User login
AGA President Brings Forth “Message Of Inclusivity”
“I was always interested in medicine. From a relatively early age I thought that’s what I would be doing,” said Dr. Kim. When his father became disillusioned with his own career as a pathologist, he encouraged his son to look in other directions.
“In college I had the opportunity to study and learn broadly and I became interested in public policy and eventually majored in that discipline,” he said.
The mentorship of the late Uwe Reinhardt, a well-respected health economist at Princeton University, had a major impact on Dr. Kim during his senior year of college. Reinhardt told him that physicians are afforded a special position in society. “They have a moral responsibility to take the lead in terms of guiding and shaping healthcare. His message made a big impression upon me,” said Dr. Kim.
Ultimately, he decided to go into clinical medicine, but maintained his interest in healthcare policy. Experiences outside of the standard approach to medicine “helped me stay in the big picture of healthcare, to make a difference beyond just my individual patients. And that’s played a big part in keeping me involved in organized medicine,” said Dr. Kim, who began his term as AGA president in May 2025.
Dr. Kim is also a partner at South Denver Gastroenterology, a 33-provider, independent gastroenterology practice in Colorado. As the first physician in Colorado with fellowship training in endoscopic ultrasound, he introduced this service line into South Denver’s advanced endoscopy practice.
Dr. Kim has served in numerous roles with AGA, among them the co-director of the AGA Clinical Congress, the Partners in Quality program, and the Nurse Practitioner and Physician Assistant Course. He is a Digestive Disease Week® abstract reviewer, has served as AGA representative to the Accreditation Association for Ambulatory Health Care and to the Alliance of Specialty Medicine. He has also served on the AGA Governing Board as clinical private practice councilor and secretary treasurer.
He discussed the high points of his career in an interview, revealing his plans as AGA president for unifying the sectors of GI medicine and fostering GI innovation and technology.
As the new AGA president, what are your goals for the society?
Dr. Kim: I want to put out a message of inclusivity. I think what’s special about AGA is that we’re the society for all gastroenterologists. Among all the other GI organizations, I think we really have the biggest tent and we work to unite clinicians, educators, and researchers – all gastroenterologists, regardless of their individual practice situation. These days, there is a tendency toward tribalism. People are starting to gravitate toward limiting their interactions to others that are from the same backgrounds. But as gastroenterologists we have more that unites us than divides us. It’s only by working together that we can make things better for everyone.
I think the second point is that we’re on the cusp of some important transformations in gastroenterology. The screening colonoscopy model that has sustained our specialty for decades is rapidly evolving. In addition, there is an increasing ability for patients as consumers to direct their own care through advances in technology, such as virtual health platforms. We’re seeing this as patients increasingly adopt things like complementary and alternative medicine outside of the standard model of physician-directed healthcare. These are two important trends that gastroenterologists need to be aware of and learn how to manage and to adapt to. I think AGA’s role is to help guide that evolution and to give physicians the tools to be able to respond.
We want to focus on innovation and we want to focus on practical solutions.
In terms of fostering innovation in gastroenterology, we’re the first medical professional society to create an incubator for new technologies. Not only do we provide that resource to our members, but we’re also putting our money where our mouth is. Through venture capital initiatives such as our GI Opportunity Fund, we directly invest in companies that we’re helping to develop.
On the practice side, we have been engaging directly with payers to foster improved communication and address pain points on both sides. I think we’re the only medical society that’s taking this type of approach and moving away from the traditional adversarial approach to dealing with payers. Recently, we had a very productive discussion with UnitedHealthcare around some of their upcoming formulary changes for inflammatory bowel disease. We used that opportunity to highlight how nonmedical switching between existing therapies can adversely impact patients, as well as increasing burden of red tape for practices.
Your practice was one of the original groups that formed the Digestive Health Physicians Association (DPHA). What accomplishments of the association are you most proud of?
Dr. Kim: DHPA formed about 10 years ago as an advocacy organization to combat a specific perceived threat, which was the in-office ancillary exception. This is the legislative pathway that allows gastroenterologists to provide ancillary services within their practice. An example of this is pathology for endoscopic procedures, which is an incredible value to patients and improves quality of care. This was under a significant legislative threat at that time. As independent physicians, DHPA took the lead in advocating against eliminating that exception.
I think the larger accomplishment was it demonstrated that gastroenterologists, specifically independent community practice gastroenterologists, could come together successfully and advocate for issues that were of importance to our specialty. AGA and DHPA have worked very well together, collaborating on shared policy interests and have worked closely on both legislative as well as regulatory issues. We’ve sponsored joint meetings that we’ve programmed together and we’re looking forward to continuing a robust partnership.
You have introduced several new clinical practice and practice management models. Can you discuss the part-time partnership model and what it has achieved?
Dr. Kim: Like many practices, South Denver Gastroenterology historically required physician partners to work full time. This conflicted with our desire and our need to attract more women gastroenterologists into our practice. The process involved careful analysis of our direct and indirect expenses, but more importantly it required a negotiation and a meeting of the minds among our partners. A lot of this ultimately came down to trust. It helped a great deal that our practice has always had strong cohesiveness. That helped us to build that trust that partners would stay engaged in the practice even if they worked part time.
Our practice has also always prioritized work-life balance. We were able to come up with a formula that allows partners to work three days per week, retaining their partnership interest and their participation in practice decisions. They stay involved but are also financially sustainable for the practice. It’s been very successful. It’s been a big draw, not just for women, but it has allowed us to create a situation where women are fully one third of our partnership. It’s something we’re all extremely proud of.
How did you get involved in AGA?
Dr. Kim: One of the first projects I participated in was the Roadmap to the Future of GI Practice. This was an initiative to help prepare GI practices for value-based care. We did things like develop quality measure sets for GI conditions such as inflammatory bowel disease and hepatitis C. We published a bundled payment model for screening colonoscopies. We also created a model for obesity management by gastroenterologists. This was 15 years ago, and I think it was about 15 years ahead of its time! It’s interesting to see how many of these changes in GI practice that we envisioned are slowly coming to pass.
I saw that AGA was interested in me as a community-based clinician. They focused on trying to develop those practical tools to help me succeed. It’s one of the reasons I’ve stayed engaged.
What is your approach to patient communication and education?
Dr. Kim: There are two things that I always tell both my staff as well as young people who come to me asking for advice. I think the first and most important is that you should always strive to treat your patients the way that you would want your family treated. Of course, we’re not perfect, but when that doesn’t happen, look at your behavior, the way that you’re interacting, but also the way the system is treating your patients and try to improve things within your own practice. And then the other thing that I tell folks is try to spend more time listening to your patients than talking or speaking at them.
What do you think is the biggest misconception about GI?
Dr. Kim: We’re not just about colonoscopies! I went into GI not just because I enjoy performing procedures, but because our specialty covers such a broad spectrum of physiology and diseases. We also have the ability as gastroenterologists to develop long-term relationships with our patients. I’ve been in practice now more than 25 years, and the greatest satisfaction in my career doesn’t come from the endoscopy center, although I still enjoy performing procedures. It comes from the clinic; it comes from the patients whom I’ve known for decades, and the interaction and conversations that I can have with them, the ability to see their families, their parents, and now in some cases their kids or even their grandkids. It’s incredibly satisfying. It makes my job fun.
What advice would you give to aspiring medical students?
Dr. Kim: One of the things I would say is stay involved in organized medicine. As physicians, we are endowed with great trust. We also have a great responsibility to help shape our healthcare care system. If we work together, we really can make a difference, not just for our profession, but also for society at large and for the patients whom we serve.
I really hope that young people don’t lose their optimism. We hear a lot these days about how much negativity and pessimism there is about the future, especially among young people in our society. But I think it’s a great time to be in medicine. Advances in medical science have made huge strides in our ability to make real differences for our patients. And the pace of technology progress is only going to continue to accelerate. Sure, there are lots of shortcomings in the practice of medicine, but honestly, that’s always been the case. I have faith that as a profession, we are smart people, we’re committed people, and we will be successful in overcoming those challenges. That’s the message that I have for young folks.
Lightning Round
Coffee or tea?
Coffee, black
What’s one hobby you’d like to pick up?
Anything except pickleball
What’s your favorite season of the year?
Winter, I’m a skier
What’s your favorite way to spend a weekend?
Doing anything outside
If you could have dinner with any historical figure, who would it be?
Ben Franklin
What’s your go-to karaoke song?
You don’t want to hear me sing
What’s one thing on your bucket list?
Skiing in South America
What’s the best piece of advice you’ve ever received?
Follow your heart
“I was always interested in medicine. From a relatively early age I thought that’s what I would be doing,” said Dr. Kim. When his father became disillusioned with his own career as a pathologist, he encouraged his son to look in other directions.
“In college I had the opportunity to study and learn broadly and I became interested in public policy and eventually majored in that discipline,” he said.
The mentorship of the late Uwe Reinhardt, a well-respected health economist at Princeton University, had a major impact on Dr. Kim during his senior year of college. Reinhardt told him that physicians are afforded a special position in society. “They have a moral responsibility to take the lead in terms of guiding and shaping healthcare. His message made a big impression upon me,” said Dr. Kim.
Ultimately, he decided to go into clinical medicine, but maintained his interest in healthcare policy. Experiences outside of the standard approach to medicine “helped me stay in the big picture of healthcare, to make a difference beyond just my individual patients. And that’s played a big part in keeping me involved in organized medicine,” said Dr. Kim, who began his term as AGA president in May 2025.
Dr. Kim is also a partner at South Denver Gastroenterology, a 33-provider, independent gastroenterology practice in Colorado. As the first physician in Colorado with fellowship training in endoscopic ultrasound, he introduced this service line into South Denver’s advanced endoscopy practice.
Dr. Kim has served in numerous roles with AGA, among them the co-director of the AGA Clinical Congress, the Partners in Quality program, and the Nurse Practitioner and Physician Assistant Course. He is a Digestive Disease Week® abstract reviewer, has served as AGA representative to the Accreditation Association for Ambulatory Health Care and to the Alliance of Specialty Medicine. He has also served on the AGA Governing Board as clinical private practice councilor and secretary treasurer.
He discussed the high points of his career in an interview, revealing his plans as AGA president for unifying the sectors of GI medicine and fostering GI innovation and technology.
As the new AGA president, what are your goals for the society?
Dr. Kim: I want to put out a message of inclusivity. I think what’s special about AGA is that we’re the society for all gastroenterologists. Among all the other GI organizations, I think we really have the biggest tent and we work to unite clinicians, educators, and researchers – all gastroenterologists, regardless of their individual practice situation. These days, there is a tendency toward tribalism. People are starting to gravitate toward limiting their interactions to others that are from the same backgrounds. But as gastroenterologists we have more that unites us than divides us. It’s only by working together that we can make things better for everyone.
I think the second point is that we’re on the cusp of some important transformations in gastroenterology. The screening colonoscopy model that has sustained our specialty for decades is rapidly evolving. In addition, there is an increasing ability for patients as consumers to direct their own care through advances in technology, such as virtual health platforms. We’re seeing this as patients increasingly adopt things like complementary and alternative medicine outside of the standard model of physician-directed healthcare. These are two important trends that gastroenterologists need to be aware of and learn how to manage and to adapt to. I think AGA’s role is to help guide that evolution and to give physicians the tools to be able to respond.
We want to focus on innovation and we want to focus on practical solutions.
In terms of fostering innovation in gastroenterology, we’re the first medical professional society to create an incubator for new technologies. Not only do we provide that resource to our members, but we’re also putting our money where our mouth is. Through venture capital initiatives such as our GI Opportunity Fund, we directly invest in companies that we’re helping to develop.
On the practice side, we have been engaging directly with payers to foster improved communication and address pain points on both sides. I think we’re the only medical society that’s taking this type of approach and moving away from the traditional adversarial approach to dealing with payers. Recently, we had a very productive discussion with UnitedHealthcare around some of their upcoming formulary changes for inflammatory bowel disease. We used that opportunity to highlight how nonmedical switching between existing therapies can adversely impact patients, as well as increasing burden of red tape for practices.
Your practice was one of the original groups that formed the Digestive Health Physicians Association (DPHA). What accomplishments of the association are you most proud of?
Dr. Kim: DHPA formed about 10 years ago as an advocacy organization to combat a specific perceived threat, which was the in-office ancillary exception. This is the legislative pathway that allows gastroenterologists to provide ancillary services within their practice. An example of this is pathology for endoscopic procedures, which is an incredible value to patients and improves quality of care. This was under a significant legislative threat at that time. As independent physicians, DHPA took the lead in advocating against eliminating that exception.
I think the larger accomplishment was it demonstrated that gastroenterologists, specifically independent community practice gastroenterologists, could come together successfully and advocate for issues that were of importance to our specialty. AGA and DHPA have worked very well together, collaborating on shared policy interests and have worked closely on both legislative as well as regulatory issues. We’ve sponsored joint meetings that we’ve programmed together and we’re looking forward to continuing a robust partnership.
You have introduced several new clinical practice and practice management models. Can you discuss the part-time partnership model and what it has achieved?
Dr. Kim: Like many practices, South Denver Gastroenterology historically required physician partners to work full time. This conflicted with our desire and our need to attract more women gastroenterologists into our practice. The process involved careful analysis of our direct and indirect expenses, but more importantly it required a negotiation and a meeting of the minds among our partners. A lot of this ultimately came down to trust. It helped a great deal that our practice has always had strong cohesiveness. That helped us to build that trust that partners would stay engaged in the practice even if they worked part time.
Our practice has also always prioritized work-life balance. We were able to come up with a formula that allows partners to work three days per week, retaining their partnership interest and their participation in practice decisions. They stay involved but are also financially sustainable for the practice. It’s been very successful. It’s been a big draw, not just for women, but it has allowed us to create a situation where women are fully one third of our partnership. It’s something we’re all extremely proud of.
How did you get involved in AGA?
Dr. Kim: One of the first projects I participated in was the Roadmap to the Future of GI Practice. This was an initiative to help prepare GI practices for value-based care. We did things like develop quality measure sets for GI conditions such as inflammatory bowel disease and hepatitis C. We published a bundled payment model for screening colonoscopies. We also created a model for obesity management by gastroenterologists. This was 15 years ago, and I think it was about 15 years ahead of its time! It’s interesting to see how many of these changes in GI practice that we envisioned are slowly coming to pass.
I saw that AGA was interested in me as a community-based clinician. They focused on trying to develop those practical tools to help me succeed. It’s one of the reasons I’ve stayed engaged.
What is your approach to patient communication and education?
Dr. Kim: There are two things that I always tell both my staff as well as young people who come to me asking for advice. I think the first and most important is that you should always strive to treat your patients the way that you would want your family treated. Of course, we’re not perfect, but when that doesn’t happen, look at your behavior, the way that you’re interacting, but also the way the system is treating your patients and try to improve things within your own practice. And then the other thing that I tell folks is try to spend more time listening to your patients than talking or speaking at them.
What do you think is the biggest misconception about GI?
Dr. Kim: We’re not just about colonoscopies! I went into GI not just because I enjoy performing procedures, but because our specialty covers such a broad spectrum of physiology and diseases. We also have the ability as gastroenterologists to develop long-term relationships with our patients. I’ve been in practice now more than 25 years, and the greatest satisfaction in my career doesn’t come from the endoscopy center, although I still enjoy performing procedures. It comes from the clinic; it comes from the patients whom I’ve known for decades, and the interaction and conversations that I can have with them, the ability to see their families, their parents, and now in some cases their kids or even their grandkids. It’s incredibly satisfying. It makes my job fun.
What advice would you give to aspiring medical students?
Dr. Kim: One of the things I would say is stay involved in organized medicine. As physicians, we are endowed with great trust. We also have a great responsibility to help shape our healthcare care system. If we work together, we really can make a difference, not just for our profession, but also for society at large and for the patients whom we serve.
I really hope that young people don’t lose their optimism. We hear a lot these days about how much negativity and pessimism there is about the future, especially among young people in our society. But I think it’s a great time to be in medicine. Advances in medical science have made huge strides in our ability to make real differences for our patients. And the pace of technology progress is only going to continue to accelerate. Sure, there are lots of shortcomings in the practice of medicine, but honestly, that’s always been the case. I have faith that as a profession, we are smart people, we’re committed people, and we will be successful in overcoming those challenges. That’s the message that I have for young folks.
Lightning Round
Coffee or tea?
Coffee, black
What’s one hobby you’d like to pick up?
Anything except pickleball
What’s your favorite season of the year?
Winter, I’m a skier
What’s your favorite way to spend a weekend?
Doing anything outside
If you could have dinner with any historical figure, who would it be?
Ben Franklin
What’s your go-to karaoke song?
You don’t want to hear me sing
What’s one thing on your bucket list?
Skiing in South America
What’s the best piece of advice you’ve ever received?
Follow your heart
“I was always interested in medicine. From a relatively early age I thought that’s what I would be doing,” said Dr. Kim. When his father became disillusioned with his own career as a pathologist, he encouraged his son to look in other directions.
“In college I had the opportunity to study and learn broadly and I became interested in public policy and eventually majored in that discipline,” he said.
The mentorship of the late Uwe Reinhardt, a well-respected health economist at Princeton University, had a major impact on Dr. Kim during his senior year of college. Reinhardt told him that physicians are afforded a special position in society. “They have a moral responsibility to take the lead in terms of guiding and shaping healthcare. His message made a big impression upon me,” said Dr. Kim.
Ultimately, he decided to go into clinical medicine, but maintained his interest in healthcare policy. Experiences outside of the standard approach to medicine “helped me stay in the big picture of healthcare, to make a difference beyond just my individual patients. And that’s played a big part in keeping me involved in organized medicine,” said Dr. Kim, who began his term as AGA president in May 2025.
Dr. Kim is also a partner at South Denver Gastroenterology, a 33-provider, independent gastroenterology practice in Colorado. As the first physician in Colorado with fellowship training in endoscopic ultrasound, he introduced this service line into South Denver’s advanced endoscopy practice.
Dr. Kim has served in numerous roles with AGA, among them the co-director of the AGA Clinical Congress, the Partners in Quality program, and the Nurse Practitioner and Physician Assistant Course. He is a Digestive Disease Week® abstract reviewer, has served as AGA representative to the Accreditation Association for Ambulatory Health Care and to the Alliance of Specialty Medicine. He has also served on the AGA Governing Board as clinical private practice councilor and secretary treasurer.
He discussed the high points of his career in an interview, revealing his plans as AGA president for unifying the sectors of GI medicine and fostering GI innovation and technology.
As the new AGA president, what are your goals for the society?
Dr. Kim: I want to put out a message of inclusivity. I think what’s special about AGA is that we’re the society for all gastroenterologists. Among all the other GI organizations, I think we really have the biggest tent and we work to unite clinicians, educators, and researchers – all gastroenterologists, regardless of their individual practice situation. These days, there is a tendency toward tribalism. People are starting to gravitate toward limiting their interactions to others that are from the same backgrounds. But as gastroenterologists we have more that unites us than divides us. It’s only by working together that we can make things better for everyone.
I think the second point is that we’re on the cusp of some important transformations in gastroenterology. The screening colonoscopy model that has sustained our specialty for decades is rapidly evolving. In addition, there is an increasing ability for patients as consumers to direct their own care through advances in technology, such as virtual health platforms. We’re seeing this as patients increasingly adopt things like complementary and alternative medicine outside of the standard model of physician-directed healthcare. These are two important trends that gastroenterologists need to be aware of and learn how to manage and to adapt to. I think AGA’s role is to help guide that evolution and to give physicians the tools to be able to respond.
We want to focus on innovation and we want to focus on practical solutions.
In terms of fostering innovation in gastroenterology, we’re the first medical professional society to create an incubator for new technologies. Not only do we provide that resource to our members, but we’re also putting our money where our mouth is. Through venture capital initiatives such as our GI Opportunity Fund, we directly invest in companies that we’re helping to develop.
On the practice side, we have been engaging directly with payers to foster improved communication and address pain points on both sides. I think we’re the only medical society that’s taking this type of approach and moving away from the traditional adversarial approach to dealing with payers. Recently, we had a very productive discussion with UnitedHealthcare around some of their upcoming formulary changes for inflammatory bowel disease. We used that opportunity to highlight how nonmedical switching between existing therapies can adversely impact patients, as well as increasing burden of red tape for practices.
Your practice was one of the original groups that formed the Digestive Health Physicians Association (DPHA). What accomplishments of the association are you most proud of?
Dr. Kim: DHPA formed about 10 years ago as an advocacy organization to combat a specific perceived threat, which was the in-office ancillary exception. This is the legislative pathway that allows gastroenterologists to provide ancillary services within their practice. An example of this is pathology for endoscopic procedures, which is an incredible value to patients and improves quality of care. This was under a significant legislative threat at that time. As independent physicians, DHPA took the lead in advocating against eliminating that exception.
I think the larger accomplishment was it demonstrated that gastroenterologists, specifically independent community practice gastroenterologists, could come together successfully and advocate for issues that were of importance to our specialty. AGA and DHPA have worked very well together, collaborating on shared policy interests and have worked closely on both legislative as well as regulatory issues. We’ve sponsored joint meetings that we’ve programmed together and we’re looking forward to continuing a robust partnership.
You have introduced several new clinical practice and practice management models. Can you discuss the part-time partnership model and what it has achieved?
Dr. Kim: Like many practices, South Denver Gastroenterology historically required physician partners to work full time. This conflicted with our desire and our need to attract more women gastroenterologists into our practice. The process involved careful analysis of our direct and indirect expenses, but more importantly it required a negotiation and a meeting of the minds among our partners. A lot of this ultimately came down to trust. It helped a great deal that our practice has always had strong cohesiveness. That helped us to build that trust that partners would stay engaged in the practice even if they worked part time.
Our practice has also always prioritized work-life balance. We were able to come up with a formula that allows partners to work three days per week, retaining their partnership interest and their participation in practice decisions. They stay involved but are also financially sustainable for the practice. It’s been very successful. It’s been a big draw, not just for women, but it has allowed us to create a situation where women are fully one third of our partnership. It’s something we’re all extremely proud of.
How did you get involved in AGA?
Dr. Kim: One of the first projects I participated in was the Roadmap to the Future of GI Practice. This was an initiative to help prepare GI practices for value-based care. We did things like develop quality measure sets for GI conditions such as inflammatory bowel disease and hepatitis C. We published a bundled payment model for screening colonoscopies. We also created a model for obesity management by gastroenterologists. This was 15 years ago, and I think it was about 15 years ahead of its time! It’s interesting to see how many of these changes in GI practice that we envisioned are slowly coming to pass.
I saw that AGA was interested in me as a community-based clinician. They focused on trying to develop those practical tools to help me succeed. It’s one of the reasons I’ve stayed engaged.
What is your approach to patient communication and education?
Dr. Kim: There are two things that I always tell both my staff as well as young people who come to me asking for advice. I think the first and most important is that you should always strive to treat your patients the way that you would want your family treated. Of course, we’re not perfect, but when that doesn’t happen, look at your behavior, the way that you’re interacting, but also the way the system is treating your patients and try to improve things within your own practice. And then the other thing that I tell folks is try to spend more time listening to your patients than talking or speaking at them.
What do you think is the biggest misconception about GI?
Dr. Kim: We’re not just about colonoscopies! I went into GI not just because I enjoy performing procedures, but because our specialty covers such a broad spectrum of physiology and diseases. We also have the ability as gastroenterologists to develop long-term relationships with our patients. I’ve been in practice now more than 25 years, and the greatest satisfaction in my career doesn’t come from the endoscopy center, although I still enjoy performing procedures. It comes from the clinic; it comes from the patients whom I’ve known for decades, and the interaction and conversations that I can have with them, the ability to see their families, their parents, and now in some cases their kids or even their grandkids. It’s incredibly satisfying. It makes my job fun.
What advice would you give to aspiring medical students?
Dr. Kim: One of the things I would say is stay involved in organized medicine. As physicians, we are endowed with great trust. We also have a great responsibility to help shape our healthcare care system. If we work together, we really can make a difference, not just for our profession, but also for society at large and for the patients whom we serve.
I really hope that young people don’t lose their optimism. We hear a lot these days about how much negativity and pessimism there is about the future, especially among young people in our society. But I think it’s a great time to be in medicine. Advances in medical science have made huge strides in our ability to make real differences for our patients. And the pace of technology progress is only going to continue to accelerate. Sure, there are lots of shortcomings in the practice of medicine, but honestly, that’s always been the case. I have faith that as a profession, we are smart people, we’re committed people, and we will be successful in overcoming those challenges. That’s the message that I have for young folks.
Lightning Round
Coffee or tea?
Coffee, black
What’s one hobby you’d like to pick up?
Anything except pickleball
What’s your favorite season of the year?
Winter, I’m a skier
What’s your favorite way to spend a weekend?
Doing anything outside
If you could have dinner with any historical figure, who would it be?
Ben Franklin
What’s your go-to karaoke song?
You don’t want to hear me sing
What’s one thing on your bucket list?
Skiing in South America
What’s the best piece of advice you’ve ever received?
Follow your heart

Patient Navigators for Serious Illnesses Can Now Bill Under New Medicare Codes
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.

Special Report II: Tackling Burnout
Last month, we introduced the epidemic of burnout and the adverse consequences for both our vascular surgery patients and ourselves. Today we will outline a framework for addressing these issues. The foundation of this framework is informed by the social and neurosciences.
From the perspective of the social scientist: Christina Maslach, the originator of the widely used Maslach Burnout Inventory, theorized that burnout arises from a chronic mismatch between people and their work setting in some or all of the following domains: Workload (too much, wrong kind); control (lack of autonomy, or insufficient control over resources); reward (insufficient financial or social rewards commensurate with achievements); community (loss of positive connection with others); fairness (lack of perceived fairness, inequity of work, pay, or promotion); and values (conflict of personal and organizational values). The reality of practicing medicine in today’s business milieu – of achieving service efficiencies by meeting performance targets – brings many of these mismatches into sharp focus.
From the perspective of the neuroscientist: Recent advances, including functional MRI, have demonstrated that the human brain is hard wired for compassion. Compassion is the deep feeling that arises when confronted with another’s suffering, coupled with a strong desire to alleviate that suffering. There are at least two neural pathways: one activated during empathy, having us experience another’s pain; and the other activated during compassion, resulting in our sense of reward. Thus, burnout is thought to occur when you know what your patient needs but you are unable to deliver it. Compassionate medical care is purposeful work, which promotes a sense of reward and mitigates burnout.
Because burnout affects all caregivers (anyone who touches the patient), a successful program addressing workforce well-being must be comprehensive and organization wide, similar to successful patient safety, CPI [continuous process improvement] and LEAN [Six Sigma] initiatives.
There are no shortcuts. Creating a culture of compassionate, collaborative care requires an understanding of the interrelationships between the individual provider, the unit or team, and organizational leadership.
1) The individual provider: There is evidence to support the use of programs that build personal resilience. A recently published meta-analysis by West and colleagues concluded that while no specific physician burnout intervention has been shown to be better than other types of interventions, mindfulness, stress management, and small-group discussions can be effective approaches to reducing burnout scores. Strategies to build individual resilience, such as mindfulness and meditation, are easy to teach but place the burden for success on the individual. No amount of resilience can withstand an unsupportive or toxic workplace environment, so both individual and organizational strategies in combination are necessary.
2) The unit or team: Scheduling time for open and honest discussion of social and emotional issues that arise in caring for patients helps nourish caregiver to caregiver compassion. The Schwartz Center for Compassionate Healthcare is a national nonprofit leading the movement to bring compassion to every patient-caregiver interaction. More than 425 health care organization are Schwartz Center members and conduct Schwartz Rounds™ to bring doctors, nurses, and other caregivers together to discuss the human side of health care. (www.theschwartzcenter.org). Team member to team member support is essential for navigating the stressors of practice. With having lunch in front of your computer being the norm, and the disappearance of traditional spaces for colleagues to connect (for example, nurses’ lounge, physician dining rooms), the opportunity for caregivers to have a safe place to escape, a place to have their own humanity reaffirmed, a place to offer support to their peers, has been eliminated.
3) Organizational Leadership: Making compassion a core value, articulating it, and establishing metrics whereby it can be measured, is a good start. The barriers to a culture of compassion are related to our systems of care. There are burgeoning administrative and documentation tasks to be performed, and productivity expectations that turn our clinics and hospitals into assembly lines. No, we cannot expect the EMR [electronic medical records] to be eliminated, but workforce well-being cannot be sustainable in the context of inadequate resources. A culture of compassionate collaborative care requires programs and policies that are implemented by the organization itself. Examples of organization-wide initiatives that support workforce well-being and provider engagement include: screening for caregiver burnout, establishing policies for managing adverse events with an eye toward the second victim, and most importantly, supporting systems that preserve work control autonomy of physicians and nurses in clinical settings. The business sector has long recognized that workplace stress is a function of how demanding a person’s job is and how much control that person has over his or her responsibilities. The business community has also recognized that the experience of the worker (provider) drives the experience of the customer (patient). In a study of hospital compassionate practices and HCAHPS [the Hospital Consumer Assessment of Healthcare Providers and Systems], McClelland and Vogus reported that how well a hospital compassionately supports it employees and rewards compassionate acts is significantly and positively is associated with that hospital’s ratings and likelihood of patients recommending it.
How does the Society of Vascular Surgery, or any professional medical/nursing society for that matter, fit into this model?
We propose that the SVS find ways to empower their members to be agents for culture change within their own health care organizations. How might this be done:
- Teach organizational leadership skills, starting with the SVS Board of Directors, the presidential line, and the chairs of committees. Offer leadership courses at the Annual Meeting.
- Develop a community of caregivers committed to creating a compassionate collaborative culture. The SVS is a founding member of the Schwartz Center Healthcare Society Leadership Council, and you, as members of the SVS benefit from reduced registration at the Annual Compassion in Action Healthcare Conference, June 24-27, 2017 in Boston. (http://compassioninactionconference.org) This conference is designed to be highly experiential, using a hands-on “how to do it” model.
- The SVS should make improving the overall wellness of its members a specific goal and find specific metrics to monitor our progress towards this goal. Members can be provided with the tools to identify, monitor, and measure burnout and compassion. Each committee and council of the SVS can reexamine their objectives through the lens of reducing burnout and improving the wellness of vascular surgeons.
- Provide members with evidence-based programs that build personal resilience. This will not be a successful initiative unless our surgeons recognize and acknowledge the symptoms of burnout, and are willing to admit vulnerability. Without doing so, it is difficult to reach out for help.
- Redesign postgraduate resident and fellowship education. Standardizing clinical care may reduce variation and promote efficiency. However, when processes such as time-limited appointment scheduling, EMR templates, and protocols that drive physician-patient interactions are embedded in Resident and Fellowship education, the result may well be inflexibility in practice, reduced face time with patients, and interactions that lack compassion; all leading to burnout. Graduate Medical Education leaders must develop programs that support the learner’s ability to connect with patients and families, cultivate and role-model skills and behaviors that strengthen compassionate interactions, and strive to develop clinical practice models that increase Resident and Fellow work control autonomy.
The SVS should work proactively to optimize workload, fairness, and reward on a larger scale for its members as it relates to the EMR, reimbursement, and systems coverage. While we may be relatively small in size, as leaders, we are perfectly poised to address these larger, global issues. Perhaps working within the current system (i.e., PAC and APM task force) and considering innovative solutions at a national leadership scale, the SVS can direct real change!
Changing culture is not easy, nor quick, nor does it have an easy-to-follow blueprint. The first step is recognizing the need. The second is taking a leadership role. The third is thinking deeply about implementation.
*The authors extend their thanks and appreciation for the guidance, resources and support of Michael Goldberg, MD, scholar in residence, Schwartz Center for Compassionate Care, Boston and clinical professor of orthopedics at Seattle Children’s Hospital.
REFERENCES
1. J Managerial Psychol. (2007) 22:309-28
2. Annu Rev Neurosci. (2012) 35:1-23
3. Medicine. (2016) 44:583-5
4. J Health Organization Manag. (2015) 29:973-87
5. De Zulueta P Developing compassionate leadership in health care: an integrative review. J Healthcare Leadership. (2016) 8:1-10
6. Dolan ED, Morh D, Lempa M et al. Using a single item to measure burnout in primary care staff: A psychometry evaluation. J Gen Intern Med. (2015) 30:582-7
7. Karasek RA Job demands, job decision latitude, and mental strain: implications for job design. Administrative Sciences Quarterly (1979) 24: 285-308
8. Lee VS, Miller T, Daniels C, et al. Creating the exceptional patient experience in one academic health system. Acad Med. (2016) 91:338-44
9. Linzer M, Levine R, Meltzer D, et al. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. (2013) 29:18-20
10. Lown BA, Manning CF The Schwartz Center Rounds: Evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. (2010) 85:1073-81
11. Lown BA, Muncer SJ, Chadwick R Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Education and Counseling (2015) 98:1005-10
12. Lown BA, McIntosh S, Gaines ME, et. al. Integrating compassionate collaborative care (“the Triple C”) into health professional education to advance the triple aim of health care. Acad Med (2016) 91:1-7
13. Lown BA A social neuroscience-informed model for teaching and practicing compassion in health care. Medical Education (2016) 50: 332-342
14. Maslach C, Schaufeli WG, Leiter MP Job burnout. Annu Rev Psychol (2001) 52:397-422
15. McClelland LE, Vogus TJ Compassion practices and HCAHPS: Does rewarding and supporting workplace compassion influence patient perceptions? HSR: Health Serv Res. (2014) 49:1670-83
16. Shanafelt TD, Noseworthy JH Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. (2016) 6:1-18
17. Shanafelt TD, Dyrbye LN, West CP Addressing physician burnout: the way forward. JAMA (2017) 317:901-2
18. Singer T, Klimecki OM Empathy and compassion Curr Biol. (2014) 24: R875-8
19. West CP, Dyrbye LN, Satele DV et. al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. (2012) 27:1445-52
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to address and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272-81
21. Wuest TK, Goldberg MJ, Kelly JD Clinical faceoff: Physician burnout-Fact, fantasy, or the fourth component of the triple aim? Clin Orthop Relat Res. (2016) doi: 10.1007/5-11999-016-5193-5
Last month, we introduced the epidemic of burnout and the adverse consequences for both our vascular surgery patients and ourselves. Today we will outline a framework for addressing these issues. The foundation of this framework is informed by the social and neurosciences.
From the perspective of the social scientist: Christina Maslach, the originator of the widely used Maslach Burnout Inventory, theorized that burnout arises from a chronic mismatch between people and their work setting in some or all of the following domains: Workload (too much, wrong kind); control (lack of autonomy, or insufficient control over resources); reward (insufficient financial or social rewards commensurate with achievements); community (loss of positive connection with others); fairness (lack of perceived fairness, inequity of work, pay, or promotion); and values (conflict of personal and organizational values). The reality of practicing medicine in today’s business milieu – of achieving service efficiencies by meeting performance targets – brings many of these mismatches into sharp focus.
From the perspective of the neuroscientist: Recent advances, including functional MRI, have demonstrated that the human brain is hard wired for compassion. Compassion is the deep feeling that arises when confronted with another’s suffering, coupled with a strong desire to alleviate that suffering. There are at least two neural pathways: one activated during empathy, having us experience another’s pain; and the other activated during compassion, resulting in our sense of reward. Thus, burnout is thought to occur when you know what your patient needs but you are unable to deliver it. Compassionate medical care is purposeful work, which promotes a sense of reward and mitigates burnout.
Because burnout affects all caregivers (anyone who touches the patient), a successful program addressing workforce well-being must be comprehensive and organization wide, similar to successful patient safety, CPI [continuous process improvement] and LEAN [Six Sigma] initiatives.
There are no shortcuts. Creating a culture of compassionate, collaborative care requires an understanding of the interrelationships between the individual provider, the unit or team, and organizational leadership.
1) The individual provider: There is evidence to support the use of programs that build personal resilience. A recently published meta-analysis by West and colleagues concluded that while no specific physician burnout intervention has been shown to be better than other types of interventions, mindfulness, stress management, and small-group discussions can be effective approaches to reducing burnout scores. Strategies to build individual resilience, such as mindfulness and meditation, are easy to teach but place the burden for success on the individual. No amount of resilience can withstand an unsupportive or toxic workplace environment, so both individual and organizational strategies in combination are necessary.
2) The unit or team: Scheduling time for open and honest discussion of social and emotional issues that arise in caring for patients helps nourish caregiver to caregiver compassion. The Schwartz Center for Compassionate Healthcare is a national nonprofit leading the movement to bring compassion to every patient-caregiver interaction. More than 425 health care organization are Schwartz Center members and conduct Schwartz Rounds™ to bring doctors, nurses, and other caregivers together to discuss the human side of health care. (www.theschwartzcenter.org). Team member to team member support is essential for navigating the stressors of practice. With having lunch in front of your computer being the norm, and the disappearance of traditional spaces for colleagues to connect (for example, nurses’ lounge, physician dining rooms), the opportunity for caregivers to have a safe place to escape, a place to have their own humanity reaffirmed, a place to offer support to their peers, has been eliminated.
3) Organizational Leadership: Making compassion a core value, articulating it, and establishing metrics whereby it can be measured, is a good start. The barriers to a culture of compassion are related to our systems of care. There are burgeoning administrative and documentation tasks to be performed, and productivity expectations that turn our clinics and hospitals into assembly lines. No, we cannot expect the EMR [electronic medical records] to be eliminated, but workforce well-being cannot be sustainable in the context of inadequate resources. A culture of compassionate collaborative care requires programs and policies that are implemented by the organization itself. Examples of organization-wide initiatives that support workforce well-being and provider engagement include: screening for caregiver burnout, establishing policies for managing adverse events with an eye toward the second victim, and most importantly, supporting systems that preserve work control autonomy of physicians and nurses in clinical settings. The business sector has long recognized that workplace stress is a function of how demanding a person’s job is and how much control that person has over his or her responsibilities. The business community has also recognized that the experience of the worker (provider) drives the experience of the customer (patient). In a study of hospital compassionate practices and HCAHPS [the Hospital Consumer Assessment of Healthcare Providers and Systems], McClelland and Vogus reported that how well a hospital compassionately supports it employees and rewards compassionate acts is significantly and positively is associated with that hospital’s ratings and likelihood of patients recommending it.
How does the Society of Vascular Surgery, or any professional medical/nursing society for that matter, fit into this model?
We propose that the SVS find ways to empower their members to be agents for culture change within their own health care organizations. How might this be done:
- Teach organizational leadership skills, starting with the SVS Board of Directors, the presidential line, and the chairs of committees. Offer leadership courses at the Annual Meeting.
- Develop a community of caregivers committed to creating a compassionate collaborative culture. The SVS is a founding member of the Schwartz Center Healthcare Society Leadership Council, and you, as members of the SVS benefit from reduced registration at the Annual Compassion in Action Healthcare Conference, June 24-27, 2017 in Boston. (http://compassioninactionconference.org) This conference is designed to be highly experiential, using a hands-on “how to do it” model.
- The SVS should make improving the overall wellness of its members a specific goal and find specific metrics to monitor our progress towards this goal. Members can be provided with the tools to identify, monitor, and measure burnout and compassion. Each committee and council of the SVS can reexamine their objectives through the lens of reducing burnout and improving the wellness of vascular surgeons.
- Provide members with evidence-based programs that build personal resilience. This will not be a successful initiative unless our surgeons recognize and acknowledge the symptoms of burnout, and are willing to admit vulnerability. Without doing so, it is difficult to reach out for help.
- Redesign postgraduate resident and fellowship education. Standardizing clinical care may reduce variation and promote efficiency. However, when processes such as time-limited appointment scheduling, EMR templates, and protocols that drive physician-patient interactions are embedded in Resident and Fellowship education, the result may well be inflexibility in practice, reduced face time with patients, and interactions that lack compassion; all leading to burnout. Graduate Medical Education leaders must develop programs that support the learner’s ability to connect with patients and families, cultivate and role-model skills and behaviors that strengthen compassionate interactions, and strive to develop clinical practice models that increase Resident and Fellow work control autonomy.
The SVS should work proactively to optimize workload, fairness, and reward on a larger scale for its members as it relates to the EMR, reimbursement, and systems coverage. While we may be relatively small in size, as leaders, we are perfectly poised to address these larger, global issues. Perhaps working within the current system (i.e., PAC and APM task force) and considering innovative solutions at a national leadership scale, the SVS can direct real change!
Changing culture is not easy, nor quick, nor does it have an easy-to-follow blueprint. The first step is recognizing the need. The second is taking a leadership role. The third is thinking deeply about implementation.
*The authors extend their thanks and appreciation for the guidance, resources and support of Michael Goldberg, MD, scholar in residence, Schwartz Center for Compassionate Care, Boston and clinical professor of orthopedics at Seattle Children’s Hospital.
REFERENCES
1. J Managerial Psychol. (2007) 22:309-28
2. Annu Rev Neurosci. (2012) 35:1-23
3. Medicine. (2016) 44:583-5
4. J Health Organization Manag. (2015) 29:973-87
5. De Zulueta P Developing compassionate leadership in health care: an integrative review. J Healthcare Leadership. (2016) 8:1-10
6. Dolan ED, Morh D, Lempa M et al. Using a single item to measure burnout in primary care staff: A psychometry evaluation. J Gen Intern Med. (2015) 30:582-7
7. Karasek RA Job demands, job decision latitude, and mental strain: implications for job design. Administrative Sciences Quarterly (1979) 24: 285-308
8. Lee VS, Miller T, Daniels C, et al. Creating the exceptional patient experience in one academic health system. Acad Med. (2016) 91:338-44
9. Linzer M, Levine R, Meltzer D, et al. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. (2013) 29:18-20
10. Lown BA, Manning CF The Schwartz Center Rounds: Evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. (2010) 85:1073-81
11. Lown BA, Muncer SJ, Chadwick R Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Education and Counseling (2015) 98:1005-10
12. Lown BA, McIntosh S, Gaines ME, et. al. Integrating compassionate collaborative care (“the Triple C”) into health professional education to advance the triple aim of health care. Acad Med (2016) 91:1-7
13. Lown BA A social neuroscience-informed model for teaching and practicing compassion in health care. Medical Education (2016) 50: 332-342
14. Maslach C, Schaufeli WG, Leiter MP Job burnout. Annu Rev Psychol (2001) 52:397-422
15. McClelland LE, Vogus TJ Compassion practices and HCAHPS: Does rewarding and supporting workplace compassion influence patient perceptions? HSR: Health Serv Res. (2014) 49:1670-83
16. Shanafelt TD, Noseworthy JH Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. (2016) 6:1-18
17. Shanafelt TD, Dyrbye LN, West CP Addressing physician burnout: the way forward. JAMA (2017) 317:901-2
18. Singer T, Klimecki OM Empathy and compassion Curr Biol. (2014) 24: R875-8
19. West CP, Dyrbye LN, Satele DV et. al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. (2012) 27:1445-52
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to address and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272-81
21. Wuest TK, Goldberg MJ, Kelly JD Clinical faceoff: Physician burnout-Fact, fantasy, or the fourth component of the triple aim? Clin Orthop Relat Res. (2016) doi: 10.1007/5-11999-016-5193-5
Last month, we introduced the epidemic of burnout and the adverse consequences for both our vascular surgery patients and ourselves. Today we will outline a framework for addressing these issues. The foundation of this framework is informed by the social and neurosciences.
From the perspective of the social scientist: Christina Maslach, the originator of the widely used Maslach Burnout Inventory, theorized that burnout arises from a chronic mismatch between people and their work setting in some or all of the following domains: Workload (too much, wrong kind); control (lack of autonomy, or insufficient control over resources); reward (insufficient financial or social rewards commensurate with achievements); community (loss of positive connection with others); fairness (lack of perceived fairness, inequity of work, pay, or promotion); and values (conflict of personal and organizational values). The reality of practicing medicine in today’s business milieu – of achieving service efficiencies by meeting performance targets – brings many of these mismatches into sharp focus.
From the perspective of the neuroscientist: Recent advances, including functional MRI, have demonstrated that the human brain is hard wired for compassion. Compassion is the deep feeling that arises when confronted with another’s suffering, coupled with a strong desire to alleviate that suffering. There are at least two neural pathways: one activated during empathy, having us experience another’s pain; and the other activated during compassion, resulting in our sense of reward. Thus, burnout is thought to occur when you know what your patient needs but you are unable to deliver it. Compassionate medical care is purposeful work, which promotes a sense of reward and mitigates burnout.
Because burnout affects all caregivers (anyone who touches the patient), a successful program addressing workforce well-being must be comprehensive and organization wide, similar to successful patient safety, CPI [continuous process improvement] and LEAN [Six Sigma] initiatives.
There are no shortcuts. Creating a culture of compassionate, collaborative care requires an understanding of the interrelationships between the individual provider, the unit or team, and organizational leadership.
1) The individual provider: There is evidence to support the use of programs that build personal resilience. A recently published meta-analysis by West and colleagues concluded that while no specific physician burnout intervention has been shown to be better than other types of interventions, mindfulness, stress management, and small-group discussions can be effective approaches to reducing burnout scores. Strategies to build individual resilience, such as mindfulness and meditation, are easy to teach but place the burden for success on the individual. No amount of resilience can withstand an unsupportive or toxic workplace environment, so both individual and organizational strategies in combination are necessary.
2) The unit or team: Scheduling time for open and honest discussion of social and emotional issues that arise in caring for patients helps nourish caregiver to caregiver compassion. The Schwartz Center for Compassionate Healthcare is a national nonprofit leading the movement to bring compassion to every patient-caregiver interaction. More than 425 health care organization are Schwartz Center members and conduct Schwartz Rounds™ to bring doctors, nurses, and other caregivers together to discuss the human side of health care. (www.theschwartzcenter.org). Team member to team member support is essential for navigating the stressors of practice. With having lunch in front of your computer being the norm, and the disappearance of traditional spaces for colleagues to connect (for example, nurses’ lounge, physician dining rooms), the opportunity for caregivers to have a safe place to escape, a place to have their own humanity reaffirmed, a place to offer support to their peers, has been eliminated.
3) Organizational Leadership: Making compassion a core value, articulating it, and establishing metrics whereby it can be measured, is a good start. The barriers to a culture of compassion are related to our systems of care. There are burgeoning administrative and documentation tasks to be performed, and productivity expectations that turn our clinics and hospitals into assembly lines. No, we cannot expect the EMR [electronic medical records] to be eliminated, but workforce well-being cannot be sustainable in the context of inadequate resources. A culture of compassionate collaborative care requires programs and policies that are implemented by the organization itself. Examples of organization-wide initiatives that support workforce well-being and provider engagement include: screening for caregiver burnout, establishing policies for managing adverse events with an eye toward the second victim, and most importantly, supporting systems that preserve work control autonomy of physicians and nurses in clinical settings. The business sector has long recognized that workplace stress is a function of how demanding a person’s job is and how much control that person has over his or her responsibilities. The business community has also recognized that the experience of the worker (provider) drives the experience of the customer (patient). In a study of hospital compassionate practices and HCAHPS [the Hospital Consumer Assessment of Healthcare Providers and Systems], McClelland and Vogus reported that how well a hospital compassionately supports it employees and rewards compassionate acts is significantly and positively is associated with that hospital’s ratings and likelihood of patients recommending it.
How does the Society of Vascular Surgery, or any professional medical/nursing society for that matter, fit into this model?
We propose that the SVS find ways to empower their members to be agents for culture change within their own health care organizations. How might this be done:
- Teach organizational leadership skills, starting with the SVS Board of Directors, the presidential line, and the chairs of committees. Offer leadership courses at the Annual Meeting.
- Develop a community of caregivers committed to creating a compassionate collaborative culture. The SVS is a founding member of the Schwartz Center Healthcare Society Leadership Council, and you, as members of the SVS benefit from reduced registration at the Annual Compassion in Action Healthcare Conference, June 24-27, 2017 in Boston. (http://compassioninactionconference.org) This conference is designed to be highly experiential, using a hands-on “how to do it” model.
- The SVS should make improving the overall wellness of its members a specific goal and find specific metrics to monitor our progress towards this goal. Members can be provided with the tools to identify, monitor, and measure burnout and compassion. Each committee and council of the SVS can reexamine their objectives through the lens of reducing burnout and improving the wellness of vascular surgeons.
- Provide members with evidence-based programs that build personal resilience. This will not be a successful initiative unless our surgeons recognize and acknowledge the symptoms of burnout, and are willing to admit vulnerability. Without doing so, it is difficult to reach out for help.
- Redesign postgraduate resident and fellowship education. Standardizing clinical care may reduce variation and promote efficiency. However, when processes such as time-limited appointment scheduling, EMR templates, and protocols that drive physician-patient interactions are embedded in Resident and Fellowship education, the result may well be inflexibility in practice, reduced face time with patients, and interactions that lack compassion; all leading to burnout. Graduate Medical Education leaders must develop programs that support the learner’s ability to connect with patients and families, cultivate and role-model skills and behaviors that strengthen compassionate interactions, and strive to develop clinical practice models that increase Resident and Fellow work control autonomy.
The SVS should work proactively to optimize workload, fairness, and reward on a larger scale for its members as it relates to the EMR, reimbursement, and systems coverage. While we may be relatively small in size, as leaders, we are perfectly poised to address these larger, global issues. Perhaps working within the current system (i.e., PAC and APM task force) and considering innovative solutions at a national leadership scale, the SVS can direct real change!
Changing culture is not easy, nor quick, nor does it have an easy-to-follow blueprint. The first step is recognizing the need. The second is taking a leadership role. The third is thinking deeply about implementation.
*The authors extend their thanks and appreciation for the guidance, resources and support of Michael Goldberg, MD, scholar in residence, Schwartz Center for Compassionate Care, Boston and clinical professor of orthopedics at Seattle Children’s Hospital.
REFERENCES
1. J Managerial Psychol. (2007) 22:309-28
2. Annu Rev Neurosci. (2012) 35:1-23
3. Medicine. (2016) 44:583-5
4. J Health Organization Manag. (2015) 29:973-87
5. De Zulueta P Developing compassionate leadership in health care: an integrative review. J Healthcare Leadership. (2016) 8:1-10
6. Dolan ED, Morh D, Lempa M et al. Using a single item to measure burnout in primary care staff: A psychometry evaluation. J Gen Intern Med. (2015) 30:582-7
7. Karasek RA Job demands, job decision latitude, and mental strain: implications for job design. Administrative Sciences Quarterly (1979) 24: 285-308
8. Lee VS, Miller T, Daniels C, et al. Creating the exceptional patient experience in one academic health system. Acad Med. (2016) 91:338-44
9. Linzer M, Levine R, Meltzer D, et al. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. (2013) 29:18-20
10. Lown BA, Manning CF The Schwartz Center Rounds: Evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. (2010) 85:1073-81
11. Lown BA, Muncer SJ, Chadwick R Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Education and Counseling (2015) 98:1005-10
12. Lown BA, McIntosh S, Gaines ME, et. al. Integrating compassionate collaborative care (“the Triple C”) into health professional education to advance the triple aim of health care. Acad Med (2016) 91:1-7
13. Lown BA A social neuroscience-informed model for teaching and practicing compassion in health care. Medical Education (2016) 50: 332-342
14. Maslach C, Schaufeli WG, Leiter MP Job burnout. Annu Rev Psychol (2001) 52:397-422
15. McClelland LE, Vogus TJ Compassion practices and HCAHPS: Does rewarding and supporting workplace compassion influence patient perceptions? HSR: Health Serv Res. (2014) 49:1670-83
16. Shanafelt TD, Noseworthy JH Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. (2016) 6:1-18
17. Shanafelt TD, Dyrbye LN, West CP Addressing physician burnout: the way forward. JAMA (2017) 317:901-2
18. Singer T, Klimecki OM Empathy and compassion Curr Biol. (2014) 24: R875-8
19. West CP, Dyrbye LN, Satele DV et. al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. (2012) 27:1445-52
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to address and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272-81
21. Wuest TK, Goldberg MJ, Kelly JD Clinical faceoff: Physician burnout-Fact, fantasy, or the fourth component of the triple aim? Clin Orthop Relat Res. (2016) doi: 10.1007/5-11999-016-5193-5
Ready for post-acute care?
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”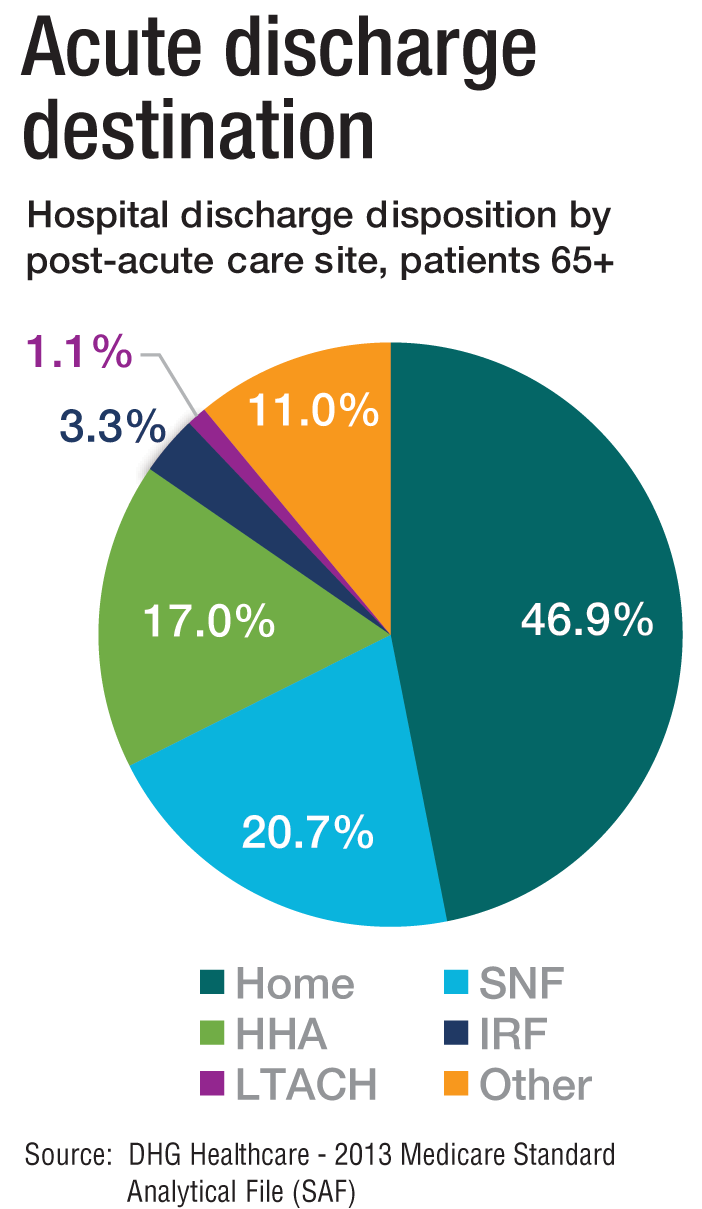
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”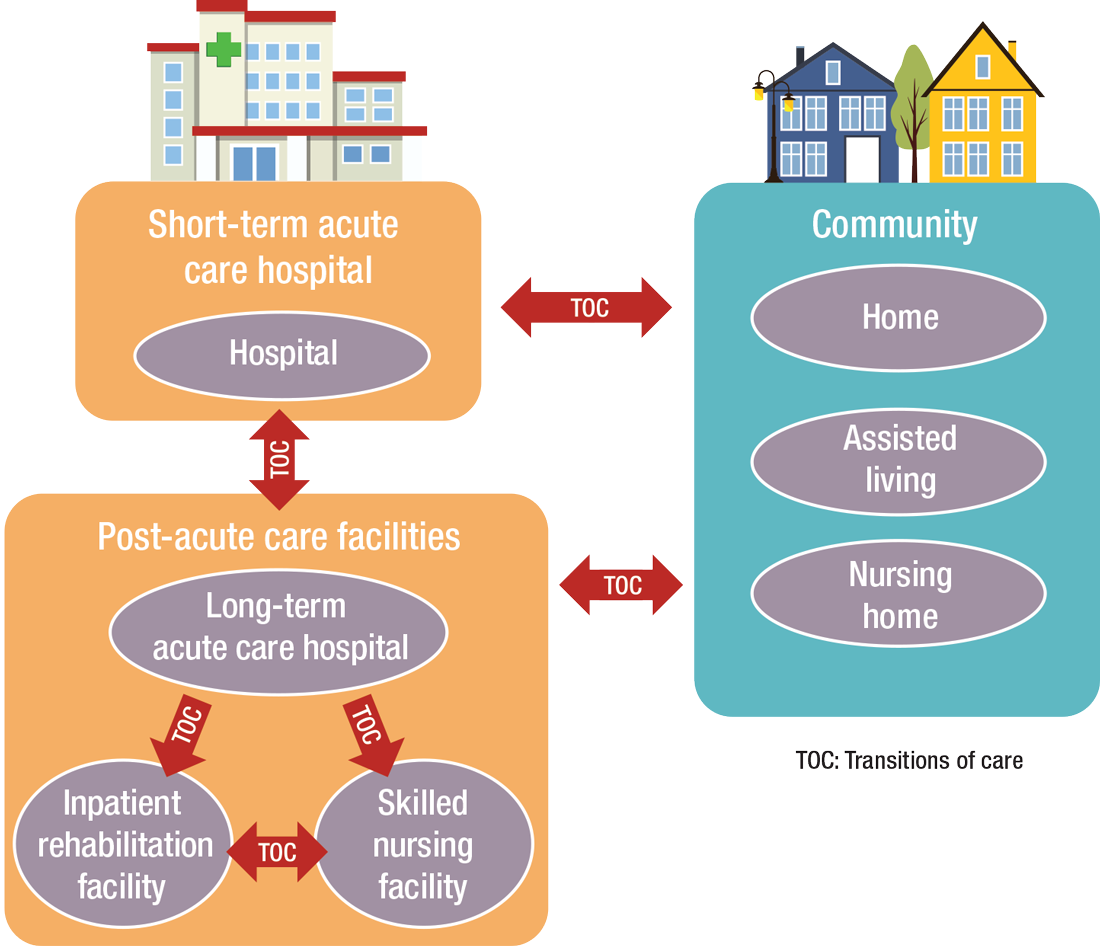
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”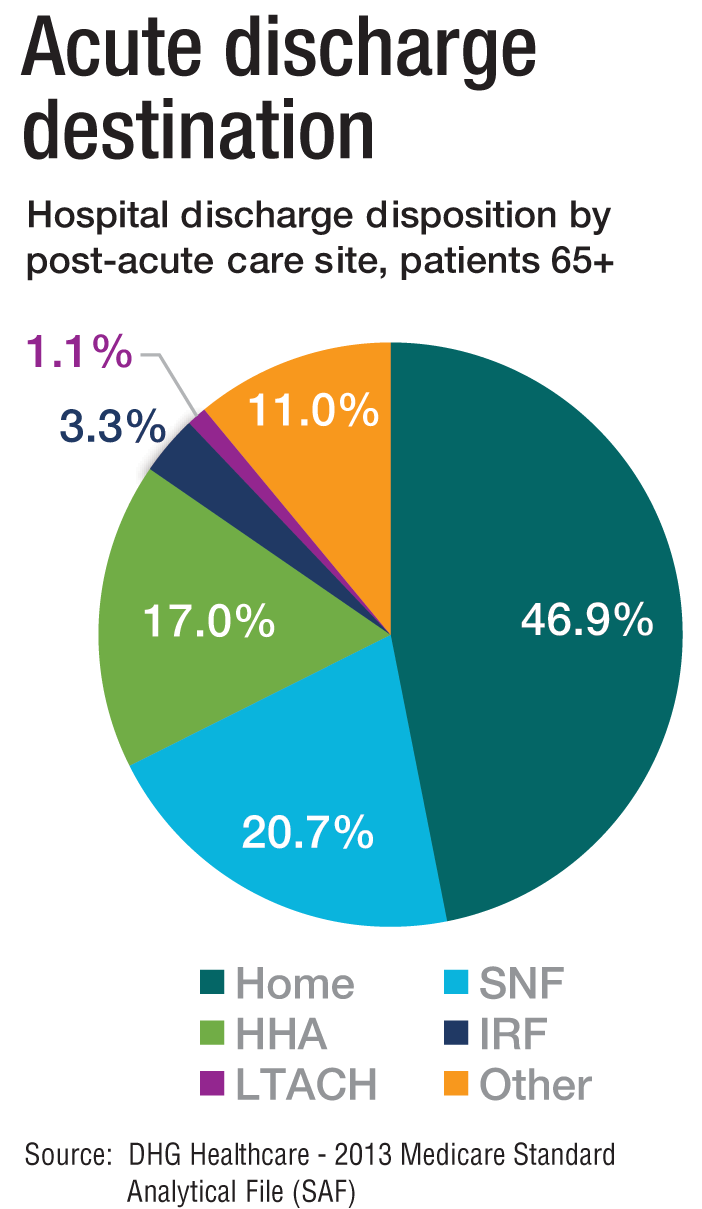
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”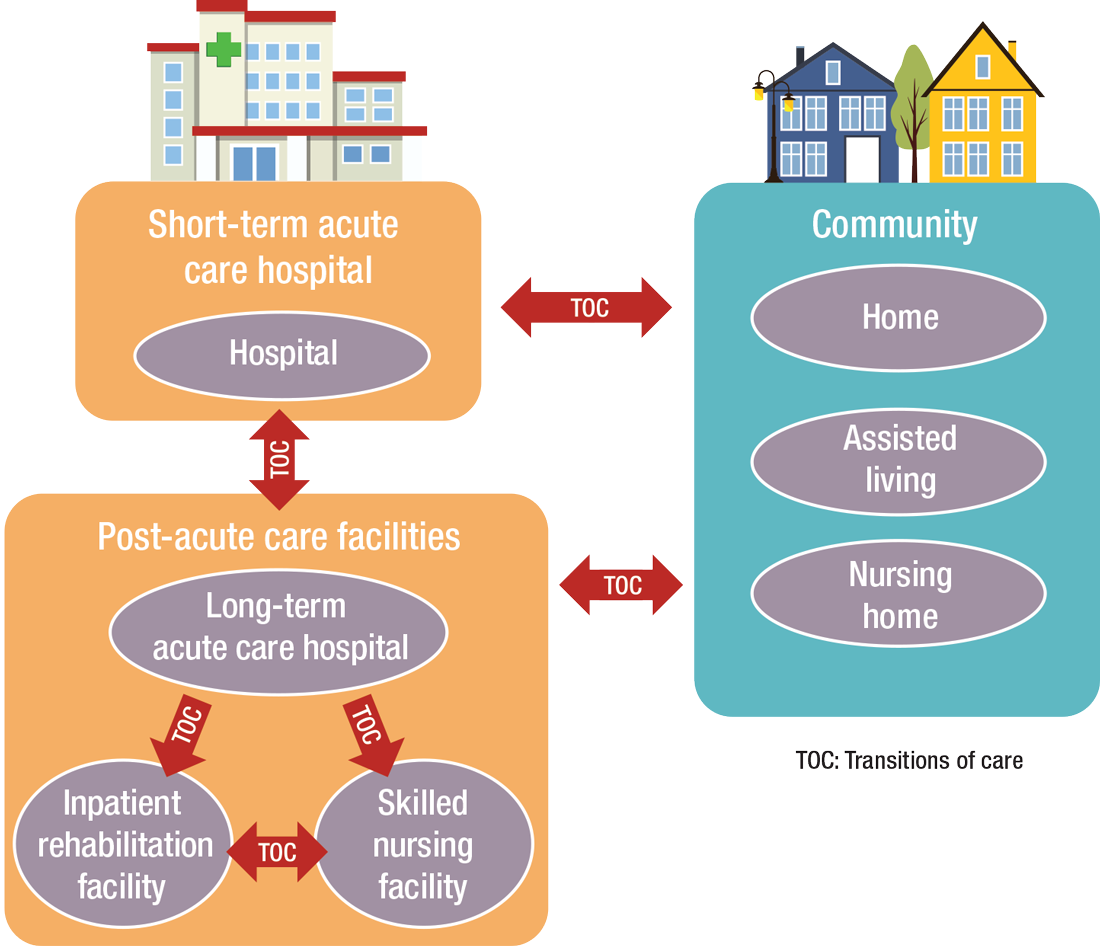
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”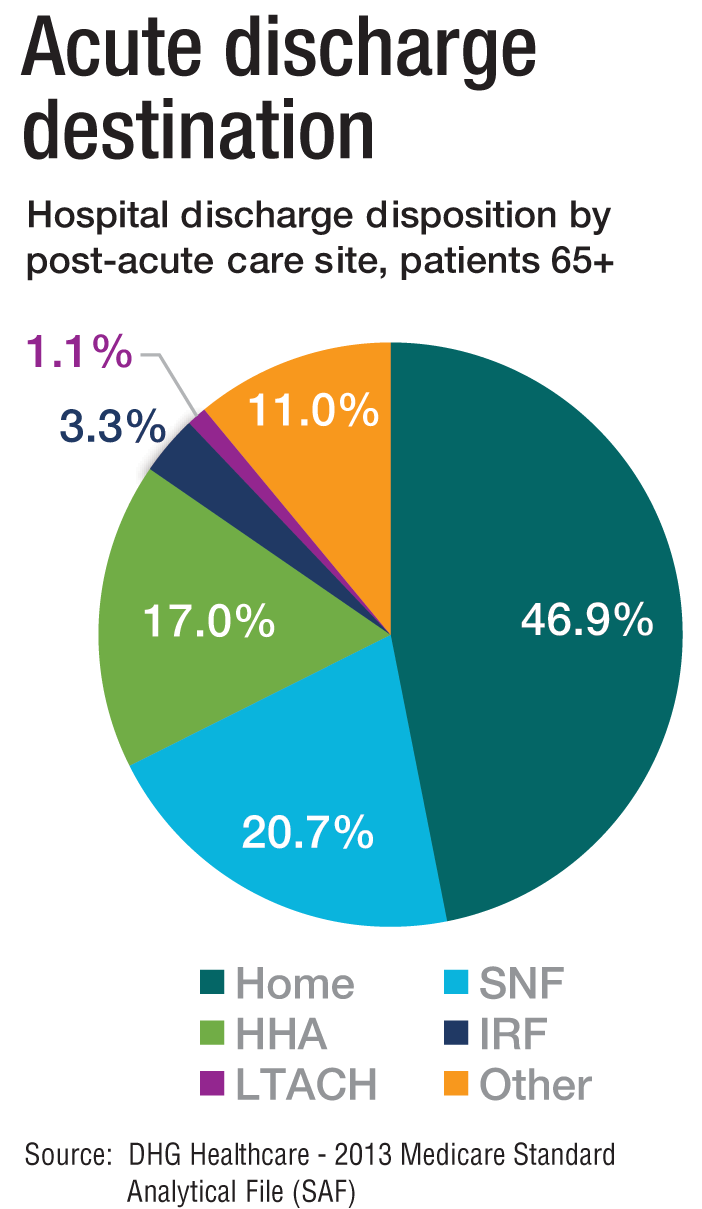
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”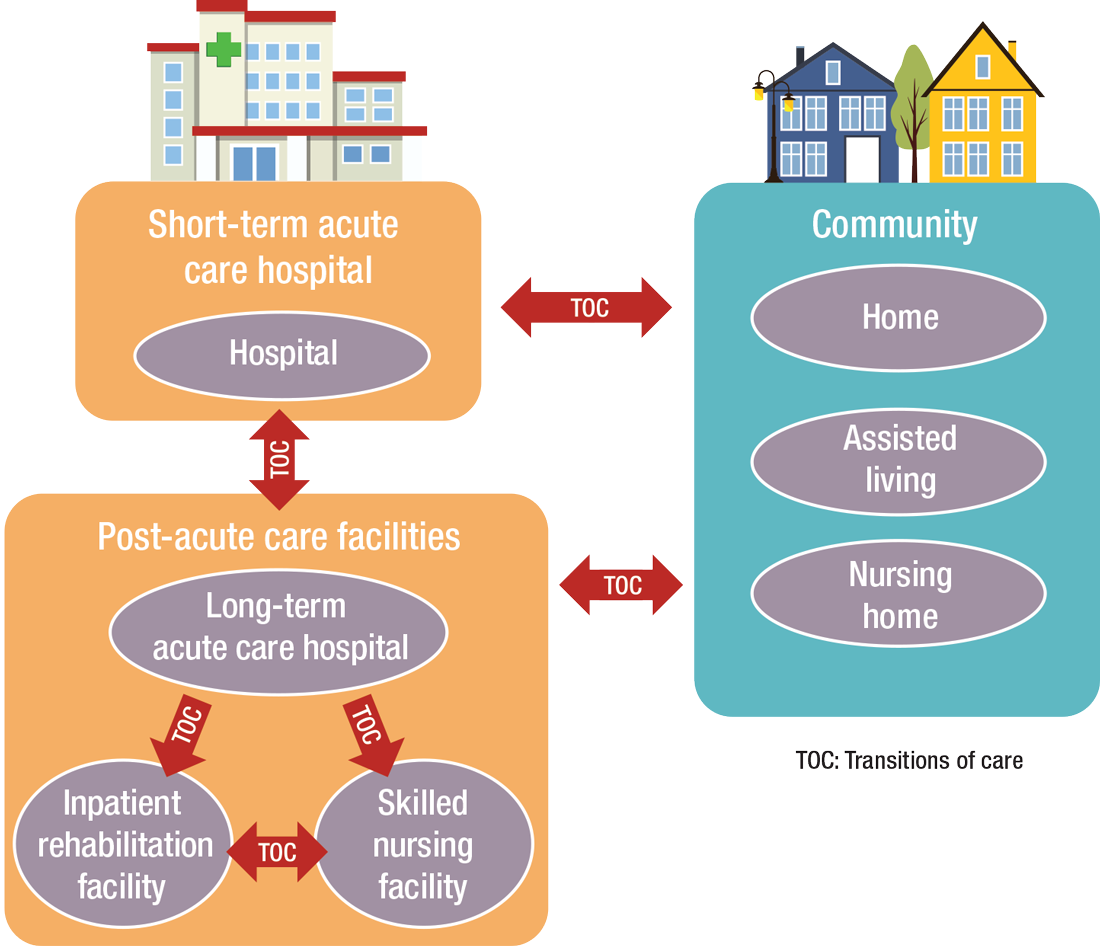
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
Office-Based Endoscopy Model Offers Way Forward for Outpatient GI
After decades of successful growth, the ambulatory surgery center (ASC) model may be turning a corner, opening up opportunity for office-based endoscopy models, according to a recent practice management editorial published in Clinical Gastroenterology and Hepatology.
Although office endoscopy has been an option, it hasn’t always felt practical or financially viable in the past. However, the paradigm appears to be shifting as ASC-based revenue streams show signs of stress and fail to keep pace with inflation. As healthcare regulatory and economic environments continue to change, gastroenterologists need a new model to support equity, efficiency, and growth in gastrointestinal (GI) care delivery, the authors wrote.
“Through the course of my 40-year career, I’ve been hit with a lot of changes related to regulations, insurance, and the market. You can’t stay entrenched in your old ways. You have to remain pivotable and come up with new strategic positions,” said Lawrence Kosinski, MD, AGAF, lead author and founder of SonarMD and VOCnomics.
During his private practice career, Kosinski built one of the largest GI practices in Illinois, which had seven ASCs and is now part of one of the largest GI groups in the country. Across 30 years of experience with ASCs, Kosinski has watched the reimbursement for professional services decline, as well as for added revenue streams such as pathology and anesthesia.
Looking for a better solution, Kosinski served on the governing board for the American Gastroenterological Association as the councilor for development and growth. During the past 3 years, he has spoken with GI practices and worked with a national anesthesia company — Ambulatory Anesthesia Care — to better understand the office endoscopy setting.
“In the ’90s, all I wanted was to have an ASC because that was in vogue,” he said. “But if you look critically at what has happened to the business of outpatient endoscopy in the past 25 years, you’ll see that professional fees haven’t kept up, and trying to replace that lost revenue is a losing battle.”
Considering Financial Shifts
Since 2001, professional reimbursement for colonoscopies has fallen by more than 40% while ASC revenue has risen, decreasing the percentage of revenue from professional fees (from 34% to 23%) and increasing the facility component (from 44% to 60%), Kosinski and colleagues wrote.
When looking at profit, compression of professional service fees appears even greater, especially with surging costs of anesthesia care due to high demand and provider shortages. Beyond that, about a third of ASCs are owned at least partially by national entities, as of 2024, leading to even lower realization of profit.
“The profit margins have really been crushed, so what is a GI doc to do? Go where there is opportunity,” Kosinski said. “The difference between hospitals and ASCs has been compressed, so what about the office?”
The proposed 2026 Medicare Physician Fee Schedule includes a 14% increase in reimbursement for office-based procedures, including endoscopy, as well as a 7% decrease for facility-based procedures.
In several states — such as Illinois, Oregon, Virginia, Washington, and Wisconsin — health plans are introducing programs to promote the transition of outpatient endoscopy to office settings rather than hospital-based or ASC-based settings due to costs, the authors wrote.
“The decision to start offering office-based endoscopy services was an easy one for our practice, as it provides a way for us to provide patients convenient, easy-to-access endoscopy that is high quality yet much more affordable than hospital-based settings,” said Neil Gupta, MD, managing partner at Midwest Digestive Health & Nutrition in Des Plaines, Illinois.
The practice has used office-based endoscopy for nearly 2 years, Gupta said, performing about 5000 GI endoscopy procedures per year.
“As we all try to find better ways to provide high-quality but affordable care for patients, office-based endoscopy is a great way to help achieve those goals,” he said. “Healthcare professionals and patients should all be asking, ‘What type of site am I getting my GI endoscopy scheduled at — hospital, surgery center, or physician’s office?’”
Regaining Autonomy and Time
Beyond the financial dynamics, , Kosinski and colleagues wrote.
Looking ahead, office-based models can also provide the agility and infrastructure to compete in value-based care models, they wrote. In turn, value-based models can create relevance and resilience in a continually changing healthcare environment.
Without the involvement of ASC managers, investors, or health system partners, physicians retain control of scheduling, clinical protocols, financial decisions, and operational workflows, the authors wrote. This could create better alignment with personal preferences, clinical judgment, and patient needs, they noted.
“GI physicians should no longer feel trapped in a hospital setting where they lack independence and influence over decision-making,” said Rock Rockett, PhD, owner and principal consultant of Rockett Healthcare Strategies, which partners with GI groups nationwide to help with development, accreditation, and payer contracting for office endoscopy.
“GI physicians should also no longer feel trapped in a ‘bad marriage’ with partners in an ASC or partners in a practice who create a difficult work environment,” he said. “The viability of office endoscopy allows them to strike out on their own or set up a new partnership on more equitable terms that are attractive for them.”
Patient safety and quality also appear to be similar or better in office-based settings, based on benchmarking data analyzed so far. Hospital transfers were lower, falls were similar, and patient experience was positive, the authors wrote.
At the same time, Kosinski and colleagues noted the difficulty in shifting to office-based models. Most practices have committed to ASCs, for instance, and adding an office-based room can be challenging. Otherwise, practices already use their available office space and don’t have extra rooms available. In that case, an office endoscopy suite may be best suited for expansion sites, allowing practices to grow into new service areas, they wrote.
“You can’t fight the market. You have to focus on what the market wants and needs,” Kosinski said. “To do that, you have to be able to pivot and change direction, looking for new ways to change your mission. This could be an option to do that.”
Kosinski, Gupta, and Rockett declared having no conflicts of interest other than their current employments.
A version of this article appeared on Medscape.com.
After decades of successful growth, the ambulatory surgery center (ASC) model may be turning a corner, opening up opportunity for office-based endoscopy models, according to a recent practice management editorial published in Clinical Gastroenterology and Hepatology.
Although office endoscopy has been an option, it hasn’t always felt practical or financially viable in the past. However, the paradigm appears to be shifting as ASC-based revenue streams show signs of stress and fail to keep pace with inflation. As healthcare regulatory and economic environments continue to change, gastroenterologists need a new model to support equity, efficiency, and growth in gastrointestinal (GI) care delivery, the authors wrote.
“Through the course of my 40-year career, I’ve been hit with a lot of changes related to regulations, insurance, and the market. You can’t stay entrenched in your old ways. You have to remain pivotable and come up with new strategic positions,” said Lawrence Kosinski, MD, AGAF, lead author and founder of SonarMD and VOCnomics.
During his private practice career, Kosinski built one of the largest GI practices in Illinois, which had seven ASCs and is now part of one of the largest GI groups in the country. Across 30 years of experience with ASCs, Kosinski has watched the reimbursement for professional services decline, as well as for added revenue streams such as pathology and anesthesia.
Looking for a better solution, Kosinski served on the governing board for the American Gastroenterological Association as the councilor for development and growth. During the past 3 years, he has spoken with GI practices and worked with a national anesthesia company — Ambulatory Anesthesia Care — to better understand the office endoscopy setting.
“In the ’90s, all I wanted was to have an ASC because that was in vogue,” he said. “But if you look critically at what has happened to the business of outpatient endoscopy in the past 25 years, you’ll see that professional fees haven’t kept up, and trying to replace that lost revenue is a losing battle.”
Considering Financial Shifts
Since 2001, professional reimbursement for colonoscopies has fallen by more than 40% while ASC revenue has risen, decreasing the percentage of revenue from professional fees (from 34% to 23%) and increasing the facility component (from 44% to 60%), Kosinski and colleagues wrote.
When looking at profit, compression of professional service fees appears even greater, especially with surging costs of anesthesia care due to high demand and provider shortages. Beyond that, about a third of ASCs are owned at least partially by national entities, as of 2024, leading to even lower realization of profit.
“The profit margins have really been crushed, so what is a GI doc to do? Go where there is opportunity,” Kosinski said. “The difference between hospitals and ASCs has been compressed, so what about the office?”
The proposed 2026 Medicare Physician Fee Schedule includes a 14% increase in reimbursement for office-based procedures, including endoscopy, as well as a 7% decrease for facility-based procedures.
In several states — such as Illinois, Oregon, Virginia, Washington, and Wisconsin — health plans are introducing programs to promote the transition of outpatient endoscopy to office settings rather than hospital-based or ASC-based settings due to costs, the authors wrote.
“The decision to start offering office-based endoscopy services was an easy one for our practice, as it provides a way for us to provide patients convenient, easy-to-access endoscopy that is high quality yet much more affordable than hospital-based settings,” said Neil Gupta, MD, managing partner at Midwest Digestive Health & Nutrition in Des Plaines, Illinois.
The practice has used office-based endoscopy for nearly 2 years, Gupta said, performing about 5000 GI endoscopy procedures per year.
“As we all try to find better ways to provide high-quality but affordable care for patients, office-based endoscopy is a great way to help achieve those goals,” he said. “Healthcare professionals and patients should all be asking, ‘What type of site am I getting my GI endoscopy scheduled at — hospital, surgery center, or physician’s office?’”
Regaining Autonomy and Time
Beyond the financial dynamics, , Kosinski and colleagues wrote.
Looking ahead, office-based models can also provide the agility and infrastructure to compete in value-based care models, they wrote. In turn, value-based models can create relevance and resilience in a continually changing healthcare environment.
Without the involvement of ASC managers, investors, or health system partners, physicians retain control of scheduling, clinical protocols, financial decisions, and operational workflows, the authors wrote. This could create better alignment with personal preferences, clinical judgment, and patient needs, they noted.
“GI physicians should no longer feel trapped in a hospital setting where they lack independence and influence over decision-making,” said Rock Rockett, PhD, owner and principal consultant of Rockett Healthcare Strategies, which partners with GI groups nationwide to help with development, accreditation, and payer contracting for office endoscopy.
“GI physicians should also no longer feel trapped in a ‘bad marriage’ with partners in an ASC or partners in a practice who create a difficult work environment,” he said. “The viability of office endoscopy allows them to strike out on their own or set up a new partnership on more equitable terms that are attractive for them.”
Patient safety and quality also appear to be similar or better in office-based settings, based on benchmarking data analyzed so far. Hospital transfers were lower, falls were similar, and patient experience was positive, the authors wrote.
At the same time, Kosinski and colleagues noted the difficulty in shifting to office-based models. Most practices have committed to ASCs, for instance, and adding an office-based room can be challenging. Otherwise, practices already use their available office space and don’t have extra rooms available. In that case, an office endoscopy suite may be best suited for expansion sites, allowing practices to grow into new service areas, they wrote.
“You can’t fight the market. You have to focus on what the market wants and needs,” Kosinski said. “To do that, you have to be able to pivot and change direction, looking for new ways to change your mission. This could be an option to do that.”
Kosinski, Gupta, and Rockett declared having no conflicts of interest other than their current employments.
A version of this article appeared on Medscape.com.
After decades of successful growth, the ambulatory surgery center (ASC) model may be turning a corner, opening up opportunity for office-based endoscopy models, according to a recent practice management editorial published in Clinical Gastroenterology and Hepatology.
Although office endoscopy has been an option, it hasn’t always felt practical or financially viable in the past. However, the paradigm appears to be shifting as ASC-based revenue streams show signs of stress and fail to keep pace with inflation. As healthcare regulatory and economic environments continue to change, gastroenterologists need a new model to support equity, efficiency, and growth in gastrointestinal (GI) care delivery, the authors wrote.
“Through the course of my 40-year career, I’ve been hit with a lot of changes related to regulations, insurance, and the market. You can’t stay entrenched in your old ways. You have to remain pivotable and come up with new strategic positions,” said Lawrence Kosinski, MD, AGAF, lead author and founder of SonarMD and VOCnomics.
During his private practice career, Kosinski built one of the largest GI practices in Illinois, which had seven ASCs and is now part of one of the largest GI groups in the country. Across 30 years of experience with ASCs, Kosinski has watched the reimbursement for professional services decline, as well as for added revenue streams such as pathology and anesthesia.
Looking for a better solution, Kosinski served on the governing board for the American Gastroenterological Association as the councilor for development and growth. During the past 3 years, he has spoken with GI practices and worked with a national anesthesia company — Ambulatory Anesthesia Care — to better understand the office endoscopy setting.
“In the ’90s, all I wanted was to have an ASC because that was in vogue,” he said. “But if you look critically at what has happened to the business of outpatient endoscopy in the past 25 years, you’ll see that professional fees haven’t kept up, and trying to replace that lost revenue is a losing battle.”
Considering Financial Shifts
Since 2001, professional reimbursement for colonoscopies has fallen by more than 40% while ASC revenue has risen, decreasing the percentage of revenue from professional fees (from 34% to 23%) and increasing the facility component (from 44% to 60%), Kosinski and colleagues wrote.
When looking at profit, compression of professional service fees appears even greater, especially with surging costs of anesthesia care due to high demand and provider shortages. Beyond that, about a third of ASCs are owned at least partially by national entities, as of 2024, leading to even lower realization of profit.
“The profit margins have really been crushed, so what is a GI doc to do? Go where there is opportunity,” Kosinski said. “The difference between hospitals and ASCs has been compressed, so what about the office?”
The proposed 2026 Medicare Physician Fee Schedule includes a 14% increase in reimbursement for office-based procedures, including endoscopy, as well as a 7% decrease for facility-based procedures.
In several states — such as Illinois, Oregon, Virginia, Washington, and Wisconsin — health plans are introducing programs to promote the transition of outpatient endoscopy to office settings rather than hospital-based or ASC-based settings due to costs, the authors wrote.
“The decision to start offering office-based endoscopy services was an easy one for our practice, as it provides a way for us to provide patients convenient, easy-to-access endoscopy that is high quality yet much more affordable than hospital-based settings,” said Neil Gupta, MD, managing partner at Midwest Digestive Health & Nutrition in Des Plaines, Illinois.
The practice has used office-based endoscopy for nearly 2 years, Gupta said, performing about 5000 GI endoscopy procedures per year.
“As we all try to find better ways to provide high-quality but affordable care for patients, office-based endoscopy is a great way to help achieve those goals,” he said. “Healthcare professionals and patients should all be asking, ‘What type of site am I getting my GI endoscopy scheduled at — hospital, surgery center, or physician’s office?’”
Regaining Autonomy and Time
Beyond the financial dynamics, , Kosinski and colleagues wrote.
Looking ahead, office-based models can also provide the agility and infrastructure to compete in value-based care models, they wrote. In turn, value-based models can create relevance and resilience in a continually changing healthcare environment.
Without the involvement of ASC managers, investors, or health system partners, physicians retain control of scheduling, clinical protocols, financial decisions, and operational workflows, the authors wrote. This could create better alignment with personal preferences, clinical judgment, and patient needs, they noted.
“GI physicians should no longer feel trapped in a hospital setting where they lack independence and influence over decision-making,” said Rock Rockett, PhD, owner and principal consultant of Rockett Healthcare Strategies, which partners with GI groups nationwide to help with development, accreditation, and payer contracting for office endoscopy.
“GI physicians should also no longer feel trapped in a ‘bad marriage’ with partners in an ASC or partners in a practice who create a difficult work environment,” he said. “The viability of office endoscopy allows them to strike out on their own or set up a new partnership on more equitable terms that are attractive for them.”
Patient safety and quality also appear to be similar or better in office-based settings, based on benchmarking data analyzed so far. Hospital transfers were lower, falls were similar, and patient experience was positive, the authors wrote.
At the same time, Kosinski and colleagues noted the difficulty in shifting to office-based models. Most practices have committed to ASCs, for instance, and adding an office-based room can be challenging. Otherwise, practices already use their available office space and don’t have extra rooms available. In that case, an office endoscopy suite may be best suited for expansion sites, allowing practices to grow into new service areas, they wrote.
“You can’t fight the market. You have to focus on what the market wants and needs,” Kosinski said. “To do that, you have to be able to pivot and change direction, looking for new ways to change your mission. This could be an option to do that.”
Kosinski, Gupta, and Rockett declared having no conflicts of interest other than their current employments.
A version of this article appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
‘So You Have an Idea…’: A Practical Guide to Tech and Device Development for the Early Career GI
You are in the middle of a busy clinic day and think, “there has to be a better way to do this.” Suddenly, a better way to do something becomes obvious. Maybe it’s a tool that simplifies documentation, a device that improves patient comfort, or an app that bridges a clinical gap. Many physicians, especially early career gastroenterologists, have ideas like this, but few know what to do next.
This article is for the curious innovator at the beginning of their clinical career. It offers practical, real-world guidance on developing a clinical product: whether that be hardware, software, or a hybrid. It outlines what questions to ask, who to consult, and how to protect your work, using personal insights and business principles learned through lived experience.
1. Understand Intellectual Property (IP): Know Its Value and Ownership
What is IP?
Intellectual property refers to your original creations: inventions, designs, software, and more. This is what you want to protect legally through patents, trademarks, or copyrights.
Who owns your idea?
This is the first and most important question to ask. If you are employed (especially by a hospital or academic center), your contract may already give your employer rights to any inventions you create, even those developed in your personal time.
What to ask:
- Does my employment contract include an “assignment of inventions” clause?
- Does the institution claim rights to anything developed with institutional resources?
- Are there moonlighting or external activity policies that affect this?
If you are developing an idea on your personal time, with your own resources, and outside your scope of clinical duties, it might still be considered “theirs” under some contracts. Early legal consultation is critical. A specialized IP attorney can help you understand what you own and how to protect it. This should be done early, ideally before you start building anything.
2. Lawyers Aren’t Optional: They’re Essential Early Partners
You do not need a full legal team, but you do need a lawyer early. An early consultation with an IP attorney can clarify your rights, guide your filing process (e.g. provisional patents), and help you avoid costly missteps.
Do this before sharing your idea publicly, including in academic presentations, pitch competitions, or even on social media. Public disclosure can start a clock ticking for application to protect your IP.
3. Build a Founding Team with Intent
Think of your startup team like a long-term relationship: you’re committing to build something together through uncertainty, tension, and change.
Strong early-stage teams often include:
- The Visionary – understands the clinical need and vision
- The Builder – engineer, developer, or designer
- The Doer – project manager or operations lead
Before forming a company, clearly define:
- Ownership (equity percentages)
- Roles and responsibilities
- Time commitments
- What happens if someone exits
Have these discussions early and document your agreements. Avoid informal “handshake” deals that can lead to serious disputes later.
4. You Don’t Need to Know Everything on Day One
You do not need to know how to write code, build a prototype, or get FDA clearance on day one. Successful innovators are humble learners. Use a Minimum Viable Product (MVP), a simple, functional version of your idea, to test assumptions and gather feedback. Iterate based on what you learn. Do not chase perfection; pursue progress. Consider using online accelerators like Y Combinator’s startup school or AGA’s Center for GI Innovation and Technology.
5. Incubators: Use them Strategically
Incubators can offer mentorship, seed funding, legal support, and technical resources, but they vary widely in value (see Table 1). Many may want equity, and not all offer when you truly need.
Ask Yourself:
- Do I need technical help, business mentorship, or just accountability?
- What does this incubator offer in terms of IP protection, exposure, and connections?
- Do I understand the equity trade-off?
- What services and funding do they provide?
- Do they take equity? How much and when?
- What’s their track record with similar ventures?
- Are their incentives aligned with your vision?
6. Academic Institutions: Partners or Pitfalls?
Universities can provide credibility, resources, and early funding through their tech transfer office (TTO).
Key Questions to Ask:
- Will my IP be managed by the TTO?
- How much say do I have in licensing decisions?
- Are there royalty-sharing agreements in place?
- Can I form a startup while employed here?
You may need to negotiate if you want to commercialize your idea independently.
7. Do it for Purpose, Not Payday
Most founders end up owning only a small percentage of their company by the time a product reaches the market. Do not expect to get rich. Do it because it solves a problem you care about. If it happens to come with a nice paycheck, then that is an added bonus.
Your clinical training and insight give you a unique edge. You already know what’s broken. Use that as your compass.
Conclusion
Innovation isn’t about brilliance, it’s about curiosity, structure, and tenacity (see Table 2). Start small. Protect your work. Choose the right partners. Most importantly, stay anchored in your mission to make GI care better.
Dr. Muratore is based at UNC Rex Digestive Health, Raleigh, North Carolina. She has no conflicts related to this article. Dr. Wechsler is based at the University of North Carolina at Chapel Hill, Chapel Hill, North Carolina. She holds a patent assigned to Trustees of Dartmouth College. Dr. Shah is based at the University of Michigan, Ann Arbor, Michigan. He consults for Ardelyx, Laborie, Neuraxis, Salix, Sanofi, and Takeda and holds a patent with the Regents of the University of Michigan.
You are in the middle of a busy clinic day and think, “there has to be a better way to do this.” Suddenly, a better way to do something becomes obvious. Maybe it’s a tool that simplifies documentation, a device that improves patient comfort, or an app that bridges a clinical gap. Many physicians, especially early career gastroenterologists, have ideas like this, but few know what to do next.
This article is for the curious innovator at the beginning of their clinical career. It offers practical, real-world guidance on developing a clinical product: whether that be hardware, software, or a hybrid. It outlines what questions to ask, who to consult, and how to protect your work, using personal insights and business principles learned through lived experience.
1. Understand Intellectual Property (IP): Know Its Value and Ownership
What is IP?
Intellectual property refers to your original creations: inventions, designs, software, and more. This is what you want to protect legally through patents, trademarks, or copyrights.
Who owns your idea?
This is the first and most important question to ask. If you are employed (especially by a hospital or academic center), your contract may already give your employer rights to any inventions you create, even those developed in your personal time.
What to ask:
- Does my employment contract include an “assignment of inventions” clause?
- Does the institution claim rights to anything developed with institutional resources?
- Are there moonlighting or external activity policies that affect this?
If you are developing an idea on your personal time, with your own resources, and outside your scope of clinical duties, it might still be considered “theirs” under some contracts. Early legal consultation is critical. A specialized IP attorney can help you understand what you own and how to protect it. This should be done early, ideally before you start building anything.
2. Lawyers Aren’t Optional: They’re Essential Early Partners
You do not need a full legal team, but you do need a lawyer early. An early consultation with an IP attorney can clarify your rights, guide your filing process (e.g. provisional patents), and help you avoid costly missteps.
Do this before sharing your idea publicly, including in academic presentations, pitch competitions, or even on social media. Public disclosure can start a clock ticking for application to protect your IP.
3. Build a Founding Team with Intent
Think of your startup team like a long-term relationship: you’re committing to build something together through uncertainty, tension, and change.
Strong early-stage teams often include:
- The Visionary – understands the clinical need and vision
- The Builder – engineer, developer, or designer
- The Doer – project manager or operations lead
Before forming a company, clearly define:
- Ownership (equity percentages)
- Roles and responsibilities
- Time commitments
- What happens if someone exits
Have these discussions early and document your agreements. Avoid informal “handshake” deals that can lead to serious disputes later.
4. You Don’t Need to Know Everything on Day One
You do not need to know how to write code, build a prototype, or get FDA clearance on day one. Successful innovators are humble learners. Use a Minimum Viable Product (MVP), a simple, functional version of your idea, to test assumptions and gather feedback. Iterate based on what you learn. Do not chase perfection; pursue progress. Consider using online accelerators like Y Combinator’s startup school or AGA’s Center for GI Innovation and Technology.
5. Incubators: Use them Strategically
Incubators can offer mentorship, seed funding, legal support, and technical resources, but they vary widely in value (see Table 1). Many may want equity, and not all offer when you truly need.
Ask Yourself:
- Do I need technical help, business mentorship, or just accountability?
- What does this incubator offer in terms of IP protection, exposure, and connections?
- Do I understand the equity trade-off?
- What services and funding do they provide?
- Do they take equity? How much and when?
- What’s their track record with similar ventures?
- Are their incentives aligned with your vision?
6. Academic Institutions: Partners or Pitfalls?
Universities can provide credibility, resources, and early funding through their tech transfer office (TTO).
Key Questions to Ask:
- Will my IP be managed by the TTO?
- How much say do I have in licensing decisions?
- Are there royalty-sharing agreements in place?
- Can I form a startup while employed here?
You may need to negotiate if you want to commercialize your idea independently.
7. Do it for Purpose, Not Payday
Most founders end up owning only a small percentage of their company by the time a product reaches the market. Do not expect to get rich. Do it because it solves a problem you care about. If it happens to come with a nice paycheck, then that is an added bonus.
Your clinical training and insight give you a unique edge. You already know what’s broken. Use that as your compass.
Conclusion
Innovation isn’t about brilliance, it’s about curiosity, structure, and tenacity (see Table 2). Start small. Protect your work. Choose the right partners. Most importantly, stay anchored in your mission to make GI care better.
Dr. Muratore is based at UNC Rex Digestive Health, Raleigh, North Carolina. She has no conflicts related to this article. Dr. Wechsler is based at the University of North Carolina at Chapel Hill, Chapel Hill, North Carolina. She holds a patent assigned to Trustees of Dartmouth College. Dr. Shah is based at the University of Michigan, Ann Arbor, Michigan. He consults for Ardelyx, Laborie, Neuraxis, Salix, Sanofi, and Takeda and holds a patent with the Regents of the University of Michigan.
You are in the middle of a busy clinic day and think, “there has to be a better way to do this.” Suddenly, a better way to do something becomes obvious. Maybe it’s a tool that simplifies documentation, a device that improves patient comfort, or an app that bridges a clinical gap. Many physicians, especially early career gastroenterologists, have ideas like this, but few know what to do next.
This article is for the curious innovator at the beginning of their clinical career. It offers practical, real-world guidance on developing a clinical product: whether that be hardware, software, or a hybrid. It outlines what questions to ask, who to consult, and how to protect your work, using personal insights and business principles learned through lived experience.
1. Understand Intellectual Property (IP): Know Its Value and Ownership
What is IP?
Intellectual property refers to your original creations: inventions, designs, software, and more. This is what you want to protect legally through patents, trademarks, or copyrights.
Who owns your idea?
This is the first and most important question to ask. If you are employed (especially by a hospital or academic center), your contract may already give your employer rights to any inventions you create, even those developed in your personal time.
What to ask:
- Does my employment contract include an “assignment of inventions” clause?
- Does the institution claim rights to anything developed with institutional resources?
- Are there moonlighting or external activity policies that affect this?
If you are developing an idea on your personal time, with your own resources, and outside your scope of clinical duties, it might still be considered “theirs” under some contracts. Early legal consultation is critical. A specialized IP attorney can help you understand what you own and how to protect it. This should be done early, ideally before you start building anything.
2. Lawyers Aren’t Optional: They’re Essential Early Partners
You do not need a full legal team, but you do need a lawyer early. An early consultation with an IP attorney can clarify your rights, guide your filing process (e.g. provisional patents), and help you avoid costly missteps.
Do this before sharing your idea publicly, including in academic presentations, pitch competitions, or even on social media. Public disclosure can start a clock ticking for application to protect your IP.
3. Build a Founding Team with Intent
Think of your startup team like a long-term relationship: you’re committing to build something together through uncertainty, tension, and change.
Strong early-stage teams often include:
- The Visionary – understands the clinical need and vision
- The Builder – engineer, developer, or designer
- The Doer – project manager or operations lead
Before forming a company, clearly define:
- Ownership (equity percentages)
- Roles and responsibilities
- Time commitments
- What happens if someone exits
Have these discussions early and document your agreements. Avoid informal “handshake” deals that can lead to serious disputes later.
4. You Don’t Need to Know Everything on Day One
You do not need to know how to write code, build a prototype, or get FDA clearance on day one. Successful innovators are humble learners. Use a Minimum Viable Product (MVP), a simple, functional version of your idea, to test assumptions and gather feedback. Iterate based on what you learn. Do not chase perfection; pursue progress. Consider using online accelerators like Y Combinator’s startup school or AGA’s Center for GI Innovation and Technology.
5. Incubators: Use them Strategically
Incubators can offer mentorship, seed funding, legal support, and technical resources, but they vary widely in value (see Table 1). Many may want equity, and not all offer when you truly need.
Ask Yourself:
- Do I need technical help, business mentorship, or just accountability?
- What does this incubator offer in terms of IP protection, exposure, and connections?
- Do I understand the equity trade-off?
- What services and funding do they provide?
- Do they take equity? How much and when?
- What’s their track record with similar ventures?
- Are their incentives aligned with your vision?
6. Academic Institutions: Partners or Pitfalls?
Universities can provide credibility, resources, and early funding through their tech transfer office (TTO).
Key Questions to Ask:
- Will my IP be managed by the TTO?
- How much say do I have in licensing decisions?
- Are there royalty-sharing agreements in place?
- Can I form a startup while employed here?
You may need to negotiate if you want to commercialize your idea independently.
7. Do it for Purpose, Not Payday
Most founders end up owning only a small percentage of their company by the time a product reaches the market. Do not expect to get rich. Do it because it solves a problem you care about. If it happens to come with a nice paycheck, then that is an added bonus.
Your clinical training and insight give you a unique edge. You already know what’s broken. Use that as your compass.
Conclusion
Innovation isn’t about brilliance, it’s about curiosity, structure, and tenacity (see Table 2). Start small. Protect your work. Choose the right partners. Most importantly, stay anchored in your mission to make GI care better.
Dr. Muratore is based at UNC Rex Digestive Health, Raleigh, North Carolina. She has no conflicts related to this article. Dr. Wechsler is based at the University of North Carolina at Chapel Hill, Chapel Hill, North Carolina. She holds a patent assigned to Trustees of Dartmouth College. Dr. Shah is based at the University of Michigan, Ann Arbor, Michigan. He consults for Ardelyx, Laborie, Neuraxis, Salix, Sanofi, and Takeda and holds a patent with the Regents of the University of Michigan.
When Your First Job Isn’t Forever: Lessons from My Journey and What Early-Career GIs Need to Know
Introduction
For many of us in gastroenterology, landing that first attending job feels like the ultimate victory lap — the reward for all those years of training. We sign the contract, relocate, and imagine this will be our “forever job.” Reality often plays out differently.
In fact, 43% of physicians change jobs within five years, while 83% changed employers at least once in their careers.1 Even within our field — which is always in demand — turnover is high; 1 in 3 gastroenterologists are planning to leave their current role within two years.2 Why does this happen? More importantly, how do we navigate this transition with clarity and confidence as an early-career GI?
My Story: When I Dared to Change My “Forever Job”
When I signed my first attending contract, I didn’t negotiate a single thing. My priorities were simple: family in Toronto and visa requirements. After a decade of medical school, residency, and fellowship, everything else felt secondary. I was happy to be back home.
The job itself was good — reasonable hours, flexible colleagues, and ample opportunity to enhance my procedural skills. As I started carving out my niche in endobariatrics, the support I needed to grow further was not there. I kept telling myself that this job fulfilled my values and I needed to be patient: “this is my forever job. I am close to my family and that’s what matters.”
Then, during a suturing course at the American Society of Gastrointestinal Endoscopy, I had a casual chat with the course director (now my boss). It took me by surprise, but as the conversation continued, he offered me a job. It was tempting: the chance to build my own endobariatrics program with real institutional backing. The catch? It was in a city I had never been to, with no family or friends around. I politely said “no, thank you, I can’t.” He smiled, gave me his number, and said, “think about it.”
For the first time, I allowed myself to ask, “could I really leave my forever job?”
The Power of a Circle and a Spreadsheet
I leaned on my circle — a close group of fellowship friends who each took a turn being someone’s lifeline. We have monthly Zoom calls to talk about jobs, family, and career aspirations. When I shared my dilemma, I realized I wasn’t alone; one friend was also unhappy with her first job. Suddenly, we were asking one another, “can we really leave?”
I hired a career consultant familiar with physician visa issues — hands down, the best money I ever invested. The job search felt like dating: each interview was a first date; some needed a second or third date before I knew if it could be a match.
After every interview, I’d jump on Zoom with my circle. We’d screen-share my giant Excel spreadsheet — our decision matrix — with columns for everything I cared about:
- Institute
- Administrative Time
- Endobariatric support
- Director Title
- Salary
- On-call
- Vacation
- Proximity to airport
- Cost of living
- RVU percentage
- Endoscopy center buy-in
- Contract duration
- Support staff
- CME
We scored each job, line by line, and not a single job checked all the boxes. As I sat there in a state of decision paralysis, it became clear that this was not a simple decision.
The GI Community: A Small, Supportive World
The GI community is incredibly close-knit and kind-hearted. At every conference, I made a point to chat with as many colleagues as I could, to hear their perspectives on jobs and how they made tough career moves. Those conversations were real — no Google search or Excel sheet could offer the perspective and insight I gained by simply asking and leaning on the GI community.
Meanwhile, the person who had first offered me that job kept checking in, catching up at conferences, and bonding over our love for food and baking. With him, I never felt like I was being ‘interviewed’ — I felt valued. It did not feel like he was trying to fill a position with just anyone to improve the call pool. He genuinely wanted to understand what my goals were and how I envisioned my future. Through those conversations, he reminded me of my original passions, which were sidelined when so immersed in the daily routine.
I’ve learned that feeling valued doesn’t come from grand gestures in recruitment. It’s in the quiet signs of respect, trust, and being seen. He wasn’t looking for just anyone; he was looking for someone whose goals aligned with his group’s and someone in whom he wanted to invest. While others might chase the highest salary, the most flexible schedule, or the strongest ancillary support, I realized I valued something I did not realize that I was lacking until then: mentorship.
What I Learned: There is No Such Thing As “The Perfect Job”
After a full year of spreadsheets, Zoom calls, conference chats, and overthinking, I came to a big realization: there’s no perfect job — there’s no such thing as an ideal “forever job.” The only constant for humans is change. Our circumstances change, our priorities shift, our interests shuffle, and our finances evolve. The best job is simply the one that fits the stage of life you’re in at that given moment. For me, mentorship and growth became my top priorities, even if it meant moving away from family.
What Physicians Value Most in a Second Job
After their first job, early-career gastroenterologists often reevaluate what really matters. Recent surveys highlight four key priorities:
- Work-life balance:
In a 2022 CompHealth Group healthcare survey, 85% of physicians ranked work-life balance as their top job priority.3
- Mentorship and growth:
Nearly 1 in 3 physicians cited lack of mentorship or career advancement as their reason for leaving a first job, per the 2023 MGMA/Jackson Physician Search report.4
- Compensation:
While not always the main reason for leaving, 77% of physicians now list compensation as a top priority — a big jump from prior years.3
- Practice support:
Poor infrastructure, administrative overload, or understaffed teams are common dealbreakers. In the second job, physicians look for well-run practices with solid support staff and reduced burnout risk.5
Conclusion
Welcome the uncertainty, talk to your circle, lean on your community, and use a spreadsheet if you need to — but don’t forget to trust your gut. There’s no forever job or the perfect path, only the next move that feels most true to who you are in that moment.
Dr. Ismail (@mayyismail) is Assistant Professor of Clinical Medicine (Gastroenterology) at Temple University in Philadelphia, Pennsylvania. She declares no conflicts of interest.
References
1. CHG Healthcare. Survey: 62% of physicians made a career change in the last two years. CHG Healthcare blog. June 10, 2024. Accessed August 5, 2025.
2. Berg S. Physicians in these 10 specialties are less likely to quit. AMA News. Published June 24, 2025. Accessed July 2025.
3. Saley C. Survey: Work/life balance is #1 priority in physicians’ job search. CHG Healthcare Insights. March 10, 2022. Accessed August 2025.
4. Medical Group Management Association; Jackson Physician Search. Early‑Career Physician Recruiting & Retention Playbook. October 23, 2023. Accessed August 2025.
5. Von Rosenvinge EC, et al. A crisis in scope: Recruitment and retention challenges reported by VA gastroenterology section chiefs. Fed Pract. 2024 Aug. doi:10.12788/fp.0504.
Introduction
For many of us in gastroenterology, landing that first attending job feels like the ultimate victory lap — the reward for all those years of training. We sign the contract, relocate, and imagine this will be our “forever job.” Reality often plays out differently.
In fact, 43% of physicians change jobs within five years, while 83% changed employers at least once in their careers.1 Even within our field — which is always in demand — turnover is high; 1 in 3 gastroenterologists are planning to leave their current role within two years.2 Why does this happen? More importantly, how do we navigate this transition with clarity and confidence as an early-career GI?
My Story: When I Dared to Change My “Forever Job”
When I signed my first attending contract, I didn’t negotiate a single thing. My priorities were simple: family in Toronto and visa requirements. After a decade of medical school, residency, and fellowship, everything else felt secondary. I was happy to be back home.
The job itself was good — reasonable hours, flexible colleagues, and ample opportunity to enhance my procedural skills. As I started carving out my niche in endobariatrics, the support I needed to grow further was not there. I kept telling myself that this job fulfilled my values and I needed to be patient: “this is my forever job. I am close to my family and that’s what matters.”
Then, during a suturing course at the American Society of Gastrointestinal Endoscopy, I had a casual chat with the course director (now my boss). It took me by surprise, but as the conversation continued, he offered me a job. It was tempting: the chance to build my own endobariatrics program with real institutional backing. The catch? It was in a city I had never been to, with no family or friends around. I politely said “no, thank you, I can’t.” He smiled, gave me his number, and said, “think about it.”
For the first time, I allowed myself to ask, “could I really leave my forever job?”
The Power of a Circle and a Spreadsheet
I leaned on my circle — a close group of fellowship friends who each took a turn being someone’s lifeline. We have monthly Zoom calls to talk about jobs, family, and career aspirations. When I shared my dilemma, I realized I wasn’t alone; one friend was also unhappy with her first job. Suddenly, we were asking one another, “can we really leave?”
I hired a career consultant familiar with physician visa issues — hands down, the best money I ever invested. The job search felt like dating: each interview was a first date; some needed a second or third date before I knew if it could be a match.
After every interview, I’d jump on Zoom with my circle. We’d screen-share my giant Excel spreadsheet — our decision matrix — with columns for everything I cared about:
- Institute
- Administrative Time
- Endobariatric support
- Director Title
- Salary
- On-call
- Vacation
- Proximity to airport
- Cost of living
- RVU percentage
- Endoscopy center buy-in
- Contract duration
- Support staff
- CME
We scored each job, line by line, and not a single job checked all the boxes. As I sat there in a state of decision paralysis, it became clear that this was not a simple decision.
The GI Community: A Small, Supportive World
The GI community is incredibly close-knit and kind-hearted. At every conference, I made a point to chat with as many colleagues as I could, to hear their perspectives on jobs and how they made tough career moves. Those conversations were real — no Google search or Excel sheet could offer the perspective and insight I gained by simply asking and leaning on the GI community.
Meanwhile, the person who had first offered me that job kept checking in, catching up at conferences, and bonding over our love for food and baking. With him, I never felt like I was being ‘interviewed’ — I felt valued. It did not feel like he was trying to fill a position with just anyone to improve the call pool. He genuinely wanted to understand what my goals were and how I envisioned my future. Through those conversations, he reminded me of my original passions, which were sidelined when so immersed in the daily routine.
I’ve learned that feeling valued doesn’t come from grand gestures in recruitment. It’s in the quiet signs of respect, trust, and being seen. He wasn’t looking for just anyone; he was looking for someone whose goals aligned with his group’s and someone in whom he wanted to invest. While others might chase the highest salary, the most flexible schedule, or the strongest ancillary support, I realized I valued something I did not realize that I was lacking until then: mentorship.
What I Learned: There is No Such Thing As “The Perfect Job”
After a full year of spreadsheets, Zoom calls, conference chats, and overthinking, I came to a big realization: there’s no perfect job — there’s no such thing as an ideal “forever job.” The only constant for humans is change. Our circumstances change, our priorities shift, our interests shuffle, and our finances evolve. The best job is simply the one that fits the stage of life you’re in at that given moment. For me, mentorship and growth became my top priorities, even if it meant moving away from family.
What Physicians Value Most in a Second Job
After their first job, early-career gastroenterologists often reevaluate what really matters. Recent surveys highlight four key priorities:
- Work-life balance:
In a 2022 CompHealth Group healthcare survey, 85% of physicians ranked work-life balance as their top job priority.3
- Mentorship and growth:
Nearly 1 in 3 physicians cited lack of mentorship or career advancement as their reason for leaving a first job, per the 2023 MGMA/Jackson Physician Search report.4
- Compensation:
While not always the main reason for leaving, 77% of physicians now list compensation as a top priority — a big jump from prior years.3
- Practice support:
Poor infrastructure, administrative overload, or understaffed teams are common dealbreakers. In the second job, physicians look for well-run practices with solid support staff and reduced burnout risk.5
Conclusion
Welcome the uncertainty, talk to your circle, lean on your community, and use a spreadsheet if you need to — but don’t forget to trust your gut. There’s no forever job or the perfect path, only the next move that feels most true to who you are in that moment.
Dr. Ismail (@mayyismail) is Assistant Professor of Clinical Medicine (Gastroenterology) at Temple University in Philadelphia, Pennsylvania. She declares no conflicts of interest.
References
1. CHG Healthcare. Survey: 62% of physicians made a career change in the last two years. CHG Healthcare blog. June 10, 2024. Accessed August 5, 2025.
2. Berg S. Physicians in these 10 specialties are less likely to quit. AMA News. Published June 24, 2025. Accessed July 2025.
3. Saley C. Survey: Work/life balance is #1 priority in physicians’ job search. CHG Healthcare Insights. March 10, 2022. Accessed August 2025.
4. Medical Group Management Association; Jackson Physician Search. Early‑Career Physician Recruiting & Retention Playbook. October 23, 2023. Accessed August 2025.
5. Von Rosenvinge EC, et al. A crisis in scope: Recruitment and retention challenges reported by VA gastroenterology section chiefs. Fed Pract. 2024 Aug. doi:10.12788/fp.0504.
Introduction
For many of us in gastroenterology, landing that first attending job feels like the ultimate victory lap — the reward for all those years of training. We sign the contract, relocate, and imagine this will be our “forever job.” Reality often plays out differently.
In fact, 43% of physicians change jobs within five years, while 83% changed employers at least once in their careers.1 Even within our field — which is always in demand — turnover is high; 1 in 3 gastroenterologists are planning to leave their current role within two years.2 Why does this happen? More importantly, how do we navigate this transition with clarity and confidence as an early-career GI?
My Story: When I Dared to Change My “Forever Job”
When I signed my first attending contract, I didn’t negotiate a single thing. My priorities were simple: family in Toronto and visa requirements. After a decade of medical school, residency, and fellowship, everything else felt secondary. I was happy to be back home.
The job itself was good — reasonable hours, flexible colleagues, and ample opportunity to enhance my procedural skills. As I started carving out my niche in endobariatrics, the support I needed to grow further was not there. I kept telling myself that this job fulfilled my values and I needed to be patient: “this is my forever job. I am close to my family and that’s what matters.”
Then, during a suturing course at the American Society of Gastrointestinal Endoscopy, I had a casual chat with the course director (now my boss). It took me by surprise, but as the conversation continued, he offered me a job. It was tempting: the chance to build my own endobariatrics program with real institutional backing. The catch? It was in a city I had never been to, with no family or friends around. I politely said “no, thank you, I can’t.” He smiled, gave me his number, and said, “think about it.”
For the first time, I allowed myself to ask, “could I really leave my forever job?”
The Power of a Circle and a Spreadsheet
I leaned on my circle — a close group of fellowship friends who each took a turn being someone’s lifeline. We have monthly Zoom calls to talk about jobs, family, and career aspirations. When I shared my dilemma, I realized I wasn’t alone; one friend was also unhappy with her first job. Suddenly, we were asking one another, “can we really leave?”
I hired a career consultant familiar with physician visa issues — hands down, the best money I ever invested. The job search felt like dating: each interview was a first date; some needed a second or third date before I knew if it could be a match.
After every interview, I’d jump on Zoom with my circle. We’d screen-share my giant Excel spreadsheet — our decision matrix — with columns for everything I cared about:
- Institute
- Administrative Time
- Endobariatric support
- Director Title
- Salary
- On-call
- Vacation
- Proximity to airport
- Cost of living
- RVU percentage
- Endoscopy center buy-in
- Contract duration
- Support staff
- CME
We scored each job, line by line, and not a single job checked all the boxes. As I sat there in a state of decision paralysis, it became clear that this was not a simple decision.
The GI Community: A Small, Supportive World
The GI community is incredibly close-knit and kind-hearted. At every conference, I made a point to chat with as many colleagues as I could, to hear their perspectives on jobs and how they made tough career moves. Those conversations were real — no Google search or Excel sheet could offer the perspective and insight I gained by simply asking and leaning on the GI community.
Meanwhile, the person who had first offered me that job kept checking in, catching up at conferences, and bonding over our love for food and baking. With him, I never felt like I was being ‘interviewed’ — I felt valued. It did not feel like he was trying to fill a position with just anyone to improve the call pool. He genuinely wanted to understand what my goals were and how I envisioned my future. Through those conversations, he reminded me of my original passions, which were sidelined when so immersed in the daily routine.
I’ve learned that feeling valued doesn’t come from grand gestures in recruitment. It’s in the quiet signs of respect, trust, and being seen. He wasn’t looking for just anyone; he was looking for someone whose goals aligned with his group’s and someone in whom he wanted to invest. While others might chase the highest salary, the most flexible schedule, or the strongest ancillary support, I realized I valued something I did not realize that I was lacking until then: mentorship.
What I Learned: There is No Such Thing As “The Perfect Job”
After a full year of spreadsheets, Zoom calls, conference chats, and overthinking, I came to a big realization: there’s no perfect job — there’s no such thing as an ideal “forever job.” The only constant for humans is change. Our circumstances change, our priorities shift, our interests shuffle, and our finances evolve. The best job is simply the one that fits the stage of life you’re in at that given moment. For me, mentorship and growth became my top priorities, even if it meant moving away from family.
What Physicians Value Most in a Second Job
After their first job, early-career gastroenterologists often reevaluate what really matters. Recent surveys highlight four key priorities:
- Work-life balance:
In a 2022 CompHealth Group healthcare survey, 85% of physicians ranked work-life balance as their top job priority.3
- Mentorship and growth:
Nearly 1 in 3 physicians cited lack of mentorship or career advancement as their reason for leaving a first job, per the 2023 MGMA/Jackson Physician Search report.4
- Compensation:
While not always the main reason for leaving, 77% of physicians now list compensation as a top priority — a big jump from prior years.3
- Practice support:
Poor infrastructure, administrative overload, or understaffed teams are common dealbreakers. In the second job, physicians look for well-run practices with solid support staff and reduced burnout risk.5
Conclusion
Welcome the uncertainty, talk to your circle, lean on your community, and use a spreadsheet if you need to — but don’t forget to trust your gut. There’s no forever job or the perfect path, only the next move that feels most true to who you are in that moment.
Dr. Ismail (@mayyismail) is Assistant Professor of Clinical Medicine (Gastroenterology) at Temple University in Philadelphia, Pennsylvania. She declares no conflicts of interest.
References
1. CHG Healthcare. Survey: 62% of physicians made a career change in the last two years. CHG Healthcare blog. June 10, 2024. Accessed August 5, 2025.
2. Berg S. Physicians in these 10 specialties are less likely to quit. AMA News. Published June 24, 2025. Accessed July 2025.
3. Saley C. Survey: Work/life balance is #1 priority in physicians’ job search. CHG Healthcare Insights. March 10, 2022. Accessed August 2025.
4. Medical Group Management Association; Jackson Physician Search. Early‑Career Physician Recruiting & Retention Playbook. October 23, 2023. Accessed August 2025.
5. Von Rosenvinge EC, et al. A crisis in scope: Recruitment and retention challenges reported by VA gastroenterology section chiefs. Fed Pract. 2024 Aug. doi:10.12788/fp.0504.
Developing the Next Generation of GI Leaders

In this episode of Private Practice Perspectives, Dr. Naresh Gunaratnam, current president and board chair of Digestive Health Physician Association, speaks with Dr. Larry Kim, current president of AGA, about .

In this episode of Private Practice Perspectives, Dr. Naresh Gunaratnam, current president and board chair of Digestive Health Physician Association, speaks with Dr. Larry Kim, current president of AGA, about .

In this episode of Private Practice Perspectives, Dr. Naresh Gunaratnam, current president and board chair of Digestive Health Physician Association, speaks with Dr. Larry Kim, current president of AGA, about .
Physician Compensation: Gains Small, Gaps Large
Few would deny that physicians today face many challenges: a growing and aging patient population, personnel shortages, mounting paperwork, regulatory and reimbursement pressures, and personal burnout. Collectively these could work to worsen patient access to care. Yet despite these headwinds, Doximity’s survey-based Physician Compensation Report 2025 found that more than three-quarters of physicians polled would still choose to enter their profession.
“Physician burnout isn’t new. It’s been a persistent problem over the past decade,” said Amit Phull, MD, chief clinical experience officer at Doximity. “In a Doximity poll of nearly 2,000 physicians conducted in May 2025, 85% reported they feel overworked, up from 73% just four years ago. As a result, about 68% of physicians said they are looking for an employment change or considering early retirement.”
Greater awareness of contemporary trends may help physicians make more-informed career decisions and more effectively advocate for both themselves and the patients who need them, the report’s authors stated.
Compensation Lag May Impact Care
A small overall average compensation increase of 3.7% from 2023 to 2024 – a slightly lower increase than the 5.9% in the prior year – has done little to close existing pay gaps across the profession.
In 2024, average compensation for men rose 5.7% over 2023, compared with just 1.7% for women – widening the gender pay gap to 26% vs 23% in 2023 and matching the gender gap seen in 2022. And significant disparities persist between physicians caring for adults vs children. In some specialties, the pay gap between pediatric and adult specialists exceeded 80% despite practitioners’ similar levels of training and clinical complexity.
Nearly 60% of respondents said reimbursement pressures could affect their ability to serve Medicare or Medicaid patients in the next year. Additionally, 81% reported that reimbursement policies have significantly contributed to the decline of private practices, and more than a third said they could stifle practice growth with compensation concerns forcing them to delay or cancel hiring or expansion plans. Almost 90% reported an adverse impact from physician shortages, with more citing an inability or limited ability to accept new patients.
Narrowing the Gap for Primary Care?
Over the past three years, the percent pay gap between primary care and specialist medicine declined modestly, the report noted. In 2024, surgical specialists earned 87% more than primary care physicians, down from 100% in 2022. Non-surgical specialists, emergency medicine physicians, and Ob/Gyns also continued to earn significantly more than primary care physicians, though the gaps have narrowed slightly.
“These trends come at a time when primary care remains critical to meeting high patient demand, especially amid ongoing physician shortages,” the report stated. “Primary care physicians continue to earn considerably less than many of their medical colleagues despite their essential role in the healthcare system.”
Significantly, many physicians believe that current reimbursement policies have contributed to the steady decline of independent practices in their fields. According to the American Medical Association, the share of physicians working in private practices dropped by 18 percentage points from 60.1% to 42.2% from 2012 to 2024.
The Specialties
This year’s review found that among 20 specialties, the highest average compensation occurred in surgical and procedural specialties, while the lowest paid were, as mentioned, pediatric medicine and primary care. Pediatric nephrology saw the largest average compensation growth in 2024 at 15.6%, yet compensation still lagged behind adult nephrology with a 40% pay gap.
By medical discipline, gastroenterologists ranked 13th overall in average annual compensation. Gastroenterology remained in the top 20 compensated specialties, with average annual compensation of $537,870 – an increase from $514,208 in 2024, representing a 4.5% growth rate over 2023. Neurosurgeons topped the list at $749,140, followed by thoracic surgeons at $689,969 and orthopedic surgeons at $679,517.
The three lowest-paid branches were all pediatric: endocrinology at $230,426, rheumatology at $231,574, and infectious diseases at $248,322. Pediatric gastroenterology paid somewhat higher at $298,457.
The largest disparities were seen in hematology and oncology, where adult specialists earned 93% more than their pediatric peers. Pediatric gastroenterology showed an 80% pay gap. There were also substantial pay differences across cardiology, pulmonology, and rheumatology. “These gaps appear to reflect a systemic lag in pay for pediatric specialty care, even as demand for pediatric subspecialists continues to rise,” the report stated.
Practice Setting and Location
Where a doctor practices impacts the bottom line, too: in 2024 the highest compensation reported for a metro area was in Rochester, Minnesota (the Mayo Clinic effect?), at $495,532, while the lowest reported was in Durham-Chapel Hill, North Carolina, at $368,782. St. Louis, Missouri ($484,883) and Los Angeles, California ($470,198) were 2nd and 3rd at the top of the list. Rochester, Minnesota, also emerged as best for annual compensation after cost-of-living adjustment, while Boston, Massachusetts, occupied the bottom rung.
The Gender Effect
With a women’s pay increase in 2024 of just 1.7%, the gender gap returned to its 2022-level disparity of 26%, with women physicians earning an average of $120,917 less than men after adjusting for specialty, location, and years of experience.
Doximity’s analysis of data from 2014 to 2019 estimated that on average men make at least $2 million more than women over the course of a 40-year career. This gap is often attributed to the fewer hours worked by female physician with their generally heavier familial responsibilities, “but Doximity’s gender wage gap analysis controls for the number of hours worked and career stage, along with specialty, work type, employment status, region, and credentials,” Phull said.
Women physicians had lower average earnings than men physicians across all specialties, a trend consistent with prior years. As a percentage of pay, the largest gender disparity was seen in pediatric nephrology (16.5%), a specialty that in fact saw the largest annual growth in physician pay. Neurosurgery had the smallest gender gap at 11.3%, while infectious diseases came in at 11.5% and oncology at 12%.
According to Maria T. Abreu, MD, AGAF, executive director of the F. Widjaja Inflammatory Bowel Disease Institute at Cedars-Sinai Medical Center in Los Angeles and past president of AGA, the remuneration gender gap in gastroenterology is being taken seriously by AGA and several other GI societies. “The discrepancies in pay start from the beginning and therefore are magnified over time. We are helping to empower women to negotiate better as well as to gather data on the roots of inequity, she told GI & Hepatology News.
The AGA Women’s Committee has developed a project to support the advancement of women in gastroenterology, Abreu said. The initiative, which includes the AGA Gender Equity Framework and Gender Equity Road Map. focuses attention on disparities in the workplace and promotes opportunities for women’s leadership, career advancement, mentorship and physician health and wellness, she added.
Are these disparities due mainly to the “motherhood penalty,” with career interruption and time lost to maternity leave and fewer hours worked owing to the greater parenting burden of physician mothers? Or are they due to the systemic effects of gender expectations around compensation?
Hours worked appear to be a factor. A 2017 study of dual physician couples found that among childless respondents men worked an average of 57 hours and women 52 hours weekly. Compared with childless men, men with children worked similar numbers of hours weekly. However, compared with childless physicians, mothers worked significantly fewer hours – roughly 40 to 43 hours weekly – depending on the age of their youngest child.
Abreu pushed back on this stereotype. “Most women physicians, including gastroenterologists, do not take the maternity leave they are allowed because they are concerned about burdening their colleagues,” she said. “Thus, it is unlikely to explain the disparities. Many systemic issues remain challenging, but we want women to be empowered to advocate for themselves at the time of hiring and along the arc of their career paths.”
In Abreu’s view, having women assume more leadership roles in the field of gastroenterology provides an opportunity to focus on reducing the disparities in compensation.
Regardless of gender, among all physicians surveyed, autonomy and work-life balance appeared to be a high priority: 77% of doctors said they would be willing to accept or have already accepted lower pay for more autonomy or work-life balance. “Overwork appears to be especially prevalent among women physicians,” said Phull, noting that 91% of women respondents reported being overworked compared with 80% of men. “This overwork has compelled 74% of women to consider making a career change, compared with 62% of men.” Differences emerged among specialties as well: 90% of primary care physicians said they are overworked compared with 84% of surgeons and 83% of non-surgical specialists.
Looking ahead, the report raised an important question. Are we relying too heavily on physicians rather than addressing the underlying need for policies that support a healthier, more sustainable future for all? “Building that future will take more than physician dedication alone,” Phull said. “It will require meaningful collaboration across the entire health care ecosystem – including health systems, hospitals, payors, and policymakers. And physicians must not only have a voice in shaping the path forward; they must have a seat at the table.”
Abreu reported no conflicts of interest in regard to her comments.
Few would deny that physicians today face many challenges: a growing and aging patient population, personnel shortages, mounting paperwork, regulatory and reimbursement pressures, and personal burnout. Collectively these could work to worsen patient access to care. Yet despite these headwinds, Doximity’s survey-based Physician Compensation Report 2025 found that more than three-quarters of physicians polled would still choose to enter their profession.
“Physician burnout isn’t new. It’s been a persistent problem over the past decade,” said Amit Phull, MD, chief clinical experience officer at Doximity. “In a Doximity poll of nearly 2,000 physicians conducted in May 2025, 85% reported they feel overworked, up from 73% just four years ago. As a result, about 68% of physicians said they are looking for an employment change or considering early retirement.”
Greater awareness of contemporary trends may help physicians make more-informed career decisions and more effectively advocate for both themselves and the patients who need them, the report’s authors stated.
Compensation Lag May Impact Care
A small overall average compensation increase of 3.7% from 2023 to 2024 – a slightly lower increase than the 5.9% in the prior year – has done little to close existing pay gaps across the profession.
In 2024, average compensation for men rose 5.7% over 2023, compared with just 1.7% for women – widening the gender pay gap to 26% vs 23% in 2023 and matching the gender gap seen in 2022. And significant disparities persist between physicians caring for adults vs children. In some specialties, the pay gap between pediatric and adult specialists exceeded 80% despite practitioners’ similar levels of training and clinical complexity.
Nearly 60% of respondents said reimbursement pressures could affect their ability to serve Medicare or Medicaid patients in the next year. Additionally, 81% reported that reimbursement policies have significantly contributed to the decline of private practices, and more than a third said they could stifle practice growth with compensation concerns forcing them to delay or cancel hiring or expansion plans. Almost 90% reported an adverse impact from physician shortages, with more citing an inability or limited ability to accept new patients.
Narrowing the Gap for Primary Care?
Over the past three years, the percent pay gap between primary care and specialist medicine declined modestly, the report noted. In 2024, surgical specialists earned 87% more than primary care physicians, down from 100% in 2022. Non-surgical specialists, emergency medicine physicians, and Ob/Gyns also continued to earn significantly more than primary care physicians, though the gaps have narrowed slightly.
“These trends come at a time when primary care remains critical to meeting high patient demand, especially amid ongoing physician shortages,” the report stated. “Primary care physicians continue to earn considerably less than many of their medical colleagues despite their essential role in the healthcare system.”
Significantly, many physicians believe that current reimbursement policies have contributed to the steady decline of independent practices in their fields. According to the American Medical Association, the share of physicians working in private practices dropped by 18 percentage points from 60.1% to 42.2% from 2012 to 2024.
The Specialties
This year’s review found that among 20 specialties, the highest average compensation occurred in surgical and procedural specialties, while the lowest paid were, as mentioned, pediatric medicine and primary care. Pediatric nephrology saw the largest average compensation growth in 2024 at 15.6%, yet compensation still lagged behind adult nephrology with a 40% pay gap.
By medical discipline, gastroenterologists ranked 13th overall in average annual compensation. Gastroenterology remained in the top 20 compensated specialties, with average annual compensation of $537,870 – an increase from $514,208 in 2024, representing a 4.5% growth rate over 2023. Neurosurgeons topped the list at $749,140, followed by thoracic surgeons at $689,969 and orthopedic surgeons at $679,517.
The three lowest-paid branches were all pediatric: endocrinology at $230,426, rheumatology at $231,574, and infectious diseases at $248,322. Pediatric gastroenterology paid somewhat higher at $298,457.
The largest disparities were seen in hematology and oncology, where adult specialists earned 93% more than their pediatric peers. Pediatric gastroenterology showed an 80% pay gap. There were also substantial pay differences across cardiology, pulmonology, and rheumatology. “These gaps appear to reflect a systemic lag in pay for pediatric specialty care, even as demand for pediatric subspecialists continues to rise,” the report stated.
Practice Setting and Location
Where a doctor practices impacts the bottom line, too: in 2024 the highest compensation reported for a metro area was in Rochester, Minnesota (the Mayo Clinic effect?), at $495,532, while the lowest reported was in Durham-Chapel Hill, North Carolina, at $368,782. St. Louis, Missouri ($484,883) and Los Angeles, California ($470,198) were 2nd and 3rd at the top of the list. Rochester, Minnesota, also emerged as best for annual compensation after cost-of-living adjustment, while Boston, Massachusetts, occupied the bottom rung.
The Gender Effect
With a women’s pay increase in 2024 of just 1.7%, the gender gap returned to its 2022-level disparity of 26%, with women physicians earning an average of $120,917 less than men after adjusting for specialty, location, and years of experience.
Doximity’s analysis of data from 2014 to 2019 estimated that on average men make at least $2 million more than women over the course of a 40-year career. This gap is often attributed to the fewer hours worked by female physician with their generally heavier familial responsibilities, “but Doximity’s gender wage gap analysis controls for the number of hours worked and career stage, along with specialty, work type, employment status, region, and credentials,” Phull said.
Women physicians had lower average earnings than men physicians across all specialties, a trend consistent with prior years. As a percentage of pay, the largest gender disparity was seen in pediatric nephrology (16.5%), a specialty that in fact saw the largest annual growth in physician pay. Neurosurgery had the smallest gender gap at 11.3%, while infectious diseases came in at 11.5% and oncology at 12%.
According to Maria T. Abreu, MD, AGAF, executive director of the F. Widjaja Inflammatory Bowel Disease Institute at Cedars-Sinai Medical Center in Los Angeles and past president of AGA, the remuneration gender gap in gastroenterology is being taken seriously by AGA and several other GI societies. “The discrepancies in pay start from the beginning and therefore are magnified over time. We are helping to empower women to negotiate better as well as to gather data on the roots of inequity, she told GI & Hepatology News.
The AGA Women’s Committee has developed a project to support the advancement of women in gastroenterology, Abreu said. The initiative, which includes the AGA Gender Equity Framework and Gender Equity Road Map. focuses attention on disparities in the workplace and promotes opportunities for women’s leadership, career advancement, mentorship and physician health and wellness, she added.
Are these disparities due mainly to the “motherhood penalty,” with career interruption and time lost to maternity leave and fewer hours worked owing to the greater parenting burden of physician mothers? Or are they due to the systemic effects of gender expectations around compensation?
Hours worked appear to be a factor. A 2017 study of dual physician couples found that among childless respondents men worked an average of 57 hours and women 52 hours weekly. Compared with childless men, men with children worked similar numbers of hours weekly. However, compared with childless physicians, mothers worked significantly fewer hours – roughly 40 to 43 hours weekly – depending on the age of their youngest child.
Abreu pushed back on this stereotype. “Most women physicians, including gastroenterologists, do not take the maternity leave they are allowed because they are concerned about burdening their colleagues,” she said. “Thus, it is unlikely to explain the disparities. Many systemic issues remain challenging, but we want women to be empowered to advocate for themselves at the time of hiring and along the arc of their career paths.”
In Abreu’s view, having women assume more leadership roles in the field of gastroenterology provides an opportunity to focus on reducing the disparities in compensation.
Regardless of gender, among all physicians surveyed, autonomy and work-life balance appeared to be a high priority: 77% of doctors said they would be willing to accept or have already accepted lower pay for more autonomy or work-life balance. “Overwork appears to be especially prevalent among women physicians,” said Phull, noting that 91% of women respondents reported being overworked compared with 80% of men. “This overwork has compelled 74% of women to consider making a career change, compared with 62% of men.” Differences emerged among specialties as well: 90% of primary care physicians said they are overworked compared with 84% of surgeons and 83% of non-surgical specialists.
Looking ahead, the report raised an important question. Are we relying too heavily on physicians rather than addressing the underlying need for policies that support a healthier, more sustainable future for all? “Building that future will take more than physician dedication alone,” Phull said. “It will require meaningful collaboration across the entire health care ecosystem – including health systems, hospitals, payors, and policymakers. And physicians must not only have a voice in shaping the path forward; they must have a seat at the table.”
Abreu reported no conflicts of interest in regard to her comments.
Few would deny that physicians today face many challenges: a growing and aging patient population, personnel shortages, mounting paperwork, regulatory and reimbursement pressures, and personal burnout. Collectively these could work to worsen patient access to care. Yet despite these headwinds, Doximity’s survey-based Physician Compensation Report 2025 found that more than three-quarters of physicians polled would still choose to enter their profession.
“Physician burnout isn’t new. It’s been a persistent problem over the past decade,” said Amit Phull, MD, chief clinical experience officer at Doximity. “In a Doximity poll of nearly 2,000 physicians conducted in May 2025, 85% reported they feel overworked, up from 73% just four years ago. As a result, about 68% of physicians said they are looking for an employment change or considering early retirement.”
Greater awareness of contemporary trends may help physicians make more-informed career decisions and more effectively advocate for both themselves and the patients who need them, the report’s authors stated.
Compensation Lag May Impact Care
A small overall average compensation increase of 3.7% from 2023 to 2024 – a slightly lower increase than the 5.9% in the prior year – has done little to close existing pay gaps across the profession.
In 2024, average compensation for men rose 5.7% over 2023, compared with just 1.7% for women – widening the gender pay gap to 26% vs 23% in 2023 and matching the gender gap seen in 2022. And significant disparities persist between physicians caring for adults vs children. In some specialties, the pay gap between pediatric and adult specialists exceeded 80% despite practitioners’ similar levels of training and clinical complexity.
Nearly 60% of respondents said reimbursement pressures could affect their ability to serve Medicare or Medicaid patients in the next year. Additionally, 81% reported that reimbursement policies have significantly contributed to the decline of private practices, and more than a third said they could stifle practice growth with compensation concerns forcing them to delay or cancel hiring or expansion plans. Almost 90% reported an adverse impact from physician shortages, with more citing an inability or limited ability to accept new patients.
Narrowing the Gap for Primary Care?
Over the past three years, the percent pay gap between primary care and specialist medicine declined modestly, the report noted. In 2024, surgical specialists earned 87% more than primary care physicians, down from 100% in 2022. Non-surgical specialists, emergency medicine physicians, and Ob/Gyns also continued to earn significantly more than primary care physicians, though the gaps have narrowed slightly.
“These trends come at a time when primary care remains critical to meeting high patient demand, especially amid ongoing physician shortages,” the report stated. “Primary care physicians continue to earn considerably less than many of their medical colleagues despite their essential role in the healthcare system.”
Significantly, many physicians believe that current reimbursement policies have contributed to the steady decline of independent practices in their fields. According to the American Medical Association, the share of physicians working in private practices dropped by 18 percentage points from 60.1% to 42.2% from 2012 to 2024.
The Specialties
This year’s review found that among 20 specialties, the highest average compensation occurred in surgical and procedural specialties, while the lowest paid were, as mentioned, pediatric medicine and primary care. Pediatric nephrology saw the largest average compensation growth in 2024 at 15.6%, yet compensation still lagged behind adult nephrology with a 40% pay gap.
By medical discipline, gastroenterologists ranked 13th overall in average annual compensation. Gastroenterology remained in the top 20 compensated specialties, with average annual compensation of $537,870 – an increase from $514,208 in 2024, representing a 4.5% growth rate over 2023. Neurosurgeons topped the list at $749,140, followed by thoracic surgeons at $689,969 and orthopedic surgeons at $679,517.
The three lowest-paid branches were all pediatric: endocrinology at $230,426, rheumatology at $231,574, and infectious diseases at $248,322. Pediatric gastroenterology paid somewhat higher at $298,457.
The largest disparities were seen in hematology and oncology, where adult specialists earned 93% more than their pediatric peers. Pediatric gastroenterology showed an 80% pay gap. There were also substantial pay differences across cardiology, pulmonology, and rheumatology. “These gaps appear to reflect a systemic lag in pay for pediatric specialty care, even as demand for pediatric subspecialists continues to rise,” the report stated.
Practice Setting and Location
Where a doctor practices impacts the bottom line, too: in 2024 the highest compensation reported for a metro area was in Rochester, Minnesota (the Mayo Clinic effect?), at $495,532, while the lowest reported was in Durham-Chapel Hill, North Carolina, at $368,782. St. Louis, Missouri ($484,883) and Los Angeles, California ($470,198) were 2nd and 3rd at the top of the list. Rochester, Minnesota, also emerged as best for annual compensation after cost-of-living adjustment, while Boston, Massachusetts, occupied the bottom rung.
The Gender Effect
With a women’s pay increase in 2024 of just 1.7%, the gender gap returned to its 2022-level disparity of 26%, with women physicians earning an average of $120,917 less than men after adjusting for specialty, location, and years of experience.
Doximity’s analysis of data from 2014 to 2019 estimated that on average men make at least $2 million more than women over the course of a 40-year career. This gap is often attributed to the fewer hours worked by female physician with their generally heavier familial responsibilities, “but Doximity’s gender wage gap analysis controls for the number of hours worked and career stage, along with specialty, work type, employment status, region, and credentials,” Phull said.
Women physicians had lower average earnings than men physicians across all specialties, a trend consistent with prior years. As a percentage of pay, the largest gender disparity was seen in pediatric nephrology (16.5%), a specialty that in fact saw the largest annual growth in physician pay. Neurosurgery had the smallest gender gap at 11.3%, while infectious diseases came in at 11.5% and oncology at 12%.
According to Maria T. Abreu, MD, AGAF, executive director of the F. Widjaja Inflammatory Bowel Disease Institute at Cedars-Sinai Medical Center in Los Angeles and past president of AGA, the remuneration gender gap in gastroenterology is being taken seriously by AGA and several other GI societies. “The discrepancies in pay start from the beginning and therefore are magnified over time. We are helping to empower women to negotiate better as well as to gather data on the roots of inequity, she told GI & Hepatology News.
The AGA Women’s Committee has developed a project to support the advancement of women in gastroenterology, Abreu said. The initiative, which includes the AGA Gender Equity Framework and Gender Equity Road Map. focuses attention on disparities in the workplace and promotes opportunities for women’s leadership, career advancement, mentorship and physician health and wellness, she added.
Are these disparities due mainly to the “motherhood penalty,” with career interruption and time lost to maternity leave and fewer hours worked owing to the greater parenting burden of physician mothers? Or are they due to the systemic effects of gender expectations around compensation?
Hours worked appear to be a factor. A 2017 study of dual physician couples found that among childless respondents men worked an average of 57 hours and women 52 hours weekly. Compared with childless men, men with children worked similar numbers of hours weekly. However, compared with childless physicians, mothers worked significantly fewer hours – roughly 40 to 43 hours weekly – depending on the age of their youngest child.
Abreu pushed back on this stereotype. “Most women physicians, including gastroenterologists, do not take the maternity leave they are allowed because they are concerned about burdening their colleagues,” she said. “Thus, it is unlikely to explain the disparities. Many systemic issues remain challenging, but we want women to be empowered to advocate for themselves at the time of hiring and along the arc of their career paths.”
In Abreu’s view, having women assume more leadership roles in the field of gastroenterology provides an opportunity to focus on reducing the disparities in compensation.
Regardless of gender, among all physicians surveyed, autonomy and work-life balance appeared to be a high priority: 77% of doctors said they would be willing to accept or have already accepted lower pay for more autonomy or work-life balance. “Overwork appears to be especially prevalent among women physicians,” said Phull, noting that 91% of women respondents reported being overworked compared with 80% of men. “This overwork has compelled 74% of women to consider making a career change, compared with 62% of men.” Differences emerged among specialties as well: 90% of primary care physicians said they are overworked compared with 84% of surgeons and 83% of non-surgical specialists.
Looking ahead, the report raised an important question. Are we relying too heavily on physicians rather than addressing the underlying need for policies that support a healthier, more sustainable future for all? “Building that future will take more than physician dedication alone,” Phull said. “It will require meaningful collaboration across the entire health care ecosystem – including health systems, hospitals, payors, and policymakers. And physicians must not only have a voice in shaping the path forward; they must have a seat at the table.”
Abreu reported no conflicts of interest in regard to her comments.
Direct Care Dermatology: Weighing the Pros and Cons for the Early-Career Physician
Direct Care Dermatology: Weighing the Pros and Cons for the Early-Career Physician
As the health care landscape continues to shift, direct care (also known as direct pay) models have emerged as attractive alternatives to traditional insurance-based practice. For dermatology residents poised to enter the workforce, the direct care model offers potential advantages in autonomy, patient relationships, and work-life balance, but not without considerable risks and operational challenges. This article explores the key benefits and drawbacks of starting a direct care dermatology practice, providing a framework to help early-career dermatologists determine whether this path aligns with their personal and professional goals.
The transition from dermatology residency to clinical practice allows for a variety of paths, from large academic institutions to private practice to corporate entities (private equity–owned groups). In recent years, the direct care model has gained traction, particularly among physicians seeking greater autonomy and a more sustainable pace of practice.
Direct care dermatology practices operate outside the constraints of third-party payers, offering patients transparent pricing and direct access to care in exchange for fees paid out of pocket. By eliminating insurance companies as the middleman, it allows for less overhead, longer visits with patients, and increased access to care; however, though this model may seem appealing, direct care practices are not without their own set of challenges, especially amid rising concerns over physician burnout and administrative burden.
This article explores the key benefits and drawbacks of starting a direct care dermatology practice, providing a framework to help early-career dermatologists determine whether this path aligns with their personal and professional goals.
Despite its appeal, starting a direct care practice is not without substantial risks and hurdles—particularly for residents just out of training. These challenges include financial risks and startup costs, market uncertainty, lack of mentorship or support, and limitations in treating complex dermatologic conditions.
Before committing to practicing via a direct care model, dermatology residents should reflect on the following:
- Risk tolerance: Are you comfortable navigating the business and financial risk?
- Location: Does your target community have patients willing and able to pay out of pocket?
- Scope of interest: Will a direct care practice align with your clinical passions?
- Support systems: Do you have access to mentors, legal and financial advisors, and operational support?
- Long-term goals: Are you building a lifestyle practice, a scalable business, or a stepping stone to a future opportunity?
Ultimately, the decision to pursue a direct care model requires careful reflection on personal values, financial preparedness, and the unique needs of the community one intends to serve.
The direct care dermatology model offers an appealing alternative to traditional practice, especially for those prioritizing autonomy, patient connection, and work-life balance; however, it demands an entrepreneurial spirit as well as careful planning and an acceptance of financial uncertainty—factors that may pose challenges for new graduates. For dermatology residents, the decision to pursue direct care should be grounded in personal values, practical considerations, and a clear understanding of both the opportunities and limitations of this evolving practice model.
- Sinsky CA, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med.
- Dorrell DN, Feldman S, Wei-ting Huang W. The most common causes of burnout among US academic dermatologists based on a survey study. J Am Acad of Dermatol. 2019;81:269-270.
- Carlasare LE. Defining the place of direct primary care in a value-based care system. WMJ. 2018;117:106-110.
As the health care landscape continues to shift, direct care (also known as direct pay) models have emerged as attractive alternatives to traditional insurance-based practice. For dermatology residents poised to enter the workforce, the direct care model offers potential advantages in autonomy, patient relationships, and work-life balance, but not without considerable risks and operational challenges. This article explores the key benefits and drawbacks of starting a direct care dermatology practice, providing a framework to help early-career dermatologists determine whether this path aligns with their personal and professional goals.
The transition from dermatology residency to clinical practice allows for a variety of paths, from large academic institutions to private practice to corporate entities (private equity–owned groups). In recent years, the direct care model has gained traction, particularly among physicians seeking greater autonomy and a more sustainable pace of practice.
Direct care dermatology practices operate outside the constraints of third-party payers, offering patients transparent pricing and direct access to care in exchange for fees paid out of pocket. By eliminating insurance companies as the middleman, it allows for less overhead, longer visits with patients, and increased access to care; however, though this model may seem appealing, direct care practices are not without their own set of challenges, especially amid rising concerns over physician burnout and administrative burden.
This article explores the key benefits and drawbacks of starting a direct care dermatology practice, providing a framework to help early-career dermatologists determine whether this path aligns with their personal and professional goals.
Despite its appeal, starting a direct care practice is not without substantial risks and hurdles—particularly for residents just out of training. These challenges include financial risks and startup costs, market uncertainty, lack of mentorship or support, and limitations in treating complex dermatologic conditions.
Before committing to practicing via a direct care model, dermatology residents should reflect on the following:
- Risk tolerance: Are you comfortable navigating the business and financial risk?
- Location: Does your target community have patients willing and able to pay out of pocket?
- Scope of interest: Will a direct care practice align with your clinical passions?
- Support systems: Do you have access to mentors, legal and financial advisors, and operational support?
- Long-term goals: Are you building a lifestyle practice, a scalable business, or a stepping stone to a future opportunity?
Ultimately, the decision to pursue a direct care model requires careful reflection on personal values, financial preparedness, and the unique needs of the community one intends to serve.
The direct care dermatology model offers an appealing alternative to traditional practice, especially for those prioritizing autonomy, patient connection, and work-life balance; however, it demands an entrepreneurial spirit as well as careful planning and an acceptance of financial uncertainty—factors that may pose challenges for new graduates. For dermatology residents, the decision to pursue direct care should be grounded in personal values, practical considerations, and a clear understanding of both the opportunities and limitations of this evolving practice model.
As the health care landscape continues to shift, direct care (also known as direct pay) models have emerged as attractive alternatives to traditional insurance-based practice. For dermatology residents poised to enter the workforce, the direct care model offers potential advantages in autonomy, patient relationships, and work-life balance, but not without considerable risks and operational challenges. This article explores the key benefits and drawbacks of starting a direct care dermatology practice, providing a framework to help early-career dermatologists determine whether this path aligns with their personal and professional goals.
The transition from dermatology residency to clinical practice allows for a variety of paths, from large academic institutions to private practice to corporate entities (private equity–owned groups). In recent years, the direct care model has gained traction, particularly among physicians seeking greater autonomy and a more sustainable pace of practice.
Direct care dermatology practices operate outside the constraints of third-party payers, offering patients transparent pricing and direct access to care in exchange for fees paid out of pocket. By eliminating insurance companies as the middleman, it allows for less overhead, longer visits with patients, and increased access to care; however, though this model may seem appealing, direct care practices are not without their own set of challenges, especially amid rising concerns over physician burnout and administrative burden.
This article explores the key benefits and drawbacks of starting a direct care dermatology practice, providing a framework to help early-career dermatologists determine whether this path aligns with their personal and professional goals.
Despite its appeal, starting a direct care practice is not without substantial risks and hurdles—particularly for residents just out of training. These challenges include financial risks and startup costs, market uncertainty, lack of mentorship or support, and limitations in treating complex dermatologic conditions.
Before committing to practicing via a direct care model, dermatology residents should reflect on the following:
- Risk tolerance: Are you comfortable navigating the business and financial risk?
- Location: Does your target community have patients willing and able to pay out of pocket?
- Scope of interest: Will a direct care practice align with your clinical passions?
- Support systems: Do you have access to mentors, legal and financial advisors, and operational support?
- Long-term goals: Are you building a lifestyle practice, a scalable business, or a stepping stone to a future opportunity?
Ultimately, the decision to pursue a direct care model requires careful reflection on personal values, financial preparedness, and the unique needs of the community one intends to serve.
The direct care dermatology model offers an appealing alternative to traditional practice, especially for those prioritizing autonomy, patient connection, and work-life balance; however, it demands an entrepreneurial spirit as well as careful planning and an acceptance of financial uncertainty—factors that may pose challenges for new graduates. For dermatology residents, the decision to pursue direct care should be grounded in personal values, practical considerations, and a clear understanding of both the opportunities and limitations of this evolving practice model.
- Sinsky CA, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med.
- Dorrell DN, Feldman S, Wei-ting Huang W. The most common causes of burnout among US academic dermatologists based on a survey study. J Am Acad of Dermatol. 2019;81:269-270.
- Carlasare LE. Defining the place of direct primary care in a value-based care system. WMJ. 2018;117:106-110.
- Sinsky CA, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med.
- Dorrell DN, Feldman S, Wei-ting Huang W. The most common causes of burnout among US academic dermatologists based on a survey study. J Am Acad of Dermatol. 2019;81:269-270.
- Carlasare LE. Defining the place of direct primary care in a value-based care system. WMJ. 2018;117:106-110.
Direct Care Dermatology: Weighing the Pros and Cons for the Early-Career Physician
Direct Care Dermatology: Weighing the Pros and Cons for the Early-Career Physician
PRACTICE POINTS
- Direct care practices may be the new horizon of health care.
- Starting a direct care practice offers autonomy but demands entrepreneurial readiness.
- New dermatologists can enjoy control over scheduling, pricing, and patient care, but success requires business acumen, financial planning, and comfort with risk.















