User login
COVID-19’s religious strain: Differentiating spirituality from pathology
As the world grapples with the coronavirus disease 2019 (COVID-19) pandemic, the search for answers, comfort, how to cope, and how to make sense of it all has become paramount. People commonly turn to their faith in times of crisis, but this recent global public health emergency is unlike many have ever seen or could have imagined.1 What happens when the well-intentioned journey for spiritual insight intersects with psychiatric symptomatology? Where does the line between these phenomena get crossed? As a psychiatric resident and person who was raised in the Pentecostal faith, I have observed faith and psychopathology come to a head in the last 6 months. COVID-19 has dealt a religious strain of undocumented cases; I hope to shed light on the topic by sharing my experience of navigating the assessment and treatment plan of patients with psychiatric symptoms whose spiritual beliefs are a cornerstone of life.
Piety, or pathology?
The following approaches have helped me to identify what is driven by faith vs what is psychopathology:
While taking the patient history. Obtaining a history from a patient who professes to have strong spiritual beliefs and presents with psychiatric symptoms is similar to a standard patient interview, but pay special attention to how the patient came to the emergency department. Was there a family member, friend, or emergency medical services present at that time? During the interview, patients often appear “normal,” which may lead a clinician to question the reason for the consult, yet considering the recent events preceding the presentation will be a good place to start gathering the appropriate information for investigation.
Next, compare the patient’s recent daily functioning with his/her baseline. If this information comes solely from the patient, it may be skewed, so try to retrieve information from a collateral source. If the patient was accompanied by someone, request permission from the patient to speak with him/her. It may also be best in some instances to speak with the collateral source out of earshot of the patient. Be aware that collateral information that comes from just one source also could be biased, so search for additional contacts to help acquire a comprehensive representation of the circumstances.
Information about a patient could come from a faith leader because people often rely on their faith leaders when they are ill, in need of support, or in crisis.2 Faith leaders may have valuable information and insight into the patient and the history of the patient’s illness. In addition, diverse sources of collateral reports may be helpful because specific spiritual views and practices can vary even within one family or congregation. What may be an abnormal practice to some followers may be normal for others.3 When approaching these situations with parishioners, it is essential to maintain confidentiality.
While performing the clinical examination. As with any psychiatric diagnosis, other causative factors (metabolic and organic) need to be ruled out. Also, assess for the use of mood-altering substances. The patient may express offense or resistance to such questions, but maintain a matter-of-fact approach and explain that assessment for substance use is a routine part of the clinical examination. Approximately 18% of people in the United States with psychiatric disorders have a comorbid substance use disorder.4 However, keep in mind that a patient who refuses substance use screening is not necessarily hiding something. The road to being thorough may lead to strained rapport with the patient, and this risk must be balanced with providing the best care. As in any other clinical situation, seek evidence to both verify and clarify information without being deterred by a patient’s vocalization of spiritual tenants.
Learn about your patients’ beliefs
Do not feel defeated if you find these interviews difficult. Religion and symptomatology can overlap and fluctuate within the same faith group, which can make these types of assessments complex.5 In an effort to understand the patient more clearly, be sensitive to their spiritual practices and receptive to learning about unfamiliar spiritual beliefs. Be transparent about not knowing a specific belief or practice, and exhibit humility. Most patients are open to sharing their religious/spiritual views with a clinician who is sincere about wanting insight. Understanding the value of spiritual care is an important skill that many medical practitioners often lack.6 This understanding is especially critical when patients express worries related to the COVID-19 pandemic and how they are coping.
Continue to: Integrate your patient's spiritual requests
Integrate your patient’s spiritual requests
If you are comfortable with certain practices that do not compromise your values or beliefs or put a patient at risk, try to integrate your patients’ spiritual request(s) in their care. For a patient who serves a higher power, admitting to a problem (eg, fears related to COVID-19) or seeking professional help for symptoms (eg, anxiety, depression) may imply spiritual doubt. Patients may believe that seeking professional assistance means they are questioning the omnipotence of their deity to prevent or heal a condition. While spiritual distress can stimulate changes in behavior, it may not be pathological.
To avoid misdiagnosis, refer to the description “V62.89 (Z65.8) Religious or Spiritual Problem” in the DSM-5.7 If you find that it is a discord in faith that is affecting the patient’s presentation, and that this has not caused a psychiatric disorder, document this appropriately and provide the necessary resources to continue supporting the patient holistically.
1. Dein S, Loewenthal K, Lewis CA, et al. COVID-19, mental health and religion: an agenda for future research. Mental Health, Religion & Culture. 2020;23(1):1-9.
2. American Psychiatric Association Foundation. Mental health: a guide for faith leaders. Arlington, VA: American Psychiatric Association Foundation; 2018.
3. Johnson CV, Friedman HL. Enlightened or delusional? Differentiating religious, spiritual, and transpersonal experiences from psychopathology. Journal of Humanistic Psychology. 2008;48(4):505-527.
4. Han B, Compton WM, Blanco C, et al. Prevalence, treatment, and unmet treatment needs of US adults with mental health and substance use disorders. Health Aff (Millwood). 2017;36(10):1739-1747.
5. Menezes Jr A, Moreira-Almeida A. Differential diagnosis between spiritual experiences and mental disorders of religious content. Rev Psiq Clín. 2009;36(2):75-82.
6. Best M, Butow P, Olver I. Doctors discussing religion and spirituality: a systematic literature review. Palliat Med. 2016;30(4):327-337.
7. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:725.
As the world grapples with the coronavirus disease 2019 (COVID-19) pandemic, the search for answers, comfort, how to cope, and how to make sense of it all has become paramount. People commonly turn to their faith in times of crisis, but this recent global public health emergency is unlike many have ever seen or could have imagined.1 What happens when the well-intentioned journey for spiritual insight intersects with psychiatric symptomatology? Where does the line between these phenomena get crossed? As a psychiatric resident and person who was raised in the Pentecostal faith, I have observed faith and psychopathology come to a head in the last 6 months. COVID-19 has dealt a religious strain of undocumented cases; I hope to shed light on the topic by sharing my experience of navigating the assessment and treatment plan of patients with psychiatric symptoms whose spiritual beliefs are a cornerstone of life.
Piety, or pathology?
The following approaches have helped me to identify what is driven by faith vs what is psychopathology:
While taking the patient history. Obtaining a history from a patient who professes to have strong spiritual beliefs and presents with psychiatric symptoms is similar to a standard patient interview, but pay special attention to how the patient came to the emergency department. Was there a family member, friend, or emergency medical services present at that time? During the interview, patients often appear “normal,” which may lead a clinician to question the reason for the consult, yet considering the recent events preceding the presentation will be a good place to start gathering the appropriate information for investigation.
Next, compare the patient’s recent daily functioning with his/her baseline. If this information comes solely from the patient, it may be skewed, so try to retrieve information from a collateral source. If the patient was accompanied by someone, request permission from the patient to speak with him/her. It may also be best in some instances to speak with the collateral source out of earshot of the patient. Be aware that collateral information that comes from just one source also could be biased, so search for additional contacts to help acquire a comprehensive representation of the circumstances.
Information about a patient could come from a faith leader because people often rely on their faith leaders when they are ill, in need of support, or in crisis.2 Faith leaders may have valuable information and insight into the patient and the history of the patient’s illness. In addition, diverse sources of collateral reports may be helpful because specific spiritual views and practices can vary even within one family or congregation. What may be an abnormal practice to some followers may be normal for others.3 When approaching these situations with parishioners, it is essential to maintain confidentiality.
While performing the clinical examination. As with any psychiatric diagnosis, other causative factors (metabolic and organic) need to be ruled out. Also, assess for the use of mood-altering substances. The patient may express offense or resistance to such questions, but maintain a matter-of-fact approach and explain that assessment for substance use is a routine part of the clinical examination. Approximately 18% of people in the United States with psychiatric disorders have a comorbid substance use disorder.4 However, keep in mind that a patient who refuses substance use screening is not necessarily hiding something. The road to being thorough may lead to strained rapport with the patient, and this risk must be balanced with providing the best care. As in any other clinical situation, seek evidence to both verify and clarify information without being deterred by a patient’s vocalization of spiritual tenants.
Learn about your patients’ beliefs
Do not feel defeated if you find these interviews difficult. Religion and symptomatology can overlap and fluctuate within the same faith group, which can make these types of assessments complex.5 In an effort to understand the patient more clearly, be sensitive to their spiritual practices and receptive to learning about unfamiliar spiritual beliefs. Be transparent about not knowing a specific belief or practice, and exhibit humility. Most patients are open to sharing their religious/spiritual views with a clinician who is sincere about wanting insight. Understanding the value of spiritual care is an important skill that many medical practitioners often lack.6 This understanding is especially critical when patients express worries related to the COVID-19 pandemic and how they are coping.
Continue to: Integrate your patient's spiritual requests
Integrate your patient’s spiritual requests
If you are comfortable with certain practices that do not compromise your values or beliefs or put a patient at risk, try to integrate your patients’ spiritual request(s) in their care. For a patient who serves a higher power, admitting to a problem (eg, fears related to COVID-19) or seeking professional help for symptoms (eg, anxiety, depression) may imply spiritual doubt. Patients may believe that seeking professional assistance means they are questioning the omnipotence of their deity to prevent or heal a condition. While spiritual distress can stimulate changes in behavior, it may not be pathological.
To avoid misdiagnosis, refer to the description “V62.89 (Z65.8) Religious or Spiritual Problem” in the DSM-5.7 If you find that it is a discord in faith that is affecting the patient’s presentation, and that this has not caused a psychiatric disorder, document this appropriately and provide the necessary resources to continue supporting the patient holistically.
As the world grapples with the coronavirus disease 2019 (COVID-19) pandemic, the search for answers, comfort, how to cope, and how to make sense of it all has become paramount. People commonly turn to their faith in times of crisis, but this recent global public health emergency is unlike many have ever seen or could have imagined.1 What happens when the well-intentioned journey for spiritual insight intersects with psychiatric symptomatology? Where does the line between these phenomena get crossed? As a psychiatric resident and person who was raised in the Pentecostal faith, I have observed faith and psychopathology come to a head in the last 6 months. COVID-19 has dealt a religious strain of undocumented cases; I hope to shed light on the topic by sharing my experience of navigating the assessment and treatment plan of patients with psychiatric symptoms whose spiritual beliefs are a cornerstone of life.
Piety, or pathology?
The following approaches have helped me to identify what is driven by faith vs what is psychopathology:
While taking the patient history. Obtaining a history from a patient who professes to have strong spiritual beliefs and presents with psychiatric symptoms is similar to a standard patient interview, but pay special attention to how the patient came to the emergency department. Was there a family member, friend, or emergency medical services present at that time? During the interview, patients often appear “normal,” which may lead a clinician to question the reason for the consult, yet considering the recent events preceding the presentation will be a good place to start gathering the appropriate information for investigation.
Next, compare the patient’s recent daily functioning with his/her baseline. If this information comes solely from the patient, it may be skewed, so try to retrieve information from a collateral source. If the patient was accompanied by someone, request permission from the patient to speak with him/her. It may also be best in some instances to speak with the collateral source out of earshot of the patient. Be aware that collateral information that comes from just one source also could be biased, so search for additional contacts to help acquire a comprehensive representation of the circumstances.
Information about a patient could come from a faith leader because people often rely on their faith leaders when they are ill, in need of support, or in crisis.2 Faith leaders may have valuable information and insight into the patient and the history of the patient’s illness. In addition, diverse sources of collateral reports may be helpful because specific spiritual views and practices can vary even within one family or congregation. What may be an abnormal practice to some followers may be normal for others.3 When approaching these situations with parishioners, it is essential to maintain confidentiality.
While performing the clinical examination. As with any psychiatric diagnosis, other causative factors (metabolic and organic) need to be ruled out. Also, assess for the use of mood-altering substances. The patient may express offense or resistance to such questions, but maintain a matter-of-fact approach and explain that assessment for substance use is a routine part of the clinical examination. Approximately 18% of people in the United States with psychiatric disorders have a comorbid substance use disorder.4 However, keep in mind that a patient who refuses substance use screening is not necessarily hiding something. The road to being thorough may lead to strained rapport with the patient, and this risk must be balanced with providing the best care. As in any other clinical situation, seek evidence to both verify and clarify information without being deterred by a patient’s vocalization of spiritual tenants.
Learn about your patients’ beliefs
Do not feel defeated if you find these interviews difficult. Religion and symptomatology can overlap and fluctuate within the same faith group, which can make these types of assessments complex.5 In an effort to understand the patient more clearly, be sensitive to their spiritual practices and receptive to learning about unfamiliar spiritual beliefs. Be transparent about not knowing a specific belief or practice, and exhibit humility. Most patients are open to sharing their religious/spiritual views with a clinician who is sincere about wanting insight. Understanding the value of spiritual care is an important skill that many medical practitioners often lack.6 This understanding is especially critical when patients express worries related to the COVID-19 pandemic and how they are coping.
Continue to: Integrate your patient's spiritual requests
Integrate your patient’s spiritual requests
If you are comfortable with certain practices that do not compromise your values or beliefs or put a patient at risk, try to integrate your patients’ spiritual request(s) in their care. For a patient who serves a higher power, admitting to a problem (eg, fears related to COVID-19) or seeking professional help for symptoms (eg, anxiety, depression) may imply spiritual doubt. Patients may believe that seeking professional assistance means they are questioning the omnipotence of their deity to prevent or heal a condition. While spiritual distress can stimulate changes in behavior, it may not be pathological.
To avoid misdiagnosis, refer to the description “V62.89 (Z65.8) Religious or Spiritual Problem” in the DSM-5.7 If you find that it is a discord in faith that is affecting the patient’s presentation, and that this has not caused a psychiatric disorder, document this appropriately and provide the necessary resources to continue supporting the patient holistically.
1. Dein S, Loewenthal K, Lewis CA, et al. COVID-19, mental health and religion: an agenda for future research. Mental Health, Religion & Culture. 2020;23(1):1-9.
2. American Psychiatric Association Foundation. Mental health: a guide for faith leaders. Arlington, VA: American Psychiatric Association Foundation; 2018.
3. Johnson CV, Friedman HL. Enlightened or delusional? Differentiating religious, spiritual, and transpersonal experiences from psychopathology. Journal of Humanistic Psychology. 2008;48(4):505-527.
4. Han B, Compton WM, Blanco C, et al. Prevalence, treatment, and unmet treatment needs of US adults with mental health and substance use disorders. Health Aff (Millwood). 2017;36(10):1739-1747.
5. Menezes Jr A, Moreira-Almeida A. Differential diagnosis between spiritual experiences and mental disorders of religious content. Rev Psiq Clín. 2009;36(2):75-82.
6. Best M, Butow P, Olver I. Doctors discussing religion and spirituality: a systematic literature review. Palliat Med. 2016;30(4):327-337.
7. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:725.
1. Dein S, Loewenthal K, Lewis CA, et al. COVID-19, mental health and religion: an agenda for future research. Mental Health, Religion & Culture. 2020;23(1):1-9.
2. American Psychiatric Association Foundation. Mental health: a guide for faith leaders. Arlington, VA: American Psychiatric Association Foundation; 2018.
3. Johnson CV, Friedman HL. Enlightened or delusional? Differentiating religious, spiritual, and transpersonal experiences from psychopathology. Journal of Humanistic Psychology. 2008;48(4):505-527.
4. Han B, Compton WM, Blanco C, et al. Prevalence, treatment, and unmet treatment needs of US adults with mental health and substance use disorders. Health Aff (Millwood). 2017;36(10):1739-1747.
5. Menezes Jr A, Moreira-Almeida A. Differential diagnosis between spiritual experiences and mental disorders of religious content. Rev Psiq Clín. 2009;36(2):75-82.
6. Best M, Butow P, Olver I. Doctors discussing religion and spirituality: a systematic literature review. Palliat Med. 2016;30(4):327-337.
7. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:725.
How much longer?
SHM has changed direction as needed during the pandemic
“How much longer?” As a kid, I can remember the long holiday car ride with my parents from my home in Annapolis, Md., to Upstate New York where my grandparents lived. At the time, the ride felt like an eternity: endless miles of frozen landscape, limited food, and a brother who constantly crossed over the invisible line that was my side of the car.
We made our parents crazy asking, “how much longer?” every few minutes. This was the late 1970s, with no GPS or Google Maps to give you arrival times to the minute, traffic warnings, or reroutes when the inevitable delays occurred. We just plowed ahead, and my parents’ answer was always something vague like, “in a few hours” or “we’re about halfway through.” They did not know when we’d arrive with certainty either.
We at SHM have that same feeling about the pandemic. How much longer? No one can tell us when the COVID-19 threat will abate. The experts’ answers are understandably vague, and the tools for forecasting are non-existent. Months? That is the best we know for now.
At SHM, we believe we will make it through this journey by adapting to roadblocks, providing tools for success to our professional community, and identifying opportunities for us to connect with each other, even if that means virtually.
Like the rest of the planet, the spring of 2020 hit SHM with a shock. Hospital Medicine 2020 (HM20) in San Diego was shaping up to be the largest Annual Conference SHM ever had, the Pediatric Hospital Medicine 2020 (PHM20) conference was well planned and expected to be a huge success, regional SHM chapters were meeting (and growing), and membership was thriving. I was transitioning out of my roles at Johns Hopkins and looking forward to my new role as CEO of SHM. All in all, March 2020 began with a fantastic outlook.
Wow, what a difference a few weeks made. We watched as the pandemic spread across regions of the country, concerned for the wellbeing of our patients and our hospitalists. We saw how our members were at the forefront of patient care during this crisis and understood that SHM had to adapt rapidly to meet their needs in real time.
By May, SHM had canceled HM20, Chapter activity was halted, PHM20 was on its way to being canceled, SHM committee work was put on hold, and I was spending my last few months at Hopkins as the chief medical officer at the Baltimore Convention Center Field Hospital (which we got up and running in less than a month)! Whew.
But just like my dad could pivot our 1970s Chevy station wagon around a traffic jam in a flash, so too did SHM leadership start navigating around the COVID-19 landscape. As soon as HM20 was canceled, SHM immediately began planning for a virtual offering in August. We had hoped to attract at least 100 attendees and we were thrilled to have more than 1,000! PHM20 was switched from an in-person to a virtual meeting with 634 attendees. We launched numerous COVID-19 webinars and made our clinical and educational offerings open access. Our Public Policy Committee was active around both COVID-19 and hospitalist-related topics – immigration, telehealth, wellbeing, and financial impacts, to name a few. (And I even met with the POTUS & advocated for PPE.) The Journal of Hospital Medicine worked with authors to get important publications out at record speed. And of course, The Hospitalist connected all of us to our professional leaders and experts.
By the fall of 2020, SHM had actively adjusted to the “new normal” of this pandemic: SHM staff have settled into their new “work from home” environments, SHM Chapters are connecting members in the virtual world, SHM’s 2021 Annual Conference will be all virtual – rebranded as “SHM Converge” – and the State of Hospital Medicine Report (our every-other-year source for trends in hospital medicine) now has a COVID-19 supplement, which was developed at lightning speed. Even our SHM Board of Directors is meeting virtually! All this while advancing the routine work at SHM, which never faltered. Our work on resources for quality improvement, the opioid epidemic, wellbeing, diversity, equity and inclusion (DEI), leadership, professional development, advocacy, and so much more is as active as ever.
I don’t know how much longer we have on this very long pandemic journey, so I’ll use my father’s answer of “we’re about halfway through.” We have been immersed in it for months already, with months still ahead. But regardless of the upcoming twists and turns COVID-19 forces you, our patients, and our larger society to take, SHM is ready to change direction faster than a 1970s Chevy. The SHM staff, leadership, and members will be sure that hospitalists receive the tools to navigate these unprecedented times. Our patients need our skills to get through this as safely as possible. While we may not be able to tell them “how much longer,” we can certainly be prepared for the long road ahead as we begin 2021.
Dr. Howell is CEO of the Society of Hospital Medicine.
SHM has changed direction as needed during the pandemic
SHM has changed direction as needed during the pandemic
“How much longer?” As a kid, I can remember the long holiday car ride with my parents from my home in Annapolis, Md., to Upstate New York where my grandparents lived. At the time, the ride felt like an eternity: endless miles of frozen landscape, limited food, and a brother who constantly crossed over the invisible line that was my side of the car.
We made our parents crazy asking, “how much longer?” every few minutes. This was the late 1970s, with no GPS or Google Maps to give you arrival times to the minute, traffic warnings, or reroutes when the inevitable delays occurred. We just plowed ahead, and my parents’ answer was always something vague like, “in a few hours” or “we’re about halfway through.” They did not know when we’d arrive with certainty either.
We at SHM have that same feeling about the pandemic. How much longer? No one can tell us when the COVID-19 threat will abate. The experts’ answers are understandably vague, and the tools for forecasting are non-existent. Months? That is the best we know for now.
At SHM, we believe we will make it through this journey by adapting to roadblocks, providing tools for success to our professional community, and identifying opportunities for us to connect with each other, even if that means virtually.
Like the rest of the planet, the spring of 2020 hit SHM with a shock. Hospital Medicine 2020 (HM20) in San Diego was shaping up to be the largest Annual Conference SHM ever had, the Pediatric Hospital Medicine 2020 (PHM20) conference was well planned and expected to be a huge success, regional SHM chapters were meeting (and growing), and membership was thriving. I was transitioning out of my roles at Johns Hopkins and looking forward to my new role as CEO of SHM. All in all, March 2020 began with a fantastic outlook.
Wow, what a difference a few weeks made. We watched as the pandemic spread across regions of the country, concerned for the wellbeing of our patients and our hospitalists. We saw how our members were at the forefront of patient care during this crisis and understood that SHM had to adapt rapidly to meet their needs in real time.
By May, SHM had canceled HM20, Chapter activity was halted, PHM20 was on its way to being canceled, SHM committee work was put on hold, and I was spending my last few months at Hopkins as the chief medical officer at the Baltimore Convention Center Field Hospital (which we got up and running in less than a month)! Whew.
But just like my dad could pivot our 1970s Chevy station wagon around a traffic jam in a flash, so too did SHM leadership start navigating around the COVID-19 landscape. As soon as HM20 was canceled, SHM immediately began planning for a virtual offering in August. We had hoped to attract at least 100 attendees and we were thrilled to have more than 1,000! PHM20 was switched from an in-person to a virtual meeting with 634 attendees. We launched numerous COVID-19 webinars and made our clinical and educational offerings open access. Our Public Policy Committee was active around both COVID-19 and hospitalist-related topics – immigration, telehealth, wellbeing, and financial impacts, to name a few. (And I even met with the POTUS & advocated for PPE.) The Journal of Hospital Medicine worked with authors to get important publications out at record speed. And of course, The Hospitalist connected all of us to our professional leaders and experts.
By the fall of 2020, SHM had actively adjusted to the “new normal” of this pandemic: SHM staff have settled into their new “work from home” environments, SHM Chapters are connecting members in the virtual world, SHM’s 2021 Annual Conference will be all virtual – rebranded as “SHM Converge” – and the State of Hospital Medicine Report (our every-other-year source for trends in hospital medicine) now has a COVID-19 supplement, which was developed at lightning speed. Even our SHM Board of Directors is meeting virtually! All this while advancing the routine work at SHM, which never faltered. Our work on resources for quality improvement, the opioid epidemic, wellbeing, diversity, equity and inclusion (DEI), leadership, professional development, advocacy, and so much more is as active as ever.
I don’t know how much longer we have on this very long pandemic journey, so I’ll use my father’s answer of “we’re about halfway through.” We have been immersed in it for months already, with months still ahead. But regardless of the upcoming twists and turns COVID-19 forces you, our patients, and our larger society to take, SHM is ready to change direction faster than a 1970s Chevy. The SHM staff, leadership, and members will be sure that hospitalists receive the tools to navigate these unprecedented times. Our patients need our skills to get through this as safely as possible. While we may not be able to tell them “how much longer,” we can certainly be prepared for the long road ahead as we begin 2021.
Dr. Howell is CEO of the Society of Hospital Medicine.
“How much longer?” As a kid, I can remember the long holiday car ride with my parents from my home in Annapolis, Md., to Upstate New York where my grandparents lived. At the time, the ride felt like an eternity: endless miles of frozen landscape, limited food, and a brother who constantly crossed over the invisible line that was my side of the car.
We made our parents crazy asking, “how much longer?” every few minutes. This was the late 1970s, with no GPS or Google Maps to give you arrival times to the minute, traffic warnings, or reroutes when the inevitable delays occurred. We just plowed ahead, and my parents’ answer was always something vague like, “in a few hours” or “we’re about halfway through.” They did not know when we’d arrive with certainty either.
We at SHM have that same feeling about the pandemic. How much longer? No one can tell us when the COVID-19 threat will abate. The experts’ answers are understandably vague, and the tools for forecasting are non-existent. Months? That is the best we know for now.
At SHM, we believe we will make it through this journey by adapting to roadblocks, providing tools for success to our professional community, and identifying opportunities for us to connect with each other, even if that means virtually.
Like the rest of the planet, the spring of 2020 hit SHM with a shock. Hospital Medicine 2020 (HM20) in San Diego was shaping up to be the largest Annual Conference SHM ever had, the Pediatric Hospital Medicine 2020 (PHM20) conference was well planned and expected to be a huge success, regional SHM chapters were meeting (and growing), and membership was thriving. I was transitioning out of my roles at Johns Hopkins and looking forward to my new role as CEO of SHM. All in all, March 2020 began with a fantastic outlook.
Wow, what a difference a few weeks made. We watched as the pandemic spread across regions of the country, concerned for the wellbeing of our patients and our hospitalists. We saw how our members were at the forefront of patient care during this crisis and understood that SHM had to adapt rapidly to meet their needs in real time.
By May, SHM had canceled HM20, Chapter activity was halted, PHM20 was on its way to being canceled, SHM committee work was put on hold, and I was spending my last few months at Hopkins as the chief medical officer at the Baltimore Convention Center Field Hospital (which we got up and running in less than a month)! Whew.
But just like my dad could pivot our 1970s Chevy station wagon around a traffic jam in a flash, so too did SHM leadership start navigating around the COVID-19 landscape. As soon as HM20 was canceled, SHM immediately began planning for a virtual offering in August. We had hoped to attract at least 100 attendees and we were thrilled to have more than 1,000! PHM20 was switched from an in-person to a virtual meeting with 634 attendees. We launched numerous COVID-19 webinars and made our clinical and educational offerings open access. Our Public Policy Committee was active around both COVID-19 and hospitalist-related topics – immigration, telehealth, wellbeing, and financial impacts, to name a few. (And I even met with the POTUS & advocated for PPE.) The Journal of Hospital Medicine worked with authors to get important publications out at record speed. And of course, The Hospitalist connected all of us to our professional leaders and experts.
By the fall of 2020, SHM had actively adjusted to the “new normal” of this pandemic: SHM staff have settled into their new “work from home” environments, SHM Chapters are connecting members in the virtual world, SHM’s 2021 Annual Conference will be all virtual – rebranded as “SHM Converge” – and the State of Hospital Medicine Report (our every-other-year source for trends in hospital medicine) now has a COVID-19 supplement, which was developed at lightning speed. Even our SHM Board of Directors is meeting virtually! All this while advancing the routine work at SHM, which never faltered. Our work on resources for quality improvement, the opioid epidemic, wellbeing, diversity, equity and inclusion (DEI), leadership, professional development, advocacy, and so much more is as active as ever.
I don’t know how much longer we have on this very long pandemic journey, so I’ll use my father’s answer of “we’re about halfway through.” We have been immersed in it for months already, with months still ahead. But regardless of the upcoming twists and turns COVID-19 forces you, our patients, and our larger society to take, SHM is ready to change direction faster than a 1970s Chevy. The SHM staff, leadership, and members will be sure that hospitalists receive the tools to navigate these unprecedented times. Our patients need our skills to get through this as safely as possible. While we may not be able to tell them “how much longer,” we can certainly be prepared for the long road ahead as we begin 2021.
Dr. Howell is CEO of the Society of Hospital Medicine.
Equitable Post-COVID-19 Care: A Practical Framework to Integrate Health Equity in Diabetes Management
From T1D Exchange, Boston, MA (Dr. Ebekozien, Dr. Odugbesan, and Nicole Rioles); Barbara Davis Center, University of Colorado, Boulder, CO (Dr. Majidi); Cincinnati Children’s Hospital Medical Center, Cincinnati, OH (Dr. Jones); and Nationwide Children’s Hospital, Columbus, OH (Dr. Kamboj)
Health equity has been described as the opportunity for all persons to obtain their highest level of health possible.1 Unfortunately, even with advances in technology and care practices, disparities persist in health care outcomes. Disparities in prevalence, prognosis, and outcomes still exist in diabetes management.2 Non-Hispanic Black and/or Hispanic populations are more likely to have worse glycemic control,3,4 to encounter more barriers in access to care,5 and to have higher levels of acute complications,4 and to use advanced technologies less frequently.4 Diabetes is one of the preexisting conditions that increase morbidity and mortality in COVID-19.6,7 Unfortunately, adverse outcomes from COVID-19 also disproportionately impact a specific vulnerable population.8,9 The urgent transition to managing diabetes remotely during the COVID-19 pandemic may exacerbate long-term inequities because some vulnerable patients might not have access to technology devices necessary for effective remote management.
Here, we describe how quality improvement (QI) tools and principles can be adapted into a framework for advancing health equity. Specifically, we describe a 10-step framework that may be applied in diabetes care management to achieve improvement, using a hypothetical example of increasing use of continuous glucose monitors (CGMs) among patients with type 1 diabetes mellitus.10 This framework was developed to address the literature gap on practical ways health care providers can address inequities using QI principles, and was implemented by 1 of the authors at a local public health department.11 The framework’s iterative and comprehensive design makes it ideal for addressing inequities in chronic diseases like diabetes, which have multiple root causes with no easy solutions. The improvement program pilot received a national model practice award.11,12
10-Step Framework
Step 1: Review program/project baseline data for existing disparities. Diabetes programs and routine QI processes encourage existing data review to determine how effective the current system is working and if the existing process has a predictable pattern.13,14 Our equity-revised framework proposes a more in-depth review to stratify baseline data based on factors that might contribute to inequities, including race, age, income levels, ethnicity, language, sexual orientation, insurance type, and zip code. This process will identify patients not served or unfairly impacted due to socioeconomic factors. For example, using the hypothetical example of improving CGM use, a team completes a preliminary data review and determines that baseline CGM use is 30% in the clinic population. However, in a review to assess for disparities, they also identify that patients on public insurance have a significantly lower CGM uptake of only 15%.
Step 2: Build an equitable project team, including patients with lived experiences. Routine projects typically have clinicians, administrative staff, and analytic staff as members of their team. In a post-COVID-19 world, every team needs to learn directly from people impacted and share decision-making power. The traditional approach to receiving feedback has generally been to collect responses using surveys or focus groups. We propose that individuals/families who are disproportionately impacted be included as active members on QI teams. For example, in the hypothetical example of the CGM project, team members would include patients with type 1 diabetes who are on public insurance and their families.
Step 3: Develop equity-focused goals. The traditional program involves the development of aims that are SMART (specific, measurable, achievable, realistic, time-bound).15 The proposed framework encourages the inclusion of equity-revised goals (SMARTer) using insights from Steps 1 and 2. For example, your typical smart goal might be to increase the percentage of patients using CGM by 20% in 6 months, while a SMARTer goal would be to increase the proportion of patients using CGM by 20% and reduce the disparities among public and private insurance patients by 30% in 6 months.
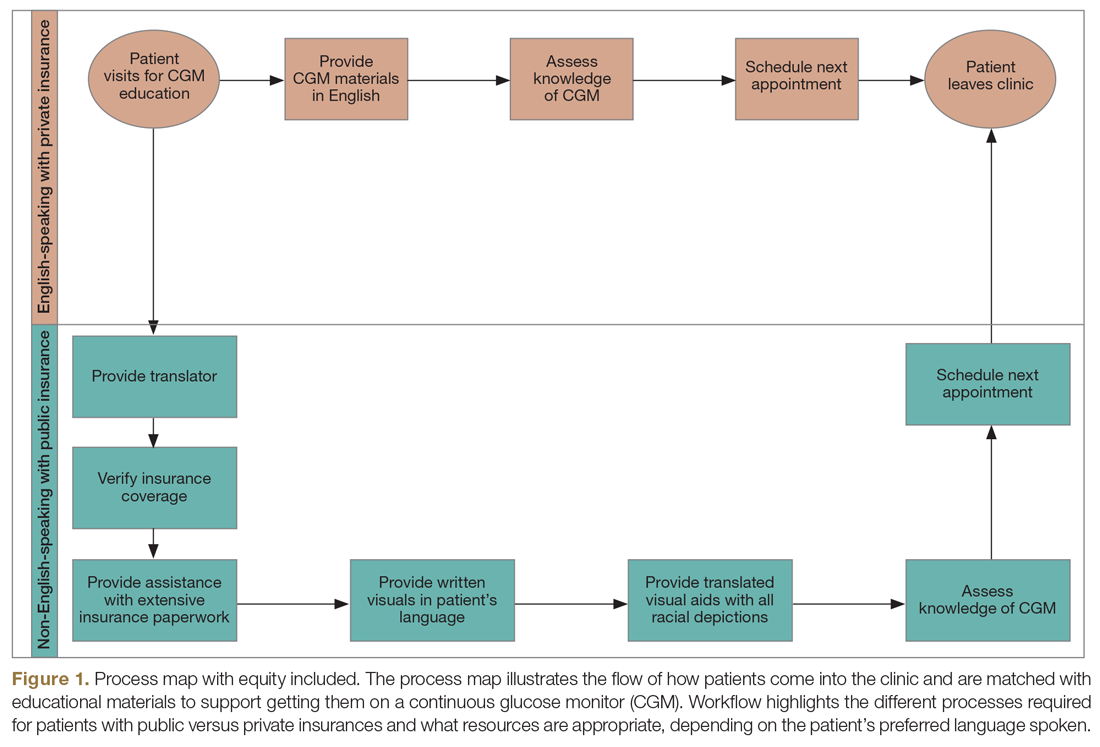
Step 4: Identify inequitable processes/pathways. Traditional QI programs might use a process map or flow diagram to depict the current state of a process visually.16 For example, in Figure 1, the process map diagram depicts some differences in the process for patients with public insurance as opposed to those with private insurance. The framework also advocates for using visual tools like process maps to depict how there might be inequitable pathways in a system. Visually identifying inequitable processes/pathways can help a team see barriers, address challenges, and pilot innovative solutions.
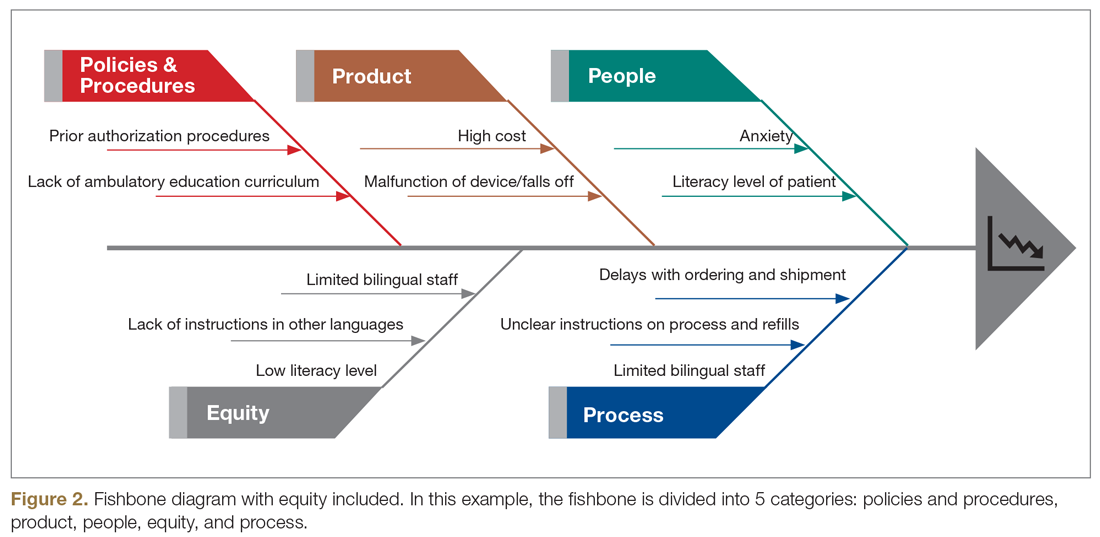
Step 5: Identify how socioeconomic factors are contributing to the current outcome. A good understanding of factors that contribute to the problem is an essential part of finding fundamental solutions. The fishbone diagram16 is a visualization tool used to identify contributing factors. When investigating contributing factors, it is commonplace to identify factors that fit into 1 of 5 categories: people, process, place, product, and policies (5 Ps). An equity-focused process will include equity as a new major factor category, and the socioeconomic impacts that contribute to inequities will be brainstormed and visually represented. For example, in the hypothetical CGM improvement example, an equity contributing factor is extensive CGM application paperwork for patients on public insurance as compared to those on private insurance. Figure 2 shows equity integrated into a fishbone diagram.
Step 6: Brainstorm possible improvements. Potential improvement ideas for the hypothetical CGM example might include redesigning the existing workflow, piloting CGM educational classes, and using a CGM barrier assessment tool to identify and address barriers to adoption.
Step 7: Use the decision matrix with equity as a criterion to prioritize improvement ideas. Decision matrix15 is a great tool that is frequently used to help teams prioritize potential ideas. Project team members must decide what criteria are important in prioritizing ideas to implement. Common criteria include implementation cost, time, and resources, but in addition to the common criteria, the team can specify ”impact on equity” as one of their criteria, alongside other standard criteria like impact.
Step 8: Test one small change at a time. This step is consistent with other traditional improvement models using the Plan, Do, Study, Act (PDSA) model for improvement.17 During this phase, the team should make predictions on the expected impact of the intervention on outcomes. For example, in the hypothetical example, the team predicts that testing and expanding CGM classes will reduce disparities among public versus private health insurance users by 5% and increase overall CGM uptake by 10%.
Step 9: Measure and compare results with predictions to identify inequitable practices or consequences. After each test of change, the team should review the results, including implementation cost considerations, and compare them to the predictions in the earlier step. The team should also document the potential reasons why their predictions were correct or inaccurate, and whether there were any unforeseen outcomes from the intervention.
Step 10: Celebrate small wins and repeat the process. Making fundamental and equitable changes takes time. This framework aimed at undoing inequities, particularly those inequities that have been amplified by the COVID-19 pandemic, is iterative and ongoing.18,19 Not every test of change will impact the outcome or reduce inequity, but over time, each change will impact the next, generating sustainable effects.
Conclusion
There are ongoing studies examining the adverse outcomes and potential health inequities for patients with diabetes impacted by COVID-19.20 Health care providers need to plan for post-COVID-19 care, keeping in mind that the pandemic might worsen already existing health disparities in diabetes management.3,4,21 This work will involve an intentional approach to address structural and systemic racism.22 Therefore, the work of building health equity solutions must be rooted in racial justice, economic equity, and equitable access to health care and education.
Initiatives like this are currently being funded through foundation grants as well as state and federal research or program grants. Regional and national payors, including the Centers for Medicare & Medicaid Services, are currently piloting long-term sustainable funding models through programs like accountable care organizations and the Accountable Health Communities Model.23
Health systems can successfully address health equity and racial justice, using a framework as described above, to identify determinants of health, develop policies to expand access to care for the most vulnerable patients, distribute decision-making power, and train staff by naming structural racism as a driver of health inequities.
Acknowledgment: The authors acknowledge the contributions of patients, families, diabetes care teams, and collaborators within the T1D Exchange Quality Improvement Collaborative, who continually seek to improve care and outcomes for people living with diabetes.
Corresponding author: Osagie Ebekozien, MD, 11 Avenue De La Fayette, Boston, MA 02115; oebekozien@t1dexchange.org.
Financial disclosures: None.
Funding: T1D Exchange QI Collaborative is funded by The Leona M. and Harry B. Helmsley Charitable Trust. No specific funding was received for this manuscript or the development of this framework.
Keywords: type 1 diabetes; quality improvement; QI framework; racial justice; health disparities.
1. American Public Health Association Health Equity web site. https://www.apha.org/topics-and-issues/health-equity. Accessed June 4, 2020.
2. Lado J, Lipman T. Racial and ethnic disparities in the incidence, treatment, and outcomes of youth with type 1 diabetes. Endocrinol Metab Clin North Am. 2016;45:453-461.
3. Kahkoska AR, Shay CM, Crandell J, et al. Association of race and ethnicity with glycemic control and hemoglobin A1c levels in youth with type 1 diabetes. JAMA Netw Open. 2018;1:e181851.
4. Willi SM, Miller KM, DiMeglio LA, et al; T1D Exchange Clinic Network. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135:424-434.
5. Valenzuela JM, Seid M, Waitzfelder B, et al. Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr. 2014;164:1369-1375.
6. Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: Knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142.
7. Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle Region - case series. N Engl J Med. 2020;382:2012-2022.
8. Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398-402.
9. Shah M, Sachdeva M, Dodiuk-Gad RP. COVID-19 and racial disparities. J Am Acad Dermatol. 2020;83:e35.
10. Ebekozien O, Rioles N, DeSalvo D, et al. Improving continuous glucose monitoring (CGM) use across national centers: results from the T1D Exchange Quality Improvement Collaborative (T1DX-QI). Diabetes. 2020;69(Supplement 1):145-LB.
11. Ebekozien O. QI methodology to address health equity. Presented at American Society of Quality BOSCON 2018; Boston, MA; March 19 and 20, 2018.
12. 2019 Model Practice Award, Building A Culture of Improvement. National Association of County and City Health Officials web site. www.naccho.org/membership/awards/model-practices. Accessed June 4, 2020.
13. Nuckols TK, Keeler E, Anderson LJ, et al. Economic evaluation of quality improvement interventions designed to improve glycemic control in diabetes: a systematic review and weighted regression analysis. Diabetes Care. 2018;41:985‐993.
14. Rossi MC, Nicolucci A, Arcangeli A, et al. Baseline quality-of-care data from a quality-improvement program implemented by a network of diabetes outpatient clinics. Diabetes Care. 2008;31:2166‐2168.
15. McQuillan RF, Silver SA, Harel Z, et al. How to measure and interpret quality improvement data. Clin J Am Soc Nephrol. 2016;11:908-914.
16. Siddiqi FS. Quality improvement in diabetes care: time for us to step up? Can J Diabetes. 2019;43:233.
17. Taylor MJ, McNicholas C, Nicolay C, et al. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23:290‐298.
18. Ferdinand KC, Nasser SA. African American COVID-19 mortality: a sentinel event. J Am Coll Cardiol. 2020;75:2746-2748..
19. Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Endocrinol Metab. 2020;318:E736-E741.
20. Ebekozien OA, Noor N, Gallagher MP, Alonso GT. Type 1 diabetes and COVID-19: preliminary findings from a multicenter surveillance study in the U.S. Diabetes Care. 2020;43:e83-e85.
21. Majidi S, Ebekozien O, Noor N, et al. Inequities in health outcomes among patients in the T1D Exchange-QI Collaborative. Diabetes. 2020;69(Supplement 1):1220-P. https://doi.org/10.2337/ db20-1220.-P.
22. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20-47.
23. Centers for Medicare & Medicaid Services. Accountable Health Communities Model. CMS.gov web site. https://innovation.cms.gov/innovation-models/ahcm. Accessed October 10, 2020.
From T1D Exchange, Boston, MA (Dr. Ebekozien, Dr. Odugbesan, and Nicole Rioles); Barbara Davis Center, University of Colorado, Boulder, CO (Dr. Majidi); Cincinnati Children’s Hospital Medical Center, Cincinnati, OH (Dr. Jones); and Nationwide Children’s Hospital, Columbus, OH (Dr. Kamboj)
Health equity has been described as the opportunity for all persons to obtain their highest level of health possible.1 Unfortunately, even with advances in technology and care practices, disparities persist in health care outcomes. Disparities in prevalence, prognosis, and outcomes still exist in diabetes management.2 Non-Hispanic Black and/or Hispanic populations are more likely to have worse glycemic control,3,4 to encounter more barriers in access to care,5 and to have higher levels of acute complications,4 and to use advanced technologies less frequently.4 Diabetes is one of the preexisting conditions that increase morbidity and mortality in COVID-19.6,7 Unfortunately, adverse outcomes from COVID-19 also disproportionately impact a specific vulnerable population.8,9 The urgent transition to managing diabetes remotely during the COVID-19 pandemic may exacerbate long-term inequities because some vulnerable patients might not have access to technology devices necessary for effective remote management.
Here, we describe how quality improvement (QI) tools and principles can be adapted into a framework for advancing health equity. Specifically, we describe a 10-step framework that may be applied in diabetes care management to achieve improvement, using a hypothetical example of increasing use of continuous glucose monitors (CGMs) among patients with type 1 diabetes mellitus.10 This framework was developed to address the literature gap on practical ways health care providers can address inequities using QI principles, and was implemented by 1 of the authors at a local public health department.11 The framework’s iterative and comprehensive design makes it ideal for addressing inequities in chronic diseases like diabetes, which have multiple root causes with no easy solutions. The improvement program pilot received a national model practice award.11,12
10-Step Framework
Step 1: Review program/project baseline data for existing disparities. Diabetes programs and routine QI processes encourage existing data review to determine how effective the current system is working and if the existing process has a predictable pattern.13,14 Our equity-revised framework proposes a more in-depth review to stratify baseline data based on factors that might contribute to inequities, including race, age, income levels, ethnicity, language, sexual orientation, insurance type, and zip code. This process will identify patients not served or unfairly impacted due to socioeconomic factors. For example, using the hypothetical example of improving CGM use, a team completes a preliminary data review and determines that baseline CGM use is 30% in the clinic population. However, in a review to assess for disparities, they also identify that patients on public insurance have a significantly lower CGM uptake of only 15%.
Step 2: Build an equitable project team, including patients with lived experiences. Routine projects typically have clinicians, administrative staff, and analytic staff as members of their team. In a post-COVID-19 world, every team needs to learn directly from people impacted and share decision-making power. The traditional approach to receiving feedback has generally been to collect responses using surveys or focus groups. We propose that individuals/families who are disproportionately impacted be included as active members on QI teams. For example, in the hypothetical example of the CGM project, team members would include patients with type 1 diabetes who are on public insurance and their families.
Step 3: Develop equity-focused goals. The traditional program involves the development of aims that are SMART (specific, measurable, achievable, realistic, time-bound).15 The proposed framework encourages the inclusion of equity-revised goals (SMARTer) using insights from Steps 1 and 2. For example, your typical smart goal might be to increase the percentage of patients using CGM by 20% in 6 months, while a SMARTer goal would be to increase the proportion of patients using CGM by 20% and reduce the disparities among public and private insurance patients by 30% in 6 months.
Step 4: Identify inequitable processes/pathways. Traditional QI programs might use a process map or flow diagram to depict the current state of a process visually.16 For example, in Figure 1, the process map diagram depicts some differences in the process for patients with public insurance as opposed to those with private insurance. The framework also advocates for using visual tools like process maps to depict how there might be inequitable pathways in a system. Visually identifying inequitable processes/pathways can help a team see barriers, address challenges, and pilot innovative solutions.
Step 5: Identify how socioeconomic factors are contributing to the current outcome. A good understanding of factors that contribute to the problem is an essential part of finding fundamental solutions. The fishbone diagram16 is a visualization tool used to identify contributing factors. When investigating contributing factors, it is commonplace to identify factors that fit into 1 of 5 categories: people, process, place, product, and policies (5 Ps). An equity-focused process will include equity as a new major factor category, and the socioeconomic impacts that contribute to inequities will be brainstormed and visually represented. For example, in the hypothetical CGM improvement example, an equity contributing factor is extensive CGM application paperwork for patients on public insurance as compared to those on private insurance. Figure 2 shows equity integrated into a fishbone diagram.
Step 6: Brainstorm possible improvements. Potential improvement ideas for the hypothetical CGM example might include redesigning the existing workflow, piloting CGM educational classes, and using a CGM barrier assessment tool to identify and address barriers to adoption.
Step 7: Use the decision matrix with equity as a criterion to prioritize improvement ideas. Decision matrix15 is a great tool that is frequently used to help teams prioritize potential ideas. Project team members must decide what criteria are important in prioritizing ideas to implement. Common criteria include implementation cost, time, and resources, but in addition to the common criteria, the team can specify ”impact on equity” as one of their criteria, alongside other standard criteria like impact.
Step 8: Test one small change at a time. This step is consistent with other traditional improvement models using the Plan, Do, Study, Act (PDSA) model for improvement.17 During this phase, the team should make predictions on the expected impact of the intervention on outcomes. For example, in the hypothetical example, the team predicts that testing and expanding CGM classes will reduce disparities among public versus private health insurance users by 5% and increase overall CGM uptake by 10%.
Step 9: Measure and compare results with predictions to identify inequitable practices or consequences. After each test of change, the team should review the results, including implementation cost considerations, and compare them to the predictions in the earlier step. The team should also document the potential reasons why their predictions were correct or inaccurate, and whether there were any unforeseen outcomes from the intervention.
Step 10: Celebrate small wins and repeat the process. Making fundamental and equitable changes takes time. This framework aimed at undoing inequities, particularly those inequities that have been amplified by the COVID-19 pandemic, is iterative and ongoing.18,19 Not every test of change will impact the outcome or reduce inequity, but over time, each change will impact the next, generating sustainable effects.
Conclusion
There are ongoing studies examining the adverse outcomes and potential health inequities for patients with diabetes impacted by COVID-19.20 Health care providers need to plan for post-COVID-19 care, keeping in mind that the pandemic might worsen already existing health disparities in diabetes management.3,4,21 This work will involve an intentional approach to address structural and systemic racism.22 Therefore, the work of building health equity solutions must be rooted in racial justice, economic equity, and equitable access to health care and education.
Initiatives like this are currently being funded through foundation grants as well as state and federal research or program grants. Regional and national payors, including the Centers for Medicare & Medicaid Services, are currently piloting long-term sustainable funding models through programs like accountable care organizations and the Accountable Health Communities Model.23
Health systems can successfully address health equity and racial justice, using a framework as described above, to identify determinants of health, develop policies to expand access to care for the most vulnerable patients, distribute decision-making power, and train staff by naming structural racism as a driver of health inequities.
Acknowledgment: The authors acknowledge the contributions of patients, families, diabetes care teams, and collaborators within the T1D Exchange Quality Improvement Collaborative, who continually seek to improve care and outcomes for people living with diabetes.
Corresponding author: Osagie Ebekozien, MD, 11 Avenue De La Fayette, Boston, MA 02115; oebekozien@t1dexchange.org.
Financial disclosures: None.
Funding: T1D Exchange QI Collaborative is funded by The Leona M. and Harry B. Helmsley Charitable Trust. No specific funding was received for this manuscript or the development of this framework.
Keywords: type 1 diabetes; quality improvement; QI framework; racial justice; health disparities.
From T1D Exchange, Boston, MA (Dr. Ebekozien, Dr. Odugbesan, and Nicole Rioles); Barbara Davis Center, University of Colorado, Boulder, CO (Dr. Majidi); Cincinnati Children’s Hospital Medical Center, Cincinnati, OH (Dr. Jones); and Nationwide Children’s Hospital, Columbus, OH (Dr. Kamboj)
Health equity has been described as the opportunity for all persons to obtain their highest level of health possible.1 Unfortunately, even with advances in technology and care practices, disparities persist in health care outcomes. Disparities in prevalence, prognosis, and outcomes still exist in diabetes management.2 Non-Hispanic Black and/or Hispanic populations are more likely to have worse glycemic control,3,4 to encounter more barriers in access to care,5 and to have higher levels of acute complications,4 and to use advanced technologies less frequently.4 Diabetes is one of the preexisting conditions that increase morbidity and mortality in COVID-19.6,7 Unfortunately, adverse outcomes from COVID-19 also disproportionately impact a specific vulnerable population.8,9 The urgent transition to managing diabetes remotely during the COVID-19 pandemic may exacerbate long-term inequities because some vulnerable patients might not have access to technology devices necessary for effective remote management.
Here, we describe how quality improvement (QI) tools and principles can be adapted into a framework for advancing health equity. Specifically, we describe a 10-step framework that may be applied in diabetes care management to achieve improvement, using a hypothetical example of increasing use of continuous glucose monitors (CGMs) among patients with type 1 diabetes mellitus.10 This framework was developed to address the literature gap on practical ways health care providers can address inequities using QI principles, and was implemented by 1 of the authors at a local public health department.11 The framework’s iterative and comprehensive design makes it ideal for addressing inequities in chronic diseases like diabetes, which have multiple root causes with no easy solutions. The improvement program pilot received a national model practice award.11,12
10-Step Framework
Step 1: Review program/project baseline data for existing disparities. Diabetes programs and routine QI processes encourage existing data review to determine how effective the current system is working and if the existing process has a predictable pattern.13,14 Our equity-revised framework proposes a more in-depth review to stratify baseline data based on factors that might contribute to inequities, including race, age, income levels, ethnicity, language, sexual orientation, insurance type, and zip code. This process will identify patients not served or unfairly impacted due to socioeconomic factors. For example, using the hypothetical example of improving CGM use, a team completes a preliminary data review and determines that baseline CGM use is 30% in the clinic population. However, in a review to assess for disparities, they also identify that patients on public insurance have a significantly lower CGM uptake of only 15%.
Step 2: Build an equitable project team, including patients with lived experiences. Routine projects typically have clinicians, administrative staff, and analytic staff as members of their team. In a post-COVID-19 world, every team needs to learn directly from people impacted and share decision-making power. The traditional approach to receiving feedback has generally been to collect responses using surveys or focus groups. We propose that individuals/families who are disproportionately impacted be included as active members on QI teams. For example, in the hypothetical example of the CGM project, team members would include patients with type 1 diabetes who are on public insurance and their families.
Step 3: Develop equity-focused goals. The traditional program involves the development of aims that are SMART (specific, measurable, achievable, realistic, time-bound).15 The proposed framework encourages the inclusion of equity-revised goals (SMARTer) using insights from Steps 1 and 2. For example, your typical smart goal might be to increase the percentage of patients using CGM by 20% in 6 months, while a SMARTer goal would be to increase the proportion of patients using CGM by 20% and reduce the disparities among public and private insurance patients by 30% in 6 months.
Step 4: Identify inequitable processes/pathways. Traditional QI programs might use a process map or flow diagram to depict the current state of a process visually.16 For example, in Figure 1, the process map diagram depicts some differences in the process for patients with public insurance as opposed to those with private insurance. The framework also advocates for using visual tools like process maps to depict how there might be inequitable pathways in a system. Visually identifying inequitable processes/pathways can help a team see barriers, address challenges, and pilot innovative solutions.
Step 5: Identify how socioeconomic factors are contributing to the current outcome. A good understanding of factors that contribute to the problem is an essential part of finding fundamental solutions. The fishbone diagram16 is a visualization tool used to identify contributing factors. When investigating contributing factors, it is commonplace to identify factors that fit into 1 of 5 categories: people, process, place, product, and policies (5 Ps). An equity-focused process will include equity as a new major factor category, and the socioeconomic impacts that contribute to inequities will be brainstormed and visually represented. For example, in the hypothetical CGM improvement example, an equity contributing factor is extensive CGM application paperwork for patients on public insurance as compared to those on private insurance. Figure 2 shows equity integrated into a fishbone diagram.
Step 6: Brainstorm possible improvements. Potential improvement ideas for the hypothetical CGM example might include redesigning the existing workflow, piloting CGM educational classes, and using a CGM barrier assessment tool to identify and address barriers to adoption.
Step 7: Use the decision matrix with equity as a criterion to prioritize improvement ideas. Decision matrix15 is a great tool that is frequently used to help teams prioritize potential ideas. Project team members must decide what criteria are important in prioritizing ideas to implement. Common criteria include implementation cost, time, and resources, but in addition to the common criteria, the team can specify ”impact on equity” as one of their criteria, alongside other standard criteria like impact.
Step 8: Test one small change at a time. This step is consistent with other traditional improvement models using the Plan, Do, Study, Act (PDSA) model for improvement.17 During this phase, the team should make predictions on the expected impact of the intervention on outcomes. For example, in the hypothetical example, the team predicts that testing and expanding CGM classes will reduce disparities among public versus private health insurance users by 5% and increase overall CGM uptake by 10%.
Step 9: Measure and compare results with predictions to identify inequitable practices or consequences. After each test of change, the team should review the results, including implementation cost considerations, and compare them to the predictions in the earlier step. The team should also document the potential reasons why their predictions were correct or inaccurate, and whether there were any unforeseen outcomes from the intervention.
Step 10: Celebrate small wins and repeat the process. Making fundamental and equitable changes takes time. This framework aimed at undoing inequities, particularly those inequities that have been amplified by the COVID-19 pandemic, is iterative and ongoing.18,19 Not every test of change will impact the outcome or reduce inequity, but over time, each change will impact the next, generating sustainable effects.
Conclusion
There are ongoing studies examining the adverse outcomes and potential health inequities for patients with diabetes impacted by COVID-19.20 Health care providers need to plan for post-COVID-19 care, keeping in mind that the pandemic might worsen already existing health disparities in diabetes management.3,4,21 This work will involve an intentional approach to address structural and systemic racism.22 Therefore, the work of building health equity solutions must be rooted in racial justice, economic equity, and equitable access to health care and education.
Initiatives like this are currently being funded through foundation grants as well as state and federal research or program grants. Regional and national payors, including the Centers for Medicare & Medicaid Services, are currently piloting long-term sustainable funding models through programs like accountable care organizations and the Accountable Health Communities Model.23
Health systems can successfully address health equity and racial justice, using a framework as described above, to identify determinants of health, develop policies to expand access to care for the most vulnerable patients, distribute decision-making power, and train staff by naming structural racism as a driver of health inequities.
Acknowledgment: The authors acknowledge the contributions of patients, families, diabetes care teams, and collaborators within the T1D Exchange Quality Improvement Collaborative, who continually seek to improve care and outcomes for people living with diabetes.
Corresponding author: Osagie Ebekozien, MD, 11 Avenue De La Fayette, Boston, MA 02115; oebekozien@t1dexchange.org.
Financial disclosures: None.
Funding: T1D Exchange QI Collaborative is funded by The Leona M. and Harry B. Helmsley Charitable Trust. No specific funding was received for this manuscript or the development of this framework.
Keywords: type 1 diabetes; quality improvement; QI framework; racial justice; health disparities.
1. American Public Health Association Health Equity web site. https://www.apha.org/topics-and-issues/health-equity. Accessed June 4, 2020.
2. Lado J, Lipman T. Racial and ethnic disparities in the incidence, treatment, and outcomes of youth with type 1 diabetes. Endocrinol Metab Clin North Am. 2016;45:453-461.
3. Kahkoska AR, Shay CM, Crandell J, et al. Association of race and ethnicity with glycemic control and hemoglobin A1c levels in youth with type 1 diabetes. JAMA Netw Open. 2018;1:e181851.
4. Willi SM, Miller KM, DiMeglio LA, et al; T1D Exchange Clinic Network. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135:424-434.
5. Valenzuela JM, Seid M, Waitzfelder B, et al. Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr. 2014;164:1369-1375.
6. Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: Knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142.
7. Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle Region - case series. N Engl J Med. 2020;382:2012-2022.
8. Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398-402.
9. Shah M, Sachdeva M, Dodiuk-Gad RP. COVID-19 and racial disparities. J Am Acad Dermatol. 2020;83:e35.
10. Ebekozien O, Rioles N, DeSalvo D, et al. Improving continuous glucose monitoring (CGM) use across national centers: results from the T1D Exchange Quality Improvement Collaborative (T1DX-QI). Diabetes. 2020;69(Supplement 1):145-LB.
11. Ebekozien O. QI methodology to address health equity. Presented at American Society of Quality BOSCON 2018; Boston, MA; March 19 and 20, 2018.
12. 2019 Model Practice Award, Building A Culture of Improvement. National Association of County and City Health Officials web site. www.naccho.org/membership/awards/model-practices. Accessed June 4, 2020.
13. Nuckols TK, Keeler E, Anderson LJ, et al. Economic evaluation of quality improvement interventions designed to improve glycemic control in diabetes: a systematic review and weighted regression analysis. Diabetes Care. 2018;41:985‐993.
14. Rossi MC, Nicolucci A, Arcangeli A, et al. Baseline quality-of-care data from a quality-improvement program implemented by a network of diabetes outpatient clinics. Diabetes Care. 2008;31:2166‐2168.
15. McQuillan RF, Silver SA, Harel Z, et al. How to measure and interpret quality improvement data. Clin J Am Soc Nephrol. 2016;11:908-914.
16. Siddiqi FS. Quality improvement in diabetes care: time for us to step up? Can J Diabetes. 2019;43:233.
17. Taylor MJ, McNicholas C, Nicolay C, et al. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23:290‐298.
18. Ferdinand KC, Nasser SA. African American COVID-19 mortality: a sentinel event. J Am Coll Cardiol. 2020;75:2746-2748..
19. Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Endocrinol Metab. 2020;318:E736-E741.
20. Ebekozien OA, Noor N, Gallagher MP, Alonso GT. Type 1 diabetes and COVID-19: preliminary findings from a multicenter surveillance study in the U.S. Diabetes Care. 2020;43:e83-e85.
21. Majidi S, Ebekozien O, Noor N, et al. Inequities in health outcomes among patients in the T1D Exchange-QI Collaborative. Diabetes. 2020;69(Supplement 1):1220-P. https://doi.org/10.2337/ db20-1220.-P.
22. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20-47.
23. Centers for Medicare & Medicaid Services. Accountable Health Communities Model. CMS.gov web site. https://innovation.cms.gov/innovation-models/ahcm. Accessed October 10, 2020.
1. American Public Health Association Health Equity web site. https://www.apha.org/topics-and-issues/health-equity. Accessed June 4, 2020.
2. Lado J, Lipman T. Racial and ethnic disparities in the incidence, treatment, and outcomes of youth with type 1 diabetes. Endocrinol Metab Clin North Am. 2016;45:453-461.
3. Kahkoska AR, Shay CM, Crandell J, et al. Association of race and ethnicity with glycemic control and hemoglobin A1c levels in youth with type 1 diabetes. JAMA Netw Open. 2018;1:e181851.
4. Willi SM, Miller KM, DiMeglio LA, et al; T1D Exchange Clinic Network. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135:424-434.
5. Valenzuela JM, Seid M, Waitzfelder B, et al. Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr. 2014;164:1369-1375.
6. Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: Knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142.
7. Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle Region - case series. N Engl J Med. 2020;382:2012-2022.
8. Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398-402.
9. Shah M, Sachdeva M, Dodiuk-Gad RP. COVID-19 and racial disparities. J Am Acad Dermatol. 2020;83:e35.
10. Ebekozien O, Rioles N, DeSalvo D, et al. Improving continuous glucose monitoring (CGM) use across national centers: results from the T1D Exchange Quality Improvement Collaborative (T1DX-QI). Diabetes. 2020;69(Supplement 1):145-LB.
11. Ebekozien O. QI methodology to address health equity. Presented at American Society of Quality BOSCON 2018; Boston, MA; March 19 and 20, 2018.
12. 2019 Model Practice Award, Building A Culture of Improvement. National Association of County and City Health Officials web site. www.naccho.org/membership/awards/model-practices. Accessed June 4, 2020.
13. Nuckols TK, Keeler E, Anderson LJ, et al. Economic evaluation of quality improvement interventions designed to improve glycemic control in diabetes: a systematic review and weighted regression analysis. Diabetes Care. 2018;41:985‐993.
14. Rossi MC, Nicolucci A, Arcangeli A, et al. Baseline quality-of-care data from a quality-improvement program implemented by a network of diabetes outpatient clinics. Diabetes Care. 2008;31:2166‐2168.
15. McQuillan RF, Silver SA, Harel Z, et al. How to measure and interpret quality improvement data. Clin J Am Soc Nephrol. 2016;11:908-914.
16. Siddiqi FS. Quality improvement in diabetes care: time for us to step up? Can J Diabetes. 2019;43:233.
17. Taylor MJ, McNicholas C, Nicolay C, et al. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23:290‐298.
18. Ferdinand KC, Nasser SA. African American COVID-19 mortality: a sentinel event. J Am Coll Cardiol. 2020;75:2746-2748..
19. Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Endocrinol Metab. 2020;318:E736-E741.
20. Ebekozien OA, Noor N, Gallagher MP, Alonso GT. Type 1 diabetes and COVID-19: preliminary findings from a multicenter surveillance study in the U.S. Diabetes Care. 2020;43:e83-e85.
21. Majidi S, Ebekozien O, Noor N, et al. Inequities in health outcomes among patients in the T1D Exchange-QI Collaborative. Diabetes. 2020;69(Supplement 1):1220-P. https://doi.org/10.2337/ db20-1220.-P.
22. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20-47.
23. Centers for Medicare & Medicaid Services. Accountable Health Communities Model. CMS.gov web site. https://innovation.cms.gov/innovation-models/ahcm. Accessed October 10, 2020.
Tips for physicians, patients to make the most of the holidays amid COVID
“We must accept finite disappointment, but never lose infinite hope,” Martin Luther King, Jr.
This holiday season will be like no other. We will remember it for the rest of our lives, and we will look back to see how we faced the holidays during a pandemic.
Like the rest of 2020, the holidays will need to be reimagined. Years and even decades of tradition will be broken as we place health above merriment.
Here are a few tips to help all of us and our patients make the most of this holiday season.
- Reprioritize: This holiday season will be about depth not breadth, quality not quantity, and less not more. Trips are canceled and gatherings have shrunk. We are not running from store to store or party to party. Instead, you will find yourself surrounded by fewer friends and family. Some will be alone to optimally protect their health and the health of others. Do your best to focus on the half-full portion.
- Embrace change: Don’t compare or try to make this year like previous years. Be creative and try to find ways to make a new format fun. Meeting during the day and limiting alcohol intake can assist in making sure everyone stays safe. It has been interesting to see how many of my patients have decreased their alcohol use during quarantine. I hope this pattern will continue over the next weeks and months.
- Practice self-care: As health care professionals, we must remember the old adage “physician, heal thyself.” This year has been so difficult for almost all of us. It was filled with unprecedented levels of personal and professional stress. Holidays are often about what we can do for others, but this year we may need to place self-care first. Do what brings you happiness.
Even though you aren’t traveling, you can still disconnect from work. Set up a schedule and stick to it making sure you take plenty of time to rest and enjoy. Many of us have been working extremely long hours and a break is so needed. Take it if you possibly can. Detox from your screen! Limit the news. Creativity and productivity will be enhanced in 2021 if we can come in recharged.
For those remaining on the front lines, be patient; the end is nearing. Take care of yourself when you are not working. We are all so grateful to those in our field who have sacrificed so much to care for others. Eat, drink, and rest well to keep your immune system strong.
- Acknowledge your negative emotions: As we all know, if you try to deny negative emotions, they continue to pop up. If we give them time and space to be felt, we will find they diminish in intensity. Long work hours may have prevented us from feeling our emotions, so don’t be surprised if they surface when we take a break.
Let yourself feel the sadness for what you have experienced this year. Be open about missing those who can’t be with you because of travel or other restrictions. Let yourself feel the disappointment about your holiday travel plans that you can’t embark upon.
You may elect to share these emotions with someone close to you or with a professional. To paraphrase Carl Jung, “what we resist, persists,” so don’t try to hide from your negative emotions. Most of us had lots of them in 2020, so don’t be shy about admitting it.
- Focus on growth: What have we learned from 2020 and how can we be better equipped in 2021 and beyond?
Trauma can bring growth not just disorder. This year has returned well-deserved prestige to our fields. We are being lauded as heroes as we have scarified our health and the health of our loved ones to serve others. Can we choose to celebrate our accomplishments?
We have become more resilient and learned to continue on in the face of great hardship. Many of us have gained confidence as we confronted this historic challenge. As we have been reminded of death daily, we learn to appreciate life more fully and not take any day for granted.
I am proud to be a physician during this pandemic, and I hope you are, too!
- Find joy: Often times, we find real happiness in smaller moments and experiences. For many, this time of year is filled with so much stress that it can be hard to carve out moments of joy. As we may be less busy socially this holiday season, might we find even more joy?
Joy can only be experienced in the present moment. Tap into all your senses. Eat slowly making sure to smell and taste every bite. Cherish those who can still gather at your table. If you find yourself alone, embrace that experience. Safety must continue to come first, and we can’t let down our guard now.
- Reflect: New Year’s Eve is always a time for reflection and hope for the future. Most of us will be glad to see 2020 in the rearview mirror. With multiple and very promising vaccines on the horizon, we can anticipate a brighter future. We must continue to work hard; remain patient; and be creative, resilient, and optimistic. Let’s try to fill our days with hope and purpose and work together to achieve a brighter future for all.
“Learn from yesterday, live for today, hope for tomorrow,” Albert Einstein
Wishing you health and happiness in this holiday season and beyond.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She also is founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world.
“We must accept finite disappointment, but never lose infinite hope,” Martin Luther King, Jr.
This holiday season will be like no other. We will remember it for the rest of our lives, and we will look back to see how we faced the holidays during a pandemic.
Like the rest of 2020, the holidays will need to be reimagined. Years and even decades of tradition will be broken as we place health above merriment.
Here are a few tips to help all of us and our patients make the most of this holiday season.
- Reprioritize: This holiday season will be about depth not breadth, quality not quantity, and less not more. Trips are canceled and gatherings have shrunk. We are not running from store to store or party to party. Instead, you will find yourself surrounded by fewer friends and family. Some will be alone to optimally protect their health and the health of others. Do your best to focus on the half-full portion.
- Embrace change: Don’t compare or try to make this year like previous years. Be creative and try to find ways to make a new format fun. Meeting during the day and limiting alcohol intake can assist in making sure everyone stays safe. It has been interesting to see how many of my patients have decreased their alcohol use during quarantine. I hope this pattern will continue over the next weeks and months.
- Practice self-care: As health care professionals, we must remember the old adage “physician, heal thyself.” This year has been so difficult for almost all of us. It was filled with unprecedented levels of personal and professional stress. Holidays are often about what we can do for others, but this year we may need to place self-care first. Do what brings you happiness.
Even though you aren’t traveling, you can still disconnect from work. Set up a schedule and stick to it making sure you take plenty of time to rest and enjoy. Many of us have been working extremely long hours and a break is so needed. Take it if you possibly can. Detox from your screen! Limit the news. Creativity and productivity will be enhanced in 2021 if we can come in recharged.
For those remaining on the front lines, be patient; the end is nearing. Take care of yourself when you are not working. We are all so grateful to those in our field who have sacrificed so much to care for others. Eat, drink, and rest well to keep your immune system strong.
- Acknowledge your negative emotions: As we all know, if you try to deny negative emotions, they continue to pop up. If we give them time and space to be felt, we will find they diminish in intensity. Long work hours may have prevented us from feeling our emotions, so don’t be surprised if they surface when we take a break.
Let yourself feel the sadness for what you have experienced this year. Be open about missing those who can’t be with you because of travel or other restrictions. Let yourself feel the disappointment about your holiday travel plans that you can’t embark upon.
You may elect to share these emotions with someone close to you or with a professional. To paraphrase Carl Jung, “what we resist, persists,” so don’t try to hide from your negative emotions. Most of us had lots of them in 2020, so don’t be shy about admitting it.
- Focus on growth: What have we learned from 2020 and how can we be better equipped in 2021 and beyond?
Trauma can bring growth not just disorder. This year has returned well-deserved prestige to our fields. We are being lauded as heroes as we have scarified our health and the health of our loved ones to serve others. Can we choose to celebrate our accomplishments?
We have become more resilient and learned to continue on in the face of great hardship. Many of us have gained confidence as we confronted this historic challenge. As we have been reminded of death daily, we learn to appreciate life more fully and not take any day for granted.
I am proud to be a physician during this pandemic, and I hope you are, too!
- Find joy: Often times, we find real happiness in smaller moments and experiences. For many, this time of year is filled with so much stress that it can be hard to carve out moments of joy. As we may be less busy socially this holiday season, might we find even more joy?
Joy can only be experienced in the present moment. Tap into all your senses. Eat slowly making sure to smell and taste every bite. Cherish those who can still gather at your table. If you find yourself alone, embrace that experience. Safety must continue to come first, and we can’t let down our guard now.
- Reflect: New Year’s Eve is always a time for reflection and hope for the future. Most of us will be glad to see 2020 in the rearview mirror. With multiple and very promising vaccines on the horizon, we can anticipate a brighter future. We must continue to work hard; remain patient; and be creative, resilient, and optimistic. Let’s try to fill our days with hope and purpose and work together to achieve a brighter future for all.
“Learn from yesterday, live for today, hope for tomorrow,” Albert Einstein
Wishing you health and happiness in this holiday season and beyond.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She also is founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world.
“We must accept finite disappointment, but never lose infinite hope,” Martin Luther King, Jr.
This holiday season will be like no other. We will remember it for the rest of our lives, and we will look back to see how we faced the holidays during a pandemic.
Like the rest of 2020, the holidays will need to be reimagined. Years and even decades of tradition will be broken as we place health above merriment.
Here are a few tips to help all of us and our patients make the most of this holiday season.
- Reprioritize: This holiday season will be about depth not breadth, quality not quantity, and less not more. Trips are canceled and gatherings have shrunk. We are not running from store to store or party to party. Instead, you will find yourself surrounded by fewer friends and family. Some will be alone to optimally protect their health and the health of others. Do your best to focus on the half-full portion.
- Embrace change: Don’t compare or try to make this year like previous years. Be creative and try to find ways to make a new format fun. Meeting during the day and limiting alcohol intake can assist in making sure everyone stays safe. It has been interesting to see how many of my patients have decreased their alcohol use during quarantine. I hope this pattern will continue over the next weeks and months.
- Practice self-care: As health care professionals, we must remember the old adage “physician, heal thyself.” This year has been so difficult for almost all of us. It was filled with unprecedented levels of personal and professional stress. Holidays are often about what we can do for others, but this year we may need to place self-care first. Do what brings you happiness.
Even though you aren’t traveling, you can still disconnect from work. Set up a schedule and stick to it making sure you take plenty of time to rest and enjoy. Many of us have been working extremely long hours and a break is so needed. Take it if you possibly can. Detox from your screen! Limit the news. Creativity and productivity will be enhanced in 2021 if we can come in recharged.
For those remaining on the front lines, be patient; the end is nearing. Take care of yourself when you are not working. We are all so grateful to those in our field who have sacrificed so much to care for others. Eat, drink, and rest well to keep your immune system strong.
- Acknowledge your negative emotions: As we all know, if you try to deny negative emotions, they continue to pop up. If we give them time and space to be felt, we will find they diminish in intensity. Long work hours may have prevented us from feeling our emotions, so don’t be surprised if they surface when we take a break.
Let yourself feel the sadness for what you have experienced this year. Be open about missing those who can’t be with you because of travel or other restrictions. Let yourself feel the disappointment about your holiday travel plans that you can’t embark upon.
You may elect to share these emotions with someone close to you or with a professional. To paraphrase Carl Jung, “what we resist, persists,” so don’t try to hide from your negative emotions. Most of us had lots of them in 2020, so don’t be shy about admitting it.
- Focus on growth: What have we learned from 2020 and how can we be better equipped in 2021 and beyond?
Trauma can bring growth not just disorder. This year has returned well-deserved prestige to our fields. We are being lauded as heroes as we have scarified our health and the health of our loved ones to serve others. Can we choose to celebrate our accomplishments?
We have become more resilient and learned to continue on in the face of great hardship. Many of us have gained confidence as we confronted this historic challenge. As we have been reminded of death daily, we learn to appreciate life more fully and not take any day for granted.
I am proud to be a physician during this pandemic, and I hope you are, too!
- Find joy: Often times, we find real happiness in smaller moments and experiences. For many, this time of year is filled with so much stress that it can be hard to carve out moments of joy. As we may be less busy socially this holiday season, might we find even more joy?
Joy can only be experienced in the present moment. Tap into all your senses. Eat slowly making sure to smell and taste every bite. Cherish those who can still gather at your table. If you find yourself alone, embrace that experience. Safety must continue to come first, and we can’t let down our guard now.
- Reflect: New Year’s Eve is always a time for reflection and hope for the future. Most of us will be glad to see 2020 in the rearview mirror. With multiple and very promising vaccines on the horizon, we can anticipate a brighter future. We must continue to work hard; remain patient; and be creative, resilient, and optimistic. Let’s try to fill our days with hope and purpose and work together to achieve a brighter future for all.
“Learn from yesterday, live for today, hope for tomorrow,” Albert Einstein
Wishing you health and happiness in this holiday season and beyond.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She also is founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world.
Escaping the daily grind
Few films have universal appeal these days, but one that comes close is the 1993 classic Groundhog Day, in which the protagonist is trapped in a time loop, doomed to living the same day over and over for many years.
One reason that this story resonates with so many, I think, is that we are all living a similar life. Not as a same-day loop, of course; but each week seems eerily similar to the last, as does each month, each year – on and on, ad infinitum. That’s why it is so important, every so often, to step out of the “loop” and reassess the bigger picture.
I write this reminder every couple of years because it’s so easy to lose sight of the overall landscape among the pressures of our daily routines. . And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of one a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a guitar, bass, or sailing lessons; or a long weekend away with my wife.
And until COVID-19 put a temporary stop to them earlier this year, we have embarked on at least one longer adventure each year, some of which have been shared in these pages. Our 2019 expedition to Easter Island remains among the most memorable, and fulfilled a dream I’ve had since I read Thor Heyerdahl’s Aku Aku in grade school. As we explored the giant stone moai – which are found nowhere else in the world – I didn’t have the time – or the slightest inclination – to worry about the office. But I did accumulate some great ideas – practical, medical, and literary. Original thoughts are hard to chase down during the daily grind; but in a refreshing environment, they will seek you out. When our trip was over, I returned ready to take on the world, and my practice, anew.
I know how some of you feel about “wasting” a day – or, God forbid, a week. Patients might go elsewhere while you’re gone, and every day the office is idle you “lose money.” That whole paradigm is wrong. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacations; it all averages out in the end.
Besides, this is much more important than money; this is breaking the routine, clearing the cobwebs, living your life. Trust me, your practice will still be there when you return. And while COVID-19 will not last forever, there are plenty of other “sharpeners” while we wait.
More than once I’ve recounted the story of Alex Müller and J. Georg Bednorz, the Swiss Nobel Laureates whose superconductivity research ground to a halt in 1986. The harder they pressed, the more elusive progress became. So Müller decided to take a break to read a new book on ceramics – a subject that had always interested him.
Nothing could have been less relevant to his work, of course; ceramics are among the poorest conductors known. But in that lower-pressure environment, Müller realized that a unique property of ceramics might apply to their project.
Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor, which in turn triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically-elevated trains, and many applications yet to be realized.
Sharpening your saw may not change the world, but it will change you; any nudge out of your comfort zone will give you fresh ideas and help you look at seemingly insoluble problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember the dying words that no one has spoken, ever: “I wish I had spent more time in my office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Few films have universal appeal these days, but one that comes close is the 1993 classic Groundhog Day, in which the protagonist is trapped in a time loop, doomed to living the same day over and over for many years.
One reason that this story resonates with so many, I think, is that we are all living a similar life. Not as a same-day loop, of course; but each week seems eerily similar to the last, as does each month, each year – on and on, ad infinitum. That’s why it is so important, every so often, to step out of the “loop” and reassess the bigger picture.
I write this reminder every couple of years because it’s so easy to lose sight of the overall landscape among the pressures of our daily routines. . And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of one a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a guitar, bass, or sailing lessons; or a long weekend away with my wife.
And until COVID-19 put a temporary stop to them earlier this year, we have embarked on at least one longer adventure each year, some of which have been shared in these pages. Our 2019 expedition to Easter Island remains among the most memorable, and fulfilled a dream I’ve had since I read Thor Heyerdahl’s Aku Aku in grade school. As we explored the giant stone moai – which are found nowhere else in the world – I didn’t have the time – or the slightest inclination – to worry about the office. But I did accumulate some great ideas – practical, medical, and literary. Original thoughts are hard to chase down during the daily grind; but in a refreshing environment, they will seek you out. When our trip was over, I returned ready to take on the world, and my practice, anew.
I know how some of you feel about “wasting” a day – or, God forbid, a week. Patients might go elsewhere while you’re gone, and every day the office is idle you “lose money.” That whole paradigm is wrong. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacations; it all averages out in the end.
Besides, this is much more important than money; this is breaking the routine, clearing the cobwebs, living your life. Trust me, your practice will still be there when you return. And while COVID-19 will not last forever, there are plenty of other “sharpeners” while we wait.
More than once I’ve recounted the story of Alex Müller and J. Georg Bednorz, the Swiss Nobel Laureates whose superconductivity research ground to a halt in 1986. The harder they pressed, the more elusive progress became. So Müller decided to take a break to read a new book on ceramics – a subject that had always interested him.
Nothing could have been less relevant to his work, of course; ceramics are among the poorest conductors known. But in that lower-pressure environment, Müller realized that a unique property of ceramics might apply to their project.
Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor, which in turn triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically-elevated trains, and many applications yet to be realized.
Sharpening your saw may not change the world, but it will change you; any nudge out of your comfort zone will give you fresh ideas and help you look at seemingly insoluble problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember the dying words that no one has spoken, ever: “I wish I had spent more time in my office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Few films have universal appeal these days, but one that comes close is the 1993 classic Groundhog Day, in which the protagonist is trapped in a time loop, doomed to living the same day over and over for many years.
One reason that this story resonates with so many, I think, is that we are all living a similar life. Not as a same-day loop, of course; but each week seems eerily similar to the last, as does each month, each year – on and on, ad infinitum. That’s why it is so important, every so often, to step out of the “loop” and reassess the bigger picture.
I write this reminder every couple of years because it’s so easy to lose sight of the overall landscape among the pressures of our daily routines. . And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of one a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a guitar, bass, or sailing lessons; or a long weekend away with my wife.
And until COVID-19 put a temporary stop to them earlier this year, we have embarked on at least one longer adventure each year, some of which have been shared in these pages. Our 2019 expedition to Easter Island remains among the most memorable, and fulfilled a dream I’ve had since I read Thor Heyerdahl’s Aku Aku in grade school. As we explored the giant stone moai – which are found nowhere else in the world – I didn’t have the time – or the slightest inclination – to worry about the office. But I did accumulate some great ideas – practical, medical, and literary. Original thoughts are hard to chase down during the daily grind; but in a refreshing environment, they will seek you out. When our trip was over, I returned ready to take on the world, and my practice, anew.
I know how some of you feel about “wasting” a day – or, God forbid, a week. Patients might go elsewhere while you’re gone, and every day the office is idle you “lose money.” That whole paradigm is wrong. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacations; it all averages out in the end.
Besides, this is much more important than money; this is breaking the routine, clearing the cobwebs, living your life. Trust me, your practice will still be there when you return. And while COVID-19 will not last forever, there are plenty of other “sharpeners” while we wait.
More than once I’ve recounted the story of Alex Müller and J. Georg Bednorz, the Swiss Nobel Laureates whose superconductivity research ground to a halt in 1986. The harder they pressed, the more elusive progress became. So Müller decided to take a break to read a new book on ceramics – a subject that had always interested him.
Nothing could have been less relevant to his work, of course; ceramics are among the poorest conductors known. But in that lower-pressure environment, Müller realized that a unique property of ceramics might apply to their project.
Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor, which in turn triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically-elevated trains, and many applications yet to be realized.
Sharpening your saw may not change the world, but it will change you; any nudge out of your comfort zone will give you fresh ideas and help you look at seemingly insoluble problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember the dying words that no one has spoken, ever: “I wish I had spent more time in my office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Using telehealth to deliver palliative care to cancer patients
Traditional delivery of palliative care to outpatients with cancer is associated with many challenges.
Telehealth can eliminate some of these challenges but comes with issues of its own, according to results of the REACH PC trial.
Jennifer S. Temel, MD, of Massachusetts General Hospital in Boston, discussed the use of telemedicine in palliative care, including results from REACH PC, during an educational session at the ASCO Virtual Quality Care Symposium 2020.
Dr. Temel noted that, for cancer patients, an in-person visit with a palliative care specialist can cost time, induce fatigue, and increase financial burden from transportation and parking expenses.
For caregivers and family, an in-person visit may necessitate absence from family and/or work, require complex scheduling to coordinate with other office visits, and result in additional transportation and/or parking expenses.
For health care systems, to have a dedicated palliative care clinic requires precious space and financial expenditures for office personnel and other resources.
These issues make it attractive to consider whether telehealth could be used for palliative care services.
Scarcity of palliative care specialists
In the United States, there is roughly 1 palliative care physician for every 20,000 older adults with a life-limiting illness, according to research published in Annual Review of Public Health in 2014.
In its 2019 state-by-state report card, the Center to Advance Palliative Care noted that only 72% of U.S. hospitals with 50 or more beds have a palliative care team.
For patients with serious illnesses and those who are socioeconomically or geographically disadvantaged, palliative care is often inaccessible.
Inefficiencies in the current system are an additional impediment. Palliative care specialists frequently see patients during a portion of the patient’s routine visit to subspecialty or primary care clinics. This limits the palliative care specialist’s ability to perform comprehensive assessments and provide patient-centered care efficiently.
Special considerations regarding telehealth for palliative care
As a specialty, palliative care involves interactions that could make the use of telehealth problematic. For example, conveyance of interest, warmth, and touch are challenging or impossible in a video format.
Palliative care specialists engage with patients regarding relatively serious topics such as prognosis and end-of-life preferences. There is uncertainty about how those discussions would be received by patients and their caregivers via video.
Furthermore, there are logistical impediments such as prescribing opioids with video or across state lines.
Despite these concerns, the ENABLE study showed that supplementing usual oncology care with weekly (transitioning to monthly) telephone-based educational palliative care produced higher quality of life and mood than did usual oncology care alone. These results were published in JAMA in 2009.
REACH PC study demonstrates feasibility of telehealth model
Dr. Temel described the ongoing REACH PC trial in which palliative care is delivered via video visits and compared with in-person palliative care for patients with advanced non–small cell lung cancer.
The primary aim of REACH PC is to determine whether telehealth palliative care is equivalent to traditional palliative care in improving quality of life as a supplement to routine oncology care.
Currently, REACH PC has enrolled 581 patients at its 20 sites, spanning a geographically diverse area. Just over half of patients approached about REACH PC agreed to enroll in it. Ultimately, 1,250 enrollees are sought.
Among patients who declined to participate, 7.6% indicated “discomfort with technology” as the reason. Most refusals were due to lack of interest in research (35.1%) and/or palliative care (22.9%).
Older adults were prominent among enrollees. More than 60% were older than 60 years of age, and more than one-third were older than 70 years.
Among patients who began the trial, there were slightly more withdrawals in the telehealth participants, in comparison with in-person participants (13.6% versus 9.1%).
When palliative care clinicians were queried about video visits, 64.3% said there were no challenges. This is comparable to the 65.5% of clinicians who had no challenges with in-person visits.
When problems occurred with video visits, they were most frequently technical (19.1%). Only 1.4% of clinicians reported difficulty addressing topics that felt uncomfortable over video, and 1.5% reported difficulty establishing rapport.
The success rates of video and in-person visits were similar. About 80% of visits accomplished planned goals.
‘Webside’ manner
Strategies such as reflective listening and summarizing what patients say (to verify an accurate understanding of the patient’s perspective) are key to successful palliative care visits, regardless of the setting.
For telehealth visits, Dr. Temel described techniques she defined as “webside manner,” to compensate for the inability of the clinician to touch a patient. These techniques include leaning in toward the camera, nodding, and pausing to be certain the patient has finished speaking before the clinician speaks again.
Is telehealth the future of palliative care?
I include myself among those oncologists who have voiced concern about moving from face-to-face to remote visits for complicated consultations such as those required for palliative care. Nonetheless, from the preliminary results of the REACH PC trial, it appears that telehealth could be a valuable tool.
To minimize differences between in-person and remote delivery of palliative care, practical strategies for ensuring rapport and facilitating a trusting relationship should be defined further and disseminated.
In addition, we need to be vigilant for widening inequities of care from rapid movement to the use of technology (i.e., an equity gap). In their telehealth experience during the COVID-19 pandemic, investigators at Houston Methodist Cancer Center found that patients declining virtual visits tended to be older, lower-income, and less likely to have commercial insurance. These results were recently published in JCO Oncology Practice.
For the foregoing reasons, hybrid systems for palliative care services will probably always be needed.
Going forward, we should heed the advice of Alvin Toffler in his book Future Shock. Mr. Toffler said, “The illiterate of the 21st century will not be those who cannot read and write, but those who cannot learn, unlearn, and relearn.”
The traditional model for delivering palliative care will almost certainly need to be reimagined and relearned.
Dr. Temel disclosed institutional research funding from Pfizer.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Traditional delivery of palliative care to outpatients with cancer is associated with many challenges.
Telehealth can eliminate some of these challenges but comes with issues of its own, according to results of the REACH PC trial.
Jennifer S. Temel, MD, of Massachusetts General Hospital in Boston, discussed the use of telemedicine in palliative care, including results from REACH PC, during an educational session at the ASCO Virtual Quality Care Symposium 2020.
Dr. Temel noted that, for cancer patients, an in-person visit with a palliative care specialist can cost time, induce fatigue, and increase financial burden from transportation and parking expenses.
For caregivers and family, an in-person visit may necessitate absence from family and/or work, require complex scheduling to coordinate with other office visits, and result in additional transportation and/or parking expenses.
For health care systems, to have a dedicated palliative care clinic requires precious space and financial expenditures for office personnel and other resources.
These issues make it attractive to consider whether telehealth could be used for palliative care services.
Scarcity of palliative care specialists
In the United States, there is roughly 1 palliative care physician for every 20,000 older adults with a life-limiting illness, according to research published in Annual Review of Public Health in 2014.
In its 2019 state-by-state report card, the Center to Advance Palliative Care noted that only 72% of U.S. hospitals with 50 or more beds have a palliative care team.
For patients with serious illnesses and those who are socioeconomically or geographically disadvantaged, palliative care is often inaccessible.
Inefficiencies in the current system are an additional impediment. Palliative care specialists frequently see patients during a portion of the patient’s routine visit to subspecialty or primary care clinics. This limits the palliative care specialist’s ability to perform comprehensive assessments and provide patient-centered care efficiently.
Special considerations regarding telehealth for palliative care
As a specialty, palliative care involves interactions that could make the use of telehealth problematic. For example, conveyance of interest, warmth, and touch are challenging or impossible in a video format.
Palliative care specialists engage with patients regarding relatively serious topics such as prognosis and end-of-life preferences. There is uncertainty about how those discussions would be received by patients and their caregivers via video.
Furthermore, there are logistical impediments such as prescribing opioids with video or across state lines.
Despite these concerns, the ENABLE study showed that supplementing usual oncology care with weekly (transitioning to monthly) telephone-based educational palliative care produced higher quality of life and mood than did usual oncology care alone. These results were published in JAMA in 2009.
REACH PC study demonstrates feasibility of telehealth model
Dr. Temel described the ongoing REACH PC trial in which palliative care is delivered via video visits and compared with in-person palliative care for patients with advanced non–small cell lung cancer.
The primary aim of REACH PC is to determine whether telehealth palliative care is equivalent to traditional palliative care in improving quality of life as a supplement to routine oncology care.
Currently, REACH PC has enrolled 581 patients at its 20 sites, spanning a geographically diverse area. Just over half of patients approached about REACH PC agreed to enroll in it. Ultimately, 1,250 enrollees are sought.
Among patients who declined to participate, 7.6% indicated “discomfort with technology” as the reason. Most refusals were due to lack of interest in research (35.1%) and/or palliative care (22.9%).
Older adults were prominent among enrollees. More than 60% were older than 60 years of age, and more than one-third were older than 70 years.
Among patients who began the trial, there were slightly more withdrawals in the telehealth participants, in comparison with in-person participants (13.6% versus 9.1%).
When palliative care clinicians were queried about video visits, 64.3% said there were no challenges. This is comparable to the 65.5% of clinicians who had no challenges with in-person visits.
When problems occurred with video visits, they were most frequently technical (19.1%). Only 1.4% of clinicians reported difficulty addressing topics that felt uncomfortable over video, and 1.5% reported difficulty establishing rapport.
The success rates of video and in-person visits were similar. About 80% of visits accomplished planned goals.
‘Webside’ manner
Strategies such as reflective listening and summarizing what patients say (to verify an accurate understanding of the patient’s perspective) are key to successful palliative care visits, regardless of the setting.
For telehealth visits, Dr. Temel described techniques she defined as “webside manner,” to compensate for the inability of the clinician to touch a patient. These techniques include leaning in toward the camera, nodding, and pausing to be certain the patient has finished speaking before the clinician speaks again.
Is telehealth the future of palliative care?
I include myself among those oncologists who have voiced concern about moving from face-to-face to remote visits for complicated consultations such as those required for palliative care. Nonetheless, from the preliminary results of the REACH PC trial, it appears that telehealth could be a valuable tool.
To minimize differences between in-person and remote delivery of palliative care, practical strategies for ensuring rapport and facilitating a trusting relationship should be defined further and disseminated.
In addition, we need to be vigilant for widening inequities of care from rapid movement to the use of technology (i.e., an equity gap). In their telehealth experience during the COVID-19 pandemic, investigators at Houston Methodist Cancer Center found that patients declining virtual visits tended to be older, lower-income, and less likely to have commercial insurance. These results were recently published in JCO Oncology Practice.
For the foregoing reasons, hybrid systems for palliative care services will probably always be needed.
Going forward, we should heed the advice of Alvin Toffler in his book Future Shock. Mr. Toffler said, “The illiterate of the 21st century will not be those who cannot read and write, but those who cannot learn, unlearn, and relearn.”
The traditional model for delivering palliative care will almost certainly need to be reimagined and relearned.
Dr. Temel disclosed institutional research funding from Pfizer.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Traditional delivery of palliative care to outpatients with cancer is associated with many challenges.
Telehealth can eliminate some of these challenges but comes with issues of its own, according to results of the REACH PC trial.
Jennifer S. Temel, MD, of Massachusetts General Hospital in Boston, discussed the use of telemedicine in palliative care, including results from REACH PC, during an educational session at the ASCO Virtual Quality Care Symposium 2020.
Dr. Temel noted that, for cancer patients, an in-person visit with a palliative care specialist can cost time, induce fatigue, and increase financial burden from transportation and parking expenses.
For caregivers and family, an in-person visit may necessitate absence from family and/or work, require complex scheduling to coordinate with other office visits, and result in additional transportation and/or parking expenses.
For health care systems, to have a dedicated palliative care clinic requires precious space and financial expenditures for office personnel and other resources.
These issues make it attractive to consider whether telehealth could be used for palliative care services.
Scarcity of palliative care specialists
In the United States, there is roughly 1 palliative care physician for every 20,000 older adults with a life-limiting illness, according to research published in Annual Review of Public Health in 2014.
In its 2019 state-by-state report card, the Center to Advance Palliative Care noted that only 72% of U.S. hospitals with 50 or more beds have a palliative care team.
For patients with serious illnesses and those who are socioeconomically or geographically disadvantaged, palliative care is often inaccessible.
Inefficiencies in the current system are an additional impediment. Palliative care specialists frequently see patients during a portion of the patient’s routine visit to subspecialty or primary care clinics. This limits the palliative care specialist’s ability to perform comprehensive assessments and provide patient-centered care efficiently.
Special considerations regarding telehealth for palliative care
As a specialty, palliative care involves interactions that could make the use of telehealth problematic. For example, conveyance of interest, warmth, and touch are challenging or impossible in a video format.
Palliative care specialists engage with patients regarding relatively serious topics such as prognosis and end-of-life preferences. There is uncertainty about how those discussions would be received by patients and their caregivers via video.
Furthermore, there are logistical impediments such as prescribing opioids with video or across state lines.
Despite these concerns, the ENABLE study showed that supplementing usual oncology care with weekly (transitioning to monthly) telephone-based educational palliative care produced higher quality of life and mood than did usual oncology care alone. These results were published in JAMA in 2009.
REACH PC study demonstrates feasibility of telehealth model
Dr. Temel described the ongoing REACH PC trial in which palliative care is delivered via video visits and compared with in-person palliative care for patients with advanced non–small cell lung cancer.
The primary aim of REACH PC is to determine whether telehealth palliative care is equivalent to traditional palliative care in improving quality of life as a supplement to routine oncology care.
Currently, REACH PC has enrolled 581 patients at its 20 sites, spanning a geographically diverse area. Just over half of patients approached about REACH PC agreed to enroll in it. Ultimately, 1,250 enrollees are sought.
Among patients who declined to participate, 7.6% indicated “discomfort with technology” as the reason. Most refusals were due to lack of interest in research (35.1%) and/or palliative care (22.9%).
Older adults were prominent among enrollees. More than 60% were older than 60 years of age, and more than one-third were older than 70 years.
Among patients who began the trial, there were slightly more withdrawals in the telehealth participants, in comparison with in-person participants (13.6% versus 9.1%).
When palliative care clinicians were queried about video visits, 64.3% said there were no challenges. This is comparable to the 65.5% of clinicians who had no challenges with in-person visits.
When problems occurred with video visits, they were most frequently technical (19.1%). Only 1.4% of clinicians reported difficulty addressing topics that felt uncomfortable over video, and 1.5% reported difficulty establishing rapport.
The success rates of video and in-person visits were similar. About 80% of visits accomplished planned goals.
‘Webside’ manner
Strategies such as reflective listening and summarizing what patients say (to verify an accurate understanding of the patient’s perspective) are key to successful palliative care visits, regardless of the setting.
For telehealth visits, Dr. Temel described techniques she defined as “webside manner,” to compensate for the inability of the clinician to touch a patient. These techniques include leaning in toward the camera, nodding, and pausing to be certain the patient has finished speaking before the clinician speaks again.
Is telehealth the future of palliative care?
I include myself among those oncologists who have voiced concern about moving from face-to-face to remote visits for complicated consultations such as those required for palliative care. Nonetheless, from the preliminary results of the REACH PC trial, it appears that telehealth could be a valuable tool.
To minimize differences between in-person and remote delivery of palliative care, practical strategies for ensuring rapport and facilitating a trusting relationship should be defined further and disseminated.
In addition, we need to be vigilant for widening inequities of care from rapid movement to the use of technology (i.e., an equity gap). In their telehealth experience during the COVID-19 pandemic, investigators at Houston Methodist Cancer Center found that patients declining virtual visits tended to be older, lower-income, and less likely to have commercial insurance. These results were recently published in JCO Oncology Practice.
For the foregoing reasons, hybrid systems for palliative care services will probably always be needed.
Going forward, we should heed the advice of Alvin Toffler in his book Future Shock. Mr. Toffler said, “The illiterate of the 21st century will not be those who cannot read and write, but those who cannot learn, unlearn, and relearn.”
The traditional model for delivering palliative care will almost certainly need to be reimagined and relearned.
Dr. Temel disclosed institutional research funding from Pfizer.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM ASCO QUALITY CARE SYMPOSIUM 2020
Practicing medicine without judgment
“What do you think of all this election stuff?” I froze. Sitting on the exam table was a 50-something-year-old woman. Her hair was long, but not gray. She was wearing a mask without distinctive markings, such as Trump lips or #BLM to identify the political leanings of the owner. She had a subtle New York accent, perhaps dating back to the Giuliani years. It was hard to know her intention. “It’s a trap!” I could hear Admiral Ackbar’s voice in my head. “Don’t engage.” We all know nothing erodes trust faster than showing your blue or red colors before you know which your patient identifies.
Instead, I replied that indeed it has been a stressful year for us all. Then I paused. She shifted a bit and tugged at the gown sleeves and admitted this was the most stress she felt in years. She was seeing me for lichen sclerosus et atrophicus, a terribly itchy, sometimes-disfiguring eruption that can occur in the vulva. She was dealing with COVID-19, kids, divorce, a new partner, working from home, parents, and now the election drama.
At this point in the visit, I knew I could help her. First, the treatment for lichen sclerosus is straightforward and mostly effective. Second, I knew I’d have 7 minutes to spare to just listen. It was a lucky break, as often no such gift of time presents itself while seeing patients in a busy clinic. We take vitals, history (typing), do an exam, make a diagnosis (more typing), and maybe a procedure (yet more typing). All of this is necessary, but sometimes not what our patient needs. Some really need just to connect and share their burden with someone who isn’t a friend or family. As physicians, we have a unique opportunity to see and hear people without judgment.
This reminds me of a recent episode from Sam Harris’s podcast, “Making Sense.” Mr. Harris, a philosopher (and “blue” all the way through) revealed his insight into Presidents Trump’s appeal. Leaving policy aside, Mr. Harris notes that people are drawn to the President because he never judges you. He is incapable of being sanctimonious, Mr. Harris argues, and therefore creates a safe space for people to continue their lives, however flawed, without expectation that they improve.
I’m unsure just how much of this theory explains the devotion of his supporters, but it resonated with me. We doctors are sanctimonious by nature. The better part of my day is spent prodding people to be better: Wear more sunscreen, exercise more, stop believing in conspiracy theories, get your flu shot, and above all, stop scratching! In doing so, I’m in a way judging them. Finger wagging: You’re lazy or poor or dumb or stubborn. “You aren’t as good as me,” is what they might feel after 15 minutes of my pep talk.
But what if that’s wrong? What if they are just fine exactly the way they are? Perhaps what my lichen sclerosis patient needs more than anything is unconditional attention? She, like most of our patients, is well aware of how her shortcomings might contribute to her own anxiety or difficulties. And now she has this rash and that’s probably somehow her fault too, she thinks.
How can I best help her? Betamethasone dipropionate b.i.d. for 2 weeks and spend the last 7 minutes just sitting and listening without judgment or advice. I don’t know who she wanted to win the election. It didn’t matter, she was exactly right to believe what she believed, either way.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“What do you think of all this election stuff?” I froze. Sitting on the exam table was a 50-something-year-old woman. Her hair was long, but not gray. She was wearing a mask without distinctive markings, such as Trump lips or #BLM to identify the political leanings of the owner. She had a subtle New York accent, perhaps dating back to the Giuliani years. It was hard to know her intention. “It’s a trap!” I could hear Admiral Ackbar’s voice in my head. “Don’t engage.” We all know nothing erodes trust faster than showing your blue or red colors before you know which your patient identifies.
Instead, I replied that indeed it has been a stressful year for us all. Then I paused. She shifted a bit and tugged at the gown sleeves and admitted this was the most stress she felt in years. She was seeing me for lichen sclerosus et atrophicus, a terribly itchy, sometimes-disfiguring eruption that can occur in the vulva. She was dealing with COVID-19, kids, divorce, a new partner, working from home, parents, and now the election drama.
At this point in the visit, I knew I could help her. First, the treatment for lichen sclerosus is straightforward and mostly effective. Second, I knew I’d have 7 minutes to spare to just listen. It was a lucky break, as often no such gift of time presents itself while seeing patients in a busy clinic. We take vitals, history (typing), do an exam, make a diagnosis (more typing), and maybe a procedure (yet more typing). All of this is necessary, but sometimes not what our patient needs. Some really need just to connect and share their burden with someone who isn’t a friend or family. As physicians, we have a unique opportunity to see and hear people without judgment.
This reminds me of a recent episode from Sam Harris’s podcast, “Making Sense.” Mr. Harris, a philosopher (and “blue” all the way through) revealed his insight into Presidents Trump’s appeal. Leaving policy aside, Mr. Harris notes that people are drawn to the President because he never judges you. He is incapable of being sanctimonious, Mr. Harris argues, and therefore creates a safe space for people to continue their lives, however flawed, without expectation that they improve.
I’m unsure just how much of this theory explains the devotion of his supporters, but it resonated with me. We doctors are sanctimonious by nature. The better part of my day is spent prodding people to be better: Wear more sunscreen, exercise more, stop believing in conspiracy theories, get your flu shot, and above all, stop scratching! In doing so, I’m in a way judging them. Finger wagging: You’re lazy or poor or dumb or stubborn. “You aren’t as good as me,” is what they might feel after 15 minutes of my pep talk.
But what if that’s wrong? What if they are just fine exactly the way they are? Perhaps what my lichen sclerosis patient needs more than anything is unconditional attention? She, like most of our patients, is well aware of how her shortcomings might contribute to her own anxiety or difficulties. And now she has this rash and that’s probably somehow her fault too, she thinks.
How can I best help her? Betamethasone dipropionate b.i.d. for 2 weeks and spend the last 7 minutes just sitting and listening without judgment or advice. I don’t know who she wanted to win the election. It didn’t matter, she was exactly right to believe what she believed, either way.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“What do you think of all this election stuff?” I froze. Sitting on the exam table was a 50-something-year-old woman. Her hair was long, but not gray. She was wearing a mask without distinctive markings, such as Trump lips or #BLM to identify the political leanings of the owner. She had a subtle New York accent, perhaps dating back to the Giuliani years. It was hard to know her intention. “It’s a trap!” I could hear Admiral Ackbar’s voice in my head. “Don’t engage.” We all know nothing erodes trust faster than showing your blue or red colors before you know which your patient identifies.
Instead, I replied that indeed it has been a stressful year for us all. Then I paused. She shifted a bit and tugged at the gown sleeves and admitted this was the most stress she felt in years. She was seeing me for lichen sclerosus et atrophicus, a terribly itchy, sometimes-disfiguring eruption that can occur in the vulva. She was dealing with COVID-19, kids, divorce, a new partner, working from home, parents, and now the election drama.
At this point in the visit, I knew I could help her. First, the treatment for lichen sclerosus is straightforward and mostly effective. Second, I knew I’d have 7 minutes to spare to just listen. It was a lucky break, as often no such gift of time presents itself while seeing patients in a busy clinic. We take vitals, history (typing), do an exam, make a diagnosis (more typing), and maybe a procedure (yet more typing). All of this is necessary, but sometimes not what our patient needs. Some really need just to connect and share their burden with someone who isn’t a friend or family. As physicians, we have a unique opportunity to see and hear people without judgment.
This reminds me of a recent episode from Sam Harris’s podcast, “Making Sense.” Mr. Harris, a philosopher (and “blue” all the way through) revealed his insight into Presidents Trump’s appeal. Leaving policy aside, Mr. Harris notes that people are drawn to the President because he never judges you. He is incapable of being sanctimonious, Mr. Harris argues, and therefore creates a safe space for people to continue their lives, however flawed, without expectation that they improve.
I’m unsure just how much of this theory explains the devotion of his supporters, but it resonated with me. We doctors are sanctimonious by nature. The better part of my day is spent prodding people to be better: Wear more sunscreen, exercise more, stop believing in conspiracy theories, get your flu shot, and above all, stop scratching! In doing so, I’m in a way judging them. Finger wagging: You’re lazy or poor or dumb or stubborn. “You aren’t as good as me,” is what they might feel after 15 minutes of my pep talk.
But what if that’s wrong? What if they are just fine exactly the way they are? Perhaps what my lichen sclerosis patient needs more than anything is unconditional attention? She, like most of our patients, is well aware of how her shortcomings might contribute to her own anxiety or difficulties. And now she has this rash and that’s probably somehow her fault too, she thinks.
How can I best help her? Betamethasone dipropionate b.i.d. for 2 weeks and spend the last 7 minutes just sitting and listening without judgment or advice. I don’t know who she wanted to win the election. It didn’t matter, she was exactly right to believe what she believed, either way.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Neurologist as patient: A missed diagnosis, poor communication, and incompetent care could have led to quadriplegia
When Steven Horowitz, MD, began experiencing neck and arm pain, numbness, and tingling following a bike ride several years ago, he immediately sought care at an elite medical center in California. As he recalls, an incompetent clinical exam and no access to highly abnormal test results done in the ED almost cost him his health. Had he listened to the doctors at that facility, he believes he would have become quadriplegic.
His training as a neurologist likely saved his life: “I was able to recover because, after arriving home, I reviewed my blood work and MRI online and recognized multiple problems.” He was able to get excellent care at his own local health care facility in Maine. The staff and leadership at the hospital in California wouldn’t admit wrongdoing, and efforts to seek recourse have proved fruitless, he said.
A lingering question nags at him: What if he had been an ordinary patient without medical expertise? What do his experiences say about the health care system’s management of medical omissions and errors?
Dr. Horowitz, 78 years old and retired, continues to teach medical students as an adjunct clinical professor of neurology at the Tufts University School of Medicine in Boston. He is also on the teaching faculty of the Maine Medical Center. He was professor and chief of neurology at a major university in the Midwest for many years.
In 2018, he visited his daughter on the West Coast, enjoying a day of biking. The neck pain began 5 or 6 hours after the ride and spread to his arms. “There was also numbness and tingling,” he said.
“I told them I was a neurologist”
The next day the pain got worse. Dr. Horowitz went to the ED of a nearby medical center with his daughter and immediately disclosed that he was a neurologist. “I did this for several reasons,” he explained. He wanted to alert staff that he had a cervical spine problem because “I wanted them to do a cervical MRI scan, and I wanted to read it because I’m capable of doing that.” He also related a past history of infection and antibiotic use and asked for C-reactive protein and erythrocyte sedimentation rate tests in addition to regular blood work. “Those inflammatory markers, if abnormal, would indicate an infection,” said Dr. Horowitz.
No reflex hammer or Babinski test
During the reflex exam with a spine consultant, Dr. Horowitz noticed that the consultant wasn’t using a reflex hammer, the clinical equivalent of evaluating the heart or lungs without a stethoscope. “I asked where the reflex hammer was, and he said he didn’t need one or own one. He used the inside of his hand. Apparently, there was some mild weakness in some muscle groups, but he didn’t address that,” said Dr. Horowitz. The consultant also didn’t test for the Babinski sign until reminded of it.
He took out a stethoscope and struck the middle of the soles of Dr. Horowitz’s feet. “I thought to myself, this consultant is the consultant for the spine service? How is it possible that he has a stethoscope and not a reflex hammer and didn’t know how to test for the Babinski sign?” The consultant also didn’t examine for gait, coordination, or hand dexterity. “He took his finger and touched my feet and legs. That was his sensory exam. He didn’t use a pin or a tuning fork” or other methods including touch, temperature, position sense, and vibration to assess sensory abnormalities that might signal spinal cord dysfunction.
An MRI at the hospital revealed a mass at the back of the neck. No contrast material was used during the MRI even though this step would have signaled the presence of infection. “Gadolinium should have been injected during the MRI because that would have strongly suggested that this mass in my neck was not a little blood clot and more likely an infection. They would have realized something more complicated than degenerative arthritis was going on. They told me that I had advanced spondylosis and that the mass was a hematoma. They told me not to worry about the blood results. Then they discharged me.”
A life-threatening discovery
Dr. Horowitz didn’t see the results of the blood work-up until returning to Maine a few days later, when he checked the online report. There was a highly elevated CRP level – 30 times above the normal limit – and elevated erythrocyte sedimentation rate and white blood cell counts. “This showed that there was an infective process going on. And it wasn’t just a localized process, it was in my bloodstream,” he said.
Alarmed by the elevated markers, he immediately went to his local hospital. “Not only did I have arthritis, but my spinal cord was compressed.” Urgent surgery was performed, including a C2-7 fusion. The mass in the back of his neck turned out to be an abscess.
His training and experience as a physician/neurologist saved him from further damage, he said. “Because the compression of the spine was at the C2, C3, C4 level, not only would I have become quadriplegic, but my diaphragm would likely have been paralyzed and I would have needed a ventilator.”
Following a month’s care in the hospital and a rehabilitation center, he wrote to the CEO of the California hospital where he received his initial care.
“I wrote about the incompetent exam, the missed infection, a discharge without information. I wrote all that out to the CEO and sent the letter registered so that he would receive it.” The CEO forwarded the letter to a patient risk manager, who interviewed staff and supervisors in the ED, radiology, and the spine program. They responded 3 months later. According to Dr. Horowitz, the spine supervisor said, “The consultant performed the exam to the best of his ability.” No one admitted to any errors in care or the lack of recognition of the infection, although the neuroradiologist did apologize for not allowing Dr. Horowitz to read his own MRI in a timely manner.
“They had promised to wheel a portable computer into my alcove so I could view the MRI.” Several hours later, after persistent complaints, he was given 1 minute to look over at least 300 images at a desktop computer in the crowded ED. They gave him the MRI images on a disk, but he wasn’t able to read it on his iMac computer.
According to Dr. Horowitz, the ED should have called in an infectious disease consultant and a neurologist or neurosurgeon to do a more complete neurologic exam. “Instead of discharging me, they should have admitted me, telling me that I had spinal cord compression, an infection, and a mass in my neck—that they don’t know what this is about, and I shouldn’t go home.”
Eventually, after long-term intravenous antibiotics and extensive physical therapy, Dr. Horowitz recovered. “I definitely had PTSD afterwards. How could a non-eventful bike ride result in an unrecognized threatening illness? I thought a healing opportunity for me and an educational opportunity for the medical staff and students at this medical center would be for me to present my case to them at a conference at their facility the next time I visited my daughter in California. I thought an experienced clinician discussing his own illness in his own specialty would be unique.”
The hospital ignored his offer.
By happenstance, a year and a half later, Dr. Horowitz made contact with a hospital administrator after hearing her speak during a TED Radio Hour in his car. “We had several telephone conversations and email correspondences in October and November 2019 but none since,” he said. In one email, she wrote that “hospitals don’t seem to know what to do with the opportunity you present. I don’t think the challenge is unique to [this institution]. A forum for these kinds of discussions – constructive, insightful patient feedback – does not exist.”
Dr. Horowitz hasn’t considered a malpractice lawsuit. “The only result would be a monetary reward based on damages. Since permanent clinical damage did not occur, the suit would have been time consuming and the reward limited. I was able to recover because I was able to review the blood work and recognize my own problem and get excellent care at my own local health care facility. I was really hoping the doctors at the California hospital would learn from this episode.”
Dr. Horowitz also wrote the Medical Board of California a detailed letter, citing relevant medical literature, guidelines on spinal care, and his test results. Nearly 2 years later, he finally got a response. The board said there was no “clear and convincing evidence that negligence took place.” In Dr. Horowitz’s opinion, “the fact that CRP was 30 times past normal is ‘clear and convincing evidence.’ That the consultant didn’t have a reflex hammer is also ‘clear and convincing evidence.’ That the clinical neurologic exam was incompetent, by any measure, is ‘clear and convincing evidence.’ Even the Medical Board, tasked with patient protection, didn’t recognize negligent medical care. They might have if I had become quadriplegic.”
A new normal?
Dr. Horowitz, who wrote of his experience in The Washington Post, said it reflects a persistent, systemic problem in health care: the inability to address medical errors and correct them. In the article, he addressed a phenomenon called the “the normalization of deviance.” Diane Vaughn wrote about this phenomenon in a 1997 book about the Space Shuttle disaster. Multiple flaws were noted in previous shuttle launches but then rationalized and “normalized” when they didn’t cause a disaster – until they ultimately did.
“That’s relevant to my situation,” Dr. Horowitz said. “The spine supervisor at this hospital excused the consultant by saying, ‘he did the exam to the best of his ability.’ Further, the response to my complaints came from hospital representatives rather than physicians, meaning that the ‘normalization’ was institutional, and it was willing to accept his poor performance without sanctions.”
He imagines that he could not be the only case handled poorly by this hospital or that particular consultant. “He could have done the same thing to another patient who didn’t have my medical knowledge,” added Dr. Horowitz.
In her book, Ms. Vaughan noted that whistleblower activity is sometimes the only device that reveals normalization of deviance.
Dr. Horowitz sees himself as a whistleblower for these types of mistakes. “The question is, how do we deal with medical errors even in sophisticated patients who see these errors, and how do you manage this in the average patient? I don’t want to see this type of medical care rendered for any patient, hence my attempt to make this situation public.”
A teachable moment lost?
Commenting on this case, Alan Rapoport, MD, said, “[it]illustrates inadequate physician evaluation in the ED, poor communication from the examining doctor about abnormal lab and MRI findings, unwillingness to call in consultants to properly evaluate the situation, and no recognition of the need to admit the patient.”
Dr. Rapoport is the editor in chief of Neurology Reviews and a clinical professor of neurology at UCLA in Los Angeles. He is a past president of the International Headache Society.
He noted that the patient is in his late 70s and needed to fly across the country to arrive at home. “Months later, when this situation was explained to the hospital via the mail, they totally failed to recognize their inadequacies and apologize for their mistakes. They were probably concerned about being sued, but I believe that their actions increased their chances of a lawsuit,” Dr. Rapoport said.
“When a teaching remedy was offered by the patient to the hospital so the doctors involved could learn from the experience, the hospital was not interested. The only party that learned from this unfortunate episode was the patient, not the doctors, or the ER, or the hospital administration,” Dr. Rapoport said.
He continued, “It is scary to think that an excellent hospital would act in this manner and refuse to learn from their mistakes. The California medical board was notified and did not investigate. It is not too late for the hospital to apologize, communicate their shortcomings, and fix the problem at multiple levels in the hospital.”
Dr. Rapoport consulted Morris Levin, MD, a professor of neurology and director of the Headache Program at UCSF, to ask what he thought, theoretically, about how a hospital should respond when they make a mistake and how much they should divulge. Dr. Levin is involved in Medical Ethics and often lectures about it at conferences.
Dr. Levin said, “When medical errors are made, to me, it is ethically sound to identify them and ‘fess up.’ There has always been reluctance to do so because of fears of lawsuits, but it turns out that when institutions do disclose errors, their liability costs actually go down.” Dr. Levin cited the University of Michigan, which tried a full disclosure policy as an experiment. “It led to reduced costs, not to mention a boost in patient satisfaction,” Dr. Levin noted.
He continued, “I think patients want and deserve to know the truth. I also believe they understand that medical errors can and will happen. It is my observation that patients have several key concerns: 1) how the error(s) happened, 2) how the error affected their health and what can be done to restore them to optimal health, and 3) what the institution is going to do to prevent this kind of error from happening to others.”
Dr. Rapoport concurs with Dr. Levin. “I am glad Dr. Horowitz has fully recovered and at least he has learned from the experience. I do not think the hospital and doctors did,” Dr. Rapoport said.
This article was updated 11/12/20.
When Steven Horowitz, MD, began experiencing neck and arm pain, numbness, and tingling following a bike ride several years ago, he immediately sought care at an elite medical center in California. As he recalls, an incompetent clinical exam and no access to highly abnormal test results done in the ED almost cost him his health. Had he listened to the doctors at that facility, he believes he would have become quadriplegic.
His training as a neurologist likely saved his life: “I was able to recover because, after arriving home, I reviewed my blood work and MRI online and recognized multiple problems.” He was able to get excellent care at his own local health care facility in Maine. The staff and leadership at the hospital in California wouldn’t admit wrongdoing, and efforts to seek recourse have proved fruitless, he said.
A lingering question nags at him: What if he had been an ordinary patient without medical expertise? What do his experiences say about the health care system’s management of medical omissions and errors?
Dr. Horowitz, 78 years old and retired, continues to teach medical students as an adjunct clinical professor of neurology at the Tufts University School of Medicine in Boston. He is also on the teaching faculty of the Maine Medical Center. He was professor and chief of neurology at a major university in the Midwest for many years.
In 2018, he visited his daughter on the West Coast, enjoying a day of biking. The neck pain began 5 or 6 hours after the ride and spread to his arms. “There was also numbness and tingling,” he said.
“I told them I was a neurologist”
The next day the pain got worse. Dr. Horowitz went to the ED of a nearby medical center with his daughter and immediately disclosed that he was a neurologist. “I did this for several reasons,” he explained. He wanted to alert staff that he had a cervical spine problem because “I wanted them to do a cervical MRI scan, and I wanted to read it because I’m capable of doing that.” He also related a past history of infection and antibiotic use and asked for C-reactive protein and erythrocyte sedimentation rate tests in addition to regular blood work. “Those inflammatory markers, if abnormal, would indicate an infection,” said Dr. Horowitz.
No reflex hammer or Babinski test
During the reflex exam with a spine consultant, Dr. Horowitz noticed that the consultant wasn’t using a reflex hammer, the clinical equivalent of evaluating the heart or lungs without a stethoscope. “I asked where the reflex hammer was, and he said he didn’t need one or own one. He used the inside of his hand. Apparently, there was some mild weakness in some muscle groups, but he didn’t address that,” said Dr. Horowitz. The consultant also didn’t test for the Babinski sign until reminded of it.
He took out a stethoscope and struck the middle of the soles of Dr. Horowitz’s feet. “I thought to myself, this consultant is the consultant for the spine service? How is it possible that he has a stethoscope and not a reflex hammer and didn’t know how to test for the Babinski sign?” The consultant also didn’t examine for gait, coordination, or hand dexterity. “He took his finger and touched my feet and legs. That was his sensory exam. He didn’t use a pin or a tuning fork” or other methods including touch, temperature, position sense, and vibration to assess sensory abnormalities that might signal spinal cord dysfunction.
An MRI at the hospital revealed a mass at the back of the neck. No contrast material was used during the MRI even though this step would have signaled the presence of infection. “Gadolinium should have been injected during the MRI because that would have strongly suggested that this mass in my neck was not a little blood clot and more likely an infection. They would have realized something more complicated than degenerative arthritis was going on. They told me that I had advanced spondylosis and that the mass was a hematoma. They told me not to worry about the blood results. Then they discharged me.”
A life-threatening discovery
Dr. Horowitz didn’t see the results of the blood work-up until returning to Maine a few days later, when he checked the online report. There was a highly elevated CRP level – 30 times above the normal limit – and elevated erythrocyte sedimentation rate and white blood cell counts. “This showed that there was an infective process going on. And it wasn’t just a localized process, it was in my bloodstream,” he said.
Alarmed by the elevated markers, he immediately went to his local hospital. “Not only did I have arthritis, but my spinal cord was compressed.” Urgent surgery was performed, including a C2-7 fusion. The mass in the back of his neck turned out to be an abscess.
His training and experience as a physician/neurologist saved him from further damage, he said. “Because the compression of the spine was at the C2, C3, C4 level, not only would I have become quadriplegic, but my diaphragm would likely have been paralyzed and I would have needed a ventilator.”
Following a month’s care in the hospital and a rehabilitation center, he wrote to the CEO of the California hospital where he received his initial care.
“I wrote about the incompetent exam, the missed infection, a discharge without information. I wrote all that out to the CEO and sent the letter registered so that he would receive it.” The CEO forwarded the letter to a patient risk manager, who interviewed staff and supervisors in the ED, radiology, and the spine program. They responded 3 months later. According to Dr. Horowitz, the spine supervisor said, “The consultant performed the exam to the best of his ability.” No one admitted to any errors in care or the lack of recognition of the infection, although the neuroradiologist did apologize for not allowing Dr. Horowitz to read his own MRI in a timely manner.
“They had promised to wheel a portable computer into my alcove so I could view the MRI.” Several hours later, after persistent complaints, he was given 1 minute to look over at least 300 images at a desktop computer in the crowded ED. They gave him the MRI images on a disk, but he wasn’t able to read it on his iMac computer.
According to Dr. Horowitz, the ED should have called in an infectious disease consultant and a neurologist or neurosurgeon to do a more complete neurologic exam. “Instead of discharging me, they should have admitted me, telling me that I had spinal cord compression, an infection, and a mass in my neck—that they don’t know what this is about, and I shouldn’t go home.”
Eventually, after long-term intravenous antibiotics and extensive physical therapy, Dr. Horowitz recovered. “I definitely had PTSD afterwards. How could a non-eventful bike ride result in an unrecognized threatening illness? I thought a healing opportunity for me and an educational opportunity for the medical staff and students at this medical center would be for me to present my case to them at a conference at their facility the next time I visited my daughter in California. I thought an experienced clinician discussing his own illness in his own specialty would be unique.”
The hospital ignored his offer.
By happenstance, a year and a half later, Dr. Horowitz made contact with a hospital administrator after hearing her speak during a TED Radio Hour in his car. “We had several telephone conversations and email correspondences in October and November 2019 but none since,” he said. In one email, she wrote that “hospitals don’t seem to know what to do with the opportunity you present. I don’t think the challenge is unique to [this institution]. A forum for these kinds of discussions – constructive, insightful patient feedback – does not exist.”
Dr. Horowitz hasn’t considered a malpractice lawsuit. “The only result would be a monetary reward based on damages. Since permanent clinical damage did not occur, the suit would have been time consuming and the reward limited. I was able to recover because I was able to review the blood work and recognize my own problem and get excellent care at my own local health care facility. I was really hoping the doctors at the California hospital would learn from this episode.”
Dr. Horowitz also wrote the Medical Board of California a detailed letter, citing relevant medical literature, guidelines on spinal care, and his test results. Nearly 2 years later, he finally got a response. The board said there was no “clear and convincing evidence that negligence took place.” In Dr. Horowitz’s opinion, “the fact that CRP was 30 times past normal is ‘clear and convincing evidence.’ That the consultant didn’t have a reflex hammer is also ‘clear and convincing evidence.’ That the clinical neurologic exam was incompetent, by any measure, is ‘clear and convincing evidence.’ Even the Medical Board, tasked with patient protection, didn’t recognize negligent medical care. They might have if I had become quadriplegic.”
A new normal?
Dr. Horowitz, who wrote of his experience in The Washington Post, said it reflects a persistent, systemic problem in health care: the inability to address medical errors and correct them. In the article, he addressed a phenomenon called the “the normalization of deviance.” Diane Vaughn wrote about this phenomenon in a 1997 book about the Space Shuttle disaster. Multiple flaws were noted in previous shuttle launches but then rationalized and “normalized” when they didn’t cause a disaster – until they ultimately did.
“That’s relevant to my situation,” Dr. Horowitz said. “The spine supervisor at this hospital excused the consultant by saying, ‘he did the exam to the best of his ability.’ Further, the response to my complaints came from hospital representatives rather than physicians, meaning that the ‘normalization’ was institutional, and it was willing to accept his poor performance without sanctions.”
He imagines that he could not be the only case handled poorly by this hospital or that particular consultant. “He could have done the same thing to another patient who didn’t have my medical knowledge,” added Dr. Horowitz.
In her book, Ms. Vaughan noted that whistleblower activity is sometimes the only device that reveals normalization of deviance.
Dr. Horowitz sees himself as a whistleblower for these types of mistakes. “The question is, how do we deal with medical errors even in sophisticated patients who see these errors, and how do you manage this in the average patient? I don’t want to see this type of medical care rendered for any patient, hence my attempt to make this situation public.”
A teachable moment lost?
Commenting on this case, Alan Rapoport, MD, said, “[it]illustrates inadequate physician evaluation in the ED, poor communication from the examining doctor about abnormal lab and MRI findings, unwillingness to call in consultants to properly evaluate the situation, and no recognition of the need to admit the patient.”
Dr. Rapoport is the editor in chief of Neurology Reviews and a clinical professor of neurology at UCLA in Los Angeles. He is a past president of the International Headache Society.
He noted that the patient is in his late 70s and needed to fly across the country to arrive at home. “Months later, when this situation was explained to the hospital via the mail, they totally failed to recognize their inadequacies and apologize for their mistakes. They were probably concerned about being sued, but I believe that their actions increased their chances of a lawsuit,” Dr. Rapoport said.
“When a teaching remedy was offered by the patient to the hospital so the doctors involved could learn from the experience, the hospital was not interested. The only party that learned from this unfortunate episode was the patient, not the doctors, or the ER, or the hospital administration,” Dr. Rapoport said.
He continued, “It is scary to think that an excellent hospital would act in this manner and refuse to learn from their mistakes. The California medical board was notified and did not investigate. It is not too late for the hospital to apologize, communicate their shortcomings, and fix the problem at multiple levels in the hospital.”
Dr. Rapoport consulted Morris Levin, MD, a professor of neurology and director of the Headache Program at UCSF, to ask what he thought, theoretically, about how a hospital should respond when they make a mistake and how much they should divulge. Dr. Levin is involved in Medical Ethics and often lectures about it at conferences.
Dr. Levin said, “When medical errors are made, to me, it is ethically sound to identify them and ‘fess up.’ There has always been reluctance to do so because of fears of lawsuits, but it turns out that when institutions do disclose errors, their liability costs actually go down.” Dr. Levin cited the University of Michigan, which tried a full disclosure policy as an experiment. “It led to reduced costs, not to mention a boost in patient satisfaction,” Dr. Levin noted.
He continued, “I think patients want and deserve to know the truth. I also believe they understand that medical errors can and will happen. It is my observation that patients have several key concerns: 1) how the error(s) happened, 2) how the error affected their health and what can be done to restore them to optimal health, and 3) what the institution is going to do to prevent this kind of error from happening to others.”
Dr. Rapoport concurs with Dr. Levin. “I am glad Dr. Horowitz has fully recovered and at least he has learned from the experience. I do not think the hospital and doctors did,” Dr. Rapoport said.
This article was updated 11/12/20.
When Steven Horowitz, MD, began experiencing neck and arm pain, numbness, and tingling following a bike ride several years ago, he immediately sought care at an elite medical center in California. As he recalls, an incompetent clinical exam and no access to highly abnormal test results done in the ED almost cost him his health. Had he listened to the doctors at that facility, he believes he would have become quadriplegic.
His training as a neurologist likely saved his life: “I was able to recover because, after arriving home, I reviewed my blood work and MRI online and recognized multiple problems.” He was able to get excellent care at his own local health care facility in Maine. The staff and leadership at the hospital in California wouldn’t admit wrongdoing, and efforts to seek recourse have proved fruitless, he said.
A lingering question nags at him: What if he had been an ordinary patient without medical expertise? What do his experiences say about the health care system’s management of medical omissions and errors?
Dr. Horowitz, 78 years old and retired, continues to teach medical students as an adjunct clinical professor of neurology at the Tufts University School of Medicine in Boston. He is also on the teaching faculty of the Maine Medical Center. He was professor and chief of neurology at a major university in the Midwest for many years.
In 2018, he visited his daughter on the West Coast, enjoying a day of biking. The neck pain began 5 or 6 hours after the ride and spread to his arms. “There was also numbness and tingling,” he said.
“I told them I was a neurologist”
The next day the pain got worse. Dr. Horowitz went to the ED of a nearby medical center with his daughter and immediately disclosed that he was a neurologist. “I did this for several reasons,” he explained. He wanted to alert staff that he had a cervical spine problem because “I wanted them to do a cervical MRI scan, and I wanted to read it because I’m capable of doing that.” He also related a past history of infection and antibiotic use and asked for C-reactive protein and erythrocyte sedimentation rate tests in addition to regular blood work. “Those inflammatory markers, if abnormal, would indicate an infection,” said Dr. Horowitz.
No reflex hammer or Babinski test
During the reflex exam with a spine consultant, Dr. Horowitz noticed that the consultant wasn’t using a reflex hammer, the clinical equivalent of evaluating the heart or lungs without a stethoscope. “I asked where the reflex hammer was, and he said he didn’t need one or own one. He used the inside of his hand. Apparently, there was some mild weakness in some muscle groups, but he didn’t address that,” said Dr. Horowitz. The consultant also didn’t test for the Babinski sign until reminded of it.
He took out a stethoscope and struck the middle of the soles of Dr. Horowitz’s feet. “I thought to myself, this consultant is the consultant for the spine service? How is it possible that he has a stethoscope and not a reflex hammer and didn’t know how to test for the Babinski sign?” The consultant also didn’t examine for gait, coordination, or hand dexterity. “He took his finger and touched my feet and legs. That was his sensory exam. He didn’t use a pin or a tuning fork” or other methods including touch, temperature, position sense, and vibration to assess sensory abnormalities that might signal spinal cord dysfunction.
An MRI at the hospital revealed a mass at the back of the neck. No contrast material was used during the MRI even though this step would have signaled the presence of infection. “Gadolinium should have been injected during the MRI because that would have strongly suggested that this mass in my neck was not a little blood clot and more likely an infection. They would have realized something more complicated than degenerative arthritis was going on. They told me that I had advanced spondylosis and that the mass was a hematoma. They told me not to worry about the blood results. Then they discharged me.”
A life-threatening discovery
Dr. Horowitz didn’t see the results of the blood work-up until returning to Maine a few days later, when he checked the online report. There was a highly elevated CRP level – 30 times above the normal limit – and elevated erythrocyte sedimentation rate and white blood cell counts. “This showed that there was an infective process going on. And it wasn’t just a localized process, it was in my bloodstream,” he said.
Alarmed by the elevated markers, he immediately went to his local hospital. “Not only did I have arthritis, but my spinal cord was compressed.” Urgent surgery was performed, including a C2-7 fusion. The mass in the back of his neck turned out to be an abscess.
His training and experience as a physician/neurologist saved him from further damage, he said. “Because the compression of the spine was at the C2, C3, C4 level, not only would I have become quadriplegic, but my diaphragm would likely have been paralyzed and I would have needed a ventilator.”
Following a month’s care in the hospital and a rehabilitation center, he wrote to the CEO of the California hospital where he received his initial care.
“I wrote about the incompetent exam, the missed infection, a discharge without information. I wrote all that out to the CEO and sent the letter registered so that he would receive it.” The CEO forwarded the letter to a patient risk manager, who interviewed staff and supervisors in the ED, radiology, and the spine program. They responded 3 months later. According to Dr. Horowitz, the spine supervisor said, “The consultant performed the exam to the best of his ability.” No one admitted to any errors in care or the lack of recognition of the infection, although the neuroradiologist did apologize for not allowing Dr. Horowitz to read his own MRI in a timely manner.
“They had promised to wheel a portable computer into my alcove so I could view the MRI.” Several hours later, after persistent complaints, he was given 1 minute to look over at least 300 images at a desktop computer in the crowded ED. They gave him the MRI images on a disk, but he wasn’t able to read it on his iMac computer.
According to Dr. Horowitz, the ED should have called in an infectious disease consultant and a neurologist or neurosurgeon to do a more complete neurologic exam. “Instead of discharging me, they should have admitted me, telling me that I had spinal cord compression, an infection, and a mass in my neck—that they don’t know what this is about, and I shouldn’t go home.”
Eventually, after long-term intravenous antibiotics and extensive physical therapy, Dr. Horowitz recovered. “I definitely had PTSD afterwards. How could a non-eventful bike ride result in an unrecognized threatening illness? I thought a healing opportunity for me and an educational opportunity for the medical staff and students at this medical center would be for me to present my case to them at a conference at their facility the next time I visited my daughter in California. I thought an experienced clinician discussing his own illness in his own specialty would be unique.”
The hospital ignored his offer.
By happenstance, a year and a half later, Dr. Horowitz made contact with a hospital administrator after hearing her speak during a TED Radio Hour in his car. “We had several telephone conversations and email correspondences in October and November 2019 but none since,” he said. In one email, she wrote that “hospitals don’t seem to know what to do with the opportunity you present. I don’t think the challenge is unique to [this institution]. A forum for these kinds of discussions – constructive, insightful patient feedback – does not exist.”
Dr. Horowitz hasn’t considered a malpractice lawsuit. “The only result would be a monetary reward based on damages. Since permanent clinical damage did not occur, the suit would have been time consuming and the reward limited. I was able to recover because I was able to review the blood work and recognize my own problem and get excellent care at my own local health care facility. I was really hoping the doctors at the California hospital would learn from this episode.”
Dr. Horowitz also wrote the Medical Board of California a detailed letter, citing relevant medical literature, guidelines on spinal care, and his test results. Nearly 2 years later, he finally got a response. The board said there was no “clear and convincing evidence that negligence took place.” In Dr. Horowitz’s opinion, “the fact that CRP was 30 times past normal is ‘clear and convincing evidence.’ That the consultant didn’t have a reflex hammer is also ‘clear and convincing evidence.’ That the clinical neurologic exam was incompetent, by any measure, is ‘clear and convincing evidence.’ Even the Medical Board, tasked with patient protection, didn’t recognize negligent medical care. They might have if I had become quadriplegic.”
A new normal?
Dr. Horowitz, who wrote of his experience in The Washington Post, said it reflects a persistent, systemic problem in health care: the inability to address medical errors and correct them. In the article, he addressed a phenomenon called the “the normalization of deviance.” Diane Vaughn wrote about this phenomenon in a 1997 book about the Space Shuttle disaster. Multiple flaws were noted in previous shuttle launches but then rationalized and “normalized” when they didn’t cause a disaster – until they ultimately did.
“That’s relevant to my situation,” Dr. Horowitz said. “The spine supervisor at this hospital excused the consultant by saying, ‘he did the exam to the best of his ability.’ Further, the response to my complaints came from hospital representatives rather than physicians, meaning that the ‘normalization’ was institutional, and it was willing to accept his poor performance without sanctions.”
He imagines that he could not be the only case handled poorly by this hospital or that particular consultant. “He could have done the same thing to another patient who didn’t have my medical knowledge,” added Dr. Horowitz.
In her book, Ms. Vaughan noted that whistleblower activity is sometimes the only device that reveals normalization of deviance.
Dr. Horowitz sees himself as a whistleblower for these types of mistakes. “The question is, how do we deal with medical errors even in sophisticated patients who see these errors, and how do you manage this in the average patient? I don’t want to see this type of medical care rendered for any patient, hence my attempt to make this situation public.”
A teachable moment lost?
Commenting on this case, Alan Rapoport, MD, said, “[it]illustrates inadequate physician evaluation in the ED, poor communication from the examining doctor about abnormal lab and MRI findings, unwillingness to call in consultants to properly evaluate the situation, and no recognition of the need to admit the patient.”
Dr. Rapoport is the editor in chief of Neurology Reviews and a clinical professor of neurology at UCLA in Los Angeles. He is a past president of the International Headache Society.
He noted that the patient is in his late 70s and needed to fly across the country to arrive at home. “Months later, when this situation was explained to the hospital via the mail, they totally failed to recognize their inadequacies and apologize for their mistakes. They were probably concerned about being sued, but I believe that their actions increased their chances of a lawsuit,” Dr. Rapoport said.
“When a teaching remedy was offered by the patient to the hospital so the doctors involved could learn from the experience, the hospital was not interested. The only party that learned from this unfortunate episode was the patient, not the doctors, or the ER, or the hospital administration,” Dr. Rapoport said.
He continued, “It is scary to think that an excellent hospital would act in this manner and refuse to learn from their mistakes. The California medical board was notified and did not investigate. It is not too late for the hospital to apologize, communicate their shortcomings, and fix the problem at multiple levels in the hospital.”
Dr. Rapoport consulted Morris Levin, MD, a professor of neurology and director of the Headache Program at UCSF, to ask what he thought, theoretically, about how a hospital should respond when they make a mistake and how much they should divulge. Dr. Levin is involved in Medical Ethics and often lectures about it at conferences.
Dr. Levin said, “When medical errors are made, to me, it is ethically sound to identify them and ‘fess up.’ There has always been reluctance to do so because of fears of lawsuits, but it turns out that when institutions do disclose errors, their liability costs actually go down.” Dr. Levin cited the University of Michigan, which tried a full disclosure policy as an experiment. “It led to reduced costs, not to mention a boost in patient satisfaction,” Dr. Levin noted.
He continued, “I think patients want and deserve to know the truth. I also believe they understand that medical errors can and will happen. It is my observation that patients have several key concerns: 1) how the error(s) happened, 2) how the error affected their health and what can be done to restore them to optimal health, and 3) what the institution is going to do to prevent this kind of error from happening to others.”
Dr. Rapoport concurs with Dr. Levin. “I am glad Dr. Horowitz has fully recovered and at least he has learned from the experience. I do not think the hospital and doctors did,” Dr. Rapoport said.
This article was updated 11/12/20.
Should our patients really go home for the holidays?
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 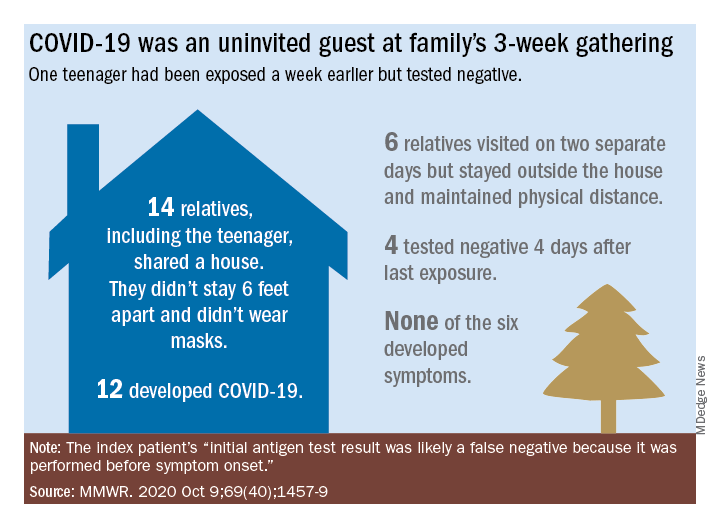
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 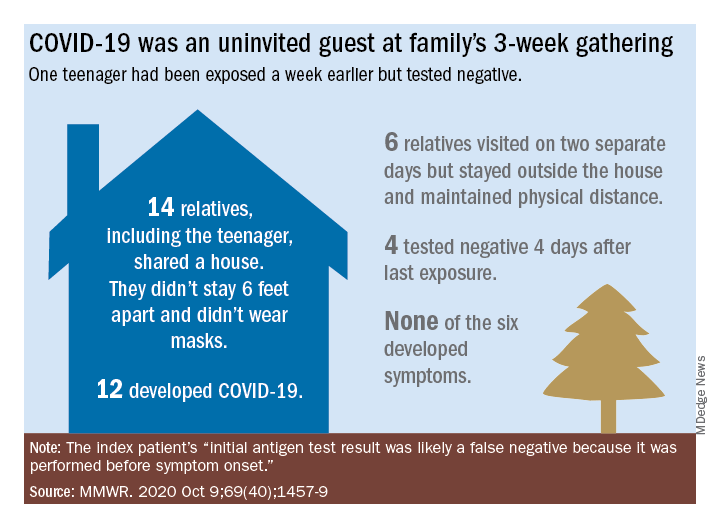
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
Medication adherence challenges and helpers
For most chronic diseases, up to 20%-30% of the pills that are prescribed are not taken. In the case of inhalers for asthma and COPD, patients miss over half of the prescribed doses.
There are many things that contribute to the problem of poor adherence, but people often just simply forget. Thankfully, there are tools designed to help remind patients of what they need to take and when. A survey of apps developed to help patients remember to take their medicines found more than 700 available in Apple and Android app stores.1 Most apps focus on medication alerts, reminders, and medication logs.2 A recent review showed that apps have some – yet limited – effectiveness in increasing adherence, with patient self-reported improvements of 7%-40%.3
Another perhaps more promising area of improving adherence involves high-tech advances in the way medications can be taken. Inhalers are a primary target as they are complicated devices. A patient has to breathe in at the correct time after the inhaler is actuated, and the inhaler works optimally only if the rate of inhalation is sufficient to carry the medication into the lungs.
A number of companies have developed attachments for inhalers (and even inhalers themselves) that can record when the medication is taken through a Bluetooth connection to a patient’s smartphone. These can also assess inspiratory flow. Reminders to take the medication are built into the app, and those reminders disappear if the medication is taken. Patients can receive feedback about the quality of their timing and inspiratory rate to maximize medication delivery to the lungs.4
We learned long ago that it is difficult to take medications three to four times a day, so extended-release tablets were developed to reduce the frequency to once or twice a day. A great deal of work is now being done behind the scenes to develop medications that decrease the need for patients to remember to take their medications. The best examples of this are the long-acting reversible contraception (LARC) devices, specifically IUDs and Nexplanon. Compared with traditional oral contraceptives that need to be taken daily, LARCs reduce the rate of pregnancy by five- to tenfold.
We also now have medications for osteoporosis that can be taken monthly, or even annually. When bisphosphonates were first developed for osteoporosis prevention, they needed to be taken daily. Then a weekly bisphosphonate was developed. Now there is a once-monthly oral bisphosphonate, Ibandronate, and even a once yearly IV bisphosphonate.
Exciting developments have also occurred in the management of diabetes. We may be tempted to take for granted how once-daily long-acting insulin, which releases insulin slowly over the course of a day, has revolutionized the diabetic treatment since its Food and Drug Administration approval in 2000. Yet progress did not end there. The first GLP-1 receptor agonist for diabetes was approved in 2005 and was a twice-a-day medicine. Shortly afterward, a daily GLP-1 was approved, and now there are three once-weekly GLP-1 receptor agonists.
Several pharmaceutical manufacturers are now working on a once-weekly insulin,5 as well as an implantable GLP-1 receptor agonist that will need to be replaced every 6-12 months.6 Imagine your patient coming in once a year to replace his or her potent glucose lowering medication – one that offers a low incidence of hypoglycemia, maintains glucose control all year long, and requires no adherence to a complicated medication regimen.
Similar technology is being used to develop a once-yearly anti-HIV prophylactic medication delivery system.7 This could help prevent the spread of HIV in areas of the world where it may be difficult for people to take daily medications.7
The many technological advances we have described may help us reduce our likelihood of missing a dose of a medication. We are hopeful that progress in this area will continue, and that one day medication adherence will require even less effort from patients than it does today.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Tabi K et al. Mobile apps for medication management: Review and analysis. JMIR Mhealth Uhealth. 2019 Sep 7(9):13608.
2. Park JYE et al. Mobile phone apps targeting medication adherence: Quality assessment and content analysis of user reviews. JMIR Mhealth Uhealth. 2019 Jan 31;7(1):e11919.
3. Pérez-Jover V et al. Mobile apps for increasing treatment adherence: Systematic review. J Med Internet Res. 2019;21(6):e12505. doi: 10.2196/12505.
4. 4 Smart inhalers that could be lifesaving for people living with asthma & COPD. MyTherapy, July 11, 2019.
5. Rosenstock J et al. Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med. 2020 Sep 22. doi: 10.1056/NEJMoa2022474.
6. GLP-1 agonists: From 2 daily injections to 1 per week and beyond. DiaTribe, Jan. 10, 2018.
7. Long-acting HIV prevention tools. Hiv.gov, July 20, 2019.
For most chronic diseases, up to 20%-30% of the pills that are prescribed are not taken. In the case of inhalers for asthma and COPD, patients miss over half of the prescribed doses.
There are many things that contribute to the problem of poor adherence, but people often just simply forget. Thankfully, there are tools designed to help remind patients of what they need to take and when. A survey of apps developed to help patients remember to take their medicines found more than 700 available in Apple and Android app stores.1 Most apps focus on medication alerts, reminders, and medication logs.2 A recent review showed that apps have some – yet limited – effectiveness in increasing adherence, with patient self-reported improvements of 7%-40%.3
Another perhaps more promising area of improving adherence involves high-tech advances in the way medications can be taken. Inhalers are a primary target as they are complicated devices. A patient has to breathe in at the correct time after the inhaler is actuated, and the inhaler works optimally only if the rate of inhalation is sufficient to carry the medication into the lungs.
A number of companies have developed attachments for inhalers (and even inhalers themselves) that can record when the medication is taken through a Bluetooth connection to a patient’s smartphone. These can also assess inspiratory flow. Reminders to take the medication are built into the app, and those reminders disappear if the medication is taken. Patients can receive feedback about the quality of their timing and inspiratory rate to maximize medication delivery to the lungs.4
We learned long ago that it is difficult to take medications three to four times a day, so extended-release tablets were developed to reduce the frequency to once or twice a day. A great deal of work is now being done behind the scenes to develop medications that decrease the need for patients to remember to take their medications. The best examples of this are the long-acting reversible contraception (LARC) devices, specifically IUDs and Nexplanon. Compared with traditional oral contraceptives that need to be taken daily, LARCs reduce the rate of pregnancy by five- to tenfold.
We also now have medications for osteoporosis that can be taken monthly, or even annually. When bisphosphonates were first developed for osteoporosis prevention, they needed to be taken daily. Then a weekly bisphosphonate was developed. Now there is a once-monthly oral bisphosphonate, Ibandronate, and even a once yearly IV bisphosphonate.
Exciting developments have also occurred in the management of diabetes. We may be tempted to take for granted how once-daily long-acting insulin, which releases insulin slowly over the course of a day, has revolutionized the diabetic treatment since its Food and Drug Administration approval in 2000. Yet progress did not end there. The first GLP-1 receptor agonist for diabetes was approved in 2005 and was a twice-a-day medicine. Shortly afterward, a daily GLP-1 was approved, and now there are three once-weekly GLP-1 receptor agonists.
Several pharmaceutical manufacturers are now working on a once-weekly insulin,5 as well as an implantable GLP-1 receptor agonist that will need to be replaced every 6-12 months.6 Imagine your patient coming in once a year to replace his or her potent glucose lowering medication – one that offers a low incidence of hypoglycemia, maintains glucose control all year long, and requires no adherence to a complicated medication regimen.
Similar technology is being used to develop a once-yearly anti-HIV prophylactic medication delivery system.7 This could help prevent the spread of HIV in areas of the world where it may be difficult for people to take daily medications.7
The many technological advances we have described may help us reduce our likelihood of missing a dose of a medication. We are hopeful that progress in this area will continue, and that one day medication adherence will require even less effort from patients than it does today.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Tabi K et al. Mobile apps for medication management: Review and analysis. JMIR Mhealth Uhealth. 2019 Sep 7(9):13608.
2. Park JYE et al. Mobile phone apps targeting medication adherence: Quality assessment and content analysis of user reviews. JMIR Mhealth Uhealth. 2019 Jan 31;7(1):e11919.
3. Pérez-Jover V et al. Mobile apps for increasing treatment adherence: Systematic review. J Med Internet Res. 2019;21(6):e12505. doi: 10.2196/12505.
4. 4 Smart inhalers that could be lifesaving for people living with asthma & COPD. MyTherapy, July 11, 2019.
5. Rosenstock J et al. Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med. 2020 Sep 22. doi: 10.1056/NEJMoa2022474.
6. GLP-1 agonists: From 2 daily injections to 1 per week and beyond. DiaTribe, Jan. 10, 2018.
7. Long-acting HIV prevention tools. Hiv.gov, July 20, 2019.
For most chronic diseases, up to 20%-30% of the pills that are prescribed are not taken. In the case of inhalers for asthma and COPD, patients miss over half of the prescribed doses.
There are many things that contribute to the problem of poor adherence, but people often just simply forget. Thankfully, there are tools designed to help remind patients of what they need to take and when. A survey of apps developed to help patients remember to take their medicines found more than 700 available in Apple and Android app stores.1 Most apps focus on medication alerts, reminders, and medication logs.2 A recent review showed that apps have some – yet limited – effectiveness in increasing adherence, with patient self-reported improvements of 7%-40%.3
Another perhaps more promising area of improving adherence involves high-tech advances in the way medications can be taken. Inhalers are a primary target as they are complicated devices. A patient has to breathe in at the correct time after the inhaler is actuated, and the inhaler works optimally only if the rate of inhalation is sufficient to carry the medication into the lungs.
A number of companies have developed attachments for inhalers (and even inhalers themselves) that can record when the medication is taken through a Bluetooth connection to a patient’s smartphone. These can also assess inspiratory flow. Reminders to take the medication are built into the app, and those reminders disappear if the medication is taken. Patients can receive feedback about the quality of their timing and inspiratory rate to maximize medication delivery to the lungs.4
We learned long ago that it is difficult to take medications three to four times a day, so extended-release tablets were developed to reduce the frequency to once or twice a day. A great deal of work is now being done behind the scenes to develop medications that decrease the need for patients to remember to take their medications. The best examples of this are the long-acting reversible contraception (LARC) devices, specifically IUDs and Nexplanon. Compared with traditional oral contraceptives that need to be taken daily, LARCs reduce the rate of pregnancy by five- to tenfold.
We also now have medications for osteoporosis that can be taken monthly, or even annually. When bisphosphonates were first developed for osteoporosis prevention, they needed to be taken daily. Then a weekly bisphosphonate was developed. Now there is a once-monthly oral bisphosphonate, Ibandronate, and even a once yearly IV bisphosphonate.
Exciting developments have also occurred in the management of diabetes. We may be tempted to take for granted how once-daily long-acting insulin, which releases insulin slowly over the course of a day, has revolutionized the diabetic treatment since its Food and Drug Administration approval in 2000. Yet progress did not end there. The first GLP-1 receptor agonist for diabetes was approved in 2005 and was a twice-a-day medicine. Shortly afterward, a daily GLP-1 was approved, and now there are three once-weekly GLP-1 receptor agonists.
Several pharmaceutical manufacturers are now working on a once-weekly insulin,5 as well as an implantable GLP-1 receptor agonist that will need to be replaced every 6-12 months.6 Imagine your patient coming in once a year to replace his or her potent glucose lowering medication – one that offers a low incidence of hypoglycemia, maintains glucose control all year long, and requires no adherence to a complicated medication regimen.
Similar technology is being used to develop a once-yearly anti-HIV prophylactic medication delivery system.7 This could help prevent the spread of HIV in areas of the world where it may be difficult for people to take daily medications.7
The many technological advances we have described may help us reduce our likelihood of missing a dose of a medication. We are hopeful that progress in this area will continue, and that one day medication adherence will require even less effort from patients than it does today.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Tabi K et al. Mobile apps for medication management: Review and analysis. JMIR Mhealth Uhealth. 2019 Sep 7(9):13608.
2. Park JYE et al. Mobile phone apps targeting medication adherence: Quality assessment and content analysis of user reviews. JMIR Mhealth Uhealth. 2019 Jan 31;7(1):e11919.
3. Pérez-Jover V et al. Mobile apps for increasing treatment adherence: Systematic review. J Med Internet Res. 2019;21(6):e12505. doi: 10.2196/12505.
4. 4 Smart inhalers that could be lifesaving for people living with asthma & COPD. MyTherapy, July 11, 2019.
5. Rosenstock J et al. Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med. 2020 Sep 22. doi: 10.1056/NEJMoa2022474.
6. GLP-1 agonists: From 2 daily injections to 1 per week and beyond. DiaTribe, Jan. 10, 2018.
7. Long-acting HIV prevention tools. Hiv.gov, July 20, 2019.