User login
TIPP the scales in managing stress
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
Focus on youth concerns at well visits
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
FROM PAS 2021
SGIM annual meeting focuses on inclusivity
In her welcome video on the opening day at the annual meeting of the Society of General Internal Medicine, meeting chair Rita Lee, MD, said she hoped that this year’s event, though virtual, will allow attendees an opportunity to “regroup, find inspiration, and celebrate the incredible strengths and diverse voices of our community.”
“We are living in an incredibly polarized world,” Dr. Lee said in an interview. “ as recent events, such as the death of George Floyd and many others, plus the disparities revealed by the COVID-19 pandemic, have brought issues of structural racism and oppression in the United States to the forefront,” she said in the interview.
“Given these circumstances, it is important now, more than ever, for generalists to move our values into action – to effect change at the health system, community, and policy levels – so our patients can achieve optimal health,” Dr. Lee emphasized.
She noted that SGIM’s vision: “A just system of care in which all people can achieve optimal health,” underlies the meeting’s sessions.
Some challenges related to adopting more antiracist training in medical education center on faculty development, Dr. Lee noted. “There are also students who don’t feel that this is part of the role of being a physician. One way to overcome these challenges is by directly linking structural competency to health outcomes for our patients,” she added. “We have evidence that structural racism impacts health and we should make that clear to our educational leaders and faculty to increase buy in. So many of our SGIM members are working on developing curricula for this.”
Two of the meeting’s workshops that addressed racism in medicine and medical education and strategies for change were “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” and “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today.” Below are some details about these.
Medical education evolves to include structural competency
In the workshop “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” participants used interactive exercises to build structural differentials for patient cases. The workshop was based in part on the experiences of including structural competency in medical education at Albert Einstein College of Medicine, New York, and the University of Pittsburgh.
During the session, participants practiced building a structural differential diagnosis in small groups, and also practiced using a structurally competent version of the 1-minute preceptor to promote structural competency in learners.
“Structural competency represents a shift in medical education towards attention to forces that influence health outcomes at levels above individual clinical interactions and develop a provider’s capacity to recognize and respond to health and illness as downstream effects of social, political and economic structures,” presenter Iman Hassan, MD, of Albert Einstein College of Medicine and Montefiore Health System, both in New York, said in an interview.
“At the same time, structural competency incorporates structural humility, which decentralizes the provider role in addressing structural factors and emphasizes collaboration with patients and communities,” she said in the interview. “Structural competency is a useful antiracism framework because it explicitly engages learners with the broader structural forces that result in health disparities, including structural racism and its downstream effects,” Dr. Hassan explained.
Addressing structural competency is important in medical education because structural and social determinants of health contribute more than half of overall health outcomes, said Dr. Hassan.
A structural competency framework equips learners to identify, discuss, and work with patients to navigate social needs such as lack of health insurance, food, or transportation, that are preventing them from accessing needed health care services, Dr. Hassan noted.
“Importantly, training in structural competency empowers physicians to be agents of change within their clinics, health systems, and communities and to recognize the value of community-led advocacy in promoting health equity,” she said.
Structural competency training also “will also allow them to engage more fully with the body of literature that exists surrounding social determinants of health and health disparities, and the use of approaches such as critical race theory through which to view health care,” she emphasized. “Importantly, understanding of the historical and structural context of medicine allows clinicians to more readily recognize when their own clinical practices, such as use of race-based clinical prediction tools, may perpetuate disparities, and work collectively to eliminate those practices.”
Recalibrating calculators for clinical care
Another workshop, “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today,” took on the challenge of inherent bias in clinical care caused by various factors, notably medical calculators such as those used to measure kidney function and pulmonary function.
Lamar K. Johnson, MD, of Christiana Care Hospital Partners/Christiana Care Pediatric Hospitalists in Newark, Del., and Celeste Newby, MD, of Tulane University, New Orleans, discussed the inherent biases in some calculators and how to take those biases into account. A stated goal of the workshop was to increase awareness of the origins of medical calculators in order to enhance equity and improve shared decision-making between patients and providers.
Addressing implicit bias in clinical practice is important because such bias has been shown to negatively affect physician behavior and clinical decision making, Dr. Johnson said in an interview.
“These effects can also negatively affect the doctor-patient relationship and lead to poorer health outcomes due to delays in or avoidance of care or avoidance of the health care system, and mistrust, resulting in nonadherence,” Dr. Johnson noted.
“Implicit bias training helps empower medical students and residents to recognize and address bias and advocate for patients. Such training can potentially be beneficial to faculty, too,” Dr. Johnson emphasized in the interview.
“Race is primarily a social, not a biological, construct, and we must be careful when we use it, as its use in the past has been largely inappropriate and not scientifically sound,” he said.
During the session, one of the presenters said removing specific mentions of race from clinical documentation can reduce racial bias in clinical practice.
The presenters also highlighted the estimated glomerular filtration rate (eGFR) which is used to estimate kidney function.
The eGFR “reports higher eGFR values for Blacks based on a faulty hypothesis that Black people have higher muscle mass. This higher estimated value can delay referral for specialist care or transplantation, leading to worse outcomes,” Dr. Johnson explained in the interview.
In response, “Many major institutions have eliminated the race modifier in eGFR, and a joint task force created by the National Kidney Foundation and American Society of Nephrology has recommended against using a race modifier as of March 2021,” Dr. Johnson said.
The presenters had no relevant financial conflicts to disclose.
In her welcome video on the opening day at the annual meeting of the Society of General Internal Medicine, meeting chair Rita Lee, MD, said she hoped that this year’s event, though virtual, will allow attendees an opportunity to “regroup, find inspiration, and celebrate the incredible strengths and diverse voices of our community.”
“We are living in an incredibly polarized world,” Dr. Lee said in an interview. “ as recent events, such as the death of George Floyd and many others, plus the disparities revealed by the COVID-19 pandemic, have brought issues of structural racism and oppression in the United States to the forefront,” she said in the interview.
“Given these circumstances, it is important now, more than ever, for generalists to move our values into action – to effect change at the health system, community, and policy levels – so our patients can achieve optimal health,” Dr. Lee emphasized.
She noted that SGIM’s vision: “A just system of care in which all people can achieve optimal health,” underlies the meeting’s sessions.
Some challenges related to adopting more antiracist training in medical education center on faculty development, Dr. Lee noted. “There are also students who don’t feel that this is part of the role of being a physician. One way to overcome these challenges is by directly linking structural competency to health outcomes for our patients,” she added. “We have evidence that structural racism impacts health and we should make that clear to our educational leaders and faculty to increase buy in. So many of our SGIM members are working on developing curricula for this.”
Two of the meeting’s workshops that addressed racism in medicine and medical education and strategies for change were “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” and “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today.” Below are some details about these.
Medical education evolves to include structural competency
In the workshop “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” participants used interactive exercises to build structural differentials for patient cases. The workshop was based in part on the experiences of including structural competency in medical education at Albert Einstein College of Medicine, New York, and the University of Pittsburgh.
During the session, participants practiced building a structural differential diagnosis in small groups, and also practiced using a structurally competent version of the 1-minute preceptor to promote structural competency in learners.
“Structural competency represents a shift in medical education towards attention to forces that influence health outcomes at levels above individual clinical interactions and develop a provider’s capacity to recognize and respond to health and illness as downstream effects of social, political and economic structures,” presenter Iman Hassan, MD, of Albert Einstein College of Medicine and Montefiore Health System, both in New York, said in an interview.
“At the same time, structural competency incorporates structural humility, which decentralizes the provider role in addressing structural factors and emphasizes collaboration with patients and communities,” she said in the interview. “Structural competency is a useful antiracism framework because it explicitly engages learners with the broader structural forces that result in health disparities, including structural racism and its downstream effects,” Dr. Hassan explained.
Addressing structural competency is important in medical education because structural and social determinants of health contribute more than half of overall health outcomes, said Dr. Hassan.
A structural competency framework equips learners to identify, discuss, and work with patients to navigate social needs such as lack of health insurance, food, or transportation, that are preventing them from accessing needed health care services, Dr. Hassan noted.
“Importantly, training in structural competency empowers physicians to be agents of change within their clinics, health systems, and communities and to recognize the value of community-led advocacy in promoting health equity,” she said.
Structural competency training also “will also allow them to engage more fully with the body of literature that exists surrounding social determinants of health and health disparities, and the use of approaches such as critical race theory through which to view health care,” she emphasized. “Importantly, understanding of the historical and structural context of medicine allows clinicians to more readily recognize when their own clinical practices, such as use of race-based clinical prediction tools, may perpetuate disparities, and work collectively to eliminate those practices.”
Recalibrating calculators for clinical care
Another workshop, “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today,” took on the challenge of inherent bias in clinical care caused by various factors, notably medical calculators such as those used to measure kidney function and pulmonary function.
Lamar K. Johnson, MD, of Christiana Care Hospital Partners/Christiana Care Pediatric Hospitalists in Newark, Del., and Celeste Newby, MD, of Tulane University, New Orleans, discussed the inherent biases in some calculators and how to take those biases into account. A stated goal of the workshop was to increase awareness of the origins of medical calculators in order to enhance equity and improve shared decision-making between patients and providers.
Addressing implicit bias in clinical practice is important because such bias has been shown to negatively affect physician behavior and clinical decision making, Dr. Johnson said in an interview.
“These effects can also negatively affect the doctor-patient relationship and lead to poorer health outcomes due to delays in or avoidance of care or avoidance of the health care system, and mistrust, resulting in nonadherence,” Dr. Johnson noted.
“Implicit bias training helps empower medical students and residents to recognize and address bias and advocate for patients. Such training can potentially be beneficial to faculty, too,” Dr. Johnson emphasized in the interview.
“Race is primarily a social, not a biological, construct, and we must be careful when we use it, as its use in the past has been largely inappropriate and not scientifically sound,” he said.
During the session, one of the presenters said removing specific mentions of race from clinical documentation can reduce racial bias in clinical practice.
The presenters also highlighted the estimated glomerular filtration rate (eGFR) which is used to estimate kidney function.
The eGFR “reports higher eGFR values for Blacks based on a faulty hypothesis that Black people have higher muscle mass. This higher estimated value can delay referral for specialist care or transplantation, leading to worse outcomes,” Dr. Johnson explained in the interview.
In response, “Many major institutions have eliminated the race modifier in eGFR, and a joint task force created by the National Kidney Foundation and American Society of Nephrology has recommended against using a race modifier as of March 2021,” Dr. Johnson said.
The presenters had no relevant financial conflicts to disclose.
In her welcome video on the opening day at the annual meeting of the Society of General Internal Medicine, meeting chair Rita Lee, MD, said she hoped that this year’s event, though virtual, will allow attendees an opportunity to “regroup, find inspiration, and celebrate the incredible strengths and diverse voices of our community.”
“We are living in an incredibly polarized world,” Dr. Lee said in an interview. “ as recent events, such as the death of George Floyd and many others, plus the disparities revealed by the COVID-19 pandemic, have brought issues of structural racism and oppression in the United States to the forefront,” she said in the interview.
“Given these circumstances, it is important now, more than ever, for generalists to move our values into action – to effect change at the health system, community, and policy levels – so our patients can achieve optimal health,” Dr. Lee emphasized.
She noted that SGIM’s vision: “A just system of care in which all people can achieve optimal health,” underlies the meeting’s sessions.
Some challenges related to adopting more antiracist training in medical education center on faculty development, Dr. Lee noted. “There are also students who don’t feel that this is part of the role of being a physician. One way to overcome these challenges is by directly linking structural competency to health outcomes for our patients,” she added. “We have evidence that structural racism impacts health and we should make that clear to our educational leaders and faculty to increase buy in. So many of our SGIM members are working on developing curricula for this.”
Two of the meeting’s workshops that addressed racism in medicine and medical education and strategies for change were “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” and “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today.” Below are some details about these.
Medical education evolves to include structural competency
In the workshop “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” participants used interactive exercises to build structural differentials for patient cases. The workshop was based in part on the experiences of including structural competency in medical education at Albert Einstein College of Medicine, New York, and the University of Pittsburgh.
During the session, participants practiced building a structural differential diagnosis in small groups, and also practiced using a structurally competent version of the 1-minute preceptor to promote structural competency in learners.
“Structural competency represents a shift in medical education towards attention to forces that influence health outcomes at levels above individual clinical interactions and develop a provider’s capacity to recognize and respond to health and illness as downstream effects of social, political and economic structures,” presenter Iman Hassan, MD, of Albert Einstein College of Medicine and Montefiore Health System, both in New York, said in an interview.
“At the same time, structural competency incorporates structural humility, which decentralizes the provider role in addressing structural factors and emphasizes collaboration with patients and communities,” she said in the interview. “Structural competency is a useful antiracism framework because it explicitly engages learners with the broader structural forces that result in health disparities, including structural racism and its downstream effects,” Dr. Hassan explained.
Addressing structural competency is important in medical education because structural and social determinants of health contribute more than half of overall health outcomes, said Dr. Hassan.
A structural competency framework equips learners to identify, discuss, and work with patients to navigate social needs such as lack of health insurance, food, or transportation, that are preventing them from accessing needed health care services, Dr. Hassan noted.
“Importantly, training in structural competency empowers physicians to be agents of change within their clinics, health systems, and communities and to recognize the value of community-led advocacy in promoting health equity,” she said.
Structural competency training also “will also allow them to engage more fully with the body of literature that exists surrounding social determinants of health and health disparities, and the use of approaches such as critical race theory through which to view health care,” she emphasized. “Importantly, understanding of the historical and structural context of medicine allows clinicians to more readily recognize when their own clinical practices, such as use of race-based clinical prediction tools, may perpetuate disparities, and work collectively to eliminate those practices.”
Recalibrating calculators for clinical care
Another workshop, “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today,” took on the challenge of inherent bias in clinical care caused by various factors, notably medical calculators such as those used to measure kidney function and pulmonary function.
Lamar K. Johnson, MD, of Christiana Care Hospital Partners/Christiana Care Pediatric Hospitalists in Newark, Del., and Celeste Newby, MD, of Tulane University, New Orleans, discussed the inherent biases in some calculators and how to take those biases into account. A stated goal of the workshop was to increase awareness of the origins of medical calculators in order to enhance equity and improve shared decision-making between patients and providers.
Addressing implicit bias in clinical practice is important because such bias has been shown to negatively affect physician behavior and clinical decision making, Dr. Johnson said in an interview.
“These effects can also negatively affect the doctor-patient relationship and lead to poorer health outcomes due to delays in or avoidance of care or avoidance of the health care system, and mistrust, resulting in nonadherence,” Dr. Johnson noted.
“Implicit bias training helps empower medical students and residents to recognize and address bias and advocate for patients. Such training can potentially be beneficial to faculty, too,” Dr. Johnson emphasized in the interview.
“Race is primarily a social, not a biological, construct, and we must be careful when we use it, as its use in the past has been largely inappropriate and not scientifically sound,” he said.
During the session, one of the presenters said removing specific mentions of race from clinical documentation can reduce racial bias in clinical practice.
The presenters also highlighted the estimated glomerular filtration rate (eGFR) which is used to estimate kidney function.
The eGFR “reports higher eGFR values for Blacks based on a faulty hypothesis that Black people have higher muscle mass. This higher estimated value can delay referral for specialist care or transplantation, leading to worse outcomes,” Dr. Johnson explained in the interview.
In response, “Many major institutions have eliminated the race modifier in eGFR, and a joint task force created by the National Kidney Foundation and American Society of Nephrology has recommended against using a race modifier as of March 2021,” Dr. Johnson said.
The presenters had no relevant financial conflicts to disclose.
FROM SGIM 2021
Transcranial brain stimulation can modulate placebo and nocebo experiences
, according to results of a new study published in the Proceedings of the National Academy of Sciences (PNAS).
“Placebo and nocebo effects are a critical component of clinical care and efficacy studies,” said senior author Jian Kong, MD, associate professor in the department of psychiatry at Massachusetts General Hospital, Charlestown campus. “Harnessing these effects in clinical practice and research could facilitate the development of new pain management methods,” he said. “Healing may involve multiple components: the self-healing properties of the body; the nonspecific effects of treatment (i.e., placebo effect); and the specific effect of a physical or pharmacologic intervention. Therefore, enhancing the placebo effect may ultimately boost the overall therapeutic effect of existing treatment,” he explained, emphasizing that the results are preliminary and should be interpreted with caution.
The authors noted that reducing nocebo effects could also be a major benefit “since patients discontinue prescribed medications, make unnecessary medical visits, and take additional medications to counteract adverse effects that are actually nocebo effects.”
Testing the hypothesis
The randomized, double-blind, sham-controlled study used transcranial direct current stimulation (tDCS), which delivers an electrical current to the brain via scalp electrodes. The aim was to see if stimulating the dorsolateral prefrontal cortex with tDCS could alter the brain’s perception of placebo and nocebo experiences.
The study included 81 participants (37 females, mean age: 27.4 years), who were randomized into one of three tDCS groups (anodal, cathodal, or sham).
All participants were first conditioned to believe that an inert cream was either lidocaine or capsaicin and that this cream could either dull the impact of a painful heat stimulus (placebo analgesia) or exacerbate it (nocebo hyperalgesia). Participants were then placed into a functional MRI scanner where tDCS was initiated. Painful stimuli were then applied to spots on their forearms where they believed they had either lidocaine, capsaicin, or a neutral control cream and they rated the pain using the Gracely Sensory Scale.
Placebo analgesia was defined as the difference between perceived pain intensity where participants believed they had lidocaine cream compared with where they believed they had control cream. Nocebo hyperalgesia was defined as the difference between perceived pain intensity where they believed they had capsaicin cream compared with where they believed they had control cream.
The researchers found that compared with sham tDCS, cathodal tDCS showed significant effects in increasing placebo analgesia and brain responses in the ventromedial prefrontal cortex (vmPFC), while anodal tDCS showed significant effects in inhibiting nocebo hyperalgesia and brain responses in the insula.
“The potential to enhance salubrious placebo effects and/or diminish treatment-interfering nocebo effects may have clinical significance,” the authors noted. “For example, clinical studies have suggested that expectancy is positively associated with chronic pain improvement, and using conditioning-like expectancy manipulation, we have shown that significantly boosting expectancy can improve treatment outcome.”
Proof of concept
Asked to comment on the study, Brian E. McGeeney, MD, of the John R. Graham Headache Center at Brigham and Women’s Faulkner Hospital in Boston, said “the findings are a proof of concept that it is possible to use noninvasive brain stimulation to modulate placebo and nocebo pain effects.”
Although the findings do not have immediate clinical application, they are “exciting” and “break new ground in expectancy research,” he said.
“It is important to recognize that the researchers are trying to utilize a purported expectancy mechanism rather than attempting to alter placebo/nocebo by verbal and other cues. It remains to be seen whether the manipulation of brief experimental pain like this can translate into altered chronic pain over time, the main clinical goal. Current tDCS therapy for various reasons is necessarily brief and one can ask whether there are meaningful changes from brief stimulation. Such results can foster speculation as to whether direct strategic placement of intracranial stimulation leads could result in more longstanding similar benefits.”
Dr. Kong holds equity in a startup company (MNT) and a pending patent to develop new peripheral neuromodulation tools, but declares no conflict of interest. All other authors declare no conflict of interest.
, according to results of a new study published in the Proceedings of the National Academy of Sciences (PNAS).
“Placebo and nocebo effects are a critical component of clinical care and efficacy studies,” said senior author Jian Kong, MD, associate professor in the department of psychiatry at Massachusetts General Hospital, Charlestown campus. “Harnessing these effects in clinical practice and research could facilitate the development of new pain management methods,” he said. “Healing may involve multiple components: the self-healing properties of the body; the nonspecific effects of treatment (i.e., placebo effect); and the specific effect of a physical or pharmacologic intervention. Therefore, enhancing the placebo effect may ultimately boost the overall therapeutic effect of existing treatment,” he explained, emphasizing that the results are preliminary and should be interpreted with caution.
The authors noted that reducing nocebo effects could also be a major benefit “since patients discontinue prescribed medications, make unnecessary medical visits, and take additional medications to counteract adverse effects that are actually nocebo effects.”
Testing the hypothesis
The randomized, double-blind, sham-controlled study used transcranial direct current stimulation (tDCS), which delivers an electrical current to the brain via scalp electrodes. The aim was to see if stimulating the dorsolateral prefrontal cortex with tDCS could alter the brain’s perception of placebo and nocebo experiences.
The study included 81 participants (37 females, mean age: 27.4 years), who were randomized into one of three tDCS groups (anodal, cathodal, or sham).
All participants were first conditioned to believe that an inert cream was either lidocaine or capsaicin and that this cream could either dull the impact of a painful heat stimulus (placebo analgesia) or exacerbate it (nocebo hyperalgesia). Participants were then placed into a functional MRI scanner where tDCS was initiated. Painful stimuli were then applied to spots on their forearms where they believed they had either lidocaine, capsaicin, or a neutral control cream and they rated the pain using the Gracely Sensory Scale.
Placebo analgesia was defined as the difference between perceived pain intensity where participants believed they had lidocaine cream compared with where they believed they had control cream. Nocebo hyperalgesia was defined as the difference between perceived pain intensity where they believed they had capsaicin cream compared with where they believed they had control cream.
The researchers found that compared with sham tDCS, cathodal tDCS showed significant effects in increasing placebo analgesia and brain responses in the ventromedial prefrontal cortex (vmPFC), while anodal tDCS showed significant effects in inhibiting nocebo hyperalgesia and brain responses in the insula.
“The potential to enhance salubrious placebo effects and/or diminish treatment-interfering nocebo effects may have clinical significance,” the authors noted. “For example, clinical studies have suggested that expectancy is positively associated with chronic pain improvement, and using conditioning-like expectancy manipulation, we have shown that significantly boosting expectancy can improve treatment outcome.”
Proof of concept
Asked to comment on the study, Brian E. McGeeney, MD, of the John R. Graham Headache Center at Brigham and Women’s Faulkner Hospital in Boston, said “the findings are a proof of concept that it is possible to use noninvasive brain stimulation to modulate placebo and nocebo pain effects.”
Although the findings do not have immediate clinical application, they are “exciting” and “break new ground in expectancy research,” he said.
“It is important to recognize that the researchers are trying to utilize a purported expectancy mechanism rather than attempting to alter placebo/nocebo by verbal and other cues. It remains to be seen whether the manipulation of brief experimental pain like this can translate into altered chronic pain over time, the main clinical goal. Current tDCS therapy for various reasons is necessarily brief and one can ask whether there are meaningful changes from brief stimulation. Such results can foster speculation as to whether direct strategic placement of intracranial stimulation leads could result in more longstanding similar benefits.”
Dr. Kong holds equity in a startup company (MNT) and a pending patent to develop new peripheral neuromodulation tools, but declares no conflict of interest. All other authors declare no conflict of interest.
, according to results of a new study published in the Proceedings of the National Academy of Sciences (PNAS).
“Placebo and nocebo effects are a critical component of clinical care and efficacy studies,” said senior author Jian Kong, MD, associate professor in the department of psychiatry at Massachusetts General Hospital, Charlestown campus. “Harnessing these effects in clinical practice and research could facilitate the development of new pain management methods,” he said. “Healing may involve multiple components: the self-healing properties of the body; the nonspecific effects of treatment (i.e., placebo effect); and the specific effect of a physical or pharmacologic intervention. Therefore, enhancing the placebo effect may ultimately boost the overall therapeutic effect of existing treatment,” he explained, emphasizing that the results are preliminary and should be interpreted with caution.
The authors noted that reducing nocebo effects could also be a major benefit “since patients discontinue prescribed medications, make unnecessary medical visits, and take additional medications to counteract adverse effects that are actually nocebo effects.”
Testing the hypothesis
The randomized, double-blind, sham-controlled study used transcranial direct current stimulation (tDCS), which delivers an electrical current to the brain via scalp electrodes. The aim was to see if stimulating the dorsolateral prefrontal cortex with tDCS could alter the brain’s perception of placebo and nocebo experiences.
The study included 81 participants (37 females, mean age: 27.4 years), who were randomized into one of three tDCS groups (anodal, cathodal, or sham).
All participants were first conditioned to believe that an inert cream was either lidocaine or capsaicin and that this cream could either dull the impact of a painful heat stimulus (placebo analgesia) or exacerbate it (nocebo hyperalgesia). Participants were then placed into a functional MRI scanner where tDCS was initiated. Painful stimuli were then applied to spots on their forearms where they believed they had either lidocaine, capsaicin, or a neutral control cream and they rated the pain using the Gracely Sensory Scale.
Placebo analgesia was defined as the difference between perceived pain intensity where participants believed they had lidocaine cream compared with where they believed they had control cream. Nocebo hyperalgesia was defined as the difference between perceived pain intensity where they believed they had capsaicin cream compared with where they believed they had control cream.
The researchers found that compared with sham tDCS, cathodal tDCS showed significant effects in increasing placebo analgesia and brain responses in the ventromedial prefrontal cortex (vmPFC), while anodal tDCS showed significant effects in inhibiting nocebo hyperalgesia and brain responses in the insula.
“The potential to enhance salubrious placebo effects and/or diminish treatment-interfering nocebo effects may have clinical significance,” the authors noted. “For example, clinical studies have suggested that expectancy is positively associated with chronic pain improvement, and using conditioning-like expectancy manipulation, we have shown that significantly boosting expectancy can improve treatment outcome.”
Proof of concept
Asked to comment on the study, Brian E. McGeeney, MD, of the John R. Graham Headache Center at Brigham and Women’s Faulkner Hospital in Boston, said “the findings are a proof of concept that it is possible to use noninvasive brain stimulation to modulate placebo and nocebo pain effects.”
Although the findings do not have immediate clinical application, they are “exciting” and “break new ground in expectancy research,” he said.
“It is important to recognize that the researchers are trying to utilize a purported expectancy mechanism rather than attempting to alter placebo/nocebo by verbal and other cues. It remains to be seen whether the manipulation of brief experimental pain like this can translate into altered chronic pain over time, the main clinical goal. Current tDCS therapy for various reasons is necessarily brief and one can ask whether there are meaningful changes from brief stimulation. Such results can foster speculation as to whether direct strategic placement of intracranial stimulation leads could result in more longstanding similar benefits.”
Dr. Kong holds equity in a startup company (MNT) and a pending patent to develop new peripheral neuromodulation tools, but declares no conflict of interest. All other authors declare no conflict of interest.
FROM PNAS
‘Malicious peer review’ destroyed doc’s career, he says
Cardiothoracic surgeon J. Marvin Smith III, MD, had always thrived on a busy practice schedule, often performing 20-30 surgeries a week. A practicing surgeon for more than 40 years, Dr. Smith said he had no plans to slow down anytime soon.
But Dr. Smith said his career was derailed when leaders at Methodist Healthcare System of San Antonio initiated a sudden peer review proceeding against him. The hospital system alleged certain surgeries performed by Dr. Smith had excessive mortality rates. When he proved the data inaccurate, Dr. Smith said administrators next claimed he was cognitively impaired and wasn’t safe to practice.
Dr. Smith has now been embroiled in a peer review dispute with the hospital system for more than 2 years and says the conflict has essentially forced him out of surgical practice. He believes the peer review was “malicious” and was really launched because of complaints he made about nurse staffing and other issues at the hospital.
“I think it is absolutely in bad faith and is disingenuous what they’ve told me along the way,” said Dr. Smith, 73. “It’s because I pointed out deficiencies in nursing care, and they want to get rid of me. It would be a lot easier for them if I had a contract and they could control me better. But the fact that I was independent, meant they had to resort to a malicious peer review to try and push me out.”
Dr. Smith had a peer review hearing with Methodist in March 2021, and in April, a panel found in Dr. Smith’s favor, according to Dr. Smith. The findings were sent to the hospital’s medical board for review, which issued a decision in early May.
Eric A. Pullen, an attorney for Dr. Smith, said he could not go into detail about the board’s decision for legal reasons, but that “the medical board’s decision did not completely resolve the matter, and Dr. Smith intends to exercise his procedural rights, which could include an appeal.”
Methodist Hospital Texsan and its parent company, Methodist Health System of San Antonio, did not respond to messages seeking comment about the case. Without hearing from the hospital system, its side is unknown and it is unclear if there is more to the story from Methodist’s view.
The problem is not new, but some experts, such as Lawrence Huntoon, MD, PhD, say the practice has become more common in recent years, particularly against independent doctors.
Dr. Huntoon believes there is a nationwide trend at many hospitals to get rid of independent physicians and replace them with employed doctors, he said.
However, because most sham peer reviews go on behind closed doors, there are no data to pinpoint its prevalence or measure its growth.
“Independent physicians are basically being purged from medical staffs across the United States,” said Dr. Huntoon, who is chair of the Association of American Physicians and Surgeons’ Committee to Combat Sham Peer Review. “The hospitals want more control over how physicians practice and who they refer to, and they do that by having employees.”
Anthony P. Weiss, MD, MBA, chief medical officer for Beth Israel Deaconess Medical Center said it has not been his experience that independent physicians are being targeted in such a way. Dr. Weiss responded to an inquiry sent to the American Hospital Association for this story.
“As the authority for peer review rests with the organized medical staff (i.e., physicians), and not formally with the hospital per se, the peer review lever is not typically available as a management tool for hospital administration,” said Dr. Weiss, who is a former member of the AHA’s Committee on Clinical Leadership, but who was speaking on behalf of himself.
A spokesman for the AHA said the organization stands behinds Dr. Weiss’ comments.
Peer review remains a foundational aspect of overseeing the safety and appropriateness of healthcare provided by physicians, Dr. Weiss said. Peer review likely varies from hospital to hospital, he added, although the Healthcare Quality Improvement Act provides some level of guidance as does the American Medical Association Code of Medical Ethics (section 9.4.1).
“In essence, both require that the evaluation be conducted in good faith with the intention to improve care, by physicians with adequate training and knowledge, using a process that is fair and inclusive of the physician under review,” he said. “I believe that most medical staffs abide by these ethical principles, but we have little data to confirm this supposition.”
Did hospital target doc for being vocal?
When members of Methodist’s medical staff first approached Dr. Smith with concerns about his surgery outcomes in November 2018, the physician says he was surprised, but that he was open to an assessment.
“They came to me and said they thought my numbers were bad, and I said: ‘Well my gosh, I certainly don’t want that to be the case. I need to see what numbers you are talking about,’ ” Dr. Smith recalled. “I’ve been president of the Bexar County Medical Society; I’ve been involved with standards and ethics for the Society of Thoracic Surgeons. Quality health care means a whole lot to me.”
The statistical information provided by hospital administrators indicated that Dr. Smith’s mortality rates for coronary artery surgery in 2018 were “excessive” and that his rates for aortic surgery were “unacceptable,” according to a lawsuit Dr. Smith filed against the hospital system. Dr. Smith, who is double boarded with the American Board of Surgery and the American Board of Thoracic Surgery, said his outcomes had never come into question in the past. Dr. Smith said the timing was suspicious to him, however, considering he had recently raised concerns with the hospital through letters about nursing performance, staffing, and compensation.
A peer review investigation was initiated. In the meantime, Dr. Smith agreed to intensivist consults on his postoperative patients and consults with the hospital’s “Heart Team” on all preoperative cardiac, valve, and aortic cases. A vocal critic of the Heart Team, Dr. Smith had long contended the entity provided no meaningful benefit to his patients in most cases and, rather, increased hospital stays and raised medical expenses. Despite his agreement, Dr. Smith was later asked to voluntarily stop performing surgeries at the hospital.
“I agreed, convinced that we’d get this all settled,” he said.
Another report issued by the hospital in 2019 also indicated elevated mortality rates associated with some of Smith’s surgeries, although the document differed from the first report, according to the lawsuit. Dr. Smith says he was ignored when he pointed out problems with the data, including a lack of appropriate risk stratification in the report, departure from Society of Thoracic Surgeons data rules, and improper inclusion of his cases in the denominator of the ratio when a comparison was made of his outcomes with those hospitalwide. A subsequent report from Methodist in March 2019 indicated Dr. Smith’s surgery outcomes were “within the expected parameters of performance,” according to court documents.
The surgery accusations were dropped, but the peer review proceeding against Dr. Smith wasn’t over. The hospital next requested that Dr. Smith undergo a competency evaluation.
“When they realized the data was bad, they then changed their argument in the peer review proceeding and essentially started to argue that Dr. Smith had some sort of cognitive disability that prevented him from continuing to practice,” said Mr. Pullen. “The way I look at it, when the initial basis for the peer review was proven false, the hospital found something else and some other reason to try to keep Dr. Smith from practicing.”
Thus began a lengthy disagreement about which entity would conduct the evaluation, who would pay, and the type of acceptable assessment. An evaluation by the hospital’s preferred organization resulted in a finding of mild cognitive impairment, Dr. Smith said. He hired his own experts who conducted separate evaluations, finding no impairment and no basis for the former evaluation’s conclusion.
“Literally, the determinant as to whether I was normal or below normal on their test was one point, which was associated with a finding that I didn’t draw a clock correctly,” Dr. Smith claimed. “The reviewer said my minute hand was a little too short and docked me a point. It was purely subjective. To me, the gold standard of whether you are learned in thoracic surgery is the American Board of Thoracic Surgery’s test. The board’s test shows my cognitive ability is entirely in keeping with my practice. That contrasts with the one point off I got for drawing a clock wrong in somebody’s estimation.”
Conflict leads to legal case
In September 2020, Dr. Smith filed a lawsuit against Methodist Healthcare System of San Antonio, alleging business disparagement by Methodist for allegedly publishing false and disparaging information about Dr. Smith and tortious interference with business relations. The latter claim stems from Methodist refusing to provide documents to other hospitals about the status of Dr. Smith’s privileges at Methodist, Mr. Pullen said.
Because Methodist refused to confirm his status, the renewal process for Baptist Health System could not be completed and Dr. Smith lost his privileges at Baptist Health System facilities, according to the lawsuit.
Notably, Dr. Smith’s legal challenge also asks the court to take a stance against alleged amendments by Methodist to its Unified Medical Staff Bylaws. The hospital allegedly proposed changes that would prevent physicians from seeking legal action against the hospital for malicious peer review, according to Dr. Smith’s lawsuit.
The amendments would make the peer review process itself the “sole and exclusive remedy with respect to any action or recommendation taken at the hospital affecting medical staff appointment and/or clinical privileges,” according to an excerpt of the proposed amendments included in Dr. Smith’s lawsuit. In addition, the changes would hold practitioners liable for lost revenues if the doctor initiates “any type of legal action challenging credentialing, privileging, or other medical peer review or professional review activity,” according to the lawsuit.
Dr. Smith’s lawsuit seeks a declaration that the proposed amendments to the bylaws are “void as against public policy,” and a declaration that the proposed amendments to the bylaws cannot take away physicians’ statutory right to bring litigation against Methodist for malicious peer review.
“The proposed amendments have a tendency to and will injure the public good,” Dr. Smith argued in the lawsuit. “The proposed amendments allow Methodist to act with malice and in bad faith in conducting peer review proceedings and face no legal repercussions.”
Regardless of the final outcome of the peer review proceeding, Mr. Pullen said the harm Dr. Smith has already endured cannot be reversed.
“Even if comes out in his favor, the damage is already done,” he said. “It will not remedy the damage Dr. Smith has incurred.”
Fighting sham peer review is difficult
Battling a malicious peer review has long been an uphill battle for physicians, according to Dr. Huntoon. That’s because the Health Care Quality Improvement Act (HCQIA), a federal law passed in 1986, provides near absolute immunity to hospitals and peer reviewers in legal disputes.
The HCQIA was created by Congress to extend immunity to good-faith peer review of doctors and to increase overall participation in peer review by removing fear of litigation. However, the act has also enabled abuse of peer review by shielding bad-faith reviewers from accountability, said Dr. Huntoon.
“The Health Care Quality Improvement Act presumes that what the hospital did was warranted and reasonable and shifts the burden to the physician to prove his innocence by a preponderance of evidence,” he said. “That’s an entirely foreign concept to most people who think a person should be considered innocent until proven guilty. Here, it’s the exact opposite.”
The HCQIA has been challenged numerous times over the years and tested at the appellate level, but continues to survive and remain settled law, added Richard B. Willner, DPM, founder and director of the Center for Peer Review Justice, which assists and counsels physicians about sham peer review.
In 2011, former Rep. Joe Heck, DO, (R-Nev.) introduced a bill that would have amended the HCQIA to prohibit a professional review entity from submitting a report to the National Practitioner Data Bank (NPDB) while the doctor was still under investigation and before the doctor was afforded adequate notice and a hearing. Although the measure had 16 cosponsors and plenty of support from the physician community, it failed.
In addition to a heavy legal burden, physicians who experience malicious peer reviews also face ramifications from being reported to the NPDB. Peer review organizations are required to report certain negative actions or findings to the NPDB.
“A databank entry is a scarlet letter on your forehead,” Dr. Willner said. “The rules at a lot of institutions are not to take anyone who has been databanked, rightfully or wrongfully. And what is the evidence necessary to databank you? None. There’s no evidence needed to databank somebody.”
Despite the bleak landscape, experts say progress has been made on a case-by-case basis by physicians who have succeeded in fighting back against questionable peer reviews in recent years.
In January 2020, Indiana ob.gyn. Rebecca Denman, MD, prevailed in her defamation lawsuit against St Vincent Carmel Hospital and St Vincent Carmel Medical Group, winning $4.75 million in damages. Dr. Denman alleged administrators failed to conduct a proper peer review investigation after a false allegation by a nurse that she was under the influence while on the job.
Indianapolis attorney Kathleen A. DeLaney, who represented Dr. Denman, said hospital leaders misled Dr. Denman into believing a peer review had occurred when no formal peer review hearing or proceeding took place.
“The CMO of the medical group claimed that he performed a peer review ‘screening,’ but he never informed the other members of the peer review executive committee of the matter until after he had placed Dr. Denman on administrative leave,” Ms. DeLaney said. “He also neglected to tell the peer review executive committee that the substance abuse policy had not been followed, or that Dr. Denman had not been tested for alcohol use – due to the 12-hour delay in report.”
Dr. Denman was ultimately required to undergo an alcohol abuse evaluation, enter a treatment program, and sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit. She claimed repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
She sued the hospital in July 2018, alleging fraud, defamation, tortious interference with an employment relationship, and negligent misrepresentation. After a 4-day trial, jurors found in her favor, awarding Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
A hospital spokesperson said Ascension St Vincent is pursuing an appeal, and that it looks “forward to the opportunity to bring this matter before the Indiana Court of Appeals in June.”
In another case, South Dakota surgeon Linda Miller, MD, was awarded $1.1 million in 2017 after a federal jury found Huron Regional Medical Center breached her contract and violated her due process rights. Dr. Miller became the subject of a peer review at Huron Regional Medical Center when the hospital began analyzing some of her surgery outcomes.
Ken Barker, an attorney for Dr. Miller, said he feels it became evident at trial that the campaign to force Dr. Miller to either resign or lose her privileges was led by the lay board of directors of the hospital and upper-level administration at the hospital.
“They began the process by ordering an unprecedented 90-day review of her medical charts, looking for errors in the medical care she provided patients,” he said. “They could find nothing, so they did a second 90-day review, waiting for a patient’s ‘bad outcome.’ As any general surgeon will say, a ‘bad outcome’ is inevitable. And so it was. Upon that occurrence, they had a medical review committee review the patient’s chart and use it as an excuse to force her to reduce her privileges. Unbeknown to Dr. Miller, an external review had been conducted on another patient’s chart, in which the external review found her care above the standards and, in some measure, ‘exemplary.’ ”
Dr. Miller was eventually pressured to resign, according to her claim. Because of reports made to the NPDB by the medical center, including a patient complication that was allegedly falsified by the hospital, Dr. Miller said she was unable to find work as a general surgeon and went to work as a wound care doctor. At trial, jurors awarded Dr. Miller $586,617 in lost wages, $343,640 for lost future earning capacity, and $250,000 for mental anguish. (The mental anguish award was subsequently struck by a district court.)
Attorneys for Huron Regional Medical Center argued the jury improperly awarded damages and requested a new trial, which was denied by an appeals court.
In the end, the evidence came to light and the jury’s verdict spoke loudly that the hospital had taken unfair advantage of Dr. Miller, Mr. Barker said. But he emphasized that such cases often end differently.
“There are a handful of cases in which physicians like Dr. Miller have challenged the system and won,” he said. “In most cases, however, it is a ‘David vs. Goliath’ scenario where the giant prevails.”
What to do if faced with malicious peer review
An important step when doctors encounter a peer review that they believe is malicious is to consult with an experienced attorney as early as possible, Dr. Huntoon said. “Not all attorneys who set themselves out to be health law attorneys necessarily have knowledge and expertise in sham peer review. And before such a thing happens, I always encourage physicians to read their medical staff bylaws. That’s where everything is set forth, [such as] the corrective action section that tells how peer review is to take place.”
Mr. Barker added that documentation is also key in the event of a potential malicious peer review.
“When a physician senses [the] administration has targeted them, they should start documenting their conversations and actions very carefully, and if possible, recruit another ‘observer’ who can provide a third-party perspective, if necessary,” Mr. Barker said.
Dr. Huntoon recently wrote an article with advice about preparedness and defense of sham peer reviews. The guidance includes that physicians educate themselves about the tactics used by some hospitals to conduct sham peer reviews and the factors that place doctors more at risk. Factors that may raise a doctor’s danger of being targeted include being in solo practice or a small group, being new on staff, or being an older physician approaching retirement as some bad-actor hospitals may view older physicians as being less likely to fight back, said Dr. Huntoon.
Doctors should also keep detailed records and a timeline in the event of a malicious peer review and insist that an independent court reporter record all peer review hearings, even if that means the physician has to pay for the reporter him or herself, according to the guidance. An independent record is invaluable should the physician ultimately issue a future legal challenge against the hospital.
Mr. Willner encourages physicians to call the Center for Peer Review Justice hotline at (504) 621-1670 or visit the website for help with peer review and NPDB issues.
As for Dr. Smith, his days are much quieter and slower today, compared with the active practice he was accustomed to for more than half his life. He misses the fast pace, the patients, and the work that always brought him great joy.
“I hope to get back to doing surgeries eventually,” he said. “I graduated medical school in 1972. Practicing surgery has been my whole life and my career. They have taken my identity and my livelihood away from me based on false numbers and false premises. I want it back.”
A version of this article first appeared on Medscape.com.
Cardiothoracic surgeon J. Marvin Smith III, MD, had always thrived on a busy practice schedule, often performing 20-30 surgeries a week. A practicing surgeon for more than 40 years, Dr. Smith said he had no plans to slow down anytime soon.
But Dr. Smith said his career was derailed when leaders at Methodist Healthcare System of San Antonio initiated a sudden peer review proceeding against him. The hospital system alleged certain surgeries performed by Dr. Smith had excessive mortality rates. When he proved the data inaccurate, Dr. Smith said administrators next claimed he was cognitively impaired and wasn’t safe to practice.
Dr. Smith has now been embroiled in a peer review dispute with the hospital system for more than 2 years and says the conflict has essentially forced him out of surgical practice. He believes the peer review was “malicious” and was really launched because of complaints he made about nurse staffing and other issues at the hospital.
“I think it is absolutely in bad faith and is disingenuous what they’ve told me along the way,” said Dr. Smith, 73. “It’s because I pointed out deficiencies in nursing care, and they want to get rid of me. It would be a lot easier for them if I had a contract and they could control me better. But the fact that I was independent, meant they had to resort to a malicious peer review to try and push me out.”
Dr. Smith had a peer review hearing with Methodist in March 2021, and in April, a panel found in Dr. Smith’s favor, according to Dr. Smith. The findings were sent to the hospital’s medical board for review, which issued a decision in early May.
Eric A. Pullen, an attorney for Dr. Smith, said he could not go into detail about the board’s decision for legal reasons, but that “the medical board’s decision did not completely resolve the matter, and Dr. Smith intends to exercise his procedural rights, which could include an appeal.”
Methodist Hospital Texsan and its parent company, Methodist Health System of San Antonio, did not respond to messages seeking comment about the case. Without hearing from the hospital system, its side is unknown and it is unclear if there is more to the story from Methodist’s view.
The problem is not new, but some experts, such as Lawrence Huntoon, MD, PhD, say the practice has become more common in recent years, particularly against independent doctors.
Dr. Huntoon believes there is a nationwide trend at many hospitals to get rid of independent physicians and replace them with employed doctors, he said.
However, because most sham peer reviews go on behind closed doors, there are no data to pinpoint its prevalence or measure its growth.
“Independent physicians are basically being purged from medical staffs across the United States,” said Dr. Huntoon, who is chair of the Association of American Physicians and Surgeons’ Committee to Combat Sham Peer Review. “The hospitals want more control over how physicians practice and who they refer to, and they do that by having employees.”
Anthony P. Weiss, MD, MBA, chief medical officer for Beth Israel Deaconess Medical Center said it has not been his experience that independent physicians are being targeted in such a way. Dr. Weiss responded to an inquiry sent to the American Hospital Association for this story.
“As the authority for peer review rests with the organized medical staff (i.e., physicians), and not formally with the hospital per se, the peer review lever is not typically available as a management tool for hospital administration,” said Dr. Weiss, who is a former member of the AHA’s Committee on Clinical Leadership, but who was speaking on behalf of himself.
A spokesman for the AHA said the organization stands behinds Dr. Weiss’ comments.
Peer review remains a foundational aspect of overseeing the safety and appropriateness of healthcare provided by physicians, Dr. Weiss said. Peer review likely varies from hospital to hospital, he added, although the Healthcare Quality Improvement Act provides some level of guidance as does the American Medical Association Code of Medical Ethics (section 9.4.1).
“In essence, both require that the evaluation be conducted in good faith with the intention to improve care, by physicians with adequate training and knowledge, using a process that is fair and inclusive of the physician under review,” he said. “I believe that most medical staffs abide by these ethical principles, but we have little data to confirm this supposition.”
Did hospital target doc for being vocal?
When members of Methodist’s medical staff first approached Dr. Smith with concerns about his surgery outcomes in November 2018, the physician says he was surprised, but that he was open to an assessment.
“They came to me and said they thought my numbers were bad, and I said: ‘Well my gosh, I certainly don’t want that to be the case. I need to see what numbers you are talking about,’ ” Dr. Smith recalled. “I’ve been president of the Bexar County Medical Society; I’ve been involved with standards and ethics for the Society of Thoracic Surgeons. Quality health care means a whole lot to me.”
The statistical information provided by hospital administrators indicated that Dr. Smith’s mortality rates for coronary artery surgery in 2018 were “excessive” and that his rates for aortic surgery were “unacceptable,” according to a lawsuit Dr. Smith filed against the hospital system. Dr. Smith, who is double boarded with the American Board of Surgery and the American Board of Thoracic Surgery, said his outcomes had never come into question in the past. Dr. Smith said the timing was suspicious to him, however, considering he had recently raised concerns with the hospital through letters about nursing performance, staffing, and compensation.
A peer review investigation was initiated. In the meantime, Dr. Smith agreed to intensivist consults on his postoperative patients and consults with the hospital’s “Heart Team” on all preoperative cardiac, valve, and aortic cases. A vocal critic of the Heart Team, Dr. Smith had long contended the entity provided no meaningful benefit to his patients in most cases and, rather, increased hospital stays and raised medical expenses. Despite his agreement, Dr. Smith was later asked to voluntarily stop performing surgeries at the hospital.
“I agreed, convinced that we’d get this all settled,” he said.
Another report issued by the hospital in 2019 also indicated elevated mortality rates associated with some of Smith’s surgeries, although the document differed from the first report, according to the lawsuit. Dr. Smith says he was ignored when he pointed out problems with the data, including a lack of appropriate risk stratification in the report, departure from Society of Thoracic Surgeons data rules, and improper inclusion of his cases in the denominator of the ratio when a comparison was made of his outcomes with those hospitalwide. A subsequent report from Methodist in March 2019 indicated Dr. Smith’s surgery outcomes were “within the expected parameters of performance,” according to court documents.
The surgery accusations were dropped, but the peer review proceeding against Dr. Smith wasn’t over. The hospital next requested that Dr. Smith undergo a competency evaluation.
“When they realized the data was bad, they then changed their argument in the peer review proceeding and essentially started to argue that Dr. Smith had some sort of cognitive disability that prevented him from continuing to practice,” said Mr. Pullen. “The way I look at it, when the initial basis for the peer review was proven false, the hospital found something else and some other reason to try to keep Dr. Smith from practicing.”
Thus began a lengthy disagreement about which entity would conduct the evaluation, who would pay, and the type of acceptable assessment. An evaluation by the hospital’s preferred organization resulted in a finding of mild cognitive impairment, Dr. Smith said. He hired his own experts who conducted separate evaluations, finding no impairment and no basis for the former evaluation’s conclusion.
“Literally, the determinant as to whether I was normal or below normal on their test was one point, which was associated with a finding that I didn’t draw a clock correctly,” Dr. Smith claimed. “The reviewer said my minute hand was a little too short and docked me a point. It was purely subjective. To me, the gold standard of whether you are learned in thoracic surgery is the American Board of Thoracic Surgery’s test. The board’s test shows my cognitive ability is entirely in keeping with my practice. That contrasts with the one point off I got for drawing a clock wrong in somebody’s estimation.”
Conflict leads to legal case
In September 2020, Dr. Smith filed a lawsuit against Methodist Healthcare System of San Antonio, alleging business disparagement by Methodist for allegedly publishing false and disparaging information about Dr. Smith and tortious interference with business relations. The latter claim stems from Methodist refusing to provide documents to other hospitals about the status of Dr. Smith’s privileges at Methodist, Mr. Pullen said.
Because Methodist refused to confirm his status, the renewal process for Baptist Health System could not be completed and Dr. Smith lost his privileges at Baptist Health System facilities, according to the lawsuit.
Notably, Dr. Smith’s legal challenge also asks the court to take a stance against alleged amendments by Methodist to its Unified Medical Staff Bylaws. The hospital allegedly proposed changes that would prevent physicians from seeking legal action against the hospital for malicious peer review, according to Dr. Smith’s lawsuit.
The amendments would make the peer review process itself the “sole and exclusive remedy with respect to any action or recommendation taken at the hospital affecting medical staff appointment and/or clinical privileges,” according to an excerpt of the proposed amendments included in Dr. Smith’s lawsuit. In addition, the changes would hold practitioners liable for lost revenues if the doctor initiates “any type of legal action challenging credentialing, privileging, or other medical peer review or professional review activity,” according to the lawsuit.
Dr. Smith’s lawsuit seeks a declaration that the proposed amendments to the bylaws are “void as against public policy,” and a declaration that the proposed amendments to the bylaws cannot take away physicians’ statutory right to bring litigation against Methodist for malicious peer review.
“The proposed amendments have a tendency to and will injure the public good,” Dr. Smith argued in the lawsuit. “The proposed amendments allow Methodist to act with malice and in bad faith in conducting peer review proceedings and face no legal repercussions.”
Regardless of the final outcome of the peer review proceeding, Mr. Pullen said the harm Dr. Smith has already endured cannot be reversed.
“Even if comes out in his favor, the damage is already done,” he said. “It will not remedy the damage Dr. Smith has incurred.”
Fighting sham peer review is difficult
Battling a malicious peer review has long been an uphill battle for physicians, according to Dr. Huntoon. That’s because the Health Care Quality Improvement Act (HCQIA), a federal law passed in 1986, provides near absolute immunity to hospitals and peer reviewers in legal disputes.
The HCQIA was created by Congress to extend immunity to good-faith peer review of doctors and to increase overall participation in peer review by removing fear of litigation. However, the act has also enabled abuse of peer review by shielding bad-faith reviewers from accountability, said Dr. Huntoon.
“The Health Care Quality Improvement Act presumes that what the hospital did was warranted and reasonable and shifts the burden to the physician to prove his innocence by a preponderance of evidence,” he said. “That’s an entirely foreign concept to most people who think a person should be considered innocent until proven guilty. Here, it’s the exact opposite.”
The HCQIA has been challenged numerous times over the years and tested at the appellate level, but continues to survive and remain settled law, added Richard B. Willner, DPM, founder and director of the Center for Peer Review Justice, which assists and counsels physicians about sham peer review.
In 2011, former Rep. Joe Heck, DO, (R-Nev.) introduced a bill that would have amended the HCQIA to prohibit a professional review entity from submitting a report to the National Practitioner Data Bank (NPDB) while the doctor was still under investigation and before the doctor was afforded adequate notice and a hearing. Although the measure had 16 cosponsors and plenty of support from the physician community, it failed.
In addition to a heavy legal burden, physicians who experience malicious peer reviews also face ramifications from being reported to the NPDB. Peer review organizations are required to report certain negative actions or findings to the NPDB.
“A databank entry is a scarlet letter on your forehead,” Dr. Willner said. “The rules at a lot of institutions are not to take anyone who has been databanked, rightfully or wrongfully. And what is the evidence necessary to databank you? None. There’s no evidence needed to databank somebody.”
Despite the bleak landscape, experts say progress has been made on a case-by-case basis by physicians who have succeeded in fighting back against questionable peer reviews in recent years.
In January 2020, Indiana ob.gyn. Rebecca Denman, MD, prevailed in her defamation lawsuit against St Vincent Carmel Hospital and St Vincent Carmel Medical Group, winning $4.75 million in damages. Dr. Denman alleged administrators failed to conduct a proper peer review investigation after a false allegation by a nurse that she was under the influence while on the job.
Indianapolis attorney Kathleen A. DeLaney, who represented Dr. Denman, said hospital leaders misled Dr. Denman into believing a peer review had occurred when no formal peer review hearing or proceeding took place.
“The CMO of the medical group claimed that he performed a peer review ‘screening,’ but he never informed the other members of the peer review executive committee of the matter until after he had placed Dr. Denman on administrative leave,” Ms. DeLaney said. “He also neglected to tell the peer review executive committee that the substance abuse policy had not been followed, or that Dr. Denman had not been tested for alcohol use – due to the 12-hour delay in report.”
Dr. Denman was ultimately required to undergo an alcohol abuse evaluation, enter a treatment program, and sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit. She claimed repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
She sued the hospital in July 2018, alleging fraud, defamation, tortious interference with an employment relationship, and negligent misrepresentation. After a 4-day trial, jurors found in her favor, awarding Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
A hospital spokesperson said Ascension St Vincent is pursuing an appeal, and that it looks “forward to the opportunity to bring this matter before the Indiana Court of Appeals in June.”
In another case, South Dakota surgeon Linda Miller, MD, was awarded $1.1 million in 2017 after a federal jury found Huron Regional Medical Center breached her contract and violated her due process rights. Dr. Miller became the subject of a peer review at Huron Regional Medical Center when the hospital began analyzing some of her surgery outcomes.
Ken Barker, an attorney for Dr. Miller, said he feels it became evident at trial that the campaign to force Dr. Miller to either resign or lose her privileges was led by the lay board of directors of the hospital and upper-level administration at the hospital.
“They began the process by ordering an unprecedented 90-day review of her medical charts, looking for errors in the medical care she provided patients,” he said. “They could find nothing, so they did a second 90-day review, waiting for a patient’s ‘bad outcome.’ As any general surgeon will say, a ‘bad outcome’ is inevitable. And so it was. Upon that occurrence, they had a medical review committee review the patient’s chart and use it as an excuse to force her to reduce her privileges. Unbeknown to Dr. Miller, an external review had been conducted on another patient’s chart, in which the external review found her care above the standards and, in some measure, ‘exemplary.’ ”
Dr. Miller was eventually pressured to resign, according to her claim. Because of reports made to the NPDB by the medical center, including a patient complication that was allegedly falsified by the hospital, Dr. Miller said she was unable to find work as a general surgeon and went to work as a wound care doctor. At trial, jurors awarded Dr. Miller $586,617 in lost wages, $343,640 for lost future earning capacity, and $250,000 for mental anguish. (The mental anguish award was subsequently struck by a district court.)
Attorneys for Huron Regional Medical Center argued the jury improperly awarded damages and requested a new trial, which was denied by an appeals court.
In the end, the evidence came to light and the jury’s verdict spoke loudly that the hospital had taken unfair advantage of Dr. Miller, Mr. Barker said. But he emphasized that such cases often end differently.
“There are a handful of cases in which physicians like Dr. Miller have challenged the system and won,” he said. “In most cases, however, it is a ‘David vs. Goliath’ scenario where the giant prevails.”
What to do if faced with malicious peer review
An important step when doctors encounter a peer review that they believe is malicious is to consult with an experienced attorney as early as possible, Dr. Huntoon said. “Not all attorneys who set themselves out to be health law attorneys necessarily have knowledge and expertise in sham peer review. And before such a thing happens, I always encourage physicians to read their medical staff bylaws. That’s where everything is set forth, [such as] the corrective action section that tells how peer review is to take place.”
Mr. Barker added that documentation is also key in the event of a potential malicious peer review.
“When a physician senses [the] administration has targeted them, they should start documenting their conversations and actions very carefully, and if possible, recruit another ‘observer’ who can provide a third-party perspective, if necessary,” Mr. Barker said.
Dr. Huntoon recently wrote an article with advice about preparedness and defense of sham peer reviews. The guidance includes that physicians educate themselves about the tactics used by some hospitals to conduct sham peer reviews and the factors that place doctors more at risk. Factors that may raise a doctor’s danger of being targeted include being in solo practice or a small group, being new on staff, or being an older physician approaching retirement as some bad-actor hospitals may view older physicians as being less likely to fight back, said Dr. Huntoon.
Doctors should also keep detailed records and a timeline in the event of a malicious peer review and insist that an independent court reporter record all peer review hearings, even if that means the physician has to pay for the reporter him or herself, according to the guidance. An independent record is invaluable should the physician ultimately issue a future legal challenge against the hospital.
Mr. Willner encourages physicians to call the Center for Peer Review Justice hotline at (504) 621-1670 or visit the website for help with peer review and NPDB issues.
As for Dr. Smith, his days are much quieter and slower today, compared with the active practice he was accustomed to for more than half his life. He misses the fast pace, the patients, and the work that always brought him great joy.
“I hope to get back to doing surgeries eventually,” he said. “I graduated medical school in 1972. Practicing surgery has been my whole life and my career. They have taken my identity and my livelihood away from me based on false numbers and false premises. I want it back.”
A version of this article first appeared on Medscape.com.
Cardiothoracic surgeon J. Marvin Smith III, MD, had always thrived on a busy practice schedule, often performing 20-30 surgeries a week. A practicing surgeon for more than 40 years, Dr. Smith said he had no plans to slow down anytime soon.
But Dr. Smith said his career was derailed when leaders at Methodist Healthcare System of San Antonio initiated a sudden peer review proceeding against him. The hospital system alleged certain surgeries performed by Dr. Smith had excessive mortality rates. When he proved the data inaccurate, Dr. Smith said administrators next claimed he was cognitively impaired and wasn’t safe to practice.
Dr. Smith has now been embroiled in a peer review dispute with the hospital system for more than 2 years and says the conflict has essentially forced him out of surgical practice. He believes the peer review was “malicious” and was really launched because of complaints he made about nurse staffing and other issues at the hospital.
“I think it is absolutely in bad faith and is disingenuous what they’ve told me along the way,” said Dr. Smith, 73. “It’s because I pointed out deficiencies in nursing care, and they want to get rid of me. It would be a lot easier for them if I had a contract and they could control me better. But the fact that I was independent, meant they had to resort to a malicious peer review to try and push me out.”
Dr. Smith had a peer review hearing with Methodist in March 2021, and in April, a panel found in Dr. Smith’s favor, according to Dr. Smith. The findings were sent to the hospital’s medical board for review, which issued a decision in early May.
Eric A. Pullen, an attorney for Dr. Smith, said he could not go into detail about the board’s decision for legal reasons, but that “the medical board’s decision did not completely resolve the matter, and Dr. Smith intends to exercise his procedural rights, which could include an appeal.”
Methodist Hospital Texsan and its parent company, Methodist Health System of San Antonio, did not respond to messages seeking comment about the case. Without hearing from the hospital system, its side is unknown and it is unclear if there is more to the story from Methodist’s view.
The problem is not new, but some experts, such as Lawrence Huntoon, MD, PhD, say the practice has become more common in recent years, particularly against independent doctors.
Dr. Huntoon believes there is a nationwide trend at many hospitals to get rid of independent physicians and replace them with employed doctors, he said.
However, because most sham peer reviews go on behind closed doors, there are no data to pinpoint its prevalence or measure its growth.
“Independent physicians are basically being purged from medical staffs across the United States,” said Dr. Huntoon, who is chair of the Association of American Physicians and Surgeons’ Committee to Combat Sham Peer Review. “The hospitals want more control over how physicians practice and who they refer to, and they do that by having employees.”
Anthony P. Weiss, MD, MBA, chief medical officer for Beth Israel Deaconess Medical Center said it has not been his experience that independent physicians are being targeted in such a way. Dr. Weiss responded to an inquiry sent to the American Hospital Association for this story.
“As the authority for peer review rests with the organized medical staff (i.e., physicians), and not formally with the hospital per se, the peer review lever is not typically available as a management tool for hospital administration,” said Dr. Weiss, who is a former member of the AHA’s Committee on Clinical Leadership, but who was speaking on behalf of himself.
A spokesman for the AHA said the organization stands behinds Dr. Weiss’ comments.
Peer review remains a foundational aspect of overseeing the safety and appropriateness of healthcare provided by physicians, Dr. Weiss said. Peer review likely varies from hospital to hospital, he added, although the Healthcare Quality Improvement Act provides some level of guidance as does the American Medical Association Code of Medical Ethics (section 9.4.1).
“In essence, both require that the evaluation be conducted in good faith with the intention to improve care, by physicians with adequate training and knowledge, using a process that is fair and inclusive of the physician under review,” he said. “I believe that most medical staffs abide by these ethical principles, but we have little data to confirm this supposition.”
Did hospital target doc for being vocal?
When members of Methodist’s medical staff first approached Dr. Smith with concerns about his surgery outcomes in November 2018, the physician says he was surprised, but that he was open to an assessment.
“They came to me and said they thought my numbers were bad, and I said: ‘Well my gosh, I certainly don’t want that to be the case. I need to see what numbers you are talking about,’ ” Dr. Smith recalled. “I’ve been president of the Bexar County Medical Society; I’ve been involved with standards and ethics for the Society of Thoracic Surgeons. Quality health care means a whole lot to me.”
The statistical information provided by hospital administrators indicated that Dr. Smith’s mortality rates for coronary artery surgery in 2018 were “excessive” and that his rates for aortic surgery were “unacceptable,” according to a lawsuit Dr. Smith filed against the hospital system. Dr. Smith, who is double boarded with the American Board of Surgery and the American Board of Thoracic Surgery, said his outcomes had never come into question in the past. Dr. Smith said the timing was suspicious to him, however, considering he had recently raised concerns with the hospital through letters about nursing performance, staffing, and compensation.
A peer review investigation was initiated. In the meantime, Dr. Smith agreed to intensivist consults on his postoperative patients and consults with the hospital’s “Heart Team” on all preoperative cardiac, valve, and aortic cases. A vocal critic of the Heart Team, Dr. Smith had long contended the entity provided no meaningful benefit to his patients in most cases and, rather, increased hospital stays and raised medical expenses. Despite his agreement, Dr. Smith was later asked to voluntarily stop performing surgeries at the hospital.
“I agreed, convinced that we’d get this all settled,” he said.
Another report issued by the hospital in 2019 also indicated elevated mortality rates associated with some of Smith’s surgeries, although the document differed from the first report, according to the lawsuit. Dr. Smith says he was ignored when he pointed out problems with the data, including a lack of appropriate risk stratification in the report, departure from Society of Thoracic Surgeons data rules, and improper inclusion of his cases in the denominator of the ratio when a comparison was made of his outcomes with those hospitalwide. A subsequent report from Methodist in March 2019 indicated Dr. Smith’s surgery outcomes were “within the expected parameters of performance,” according to court documents.
The surgery accusations were dropped, but the peer review proceeding against Dr. Smith wasn’t over. The hospital next requested that Dr. Smith undergo a competency evaluation.
“When they realized the data was bad, they then changed their argument in the peer review proceeding and essentially started to argue that Dr. Smith had some sort of cognitive disability that prevented him from continuing to practice,” said Mr. Pullen. “The way I look at it, when the initial basis for the peer review was proven false, the hospital found something else and some other reason to try to keep Dr. Smith from practicing.”
Thus began a lengthy disagreement about which entity would conduct the evaluation, who would pay, and the type of acceptable assessment. An evaluation by the hospital’s preferred organization resulted in a finding of mild cognitive impairment, Dr. Smith said. He hired his own experts who conducted separate evaluations, finding no impairment and no basis for the former evaluation’s conclusion.
“Literally, the determinant as to whether I was normal or below normal on their test was one point, which was associated with a finding that I didn’t draw a clock correctly,” Dr. Smith claimed. “The reviewer said my minute hand was a little too short and docked me a point. It was purely subjective. To me, the gold standard of whether you are learned in thoracic surgery is the American Board of Thoracic Surgery’s test. The board’s test shows my cognitive ability is entirely in keeping with my practice. That contrasts with the one point off I got for drawing a clock wrong in somebody’s estimation.”
Conflict leads to legal case
In September 2020, Dr. Smith filed a lawsuit against Methodist Healthcare System of San Antonio, alleging business disparagement by Methodist for allegedly publishing false and disparaging information about Dr. Smith and tortious interference with business relations. The latter claim stems from Methodist refusing to provide documents to other hospitals about the status of Dr. Smith’s privileges at Methodist, Mr. Pullen said.
Because Methodist refused to confirm his status, the renewal process for Baptist Health System could not be completed and Dr. Smith lost his privileges at Baptist Health System facilities, according to the lawsuit.
Notably, Dr. Smith’s legal challenge also asks the court to take a stance against alleged amendments by Methodist to its Unified Medical Staff Bylaws. The hospital allegedly proposed changes that would prevent physicians from seeking legal action against the hospital for malicious peer review, according to Dr. Smith’s lawsuit.
The amendments would make the peer review process itself the “sole and exclusive remedy with respect to any action or recommendation taken at the hospital affecting medical staff appointment and/or clinical privileges,” according to an excerpt of the proposed amendments included in Dr. Smith’s lawsuit. In addition, the changes would hold practitioners liable for lost revenues if the doctor initiates “any type of legal action challenging credentialing, privileging, or other medical peer review or professional review activity,” according to the lawsuit.
Dr. Smith’s lawsuit seeks a declaration that the proposed amendments to the bylaws are “void as against public policy,” and a declaration that the proposed amendments to the bylaws cannot take away physicians’ statutory right to bring litigation against Methodist for malicious peer review.
“The proposed amendments have a tendency to and will injure the public good,” Dr. Smith argued in the lawsuit. “The proposed amendments allow Methodist to act with malice and in bad faith in conducting peer review proceedings and face no legal repercussions.”
Regardless of the final outcome of the peer review proceeding, Mr. Pullen said the harm Dr. Smith has already endured cannot be reversed.
“Even if comes out in his favor, the damage is already done,” he said. “It will not remedy the damage Dr. Smith has incurred.”
Fighting sham peer review is difficult
Battling a malicious peer review has long been an uphill battle for physicians, according to Dr. Huntoon. That’s because the Health Care Quality Improvement Act (HCQIA), a federal law passed in 1986, provides near absolute immunity to hospitals and peer reviewers in legal disputes.
The HCQIA was created by Congress to extend immunity to good-faith peer review of doctors and to increase overall participation in peer review by removing fear of litigation. However, the act has also enabled abuse of peer review by shielding bad-faith reviewers from accountability, said Dr. Huntoon.
“The Health Care Quality Improvement Act presumes that what the hospital did was warranted and reasonable and shifts the burden to the physician to prove his innocence by a preponderance of evidence,” he said. “That’s an entirely foreign concept to most people who think a person should be considered innocent until proven guilty. Here, it’s the exact opposite.”
The HCQIA has been challenged numerous times over the years and tested at the appellate level, but continues to survive and remain settled law, added Richard B. Willner, DPM, founder and director of the Center for Peer Review Justice, which assists and counsels physicians about sham peer review.
In 2011, former Rep. Joe Heck, DO, (R-Nev.) introduced a bill that would have amended the HCQIA to prohibit a professional review entity from submitting a report to the National Practitioner Data Bank (NPDB) while the doctor was still under investigation and before the doctor was afforded adequate notice and a hearing. Although the measure had 16 cosponsors and plenty of support from the physician community, it failed.
In addition to a heavy legal burden, physicians who experience malicious peer reviews also face ramifications from being reported to the NPDB. Peer review organizations are required to report certain negative actions or findings to the NPDB.
“A databank entry is a scarlet letter on your forehead,” Dr. Willner said. “The rules at a lot of institutions are not to take anyone who has been databanked, rightfully or wrongfully. And what is the evidence necessary to databank you? None. There’s no evidence needed to databank somebody.”
Despite the bleak landscape, experts say progress has been made on a case-by-case basis by physicians who have succeeded in fighting back against questionable peer reviews in recent years.
In January 2020, Indiana ob.gyn. Rebecca Denman, MD, prevailed in her defamation lawsuit against St Vincent Carmel Hospital and St Vincent Carmel Medical Group, winning $4.75 million in damages. Dr. Denman alleged administrators failed to conduct a proper peer review investigation after a false allegation by a nurse that she was under the influence while on the job.
Indianapolis attorney Kathleen A. DeLaney, who represented Dr. Denman, said hospital leaders misled Dr. Denman into believing a peer review had occurred when no formal peer review hearing or proceeding took place.
“The CMO of the medical group claimed that he performed a peer review ‘screening,’ but he never informed the other members of the peer review executive committee of the matter until after he had placed Dr. Denman on administrative leave,” Ms. DeLaney said. “He also neglected to tell the peer review executive committee that the substance abuse policy had not been followed, or that Dr. Denman had not been tested for alcohol use – due to the 12-hour delay in report.”
Dr. Denman was ultimately required to undergo an alcohol abuse evaluation, enter a treatment program, and sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit. She claimed repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
She sued the hospital in July 2018, alleging fraud, defamation, tortious interference with an employment relationship, and negligent misrepresentation. After a 4-day trial, jurors found in her favor, awarding Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
A hospital spokesperson said Ascension St Vincent is pursuing an appeal, and that it looks “forward to the opportunity to bring this matter before the Indiana Court of Appeals in June.”
In another case, South Dakota surgeon Linda Miller, MD, was awarded $1.1 million in 2017 after a federal jury found Huron Regional Medical Center breached her contract and violated her due process rights. Dr. Miller became the subject of a peer review at Huron Regional Medical Center when the hospital began analyzing some of her surgery outcomes.
Ken Barker, an attorney for Dr. Miller, said he feels it became evident at trial that the campaign to force Dr. Miller to either resign or lose her privileges was led by the lay board of directors of the hospital and upper-level administration at the hospital.
“They began the process by ordering an unprecedented 90-day review of her medical charts, looking for errors in the medical care she provided patients,” he said. “They could find nothing, so they did a second 90-day review, waiting for a patient’s ‘bad outcome.’ As any general surgeon will say, a ‘bad outcome’ is inevitable. And so it was. Upon that occurrence, they had a medical review committee review the patient’s chart and use it as an excuse to force her to reduce her privileges. Unbeknown to Dr. Miller, an external review had been conducted on another patient’s chart, in which the external review found her care above the standards and, in some measure, ‘exemplary.’ ”
Dr. Miller was eventually pressured to resign, according to her claim. Because of reports made to the NPDB by the medical center, including a patient complication that was allegedly falsified by the hospital, Dr. Miller said she was unable to find work as a general surgeon and went to work as a wound care doctor. At trial, jurors awarded Dr. Miller $586,617 in lost wages, $343,640 for lost future earning capacity, and $250,000 for mental anguish. (The mental anguish award was subsequently struck by a district court.)
Attorneys for Huron Regional Medical Center argued the jury improperly awarded damages and requested a new trial, which was denied by an appeals court.
In the end, the evidence came to light and the jury’s verdict spoke loudly that the hospital had taken unfair advantage of Dr. Miller, Mr. Barker said. But he emphasized that such cases often end differently.
“There are a handful of cases in which physicians like Dr. Miller have challenged the system and won,” he said. “In most cases, however, it is a ‘David vs. Goliath’ scenario where the giant prevails.”
What to do if faced with malicious peer review
An important step when doctors encounter a peer review that they believe is malicious is to consult with an experienced attorney as early as possible, Dr. Huntoon said. “Not all attorneys who set themselves out to be health law attorneys necessarily have knowledge and expertise in sham peer review. And before such a thing happens, I always encourage physicians to read their medical staff bylaws. That’s where everything is set forth, [such as] the corrective action section that tells how peer review is to take place.”
Mr. Barker added that documentation is also key in the event of a potential malicious peer review.
“When a physician senses [the] administration has targeted them, they should start documenting their conversations and actions very carefully, and if possible, recruit another ‘observer’ who can provide a third-party perspective, if necessary,” Mr. Barker said.
Dr. Huntoon recently wrote an article with advice about preparedness and defense of sham peer reviews. The guidance includes that physicians educate themselves about the tactics used by some hospitals to conduct sham peer reviews and the factors that place doctors more at risk. Factors that may raise a doctor’s danger of being targeted include being in solo practice or a small group, being new on staff, or being an older physician approaching retirement as some bad-actor hospitals may view older physicians as being less likely to fight back, said Dr. Huntoon.
Doctors should also keep detailed records and a timeline in the event of a malicious peer review and insist that an independent court reporter record all peer review hearings, even if that means the physician has to pay for the reporter him or herself, according to the guidance. An independent record is invaluable should the physician ultimately issue a future legal challenge against the hospital.
Mr. Willner encourages physicians to call the Center for Peer Review Justice hotline at (504) 621-1670 or visit the website for help with peer review and NPDB issues.
As for Dr. Smith, his days are much quieter and slower today, compared with the active practice he was accustomed to for more than half his life. He misses the fast pace, the patients, and the work that always brought him great joy.
“I hope to get back to doing surgeries eventually,” he said. “I graduated medical school in 1972. Practicing surgery has been my whole life and my career. They have taken my identity and my livelihood away from me based on false numbers and false premises. I want it back.”
A version of this article first appeared on Medscape.com.
Study supports intensifying chemoradiotherapy for head and neck cancer
Of the 16 treatment options compared and ranked, HFCRT topped the list for overall survival, event-free survival, locoregional control, and cancer-specific death.
The results also suggested that taxane-based induction chemotherapy followed by locoregional therapy, especially with concomitant chemotherapy, “is another good option in selected patients with a good performance status and minor comorbidities,” according to investigator Claire Petit, MD, PhD, of Centre hospitalier de l’Université de Montréal in Canada, and colleagues.
The investigators concluded that further intensifying chemoradiotherapy with these approaches “could improve outcomes over chemoradiotherapy.”
The findings, published in The Lancet Oncology, “could help to guide clinical decision-making in locally advanced head and neck cancer with a high risk of locoregional failure, especially human papillomavirus–negative tumours,” the authors wrote.
However, Jared Weiss, MD, of the University of North Carolina, Chapel Hill, cautioned that this “study is an individual patient data network meta-analysis, not a randomized controlled trial. As the authors note, it can help frame existing data but cannot define standard of care.”
Still, “it does support the efficacy of two commonly considered intensification strategies for high-risk patients – hyperfractionation of the radiation and the addition of preceding induction chemotherapy. Both of these intensifications substantially increase the time commitment from the patient, and many patients find this unacceptable. But, for select patients, hyperfractionation and induction chemotherapy have a role and may be considered for patients at high risk of treatment failure,” Dr. Weiss said.
Study details
The goal of this study was to find the best option among many chemoradiation approaches for head and neck cancer. The investigators pulled together and reanalyzed individual patient data from recently updated meta-analyses.
The current analysis included 115 randomized trials that enrolled patients between Jan. 1, 1980, and April 30, 2012. This encompassed 28,978 patients with 20,579 progression events and 19,253 deaths over a median follow-up of 6.6 years.
Treatments were ranked by P score, with higher scores indicating more effective therapies.
For overall survival, HFCRT had a P score of 97%. The hazard ratio (HR) was 0.63 for the comparison with locoregional therapy alone (surgery, radiotherapy, or both). The absolute benefit at 5 years, compared with locoregional therapy alone, was 16.7% with HFCRT.
The P score for the second most effective treatment option – induction chemotherapy with taxane, cisplatin, and fluorouracil followed by locoregional therapy (ICTaxPF-LRT) – was 89%, with a hazard ratio of 0.69 and an absolute benefit at 5 years of 13.4%, versus locoregional therapy.
The HR of HFCRT versus the accepted standard of care worldwide – locoregional therapy with concomitant platinum-based chemotherapy and radiotherapy (CLRTP) – was 0.82 in favor of HFCRT for overall survival and 0.80 for event-free survival.
For overall survival, the P score for CLRTP was 78%. Three other treatment options had a better P score than CLRTP but not a better HR (0.77). These included ICTaxPF-LRT (P score, 89%; HR, 0.69), accelerated radiotherapy with concomitant chemotherapy (P score, 82%; HR, 0.75), and ICTaxPF-LRT followed by CLRTP (P score, 80%; HR, 0.75).
In the end, the investigators found “superiority of HFCRT over other treatments,” but noted it can be difficult to implement HFCRT in the era of intensity-modulated radiotherapy for head and neck cancer. Even so, HFCRT “could be considered as an option for tertiary centres with a high throughput of patients,” the investigators wrote.
The team noted that one of the limitations of this study is that cancer care has improved substantially since the very earliest trials that were included in the analysis. This introduces potential confounders, including that patients in older trials might have been understaged so that even an experimental local therapy would have been less effective.
Toxicity wasn’t part of this analysis but must be taken into account when making therapeutic decisions, “especially because HFCRT and induction chemotherapy based on taxane, cisplatin, and fluorouracil are known to be toxic,” the investigators wrote.
This research was funded by the French Institut National du Cancer, French Ligue Nationale Contre le Cancer, and Fondation ARC. The authors disclosed relationships with numerous companies, including AbbVie, Lilly, and Merck. Dr. Weiss did not report any relevant conflicts.
Of the 16 treatment options compared and ranked, HFCRT topped the list for overall survival, event-free survival, locoregional control, and cancer-specific death.
The results also suggested that taxane-based induction chemotherapy followed by locoregional therapy, especially with concomitant chemotherapy, “is another good option in selected patients with a good performance status and minor comorbidities,” according to investigator Claire Petit, MD, PhD, of Centre hospitalier de l’Université de Montréal in Canada, and colleagues.
The investigators concluded that further intensifying chemoradiotherapy with these approaches “could improve outcomes over chemoradiotherapy.”
The findings, published in The Lancet Oncology, “could help to guide clinical decision-making in locally advanced head and neck cancer with a high risk of locoregional failure, especially human papillomavirus–negative tumours,” the authors wrote.
However, Jared Weiss, MD, of the University of North Carolina, Chapel Hill, cautioned that this “study is an individual patient data network meta-analysis, not a randomized controlled trial. As the authors note, it can help frame existing data but cannot define standard of care.”
Still, “it does support the efficacy of two commonly considered intensification strategies for high-risk patients – hyperfractionation of the radiation and the addition of preceding induction chemotherapy. Both of these intensifications substantially increase the time commitment from the patient, and many patients find this unacceptable. But, for select patients, hyperfractionation and induction chemotherapy have a role and may be considered for patients at high risk of treatment failure,” Dr. Weiss said.
Study details
The goal of this study was to find the best option among many chemoradiation approaches for head and neck cancer. The investigators pulled together and reanalyzed individual patient data from recently updated meta-analyses.
The current analysis included 115 randomized trials that enrolled patients between Jan. 1, 1980, and April 30, 2012. This encompassed 28,978 patients with 20,579 progression events and 19,253 deaths over a median follow-up of 6.6 years.
Treatments were ranked by P score, with higher scores indicating more effective therapies.
For overall survival, HFCRT had a P score of 97%. The hazard ratio (HR) was 0.63 for the comparison with locoregional therapy alone (surgery, radiotherapy, or both). The absolute benefit at 5 years, compared with locoregional therapy alone, was 16.7% with HFCRT.
The P score for the second most effective treatment option – induction chemotherapy with taxane, cisplatin, and fluorouracil followed by locoregional therapy (ICTaxPF-LRT) – was 89%, with a hazard ratio of 0.69 and an absolute benefit at 5 years of 13.4%, versus locoregional therapy.
The HR of HFCRT versus the accepted standard of care worldwide – locoregional therapy with concomitant platinum-based chemotherapy and radiotherapy (CLRTP) – was 0.82 in favor of HFCRT for overall survival and 0.80 for event-free survival.
For overall survival, the P score for CLRTP was 78%. Three other treatment options had a better P score than CLRTP but not a better HR (0.77). These included ICTaxPF-LRT (P score, 89%; HR, 0.69), accelerated radiotherapy with concomitant chemotherapy (P score, 82%; HR, 0.75), and ICTaxPF-LRT followed by CLRTP (P score, 80%; HR, 0.75).
In the end, the investigators found “superiority of HFCRT over other treatments,” but noted it can be difficult to implement HFCRT in the era of intensity-modulated radiotherapy for head and neck cancer. Even so, HFCRT “could be considered as an option for tertiary centres with a high throughput of patients,” the investigators wrote.
The team noted that one of the limitations of this study is that cancer care has improved substantially since the very earliest trials that were included in the analysis. This introduces potential confounders, including that patients in older trials might have been understaged so that even an experimental local therapy would have been less effective.
Toxicity wasn’t part of this analysis but must be taken into account when making therapeutic decisions, “especially because HFCRT and induction chemotherapy based on taxane, cisplatin, and fluorouracil are known to be toxic,” the investigators wrote.
This research was funded by the French Institut National du Cancer, French Ligue Nationale Contre le Cancer, and Fondation ARC. The authors disclosed relationships with numerous companies, including AbbVie, Lilly, and Merck. Dr. Weiss did not report any relevant conflicts.
Of the 16 treatment options compared and ranked, HFCRT topped the list for overall survival, event-free survival, locoregional control, and cancer-specific death.
The results also suggested that taxane-based induction chemotherapy followed by locoregional therapy, especially with concomitant chemotherapy, “is another good option in selected patients with a good performance status and minor comorbidities,” according to investigator Claire Petit, MD, PhD, of Centre hospitalier de l’Université de Montréal in Canada, and colleagues.
The investigators concluded that further intensifying chemoradiotherapy with these approaches “could improve outcomes over chemoradiotherapy.”
The findings, published in The Lancet Oncology, “could help to guide clinical decision-making in locally advanced head and neck cancer with a high risk of locoregional failure, especially human papillomavirus–negative tumours,” the authors wrote.
However, Jared Weiss, MD, of the University of North Carolina, Chapel Hill, cautioned that this “study is an individual patient data network meta-analysis, not a randomized controlled trial. As the authors note, it can help frame existing data but cannot define standard of care.”
Still, “it does support the efficacy of two commonly considered intensification strategies for high-risk patients – hyperfractionation of the radiation and the addition of preceding induction chemotherapy. Both of these intensifications substantially increase the time commitment from the patient, and many patients find this unacceptable. But, for select patients, hyperfractionation and induction chemotherapy have a role and may be considered for patients at high risk of treatment failure,” Dr. Weiss said.
Study details
The goal of this study was to find the best option among many chemoradiation approaches for head and neck cancer. The investigators pulled together and reanalyzed individual patient data from recently updated meta-analyses.
The current analysis included 115 randomized trials that enrolled patients between Jan. 1, 1980, and April 30, 2012. This encompassed 28,978 patients with 20,579 progression events and 19,253 deaths over a median follow-up of 6.6 years.
Treatments were ranked by P score, with higher scores indicating more effective therapies.
For overall survival, HFCRT had a P score of 97%. The hazard ratio (HR) was 0.63 for the comparison with locoregional therapy alone (surgery, radiotherapy, or both). The absolute benefit at 5 years, compared with locoregional therapy alone, was 16.7% with HFCRT.
The P score for the second most effective treatment option – induction chemotherapy with taxane, cisplatin, and fluorouracil followed by locoregional therapy (ICTaxPF-LRT) – was 89%, with a hazard ratio of 0.69 and an absolute benefit at 5 years of 13.4%, versus locoregional therapy.
The HR of HFCRT versus the accepted standard of care worldwide – locoregional therapy with concomitant platinum-based chemotherapy and radiotherapy (CLRTP) – was 0.82 in favor of HFCRT for overall survival and 0.80 for event-free survival.
For overall survival, the P score for CLRTP was 78%. Three other treatment options had a better P score than CLRTP but not a better HR (0.77). These included ICTaxPF-LRT (P score, 89%; HR, 0.69), accelerated radiotherapy with concomitant chemotherapy (P score, 82%; HR, 0.75), and ICTaxPF-LRT followed by CLRTP (P score, 80%; HR, 0.75).
In the end, the investigators found “superiority of HFCRT over other treatments,” but noted it can be difficult to implement HFCRT in the era of intensity-modulated radiotherapy for head and neck cancer. Even so, HFCRT “could be considered as an option for tertiary centres with a high throughput of patients,” the investigators wrote.
The team noted that one of the limitations of this study is that cancer care has improved substantially since the very earliest trials that were included in the analysis. This introduces potential confounders, including that patients in older trials might have been understaged so that even an experimental local therapy would have been less effective.
Toxicity wasn’t part of this analysis but must be taken into account when making therapeutic decisions, “especially because HFCRT and induction chemotherapy based on taxane, cisplatin, and fluorouracil are known to be toxic,” the investigators wrote.
This research was funded by the French Institut National du Cancer, French Ligue Nationale Contre le Cancer, and Fondation ARC. The authors disclosed relationships with numerous companies, including AbbVie, Lilly, and Merck. Dr. Weiss did not report any relevant conflicts.
FROM THE LANCET ONCOLOGY
The problem with samples
Ubrelvy and Nurtec are the latest in acute migraine treatment, both with solid data to back them up.
As with the triptans 25 years ago, my sample cabinet (and probably everyone else’s) is loaded with them, and friendly sales reps bringing coupon cards are a frequent occurrence.
Unfortunately, samples also bring up the same conundrum I faced with the triptans earlier in my career. It’s one thing to give patients samples to see if they work. It’s quite another to get them covered if they do.
This is an ongoing issue in modern medicine. It’s hard to resist the temptation to just hand something out when it’s conveniently at hand. It saves the patient a trip to the pharmacy and a medication copay up front, which is great.
But if it works, you have a whole new set of issues. The patient wants a real prescription now. So you call it in, then get a denial back saying it isn’t covered. It tells you to call a number, or try CoverMyMeds.
You do that, but the patient has to have failed three triptans, two NSAIDs, and a partridge in a pear tree to get it approved. The “copay assistance cards” don’t help if the medication isn’t covered at all. Each of these new medications is currently listed at roughly $900/month on GoodRx.com. Inevitably, your staff gets an earful when a patient with sticker shock calls your office.
One manufacturer is now eating the cost of the first script, so the patient leaves the pharmacy with a 1-month supply, under the impression that it was covered by insurance. This only kicks the can down the road 4-6 weeks, until they call for a refill.
To the chagrin of my sales reps (who are certainly going to read this), I’ve been burned on this and similar issues many times in my career, so I don’t even bother playing the game.
Certainly, there are cases where handing out a sample of Ubrelvy or Nurtec is indicated – some patients have already failed other agents, or have medical contraindications to them – but most don’t. So I start with triptans, currently going for $15/month. That doesn’t mean I’m not open to a newer agent at some point, but leaping directly to them quickly becomes an exercise in frustration.
Which brings up another issue I’ve encountered. While I try to be aware of this sort of thing, many other docs aren’t. Especially my already overburdened colleagues in primary care, who have enough on their plate with COVID-19, insurance regulations, paperwork, and an insanely busy schedule. In the controlled chaos of a general practice, it’s often easier for the staff to just hand out a sample at the same time they refer to a neurologist. So when the patient comes to me, they’re expecting I’ll be able to get it covered. After all, I’m the specialist. Getting expensive tests and medications covered seem to be something that’s expected for the higher copay to see me.
It doesn’t work that way, either.
I have nothing against new drugs. It’s the breakthroughs that keep medicine moving forward (like the COVID-19 vaccines). Nor do I have anything against samples or sales reps.
But in many cases, the time you save handing out samples isn’t worth the time you have to spend on them down the line.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Ubrelvy and Nurtec are the latest in acute migraine treatment, both with solid data to back them up.
As with the triptans 25 years ago, my sample cabinet (and probably everyone else’s) is loaded with them, and friendly sales reps bringing coupon cards are a frequent occurrence.
Unfortunately, samples also bring up the same conundrum I faced with the triptans earlier in my career. It’s one thing to give patients samples to see if they work. It’s quite another to get them covered if they do.
This is an ongoing issue in modern medicine. It’s hard to resist the temptation to just hand something out when it’s conveniently at hand. It saves the patient a trip to the pharmacy and a medication copay up front, which is great.
But if it works, you have a whole new set of issues. The patient wants a real prescription now. So you call it in, then get a denial back saying it isn’t covered. It tells you to call a number, or try CoverMyMeds.
You do that, but the patient has to have failed three triptans, two NSAIDs, and a partridge in a pear tree to get it approved. The “copay assistance cards” don’t help if the medication isn’t covered at all. Each of these new medications is currently listed at roughly $900/month on GoodRx.com. Inevitably, your staff gets an earful when a patient with sticker shock calls your office.
One manufacturer is now eating the cost of the first script, so the patient leaves the pharmacy with a 1-month supply, under the impression that it was covered by insurance. This only kicks the can down the road 4-6 weeks, until they call for a refill.
To the chagrin of my sales reps (who are certainly going to read this), I’ve been burned on this and similar issues many times in my career, so I don’t even bother playing the game.
Certainly, there are cases where handing out a sample of Ubrelvy or Nurtec is indicated – some patients have already failed other agents, or have medical contraindications to them – but most don’t. So I start with triptans, currently going for $15/month. That doesn’t mean I’m not open to a newer agent at some point, but leaping directly to them quickly becomes an exercise in frustration.
Which brings up another issue I’ve encountered. While I try to be aware of this sort of thing, many other docs aren’t. Especially my already overburdened colleagues in primary care, who have enough on their plate with COVID-19, insurance regulations, paperwork, and an insanely busy schedule. In the controlled chaos of a general practice, it’s often easier for the staff to just hand out a sample at the same time they refer to a neurologist. So when the patient comes to me, they’re expecting I’ll be able to get it covered. After all, I’m the specialist. Getting expensive tests and medications covered seem to be something that’s expected for the higher copay to see me.
It doesn’t work that way, either.
I have nothing against new drugs. It’s the breakthroughs that keep medicine moving forward (like the COVID-19 vaccines). Nor do I have anything against samples or sales reps.
But in many cases, the time you save handing out samples isn’t worth the time you have to spend on them down the line.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Ubrelvy and Nurtec are the latest in acute migraine treatment, both with solid data to back them up.
As with the triptans 25 years ago, my sample cabinet (and probably everyone else’s) is loaded with them, and friendly sales reps bringing coupon cards are a frequent occurrence.
Unfortunately, samples also bring up the same conundrum I faced with the triptans earlier in my career. It’s one thing to give patients samples to see if they work. It’s quite another to get them covered if they do.
This is an ongoing issue in modern medicine. It’s hard to resist the temptation to just hand something out when it’s conveniently at hand. It saves the patient a trip to the pharmacy and a medication copay up front, which is great.
But if it works, you have a whole new set of issues. The patient wants a real prescription now. So you call it in, then get a denial back saying it isn’t covered. It tells you to call a number, or try CoverMyMeds.
You do that, but the patient has to have failed three triptans, two NSAIDs, and a partridge in a pear tree to get it approved. The “copay assistance cards” don’t help if the medication isn’t covered at all. Each of these new medications is currently listed at roughly $900/month on GoodRx.com. Inevitably, your staff gets an earful when a patient with sticker shock calls your office.
One manufacturer is now eating the cost of the first script, so the patient leaves the pharmacy with a 1-month supply, under the impression that it was covered by insurance. This only kicks the can down the road 4-6 weeks, until they call for a refill.
To the chagrin of my sales reps (who are certainly going to read this), I’ve been burned on this and similar issues many times in my career, so I don’t even bother playing the game.
Certainly, there are cases where handing out a sample of Ubrelvy or Nurtec is indicated – some patients have already failed other agents, or have medical contraindications to them – but most don’t. So I start with triptans, currently going for $15/month. That doesn’t mean I’m not open to a newer agent at some point, but leaping directly to them quickly becomes an exercise in frustration.
Which brings up another issue I’ve encountered. While I try to be aware of this sort of thing, many other docs aren’t. Especially my already overburdened colleagues in primary care, who have enough on their plate with COVID-19, insurance regulations, paperwork, and an insanely busy schedule. In the controlled chaos of a general practice, it’s often easier for the staff to just hand out a sample at the same time they refer to a neurologist. So when the patient comes to me, they’re expecting I’ll be able to get it covered. After all, I’m the specialist. Getting expensive tests and medications covered seem to be something that’s expected for the higher copay to see me.
It doesn’t work that way, either.
I have nothing against new drugs. It’s the breakthroughs that keep medicine moving forward (like the COVID-19 vaccines). Nor do I have anything against samples or sales reps.
But in many cases, the time you save handing out samples isn’t worth the time you have to spend on them down the line.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mohs Micrographic Surgery During the COVID-19 Pandemic: Considering the Patient Perspective
Guidelines on Skin Cancer Surgeries During the COVID-19 Pandemic
At the start of the COVID-19 pandemic, the Centers for Disease Control and Prevention issued recommendations to decrease the spread of SARS-CoV-2 and optimize the use of personal protective equipment (PPE) for frontline workers.1 In the field of dermatologic surgery, the American College of Mohs Surgery, the National Comprehensive Cancer Network, the American Society for Dermatologic Surgery, and the American Academy of Dermatology made recommendations to postpone nonessential and nonurgent procedures.2-4 The initial guidelines of the American College of Mohs Surgery advised cancellation of all elective surgeries and deferred treatment of most cases of basal cell carcinoma for as long as 3 months; low-risk squamous cell carcinoma (SCC) and melanoma in situ treatment was deferred for as long as 2 or 3 months.3 Additional recommendations were made to reserve inpatient visits for suspicious lesions and high-risk cancers, postpone other nonessential and nonurgent appointments, and utilize telemedicine whenever possible.5
These recommendations led to great uncertainty and stress for patients and providers. Although numerous important variables, such as patient risk factors, severity of disease, availability of PPE and staff, and patient-to-provider transmission were considered when creating these guidelines, the patient’s experience likely was not a contributing factor.
COVID-19 Transmission During Mohs Surgery
There have been concerns that surgeons performing Mohs micrographic surgery (MMS) might be at an increased risk for COVID-19, given their close contact with high-risk sites (ie, nose, mouth) and cautery-generated aerosols; most of the estimated transmission risk associated with MMS has been based on head and neck surgery experience and publications.6-8 Tee and colleagues9 recently published their institution’s MMS COVID-19 preventive measures, which, to their knowledge, have prevented all intraoperative transmission of SARS-CoV-2, even in disease-positive patients. Currently, evidence is lacking to support a high risk for SARS-CoV-2 transmission during MMS when proper PPE and personal hygiene measures as well as strict infection control protocols—presurgical COVID-19 testing in high-risk cases, COVID-19 screening optimization, visitor restrictions, and appropriate disinfection between patients—are in place.
The Impact of Postponing Treatment on Patients
Although studies have focused on the effects of the COVID-19 pandemic on physicians practicing MMS,10 little is known about the effects of delays in skin cancer treatment on patients. A survey conducted in the United Kingdom investigating the patient’s perspective found that patients expressed worry and concern about the possibility that their MMS would be postponed and greatly appreciated continuation of treatment during the pandemic.11
Other medical specialties have reported their patient experiences during the pandemic. In a study examining patient perception of postponed surgical treatment of pelvic floor disorders due to COVID-19, nearly half of survey respondents were unhappy with the delay in receiving care. Furthermore, patients who reported being unhappy were more likely to report feelings of isolation and anxiety because their surgery was postponed.12 In another study involving patients with lung cancer, 9.1% (N=15) of patients postponed their treatment during the COVID-19 pandemic because of pandemic-related anxiety.13
With the goal of improving care at our institution, we conducted a brief institutional review board–approved survey to evaluate how postponing MMS treatment due to the COVID-19 pandemic affected patients. All MMS patients undergoing surgery in June 2020 and July 2020 (N=99) were asked to complete our voluntary and anonymous 23-question survey in person during their procedure. We obtained 88 responses (response rate, 89%). Twenty percent of surveyed patients (n=18) reported that their MMS had been postponed; 78% of those whose MMS was postponed (n=14) indicated some level of anxiety during the waiting period. It was unclear which patients had their treatment postponed based on national guidelines and which ones elected to postpone surgery.
Tips for Health Care Providers
Patient-provider communication highlighting specific skin cancer risk and the risk vs benefit of postponing treatment might reduce anxiety and stress during the waiting period.14 A study found that COVID-19 posed a bigger threat than most noninvasive skin cancers; therefore, the authors of that study concluded that treatment for most skin cancers could be safely postponed.15 Specifically, those authors recommended prioritizing treatment for Merkel cell carcinoma, invasive SCC, and melanoma with positive margins or macroscopic residual disease. They proposed that all other skin cancers, including basal cell carcinoma, SCC in situ, and melanoma with negative margins and no macroscopic residual disease, could be safely delayed for as long as 3 months.15
For patients with multiple risk factors for COVID-19–related morbidity or mortality, delaying skin cancer treatment likely has less risk than contracting the virus.15 This information should be communicated with patients. Investigation of specific patient concerns is warranted, and case-by-case evaluation of patients’ risk factors and skin cancer risk should be considered.
Based on the current, though limited, literature, delaying medical treatment can have a negative impact on the patient experience. Furthermore, proper precautions have been shown to limit intraoperative transmission of SARS-CoV-2 during MMS, but research is lacking. Practitioners should utilize shared decision-making and evaluate a given patient’s risk factors and concerns when deciding whether to postpone treatment. We encourage other institutions to evaluate the effects that delaying MMS has had on their patients, as further studies would improve understanding of patients’ experiences during a pandemic and potentially influence future dermatology guidelines.
- Center for Disease Control and Prevention. COVID-19. Accessed April 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/index.html
- American College of Mohs Surgery. Mohs surgery ambulatory protocol during COVID pandemic (version 6-3-20). June 4, 2020. Accessed April 20, 2021. http://staging.mohscollege.org/UserFiles/AM20/Member%20Alert/MohsSurgeryAmbulatoryProtocolDuringCOVIDPandemicFinal.pdf
- COVID-19 resources. National Comprehensive Cancer Network website. Accessed April 20, 2021. https://www.nccn.org/covid-19
- Narla S, Alam M, Ozog DM, et al. American Society of Dermatologic Surgery Association (ASDSA) and American Society for Laser Medicine & Surgery (ASLMS) guidance for cosmetic dermatology practices during COVID-19. Updated January 11, 2021. Accessed April 10, 2021. https://www.asds.net/Portals/0/PDF/asdsa/asdsa-aslms-cosmetic-reopening-guidance.pdf
- Geskin LJ, Trager MH, Aasi SZ, et al. Perspectives on the recommendations for skin cancer management during the COVID-19 pandemic.J Am Acad Dermatol. 2020;83:295-296. doi:10.1016/j.jaad.2020.05.002
- Yuan JT, Jiang SIB. Urgent safety considerations for dermatologic surgeons in the COVID-19 pandemic. Dermatol Online J. 2020;26:1. Accessed April 20, 2021. http://escholarship.org/uc/item/2qr3w771
- Otolaryngologists may contract COVID-19 during surgery. ENTtoday. March 20, 2020. Accessed April 20, 2021. https://www.enttoday.org/article/otolaryngologists-may-contract-covid-19-during-surgery/
- Howard BE. High-risk aerosol-generating procedures in COVID-19: respiratory protective equipment considerations. Otolaryngol Head Neck Surg. 2020;163:98-103. doi:10.1177/0194599820927335
- Tee MW, Stewart C, Aliessa S, et al. Dermatological surgery during the COVID-19 pandemic: experience of a large academic center. J Am Acad Dermatol. 2021;84:1094-1096. doi:10.1016/j.jaad.2020.12.003
- Hooper J, Feng H. The impact of COVID-19 on micrographic surgery and dermatologic oncology fellows. Dermatol Surg. 2020;46:1762-1763. doi:10.1097/DSS.0000000000002766
- Nicholson P, Ali FR, Patalay R, et al. Patient perceptions of Mohs micrographic surgery during the COVID-19 pandemic and lessons for the next outbreak. Clin Exp Dermatol. 2021;46:179-180. doi:10.1111/ced.14423
- Mou T, Brown O, Gillingham A, et al. Patients’ perceptions on surgical care suspension for pelvic floor disorders during the COVID-19 pandemic. Female Pelvic Med Reconstr Surg. 2020;26:477-482. doi:10.1097/SPV.0000000000000918
- Fujita K, Ito T, Saito Z, et al. Impact of COVID-19 pandemic on lung cancer treatment scheduling. Thorac Cancer. 2020;11:2983-2986. doi:10.1111/1759-7714.13615
- Nikumb VB, Banerjee A, Kaur G, et al. Impact of doctor-patient communication on preoperative anxiety: study at industrial township, Pimpri, Pune. Ind Psychiatry J. 2009;18:19-21. doi:10.4103/0972-6748.57852
- Baumann BC, MacArthur KM, Brewer JD, et al. Management of primary skin cancer during a pandemic: multidisciplinary recommendations. Cancer. 2020;126:3900-3906. doi:10.1002/cncr.32969
Guidelines on Skin Cancer Surgeries During the COVID-19 Pandemic
At the start of the COVID-19 pandemic, the Centers for Disease Control and Prevention issued recommendations to decrease the spread of SARS-CoV-2 and optimize the use of personal protective equipment (PPE) for frontline workers.1 In the field of dermatologic surgery, the American College of Mohs Surgery, the National Comprehensive Cancer Network, the American Society for Dermatologic Surgery, and the American Academy of Dermatology made recommendations to postpone nonessential and nonurgent procedures.2-4 The initial guidelines of the American College of Mohs Surgery advised cancellation of all elective surgeries and deferred treatment of most cases of basal cell carcinoma for as long as 3 months; low-risk squamous cell carcinoma (SCC) and melanoma in situ treatment was deferred for as long as 2 or 3 months.3 Additional recommendations were made to reserve inpatient visits for suspicious lesions and high-risk cancers, postpone other nonessential and nonurgent appointments, and utilize telemedicine whenever possible.5
These recommendations led to great uncertainty and stress for patients and providers. Although numerous important variables, such as patient risk factors, severity of disease, availability of PPE and staff, and patient-to-provider transmission were considered when creating these guidelines, the patient’s experience likely was not a contributing factor.
COVID-19 Transmission During Mohs Surgery
There have been concerns that surgeons performing Mohs micrographic surgery (MMS) might be at an increased risk for COVID-19, given their close contact with high-risk sites (ie, nose, mouth) and cautery-generated aerosols; most of the estimated transmission risk associated with MMS has been based on head and neck surgery experience and publications.6-8 Tee and colleagues9 recently published their institution’s MMS COVID-19 preventive measures, which, to their knowledge, have prevented all intraoperative transmission of SARS-CoV-2, even in disease-positive patients. Currently, evidence is lacking to support a high risk for SARS-CoV-2 transmission during MMS when proper PPE and personal hygiene measures as well as strict infection control protocols—presurgical COVID-19 testing in high-risk cases, COVID-19 screening optimization, visitor restrictions, and appropriate disinfection between patients—are in place.
The Impact of Postponing Treatment on Patients
Although studies have focused on the effects of the COVID-19 pandemic on physicians practicing MMS,10 little is known about the effects of delays in skin cancer treatment on patients. A survey conducted in the United Kingdom investigating the patient’s perspective found that patients expressed worry and concern about the possibility that their MMS would be postponed and greatly appreciated continuation of treatment during the pandemic.11
Other medical specialties have reported their patient experiences during the pandemic. In a study examining patient perception of postponed surgical treatment of pelvic floor disorders due to COVID-19, nearly half of survey respondents were unhappy with the delay in receiving care. Furthermore, patients who reported being unhappy were more likely to report feelings of isolation and anxiety because their surgery was postponed.12 In another study involving patients with lung cancer, 9.1% (N=15) of patients postponed their treatment during the COVID-19 pandemic because of pandemic-related anxiety.13
With the goal of improving care at our institution, we conducted a brief institutional review board–approved survey to evaluate how postponing MMS treatment due to the COVID-19 pandemic affected patients. All MMS patients undergoing surgery in June 2020 and July 2020 (N=99) were asked to complete our voluntary and anonymous 23-question survey in person during their procedure. We obtained 88 responses (response rate, 89%). Twenty percent of surveyed patients (n=18) reported that their MMS had been postponed; 78% of those whose MMS was postponed (n=14) indicated some level of anxiety during the waiting period. It was unclear which patients had their treatment postponed based on national guidelines and which ones elected to postpone surgery.
Tips for Health Care Providers
Patient-provider communication highlighting specific skin cancer risk and the risk vs benefit of postponing treatment might reduce anxiety and stress during the waiting period.14 A study found that COVID-19 posed a bigger threat than most noninvasive skin cancers; therefore, the authors of that study concluded that treatment for most skin cancers could be safely postponed.15 Specifically, those authors recommended prioritizing treatment for Merkel cell carcinoma, invasive SCC, and melanoma with positive margins or macroscopic residual disease. They proposed that all other skin cancers, including basal cell carcinoma, SCC in situ, and melanoma with negative margins and no macroscopic residual disease, could be safely delayed for as long as 3 months.15
For patients with multiple risk factors for COVID-19–related morbidity or mortality, delaying skin cancer treatment likely has less risk than contracting the virus.15 This information should be communicated with patients. Investigation of specific patient concerns is warranted, and case-by-case evaluation of patients’ risk factors and skin cancer risk should be considered.
Based on the current, though limited, literature, delaying medical treatment can have a negative impact on the patient experience. Furthermore, proper precautions have been shown to limit intraoperative transmission of SARS-CoV-2 during MMS, but research is lacking. Practitioners should utilize shared decision-making and evaluate a given patient’s risk factors and concerns when deciding whether to postpone treatment. We encourage other institutions to evaluate the effects that delaying MMS has had on their patients, as further studies would improve understanding of patients’ experiences during a pandemic and potentially influence future dermatology guidelines.
Guidelines on Skin Cancer Surgeries During the COVID-19 Pandemic
At the start of the COVID-19 pandemic, the Centers for Disease Control and Prevention issued recommendations to decrease the spread of SARS-CoV-2 and optimize the use of personal protective equipment (PPE) for frontline workers.1 In the field of dermatologic surgery, the American College of Mohs Surgery, the National Comprehensive Cancer Network, the American Society for Dermatologic Surgery, and the American Academy of Dermatology made recommendations to postpone nonessential and nonurgent procedures.2-4 The initial guidelines of the American College of Mohs Surgery advised cancellation of all elective surgeries and deferred treatment of most cases of basal cell carcinoma for as long as 3 months; low-risk squamous cell carcinoma (SCC) and melanoma in situ treatment was deferred for as long as 2 or 3 months.3 Additional recommendations were made to reserve inpatient visits for suspicious lesions and high-risk cancers, postpone other nonessential and nonurgent appointments, and utilize telemedicine whenever possible.5
These recommendations led to great uncertainty and stress for patients and providers. Although numerous important variables, such as patient risk factors, severity of disease, availability of PPE and staff, and patient-to-provider transmission were considered when creating these guidelines, the patient’s experience likely was not a contributing factor.
COVID-19 Transmission During Mohs Surgery
There have been concerns that surgeons performing Mohs micrographic surgery (MMS) might be at an increased risk for COVID-19, given their close contact with high-risk sites (ie, nose, mouth) and cautery-generated aerosols; most of the estimated transmission risk associated with MMS has been based on head and neck surgery experience and publications.6-8 Tee and colleagues9 recently published their institution’s MMS COVID-19 preventive measures, which, to their knowledge, have prevented all intraoperative transmission of SARS-CoV-2, even in disease-positive patients. Currently, evidence is lacking to support a high risk for SARS-CoV-2 transmission during MMS when proper PPE and personal hygiene measures as well as strict infection control protocols—presurgical COVID-19 testing in high-risk cases, COVID-19 screening optimization, visitor restrictions, and appropriate disinfection between patients—are in place.
The Impact of Postponing Treatment on Patients
Although studies have focused on the effects of the COVID-19 pandemic on physicians practicing MMS,10 little is known about the effects of delays in skin cancer treatment on patients. A survey conducted in the United Kingdom investigating the patient’s perspective found that patients expressed worry and concern about the possibility that their MMS would be postponed and greatly appreciated continuation of treatment during the pandemic.11
Other medical specialties have reported their patient experiences during the pandemic. In a study examining patient perception of postponed surgical treatment of pelvic floor disorders due to COVID-19, nearly half of survey respondents were unhappy with the delay in receiving care. Furthermore, patients who reported being unhappy were more likely to report feelings of isolation and anxiety because their surgery was postponed.12 In another study involving patients with lung cancer, 9.1% (N=15) of patients postponed their treatment during the COVID-19 pandemic because of pandemic-related anxiety.13
With the goal of improving care at our institution, we conducted a brief institutional review board–approved survey to evaluate how postponing MMS treatment due to the COVID-19 pandemic affected patients. All MMS patients undergoing surgery in June 2020 and July 2020 (N=99) were asked to complete our voluntary and anonymous 23-question survey in person during their procedure. We obtained 88 responses (response rate, 89%). Twenty percent of surveyed patients (n=18) reported that their MMS had been postponed; 78% of those whose MMS was postponed (n=14) indicated some level of anxiety during the waiting period. It was unclear which patients had their treatment postponed based on national guidelines and which ones elected to postpone surgery.
Tips for Health Care Providers
Patient-provider communication highlighting specific skin cancer risk and the risk vs benefit of postponing treatment might reduce anxiety and stress during the waiting period.14 A study found that COVID-19 posed a bigger threat than most noninvasive skin cancers; therefore, the authors of that study concluded that treatment for most skin cancers could be safely postponed.15 Specifically, those authors recommended prioritizing treatment for Merkel cell carcinoma, invasive SCC, and melanoma with positive margins or macroscopic residual disease. They proposed that all other skin cancers, including basal cell carcinoma, SCC in situ, and melanoma with negative margins and no macroscopic residual disease, could be safely delayed for as long as 3 months.15
For patients with multiple risk factors for COVID-19–related morbidity or mortality, delaying skin cancer treatment likely has less risk than contracting the virus.15 This information should be communicated with patients. Investigation of specific patient concerns is warranted, and case-by-case evaluation of patients’ risk factors and skin cancer risk should be considered.
Based on the current, though limited, literature, delaying medical treatment can have a negative impact on the patient experience. Furthermore, proper precautions have been shown to limit intraoperative transmission of SARS-CoV-2 during MMS, but research is lacking. Practitioners should utilize shared decision-making and evaluate a given patient’s risk factors and concerns when deciding whether to postpone treatment. We encourage other institutions to evaluate the effects that delaying MMS has had on their patients, as further studies would improve understanding of patients’ experiences during a pandemic and potentially influence future dermatology guidelines.
- Center for Disease Control and Prevention. COVID-19. Accessed April 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/index.html
- American College of Mohs Surgery. Mohs surgery ambulatory protocol during COVID pandemic (version 6-3-20). June 4, 2020. Accessed April 20, 2021. http://staging.mohscollege.org/UserFiles/AM20/Member%20Alert/MohsSurgeryAmbulatoryProtocolDuringCOVIDPandemicFinal.pdf
- COVID-19 resources. National Comprehensive Cancer Network website. Accessed April 20, 2021. https://www.nccn.org/covid-19
- Narla S, Alam M, Ozog DM, et al. American Society of Dermatologic Surgery Association (ASDSA) and American Society for Laser Medicine & Surgery (ASLMS) guidance for cosmetic dermatology practices during COVID-19. Updated January 11, 2021. Accessed April 10, 2021. https://www.asds.net/Portals/0/PDF/asdsa/asdsa-aslms-cosmetic-reopening-guidance.pdf
- Geskin LJ, Trager MH, Aasi SZ, et al. Perspectives on the recommendations for skin cancer management during the COVID-19 pandemic.J Am Acad Dermatol. 2020;83:295-296. doi:10.1016/j.jaad.2020.05.002
- Yuan JT, Jiang SIB. Urgent safety considerations for dermatologic surgeons in the COVID-19 pandemic. Dermatol Online J. 2020;26:1. Accessed April 20, 2021. http://escholarship.org/uc/item/2qr3w771
- Otolaryngologists may contract COVID-19 during surgery. ENTtoday. March 20, 2020. Accessed April 20, 2021. https://www.enttoday.org/article/otolaryngologists-may-contract-covid-19-during-surgery/
- Howard BE. High-risk aerosol-generating procedures in COVID-19: respiratory protective equipment considerations. Otolaryngol Head Neck Surg. 2020;163:98-103. doi:10.1177/0194599820927335
- Tee MW, Stewart C, Aliessa S, et al. Dermatological surgery during the COVID-19 pandemic: experience of a large academic center. J Am Acad Dermatol. 2021;84:1094-1096. doi:10.1016/j.jaad.2020.12.003
- Hooper J, Feng H. The impact of COVID-19 on micrographic surgery and dermatologic oncology fellows. Dermatol Surg. 2020;46:1762-1763. doi:10.1097/DSS.0000000000002766
- Nicholson P, Ali FR, Patalay R, et al. Patient perceptions of Mohs micrographic surgery during the COVID-19 pandemic and lessons for the next outbreak. Clin Exp Dermatol. 2021;46:179-180. doi:10.1111/ced.14423
- Mou T, Brown O, Gillingham A, et al. Patients’ perceptions on surgical care suspension for pelvic floor disorders during the COVID-19 pandemic. Female Pelvic Med Reconstr Surg. 2020;26:477-482. doi:10.1097/SPV.0000000000000918
- Fujita K, Ito T, Saito Z, et al. Impact of COVID-19 pandemic on lung cancer treatment scheduling. Thorac Cancer. 2020;11:2983-2986. doi:10.1111/1759-7714.13615
- Nikumb VB, Banerjee A, Kaur G, et al. Impact of doctor-patient communication on preoperative anxiety: study at industrial township, Pimpri, Pune. Ind Psychiatry J. 2009;18:19-21. doi:10.4103/0972-6748.57852
- Baumann BC, MacArthur KM, Brewer JD, et al. Management of primary skin cancer during a pandemic: multidisciplinary recommendations. Cancer. 2020;126:3900-3906. doi:10.1002/cncr.32969
- Center for Disease Control and Prevention. COVID-19. Accessed April 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/index.html
- American College of Mohs Surgery. Mohs surgery ambulatory protocol during COVID pandemic (version 6-3-20). June 4, 2020. Accessed April 20, 2021. http://staging.mohscollege.org/UserFiles/AM20/Member%20Alert/MohsSurgeryAmbulatoryProtocolDuringCOVIDPandemicFinal.pdf
- COVID-19 resources. National Comprehensive Cancer Network website. Accessed April 20, 2021. https://www.nccn.org/covid-19
- Narla S, Alam M, Ozog DM, et al. American Society of Dermatologic Surgery Association (ASDSA) and American Society for Laser Medicine & Surgery (ASLMS) guidance for cosmetic dermatology practices during COVID-19. Updated January 11, 2021. Accessed April 10, 2021. https://www.asds.net/Portals/0/PDF/asdsa/asdsa-aslms-cosmetic-reopening-guidance.pdf
- Geskin LJ, Trager MH, Aasi SZ, et al. Perspectives on the recommendations for skin cancer management during the COVID-19 pandemic.J Am Acad Dermatol. 2020;83:295-296. doi:10.1016/j.jaad.2020.05.002
- Yuan JT, Jiang SIB. Urgent safety considerations for dermatologic surgeons in the COVID-19 pandemic. Dermatol Online J. 2020;26:1. Accessed April 20, 2021. http://escholarship.org/uc/item/2qr3w771
- Otolaryngologists may contract COVID-19 during surgery. ENTtoday. March 20, 2020. Accessed April 20, 2021. https://www.enttoday.org/article/otolaryngologists-may-contract-covid-19-during-surgery/
- Howard BE. High-risk aerosol-generating procedures in COVID-19: respiratory protective equipment considerations. Otolaryngol Head Neck Surg. 2020;163:98-103. doi:10.1177/0194599820927335
- Tee MW, Stewart C, Aliessa S, et al. Dermatological surgery during the COVID-19 pandemic: experience of a large academic center. J Am Acad Dermatol. 2021;84:1094-1096. doi:10.1016/j.jaad.2020.12.003
- Hooper J, Feng H. The impact of COVID-19 on micrographic surgery and dermatologic oncology fellows. Dermatol Surg. 2020;46:1762-1763. doi:10.1097/DSS.0000000000002766
- Nicholson P, Ali FR, Patalay R, et al. Patient perceptions of Mohs micrographic surgery during the COVID-19 pandemic and lessons for the next outbreak. Clin Exp Dermatol. 2021;46:179-180. doi:10.1111/ced.14423
- Mou T, Brown O, Gillingham A, et al. Patients’ perceptions on surgical care suspension for pelvic floor disorders during the COVID-19 pandemic. Female Pelvic Med Reconstr Surg. 2020;26:477-482. doi:10.1097/SPV.0000000000000918
- Fujita K, Ito T, Saito Z, et al. Impact of COVID-19 pandemic on lung cancer treatment scheduling. Thorac Cancer. 2020;11:2983-2986. doi:10.1111/1759-7714.13615
- Nikumb VB, Banerjee A, Kaur G, et al. Impact of doctor-patient communication on preoperative anxiety: study at industrial township, Pimpri, Pune. Ind Psychiatry J. 2009;18:19-21. doi:10.4103/0972-6748.57852
- Baumann BC, MacArthur KM, Brewer JD, et al. Management of primary skin cancer during a pandemic: multidisciplinary recommendations. Cancer. 2020;126:3900-3906. doi:10.1002/cncr.32969
Practice Points
- There is little evidence that supports a high risk for SARS-CoV-2 transmission during Mohs micrographic surgery when proper personal protective equipment and strict infection control protocols are in place.
- The effects of treatment delays due to COVID-19 on the patient experience have not been well studied, but the limited literature suggests a negative association.
- Shared decision-making and evaluation of individual patient risk factors and concerns should be considered when deciding whether to postpone skin cancer treatment.
Possible obesity effect detected in cancer death rates
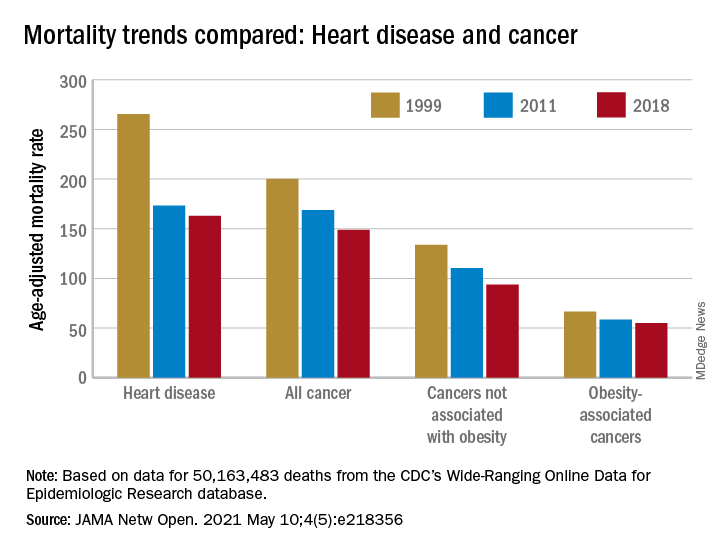
“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.
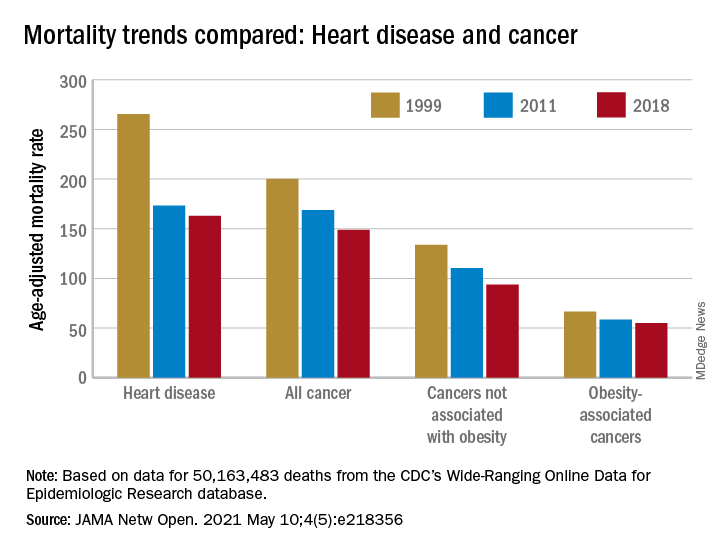
“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.
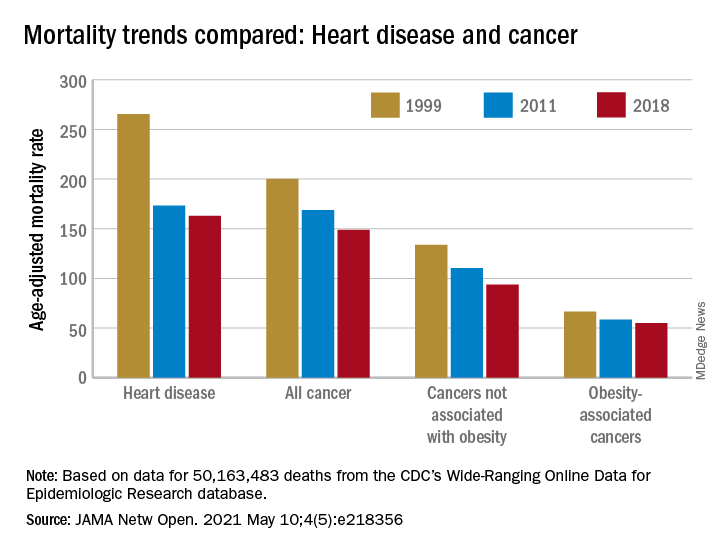
“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.
FROM JAMA NETWORK OPEN
Combination Therapy for Severe Asthma
Patients with severe asthma often experience symptoms and exacerbations that can interfere with daily life and further compromise lung function.
These patients often need combination therapy to achieve optimal control. This typically includes a low-dose inhaled corticosteroid (ICS) plus a long-acting beta-agonist (LABA).
For some patients, however, adherence to these therapies will not result in optimal outcomes.
Dr Monica Kraft, of the University of Arizona Health Sciences Center, discusses additional therapeutic options for these patients, which include increasing the dose of ICS or adding an oral corticosteroid such as prednisone or methylprednisolone.
When treatment-adherent patients are still unable to maintain control of their asthma symptoms, it may be optimal to move to biologic therapy.
There are currently five available biologics that work against IgE, IL-4/IL-13, IL-5, and IL-5R. Biomarker testing for blood eosinophils, exhaled nitric oxide, and serum IgE can help determine which biologic is best suited to each individual patient.
--
Robert and Irene Flinn Professor, Department of Medicine, Banner University Medical Center, North Campus; Chair, Department of Medicine, University of Arizona Health Sciences Center, Tucson, Arizona.
Monica Kraft, MD, has disclosed the following relevant financial relationships:
Serve(d) as a consultant for: AstraZeneca; Genentech; Chiesi; Sanofi
Serve(d) as Chief Medical Officer for: RaeSedo, LLC
Received research grant from: National Institutes of Health; American Lung Association; Sanofi; AstraZeneca; Chiesi
received income in an amount equal to or greater than $250 from: AstraZeneca; Genentech; Chiesi; Sanof.
Patients with severe asthma often experience symptoms and exacerbations that can interfere with daily life and further compromise lung function.
These patients often need combination therapy to achieve optimal control. This typically includes a low-dose inhaled corticosteroid (ICS) plus a long-acting beta-agonist (LABA).
For some patients, however, adherence to these therapies will not result in optimal outcomes.
Dr Monica Kraft, of the University of Arizona Health Sciences Center, discusses additional therapeutic options for these patients, which include increasing the dose of ICS or adding an oral corticosteroid such as prednisone or methylprednisolone.
When treatment-adherent patients are still unable to maintain control of their asthma symptoms, it may be optimal to move to biologic therapy.
There are currently five available biologics that work against IgE, IL-4/IL-13, IL-5, and IL-5R. Biomarker testing for blood eosinophils, exhaled nitric oxide, and serum IgE can help determine which biologic is best suited to each individual patient.
--
Robert and Irene Flinn Professor, Department of Medicine, Banner University Medical Center, North Campus; Chair, Department of Medicine, University of Arizona Health Sciences Center, Tucson, Arizona.
Monica Kraft, MD, has disclosed the following relevant financial relationships:
Serve(d) as a consultant for: AstraZeneca; Genentech; Chiesi; Sanofi
Serve(d) as Chief Medical Officer for: RaeSedo, LLC
Received research grant from: National Institutes of Health; American Lung Association; Sanofi; AstraZeneca; Chiesi
received income in an amount equal to or greater than $250 from: AstraZeneca; Genentech; Chiesi; Sanof.
Patients with severe asthma often experience symptoms and exacerbations that can interfere with daily life and further compromise lung function.
These patients often need combination therapy to achieve optimal control. This typically includes a low-dose inhaled corticosteroid (ICS) plus a long-acting beta-agonist (LABA).
For some patients, however, adherence to these therapies will not result in optimal outcomes.
Dr Monica Kraft, of the University of Arizona Health Sciences Center, discusses additional therapeutic options for these patients, which include increasing the dose of ICS or adding an oral corticosteroid such as prednisone or methylprednisolone.
When treatment-adherent patients are still unable to maintain control of their asthma symptoms, it may be optimal to move to biologic therapy.
There are currently five available biologics that work against IgE, IL-4/IL-13, IL-5, and IL-5R. Biomarker testing for blood eosinophils, exhaled nitric oxide, and serum IgE can help determine which biologic is best suited to each individual patient.
--
Robert and Irene Flinn Professor, Department of Medicine, Banner University Medical Center, North Campus; Chair, Department of Medicine, University of Arizona Health Sciences Center, Tucson, Arizona.
Monica Kraft, MD, has disclosed the following relevant financial relationships:
Serve(d) as a consultant for: AstraZeneca; Genentech; Chiesi; Sanofi
Serve(d) as Chief Medical Officer for: RaeSedo, LLC
Received research grant from: National Institutes of Health; American Lung Association; Sanofi; AstraZeneca; Chiesi
received income in an amount equal to or greater than $250 from: AstraZeneca; Genentech; Chiesi; Sanof.




