User login
For MD-IQ use only
Brain differences suggest therapeutic targets in Takotsubo
A new study has identified differences in the brain present in patients with the cardiac disorder Takotsubo syndrome versus control scans, which may lead to new therapeutic targets.
Takotsubo syndrome is an acute heart failure cardiomyopathy mimicking an acute myocardial infarction in its presentation, but on investigation, no obstructive coronary disease is present. The syndrome, which mainly affects women, typically occurs in the aftermath of intense emotional or physical stress and has become known as “broken heart syndrome.”
The mechanism by which emotional processing in the context of stress leads to significant cardiac injury and acute left ventricular dysfunction is not understood. So, the current study examined both structural and functional effects in the brain in patients with Takotsubo syndrome to shed more light on the issue.
“The abnormalities in the thalamus-amygdala-insula and basal ganglia support the concept of involvement of higher-level function centers in Takotsubo syndrome, and interventions aimed at modulating these may be of benefit,” the authors conclude.
The study was published online in JACC: Heart Failure.
Lead author Hilal Khan, MB BCh, BAO, from the University of Aberdeen (Scotland), explained to this news organization that patients with Takotsubo syndrome have a substantial drop in heart function and show an apical ballooning of the heart.
It is a relatively newly defined condition and was first described in 1990 in Japan, and so named because the heart was thought to resemble the Takotsubo pot used by Japanese fishermen to trap octopus.
Although uncommon, the condition is not rare. Dr. Khan estimates that about 1 in 20 women with suspected MI turn out to have Takotsubo syndrome, with cases increasing in times of global stress such as in the recent pandemic.
While patients tend to recover in a few weeks and the pumping function of the heart usually returns to normal, there are some long-term cardiac complications including a reduction in global longitudinal strain, and patients have similar long-term outcomes as those with MI.
“It is believed that these cardiac changes may be triggered by changes in the brain caused by emotional stress, so we wanted to look at this more closely,” Dr. Khan said.
There have been a couple of studies published previously looking at brain changes in Takotsubo syndrome, but they haven’t reported patients in the acute stage of the condition and they haven’t compared the patients to controls, he noted.
For the current study, the researchers looked at brain scans for 25 acute Takotsubo patients and in 25 controls matched for age, gender, comorbidities, and medications. All the patients and controls were examined using the same MRI scanner in the same hospital.
“This is the largest structural and functional brain study of acute Takotsubo syndrome patients compared with matched control subjects,” Dr. Khan said.
The researchers looked at many different factors including brain volume in different regions, cortical thickness, small-vessel disease, and functional and structural connectivity to try and obtain a complete holistic view of the brain.
Key findings were that patients with Takotsubo syndrome had smaller brain volumes, compared with matched controls, driven by a reduction in brain surface area. In contrast, the insula and thalamus regions were larger.
“A reduction in brain volume could be caused by inflammation; this is often seen in depression,” Dr. Khan commented.
The researchers also found that certain areas of the brain had a reduction in functional connectivity, particularly the thalamus – the central autonomic area of the brain, which regulates the autonomic nervous system – and also the insula region, which is also involved in the autonomic regulation of the heart.
They suggest that there may be a loss of parasympathetic inhibition in Takotsubo syndrome, which would fit the theory that Takotsubo brings with it a surge of catecholamines, which could injure the heart.
Reduced functional connectivity was also seen in parts of the basal ganglia, abnormalities of which have been associated with an increased risk of both arrhythmias, and in the amygdala, similar to patients with a tendency to catastrophize events.
The other observation was that there appeared to be an increase in structural connectivity in certain areas of the brain.
“Structural pathways seem to be increased but functional connectivity was reduced, so while physical pathways are enhanced, they don’t seem to be doing anything,” Dr. Khan said. “We don’t know why this occurs, or if this has happened over time and made the brain and heart more vulnerable in some way.”
One possibility is that ,under a significant emotional stress, the brain may divert function from some areas to others to be able to cope, and that this results in reduced functioning in areas of the brain responsible for regulating the heart, Dr. Khan suggested.
“We believe this study confirms that the brain is involved in Takotsubo syndrome, and we have identified markers in the brain that may be contributing to the condition,” he said.
The researchers are planning to further study these markers and whether it might be possible to modulate these changes with various interventions such as exercise or mindfulness.
“We believe there is some interface between the brain changes and the impact on the heart. We don’t think it is just the release of catecholamines that causes damage to the heart. We think there is something else happening as well,” Dr. Khan commented.
It is also possible that the hearts of patients with Takotsubo syndrome are predisposed in some way and more vulnerable to this condition occurring.
“It will be important to obtain a greater understanding of the triggers and identify people who may be vulnerable,” Dr. Khan noted. “Around 10% of individuals who experience Takotsubo syndrome will have a recurrence, so we need to try and develop preventative strategies to reduce this.”
He suggested that possible preventive or therapeutic approaches may involve interventions such as exercise or mindfulness.
This work was supported by National Health Service Grampian Endowment. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study has identified differences in the brain present in patients with the cardiac disorder Takotsubo syndrome versus control scans, which may lead to new therapeutic targets.
Takotsubo syndrome is an acute heart failure cardiomyopathy mimicking an acute myocardial infarction in its presentation, but on investigation, no obstructive coronary disease is present. The syndrome, which mainly affects women, typically occurs in the aftermath of intense emotional or physical stress and has become known as “broken heart syndrome.”
The mechanism by which emotional processing in the context of stress leads to significant cardiac injury and acute left ventricular dysfunction is not understood. So, the current study examined both structural and functional effects in the brain in patients with Takotsubo syndrome to shed more light on the issue.
“The abnormalities in the thalamus-amygdala-insula and basal ganglia support the concept of involvement of higher-level function centers in Takotsubo syndrome, and interventions aimed at modulating these may be of benefit,” the authors conclude.
The study was published online in JACC: Heart Failure.
Lead author Hilal Khan, MB BCh, BAO, from the University of Aberdeen (Scotland), explained to this news organization that patients with Takotsubo syndrome have a substantial drop in heart function and show an apical ballooning of the heart.
It is a relatively newly defined condition and was first described in 1990 in Japan, and so named because the heart was thought to resemble the Takotsubo pot used by Japanese fishermen to trap octopus.
Although uncommon, the condition is not rare. Dr. Khan estimates that about 1 in 20 women with suspected MI turn out to have Takotsubo syndrome, with cases increasing in times of global stress such as in the recent pandemic.
While patients tend to recover in a few weeks and the pumping function of the heart usually returns to normal, there are some long-term cardiac complications including a reduction in global longitudinal strain, and patients have similar long-term outcomes as those with MI.
“It is believed that these cardiac changes may be triggered by changes in the brain caused by emotional stress, so we wanted to look at this more closely,” Dr. Khan said.
There have been a couple of studies published previously looking at brain changes in Takotsubo syndrome, but they haven’t reported patients in the acute stage of the condition and they haven’t compared the patients to controls, he noted.
For the current study, the researchers looked at brain scans for 25 acute Takotsubo patients and in 25 controls matched for age, gender, comorbidities, and medications. All the patients and controls were examined using the same MRI scanner in the same hospital.
“This is the largest structural and functional brain study of acute Takotsubo syndrome patients compared with matched control subjects,” Dr. Khan said.
The researchers looked at many different factors including brain volume in different regions, cortical thickness, small-vessel disease, and functional and structural connectivity to try and obtain a complete holistic view of the brain.
Key findings were that patients with Takotsubo syndrome had smaller brain volumes, compared with matched controls, driven by a reduction in brain surface area. In contrast, the insula and thalamus regions were larger.
“A reduction in brain volume could be caused by inflammation; this is often seen in depression,” Dr. Khan commented.
The researchers also found that certain areas of the brain had a reduction in functional connectivity, particularly the thalamus – the central autonomic area of the brain, which regulates the autonomic nervous system – and also the insula region, which is also involved in the autonomic regulation of the heart.
They suggest that there may be a loss of parasympathetic inhibition in Takotsubo syndrome, which would fit the theory that Takotsubo brings with it a surge of catecholamines, which could injure the heart.
Reduced functional connectivity was also seen in parts of the basal ganglia, abnormalities of which have been associated with an increased risk of both arrhythmias, and in the amygdala, similar to patients with a tendency to catastrophize events.
The other observation was that there appeared to be an increase in structural connectivity in certain areas of the brain.
“Structural pathways seem to be increased but functional connectivity was reduced, so while physical pathways are enhanced, they don’t seem to be doing anything,” Dr. Khan said. “We don’t know why this occurs, or if this has happened over time and made the brain and heart more vulnerable in some way.”
One possibility is that ,under a significant emotional stress, the brain may divert function from some areas to others to be able to cope, and that this results in reduced functioning in areas of the brain responsible for regulating the heart, Dr. Khan suggested.
“We believe this study confirms that the brain is involved in Takotsubo syndrome, and we have identified markers in the brain that may be contributing to the condition,” he said.
The researchers are planning to further study these markers and whether it might be possible to modulate these changes with various interventions such as exercise or mindfulness.
“We believe there is some interface between the brain changes and the impact on the heart. We don’t think it is just the release of catecholamines that causes damage to the heart. We think there is something else happening as well,” Dr. Khan commented.
It is also possible that the hearts of patients with Takotsubo syndrome are predisposed in some way and more vulnerable to this condition occurring.
“It will be important to obtain a greater understanding of the triggers and identify people who may be vulnerable,” Dr. Khan noted. “Around 10% of individuals who experience Takotsubo syndrome will have a recurrence, so we need to try and develop preventative strategies to reduce this.”
He suggested that possible preventive or therapeutic approaches may involve interventions such as exercise or mindfulness.
This work was supported by National Health Service Grampian Endowment. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study has identified differences in the brain present in patients with the cardiac disorder Takotsubo syndrome versus control scans, which may lead to new therapeutic targets.
Takotsubo syndrome is an acute heart failure cardiomyopathy mimicking an acute myocardial infarction in its presentation, but on investigation, no obstructive coronary disease is present. The syndrome, which mainly affects women, typically occurs in the aftermath of intense emotional or physical stress and has become known as “broken heart syndrome.”
The mechanism by which emotional processing in the context of stress leads to significant cardiac injury and acute left ventricular dysfunction is not understood. So, the current study examined both structural and functional effects in the brain in patients with Takotsubo syndrome to shed more light on the issue.
“The abnormalities in the thalamus-amygdala-insula and basal ganglia support the concept of involvement of higher-level function centers in Takotsubo syndrome, and interventions aimed at modulating these may be of benefit,” the authors conclude.
The study was published online in JACC: Heart Failure.
Lead author Hilal Khan, MB BCh, BAO, from the University of Aberdeen (Scotland), explained to this news organization that patients with Takotsubo syndrome have a substantial drop in heart function and show an apical ballooning of the heart.
It is a relatively newly defined condition and was first described in 1990 in Japan, and so named because the heart was thought to resemble the Takotsubo pot used by Japanese fishermen to trap octopus.
Although uncommon, the condition is not rare. Dr. Khan estimates that about 1 in 20 women with suspected MI turn out to have Takotsubo syndrome, with cases increasing in times of global stress such as in the recent pandemic.
While patients tend to recover in a few weeks and the pumping function of the heart usually returns to normal, there are some long-term cardiac complications including a reduction in global longitudinal strain, and patients have similar long-term outcomes as those with MI.
“It is believed that these cardiac changes may be triggered by changes in the brain caused by emotional stress, so we wanted to look at this more closely,” Dr. Khan said.
There have been a couple of studies published previously looking at brain changes in Takotsubo syndrome, but they haven’t reported patients in the acute stage of the condition and they haven’t compared the patients to controls, he noted.
For the current study, the researchers looked at brain scans for 25 acute Takotsubo patients and in 25 controls matched for age, gender, comorbidities, and medications. All the patients and controls were examined using the same MRI scanner in the same hospital.
“This is the largest structural and functional brain study of acute Takotsubo syndrome patients compared with matched control subjects,” Dr. Khan said.
The researchers looked at many different factors including brain volume in different regions, cortical thickness, small-vessel disease, and functional and structural connectivity to try and obtain a complete holistic view of the brain.
Key findings were that patients with Takotsubo syndrome had smaller brain volumes, compared with matched controls, driven by a reduction in brain surface area. In contrast, the insula and thalamus regions were larger.
“A reduction in brain volume could be caused by inflammation; this is often seen in depression,” Dr. Khan commented.
The researchers also found that certain areas of the brain had a reduction in functional connectivity, particularly the thalamus – the central autonomic area of the brain, which regulates the autonomic nervous system – and also the insula region, which is also involved in the autonomic regulation of the heart.
They suggest that there may be a loss of parasympathetic inhibition in Takotsubo syndrome, which would fit the theory that Takotsubo brings with it a surge of catecholamines, which could injure the heart.
Reduced functional connectivity was also seen in parts of the basal ganglia, abnormalities of which have been associated with an increased risk of both arrhythmias, and in the amygdala, similar to patients with a tendency to catastrophize events.
The other observation was that there appeared to be an increase in structural connectivity in certain areas of the brain.
“Structural pathways seem to be increased but functional connectivity was reduced, so while physical pathways are enhanced, they don’t seem to be doing anything,” Dr. Khan said. “We don’t know why this occurs, or if this has happened over time and made the brain and heart more vulnerable in some way.”
One possibility is that ,under a significant emotional stress, the brain may divert function from some areas to others to be able to cope, and that this results in reduced functioning in areas of the brain responsible for regulating the heart, Dr. Khan suggested.
“We believe this study confirms that the brain is involved in Takotsubo syndrome, and we have identified markers in the brain that may be contributing to the condition,” he said.
The researchers are planning to further study these markers and whether it might be possible to modulate these changes with various interventions such as exercise or mindfulness.
“We believe there is some interface between the brain changes and the impact on the heart. We don’t think it is just the release of catecholamines that causes damage to the heart. We think there is something else happening as well,” Dr. Khan commented.
It is also possible that the hearts of patients with Takotsubo syndrome are predisposed in some way and more vulnerable to this condition occurring.
“It will be important to obtain a greater understanding of the triggers and identify people who may be vulnerable,” Dr. Khan noted. “Around 10% of individuals who experience Takotsubo syndrome will have a recurrence, so we need to try and develop preventative strategies to reduce this.”
He suggested that possible preventive or therapeutic approaches may involve interventions such as exercise or mindfulness.
This work was supported by National Health Service Grampian Endowment. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JACC: HEART FAILURE
It’s all about the brains: Guilt placebos, transplants, and negative feelings
Guilt reduction, now in deceptive and open-secret forms
Guilt plagues a lot of us, sometimes regularly. Maybe you felt bad about eating the leftovers that your partner was looking forward to eating at the end of the day. Or for not saving a seat for your friend who was running late to the movies. Maybe even hiding a secret that you know would hurt a person’s feelings. We’ve all felt it, and it doesn’t feel good.
But what if there was a pill that would make those feelings seem to hurt less? There’s already a pill for almost everything, right?
Well, researchers from the University of Basel are on the case and have conducted a study suggesting that a placebo might work. They asked participants to write down a time they felt super guilty about something, just to stir up those feelings again, then they were divided into three groups. One group was told they would receive real medication that was actually a placebo, one was told they would get a placebo, and one got nothing. The subjects’ guilty feelings were reduced in both the medication-that-was-really-a-placebo group and placebo-that-was-a-placebo group.
“Our study therefore supports the intriguing finding that placebos work even when they are administered openly, and that explanation of the treatment is key to its effectiveness,” lead author Dilan Sezer said in a written statement.
More research is needed, but the human mind is a very interesting place. It seems like we can convince ourselves of just about anything. Especially to feel less guilty.
It’s a mad, mad, mad, mad scientist’s world
Mad scientists. Life’s just more interesting with a few of them running around, but they’re mostly relegated to works of fiction. Real life is boring; we don’t actually have neurosurgeons going around claiming human brain transplant is technically feasible.
Best of all, this isn’t even Dr. Sergio Canavero’s first rodeo with mad science: In 2015 he claimed human head transplants were technically feasible, and in the past few years has claimed to have rehearsed head transplants on cadavers and successfully repaired spinal cord injuries in animals. Lots of claims in there, but precious little evidence. And contrary to what everyone at the head enhancement clinic says, people will notice if you start going around with a new head.
But let’s get back to brains. Ignoring the fact that brain transplant sounds like a zombie with a PhD nibbling on your skull, the article does appear in a peer-reviewed journal. So surely there’s some level of legitimacy. After all, it’s not like Dr. Canavero is an editor for this journal. [Editor’s note: By that we mean he is an editor for the journal.]
Man, he’s taking all the fun out of this.
Anyway, now that we’ve prefaced this with the mother of all caveats, what exactly is Dr. Canavero proposing with his brain transplant? It’s pretty simple: Just have a robot scoop out the first brain and place it into a fresh body, either a donated but moribund younger body or a cloned body. Reconnect all the nerves and vasculature and you’re good to go. Enjoy your wine and laugh in the face of death.
Naturally, such a … bold proposal is lacking in the details, but who cares about details, anyway? This is mad science, not respectable science. Professionals have standards. And if we hear that a human brain transplant was successfully completed on a non–dark and stormy night and the doctor didn’t cackle madly “It’s alive! It’s alive!” then honestly, what even was the point?
Ambivalence rules!
As the office’s unofficial Sith lord/Star Wars nerd, LOTME takes notice when science extols the benefits of unhappiness: “It’s good to be grumpy: Bad moods make us more detail-oriented, study shows.”
The investigators manipulated the emotions of participants by having them watch a clip from “Sophie’s Choice” or one from “Friends.” Then the subjects listened to short, emotionally neutral stories, some of which contained inconsistencies, with the text displayed on a computer screen. Sorry to say, gang at Central Perk, but round one went to the sad movie.
“When people are in a negative mood, they are more careful and analytical. They scrutinize what’s actually stated in a text, and they don’t just fall back on their default world knowledge,” lead author Vicky Lai, PhD, of the University of Arizona said in a statement from the school.
Negative mood. Careful and analytical. Grumpy is good.
You’ve fallen into Darth Science’s little trap, and we have you now.
A study conducted at the University of Geneva offers a slightly different conclusion. And by slightly different, we mean completely different. People over age 65 who watched a series of short TV clips depicting people in a state of emotional suffering experienced excessive modification of their neuronal connections, compared with those who watched emotionally neutral videos.
The brains of these subjects remained “frozen in a negative state by relating the suffering of others to their own emotional memories,” lead author Sebastian Baez Lugo said in a written release from the university.
Emotional suffering. Frozen brains. Grumpy is … not good?
So there you have it. Darth Science’s lesson for the day: A negative mood makes you careful and analytical, but negative thoughts are bad for your brain.
Guilt reduction, now in deceptive and open-secret forms
Guilt plagues a lot of us, sometimes regularly. Maybe you felt bad about eating the leftovers that your partner was looking forward to eating at the end of the day. Or for not saving a seat for your friend who was running late to the movies. Maybe even hiding a secret that you know would hurt a person’s feelings. We’ve all felt it, and it doesn’t feel good.
But what if there was a pill that would make those feelings seem to hurt less? There’s already a pill for almost everything, right?
Well, researchers from the University of Basel are on the case and have conducted a study suggesting that a placebo might work. They asked participants to write down a time they felt super guilty about something, just to stir up those feelings again, then they were divided into three groups. One group was told they would receive real medication that was actually a placebo, one was told they would get a placebo, and one got nothing. The subjects’ guilty feelings were reduced in both the medication-that-was-really-a-placebo group and placebo-that-was-a-placebo group.
“Our study therefore supports the intriguing finding that placebos work even when they are administered openly, and that explanation of the treatment is key to its effectiveness,” lead author Dilan Sezer said in a written statement.
More research is needed, but the human mind is a very interesting place. It seems like we can convince ourselves of just about anything. Especially to feel less guilty.
It’s a mad, mad, mad, mad scientist’s world
Mad scientists. Life’s just more interesting with a few of them running around, but they’re mostly relegated to works of fiction. Real life is boring; we don’t actually have neurosurgeons going around claiming human brain transplant is technically feasible.
Best of all, this isn’t even Dr. Sergio Canavero’s first rodeo with mad science: In 2015 he claimed human head transplants were technically feasible, and in the past few years has claimed to have rehearsed head transplants on cadavers and successfully repaired spinal cord injuries in animals. Lots of claims in there, but precious little evidence. And contrary to what everyone at the head enhancement clinic says, people will notice if you start going around with a new head.
But let’s get back to brains. Ignoring the fact that brain transplant sounds like a zombie with a PhD nibbling on your skull, the article does appear in a peer-reviewed journal. So surely there’s some level of legitimacy. After all, it’s not like Dr. Canavero is an editor for this journal. [Editor’s note: By that we mean he is an editor for the journal.]
Man, he’s taking all the fun out of this.
Anyway, now that we’ve prefaced this with the mother of all caveats, what exactly is Dr. Canavero proposing with his brain transplant? It’s pretty simple: Just have a robot scoop out the first brain and place it into a fresh body, either a donated but moribund younger body or a cloned body. Reconnect all the nerves and vasculature and you’re good to go. Enjoy your wine and laugh in the face of death.
Naturally, such a … bold proposal is lacking in the details, but who cares about details, anyway? This is mad science, not respectable science. Professionals have standards. And if we hear that a human brain transplant was successfully completed on a non–dark and stormy night and the doctor didn’t cackle madly “It’s alive! It’s alive!” then honestly, what even was the point?
Ambivalence rules!
As the office’s unofficial Sith lord/Star Wars nerd, LOTME takes notice when science extols the benefits of unhappiness: “It’s good to be grumpy: Bad moods make us more detail-oriented, study shows.”
The investigators manipulated the emotions of participants by having them watch a clip from “Sophie’s Choice” or one from “Friends.” Then the subjects listened to short, emotionally neutral stories, some of which contained inconsistencies, with the text displayed on a computer screen. Sorry to say, gang at Central Perk, but round one went to the sad movie.
“When people are in a negative mood, they are more careful and analytical. They scrutinize what’s actually stated in a text, and they don’t just fall back on their default world knowledge,” lead author Vicky Lai, PhD, of the University of Arizona said in a statement from the school.
Negative mood. Careful and analytical. Grumpy is good.
You’ve fallen into Darth Science’s little trap, and we have you now.
A study conducted at the University of Geneva offers a slightly different conclusion. And by slightly different, we mean completely different. People over age 65 who watched a series of short TV clips depicting people in a state of emotional suffering experienced excessive modification of their neuronal connections, compared with those who watched emotionally neutral videos.
The brains of these subjects remained “frozen in a negative state by relating the suffering of others to their own emotional memories,” lead author Sebastian Baez Lugo said in a written release from the university.
Emotional suffering. Frozen brains. Grumpy is … not good?
So there you have it. Darth Science’s lesson for the day: A negative mood makes you careful and analytical, but negative thoughts are bad for your brain.
Guilt reduction, now in deceptive and open-secret forms
Guilt plagues a lot of us, sometimes regularly. Maybe you felt bad about eating the leftovers that your partner was looking forward to eating at the end of the day. Or for not saving a seat for your friend who was running late to the movies. Maybe even hiding a secret that you know would hurt a person’s feelings. We’ve all felt it, and it doesn’t feel good.
But what if there was a pill that would make those feelings seem to hurt less? There’s already a pill for almost everything, right?
Well, researchers from the University of Basel are on the case and have conducted a study suggesting that a placebo might work. They asked participants to write down a time they felt super guilty about something, just to stir up those feelings again, then they were divided into three groups. One group was told they would receive real medication that was actually a placebo, one was told they would get a placebo, and one got nothing. The subjects’ guilty feelings were reduced in both the medication-that-was-really-a-placebo group and placebo-that-was-a-placebo group.
“Our study therefore supports the intriguing finding that placebos work even when they are administered openly, and that explanation of the treatment is key to its effectiveness,” lead author Dilan Sezer said in a written statement.
More research is needed, but the human mind is a very interesting place. It seems like we can convince ourselves of just about anything. Especially to feel less guilty.
It’s a mad, mad, mad, mad scientist’s world
Mad scientists. Life’s just more interesting with a few of them running around, but they’re mostly relegated to works of fiction. Real life is boring; we don’t actually have neurosurgeons going around claiming human brain transplant is technically feasible.
Best of all, this isn’t even Dr. Sergio Canavero’s first rodeo with mad science: In 2015 he claimed human head transplants were technically feasible, and in the past few years has claimed to have rehearsed head transplants on cadavers and successfully repaired spinal cord injuries in animals. Lots of claims in there, but precious little evidence. And contrary to what everyone at the head enhancement clinic says, people will notice if you start going around with a new head.
But let’s get back to brains. Ignoring the fact that brain transplant sounds like a zombie with a PhD nibbling on your skull, the article does appear in a peer-reviewed journal. So surely there’s some level of legitimacy. After all, it’s not like Dr. Canavero is an editor for this journal. [Editor’s note: By that we mean he is an editor for the journal.]
Man, he’s taking all the fun out of this.
Anyway, now that we’ve prefaced this with the mother of all caveats, what exactly is Dr. Canavero proposing with his brain transplant? It’s pretty simple: Just have a robot scoop out the first brain and place it into a fresh body, either a donated but moribund younger body or a cloned body. Reconnect all the nerves and vasculature and you’re good to go. Enjoy your wine and laugh in the face of death.
Naturally, such a … bold proposal is lacking in the details, but who cares about details, anyway? This is mad science, not respectable science. Professionals have standards. And if we hear that a human brain transplant was successfully completed on a non–dark and stormy night and the doctor didn’t cackle madly “It’s alive! It’s alive!” then honestly, what even was the point?
Ambivalence rules!
As the office’s unofficial Sith lord/Star Wars nerd, LOTME takes notice when science extols the benefits of unhappiness: “It’s good to be grumpy: Bad moods make us more detail-oriented, study shows.”
The investigators manipulated the emotions of participants by having them watch a clip from “Sophie’s Choice” or one from “Friends.” Then the subjects listened to short, emotionally neutral stories, some of which contained inconsistencies, with the text displayed on a computer screen. Sorry to say, gang at Central Perk, but round one went to the sad movie.
“When people are in a negative mood, they are more careful and analytical. They scrutinize what’s actually stated in a text, and they don’t just fall back on their default world knowledge,” lead author Vicky Lai, PhD, of the University of Arizona said in a statement from the school.
Negative mood. Careful and analytical. Grumpy is good.
You’ve fallen into Darth Science’s little trap, and we have you now.
A study conducted at the University of Geneva offers a slightly different conclusion. And by slightly different, we mean completely different. People over age 65 who watched a series of short TV clips depicting people in a state of emotional suffering experienced excessive modification of their neuronal connections, compared with those who watched emotionally neutral videos.
The brains of these subjects remained “frozen in a negative state by relating the suffering of others to their own emotional memories,” lead author Sebastian Baez Lugo said in a written release from the university.
Emotional suffering. Frozen brains. Grumpy is … not good?
So there you have it. Darth Science’s lesson for the day: A negative mood makes you careful and analytical, but negative thoughts are bad for your brain.
How to talk with patients in ways that help them feel heard and understood
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
Adverse events reported in one-quarter of inpatient admissions
as indicated from data from 2,809 admissions at 11 hospitals.
The 1991 Harvard Medical Practice Study, which focused on medical injury and litigation, documented an adverse event rate of 3.7 events per 100 admissions; 28% of those events were attributed to negligence, write David W. Bates, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
Although patient safety has changed significantly since 1991, documenting improvements has been challenging, the researchers say. Several reports have shown a decrease in health care–associated infections. However, other aspects of safety – notably, adverse drug events, defined as injuries resulting from drugs taken – are not easily measured and tracked, the researchers say.
“We have not had good estimates of how much harm is being caused by care in hospitals in an ongoing way that looked across all types of adverse events,” and the current review is therefore important, Dr. Bates said in an interview.
In a study recently published in the New England Journal of Medicine, the researchers analyzed a random sample of 2,809 hospital admissions from 11 hospitals in Massachusetts during the 2018 calendar year. The hospitals ranged in size from fewer than 100 beds to more than 700 beds; all patients were aged 18 years and older. A panel of nine nurses reviewed the admissions records to identify potential adverse events, and eight physicians reviewed the adverse event summaries and either agreed or disagreed with the adverse event type. The severity of each event was ranked using a general severity scale into categories of significant, serious, life-threatening, or fatal.
Overall, at least one adverse event was identified in 23.6% of the hospital admissions. A total of 978 adverse events were deemed to have occurred during the index admission, and 222 of these (22.7%) were deemed preventable. Among the preventable adverse events, 19.7% were classified as serious, 3.3% as life-threatening, and 0.5% as fatal.
A total of 523 admissions (18.6%) involved at least one significant adverse event, defined as an event that caused unnecessary harm but from which recovery was rapid. A total of 211 admissions involved a serious adverse event, defined as harm resulting in substantial intervention or prolonged recovery; 34 included at least one life-threatening event; and seven admissions involved a fatal adverse event.
A total of 191 admissions involved at least one adverse event deemed preventable. Of those, 29 involved at least one preventable adverse event that was serious, life-threatening, or fatal, the researchers write. Of the seven deaths in the study population, one was deemed preventable.
The most common adverse events were adverse drug events, which accounted for 39.0% of the adverse events; surgical or other procedural events accounted for 30.4%; patient care events (including falls and pressure ulcers) accounted for 15.0%; and health care–associated infections accounted for 11.9%.
Overcoming barriers to better safety
“The overall level of harm, with nearly 1 in 4 patients suffering an adverse event, was higher than I expected it might be,” Dr. Bates told this news organization. However, techniques for identifying adverse events have improved, and “it is easier to find them in electronic records than in paper records,” he noted.
“Hospitals have many issues they are currently dealing with since COVID, and one issue is simply prioritization,” Dr. Bates said. “But it is now possible to measure harm for all patients using electronic tools, and if hospitals know how much harm they are having in specific areas, they can make choices about which ones to focus on.”
“We now have effective prevention strategies for most of the main kinds of harm,” he said. Generally, rates of harm are high because these strategies are not being used effectively, he said. “In addition, there are new tools that can be used – for example, to identify patients who are decompensating earlier,” he noted.
As for additional research, some specific types of harm that have been resistant to interventions, such as pressure ulcers, deserve more attention, said Dr. Bates. “In addition, diagnostic errors appear to cause a great deal of harm, but we don’t yet have good strategies for preventing these,” he said.
The study findings were limited by several factors, including the use of data from hospitals that might not represent hospitals at large and by the inclusion mainly of patients with private insurance, the researchers write. Other limitations include the likelihood that some adverse events were missed and the level of agreement on adverse events between adjudicators was only fair.
However, the findings serve as a reminder to health care professionals of the need for continued attention to improving patient safety, and measuring adverse events remains a critical part of guiding these improvements, the researchers conclude.
Timely reassessment and opportunities to improve
In the decades since the publication of the report, “To Err Is Human,” by the National Academies in 2000, significant attention has been paid to improving patient safety during hospitalizations, and health care systems have increased in both system and disease complexity, Said Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview. “Therefore, this study is important in reassessing the safety of inpatient care at the current time,” he said.
“The findings of this study showing preventable adverse events in approximately 7% of all admissions; while concerning, is not surprising, as it is consistent with other studies over time, as the authors have also noted in their discussion,” said Dr. Pal. The current findings “underscore the importance of continuous quality improvement efforts to increase the safety of patient care for hospitalized patients,” he noted.
“The increasing complexity of medical care, fragmentation of health care, structural inequities of health systems, and more recent widespread public health challenges such as the COVID-19 pandemic have been, in my opinion, barriers to improving patient safety,” Dr. Pal said. “The use of innovation and an interdisciplinary approach to patient safety and quality improvement in hospital-based care, such as the use of machine learning to monitor trends and predict the individualized risk of harm, could be a potential way out” to help reduce barriers and improve safety, he said.
“Additional research is needed to understand the key drivers of preventable harm for hospitalized patients in the United States,” said Dr. Pal. “When planning for change, keen attention must be paid to understanding how these [drivers] may differ for patients who have been historically marginalized or are otherwise underserved so as to not exacerbate health care inequities,” he added.
The study was funded by the Controlled Risk Insurance Company and the Risk Management Foundation of the Harvard Medical Institutions. Dr. Bates owns stock options with AESOP, Clew, FeelBetter, Guided Clinical Solutions, MDClone, and ValeraHealth and has grants/contracts from IBM Watson and EarlySense. He has also served as a consultant for CDI Negev. Dr. Pal has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
as indicated from data from 2,809 admissions at 11 hospitals.
The 1991 Harvard Medical Practice Study, which focused on medical injury and litigation, documented an adverse event rate of 3.7 events per 100 admissions; 28% of those events were attributed to negligence, write David W. Bates, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
Although patient safety has changed significantly since 1991, documenting improvements has been challenging, the researchers say. Several reports have shown a decrease in health care–associated infections. However, other aspects of safety – notably, adverse drug events, defined as injuries resulting from drugs taken – are not easily measured and tracked, the researchers say.
“We have not had good estimates of how much harm is being caused by care in hospitals in an ongoing way that looked across all types of adverse events,” and the current review is therefore important, Dr. Bates said in an interview.
In a study recently published in the New England Journal of Medicine, the researchers analyzed a random sample of 2,809 hospital admissions from 11 hospitals in Massachusetts during the 2018 calendar year. The hospitals ranged in size from fewer than 100 beds to more than 700 beds; all patients were aged 18 years and older. A panel of nine nurses reviewed the admissions records to identify potential adverse events, and eight physicians reviewed the adverse event summaries and either agreed or disagreed with the adverse event type. The severity of each event was ranked using a general severity scale into categories of significant, serious, life-threatening, or fatal.
Overall, at least one adverse event was identified in 23.6% of the hospital admissions. A total of 978 adverse events were deemed to have occurred during the index admission, and 222 of these (22.7%) were deemed preventable. Among the preventable adverse events, 19.7% were classified as serious, 3.3% as life-threatening, and 0.5% as fatal.
A total of 523 admissions (18.6%) involved at least one significant adverse event, defined as an event that caused unnecessary harm but from which recovery was rapid. A total of 211 admissions involved a serious adverse event, defined as harm resulting in substantial intervention or prolonged recovery; 34 included at least one life-threatening event; and seven admissions involved a fatal adverse event.
A total of 191 admissions involved at least one adverse event deemed preventable. Of those, 29 involved at least one preventable adverse event that was serious, life-threatening, or fatal, the researchers write. Of the seven deaths in the study population, one was deemed preventable.
The most common adverse events were adverse drug events, which accounted for 39.0% of the adverse events; surgical or other procedural events accounted for 30.4%; patient care events (including falls and pressure ulcers) accounted for 15.0%; and health care–associated infections accounted for 11.9%.
Overcoming barriers to better safety
“The overall level of harm, with nearly 1 in 4 patients suffering an adverse event, was higher than I expected it might be,” Dr. Bates told this news organization. However, techniques for identifying adverse events have improved, and “it is easier to find them in electronic records than in paper records,” he noted.
“Hospitals have many issues they are currently dealing with since COVID, and one issue is simply prioritization,” Dr. Bates said. “But it is now possible to measure harm for all patients using electronic tools, and if hospitals know how much harm they are having in specific areas, they can make choices about which ones to focus on.”
“We now have effective prevention strategies for most of the main kinds of harm,” he said. Generally, rates of harm are high because these strategies are not being used effectively, he said. “In addition, there are new tools that can be used – for example, to identify patients who are decompensating earlier,” he noted.
As for additional research, some specific types of harm that have been resistant to interventions, such as pressure ulcers, deserve more attention, said Dr. Bates. “In addition, diagnostic errors appear to cause a great deal of harm, but we don’t yet have good strategies for preventing these,” he said.
The study findings were limited by several factors, including the use of data from hospitals that might not represent hospitals at large and by the inclusion mainly of patients with private insurance, the researchers write. Other limitations include the likelihood that some adverse events were missed and the level of agreement on adverse events between adjudicators was only fair.
However, the findings serve as a reminder to health care professionals of the need for continued attention to improving patient safety, and measuring adverse events remains a critical part of guiding these improvements, the researchers conclude.
Timely reassessment and opportunities to improve
In the decades since the publication of the report, “To Err Is Human,” by the National Academies in 2000, significant attention has been paid to improving patient safety during hospitalizations, and health care systems have increased in both system and disease complexity, Said Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview. “Therefore, this study is important in reassessing the safety of inpatient care at the current time,” he said.
“The findings of this study showing preventable adverse events in approximately 7% of all admissions; while concerning, is not surprising, as it is consistent with other studies over time, as the authors have also noted in their discussion,” said Dr. Pal. The current findings “underscore the importance of continuous quality improvement efforts to increase the safety of patient care for hospitalized patients,” he noted.
“The increasing complexity of medical care, fragmentation of health care, structural inequities of health systems, and more recent widespread public health challenges such as the COVID-19 pandemic have been, in my opinion, barriers to improving patient safety,” Dr. Pal said. “The use of innovation and an interdisciplinary approach to patient safety and quality improvement in hospital-based care, such as the use of machine learning to monitor trends and predict the individualized risk of harm, could be a potential way out” to help reduce barriers and improve safety, he said.
“Additional research is needed to understand the key drivers of preventable harm for hospitalized patients in the United States,” said Dr. Pal. “When planning for change, keen attention must be paid to understanding how these [drivers] may differ for patients who have been historically marginalized or are otherwise underserved so as to not exacerbate health care inequities,” he added.
The study was funded by the Controlled Risk Insurance Company and the Risk Management Foundation of the Harvard Medical Institutions. Dr. Bates owns stock options with AESOP, Clew, FeelBetter, Guided Clinical Solutions, MDClone, and ValeraHealth and has grants/contracts from IBM Watson and EarlySense. He has also served as a consultant for CDI Negev. Dr. Pal has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
as indicated from data from 2,809 admissions at 11 hospitals.
The 1991 Harvard Medical Practice Study, which focused on medical injury and litigation, documented an adverse event rate of 3.7 events per 100 admissions; 28% of those events were attributed to negligence, write David W. Bates, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
Although patient safety has changed significantly since 1991, documenting improvements has been challenging, the researchers say. Several reports have shown a decrease in health care–associated infections. However, other aspects of safety – notably, adverse drug events, defined as injuries resulting from drugs taken – are not easily measured and tracked, the researchers say.
“We have not had good estimates of how much harm is being caused by care in hospitals in an ongoing way that looked across all types of adverse events,” and the current review is therefore important, Dr. Bates said in an interview.
In a study recently published in the New England Journal of Medicine, the researchers analyzed a random sample of 2,809 hospital admissions from 11 hospitals in Massachusetts during the 2018 calendar year. The hospitals ranged in size from fewer than 100 beds to more than 700 beds; all patients were aged 18 years and older. A panel of nine nurses reviewed the admissions records to identify potential adverse events, and eight physicians reviewed the adverse event summaries and either agreed or disagreed with the adverse event type. The severity of each event was ranked using a general severity scale into categories of significant, serious, life-threatening, or fatal.
Overall, at least one adverse event was identified in 23.6% of the hospital admissions. A total of 978 adverse events were deemed to have occurred during the index admission, and 222 of these (22.7%) were deemed preventable. Among the preventable adverse events, 19.7% were classified as serious, 3.3% as life-threatening, and 0.5% as fatal.
A total of 523 admissions (18.6%) involved at least one significant adverse event, defined as an event that caused unnecessary harm but from which recovery was rapid. A total of 211 admissions involved a serious adverse event, defined as harm resulting in substantial intervention or prolonged recovery; 34 included at least one life-threatening event; and seven admissions involved a fatal adverse event.
A total of 191 admissions involved at least one adverse event deemed preventable. Of those, 29 involved at least one preventable adverse event that was serious, life-threatening, or fatal, the researchers write. Of the seven deaths in the study population, one was deemed preventable.
The most common adverse events were adverse drug events, which accounted for 39.0% of the adverse events; surgical or other procedural events accounted for 30.4%; patient care events (including falls and pressure ulcers) accounted for 15.0%; and health care–associated infections accounted for 11.9%.
Overcoming barriers to better safety
“The overall level of harm, with nearly 1 in 4 patients suffering an adverse event, was higher than I expected it might be,” Dr. Bates told this news organization. However, techniques for identifying adverse events have improved, and “it is easier to find them in electronic records than in paper records,” he noted.
“Hospitals have many issues they are currently dealing with since COVID, and one issue is simply prioritization,” Dr. Bates said. “But it is now possible to measure harm for all patients using electronic tools, and if hospitals know how much harm they are having in specific areas, they can make choices about which ones to focus on.”
“We now have effective prevention strategies for most of the main kinds of harm,” he said. Generally, rates of harm are high because these strategies are not being used effectively, he said. “In addition, there are new tools that can be used – for example, to identify patients who are decompensating earlier,” he noted.
As for additional research, some specific types of harm that have been resistant to interventions, such as pressure ulcers, deserve more attention, said Dr. Bates. “In addition, diagnostic errors appear to cause a great deal of harm, but we don’t yet have good strategies for preventing these,” he said.
The study findings were limited by several factors, including the use of data from hospitals that might not represent hospitals at large and by the inclusion mainly of patients with private insurance, the researchers write. Other limitations include the likelihood that some adverse events were missed and the level of agreement on adverse events between adjudicators was only fair.
However, the findings serve as a reminder to health care professionals of the need for continued attention to improving patient safety, and measuring adverse events remains a critical part of guiding these improvements, the researchers conclude.
Timely reassessment and opportunities to improve
In the decades since the publication of the report, “To Err Is Human,” by the National Academies in 2000, significant attention has been paid to improving patient safety during hospitalizations, and health care systems have increased in both system and disease complexity, Said Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview. “Therefore, this study is important in reassessing the safety of inpatient care at the current time,” he said.
“The findings of this study showing preventable adverse events in approximately 7% of all admissions; while concerning, is not surprising, as it is consistent with other studies over time, as the authors have also noted in their discussion,” said Dr. Pal. The current findings “underscore the importance of continuous quality improvement efforts to increase the safety of patient care for hospitalized patients,” he noted.
“The increasing complexity of medical care, fragmentation of health care, structural inequities of health systems, and more recent widespread public health challenges such as the COVID-19 pandemic have been, in my opinion, barriers to improving patient safety,” Dr. Pal said. “The use of innovation and an interdisciplinary approach to patient safety and quality improvement in hospital-based care, such as the use of machine learning to monitor trends and predict the individualized risk of harm, could be a potential way out” to help reduce barriers and improve safety, he said.
“Additional research is needed to understand the key drivers of preventable harm for hospitalized patients in the United States,” said Dr. Pal. “When planning for change, keen attention must be paid to understanding how these [drivers] may differ for patients who have been historically marginalized or are otherwise underserved so as to not exacerbate health care inequities,” he added.
The study was funded by the Controlled Risk Insurance Company and the Risk Management Foundation of the Harvard Medical Institutions. Dr. Bates owns stock options with AESOP, Clew, FeelBetter, Guided Clinical Solutions, MDClone, and ValeraHealth and has grants/contracts from IBM Watson and EarlySense. He has also served as a consultant for CDI Negev. Dr. Pal has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Manicure gone wrong leads to cancer diagnosis
. Now, she and her doctor are spreading the word about her ordeal as a lesson that speed and persistence in seeking treatment are the keys that make her type of cancer – squamous cell carcinoma – completely curable.
“She cut me, and the cut wasn’t just a regular cuticle cut. She cut me deep, and that was one of the first times that happened to me,” Grace Garcia, 50, told TODAY.com, recalling the November 2021 incident.
Ms. Garcia had been getting her nails done regularly for 20 years, she said, but happened to go to a different salon than her usual spot because she couldn’t get an appointment during the busy pre-Thanksgiving season. She doesn’t recall whether the technician opened packaging that signals unused tools.
She put antibiotic ointment on the cut, but it didn’t heal after a few days. Eventually, the skin closed and a darkened bump formed. It was painful. She went to her doctor, who said it was a “callus from writing,” she told TODAY.com. But it was on her ring finger, which didn’t seem connected to writing. Her doctor said to keep an eye on it.
Five months after the cut occurred, she mentioned it during a gynecology appointment and was referred to a dermatologist, who also advised keeping an eye on it. A wart developed. She went back to her primary care physician and then to another dermatologist. The spot was biopsied.
Squamous cell carcinoma is a common type of skin cancer, according to the American Academy of Dermatology. It can have many causes, but the cause in Ms. Garcia’s case was both very common and very rare: human papillomavirus, or HPV. HPV is a virus that infects millions of people every year, but it’s not a typical cause of skin cancer.
“It’s pretty rare for several reasons. Generally speaking, the strains that cause cancer from an HPV standpoint tend to be more sexually transmitted,” dermatologist Teo Soleymani told TODAY.com. “In Grace’s case, she had an injury, which became the portal of entry. So that thick skin that we have on our hands and feet that acts as a natural barrier against infections and things like that was no longer the case, and the virus was able to infect her skin.”
Dr. Soleymani said Ms. Garcia’s persistence to get answers likely saved her from losing a finger.
“Your outcomes are entirely dictated by how early you catch them, and very often they’re completely curable,” he said. “Her persistence – not only was she able to have a great outcome, she probably saved herself from having her finger amputated.”
. Now, she and her doctor are spreading the word about her ordeal as a lesson that speed and persistence in seeking treatment are the keys that make her type of cancer – squamous cell carcinoma – completely curable.
“She cut me, and the cut wasn’t just a regular cuticle cut. She cut me deep, and that was one of the first times that happened to me,” Grace Garcia, 50, told TODAY.com, recalling the November 2021 incident.
Ms. Garcia had been getting her nails done regularly for 20 years, she said, but happened to go to a different salon than her usual spot because she couldn’t get an appointment during the busy pre-Thanksgiving season. She doesn’t recall whether the technician opened packaging that signals unused tools.
She put antibiotic ointment on the cut, but it didn’t heal after a few days. Eventually, the skin closed and a darkened bump formed. It was painful. She went to her doctor, who said it was a “callus from writing,” she told TODAY.com. But it was on her ring finger, which didn’t seem connected to writing. Her doctor said to keep an eye on it.
Five months after the cut occurred, she mentioned it during a gynecology appointment and was referred to a dermatologist, who also advised keeping an eye on it. A wart developed. She went back to her primary care physician and then to another dermatologist. The spot was biopsied.
Squamous cell carcinoma is a common type of skin cancer, according to the American Academy of Dermatology. It can have many causes, but the cause in Ms. Garcia’s case was both very common and very rare: human papillomavirus, or HPV. HPV is a virus that infects millions of people every year, but it’s not a typical cause of skin cancer.
“It’s pretty rare for several reasons. Generally speaking, the strains that cause cancer from an HPV standpoint tend to be more sexually transmitted,” dermatologist Teo Soleymani told TODAY.com. “In Grace’s case, she had an injury, which became the portal of entry. So that thick skin that we have on our hands and feet that acts as a natural barrier against infections and things like that was no longer the case, and the virus was able to infect her skin.”
Dr. Soleymani said Ms. Garcia’s persistence to get answers likely saved her from losing a finger.
“Your outcomes are entirely dictated by how early you catch them, and very often they’re completely curable,” he said. “Her persistence – not only was she able to have a great outcome, she probably saved herself from having her finger amputated.”
. Now, she and her doctor are spreading the word about her ordeal as a lesson that speed and persistence in seeking treatment are the keys that make her type of cancer – squamous cell carcinoma – completely curable.
“She cut me, and the cut wasn’t just a regular cuticle cut. She cut me deep, and that was one of the first times that happened to me,” Grace Garcia, 50, told TODAY.com, recalling the November 2021 incident.
Ms. Garcia had been getting her nails done regularly for 20 years, she said, but happened to go to a different salon than her usual spot because she couldn’t get an appointment during the busy pre-Thanksgiving season. She doesn’t recall whether the technician opened packaging that signals unused tools.
She put antibiotic ointment on the cut, but it didn’t heal after a few days. Eventually, the skin closed and a darkened bump formed. It was painful. She went to her doctor, who said it was a “callus from writing,” she told TODAY.com. But it was on her ring finger, which didn’t seem connected to writing. Her doctor said to keep an eye on it.
Five months after the cut occurred, she mentioned it during a gynecology appointment and was referred to a dermatologist, who also advised keeping an eye on it. A wart developed. She went back to her primary care physician and then to another dermatologist. The spot was biopsied.
Squamous cell carcinoma is a common type of skin cancer, according to the American Academy of Dermatology. It can have many causes, but the cause in Ms. Garcia’s case was both very common and very rare: human papillomavirus, or HPV. HPV is a virus that infects millions of people every year, but it’s not a typical cause of skin cancer.
“It’s pretty rare for several reasons. Generally speaking, the strains that cause cancer from an HPV standpoint tend to be more sexually transmitted,” dermatologist Teo Soleymani told TODAY.com. “In Grace’s case, she had an injury, which became the portal of entry. So that thick skin that we have on our hands and feet that acts as a natural barrier against infections and things like that was no longer the case, and the virus was able to infect her skin.”
Dr. Soleymani said Ms. Garcia’s persistence to get answers likely saved her from losing a finger.
“Your outcomes are entirely dictated by how early you catch them, and very often they’re completely curable,” he said. “Her persistence – not only was she able to have a great outcome, she probably saved herself from having her finger amputated.”
Black Veterans Disproportionately Denied VA Benefits
Black veterans are less likely to have their benefits claims processed and paid than are their White peers because of systemic problems within the US Department of Veterans Affairs, according to a lawsuit filed against the agency.
“A Black veteran who served honorably can walk into the VA, file a disability claim, and be at a significantly higher likelihood of having that claim denied,” said Adam Henderson, a student working with the Yale Law School Veterans Legal Services Clinic, one of several groups connected to the lawsuit.
“The VA has denied countless meritorious applications of Black veterans and thus deprived them and their families of the support that they are entitled to.”
The suit, filed in federal court by the clinic on behalf of Vietnam War veteran Conley Monk Jr., asks for “redress for the harms caused by the failure of VA staff and leaders to administer these benefits programs in a manner free from racial discrimination against Black veterans.”
In a press conference announcing the lawsuit, the effort received backing from Sen. Richard Blumenthal (D, Connecticut) who called it an “unacceptable” situation.
“Black veterans are denied benefits at a very significantly disproportionate rate,” he said. “We know the results. We want to know the reason why.”
The suit stems from an analysis of VA claims records released by the department following an earlier legal action. Between 2001 and 2020, the average denial rate for disability claims filed for Black veterans was 29.5%, significantly above the 24.2% for White veterans.
Attorneys allege the problems date back even further and that VA officials should have known about the racial disparities in the system from previous complaints.
“The negligence of VA leadership, and their failure to train, supervise, monitor and instruct agency officials to take steps to identify and correct racial disparities, led to systematic benefits obstruction for Black veterans,” the suit states.
Monk is a Black disabled Marine Corps veteran who previously sued the military to overturn his less-than-honorable military discharge due to complications from undiagnosed posttraumatic stress disorder.
He was subsequently granted access to a host of veterans benefits but not to retroactive payouts for claims he was denied in the 1970s.
“They didn’t fully compensate me or my family,” he said. “I wasn’t able to give my kids my educational benefits. We should have been receiving checks while they were growing up.”
Along with potential past benefits for Monk, individuals involved with the lawsuit said the move could force the VA to reassess thousands of other unfairly dismissed cases. “For decades [the US government] has allowed racially discriminatory practices to obstruct Black veterans from easily accessing veterans housing, education, and health care benefits with wide-reaching economic consequences for Black veterans and their families,” said Richard Brookshire, executive director of the Black Veterans Project.
“This lawsuit reckons with the shameful history of racism by the Department of Veteran Affairs and seeks to redress long-standing improprieties reverberating across generations of Black military service.”
In a statement, VA press secretary Terrence Hayes did not directly respond to the lawsuit but noted that “throughout history, there have been unacceptable disparities in both VA benefits decisions and military discharge status due to racism, which have wrongly left Black veterans without access to VA care and benefits.”
“We are actively working to right these wrongs, and we will stop at nothing to ensure that all Black veterans get the VA services they have earned and deserve,” he said. “We are currently studying racial disparities in benefits claims decisions, and we will publish the results of that study as soon as they are available.”
Hayes said the department has already begun targeted outreach to Black veterans to help them with claims and is “taking steps to ensure that our claims process combats institutional racism, rather than perpetuating it.”
Black veterans are less likely to have their benefits claims processed and paid than are their White peers because of systemic problems within the US Department of Veterans Affairs, according to a lawsuit filed against the agency.
“A Black veteran who served honorably can walk into the VA, file a disability claim, and be at a significantly higher likelihood of having that claim denied,” said Adam Henderson, a student working with the Yale Law School Veterans Legal Services Clinic, one of several groups connected to the lawsuit.
“The VA has denied countless meritorious applications of Black veterans and thus deprived them and their families of the support that they are entitled to.”
The suit, filed in federal court by the clinic on behalf of Vietnam War veteran Conley Monk Jr., asks for “redress for the harms caused by the failure of VA staff and leaders to administer these benefits programs in a manner free from racial discrimination against Black veterans.”
In a press conference announcing the lawsuit, the effort received backing from Sen. Richard Blumenthal (D, Connecticut) who called it an “unacceptable” situation.
“Black veterans are denied benefits at a very significantly disproportionate rate,” he said. “We know the results. We want to know the reason why.”
The suit stems from an analysis of VA claims records released by the department following an earlier legal action. Between 2001 and 2020, the average denial rate for disability claims filed for Black veterans was 29.5%, significantly above the 24.2% for White veterans.
Attorneys allege the problems date back even further and that VA officials should have known about the racial disparities in the system from previous complaints.
“The negligence of VA leadership, and their failure to train, supervise, monitor and instruct agency officials to take steps to identify and correct racial disparities, led to systematic benefits obstruction for Black veterans,” the suit states.
Monk is a Black disabled Marine Corps veteran who previously sued the military to overturn his less-than-honorable military discharge due to complications from undiagnosed posttraumatic stress disorder.
He was subsequently granted access to a host of veterans benefits but not to retroactive payouts for claims he was denied in the 1970s.
“They didn’t fully compensate me or my family,” he said. “I wasn’t able to give my kids my educational benefits. We should have been receiving checks while they were growing up.”
Along with potential past benefits for Monk, individuals involved with the lawsuit said the move could force the VA to reassess thousands of other unfairly dismissed cases. “For decades [the US government] has allowed racially discriminatory practices to obstruct Black veterans from easily accessing veterans housing, education, and health care benefits with wide-reaching economic consequences for Black veterans and their families,” said Richard Brookshire, executive director of the Black Veterans Project.
“This lawsuit reckons with the shameful history of racism by the Department of Veteran Affairs and seeks to redress long-standing improprieties reverberating across generations of Black military service.”
In a statement, VA press secretary Terrence Hayes did not directly respond to the lawsuit but noted that “throughout history, there have been unacceptable disparities in both VA benefits decisions and military discharge status due to racism, which have wrongly left Black veterans without access to VA care and benefits.”
“We are actively working to right these wrongs, and we will stop at nothing to ensure that all Black veterans get the VA services they have earned and deserve,” he said. “We are currently studying racial disparities in benefits claims decisions, and we will publish the results of that study as soon as they are available.”
Hayes said the department has already begun targeted outreach to Black veterans to help them with claims and is “taking steps to ensure that our claims process combats institutional racism, rather than perpetuating it.”
Black veterans are less likely to have their benefits claims processed and paid than are their White peers because of systemic problems within the US Department of Veterans Affairs, according to a lawsuit filed against the agency.
“A Black veteran who served honorably can walk into the VA, file a disability claim, and be at a significantly higher likelihood of having that claim denied,” said Adam Henderson, a student working with the Yale Law School Veterans Legal Services Clinic, one of several groups connected to the lawsuit.
“The VA has denied countless meritorious applications of Black veterans and thus deprived them and their families of the support that they are entitled to.”
The suit, filed in federal court by the clinic on behalf of Vietnam War veteran Conley Monk Jr., asks for “redress for the harms caused by the failure of VA staff and leaders to administer these benefits programs in a manner free from racial discrimination against Black veterans.”
In a press conference announcing the lawsuit, the effort received backing from Sen. Richard Blumenthal (D, Connecticut) who called it an “unacceptable” situation.
“Black veterans are denied benefits at a very significantly disproportionate rate,” he said. “We know the results. We want to know the reason why.”
The suit stems from an analysis of VA claims records released by the department following an earlier legal action. Between 2001 and 2020, the average denial rate for disability claims filed for Black veterans was 29.5%, significantly above the 24.2% for White veterans.
Attorneys allege the problems date back even further and that VA officials should have known about the racial disparities in the system from previous complaints.
“The negligence of VA leadership, and their failure to train, supervise, monitor and instruct agency officials to take steps to identify and correct racial disparities, led to systematic benefits obstruction for Black veterans,” the suit states.
Monk is a Black disabled Marine Corps veteran who previously sued the military to overturn his less-than-honorable military discharge due to complications from undiagnosed posttraumatic stress disorder.
He was subsequently granted access to a host of veterans benefits but not to retroactive payouts for claims he was denied in the 1970s.
“They didn’t fully compensate me or my family,” he said. “I wasn’t able to give my kids my educational benefits. We should have been receiving checks while they were growing up.”
Along with potential past benefits for Monk, individuals involved with the lawsuit said the move could force the VA to reassess thousands of other unfairly dismissed cases. “For decades [the US government] has allowed racially discriminatory practices to obstruct Black veterans from easily accessing veterans housing, education, and health care benefits with wide-reaching economic consequences for Black veterans and their families,” said Richard Brookshire, executive director of the Black Veterans Project.
“This lawsuit reckons with the shameful history of racism by the Department of Veteran Affairs and seeks to redress long-standing improprieties reverberating across generations of Black military service.”
In a statement, VA press secretary Terrence Hayes did not directly respond to the lawsuit but noted that “throughout history, there have been unacceptable disparities in both VA benefits decisions and military discharge status due to racism, which have wrongly left Black veterans without access to VA care and benefits.”
“We are actively working to right these wrongs, and we will stop at nothing to ensure that all Black veterans get the VA services they have earned and deserve,” he said. “We are currently studying racial disparities in benefits claims decisions, and we will publish the results of that study as soon as they are available.”
Hayes said the department has already begun targeted outreach to Black veterans to help them with claims and is “taking steps to ensure that our claims process combats institutional racism, rather than perpetuating it.”
Simulating psychoanalysis: A review of Freud’s Bones
While psychiatry has been the subject of many films, video games are not a medium commonly known for examining mental illness.1 There have been PC games over the years with psychiatric themes, such as Sanitarium (1998), Depression Quest (2013), Fran Bow (2015), and Night in the Woods (2017). Now for perhaps the first time a game has been developed with the practice of psychiatry as its primary focus.
Freud’s Bones is a 2022 game developed by independent Italian game studio Fortuna Imperatore. The result of a successful Kickstarter crowdfunding campaign, Freud’s Bones is advertised as “the first point & click narrative-drive game to pay homage to the birth of psychoanalysis and its founder, addressing the themes of sexuality and neuroses filled with existential doubts.”
In Freud’s Bones, you take control of Sigmund Freud and guide him through his daily tasks. Gameplay is of the simple point-and-click variety, modeled after classic LucasArts-style adventure games of the 1990s such as The Secret of Monkey Island or Day of the Tentacle. Prior to seeing your first patient, the game provides several documents the player can peruse to become familiar with basic concepts of psychoanalysis. Although the game was originally written in Italian (and translation gaffes occasionally arise), generally the English wording is easy to read. However, some players may feel intimidated or bored by the sheer quantity of text the game provides. All in-game text, including books and spoken words, are written and there is no recorded voice acting. Audio consists largely of unintrusive background music and occasional sound effects. The graphical style is simple and cartoonish but pleasant.
Freud’s personal life is a major focus of the game. His real life dog Jofi is a constant presence in Freud’s office. At various times the player will witness Freud’s dreams, act as a voice inside his head, and attempt to interpret mystical Egyptian messages he receives. Players are also tasked with managing Freud’s reputation in the scientific community. This is apparently intended as a reflection of in-game clinical acumen, but it was sometimes difficult to tell what direct influence my actions had on Freud’s reputation.
Freud’s energy may flag at various points during the game, and the player may choose to give him a cigar or a dose of cocaine to stimulate him. These options sound interesting on the surface, but I found the effect of these substances on the game’s actual outcome to be minimal. Some tasks are presented in a less than user-friendly manner. For example, on my initial playthrough I could not figure out how to complete several optional errands such as shopping for more tobacco or selecting a cover for Freud’s books. The player is also given the opportunity to make choices that affect Freud’s personal life, such as whether to pursue an extramarital affair. The game does have a few narrative surprises, including appearances from some of Freud’s well-known contemporaries. One particularly vivid sequence late in the game involves navigating Freud through a hallucination with some bizarre, but very Freudian, imagery.
By far the most interesting and enjoyable part of the game is the psychoanalysis sessions. The player guides Freud through multiple sessions with four different patients. Each of them has a unique story and associated symptoms, and the player can choose a variety of responses. For example, will you take a comforting, paternalistic approach to the patient uncomfortable with her first appointment? Or will you take the more stoic, quiet approach of the analyst and allow the patient to speak without prompting? Part of the player’s quest in guiding Freud through these sessions is to help patients bring their unconscious thoughts to conscious awareness. This is depicted graphically as the thought moves vertically through images representing the id, superego, and ego. Skillful questioning can bring these thoughts to the surface, but poor choices can leave valuable insights buried in the unconscious.
These therapy sessions were unique and engaging, and I wish they constituted a larger portion of the gameplay in Freud’s Bones. More patients, more sessions with each patient, and longer sessions would all have been welcome additions. These analytic sessions eventually culminate in an opportunity to offer a diagnosis, and the player’s accuracy in treatment can result in divergent outcomes for each patient. The game is not lengthy, as it can be played in its entirety in roughly 5-6 hours. Selecting different options for Freud’s personal life and the analysis sessions provides some replay value for subsequent playthroughs.
Overall, Freud’s Bones is a worthy effort for being uniquely designed as interactive entertainment simulating psychoanalysis. It provides an experience of interest to psychiatrists but is also accessible to the general public. While the game has flaws in that it can be overly text-heavy and goals are not always clear, it shines in the moments where it allows the player to participate directly in the process of psychoanalysis. Freud’s Bones is available for purchase on Steam (currently priced at $13.99) and can be played on Windows PCs.
Dr. Weber is a psychiatrist at Intermountain Logan Regional Hospital in Logan, Utah. He disclosed no relevant financial relationships.
References
1. See, for example, Gabbard GO, Gabbard K. Psychiatry and the Cinema, 2nd ed. American Psychiatric Press, Inc.; 1999.
While psychiatry has been the subject of many films, video games are not a medium commonly known for examining mental illness.1 There have been PC games over the years with psychiatric themes, such as Sanitarium (1998), Depression Quest (2013), Fran Bow (2015), and Night in the Woods (2017). Now for perhaps the first time a game has been developed with the practice of psychiatry as its primary focus.
Freud’s Bones is a 2022 game developed by independent Italian game studio Fortuna Imperatore. The result of a successful Kickstarter crowdfunding campaign, Freud’s Bones is advertised as “the first point & click narrative-drive game to pay homage to the birth of psychoanalysis and its founder, addressing the themes of sexuality and neuroses filled with existential doubts.”
In Freud’s Bones, you take control of Sigmund Freud and guide him through his daily tasks. Gameplay is of the simple point-and-click variety, modeled after classic LucasArts-style adventure games of the 1990s such as The Secret of Monkey Island or Day of the Tentacle. Prior to seeing your first patient, the game provides several documents the player can peruse to become familiar with basic concepts of psychoanalysis. Although the game was originally written in Italian (and translation gaffes occasionally arise), generally the English wording is easy to read. However, some players may feel intimidated or bored by the sheer quantity of text the game provides. All in-game text, including books and spoken words, are written and there is no recorded voice acting. Audio consists largely of unintrusive background music and occasional sound effects. The graphical style is simple and cartoonish but pleasant.
Freud’s personal life is a major focus of the game. His real life dog Jofi is a constant presence in Freud’s office. At various times the player will witness Freud’s dreams, act as a voice inside his head, and attempt to interpret mystical Egyptian messages he receives. Players are also tasked with managing Freud’s reputation in the scientific community. This is apparently intended as a reflection of in-game clinical acumen, but it was sometimes difficult to tell what direct influence my actions had on Freud’s reputation.
Freud’s energy may flag at various points during the game, and the player may choose to give him a cigar or a dose of cocaine to stimulate him. These options sound interesting on the surface, but I found the effect of these substances on the game’s actual outcome to be minimal. Some tasks are presented in a less than user-friendly manner. For example, on my initial playthrough I could not figure out how to complete several optional errands such as shopping for more tobacco or selecting a cover for Freud’s books. The player is also given the opportunity to make choices that affect Freud’s personal life, such as whether to pursue an extramarital affair. The game does have a few narrative surprises, including appearances from some of Freud’s well-known contemporaries. One particularly vivid sequence late in the game involves navigating Freud through a hallucination with some bizarre, but very Freudian, imagery.
By far the most interesting and enjoyable part of the game is the psychoanalysis sessions. The player guides Freud through multiple sessions with four different patients. Each of them has a unique story and associated symptoms, and the player can choose a variety of responses. For example, will you take a comforting, paternalistic approach to the patient uncomfortable with her first appointment? Or will you take the more stoic, quiet approach of the analyst and allow the patient to speak without prompting? Part of the player’s quest in guiding Freud through these sessions is to help patients bring their unconscious thoughts to conscious awareness. This is depicted graphically as the thought moves vertically through images representing the id, superego, and ego. Skillful questioning can bring these thoughts to the surface, but poor choices can leave valuable insights buried in the unconscious.
These therapy sessions were unique and engaging, and I wish they constituted a larger portion of the gameplay in Freud’s Bones. More patients, more sessions with each patient, and longer sessions would all have been welcome additions. These analytic sessions eventually culminate in an opportunity to offer a diagnosis, and the player’s accuracy in treatment can result in divergent outcomes for each patient. The game is not lengthy, as it can be played in its entirety in roughly 5-6 hours. Selecting different options for Freud’s personal life and the analysis sessions provides some replay value for subsequent playthroughs.
Overall, Freud’s Bones is a worthy effort for being uniquely designed as interactive entertainment simulating psychoanalysis. It provides an experience of interest to psychiatrists but is also accessible to the general public. While the game has flaws in that it can be overly text-heavy and goals are not always clear, it shines in the moments where it allows the player to participate directly in the process of psychoanalysis. Freud’s Bones is available for purchase on Steam (currently priced at $13.99) and can be played on Windows PCs.
Dr. Weber is a psychiatrist at Intermountain Logan Regional Hospital in Logan, Utah. He disclosed no relevant financial relationships.
References
1. See, for example, Gabbard GO, Gabbard K. Psychiatry and the Cinema, 2nd ed. American Psychiatric Press, Inc.; 1999.
While psychiatry has been the subject of many films, video games are not a medium commonly known for examining mental illness.1 There have been PC games over the years with psychiatric themes, such as Sanitarium (1998), Depression Quest (2013), Fran Bow (2015), and Night in the Woods (2017). Now for perhaps the first time a game has been developed with the practice of psychiatry as its primary focus.
Freud’s Bones is a 2022 game developed by independent Italian game studio Fortuna Imperatore. The result of a successful Kickstarter crowdfunding campaign, Freud’s Bones is advertised as “the first point & click narrative-drive game to pay homage to the birth of psychoanalysis and its founder, addressing the themes of sexuality and neuroses filled with existential doubts.”
In Freud’s Bones, you take control of Sigmund Freud and guide him through his daily tasks. Gameplay is of the simple point-and-click variety, modeled after classic LucasArts-style adventure games of the 1990s such as The Secret of Monkey Island or Day of the Tentacle. Prior to seeing your first patient, the game provides several documents the player can peruse to become familiar with basic concepts of psychoanalysis. Although the game was originally written in Italian (and translation gaffes occasionally arise), generally the English wording is easy to read. However, some players may feel intimidated or bored by the sheer quantity of text the game provides. All in-game text, including books and spoken words, are written and there is no recorded voice acting. Audio consists largely of unintrusive background music and occasional sound effects. The graphical style is simple and cartoonish but pleasant.
Freud’s personal life is a major focus of the game. His real life dog Jofi is a constant presence in Freud’s office. At various times the player will witness Freud’s dreams, act as a voice inside his head, and attempt to interpret mystical Egyptian messages he receives. Players are also tasked with managing Freud’s reputation in the scientific community. This is apparently intended as a reflection of in-game clinical acumen, but it was sometimes difficult to tell what direct influence my actions had on Freud’s reputation.
Freud’s energy may flag at various points during the game, and the player may choose to give him a cigar or a dose of cocaine to stimulate him. These options sound interesting on the surface, but I found the effect of these substances on the game’s actual outcome to be minimal. Some tasks are presented in a less than user-friendly manner. For example, on my initial playthrough I could not figure out how to complete several optional errands such as shopping for more tobacco or selecting a cover for Freud’s books. The player is also given the opportunity to make choices that affect Freud’s personal life, such as whether to pursue an extramarital affair. The game does have a few narrative surprises, including appearances from some of Freud’s well-known contemporaries. One particularly vivid sequence late in the game involves navigating Freud through a hallucination with some bizarre, but very Freudian, imagery.
By far the most interesting and enjoyable part of the game is the psychoanalysis sessions. The player guides Freud through multiple sessions with four different patients. Each of them has a unique story and associated symptoms, and the player can choose a variety of responses. For example, will you take a comforting, paternalistic approach to the patient uncomfortable with her first appointment? Or will you take the more stoic, quiet approach of the analyst and allow the patient to speak without prompting? Part of the player’s quest in guiding Freud through these sessions is to help patients bring their unconscious thoughts to conscious awareness. This is depicted graphically as the thought moves vertically through images representing the id, superego, and ego. Skillful questioning can bring these thoughts to the surface, but poor choices can leave valuable insights buried in the unconscious.
These therapy sessions were unique and engaging, and I wish they constituted a larger portion of the gameplay in Freud’s Bones. More patients, more sessions with each patient, and longer sessions would all have been welcome additions. These analytic sessions eventually culminate in an opportunity to offer a diagnosis, and the player’s accuracy in treatment can result in divergent outcomes for each patient. The game is not lengthy, as it can be played in its entirety in roughly 5-6 hours. Selecting different options for Freud’s personal life and the analysis sessions provides some replay value for subsequent playthroughs.
Overall, Freud’s Bones is a worthy effort for being uniquely designed as interactive entertainment simulating psychoanalysis. It provides an experience of interest to psychiatrists but is also accessible to the general public. While the game has flaws in that it can be overly text-heavy and goals are not always clear, it shines in the moments where it allows the player to participate directly in the process of psychoanalysis. Freud’s Bones is available for purchase on Steam (currently priced at $13.99) and can be played on Windows PCs.
Dr. Weber is a psychiatrist at Intermountain Logan Regional Hospital in Logan, Utah. He disclosed no relevant financial relationships.
References
1. See, for example, Gabbard GO, Gabbard K. Psychiatry and the Cinema, 2nd ed. American Psychiatric Press, Inc.; 1999.
By the numbers: Cardiology slow to add women, IMGs join more quickly
Despite Mark Twain’s assertion that “there are three kinds of lies: lies, damned lies, and statistics,” we’re going to dive into 20 years’ worth of data and, hopefully, come up with a few statistics that shed some light on the specialty’s workforce since Cardiology News published its first issue in February 2003.
We start with a major issue over these last 20 years: The participation of women in the specialty.
Back in July of 2002, just a few months before the first issue of Cardiology News was published, W. Bruce Fye, MD, then-president of the American College of Cardiology, wrote, “We need to do more to attract female medical graduates to our specialty because they represent almost one-half of the new doctors trained in this country. Cardiology needs to take full advantage of this large talent pool”
Data from the American Medical Association confirm that assertion: Of the nearly 20,000 postgraduate cardiologists in practice that year, only 7.8% were women. And that was at a time when more than 42% of medical school graduates were women, Dr. Fye noted, while also pointing out that “only 10% of cardiology trainees are female, and just 6% of ACC fellows are women.”
The gap between men and women has closed somewhat in the last 20 years, but the specialty continues to lag behind the profession as a whole. Women represented 16.7% of cardiologists in 2022, versus 37% of physicians overall, AMA data show. In 2019, for the first time, the majority of U.S. medical school students (50.5%) were women, according to the Association of American Medical Colleges.
A look at residency numbers from the Accreditation Council for Graduate Medical Education shows that continued slow improvement in the number of women can be expected, as 25.5% of cardiovascular disease residents were women during the 2021-2022 academic year. Only 2 of the 19 other internal medicine subspecialties were lower, and they happened to be interventional cardiology (20.1%) and clinical cardiac electrophysiology (14.5%).
When men are added to the mix, cardiovascular disease had a total of 3,320 active residents training in 268 programs in 2021-2022, making it the largest of the IM subspecialties in both respects. The resident total is up 57% since 2003, when it came in at 2,117, while programs have increased 55% from the 173 that were operating 2 decades ago. During the year in the middle (2011-2012), there were 2,521 residents in 187 programs, so a larger share of the growth has occurred in the last 10 years, the ACGME data indicate.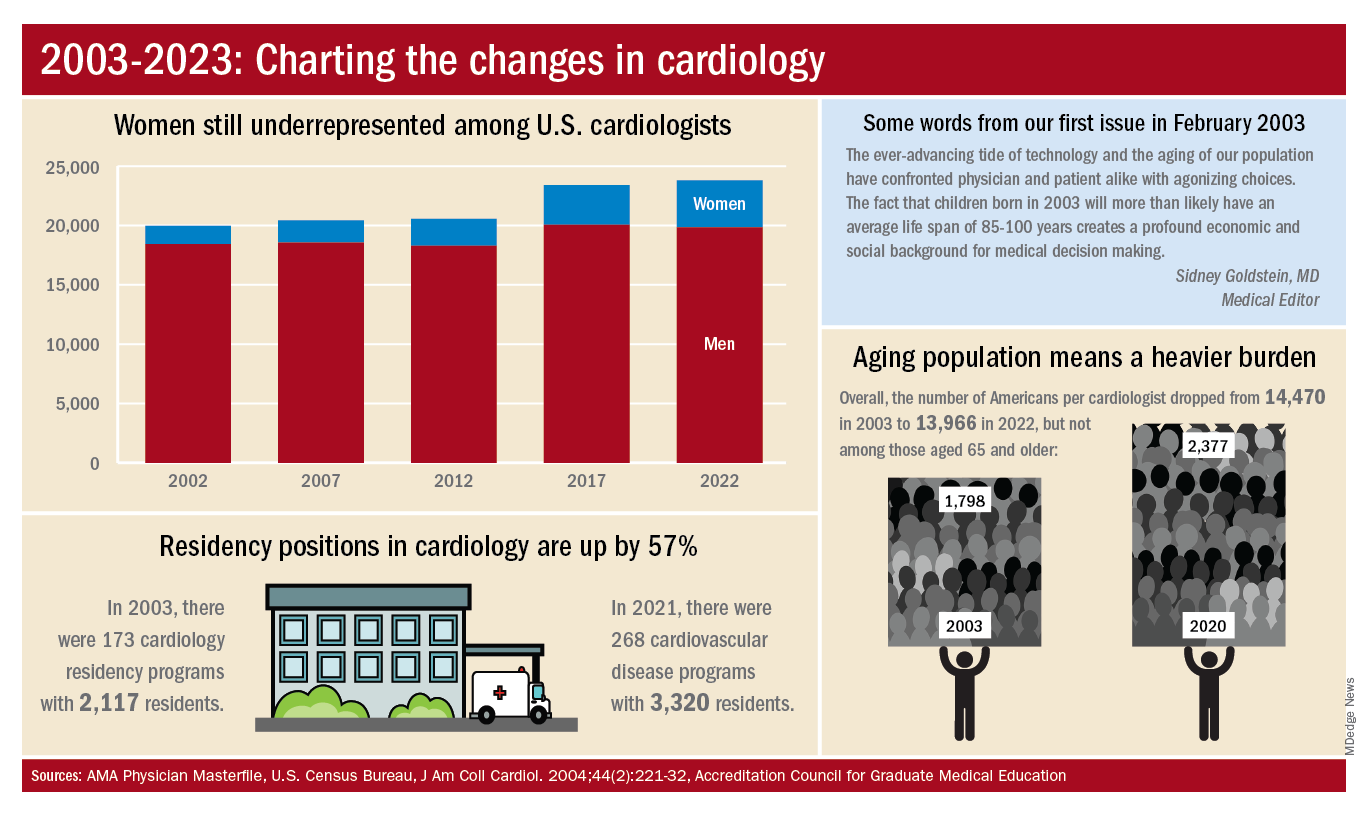
The shortage of cardiologists that Dr. Fye and others wrote about 20 years ago has not gone away. A 2018 report from health consulting firm PYA noted the increase in obesity and the low number of medical school graduates choosing the specialty. “Older and fewer physicians specializing in cardiology, coupled with the aging of baby boomers and gravitation toward practice in urban areas, will continue to exacerbate shortages in physician services in the specialty of cardiology, especially in rural areas, over the next decade,” PYA principal Lyle Oelrich wrote.
A little math appears to back up the claims of a cardiologist shortage. Based on census figures for the U.S. population in 2003, there were 14,470 Americans for each of the cardiologists reported by the AMA. That figure dropped to 13,966 by 2022, which seems like an improvement, but it comes with a caveat. The number of Americans aged 65 years and older increased from 1,798 to 2,377 per cardiologist as of 2020, the latest year for which population data were available by age.
One source of growth in the cardiology workforce has been perhaps its most significant minority: international medical graduates. Even by 2004, IMGs represented a much larger segment of all cardiologists (30.0%) than did women (9.3%), based on AMA data. To put it another way, there were more IMGs specializing in cardiovascular disease (6,615) in 2004 than there were women (3,963) in 2022.
The latest data on cardiology training programs – overall numbers were not available – put IMGs at 39.2% for the 2019-2020 academic year. The 2022 fellowship match provides a slightly smaller proportion of IMGs (37.4%) filling cardiovascular disease positions, according to the National Resident Matching Program.
Despite Mark Twain’s assertion that “there are three kinds of lies: lies, damned lies, and statistics,” we’re going to dive into 20 years’ worth of data and, hopefully, come up with a few statistics that shed some light on the specialty’s workforce since Cardiology News published its first issue in February 2003.
We start with a major issue over these last 20 years: The participation of women in the specialty.
Back in July of 2002, just a few months before the first issue of Cardiology News was published, W. Bruce Fye, MD, then-president of the American College of Cardiology, wrote, “We need to do more to attract female medical graduates to our specialty because they represent almost one-half of the new doctors trained in this country. Cardiology needs to take full advantage of this large talent pool”
Data from the American Medical Association confirm that assertion: Of the nearly 20,000 postgraduate cardiologists in practice that year, only 7.8% were women. And that was at a time when more than 42% of medical school graduates were women, Dr. Fye noted, while also pointing out that “only 10% of cardiology trainees are female, and just 6% of ACC fellows are women.”
The gap between men and women has closed somewhat in the last 20 years, but the specialty continues to lag behind the profession as a whole. Women represented 16.7% of cardiologists in 2022, versus 37% of physicians overall, AMA data show. In 2019, for the first time, the majority of U.S. medical school students (50.5%) were women, according to the Association of American Medical Colleges.
A look at residency numbers from the Accreditation Council for Graduate Medical Education shows that continued slow improvement in the number of women can be expected, as 25.5% of cardiovascular disease residents were women during the 2021-2022 academic year. Only 2 of the 19 other internal medicine subspecialties were lower, and they happened to be interventional cardiology (20.1%) and clinical cardiac electrophysiology (14.5%).
When men are added to the mix, cardiovascular disease had a total of 3,320 active residents training in 268 programs in 2021-2022, making it the largest of the IM subspecialties in both respects. The resident total is up 57% since 2003, when it came in at 2,117, while programs have increased 55% from the 173 that were operating 2 decades ago. During the year in the middle (2011-2012), there were 2,521 residents in 187 programs, so a larger share of the growth has occurred in the last 10 years, the ACGME data indicate.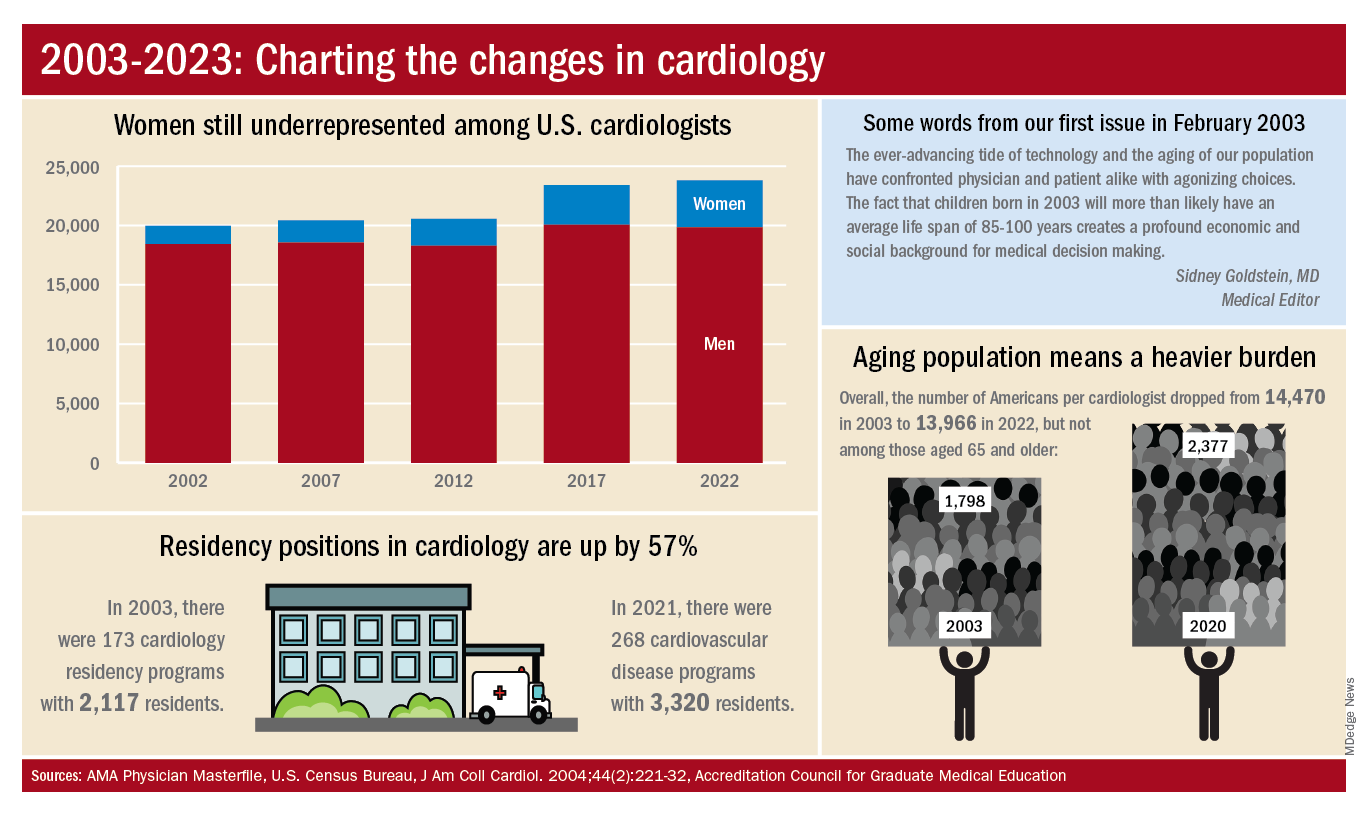
The shortage of cardiologists that Dr. Fye and others wrote about 20 years ago has not gone away. A 2018 report from health consulting firm PYA noted the increase in obesity and the low number of medical school graduates choosing the specialty. “Older and fewer physicians specializing in cardiology, coupled with the aging of baby boomers and gravitation toward practice in urban areas, will continue to exacerbate shortages in physician services in the specialty of cardiology, especially in rural areas, over the next decade,” PYA principal Lyle Oelrich wrote.
A little math appears to back up the claims of a cardiologist shortage. Based on census figures for the U.S. population in 2003, there were 14,470 Americans for each of the cardiologists reported by the AMA. That figure dropped to 13,966 by 2022, which seems like an improvement, but it comes with a caveat. The number of Americans aged 65 years and older increased from 1,798 to 2,377 per cardiologist as of 2020, the latest year for which population data were available by age.
One source of growth in the cardiology workforce has been perhaps its most significant minority: international medical graduates. Even by 2004, IMGs represented a much larger segment of all cardiologists (30.0%) than did women (9.3%), based on AMA data. To put it another way, there were more IMGs specializing in cardiovascular disease (6,615) in 2004 than there were women (3,963) in 2022.
The latest data on cardiology training programs – overall numbers were not available – put IMGs at 39.2% for the 2019-2020 academic year. The 2022 fellowship match provides a slightly smaller proportion of IMGs (37.4%) filling cardiovascular disease positions, according to the National Resident Matching Program.
Despite Mark Twain’s assertion that “there are three kinds of lies: lies, damned lies, and statistics,” we’re going to dive into 20 years’ worth of data and, hopefully, come up with a few statistics that shed some light on the specialty’s workforce since Cardiology News published its first issue in February 2003.
We start with a major issue over these last 20 years: The participation of women in the specialty.
Back in July of 2002, just a few months before the first issue of Cardiology News was published, W. Bruce Fye, MD, then-president of the American College of Cardiology, wrote, “We need to do more to attract female medical graduates to our specialty because they represent almost one-half of the new doctors trained in this country. Cardiology needs to take full advantage of this large talent pool”
Data from the American Medical Association confirm that assertion: Of the nearly 20,000 postgraduate cardiologists in practice that year, only 7.8% were women. And that was at a time when more than 42% of medical school graduates were women, Dr. Fye noted, while also pointing out that “only 10% of cardiology trainees are female, and just 6% of ACC fellows are women.”
The gap between men and women has closed somewhat in the last 20 years, but the specialty continues to lag behind the profession as a whole. Women represented 16.7% of cardiologists in 2022, versus 37% of physicians overall, AMA data show. In 2019, for the first time, the majority of U.S. medical school students (50.5%) were women, according to the Association of American Medical Colleges.
A look at residency numbers from the Accreditation Council for Graduate Medical Education shows that continued slow improvement in the number of women can be expected, as 25.5% of cardiovascular disease residents were women during the 2021-2022 academic year. Only 2 of the 19 other internal medicine subspecialties were lower, and they happened to be interventional cardiology (20.1%) and clinical cardiac electrophysiology (14.5%).
When men are added to the mix, cardiovascular disease had a total of 3,320 active residents training in 268 programs in 2021-2022, making it the largest of the IM subspecialties in both respects. The resident total is up 57% since 2003, when it came in at 2,117, while programs have increased 55% from the 173 that were operating 2 decades ago. During the year in the middle (2011-2012), there were 2,521 residents in 187 programs, so a larger share of the growth has occurred in the last 10 years, the ACGME data indicate.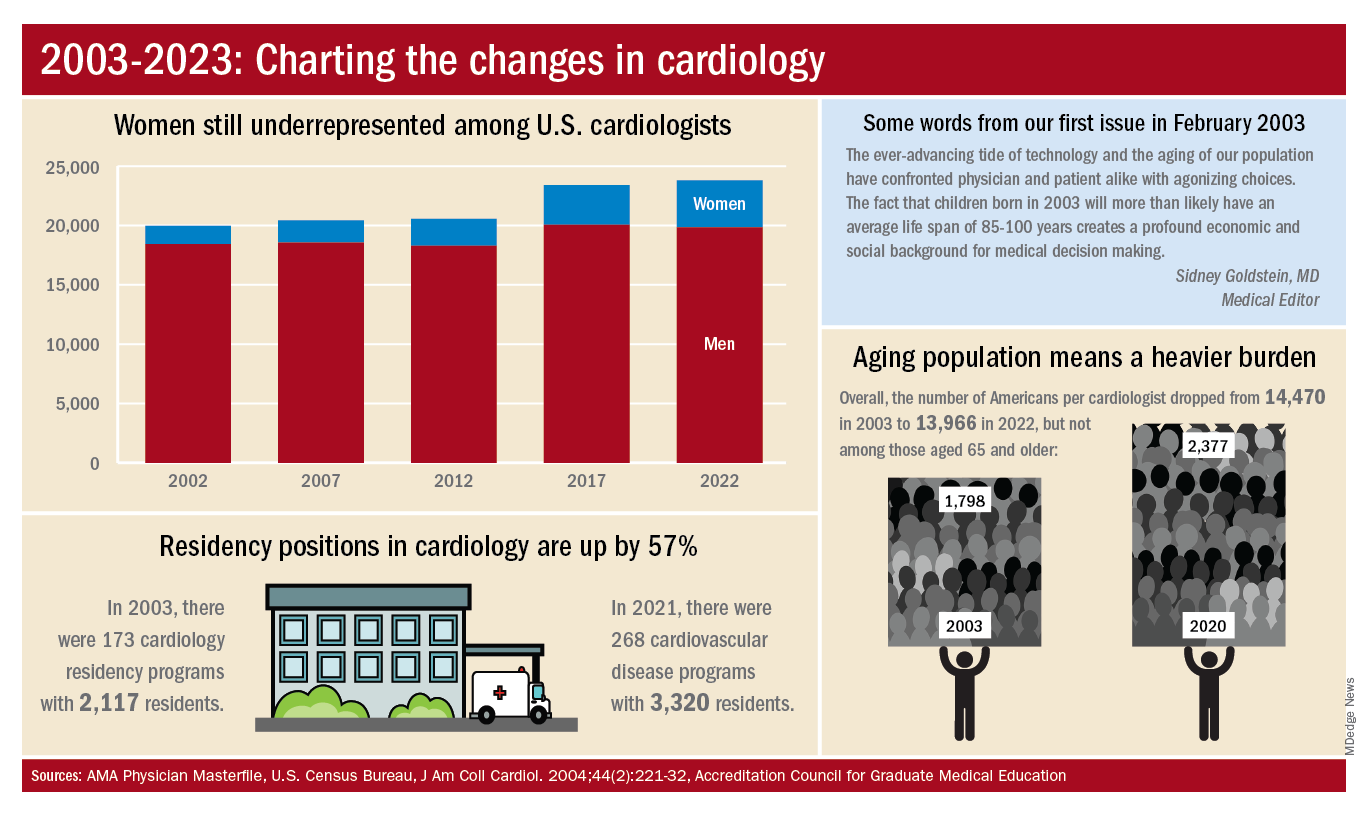
The shortage of cardiologists that Dr. Fye and others wrote about 20 years ago has not gone away. A 2018 report from health consulting firm PYA noted the increase in obesity and the low number of medical school graduates choosing the specialty. “Older and fewer physicians specializing in cardiology, coupled with the aging of baby boomers and gravitation toward practice in urban areas, will continue to exacerbate shortages in physician services in the specialty of cardiology, especially in rural areas, over the next decade,” PYA principal Lyle Oelrich wrote.
A little math appears to back up the claims of a cardiologist shortage. Based on census figures for the U.S. population in 2003, there were 14,470 Americans for each of the cardiologists reported by the AMA. That figure dropped to 13,966 by 2022, which seems like an improvement, but it comes with a caveat. The number of Americans aged 65 years and older increased from 1,798 to 2,377 per cardiologist as of 2020, the latest year for which population data were available by age.
One source of growth in the cardiology workforce has been perhaps its most significant minority: international medical graduates. Even by 2004, IMGs represented a much larger segment of all cardiologists (30.0%) than did women (9.3%), based on AMA data. To put it another way, there were more IMGs specializing in cardiovascular disease (6,615) in 2004 than there were women (3,963) in 2022.
The latest data on cardiology training programs – overall numbers were not available – put IMGs at 39.2% for the 2019-2020 academic year. The 2022 fellowship match provides a slightly smaller proportion of IMGs (37.4%) filling cardiovascular disease positions, according to the National Resident Matching Program.
A Better Way to Breathe: Combining Allergy and Pulmonary Care Into One Clinic
Asthma affects more than 300 million people worldwide.1 While many of these cases can achieve control with standard therapy, 5% to 10% of these cases are classified as severe asthma, remaining poorly controlled despite treatment with inhaled corticosteroids (ICS) and long-acting β agonists (LABA).2 These patients also account for the majority of morbidity and mortality associated with the disease, with increased hospitalizations, intensive care unit (ICU) stays, detrimental adverse effects of oral corticosteroids (OCS), and lower quality of life.3-6 Additionally, the financial repercussions of severe asthma are notable; in the United States, the estimated cost of asthma management is $82 billion annually, with $3 billion accounting for asthma-related work/school absences.7
In the past several years, the use of anti-immunoglobulin E (IgE), anti-interleukin-4 (IL-4), and anti-IL-5 biologic agents for severe asthma has been shown to decrease asthma exacerbations, improve lung function, reduce corticosteroid use, and decrease hospitalizations, especially for type 2 helper T cell (TH2-high) asthma.8-10 However, clinicians have observed significant barriers to the implementation and widespread use of biologics, including insurance coverage, long wait times, follow-up, and limited access for lower income groups.11,12
This article describes a unique model for a severe asthma clinic located at the Washington DC Veterans Affairs Medical Center (WDCVAMC) that is dually staffed by an allergist and pulmonologist. This clinic uses biologic agents for patients with difficult-to-treat asthma, many of whom require repeated or prolonged steroid use, in addition to prolonged and recurrent hospitalizations for exacerbations. The objective of this clinic is to provide a standardized approach to the management of severe asthma with the perspective of both an allergist and pulmonologist, thereby reducing the need to schedule appointments with multiple specialties and reducing delays in initiating biologics. This article presents the preliminary findings of 30 months of severe asthma management with various biologic agents, examining the impact of these therapies on hospitalizations, asthma exacerbations, ICU stays, and OCS use. The findings of this study support the benefits of biologics and suggest that the use of these agents within a dually staffed clinic may be a particularly effective model through which to manage severe asthma.
Background
Asthma affects approximately 20 million adults in the United States.13 Veterans are a population particularly impacted by asthma. Between 2015 and 2018, 10.9% of all veterans reported being diagnosed with asthma and 5.1% stated that they currently have asthma, compared with 13.4% and 8.0% of nonveterans, respectively.14 Veterans are susceptible to many of the factors that can trigger exacerbations while engaging in military service, such as chemical and environmental exposures both abroad and domestically.15,16 Additionally, medication adherence is often challenging among the veteran population, particularly with more involved therapy, such as inhaler use.17 Such factors contribute to asthma exacerbations, with 2.9% of veterans reporting at least 1 asthma exacerbation in the past 12 months.14
Over the past several years, the development and use of biologic agents have transformed the management of severe asthma.8 Before the development of biologic agents for severe asthma, treatment options for patients were limited. While OCS are frequently used for asthma exacerbations, they are associated with a multiplicity of undesirable adverse effects, including weight gain, mood lability, gastrointestinal upset, hyperglycemia, risk of bone fractures, and hypertension.18-20 The regular use of OCS are particularly problematic among other medical comorbidities commonly affecting the veteran population, such as diabetes and hypertension.21-22
The WDCVAMC severe allergy clinic used 3 biologic agents: omalizumab (anti-IgE), benralizumab (anti-IL-5), and agent dupilumab (anti-IL-4). These medications have shown significant improvements in quality of life, reduction in asthma exacerbations and hospitalizations, and decreased use of OCS.8,9 While research has firmly established the medical benefits of the use of biologic agents in severe asthma, several barriers exist in implementing widespread use.11,12
In Gelhorn and colleagues’ study examining both physician and patient challenges in the use of biologics for severe asthma, scheduling, administrative time, and insurance costs were found to be major barriers to the use of these medications.12 Patients expressed a preference for the administration of these medications in a specialist’s office but cited long wait times and scheduling difficulties as barriers. One of the most notable challenges from the physician perspective was the difficulty in obtaining reimbursement from insurance companies, requiring them to devote significant portions of time to prior authorizations and documentation.12
This article examines a dual specialty clinic that focuses on the treatment of severe asthma with biologic agents. This model is unique for several reasons. First, given the US Department of Veterans Affairs (VA) health care model, the health care practitioners (HCPs) in this clinic can avoid much of the administrative burden of obtaining reimbursement or working with insurance companies. Additionally, by dedicating specific days to the severe asthma clinic, patients do not experience long wait times to see both an allergist and pulmonologist. By seeing both clinicians, concurrent allergic and pulmonary issues can be addressed in the same visit, rather than delaying treatment by waiting on 2 specialist appointments.
Severe Asthma Clinic
The severe asthma clinic was started in September 2017 by a pulmonologist and an allergist at WDCVAMC. After experiencing substantial delays with the initiation of biologics for their patients and multiple referrals between their clinics, these physicians wanted to start a dually staffed asthma clinic to specifically focus on evaluating and treating severe asthma. A dedicated severe asthma clinic allowed the allergist and pulmonologist to streamline resources and collaborate to advocate for patients with the pharmacy section. Additionally, patients can benefit from the perspective of both specialists, as both the pulmonologist and allergist evaluate each patient and discuss the next steps of management.
This clinic is composed of 4 registered nurses, an allergist, and a pulmonologist. Clinic is held twice monthly through both telemedicine and in-office visits. The VA has strict guidelines for the use of certain biologics, including blood eosinophil count > 150 cells/µL, failure of traditional therapy, and frequent use of OCS. Additionally, to ensure these biologic agents are prescribed to patients that will benefit from them, the patients enrolled in this clinic are already on maximum therapy for their asthma, meaning all other therapeutic options (inhalers and oral medications) are being used. The clinic services all patients with severe asthma, not just patients who are on biologic therapy. Often, patients are referred to the severe allergy clinic late in their disease course given a lack of familiarity with biologic agents from prescribers and both institutional and insurance barriers.
Before the COVID-19 pandemic, spirometry and fractional exhaled nitric oxide (FENO) tests were recorded at each visit. Initially during the pandemic, the clinic transitioned to primarily telemedicine visits due to patients’ hesitance to seek in-person care. More recently, the clinic has transitioned back to primarily office visits; patients are seen in clinic on average every 3 months. At each visit, the patient is seen by both the pulmonologist and allergist. Additionally, the nursing staff reviews inhaler adherence with patients, spacer use, documents, Asthma Control Test (ACT) scores, and schedules follow-up visits.
Every 4 to 8 weeks, patients receive biologics agent at the WDCVAMC infusion center depending on the agent. The infusion center also instructs patients how to handle self-administered medications, like benralizumab, if the patient expresses a preference for taking it at home. Omalizumab has a boxed warning for anaphylaxis, although the other biologics in this study have a low risk of anaphylaxis. All patients receiving omalizumab, benralizumab, and dupilumab were provided with epinephrine injection devices in case of an allergic reaction and were taught how to use them in the clinic.23,24
If patients continued to experience asthma exacerbations after the initiation of a biologic, a change in agent was considered after 4 to 6 months. Additionally, a complete blood count, respiratory allergy panel, and pulmonary function tests (PFTs) were completed.
Clinic Patients
Preliminary data were obtained from a retrospective chart review of 15 patients enrolled in the severe asthma clinic over 30 months. The inclusion criteria for chart review consisted of patients aged > 18 years receiving a biologic agent for > 3 months for the treatment of severe asthma. The outcomes examined included steroid use, emergency department (ED) visits, hospitalizations, FEV1, and ICU stays.
Seven patients used benralizumab, 6 used dupilumab, and 2 used omalizumab (Table).
There was a notable clinical improvement in these patients. Before starting a biologic agent, all the patients in this study were prescribed steroids at least once a year for an asthma exacerbation, with a mean of 4.2 steroid tapers per year.
The initiation of a biologic agent also resulted in fewer ED visits and hospitalizations. Two patients had an ED visit for an asthma exacerbation since starting a biologic agent and 1 patient had a hospital admission for an asthma exacerbation. No patients were hospitalized in the ICU after starting a biologic agent.
Discussion
The 15 patients in this initial data were referred to the severe asthma clinic by pulmonology, ear, nose, and throat (ENT), primary care, and a hospitalist during an in-patient stay. As the enrollment in our clinic grows, an increasing number of patients are referred from the allergy clinic as well. Patients in the severe asthma clinic also are referred by regional centers as news of the clinic is spread by word of mouth to surrounding VA facilities. As our clinic gains the capacity to serve more patients, we hope to contact WDCVAMC primary care, pulmonology, allergy, and ENT departments to raise awareness of the clinic.
Benralizumab and dupilumab were the most used agents in this preliminary data. This finding was largely due to the ability of patients to self-administer benralizumab, which was particularly beneficial during the COVID-19 pandemic. Of note, 5 patients in this study switched from another biologic agent to benralizumab due to the ability to self-administer. Three of 5 patients that required steroids after initiating benralizumab used fewer steroids than they had previously. This finding suggests benralizumab may be the preferred agent when travel time to health care is a challenge, reducing the need for frequent clinic visits and transportation.
This preliminary data supports previous studies that have demonstrated that biologic agents improve clinical outcomes by reducing asthma exacerbations, OCS use, hospitalizations, and ICU stays for patients on all 4 biologic agents. In addition to improving patient health through avoiding complications of prolonged OCS use and hospital stays, the decrease in ED visits and hospitalizations provides a substantial cost reduction to the health care system.
These findings highlight the strength of a unique model of a combined allergy/pulmonary clinic. Before this combined clinic model, both pulmonology and allergy clinics noted delays in the initiation of biologics for patients who were potential candidates. Impediments include referrals between each specialty for evaluation of concurrent pulmonary conditions or allergy testing, overlap in asthma management, and a delay in coordination with the pharmacy department to start biologic agents. A dedicated severe asthma clinic staffed by both an allergist and pulmonologist provides a convenient option for patients to be seen by both specialists, reducing the need for separate appointments with each specialty, transportation to those appointments, and clinical time. This is particularly beneficial in a clinic such as this model, as this clinic serves patients from 4 states and Washington, DC. An additional benefit of this model is trained staff who directly communicate with the pharmacy in the initiation of these agents, allocate time to educating patients in biologic use, and coordinate follow-up.
Limitations
There were several limitations to this report. First, the number of patients examined in this preliminary data set is small. Due to the COVID-19 pandemic, there was a limited ability to see patients in person, and patients were seen exclusively over telemedicine for several months. For this reason, collecting data such as patient surveys and laboratory work following the initiation of a biologic was a challenge. Additionally, during the height of COVID-19, WDCVAMC did not perform aerosolizing procedures, such as PFTs and FENOs; thus, peak flows were obtained instead. Examining metrics, such as FENOs and IgE levels, and expanding PFT data would provide additional insight into the impact of biologic agents on clinical outcomes. Patient survey data in the form of ACTs or satisfaction surveys would also yield important data examining the impact of this clinic design and biologic use on patient experience. As of December 2022, 114 patients are enrolled in the clinic. We are working to collect the above laboratory results and spirometry for these patients so that these results can be published with a more robust data set. Another limitation of the information presented is that it is a retrospective data analysis; the data collected was contingent upon documentation and the assumption that these patients were exclusively receiving care through the VA. For example, steroid use before and after initiation of biologic was taken from asthma clinic notes and the patient’s medication list. Therefore, there is a possibility that not all instances were accounted for if that patient sought care outside the VA or whether it was not documented in a follow-up note.
Conclusions
The model of a combined allergy/pulmonology clinic can be particularly efficacious in the treatment of severe asthma, as it reduces the need for multiple appointments with different specialties, reduces wait time before starting a biologic agent, and offers the perspective of 2 specialists. This kind of model could be an example to many clinics in the VA. With a rapid increase in telemedicine due to the COVID-19 pandemic, multiple physicians consulting simultaneously is becoming a more feasible possibility across multiple specialties. As the use of biologics becomes more widespread, a combined clinic design is an efficient and promising method to improve severe asthma management.
This preliminary data continue to support previous research that shows biologic agents have led to better clinical outcomes through the reduction of asthma exacerbations, hospitalizations, and improved PFTs. While this initial data set highlights the results for 15 patients, there are 86 patients currently enrolled in this clinic. We are collecting additional data to publish more comprehensive results.
1. Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol. 2015;16(1):45-56. doi:10.1038/ni.3049
2. Moore WC, Bleecker ER, Curran-Everett D, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. J Allergy Clin Immunol. 2007;119(2):405-413. doi:10.1016/j.jaci.2006.11.639
3. Barnes PJ, Jonsson B, Klim JB. The costs of asthma. Eur Respir J. 1996;9(4):636-642. doi:10.1183/09031936.96.09040636
4. Bourdin A, Charriot J, Boissin C, et al. Will the asthma revolution fostered by biologics also benefit adult ICU patients?. Allergy. 2021;76(8):2395-2406. doi:10.1111/all.14688
5. Lloyd A, Price D, Brown R. The impact of asthma exacerbations on health-related quality of life in moderate to severe asthma patients in the UK. Prim Care Respir J. 2007;16(1):22-27. doi:10.3132/pcrj.2007.00002
6. Eisner MD, Yelin EH, Katz PP, Lactao G, Iribarren C, Blanc PD. Risk factors for work disability in severe adult asthma. Am J Med. 2006;119(10):884-891. doi:10.1016/j.amjmed.2006.01.016
7. Nurmagambetov T, Kuwahara R, Garbe P. The Economic Burden of Asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018;15(3):348-356. doi:10.1513/AnnalsATS.201703-259OC
8. McGregor MC, Krings JG, Nair P, Castro M. Role of biologics in asthma. Am J Respir Crit Care Med. 2019;199(4):433-445. doi:10.1164/rccm.201810-1944CI
9. Bice JB, Leechawengwongs E, Montanaro A. Biologic targeted therapy in allergic asthma. Ann Allergy Asthma Immunol. 2014;112(2):108-115. doi:10.1016/j.anai.2013.12.013
10. Darveaux J, Busse WW. Biologics in asthma--the next step toward personalized treatment. J Allergy Clin Immunol Pract. 2015;3(2):152-161. doi:10.1016/j.jaip.2014.09.014
11. Inselman JW, Jeffery MM, Maddux JT, Shah ND, Rank MA. Trends and disparities in asthma biologic use in the United States. J Allergy Clin Immunol Pract. 2020;8(2):549-554.e1. doi:10.1016/j.jaip.2019.08.024
12. Gelhorn HL, Balantac Z, Ambrose CS, Chung YN, Stone B. Patient and physician preferences for attributes of biologic medications for severe asthma. Patient Prefer Adherence. 2019;13:1253-1268. Published 2019 Jul 25. doi:10.2147/PPA.S198953
13. Centers for Disease Control and Prevention, National Center for Environmental Health. 2019 National Health Interview Survey (NHIS) data. Accessed December 6, 2022. https://www.cdc.gov/asthma/nhis/2019/data.htm
14. Zelaya CE BP, Moy E. Crude and age-adjusted percent distribution of respondent-assessed health status among adults aged 20 and over, by veteran status and other selected characteristics: United States, 2015-2018. National Center for Health Statistic. Updated June 19, 2020. Accessed December 12, 2022. https://www.cdc.gov/nchs/nhis/veterans_health_statistics/tables.htm
15. Szema AM, Peters MC, Weissinger KM, Gagliano CA, Chen JJ. New-onset asthma among soldiers serving in Iraq and Afghanistan. Allergy Asthma Proc. 2010;31(5):67-71. doi:10.2500/aap.2010.31.3383
16. Yi SW, Hong JS, Ohrr H, Yi JJ. Agent Orange exposure and disease prevalence in Korean Vietnam veterans: the Korean veterans health study. Environ Res. 2014;133:56-65. doi:10.1016/j.envres.2014.04.027
17. Huetsch JC, Uman JE, Udris EM, Au DH. Predictors of adherence to inhaled medications among veterans with COPD. J Gen Intern Med. 2012;27(11):1506-1512. doi:10.1007/s11606-012-2130-5
18. Mundell L, Lindemann R, Douglas J. Monitoring long-term oral corticosteroids. BMJ Open Qual. 2017;6(2):e000209. Published 2017 Nov 8. doi:10.1136/bmjoq-2017-000209
19. Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C. Use of oral corticosteroids and risk of fractures. J Bone Miner Res. 2005;20(8):1487-1486. doi:10.1359/jbmr.2005.20.8.1486
20. Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81(10):1361-1367. doi:10.4065/81.10.1361
21. Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(suppl 2):B10-B21. doi:10.2337/diacare.27.suppl_2.b10
22. Acharya T, Tringali S, Singh M, Huang J. Resistant hypertension and associated comorbidities in a Veterans Affairs population. J Clin Hypertens (Greenwich). 2014;16(10):741-745. doi:10.1111/jch.12410
23. Dupixent (dupilumab). Prescribing information. Sanofi and Regeneron Pharmaceuticals; 2022. Accessed December 6, 2022. https://www.dupixenthcp.com/asthma/efficacy/safety-data
24. Li L, Wang Z, Cui L, Xu Y, Guan K, Zhao B. Anaphylactic risk related to omalizumab, benralizumab, reslizumab, mepolizumab, and dupilumab. Clin Transl Allergy. 2021;11(4):e12038. Published 2021 Jun 3. doi:10.1002/clt2.12038
Asthma affects more than 300 million people worldwide.1 While many of these cases can achieve control with standard therapy, 5% to 10% of these cases are classified as severe asthma, remaining poorly controlled despite treatment with inhaled corticosteroids (ICS) and long-acting β agonists (LABA).2 These patients also account for the majority of morbidity and mortality associated with the disease, with increased hospitalizations, intensive care unit (ICU) stays, detrimental adverse effects of oral corticosteroids (OCS), and lower quality of life.3-6 Additionally, the financial repercussions of severe asthma are notable; in the United States, the estimated cost of asthma management is $82 billion annually, with $3 billion accounting for asthma-related work/school absences.7
In the past several years, the use of anti-immunoglobulin E (IgE), anti-interleukin-4 (IL-4), and anti-IL-5 biologic agents for severe asthma has been shown to decrease asthma exacerbations, improve lung function, reduce corticosteroid use, and decrease hospitalizations, especially for type 2 helper T cell (TH2-high) asthma.8-10 However, clinicians have observed significant barriers to the implementation and widespread use of biologics, including insurance coverage, long wait times, follow-up, and limited access for lower income groups.11,12
This article describes a unique model for a severe asthma clinic located at the Washington DC Veterans Affairs Medical Center (WDCVAMC) that is dually staffed by an allergist and pulmonologist. This clinic uses biologic agents for patients with difficult-to-treat asthma, many of whom require repeated or prolonged steroid use, in addition to prolonged and recurrent hospitalizations for exacerbations. The objective of this clinic is to provide a standardized approach to the management of severe asthma with the perspective of both an allergist and pulmonologist, thereby reducing the need to schedule appointments with multiple specialties and reducing delays in initiating biologics. This article presents the preliminary findings of 30 months of severe asthma management with various biologic agents, examining the impact of these therapies on hospitalizations, asthma exacerbations, ICU stays, and OCS use. The findings of this study support the benefits of biologics and suggest that the use of these agents within a dually staffed clinic may be a particularly effective model through which to manage severe asthma.
Background
Asthma affects approximately 20 million adults in the United States.13 Veterans are a population particularly impacted by asthma. Between 2015 and 2018, 10.9% of all veterans reported being diagnosed with asthma and 5.1% stated that they currently have asthma, compared with 13.4% and 8.0% of nonveterans, respectively.14 Veterans are susceptible to many of the factors that can trigger exacerbations while engaging in military service, such as chemical and environmental exposures both abroad and domestically.15,16 Additionally, medication adherence is often challenging among the veteran population, particularly with more involved therapy, such as inhaler use.17 Such factors contribute to asthma exacerbations, with 2.9% of veterans reporting at least 1 asthma exacerbation in the past 12 months.14
Over the past several years, the development and use of biologic agents have transformed the management of severe asthma.8 Before the development of biologic agents for severe asthma, treatment options for patients were limited. While OCS are frequently used for asthma exacerbations, they are associated with a multiplicity of undesirable adverse effects, including weight gain, mood lability, gastrointestinal upset, hyperglycemia, risk of bone fractures, and hypertension.18-20 The regular use of OCS are particularly problematic among other medical comorbidities commonly affecting the veteran population, such as diabetes and hypertension.21-22
The WDCVAMC severe allergy clinic used 3 biologic agents: omalizumab (anti-IgE), benralizumab (anti-IL-5), and agent dupilumab (anti-IL-4). These medications have shown significant improvements in quality of life, reduction in asthma exacerbations and hospitalizations, and decreased use of OCS.8,9 While research has firmly established the medical benefits of the use of biologic agents in severe asthma, several barriers exist in implementing widespread use.11,12
In Gelhorn and colleagues’ study examining both physician and patient challenges in the use of biologics for severe asthma, scheduling, administrative time, and insurance costs were found to be major barriers to the use of these medications.12 Patients expressed a preference for the administration of these medications in a specialist’s office but cited long wait times and scheduling difficulties as barriers. One of the most notable challenges from the physician perspective was the difficulty in obtaining reimbursement from insurance companies, requiring them to devote significant portions of time to prior authorizations and documentation.12
This article examines a dual specialty clinic that focuses on the treatment of severe asthma with biologic agents. This model is unique for several reasons. First, given the US Department of Veterans Affairs (VA) health care model, the health care practitioners (HCPs) in this clinic can avoid much of the administrative burden of obtaining reimbursement or working with insurance companies. Additionally, by dedicating specific days to the severe asthma clinic, patients do not experience long wait times to see both an allergist and pulmonologist. By seeing both clinicians, concurrent allergic and pulmonary issues can be addressed in the same visit, rather than delaying treatment by waiting on 2 specialist appointments.
Severe Asthma Clinic
The severe asthma clinic was started in September 2017 by a pulmonologist and an allergist at WDCVAMC. After experiencing substantial delays with the initiation of biologics for their patients and multiple referrals between their clinics, these physicians wanted to start a dually staffed asthma clinic to specifically focus on evaluating and treating severe asthma. A dedicated severe asthma clinic allowed the allergist and pulmonologist to streamline resources and collaborate to advocate for patients with the pharmacy section. Additionally, patients can benefit from the perspective of both specialists, as both the pulmonologist and allergist evaluate each patient and discuss the next steps of management.
This clinic is composed of 4 registered nurses, an allergist, and a pulmonologist. Clinic is held twice monthly through both telemedicine and in-office visits. The VA has strict guidelines for the use of certain biologics, including blood eosinophil count > 150 cells/µL, failure of traditional therapy, and frequent use of OCS. Additionally, to ensure these biologic agents are prescribed to patients that will benefit from them, the patients enrolled in this clinic are already on maximum therapy for their asthma, meaning all other therapeutic options (inhalers and oral medications) are being used. The clinic services all patients with severe asthma, not just patients who are on biologic therapy. Often, patients are referred to the severe allergy clinic late in their disease course given a lack of familiarity with biologic agents from prescribers and both institutional and insurance barriers.
Before the COVID-19 pandemic, spirometry and fractional exhaled nitric oxide (FENO) tests were recorded at each visit. Initially during the pandemic, the clinic transitioned to primarily telemedicine visits due to patients’ hesitance to seek in-person care. More recently, the clinic has transitioned back to primarily office visits; patients are seen in clinic on average every 3 months. At each visit, the patient is seen by both the pulmonologist and allergist. Additionally, the nursing staff reviews inhaler adherence with patients, spacer use, documents, Asthma Control Test (ACT) scores, and schedules follow-up visits.
Every 4 to 8 weeks, patients receive biologics agent at the WDCVAMC infusion center depending on the agent. The infusion center also instructs patients how to handle self-administered medications, like benralizumab, if the patient expresses a preference for taking it at home. Omalizumab has a boxed warning for anaphylaxis, although the other biologics in this study have a low risk of anaphylaxis. All patients receiving omalizumab, benralizumab, and dupilumab were provided with epinephrine injection devices in case of an allergic reaction and were taught how to use them in the clinic.23,24
If patients continued to experience asthma exacerbations after the initiation of a biologic, a change in agent was considered after 4 to 6 months. Additionally, a complete blood count, respiratory allergy panel, and pulmonary function tests (PFTs) were completed.
Clinic Patients
Preliminary data were obtained from a retrospective chart review of 15 patients enrolled in the severe asthma clinic over 30 months. The inclusion criteria for chart review consisted of patients aged > 18 years receiving a biologic agent for > 3 months for the treatment of severe asthma. The outcomes examined included steroid use, emergency department (ED) visits, hospitalizations, FEV1, and ICU stays.
Seven patients used benralizumab, 6 used dupilumab, and 2 used omalizumab (Table).
There was a notable clinical improvement in these patients. Before starting a biologic agent, all the patients in this study were prescribed steroids at least once a year for an asthma exacerbation, with a mean of 4.2 steroid tapers per year.
The initiation of a biologic agent also resulted in fewer ED visits and hospitalizations. Two patients had an ED visit for an asthma exacerbation since starting a biologic agent and 1 patient had a hospital admission for an asthma exacerbation. No patients were hospitalized in the ICU after starting a biologic agent.
Discussion
The 15 patients in this initial data were referred to the severe asthma clinic by pulmonology, ear, nose, and throat (ENT), primary care, and a hospitalist during an in-patient stay. As the enrollment in our clinic grows, an increasing number of patients are referred from the allergy clinic as well. Patients in the severe asthma clinic also are referred by regional centers as news of the clinic is spread by word of mouth to surrounding VA facilities. As our clinic gains the capacity to serve more patients, we hope to contact WDCVAMC primary care, pulmonology, allergy, and ENT departments to raise awareness of the clinic.
Benralizumab and dupilumab were the most used agents in this preliminary data. This finding was largely due to the ability of patients to self-administer benralizumab, which was particularly beneficial during the COVID-19 pandemic. Of note, 5 patients in this study switched from another biologic agent to benralizumab due to the ability to self-administer. Three of 5 patients that required steroids after initiating benralizumab used fewer steroids than they had previously. This finding suggests benralizumab may be the preferred agent when travel time to health care is a challenge, reducing the need for frequent clinic visits and transportation.
This preliminary data supports previous studies that have demonstrated that biologic agents improve clinical outcomes by reducing asthma exacerbations, OCS use, hospitalizations, and ICU stays for patients on all 4 biologic agents. In addition to improving patient health through avoiding complications of prolonged OCS use and hospital stays, the decrease in ED visits and hospitalizations provides a substantial cost reduction to the health care system.
These findings highlight the strength of a unique model of a combined allergy/pulmonary clinic. Before this combined clinic model, both pulmonology and allergy clinics noted delays in the initiation of biologics for patients who were potential candidates. Impediments include referrals between each specialty for evaluation of concurrent pulmonary conditions or allergy testing, overlap in asthma management, and a delay in coordination with the pharmacy department to start biologic agents. A dedicated severe asthma clinic staffed by both an allergist and pulmonologist provides a convenient option for patients to be seen by both specialists, reducing the need for separate appointments with each specialty, transportation to those appointments, and clinical time. This is particularly beneficial in a clinic such as this model, as this clinic serves patients from 4 states and Washington, DC. An additional benefit of this model is trained staff who directly communicate with the pharmacy in the initiation of these agents, allocate time to educating patients in biologic use, and coordinate follow-up.
Limitations
There were several limitations to this report. First, the number of patients examined in this preliminary data set is small. Due to the COVID-19 pandemic, there was a limited ability to see patients in person, and patients were seen exclusively over telemedicine for several months. For this reason, collecting data such as patient surveys and laboratory work following the initiation of a biologic was a challenge. Additionally, during the height of COVID-19, WDCVAMC did not perform aerosolizing procedures, such as PFTs and FENOs; thus, peak flows were obtained instead. Examining metrics, such as FENOs and IgE levels, and expanding PFT data would provide additional insight into the impact of biologic agents on clinical outcomes. Patient survey data in the form of ACTs or satisfaction surveys would also yield important data examining the impact of this clinic design and biologic use on patient experience. As of December 2022, 114 patients are enrolled in the clinic. We are working to collect the above laboratory results and spirometry for these patients so that these results can be published with a more robust data set. Another limitation of the information presented is that it is a retrospective data analysis; the data collected was contingent upon documentation and the assumption that these patients were exclusively receiving care through the VA. For example, steroid use before and after initiation of biologic was taken from asthma clinic notes and the patient’s medication list. Therefore, there is a possibility that not all instances were accounted for if that patient sought care outside the VA or whether it was not documented in a follow-up note.
Conclusions
The model of a combined allergy/pulmonology clinic can be particularly efficacious in the treatment of severe asthma, as it reduces the need for multiple appointments with different specialties, reduces wait time before starting a biologic agent, and offers the perspective of 2 specialists. This kind of model could be an example to many clinics in the VA. With a rapid increase in telemedicine due to the COVID-19 pandemic, multiple physicians consulting simultaneously is becoming a more feasible possibility across multiple specialties. As the use of biologics becomes more widespread, a combined clinic design is an efficient and promising method to improve severe asthma management.
This preliminary data continue to support previous research that shows biologic agents have led to better clinical outcomes through the reduction of asthma exacerbations, hospitalizations, and improved PFTs. While this initial data set highlights the results for 15 patients, there are 86 patients currently enrolled in this clinic. We are collecting additional data to publish more comprehensive results.
Asthma affects more than 300 million people worldwide.1 While many of these cases can achieve control with standard therapy, 5% to 10% of these cases are classified as severe asthma, remaining poorly controlled despite treatment with inhaled corticosteroids (ICS) and long-acting β agonists (LABA).2 These patients also account for the majority of morbidity and mortality associated with the disease, with increased hospitalizations, intensive care unit (ICU) stays, detrimental adverse effects of oral corticosteroids (OCS), and lower quality of life.3-6 Additionally, the financial repercussions of severe asthma are notable; in the United States, the estimated cost of asthma management is $82 billion annually, with $3 billion accounting for asthma-related work/school absences.7
In the past several years, the use of anti-immunoglobulin E (IgE), anti-interleukin-4 (IL-4), and anti-IL-5 biologic agents for severe asthma has been shown to decrease asthma exacerbations, improve lung function, reduce corticosteroid use, and decrease hospitalizations, especially for type 2 helper T cell (TH2-high) asthma.8-10 However, clinicians have observed significant barriers to the implementation and widespread use of biologics, including insurance coverage, long wait times, follow-up, and limited access for lower income groups.11,12
This article describes a unique model for a severe asthma clinic located at the Washington DC Veterans Affairs Medical Center (WDCVAMC) that is dually staffed by an allergist and pulmonologist. This clinic uses biologic agents for patients with difficult-to-treat asthma, many of whom require repeated or prolonged steroid use, in addition to prolonged and recurrent hospitalizations for exacerbations. The objective of this clinic is to provide a standardized approach to the management of severe asthma with the perspective of both an allergist and pulmonologist, thereby reducing the need to schedule appointments with multiple specialties and reducing delays in initiating biologics. This article presents the preliminary findings of 30 months of severe asthma management with various biologic agents, examining the impact of these therapies on hospitalizations, asthma exacerbations, ICU stays, and OCS use. The findings of this study support the benefits of biologics and suggest that the use of these agents within a dually staffed clinic may be a particularly effective model through which to manage severe asthma.
Background
Asthma affects approximately 20 million adults in the United States.13 Veterans are a population particularly impacted by asthma. Between 2015 and 2018, 10.9% of all veterans reported being diagnosed with asthma and 5.1% stated that they currently have asthma, compared with 13.4% and 8.0% of nonveterans, respectively.14 Veterans are susceptible to many of the factors that can trigger exacerbations while engaging in military service, such as chemical and environmental exposures both abroad and domestically.15,16 Additionally, medication adherence is often challenging among the veteran population, particularly with more involved therapy, such as inhaler use.17 Such factors contribute to asthma exacerbations, with 2.9% of veterans reporting at least 1 asthma exacerbation in the past 12 months.14
Over the past several years, the development and use of biologic agents have transformed the management of severe asthma.8 Before the development of biologic agents for severe asthma, treatment options for patients were limited. While OCS are frequently used for asthma exacerbations, they are associated with a multiplicity of undesirable adverse effects, including weight gain, mood lability, gastrointestinal upset, hyperglycemia, risk of bone fractures, and hypertension.18-20 The regular use of OCS are particularly problematic among other medical comorbidities commonly affecting the veteran population, such as diabetes and hypertension.21-22
The WDCVAMC severe allergy clinic used 3 biologic agents: omalizumab (anti-IgE), benralizumab (anti-IL-5), and agent dupilumab (anti-IL-4). These medications have shown significant improvements in quality of life, reduction in asthma exacerbations and hospitalizations, and decreased use of OCS.8,9 While research has firmly established the medical benefits of the use of biologic agents in severe asthma, several barriers exist in implementing widespread use.11,12
In Gelhorn and colleagues’ study examining both physician and patient challenges in the use of biologics for severe asthma, scheduling, administrative time, and insurance costs were found to be major barriers to the use of these medications.12 Patients expressed a preference for the administration of these medications in a specialist’s office but cited long wait times and scheduling difficulties as barriers. One of the most notable challenges from the physician perspective was the difficulty in obtaining reimbursement from insurance companies, requiring them to devote significant portions of time to prior authorizations and documentation.12
This article examines a dual specialty clinic that focuses on the treatment of severe asthma with biologic agents. This model is unique for several reasons. First, given the US Department of Veterans Affairs (VA) health care model, the health care practitioners (HCPs) in this clinic can avoid much of the administrative burden of obtaining reimbursement or working with insurance companies. Additionally, by dedicating specific days to the severe asthma clinic, patients do not experience long wait times to see both an allergist and pulmonologist. By seeing both clinicians, concurrent allergic and pulmonary issues can be addressed in the same visit, rather than delaying treatment by waiting on 2 specialist appointments.
Severe Asthma Clinic
The severe asthma clinic was started in September 2017 by a pulmonologist and an allergist at WDCVAMC. After experiencing substantial delays with the initiation of biologics for their patients and multiple referrals between their clinics, these physicians wanted to start a dually staffed asthma clinic to specifically focus on evaluating and treating severe asthma. A dedicated severe asthma clinic allowed the allergist and pulmonologist to streamline resources and collaborate to advocate for patients with the pharmacy section. Additionally, patients can benefit from the perspective of both specialists, as both the pulmonologist and allergist evaluate each patient and discuss the next steps of management.
This clinic is composed of 4 registered nurses, an allergist, and a pulmonologist. Clinic is held twice monthly through both telemedicine and in-office visits. The VA has strict guidelines for the use of certain biologics, including blood eosinophil count > 150 cells/µL, failure of traditional therapy, and frequent use of OCS. Additionally, to ensure these biologic agents are prescribed to patients that will benefit from them, the patients enrolled in this clinic are already on maximum therapy for their asthma, meaning all other therapeutic options (inhalers and oral medications) are being used. The clinic services all patients with severe asthma, not just patients who are on biologic therapy. Often, patients are referred to the severe allergy clinic late in their disease course given a lack of familiarity with biologic agents from prescribers and both institutional and insurance barriers.
Before the COVID-19 pandemic, spirometry and fractional exhaled nitric oxide (FENO) tests were recorded at each visit. Initially during the pandemic, the clinic transitioned to primarily telemedicine visits due to patients’ hesitance to seek in-person care. More recently, the clinic has transitioned back to primarily office visits; patients are seen in clinic on average every 3 months. At each visit, the patient is seen by both the pulmonologist and allergist. Additionally, the nursing staff reviews inhaler adherence with patients, spacer use, documents, Asthma Control Test (ACT) scores, and schedules follow-up visits.
Every 4 to 8 weeks, patients receive biologics agent at the WDCVAMC infusion center depending on the agent. The infusion center also instructs patients how to handle self-administered medications, like benralizumab, if the patient expresses a preference for taking it at home. Omalizumab has a boxed warning for anaphylaxis, although the other biologics in this study have a low risk of anaphylaxis. All patients receiving omalizumab, benralizumab, and dupilumab were provided with epinephrine injection devices in case of an allergic reaction and were taught how to use them in the clinic.23,24
If patients continued to experience asthma exacerbations after the initiation of a biologic, a change in agent was considered after 4 to 6 months. Additionally, a complete blood count, respiratory allergy panel, and pulmonary function tests (PFTs) were completed.
Clinic Patients
Preliminary data were obtained from a retrospective chart review of 15 patients enrolled in the severe asthma clinic over 30 months. The inclusion criteria for chart review consisted of patients aged > 18 years receiving a biologic agent for > 3 months for the treatment of severe asthma. The outcomes examined included steroid use, emergency department (ED) visits, hospitalizations, FEV1, and ICU stays.
Seven patients used benralizumab, 6 used dupilumab, and 2 used omalizumab (Table).
There was a notable clinical improvement in these patients. Before starting a biologic agent, all the patients in this study were prescribed steroids at least once a year for an asthma exacerbation, with a mean of 4.2 steroid tapers per year.
The initiation of a biologic agent also resulted in fewer ED visits and hospitalizations. Two patients had an ED visit for an asthma exacerbation since starting a biologic agent and 1 patient had a hospital admission for an asthma exacerbation. No patients were hospitalized in the ICU after starting a biologic agent.
Discussion
The 15 patients in this initial data were referred to the severe asthma clinic by pulmonology, ear, nose, and throat (ENT), primary care, and a hospitalist during an in-patient stay. As the enrollment in our clinic grows, an increasing number of patients are referred from the allergy clinic as well. Patients in the severe asthma clinic also are referred by regional centers as news of the clinic is spread by word of mouth to surrounding VA facilities. As our clinic gains the capacity to serve more patients, we hope to contact WDCVAMC primary care, pulmonology, allergy, and ENT departments to raise awareness of the clinic.
Benralizumab and dupilumab were the most used agents in this preliminary data. This finding was largely due to the ability of patients to self-administer benralizumab, which was particularly beneficial during the COVID-19 pandemic. Of note, 5 patients in this study switched from another biologic agent to benralizumab due to the ability to self-administer. Three of 5 patients that required steroids after initiating benralizumab used fewer steroids than they had previously. This finding suggests benralizumab may be the preferred agent when travel time to health care is a challenge, reducing the need for frequent clinic visits and transportation.
This preliminary data supports previous studies that have demonstrated that biologic agents improve clinical outcomes by reducing asthma exacerbations, OCS use, hospitalizations, and ICU stays for patients on all 4 biologic agents. In addition to improving patient health through avoiding complications of prolonged OCS use and hospital stays, the decrease in ED visits and hospitalizations provides a substantial cost reduction to the health care system.
These findings highlight the strength of a unique model of a combined allergy/pulmonary clinic. Before this combined clinic model, both pulmonology and allergy clinics noted delays in the initiation of biologics for patients who were potential candidates. Impediments include referrals between each specialty for evaluation of concurrent pulmonary conditions or allergy testing, overlap in asthma management, and a delay in coordination with the pharmacy department to start biologic agents. A dedicated severe asthma clinic staffed by both an allergist and pulmonologist provides a convenient option for patients to be seen by both specialists, reducing the need for separate appointments with each specialty, transportation to those appointments, and clinical time. This is particularly beneficial in a clinic such as this model, as this clinic serves patients from 4 states and Washington, DC. An additional benefit of this model is trained staff who directly communicate with the pharmacy in the initiation of these agents, allocate time to educating patients in biologic use, and coordinate follow-up.
Limitations
There were several limitations to this report. First, the number of patients examined in this preliminary data set is small. Due to the COVID-19 pandemic, there was a limited ability to see patients in person, and patients were seen exclusively over telemedicine for several months. For this reason, collecting data such as patient surveys and laboratory work following the initiation of a biologic was a challenge. Additionally, during the height of COVID-19, WDCVAMC did not perform aerosolizing procedures, such as PFTs and FENOs; thus, peak flows were obtained instead. Examining metrics, such as FENOs and IgE levels, and expanding PFT data would provide additional insight into the impact of biologic agents on clinical outcomes. Patient survey data in the form of ACTs or satisfaction surveys would also yield important data examining the impact of this clinic design and biologic use on patient experience. As of December 2022, 114 patients are enrolled in the clinic. We are working to collect the above laboratory results and spirometry for these patients so that these results can be published with a more robust data set. Another limitation of the information presented is that it is a retrospective data analysis; the data collected was contingent upon documentation and the assumption that these patients were exclusively receiving care through the VA. For example, steroid use before and after initiation of biologic was taken from asthma clinic notes and the patient’s medication list. Therefore, there is a possibility that not all instances were accounted for if that patient sought care outside the VA or whether it was not documented in a follow-up note.
Conclusions
The model of a combined allergy/pulmonology clinic can be particularly efficacious in the treatment of severe asthma, as it reduces the need for multiple appointments with different specialties, reduces wait time before starting a biologic agent, and offers the perspective of 2 specialists. This kind of model could be an example to many clinics in the VA. With a rapid increase in telemedicine due to the COVID-19 pandemic, multiple physicians consulting simultaneously is becoming a more feasible possibility across multiple specialties. As the use of biologics becomes more widespread, a combined clinic design is an efficient and promising method to improve severe asthma management.
This preliminary data continue to support previous research that shows biologic agents have led to better clinical outcomes through the reduction of asthma exacerbations, hospitalizations, and improved PFTs. While this initial data set highlights the results for 15 patients, there are 86 patients currently enrolled in this clinic. We are collecting additional data to publish more comprehensive results.
1. Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol. 2015;16(1):45-56. doi:10.1038/ni.3049
2. Moore WC, Bleecker ER, Curran-Everett D, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. J Allergy Clin Immunol. 2007;119(2):405-413. doi:10.1016/j.jaci.2006.11.639
3. Barnes PJ, Jonsson B, Klim JB. The costs of asthma. Eur Respir J. 1996;9(4):636-642. doi:10.1183/09031936.96.09040636
4. Bourdin A, Charriot J, Boissin C, et al. Will the asthma revolution fostered by biologics also benefit adult ICU patients?. Allergy. 2021;76(8):2395-2406. doi:10.1111/all.14688
5. Lloyd A, Price D, Brown R. The impact of asthma exacerbations on health-related quality of life in moderate to severe asthma patients in the UK. Prim Care Respir J. 2007;16(1):22-27. doi:10.3132/pcrj.2007.00002
6. Eisner MD, Yelin EH, Katz PP, Lactao G, Iribarren C, Blanc PD. Risk factors for work disability in severe adult asthma. Am J Med. 2006;119(10):884-891. doi:10.1016/j.amjmed.2006.01.016
7. Nurmagambetov T, Kuwahara R, Garbe P. The Economic Burden of Asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018;15(3):348-356. doi:10.1513/AnnalsATS.201703-259OC
8. McGregor MC, Krings JG, Nair P, Castro M. Role of biologics in asthma. Am J Respir Crit Care Med. 2019;199(4):433-445. doi:10.1164/rccm.201810-1944CI
9. Bice JB, Leechawengwongs E, Montanaro A. Biologic targeted therapy in allergic asthma. Ann Allergy Asthma Immunol. 2014;112(2):108-115. doi:10.1016/j.anai.2013.12.013
10. Darveaux J, Busse WW. Biologics in asthma--the next step toward personalized treatment. J Allergy Clin Immunol Pract. 2015;3(2):152-161. doi:10.1016/j.jaip.2014.09.014
11. Inselman JW, Jeffery MM, Maddux JT, Shah ND, Rank MA. Trends and disparities in asthma biologic use in the United States. J Allergy Clin Immunol Pract. 2020;8(2):549-554.e1. doi:10.1016/j.jaip.2019.08.024
12. Gelhorn HL, Balantac Z, Ambrose CS, Chung YN, Stone B. Patient and physician preferences for attributes of biologic medications for severe asthma. Patient Prefer Adherence. 2019;13:1253-1268. Published 2019 Jul 25. doi:10.2147/PPA.S198953
13. Centers for Disease Control and Prevention, National Center for Environmental Health. 2019 National Health Interview Survey (NHIS) data. Accessed December 6, 2022. https://www.cdc.gov/asthma/nhis/2019/data.htm
14. Zelaya CE BP, Moy E. Crude and age-adjusted percent distribution of respondent-assessed health status among adults aged 20 and over, by veteran status and other selected characteristics: United States, 2015-2018. National Center for Health Statistic. Updated June 19, 2020. Accessed December 12, 2022. https://www.cdc.gov/nchs/nhis/veterans_health_statistics/tables.htm
15. Szema AM, Peters MC, Weissinger KM, Gagliano CA, Chen JJ. New-onset asthma among soldiers serving in Iraq and Afghanistan. Allergy Asthma Proc. 2010;31(5):67-71. doi:10.2500/aap.2010.31.3383
16. Yi SW, Hong JS, Ohrr H, Yi JJ. Agent Orange exposure and disease prevalence in Korean Vietnam veterans: the Korean veterans health study. Environ Res. 2014;133:56-65. doi:10.1016/j.envres.2014.04.027
17. Huetsch JC, Uman JE, Udris EM, Au DH. Predictors of adherence to inhaled medications among veterans with COPD. J Gen Intern Med. 2012;27(11):1506-1512. doi:10.1007/s11606-012-2130-5
18. Mundell L, Lindemann R, Douglas J. Monitoring long-term oral corticosteroids. BMJ Open Qual. 2017;6(2):e000209. Published 2017 Nov 8. doi:10.1136/bmjoq-2017-000209
19. Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C. Use of oral corticosteroids and risk of fractures. J Bone Miner Res. 2005;20(8):1487-1486. doi:10.1359/jbmr.2005.20.8.1486
20. Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81(10):1361-1367. doi:10.4065/81.10.1361
21. Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(suppl 2):B10-B21. doi:10.2337/diacare.27.suppl_2.b10
22. Acharya T, Tringali S, Singh M, Huang J. Resistant hypertension and associated comorbidities in a Veterans Affairs population. J Clin Hypertens (Greenwich). 2014;16(10):741-745. doi:10.1111/jch.12410
23. Dupixent (dupilumab). Prescribing information. Sanofi and Regeneron Pharmaceuticals; 2022. Accessed December 6, 2022. https://www.dupixenthcp.com/asthma/efficacy/safety-data
24. Li L, Wang Z, Cui L, Xu Y, Guan K, Zhao B. Anaphylactic risk related to omalizumab, benralizumab, reslizumab, mepolizumab, and dupilumab. Clin Transl Allergy. 2021;11(4):e12038. Published 2021 Jun 3. doi:10.1002/clt2.12038
1. Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol. 2015;16(1):45-56. doi:10.1038/ni.3049
2. Moore WC, Bleecker ER, Curran-Everett D, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. J Allergy Clin Immunol. 2007;119(2):405-413. doi:10.1016/j.jaci.2006.11.639
3. Barnes PJ, Jonsson B, Klim JB. The costs of asthma. Eur Respir J. 1996;9(4):636-642. doi:10.1183/09031936.96.09040636
4. Bourdin A, Charriot J, Boissin C, et al. Will the asthma revolution fostered by biologics also benefit adult ICU patients?. Allergy. 2021;76(8):2395-2406. doi:10.1111/all.14688
5. Lloyd A, Price D, Brown R. The impact of asthma exacerbations on health-related quality of life in moderate to severe asthma patients in the UK. Prim Care Respir J. 2007;16(1):22-27. doi:10.3132/pcrj.2007.00002
6. Eisner MD, Yelin EH, Katz PP, Lactao G, Iribarren C, Blanc PD. Risk factors for work disability in severe adult asthma. Am J Med. 2006;119(10):884-891. doi:10.1016/j.amjmed.2006.01.016
7. Nurmagambetov T, Kuwahara R, Garbe P. The Economic Burden of Asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018;15(3):348-356. doi:10.1513/AnnalsATS.201703-259OC
8. McGregor MC, Krings JG, Nair P, Castro M. Role of biologics in asthma. Am J Respir Crit Care Med. 2019;199(4):433-445. doi:10.1164/rccm.201810-1944CI
9. Bice JB, Leechawengwongs E, Montanaro A. Biologic targeted therapy in allergic asthma. Ann Allergy Asthma Immunol. 2014;112(2):108-115. doi:10.1016/j.anai.2013.12.013
10. Darveaux J, Busse WW. Biologics in asthma--the next step toward personalized treatment. J Allergy Clin Immunol Pract. 2015;3(2):152-161. doi:10.1016/j.jaip.2014.09.014
11. Inselman JW, Jeffery MM, Maddux JT, Shah ND, Rank MA. Trends and disparities in asthma biologic use in the United States. J Allergy Clin Immunol Pract. 2020;8(2):549-554.e1. doi:10.1016/j.jaip.2019.08.024
12. Gelhorn HL, Balantac Z, Ambrose CS, Chung YN, Stone B. Patient and physician preferences for attributes of biologic medications for severe asthma. Patient Prefer Adherence. 2019;13:1253-1268. Published 2019 Jul 25. doi:10.2147/PPA.S198953
13. Centers for Disease Control and Prevention, National Center for Environmental Health. 2019 National Health Interview Survey (NHIS) data. Accessed December 6, 2022. https://www.cdc.gov/asthma/nhis/2019/data.htm
14. Zelaya CE BP, Moy E. Crude and age-adjusted percent distribution of respondent-assessed health status among adults aged 20 and over, by veteran status and other selected characteristics: United States, 2015-2018. National Center for Health Statistic. Updated June 19, 2020. Accessed December 12, 2022. https://www.cdc.gov/nchs/nhis/veterans_health_statistics/tables.htm
15. Szema AM, Peters MC, Weissinger KM, Gagliano CA, Chen JJ. New-onset asthma among soldiers serving in Iraq and Afghanistan. Allergy Asthma Proc. 2010;31(5):67-71. doi:10.2500/aap.2010.31.3383
16. Yi SW, Hong JS, Ohrr H, Yi JJ. Agent Orange exposure and disease prevalence in Korean Vietnam veterans: the Korean veterans health study. Environ Res. 2014;133:56-65. doi:10.1016/j.envres.2014.04.027
17. Huetsch JC, Uman JE, Udris EM, Au DH. Predictors of adherence to inhaled medications among veterans with COPD. J Gen Intern Med. 2012;27(11):1506-1512. doi:10.1007/s11606-012-2130-5
18. Mundell L, Lindemann R, Douglas J. Monitoring long-term oral corticosteroids. BMJ Open Qual. 2017;6(2):e000209. Published 2017 Nov 8. doi:10.1136/bmjoq-2017-000209
19. Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C. Use of oral corticosteroids and risk of fractures. J Bone Miner Res. 2005;20(8):1487-1486. doi:10.1359/jbmr.2005.20.8.1486
20. Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81(10):1361-1367. doi:10.4065/81.10.1361
21. Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(suppl 2):B10-B21. doi:10.2337/diacare.27.suppl_2.b10
22. Acharya T, Tringali S, Singh M, Huang J. Resistant hypertension and associated comorbidities in a Veterans Affairs population. J Clin Hypertens (Greenwich). 2014;16(10):741-745. doi:10.1111/jch.12410
23. Dupixent (dupilumab). Prescribing information. Sanofi and Regeneron Pharmaceuticals; 2022. Accessed December 6, 2022. https://www.dupixenthcp.com/asthma/efficacy/safety-data
24. Li L, Wang Z, Cui L, Xu Y, Guan K, Zhao B. Anaphylactic risk related to omalizumab, benralizumab, reslizumab, mepolizumab, and dupilumab. Clin Transl Allergy. 2021;11(4):e12038. Published 2021 Jun 3. doi:10.1002/clt2.12038
February 2023 - ICYMI
Gastroenterology
October 2022
Cryer B et al. Bridging the Racial, Ethnic, and Gender Gap in Gastroenterology. Gastroenterology. 2022 Oct;163(4):800-5. doi: 10.1053/j.gastro.2022.08.037. PMID: 36137708.
Bajaj JS and Nagy LE. Natural History of Alcohol-Associated Liver Disease: Understanding the Changing Landscape of Pathophysiology and Patient Care. Gastroenterology. 2022 Oct;163(4):840-51. doi: 10.1053/j.gastro.2022.05.031. Epub 2022 May 19. PMID: 35598629; PMCID: PMC9509416.
November 2022
Grunvald E et al; AGA Clinical Guidelines Committee. AGA Clinical Practice Guideline on Pharmacological Interventions for Adults With Obesity. Gastroenterology. 2022 Nov;163(5):1198-225. doi: 10.1053/j.gastro.2022.08.045. Epub 2022 Oct 20. PMID: 36273831.
December 2022
Blackett JW et al. Comparison of Anorectal Manometry, Rectal Balloon Expulsion Test, and Defecography for Diagnosing Defecatory Disorders. Gastroenterology. 2022 Dec;163(6):1582-92.e2. doi: 10.1053/j.gastro.2022.08.034. Epub 2022 Aug 19. PMID: 35995074; PMCID: PMC9691522.
de Voogd F et al. Intestinal Ultrasound Is Accurate to Determine Endoscopic Response and Remission in Patients With Moderate to Severe Ulcerative Colitis: A Longitudinal Prospective Cohort Study. Gastroenterology. 2022 Dec;163(6):1569-81. doi: 10.1053/j.gastro.2022.08.038. Epub 2022 Aug 24. PMID: 36030056.
Clinical Gastroenterology and Hepatology
October 2022
Bhavsar-Burke I et al. How to Promote Professional Identity Development and Support Fellows-In-Training Through Teaching, Coaching, Mentorship, and Sponsorship. Clin Gastroenterol Hepatol. 2022 Oct;20(10):2166-9. doi: 10.1016/j.cgh.2022.05.043. Epub 2022 Aug 7. PMID: 35948073.
van Megen F et al. A Low FODMAP Diet Reduces Symptoms in Treated Celiac Patients With Ongoing Symptoms – A Randomized Controlled Trial. Clin Gastroenterol Hepatol. 2022 Oct;20(10):2258-66.e3. doi: 10.1016/j.cgh.2022.01.011. Epub 2022 Jan 17. PMID: 35051648.
November 2022
Sharzehi K et al. AGA Clinical Practice Update on Management of Subepithelial Lesions Encountered During Routine Endoscopy: Expert Review. Clin Gastroenterol Hepatol. 2022 Nov;20(11):2435-43.e4. doi: 10.1016/j.cgh.2022.05.054. Epub 2022 Jul 13. PMID: 35842117.
December 2022
Kardashian A et al. Food Insecurity is Associated With Mortality Among U.S. Adults With Nonalcoholic Fatty Liver Disease and Advanced Fibrosis. Clin Gastroenterol Hepatol. 2022 Dec;20(12):2790-9.e4. doi: 10.1016/j.cgh.2021.11.029. Epub 2021 Dec 16. PMID: 34958747.
Schuitenmaker JM et al. Sleep Positional Therapy for Nocturnal Gastroesophageal Reflux: A Double-Blind, Randomized, Sham-Controlled Trial. Clin Gastroenterol Hepatol. 2022 Dec;20(12):2753-62.e2. doi: 10.1016/j.cgh.2022.02.058. Epub 2022 Mar 14. PMID: 35301135.
Techniques and Innovations in Gastrointestinal Endoscopy
Azizian JM et al. Yield of Post-Acute Diverticulitis Colonoscopy for Ruling Out Colorectal Cancer. Tech Innov Gastrointest Endosc. 2022;24(3):254-61. doi: 10.1016/j.tige.2022.04.001. Epub 2022 Apr 18. PMID: 36540108; PMCID: PMC9762736.
Gastro Hep Advances
Kim RW et al. Timely Albumin Improves Survival in Patients With Cirrhosis on Diuretic Therapy Who Develop Acute Kidney Injury: Real-World Evidence in the United States. Gastro Hep Advances. 2023;2(2):252-60. doi: 10.1016/j.gastha.2022.10.008.
Gastroenterology
October 2022
Cryer B et al. Bridging the Racial, Ethnic, and Gender Gap in Gastroenterology. Gastroenterology. 2022 Oct;163(4):800-5. doi: 10.1053/j.gastro.2022.08.037. PMID: 36137708.
Bajaj JS and Nagy LE. Natural History of Alcohol-Associated Liver Disease: Understanding the Changing Landscape of Pathophysiology and Patient Care. Gastroenterology. 2022 Oct;163(4):840-51. doi: 10.1053/j.gastro.2022.05.031. Epub 2022 May 19. PMID: 35598629; PMCID: PMC9509416.
November 2022
Grunvald E et al; AGA Clinical Guidelines Committee. AGA Clinical Practice Guideline on Pharmacological Interventions for Adults With Obesity. Gastroenterology. 2022 Nov;163(5):1198-225. doi: 10.1053/j.gastro.2022.08.045. Epub 2022 Oct 20. PMID: 36273831.
December 2022
Blackett JW et al. Comparison of Anorectal Manometry, Rectal Balloon Expulsion Test, and Defecography for Diagnosing Defecatory Disorders. Gastroenterology. 2022 Dec;163(6):1582-92.e2. doi: 10.1053/j.gastro.2022.08.034. Epub 2022 Aug 19. PMID: 35995074; PMCID: PMC9691522.
de Voogd F et al. Intestinal Ultrasound Is Accurate to Determine Endoscopic Response and Remission in Patients With Moderate to Severe Ulcerative Colitis: A Longitudinal Prospective Cohort Study. Gastroenterology. 2022 Dec;163(6):1569-81. doi: 10.1053/j.gastro.2022.08.038. Epub 2022 Aug 24. PMID: 36030056.
Clinical Gastroenterology and Hepatology
October 2022
Bhavsar-Burke I et al. How to Promote Professional Identity Development and Support Fellows-In-Training Through Teaching, Coaching, Mentorship, and Sponsorship. Clin Gastroenterol Hepatol. 2022 Oct;20(10):2166-9. doi: 10.1016/j.cgh.2022.05.043. Epub 2022 Aug 7. PMID: 35948073.
van Megen F et al. A Low FODMAP Diet Reduces Symptoms in Treated Celiac Patients With Ongoing Symptoms – A Randomized Controlled Trial. Clin Gastroenterol Hepatol. 2022 Oct;20(10):2258-66.e3. doi: 10.1016/j.cgh.2022.01.011. Epub 2022 Jan 17. PMID: 35051648.
November 2022
Sharzehi K et al. AGA Clinical Practice Update on Management of Subepithelial Lesions Encountered During Routine Endoscopy: Expert Review. Clin Gastroenterol Hepatol. 2022 Nov;20(11):2435-43.e4. doi: 10.1016/j.cgh.2022.05.054. Epub 2022 Jul 13. PMID: 35842117.
December 2022
Kardashian A et al. Food Insecurity is Associated With Mortality Among U.S. Adults With Nonalcoholic Fatty Liver Disease and Advanced Fibrosis. Clin Gastroenterol Hepatol. 2022 Dec;20(12):2790-9.e4. doi: 10.1016/j.cgh.2021.11.029. Epub 2021 Dec 16. PMID: 34958747.
Schuitenmaker JM et al. Sleep Positional Therapy for Nocturnal Gastroesophageal Reflux: A Double-Blind, Randomized, Sham-Controlled Trial. Clin Gastroenterol Hepatol. 2022 Dec;20(12):2753-62.e2. doi: 10.1016/j.cgh.2022.02.058. Epub 2022 Mar 14. PMID: 35301135.
Techniques and Innovations in Gastrointestinal Endoscopy
Azizian JM et al. Yield of Post-Acute Diverticulitis Colonoscopy for Ruling Out Colorectal Cancer. Tech Innov Gastrointest Endosc. 2022;24(3):254-61. doi: 10.1016/j.tige.2022.04.001. Epub 2022 Apr 18. PMID: 36540108; PMCID: PMC9762736.
Gastro Hep Advances
Kim RW et al. Timely Albumin Improves Survival in Patients With Cirrhosis on Diuretic Therapy Who Develop Acute Kidney Injury: Real-World Evidence in the United States. Gastro Hep Advances. 2023;2(2):252-60. doi: 10.1016/j.gastha.2022.10.008.
Gastroenterology
October 2022
Cryer B et al. Bridging the Racial, Ethnic, and Gender Gap in Gastroenterology. Gastroenterology. 2022 Oct;163(4):800-5. doi: 10.1053/j.gastro.2022.08.037. PMID: 36137708.
Bajaj JS and Nagy LE. Natural History of Alcohol-Associated Liver Disease: Understanding the Changing Landscape of Pathophysiology and Patient Care. Gastroenterology. 2022 Oct;163(4):840-51. doi: 10.1053/j.gastro.2022.05.031. Epub 2022 May 19. PMID: 35598629; PMCID: PMC9509416.
November 2022
Grunvald E et al; AGA Clinical Guidelines Committee. AGA Clinical Practice Guideline on Pharmacological Interventions for Adults With Obesity. Gastroenterology. 2022 Nov;163(5):1198-225. doi: 10.1053/j.gastro.2022.08.045. Epub 2022 Oct 20. PMID: 36273831.
December 2022
Blackett JW et al. Comparison of Anorectal Manometry, Rectal Balloon Expulsion Test, and Defecography for Diagnosing Defecatory Disorders. Gastroenterology. 2022 Dec;163(6):1582-92.e2. doi: 10.1053/j.gastro.2022.08.034. Epub 2022 Aug 19. PMID: 35995074; PMCID: PMC9691522.
de Voogd F et al. Intestinal Ultrasound Is Accurate to Determine Endoscopic Response and Remission in Patients With Moderate to Severe Ulcerative Colitis: A Longitudinal Prospective Cohort Study. Gastroenterology. 2022 Dec;163(6):1569-81. doi: 10.1053/j.gastro.2022.08.038. Epub 2022 Aug 24. PMID: 36030056.
Clinical Gastroenterology and Hepatology
October 2022
Bhavsar-Burke I et al. How to Promote Professional Identity Development and Support Fellows-In-Training Through Teaching, Coaching, Mentorship, and Sponsorship. Clin Gastroenterol Hepatol. 2022 Oct;20(10):2166-9. doi: 10.1016/j.cgh.2022.05.043. Epub 2022 Aug 7. PMID: 35948073.
van Megen F et al. A Low FODMAP Diet Reduces Symptoms in Treated Celiac Patients With Ongoing Symptoms – A Randomized Controlled Trial. Clin Gastroenterol Hepatol. 2022 Oct;20(10):2258-66.e3. doi: 10.1016/j.cgh.2022.01.011. Epub 2022 Jan 17. PMID: 35051648.
November 2022
Sharzehi K et al. AGA Clinical Practice Update on Management of Subepithelial Lesions Encountered During Routine Endoscopy: Expert Review. Clin Gastroenterol Hepatol. 2022 Nov;20(11):2435-43.e4. doi: 10.1016/j.cgh.2022.05.054. Epub 2022 Jul 13. PMID: 35842117.
December 2022
Kardashian A et al. Food Insecurity is Associated With Mortality Among U.S. Adults With Nonalcoholic Fatty Liver Disease and Advanced Fibrosis. Clin Gastroenterol Hepatol. 2022 Dec;20(12):2790-9.e4. doi: 10.1016/j.cgh.2021.11.029. Epub 2021 Dec 16. PMID: 34958747.
Schuitenmaker JM et al. Sleep Positional Therapy for Nocturnal Gastroesophageal Reflux: A Double-Blind, Randomized, Sham-Controlled Trial. Clin Gastroenterol Hepatol. 2022 Dec;20(12):2753-62.e2. doi: 10.1016/j.cgh.2022.02.058. Epub 2022 Mar 14. PMID: 35301135.
Techniques and Innovations in Gastrointestinal Endoscopy
Azizian JM et al. Yield of Post-Acute Diverticulitis Colonoscopy for Ruling Out Colorectal Cancer. Tech Innov Gastrointest Endosc. 2022;24(3):254-61. doi: 10.1016/j.tige.2022.04.001. Epub 2022 Apr 18. PMID: 36540108; PMCID: PMC9762736.
Gastro Hep Advances
Kim RW et al. Timely Albumin Improves Survival in Patients With Cirrhosis on Diuretic Therapy Who Develop Acute Kidney Injury: Real-World Evidence in the United States. Gastro Hep Advances. 2023;2(2):252-60. doi: 10.1016/j.gastha.2022.10.008.