User login
What’s Eating You? Rhipicephalus Ticks Revisited
Characteristics
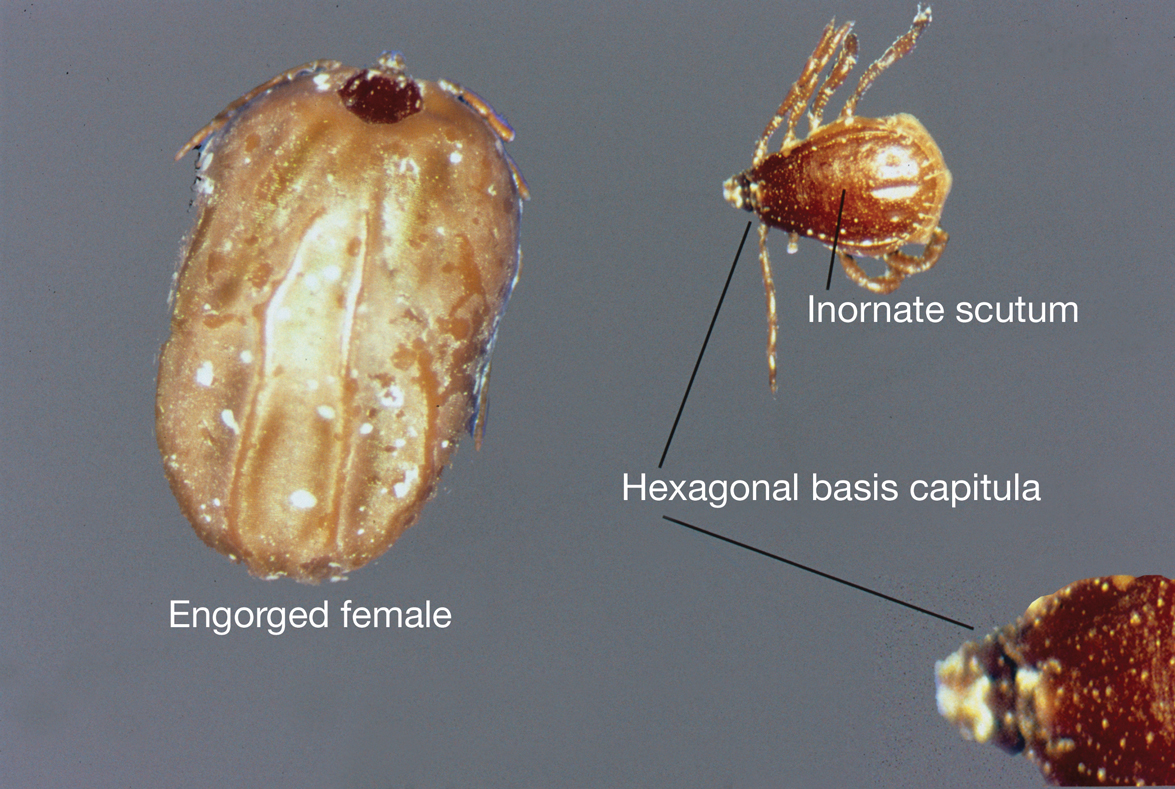
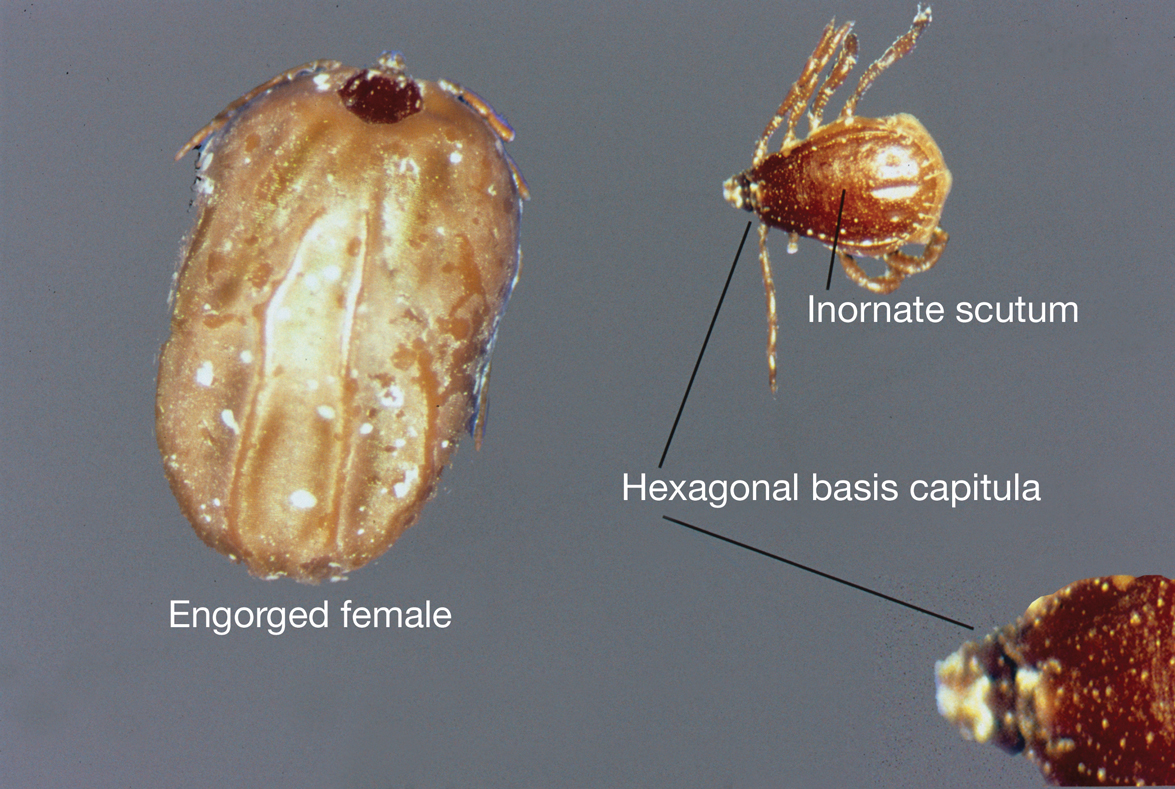
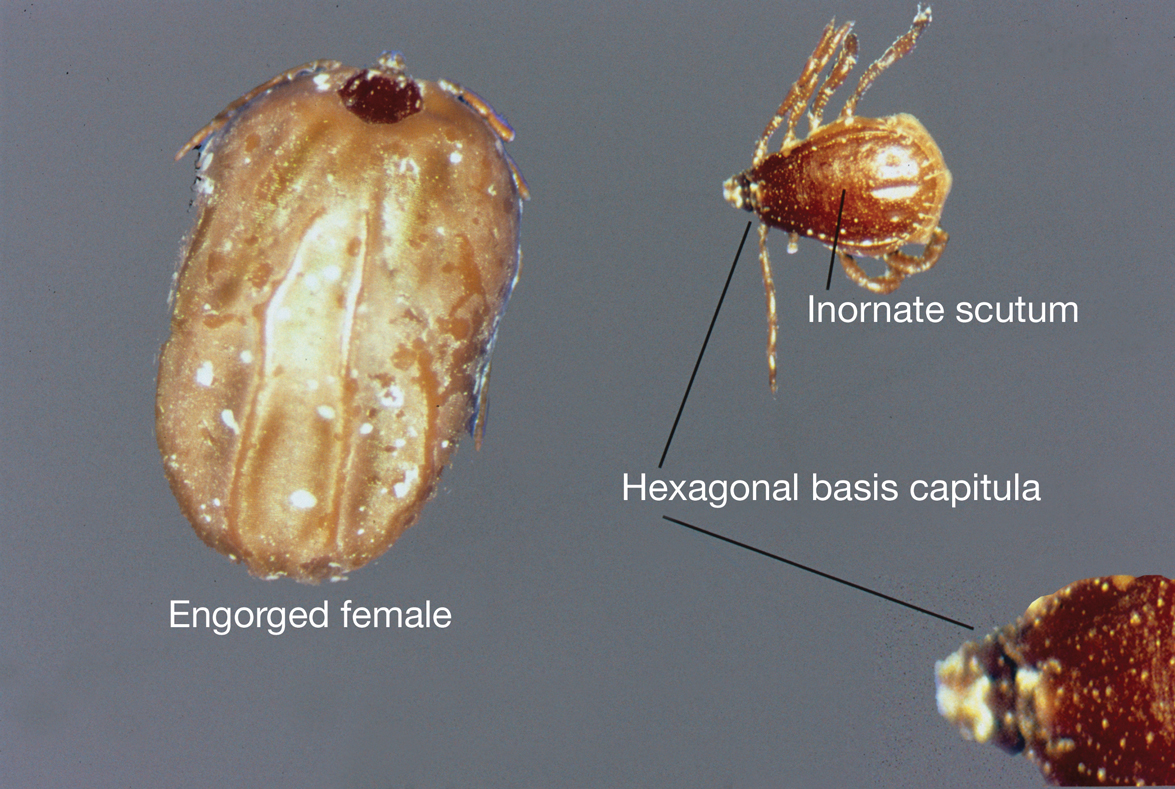
Rhipicephalus ticks belong to the Ixodidae family of hard-bodied ticks. They are large and teardrop shaped with an inornate scutum (hard dorsal plate) and relatively short mouthparts attached at a hexagonal basis capitulum (base of the head to which mouthparts are attached)(Figure).1 Widely spaced eyes and festoons also are present. The first pair of coxae—attachment base for the first pair of legs—are characteristically bifid; males have a pair of sclerotized adanal plates on the ventral surface adjacent to the anus as well as accessory adanal shields.2 Rhipicephalus (formerly Boophilus) microplus (the so-called cattle tick) is a newly added species; it lacks posterior festoons, and the anal groove is absent.3
Almost all Rhipicephalus ticks, except for R microplus, are 3-host ticks in which a single blood meal is consumed from a vertebrate host at each active life stage—larva, nymph, and adult—to complete development.4,5 In contrast to most ixodid ticks, which are exophilic (living outside of human habitation), the Rhipicephalus sanguineus sensu lato species (the brown dog tick) is highly endophilic (adapted to indoor living) and often can be found hidden in cracks and crevices of walls in homes and peridomestic structures.6 It is predominately monotropic (all developmental stages feed on the same host species) and has a strong host preference for dogs, though it occasionally feeds on other hosts (eg, humans).7 Although most common in tropical and subtropical climates, they can be found anywhere there are dogs due to their ability to colonize indoor dwellings.8 In contrast, R microplus ticks have a predilection for cattle and livestock rather than humans, posing a notable concern to livestock worldwide. Infestation results in transmission of disease-causing pathogens, such as Babesia and Anaplasma species, which costs the cattle industry billions of dollars annually.9
Clinical Manifestations and Treatment
Tick bites usually manifest as intensely pruritic, erythematous papules at the site of tick attachment due to a local type IV hypersensitivity reaction to antigens in the tick’s saliva. This reaction can be long-lasting. In addition to pruritic papules following a bite, an attached tick can be mistaken for a skin neoplasm or nevus. Given that ticks are small, especially during the larval stage, dermoscopy may be helpful in making a diagnosis.10 Symptomatic relief usually can be achieved with topical antipruritics or oral antihistamines.
Of public health concern, brown dog ticks are important vectors of Rickettsia rickettsii (the causative organism of Rocky Mountain spotted fever [RMSF]) in the Western hemisphere, and Rickettsia conorii (the causative organism of Mediterranean spotted fever [MSF][also known as Boutonneuse fever]) in the Eastern hemisphere.11 Bites by ticks carrying rickettsial disease classically manifest with early symptoms of fever, headache, and myalgia, followed by a rash or by a localized eschar or tache noire (a black, necrotic, scabbed lesion) that represents direct endothelial invasion and vascular damage by Rickettsia.12 Rocky Mountain spotted fever and MSF are more prevalent during summer, likely due, in part, to the combination of increased outdoor activity and a higher rate of tick-questing (host-seeking) behavior in warmer climates.4,7
Rocky Mountain Spotted Fever—Dermacentor variabilis is the primary vector of RMSF in the southeastern United States; Dermacentor andersoni is the major vector of RMSF in Rocky Mountain states. Rhipicephalus sanguineus sensu lato is an important vector of RMSF in the southwestern United States, Mexico, and Central America.11,13
Early symptoms of RMSF are nonspecific and can include fever, headache, arthralgia, myalgia, and malaise. Gastrointestinal tract symptoms (eg, nausea, vomiting, anorexia) may occur; notable abdominal pain occurs in some patients, particularly children. A characteristic petechial rash occurs in as many as 90% of patients, typically at the third to fifth day of illness, and classically begins on the wrists and ankles, with progression to the palms and soles before spreading centripetally to the arms, legs, and trunk.14 An eschar at the inoculation site is uncommon in RMSF; when present, it is more suggestive of MSF.15
The classic triad of fever, headache, and rash is present in 3% of patients during the first 3 days after a tick bite and in 60% to 70% within 2 weeks.16 A rash often is absent when patients first seek medical attention and may not develop (absent in 9% to 12% of cases; so-called spotless RMSF). Therefore, absence of rash should not be a reason to withhold treatment.16 Empiric treatment with doxycycline should be started promptly for all suspected cases of RMSF because of the rapid progression of disease and an increased risk for morbidity and mortality with delayed diagnosis.
Patients do not become antibody positive until 7 to 10 days after symptoms begin; therefore, treatment should not be delayed while awaiting serologic test results. The case fatality rate in the United States is estimated to be 5% to 10% overall and as high as 40% to 50% among patients who are not treated until day 8 or 9 of illness.17
Cutaneous complications include skin necrosis and gangrene due to continuous tissue damage in severe cases.16 Severe infection also may manifest with signs of multiorgan system damage, including altered mental status, cerebral edema, meningismus, transient deafness, myocarditis, pulmonary hemorrhage and edema, conjunctivitis, retinal abnormalities, and acute renal failure.14,16 Risk factors for more severe illness include delayed treatment, age 40 years or older or younger than 10 years, and underlying medical conditions such as alcoholic liver disease and glucose-6-phosphate dehydrogenase deficiency. However, even some healthy young patients die of this disease.17
Mediterranean Spotted Fever—Rhipicephalus sanguineus sensu lato is the primary vector of MSF, which is prevalent in areas adjacent to the Mediterranean Sea, including southern Europe, Africa, and Central Asia; Sicily is the most highly affected region.18 Findings with MSF are nearly identical to those of RMSF, except that tache noire is more common, present in as many as 70% of cases at the site of the inoculating tick bite, and MSF typically follows a less severe clinical course.12 Similar to other rickettsial diseases, the pathogenesis of MSF involves direct injury to vascular endothelial cells, causing a vasculitis that is responsible for the clinical abnormalities observed.
Patients with severe MSF experience complications similar to severe RMSF, including neurologic manifestations and multiorgan damage.18 Risk factors include advanced age, immunocompromised state, cardiac disease, chronic alcoholism, diabetes mellitus, glucose-6-phosphate dehydrogenase deficiency, respiratory insufficiency, and delayed treatment.18
Treatment—For all spotted fever group rickettsial infections, doxycycline is the treatment of choice for all patients, including children and pregnant women. Treatment should be started without delay; recommended dosages are 100 mg twice daily for children weighing more than 45 kg and adults, and 2.2 mg/kg twice daily for children weighing 45 kg or less.12
Rhipicephalus tick bites rarely can result in paralysis; however, Dermacentor ticks are responsible for most cases of tick-related paralysis in North America. Other pathogens proven or reputed to be transmitted by Rhipicephalus sanguineus sensu lato with zoonotic potential include but are not limited to Rickettsia massiliae, Coxiella burnetti, Anaplasma platys, Leishmania infantum, and Crimean-Congo hemorrhagic fever virus (Nairovirus).19
Environmental Treatment and Prevention
The most effective way to prevent tick-borne illness is avoidance of tick bites. Primary prevention methods include vector control, use of repellents (eg, N,N-diethyl-meta-toluamide [DEET]), picaridin, permethrin), avoidance of areas with a high tick burden, use of protective clothing, and detection and removal of ticks as soon as possible.
Environmental and veterinary controls also are important methods of tick-bite prevention. A veterinarian can recommend a variety of agents for dogs and cats that prevent attachment of ticks. Environmental controls include synthetic or natural product-based chemical acaricides and nonchemical methods, such as landscape management (eg, sealing cracks and crevices in homes and controlling tall grasses, weeds, and leaf debris) to minimize potential tick habitat.20 Secondary prevention includes antibiotics for prophylaxis or for treatment of tick-borne disease, when indicated.
Numerous tick repellents are available commercially; others are being studied. DEET, the most widely used topical repellent, has a broad spectrum of activity against many tick species.21 In addition, DEET has a well-known safety and toxicity profile, with rare adverse effects, and is safe for use in pregnant women and children older than 2 years. Alternative repellents, such as those containing picaridin, ethyl butylacetylaminopropionate (IR3535 [Merck]), oil of lemon eucalyptus, and 2-undecanone can be effective; some show efficacy comparable to that of DEET.22 Permethrin, a synthetic pyrethroid, is a highly efficacious tick repellent and insecticide, especially when used in conjunction with a topical repellent such as DEET. Unlike topically applied repellents, permethrin spray is applied to fabric (eg, clothing, shoes, bed nets, camping gear), not to skin.
Indiscriminate use of acaricides worldwide has led to increasing selection of acaricide resistance in Rhipicephalus tick species, which is especially true with the use of acaricides in controlling R microplus livestock infestations; several tick populations now show resistance to all major classes of these compounds.23-25 For that reason, there has been an increasing effort to develop new chemical and nonchemical approaches to tick control that are more environmentally sustainable and strategies to minimize development and progression of resistance such as rotation of acaricides; reducing the frequency of their application; use of pesticide mixtures, synergists, or both; and increasing use of nonacaricidal methods of control.26
Prompt removal of ticks is important for preventing the transmission of tick-borne disease. Proper removal involves rubbing the tick in a circular motion with a moist gauze pad or using fine-tipped tweezers to grasp the tick as close to the skin surface as possible and pulling upward with a steady pressure.17,27 It is important not to jerk, twist, squeeze, smash, or burn the tick, as this can result in insufficient removal of mouthparts or spread contaminated tick fluids to mucous membranes, increasing the risk for infection. Application of petroleum jelly or nail polish to aid in tick removal have not been shown to be effective and are not recommended.16,28
- Dantas-Torres F. The brown dog tick, Rhipicephalus sanguineus (Latreille, 1806) (Acari: Ixodidae): from taxonomy to control. Vet Parasitol. 2008;152:173-185. doi:10.1016/j.vetpar.2007.12.030
- Madder M, Fourie JJ, Schetters TPM. Arachnida, Metastigmata, Ixodidae (except Ixodes holocyclus). In: Marchiondo AA, Cruthers LR, Fourie JJ, eds. Parasiticide Screening: In Vitro and In Vivo Tests With Relevant Parasite Rearing and Host Infection/Infestation Methods. Volume 1. Elsevier Academic Press; 2019:19-20.
- Burger TD, Shao R, Barker SC. Phylogenetic analysis of mitochondrial genome sequences indicates that the cattle tick, Rhipicephalus (Boophilus) microplus, contains a cryptic species. Mol Phylogenet Evol. 2014;76:241-253. doi:10.1016/j.ympev.2014.03.017
- Gray J, Dantas-Torres F, Estrada-Peña A, et al. Systematics and ecology of the brown dog tick, Rhipicephalus sanguineus. Ticks Tick Borne Dis. 2013;4:171-180. doi:10.1016/j.ttbdis.2012.12.003
- Tian Y, Lord CC, Kaufman PE. Brown dog tick, Rhipicephalus Sanguineus Latrielle (Arachnida: Acari: Ixodidae): EENY-221/IN378. EDIS. March 26, 2020. Accessed January 3, 2024. https://doi.org/10.32473/edis-in378-2020
- Saleh MN, Allen KE, Lineberry MW, et al. Ticks infesting dogs and cats in North America: biology, geographic distribution, and pathogen transmission. Vet Parasitol. 2021;294:109392. doi:10.1016/j.vetpar.2021.109392
- Dantas-Torres F. Biology and ecology of the brown dog tick, Rhipicephalus sanguineus. Parasit Vectors. 2010;3:26. doi:10.1186/1756-3305-3-26
- Dryden MW, Payne PA. Biology and control of ticks infesting dogs and cats in North America. Vet Ther. 2004;5:139-154.
- Nyangiwe N, Yawa M, Muchenje V. Driving forces for changes in geographic range of cattle ticks (Acari: Ixodidae) in Africa: a Review. S Afr J Anim Sci. 2018;48:829. doi:10.4314/sajas.v48i5.4
- Ramot Y, Zlotogorski A, Mumcuoglu KY. Brown dog tick (Rhipicephalus sanguineus) infestation of the penis detected by dermoscopy. Int J Dermatol. 2012;51:1402-1403. doi:10.1111/j.1365-4632.2010.04756.x
- Tucker NSG, Weeks ENI, Beati L, et al. Prevalence and distribution of pathogen infection and permethrin resistance in tropical and temperate populations of Rhipicephalus sanguineus s.l. collected worldwide. Med Vet Entomol. 2021;35:147-157. doi:10.1111/mve.12479
- McClain MT, Sexton DJ, Hall KK, eds. Other spotted fever group rickettsial infections. UpToDate. Updated October 10, 2022. Accessed January 3, 2024. https://www.uptodate.com/contents/other-spotted-fever-group-rickettsial-infections
- Ribeiro CM, Carvalho JLB, Bastos PAS, et al. Prevalence of Rickettsia rickettsii in ticks: systematic review and meta-analysis. Vector Borne Zoonotic Dis. 2021;21:557-565. doi:10.1089/vbz.2021.0004
- Pace EJ, O’Reilly M. Tickborne diseases: diagnosis and management. Am Fam Physician. 2020;101:530-540.
- Patterson JW. Weedon’s Skin Pathology. 5th ed. Elsevier; 2020.
- Dantas-Torres F. Rocky Mountain spotted fever. Lancet Infect Dis. 2007;7:724-732. doi:10.1016/S1473-3099(07)70261-X
- Biggs HM, Behravesh CB, Bradley KK, et al. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever and other spotted fever group rickettsioses, ehrlichioses, and anaplasmosis—United States. MMWR Recomm Rep. 2016;65:1-44. doi:10.15585/mmwr.rr6502a1
- Rossio R, Conalbi V, Castagna V, et al. Mediterranean spotted fever and hearing impairment: a rare complication. Int J Infect Dis. 2015;35:34-36. doi:10.1016/j.ijid.2015.04.005
- Dantas-Torres F, Otranto D. Further thoughts on the taxonomy and vector role of Rhipicephalus sanguineus group ticks. Vet Parasitol. 2015;208:9-13. doi:10.1016/j.vetpar.2014.12.014
- Eisen RJ, Kugeler KJ, Eisen L, et al. Tick-borne zoonoses in the United States: persistent and emerging threats to human health. ILAR J. 2017;58:319-335. doi:10.1093/ilar/ilx005
- Nguyen QD, Vu MN, Hebert AA. Insect repellents: an updated review for the clinician. J Am Acad Dermatol. 2018;88:123-130. doi:10.1016/j.jaad.2018.10.053
- Pages F, Dautel H, Duvallet G, et al. Tick repellents for human use: prevention of tick bites and tick-borne diseases. Vector Borne Zoonotic Dis. 2014;14:85-93. doi:10.1089/vbz.2013.1410
- Rodriguez-Vivas RI, Alonso-Díaz MA, et al. Prevalence and potential risk factors for organophosphate and pyrethroid resistance in Boophilus microplus ticks on cattle ranches from the State of Yucatan, Mexico. Vet Parasitol. 2006;136:335-342. doi:10.1016/j.vetpar.2005.05.069
- Rodríguez-Vivas RI, Rodríguez-Arevalo F, Alonso-Díaz MA, et al. Prevalence and potential risk factors for amitraz resistance in Boophilus microplus ticks in cattle farms in the State of Yucatan, Mexico. Prev Vet Med. 2006;75:280-286. doi:10.1016/j.prevetmed.2006.04.001
- Perez-Cogollo LC, Rodriguez-Vivas RI, Ramirez-Cruz GT, et al. First report of the cattle tick Rhipicephalus microplus resistant to ivermectin in Mexico. Vet Parasitol. 2010;168:165-169. doi:10.1016/j.vetpar.2009.10.021
- Rodriguez-Vivas RI, Jonsson NN, Bhushan C. Strategies for the control of Rhipicephalus microplus ticks in a world of conventional acaricide and macrocyclic lactone resistance. Parasitol Res.2018;117:3-29. doi:10.1007/s00436-017-5677-6
- Centers for Disease Control and Prevention. Tick removal. Updated May 13, 2022. Accessed January 3, 2024. https://www.cdc.gov/ticks/removing_a_tick.html
- Diaz JH. Chemical and plant-based insect repellents: efficacy, safety, and toxicity. Wilderness Environ Med. 2016;27:153-163. doi:10.1016/j.wem.2015.11.007
Characteristics
Rhipicephalus ticks belong to the Ixodidae family of hard-bodied ticks. They are large and teardrop shaped with an inornate scutum (hard dorsal plate) and relatively short mouthparts attached at a hexagonal basis capitulum (base of the head to which mouthparts are attached)(Figure).1 Widely spaced eyes and festoons also are present. The first pair of coxae—attachment base for the first pair of legs—are characteristically bifid; males have a pair of sclerotized adanal plates on the ventral surface adjacent to the anus as well as accessory adanal shields.2 Rhipicephalus (formerly Boophilus) microplus (the so-called cattle tick) is a newly added species; it lacks posterior festoons, and the anal groove is absent.3
Almost all Rhipicephalus ticks, except for R microplus, are 3-host ticks in which a single blood meal is consumed from a vertebrate host at each active life stage—larva, nymph, and adult—to complete development.4,5 In contrast to most ixodid ticks, which are exophilic (living outside of human habitation), the Rhipicephalus sanguineus sensu lato species (the brown dog tick) is highly endophilic (adapted to indoor living) and often can be found hidden in cracks and crevices of walls in homes and peridomestic structures.6 It is predominately monotropic (all developmental stages feed on the same host species) and has a strong host preference for dogs, though it occasionally feeds on other hosts (eg, humans).7 Although most common in tropical and subtropical climates, they can be found anywhere there are dogs due to their ability to colonize indoor dwellings.8 In contrast, R microplus ticks have a predilection for cattle and livestock rather than humans, posing a notable concern to livestock worldwide. Infestation results in transmission of disease-causing pathogens, such as Babesia and Anaplasma species, which costs the cattle industry billions of dollars annually.9
Clinical Manifestations and Treatment
Tick bites usually manifest as intensely pruritic, erythematous papules at the site of tick attachment due to a local type IV hypersensitivity reaction to antigens in the tick’s saliva. This reaction can be long-lasting. In addition to pruritic papules following a bite, an attached tick can be mistaken for a skin neoplasm or nevus. Given that ticks are small, especially during the larval stage, dermoscopy may be helpful in making a diagnosis.10 Symptomatic relief usually can be achieved with topical antipruritics or oral antihistamines.
Of public health concern, brown dog ticks are important vectors of Rickettsia rickettsii (the causative organism of Rocky Mountain spotted fever [RMSF]) in the Western hemisphere, and Rickettsia conorii (the causative organism of Mediterranean spotted fever [MSF][also known as Boutonneuse fever]) in the Eastern hemisphere.11 Bites by ticks carrying rickettsial disease classically manifest with early symptoms of fever, headache, and myalgia, followed by a rash or by a localized eschar or tache noire (a black, necrotic, scabbed lesion) that represents direct endothelial invasion and vascular damage by Rickettsia.12 Rocky Mountain spotted fever and MSF are more prevalent during summer, likely due, in part, to the combination of increased outdoor activity and a higher rate of tick-questing (host-seeking) behavior in warmer climates.4,7
Rocky Mountain Spotted Fever—Dermacentor variabilis is the primary vector of RMSF in the southeastern United States; Dermacentor andersoni is the major vector of RMSF in Rocky Mountain states. Rhipicephalus sanguineus sensu lato is an important vector of RMSF in the southwestern United States, Mexico, and Central America.11,13
Early symptoms of RMSF are nonspecific and can include fever, headache, arthralgia, myalgia, and malaise. Gastrointestinal tract symptoms (eg, nausea, vomiting, anorexia) may occur; notable abdominal pain occurs in some patients, particularly children. A characteristic petechial rash occurs in as many as 90% of patients, typically at the third to fifth day of illness, and classically begins on the wrists and ankles, with progression to the palms and soles before spreading centripetally to the arms, legs, and trunk.14 An eschar at the inoculation site is uncommon in RMSF; when present, it is more suggestive of MSF.15
The classic triad of fever, headache, and rash is present in 3% of patients during the first 3 days after a tick bite and in 60% to 70% within 2 weeks.16 A rash often is absent when patients first seek medical attention and may not develop (absent in 9% to 12% of cases; so-called spotless RMSF). Therefore, absence of rash should not be a reason to withhold treatment.16 Empiric treatment with doxycycline should be started promptly for all suspected cases of RMSF because of the rapid progression of disease and an increased risk for morbidity and mortality with delayed diagnosis.
Patients do not become antibody positive until 7 to 10 days after symptoms begin; therefore, treatment should not be delayed while awaiting serologic test results. The case fatality rate in the United States is estimated to be 5% to 10% overall and as high as 40% to 50% among patients who are not treated until day 8 or 9 of illness.17
Cutaneous complications include skin necrosis and gangrene due to continuous tissue damage in severe cases.16 Severe infection also may manifest with signs of multiorgan system damage, including altered mental status, cerebral edema, meningismus, transient deafness, myocarditis, pulmonary hemorrhage and edema, conjunctivitis, retinal abnormalities, and acute renal failure.14,16 Risk factors for more severe illness include delayed treatment, age 40 years or older or younger than 10 years, and underlying medical conditions such as alcoholic liver disease and glucose-6-phosphate dehydrogenase deficiency. However, even some healthy young patients die of this disease.17
Mediterranean Spotted Fever—Rhipicephalus sanguineus sensu lato is the primary vector of MSF, which is prevalent in areas adjacent to the Mediterranean Sea, including southern Europe, Africa, and Central Asia; Sicily is the most highly affected region.18 Findings with MSF are nearly identical to those of RMSF, except that tache noire is more common, present in as many as 70% of cases at the site of the inoculating tick bite, and MSF typically follows a less severe clinical course.12 Similar to other rickettsial diseases, the pathogenesis of MSF involves direct injury to vascular endothelial cells, causing a vasculitis that is responsible for the clinical abnormalities observed.
Patients with severe MSF experience complications similar to severe RMSF, including neurologic manifestations and multiorgan damage.18 Risk factors include advanced age, immunocompromised state, cardiac disease, chronic alcoholism, diabetes mellitus, glucose-6-phosphate dehydrogenase deficiency, respiratory insufficiency, and delayed treatment.18
Treatment—For all spotted fever group rickettsial infections, doxycycline is the treatment of choice for all patients, including children and pregnant women. Treatment should be started without delay; recommended dosages are 100 mg twice daily for children weighing more than 45 kg and adults, and 2.2 mg/kg twice daily for children weighing 45 kg or less.12
Rhipicephalus tick bites rarely can result in paralysis; however, Dermacentor ticks are responsible for most cases of tick-related paralysis in North America. Other pathogens proven or reputed to be transmitted by Rhipicephalus sanguineus sensu lato with zoonotic potential include but are not limited to Rickettsia massiliae, Coxiella burnetti, Anaplasma platys, Leishmania infantum, and Crimean-Congo hemorrhagic fever virus (Nairovirus).19
Environmental Treatment and Prevention
The most effective way to prevent tick-borne illness is avoidance of tick bites. Primary prevention methods include vector control, use of repellents (eg, N,N-diethyl-meta-toluamide [DEET]), picaridin, permethrin), avoidance of areas with a high tick burden, use of protective clothing, and detection and removal of ticks as soon as possible.
Environmental and veterinary controls also are important methods of tick-bite prevention. A veterinarian can recommend a variety of agents for dogs and cats that prevent attachment of ticks. Environmental controls include synthetic or natural product-based chemical acaricides and nonchemical methods, such as landscape management (eg, sealing cracks and crevices in homes and controlling tall grasses, weeds, and leaf debris) to minimize potential tick habitat.20 Secondary prevention includes antibiotics for prophylaxis or for treatment of tick-borne disease, when indicated.
Numerous tick repellents are available commercially; others are being studied. DEET, the most widely used topical repellent, has a broad spectrum of activity against many tick species.21 In addition, DEET has a well-known safety and toxicity profile, with rare adverse effects, and is safe for use in pregnant women and children older than 2 years. Alternative repellents, such as those containing picaridin, ethyl butylacetylaminopropionate (IR3535 [Merck]), oil of lemon eucalyptus, and 2-undecanone can be effective; some show efficacy comparable to that of DEET.22 Permethrin, a synthetic pyrethroid, is a highly efficacious tick repellent and insecticide, especially when used in conjunction with a topical repellent such as DEET. Unlike topically applied repellents, permethrin spray is applied to fabric (eg, clothing, shoes, bed nets, camping gear), not to skin.
Indiscriminate use of acaricides worldwide has led to increasing selection of acaricide resistance in Rhipicephalus tick species, which is especially true with the use of acaricides in controlling R microplus livestock infestations; several tick populations now show resistance to all major classes of these compounds.23-25 For that reason, there has been an increasing effort to develop new chemical and nonchemical approaches to tick control that are more environmentally sustainable and strategies to minimize development and progression of resistance such as rotation of acaricides; reducing the frequency of their application; use of pesticide mixtures, synergists, or both; and increasing use of nonacaricidal methods of control.26
Prompt removal of ticks is important for preventing the transmission of tick-borne disease. Proper removal involves rubbing the tick in a circular motion with a moist gauze pad or using fine-tipped tweezers to grasp the tick as close to the skin surface as possible and pulling upward with a steady pressure.17,27 It is important not to jerk, twist, squeeze, smash, or burn the tick, as this can result in insufficient removal of mouthparts or spread contaminated tick fluids to mucous membranes, increasing the risk for infection. Application of petroleum jelly or nail polish to aid in tick removal have not been shown to be effective and are not recommended.16,28
Characteristics
Rhipicephalus ticks belong to the Ixodidae family of hard-bodied ticks. They are large and teardrop shaped with an inornate scutum (hard dorsal plate) and relatively short mouthparts attached at a hexagonal basis capitulum (base of the head to which mouthparts are attached)(Figure).1 Widely spaced eyes and festoons also are present. The first pair of coxae—attachment base for the first pair of legs—are characteristically bifid; males have a pair of sclerotized adanal plates on the ventral surface adjacent to the anus as well as accessory adanal shields.2 Rhipicephalus (formerly Boophilus) microplus (the so-called cattle tick) is a newly added species; it lacks posterior festoons, and the anal groove is absent.3
Almost all Rhipicephalus ticks, except for R microplus, are 3-host ticks in which a single blood meal is consumed from a vertebrate host at each active life stage—larva, nymph, and adult—to complete development.4,5 In contrast to most ixodid ticks, which are exophilic (living outside of human habitation), the Rhipicephalus sanguineus sensu lato species (the brown dog tick) is highly endophilic (adapted to indoor living) and often can be found hidden in cracks and crevices of walls in homes and peridomestic structures.6 It is predominately monotropic (all developmental stages feed on the same host species) and has a strong host preference for dogs, though it occasionally feeds on other hosts (eg, humans).7 Although most common in tropical and subtropical climates, they can be found anywhere there are dogs due to their ability to colonize indoor dwellings.8 In contrast, R microplus ticks have a predilection for cattle and livestock rather than humans, posing a notable concern to livestock worldwide. Infestation results in transmission of disease-causing pathogens, such as Babesia and Anaplasma species, which costs the cattle industry billions of dollars annually.9
Clinical Manifestations and Treatment
Tick bites usually manifest as intensely pruritic, erythematous papules at the site of tick attachment due to a local type IV hypersensitivity reaction to antigens in the tick’s saliva. This reaction can be long-lasting. In addition to pruritic papules following a bite, an attached tick can be mistaken for a skin neoplasm or nevus. Given that ticks are small, especially during the larval stage, dermoscopy may be helpful in making a diagnosis.10 Symptomatic relief usually can be achieved with topical antipruritics or oral antihistamines.
Of public health concern, brown dog ticks are important vectors of Rickettsia rickettsii (the causative organism of Rocky Mountain spotted fever [RMSF]) in the Western hemisphere, and Rickettsia conorii (the causative organism of Mediterranean spotted fever [MSF][also known as Boutonneuse fever]) in the Eastern hemisphere.11 Bites by ticks carrying rickettsial disease classically manifest with early symptoms of fever, headache, and myalgia, followed by a rash or by a localized eschar or tache noire (a black, necrotic, scabbed lesion) that represents direct endothelial invasion and vascular damage by Rickettsia.12 Rocky Mountain spotted fever and MSF are more prevalent during summer, likely due, in part, to the combination of increased outdoor activity and a higher rate of tick-questing (host-seeking) behavior in warmer climates.4,7
Rocky Mountain Spotted Fever—Dermacentor variabilis is the primary vector of RMSF in the southeastern United States; Dermacentor andersoni is the major vector of RMSF in Rocky Mountain states. Rhipicephalus sanguineus sensu lato is an important vector of RMSF in the southwestern United States, Mexico, and Central America.11,13
Early symptoms of RMSF are nonspecific and can include fever, headache, arthralgia, myalgia, and malaise. Gastrointestinal tract symptoms (eg, nausea, vomiting, anorexia) may occur; notable abdominal pain occurs in some patients, particularly children. A characteristic petechial rash occurs in as many as 90% of patients, typically at the third to fifth day of illness, and classically begins on the wrists and ankles, with progression to the palms and soles before spreading centripetally to the arms, legs, and trunk.14 An eschar at the inoculation site is uncommon in RMSF; when present, it is more suggestive of MSF.15
The classic triad of fever, headache, and rash is present in 3% of patients during the first 3 days after a tick bite and in 60% to 70% within 2 weeks.16 A rash often is absent when patients first seek medical attention and may not develop (absent in 9% to 12% of cases; so-called spotless RMSF). Therefore, absence of rash should not be a reason to withhold treatment.16 Empiric treatment with doxycycline should be started promptly for all suspected cases of RMSF because of the rapid progression of disease and an increased risk for morbidity and mortality with delayed diagnosis.
Patients do not become antibody positive until 7 to 10 days after symptoms begin; therefore, treatment should not be delayed while awaiting serologic test results. The case fatality rate in the United States is estimated to be 5% to 10% overall and as high as 40% to 50% among patients who are not treated until day 8 or 9 of illness.17
Cutaneous complications include skin necrosis and gangrene due to continuous tissue damage in severe cases.16 Severe infection also may manifest with signs of multiorgan system damage, including altered mental status, cerebral edema, meningismus, transient deafness, myocarditis, pulmonary hemorrhage and edema, conjunctivitis, retinal abnormalities, and acute renal failure.14,16 Risk factors for more severe illness include delayed treatment, age 40 years or older or younger than 10 years, and underlying medical conditions such as alcoholic liver disease and glucose-6-phosphate dehydrogenase deficiency. However, even some healthy young patients die of this disease.17
Mediterranean Spotted Fever—Rhipicephalus sanguineus sensu lato is the primary vector of MSF, which is prevalent in areas adjacent to the Mediterranean Sea, including southern Europe, Africa, and Central Asia; Sicily is the most highly affected region.18 Findings with MSF are nearly identical to those of RMSF, except that tache noire is more common, present in as many as 70% of cases at the site of the inoculating tick bite, and MSF typically follows a less severe clinical course.12 Similar to other rickettsial diseases, the pathogenesis of MSF involves direct injury to vascular endothelial cells, causing a vasculitis that is responsible for the clinical abnormalities observed.
Patients with severe MSF experience complications similar to severe RMSF, including neurologic manifestations and multiorgan damage.18 Risk factors include advanced age, immunocompromised state, cardiac disease, chronic alcoholism, diabetes mellitus, glucose-6-phosphate dehydrogenase deficiency, respiratory insufficiency, and delayed treatment.18
Treatment—For all spotted fever group rickettsial infections, doxycycline is the treatment of choice for all patients, including children and pregnant women. Treatment should be started without delay; recommended dosages are 100 mg twice daily for children weighing more than 45 kg and adults, and 2.2 mg/kg twice daily for children weighing 45 kg or less.12
Rhipicephalus tick bites rarely can result in paralysis; however, Dermacentor ticks are responsible for most cases of tick-related paralysis in North America. Other pathogens proven or reputed to be transmitted by Rhipicephalus sanguineus sensu lato with zoonotic potential include but are not limited to Rickettsia massiliae, Coxiella burnetti, Anaplasma platys, Leishmania infantum, and Crimean-Congo hemorrhagic fever virus (Nairovirus).19
Environmental Treatment and Prevention
The most effective way to prevent tick-borne illness is avoidance of tick bites. Primary prevention methods include vector control, use of repellents (eg, N,N-diethyl-meta-toluamide [DEET]), picaridin, permethrin), avoidance of areas with a high tick burden, use of protective clothing, and detection and removal of ticks as soon as possible.
Environmental and veterinary controls also are important methods of tick-bite prevention. A veterinarian can recommend a variety of agents for dogs and cats that prevent attachment of ticks. Environmental controls include synthetic or natural product-based chemical acaricides and nonchemical methods, such as landscape management (eg, sealing cracks and crevices in homes and controlling tall grasses, weeds, and leaf debris) to minimize potential tick habitat.20 Secondary prevention includes antibiotics for prophylaxis or for treatment of tick-borne disease, when indicated.
Numerous tick repellents are available commercially; others are being studied. DEET, the most widely used topical repellent, has a broad spectrum of activity against many tick species.21 In addition, DEET has a well-known safety and toxicity profile, with rare adverse effects, and is safe for use in pregnant women and children older than 2 years. Alternative repellents, such as those containing picaridin, ethyl butylacetylaminopropionate (IR3535 [Merck]), oil of lemon eucalyptus, and 2-undecanone can be effective; some show efficacy comparable to that of DEET.22 Permethrin, a synthetic pyrethroid, is a highly efficacious tick repellent and insecticide, especially when used in conjunction with a topical repellent such as DEET. Unlike topically applied repellents, permethrin spray is applied to fabric (eg, clothing, shoes, bed nets, camping gear), not to skin.
Indiscriminate use of acaricides worldwide has led to increasing selection of acaricide resistance in Rhipicephalus tick species, which is especially true with the use of acaricides in controlling R microplus livestock infestations; several tick populations now show resistance to all major classes of these compounds.23-25 For that reason, there has been an increasing effort to develop new chemical and nonchemical approaches to tick control that are more environmentally sustainable and strategies to minimize development and progression of resistance such as rotation of acaricides; reducing the frequency of their application; use of pesticide mixtures, synergists, or both; and increasing use of nonacaricidal methods of control.26
Prompt removal of ticks is important for preventing the transmission of tick-borne disease. Proper removal involves rubbing the tick in a circular motion with a moist gauze pad or using fine-tipped tweezers to grasp the tick as close to the skin surface as possible and pulling upward with a steady pressure.17,27 It is important not to jerk, twist, squeeze, smash, or burn the tick, as this can result in insufficient removal of mouthparts or spread contaminated tick fluids to mucous membranes, increasing the risk for infection. Application of petroleum jelly or nail polish to aid in tick removal have not been shown to be effective and are not recommended.16,28
- Dantas-Torres F. The brown dog tick, Rhipicephalus sanguineus (Latreille, 1806) (Acari: Ixodidae): from taxonomy to control. Vet Parasitol. 2008;152:173-185. doi:10.1016/j.vetpar.2007.12.030
- Madder M, Fourie JJ, Schetters TPM. Arachnida, Metastigmata, Ixodidae (except Ixodes holocyclus). In: Marchiondo AA, Cruthers LR, Fourie JJ, eds. Parasiticide Screening: In Vitro and In Vivo Tests With Relevant Parasite Rearing and Host Infection/Infestation Methods. Volume 1. Elsevier Academic Press; 2019:19-20.
- Burger TD, Shao R, Barker SC. Phylogenetic analysis of mitochondrial genome sequences indicates that the cattle tick, Rhipicephalus (Boophilus) microplus, contains a cryptic species. Mol Phylogenet Evol. 2014;76:241-253. doi:10.1016/j.ympev.2014.03.017
- Gray J, Dantas-Torres F, Estrada-Peña A, et al. Systematics and ecology of the brown dog tick, Rhipicephalus sanguineus. Ticks Tick Borne Dis. 2013;4:171-180. doi:10.1016/j.ttbdis.2012.12.003
- Tian Y, Lord CC, Kaufman PE. Brown dog tick, Rhipicephalus Sanguineus Latrielle (Arachnida: Acari: Ixodidae): EENY-221/IN378. EDIS. March 26, 2020. Accessed January 3, 2024. https://doi.org/10.32473/edis-in378-2020
- Saleh MN, Allen KE, Lineberry MW, et al. Ticks infesting dogs and cats in North America: biology, geographic distribution, and pathogen transmission. Vet Parasitol. 2021;294:109392. doi:10.1016/j.vetpar.2021.109392
- Dantas-Torres F. Biology and ecology of the brown dog tick, Rhipicephalus sanguineus. Parasit Vectors. 2010;3:26. doi:10.1186/1756-3305-3-26
- Dryden MW, Payne PA. Biology and control of ticks infesting dogs and cats in North America. Vet Ther. 2004;5:139-154.
- Nyangiwe N, Yawa M, Muchenje V. Driving forces for changes in geographic range of cattle ticks (Acari: Ixodidae) in Africa: a Review. S Afr J Anim Sci. 2018;48:829. doi:10.4314/sajas.v48i5.4
- Ramot Y, Zlotogorski A, Mumcuoglu KY. Brown dog tick (Rhipicephalus sanguineus) infestation of the penis detected by dermoscopy. Int J Dermatol. 2012;51:1402-1403. doi:10.1111/j.1365-4632.2010.04756.x
- Tucker NSG, Weeks ENI, Beati L, et al. Prevalence and distribution of pathogen infection and permethrin resistance in tropical and temperate populations of Rhipicephalus sanguineus s.l. collected worldwide. Med Vet Entomol. 2021;35:147-157. doi:10.1111/mve.12479
- McClain MT, Sexton DJ, Hall KK, eds. Other spotted fever group rickettsial infections. UpToDate. Updated October 10, 2022. Accessed January 3, 2024. https://www.uptodate.com/contents/other-spotted-fever-group-rickettsial-infections
- Ribeiro CM, Carvalho JLB, Bastos PAS, et al. Prevalence of Rickettsia rickettsii in ticks: systematic review and meta-analysis. Vector Borne Zoonotic Dis. 2021;21:557-565. doi:10.1089/vbz.2021.0004
- Pace EJ, O’Reilly M. Tickborne diseases: diagnosis and management. Am Fam Physician. 2020;101:530-540.
- Patterson JW. Weedon’s Skin Pathology. 5th ed. Elsevier; 2020.
- Dantas-Torres F. Rocky Mountain spotted fever. Lancet Infect Dis. 2007;7:724-732. doi:10.1016/S1473-3099(07)70261-X
- Biggs HM, Behravesh CB, Bradley KK, et al. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever and other spotted fever group rickettsioses, ehrlichioses, and anaplasmosis—United States. MMWR Recomm Rep. 2016;65:1-44. doi:10.15585/mmwr.rr6502a1
- Rossio R, Conalbi V, Castagna V, et al. Mediterranean spotted fever and hearing impairment: a rare complication. Int J Infect Dis. 2015;35:34-36. doi:10.1016/j.ijid.2015.04.005
- Dantas-Torres F, Otranto D. Further thoughts on the taxonomy and vector role of Rhipicephalus sanguineus group ticks. Vet Parasitol. 2015;208:9-13. doi:10.1016/j.vetpar.2014.12.014
- Eisen RJ, Kugeler KJ, Eisen L, et al. Tick-borne zoonoses in the United States: persistent and emerging threats to human health. ILAR J. 2017;58:319-335. doi:10.1093/ilar/ilx005
- Nguyen QD, Vu MN, Hebert AA. Insect repellents: an updated review for the clinician. J Am Acad Dermatol. 2018;88:123-130. doi:10.1016/j.jaad.2018.10.053
- Pages F, Dautel H, Duvallet G, et al. Tick repellents for human use: prevention of tick bites and tick-borne diseases. Vector Borne Zoonotic Dis. 2014;14:85-93. doi:10.1089/vbz.2013.1410
- Rodriguez-Vivas RI, Alonso-Díaz MA, et al. Prevalence and potential risk factors for organophosphate and pyrethroid resistance in Boophilus microplus ticks on cattle ranches from the State of Yucatan, Mexico. Vet Parasitol. 2006;136:335-342. doi:10.1016/j.vetpar.2005.05.069
- Rodríguez-Vivas RI, Rodríguez-Arevalo F, Alonso-Díaz MA, et al. Prevalence and potential risk factors for amitraz resistance in Boophilus microplus ticks in cattle farms in the State of Yucatan, Mexico. Prev Vet Med. 2006;75:280-286. doi:10.1016/j.prevetmed.2006.04.001
- Perez-Cogollo LC, Rodriguez-Vivas RI, Ramirez-Cruz GT, et al. First report of the cattle tick Rhipicephalus microplus resistant to ivermectin in Mexico. Vet Parasitol. 2010;168:165-169. doi:10.1016/j.vetpar.2009.10.021
- Rodriguez-Vivas RI, Jonsson NN, Bhushan C. Strategies for the control of Rhipicephalus microplus ticks in a world of conventional acaricide and macrocyclic lactone resistance. Parasitol Res.2018;117:3-29. doi:10.1007/s00436-017-5677-6
- Centers for Disease Control and Prevention. Tick removal. Updated May 13, 2022. Accessed January 3, 2024. https://www.cdc.gov/ticks/removing_a_tick.html
- Diaz JH. Chemical and plant-based insect repellents: efficacy, safety, and toxicity. Wilderness Environ Med. 2016;27:153-163. doi:10.1016/j.wem.2015.11.007
- Dantas-Torres F. The brown dog tick, Rhipicephalus sanguineus (Latreille, 1806) (Acari: Ixodidae): from taxonomy to control. Vet Parasitol. 2008;152:173-185. doi:10.1016/j.vetpar.2007.12.030
- Madder M, Fourie JJ, Schetters TPM. Arachnida, Metastigmata, Ixodidae (except Ixodes holocyclus). In: Marchiondo AA, Cruthers LR, Fourie JJ, eds. Parasiticide Screening: In Vitro and In Vivo Tests With Relevant Parasite Rearing and Host Infection/Infestation Methods. Volume 1. Elsevier Academic Press; 2019:19-20.
- Burger TD, Shao R, Barker SC. Phylogenetic analysis of mitochondrial genome sequences indicates that the cattle tick, Rhipicephalus (Boophilus) microplus, contains a cryptic species. Mol Phylogenet Evol. 2014;76:241-253. doi:10.1016/j.ympev.2014.03.017
- Gray J, Dantas-Torres F, Estrada-Peña A, et al. Systematics and ecology of the brown dog tick, Rhipicephalus sanguineus. Ticks Tick Borne Dis. 2013;4:171-180. doi:10.1016/j.ttbdis.2012.12.003
- Tian Y, Lord CC, Kaufman PE. Brown dog tick, Rhipicephalus Sanguineus Latrielle (Arachnida: Acari: Ixodidae): EENY-221/IN378. EDIS. March 26, 2020. Accessed January 3, 2024. https://doi.org/10.32473/edis-in378-2020
- Saleh MN, Allen KE, Lineberry MW, et al. Ticks infesting dogs and cats in North America: biology, geographic distribution, and pathogen transmission. Vet Parasitol. 2021;294:109392. doi:10.1016/j.vetpar.2021.109392
- Dantas-Torres F. Biology and ecology of the brown dog tick, Rhipicephalus sanguineus. Parasit Vectors. 2010;3:26. doi:10.1186/1756-3305-3-26
- Dryden MW, Payne PA. Biology and control of ticks infesting dogs and cats in North America. Vet Ther. 2004;5:139-154.
- Nyangiwe N, Yawa M, Muchenje V. Driving forces for changes in geographic range of cattle ticks (Acari: Ixodidae) in Africa: a Review. S Afr J Anim Sci. 2018;48:829. doi:10.4314/sajas.v48i5.4
- Ramot Y, Zlotogorski A, Mumcuoglu KY. Brown dog tick (Rhipicephalus sanguineus) infestation of the penis detected by dermoscopy. Int J Dermatol. 2012;51:1402-1403. doi:10.1111/j.1365-4632.2010.04756.x
- Tucker NSG, Weeks ENI, Beati L, et al. Prevalence and distribution of pathogen infection and permethrin resistance in tropical and temperate populations of Rhipicephalus sanguineus s.l. collected worldwide. Med Vet Entomol. 2021;35:147-157. doi:10.1111/mve.12479
- McClain MT, Sexton DJ, Hall KK, eds. Other spotted fever group rickettsial infections. UpToDate. Updated October 10, 2022. Accessed January 3, 2024. https://www.uptodate.com/contents/other-spotted-fever-group-rickettsial-infections
- Ribeiro CM, Carvalho JLB, Bastos PAS, et al. Prevalence of Rickettsia rickettsii in ticks: systematic review and meta-analysis. Vector Borne Zoonotic Dis. 2021;21:557-565. doi:10.1089/vbz.2021.0004
- Pace EJ, O’Reilly M. Tickborne diseases: diagnosis and management. Am Fam Physician. 2020;101:530-540.
- Patterson JW. Weedon’s Skin Pathology. 5th ed. Elsevier; 2020.
- Dantas-Torres F. Rocky Mountain spotted fever. Lancet Infect Dis. 2007;7:724-732. doi:10.1016/S1473-3099(07)70261-X
- Biggs HM, Behravesh CB, Bradley KK, et al. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever and other spotted fever group rickettsioses, ehrlichioses, and anaplasmosis—United States. MMWR Recomm Rep. 2016;65:1-44. doi:10.15585/mmwr.rr6502a1
- Rossio R, Conalbi V, Castagna V, et al. Mediterranean spotted fever and hearing impairment: a rare complication. Int J Infect Dis. 2015;35:34-36. doi:10.1016/j.ijid.2015.04.005
- Dantas-Torres F, Otranto D. Further thoughts on the taxonomy and vector role of Rhipicephalus sanguineus group ticks. Vet Parasitol. 2015;208:9-13. doi:10.1016/j.vetpar.2014.12.014
- Eisen RJ, Kugeler KJ, Eisen L, et al. Tick-borne zoonoses in the United States: persistent and emerging threats to human health. ILAR J. 2017;58:319-335. doi:10.1093/ilar/ilx005
- Nguyen QD, Vu MN, Hebert AA. Insect repellents: an updated review for the clinician. J Am Acad Dermatol. 2018;88:123-130. doi:10.1016/j.jaad.2018.10.053
- Pages F, Dautel H, Duvallet G, et al. Tick repellents for human use: prevention of tick bites and tick-borne diseases. Vector Borne Zoonotic Dis. 2014;14:85-93. doi:10.1089/vbz.2013.1410
- Rodriguez-Vivas RI, Alonso-Díaz MA, et al. Prevalence and potential risk factors for organophosphate and pyrethroid resistance in Boophilus microplus ticks on cattle ranches from the State of Yucatan, Mexico. Vet Parasitol. 2006;136:335-342. doi:10.1016/j.vetpar.2005.05.069
- Rodríguez-Vivas RI, Rodríguez-Arevalo F, Alonso-Díaz MA, et al. Prevalence and potential risk factors for amitraz resistance in Boophilus microplus ticks in cattle farms in the State of Yucatan, Mexico. Prev Vet Med. 2006;75:280-286. doi:10.1016/j.prevetmed.2006.04.001
- Perez-Cogollo LC, Rodriguez-Vivas RI, Ramirez-Cruz GT, et al. First report of the cattle tick Rhipicephalus microplus resistant to ivermectin in Mexico. Vet Parasitol. 2010;168:165-169. doi:10.1016/j.vetpar.2009.10.021
- Rodriguez-Vivas RI, Jonsson NN, Bhushan C. Strategies for the control of Rhipicephalus microplus ticks in a world of conventional acaricide and macrocyclic lactone resistance. Parasitol Res.2018;117:3-29. doi:10.1007/s00436-017-5677-6
- Centers for Disease Control and Prevention. Tick removal. Updated May 13, 2022. Accessed January 3, 2024. https://www.cdc.gov/ticks/removing_a_tick.html
- Diaz JH. Chemical and plant-based insect repellents: efficacy, safety, and toxicity. Wilderness Environ Med. 2016;27:153-163. doi:10.1016/j.wem.2015.11.007
PRACTICE POINTS
- Rhipicephalus ticks are vectors of a variety of diseases, including the rickettsial diseases Rocky Mountain spotted fever and Mediterranean spotted fever.
- Presenting symptoms of a tick bite include intensely pruritic, erythematous papules and nodules at the site of tick attachment.
- If rickettsial disease is suspected, treatment with doxycycline should be initiated immediately; do not delay treatment to await results of confirmatory tests or because of the absence of a rash.
- Primary methods of prevention of tick-borne disease include repellents, protective clothing, vector control, and prompt removal of the tick.
New Guideline Offers Recommendations for Alcohol-Associated Liver Disease
according to a new clinical guideline from the American College of Gastroenterology.
In addition, health systems need to overcome barriers to treating alcohol use disorder (AUD) and commit to creating a multidisciplinary care model with behavioral interventions and pharmacotherapy for patients.
Experts were convened to develop these guidelines because it was “imperative to provide an up-to-date, evidence-based blueprint for how to care for patients, as well as guide prevention and research efforts in the field of ALD for the coming years,” said the first author, Loretta Jophlin, MD, PhD, assistant professor of medicine in gastroenterology, hepatology, and nutrition and medical director of liver transplantation at the University of Louisville in Kentucky.
“In recent years, perhaps fueled by the COVID-19 pandemic, alcohol use has been normalized in an increasing number of situations,” she said. “Drinking was normalized as a coping mechanism to deal with many of the sorrows we experienced during the pandemic, including loss of purposeful work and social isolation, and many more people are struggling with AUD. So many aspects of our culture have been inundated by the presence of alcohol use, and we need to work hard to denormalize this, first focusing on at-risk populations.”
The guideline was published in the January issue of the American Journal of Gastroenterology.
Updating ALD Recommendations
With ALD as the most common cause of advanced hepatic disease and a frequent indicator of eventual liver transplantation, the rising incidence of alcohol use during the past decade has led to rapid growth in ALD-related healthcare burdens, the guideline authors wrote.
In particular, those with ALD tend to present at an advanced stage and progress faster, which can lead to progressive fibrosis, cirrhosis, and hepatocellular carcinoma. This can include alcohol-associated hepatitis (AH), which often presents with a rapid onset or worsening of jaundice and can lead to acute or chronic liver failure.
To update the guideline, Dr. Jophlin and colleagues analyzed data based on a patient-intervention-comparison-outcome format, resulting in 34 key concepts or statements and 21 recommendations.
Among them, the authors recommended screening and treating AUD with the goal of helping patients who have not yet developed significant liver injury and preventing progression to advanced stages of ALD, particularly among at-risk groups who have had an increasing prevalence of severe AUD, including women, younger people, and Hispanic and American Indian patients.
“So many patients are still told to ‘stop drinking’ or ‘cut back’ but are provided no additional resources. Without offering referrals to treatment programs or pharmacologic therapies to assist in abstinence, many patients are not successful,” Dr. Jophlin said. “We hope these guidelines empower providers to consider selected [Food and Drug Administration]-approved medications, well-studied off-label therapies, and nonpharmacologic interventions to aid their patients’ journeys to abstinence and hopefully avert the progression of ALD.”
In addition, the guidelines provide recommendations for AH treatment. In patients with severe AH, the authors offered strong recommendations against the use of pentoxifylline and prophylactic antibiotics, and in support of corticosteroid therapy and intravenous N-acetyl cysteine as an adjuvant to corticosteroids.
Liver transplantation, which may be recommended for carefully selected patients, is being performed at many centers but remains relatively controversial, Dr. Jophlin said.
“Questions remain about ideal patient selection as center practices vary considerably, yet we have started to realize the impacts of relapse after transplantation,” she said. “The guidelines highlight the knowns and unknowns in this area and will hopefully serve as a catalyst for the dissemination of centers’ experiences and the development of a universal set of ethically sound, evidence-based guidelines to be used by all transplant centers.”
Policy Implications
Dr. Jophlin and colleagues noted the importance of policy aimed at alcohol use reduction, multidisciplinary care for AUD and ALD, and additional research around severe AH.
“As a practicing transplant hepatologist and medical director of a liver transplant program in the heart of Bourbon country, I am a part of just one healthcare team experiencing ALD, particularly AH, as a mass casualty event. Healthcare teams are fighting an unrelenting fire that the alcohol industry is pouring gasoline on,” Dr. Jophlin said. “It is imperative that healthcare providers have a voice in the policies that shape this preventable disease. We hope these guidelines inspire practitioners to explore our influence on how alcohol is regulated, marketed, and distributed.”
Additional interventions and public policy considerations could help reduce alcohol-related morbidity and mortality at a moment when the characteristics of those who present with AUD appear to be evolving.
“The typical person I’m seeing now is not someone who has been drinking heavily for decades. Rather, it’s a young person who has been drinking heavily for many months or a couple of years,” said James Burton, MD, a professor of medicine at the University of Colorado School of Medicine and medical director of liver transplantation at the University of Colorado Hospital’s Anschutz Medical Campus in Aurora.
Dr. Burton, who wasn’t involved with the guideline, noted it’s become more common for people to drink multiple alcoholic drinks per day for multiple times per week. Patients often don’t think it’s a problem, even as he discusses their liver-related issues.
“We can’t just keep living and working the way we were 10 years ago,” he said. “We’ve got to change how we approach treatment. We have to treat liver disease and AUD.”
The guideline was supported by several National Institutes of Health grants and an American College of Gastroenterology faculty development grant. The authors declared potential competing interests with various pharmaceutical companies. Dr. Burton reported no financial disclosures.
A version of this article appeared on Medscape.com.
according to a new clinical guideline from the American College of Gastroenterology.
In addition, health systems need to overcome barriers to treating alcohol use disorder (AUD) and commit to creating a multidisciplinary care model with behavioral interventions and pharmacotherapy for patients.
Experts were convened to develop these guidelines because it was “imperative to provide an up-to-date, evidence-based blueprint for how to care for patients, as well as guide prevention and research efforts in the field of ALD for the coming years,” said the first author, Loretta Jophlin, MD, PhD, assistant professor of medicine in gastroenterology, hepatology, and nutrition and medical director of liver transplantation at the University of Louisville in Kentucky.
“In recent years, perhaps fueled by the COVID-19 pandemic, alcohol use has been normalized in an increasing number of situations,” she said. “Drinking was normalized as a coping mechanism to deal with many of the sorrows we experienced during the pandemic, including loss of purposeful work and social isolation, and many more people are struggling with AUD. So many aspects of our culture have been inundated by the presence of alcohol use, and we need to work hard to denormalize this, first focusing on at-risk populations.”
The guideline was published in the January issue of the American Journal of Gastroenterology.
Updating ALD Recommendations
With ALD as the most common cause of advanced hepatic disease and a frequent indicator of eventual liver transplantation, the rising incidence of alcohol use during the past decade has led to rapid growth in ALD-related healthcare burdens, the guideline authors wrote.
In particular, those with ALD tend to present at an advanced stage and progress faster, which can lead to progressive fibrosis, cirrhosis, and hepatocellular carcinoma. This can include alcohol-associated hepatitis (AH), which often presents with a rapid onset or worsening of jaundice and can lead to acute or chronic liver failure.
To update the guideline, Dr. Jophlin and colleagues analyzed data based on a patient-intervention-comparison-outcome format, resulting in 34 key concepts or statements and 21 recommendations.
Among them, the authors recommended screening and treating AUD with the goal of helping patients who have not yet developed significant liver injury and preventing progression to advanced stages of ALD, particularly among at-risk groups who have had an increasing prevalence of severe AUD, including women, younger people, and Hispanic and American Indian patients.
“So many patients are still told to ‘stop drinking’ or ‘cut back’ but are provided no additional resources. Without offering referrals to treatment programs or pharmacologic therapies to assist in abstinence, many patients are not successful,” Dr. Jophlin said. “We hope these guidelines empower providers to consider selected [Food and Drug Administration]-approved medications, well-studied off-label therapies, and nonpharmacologic interventions to aid their patients’ journeys to abstinence and hopefully avert the progression of ALD.”
In addition, the guidelines provide recommendations for AH treatment. In patients with severe AH, the authors offered strong recommendations against the use of pentoxifylline and prophylactic antibiotics, and in support of corticosteroid therapy and intravenous N-acetyl cysteine as an adjuvant to corticosteroids.
Liver transplantation, which may be recommended for carefully selected patients, is being performed at many centers but remains relatively controversial, Dr. Jophlin said.
“Questions remain about ideal patient selection as center practices vary considerably, yet we have started to realize the impacts of relapse after transplantation,” she said. “The guidelines highlight the knowns and unknowns in this area and will hopefully serve as a catalyst for the dissemination of centers’ experiences and the development of a universal set of ethically sound, evidence-based guidelines to be used by all transplant centers.”
Policy Implications
Dr. Jophlin and colleagues noted the importance of policy aimed at alcohol use reduction, multidisciplinary care for AUD and ALD, and additional research around severe AH.
“As a practicing transplant hepatologist and medical director of a liver transplant program in the heart of Bourbon country, I am a part of just one healthcare team experiencing ALD, particularly AH, as a mass casualty event. Healthcare teams are fighting an unrelenting fire that the alcohol industry is pouring gasoline on,” Dr. Jophlin said. “It is imperative that healthcare providers have a voice in the policies that shape this preventable disease. We hope these guidelines inspire practitioners to explore our influence on how alcohol is regulated, marketed, and distributed.”
Additional interventions and public policy considerations could help reduce alcohol-related morbidity and mortality at a moment when the characteristics of those who present with AUD appear to be evolving.
“The typical person I’m seeing now is not someone who has been drinking heavily for decades. Rather, it’s a young person who has been drinking heavily for many months or a couple of years,” said James Burton, MD, a professor of medicine at the University of Colorado School of Medicine and medical director of liver transplantation at the University of Colorado Hospital’s Anschutz Medical Campus in Aurora.
Dr. Burton, who wasn’t involved with the guideline, noted it’s become more common for people to drink multiple alcoholic drinks per day for multiple times per week. Patients often don’t think it’s a problem, even as he discusses their liver-related issues.
“We can’t just keep living and working the way we were 10 years ago,” he said. “We’ve got to change how we approach treatment. We have to treat liver disease and AUD.”
The guideline was supported by several National Institutes of Health grants and an American College of Gastroenterology faculty development grant. The authors declared potential competing interests with various pharmaceutical companies. Dr. Burton reported no financial disclosures.
A version of this article appeared on Medscape.com.
according to a new clinical guideline from the American College of Gastroenterology.
In addition, health systems need to overcome barriers to treating alcohol use disorder (AUD) and commit to creating a multidisciplinary care model with behavioral interventions and pharmacotherapy for patients.
Experts were convened to develop these guidelines because it was “imperative to provide an up-to-date, evidence-based blueprint for how to care for patients, as well as guide prevention and research efforts in the field of ALD for the coming years,” said the first author, Loretta Jophlin, MD, PhD, assistant professor of medicine in gastroenterology, hepatology, and nutrition and medical director of liver transplantation at the University of Louisville in Kentucky.
“In recent years, perhaps fueled by the COVID-19 pandemic, alcohol use has been normalized in an increasing number of situations,” she said. “Drinking was normalized as a coping mechanism to deal with many of the sorrows we experienced during the pandemic, including loss of purposeful work and social isolation, and many more people are struggling with AUD. So many aspects of our culture have been inundated by the presence of alcohol use, and we need to work hard to denormalize this, first focusing on at-risk populations.”
The guideline was published in the January issue of the American Journal of Gastroenterology.
Updating ALD Recommendations
With ALD as the most common cause of advanced hepatic disease and a frequent indicator of eventual liver transplantation, the rising incidence of alcohol use during the past decade has led to rapid growth in ALD-related healthcare burdens, the guideline authors wrote.
In particular, those with ALD tend to present at an advanced stage and progress faster, which can lead to progressive fibrosis, cirrhosis, and hepatocellular carcinoma. This can include alcohol-associated hepatitis (AH), which often presents with a rapid onset or worsening of jaundice and can lead to acute or chronic liver failure.
To update the guideline, Dr. Jophlin and colleagues analyzed data based on a patient-intervention-comparison-outcome format, resulting in 34 key concepts or statements and 21 recommendations.
Among them, the authors recommended screening and treating AUD with the goal of helping patients who have not yet developed significant liver injury and preventing progression to advanced stages of ALD, particularly among at-risk groups who have had an increasing prevalence of severe AUD, including women, younger people, and Hispanic and American Indian patients.
“So many patients are still told to ‘stop drinking’ or ‘cut back’ but are provided no additional resources. Without offering referrals to treatment programs or pharmacologic therapies to assist in abstinence, many patients are not successful,” Dr. Jophlin said. “We hope these guidelines empower providers to consider selected [Food and Drug Administration]-approved medications, well-studied off-label therapies, and nonpharmacologic interventions to aid their patients’ journeys to abstinence and hopefully avert the progression of ALD.”
In addition, the guidelines provide recommendations for AH treatment. In patients with severe AH, the authors offered strong recommendations against the use of pentoxifylline and prophylactic antibiotics, and in support of corticosteroid therapy and intravenous N-acetyl cysteine as an adjuvant to corticosteroids.
Liver transplantation, which may be recommended for carefully selected patients, is being performed at many centers but remains relatively controversial, Dr. Jophlin said.
“Questions remain about ideal patient selection as center practices vary considerably, yet we have started to realize the impacts of relapse after transplantation,” she said. “The guidelines highlight the knowns and unknowns in this area and will hopefully serve as a catalyst for the dissemination of centers’ experiences and the development of a universal set of ethically sound, evidence-based guidelines to be used by all transplant centers.”
Policy Implications
Dr. Jophlin and colleagues noted the importance of policy aimed at alcohol use reduction, multidisciplinary care for AUD and ALD, and additional research around severe AH.
“As a practicing transplant hepatologist and medical director of a liver transplant program in the heart of Bourbon country, I am a part of just one healthcare team experiencing ALD, particularly AH, as a mass casualty event. Healthcare teams are fighting an unrelenting fire that the alcohol industry is pouring gasoline on,” Dr. Jophlin said. “It is imperative that healthcare providers have a voice in the policies that shape this preventable disease. We hope these guidelines inspire practitioners to explore our influence on how alcohol is regulated, marketed, and distributed.”
Additional interventions and public policy considerations could help reduce alcohol-related morbidity and mortality at a moment when the characteristics of those who present with AUD appear to be evolving.
“The typical person I’m seeing now is not someone who has been drinking heavily for decades. Rather, it’s a young person who has been drinking heavily for many months or a couple of years,” said James Burton, MD, a professor of medicine at the University of Colorado School of Medicine and medical director of liver transplantation at the University of Colorado Hospital’s Anschutz Medical Campus in Aurora.
Dr. Burton, who wasn’t involved with the guideline, noted it’s become more common for people to drink multiple alcoholic drinks per day for multiple times per week. Patients often don’t think it’s a problem, even as he discusses their liver-related issues.
“We can’t just keep living and working the way we were 10 years ago,” he said. “We’ve got to change how we approach treatment. We have to treat liver disease and AUD.”
The guideline was supported by several National Institutes of Health grants and an American College of Gastroenterology faculty development grant. The authors declared potential competing interests with various pharmaceutical companies. Dr. Burton reported no financial disclosures.
A version of this article appeared on Medscape.com.
Psychotherapy as Effective as Drugs for Depression in HF
TOPLINE:
, a comparative trial of these interventions found.
METHODOLOGY:
- The study included 416 patients with HF and a confirmed depressive disorder from the Cedars-Sinai Health System, with a mean age of 60.71 years, including nearly 42% women and 30% Black individuals, who were randomized to receive one of two evidence-based treatments for depression in HF: Antidepressant medication management (MEDS) or behavioral activation (BA) psychotherapy. BA therapy promotes engaging in pleasurable and rewarding activities without delving into complex cognitive domains explored in cognitive behavioral therapy, another psychotherapy type.
- All patients received 12 weekly sessions delivered via video or telephone, followed by monthly sessions for 3 months, and were then contacted as needed for an additional 6 months.
- The primary outcome was depressive symptom severity at 6 months, measured by the Patient Health Questionnaire 9-Item (PHQ-9), and secondary outcomes included three measures of health-related quality of life (HRQOL) — caregiver burden, morbidity, and mortality — collected at 3, 6, and 12 months.
- Physical and mental HRQOL were measured with the 12-Item Short-Form Medical Outcomes Study (SF-12), HF-specific HRQOL with the 23-item patient-reported Kansas City Cardiomyopathy Questionnaire, caregiver burden with the 26-item Caregiver Burden Questionnaire for HF, morbidity by ED visits, hospital readmissions, and days hospitalized, and mortality data came from medical records and family or caregiver reports, with survival assessed using Kaplan-Meier plots at 3, 6, and 12 months.
- Covariates included age, sex, race, ethnicity, marital status, employment, education, insurance type, recruitment site (inpatient or outpatient), ejection fraction (preserved or reduced), New York Heart Association class, medical history, and medications.
TAKEAWAY:
- Depressive symptom severity was reduced at 6 months by nearly 50% for both BA (mean PHQ-9 score, 7.53; P vs baseline < .001) and MEDS (mean PHQ-9 score, 8.09; P vs baseline < .001) participants, with reductions persisting at 12 months and no significant difference between groups.
- Compared with MEDS recipients, those who received BA had slightly higher improvement in physical HRQOL at 6 months (multivariable mean difference without imputation, 2.13; 95% CI, 0.06-4.20; P = .04), but there were no statistically significant differences between groups in mental HRQOL, HF-specific HRQOL, or caregiver burden at 3, 6, or 12 months.
- Patients who received BA were significantly less likely than those in the MEDS group to have ED visits and spent fewer days in hospital at 3, 6, and 12 months, but there was no significant difference in number of hospital readmissions or in mortality at 3, 6, or 12 months.
IN PRACTICE:
“Our findings of comparable primary effects between BA and MEDS suggest both options are effective and that personal preferences, patient values, and availability of services could inform decisions,” the authors wrote. They noted BA has no pharmacological adverse effects but requires more engagement than drug therapy and might be less accessible.
SOURCE:
The study was conducted by Waguih William IsHak, MD, Department of Psychiatry and Behavioral Neurosciences, Cedars-Sinai Medical Center, Los Angeles, and others. It was published online on January 17, 2024, in JAMA Network Open.
LIMITATIONS:
As the study had no control group, such as a waiting list, it was impossible to draw conclusions about the natural course of depressive symptoms in HF. However, the authors noted improvements were sustained at 12 months despite substantially diminished contact with intervention teams after 6 months. Researchers were unable to collect data for ED visits, readmissions, and hospital stays outside of California and didn’t assess treatment preference at enrollment, which could have helped inform the association with outcomes and adherence.
DISCLOSURES:
The study was funded by the Patient-Centered Outcome Research Institute, paid to Cedars-Sinai Medical Center. Dr. IsHak reported receiving royalties from Springer Nature and Cambridge University Press. No other disclosures were reported.
A version of this article appeared on Medscape.com.
TOPLINE:
, a comparative trial of these interventions found.
METHODOLOGY:
- The study included 416 patients with HF and a confirmed depressive disorder from the Cedars-Sinai Health System, with a mean age of 60.71 years, including nearly 42% women and 30% Black individuals, who were randomized to receive one of two evidence-based treatments for depression in HF: Antidepressant medication management (MEDS) or behavioral activation (BA) psychotherapy. BA therapy promotes engaging in pleasurable and rewarding activities without delving into complex cognitive domains explored in cognitive behavioral therapy, another psychotherapy type.
- All patients received 12 weekly sessions delivered via video or telephone, followed by monthly sessions for 3 months, and were then contacted as needed for an additional 6 months.
- The primary outcome was depressive symptom severity at 6 months, measured by the Patient Health Questionnaire 9-Item (PHQ-9), and secondary outcomes included three measures of health-related quality of life (HRQOL) — caregiver burden, morbidity, and mortality — collected at 3, 6, and 12 months.
- Physical and mental HRQOL were measured with the 12-Item Short-Form Medical Outcomes Study (SF-12), HF-specific HRQOL with the 23-item patient-reported Kansas City Cardiomyopathy Questionnaire, caregiver burden with the 26-item Caregiver Burden Questionnaire for HF, morbidity by ED visits, hospital readmissions, and days hospitalized, and mortality data came from medical records and family or caregiver reports, with survival assessed using Kaplan-Meier plots at 3, 6, and 12 months.
- Covariates included age, sex, race, ethnicity, marital status, employment, education, insurance type, recruitment site (inpatient or outpatient), ejection fraction (preserved or reduced), New York Heart Association class, medical history, and medications.
TAKEAWAY:
- Depressive symptom severity was reduced at 6 months by nearly 50% for both BA (mean PHQ-9 score, 7.53; P vs baseline < .001) and MEDS (mean PHQ-9 score, 8.09; P vs baseline < .001) participants, with reductions persisting at 12 months and no significant difference between groups.
- Compared with MEDS recipients, those who received BA had slightly higher improvement in physical HRQOL at 6 months (multivariable mean difference without imputation, 2.13; 95% CI, 0.06-4.20; P = .04), but there were no statistically significant differences between groups in mental HRQOL, HF-specific HRQOL, or caregiver burden at 3, 6, or 12 months.
- Patients who received BA were significantly less likely than those in the MEDS group to have ED visits and spent fewer days in hospital at 3, 6, and 12 months, but there was no significant difference in number of hospital readmissions or in mortality at 3, 6, or 12 months.
IN PRACTICE:
“Our findings of comparable primary effects between BA and MEDS suggest both options are effective and that personal preferences, patient values, and availability of services could inform decisions,” the authors wrote. They noted BA has no pharmacological adverse effects but requires more engagement than drug therapy and might be less accessible.
SOURCE:
The study was conducted by Waguih William IsHak, MD, Department of Psychiatry and Behavioral Neurosciences, Cedars-Sinai Medical Center, Los Angeles, and others. It was published online on January 17, 2024, in JAMA Network Open.
LIMITATIONS:
As the study had no control group, such as a waiting list, it was impossible to draw conclusions about the natural course of depressive symptoms in HF. However, the authors noted improvements were sustained at 12 months despite substantially diminished contact with intervention teams after 6 months. Researchers were unable to collect data for ED visits, readmissions, and hospital stays outside of California and didn’t assess treatment preference at enrollment, which could have helped inform the association with outcomes and adherence.
DISCLOSURES:
The study was funded by the Patient-Centered Outcome Research Institute, paid to Cedars-Sinai Medical Center. Dr. IsHak reported receiving royalties from Springer Nature and Cambridge University Press. No other disclosures were reported.
A version of this article appeared on Medscape.com.
TOPLINE:
, a comparative trial of these interventions found.
METHODOLOGY:
- The study included 416 patients with HF and a confirmed depressive disorder from the Cedars-Sinai Health System, with a mean age of 60.71 years, including nearly 42% women and 30% Black individuals, who were randomized to receive one of two evidence-based treatments for depression in HF: Antidepressant medication management (MEDS) or behavioral activation (BA) psychotherapy. BA therapy promotes engaging in pleasurable and rewarding activities without delving into complex cognitive domains explored in cognitive behavioral therapy, another psychotherapy type.
- All patients received 12 weekly sessions delivered via video or telephone, followed by monthly sessions for 3 months, and were then contacted as needed for an additional 6 months.
- The primary outcome was depressive symptom severity at 6 months, measured by the Patient Health Questionnaire 9-Item (PHQ-9), and secondary outcomes included three measures of health-related quality of life (HRQOL) — caregiver burden, morbidity, and mortality — collected at 3, 6, and 12 months.
- Physical and mental HRQOL were measured with the 12-Item Short-Form Medical Outcomes Study (SF-12), HF-specific HRQOL with the 23-item patient-reported Kansas City Cardiomyopathy Questionnaire, caregiver burden with the 26-item Caregiver Burden Questionnaire for HF, morbidity by ED visits, hospital readmissions, and days hospitalized, and mortality data came from medical records and family or caregiver reports, with survival assessed using Kaplan-Meier plots at 3, 6, and 12 months.
- Covariates included age, sex, race, ethnicity, marital status, employment, education, insurance type, recruitment site (inpatient or outpatient), ejection fraction (preserved or reduced), New York Heart Association class, medical history, and medications.
TAKEAWAY:
- Depressive symptom severity was reduced at 6 months by nearly 50% for both BA (mean PHQ-9 score, 7.53; P vs baseline < .001) and MEDS (mean PHQ-9 score, 8.09; P vs baseline < .001) participants, with reductions persisting at 12 months and no significant difference between groups.
- Compared with MEDS recipients, those who received BA had slightly higher improvement in physical HRQOL at 6 months (multivariable mean difference without imputation, 2.13; 95% CI, 0.06-4.20; P = .04), but there were no statistically significant differences between groups in mental HRQOL, HF-specific HRQOL, or caregiver burden at 3, 6, or 12 months.
- Patients who received BA were significantly less likely than those in the MEDS group to have ED visits and spent fewer days in hospital at 3, 6, and 12 months, but there was no significant difference in number of hospital readmissions or in mortality at 3, 6, or 12 months.
IN PRACTICE:
“Our findings of comparable primary effects between BA and MEDS suggest both options are effective and that personal preferences, patient values, and availability of services could inform decisions,” the authors wrote. They noted BA has no pharmacological adverse effects but requires more engagement than drug therapy and might be less accessible.
SOURCE:
The study was conducted by Waguih William IsHak, MD, Department of Psychiatry and Behavioral Neurosciences, Cedars-Sinai Medical Center, Los Angeles, and others. It was published online on January 17, 2024, in JAMA Network Open.
LIMITATIONS:
As the study had no control group, such as a waiting list, it was impossible to draw conclusions about the natural course of depressive symptoms in HF. However, the authors noted improvements were sustained at 12 months despite substantially diminished contact with intervention teams after 6 months. Researchers were unable to collect data for ED visits, readmissions, and hospital stays outside of California and didn’t assess treatment preference at enrollment, which could have helped inform the association with outcomes and adherence.
DISCLOSURES:
The study was funded by the Patient-Centered Outcome Research Institute, paid to Cedars-Sinai Medical Center. Dr. IsHak reported receiving royalties from Springer Nature and Cambridge University Press. No other disclosures were reported.
A version of this article appeared on Medscape.com.
Surveillance for 21 Possible Effects of Endocrine Disruptors
Santé Publique France (SPF), the French national public health agency, has released the findings of the PEPS’PE study, which was launched in 2021. The study aims to prioritize, following extensive consultation, the health effects to be monitored for their potential link to endocrine disruptors (EDs). Out of 59 health effects suspected to be associated with exposure to EDs, 21 have been considered a priority for surveillance. Based on these results and others, SPF will expand the scope of the Agency’s surveillance by incorporating new pathologies.
As part of its environmental health program and the National Strategy on EDs, To incorporate new scientific knowledge, the PEPS’PE project aims to prioritize health effects related to EDs and identify health events to integrate into the agency’s current surveillance. The 59 health effects suspected to be associated with exposure to EDs were to be evaluated based on two criteria: The weight of evidence and the epidemiological and societal impact of the health effect. A diverse panel of international experts and French stakeholders in the field of EDs classified 21 health effects as a priority for surveillance.
Among these effects, six reproductive health effects are already monitored in the surveillance program: Cryptorchidism, hypospadias, early puberty, testicular cancer, alteration of sperm quality, and endometriosis. In addition, infertility and decreased fertility (which are not currently monitored for their link to EDs) have been included.
Metabolic effects (including overweight and obesity, cardiovascular diseases, type 2 diabetes, and metabolic syndrome), child neurodevelopmental disorders (including behavioral disorders, intellectual deficits, and attention-deficit disorders), cancers (including breast cancer, prostate cancer, lymphomas, and leukemias in children), and asthma have also been highlighted.
Furthermore, 22 effects were considered low priorities or deemed nonpriorities when, for example, they presented weak or moderate evidence with varying levels of interest in implementing surveillance. Finally, 16 health effects could not be prioritized because of a lack of scientific experts on these topics and a failure to achieve consensus (eg, bone disorders, adrenal disorders, and skin and eye disorders). Consensus was sought during this consultation using a Delphi method.
“These results indicate the need to expand the scope of the Agency’s surveillance beyond reproductive health, incorporating new pathologies when surveillance data are available,” SPF declared in a press release.
“With the initial decision elements obtained through this study, Santé Publique France will analyze the feasibility of implementing surveillance for effects classified as priorities.”
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
Santé Publique France (SPF), the French national public health agency, has released the findings of the PEPS’PE study, which was launched in 2021. The study aims to prioritize, following extensive consultation, the health effects to be monitored for their potential link to endocrine disruptors (EDs). Out of 59 health effects suspected to be associated with exposure to EDs, 21 have been considered a priority for surveillance. Based on these results and others, SPF will expand the scope of the Agency’s surveillance by incorporating new pathologies.
As part of its environmental health program and the National Strategy on EDs, To incorporate new scientific knowledge, the PEPS’PE project aims to prioritize health effects related to EDs and identify health events to integrate into the agency’s current surveillance. The 59 health effects suspected to be associated with exposure to EDs were to be evaluated based on two criteria: The weight of evidence and the epidemiological and societal impact of the health effect. A diverse panel of international experts and French stakeholders in the field of EDs classified 21 health effects as a priority for surveillance.
Among these effects, six reproductive health effects are already monitored in the surveillance program: Cryptorchidism, hypospadias, early puberty, testicular cancer, alteration of sperm quality, and endometriosis. In addition, infertility and decreased fertility (which are not currently monitored for their link to EDs) have been included.
Metabolic effects (including overweight and obesity, cardiovascular diseases, type 2 diabetes, and metabolic syndrome), child neurodevelopmental disorders (including behavioral disorders, intellectual deficits, and attention-deficit disorders), cancers (including breast cancer, prostate cancer, lymphomas, and leukemias in children), and asthma have also been highlighted.
Furthermore, 22 effects were considered low priorities or deemed nonpriorities when, for example, they presented weak or moderate evidence with varying levels of interest in implementing surveillance. Finally, 16 health effects could not be prioritized because of a lack of scientific experts on these topics and a failure to achieve consensus (eg, bone disorders, adrenal disorders, and skin and eye disorders). Consensus was sought during this consultation using a Delphi method.
“These results indicate the need to expand the scope of the Agency’s surveillance beyond reproductive health, incorporating new pathologies when surveillance data are available,” SPF declared in a press release.
“With the initial decision elements obtained through this study, Santé Publique France will analyze the feasibility of implementing surveillance for effects classified as priorities.”
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
Santé Publique France (SPF), the French national public health agency, has released the findings of the PEPS’PE study, which was launched in 2021. The study aims to prioritize, following extensive consultation, the health effects to be monitored for their potential link to endocrine disruptors (EDs). Out of 59 health effects suspected to be associated with exposure to EDs, 21 have been considered a priority for surveillance. Based on these results and others, SPF will expand the scope of the Agency’s surveillance by incorporating new pathologies.
As part of its environmental health program and the National Strategy on EDs, To incorporate new scientific knowledge, the PEPS’PE project aims to prioritize health effects related to EDs and identify health events to integrate into the agency’s current surveillance. The 59 health effects suspected to be associated with exposure to EDs were to be evaluated based on two criteria: The weight of evidence and the epidemiological and societal impact of the health effect. A diverse panel of international experts and French stakeholders in the field of EDs classified 21 health effects as a priority for surveillance.
Among these effects, six reproductive health effects are already monitored in the surveillance program: Cryptorchidism, hypospadias, early puberty, testicular cancer, alteration of sperm quality, and endometriosis. In addition, infertility and decreased fertility (which are not currently monitored for their link to EDs) have been included.
Metabolic effects (including overweight and obesity, cardiovascular diseases, type 2 diabetes, and metabolic syndrome), child neurodevelopmental disorders (including behavioral disorders, intellectual deficits, and attention-deficit disorders), cancers (including breast cancer, prostate cancer, lymphomas, and leukemias in children), and asthma have also been highlighted.
Furthermore, 22 effects were considered low priorities or deemed nonpriorities when, for example, they presented weak or moderate evidence with varying levels of interest in implementing surveillance. Finally, 16 health effects could not be prioritized because of a lack of scientific experts on these topics and a failure to achieve consensus (eg, bone disorders, adrenal disorders, and skin and eye disorders). Consensus was sought during this consultation using a Delphi method.
“These results indicate the need to expand the scope of the Agency’s surveillance beyond reproductive health, incorporating new pathologies when surveillance data are available,” SPF declared in a press release.
“With the initial decision elements obtained through this study, Santé Publique France will analyze the feasibility of implementing surveillance for effects classified as priorities.”
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
Top 5 Medications That Can Increase Blood Glucose Levels
It’s that time of the year, when social media is rife with many top 5 and top 10 lists. Let’s revisit some of the most commonly used medications known to increase glucose levels and look at some practical tips on overcoming these.
1. Glucocorticoids
Without a doubt, corticosteroids are at the top of the list when it comes to the potential for increasing blood glucose levels. High-dose glucocorticoid therapy is known to lead to new-onset diabetes (steroid-induced diabetes). Similarly, people with preexisting diabetes may notice significant worsening of glycemic control when they start on glucocorticoid therapy. The extent of glucose elevation depends on their glycemic status prior to initiation on steroids, the dose and duration of glucocorticoid therapy, and comorbid conditions, among other factors.
Management tip: For those with previously well-controlled diabetes or borderline diabetes, glucocorticoid-induced hyperglycemia may be managed by metformin with or without sulfonylurea therapy, especially if corticosteroid treatment is low-dose and for a shorter duration. However, for many individuals with preexisting poorly controlled diabetes or those initiated on high-dose corticosteroids, insulin therapy would perhaps be the treatment of choice. Glucocorticoid therapy generally leads to more pronounced postprandial hyperglycemia compared with fasting hyperglycemia; hence, the use of short-acting insulin therapy or perhaps NPH insulin in the morning might be a better option for many individuals. Dietary modification plays an important role in limiting the extent of postprandial hyperglycemia. Use of continuous glucose monitoring (CGM) devices may also be very helpful for understanding glycemic excursions and how to adjust insulin. In individuals for whom glucocorticoid therapy is tapered down, it is important to adjust the dose of medications with potential to cause hypoglycemia, such as insulin/sulfonylurea therapy, as the degree of hyperglycemia may decrease with decreased dose of the glucocorticoid therapy.
2. Antipsychotic Therapy
Antipsychotic medications can be obesogenic; between 15% and 72% of people who take second-generation antipsychotics experience weight gain of 7% or more. Increases in weight are not the only factor contributing to an elevated risk of developing type 2 diabetes. Antipsychotics are thought to cause downregulation of intracellular insulin signaling, leading to insulin resistance. At the same time, there seems to be a direct effect on the pancreatic beta cells. Antagonism of the dopamine D2, serotonin 5-HT2C, and muscarinic M3 receptors impairs beta-cell response to changes in blood glucose. In addition to the pharmacologic effects, cell culture experiments have shown that antipsychotics increase apoptosis of beta cells. Increased weight and concomitant development of type 2 diabetes is seen particularly in agents that exhibit high muscarinic M3 and histamine H1 receptor blockade. The effect on glucose metabolism is seen the most with agents such as clozapine, olanzapine, and haloperidol and the least with agents such as ziprasidone.
Management tip: Given the ongoing change in the understanding of increases in weight and their association with the risk of developing type 2 diabetes, a metabolically safer approach involves starting with medications that have a lower propensity for weight gain, and the partial agonists/third-generation antipsychotics as a family presently have the best overall data.
3. Thiazide Diuretics
Thiazide diuretics are commonly used for the management of hypertension and are associated with metabolic complications including hypokalemia; higher cholesterol, triglycerides, and other circulating lipids; and elevated glucose. It’s thought that the reduced potassium level occurring as a result of these medications might contribute to new-onset diabetes. The hypokalemia occurring from these medications is thought to lead to a decrease in insulin secretion and sensitivity, which is dose dependent. Studies show that the number needed to harm for chlorthalidone-induced diabetes is 29 over 1 year. There is believed to be no additional risk beyond 1 year.
Management tip: It’s important to monitor potassium levels for those initiated on thiazide diuretics. If hypokalemia occurs, it would be pertinent to correct the hypokalemia with potassium supplements to mitigate the risk for new-onset diabetes.
4. Statin Therapy
Statin therapy is thought to be associated with decreased insulin sensitivity and impairment in insulin secretion. The overall incidence of diabetes is pegged to be between 9% and 12% on statin therapy on the basis of meta-analysis studies, and higher on the basis of population-based studies. Overall, the estimated number needed to harm is: 1 out of every 255 patients on statin therapy for 4 years may develop new-onset diabetes. Compare this with the extremely strong evidence for number needed to treat being 39 for 5 years with statin therapy in patients with preexisting heart disease to prevent one occurrence of a nonfatal myocardial infarction.
Management tip: Although statins are associated with a small incident increase in the risk of developing diabetes, the potential benefits of using statin therapy for both primary and secondary prevention of cardiovascular disease significantly outweigh any of the potential risks associated with hyperglycemia. This is an important discussion to have with patients who are reluctant to use statin therapy because of the potential risk for new-onset diabetes as a side effect.
5. Beta-Blockers
Beta-blockers are another commonly used group of medications for managing hypertension, heart failure, coronary artery disease, and arrhythmia. Nonvasodilating beta-blockers such as metoprolol and atenolol are more likely to be associated with increases in A1c, mean plasma glucose, body weight, and triglycerides compared with vasodilating beta-blockers such as carvedilol, nebivolol, and labetalol (Bakris GL et al; Giugliano D et al). Similarly, studies have also shown that atenolol and metoprolol are associated with increased odds of hypoglycemia compared with carvedilol. People on beta-blockers may have masking of some of the symptoms of hypoglycemia, such as tremor, irritability, and palpitations, while other symptoms such as diaphoresis may remain unaffected on beta-blockers.
Management tip: Education on recognizing and managing hypoglycemia would be important when starting patients on beta-blockers if they are on preexisting insulin/sulfonylurea therapy. Use of CGM devices may be helpful if there is a high risk for hypoglycemia, especially as symptoms of hypoglycemia are often masked.
Honorable Mention
Several other medications — including antiretroviral therapy, tyrosine kinase inhibitors, mechanistic target of rapamycin (mTOR) inhibitors, immunosuppressants, and interferon alpha — are associated with worsening glycemic control and new-onset diabetes. Consider these agents’ effects on blood glucose, especially in people with an elevated risk of developing diabetes or those with preexisting diabetes, when prescribing.
A special mention should also be made of androgen deprivation therapy. These include treatment options like goserelin and leuprolide, which are gonadotropin-releasing hormone (GnRH) agonist therapies and are commonly used for prostate cancer management. Depending on the patient, these agents may be used for prolonged duration. Androgen deprivation therapy, by definition, decreases testosterone levels in men, thereby leading to worsening insulin resistance. Increase in fat mass and concomitant muscle wasting have been associated with the use of these medications; these, in turn, lead to peripheral insulin resistance. Nearly 1 out of every 5 men treated with long-term androgen deprivation therapy may be prone to developing worsening of A1c by 1% or more.
Management tip: Men on androgen deprivation therapy should be encouraged to participate in regular physical activity to reduce the burden of insulin resistance and to promote cardiovascular health.
Drug-induced diabetes is potentially reversible in many cases. Similarly, worsening of glycemic control due to medications in people with preexisting diabetes may also attenuate once the effect of the drug wears off. Blood glucose should be monitored on an ongoing basis so that diabetes medications can be adjusted. For some individuals, however, the worsening of glycemic status may be more chronic and may require long-term use of antihyperglycemic agents, especially if the benefits of continuation of the medication leading to hyperglycemia far exceed any potential risks.
Dr. Jain is Clinical Instructor, Department of Endocrinology, University of British Columbia; Endocrinologist, Fraser River Endocrinology, Vancouver, British Columbia, Canada. He disclosed ties with Abbott, Amgen, Boehringer Ingelheim, Dexcom, Eli Lilly, Janssen, Medtronic, Merck, and Novo Nordisk.
A version of this article appeared on Medscape.com.
It’s that time of the year, when social media is rife with many top 5 and top 10 lists. Let’s revisit some of the most commonly used medications known to increase glucose levels and look at some practical tips on overcoming these.
1. Glucocorticoids
Without a doubt, corticosteroids are at the top of the list when it comes to the potential for increasing blood glucose levels. High-dose glucocorticoid therapy is known to lead to new-onset diabetes (steroid-induced diabetes). Similarly, people with preexisting diabetes may notice significant worsening of glycemic control when they start on glucocorticoid therapy. The extent of glucose elevation depends on their glycemic status prior to initiation on steroids, the dose and duration of glucocorticoid therapy, and comorbid conditions, among other factors.
Management tip: For those with previously well-controlled diabetes or borderline diabetes, glucocorticoid-induced hyperglycemia may be managed by metformin with or without sulfonylurea therapy, especially if corticosteroid treatment is low-dose and for a shorter duration. However, for many individuals with preexisting poorly controlled diabetes or those initiated on high-dose corticosteroids, insulin therapy would perhaps be the treatment of choice. Glucocorticoid therapy generally leads to more pronounced postprandial hyperglycemia compared with fasting hyperglycemia; hence, the use of short-acting insulin therapy or perhaps NPH insulin in the morning might be a better option for many individuals. Dietary modification plays an important role in limiting the extent of postprandial hyperglycemia. Use of continuous glucose monitoring (CGM) devices may also be very helpful for understanding glycemic excursions and how to adjust insulin. In individuals for whom glucocorticoid therapy is tapered down, it is important to adjust the dose of medications with potential to cause hypoglycemia, such as insulin/sulfonylurea therapy, as the degree of hyperglycemia may decrease with decreased dose of the glucocorticoid therapy.
2. Antipsychotic Therapy
Antipsychotic medications can be obesogenic; between 15% and 72% of people who take second-generation antipsychotics experience weight gain of 7% or more. Increases in weight are not the only factor contributing to an elevated risk of developing type 2 diabetes. Antipsychotics are thought to cause downregulation of intracellular insulin signaling, leading to insulin resistance. At the same time, there seems to be a direct effect on the pancreatic beta cells. Antagonism of the dopamine D2, serotonin 5-HT2C, and muscarinic M3 receptors impairs beta-cell response to changes in blood glucose. In addition to the pharmacologic effects, cell culture experiments have shown that antipsychotics increase apoptosis of beta cells. Increased weight and concomitant development of type 2 diabetes is seen particularly in agents that exhibit high muscarinic M3 and histamine H1 receptor blockade. The effect on glucose metabolism is seen the most with agents such as clozapine, olanzapine, and haloperidol and the least with agents such as ziprasidone.
Management tip: Given the ongoing change in the understanding of increases in weight and their association with the risk of developing type 2 diabetes, a metabolically safer approach involves starting with medications that have a lower propensity for weight gain, and the partial agonists/third-generation antipsychotics as a family presently have the best overall data.
3. Thiazide Diuretics
Thiazide diuretics are commonly used for the management of hypertension and are associated with metabolic complications including hypokalemia; higher cholesterol, triglycerides, and other circulating lipids; and elevated glucose. It’s thought that the reduced potassium level occurring as a result of these medications might contribute to new-onset diabetes. The hypokalemia occurring from these medications is thought to lead to a decrease in insulin secretion and sensitivity, which is dose dependent. Studies show that the number needed to harm for chlorthalidone-induced diabetes is 29 over 1 year. There is believed to be no additional risk beyond 1 year.
Management tip: It’s important to monitor potassium levels for those initiated on thiazide diuretics. If hypokalemia occurs, it would be pertinent to correct the hypokalemia with potassium supplements to mitigate the risk for new-onset diabetes.
4. Statin Therapy
Statin therapy is thought to be associated with decreased insulin sensitivity and impairment in insulin secretion. The overall incidence of diabetes is pegged to be between 9% and 12% on statin therapy on the basis of meta-analysis studies, and higher on the basis of population-based studies. Overall, the estimated number needed to harm is: 1 out of every 255 patients on statin therapy for 4 years may develop new-onset diabetes. Compare this with the extremely strong evidence for number needed to treat being 39 for 5 years with statin therapy in patients with preexisting heart disease to prevent one occurrence of a nonfatal myocardial infarction.
Management tip: Although statins are associated with a small incident increase in the risk of developing diabetes, the potential benefits of using statin therapy for both primary and secondary prevention of cardiovascular disease significantly outweigh any of the potential risks associated with hyperglycemia. This is an important discussion to have with patients who are reluctant to use statin therapy because of the potential risk for new-onset diabetes as a side effect.
5. Beta-Blockers
Beta-blockers are another commonly used group of medications for managing hypertension, heart failure, coronary artery disease, and arrhythmia. Nonvasodilating beta-blockers such as metoprolol and atenolol are more likely to be associated with increases in A1c, mean plasma glucose, body weight, and triglycerides compared with vasodilating beta-blockers such as carvedilol, nebivolol, and labetalol (Bakris GL et al; Giugliano D et al). Similarly, studies have also shown that atenolol and metoprolol are associated with increased odds of hypoglycemia compared with carvedilol. People on beta-blockers may have masking of some of the symptoms of hypoglycemia, such as tremor, irritability, and palpitations, while other symptoms such as diaphoresis may remain unaffected on beta-blockers.
Management tip: Education on recognizing and managing hypoglycemia would be important when starting patients on beta-blockers if they are on preexisting insulin/sulfonylurea therapy. Use of CGM devices may be helpful if there is a high risk for hypoglycemia, especially as symptoms of hypoglycemia are often masked.
Honorable Mention
Several other medications — including antiretroviral therapy, tyrosine kinase inhibitors, mechanistic target of rapamycin (mTOR) inhibitors, immunosuppressants, and interferon alpha — are associated with worsening glycemic control and new-onset diabetes. Consider these agents’ effects on blood glucose, especially in people with an elevated risk of developing diabetes or those with preexisting diabetes, when prescribing.
A special mention should also be made of androgen deprivation therapy. These include treatment options like goserelin and leuprolide, which are gonadotropin-releasing hormone (GnRH) agonist therapies and are commonly used for prostate cancer management. Depending on the patient, these agents may be used for prolonged duration. Androgen deprivation therapy, by definition, decreases testosterone levels in men, thereby leading to worsening insulin resistance. Increase in fat mass and concomitant muscle wasting have been associated with the use of these medications; these, in turn, lead to peripheral insulin resistance. Nearly 1 out of every 5 men treated with long-term androgen deprivation therapy may be prone to developing worsening of A1c by 1% or more.
Management tip: Men on androgen deprivation therapy should be encouraged to participate in regular physical activity to reduce the burden of insulin resistance and to promote cardiovascular health.
Drug-induced diabetes is potentially reversible in many cases. Similarly, worsening of glycemic control due to medications in people with preexisting diabetes may also attenuate once the effect of the drug wears off. Blood glucose should be monitored on an ongoing basis so that diabetes medications can be adjusted. For some individuals, however, the worsening of glycemic status may be more chronic and may require long-term use of antihyperglycemic agents, especially if the benefits of continuation of the medication leading to hyperglycemia far exceed any potential risks.
Dr. Jain is Clinical Instructor, Department of Endocrinology, University of British Columbia; Endocrinologist, Fraser River Endocrinology, Vancouver, British Columbia, Canada. He disclosed ties with Abbott, Amgen, Boehringer Ingelheim, Dexcom, Eli Lilly, Janssen, Medtronic, Merck, and Novo Nordisk.
A version of this article appeared on Medscape.com.
It’s that time of the year, when social media is rife with many top 5 and top 10 lists. Let’s revisit some of the most commonly used medications known to increase glucose levels and look at some practical tips on overcoming these.
1. Glucocorticoids
Without a doubt, corticosteroids are at the top of the list when it comes to the potential for increasing blood glucose levels. High-dose glucocorticoid therapy is known to lead to new-onset diabetes (steroid-induced diabetes). Similarly, people with preexisting diabetes may notice significant worsening of glycemic control when they start on glucocorticoid therapy. The extent of glucose elevation depends on their glycemic status prior to initiation on steroids, the dose and duration of glucocorticoid therapy, and comorbid conditions, among other factors.
Management tip: For those with previously well-controlled diabetes or borderline diabetes, glucocorticoid-induced hyperglycemia may be managed by metformin with or without sulfonylurea therapy, especially if corticosteroid treatment is low-dose and for a shorter duration. However, for many individuals with preexisting poorly controlled diabetes or those initiated on high-dose corticosteroids, insulin therapy would perhaps be the treatment of choice. Glucocorticoid therapy generally leads to more pronounced postprandial hyperglycemia compared with fasting hyperglycemia; hence, the use of short-acting insulin therapy or perhaps NPH insulin in the morning might be a better option for many individuals. Dietary modification plays an important role in limiting the extent of postprandial hyperglycemia. Use of continuous glucose monitoring (CGM) devices may also be very helpful for understanding glycemic excursions and how to adjust insulin. In individuals for whom glucocorticoid therapy is tapered down, it is important to adjust the dose of medications with potential to cause hypoglycemia, such as insulin/sulfonylurea therapy, as the degree of hyperglycemia may decrease with decreased dose of the glucocorticoid therapy.
2. Antipsychotic Therapy
Antipsychotic medications can be obesogenic; between 15% and 72% of people who take second-generation antipsychotics experience weight gain of 7% or more. Increases in weight are not the only factor contributing to an elevated risk of developing type 2 diabetes. Antipsychotics are thought to cause downregulation of intracellular insulin signaling, leading to insulin resistance. At the same time, there seems to be a direct effect on the pancreatic beta cells. Antagonism of the dopamine D2, serotonin 5-HT2C, and muscarinic M3 receptors impairs beta-cell response to changes in blood glucose. In addition to the pharmacologic effects, cell culture experiments have shown that antipsychotics increase apoptosis of beta cells. Increased weight and concomitant development of type 2 diabetes is seen particularly in agents that exhibit high muscarinic M3 and histamine H1 receptor blockade. The effect on glucose metabolism is seen the most with agents such as clozapine, olanzapine, and haloperidol and the least with agents such as ziprasidone.
Management tip: Given the ongoing change in the understanding of increases in weight and their association with the risk of developing type 2 diabetes, a metabolically safer approach involves starting with medications that have a lower propensity for weight gain, and the partial agonists/third-generation antipsychotics as a family presently have the best overall data.
3. Thiazide Diuretics
Thiazide diuretics are commonly used for the management of hypertension and are associated with metabolic complications including hypokalemia; higher cholesterol, triglycerides, and other circulating lipids; and elevated glucose. It’s thought that the reduced potassium level occurring as a result of these medications might contribute to new-onset diabetes. The hypokalemia occurring from these medications is thought to lead to a decrease in insulin secretion and sensitivity, which is dose dependent. Studies show that the number needed to harm for chlorthalidone-induced diabetes is 29 over 1 year. There is believed to be no additional risk beyond 1 year.
Management tip: It’s important to monitor potassium levels for those initiated on thiazide diuretics. If hypokalemia occurs, it would be pertinent to correct the hypokalemia with potassium supplements to mitigate the risk for new-onset diabetes.
4. Statin Therapy
Statin therapy is thought to be associated with decreased insulin sensitivity and impairment in insulin secretion. The overall incidence of diabetes is pegged to be between 9% and 12% on statin therapy on the basis of meta-analysis studies, and higher on the basis of population-based studies. Overall, the estimated number needed to harm is: 1 out of every 255 patients on statin therapy for 4 years may develop new-onset diabetes. Compare this with the extremely strong evidence for number needed to treat being 39 for 5 years with statin therapy in patients with preexisting heart disease to prevent one occurrence of a nonfatal myocardial infarction.
Management tip: Although statins are associated with a small incident increase in the risk of developing diabetes, the potential benefits of using statin therapy for both primary and secondary prevention of cardiovascular disease significantly outweigh any of the potential risks associated with hyperglycemia. This is an important discussion to have with patients who are reluctant to use statin therapy because of the potential risk for new-onset diabetes as a side effect.
5. Beta-Blockers
Beta-blockers are another commonly used group of medications for managing hypertension, heart failure, coronary artery disease, and arrhythmia. Nonvasodilating beta-blockers such as metoprolol and atenolol are more likely to be associated with increases in A1c, mean plasma glucose, body weight, and triglycerides compared with vasodilating beta-blockers such as carvedilol, nebivolol, and labetalol (Bakris GL et al; Giugliano D et al). Similarly, studies have also shown that atenolol and metoprolol are associated with increased odds of hypoglycemia compared with carvedilol. People on beta-blockers may have masking of some of the symptoms of hypoglycemia, such as tremor, irritability, and palpitations, while other symptoms such as diaphoresis may remain unaffected on beta-blockers.
Management tip: Education on recognizing and managing hypoglycemia would be important when starting patients on beta-blockers if they are on preexisting insulin/sulfonylurea therapy. Use of CGM devices may be helpful if there is a high risk for hypoglycemia, especially as symptoms of hypoglycemia are often masked.
Honorable Mention
Several other medications — including antiretroviral therapy, tyrosine kinase inhibitors, mechanistic target of rapamycin (mTOR) inhibitors, immunosuppressants, and interferon alpha — are associated with worsening glycemic control and new-onset diabetes. Consider these agents’ effects on blood glucose, especially in people with an elevated risk of developing diabetes or those with preexisting diabetes, when prescribing.
A special mention should also be made of androgen deprivation therapy. These include treatment options like goserelin and leuprolide, which are gonadotropin-releasing hormone (GnRH) agonist therapies and are commonly used for prostate cancer management. Depending on the patient, these agents may be used for prolonged duration. Androgen deprivation therapy, by definition, decreases testosterone levels in men, thereby leading to worsening insulin resistance. Increase in fat mass and concomitant muscle wasting have been associated with the use of these medications; these, in turn, lead to peripheral insulin resistance. Nearly 1 out of every 5 men treated with long-term androgen deprivation therapy may be prone to developing worsening of A1c by 1% or more.
Management tip: Men on androgen deprivation therapy should be encouraged to participate in regular physical activity to reduce the burden of insulin resistance and to promote cardiovascular health.
Drug-induced diabetes is potentially reversible in many cases. Similarly, worsening of glycemic control due to medications in people with preexisting diabetes may also attenuate once the effect of the drug wears off. Blood glucose should be monitored on an ongoing basis so that diabetes medications can be adjusted. For some individuals, however, the worsening of glycemic status may be more chronic and may require long-term use of antihyperglycemic agents, especially if the benefits of continuation of the medication leading to hyperglycemia far exceed any potential risks.
Dr. Jain is Clinical Instructor, Department of Endocrinology, University of British Columbia; Endocrinologist, Fraser River Endocrinology, Vancouver, British Columbia, Canada. He disclosed ties with Abbott, Amgen, Boehringer Ingelheim, Dexcom, Eli Lilly, Janssen, Medtronic, Merck, and Novo Nordisk.
A version of this article appeared on Medscape.com.
Migraine Associated With Increased Risk for IBD
TOPLINE:
Migraine is associated with a significantly increased risk of developing inflammatory bowel disease (IBD), including both Crohn’s disease (CD) and ulcerative colitis (UC), a new nationwide, population-based cohort study showed.
METHODOLOGY:
- Investigators analyzed data from South Korea’s National Health Insurance Service (NHIS) database, which houses data for the nationwide obligatory health system for South Korean citizens.
- Individuals aged ≥ 20 years who had at least one national health screening in 2009 were enrolled in the study and followed until December 2019.
- Investigators searched the data for International Classification of Diseases (10th Revision) codes corresponding to migraine and IBD. IBD diagnoses were also based on clinical manifestation, endoscopic findings, and pathologic findings.
TAKEAWAY:
- More than 10 million people were enrolled in the study (55% male; mean age, 47 years), and of these, 2.8% were diagnosed with migraine during the study period.
- During a median follow-up of 10 years, the incidence of IBD was significantly higher in patients with migraine (adjusted hazard ratio [aHR], 1.31; P < .001), CD (aHR, 1.58; P < .001) and UC (aHR, 1.26; P < .001) than in those without migraine.
- in men vs women (aHR, 1.43 vs 1.12; P = .042).
- Investigators could only speculate about the mechanisms underlying the association between migraine and IBD but suggest pathological processes underlying both migraine and IBD, including proinflammatory cytokines and tumor necrosis factor alpha, may be involved.
IN PRACTICE:
“Clinicians should be aware of the potential risk of IBD in patients diagnosed with migraine especially in men for the development of UC and in migraineurs with a long disease duration for a further risk of CD,” the authors wrote.
SOURCE:
Hyunjung Lee, MD, of Seoul National University College of Medicine, Seoul, South Korea, led the study, which was published online on January 12, 2024, in Scientific Reports.
LIMITATIONS:
Disease severity of migraine and IBD was not available. In addition, certain medications taken to relieve migraine, such as nonsteroidal anti-inflammatory drugs like ibuprofen, could cause intestinal inflammation, but there was no medication information available.
DISCLOSURES:
There was no information about study funding nor disclosures from study authors.
A version of this article appeared on Medscape.com.
TOPLINE:
Migraine is associated with a significantly increased risk of developing inflammatory bowel disease (IBD), including both Crohn’s disease (CD) and ulcerative colitis (UC), a new nationwide, population-based cohort study showed.
METHODOLOGY:
- Investigators analyzed data from South Korea’s National Health Insurance Service (NHIS) database, which houses data for the nationwide obligatory health system for South Korean citizens.
- Individuals aged ≥ 20 years who had at least one national health screening in 2009 were enrolled in the study and followed until December 2019.
- Investigators searched the data for International Classification of Diseases (10th Revision) codes corresponding to migraine and IBD. IBD diagnoses were also based on clinical manifestation, endoscopic findings, and pathologic findings.
TAKEAWAY:
- More than 10 million people were enrolled in the study (55% male; mean age, 47 years), and of these, 2.8% were diagnosed with migraine during the study period.
- During a median follow-up of 10 years, the incidence of IBD was significantly higher in patients with migraine (adjusted hazard ratio [aHR], 1.31; P < .001), CD (aHR, 1.58; P < .001) and UC (aHR, 1.26; P < .001) than in those without migraine.
- in men vs women (aHR, 1.43 vs 1.12; P = .042).
- Investigators could only speculate about the mechanisms underlying the association between migraine and IBD but suggest pathological processes underlying both migraine and IBD, including proinflammatory cytokines and tumor necrosis factor alpha, may be involved.
IN PRACTICE:
“Clinicians should be aware of the potential risk of IBD in patients diagnosed with migraine especially in men for the development of UC and in migraineurs with a long disease duration for a further risk of CD,” the authors wrote.
SOURCE:
Hyunjung Lee, MD, of Seoul National University College of Medicine, Seoul, South Korea, led the study, which was published online on January 12, 2024, in Scientific Reports.
LIMITATIONS:
Disease severity of migraine and IBD was not available. In addition, certain medications taken to relieve migraine, such as nonsteroidal anti-inflammatory drugs like ibuprofen, could cause intestinal inflammation, but there was no medication information available.
DISCLOSURES:
There was no information about study funding nor disclosures from study authors.
A version of this article appeared on Medscape.com.
TOPLINE:
Migraine is associated with a significantly increased risk of developing inflammatory bowel disease (IBD), including both Crohn’s disease (CD) and ulcerative colitis (UC), a new nationwide, population-based cohort study showed.
METHODOLOGY:
- Investigators analyzed data from South Korea’s National Health Insurance Service (NHIS) database, which houses data for the nationwide obligatory health system for South Korean citizens.
- Individuals aged ≥ 20 years who had at least one national health screening in 2009 were enrolled in the study and followed until December 2019.
- Investigators searched the data for International Classification of Diseases (10th Revision) codes corresponding to migraine and IBD. IBD diagnoses were also based on clinical manifestation, endoscopic findings, and pathologic findings.
TAKEAWAY:
- More than 10 million people were enrolled in the study (55% male; mean age, 47 years), and of these, 2.8% were diagnosed with migraine during the study period.
- During a median follow-up of 10 years, the incidence of IBD was significantly higher in patients with migraine (adjusted hazard ratio [aHR], 1.31; P < .001), CD (aHR, 1.58; P < .001) and UC (aHR, 1.26; P < .001) than in those without migraine.
- in men vs women (aHR, 1.43 vs 1.12; P = .042).
- Investigators could only speculate about the mechanisms underlying the association between migraine and IBD but suggest pathological processes underlying both migraine and IBD, including proinflammatory cytokines and tumor necrosis factor alpha, may be involved.
IN PRACTICE:
“Clinicians should be aware of the potential risk of IBD in patients diagnosed with migraine especially in men for the development of UC and in migraineurs with a long disease duration for a further risk of CD,” the authors wrote.
SOURCE:
Hyunjung Lee, MD, of Seoul National University College of Medicine, Seoul, South Korea, led the study, which was published online on January 12, 2024, in Scientific Reports.
LIMITATIONS:
Disease severity of migraine and IBD was not available. In addition, certain medications taken to relieve migraine, such as nonsteroidal anti-inflammatory drugs like ibuprofen, could cause intestinal inflammation, but there was no medication information available.
DISCLOSURES:
There was no information about study funding nor disclosures from study authors.
A version of this article appeared on Medscape.com.
Commentary: PsA in Women, February 2024
Another study investigated the persistence of targeted therapies for PsA in women compared with men. In a nationwide cohort study using administrative information from French health insurance, the study looked at 14,778 patients (57% women) with PsA who were new users of targeted therapies. The study showed that women had 20%-40% lower treatment persistence rates than men for tumour necrosis factor (TNF) inhibitors (adjusted hazard ratio [aHR] 1.4; 99% CI 1.3-1.5) and interleukin (IL)-17 inhibitors (aHR 1.2; 99% CI 1.1-1.3). However, the treatment persistence between both sexes was comparable for IL-12/23 inhibitor (aHR 1.1; 99% CI 0.9-1.3), IL-23 inhibitor (aHR 1.1; 99% CI 0.7-1.5), and Janus kinase (JAK) inhibitor (aHR 1.2; 99% CI 0.9-1.6) therapies. The paradigm that women have lower treatment persistence is based on studies done primarily in patients treated with TNF inhibitors. This study and a few other recent studies challenge this paradigm by indicating that other targeted therapies, especially JAK inhibitors, may not have lower persistence in women. Sex should be taken into consideration while choosing and counseling women about PsA therapies.
There are few studies on exercise and its impact on PsA. Functional training (FT) and resistance training (RT) may improve functional capacity and quality of life of patients with PsA. The safety of exercise is also not known, given that (micro)trauma is a risk factor for PsA. To evaluate this, Silva and colleagues conducted a 12-week, single-blind trial including 41 patients with PsA who were randomly assigned to undergo FT with elastic bands or RT with weight machines. They demonstrated that FT and RT led to similar improvements in functional capacity measured by the Bath Ankylosing Spondylitis Functional Index (P = .919), functional status measured by the Health Assessment Questionnaire for Spondyloarthritis (P = .932), disease activity measured by the Bath Ankylosing Spondylitis Disease Activity Index (P = .700), and muscle strength. No adverse events occurred in either group. Thus, FT and RT improved functional capacity, functional status, disease activity, and muscle strength to a comparable extent in patients with PsA, with no adverse events. Both modalities may be recommended for PsA patients.
Finally, a cross-sectional study that included 503 patients with PsA, of whom 160 patients underwent treatment escalation, evaluated whether the patient-reported outcome (PsA Impact of Disease questionnaire [PsAID-12]) affected treatment decisions by the treating rheumatologist. Coyle and colleagues demonstrated that although PsAID-12 scores were higher in patients who did vs did not have a treatment escalation, physicians relied more on their assessment of disease activity rather than the PsAID-12 scores when making treatment-related decisions. Of note, physicians also reported that PsAID-12 scores influenced treatment reduction decisions.
Another study investigated the persistence of targeted therapies for PsA in women compared with men. In a nationwide cohort study using administrative information from French health insurance, the study looked at 14,778 patients (57% women) with PsA who were new users of targeted therapies. The study showed that women had 20%-40% lower treatment persistence rates than men for tumour necrosis factor (TNF) inhibitors (adjusted hazard ratio [aHR] 1.4; 99% CI 1.3-1.5) and interleukin (IL)-17 inhibitors (aHR 1.2; 99% CI 1.1-1.3). However, the treatment persistence between both sexes was comparable for IL-12/23 inhibitor (aHR 1.1; 99% CI 0.9-1.3), IL-23 inhibitor (aHR 1.1; 99% CI 0.7-1.5), and Janus kinase (JAK) inhibitor (aHR 1.2; 99% CI 0.9-1.6) therapies. The paradigm that women have lower treatment persistence is based on studies done primarily in patients treated with TNF inhibitors. This study and a few other recent studies challenge this paradigm by indicating that other targeted therapies, especially JAK inhibitors, may not have lower persistence in women. Sex should be taken into consideration while choosing and counseling women about PsA therapies.
There are few studies on exercise and its impact on PsA. Functional training (FT) and resistance training (RT) may improve functional capacity and quality of life of patients with PsA. The safety of exercise is also not known, given that (micro)trauma is a risk factor for PsA. To evaluate this, Silva and colleagues conducted a 12-week, single-blind trial including 41 patients with PsA who were randomly assigned to undergo FT with elastic bands or RT with weight machines. They demonstrated that FT and RT led to similar improvements in functional capacity measured by the Bath Ankylosing Spondylitis Functional Index (P = .919), functional status measured by the Health Assessment Questionnaire for Spondyloarthritis (P = .932), disease activity measured by the Bath Ankylosing Spondylitis Disease Activity Index (P = .700), and muscle strength. No adverse events occurred in either group. Thus, FT and RT improved functional capacity, functional status, disease activity, and muscle strength to a comparable extent in patients with PsA, with no adverse events. Both modalities may be recommended for PsA patients.
Finally, a cross-sectional study that included 503 patients with PsA, of whom 160 patients underwent treatment escalation, evaluated whether the patient-reported outcome (PsA Impact of Disease questionnaire [PsAID-12]) affected treatment decisions by the treating rheumatologist. Coyle and colleagues demonstrated that although PsAID-12 scores were higher in patients who did vs did not have a treatment escalation, physicians relied more on their assessment of disease activity rather than the PsAID-12 scores when making treatment-related decisions. Of note, physicians also reported that PsAID-12 scores influenced treatment reduction decisions.
Another study investigated the persistence of targeted therapies for PsA in women compared with men. In a nationwide cohort study using administrative information from French health insurance, the study looked at 14,778 patients (57% women) with PsA who were new users of targeted therapies. The study showed that women had 20%-40% lower treatment persistence rates than men for tumour necrosis factor (TNF) inhibitors (adjusted hazard ratio [aHR] 1.4; 99% CI 1.3-1.5) and interleukin (IL)-17 inhibitors (aHR 1.2; 99% CI 1.1-1.3). However, the treatment persistence between both sexes was comparable for IL-12/23 inhibitor (aHR 1.1; 99% CI 0.9-1.3), IL-23 inhibitor (aHR 1.1; 99% CI 0.7-1.5), and Janus kinase (JAK) inhibitor (aHR 1.2; 99% CI 0.9-1.6) therapies. The paradigm that women have lower treatment persistence is based on studies done primarily in patients treated with TNF inhibitors. This study and a few other recent studies challenge this paradigm by indicating that other targeted therapies, especially JAK inhibitors, may not have lower persistence in women. Sex should be taken into consideration while choosing and counseling women about PsA therapies.
There are few studies on exercise and its impact on PsA. Functional training (FT) and resistance training (RT) may improve functional capacity and quality of life of patients with PsA. The safety of exercise is also not known, given that (micro)trauma is a risk factor for PsA. To evaluate this, Silva and colleagues conducted a 12-week, single-blind trial including 41 patients with PsA who were randomly assigned to undergo FT with elastic bands or RT with weight machines. They demonstrated that FT and RT led to similar improvements in functional capacity measured by the Bath Ankylosing Spondylitis Functional Index (P = .919), functional status measured by the Health Assessment Questionnaire for Spondyloarthritis (P = .932), disease activity measured by the Bath Ankylosing Spondylitis Disease Activity Index (P = .700), and muscle strength. No adverse events occurred in either group. Thus, FT and RT improved functional capacity, functional status, disease activity, and muscle strength to a comparable extent in patients with PsA, with no adverse events. Both modalities may be recommended for PsA patients.
Finally, a cross-sectional study that included 503 patients with PsA, of whom 160 patients underwent treatment escalation, evaluated whether the patient-reported outcome (PsA Impact of Disease questionnaire [PsAID-12]) affected treatment decisions by the treating rheumatologist. Coyle and colleagues demonstrated that although PsAID-12 scores were higher in patients who did vs did not have a treatment escalation, physicians relied more on their assessment of disease activity rather than the PsAID-12 scores when making treatment-related decisions. Of note, physicians also reported that PsAID-12 scores influenced treatment reduction decisions.
Respiratory Virus Surge: Diagnosing COVID-19 vs RSV, Flu
Amid the current wave of winter respiratory virus cases, influenza (types A and B) leads the way with the highest number of emergency room visits, followed closely by COVID-19, thanks to the JN.1 variant, and respiratory syncytial virus (RSV). With various similarities and differences in disease presentations, how challenging is it for physician’s to distinguish between, diagnose, and treat COVID-19 vs RSV and influenza?
While these three respiratory viruses often have similar presentations, you may often find that patients with COVID-19 experience more fever, dry cough, and labored breathing, according to Cyrus Munguti, MD, assistant professor of medicine at KU Medical Center and hospitalist at Wesley Medical Center, Wichita, Kansas.
“COVID-19 patients tend to have trouble breathing because the alveoli are affected and get inflammation and fluid accumulating in the lungs, and they end up having little to no oxygen,” said Dr. Munguti. “When we check their vital signs, patients with COVID tend to have hypoxemia [meaning saturations are less than 88% or 90% depending on the guidelines you follow].”
Patients with RSV and influenza tend to have more upper respiratory symptoms, like runny nose, sternutation — which later can progress to a cough in the upper airways, Dr. Munguti said. Unlike with COVID-19, patients with RSV and influenza — generally until they are very sick — often do not experience hypoxemia.
Inflammation in the airways can form as a result of all three viruses. Furthermore, bacteria that live in these airways could lead to a secondary bacterial infection in the upper respiratory and lower respiratory tracts — which could then cause pneumonia, Dr. Munguti said.
Another note: , according to Panagis Galiatsatos, MD, pulmonologist and associate professor at Johns Hopkins Medicine. “The Alpha through Delta variants really were a lot more lung tissue invading,” Dr. Galiatsatos said. “With the COVID-19 Omicron family — its capabilities are similar to what flu and RSV have done over the years. It’s more airway-invading.”
It’s critical to understand that diagnosing these diseases based on symptoms alone can be quite fickle, according to Dr. Galiatsatos. Objective tests, either at home or in a laboratory, are preferred. This is largely because disease presentation can depend on the host factor that the virus enters into, said Dr. Galiatsatos. For example, virus symptoms may look different for a patient with asthma and for someone with heart disease.
With children being among the most vulnerable for severe respiratory illness, testing and treatment are paramount and can be quite accurate in seasons where respiratory viruses thrive, according to Stan Spinner, MD, chief medical officer at Texas Children’s Pediatrics and Urgent Care. “When individuals are tested for either of these conditions when the prevalence in the community is low, we tend to see false positive results.”
Texas Children’s Pediatrics and Urgent Care’s 12 sites offer COVID-19 and influenza antigen tests that have results ready in around 10 minutes. RSV testing, on the other hand, is limited to around half of the Texas Children’s Pediatrics and none of the urgent care locations, as the test can only be administered through a nasal swab conducted by a physician. As there is no specific treatment or therapy for RSV, the benefits of RSV testing can actually be quite low — often leading to frustrated parents regarding next steps after diagnosis.
“There are a number of respiratory viruses that may present with similar symptoms as RSV, and some of these viruses may even lead to much of the same adverse outcomes as the RSV virus,” Dr. Galiatsatos said. “Consequently, our physicians need to help parents understand this and give them guidance as to when to seek medical attention for worsening symptoms.”
There are two new RSV immunizations to treat certain demographics of patients, Dr. Spinner added. One is an RSV vaccine for infants under 8 months old, though there is limited supply. There is also an RSV vaccine available for pregnant women (between 32 and 36 weeks gestation) that has proved to be effective in fending off RSV infections in newborns up to 6 months old.
Physicians should remain diligent in stressing to patients that vaccinations against COVID-19 and influenza play a key role in keeping their families safe during seasons of staggering respiratory infections.
“These vaccines are extremely safe, and while they may not always prevent infection, these vaccines are extremely effective in preventing more serious consequences, such as hospitalization or death,” Dr. Galiatsatos said.
A version of this article appeared on Medscape.com.
Amid the current wave of winter respiratory virus cases, influenza (types A and B) leads the way with the highest number of emergency room visits, followed closely by COVID-19, thanks to the JN.1 variant, and respiratory syncytial virus (RSV). With various similarities and differences in disease presentations, how challenging is it for physician’s to distinguish between, diagnose, and treat COVID-19 vs RSV and influenza?
While these three respiratory viruses often have similar presentations, you may often find that patients with COVID-19 experience more fever, dry cough, and labored breathing, according to Cyrus Munguti, MD, assistant professor of medicine at KU Medical Center and hospitalist at Wesley Medical Center, Wichita, Kansas.
“COVID-19 patients tend to have trouble breathing because the alveoli are affected and get inflammation and fluid accumulating in the lungs, and they end up having little to no oxygen,” said Dr. Munguti. “When we check their vital signs, patients with COVID tend to have hypoxemia [meaning saturations are less than 88% or 90% depending on the guidelines you follow].”
Patients with RSV and influenza tend to have more upper respiratory symptoms, like runny nose, sternutation — which later can progress to a cough in the upper airways, Dr. Munguti said. Unlike with COVID-19, patients with RSV and influenza — generally until they are very sick — often do not experience hypoxemia.
Inflammation in the airways can form as a result of all three viruses. Furthermore, bacteria that live in these airways could lead to a secondary bacterial infection in the upper respiratory and lower respiratory tracts — which could then cause pneumonia, Dr. Munguti said.
Another note: , according to Panagis Galiatsatos, MD, pulmonologist and associate professor at Johns Hopkins Medicine. “The Alpha through Delta variants really were a lot more lung tissue invading,” Dr. Galiatsatos said. “With the COVID-19 Omicron family — its capabilities are similar to what flu and RSV have done over the years. It’s more airway-invading.”
It’s critical to understand that diagnosing these diseases based on symptoms alone can be quite fickle, according to Dr. Galiatsatos. Objective tests, either at home or in a laboratory, are preferred. This is largely because disease presentation can depend on the host factor that the virus enters into, said Dr. Galiatsatos. For example, virus symptoms may look different for a patient with asthma and for someone with heart disease.
With children being among the most vulnerable for severe respiratory illness, testing and treatment are paramount and can be quite accurate in seasons where respiratory viruses thrive, according to Stan Spinner, MD, chief medical officer at Texas Children’s Pediatrics and Urgent Care. “When individuals are tested for either of these conditions when the prevalence in the community is low, we tend to see false positive results.”
Texas Children’s Pediatrics and Urgent Care’s 12 sites offer COVID-19 and influenza antigen tests that have results ready in around 10 minutes. RSV testing, on the other hand, is limited to around half of the Texas Children’s Pediatrics and none of the urgent care locations, as the test can only be administered through a nasal swab conducted by a physician. As there is no specific treatment or therapy for RSV, the benefits of RSV testing can actually be quite low — often leading to frustrated parents regarding next steps after diagnosis.
“There are a number of respiratory viruses that may present with similar symptoms as RSV, and some of these viruses may even lead to much of the same adverse outcomes as the RSV virus,” Dr. Galiatsatos said. “Consequently, our physicians need to help parents understand this and give them guidance as to when to seek medical attention for worsening symptoms.”
There are two new RSV immunizations to treat certain demographics of patients, Dr. Spinner added. One is an RSV vaccine for infants under 8 months old, though there is limited supply. There is also an RSV vaccine available for pregnant women (between 32 and 36 weeks gestation) that has proved to be effective in fending off RSV infections in newborns up to 6 months old.
Physicians should remain diligent in stressing to patients that vaccinations against COVID-19 and influenza play a key role in keeping their families safe during seasons of staggering respiratory infections.
“These vaccines are extremely safe, and while they may not always prevent infection, these vaccines are extremely effective in preventing more serious consequences, such as hospitalization or death,” Dr. Galiatsatos said.
A version of this article appeared on Medscape.com.
Amid the current wave of winter respiratory virus cases, influenza (types A and B) leads the way with the highest number of emergency room visits, followed closely by COVID-19, thanks to the JN.1 variant, and respiratory syncytial virus (RSV). With various similarities and differences in disease presentations, how challenging is it for physician’s to distinguish between, diagnose, and treat COVID-19 vs RSV and influenza?
While these three respiratory viruses often have similar presentations, you may often find that patients with COVID-19 experience more fever, dry cough, and labored breathing, according to Cyrus Munguti, MD, assistant professor of medicine at KU Medical Center and hospitalist at Wesley Medical Center, Wichita, Kansas.
“COVID-19 patients tend to have trouble breathing because the alveoli are affected and get inflammation and fluid accumulating in the lungs, and they end up having little to no oxygen,” said Dr. Munguti. “When we check their vital signs, patients with COVID tend to have hypoxemia [meaning saturations are less than 88% or 90% depending on the guidelines you follow].”
Patients with RSV and influenza tend to have more upper respiratory symptoms, like runny nose, sternutation — which later can progress to a cough in the upper airways, Dr. Munguti said. Unlike with COVID-19, patients with RSV and influenza — generally until they are very sick — often do not experience hypoxemia.
Inflammation in the airways can form as a result of all three viruses. Furthermore, bacteria that live in these airways could lead to a secondary bacterial infection in the upper respiratory and lower respiratory tracts — which could then cause pneumonia, Dr. Munguti said.
Another note: , according to Panagis Galiatsatos, MD, pulmonologist and associate professor at Johns Hopkins Medicine. “The Alpha through Delta variants really were a lot more lung tissue invading,” Dr. Galiatsatos said. “With the COVID-19 Omicron family — its capabilities are similar to what flu and RSV have done over the years. It’s more airway-invading.”
It’s critical to understand that diagnosing these diseases based on symptoms alone can be quite fickle, according to Dr. Galiatsatos. Objective tests, either at home or in a laboratory, are preferred. This is largely because disease presentation can depend on the host factor that the virus enters into, said Dr. Galiatsatos. For example, virus symptoms may look different for a patient with asthma and for someone with heart disease.
With children being among the most vulnerable for severe respiratory illness, testing and treatment are paramount and can be quite accurate in seasons where respiratory viruses thrive, according to Stan Spinner, MD, chief medical officer at Texas Children’s Pediatrics and Urgent Care. “When individuals are tested for either of these conditions when the prevalence in the community is low, we tend to see false positive results.”
Texas Children’s Pediatrics and Urgent Care’s 12 sites offer COVID-19 and influenza antigen tests that have results ready in around 10 minutes. RSV testing, on the other hand, is limited to around half of the Texas Children’s Pediatrics and none of the urgent care locations, as the test can only be administered through a nasal swab conducted by a physician. As there is no specific treatment or therapy for RSV, the benefits of RSV testing can actually be quite low — often leading to frustrated parents regarding next steps after diagnosis.
“There are a number of respiratory viruses that may present with similar symptoms as RSV, and some of these viruses may even lead to much of the same adverse outcomes as the RSV virus,” Dr. Galiatsatos said. “Consequently, our physicians need to help parents understand this and give them guidance as to when to seek medical attention for worsening symptoms.”
There are two new RSV immunizations to treat certain demographics of patients, Dr. Spinner added. One is an RSV vaccine for infants under 8 months old, though there is limited supply. There is also an RSV vaccine available for pregnant women (between 32 and 36 weeks gestation) that has proved to be effective in fending off RSV infections in newborns up to 6 months old.
Physicians should remain diligent in stressing to patients that vaccinations against COVID-19 and influenza play a key role in keeping their families safe during seasons of staggering respiratory infections.
“These vaccines are extremely safe, and while they may not always prevent infection, these vaccines are extremely effective in preventing more serious consequences, such as hospitalization or death,” Dr. Galiatsatos said.
A version of this article appeared on Medscape.com.
OCD Tied to a Twofold Increased Risk for All-Cause Mortality
TOPLINE:
Obsessive-compulsive disorder (OCD) is linked to a twofold increased risk for all-cause mortality and a heightened risk for death from both natural and unnatural causes, a new study showed.
METHODOLOGY:
- Investigators studied a population-based cohort (58% female) of 61,378 people with OCD and 613,780 unaffected individuals from several Swedish population registers and a sibling cohort of 34,085 people with OCD (58% female) and 47,874 unaffected full siblings (48% female).
- The median 8.1-year follow-up and median age at first diagnosis of OCD were 27 years.
- The researchers used Cox proportional hazard models, adjusting for birth year, sex, county, country of birth (Sweden vs abroad), and sociodemographic variables.
TAKEAWAY:
- (adjusted hazard ratio [aHR], 1.82; 95% CI, 1.76-1.89), an almost threefold higher risk for mortality due to unnatural causes (aHR, 3.30; 95% CI, 3.05-3.57), and a higher risk for mortality due to natural causes (aHR, 1.31; 95% CI, 1.24-1.37).
- Of all the unnatural causes of death, suicide was most common (hazard ratio [HR], 4.90; 95% CI, 4.40-5.46), followed by accidents (HR, 1.92; 95% CI, 1.68-2.19).
- Similar results were found in the sibling comparison, where the HR of all-cause mortality was 1.85 (95% CI, 1.67-2.03), death from natural causes was 1.51 (95% CI, 1.35-1.68), and death from unnatural causes was 3.10 (95% CI, 2.52-3.80).
- Natural causes of death that were higher in the OCD vs non-OCD cohort included endocrine, nutritional, and metabolic diseases; mental and behavioral disorders; and diseases of the nervous, circulatory, respiratory, digestive, and genitourinary systems.
IN PRACTICE:
“Better surveillance, prevention, and early intervention strategies should be implemented to reduce the risk of fatal outcomes in people with OCD,” the authors wrote.
SOURCE:
Lorena Fernández de la Cruz, PhD, of Karolinska Institutet, Solna, Sweden, led the study, which was published online on January 17 in the British Medical Journal.
LIMITATIONS:
The study does not establish causality. Registry data used by the investigators only included diagnoses made in specialist care and may not have included diagnoses made in other settings. It is also unclear whether the findings, derived from a Swedish population, can be generalized to other populations, health systems, and medical practices.
DISCLOSURES:
The study was funded by the Swedish Council for Health, Working Life and Welfare, Region Stockholm, the Swedish Society of Medicine, and Karolinska Institutet. Dr. de la Cruz received royalties for contributing articles to UpToDate and Wolters Kluwer Health and for editorial work from Elsevier outside the submitted work. See the paper for disclosures of the other authors.
A version of this article appeared on Medscape.com.
TOPLINE:
Obsessive-compulsive disorder (OCD) is linked to a twofold increased risk for all-cause mortality and a heightened risk for death from both natural and unnatural causes, a new study showed.
METHODOLOGY:
- Investigators studied a population-based cohort (58% female) of 61,378 people with OCD and 613,780 unaffected individuals from several Swedish population registers and a sibling cohort of 34,085 people with OCD (58% female) and 47,874 unaffected full siblings (48% female).
- The median 8.1-year follow-up and median age at first diagnosis of OCD were 27 years.
- The researchers used Cox proportional hazard models, adjusting for birth year, sex, county, country of birth (Sweden vs abroad), and sociodemographic variables.
TAKEAWAY:
- (adjusted hazard ratio [aHR], 1.82; 95% CI, 1.76-1.89), an almost threefold higher risk for mortality due to unnatural causes (aHR, 3.30; 95% CI, 3.05-3.57), and a higher risk for mortality due to natural causes (aHR, 1.31; 95% CI, 1.24-1.37).
- Of all the unnatural causes of death, suicide was most common (hazard ratio [HR], 4.90; 95% CI, 4.40-5.46), followed by accidents (HR, 1.92; 95% CI, 1.68-2.19).
- Similar results were found in the sibling comparison, where the HR of all-cause mortality was 1.85 (95% CI, 1.67-2.03), death from natural causes was 1.51 (95% CI, 1.35-1.68), and death from unnatural causes was 3.10 (95% CI, 2.52-3.80).
- Natural causes of death that were higher in the OCD vs non-OCD cohort included endocrine, nutritional, and metabolic diseases; mental and behavioral disorders; and diseases of the nervous, circulatory, respiratory, digestive, and genitourinary systems.
IN PRACTICE:
“Better surveillance, prevention, and early intervention strategies should be implemented to reduce the risk of fatal outcomes in people with OCD,” the authors wrote.
SOURCE:
Lorena Fernández de la Cruz, PhD, of Karolinska Institutet, Solna, Sweden, led the study, which was published online on January 17 in the British Medical Journal.
LIMITATIONS:
The study does not establish causality. Registry data used by the investigators only included diagnoses made in specialist care and may not have included diagnoses made in other settings. It is also unclear whether the findings, derived from a Swedish population, can be generalized to other populations, health systems, and medical practices.
DISCLOSURES:
The study was funded by the Swedish Council for Health, Working Life and Welfare, Region Stockholm, the Swedish Society of Medicine, and Karolinska Institutet. Dr. de la Cruz received royalties for contributing articles to UpToDate and Wolters Kluwer Health and for editorial work from Elsevier outside the submitted work. See the paper for disclosures of the other authors.
A version of this article appeared on Medscape.com.
TOPLINE:
Obsessive-compulsive disorder (OCD) is linked to a twofold increased risk for all-cause mortality and a heightened risk for death from both natural and unnatural causes, a new study showed.
METHODOLOGY:
- Investigators studied a population-based cohort (58% female) of 61,378 people with OCD and 613,780 unaffected individuals from several Swedish population registers and a sibling cohort of 34,085 people with OCD (58% female) and 47,874 unaffected full siblings (48% female).
- The median 8.1-year follow-up and median age at first diagnosis of OCD were 27 years.
- The researchers used Cox proportional hazard models, adjusting for birth year, sex, county, country of birth (Sweden vs abroad), and sociodemographic variables.
TAKEAWAY:
- (adjusted hazard ratio [aHR], 1.82; 95% CI, 1.76-1.89), an almost threefold higher risk for mortality due to unnatural causes (aHR, 3.30; 95% CI, 3.05-3.57), and a higher risk for mortality due to natural causes (aHR, 1.31; 95% CI, 1.24-1.37).
- Of all the unnatural causes of death, suicide was most common (hazard ratio [HR], 4.90; 95% CI, 4.40-5.46), followed by accidents (HR, 1.92; 95% CI, 1.68-2.19).
- Similar results were found in the sibling comparison, where the HR of all-cause mortality was 1.85 (95% CI, 1.67-2.03), death from natural causes was 1.51 (95% CI, 1.35-1.68), and death from unnatural causes was 3.10 (95% CI, 2.52-3.80).
- Natural causes of death that were higher in the OCD vs non-OCD cohort included endocrine, nutritional, and metabolic diseases; mental and behavioral disorders; and diseases of the nervous, circulatory, respiratory, digestive, and genitourinary systems.
IN PRACTICE:
“Better surveillance, prevention, and early intervention strategies should be implemented to reduce the risk of fatal outcomes in people with OCD,” the authors wrote.
SOURCE:
Lorena Fernández de la Cruz, PhD, of Karolinska Institutet, Solna, Sweden, led the study, which was published online on January 17 in the British Medical Journal.
LIMITATIONS:
The study does not establish causality. Registry data used by the investigators only included diagnoses made in specialist care and may not have included diagnoses made in other settings. It is also unclear whether the findings, derived from a Swedish population, can be generalized to other populations, health systems, and medical practices.
DISCLOSURES:
The study was funded by the Swedish Council for Health, Working Life and Welfare, Region Stockholm, the Swedish Society of Medicine, and Karolinska Institutet. Dr. de la Cruz received royalties for contributing articles to UpToDate and Wolters Kluwer Health and for editorial work from Elsevier outside the submitted work. See the paper for disclosures of the other authors.
A version of this article appeared on Medscape.com.
Commentary: Benign Breast Disease, PD-L1+ TNBC, and Exercise in BC, February 2024
The benefit of immunotherapy in combination with chemotherapy for programmed death–ligand 1–positive (PD-L1+) metastatic triple-negative breast cancer (mTNBC) has been shown in both the IMpassion130 and KEYNOTE-355 trials.[2,3] However, the IMpassion131 trial, which evaluated atezolizumab plus paclitaxel, did not show a progression-free survival (PFS) or overall survival (OS) benefit vs paclitaxel alone in PD-L1+ mTNBC.[4] Various explanations for these divergent results have been proposed, including the inherent properties of the chemotherapy backbone, patient populations, and the heterogenous nature of TNBC, which can affect response to immunotherapy. Of present, the various KEYNOTE-355 regimens (pembrolizumab plus investigator's choice chemotherapy [nab-paclitaxel, paclitaxel, or gemcitabine-carboplatin]) are US Food and Drug Administration approved for PD-L1+ mTNBC in the first-line setting. The phase 2 randomized TBCRC 043 trial investigated the effect of atezolizumab with carboplatin in patients with mTNBC and further looked at clinical and molecular correlates of response (Lehmann et al). A total of 106 patients were randomly assigned to carboplatin or carboplatin plus atezolizumab; the combination improved PFS (median PFS, 4.1 vs 2.2 mo; hazard ratio [HR] 0.66; P = .05) and OS (12.6 vs 8.6 mo; HR 0.60; P = .03). Grade 3/4 serious adverse events were more common with carboplatin-atezolizumab vs carboplatin alone (41% vs 8%). In addition, an association of better responses with PD-L1 immunotherapy was seen in patients with obesity, uncontrolled blood glucose levels, high tumor mutation burden, and increased tumor infiltrating lymphocytes. These data support the role of immunotherapy in mTNBC, highlight tumor heterogeneity within this subtype and encourage correlative studies to better define which patients benefit from immunotherapy.
Various studies have demonstrated the favorable impact of physical activity on breast cancer risk in postmenopausal women.[5] However, data in premenopausal women is less clear. Various mechanisms connecting physical activity to premenopausal breast cancer risk have been proposed including the effect of exercise on sex steroid hormones, fasting insulin levels, and inflammation.[6] A pooled analysis from 19 cohort studies including 547,601 premenopausal women, with 10,231 incident cases of breast cancer, aimed to examine the relationship between leisure-time physical activity (sports, exercise, recreational walking) and breast cancer risk in young women (Timmins et al). Higher (90th percentile) vs lower (10th percentile) levels of leisure-time physical activity were associated with a 10% reduction in breast cancer risk after adjustment for body mass index (BMI; adjusted HR 0.90; 95% CI 0.85-0.95; P < .001). They also found a significant reduction in risk: 32% (HR 0.68; P = .01) and 9% (HR 0.91; P = .005) for women with underweight (BMI < 18.5) and with average weight (BMI 18.5-24.9), respectively. Further, the effect of physical activity was most pronounced in the human epidermal growth factor receptor 2 (HER2)–enriched breast cancer subtype, wherein higher vs lower levels of activity were associated with an estimated 45% reduction in breast cancer risk (adjusted HR 0.55; 95% CI 0.37-0.82). These findings support the beneficial role of aerobic exercise and healthy body weight on breast cancer risk among premenopausal women and highlight the value of incorporating this information into counseling for our patients.
Additional References
- Figueroa JD, Gierach GL, Duggan MA, et al. Risk factors for breast cancer development by tumor characteristics among women with benign breast disease. Breast Cancer Res. 2021;23:34. doi: 10.1186/s13058-021-01410-1 Source
- Schmid P, Adams S, Rugo HS, et al, for the IMpassion130 Trial Investigators. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med. 2018;379:2108-2121. doi: 10.1056/nejmoa1809615 Source
- Cortes J, Rugo HS, Cescon DW, et al, for the KEYNOTE-355 Investigators. Pembrolizumab plus chemotherapy in advanced triple-negative breast cancer. N Engl J Med. 2022;387:217-226. doi: 10.1056/NEJMoa2202809 Source
- Miles D, Gligorov J, André F, et al, on behalf of the IMpassion131 investigators. Primary results from IMpassion131, a double-blind, placebo-controlled, randomised phase III trial of first-line paclitaxel with or without atezolizumab for unresectable locally advanced/metastatic triple-negative breast cancer. Ann Oncol. 2021;32:994-1004. doi: 10.1016/j.annonc.2021.05.801 Source
- Eliassen AH, Hankinson SE, Rosner B, et al. Physical activity and risk of breast cancer among postmenopausal women. Arch Intern Med. 2010;170:1758-1764. doi: 10.1001/archinternmed.2010.363 Source
- Swain CTV, Drummond AE, Boing L, et al. Linking physical activity to breast cancer via sex hormones, part 1: The effect of physical activity on sex steroid hormones. Cancer Epidemiol Biomarkers Prev. 2022;31:16-27. doi: 10.1158/1055-9965.EPI-21-0437 Source
The benefit of immunotherapy in combination with chemotherapy for programmed death–ligand 1–positive (PD-L1+) metastatic triple-negative breast cancer (mTNBC) has been shown in both the IMpassion130 and KEYNOTE-355 trials.[2,3] However, the IMpassion131 trial, which evaluated atezolizumab plus paclitaxel, did not show a progression-free survival (PFS) or overall survival (OS) benefit vs paclitaxel alone in PD-L1+ mTNBC.[4] Various explanations for these divergent results have been proposed, including the inherent properties of the chemotherapy backbone, patient populations, and the heterogenous nature of TNBC, which can affect response to immunotherapy. Of present, the various KEYNOTE-355 regimens (pembrolizumab plus investigator's choice chemotherapy [nab-paclitaxel, paclitaxel, or gemcitabine-carboplatin]) are US Food and Drug Administration approved for PD-L1+ mTNBC in the first-line setting. The phase 2 randomized TBCRC 043 trial investigated the effect of atezolizumab with carboplatin in patients with mTNBC and further looked at clinical and molecular correlates of response (Lehmann et al). A total of 106 patients were randomly assigned to carboplatin or carboplatin plus atezolizumab; the combination improved PFS (median PFS, 4.1 vs 2.2 mo; hazard ratio [HR] 0.66; P = .05) and OS (12.6 vs 8.6 mo; HR 0.60; P = .03). Grade 3/4 serious adverse events were more common with carboplatin-atezolizumab vs carboplatin alone (41% vs 8%). In addition, an association of better responses with PD-L1 immunotherapy was seen in patients with obesity, uncontrolled blood glucose levels, high tumor mutation burden, and increased tumor infiltrating lymphocytes. These data support the role of immunotherapy in mTNBC, highlight tumor heterogeneity within this subtype and encourage correlative studies to better define which patients benefit from immunotherapy.
Various studies have demonstrated the favorable impact of physical activity on breast cancer risk in postmenopausal women.[5] However, data in premenopausal women is less clear. Various mechanisms connecting physical activity to premenopausal breast cancer risk have been proposed including the effect of exercise on sex steroid hormones, fasting insulin levels, and inflammation.[6] A pooled analysis from 19 cohort studies including 547,601 premenopausal women, with 10,231 incident cases of breast cancer, aimed to examine the relationship between leisure-time physical activity (sports, exercise, recreational walking) and breast cancer risk in young women (Timmins et al). Higher (90th percentile) vs lower (10th percentile) levels of leisure-time physical activity were associated with a 10% reduction in breast cancer risk after adjustment for body mass index (BMI; adjusted HR 0.90; 95% CI 0.85-0.95; P < .001). They also found a significant reduction in risk: 32% (HR 0.68; P = .01) and 9% (HR 0.91; P = .005) for women with underweight (BMI < 18.5) and with average weight (BMI 18.5-24.9), respectively. Further, the effect of physical activity was most pronounced in the human epidermal growth factor receptor 2 (HER2)–enriched breast cancer subtype, wherein higher vs lower levels of activity were associated with an estimated 45% reduction in breast cancer risk (adjusted HR 0.55; 95% CI 0.37-0.82). These findings support the beneficial role of aerobic exercise and healthy body weight on breast cancer risk among premenopausal women and highlight the value of incorporating this information into counseling for our patients.
Additional References
- Figueroa JD, Gierach GL, Duggan MA, et al. Risk factors for breast cancer development by tumor characteristics among women with benign breast disease. Breast Cancer Res. 2021;23:34. doi: 10.1186/s13058-021-01410-1 Source
- Schmid P, Adams S, Rugo HS, et al, for the IMpassion130 Trial Investigators. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med. 2018;379:2108-2121. doi: 10.1056/nejmoa1809615 Source
- Cortes J, Rugo HS, Cescon DW, et al, for the KEYNOTE-355 Investigators. Pembrolizumab plus chemotherapy in advanced triple-negative breast cancer. N Engl J Med. 2022;387:217-226. doi: 10.1056/NEJMoa2202809 Source
- Miles D, Gligorov J, André F, et al, on behalf of the IMpassion131 investigators. Primary results from IMpassion131, a double-blind, placebo-controlled, randomised phase III trial of first-line paclitaxel with or without atezolizumab for unresectable locally advanced/metastatic triple-negative breast cancer. Ann Oncol. 2021;32:994-1004. doi: 10.1016/j.annonc.2021.05.801 Source
- Eliassen AH, Hankinson SE, Rosner B, et al. Physical activity and risk of breast cancer among postmenopausal women. Arch Intern Med. 2010;170:1758-1764. doi: 10.1001/archinternmed.2010.363 Source
- Swain CTV, Drummond AE, Boing L, et al. Linking physical activity to breast cancer via sex hormones, part 1: The effect of physical activity on sex steroid hormones. Cancer Epidemiol Biomarkers Prev. 2022;31:16-27. doi: 10.1158/1055-9965.EPI-21-0437 Source
The benefit of immunotherapy in combination with chemotherapy for programmed death–ligand 1–positive (PD-L1+) metastatic triple-negative breast cancer (mTNBC) has been shown in both the IMpassion130 and KEYNOTE-355 trials.[2,3] However, the IMpassion131 trial, which evaluated atezolizumab plus paclitaxel, did not show a progression-free survival (PFS) or overall survival (OS) benefit vs paclitaxel alone in PD-L1+ mTNBC.[4] Various explanations for these divergent results have been proposed, including the inherent properties of the chemotherapy backbone, patient populations, and the heterogenous nature of TNBC, which can affect response to immunotherapy. Of present, the various KEYNOTE-355 regimens (pembrolizumab plus investigator's choice chemotherapy [nab-paclitaxel, paclitaxel, or gemcitabine-carboplatin]) are US Food and Drug Administration approved for PD-L1+ mTNBC in the first-line setting. The phase 2 randomized TBCRC 043 trial investigated the effect of atezolizumab with carboplatin in patients with mTNBC and further looked at clinical and molecular correlates of response (Lehmann et al). A total of 106 patients were randomly assigned to carboplatin or carboplatin plus atezolizumab; the combination improved PFS (median PFS, 4.1 vs 2.2 mo; hazard ratio [HR] 0.66; P = .05) and OS (12.6 vs 8.6 mo; HR 0.60; P = .03). Grade 3/4 serious adverse events were more common with carboplatin-atezolizumab vs carboplatin alone (41% vs 8%). In addition, an association of better responses with PD-L1 immunotherapy was seen in patients with obesity, uncontrolled blood glucose levels, high tumor mutation burden, and increased tumor infiltrating lymphocytes. These data support the role of immunotherapy in mTNBC, highlight tumor heterogeneity within this subtype and encourage correlative studies to better define which patients benefit from immunotherapy.
Various studies have demonstrated the favorable impact of physical activity on breast cancer risk in postmenopausal women.[5] However, data in premenopausal women is less clear. Various mechanisms connecting physical activity to premenopausal breast cancer risk have been proposed including the effect of exercise on sex steroid hormones, fasting insulin levels, and inflammation.[6] A pooled analysis from 19 cohort studies including 547,601 premenopausal women, with 10,231 incident cases of breast cancer, aimed to examine the relationship between leisure-time physical activity (sports, exercise, recreational walking) and breast cancer risk in young women (Timmins et al). Higher (90th percentile) vs lower (10th percentile) levels of leisure-time physical activity were associated with a 10% reduction in breast cancer risk after adjustment for body mass index (BMI; adjusted HR 0.90; 95% CI 0.85-0.95; P < .001). They also found a significant reduction in risk: 32% (HR 0.68; P = .01) and 9% (HR 0.91; P = .005) for women with underweight (BMI < 18.5) and with average weight (BMI 18.5-24.9), respectively. Further, the effect of physical activity was most pronounced in the human epidermal growth factor receptor 2 (HER2)–enriched breast cancer subtype, wherein higher vs lower levels of activity were associated with an estimated 45% reduction in breast cancer risk (adjusted HR 0.55; 95% CI 0.37-0.82). These findings support the beneficial role of aerobic exercise and healthy body weight on breast cancer risk among premenopausal women and highlight the value of incorporating this information into counseling for our patients.
Additional References
- Figueroa JD, Gierach GL, Duggan MA, et al. Risk factors for breast cancer development by tumor characteristics among women with benign breast disease. Breast Cancer Res. 2021;23:34. doi: 10.1186/s13058-021-01410-1 Source
- Schmid P, Adams S, Rugo HS, et al, for the IMpassion130 Trial Investigators. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med. 2018;379:2108-2121. doi: 10.1056/nejmoa1809615 Source
- Cortes J, Rugo HS, Cescon DW, et al, for the KEYNOTE-355 Investigators. Pembrolizumab plus chemotherapy in advanced triple-negative breast cancer. N Engl J Med. 2022;387:217-226. doi: 10.1056/NEJMoa2202809 Source
- Miles D, Gligorov J, André F, et al, on behalf of the IMpassion131 investigators. Primary results from IMpassion131, a double-blind, placebo-controlled, randomised phase III trial of first-line paclitaxel with or without atezolizumab for unresectable locally advanced/metastatic triple-negative breast cancer. Ann Oncol. 2021;32:994-1004. doi: 10.1016/j.annonc.2021.05.801 Source
- Eliassen AH, Hankinson SE, Rosner B, et al. Physical activity and risk of breast cancer among postmenopausal women. Arch Intern Med. 2010;170:1758-1764. doi: 10.1001/archinternmed.2010.363 Source
- Swain CTV, Drummond AE, Boing L, et al. Linking physical activity to breast cancer via sex hormones, part 1: The effect of physical activity on sex steroid hormones. Cancer Epidemiol Biomarkers Prev. 2022;31:16-27. doi: 10.1158/1055-9965.EPI-21-0437 Source


