User login
Can Changes to Chemo Regimens Improve Drug Tolerability in Older Patients?
TOPLINE:
Treatment modifications, such as dose reductions, schedule changes, or use of less toxic regimens, can improve how well older patients with advanced cancer and aging-related conditions tolerate chemotherapy regimens.
METHODOLOGY:
- Older patients are underrepresented in clinical trials, which means the reported risks associated with standard-of-care regimens typically reflect outcomes in younger, healthier patients. This underrepresentation in clinical trials has also led to uncertainties about the safety of standard chemotherapy regimens in older patients who often have other health conditions to manage, alongside cancer.
- In this secondary analysis, researchers evaluated the association between primary treatment modifications to standard-of-care chemotherapy regimens and treatment tolerability.
- The trial included 609 patients aged ≥ 70 years who had advanced cancer alongside at least one age-related condition, such as impaired cognition, and planned to start a new palliative chemotherapy regimen in the community oncology setting. The most common cancer types were gastrointestinal cancer (37.4%) and lung cancer (28.6%).
- The primary outcome was grade 3-5 adverse events within 3 months of chemotherapy initiation.
- Secondary outcomes included patient-reported functional decline and combined adverse outcomes, which incorporated clinician-rated toxic effects, patient-reported functional decline, and 6-month overall survival.
TAKEAWAY:
- Overall, 281 patients (46.1%) received a primary treatment modification, most often a dose reduction (71.9%) or a scheduling change (11.7%).
- Patients who received primary treatment modifications had a 15% lower risk for grades 3-5 adverse effects (relative risk [RR], 0.85) and a 20% lower risk for patient-reported functional decline (RR, 0.80) than those who received standard treatment.
- Patients receiving treatment modifications had 32% lower risk for a worse combined adverse outcome (odds ratio, 0.68).
- Cancer type may matter as well. When looking at outcomes by cancer type, patients with gastrointestinal cancers who received a primary treatment modification had a lower risk for toxic effects (RR, 0.82), whereas patients with lung cancer did not (RR, 1.03; 95% CI, 0.88-1.20).
IN PRACTICE:
These findings “can help oncologists to choose the optimal drug regimen, select a safe and effective initial dose, and undertake appropriate monitoring strategies to manage the clinical care of older people with advanced cancer,” the authors said.
SOURCE:
This study, led by Mostafa R. Mohamed from University of Rochester, New York, was published February 15 in JAMA Network Open.
LIMITATIONS:
Residual confounding may be present. Extremely healthy older patients may have been excluded due to study criteria, limiting generalizability. There may be variation in toxicities due to inclusion of patients with multiple heterogeneous cancer.
DISCLOSURES:
This work was supported by the National Cancer Institute and the University of Rochester, New York. The authors disclosed financial relationships outside this work.
A version of this article first appeared on Medscape.com.
TOPLINE:
Treatment modifications, such as dose reductions, schedule changes, or use of less toxic regimens, can improve how well older patients with advanced cancer and aging-related conditions tolerate chemotherapy regimens.
METHODOLOGY:
- Older patients are underrepresented in clinical trials, which means the reported risks associated with standard-of-care regimens typically reflect outcomes in younger, healthier patients. This underrepresentation in clinical trials has also led to uncertainties about the safety of standard chemotherapy regimens in older patients who often have other health conditions to manage, alongside cancer.
- In this secondary analysis, researchers evaluated the association between primary treatment modifications to standard-of-care chemotherapy regimens and treatment tolerability.
- The trial included 609 patients aged ≥ 70 years who had advanced cancer alongside at least one age-related condition, such as impaired cognition, and planned to start a new palliative chemotherapy regimen in the community oncology setting. The most common cancer types were gastrointestinal cancer (37.4%) and lung cancer (28.6%).
- The primary outcome was grade 3-5 adverse events within 3 months of chemotherapy initiation.
- Secondary outcomes included patient-reported functional decline and combined adverse outcomes, which incorporated clinician-rated toxic effects, patient-reported functional decline, and 6-month overall survival.
TAKEAWAY:
- Overall, 281 patients (46.1%) received a primary treatment modification, most often a dose reduction (71.9%) or a scheduling change (11.7%).
- Patients who received primary treatment modifications had a 15% lower risk for grades 3-5 adverse effects (relative risk [RR], 0.85) and a 20% lower risk for patient-reported functional decline (RR, 0.80) than those who received standard treatment.
- Patients receiving treatment modifications had 32% lower risk for a worse combined adverse outcome (odds ratio, 0.68).
- Cancer type may matter as well. When looking at outcomes by cancer type, patients with gastrointestinal cancers who received a primary treatment modification had a lower risk for toxic effects (RR, 0.82), whereas patients with lung cancer did not (RR, 1.03; 95% CI, 0.88-1.20).
IN PRACTICE:
These findings “can help oncologists to choose the optimal drug regimen, select a safe and effective initial dose, and undertake appropriate monitoring strategies to manage the clinical care of older people with advanced cancer,” the authors said.
SOURCE:
This study, led by Mostafa R. Mohamed from University of Rochester, New York, was published February 15 in JAMA Network Open.
LIMITATIONS:
Residual confounding may be present. Extremely healthy older patients may have been excluded due to study criteria, limiting generalizability. There may be variation in toxicities due to inclusion of patients with multiple heterogeneous cancer.
DISCLOSURES:
This work was supported by the National Cancer Institute and the University of Rochester, New York. The authors disclosed financial relationships outside this work.
A version of this article first appeared on Medscape.com.
TOPLINE:
Treatment modifications, such as dose reductions, schedule changes, or use of less toxic regimens, can improve how well older patients with advanced cancer and aging-related conditions tolerate chemotherapy regimens.
METHODOLOGY:
- Older patients are underrepresented in clinical trials, which means the reported risks associated with standard-of-care regimens typically reflect outcomes in younger, healthier patients. This underrepresentation in clinical trials has also led to uncertainties about the safety of standard chemotherapy regimens in older patients who often have other health conditions to manage, alongside cancer.
- In this secondary analysis, researchers evaluated the association between primary treatment modifications to standard-of-care chemotherapy regimens and treatment tolerability.
- The trial included 609 patients aged ≥ 70 years who had advanced cancer alongside at least one age-related condition, such as impaired cognition, and planned to start a new palliative chemotherapy regimen in the community oncology setting. The most common cancer types were gastrointestinal cancer (37.4%) and lung cancer (28.6%).
- The primary outcome was grade 3-5 adverse events within 3 months of chemotherapy initiation.
- Secondary outcomes included patient-reported functional decline and combined adverse outcomes, which incorporated clinician-rated toxic effects, patient-reported functional decline, and 6-month overall survival.
TAKEAWAY:
- Overall, 281 patients (46.1%) received a primary treatment modification, most often a dose reduction (71.9%) or a scheduling change (11.7%).
- Patients who received primary treatment modifications had a 15% lower risk for grades 3-5 adverse effects (relative risk [RR], 0.85) and a 20% lower risk for patient-reported functional decline (RR, 0.80) than those who received standard treatment.
- Patients receiving treatment modifications had 32% lower risk for a worse combined adverse outcome (odds ratio, 0.68).
- Cancer type may matter as well. When looking at outcomes by cancer type, patients with gastrointestinal cancers who received a primary treatment modification had a lower risk for toxic effects (RR, 0.82), whereas patients with lung cancer did not (RR, 1.03; 95% CI, 0.88-1.20).
IN PRACTICE:
These findings “can help oncologists to choose the optimal drug regimen, select a safe and effective initial dose, and undertake appropriate monitoring strategies to manage the clinical care of older people with advanced cancer,” the authors said.
SOURCE:
This study, led by Mostafa R. Mohamed from University of Rochester, New York, was published February 15 in JAMA Network Open.
LIMITATIONS:
Residual confounding may be present. Extremely healthy older patients may have been excluded due to study criteria, limiting generalizability. There may be variation in toxicities due to inclusion of patients with multiple heterogeneous cancer.
DISCLOSURES:
This work was supported by the National Cancer Institute and the University of Rochester, New York. The authors disclosed financial relationships outside this work.
A version of this article first appeared on Medscape.com.
Effect of Metformin Across Renal Function States in Diabetes
TOPLINE:
Metformin cuts the risk for diabetic nephropathy (DN) and major kidney and cardiovascular events in patients with newly diagnosed type 2 diabetes (T2D) across various renal function states.
METHODOLOGY:
Metformin is a first-line treatment in US and South Korean T2D management guidelines, except for patients with advanced chronic kidney disease (CKD) (stage, ≥ 4; estimated glomerular filtration rate [eGFR], < 30).
The study used data from the databases of three tertiary hospitals in South Korea to assess the effect of metformin on long-term renal and cardiovascular outcomes across various renal function states in patients with newly diagnosed T2D.
Four groups of treatment-control comparative cohorts were identified at each hospital: Patients who had not yet developed DN at T2D diagnosis (mean age in treatment and control cohorts, 61-65 years) and those with reduced renal function (CKD stages 3A, 3B, and 4).
Patients who continuously received metformin after T2D diagnosis and beyond the observation period were 1:1 propensity score matched with controls who were prescribed oral hypoglycemic agents other than metformin.
Primary outcomes were net major adverse cardiovascular events including strokes (MACEs) or in-hospital death and a composite of major adverse kidney events (MAKEs) or in-hospital death.
TAKEAWAY:
Among patients without DN at T2D diagnosis, the continuous use of metformin vs other oral hypoglycemic agents was associated with a lower risk for:
Overt DN (incidence rate ratio [IRR], 0.82; 95% CI, 0.71-0.95),
MACEs (IRR, 0.76; 95% CI, 0.64-0.92), and
MAKEs (IRR, 0.45; 95% CI, 0.33-0.62).
Compared with non-metformin or discontinued metformin use, the continuous use of metformin was associated with a lower risk for MACE across CKD stages 3A (IRR, 0.70; 95% CI, 0.57-0.87), 3B (IRR, 0.83; 95% CI, 0.74-0.93), and 4 (IRR, 0.71; 95% CI, 0.60-0.85).
Similarly, the risk for MAKE was lower among continuous metformin users than in nonusers or discontinuous metformin users across CKD stage 3A (IRR, 0.39; 95% CI, 0.35-0.43), 3B (IRR, 0.44; 95% CI, 0.40-0.48), and 4 (IRR, 0.45; 95% CI, 0.39-0.51).
IN PRACTICE:
“The significance of the current study is highlighted by its integration of real-world clinical data, which encompasses patients diagnosed with CDK4 [eGRF, 15-29 mL/min/1.73 m2], a group currently considered contraindicated,” the authors wrote.
SOURCE:
The study, led by Yongjin Yi, MD, PhD, Department of Internal Medicine, Dankook University College of Medicine, Cheonan-si, Republic of Korea, was published in Scientific Reports.
LIMITATIONS:
There may be a possibility of selection bias because of the retrospective and observational nature of this study. Despite achieving a 1:1 propensity score matching to address the confounding factors, some variables, such as serum albumin and A1c levels, remained unbalanced after matching. The paper did not include observation length or patient numbers, but in response to an email query from Medscape, Yi notes that in one hospital, the mean duration of observation for the control and treatment groups was about 6.5 years, and the total number in the treatment groups across data from three hospitals was 11,675, with the same number of matched controls.
DISCLOSURES:
This study was supported by a Young Investigator Research Grant from the Korean Society of Nephrology, a grant from the Seoul National University Bundang Hospital Research Fund, and the Bio&Medical Technology Development Program of the National Research Foundation funded by the Korean government. The authors disclosed no competing interests.
A version of this article appeared on Medscape.com.
TOPLINE:
Metformin cuts the risk for diabetic nephropathy (DN) and major kidney and cardiovascular events in patients with newly diagnosed type 2 diabetes (T2D) across various renal function states.
METHODOLOGY:
Metformin is a first-line treatment in US and South Korean T2D management guidelines, except for patients with advanced chronic kidney disease (CKD) (stage, ≥ 4; estimated glomerular filtration rate [eGFR], < 30).
The study used data from the databases of three tertiary hospitals in South Korea to assess the effect of metformin on long-term renal and cardiovascular outcomes across various renal function states in patients with newly diagnosed T2D.
Four groups of treatment-control comparative cohorts were identified at each hospital: Patients who had not yet developed DN at T2D diagnosis (mean age in treatment and control cohorts, 61-65 years) and those with reduced renal function (CKD stages 3A, 3B, and 4).
Patients who continuously received metformin after T2D diagnosis and beyond the observation period were 1:1 propensity score matched with controls who were prescribed oral hypoglycemic agents other than metformin.
Primary outcomes were net major adverse cardiovascular events including strokes (MACEs) or in-hospital death and a composite of major adverse kidney events (MAKEs) or in-hospital death.
TAKEAWAY:
Among patients without DN at T2D diagnosis, the continuous use of metformin vs other oral hypoglycemic agents was associated with a lower risk for:
Overt DN (incidence rate ratio [IRR], 0.82; 95% CI, 0.71-0.95),
MACEs (IRR, 0.76; 95% CI, 0.64-0.92), and
MAKEs (IRR, 0.45; 95% CI, 0.33-0.62).
Compared with non-metformin or discontinued metformin use, the continuous use of metformin was associated with a lower risk for MACE across CKD stages 3A (IRR, 0.70; 95% CI, 0.57-0.87), 3B (IRR, 0.83; 95% CI, 0.74-0.93), and 4 (IRR, 0.71; 95% CI, 0.60-0.85).
Similarly, the risk for MAKE was lower among continuous metformin users than in nonusers or discontinuous metformin users across CKD stage 3A (IRR, 0.39; 95% CI, 0.35-0.43), 3B (IRR, 0.44; 95% CI, 0.40-0.48), and 4 (IRR, 0.45; 95% CI, 0.39-0.51).
IN PRACTICE:
“The significance of the current study is highlighted by its integration of real-world clinical data, which encompasses patients diagnosed with CDK4 [eGRF, 15-29 mL/min/1.73 m2], a group currently considered contraindicated,” the authors wrote.
SOURCE:
The study, led by Yongjin Yi, MD, PhD, Department of Internal Medicine, Dankook University College of Medicine, Cheonan-si, Republic of Korea, was published in Scientific Reports.
LIMITATIONS:
There may be a possibility of selection bias because of the retrospective and observational nature of this study. Despite achieving a 1:1 propensity score matching to address the confounding factors, some variables, such as serum albumin and A1c levels, remained unbalanced after matching. The paper did not include observation length or patient numbers, but in response to an email query from Medscape, Yi notes that in one hospital, the mean duration of observation for the control and treatment groups was about 6.5 years, and the total number in the treatment groups across data from three hospitals was 11,675, with the same number of matched controls.
DISCLOSURES:
This study was supported by a Young Investigator Research Grant from the Korean Society of Nephrology, a grant from the Seoul National University Bundang Hospital Research Fund, and the Bio&Medical Technology Development Program of the National Research Foundation funded by the Korean government. The authors disclosed no competing interests.
A version of this article appeared on Medscape.com.
TOPLINE:
Metformin cuts the risk for diabetic nephropathy (DN) and major kidney and cardiovascular events in patients with newly diagnosed type 2 diabetes (T2D) across various renal function states.
METHODOLOGY:
Metformin is a first-line treatment in US and South Korean T2D management guidelines, except for patients with advanced chronic kidney disease (CKD) (stage, ≥ 4; estimated glomerular filtration rate [eGFR], < 30).
The study used data from the databases of three tertiary hospitals in South Korea to assess the effect of metformin on long-term renal and cardiovascular outcomes across various renal function states in patients with newly diagnosed T2D.
Four groups of treatment-control comparative cohorts were identified at each hospital: Patients who had not yet developed DN at T2D diagnosis (mean age in treatment and control cohorts, 61-65 years) and those with reduced renal function (CKD stages 3A, 3B, and 4).
Patients who continuously received metformin after T2D diagnosis and beyond the observation period were 1:1 propensity score matched with controls who were prescribed oral hypoglycemic agents other than metformin.
Primary outcomes were net major adverse cardiovascular events including strokes (MACEs) or in-hospital death and a composite of major adverse kidney events (MAKEs) or in-hospital death.
TAKEAWAY:
Among patients without DN at T2D diagnosis, the continuous use of metformin vs other oral hypoglycemic agents was associated with a lower risk for:
Overt DN (incidence rate ratio [IRR], 0.82; 95% CI, 0.71-0.95),
MACEs (IRR, 0.76; 95% CI, 0.64-0.92), and
MAKEs (IRR, 0.45; 95% CI, 0.33-0.62).
Compared with non-metformin or discontinued metformin use, the continuous use of metformin was associated with a lower risk for MACE across CKD stages 3A (IRR, 0.70; 95% CI, 0.57-0.87), 3B (IRR, 0.83; 95% CI, 0.74-0.93), and 4 (IRR, 0.71; 95% CI, 0.60-0.85).
Similarly, the risk for MAKE was lower among continuous metformin users than in nonusers or discontinuous metformin users across CKD stage 3A (IRR, 0.39; 95% CI, 0.35-0.43), 3B (IRR, 0.44; 95% CI, 0.40-0.48), and 4 (IRR, 0.45; 95% CI, 0.39-0.51).
IN PRACTICE:
“The significance of the current study is highlighted by its integration of real-world clinical data, which encompasses patients diagnosed with CDK4 [eGRF, 15-29 mL/min/1.73 m2], a group currently considered contraindicated,” the authors wrote.
SOURCE:
The study, led by Yongjin Yi, MD, PhD, Department of Internal Medicine, Dankook University College of Medicine, Cheonan-si, Republic of Korea, was published in Scientific Reports.
LIMITATIONS:
There may be a possibility of selection bias because of the retrospective and observational nature of this study. Despite achieving a 1:1 propensity score matching to address the confounding factors, some variables, such as serum albumin and A1c levels, remained unbalanced after matching. The paper did not include observation length or patient numbers, but in response to an email query from Medscape, Yi notes that in one hospital, the mean duration of observation for the control and treatment groups was about 6.5 years, and the total number in the treatment groups across data from three hospitals was 11,675, with the same number of matched controls.
DISCLOSURES:
This study was supported by a Young Investigator Research Grant from the Korean Society of Nephrology, a grant from the Seoul National University Bundang Hospital Research Fund, and the Bio&Medical Technology Development Program of the National Research Foundation funded by the Korean government. The authors disclosed no competing interests.
A version of this article appeared on Medscape.com.
Increased Risk of New Rheumatic Disease Follows COVID-19 Infection
The risk of developing a new autoimmune inflammatory rheumatic disease (AIRD) is greater following a COVID-19 infection than after an influenza infection or in the general population, according to a study published March 5 in Annals of Internal Medicine. More severe COVID-19 infections were linked to a greater risk of incident rheumatic disease, but vaccination appeared protective against development of a new AIRD.
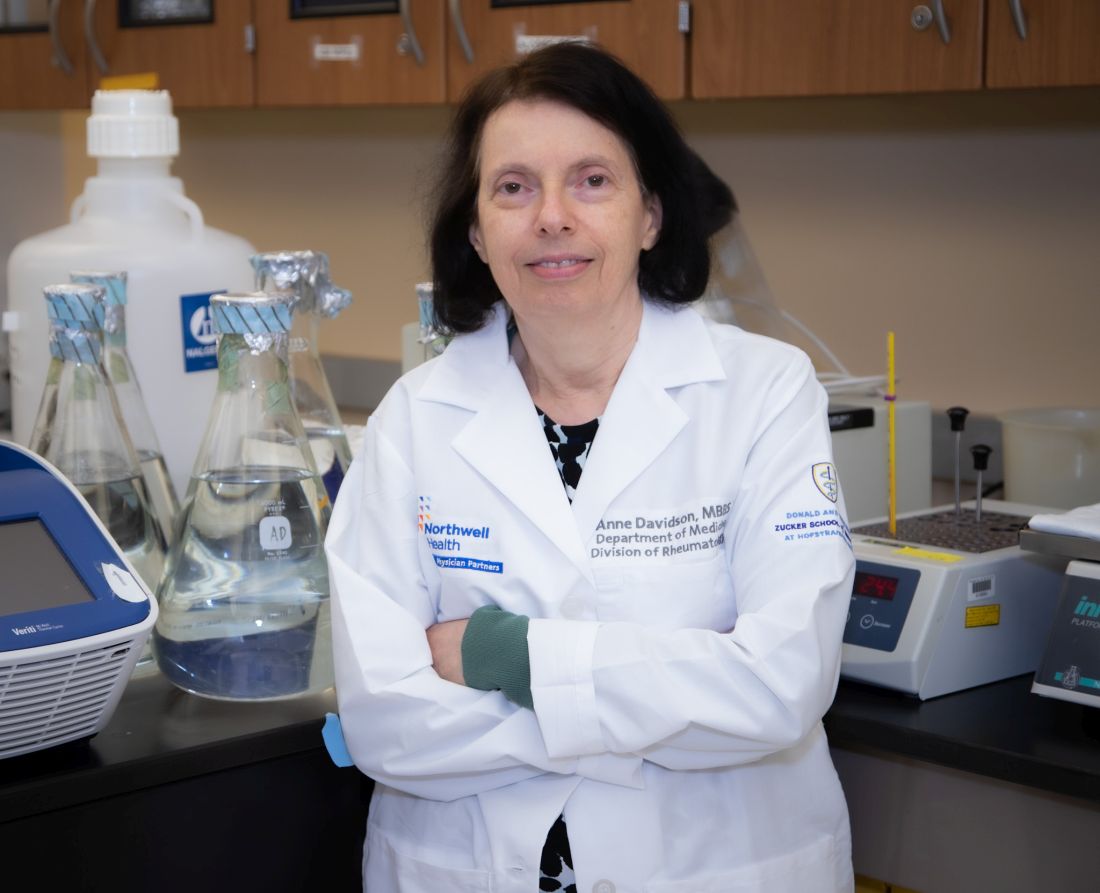
“Importantly, this study shows the value of vaccination to prevent severe disease and these types of sequelae,” Anne Davidson, MBBS, a professor in the Institute of Molecular Medicine at The Feinstein Institutes for Medical Research in Manhasset, New York, who was not involved in the study, said in an interview.
Previous research had already identified the likelihood of an association between SARS-CoV-2 infection and subsequent development of a new AIRD. This new study, however, includes much larger cohorts from two different countries and relies on more robust methodology than previous studies, experts said.
“Unique steps were taken by the study authors to make sure that what they were looking at in terms of signal was most likely true,” Alfred Kim, MD, PhD, assistant professor of medicine in rheumatology at Washington University in St. Louis, who was not involved in the study, said in an interview. Dr. Davidson agreed, noting that these authors “were a bit more rigorous with ascertainment of the autoimmune diagnosis, using two codes and also checking that appropriate medications were administered.”
More Robust and Rigorous Research
Past cohort studies finding an increased risk of rheumatic disease after COVID-19 “based their findings solely on comparisons between infected and uninfected groups, which could be influenced by ascertainment bias due to disparities in care, differences in health-seeking tendencies, and inherent risks among the groups,” Min Seo Kim, MD, of the Broad Institute of MIT and Harvard, Cambridge, Massachusetts, and his colleagues reported. Their study, however, required at least two claims with codes for rheumatic disease and compared patients with COVID-19 to those with flu “to adjust for the potentially heightened detection of AIRD in SARS-CoV-2–infected persons owing to their interactions with the health care system.”
Dr. Alfred Kim said the fact that they used at least two claims codes “gives a little more credence that the patients were actually experiencing some sort of autoimmune inflammatory condition as opposed to a very transient issue post COVID that just went away on its own.”
He acknowledged that the previous research was reasonably strong, “especially in light of the fact that there has been so much work done on a molecular level demonstrating that COVID-19 is associated with a substantial increase in autoantibodies in a significant proportion of patients, so this always opened up the possibility that this could associate with some sort of autoimmune disease downstream.”
While the study is well done with a large population, “it still has limitations that might overestimate the effect,” Kevin W. Byram, MD, associate professor of medicine in rheumatology and immunology at Vanderbilt University Medical Center in Nashville, Tennessee, who was not involved in the study, said in an interview. “We certainly have seen individual cases of new rheumatic disease where COVID-19 infection is likely the trigger,” but the phenomenon is not new, he added.
“Many autoimmune diseases are spurred by a loss of tolerance that might be induced by a pathogen of some sort,” Dr. Byram said. “The study is right to point out different forms of bias that might be at play. One in particular that is important to consider in a study like this is the lack of case-level adjudication regarding the diagnosis of rheumatic disease” since the study relied on available ICD-10 codes and medication prescriptions.
The researchers used national claims data to compare risk of incident AIRD in 10,027,506 South Korean and 12,218,680 Japanese adults, aged 20 and older, at 1 month, 6 months, and 12 months after COVID-19 infection, influenza infection, or a matched index date for uninfected control participants. Only patients with at least two claims for AIRD were considered to have a new diagnosis.
Patients who had COVID-19 between January 2020 and December 2021, confirmed by PCR or antigen testing, were matched 1:1 with patients who had test-confirmed influenza during that time and 1:4 with uninfected control participants, whose index date was set to the infection date of their matched COVID-19 patient.
The propensity score matching was based on age, sex, household income, urban versus rural residence, and various clinical characteristics and history: body mass index; blood pressure; fasting blood glucose; glomerular filtration rate; smoking status; alcohol consumption; weekly aerobic physical activity; comorbidity index; hospitalizations and outpatient visits in the previous year; past use of diabetes, hyperlipidemia, or hypertension medication; and history of cardiovascular disease, chronic kidney disease, chronic obstructive pulmonary disease, or respiratory infectious disease.
Patients with a history of AIRD or with coinfection or reinfection of COVID-19 and influenza were excluded, as were patients diagnosed with rheumatic disease within a month of COVID-19 infection.
Risk Varied With Disease Severity and Vaccination Status
Among the Korean patients, 3.9% had a COVID-19 infection and 0.98% had an influenza infection. After matching, the comparison populations included 94,504 patients with COVID-19 versus 94,504 patients with flu, and 177,083 patients with COVID-19 versus 675,750 uninfected controls.
The risk of developing an AIRD at least 1 month after infection in South Korean patients with COVID-19 was 25% higher than in uninfected control participants (adjusted hazard ratio [aHR], 1.25; 95% CI, 1.18–1.31; P < .05) and 30% higher than in influenza patients (aHR, 1.3; 95% CI, 1.02–1.59; P < .05). Specifically, risk in South Korean patients with COVID-19 was significantly increased for connective tissue disease and both treated and untreated AIRD but not for inflammatory arthritis.
Among the Japanese patients, 8.2% had COVID-19 and 0.99% had flu, resulting in matched populations of 115,003 with COVID-19 versus 110,310 with flu, and 960,849 with COVID-19 versus 1,606,873 uninfected patients. The effect size was larger in Japanese patients, with a 79% increased risk for AIRD in patients with COVID-19, compared with the general population (aHR, 1.79; 95% CI, 1.77–1.82; P < .05) and a 14% increased risk, compared with patients with influenza infection (aHR, 1.14; 95% CI, 1.10–1.17; P < .05). In Japanese patients, risk was increased across all four categories, including a doubled risk for inflammatory arthritis (aHR, 2.02; 95% CI, 1.96–2.07; P < .05), compared with the general population.
The researchers had data only from the South Korean cohort to calculate risk based on vaccination status, SARS-CoV-2 variant (wild type versus Delta), and COVID-19 severity. Researchers determined a COVID-19 infection to be moderate-to-severe based on billing codes for ICU admission or requiring oxygen therapy, extracorporeal membrane oxygenation, renal replacement, or CPR.
Infection with both the original strain and the Delta variant were linked to similar increased risks for AIRD, but moderate to severe COVID-19 infections had greater risk of subsequent AIRD (aHR, 1.42; P < .05) than mild infections (aHR, 1.22; P < .05). Vaccination was linked to a lower risk of AIRD within the COVID-19 patient population: One dose was linked to a 41% reduced risk (HR, 0.59; P < .05) and two doses were linked to a 58% reduced risk (HR, 0.42; P < .05), regardless of the vaccine type, compared with unvaccinated patients with COVID-19. The apparent protective effect of vaccination was true only for patients with mild COVID-19, not those with moderate to severe infection.
“One has to wonder whether or not these people were at much higher risk of developing autoimmune disease that just got exposed because they got COVID, so that a fraction of these would have gotten an autoimmune disease downstream,” Dr. Alfred Kim said. Regardless, one clinical implication of the findings is the reduced risk in vaccinated patients, regardless of the vaccine type, given the fact that “mRNA vaccination in particular has not been associated with any autoantibody development,” he said.
Though the correlations in the study cannot translate to causation, several mechanisms might be at play in a viral infection contributing to autoimmune risk, Dr. Davidson said. Given that viral nucleic acids also recognize self-nucleic acids, “a large load of viral nucleic acid may break tolerance,” or “viral proteins could also mimic self-proteins,” she said. “In addition, tolerance may be broken by a highly inflammatory environment associated with the release of cytokines and other inflammatory mediators.”
The association between new-onset autoimmune disease and severe COVID-19 infection suggests multiple mechanisms may be involved in excess immune stimulation, Dr. Davidson said. But she added that it’s unclear how these findings, involving the original strain and Delta variant of SARS-CoV-2, might relate to currently circulating variants.
The research was funded by the National Research Foundation of Korea, the Korea Health Industry Development Institute, and the Ministry of Food and Drug Safety of the Republic of Korea. The authors reported no relevant financial relationships with industry. Dr. Alfred Kim has sponsored research agreements with AstraZeneca, Bristol-Myers Squibb, and Novartis; receives royalties from a patent with Kypha Inc.; and has done consulting or speaking for Amgen, ANI Pharmaceuticals, Aurinia Pharmaceuticals, Exagen Diagnostics, GlaxoSmithKline, Kypha, Miltenyi Biotech, Pfizer, Rheumatology & Arthritis Learning Network, Synthekine, Techtonic Therapeutics, and UpToDate. Dr. Byram reported consulting for TenSixteen Bio. Dr. Davidson had no disclosures.
The risk of developing a new autoimmune inflammatory rheumatic disease (AIRD) is greater following a COVID-19 infection than after an influenza infection or in the general population, according to a study published March 5 in Annals of Internal Medicine. More severe COVID-19 infections were linked to a greater risk of incident rheumatic disease, but vaccination appeared protective against development of a new AIRD.
“Importantly, this study shows the value of vaccination to prevent severe disease and these types of sequelae,” Anne Davidson, MBBS, a professor in the Institute of Molecular Medicine at The Feinstein Institutes for Medical Research in Manhasset, New York, who was not involved in the study, said in an interview.
Previous research had already identified the likelihood of an association between SARS-CoV-2 infection and subsequent development of a new AIRD. This new study, however, includes much larger cohorts from two different countries and relies on more robust methodology than previous studies, experts said.
“Unique steps were taken by the study authors to make sure that what they were looking at in terms of signal was most likely true,” Alfred Kim, MD, PhD, assistant professor of medicine in rheumatology at Washington University in St. Louis, who was not involved in the study, said in an interview. Dr. Davidson agreed, noting that these authors “were a bit more rigorous with ascertainment of the autoimmune diagnosis, using two codes and also checking that appropriate medications were administered.”
More Robust and Rigorous Research
Past cohort studies finding an increased risk of rheumatic disease after COVID-19 “based their findings solely on comparisons between infected and uninfected groups, which could be influenced by ascertainment bias due to disparities in care, differences in health-seeking tendencies, and inherent risks among the groups,” Min Seo Kim, MD, of the Broad Institute of MIT and Harvard, Cambridge, Massachusetts, and his colleagues reported. Their study, however, required at least two claims with codes for rheumatic disease and compared patients with COVID-19 to those with flu “to adjust for the potentially heightened detection of AIRD in SARS-CoV-2–infected persons owing to their interactions with the health care system.”
Dr. Alfred Kim said the fact that they used at least two claims codes “gives a little more credence that the patients were actually experiencing some sort of autoimmune inflammatory condition as opposed to a very transient issue post COVID that just went away on its own.”
He acknowledged that the previous research was reasonably strong, “especially in light of the fact that there has been so much work done on a molecular level demonstrating that COVID-19 is associated with a substantial increase in autoantibodies in a significant proportion of patients, so this always opened up the possibility that this could associate with some sort of autoimmune disease downstream.”
While the study is well done with a large population, “it still has limitations that might overestimate the effect,” Kevin W. Byram, MD, associate professor of medicine in rheumatology and immunology at Vanderbilt University Medical Center in Nashville, Tennessee, who was not involved in the study, said in an interview. “We certainly have seen individual cases of new rheumatic disease where COVID-19 infection is likely the trigger,” but the phenomenon is not new, he added.
“Many autoimmune diseases are spurred by a loss of tolerance that might be induced by a pathogen of some sort,” Dr. Byram said. “The study is right to point out different forms of bias that might be at play. One in particular that is important to consider in a study like this is the lack of case-level adjudication regarding the diagnosis of rheumatic disease” since the study relied on available ICD-10 codes and medication prescriptions.
The researchers used national claims data to compare risk of incident AIRD in 10,027,506 South Korean and 12,218,680 Japanese adults, aged 20 and older, at 1 month, 6 months, and 12 months after COVID-19 infection, influenza infection, or a matched index date for uninfected control participants. Only patients with at least two claims for AIRD were considered to have a new diagnosis.
Patients who had COVID-19 between January 2020 and December 2021, confirmed by PCR or antigen testing, were matched 1:1 with patients who had test-confirmed influenza during that time and 1:4 with uninfected control participants, whose index date was set to the infection date of their matched COVID-19 patient.
The propensity score matching was based on age, sex, household income, urban versus rural residence, and various clinical characteristics and history: body mass index; blood pressure; fasting blood glucose; glomerular filtration rate; smoking status; alcohol consumption; weekly aerobic physical activity; comorbidity index; hospitalizations and outpatient visits in the previous year; past use of diabetes, hyperlipidemia, or hypertension medication; and history of cardiovascular disease, chronic kidney disease, chronic obstructive pulmonary disease, or respiratory infectious disease.
Patients with a history of AIRD or with coinfection or reinfection of COVID-19 and influenza were excluded, as were patients diagnosed with rheumatic disease within a month of COVID-19 infection.
Risk Varied With Disease Severity and Vaccination Status
Among the Korean patients, 3.9% had a COVID-19 infection and 0.98% had an influenza infection. After matching, the comparison populations included 94,504 patients with COVID-19 versus 94,504 patients with flu, and 177,083 patients with COVID-19 versus 675,750 uninfected controls.
The risk of developing an AIRD at least 1 month after infection in South Korean patients with COVID-19 was 25% higher than in uninfected control participants (adjusted hazard ratio [aHR], 1.25; 95% CI, 1.18–1.31; P < .05) and 30% higher than in influenza patients (aHR, 1.3; 95% CI, 1.02–1.59; P < .05). Specifically, risk in South Korean patients with COVID-19 was significantly increased for connective tissue disease and both treated and untreated AIRD but not for inflammatory arthritis.
Among the Japanese patients, 8.2% had COVID-19 and 0.99% had flu, resulting in matched populations of 115,003 with COVID-19 versus 110,310 with flu, and 960,849 with COVID-19 versus 1,606,873 uninfected patients. The effect size was larger in Japanese patients, with a 79% increased risk for AIRD in patients with COVID-19, compared with the general population (aHR, 1.79; 95% CI, 1.77–1.82; P < .05) and a 14% increased risk, compared with patients with influenza infection (aHR, 1.14; 95% CI, 1.10–1.17; P < .05). In Japanese patients, risk was increased across all four categories, including a doubled risk for inflammatory arthritis (aHR, 2.02; 95% CI, 1.96–2.07; P < .05), compared with the general population.
The researchers had data only from the South Korean cohort to calculate risk based on vaccination status, SARS-CoV-2 variant (wild type versus Delta), and COVID-19 severity. Researchers determined a COVID-19 infection to be moderate-to-severe based on billing codes for ICU admission or requiring oxygen therapy, extracorporeal membrane oxygenation, renal replacement, or CPR.
Infection with both the original strain and the Delta variant were linked to similar increased risks for AIRD, but moderate to severe COVID-19 infections had greater risk of subsequent AIRD (aHR, 1.42; P < .05) than mild infections (aHR, 1.22; P < .05). Vaccination was linked to a lower risk of AIRD within the COVID-19 patient population: One dose was linked to a 41% reduced risk (HR, 0.59; P < .05) and two doses were linked to a 58% reduced risk (HR, 0.42; P < .05), regardless of the vaccine type, compared with unvaccinated patients with COVID-19. The apparent protective effect of vaccination was true only for patients with mild COVID-19, not those with moderate to severe infection.
“One has to wonder whether or not these people were at much higher risk of developing autoimmune disease that just got exposed because they got COVID, so that a fraction of these would have gotten an autoimmune disease downstream,” Dr. Alfred Kim said. Regardless, one clinical implication of the findings is the reduced risk in vaccinated patients, regardless of the vaccine type, given the fact that “mRNA vaccination in particular has not been associated with any autoantibody development,” he said.
Though the correlations in the study cannot translate to causation, several mechanisms might be at play in a viral infection contributing to autoimmune risk, Dr. Davidson said. Given that viral nucleic acids also recognize self-nucleic acids, “a large load of viral nucleic acid may break tolerance,” or “viral proteins could also mimic self-proteins,” she said. “In addition, tolerance may be broken by a highly inflammatory environment associated with the release of cytokines and other inflammatory mediators.”
The association between new-onset autoimmune disease and severe COVID-19 infection suggests multiple mechanisms may be involved in excess immune stimulation, Dr. Davidson said. But she added that it’s unclear how these findings, involving the original strain and Delta variant of SARS-CoV-2, might relate to currently circulating variants.
The research was funded by the National Research Foundation of Korea, the Korea Health Industry Development Institute, and the Ministry of Food and Drug Safety of the Republic of Korea. The authors reported no relevant financial relationships with industry. Dr. Alfred Kim has sponsored research agreements with AstraZeneca, Bristol-Myers Squibb, and Novartis; receives royalties from a patent with Kypha Inc.; and has done consulting or speaking for Amgen, ANI Pharmaceuticals, Aurinia Pharmaceuticals, Exagen Diagnostics, GlaxoSmithKline, Kypha, Miltenyi Biotech, Pfizer, Rheumatology & Arthritis Learning Network, Synthekine, Techtonic Therapeutics, and UpToDate. Dr. Byram reported consulting for TenSixteen Bio. Dr. Davidson had no disclosures.
The risk of developing a new autoimmune inflammatory rheumatic disease (AIRD) is greater following a COVID-19 infection than after an influenza infection or in the general population, according to a study published March 5 in Annals of Internal Medicine. More severe COVID-19 infections were linked to a greater risk of incident rheumatic disease, but vaccination appeared protective against development of a new AIRD.
“Importantly, this study shows the value of vaccination to prevent severe disease and these types of sequelae,” Anne Davidson, MBBS, a professor in the Institute of Molecular Medicine at The Feinstein Institutes for Medical Research in Manhasset, New York, who was not involved in the study, said in an interview.
Previous research had already identified the likelihood of an association between SARS-CoV-2 infection and subsequent development of a new AIRD. This new study, however, includes much larger cohorts from two different countries and relies on more robust methodology than previous studies, experts said.
“Unique steps were taken by the study authors to make sure that what they were looking at in terms of signal was most likely true,” Alfred Kim, MD, PhD, assistant professor of medicine in rheumatology at Washington University in St. Louis, who was not involved in the study, said in an interview. Dr. Davidson agreed, noting that these authors “were a bit more rigorous with ascertainment of the autoimmune diagnosis, using two codes and also checking that appropriate medications were administered.”
More Robust and Rigorous Research
Past cohort studies finding an increased risk of rheumatic disease after COVID-19 “based their findings solely on comparisons between infected and uninfected groups, which could be influenced by ascertainment bias due to disparities in care, differences in health-seeking tendencies, and inherent risks among the groups,” Min Seo Kim, MD, of the Broad Institute of MIT and Harvard, Cambridge, Massachusetts, and his colleagues reported. Their study, however, required at least two claims with codes for rheumatic disease and compared patients with COVID-19 to those with flu “to adjust for the potentially heightened detection of AIRD in SARS-CoV-2–infected persons owing to their interactions with the health care system.”
Dr. Alfred Kim said the fact that they used at least two claims codes “gives a little more credence that the patients were actually experiencing some sort of autoimmune inflammatory condition as opposed to a very transient issue post COVID that just went away on its own.”
He acknowledged that the previous research was reasonably strong, “especially in light of the fact that there has been so much work done on a molecular level demonstrating that COVID-19 is associated with a substantial increase in autoantibodies in a significant proportion of patients, so this always opened up the possibility that this could associate with some sort of autoimmune disease downstream.”
While the study is well done with a large population, “it still has limitations that might overestimate the effect,” Kevin W. Byram, MD, associate professor of medicine in rheumatology and immunology at Vanderbilt University Medical Center in Nashville, Tennessee, who was not involved in the study, said in an interview. “We certainly have seen individual cases of new rheumatic disease where COVID-19 infection is likely the trigger,” but the phenomenon is not new, he added.
“Many autoimmune diseases are spurred by a loss of tolerance that might be induced by a pathogen of some sort,” Dr. Byram said. “The study is right to point out different forms of bias that might be at play. One in particular that is important to consider in a study like this is the lack of case-level adjudication regarding the diagnosis of rheumatic disease” since the study relied on available ICD-10 codes and medication prescriptions.
The researchers used national claims data to compare risk of incident AIRD in 10,027,506 South Korean and 12,218,680 Japanese adults, aged 20 and older, at 1 month, 6 months, and 12 months after COVID-19 infection, influenza infection, or a matched index date for uninfected control participants. Only patients with at least two claims for AIRD were considered to have a new diagnosis.
Patients who had COVID-19 between January 2020 and December 2021, confirmed by PCR or antigen testing, were matched 1:1 with patients who had test-confirmed influenza during that time and 1:4 with uninfected control participants, whose index date was set to the infection date of their matched COVID-19 patient.
The propensity score matching was based on age, sex, household income, urban versus rural residence, and various clinical characteristics and history: body mass index; blood pressure; fasting blood glucose; glomerular filtration rate; smoking status; alcohol consumption; weekly aerobic physical activity; comorbidity index; hospitalizations and outpatient visits in the previous year; past use of diabetes, hyperlipidemia, or hypertension medication; and history of cardiovascular disease, chronic kidney disease, chronic obstructive pulmonary disease, or respiratory infectious disease.
Patients with a history of AIRD or with coinfection or reinfection of COVID-19 and influenza were excluded, as were patients diagnosed with rheumatic disease within a month of COVID-19 infection.
Risk Varied With Disease Severity and Vaccination Status
Among the Korean patients, 3.9% had a COVID-19 infection and 0.98% had an influenza infection. After matching, the comparison populations included 94,504 patients with COVID-19 versus 94,504 patients with flu, and 177,083 patients with COVID-19 versus 675,750 uninfected controls.
The risk of developing an AIRD at least 1 month after infection in South Korean patients with COVID-19 was 25% higher than in uninfected control participants (adjusted hazard ratio [aHR], 1.25; 95% CI, 1.18–1.31; P < .05) and 30% higher than in influenza patients (aHR, 1.3; 95% CI, 1.02–1.59; P < .05). Specifically, risk in South Korean patients with COVID-19 was significantly increased for connective tissue disease and both treated and untreated AIRD but not for inflammatory arthritis.
Among the Japanese patients, 8.2% had COVID-19 and 0.99% had flu, resulting in matched populations of 115,003 with COVID-19 versus 110,310 with flu, and 960,849 with COVID-19 versus 1,606,873 uninfected patients. The effect size was larger in Japanese patients, with a 79% increased risk for AIRD in patients with COVID-19, compared with the general population (aHR, 1.79; 95% CI, 1.77–1.82; P < .05) and a 14% increased risk, compared with patients with influenza infection (aHR, 1.14; 95% CI, 1.10–1.17; P < .05). In Japanese patients, risk was increased across all four categories, including a doubled risk for inflammatory arthritis (aHR, 2.02; 95% CI, 1.96–2.07; P < .05), compared with the general population.
The researchers had data only from the South Korean cohort to calculate risk based on vaccination status, SARS-CoV-2 variant (wild type versus Delta), and COVID-19 severity. Researchers determined a COVID-19 infection to be moderate-to-severe based on billing codes for ICU admission or requiring oxygen therapy, extracorporeal membrane oxygenation, renal replacement, or CPR.
Infection with both the original strain and the Delta variant were linked to similar increased risks for AIRD, but moderate to severe COVID-19 infections had greater risk of subsequent AIRD (aHR, 1.42; P < .05) than mild infections (aHR, 1.22; P < .05). Vaccination was linked to a lower risk of AIRD within the COVID-19 patient population: One dose was linked to a 41% reduced risk (HR, 0.59; P < .05) and two doses were linked to a 58% reduced risk (HR, 0.42; P < .05), regardless of the vaccine type, compared with unvaccinated patients with COVID-19. The apparent protective effect of vaccination was true only for patients with mild COVID-19, not those with moderate to severe infection.
“One has to wonder whether or not these people were at much higher risk of developing autoimmune disease that just got exposed because they got COVID, so that a fraction of these would have gotten an autoimmune disease downstream,” Dr. Alfred Kim said. Regardless, one clinical implication of the findings is the reduced risk in vaccinated patients, regardless of the vaccine type, given the fact that “mRNA vaccination in particular has not been associated with any autoantibody development,” he said.
Though the correlations in the study cannot translate to causation, several mechanisms might be at play in a viral infection contributing to autoimmune risk, Dr. Davidson said. Given that viral nucleic acids also recognize self-nucleic acids, “a large load of viral nucleic acid may break tolerance,” or “viral proteins could also mimic self-proteins,” she said. “In addition, tolerance may be broken by a highly inflammatory environment associated with the release of cytokines and other inflammatory mediators.”
The association between new-onset autoimmune disease and severe COVID-19 infection suggests multiple mechanisms may be involved in excess immune stimulation, Dr. Davidson said. But she added that it’s unclear how these findings, involving the original strain and Delta variant of SARS-CoV-2, might relate to currently circulating variants.
The research was funded by the National Research Foundation of Korea, the Korea Health Industry Development Institute, and the Ministry of Food and Drug Safety of the Republic of Korea. The authors reported no relevant financial relationships with industry. Dr. Alfred Kim has sponsored research agreements with AstraZeneca, Bristol-Myers Squibb, and Novartis; receives royalties from a patent with Kypha Inc.; and has done consulting or speaking for Amgen, ANI Pharmaceuticals, Aurinia Pharmaceuticals, Exagen Diagnostics, GlaxoSmithKline, Kypha, Miltenyi Biotech, Pfizer, Rheumatology & Arthritis Learning Network, Synthekine, Techtonic Therapeutics, and UpToDate. Dr. Byram reported consulting for TenSixteen Bio. Dr. Davidson had no disclosures.
FROM ANNALS OF INTERNAL MEDICINE
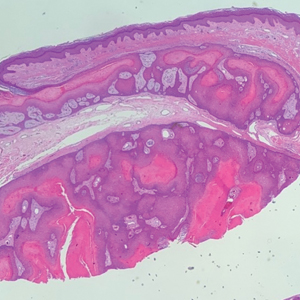
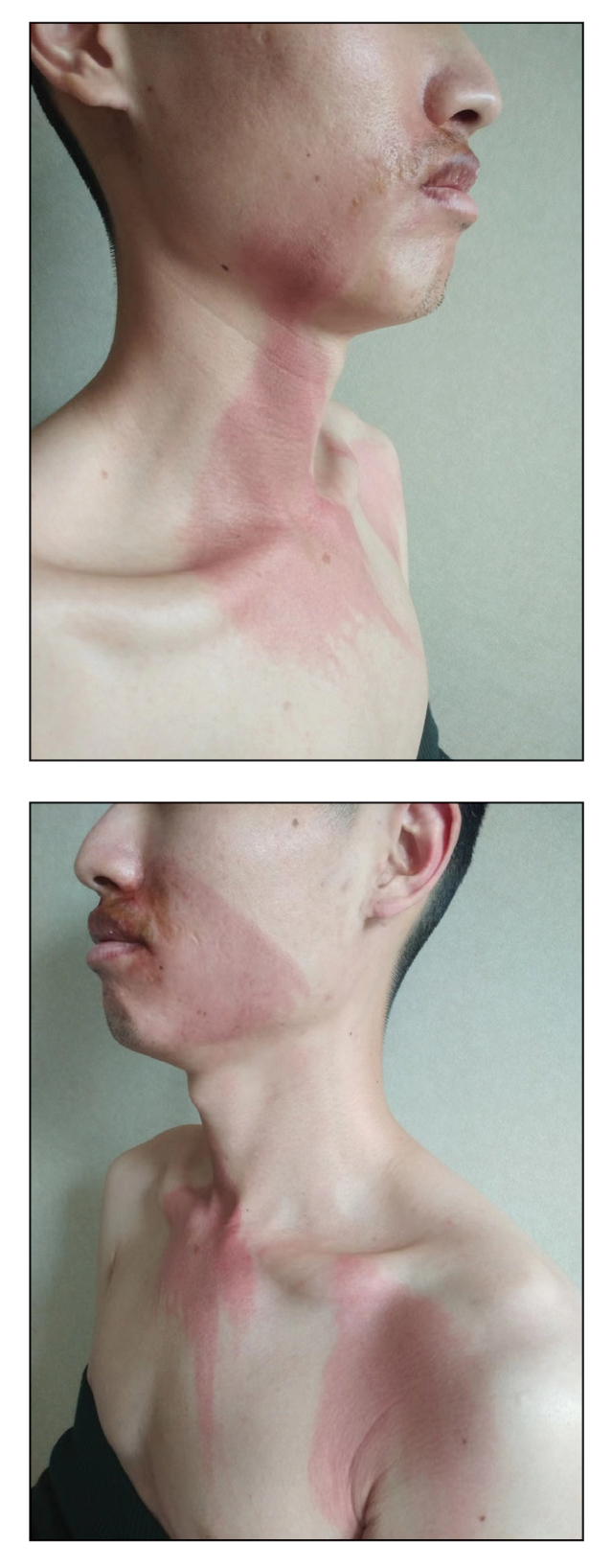
Burning Skin Patches on the Face, Neck, and Chest
The Diagnosis: Gastric Acid Dermatitis
After further discussion, the patient indicated that he had vomited during the night of alcohol consumption, and the vomitus remained on the affected areas until the next morning, indicating that excessive alcohol ingestion stimulated abundant secretion of gastric acid, which caused the symptoms. Additionally, the presence of clothing acted as a buffer in the unaffected areas, which helped make the final diagnosis of gastric acid dermatitis. The patient was treated with external application of recombinant bovine basic fibroblast growth factor gel (21,000 IU/5 g) once daily, and the lesions greatly improved within 7 days. The burning pain of the throat, stomach, and esophagus resolved after consultation with an otolaryngologist and a gastroenterologist.
Gastric acid dermatitis is a new term used to describe an acute skin burn caused by the patient's own gastric acid. Generally, the pH of human gastric acid is between 0.9 and 1.8 but will be diluted after eating and will gradually increase to approximately 3.5, which is not enough to induce burns on the skin.1 In addition, the skin barrier is capable of preventing transient gastric acid corrosion.2,3 However, the release of a large amount of gastric acid after excessive alcohol ingestion coupled with 1 night of lethargy left enough acid and time to induce skin burns in our patient.
Dermatitis caused by other allergic or chemical factors, such as Paederus dermatitis, was excluded, as the patient’s manifestation occurred during the inactive period of Paederus fuscipes. Furthermore, the patient denied any history of contact with chemicals in the last month. Food eruptions primarily manifest as systemic anaphylaxis with eruptive and pruritic rashes after consumption of seafood, eggs, milk, or other proteins, while alcoholic contact dermatitis is a form of irritating dermatitis that could be easily induced again by direct skin contact with alcohol.
Management of gastric acid dermatitis is similar to that for other chemical burns. Because scarring seldom occurs, the central issue is to restore the skin barrier as quickly as possible and to avoid or alleviate postinflammatory hyperpigmentation. Treatments to restore the skin barrier include recombinant bovine or human-derived basic fibroblast growth factor gel, moist exposed burn ointment, and medical sodium hyaluronate gelatin. To treat postinflammatory hyperpigmentation, some whitening agents such as compound superoxide dismutase arbutin cream and hydroquinone cream as well as the Q-switched Nd:YAG laser are effective to ameliorate the skin condition. If skin burns are on sun-exposed areas, photoprotection is necessary to prevent hyperpigmentation.
Acknowledgment—We thank the patient for granting permission to publish this information.
- Ergun P, Kipcak S, Dettmar PW, et al. Pepsin and pH of gastric juice in patients with gastrointestinal reflux disease and subgroups. J Clin Gastroenterol. 2022;56:512-517. doi:10.1097 /MCG.0000000000001560
- Mitamura Y, Ogulur I, Pat Y, et al. Dysregulation of the epithelial barrier by environmental and other exogenous factors. Contact Dermatitis. 2021;85:615-626. doi:10.1111/cod.13959
- Kuo SH, Shen CJ, Shen CF, et al. Role of pH value in clinically relevant diagnosis. Diagnostics (Basel). 2020;10:107. doi:10.3390 /diagnostics10020107
The Diagnosis: Gastric Acid Dermatitis
After further discussion, the patient indicated that he had vomited during the night of alcohol consumption, and the vomitus remained on the affected areas until the next morning, indicating that excessive alcohol ingestion stimulated abundant secretion of gastric acid, which caused the symptoms. Additionally, the presence of clothing acted as a buffer in the unaffected areas, which helped make the final diagnosis of gastric acid dermatitis. The patient was treated with external application of recombinant bovine basic fibroblast growth factor gel (21,000 IU/5 g) once daily, and the lesions greatly improved within 7 days. The burning pain of the throat, stomach, and esophagus resolved after consultation with an otolaryngologist and a gastroenterologist.
Gastric acid dermatitis is a new term used to describe an acute skin burn caused by the patient's own gastric acid. Generally, the pH of human gastric acid is between 0.9 and 1.8 but will be diluted after eating and will gradually increase to approximately 3.5, which is not enough to induce burns on the skin.1 In addition, the skin barrier is capable of preventing transient gastric acid corrosion.2,3 However, the release of a large amount of gastric acid after excessive alcohol ingestion coupled with 1 night of lethargy left enough acid and time to induce skin burns in our patient.
Dermatitis caused by other allergic or chemical factors, such as Paederus dermatitis, was excluded, as the patient’s manifestation occurred during the inactive period of Paederus fuscipes. Furthermore, the patient denied any history of contact with chemicals in the last month. Food eruptions primarily manifest as systemic anaphylaxis with eruptive and pruritic rashes after consumption of seafood, eggs, milk, or other proteins, while alcoholic contact dermatitis is a form of irritating dermatitis that could be easily induced again by direct skin contact with alcohol.
Management of gastric acid dermatitis is similar to that for other chemical burns. Because scarring seldom occurs, the central issue is to restore the skin barrier as quickly as possible and to avoid or alleviate postinflammatory hyperpigmentation. Treatments to restore the skin barrier include recombinant bovine or human-derived basic fibroblast growth factor gel, moist exposed burn ointment, and medical sodium hyaluronate gelatin. To treat postinflammatory hyperpigmentation, some whitening agents such as compound superoxide dismutase arbutin cream and hydroquinone cream as well as the Q-switched Nd:YAG laser are effective to ameliorate the skin condition. If skin burns are on sun-exposed areas, photoprotection is necessary to prevent hyperpigmentation.
Acknowledgment—We thank the patient for granting permission to publish this information.
The Diagnosis: Gastric Acid Dermatitis
After further discussion, the patient indicated that he had vomited during the night of alcohol consumption, and the vomitus remained on the affected areas until the next morning, indicating that excessive alcohol ingestion stimulated abundant secretion of gastric acid, which caused the symptoms. Additionally, the presence of clothing acted as a buffer in the unaffected areas, which helped make the final diagnosis of gastric acid dermatitis. The patient was treated with external application of recombinant bovine basic fibroblast growth factor gel (21,000 IU/5 g) once daily, and the lesions greatly improved within 7 days. The burning pain of the throat, stomach, and esophagus resolved after consultation with an otolaryngologist and a gastroenterologist.
Gastric acid dermatitis is a new term used to describe an acute skin burn caused by the patient's own gastric acid. Generally, the pH of human gastric acid is between 0.9 and 1.8 but will be diluted after eating and will gradually increase to approximately 3.5, which is not enough to induce burns on the skin.1 In addition, the skin barrier is capable of preventing transient gastric acid corrosion.2,3 However, the release of a large amount of gastric acid after excessive alcohol ingestion coupled with 1 night of lethargy left enough acid and time to induce skin burns in our patient.
Dermatitis caused by other allergic or chemical factors, such as Paederus dermatitis, was excluded, as the patient’s manifestation occurred during the inactive period of Paederus fuscipes. Furthermore, the patient denied any history of contact with chemicals in the last month. Food eruptions primarily manifest as systemic anaphylaxis with eruptive and pruritic rashes after consumption of seafood, eggs, milk, or other proteins, while alcoholic contact dermatitis is a form of irritating dermatitis that could be easily induced again by direct skin contact with alcohol.
Management of gastric acid dermatitis is similar to that for other chemical burns. Because scarring seldom occurs, the central issue is to restore the skin barrier as quickly as possible and to avoid or alleviate postinflammatory hyperpigmentation. Treatments to restore the skin barrier include recombinant bovine or human-derived basic fibroblast growth factor gel, moist exposed burn ointment, and medical sodium hyaluronate gelatin. To treat postinflammatory hyperpigmentation, some whitening agents such as compound superoxide dismutase arbutin cream and hydroquinone cream as well as the Q-switched Nd:YAG laser are effective to ameliorate the skin condition. If skin burns are on sun-exposed areas, photoprotection is necessary to prevent hyperpigmentation.
Acknowledgment—We thank the patient for granting permission to publish this information.
- Ergun P, Kipcak S, Dettmar PW, et al. Pepsin and pH of gastric juice in patients with gastrointestinal reflux disease and subgroups. J Clin Gastroenterol. 2022;56:512-517. doi:10.1097 /MCG.0000000000001560
- Mitamura Y, Ogulur I, Pat Y, et al. Dysregulation of the epithelial barrier by environmental and other exogenous factors. Contact Dermatitis. 2021;85:615-626. doi:10.1111/cod.13959
- Kuo SH, Shen CJ, Shen CF, et al. Role of pH value in clinically relevant diagnosis. Diagnostics (Basel). 2020;10:107. doi:10.3390 /diagnostics10020107
- Ergun P, Kipcak S, Dettmar PW, et al. Pepsin and pH of gastric juice in patients with gastrointestinal reflux disease and subgroups. J Clin Gastroenterol. 2022;56:512-517. doi:10.1097 /MCG.0000000000001560
- Mitamura Y, Ogulur I, Pat Y, et al. Dysregulation of the epithelial barrier by environmental and other exogenous factors. Contact Dermatitis. 2021;85:615-626. doi:10.1111/cod.13959
- Kuo SH, Shen CJ, Shen CF, et al. Role of pH value in clinically relevant diagnosis. Diagnostics (Basel). 2020;10:107. doi:10.3390 /diagnostics10020107
A 26-year-old man presented with a burning skin rash around the mouth, neck, and chest after 1 night of lethargy due to excessive alcohol consumption 2 days prior. He also reported a sore throat and burning pain in the stomach and esophagus. Physical examination revealed signs of severe epidermal necrosis, including erythema, blisters, serous discharge, and superficial crusts on the perioral region, as well as well-defined erythema on the anterior neck and chest. Gastroscopy and laryngoscopy showed extensive mucosal erosion. A laboratory workup revealed no abnormalities.
Longitudinal Melanonychia

THE COMPARISON
A Melanoma in situ manifesting as longitudinal melanonychia (LM) in a single digit in a Black man. Dermoscopy showed irregular dark bands of brown pigmentation and micro-Hutchinson sign on the cuticle (inset).
B Melanoma manifesting as LM with a prominent Hutchinson sign in a Hispanic man, with variable shades of brown covering more than 50% of the nail width.
C Longitudinal melanonychia of at least 2 nails with a pseudo-Hutchinson sign (pigment on the nail folds in a benign case of LM) in a young Black man demonstrating ethnic/racial melanosis. The longitudinal bands, which were caused by benign melanocytic activation, are more gray than brown and are less than 3 mm wide.
Longitudinal melanonychia (LM) is a pigmented linear band—brown, black, or gray—spanning the length of the nail plate due to the presence of excess melanin, which may be attributed to a benign or malignant process and may warrant further investigation.1,2 The majority of patients who present with LM are diagnosed with melanocytic activation of the nail matrix due to their inherent darker skin tone or various triggers including trauma, infection, and medications. Longitudinal melanonychia secondary to melanocytic activation often occurs spontaneously in patients with skin of color.3 Less commonly, LM is caused by a nail matrix nevus or lentigo; however, LM may arise secondary to subungual melanoma, a more dangerous cause.
A thorough clinical history including duration, recent changes in LM manifestation, nail trauma, or infection is helpful in evaluating patients with LM; however, a history of nail trauma can be misleading, as nail changes attributed to the trauma may in fact be melanoma. Irregularly spaced vertical lines of pigmentation ranging from brown to black with variations in spacing and width are characteristic of subungual melanoma.4 Nail dystrophy, granular hyperpigmentation, and Hutchinson sign (extension of pigmentation to the nail folds) also are worrisome features.5 In recent years, dermoscopy has become an important tool in the clinical examination of LM, with the development of criteria based on color and pattern recognition.5,6 Dermoscopy can be useful in screening potential candidates for biopsy. Although clinical examination and dermoscopy are essential to evaluating LM, the gold-standard diagnostic test when malignancy is suspected is a nail matrix biopsy.1,2,6,7
Epidemiology
It is not unusual for patients with darker skin tones to develop LM due to melanocytic activation of multiple nails with age. This finding can be seen in approximately 80% of African American individuals, 30% of Japanese individuals, and 50% of Hispanic individuals.2 It has even been reported that approximately 100% of Black patients older than 50 years will have evidence of LM.3
In a retrospective analysis, children presenting with LM tend to have a higher prevalence of nail matrix nevi compared to adults (56.1% [60/106] vs 34.3% [23/66]; P=.005).8 Involvement of a single digit in children is most likely indicative of a nevus; however, when an adult presents with LM in a single digit, suspicion for subungual melanoma should be raised.2,3,9
Two separate single-center retrospective studies showed the prevalence of subungual melanoma in patients presenting with melanonychia in Asia. Jin et al10 reported subungual melanoma in 6.2% (17/275) of Korean patients presenting with melanonychia at a general dermatology clinic from 2002 to 2014. Lyu et al8 studied LM in 172 Chinese patients in a dermatology clinic from 2018 to 2021 and reported 9% (6/66) of adults (aged ≥18 years) with subungual melanoma, with no reported cases in childhood (aged <18 years).
Although the prevalence of subungual melanoma in patients with LM is low, it is an important diagnosis that should not be missed. In confirmed cases of subungual melanoma, two-thirds of lesions manifested as LM.3,10,11 Thus, LM arising in an adult in a single digit is more concerning for malignancy.2,3,7,9
Individuals of African and Asian descent as well as American Indian individuals are at highest risk for subungual melanoma with a poor prognosis compared to other types of melanoma, largely due to diagnosis at an advanced stage of disease.3,9 In a retrospective study of 25 patients with surgically treated subungual melanoma, the mean recurrence-free survival was 33.6 months. The recurrence-free survival was 66% at 1 year and 40% at 3 years, and the overall survival rate was 37% at 3 years.12
Key clinical features in individuals with darker skin tones
- In patients with darker skin tones, LM tends to occur on multiple nails as a result of melanocytic activation.2,13
- Several longitudinal bands may be noted on the same nail and the pigmentation of the bands may vary. With age, these longitudinal bands typically increase in number and width.13
- Pseudo-Hutchinson sign may be present due to ethnic melanosis of the proximal nail fold.13,14
- Dermoscopic findings of LM in patients with skin of color include wider bands (P=.0125), lower band brightness (P<.032), and higher frequency of changing appearance of bands (P=.0071).15
Worth noting
When patients present with LM, thorough examination of the nail plate, periungual skin, and distal pulp of all digits on all extremities with adequate lighting is important.2 Dermoscopy is useful, and a gel interface helps for examining the nail plates.7
Clinicians should be encouraged to biopsy or immediately refer patients with concerning nail unit lesions. Cases of LM most likely are benign, but if some doubt exists, the lesions should be biopsied or tracked closely with clinical and dermoscopic images, with a biopsy if changes occur.16 In conjunction with evaluation by a qualified clinician, patients also should be encouraged to take photographs, as the evolution of nail changes is a critical part of clinical decision-making on the need for a biopsy or referral.
Health disparity highlight
Despite the disproportionately high mortality rates from subungual melanoma in Black and Hispanic populations,3,9 studies often do not adequately represent these populations. Although subungual melanoma is rare, a delay in the diagnosis contributes to high morbidity and mortality rates.
- Tosti A, Piraccini BM, de Farias DC. Dealing with melanonychia. Semin Cutan Med Surg. 2009;28:49-54. doi:10.1016/j.sder.2008.12.004
- Piraccini BM, Dika E, Fanti PA. Tips for diagnosis and treatment of nail pigmentation with practical algorithm. Dermatol Clin. 2015;33:185-195. doi:10.1016/j.det.2014.12.002
- Halteh P, Scher R, Artis A, et al. Assessment of patient knowledge of longitudinal melanonychia: a survey study of patients in outpatient clinics. Skin Appendage Disord. 2016;2:156-161. doi:10.1159/000452673
- Singal A, Bisherwal K. Melanonychia: etiology, diagnosis, and treatment. Indian Dermatol J Online. 2020;11:1-11. doi:10.4103/idoj.IDOJ_167_19
- Benati E, Ribero S, Longo C, et al. Clinical and dermoscopic clues to differentiate pigmented nail bands: an International Dermoscopy Society study. J Eur Acad Dermatol Venereol. 2017; 31:732-736. doi:10.1111/jdv.13991
- Sawada M, Yokota K, Matsumoto T, et al. Proposed classification of longitudinal melanonychia based on clinical and dermoscopic criteria. Int J Dermatol. 2014;53:581-585. doi:10.1111/ijd.12001
- Starace M, Alessandrini A, Brandi N, et al. Use of nail dermoscopy in the management of melanonychia. Dermatol Pract Concept. 2019; 9:38-43. doi:10.5826/dpc.0901a10
- Lyu A, Hou Y, Wang Q. Retrospective analysis of longitudinal melanonychia: a Chinese experience. Front Pediatr. 2023;10:1065758. doi:10.3389/fped.2022.1065758
- Williams NM, Obayomi AO, Diaz-Perez, JA, et al. Monodactylous longitudinal melanonychia: a sign of Bowen’s disease in skin of color. Skin Appendage Disord. 2021;7:306-310. doi:10.1159/000514221
- Jin H, Kim JM, Kim GW, et al. Diagnostic criteria for and clinical review of melanonychia in Korean patients. J Am Acad Dermatol. 2016;74,1121-1127. doi:10.1016/j.jaad.2015.12.039
- Halteh P, Scher R, Artis A, et al. A survey-based study of management of longitudinal melanonychia amongst attending and resident dermatologists. J Am Acad Dermatol. 2017;76:994-996. doi:10.1016 /j.jaad.2016.11.053
- LaRocca CJ, Lai L, Nelson RA, et al. Subungual melanoma: a single institution experience. Med Sci (Basel). 2021;9:57. doi:10.3390 /medsci9030057
- Baran LR, Ruben BS, Kechijian P, et al. Non‐melanoma Hutchinson’s sign: a reappraisal of this important, remarkable melanoma simulant. J Eur Acad Dermatol Venereol. 2018;32:495-501. doi:10.1111/jdv.14715
- Sladden MJ, Mortimer NJ, Osborne JE. Longitudinal melanonychia and pseudo‐Hutchinson sign associated with amlodipine. Br J Dermatol. 2005;153:219-220. doi:10.1111/j.1365-2133.2005.06668.x
- Lee DK, Chang MJ, Desai AD, et al. Clinical and dermoscopic findings of benign longitudinal melanonychia due to melanocytic activation differ by skin type and predict likelihood of nail matrix biopsy. J Am Acad Dermatol. 2022;87:792-799. doi:10.1016/j.jaad.2022.06.1165
- Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi:10.1016/j.det.2019.05.009

THE COMPARISON
A Melanoma in situ manifesting as longitudinal melanonychia (LM) in a single digit in a Black man. Dermoscopy showed irregular dark bands of brown pigmentation and micro-Hutchinson sign on the cuticle (inset).
B Melanoma manifesting as LM with a prominent Hutchinson sign in a Hispanic man, with variable shades of brown covering more than 50% of the nail width.
C Longitudinal melanonychia of at least 2 nails with a pseudo-Hutchinson sign (pigment on the nail folds in a benign case of LM) in a young Black man demonstrating ethnic/racial melanosis. The longitudinal bands, which were caused by benign melanocytic activation, are more gray than brown and are less than 3 mm wide.
Longitudinal melanonychia (LM) is a pigmented linear band—brown, black, or gray—spanning the length of the nail plate due to the presence of excess melanin, which may be attributed to a benign or malignant process and may warrant further investigation.1,2 The majority of patients who present with LM are diagnosed with melanocytic activation of the nail matrix due to their inherent darker skin tone or various triggers including trauma, infection, and medications. Longitudinal melanonychia secondary to melanocytic activation often occurs spontaneously in patients with skin of color.3 Less commonly, LM is caused by a nail matrix nevus or lentigo; however, LM may arise secondary to subungual melanoma, a more dangerous cause.
A thorough clinical history including duration, recent changes in LM manifestation, nail trauma, or infection is helpful in evaluating patients with LM; however, a history of nail trauma can be misleading, as nail changes attributed to the trauma may in fact be melanoma. Irregularly spaced vertical lines of pigmentation ranging from brown to black with variations in spacing and width are characteristic of subungual melanoma.4 Nail dystrophy, granular hyperpigmentation, and Hutchinson sign (extension of pigmentation to the nail folds) also are worrisome features.5 In recent years, dermoscopy has become an important tool in the clinical examination of LM, with the development of criteria based on color and pattern recognition.5,6 Dermoscopy can be useful in screening potential candidates for biopsy. Although clinical examination and dermoscopy are essential to evaluating LM, the gold-standard diagnostic test when malignancy is suspected is a nail matrix biopsy.1,2,6,7
Epidemiology
It is not unusual for patients with darker skin tones to develop LM due to melanocytic activation of multiple nails with age. This finding can be seen in approximately 80% of African American individuals, 30% of Japanese individuals, and 50% of Hispanic individuals.2 It has even been reported that approximately 100% of Black patients older than 50 years will have evidence of LM.3
In a retrospective analysis, children presenting with LM tend to have a higher prevalence of nail matrix nevi compared to adults (56.1% [60/106] vs 34.3% [23/66]; P=.005).8 Involvement of a single digit in children is most likely indicative of a nevus; however, when an adult presents with LM in a single digit, suspicion for subungual melanoma should be raised.2,3,9
Two separate single-center retrospective studies showed the prevalence of subungual melanoma in patients presenting with melanonychia in Asia. Jin et al10 reported subungual melanoma in 6.2% (17/275) of Korean patients presenting with melanonychia at a general dermatology clinic from 2002 to 2014. Lyu et al8 studied LM in 172 Chinese patients in a dermatology clinic from 2018 to 2021 and reported 9% (6/66) of adults (aged ≥18 years) with subungual melanoma, with no reported cases in childhood (aged <18 years).
Although the prevalence of subungual melanoma in patients with LM is low, it is an important diagnosis that should not be missed. In confirmed cases of subungual melanoma, two-thirds of lesions manifested as LM.3,10,11 Thus, LM arising in an adult in a single digit is more concerning for malignancy.2,3,7,9
Individuals of African and Asian descent as well as American Indian individuals are at highest risk for subungual melanoma with a poor prognosis compared to other types of melanoma, largely due to diagnosis at an advanced stage of disease.3,9 In a retrospective study of 25 patients with surgically treated subungual melanoma, the mean recurrence-free survival was 33.6 months. The recurrence-free survival was 66% at 1 year and 40% at 3 years, and the overall survival rate was 37% at 3 years.12
Key clinical features in individuals with darker skin tones
- In patients with darker skin tones, LM tends to occur on multiple nails as a result of melanocytic activation.2,13
- Several longitudinal bands may be noted on the same nail and the pigmentation of the bands may vary. With age, these longitudinal bands typically increase in number and width.13
- Pseudo-Hutchinson sign may be present due to ethnic melanosis of the proximal nail fold.13,14
- Dermoscopic findings of LM in patients with skin of color include wider bands (P=.0125), lower band brightness (P<.032), and higher frequency of changing appearance of bands (P=.0071).15
Worth noting
When patients present with LM, thorough examination of the nail plate, periungual skin, and distal pulp of all digits on all extremities with adequate lighting is important.2 Dermoscopy is useful, and a gel interface helps for examining the nail plates.7
Clinicians should be encouraged to biopsy or immediately refer patients with concerning nail unit lesions. Cases of LM most likely are benign, but if some doubt exists, the lesions should be biopsied or tracked closely with clinical and dermoscopic images, with a biopsy if changes occur.16 In conjunction with evaluation by a qualified clinician, patients also should be encouraged to take photographs, as the evolution of nail changes is a critical part of clinical decision-making on the need for a biopsy or referral.
Health disparity highlight
Despite the disproportionately high mortality rates from subungual melanoma in Black and Hispanic populations,3,9 studies often do not adequately represent these populations. Although subungual melanoma is rare, a delay in the diagnosis contributes to high morbidity and mortality rates.

THE COMPARISON
A Melanoma in situ manifesting as longitudinal melanonychia (LM) in a single digit in a Black man. Dermoscopy showed irregular dark bands of brown pigmentation and micro-Hutchinson sign on the cuticle (inset).
B Melanoma manifesting as LM with a prominent Hutchinson sign in a Hispanic man, with variable shades of brown covering more than 50% of the nail width.
C Longitudinal melanonychia of at least 2 nails with a pseudo-Hutchinson sign (pigment on the nail folds in a benign case of LM) in a young Black man demonstrating ethnic/racial melanosis. The longitudinal bands, which were caused by benign melanocytic activation, are more gray than brown and are less than 3 mm wide.
Longitudinal melanonychia (LM) is a pigmented linear band—brown, black, or gray—spanning the length of the nail plate due to the presence of excess melanin, which may be attributed to a benign or malignant process and may warrant further investigation.1,2 The majority of patients who present with LM are diagnosed with melanocytic activation of the nail matrix due to their inherent darker skin tone or various triggers including trauma, infection, and medications. Longitudinal melanonychia secondary to melanocytic activation often occurs spontaneously in patients with skin of color.3 Less commonly, LM is caused by a nail matrix nevus or lentigo; however, LM may arise secondary to subungual melanoma, a more dangerous cause.
A thorough clinical history including duration, recent changes in LM manifestation, nail trauma, or infection is helpful in evaluating patients with LM; however, a history of nail trauma can be misleading, as nail changes attributed to the trauma may in fact be melanoma. Irregularly spaced vertical lines of pigmentation ranging from brown to black with variations in spacing and width are characteristic of subungual melanoma.4 Nail dystrophy, granular hyperpigmentation, and Hutchinson sign (extension of pigmentation to the nail folds) also are worrisome features.5 In recent years, dermoscopy has become an important tool in the clinical examination of LM, with the development of criteria based on color and pattern recognition.5,6 Dermoscopy can be useful in screening potential candidates for biopsy. Although clinical examination and dermoscopy are essential to evaluating LM, the gold-standard diagnostic test when malignancy is suspected is a nail matrix biopsy.1,2,6,7
Epidemiology
It is not unusual for patients with darker skin tones to develop LM due to melanocytic activation of multiple nails with age. This finding can be seen in approximately 80% of African American individuals, 30% of Japanese individuals, and 50% of Hispanic individuals.2 It has even been reported that approximately 100% of Black patients older than 50 years will have evidence of LM.3
In a retrospective analysis, children presenting with LM tend to have a higher prevalence of nail matrix nevi compared to adults (56.1% [60/106] vs 34.3% [23/66]; P=.005).8 Involvement of a single digit in children is most likely indicative of a nevus; however, when an adult presents with LM in a single digit, suspicion for subungual melanoma should be raised.2,3,9
Two separate single-center retrospective studies showed the prevalence of subungual melanoma in patients presenting with melanonychia in Asia. Jin et al10 reported subungual melanoma in 6.2% (17/275) of Korean patients presenting with melanonychia at a general dermatology clinic from 2002 to 2014. Lyu et al8 studied LM in 172 Chinese patients in a dermatology clinic from 2018 to 2021 and reported 9% (6/66) of adults (aged ≥18 years) with subungual melanoma, with no reported cases in childhood (aged <18 years).
Although the prevalence of subungual melanoma in patients with LM is low, it is an important diagnosis that should not be missed. In confirmed cases of subungual melanoma, two-thirds of lesions manifested as LM.3,10,11 Thus, LM arising in an adult in a single digit is more concerning for malignancy.2,3,7,9
Individuals of African and Asian descent as well as American Indian individuals are at highest risk for subungual melanoma with a poor prognosis compared to other types of melanoma, largely due to diagnosis at an advanced stage of disease.3,9 In a retrospective study of 25 patients with surgically treated subungual melanoma, the mean recurrence-free survival was 33.6 months. The recurrence-free survival was 66% at 1 year and 40% at 3 years, and the overall survival rate was 37% at 3 years.12
Key clinical features in individuals with darker skin tones
- In patients with darker skin tones, LM tends to occur on multiple nails as a result of melanocytic activation.2,13
- Several longitudinal bands may be noted on the same nail and the pigmentation of the bands may vary. With age, these longitudinal bands typically increase in number and width.13
- Pseudo-Hutchinson sign may be present due to ethnic melanosis of the proximal nail fold.13,14
- Dermoscopic findings of LM in patients with skin of color include wider bands (P=.0125), lower band brightness (P<.032), and higher frequency of changing appearance of bands (P=.0071).15
Worth noting
When patients present with LM, thorough examination of the nail plate, periungual skin, and distal pulp of all digits on all extremities with adequate lighting is important.2 Dermoscopy is useful, and a gel interface helps for examining the nail plates.7
Clinicians should be encouraged to biopsy or immediately refer patients with concerning nail unit lesions. Cases of LM most likely are benign, but if some doubt exists, the lesions should be biopsied or tracked closely with clinical and dermoscopic images, with a biopsy if changes occur.16 In conjunction with evaluation by a qualified clinician, patients also should be encouraged to take photographs, as the evolution of nail changes is a critical part of clinical decision-making on the need for a biopsy or referral.
Health disparity highlight
Despite the disproportionately high mortality rates from subungual melanoma in Black and Hispanic populations,3,9 studies often do not adequately represent these populations. Although subungual melanoma is rare, a delay in the diagnosis contributes to high morbidity and mortality rates.
- Tosti A, Piraccini BM, de Farias DC. Dealing with melanonychia. Semin Cutan Med Surg. 2009;28:49-54. doi:10.1016/j.sder.2008.12.004
- Piraccini BM, Dika E, Fanti PA. Tips for diagnosis and treatment of nail pigmentation with practical algorithm. Dermatol Clin. 2015;33:185-195. doi:10.1016/j.det.2014.12.002
- Halteh P, Scher R, Artis A, et al. Assessment of patient knowledge of longitudinal melanonychia: a survey study of patients in outpatient clinics. Skin Appendage Disord. 2016;2:156-161. doi:10.1159/000452673
- Singal A, Bisherwal K. Melanonychia: etiology, diagnosis, and treatment. Indian Dermatol J Online. 2020;11:1-11. doi:10.4103/idoj.IDOJ_167_19
- Benati E, Ribero S, Longo C, et al. Clinical and dermoscopic clues to differentiate pigmented nail bands: an International Dermoscopy Society study. J Eur Acad Dermatol Venereol. 2017; 31:732-736. doi:10.1111/jdv.13991
- Sawada M, Yokota K, Matsumoto T, et al. Proposed classification of longitudinal melanonychia based on clinical and dermoscopic criteria. Int J Dermatol. 2014;53:581-585. doi:10.1111/ijd.12001
- Starace M, Alessandrini A, Brandi N, et al. Use of nail dermoscopy in the management of melanonychia. Dermatol Pract Concept. 2019; 9:38-43. doi:10.5826/dpc.0901a10
- Lyu A, Hou Y, Wang Q. Retrospective analysis of longitudinal melanonychia: a Chinese experience. Front Pediatr. 2023;10:1065758. doi:10.3389/fped.2022.1065758
- Williams NM, Obayomi AO, Diaz-Perez, JA, et al. Monodactylous longitudinal melanonychia: a sign of Bowen’s disease in skin of color. Skin Appendage Disord. 2021;7:306-310. doi:10.1159/000514221
- Jin H, Kim JM, Kim GW, et al. Diagnostic criteria for and clinical review of melanonychia in Korean patients. J Am Acad Dermatol. 2016;74,1121-1127. doi:10.1016/j.jaad.2015.12.039
- Halteh P, Scher R, Artis A, et al. A survey-based study of management of longitudinal melanonychia amongst attending and resident dermatologists. J Am Acad Dermatol. 2017;76:994-996. doi:10.1016 /j.jaad.2016.11.053
- LaRocca CJ, Lai L, Nelson RA, et al. Subungual melanoma: a single institution experience. Med Sci (Basel). 2021;9:57. doi:10.3390 /medsci9030057
- Baran LR, Ruben BS, Kechijian P, et al. Non‐melanoma Hutchinson’s sign: a reappraisal of this important, remarkable melanoma simulant. J Eur Acad Dermatol Venereol. 2018;32:495-501. doi:10.1111/jdv.14715
- Sladden MJ, Mortimer NJ, Osborne JE. Longitudinal melanonychia and pseudo‐Hutchinson sign associated with amlodipine. Br J Dermatol. 2005;153:219-220. doi:10.1111/j.1365-2133.2005.06668.x
- Lee DK, Chang MJ, Desai AD, et al. Clinical and dermoscopic findings of benign longitudinal melanonychia due to melanocytic activation differ by skin type and predict likelihood of nail matrix biopsy. J Am Acad Dermatol. 2022;87:792-799. doi:10.1016/j.jaad.2022.06.1165
- Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi:10.1016/j.det.2019.05.009
- Tosti A, Piraccini BM, de Farias DC. Dealing with melanonychia. Semin Cutan Med Surg. 2009;28:49-54. doi:10.1016/j.sder.2008.12.004
- Piraccini BM, Dika E, Fanti PA. Tips for diagnosis and treatment of nail pigmentation with practical algorithm. Dermatol Clin. 2015;33:185-195. doi:10.1016/j.det.2014.12.002
- Halteh P, Scher R, Artis A, et al. Assessment of patient knowledge of longitudinal melanonychia: a survey study of patients in outpatient clinics. Skin Appendage Disord. 2016;2:156-161. doi:10.1159/000452673
- Singal A, Bisherwal K. Melanonychia: etiology, diagnosis, and treatment. Indian Dermatol J Online. 2020;11:1-11. doi:10.4103/idoj.IDOJ_167_19
- Benati E, Ribero S, Longo C, et al. Clinical and dermoscopic clues to differentiate pigmented nail bands: an International Dermoscopy Society study. J Eur Acad Dermatol Venereol. 2017; 31:732-736. doi:10.1111/jdv.13991
- Sawada M, Yokota K, Matsumoto T, et al. Proposed classification of longitudinal melanonychia based on clinical and dermoscopic criteria. Int J Dermatol. 2014;53:581-585. doi:10.1111/ijd.12001
- Starace M, Alessandrini A, Brandi N, et al. Use of nail dermoscopy in the management of melanonychia. Dermatol Pract Concept. 2019; 9:38-43. doi:10.5826/dpc.0901a10
- Lyu A, Hou Y, Wang Q. Retrospective analysis of longitudinal melanonychia: a Chinese experience. Front Pediatr. 2023;10:1065758. doi:10.3389/fped.2022.1065758
- Williams NM, Obayomi AO, Diaz-Perez, JA, et al. Monodactylous longitudinal melanonychia: a sign of Bowen’s disease in skin of color. Skin Appendage Disord. 2021;7:306-310. doi:10.1159/000514221
- Jin H, Kim JM, Kim GW, et al. Diagnostic criteria for and clinical review of melanonychia in Korean patients. J Am Acad Dermatol. 2016;74,1121-1127. doi:10.1016/j.jaad.2015.12.039
- Halteh P, Scher R, Artis A, et al. A survey-based study of management of longitudinal melanonychia amongst attending and resident dermatologists. J Am Acad Dermatol. 2017;76:994-996. doi:10.1016 /j.jaad.2016.11.053
- LaRocca CJ, Lai L, Nelson RA, et al. Subungual melanoma: a single institution experience. Med Sci (Basel). 2021;9:57. doi:10.3390 /medsci9030057
- Baran LR, Ruben BS, Kechijian P, et al. Non‐melanoma Hutchinson’s sign: a reappraisal of this important, remarkable melanoma simulant. J Eur Acad Dermatol Venereol. 2018;32:495-501. doi:10.1111/jdv.14715
- Sladden MJ, Mortimer NJ, Osborne JE. Longitudinal melanonychia and pseudo‐Hutchinson sign associated with amlodipine. Br J Dermatol. 2005;153:219-220. doi:10.1111/j.1365-2133.2005.06668.x
- Lee DK, Chang MJ, Desai AD, et al. Clinical and dermoscopic findings of benign longitudinal melanonychia due to melanocytic activation differ by skin type and predict likelihood of nail matrix biopsy. J Am Acad Dermatol. 2022;87:792-799. doi:10.1016/j.jaad.2022.06.1165
- Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi:10.1016/j.det.2019.05.009
Depression As a Potential Contributing Factor in Hidradenitis Suppurativa and Associated Racial Gaps
Hidradenitis suppurativa (HS)—a chronic, relapsing, inflammatory disorder involving terminal hair follicles in apocrine gland–rich skin—manifests as tender inflamed nodules that transform into abscesses, sinus tracts, and scarring.1,2 The etiology of HS is multifactorial, encompassing lifestyle, microbiota, hormonal status, and genetic and environmental factors. These factors activate the immune system around the terminal hair follicles and lead to hyperkeratosis of the infundibulum of the hair follicles in intertriginous regions. This progresses to follicular occlusion, stasis, and eventual rupture. Bacterial multiplication within the plugged pilosebaceous units further boosts immune activation. Resident and migrated cells of the innate and adaptive immune system then release proinflammatory cytokines such as tumor necrosis factor, IL-1β, and IL-17, which further enhance immune cell influx and inflammation.3,4 This aberrant immune response propagates the production of deep-seated inflammatory nodules and abscesses.3-8
The estimated prevalence of HS is 1% worldwide.9 It is more prevalent in female and Black patients (0.30%) than White patients (0.09%) and is intermediate in prevalence in the biracial population (0.22%).10 Hidradenitis suppurativa is thought to be associated with lower socioeconomic status (SES). In a retrospective analysis of HS patients (N=375), approximately one-third of patients were Black, had advanced disease, and had a notably lower SES.11 Furthermore, HS has been reported to be associated with systemic inflammation and comorbidities such as morbid obesity (38.3%) and hypertension (39.6%) as well as other metabolic syndrome–related disorders and depression (48.1%).1
Hidradenitis suppurativa may contribute to the risk for depression through its substantial impact on health-related quality of life, which culminates in social withdrawal, unemployment, and suicidal thoughts.12 The high prevalence of depression in individuals with HS1 and its association with systemic inflammation13 increases the likelihood that a common genetic predisposition also may exist between both conditions. Because depression frequently has been discovered as a concomitant diagnosis in patients with HS, we hypothesize that a shared genetic susceptibility also may exist between the 2 disorders. Our study sought to explore data on the co-occurrence of depression with HS, including its demographics and racial data.
Methods
We conducted a PubMed search of articles indexed for MEDLINE as well as Google Scholar using the terms depression and hidradenitis suppurativa to obtain all research articles published from 2000 to 2022. Articles were selected based on relevance to the topic of exploration. English-language articles that directly addressed the epidemiology, etiology, pathophysiology, and co-occurrence of both depression and HS with numerical data were included. Articles were excluded if they did not explore the information of interest on these 2 disorders or did not contain clear statistical data of patients with the 2 concurrent medical conditions.
Results
Twenty-two cross-sectional, prospective, and retrospective studies that fit the search criteria were identified and included in the analysis (eTable).1,14-34 Sixteen (72.7%) studies were cross-sectional, 5 (22.7%) were retrospective, and only 1 (4.5%) was a prospective study. Only 6 of the studies provided racial data,1,14,17,26,28,32 and of them, 4 had predominately White patients,1,14,26,32 whereas the other 2 had predominantly Black patients.17,28
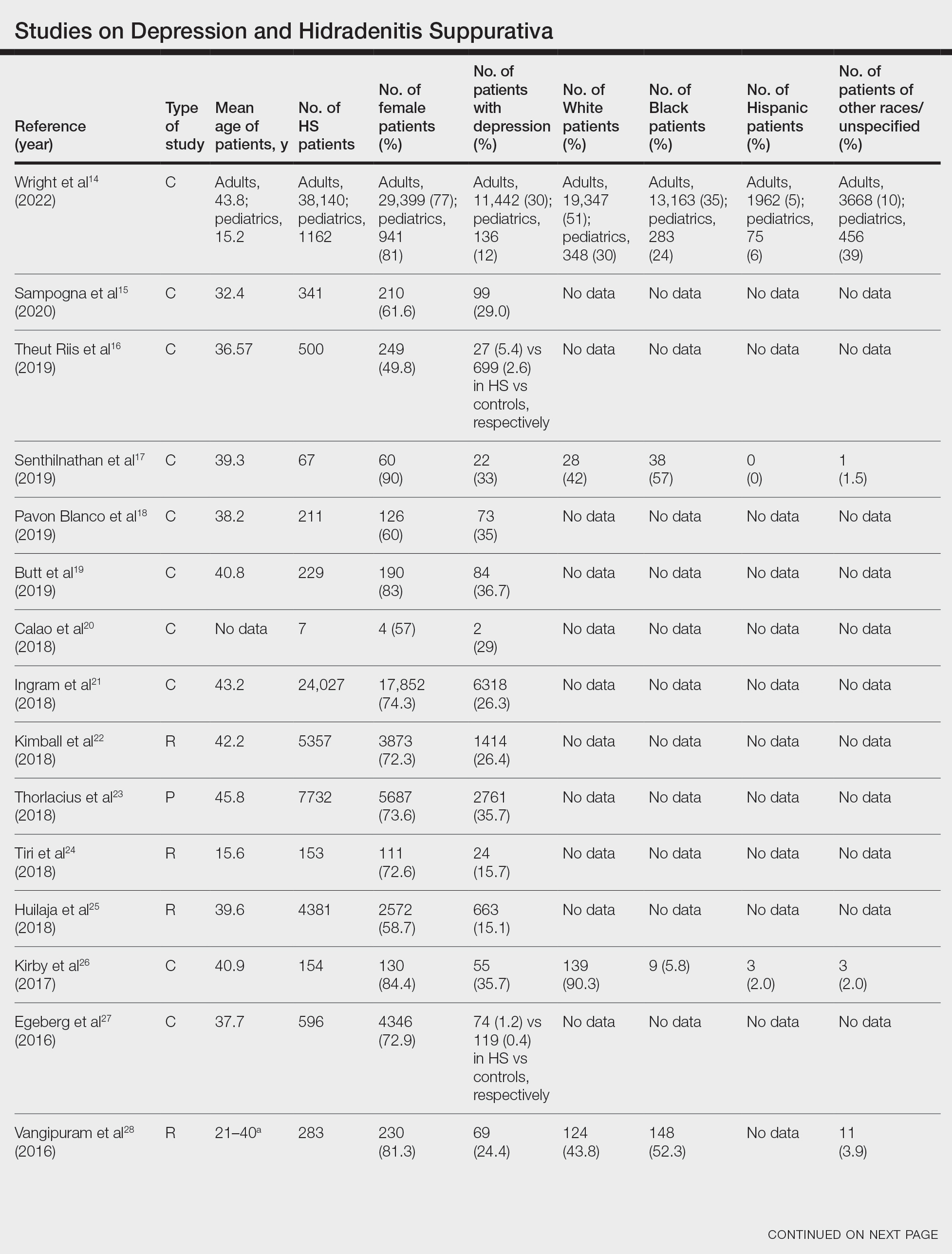
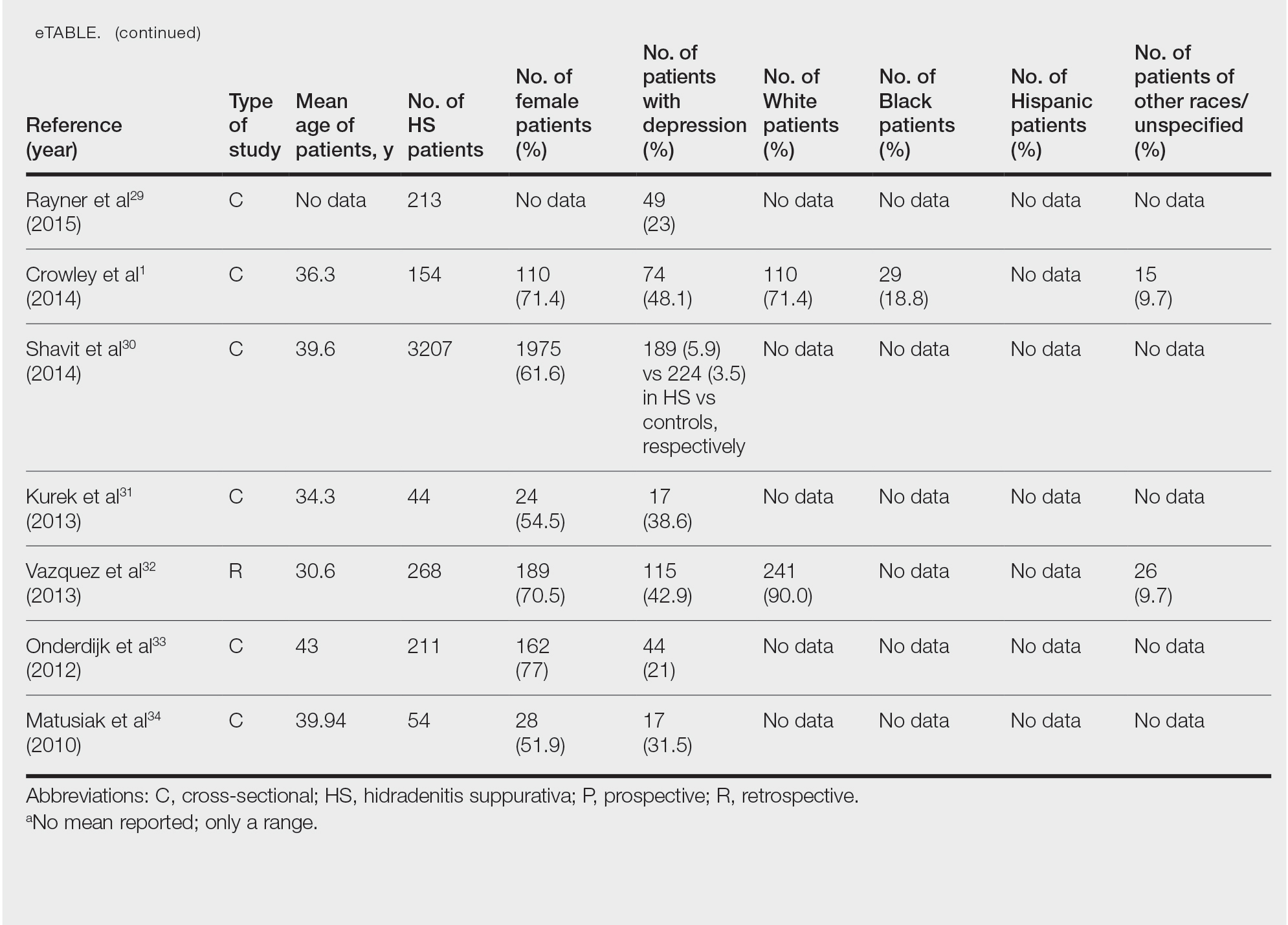
Hidradenitis suppurativa was found to coexist with depression in all the studies, with a prevalence of 1.2% to 48.1%. There also was a higher prevalence of depression in HS patients than in the control patients without HS. Furthermore, a recent study by Wright and colleagues14 stratified the depression prevalence data by age and found a higher prevalence of depression in adults vs children with HS (30% vs 12%).
Comment
Major depression—a chronic and debilitating illness—is the chief cause of disability globally and in the United States alone and has a global lifetime prevalence of 17%.35 In a study of 388 patients diagnosed with depression and 404 community-matched controls who were observed for 10 years, depressed patients had a two-thirds higher likelihood of developing a serious physical illness than controls. The depression-associated elevated risk for serious physical illness persisted after controlling for confounding variables such as alcohol abuse, smoking, and level of physical activity.36 Studies also have demonstrated that HS is more prevalent in Black individuals10 and in individuals of low SES,37 who are mostly the Black and Hispanic populations that experience the highest burden of racial microaggression38 and disparities in health access and outcomes.39,40 The severity and chronicity of major depressive disorder also is higher in Black patients compared with White patients (57% vs 39%).41 Because major depression and HS are most common among Black patients who experience the highest-burden negative financial and health disparities, there may be a shared genetic disposition to both medical conditions.
Moreover, the common detrimental lifestyle choices associated with patients with depression and HS also suggest the possibility of a collective genetic susceptibility. Patients with depression also report increased consumption of alcohol, tobacco, and illicit substances; sedentary lifestyle leading to obesity; and poor compliance with prescribed medical treatment.42 Smoking and obesity are known contributors to the pathogenesis of HS, and their modification also is known to positively impact the disease course. In a retrospective single-cohort study, 50% of obese HS patients (n=35) reported a substantial decrease in disease severity after a reduction of more than 15% in body mass index over 2 years following bariatric surgery (n=35).43 Patients with HS also have reported disease remission following extensive weight loss.44 In addition, evidence has supported smoking cessation in improving the disease course of HS.43 Because these detrimental lifestyle choices are prevalent in both patients with HS and those with depression, a co-genetic susceptibility also may exist.
Furthermore, depression is characterized by a persistent inflammatory state,13,45 similar to HS.46 Elevated levels of a variety of inflammatory markers, such as C-reactive protein (CRP), IL-6, and soluble intercellular adhesion molecule 1, have been reported in patients with depression compared with healthy controls.13,45 Further analysis found a positive correlation and a strong association between depression and these inflammatory markers.47 Moreover, adipokines regulate inflammatory responses, and adipokines play a role in the pathogenesis of HS. Adipokine levels such as elevated omentin-1 (a recently identified adipokine) were found to be altered in patients with HS compared with controls.48 Results from clinical studies and meta-analyses of patients with depression also have demonstrated that adipokines are dysregulated in this population,49,50 which may be another potential genetic link between depression and HS.
In addition, genetic susceptibility to depression and HS may be shared because the inflammatory markers that have a strong association with depression also have been found to play an important role in HS treatment and disease severity prediction. In a retrospective cohort study of 404 patients, CRP or IL-6 levels were found to be reliable predictors of HS disease severity, which may explain why anti–tumor necrosis factor antibody regimens such as adalimumab and infliximab have clinically ameliorated disease activity in several cases of HS.51 In a study evaluating these drugs, high baseline levels of high-sensitivity CRP and IL-6 were predictive of patient response to infliximab.52 In a meta-analysis evaluating 20,791 participants, an association was found between concurrent depression and CRP. Furthermore, inflammation measured by high levels of CRP or IL-6 was observed to predict future depression.53 If the same inflammatory markers—CRP and IL-6—both play a major role in the disease activity of depression and HS, then a concurrent genetic predisposition may exist.
Conclusion
Understanding the comorbidities, etiologies, and risk factors for the development and progression of HS is an important step toward improved disease management. Available studies on comorbid depression in HS largely involve White patients, and more studies are needed in patients with skin of color, particularly the Black population, who have the highest prevalence of HS.10 Given the evidence for an association between depression and HS, we suggest a large-scale investigation of this patient population that includes a complete medical history, onset of HS in comparison to the onset of depression, and specific measures of disease progress and lifetime management of depression, which may help to increase knowledge about the role of depression in HS and encourage more research in this area. If shared genetic susceptibility is established, aggressive management of depression in patients at risk for HS may reduce disease incidence and severity as well as the psychological burden on patients.
- Crowley JJ, Mekkes JR, Zouboulis CC, et al. Association of hidradenitis suppurativa disease severity with increased risk for systemic comorbidities. Br J Dermatol. 2014;171:1561-1565.
- Napolitano M, Megna M, Timoshchuk EA, et al. Hidradenitis suppurativa: from pathogenesis to diagnosis and treatment. Clin Cosmet Investig Dermatol. 2017;10:105-115.
- Sabat R, Jemec GBE, Matusiak Ł, et al. Hidradenitis suppurativa. Nat Rev Dis Prim. 2020;6:1-20.
- Wolk K, Warszawska K, Hoeflich C, et al. Deficiency of IL-22 contributes to a chronic inflammatory disease: pathogenetic mechanisms in acne inversa. J Immunol. 2011;186:1228-1239.
- von Laffert M, Helmbold P, Wohlrab J, et al. Hidradenitis suppurativa (acne inversa): early inflammatory events at terminal follicles and at interfollicular epidermis. Exp Dermatol. 2010;19:533-537.
- Van Der Zee HH, De Ruiter L, Van Den Broecke DG, et al. Elevated levels of tumour necrosis factor (TNF)-α, interleukin (IL)-1β and IL-10 in hidradenitis suppurativa skin: a rationale for targeting TNF-α and IL-1β. Br J Dermatol. 2011;164:1292-1298.
- Schlapbach C, Hänni T, Yawalkar N, et al. Expression of the IL-23/Th17 pathway in lesions of hidradenitis suppurativa. J Am Acad Dermatol. 2011;65:790-798.
- Kelly G, Hughes R, McGarry T, et al. Dysregulated cytokine expression in lesional and nonlesional skin in hidradenitis suppurativa. Br J Dermatol. 2015;173:1431-1439.
- Jemec GBE, Kimball AB. Hidradenitis suppurativa: epidemiology and scope of the problem. J Am Acad Dermatol. 2015;73(5 Suppl 1):S4-S7.
- Garg A, Kirby JS, Lavian J, et al. Sex- and age-adjusted population analysis of prevalence estimates for hidradenitis suppurativa in the United States. JAMA Dermatol. 2017;153:760-764.
- Soliman YS, Hoffman LK, Guzman AK, et al. African American patients with hidradenitis suppurativa have significant health care disparities: a retrospective study. J Cutan Med Surg. 2019;23:334-336.
- Garg A, Malviya N, Strunk A, et al. Comorbidity screening in hidradenitis suppurativa: evidence-based recommendations from the US and Canadian Hidradenitis Suppurativa Foundations. J Am Acad Dermatol. 2022;86:1092-1101.
- Beatriz Currier M, Nemeroff CB. Inflammation and mood disorders: proinflammatory cytokines and the pathogenesis of depression. Antiinflamm Antiallergy Agents Med Chem. 2012;9:212-220.
- Wright S, Strunk A, Garg A. Prevalence of depression among children, adolescents, and adults with hidradenitis suppurativa. J Am Acad Dermatol. 2022;86:55-60.
- Sampogna F, Fania L, Mastroeni S, et al. Correlation between depression, quality of life and clinical severity in patients with hidradenitis suppurativa. Acta Derm Venereol. 2020;100:1-6.
- Theut Riis P, Pedersen OB, Sigsgaard V, et al. Prevalence of patients with self-reported hidradenitis suppurativa in a cohort of Danish blood donors: a cross-sectional study. Br J Dermatol. 2019;180:774-781.
- Senthilnathan A, Kolli SS, Cardwell LA, et al. Depression in hidradenitis suppurativa. Br J Dermatol. 2019;181:1087-1088.
- Pavon Blanco A, Turner MA, Petrof G, et al. To what extent do disease severity and illness perceptions explain depression, anxiety and quality of life in hidradenitis suppurativa? Br J Dermatol. 2019;180:338-345.
- Butt M, Sisic M, Silva C, et al. The associations of depression and coping methods on health-related quality of life for those with hidradenitis suppurativa. J Am Acad Dermatol. 2019;80:1137-1139.
- Calao M, Wilson JL, Spelman L, et al. Hidradenitis suppurativa (HS) prevalence, demographics and management pathways in Australia: a population-based cross-sectional study. PLoS One. 2018;13:e0200683.
- Ingram JR, Jenkins-Jones S, Knipe DW, et al. Population-based Clinical Practice Research Datalink study using algorithm modelling to identify the true burden of hidradenitis suppurativa. Br J Dermatol. 2018;178:917-924.
- Kimball AB, Sundaram M, Gauthier G, et al. The comorbidity burden of hidradenitis suppurativa in the United States: a claims data analysis. Dermatol Ther (Heidelb). 2018;8:557.
- Thorlacius L, Cohen AD, Gislason GH, et al. Increased suicide risk in patients with hidradenitis suppurativa. J Invest Dermatol. 2018;138:52-57.
- Tiri H, Jokelainen J, Timonen M, et al. Somatic and psychiatric comorbidities of hidradenitis suppurativa in children and adolescents. J Am Acad Dermatol. 2018;79:514-519.
- Huilaja L, Tiri H, Jokelainen J, et al. Patients with hidradenitis suppurativa have a high psychiatric disease burden: a Finnish nationwide registry study. J Invest Dermatol. 2018;138:46-51.
- Kirby JS, Butt M, Esmann S, et al. Association of resilience with depression and health-related quality of life for patients with hidradenitis suppurativa. JAMA Dermatol. 2017;153:1263.
- Egeberg A, Gislason GH, Hansen PR. Risk of major adverse cardiovascular events and all-cause mortality in patients with hidradenitis suppurativa. JAMA Dermatol. 2016;152:429-434.
- Vangipuram R, Vaidya T, Jandarov R, et al. Factors contributing to depression and chronic pain in patients with hidradenitis suppurativa: results from a single-center retrospective review. Dermatology. 2016;232:692-695.
- Rayner L, Jackson K, Turner M, et al. Integrated mental health assessment in a tertiary medical dermatology service: feasibility and the prevalence of common mental disorder. Br J Dermatol. 2015;173:201.
- Shavit E, Dreiher J, Freud T, et al. Psychiatric comorbidities in 3207 patients with hidradenitis suppurativa [published online June 9, 2014]. J Eur Acad Dermatol Venereol. 2015;29:371-376.
- Kurek A, Johanne Peters EM, Sabat R, et al. Depression is a frequent co-morbidity in patients with acne inversa. J Dtsch Dermatol Ges. 2013;11:743-749.
- Vazquez BG, Alikhan A, Weaver AL, et al. Incidence of hidradenitis suppurativa and associated factors: a population-based study of Olmsted County, Minnesota. J Invest Dermatol. 2013;133:97.
- Onderdijk AJ, Van Der Zee HH, Esmann S, et al. Depression in patients with hidradenitis suppurativa [published online February 20, 2012]. J Eur Acad Dermatol Venereol. 2013;27:473-478.
- Matusiak Ł, Bieniek A, Szepietowski JC. Psychophysical aspects of hidradenitis suppurativa. Acta Derm Venereol. 2010;90:264-268.
- Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617-627.
- Holahan CJ, Pahl SA, Cronkite RC, et al. Depression and vulnerability to incident physical illness across 10 years. J Affect Disord. 2009;123:222-229.
- Deckers IE, Janse IC, van der Zee HH, et al. Hidradenitis suppurativa (HS) is associated with low socioeconomic status (SES): a cross-sectional reference study. J Am Acad Dermatol. 2016;75:755-759.e1.
- Williams MT, Skinta MD, Kanter JW, et al. A qualitative study of microaggressions against African Americans on predominantly White campuses. BMC Psychol. 2020;8:1-13.
- Dunlop DD, Song J, Lyons JS, et al. Racial/ethnic differences in rates of depression among preretirement adults. Am J Public Health. 2003;93:1945-1952.
- Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol. 2016;35:407-411.
- Williams DR, González HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and Non-Hispanic Whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305-315.
- Druss BG, Bradford DW, Rosenheck RA, et al. Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA. 2000;283:506-511.
- Kromann CB, Deckers IE, Esmann S, et al. Risk factors, clinical course and long-term prognosis in hidradenitis suppurativa: a cross-sectional study. Br J Dermatol. 2014;171:819-824.
- Sivanand A, Gulliver WP, Josan CK, et al. Weight loss and dietary interventions for hidradenitis suppurativa: a systematic review. J Cutan Med Surg . 2020;24:64-72.
- Raedler TJ. Inflammatory mechanisms in major depressive disorder. Curr Opin Psychiatry. 2011;24:519-525.
- Rocha VZ, Libby P. Obesity, inflammation, and atherosclerosis. Nat Rev Cardiol. 2009;6:399-409.
- Davidson KW, Schwartz JE, Kirkland SA, et al. Relation of inflammation to depression and incident coronary heart disease (from the Canadian Nova Scotia Health Survey [NSHS95] Prospective Population Study). Am J Cardiol. 2009;103:755-761.
- González-López MA, Ocejo-Viñals JG, Mata C, et al. Evaluation of serum omentin-1 and apelin concentrations in patients with hidradenitis suppurativa. Postepy Dermatol Alergol. 2021;38:450-454.
- Taylor VH, Macqueen GM. The role of adipokines in understanding the associations between obesity and depression. J Obes. 2010;2010:748048.
- Setayesh L, Ebrahimi R, Pooyan S, et al. The possible mediatory role of adipokines in the association between low carbohydrate diet and depressive symptoms among overweight and obese women. PLoS One. 2021;16:e0257275 .
- Andriano TM, Benesh G, Babbush KM, et al. Serum inflammatory markers and leukocyte profiles accurately describe hidradenitis suppurativa disease severity. Int J Dermatol. 2022;61:1270-1275.
- Montaudié H, Seitz-Polski B, Cornille A, et al. Interleukin 6 and high-sensitivity C-reactive protein are potential predictive markers of response to infliximab in hidradenitis suppurativa. J Am Acad Dermatol. 2017;6:156-158.
- Colasanto M, Madigan S, Korczak DJ. Depression and inflammation among children and adolescents: a meta-analysis. J Affect Disord. 2020;277:940-948.
Hidradenitis suppurativa (HS)—a chronic, relapsing, inflammatory disorder involving terminal hair follicles in apocrine gland–rich skin—manifests as tender inflamed nodules that transform into abscesses, sinus tracts, and scarring.1,2 The etiology of HS is multifactorial, encompassing lifestyle, microbiota, hormonal status, and genetic and environmental factors. These factors activate the immune system around the terminal hair follicles and lead to hyperkeratosis of the infundibulum of the hair follicles in intertriginous regions. This progresses to follicular occlusion, stasis, and eventual rupture. Bacterial multiplication within the plugged pilosebaceous units further boosts immune activation. Resident and migrated cells of the innate and adaptive immune system then release proinflammatory cytokines such as tumor necrosis factor, IL-1β, and IL-17, which further enhance immune cell influx and inflammation.3,4 This aberrant immune response propagates the production of deep-seated inflammatory nodules and abscesses.3-8
The estimated prevalence of HS is 1% worldwide.9 It is more prevalent in female and Black patients (0.30%) than White patients (0.09%) and is intermediate in prevalence in the biracial population (0.22%).10 Hidradenitis suppurativa is thought to be associated with lower socioeconomic status (SES). In a retrospective analysis of HS patients (N=375), approximately one-third of patients were Black, had advanced disease, and had a notably lower SES.11 Furthermore, HS has been reported to be associated with systemic inflammation and comorbidities such as morbid obesity (38.3%) and hypertension (39.6%) as well as other metabolic syndrome–related disorders and depression (48.1%).1
Hidradenitis suppurativa may contribute to the risk for depression through its substantial impact on health-related quality of life, which culminates in social withdrawal, unemployment, and suicidal thoughts.12 The high prevalence of depression in individuals with HS1 and its association with systemic inflammation13 increases the likelihood that a common genetic predisposition also may exist between both conditions. Because depression frequently has been discovered as a concomitant diagnosis in patients with HS, we hypothesize that a shared genetic susceptibility also may exist between the 2 disorders. Our study sought to explore data on the co-occurrence of depression with HS, including its demographics and racial data.
Methods
We conducted a PubMed search of articles indexed for MEDLINE as well as Google Scholar using the terms depression and hidradenitis suppurativa to obtain all research articles published from 2000 to 2022. Articles were selected based on relevance to the topic of exploration. English-language articles that directly addressed the epidemiology, etiology, pathophysiology, and co-occurrence of both depression and HS with numerical data were included. Articles were excluded if they did not explore the information of interest on these 2 disorders or did not contain clear statistical data of patients with the 2 concurrent medical conditions.
Results
Twenty-two cross-sectional, prospective, and retrospective studies that fit the search criteria were identified and included in the analysis (eTable).1,14-34 Sixteen (72.7%) studies were cross-sectional, 5 (22.7%) were retrospective, and only 1 (4.5%) was a prospective study. Only 6 of the studies provided racial data,1,14,17,26,28,32 and of them, 4 had predominately White patients,1,14,26,32 whereas the other 2 had predominantly Black patients.17,28
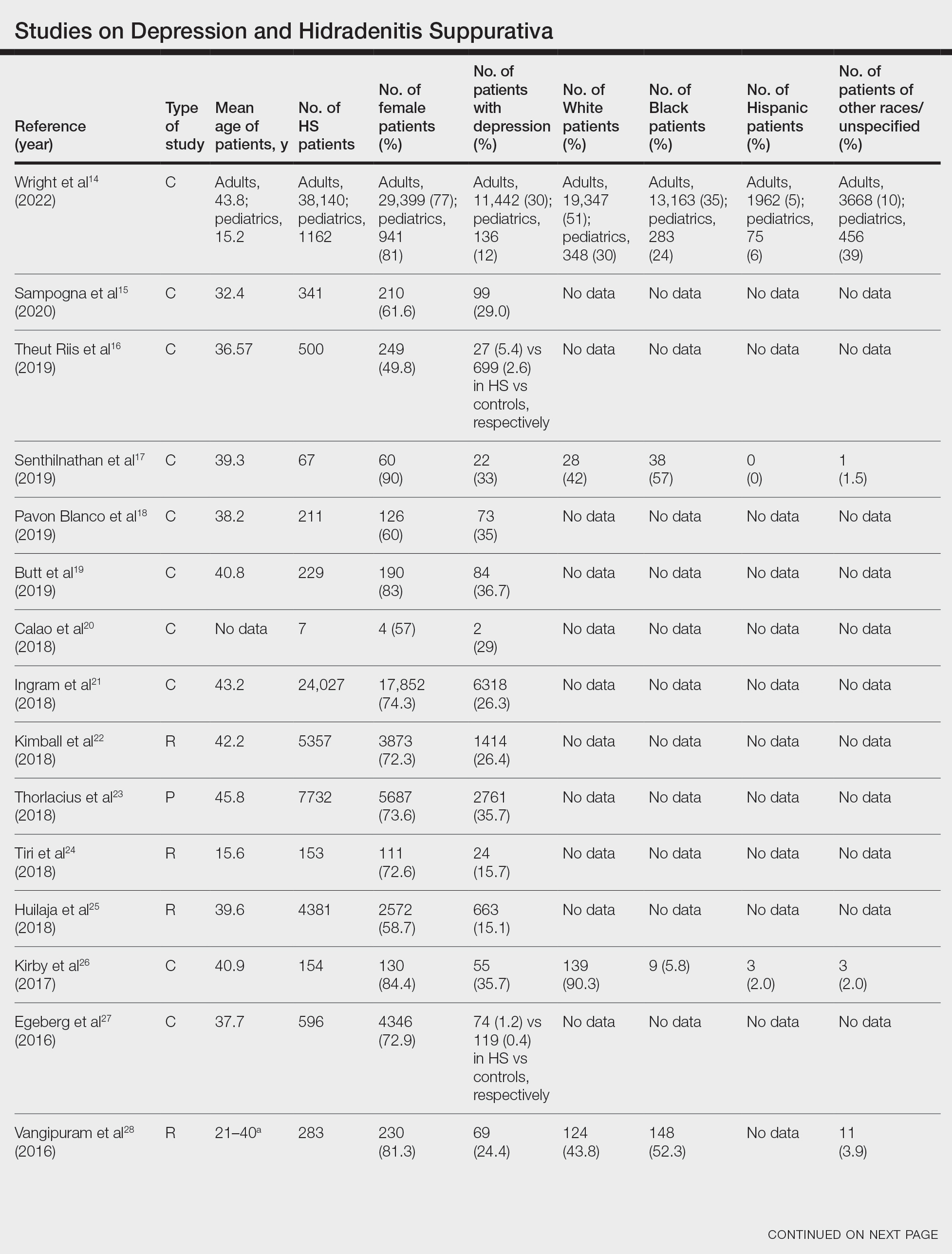
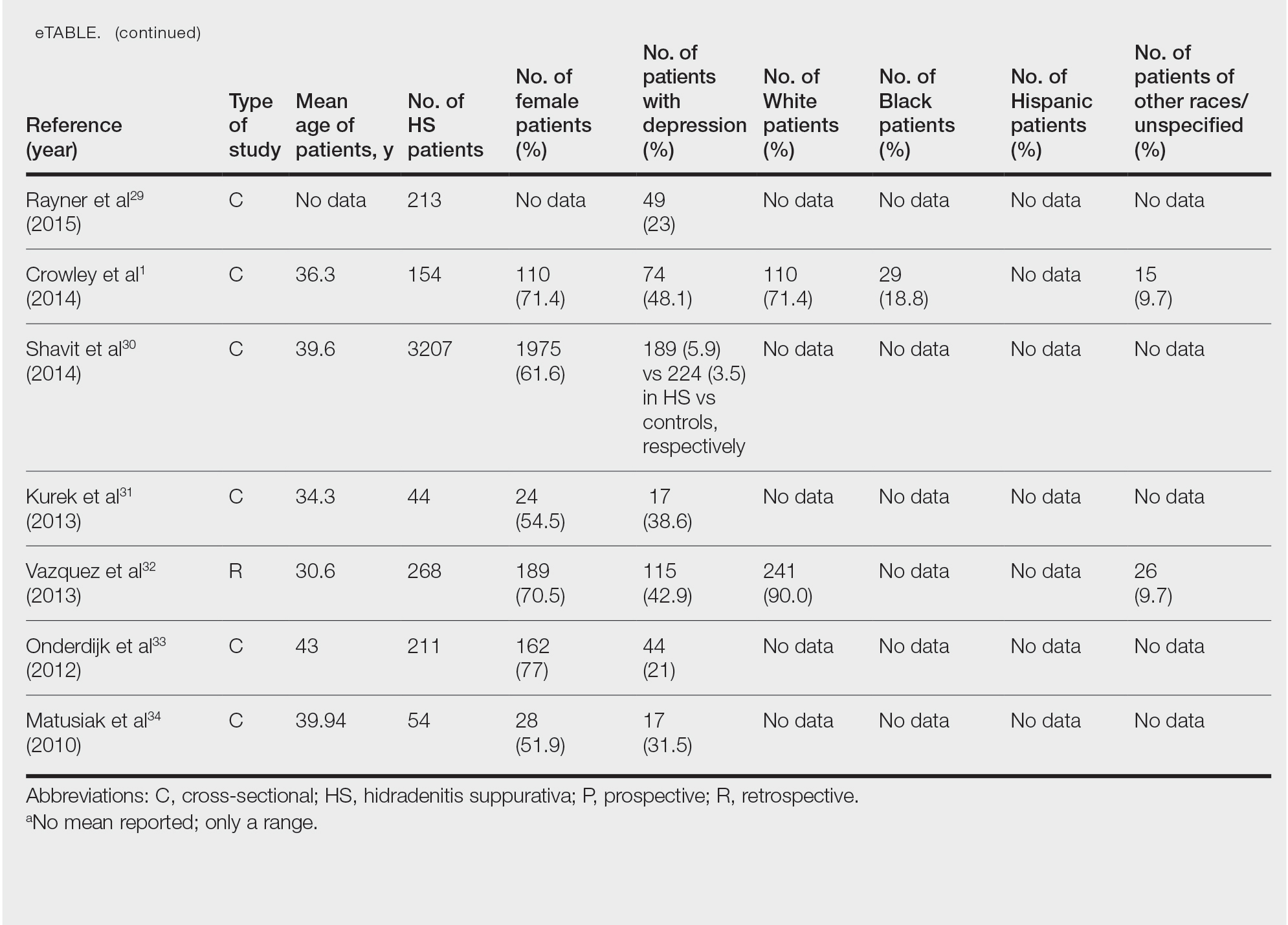
Hidradenitis suppurativa was found to coexist with depression in all the studies, with a prevalence of 1.2% to 48.1%. There also was a higher prevalence of depression in HS patients than in the control patients without HS. Furthermore, a recent study by Wright and colleagues14 stratified the depression prevalence data by age and found a higher prevalence of depression in adults vs children with HS (30% vs 12%).
Comment
Major depression—a chronic and debilitating illness—is the chief cause of disability globally and in the United States alone and has a global lifetime prevalence of 17%.35 In a study of 388 patients diagnosed with depression and 404 community-matched controls who were observed for 10 years, depressed patients had a two-thirds higher likelihood of developing a serious physical illness than controls. The depression-associated elevated risk for serious physical illness persisted after controlling for confounding variables such as alcohol abuse, smoking, and level of physical activity.36 Studies also have demonstrated that HS is more prevalent in Black individuals10 and in individuals of low SES,37 who are mostly the Black and Hispanic populations that experience the highest burden of racial microaggression38 and disparities in health access and outcomes.39,40 The severity and chronicity of major depressive disorder also is higher in Black patients compared with White patients (57% vs 39%).41 Because major depression and HS are most common among Black patients who experience the highest-burden negative financial and health disparities, there may be a shared genetic disposition to both medical conditions.
Moreover, the common detrimental lifestyle choices associated with patients with depression and HS also suggest the possibility of a collective genetic susceptibility. Patients with depression also report increased consumption of alcohol, tobacco, and illicit substances; sedentary lifestyle leading to obesity; and poor compliance with prescribed medical treatment.42 Smoking and obesity are known contributors to the pathogenesis of HS, and their modification also is known to positively impact the disease course. In a retrospective single-cohort study, 50% of obese HS patients (n=35) reported a substantial decrease in disease severity after a reduction of more than 15% in body mass index over 2 years following bariatric surgery (n=35).43 Patients with HS also have reported disease remission following extensive weight loss.44 In addition, evidence has supported smoking cessation in improving the disease course of HS.43 Because these detrimental lifestyle choices are prevalent in both patients with HS and those with depression, a co-genetic susceptibility also may exist.
Furthermore, depression is characterized by a persistent inflammatory state,13,45 similar to HS.46 Elevated levels of a variety of inflammatory markers, such as C-reactive protein (CRP), IL-6, and soluble intercellular adhesion molecule 1, have been reported in patients with depression compared with healthy controls.13,45 Further analysis found a positive correlation and a strong association between depression and these inflammatory markers.47 Moreover, adipokines regulate inflammatory responses, and adipokines play a role in the pathogenesis of HS. Adipokine levels such as elevated omentin-1 (a recently identified adipokine) were found to be altered in patients with HS compared with controls.48 Results from clinical studies and meta-analyses of patients with depression also have demonstrated that adipokines are dysregulated in this population,49,50 which may be another potential genetic link between depression and HS.
In addition, genetic susceptibility to depression and HS may be shared because the inflammatory markers that have a strong association with depression also have been found to play an important role in HS treatment and disease severity prediction. In a retrospective cohort study of 404 patients, CRP or IL-6 levels were found to be reliable predictors of HS disease severity, which may explain why anti–tumor necrosis factor antibody regimens such as adalimumab and infliximab have clinically ameliorated disease activity in several cases of HS.51 In a study evaluating these drugs, high baseline levels of high-sensitivity CRP and IL-6 were predictive of patient response to infliximab.52 In a meta-analysis evaluating 20,791 participants, an association was found between concurrent depression and CRP. Furthermore, inflammation measured by high levels of CRP or IL-6 was observed to predict future depression.53 If the same inflammatory markers—CRP and IL-6—both play a major role in the disease activity of depression and HS, then a concurrent genetic predisposition may exist.
Conclusion
Understanding the comorbidities, etiologies, and risk factors for the development and progression of HS is an important step toward improved disease management. Available studies on comorbid depression in HS largely involve White patients, and more studies are needed in patients with skin of color, particularly the Black population, who have the highest prevalence of HS.10 Given the evidence for an association between depression and HS, we suggest a large-scale investigation of this patient population that includes a complete medical history, onset of HS in comparison to the onset of depression, and specific measures of disease progress and lifetime management of depression, which may help to increase knowledge about the role of depression in HS and encourage more research in this area. If shared genetic susceptibility is established, aggressive management of depression in patients at risk for HS may reduce disease incidence and severity as well as the psychological burden on patients.
Hidradenitis suppurativa (HS)—a chronic, relapsing, inflammatory disorder involving terminal hair follicles in apocrine gland–rich skin—manifests as tender inflamed nodules that transform into abscesses, sinus tracts, and scarring.1,2 The etiology of HS is multifactorial, encompassing lifestyle, microbiota, hormonal status, and genetic and environmental factors. These factors activate the immune system around the terminal hair follicles and lead to hyperkeratosis of the infundibulum of the hair follicles in intertriginous regions. This progresses to follicular occlusion, stasis, and eventual rupture. Bacterial multiplication within the plugged pilosebaceous units further boosts immune activation. Resident and migrated cells of the innate and adaptive immune system then release proinflammatory cytokines such as tumor necrosis factor, IL-1β, and IL-17, which further enhance immune cell influx and inflammation.3,4 This aberrant immune response propagates the production of deep-seated inflammatory nodules and abscesses.3-8
The estimated prevalence of HS is 1% worldwide.9 It is more prevalent in female and Black patients (0.30%) than White patients (0.09%) and is intermediate in prevalence in the biracial population (0.22%).10 Hidradenitis suppurativa is thought to be associated with lower socioeconomic status (SES). In a retrospective analysis of HS patients (N=375), approximately one-third of patients were Black, had advanced disease, and had a notably lower SES.11 Furthermore, HS has been reported to be associated with systemic inflammation and comorbidities such as morbid obesity (38.3%) and hypertension (39.6%) as well as other metabolic syndrome–related disorders and depression (48.1%).1
Hidradenitis suppurativa may contribute to the risk for depression through its substantial impact on health-related quality of life, which culminates in social withdrawal, unemployment, and suicidal thoughts.12 The high prevalence of depression in individuals with HS1 and its association with systemic inflammation13 increases the likelihood that a common genetic predisposition also may exist between both conditions. Because depression frequently has been discovered as a concomitant diagnosis in patients with HS, we hypothesize that a shared genetic susceptibility also may exist between the 2 disorders. Our study sought to explore data on the co-occurrence of depression with HS, including its demographics and racial data.
Methods
We conducted a PubMed search of articles indexed for MEDLINE as well as Google Scholar using the terms depression and hidradenitis suppurativa to obtain all research articles published from 2000 to 2022. Articles were selected based on relevance to the topic of exploration. English-language articles that directly addressed the epidemiology, etiology, pathophysiology, and co-occurrence of both depression and HS with numerical data were included. Articles were excluded if they did not explore the information of interest on these 2 disorders or did not contain clear statistical data of patients with the 2 concurrent medical conditions.
Results
Twenty-two cross-sectional, prospective, and retrospective studies that fit the search criteria were identified and included in the analysis (eTable).1,14-34 Sixteen (72.7%) studies were cross-sectional, 5 (22.7%) were retrospective, and only 1 (4.5%) was a prospective study. Only 6 of the studies provided racial data,1,14,17,26,28,32 and of them, 4 had predominately White patients,1,14,26,32 whereas the other 2 had predominantly Black patients.17,28
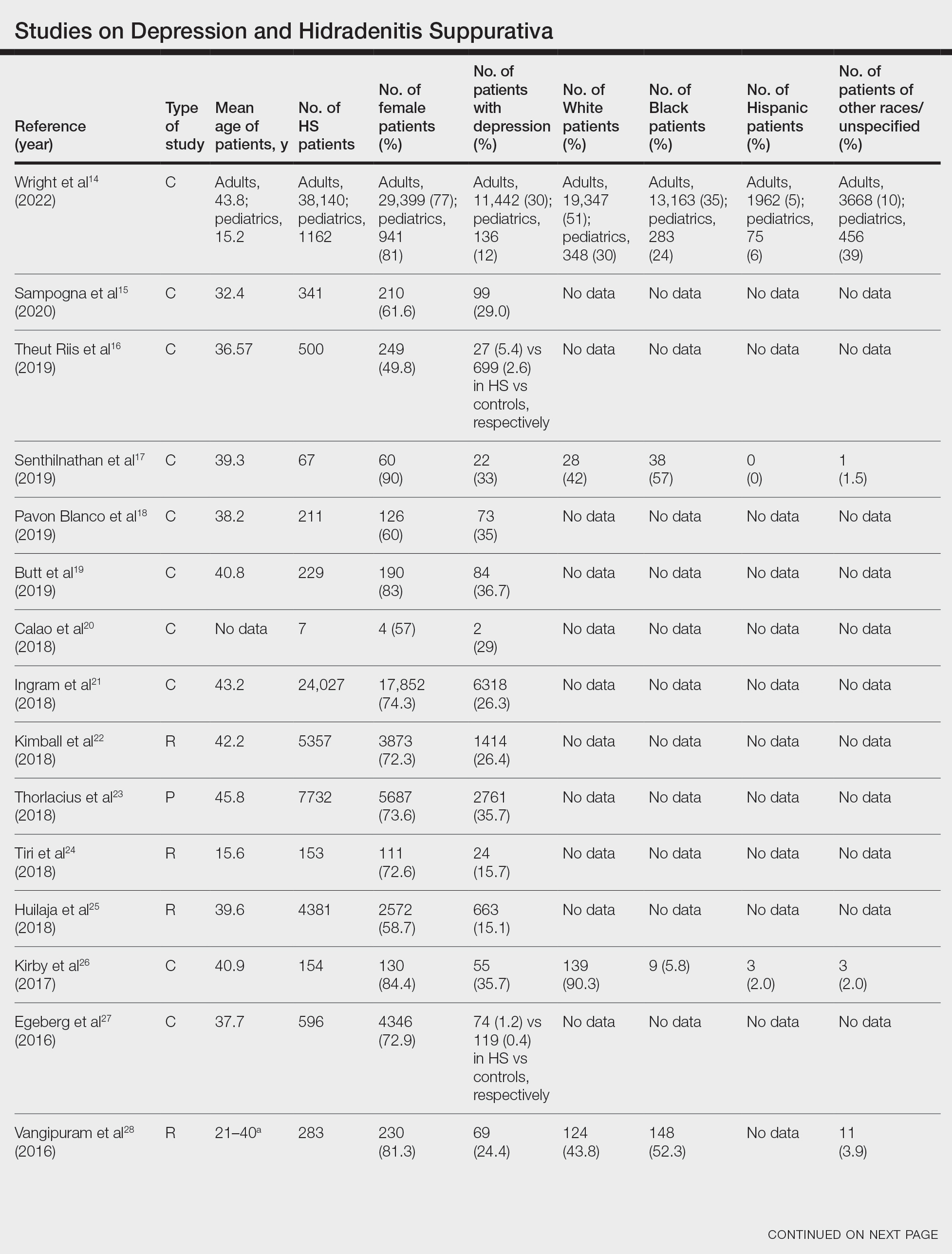
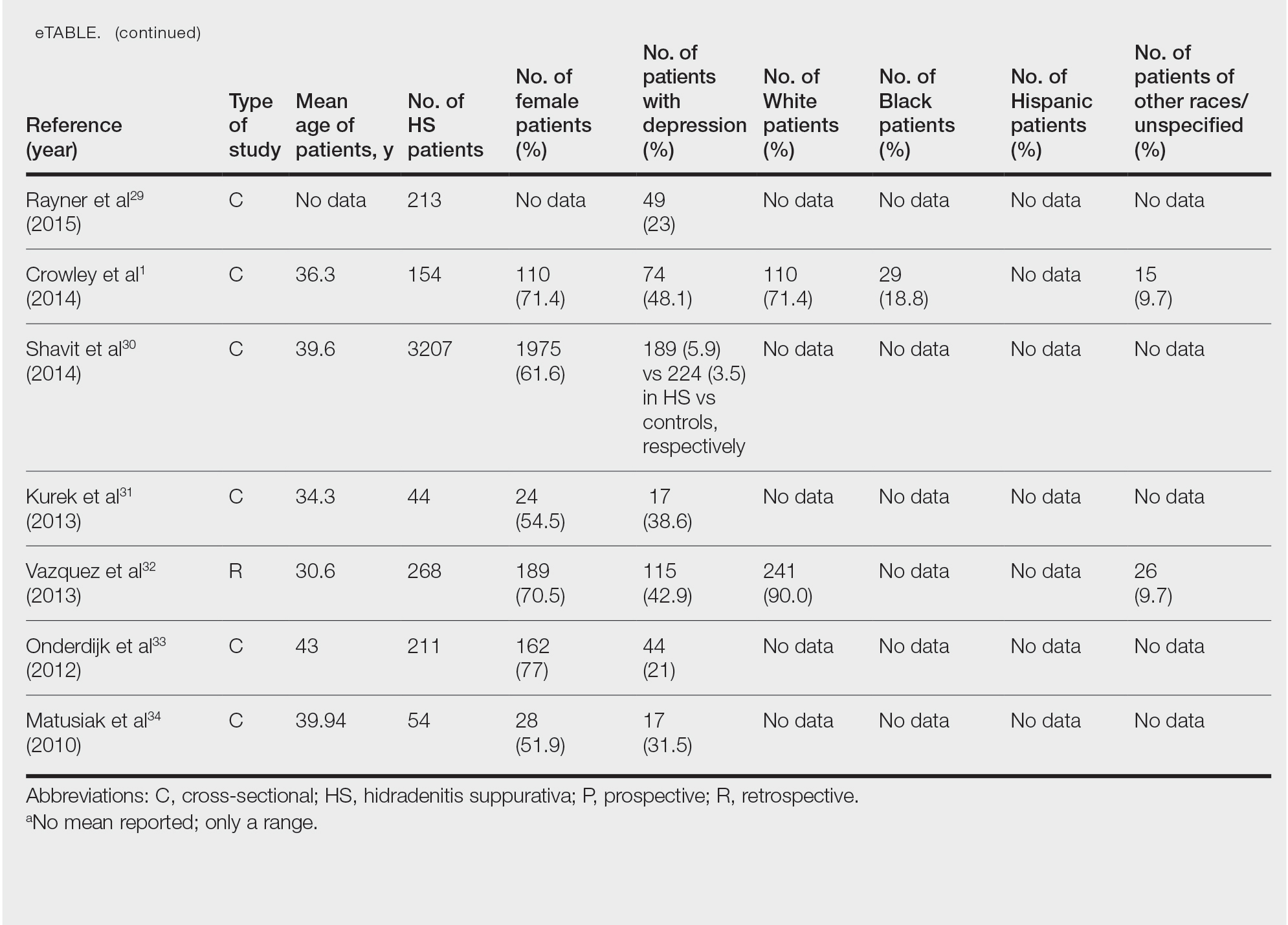
Hidradenitis suppurativa was found to coexist with depression in all the studies, with a prevalence of 1.2% to 48.1%. There also was a higher prevalence of depression in HS patients than in the control patients without HS. Furthermore, a recent study by Wright and colleagues14 stratified the depression prevalence data by age and found a higher prevalence of depression in adults vs children with HS (30% vs 12%).
Comment
Major depression—a chronic and debilitating illness—is the chief cause of disability globally and in the United States alone and has a global lifetime prevalence of 17%.35 In a study of 388 patients diagnosed with depression and 404 community-matched controls who were observed for 10 years, depressed patients had a two-thirds higher likelihood of developing a serious physical illness than controls. The depression-associated elevated risk for serious physical illness persisted after controlling for confounding variables such as alcohol abuse, smoking, and level of physical activity.36 Studies also have demonstrated that HS is more prevalent in Black individuals10 and in individuals of low SES,37 who are mostly the Black and Hispanic populations that experience the highest burden of racial microaggression38 and disparities in health access and outcomes.39,40 The severity and chronicity of major depressive disorder also is higher in Black patients compared with White patients (57% vs 39%).41 Because major depression and HS are most common among Black patients who experience the highest-burden negative financial and health disparities, there may be a shared genetic disposition to both medical conditions.
Moreover, the common detrimental lifestyle choices associated with patients with depression and HS also suggest the possibility of a collective genetic susceptibility. Patients with depression also report increased consumption of alcohol, tobacco, and illicit substances; sedentary lifestyle leading to obesity; and poor compliance with prescribed medical treatment.42 Smoking and obesity are known contributors to the pathogenesis of HS, and their modification also is known to positively impact the disease course. In a retrospective single-cohort study, 50% of obese HS patients (n=35) reported a substantial decrease in disease severity after a reduction of more than 15% in body mass index over 2 years following bariatric surgery (n=35).43 Patients with HS also have reported disease remission following extensive weight loss.44 In addition, evidence has supported smoking cessation in improving the disease course of HS.43 Because these detrimental lifestyle choices are prevalent in both patients with HS and those with depression, a co-genetic susceptibility also may exist.
Furthermore, depression is characterized by a persistent inflammatory state,13,45 similar to HS.46 Elevated levels of a variety of inflammatory markers, such as C-reactive protein (CRP), IL-6, and soluble intercellular adhesion molecule 1, have been reported in patients with depression compared with healthy controls.13,45 Further analysis found a positive correlation and a strong association between depression and these inflammatory markers.47 Moreover, adipokines regulate inflammatory responses, and adipokines play a role in the pathogenesis of HS. Adipokine levels such as elevated omentin-1 (a recently identified adipokine) were found to be altered in patients with HS compared with controls.48 Results from clinical studies and meta-analyses of patients with depression also have demonstrated that adipokines are dysregulated in this population,49,50 which may be another potential genetic link between depression and HS.
In addition, genetic susceptibility to depression and HS may be shared because the inflammatory markers that have a strong association with depression also have been found to play an important role in HS treatment and disease severity prediction. In a retrospective cohort study of 404 patients, CRP or IL-6 levels were found to be reliable predictors of HS disease severity, which may explain why anti–tumor necrosis factor antibody regimens such as adalimumab and infliximab have clinically ameliorated disease activity in several cases of HS.51 In a study evaluating these drugs, high baseline levels of high-sensitivity CRP and IL-6 were predictive of patient response to infliximab.52 In a meta-analysis evaluating 20,791 participants, an association was found between concurrent depression and CRP. Furthermore, inflammation measured by high levels of CRP or IL-6 was observed to predict future depression.53 If the same inflammatory markers—CRP and IL-6—both play a major role in the disease activity of depression and HS, then a concurrent genetic predisposition may exist.
Conclusion
Understanding the comorbidities, etiologies, and risk factors for the development and progression of HS is an important step toward improved disease management. Available studies on comorbid depression in HS largely involve White patients, and more studies are needed in patients with skin of color, particularly the Black population, who have the highest prevalence of HS.10 Given the evidence for an association between depression and HS, we suggest a large-scale investigation of this patient population that includes a complete medical history, onset of HS in comparison to the onset of depression, and specific measures of disease progress and lifetime management of depression, which may help to increase knowledge about the role of depression in HS and encourage more research in this area. If shared genetic susceptibility is established, aggressive management of depression in patients at risk for HS may reduce disease incidence and severity as well as the psychological burden on patients.
- Crowley JJ, Mekkes JR, Zouboulis CC, et al. Association of hidradenitis suppurativa disease severity with increased risk for systemic comorbidities. Br J Dermatol. 2014;171:1561-1565.
- Napolitano M, Megna M, Timoshchuk EA, et al. Hidradenitis suppurativa: from pathogenesis to diagnosis and treatment. Clin Cosmet Investig Dermatol. 2017;10:105-115.
- Sabat R, Jemec GBE, Matusiak Ł, et al. Hidradenitis suppurativa. Nat Rev Dis Prim. 2020;6:1-20.
- Wolk K, Warszawska K, Hoeflich C, et al. Deficiency of IL-22 contributes to a chronic inflammatory disease: pathogenetic mechanisms in acne inversa. J Immunol. 2011;186:1228-1239.
- von Laffert M, Helmbold P, Wohlrab J, et al. Hidradenitis suppurativa (acne inversa): early inflammatory events at terminal follicles and at interfollicular epidermis. Exp Dermatol. 2010;19:533-537.
- Van Der Zee HH, De Ruiter L, Van Den Broecke DG, et al. Elevated levels of tumour necrosis factor (TNF)-α, interleukin (IL)-1β and IL-10 in hidradenitis suppurativa skin: a rationale for targeting TNF-α and IL-1β. Br J Dermatol. 2011;164:1292-1298.
- Schlapbach C, Hänni T, Yawalkar N, et al. Expression of the IL-23/Th17 pathway in lesions of hidradenitis suppurativa. J Am Acad Dermatol. 2011;65:790-798.
- Kelly G, Hughes R, McGarry T, et al. Dysregulated cytokine expression in lesional and nonlesional skin in hidradenitis suppurativa. Br J Dermatol. 2015;173:1431-1439.
- Jemec GBE, Kimball AB. Hidradenitis suppurativa: epidemiology and scope of the problem. J Am Acad Dermatol. 2015;73(5 Suppl 1):S4-S7.
- Garg A, Kirby JS, Lavian J, et al. Sex- and age-adjusted population analysis of prevalence estimates for hidradenitis suppurativa in the United States. JAMA Dermatol. 2017;153:760-764.
- Soliman YS, Hoffman LK, Guzman AK, et al. African American patients with hidradenitis suppurativa have significant health care disparities: a retrospective study. J Cutan Med Surg. 2019;23:334-336.
- Garg A, Malviya N, Strunk A, et al. Comorbidity screening in hidradenitis suppurativa: evidence-based recommendations from the US and Canadian Hidradenitis Suppurativa Foundations. J Am Acad Dermatol. 2022;86:1092-1101.
- Beatriz Currier M, Nemeroff CB. Inflammation and mood disorders: proinflammatory cytokines and the pathogenesis of depression. Antiinflamm Antiallergy Agents Med Chem. 2012;9:212-220.
- Wright S, Strunk A, Garg A. Prevalence of depression among children, adolescents, and adults with hidradenitis suppurativa. J Am Acad Dermatol. 2022;86:55-60.
- Sampogna F, Fania L, Mastroeni S, et al. Correlation between depression, quality of life and clinical severity in patients with hidradenitis suppurativa. Acta Derm Venereol. 2020;100:1-6.
- Theut Riis P, Pedersen OB, Sigsgaard V, et al. Prevalence of patients with self-reported hidradenitis suppurativa in a cohort of Danish blood donors: a cross-sectional study. Br J Dermatol. 2019;180:774-781.
- Senthilnathan A, Kolli SS, Cardwell LA, et al. Depression in hidradenitis suppurativa. Br J Dermatol. 2019;181:1087-1088.
- Pavon Blanco A, Turner MA, Petrof G, et al. To what extent do disease severity and illness perceptions explain depression, anxiety and quality of life in hidradenitis suppurativa? Br J Dermatol. 2019;180:338-345.
- Butt M, Sisic M, Silva C, et al. The associations of depression and coping methods on health-related quality of life for those with hidradenitis suppurativa. J Am Acad Dermatol. 2019;80:1137-1139.
- Calao M, Wilson JL, Spelman L, et al. Hidradenitis suppurativa (HS) prevalence, demographics and management pathways in Australia: a population-based cross-sectional study. PLoS One. 2018;13:e0200683.
- Ingram JR, Jenkins-Jones S, Knipe DW, et al. Population-based Clinical Practice Research Datalink study using algorithm modelling to identify the true burden of hidradenitis suppurativa. Br J Dermatol. 2018;178:917-924.
- Kimball AB, Sundaram M, Gauthier G, et al. The comorbidity burden of hidradenitis suppurativa in the United States: a claims data analysis. Dermatol Ther (Heidelb). 2018;8:557.
- Thorlacius L, Cohen AD, Gislason GH, et al. Increased suicide risk in patients with hidradenitis suppurativa. J Invest Dermatol. 2018;138:52-57.
- Tiri H, Jokelainen J, Timonen M, et al. Somatic and psychiatric comorbidities of hidradenitis suppurativa in children and adolescents. J Am Acad Dermatol. 2018;79:514-519.
- Huilaja L, Tiri H, Jokelainen J, et al. Patients with hidradenitis suppurativa have a high psychiatric disease burden: a Finnish nationwide registry study. J Invest Dermatol. 2018;138:46-51.
- Kirby JS, Butt M, Esmann S, et al. Association of resilience with depression and health-related quality of life for patients with hidradenitis suppurativa. JAMA Dermatol. 2017;153:1263.
- Egeberg A, Gislason GH, Hansen PR. Risk of major adverse cardiovascular events and all-cause mortality in patients with hidradenitis suppurativa. JAMA Dermatol. 2016;152:429-434.
- Vangipuram R, Vaidya T, Jandarov R, et al. Factors contributing to depression and chronic pain in patients with hidradenitis suppurativa: results from a single-center retrospective review. Dermatology. 2016;232:692-695.
- Rayner L, Jackson K, Turner M, et al. Integrated mental health assessment in a tertiary medical dermatology service: feasibility and the prevalence of common mental disorder. Br J Dermatol. 2015;173:201.
- Shavit E, Dreiher J, Freud T, et al. Psychiatric comorbidities in 3207 patients with hidradenitis suppurativa [published online June 9, 2014]. J Eur Acad Dermatol Venereol. 2015;29:371-376.
- Kurek A, Johanne Peters EM, Sabat R, et al. Depression is a frequent co-morbidity in patients with acne inversa. J Dtsch Dermatol Ges. 2013;11:743-749.
- Vazquez BG, Alikhan A, Weaver AL, et al. Incidence of hidradenitis suppurativa and associated factors: a population-based study of Olmsted County, Minnesota. J Invest Dermatol. 2013;133:97.
- Onderdijk AJ, Van Der Zee HH, Esmann S, et al. Depression in patients with hidradenitis suppurativa [published online February 20, 2012]. J Eur Acad Dermatol Venereol. 2013;27:473-478.
- Matusiak Ł, Bieniek A, Szepietowski JC. Psychophysical aspects of hidradenitis suppurativa. Acta Derm Venereol. 2010;90:264-268.
- Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617-627.
- Holahan CJ, Pahl SA, Cronkite RC, et al. Depression and vulnerability to incident physical illness across 10 years. J Affect Disord. 2009;123:222-229.
- Deckers IE, Janse IC, van der Zee HH, et al. Hidradenitis suppurativa (HS) is associated with low socioeconomic status (SES): a cross-sectional reference study. J Am Acad Dermatol. 2016;75:755-759.e1.
- Williams MT, Skinta MD, Kanter JW, et al. A qualitative study of microaggressions against African Americans on predominantly White campuses. BMC Psychol. 2020;8:1-13.
- Dunlop DD, Song J, Lyons JS, et al. Racial/ethnic differences in rates of depression among preretirement adults. Am J Public Health. 2003;93:1945-1952.
- Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol. 2016;35:407-411.
- Williams DR, González HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and Non-Hispanic Whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305-315.
- Druss BG, Bradford DW, Rosenheck RA, et al. Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA. 2000;283:506-511.
- Kromann CB, Deckers IE, Esmann S, et al. Risk factors, clinical course and long-term prognosis in hidradenitis suppurativa: a cross-sectional study. Br J Dermatol. 2014;171:819-824.
- Sivanand A, Gulliver WP, Josan CK, et al. Weight loss and dietary interventions for hidradenitis suppurativa: a systematic review. J Cutan Med Surg . 2020;24:64-72.
- Raedler TJ. Inflammatory mechanisms in major depressive disorder. Curr Opin Psychiatry. 2011;24:519-525.
- Rocha VZ, Libby P. Obesity, inflammation, and atherosclerosis. Nat Rev Cardiol. 2009;6:399-409.
- Davidson KW, Schwartz JE, Kirkland SA, et al. Relation of inflammation to depression and incident coronary heart disease (from the Canadian Nova Scotia Health Survey [NSHS95] Prospective Population Study). Am J Cardiol. 2009;103:755-761.
- González-López MA, Ocejo-Viñals JG, Mata C, et al. Evaluation of serum omentin-1 and apelin concentrations in patients with hidradenitis suppurativa. Postepy Dermatol Alergol. 2021;38:450-454.
- Taylor VH, Macqueen GM. The role of adipokines in understanding the associations between obesity and depression. J Obes. 2010;2010:748048.
- Setayesh L, Ebrahimi R, Pooyan S, et al. The possible mediatory role of adipokines in the association between low carbohydrate diet and depressive symptoms among overweight and obese women. PLoS One. 2021;16:e0257275 .
- Andriano TM, Benesh G, Babbush KM, et al. Serum inflammatory markers and leukocyte profiles accurately describe hidradenitis suppurativa disease severity. Int J Dermatol. 2022;61:1270-1275.
- Montaudié H, Seitz-Polski B, Cornille A, et al. Interleukin 6 and high-sensitivity C-reactive protein are potential predictive markers of response to infliximab in hidradenitis suppurativa. J Am Acad Dermatol. 2017;6:156-158.
- Colasanto M, Madigan S, Korczak DJ. Depression and inflammation among children and adolescents: a meta-analysis. J Affect Disord. 2020;277:940-948.
- Crowley JJ, Mekkes JR, Zouboulis CC, et al. Association of hidradenitis suppurativa disease severity with increased risk for systemic comorbidities. Br J Dermatol. 2014;171:1561-1565.
- Napolitano M, Megna M, Timoshchuk EA, et al. Hidradenitis suppurativa: from pathogenesis to diagnosis and treatment. Clin Cosmet Investig Dermatol. 2017;10:105-115.
- Sabat R, Jemec GBE, Matusiak Ł, et al. Hidradenitis suppurativa. Nat Rev Dis Prim. 2020;6:1-20.
- Wolk K, Warszawska K, Hoeflich C, et al. Deficiency of IL-22 contributes to a chronic inflammatory disease: pathogenetic mechanisms in acne inversa. J Immunol. 2011;186:1228-1239.
- von Laffert M, Helmbold P, Wohlrab J, et al. Hidradenitis suppurativa (acne inversa): early inflammatory events at terminal follicles and at interfollicular epidermis. Exp Dermatol. 2010;19:533-537.
- Van Der Zee HH, De Ruiter L, Van Den Broecke DG, et al. Elevated levels of tumour necrosis factor (TNF)-α, interleukin (IL)-1β and IL-10 in hidradenitis suppurativa skin: a rationale for targeting TNF-α and IL-1β. Br J Dermatol. 2011;164:1292-1298.
- Schlapbach C, Hänni T, Yawalkar N, et al. Expression of the IL-23/Th17 pathway in lesions of hidradenitis suppurativa. J Am Acad Dermatol. 2011;65:790-798.
- Kelly G, Hughes R, McGarry T, et al. Dysregulated cytokine expression in lesional and nonlesional skin in hidradenitis suppurativa. Br J Dermatol. 2015;173:1431-1439.
- Jemec GBE, Kimball AB. Hidradenitis suppurativa: epidemiology and scope of the problem. J Am Acad Dermatol. 2015;73(5 Suppl 1):S4-S7.
- Garg A, Kirby JS, Lavian J, et al. Sex- and age-adjusted population analysis of prevalence estimates for hidradenitis suppurativa in the United States. JAMA Dermatol. 2017;153:760-764.
- Soliman YS, Hoffman LK, Guzman AK, et al. African American patients with hidradenitis suppurativa have significant health care disparities: a retrospective study. J Cutan Med Surg. 2019;23:334-336.
- Garg A, Malviya N, Strunk A, et al. Comorbidity screening in hidradenitis suppurativa: evidence-based recommendations from the US and Canadian Hidradenitis Suppurativa Foundations. J Am Acad Dermatol. 2022;86:1092-1101.
- Beatriz Currier M, Nemeroff CB. Inflammation and mood disorders: proinflammatory cytokines and the pathogenesis of depression. Antiinflamm Antiallergy Agents Med Chem. 2012;9:212-220.
- Wright S, Strunk A, Garg A. Prevalence of depression among children, adolescents, and adults with hidradenitis suppurativa. J Am Acad Dermatol. 2022;86:55-60.
- Sampogna F, Fania L, Mastroeni S, et al. Correlation between depression, quality of life and clinical severity in patients with hidradenitis suppurativa. Acta Derm Venereol. 2020;100:1-6.
- Theut Riis P, Pedersen OB, Sigsgaard V, et al. Prevalence of patients with self-reported hidradenitis suppurativa in a cohort of Danish blood donors: a cross-sectional study. Br J Dermatol. 2019;180:774-781.
- Senthilnathan A, Kolli SS, Cardwell LA, et al. Depression in hidradenitis suppurativa. Br J Dermatol. 2019;181:1087-1088.
- Pavon Blanco A, Turner MA, Petrof G, et al. To what extent do disease severity and illness perceptions explain depression, anxiety and quality of life in hidradenitis suppurativa? Br J Dermatol. 2019;180:338-345.
- Butt M, Sisic M, Silva C, et al. The associations of depression and coping methods on health-related quality of life for those with hidradenitis suppurativa. J Am Acad Dermatol. 2019;80:1137-1139.
- Calao M, Wilson JL, Spelman L, et al. Hidradenitis suppurativa (HS) prevalence, demographics and management pathways in Australia: a population-based cross-sectional study. PLoS One. 2018;13:e0200683.
- Ingram JR, Jenkins-Jones S, Knipe DW, et al. Population-based Clinical Practice Research Datalink study using algorithm modelling to identify the true burden of hidradenitis suppurativa. Br J Dermatol. 2018;178:917-924.
- Kimball AB, Sundaram M, Gauthier G, et al. The comorbidity burden of hidradenitis suppurativa in the United States: a claims data analysis. Dermatol Ther (Heidelb). 2018;8:557.
- Thorlacius L, Cohen AD, Gislason GH, et al. Increased suicide risk in patients with hidradenitis suppurativa. J Invest Dermatol. 2018;138:52-57.
- Tiri H, Jokelainen J, Timonen M, et al. Somatic and psychiatric comorbidities of hidradenitis suppurativa in children and adolescents. J Am Acad Dermatol. 2018;79:514-519.
- Huilaja L, Tiri H, Jokelainen J, et al. Patients with hidradenitis suppurativa have a high psychiatric disease burden: a Finnish nationwide registry study. J Invest Dermatol. 2018;138:46-51.
- Kirby JS, Butt M, Esmann S, et al. Association of resilience with depression and health-related quality of life for patients with hidradenitis suppurativa. JAMA Dermatol. 2017;153:1263.
- Egeberg A, Gislason GH, Hansen PR. Risk of major adverse cardiovascular events and all-cause mortality in patients with hidradenitis suppurativa. JAMA Dermatol. 2016;152:429-434.
- Vangipuram R, Vaidya T, Jandarov R, et al. Factors contributing to depression and chronic pain in patients with hidradenitis suppurativa: results from a single-center retrospective review. Dermatology. 2016;232:692-695.
- Rayner L, Jackson K, Turner M, et al. Integrated mental health assessment in a tertiary medical dermatology service: feasibility and the prevalence of common mental disorder. Br J Dermatol. 2015;173:201.
- Shavit E, Dreiher J, Freud T, et al. Psychiatric comorbidities in 3207 patients with hidradenitis suppurativa [published online June 9, 2014]. J Eur Acad Dermatol Venereol. 2015;29:371-376.
- Kurek A, Johanne Peters EM, Sabat R, et al. Depression is a frequent co-morbidity in patients with acne inversa. J Dtsch Dermatol Ges. 2013;11:743-749.
- Vazquez BG, Alikhan A, Weaver AL, et al. Incidence of hidradenitis suppurativa and associated factors: a population-based study of Olmsted County, Minnesota. J Invest Dermatol. 2013;133:97.
- Onderdijk AJ, Van Der Zee HH, Esmann S, et al. Depression in patients with hidradenitis suppurativa [published online February 20, 2012]. J Eur Acad Dermatol Venereol. 2013;27:473-478.
- Matusiak Ł, Bieniek A, Szepietowski JC. Psychophysical aspects of hidradenitis suppurativa. Acta Derm Venereol. 2010;90:264-268.
- Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617-627.
- Holahan CJ, Pahl SA, Cronkite RC, et al. Depression and vulnerability to incident physical illness across 10 years. J Affect Disord. 2009;123:222-229.
- Deckers IE, Janse IC, van der Zee HH, et al. Hidradenitis suppurativa (HS) is associated with low socioeconomic status (SES): a cross-sectional reference study. J Am Acad Dermatol. 2016;75:755-759.e1.
- Williams MT, Skinta MD, Kanter JW, et al. A qualitative study of microaggressions against African Americans on predominantly White campuses. BMC Psychol. 2020;8:1-13.
- Dunlop DD, Song J, Lyons JS, et al. Racial/ethnic differences in rates of depression among preretirement adults. Am J Public Health. 2003;93:1945-1952.
- Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol. 2016;35:407-411.
- Williams DR, González HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and Non-Hispanic Whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305-315.
- Druss BG, Bradford DW, Rosenheck RA, et al. Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA. 2000;283:506-511.
- Kromann CB, Deckers IE, Esmann S, et al. Risk factors, clinical course and long-term prognosis in hidradenitis suppurativa: a cross-sectional study. Br J Dermatol. 2014;171:819-824.
- Sivanand A, Gulliver WP, Josan CK, et al. Weight loss and dietary interventions for hidradenitis suppurativa: a systematic review. J Cutan Med Surg . 2020;24:64-72.
- Raedler TJ. Inflammatory mechanisms in major depressive disorder. Curr Opin Psychiatry. 2011;24:519-525.
- Rocha VZ, Libby P. Obesity, inflammation, and atherosclerosis. Nat Rev Cardiol. 2009;6:399-409.
- Davidson KW, Schwartz JE, Kirkland SA, et al. Relation of inflammation to depression and incident coronary heart disease (from the Canadian Nova Scotia Health Survey [NSHS95] Prospective Population Study). Am J Cardiol. 2009;103:755-761.
- González-López MA, Ocejo-Viñals JG, Mata C, et al. Evaluation of serum omentin-1 and apelin concentrations in patients with hidradenitis suppurativa. Postepy Dermatol Alergol. 2021;38:450-454.
- Taylor VH, Macqueen GM. The role of adipokines in understanding the associations between obesity and depression. J Obes. 2010;2010:748048.
- Setayesh L, Ebrahimi R, Pooyan S, et al. The possible mediatory role of adipokines in the association between low carbohydrate diet and depressive symptoms among overweight and obese women. PLoS One. 2021;16:e0257275 .
- Andriano TM, Benesh G, Babbush KM, et al. Serum inflammatory markers and leukocyte profiles accurately describe hidradenitis suppurativa disease severity. Int J Dermatol. 2022;61:1270-1275.
- Montaudié H, Seitz-Polski B, Cornille A, et al. Interleukin 6 and high-sensitivity C-reactive protein are potential predictive markers of response to infliximab in hidradenitis suppurativa. J Am Acad Dermatol. 2017;6:156-158.
- Colasanto M, Madigan S, Korczak DJ. Depression and inflammation among children and adolescents: a meta-analysis. J Affect Disord. 2020;277:940-948.
Practice Points
- Hidradenitis suppurativa (HS) is known to be associated with systemic inflammation and comorbidities, including depression.
- Depression may be a potential contributing factor to HS in affected patients, and studies on HS with comorbid depression in patients with skin of color are lacking.
Hyperkeratotic Nodule on the Knee in a Patient With KID Syndrome
The Diagnosis: Proliferating Pilar Cyst
Histopathology revealed an extensive lobulated epithelial proliferation in a characteristic “rolls and scrolls” pattern (Figure 1). This finding along with the patient’s prior diagnosis of keratitis-ichthyosisdeafness (KID) syndrome supported the diagnosis of a proliferating pilar cyst.
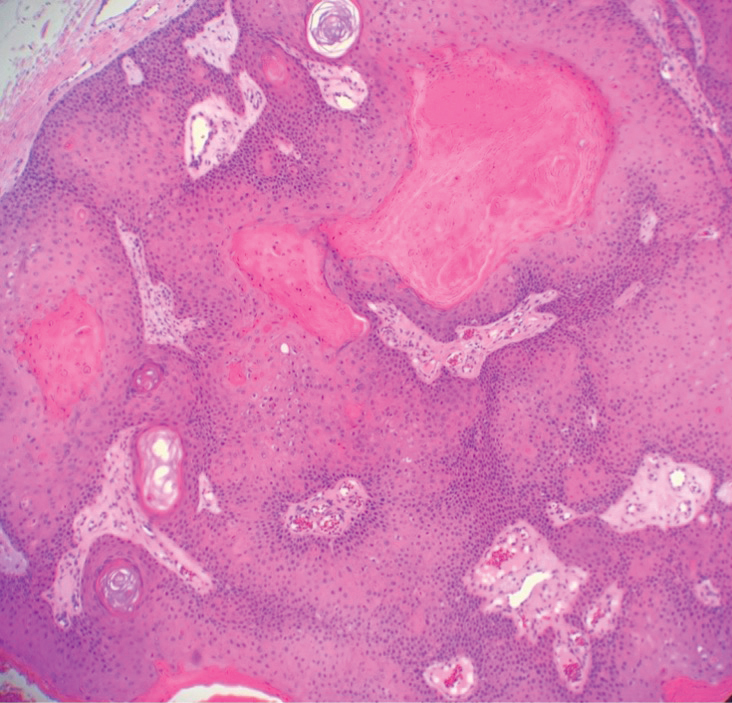
Pilar (or trichilemmal) cysts are common dermal cysts typically found on the outer root sheath of hair follicles. They clinically manifest as multiple yellow dome-shaped nodules without central puncta. They are slow growing and histologically are characterized as cysts with a stratified squamous epithelium demonstrating lack of a granular layer (trichilemmal keratinization) with bright red keratin contents and central focal calcification (Figure 2). Pilar cysts are more common in adult women and may be inherited through an autosomal-dominant pattern.1
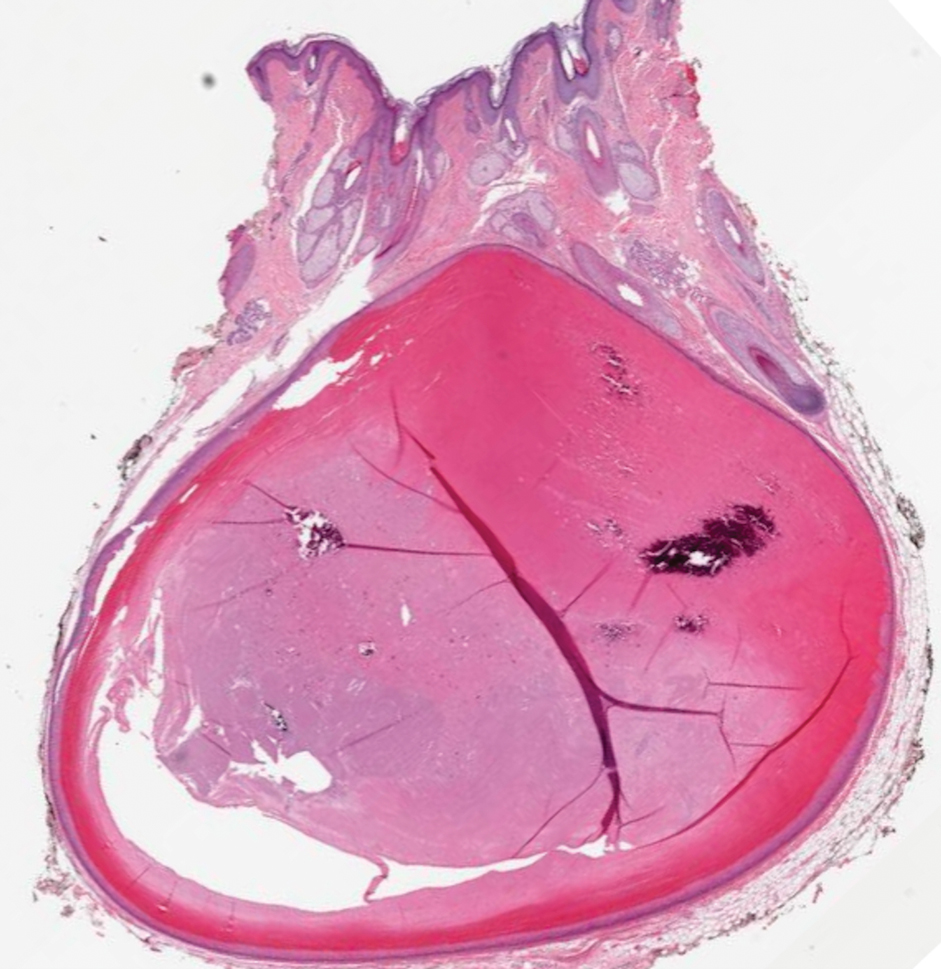
Proliferating pilar cysts represent less than 3% of all pilar cysts.2 In addition to the characteristic features of a pilar cyst, proliferating pilar cysts generally are larger (can be >6-cm wide) and are more ulcerative.3 Histopathology of proliferating pilar cysts reveals a more extensive epithelial proliferation, yielding a rolls and scrolls appearance, and may demonstrate nuclear atypia.4 Proliferating pilar cysts classically manifest as large, raised, smooth and/or ulcerated nodules on the scalp accompanied by areas of excessive hair growth in older women. They generally arise from pre-existing pilar cysts but also may occur sporadically.4
The development of multiple proliferating pilar cysts has been observed in patients with KID syndrome, a rare congenital ectodermal disorder characterized by a triad of vascularizing keratitis, hyperkeratosis, and sensorineural deafness.5,6 It is caused by a missense mutation of the GJB2 gene encoding for connexin 26, a gap junction that facilitates intercellular signaling and is expressed in a variety of structures including the cochlea, cornea, sweat glands, and inner and outer root sheaths of hair follicles.7
The differential diagnosis for proliferating pilar cysts includes pilomatrixomas, squamous cell carcinomas, and malignant proliferating pilar tumors. Pilomatrixomas (or calcifying epitheliomas of Malherbe) are the most common adnexal skin tumors in the pediatric population and most commonly present on the head, neck, and arms.8 They also can manifest in adults. Pilomatrixomas are benign dermal-subcutaneous tumors encapsulated by connective tissue that are found on the hair matrix and are histologically characterized by basaloid cells, shadow (or ghost) cells, dystrophic calcifications, and giant cells.9 The amount of basaloid cells and shadow cells can vary. Tumor progression results in the enucleation of the basaloid cells to form eosinophilic shadow cells in which calcification can occur. Giant cell granulomas may form contiguous with the calcifications. Both proliferating pilar cysts and pilomatrixomas have a rolls and scrolls appearance on low-power microscopy, but the latter are differentiated by their shadow cells and basaloid areas (Figure 3).
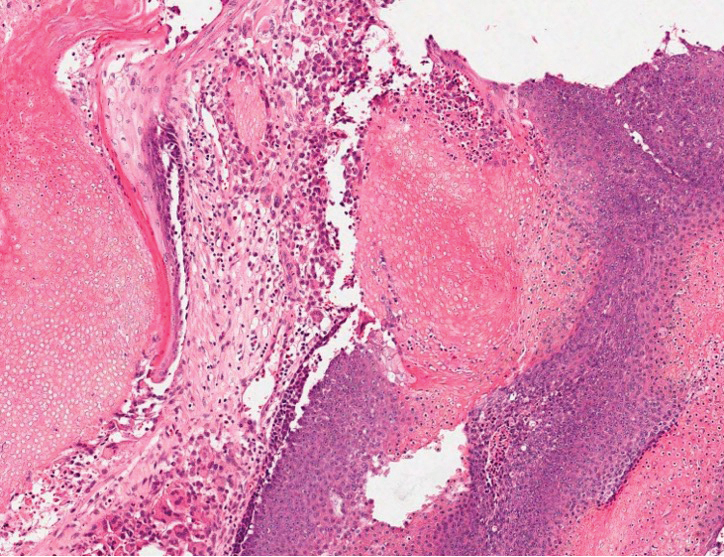
Squamous cell carcinoma (SCC) is the second most common nonmelanoma skin cancer and more commonly affects men. Risk factors for SCC include immunosuppression and exposure to UV radiation. Histopathology of well-differentiated SCCs reveals invasive squamous cells with larger nuclei and a glassy appearance in addition to possible mitotic figures and keratin pearls (Figure 4). They typically manifest in sun-exposed areas such as the scalp, face, forearms, dorsal aspects of the hands, and lower legs.10 Proliferating pilar tumors often lack the nuclear atypia and invasive architecture of a well-differentiated SCC.
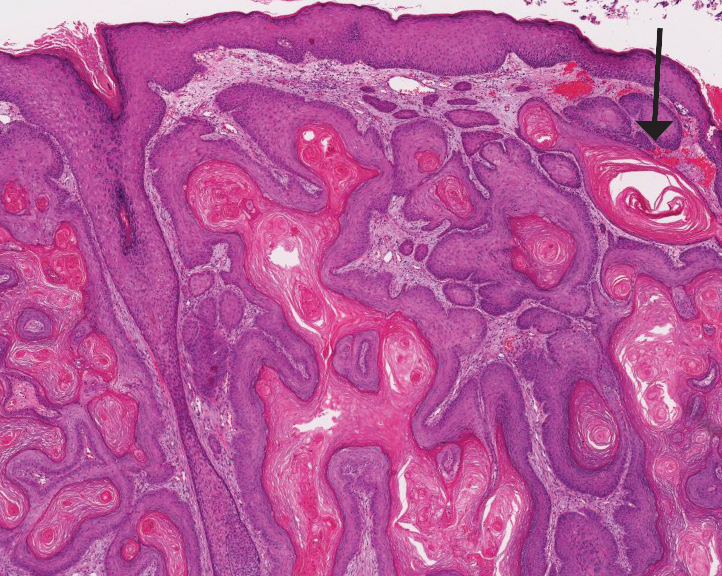
Features of malignant proliferating pilar tumors overlap with proliferating pilar cysts. In addition to the proliferative epithelium with abrupt trichilemmal keratinization that is typical of a proliferating pilar cyst, a malignant proliferating pilar tumor will demonstrate invasion into the surrounding tissue and lymph nodes, mitotic and architectural atypia, and necrosis (Figure 5).11 Malignant proliferating pilar tumors grow rapidly, ranging in size from 1 to 10 cm, and may develop from pre-existing or proliferating pilar cysts or de novo.
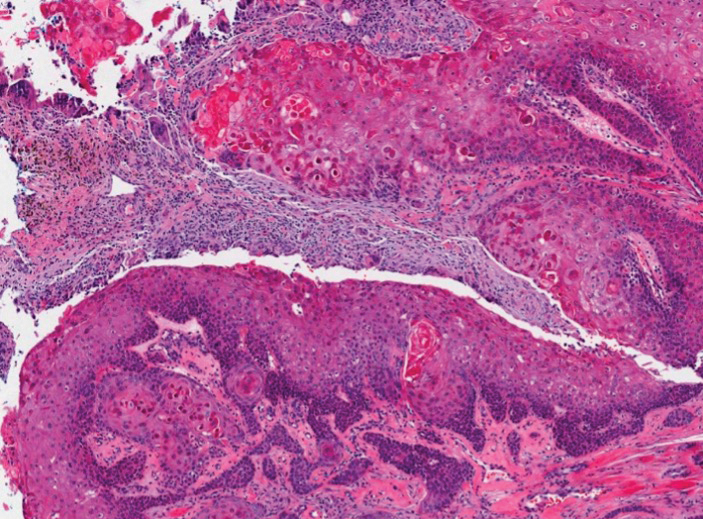
The development of multiple proliferating pilar cysts and thus increased risk for progression to malignant proliferating pilar tumors has been observed in patients with KID syndrome.6 Our case highlights the importance of early screening and recognition of proliferating pilar tumors in patients with this condition.
- Poiares Baptista A, Garcia E Silva L, Born MC. Proliferating trichilemmal cyst. J Cutan Pathol. 1983;10:178-187.
- Al Aboud DM, Yarrarapu SNS, Patel BC. Pilar cyst. StatPearls. StatPearls Publishing; 2023.
- Kim UG, Kook DB, Kim TH, et al. Trichilemmal carcinoma from proliferating trichilemmal cyst on the posterior neck [published online March 25, 2017]. Arch Craniofac Surg. 2017;18:50-53. doi:10.7181/acfs.2017.18.1.50
- Folpe AL, Reisenauer AK, Mentzel T, et al. Proliferating trichilemmal tumors: clinicopathologic evaluation is a guide to biologic behavior. J Cutan Pathol. 2003;30:492-498.
- Alsabbagh M. Keratitis-ichthyosis-deafness syndrome: a comprehensive review of cutaneous and systemic manifestations. Pediatr Dermatol. 2023;40:19-27.
- Nyquist GG, Mumm C, Grau R, et al. Malignant proliferating pilar tumors arising in KID syndrome: a report of two patients. Am J Med Genet A. 2007;143A:734-741.
- Richard G, Rouan F, Willoughby CE, et al. Missense mutations in GJB2 encoding connexin-26 cause the ectodermal dysplasia keratitis-ichthyosis-deafness syndrome. Am J Hum Genet. 2002;70: 1341-1348.
- Lee SI, Choi JH, Sung KY, et al. Proliferating pilar tumor of the cheek misdiagnosed as squamous cell carcinoma. Indian J Dermatol. 2022;67:207.
- Thompson LD. Pilomatricoma. Ear Nose Throat J. 2012;91:18-20.
- Waldman A, Schmults C. Cutaneous squamous cell carcinoma. Hematol Oncol Clin North Am. 2019;33:1-12.
- Cavanagh G, Negbenebor NA, Robinson-Bostom L, et al. Two cases of malignant proliferating trichilemmal tumor (MPTT) and review of literature. R I Med J (2013). 2022;105:12-16.
The Diagnosis: Proliferating Pilar Cyst
Histopathology revealed an extensive lobulated epithelial proliferation in a characteristic “rolls and scrolls” pattern (Figure 1). This finding along with the patient’s prior diagnosis of keratitis-ichthyosisdeafness (KID) syndrome supported the diagnosis of a proliferating pilar cyst.
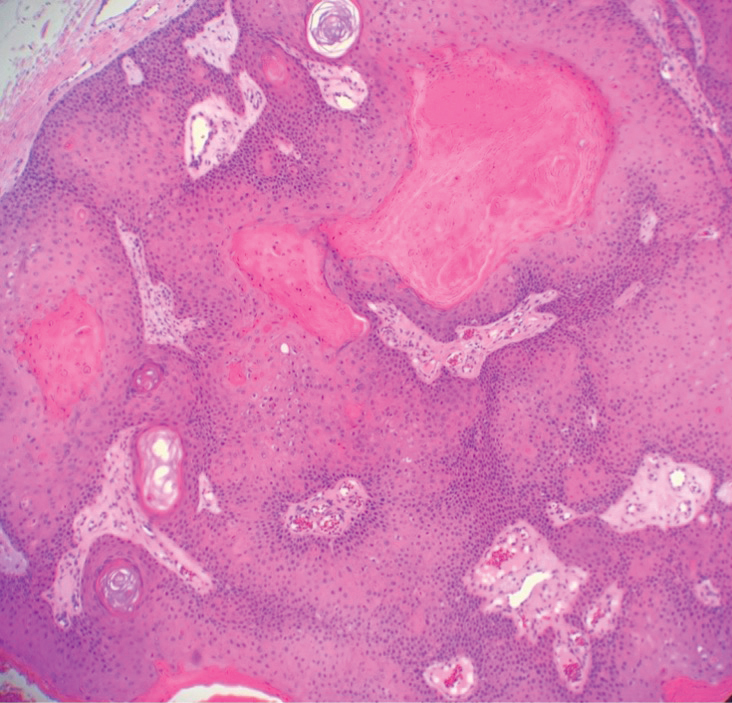
Pilar (or trichilemmal) cysts are common dermal cysts typically found on the outer root sheath of hair follicles. They clinically manifest as multiple yellow dome-shaped nodules without central puncta. They are slow growing and histologically are characterized as cysts with a stratified squamous epithelium demonstrating lack of a granular layer (trichilemmal keratinization) with bright red keratin contents and central focal calcification (Figure 2). Pilar cysts are more common in adult women and may be inherited through an autosomal-dominant pattern.1
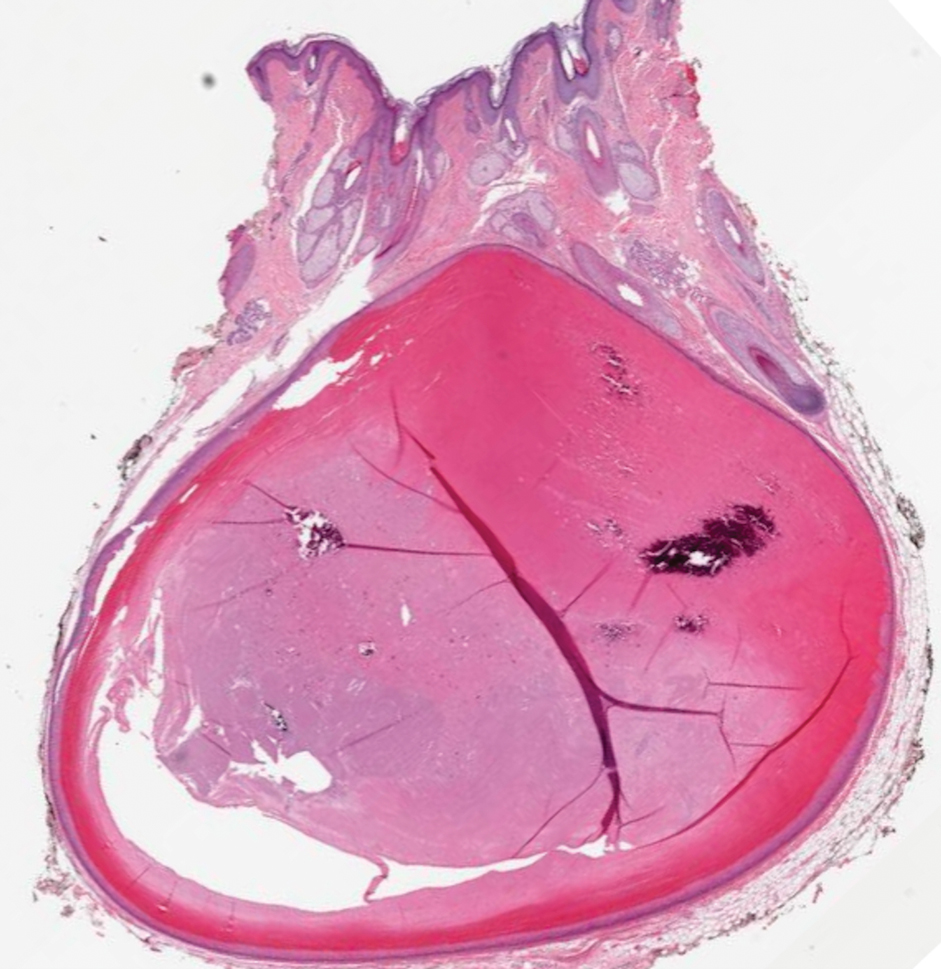
Proliferating pilar cysts represent less than 3% of all pilar cysts.2 In addition to the characteristic features of a pilar cyst, proliferating pilar cysts generally are larger (can be >6-cm wide) and are more ulcerative.3 Histopathology of proliferating pilar cysts reveals a more extensive epithelial proliferation, yielding a rolls and scrolls appearance, and may demonstrate nuclear atypia.4 Proliferating pilar cysts classically manifest as large, raised, smooth and/or ulcerated nodules on the scalp accompanied by areas of excessive hair growth in older women. They generally arise from pre-existing pilar cysts but also may occur sporadically.4
The development of multiple proliferating pilar cysts has been observed in patients with KID syndrome, a rare congenital ectodermal disorder characterized by a triad of vascularizing keratitis, hyperkeratosis, and sensorineural deafness.5,6 It is caused by a missense mutation of the GJB2 gene encoding for connexin 26, a gap junction that facilitates intercellular signaling and is expressed in a variety of structures including the cochlea, cornea, sweat glands, and inner and outer root sheaths of hair follicles.7
The differential diagnosis for proliferating pilar cysts includes pilomatrixomas, squamous cell carcinomas, and malignant proliferating pilar tumors. Pilomatrixomas (or calcifying epitheliomas of Malherbe) are the most common adnexal skin tumors in the pediatric population and most commonly present on the head, neck, and arms.8 They also can manifest in adults. Pilomatrixomas are benign dermal-subcutaneous tumors encapsulated by connective tissue that are found on the hair matrix and are histologically characterized by basaloid cells, shadow (or ghost) cells, dystrophic calcifications, and giant cells.9 The amount of basaloid cells and shadow cells can vary. Tumor progression results in the enucleation of the basaloid cells to form eosinophilic shadow cells in which calcification can occur. Giant cell granulomas may form contiguous with the calcifications. Both proliferating pilar cysts and pilomatrixomas have a rolls and scrolls appearance on low-power microscopy, but the latter are differentiated by their shadow cells and basaloid areas (Figure 3).
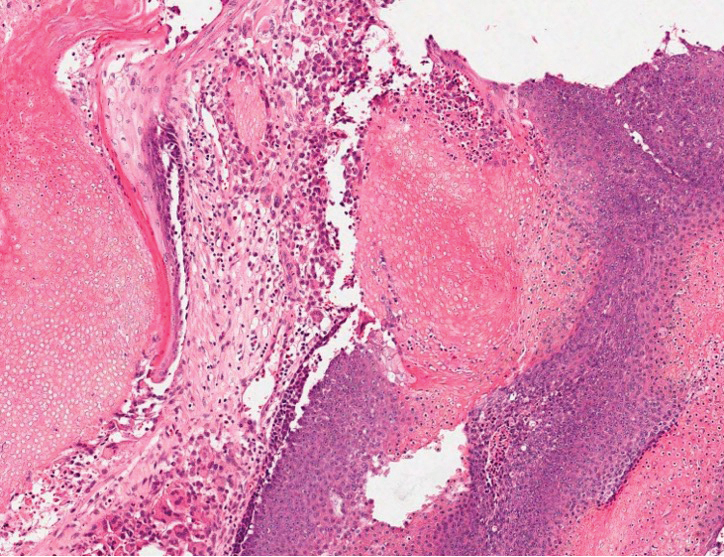
Squamous cell carcinoma (SCC) is the second most common nonmelanoma skin cancer and more commonly affects men. Risk factors for SCC include immunosuppression and exposure to UV radiation. Histopathology of well-differentiated SCCs reveals invasive squamous cells with larger nuclei and a glassy appearance in addition to possible mitotic figures and keratin pearls (Figure 4). They typically manifest in sun-exposed areas such as the scalp, face, forearms, dorsal aspects of the hands, and lower legs.10 Proliferating pilar tumors often lack the nuclear atypia and invasive architecture of a well-differentiated SCC.
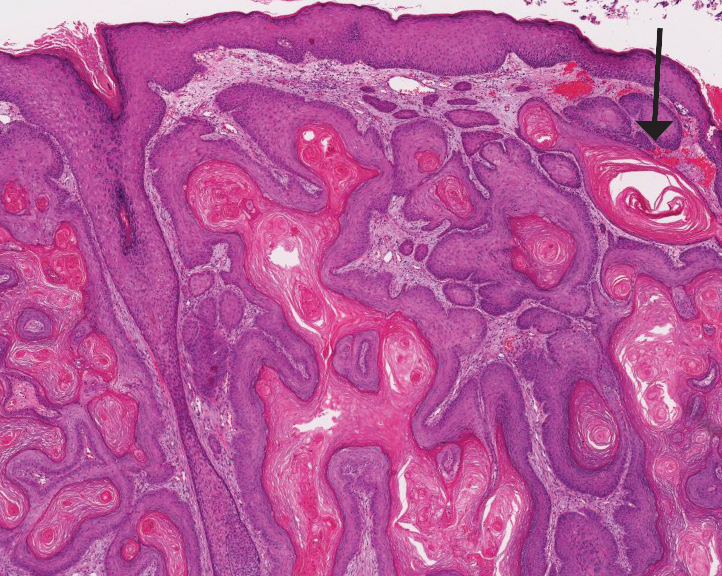
Features of malignant proliferating pilar tumors overlap with proliferating pilar cysts. In addition to the proliferative epithelium with abrupt trichilemmal keratinization that is typical of a proliferating pilar cyst, a malignant proliferating pilar tumor will demonstrate invasion into the surrounding tissue and lymph nodes, mitotic and architectural atypia, and necrosis (Figure 5).11 Malignant proliferating pilar tumors grow rapidly, ranging in size from 1 to 10 cm, and may develop from pre-existing or proliferating pilar cysts or de novo.
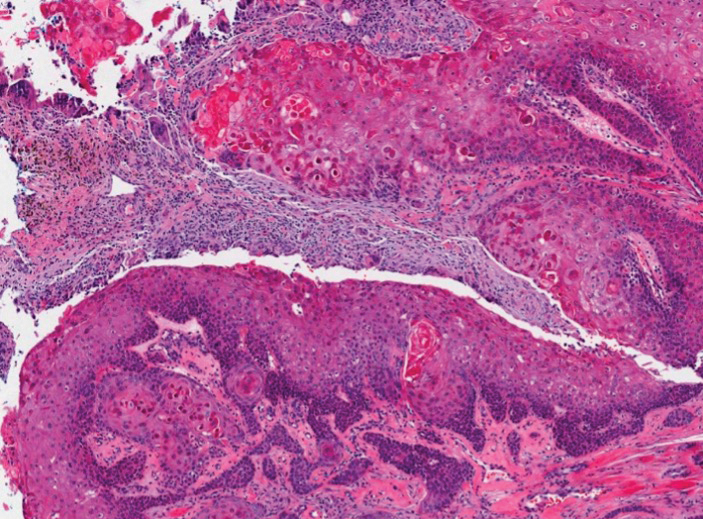
The development of multiple proliferating pilar cysts and thus increased risk for progression to malignant proliferating pilar tumors has been observed in patients with KID syndrome.6 Our case highlights the importance of early screening and recognition of proliferating pilar tumors in patients with this condition.
The Diagnosis: Proliferating Pilar Cyst
Histopathology revealed an extensive lobulated epithelial proliferation in a characteristic “rolls and scrolls” pattern (Figure 1). This finding along with the patient’s prior diagnosis of keratitis-ichthyosisdeafness (KID) syndrome supported the diagnosis of a proliferating pilar cyst.
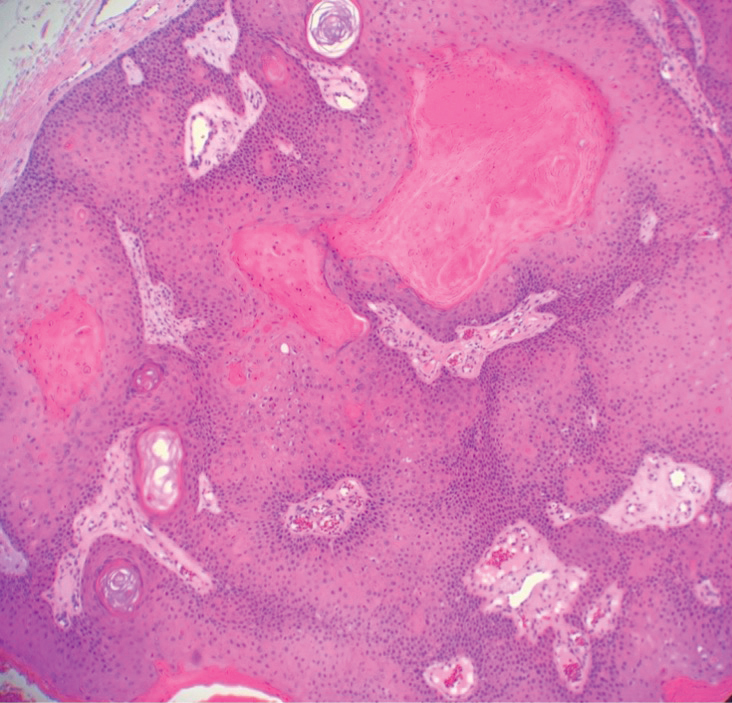
Pilar (or trichilemmal) cysts are common dermal cysts typically found on the outer root sheath of hair follicles. They clinically manifest as multiple yellow dome-shaped nodules without central puncta. They are slow growing and histologically are characterized as cysts with a stratified squamous epithelium demonstrating lack of a granular layer (trichilemmal keratinization) with bright red keratin contents and central focal calcification (Figure 2). Pilar cysts are more common in adult women and may be inherited through an autosomal-dominant pattern.1
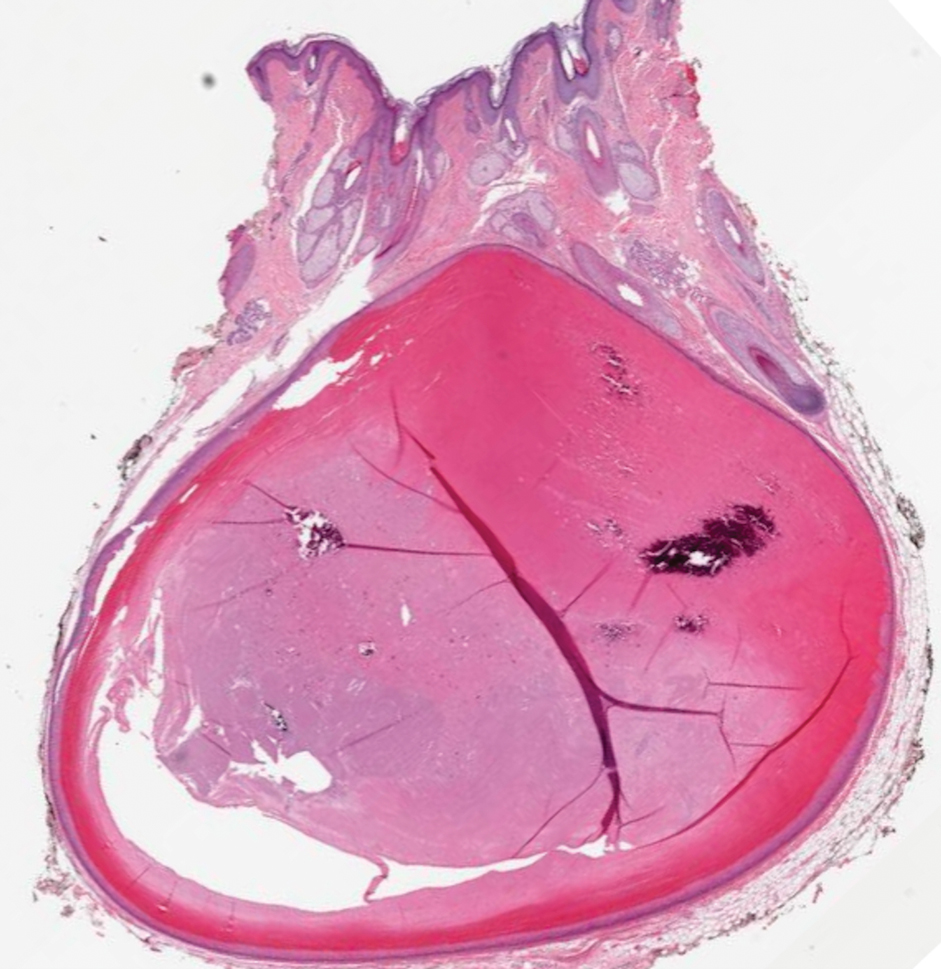
Proliferating pilar cysts represent less than 3% of all pilar cysts.2 In addition to the characteristic features of a pilar cyst, proliferating pilar cysts generally are larger (can be >6-cm wide) and are more ulcerative.3 Histopathology of proliferating pilar cysts reveals a more extensive epithelial proliferation, yielding a rolls and scrolls appearance, and may demonstrate nuclear atypia.4 Proliferating pilar cysts classically manifest as large, raised, smooth and/or ulcerated nodules on the scalp accompanied by areas of excessive hair growth in older women. They generally arise from pre-existing pilar cysts but also may occur sporadically.4
The development of multiple proliferating pilar cysts has been observed in patients with KID syndrome, a rare congenital ectodermal disorder characterized by a triad of vascularizing keratitis, hyperkeratosis, and sensorineural deafness.5,6 It is caused by a missense mutation of the GJB2 gene encoding for connexin 26, a gap junction that facilitates intercellular signaling and is expressed in a variety of structures including the cochlea, cornea, sweat glands, and inner and outer root sheaths of hair follicles.7
The differential diagnosis for proliferating pilar cysts includes pilomatrixomas, squamous cell carcinomas, and malignant proliferating pilar tumors. Pilomatrixomas (or calcifying epitheliomas of Malherbe) are the most common adnexal skin tumors in the pediatric population and most commonly present on the head, neck, and arms.8 They also can manifest in adults. Pilomatrixomas are benign dermal-subcutaneous tumors encapsulated by connective tissue that are found on the hair matrix and are histologically characterized by basaloid cells, shadow (or ghost) cells, dystrophic calcifications, and giant cells.9 The amount of basaloid cells and shadow cells can vary. Tumor progression results in the enucleation of the basaloid cells to form eosinophilic shadow cells in which calcification can occur. Giant cell granulomas may form contiguous with the calcifications. Both proliferating pilar cysts and pilomatrixomas have a rolls and scrolls appearance on low-power microscopy, but the latter are differentiated by their shadow cells and basaloid areas (Figure 3).
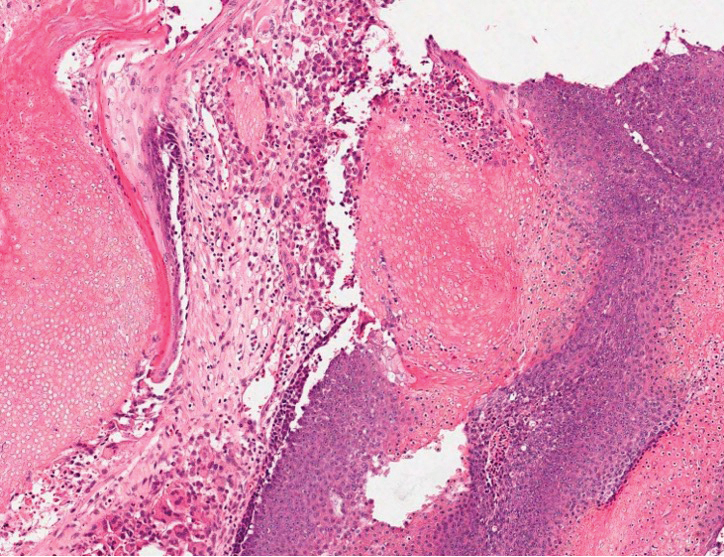
Squamous cell carcinoma (SCC) is the second most common nonmelanoma skin cancer and more commonly affects men. Risk factors for SCC include immunosuppression and exposure to UV radiation. Histopathology of well-differentiated SCCs reveals invasive squamous cells with larger nuclei and a glassy appearance in addition to possible mitotic figures and keratin pearls (Figure 4). They typically manifest in sun-exposed areas such as the scalp, face, forearms, dorsal aspects of the hands, and lower legs.10 Proliferating pilar tumors often lack the nuclear atypia and invasive architecture of a well-differentiated SCC.
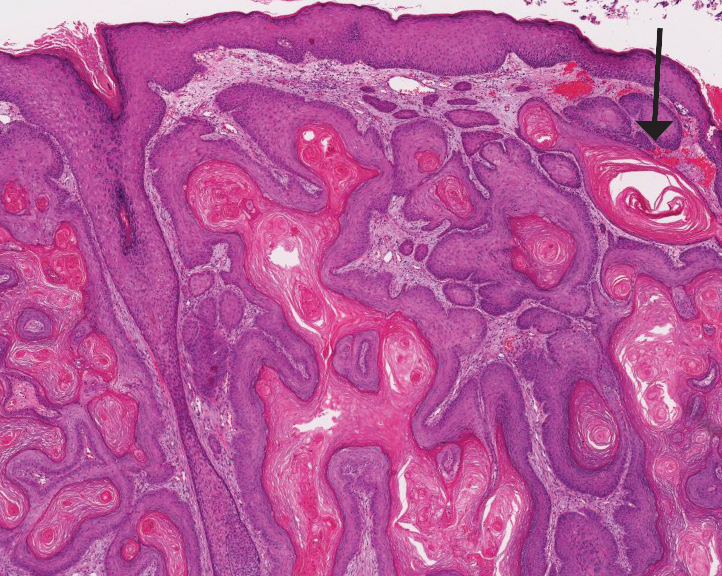
Features of malignant proliferating pilar tumors overlap with proliferating pilar cysts. In addition to the proliferative epithelium with abrupt trichilemmal keratinization that is typical of a proliferating pilar cyst, a malignant proliferating pilar tumor will demonstrate invasion into the surrounding tissue and lymph nodes, mitotic and architectural atypia, and necrosis (Figure 5).11 Malignant proliferating pilar tumors grow rapidly, ranging in size from 1 to 10 cm, and may develop from pre-existing or proliferating pilar cysts or de novo.
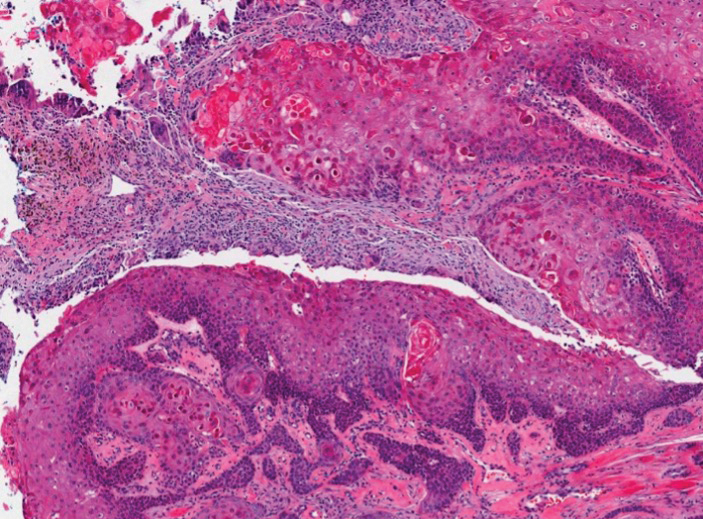
The development of multiple proliferating pilar cysts and thus increased risk for progression to malignant proliferating pilar tumors has been observed in patients with KID syndrome.6 Our case highlights the importance of early screening and recognition of proliferating pilar tumors in patients with this condition.
- Poiares Baptista A, Garcia E Silva L, Born MC. Proliferating trichilemmal cyst. J Cutan Pathol. 1983;10:178-187.
- Al Aboud DM, Yarrarapu SNS, Patel BC. Pilar cyst. StatPearls. StatPearls Publishing; 2023.
- Kim UG, Kook DB, Kim TH, et al. Trichilemmal carcinoma from proliferating trichilemmal cyst on the posterior neck [published online March 25, 2017]. Arch Craniofac Surg. 2017;18:50-53. doi:10.7181/acfs.2017.18.1.50
- Folpe AL, Reisenauer AK, Mentzel T, et al. Proliferating trichilemmal tumors: clinicopathologic evaluation is a guide to biologic behavior. J Cutan Pathol. 2003;30:492-498.
- Alsabbagh M. Keratitis-ichthyosis-deafness syndrome: a comprehensive review of cutaneous and systemic manifestations. Pediatr Dermatol. 2023;40:19-27.
- Nyquist GG, Mumm C, Grau R, et al. Malignant proliferating pilar tumors arising in KID syndrome: a report of two patients. Am J Med Genet A. 2007;143A:734-741.
- Richard G, Rouan F, Willoughby CE, et al. Missense mutations in GJB2 encoding connexin-26 cause the ectodermal dysplasia keratitis-ichthyosis-deafness syndrome. Am J Hum Genet. 2002;70: 1341-1348.
- Lee SI, Choi JH, Sung KY, et al. Proliferating pilar tumor of the cheek misdiagnosed as squamous cell carcinoma. Indian J Dermatol. 2022;67:207.
- Thompson LD. Pilomatricoma. Ear Nose Throat J. 2012;91:18-20.
- Waldman A, Schmults C. Cutaneous squamous cell carcinoma. Hematol Oncol Clin North Am. 2019;33:1-12.
- Cavanagh G, Negbenebor NA, Robinson-Bostom L, et al. Two cases of malignant proliferating trichilemmal tumor (MPTT) and review of literature. R I Med J (2013). 2022;105:12-16.
- Poiares Baptista A, Garcia E Silva L, Born MC. Proliferating trichilemmal cyst. J Cutan Pathol. 1983;10:178-187.
- Al Aboud DM, Yarrarapu SNS, Patel BC. Pilar cyst. StatPearls. StatPearls Publishing; 2023.
- Kim UG, Kook DB, Kim TH, et al. Trichilemmal carcinoma from proliferating trichilemmal cyst on the posterior neck [published online March 25, 2017]. Arch Craniofac Surg. 2017;18:50-53. doi:10.7181/acfs.2017.18.1.50
- Folpe AL, Reisenauer AK, Mentzel T, et al. Proliferating trichilemmal tumors: clinicopathologic evaluation is a guide to biologic behavior. J Cutan Pathol. 2003;30:492-498.
- Alsabbagh M. Keratitis-ichthyosis-deafness syndrome: a comprehensive review of cutaneous and systemic manifestations. Pediatr Dermatol. 2023;40:19-27.
- Nyquist GG, Mumm C, Grau R, et al. Malignant proliferating pilar tumors arising in KID syndrome: a report of two patients. Am J Med Genet A. 2007;143A:734-741.
- Richard G, Rouan F, Willoughby CE, et al. Missense mutations in GJB2 encoding connexin-26 cause the ectodermal dysplasia keratitis-ichthyosis-deafness syndrome. Am J Hum Genet. 2002;70: 1341-1348.
- Lee SI, Choi JH, Sung KY, et al. Proliferating pilar tumor of the cheek misdiagnosed as squamous cell carcinoma. Indian J Dermatol. 2022;67:207.
- Thompson LD. Pilomatricoma. Ear Nose Throat J. 2012;91:18-20.
- Waldman A, Schmults C. Cutaneous squamous cell carcinoma. Hematol Oncol Clin North Am. 2019;33:1-12.
- Cavanagh G, Negbenebor NA, Robinson-Bostom L, et al. Two cases of malignant proliferating trichilemmal tumor (MPTT) and review of literature. R I Med J (2013). 2022;105:12-16.
A 28-year-old man presented with an 8-mm, tender, mildly hyperkeratotic nodule on the right knee (top) of unknown duration. He had a history of mild keratitis-ichthyosis-deafness (KID) syndrome that was diagnosed based on the presence of congenital erythrokeratoderma, hearing issues identified at 2 years of age, palmoplantar keratoderma, keratitis, photophobia, chronic fungal nail infections, and alopecia and later was confirmed with a chromosome microarray for the GJB2 gene, which is associated with a connexin 26 mutation. A shave biopsy of the nodule was performed (bottom).
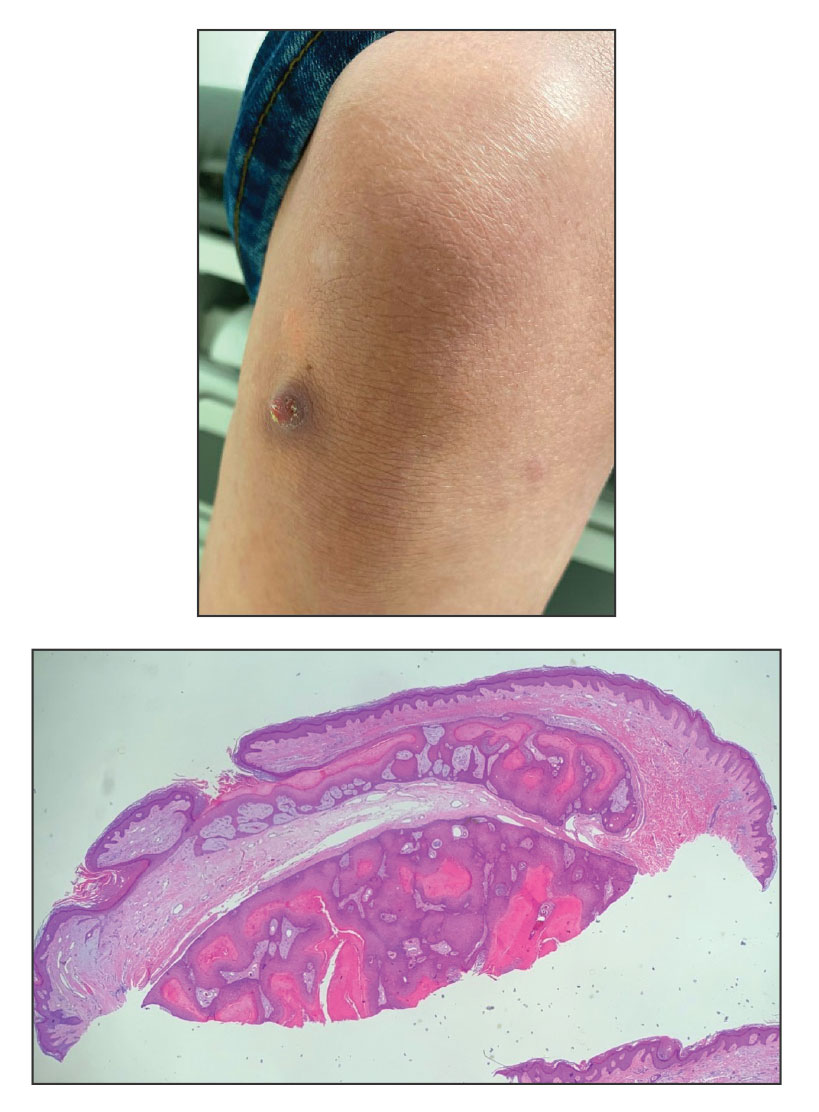
Aquatic Antagonists: Scorpionfish Envenomation
With the growing popularity of water sports and a proliferation of invasive species, human injuries from marine animal envenomation continue to rise.1-3 Members of the scorpionfish family Scorpaenidae are second only to stingrays as the leading cause of the 40,000 to 50,000 injuries annually from marine life worldwide.4 Because scorpionfish represent a growing threat and competition with native species, it has been suggested that they could replace endangered species on restaurant menus.5-8 Scorpionfish have been introduced by humans from tropical to temperate seas and are now common off the coast of California and the eastern coast from New York to Florida, as well as in the Caribbean, the Bahamas, and off the southern coast of Brazil. Victims of scorpionfish stings experience considerable pain and may require days to weeks to fully recover, highlighting the socioeconomic costs and burden of scorpionfish envenomation.9,10 Fishers, divers, swimmers, and aquarium owners are most often affected.
Family
The common term scorpionfish refers to both the family Scorpaenidae and the genus Scorpaena. Members of this family possess similar dorsal, anal, and pelvic fins, though they vary between genera in their size and the potency of the venom they insulate. Other familiar members include the genus Pterois (lionfish) and Synanceja (stonefish). Synanceja are the most venomous within the group, but scorpionfish stings more commonly arise from Pterois and Scorpaena.8 Because of the rare shapes and vibrant colors of scorpionfish, some traders and aquarium owners will seek and pay high prices for these fish, providing further opportunity for envenomation.11,12
Characteristics
Scorpionfish have with a high variation in color, ranging from lighter grays to intense reds depending on their geographic location and habitat. Synanceja are bland in coloration, blending in with rocks and gravel, but the more dramatic-appearing Scorpaena exhibit a large cranium and wide range of multicolored patterns (Figure 1).13 Pterois serve as the most conspicuous member of the group with brightly colored red and white stripes (Figure 2). Scorpionfish commonly grow up to 19 inches long and boast 12 dorsal, 2 pelvic, and 3 anal spines housing 5 to 10 mg of venom.14 An integumentary sheath encapsulates each spine housing the glandular tissue that produces the potent venom.

Toxin Properties
Unlike Pterois and Synanceja, Scorpaena do not have venom ducts around their glands, complicating the work of marine biologists aiming to extract and study the venomous toxins. Several studies have managed to isolate scorpionfish venom and overcome its unstable heat-labile nature to investigate its biologic properties.15-20 Several high-molecular-weight proteins (50–800 kDa) comprise the venom, including hyaluronidase, integrin-inhibiting factors, capillary permeability factor, proteases, and some less-understood cytolytic toxins. These factors provoke the inflammatory, proteolytic, hemorrhagic, cardiovascular, and hemolytic biologic activities at both the local and systemic levels, directing damage to wounded tissues and inducing vascular and tissue permeability to reach cellular processes far and wide. Mediators of inflammation include tumor necrosis factor, IL-6, and monocyte chemoattractant protein 1, followed by neutrophils and other mononuclear cells, initiating the immune response at the wound site. Toxin potency remains for up to 2 days after fish death.1

Clinical Manifestation
Physicians may be guided by clinical symptoms in identifying scorpionfish stings, as the patient may not know the identity of their marine assailant. Initially, individuals punctured by scorpionfish spikes will experience an acute pain and burning sensation at the puncture site that may be accompanied by systemic symptoms such as nausea, vomiting, diarrhea, tachycardia, hypotension, loss of consciousness, difficulty breathing, and delirium.9,21-23 The pain will intensify and radiate distal to the site of envenomation, and the wound may exhibit vesiculation, erythema, bruising, pallor, and notable edema.4,24 Pain intensity peaks at 30 to 90 minutes after envenomation, and other systemic symptoms generally last for 24 to 48 hours.25 If patients do not seek prompt treatment, secondary infection may ensue, and the lingering venom in the blister may cause dermal necrosis, paresthesia, and anesthesia. Chronic sequelae may include joint contractures, compartment syndrome, necrotic ulcers, and chronic neuropathy.1
Management
Treatment of scorpionfish stings primarily is palliative and aimed at symptom reduction. Patients should immediately treat wounds with hot but not scalding water immersion.26,27 Given the thermolabile components of scorpionfish venom, the most effective treatment is to soak the affected limb in water 42 °C to 45 °C for 30 to 90 minutes. Any higher temperature may pose risk for scalding burns. Children should be monitored throughout treatment.28 If hot water immersion does not provide relief, oral analgesics may be considered. Stonefish antivenom is available and may be used for any scorpionfish sting given the shared biologic properties between genera. Providers evaluating stings could use sterile irrigation to clean wounds and search for foreign bodies including spine fragments; probing should be accomplished by instruments rather than a gloved finger. Providers should consider culturing wounds and prescribing antibiotics for suspected secondary infections. A tetanus toxoid history also should be elicited, and patients may have a booster administered, as indicated.29
- Rensch G, Murphy-Lavoie HM. Lionfish, scorpionfish, and stonefish toxicity. StatPearls. StatPearls Publishing; May 10, 2022.
- Cearnal L. Red lionfish and ciguatoxin: menace spreading through western hemisphere. Ann Emerg Med. 2012;60:21A-22A. doi:10.1016/j.annemergmed.2012.05.022
- Côté IM, Green SJ. Potential effects of climate change on a marine invasion: the importance of current context. Curr Zool. 2012;58:1-8. doi:10.1093/czoolo/58.1.1
- Venomology of scorpionfishes. In: Santhanam R. Biology and Ecology of Venomous Marine Scorpionfishes. Academic Press; 2019:263-278.
- Ferri J, Staglicˇic´ N, Matić-Skoko S. The black scorpionfish, Scorpaena porcus (Scorpaenidae): could it serve as reliable indicator of Mediterranean coastal communities’ health? Ecol Indicators. 2012;18:25-30. doi:10.1016/j.ecolind.2011.11.004
- Santhanam R. Biology and Ecology of Venomous Marine Scorpionfishes. Academic Press; 2019.
- Morris JA, Akins JL. Feeding ecology of invasive lionfish (Pterois volitans) in the Bahamian Archipelago. Environ Biol Fishes. 2009;86:389-398. doi:10.1007/s10641-009-9538-8
- Albins MA, Hixon MA. Worst case scenario: potential long-term effects of invasive predatory lionfish (Pterois volitans) on Atlantic and Caribbean coral-reef communities. Environ Biol Fishes. 2013;96:1151–1157. doi:10.1007/s10641-011-9795-1
- Haddad V Jr, Martins IA, Makyama HM. Injuries caused by scorpionfishes (Scorpaena plumieri Bloch, 1789 and Scorpaena brasiliensis Cuvier, 1829) in the Southwestern Atlantic Ocean (Brazilian coast): epidemiologic, clinic and therapeutic aspects of 23 stings in humans. Toxicon. 2003;42:79-83. doi:10.1016/s0041-0101(03)00103-x
- Campos FV, Menezes TN, Malacarne PF, et al. A review on the Scorpaena plumieri fish venom and its bioactive compounds. J Venom Anim Toxins Incl Trop Dis. 2016;22:35. doi:10.1186/s40409-016-0090-7
- Needleman RK, Neylan IP, Erickson TB. Environmental and ecological effects of climate change on venomous marine and amphibious species in the wilderness. Wilderness Environ Med. 2018;29:343-356. doi:10.1016/j.wem.2018.04.003
- Aldred B, Erickson T, Lipscomb J. Lionfish envenomations in an urban wilderness. Wilderness Environ Med. 1996;7:291-296. doi:10.1580/1080-6032(1996)007[0291:leiauw]2.3.co;2
- Stewart J, Hughes JM. Life-history traits of the southern hemisphere eastern red scorpionfish, Scorpaena cardinalis (Scorpaenidae: Scorpaeninae). Mar Freshw Res. 2010;61:1290-1297. doi:10.1071/MF10040
- Auerbach PS. Marine envenomations. N Engl J Med. 1991;325:486-493. doi:10.1056/NEJM199108153250707
- Andrich F, Carnielli JB, Cassoli JS, et al. A potent vasoactive cytolysin isolated from Scorpaena plumieri scorpionfish venom. Toxicon. 2010;56:487-496. doi:10.1016/j.toxicon.2010.05.003
- Gomes HL, Andrich F, Mauad H, et al. Cardiovascular effects of scorpionfish (Scorpaena plumieri) venom. Toxicon. 2010;55(2-3):580-589. doi:10.1016/j.toxicon.2009.10.012
- Menezes TN, Carnielli JB, Gomes HL, et al. Local inflammatory response induced by scorpionfish Scorpaena plumieri venom in mice. Toxicon. 2012;60:4-11. doi:10.1016/j.toxicon.2012.03.008
- Schaeffer RC Jr, Carlson RW, Russell FE. Some chemical properties of the venom of the scorpionfish Scorpaena guttata. Toxicon. 1971;9:69-78. doi:10.1016/0041-0101(71)90045-6
- Khalil AM, Wahsha MA, Abu Khadra KM, et al. Biochemical and histopathological effects of the stonefish (Synanceia verrucosa) venom in rats. Toxicon. 2018;142:45-51. doi:10.1016/j.toxicon.2017.12.052
- Mouchbahani-Constance S, Lesperance LS, Petitjean H, et al. Lionfish venom elicits pain predominantly through the activation of nonpeptidergic nociceptors. Pain. 2018;159:2255-2266. doi:10.1097/j.pain.0000000000001326
- Ottuso P. Aquatic dermatology: encounters with the denizens of the deep (and not so deep)—a review. part II: the vertebrates, single-celled organisms, and aquatic biotoxins. Int J Dermatol. 2013;52:268-278. doi:10.1111/j.1365-4632.2011.05426.x
- Bayley HH. Injuries caused by scorpion fish. Trans R Soc Trop Med Hyg. 1940;34:227-230. doi:10.1016/s0035-9203(40)90072-4
- González D. Epidemiological and clinical aspects of certain venomous animals of Spain. Toxicon. 1982;20:925-928. doi:10.1016/0041-0101(82)90080-0
- Halstead BW. Injurious effects from the sting of the scorpionfish, Scorpaena guttata. with report of a case. Calif Med. 1951;74:395-396.
- Vasievich MP, Villarreal JD, Tomecki KJ. Got the travel bug? a review of common infections, infestations, bites, and stings among returning travelers. Am J Clin Dermatol. 2016;17:451-462. doi:10.1007/s40257-016-0203-7
- Barnett S, Saggiomo S, Smout M, et al. Heat deactivation of the stonefish Synanceia horrida venom—implications for first-aid management. Diving Hyperb Med. 2017;47:155-158. doi:10.28920/dhm47.3.155-158
- Russell FE. Weever fish sting: the last word. Br Med J (Clin Res Ed). 1983;287:981-982. doi:10.1136/bmj.287.6397.981-c
- Tomlinson H, Elston DM. Aquatic antagonists: lionfish (Pterois volitans). Cutis. 2018;102:232-234.
- Hornbeak KB, Auerbach PS. Marine envenomation. Emerg Med Clin North Am. 2017;35:321-337. doi:10.1016/j.emc.2016.12.004
With the growing popularity of water sports and a proliferation of invasive species, human injuries from marine animal envenomation continue to rise.1-3 Members of the scorpionfish family Scorpaenidae are second only to stingrays as the leading cause of the 40,000 to 50,000 injuries annually from marine life worldwide.4 Because scorpionfish represent a growing threat and competition with native species, it has been suggested that they could replace endangered species on restaurant menus.5-8 Scorpionfish have been introduced by humans from tropical to temperate seas and are now common off the coast of California and the eastern coast from New York to Florida, as well as in the Caribbean, the Bahamas, and off the southern coast of Brazil. Victims of scorpionfish stings experience considerable pain and may require days to weeks to fully recover, highlighting the socioeconomic costs and burden of scorpionfish envenomation.9,10 Fishers, divers, swimmers, and aquarium owners are most often affected.
Family
The common term scorpionfish refers to both the family Scorpaenidae and the genus Scorpaena. Members of this family possess similar dorsal, anal, and pelvic fins, though they vary between genera in their size and the potency of the venom they insulate. Other familiar members include the genus Pterois (lionfish) and Synanceja (stonefish). Synanceja are the most venomous within the group, but scorpionfish stings more commonly arise from Pterois and Scorpaena.8 Because of the rare shapes and vibrant colors of scorpionfish, some traders and aquarium owners will seek and pay high prices for these fish, providing further opportunity for envenomation.11,12
Characteristics
Scorpionfish have with a high variation in color, ranging from lighter grays to intense reds depending on their geographic location and habitat. Synanceja are bland in coloration, blending in with rocks and gravel, but the more dramatic-appearing Scorpaena exhibit a large cranium and wide range of multicolored patterns (Figure 1).13 Pterois serve as the most conspicuous member of the group with brightly colored red and white stripes (Figure 2). Scorpionfish commonly grow up to 19 inches long and boast 12 dorsal, 2 pelvic, and 3 anal spines housing 5 to 10 mg of venom.14 An integumentary sheath encapsulates each spine housing the glandular tissue that produces the potent venom.

Toxin Properties
Unlike Pterois and Synanceja, Scorpaena do not have venom ducts around their glands, complicating the work of marine biologists aiming to extract and study the venomous toxins. Several studies have managed to isolate scorpionfish venom and overcome its unstable heat-labile nature to investigate its biologic properties.15-20 Several high-molecular-weight proteins (50–800 kDa) comprise the venom, including hyaluronidase, integrin-inhibiting factors, capillary permeability factor, proteases, and some less-understood cytolytic toxins. These factors provoke the inflammatory, proteolytic, hemorrhagic, cardiovascular, and hemolytic biologic activities at both the local and systemic levels, directing damage to wounded tissues and inducing vascular and tissue permeability to reach cellular processes far and wide. Mediators of inflammation include tumor necrosis factor, IL-6, and monocyte chemoattractant protein 1, followed by neutrophils and other mononuclear cells, initiating the immune response at the wound site. Toxin potency remains for up to 2 days after fish death.1

Clinical Manifestation
Physicians may be guided by clinical symptoms in identifying scorpionfish stings, as the patient may not know the identity of their marine assailant. Initially, individuals punctured by scorpionfish spikes will experience an acute pain and burning sensation at the puncture site that may be accompanied by systemic symptoms such as nausea, vomiting, diarrhea, tachycardia, hypotension, loss of consciousness, difficulty breathing, and delirium.9,21-23 The pain will intensify and radiate distal to the site of envenomation, and the wound may exhibit vesiculation, erythema, bruising, pallor, and notable edema.4,24 Pain intensity peaks at 30 to 90 minutes after envenomation, and other systemic symptoms generally last for 24 to 48 hours.25 If patients do not seek prompt treatment, secondary infection may ensue, and the lingering venom in the blister may cause dermal necrosis, paresthesia, and anesthesia. Chronic sequelae may include joint contractures, compartment syndrome, necrotic ulcers, and chronic neuropathy.1
Management
Treatment of scorpionfish stings primarily is palliative and aimed at symptom reduction. Patients should immediately treat wounds with hot but not scalding water immersion.26,27 Given the thermolabile components of scorpionfish venom, the most effective treatment is to soak the affected limb in water 42 °C to 45 °C for 30 to 90 minutes. Any higher temperature may pose risk for scalding burns. Children should be monitored throughout treatment.28 If hot water immersion does not provide relief, oral analgesics may be considered. Stonefish antivenom is available and may be used for any scorpionfish sting given the shared biologic properties between genera. Providers evaluating stings could use sterile irrigation to clean wounds and search for foreign bodies including spine fragments; probing should be accomplished by instruments rather than a gloved finger. Providers should consider culturing wounds and prescribing antibiotics for suspected secondary infections. A tetanus toxoid history also should be elicited, and patients may have a booster administered, as indicated.29
With the growing popularity of water sports and a proliferation of invasive species, human injuries from marine animal envenomation continue to rise.1-3 Members of the scorpionfish family Scorpaenidae are second only to stingrays as the leading cause of the 40,000 to 50,000 injuries annually from marine life worldwide.4 Because scorpionfish represent a growing threat and competition with native species, it has been suggested that they could replace endangered species on restaurant menus.5-8 Scorpionfish have been introduced by humans from tropical to temperate seas and are now common off the coast of California and the eastern coast from New York to Florida, as well as in the Caribbean, the Bahamas, and off the southern coast of Brazil. Victims of scorpionfish stings experience considerable pain and may require days to weeks to fully recover, highlighting the socioeconomic costs and burden of scorpionfish envenomation.9,10 Fishers, divers, swimmers, and aquarium owners are most often affected.
Family
The common term scorpionfish refers to both the family Scorpaenidae and the genus Scorpaena. Members of this family possess similar dorsal, anal, and pelvic fins, though they vary between genera in their size and the potency of the venom they insulate. Other familiar members include the genus Pterois (lionfish) and Synanceja (stonefish). Synanceja are the most venomous within the group, but scorpionfish stings more commonly arise from Pterois and Scorpaena.8 Because of the rare shapes and vibrant colors of scorpionfish, some traders and aquarium owners will seek and pay high prices for these fish, providing further opportunity for envenomation.11,12
Characteristics
Scorpionfish have with a high variation in color, ranging from lighter grays to intense reds depending on their geographic location and habitat. Synanceja are bland in coloration, blending in with rocks and gravel, but the more dramatic-appearing Scorpaena exhibit a large cranium and wide range of multicolored patterns (Figure 1).13 Pterois serve as the most conspicuous member of the group with brightly colored red and white stripes (Figure 2). Scorpionfish commonly grow up to 19 inches long and boast 12 dorsal, 2 pelvic, and 3 anal spines housing 5 to 10 mg of venom.14 An integumentary sheath encapsulates each spine housing the glandular tissue that produces the potent venom.

Toxin Properties
Unlike Pterois and Synanceja, Scorpaena do not have venom ducts around their glands, complicating the work of marine biologists aiming to extract and study the venomous toxins. Several studies have managed to isolate scorpionfish venom and overcome its unstable heat-labile nature to investigate its biologic properties.15-20 Several high-molecular-weight proteins (50–800 kDa) comprise the venom, including hyaluronidase, integrin-inhibiting factors, capillary permeability factor, proteases, and some less-understood cytolytic toxins. These factors provoke the inflammatory, proteolytic, hemorrhagic, cardiovascular, and hemolytic biologic activities at both the local and systemic levels, directing damage to wounded tissues and inducing vascular and tissue permeability to reach cellular processes far and wide. Mediators of inflammation include tumor necrosis factor, IL-6, and monocyte chemoattractant protein 1, followed by neutrophils and other mononuclear cells, initiating the immune response at the wound site. Toxin potency remains for up to 2 days after fish death.1

Clinical Manifestation
Physicians may be guided by clinical symptoms in identifying scorpionfish stings, as the patient may not know the identity of their marine assailant. Initially, individuals punctured by scorpionfish spikes will experience an acute pain and burning sensation at the puncture site that may be accompanied by systemic symptoms such as nausea, vomiting, diarrhea, tachycardia, hypotension, loss of consciousness, difficulty breathing, and delirium.9,21-23 The pain will intensify and radiate distal to the site of envenomation, and the wound may exhibit vesiculation, erythema, bruising, pallor, and notable edema.4,24 Pain intensity peaks at 30 to 90 minutes after envenomation, and other systemic symptoms generally last for 24 to 48 hours.25 If patients do not seek prompt treatment, secondary infection may ensue, and the lingering venom in the blister may cause dermal necrosis, paresthesia, and anesthesia. Chronic sequelae may include joint contractures, compartment syndrome, necrotic ulcers, and chronic neuropathy.1
Management
Treatment of scorpionfish stings primarily is palliative and aimed at symptom reduction. Patients should immediately treat wounds with hot but not scalding water immersion.26,27 Given the thermolabile components of scorpionfish venom, the most effective treatment is to soak the affected limb in water 42 °C to 45 °C for 30 to 90 minutes. Any higher temperature may pose risk for scalding burns. Children should be monitored throughout treatment.28 If hot water immersion does not provide relief, oral analgesics may be considered. Stonefish antivenom is available and may be used for any scorpionfish sting given the shared biologic properties between genera. Providers evaluating stings could use sterile irrigation to clean wounds and search for foreign bodies including spine fragments; probing should be accomplished by instruments rather than a gloved finger. Providers should consider culturing wounds and prescribing antibiotics for suspected secondary infections. A tetanus toxoid history also should be elicited, and patients may have a booster administered, as indicated.29
- Rensch G, Murphy-Lavoie HM. Lionfish, scorpionfish, and stonefish toxicity. StatPearls. StatPearls Publishing; May 10, 2022.
- Cearnal L. Red lionfish and ciguatoxin: menace spreading through western hemisphere. Ann Emerg Med. 2012;60:21A-22A. doi:10.1016/j.annemergmed.2012.05.022
- Côté IM, Green SJ. Potential effects of climate change on a marine invasion: the importance of current context. Curr Zool. 2012;58:1-8. doi:10.1093/czoolo/58.1.1
- Venomology of scorpionfishes. In: Santhanam R. Biology and Ecology of Venomous Marine Scorpionfishes. Academic Press; 2019:263-278.
- Ferri J, Staglicˇic´ N, Matić-Skoko S. The black scorpionfish, Scorpaena porcus (Scorpaenidae): could it serve as reliable indicator of Mediterranean coastal communities’ health? Ecol Indicators. 2012;18:25-30. doi:10.1016/j.ecolind.2011.11.004
- Santhanam R. Biology and Ecology of Venomous Marine Scorpionfishes. Academic Press; 2019.
- Morris JA, Akins JL. Feeding ecology of invasive lionfish (Pterois volitans) in the Bahamian Archipelago. Environ Biol Fishes. 2009;86:389-398. doi:10.1007/s10641-009-9538-8
- Albins MA, Hixon MA. Worst case scenario: potential long-term effects of invasive predatory lionfish (Pterois volitans) on Atlantic and Caribbean coral-reef communities. Environ Biol Fishes. 2013;96:1151–1157. doi:10.1007/s10641-011-9795-1
- Haddad V Jr, Martins IA, Makyama HM. Injuries caused by scorpionfishes (Scorpaena plumieri Bloch, 1789 and Scorpaena brasiliensis Cuvier, 1829) in the Southwestern Atlantic Ocean (Brazilian coast): epidemiologic, clinic and therapeutic aspects of 23 stings in humans. Toxicon. 2003;42:79-83. doi:10.1016/s0041-0101(03)00103-x
- Campos FV, Menezes TN, Malacarne PF, et al. A review on the Scorpaena plumieri fish venom and its bioactive compounds. J Venom Anim Toxins Incl Trop Dis. 2016;22:35. doi:10.1186/s40409-016-0090-7
- Needleman RK, Neylan IP, Erickson TB. Environmental and ecological effects of climate change on venomous marine and amphibious species in the wilderness. Wilderness Environ Med. 2018;29:343-356. doi:10.1016/j.wem.2018.04.003
- Aldred B, Erickson T, Lipscomb J. Lionfish envenomations in an urban wilderness. Wilderness Environ Med. 1996;7:291-296. doi:10.1580/1080-6032(1996)007[0291:leiauw]2.3.co;2
- Stewart J, Hughes JM. Life-history traits of the southern hemisphere eastern red scorpionfish, Scorpaena cardinalis (Scorpaenidae: Scorpaeninae). Mar Freshw Res. 2010;61:1290-1297. doi:10.1071/MF10040
- Auerbach PS. Marine envenomations. N Engl J Med. 1991;325:486-493. doi:10.1056/NEJM199108153250707
- Andrich F, Carnielli JB, Cassoli JS, et al. A potent vasoactive cytolysin isolated from Scorpaena plumieri scorpionfish venom. Toxicon. 2010;56:487-496. doi:10.1016/j.toxicon.2010.05.003
- Gomes HL, Andrich F, Mauad H, et al. Cardiovascular effects of scorpionfish (Scorpaena plumieri) venom. Toxicon. 2010;55(2-3):580-589. doi:10.1016/j.toxicon.2009.10.012
- Menezes TN, Carnielli JB, Gomes HL, et al. Local inflammatory response induced by scorpionfish Scorpaena plumieri venom in mice. Toxicon. 2012;60:4-11. doi:10.1016/j.toxicon.2012.03.008
- Schaeffer RC Jr, Carlson RW, Russell FE. Some chemical properties of the venom of the scorpionfish Scorpaena guttata. Toxicon. 1971;9:69-78. doi:10.1016/0041-0101(71)90045-6
- Khalil AM, Wahsha MA, Abu Khadra KM, et al. Biochemical and histopathological effects of the stonefish (Synanceia verrucosa) venom in rats. Toxicon. 2018;142:45-51. doi:10.1016/j.toxicon.2017.12.052
- Mouchbahani-Constance S, Lesperance LS, Petitjean H, et al. Lionfish venom elicits pain predominantly through the activation of nonpeptidergic nociceptors. Pain. 2018;159:2255-2266. doi:10.1097/j.pain.0000000000001326
- Ottuso P. Aquatic dermatology: encounters with the denizens of the deep (and not so deep)—a review. part II: the vertebrates, single-celled organisms, and aquatic biotoxins. Int J Dermatol. 2013;52:268-278. doi:10.1111/j.1365-4632.2011.05426.x
- Bayley HH. Injuries caused by scorpion fish. Trans R Soc Trop Med Hyg. 1940;34:227-230. doi:10.1016/s0035-9203(40)90072-4
- González D. Epidemiological and clinical aspects of certain venomous animals of Spain. Toxicon. 1982;20:925-928. doi:10.1016/0041-0101(82)90080-0
- Halstead BW. Injurious effects from the sting of the scorpionfish, Scorpaena guttata. with report of a case. Calif Med. 1951;74:395-396.
- Vasievich MP, Villarreal JD, Tomecki KJ. Got the travel bug? a review of common infections, infestations, bites, and stings among returning travelers. Am J Clin Dermatol. 2016;17:451-462. doi:10.1007/s40257-016-0203-7
- Barnett S, Saggiomo S, Smout M, et al. Heat deactivation of the stonefish Synanceia horrida venom—implications for first-aid management. Diving Hyperb Med. 2017;47:155-158. doi:10.28920/dhm47.3.155-158
- Russell FE. Weever fish sting: the last word. Br Med J (Clin Res Ed). 1983;287:981-982. doi:10.1136/bmj.287.6397.981-c
- Tomlinson H, Elston DM. Aquatic antagonists: lionfish (Pterois volitans). Cutis. 2018;102:232-234.
- Hornbeak KB, Auerbach PS. Marine envenomation. Emerg Med Clin North Am. 2017;35:321-337. doi:10.1016/j.emc.2016.12.004
- Rensch G, Murphy-Lavoie HM. Lionfish, scorpionfish, and stonefish toxicity. StatPearls. StatPearls Publishing; May 10, 2022.
- Cearnal L. Red lionfish and ciguatoxin: menace spreading through western hemisphere. Ann Emerg Med. 2012;60:21A-22A. doi:10.1016/j.annemergmed.2012.05.022
- Côté IM, Green SJ. Potential effects of climate change on a marine invasion: the importance of current context. Curr Zool. 2012;58:1-8. doi:10.1093/czoolo/58.1.1
- Venomology of scorpionfishes. In: Santhanam R. Biology and Ecology of Venomous Marine Scorpionfishes. Academic Press; 2019:263-278.
- Ferri J, Staglicˇic´ N, Matić-Skoko S. The black scorpionfish, Scorpaena porcus (Scorpaenidae): could it serve as reliable indicator of Mediterranean coastal communities’ health? Ecol Indicators. 2012;18:25-30. doi:10.1016/j.ecolind.2011.11.004
- Santhanam R. Biology and Ecology of Venomous Marine Scorpionfishes. Academic Press; 2019.
- Morris JA, Akins JL. Feeding ecology of invasive lionfish (Pterois volitans) in the Bahamian Archipelago. Environ Biol Fishes. 2009;86:389-398. doi:10.1007/s10641-009-9538-8
- Albins MA, Hixon MA. Worst case scenario: potential long-term effects of invasive predatory lionfish (Pterois volitans) on Atlantic and Caribbean coral-reef communities. Environ Biol Fishes. 2013;96:1151–1157. doi:10.1007/s10641-011-9795-1
- Haddad V Jr, Martins IA, Makyama HM. Injuries caused by scorpionfishes (Scorpaena plumieri Bloch, 1789 and Scorpaena brasiliensis Cuvier, 1829) in the Southwestern Atlantic Ocean (Brazilian coast): epidemiologic, clinic and therapeutic aspects of 23 stings in humans. Toxicon. 2003;42:79-83. doi:10.1016/s0041-0101(03)00103-x
- Campos FV, Menezes TN, Malacarne PF, et al. A review on the Scorpaena plumieri fish venom and its bioactive compounds. J Venom Anim Toxins Incl Trop Dis. 2016;22:35. doi:10.1186/s40409-016-0090-7
- Needleman RK, Neylan IP, Erickson TB. Environmental and ecological effects of climate change on venomous marine and amphibious species in the wilderness. Wilderness Environ Med. 2018;29:343-356. doi:10.1016/j.wem.2018.04.003
- Aldred B, Erickson T, Lipscomb J. Lionfish envenomations in an urban wilderness. Wilderness Environ Med. 1996;7:291-296. doi:10.1580/1080-6032(1996)007[0291:leiauw]2.3.co;2
- Stewart J, Hughes JM. Life-history traits of the southern hemisphere eastern red scorpionfish, Scorpaena cardinalis (Scorpaenidae: Scorpaeninae). Mar Freshw Res. 2010;61:1290-1297. doi:10.1071/MF10040
- Auerbach PS. Marine envenomations. N Engl J Med. 1991;325:486-493. doi:10.1056/NEJM199108153250707
- Andrich F, Carnielli JB, Cassoli JS, et al. A potent vasoactive cytolysin isolated from Scorpaena plumieri scorpionfish venom. Toxicon. 2010;56:487-496. doi:10.1016/j.toxicon.2010.05.003
- Gomes HL, Andrich F, Mauad H, et al. Cardiovascular effects of scorpionfish (Scorpaena plumieri) venom. Toxicon. 2010;55(2-3):580-589. doi:10.1016/j.toxicon.2009.10.012
- Menezes TN, Carnielli JB, Gomes HL, et al. Local inflammatory response induced by scorpionfish Scorpaena plumieri venom in mice. Toxicon. 2012;60:4-11. doi:10.1016/j.toxicon.2012.03.008
- Schaeffer RC Jr, Carlson RW, Russell FE. Some chemical properties of the venom of the scorpionfish Scorpaena guttata. Toxicon. 1971;9:69-78. doi:10.1016/0041-0101(71)90045-6
- Khalil AM, Wahsha MA, Abu Khadra KM, et al. Biochemical and histopathological effects of the stonefish (Synanceia verrucosa) venom in rats. Toxicon. 2018;142:45-51. doi:10.1016/j.toxicon.2017.12.052
- Mouchbahani-Constance S, Lesperance LS, Petitjean H, et al. Lionfish venom elicits pain predominantly through the activation of nonpeptidergic nociceptors. Pain. 2018;159:2255-2266. doi:10.1097/j.pain.0000000000001326
- Ottuso P. Aquatic dermatology: encounters with the denizens of the deep (and not so deep)—a review. part II: the vertebrates, single-celled organisms, and aquatic biotoxins. Int J Dermatol. 2013;52:268-278. doi:10.1111/j.1365-4632.2011.05426.x
- Bayley HH. Injuries caused by scorpion fish. Trans R Soc Trop Med Hyg. 1940;34:227-230. doi:10.1016/s0035-9203(40)90072-4
- González D. Epidemiological and clinical aspects of certain venomous animals of Spain. Toxicon. 1982;20:925-928. doi:10.1016/0041-0101(82)90080-0
- Halstead BW. Injurious effects from the sting of the scorpionfish, Scorpaena guttata. with report of a case. Calif Med. 1951;74:395-396.
- Vasievich MP, Villarreal JD, Tomecki KJ. Got the travel bug? a review of common infections, infestations, bites, and stings among returning travelers. Am J Clin Dermatol. 2016;17:451-462. doi:10.1007/s40257-016-0203-7
- Barnett S, Saggiomo S, Smout M, et al. Heat deactivation of the stonefish Synanceia horrida venom—implications for first-aid management. Diving Hyperb Med. 2017;47:155-158. doi:10.28920/dhm47.3.155-158
- Russell FE. Weever fish sting: the last word. Br Med J (Clin Res Ed). 1983;287:981-982. doi:10.1136/bmj.287.6397.981-c
- Tomlinson H, Elston DM. Aquatic antagonists: lionfish (Pterois volitans). Cutis. 2018;102:232-234.
- Hornbeak KB, Auerbach PS. Marine envenomation. Emerg Med Clin North Am. 2017;35:321-337. doi:10.1016/j.emc.2016.12.004
Practice Points
- As some species of scorpionfish proliferate, providers may see an increase in envenomation cases.
- Physicians should suspect scorpionfish stings based on clinical symptoms and physical examination.
- Scorpionfish toxins are thermolabile, and patients can find symptom relief by immediately immersing the affected area in hot water (42 °C–45 °C) for 30 to 90 minutes.
Wound Healing: Cellular Review With Specific Attention to Postamputation Care
Restoring skin integrity and balance after injury is vital for survival, serving as a crucial defense mechanism against potential infections by preventing the entry of harmful pathogens. Moreover, proper healing is essential for restoring normal tissue function, allowing damaged tissues to repair and, in an ideal scenario, regenerate. Timely healing helps reduce the risk for complications, such as chronic wounds, which could lead to more severe issues if left untreated. Additionally, pain relief often is associated with effective wound healing as inflammatory responses diminish during the repair process.
The immune system plays a pivotal role in wound healing, influencing various repair mechanisms and ultimately determining the extent of scarring. Although inflammation is present throughout the repair response, recent studies have challenged the conventional belief of an inverse correlation between the intensity of inflammation and regenerative capacity. Inflammatory signals were found to be crucial for timely repair and fundamental processes in regeneration, possibly presenting a paradigm shift in the understanding of immunology.1-4 The complexities of wound healing are exemplified when evaluating and treating postamputation wounds. To address such a task, one needs a firm understanding of the science behind healing wounds and what can go wrong along the way.
Phases of Wound Healing
Wound healing is a complex process that involves a series of sequential yet overlapping phases, including hemostasis/inflammation, proliferation, and remodeling.
Hemostasis/Inflammation—The initial stage of wound healing involves hemostasis, in which the primary objective is to prevent blood loss and initiate inflammation. Platelets arrive at the wound site, forming a provisional clot that is crucial for subsequent healing phases.4-6 Platelets halt bleeding as well as act as a medium for cell migration and adhesion; they also are a source of growth factors and proinflammatory cytokines that herald the inflammatory response.4-7
Inflammation is characterized by the infiltration of immune cells, particularly neutrophils and macrophages. Neutrophils act as the first line of defense, clearing debris and preventing infection. Macrophages follow, phagocytizing apoptotic cells and releasing growth factors such as tumor necrosis factor α, vascular endothelial growth factor, and matrix metalloprotease 9, which stimulate the next phase.4-6,8 Typically, the hemostasis and inflammatory phase starts approximately 6 to 8 hours after wound origin and lasts 3 to 4 days.4,6,7
Proliferation—Following hemostasis and inflammation, the wound transitions into the proliferation phase, which is marked by the development of granulation tissue—a dynamic amalgamation of fibroblasts, endothelial cells, and inflammatory cells.1,4-8 Fibroblasts play a central role in synthesizing collagen, the primary structural protein in connective tissue. They also orchestrate synthesis of vitronectin, fibronectin, fibrin, and tenascin.4-6,8 Simultaneously, angiogenesis takes place, involving the creation of new blood vessels to supply essential nutrients and oxygen to the healing tissue.4,7,9 Growth factors such as transforming growth factor β and vascular endothelial growth factor coordinate cellular activities and foster tissue repair.4-6,8 The proliferation phase extends over days to weeks, laying the groundwork for subsequent tissue restructuring.
Remodeling—The final stage of wound healing is remodeling, an extended process that may persist for several months or, in some cases, years. Throughout this phase, the initially deposited collagen, predominantly type III collagen, undergoes transformation into mature type I collagen.4-6,8 This transformation is critical for reinstating the tissue’s strength and functionality. The balance between collagen synthesis and degradation is delicate, regulated by matrix metalloproteinases and inhibitors of metalloproteinases.4-8 Fibroblasts, myofibroblasts, and other cells coordinate this intricate process of tissue reorganization.4-7
The eventual outcome of the remodeling phase determines the appearance and functionality of the healed tissue. Any disruption in this phase can lead to complications, such as chronic wounds and hypertrophic scars/keloids.4-6 These abnormal healing processes are characterized by localized inflammation, heightened fibroblast function, and excessive accumulation of the extracellular matrix.4-8
Molecular Mechanisms
Comprehensive investigations—both in vivo and in vitro—have explored the intricate molecular mechanisms involved in heightened wound healing. Transforming growth factor β takes center stage as a crucial factor, prompting the transformation of fibroblasts into myofibroblasts and contributing to the deposition of extracellular matrix.2,4-8,10 Transforming growth factor β activates non-Smad signaling pathways, such as MAPK (mitogen-activated protein kinase) and PI3K (phosphoinositide 3-kinase), influencing processes associated with fibrosis.5,11 Furthermore, microRNAs play a pivotal role in posttranscriptional regulation, influencing both transforming growth factor β signaling and fibroblast behavior.12-16
The involvement of prostaglandins is crucial in wound healing. Prostaglandin E2 plays a notable role and is positively correlated with the rate of wound healing.5 The cyclooxygenase pathway, pivotal for prostaglandin synthesis, becomes a target for inflammation control.4,5,10 Although aspirin and nonsteroidal anti-inflammatory drugs commonly are employed, their impact on wound healing remains controversial, as inhibition of cyclooxygenase may disrupt normal repair processes.5,17,18
Wound healing exhibits variations depending on age. Fetal skin regeneration is marked by the restoration of normal dermal architecture, including adnexal structures, nerves, vessels, and muscle.4-6 The distinctive characteristics of fetal wound healing include a unique profile of growth factors, a diminished inflammatory response, reduced biomechanical stress, and a distinct extracellular matrix composition.19 These factors contribute to a lower propensity for scar formation compared to the healing processes observed in adults. Fetal and adult wound healing differ fundamentally in their extracellular matrix composition, inflammatory cells, and cytokine levels.4-6,19 Adult wounds feature myofibroblasts, which are absent in fetal wounds, contributing to heightened mechanical tension.5 Delving deeper into the biochemical basis of fetal wound healing holds promise for mitigating scar formation in adults.
Takeaways From Other Species
Much of the biochemical knowledge of wound healing, especially regenerative wound healing, is known from other species. Geckos provide a unique model for studying regenerative repair in tails and nonregenerative healing in limbs after amputation. Scar-free wound healing is characterized by rapid wound closure, delayed blood vessel development, and collagen deposition, which contrasts with the hypervascular granulation tissue seen in scarring wounds.20 Scar-free wound healing and regeneration are intrinsic properties of the lizard tail and are unaffected by the location or method of detachment.21
Compared to amphibians with extraordinary regenerative capacity, data suggest the lack of regenerative capacity in mammals may come from a desynchronization of the fine-tuned interplay of progenitor cells such as blastema and differentiated cells.22,23 In mice, the response to amputation is specific to the level: cutting through the distal third of the terminal phalanx elicits a regeneration response, yielding a new digit tip resembling the lost one, while an amputation through the distal third of the intermediate phalanx triggers a wound healing and scarring response.24
Wound Healing Following Limb Amputation
Limb amputation represents a profound change in an individual’s life, impacting daily activities and overall well-being. There are many causes of amputation, but the most common include cardiovascular diseases, diabetes mellitus, cancer, and trauma.25-27 Trauma represents a relatively common cause within the US Military due to the overall young population as well as inherent risks of uniformed service.25,27 Advances in protective gear and combat casualty care have led to an increased number of individuals surviving with extremity injuries requiring amputation, particularly among younger service members, with a subgroup experiencing multiple amputations.27-29
Numerous factors play a crucial role in the healing and function of postamputation wounds. The level of amputation is a key determinant influencing both functional outcomes and the healing process. Achieving a balance between preserving function and removing damaged tissue is essential. A study investigating cardiac function and oxygen consumption in 25 patients with peripheral vascular disease found higher-level amputations resulted in decreased walking speed and cadence, along with increased oxygen consumption per meter walked.30
Selecting the appropriate amputation level is vital to optimize functional outcomes without compromising wound healing. Successful prosthetic limb fitting depends largely on the length of the residual stump to support the body load and suspend the prosthesis. For long bone amputations, maintaining at least 12-cm clearance above the knee joint in transfemoral amputees and 10-cm below the knee joint in transtibial amputees is critical for maximizing functional outcomes.31
Surgical technique also is paramount. The goal is to minimize the risk for pressure ulcers by avoiding bony spurs and muscle imbalances. Shaping the muscle and residual limb is essential for proper prosthesis fitting. Attention to neurovascular structures, such as burying nerve ends to prevent neuropathic pain during prosthesis wear, is crucial.32 In extremity amputations, surgeons often resort to free flap transfer techniques for stump reconstruction. In a study of 31 patients with severe lower extremity injuries undergoing various amputations, the use of latissimus dorsi myocutaneous flaps, alone or in combination with serratus anterior muscle flaps, resulted in fewer instances of deep ulceration and allowed for earlier prosthesis wear.33
Addressing Barriers to Wound Healing
Multiple barriers to successful wound healing are encountered in the amputee population. Amputations from trauma have a less-controlled initiation, which carries with it a higher risk for infection, poor wound healing, and other complications.
Infection—Infection often is one of the first hurdles encountered in postamputation wound healing. Critical first steps in infection prevention include thorough cleaning of soiled traumatic wounds and appropriate tissue debridement coupled with scrupulous sterile technique and postoperative monitoring for signs and symptoms of infection.
In a retrospective study of 223 combat-related major lower extremity amputations (initial and revision) between 2009 and 2015, the use of intrawound antibiotic powder at the time of closure demonstrated a 13% absolute risk reduction in deep infection rates, which was particularly notable in revision amputations, with a number needed to treat of 8 for initial amputations and 4 for revision amputations on previously infected limbs.34 Intra-operative antibiotic powder may represent a cheap and easy consideration for this special population of amputees. Postamputation antibiotic prophylaxis for infection prevention is an area of controversy. For nontraumatic infections, data suggest antibiotic prophylaxis may not decrease infection rates in these patients.35,36
Interestingly, a study by Azarbal et al37 aimed to investigate the correlation between nasal methicillin-resistant Staphylococcus aureus (MRSA) colonization and other patient factors with wound occurrence following major lower extremity amputation. The study found MRSA colonization was associated with higher rates of overall wound occurrence as well as wound occurrence due to wound infection. These data suggest nasal MRSA eradication may improve postoperative wound outcomes after major lower extremity amputation.37
Dressing Choice—The dressing chosen for a residual limb also is of paramount importance following amputation. The personalized and dynamic management of postamputation wounds and skin involves achieving optimal healing through a dressing that sustains appropriate moisture levels, addresses edema, helps prevent contractures, and safeguards the limb.38 From the start, using negative pressure wound dressings after surgical amputation can decrease wound-related complications.39
Topical oxygen therapy following amputation also shows promise. In a retrospective case series by Kalliainen et al,40 topical oxygen therapy applied to 58 wounds in 32 patients over 9 months demonstrated positive outcomes in promoting wound healing, with 38 wounds (66%) healing completely with the use of topical oxygen. Minimal complications and no detrimental effects were observed.40
Current recommendations suggest that non–weight-bearing removable rigid dressings are the superior postoperative management for transtibial amputations compared to soft dressings, offering benefits such as faster healing, reduced limb edema, earlier ambulation, preparatory shaping for prosthetic use, and prevention of knee flexion contractures.41-46 Similarly, adding a silicone liner following amputation significantly reduced the duration of prosthetic rehabilitation compared with a conventional soft dressing program in one study (P<.05).47
Specifically targeting wound edema, a case series by Hoskins et al48 investigated the impact of prostheses with vacuum-assisted suspension on the size of residual limb wounds in individuals with transtibial amputation. Well-fitting sockets with vacuum-assisted suspension did not impede wound healing, and the results suggest the potential for continued prosthesis use during the healing process.48 However, a study by Johannesson et al49 compared the outcomes of transtibial amputation patients using a vacuum-formed rigid dressing and a conventional rigid plaster dressing, finding no significant differences in wound healing, time to prosthetic fitting, or functional outcomes with the prosthesis between the 2 groups. When comparing elastic bandaging, pneumatic prosthesis, and temporary prosthesis on postoperative stump management, temporary prosthesis led to a decrease in stump volume, quicker transition to a permanent prosthesis, and improved quality of life compared with elastic bandaging and pneumatic prosthetics.50
The type of material in dressings may contribute to utility in amputation wounds. Keratin-based wound dressings show promise for wound healing, especially in recalcitrant vascular wounds.51 There also are numerous proprietary wound dressings available for patients, at least one of which has particularly thorough data. In a retrospective study of more than 2 million lower extremity wounds across 644 institutions, a proprietary bioactive human skin allograft (TheraSkin [LifeNet Health]) demonstrated higher healing rates, greater percentage area reductions, lower amputations, reduced recidivism, higher treatment completion, and fewer medical transfers compared with standard of care alone.52
Postamputation Dermatologic Concerns
After the postamputation wound heals, a notable concern is the prevalence of skin diseases affecting residual limbs. The stump site in amputees, marked by a delicate cutaneous landscape vulnerable to skin diseases, faces challenges arising from amputation-induced damage to various structures.53
When integrated into a prosthesis socket, the altered skin must acclimate to a humid environment and endure forces for which it is not well suited, especially during movement.53 Amputation remarkably alters normal tissue perfusion, which can lead to aberrant blood and lymphatic circulation in residual limbs.27,53 This compromised skin, often associated with a history of vascular disease, diabetes mellitus, or malignancy, becomes immunocompromised, heightening the risk for dermatologic issues such as inflammation, infection, and malignancies.53 Unlike the resilient volar skin on palms and soles, stump skin lacks adaptation to withstand the compressive forces generated during ambulation, sometimes leading to skin disease and pain that result in abandonment of the prosthesis.53,54 Mechanical forces on the skin, especially in active patients eager to resume pre-injury lifestyles, contribute to skin breakdown. The dynamic nature of the residual limb, including muscle atrophy, gait changes, and weight fluctuations, complicates the prosthetic fitting process. Prosthesis abandonment remains a challenge, despite modern technologic advancements.
The occurrence of heterotopic ossification (extraskeletal bone formation) is another notable issue in military amputees.27,55-57 Poor prosthetic fit can lead to skin degradation, necessitating further surgery to address mispositioned bone formations. Orthopedic monitoring supplemented by appropriate imaging studies can benefit postamputation patients by detecting and preventing heterotopic ossification in its early stages.
Dermatologic issues, especially among lower limb amputees, are noteworthy, with a substantial percentage experiencing complications related to socket prosthetics, such as heat, sweating, sores, and skin irritation. Up to 41% of patients are seen regularly for a secondary skin disorder following amputation.58 As one might expect, persistent wounds, blisters, ulcers, and abscesses are some of the most typical cutaneous abnormalities affecting residual limbs with prostheses.27,58 More rare skin conditions also are documented in residual limbs, including cutaneous granuloma, verrucous carcinoma, bullous pemphigoid, and angiodermatitis.27,59-61
Treatments offered in the dermatology clinic often are similar to patients who have not had an amputation. For instance, hyperhidrosis can be treated with prescription antiperspirant, topical aluminum chloride, topical glycopyrronium, botulinum toxin, and iontophoresis, which can greatly decrease skin irritation and malodor. Subcutaneous neurotoxins such as botulinum toxin are especially useful for hyperhidrosis following amputation because a single treatment can last 3 to 6 months, whereas topicals must be applied multiple times per day and can be inherently irritating to the skin.27,62 Furthermore, ablative fractional resurfacing lasers also can help stimulate new collagen growth, increase skin mobility on residual limbs, smooth jagged scars, and aid prosthetic fitting.27,63 Perforated prosthetic liners also may be useful to address issues such as excessive sweating, demonstrating improvements in skin health, reduced sweating problems, and potential avoidance of surgical interventions.64
When comorbid skin conditions are at bay, preventive measures for excessive wound healing necessitate early recognition and timely intervention for residual limbs. Preventive techniques encompass the use of silicone gel sheeting, hypoallergenic microporous tape, and intralesional steroid injections.
Psychological Concerns—An overarching issue following amputation is the psychological toll the process imposes on the patient. Psychological concerns, including anxiety and depression, present additional challenges impacting residual limb hygiene and prosthetic maintenance. Chronic wounds are devastating to patients. These patients consistently express feeling ostracized from their community and anxious about unemployment, leaking fluid, or odor from the wound, as well as other social stigmata.62 Depression and anxiety can hinder a patient’s ability to care for their wound and make them more susceptible to the myriad issues that can ensue.
Recent Developments in Wound Healing
Wound healing is ripe for innovation that could assuage ailments that impact patients following amputation. A 2022 study by Abu El Hawa et al65 illustrated advanced progression in wound healing for patients taking statins, even though the statin group had increased age and number of comorbidities compared with patients not taking statins.
Nasseri and Sharifi66 showed the potential of antimicrobial peptides—small proteins with cationic charges and amphipathic structures exhibiting electrostatic interaction with microbial cell membranes—in promoting wound healing, particularly defensins and cathelicidin LL-37.They also discussed innovative delivery systems, such as nanoparticles and electrospun fibrous scaffolds, highlighting their potential as possibly more effective therapeutics than antibiotics, especially in the context of diabetic wound closure.66 Aimed at increased angiogenesis in the proliferative phase, there is evidence that N-acetylcysteine can increase amputation stump perfusion with the goal of better long-term wound healing and more efficient scar formation.67
Stem cell therapy, particularly employing cells from the human amniotic membrane, represents an auspicious avenue for antifibrotic treatment. Amniotic epithelial cells and amniotic mesenchymal cells, with their self-renewal and multilineage differentiation capabilities, exhibit anti-inflammatory and antifibrotic properties.4,5 A study by Dong et al68 aimed to assess the efficacy of cell therapy, particularly differentiated progenitor cell–based graft transplantation or autologous stem cell injection, in treating refractory skin injuries such as nonrevascularizable critical limb ischemic ulcers, venous leg ulcers, and diabetic lower limb ulcers. The findings demonstrated cell therapy effectively reduced the size of ulcers, improved wound closure rates, and decreased major amputation rates compared with standard therapy. Of note, cell therapy had limited impact on alleviating pain in patients with critical limb ischemia-related cutaneous ulcers.68
Final Thoughts
Wound care following amputation is a multidisciplinary endeavor, necessitating collaboration between many health care professionals. Dermatologists play a crucial role in providing routine care as well as addressing wound healing and related skin issues among amputation patients. As the field progresses, dermatologists are well positioned to make notable contributions and ensure enhanced outcomes, resulting in a better quality of life for patients facing the challenges of limb amputation and prosthetic use.
- Brockes JP, Kumar A. Comparative aspects of animal regeneration. Annu Rev Cell Dev Biol. 2008;24:525-549. doi:10.1146/annurev.cellbio.24.110707.175336
- Eming SA, Hammerschmidt M, Krieg T, et al. Interrelation of immunity and tissue repair or regeneration. Semin Cell Dev Biol. 2009;20:517-527. doi:10.1016/j.semcdb.2009.04.009
- Eming SA. Evolution of immune pathways in regeneration and repair: recent concepts and translational perspectives. Semin Immunol. 2014;26:275-276. doi:10.1016/j.smim.2014.09.001
- Bolognia JL, Jorizzo JJ, Schaffer JV, et al. Dermatology. 4th edition. Elsevier; 2018.
- Wang PH, Huang BS, Horng HC, et al. Wound healing. J Chin Med Assoc JCMA. 2018;81:94-101. doi:10.1016/j.jcma.2017.11.002
- Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009;37:1528-1542. doi:10.1177/147323000903700531
- Gurtner GC, Werner S, Barrandon Y, et al. Wound repair and regeneration. Nature. 2008;453:314-321. doi:10.1038/nature07039
- Eming SA, Martin P, Tomic-Canic M. Wound repair and regeneration: mechanisms, signaling, and translation. Sci Transl Med. 2014;6:265sr6. doi:10.1126/scitranslmed.3009337
- Eming SA, Brachvogel B, Odorisio T, et al. Regulation of angiogenesis: wound healing as a model. Prog Histochem Cytochem. 2007;42:115-170. doi:10.1016/j.proghi.2007.06.001
- Janis JE, Harrison B. Wound healing: part I. basic science. Plast Reconstr Surg. 2016;138(3 suppl):9S-17S. doi:10.1097/PRS.0000000000002773
- Profyris C, Tziotzios C, Do Vale I. Cutaneous scarring: pathophysiology, molecular mechanisms, and scar reduction therapeutics. part I: the molecular basis of scar formation. J Am Acad Dermatol. 2012;66:1-10; quiz 11-12. doi:10.1016/j.jaad.2011.05.055
- Kwan P, Ding J, Tredget EE. MicroRNA 181b regulates decorin production by dermal fibroblasts and may be a potential therapy for hypertrophic scar. PLoS One. 2015;10:e0123054. doi:10.1371/journal.pone.0123054
- Ben W, Yang Y, Yuan J, et al. Human papillomavirus 16 E6 modulates the expression of host microRNAs in cervical cancer. Taiwan J Obstet Gynecol. 2015;54:364-370. doi:10.1016/j.tjog.2014.06.007
- Yu EH, Tu HF, Wu CH, et al. MicroRNA-21 promotes perineural invasion and impacts survival in patients with oral carcinoma. J Chin Med Assoc JCMA. 2017;80:383-388. doi:10.1016/j.jcma.2017.01.003
- Wen KC, Sung PL, Yen MS, et al. MicroRNAs regulate several functions of normal tissues and malignancies. Taiwan J Obstet Gynecol. 2013;52:465-469. doi:10.1016/j.tjog.2013.10.002
- Babalola O, Mamalis A, Lev-Tov H, et al. The role of microRNAs in skin fibrosis. Arch Dermatol Res. 2013;305:763-776. doi:10.1007/s00403-013-1410-1
- Hofer M, Hoferová Z, Falk M. Pharmacological modulation of radiation damage. does it exist a chance for other substances than hematopoietic growth factors and cytokines? Int J Mol Sci. 2017;18:1385. doi:10.3390/ijms18071385
- Darby IA, Weller CD. Aspirin treatment for chronic wounds: potential beneficial and inhibitory effects. Wound Repair Regen. 2017;25:7-12. doi:10.1111/wrr.12502
- Khalid KA, Nawi AFM, Zulkifli N, et al. Aging and wound healing of the skin: a review of clinical and pathophysiological hallmarks. Life. 2022;12:2142. doi:10.3390/life12122142
- Peacock HM, Gilbert EAB, Vickaryous MK. Scar‐free cutaneous wound healing in the leopard gecko, Eublepharis macularius. J Anat. 2015;227:596-610. doi:10.1111/joa.12368
- Delorme SL, Lungu IM, Vickaryous MK. Scar‐free wound healing and regeneration following tail loss in the leopard gecko, Eublepharis macularius. Anat Rec. 2012;295:1575-1595. doi:10.1002/ar.22490
- Brunauer R, Xia IG, Asrar SN, et al. Aging delays epimorphic regeneration in mice. J Gerontol Ser A Biol Sci Med Sci. 2021;76:1726-1733. doi:10.1093/gerona/glab131
- Dolan CP, Yang TJ, Zimmel K, et al. Epimorphic regeneration of the mouse digit tip is finite. Stem Cell Res Ther. 2022;13:62. doi:10.1186/s13287-022-02741-2
- Simkin J, Han M, Yu L, et al. The mouse digit tip: from wound healing to regeneration. Methods Mol Biol Clifton NJ. 2013;1037:419-435. doi:10.1007/978-1-62703-505-7_24
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429. doi:10.1016/j.apmr.2007.11.005
- Dudek NL, Marks MB, Marshall SC, et al. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch Phys Med Rehabil. 2005;86:659-663. doi:10.1016/j.apmr.2004.09.003
- Lannan FM, Meyerle JH. The dermatologist’s role in amputee skin care. Cutis. 2019;103:86-90.
- Dougherty AL, Mohrle CR, Galarneau MR, et al. Battlefield extremity injuries in Operation Iraqi Freedom. Injury. 2009;40:772-777. doi:10.1016/j.injury.2009.02.014
- Epstein RA, Heinemann AW, McFarland LV. Quality of life for veterans and servicemembers with major traumatic limb loss from Vietnam and OIF/OEF conflicts. J Rehabil Res Dev. 2010;47:373-385. doi:10.1682/jrrd.2009.03.0023
- Pinzur MS, Gold J, Schwartz D, et al. Energy demands for walking in dysvascular amputees as related to the level of amputation. Orthopedics. 1992;15:1033-1036; discussion 1036-1037. doi:10.3928/0147-7447-19920901-07
- Robinson V, Sansam K, Hirst L, et al. Major lower limb amputation–what, why and how to achieve the best results. Orthop Trauma. 2010;24:276-285. doi:10.1016/j.mporth.2010.03.017
- Lu S, Wang C, Zhong W, et al. Amputation stump revision using a free sural neurocutaneous perforator flap. Ann Plast Surg. 2016;76:83-87. doi:10.1097/SAP.0000000000000211
- Kim SW, Jeon SB, Hwang KT, et al. Coverage of amputation stumps using a latissimus dorsi flap with a serratus anterior muscle flap: a comparative study. Ann Plast Surg. 2016;76:88-93. doi:10.1097/SAP.0000000000000220
- Pavey GJ, Formby PM, Hoyt BW, et al. Intrawound antibiotic powder decreases frequency of deep infection and severity of heterotopic ossification in combat lower extremity amputations. Clin Orthop. 2019;477:802-810. doi:10.1007/s11999.0000000000000090
- Dunkel N, Belaieff W, Assal M, et al. Wound dehiscence and stump infection after lower limb amputation: risk factors and association with antibiotic use. J Orthop Sci Off J Jpn Orthop Assoc. 2012;17:588-594. doi:10.1007/s00776-012-0245-5
- Rubin G, Orbach H, Rinott M, et al. The use of prophylactic antibiotics in treatment of fingertip amputation: a randomized prospective trial. Am J Emerg Med. 2015;33:645-647. doi:10.1016/j.ajem.2015.02.002
- Azarbal AF, Harris S, Mitchell EL, et al. Nasal methicillin-resistant Staphylococcus aureus colonization is associated with increased wound occurrence after major lower extremity amputation. J Vasc Surg. 2015;62:401-405. doi:10.1016/j.jvs.2015.02.052
- Kwasniewski M, Mitchel D. Post amputation skin and wound care. Phys Med Rehabil Clin N Am. 2022;33:857-870. doi:10.1016/j.pmr.2022.06.010
- Chang H, Maldonado TS, Rockman CB, et al. Closed incision negative pressure wound therapy may decrease wound complications in major lower extremity amputations. J Vasc Surg. 2021;73:1041-1047. doi:10.1016/j.jvs.2020.07.061
- Kalliainen LK, Gordillo GM, Schlanger R, et al. Topical oxygen as an adjunct to wound healing: a clinical case series. Pathophysiol Off J Int Soc Pathophysiol. 2003;9:81-87. doi:10.1016/s0928-4680(02)00079-2
- Reichmann JP, Stevens PM, Rheinstein J, et al. Removable rigid dressings for postoperative management of transtibial amputations: a review of published evidence. PM R. 2018;10:516-523. doi:10.1016/j.pmrj.2017.10.002
- MacLean N, Fick GH. The effect of semirigid dressings on below-knee amputations. Phys Ther. 1994;74:668-673. doi:10.1093/ptj/74.7.668
- Koonalinthip N, Sukthongsa A, Janchai S. Comparison of removable rigid dressing and elastic bandage for residual limb maturation in transtibial amputees: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101:1683-1688. doi:10.1016/j.apmr.2020.05.009
- Taylor L, Cavenett S, Stepien JM, et al. Removable rigid dressings: a retrospective case-note audit to determine the validity of post-amputation application. Prosthet Orthot Int. 2008;32:223-230. doi:10.1080/03093640802016795
- Sumpio B, Shine SR, Mahler D, et al. A comparison of immediate postoperative rigid and soft dressings for below-knee amputations. Ann Vasc Surg. 2013;27:774-780. doi:10.1016/j.avsg.2013.03.007
- van Velzen AD, Nederhand MJ, Emmelot CH, et al. Early treatment of trans-tibial amputees: retrospective analysis of early fitting and elastic bandaging. Prosthet Orthot Int. 2005;29:3-12. doi:10.1080/17461550500069588
- Chin T, Toda M. Results of prosthetic rehabilitation on managing transtibial vascular amputation with silicone liner after wound closure. J Int Med Res. 2016;44:957-967. doi:10.1177/0300060516647554
- Hoskins RD, Sutton EE, Kinor D, et al. Using vacuum-assisted suspension to manage residual limb wounds in persons with transtibial amputation: a case series. Prosthet Orthot Int. 2014;38:68-74. doi:10.1177/0309364613487547
- Johannesson A, Larsson GU, Oberg T, et al. Comparison of vacuum-formed removable rigid dressing with conventional rigid dressing after transtibial amputation: similar outcome in a randomized controlled trial involving 27 patients. Acta Orthop. 2008;79:361-369. doi:10.1080/17453670710015265
- Alsancak S, Köse SK, Altınkaynak H. Effect of elastic bandaging and prosthesis on the decrease in stump volume. Acta Orthop Traumatol Turc. 2011;45:14-22. doi:10.3944/AOTT.2011.2365
- Than MP, Smith RA, Hammond C, et al. Keratin-based wound care products for treatment of resistant vascular wounds. J Clin Aesthetic Dermatol. 2012;5:31-35.
- Gurtner GC, Garcia AD, Bakewell K, et al. A retrospective matched‐cohort study of 3994 lower extremity wounds of multiple etiologies across 644 institutions comparing a bioactive human skin allograft, TheraSkin, plus standard of care, to standard of care alone. Int Wound J. 2020;17:55-64. doi:10.1111/iwj.13231
- Buikema KES, Meyerle JH. Amputation stump: privileged harbor for infections, tumors, and immune disorders. Clin Dermatol. 2014;32:670-677. doi:10.1016/j.clindermatol.2014.04.015
- Yang NB, Garza LA, Foote CE, et al. High prevalence of stump dermatoses 38 years or more after amputation. Arch Dermatol. 2012;148:1283-1286. doi:10.1001/archdermatol.2012.3004
- Potter BK, Burns TC, Lacap AP, et al. Heterotopic ossification following traumatic and combat-related amputations. Prevalence, risk factors, and preliminary results of excision. J Bone Joint Surg Am. 2007;89:476-486. doi:10.2106/JBJS.F.00412
- Edwards DS, Kuhn KM, Potter BK, et al. Heterotopic ossification: a review of current understanding, treatment, and future. J Orthop Trauma. 2016;30(suppl 3):S27-S30. doi:10.1097/BOT.0000000000000666
- Tintle SM, Shawen SB, Forsberg JA, et al. Reoperation after combat-related major lower extremity amputations. J Orthop Trauma. 2014;28:232-237. doi:10.1097/BOT.0b013e3182a53130
- Bui KM, Raugi GJ, Nguyen VQ, et al. Skin problems in individuals with lower-limb loss: literature review and proposed classification system. J Rehabil Res Dev. 2009;46:1085-1090. doi:10.1682/jrrd.2009.04.0052
- Turan H, Bas¸kan EB, Adim SB, et al. Acroangiodermatitis in a below-knee amputation stump. Clin Exp Dermatol. 2011;36:560-561. doi:10.1111/j.1365-2230.2011.04037.x
- Lin CH, Ma H, Chung MT, et al. Granulomatous cutaneous lesions associated with risperidone-induced hyperprolactinemia in an amputated upper limb. Int J Dermatol. 2012;51:75-78. doi:10.1111/j.1365-4632.2011.04906.x
- Schwartz RA, Bagley MP, Janniger CK, et al. Verrucous carcinoma of a leg amputation stump. Dermatologica. 1991;182:193-195. doi:10.1159/000247782
- Campanati A, Diotallevi F, Radi G, et al. Efficacy and safety of botulinum toxin B in focal hyperhidrosis: a narrative review. Toxins. 2023;15:147. doi:10.3390/toxins15020147
- Anderson RR, Donelan MB, Hivnor C, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol. 2014;150:187-193. doi:10.1001/jamadermatol.2013.7761
- McGrath M, McCarthy J, Gallego A, et al. The influence of perforated prosthetic liners on residual limb wound healing: a case report. Can Prosthet Orthot J. 2019;2:32723. doi:10.33137/cpoj.v2i1.32723
- Abu El Hawa AA, Klein D, Bekeny JC, et al. The impact of statins on wound healing: an ally in treating the highly comorbid patient. J Wound Care. 2022;31(suppl 2):S36-S41. doi:10.12968/jowc.2022.31.Sup2.S36
- Nasseri S, Sharifi M. Therapeutic potential of antimicrobial peptides for wound healing. Int J Pept Res Ther. 2022;28:38. doi:10.1007/s10989-021-10350-5
- Lee JV, Engel C, Tay S, et al. N-Acetyl-Cysteine treatment after lower extremity amputation improves areas of perfusion defect and wound healing outcomes. J Vasc Surg. 2021;73:39-40. doi:10.1016/j.jvs.2020.12.025
- Dong Y, Yang Q, Sun X. Comprehensive analysis of cell therapy on chronic skin wound healing: a meta-analysis. Hum Gene Ther. 2021;32:787-795. doi:10.1089/hum.2020.275
Restoring skin integrity and balance after injury is vital for survival, serving as a crucial defense mechanism against potential infections by preventing the entry of harmful pathogens. Moreover, proper healing is essential for restoring normal tissue function, allowing damaged tissues to repair and, in an ideal scenario, regenerate. Timely healing helps reduce the risk for complications, such as chronic wounds, which could lead to more severe issues if left untreated. Additionally, pain relief often is associated with effective wound healing as inflammatory responses diminish during the repair process.
The immune system plays a pivotal role in wound healing, influencing various repair mechanisms and ultimately determining the extent of scarring. Although inflammation is present throughout the repair response, recent studies have challenged the conventional belief of an inverse correlation between the intensity of inflammation and regenerative capacity. Inflammatory signals were found to be crucial for timely repair and fundamental processes in regeneration, possibly presenting a paradigm shift in the understanding of immunology.1-4 The complexities of wound healing are exemplified when evaluating and treating postamputation wounds. To address such a task, one needs a firm understanding of the science behind healing wounds and what can go wrong along the way.
Phases of Wound Healing
Wound healing is a complex process that involves a series of sequential yet overlapping phases, including hemostasis/inflammation, proliferation, and remodeling.
Hemostasis/Inflammation—The initial stage of wound healing involves hemostasis, in which the primary objective is to prevent blood loss and initiate inflammation. Platelets arrive at the wound site, forming a provisional clot that is crucial for subsequent healing phases.4-6 Platelets halt bleeding as well as act as a medium for cell migration and adhesion; they also are a source of growth factors and proinflammatory cytokines that herald the inflammatory response.4-7
Inflammation is characterized by the infiltration of immune cells, particularly neutrophils and macrophages. Neutrophils act as the first line of defense, clearing debris and preventing infection. Macrophages follow, phagocytizing apoptotic cells and releasing growth factors such as tumor necrosis factor α, vascular endothelial growth factor, and matrix metalloprotease 9, which stimulate the next phase.4-6,8 Typically, the hemostasis and inflammatory phase starts approximately 6 to 8 hours after wound origin and lasts 3 to 4 days.4,6,7
Proliferation—Following hemostasis and inflammation, the wound transitions into the proliferation phase, which is marked by the development of granulation tissue—a dynamic amalgamation of fibroblasts, endothelial cells, and inflammatory cells.1,4-8 Fibroblasts play a central role in synthesizing collagen, the primary structural protein in connective tissue. They also orchestrate synthesis of vitronectin, fibronectin, fibrin, and tenascin.4-6,8 Simultaneously, angiogenesis takes place, involving the creation of new blood vessels to supply essential nutrients and oxygen to the healing tissue.4,7,9 Growth factors such as transforming growth factor β and vascular endothelial growth factor coordinate cellular activities and foster tissue repair.4-6,8 The proliferation phase extends over days to weeks, laying the groundwork for subsequent tissue restructuring.
Remodeling—The final stage of wound healing is remodeling, an extended process that may persist for several months or, in some cases, years. Throughout this phase, the initially deposited collagen, predominantly type III collagen, undergoes transformation into mature type I collagen.4-6,8 This transformation is critical for reinstating the tissue’s strength and functionality. The balance between collagen synthesis and degradation is delicate, regulated by matrix metalloproteinases and inhibitors of metalloproteinases.4-8 Fibroblasts, myofibroblasts, and other cells coordinate this intricate process of tissue reorganization.4-7
The eventual outcome of the remodeling phase determines the appearance and functionality of the healed tissue. Any disruption in this phase can lead to complications, such as chronic wounds and hypertrophic scars/keloids.4-6 These abnormal healing processes are characterized by localized inflammation, heightened fibroblast function, and excessive accumulation of the extracellular matrix.4-8
Molecular Mechanisms
Comprehensive investigations—both in vivo and in vitro—have explored the intricate molecular mechanisms involved in heightened wound healing. Transforming growth factor β takes center stage as a crucial factor, prompting the transformation of fibroblasts into myofibroblasts and contributing to the deposition of extracellular matrix.2,4-8,10 Transforming growth factor β activates non-Smad signaling pathways, such as MAPK (mitogen-activated protein kinase) and PI3K (phosphoinositide 3-kinase), influencing processes associated with fibrosis.5,11 Furthermore, microRNAs play a pivotal role in posttranscriptional regulation, influencing both transforming growth factor β signaling and fibroblast behavior.12-16
The involvement of prostaglandins is crucial in wound healing. Prostaglandin E2 plays a notable role and is positively correlated with the rate of wound healing.5 The cyclooxygenase pathway, pivotal for prostaglandin synthesis, becomes a target for inflammation control.4,5,10 Although aspirin and nonsteroidal anti-inflammatory drugs commonly are employed, their impact on wound healing remains controversial, as inhibition of cyclooxygenase may disrupt normal repair processes.5,17,18
Wound healing exhibits variations depending on age. Fetal skin regeneration is marked by the restoration of normal dermal architecture, including adnexal structures, nerves, vessels, and muscle.4-6 The distinctive characteristics of fetal wound healing include a unique profile of growth factors, a diminished inflammatory response, reduced biomechanical stress, and a distinct extracellular matrix composition.19 These factors contribute to a lower propensity for scar formation compared to the healing processes observed in adults. Fetal and adult wound healing differ fundamentally in their extracellular matrix composition, inflammatory cells, and cytokine levels.4-6,19 Adult wounds feature myofibroblasts, which are absent in fetal wounds, contributing to heightened mechanical tension.5 Delving deeper into the biochemical basis of fetal wound healing holds promise for mitigating scar formation in adults.
Takeaways From Other Species
Much of the biochemical knowledge of wound healing, especially regenerative wound healing, is known from other species. Geckos provide a unique model for studying regenerative repair in tails and nonregenerative healing in limbs after amputation. Scar-free wound healing is characterized by rapid wound closure, delayed blood vessel development, and collagen deposition, which contrasts with the hypervascular granulation tissue seen in scarring wounds.20 Scar-free wound healing and regeneration are intrinsic properties of the lizard tail and are unaffected by the location or method of detachment.21
Compared to amphibians with extraordinary regenerative capacity, data suggest the lack of regenerative capacity in mammals may come from a desynchronization of the fine-tuned interplay of progenitor cells such as blastema and differentiated cells.22,23 In mice, the response to amputation is specific to the level: cutting through the distal third of the terminal phalanx elicits a regeneration response, yielding a new digit tip resembling the lost one, while an amputation through the distal third of the intermediate phalanx triggers a wound healing and scarring response.24
Wound Healing Following Limb Amputation
Limb amputation represents a profound change in an individual’s life, impacting daily activities and overall well-being. There are many causes of amputation, but the most common include cardiovascular diseases, diabetes mellitus, cancer, and trauma.25-27 Trauma represents a relatively common cause within the US Military due to the overall young population as well as inherent risks of uniformed service.25,27 Advances in protective gear and combat casualty care have led to an increased number of individuals surviving with extremity injuries requiring amputation, particularly among younger service members, with a subgroup experiencing multiple amputations.27-29
Numerous factors play a crucial role in the healing and function of postamputation wounds. The level of amputation is a key determinant influencing both functional outcomes and the healing process. Achieving a balance between preserving function and removing damaged tissue is essential. A study investigating cardiac function and oxygen consumption in 25 patients with peripheral vascular disease found higher-level amputations resulted in decreased walking speed and cadence, along with increased oxygen consumption per meter walked.30
Selecting the appropriate amputation level is vital to optimize functional outcomes without compromising wound healing. Successful prosthetic limb fitting depends largely on the length of the residual stump to support the body load and suspend the prosthesis. For long bone amputations, maintaining at least 12-cm clearance above the knee joint in transfemoral amputees and 10-cm below the knee joint in transtibial amputees is critical for maximizing functional outcomes.31
Surgical technique also is paramount. The goal is to minimize the risk for pressure ulcers by avoiding bony spurs and muscle imbalances. Shaping the muscle and residual limb is essential for proper prosthesis fitting. Attention to neurovascular structures, such as burying nerve ends to prevent neuropathic pain during prosthesis wear, is crucial.32 In extremity amputations, surgeons often resort to free flap transfer techniques for stump reconstruction. In a study of 31 patients with severe lower extremity injuries undergoing various amputations, the use of latissimus dorsi myocutaneous flaps, alone or in combination with serratus anterior muscle flaps, resulted in fewer instances of deep ulceration and allowed for earlier prosthesis wear.33
Addressing Barriers to Wound Healing
Multiple barriers to successful wound healing are encountered in the amputee population. Amputations from trauma have a less-controlled initiation, which carries with it a higher risk for infection, poor wound healing, and other complications.
Infection—Infection often is one of the first hurdles encountered in postamputation wound healing. Critical first steps in infection prevention include thorough cleaning of soiled traumatic wounds and appropriate tissue debridement coupled with scrupulous sterile technique and postoperative monitoring for signs and symptoms of infection.
In a retrospective study of 223 combat-related major lower extremity amputations (initial and revision) between 2009 and 2015, the use of intrawound antibiotic powder at the time of closure demonstrated a 13% absolute risk reduction in deep infection rates, which was particularly notable in revision amputations, with a number needed to treat of 8 for initial amputations and 4 for revision amputations on previously infected limbs.34 Intra-operative antibiotic powder may represent a cheap and easy consideration for this special population of amputees. Postamputation antibiotic prophylaxis for infection prevention is an area of controversy. For nontraumatic infections, data suggest antibiotic prophylaxis may not decrease infection rates in these patients.35,36
Interestingly, a study by Azarbal et al37 aimed to investigate the correlation between nasal methicillin-resistant Staphylococcus aureus (MRSA) colonization and other patient factors with wound occurrence following major lower extremity amputation. The study found MRSA colonization was associated with higher rates of overall wound occurrence as well as wound occurrence due to wound infection. These data suggest nasal MRSA eradication may improve postoperative wound outcomes after major lower extremity amputation.37
Dressing Choice—The dressing chosen for a residual limb also is of paramount importance following amputation. The personalized and dynamic management of postamputation wounds and skin involves achieving optimal healing through a dressing that sustains appropriate moisture levels, addresses edema, helps prevent contractures, and safeguards the limb.38 From the start, using negative pressure wound dressings after surgical amputation can decrease wound-related complications.39
Topical oxygen therapy following amputation also shows promise. In a retrospective case series by Kalliainen et al,40 topical oxygen therapy applied to 58 wounds in 32 patients over 9 months demonstrated positive outcomes in promoting wound healing, with 38 wounds (66%) healing completely with the use of topical oxygen. Minimal complications and no detrimental effects were observed.40
Current recommendations suggest that non–weight-bearing removable rigid dressings are the superior postoperative management for transtibial amputations compared to soft dressings, offering benefits such as faster healing, reduced limb edema, earlier ambulation, preparatory shaping for prosthetic use, and prevention of knee flexion contractures.41-46 Similarly, adding a silicone liner following amputation significantly reduced the duration of prosthetic rehabilitation compared with a conventional soft dressing program in one study (P<.05).47
Specifically targeting wound edema, a case series by Hoskins et al48 investigated the impact of prostheses with vacuum-assisted suspension on the size of residual limb wounds in individuals with transtibial amputation. Well-fitting sockets with vacuum-assisted suspension did not impede wound healing, and the results suggest the potential for continued prosthesis use during the healing process.48 However, a study by Johannesson et al49 compared the outcomes of transtibial amputation patients using a vacuum-formed rigid dressing and a conventional rigid plaster dressing, finding no significant differences in wound healing, time to prosthetic fitting, or functional outcomes with the prosthesis between the 2 groups. When comparing elastic bandaging, pneumatic prosthesis, and temporary prosthesis on postoperative stump management, temporary prosthesis led to a decrease in stump volume, quicker transition to a permanent prosthesis, and improved quality of life compared with elastic bandaging and pneumatic prosthetics.50
The type of material in dressings may contribute to utility in amputation wounds. Keratin-based wound dressings show promise for wound healing, especially in recalcitrant vascular wounds.51 There also are numerous proprietary wound dressings available for patients, at least one of which has particularly thorough data. In a retrospective study of more than 2 million lower extremity wounds across 644 institutions, a proprietary bioactive human skin allograft (TheraSkin [LifeNet Health]) demonstrated higher healing rates, greater percentage area reductions, lower amputations, reduced recidivism, higher treatment completion, and fewer medical transfers compared with standard of care alone.52
Postamputation Dermatologic Concerns
After the postamputation wound heals, a notable concern is the prevalence of skin diseases affecting residual limbs. The stump site in amputees, marked by a delicate cutaneous landscape vulnerable to skin diseases, faces challenges arising from amputation-induced damage to various structures.53
When integrated into a prosthesis socket, the altered skin must acclimate to a humid environment and endure forces for which it is not well suited, especially during movement.53 Amputation remarkably alters normal tissue perfusion, which can lead to aberrant blood and lymphatic circulation in residual limbs.27,53 This compromised skin, often associated with a history of vascular disease, diabetes mellitus, or malignancy, becomes immunocompromised, heightening the risk for dermatologic issues such as inflammation, infection, and malignancies.53 Unlike the resilient volar skin on palms and soles, stump skin lacks adaptation to withstand the compressive forces generated during ambulation, sometimes leading to skin disease and pain that result in abandonment of the prosthesis.53,54 Mechanical forces on the skin, especially in active patients eager to resume pre-injury lifestyles, contribute to skin breakdown. The dynamic nature of the residual limb, including muscle atrophy, gait changes, and weight fluctuations, complicates the prosthetic fitting process. Prosthesis abandonment remains a challenge, despite modern technologic advancements.
The occurrence of heterotopic ossification (extraskeletal bone formation) is another notable issue in military amputees.27,55-57 Poor prosthetic fit can lead to skin degradation, necessitating further surgery to address mispositioned bone formations. Orthopedic monitoring supplemented by appropriate imaging studies can benefit postamputation patients by detecting and preventing heterotopic ossification in its early stages.
Dermatologic issues, especially among lower limb amputees, are noteworthy, with a substantial percentage experiencing complications related to socket prosthetics, such as heat, sweating, sores, and skin irritation. Up to 41% of patients are seen regularly for a secondary skin disorder following amputation.58 As one might expect, persistent wounds, blisters, ulcers, and abscesses are some of the most typical cutaneous abnormalities affecting residual limbs with prostheses.27,58 More rare skin conditions also are documented in residual limbs, including cutaneous granuloma, verrucous carcinoma, bullous pemphigoid, and angiodermatitis.27,59-61
Treatments offered in the dermatology clinic often are similar to patients who have not had an amputation. For instance, hyperhidrosis can be treated with prescription antiperspirant, topical aluminum chloride, topical glycopyrronium, botulinum toxin, and iontophoresis, which can greatly decrease skin irritation and malodor. Subcutaneous neurotoxins such as botulinum toxin are especially useful for hyperhidrosis following amputation because a single treatment can last 3 to 6 months, whereas topicals must be applied multiple times per day and can be inherently irritating to the skin.27,62 Furthermore, ablative fractional resurfacing lasers also can help stimulate new collagen growth, increase skin mobility on residual limbs, smooth jagged scars, and aid prosthetic fitting.27,63 Perforated prosthetic liners also may be useful to address issues such as excessive sweating, demonstrating improvements in skin health, reduced sweating problems, and potential avoidance of surgical interventions.64
When comorbid skin conditions are at bay, preventive measures for excessive wound healing necessitate early recognition and timely intervention for residual limbs. Preventive techniques encompass the use of silicone gel sheeting, hypoallergenic microporous tape, and intralesional steroid injections.
Psychological Concerns—An overarching issue following amputation is the psychological toll the process imposes on the patient. Psychological concerns, including anxiety and depression, present additional challenges impacting residual limb hygiene and prosthetic maintenance. Chronic wounds are devastating to patients. These patients consistently express feeling ostracized from their community and anxious about unemployment, leaking fluid, or odor from the wound, as well as other social stigmata.62 Depression and anxiety can hinder a patient’s ability to care for their wound and make them more susceptible to the myriad issues that can ensue.
Recent Developments in Wound Healing
Wound healing is ripe for innovation that could assuage ailments that impact patients following amputation. A 2022 study by Abu El Hawa et al65 illustrated advanced progression in wound healing for patients taking statins, even though the statin group had increased age and number of comorbidities compared with patients not taking statins.
Nasseri and Sharifi66 showed the potential of antimicrobial peptides—small proteins with cationic charges and amphipathic structures exhibiting electrostatic interaction with microbial cell membranes—in promoting wound healing, particularly defensins and cathelicidin LL-37.They also discussed innovative delivery systems, such as nanoparticles and electrospun fibrous scaffolds, highlighting their potential as possibly more effective therapeutics than antibiotics, especially in the context of diabetic wound closure.66 Aimed at increased angiogenesis in the proliferative phase, there is evidence that N-acetylcysteine can increase amputation stump perfusion with the goal of better long-term wound healing and more efficient scar formation.67
Stem cell therapy, particularly employing cells from the human amniotic membrane, represents an auspicious avenue for antifibrotic treatment. Amniotic epithelial cells and amniotic mesenchymal cells, with their self-renewal and multilineage differentiation capabilities, exhibit anti-inflammatory and antifibrotic properties.4,5 A study by Dong et al68 aimed to assess the efficacy of cell therapy, particularly differentiated progenitor cell–based graft transplantation or autologous stem cell injection, in treating refractory skin injuries such as nonrevascularizable critical limb ischemic ulcers, venous leg ulcers, and diabetic lower limb ulcers. The findings demonstrated cell therapy effectively reduced the size of ulcers, improved wound closure rates, and decreased major amputation rates compared with standard therapy. Of note, cell therapy had limited impact on alleviating pain in patients with critical limb ischemia-related cutaneous ulcers.68
Final Thoughts
Wound care following amputation is a multidisciplinary endeavor, necessitating collaboration between many health care professionals. Dermatologists play a crucial role in providing routine care as well as addressing wound healing and related skin issues among amputation patients. As the field progresses, dermatologists are well positioned to make notable contributions and ensure enhanced outcomes, resulting in a better quality of life for patients facing the challenges of limb amputation and prosthetic use.
Restoring skin integrity and balance after injury is vital for survival, serving as a crucial defense mechanism against potential infections by preventing the entry of harmful pathogens. Moreover, proper healing is essential for restoring normal tissue function, allowing damaged tissues to repair and, in an ideal scenario, regenerate. Timely healing helps reduce the risk for complications, such as chronic wounds, which could lead to more severe issues if left untreated. Additionally, pain relief often is associated with effective wound healing as inflammatory responses diminish during the repair process.
The immune system plays a pivotal role in wound healing, influencing various repair mechanisms and ultimately determining the extent of scarring. Although inflammation is present throughout the repair response, recent studies have challenged the conventional belief of an inverse correlation between the intensity of inflammation and regenerative capacity. Inflammatory signals were found to be crucial for timely repair and fundamental processes in regeneration, possibly presenting a paradigm shift in the understanding of immunology.1-4 The complexities of wound healing are exemplified when evaluating and treating postamputation wounds. To address such a task, one needs a firm understanding of the science behind healing wounds and what can go wrong along the way.
Phases of Wound Healing
Wound healing is a complex process that involves a series of sequential yet overlapping phases, including hemostasis/inflammation, proliferation, and remodeling.
Hemostasis/Inflammation—The initial stage of wound healing involves hemostasis, in which the primary objective is to prevent blood loss and initiate inflammation. Platelets arrive at the wound site, forming a provisional clot that is crucial for subsequent healing phases.4-6 Platelets halt bleeding as well as act as a medium for cell migration and adhesion; they also are a source of growth factors and proinflammatory cytokines that herald the inflammatory response.4-7
Inflammation is characterized by the infiltration of immune cells, particularly neutrophils and macrophages. Neutrophils act as the first line of defense, clearing debris and preventing infection. Macrophages follow, phagocytizing apoptotic cells and releasing growth factors such as tumor necrosis factor α, vascular endothelial growth factor, and matrix metalloprotease 9, which stimulate the next phase.4-6,8 Typically, the hemostasis and inflammatory phase starts approximately 6 to 8 hours after wound origin and lasts 3 to 4 days.4,6,7
Proliferation—Following hemostasis and inflammation, the wound transitions into the proliferation phase, which is marked by the development of granulation tissue—a dynamic amalgamation of fibroblasts, endothelial cells, and inflammatory cells.1,4-8 Fibroblasts play a central role in synthesizing collagen, the primary structural protein in connective tissue. They also orchestrate synthesis of vitronectin, fibronectin, fibrin, and tenascin.4-6,8 Simultaneously, angiogenesis takes place, involving the creation of new blood vessels to supply essential nutrients and oxygen to the healing tissue.4,7,9 Growth factors such as transforming growth factor β and vascular endothelial growth factor coordinate cellular activities and foster tissue repair.4-6,8 The proliferation phase extends over days to weeks, laying the groundwork for subsequent tissue restructuring.
Remodeling—The final stage of wound healing is remodeling, an extended process that may persist for several months or, in some cases, years. Throughout this phase, the initially deposited collagen, predominantly type III collagen, undergoes transformation into mature type I collagen.4-6,8 This transformation is critical for reinstating the tissue’s strength and functionality. The balance between collagen synthesis and degradation is delicate, regulated by matrix metalloproteinases and inhibitors of metalloproteinases.4-8 Fibroblasts, myofibroblasts, and other cells coordinate this intricate process of tissue reorganization.4-7
The eventual outcome of the remodeling phase determines the appearance and functionality of the healed tissue. Any disruption in this phase can lead to complications, such as chronic wounds and hypertrophic scars/keloids.4-6 These abnormal healing processes are characterized by localized inflammation, heightened fibroblast function, and excessive accumulation of the extracellular matrix.4-8
Molecular Mechanisms
Comprehensive investigations—both in vivo and in vitro—have explored the intricate molecular mechanisms involved in heightened wound healing. Transforming growth factor β takes center stage as a crucial factor, prompting the transformation of fibroblasts into myofibroblasts and contributing to the deposition of extracellular matrix.2,4-8,10 Transforming growth factor β activates non-Smad signaling pathways, such as MAPK (mitogen-activated protein kinase) and PI3K (phosphoinositide 3-kinase), influencing processes associated with fibrosis.5,11 Furthermore, microRNAs play a pivotal role in posttranscriptional regulation, influencing both transforming growth factor β signaling and fibroblast behavior.12-16
The involvement of prostaglandins is crucial in wound healing. Prostaglandin E2 plays a notable role and is positively correlated with the rate of wound healing.5 The cyclooxygenase pathway, pivotal for prostaglandin synthesis, becomes a target for inflammation control.4,5,10 Although aspirin and nonsteroidal anti-inflammatory drugs commonly are employed, their impact on wound healing remains controversial, as inhibition of cyclooxygenase may disrupt normal repair processes.5,17,18
Wound healing exhibits variations depending on age. Fetal skin regeneration is marked by the restoration of normal dermal architecture, including adnexal structures, nerves, vessels, and muscle.4-6 The distinctive characteristics of fetal wound healing include a unique profile of growth factors, a diminished inflammatory response, reduced biomechanical stress, and a distinct extracellular matrix composition.19 These factors contribute to a lower propensity for scar formation compared to the healing processes observed in adults. Fetal and adult wound healing differ fundamentally in their extracellular matrix composition, inflammatory cells, and cytokine levels.4-6,19 Adult wounds feature myofibroblasts, which are absent in fetal wounds, contributing to heightened mechanical tension.5 Delving deeper into the biochemical basis of fetal wound healing holds promise for mitigating scar formation in adults.
Takeaways From Other Species
Much of the biochemical knowledge of wound healing, especially regenerative wound healing, is known from other species. Geckos provide a unique model for studying regenerative repair in tails and nonregenerative healing in limbs after amputation. Scar-free wound healing is characterized by rapid wound closure, delayed blood vessel development, and collagen deposition, which contrasts with the hypervascular granulation tissue seen in scarring wounds.20 Scar-free wound healing and regeneration are intrinsic properties of the lizard tail and are unaffected by the location or method of detachment.21
Compared to amphibians with extraordinary regenerative capacity, data suggest the lack of regenerative capacity in mammals may come from a desynchronization of the fine-tuned interplay of progenitor cells such as blastema and differentiated cells.22,23 In mice, the response to amputation is specific to the level: cutting through the distal third of the terminal phalanx elicits a regeneration response, yielding a new digit tip resembling the lost one, while an amputation through the distal third of the intermediate phalanx triggers a wound healing and scarring response.24
Wound Healing Following Limb Amputation
Limb amputation represents a profound change in an individual’s life, impacting daily activities and overall well-being. There are many causes of amputation, but the most common include cardiovascular diseases, diabetes mellitus, cancer, and trauma.25-27 Trauma represents a relatively common cause within the US Military due to the overall young population as well as inherent risks of uniformed service.25,27 Advances in protective gear and combat casualty care have led to an increased number of individuals surviving with extremity injuries requiring amputation, particularly among younger service members, with a subgroup experiencing multiple amputations.27-29
Numerous factors play a crucial role in the healing and function of postamputation wounds. The level of amputation is a key determinant influencing both functional outcomes and the healing process. Achieving a balance between preserving function and removing damaged tissue is essential. A study investigating cardiac function and oxygen consumption in 25 patients with peripheral vascular disease found higher-level amputations resulted in decreased walking speed and cadence, along with increased oxygen consumption per meter walked.30
Selecting the appropriate amputation level is vital to optimize functional outcomes without compromising wound healing. Successful prosthetic limb fitting depends largely on the length of the residual stump to support the body load and suspend the prosthesis. For long bone amputations, maintaining at least 12-cm clearance above the knee joint in transfemoral amputees and 10-cm below the knee joint in transtibial amputees is critical for maximizing functional outcomes.31
Surgical technique also is paramount. The goal is to minimize the risk for pressure ulcers by avoiding bony spurs and muscle imbalances. Shaping the muscle and residual limb is essential for proper prosthesis fitting. Attention to neurovascular structures, such as burying nerve ends to prevent neuropathic pain during prosthesis wear, is crucial.32 In extremity amputations, surgeons often resort to free flap transfer techniques for stump reconstruction. In a study of 31 patients with severe lower extremity injuries undergoing various amputations, the use of latissimus dorsi myocutaneous flaps, alone or in combination with serratus anterior muscle flaps, resulted in fewer instances of deep ulceration and allowed for earlier prosthesis wear.33
Addressing Barriers to Wound Healing
Multiple barriers to successful wound healing are encountered in the amputee population. Amputations from trauma have a less-controlled initiation, which carries with it a higher risk for infection, poor wound healing, and other complications.
Infection—Infection often is one of the first hurdles encountered in postamputation wound healing. Critical first steps in infection prevention include thorough cleaning of soiled traumatic wounds and appropriate tissue debridement coupled with scrupulous sterile technique and postoperative monitoring for signs and symptoms of infection.
In a retrospective study of 223 combat-related major lower extremity amputations (initial and revision) between 2009 and 2015, the use of intrawound antibiotic powder at the time of closure demonstrated a 13% absolute risk reduction in deep infection rates, which was particularly notable in revision amputations, with a number needed to treat of 8 for initial amputations and 4 for revision amputations on previously infected limbs.34 Intra-operative antibiotic powder may represent a cheap and easy consideration for this special population of amputees. Postamputation antibiotic prophylaxis for infection prevention is an area of controversy. For nontraumatic infections, data suggest antibiotic prophylaxis may not decrease infection rates in these patients.35,36
Interestingly, a study by Azarbal et al37 aimed to investigate the correlation between nasal methicillin-resistant Staphylococcus aureus (MRSA) colonization and other patient factors with wound occurrence following major lower extremity amputation. The study found MRSA colonization was associated with higher rates of overall wound occurrence as well as wound occurrence due to wound infection. These data suggest nasal MRSA eradication may improve postoperative wound outcomes after major lower extremity amputation.37
Dressing Choice—The dressing chosen for a residual limb also is of paramount importance following amputation. The personalized and dynamic management of postamputation wounds and skin involves achieving optimal healing through a dressing that sustains appropriate moisture levels, addresses edema, helps prevent contractures, and safeguards the limb.38 From the start, using negative pressure wound dressings after surgical amputation can decrease wound-related complications.39
Topical oxygen therapy following amputation also shows promise. In a retrospective case series by Kalliainen et al,40 topical oxygen therapy applied to 58 wounds in 32 patients over 9 months demonstrated positive outcomes in promoting wound healing, with 38 wounds (66%) healing completely with the use of topical oxygen. Minimal complications and no detrimental effects were observed.40
Current recommendations suggest that non–weight-bearing removable rigid dressings are the superior postoperative management for transtibial amputations compared to soft dressings, offering benefits such as faster healing, reduced limb edema, earlier ambulation, preparatory shaping for prosthetic use, and prevention of knee flexion contractures.41-46 Similarly, adding a silicone liner following amputation significantly reduced the duration of prosthetic rehabilitation compared with a conventional soft dressing program in one study (P<.05).47
Specifically targeting wound edema, a case series by Hoskins et al48 investigated the impact of prostheses with vacuum-assisted suspension on the size of residual limb wounds in individuals with transtibial amputation. Well-fitting sockets with vacuum-assisted suspension did not impede wound healing, and the results suggest the potential for continued prosthesis use during the healing process.48 However, a study by Johannesson et al49 compared the outcomes of transtibial amputation patients using a vacuum-formed rigid dressing and a conventional rigid plaster dressing, finding no significant differences in wound healing, time to prosthetic fitting, or functional outcomes with the prosthesis between the 2 groups. When comparing elastic bandaging, pneumatic prosthesis, and temporary prosthesis on postoperative stump management, temporary prosthesis led to a decrease in stump volume, quicker transition to a permanent prosthesis, and improved quality of life compared with elastic bandaging and pneumatic prosthetics.50
The type of material in dressings may contribute to utility in amputation wounds. Keratin-based wound dressings show promise for wound healing, especially in recalcitrant vascular wounds.51 There also are numerous proprietary wound dressings available for patients, at least one of which has particularly thorough data. In a retrospective study of more than 2 million lower extremity wounds across 644 institutions, a proprietary bioactive human skin allograft (TheraSkin [LifeNet Health]) demonstrated higher healing rates, greater percentage area reductions, lower amputations, reduced recidivism, higher treatment completion, and fewer medical transfers compared with standard of care alone.52
Postamputation Dermatologic Concerns
After the postamputation wound heals, a notable concern is the prevalence of skin diseases affecting residual limbs. The stump site in amputees, marked by a delicate cutaneous landscape vulnerable to skin diseases, faces challenges arising from amputation-induced damage to various structures.53
When integrated into a prosthesis socket, the altered skin must acclimate to a humid environment and endure forces for which it is not well suited, especially during movement.53 Amputation remarkably alters normal tissue perfusion, which can lead to aberrant blood and lymphatic circulation in residual limbs.27,53 This compromised skin, often associated with a history of vascular disease, diabetes mellitus, or malignancy, becomes immunocompromised, heightening the risk for dermatologic issues such as inflammation, infection, and malignancies.53 Unlike the resilient volar skin on palms and soles, stump skin lacks adaptation to withstand the compressive forces generated during ambulation, sometimes leading to skin disease and pain that result in abandonment of the prosthesis.53,54 Mechanical forces on the skin, especially in active patients eager to resume pre-injury lifestyles, contribute to skin breakdown. The dynamic nature of the residual limb, including muscle atrophy, gait changes, and weight fluctuations, complicates the prosthetic fitting process. Prosthesis abandonment remains a challenge, despite modern technologic advancements.
The occurrence of heterotopic ossification (extraskeletal bone formation) is another notable issue in military amputees.27,55-57 Poor prosthetic fit can lead to skin degradation, necessitating further surgery to address mispositioned bone formations. Orthopedic monitoring supplemented by appropriate imaging studies can benefit postamputation patients by detecting and preventing heterotopic ossification in its early stages.
Dermatologic issues, especially among lower limb amputees, are noteworthy, with a substantial percentage experiencing complications related to socket prosthetics, such as heat, sweating, sores, and skin irritation. Up to 41% of patients are seen regularly for a secondary skin disorder following amputation.58 As one might expect, persistent wounds, blisters, ulcers, and abscesses are some of the most typical cutaneous abnormalities affecting residual limbs with prostheses.27,58 More rare skin conditions also are documented in residual limbs, including cutaneous granuloma, verrucous carcinoma, bullous pemphigoid, and angiodermatitis.27,59-61
Treatments offered in the dermatology clinic often are similar to patients who have not had an amputation. For instance, hyperhidrosis can be treated with prescription antiperspirant, topical aluminum chloride, topical glycopyrronium, botulinum toxin, and iontophoresis, which can greatly decrease skin irritation and malodor. Subcutaneous neurotoxins such as botulinum toxin are especially useful for hyperhidrosis following amputation because a single treatment can last 3 to 6 months, whereas topicals must be applied multiple times per day and can be inherently irritating to the skin.27,62 Furthermore, ablative fractional resurfacing lasers also can help stimulate new collagen growth, increase skin mobility on residual limbs, smooth jagged scars, and aid prosthetic fitting.27,63 Perforated prosthetic liners also may be useful to address issues such as excessive sweating, demonstrating improvements in skin health, reduced sweating problems, and potential avoidance of surgical interventions.64
When comorbid skin conditions are at bay, preventive measures for excessive wound healing necessitate early recognition and timely intervention for residual limbs. Preventive techniques encompass the use of silicone gel sheeting, hypoallergenic microporous tape, and intralesional steroid injections.
Psychological Concerns—An overarching issue following amputation is the psychological toll the process imposes on the patient. Psychological concerns, including anxiety and depression, present additional challenges impacting residual limb hygiene and prosthetic maintenance. Chronic wounds are devastating to patients. These patients consistently express feeling ostracized from their community and anxious about unemployment, leaking fluid, or odor from the wound, as well as other social stigmata.62 Depression and anxiety can hinder a patient’s ability to care for their wound and make them more susceptible to the myriad issues that can ensue.
Recent Developments in Wound Healing
Wound healing is ripe for innovation that could assuage ailments that impact patients following amputation. A 2022 study by Abu El Hawa et al65 illustrated advanced progression in wound healing for patients taking statins, even though the statin group had increased age and number of comorbidities compared with patients not taking statins.
Nasseri and Sharifi66 showed the potential of antimicrobial peptides—small proteins with cationic charges and amphipathic structures exhibiting electrostatic interaction with microbial cell membranes—in promoting wound healing, particularly defensins and cathelicidin LL-37.They also discussed innovative delivery systems, such as nanoparticles and electrospun fibrous scaffolds, highlighting their potential as possibly more effective therapeutics than antibiotics, especially in the context of diabetic wound closure.66 Aimed at increased angiogenesis in the proliferative phase, there is evidence that N-acetylcysteine can increase amputation stump perfusion with the goal of better long-term wound healing and more efficient scar formation.67
Stem cell therapy, particularly employing cells from the human amniotic membrane, represents an auspicious avenue for antifibrotic treatment. Amniotic epithelial cells and amniotic mesenchymal cells, with their self-renewal and multilineage differentiation capabilities, exhibit anti-inflammatory and antifibrotic properties.4,5 A study by Dong et al68 aimed to assess the efficacy of cell therapy, particularly differentiated progenitor cell–based graft transplantation or autologous stem cell injection, in treating refractory skin injuries such as nonrevascularizable critical limb ischemic ulcers, venous leg ulcers, and diabetic lower limb ulcers. The findings demonstrated cell therapy effectively reduced the size of ulcers, improved wound closure rates, and decreased major amputation rates compared with standard therapy. Of note, cell therapy had limited impact on alleviating pain in patients with critical limb ischemia-related cutaneous ulcers.68
Final Thoughts
Wound care following amputation is a multidisciplinary endeavor, necessitating collaboration between many health care professionals. Dermatologists play a crucial role in providing routine care as well as addressing wound healing and related skin issues among amputation patients. As the field progresses, dermatologists are well positioned to make notable contributions and ensure enhanced outcomes, resulting in a better quality of life for patients facing the challenges of limb amputation and prosthetic use.
- Brockes JP, Kumar A. Comparative aspects of animal regeneration. Annu Rev Cell Dev Biol. 2008;24:525-549. doi:10.1146/annurev.cellbio.24.110707.175336
- Eming SA, Hammerschmidt M, Krieg T, et al. Interrelation of immunity and tissue repair or regeneration. Semin Cell Dev Biol. 2009;20:517-527. doi:10.1016/j.semcdb.2009.04.009
- Eming SA. Evolution of immune pathways in regeneration and repair: recent concepts and translational perspectives. Semin Immunol. 2014;26:275-276. doi:10.1016/j.smim.2014.09.001
- Bolognia JL, Jorizzo JJ, Schaffer JV, et al. Dermatology. 4th edition. Elsevier; 2018.
- Wang PH, Huang BS, Horng HC, et al. Wound healing. J Chin Med Assoc JCMA. 2018;81:94-101. doi:10.1016/j.jcma.2017.11.002
- Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009;37:1528-1542. doi:10.1177/147323000903700531
- Gurtner GC, Werner S, Barrandon Y, et al. Wound repair and regeneration. Nature. 2008;453:314-321. doi:10.1038/nature07039
- Eming SA, Martin P, Tomic-Canic M. Wound repair and regeneration: mechanisms, signaling, and translation. Sci Transl Med. 2014;6:265sr6. doi:10.1126/scitranslmed.3009337
- Eming SA, Brachvogel B, Odorisio T, et al. Regulation of angiogenesis: wound healing as a model. Prog Histochem Cytochem. 2007;42:115-170. doi:10.1016/j.proghi.2007.06.001
- Janis JE, Harrison B. Wound healing: part I. basic science. Plast Reconstr Surg. 2016;138(3 suppl):9S-17S. doi:10.1097/PRS.0000000000002773
- Profyris C, Tziotzios C, Do Vale I. Cutaneous scarring: pathophysiology, molecular mechanisms, and scar reduction therapeutics. part I: the molecular basis of scar formation. J Am Acad Dermatol. 2012;66:1-10; quiz 11-12. doi:10.1016/j.jaad.2011.05.055
- Kwan P, Ding J, Tredget EE. MicroRNA 181b regulates decorin production by dermal fibroblasts and may be a potential therapy for hypertrophic scar. PLoS One. 2015;10:e0123054. doi:10.1371/journal.pone.0123054
- Ben W, Yang Y, Yuan J, et al. Human papillomavirus 16 E6 modulates the expression of host microRNAs in cervical cancer. Taiwan J Obstet Gynecol. 2015;54:364-370. doi:10.1016/j.tjog.2014.06.007
- Yu EH, Tu HF, Wu CH, et al. MicroRNA-21 promotes perineural invasion and impacts survival in patients with oral carcinoma. J Chin Med Assoc JCMA. 2017;80:383-388. doi:10.1016/j.jcma.2017.01.003
- Wen KC, Sung PL, Yen MS, et al. MicroRNAs regulate several functions of normal tissues and malignancies. Taiwan J Obstet Gynecol. 2013;52:465-469. doi:10.1016/j.tjog.2013.10.002
- Babalola O, Mamalis A, Lev-Tov H, et al. The role of microRNAs in skin fibrosis. Arch Dermatol Res. 2013;305:763-776. doi:10.1007/s00403-013-1410-1
- Hofer M, Hoferová Z, Falk M. Pharmacological modulation of radiation damage. does it exist a chance for other substances than hematopoietic growth factors and cytokines? Int J Mol Sci. 2017;18:1385. doi:10.3390/ijms18071385
- Darby IA, Weller CD. Aspirin treatment for chronic wounds: potential beneficial and inhibitory effects. Wound Repair Regen. 2017;25:7-12. doi:10.1111/wrr.12502
- Khalid KA, Nawi AFM, Zulkifli N, et al. Aging and wound healing of the skin: a review of clinical and pathophysiological hallmarks. Life. 2022;12:2142. doi:10.3390/life12122142
- Peacock HM, Gilbert EAB, Vickaryous MK. Scar‐free cutaneous wound healing in the leopard gecko, Eublepharis macularius. J Anat. 2015;227:596-610. doi:10.1111/joa.12368
- Delorme SL, Lungu IM, Vickaryous MK. Scar‐free wound healing and regeneration following tail loss in the leopard gecko, Eublepharis macularius. Anat Rec. 2012;295:1575-1595. doi:10.1002/ar.22490
- Brunauer R, Xia IG, Asrar SN, et al. Aging delays epimorphic regeneration in mice. J Gerontol Ser A Biol Sci Med Sci. 2021;76:1726-1733. doi:10.1093/gerona/glab131
- Dolan CP, Yang TJ, Zimmel K, et al. Epimorphic regeneration of the mouse digit tip is finite. Stem Cell Res Ther. 2022;13:62. doi:10.1186/s13287-022-02741-2
- Simkin J, Han M, Yu L, et al. The mouse digit tip: from wound healing to regeneration. Methods Mol Biol Clifton NJ. 2013;1037:419-435. doi:10.1007/978-1-62703-505-7_24
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429. doi:10.1016/j.apmr.2007.11.005
- Dudek NL, Marks MB, Marshall SC, et al. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch Phys Med Rehabil. 2005;86:659-663. doi:10.1016/j.apmr.2004.09.003
- Lannan FM, Meyerle JH. The dermatologist’s role in amputee skin care. Cutis. 2019;103:86-90.
- Dougherty AL, Mohrle CR, Galarneau MR, et al. Battlefield extremity injuries in Operation Iraqi Freedom. Injury. 2009;40:772-777. doi:10.1016/j.injury.2009.02.014
- Epstein RA, Heinemann AW, McFarland LV. Quality of life for veterans and servicemembers with major traumatic limb loss from Vietnam and OIF/OEF conflicts. J Rehabil Res Dev. 2010;47:373-385. doi:10.1682/jrrd.2009.03.0023
- Pinzur MS, Gold J, Schwartz D, et al. Energy demands for walking in dysvascular amputees as related to the level of amputation. Orthopedics. 1992;15:1033-1036; discussion 1036-1037. doi:10.3928/0147-7447-19920901-07
- Robinson V, Sansam K, Hirst L, et al. Major lower limb amputation–what, why and how to achieve the best results. Orthop Trauma. 2010;24:276-285. doi:10.1016/j.mporth.2010.03.017
- Lu S, Wang C, Zhong W, et al. Amputation stump revision using a free sural neurocutaneous perforator flap. Ann Plast Surg. 2016;76:83-87. doi:10.1097/SAP.0000000000000211
- Kim SW, Jeon SB, Hwang KT, et al. Coverage of amputation stumps using a latissimus dorsi flap with a serratus anterior muscle flap: a comparative study. Ann Plast Surg. 2016;76:88-93. doi:10.1097/SAP.0000000000000220
- Pavey GJ, Formby PM, Hoyt BW, et al. Intrawound antibiotic powder decreases frequency of deep infection and severity of heterotopic ossification in combat lower extremity amputations. Clin Orthop. 2019;477:802-810. doi:10.1007/s11999.0000000000000090
- Dunkel N, Belaieff W, Assal M, et al. Wound dehiscence and stump infection after lower limb amputation: risk factors and association with antibiotic use. J Orthop Sci Off J Jpn Orthop Assoc. 2012;17:588-594. doi:10.1007/s00776-012-0245-5
- Rubin G, Orbach H, Rinott M, et al. The use of prophylactic antibiotics in treatment of fingertip amputation: a randomized prospective trial. Am J Emerg Med. 2015;33:645-647. doi:10.1016/j.ajem.2015.02.002
- Azarbal AF, Harris S, Mitchell EL, et al. Nasal methicillin-resistant Staphylococcus aureus colonization is associated with increased wound occurrence after major lower extremity amputation. J Vasc Surg. 2015;62:401-405. doi:10.1016/j.jvs.2015.02.052
- Kwasniewski M, Mitchel D. Post amputation skin and wound care. Phys Med Rehabil Clin N Am. 2022;33:857-870. doi:10.1016/j.pmr.2022.06.010
- Chang H, Maldonado TS, Rockman CB, et al. Closed incision negative pressure wound therapy may decrease wound complications in major lower extremity amputations. J Vasc Surg. 2021;73:1041-1047. doi:10.1016/j.jvs.2020.07.061
- Kalliainen LK, Gordillo GM, Schlanger R, et al. Topical oxygen as an adjunct to wound healing: a clinical case series. Pathophysiol Off J Int Soc Pathophysiol. 2003;9:81-87. doi:10.1016/s0928-4680(02)00079-2
- Reichmann JP, Stevens PM, Rheinstein J, et al. Removable rigid dressings for postoperative management of transtibial amputations: a review of published evidence. PM R. 2018;10:516-523. doi:10.1016/j.pmrj.2017.10.002
- MacLean N, Fick GH. The effect of semirigid dressings on below-knee amputations. Phys Ther. 1994;74:668-673. doi:10.1093/ptj/74.7.668
- Koonalinthip N, Sukthongsa A, Janchai S. Comparison of removable rigid dressing and elastic bandage for residual limb maturation in transtibial amputees: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101:1683-1688. doi:10.1016/j.apmr.2020.05.009
- Taylor L, Cavenett S, Stepien JM, et al. Removable rigid dressings: a retrospective case-note audit to determine the validity of post-amputation application. Prosthet Orthot Int. 2008;32:223-230. doi:10.1080/03093640802016795
- Sumpio B, Shine SR, Mahler D, et al. A comparison of immediate postoperative rigid and soft dressings for below-knee amputations. Ann Vasc Surg. 2013;27:774-780. doi:10.1016/j.avsg.2013.03.007
- van Velzen AD, Nederhand MJ, Emmelot CH, et al. Early treatment of trans-tibial amputees: retrospective analysis of early fitting and elastic bandaging. Prosthet Orthot Int. 2005;29:3-12. doi:10.1080/17461550500069588
- Chin T, Toda M. Results of prosthetic rehabilitation on managing transtibial vascular amputation with silicone liner after wound closure. J Int Med Res. 2016;44:957-967. doi:10.1177/0300060516647554
- Hoskins RD, Sutton EE, Kinor D, et al. Using vacuum-assisted suspension to manage residual limb wounds in persons with transtibial amputation: a case series. Prosthet Orthot Int. 2014;38:68-74. doi:10.1177/0309364613487547
- Johannesson A, Larsson GU, Oberg T, et al. Comparison of vacuum-formed removable rigid dressing with conventional rigid dressing after transtibial amputation: similar outcome in a randomized controlled trial involving 27 patients. Acta Orthop. 2008;79:361-369. doi:10.1080/17453670710015265
- Alsancak S, Köse SK, Altınkaynak H. Effect of elastic bandaging and prosthesis on the decrease in stump volume. Acta Orthop Traumatol Turc. 2011;45:14-22. doi:10.3944/AOTT.2011.2365
- Than MP, Smith RA, Hammond C, et al. Keratin-based wound care products for treatment of resistant vascular wounds. J Clin Aesthetic Dermatol. 2012;5:31-35.
- Gurtner GC, Garcia AD, Bakewell K, et al. A retrospective matched‐cohort study of 3994 lower extremity wounds of multiple etiologies across 644 institutions comparing a bioactive human skin allograft, TheraSkin, plus standard of care, to standard of care alone. Int Wound J. 2020;17:55-64. doi:10.1111/iwj.13231
- Buikema KES, Meyerle JH. Amputation stump: privileged harbor for infections, tumors, and immune disorders. Clin Dermatol. 2014;32:670-677. doi:10.1016/j.clindermatol.2014.04.015
- Yang NB, Garza LA, Foote CE, et al. High prevalence of stump dermatoses 38 years or more after amputation. Arch Dermatol. 2012;148:1283-1286. doi:10.1001/archdermatol.2012.3004
- Potter BK, Burns TC, Lacap AP, et al. Heterotopic ossification following traumatic and combat-related amputations. Prevalence, risk factors, and preliminary results of excision. J Bone Joint Surg Am. 2007;89:476-486. doi:10.2106/JBJS.F.00412
- Edwards DS, Kuhn KM, Potter BK, et al. Heterotopic ossification: a review of current understanding, treatment, and future. J Orthop Trauma. 2016;30(suppl 3):S27-S30. doi:10.1097/BOT.0000000000000666
- Tintle SM, Shawen SB, Forsberg JA, et al. Reoperation after combat-related major lower extremity amputations. J Orthop Trauma. 2014;28:232-237. doi:10.1097/BOT.0b013e3182a53130
- Bui KM, Raugi GJ, Nguyen VQ, et al. Skin problems in individuals with lower-limb loss: literature review and proposed classification system. J Rehabil Res Dev. 2009;46:1085-1090. doi:10.1682/jrrd.2009.04.0052
- Turan H, Bas¸kan EB, Adim SB, et al. Acroangiodermatitis in a below-knee amputation stump. Clin Exp Dermatol. 2011;36:560-561. doi:10.1111/j.1365-2230.2011.04037.x
- Lin CH, Ma H, Chung MT, et al. Granulomatous cutaneous lesions associated with risperidone-induced hyperprolactinemia in an amputated upper limb. Int J Dermatol. 2012;51:75-78. doi:10.1111/j.1365-4632.2011.04906.x
- Schwartz RA, Bagley MP, Janniger CK, et al. Verrucous carcinoma of a leg amputation stump. Dermatologica. 1991;182:193-195. doi:10.1159/000247782
- Campanati A, Diotallevi F, Radi G, et al. Efficacy and safety of botulinum toxin B in focal hyperhidrosis: a narrative review. Toxins. 2023;15:147. doi:10.3390/toxins15020147
- Anderson RR, Donelan MB, Hivnor C, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol. 2014;150:187-193. doi:10.1001/jamadermatol.2013.7761
- McGrath M, McCarthy J, Gallego A, et al. The influence of perforated prosthetic liners on residual limb wound healing: a case report. Can Prosthet Orthot J. 2019;2:32723. doi:10.33137/cpoj.v2i1.32723
- Abu El Hawa AA, Klein D, Bekeny JC, et al. The impact of statins on wound healing: an ally in treating the highly comorbid patient. J Wound Care. 2022;31(suppl 2):S36-S41. doi:10.12968/jowc.2022.31.Sup2.S36
- Nasseri S, Sharifi M. Therapeutic potential of antimicrobial peptides for wound healing. Int J Pept Res Ther. 2022;28:38. doi:10.1007/s10989-021-10350-5
- Lee JV, Engel C, Tay S, et al. N-Acetyl-Cysteine treatment after lower extremity amputation improves areas of perfusion defect and wound healing outcomes. J Vasc Surg. 2021;73:39-40. doi:10.1016/j.jvs.2020.12.025
- Dong Y, Yang Q, Sun X. Comprehensive analysis of cell therapy on chronic skin wound healing: a meta-analysis. Hum Gene Ther. 2021;32:787-795. doi:10.1089/hum.2020.275
- Brockes JP, Kumar A. Comparative aspects of animal regeneration. Annu Rev Cell Dev Biol. 2008;24:525-549. doi:10.1146/annurev.cellbio.24.110707.175336
- Eming SA, Hammerschmidt M, Krieg T, et al. Interrelation of immunity and tissue repair or regeneration. Semin Cell Dev Biol. 2009;20:517-527. doi:10.1016/j.semcdb.2009.04.009
- Eming SA. Evolution of immune pathways in regeneration and repair: recent concepts and translational perspectives. Semin Immunol. 2014;26:275-276. doi:10.1016/j.smim.2014.09.001
- Bolognia JL, Jorizzo JJ, Schaffer JV, et al. Dermatology. 4th edition. Elsevier; 2018.
- Wang PH, Huang BS, Horng HC, et al. Wound healing. J Chin Med Assoc JCMA. 2018;81:94-101. doi:10.1016/j.jcma.2017.11.002
- Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009;37:1528-1542. doi:10.1177/147323000903700531
- Gurtner GC, Werner S, Barrandon Y, et al. Wound repair and regeneration. Nature. 2008;453:314-321. doi:10.1038/nature07039
- Eming SA, Martin P, Tomic-Canic M. Wound repair and regeneration: mechanisms, signaling, and translation. Sci Transl Med. 2014;6:265sr6. doi:10.1126/scitranslmed.3009337
- Eming SA, Brachvogel B, Odorisio T, et al. Regulation of angiogenesis: wound healing as a model. Prog Histochem Cytochem. 2007;42:115-170. doi:10.1016/j.proghi.2007.06.001
- Janis JE, Harrison B. Wound healing: part I. basic science. Plast Reconstr Surg. 2016;138(3 suppl):9S-17S. doi:10.1097/PRS.0000000000002773
- Profyris C, Tziotzios C, Do Vale I. Cutaneous scarring: pathophysiology, molecular mechanisms, and scar reduction therapeutics. part I: the molecular basis of scar formation. J Am Acad Dermatol. 2012;66:1-10; quiz 11-12. doi:10.1016/j.jaad.2011.05.055
- Kwan P, Ding J, Tredget EE. MicroRNA 181b regulates decorin production by dermal fibroblasts and may be a potential therapy for hypertrophic scar. PLoS One. 2015;10:e0123054. doi:10.1371/journal.pone.0123054
- Ben W, Yang Y, Yuan J, et al. Human papillomavirus 16 E6 modulates the expression of host microRNAs in cervical cancer. Taiwan J Obstet Gynecol. 2015;54:364-370. doi:10.1016/j.tjog.2014.06.007
- Yu EH, Tu HF, Wu CH, et al. MicroRNA-21 promotes perineural invasion and impacts survival in patients with oral carcinoma. J Chin Med Assoc JCMA. 2017;80:383-388. doi:10.1016/j.jcma.2017.01.003
- Wen KC, Sung PL, Yen MS, et al. MicroRNAs regulate several functions of normal tissues and malignancies. Taiwan J Obstet Gynecol. 2013;52:465-469. doi:10.1016/j.tjog.2013.10.002
- Babalola O, Mamalis A, Lev-Tov H, et al. The role of microRNAs in skin fibrosis. Arch Dermatol Res. 2013;305:763-776. doi:10.1007/s00403-013-1410-1
- Hofer M, Hoferová Z, Falk M. Pharmacological modulation of radiation damage. does it exist a chance for other substances than hematopoietic growth factors and cytokines? Int J Mol Sci. 2017;18:1385. doi:10.3390/ijms18071385
- Darby IA, Weller CD. Aspirin treatment for chronic wounds: potential beneficial and inhibitory effects. Wound Repair Regen. 2017;25:7-12. doi:10.1111/wrr.12502
- Khalid KA, Nawi AFM, Zulkifli N, et al. Aging and wound healing of the skin: a review of clinical and pathophysiological hallmarks. Life. 2022;12:2142. doi:10.3390/life12122142
- Peacock HM, Gilbert EAB, Vickaryous MK. Scar‐free cutaneous wound healing in the leopard gecko, Eublepharis macularius. J Anat. 2015;227:596-610. doi:10.1111/joa.12368
- Delorme SL, Lungu IM, Vickaryous MK. Scar‐free wound healing and regeneration following tail loss in the leopard gecko, Eublepharis macularius. Anat Rec. 2012;295:1575-1595. doi:10.1002/ar.22490
- Brunauer R, Xia IG, Asrar SN, et al. Aging delays epimorphic regeneration in mice. J Gerontol Ser A Biol Sci Med Sci. 2021;76:1726-1733. doi:10.1093/gerona/glab131
- Dolan CP, Yang TJ, Zimmel K, et al. Epimorphic regeneration of the mouse digit tip is finite. Stem Cell Res Ther. 2022;13:62. doi:10.1186/s13287-022-02741-2
- Simkin J, Han M, Yu L, et al. The mouse digit tip: from wound healing to regeneration. Methods Mol Biol Clifton NJ. 2013;1037:419-435. doi:10.1007/978-1-62703-505-7_24
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429. doi:10.1016/j.apmr.2007.11.005
- Dudek NL, Marks MB, Marshall SC, et al. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch Phys Med Rehabil. 2005;86:659-663. doi:10.1016/j.apmr.2004.09.003
- Lannan FM, Meyerle JH. The dermatologist’s role in amputee skin care. Cutis. 2019;103:86-90.
- Dougherty AL, Mohrle CR, Galarneau MR, et al. Battlefield extremity injuries in Operation Iraqi Freedom. Injury. 2009;40:772-777. doi:10.1016/j.injury.2009.02.014
- Epstein RA, Heinemann AW, McFarland LV. Quality of life for veterans and servicemembers with major traumatic limb loss from Vietnam and OIF/OEF conflicts. J Rehabil Res Dev. 2010;47:373-385. doi:10.1682/jrrd.2009.03.0023
- Pinzur MS, Gold J, Schwartz D, et al. Energy demands for walking in dysvascular amputees as related to the level of amputation. Orthopedics. 1992;15:1033-1036; discussion 1036-1037. doi:10.3928/0147-7447-19920901-07
- Robinson V, Sansam K, Hirst L, et al. Major lower limb amputation–what, why and how to achieve the best results. Orthop Trauma. 2010;24:276-285. doi:10.1016/j.mporth.2010.03.017
- Lu S, Wang C, Zhong W, et al. Amputation stump revision using a free sural neurocutaneous perforator flap. Ann Plast Surg. 2016;76:83-87. doi:10.1097/SAP.0000000000000211
- Kim SW, Jeon SB, Hwang KT, et al. Coverage of amputation stumps using a latissimus dorsi flap with a serratus anterior muscle flap: a comparative study. Ann Plast Surg. 2016;76:88-93. doi:10.1097/SAP.0000000000000220
- Pavey GJ, Formby PM, Hoyt BW, et al. Intrawound antibiotic powder decreases frequency of deep infection and severity of heterotopic ossification in combat lower extremity amputations. Clin Orthop. 2019;477:802-810. doi:10.1007/s11999.0000000000000090
- Dunkel N, Belaieff W, Assal M, et al. Wound dehiscence and stump infection after lower limb amputation: risk factors and association with antibiotic use. J Orthop Sci Off J Jpn Orthop Assoc. 2012;17:588-594. doi:10.1007/s00776-012-0245-5
- Rubin G, Orbach H, Rinott M, et al. The use of prophylactic antibiotics in treatment of fingertip amputation: a randomized prospective trial. Am J Emerg Med. 2015;33:645-647. doi:10.1016/j.ajem.2015.02.002
- Azarbal AF, Harris S, Mitchell EL, et al. Nasal methicillin-resistant Staphylococcus aureus colonization is associated with increased wound occurrence after major lower extremity amputation. J Vasc Surg. 2015;62:401-405. doi:10.1016/j.jvs.2015.02.052
- Kwasniewski M, Mitchel D. Post amputation skin and wound care. Phys Med Rehabil Clin N Am. 2022;33:857-870. doi:10.1016/j.pmr.2022.06.010
- Chang H, Maldonado TS, Rockman CB, et al. Closed incision negative pressure wound therapy may decrease wound complications in major lower extremity amputations. J Vasc Surg. 2021;73:1041-1047. doi:10.1016/j.jvs.2020.07.061
- Kalliainen LK, Gordillo GM, Schlanger R, et al. Topical oxygen as an adjunct to wound healing: a clinical case series. Pathophysiol Off J Int Soc Pathophysiol. 2003;9:81-87. doi:10.1016/s0928-4680(02)00079-2
- Reichmann JP, Stevens PM, Rheinstein J, et al. Removable rigid dressings for postoperative management of transtibial amputations: a review of published evidence. PM R. 2018;10:516-523. doi:10.1016/j.pmrj.2017.10.002
- MacLean N, Fick GH. The effect of semirigid dressings on below-knee amputations. Phys Ther. 1994;74:668-673. doi:10.1093/ptj/74.7.668
- Koonalinthip N, Sukthongsa A, Janchai S. Comparison of removable rigid dressing and elastic bandage for residual limb maturation in transtibial amputees: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101:1683-1688. doi:10.1016/j.apmr.2020.05.009
- Taylor L, Cavenett S, Stepien JM, et al. Removable rigid dressings: a retrospective case-note audit to determine the validity of post-amputation application. Prosthet Orthot Int. 2008;32:223-230. doi:10.1080/03093640802016795
- Sumpio B, Shine SR, Mahler D, et al. A comparison of immediate postoperative rigid and soft dressings for below-knee amputations. Ann Vasc Surg. 2013;27:774-780. doi:10.1016/j.avsg.2013.03.007
- van Velzen AD, Nederhand MJ, Emmelot CH, et al. Early treatment of trans-tibial amputees: retrospective analysis of early fitting and elastic bandaging. Prosthet Orthot Int. 2005;29:3-12. doi:10.1080/17461550500069588
- Chin T, Toda M. Results of prosthetic rehabilitation on managing transtibial vascular amputation with silicone liner after wound closure. J Int Med Res. 2016;44:957-967. doi:10.1177/0300060516647554
- Hoskins RD, Sutton EE, Kinor D, et al. Using vacuum-assisted suspension to manage residual limb wounds in persons with transtibial amputation: a case series. Prosthet Orthot Int. 2014;38:68-74. doi:10.1177/0309364613487547
- Johannesson A, Larsson GU, Oberg T, et al. Comparison of vacuum-formed removable rigid dressing with conventional rigid dressing after transtibial amputation: similar outcome in a randomized controlled trial involving 27 patients. Acta Orthop. 2008;79:361-369. doi:10.1080/17453670710015265
- Alsancak S, Köse SK, Altınkaynak H. Effect of elastic bandaging and prosthesis on the decrease in stump volume. Acta Orthop Traumatol Turc. 2011;45:14-22. doi:10.3944/AOTT.2011.2365
- Than MP, Smith RA, Hammond C, et al. Keratin-based wound care products for treatment of resistant vascular wounds. J Clin Aesthetic Dermatol. 2012;5:31-35.
- Gurtner GC, Garcia AD, Bakewell K, et al. A retrospective matched‐cohort study of 3994 lower extremity wounds of multiple etiologies across 644 institutions comparing a bioactive human skin allograft, TheraSkin, plus standard of care, to standard of care alone. Int Wound J. 2020;17:55-64. doi:10.1111/iwj.13231
- Buikema KES, Meyerle JH. Amputation stump: privileged harbor for infections, tumors, and immune disorders. Clin Dermatol. 2014;32:670-677. doi:10.1016/j.clindermatol.2014.04.015
- Yang NB, Garza LA, Foote CE, et al. High prevalence of stump dermatoses 38 years or more after amputation. Arch Dermatol. 2012;148:1283-1286. doi:10.1001/archdermatol.2012.3004
- Potter BK, Burns TC, Lacap AP, et al. Heterotopic ossification following traumatic and combat-related amputations. Prevalence, risk factors, and preliminary results of excision. J Bone Joint Surg Am. 2007;89:476-486. doi:10.2106/JBJS.F.00412
- Edwards DS, Kuhn KM, Potter BK, et al. Heterotopic ossification: a review of current understanding, treatment, and future. J Orthop Trauma. 2016;30(suppl 3):S27-S30. doi:10.1097/BOT.0000000000000666
- Tintle SM, Shawen SB, Forsberg JA, et al. Reoperation after combat-related major lower extremity amputations. J Orthop Trauma. 2014;28:232-237. doi:10.1097/BOT.0b013e3182a53130
- Bui KM, Raugi GJ, Nguyen VQ, et al. Skin problems in individuals with lower-limb loss: literature review and proposed classification system. J Rehabil Res Dev. 2009;46:1085-1090. doi:10.1682/jrrd.2009.04.0052
- Turan H, Bas¸kan EB, Adim SB, et al. Acroangiodermatitis in a below-knee amputation stump. Clin Exp Dermatol. 2011;36:560-561. doi:10.1111/j.1365-2230.2011.04037.x
- Lin CH, Ma H, Chung MT, et al. Granulomatous cutaneous lesions associated with risperidone-induced hyperprolactinemia in an amputated upper limb. Int J Dermatol. 2012;51:75-78. doi:10.1111/j.1365-4632.2011.04906.x
- Schwartz RA, Bagley MP, Janniger CK, et al. Verrucous carcinoma of a leg amputation stump. Dermatologica. 1991;182:193-195. doi:10.1159/000247782
- Campanati A, Diotallevi F, Radi G, et al. Efficacy and safety of botulinum toxin B in focal hyperhidrosis: a narrative review. Toxins. 2023;15:147. doi:10.3390/toxins15020147
- Anderson RR, Donelan MB, Hivnor C, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol. 2014;150:187-193. doi:10.1001/jamadermatol.2013.7761
- McGrath M, McCarthy J, Gallego A, et al. The influence of perforated prosthetic liners on residual limb wound healing: a case report. Can Prosthet Orthot J. 2019;2:32723. doi:10.33137/cpoj.v2i1.32723
- Abu El Hawa AA, Klein D, Bekeny JC, et al. The impact of statins on wound healing: an ally in treating the highly comorbid patient. J Wound Care. 2022;31(suppl 2):S36-S41. doi:10.12968/jowc.2022.31.Sup2.S36
- Nasseri S, Sharifi M. Therapeutic potential of antimicrobial peptides for wound healing. Int J Pept Res Ther. 2022;28:38. doi:10.1007/s10989-021-10350-5
- Lee JV, Engel C, Tay S, et al. N-Acetyl-Cysteine treatment after lower extremity amputation improves areas of perfusion defect and wound healing outcomes. J Vasc Surg. 2021;73:39-40. doi:10.1016/j.jvs.2020.12.025
- Dong Y, Yang Q, Sun X. Comprehensive analysis of cell therapy on chronic skin wound healing: a meta-analysis. Hum Gene Ther. 2021;32:787-795. doi:10.1089/hum.2020.275
Practice Points
- Wound healing in adults is a complex dynamic process that usually takes the greater part of 1 year to completely resolve and is marked by the end of scar formation.
- Postamputation residual limbs are subject to mechanical and biophysical stress to which the overlying skin is not accustomed. Skin treatment aims at mitigating these stresses.
- The major dermatologic barriers to successful wound healing following amputation include infection, skin breakdown, formation of chronic wounds and granulation tissue, heterotopic ossification, and hyperhidrosis.
Tangled Truths: Unraveling the Link Between Frontal Fibrosing Alopecia and Allergic Contact Dermatitis
Frontal fibrosing alopecia (FFA) is an increasingly common diagnosis, especially in middle-aged women, and was first described by Kossard1 in 1994. It is a variant of lichen planopilaris (LPP), a progressive scarring cicatricial alopecia that affects the frontotemporal area of the scalp, eyebrows, and sometimes even body hair.1 Although its etiology remains unclear, genetic causes, drugs, hormones, and environmental exposures—including certain chemicals found in sunscreens—have been implicated in its pathogenesis.2,3 An association between contact allergy to ingredients in personal care products and FFA diagnosis has been suggested; however, there is no evidence of causality to date. In this article, we highlight the potential relationship between contact allergy and FFA as well as clinical considerations for management.
Clinical Features and Diagnosis
Frontal fibrosing alopecia typically manifests with gradual symmetric recession of the frontal hairline leading to bandlike hair loss along the forehead, sometimes extending to the temporal region.4 Some patients may experience symptoms of scalp itching, burning, or tenderness that may precede or accompany the hair loss. Perifollicular erythema may be visible during the early stages and can be visualized on trichoscopy. The affected skin may appear pale and shiny and may have a smooth texture with a distinct lack of follicular openings. Aside from scalp involvement, other manifestations may include lichen planus pigmentosus, facial papules, body hair involvement, hypochromic lesions, diffuse redness on the face and neck, and prominent frontal veins.5 Although most FFA cases have characteristic clinical features and trichoscopic findings, biopsy for histopathologic examination is still recommended to confirm the diagnosis and ensure appropriate treatment.4 Classic histopathologic features include perifollicular lymphocytic inflammation, follicular destruction, and scarring.
Pathophysiology of FFA
The pathogenesis of FFA is thought to involve a variety of triggers, including immune-mediated inflammation, stress, genetics, hormones, and possibly environmental factors.6 Frontal fibrosing alopecia demonstrates considerable upregulation in cytotoxic helper T cells (TH1) and IFN-γ activity resulting in epithelial hair follicle stem cell apoptosis and replacement of normal epithelial tissue with fibrous tissue.7 There is some suspicion of genetic susceptibility in the onset of FFA as suggested by familial reports and genome-wide association studies.8-10 Hormonal and autoimmune factors also have been linked to FFA, including an increased risk for thyroid disease and the postmenopausal rise of androgen levels.6
Allergic Contact Dermatitis and FFA
Although they are 2 distinct conditions with differing etiologies, allergic contact dermatitis (ACD) and FFA may share environmental triggers, especially in susceptible individuals. This may support the coexistence and potential association between ACD and FFA.
In one case report, a woman who developed facial eczema followed by FFA showed positive patch tests to the UV filters drometrizole trisiloxane and ethylhexyl salicylate, which were listed as ingredients in her sunscreens. Avoidance of these allergens reportedly led to notable improvement of the symptoms.11 Case-control studies have found an association between the use of facial sunscreen and risk for FFA.12 A 2016 questionnaire that assessed a wide range of lifestyle, social, and medical factors related to FFA found that the use of sunscreens was significantly higher in patients with FFA than controls (P<.001), pointing to sunscreens as a potential contributing factor, but further research has been inconclusive. A higher frequency of positive patch tests to hydroperoxides of linalool and balsam of Peru (BoP) in patients with FFA have been documented; however, a direct cause cannot be established.2
In a 2020 prospective study conducted at multiple international centers, 65% (13/20) of FFA patients and 37.5% (9/24) of the control group had a positive patch test reaction to one or more allergens (P=.003). The most common allergens that were identified included cobalt chloride (positive in 35% [7/20] of patients with FFA), nickel sulfate (25% [5/20]), and potassium dichromate (15% [3/20]).13 In a recent 2-year cohort study of 42 patients with FFA who were referred for patch testing, the most common allergens included gallates, hydroperoxides of linalool, and other fragrances.14 After a 3-month period of allergen avoidance, 70% (29/42) of patients had decreased scalp erythema on examination, indicating that avoiding relevant allergens may reduce local inflammation. Furthermore, 76.2% (32/42) of patients with FFA showed delayed-type hypersensitivity to allergens found in daily personal care products such as shampoos, sunscreens, and moisturizers, among others.14 Notably, the study lacked a control group. A case-control study of 36 Hispanic women conducted in Mexico also resulted in 83.3% (15/18) of patients with FFA and 55.5% (10/18) of controls having at least 1 positive patch test; in the FFA group, these included iodopropynyl butylcarbamate (16.7% [3/18]) and propolis (16.7% [3/18]).15
Most recently, a retrospective study conducted by Shtaynberger et al16 included 12 patients with LPP or FFA diagnosed via clinical findings or biopsy. It also included an age- and temporally matched control group tested with identical allergens. Among the 12 patients who had FFA/LPP, all had at least 1 allergen identified on patch testing. The most common allergens identified were propolis (positive in 50% [6/12] of patients with FFA/LPP), fragrance mix I (16%), and methylisothiazolinone (16% [2/12]). Follow-up data were available for 9 of these patients, of whom 6 (66.7%) experienced symptom improvement after 6 months of allergen avoidance. Four (44.4%) patients experienced decreased follicular redness or scaling, 2 (22.2%) patients experienced improved scalp pain/itch, 2 (22.2%) patients had stable/improved hair density, and 1 (1.1%) patient had decreased hair shedding. Although this suggests an environmental trigger for FFA/LPP, the authors stated that changes in patient treatment plans could have contributed to their improvement. The study also was limited by its small size and its overall generalizability.16
These studies have underscored the significance of patch testing in individuals diagnosed with FFA and have identified common allergens prevalent in this patient population. They have suggested that patients with FFA are more likely to have positive patch tests, and in some cases patients could experience improvements in scalp pruritus and erythema with allergen avoidance; however, we emphasize that a causal association between contact allergy and FFA remains unproven to date.
Most Common Allergens Pertinent to FFA
Preservatives—In some studies, patients with FFA have had positive patch tests to preservatives such as gallates and methylchloroisothiazolinone/methylisothiazolinone (MCI/MI).14 Gallates are antioxidants that are used in food preservation, pharmaceuticals, and cosmetics due to their ability to inhibit oxidation and rancidity of fats and oils.17 The most common gallates include propyl gallate, octyl gallate, and dodecyl gallate. Propyl gallate is utilized in some waxy or oily cosmetics and personal care items including sunscreens, shampoos, conditioners, bar soaps, facial cleansers, and moisturizers.18 Typically, if patients have a positive patch test to one gallate, they should be advised to avoid all gallate compounds, as they can cross-react.
Similarly, MCI/MI can prevent product degradation through their antibacterial and antifungal properties. This combination of MCI and MI is used as an effective method of prolonging the shelf life of cosmetic products and commonly is found in sunscreens, facial moisturizing creams, shampoos, and conditioners19; it is banned from use in leave-on products in the European Union and Canada due to increased rates of contact allergy.20 In patients with FFA who commonly use facial sunscreen, preservatives can be a potential allergen exposure to consider.
Iodopropynyl butylcarbamate also is a preservative used in cosmetic formulations. Similar to MCI/MI, it is a potent fungicide and bactericide. This allergen can be found in hair care products, bodywashes, and other personal products.21
UV Light–Absorbing Agents—A systematic review and meta-analysis conducted in 2022 showed a significant (P<.001) association between sunscreen use and FFA.22 A majority of allergens identified on patch testing included UVA- and UVB-absorbing agents found in sunscreens and other products including cosmetics,11,12 such as drometrizole trisiloxane, ethylhexyl salicylate, avobenzone, and benzophenone-4. Drometrizole trisiloxane is a photostabilizer and a broad-spectrum UV filter that is not approved for use in sunscreens in the United States.23 It also is effective in stabilizing and preventing the degradation of avobenzone, a commonly used UVA filter.24
Fragrances—Fragrances are present in nearly every personal and cosmetic product, sometimes even in those advertised as being “fragrance free.” Hydroperoxides of linalool, BoP, and fragrance mix are common allergens that are found in a variety of personal care products including perfumes, cosmetics, and even household cleaning supplies.25 Simultaneous positive patch tests to BoP and fragrance mix are common due to shared components. Linalool can be found in various plants such as lavender, rose, bergamot, and jasmine.26 Upon air exposure, linalool auto-oxidizes to form allergenic hydroperoxides of linalool. Among patients with FFA, positive patch test reactions to fragrance chemicals are common and could be attributed to the use of fragranced hair products and facial cosmetics.
Hair Dyes and Bleaches—Allergic reactions to hair dyes and bleaches can result in severe ACD of the head/neck and, in rare cases, scarring alopecia.27 Chemicals found in these products include paraphenylenediamine (PPD) and ammonium persulfate. The most common hair dye allergen, PPD also is used in some rubbers and plastics. Ammonium persulfate is a chemical used in hair bleaches and to deodorize oils. One case study reported a patient with FFA who developed chemically induced vitiligo immediately after the use of a hair color product that contained PPD.28 However, without patch testing to confirm the presence of contact allergy, other patient-specific and environmental risk factors could have contributed to FFA in this case.
A Knot in the Truth
In this endeavor to untangle the truth, it should be remembered that at the time of writing, the purported association between FFA and ACD remains debatable. Contact dermatitis specialists have voiced that the association between FFA and ACD, especially with regard to sunscreen, cannot be supported due to the lack of sufficient evidence.29 A large majority of the research conducted on FFA and ACD is based on case reports and studies limited to a small sample size, and most of these patch test studies lack a control group. Felmingham et al30 noted that the recent epidemiology of FFA aligns with increased sunscreen use. They also highlighted the limitations of the aforementioned studies, which include misclassification of exposures in the control group2 and recall bias in questionnaire participants.2,12 The most pressing limitation that permeates through most of these studies is the temporal ambiguity associated with sunscreen use. A study by Dhana et al31 failed to specify whether increased sunscreen use preceded the diagnosis of FFA or if it stems from the need to protect more exposed skin as a consequence of disease. Broad sunscreen avoidance due to concern for a possible association with hair loss could have detrimental health implications by increasing the risk for photodamage and skin cancer.
FFA Patch Testing
The avoidance of pertinent allergens could be effective in reducing local inflammation, pruritus, and erythema in FFA.9,14,32 At our institution, we selectively patch test patients with FFA when there is a suspected contact allergy. Clinical features that may allude to a potential contact allergy include an erythematous or eczematous dermatitis or symptoms of pruritus along the scalp or eyebrows. If patients recall hair loss or symptoms after using a hair or facial product, then a potential contact allergy to these products could be considered. Patch testing in patients with FFA includes the North American 80 Comprehensive Series and the cosmetic and hairdresser supplemental series, as well as an additional customized panel of 8 allergens as determined by patch testing experts at the University of Massachusetts, Brigham and Women’s Hospital, and Massachusetts General Hospital (private email communication, November 2017). Patch test readings are performed at 48 and 96 or 120 hours. Using the American Contact Dermatitis Society’s Contact Allergen Management Program, patients are provided personalized safe product lists and avoidance strategies are discussed.
Final Interpretation
In a world where cosmetic products are ubiquitous, it is hard to define the potential role of contact allergens in the entangled pathogenesis of FFA and ACD. As evidenced by emerging literature that correlates the 2 conditions and their exacerbating factors, it is important for physicians to have a comprehensive diagnostic approach and heightened awareness for potential allergens at play in FFA (Table). The identification of certain chemicals and preservatives as potential triggers for FFA should emphasize the importance of patch testing in these patients; however, whether the positive reactions are relevant to the pathogenesis or disease course of FFA still is unknown. While these findings begin to unravel the intertwined causes of FFA and ACD, further research encompassing larger cohorts and prospective studies is imperative to solidify these associations, define concrete guidelines, and improve patient outcomes.
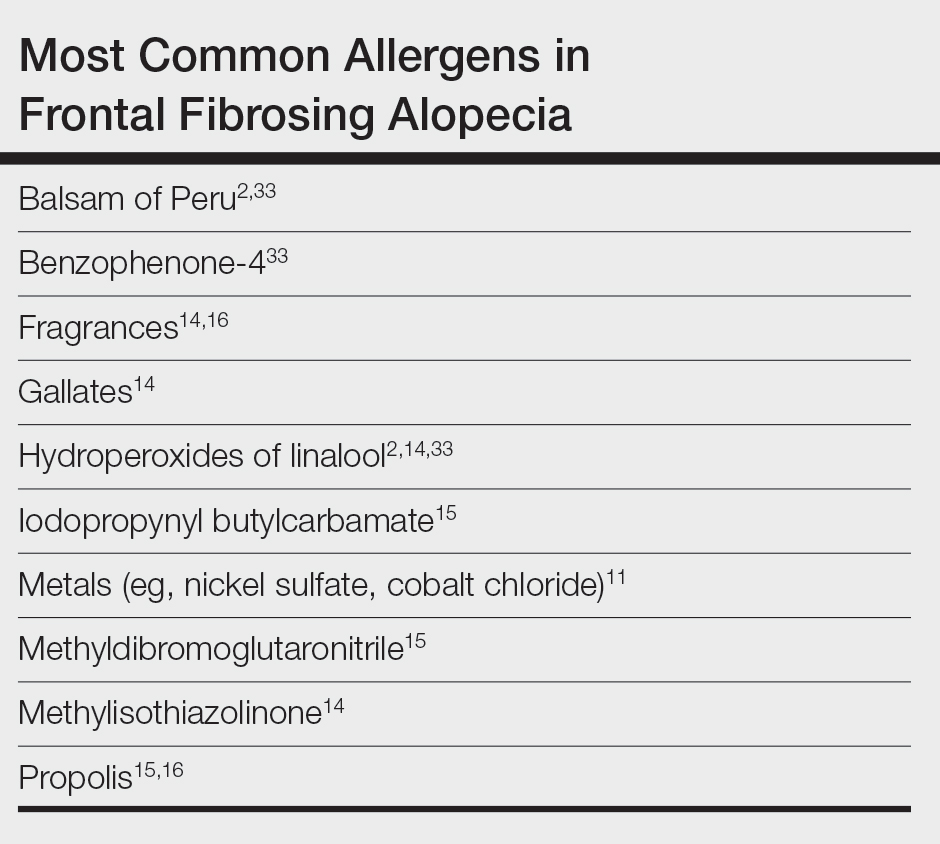
- Kossard S. Postmenopausal frontal fibrosing alopecia: scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770-774. doi:10.1001/archderm.1994.01690060100013
- Aldoori N, Dobson K, Holden CR, et al. Frontal fibrosing alopecia: possible association with leave-on facial skin care products and sunscreens; a questionnaire study. Br J Dermatol. 2016;175:762-767. doi:10.1111/bjd.14535
- Debroy Kidambi A, Dobson K, Holmes S, et al. Frontal fibrosing alopecia in men: an association with facial moisturizers and sunscreens. Br J Dermatol. 2017;177:260-261. doi:10.1111/bjd.15311
- Starace M, Orlando G, Iorizzo M, et al. Clinical and dermoscopic approaches to diagnosis of frontal fibrosing alopecia: results from a multicenter study of the International Dermoscopy Society. Dermatol Pract Concept. 2022;12:E2022080. doi:10.5826/dpc.1201a80
- Fechine COC, Valente NYS, Romiti R. Lichen planopilaris and frontal fibrosing alopecia: review and update of diagnostic and therapeutic features. An Bras Dermatol. 2022;97:348-357. doi:10.1016/j.abd.2021.08.008
- Frontal fibrosing alopecia: a review of disease pathogenesis. Front Med (Lausanne). 2022;9:911944. doi:10.3389/fmed.2022.911944
- Del Duca E, Ruano Ruiz J, Pavel AB, et al. Frontal fibrosing alopecia shows robust T helper 1 and Janus kinase 3 skewing. Br J Dermatol. 2020;183:1083-1093. doi:10.1111/bjd.19040
- Tziotzios C, Petridis C, Dand N, et al. Genome-wide association study in frontal fibrosing alopecia identifies four susceptibility loci including HLA-B*07:02. Nat Commun. 2019;10:1150. doi:10.1038/s41467-019-09117-w
- Navarro‐Belmonte MR, Navarro‐López V, Ramírez‐Boscà A, et al. Case series of familial frontal fibrosing alopecia and a review of the literature. J Cosmet Dermatol. 2015;14:64-69. doi:10.1111/jocd.12125
- Cuenca-Barrales C, Ruiz-Villaverde R, Molina-Leyva A. Familial frontal fibrosing alopecia. Sultan Qaboos Univ Med J. 2021;21:E320-E323. doi:10.18295/squmj.2021.21.02.025
- Pastor-Nieto MA, Gatica-Ortega ME. Allergic contact dermatitis to drometrizole trisiloxane in a woman thereafter diagnosed with frontal fibrosing alopecia. Contact Dermatitis. 2023;89:215-217. doi:10.1111/cod.14370
- Moreno-Arrones OM, Saceda-Corralo D, Rodrigues-Barata AR, et al. Risk factors associated with frontal fibrosing alopecia: a multicentre case–control study. Clin Exp Dermatol. 2019;44:404-410. doi:10.1111/ced.13785
- Rudnicka L, Rokni GR, Lotti T, et al. Allergic contact dermatitis in patients with frontal fibrosing alopecia: an international multi-center study. Dermatol Ther. 2020;33:E13560. doi:10.1111/dth.13560
- Prasad S, Marks DH, Burns LJ, et al. Patch testing and contact allergen avoidance in patients with lichen planopilaris and/or frontal fibrosing alopecia: a cohort study. J Am Acad Dermatol. 2020;83:659-661. doi:10.1016/j.jaad.2020.01.026
- Ocampo-Garza SS, Herz-Ruelas ME, Chavez-Alvarez S, et al. Association of frontal fibrosing alopecia and contact allergens in everyday skincare products in Hispanic females: a case-control study. An Bras Dermatol. 2021;96:776-778. doi:10.1016/j.abd.2020.09.013
- Shtaynberger B, Bruder P, Zippin JH. The prevalence of type iv hypersensitivity in patients with lichen planopilaris and frontal fibrosing alopecia. Dermatitis. 2023;34:351-352. doi:10.1097/DER.0000000000000965
- Kahkeshani N, Farzaei F, Fotouhi M, et al. Pharmacological effects of gallic acid in health and diseases: a mechanistic review. Iran J Basic Med Sci. 2019;22:225-237. doi:10.22038/ijbms.2019.32806.7897
- Holcomb ZE, Van Noord MG, Atwater AR. Gallate contact dermatitis: product update and systematic review. Dermatitis. 2017;28:115-127. doi:10.1097/DER.0000000000000263
- Gorris A, Valencak J, Schremser V, et al. Contact allergy to methylisothiazolinone with three clinical presentations in one patient. Contact Dermatitis. 2020;82:162-164. doi:10.1111/cod.13384
- Uter W, Aalto-Korte K, Agner T, et al. The epidemic of methylisothiazolinone contact allergy in Europe: follow-up on changing exposures. J Eur Acad Dermatol Venereol. 2020;34:333-339. doi:10.1111/jdv.15875
- Batista M, Morgado F, Gonçalo M. Patch test reactivity to iodopropynyl butylcarbamate in consecutive patients during a period of 7 years. Contact Dermatitis. 2019;81:54-55. doi:10.1111/cod.13213
- Maghfour J, Ceresnie M, Olson J, et al. The association between frontal fibrosing alopecia, sunscreen, and moisturizers: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;87:395-396. doi:10.1016/j.jaad.2021.12.058
- Drometrizole trisiloxane. PubChem website. Accessed February 21, 2024. https://pubchem.ncbi.nlm.nih.gov/compound/9848888
- Hughes TM, Martin JA, Lewis VJ, et al. Allergic contact dermatitis to drometrizole trisiloxane in a sunscreen with concomitant sensitivities to other sunscreens. Contact Dermatitis. 2005;52:226-227. doi:10.1111/j.0105-1873.2005.0566a.x
- de Groot AC. Myroxylon pereirae resin (balsam of Peru)—a critical review of the literature and assessment of the significance of positive patch test reactions and the usefulness of restrictive diets. Contact Dermatitis. 2019;80:335-353. doi:10.1111/cod.13263
- Sköld M, Börje A, Matura M, et al. Studies on the autoxidation and sensitizing capacity of the fragrance chemical linalool, identifying a linalool hydroperoxide. Contact Dermatitis. 2002;46:267-272. doi:10.1034/j.1600-0536.2002.460504.x
- Dev T, Khan E, Patel U, et al. Cicatricial alopecia following allergic contact dermatitis from hair dyes: a rare clinical presentation. Contact Dermatitis. 2022;86:59-61. doi:10.1111/cod.13974
- De Souza B, Burns L, Senna MM. Frontal fibrosing alopecia preceding the development of vitiligo: a case report. JAAD Case Rep. 2020;6:154-155. doi:10.1016/j.jdcr.2019.12.011
- Abuav R, Shon W. Are sunscreen particles involved in frontal fibrosing alopecia?—a TEM-EDXS analysis on formalin-fixed paraffin-embedded alopecia biopsies (pilot study). Am J Dermatopathol. 2022;44:E135. doi:10.1097/DAD.0000000000002317
- Felmingham C, Yip L, Tam M, et al. Allergy to sunscreen and leave-on facial products is not a likely causative mechanism in frontal fibrosing alopecia: perspective from contact allergy experts. Br J Dermatol. 2020;182:481-482. doi:10.1111/bjd.18380
- Dhana A, Gumedze F, Khumalo N. Regarding “frontal fibrosing alopecia: possible association with leave-on facial skincare products and sunscreens; a questionnaire study.” Br J Dermatol. 2016;176:836-837. doi:10.1111/bjd.15197
- Pastor-Nieto MA, Gatica-Ortega ME, Sánchez-Herreros C, et al. Sensitization to benzyl salicylate and other allergens in patients with frontal fibrosing alopecia. Contact Dermatitis. 2021;84:423-430. doi:10.1111/cod.13763
- Rocha VB, Donati A, Contin LA, et al. Photopatch and patch testing in 63 patients with frontal fibrosing alopecia: a case series. Br J Dermatol. 2018;179:1402-1403. doi:10.1111/bjd.16933
Frontal fibrosing alopecia (FFA) is an increasingly common diagnosis, especially in middle-aged women, and was first described by Kossard1 in 1994. It is a variant of lichen planopilaris (LPP), a progressive scarring cicatricial alopecia that affects the frontotemporal area of the scalp, eyebrows, and sometimes even body hair.1 Although its etiology remains unclear, genetic causes, drugs, hormones, and environmental exposures—including certain chemicals found in sunscreens—have been implicated in its pathogenesis.2,3 An association between contact allergy to ingredients in personal care products and FFA diagnosis has been suggested; however, there is no evidence of causality to date. In this article, we highlight the potential relationship between contact allergy and FFA as well as clinical considerations for management.
Clinical Features and Diagnosis
Frontal fibrosing alopecia typically manifests with gradual symmetric recession of the frontal hairline leading to bandlike hair loss along the forehead, sometimes extending to the temporal region.4 Some patients may experience symptoms of scalp itching, burning, or tenderness that may precede or accompany the hair loss. Perifollicular erythema may be visible during the early stages and can be visualized on trichoscopy. The affected skin may appear pale and shiny and may have a smooth texture with a distinct lack of follicular openings. Aside from scalp involvement, other manifestations may include lichen planus pigmentosus, facial papules, body hair involvement, hypochromic lesions, diffuse redness on the face and neck, and prominent frontal veins.5 Although most FFA cases have characteristic clinical features and trichoscopic findings, biopsy for histopathologic examination is still recommended to confirm the diagnosis and ensure appropriate treatment.4 Classic histopathologic features include perifollicular lymphocytic inflammation, follicular destruction, and scarring.
Pathophysiology of FFA
The pathogenesis of FFA is thought to involve a variety of triggers, including immune-mediated inflammation, stress, genetics, hormones, and possibly environmental factors.6 Frontal fibrosing alopecia demonstrates considerable upregulation in cytotoxic helper T cells (TH1) and IFN-γ activity resulting in epithelial hair follicle stem cell apoptosis and replacement of normal epithelial tissue with fibrous tissue.7 There is some suspicion of genetic susceptibility in the onset of FFA as suggested by familial reports and genome-wide association studies.8-10 Hormonal and autoimmune factors also have been linked to FFA, including an increased risk for thyroid disease and the postmenopausal rise of androgen levels.6
Allergic Contact Dermatitis and FFA
Although they are 2 distinct conditions with differing etiologies, allergic contact dermatitis (ACD) and FFA may share environmental triggers, especially in susceptible individuals. This may support the coexistence and potential association between ACD and FFA.
In one case report, a woman who developed facial eczema followed by FFA showed positive patch tests to the UV filters drometrizole trisiloxane and ethylhexyl salicylate, which were listed as ingredients in her sunscreens. Avoidance of these allergens reportedly led to notable improvement of the symptoms.11 Case-control studies have found an association between the use of facial sunscreen and risk for FFA.12 A 2016 questionnaire that assessed a wide range of lifestyle, social, and medical factors related to FFA found that the use of sunscreens was significantly higher in patients with FFA than controls (P<.001), pointing to sunscreens as a potential contributing factor, but further research has been inconclusive. A higher frequency of positive patch tests to hydroperoxides of linalool and balsam of Peru (BoP) in patients with FFA have been documented; however, a direct cause cannot be established.2
In a 2020 prospective study conducted at multiple international centers, 65% (13/20) of FFA patients and 37.5% (9/24) of the control group had a positive patch test reaction to one or more allergens (P=.003). The most common allergens that were identified included cobalt chloride (positive in 35% [7/20] of patients with FFA), nickel sulfate (25% [5/20]), and potassium dichromate (15% [3/20]).13 In a recent 2-year cohort study of 42 patients with FFA who were referred for patch testing, the most common allergens included gallates, hydroperoxides of linalool, and other fragrances.14 After a 3-month period of allergen avoidance, 70% (29/42) of patients had decreased scalp erythema on examination, indicating that avoiding relevant allergens may reduce local inflammation. Furthermore, 76.2% (32/42) of patients with FFA showed delayed-type hypersensitivity to allergens found in daily personal care products such as shampoos, sunscreens, and moisturizers, among others.14 Notably, the study lacked a control group. A case-control study of 36 Hispanic women conducted in Mexico also resulted in 83.3% (15/18) of patients with FFA and 55.5% (10/18) of controls having at least 1 positive patch test; in the FFA group, these included iodopropynyl butylcarbamate (16.7% [3/18]) and propolis (16.7% [3/18]).15
Most recently, a retrospective study conducted by Shtaynberger et al16 included 12 patients with LPP or FFA diagnosed via clinical findings or biopsy. It also included an age- and temporally matched control group tested with identical allergens. Among the 12 patients who had FFA/LPP, all had at least 1 allergen identified on patch testing. The most common allergens identified were propolis (positive in 50% [6/12] of patients with FFA/LPP), fragrance mix I (16%), and methylisothiazolinone (16% [2/12]). Follow-up data were available for 9 of these patients, of whom 6 (66.7%) experienced symptom improvement after 6 months of allergen avoidance. Four (44.4%) patients experienced decreased follicular redness or scaling, 2 (22.2%) patients experienced improved scalp pain/itch, 2 (22.2%) patients had stable/improved hair density, and 1 (1.1%) patient had decreased hair shedding. Although this suggests an environmental trigger for FFA/LPP, the authors stated that changes in patient treatment plans could have contributed to their improvement. The study also was limited by its small size and its overall generalizability.16
These studies have underscored the significance of patch testing in individuals diagnosed with FFA and have identified common allergens prevalent in this patient population. They have suggested that patients with FFA are more likely to have positive patch tests, and in some cases patients could experience improvements in scalp pruritus and erythema with allergen avoidance; however, we emphasize that a causal association between contact allergy and FFA remains unproven to date.
Most Common Allergens Pertinent to FFA
Preservatives—In some studies, patients with FFA have had positive patch tests to preservatives such as gallates and methylchloroisothiazolinone/methylisothiazolinone (MCI/MI).14 Gallates are antioxidants that are used in food preservation, pharmaceuticals, and cosmetics due to their ability to inhibit oxidation and rancidity of fats and oils.17 The most common gallates include propyl gallate, octyl gallate, and dodecyl gallate. Propyl gallate is utilized in some waxy or oily cosmetics and personal care items including sunscreens, shampoos, conditioners, bar soaps, facial cleansers, and moisturizers.18 Typically, if patients have a positive patch test to one gallate, they should be advised to avoid all gallate compounds, as they can cross-react.
Similarly, MCI/MI can prevent product degradation through their antibacterial and antifungal properties. This combination of MCI and MI is used as an effective method of prolonging the shelf life of cosmetic products and commonly is found in sunscreens, facial moisturizing creams, shampoos, and conditioners19; it is banned from use in leave-on products in the European Union and Canada due to increased rates of contact allergy.20 In patients with FFA who commonly use facial sunscreen, preservatives can be a potential allergen exposure to consider.
Iodopropynyl butylcarbamate also is a preservative used in cosmetic formulations. Similar to MCI/MI, it is a potent fungicide and bactericide. This allergen can be found in hair care products, bodywashes, and other personal products.21
UV Light–Absorbing Agents—A systematic review and meta-analysis conducted in 2022 showed a significant (P<.001) association between sunscreen use and FFA.22 A majority of allergens identified on patch testing included UVA- and UVB-absorbing agents found in sunscreens and other products including cosmetics,11,12 such as drometrizole trisiloxane, ethylhexyl salicylate, avobenzone, and benzophenone-4. Drometrizole trisiloxane is a photostabilizer and a broad-spectrum UV filter that is not approved for use in sunscreens in the United States.23 It also is effective in stabilizing and preventing the degradation of avobenzone, a commonly used UVA filter.24
Fragrances—Fragrances are present in nearly every personal and cosmetic product, sometimes even in those advertised as being “fragrance free.” Hydroperoxides of linalool, BoP, and fragrance mix are common allergens that are found in a variety of personal care products including perfumes, cosmetics, and even household cleaning supplies.25 Simultaneous positive patch tests to BoP and fragrance mix are common due to shared components. Linalool can be found in various plants such as lavender, rose, bergamot, and jasmine.26 Upon air exposure, linalool auto-oxidizes to form allergenic hydroperoxides of linalool. Among patients with FFA, positive patch test reactions to fragrance chemicals are common and could be attributed to the use of fragranced hair products and facial cosmetics.
Hair Dyes and Bleaches—Allergic reactions to hair dyes and bleaches can result in severe ACD of the head/neck and, in rare cases, scarring alopecia.27 Chemicals found in these products include paraphenylenediamine (PPD) and ammonium persulfate. The most common hair dye allergen, PPD also is used in some rubbers and plastics. Ammonium persulfate is a chemical used in hair bleaches and to deodorize oils. One case study reported a patient with FFA who developed chemically induced vitiligo immediately after the use of a hair color product that contained PPD.28 However, without patch testing to confirm the presence of contact allergy, other patient-specific and environmental risk factors could have contributed to FFA in this case.
A Knot in the Truth
In this endeavor to untangle the truth, it should be remembered that at the time of writing, the purported association between FFA and ACD remains debatable. Contact dermatitis specialists have voiced that the association between FFA and ACD, especially with regard to sunscreen, cannot be supported due to the lack of sufficient evidence.29 A large majority of the research conducted on FFA and ACD is based on case reports and studies limited to a small sample size, and most of these patch test studies lack a control group. Felmingham et al30 noted that the recent epidemiology of FFA aligns with increased sunscreen use. They also highlighted the limitations of the aforementioned studies, which include misclassification of exposures in the control group2 and recall bias in questionnaire participants.2,12 The most pressing limitation that permeates through most of these studies is the temporal ambiguity associated with sunscreen use. A study by Dhana et al31 failed to specify whether increased sunscreen use preceded the diagnosis of FFA or if it stems from the need to protect more exposed skin as a consequence of disease. Broad sunscreen avoidance due to concern for a possible association with hair loss could have detrimental health implications by increasing the risk for photodamage and skin cancer.
FFA Patch Testing
The avoidance of pertinent allergens could be effective in reducing local inflammation, pruritus, and erythema in FFA.9,14,32 At our institution, we selectively patch test patients with FFA when there is a suspected contact allergy. Clinical features that may allude to a potential contact allergy include an erythematous or eczematous dermatitis or symptoms of pruritus along the scalp or eyebrows. If patients recall hair loss or symptoms after using a hair or facial product, then a potential contact allergy to these products could be considered. Patch testing in patients with FFA includes the North American 80 Comprehensive Series and the cosmetic and hairdresser supplemental series, as well as an additional customized panel of 8 allergens as determined by patch testing experts at the University of Massachusetts, Brigham and Women’s Hospital, and Massachusetts General Hospital (private email communication, November 2017). Patch test readings are performed at 48 and 96 or 120 hours. Using the American Contact Dermatitis Society’s Contact Allergen Management Program, patients are provided personalized safe product lists and avoidance strategies are discussed.
Final Interpretation
In a world where cosmetic products are ubiquitous, it is hard to define the potential role of contact allergens in the entangled pathogenesis of FFA and ACD. As evidenced by emerging literature that correlates the 2 conditions and their exacerbating factors, it is important for physicians to have a comprehensive diagnostic approach and heightened awareness for potential allergens at play in FFA (Table). The identification of certain chemicals and preservatives as potential triggers for FFA should emphasize the importance of patch testing in these patients; however, whether the positive reactions are relevant to the pathogenesis or disease course of FFA still is unknown. While these findings begin to unravel the intertwined causes of FFA and ACD, further research encompassing larger cohorts and prospective studies is imperative to solidify these associations, define concrete guidelines, and improve patient outcomes.
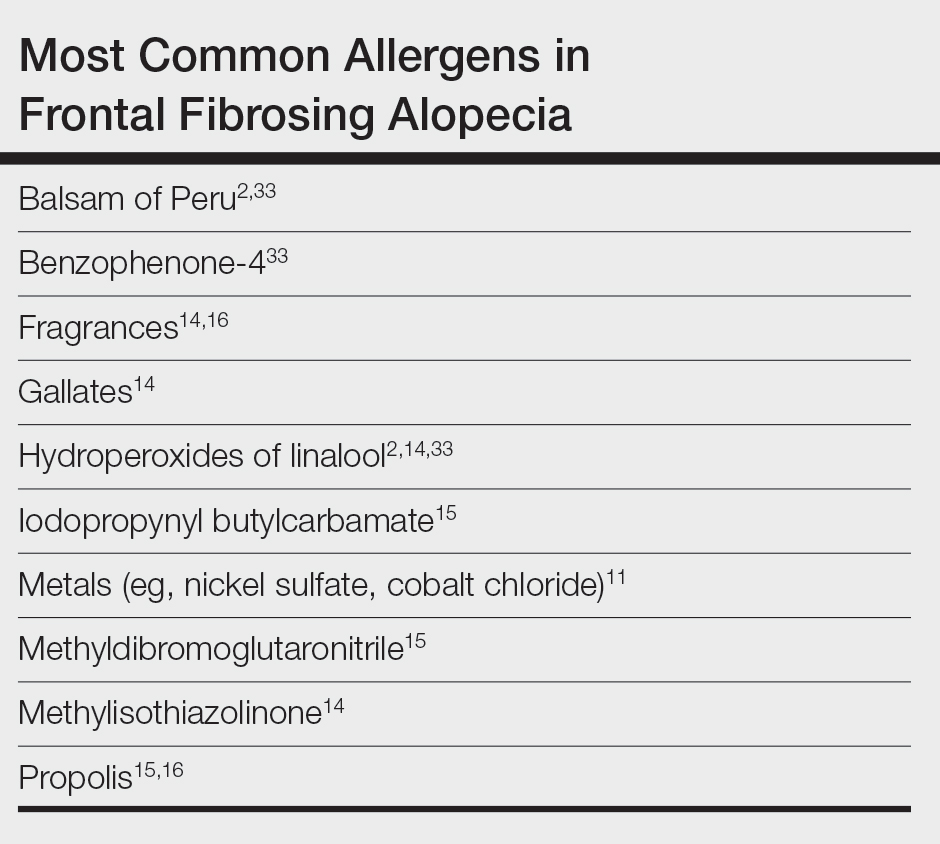
Frontal fibrosing alopecia (FFA) is an increasingly common diagnosis, especially in middle-aged women, and was first described by Kossard1 in 1994. It is a variant of lichen planopilaris (LPP), a progressive scarring cicatricial alopecia that affects the frontotemporal area of the scalp, eyebrows, and sometimes even body hair.1 Although its etiology remains unclear, genetic causes, drugs, hormones, and environmental exposures—including certain chemicals found in sunscreens—have been implicated in its pathogenesis.2,3 An association between contact allergy to ingredients in personal care products and FFA diagnosis has been suggested; however, there is no evidence of causality to date. In this article, we highlight the potential relationship between contact allergy and FFA as well as clinical considerations for management.
Clinical Features and Diagnosis
Frontal fibrosing alopecia typically manifests with gradual symmetric recession of the frontal hairline leading to bandlike hair loss along the forehead, sometimes extending to the temporal region.4 Some patients may experience symptoms of scalp itching, burning, or tenderness that may precede or accompany the hair loss. Perifollicular erythema may be visible during the early stages and can be visualized on trichoscopy. The affected skin may appear pale and shiny and may have a smooth texture with a distinct lack of follicular openings. Aside from scalp involvement, other manifestations may include lichen planus pigmentosus, facial papules, body hair involvement, hypochromic lesions, diffuse redness on the face and neck, and prominent frontal veins.5 Although most FFA cases have characteristic clinical features and trichoscopic findings, biopsy for histopathologic examination is still recommended to confirm the diagnosis and ensure appropriate treatment.4 Classic histopathologic features include perifollicular lymphocytic inflammation, follicular destruction, and scarring.
Pathophysiology of FFA
The pathogenesis of FFA is thought to involve a variety of triggers, including immune-mediated inflammation, stress, genetics, hormones, and possibly environmental factors.6 Frontal fibrosing alopecia demonstrates considerable upregulation in cytotoxic helper T cells (TH1) and IFN-γ activity resulting in epithelial hair follicle stem cell apoptosis and replacement of normal epithelial tissue with fibrous tissue.7 There is some suspicion of genetic susceptibility in the onset of FFA as suggested by familial reports and genome-wide association studies.8-10 Hormonal and autoimmune factors also have been linked to FFA, including an increased risk for thyroid disease and the postmenopausal rise of androgen levels.6
Allergic Contact Dermatitis and FFA
Although they are 2 distinct conditions with differing etiologies, allergic contact dermatitis (ACD) and FFA may share environmental triggers, especially in susceptible individuals. This may support the coexistence and potential association between ACD and FFA.
In one case report, a woman who developed facial eczema followed by FFA showed positive patch tests to the UV filters drometrizole trisiloxane and ethylhexyl salicylate, which were listed as ingredients in her sunscreens. Avoidance of these allergens reportedly led to notable improvement of the symptoms.11 Case-control studies have found an association between the use of facial sunscreen and risk for FFA.12 A 2016 questionnaire that assessed a wide range of lifestyle, social, and medical factors related to FFA found that the use of sunscreens was significantly higher in patients with FFA than controls (P<.001), pointing to sunscreens as a potential contributing factor, but further research has been inconclusive. A higher frequency of positive patch tests to hydroperoxides of linalool and balsam of Peru (BoP) in patients with FFA have been documented; however, a direct cause cannot be established.2
In a 2020 prospective study conducted at multiple international centers, 65% (13/20) of FFA patients and 37.5% (9/24) of the control group had a positive patch test reaction to one or more allergens (P=.003). The most common allergens that were identified included cobalt chloride (positive in 35% [7/20] of patients with FFA), nickel sulfate (25% [5/20]), and potassium dichromate (15% [3/20]).13 In a recent 2-year cohort study of 42 patients with FFA who were referred for patch testing, the most common allergens included gallates, hydroperoxides of linalool, and other fragrances.14 After a 3-month period of allergen avoidance, 70% (29/42) of patients had decreased scalp erythema on examination, indicating that avoiding relevant allergens may reduce local inflammation. Furthermore, 76.2% (32/42) of patients with FFA showed delayed-type hypersensitivity to allergens found in daily personal care products such as shampoos, sunscreens, and moisturizers, among others.14 Notably, the study lacked a control group. A case-control study of 36 Hispanic women conducted in Mexico also resulted in 83.3% (15/18) of patients with FFA and 55.5% (10/18) of controls having at least 1 positive patch test; in the FFA group, these included iodopropynyl butylcarbamate (16.7% [3/18]) and propolis (16.7% [3/18]).15
Most recently, a retrospective study conducted by Shtaynberger et al16 included 12 patients with LPP or FFA diagnosed via clinical findings or biopsy. It also included an age- and temporally matched control group tested with identical allergens. Among the 12 patients who had FFA/LPP, all had at least 1 allergen identified on patch testing. The most common allergens identified were propolis (positive in 50% [6/12] of patients with FFA/LPP), fragrance mix I (16%), and methylisothiazolinone (16% [2/12]). Follow-up data were available for 9 of these patients, of whom 6 (66.7%) experienced symptom improvement after 6 months of allergen avoidance. Four (44.4%) patients experienced decreased follicular redness or scaling, 2 (22.2%) patients experienced improved scalp pain/itch, 2 (22.2%) patients had stable/improved hair density, and 1 (1.1%) patient had decreased hair shedding. Although this suggests an environmental trigger for FFA/LPP, the authors stated that changes in patient treatment plans could have contributed to their improvement. The study also was limited by its small size and its overall generalizability.16
These studies have underscored the significance of patch testing in individuals diagnosed with FFA and have identified common allergens prevalent in this patient population. They have suggested that patients with FFA are more likely to have positive patch tests, and in some cases patients could experience improvements in scalp pruritus and erythema with allergen avoidance; however, we emphasize that a causal association between contact allergy and FFA remains unproven to date.
Most Common Allergens Pertinent to FFA
Preservatives—In some studies, patients with FFA have had positive patch tests to preservatives such as gallates and methylchloroisothiazolinone/methylisothiazolinone (MCI/MI).14 Gallates are antioxidants that are used in food preservation, pharmaceuticals, and cosmetics due to their ability to inhibit oxidation and rancidity of fats and oils.17 The most common gallates include propyl gallate, octyl gallate, and dodecyl gallate. Propyl gallate is utilized in some waxy or oily cosmetics and personal care items including sunscreens, shampoos, conditioners, bar soaps, facial cleansers, and moisturizers.18 Typically, if patients have a positive patch test to one gallate, they should be advised to avoid all gallate compounds, as they can cross-react.
Similarly, MCI/MI can prevent product degradation through their antibacterial and antifungal properties. This combination of MCI and MI is used as an effective method of prolonging the shelf life of cosmetic products and commonly is found in sunscreens, facial moisturizing creams, shampoos, and conditioners19; it is banned from use in leave-on products in the European Union and Canada due to increased rates of contact allergy.20 In patients with FFA who commonly use facial sunscreen, preservatives can be a potential allergen exposure to consider.
Iodopropynyl butylcarbamate also is a preservative used in cosmetic formulations. Similar to MCI/MI, it is a potent fungicide and bactericide. This allergen can be found in hair care products, bodywashes, and other personal products.21
UV Light–Absorbing Agents—A systematic review and meta-analysis conducted in 2022 showed a significant (P<.001) association between sunscreen use and FFA.22 A majority of allergens identified on patch testing included UVA- and UVB-absorbing agents found in sunscreens and other products including cosmetics,11,12 such as drometrizole trisiloxane, ethylhexyl salicylate, avobenzone, and benzophenone-4. Drometrizole trisiloxane is a photostabilizer and a broad-spectrum UV filter that is not approved for use in sunscreens in the United States.23 It also is effective in stabilizing and preventing the degradation of avobenzone, a commonly used UVA filter.24
Fragrances—Fragrances are present in nearly every personal and cosmetic product, sometimes even in those advertised as being “fragrance free.” Hydroperoxides of linalool, BoP, and fragrance mix are common allergens that are found in a variety of personal care products including perfumes, cosmetics, and even household cleaning supplies.25 Simultaneous positive patch tests to BoP and fragrance mix are common due to shared components. Linalool can be found in various plants such as lavender, rose, bergamot, and jasmine.26 Upon air exposure, linalool auto-oxidizes to form allergenic hydroperoxides of linalool. Among patients with FFA, positive patch test reactions to fragrance chemicals are common and could be attributed to the use of fragranced hair products and facial cosmetics.
Hair Dyes and Bleaches—Allergic reactions to hair dyes and bleaches can result in severe ACD of the head/neck and, in rare cases, scarring alopecia.27 Chemicals found in these products include paraphenylenediamine (PPD) and ammonium persulfate. The most common hair dye allergen, PPD also is used in some rubbers and plastics. Ammonium persulfate is a chemical used in hair bleaches and to deodorize oils. One case study reported a patient with FFA who developed chemically induced vitiligo immediately after the use of a hair color product that contained PPD.28 However, without patch testing to confirm the presence of contact allergy, other patient-specific and environmental risk factors could have contributed to FFA in this case.
A Knot in the Truth
In this endeavor to untangle the truth, it should be remembered that at the time of writing, the purported association between FFA and ACD remains debatable. Contact dermatitis specialists have voiced that the association between FFA and ACD, especially with regard to sunscreen, cannot be supported due to the lack of sufficient evidence.29 A large majority of the research conducted on FFA and ACD is based on case reports and studies limited to a small sample size, and most of these patch test studies lack a control group. Felmingham et al30 noted that the recent epidemiology of FFA aligns with increased sunscreen use. They also highlighted the limitations of the aforementioned studies, which include misclassification of exposures in the control group2 and recall bias in questionnaire participants.2,12 The most pressing limitation that permeates through most of these studies is the temporal ambiguity associated with sunscreen use. A study by Dhana et al31 failed to specify whether increased sunscreen use preceded the diagnosis of FFA or if it stems from the need to protect more exposed skin as a consequence of disease. Broad sunscreen avoidance due to concern for a possible association with hair loss could have detrimental health implications by increasing the risk for photodamage and skin cancer.
FFA Patch Testing
The avoidance of pertinent allergens could be effective in reducing local inflammation, pruritus, and erythema in FFA.9,14,32 At our institution, we selectively patch test patients with FFA when there is a suspected contact allergy. Clinical features that may allude to a potential contact allergy include an erythematous or eczematous dermatitis or symptoms of pruritus along the scalp or eyebrows. If patients recall hair loss or symptoms after using a hair or facial product, then a potential contact allergy to these products could be considered. Patch testing in patients with FFA includes the North American 80 Comprehensive Series and the cosmetic and hairdresser supplemental series, as well as an additional customized panel of 8 allergens as determined by patch testing experts at the University of Massachusetts, Brigham and Women’s Hospital, and Massachusetts General Hospital (private email communication, November 2017). Patch test readings are performed at 48 and 96 or 120 hours. Using the American Contact Dermatitis Society’s Contact Allergen Management Program, patients are provided personalized safe product lists and avoidance strategies are discussed.
Final Interpretation
In a world where cosmetic products are ubiquitous, it is hard to define the potential role of contact allergens in the entangled pathogenesis of FFA and ACD. As evidenced by emerging literature that correlates the 2 conditions and their exacerbating factors, it is important for physicians to have a comprehensive diagnostic approach and heightened awareness for potential allergens at play in FFA (Table). The identification of certain chemicals and preservatives as potential triggers for FFA should emphasize the importance of patch testing in these patients; however, whether the positive reactions are relevant to the pathogenesis or disease course of FFA still is unknown. While these findings begin to unravel the intertwined causes of FFA and ACD, further research encompassing larger cohorts and prospective studies is imperative to solidify these associations, define concrete guidelines, and improve patient outcomes.
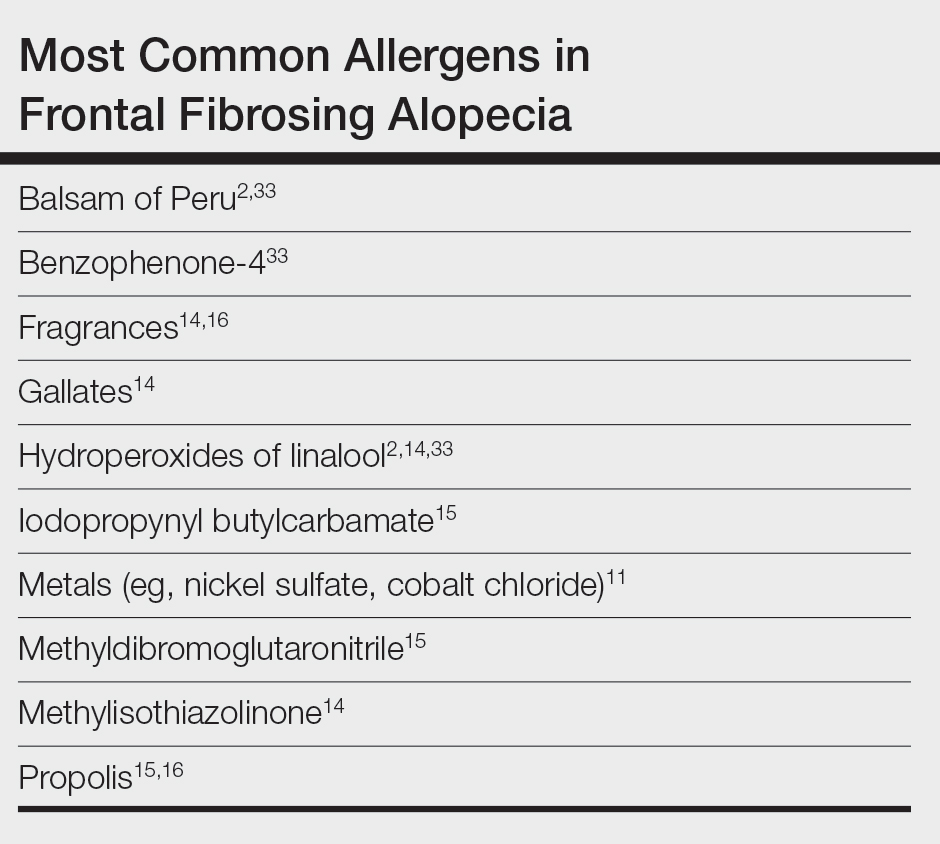
- Kossard S. Postmenopausal frontal fibrosing alopecia: scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770-774. doi:10.1001/archderm.1994.01690060100013
- Aldoori N, Dobson K, Holden CR, et al. Frontal fibrosing alopecia: possible association with leave-on facial skin care products and sunscreens; a questionnaire study. Br J Dermatol. 2016;175:762-767. doi:10.1111/bjd.14535
- Debroy Kidambi A, Dobson K, Holmes S, et al. Frontal fibrosing alopecia in men: an association with facial moisturizers and sunscreens. Br J Dermatol. 2017;177:260-261. doi:10.1111/bjd.15311
- Starace M, Orlando G, Iorizzo M, et al. Clinical and dermoscopic approaches to diagnosis of frontal fibrosing alopecia: results from a multicenter study of the International Dermoscopy Society. Dermatol Pract Concept. 2022;12:E2022080. doi:10.5826/dpc.1201a80
- Fechine COC, Valente NYS, Romiti R. Lichen planopilaris and frontal fibrosing alopecia: review and update of diagnostic and therapeutic features. An Bras Dermatol. 2022;97:348-357. doi:10.1016/j.abd.2021.08.008
- Frontal fibrosing alopecia: a review of disease pathogenesis. Front Med (Lausanne). 2022;9:911944. doi:10.3389/fmed.2022.911944
- Del Duca E, Ruano Ruiz J, Pavel AB, et al. Frontal fibrosing alopecia shows robust T helper 1 and Janus kinase 3 skewing. Br J Dermatol. 2020;183:1083-1093. doi:10.1111/bjd.19040
- Tziotzios C, Petridis C, Dand N, et al. Genome-wide association study in frontal fibrosing alopecia identifies four susceptibility loci including HLA-B*07:02. Nat Commun. 2019;10:1150. doi:10.1038/s41467-019-09117-w
- Navarro‐Belmonte MR, Navarro‐López V, Ramírez‐Boscà A, et al. Case series of familial frontal fibrosing alopecia and a review of the literature. J Cosmet Dermatol. 2015;14:64-69. doi:10.1111/jocd.12125
- Cuenca-Barrales C, Ruiz-Villaverde R, Molina-Leyva A. Familial frontal fibrosing alopecia. Sultan Qaboos Univ Med J. 2021;21:E320-E323. doi:10.18295/squmj.2021.21.02.025
- Pastor-Nieto MA, Gatica-Ortega ME. Allergic contact dermatitis to drometrizole trisiloxane in a woman thereafter diagnosed with frontal fibrosing alopecia. Contact Dermatitis. 2023;89:215-217. doi:10.1111/cod.14370
- Moreno-Arrones OM, Saceda-Corralo D, Rodrigues-Barata AR, et al. Risk factors associated with frontal fibrosing alopecia: a multicentre case–control study. Clin Exp Dermatol. 2019;44:404-410. doi:10.1111/ced.13785
- Rudnicka L, Rokni GR, Lotti T, et al. Allergic contact dermatitis in patients with frontal fibrosing alopecia: an international multi-center study. Dermatol Ther. 2020;33:E13560. doi:10.1111/dth.13560
- Prasad S, Marks DH, Burns LJ, et al. Patch testing and contact allergen avoidance in patients with lichen planopilaris and/or frontal fibrosing alopecia: a cohort study. J Am Acad Dermatol. 2020;83:659-661. doi:10.1016/j.jaad.2020.01.026
- Ocampo-Garza SS, Herz-Ruelas ME, Chavez-Alvarez S, et al. Association of frontal fibrosing alopecia and contact allergens in everyday skincare products in Hispanic females: a case-control study. An Bras Dermatol. 2021;96:776-778. doi:10.1016/j.abd.2020.09.013
- Shtaynberger B, Bruder P, Zippin JH. The prevalence of type iv hypersensitivity in patients with lichen planopilaris and frontal fibrosing alopecia. Dermatitis. 2023;34:351-352. doi:10.1097/DER.0000000000000965
- Kahkeshani N, Farzaei F, Fotouhi M, et al. Pharmacological effects of gallic acid in health and diseases: a mechanistic review. Iran J Basic Med Sci. 2019;22:225-237. doi:10.22038/ijbms.2019.32806.7897
- Holcomb ZE, Van Noord MG, Atwater AR. Gallate contact dermatitis: product update and systematic review. Dermatitis. 2017;28:115-127. doi:10.1097/DER.0000000000000263
- Gorris A, Valencak J, Schremser V, et al. Contact allergy to methylisothiazolinone with three clinical presentations in one patient. Contact Dermatitis. 2020;82:162-164. doi:10.1111/cod.13384
- Uter W, Aalto-Korte K, Agner T, et al. The epidemic of methylisothiazolinone contact allergy in Europe: follow-up on changing exposures. J Eur Acad Dermatol Venereol. 2020;34:333-339. doi:10.1111/jdv.15875
- Batista M, Morgado F, Gonçalo M. Patch test reactivity to iodopropynyl butylcarbamate in consecutive patients during a period of 7 years. Contact Dermatitis. 2019;81:54-55. doi:10.1111/cod.13213
- Maghfour J, Ceresnie M, Olson J, et al. The association between frontal fibrosing alopecia, sunscreen, and moisturizers: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;87:395-396. doi:10.1016/j.jaad.2021.12.058
- Drometrizole trisiloxane. PubChem website. Accessed February 21, 2024. https://pubchem.ncbi.nlm.nih.gov/compound/9848888
- Hughes TM, Martin JA, Lewis VJ, et al. Allergic contact dermatitis to drometrizole trisiloxane in a sunscreen with concomitant sensitivities to other sunscreens. Contact Dermatitis. 2005;52:226-227. doi:10.1111/j.0105-1873.2005.0566a.x
- de Groot AC. Myroxylon pereirae resin (balsam of Peru)—a critical review of the literature and assessment of the significance of positive patch test reactions and the usefulness of restrictive diets. Contact Dermatitis. 2019;80:335-353. doi:10.1111/cod.13263
- Sköld M, Börje A, Matura M, et al. Studies on the autoxidation and sensitizing capacity of the fragrance chemical linalool, identifying a linalool hydroperoxide. Contact Dermatitis. 2002;46:267-272. doi:10.1034/j.1600-0536.2002.460504.x
- Dev T, Khan E, Patel U, et al. Cicatricial alopecia following allergic contact dermatitis from hair dyes: a rare clinical presentation. Contact Dermatitis. 2022;86:59-61. doi:10.1111/cod.13974
- De Souza B, Burns L, Senna MM. Frontal fibrosing alopecia preceding the development of vitiligo: a case report. JAAD Case Rep. 2020;6:154-155. doi:10.1016/j.jdcr.2019.12.011
- Abuav R, Shon W. Are sunscreen particles involved in frontal fibrosing alopecia?—a TEM-EDXS analysis on formalin-fixed paraffin-embedded alopecia biopsies (pilot study). Am J Dermatopathol. 2022;44:E135. doi:10.1097/DAD.0000000000002317
- Felmingham C, Yip L, Tam M, et al. Allergy to sunscreen and leave-on facial products is not a likely causative mechanism in frontal fibrosing alopecia: perspective from contact allergy experts. Br J Dermatol. 2020;182:481-482. doi:10.1111/bjd.18380
- Dhana A, Gumedze F, Khumalo N. Regarding “frontal fibrosing alopecia: possible association with leave-on facial skincare products and sunscreens; a questionnaire study.” Br J Dermatol. 2016;176:836-837. doi:10.1111/bjd.15197
- Pastor-Nieto MA, Gatica-Ortega ME, Sánchez-Herreros C, et al. Sensitization to benzyl salicylate and other allergens in patients with frontal fibrosing alopecia. Contact Dermatitis. 2021;84:423-430. doi:10.1111/cod.13763
- Rocha VB, Donati A, Contin LA, et al. Photopatch and patch testing in 63 patients with frontal fibrosing alopecia: a case series. Br J Dermatol. 2018;179:1402-1403. doi:10.1111/bjd.16933
- Kossard S. Postmenopausal frontal fibrosing alopecia: scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770-774. doi:10.1001/archderm.1994.01690060100013
- Aldoori N, Dobson K, Holden CR, et al. Frontal fibrosing alopecia: possible association with leave-on facial skin care products and sunscreens; a questionnaire study. Br J Dermatol. 2016;175:762-767. doi:10.1111/bjd.14535
- Debroy Kidambi A, Dobson K, Holmes S, et al. Frontal fibrosing alopecia in men: an association with facial moisturizers and sunscreens. Br J Dermatol. 2017;177:260-261. doi:10.1111/bjd.15311
- Starace M, Orlando G, Iorizzo M, et al. Clinical and dermoscopic approaches to diagnosis of frontal fibrosing alopecia: results from a multicenter study of the International Dermoscopy Society. Dermatol Pract Concept. 2022;12:E2022080. doi:10.5826/dpc.1201a80
- Fechine COC, Valente NYS, Romiti R. Lichen planopilaris and frontal fibrosing alopecia: review and update of diagnostic and therapeutic features. An Bras Dermatol. 2022;97:348-357. doi:10.1016/j.abd.2021.08.008
- Frontal fibrosing alopecia: a review of disease pathogenesis. Front Med (Lausanne). 2022;9:911944. doi:10.3389/fmed.2022.911944
- Del Duca E, Ruano Ruiz J, Pavel AB, et al. Frontal fibrosing alopecia shows robust T helper 1 and Janus kinase 3 skewing. Br J Dermatol. 2020;183:1083-1093. doi:10.1111/bjd.19040
- Tziotzios C, Petridis C, Dand N, et al. Genome-wide association study in frontal fibrosing alopecia identifies four susceptibility loci including HLA-B*07:02. Nat Commun. 2019;10:1150. doi:10.1038/s41467-019-09117-w
- Navarro‐Belmonte MR, Navarro‐López V, Ramírez‐Boscà A, et al. Case series of familial frontal fibrosing alopecia and a review of the literature. J Cosmet Dermatol. 2015;14:64-69. doi:10.1111/jocd.12125
- Cuenca-Barrales C, Ruiz-Villaverde R, Molina-Leyva A. Familial frontal fibrosing alopecia. Sultan Qaboos Univ Med J. 2021;21:E320-E323. doi:10.18295/squmj.2021.21.02.025
- Pastor-Nieto MA, Gatica-Ortega ME. Allergic contact dermatitis to drometrizole trisiloxane in a woman thereafter diagnosed with frontal fibrosing alopecia. Contact Dermatitis. 2023;89:215-217. doi:10.1111/cod.14370
- Moreno-Arrones OM, Saceda-Corralo D, Rodrigues-Barata AR, et al. Risk factors associated with frontal fibrosing alopecia: a multicentre case–control study. Clin Exp Dermatol. 2019;44:404-410. doi:10.1111/ced.13785
- Rudnicka L, Rokni GR, Lotti T, et al. Allergic contact dermatitis in patients with frontal fibrosing alopecia: an international multi-center study. Dermatol Ther. 2020;33:E13560. doi:10.1111/dth.13560
- Prasad S, Marks DH, Burns LJ, et al. Patch testing and contact allergen avoidance in patients with lichen planopilaris and/or frontal fibrosing alopecia: a cohort study. J Am Acad Dermatol. 2020;83:659-661. doi:10.1016/j.jaad.2020.01.026
- Ocampo-Garza SS, Herz-Ruelas ME, Chavez-Alvarez S, et al. Association of frontal fibrosing alopecia and contact allergens in everyday skincare products in Hispanic females: a case-control study. An Bras Dermatol. 2021;96:776-778. doi:10.1016/j.abd.2020.09.013
- Shtaynberger B, Bruder P, Zippin JH. The prevalence of type iv hypersensitivity in patients with lichen planopilaris and frontal fibrosing alopecia. Dermatitis. 2023;34:351-352. doi:10.1097/DER.0000000000000965
- Kahkeshani N, Farzaei F, Fotouhi M, et al. Pharmacological effects of gallic acid in health and diseases: a mechanistic review. Iran J Basic Med Sci. 2019;22:225-237. doi:10.22038/ijbms.2019.32806.7897
- Holcomb ZE, Van Noord MG, Atwater AR. Gallate contact dermatitis: product update and systematic review. Dermatitis. 2017;28:115-127. doi:10.1097/DER.0000000000000263
- Gorris A, Valencak J, Schremser V, et al. Contact allergy to methylisothiazolinone with three clinical presentations in one patient. Contact Dermatitis. 2020;82:162-164. doi:10.1111/cod.13384
- Uter W, Aalto-Korte K, Agner T, et al. The epidemic of methylisothiazolinone contact allergy in Europe: follow-up on changing exposures. J Eur Acad Dermatol Venereol. 2020;34:333-339. doi:10.1111/jdv.15875
- Batista M, Morgado F, Gonçalo M. Patch test reactivity to iodopropynyl butylcarbamate in consecutive patients during a period of 7 years. Contact Dermatitis. 2019;81:54-55. doi:10.1111/cod.13213
- Maghfour J, Ceresnie M, Olson J, et al. The association between frontal fibrosing alopecia, sunscreen, and moisturizers: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;87:395-396. doi:10.1016/j.jaad.2021.12.058
- Drometrizole trisiloxane. PubChem website. Accessed February 21, 2024. https://pubchem.ncbi.nlm.nih.gov/compound/9848888
- Hughes TM, Martin JA, Lewis VJ, et al. Allergic contact dermatitis to drometrizole trisiloxane in a sunscreen with concomitant sensitivities to other sunscreens. Contact Dermatitis. 2005;52:226-227. doi:10.1111/j.0105-1873.2005.0566a.x
- de Groot AC. Myroxylon pereirae resin (balsam of Peru)—a critical review of the literature and assessment of the significance of positive patch test reactions and the usefulness of restrictive diets. Contact Dermatitis. 2019;80:335-353. doi:10.1111/cod.13263
- Sköld M, Börje A, Matura M, et al. Studies on the autoxidation and sensitizing capacity of the fragrance chemical linalool, identifying a linalool hydroperoxide. Contact Dermatitis. 2002;46:267-272. doi:10.1034/j.1600-0536.2002.460504.x
- Dev T, Khan E, Patel U, et al. Cicatricial alopecia following allergic contact dermatitis from hair dyes: a rare clinical presentation. Contact Dermatitis. 2022;86:59-61. doi:10.1111/cod.13974
- De Souza B, Burns L, Senna MM. Frontal fibrosing alopecia preceding the development of vitiligo: a case report. JAAD Case Rep. 2020;6:154-155. doi:10.1016/j.jdcr.2019.12.011
- Abuav R, Shon W. Are sunscreen particles involved in frontal fibrosing alopecia?—a TEM-EDXS analysis on formalin-fixed paraffin-embedded alopecia biopsies (pilot study). Am J Dermatopathol. 2022;44:E135. doi:10.1097/DAD.0000000000002317
- Felmingham C, Yip L, Tam M, et al. Allergy to sunscreen and leave-on facial products is not a likely causative mechanism in frontal fibrosing alopecia: perspective from contact allergy experts. Br J Dermatol. 2020;182:481-482. doi:10.1111/bjd.18380
- Dhana A, Gumedze F, Khumalo N. Regarding “frontal fibrosing alopecia: possible association with leave-on facial skincare products and sunscreens; a questionnaire study.” Br J Dermatol. 2016;176:836-837. doi:10.1111/bjd.15197
- Pastor-Nieto MA, Gatica-Ortega ME, Sánchez-Herreros C, et al. Sensitization to benzyl salicylate and other allergens in patients with frontal fibrosing alopecia. Contact Dermatitis. 2021;84:423-430. doi:10.1111/cod.13763
- Rocha VB, Donati A, Contin LA, et al. Photopatch and patch testing in 63 patients with frontal fibrosing alopecia: a case series. Br J Dermatol. 2018;179:1402-1403. doi:10.1111/bjd.16933
Practice Points
- Frontal fibrosing alopecia (FFA), a variant of lichen planopilaris (LPP), is an increasingly prevalent type of scarring alopecia that may have a closer relationship to contact allergy than was previously understood. However, there is no evidence of a causal association to date.
- When evaluating for FFA/LPP, clinicians should assess for use of cosmetic products or sunscreens that may have a potential impact on the disease course.