User login
The triple overlap: COPD-OSA-OHS. Is it time for new definitions?
In our current society, it is likely that the “skinny patient with COPD” who walks into your clinic is less and less your “traditional” patient with COPD. We are seeing in our health care systems more of the “blue bloaters” – patients with COPD and significant obesity. This phenotype is representing what we are seeing worldwide as a consequence of the rising obesity prevalence. In the United States, the prepandemic (2017-2020) estimated percentage of adults over the age of 40 with obesity, defined as a body mass index (BMI) of at least 30 kg/m2, was over 40%. Moreover, the estimated percentage of adults with morbid obesity (BMI at least 40 kg/m2) is close to 10% (Akinbami, LJ et al. Vital Health Stat. 2022:190:1-36) and trending up. These patients with the “triple overlap” of morbid obesity, COPD, and awake daytime hypercapnia are being seen in clinics and in-hospital settings with increasing frequency, often presenting with complicating comorbidities such as acute respiratory failure, acute heart failure, kidney disease, or pulmonary hypertension. We are now faced with managing these patients with complex disease.
The obesity paradox does not seem applicable in the triple overlap phenotype. Patients with COPD who are overweight, defined as “mild obesity,” have lower mortality when compared with normal weight and underweight patients with COPD; however, this effect diminishes when BMI increases beyond 32 kg/m2. With increasing obesity severity and aging, the risk of both obstructive sleep apnea (OSA) and hypoventilation increases. It is well documented that COPD-OSA overlap is linked to worse outcomes and that continuous positive airway pressure (CPAP) as first-line therapy decreases readmission rates and mortality. The pathophysiology of hypoventilation in obesity is complex and multifactorial, and, although significant overlaps likely exist with comorbid COPD, by current definitions, to establish a diagnosis of obesity hypoventilation syndrome (OHS), one must have excluded other causes of hypoventilation, such as COPD.
These patients with the triple overlap of morbid obesity, awake daytime hypercapnia, and COPD are the subset of patients that providers struggle to fit in a diagnosis or in clinical research trials.
The triple overlap is a distinct syndrome
Different labels have been used in the medical literature: hypercapnic OSA-COPD overlap, morbid obesity and OSA-COPD overlap, hypercapnic morbidly obese COPD and OHS-COPD overlap. A better characterization of this distinctive phenotype is much needed. Patients with OSA-COPD overlap, for example, have an increased propensity to develop hypercapnia at higher FEV1 when compared with COPD without OSA – but this is thought to be a consequence of prolonged and frequent apneas and hypopneas compounded with obesity-related central hypoventilation. We found that morbidly obese patients with OSA-COPD overlap have a higher hypoxia burden, more severe OSA, and are frequently prescribed noninvasive ventilation after a failed titration polysomnogram (Htun ZM, et al. Am J Respir Crit Care Med. 2019;199:A1382), perhaps signaling a distinctive phenotype with worse outcomes, but the study had the inherent limitations of a single-center, retrospective design lacking data on awake hypercapnia. On the other side, the term OHS-COPD is contradictory and confusing based on current OHS diagnostic criteria.
In standardizing diagnostic criteria for patients with this triple overlap syndrome, challenges remain: would the patient with a BMI of 70 kg/m2 and fixed chronic airflow obstruction with FEV1 72% fall under the category of hypercapnic COPD vs OHS? Do these patients have worse outcomes regardless of their predominant feature? Would outcomes change if the apnea hypopnea index (AHI) is 10/h vs 65/h? More importantly, do patients with the triple overlap of COPD, morbid obesity, and daytime hypercapnia have worse outcomes when compared with hypercapnic COPD, or OHS with/without OSA? These questions can be better addressed once we agree on a definition. The patients with triple overlap syndrome have been traditionally excluded from clinical trials: the patient with morbid obesity has been excluded from chronic hypercapnic COPD clinical trials, and the patient with COPD has been excluded from OHS trials.
There are no specific clinical guidelines for this triple overlap phenotype. Positive airway pressure is the mainstay of treatment. CPAP is recommended as first-line therapy for patients with OSA-COPD overlap syndrome, while noninvasive ventilation (NIV) with bilevel positive airway pressure (BPAP) is recommended as first-line for the stable ambulatory hypercapnic patient with COPD. It is unclear if NIV is superior to CPAP in patients with triple overlap syndrome, although recently published data showed greater efficacy in reducing carbon dioxide (PaCO2) and improving quality of life in a small group of subjects (Zheng et al. J Clin Sleep Med. 2022;18[1]:99-107). To take a step further, the subtleties of NIV set up, such as rise time and minimum inspiratory time, are contradictory: the goal in ventilating patients with COPD is to shorten inspiratory time, prolonging expiratory time, therefore allowing a shortened inspiratory cycle. In obesity, ventilation strategies aim to prolong and sustain inspiratory time to improve ventilation and dependent atelectasis. Another area of uncertainty is device selection. Should we aim to provide a respiratory assist device (RAD): the traditional, rent to own bilevel PAP without auto-expiratory positive airway pressure (EPAP) capabilities and lower maximum inspiratory pressure delivery capacity, vs a home mechanical ventilator at a higher expense, life-time rental, and one-way only data monitoring, which limits remote prescription adjustments, but allow auto-EPAP settings for patients with comorbid OSA? More importantly, how do we get these patients, who do not fit in any of the specified insurance criteria for PAP therapy approved for treatment?
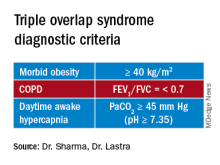
A uniform diagnostic definition and clear taxonomy allows for resource allocation, from government funded grants for clinical trials to a better-informed distribution of health care systems resources and support health care policy changes to improve patient-centric outcomes. Here, we propose that the morbidly obese patient (BMI >40 kg/m2) with chronic airflow obstruction and a forced expiratory ratio (FEV1/FVC) <0.7 with awake daytime hypercapnia (PaCO2 > 45 mm Hg) represents a different entity/phenotype and fits best under the triple overlap syndrome taxonomy.
We suspect that these patients have worse outcomes, including comorbidity burden, quality of life, exacerbation rates, longer hospital length-of-stay, and respiratory and all-cause mortality. Large, multicenter, controlled trials comparing the long-term effectiveness of NIV and CPAP: measurements of respiratory function, gas exchange, blood pressure, and health related quality of life are needed. This is a group of patients that may specifically benefit from volume-targeted pressure support mode ventilation with auto-EPAP capabilities upon discharge from the hospital after an acute exacerbation.
Inpatient (sleep medicine) and outpatient transitions
In patients hospitalized with the triple overlap syndrome, there are certain considerations that are of special interest. Given comorbid hypercapnia and limited data on NIV superiority over CPAP, a sleep study should not be needed for NIV qualification. In addition, the medical team may consider the following (Figure 1):
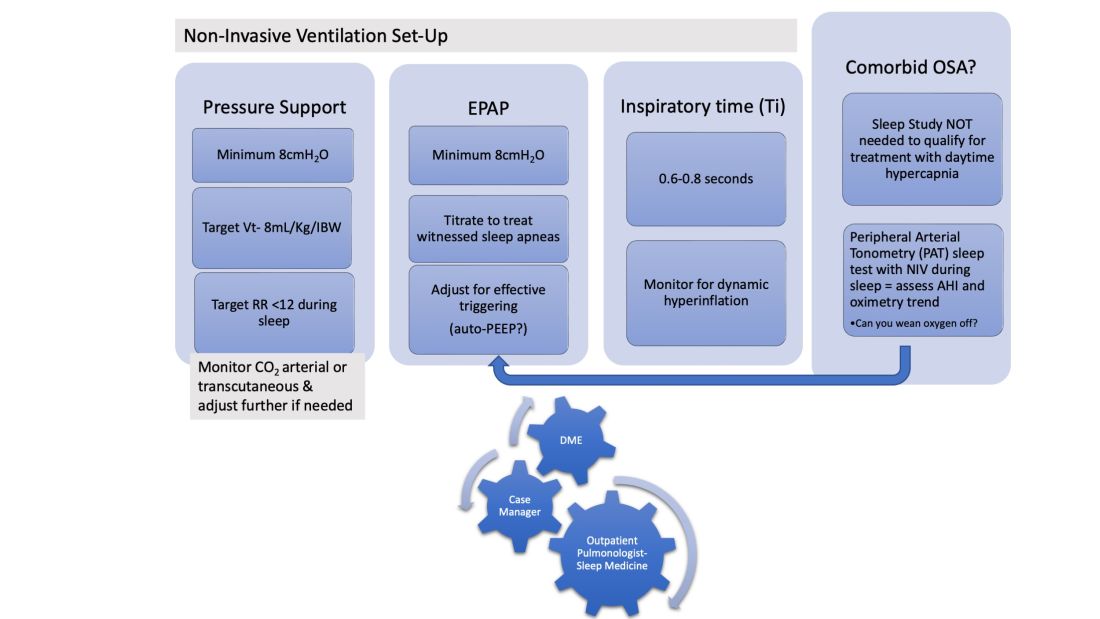
1. Noninvasive Ventilation:
a. Maintaining a high-pressure support differential between inspiratory positive airway pressure (IPAP) and EPAP. This can usually be achieved at 8-10 cm H2O, further adjusting to target a tidal volume (Vt) of 8 mL/kg of ideal body weight (IBW).
b. Higher EPAP: To overcome dependent atelectasis, improve ventilation-perfusion (VQ) matching, and better treat upper airway resistance both during wakefulness and sleep. Also, adjustments of EPAP at bedside should be considered to counteract auto-PEEP-related ineffective triggering if observed.
c. OSA screening and EPAP adjustment: for high residual obstructive apneas or hypopneas if data are available on the NIV device, or with the use of peripheral arterial tonometry sleep testing devices with NIV on overnight before discharge.
d. Does the patient meet criteria for oxygen supplementation at home? Wean oxygen off, if possible.
2. Case-managers can help establish services with a durable medical equipment provider with expertise in advanced PAP devices.3. Obesity management, Consider referral to an obesity management program for lifestyle/dietary modifications along with pharmacotherapy or bariatric surgery interventions.
4. Close follow-up, track exacerbations. Device download data are crucial to monitor adherence/tolerance and treatment effectiveness with particular interest in AHI, oximetry, and CO2 trends monitoring. Some patients may need dedicated titration polysomnograms to adjust ventilation settings, for optimization of residual OSA or for oxygen addition or discontinuation.
Conclusion
Patients with the triple overlap phenotype have not been systematically defined, studied, or included in clinical trials. We anticipate that these patients have worse outcomes: quality of life, symptom and comorbidity burden, exacerbation rates, in-hospital mortality, longer hospital stay and ICU stay, and respiratory and all-cause mortality. This is a group of patients that may specifically benefit from domiciliary NIV set-up upon discharge from the hospital with close follow-up. Properly identifying these patients will help pulmonologists and health care systems direct resources to optimally manage this complex group of patients. Funding of research trials to support clinical guidelines development should be prioritized. Triple overlap syndrome is different from COPD-OSA overlap, OHS with moderate to severe OSA, or OHS without significant OSA.
In our current society, it is likely that the “skinny patient with COPD” who walks into your clinic is less and less your “traditional” patient with COPD. We are seeing in our health care systems more of the “blue bloaters” – patients with COPD and significant obesity. This phenotype is representing what we are seeing worldwide as a consequence of the rising obesity prevalence. In the United States, the prepandemic (2017-2020) estimated percentage of adults over the age of 40 with obesity, defined as a body mass index (BMI) of at least 30 kg/m2, was over 40%. Moreover, the estimated percentage of adults with morbid obesity (BMI at least 40 kg/m2) is close to 10% (Akinbami, LJ et al. Vital Health Stat. 2022:190:1-36) and trending up. These patients with the “triple overlap” of morbid obesity, COPD, and awake daytime hypercapnia are being seen in clinics and in-hospital settings with increasing frequency, often presenting with complicating comorbidities such as acute respiratory failure, acute heart failure, kidney disease, or pulmonary hypertension. We are now faced with managing these patients with complex disease.
The obesity paradox does not seem applicable in the triple overlap phenotype. Patients with COPD who are overweight, defined as “mild obesity,” have lower mortality when compared with normal weight and underweight patients with COPD; however, this effect diminishes when BMI increases beyond 32 kg/m2. With increasing obesity severity and aging, the risk of both obstructive sleep apnea (OSA) and hypoventilation increases. It is well documented that COPD-OSA overlap is linked to worse outcomes and that continuous positive airway pressure (CPAP) as first-line therapy decreases readmission rates and mortality. The pathophysiology of hypoventilation in obesity is complex and multifactorial, and, although significant overlaps likely exist with comorbid COPD, by current definitions, to establish a diagnosis of obesity hypoventilation syndrome (OHS), one must have excluded other causes of hypoventilation, such as COPD.
These patients with the triple overlap of morbid obesity, awake daytime hypercapnia, and COPD are the subset of patients that providers struggle to fit in a diagnosis or in clinical research trials.
The triple overlap is a distinct syndrome
Different labels have been used in the medical literature: hypercapnic OSA-COPD overlap, morbid obesity and OSA-COPD overlap, hypercapnic morbidly obese COPD and OHS-COPD overlap. A better characterization of this distinctive phenotype is much needed. Patients with OSA-COPD overlap, for example, have an increased propensity to develop hypercapnia at higher FEV1 when compared with COPD without OSA – but this is thought to be a consequence of prolonged and frequent apneas and hypopneas compounded with obesity-related central hypoventilation. We found that morbidly obese patients with OSA-COPD overlap have a higher hypoxia burden, more severe OSA, and are frequently prescribed noninvasive ventilation after a failed titration polysomnogram (Htun ZM, et al. Am J Respir Crit Care Med. 2019;199:A1382), perhaps signaling a distinctive phenotype with worse outcomes, but the study had the inherent limitations of a single-center, retrospective design lacking data on awake hypercapnia. On the other side, the term OHS-COPD is contradictory and confusing based on current OHS diagnostic criteria.
In standardizing diagnostic criteria for patients with this triple overlap syndrome, challenges remain: would the patient with a BMI of 70 kg/m2 and fixed chronic airflow obstruction with FEV1 72% fall under the category of hypercapnic COPD vs OHS? Do these patients have worse outcomes regardless of their predominant feature? Would outcomes change if the apnea hypopnea index (AHI) is 10/h vs 65/h? More importantly, do patients with the triple overlap of COPD, morbid obesity, and daytime hypercapnia have worse outcomes when compared with hypercapnic COPD, or OHS with/without OSA? These questions can be better addressed once we agree on a definition. The patients with triple overlap syndrome have been traditionally excluded from clinical trials: the patient with morbid obesity has been excluded from chronic hypercapnic COPD clinical trials, and the patient with COPD has been excluded from OHS trials.
There are no specific clinical guidelines for this triple overlap phenotype. Positive airway pressure is the mainstay of treatment. CPAP is recommended as first-line therapy for patients with OSA-COPD overlap syndrome, while noninvasive ventilation (NIV) with bilevel positive airway pressure (BPAP) is recommended as first-line for the stable ambulatory hypercapnic patient with COPD. It is unclear if NIV is superior to CPAP in patients with triple overlap syndrome, although recently published data showed greater efficacy in reducing carbon dioxide (PaCO2) and improving quality of life in a small group of subjects (Zheng et al. J Clin Sleep Med. 2022;18[1]:99-107). To take a step further, the subtleties of NIV set up, such as rise time and minimum inspiratory time, are contradictory: the goal in ventilating patients with COPD is to shorten inspiratory time, prolonging expiratory time, therefore allowing a shortened inspiratory cycle. In obesity, ventilation strategies aim to prolong and sustain inspiratory time to improve ventilation and dependent atelectasis. Another area of uncertainty is device selection. Should we aim to provide a respiratory assist device (RAD): the traditional, rent to own bilevel PAP without auto-expiratory positive airway pressure (EPAP) capabilities and lower maximum inspiratory pressure delivery capacity, vs a home mechanical ventilator at a higher expense, life-time rental, and one-way only data monitoring, which limits remote prescription adjustments, but allow auto-EPAP settings for patients with comorbid OSA? More importantly, how do we get these patients, who do not fit in any of the specified insurance criteria for PAP therapy approved for treatment?
A uniform diagnostic definition and clear taxonomy allows for resource allocation, from government funded grants for clinical trials to a better-informed distribution of health care systems resources and support health care policy changes to improve patient-centric outcomes. Here, we propose that the morbidly obese patient (BMI >40 kg/m2) with chronic airflow obstruction and a forced expiratory ratio (FEV1/FVC) <0.7 with awake daytime hypercapnia (PaCO2 > 45 mm Hg) represents a different entity/phenotype and fits best under the triple overlap syndrome taxonomy.
We suspect that these patients have worse outcomes, including comorbidity burden, quality of life, exacerbation rates, longer hospital length-of-stay, and respiratory and all-cause mortality. Large, multicenter, controlled trials comparing the long-term effectiveness of NIV and CPAP: measurements of respiratory function, gas exchange, blood pressure, and health related quality of life are needed. This is a group of patients that may specifically benefit from volume-targeted pressure support mode ventilation with auto-EPAP capabilities upon discharge from the hospital after an acute exacerbation.
Inpatient (sleep medicine) and outpatient transitions
In patients hospitalized with the triple overlap syndrome, there are certain considerations that are of special interest. Given comorbid hypercapnia and limited data on NIV superiority over CPAP, a sleep study should not be needed for NIV qualification. In addition, the medical team may consider the following (Figure 1):
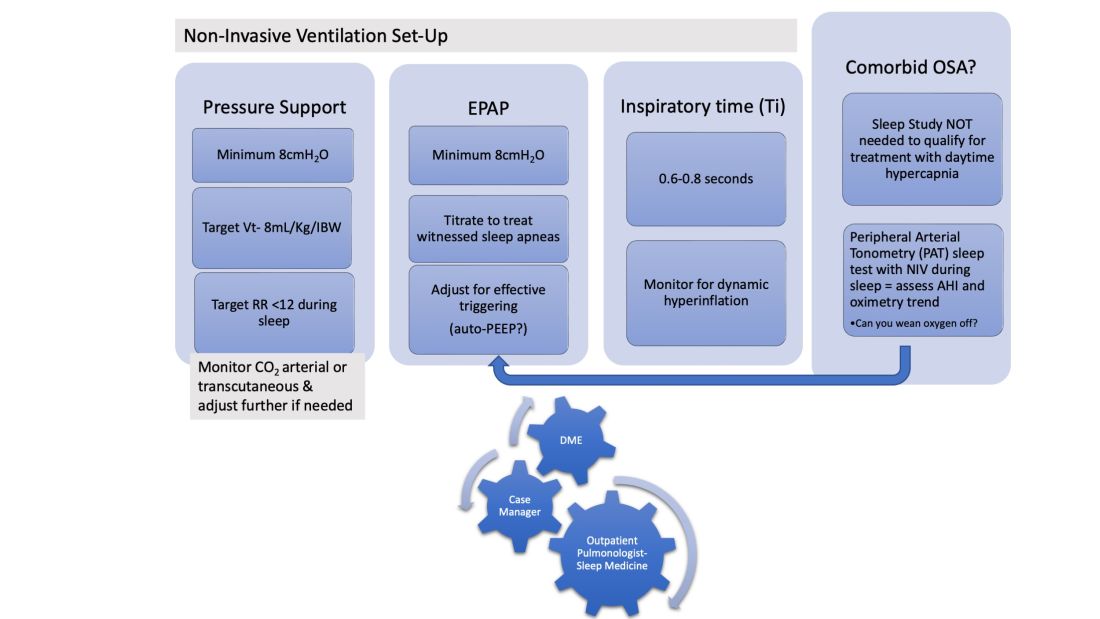
1. Noninvasive Ventilation:
a. Maintaining a high-pressure support differential between inspiratory positive airway pressure (IPAP) and EPAP. This can usually be achieved at 8-10 cm H2O, further adjusting to target a tidal volume (Vt) of 8 mL/kg of ideal body weight (IBW).
b. Higher EPAP: To overcome dependent atelectasis, improve ventilation-perfusion (VQ) matching, and better treat upper airway resistance both during wakefulness and sleep. Also, adjustments of EPAP at bedside should be considered to counteract auto-PEEP-related ineffective triggering if observed.
c. OSA screening and EPAP adjustment: for high residual obstructive apneas or hypopneas if data are available on the NIV device, or with the use of peripheral arterial tonometry sleep testing devices with NIV on overnight before discharge.
d. Does the patient meet criteria for oxygen supplementation at home? Wean oxygen off, if possible.
2. Case-managers can help establish services with a durable medical equipment provider with expertise in advanced PAP devices.3. Obesity management, Consider referral to an obesity management program for lifestyle/dietary modifications along with pharmacotherapy or bariatric surgery interventions.
4. Close follow-up, track exacerbations. Device download data are crucial to monitor adherence/tolerance and treatment effectiveness with particular interest in AHI, oximetry, and CO2 trends monitoring. Some patients may need dedicated titration polysomnograms to adjust ventilation settings, for optimization of residual OSA or for oxygen addition or discontinuation.
Conclusion
Patients with the triple overlap phenotype have not been systematically defined, studied, or included in clinical trials. We anticipate that these patients have worse outcomes: quality of life, symptom and comorbidity burden, exacerbation rates, in-hospital mortality, longer hospital stay and ICU stay, and respiratory and all-cause mortality. This is a group of patients that may specifically benefit from domiciliary NIV set-up upon discharge from the hospital with close follow-up. Properly identifying these patients will help pulmonologists and health care systems direct resources to optimally manage this complex group of patients. Funding of research trials to support clinical guidelines development should be prioritized. Triple overlap syndrome is different from COPD-OSA overlap, OHS with moderate to severe OSA, or OHS without significant OSA.
In our current society, it is likely that the “skinny patient with COPD” who walks into your clinic is less and less your “traditional” patient with COPD. We are seeing in our health care systems more of the “blue bloaters” – patients with COPD and significant obesity. This phenotype is representing what we are seeing worldwide as a consequence of the rising obesity prevalence. In the United States, the prepandemic (2017-2020) estimated percentage of adults over the age of 40 with obesity, defined as a body mass index (BMI) of at least 30 kg/m2, was over 40%. Moreover, the estimated percentage of adults with morbid obesity (BMI at least 40 kg/m2) is close to 10% (Akinbami, LJ et al. Vital Health Stat. 2022:190:1-36) and trending up. These patients with the “triple overlap” of morbid obesity, COPD, and awake daytime hypercapnia are being seen in clinics and in-hospital settings with increasing frequency, often presenting with complicating comorbidities such as acute respiratory failure, acute heart failure, kidney disease, or pulmonary hypertension. We are now faced with managing these patients with complex disease.
The obesity paradox does not seem applicable in the triple overlap phenotype. Patients with COPD who are overweight, defined as “mild obesity,” have lower mortality when compared with normal weight and underweight patients with COPD; however, this effect diminishes when BMI increases beyond 32 kg/m2. With increasing obesity severity and aging, the risk of both obstructive sleep apnea (OSA) and hypoventilation increases. It is well documented that COPD-OSA overlap is linked to worse outcomes and that continuous positive airway pressure (CPAP) as first-line therapy decreases readmission rates and mortality. The pathophysiology of hypoventilation in obesity is complex and multifactorial, and, although significant overlaps likely exist with comorbid COPD, by current definitions, to establish a diagnosis of obesity hypoventilation syndrome (OHS), one must have excluded other causes of hypoventilation, such as COPD.
These patients with the triple overlap of morbid obesity, awake daytime hypercapnia, and COPD are the subset of patients that providers struggle to fit in a diagnosis or in clinical research trials.
The triple overlap is a distinct syndrome
Different labels have been used in the medical literature: hypercapnic OSA-COPD overlap, morbid obesity and OSA-COPD overlap, hypercapnic morbidly obese COPD and OHS-COPD overlap. A better characterization of this distinctive phenotype is much needed. Patients with OSA-COPD overlap, for example, have an increased propensity to develop hypercapnia at higher FEV1 when compared with COPD without OSA – but this is thought to be a consequence of prolonged and frequent apneas and hypopneas compounded with obesity-related central hypoventilation. We found that morbidly obese patients with OSA-COPD overlap have a higher hypoxia burden, more severe OSA, and are frequently prescribed noninvasive ventilation after a failed titration polysomnogram (Htun ZM, et al. Am J Respir Crit Care Med. 2019;199:A1382), perhaps signaling a distinctive phenotype with worse outcomes, but the study had the inherent limitations of a single-center, retrospective design lacking data on awake hypercapnia. On the other side, the term OHS-COPD is contradictory and confusing based on current OHS diagnostic criteria.
In standardizing diagnostic criteria for patients with this triple overlap syndrome, challenges remain: would the patient with a BMI of 70 kg/m2 and fixed chronic airflow obstruction with FEV1 72% fall under the category of hypercapnic COPD vs OHS? Do these patients have worse outcomes regardless of their predominant feature? Would outcomes change if the apnea hypopnea index (AHI) is 10/h vs 65/h? More importantly, do patients with the triple overlap of COPD, morbid obesity, and daytime hypercapnia have worse outcomes when compared with hypercapnic COPD, or OHS with/without OSA? These questions can be better addressed once we agree on a definition. The patients with triple overlap syndrome have been traditionally excluded from clinical trials: the patient with morbid obesity has been excluded from chronic hypercapnic COPD clinical trials, and the patient with COPD has been excluded from OHS trials.
There are no specific clinical guidelines for this triple overlap phenotype. Positive airway pressure is the mainstay of treatment. CPAP is recommended as first-line therapy for patients with OSA-COPD overlap syndrome, while noninvasive ventilation (NIV) with bilevel positive airway pressure (BPAP) is recommended as first-line for the stable ambulatory hypercapnic patient with COPD. It is unclear if NIV is superior to CPAP in patients with triple overlap syndrome, although recently published data showed greater efficacy in reducing carbon dioxide (PaCO2) and improving quality of life in a small group of subjects (Zheng et al. J Clin Sleep Med. 2022;18[1]:99-107). To take a step further, the subtleties of NIV set up, such as rise time and minimum inspiratory time, are contradictory: the goal in ventilating patients with COPD is to shorten inspiratory time, prolonging expiratory time, therefore allowing a shortened inspiratory cycle. In obesity, ventilation strategies aim to prolong and sustain inspiratory time to improve ventilation and dependent atelectasis. Another area of uncertainty is device selection. Should we aim to provide a respiratory assist device (RAD): the traditional, rent to own bilevel PAP without auto-expiratory positive airway pressure (EPAP) capabilities and lower maximum inspiratory pressure delivery capacity, vs a home mechanical ventilator at a higher expense, life-time rental, and one-way only data monitoring, which limits remote prescription adjustments, but allow auto-EPAP settings for patients with comorbid OSA? More importantly, how do we get these patients, who do not fit in any of the specified insurance criteria for PAP therapy approved for treatment?
A uniform diagnostic definition and clear taxonomy allows for resource allocation, from government funded grants for clinical trials to a better-informed distribution of health care systems resources and support health care policy changes to improve patient-centric outcomes. Here, we propose that the morbidly obese patient (BMI >40 kg/m2) with chronic airflow obstruction and a forced expiratory ratio (FEV1/FVC) <0.7 with awake daytime hypercapnia (PaCO2 > 45 mm Hg) represents a different entity/phenotype and fits best under the triple overlap syndrome taxonomy.
We suspect that these patients have worse outcomes, including comorbidity burden, quality of life, exacerbation rates, longer hospital length-of-stay, and respiratory and all-cause mortality. Large, multicenter, controlled trials comparing the long-term effectiveness of NIV and CPAP: measurements of respiratory function, gas exchange, blood pressure, and health related quality of life are needed. This is a group of patients that may specifically benefit from volume-targeted pressure support mode ventilation with auto-EPAP capabilities upon discharge from the hospital after an acute exacerbation.
Inpatient (sleep medicine) and outpatient transitions
In patients hospitalized with the triple overlap syndrome, there are certain considerations that are of special interest. Given comorbid hypercapnia and limited data on NIV superiority over CPAP, a sleep study should not be needed for NIV qualification. In addition, the medical team may consider the following (Figure 1):
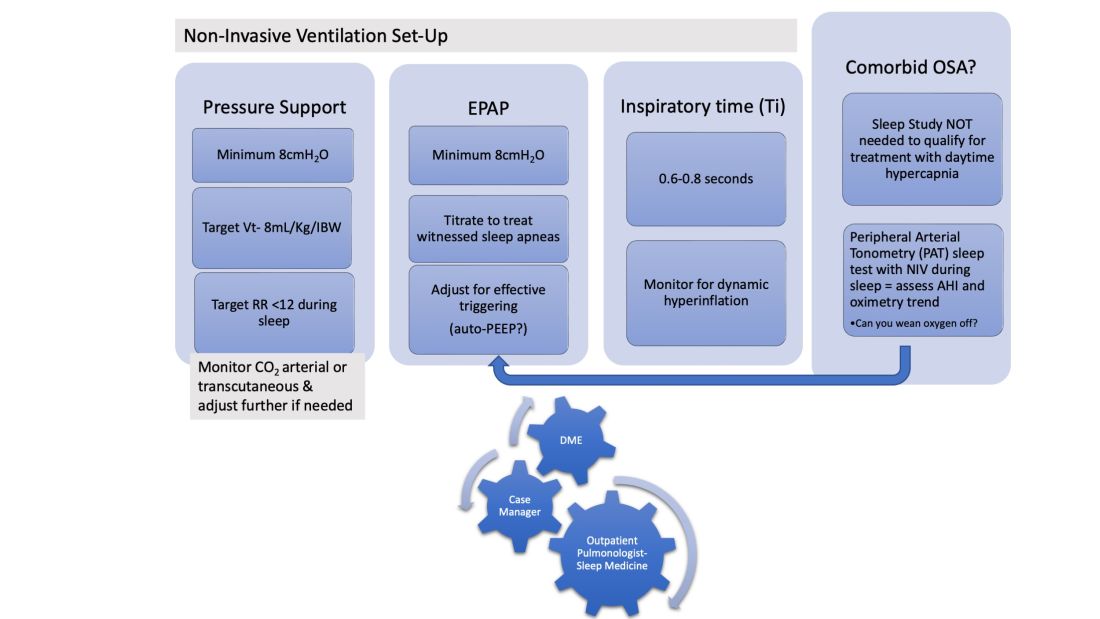
1. Noninvasive Ventilation:
a. Maintaining a high-pressure support differential between inspiratory positive airway pressure (IPAP) and EPAP. This can usually be achieved at 8-10 cm H2O, further adjusting to target a tidal volume (Vt) of 8 mL/kg of ideal body weight (IBW).
b. Higher EPAP: To overcome dependent atelectasis, improve ventilation-perfusion (VQ) matching, and better treat upper airway resistance both during wakefulness and sleep. Also, adjustments of EPAP at bedside should be considered to counteract auto-PEEP-related ineffective triggering if observed.
c. OSA screening and EPAP adjustment: for high residual obstructive apneas or hypopneas if data are available on the NIV device, or with the use of peripheral arterial tonometry sleep testing devices with NIV on overnight before discharge.
d. Does the patient meet criteria for oxygen supplementation at home? Wean oxygen off, if possible.
2. Case-managers can help establish services with a durable medical equipment provider with expertise in advanced PAP devices.3. Obesity management, Consider referral to an obesity management program for lifestyle/dietary modifications along with pharmacotherapy or bariatric surgery interventions.
4. Close follow-up, track exacerbations. Device download data are crucial to monitor adherence/tolerance and treatment effectiveness with particular interest in AHI, oximetry, and CO2 trends monitoring. Some patients may need dedicated titration polysomnograms to adjust ventilation settings, for optimization of residual OSA or for oxygen addition or discontinuation.
Conclusion
Patients with the triple overlap phenotype have not been systematically defined, studied, or included in clinical trials. We anticipate that these patients have worse outcomes: quality of life, symptom and comorbidity burden, exacerbation rates, in-hospital mortality, longer hospital stay and ICU stay, and respiratory and all-cause mortality. This is a group of patients that may specifically benefit from domiciliary NIV set-up upon discharge from the hospital with close follow-up. Properly identifying these patients will help pulmonologists and health care systems direct resources to optimally manage this complex group of patients. Funding of research trials to support clinical guidelines development should be prioritized. Triple overlap syndrome is different from COPD-OSA overlap, OHS with moderate to severe OSA, or OHS without significant OSA.
Introducing CHEST President-Designate John A. Howington, MD, MBA, FCCP
John A. Howington, MD, MBA, FCCP, is a cardiothoracic surgeon currently serving as Chief of Oncology Services and Chair of Thoracic Surgery at Ascension Saint Thomas Health and a professor at the University of Tennessee Health Sciences Center in Nashville, Tennessee.
Dr. Howington received his undergraduate degree from Tennessee Technological University and medical degree from the University of Tennessee. He completed his general surgery residency at the University of Missouri, Kansas City and thoracic surgery residency at Vanderbilt University Medical Center.
Most recently, he received his Physician Executive MBA from the University of Tennessee.
As a passionate thoracic surgeon, he has lent his knowledge to the extensive CHEST lung cancer guideline portfolio for more than a decade. He offers regular leadership in multidisciplinary and executive forums and has spearheaded a series of quality improvement initiatives at Ascension. He has served in a variety of leadership roles with CHEST and with other national thoracic surgery societies.
Dr. Howington began his CHEST leadership journey with the Networks, as a member of the Interventional Chest Medicine Steering Committee and then as the Thoracic Oncology Network Chair (2008-2010).
Other leadership positions include serving as the President of the CHEST Foundation (2014-2016), member of the Scientific Program Committee and Membership Committee, and, recently, as the Chair of the Finance Committee from 2018-2021.
Since 2017, he has served on the Board of Regents as a Member at Large. Dr. Howington will serve as the 87th CHEST President in 2025.
John A. Howington, MD, MBA, FCCP, is a cardiothoracic surgeon currently serving as Chief of Oncology Services and Chair of Thoracic Surgery at Ascension Saint Thomas Health and a professor at the University of Tennessee Health Sciences Center in Nashville, Tennessee.
Dr. Howington received his undergraduate degree from Tennessee Technological University and medical degree from the University of Tennessee. He completed his general surgery residency at the University of Missouri, Kansas City and thoracic surgery residency at Vanderbilt University Medical Center.
Most recently, he received his Physician Executive MBA from the University of Tennessee.
As a passionate thoracic surgeon, he has lent his knowledge to the extensive CHEST lung cancer guideline portfolio for more than a decade. He offers regular leadership in multidisciplinary and executive forums and has spearheaded a series of quality improvement initiatives at Ascension. He has served in a variety of leadership roles with CHEST and with other national thoracic surgery societies.
Dr. Howington began his CHEST leadership journey with the Networks, as a member of the Interventional Chest Medicine Steering Committee and then as the Thoracic Oncology Network Chair (2008-2010).
Other leadership positions include serving as the President of the CHEST Foundation (2014-2016), member of the Scientific Program Committee and Membership Committee, and, recently, as the Chair of the Finance Committee from 2018-2021.
Since 2017, he has served on the Board of Regents as a Member at Large. Dr. Howington will serve as the 87th CHEST President in 2025.
John A. Howington, MD, MBA, FCCP, is a cardiothoracic surgeon currently serving as Chief of Oncology Services and Chair of Thoracic Surgery at Ascension Saint Thomas Health and a professor at the University of Tennessee Health Sciences Center in Nashville, Tennessee.
Dr. Howington received his undergraduate degree from Tennessee Technological University and medical degree from the University of Tennessee. He completed his general surgery residency at the University of Missouri, Kansas City and thoracic surgery residency at Vanderbilt University Medical Center.
Most recently, he received his Physician Executive MBA from the University of Tennessee.
As a passionate thoracic surgeon, he has lent his knowledge to the extensive CHEST lung cancer guideline portfolio for more than a decade. He offers regular leadership in multidisciplinary and executive forums and has spearheaded a series of quality improvement initiatives at Ascension. He has served in a variety of leadership roles with CHEST and with other national thoracic surgery societies.
Dr. Howington began his CHEST leadership journey with the Networks, as a member of the Interventional Chest Medicine Steering Committee and then as the Thoracic Oncology Network Chair (2008-2010).
Other leadership positions include serving as the President of the CHEST Foundation (2014-2016), member of the Scientific Program Committee and Membership Committee, and, recently, as the Chair of the Finance Committee from 2018-2021.
Since 2017, he has served on the Board of Regents as a Member at Large. Dr. Howington will serve as the 87th CHEST President in 2025.
Three surprising studies on exercise restriction and an exercise sweet spot
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
FDA strengthens mammography regulations: Final rule
A final rule, updating the regulations issued under the Mammography Quality Standards Act of 1992, requires that mammography facilities notify patients about the density of their breasts, strengthens the FDA’s oversight of facilities, and provides guidance to help physicians better categorize and assess mammograms, according to a March 9 press release.
The rule requires implementation of the changes within 18 months.
According to the final rule document, the updates are “intended to improve the delivery of mammography services” in ways that reflect changes in mammography technology, quality standards, and the way results are categorized, reported, and communicated to patients and providers.
For instance, mammography reports must include an assessment of breast density to provide greater detail on the potential limitations of the mammogram results and allow patients and physicians to make more informed decisions, such as the possibility of additional imaging for women with dense breast tissue.
“Today’s action represents the agency’s broader commitment to support innovation to prevent, detect and treat cancer,” said Hilary Marston, MD, MPH, FDA’s chief medical officer, in the agency’s press release. The FDA remains “committed to advancing efforts to improve the health of women and strengthen the fight against breast cancer.”
A version of this article first appeared on Medscape.com.
A final rule, updating the regulations issued under the Mammography Quality Standards Act of 1992, requires that mammography facilities notify patients about the density of their breasts, strengthens the FDA’s oversight of facilities, and provides guidance to help physicians better categorize and assess mammograms, according to a March 9 press release.
The rule requires implementation of the changes within 18 months.
According to the final rule document, the updates are “intended to improve the delivery of mammography services” in ways that reflect changes in mammography technology, quality standards, and the way results are categorized, reported, and communicated to patients and providers.
For instance, mammography reports must include an assessment of breast density to provide greater detail on the potential limitations of the mammogram results and allow patients and physicians to make more informed decisions, such as the possibility of additional imaging for women with dense breast tissue.
“Today’s action represents the agency’s broader commitment to support innovation to prevent, detect and treat cancer,” said Hilary Marston, MD, MPH, FDA’s chief medical officer, in the agency’s press release. The FDA remains “committed to advancing efforts to improve the health of women and strengthen the fight against breast cancer.”
A version of this article first appeared on Medscape.com.
A final rule, updating the regulations issued under the Mammography Quality Standards Act of 1992, requires that mammography facilities notify patients about the density of their breasts, strengthens the FDA’s oversight of facilities, and provides guidance to help physicians better categorize and assess mammograms, according to a March 9 press release.
The rule requires implementation of the changes within 18 months.
According to the final rule document, the updates are “intended to improve the delivery of mammography services” in ways that reflect changes in mammography technology, quality standards, and the way results are categorized, reported, and communicated to patients and providers.
For instance, mammography reports must include an assessment of breast density to provide greater detail on the potential limitations of the mammogram results and allow patients and physicians to make more informed decisions, such as the possibility of additional imaging for women with dense breast tissue.
“Today’s action represents the agency’s broader commitment to support innovation to prevent, detect and treat cancer,” said Hilary Marston, MD, MPH, FDA’s chief medical officer, in the agency’s press release. The FDA remains “committed to advancing efforts to improve the health of women and strengthen the fight against breast cancer.”
A version of this article first appeared on Medscape.com.
Racial morphing: A conundrum in cosmetic dermatology
HONOLULU – In the opinion of Nazanin A. Saedi, MD, social media-induced dissatisfaction with appearance is getting out of hand in the field of cosmetic dermatology, with the emergence of apps to filter and edit images to the patient’s liking.
This, coupled with
“Overexposure of celebrity images and altered faces on social media have led to a trend of overarching brows, sculpted noses, enlarged cheeks, and sharply defined jawlines,” Dr. Saedi, cochair of the laser and aesthetics surgery center at Dermatology Associates of Plymouth Meeting, Pa., said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! “These trends have made people of different ethnicities morph into a similar appearance.”
At the meeting, she showed early career images of celebrities from different ethnic backgrounds, “and they all have unique features that make them look great,” said Dr. Saedi, clinical associate professor of dermatology at Thomas Jefferson University, Philadelphia. She then showed images of the same celebrities after they had undergone cosmetic procedures, “and they look so much more similar,” with overarched brows, sculpted noses, enlarged cheeks, and sharply defined jawlines. “Whereas they were all beautiful before individually, now they look very similar,” she said. “This is what we see on social media.”
Referring to the Kardashians as an example of celebrities who have had a lot of aesthetic treatments, look different than they did years ago, and are seen “more and more,” she added, “it’s this repeated overexposure to people on social media, to celebrities, that’s created this different trend of attractiveness.”
This trend also affects patients seeking cosmetic treatments, she noted. Individuals can use an app to alter their appearance, “changing the way they look to create the best version of themselves, they might say, or a filtered version of themselves,” said Dr. Saedi, one of the authors of a commentary on patient perception of beauty on social media published several years ago.
“I tell people, ‘Don’t use filters in your photos. Embrace your beauty.’ I have patients coming in who want to look like the social media photos they’ve curated, maybe larger lips or more definition in their jawline. What they don’t understand is that it takes a long time for that to happen. It’s a process.” In other cases, their desired outcome is not possible due to limits of their individual facial anatomy.
In a study published almost 20 years ago in the journal Perception, Irish researchers manipulated the familiarity of typical and distinctive faces to measure the effect on attractiveness. They found that episodic familiarity affects attractiveness ratings independently of general or structural familiarity.
“So, the more you saw a face, the more familiar that face was to you,” said Dr. Saedi, who was not involved with the study. “Over time, you felt that to be more attractive. I think that’s a lot of what’s going on in the trends that we’re seeing – both in real life and on social media. I do think we need to be more mindful of maintaining features that make an individual unique, while also maintaining their ethnic beauty.”
In an interview at the meeting, Jacqueline D. Watchmaker, MD, a board-certified cosmetic and medical dermatologist who practices in Scottsdale, Ariz., said that she identifies with the notion of racial morphing in her own clinical experience. “Patients come in and specifically ask for chiseled jawlines, high cheekbones, and bigger lips,” Dr. Watchmaker said. “It’s a tricky situation when they ask for [a treatment] you don’t think they need. I prefer a more staged approach to maintain their individuality while giving them a little bit of the aesthetic benefit that they’re looking for.”
Dr. Saedi disclosed ties with AbbVie, Aerolase, Allergan, Alma, Cartessa, Cynosure, Galderma Laboratories, LP, Grand Cosmetics, Revelle Aesthetics, and Revision Skincare. Dr. Watchmaker reported having no financial disclosures.
Medscape and this news organization are owned by the same parent company.
HONOLULU – In the opinion of Nazanin A. Saedi, MD, social media-induced dissatisfaction with appearance is getting out of hand in the field of cosmetic dermatology, with the emergence of apps to filter and edit images to the patient’s liking.
This, coupled with
“Overexposure of celebrity images and altered faces on social media have led to a trend of overarching brows, sculpted noses, enlarged cheeks, and sharply defined jawlines,” Dr. Saedi, cochair of the laser and aesthetics surgery center at Dermatology Associates of Plymouth Meeting, Pa., said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! “These trends have made people of different ethnicities morph into a similar appearance.”
At the meeting, she showed early career images of celebrities from different ethnic backgrounds, “and they all have unique features that make them look great,” said Dr. Saedi, clinical associate professor of dermatology at Thomas Jefferson University, Philadelphia. She then showed images of the same celebrities after they had undergone cosmetic procedures, “and they look so much more similar,” with overarched brows, sculpted noses, enlarged cheeks, and sharply defined jawlines. “Whereas they were all beautiful before individually, now they look very similar,” she said. “This is what we see on social media.”
Referring to the Kardashians as an example of celebrities who have had a lot of aesthetic treatments, look different than they did years ago, and are seen “more and more,” she added, “it’s this repeated overexposure to people on social media, to celebrities, that’s created this different trend of attractiveness.”
This trend also affects patients seeking cosmetic treatments, she noted. Individuals can use an app to alter their appearance, “changing the way they look to create the best version of themselves, they might say, or a filtered version of themselves,” said Dr. Saedi, one of the authors of a commentary on patient perception of beauty on social media published several years ago.
“I tell people, ‘Don’t use filters in your photos. Embrace your beauty.’ I have patients coming in who want to look like the social media photos they’ve curated, maybe larger lips or more definition in their jawline. What they don’t understand is that it takes a long time for that to happen. It’s a process.” In other cases, their desired outcome is not possible due to limits of their individual facial anatomy.
In a study published almost 20 years ago in the journal Perception, Irish researchers manipulated the familiarity of typical and distinctive faces to measure the effect on attractiveness. They found that episodic familiarity affects attractiveness ratings independently of general or structural familiarity.
“So, the more you saw a face, the more familiar that face was to you,” said Dr. Saedi, who was not involved with the study. “Over time, you felt that to be more attractive. I think that’s a lot of what’s going on in the trends that we’re seeing – both in real life and on social media. I do think we need to be more mindful of maintaining features that make an individual unique, while also maintaining their ethnic beauty.”
In an interview at the meeting, Jacqueline D. Watchmaker, MD, a board-certified cosmetic and medical dermatologist who practices in Scottsdale, Ariz., said that she identifies with the notion of racial morphing in her own clinical experience. “Patients come in and specifically ask for chiseled jawlines, high cheekbones, and bigger lips,” Dr. Watchmaker said. “It’s a tricky situation when they ask for [a treatment] you don’t think they need. I prefer a more staged approach to maintain their individuality while giving them a little bit of the aesthetic benefit that they’re looking for.”
Dr. Saedi disclosed ties with AbbVie, Aerolase, Allergan, Alma, Cartessa, Cynosure, Galderma Laboratories, LP, Grand Cosmetics, Revelle Aesthetics, and Revision Skincare. Dr. Watchmaker reported having no financial disclosures.
Medscape and this news organization are owned by the same parent company.
HONOLULU – In the opinion of Nazanin A. Saedi, MD, social media-induced dissatisfaction with appearance is getting out of hand in the field of cosmetic dermatology, with the emergence of apps to filter and edit images to the patient’s liking.
This, coupled with
“Overexposure of celebrity images and altered faces on social media have led to a trend of overarching brows, sculpted noses, enlarged cheeks, and sharply defined jawlines,” Dr. Saedi, cochair of the laser and aesthetics surgery center at Dermatology Associates of Plymouth Meeting, Pa., said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! “These trends have made people of different ethnicities morph into a similar appearance.”
At the meeting, she showed early career images of celebrities from different ethnic backgrounds, “and they all have unique features that make them look great,” said Dr. Saedi, clinical associate professor of dermatology at Thomas Jefferson University, Philadelphia. She then showed images of the same celebrities after they had undergone cosmetic procedures, “and they look so much more similar,” with overarched brows, sculpted noses, enlarged cheeks, and sharply defined jawlines. “Whereas they were all beautiful before individually, now they look very similar,” she said. “This is what we see on social media.”
Referring to the Kardashians as an example of celebrities who have had a lot of aesthetic treatments, look different than they did years ago, and are seen “more and more,” she added, “it’s this repeated overexposure to people on social media, to celebrities, that’s created this different trend of attractiveness.”
This trend also affects patients seeking cosmetic treatments, she noted. Individuals can use an app to alter their appearance, “changing the way they look to create the best version of themselves, they might say, or a filtered version of themselves,” said Dr. Saedi, one of the authors of a commentary on patient perception of beauty on social media published several years ago.
“I tell people, ‘Don’t use filters in your photos. Embrace your beauty.’ I have patients coming in who want to look like the social media photos they’ve curated, maybe larger lips or more definition in their jawline. What they don’t understand is that it takes a long time for that to happen. It’s a process.” In other cases, their desired outcome is not possible due to limits of their individual facial anatomy.
In a study published almost 20 years ago in the journal Perception, Irish researchers manipulated the familiarity of typical and distinctive faces to measure the effect on attractiveness. They found that episodic familiarity affects attractiveness ratings independently of general or structural familiarity.
“So, the more you saw a face, the more familiar that face was to you,” said Dr. Saedi, who was not involved with the study. “Over time, you felt that to be more attractive. I think that’s a lot of what’s going on in the trends that we’re seeing – both in real life and on social media. I do think we need to be more mindful of maintaining features that make an individual unique, while also maintaining their ethnic beauty.”
In an interview at the meeting, Jacqueline D. Watchmaker, MD, a board-certified cosmetic and medical dermatologist who practices in Scottsdale, Ariz., said that she identifies with the notion of racial morphing in her own clinical experience. “Patients come in and specifically ask for chiseled jawlines, high cheekbones, and bigger lips,” Dr. Watchmaker said. “It’s a tricky situation when they ask for [a treatment] you don’t think they need. I prefer a more staged approach to maintain their individuality while giving them a little bit of the aesthetic benefit that they’re looking for.”
Dr. Saedi disclosed ties with AbbVie, Aerolase, Allergan, Alma, Cartessa, Cynosure, Galderma Laboratories, LP, Grand Cosmetics, Revelle Aesthetics, and Revision Skincare. Dr. Watchmaker reported having no financial disclosures.
Medscape and this news organization are owned by the same parent company.
AT THE MEDSCAPELIVE! HAWAII DERMATOLOGY SEMINAR
Cancer clinical trials: Can industry stack the deck?
A year before the COVID-19 pandemic began, a team of clinical statisticians at the University of Texas MD Anderson Cancer Center sat together in small office for a year, painstakingly hand coding data from the U.S. clinical trials database, www.clinicaltrials.gov.
“We found marked disparities across different disease sites. ... The patients that are enrolling on studies are markedly younger than the average patient seen in the population with those same conditions,” said team leader Ethan Ludmir, MD, assistant professor, Division of Radiation Oncology at the University of Texas.
And this age disparity was significantly greater in industry-funded trials.
Researchers have known for 20 years that cancer trial participants are not representative of the wider cancer population, and numerous government guidance documents have been issued on the matter. However, this Texas team’s findings were the first unambiguous evidence that pharmaceutical companies seem to be selecting younger patients to test their drugs.
“If we’re being generous then perhaps the answer is: They’re looking for some element of homogeneity, which is to say they don’t want competing risks to make the signal-to-noise ratio uninterpretable,” said Dr. Ludmir.
Dr. Laura Bothwell, PhD, assistant professor, Yale School of Public Health, recently coauthored a 259-page consensus report for the National Academies of Sciences, Engineering and Medicine on how to increase the research involvement of under-represented groups.
Dr. Bothwell said, “The problem with industry funded research is that ... it’s an inevitable conflict of interest that exists. They want the research to show that their products work. And older populations ... have a lot more complications, which leads to potentially less favorable results.”
The MD Anderson findings were published in JAMA Oncology. “That was the starting point in our journey,” said Dr. Ludmir. For the next 3 years, the researchers mined their painstakingly constructed database to understand what was preventing greater numbers of older patients from enrollment in cancer trials.
Meanwhile, answers were coming from elsewhere. In parallel with the work at MD Anderson, a team in California led by Mina Sedrak, MD, a medical oncologist at the City of Hope National Medical Center, had also started investigating age disparities in clinical trials.
Dr. Sedrak, who also serves as deputy director of Clinical Trials at the Center for Cancer and Aging, said he had become increasingly concerned that he did not have adequate information on new cancer therapies for his older patients.
“I was caring for a large number of people who were ... older adults,” said Dr. Sedrak, “But the data that was being used to get the standard-of-care treatment for cancer did not include older adults. And so there was this lack of applicability.”
He summed up the challenges in a 2021 review paper: “Most of what we know about cancer therapeutics is based on clinical trials conducted in younger, healthier patients.”
By 2030, it is estimated that 70% of all new cancer diagnoses will be in patients 65 years old and older. By contrast, patients over age 65 still account for only 40% of patients in cancer trials registered with the FDA (2015 figures) and older adults make up only 44% of participants in practice-changing cancer trials, according to a 2022 study.
So what is going on? Are studies specifically designed to squeeze out older patients?
Surprisingly, patients are not being kept out of trials by formal age limits, according to Dr. Ludmir. His team found that only 10% of phase 3 trials over the past 30 years had an upper limit for age, and age restrictions have been dropping by 1% a year. (For example, 16% of trials that enrolled in 2002-2005 had an upper age limit, compared with just 8% of trials that started in 2010-2014.)
Dr. Sedrak’s team found that “clinician bias” may be a factor, a situation in which trial investigators – particularly academic oncologists – are subconsciously picking younger, healthier patients for trials and excluding older, sicker patients to protect them from drug toxicities.
Dr. Ludmir said this was understandable, especially in the case of industry-driven trials, which tend to have demanding endpoints and “an overall posture of more treatment aggressiveness.”
“These are typically not trials where they’re saying, `Hey, if we add acupuncture ... are we going to see improved patient reported outcomes?’” Dr. Ludmir explained. “You’re asking ... I’ve got this cocktail of two pretty rough chemos: I want to see what happens if I add an immunotherapy to that. If I’m the clinician in clinic, I might reasonably, subconsciously, say, is the 75-year-old really who I want on this?”
What about patient bias? Perhaps fewer older patients wish to join clinical trials?
Not so, at least not at community cancer centers, said Dr. Sedrak. His team’s analysis of the National Cancer Institute Community Oncology Research Program database for 2016-2019 revealed that older patients were just as keen as the younger patients to participate in trials (68% of patients aged 50-69 years and 65% of patients 70+; P = .28).
However, drug companies may be excluding older patients by more subtle means. One-fifth of patients over 65 have had a prior cancer. Dr. Ludmir and coauthor Roshal Patel, MD, used their hand-coded www.clinicaltrials.gov database to look at prior malignancy exclusion criteria (PMEC). The analysis found “pervasive utilization” of PMEC in phase 3 trials, cropping up in 41% of studies over the past 30 years.
PMEC was significantly associated with age disparities and was significantly more common in industry-funded trials.
When asked whether PMEC are “age restriction by stealth” on the part of drug companies, Dr. Ludmir was reluctant to assign blame, but stood by his data: “The wider you restrict people in terms of having a prior cancer, the wider the age disparities in the subsequent studies, which to me is about as strong, in terms of causal understanding of these phenomena, as you can reasonably get at this level.”
In March the FDA released a guidance document titled Inclusion of Older Adults in Cancer Clinical Trials. However, its recommendations are “nonbinding” and “do not have the force and effect of law.”
To fix the issues, said Dr. Sedrak, the FDA must be given teeth.
“Okay, you write guidelines,” he said. “But if you don’t actually hold people accountable to following the guidelines, how are we going to implement and make sure that we’re transforming policy into action?”
Dr. Bothwell of Yale’s School of Public Health agreed. “Accountability has been the weakest link for decades now.”
She concluded, “In medicine there’s a tendency to believe that a therapy, because it exists and it has been tested and it’s shown some efficacy, it’s useful. But we don’t know the answer to that question unless we have statistically valid research in the population that we’re using it in.”
Dr. Bothwell and Dr. Ludmir report no conflicts of interest. In his publications, Dr. Sedrak reports industry grants from Seattle Genetics, Eli Lilly, Novartis, and Pfizer Foundation.
A year before the COVID-19 pandemic began, a team of clinical statisticians at the University of Texas MD Anderson Cancer Center sat together in small office for a year, painstakingly hand coding data from the U.S. clinical trials database, www.clinicaltrials.gov.
“We found marked disparities across different disease sites. ... The patients that are enrolling on studies are markedly younger than the average patient seen in the population with those same conditions,” said team leader Ethan Ludmir, MD, assistant professor, Division of Radiation Oncology at the University of Texas.
And this age disparity was significantly greater in industry-funded trials.
Researchers have known for 20 years that cancer trial participants are not representative of the wider cancer population, and numerous government guidance documents have been issued on the matter. However, this Texas team’s findings were the first unambiguous evidence that pharmaceutical companies seem to be selecting younger patients to test their drugs.
“If we’re being generous then perhaps the answer is: They’re looking for some element of homogeneity, which is to say they don’t want competing risks to make the signal-to-noise ratio uninterpretable,” said Dr. Ludmir.
Dr. Laura Bothwell, PhD, assistant professor, Yale School of Public Health, recently coauthored a 259-page consensus report for the National Academies of Sciences, Engineering and Medicine on how to increase the research involvement of under-represented groups.
Dr. Bothwell said, “The problem with industry funded research is that ... it’s an inevitable conflict of interest that exists. They want the research to show that their products work. And older populations ... have a lot more complications, which leads to potentially less favorable results.”
The MD Anderson findings were published in JAMA Oncology. “That was the starting point in our journey,” said Dr. Ludmir. For the next 3 years, the researchers mined their painstakingly constructed database to understand what was preventing greater numbers of older patients from enrollment in cancer trials.
Meanwhile, answers were coming from elsewhere. In parallel with the work at MD Anderson, a team in California led by Mina Sedrak, MD, a medical oncologist at the City of Hope National Medical Center, had also started investigating age disparities in clinical trials.
Dr. Sedrak, who also serves as deputy director of Clinical Trials at the Center for Cancer and Aging, said he had become increasingly concerned that he did not have adequate information on new cancer therapies for his older patients.
“I was caring for a large number of people who were ... older adults,” said Dr. Sedrak, “But the data that was being used to get the standard-of-care treatment for cancer did not include older adults. And so there was this lack of applicability.”
He summed up the challenges in a 2021 review paper: “Most of what we know about cancer therapeutics is based on clinical trials conducted in younger, healthier patients.”
By 2030, it is estimated that 70% of all new cancer diagnoses will be in patients 65 years old and older. By contrast, patients over age 65 still account for only 40% of patients in cancer trials registered with the FDA (2015 figures) and older adults make up only 44% of participants in practice-changing cancer trials, according to a 2022 study.
So what is going on? Are studies specifically designed to squeeze out older patients?
Surprisingly, patients are not being kept out of trials by formal age limits, according to Dr. Ludmir. His team found that only 10% of phase 3 trials over the past 30 years had an upper limit for age, and age restrictions have been dropping by 1% a year. (For example, 16% of trials that enrolled in 2002-2005 had an upper age limit, compared with just 8% of trials that started in 2010-2014.)
Dr. Sedrak’s team found that “clinician bias” may be a factor, a situation in which trial investigators – particularly academic oncologists – are subconsciously picking younger, healthier patients for trials and excluding older, sicker patients to protect them from drug toxicities.
Dr. Ludmir said this was understandable, especially in the case of industry-driven trials, which tend to have demanding endpoints and “an overall posture of more treatment aggressiveness.”
“These are typically not trials where they’re saying, `Hey, if we add acupuncture ... are we going to see improved patient reported outcomes?’” Dr. Ludmir explained. “You’re asking ... I’ve got this cocktail of two pretty rough chemos: I want to see what happens if I add an immunotherapy to that. If I’m the clinician in clinic, I might reasonably, subconsciously, say, is the 75-year-old really who I want on this?”
What about patient bias? Perhaps fewer older patients wish to join clinical trials?
Not so, at least not at community cancer centers, said Dr. Sedrak. His team’s analysis of the National Cancer Institute Community Oncology Research Program database for 2016-2019 revealed that older patients were just as keen as the younger patients to participate in trials (68% of patients aged 50-69 years and 65% of patients 70+; P = .28).
However, drug companies may be excluding older patients by more subtle means. One-fifth of patients over 65 have had a prior cancer. Dr. Ludmir and coauthor Roshal Patel, MD, used their hand-coded www.clinicaltrials.gov database to look at prior malignancy exclusion criteria (PMEC). The analysis found “pervasive utilization” of PMEC in phase 3 trials, cropping up in 41% of studies over the past 30 years.
PMEC was significantly associated with age disparities and was significantly more common in industry-funded trials.
When asked whether PMEC are “age restriction by stealth” on the part of drug companies, Dr. Ludmir was reluctant to assign blame, but stood by his data: “The wider you restrict people in terms of having a prior cancer, the wider the age disparities in the subsequent studies, which to me is about as strong, in terms of causal understanding of these phenomena, as you can reasonably get at this level.”
In March the FDA released a guidance document titled Inclusion of Older Adults in Cancer Clinical Trials. However, its recommendations are “nonbinding” and “do not have the force and effect of law.”
To fix the issues, said Dr. Sedrak, the FDA must be given teeth.
“Okay, you write guidelines,” he said. “But if you don’t actually hold people accountable to following the guidelines, how are we going to implement and make sure that we’re transforming policy into action?”
Dr. Bothwell of Yale’s School of Public Health agreed. “Accountability has been the weakest link for decades now.”
She concluded, “In medicine there’s a tendency to believe that a therapy, because it exists and it has been tested and it’s shown some efficacy, it’s useful. But we don’t know the answer to that question unless we have statistically valid research in the population that we’re using it in.”
Dr. Bothwell and Dr. Ludmir report no conflicts of interest. In his publications, Dr. Sedrak reports industry grants from Seattle Genetics, Eli Lilly, Novartis, and Pfizer Foundation.
A year before the COVID-19 pandemic began, a team of clinical statisticians at the University of Texas MD Anderson Cancer Center sat together in small office for a year, painstakingly hand coding data from the U.S. clinical trials database, www.clinicaltrials.gov.
“We found marked disparities across different disease sites. ... The patients that are enrolling on studies are markedly younger than the average patient seen in the population with those same conditions,” said team leader Ethan Ludmir, MD, assistant professor, Division of Radiation Oncology at the University of Texas.
And this age disparity was significantly greater in industry-funded trials.
Researchers have known for 20 years that cancer trial participants are not representative of the wider cancer population, and numerous government guidance documents have been issued on the matter. However, this Texas team’s findings were the first unambiguous evidence that pharmaceutical companies seem to be selecting younger patients to test their drugs.
“If we’re being generous then perhaps the answer is: They’re looking for some element of homogeneity, which is to say they don’t want competing risks to make the signal-to-noise ratio uninterpretable,” said Dr. Ludmir.
Dr. Laura Bothwell, PhD, assistant professor, Yale School of Public Health, recently coauthored a 259-page consensus report for the National Academies of Sciences, Engineering and Medicine on how to increase the research involvement of under-represented groups.
Dr. Bothwell said, “The problem with industry funded research is that ... it’s an inevitable conflict of interest that exists. They want the research to show that their products work. And older populations ... have a lot more complications, which leads to potentially less favorable results.”
The MD Anderson findings were published in JAMA Oncology. “That was the starting point in our journey,” said Dr. Ludmir. For the next 3 years, the researchers mined their painstakingly constructed database to understand what was preventing greater numbers of older patients from enrollment in cancer trials.
Meanwhile, answers were coming from elsewhere. In parallel with the work at MD Anderson, a team in California led by Mina Sedrak, MD, a medical oncologist at the City of Hope National Medical Center, had also started investigating age disparities in clinical trials.
Dr. Sedrak, who also serves as deputy director of Clinical Trials at the Center for Cancer and Aging, said he had become increasingly concerned that he did not have adequate information on new cancer therapies for his older patients.
“I was caring for a large number of people who were ... older adults,” said Dr. Sedrak, “But the data that was being used to get the standard-of-care treatment for cancer did not include older adults. And so there was this lack of applicability.”
He summed up the challenges in a 2021 review paper: “Most of what we know about cancer therapeutics is based on clinical trials conducted in younger, healthier patients.”
By 2030, it is estimated that 70% of all new cancer diagnoses will be in patients 65 years old and older. By contrast, patients over age 65 still account for only 40% of patients in cancer trials registered with the FDA (2015 figures) and older adults make up only 44% of participants in practice-changing cancer trials, according to a 2022 study.
So what is going on? Are studies specifically designed to squeeze out older patients?
Surprisingly, patients are not being kept out of trials by formal age limits, according to Dr. Ludmir. His team found that only 10% of phase 3 trials over the past 30 years had an upper limit for age, and age restrictions have been dropping by 1% a year. (For example, 16% of trials that enrolled in 2002-2005 had an upper age limit, compared with just 8% of trials that started in 2010-2014.)
Dr. Sedrak’s team found that “clinician bias” may be a factor, a situation in which trial investigators – particularly academic oncologists – are subconsciously picking younger, healthier patients for trials and excluding older, sicker patients to protect them from drug toxicities.
Dr. Ludmir said this was understandable, especially in the case of industry-driven trials, which tend to have demanding endpoints and “an overall posture of more treatment aggressiveness.”
“These are typically not trials where they’re saying, `Hey, if we add acupuncture ... are we going to see improved patient reported outcomes?’” Dr. Ludmir explained. “You’re asking ... I’ve got this cocktail of two pretty rough chemos: I want to see what happens if I add an immunotherapy to that. If I’m the clinician in clinic, I might reasonably, subconsciously, say, is the 75-year-old really who I want on this?”
What about patient bias? Perhaps fewer older patients wish to join clinical trials?
Not so, at least not at community cancer centers, said Dr. Sedrak. His team’s analysis of the National Cancer Institute Community Oncology Research Program database for 2016-2019 revealed that older patients were just as keen as the younger patients to participate in trials (68% of patients aged 50-69 years and 65% of patients 70+; P = .28).
However, drug companies may be excluding older patients by more subtle means. One-fifth of patients over 65 have had a prior cancer. Dr. Ludmir and coauthor Roshal Patel, MD, used their hand-coded www.clinicaltrials.gov database to look at prior malignancy exclusion criteria (PMEC). The analysis found “pervasive utilization” of PMEC in phase 3 trials, cropping up in 41% of studies over the past 30 years.
PMEC was significantly associated with age disparities and was significantly more common in industry-funded trials.
When asked whether PMEC are “age restriction by stealth” on the part of drug companies, Dr. Ludmir was reluctant to assign blame, but stood by his data: “The wider you restrict people in terms of having a prior cancer, the wider the age disparities in the subsequent studies, which to me is about as strong, in terms of causal understanding of these phenomena, as you can reasonably get at this level.”
In March the FDA released a guidance document titled Inclusion of Older Adults in Cancer Clinical Trials. However, its recommendations are “nonbinding” and “do not have the force and effect of law.”
To fix the issues, said Dr. Sedrak, the FDA must be given teeth.
“Okay, you write guidelines,” he said. “But if you don’t actually hold people accountable to following the guidelines, how are we going to implement and make sure that we’re transforming policy into action?”
Dr. Bothwell of Yale’s School of Public Health agreed. “Accountability has been the weakest link for decades now.”
She concluded, “In medicine there’s a tendency to believe that a therapy, because it exists and it has been tested and it’s shown some efficacy, it’s useful. But we don’t know the answer to that question unless we have statistically valid research in the population that we’re using it in.”
Dr. Bothwell and Dr. Ludmir report no conflicts of interest. In his publications, Dr. Sedrak reports industry grants from Seattle Genetics, Eli Lilly, Novartis, and Pfizer Foundation.
Ob.gyns. reveal heavier suicide ideation burden than most specialists
Obstetricians and gynecologists are more likely than most specialists to have thoughts of suicide, and almost of quarter of physicians in general reported that they were depressed in a recent survey conducted by Medscape.
“Too much work with too little control is a recipe for depression in anyone,” Andrea Giedinghagen, MD, of Washington University, St. Louis, said in the Medscape Physician Suicide Report: Doctors’ Burden 2023. “Physicians are also still coping with a pandemic – the trauma from COVID-19 didn’t disappear just because the full ICUs did – and with a fractured health care system that virtually guarantees moral distress.”
About 23% of the almost 9,200 survey respondents said that they were depressed in 2022, compared with 21% the previous year. Suicide ideation was down in 2022, however, with 9% of all responding physicians reporting contemplation versus 13% in 2021, based on the results of the latest survey, which was conducted from June 28, 2022, to Oct. 2, 2022.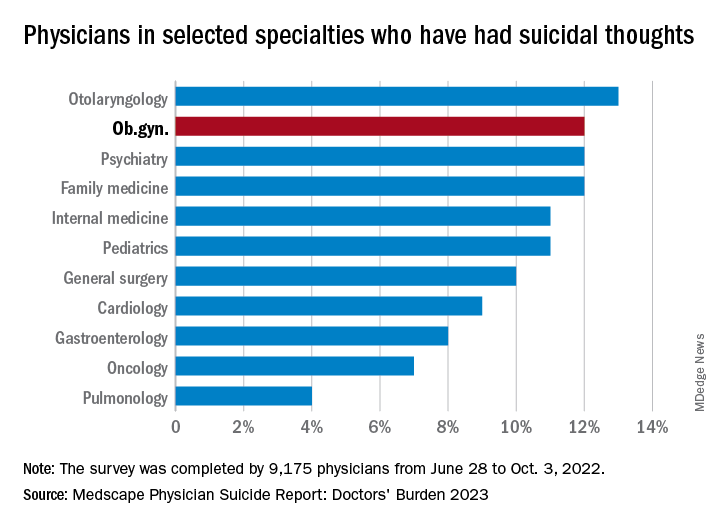
Ob.gyns. were above that average, with 12% reporting suicidal thoughts over the past year, equaling psychiatrists, family physicians, anesthesiologists, and emergency physicians and trailing only the otolaryngologists at 13%. The lowest rate among the 29 specialties included in the report was 4% for pulmonary medicine.
Differences between physicians, general population
Comparisons with the general U.S. population show that physicians are about twice as likely to report thoughts of suicide (9% vs. 4.9%) and to attempt it (1% vs. 0.5%). Among the overall population, however, “females are two to three times more likely to attempt suicide than males are,” noted Perry Lin, MD, national cochair of the American Association of Suicidology’s Physician Suicide Awareness Committee. That was not the case for survey respondents, as men and women both had an attempt rate of 1% and women were slightly ahead in ideation (11% to 9%).
There was a somewhat larger gap when age group was considered. Among physicians aged 57-75 years, 8% had thought about suicide, compared with 10% of those aged 42-56 years and 12% of respondents aged 27-41. This, again, runs counter to the general population, where older men typically deal with higher suicide rates, Michael F. Myers of the State University of New York, Brooklyn, said in the Medscape report.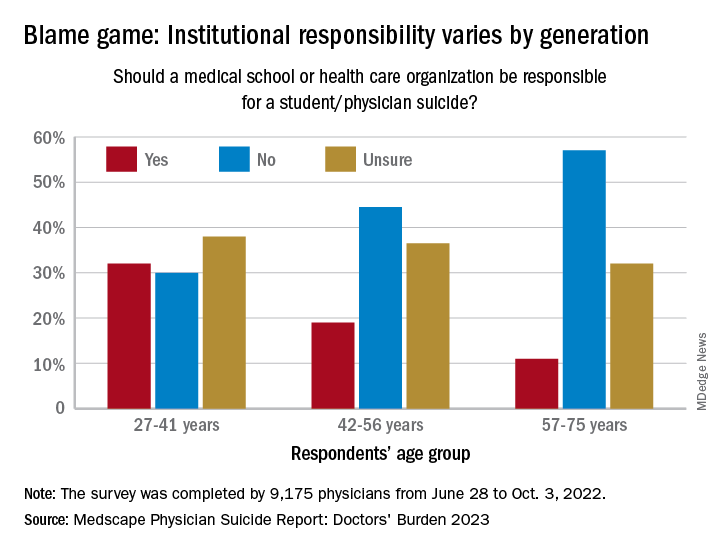
Age also was a factor when responsibility was brought into the equation. Over 30% of the youngest group of respondents (age 27-41) said that medical schools and health care organizations should be held responsible for an individual’s suicide, compared with 19% of those aged 42-56 and 11% of the 57- to 75-year-olds.
That trend was concerning to Dr. Myers: “Most suicides are multifactorial, many stressors coming together all at once in a person’s life, a so-called ‘perfect storm.’ ... But there are suicides each year involving medical students and physicians that have nothing to do with the medical school or place of work.”
Reasons to avoid professional help
Many of the survey respondents also were thinking about third parties when asked why they might not seek professional help for their suicidal thoughts. The most common response, cited by 52%, was that they didn’t need professional help, but 42% didn’t want to risk disclosure to a medical board, 33% were concerned about it being on their insurance record, and 25% were concerned about colleagues finding out.
“Doctors are willing and able to treat suicidal ideation among patients but appear fearful to seek such help themselves. We must do better,” Dr. Lin said in an interview.
Exact numbers of survey respondents were not given by specialty, but about 5% of the 9,175 total responses were completed by ob.gyns. The margin of error for the survey was ±1.02% at the 95% confidence interval.
Obstetricians and gynecologists are more likely than most specialists to have thoughts of suicide, and almost of quarter of physicians in general reported that they were depressed in a recent survey conducted by Medscape.
“Too much work with too little control is a recipe for depression in anyone,” Andrea Giedinghagen, MD, of Washington University, St. Louis, said in the Medscape Physician Suicide Report: Doctors’ Burden 2023. “Physicians are also still coping with a pandemic – the trauma from COVID-19 didn’t disappear just because the full ICUs did – and with a fractured health care system that virtually guarantees moral distress.”
About 23% of the almost 9,200 survey respondents said that they were depressed in 2022, compared with 21% the previous year. Suicide ideation was down in 2022, however, with 9% of all responding physicians reporting contemplation versus 13% in 2021, based on the results of the latest survey, which was conducted from June 28, 2022, to Oct. 2, 2022.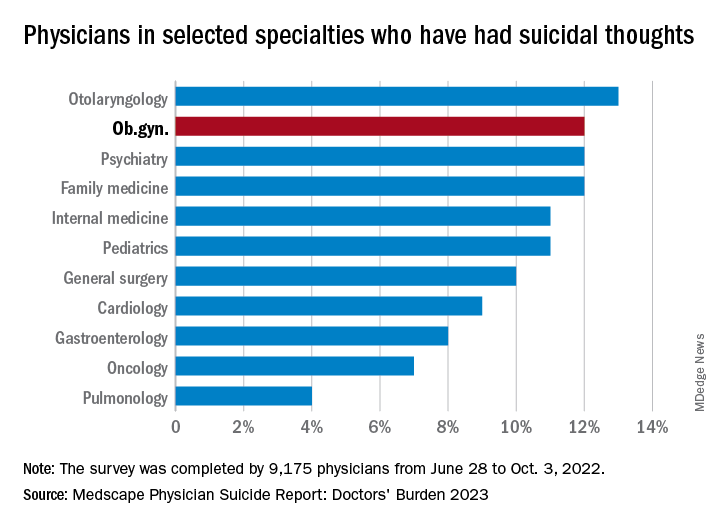
Ob.gyns. were above that average, with 12% reporting suicidal thoughts over the past year, equaling psychiatrists, family physicians, anesthesiologists, and emergency physicians and trailing only the otolaryngologists at 13%. The lowest rate among the 29 specialties included in the report was 4% for pulmonary medicine.
Differences between physicians, general population
Comparisons with the general U.S. population show that physicians are about twice as likely to report thoughts of suicide (9% vs. 4.9%) and to attempt it (1% vs. 0.5%). Among the overall population, however, “females are two to three times more likely to attempt suicide than males are,” noted Perry Lin, MD, national cochair of the American Association of Suicidology’s Physician Suicide Awareness Committee. That was not the case for survey respondents, as men and women both had an attempt rate of 1% and women were slightly ahead in ideation (11% to 9%).
There was a somewhat larger gap when age group was considered. Among physicians aged 57-75 years, 8% had thought about suicide, compared with 10% of those aged 42-56 years and 12% of respondents aged 27-41. This, again, runs counter to the general population, where older men typically deal with higher suicide rates, Michael F. Myers of the State University of New York, Brooklyn, said in the Medscape report.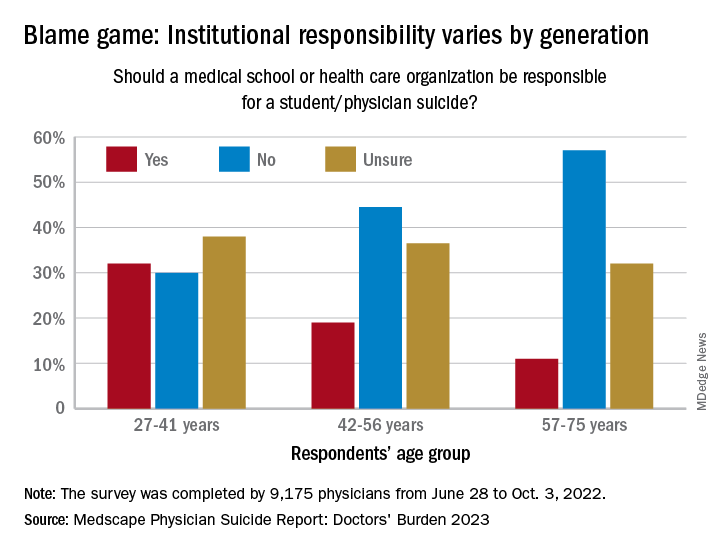
Age also was a factor when responsibility was brought into the equation. Over 30% of the youngest group of respondents (age 27-41) said that medical schools and health care organizations should be held responsible for an individual’s suicide, compared with 19% of those aged 42-56 and 11% of the 57- to 75-year-olds.
That trend was concerning to Dr. Myers: “Most suicides are multifactorial, many stressors coming together all at once in a person’s life, a so-called ‘perfect storm.’ ... But there are suicides each year involving medical students and physicians that have nothing to do with the medical school or place of work.”
Reasons to avoid professional help
Many of the survey respondents also were thinking about third parties when asked why they might not seek professional help for their suicidal thoughts. The most common response, cited by 52%, was that they didn’t need professional help, but 42% didn’t want to risk disclosure to a medical board, 33% were concerned about it being on their insurance record, and 25% were concerned about colleagues finding out.
“Doctors are willing and able to treat suicidal ideation among patients but appear fearful to seek such help themselves. We must do better,” Dr. Lin said in an interview.
Exact numbers of survey respondents were not given by specialty, but about 5% of the 9,175 total responses were completed by ob.gyns. The margin of error for the survey was ±1.02% at the 95% confidence interval.
Obstetricians and gynecologists are more likely than most specialists to have thoughts of suicide, and almost of quarter of physicians in general reported that they were depressed in a recent survey conducted by Medscape.
“Too much work with too little control is a recipe for depression in anyone,” Andrea Giedinghagen, MD, of Washington University, St. Louis, said in the Medscape Physician Suicide Report: Doctors’ Burden 2023. “Physicians are also still coping with a pandemic – the trauma from COVID-19 didn’t disappear just because the full ICUs did – and with a fractured health care system that virtually guarantees moral distress.”
About 23% of the almost 9,200 survey respondents said that they were depressed in 2022, compared with 21% the previous year. Suicide ideation was down in 2022, however, with 9% of all responding physicians reporting contemplation versus 13% in 2021, based on the results of the latest survey, which was conducted from June 28, 2022, to Oct. 2, 2022.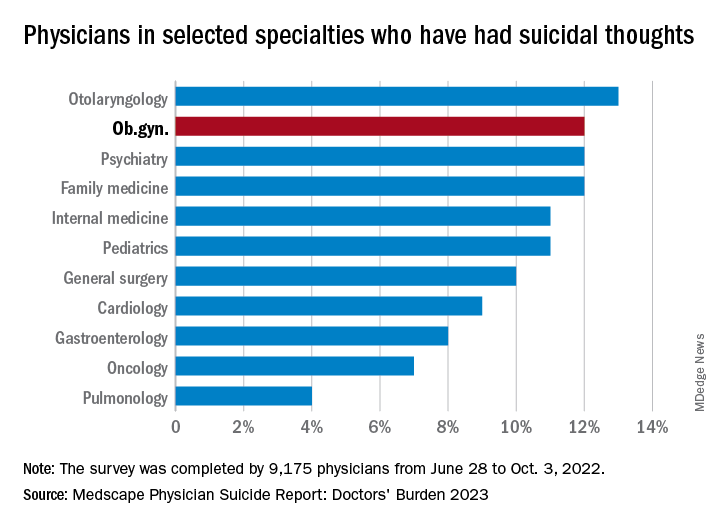
Ob.gyns. were above that average, with 12% reporting suicidal thoughts over the past year, equaling psychiatrists, family physicians, anesthesiologists, and emergency physicians and trailing only the otolaryngologists at 13%. The lowest rate among the 29 specialties included in the report was 4% for pulmonary medicine.
Differences between physicians, general population
Comparisons with the general U.S. population show that physicians are about twice as likely to report thoughts of suicide (9% vs. 4.9%) and to attempt it (1% vs. 0.5%). Among the overall population, however, “females are two to three times more likely to attempt suicide than males are,” noted Perry Lin, MD, national cochair of the American Association of Suicidology’s Physician Suicide Awareness Committee. That was not the case for survey respondents, as men and women both had an attempt rate of 1% and women were slightly ahead in ideation (11% to 9%).
There was a somewhat larger gap when age group was considered. Among physicians aged 57-75 years, 8% had thought about suicide, compared with 10% of those aged 42-56 years and 12% of respondents aged 27-41. This, again, runs counter to the general population, where older men typically deal with higher suicide rates, Michael F. Myers of the State University of New York, Brooklyn, said in the Medscape report.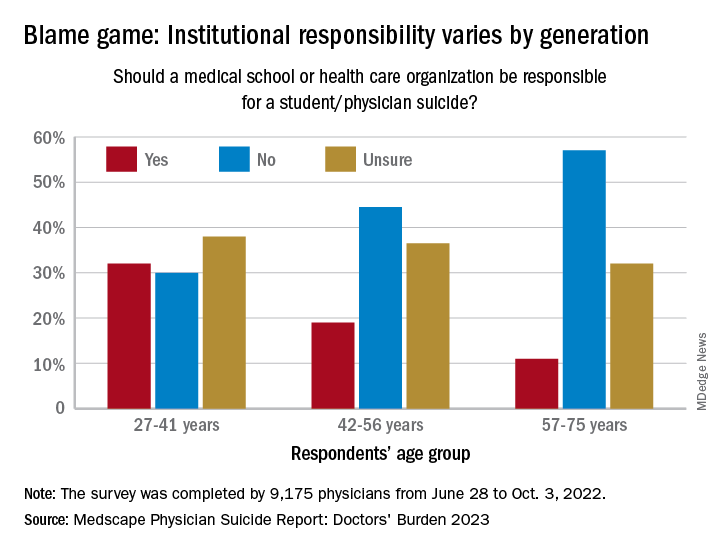
Age also was a factor when responsibility was brought into the equation. Over 30% of the youngest group of respondents (age 27-41) said that medical schools and health care organizations should be held responsible for an individual’s suicide, compared with 19% of those aged 42-56 and 11% of the 57- to 75-year-olds.
That trend was concerning to Dr. Myers: “Most suicides are multifactorial, many stressors coming together all at once in a person’s life, a so-called ‘perfect storm.’ ... But there are suicides each year involving medical students and physicians that have nothing to do with the medical school or place of work.”
Reasons to avoid professional help
Many of the survey respondents also were thinking about third parties when asked why they might not seek professional help for their suicidal thoughts. The most common response, cited by 52%, was that they didn’t need professional help, but 42% didn’t want to risk disclosure to a medical board, 33% were concerned about it being on their insurance record, and 25% were concerned about colleagues finding out.
“Doctors are willing and able to treat suicidal ideation among patients but appear fearful to seek such help themselves. We must do better,” Dr. Lin said in an interview.
Exact numbers of survey respondents were not given by specialty, but about 5% of the 9,175 total responses were completed by ob.gyns. The margin of error for the survey was ±1.02% at the 95% confidence interval.
Defensiveness may drive refusal for colon cancer screening
An Irish study attempting to get at the root of why men and women delay colon cancer screening found that, despite an uptick in colon cancer cases among younger adults, screening isn’t a priority for some adults while others are under the impression that a healthy diet with regular bowel movements negates the need for regular screening.
The findings are based on a survey of over 2,000 adults who participated in a population-based fecal immunochemical test (FIT) screening program. The authors found that denying the immediacy of the need to be tested and self-exempting from screening because of a belief in a healthy lifestyle were key drivers for opting out of FIT screening.
“What we found was that people who didn’t take part [in the survey] responded much more defensively to the invitation,” said Nicholas Clarke, PhD, a researcher at Dublin City University, who served as the lead author of the study published in the journal Cancer.
The domain of denying immediacy, which covers decisions like putting off a test because of more pressing life events, was associated with a 47% reduction in screening probability. “That’s quite a high percentage. They’re not saying I won’t do it. They’re saying: ‘I’ll wait to get tested for colon cancer until my other health concerns are under control, or until there’s a better test,’ ” he said.
The other suppression category of self-exempting was associated with a 20% reduction in the odds of participation. “They’re saying: ‘I don’t need to be tested because I have enough vegetables in my diet or because I have regular bowel movements,’ ” Dr. Clarke said.
Despite the proven efficacy of screening, many individuals still resist screening. In previous research, Dr. Clarke found that men in Ireland were less likely than women to undergo screening.
FIT works by identifying small amounts of blood in the stool that could suggest the presence of a tumor or precancerous polyps. The test also looks for methylation and DNA mutations that are indicative of precancer polyps or tumors. A positive test calls for a follow-up procedure such as a colonoscopy, where precancerous polyps can be removed to prevent them from developing into tumors.
FIT has similar sensitivity to colonoscopy in detecting cancers (93% vs. 95%), but is less effective with respect to polyps (42% vs. 75%-93%). For average risk adults between 50-75 years old, the U.S Preventive Services Task Force recommends colonoscopy every 10 years; flexible sigmoidoscopy or CT colonography every 5 years, or flexible sigmoidoscopy every 10 years plus fecal immunochemical test (FIT) every year; FIT DNA test every 3 years; guaiac-based fecal occult blood test or FIT test annually.
Findings from the new study
In the new study, researchers contacted both 2,299 responders and nonresponders to FIT tests that had been mailed out as part of a Dublin colorectal cancer screening program between 2008 and 2012. Researchers employed the McQueen defensive information processing (DIP) measure, which includes four domains of defensive attitudes that include information avoidance, mental disengagement or denial, suppression through belief that one is immune, and arguing against the evidence.
In this study, 7,476 men and women in Dublin were invited to participate in a population‐based FIT screening program. In follow-up questionnaires sent to those who did or did not complete FIT, 53% of those who completed FIT screening answered the questionnaire, while 8% of those who did not complete the screening returned the questionnaire. Those who didn’t complete the FIT test had higher DIP scores suggesting more rates of opting out of receiving health information, avoiding doctor visits, prevention avoidance, continually delaying screening, either claiming colon cancer is rare or normalizing cancer risk, and falsely aligning regular bowel movements with good health which was directly associated with less screening.
Increasing rates of early onset colorectal cancer
The research may shed light on reasons for increasing rates of early-onset colorectal cancer. “Often younger people feel invincible and as Beverly Green, MD, MPH, pointed out in an editorial on defensive information processing, invincibility is a good example of self-exemption DIP,” Dr. Clarke said.
“I think what’s underlying these two pieces is a lack of awareness of the trajectory of colorectal cancer, but it’s also the future consequences of not taking part [in screening]. A person can have their colorectal cancer for about 10 years before they begin to feel any symptoms from it, and usually at that point, the disease has gone to an advanced stage, so it’s much more difficult to treat, and the person will have much poorer outcomes. If it’s detected at stage 1, the outcomes are far better,” Dr. Clarke said.
Doctors should react calmly to defensiveness and listen to the patient’s concerns. “Informing them of the aim of screening, i.e. to detect it when its precancerous or at the earliest possible stage, is very important. Letting them know they are taking responsibility for their own health and giving them the best chance of a healthy old age may be a good way of counteracting defensiveness,” he said.
Dr. Green noted that nonresponders claiming lack of immediacy could be swayed with the right approach. She has conducted similar research and subjects themselves suggested the use of marketing techniques “like what happens on Amazon. People remind you frequently the same thing when they get a clue that you have an interest in that behavior. Or, they tell you it’s on sale, and you might lose out from that big bargain if you don’t buy it now. There’s a deadline. I think a lot of the things we might do to nudge people are similar to what’s already happening in marketing,” said Dr. Green, who is a family physician and a researcher at the Kaiser Permanente Washington Health Research Institute.
Dr. Clarke and Dr. Green have no relevant financial disclosures.
An Irish study attempting to get at the root of why men and women delay colon cancer screening found that, despite an uptick in colon cancer cases among younger adults, screening isn’t a priority for some adults while others are under the impression that a healthy diet with regular bowel movements negates the need for regular screening.
The findings are based on a survey of over 2,000 adults who participated in a population-based fecal immunochemical test (FIT) screening program. The authors found that denying the immediacy of the need to be tested and self-exempting from screening because of a belief in a healthy lifestyle were key drivers for opting out of FIT screening.
“What we found was that people who didn’t take part [in the survey] responded much more defensively to the invitation,” said Nicholas Clarke, PhD, a researcher at Dublin City University, who served as the lead author of the study published in the journal Cancer.
The domain of denying immediacy, which covers decisions like putting off a test because of more pressing life events, was associated with a 47% reduction in screening probability. “That’s quite a high percentage. They’re not saying I won’t do it. They’re saying: ‘I’ll wait to get tested for colon cancer until my other health concerns are under control, or until there’s a better test,’ ” he said.
The other suppression category of self-exempting was associated with a 20% reduction in the odds of participation. “They’re saying: ‘I don’t need to be tested because I have enough vegetables in my diet or because I have regular bowel movements,’ ” Dr. Clarke said.
Despite the proven efficacy of screening, many individuals still resist screening. In previous research, Dr. Clarke found that men in Ireland were less likely than women to undergo screening.
FIT works by identifying small amounts of blood in the stool that could suggest the presence of a tumor or precancerous polyps. The test also looks for methylation and DNA mutations that are indicative of precancer polyps or tumors. A positive test calls for a follow-up procedure such as a colonoscopy, where precancerous polyps can be removed to prevent them from developing into tumors.
FIT has similar sensitivity to colonoscopy in detecting cancers (93% vs. 95%), but is less effective with respect to polyps (42% vs. 75%-93%). For average risk adults between 50-75 years old, the U.S Preventive Services Task Force recommends colonoscopy every 10 years; flexible sigmoidoscopy or CT colonography every 5 years, or flexible sigmoidoscopy every 10 years plus fecal immunochemical test (FIT) every year; FIT DNA test every 3 years; guaiac-based fecal occult blood test or FIT test annually.
Findings from the new study
In the new study, researchers contacted both 2,299 responders and nonresponders to FIT tests that had been mailed out as part of a Dublin colorectal cancer screening program between 2008 and 2012. Researchers employed the McQueen defensive information processing (DIP) measure, which includes four domains of defensive attitudes that include information avoidance, mental disengagement or denial, suppression through belief that one is immune, and arguing against the evidence.
In this study, 7,476 men and women in Dublin were invited to participate in a population‐based FIT screening program. In follow-up questionnaires sent to those who did or did not complete FIT, 53% of those who completed FIT screening answered the questionnaire, while 8% of those who did not complete the screening returned the questionnaire. Those who didn’t complete the FIT test had higher DIP scores suggesting more rates of opting out of receiving health information, avoiding doctor visits, prevention avoidance, continually delaying screening, either claiming colon cancer is rare or normalizing cancer risk, and falsely aligning regular bowel movements with good health which was directly associated with less screening.
Increasing rates of early onset colorectal cancer
The research may shed light on reasons for increasing rates of early-onset colorectal cancer. “Often younger people feel invincible and as Beverly Green, MD, MPH, pointed out in an editorial on defensive information processing, invincibility is a good example of self-exemption DIP,” Dr. Clarke said.
“I think what’s underlying these two pieces is a lack of awareness of the trajectory of colorectal cancer, but it’s also the future consequences of not taking part [in screening]. A person can have their colorectal cancer for about 10 years before they begin to feel any symptoms from it, and usually at that point, the disease has gone to an advanced stage, so it’s much more difficult to treat, and the person will have much poorer outcomes. If it’s detected at stage 1, the outcomes are far better,” Dr. Clarke said.
Doctors should react calmly to defensiveness and listen to the patient’s concerns. “Informing them of the aim of screening, i.e. to detect it when its precancerous or at the earliest possible stage, is very important. Letting them know they are taking responsibility for their own health and giving them the best chance of a healthy old age may be a good way of counteracting defensiveness,” he said.
Dr. Green noted that nonresponders claiming lack of immediacy could be swayed with the right approach. She has conducted similar research and subjects themselves suggested the use of marketing techniques “like what happens on Amazon. People remind you frequently the same thing when they get a clue that you have an interest in that behavior. Or, they tell you it’s on sale, and you might lose out from that big bargain if you don’t buy it now. There’s a deadline. I think a lot of the things we might do to nudge people are similar to what’s already happening in marketing,” said Dr. Green, who is a family physician and a researcher at the Kaiser Permanente Washington Health Research Institute.
Dr. Clarke and Dr. Green have no relevant financial disclosures.
An Irish study attempting to get at the root of why men and women delay colon cancer screening found that, despite an uptick in colon cancer cases among younger adults, screening isn’t a priority for some adults while others are under the impression that a healthy diet with regular bowel movements negates the need for regular screening.
The findings are based on a survey of over 2,000 adults who participated in a population-based fecal immunochemical test (FIT) screening program. The authors found that denying the immediacy of the need to be tested and self-exempting from screening because of a belief in a healthy lifestyle were key drivers for opting out of FIT screening.
“What we found was that people who didn’t take part [in the survey] responded much more defensively to the invitation,” said Nicholas Clarke, PhD, a researcher at Dublin City University, who served as the lead author of the study published in the journal Cancer.
The domain of denying immediacy, which covers decisions like putting off a test because of more pressing life events, was associated with a 47% reduction in screening probability. “That’s quite a high percentage. They’re not saying I won’t do it. They’re saying: ‘I’ll wait to get tested for colon cancer until my other health concerns are under control, or until there’s a better test,’ ” he said.
The other suppression category of self-exempting was associated with a 20% reduction in the odds of participation. “They’re saying: ‘I don’t need to be tested because I have enough vegetables in my diet or because I have regular bowel movements,’ ” Dr. Clarke said.
Despite the proven efficacy of screening, many individuals still resist screening. In previous research, Dr. Clarke found that men in Ireland were less likely than women to undergo screening.
FIT works by identifying small amounts of blood in the stool that could suggest the presence of a tumor or precancerous polyps. The test also looks for methylation and DNA mutations that are indicative of precancer polyps or tumors. A positive test calls for a follow-up procedure such as a colonoscopy, where precancerous polyps can be removed to prevent them from developing into tumors.
FIT has similar sensitivity to colonoscopy in detecting cancers (93% vs. 95%), but is less effective with respect to polyps (42% vs. 75%-93%). For average risk adults between 50-75 years old, the U.S Preventive Services Task Force recommends colonoscopy every 10 years; flexible sigmoidoscopy or CT colonography every 5 years, or flexible sigmoidoscopy every 10 years plus fecal immunochemical test (FIT) every year; FIT DNA test every 3 years; guaiac-based fecal occult blood test or FIT test annually.
Findings from the new study
In the new study, researchers contacted both 2,299 responders and nonresponders to FIT tests that had been mailed out as part of a Dublin colorectal cancer screening program between 2008 and 2012. Researchers employed the McQueen defensive information processing (DIP) measure, which includes four domains of defensive attitudes that include information avoidance, mental disengagement or denial, suppression through belief that one is immune, and arguing against the evidence.
In this study, 7,476 men and women in Dublin were invited to participate in a population‐based FIT screening program. In follow-up questionnaires sent to those who did or did not complete FIT, 53% of those who completed FIT screening answered the questionnaire, while 8% of those who did not complete the screening returned the questionnaire. Those who didn’t complete the FIT test had higher DIP scores suggesting more rates of opting out of receiving health information, avoiding doctor visits, prevention avoidance, continually delaying screening, either claiming colon cancer is rare or normalizing cancer risk, and falsely aligning regular bowel movements with good health which was directly associated with less screening.
Increasing rates of early onset colorectal cancer
The research may shed light on reasons for increasing rates of early-onset colorectal cancer. “Often younger people feel invincible and as Beverly Green, MD, MPH, pointed out in an editorial on defensive information processing, invincibility is a good example of self-exemption DIP,” Dr. Clarke said.
“I think what’s underlying these two pieces is a lack of awareness of the trajectory of colorectal cancer, but it’s also the future consequences of not taking part [in screening]. A person can have their colorectal cancer for about 10 years before they begin to feel any symptoms from it, and usually at that point, the disease has gone to an advanced stage, so it’s much more difficult to treat, and the person will have much poorer outcomes. If it’s detected at stage 1, the outcomes are far better,” Dr. Clarke said.
Doctors should react calmly to defensiveness and listen to the patient’s concerns. “Informing them of the aim of screening, i.e. to detect it when its precancerous or at the earliest possible stage, is very important. Letting them know they are taking responsibility for their own health and giving them the best chance of a healthy old age may be a good way of counteracting defensiveness,” he said.
Dr. Green noted that nonresponders claiming lack of immediacy could be swayed with the right approach. She has conducted similar research and subjects themselves suggested the use of marketing techniques “like what happens on Amazon. People remind you frequently the same thing when they get a clue that you have an interest in that behavior. Or, they tell you it’s on sale, and you might lose out from that big bargain if you don’t buy it now. There’s a deadline. I think a lot of the things we might do to nudge people are similar to what’s already happening in marketing,” said Dr. Green, who is a family physician and a researcher at the Kaiser Permanente Washington Health Research Institute.
Dr. Clarke and Dr. Green have no relevant financial disclosures.
FROM CANCER
In utero exposure to asthma medication not tied to risks of neurodevelopmental disorders
The drugs included in the study were leukotriene-receptor antagonists (LTRAs), which are often used to treat allergic airway diseases, including asthma and allergic rhinitis.
“Over the years, the U.S. Food and Drug Administration has monitored post-marketing data about the potential harm of neuropsychiatric events (NEs) associated with montelukast, the first type of LTRAs, and issued boxed warnings about serious mental health side effects for montelukast in 2020,” said corresponding author Tsung-Chieh Yao, MD, of Chang Gung Memorial Hospital, Taiwan, in an interview.
However, evidence of a link between NEs and LTRA use has been inconsistent, according to Dr. Yao and colleagues.
“To date, it remains totally unknown whether the exposure to LTRAs during pregnancy is associated with the risk of neuropsychiatric events in offspring,” said Dr. Yao.
To address this question, the researchers used data from National Health Insurance Research Database in Taiwan to identify pregnant women and their offspring from 2009 to 2019. The initial study population included 576,157 mother-offspring pairs, including 1,995 LTRA-exposed and 574,162 nonexposed children.
The women had a diagnosis of asthma or allergic rhinitis; multiple births and children with congenital malformations were excluded. LTRA exposure was defined as any dispensed prescription for LTRAs during pregnancy. Approximately two-thirds of the mothers were aged 30-40 years at the time of delivery.
The findings were published in a research letter in JAMA Network Open.
In the study population at large, the incidence of the three neurodevelopmental disorders ADHD, autism spectrum disorder (ASD), and Tourette syndrome was not significantly different between those children exposed to LTRAs and those not exposed to LTRAs in utero (1.25% vs. 1.32%; 3.31% vs. 4.36%; and 0.45% vs. 0.83%, respectively).
After propensity score matching, the study population included 1,988 LTRA-exposed children and 19,863 nonexposed children. In this group, no significant associations appeared between prenatal LTRA exposure and the risk of attention-deficit/hyperactivity disorder (adjusted hazard ratio, 1.03), autism spectrum disorder (AHR, 1.01), and Tourette syndrome (AHR, 0.63).
Neither duration nor cumulative dose of LTRA use during pregnancy showed an association with ADHD, ASD, or Tourette syndrome in offspring. Duration of LTRA use was categorized as shorter or longer periods of 1-4 weeks vs. more than 4 weeks; cumulative dose was categorized as 1-170 mg vs. 170 mg or higher.
The findings were limited by the lack of randomization, inability to detect long-term risk, and potential lack of generalizability to non-Asian populations, and more research is needed to replicate the results, the researchers noted. However, the current findings were strengthened by the large study population, and suggest that LTRA use in pregnancy does not present a significant risk for NEs in children, which should be reassuring to clinicians and patients, they concluded.
The current study is the first to use the whole of Taiwan population data and extends previous studies by examining the association between LTRA use during pregnancy and risk of neuropsychiatric events in offspring, Dr. Yao said in an interview. “The possibly surprising, but reassuring, finding is that prenatal LTRA exposure did not increase risk of ADHD, ASD, and Tourette syndrome in offspring,” he said.
“Clinicians prescribing LTRAs such as montelukast (Singulair and generics) to pregnant women with asthma or allergic rhinitis may be reassured by our findings,” Dr. Yao added. The results offer real-world evidence to help inform decision-making about the use of LTRAs during pregnancy, although additional research is needed to replicate the study findings in other populations, he said.
The study was supported by the National Health Research Institutes, Taiwan, the Ministry of Science and Technology of Taiwan, the National Science and Technology Council of Taiwan, and the Chang Gung Medical Foundation. The researchers had no financial conflicts to disclose.
The drugs included in the study were leukotriene-receptor antagonists (LTRAs), which are often used to treat allergic airway diseases, including asthma and allergic rhinitis.
“Over the years, the U.S. Food and Drug Administration has monitored post-marketing data about the potential harm of neuropsychiatric events (NEs) associated with montelukast, the first type of LTRAs, and issued boxed warnings about serious mental health side effects for montelukast in 2020,” said corresponding author Tsung-Chieh Yao, MD, of Chang Gung Memorial Hospital, Taiwan, in an interview.
However, evidence of a link between NEs and LTRA use has been inconsistent, according to Dr. Yao and colleagues.
“To date, it remains totally unknown whether the exposure to LTRAs during pregnancy is associated with the risk of neuropsychiatric events in offspring,” said Dr. Yao.
To address this question, the researchers used data from National Health Insurance Research Database in Taiwan to identify pregnant women and their offspring from 2009 to 2019. The initial study population included 576,157 mother-offspring pairs, including 1,995 LTRA-exposed and 574,162 nonexposed children.
The women had a diagnosis of asthma or allergic rhinitis; multiple births and children with congenital malformations were excluded. LTRA exposure was defined as any dispensed prescription for LTRAs during pregnancy. Approximately two-thirds of the mothers were aged 30-40 years at the time of delivery.
The findings were published in a research letter in JAMA Network Open.
In the study population at large, the incidence of the three neurodevelopmental disorders ADHD, autism spectrum disorder (ASD), and Tourette syndrome was not significantly different between those children exposed to LTRAs and those not exposed to LTRAs in utero (1.25% vs. 1.32%; 3.31% vs. 4.36%; and 0.45% vs. 0.83%, respectively).
After propensity score matching, the study population included 1,988 LTRA-exposed children and 19,863 nonexposed children. In this group, no significant associations appeared between prenatal LTRA exposure and the risk of attention-deficit/hyperactivity disorder (adjusted hazard ratio, 1.03), autism spectrum disorder (AHR, 1.01), and Tourette syndrome (AHR, 0.63).
Neither duration nor cumulative dose of LTRA use during pregnancy showed an association with ADHD, ASD, or Tourette syndrome in offspring. Duration of LTRA use was categorized as shorter or longer periods of 1-4 weeks vs. more than 4 weeks; cumulative dose was categorized as 1-170 mg vs. 170 mg or higher.
The findings were limited by the lack of randomization, inability to detect long-term risk, and potential lack of generalizability to non-Asian populations, and more research is needed to replicate the results, the researchers noted. However, the current findings were strengthened by the large study population, and suggest that LTRA use in pregnancy does not present a significant risk for NEs in children, which should be reassuring to clinicians and patients, they concluded.
The current study is the first to use the whole of Taiwan population data and extends previous studies by examining the association between LTRA use during pregnancy and risk of neuropsychiatric events in offspring, Dr. Yao said in an interview. “The possibly surprising, but reassuring, finding is that prenatal LTRA exposure did not increase risk of ADHD, ASD, and Tourette syndrome in offspring,” he said.
“Clinicians prescribing LTRAs such as montelukast (Singulair and generics) to pregnant women with asthma or allergic rhinitis may be reassured by our findings,” Dr. Yao added. The results offer real-world evidence to help inform decision-making about the use of LTRAs during pregnancy, although additional research is needed to replicate the study findings in other populations, he said.
The study was supported by the National Health Research Institutes, Taiwan, the Ministry of Science and Technology of Taiwan, the National Science and Technology Council of Taiwan, and the Chang Gung Medical Foundation. The researchers had no financial conflicts to disclose.
The drugs included in the study were leukotriene-receptor antagonists (LTRAs), which are often used to treat allergic airway diseases, including asthma and allergic rhinitis.
“Over the years, the U.S. Food and Drug Administration has monitored post-marketing data about the potential harm of neuropsychiatric events (NEs) associated with montelukast, the first type of LTRAs, and issued boxed warnings about serious mental health side effects for montelukast in 2020,” said corresponding author Tsung-Chieh Yao, MD, of Chang Gung Memorial Hospital, Taiwan, in an interview.
However, evidence of a link between NEs and LTRA use has been inconsistent, according to Dr. Yao and colleagues.
“To date, it remains totally unknown whether the exposure to LTRAs during pregnancy is associated with the risk of neuropsychiatric events in offspring,” said Dr. Yao.
To address this question, the researchers used data from National Health Insurance Research Database in Taiwan to identify pregnant women and their offspring from 2009 to 2019. The initial study population included 576,157 mother-offspring pairs, including 1,995 LTRA-exposed and 574,162 nonexposed children.
The women had a diagnosis of asthma or allergic rhinitis; multiple births and children with congenital malformations were excluded. LTRA exposure was defined as any dispensed prescription for LTRAs during pregnancy. Approximately two-thirds of the mothers were aged 30-40 years at the time of delivery.
The findings were published in a research letter in JAMA Network Open.
In the study population at large, the incidence of the three neurodevelopmental disorders ADHD, autism spectrum disorder (ASD), and Tourette syndrome was not significantly different between those children exposed to LTRAs and those not exposed to LTRAs in utero (1.25% vs. 1.32%; 3.31% vs. 4.36%; and 0.45% vs. 0.83%, respectively).
After propensity score matching, the study population included 1,988 LTRA-exposed children and 19,863 nonexposed children. In this group, no significant associations appeared between prenatal LTRA exposure and the risk of attention-deficit/hyperactivity disorder (adjusted hazard ratio, 1.03), autism spectrum disorder (AHR, 1.01), and Tourette syndrome (AHR, 0.63).
Neither duration nor cumulative dose of LTRA use during pregnancy showed an association with ADHD, ASD, or Tourette syndrome in offspring. Duration of LTRA use was categorized as shorter or longer periods of 1-4 weeks vs. more than 4 weeks; cumulative dose was categorized as 1-170 mg vs. 170 mg or higher.
The findings were limited by the lack of randomization, inability to detect long-term risk, and potential lack of generalizability to non-Asian populations, and more research is needed to replicate the results, the researchers noted. However, the current findings were strengthened by the large study population, and suggest that LTRA use in pregnancy does not present a significant risk for NEs in children, which should be reassuring to clinicians and patients, they concluded.
The current study is the first to use the whole of Taiwan population data and extends previous studies by examining the association between LTRA use during pregnancy and risk of neuropsychiatric events in offspring, Dr. Yao said in an interview. “The possibly surprising, but reassuring, finding is that prenatal LTRA exposure did not increase risk of ADHD, ASD, and Tourette syndrome in offspring,” he said.
“Clinicians prescribing LTRAs such as montelukast (Singulair and generics) to pregnant women with asthma or allergic rhinitis may be reassured by our findings,” Dr. Yao added. The results offer real-world evidence to help inform decision-making about the use of LTRAs during pregnancy, although additional research is needed to replicate the study findings in other populations, he said.
The study was supported by the National Health Research Institutes, Taiwan, the Ministry of Science and Technology of Taiwan, the National Science and Technology Council of Taiwan, and the Chang Gung Medical Foundation. The researchers had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
Phase 3 results: Ponatinib bests imatinib for Ph+ALL
The agents were evaluated in the randomized, open-label, phase 3 PhALLCON study, the first head-to-head comparison of ponatinib and imatinib in combination with reduced-intensity chemotherapy in the Ph+ALL population.
Overall, patients in the ponatinib arm experienced a significantly higher minimal residual disease (MRD)–negative complete response rate as well as deeper and more durable responses compared with those in the imatinib arm, the investigators reported.
The findings were presented during an American Society of Clinical Oncology virtual plenary session.
In adults with ALL, Ph+ disease is the most frequent genetic subtype, accounting for about one third of cases. The current standard of care for newly diagnosed Ph+ALL, also known as BCR-ABL-1–positive ALL, is BCR-ABL1 TKIs in combination with chemotherapy or steroids. However, when treated with first- or second-generation TKIs, patients eventually progress due to the emergence of treatment resistance.
Before the advent of TKI therapies, Ph+ALL had a very poor prognosis, but the development of imatinib in 2001 was transformative, said Marlise R. Luskin, MD, a senior physician at Dana-Farber Cancer Institute, Boston, in the ASCO plenary session, exploring the state of the science.
Added to “backbone” chemotherapy regimens, imatinib improved complete response rates, increased eligibility for stem cell transplantation, and improved overall survival. Second-generation TKIs, including dasatinib and nilotinib further improved outcomes, said Dr. Luskin, also assistant professor at Harvard Medical School, Boston.
More recently, ponatinib has emerged as a promising treatment given its unique action against the ABLA1 T315I KD mutation present in about 75% of cases that relapse as well as the findings of improved MRD-negative complete response rates and event-free survival in retrospective studies, Dr. Luskin said.
The PhALLCON study was designed to further investigate promising results seen in retrospective studies of ponatinib.
To assess ponatinib versus imatinib, patients were enrolled and randomized two to one to receive either a 30-mg once-daily starting dose of ponatinib or a once-daily 600 mg dose of imatinib plus reduced-intensity chemotherapy. After cycle 20, patients received single agent ponatinib or imatinib until disease progression or unacceptable toxicity.
Of the 245 enrolled, 78 remained on treatment at the August 2022 data cutoff, including 42% of those in the ponatinib arm and 12% in the imatinib arm. The most common reasons for discontinuation included hematopoietic stem cell transplantation (31% for ponatinib and 37% for imatinib), adverse events (12% in both arms), and lack of efficacy (7% and 26%, respectively).
At median follow-up of 20 months among 164 patients in the ponatinib arm and 18 months among 81 patients in the imatinib arm, the MRD-negative complete response rates were 34.4% and 16.7%, respectively, said first author Elias J. Jabbour, MD, a professor of medicine at the University of Texas MD Anderson Cancer Center, Houston.
A trend toward improved event-free survival was also observed in the ponatinib arm, but the data were not mature at the time of the analysis, Dr. Jabbour noted.
The two treatments showed comparable safety. Treatment-emergent adverse event rates of any grade and of grade 3 or higher were similar in the two study arms. Arterial occlusive events were infrequent and were also similar between the arms.
“Taken together, for this patient population, the efficacy and safety results demonstrate a favorable risk-benefit assessment for ponatinib, which should be considered a standard of care for frontline therapy in patents with newly diagnosed Ph+ALL,” Dr. Jabbour said.
Although the PhALLCON findings are encouraging, invited discussant Anjali S. Advani, MD, of the Cleveland Clinic, noted some study “pitfalls and caveats,” including the generally younger age and low incidence of cardiovascular risk factors in the study population, which raises questions about the ability to extrapolate the findings to “the larger population, which may be older and have more comorbidities.”
Dr. Advani also said that the ponatinib versus imatinib comparison is a reasonable one, but that most clinicians are now using dasatinib, so “it would have been nice to have this comparison.”
Additionally, “the landscape is now changing with the use of blinatumomab plus TKIs – either dasatinib or ponatinib – in the up-front setting.”
“There is data now from various groups ... showing excellent results, although longer follow-up is needed on all of these,” she said.
One such study is the GIMEMA ALL2820 trial looking at ponatinib plus blinatumomab versus imatinib plus chemotherapy, said Nicolas Boissel, MD, PhD, of Hôpital Saint-Louis in Paris, an invited discussant who addressed the European perspective on the PhALLCON results.
“It is expected that access to ponatinib will be delayed in Europe, compared with the U.S., so meanwhile, clinical trials remain a good option to give access to ponatinib frontline,” he said.
Going forward, Dr. Boissel said it will be important to determine the role of second-generation TKIs in patients who are ineligible to receive ponatinib, the treatment duration needed to reduce long-term risk of relapse, and the potential for eliminating the need for postremission chemotherapy and stem cell transplantation in certain patients.
Dr. Advani added that when evaluating and comparing treatments, it will be important to look at genomic alterations and BCR-ABL mutation status, age and comorbidities, and patterns of disease relapse, including relapse sites and genomics. Longer follow-up results for event-free survival and overall survival are also needed.
“I think, particularly in younger patients with relatively few or no cardiovascular comorbidities, [ponatinib plus reduced-intensity chemotherapy] represents a really exciting option,” Dr. Advani said. “What’s difficult is that the landscape is changing quickly in this field, and so is the standard of care. I think what we struggle with is whether we should be using antibody-based therapies plus TKIs or look at an approach such as this, and further studies are going to be needed to answer that question.”
Dr. Jabbour disclosed ties with Pfizer, Takeda, Amgen, AbbVie, Bristol-Myers Squibb, Incyte, Adaptive Biotechnologies, Astellas Pharma, Genentech, and Ascentage Pharma. Dr. Luskin reported relationships with Pfizer, Novartis, and Abbvie. Dr. Advani disclosed ties with Novartis, Glycomimetics, Kite Pharma, Seattle Genetics, Amgen, Beam Therapeutics, Mkarta, Taiho Oncology, Jazz Pharmaceuticals, Pfizer, and Kura Oncology. Dr. Boissel reported relationships with Amgen, ARIAD/Incyte, Novartis, SERVIER, and Astellas Pharma.
A version of this article originally appeared on Medscape.com.
The agents were evaluated in the randomized, open-label, phase 3 PhALLCON study, the first head-to-head comparison of ponatinib and imatinib in combination with reduced-intensity chemotherapy in the Ph+ALL population.
Overall, patients in the ponatinib arm experienced a significantly higher minimal residual disease (MRD)–negative complete response rate as well as deeper and more durable responses compared with those in the imatinib arm, the investigators reported.
The findings were presented during an American Society of Clinical Oncology virtual plenary session.
In adults with ALL, Ph+ disease is the most frequent genetic subtype, accounting for about one third of cases. The current standard of care for newly diagnosed Ph+ALL, also known as BCR-ABL-1–positive ALL, is BCR-ABL1 TKIs in combination with chemotherapy or steroids. However, when treated with first- or second-generation TKIs, patients eventually progress due to the emergence of treatment resistance.
Before the advent of TKI therapies, Ph+ALL had a very poor prognosis, but the development of imatinib in 2001 was transformative, said Marlise R. Luskin, MD, a senior physician at Dana-Farber Cancer Institute, Boston, in the ASCO plenary session, exploring the state of the science.
Added to “backbone” chemotherapy regimens, imatinib improved complete response rates, increased eligibility for stem cell transplantation, and improved overall survival. Second-generation TKIs, including dasatinib and nilotinib further improved outcomes, said Dr. Luskin, also assistant professor at Harvard Medical School, Boston.
More recently, ponatinib has emerged as a promising treatment given its unique action against the ABLA1 T315I KD mutation present in about 75% of cases that relapse as well as the findings of improved MRD-negative complete response rates and event-free survival in retrospective studies, Dr. Luskin said.
The PhALLCON study was designed to further investigate promising results seen in retrospective studies of ponatinib.
To assess ponatinib versus imatinib, patients were enrolled and randomized two to one to receive either a 30-mg once-daily starting dose of ponatinib or a once-daily 600 mg dose of imatinib plus reduced-intensity chemotherapy. After cycle 20, patients received single agent ponatinib or imatinib until disease progression or unacceptable toxicity.
Of the 245 enrolled, 78 remained on treatment at the August 2022 data cutoff, including 42% of those in the ponatinib arm and 12% in the imatinib arm. The most common reasons for discontinuation included hematopoietic stem cell transplantation (31% for ponatinib and 37% for imatinib), adverse events (12% in both arms), and lack of efficacy (7% and 26%, respectively).
At median follow-up of 20 months among 164 patients in the ponatinib arm and 18 months among 81 patients in the imatinib arm, the MRD-negative complete response rates were 34.4% and 16.7%, respectively, said first author Elias J. Jabbour, MD, a professor of medicine at the University of Texas MD Anderson Cancer Center, Houston.
A trend toward improved event-free survival was also observed in the ponatinib arm, but the data were not mature at the time of the analysis, Dr. Jabbour noted.
The two treatments showed comparable safety. Treatment-emergent adverse event rates of any grade and of grade 3 or higher were similar in the two study arms. Arterial occlusive events were infrequent and were also similar between the arms.
“Taken together, for this patient population, the efficacy and safety results demonstrate a favorable risk-benefit assessment for ponatinib, which should be considered a standard of care for frontline therapy in patents with newly diagnosed Ph+ALL,” Dr. Jabbour said.
Although the PhALLCON findings are encouraging, invited discussant Anjali S. Advani, MD, of the Cleveland Clinic, noted some study “pitfalls and caveats,” including the generally younger age and low incidence of cardiovascular risk factors in the study population, which raises questions about the ability to extrapolate the findings to “the larger population, which may be older and have more comorbidities.”
Dr. Advani also said that the ponatinib versus imatinib comparison is a reasonable one, but that most clinicians are now using dasatinib, so “it would have been nice to have this comparison.”
Additionally, “the landscape is now changing with the use of blinatumomab plus TKIs – either dasatinib or ponatinib – in the up-front setting.”
“There is data now from various groups ... showing excellent results, although longer follow-up is needed on all of these,” she said.
One such study is the GIMEMA ALL2820 trial looking at ponatinib plus blinatumomab versus imatinib plus chemotherapy, said Nicolas Boissel, MD, PhD, of Hôpital Saint-Louis in Paris, an invited discussant who addressed the European perspective on the PhALLCON results.
“It is expected that access to ponatinib will be delayed in Europe, compared with the U.S., so meanwhile, clinical trials remain a good option to give access to ponatinib frontline,” he said.
Going forward, Dr. Boissel said it will be important to determine the role of second-generation TKIs in patients who are ineligible to receive ponatinib, the treatment duration needed to reduce long-term risk of relapse, and the potential for eliminating the need for postremission chemotherapy and stem cell transplantation in certain patients.
Dr. Advani added that when evaluating and comparing treatments, it will be important to look at genomic alterations and BCR-ABL mutation status, age and comorbidities, and patterns of disease relapse, including relapse sites and genomics. Longer follow-up results for event-free survival and overall survival are also needed.
“I think, particularly in younger patients with relatively few or no cardiovascular comorbidities, [ponatinib plus reduced-intensity chemotherapy] represents a really exciting option,” Dr. Advani said. “What’s difficult is that the landscape is changing quickly in this field, and so is the standard of care. I think what we struggle with is whether we should be using antibody-based therapies plus TKIs or look at an approach such as this, and further studies are going to be needed to answer that question.”
Dr. Jabbour disclosed ties with Pfizer, Takeda, Amgen, AbbVie, Bristol-Myers Squibb, Incyte, Adaptive Biotechnologies, Astellas Pharma, Genentech, and Ascentage Pharma. Dr. Luskin reported relationships with Pfizer, Novartis, and Abbvie. Dr. Advani disclosed ties with Novartis, Glycomimetics, Kite Pharma, Seattle Genetics, Amgen, Beam Therapeutics, Mkarta, Taiho Oncology, Jazz Pharmaceuticals, Pfizer, and Kura Oncology. Dr. Boissel reported relationships with Amgen, ARIAD/Incyte, Novartis, SERVIER, and Astellas Pharma.
A version of this article originally appeared on Medscape.com.
The agents were evaluated in the randomized, open-label, phase 3 PhALLCON study, the first head-to-head comparison of ponatinib and imatinib in combination with reduced-intensity chemotherapy in the Ph+ALL population.
Overall, patients in the ponatinib arm experienced a significantly higher minimal residual disease (MRD)–negative complete response rate as well as deeper and more durable responses compared with those in the imatinib arm, the investigators reported.
The findings were presented during an American Society of Clinical Oncology virtual plenary session.
In adults with ALL, Ph+ disease is the most frequent genetic subtype, accounting for about one third of cases. The current standard of care for newly diagnosed Ph+ALL, also known as BCR-ABL-1–positive ALL, is BCR-ABL1 TKIs in combination with chemotherapy or steroids. However, when treated with first- or second-generation TKIs, patients eventually progress due to the emergence of treatment resistance.
Before the advent of TKI therapies, Ph+ALL had a very poor prognosis, but the development of imatinib in 2001 was transformative, said Marlise R. Luskin, MD, a senior physician at Dana-Farber Cancer Institute, Boston, in the ASCO plenary session, exploring the state of the science.
Added to “backbone” chemotherapy regimens, imatinib improved complete response rates, increased eligibility for stem cell transplantation, and improved overall survival. Second-generation TKIs, including dasatinib and nilotinib further improved outcomes, said Dr. Luskin, also assistant professor at Harvard Medical School, Boston.
More recently, ponatinib has emerged as a promising treatment given its unique action against the ABLA1 T315I KD mutation present in about 75% of cases that relapse as well as the findings of improved MRD-negative complete response rates and event-free survival in retrospective studies, Dr. Luskin said.
The PhALLCON study was designed to further investigate promising results seen in retrospective studies of ponatinib.
To assess ponatinib versus imatinib, patients were enrolled and randomized two to one to receive either a 30-mg once-daily starting dose of ponatinib or a once-daily 600 mg dose of imatinib plus reduced-intensity chemotherapy. After cycle 20, patients received single agent ponatinib or imatinib until disease progression or unacceptable toxicity.
Of the 245 enrolled, 78 remained on treatment at the August 2022 data cutoff, including 42% of those in the ponatinib arm and 12% in the imatinib arm. The most common reasons for discontinuation included hematopoietic stem cell transplantation (31% for ponatinib and 37% for imatinib), adverse events (12% in both arms), and lack of efficacy (7% and 26%, respectively).
At median follow-up of 20 months among 164 patients in the ponatinib arm and 18 months among 81 patients in the imatinib arm, the MRD-negative complete response rates were 34.4% and 16.7%, respectively, said first author Elias J. Jabbour, MD, a professor of medicine at the University of Texas MD Anderson Cancer Center, Houston.
A trend toward improved event-free survival was also observed in the ponatinib arm, but the data were not mature at the time of the analysis, Dr. Jabbour noted.
The two treatments showed comparable safety. Treatment-emergent adverse event rates of any grade and of grade 3 or higher were similar in the two study arms. Arterial occlusive events were infrequent and were also similar between the arms.
“Taken together, for this patient population, the efficacy and safety results demonstrate a favorable risk-benefit assessment for ponatinib, which should be considered a standard of care for frontline therapy in patents with newly diagnosed Ph+ALL,” Dr. Jabbour said.
Although the PhALLCON findings are encouraging, invited discussant Anjali S. Advani, MD, of the Cleveland Clinic, noted some study “pitfalls and caveats,” including the generally younger age and low incidence of cardiovascular risk factors in the study population, which raises questions about the ability to extrapolate the findings to “the larger population, which may be older and have more comorbidities.”
Dr. Advani also said that the ponatinib versus imatinib comparison is a reasonable one, but that most clinicians are now using dasatinib, so “it would have been nice to have this comparison.”
Additionally, “the landscape is now changing with the use of blinatumomab plus TKIs – either dasatinib or ponatinib – in the up-front setting.”
“There is data now from various groups ... showing excellent results, although longer follow-up is needed on all of these,” she said.
One such study is the GIMEMA ALL2820 trial looking at ponatinib plus blinatumomab versus imatinib plus chemotherapy, said Nicolas Boissel, MD, PhD, of Hôpital Saint-Louis in Paris, an invited discussant who addressed the European perspective on the PhALLCON results.
“It is expected that access to ponatinib will be delayed in Europe, compared with the U.S., so meanwhile, clinical trials remain a good option to give access to ponatinib frontline,” he said.
Going forward, Dr. Boissel said it will be important to determine the role of second-generation TKIs in patients who are ineligible to receive ponatinib, the treatment duration needed to reduce long-term risk of relapse, and the potential for eliminating the need for postremission chemotherapy and stem cell transplantation in certain patients.
Dr. Advani added that when evaluating and comparing treatments, it will be important to look at genomic alterations and BCR-ABL mutation status, age and comorbidities, and patterns of disease relapse, including relapse sites and genomics. Longer follow-up results for event-free survival and overall survival are also needed.
“I think, particularly in younger patients with relatively few or no cardiovascular comorbidities, [ponatinib plus reduced-intensity chemotherapy] represents a really exciting option,” Dr. Advani said. “What’s difficult is that the landscape is changing quickly in this field, and so is the standard of care. I think what we struggle with is whether we should be using antibody-based therapies plus TKIs or look at an approach such as this, and further studies are going to be needed to answer that question.”
Dr. Jabbour disclosed ties with Pfizer, Takeda, Amgen, AbbVie, Bristol-Myers Squibb, Incyte, Adaptive Biotechnologies, Astellas Pharma, Genentech, and Ascentage Pharma. Dr. Luskin reported relationships with Pfizer, Novartis, and Abbvie. Dr. Advani disclosed ties with Novartis, Glycomimetics, Kite Pharma, Seattle Genetics, Amgen, Beam Therapeutics, Mkarta, Taiho Oncology, Jazz Pharmaceuticals, Pfizer, and Kura Oncology. Dr. Boissel reported relationships with Amgen, ARIAD/Incyte, Novartis, SERVIER, and Astellas Pharma.
A version of this article originally appeared on Medscape.com.