting C-peptide, 2-hour glucose, fasting glucose, and body mass index (BMI), among other baseline characteristics.
TAKEAWAY:
- Thirty-six children (6.5%) progressed to T2D during the duration of the study period.
- The average time to T2D diagnosis was much longer in patients taking metformin (43 months), compared with those not taking the prescribed medication (28 months).
- Worsening obesity was strongly associated with T2D progression – patients who progressed to T2D had a higher BMI at baseline and had continued weight gain.
- A higher baseline A1c, fasting C-peptide, and 2-hour glucose were also associated with progression to T2D.
- In the multivariable analysis, both A1c and 2-hour glucose were strong independent predictors of progression.
- Fasting plasma glucose was not associated with progression to T2D.
IN PRACTICE:
“Weight stabilization and metformin therapy could be important interventions for diabetes prevention in children,” study author Ashley H. Shoemaker, MD, MSci, a pediatric endocrinologist at Vanderbilt University Medical Center in Nashville, Tenn., said in a press release.
In addition, A1c plus a nonfasting glucose may be a feasible way to identify high-risk pediatric patients in a clinical setting.
SOURCE:
This study was performed by Natasha Belsky, Jaclyn Tamaroff, and Ashley H. Shoemaker of the Vanderbilt University Medical Center and the Vanderbilt University School of Medicine in Nashville, Tenn. It was published October 12, 2023, in the Journal of the Endocrine Society
LIMITATIONS:
Additional patients who developed T2D may have been lost to follow-up, since the authors did not contact patients to confirm their disease status. The authors were also unable to establish racial differences in the progression to T2D because of missing data.
DISCLOSURES:
Funding for this study was provided by the National Center for Advancing Translational Sciences. One author has research contracts with Novo Nordisk and Boehringer Ingelheim.
A version of this article first appeared on Medscape.com.
TOPLINE:
Nearly one in five adolescents are living with prediabetes, a condition where blood glucose levels are elevated, but are not high enough for a type 2 diabetes (T2D) diagnosis. According to a new study, higher levels of nonfasting glucose and hemoglobin A1c, and worsening obesity are important predictors of progression to T2D. In addition, metformin and weight stabilization may prove to be important interventions for preventing T2D in kids.
METHODOLOGY:
- Researchers did a retrospective chart review of patient data from Vanderbilt University Medical Center Pediatric Prediabetes Clinic, Nashville, Tenn., from May 2015 to August 2022.
- The study included 552 children with prediabetes, defined as abnormal blood glucose (fasting plasma glucose [FPG] ≥ 100 mg/dL, random glucose ≥ 150 mg/dL), or hemoglobin A1c equal to or greater than 5.9%.
- Based on follow-up visits, patients were classified as having progressed to T2D, or nonprogression.
- Researchers analyzed the patients’ initial visit A1c, fasting C-peptide, 2-hour glucose, fasting glucose, and body mass index (BMI), among other baseline characteristics.
TAKEAWAY:
- Thirty-six children (6.5%) progressed to T2D during the duration of the study period.
- The average time to T2D diagnosis was much longer in patients taking metformin (43 months), compared with those not taking the prescribed medication (28 months).
- Worsening obesity was strongly associated with T2D progression – patients who progressed to T2D had a higher BMI at baseline and had continued weight gain.
- A higher baseline A1c, fasting C-peptide, and 2-hour glucose were also associated with progression to T2D.
- In the multivariable analysis, both A1c and 2-hour glucose were strong independent predictors of progression.
- Fasting plasma glucose was not associated with progression to T2D.
IN PRACTICE:
“Weight stabilization and metformin therapy could be important interventions for diabetes prevention in children,” study author Ashley H. Shoemaker, MD, MSci, a pediatric endocrinologist at Vanderbilt University Medical Center in Nashville, Tenn., said in a press release.
In addition, A1c plus a nonfasting glucose may be a feasible way to identify high-risk pediatric patients in a clinical setting.
SOURCE:
This study was performed by Natasha Belsky, Jaclyn Tamaroff, and Ashley H. Shoemaker of the Vanderbilt University Medical Center and the Vanderbilt University School of Medicine in Nashville, Tenn. It was published October 12, 2023, in the Journal of the Endocrine Society
LIMITATIONS:
Additional patients who developed T2D may have been lost to follow-up, since the authors did not contact patients to confirm their disease status. The authors were also unable to establish racial differences in the progression to T2D because of missing data.
DISCLOSURES:
Funding for this study was provided by the National Center for Advancing Translational Sciences. One author has research contracts with Novo Nordisk and Boehringer Ingelheim.
A version of this article first appeared on Medscape.com.
TOPLINE:
Nearly one in five adolescents are living with prediabetes, a condition where blood glucose levels are elevated, but are not high enough for a type 2 diabetes (T2D) diagnosis. According to a new study, higher levels of nonfasting glucose and hemoglobin A1c, and worsening obesity are important predictors of progression to T2D. In addition, metformin and weight stabilization may prove to be important interventions for preventing T2D in kids.
METHODOLOGY:
- Researchers did a retrospective chart review of patient data from Vanderbilt University Medical Center Pediatric Prediabetes Clinic, Nashville, Tenn., from May 2015 to August 2022.
- The study included 552 children with prediabetes, defined as abnormal blood glucose (fasting plasma glucose [FPG] ≥ 100 mg/dL, random glucose ≥ 150 mg/dL), or hemoglobin A1c equal to or greater than 5.9%.
- Based on follow-up visits, patients were classified as having progressed to T2D, or nonprogression.
- Researchers analyzed the patients’ initial visit A1c, fasting C-peptide, 2-hour glucose, fasting glucose, and body mass index (BMI), among other baseline characteristics.
TAKEAWAY:
- Thirty-six children (6.5%) progressed to T2D during the duration of the study period.
- The average time to T2D diagnosis was much longer in patients taking metformin (43 months), compared with those not taking the prescribed medication (28 months).
- Worsening obesity was strongly associated with T2D progression – patients who progressed to T2D had a higher BMI at baseline and had continued weight gain.
- A higher baseline A1c, fasting C-peptide, and 2-hour glucose were also associated with progression to T2D.
- In the multivariable analysis, both A1c and 2-hour glucose were strong independent predictors of progression.
- Fasting plasma glucose was not associated with progression to T2D.
IN PRACTICE:
“Weight stabilization and metformin therapy could be important interventions for diabetes prevention in children,” study author Ashley H. Shoemaker, MD, MSci, a pediatric endocrinologist at Vanderbilt University Medical Center in Nashville, Tenn., said in a press release.
In addition, A1c plus a nonfasting glucose may be a feasible way to identify high-risk pediatric patients in a clinical setting.
SOURCE:
This study was performed by Natasha Belsky, Jaclyn Tamaroff, and Ashley H. Shoemaker of the Vanderbilt University Medical Center and the Vanderbilt University School of Medicine in Nashville, Tenn. It was published October 12, 2023, in the Journal of the Endocrine Society
LIMITATIONS:
Additional patients who developed T2D may have been lost to follow-up, since the authors did not contact patients to confirm their disease status. The authors were also unable to establish racial differences in the progression to T2D because of missing data.
DISCLOSURES:
Funding for this study was provided by the National Center for Advancing Translational Sciences. One author has research contracts with Novo Nordisk and Boehringer Ingelheim.
A version of this article first appeared on Medscape.com.
New ‘twincretin’ pemvidutide: Another option for obesity
HAMBURG, GERMANY – , adding a different type of “twincretin” to a growing mix of incretin-based weight-loss drugs in development that also offer additional benefits.
Pemvidutide (Altimmune Inc) is a long-acting “balanced” dual agonist of both glucagon-like peptide 1 (GLP-1) and glucagon that is in development for the treatment of obesity and nonalcoholic steatohepatitis (NASH) but not type 2 diabetes, as its effect on glucose is neutral. Phase 1 data for pemvidutide’s liver effect were presented in 2022.
In contrast, the dual GLP-1-glucose-dependent insulinotropic polypeptide (GIP) agonist tirzepatide (Mounjaro, Lilly) has been approved for the treatment of type 2 diabetes. It awaits an indication for obesity.
“When you look [at] the results for any given agent, think about obesity as a series of problems. Some overlap, and some don’t. While about 20%-25% of people with obesity also have type 2 diabetes, not everybody does. So the compounds that don’t lower glucose ... those will be great for others who have [fatty liver disease] or hyperlipidemia. ... It’s not going to be one compound for everybody,” said Louis J. Aronne, MD, director of the center for weight management and metabolic clinical research, Weill Cornell Medicine, New York.
Results of a new 24-week interim analysis of data from the phase 2 pemvidutide trial, called MOMENTUM, were presented at the annual meeting of the European Association for the Study of Diabetes by Dr. Aronne.
Included in that session were encore presentations of data for another GLP-1-glucagon dual agonist, survodutide, as well as data for Eli Lilly’s GLP-1-GIP-glucagon “triagonist,” retatrutide. Retatrutide is in development to induce weight loss, while survodutide (Boehringer Ingelheim and Zealand Pharma), like pemvidutide, is in development to induce weight loss and treat fatty liver disease.
Added Dr. Aronne, “As good as [the triple agonist] retatrutide looks, I doubt that every single person with obesity in the world will be treated with it. ... Think about this as a field, the way you treat diabetes and every other chronic illness.”
Asked to comment, session moderator Rajna Golubic, PhD, of the Oxford (England) Centre for Diabetes, Endocrinology and Metabolism, told this news organization, “We need to think in terms of treating beyond weight loss. ... We need to look at the person holistically and at other aspects of cardiometabolic health and treat in a personalized way and choose treatments according to the comorbidities people have.”
Regarding the dual GLP-1-glucagon agonists, including pemvidutide, Dr. Golubic pointed out that the glucagon agonism does the opposite of glucose-lowering agents but that the compound is “balanced for greater affinity for the GLP-1 receptor vs. glucagon, so that the beneficial effects outweigh the effect for glucose but it still harnesses the benefits of glucagon on liver with a decrease in liver fat, with positive effects on heart, positive effects on kidneys, and other beneficial metabolic effects.”
Pemvidutide lowers weight, LDL cholesterol, triglycerides, and blood pressure
Dr. Aronne began his presentation by noting that dyslipidemia, fatty liver disease, and hypertension are the most significant comorbidities of obesity, occurring in 66%-70%, 58%-75%, and 45%-55% of patients, respectively, while type 2 diabetes is less common, at 19%-23%.
Pemvidutide’s GLP-1 receptor agonism reduces appetite, inflammation, and gastric emptying, while glucagon agonism increases lipolysis, mobilizes fat, and increases energy expenditure, Dr. Aronne explained.
The 48-week phase 2 MOMENTUM trial randomly assigned 320 participants with overweight or obesity and at least one obesity-related comorbidity but not diabetes to receive weekly doses of 1.2 mg, 1.8 mg, or 2.4 mg of pemvidutide or placebo. The two lower pemvidutide doses were initiated immediately without titration, while the 2.4-mg dose was titrated rapidly over 4 weeks.
In a prespecified interim analysis of 160 participants, the percent body weight loss at 24 weeks was 10.7%, 9.4%, and 7.3% with the 2.4-mg, 1.8-mg, and 1.2-mg doses, respectively (P < .001). All weight loss values were significant; weight loss with placebo was a nonsignificant 1%.
The proportions of patients who lost at least 5% of their body weight were 84.6%, 66.7%, and 66.7%, respectively, vs. 25% with placebo. Half of the patients who received the 2.4-mg and 1.8-mg doses lost at least 10% of their body weight. Reductions in waist circumference followed suit; the patients who received the 2.4-mg dose lost an average of 10.2 cm, or “in the U.S., about 4 inches or 4 belt loops. That’s pretty good, you need a new belt,” Dr. Aronne commented.
Significant reductions in total cholesterol and triglyceride levels were also seen at week 24 by 16.5% and 25.0%, respectively, with the 2.4-mg dose. Low-density lipoprotein cholesterol levels also dropped, although not significantly; high-density lipoprotein levels dropped significantly.
Systolic blood pressure dropped by 5.5 mm Hg, and diastolic blood pressure dropped by 1.8 mm Hg in the 2.4-mg group and by lesser degrees among the patients who received lower doses. There were no significant changes in heart rate, Dr. Aronne noted.
Glucose homeostasis was preserved in all groups throughout the 24 weeks.
As with all drugs in the incretin class, gastrointestinal adverse events were common. Severe vomiting occurred in one person in the 1.8-mg group and in four with 2.4 mg. Efforts will be made to reduce that in subsequent trials, Dr. Aronne said.
“We have learned over time that going more gradually in titrating up these agents is a better strategy, allowing dose reduction may be a better strategy, and allowing antiemetics temporarily as we increase the dose is a lesson that many have learned doing these trials and of course in our clinical practices,” he commented.
Dr. Golubic told this news organization that the recent emergence of potent incretin-based weight loss drugs is “a huge paradigm shift. The prevalence of obesity will be 35% or higher by 2035. Bariatric surgery isn’t feasible for everyone, and it’s very expensive, so we need drugs to provide benefits in terms of lowering weight, glucose, and other cardiometabolic risk factors.”
The full 48-week data for MOMENTUM will be announced in the fourth quarter of 2023.
Dr. Aronne has received consulting fees from and serves on advisory boards for Allurion, Altimmune, Atria, Gelesis, Jamieson Wellness, Janssen Pharmaceuticals, Jazz Pharmaceuticals, Novo Nordisk, Pfizer, Optum, Eli Lilly, Senda Biosciences, and Versanis; has received research funding from Allurion, AstraZeneca, Gelesis, Janssen Pharmaceuticals, Novo Nordisk, and Eli Lilly; has equity interests in Allurion, ERX Pharmaceuticals, Gelesis, Intellihealth, Jamieson Wellness, and Myos Corp; and serves on a board of directors for ERX Pharmaceuticals, Intellihealth, and Jamieson Wellness. Dr. Golubic has received research support from AstraZeneca.
A version of this article first appeared on Medscape.com.
HAMBURG, GERMANY – , adding a different type of “twincretin” to a growing mix of incretin-based weight-loss drugs in development that also offer additional benefits.
Pemvidutide (Altimmune Inc) is a long-acting “balanced” dual agonist of both glucagon-like peptide 1 (GLP-1) and glucagon that is in development for the treatment of obesity and nonalcoholic steatohepatitis (NASH) but not type 2 diabetes, as its effect on glucose is neutral. Phase 1 data for pemvidutide’s liver effect were presented in 2022.
In contrast, the dual GLP-1-glucose-dependent insulinotropic polypeptide (GIP) agonist tirzepatide (Mounjaro, Lilly) has been approved for the treatment of type 2 diabetes. It awaits an indication for obesity.
“When you look [at] the results for any given agent, think about obesity as a series of problems. Some overlap, and some don’t. While about 20%-25% of people with obesity also have type 2 diabetes, not everybody does. So the compounds that don’t lower glucose ... those will be great for others who have [fatty liver disease] or hyperlipidemia. ... It’s not going to be one compound for everybody,” said Louis J. Aronne, MD, director of the center for weight management and metabolic clinical research, Weill Cornell Medicine, New York.
Results of a new 24-week interim analysis of data from the phase 2 pemvidutide trial, called MOMENTUM, were presented at the annual meeting of the European Association for the Study of Diabetes by Dr. Aronne.
Included in that session were encore presentations of data for another GLP-1-glucagon dual agonist, survodutide, as well as data for Eli Lilly’s GLP-1-GIP-glucagon “triagonist,” retatrutide. Retatrutide is in development to induce weight loss, while survodutide (Boehringer Ingelheim and Zealand Pharma), like pemvidutide, is in development to induce weight loss and treat fatty liver disease.
Added Dr. Aronne, “As good as [the triple agonist] retatrutide looks, I doubt that every single person with obesity in the world will be treated with it. ... Think about this as a field, the way you treat diabetes and every other chronic illness.”
Asked to comment, session moderator Rajna Golubic, PhD, of the Oxford (England) Centre for Diabetes, Endocrinology and Metabolism, told this news organization, “We need to think in terms of treating beyond weight loss. ... We need to look at the person holistically and at other aspects of cardiometabolic health and treat in a personalized way and choose treatments according to the comorbidities people have.”
Regarding the dual GLP-1-glucagon agonists, including pemvidutide, Dr. Golubic pointed out that the glucagon agonism does the opposite of glucose-lowering agents but that the compound is “balanced for greater affinity for the GLP-1 receptor vs. glucagon, so that the beneficial effects outweigh the effect for glucose but it still harnesses the benefits of glucagon on liver with a decrease in liver fat, with positive effects on heart, positive effects on kidneys, and other beneficial metabolic effects.”
Pemvidutide lowers weight, LDL cholesterol, triglycerides, and blood pressure
Dr. Aronne began his presentation by noting that dyslipidemia, fatty liver disease, and hypertension are the most significant comorbidities of obesity, occurring in 66%-70%, 58%-75%, and 45%-55% of patients, respectively, while type 2 diabetes is less common, at 19%-23%.
Pemvidutide’s GLP-1 receptor agonism reduces appetite, inflammation, and gastric emptying, while glucagon agonism increases lipolysis, mobilizes fat, and increases energy expenditure, Dr. Aronne explained.
The 48-week phase 2 MOMENTUM trial randomly assigned 320 participants with overweight or obesity and at least one obesity-related comorbidity but not diabetes to receive weekly doses of 1.2 mg, 1.8 mg, or 2.4 mg of pemvidutide or placebo. The two lower pemvidutide doses were initiated immediately without titration, while the 2.4-mg dose was titrated rapidly over 4 weeks.
In a prespecified interim analysis of 160 participants, the percent body weight loss at 24 weeks was 10.7%, 9.4%, and 7.3% with the 2.4-mg, 1.8-mg, and 1.2-mg doses, respectively (P < .001). All weight loss values were significant; weight loss with placebo was a nonsignificant 1%.
The proportions of patients who lost at least 5% of their body weight were 84.6%, 66.7%, and 66.7%, respectively, vs. 25% with placebo. Half of the patients who received the 2.4-mg and 1.8-mg doses lost at least 10% of their body weight. Reductions in waist circumference followed suit; the patients who received the 2.4-mg dose lost an average of 10.2 cm, or “in the U.S., about 4 inches or 4 belt loops. That’s pretty good, you need a new belt,” Dr. Aronne commented.
Significant reductions in total cholesterol and triglyceride levels were also seen at week 24 by 16.5% and 25.0%, respectively, with the 2.4-mg dose. Low-density lipoprotein cholesterol levels also dropped, although not significantly; high-density lipoprotein levels dropped significantly.
Systolic blood pressure dropped by 5.5 mm Hg, and diastolic blood pressure dropped by 1.8 mm Hg in the 2.4-mg group and by lesser degrees among the patients who received lower doses. There were no significant changes in heart rate, Dr. Aronne noted.
Glucose homeostasis was preserved in all groups throughout the 24 weeks.
As with all drugs in the incretin class, gastrointestinal adverse events were common. Severe vomiting occurred in one person in the 1.8-mg group and in four with 2.4 mg. Efforts will be made to reduce that in subsequent trials, Dr. Aronne said.
“We have learned over time that going more gradually in titrating up these agents is a better strategy, allowing dose reduction may be a better strategy, and allowing antiemetics temporarily as we increase the dose is a lesson that many have learned doing these trials and of course in our clinical practices,” he commented.
Dr. Golubic told this news organization that the recent emergence of potent incretin-based weight loss drugs is “a huge paradigm shift. The prevalence of obesity will be 35% or higher by 2035. Bariatric surgery isn’t feasible for everyone, and it’s very expensive, so we need drugs to provide benefits in terms of lowering weight, glucose, and other cardiometabolic risk factors.”
The full 48-week data for MOMENTUM will be announced in the fourth quarter of 2023.
Dr. Aronne has received consulting fees from and serves on advisory boards for Allurion, Altimmune, Atria, Gelesis, Jamieson Wellness, Janssen Pharmaceuticals, Jazz Pharmaceuticals, Novo Nordisk, Pfizer, Optum, Eli Lilly, Senda Biosciences, and Versanis; has received research funding from Allurion, AstraZeneca, Gelesis, Janssen Pharmaceuticals, Novo Nordisk, and Eli Lilly; has equity interests in Allurion, ERX Pharmaceuticals, Gelesis, Intellihealth, Jamieson Wellness, and Myos Corp; and serves on a board of directors for ERX Pharmaceuticals, Intellihealth, and Jamieson Wellness. Dr. Golubic has received research support from AstraZeneca.
A version of this article first appeared on Medscape.com.
HAMBURG, GERMANY – , adding a different type of “twincretin” to a growing mix of incretin-based weight-loss drugs in development that also offer additional benefits.
Pemvidutide (Altimmune Inc) is a long-acting “balanced” dual agonist of both glucagon-like peptide 1 (GLP-1) and glucagon that is in development for the treatment of obesity and nonalcoholic steatohepatitis (NASH) but not type 2 diabetes, as its effect on glucose is neutral. Phase 1 data for pemvidutide’s liver effect were presented in 2022.
In contrast, the dual GLP-1-glucose-dependent insulinotropic polypeptide (GIP) agonist tirzepatide (Mounjaro, Lilly) has been approved for the treatment of type 2 diabetes. It awaits an indication for obesity.
“When you look [at] the results for any given agent, think about obesity as a series of problems. Some overlap, and some don’t. While about 20%-25% of people with obesity also have type 2 diabetes, not everybody does. So the compounds that don’t lower glucose ... those will be great for others who have [fatty liver disease] or hyperlipidemia. ... It’s not going to be one compound for everybody,” said Louis J. Aronne, MD, director of the center for weight management and metabolic clinical research, Weill Cornell Medicine, New York.
Results of a new 24-week interim analysis of data from the phase 2 pemvidutide trial, called MOMENTUM, were presented at the annual meeting of the European Association for the Study of Diabetes by Dr. Aronne.
Included in that session were encore presentations of data for another GLP-1-glucagon dual agonist, survodutide, as well as data for Eli Lilly’s GLP-1-GIP-glucagon “triagonist,” retatrutide. Retatrutide is in development to induce weight loss, while survodutide (Boehringer Ingelheim and Zealand Pharma), like pemvidutide, is in development to induce weight loss and treat fatty liver disease.
Added Dr. Aronne, “As good as [the triple agonist] retatrutide looks, I doubt that every single person with obesity in the world will be treated with it. ... Think about this as a field, the way you treat diabetes and every other chronic illness.”
Asked to comment, session moderator Rajna Golubic, PhD, of the Oxford (England) Centre for Diabetes, Endocrinology and Metabolism, told this news organization, “We need to think in terms of treating beyond weight loss. ... We need to look at the person holistically and at other aspects of cardiometabolic health and treat in a personalized way and choose treatments according to the comorbidities people have.”
Regarding the dual GLP-1-glucagon agonists, including pemvidutide, Dr. Golubic pointed out that the glucagon agonism does the opposite of glucose-lowering agents but that the compound is “balanced for greater affinity for the GLP-1 receptor vs. glucagon, so that the beneficial effects outweigh the effect for glucose but it still harnesses the benefits of glucagon on liver with a decrease in liver fat, with positive effects on heart, positive effects on kidneys, and other beneficial metabolic effects.”
Pemvidutide lowers weight, LDL cholesterol, triglycerides, and blood pressure
Dr. Aronne began his presentation by noting that dyslipidemia, fatty liver disease, and hypertension are the most significant comorbidities of obesity, occurring in 66%-70%, 58%-75%, and 45%-55% of patients, respectively, while type 2 diabetes is less common, at 19%-23%.
Pemvidutide’s GLP-1 receptor agonism reduces appetite, inflammation, and gastric emptying, while glucagon agonism increases lipolysis, mobilizes fat, and increases energy expenditure, Dr. Aronne explained.
The 48-week phase 2 MOMENTUM trial randomly assigned 320 participants with overweight or obesity and at least one obesity-related comorbidity but not diabetes to receive weekly doses of 1.2 mg, 1.8 mg, or 2.4 mg of pemvidutide or placebo. The two lower pemvidutide doses were initiated immediately without titration, while the 2.4-mg dose was titrated rapidly over 4 weeks.
In a prespecified interim analysis of 160 participants, the percent body weight loss at 24 weeks was 10.7%, 9.4%, and 7.3% with the 2.4-mg, 1.8-mg, and 1.2-mg doses, respectively (P < .001). All weight loss values were significant; weight loss with placebo was a nonsignificant 1%.
The proportions of patients who lost at least 5% of their body weight were 84.6%, 66.7%, and 66.7%, respectively, vs. 25% with placebo. Half of the patients who received the 2.4-mg and 1.8-mg doses lost at least 10% of their body weight. Reductions in waist circumference followed suit; the patients who received the 2.4-mg dose lost an average of 10.2 cm, or “in the U.S., about 4 inches or 4 belt loops. That’s pretty good, you need a new belt,” Dr. Aronne commented.
Significant reductions in total cholesterol and triglyceride levels were also seen at week 24 by 16.5% and 25.0%, respectively, with the 2.4-mg dose. Low-density lipoprotein cholesterol levels also dropped, although not significantly; high-density lipoprotein levels dropped significantly.
Systolic blood pressure dropped by 5.5 mm Hg, and diastolic blood pressure dropped by 1.8 mm Hg in the 2.4-mg group and by lesser degrees among the patients who received lower doses. There were no significant changes in heart rate, Dr. Aronne noted.
Glucose homeostasis was preserved in all groups throughout the 24 weeks.
As with all drugs in the incretin class, gastrointestinal adverse events were common. Severe vomiting occurred in one person in the 1.8-mg group and in four with 2.4 mg. Efforts will be made to reduce that in subsequent trials, Dr. Aronne said.
“We have learned over time that going more gradually in titrating up these agents is a better strategy, allowing dose reduction may be a better strategy, and allowing antiemetics temporarily as we increase the dose is a lesson that many have learned doing these trials and of course in our clinical practices,” he commented.
Dr. Golubic told this news organization that the recent emergence of potent incretin-based weight loss drugs is “a huge paradigm shift. The prevalence of obesity will be 35% or higher by 2035. Bariatric surgery isn’t feasible for everyone, and it’s very expensive, so we need drugs to provide benefits in terms of lowering weight, glucose, and other cardiometabolic risk factors.”
The full 48-week data for MOMENTUM will be announced in the fourth quarter of 2023.
Dr. Aronne has received consulting fees from and serves on advisory boards for Allurion, Altimmune, Atria, Gelesis, Jamieson Wellness, Janssen Pharmaceuticals, Jazz Pharmaceuticals, Novo Nordisk, Pfizer, Optum, Eli Lilly, Senda Biosciences, and Versanis; has received research funding from Allurion, AstraZeneca, Gelesis, Janssen Pharmaceuticals, Novo Nordisk, and Eli Lilly; has equity interests in Allurion, ERX Pharmaceuticals, Gelesis, Intellihealth, Jamieson Wellness, and Myos Corp; and serves on a board of directors for ERX Pharmaceuticals, Intellihealth, and Jamieson Wellness. Dr. Golubic has received research support from AstraZeneca.
A version of this article first appeared on Medscape.com.
AT EASD 2023
Lack of time is damaging women’s health
Various speakers at the VII National Conference of the Onda Foundation, Italy’s National Observatory for Women and Gender’s Health, focused on this topic. The conference was dedicated to the social factors that determine health within the context of gender medicine.
In our society, housework and raising a family are responsibilities placed predominantly on the shoulders of women. These responsibilities contribute significantly to women’s daily workload. The most overburdened women are working mothers (according to ISTAT, Italy’s Office for National Statistics, 2019), who are forced to combine their professional responsibilities with family life, dedicating 8 hours and 20 minutes per day to paid and unpaid work overall, compared with the 7 hours and 29 minutes spent by working fathers. Working mothers between ages 25 and 44 years have on average 2 hours and 35 minutes of free time per day.
Stress and sleep deprivation
“Under these conditions, the risk of chronic stress is raised, and stress leads to depression. The rate of depression in the female population is double that of the male population,” said Claudio Mencacci, MD, chair of the Italian Society of Neuropsychopharmacology and the Onda Foundation. “What’s more, stress increases the risk of cardiovascular and metabolic diseases, asthma, arthritis, and autoimmune diseases.”
The one thing that is especially damaging to physical and mental health is sleep deprivation, and working mothers get less sleep than do working fathers. “This is partially due to biological factors: hormonal changes that take place toward the end of adolescence in women during the premenstrual period are responsible for an increased rate of sleep disturbance and insomnia,” said Dr. Mencacci. “During pregnancy and the postpartum period, female sex hormones make sleep lighter, reducing time spent in the REM sleep stage. Then there’s the social aspect that plays a decisive role: by and large, it’s mothers who take care of the youngest children at night.”
According to a 2019 German study, during the first 6 years of life of the first child, a mother loses on average 44 minutes sleep per night, compared with the average time spent sleeping before pregnancy; a father loses 14 minutes.
“Another aspect to bear in mind is that, for cultural reasons, women tend to overlook the issue and not seek help, deeming sleep deprivation normal,” said Dr. Mencacci.
Caregivers at greatest risk
The negative effects of stress are evident in people continuously caring for a dependent older or disabled family member, so-called caregivers. This is, “A group predominantly made up of women aged between 45 and 55 years,” said Marina Petrini, PhD, of the Italian Health Institute’s Gender Medicine Center of Excellence. Dr. Petrini coordinated a study on stress and health in family caregivers.
“The results obtained reveal a high level of stress, especially among female caregivers, who are more exposed to the risk of severe symptoms of depression, physical disorders, especially those affecting the nervous and immune systems, and who tend to adopt irregular eating patterns and sedentary habits,” said Dr. Petrini.
Limited treatment access
Another study presented at the Onda Foundation’s conference, which shows just how much a lack of “me time” can damage your health, is the Access to Diagnostic Medicine and Treatment by Region: the Patient’s Perspective Survey, conducted by market research agency Elma Research on a sample of cancer patients requiring specialist treatment.
“Forty percent of them had to move to a different region from the one they live in to get the care they needed,” said Massimo Massagrande, CEO of Elma Research. “Of that group, 40% had to move to an area not neighboring their own. The impact of area of residence is heavy, in terms of money and logistics – so much so that a large proportion of patients interviewed were forced to turn their back on the best available treatments. For women responding to our survey, the biggest obstacle is the impossibility of reconciling the effects of a move or the prospective of a temporary transfer to another region with their responsibilities for looking after their family.”
This article was translated from Univadis Italy. A version appeared on Medscape.com.
Various speakers at the VII National Conference of the Onda Foundation, Italy’s National Observatory for Women and Gender’s Health, focused on this topic. The conference was dedicated to the social factors that determine health within the context of gender medicine.
In our society, housework and raising a family are responsibilities placed predominantly on the shoulders of women. These responsibilities contribute significantly to women’s daily workload. The most overburdened women are working mothers (according to ISTAT, Italy’s Office for National Statistics, 2019), who are forced to combine their professional responsibilities with family life, dedicating 8 hours and 20 minutes per day to paid and unpaid work overall, compared with the 7 hours and 29 minutes spent by working fathers. Working mothers between ages 25 and 44 years have on average 2 hours and 35 minutes of free time per day.
Stress and sleep deprivation
“Under these conditions, the risk of chronic stress is raised, and stress leads to depression. The rate of depression in the female population is double that of the male population,” said Claudio Mencacci, MD, chair of the Italian Society of Neuropsychopharmacology and the Onda Foundation. “What’s more, stress increases the risk of cardiovascular and metabolic diseases, asthma, arthritis, and autoimmune diseases.”
The one thing that is especially damaging to physical and mental health is sleep deprivation, and working mothers get less sleep than do working fathers. “This is partially due to biological factors: hormonal changes that take place toward the end of adolescence in women during the premenstrual period are responsible for an increased rate of sleep disturbance and insomnia,” said Dr. Mencacci. “During pregnancy and the postpartum period, female sex hormones make sleep lighter, reducing time spent in the REM sleep stage. Then there’s the social aspect that plays a decisive role: by and large, it’s mothers who take care of the youngest children at night.”
According to a 2019 German study, during the first 6 years of life of the first child, a mother loses on average 44 minutes sleep per night, compared with the average time spent sleeping before pregnancy; a father loses 14 minutes.
“Another aspect to bear in mind is that, for cultural reasons, women tend to overlook the issue and not seek help, deeming sleep deprivation normal,” said Dr. Mencacci.
Caregivers at greatest risk
The negative effects of stress are evident in people continuously caring for a dependent older or disabled family member, so-called caregivers. This is, “A group predominantly made up of women aged between 45 and 55 years,” said Marina Petrini, PhD, of the Italian Health Institute’s Gender Medicine Center of Excellence. Dr. Petrini coordinated a study on stress and health in family caregivers.
“The results obtained reveal a high level of stress, especially among female caregivers, who are more exposed to the risk of severe symptoms of depression, physical disorders, especially those affecting the nervous and immune systems, and who tend to adopt irregular eating patterns and sedentary habits,” said Dr. Petrini.
Limited treatment access
Another study presented at the Onda Foundation’s conference, which shows just how much a lack of “me time” can damage your health, is the Access to Diagnostic Medicine and Treatment by Region: the Patient’s Perspective Survey, conducted by market research agency Elma Research on a sample of cancer patients requiring specialist treatment.
“Forty percent of them had to move to a different region from the one they live in to get the care they needed,” said Massimo Massagrande, CEO of Elma Research. “Of that group, 40% had to move to an area not neighboring their own. The impact of area of residence is heavy, in terms of money and logistics – so much so that a large proportion of patients interviewed were forced to turn their back on the best available treatments. For women responding to our survey, the biggest obstacle is the impossibility of reconciling the effects of a move or the prospective of a temporary transfer to another region with their responsibilities for looking after their family.”
This article was translated from Univadis Italy. A version appeared on Medscape.com.
Various speakers at the VII National Conference of the Onda Foundation, Italy’s National Observatory for Women and Gender’s Health, focused on this topic. The conference was dedicated to the social factors that determine health within the context of gender medicine.
In our society, housework and raising a family are responsibilities placed predominantly on the shoulders of women. These responsibilities contribute significantly to women’s daily workload. The most overburdened women are working mothers (according to ISTAT, Italy’s Office for National Statistics, 2019), who are forced to combine their professional responsibilities with family life, dedicating 8 hours and 20 minutes per day to paid and unpaid work overall, compared with the 7 hours and 29 minutes spent by working fathers. Working mothers between ages 25 and 44 years have on average 2 hours and 35 minutes of free time per day.
Stress and sleep deprivation
“Under these conditions, the risk of chronic stress is raised, and stress leads to depression. The rate of depression in the female population is double that of the male population,” said Claudio Mencacci, MD, chair of the Italian Society of Neuropsychopharmacology and the Onda Foundation. “What’s more, stress increases the risk of cardiovascular and metabolic diseases, asthma, arthritis, and autoimmune diseases.”
The one thing that is especially damaging to physical and mental health is sleep deprivation, and working mothers get less sleep than do working fathers. “This is partially due to biological factors: hormonal changes that take place toward the end of adolescence in women during the premenstrual period are responsible for an increased rate of sleep disturbance and insomnia,” said Dr. Mencacci. “During pregnancy and the postpartum period, female sex hormones make sleep lighter, reducing time spent in the REM sleep stage. Then there’s the social aspect that plays a decisive role: by and large, it’s mothers who take care of the youngest children at night.”
According to a 2019 German study, during the first 6 years of life of the first child, a mother loses on average 44 minutes sleep per night, compared with the average time spent sleeping before pregnancy; a father loses 14 minutes.
“Another aspect to bear in mind is that, for cultural reasons, women tend to overlook the issue and not seek help, deeming sleep deprivation normal,” said Dr. Mencacci.
Caregivers at greatest risk
The negative effects of stress are evident in people continuously caring for a dependent older or disabled family member, so-called caregivers. This is, “A group predominantly made up of women aged between 45 and 55 years,” said Marina Petrini, PhD, of the Italian Health Institute’s Gender Medicine Center of Excellence. Dr. Petrini coordinated a study on stress and health in family caregivers.
“The results obtained reveal a high level of stress, especially among female caregivers, who are more exposed to the risk of severe symptoms of depression, physical disorders, especially those affecting the nervous and immune systems, and who tend to adopt irregular eating patterns and sedentary habits,” said Dr. Petrini.
Limited treatment access
Another study presented at the Onda Foundation’s conference, which shows just how much a lack of “me time” can damage your health, is the Access to Diagnostic Medicine and Treatment by Region: the Patient’s Perspective Survey, conducted by market research agency Elma Research on a sample of cancer patients requiring specialist treatment.
“Forty percent of them had to move to a different region from the one they live in to get the care they needed,” said Massimo Massagrande, CEO of Elma Research. “Of that group, 40% had to move to an area not neighboring their own. The impact of area of residence is heavy, in terms of money and logistics – so much so that a large proportion of patients interviewed were forced to turn their back on the best available treatments. For women responding to our survey, the biggest obstacle is the impossibility of reconciling the effects of a move or the prospective of a temporary transfer to another region with their responsibilities for looking after their family.”
This article was translated from Univadis Italy. A version appeared on Medscape.com.
Tender Nodular Lesions in the Axilla and Vulva
The Diagnosis: Cutaneous Langerhans Cell Histiocytosis
Histopathologic findings of the left axillary lesion included a diffuse infiltrate of irregular hematolymphoid cells with reniform nuclei that strongly and diffusely stained positively with CD1a and S-100 but were negative for CD138 and CD163 (Figure). Numerous eosinophils also were present. The surrounding lymphocytic infiltrate stained positively with CD45. Polymerase chain reaction of the vaginal lesion was negative for herpes simplex virus types 1 and 2. Biopsy of the vaginal lesion revealed a mildly acanthotic epidermis and an aggregation of epithelioid cells with reniform nuclei in the papillary dermis. Positron emission tomography revealed widely disseminated disease. Sequencing of the mitogen-activated protein kinase/extracellular signalregulated kinase pathway showed amplified expression of these genes but found no mutations. These results led to a diagnosis of cutaneous Langerhans cell histiocytosis (LCH) with a background of hidradenitis suppurativa (HS). Our patient has since initiated therapy with trametinib leading to disease improvement without known recurrence.

Langerhans cell histiocytosis is a rare disease of clonal dendritic cells (Langerhans cells) that can present in any organ.1 Most LCH diagnoses are made in pediatric patients, most often presenting in the bones, with other presentations in the skin, hypophysis, liver, lymph nodes, lungs, and spleen occurring less commonly.2 Proto-oncogene BRAF V600E mutations are a common determinant of LCH, with half of cases linked with this mutation that leads to enhanced activation of the mitogen-activated protein kinase pathway, though other mutations have been reported.3,4 These genetic alterations suggest LCH is neoplastic in nature; however, this is controversial, as spontaneous regression among pulmonary LCH has been observed, pointing to a reactive inflammatory process.5 Cutaneous LCH can present as a distinct papular or nodular lesion or multiple lesions with possible ulceration, but it is rare that LCH first presents on the skin.2,6 There is a substantial association of cutaneous LCH with the development of systemically disseminated LCH as well as other blood tumors, such as myelomonocytic leukemia, histiocytic sarcoma, and multiple lymphomas; this association is thought to be due to the common origin of LCH and other blood diseases in the bone marrow.6
Histopathology of LCH shows a diffuse papillary dermal infiltrate of clonal proliferation of reniform or cleaved histiocytes.5 Epidermal ulceration and epidermotropism also are common. Neoplastic cells are found admixed with variable levels of eosinophils, lymphocytes, plasma cells, and neutrophils, though eosinophils typically are elevated. Immunohistochemistry characteristically shows the expression of CD1a, S-100, and/or CD207, and the absence of CD163 expression.
Treatment of LCH is primarily dependent on disease dissemination status, with splenic and hepatic involvement, genetic panel results, and central nervous system risk considered in the treatment plan.5 Langerhans cell histiocytosis localized to the skin may require follow-up and monitoring, as spontaneous regression of cutaneous LCH is common. However, topical steroids or psoralen and long-wave UV radiation are potential treatments. Physicians who diagnose unifocal cutaneous LCH should have high clinical suspicion of disseminated LCH, and laboratory and radiographic evaluation may be necessary to rule out systemic disease, as more than 40% of patients with cutaneous LCH have systemic disease upon full evaluation.7 With systemic involvement, systemic chemotherapy may reduce morbidity and mortality, but clinical response should be monitored after 6 weeks of treatment, as results are variably effective. Vinblastine is the most common chemotherapy regimen, with an 84% survival rate and 51.5% event-free survival rate after 8 years.8 Targeted therapy for common genetic mutations also is possible, as vemurafenib has been used to treat patients with the BRAF V600E mutation.
Due to the variable clinical presentation of cutaneous LCH, the lesions can mimic other common skin diseases such as eczema or seborrheic dermatitis.7 However, there are limited data on LCH presenting in infiltrative skin disease. Langerhans cell histiocytosis that was misdiagnosed as HS has been reported,9-11 but LCH presenting alongside long-standing HS is rare. Although LCH often mimics infiltrative skin diseases, its simultaneous presentation with a previously confirmed diagnosis of HS was notable in our patient.
In our patient, the differential diagnosis included HS, Actinomyces infection, lymphomatoid papulosis, and dermatofibrosarcoma protuberans. Cutaneous findings in HS include chronic acneform nodules with follicular plugging, ruptured ducts leading to epithelized sinuses, inflammation, and abscesses in the axillae or inguinal and perineal areas.11 Histopathology reveals follicular occlusion and hyperkeratinization, which cause destruction of the pilosebaceous glands. Hidradenitis suppurativa features on immunohistochemistry often are conflicting, but there consistently is co-localization of keratinocyte hyperplasia with CD3-, CD4-, CD8-, and CD68-positive staining of cells that produce tumor necrosis factor α, IL-12, IL-23, and IL-32, with CD1a staining variable.12 An infection with Actinomyces, a slow-progressing anaerobic or microaerophilic bacteria, may present in the skin with chronic suppurative inflammation on the neck, trunk, and abdomen. The classic presentation is subcutaneous nodules with localized infiltration of abscesses, fistulas, and draining sinuses.13 Morphologically, Actinomyces causes chronic granulomatous infection with 0.1- to 1-mm sulfur granules, which are seen as basophilic masses with eosinophilic terminal clubs on hematoxylin and eosin staining.14 Histopathology reveals grampositive filamentous Actinomyces bacteria that branch at the edge of the granules. Lymphomatoid papulosis, a nonaggressive T-cell lymphoma, presents as papulonodular and sometimes necrotic disseminated lesions that spontaneously can regress or can cause a higher risk for the development of more aggressive lymphomas.15 Histopathology shows consistently dense, dermal, lymphocytic infiltration. Immunohistochemistry is characterized by lymphocytes expressing CD30 of varying degrees: type A with many CD30 staining cells, type B presenting similar to mycosis fungoides with little CD30 staining, and type C with lymphocytic CD30-staining plaques. Dermatofibrosarcoma protuberans is a low-grade soft-tissue malignant tumor with extensive local infiltration characterized by asymptomatic plaques on the trunk and proximal extremities that are indurated and adhered to the skin.16 Histopathology shows extensive invasion into the adjacent tissue far from the original focus of the tumor.
- Girschikofsky M, Arico M, Castillo D, et al. Management of adult patients with Langerhans cell histiocytosis: recommendations from an expert panel on behalf of Euro-Histio-Net. Orphanet J Rare Dis. 2013;8:72. doi:10.1186/1750-1172-8-72
- Flores-Terry MA, Sanz-Trenado JL, García-Arpa M, et al. Cutaneous Langerhans cell histiocytosis presenting in adulthood. Actas Dermosifiliogr (Engl Ed). 2019;110:167-169. doi:10.1016/j .adengl.2018.12.005
- Emile J-F, Abla O, Fraitag S, et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016;127:2672-2681. doi:10.1182/blood-2016-01-690636
- Badalian-Very G, Vergilio J-A, Degar BA, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116:1919-1923. doi:10.1182/blood-2010-04-279083
- Bohn OL, Teruya-Feldstein J, Sanchez-Sosa S. Skin biopsy diagnosis of Langerhans cell neoplasms. In: Fernando S, ed. Skin Biopsy: Diagnosis and Treatment [Internet]. InTechOpen; 2013. http://dx.doi .org/10.5772/55893
- Edelbroek JR, Vermeer MH, Jansen PM, et al. Langerhans cell histiocytosis first presenting in the skin in adults: frequent association with a second haematological malignancy. Br J Dermatol. 2012;167:1287-1294. doi:10.1111/j.1365-2133.2012.11169.x
- Simko SJ, Garmezy B, Abhyankar H, et al. Differentiating skin-limited and multisystem Langerhans cell histiocytosis. J Pediatr. 2014;165: 990-996. doi:10.1016/j.jpeds.2014.07.063
- Yag˘ ci B, Varan A, Cag˘ lar M, et al. Langerhans cell histiocytosis: retrospective analysis of 217 cases in a single center. Pediatr Hematol Oncol. 2008;25:399-408. doi:10.1080/08880010802107356
- Kalen JE, Shokeen D, Mislankar M, et al. Langerhans cell histiocytosis with clinical and histologic features of hidradenitis suppurativa: brief report and review. Am J Dermatopathol. 2018;40:502-505. doi:10.1097/dad.0000000000001005
- Chertoff J, Chung J, Ataya A. Adult Langerhans cell histiocytosis masquerading as hidradenitis suppurativa. Am J Respir Crit Care Med. 2017;195:E34-E36. doi:10.1164/rccm.201610-2082IM
- St. Claire K, Bunney R, Ashack KA, et al. Langerhans cell histiocytosis: a great imitator. Clin Dermatol. 2020;38:223-234. doi:10.1016/j.clindermatol.2019.10.007
- Frew JW, Hawkes JE, Krueger JG. A systematic review and critical evaluation of immunohistochemical associations in hidradenitis suppurativa. F1000Research. 2019;7:1923. doi:10.12688/f1000research.17268.2
- Robati RM, Niknezhad N, Bidari-Zerehpoush F, et al. Primary cutaneous actinomycosis along with the surgical scar on the hand [published online November 9, 2016]. Case Rep Infect Dis. doi:10.1155/2016/5943932
- Ferry T, Valour F, Karsenty J, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Res. 2014;2014:183-197. doi:10.2147/idr.s39601
- Willemze R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005;105:3768-3785. doi:10.1182 /blood-2004-09-3502
- Tsai Y, Lin P, Chew K, et al. Dermatofibrosarcoma protuberans in children and adolescents: clinical presentation, histology, treatment, and review of the literature. J Plast Reconstr Aesthet Surg. 2014;67:1222-1229. doi:10.1016/j.bjps.2014.05.03
The Diagnosis: Cutaneous Langerhans Cell Histiocytosis
Histopathologic findings of the left axillary lesion included a diffuse infiltrate of irregular hematolymphoid cells with reniform nuclei that strongly and diffusely stained positively with CD1a and S-100 but were negative for CD138 and CD163 (Figure). Numerous eosinophils also were present. The surrounding lymphocytic infiltrate stained positively with CD45. Polymerase chain reaction of the vaginal lesion was negative for herpes simplex virus types 1 and 2. Biopsy of the vaginal lesion revealed a mildly acanthotic epidermis and an aggregation of epithelioid cells with reniform nuclei in the papillary dermis. Positron emission tomography revealed widely disseminated disease. Sequencing of the mitogen-activated protein kinase/extracellular signalregulated kinase pathway showed amplified expression of these genes but found no mutations. These results led to a diagnosis of cutaneous Langerhans cell histiocytosis (LCH) with a background of hidradenitis suppurativa (HS). Our patient has since initiated therapy with trametinib leading to disease improvement without known recurrence.

Langerhans cell histiocytosis is a rare disease of clonal dendritic cells (Langerhans cells) that can present in any organ.1 Most LCH diagnoses are made in pediatric patients, most often presenting in the bones, with other presentations in the skin, hypophysis, liver, lymph nodes, lungs, and spleen occurring less commonly.2 Proto-oncogene BRAF V600E mutations are a common determinant of LCH, with half of cases linked with this mutation that leads to enhanced activation of the mitogen-activated protein kinase pathway, though other mutations have been reported.3,4 These genetic alterations suggest LCH is neoplastic in nature; however, this is controversial, as spontaneous regression among pulmonary LCH has been observed, pointing to a reactive inflammatory process.5 Cutaneous LCH can present as a distinct papular or nodular lesion or multiple lesions with possible ulceration, but it is rare that LCH first presents on the skin.2,6 There is a substantial association of cutaneous LCH with the development of systemically disseminated LCH as well as other blood tumors, such as myelomonocytic leukemia, histiocytic sarcoma, and multiple lymphomas; this association is thought to be due to the common origin of LCH and other blood diseases in the bone marrow.6
Histopathology of LCH shows a diffuse papillary dermal infiltrate of clonal proliferation of reniform or cleaved histiocytes.5 Epidermal ulceration and epidermotropism also are common. Neoplastic cells are found admixed with variable levels of eosinophils, lymphocytes, plasma cells, and neutrophils, though eosinophils typically are elevated. Immunohistochemistry characteristically shows the expression of CD1a, S-100, and/or CD207, and the absence of CD163 expression.
Treatment of LCH is primarily dependent on disease dissemination status, with splenic and hepatic involvement, genetic panel results, and central nervous system risk considered in the treatment plan.5 Langerhans cell histiocytosis localized to the skin may require follow-up and monitoring, as spontaneous regression of cutaneous LCH is common. However, topical steroids or psoralen and long-wave UV radiation are potential treatments. Physicians who diagnose unifocal cutaneous LCH should have high clinical suspicion of disseminated LCH, and laboratory and radiographic evaluation may be necessary to rule out systemic disease, as more than 40% of patients with cutaneous LCH have systemic disease upon full evaluation.7 With systemic involvement, systemic chemotherapy may reduce morbidity and mortality, but clinical response should be monitored after 6 weeks of treatment, as results are variably effective. Vinblastine is the most common chemotherapy regimen, with an 84% survival rate and 51.5% event-free survival rate after 8 years.8 Targeted therapy for common genetic mutations also is possible, as vemurafenib has been used to treat patients with the BRAF V600E mutation.
Due to the variable clinical presentation of cutaneous LCH, the lesions can mimic other common skin diseases such as eczema or seborrheic dermatitis.7 However, there are limited data on LCH presenting in infiltrative skin disease. Langerhans cell histiocytosis that was misdiagnosed as HS has been reported,9-11 but LCH presenting alongside long-standing HS is rare. Although LCH often mimics infiltrative skin diseases, its simultaneous presentation with a previously confirmed diagnosis of HS was notable in our patient.
In our patient, the differential diagnosis included HS, Actinomyces infection, lymphomatoid papulosis, and dermatofibrosarcoma protuberans. Cutaneous findings in HS include chronic acneform nodules with follicular plugging, ruptured ducts leading to epithelized sinuses, inflammation, and abscesses in the axillae or inguinal and perineal areas.11 Histopathology reveals follicular occlusion and hyperkeratinization, which cause destruction of the pilosebaceous glands. Hidradenitis suppurativa features on immunohistochemistry often are conflicting, but there consistently is co-localization of keratinocyte hyperplasia with CD3-, CD4-, CD8-, and CD68-positive staining of cells that produce tumor necrosis factor α, IL-12, IL-23, and IL-32, with CD1a staining variable.12 An infection with Actinomyces, a slow-progressing anaerobic or microaerophilic bacteria, may present in the skin with chronic suppurative inflammation on the neck, trunk, and abdomen. The classic presentation is subcutaneous nodules with localized infiltration of abscesses, fistulas, and draining sinuses.13 Morphologically, Actinomyces causes chronic granulomatous infection with 0.1- to 1-mm sulfur granules, which are seen as basophilic masses with eosinophilic terminal clubs on hematoxylin and eosin staining.14 Histopathology reveals grampositive filamentous Actinomyces bacteria that branch at the edge of the granules. Lymphomatoid papulosis, a nonaggressive T-cell lymphoma, presents as papulonodular and sometimes necrotic disseminated lesions that spontaneously can regress or can cause a higher risk for the development of more aggressive lymphomas.15 Histopathology shows consistently dense, dermal, lymphocytic infiltration. Immunohistochemistry is characterized by lymphocytes expressing CD30 of varying degrees: type A with many CD30 staining cells, type B presenting similar to mycosis fungoides with little CD30 staining, and type C with lymphocytic CD30-staining plaques. Dermatofibrosarcoma protuberans is a low-grade soft-tissue malignant tumor with extensive local infiltration characterized by asymptomatic plaques on the trunk and proximal extremities that are indurated and adhered to the skin.16 Histopathology shows extensive invasion into the adjacent tissue far from the original focus of the tumor.
The Diagnosis: Cutaneous Langerhans Cell Histiocytosis
Histopathologic findings of the left axillary lesion included a diffuse infiltrate of irregular hematolymphoid cells with reniform nuclei that strongly and diffusely stained positively with CD1a and S-100 but were negative for CD138 and CD163 (Figure). Numerous eosinophils also were present. The surrounding lymphocytic infiltrate stained positively with CD45. Polymerase chain reaction of the vaginal lesion was negative for herpes simplex virus types 1 and 2. Biopsy of the vaginal lesion revealed a mildly acanthotic epidermis and an aggregation of epithelioid cells with reniform nuclei in the papillary dermis. Positron emission tomography revealed widely disseminated disease. Sequencing of the mitogen-activated protein kinase/extracellular signalregulated kinase pathway showed amplified expression of these genes but found no mutations. These results led to a diagnosis of cutaneous Langerhans cell histiocytosis (LCH) with a background of hidradenitis suppurativa (HS). Our patient has since initiated therapy with trametinib leading to disease improvement without known recurrence.

Langerhans cell histiocytosis is a rare disease of clonal dendritic cells (Langerhans cells) that can present in any organ.1 Most LCH diagnoses are made in pediatric patients, most often presenting in the bones, with other presentations in the skin, hypophysis, liver, lymph nodes, lungs, and spleen occurring less commonly.2 Proto-oncogene BRAF V600E mutations are a common determinant of LCH, with half of cases linked with this mutation that leads to enhanced activation of the mitogen-activated protein kinase pathway, though other mutations have been reported.3,4 These genetic alterations suggest LCH is neoplastic in nature; however, this is controversial, as spontaneous regression among pulmonary LCH has been observed, pointing to a reactive inflammatory process.5 Cutaneous LCH can present as a distinct papular or nodular lesion or multiple lesions with possible ulceration, but it is rare that LCH first presents on the skin.2,6 There is a substantial association of cutaneous LCH with the development of systemically disseminated LCH as well as other blood tumors, such as myelomonocytic leukemia, histiocytic sarcoma, and multiple lymphomas; this association is thought to be due to the common origin of LCH and other blood diseases in the bone marrow.6
Histopathology of LCH shows a diffuse papillary dermal infiltrate of clonal proliferation of reniform or cleaved histiocytes.5 Epidermal ulceration and epidermotropism also are common. Neoplastic cells are found admixed with variable levels of eosinophils, lymphocytes, plasma cells, and neutrophils, though eosinophils typically are elevated. Immunohistochemistry characteristically shows the expression of CD1a, S-100, and/or CD207, and the absence of CD163 expression.
Treatment of LCH is primarily dependent on disease dissemination status, with splenic and hepatic involvement, genetic panel results, and central nervous system risk considered in the treatment plan.5 Langerhans cell histiocytosis localized to the skin may require follow-up and monitoring, as spontaneous regression of cutaneous LCH is common. However, topical steroids or psoralen and long-wave UV radiation are potential treatments. Physicians who diagnose unifocal cutaneous LCH should have high clinical suspicion of disseminated LCH, and laboratory and radiographic evaluation may be necessary to rule out systemic disease, as more than 40% of patients with cutaneous LCH have systemic disease upon full evaluation.7 With systemic involvement, systemic chemotherapy may reduce morbidity and mortality, but clinical response should be monitored after 6 weeks of treatment, as results are variably effective. Vinblastine is the most common chemotherapy regimen, with an 84% survival rate and 51.5% event-free survival rate after 8 years.8 Targeted therapy for common genetic mutations also is possible, as vemurafenib has been used to treat patients with the BRAF V600E mutation.
Due to the variable clinical presentation of cutaneous LCH, the lesions can mimic other common skin diseases such as eczema or seborrheic dermatitis.7 However, there are limited data on LCH presenting in infiltrative skin disease. Langerhans cell histiocytosis that was misdiagnosed as HS has been reported,9-11 but LCH presenting alongside long-standing HS is rare. Although LCH often mimics infiltrative skin diseases, its simultaneous presentation with a previously confirmed diagnosis of HS was notable in our patient.
In our patient, the differential diagnosis included HS, Actinomyces infection, lymphomatoid papulosis, and dermatofibrosarcoma protuberans. Cutaneous findings in HS include chronic acneform nodules with follicular plugging, ruptured ducts leading to epithelized sinuses, inflammation, and abscesses in the axillae or inguinal and perineal areas.11 Histopathology reveals follicular occlusion and hyperkeratinization, which cause destruction of the pilosebaceous glands. Hidradenitis suppurativa features on immunohistochemistry often are conflicting, but there consistently is co-localization of keratinocyte hyperplasia with CD3-, CD4-, CD8-, and CD68-positive staining of cells that produce tumor necrosis factor α, IL-12, IL-23, and IL-32, with CD1a staining variable.12 An infection with Actinomyces, a slow-progressing anaerobic or microaerophilic bacteria, may present in the skin with chronic suppurative inflammation on the neck, trunk, and abdomen. The classic presentation is subcutaneous nodules with localized infiltration of abscesses, fistulas, and draining sinuses.13 Morphologically, Actinomyces causes chronic granulomatous infection with 0.1- to 1-mm sulfur granules, which are seen as basophilic masses with eosinophilic terminal clubs on hematoxylin and eosin staining.14 Histopathology reveals grampositive filamentous Actinomyces bacteria that branch at the edge of the granules. Lymphomatoid papulosis, a nonaggressive T-cell lymphoma, presents as papulonodular and sometimes necrotic disseminated lesions that spontaneously can regress or can cause a higher risk for the development of more aggressive lymphomas.15 Histopathology shows consistently dense, dermal, lymphocytic infiltration. Immunohistochemistry is characterized by lymphocytes expressing CD30 of varying degrees: type A with many CD30 staining cells, type B presenting similar to mycosis fungoides with little CD30 staining, and type C with lymphocytic CD30-staining plaques. Dermatofibrosarcoma protuberans is a low-grade soft-tissue malignant tumor with extensive local infiltration characterized by asymptomatic plaques on the trunk and proximal extremities that are indurated and adhered to the skin.16 Histopathology shows extensive invasion into the adjacent tissue far from the original focus of the tumor.
- Girschikofsky M, Arico M, Castillo D, et al. Management of adult patients with Langerhans cell histiocytosis: recommendations from an expert panel on behalf of Euro-Histio-Net. Orphanet J Rare Dis. 2013;8:72. doi:10.1186/1750-1172-8-72
- Flores-Terry MA, Sanz-Trenado JL, García-Arpa M, et al. Cutaneous Langerhans cell histiocytosis presenting in adulthood. Actas Dermosifiliogr (Engl Ed). 2019;110:167-169. doi:10.1016/j .adengl.2018.12.005
- Emile J-F, Abla O, Fraitag S, et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016;127:2672-2681. doi:10.1182/blood-2016-01-690636
- Badalian-Very G, Vergilio J-A, Degar BA, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116:1919-1923. doi:10.1182/blood-2010-04-279083
- Bohn OL, Teruya-Feldstein J, Sanchez-Sosa S. Skin biopsy diagnosis of Langerhans cell neoplasms. In: Fernando S, ed. Skin Biopsy: Diagnosis and Treatment [Internet]. InTechOpen; 2013. http://dx.doi .org/10.5772/55893
- Edelbroek JR, Vermeer MH, Jansen PM, et al. Langerhans cell histiocytosis first presenting in the skin in adults: frequent association with a second haematological malignancy. Br J Dermatol. 2012;167:1287-1294. doi:10.1111/j.1365-2133.2012.11169.x
- Simko SJ, Garmezy B, Abhyankar H, et al. Differentiating skin-limited and multisystem Langerhans cell histiocytosis. J Pediatr. 2014;165: 990-996. doi:10.1016/j.jpeds.2014.07.063
- Yag˘ ci B, Varan A, Cag˘ lar M, et al. Langerhans cell histiocytosis: retrospective analysis of 217 cases in a single center. Pediatr Hematol Oncol. 2008;25:399-408. doi:10.1080/08880010802107356
- Kalen JE, Shokeen D, Mislankar M, et al. Langerhans cell histiocytosis with clinical and histologic features of hidradenitis suppurativa: brief report and review. Am J Dermatopathol. 2018;40:502-505. doi:10.1097/dad.0000000000001005
- Chertoff J, Chung J, Ataya A. Adult Langerhans cell histiocytosis masquerading as hidradenitis suppurativa. Am J Respir Crit Care Med. 2017;195:E34-E36. doi:10.1164/rccm.201610-2082IM
- St. Claire K, Bunney R, Ashack KA, et al. Langerhans cell histiocytosis: a great imitator. Clin Dermatol. 2020;38:223-234. doi:10.1016/j.clindermatol.2019.10.007
- Frew JW, Hawkes JE, Krueger JG. A systematic review and critical evaluation of immunohistochemical associations in hidradenitis suppurativa. F1000Research. 2019;7:1923. doi:10.12688/f1000research.17268.2
- Robati RM, Niknezhad N, Bidari-Zerehpoush F, et al. Primary cutaneous actinomycosis along with the surgical scar on the hand [published online November 9, 2016]. Case Rep Infect Dis. doi:10.1155/2016/5943932
- Ferry T, Valour F, Karsenty J, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Res. 2014;2014:183-197. doi:10.2147/idr.s39601
- Willemze R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005;105:3768-3785. doi:10.1182 /blood-2004-09-3502
- Tsai Y, Lin P, Chew K, et al. Dermatofibrosarcoma protuberans in children and adolescents: clinical presentation, histology, treatment, and review of the literature. J Plast Reconstr Aesthet Surg. 2014;67:1222-1229. doi:10.1016/j.bjps.2014.05.03
- Girschikofsky M, Arico M, Castillo D, et al. Management of adult patients with Langerhans cell histiocytosis: recommendations from an expert panel on behalf of Euro-Histio-Net. Orphanet J Rare Dis. 2013;8:72. doi:10.1186/1750-1172-8-72
- Flores-Terry MA, Sanz-Trenado JL, García-Arpa M, et al. Cutaneous Langerhans cell histiocytosis presenting in adulthood. Actas Dermosifiliogr (Engl Ed). 2019;110:167-169. doi:10.1016/j .adengl.2018.12.005
- Emile J-F, Abla O, Fraitag S, et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016;127:2672-2681. doi:10.1182/blood-2016-01-690636
- Badalian-Very G, Vergilio J-A, Degar BA, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116:1919-1923. doi:10.1182/blood-2010-04-279083
- Bohn OL, Teruya-Feldstein J, Sanchez-Sosa S. Skin biopsy diagnosis of Langerhans cell neoplasms. In: Fernando S, ed. Skin Biopsy: Diagnosis and Treatment [Internet]. InTechOpen; 2013. http://dx.doi .org/10.5772/55893
- Edelbroek JR, Vermeer MH, Jansen PM, et al. Langerhans cell histiocytosis first presenting in the skin in adults: frequent association with a second haematological malignancy. Br J Dermatol. 2012;167:1287-1294. doi:10.1111/j.1365-2133.2012.11169.x
- Simko SJ, Garmezy B, Abhyankar H, et al. Differentiating skin-limited and multisystem Langerhans cell histiocytosis. J Pediatr. 2014;165: 990-996. doi:10.1016/j.jpeds.2014.07.063
- Yag˘ ci B, Varan A, Cag˘ lar M, et al. Langerhans cell histiocytosis: retrospective analysis of 217 cases in a single center. Pediatr Hematol Oncol. 2008;25:399-408. doi:10.1080/08880010802107356
- Kalen JE, Shokeen D, Mislankar M, et al. Langerhans cell histiocytosis with clinical and histologic features of hidradenitis suppurativa: brief report and review. Am J Dermatopathol. 2018;40:502-505. doi:10.1097/dad.0000000000001005
- Chertoff J, Chung J, Ataya A. Adult Langerhans cell histiocytosis masquerading as hidradenitis suppurativa. Am J Respir Crit Care Med. 2017;195:E34-E36. doi:10.1164/rccm.201610-2082IM
- St. Claire K, Bunney R, Ashack KA, et al. Langerhans cell histiocytosis: a great imitator. Clin Dermatol. 2020;38:223-234. doi:10.1016/j.clindermatol.2019.10.007
- Frew JW, Hawkes JE, Krueger JG. A systematic review and critical evaluation of immunohistochemical associations in hidradenitis suppurativa. F1000Research. 2019;7:1923. doi:10.12688/f1000research.17268.2
- Robati RM, Niknezhad N, Bidari-Zerehpoush F, et al. Primary cutaneous actinomycosis along with the surgical scar on the hand [published online November 9, 2016]. Case Rep Infect Dis. doi:10.1155/2016/5943932
- Ferry T, Valour F, Karsenty J, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Res. 2014;2014:183-197. doi:10.2147/idr.s39601
- Willemze R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005;105:3768-3785. doi:10.1182 /blood-2004-09-3502
- Tsai Y, Lin P, Chew K, et al. Dermatofibrosarcoma protuberans in children and adolescents: clinical presentation, histology, treatment, and review of the literature. J Plast Reconstr Aesthet Surg. 2014;67:1222-1229. doi:10.1016/j.bjps.2014.05.03
A 28-year-old woman presented with tender burning lesions of the left axillary and vaginal skin that had worsened over the last year. Her medical history was notable for hidradenitis suppurativa, which had been present since adolescence, as well as pulmonary Langerhans cell histiocytosis diagnosed 7 years prior to the current presentation after a spontaneous pneumothorax that eventually led to a pulmonary transplantation 3 years prior. The patient’s Langerhans cell histiocytosis was believed to have resolved without treatment after smoking cessation. Physical examination revealed nodular inflammation and scarring with deep undermining along the left axilla as well as swelling of the mons pubis with erosive skin lesions in the surrounding vaginal area. Bilateral cervical, axillary, inguinal, supraclavicular, and femoral lymph node chains were negative for adenopathy. A shave biopsy was performed on the axillary nodule.





